User login
FDA approves oral dacomitinib for some metastatic NSCLC
The Food and Drug Administration has approved dacomitinib tablets (VIZIMPRO) for the first-line treatment of metastatic non-small cell lung cancer in patients with epidermal growth factor receptor (EGFR) exon 19 deletion or exon 21 L858R substitution mutations.
The second-generation, irreversible EGFR tyrosine kinase inhibitor (TKI) has a recommended dose of 45 mg once daily with or without food.
The approval is based on the randomized, active-controlled 452-patient ARCHER 1050 trial, in which the drug showed improvement in progression-free survival (PFS) versus gefitinib. The median PFS was 14.7 in the dacomitinib arm, compared with 9.2 months in the gefitinib arm (hazard ratio 0.59).
ARCHER 1050 trial participants had good performance status, no prior therapy for metastatic disease or recurrent disease and were disease-free for at least 12 months following systemic non-EGFR TKI-containing therapy. Dacomitinib and gefitinib were given once-daily at 45 mg and 250 mg oral doses, respectively, until disease progression or unacceptable toxicity.
No improvement was seen in overall response rate or overall survival with dacomitinib vs. gefitinib.
Of 394 patients who received dacomitinib, 27% experienced serious adverse reactions – most often diarrhea, rash, paronychia, stomatitis, decreased appetite, dry skin, decreased weight, alopecia, cough, and pruritus, according to the FDA. Those that most often lead to discontinuation were diarrhea and interstitial lung disease. Prescribing information for dacomitinib contains warnings and precautions for interstitial lung disease, diarrhea, and dermatologic adverse reactions.
The Food and Drug Administration has approved dacomitinib tablets (VIZIMPRO) for the first-line treatment of metastatic non-small cell lung cancer in patients with epidermal growth factor receptor (EGFR) exon 19 deletion or exon 21 L858R substitution mutations.
The second-generation, irreversible EGFR tyrosine kinase inhibitor (TKI) has a recommended dose of 45 mg once daily with or without food.
The approval is based on the randomized, active-controlled 452-patient ARCHER 1050 trial, in which the drug showed improvement in progression-free survival (PFS) versus gefitinib. The median PFS was 14.7 in the dacomitinib arm, compared with 9.2 months in the gefitinib arm (hazard ratio 0.59).
ARCHER 1050 trial participants had good performance status, no prior therapy for metastatic disease or recurrent disease and were disease-free for at least 12 months following systemic non-EGFR TKI-containing therapy. Dacomitinib and gefitinib were given once-daily at 45 mg and 250 mg oral doses, respectively, until disease progression or unacceptable toxicity.
No improvement was seen in overall response rate or overall survival with dacomitinib vs. gefitinib.
Of 394 patients who received dacomitinib, 27% experienced serious adverse reactions – most often diarrhea, rash, paronychia, stomatitis, decreased appetite, dry skin, decreased weight, alopecia, cough, and pruritus, according to the FDA. Those that most often lead to discontinuation were diarrhea and interstitial lung disease. Prescribing information for dacomitinib contains warnings and precautions for interstitial lung disease, diarrhea, and dermatologic adverse reactions.
The Food and Drug Administration has approved dacomitinib tablets (VIZIMPRO) for the first-line treatment of metastatic non-small cell lung cancer in patients with epidermal growth factor receptor (EGFR) exon 19 deletion or exon 21 L858R substitution mutations.
The second-generation, irreversible EGFR tyrosine kinase inhibitor (TKI) has a recommended dose of 45 mg once daily with or without food.
The approval is based on the randomized, active-controlled 452-patient ARCHER 1050 trial, in which the drug showed improvement in progression-free survival (PFS) versus gefitinib. The median PFS was 14.7 in the dacomitinib arm, compared with 9.2 months in the gefitinib arm (hazard ratio 0.59).
ARCHER 1050 trial participants had good performance status, no prior therapy for metastatic disease or recurrent disease and were disease-free for at least 12 months following systemic non-EGFR TKI-containing therapy. Dacomitinib and gefitinib were given once-daily at 45 mg and 250 mg oral doses, respectively, until disease progression or unacceptable toxicity.
No improvement was seen in overall response rate or overall survival with dacomitinib vs. gefitinib.
Of 394 patients who received dacomitinib, 27% experienced serious adverse reactions – most often diarrhea, rash, paronychia, stomatitis, decreased appetite, dry skin, decreased weight, alopecia, cough, and pruritus, according to the FDA. Those that most often lead to discontinuation were diarrhea and interstitial lung disease. Prescribing information for dacomitinib contains warnings and precautions for interstitial lung disease, diarrhea, and dermatologic adverse reactions.
PACIFIC trial: Durvalumab improves both OS and PFS in stage III NSCLC
TORONTO – The programmed death-ligand 1 (PD-L1) inhibitor durvalumab significantly improves overall survival in patients with stage III unresectable non–small-cell lung cancer without progression after chemoradiotherapy, according to updated results from the global phase 3 PACIFIC study.
The findings, presented at the World Conference on Lung Cancer, follow a prior report from the study showing improved progression-free survival (PFS) in durvalumab-treated patients (stratified hazard ratio, 0.52), and together these survival benefits mark the first major advance in this disease setting in decades,” Scott J. Antonia, MD, reported at the conference, sponsored by the International Association for the Study of Lung Cancer (IASLC).
“The fact is this is a new standard of care treatment for the patients with this disease,” he said, adding that “in all likelihood we are improving the cure rate for the patients with this disease.”
The findings were published simultaneously in the New England Journal of Medicine.
Overall survival at a median follow-up of 25.2 months in 473 patients randomized to receive durvalumab was significantly greater than among 236 who received placebo (stratified HR, 0.68; median survival not reached vs. 28.7 months in the groups, respectively), said Dr. Antonia of the H. Lee Moffitt Cancer Center and Research Institute, and professor of oncologic sciences at the University of South Florida, Tampa.
Durvalumab also improved overall survival in all prespecified subgroups, and PFS was similar to that in previous reports (stratified HR 0.51; median of 17.2 vs. 5.6 months with durvalumab and placebo, respectively), he said, noting that “interestingly, patients who were nonsmokers did benefit from durvalumab.”
This is notable because prior research suggests that never-smokers with advanced stage cancer have less of a chance of responding to immunotherapy (although they should still be offered immunotherapy), he explained.
“Also interestingly, it appears as if cisplatin was the better drug to use in the conventional therapy portion of the treatment,” he said.
Durvalumab also provided continued improvement vs. placebo in time to death or distant metastasis (stratified HR, 0.53), time to second progression (stratified HR, 0.58), time to first subsequent therapy or death (stratified HR, 0.58), and time to second subsequent therapy or death (stratified HR, 0.63).
Study subjects were patients with World Health Organization Performance Status scores of 0 or 1 with any PD-L1 tumor status, who received at least two cycles of conventional standard-of-care platinum-based chemoradiotherapy (CRT). They were randomized between May 2014 and April 2016 – at 1-42 days after CRT – to receive intravenous durvalumab at a dose of 10 mg/kg given intravenously every 2 weeks or placebo, and were stratified by age, gender, and smoking history.
Durvalumab was well tolerated; 30.5% and 26.1% of treatment and placebo patients, respectively, had grade 3/4 adverse events, and 15.4% and 9.8%, respectively, discontinued because of adverse events.
“There were no new safety signals with this longer follow-up,” Dr. Antonia said.
After study treatment ended, 41% and 54% in the groups, respectively, received additional anticancer therapy, and 8% and 22.4%, respectively, received additional immunotherapy, he noted.
The results are not only statistically significant, but clinically meaningful, and they offer new hope for patients with a disease that, in those who receive chemoradiotherapy, has a 3-year survival rate of only about 27%, he said.
During a press briefing at the conference, moderator Frances Shepherd, MD, a medical oncologist at Princess Margaret Cancer Centre in Toronto and a past president of the International Association for the Study of Lung Cancer, called the results “very exciting” given that this type of cancer represents about a third of all lung cancers and therefore affects an “enormous number of patients in Canada and globally.”
The PACIFIC trial was sponsored by AstraZeneca. Dr. Antonia reported being a speaker or advisory board member or receiving funding support from AstraZeneca and numerous other companies. Dr. Shepherd reported receiving honoraria and support from AstraZeneca and others. She is a speaker or advisory board member for Eli Lilly, AstraZeneca, and Merck, and she has ownership Interest in Eli Lilly and AstraZeneca.
SOURCE: Antonia S et al., WCLC 2018 Abstract PL02.01.
TORONTO – The programmed death-ligand 1 (PD-L1) inhibitor durvalumab significantly improves overall survival in patients with stage III unresectable non–small-cell lung cancer without progression after chemoradiotherapy, according to updated results from the global phase 3 PACIFIC study.
The findings, presented at the World Conference on Lung Cancer, follow a prior report from the study showing improved progression-free survival (PFS) in durvalumab-treated patients (stratified hazard ratio, 0.52), and together these survival benefits mark the first major advance in this disease setting in decades,” Scott J. Antonia, MD, reported at the conference, sponsored by the International Association for the Study of Lung Cancer (IASLC).
“The fact is this is a new standard of care treatment for the patients with this disease,” he said, adding that “in all likelihood we are improving the cure rate for the patients with this disease.”
The findings were published simultaneously in the New England Journal of Medicine.
Overall survival at a median follow-up of 25.2 months in 473 patients randomized to receive durvalumab was significantly greater than among 236 who received placebo (stratified HR, 0.68; median survival not reached vs. 28.7 months in the groups, respectively), said Dr. Antonia of the H. Lee Moffitt Cancer Center and Research Institute, and professor of oncologic sciences at the University of South Florida, Tampa.
Durvalumab also improved overall survival in all prespecified subgroups, and PFS was similar to that in previous reports (stratified HR 0.51; median of 17.2 vs. 5.6 months with durvalumab and placebo, respectively), he said, noting that “interestingly, patients who were nonsmokers did benefit from durvalumab.”
This is notable because prior research suggests that never-smokers with advanced stage cancer have less of a chance of responding to immunotherapy (although they should still be offered immunotherapy), he explained.
“Also interestingly, it appears as if cisplatin was the better drug to use in the conventional therapy portion of the treatment,” he said.
Durvalumab also provided continued improvement vs. placebo in time to death or distant metastasis (stratified HR, 0.53), time to second progression (stratified HR, 0.58), time to first subsequent therapy or death (stratified HR, 0.58), and time to second subsequent therapy or death (stratified HR, 0.63).
Study subjects were patients with World Health Organization Performance Status scores of 0 or 1 with any PD-L1 tumor status, who received at least two cycles of conventional standard-of-care platinum-based chemoradiotherapy (CRT). They were randomized between May 2014 and April 2016 – at 1-42 days after CRT – to receive intravenous durvalumab at a dose of 10 mg/kg given intravenously every 2 weeks or placebo, and were stratified by age, gender, and smoking history.
Durvalumab was well tolerated; 30.5% and 26.1% of treatment and placebo patients, respectively, had grade 3/4 adverse events, and 15.4% and 9.8%, respectively, discontinued because of adverse events.
“There were no new safety signals with this longer follow-up,” Dr. Antonia said.
After study treatment ended, 41% and 54% in the groups, respectively, received additional anticancer therapy, and 8% and 22.4%, respectively, received additional immunotherapy, he noted.
The results are not only statistically significant, but clinically meaningful, and they offer new hope for patients with a disease that, in those who receive chemoradiotherapy, has a 3-year survival rate of only about 27%, he said.
During a press briefing at the conference, moderator Frances Shepherd, MD, a medical oncologist at Princess Margaret Cancer Centre in Toronto and a past president of the International Association for the Study of Lung Cancer, called the results “very exciting” given that this type of cancer represents about a third of all lung cancers and therefore affects an “enormous number of patients in Canada and globally.”
The PACIFIC trial was sponsored by AstraZeneca. Dr. Antonia reported being a speaker or advisory board member or receiving funding support from AstraZeneca and numerous other companies. Dr. Shepherd reported receiving honoraria and support from AstraZeneca and others. She is a speaker or advisory board member for Eli Lilly, AstraZeneca, and Merck, and she has ownership Interest in Eli Lilly and AstraZeneca.
SOURCE: Antonia S et al., WCLC 2018 Abstract PL02.01.
TORONTO – The programmed death-ligand 1 (PD-L1) inhibitor durvalumab significantly improves overall survival in patients with stage III unresectable non–small-cell lung cancer without progression after chemoradiotherapy, according to updated results from the global phase 3 PACIFIC study.
The findings, presented at the World Conference on Lung Cancer, follow a prior report from the study showing improved progression-free survival (PFS) in durvalumab-treated patients (stratified hazard ratio, 0.52), and together these survival benefits mark the first major advance in this disease setting in decades,” Scott J. Antonia, MD, reported at the conference, sponsored by the International Association for the Study of Lung Cancer (IASLC).
“The fact is this is a new standard of care treatment for the patients with this disease,” he said, adding that “in all likelihood we are improving the cure rate for the patients with this disease.”
The findings were published simultaneously in the New England Journal of Medicine.
Overall survival at a median follow-up of 25.2 months in 473 patients randomized to receive durvalumab was significantly greater than among 236 who received placebo (stratified HR, 0.68; median survival not reached vs. 28.7 months in the groups, respectively), said Dr. Antonia of the H. Lee Moffitt Cancer Center and Research Institute, and professor of oncologic sciences at the University of South Florida, Tampa.
Durvalumab also improved overall survival in all prespecified subgroups, and PFS was similar to that in previous reports (stratified HR 0.51; median of 17.2 vs. 5.6 months with durvalumab and placebo, respectively), he said, noting that “interestingly, patients who were nonsmokers did benefit from durvalumab.”
This is notable because prior research suggests that never-smokers with advanced stage cancer have less of a chance of responding to immunotherapy (although they should still be offered immunotherapy), he explained.
“Also interestingly, it appears as if cisplatin was the better drug to use in the conventional therapy portion of the treatment,” he said.
Durvalumab also provided continued improvement vs. placebo in time to death or distant metastasis (stratified HR, 0.53), time to second progression (stratified HR, 0.58), time to first subsequent therapy or death (stratified HR, 0.58), and time to second subsequent therapy or death (stratified HR, 0.63).
Study subjects were patients with World Health Organization Performance Status scores of 0 or 1 with any PD-L1 tumor status, who received at least two cycles of conventional standard-of-care platinum-based chemoradiotherapy (CRT). They were randomized between May 2014 and April 2016 – at 1-42 days after CRT – to receive intravenous durvalumab at a dose of 10 mg/kg given intravenously every 2 weeks or placebo, and were stratified by age, gender, and smoking history.
Durvalumab was well tolerated; 30.5% and 26.1% of treatment and placebo patients, respectively, had grade 3/4 adverse events, and 15.4% and 9.8%, respectively, discontinued because of adverse events.
“There were no new safety signals with this longer follow-up,” Dr. Antonia said.
After study treatment ended, 41% and 54% in the groups, respectively, received additional anticancer therapy, and 8% and 22.4%, respectively, received additional immunotherapy, he noted.
The results are not only statistically significant, but clinically meaningful, and they offer new hope for patients with a disease that, in those who receive chemoradiotherapy, has a 3-year survival rate of only about 27%, he said.
During a press briefing at the conference, moderator Frances Shepherd, MD, a medical oncologist at Princess Margaret Cancer Centre in Toronto and a past president of the International Association for the Study of Lung Cancer, called the results “very exciting” given that this type of cancer represents about a third of all lung cancers and therefore affects an “enormous number of patients in Canada and globally.”
The PACIFIC trial was sponsored by AstraZeneca. Dr. Antonia reported being a speaker or advisory board member or receiving funding support from AstraZeneca and numerous other companies. Dr. Shepherd reported receiving honoraria and support from AstraZeneca and others. She is a speaker or advisory board member for Eli Lilly, AstraZeneca, and Merck, and she has ownership Interest in Eli Lilly and AstraZeneca.
SOURCE: Antonia S et al., WCLC 2018 Abstract PL02.01.
REPORTING FROM WCLC 2018
Key clinical point: Durvalumab improves survival in stage III unresectable NSCLC patients without progression after CRT.
Major finding: Median overall survival not reached vs. 28.7 months for durvalumab compared with placebo (stratified HR, 0.58).
Study details: The global, randomized, placebo-controlled phase 3 PACIFIC trial of 709 patients.
Disclosures: The PACIFIC trial was sponsored by AstraZeneca. Dr. Antonia reported being a speaker or advisory board member or receiving funding support from AstraZeneca and numerous other companies. Dr. Shepherd reported receiving honoraria and support from AstraZeneca and others. She is a speaker or advisory board member for Eli Lilly, AstraZeneca, and Merck, and she has ownership Interest in Eli Lilly and AstraZeneca.
Source: Antonia S et al. WCLC 2018 Abstract PL02.01.
Erythematous Verrucous Plaque on the Hand
The Diagnosis: Chromomycosis
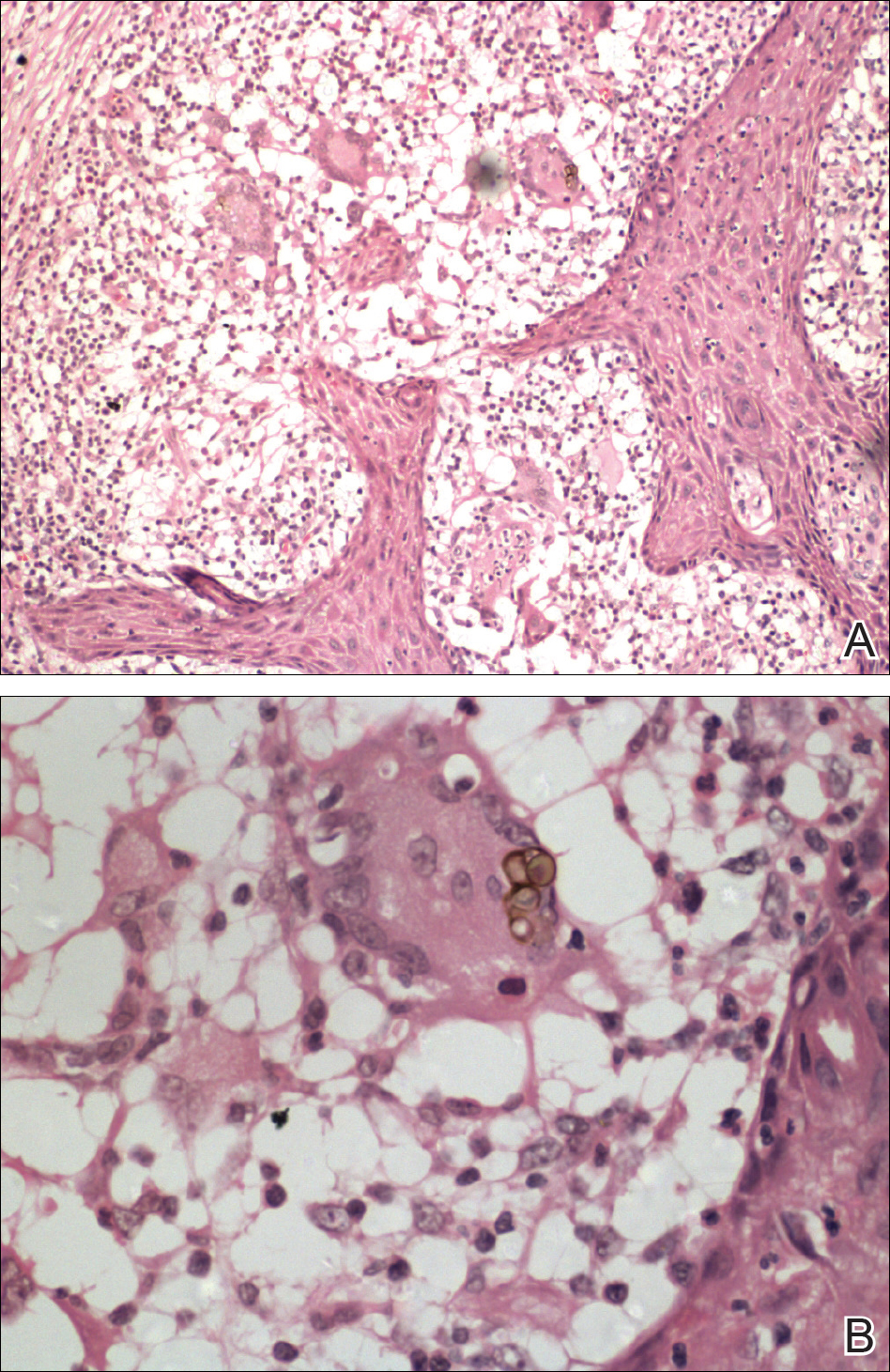
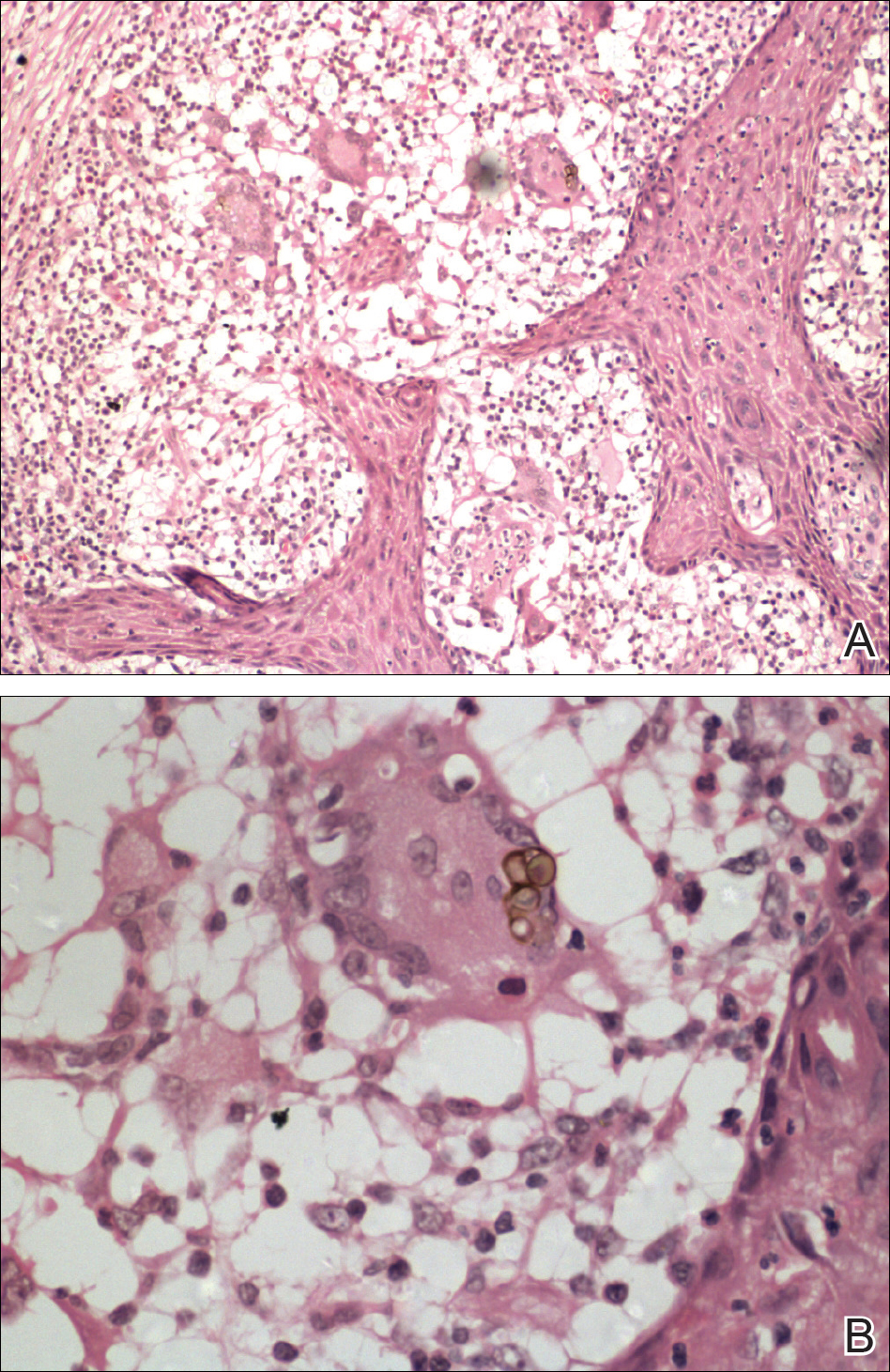
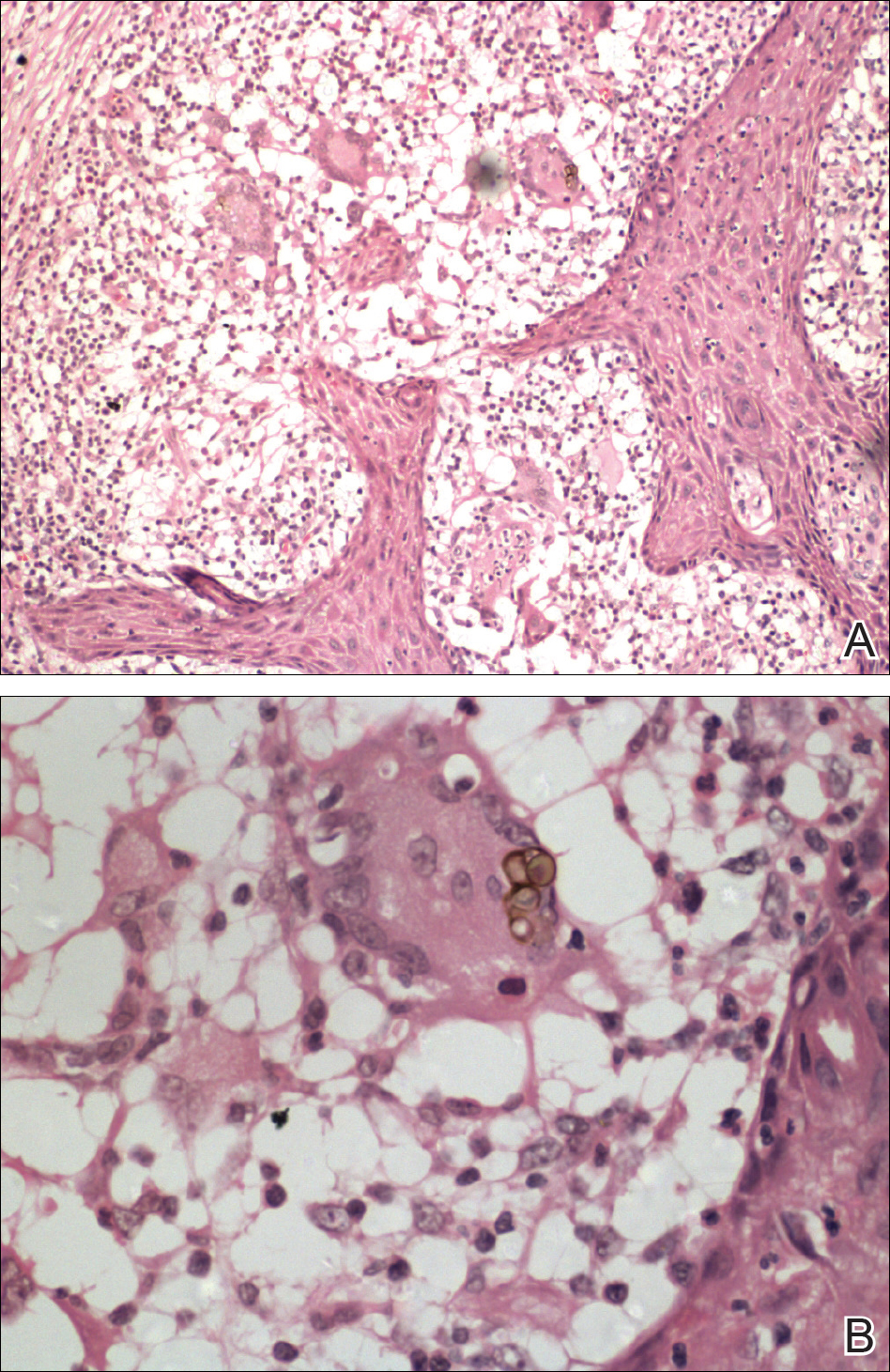
Skin scrapings revealed brownish sclerotic bodies. A review of the skin biopsy performed 4 years prior showed florid pseudoepitheliomatous hyperplasia overlying dense mixed inflammatory infiltrates of predominantly granulomatous microabscesses in the dermis. Numerous sclerotic bodies were evident within multinucleated giant cells and scattered among epidermal and dermal microabscesses (Figure). Few atypical basal keratinocytes were noted, but frank pleomorphism and aberrant mitosis was absent.
Chromomycosis is a chronic subcutaneous fungal infection caused by pigmented (dematiaceous) fungi growing in soil, decaying vegetables, and rotting wood. Infection usually occurs via traumatic inoculation from splinters and thorns. Some of the agents responsible include Fonsecaea pedrosoi, Cladophialophora carrionii, and Phialophora verrucosa.1
Diverse cutaneous manifestations have been observed with 5 different clinical forms: nodules, verrucous hyperkeratotic plaques, cicatricial lesions with central sparing, scaly plaques, and tumoral (cauliflowerlike) lesions.2 Of these clinical presentations, verrucous hyperkeratotic plaques are the most common, as seen in our patient. However, this presentation is not exclusive to chromomycosis because many conditions appear similarly, including sporotrichosis, nontuberculous mycobacterial infection, tuberculosis verrucosa cutis, and squamous cell carcinoma (SCC). The presence of small ulcerations may appear as the black dots seen on the plaques of chromomycosis, distinguishing chromomycosis from other conditions. Although this feature may be a fundamental clue for diagnosis, it should be emphasized that in many occasions, clinical differences between chromomycosis and its differentials are subtle. A study involving 9 patients with chromomycosis reported that only 1 was given the initial diagnosis of mycosis. Six patients initially were diagnosed with cutaneous malignancies, 1 patient with viral warts, and another patient with ganglion.3 Therefore, unless there is a high index of suspicion, these conditions may easily be mistaken for others by clinicians who are unfamiliar with their presentations, particularly in the setting of a busy clinic.
Chromomycosis routinely is diagnosed based on histologic examination and culture. Apart from sclerotic bodies, other histopathologic features include an inflammatory infiltrate characterized by neutrophilic microabscesses, multinucleated cells, fibrosis, acanthosis, papillomatosis, hyperkeratosis, and pseudoepitheliomatous hyperplasia (PEH).2 Pseudoepitheliomatous hyperplasia is an exaggerated proliferation of the epidermis, usually secondary to chronic inflammatory skin conditions.4 Because most verrucous lesions are thought to be neoplastic and carcinomas more commonly are seen and expected in dermatopathology, PEH can sometimes be mistaken for SCC. At times, the squamous epithelium of PEH can appear infiltrative, giving the illusion of well-differentiated SCC.5 However, absence of marked cellular atypia and abnormal mitotic activity should suggest otherwise. Thorough scrutiny for a concomitant infective process is necessary to avoid the overdiagnosis of SCC. Special stains for infectious agents such as periodic acid-Schiff and Grocott-Gomori methenamine-silver for fungal spores and Ziehl-Neelsen for acid-fast bacilli may reveal infectious organisms. Multilevel sections of deeper levels also may be essential to uncover sparse organisms.6
There is no standard treatment of chromomycosis. Some treatment options are available based on few open clinical studies and expert opinions. Systemic antifungals such as itraconazole or terbinafine most commonly are used with 15% to 80% cure rates.7 In invasive refractory cases, a combination of itraconazole and terbinafine has been employed as salvage therapy. Recently, the use of newer azoles such as posaconazole is favored due to its expanded-spectrum profile along with better pharmacodynamics and pharmacokinetic profile versus itraconazole. Physical methods such as cryotherapy, heat therapy, laser therapy, and photodynamic therapy frequently are practiced in conjunction with systemic antifungal therapy.8 Surgical procedures such as photocoagulation, Mohs micrographic surgery, and curettage sometimes are recommended for smaller well-defined lesions. Amputation, however, is rarely ever indicated, as there rarely is deep tissue involvement.2
Our case highlights the importance of clinicopathologic correlation in diagnosing squamous epithelial lesions. A high index of clinical suspicion and a wider list of differential diagnoses of verrucous plaques are necessary to minimize pitfalls in diagnosing lesions with squamous proliferation and therefore reduces the need for unnecessary interventions.
- Queiroz-Telles F, Esterre P, Perez-Blanco M, et al. Chromoblastomycosis: an overview of clinical manifestations, diagnosis and treatment. Med Mycol. 2009;47:3-15.
- Krzyściak PM, Pindycka-Piaszczyńska M, Piaszczyński M. Chromoblastomycosis. Postepy Dermatol Allergol. 2014;31:310-321.
- Jayalakshmi P, Looi LM, Soo-Hoo TS. Chromoblastomycosis in Malaysia. Mycopathologica. 1990;109:27-31.
- Zayour M, Lazova R. Pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2011;33:112-126.
- El-Khoury J, Kibbi AG, Abbas O. Mucocutaneous pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2012;34:165-175.
- Tan KB, Tan SH, Aw DC, et al. Simulators of squamous cell carcinoma of the skin: diagnostic challenges on small biopsies and clinicopathological correlation [published online June 25, 2013]. J Skin Cancer. 2013;2013:752864.
- Queiroz-Telles F, Santos DW. Challenges in the therapy of chromoblastomycosis. Mycopathologia. 2013;175:477-488.
- Queiroz-Telles F, de Hoog S, Santos DW, et al. Chromoblastomycosis. Clin Microbiol Rev. 2017;30:233-276.
The Diagnosis: Chromomycosis
Skin scrapings revealed brownish sclerotic bodies. A review of the skin biopsy performed 4 years prior showed florid pseudoepitheliomatous hyperplasia overlying dense mixed inflammatory infiltrates of predominantly granulomatous microabscesses in the dermis. Numerous sclerotic bodies were evident within multinucleated giant cells and scattered among epidermal and dermal microabscesses (Figure). Few atypical basal keratinocytes were noted, but frank pleomorphism and aberrant mitosis was absent.
Chromomycosis is a chronic subcutaneous fungal infection caused by pigmented (dematiaceous) fungi growing in soil, decaying vegetables, and rotting wood. Infection usually occurs via traumatic inoculation from splinters and thorns. Some of the agents responsible include Fonsecaea pedrosoi, Cladophialophora carrionii, and Phialophora verrucosa.1
Diverse cutaneous manifestations have been observed with 5 different clinical forms: nodules, verrucous hyperkeratotic plaques, cicatricial lesions with central sparing, scaly plaques, and tumoral (cauliflowerlike) lesions.2 Of these clinical presentations, verrucous hyperkeratotic plaques are the most common, as seen in our patient. However, this presentation is not exclusive to chromomycosis because many conditions appear similarly, including sporotrichosis, nontuberculous mycobacterial infection, tuberculosis verrucosa cutis, and squamous cell carcinoma (SCC). The presence of small ulcerations may appear as the black dots seen on the plaques of chromomycosis, distinguishing chromomycosis from other conditions. Although this feature may be a fundamental clue for diagnosis, it should be emphasized that in many occasions, clinical differences between chromomycosis and its differentials are subtle. A study involving 9 patients with chromomycosis reported that only 1 was given the initial diagnosis of mycosis. Six patients initially were diagnosed with cutaneous malignancies, 1 patient with viral warts, and another patient with ganglion.3 Therefore, unless there is a high index of suspicion, these conditions may easily be mistaken for others by clinicians who are unfamiliar with their presentations, particularly in the setting of a busy clinic.
Chromomycosis routinely is diagnosed based on histologic examination and culture. Apart from sclerotic bodies, other histopathologic features include an inflammatory infiltrate characterized by neutrophilic microabscesses, multinucleated cells, fibrosis, acanthosis, papillomatosis, hyperkeratosis, and pseudoepitheliomatous hyperplasia (PEH).2 Pseudoepitheliomatous hyperplasia is an exaggerated proliferation of the epidermis, usually secondary to chronic inflammatory skin conditions.4 Because most verrucous lesions are thought to be neoplastic and carcinomas more commonly are seen and expected in dermatopathology, PEH can sometimes be mistaken for SCC. At times, the squamous epithelium of PEH can appear infiltrative, giving the illusion of well-differentiated SCC.5 However, absence of marked cellular atypia and abnormal mitotic activity should suggest otherwise. Thorough scrutiny for a concomitant infective process is necessary to avoid the overdiagnosis of SCC. Special stains for infectious agents such as periodic acid-Schiff and Grocott-Gomori methenamine-silver for fungal spores and Ziehl-Neelsen for acid-fast bacilli may reveal infectious organisms. Multilevel sections of deeper levels also may be essential to uncover sparse organisms.6
There is no standard treatment of chromomycosis. Some treatment options are available based on few open clinical studies and expert opinions. Systemic antifungals such as itraconazole or terbinafine most commonly are used with 15% to 80% cure rates.7 In invasive refractory cases, a combination of itraconazole and terbinafine has been employed as salvage therapy. Recently, the use of newer azoles such as posaconazole is favored due to its expanded-spectrum profile along with better pharmacodynamics and pharmacokinetic profile versus itraconazole. Physical methods such as cryotherapy, heat therapy, laser therapy, and photodynamic therapy frequently are practiced in conjunction with systemic antifungal therapy.8 Surgical procedures such as photocoagulation, Mohs micrographic surgery, and curettage sometimes are recommended for smaller well-defined lesions. Amputation, however, is rarely ever indicated, as there rarely is deep tissue involvement.2
Our case highlights the importance of clinicopathologic correlation in diagnosing squamous epithelial lesions. A high index of clinical suspicion and a wider list of differential diagnoses of verrucous plaques are necessary to minimize pitfalls in diagnosing lesions with squamous proliferation and therefore reduces the need for unnecessary interventions.
The Diagnosis: Chromomycosis
Skin scrapings revealed brownish sclerotic bodies. A review of the skin biopsy performed 4 years prior showed florid pseudoepitheliomatous hyperplasia overlying dense mixed inflammatory infiltrates of predominantly granulomatous microabscesses in the dermis. Numerous sclerotic bodies were evident within multinucleated giant cells and scattered among epidermal and dermal microabscesses (Figure). Few atypical basal keratinocytes were noted, but frank pleomorphism and aberrant mitosis was absent.
Chromomycosis is a chronic subcutaneous fungal infection caused by pigmented (dematiaceous) fungi growing in soil, decaying vegetables, and rotting wood. Infection usually occurs via traumatic inoculation from splinters and thorns. Some of the agents responsible include Fonsecaea pedrosoi, Cladophialophora carrionii, and Phialophora verrucosa.1
Diverse cutaneous manifestations have been observed with 5 different clinical forms: nodules, verrucous hyperkeratotic plaques, cicatricial lesions with central sparing, scaly plaques, and tumoral (cauliflowerlike) lesions.2 Of these clinical presentations, verrucous hyperkeratotic plaques are the most common, as seen in our patient. However, this presentation is not exclusive to chromomycosis because many conditions appear similarly, including sporotrichosis, nontuberculous mycobacterial infection, tuberculosis verrucosa cutis, and squamous cell carcinoma (SCC). The presence of small ulcerations may appear as the black dots seen on the plaques of chromomycosis, distinguishing chromomycosis from other conditions. Although this feature may be a fundamental clue for diagnosis, it should be emphasized that in many occasions, clinical differences between chromomycosis and its differentials are subtle. A study involving 9 patients with chromomycosis reported that only 1 was given the initial diagnosis of mycosis. Six patients initially were diagnosed with cutaneous malignancies, 1 patient with viral warts, and another patient with ganglion.3 Therefore, unless there is a high index of suspicion, these conditions may easily be mistaken for others by clinicians who are unfamiliar with their presentations, particularly in the setting of a busy clinic.
Chromomycosis routinely is diagnosed based on histologic examination and culture. Apart from sclerotic bodies, other histopathologic features include an inflammatory infiltrate characterized by neutrophilic microabscesses, multinucleated cells, fibrosis, acanthosis, papillomatosis, hyperkeratosis, and pseudoepitheliomatous hyperplasia (PEH).2 Pseudoepitheliomatous hyperplasia is an exaggerated proliferation of the epidermis, usually secondary to chronic inflammatory skin conditions.4 Because most verrucous lesions are thought to be neoplastic and carcinomas more commonly are seen and expected in dermatopathology, PEH can sometimes be mistaken for SCC. At times, the squamous epithelium of PEH can appear infiltrative, giving the illusion of well-differentiated SCC.5 However, absence of marked cellular atypia and abnormal mitotic activity should suggest otherwise. Thorough scrutiny for a concomitant infective process is necessary to avoid the overdiagnosis of SCC. Special stains for infectious agents such as periodic acid-Schiff and Grocott-Gomori methenamine-silver for fungal spores and Ziehl-Neelsen for acid-fast bacilli may reveal infectious organisms. Multilevel sections of deeper levels also may be essential to uncover sparse organisms.6
There is no standard treatment of chromomycosis. Some treatment options are available based on few open clinical studies and expert opinions. Systemic antifungals such as itraconazole or terbinafine most commonly are used with 15% to 80% cure rates.7 In invasive refractory cases, a combination of itraconazole and terbinafine has been employed as salvage therapy. Recently, the use of newer azoles such as posaconazole is favored due to its expanded-spectrum profile along with better pharmacodynamics and pharmacokinetic profile versus itraconazole. Physical methods such as cryotherapy, heat therapy, laser therapy, and photodynamic therapy frequently are practiced in conjunction with systemic antifungal therapy.8 Surgical procedures such as photocoagulation, Mohs micrographic surgery, and curettage sometimes are recommended for smaller well-defined lesions. Amputation, however, is rarely ever indicated, as there rarely is deep tissue involvement.2
Our case highlights the importance of clinicopathologic correlation in diagnosing squamous epithelial lesions. A high index of clinical suspicion and a wider list of differential diagnoses of verrucous plaques are necessary to minimize pitfalls in diagnosing lesions with squamous proliferation and therefore reduces the need for unnecessary interventions.
- Queiroz-Telles F, Esterre P, Perez-Blanco M, et al. Chromoblastomycosis: an overview of clinical manifestations, diagnosis and treatment. Med Mycol. 2009;47:3-15.
- Krzyściak PM, Pindycka-Piaszczyńska M, Piaszczyński M. Chromoblastomycosis. Postepy Dermatol Allergol. 2014;31:310-321.
- Jayalakshmi P, Looi LM, Soo-Hoo TS. Chromoblastomycosis in Malaysia. Mycopathologica. 1990;109:27-31.
- Zayour M, Lazova R. Pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2011;33:112-126.
- El-Khoury J, Kibbi AG, Abbas O. Mucocutaneous pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2012;34:165-175.
- Tan KB, Tan SH, Aw DC, et al. Simulators of squamous cell carcinoma of the skin: diagnostic challenges on small biopsies and clinicopathological correlation [published online June 25, 2013]. J Skin Cancer. 2013;2013:752864.
- Queiroz-Telles F, Santos DW. Challenges in the therapy of chromoblastomycosis. Mycopathologia. 2013;175:477-488.
- Queiroz-Telles F, de Hoog S, Santos DW, et al. Chromoblastomycosis. Clin Microbiol Rev. 2017;30:233-276.
- Queiroz-Telles F, Esterre P, Perez-Blanco M, et al. Chromoblastomycosis: an overview of clinical manifestations, diagnosis and treatment. Med Mycol. 2009;47:3-15.
- Krzyściak PM, Pindycka-Piaszczyńska M, Piaszczyński M. Chromoblastomycosis. Postepy Dermatol Allergol. 2014;31:310-321.
- Jayalakshmi P, Looi LM, Soo-Hoo TS. Chromoblastomycosis in Malaysia. Mycopathologica. 1990;109:27-31.
- Zayour M, Lazova R. Pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2011;33:112-126.
- El-Khoury J, Kibbi AG, Abbas O. Mucocutaneous pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2012;34:165-175.
- Tan KB, Tan SH, Aw DC, et al. Simulators of squamous cell carcinoma of the skin: diagnostic challenges on small biopsies and clinicopathological correlation [published online June 25, 2013]. J Skin Cancer. 2013;2013:752864.
- Queiroz-Telles F, Santos DW. Challenges in the therapy of chromoblastomycosis. Mycopathologia. 2013;175:477-488.
- Queiroz-Telles F, de Hoog S, Santos DW, et al. Chromoblastomycosis. Clin Microbiol Rev. 2017;30:233-276.

A 75-year-old retired farmer presented with an erythematous verrucous plaque on the dorsal aspect of the left hand of 4 years' duration. Superficial biopsies from the lesion 4 years prior to presentation revealed pseudoepitheliomatous hyperplasia suggestive of squamous cell carcinoma, which led to the excision of the lesion along with 2 digits of the left hand. Despite surgery, the lesions promptly recurred and continued to progress. Physical examination revealed a verrucous plaque with crusting and small ulcerations (black dots) over the extensor aspect of the left hand and forearm.
Identifying and Treating CNS Vasculitis
Often difficult to diagnose, CNS vasculitis is a serious condition that can be treated effectively if addressed early.
HILTON HEAD, SC—Vasculitis is a general term for a group of uncommon diseases involving inflammation of blood vessels, which can lead to the occlusion or destruction of the vessels and to ischemia of the tissues supplied by those vessels. CNS vasculitis can be a primary disease or occur secondary to infections or as part of a systemic vasculitis or systemic inflammatory (eg, rheumatologic) disease. Without prompt diagnosis and treatment, patients are at high risk of permanent neurologic disability or death, according to a presentation at the 41st Annual Contemporary Clinical Neurology Symposium.
If diagnosed and treated early, CNS vasculitis has a good prognosis, but delayed intervention can result in severe morbidity or mortality, said Siddharama Pawate, MD, Associate Professor of Neurology at the Vanderbilt University Medical Center in Nashville. “You have to do extensive workups sometimes before you can make a diagnosis,” he said, citing the need for neurology, rheumatology, and infectious disease input. “Investigations include serologic testing, CSF analysis, MRI, and brain biopsy.”
Rare But With a High Risk of Morbidity
The 2012 International Chapel Hill Consensus Conference on the Nomenclature of Vasculitis adopted an extensive list of names for the numerous manifestations of vasculitis. These include the following:
• Large-vessel vasculitis (eg, giant cell arteritis [GCA])
• Medium-vessel vasculitis (eg, polyarteritis nodosa)
• Small-vessel vasculitis (eg, microscopic polyangiitis and granulomatosis with polyangiitis [Wegener’s granulomatosis])
• Variable-vessel vasculitis (eg, Behçet’s disease)
• Single-organ vasculitis (eg, primary CNS vasculitis)
• Vasculitis associated with systemic disease (eg, rheumatoid vasculitis)
• Vasculitis associated with probable etiology (eg, hepatitis B virus-associated or cancer-associated vasculitis).
CNS vasculitis may be grouped into two larger categories—infectious CNS vasculitis and immune-mediated CNS vasculitis. Dr. Pawate provided a brief overview of infectious causes of vasculitis including bacteria, mycobacteria, varicella-zoster, fungi, and neurocysticercosis, but devoted the main part of his presentation to the latter of the two categories, including a focus on primary CNS vasculitis (PCNSV), which is also known as primary angiitis of the CNS (PACNS). Dr. Pawate offered an analysis of what is entailed in the recognition, diagnosis, and treatment of CNS vasculitis in general and its immune-mediated variants more specifically.
CNS vasculitis may occur as part of a broader systemic vasculitis. GCA is a medical emergency that can cause permanent visual loss if not diagnosed and treated early. Vision loss occurs most often due to anterior ischemic optic neuropathy but also central retinal artery occlusion and posterior ischemic optic neuropathy. The American College of Rheumatology criteria for GCA diagnosis include three of the five following core features: age 50 or older at onset, new-onset headaches, temporal artery abnormality, elevated erythrocyte sedimentation rate of at least 50 mm/h, and abnormal temporal artery biopsy. High-dose steroids should be started if there is suspicion, without waiting for biopsy results. Recently, the anti-IL6 monoclonal antibody tocilizumab was approved by the FDA as a treatment for GCA. Granulomatosis with polyangiitis most often causes peripheral neuropathy, but can cause a small or medium vessel CNS vasculitis. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome) is characterized by the triad of asthma, hypereosinophilia, and necrotizing vasculitis, usually in that order. CNS involvement is common as part of the vasculitis. CNS vasculitis may also be seen in Behçet’s disease manifesting as dural sinus thrombosis and arterial occlusion or aneurysm.
In systemic lupus erythematosus, vasculitis has a prevalence ranging between 11% and 36%, but CNS involvement is much less common. Case reports of CNS vasculitis in patients with rheumatoid arthritis are rare.
Primary CNS Vasculitis
Primary CNS vasculitis causes inflammation of mostly small- to medium-sized leptomeningeal and parenchymal arterial vessels. It is rare—a 2007 retrospective analysis by Salvarani et al of 101 cases estimated the average annual incidence to be 2.4 cases per one million person-years. Onset tends to occur in middle age, with a median age at diagnosis of 50 and a similar frequency in males and females.
Clinical presentation of PCNSV can be acute, subacute, chronic, or recurrent. Depending on the area of the brain or spinal cord that is affected, patients can present with a wide variety of neurologic complaints. Headache is the most common symptom—found in 50% to 78% of patients—followed by altered cognition and persistent neurologic deficits. Stroke and transient ischemic attack involving multiple vascular areas occur in 30% to 50% of patients.
The diagnostic gold standard for PCNSV is brain parenchymal/leptomeningeal biopsy. The most common diagnoses are granulomatous angiitis of the CNS (58%), lymphocytic PACNS (28%), and necrotizing vasculitis (14%). More than 90% of patients have abnormalities on MRI, and the most common imaging findings are cortical and subcortical infarcts, leptomeningeal enhancement, intracranial hemorrhage, and areas of increased signal on FLAIR and T2-weighted sequences. It has been increasingly recognized that differential diagnosis for PCNSV should include reversible cerebral vasoconstriction syndrome (RCVS), which is characterized by reversible multifocal narrowing of the cerebral arteries—typically preceded by sudden, severe thunderclap headaches with or without associated neurologic deficits. RCVS typically resolves in approximately 12 weeks.
Regarding treatment for PCNSV, Dr. Pawate recommended starting with high-dose steroids—eg, IV methylprednisolone, 1,000 mg daily for five days, with a prolonged oral prednisone taper starting at 1 mg/kg/day—and six to nine months of IV cyclophosphamide pulse therapy, 500–750 mg/m2 every two to four weeks for more severe cases. Case studies have shown rituximab and mycophenolate to be effective. “I had one patient initially on cyclophosphamide for six months who we [then] maintained on mycophenolate for five years and then stopped immunosuppression,” Dr. Pawate said. “She did quite well.”
—Fred Balzac
Suggested Reading
Abdel Razek AA, Alvarez H, Bagg S, et al. Imaging spectrum of CNS vasculitis. Radiographics. 2014;34(4):873-894.
Chow FC, Marra CM, Cho TA. Cerebrovascular disease in central nervous system infections. Semin Neurol. 2011;31(3):286-306.
Hajj-Ali RA, Calabrese LH. Diagnosis and classification of central nervous system vasculitis. J Autoimmun. 2014;48-49:149-152.
Jennette JC, Falk RJ, Bacon PA, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1-11.
Salvarani C, Brown RD Jr, Calamia KT, et al. Primary central nervous system vasculitis: analysis of 101 patients. Ann Neurol. 2007;62(5):442-451.
Scolding NJ. Central nervous system vasculitis. Semin Immunopathol. 2009;31(4):527-536.
Often difficult to diagnose, CNS vasculitis is a serious condition that can be treated effectively if addressed early.
Often difficult to diagnose, CNS vasculitis is a serious condition that can be treated effectively if addressed early.
HILTON HEAD, SC—Vasculitis is a general term for a group of uncommon diseases involving inflammation of blood vessels, which can lead to the occlusion or destruction of the vessels and to ischemia of the tissues supplied by those vessels. CNS vasculitis can be a primary disease or occur secondary to infections or as part of a systemic vasculitis or systemic inflammatory (eg, rheumatologic) disease. Without prompt diagnosis and treatment, patients are at high risk of permanent neurologic disability or death, according to a presentation at the 41st Annual Contemporary Clinical Neurology Symposium.
If diagnosed and treated early, CNS vasculitis has a good prognosis, but delayed intervention can result in severe morbidity or mortality, said Siddharama Pawate, MD, Associate Professor of Neurology at the Vanderbilt University Medical Center in Nashville. “You have to do extensive workups sometimes before you can make a diagnosis,” he said, citing the need for neurology, rheumatology, and infectious disease input. “Investigations include serologic testing, CSF analysis, MRI, and brain biopsy.”
Rare But With a High Risk of Morbidity
The 2012 International Chapel Hill Consensus Conference on the Nomenclature of Vasculitis adopted an extensive list of names for the numerous manifestations of vasculitis. These include the following:
• Large-vessel vasculitis (eg, giant cell arteritis [GCA])
• Medium-vessel vasculitis (eg, polyarteritis nodosa)
• Small-vessel vasculitis (eg, microscopic polyangiitis and granulomatosis with polyangiitis [Wegener’s granulomatosis])
• Variable-vessel vasculitis (eg, Behçet’s disease)
• Single-organ vasculitis (eg, primary CNS vasculitis)
• Vasculitis associated with systemic disease (eg, rheumatoid vasculitis)
• Vasculitis associated with probable etiology (eg, hepatitis B virus-associated or cancer-associated vasculitis).
CNS vasculitis may be grouped into two larger categories—infectious CNS vasculitis and immune-mediated CNS vasculitis. Dr. Pawate provided a brief overview of infectious causes of vasculitis including bacteria, mycobacteria, varicella-zoster, fungi, and neurocysticercosis, but devoted the main part of his presentation to the latter of the two categories, including a focus on primary CNS vasculitis (PCNSV), which is also known as primary angiitis of the CNS (PACNS). Dr. Pawate offered an analysis of what is entailed in the recognition, diagnosis, and treatment of CNS vasculitis in general and its immune-mediated variants more specifically.
CNS vasculitis may occur as part of a broader systemic vasculitis. GCA is a medical emergency that can cause permanent visual loss if not diagnosed and treated early. Vision loss occurs most often due to anterior ischemic optic neuropathy but also central retinal artery occlusion and posterior ischemic optic neuropathy. The American College of Rheumatology criteria for GCA diagnosis include three of the five following core features: age 50 or older at onset, new-onset headaches, temporal artery abnormality, elevated erythrocyte sedimentation rate of at least 50 mm/h, and abnormal temporal artery biopsy. High-dose steroids should be started if there is suspicion, without waiting for biopsy results. Recently, the anti-IL6 monoclonal antibody tocilizumab was approved by the FDA as a treatment for GCA. Granulomatosis with polyangiitis most often causes peripheral neuropathy, but can cause a small or medium vessel CNS vasculitis. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome) is characterized by the triad of asthma, hypereosinophilia, and necrotizing vasculitis, usually in that order. CNS involvement is common as part of the vasculitis. CNS vasculitis may also be seen in Behçet’s disease manifesting as dural sinus thrombosis and arterial occlusion or aneurysm.
In systemic lupus erythematosus, vasculitis has a prevalence ranging between 11% and 36%, but CNS involvement is much less common. Case reports of CNS vasculitis in patients with rheumatoid arthritis are rare.
Primary CNS Vasculitis
Primary CNS vasculitis causes inflammation of mostly small- to medium-sized leptomeningeal and parenchymal arterial vessels. It is rare—a 2007 retrospective analysis by Salvarani et al of 101 cases estimated the average annual incidence to be 2.4 cases per one million person-years. Onset tends to occur in middle age, with a median age at diagnosis of 50 and a similar frequency in males and females.
Clinical presentation of PCNSV can be acute, subacute, chronic, or recurrent. Depending on the area of the brain or spinal cord that is affected, patients can present with a wide variety of neurologic complaints. Headache is the most common symptom—found in 50% to 78% of patients—followed by altered cognition and persistent neurologic deficits. Stroke and transient ischemic attack involving multiple vascular areas occur in 30% to 50% of patients.
The diagnostic gold standard for PCNSV is brain parenchymal/leptomeningeal biopsy. The most common diagnoses are granulomatous angiitis of the CNS (58%), lymphocytic PACNS (28%), and necrotizing vasculitis (14%). More than 90% of patients have abnormalities on MRI, and the most common imaging findings are cortical and subcortical infarcts, leptomeningeal enhancement, intracranial hemorrhage, and areas of increased signal on FLAIR and T2-weighted sequences. It has been increasingly recognized that differential diagnosis for PCNSV should include reversible cerebral vasoconstriction syndrome (RCVS), which is characterized by reversible multifocal narrowing of the cerebral arteries—typically preceded by sudden, severe thunderclap headaches with or without associated neurologic deficits. RCVS typically resolves in approximately 12 weeks.
Regarding treatment for PCNSV, Dr. Pawate recommended starting with high-dose steroids—eg, IV methylprednisolone, 1,000 mg daily for five days, with a prolonged oral prednisone taper starting at 1 mg/kg/day—and six to nine months of IV cyclophosphamide pulse therapy, 500–750 mg/m2 every two to four weeks for more severe cases. Case studies have shown rituximab and mycophenolate to be effective. “I had one patient initially on cyclophosphamide for six months who we [then] maintained on mycophenolate for five years and then stopped immunosuppression,” Dr. Pawate said. “She did quite well.”
—Fred Balzac
Suggested Reading
Abdel Razek AA, Alvarez H, Bagg S, et al. Imaging spectrum of CNS vasculitis. Radiographics. 2014;34(4):873-894.
Chow FC, Marra CM, Cho TA. Cerebrovascular disease in central nervous system infections. Semin Neurol. 2011;31(3):286-306.
Hajj-Ali RA, Calabrese LH. Diagnosis and classification of central nervous system vasculitis. J Autoimmun. 2014;48-49:149-152.
Jennette JC, Falk RJ, Bacon PA, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1-11.
Salvarani C, Brown RD Jr, Calamia KT, et al. Primary central nervous system vasculitis: analysis of 101 patients. Ann Neurol. 2007;62(5):442-451.
Scolding NJ. Central nervous system vasculitis. Semin Immunopathol. 2009;31(4):527-536.
HILTON HEAD, SC—Vasculitis is a general term for a group of uncommon diseases involving inflammation of blood vessels, which can lead to the occlusion or destruction of the vessels and to ischemia of the tissues supplied by those vessels. CNS vasculitis can be a primary disease or occur secondary to infections or as part of a systemic vasculitis or systemic inflammatory (eg, rheumatologic) disease. Without prompt diagnosis and treatment, patients are at high risk of permanent neurologic disability or death, according to a presentation at the 41st Annual Contemporary Clinical Neurology Symposium.
If diagnosed and treated early, CNS vasculitis has a good prognosis, but delayed intervention can result in severe morbidity or mortality, said Siddharama Pawate, MD, Associate Professor of Neurology at the Vanderbilt University Medical Center in Nashville. “You have to do extensive workups sometimes before you can make a diagnosis,” he said, citing the need for neurology, rheumatology, and infectious disease input. “Investigations include serologic testing, CSF analysis, MRI, and brain biopsy.”
Rare But With a High Risk of Morbidity
The 2012 International Chapel Hill Consensus Conference on the Nomenclature of Vasculitis adopted an extensive list of names for the numerous manifestations of vasculitis. These include the following:
• Large-vessel vasculitis (eg, giant cell arteritis [GCA])
• Medium-vessel vasculitis (eg, polyarteritis nodosa)
• Small-vessel vasculitis (eg, microscopic polyangiitis and granulomatosis with polyangiitis [Wegener’s granulomatosis])
• Variable-vessel vasculitis (eg, Behçet’s disease)
• Single-organ vasculitis (eg, primary CNS vasculitis)
• Vasculitis associated with systemic disease (eg, rheumatoid vasculitis)
• Vasculitis associated with probable etiology (eg, hepatitis B virus-associated or cancer-associated vasculitis).
CNS vasculitis may be grouped into two larger categories—infectious CNS vasculitis and immune-mediated CNS vasculitis. Dr. Pawate provided a brief overview of infectious causes of vasculitis including bacteria, mycobacteria, varicella-zoster, fungi, and neurocysticercosis, but devoted the main part of his presentation to the latter of the two categories, including a focus on primary CNS vasculitis (PCNSV), which is also known as primary angiitis of the CNS (PACNS). Dr. Pawate offered an analysis of what is entailed in the recognition, diagnosis, and treatment of CNS vasculitis in general and its immune-mediated variants more specifically.
CNS vasculitis may occur as part of a broader systemic vasculitis. GCA is a medical emergency that can cause permanent visual loss if not diagnosed and treated early. Vision loss occurs most often due to anterior ischemic optic neuropathy but also central retinal artery occlusion and posterior ischemic optic neuropathy. The American College of Rheumatology criteria for GCA diagnosis include three of the five following core features: age 50 or older at onset, new-onset headaches, temporal artery abnormality, elevated erythrocyte sedimentation rate of at least 50 mm/h, and abnormal temporal artery biopsy. High-dose steroids should be started if there is suspicion, without waiting for biopsy results. Recently, the anti-IL6 monoclonal antibody tocilizumab was approved by the FDA as a treatment for GCA. Granulomatosis with polyangiitis most often causes peripheral neuropathy, but can cause a small or medium vessel CNS vasculitis. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome) is characterized by the triad of asthma, hypereosinophilia, and necrotizing vasculitis, usually in that order. CNS involvement is common as part of the vasculitis. CNS vasculitis may also be seen in Behçet’s disease manifesting as dural sinus thrombosis and arterial occlusion or aneurysm.
In systemic lupus erythematosus, vasculitis has a prevalence ranging between 11% and 36%, but CNS involvement is much less common. Case reports of CNS vasculitis in patients with rheumatoid arthritis are rare.
Primary CNS Vasculitis
Primary CNS vasculitis causes inflammation of mostly small- to medium-sized leptomeningeal and parenchymal arterial vessels. It is rare—a 2007 retrospective analysis by Salvarani et al of 101 cases estimated the average annual incidence to be 2.4 cases per one million person-years. Onset tends to occur in middle age, with a median age at diagnosis of 50 and a similar frequency in males and females.
Clinical presentation of PCNSV can be acute, subacute, chronic, or recurrent. Depending on the area of the brain or spinal cord that is affected, patients can present with a wide variety of neurologic complaints. Headache is the most common symptom—found in 50% to 78% of patients—followed by altered cognition and persistent neurologic deficits. Stroke and transient ischemic attack involving multiple vascular areas occur in 30% to 50% of patients.
The diagnostic gold standard for PCNSV is brain parenchymal/leptomeningeal biopsy. The most common diagnoses are granulomatous angiitis of the CNS (58%), lymphocytic PACNS (28%), and necrotizing vasculitis (14%). More than 90% of patients have abnormalities on MRI, and the most common imaging findings are cortical and subcortical infarcts, leptomeningeal enhancement, intracranial hemorrhage, and areas of increased signal on FLAIR and T2-weighted sequences. It has been increasingly recognized that differential diagnosis for PCNSV should include reversible cerebral vasoconstriction syndrome (RCVS), which is characterized by reversible multifocal narrowing of the cerebral arteries—typically preceded by sudden, severe thunderclap headaches with or without associated neurologic deficits. RCVS typically resolves in approximately 12 weeks.
Regarding treatment for PCNSV, Dr. Pawate recommended starting with high-dose steroids—eg, IV methylprednisolone, 1,000 mg daily for five days, with a prolonged oral prednisone taper starting at 1 mg/kg/day—and six to nine months of IV cyclophosphamide pulse therapy, 500–750 mg/m2 every two to four weeks for more severe cases. Case studies have shown rituximab and mycophenolate to be effective. “I had one patient initially on cyclophosphamide for six months who we [then] maintained on mycophenolate for five years and then stopped immunosuppression,” Dr. Pawate said. “She did quite well.”
—Fred Balzac
Suggested Reading
Abdel Razek AA, Alvarez H, Bagg S, et al. Imaging spectrum of CNS vasculitis. Radiographics. 2014;34(4):873-894.
Chow FC, Marra CM, Cho TA. Cerebrovascular disease in central nervous system infections. Semin Neurol. 2011;31(3):286-306.
Hajj-Ali RA, Calabrese LH. Diagnosis and classification of central nervous system vasculitis. J Autoimmun. 2014;48-49:149-152.
Jennette JC, Falk RJ, Bacon PA, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1-11.
Salvarani C, Brown RD Jr, Calamia KT, et al. Primary central nervous system vasculitis: analysis of 101 patients. Ann Neurol. 2007;62(5):442-451.
Scolding NJ. Central nervous system vasculitis. Semin Immunopathol. 2009;31(4):527-536.
How to Correct a Misdiagnosis of MS
Build rapport with patients and recognize that they may be emotionally and financially invested in the diagnosis, one neurologist suggests.
HILTON HEAD, SC—Given the lack of a definitive diagnostic test for multiple sclerosis (MS), diagnosing the disease can prove difficult. When considering symptoms, signs, and MRI findings that are suggestive of MS, clinicians must rely on their clinical judgment and experience, skillful interpretation of tests, and knowledge of and willingness to consider alternative diagnoses. Because of the subjective judgments involved and the many conditions that may mimic MS, it is not surprising that physicians sometimes misdiagnose MS, said Harold Moses, MD, at Vanderbilt University’s 41st Annual Contemporary Clinical Neurology Symposium.
A study by Solomon et al suggests ways to reduce the likelihood of misdiagnosis, said Dr. Moses, Associate Professor of Neurology at Vanderbilt University in Nashville. “Neurologists should … avoid overreliance on MRI changes as the principal support for an MS diagnosis,” he said. “Nonspecific or atypical MRI findings should be interpreted cautiously. A diagnosis of MS should not be made or reinforced in patients with psychiatric conditions without evidence for MS.”
For patients with emotional distress and psychologically based functional disability who do not meet diagnostic criteria for MS, a diagnosis of MS should be avoided. When MS remains a possibility, the patient should be informed of that fact and followed with clinical assessment and, if appropriate, MRI, Dr. Moses added. “Neurologists should be open in admitting and discussing uncertainty with patients,” he said. “It’s important to be honest in … indicating the need for further testing or observation over time. When emotional factors are thought to contribute [to a patient’s symptoms], treatments should be directed at these issues concurrently.”
First, Do No Harm
Psychiatrists and other therapists may be able to help patients when the diagnosis remains an open question. “MS disease-modifying drugs should be prescribed only for patients who have definitive evidence for MS or for those who present with classical clinically isolated syndromes—optic neuritis, transverse myelitis, and brainstem events—accompanied by appropriate changes on MRI,” Dr. Moses said.
Challenging cases include asymptomatic patients with MRI findings; patients with a first occurrence of symptoms, especially when the presentation is atypical; and patients with mimics of MS, such as vasculitis. Neurologists should be vigilant to identify mimics, particularly because these conditions may be treatable. The presence of psychiatric illness also may create challenging clinical scenarios.
“Psychologic and psychiatric factors may be present, but that patient may still have MS…. The question is, how do you tease out why that person is not doing well—that discordance, if you will, between how their MRI and exam are versus how they feel and how they are functioning.”
A Survey of Specialists
Solomon et al conducted a cross-sectional, internet-based survey of 242 MS specialists. Of the 50.4% of physicians who responded, 95% reported evaluating within the past year at least one patient who had been diagnosed with MS but who they felt strongly did not have the disease. More than 90% of respondents reported the use of disease-modifying therapy (DMT) in a proportion of these patients, and 94% found clinical encounters with these patients to be of an equal or greater challenge than making a new diagnosis of MS. A smaller proportion of respondents (14%) reported that, in some cases, they withheld telling a patient their opinion that the patient did not have MS.
As the study’s authors observed, evidence of therapeutic benefit from early initiation of DMT in patients with MS generates a sense of urgency to diagnose the disease early and begin therapy, Dr. Moses said. However, misdiagnosis in many cases may have resulted from—in place of prudent clinical and laboratory monitoring—an overreliance on MRI findings in patients with syndromes for which established MS diagnostic imaging criteria have not been validated. “Ultimately, MS remains a clinical diagnosis,” said Dr. Moses. “You use an MRI as an adjunct to help you confirm a diagnosis.”
Misdiagnosis of MS can cause serious harm. For example, conditions such as neuromyelitis optica and cervical spondylosis can lead to irreversible disability if unrecognized and inappropriately treated. Use of DMT in patients without MS exposes them to unnecessary health risks and financial costs. Dr. Moses cited the case of a 45-year-old woman who probably did not have MS but whose treatment with interferon beta-1a likely resulted in her going on dialysis. “These drugs are not benign,” he said. “[Such an outcome] is a very rare thing, but keep in mind that if a patient does not have MS, he or she should not be on MS therapy.”
Invested in the Diagnosis
As discussed by Boissy and Ford, neurologists may be inclined to use a medically inaccurate label, such as “a touch of MS,” “mild MS,” “benign MS,” or “MS by history,” when talking with patients who have received a misdiagnosis of MS, Dr. Moses said. Patients who have attributed psychogenic symptoms to misdiagnosed MS often resist a psychogenic explanation. In addition, they may be invested physically, emotionally, and financially in the diagnosis of MS—making treatment challenging for clinicians, Dr. Moses said.
Therapeutic mislabeling raises ethical issues, however. Mislabeling may expose patients to risky therapies, lead to an inappropriate use of resources, compromise the credibility of the clinician, and cause psychologic harm to the patient.
Neurologists would do better to consider scheduling multiple visits to explore psychogenic factors, as well as the patient’s fears and emotions, with the aim of developing a rapport and encouraging appropriate evaluations, Dr. Moses said. “If physicians endorse an inaccurate diagnosis, this undoubtedly conflicts with their professional obligations for truth telling, avoiding harming patients, … acting in the patient’s best interest, and stewardship of medical resources,” he said.
—Fred Balzac
Suggested Reading
Boissy AR, Ford PJ. A touch of MS: therapeutic mislabeling. Neurology. 2012;78(24):1981-1985.
Solomon AJ, Bourdette DN, Cross AH, et al. The contemporary spectrum of multiple sclerosis misdiagnosis: a multicenter study. Neurology. 2016;87(13):1393-1399.
Solomon AJ, Klein EP, Bourdette D. “Undiagnosing” multiple sclerosis: the challenge of misdiagnosis in MS. Neurology. 2012;78(24):1986-1991.
Build rapport with patients and recognize that they may be emotionally and financially invested in the diagnosis, one neurologist suggests.
Build rapport with patients and recognize that they may be emotionally and financially invested in the diagnosis, one neurologist suggests.
HILTON HEAD, SC—Given the lack of a definitive diagnostic test for multiple sclerosis (MS), diagnosing the disease can prove difficult. When considering symptoms, signs, and MRI findings that are suggestive of MS, clinicians must rely on their clinical judgment and experience, skillful interpretation of tests, and knowledge of and willingness to consider alternative diagnoses. Because of the subjective judgments involved and the many conditions that may mimic MS, it is not surprising that physicians sometimes misdiagnose MS, said Harold Moses, MD, at Vanderbilt University’s 41st Annual Contemporary Clinical Neurology Symposium.
A study by Solomon et al suggests ways to reduce the likelihood of misdiagnosis, said Dr. Moses, Associate Professor of Neurology at Vanderbilt University in Nashville. “Neurologists should … avoid overreliance on MRI changes as the principal support for an MS diagnosis,” he said. “Nonspecific or atypical MRI findings should be interpreted cautiously. A diagnosis of MS should not be made or reinforced in patients with psychiatric conditions without evidence for MS.”
For patients with emotional distress and psychologically based functional disability who do not meet diagnostic criteria for MS, a diagnosis of MS should be avoided. When MS remains a possibility, the patient should be informed of that fact and followed with clinical assessment and, if appropriate, MRI, Dr. Moses added. “Neurologists should be open in admitting and discussing uncertainty with patients,” he said. “It’s important to be honest in … indicating the need for further testing or observation over time. When emotional factors are thought to contribute [to a patient’s symptoms], treatments should be directed at these issues concurrently.”
First, Do No Harm
Psychiatrists and other therapists may be able to help patients when the diagnosis remains an open question. “MS disease-modifying drugs should be prescribed only for patients who have definitive evidence for MS or for those who present with classical clinically isolated syndromes—optic neuritis, transverse myelitis, and brainstem events—accompanied by appropriate changes on MRI,” Dr. Moses said.
Challenging cases include asymptomatic patients with MRI findings; patients with a first occurrence of symptoms, especially when the presentation is atypical; and patients with mimics of MS, such as vasculitis. Neurologists should be vigilant to identify mimics, particularly because these conditions may be treatable. The presence of psychiatric illness also may create challenging clinical scenarios.
“Psychologic and psychiatric factors may be present, but that patient may still have MS…. The question is, how do you tease out why that person is not doing well—that discordance, if you will, between how their MRI and exam are versus how they feel and how they are functioning.”
A Survey of Specialists
Solomon et al conducted a cross-sectional, internet-based survey of 242 MS specialists. Of the 50.4% of physicians who responded, 95% reported evaluating within the past year at least one patient who had been diagnosed with MS but who they felt strongly did not have the disease. More than 90% of respondents reported the use of disease-modifying therapy (DMT) in a proportion of these patients, and 94% found clinical encounters with these patients to be of an equal or greater challenge than making a new diagnosis of MS. A smaller proportion of respondents (14%) reported that, in some cases, they withheld telling a patient their opinion that the patient did not have MS.
As the study’s authors observed, evidence of therapeutic benefit from early initiation of DMT in patients with MS generates a sense of urgency to diagnose the disease early and begin therapy, Dr. Moses said. However, misdiagnosis in many cases may have resulted from—in place of prudent clinical and laboratory monitoring—an overreliance on MRI findings in patients with syndromes for which established MS diagnostic imaging criteria have not been validated. “Ultimately, MS remains a clinical diagnosis,” said Dr. Moses. “You use an MRI as an adjunct to help you confirm a diagnosis.”
Misdiagnosis of MS can cause serious harm. For example, conditions such as neuromyelitis optica and cervical spondylosis can lead to irreversible disability if unrecognized and inappropriately treated. Use of DMT in patients without MS exposes them to unnecessary health risks and financial costs. Dr. Moses cited the case of a 45-year-old woman who probably did not have MS but whose treatment with interferon beta-1a likely resulted in her going on dialysis. “These drugs are not benign,” he said. “[Such an outcome] is a very rare thing, but keep in mind that if a patient does not have MS, he or she should not be on MS therapy.”
Invested in the Diagnosis
As discussed by Boissy and Ford, neurologists may be inclined to use a medically inaccurate label, such as “a touch of MS,” “mild MS,” “benign MS,” or “MS by history,” when talking with patients who have received a misdiagnosis of MS, Dr. Moses said. Patients who have attributed psychogenic symptoms to misdiagnosed MS often resist a psychogenic explanation. In addition, they may be invested physically, emotionally, and financially in the diagnosis of MS—making treatment challenging for clinicians, Dr. Moses said.
Therapeutic mislabeling raises ethical issues, however. Mislabeling may expose patients to risky therapies, lead to an inappropriate use of resources, compromise the credibility of the clinician, and cause psychologic harm to the patient.
Neurologists would do better to consider scheduling multiple visits to explore psychogenic factors, as well as the patient’s fears and emotions, with the aim of developing a rapport and encouraging appropriate evaluations, Dr. Moses said. “If physicians endorse an inaccurate diagnosis, this undoubtedly conflicts with their professional obligations for truth telling, avoiding harming patients, … acting in the patient’s best interest, and stewardship of medical resources,” he said.
—Fred Balzac
Suggested Reading
Boissy AR, Ford PJ. A touch of MS: therapeutic mislabeling. Neurology. 2012;78(24):1981-1985.
Solomon AJ, Bourdette DN, Cross AH, et al. The contemporary spectrum of multiple sclerosis misdiagnosis: a multicenter study. Neurology. 2016;87(13):1393-1399.
Solomon AJ, Klein EP, Bourdette D. “Undiagnosing” multiple sclerosis: the challenge of misdiagnosis in MS. Neurology. 2012;78(24):1986-1991.
HILTON HEAD, SC—Given the lack of a definitive diagnostic test for multiple sclerosis (MS), diagnosing the disease can prove difficult. When considering symptoms, signs, and MRI findings that are suggestive of MS, clinicians must rely on their clinical judgment and experience, skillful interpretation of tests, and knowledge of and willingness to consider alternative diagnoses. Because of the subjective judgments involved and the many conditions that may mimic MS, it is not surprising that physicians sometimes misdiagnose MS, said Harold Moses, MD, at Vanderbilt University’s 41st Annual Contemporary Clinical Neurology Symposium.
A study by Solomon et al suggests ways to reduce the likelihood of misdiagnosis, said Dr. Moses, Associate Professor of Neurology at Vanderbilt University in Nashville. “Neurologists should … avoid overreliance on MRI changes as the principal support for an MS diagnosis,” he said. “Nonspecific or atypical MRI findings should be interpreted cautiously. A diagnosis of MS should not be made or reinforced in patients with psychiatric conditions without evidence for MS.”
For patients with emotional distress and psychologically based functional disability who do not meet diagnostic criteria for MS, a diagnosis of MS should be avoided. When MS remains a possibility, the patient should be informed of that fact and followed with clinical assessment and, if appropriate, MRI, Dr. Moses added. “Neurologists should be open in admitting and discussing uncertainty with patients,” he said. “It’s important to be honest in … indicating the need for further testing or observation over time. When emotional factors are thought to contribute [to a patient’s symptoms], treatments should be directed at these issues concurrently.”
First, Do No Harm
Psychiatrists and other therapists may be able to help patients when the diagnosis remains an open question. “MS disease-modifying drugs should be prescribed only for patients who have definitive evidence for MS or for those who present with classical clinically isolated syndromes—optic neuritis, transverse myelitis, and brainstem events—accompanied by appropriate changes on MRI,” Dr. Moses said.
Challenging cases include asymptomatic patients with MRI findings; patients with a first occurrence of symptoms, especially when the presentation is atypical; and patients with mimics of MS, such as vasculitis. Neurologists should be vigilant to identify mimics, particularly because these conditions may be treatable. The presence of psychiatric illness also may create challenging clinical scenarios.
“Psychologic and psychiatric factors may be present, but that patient may still have MS…. The question is, how do you tease out why that person is not doing well—that discordance, if you will, between how their MRI and exam are versus how they feel and how they are functioning.”
A Survey of Specialists
Solomon et al conducted a cross-sectional, internet-based survey of 242 MS specialists. Of the 50.4% of physicians who responded, 95% reported evaluating within the past year at least one patient who had been diagnosed with MS but who they felt strongly did not have the disease. More than 90% of respondents reported the use of disease-modifying therapy (DMT) in a proportion of these patients, and 94% found clinical encounters with these patients to be of an equal or greater challenge than making a new diagnosis of MS. A smaller proportion of respondents (14%) reported that, in some cases, they withheld telling a patient their opinion that the patient did not have MS.
As the study’s authors observed, evidence of therapeutic benefit from early initiation of DMT in patients with MS generates a sense of urgency to diagnose the disease early and begin therapy, Dr. Moses said. However, misdiagnosis in many cases may have resulted from—in place of prudent clinical and laboratory monitoring—an overreliance on MRI findings in patients with syndromes for which established MS diagnostic imaging criteria have not been validated. “Ultimately, MS remains a clinical diagnosis,” said Dr. Moses. “You use an MRI as an adjunct to help you confirm a diagnosis.”
Misdiagnosis of MS can cause serious harm. For example, conditions such as neuromyelitis optica and cervical spondylosis can lead to irreversible disability if unrecognized and inappropriately treated. Use of DMT in patients without MS exposes them to unnecessary health risks and financial costs. Dr. Moses cited the case of a 45-year-old woman who probably did not have MS but whose treatment with interferon beta-1a likely resulted in her going on dialysis. “These drugs are not benign,” he said. “[Such an outcome] is a very rare thing, but keep in mind that if a patient does not have MS, he or she should not be on MS therapy.”
Invested in the Diagnosis
As discussed by Boissy and Ford, neurologists may be inclined to use a medically inaccurate label, such as “a touch of MS,” “mild MS,” “benign MS,” or “MS by history,” when talking with patients who have received a misdiagnosis of MS, Dr. Moses said. Patients who have attributed psychogenic symptoms to misdiagnosed MS often resist a psychogenic explanation. In addition, they may be invested physically, emotionally, and financially in the diagnosis of MS—making treatment challenging for clinicians, Dr. Moses said.
Therapeutic mislabeling raises ethical issues, however. Mislabeling may expose patients to risky therapies, lead to an inappropriate use of resources, compromise the credibility of the clinician, and cause psychologic harm to the patient.
Neurologists would do better to consider scheduling multiple visits to explore psychogenic factors, as well as the patient’s fears and emotions, with the aim of developing a rapport and encouraging appropriate evaluations, Dr. Moses said. “If physicians endorse an inaccurate diagnosis, this undoubtedly conflicts with their professional obligations for truth telling, avoiding harming patients, … acting in the patient’s best interest, and stewardship of medical resources,” he said.
—Fred Balzac
Suggested Reading
Boissy AR, Ford PJ. A touch of MS: therapeutic mislabeling. Neurology. 2012;78(24):1981-1985.
Solomon AJ, Bourdette DN, Cross AH, et al. The contemporary spectrum of multiple sclerosis misdiagnosis: a multicenter study. Neurology. 2016;87(13):1393-1399.
Solomon AJ, Klein EP, Bourdette D. “Undiagnosing” multiple sclerosis: the challenge of misdiagnosis in MS. Neurology. 2012;78(24):1986-1991.
Study Examines Dementia Epidemiology in the LGB Population
Among older adults who are lesbian, gay, or bisexual, depression nearly triples the risk of dementia.
CHICAGO—The first large-scale analysis of dementia prevalence among sexual minorities found a rate of 8% in adults age 60 or older who are lesbian, gay, or bisexual (LGB), according to research presented at AAIC 2018.
The crude dementia prevalence was lower than the 9% prevalence among a heterosexual comparator group. Subjects in the LGB group, however, were younger, more likely to be male, and more likely to have a college education, compared with subjects in the heterosexual group, said Jason Flatt, PhD.
The analysis of a large California health care database is the first step in learning more about dementia in this diverse population, said Dr. Flatt, Assistant Professor at the Institute for Health & Aging at the University of California, San Francisco.
A Gap in the Literature
Between two million and three million people age 60 or older in the United States identify as LGB. “With the continued aging of our entire population, we expect this number to increase to about six million by 2040,” Dr. Flatt said. “Given the gaps in collection of sexual orientation and gender identification, we have not been able to look at this issue before.”
Sexual minorities may face unique dementia risks. They are less likely to marry and have children than are heterosexuals, and twice as likely to live alone. “They often have little or no caregiver support, and are likely to have experienced stigma, discrimination, trauma, and high lifelong stress,” he said. These experiences make the LGB population less likely to seek out medical care. “All of these things impact health over the life course,” he said.
To examine the prevalence of dementia and potential risk factors in a sample of LGB older adults, Dr. Flatt and his colleagues analyzed data from the Kaiser Permanente Research Program on Genes, Environment, and Health. Their study examined dementia prevalence and comorbidities among 4,337 LGB subjects and 195,264 heterosexual subjects aged 60 or older. Dementia diagnoses occurred between 1996 and 2015, and the mean follow-up time was nine years. A quarter of the LGB sample identified as lesbian, 37% identified as gay men, and 38% identified as bisexual. Depression was more common in the LGB group (35% vs 28%), as was posttraumatic stress disorder (1.9% vs 1%). Both are well-documented risk factors for dementia.
The LGB group had a younger mean age, compared with the heterosexual group (69 vs 71). In addition, a greater percentage of LGB subjects identified as male (63% vs 44%) and had a college education (62% vs 40%).
Other risk factors such as hypertension, stroke, and heart disease did not significantly differ between the groups. Dr. Flatt and his associates plan to examine midlife obesity, physical inactivity, and low educational attainment in a future analysis.
Depression Nearly Tripled the Risk
A dementia diagnosis occurred in 343 subjects (7.9%) in the LGB group and in 18,060 subjects (9.2%) in the heterosexual group.
Higher education did not seem to be as protective in the LGB population, Dr. Flatt said.
In a regression analysis that adjusted for age and education, depression almost tripled the risk of dementia among sexual minorities (odds ratio, 2.7). Depression was also a significant dementia risk factor for heterosexual subjects (odds ratio, 2.5).
These initial findings highlight the need for more research into this population, Dr. Flatt said.
“We need to provide more LGB-affirming health care services, and this means training health care providers to meet these needs,” he said. Such efforts might include improved community outreach that could result in earlier detection and treatment, as well as training medical staff to provide more culturally sensitive care.
—Michele G. Sullivan
Among older adults who are lesbian, gay, or bisexual, depression nearly triples the risk of dementia.
Among older adults who are lesbian, gay, or bisexual, depression nearly triples the risk of dementia.
CHICAGO—The first large-scale analysis of dementia prevalence among sexual minorities found a rate of 8% in adults age 60 or older who are lesbian, gay, or bisexual (LGB), according to research presented at AAIC 2018.
The crude dementia prevalence was lower than the 9% prevalence among a heterosexual comparator group. Subjects in the LGB group, however, were younger, more likely to be male, and more likely to have a college education, compared with subjects in the heterosexual group, said Jason Flatt, PhD.
The analysis of a large California health care database is the first step in learning more about dementia in this diverse population, said Dr. Flatt, Assistant Professor at the Institute for Health & Aging at the University of California, San Francisco.
A Gap in the Literature
Between two million and three million people age 60 or older in the United States identify as LGB. “With the continued aging of our entire population, we expect this number to increase to about six million by 2040,” Dr. Flatt said. “Given the gaps in collection of sexual orientation and gender identification, we have not been able to look at this issue before.”
Sexual minorities may face unique dementia risks. They are less likely to marry and have children than are heterosexuals, and twice as likely to live alone. “They often have little or no caregiver support, and are likely to have experienced stigma, discrimination, trauma, and high lifelong stress,” he said. These experiences make the LGB population less likely to seek out medical care. “All of these things impact health over the life course,” he said.
To examine the prevalence of dementia and potential risk factors in a sample of LGB older adults, Dr. Flatt and his colleagues analyzed data from the Kaiser Permanente Research Program on Genes, Environment, and Health. Their study examined dementia prevalence and comorbidities among 4,337 LGB subjects and 195,264 heterosexual subjects aged 60 or older. Dementia diagnoses occurred between 1996 and 2015, and the mean follow-up time was nine years. A quarter of the LGB sample identified as lesbian, 37% identified as gay men, and 38% identified as bisexual. Depression was more common in the LGB group (35% vs 28%), as was posttraumatic stress disorder (1.9% vs 1%). Both are well-documented risk factors for dementia.
The LGB group had a younger mean age, compared with the heterosexual group (69 vs 71). In addition, a greater percentage of LGB subjects identified as male (63% vs 44%) and had a college education (62% vs 40%).
Other risk factors such as hypertension, stroke, and heart disease did not significantly differ between the groups. Dr. Flatt and his associates plan to examine midlife obesity, physical inactivity, and low educational attainment in a future analysis.
Depression Nearly Tripled the Risk
A dementia diagnosis occurred in 343 subjects (7.9%) in the LGB group and in 18,060 subjects (9.2%) in the heterosexual group.
Higher education did not seem to be as protective in the LGB population, Dr. Flatt said.
In a regression analysis that adjusted for age and education, depression almost tripled the risk of dementia among sexual minorities (odds ratio, 2.7). Depression was also a significant dementia risk factor for heterosexual subjects (odds ratio, 2.5).
These initial findings highlight the need for more research into this population, Dr. Flatt said.
“We need to provide more LGB-affirming health care services, and this means training health care providers to meet these needs,” he said. Such efforts might include improved community outreach that could result in earlier detection and treatment, as well as training medical staff to provide more culturally sensitive care.
—Michele G. Sullivan
CHICAGO—The first large-scale analysis of dementia prevalence among sexual minorities found a rate of 8% in adults age 60 or older who are lesbian, gay, or bisexual (LGB), according to research presented at AAIC 2018.
The crude dementia prevalence was lower than the 9% prevalence among a heterosexual comparator group. Subjects in the LGB group, however, were younger, more likely to be male, and more likely to have a college education, compared with subjects in the heterosexual group, said Jason Flatt, PhD.
The analysis of a large California health care database is the first step in learning more about dementia in this diverse population, said Dr. Flatt, Assistant Professor at the Institute for Health & Aging at the University of California, San Francisco.
A Gap in the Literature
Between two million and three million people age 60 or older in the United States identify as LGB. “With the continued aging of our entire population, we expect this number to increase to about six million by 2040,” Dr. Flatt said. “Given the gaps in collection of sexual orientation and gender identification, we have not been able to look at this issue before.”
Sexual minorities may face unique dementia risks. They are less likely to marry and have children than are heterosexuals, and twice as likely to live alone. “They often have little or no caregiver support, and are likely to have experienced stigma, discrimination, trauma, and high lifelong stress,” he said. These experiences make the LGB population less likely to seek out medical care. “All of these things impact health over the life course,” he said.
To examine the prevalence of dementia and potential risk factors in a sample of LGB older adults, Dr. Flatt and his colleagues analyzed data from the Kaiser Permanente Research Program on Genes, Environment, and Health. Their study examined dementia prevalence and comorbidities among 4,337 LGB subjects and 195,264 heterosexual subjects aged 60 or older. Dementia diagnoses occurred between 1996 and 2015, and the mean follow-up time was nine years. A quarter of the LGB sample identified as lesbian, 37% identified as gay men, and 38% identified as bisexual. Depression was more common in the LGB group (35% vs 28%), as was posttraumatic stress disorder (1.9% vs 1%). Both are well-documented risk factors for dementia.
The LGB group had a younger mean age, compared with the heterosexual group (69 vs 71). In addition, a greater percentage of LGB subjects identified as male (63% vs 44%) and had a college education (62% vs 40%).
Other risk factors such as hypertension, stroke, and heart disease did not significantly differ between the groups. Dr. Flatt and his associates plan to examine midlife obesity, physical inactivity, and low educational attainment in a future analysis.
Depression Nearly Tripled the Risk
A dementia diagnosis occurred in 343 subjects (7.9%) in the LGB group and in 18,060 subjects (9.2%) in the heterosexual group.
Higher education did not seem to be as protective in the LGB population, Dr. Flatt said.
In a regression analysis that adjusted for age and education, depression almost tripled the risk of dementia among sexual minorities (odds ratio, 2.7). Depression was also a significant dementia risk factor for heterosexual subjects (odds ratio, 2.5).
These initial findings highlight the need for more research into this population, Dr. Flatt said.
“We need to provide more LGB-affirming health care services, and this means training health care providers to meet these needs,” he said. Such efforts might include improved community outreach that could result in earlier detection and treatment, as well as training medical staff to provide more culturally sensitive care.
—Michele G. Sullivan
Alan M. Rapoport, MD, on Medication Overuse Headache
Neurology Reviews recently shared two poll questions with our Facebook followers about treatment medication overuse headache (MOH). I was very interested to see the results of our poll. While the number of responses was somewhat low, we do get some sense of what respondents are saying. In this commentary, I will first tell you my perspective on the answers and then we will see what some other headache specialists say about the answers to these questions.
Poll Results:
Can MOH be treated with preventive medications without detoxification?
33 votes
YES, 39%
NO, 61%
Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor) without detoxification?
26 votes
YES, 38%
NO, 62%
My Commentary:
Let me explain in more detail my thoughts on the first question, “Can MOH be treated with preventive medications without detoxification?”
If a patient had the diagnosis of MOH – meaning 15 or more headache days per month for at least 3 months, with use of stronger medications (triptans, ergots, opiates, butalbital-containing medications) for 10 days per month or milder treatment (aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs]) for 15 days per month – can they improve by being put on a traditional preventive medication without intentionally reducing their overused acute medications by a detoxification protocol ordered by a doctor or nurse?
Only 39% of our audience said yes. Yet some studies have shown that patients placed on onabotulinumtoxinA or topiramate might improve without them going through a detoxification of the overused medications. As a physician, I would suggest simultaneously decreasing in their acute medications. I think in some cases this approach creates additional improvement and makes the patient feel better. It would be better for their quality of life, as well as for their kidneys and possibly even their brains.
Here are my thoughts on the second question, “Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor), without detoxification?”
If a patient has MOH, can you expect them to improve after being placed on 1 of the 4 monoclonal antibodies to CGRP ligand or its receptor – all of which are either recently approved or currently in development – without suggesting that they decrease their overused acute care medications? Note that erenumab (Aimovig-aaoe) has been approved by the FDA and marketed as of the time of this writing; we expect 2 more products to be approved very soon.
Almost an identical percentage of our audience (38%) said yes. There is evidence in published clinical trials that those patients given these new medications did about as well with or without the presence of MOH, and both groups did better than the placebo patients. Note that most trials prohibited overuse of opiates and butalbital.
I am a firm believer of detoxifying patients from their overused over-the-counter (OTC) or prescription medications. I believe that opiates and butalbital-containing medications, when overused, are worse for patients than OTCs, NSAIDs, ergot and triptans, but all of these can cause MOH. There are many studies showing that both inpatient and outpatient detoxification alone can really help. However, it is difficult to detoxify patients and some refuse to try this approach.
So, what should we do as physicians? If a patient has MOH, I educate them, try to detoxify them slowly on an outpatient basis, and if I feel it will help, start them on a preventive medication, even before the detoxification begins so they can reach therapeutic levels. In the future, will I use one of the standard preventives, approved or off-label, for migraine prevention (beta blockers, topiramate and other anticonvulsants, antidepressants, angiotensin receptor blockers, onabotulinumtoxinA and others)? It remains to be seen. I am leaning towards the anti CGRP ligand and receptor monoclonal antibodies and preventive small molecule oral CGRP receptor blockers. While that might be enough to start with, I will continue explaining to my patients why they should actively begin a slow detoxification.
Let us see what some headache specialists said about both questions.
Robert Cowan, MD, FAAN:
There have been studies that show migraine can improve without the discontinuation of medication overuse. But that is not what the question asks. The question as posed is whether MOH can be treated with a preventive medication without detoxification. Since the diagnosis of MOH has, in the past, required the cessation of overuse leading to an improvement in the underlying headache, then technically, the answer would be “no.” But that being said, there is ample evidence that the number of headache days/months and other measures of headache can, in fact, improve with the introduction of a preventive, along with other measures such as lifestyle modification. The other ambiguity in the question has to do with what is meant by “detoxification.” Is this a hospital-based detox, or is a gradual decrease in the offending medicine in combination with the addition of a preventive, still considered “detoxification?” Also, does the response imply a sequential relationship between the detoxification and initiation of the preventive? Without further clarification, this response ratio to the question is very difficult to interpret.
There is animal data that suggests acute migraine medications may promote MOH in susceptible individuals through CGRP-dependent mechanisms and anti-CGRP antibodies may be useful for the MOH (Cephalalgia. 2017;37(6):560-570. doi: 10.1177/0333102416650702). While there are no published CGRP antibody studies that did not exclude MOH patients to my knowledge, an abstract by Silberstein et al at the recent AHS Scientific Meeting reported decreased use of overused medication with fremanazumab (Headache. 2018;58(S2):76-78).
Ira Turner, MD
There is clear data to suggest that it is not necessary to detoxify these patients before starting preventive therapy. This is true for the older and newer medications. In fact, not only do these preventive therapies still work in the presence of medication overuse, but they also help to reduce medication overuse. The one caveat that must be mentioned is that this may not apply to opiate overuse. Opiate over-users were excluded from these studies.
While it is of course our goal to reduce and stop acute medication overuse, it should not be done at the expense of delaying preventive therapy. In fact, it is desirable to do both simultaneously. This applies to oral preventive medications, botulinum toxin and CGRP monoclonal antibodies.
In view of this well-established data, it was quite surprising to me to see the results of the 2 polls cited. It seems as if we still have a lot of educating to do regarding migraine prevention in general and with medication overuse in migraine in particular.
Stewart Tepper, MD
Dr. Tepper did not have time to comment, but suggested we show you an abstract presented at the recent AHS meeting. It shows that erenumab-aaoe helps patients with MOH who have not been detoxified (Headache. 2018;58(S2):160-162).
###
Please write to us at Neurology Reviews Migraine Resource Center ([email protected]) with your opinions.
Alan M. Rapoport, MD
Editor-in-Chief
Migraine Resource Center
Clinical Professor of Neurology
The David Geffen School of Medicine at UCLA
Los Angeles, California
Neurology Reviews recently shared two poll questions with our Facebook followers about treatment medication overuse headache (MOH). I was very interested to see the results of our poll. While the number of responses was somewhat low, we do get some sense of what respondents are saying. In this commentary, I will first tell you my perspective on the answers and then we will see what some other headache specialists say about the answers to these questions.
Poll Results:
Can MOH be treated with preventive medications without detoxification?
33 votes
YES, 39%
NO, 61%
Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor) without detoxification?
26 votes
YES, 38%
NO, 62%
My Commentary:
Let me explain in more detail my thoughts on the first question, “Can MOH be treated with preventive medications without detoxification?”
If a patient had the diagnosis of MOH – meaning 15 or more headache days per month for at least 3 months, with use of stronger medications (triptans, ergots, opiates, butalbital-containing medications) for 10 days per month or milder treatment (aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs]) for 15 days per month – can they improve by being put on a traditional preventive medication without intentionally reducing their overused acute medications by a detoxification protocol ordered by a doctor or nurse?
Only 39% of our audience said yes. Yet some studies have shown that patients placed on onabotulinumtoxinA or topiramate might improve without them going through a detoxification of the overused medications. As a physician, I would suggest simultaneously decreasing in their acute medications. I think in some cases this approach creates additional improvement and makes the patient feel better. It would be better for their quality of life, as well as for their kidneys and possibly even their brains.
Here are my thoughts on the second question, “Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor), without detoxification?”
If a patient has MOH, can you expect them to improve after being placed on 1 of the 4 monoclonal antibodies to CGRP ligand or its receptor – all of which are either recently approved or currently in development – without suggesting that they decrease their overused acute care medications? Note that erenumab (Aimovig-aaoe) has been approved by the FDA and marketed as of the time of this writing; we expect 2 more products to be approved very soon.
Almost an identical percentage of our audience (38%) said yes. There is evidence in published clinical trials that those patients given these new medications did about as well with or without the presence of MOH, and both groups did better than the placebo patients. Note that most trials prohibited overuse of opiates and butalbital.
I am a firm believer of detoxifying patients from their overused over-the-counter (OTC) or prescription medications. I believe that opiates and butalbital-containing medications, when overused, are worse for patients than OTCs, NSAIDs, ergot and triptans, but all of these can cause MOH. There are many studies showing that both inpatient and outpatient detoxification alone can really help. However, it is difficult to detoxify patients and some refuse to try this approach.
So, what should we do as physicians? If a patient has MOH, I educate them, try to detoxify them slowly on an outpatient basis, and if I feel it will help, start them on a preventive medication, even before the detoxification begins so they can reach therapeutic levels. In the future, will I use one of the standard preventives, approved or off-label, for migraine prevention (beta blockers, topiramate and other anticonvulsants, antidepressants, angiotensin receptor blockers, onabotulinumtoxinA and others)? It remains to be seen. I am leaning towards the anti CGRP ligand and receptor monoclonal antibodies and preventive small molecule oral CGRP receptor blockers. While that might be enough to start with, I will continue explaining to my patients why they should actively begin a slow detoxification.
Let us see what some headache specialists said about both questions.
Robert Cowan, MD, FAAN:
There have been studies that show migraine can improve without the discontinuation of medication overuse. But that is not what the question asks. The question as posed is whether MOH can be treated with a preventive medication without detoxification. Since the diagnosis of MOH has, in the past, required the cessation of overuse leading to an improvement in the underlying headache, then technically, the answer would be “no.” But that being said, there is ample evidence that the number of headache days/months and other measures of headache can, in fact, improve with the introduction of a preventive, along with other measures such as lifestyle modification. The other ambiguity in the question has to do with what is meant by “detoxification.” Is this a hospital-based detox, or is a gradual decrease in the offending medicine in combination with the addition of a preventive, still considered “detoxification?” Also, does the response imply a sequential relationship between the detoxification and initiation of the preventive? Without further clarification, this response ratio to the question is very difficult to interpret.
There is animal data that suggests acute migraine medications may promote MOH in susceptible individuals through CGRP-dependent mechanisms and anti-CGRP antibodies may be useful for the MOH (Cephalalgia. 2017;37(6):560-570. doi: 10.1177/0333102416650702). While there are no published CGRP antibody studies that did not exclude MOH patients to my knowledge, an abstract by Silberstein et al at the recent AHS Scientific Meeting reported decreased use of overused medication with fremanazumab (Headache. 2018;58(S2):76-78).
Ira Turner, MD
There is clear data to suggest that it is not necessary to detoxify these patients before starting preventive therapy. This is true for the older and newer medications. In fact, not only do these preventive therapies still work in the presence of medication overuse, but they also help to reduce medication overuse. The one caveat that must be mentioned is that this may not apply to opiate overuse. Opiate over-users were excluded from these studies.
While it is of course our goal to reduce and stop acute medication overuse, it should not be done at the expense of delaying preventive therapy. In fact, it is desirable to do both simultaneously. This applies to oral preventive medications, botulinum toxin and CGRP monoclonal antibodies.
In view of this well-established data, it was quite surprising to me to see the results of the 2 polls cited. It seems as if we still have a lot of educating to do regarding migraine prevention in general and with medication overuse in migraine in particular.
Stewart Tepper, MD
Dr. Tepper did not have time to comment, but suggested we show you an abstract presented at the recent AHS meeting. It shows that erenumab-aaoe helps patients with MOH who have not been detoxified (Headache. 2018;58(S2):160-162).
###
Please write to us at Neurology Reviews Migraine Resource Center ([email protected]) with your opinions.
Alan M. Rapoport, MD
Editor-in-Chief
Migraine Resource Center
Clinical Professor of Neurology
The David Geffen School of Medicine at UCLA
Los Angeles, California
Neurology Reviews recently shared two poll questions with our Facebook followers about treatment medication overuse headache (MOH). I was very interested to see the results of our poll. While the number of responses was somewhat low, we do get some sense of what respondents are saying. In this commentary, I will first tell you my perspective on the answers and then we will see what some other headache specialists say about the answers to these questions.
Poll Results:
Can MOH be treated with preventive medications without detoxification?
33 votes
YES, 39%
NO, 61%
Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor) without detoxification?
26 votes
YES, 38%
NO, 62%
My Commentary:
Let me explain in more detail my thoughts on the first question, “Can MOH be treated with preventive medications without detoxification?”
If a patient had the diagnosis of MOH – meaning 15 or more headache days per month for at least 3 months, with use of stronger medications (triptans, ergots, opiates, butalbital-containing medications) for 10 days per month or milder treatment (aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs]) for 15 days per month – can they improve by being put on a traditional preventive medication without intentionally reducing their overused acute medications by a detoxification protocol ordered by a doctor or nurse?
Only 39% of our audience said yes. Yet some studies have shown that patients placed on onabotulinumtoxinA or topiramate might improve without them going through a detoxification of the overused medications. As a physician, I would suggest simultaneously decreasing in their acute medications. I think in some cases this approach creates additional improvement and makes the patient feel better. It would be better for their quality of life, as well as for their kidneys and possibly even their brains.
Here are my thoughts on the second question, “Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor), without detoxification?”
If a patient has MOH, can you expect them to improve after being placed on 1 of the 4 monoclonal antibodies to CGRP ligand or its receptor – all of which are either recently approved or currently in development – without suggesting that they decrease their overused acute care medications? Note that erenumab (Aimovig-aaoe) has been approved by the FDA and marketed as of the time of this writing; we expect 2 more products to be approved very soon.
Almost an identical percentage of our audience (38%) said yes. There is evidence in published clinical trials that those patients given these new medications did about as well with or without the presence of MOH, and both groups did better than the placebo patients. Note that most trials prohibited overuse of opiates and butalbital.
I am a firm believer of detoxifying patients from their overused over-the-counter (OTC) or prescription medications. I believe that opiates and butalbital-containing medications, when overused, are worse for patients than OTCs, NSAIDs, ergot and triptans, but all of these can cause MOH. There are many studies showing that both inpatient and outpatient detoxification alone can really help. However, it is difficult to detoxify patients and some refuse to try this approach.
So, what should we do as physicians? If a patient has MOH, I educate them, try to detoxify them slowly on an outpatient basis, and if I feel it will help, start them on a preventive medication, even before the detoxification begins so they can reach therapeutic levels. In the future, will I use one of the standard preventives, approved or off-label, for migraine prevention (beta blockers, topiramate and other anticonvulsants, antidepressants, angiotensin receptor blockers, onabotulinumtoxinA and others)? It remains to be seen. I am leaning towards the anti CGRP ligand and receptor monoclonal antibodies and preventive small molecule oral CGRP receptor blockers. While that might be enough to start with, I will continue explaining to my patients why they should actively begin a slow detoxification.
Let us see what some headache specialists said about both questions.
Robert Cowan, MD, FAAN:
There have been studies that show migraine can improve without the discontinuation of medication overuse. But that is not what the question asks. The question as posed is whether MOH can be treated with a preventive medication without detoxification. Since the diagnosis of MOH has, in the past, required the cessation of overuse leading to an improvement in the underlying headache, then technically, the answer would be “no.” But that being said, there is ample evidence that the number of headache days/months and other measures of headache can, in fact, improve with the introduction of a preventive, along with other measures such as lifestyle modification. The other ambiguity in the question has to do with what is meant by “detoxification.” Is this a hospital-based detox, or is a gradual decrease in the offending medicine in combination with the addition of a preventive, still considered “detoxification?” Also, does the response imply a sequential relationship between the detoxification and initiation of the preventive? Without further clarification, this response ratio to the question is very difficult to interpret.
There is animal data that suggests acute migraine medications may promote MOH in susceptible individuals through CGRP-dependent mechanisms and anti-CGRP antibodies may be useful for the MOH (Cephalalgia. 2017;37(6):560-570. doi: 10.1177/0333102416650702). While there are no published CGRP antibody studies that did not exclude MOH patients to my knowledge, an abstract by Silberstein et al at the recent AHS Scientific Meeting reported decreased use of overused medication with fremanazumab (Headache. 2018;58(S2):76-78).
Ira Turner, MD
There is clear data to suggest that it is not necessary to detoxify these patients before starting preventive therapy. This is true for the older and newer medications. In fact, not only do these preventive therapies still work in the presence of medication overuse, but they also help to reduce medication overuse. The one caveat that must be mentioned is that this may not apply to opiate overuse. Opiate over-users were excluded from these studies.
While it is of course our goal to reduce and stop acute medication overuse, it should not be done at the expense of delaying preventive therapy. In fact, it is desirable to do both simultaneously. This applies to oral preventive medications, botulinum toxin and CGRP monoclonal antibodies.
In view of this well-established data, it was quite surprising to me to see the results of the 2 polls cited. It seems as if we still have a lot of educating to do regarding migraine prevention in general and with medication overuse in migraine in particular.
Stewart Tepper, MD
Dr. Tepper did not have time to comment, but suggested we show you an abstract presented at the recent AHS meeting. It shows that erenumab-aaoe helps patients with MOH who have not been detoxified (Headache. 2018;58(S2):160-162).
###
Please write to us at Neurology Reviews Migraine Resource Center ([email protected]) with your opinions.
Alan M. Rapoport, MD
Editor-in-Chief
Migraine Resource Center
Clinical Professor of Neurology
The David Geffen School of Medicine at UCLA
Los Angeles, California
Breast cancer patients getting unnecessary scans against recommendations
PHOENIX – Despite clear guidance on lack of benefit and potential harms, many patients with early-stage breast cancers at low metastasis risk have undergone imaging tests for staging, recent retrospective studies have shown.
Nearly one-third of early-stage breast cancer patients received the unnecessary and potentially harmful interventions in one of the two studies presented at a symposium on quality care sponsored by the American Society of Clinical Oncology (ASCO).
Low-risk patients in that study were more likely to undergo imaging if they were younger or had triple-negative disease, among other factors, said researcher Brett Barlow, of the University of Alabama at Birmingham.
Physicians should be further educated about the low-risk nature of early-stage breast cancer, even in subgroups that are perceived to be higher risk, Mr. Barlow said in an interview.
“I think we can reassure physicians that these patients will do well and that these guidelines are based on good data,” he said “There could potentially be an element of distrust in these guidelines in these higher-risk patients, and that may be what’s driving some of these extra tests.”
According to Mr. Barlow, imaging low-risk patients is inconsistent with guidance from Choosing Wisely, an initiative designed to promote discussions between clinicians and patients about medical tests or procedures that are unnecessary.
As part of that initiative, ASCO recommended that PET, CT, and radionuclide bone scans should not be performed for staging of early-stage breast cancer at low risk for metastasis.
There is a lack of evidence that demonstrates a benefit for those imaging modalities in patients with newly identified ductal carcinoma in situ (DCIS) or clinical stage I or II disease, the society said at the time.
Unnecessary imaging can result in unnecessary invasive procedures, overtreatment, radiation exposure, and misdiagnosis, the society said in the guidance, which was published in 2012.
Despite the guidance, 262 out of 872 patients with stage 0-II breast cancer (30%) seen during 2013-2015 underwent imaging, according to results of the single-center retrospective cohort study Mr. Barlow and his coauthors described in a poster presentation.
The median age of the patients who underwent unnecessary imaging was 55 years versus 60 years for patients who did not, according to the researchers.
Risk of inappropriate imaging was increased in younger patients, those with triple-negative disease versus those with any hormone receptor–positive disease, those with higher-stage breast cancer, and those without Medicare insurance, investigators found.
Although it’s unclear whether there were any formal, institution-level efforts to promote the ASCO recommendations during the 2013-2015 period, it was “definitely a topic of debate at the time,” Mr. Barlow said.
“Something we hope to evaluate further is whether we have improved,” he said. “It’s important to set a baseline and see how we did in this area. We look forward to reevaluating that in a few years to see.”
In a separate study, investigators reviewed records from Mount Sinai Health System in New York and found that unnecessary scans were performed in 19% of patients diagnosed with stage I-II breast cancer during 2014-2015.
No cases of metastatic disease were found in 733 patients included in the study, and 43% had false-positive findings, according to Ana I. Velazquez Manana, MD, MS, of Mount Sinai Beth Israel Foundation, New York, and her coinvestigators.
Imaging increased costs by $4,480 per patient, according to the investigators, who found in multivariate analysis that the unnecessary scans were associated with young age, presence of T2 tumor, positive lymph nodes, and triple-negative disease.
“Further educational efforts are needed to avoid unnecessary scans in patients with early-stage breast cancer,” the researchers wrote in an abstract describing the results.
Mr. Barlow reported no disclosures, while one coauthor reported disclosures related to Carevive Systems, Genentech/Roche, Medscape, Pack Health, and Pfizer. Dr. Velazquez Manana and her coauthors had no relationships to disclose, and their study was funded by the Medical Student Rotation for Underrepresented Populations.
SOURCE: Barlow B et al. Quality Care Symposium, Abstract 51. Velazquez Manana AI et al. Quality Care Symposium, Abstract 52.
PHOENIX – Despite clear guidance on lack of benefit and potential harms, many patients with early-stage breast cancers at low metastasis risk have undergone imaging tests for staging, recent retrospective studies have shown.
Nearly one-third of early-stage breast cancer patients received the unnecessary and potentially harmful interventions in one of the two studies presented at a symposium on quality care sponsored by the American Society of Clinical Oncology (ASCO).
Low-risk patients in that study were more likely to undergo imaging if they were younger or had triple-negative disease, among other factors, said researcher Brett Barlow, of the University of Alabama at Birmingham.
Physicians should be further educated about the low-risk nature of early-stage breast cancer, even in subgroups that are perceived to be higher risk, Mr. Barlow said in an interview.
“I think we can reassure physicians that these patients will do well and that these guidelines are based on good data,” he said “There could potentially be an element of distrust in these guidelines in these higher-risk patients, and that may be what’s driving some of these extra tests.”
According to Mr. Barlow, imaging low-risk patients is inconsistent with guidance from Choosing Wisely, an initiative designed to promote discussions between clinicians and patients about medical tests or procedures that are unnecessary.
As part of that initiative, ASCO recommended that PET, CT, and radionuclide bone scans should not be performed for staging of early-stage breast cancer at low risk for metastasis.
There is a lack of evidence that demonstrates a benefit for those imaging modalities in patients with newly identified ductal carcinoma in situ (DCIS) or clinical stage I or II disease, the society said at the time.
Unnecessary imaging can result in unnecessary invasive procedures, overtreatment, radiation exposure, and misdiagnosis, the society said in the guidance, which was published in 2012.
Despite the guidance, 262 out of 872 patients with stage 0-II breast cancer (30%) seen during 2013-2015 underwent imaging, according to results of the single-center retrospective cohort study Mr. Barlow and his coauthors described in a poster presentation.
The median age of the patients who underwent unnecessary imaging was 55 years versus 60 years for patients who did not, according to the researchers.
Risk of inappropriate imaging was increased in younger patients, those with triple-negative disease versus those with any hormone receptor–positive disease, those with higher-stage breast cancer, and those without Medicare insurance, investigators found.
Although it’s unclear whether there were any formal, institution-level efforts to promote the ASCO recommendations during the 2013-2015 period, it was “definitely a topic of debate at the time,” Mr. Barlow said.
“Something we hope to evaluate further is whether we have improved,” he said. “It’s important to set a baseline and see how we did in this area. We look forward to reevaluating that in a few years to see.”
In a separate study, investigators reviewed records from Mount Sinai Health System in New York and found that unnecessary scans were performed in 19% of patients diagnosed with stage I-II breast cancer during 2014-2015.
No cases of metastatic disease were found in 733 patients included in the study, and 43% had false-positive findings, according to Ana I. Velazquez Manana, MD, MS, of Mount Sinai Beth Israel Foundation, New York, and her coinvestigators.
Imaging increased costs by $4,480 per patient, according to the investigators, who found in multivariate analysis that the unnecessary scans were associated with young age, presence of T2 tumor, positive lymph nodes, and triple-negative disease.
“Further educational efforts are needed to avoid unnecessary scans in patients with early-stage breast cancer,” the researchers wrote in an abstract describing the results.
Mr. Barlow reported no disclosures, while one coauthor reported disclosures related to Carevive Systems, Genentech/Roche, Medscape, Pack Health, and Pfizer. Dr. Velazquez Manana and her coauthors had no relationships to disclose, and their study was funded by the Medical Student Rotation for Underrepresented Populations.
SOURCE: Barlow B et al. Quality Care Symposium, Abstract 51. Velazquez Manana AI et al. Quality Care Symposium, Abstract 52.
PHOENIX – Despite clear guidance on lack of benefit and potential harms, many patients with early-stage breast cancers at low metastasis risk have undergone imaging tests for staging, recent retrospective studies have shown.
Nearly one-third of early-stage breast cancer patients received the unnecessary and potentially harmful interventions in one of the two studies presented at a symposium on quality care sponsored by the American Society of Clinical Oncology (ASCO).
Low-risk patients in that study were more likely to undergo imaging if they were younger or had triple-negative disease, among other factors, said researcher Brett Barlow, of the University of Alabama at Birmingham.
Physicians should be further educated about the low-risk nature of early-stage breast cancer, even in subgroups that are perceived to be higher risk, Mr. Barlow said in an interview.
“I think we can reassure physicians that these patients will do well and that these guidelines are based on good data,” he said “There could potentially be an element of distrust in these guidelines in these higher-risk patients, and that may be what’s driving some of these extra tests.”
According to Mr. Barlow, imaging low-risk patients is inconsistent with guidance from Choosing Wisely, an initiative designed to promote discussions between clinicians and patients about medical tests or procedures that are unnecessary.
As part of that initiative, ASCO recommended that PET, CT, and radionuclide bone scans should not be performed for staging of early-stage breast cancer at low risk for metastasis.
There is a lack of evidence that demonstrates a benefit for those imaging modalities in patients with newly identified ductal carcinoma in situ (DCIS) or clinical stage I or II disease, the society said at the time.
Unnecessary imaging can result in unnecessary invasive procedures, overtreatment, radiation exposure, and misdiagnosis, the society said in the guidance, which was published in 2012.
Despite the guidance, 262 out of 872 patients with stage 0-II breast cancer (30%) seen during 2013-2015 underwent imaging, according to results of the single-center retrospective cohort study Mr. Barlow and his coauthors described in a poster presentation.
The median age of the patients who underwent unnecessary imaging was 55 years versus 60 years for patients who did not, according to the researchers.
Risk of inappropriate imaging was increased in younger patients, those with triple-negative disease versus those with any hormone receptor–positive disease, those with higher-stage breast cancer, and those without Medicare insurance, investigators found.
Although it’s unclear whether there were any formal, institution-level efforts to promote the ASCO recommendations during the 2013-2015 period, it was “definitely a topic of debate at the time,” Mr. Barlow said.
“Something we hope to evaluate further is whether we have improved,” he said. “It’s important to set a baseline and see how we did in this area. We look forward to reevaluating that in a few years to see.”
In a separate study, investigators reviewed records from Mount Sinai Health System in New York and found that unnecessary scans were performed in 19% of patients diagnosed with stage I-II breast cancer during 2014-2015.
No cases of metastatic disease were found in 733 patients included in the study, and 43% had false-positive findings, according to Ana I. Velazquez Manana, MD, MS, of Mount Sinai Beth Israel Foundation, New York, and her coinvestigators.
Imaging increased costs by $4,480 per patient, according to the investigators, who found in multivariate analysis that the unnecessary scans were associated with young age, presence of T2 tumor, positive lymph nodes, and triple-negative disease.
“Further educational efforts are needed to avoid unnecessary scans in patients with early-stage breast cancer,” the researchers wrote in an abstract describing the results.
Mr. Barlow reported no disclosures, while one coauthor reported disclosures related to Carevive Systems, Genentech/Roche, Medscape, Pack Health, and Pfizer. Dr. Velazquez Manana and her coauthors had no relationships to disclose, and their study was funded by the Medical Student Rotation for Underrepresented Populations.
SOURCE: Barlow B et al. Quality Care Symposium, Abstract 51. Velazquez Manana AI et al. Quality Care Symposium, Abstract 52.
REPORTING FROM THE QUALITY CARE SYMPOSIUM
Key clinical point: Many patients with early breast cancers at low metastasis risk received imaging tests for staging despite ASCO recommendations against such testing.
Major finding: In two studies, 30% and 19% of low-risk breast cancer patients underwent imaging for staging.
Study details: Two single-center, retrospective cohort studies that included 872 and 733 patients, respectively.
Disclosures: In one study, researchers reported disclosures related to Carevive Systems, Genentech/Roche, Medscape, Pack Health, and Pfizer. The second study was funded by the Medical Student Rotation for Underrepresented Populations.
Source: Barlow B et al. Quality Care Symposium, Abstract 51; Velazquez Manana AI et al. Quality Care Symposium, Abstract 52.
No evidence of subclinical axial involvement seen in skin psoriasis
A study of individuals with longstanding skin psoriasis but no clinical arthritis or spondylitis has found no evidence of subclinical involvement of the sacroiliac joint or spine.
The prevalence of sacroiliac lesions on blinded MRI assessment was similar in 20 patients who had skin psoriasis for a median of 23 years and in 22 healthy controls, and no sacroiliac ankylosis was seen in either group. Similarly, there was no significant difference between the two groups in spinal lesions on MRI, nor in any of the five levels of lesion frequency, Vlad A. Bratu, MD, of the department of radiology at University Hospital Basel (Switzerland) and his coauthors reported in Arthritis Care & Research.
On blinded MRI assessment, five (25%) patients with skin psoriasis and two (9.1%) controls were classified as having inflammation of the sacroiliac joint. Three of these patients in the psoriasis group and one in the control group were older than 50, and the three with psoriasis had had the condition for 26-35 years.
Dr. Bratu and his colleagues said that subclinical peripheral joint inflammation on MRI had previously been a common finding in patients who had skin psoriasis but no clinical signs of psoriatic arthritis. But given the limited evidence of concomitant subclinical axial or spinal inflammation in their study, the authors argued there was no support for routine screening for potential subclinical axial inflammation in patients with longstanding skin psoriasis.
They noted that bone marrow edema lesions in at least two sacroiliac joint quadrants were seen in 35% of patients with psoriasis and 23% of healthy controls, a finding that reflected those seen in other studies in healthy individuals.
“If a specificity threshold for a given MRI lesion of at least 0.9 is applied for axial MRI to discriminate between axial SpA [spondyloarthritis] and background variation in healthy controls or in differential diagnostic conditions, no more than 10% of healthy controls in our study should meet this criterion by an individual level data analysis,” they wrote.
The authors also pointed out the impact of age on lesion frequency, which was more evident in spinal lesions.
“This observation supports the hypothesis that some spinal alterations in higher age may reflect degenerative rather than inflammatory changes,” they wrote. “However, there is a gap in knowledge with virtually no evidence about presence and pattern of degenerative versus inflammatory spinal lesions in subjects beyond 50 years of age.”
The study was supported by the Gottfried and Julia Bangerter-Rhyner Foundation. No conflicts of interest were declared.
SOURCE: Bratu V et al. Arthritis Care Res. 2018 Sep 22. doi: 10.1002/acr.23767.
A study of individuals with longstanding skin psoriasis but no clinical arthritis or spondylitis has found no evidence of subclinical involvement of the sacroiliac joint or spine.
The prevalence of sacroiliac lesions on blinded MRI assessment was similar in 20 patients who had skin psoriasis for a median of 23 years and in 22 healthy controls, and no sacroiliac ankylosis was seen in either group. Similarly, there was no significant difference between the two groups in spinal lesions on MRI, nor in any of the five levels of lesion frequency, Vlad A. Bratu, MD, of the department of radiology at University Hospital Basel (Switzerland) and his coauthors reported in Arthritis Care & Research.
On blinded MRI assessment, five (25%) patients with skin psoriasis and two (9.1%) controls were classified as having inflammation of the sacroiliac joint. Three of these patients in the psoriasis group and one in the control group were older than 50, and the three with psoriasis had had the condition for 26-35 years.
Dr. Bratu and his colleagues said that subclinical peripheral joint inflammation on MRI had previously been a common finding in patients who had skin psoriasis but no clinical signs of psoriatic arthritis. But given the limited evidence of concomitant subclinical axial or spinal inflammation in their study, the authors argued there was no support for routine screening for potential subclinical axial inflammation in patients with longstanding skin psoriasis.
They noted that bone marrow edema lesions in at least two sacroiliac joint quadrants were seen in 35% of patients with psoriasis and 23% of healthy controls, a finding that reflected those seen in other studies in healthy individuals.
“If a specificity threshold for a given MRI lesion of at least 0.9 is applied for axial MRI to discriminate between axial SpA [spondyloarthritis] and background variation in healthy controls or in differential diagnostic conditions, no more than 10% of healthy controls in our study should meet this criterion by an individual level data analysis,” they wrote.
The authors also pointed out the impact of age on lesion frequency, which was more evident in spinal lesions.
“This observation supports the hypothesis that some spinal alterations in higher age may reflect degenerative rather than inflammatory changes,” they wrote. “However, there is a gap in knowledge with virtually no evidence about presence and pattern of degenerative versus inflammatory spinal lesions in subjects beyond 50 years of age.”
The study was supported by the Gottfried and Julia Bangerter-Rhyner Foundation. No conflicts of interest were declared.
SOURCE: Bratu V et al. Arthritis Care Res. 2018 Sep 22. doi: 10.1002/acr.23767.
A study of individuals with longstanding skin psoriasis but no clinical arthritis or spondylitis has found no evidence of subclinical involvement of the sacroiliac joint or spine.
The prevalence of sacroiliac lesions on blinded MRI assessment was similar in 20 patients who had skin psoriasis for a median of 23 years and in 22 healthy controls, and no sacroiliac ankylosis was seen in either group. Similarly, there was no significant difference between the two groups in spinal lesions on MRI, nor in any of the five levels of lesion frequency, Vlad A. Bratu, MD, of the department of radiology at University Hospital Basel (Switzerland) and his coauthors reported in Arthritis Care & Research.
On blinded MRI assessment, five (25%) patients with skin psoriasis and two (9.1%) controls were classified as having inflammation of the sacroiliac joint. Three of these patients in the psoriasis group and one in the control group were older than 50, and the three with psoriasis had had the condition for 26-35 years.
Dr. Bratu and his colleagues said that subclinical peripheral joint inflammation on MRI had previously been a common finding in patients who had skin psoriasis but no clinical signs of psoriatic arthritis. But given the limited evidence of concomitant subclinical axial or spinal inflammation in their study, the authors argued there was no support for routine screening for potential subclinical axial inflammation in patients with longstanding skin psoriasis.
They noted that bone marrow edema lesions in at least two sacroiliac joint quadrants were seen in 35% of patients with psoriasis and 23% of healthy controls, a finding that reflected those seen in other studies in healthy individuals.
“If a specificity threshold for a given MRI lesion of at least 0.9 is applied for axial MRI to discriminate between axial SpA [spondyloarthritis] and background variation in healthy controls or in differential diagnostic conditions, no more than 10% of healthy controls in our study should meet this criterion by an individual level data analysis,” they wrote.
The authors also pointed out the impact of age on lesion frequency, which was more evident in spinal lesions.
“This observation supports the hypothesis that some spinal alterations in higher age may reflect degenerative rather than inflammatory changes,” they wrote. “However, there is a gap in knowledge with virtually no evidence about presence and pattern of degenerative versus inflammatory spinal lesions in subjects beyond 50 years of age.”
The study was supported by the Gottfried and Julia Bangerter-Rhyner Foundation. No conflicts of interest were declared.
SOURCE: Bratu V et al. Arthritis Care Res. 2018 Sep 22. doi: 10.1002/acr.23767.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point:
Major finding: The prevalence of sacroiliac bone marrow lesions was similar between patients with skin psoriasis and healthy controls.
Study details: Case-control study in 20 patients with skin psoriasis and 22 healthy controls.
Disclosures: The study was supported by the Gottfried and Julia Bangerter-Rhyner Foundation. No conflicts of interest were declared.
Source: Bratu V et al. Arthritis Care Res. 2018 Sep 22. doi: 10.1002/acr.23767.
Conference News Roundup—European Society of Cardiology
Patients With High Blood Pressure Should Undergo Clock Drawing Test
A clock drawing test for detecting cognitive dysfunction should be conducted routinely in patients with high blood pressure, according to researchers.
Patients with high blood pressure who have impaired cognitive function are at increased risk of developing dementia within five years. Despite this known link, cognitive function is not routinely measured in patients with high blood pressure.
“The ability to draw the numbers of a clock and a particular time is an easy way to find out if a patient with high blood pressure has cognitive impairment,” said Augusto Vicario, MD, a cardiologist at the Cardiovascular Institute of Buenos Aires. “Identifying these patients provides the opportunity to intervene before dementia develops.”
The Heart-Brain Study in Argentina evaluated the usefulness of the clock drawing test, compared with the Mini-Mental State Examination (MMSE), to detect cognitive impairment in 1,414 adults with high blood pressure recruited from 18 cardiology centers in Argentina. The population’s average blood pressure was 144/84 mm Hg, average age was 60, and 62% were women.
For the clock drawing test, patients were given a piece of paper with a circle on it (diameter, 10 cm). They were asked to write the numbers of the clock in the correct positions inside the circle and draw hands on the clock indicating the time “20 to four.” Patients were scored as having normal cognition or moderate or severe cognitive impairment.
The researchers found a higher prevalence of cognitive impairment with the clock drawing test (36%), compared with the MMSE (21%). Three of 10 patients who had a normal MMSE score had an abnormal clock drawing result. The disparity in results between the two tests was greatest in middle-aged patients.
“Untreated high blood pressure silently and progressively damages the arteries in the subcortex of the brain and stops communication between the subcortex and frontal lobe,” said Dr. Vicario. “This disconnect leads to impaired executive functions such as planning, visuospatial abilities, remembering details, and decision-making. The clock drawing test is known to evaluate executive functions. The MMSE evaluates several other cognitive abilities but is weakly correlated with executive functions.
“Our study suggests that the clock drawing test should be preferred over the MMSE for early detection of executive dysfunction in patients with high blood pressure, particularly in middle age. We think the score on the clock drawing test can be considered a surrogate measure of silent vascular damage in the brain and identifies patients at greater risk of developing dementia. In our study, more than one-third of patients were at risk.
“The clock drawing test should be adopted as a routine screening tool for cognitive decline in patients with high blood pressure. Further studies are needed to determine whether lowering blood pressure can prevent progression to dementia,” Dr. Vicario concluded.
Short Sleep Associated With Doubled Risk of Cardiovascular Disease
Middle-aged men who sleep for five hours or fewer per night have twice the risk of developing a major cardiovascular event during the following two decades, compared with men who sleep for seven to eight hours, according to a study.
“For people with busy lives, sleeping may feel like a waste of time, but our study suggests that short sleep could be linked with future cardiovascular disease,” said Moa Bengtsson of the University of Gothenburg, Sweden.
Previous studies have generated conflicting evidence on whether short sleep is associated with a greater chance of having a future cardiovascular event. This study investigated this relationship in 50-year-old men.
In 1993, 50% of all men born in 1943 and living in Gothenburg were randomly selected to participate in the study. Of the 1,463 invited, 798 (55%) men agreed to take part. Participants underwent a physical examination and completed a questionnaire on current health conditions, average sleep duration, physical activity, and smoking. The men were divided into four groups according to their self-estimated average sleep duration at the start of the study: five or fewer hours, six hours, seven to eight hours (considered normal sleep duration), and more than eight hours.
Participants were followed up for 21 years for the occurrence of major cardiovascular events, which included heart attack, stroke, hospitalization due to heart failure, coronary revascularization, or death from cardiovascular disease. Data on cardiovascular events were collected from medical records, the Swedish Hospital Discharge Registry, and the Swedish Cause of Death Register.
Men with incomplete data on sleep duration, incomplete follow-up information, or who had a major cardiovascular event before the start of the study were excluded, leaving a total of 759 men for the analyses.
High blood pressure, diabetes, obesity, current smoking, low physical activity, and poor sleep quality were more common in men who slept for five or fewer hours per night, compared with those who slept for seven to eight hours.
Compared with those with normal sleep duration, men who slept for five or fewer hours per night had a twofold higher risk of having a major cardiovascular event by age 71. The risk remained doubled after adjusting for cardiovascular risk factors at the start of the study, including obesity, diabetes, and smoking.
“Men with the shortest sleep duration at the age of 50 were twice as likely to have had a cardiovascular event by age 71 as those who slept a normal amount, even when other risk factors were taken into account,” said Ms. Bengtsson.
“In our study, the magnitude of increased cardiovascular risk associated with insufficient sleep is similar to that of smoking or having diabetes at age 50. This was an observational study, so, based on our findings, we cannot conclude that short sleep causes cardiovascular disease or say definitively that sleeping more will reduce risk. However, the findings do suggest that sleep is important, and that should be a wake-up call to all of us.”
How Long Is a Good Night’s Sleep?
Researchers have found that a sweet spot of six to eight hours’ sleep per night is most beneficial for heart health. More or less sleep is detrimental.
“We spend one-third of our lives sleeping, yet we know little about the impact of this biologic need on the cardiovascular system,” said Epameinondas Fountas, MD, of the Onassis Cardiac Surgery Centre in Athens.
The study investigated the relationship between sleep duration and cardiovascular disease using a meta-analysis that included 11 prospective studies published within the past five years of more than one million adults without cardiovascular disease.
Two groups, one with short (ie, fewer than six hours) and another with long (ie, more than eight hours) nightly sleep duration, were compared with the reference group (ie, six to eight hours’ sleep).
Short and long sleepers had a greater risk of developing or dying from coronary artery disease or stroke. Compared with adults who slept for six to eight hours per night, short and long sleepers had 11% and 33% greater risks, respectively, of developing or dying from coronary artery disease or stroke during an average follow-up of 9.3 years.
“Our findings suggest that too much or too little sleep may be bad for the heart,” said Dr. Fountas. “More research is needed to clarify exactly why, but we do know that sleep influences biologic processes like glucose metabolism, blood pressure, and inflammation, all of which have an impact on cardiovascular disease.”
A strength of the current analysis is that only prospective studies were included, noted Dr. Fountas. This technique avoids recall bias.
“Having the odd short night or lie-in is unlikely to be detrimental to health, but evidence is accumulating that prolonged nightly sleep deprivation or excessive sleeping should be avoided,” said Dr. Fountas. “The good news is that there are plenty of ways to get into the habit of getting six to eight hours a night: for example, by going to bed and getting up at the same time every day, avoiding alcohol and caffeine before bed, eating healthily, and being physically active. Getting the right amount of sleep is an important part of a healthy lifestyle.”
Four in 10 Patients With Atrial Fibrillation Have Unrecognized Brain Damage
Four out of 10 patients with atrial fibrillation but no history of stroke or transient ischemic attack have previously unrecognized brain damage, according to the first results of the Swiss Atrial Fibrillation Cohort Study (Swiss-AF).
“Our results suggest that clinically unrecognized brain damage may explain the association between dementia and atrial fibrillation in patients without prior stroke,” said David Conen, MD, MPH, Associate Professor of Cardiology at McMaster University in Hamilton, Canada.
Patients with atrial fibrillation have a significantly increased risk of stroke, which is why most are treated with oral anticoagulation. This increased stroke risk is probably the main reason why patients with atrial fibrillation also face an increased risk of cognitive dysfunction and dementia. The relationship between atrial fibrillation and dementia has also been shown among patients without prior strokes, however, meaning that additional mechanisms must be involved. Clarifying the mechanisms by which atrial fibrillation increases the risk of cognitive dysfunction and dementia is a first step towards developing preventive measures.
Swiss-AF is a prospective, observational study designed to pinpoint the mechanisms of cognitive decline in patients with atrial fibrillation. Dr. Conen’s analysis investigated the prevalence of silent brain damage in patients with atrial fibrillation.
The study enrolled 2,415 patients older than 65 with atrial fibrillation between 2014 and 2017 from 14 centers in Switzerland. All patients without contraindications underwent standardized brain MRI, and the images were analyzed in a central core laboratory. Scans were available in 1,736 patients. Of those patients, 347 (20%) had a history of stroke or transient ischemic attack and were excluded from the analysis.
The final analysis included 1,389 patients with atrial fibrillation but no history of stroke or transient ischemic attack. The average age of participants was 72, and 26% were women. The scans showed that 569 (41%) patients had at least one type of previously unrecognized brain damage: 207 (15%) had a cerebral infarct, 269 (19%) had microbleeds, and 222 (16%) had lacunes.
“Four in 10 patients with atrial fibrillation but no history of stroke or transient ischemic attack had clinically unrecognized silent brain lesions,” said Dr. Conen. “This brain damage could trigger cognitive decline.”
Most study participants (1,234; 89%) were treated with oral anticoagulants. Stefan Osswald, MD, Chief of Cardiology at University Hospital Basel in Switzerland, noted that the cross-sectional analysis looked at the data at a single point in time and cannot address the question of whether the cerebral infarcts and other brain lesions occurred before or after initiation of oral anticoagulation. “The findings nevertheless raise the issue that oral anticoagulation might not prevent all brain damage in patients with atrial fibrillation,” he said.
“All Swiss-AF participants underwent extensive cognitive testing. These data will be analyzed to see whether patients with silent brain lesions also have impaired cognitive function,” said Dr. Conen. Collaborations with other study groups will help determine whether these findings are specific to patients with atrial fibrillation.
Impaired Mental Status Doubles Elderly’s Risk of Death After Heart Attack
Impaired mental status is associated with a doubled risk of death one year after a heart attack in elderly patients, according to researchers.
“Cardiologists should consider conducting simple tests to assess mental status in elderly people after a heart attack,” said Farzin Beygui, MD, hospital practitioner at Caen University Hospital in France. “Patients with reduced mental status can then receive more intensive management such as regular follow-up appointments with their general practitioners or nurses, more specific assessment for an early diagnosis of dementia, and tailored therapy.”
The risks of dementia, Alzheimer’s disease, confusion, and delirium increase with age. Elderly people are also at higher risk of having a heart attack and dying afterwards. People aged 75 and older account for approximately one-third of heart attack admissions and more than half of those dying in the hospital after admission for a heart attack. Until now, it was not known whether impaired mental status affected the prognosis of elderly patients with heart attack.
This study assessed the impact of mental status on the risk of death in 600 patients age 75 and above consecutively admitted for heart attack and followed up for at least one year. Mental status was assessed using the Mini-Mental State Examination (MMSE) and the Confusion Assessment Method (CAM).Cognitive impairment was detected in 174 (29%) patients. Patients with impaired mental function were more than twice as likely to be dead one year after their heart attack than those with healthy mental function. The association was independent of other potential predictors of death such as age, sex, invasive treatment, type of myocardial infarction, heart failure, and severity of the heart attack.
Impaired mental status was also associated with a nearly fourfold higher rate of bleeding complications while in the hospital and a more than twofold higher risk of being readmitted to the hospital for cardiovascular causes within three months after discharge.
“Almost one-third of elderly heart attack patients in our study had reduced mental capacity,” said Dr. Beygui. “These patients had higher risks of bleeding, rehospitalization, and death. This may be because they forget to take their medicines or take them more than prescribed, rather than because of poor cognitive function itself.
“Assessing mental status is a simple way to identify elderly patients at particularly high risk of poor outcomes following a heart attack. Identifying these patients may help us target treatment to those who need it most.”
Patients With High Blood Pressure Should Undergo Clock Drawing Test
A clock drawing test for detecting cognitive dysfunction should be conducted routinely in patients with high blood pressure, according to researchers.
Patients with high blood pressure who have impaired cognitive function are at increased risk of developing dementia within five years. Despite this known link, cognitive function is not routinely measured in patients with high blood pressure.
“The ability to draw the numbers of a clock and a particular time is an easy way to find out if a patient with high blood pressure has cognitive impairment,” said Augusto Vicario, MD, a cardiologist at the Cardiovascular Institute of Buenos Aires. “Identifying these patients provides the opportunity to intervene before dementia develops.”
The Heart-Brain Study in Argentina evaluated the usefulness of the clock drawing test, compared with the Mini-Mental State Examination (MMSE), to detect cognitive impairment in 1,414 adults with high blood pressure recruited from 18 cardiology centers in Argentina. The population’s average blood pressure was 144/84 mm Hg, average age was 60, and 62% were women.
For the clock drawing test, patients were given a piece of paper with a circle on it (diameter, 10 cm). They were asked to write the numbers of the clock in the correct positions inside the circle and draw hands on the clock indicating the time “20 to four.” Patients were scored as having normal cognition or moderate or severe cognitive impairment.
The researchers found a higher prevalence of cognitive impairment with the clock drawing test (36%), compared with the MMSE (21%). Three of 10 patients who had a normal MMSE score had an abnormal clock drawing result. The disparity in results between the two tests was greatest in middle-aged patients.
“Untreated high blood pressure silently and progressively damages the arteries in the subcortex of the brain and stops communication between the subcortex and frontal lobe,” said Dr. Vicario. “This disconnect leads to impaired executive functions such as planning, visuospatial abilities, remembering details, and decision-making. The clock drawing test is known to evaluate executive functions. The MMSE evaluates several other cognitive abilities but is weakly correlated with executive functions.
“Our study suggests that the clock drawing test should be preferred over the MMSE for early detection of executive dysfunction in patients with high blood pressure, particularly in middle age. We think the score on the clock drawing test can be considered a surrogate measure of silent vascular damage in the brain and identifies patients at greater risk of developing dementia. In our study, more than one-third of patients were at risk.
“The clock drawing test should be adopted as a routine screening tool for cognitive decline in patients with high blood pressure. Further studies are needed to determine whether lowering blood pressure can prevent progression to dementia,” Dr. Vicario concluded.
Short Sleep Associated With Doubled Risk of Cardiovascular Disease
Middle-aged men who sleep for five hours or fewer per night have twice the risk of developing a major cardiovascular event during the following two decades, compared with men who sleep for seven to eight hours, according to a study.
“For people with busy lives, sleeping may feel like a waste of time, but our study suggests that short sleep could be linked with future cardiovascular disease,” said Moa Bengtsson of the University of Gothenburg, Sweden.
Previous studies have generated conflicting evidence on whether short sleep is associated with a greater chance of having a future cardiovascular event. This study investigated this relationship in 50-year-old men.
In 1993, 50% of all men born in 1943 and living in Gothenburg were randomly selected to participate in the study. Of the 1,463 invited, 798 (55%) men agreed to take part. Participants underwent a physical examination and completed a questionnaire on current health conditions, average sleep duration, physical activity, and smoking. The men were divided into four groups according to their self-estimated average sleep duration at the start of the study: five or fewer hours, six hours, seven to eight hours (considered normal sleep duration), and more than eight hours.
Participants were followed up for 21 years for the occurrence of major cardiovascular events, which included heart attack, stroke, hospitalization due to heart failure, coronary revascularization, or death from cardiovascular disease. Data on cardiovascular events were collected from medical records, the Swedish Hospital Discharge Registry, and the Swedish Cause of Death Register.
Men with incomplete data on sleep duration, incomplete follow-up information, or who had a major cardiovascular event before the start of the study were excluded, leaving a total of 759 men for the analyses.
High blood pressure, diabetes, obesity, current smoking, low physical activity, and poor sleep quality were more common in men who slept for five or fewer hours per night, compared with those who slept for seven to eight hours.
Compared with those with normal sleep duration, men who slept for five or fewer hours per night had a twofold higher risk of having a major cardiovascular event by age 71. The risk remained doubled after adjusting for cardiovascular risk factors at the start of the study, including obesity, diabetes, and smoking.
“Men with the shortest sleep duration at the age of 50 were twice as likely to have had a cardiovascular event by age 71 as those who slept a normal amount, even when other risk factors were taken into account,” said Ms. Bengtsson.
“In our study, the magnitude of increased cardiovascular risk associated with insufficient sleep is similar to that of smoking or having diabetes at age 50. This was an observational study, so, based on our findings, we cannot conclude that short sleep causes cardiovascular disease or say definitively that sleeping more will reduce risk. However, the findings do suggest that sleep is important, and that should be a wake-up call to all of us.”
How Long Is a Good Night’s Sleep?
Researchers have found that a sweet spot of six to eight hours’ sleep per night is most beneficial for heart health. More or less sleep is detrimental.
“We spend one-third of our lives sleeping, yet we know little about the impact of this biologic need on the cardiovascular system,” said Epameinondas Fountas, MD, of the Onassis Cardiac Surgery Centre in Athens.
The study investigated the relationship between sleep duration and cardiovascular disease using a meta-analysis that included 11 prospective studies published within the past five years of more than one million adults without cardiovascular disease.
Two groups, one with short (ie, fewer than six hours) and another with long (ie, more than eight hours) nightly sleep duration, were compared with the reference group (ie, six to eight hours’ sleep).
Short and long sleepers had a greater risk of developing or dying from coronary artery disease or stroke. Compared with adults who slept for six to eight hours per night, short and long sleepers had 11% and 33% greater risks, respectively, of developing or dying from coronary artery disease or stroke during an average follow-up of 9.3 years.
“Our findings suggest that too much or too little sleep may be bad for the heart,” said Dr. Fountas. “More research is needed to clarify exactly why, but we do know that sleep influences biologic processes like glucose metabolism, blood pressure, and inflammation, all of which have an impact on cardiovascular disease.”
A strength of the current analysis is that only prospective studies were included, noted Dr. Fountas. This technique avoids recall bias.
“Having the odd short night or lie-in is unlikely to be detrimental to health, but evidence is accumulating that prolonged nightly sleep deprivation or excessive sleeping should be avoided,” said Dr. Fountas. “The good news is that there are plenty of ways to get into the habit of getting six to eight hours a night: for example, by going to bed and getting up at the same time every day, avoiding alcohol and caffeine before bed, eating healthily, and being physically active. Getting the right amount of sleep is an important part of a healthy lifestyle.”
Four in 10 Patients With Atrial Fibrillation Have Unrecognized Brain Damage
Four out of 10 patients with atrial fibrillation but no history of stroke or transient ischemic attack have previously unrecognized brain damage, according to the first results of the Swiss Atrial Fibrillation Cohort Study (Swiss-AF).
“Our results suggest that clinically unrecognized brain damage may explain the association between dementia and atrial fibrillation in patients without prior stroke,” said David Conen, MD, MPH, Associate Professor of Cardiology at McMaster University in Hamilton, Canada.
Patients with atrial fibrillation have a significantly increased risk of stroke, which is why most are treated with oral anticoagulation. This increased stroke risk is probably the main reason why patients with atrial fibrillation also face an increased risk of cognitive dysfunction and dementia. The relationship between atrial fibrillation and dementia has also been shown among patients without prior strokes, however, meaning that additional mechanisms must be involved. Clarifying the mechanisms by which atrial fibrillation increases the risk of cognitive dysfunction and dementia is a first step towards developing preventive measures.
Swiss-AF is a prospective, observational study designed to pinpoint the mechanisms of cognitive decline in patients with atrial fibrillation. Dr. Conen’s analysis investigated the prevalence of silent brain damage in patients with atrial fibrillation.
The study enrolled 2,415 patients older than 65 with atrial fibrillation between 2014 and 2017 from 14 centers in Switzerland. All patients without contraindications underwent standardized brain MRI, and the images were analyzed in a central core laboratory. Scans were available in 1,736 patients. Of those patients, 347 (20%) had a history of stroke or transient ischemic attack and were excluded from the analysis.
The final analysis included 1,389 patients with atrial fibrillation but no history of stroke or transient ischemic attack. The average age of participants was 72, and 26% were women. The scans showed that 569 (41%) patients had at least one type of previously unrecognized brain damage: 207 (15%) had a cerebral infarct, 269 (19%) had microbleeds, and 222 (16%) had lacunes.
“Four in 10 patients with atrial fibrillation but no history of stroke or transient ischemic attack had clinically unrecognized silent brain lesions,” said Dr. Conen. “This brain damage could trigger cognitive decline.”
Most study participants (1,234; 89%) were treated with oral anticoagulants. Stefan Osswald, MD, Chief of Cardiology at University Hospital Basel in Switzerland, noted that the cross-sectional analysis looked at the data at a single point in time and cannot address the question of whether the cerebral infarcts and other brain lesions occurred before or after initiation of oral anticoagulation. “The findings nevertheless raise the issue that oral anticoagulation might not prevent all brain damage in patients with atrial fibrillation,” he said.
“All Swiss-AF participants underwent extensive cognitive testing. These data will be analyzed to see whether patients with silent brain lesions also have impaired cognitive function,” said Dr. Conen. Collaborations with other study groups will help determine whether these findings are specific to patients with atrial fibrillation.
Impaired Mental Status Doubles Elderly’s Risk of Death After Heart Attack
Impaired mental status is associated with a doubled risk of death one year after a heart attack in elderly patients, according to researchers.
“Cardiologists should consider conducting simple tests to assess mental status in elderly people after a heart attack,” said Farzin Beygui, MD, hospital practitioner at Caen University Hospital in France. “Patients with reduced mental status can then receive more intensive management such as regular follow-up appointments with their general practitioners or nurses, more specific assessment for an early diagnosis of dementia, and tailored therapy.”
The risks of dementia, Alzheimer’s disease, confusion, and delirium increase with age. Elderly people are also at higher risk of having a heart attack and dying afterwards. People aged 75 and older account for approximately one-third of heart attack admissions and more than half of those dying in the hospital after admission for a heart attack. Until now, it was not known whether impaired mental status affected the prognosis of elderly patients with heart attack.
This study assessed the impact of mental status on the risk of death in 600 patients age 75 and above consecutively admitted for heart attack and followed up for at least one year. Mental status was assessed using the Mini-Mental State Examination (MMSE) and the Confusion Assessment Method (CAM).Cognitive impairment was detected in 174 (29%) patients. Patients with impaired mental function were more than twice as likely to be dead one year after their heart attack than those with healthy mental function. The association was independent of other potential predictors of death such as age, sex, invasive treatment, type of myocardial infarction, heart failure, and severity of the heart attack.
Impaired mental status was also associated with a nearly fourfold higher rate of bleeding complications while in the hospital and a more than twofold higher risk of being readmitted to the hospital for cardiovascular causes within three months after discharge.
“Almost one-third of elderly heart attack patients in our study had reduced mental capacity,” said Dr. Beygui. “These patients had higher risks of bleeding, rehospitalization, and death. This may be because they forget to take their medicines or take them more than prescribed, rather than because of poor cognitive function itself.
“Assessing mental status is a simple way to identify elderly patients at particularly high risk of poor outcomes following a heart attack. Identifying these patients may help us target treatment to those who need it most.”
Patients With High Blood Pressure Should Undergo Clock Drawing Test
A clock drawing test for detecting cognitive dysfunction should be conducted routinely in patients with high blood pressure, according to researchers.
Patients with high blood pressure who have impaired cognitive function are at increased risk of developing dementia within five years. Despite this known link, cognitive function is not routinely measured in patients with high blood pressure.
“The ability to draw the numbers of a clock and a particular time is an easy way to find out if a patient with high blood pressure has cognitive impairment,” said Augusto Vicario, MD, a cardiologist at the Cardiovascular Institute of Buenos Aires. “Identifying these patients provides the opportunity to intervene before dementia develops.”
The Heart-Brain Study in Argentina evaluated the usefulness of the clock drawing test, compared with the Mini-Mental State Examination (MMSE), to detect cognitive impairment in 1,414 adults with high blood pressure recruited from 18 cardiology centers in Argentina. The population’s average blood pressure was 144/84 mm Hg, average age was 60, and 62% were women.
For the clock drawing test, patients were given a piece of paper with a circle on it (diameter, 10 cm). They were asked to write the numbers of the clock in the correct positions inside the circle and draw hands on the clock indicating the time “20 to four.” Patients were scored as having normal cognition or moderate or severe cognitive impairment.
The researchers found a higher prevalence of cognitive impairment with the clock drawing test (36%), compared with the MMSE (21%). Three of 10 patients who had a normal MMSE score had an abnormal clock drawing result. The disparity in results between the two tests was greatest in middle-aged patients.
“Untreated high blood pressure silently and progressively damages the arteries in the subcortex of the brain and stops communication between the subcortex and frontal lobe,” said Dr. Vicario. “This disconnect leads to impaired executive functions such as planning, visuospatial abilities, remembering details, and decision-making. The clock drawing test is known to evaluate executive functions. The MMSE evaluates several other cognitive abilities but is weakly correlated with executive functions.
“Our study suggests that the clock drawing test should be preferred over the MMSE for early detection of executive dysfunction in patients with high blood pressure, particularly in middle age. We think the score on the clock drawing test can be considered a surrogate measure of silent vascular damage in the brain and identifies patients at greater risk of developing dementia. In our study, more than one-third of patients were at risk.
“The clock drawing test should be adopted as a routine screening tool for cognitive decline in patients with high blood pressure. Further studies are needed to determine whether lowering blood pressure can prevent progression to dementia,” Dr. Vicario concluded.
Short Sleep Associated With Doubled Risk of Cardiovascular Disease
Middle-aged men who sleep for five hours or fewer per night have twice the risk of developing a major cardiovascular event during the following two decades, compared with men who sleep for seven to eight hours, according to a study.
“For people with busy lives, sleeping may feel like a waste of time, but our study suggests that short sleep could be linked with future cardiovascular disease,” said Moa Bengtsson of the University of Gothenburg, Sweden.
Previous studies have generated conflicting evidence on whether short sleep is associated with a greater chance of having a future cardiovascular event. This study investigated this relationship in 50-year-old men.
In 1993, 50% of all men born in 1943 and living in Gothenburg were randomly selected to participate in the study. Of the 1,463 invited, 798 (55%) men agreed to take part. Participants underwent a physical examination and completed a questionnaire on current health conditions, average sleep duration, physical activity, and smoking. The men were divided into four groups according to their self-estimated average sleep duration at the start of the study: five or fewer hours, six hours, seven to eight hours (considered normal sleep duration), and more than eight hours.
Participants were followed up for 21 years for the occurrence of major cardiovascular events, which included heart attack, stroke, hospitalization due to heart failure, coronary revascularization, or death from cardiovascular disease. Data on cardiovascular events were collected from medical records, the Swedish Hospital Discharge Registry, and the Swedish Cause of Death Register.
Men with incomplete data on sleep duration, incomplete follow-up information, or who had a major cardiovascular event before the start of the study were excluded, leaving a total of 759 men for the analyses.
High blood pressure, diabetes, obesity, current smoking, low physical activity, and poor sleep quality were more common in men who slept for five or fewer hours per night, compared with those who slept for seven to eight hours.
Compared with those with normal sleep duration, men who slept for five or fewer hours per night had a twofold higher risk of having a major cardiovascular event by age 71. The risk remained doubled after adjusting for cardiovascular risk factors at the start of the study, including obesity, diabetes, and smoking.
“Men with the shortest sleep duration at the age of 50 were twice as likely to have had a cardiovascular event by age 71 as those who slept a normal amount, even when other risk factors were taken into account,” said Ms. Bengtsson.
“In our study, the magnitude of increased cardiovascular risk associated with insufficient sleep is similar to that of smoking or having diabetes at age 50. This was an observational study, so, based on our findings, we cannot conclude that short sleep causes cardiovascular disease or say definitively that sleeping more will reduce risk. However, the findings do suggest that sleep is important, and that should be a wake-up call to all of us.”
How Long Is a Good Night’s Sleep?
Researchers have found that a sweet spot of six to eight hours’ sleep per night is most beneficial for heart health. More or less sleep is detrimental.
“We spend one-third of our lives sleeping, yet we know little about the impact of this biologic need on the cardiovascular system,” said Epameinondas Fountas, MD, of the Onassis Cardiac Surgery Centre in Athens.
The study investigated the relationship between sleep duration and cardiovascular disease using a meta-analysis that included 11 prospective studies published within the past five years of more than one million adults without cardiovascular disease.
Two groups, one with short (ie, fewer than six hours) and another with long (ie, more than eight hours) nightly sleep duration, were compared with the reference group (ie, six to eight hours’ sleep).
Short and long sleepers had a greater risk of developing or dying from coronary artery disease or stroke. Compared with adults who slept for six to eight hours per night, short and long sleepers had 11% and 33% greater risks, respectively, of developing or dying from coronary artery disease or stroke during an average follow-up of 9.3 years.
“Our findings suggest that too much or too little sleep may be bad for the heart,” said Dr. Fountas. “More research is needed to clarify exactly why, but we do know that sleep influences biologic processes like glucose metabolism, blood pressure, and inflammation, all of which have an impact on cardiovascular disease.”
A strength of the current analysis is that only prospective studies were included, noted Dr. Fountas. This technique avoids recall bias.
“Having the odd short night or lie-in is unlikely to be detrimental to health, but evidence is accumulating that prolonged nightly sleep deprivation or excessive sleeping should be avoided,” said Dr. Fountas. “The good news is that there are plenty of ways to get into the habit of getting six to eight hours a night: for example, by going to bed and getting up at the same time every day, avoiding alcohol and caffeine before bed, eating healthily, and being physically active. Getting the right amount of sleep is an important part of a healthy lifestyle.”
Four in 10 Patients With Atrial Fibrillation Have Unrecognized Brain Damage
Four out of 10 patients with atrial fibrillation but no history of stroke or transient ischemic attack have previously unrecognized brain damage, according to the first results of the Swiss Atrial Fibrillation Cohort Study (Swiss-AF).
“Our results suggest that clinically unrecognized brain damage may explain the association between dementia and atrial fibrillation in patients without prior stroke,” said David Conen, MD, MPH, Associate Professor of Cardiology at McMaster University in Hamilton, Canada.
Patients with atrial fibrillation have a significantly increased risk of stroke, which is why most are treated with oral anticoagulation. This increased stroke risk is probably the main reason why patients with atrial fibrillation also face an increased risk of cognitive dysfunction and dementia. The relationship between atrial fibrillation and dementia has also been shown among patients without prior strokes, however, meaning that additional mechanisms must be involved. Clarifying the mechanisms by which atrial fibrillation increases the risk of cognitive dysfunction and dementia is a first step towards developing preventive measures.
Swiss-AF is a prospective, observational study designed to pinpoint the mechanisms of cognitive decline in patients with atrial fibrillation. Dr. Conen’s analysis investigated the prevalence of silent brain damage in patients with atrial fibrillation.
The study enrolled 2,415 patients older than 65 with atrial fibrillation between 2014 and 2017 from 14 centers in Switzerland. All patients without contraindications underwent standardized brain MRI, and the images were analyzed in a central core laboratory. Scans were available in 1,736 patients. Of those patients, 347 (20%) had a history of stroke or transient ischemic attack and were excluded from the analysis.
The final analysis included 1,389 patients with atrial fibrillation but no history of stroke or transient ischemic attack. The average age of participants was 72, and 26% were women. The scans showed that 569 (41%) patients had at least one type of previously unrecognized brain damage: 207 (15%) had a cerebral infarct, 269 (19%) had microbleeds, and 222 (16%) had lacunes.
“Four in 10 patients with atrial fibrillation but no history of stroke or transient ischemic attack had clinically unrecognized silent brain lesions,” said Dr. Conen. “This brain damage could trigger cognitive decline.”
Most study participants (1,234; 89%) were treated with oral anticoagulants. Stefan Osswald, MD, Chief of Cardiology at University Hospital Basel in Switzerland, noted that the cross-sectional analysis looked at the data at a single point in time and cannot address the question of whether the cerebral infarcts and other brain lesions occurred before or after initiation of oral anticoagulation. “The findings nevertheless raise the issue that oral anticoagulation might not prevent all brain damage in patients with atrial fibrillation,” he said.
“All Swiss-AF participants underwent extensive cognitive testing. These data will be analyzed to see whether patients with silent brain lesions also have impaired cognitive function,” said Dr. Conen. Collaborations with other study groups will help determine whether these findings are specific to patients with atrial fibrillation.
Impaired Mental Status Doubles Elderly’s Risk of Death After Heart Attack
Impaired mental status is associated with a doubled risk of death one year after a heart attack in elderly patients, according to researchers.
“Cardiologists should consider conducting simple tests to assess mental status in elderly people after a heart attack,” said Farzin Beygui, MD, hospital practitioner at Caen University Hospital in France. “Patients with reduced mental status can then receive more intensive management such as regular follow-up appointments with their general practitioners or nurses, more specific assessment for an early diagnosis of dementia, and tailored therapy.”
The risks of dementia, Alzheimer’s disease, confusion, and delirium increase with age. Elderly people are also at higher risk of having a heart attack and dying afterwards. People aged 75 and older account for approximately one-third of heart attack admissions and more than half of those dying in the hospital after admission for a heart attack. Until now, it was not known whether impaired mental status affected the prognosis of elderly patients with heart attack.
This study assessed the impact of mental status on the risk of death in 600 patients age 75 and above consecutively admitted for heart attack and followed up for at least one year. Mental status was assessed using the Mini-Mental State Examination (MMSE) and the Confusion Assessment Method (CAM).Cognitive impairment was detected in 174 (29%) patients. Patients with impaired mental function were more than twice as likely to be dead one year after their heart attack than those with healthy mental function. The association was independent of other potential predictors of death such as age, sex, invasive treatment, type of myocardial infarction, heart failure, and severity of the heart attack.
Impaired mental status was also associated with a nearly fourfold higher rate of bleeding complications while in the hospital and a more than twofold higher risk of being readmitted to the hospital for cardiovascular causes within three months after discharge.
“Almost one-third of elderly heart attack patients in our study had reduced mental capacity,” said Dr. Beygui. “These patients had higher risks of bleeding, rehospitalization, and death. This may be because they forget to take their medicines or take them more than prescribed, rather than because of poor cognitive function itself.
“Assessing mental status is a simple way to identify elderly patients at particularly high risk of poor outcomes following a heart attack. Identifying these patients may help us target treatment to those who need it most.”