User login
With Proper Training, AI Can Be a Useful Tool in Epilepsy Management
ORLANDO — Experts shed light on the applications, benefits, and pitfalls of artificial intelligence (AI) during the Merrit-Putnam Symposium at the annual meeting of the American Epilepsy Society (AES).
In a session titled “Artificial Intelligence Fundamentals and Breakthrough Applications in Epilepsy,” University of Pittsburgh neurologist and assistant professor Wesley Kerr, MD, PhD, provided an overview of AI as well its applications in neurology. He began by addressing perhaps one of the most controversial topics regarding AI in the medical community: clinicians’ fear of being replaced by technology.
he told the audience.
To Optimize AI, Clinicians Must Lay the Proper Foundation
Dr. Kerr’s presentation focused on providing audience members with tools to help them evaluate new technologies, recognize benefits, and identify key costs and limitations associated with AI implementation and integration into clinical practice.
Before delving deeper, one must first understand basic terminology regarding AI. Without this knowledge, clinicians may inadvertently introduce bias or errata or fail to understand how to best leverage the technology to enhance the quality of the practice while improving patient outcomes.
Machine learning (ML) describes the process of using data to learn a specific task. Deep learning (DL) stacks multiple layers of ML to improve performance on the task. Lastly, generative AI generates content such as text, images, and media.
Utilizing AI effectively in clinical applications involves tapping into select features most related to prediction (for example, disease factors) and grouping features into categories based on measuring commonalities such as factor composition in a population. This information should be used in training data only.
Fully understanding ML/AI allows clinicians to use it as a diagnostic test by exploiting a combination of accuracy, sensitivity, and specificity, along with positive and negative predictive values.
Data Fidelity and Integrity Hinge on Optimal Data Inputs
In the case of epilepsy, calibration curves can provide practical guidance in terms of predicting impending seizures.
“ML/AI needs gold-standard labels for evaluation,” Dr. Kerr said. He went on to stress the importance of quality data inputs to optimize the fidelity of AI’s predictive analytics.
“If you input garbage, you’ll get garbage out,” he said. “So a lot of garbage going in means a lot of garbage out.”
Such “garbage” can result in missed or erroneous diagnoses, or even faulty predictions. Even when the data are complete, AI can draw incorrect conclusions based on trends for which it lacks proper context.
Dr. Kerr used epilepsy trends in the Black population to illustrate this problem.
“One potential bias is that AI can figure out a patient is Black without being told, and based on data that Black patients are less likely to get epilepsy surgery,” he said, “AI would say they don’t need it because they’re Black, which isn’t true.”
In other words, ML/AI can use systematic determinants of health, such as race, to learn what Dr. Kerr referred to as an “inappropriate association.”
For that reason, ML/AI users must test for bias.
Such data are often retrieved from electronic health records (EHR), which serve as an important source of data ML/AI input. Using EHR makes sense, as they are a major source of missed potential in improving prompt treatment. According to Dr. Kerr, 20% of academic neurologists’ notes miss seizure frequency, and 30% miss the age of onset.
In addition, International Classification of Diseases (ICD) codes create another hurdle depending on the type of code used. For example, epilepsy with G40 or 2 codes of R56 is reliable, while focal to bilateral versus generalized epilepsy proves more challenging.
AI Improves Efficiency in National Language Generation
Large language models (LLM) look at first drafts and can save time on formatting, image selection, and construction. Perhaps ChatGPT is the most famous LLM, but other tools in this category include Open AI and Bard. LLMs are trained on “the whole internet” and use publicly accessible text.
In these cases, prompts serve as input data. Output data are predictions of the first and subsequent words.
Many users appreciate the foundation LLMs provide in terms of facilitating and collating research and summarizing ideas. The LLM-generated text actually serves as a first draft, saving users time on more clerical tasks such as formatting, image selection, and structure. Notwithstanding, these tools still require human supervision to screen for hallucinations or to add specialized content.
“LLMs are a great starting place to save time but are loaded with errors,” Dr. Kerr said.
Even if the tools could produce error-free content, ethics still come into play when using AI-generated content without any alterations. Any ML/AI that has not been modified or supervised is considered plagiarism.
Yet, interestingly enough, Dr. Kerr found that patients respond more positively to AI than physicians when interacting.
“Patients felt that AI was more sensitive and compassionate because it was longer-winded and humans are short,” he said. He went on to argue that AI might actually prove useful in helping physicians to improve the quality of their patient interactions.
Dr. Kerr left the audience with these key takeaways:
- ML/AI is just one type of clinical tool with benefits and limitations. The technology conveys the advantages of freeing up the clinician’s time to focus on more human-centered tasks, improving clinical decisions in challenging situations, and improving efficiency.
- However, healthcare systems should understand that ML/AI is not 100% foolproof, as the software’s knowledge is limited to its training exposure, and proper use requires supervision.
ORLANDO — Experts shed light on the applications, benefits, and pitfalls of artificial intelligence (AI) during the Merrit-Putnam Symposium at the annual meeting of the American Epilepsy Society (AES).
In a session titled “Artificial Intelligence Fundamentals and Breakthrough Applications in Epilepsy,” University of Pittsburgh neurologist and assistant professor Wesley Kerr, MD, PhD, provided an overview of AI as well its applications in neurology. He began by addressing perhaps one of the most controversial topics regarding AI in the medical community: clinicians’ fear of being replaced by technology.
he told the audience.
To Optimize AI, Clinicians Must Lay the Proper Foundation
Dr. Kerr’s presentation focused on providing audience members with tools to help them evaluate new technologies, recognize benefits, and identify key costs and limitations associated with AI implementation and integration into clinical practice.
Before delving deeper, one must first understand basic terminology regarding AI. Without this knowledge, clinicians may inadvertently introduce bias or errata or fail to understand how to best leverage the technology to enhance the quality of the practice while improving patient outcomes.
Machine learning (ML) describes the process of using data to learn a specific task. Deep learning (DL) stacks multiple layers of ML to improve performance on the task. Lastly, generative AI generates content such as text, images, and media.
Utilizing AI effectively in clinical applications involves tapping into select features most related to prediction (for example, disease factors) and grouping features into categories based on measuring commonalities such as factor composition in a population. This information should be used in training data only.
Fully understanding ML/AI allows clinicians to use it as a diagnostic test by exploiting a combination of accuracy, sensitivity, and specificity, along with positive and negative predictive values.
Data Fidelity and Integrity Hinge on Optimal Data Inputs
In the case of epilepsy, calibration curves can provide practical guidance in terms of predicting impending seizures.
“ML/AI needs gold-standard labels for evaluation,” Dr. Kerr said. He went on to stress the importance of quality data inputs to optimize the fidelity of AI’s predictive analytics.
“If you input garbage, you’ll get garbage out,” he said. “So a lot of garbage going in means a lot of garbage out.”
Such “garbage” can result in missed or erroneous diagnoses, or even faulty predictions. Even when the data are complete, AI can draw incorrect conclusions based on trends for which it lacks proper context.
Dr. Kerr used epilepsy trends in the Black population to illustrate this problem.
“One potential bias is that AI can figure out a patient is Black without being told, and based on data that Black patients are less likely to get epilepsy surgery,” he said, “AI would say they don’t need it because they’re Black, which isn’t true.”
In other words, ML/AI can use systematic determinants of health, such as race, to learn what Dr. Kerr referred to as an “inappropriate association.”
For that reason, ML/AI users must test for bias.
Such data are often retrieved from electronic health records (EHR), which serve as an important source of data ML/AI input. Using EHR makes sense, as they are a major source of missed potential in improving prompt treatment. According to Dr. Kerr, 20% of academic neurologists’ notes miss seizure frequency, and 30% miss the age of onset.
In addition, International Classification of Diseases (ICD) codes create another hurdle depending on the type of code used. For example, epilepsy with G40 or 2 codes of R56 is reliable, while focal to bilateral versus generalized epilepsy proves more challenging.
AI Improves Efficiency in National Language Generation
Large language models (LLM) look at first drafts and can save time on formatting, image selection, and construction. Perhaps ChatGPT is the most famous LLM, but other tools in this category include Open AI and Bard. LLMs are trained on “the whole internet” and use publicly accessible text.
In these cases, prompts serve as input data. Output data are predictions of the first and subsequent words.
Many users appreciate the foundation LLMs provide in terms of facilitating and collating research and summarizing ideas. The LLM-generated text actually serves as a first draft, saving users time on more clerical tasks such as formatting, image selection, and structure. Notwithstanding, these tools still require human supervision to screen for hallucinations or to add specialized content.
“LLMs are a great starting place to save time but are loaded with errors,” Dr. Kerr said.
Even if the tools could produce error-free content, ethics still come into play when using AI-generated content without any alterations. Any ML/AI that has not been modified or supervised is considered plagiarism.
Yet, interestingly enough, Dr. Kerr found that patients respond more positively to AI than physicians when interacting.
“Patients felt that AI was more sensitive and compassionate because it was longer-winded and humans are short,” he said. He went on to argue that AI might actually prove useful in helping physicians to improve the quality of their patient interactions.
Dr. Kerr left the audience with these key takeaways:
- ML/AI is just one type of clinical tool with benefits and limitations. The technology conveys the advantages of freeing up the clinician’s time to focus on more human-centered tasks, improving clinical decisions in challenging situations, and improving efficiency.
- However, healthcare systems should understand that ML/AI is not 100% foolproof, as the software’s knowledge is limited to its training exposure, and proper use requires supervision.
ORLANDO — Experts shed light on the applications, benefits, and pitfalls of artificial intelligence (AI) during the Merrit-Putnam Symposium at the annual meeting of the American Epilepsy Society (AES).
In a session titled “Artificial Intelligence Fundamentals and Breakthrough Applications in Epilepsy,” University of Pittsburgh neurologist and assistant professor Wesley Kerr, MD, PhD, provided an overview of AI as well its applications in neurology. He began by addressing perhaps one of the most controversial topics regarding AI in the medical community: clinicians’ fear of being replaced by technology.
he told the audience.
To Optimize AI, Clinicians Must Lay the Proper Foundation
Dr. Kerr’s presentation focused on providing audience members with tools to help them evaluate new technologies, recognize benefits, and identify key costs and limitations associated with AI implementation and integration into clinical practice.
Before delving deeper, one must first understand basic terminology regarding AI. Without this knowledge, clinicians may inadvertently introduce bias or errata or fail to understand how to best leverage the technology to enhance the quality of the practice while improving patient outcomes.
Machine learning (ML) describes the process of using data to learn a specific task. Deep learning (DL) stacks multiple layers of ML to improve performance on the task. Lastly, generative AI generates content such as text, images, and media.
Utilizing AI effectively in clinical applications involves tapping into select features most related to prediction (for example, disease factors) and grouping features into categories based on measuring commonalities such as factor composition in a population. This information should be used in training data only.
Fully understanding ML/AI allows clinicians to use it as a diagnostic test by exploiting a combination of accuracy, sensitivity, and specificity, along with positive and negative predictive values.
Data Fidelity and Integrity Hinge on Optimal Data Inputs
In the case of epilepsy, calibration curves can provide practical guidance in terms of predicting impending seizures.
“ML/AI needs gold-standard labels for evaluation,” Dr. Kerr said. He went on to stress the importance of quality data inputs to optimize the fidelity of AI’s predictive analytics.
“If you input garbage, you’ll get garbage out,” he said. “So a lot of garbage going in means a lot of garbage out.”
Such “garbage” can result in missed or erroneous diagnoses, or even faulty predictions. Even when the data are complete, AI can draw incorrect conclusions based on trends for which it lacks proper context.
Dr. Kerr used epilepsy trends in the Black population to illustrate this problem.
“One potential bias is that AI can figure out a patient is Black without being told, and based on data that Black patients are less likely to get epilepsy surgery,” he said, “AI would say they don’t need it because they’re Black, which isn’t true.”
In other words, ML/AI can use systematic determinants of health, such as race, to learn what Dr. Kerr referred to as an “inappropriate association.”
For that reason, ML/AI users must test for bias.
Such data are often retrieved from electronic health records (EHR), which serve as an important source of data ML/AI input. Using EHR makes sense, as they are a major source of missed potential in improving prompt treatment. According to Dr. Kerr, 20% of academic neurologists’ notes miss seizure frequency, and 30% miss the age of onset.
In addition, International Classification of Diseases (ICD) codes create another hurdle depending on the type of code used. For example, epilepsy with G40 or 2 codes of R56 is reliable, while focal to bilateral versus generalized epilepsy proves more challenging.
AI Improves Efficiency in National Language Generation
Large language models (LLM) look at first drafts and can save time on formatting, image selection, and construction. Perhaps ChatGPT is the most famous LLM, but other tools in this category include Open AI and Bard. LLMs are trained on “the whole internet” and use publicly accessible text.
In these cases, prompts serve as input data. Output data are predictions of the first and subsequent words.
Many users appreciate the foundation LLMs provide in terms of facilitating and collating research and summarizing ideas. The LLM-generated text actually serves as a first draft, saving users time on more clerical tasks such as formatting, image selection, and structure. Notwithstanding, these tools still require human supervision to screen for hallucinations or to add specialized content.
“LLMs are a great starting place to save time but are loaded with errors,” Dr. Kerr said.
Even if the tools could produce error-free content, ethics still come into play when using AI-generated content without any alterations. Any ML/AI that has not been modified or supervised is considered plagiarism.
Yet, interestingly enough, Dr. Kerr found that patients respond more positively to AI than physicians when interacting.
“Patients felt that AI was more sensitive and compassionate because it was longer-winded and humans are short,” he said. He went on to argue that AI might actually prove useful in helping physicians to improve the quality of their patient interactions.
Dr. Kerr left the audience with these key takeaways:
- ML/AI is just one type of clinical tool with benefits and limitations. The technology conveys the advantages of freeing up the clinician’s time to focus on more human-centered tasks, improving clinical decisions in challenging situations, and improving efficiency.
- However, healthcare systems should understand that ML/AI is not 100% foolproof, as the software’s knowledge is limited to its training exposure, and proper use requires supervision.
FROM AES 2023
Magic Wand Initiative Empowers Dermatologists to Innovate
NEW YORK – .
The program was founded in 2013 by two Harvard Medical School dermatologists, Lilit Garibyan, MD, PhD, the program director, and her mentor R. Rox Anderson MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital (MGH), Boston. It was based on the idea that clinicians are in a unique position to identify gaps in patient care and should be active in developing medical solutions to address those gaps.
“I truly believe that if we do a better job educating, training, and empowering our clinicians to become innovators, this will benefit patients and hospitals and physicians,” Dr. Garibyan said at the 26th annual Mount Sinai Winter Symposium — Advances in Medical and Surgical Dermatology.
One of the seeds for the project was her own experience with cryolipolysis which involves topical cooling, a noninvasive method of removing subcutaneous fat for body contouring, which relies on conducting heat from subcutaneous fat across the skin and therefore, does not reach fat far from the dermis. With Dr. Anderson’s mentorship, she developed injectable cooling technology (ICT), a procedure where “ice slurry,” composed of normal saline and glycerol, is directly injected into adipose tissue, possibly leading to more efficient and effective cryolipolysis.
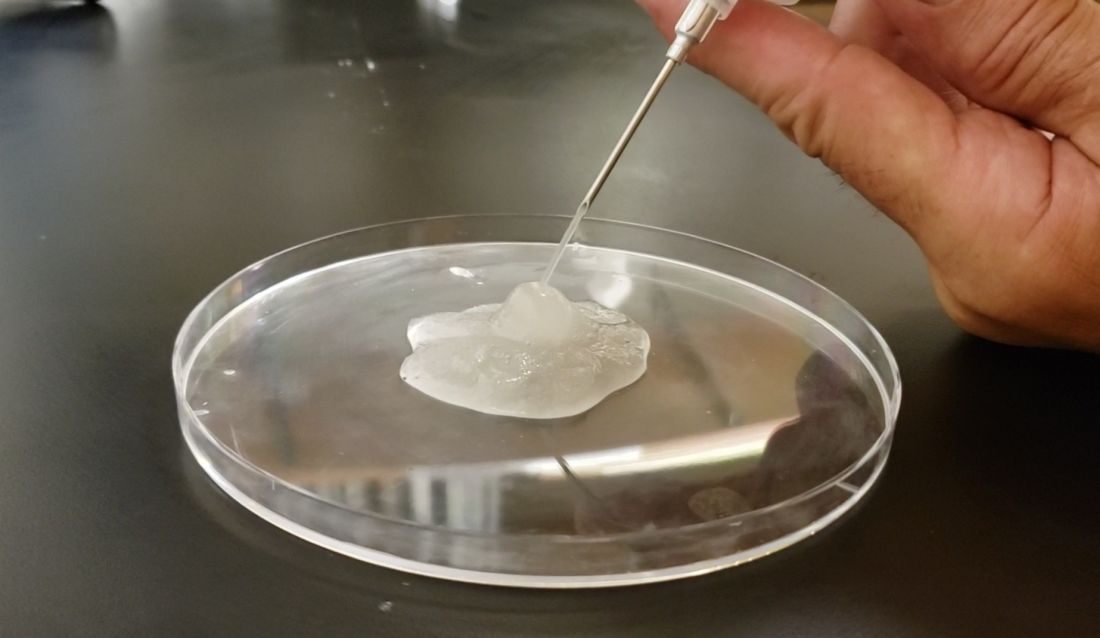
After nearly 10 years of animal studies at MGH, led by Dr. Garibyan as proof of concept trials, ice slurry (Coolio Therapy) recently received FDA breakthrough designation for long-term pain control and early-stage human trials of clinical applications are underway, she noted.
Magic Wand Program
In the Magic Wand program, participating physicians start by recording areas of unmet needs in their day-to-day practices, and in groups, engage in clinician-only brainstorming sessions to screen ideas, define problems, and generate lists of specifications and tools needed to address clinical problems. After working together to define challenges and possible solutions, they take their ideas to a development team, where scientists, engineers, regulatory experts, and industry professionals meet and help clinicians start pilot proof-of-concept projects, develop prototypes, and gain support for studies, followed by pilot feasibility studies.
Part of the project is the Virtual Magic Wand (VMW) Initiative, a 10-month online instructive and interactive course open to clinicians in the United States and Europe, designed to bring together dermatologists “interested in deeply understanding a dermatologic clinical problem worth solving,” according to Dr. Garibyan. Currently, there are more than 86 VMW scholars from 46 institutions, and military and private practice sites in the United States. The VMW was expanded to Europe in 2021 and there are plans to expand to Asia as well, she said.
The success of the program is not only attributed to its clinical methods but the fact that it provides a benefit to doctors at all stages of their careers, patients, and industry. “This is the only program that aims to engage in innovation from resident to full professor. We provide ideas that industry can then support and bring to market. Everyone including patients, doctors, and healthcare companies can benefit from active, engaged, and innovative physicians,” Dr. Garibyan said.
One of the success stories is that of Veradermics, a company founded by Kansas City dermatologist, Reid A. Waldman, MD, the company’s CEO, and Tim Durso, MD, the president, who met while participating in the VMW program in 2020, which eventually led them to start a company addressing an unmet need in dermatology, a kid-friendly treatment of warts.
In an interview with this news organization, Dr. Waldman explained how the program informed his company’s ethos. “Magic Wand Initiative is about identifying problems worth solving,” he said. At the company, “we find problems or unmet needs that are large enough to motivate prescribing changes, so we’ve really taken the philosophy I learned in the program into this company and building our portfolio.”
One of the first needs that Veradermics addressed was the fact that treatment for common warts, cryotherapy with liquid nitrogen, is painful and can frighten children, and, with a response rate of “at best, 50%,” Dr. Waldman said. Veradermics is in the process of creating a nearly painless, child-friendly wart treatment: an “immunostimulatory dissolvable microarray” patch that contains Candida antigen extract, which is currently being evaluated for treating warts in a phase 2 clinical trial started in 2023.
Although the Magic Wand Initiative was initially restricted to dermatologists at MGH, stories like that of Veradermics have made the program so popular that it has branched out to include anesthesiologists and otolaryngologists, as well as general and orthopedic surgeons at MGH, Dr. Garibyan said at the Mount Sinai meeting.
Dr. Garibyan disclosed that she is a cofounder of and has equity in Brixton Biosciences and EyeCool, and is a consultant for and/or investor in Brixton and Clarity Cosmetics. Royalties/inventorship are assigned to MGH.
NEW YORK – .
The program was founded in 2013 by two Harvard Medical School dermatologists, Lilit Garibyan, MD, PhD, the program director, and her mentor R. Rox Anderson MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital (MGH), Boston. It was based on the idea that clinicians are in a unique position to identify gaps in patient care and should be active in developing medical solutions to address those gaps.
“I truly believe that if we do a better job educating, training, and empowering our clinicians to become innovators, this will benefit patients and hospitals and physicians,” Dr. Garibyan said at the 26th annual Mount Sinai Winter Symposium — Advances in Medical and Surgical Dermatology.
One of the seeds for the project was her own experience with cryolipolysis which involves topical cooling, a noninvasive method of removing subcutaneous fat for body contouring, which relies on conducting heat from subcutaneous fat across the skin and therefore, does not reach fat far from the dermis. With Dr. Anderson’s mentorship, she developed injectable cooling technology (ICT), a procedure where “ice slurry,” composed of normal saline and glycerol, is directly injected into adipose tissue, possibly leading to more efficient and effective cryolipolysis.
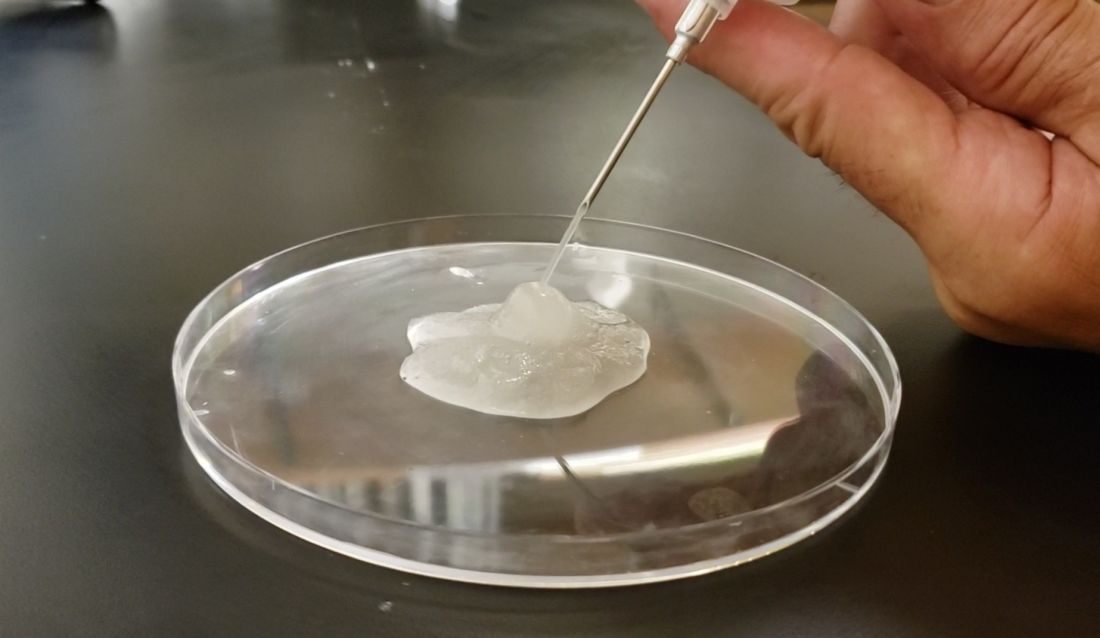
After nearly 10 years of animal studies at MGH, led by Dr. Garibyan as proof of concept trials, ice slurry (Coolio Therapy) recently received FDA breakthrough designation for long-term pain control and early-stage human trials of clinical applications are underway, she noted.
Magic Wand Program
In the Magic Wand program, participating physicians start by recording areas of unmet needs in their day-to-day practices, and in groups, engage in clinician-only brainstorming sessions to screen ideas, define problems, and generate lists of specifications and tools needed to address clinical problems. After working together to define challenges and possible solutions, they take their ideas to a development team, where scientists, engineers, regulatory experts, and industry professionals meet and help clinicians start pilot proof-of-concept projects, develop prototypes, and gain support for studies, followed by pilot feasibility studies.
Part of the project is the Virtual Magic Wand (VMW) Initiative, a 10-month online instructive and interactive course open to clinicians in the United States and Europe, designed to bring together dermatologists “interested in deeply understanding a dermatologic clinical problem worth solving,” according to Dr. Garibyan. Currently, there are more than 86 VMW scholars from 46 institutions, and military and private practice sites in the United States. The VMW was expanded to Europe in 2021 and there are plans to expand to Asia as well, she said.
The success of the program is not only attributed to its clinical methods but the fact that it provides a benefit to doctors at all stages of their careers, patients, and industry. “This is the only program that aims to engage in innovation from resident to full professor. We provide ideas that industry can then support and bring to market. Everyone including patients, doctors, and healthcare companies can benefit from active, engaged, and innovative physicians,” Dr. Garibyan said.
One of the success stories is that of Veradermics, a company founded by Kansas City dermatologist, Reid A. Waldman, MD, the company’s CEO, and Tim Durso, MD, the president, who met while participating in the VMW program in 2020, which eventually led them to start a company addressing an unmet need in dermatology, a kid-friendly treatment of warts.
In an interview with this news organization, Dr. Waldman explained how the program informed his company’s ethos. “Magic Wand Initiative is about identifying problems worth solving,” he said. At the company, “we find problems or unmet needs that are large enough to motivate prescribing changes, so we’ve really taken the philosophy I learned in the program into this company and building our portfolio.”
One of the first needs that Veradermics addressed was the fact that treatment for common warts, cryotherapy with liquid nitrogen, is painful and can frighten children, and, with a response rate of “at best, 50%,” Dr. Waldman said. Veradermics is in the process of creating a nearly painless, child-friendly wart treatment: an “immunostimulatory dissolvable microarray” patch that contains Candida antigen extract, which is currently being evaluated for treating warts in a phase 2 clinical trial started in 2023.
Although the Magic Wand Initiative was initially restricted to dermatologists at MGH, stories like that of Veradermics have made the program so popular that it has branched out to include anesthesiologists and otolaryngologists, as well as general and orthopedic surgeons at MGH, Dr. Garibyan said at the Mount Sinai meeting.
Dr. Garibyan disclosed that she is a cofounder of and has equity in Brixton Biosciences and EyeCool, and is a consultant for and/or investor in Brixton and Clarity Cosmetics. Royalties/inventorship are assigned to MGH.
NEW YORK – .
The program was founded in 2013 by two Harvard Medical School dermatologists, Lilit Garibyan, MD, PhD, the program director, and her mentor R. Rox Anderson MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital (MGH), Boston. It was based on the idea that clinicians are in a unique position to identify gaps in patient care and should be active in developing medical solutions to address those gaps.
“I truly believe that if we do a better job educating, training, and empowering our clinicians to become innovators, this will benefit patients and hospitals and physicians,” Dr. Garibyan said at the 26th annual Mount Sinai Winter Symposium — Advances in Medical and Surgical Dermatology.
One of the seeds for the project was her own experience with cryolipolysis which involves topical cooling, a noninvasive method of removing subcutaneous fat for body contouring, which relies on conducting heat from subcutaneous fat across the skin and therefore, does not reach fat far from the dermis. With Dr. Anderson’s mentorship, she developed injectable cooling technology (ICT), a procedure where “ice slurry,” composed of normal saline and glycerol, is directly injected into adipose tissue, possibly leading to more efficient and effective cryolipolysis.
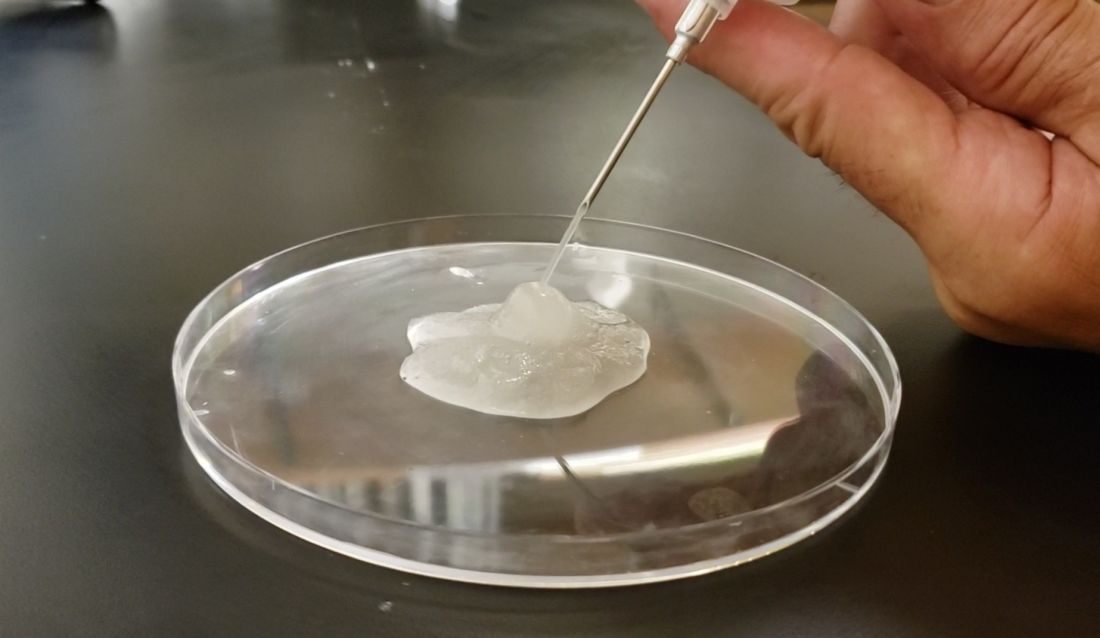
After nearly 10 years of animal studies at MGH, led by Dr. Garibyan as proof of concept trials, ice slurry (Coolio Therapy) recently received FDA breakthrough designation for long-term pain control and early-stage human trials of clinical applications are underway, she noted.
Magic Wand Program
In the Magic Wand program, participating physicians start by recording areas of unmet needs in their day-to-day practices, and in groups, engage in clinician-only brainstorming sessions to screen ideas, define problems, and generate lists of specifications and tools needed to address clinical problems. After working together to define challenges and possible solutions, they take their ideas to a development team, where scientists, engineers, regulatory experts, and industry professionals meet and help clinicians start pilot proof-of-concept projects, develop prototypes, and gain support for studies, followed by pilot feasibility studies.
Part of the project is the Virtual Magic Wand (VMW) Initiative, a 10-month online instructive and interactive course open to clinicians in the United States and Europe, designed to bring together dermatologists “interested in deeply understanding a dermatologic clinical problem worth solving,” according to Dr. Garibyan. Currently, there are more than 86 VMW scholars from 46 institutions, and military and private practice sites in the United States. The VMW was expanded to Europe in 2021 and there are plans to expand to Asia as well, she said.
The success of the program is not only attributed to its clinical methods but the fact that it provides a benefit to doctors at all stages of their careers, patients, and industry. “This is the only program that aims to engage in innovation from resident to full professor. We provide ideas that industry can then support and bring to market. Everyone including patients, doctors, and healthcare companies can benefit from active, engaged, and innovative physicians,” Dr. Garibyan said.
One of the success stories is that of Veradermics, a company founded by Kansas City dermatologist, Reid A. Waldman, MD, the company’s CEO, and Tim Durso, MD, the president, who met while participating in the VMW program in 2020, which eventually led them to start a company addressing an unmet need in dermatology, a kid-friendly treatment of warts.
In an interview with this news organization, Dr. Waldman explained how the program informed his company’s ethos. “Magic Wand Initiative is about identifying problems worth solving,” he said. At the company, “we find problems or unmet needs that are large enough to motivate prescribing changes, so we’ve really taken the philosophy I learned in the program into this company and building our portfolio.”
One of the first needs that Veradermics addressed was the fact that treatment for common warts, cryotherapy with liquid nitrogen, is painful and can frighten children, and, with a response rate of “at best, 50%,” Dr. Waldman said. Veradermics is in the process of creating a nearly painless, child-friendly wart treatment: an “immunostimulatory dissolvable microarray” patch that contains Candida antigen extract, which is currently being evaluated for treating warts in a phase 2 clinical trial started in 2023.
Although the Magic Wand Initiative was initially restricted to dermatologists at MGH, stories like that of Veradermics have made the program so popular that it has branched out to include anesthesiologists and otolaryngologists, as well as general and orthopedic surgeons at MGH, Dr. Garibyan said at the Mount Sinai meeting.
Dr. Garibyan disclosed that she is a cofounder of and has equity in Brixton Biosciences and EyeCool, and is a consultant for and/or investor in Brixton and Clarity Cosmetics. Royalties/inventorship are assigned to MGH.
Biosimilar Business Deals Keep Up ‘Musical Chairs’ Game of Formulary Construction
As the saying goes, “The more things change, the more they stay the same.” That is particularly true when it comes to the affordability of drugs for our patients even after the launch of so many Humira biosimilars. And we still have the “musical chairs” game of formulary construction — when the music stops, who knows whether your patient’s drug found a chair to sit on. There seems to be only a few chairs available for the many adalimumab biosimilars playing the game.
Nothing has changed since my testimony before the FDA Arthritis Advisory Committee in July 2016 during the approval hearing of the first Humira biosimilar. Below is a quote from that meeting where I was speaking predominantly about the pharmacy side of drugs.
“I’d like to highlight the term ‘access’ because none of us are really naive enough to believe that just approving a biosimilar gives a patient true, hands-on access to the medication, because even if the biosimilar is offered at a 30% discount, I don’t have any patients that can afford it. This means that access is ultimately controlled by third-party payers.”
My prediction, that approving and launching biosimilars with lower prices would not ensure patient access to the drug unless it is paid for by insurance, is now our reality. Today, a drug with an 85% discount on the price of Humira is still unattainable for patients without a “payer.”
Competition and Lower Prices
Lawmakers and some in the media cry for more competition to lower prices. This is the main reason that there has been such a push to get biosimilars to the market as quickly as possible. It is abundantly clear that competition to get on the formulary is fierce. Placement of a medication on a formulary can make or break a manufacturer’s ability to get a return on the R&D and make a profit on that medication. For a small biotech manufacturer, it can be the difference between “life and death” of the company.
Does anyone remember when the first interchangeable biosimilar for the reference insulin glargine product Lantus (insulin glargine-yfgn; Semglee) came to market in 2021? Janet Woodcock, MD, then acting FDA commissioner, called it a “momentous day” and further said, “Today’s approval of the first interchangeable biosimilar product furthers FDA’s longstanding commitment to support a competitive marketplace for biological products and ultimately empowers patients by helping to increase access to safe, effective and high-quality medications at potentially lower cost.” There was a high-priced interchangeable biosimilar and an identical unbranded low-priced interchangeable biosimilar, and the only one that could get formulary placement was the high-priced drug.
Patients pay their cost share on the list price of the drug, and because most pharmacy benefit managers’ (PBMs’) formularies cover only the high-priced biosimilar, patients never share in the savings. So much for the “competitive marketplace” creating lower costs for patients. This is just one of hundreds of examples in which lower-priced drugs are excluded from the formulary. It is unfortunate that the bidding process from manufacturers to PBMs to “win” preferred formulary placement is like an art auction, where the highest bidder wins.
Biosimilars and Formulary Construction
For those of us who have been looking into PBMs for many years, it is no surprise that PBMs’ formulary construction has become a profit center for them. Now, with so many adalimumab biosimilars having entered the market, it has become the Wild West where only those with the most money to fork over to the PBMs get preferred placement. Unfortunately, many of the choices that make money for the PBM cost employers and patients more.
How did we get here? In the 1980s and 90s, the price of medications began to increase to the point that many were not affordable without insurance. And who better to construct the list of drugs that would be covered by insurance (formulary) than the PBMs who were already adjudicating the claims for these drugs. The Federal Trade Commission (FTC) realized the power inherent in constructing this list of medications known as the formulary. So when the manufacturer Merck acquired the PBM Medco in the mid-1990s, the FTC stepped in. The FTC surmised that making the drugs and deciding which ones will be paid for created a “conflict of interest” with anticompetitive ramifications.
So, in 1998, William J. Baer, director of the FTC’s Bureau of Competition, said, “Our investigation into the PBM industry has revealed that Merck’s acquisition of Medco has reduced competition in the market for pharmaceutical products … We have found that Medco has given favorable treatment to Merck drugs. As a result, in some cases, consumers have been denied access to the drugs of competing manufacturers. In addition, the merger has made it possible for Medco to share with Merck sensitive pricing information it gets from Merck’s competitors, which could foster collusion among drug manufacturers.” Wow!
These anticompetitive behaviors and conflicts of interest resulting from the Medco acquisition led the FTC to propose a consent agreement.
The agreement would require Merck-Medco to maintain an “open formulary” — one that includes drugs selected and approved by an independent Pharmacy and Therapeutics Committee regardless of the manufacturer. Medco would have to accept rebates and other price concessions and reflect these in the ranking of the drugs on the formulary. Merck would have to make known the availability of the open formulary to any drug maker with an agreement with Medco.
Let’s hope the FTC of 2024 remembers the stance of the FTC in the 1990s regarding anticompetitive behavior involved in formulary construction.
Conflicts of Interest
But today it is apparent that crafting formularies that pay only for the drugs that make the most money for the PBM is not a conflict of interest. In its policy manual, Cigna directly tells employers and employees that they are collecting and keeping rebates and fees on medical pharmaceuticals, and they are not for the benefit of the employer or the plan.
And now, in August 2023, CVS launched Cordavis, a subsidiary wholly owned by CVS. Cordavis/CVS has partnered with Sandoz, which makes Hyrimoz, an adalimumab biosimilar. There is a high-priced version that is discounted 5% from Humira, a lower-cost unbranded version that is discounted 80% off the list price of Humira, and a co-branded CVS/Sandoz version of Hyrimoz that is lower priced as well.
It isn’t a surprise that CVS’ Standard and Advanced Commercial and Chart formularies are offering only Sandoz adalimumab biosimilar products. While these formularies have excluded Humira, CVS has entered into an agreement with AbbVie to allow Humira on a number of their other formularies. It can be very confusing.
As stated earlier, in the 1990s, the FTC frowned upon manufacturers owning PBMs and allowing them to construct their own formularies. Here we have CVS Health, mothership for the PBM CVS Caremark, owning a company that will be co-producing biosimilars with other manufacturers and then determining which biosimilars are on their formularies. The FTC knew back then that the tendency would be to offer only their own drugs for coverage, thus reducing competition. This is exactly what the CVS-Cordavis-Sandoz partnership has done for their Standard and Advanced Commercial and Chart formularies. It is perhaps anti-competitive but certainly profitable.
Perhaps the FTC should require the same consent agreement that was given to Merck in 1998. CVS Caremark would then have to open their formularies to all competitors of their co-branded, co-produced Sandoz biosimilar.
Summary
It is the same old adage, “The more things change, the more they stay the same.” PBMs are still constructing formularies with biosimilars based on their profitability, with huge differences between gross and net cost. Patients still pay their cost share on the list (gross) price. With the CVS-Cordavis-Sandoz partnership, more vertical integration has led to yet another profit river. Self-funded employers are still getting the wool pulled over their eyes by the big three PBMs who threaten to take away rebates if they don’t choose the preferred formularies. The employers don’t realize that sometimes it is less expensive to choose the lower-priced drugs with no rebates, and that holds true for biosimilars as well.
Let’s hope that the FTC investigates the situation of a PBM partnering with a manufacturer and then choosing only that manufacturer’s drugs for many of their formularies.
We need to continue our advocacy for our patients because the medication that has kept them stable for so long may find itself without a chair the next time the music stops.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
As the saying goes, “The more things change, the more they stay the same.” That is particularly true when it comes to the affordability of drugs for our patients even after the launch of so many Humira biosimilars. And we still have the “musical chairs” game of formulary construction — when the music stops, who knows whether your patient’s drug found a chair to sit on. There seems to be only a few chairs available for the many adalimumab biosimilars playing the game.
Nothing has changed since my testimony before the FDA Arthritis Advisory Committee in July 2016 during the approval hearing of the first Humira biosimilar. Below is a quote from that meeting where I was speaking predominantly about the pharmacy side of drugs.
“I’d like to highlight the term ‘access’ because none of us are really naive enough to believe that just approving a biosimilar gives a patient true, hands-on access to the medication, because even if the biosimilar is offered at a 30% discount, I don’t have any patients that can afford it. This means that access is ultimately controlled by third-party payers.”
My prediction, that approving and launching biosimilars with lower prices would not ensure patient access to the drug unless it is paid for by insurance, is now our reality. Today, a drug with an 85% discount on the price of Humira is still unattainable for patients without a “payer.”
Competition and Lower Prices
Lawmakers and some in the media cry for more competition to lower prices. This is the main reason that there has been such a push to get biosimilars to the market as quickly as possible. It is abundantly clear that competition to get on the formulary is fierce. Placement of a medication on a formulary can make or break a manufacturer’s ability to get a return on the R&D and make a profit on that medication. For a small biotech manufacturer, it can be the difference between “life and death” of the company.
Does anyone remember when the first interchangeable biosimilar for the reference insulin glargine product Lantus (insulin glargine-yfgn; Semglee) came to market in 2021? Janet Woodcock, MD, then acting FDA commissioner, called it a “momentous day” and further said, “Today’s approval of the first interchangeable biosimilar product furthers FDA’s longstanding commitment to support a competitive marketplace for biological products and ultimately empowers patients by helping to increase access to safe, effective and high-quality medications at potentially lower cost.” There was a high-priced interchangeable biosimilar and an identical unbranded low-priced interchangeable biosimilar, and the only one that could get formulary placement was the high-priced drug.
Patients pay their cost share on the list price of the drug, and because most pharmacy benefit managers’ (PBMs’) formularies cover only the high-priced biosimilar, patients never share in the savings. So much for the “competitive marketplace” creating lower costs for patients. This is just one of hundreds of examples in which lower-priced drugs are excluded from the formulary. It is unfortunate that the bidding process from manufacturers to PBMs to “win” preferred formulary placement is like an art auction, where the highest bidder wins.
Biosimilars and Formulary Construction
For those of us who have been looking into PBMs for many years, it is no surprise that PBMs’ formulary construction has become a profit center for them. Now, with so many adalimumab biosimilars having entered the market, it has become the Wild West where only those with the most money to fork over to the PBMs get preferred placement. Unfortunately, many of the choices that make money for the PBM cost employers and patients more.
How did we get here? In the 1980s and 90s, the price of medications began to increase to the point that many were not affordable without insurance. And who better to construct the list of drugs that would be covered by insurance (formulary) than the PBMs who were already adjudicating the claims for these drugs. The Federal Trade Commission (FTC) realized the power inherent in constructing this list of medications known as the formulary. So when the manufacturer Merck acquired the PBM Medco in the mid-1990s, the FTC stepped in. The FTC surmised that making the drugs and deciding which ones will be paid for created a “conflict of interest” with anticompetitive ramifications.
So, in 1998, William J. Baer, director of the FTC’s Bureau of Competition, said, “Our investigation into the PBM industry has revealed that Merck’s acquisition of Medco has reduced competition in the market for pharmaceutical products … We have found that Medco has given favorable treatment to Merck drugs. As a result, in some cases, consumers have been denied access to the drugs of competing manufacturers. In addition, the merger has made it possible for Medco to share with Merck sensitive pricing information it gets from Merck’s competitors, which could foster collusion among drug manufacturers.” Wow!
These anticompetitive behaviors and conflicts of interest resulting from the Medco acquisition led the FTC to propose a consent agreement.
The agreement would require Merck-Medco to maintain an “open formulary” — one that includes drugs selected and approved by an independent Pharmacy and Therapeutics Committee regardless of the manufacturer. Medco would have to accept rebates and other price concessions and reflect these in the ranking of the drugs on the formulary. Merck would have to make known the availability of the open formulary to any drug maker with an agreement with Medco.
Let’s hope the FTC of 2024 remembers the stance of the FTC in the 1990s regarding anticompetitive behavior involved in formulary construction.
Conflicts of Interest
But today it is apparent that crafting formularies that pay only for the drugs that make the most money for the PBM is not a conflict of interest. In its policy manual, Cigna directly tells employers and employees that they are collecting and keeping rebates and fees on medical pharmaceuticals, and they are not for the benefit of the employer or the plan.
And now, in August 2023, CVS launched Cordavis, a subsidiary wholly owned by CVS. Cordavis/CVS has partnered with Sandoz, which makes Hyrimoz, an adalimumab biosimilar. There is a high-priced version that is discounted 5% from Humira, a lower-cost unbranded version that is discounted 80% off the list price of Humira, and a co-branded CVS/Sandoz version of Hyrimoz that is lower priced as well.
It isn’t a surprise that CVS’ Standard and Advanced Commercial and Chart formularies are offering only Sandoz adalimumab biosimilar products. While these formularies have excluded Humira, CVS has entered into an agreement with AbbVie to allow Humira on a number of their other formularies. It can be very confusing.
As stated earlier, in the 1990s, the FTC frowned upon manufacturers owning PBMs and allowing them to construct their own formularies. Here we have CVS Health, mothership for the PBM CVS Caremark, owning a company that will be co-producing biosimilars with other manufacturers and then determining which biosimilars are on their formularies. The FTC knew back then that the tendency would be to offer only their own drugs for coverage, thus reducing competition. This is exactly what the CVS-Cordavis-Sandoz partnership has done for their Standard and Advanced Commercial and Chart formularies. It is perhaps anti-competitive but certainly profitable.
Perhaps the FTC should require the same consent agreement that was given to Merck in 1998. CVS Caremark would then have to open their formularies to all competitors of their co-branded, co-produced Sandoz biosimilar.
Summary
It is the same old adage, “The more things change, the more they stay the same.” PBMs are still constructing formularies with biosimilars based on their profitability, with huge differences between gross and net cost. Patients still pay their cost share on the list (gross) price. With the CVS-Cordavis-Sandoz partnership, more vertical integration has led to yet another profit river. Self-funded employers are still getting the wool pulled over their eyes by the big three PBMs who threaten to take away rebates if they don’t choose the preferred formularies. The employers don’t realize that sometimes it is less expensive to choose the lower-priced drugs with no rebates, and that holds true for biosimilars as well.
Let’s hope that the FTC investigates the situation of a PBM partnering with a manufacturer and then choosing only that manufacturer’s drugs for many of their formularies.
We need to continue our advocacy for our patients because the medication that has kept them stable for so long may find itself without a chair the next time the music stops.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
As the saying goes, “The more things change, the more they stay the same.” That is particularly true when it comes to the affordability of drugs for our patients even after the launch of so many Humira biosimilars. And we still have the “musical chairs” game of formulary construction — when the music stops, who knows whether your patient’s drug found a chair to sit on. There seems to be only a few chairs available for the many adalimumab biosimilars playing the game.
Nothing has changed since my testimony before the FDA Arthritis Advisory Committee in July 2016 during the approval hearing of the first Humira biosimilar. Below is a quote from that meeting where I was speaking predominantly about the pharmacy side of drugs.
“I’d like to highlight the term ‘access’ because none of us are really naive enough to believe that just approving a biosimilar gives a patient true, hands-on access to the medication, because even if the biosimilar is offered at a 30% discount, I don’t have any patients that can afford it. This means that access is ultimately controlled by third-party payers.”
My prediction, that approving and launching biosimilars with lower prices would not ensure patient access to the drug unless it is paid for by insurance, is now our reality. Today, a drug with an 85% discount on the price of Humira is still unattainable for patients without a “payer.”
Competition and Lower Prices
Lawmakers and some in the media cry for more competition to lower prices. This is the main reason that there has been such a push to get biosimilars to the market as quickly as possible. It is abundantly clear that competition to get on the formulary is fierce. Placement of a medication on a formulary can make or break a manufacturer’s ability to get a return on the R&D and make a profit on that medication. For a small biotech manufacturer, it can be the difference between “life and death” of the company.
Does anyone remember when the first interchangeable biosimilar for the reference insulin glargine product Lantus (insulin glargine-yfgn; Semglee) came to market in 2021? Janet Woodcock, MD, then acting FDA commissioner, called it a “momentous day” and further said, “Today’s approval of the first interchangeable biosimilar product furthers FDA’s longstanding commitment to support a competitive marketplace for biological products and ultimately empowers patients by helping to increase access to safe, effective and high-quality medications at potentially lower cost.” There was a high-priced interchangeable biosimilar and an identical unbranded low-priced interchangeable biosimilar, and the only one that could get formulary placement was the high-priced drug.
Patients pay their cost share on the list price of the drug, and because most pharmacy benefit managers’ (PBMs’) formularies cover only the high-priced biosimilar, patients never share in the savings. So much for the “competitive marketplace” creating lower costs for patients. This is just one of hundreds of examples in which lower-priced drugs are excluded from the formulary. It is unfortunate that the bidding process from manufacturers to PBMs to “win” preferred formulary placement is like an art auction, where the highest bidder wins.
Biosimilars and Formulary Construction
For those of us who have been looking into PBMs for many years, it is no surprise that PBMs’ formulary construction has become a profit center for them. Now, with so many adalimumab biosimilars having entered the market, it has become the Wild West where only those with the most money to fork over to the PBMs get preferred placement. Unfortunately, many of the choices that make money for the PBM cost employers and patients more.
How did we get here? In the 1980s and 90s, the price of medications began to increase to the point that many were not affordable without insurance. And who better to construct the list of drugs that would be covered by insurance (formulary) than the PBMs who were already adjudicating the claims for these drugs. The Federal Trade Commission (FTC) realized the power inherent in constructing this list of medications known as the formulary. So when the manufacturer Merck acquired the PBM Medco in the mid-1990s, the FTC stepped in. The FTC surmised that making the drugs and deciding which ones will be paid for created a “conflict of interest” with anticompetitive ramifications.
So, in 1998, William J. Baer, director of the FTC’s Bureau of Competition, said, “Our investigation into the PBM industry has revealed that Merck’s acquisition of Medco has reduced competition in the market for pharmaceutical products … We have found that Medco has given favorable treatment to Merck drugs. As a result, in some cases, consumers have been denied access to the drugs of competing manufacturers. In addition, the merger has made it possible for Medco to share with Merck sensitive pricing information it gets from Merck’s competitors, which could foster collusion among drug manufacturers.” Wow!
These anticompetitive behaviors and conflicts of interest resulting from the Medco acquisition led the FTC to propose a consent agreement.
The agreement would require Merck-Medco to maintain an “open formulary” — one that includes drugs selected and approved by an independent Pharmacy and Therapeutics Committee regardless of the manufacturer. Medco would have to accept rebates and other price concessions and reflect these in the ranking of the drugs on the formulary. Merck would have to make known the availability of the open formulary to any drug maker with an agreement with Medco.
Let’s hope the FTC of 2024 remembers the stance of the FTC in the 1990s regarding anticompetitive behavior involved in formulary construction.
Conflicts of Interest
But today it is apparent that crafting formularies that pay only for the drugs that make the most money for the PBM is not a conflict of interest. In its policy manual, Cigna directly tells employers and employees that they are collecting and keeping rebates and fees on medical pharmaceuticals, and they are not for the benefit of the employer or the plan.
And now, in August 2023, CVS launched Cordavis, a subsidiary wholly owned by CVS. Cordavis/CVS has partnered with Sandoz, which makes Hyrimoz, an adalimumab biosimilar. There is a high-priced version that is discounted 5% from Humira, a lower-cost unbranded version that is discounted 80% off the list price of Humira, and a co-branded CVS/Sandoz version of Hyrimoz that is lower priced as well.
It isn’t a surprise that CVS’ Standard and Advanced Commercial and Chart formularies are offering only Sandoz adalimumab biosimilar products. While these formularies have excluded Humira, CVS has entered into an agreement with AbbVie to allow Humira on a number of their other formularies. It can be very confusing.
As stated earlier, in the 1990s, the FTC frowned upon manufacturers owning PBMs and allowing them to construct their own formularies. Here we have CVS Health, mothership for the PBM CVS Caremark, owning a company that will be co-producing biosimilars with other manufacturers and then determining which biosimilars are on their formularies. The FTC knew back then that the tendency would be to offer only their own drugs for coverage, thus reducing competition. This is exactly what the CVS-Cordavis-Sandoz partnership has done for their Standard and Advanced Commercial and Chart formularies. It is perhaps anti-competitive but certainly profitable.
Perhaps the FTC should require the same consent agreement that was given to Merck in 1998. CVS Caremark would then have to open their formularies to all competitors of their co-branded, co-produced Sandoz biosimilar.
Summary
It is the same old adage, “The more things change, the more they stay the same.” PBMs are still constructing formularies with biosimilars based on their profitability, with huge differences between gross and net cost. Patients still pay their cost share on the list (gross) price. With the CVS-Cordavis-Sandoz partnership, more vertical integration has led to yet another profit river. Self-funded employers are still getting the wool pulled over their eyes by the big three PBMs who threaten to take away rebates if they don’t choose the preferred formularies. The employers don’t realize that sometimes it is less expensive to choose the lower-priced drugs with no rebates, and that holds true for biosimilars as well.
Let’s hope that the FTC investigates the situation of a PBM partnering with a manufacturer and then choosing only that manufacturer’s drugs for many of their formularies.
We need to continue our advocacy for our patients because the medication that has kept them stable for so long may find itself without a chair the next time the music stops.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
Acidogenic diet may be negative in patients with PsA
Key clinical point: In patients with psoriatic arthritis (PsA), a high dietary acid load (DAL), evaluated through potential renal acid load (PRAL) and net endogenous acid production (NEAP), was associated with increased disease activity and inflammation.
Major finding: The mean Disease Activity Index for PsA scores were higher in patients with PsA who had high vs low PRAL (19.8 vs 14.0; P = .006) and high vs low NEAP (20.3 vs 13.5; P = .001). In addition, patients in the high vs low PRAL and NEAP groups had significantly higher C-reactive protein levels (P = .024 and P = .020, respectively), indicating increased inflammation.
Study details: Findings are from a cross-sectional study that included 58 patients with overweight or obesity and a diagnosis of PsA.
Disclosures: This study did not disclose any funding. The authors declared no conflicts of interest.
Source: Öteleş S et al. The dietary acid load is associated with disease severity in psoriatic arthritis. Mod Rheumatol. 2023 (Nov 10). doi: 10.1093/mr/road107
Key clinical point: In patients with psoriatic arthritis (PsA), a high dietary acid load (DAL), evaluated through potential renal acid load (PRAL) and net endogenous acid production (NEAP), was associated with increased disease activity and inflammation.
Major finding: The mean Disease Activity Index for PsA scores were higher in patients with PsA who had high vs low PRAL (19.8 vs 14.0; P = .006) and high vs low NEAP (20.3 vs 13.5; P = .001). In addition, patients in the high vs low PRAL and NEAP groups had significantly higher C-reactive protein levels (P = .024 and P = .020, respectively), indicating increased inflammation.
Study details: Findings are from a cross-sectional study that included 58 patients with overweight or obesity and a diagnosis of PsA.
Disclosures: This study did not disclose any funding. The authors declared no conflicts of interest.
Source: Öteleş S et al. The dietary acid load is associated with disease severity in psoriatic arthritis. Mod Rheumatol. 2023 (Nov 10). doi: 10.1093/mr/road107
Key clinical point: In patients with psoriatic arthritis (PsA), a high dietary acid load (DAL), evaluated through potential renal acid load (PRAL) and net endogenous acid production (NEAP), was associated with increased disease activity and inflammation.
Major finding: The mean Disease Activity Index for PsA scores were higher in patients with PsA who had high vs low PRAL (19.8 vs 14.0; P = .006) and high vs low NEAP (20.3 vs 13.5; P = .001). In addition, patients in the high vs low PRAL and NEAP groups had significantly higher C-reactive protein levels (P = .024 and P = .020, respectively), indicating increased inflammation.
Study details: Findings are from a cross-sectional study that included 58 patients with overweight or obesity and a diagnosis of PsA.
Disclosures: This study did not disclose any funding. The authors declared no conflicts of interest.
Source: Öteleş S et al. The dietary acid load is associated with disease severity in psoriatic arthritis. Mod Rheumatol. 2023 (Nov 10). doi: 10.1093/mr/road107
Age at natural menopause and reproductive lifespan tied to PsA risk
Key clinical point: The risk for late-onset psoriatic arthritis (PsA) was higher in women who attained early natural menopause and had shorter reproductive years.
Major finding: The risk for incident PsA reduced by 46% and 34% in women who reached natural menopause at ≥55 vs <45 years of age and had a reproductive lifespan of ≥38 vs <38 years, respectively (P ≤ .006 for all). The partial population-attributable risk estimated that approximately 1/5 of late-onset PsA incidences could be prevented if women went through menopause after the age of 55 years.
Study details: This prospective cohort study included postmenopausal women without psoriatic diseases from the UK Biobank, who were investigated for incident psoriasis (n = 139,572) or PsA (n = 142,329).
Disclosures: This study was supported by the National Natural Science Foundation of China and the Huxiang Youth Talent Supporting Program of Hunan. The authors declared no conflicts of interest.
Source: Xiao Y et al. Age at natural menopause, reproductive lifespan and the risk of late-onset psoriasis and psoriatic arthritis in women: A prospective cohort study. J Invest Dermatol. 2023 (Dec 9). doi: 10.1016/j.jid.2023.11.010
Key clinical point: The risk for late-onset psoriatic arthritis (PsA) was higher in women who attained early natural menopause and had shorter reproductive years.
Major finding: The risk for incident PsA reduced by 46% and 34% in women who reached natural menopause at ≥55 vs <45 years of age and had a reproductive lifespan of ≥38 vs <38 years, respectively (P ≤ .006 for all). The partial population-attributable risk estimated that approximately 1/5 of late-onset PsA incidences could be prevented if women went through menopause after the age of 55 years.
Study details: This prospective cohort study included postmenopausal women without psoriatic diseases from the UK Biobank, who were investigated for incident psoriasis (n = 139,572) or PsA (n = 142,329).
Disclosures: This study was supported by the National Natural Science Foundation of China and the Huxiang Youth Talent Supporting Program of Hunan. The authors declared no conflicts of interest.
Source: Xiao Y et al. Age at natural menopause, reproductive lifespan and the risk of late-onset psoriasis and psoriatic arthritis in women: A prospective cohort study. J Invest Dermatol. 2023 (Dec 9). doi: 10.1016/j.jid.2023.11.010
Key clinical point: The risk for late-onset psoriatic arthritis (PsA) was higher in women who attained early natural menopause and had shorter reproductive years.
Major finding: The risk for incident PsA reduced by 46% and 34% in women who reached natural menopause at ≥55 vs <45 years of age and had a reproductive lifespan of ≥38 vs <38 years, respectively (P ≤ .006 for all). The partial population-attributable risk estimated that approximately 1/5 of late-onset PsA incidences could be prevented if women went through menopause after the age of 55 years.
Study details: This prospective cohort study included postmenopausal women without psoriatic diseases from the UK Biobank, who were investigated for incident psoriasis (n = 139,572) or PsA (n = 142,329).
Disclosures: This study was supported by the National Natural Science Foundation of China and the Huxiang Youth Talent Supporting Program of Hunan. The authors declared no conflicts of interest.
Source: Xiao Y et al. Age at natural menopause, reproductive lifespan and the risk of late-onset psoriasis and psoriatic arthritis in women: A prospective cohort study. J Invest Dermatol. 2023 (Dec 9). doi: 10.1016/j.jid.2023.11.010
Factors associated with poor sleep quality in PsA
Key clinical point: Poor sleep quality was a very common phenomenon in patients with psoriatic arthritis (PsA) and associated with increased disease activity and higher levels of pain, fatigue, anxiety, and depression.
Major finding: A majority (63%) of patients with PsA experienced poor sleep quality, with factors like higher Disease Activity Index for PsA scores, pain, fatigue, anxiety, and depression (P < .01 for all) associated with poorer sleep quality. Patients with vs without fibromyalgia also reported poorer sleep quality (P < .001).
Study details: Findings are from a single-center cross-sectional study that included 247 patients with PsA.
Disclosures: This study received medical writing/editorial assistance from the Spanish Foundation of Rheumatology. The authors declared no conflicts of interest.
Source: Toledano E et al. SLEEP quality in patients with psoriatic arthritis and its relationship with disease activity and comorbidities: A cross-sectional study. Sci Rep. 2023;13:22927 (Dec 21). doi: 10.1038/s41598-023-48723-z
Key clinical point: Poor sleep quality was a very common phenomenon in patients with psoriatic arthritis (PsA) and associated with increased disease activity and higher levels of pain, fatigue, anxiety, and depression.
Major finding: A majority (63%) of patients with PsA experienced poor sleep quality, with factors like higher Disease Activity Index for PsA scores, pain, fatigue, anxiety, and depression (P < .01 for all) associated with poorer sleep quality. Patients with vs without fibromyalgia also reported poorer sleep quality (P < .001).
Study details: Findings are from a single-center cross-sectional study that included 247 patients with PsA.
Disclosures: This study received medical writing/editorial assistance from the Spanish Foundation of Rheumatology. The authors declared no conflicts of interest.
Source: Toledano E et al. SLEEP quality in patients with psoriatic arthritis and its relationship with disease activity and comorbidities: A cross-sectional study. Sci Rep. 2023;13:22927 (Dec 21). doi: 10.1038/s41598-023-48723-z
Key clinical point: Poor sleep quality was a very common phenomenon in patients with psoriatic arthritis (PsA) and associated with increased disease activity and higher levels of pain, fatigue, anxiety, and depression.
Major finding: A majority (63%) of patients with PsA experienced poor sleep quality, with factors like higher Disease Activity Index for PsA scores, pain, fatigue, anxiety, and depression (P < .01 for all) associated with poorer sleep quality. Patients with vs without fibromyalgia also reported poorer sleep quality (P < .001).
Study details: Findings are from a single-center cross-sectional study that included 247 patients with PsA.
Disclosures: This study received medical writing/editorial assistance from the Spanish Foundation of Rheumatology. The authors declared no conflicts of interest.
Source: Toledano E et al. SLEEP quality in patients with psoriatic arthritis and its relationship with disease activity and comorbidities: A cross-sectional study. Sci Rep. 2023;13:22927 (Dec 21). doi: 10.1038/s41598-023-48723-z
Novel targeted therapies linked with the risk for melanoma and nonmelanoma skin cancer in PsA
Key clinical point: Adult patients with psoriatic arthritis (PsA) who received biologics, such as interleukin (IL)-12/23, IL-23, and IL-17 inhibitors, or small molecules, such as Janus kinase inhibitors, reported a risk for melanoma and nonmelanoma skin cancer (NMSC).
Major finding: In patients with PsA, the incidence rate of melanoma was 0.09 (95% CI 0.04-0.19) events per 100 patient years (PY) whereas that of NMSC was 0.47 (95% CI 0.28-0.81) events per 100 PY.
Study details: Findings are from a meta-analysis of 19 studies that included 13,739 patients with psoriasis and PsA who were treated with biologics or small molecules tested against an active or placebo comparator.
Disclosures: This study was funded by a research grant from Faculty of Medicine and Health Sciences, Andrzej Frycz Modrzewski Krakow University, Kraków, Poland. P Brzewski declared receiving honoraria or consultation fees from various sources.
Source: Krzysztofik M et al. Risk of melanoma and nonmelanoma skin cancer in patients with psoriasis and psoriatic arthritis treated with targeted therapies: A systematic review and meta-analysis. Pharmaceuticals. 2023;17(1):14 (Dec 21). doi: 10.3390/ph17010014
Key clinical point: Adult patients with psoriatic arthritis (PsA) who received biologics, such as interleukin (IL)-12/23, IL-23, and IL-17 inhibitors, or small molecules, such as Janus kinase inhibitors, reported a risk for melanoma and nonmelanoma skin cancer (NMSC).
Major finding: In patients with PsA, the incidence rate of melanoma was 0.09 (95% CI 0.04-0.19) events per 100 patient years (PY) whereas that of NMSC was 0.47 (95% CI 0.28-0.81) events per 100 PY.
Study details: Findings are from a meta-analysis of 19 studies that included 13,739 patients with psoriasis and PsA who were treated with biologics or small molecules tested against an active or placebo comparator.
Disclosures: This study was funded by a research grant from Faculty of Medicine and Health Sciences, Andrzej Frycz Modrzewski Krakow University, Kraków, Poland. P Brzewski declared receiving honoraria or consultation fees from various sources.
Source: Krzysztofik M et al. Risk of melanoma and nonmelanoma skin cancer in patients with psoriasis and psoriatic arthritis treated with targeted therapies: A systematic review and meta-analysis. Pharmaceuticals. 2023;17(1):14 (Dec 21). doi: 10.3390/ph17010014
Key clinical point: Adult patients with psoriatic arthritis (PsA) who received biologics, such as interleukin (IL)-12/23, IL-23, and IL-17 inhibitors, or small molecules, such as Janus kinase inhibitors, reported a risk for melanoma and nonmelanoma skin cancer (NMSC).
Major finding: In patients with PsA, the incidence rate of melanoma was 0.09 (95% CI 0.04-0.19) events per 100 patient years (PY) whereas that of NMSC was 0.47 (95% CI 0.28-0.81) events per 100 PY.
Study details: Findings are from a meta-analysis of 19 studies that included 13,739 patients with psoriasis and PsA who were treated with biologics or small molecules tested against an active or placebo comparator.
Disclosures: This study was funded by a research grant from Faculty of Medicine and Health Sciences, Andrzej Frycz Modrzewski Krakow University, Kraków, Poland. P Brzewski declared receiving honoraria or consultation fees from various sources.
Source: Krzysztofik M et al. Risk of melanoma and nonmelanoma skin cancer in patients with psoriasis and psoriatic arthritis treated with targeted therapies: A systematic review and meta-analysis. Pharmaceuticals. 2023;17(1):14 (Dec 21). doi: 10.3390/ph17010014
Dermatological manifestations vary in pediatric psoriasis vs PsA
Key clinical point: In pediatric patients, psoriasis vs psoriatic arthritis (PsA) was associated with greater body surface area (BSA) involvement particularly in the extremities, scalp, trunk, genitals, face, skin folds, and nails.
Major finding: The median BSA affected by psoriasis was higher in patients with psoriasis vs PsA (19.7% vs 6.1%; P = .029), with significantly greater disease distribution observed in extremities (75% vs 24%), scalp (61% vs 28%), trunk (58% vs 10%), and genitals (38% vs 10%; P < .05 for all).
Study details: Findings are from a retrospective case-control study that included pediatric patients (age < 18 years) with psoriasis (n = 64) or PsA (n = 29) who were matched by age and sex.
Disclosures: This study did not receive any external funding. The authors declared no conflicts of interest.
Source: Ollech A et al. Pediatric psoriasis with or without arthritis: Does it make a difference? J Clin Med. 2023;13(1):242 (Dec 31). doi: 10.3390/jcm13010242
Key clinical point: In pediatric patients, psoriasis vs psoriatic arthritis (PsA) was associated with greater body surface area (BSA) involvement particularly in the extremities, scalp, trunk, genitals, face, skin folds, and nails.
Major finding: The median BSA affected by psoriasis was higher in patients with psoriasis vs PsA (19.7% vs 6.1%; P = .029), with significantly greater disease distribution observed in extremities (75% vs 24%), scalp (61% vs 28%), trunk (58% vs 10%), and genitals (38% vs 10%; P < .05 for all).
Study details: Findings are from a retrospective case-control study that included pediatric patients (age < 18 years) with psoriasis (n = 64) or PsA (n = 29) who were matched by age and sex.
Disclosures: This study did not receive any external funding. The authors declared no conflicts of interest.
Source: Ollech A et al. Pediatric psoriasis with or without arthritis: Does it make a difference? J Clin Med. 2023;13(1):242 (Dec 31). doi: 10.3390/jcm13010242
Key clinical point: In pediatric patients, psoriasis vs psoriatic arthritis (PsA) was associated with greater body surface area (BSA) involvement particularly in the extremities, scalp, trunk, genitals, face, skin folds, and nails.
Major finding: The median BSA affected by psoriasis was higher in patients with psoriasis vs PsA (19.7% vs 6.1%; P = .029), with significantly greater disease distribution observed in extremities (75% vs 24%), scalp (61% vs 28%), trunk (58% vs 10%), and genitals (38% vs 10%; P < .05 for all).
Study details: Findings are from a retrospective case-control study that included pediatric patients (age < 18 years) with psoriasis (n = 64) or PsA (n = 29) who were matched by age and sex.
Disclosures: This study did not receive any external funding. The authors declared no conflicts of interest.
Source: Ollech A et al. Pediatric psoriasis with or without arthritis: Does it make a difference? J Clin Med. 2023;13(1):242 (Dec 31). doi: 10.3390/jcm13010242
Study identifies risk factors for uveitis in a PsA cohort
Key clinical point: The risk for uveitis was increased by more than double in patients with psoriatic arthritis (PsA), with past uveitis events and etanercept treatment being significant risk factors.
Major finding: The risk for uveitis was higher in patients with PsA vs matched control individuals without PsA (adjusted hazard ratio 2.38; 95% CI 1.80-3.15). Among patients with PsA, past events of uveitis (adjusted odds ratio [aOR] 136.4; 95% CI 27.38-679.88) and treatment with etanercept (aOR 2.57; 95% CI 1.45-4.57) were associated with an increased risk for uveitis.
Study details: This retrospective matched cohort study included 6147 patients with newly diagnosed PsA and 23,999 matched control individuals without PsA.
Disclosures: This study did not disclose the funding source. The authors declared no conflicts of interest.
Source: Hijazi N et al. The risk factors for uveitis among psoriatic arthritis patients: A population-based cohort study. Clin Rheumatol. 2023 (Dec 11). doi: 10.1007/s10067-023-06834-y
Key clinical point: The risk for uveitis was increased by more than double in patients with psoriatic arthritis (PsA), with past uveitis events and etanercept treatment being significant risk factors.
Major finding: The risk for uveitis was higher in patients with PsA vs matched control individuals without PsA (adjusted hazard ratio 2.38; 95% CI 1.80-3.15). Among patients with PsA, past events of uveitis (adjusted odds ratio [aOR] 136.4; 95% CI 27.38-679.88) and treatment with etanercept (aOR 2.57; 95% CI 1.45-4.57) were associated with an increased risk for uveitis.
Study details: This retrospective matched cohort study included 6147 patients with newly diagnosed PsA and 23,999 matched control individuals without PsA.
Disclosures: This study did not disclose the funding source. The authors declared no conflicts of interest.
Source: Hijazi N et al. The risk factors for uveitis among psoriatic arthritis patients: A population-based cohort study. Clin Rheumatol. 2023 (Dec 11). doi: 10.1007/s10067-023-06834-y
Key clinical point: The risk for uveitis was increased by more than double in patients with psoriatic arthritis (PsA), with past uveitis events and etanercept treatment being significant risk factors.
Major finding: The risk for uveitis was higher in patients with PsA vs matched control individuals without PsA (adjusted hazard ratio 2.38; 95% CI 1.80-3.15). Among patients with PsA, past events of uveitis (adjusted odds ratio [aOR] 136.4; 95% CI 27.38-679.88) and treatment with etanercept (aOR 2.57; 95% CI 1.45-4.57) were associated with an increased risk for uveitis.
Study details: This retrospective matched cohort study included 6147 patients with newly diagnosed PsA and 23,999 matched control individuals without PsA.
Disclosures: This study did not disclose the funding source. The authors declared no conflicts of interest.
Source: Hijazi N et al. The risk factors for uveitis among psoriatic arthritis patients: A population-based cohort study. Clin Rheumatol. 2023 (Dec 11). doi: 10.1007/s10067-023-06834-y
Both functional training and resistance exercise improve strength and function in PsA
Key clinical point: Functional training (FT) and resistance exercise (RE) improved functional capacity, functional status, disease activity, and muscle strength to a comparable extent in patients with psoriatic arthritis (PsA).
Major finding: FT and RE led to similar improvements in functional capacity measured by the Bath Ankylosing Spondylitis Functional Index (P = .919), functional status measured by the Health Assessment Questionnaire for the Spondyloarthropathies (P = 0.932), disease activity measured by the Bath Ankylosing Spondylitis Disease Activity Index (P = .700), and muscle strength in patients with PsA. No adverse event occurred in either group.
Study details: Findings are from a 12-week, single-blind trial that included 41 patients with PsA who were randomly assigned to undergo FT with elastic bands or RE with weight machines.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Silva DR et al. Effectiveness of functional training versus resistance exercise in patients with psoriatic arthritis: Randomized controlled trial. Adv Rheumatol. 2023;63:58. (Dec 13). doi: 10.1186/s42358-023-00342-y
Key clinical point: Functional training (FT) and resistance exercise (RE) improved functional capacity, functional status, disease activity, and muscle strength to a comparable extent in patients with psoriatic arthritis (PsA).
Major finding: FT and RE led to similar improvements in functional capacity measured by the Bath Ankylosing Spondylitis Functional Index (P = .919), functional status measured by the Health Assessment Questionnaire for the Spondyloarthropathies (P = 0.932), disease activity measured by the Bath Ankylosing Spondylitis Disease Activity Index (P = .700), and muscle strength in patients with PsA. No adverse event occurred in either group.
Study details: Findings are from a 12-week, single-blind trial that included 41 patients with PsA who were randomly assigned to undergo FT with elastic bands or RE with weight machines.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Silva DR et al. Effectiveness of functional training versus resistance exercise in patients with psoriatic arthritis: Randomized controlled trial. Adv Rheumatol. 2023;63:58. (Dec 13). doi: 10.1186/s42358-023-00342-y
Key clinical point: Functional training (FT) and resistance exercise (RE) improved functional capacity, functional status, disease activity, and muscle strength to a comparable extent in patients with psoriatic arthritis (PsA).
Major finding: FT and RE led to similar improvements in functional capacity measured by the Bath Ankylosing Spondylitis Functional Index (P = .919), functional status measured by the Health Assessment Questionnaire for the Spondyloarthropathies (P = 0.932), disease activity measured by the Bath Ankylosing Spondylitis Disease Activity Index (P = .700), and muscle strength in patients with PsA. No adverse event occurred in either group.
Study details: Findings are from a 12-week, single-blind trial that included 41 patients with PsA who were randomly assigned to undergo FT with elastic bands or RE with weight machines.
Disclosures: This study did not receive any funding. The authors declared no conflicts of interest.
Source: Silva DR et al. Effectiveness of functional training versus resistance exercise in patients with psoriatic arthritis: Randomized controlled trial. Adv Rheumatol. 2023;63:58. (Dec 13). doi: 10.1186/s42358-023-00342-y


