User login
Robot sperm, CRISPR-Cas9 parenting, eavesdropping on brains
Life (and mice) find a way
Apparently we have learned nothing from “Jurassic Park.” This time, though, we might get a world overrun by ... mice? Researchers in China have utilized the complex science of gene editing to help same-sex mice couples bear offspring. This is the first time both female-female and male-male pairs have produced pups (previously, only the female pairs were able to carry to full term) using CRISPR-Cas9. The experiment also served as a study in the relative uselessness of males: All the pups born of male pairs died shortly after birth. Researchers are hopeful to move on to bigger mammals including monkeys, which could eventually turn this “Jurassic Park” adventure into a full-on “Planet of the Apes” nightmare. Best of luck to them!
Hold me closer, tiny robot
Gentleman, we’ve all been put on notice. A team from the University of Exeter in England has taken the next step toward redundancy for the male of the species: robot sperm. Now that we’ve got your attention, take a deep breath and relax. It’s not that bad. The idea is for the robot sperm, or “torque-driven ferromagnetic swimmers,” to be used to deliver drugs, not DNA, the investigators explained. Each millimeter-long device consists “of a magnetic head and flexible tail that allows them to ‘swim’ to a specific location when activated by a magnetic field,” they said. “Developing this technology could radically change the way we do medicine. The swimmers could one day be used to direct drugs to the right areas of the body by swimming through blood vessels,” senior investigator Feodor Ogrin said. So, it looks like it’s going to be okay for men after all. Still, we have to wonder, how long will it be before Siri and Alexa try to make a withdrawal from the robot sperm bank?
Eavesdropping on the brain
Does this count as mind reading? A team of scientists and clinicians from the University of Cambridge has created a new method of testing brain function after tumor removal. The current method of running through cognitive tests while a patient is awake and the brain is exposed is painless (albeit objectively horrifying) but can be risky, and the current cognitive tests can be limited. This new approach is much safer – everyone wears protective gloves and gently massages the brain while singing “Kumbaya” ... Just kidding. Clinicians actually use MRI to examine the brain before surgery and determine how different regions of that ball of gray matter communicate with each other. A 3D-printed model of the patient’s brain is also provided, both as a handy 3D map and a fun souvenir! Because that’s what the world of medicine is missing: a gift shop.
Cannabinoids. Period.
When other medical news columns go high, we go low. How anatomically low? “Cannabis-infused vaginal suppositories.” Those of you about to be made reproductively moot by robot sperm and CRISPR-Cas9 should stop with the junior-high smirking. Because our more mature readers may be interested in an upcoming study. Foria Wellness is ready to put its cannabinoid-infused menstrual pain relief product, Foria Relief, to the test this fall in an observational study of 400 women. The suppositories deliver 60 mg of tetrahydrocannabinol and 10 mg of cannabidiol to their target. The company claims it’s a natural, side-effect–free analgesic alternative to hormonal birth control, ibuprofen, and opioids. And unlike unsuppositoried cannabinoid pain products that waft from place to place around a user’s system, Foria Relief promises sustained focus on its specific task. A quality that smirking junior-high types often lack.
Life (and mice) find a way
Apparently we have learned nothing from “Jurassic Park.” This time, though, we might get a world overrun by ... mice? Researchers in China have utilized the complex science of gene editing to help same-sex mice couples bear offspring. This is the first time both female-female and male-male pairs have produced pups (previously, only the female pairs were able to carry to full term) using CRISPR-Cas9. The experiment also served as a study in the relative uselessness of males: All the pups born of male pairs died shortly after birth. Researchers are hopeful to move on to bigger mammals including monkeys, which could eventually turn this “Jurassic Park” adventure into a full-on “Planet of the Apes” nightmare. Best of luck to them!
Hold me closer, tiny robot
Gentleman, we’ve all been put on notice. A team from the University of Exeter in England has taken the next step toward redundancy for the male of the species: robot sperm. Now that we’ve got your attention, take a deep breath and relax. It’s not that bad. The idea is for the robot sperm, or “torque-driven ferromagnetic swimmers,” to be used to deliver drugs, not DNA, the investigators explained. Each millimeter-long device consists “of a magnetic head and flexible tail that allows them to ‘swim’ to a specific location when activated by a magnetic field,” they said. “Developing this technology could radically change the way we do medicine. The swimmers could one day be used to direct drugs to the right areas of the body by swimming through blood vessels,” senior investigator Feodor Ogrin said. So, it looks like it’s going to be okay for men after all. Still, we have to wonder, how long will it be before Siri and Alexa try to make a withdrawal from the robot sperm bank?
Eavesdropping on the brain
Does this count as mind reading? A team of scientists and clinicians from the University of Cambridge has created a new method of testing brain function after tumor removal. The current method of running through cognitive tests while a patient is awake and the brain is exposed is painless (albeit objectively horrifying) but can be risky, and the current cognitive tests can be limited. This new approach is much safer – everyone wears protective gloves and gently massages the brain while singing “Kumbaya” ... Just kidding. Clinicians actually use MRI to examine the brain before surgery and determine how different regions of that ball of gray matter communicate with each other. A 3D-printed model of the patient’s brain is also provided, both as a handy 3D map and a fun souvenir! Because that’s what the world of medicine is missing: a gift shop.
Cannabinoids. Period.
When other medical news columns go high, we go low. How anatomically low? “Cannabis-infused vaginal suppositories.” Those of you about to be made reproductively moot by robot sperm and CRISPR-Cas9 should stop with the junior-high smirking. Because our more mature readers may be interested in an upcoming study. Foria Wellness is ready to put its cannabinoid-infused menstrual pain relief product, Foria Relief, to the test this fall in an observational study of 400 women. The suppositories deliver 60 mg of tetrahydrocannabinol and 10 mg of cannabidiol to their target. The company claims it’s a natural, side-effect–free analgesic alternative to hormonal birth control, ibuprofen, and opioids. And unlike unsuppositoried cannabinoid pain products that waft from place to place around a user’s system, Foria Relief promises sustained focus on its specific task. A quality that smirking junior-high types often lack.
Life (and mice) find a way
Apparently we have learned nothing from “Jurassic Park.” This time, though, we might get a world overrun by ... mice? Researchers in China have utilized the complex science of gene editing to help same-sex mice couples bear offspring. This is the first time both female-female and male-male pairs have produced pups (previously, only the female pairs were able to carry to full term) using CRISPR-Cas9. The experiment also served as a study in the relative uselessness of males: All the pups born of male pairs died shortly after birth. Researchers are hopeful to move on to bigger mammals including monkeys, which could eventually turn this “Jurassic Park” adventure into a full-on “Planet of the Apes” nightmare. Best of luck to them!
Hold me closer, tiny robot
Gentleman, we’ve all been put on notice. A team from the University of Exeter in England has taken the next step toward redundancy for the male of the species: robot sperm. Now that we’ve got your attention, take a deep breath and relax. It’s not that bad. The idea is for the robot sperm, or “torque-driven ferromagnetic swimmers,” to be used to deliver drugs, not DNA, the investigators explained. Each millimeter-long device consists “of a magnetic head and flexible tail that allows them to ‘swim’ to a specific location when activated by a magnetic field,” they said. “Developing this technology could radically change the way we do medicine. The swimmers could one day be used to direct drugs to the right areas of the body by swimming through blood vessels,” senior investigator Feodor Ogrin said. So, it looks like it’s going to be okay for men after all. Still, we have to wonder, how long will it be before Siri and Alexa try to make a withdrawal from the robot sperm bank?
Eavesdropping on the brain
Does this count as mind reading? A team of scientists and clinicians from the University of Cambridge has created a new method of testing brain function after tumor removal. The current method of running through cognitive tests while a patient is awake and the brain is exposed is painless (albeit objectively horrifying) but can be risky, and the current cognitive tests can be limited. This new approach is much safer – everyone wears protective gloves and gently massages the brain while singing “Kumbaya” ... Just kidding. Clinicians actually use MRI to examine the brain before surgery and determine how different regions of that ball of gray matter communicate with each other. A 3D-printed model of the patient’s brain is also provided, both as a handy 3D map and a fun souvenir! Because that’s what the world of medicine is missing: a gift shop.
Cannabinoids. Period.
When other medical news columns go high, we go low. How anatomically low? “Cannabis-infused vaginal suppositories.” Those of you about to be made reproductively moot by robot sperm and CRISPR-Cas9 should stop with the junior-high smirking. Because our more mature readers may be interested in an upcoming study. Foria Wellness is ready to put its cannabinoid-infused menstrual pain relief product, Foria Relief, to the test this fall in an observational study of 400 women. The suppositories deliver 60 mg of tetrahydrocannabinol and 10 mg of cannabidiol to their target. The company claims it’s a natural, side-effect–free analgesic alternative to hormonal birth control, ibuprofen, and opioids. And unlike unsuppositoried cannabinoid pain products that waft from place to place around a user’s system, Foria Relief promises sustained focus on its specific task. A quality that smirking junior-high types often lack.
Big drinkers face newly appreciated massive health burden
BARCELONA – Individuals who regularly consume alcohol in quantities defined by the World Health Organization as “very high risk” face a daunting and yet widely underappreciated health burden, Rainer Spanagel, MD, observed at the annual congress of the European College of Neuropsychopharmacology.
He cited a recent study led by Jürgen Rehm, PhD, of the Centre for Addiction and Mental Health in Toronto in which the investigators estimated the prevalence of what the WHO has defined as a “very-high-risk drinking level” among people aged 15-65 years in 13 E.U. countries. The researchers then went on to determine the associated annual risk of disease and injury, as well as the effects on life expectancy.
“The numbers are so shocking that you have to take it seriously,” said Dr. Spanagel, chair of the department of psychopharmacology at the Central Institute of Mental Health in Mannheim, Germany.
Nearly 2 decades ago, the WHO defined very-high-risk level of alcohol consumption as more than 100 g/day of ethanol for men and more than 60 g/day for women. That translates to a threshold of 7.1 and 4.3 standard drinks – a 12-ounce beer, 5-ounce glass of wine, or 1.5-ounce serving of liquor – on a daily basis.
“This WHO categorization of drinking risk levels has been pretty much ignored in clinical trials and epidemiologic studies until 3 or 4 years ago,” according to Dr. Spanagel.
The study by Dr. Rehm and his colleagues suggests this has been a serious mistake. By using data from the WHO’s Global Information System on Alcohol and Health, as well as from clinical trials, the investigators determined that the prevalence of this level of alcohol consumption was less than 1% overall across 13 European countries. However, rates varied markedly: in excess of 4% in Ireland and more than 3.5% in the United Kingdom, compared with less than 0.5% in Germany, Sweden, Denmark, Finland, Hungary, and the Netherlands. The Czech Republic came in at about 3%, while Italy, Spain, France, and Austria had rates of more than 0.5% but less than 1%.
The investigators estimated that the risk of disease or injury associated with this very-high-risk drinking level was 13.5% per year. Based on data from nine E.U. countries, Dr. Rehm and his colleagues found that a very-high-risk level of alcohol consumption caused nearly 54% of all cases of hepatic cirrhosis in those countries, 41% of esophageal and oral cancers, and 44% of pancreatitis.
Life expectancy in the European Union stands at 80.6 years. compared with the general population. By comparison, all cancers considered together resulted in 10 years of life lost.
Dr. Spanagel is editor in chief of the journal Addiction Biology, in which this study appeared (Addict Biol. 2018 Jul;23[4]:961-8).
BARCELONA – Individuals who regularly consume alcohol in quantities defined by the World Health Organization as “very high risk” face a daunting and yet widely underappreciated health burden, Rainer Spanagel, MD, observed at the annual congress of the European College of Neuropsychopharmacology.
He cited a recent study led by Jürgen Rehm, PhD, of the Centre for Addiction and Mental Health in Toronto in which the investigators estimated the prevalence of what the WHO has defined as a “very-high-risk drinking level” among people aged 15-65 years in 13 E.U. countries. The researchers then went on to determine the associated annual risk of disease and injury, as well as the effects on life expectancy.
“The numbers are so shocking that you have to take it seriously,” said Dr. Spanagel, chair of the department of psychopharmacology at the Central Institute of Mental Health in Mannheim, Germany.
Nearly 2 decades ago, the WHO defined very-high-risk level of alcohol consumption as more than 100 g/day of ethanol for men and more than 60 g/day for women. That translates to a threshold of 7.1 and 4.3 standard drinks – a 12-ounce beer, 5-ounce glass of wine, or 1.5-ounce serving of liquor – on a daily basis.
“This WHO categorization of drinking risk levels has been pretty much ignored in clinical trials and epidemiologic studies until 3 or 4 years ago,” according to Dr. Spanagel.
The study by Dr. Rehm and his colleagues suggests this has been a serious mistake. By using data from the WHO’s Global Information System on Alcohol and Health, as well as from clinical trials, the investigators determined that the prevalence of this level of alcohol consumption was less than 1% overall across 13 European countries. However, rates varied markedly: in excess of 4% in Ireland and more than 3.5% in the United Kingdom, compared with less than 0.5% in Germany, Sweden, Denmark, Finland, Hungary, and the Netherlands. The Czech Republic came in at about 3%, while Italy, Spain, France, and Austria had rates of more than 0.5% but less than 1%.
The investigators estimated that the risk of disease or injury associated with this very-high-risk drinking level was 13.5% per year. Based on data from nine E.U. countries, Dr. Rehm and his colleagues found that a very-high-risk level of alcohol consumption caused nearly 54% of all cases of hepatic cirrhosis in those countries, 41% of esophageal and oral cancers, and 44% of pancreatitis.
Life expectancy in the European Union stands at 80.6 years. compared with the general population. By comparison, all cancers considered together resulted in 10 years of life lost.
Dr. Spanagel is editor in chief of the journal Addiction Biology, in which this study appeared (Addict Biol. 2018 Jul;23[4]:961-8).
BARCELONA – Individuals who regularly consume alcohol in quantities defined by the World Health Organization as “very high risk” face a daunting and yet widely underappreciated health burden, Rainer Spanagel, MD, observed at the annual congress of the European College of Neuropsychopharmacology.
He cited a recent study led by Jürgen Rehm, PhD, of the Centre for Addiction and Mental Health in Toronto in which the investigators estimated the prevalence of what the WHO has defined as a “very-high-risk drinking level” among people aged 15-65 years in 13 E.U. countries. The researchers then went on to determine the associated annual risk of disease and injury, as well as the effects on life expectancy.
“The numbers are so shocking that you have to take it seriously,” said Dr. Spanagel, chair of the department of psychopharmacology at the Central Institute of Mental Health in Mannheim, Germany.
Nearly 2 decades ago, the WHO defined very-high-risk level of alcohol consumption as more than 100 g/day of ethanol for men and more than 60 g/day for women. That translates to a threshold of 7.1 and 4.3 standard drinks – a 12-ounce beer, 5-ounce glass of wine, or 1.5-ounce serving of liquor – on a daily basis.
“This WHO categorization of drinking risk levels has been pretty much ignored in clinical trials and epidemiologic studies until 3 or 4 years ago,” according to Dr. Spanagel.
The study by Dr. Rehm and his colleagues suggests this has been a serious mistake. By using data from the WHO’s Global Information System on Alcohol and Health, as well as from clinical trials, the investigators determined that the prevalence of this level of alcohol consumption was less than 1% overall across 13 European countries. However, rates varied markedly: in excess of 4% in Ireland and more than 3.5% in the United Kingdom, compared with less than 0.5% in Germany, Sweden, Denmark, Finland, Hungary, and the Netherlands. The Czech Republic came in at about 3%, while Italy, Spain, France, and Austria had rates of more than 0.5% but less than 1%.
The investigators estimated that the risk of disease or injury associated with this very-high-risk drinking level was 13.5% per year. Based on data from nine E.U. countries, Dr. Rehm and his colleagues found that a very-high-risk level of alcohol consumption caused nearly 54% of all cases of hepatic cirrhosis in those countries, 41% of esophageal and oral cancers, and 44% of pancreatitis.
Life expectancy in the European Union stands at 80.6 years. compared with the general population. By comparison, all cancers considered together resulted in 10 years of life lost.
Dr. Spanagel is editor in chief of the journal Addiction Biology, in which this study appeared (Addict Biol. 2018 Jul;23[4]:961-8).
REPORTING FROM THE ECNP CONGRESS
This year’s top papers on mood disorders
BARCELONA – Among the handful of top publications on mood disorders during the first three-quarters of 2018 was a landmark comparison of the efficacy and acceptability of 21 antidepressants for acute treatment of major depressive disorder, Íria Grande, MD, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
Dr. Grande, a psychiatrist at the bipolar disorders clinic of the University of Barcelona, shared her personal top picks.
‘Antidepressants work’
This epic systematic review and network meta-analysis (Lancet. 2018 Apr 7;391[10128]:1357-66) encompassed 522 randomized double-blind trials with 116,477 participants with major depressive disorder assigned to 21 antidepressants or placebo, in some instances with an additional active comparator antidepressant arm. The report is a major extension of previous work by the same multinational group of investigators (Lancet. 2009 Feb 28;373[9665]:746-58), who initially scrutinized 12 older antidepressants in a total population only one-quarter the size of the updated analysis.
Based upon this vast randomized trial evidence, some of which came from unpublished studies tracked down by the investigators, the 21 antidepressants were rank-ordered in terms of effectiveness and acceptability. But in Dr. Grande’s view, the most important study finding wasn’t which antidepressant donned the crown of most effective or patient acceptable, it was the fact that all 21 drugs proved significantly more effective than placebo, with odds ratios ranging from 2.13 at the top end to 1.37 for reboxetine.
“The results showed antidepressants work. All of the antipsychiatry system is trying to show us that antidepressants do not work in major depression. Well, in this study, it has been proven that all antidepressants are more effective than placebo in major depressive disorder. I think social media should be made aware of that. (Lead investigator) Dr. Andrea Cipriani talked on the BBC about this article, and it had a high impact,” according to Dr. Grande.
All but three of the 21 antidepressants were deemed to be as acceptable as placebo, based upon study dropout rates. The exceptions were agomelatine and fluoxetine, which were 12%-14% more acceptable than placebo. “That’s strange, I think, but that’s what the clinical trial results showed,” she noted. The findings on clomipramine, which was 30% less acceptable than placebo, make sense, Dr. Grande said, “due to its muscarinic effects.”
She took issue with some of the specific study findings. For example, the two top-rated antidepressants in terms of efficacy were amitriptyline and mirtazapine, with odds ratios of 2.13 and 1.89, respectively.
“As a clinician, I don’t consider mirtazapine to be one of the best antidepressants, especially in major depression,” she said. “But these are the results, and as always, we have to adapt the evidence-based medicine and consider it from our clinical point of view.”
The investigators conducted a subanalysis restricted to placebo-controlled head-to-head studies with a comparator antidepressant which Dr. Grande found more interesting and informative than the overall analysis. In the head-to-head analysis, vortioxetine emerged as the top-rated antidepressant, both in efficacy, with an odds ratio of 2.0, as well as in acceptability.
Lithium vs. quetiapine
Finnish investigators used prospective national databases to examine the rates of psychiatric and all-cause hospitalization during a mean 7.2 years of follow-up in all 18,018 Finns hospitalized for bipolar disorder. The purpose was to assess the impact of various mood stabilizers on overall health outcomes in a real-world setting.
The big winner was lithium. In an analysis adjusted for concomitant psychotropic medications, duration of bipolar illness, and intervals of drug exposure and nonexposure, lithium was associated with the lowest risks of psychiatric rehospitalization and all-cause hospitalization, with relative risk reductions of 33% and 29%, respectively. In contrast, quetiapine, the most widely used antipsychotic agent, paled by comparison, achieving only an 8% reduction in the risk of psychiatric rehospitalization and a 7% decrease in all-cause hospitalization (JAMA Psychiatry. 2018 Apr 1;75[4]:347-55).
In addition, long-acting injectable antipsychotics were significantly more effective for prevention of hospitalization than oral antipsychotics.
“That is kind of shocking, because in some countries, long-acting injectables are not authorized and cannot be used. But I think after this article some regulatory changes are going to take place as a result,” Dr. Grande predicted.
“Another issue I thought was interesting, although it was not the main aim of the study, involved benzodiazepines. They increased the risk of hospitalizations, both for psychiatric illness and all other causes. So apart from giving lithium and long-acting injectable antipsychotics to our bipolar patients, we should also be really careful about the use of benzodiazepines,” she commented.
Intranasal esketamine for suicidality?
Esketamine nasal spray, a fast-acting N-methyl-D-aspartate antagonist whose application for marketing approval in combination with a standard oral antidepressant in treatment-resistant depression is now under Food and Drug Administration review, also is being developed for another indication: reduction of suicidality in patients at imminent suicide risk. In a proof-of-concept study, intranasal esketamine resulted in a significant reduction in suicidal thoughts 4 hours after administration, compared with usual care – but not at 24 hours (Am J Psychiatry. 2018 Jul 1;175[7]:620-30).
New and effective medications for this indication are sorely needed. The only drug approved for the indication of suicide prevention is clozapine.
‘Latest thinking’ on bipolar disorders
Dr. Grande coauthored a comprehensive review article on bipolar disorders that she recommended as worthwhile reading (Nat Rev Dis Primers. 2018 Mar 8;4:18008. doi: 10.1038/nrdp.2018.8).
“It covers all the latest thinking. It focuses on the early stages of the disorder, how epigenetic factors are essential, and many other topics, including the bipolarity index being developed at the University of Barcelona to classify drugs in terms of their capacity to prevent episodes of mania or depression in terms of number needed to treat and number needed to harm. It emphasizes the importance of intervening early and focusing on cognitive dysfunction,” Dr Grande said.
Psychedelics making a comeback
German and Swiss investigators used a facial expression discrimination task to demonstrate that psilocybin, a 5-hydroxytryptamine2A–receptor agonist, decreases connectivity between the amygdala and regions of the brain important in emotion processing, including the striatum and frontal pole. The investigators theorized that this might be the mechanism for the psychedelic’s apparent antidepressant effects (Eur Neuropsychopharmacol. 2018 Jun;28[6]:691-700).
Dr. Grande included this study in her top publications list because it reflects the rapidly growing rebirth of interest in psychedelics research among European psychiatrists.
Indeed, elsewhere at the ECNP congress David J. Nutt, DM, declared, “We now have the beginnings of some swinging of the pendulum back in a modern direction. Over the last 10 years there have been a small number of open studies, all done with psilocybin, which is somewhat easier to use than LSD. There are studies in OCD [obsessive-compulsive disorder], tobacco dependence, alcoholism, resistant depression, end-of-life mood changes with cancer and other terminal diseases, and at least two ongoing randomized trials in resistant depression.”
Dr. Nutt, professor of neuropsychopharmacology at Imperial College London, was senior author of the first proof-of-concept study of psilocybin accompanied by psychologic support as a novel therapy for moderate to severe treatment-resistant major depression (Lancet Psychiatry. 2016 Jul;3[7]:619-27).
Methylphenidate ineffective for treatment of acute mania
The MEMAP study was a randomized, double-blind, placebo-controlled multicenter clinical trial testing what has been called the vigilance regulation model of mania. This model hypothesized that unstable regulation of wakefulness figures prominently in the pathogenesis of both mania and attention-deficit/hyperactivity disorder. If true, investigators reasoned, then 2.5 days of methylphenidate at 20-40 mg/day should have a rapid antimanic effect similar to the drug’s benefits in ADHD. Dr. Grande had been a skeptic, and indeed, the trial was halted early for futility (Eur Neuropsychopharmacol. 2018 Jan;28[1]:185-94).
She reported serving as a paid speaker for Lunbeck, Ferrer, GlaxoSmithKline, and Janssen. Her own research is funded by the Spanish Ministry of Economy and Competitiveness.
BARCELONA – Among the handful of top publications on mood disorders during the first three-quarters of 2018 was a landmark comparison of the efficacy and acceptability of 21 antidepressants for acute treatment of major depressive disorder, Íria Grande, MD, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
Dr. Grande, a psychiatrist at the bipolar disorders clinic of the University of Barcelona, shared her personal top picks.
‘Antidepressants work’
This epic systematic review and network meta-analysis (Lancet. 2018 Apr 7;391[10128]:1357-66) encompassed 522 randomized double-blind trials with 116,477 participants with major depressive disorder assigned to 21 antidepressants or placebo, in some instances with an additional active comparator antidepressant arm. The report is a major extension of previous work by the same multinational group of investigators (Lancet. 2009 Feb 28;373[9665]:746-58), who initially scrutinized 12 older antidepressants in a total population only one-quarter the size of the updated analysis.
Based upon this vast randomized trial evidence, some of which came from unpublished studies tracked down by the investigators, the 21 antidepressants were rank-ordered in terms of effectiveness and acceptability. But in Dr. Grande’s view, the most important study finding wasn’t which antidepressant donned the crown of most effective or patient acceptable, it was the fact that all 21 drugs proved significantly more effective than placebo, with odds ratios ranging from 2.13 at the top end to 1.37 for reboxetine.
“The results showed antidepressants work. All of the antipsychiatry system is trying to show us that antidepressants do not work in major depression. Well, in this study, it has been proven that all antidepressants are more effective than placebo in major depressive disorder. I think social media should be made aware of that. (Lead investigator) Dr. Andrea Cipriani talked on the BBC about this article, and it had a high impact,” according to Dr. Grande.
All but three of the 21 antidepressants were deemed to be as acceptable as placebo, based upon study dropout rates. The exceptions were agomelatine and fluoxetine, which were 12%-14% more acceptable than placebo. “That’s strange, I think, but that’s what the clinical trial results showed,” she noted. The findings on clomipramine, which was 30% less acceptable than placebo, make sense, Dr. Grande said, “due to its muscarinic effects.”
She took issue with some of the specific study findings. For example, the two top-rated antidepressants in terms of efficacy were amitriptyline and mirtazapine, with odds ratios of 2.13 and 1.89, respectively.
“As a clinician, I don’t consider mirtazapine to be one of the best antidepressants, especially in major depression,” she said. “But these are the results, and as always, we have to adapt the evidence-based medicine and consider it from our clinical point of view.”
The investigators conducted a subanalysis restricted to placebo-controlled head-to-head studies with a comparator antidepressant which Dr. Grande found more interesting and informative than the overall analysis. In the head-to-head analysis, vortioxetine emerged as the top-rated antidepressant, both in efficacy, with an odds ratio of 2.0, as well as in acceptability.
Lithium vs. quetiapine
Finnish investigators used prospective national databases to examine the rates of psychiatric and all-cause hospitalization during a mean 7.2 years of follow-up in all 18,018 Finns hospitalized for bipolar disorder. The purpose was to assess the impact of various mood stabilizers on overall health outcomes in a real-world setting.
The big winner was lithium. In an analysis adjusted for concomitant psychotropic medications, duration of bipolar illness, and intervals of drug exposure and nonexposure, lithium was associated with the lowest risks of psychiatric rehospitalization and all-cause hospitalization, with relative risk reductions of 33% and 29%, respectively. In contrast, quetiapine, the most widely used antipsychotic agent, paled by comparison, achieving only an 8% reduction in the risk of psychiatric rehospitalization and a 7% decrease in all-cause hospitalization (JAMA Psychiatry. 2018 Apr 1;75[4]:347-55).
In addition, long-acting injectable antipsychotics were significantly more effective for prevention of hospitalization than oral antipsychotics.
“That is kind of shocking, because in some countries, long-acting injectables are not authorized and cannot be used. But I think after this article some regulatory changes are going to take place as a result,” Dr. Grande predicted.
“Another issue I thought was interesting, although it was not the main aim of the study, involved benzodiazepines. They increased the risk of hospitalizations, both for psychiatric illness and all other causes. So apart from giving lithium and long-acting injectable antipsychotics to our bipolar patients, we should also be really careful about the use of benzodiazepines,” she commented.
Intranasal esketamine for suicidality?
Esketamine nasal spray, a fast-acting N-methyl-D-aspartate antagonist whose application for marketing approval in combination with a standard oral antidepressant in treatment-resistant depression is now under Food and Drug Administration review, also is being developed for another indication: reduction of suicidality in patients at imminent suicide risk. In a proof-of-concept study, intranasal esketamine resulted in a significant reduction in suicidal thoughts 4 hours after administration, compared with usual care – but not at 24 hours (Am J Psychiatry. 2018 Jul 1;175[7]:620-30).
New and effective medications for this indication are sorely needed. The only drug approved for the indication of suicide prevention is clozapine.
‘Latest thinking’ on bipolar disorders
Dr. Grande coauthored a comprehensive review article on bipolar disorders that she recommended as worthwhile reading (Nat Rev Dis Primers. 2018 Mar 8;4:18008. doi: 10.1038/nrdp.2018.8).
“It covers all the latest thinking. It focuses on the early stages of the disorder, how epigenetic factors are essential, and many other topics, including the bipolarity index being developed at the University of Barcelona to classify drugs in terms of their capacity to prevent episodes of mania or depression in terms of number needed to treat and number needed to harm. It emphasizes the importance of intervening early and focusing on cognitive dysfunction,” Dr Grande said.
Psychedelics making a comeback
German and Swiss investigators used a facial expression discrimination task to demonstrate that psilocybin, a 5-hydroxytryptamine2A–receptor agonist, decreases connectivity between the amygdala and regions of the brain important in emotion processing, including the striatum and frontal pole. The investigators theorized that this might be the mechanism for the psychedelic’s apparent antidepressant effects (Eur Neuropsychopharmacol. 2018 Jun;28[6]:691-700).
Dr. Grande included this study in her top publications list because it reflects the rapidly growing rebirth of interest in psychedelics research among European psychiatrists.
Indeed, elsewhere at the ECNP congress David J. Nutt, DM, declared, “We now have the beginnings of some swinging of the pendulum back in a modern direction. Over the last 10 years there have been a small number of open studies, all done with psilocybin, which is somewhat easier to use than LSD. There are studies in OCD [obsessive-compulsive disorder], tobacco dependence, alcoholism, resistant depression, end-of-life mood changes with cancer and other terminal diseases, and at least two ongoing randomized trials in resistant depression.”
Dr. Nutt, professor of neuropsychopharmacology at Imperial College London, was senior author of the first proof-of-concept study of psilocybin accompanied by psychologic support as a novel therapy for moderate to severe treatment-resistant major depression (Lancet Psychiatry. 2016 Jul;3[7]:619-27).
Methylphenidate ineffective for treatment of acute mania
The MEMAP study was a randomized, double-blind, placebo-controlled multicenter clinical trial testing what has been called the vigilance regulation model of mania. This model hypothesized that unstable regulation of wakefulness figures prominently in the pathogenesis of both mania and attention-deficit/hyperactivity disorder. If true, investigators reasoned, then 2.5 days of methylphenidate at 20-40 mg/day should have a rapid antimanic effect similar to the drug’s benefits in ADHD. Dr. Grande had been a skeptic, and indeed, the trial was halted early for futility (Eur Neuropsychopharmacol. 2018 Jan;28[1]:185-94).
She reported serving as a paid speaker for Lunbeck, Ferrer, GlaxoSmithKline, and Janssen. Her own research is funded by the Spanish Ministry of Economy and Competitiveness.
BARCELONA – Among the handful of top publications on mood disorders during the first three-quarters of 2018 was a landmark comparison of the efficacy and acceptability of 21 antidepressants for acute treatment of major depressive disorder, Íria Grande, MD, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
Dr. Grande, a psychiatrist at the bipolar disorders clinic of the University of Barcelona, shared her personal top picks.
‘Antidepressants work’
This epic systematic review and network meta-analysis (Lancet. 2018 Apr 7;391[10128]:1357-66) encompassed 522 randomized double-blind trials with 116,477 participants with major depressive disorder assigned to 21 antidepressants or placebo, in some instances with an additional active comparator antidepressant arm. The report is a major extension of previous work by the same multinational group of investigators (Lancet. 2009 Feb 28;373[9665]:746-58), who initially scrutinized 12 older antidepressants in a total population only one-quarter the size of the updated analysis.
Based upon this vast randomized trial evidence, some of which came from unpublished studies tracked down by the investigators, the 21 antidepressants were rank-ordered in terms of effectiveness and acceptability. But in Dr. Grande’s view, the most important study finding wasn’t which antidepressant donned the crown of most effective or patient acceptable, it was the fact that all 21 drugs proved significantly more effective than placebo, with odds ratios ranging from 2.13 at the top end to 1.37 for reboxetine.
“The results showed antidepressants work. All of the antipsychiatry system is trying to show us that antidepressants do not work in major depression. Well, in this study, it has been proven that all antidepressants are more effective than placebo in major depressive disorder. I think social media should be made aware of that. (Lead investigator) Dr. Andrea Cipriani talked on the BBC about this article, and it had a high impact,” according to Dr. Grande.
All but three of the 21 antidepressants were deemed to be as acceptable as placebo, based upon study dropout rates. The exceptions were agomelatine and fluoxetine, which were 12%-14% more acceptable than placebo. “That’s strange, I think, but that’s what the clinical trial results showed,” she noted. The findings on clomipramine, which was 30% less acceptable than placebo, make sense, Dr. Grande said, “due to its muscarinic effects.”
She took issue with some of the specific study findings. For example, the two top-rated antidepressants in terms of efficacy were amitriptyline and mirtazapine, with odds ratios of 2.13 and 1.89, respectively.
“As a clinician, I don’t consider mirtazapine to be one of the best antidepressants, especially in major depression,” she said. “But these are the results, and as always, we have to adapt the evidence-based medicine and consider it from our clinical point of view.”
The investigators conducted a subanalysis restricted to placebo-controlled head-to-head studies with a comparator antidepressant which Dr. Grande found more interesting and informative than the overall analysis. In the head-to-head analysis, vortioxetine emerged as the top-rated antidepressant, both in efficacy, with an odds ratio of 2.0, as well as in acceptability.
Lithium vs. quetiapine
Finnish investigators used prospective national databases to examine the rates of psychiatric and all-cause hospitalization during a mean 7.2 years of follow-up in all 18,018 Finns hospitalized for bipolar disorder. The purpose was to assess the impact of various mood stabilizers on overall health outcomes in a real-world setting.
The big winner was lithium. In an analysis adjusted for concomitant psychotropic medications, duration of bipolar illness, and intervals of drug exposure and nonexposure, lithium was associated with the lowest risks of psychiatric rehospitalization and all-cause hospitalization, with relative risk reductions of 33% and 29%, respectively. In contrast, quetiapine, the most widely used antipsychotic agent, paled by comparison, achieving only an 8% reduction in the risk of psychiatric rehospitalization and a 7% decrease in all-cause hospitalization (JAMA Psychiatry. 2018 Apr 1;75[4]:347-55).
In addition, long-acting injectable antipsychotics were significantly more effective for prevention of hospitalization than oral antipsychotics.
“That is kind of shocking, because in some countries, long-acting injectables are not authorized and cannot be used. But I think after this article some regulatory changes are going to take place as a result,” Dr. Grande predicted.
“Another issue I thought was interesting, although it was not the main aim of the study, involved benzodiazepines. They increased the risk of hospitalizations, both for psychiatric illness and all other causes. So apart from giving lithium and long-acting injectable antipsychotics to our bipolar patients, we should also be really careful about the use of benzodiazepines,” she commented.
Intranasal esketamine for suicidality?
Esketamine nasal spray, a fast-acting N-methyl-D-aspartate antagonist whose application for marketing approval in combination with a standard oral antidepressant in treatment-resistant depression is now under Food and Drug Administration review, also is being developed for another indication: reduction of suicidality in patients at imminent suicide risk. In a proof-of-concept study, intranasal esketamine resulted in a significant reduction in suicidal thoughts 4 hours after administration, compared with usual care – but not at 24 hours (Am J Psychiatry. 2018 Jul 1;175[7]:620-30).
New and effective medications for this indication are sorely needed. The only drug approved for the indication of suicide prevention is clozapine.
‘Latest thinking’ on bipolar disorders
Dr. Grande coauthored a comprehensive review article on bipolar disorders that she recommended as worthwhile reading (Nat Rev Dis Primers. 2018 Mar 8;4:18008. doi: 10.1038/nrdp.2018.8).
“It covers all the latest thinking. It focuses on the early stages of the disorder, how epigenetic factors are essential, and many other topics, including the bipolarity index being developed at the University of Barcelona to classify drugs in terms of their capacity to prevent episodes of mania or depression in terms of number needed to treat and number needed to harm. It emphasizes the importance of intervening early and focusing on cognitive dysfunction,” Dr Grande said.
Psychedelics making a comeback
German and Swiss investigators used a facial expression discrimination task to demonstrate that psilocybin, a 5-hydroxytryptamine2A–receptor agonist, decreases connectivity between the amygdala and regions of the brain important in emotion processing, including the striatum and frontal pole. The investigators theorized that this might be the mechanism for the psychedelic’s apparent antidepressant effects (Eur Neuropsychopharmacol. 2018 Jun;28[6]:691-700).
Dr. Grande included this study in her top publications list because it reflects the rapidly growing rebirth of interest in psychedelics research among European psychiatrists.
Indeed, elsewhere at the ECNP congress David J. Nutt, DM, declared, “We now have the beginnings of some swinging of the pendulum back in a modern direction. Over the last 10 years there have been a small number of open studies, all done with psilocybin, which is somewhat easier to use than LSD. There are studies in OCD [obsessive-compulsive disorder], tobacco dependence, alcoholism, resistant depression, end-of-life mood changes with cancer and other terminal diseases, and at least two ongoing randomized trials in resistant depression.”
Dr. Nutt, professor of neuropsychopharmacology at Imperial College London, was senior author of the first proof-of-concept study of psilocybin accompanied by psychologic support as a novel therapy for moderate to severe treatment-resistant major depression (Lancet Psychiatry. 2016 Jul;3[7]:619-27).
Methylphenidate ineffective for treatment of acute mania
The MEMAP study was a randomized, double-blind, placebo-controlled multicenter clinical trial testing what has been called the vigilance regulation model of mania. This model hypothesized that unstable regulation of wakefulness figures prominently in the pathogenesis of both mania and attention-deficit/hyperactivity disorder. If true, investigators reasoned, then 2.5 days of methylphenidate at 20-40 mg/day should have a rapid antimanic effect similar to the drug’s benefits in ADHD. Dr. Grande had been a skeptic, and indeed, the trial was halted early for futility (Eur Neuropsychopharmacol. 2018 Jan;28[1]:185-94).
She reported serving as a paid speaker for Lunbeck, Ferrer, GlaxoSmithKline, and Janssen. Her own research is funded by the Spanish Ministry of Economy and Competitiveness.
REPORTING FROM THE ECNP CONGRESS
Novel score predicts esophageal varices in patients with cirrhosis prior to EGD
PHILADELPHIA – A novel score accurately predicted the size and presence of esophageal varices in a noninvasive manner, which may help clinicians avoid unnecessary esophagogastroduodenoscopy in patients with cirrhosis, according to a recent award-winning presentation at the annual meeting of the American College of Gastroenterology.
Although there are two validated scores for predicting esophageal varices (EV), platelet count to spleen diameter ratio and Baveno VI criteria, they have drawbacks, Tien Dong, MD, from the University of California, Los Angeles said.
“The limitations to these existing scores and criteria are both of them require imaging to do, so because of that, they oftentimes are limited in national clinical use,” Dr. Dong said in his presentation of his team’s abstract, which won the ACG Governors Award for Excellence in Clinical Research. “The other thing is that, even though it’s recommended, sometimes spleen diameter on a normal ultrasound is not reported. Furthermore, elastography – even though it’s becoming more and more common – is still not yet readily available across the country.”
Dr. Dong and his colleagues sought to identify noninvasive clinical predictors of EV to create a predictive score to identify EV to overcome these drawbacks. They gathered endoscopy data from the Olive View–UCLA and West Los Angeles Veterans Affairs Hospital to create a discovery cohort (165 patients) and tested the score on patients from Ronald Reagan UCLA Medical Center in a validation cohort (73 patients).
They used a random forest classifier machine learning algorithm “to create a forest of decision trees so that it can tell us which variables it believes to be the most predictive of our outcomes of interest,” Dr. Dong said.
The algorithm identified several variables that appeared to be predictive of EV presence, such as international normalized ratio, aminotransferase, platelet mean, hemoglobin, albumin and blood urea nitrogen less than or equal to 3, which the researchers used to create an EV-endoscopy (EV-Endo) score.
In the discovery cohort, area under the curve (AUC) for the presence of EV was 0.81, compared with an AUC of 0.82 in the validation cohort, while there was an AUC of 0.77 in the discovery cohort and an AUC of 0.79 for small/absent vs. medium/large EV. Patients with Child-Pugh class A cirrhosis had an AUC of 0.81 for EV presence and an AUC of 0.77 for EV size. The researchers then created a cutoff score of 3.48 or less and 7.70 or more for EV presence, which had a sensitivity and specificity of 93.9% and 97.5%, respectively. EV-Endo score EV size cutoff scores were also 3.48 or less and 7.70 or more, with a sensitivity of 95.8% and specificity of 95.0%.
Dr. Dong reports no conflicts of interest.
SOURCE: Hauer M et al. ACG 2018. Presentation 31.
PHILADELPHIA – A novel score accurately predicted the size and presence of esophageal varices in a noninvasive manner, which may help clinicians avoid unnecessary esophagogastroduodenoscopy in patients with cirrhosis, according to a recent award-winning presentation at the annual meeting of the American College of Gastroenterology.
Although there are two validated scores for predicting esophageal varices (EV), platelet count to spleen diameter ratio and Baveno VI criteria, they have drawbacks, Tien Dong, MD, from the University of California, Los Angeles said.
“The limitations to these existing scores and criteria are both of them require imaging to do, so because of that, they oftentimes are limited in national clinical use,” Dr. Dong said in his presentation of his team’s abstract, which won the ACG Governors Award for Excellence in Clinical Research. “The other thing is that, even though it’s recommended, sometimes spleen diameter on a normal ultrasound is not reported. Furthermore, elastography – even though it’s becoming more and more common – is still not yet readily available across the country.”
Dr. Dong and his colleagues sought to identify noninvasive clinical predictors of EV to create a predictive score to identify EV to overcome these drawbacks. They gathered endoscopy data from the Olive View–UCLA and West Los Angeles Veterans Affairs Hospital to create a discovery cohort (165 patients) and tested the score on patients from Ronald Reagan UCLA Medical Center in a validation cohort (73 patients).
They used a random forest classifier machine learning algorithm “to create a forest of decision trees so that it can tell us which variables it believes to be the most predictive of our outcomes of interest,” Dr. Dong said.
The algorithm identified several variables that appeared to be predictive of EV presence, such as international normalized ratio, aminotransferase, platelet mean, hemoglobin, albumin and blood urea nitrogen less than or equal to 3, which the researchers used to create an EV-endoscopy (EV-Endo) score.
In the discovery cohort, area under the curve (AUC) for the presence of EV was 0.81, compared with an AUC of 0.82 in the validation cohort, while there was an AUC of 0.77 in the discovery cohort and an AUC of 0.79 for small/absent vs. medium/large EV. Patients with Child-Pugh class A cirrhosis had an AUC of 0.81 for EV presence and an AUC of 0.77 for EV size. The researchers then created a cutoff score of 3.48 or less and 7.70 or more for EV presence, which had a sensitivity and specificity of 93.9% and 97.5%, respectively. EV-Endo score EV size cutoff scores were also 3.48 or less and 7.70 or more, with a sensitivity of 95.8% and specificity of 95.0%.
Dr. Dong reports no conflicts of interest.
SOURCE: Hauer M et al. ACG 2018. Presentation 31.
PHILADELPHIA – A novel score accurately predicted the size and presence of esophageal varices in a noninvasive manner, which may help clinicians avoid unnecessary esophagogastroduodenoscopy in patients with cirrhosis, according to a recent award-winning presentation at the annual meeting of the American College of Gastroenterology.
Although there are two validated scores for predicting esophageal varices (EV), platelet count to spleen diameter ratio and Baveno VI criteria, they have drawbacks, Tien Dong, MD, from the University of California, Los Angeles said.
“The limitations to these existing scores and criteria are both of them require imaging to do, so because of that, they oftentimes are limited in national clinical use,” Dr. Dong said in his presentation of his team’s abstract, which won the ACG Governors Award for Excellence in Clinical Research. “The other thing is that, even though it’s recommended, sometimes spleen diameter on a normal ultrasound is not reported. Furthermore, elastography – even though it’s becoming more and more common – is still not yet readily available across the country.”
Dr. Dong and his colleagues sought to identify noninvasive clinical predictors of EV to create a predictive score to identify EV to overcome these drawbacks. They gathered endoscopy data from the Olive View–UCLA and West Los Angeles Veterans Affairs Hospital to create a discovery cohort (165 patients) and tested the score on patients from Ronald Reagan UCLA Medical Center in a validation cohort (73 patients).
They used a random forest classifier machine learning algorithm “to create a forest of decision trees so that it can tell us which variables it believes to be the most predictive of our outcomes of interest,” Dr. Dong said.
The algorithm identified several variables that appeared to be predictive of EV presence, such as international normalized ratio, aminotransferase, platelet mean, hemoglobin, albumin and blood urea nitrogen less than or equal to 3, which the researchers used to create an EV-endoscopy (EV-Endo) score.
In the discovery cohort, area under the curve (AUC) for the presence of EV was 0.81, compared with an AUC of 0.82 in the validation cohort, while there was an AUC of 0.77 in the discovery cohort and an AUC of 0.79 for small/absent vs. medium/large EV. Patients with Child-Pugh class A cirrhosis had an AUC of 0.81 for EV presence and an AUC of 0.77 for EV size. The researchers then created a cutoff score of 3.48 or less and 7.70 or more for EV presence, which had a sensitivity and specificity of 93.9% and 97.5%, respectively. EV-Endo score EV size cutoff scores were also 3.48 or less and 7.70 or more, with a sensitivity of 95.8% and specificity of 95.0%.
Dr. Dong reports no conflicts of interest.
SOURCE: Hauer M et al. ACG 2018. Presentation 31.
REPORTING FROM ACG 2018
November 2018
Gastroenterology
How and when to consider genetic testing for colon cancer? Ballester V; Cruz-Correa M. 2018 Oct;155(4):955-9. doi: 10.1053/j.gastro.2018.08.031.
How to approach a patient with eosinophilic esophagitis. Hirano I. 2018 Sept;155(3):601-6. doi: 10.1053/j.gastro.2018.08.001.
How to ensure patient adherence to colorectal cancer screening and surveillance in your practice. Hassan C; Kaminski MF; Repici A. 2018 Aug;155(2):252-7. doi: 10.1053/j.gastro.2018.06.051.
How to approach difficult patient encounters: ROAR. McCarthy JG; Cheatham JG; Singla M. 2018 Aug;155(2):258-61. doi: 10.1053/j.gastro.2018.06.052.
An inside view: AGA advocacy priorities. Jain R. 2018 Aug;155(2):572-3. doi: 10.1053/j.gastro.2018.06.028.
Clin Gastro Hepatol
Adding value to the conversation about colorectal cancer screening: Practical pearls for gastroenterologists. Maratt JK; Naylor K; Saini SD. 2018 Oct;16(10):1545–8. doi: 10.1016/j.cgh.2018.07.002.
Credentialing for endoscopic practice: The Mayo Clinic model. Kane SV; Chandrasekhara V; Sedlack RE; Buttar NS. 2018 Sept;16(9):1370–3.e1 doi: 10.1016/j.cgh.2018.06.020.
Gastroenterology
How and when to consider genetic testing for colon cancer? Ballester V; Cruz-Correa M. 2018 Oct;155(4):955-9. doi: 10.1053/j.gastro.2018.08.031.
How to approach a patient with eosinophilic esophagitis. Hirano I. 2018 Sept;155(3):601-6. doi: 10.1053/j.gastro.2018.08.001.
How to ensure patient adherence to colorectal cancer screening and surveillance in your practice. Hassan C; Kaminski MF; Repici A. 2018 Aug;155(2):252-7. doi: 10.1053/j.gastro.2018.06.051.
How to approach difficult patient encounters: ROAR. McCarthy JG; Cheatham JG; Singla M. 2018 Aug;155(2):258-61. doi: 10.1053/j.gastro.2018.06.052.
An inside view: AGA advocacy priorities. Jain R. 2018 Aug;155(2):572-3. doi: 10.1053/j.gastro.2018.06.028.
Clin Gastro Hepatol
Adding value to the conversation about colorectal cancer screening: Practical pearls for gastroenterologists. Maratt JK; Naylor K; Saini SD. 2018 Oct;16(10):1545–8. doi: 10.1016/j.cgh.2018.07.002.
Credentialing for endoscopic practice: The Mayo Clinic model. Kane SV; Chandrasekhara V; Sedlack RE; Buttar NS. 2018 Sept;16(9):1370–3.e1 doi: 10.1016/j.cgh.2018.06.020.
Gastroenterology
How and when to consider genetic testing for colon cancer? Ballester V; Cruz-Correa M. 2018 Oct;155(4):955-9. doi: 10.1053/j.gastro.2018.08.031.
How to approach a patient with eosinophilic esophagitis. Hirano I. 2018 Sept;155(3):601-6. doi: 10.1053/j.gastro.2018.08.001.
How to ensure patient adherence to colorectal cancer screening and surveillance in your practice. Hassan C; Kaminski MF; Repici A. 2018 Aug;155(2):252-7. doi: 10.1053/j.gastro.2018.06.051.
How to approach difficult patient encounters: ROAR. McCarthy JG; Cheatham JG; Singla M. 2018 Aug;155(2):258-61. doi: 10.1053/j.gastro.2018.06.052.
An inside view: AGA advocacy priorities. Jain R. 2018 Aug;155(2):572-3. doi: 10.1053/j.gastro.2018.06.028.
Clin Gastro Hepatol
Adding value to the conversation about colorectal cancer screening: Practical pearls for gastroenterologists. Maratt JK; Naylor K; Saini SD. 2018 Oct;16(10):1545–8. doi: 10.1016/j.cgh.2018.07.002.
Credentialing for endoscopic practice: The Mayo Clinic model. Kane SV; Chandrasekhara V; Sedlack RE; Buttar NS. 2018 Sept;16(9):1370–3.e1 doi: 10.1016/j.cgh.2018.06.020.
HF unlikely in pregnant cancer survivors without history of cardiotoxicity
The risk of adverse cardiac events in female cancer survivors during pregnancy is low unless there is a history of cardiotoxicity, according to Shiying Liu, MD, of the University of Toronto, and her associates.
In a research letter published in the Journal of the American College of Cardiology, Dr. Liu and her associates reported on a retrospective chart review of 78 women with 94 pregnancies who had previously received cancer therapy who were seen at Mount Sinai Hospital between 2005 and 2015. Of these, 15 pregnancies occurred in 13 women with a prior history of cardiotoxicity. The primary outcome was a composite of cardiac events including cardiac death, heart failure (HF), acute coronary syndrome, and sustained arrhythmia.
HF occurred during five pregnancies in four women; no other adverse cardiac events occurred during the study period. All four of the women who experienced HF had a history of cardiotoxicity. There was no difference in age at cancer diagnosis, age at pregnancy, cancer type, or exposure to anthracyclines between those who did and did not experience HF, but women who developed HF were more likely to have left ventricular systolic dysfunction at the first antenatal visit (75% vs. 8%; P = .004) and to be on cardiac medications (50% vs. 8%; P = .026).
“The risk of developing [HF] during pregnancy is rare in female cancer survivors without a history of cardiotoxicity. These women can be reassured that they are at a very low risk of developing [HF] during pregnancy. Women who have a history of cardiotoxicity have an approximately one in three chance of developing [HF] during pregnancy and should receive close cardiac surveillance during pregnancy at a center with expertise in cardiac disease in pregnancy,” the authors concluded.
Coauthor Paaladinesh Thavendiranathan, MD, reported support from the Canadian Institutes of Health Research New Investigator Award. None of the other authors had any relevant financial disclosures.
SOURCE: Liu S et al. J Am Coll Cardiol. 2018 Oct 15. doi: 10.1016/j.jacc.2018.07.085.
The risk of adverse cardiac events in female cancer survivors during pregnancy is low unless there is a history of cardiotoxicity, according to Shiying Liu, MD, of the University of Toronto, and her associates.
In a research letter published in the Journal of the American College of Cardiology, Dr. Liu and her associates reported on a retrospective chart review of 78 women with 94 pregnancies who had previously received cancer therapy who were seen at Mount Sinai Hospital between 2005 and 2015. Of these, 15 pregnancies occurred in 13 women with a prior history of cardiotoxicity. The primary outcome was a composite of cardiac events including cardiac death, heart failure (HF), acute coronary syndrome, and sustained arrhythmia.
HF occurred during five pregnancies in four women; no other adverse cardiac events occurred during the study period. All four of the women who experienced HF had a history of cardiotoxicity. There was no difference in age at cancer diagnosis, age at pregnancy, cancer type, or exposure to anthracyclines between those who did and did not experience HF, but women who developed HF were more likely to have left ventricular systolic dysfunction at the first antenatal visit (75% vs. 8%; P = .004) and to be on cardiac medications (50% vs. 8%; P = .026).
“The risk of developing [HF] during pregnancy is rare in female cancer survivors without a history of cardiotoxicity. These women can be reassured that they are at a very low risk of developing [HF] during pregnancy. Women who have a history of cardiotoxicity have an approximately one in three chance of developing [HF] during pregnancy and should receive close cardiac surveillance during pregnancy at a center with expertise in cardiac disease in pregnancy,” the authors concluded.
Coauthor Paaladinesh Thavendiranathan, MD, reported support from the Canadian Institutes of Health Research New Investigator Award. None of the other authors had any relevant financial disclosures.
SOURCE: Liu S et al. J Am Coll Cardiol. 2018 Oct 15. doi: 10.1016/j.jacc.2018.07.085.
The risk of adverse cardiac events in female cancer survivors during pregnancy is low unless there is a history of cardiotoxicity, according to Shiying Liu, MD, of the University of Toronto, and her associates.
In a research letter published in the Journal of the American College of Cardiology, Dr. Liu and her associates reported on a retrospective chart review of 78 women with 94 pregnancies who had previously received cancer therapy who were seen at Mount Sinai Hospital between 2005 and 2015. Of these, 15 pregnancies occurred in 13 women with a prior history of cardiotoxicity. The primary outcome was a composite of cardiac events including cardiac death, heart failure (HF), acute coronary syndrome, and sustained arrhythmia.
HF occurred during five pregnancies in four women; no other adverse cardiac events occurred during the study period. All four of the women who experienced HF had a history of cardiotoxicity. There was no difference in age at cancer diagnosis, age at pregnancy, cancer type, or exposure to anthracyclines between those who did and did not experience HF, but women who developed HF were more likely to have left ventricular systolic dysfunction at the first antenatal visit (75% vs. 8%; P = .004) and to be on cardiac medications (50% vs. 8%; P = .026).
“The risk of developing [HF] during pregnancy is rare in female cancer survivors without a history of cardiotoxicity. These women can be reassured that they are at a very low risk of developing [HF] during pregnancy. Women who have a history of cardiotoxicity have an approximately one in three chance of developing [HF] during pregnancy and should receive close cardiac surveillance during pregnancy at a center with expertise in cardiac disease in pregnancy,” the authors concluded.
Coauthor Paaladinesh Thavendiranathan, MD, reported support from the Canadian Institutes of Health Research New Investigator Award. None of the other authors had any relevant financial disclosures.
SOURCE: Liu S et al. J Am Coll Cardiol. 2018 Oct 15. doi: 10.1016/j.jacc.2018.07.085.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
States act to safeguard young cancer patients’ chances to have children
When Katherine Frega was diagnosed with Hodgkin lymphoma 8 years ago at the age 17 years, she was so sick that all she could focus on was starting chemotherapy to treat her aggressive blood cancer. It was her dad who thought to ask the oncologist, “How is this treatment going to affect her ability to have children?”
The oncologist discussed the risks but stressed that Ms. Frega needed to start treatment right away.
The question of fertility is often overlooked when young cancer patients are battling a life-threatening illness. And since health insurance doesn’t typically cover fertility preservation care, patients and their families may be deterred by the cost.
But a growing number of states now require plans to cover such services when medically necessary treatment jeopardizes fertility.
Treatment for cancer and other serious conditions involves toxic chemotherapy drugs, radiation, and surgery that can cause infertility in women and men.
The cost to freeze patients’ healthy eggs, sperm, or embryos for future use can be a major barrier, said Eden Cardozo, MD, a reproductive endocrinologist and director of the fertility preservation program at the Women & Infants Fertility Center in Providence, R.I. Dr. Cardozo was instrumental in getting Rhode Island’s law passed last year.
“[Patients] have to move quickly,” she said. “They don’t have time to raise funds from family and friends. They don’t have time to petition their insurance company.”
Reproductive health advocates argue that fertility preservation should be viewed as a core component of cancer care in younger people, not as an optional infertility offering. Some compare this type of coverage with the federal Women’s Health and Cancer Rights Act, which requires plans that cover a patient’s mastectomy to also provide for breast reconstruction.
New laws in Delaware, Illinois, and Maryland require plans to include this benefit. The Delaware law applies to plans issued or renewed after June of this year; the requirement in the other two states starts in 2019. Connecticut and Rhode Island passed similar laws last year. New Jersey lawmakers are considering a bill and advocates in New York plan to make another attempt after both legislative chambers passed fertility preservation bills in the last session but failed to reconcile them.
The state measures don’t apply to companies that are self-funded, meaning they pay their employee claims directly rather than buying state-regulated insurance policies for that purpose. They also don’t apply to government-funded programs such as Medicaid or Tricare.
Although freezing sperm and embryos has been common medical practice for decades, egg freezing was considered experimental by professional groups until 2012. As the technology has improved, the need for insurance coverage has grown, said Joyce Reinecke, executive director of the Alliance for Fertility Preservation, an advocacy group for cancer patients.
When Ms. Frega’s cancer didn’t respond to chemotherapy, her doctors recommended a bone marrow transplant in January 2012. Even if her eggs hadn’t been damaged by the chemotherapy, the transplant would likely cause permanent infertility, she was told. So she took hormones to stimulate her ovaries to produce more eggs, among other things, and seven were retrieved during an outpatient procedure days before her transplant.
Ms. Frega’s parents paid $10,000 for the medications and egg retrieval, a significant amount but less than what many pay. They were aided by Livestrong Fertility, a nonprofit group that provides access to discounted fertility preservation services for cancer patients who meet income guidelines.
Ms. Frega has good insurance through her mother’s employer plan. “They covered everything else, except for this,” she said. “They considered it not medically necessary.”
Cancer-free following two bone marrow transplants, Ms. Frega, now 25 years old, is a third-year medical student at the Upstate Medical University in Syracuse, N.Y. She plans to specialize in oncology.
Between 20% and 70% of cancer patients experience some degree of fertility impairment, according to Dr. Cardozo in Rhode Island. Though they make up the largest at-risk group, the complication isn’t unique to cancer patients. People with other conditions such as lupus and rheumatoid arthritis who are treated with chemotherapy drugs may be affected, as may patients with conditions such as endometriosis who require surgery.
Despite the much-ballyhooed examples of tech companies like Facebook, Apple, and Google that offer egg freezing as an employee perk, cryopreservation, as it’s called, isn’t a typical employee benefit.
Only 6% of large companies with 500 or more workers offer egg freezing for employees or their spouses, according to the 2017 annual employer survey by benefits consultant Mercer. About a quarter cover in vitro fertilization (IVF). About 44% of large employers don’t offer any infertility services, the survey found.
Men face the same infertility risk when they need cancer treatment.
When Blake Hornbrook, an Army medic at Fort Campbell, Ky., had surgery to remove a cancerous testicle in the fall of 2015, he and his wife, Kelsey, were stationed in Germany. Mr. Hornbrook, then 26 years old, looked into fertility preservation while overseas, but the annual storage fee of 1,000 euros (about $1,150) deterred the couple.
He required a second surgery several months later to see if the cancer had spread to his lymph nodes. The couple returned to the United States and drove directly from the airport to a sperm bank in Fairfax, Va. It cost roughly $400 for the initial appointment to provide a sperm specimen and store it, Mr. Hornbrook said.
Tricare covered Mr. Hornbrook’s cancer treatment, but it didn’t pay for fertility preservation or for IVF, which he estimated cost the couple $6,500 in clinic fees. Tricare provided discounts on some of the fertility drugs.
Their daughter, Harper, was born 7 months ago, and Mr. Hornbrook’s cancer remains in remission.
For young cancer patients, the cost of storing the eggs or sperm that have been preserved can add up. Even if a state has a fertility preservation law, it typically doesn’t cover those costs, Ms. Reinecke said.
The Hornbrooks pay $480 annually to store his sperm and $375 to store their remaining embryos. Ms. Frega pays $1,000 annually to store her eggs.
Ms. Frega hopes to be able to conceive naturally and knowing she has frozen eggs available is “relieving, but also anxiety producing,” she said. If she can’t get pregnant later on, she may have to pay $10,000 or more for IVF as well. “That’s what lies ahead,” she said.
A total of 16 states require insurers to offer or cover infertility services to some extent, according to infertility advocacy organization Resolve. Requirements vary: Insurers may have to cover diagnosis or testing for infertility, for example, but not treatments like IVF or fertility medications, said Barbara Collura, president and CEO of Resolve.
Typically, state infertility coverage laws require couples to try to get pregnant for a year or two before they’re eligible for insurance coverage of IVF or other treatments.
That requirement makes little sense for patients trying to preserve their fertility before undergoing medically necessary cancer or other treatment.
“These people aren’t infertile,” said Ms. Collura. “They need to undergo some sort of intervention that is going to impair their future fertility, and what we say is that if it’s medically necessary, they should have a right to have it covered.”
KHN’s coverage of women’s health care issues is supported in part by The David and Lucile Packard Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
When Katherine Frega was diagnosed with Hodgkin lymphoma 8 years ago at the age 17 years, she was so sick that all she could focus on was starting chemotherapy to treat her aggressive blood cancer. It was her dad who thought to ask the oncologist, “How is this treatment going to affect her ability to have children?”
The oncologist discussed the risks but stressed that Ms. Frega needed to start treatment right away.
The question of fertility is often overlooked when young cancer patients are battling a life-threatening illness. And since health insurance doesn’t typically cover fertility preservation care, patients and their families may be deterred by the cost.
But a growing number of states now require plans to cover such services when medically necessary treatment jeopardizes fertility.
Treatment for cancer and other serious conditions involves toxic chemotherapy drugs, radiation, and surgery that can cause infertility in women and men.
The cost to freeze patients’ healthy eggs, sperm, or embryos for future use can be a major barrier, said Eden Cardozo, MD, a reproductive endocrinologist and director of the fertility preservation program at the Women & Infants Fertility Center in Providence, R.I. Dr. Cardozo was instrumental in getting Rhode Island’s law passed last year.
“[Patients] have to move quickly,” she said. “They don’t have time to raise funds from family and friends. They don’t have time to petition their insurance company.”
Reproductive health advocates argue that fertility preservation should be viewed as a core component of cancer care in younger people, not as an optional infertility offering. Some compare this type of coverage with the federal Women’s Health and Cancer Rights Act, which requires plans that cover a patient’s mastectomy to also provide for breast reconstruction.
New laws in Delaware, Illinois, and Maryland require plans to include this benefit. The Delaware law applies to plans issued or renewed after June of this year; the requirement in the other two states starts in 2019. Connecticut and Rhode Island passed similar laws last year. New Jersey lawmakers are considering a bill and advocates in New York plan to make another attempt after both legislative chambers passed fertility preservation bills in the last session but failed to reconcile them.
The state measures don’t apply to companies that are self-funded, meaning they pay their employee claims directly rather than buying state-regulated insurance policies for that purpose. They also don’t apply to government-funded programs such as Medicaid or Tricare.
Although freezing sperm and embryos has been common medical practice for decades, egg freezing was considered experimental by professional groups until 2012. As the technology has improved, the need for insurance coverage has grown, said Joyce Reinecke, executive director of the Alliance for Fertility Preservation, an advocacy group for cancer patients.
When Ms. Frega’s cancer didn’t respond to chemotherapy, her doctors recommended a bone marrow transplant in January 2012. Even if her eggs hadn’t been damaged by the chemotherapy, the transplant would likely cause permanent infertility, she was told. So she took hormones to stimulate her ovaries to produce more eggs, among other things, and seven were retrieved during an outpatient procedure days before her transplant.
Ms. Frega’s parents paid $10,000 for the medications and egg retrieval, a significant amount but less than what many pay. They were aided by Livestrong Fertility, a nonprofit group that provides access to discounted fertility preservation services for cancer patients who meet income guidelines.
Ms. Frega has good insurance through her mother’s employer plan. “They covered everything else, except for this,” she said. “They considered it not medically necessary.”
Cancer-free following two bone marrow transplants, Ms. Frega, now 25 years old, is a third-year medical student at the Upstate Medical University in Syracuse, N.Y. She plans to specialize in oncology.
Between 20% and 70% of cancer patients experience some degree of fertility impairment, according to Dr. Cardozo in Rhode Island. Though they make up the largest at-risk group, the complication isn’t unique to cancer patients. People with other conditions such as lupus and rheumatoid arthritis who are treated with chemotherapy drugs may be affected, as may patients with conditions such as endometriosis who require surgery.
Despite the much-ballyhooed examples of tech companies like Facebook, Apple, and Google that offer egg freezing as an employee perk, cryopreservation, as it’s called, isn’t a typical employee benefit.
Only 6% of large companies with 500 or more workers offer egg freezing for employees or their spouses, according to the 2017 annual employer survey by benefits consultant Mercer. About a quarter cover in vitro fertilization (IVF). About 44% of large employers don’t offer any infertility services, the survey found.
Men face the same infertility risk when they need cancer treatment.
When Blake Hornbrook, an Army medic at Fort Campbell, Ky., had surgery to remove a cancerous testicle in the fall of 2015, he and his wife, Kelsey, were stationed in Germany. Mr. Hornbrook, then 26 years old, looked into fertility preservation while overseas, but the annual storage fee of 1,000 euros (about $1,150) deterred the couple.
He required a second surgery several months later to see if the cancer had spread to his lymph nodes. The couple returned to the United States and drove directly from the airport to a sperm bank in Fairfax, Va. It cost roughly $400 for the initial appointment to provide a sperm specimen and store it, Mr. Hornbrook said.
Tricare covered Mr. Hornbrook’s cancer treatment, but it didn’t pay for fertility preservation or for IVF, which he estimated cost the couple $6,500 in clinic fees. Tricare provided discounts on some of the fertility drugs.
Their daughter, Harper, was born 7 months ago, and Mr. Hornbrook’s cancer remains in remission.
For young cancer patients, the cost of storing the eggs or sperm that have been preserved can add up. Even if a state has a fertility preservation law, it typically doesn’t cover those costs, Ms. Reinecke said.
The Hornbrooks pay $480 annually to store his sperm and $375 to store their remaining embryos. Ms. Frega pays $1,000 annually to store her eggs.
Ms. Frega hopes to be able to conceive naturally and knowing she has frozen eggs available is “relieving, but also anxiety producing,” she said. If she can’t get pregnant later on, she may have to pay $10,000 or more for IVF as well. “That’s what lies ahead,” she said.
A total of 16 states require insurers to offer or cover infertility services to some extent, according to infertility advocacy organization Resolve. Requirements vary: Insurers may have to cover diagnosis or testing for infertility, for example, but not treatments like IVF or fertility medications, said Barbara Collura, president and CEO of Resolve.
Typically, state infertility coverage laws require couples to try to get pregnant for a year or two before they’re eligible for insurance coverage of IVF or other treatments.
That requirement makes little sense for patients trying to preserve their fertility before undergoing medically necessary cancer or other treatment.
“These people aren’t infertile,” said Ms. Collura. “They need to undergo some sort of intervention that is going to impair their future fertility, and what we say is that if it’s medically necessary, they should have a right to have it covered.”
KHN’s coverage of women’s health care issues is supported in part by The David and Lucile Packard Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
When Katherine Frega was diagnosed with Hodgkin lymphoma 8 years ago at the age 17 years, she was so sick that all she could focus on was starting chemotherapy to treat her aggressive blood cancer. It was her dad who thought to ask the oncologist, “How is this treatment going to affect her ability to have children?”
The oncologist discussed the risks but stressed that Ms. Frega needed to start treatment right away.
The question of fertility is often overlooked when young cancer patients are battling a life-threatening illness. And since health insurance doesn’t typically cover fertility preservation care, patients and their families may be deterred by the cost.
But a growing number of states now require plans to cover such services when medically necessary treatment jeopardizes fertility.
Treatment for cancer and other serious conditions involves toxic chemotherapy drugs, radiation, and surgery that can cause infertility in women and men.
The cost to freeze patients’ healthy eggs, sperm, or embryos for future use can be a major barrier, said Eden Cardozo, MD, a reproductive endocrinologist and director of the fertility preservation program at the Women & Infants Fertility Center in Providence, R.I. Dr. Cardozo was instrumental in getting Rhode Island’s law passed last year.
“[Patients] have to move quickly,” she said. “They don’t have time to raise funds from family and friends. They don’t have time to petition their insurance company.”
Reproductive health advocates argue that fertility preservation should be viewed as a core component of cancer care in younger people, not as an optional infertility offering. Some compare this type of coverage with the federal Women’s Health and Cancer Rights Act, which requires plans that cover a patient’s mastectomy to also provide for breast reconstruction.
New laws in Delaware, Illinois, and Maryland require plans to include this benefit. The Delaware law applies to plans issued or renewed after June of this year; the requirement in the other two states starts in 2019. Connecticut and Rhode Island passed similar laws last year. New Jersey lawmakers are considering a bill and advocates in New York plan to make another attempt after both legislative chambers passed fertility preservation bills in the last session but failed to reconcile them.
The state measures don’t apply to companies that are self-funded, meaning they pay their employee claims directly rather than buying state-regulated insurance policies for that purpose. They also don’t apply to government-funded programs such as Medicaid or Tricare.
Although freezing sperm and embryos has been common medical practice for decades, egg freezing was considered experimental by professional groups until 2012. As the technology has improved, the need for insurance coverage has grown, said Joyce Reinecke, executive director of the Alliance for Fertility Preservation, an advocacy group for cancer patients.
When Ms. Frega’s cancer didn’t respond to chemotherapy, her doctors recommended a bone marrow transplant in January 2012. Even if her eggs hadn’t been damaged by the chemotherapy, the transplant would likely cause permanent infertility, she was told. So she took hormones to stimulate her ovaries to produce more eggs, among other things, and seven were retrieved during an outpatient procedure days before her transplant.
Ms. Frega’s parents paid $10,000 for the medications and egg retrieval, a significant amount but less than what many pay. They were aided by Livestrong Fertility, a nonprofit group that provides access to discounted fertility preservation services for cancer patients who meet income guidelines.
Ms. Frega has good insurance through her mother’s employer plan. “They covered everything else, except for this,” she said. “They considered it not medically necessary.”
Cancer-free following two bone marrow transplants, Ms. Frega, now 25 years old, is a third-year medical student at the Upstate Medical University in Syracuse, N.Y. She plans to specialize in oncology.
Between 20% and 70% of cancer patients experience some degree of fertility impairment, according to Dr. Cardozo in Rhode Island. Though they make up the largest at-risk group, the complication isn’t unique to cancer patients. People with other conditions such as lupus and rheumatoid arthritis who are treated with chemotherapy drugs may be affected, as may patients with conditions such as endometriosis who require surgery.
Despite the much-ballyhooed examples of tech companies like Facebook, Apple, and Google that offer egg freezing as an employee perk, cryopreservation, as it’s called, isn’t a typical employee benefit.
Only 6% of large companies with 500 or more workers offer egg freezing for employees or their spouses, according to the 2017 annual employer survey by benefits consultant Mercer. About a quarter cover in vitro fertilization (IVF). About 44% of large employers don’t offer any infertility services, the survey found.
Men face the same infertility risk when they need cancer treatment.
When Blake Hornbrook, an Army medic at Fort Campbell, Ky., had surgery to remove a cancerous testicle in the fall of 2015, he and his wife, Kelsey, were stationed in Germany. Mr. Hornbrook, then 26 years old, looked into fertility preservation while overseas, but the annual storage fee of 1,000 euros (about $1,150) deterred the couple.
He required a second surgery several months later to see if the cancer had spread to his lymph nodes. The couple returned to the United States and drove directly from the airport to a sperm bank in Fairfax, Va. It cost roughly $400 for the initial appointment to provide a sperm specimen and store it, Mr. Hornbrook said.
Tricare covered Mr. Hornbrook’s cancer treatment, but it didn’t pay for fertility preservation or for IVF, which he estimated cost the couple $6,500 in clinic fees. Tricare provided discounts on some of the fertility drugs.
Their daughter, Harper, was born 7 months ago, and Mr. Hornbrook’s cancer remains in remission.
For young cancer patients, the cost of storing the eggs or sperm that have been preserved can add up. Even if a state has a fertility preservation law, it typically doesn’t cover those costs, Ms. Reinecke said.
The Hornbrooks pay $480 annually to store his sperm and $375 to store their remaining embryos. Ms. Frega pays $1,000 annually to store her eggs.
Ms. Frega hopes to be able to conceive naturally and knowing she has frozen eggs available is “relieving, but also anxiety producing,” she said. If she can’t get pregnant later on, she may have to pay $10,000 or more for IVF as well. “That’s what lies ahead,” she said.
A total of 16 states require insurers to offer or cover infertility services to some extent, according to infertility advocacy organization Resolve. Requirements vary: Insurers may have to cover diagnosis or testing for infertility, for example, but not treatments like IVF or fertility medications, said Barbara Collura, president and CEO of Resolve.
Typically, state infertility coverage laws require couples to try to get pregnant for a year or two before they’re eligible for insurance coverage of IVF or other treatments.
That requirement makes little sense for patients trying to preserve their fertility before undergoing medically necessary cancer or other treatment.
“These people aren’t infertile,” said Ms. Collura. “They need to undergo some sort of intervention that is going to impair their future fertility, and what we say is that if it’s medically necessary, they should have a right to have it covered.”
KHN’s coverage of women’s health care issues is supported in part by The David and Lucile Packard Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Researchers consider R/R ALL drugs in the first-line setting
CHICAGO – Novel antibodies are improving outcomes in relapsed and refractory acute lymphoblastic leukemia (ALL), and the hope is that they will also show benefit in the up-front treatment setting and thereby improve overall outcomes, according to Anjali Advani, MD.
“It has been a really exciting time in ALL because several drugs have now been FDA approved: blinatumomab, inotuzumab, and now – for patients who are less than 26 years of age – we actually have CAR [chimeric antigen receptor] T cells that have been approved,” Dr. Advani, a hematologist and director of the inpatient leukemia program at the Cleveland Clinic said at the American Society of Hematology Meeting on Hematologic Malignancies.
At the time of relapse, however, the only known cure is allogeneic bone marrow transplant. That may change as more data regarding CAR T cells become available, but the typical goal at this time is to get patients into remission and then to transplant, she said.
Blinatumomab
“Blinatumomab is a very interesting antibody,” Dr. Advani said, explaining that it is a bispecific, T cell–engaging antibody with an anti-CD3 arm that engages the T cell and an anti-CD19 antibody that engages the B lymphoblast.
“Basically this drug then acts as a bridge between the lymphoblast and the T cell to lead to proliferation of the cytotoxic T cell and apoptosis of the lymphoblast,” she said. “It’s interesting because it’s an antibody but it actually works through the immune system through the T cells.”
The largest study to date of blinatumomab in the relapsed/refractory ALL setting showed a 43% complete remission (CR) or CR with partial hematological recovery of peripheral blood counts (CRi) in 189 treated patients with Philadelphia chromosome–negative ALL. It also demonstrated and a 39% rate of salvage status 2 or higher, she said, noting that the response was impressive given that about 30% of participants had a prior transplant (Lancet. 2015 Jan 1;16[1]:57-66).
Of the responders, 40% went on to allogeneic transplant. This was a “fairly impressive” rate given the 30% prior-transplant rate, Dr. Advani said.
“There also was a high minimal residual disease response in those patients achieving CR,” she said, adding that the only significant predictor of response was bone marrow blast count; patients with 50% or more blasts in the bone marrow had a reduced likelihood of responding to blinatumomab.
The agent was approved by the Food and Drug Administration in December 2014 based on these phase 2 findings.
Adverse events mainly included toxicities that are expected in leukemia patients; the most frequent were febrile neutropenia, neutropenia, and anemia. Two patients developed cytokine release syndrome, and about half of the blinatumomab-treated patients experienced neurological events, although the majority of those were grade 1 or 2 and were easily manageable, she noted.
Blinatumomab was further evaluated in the phase 3 TOWER study (NCT02013167), which compared it with standard-of-care chemotherapy regimens. This study showed much higher response rates with blinatumomab than with the chemotherapy regimens (CR with full, partial, or incomplete hematologic recovery, 44% vs. 25%, respectively), Dr. Advani said (N Engl J Med. 2017 Mar 2;376[9]:836-47).
“The main things to remember [are that blinatumomab is] generally very well tolerated and it has been shown to be superior over standard chemotherapy,” she said. “I think it’s a very good drug to use as a bridge to transplant.”
One setting where blinatumomab perhaps should not be used is in patients with central nervous system disease, she noted.
“There is some concern, at least theoretically, that if you have to use concurrent intrathecal chemo along with blinatumomab, there could be some neurotoxicity,” Dr. Advani said, adding that there are no clear data in that setting because patients with CNS disease were not included in the trials.
Patients with high tumor burden may also be poor candidates for blinatumomab because they tend to have lower response rates.
“That doesn’t mean you can’t use it, but you have to kind of think about what the best option would be,” she said.
Additionally, patients treated with CAR T-cell therapy may develop CD19 loss or CD19-negative disease, and blinatumomab should be avoided in these patients.
“The nice thing ... is you don’t have to worry about veno-occlusive disease [VOD] in patients who are proceeding to transplant,” she said, explaining that no increased risk of VOD was seen in these trials.
Inotuzumab
Inotuzumab, which was approved in 2017, differs from blinatumomab in that it is an anti-CD22-calicheamicin conjugate; however, it also showed high response rates in the initial phase 2 trial in relapsed/refractory ALL. The overall response rate was 57%, with 18% achieving a complete response and 63% achieving complete molecular remission.
Of 49 treated patients, 22 patients proceeded to allogeneic transplant, and 5 of those developed VOD.
“Interestingly, four out of five of these patients had received a clofarabine-based preparative regimen, and this likely explains why there was a higher risk of VOD in this study,” she said, noting that the VOD risk has been lower in subsequent studies of inotuzumab.
The international INO-VATE ALL study (NCT01564784) that led to FDA approval was similar in design to the TOWER study in that it compared inotuzumab with standard chemotherapy regimens, and response rates were clearly higher (81% vs. 33%) with inotuzumab (N Engl J Med. 2016 Aug 25;375[8]:740-53).
The VOD risk in the INO-VATE trial was 11%, and it seemed to be higher in those who received dual alkylator–conditioning regimens, which are commonly used in Europe.
Longer-term outcomes after transplant in INO-VATE participants show that median survival has not been reached.
“It’s encouraging that with longer follow-up these patients actually look like they’re doing well,” Dr. Advani said, adding that inotuzumab is a good treatment option for relapsed patients with high disease burden or with CNS disease.
The continuous hookup required for this treatment may be problematic for some younger and older patients, but it is generally not an issue, she noted.
It is important, though, to give as few cycles prior to transplant as possible and to “really think about the preparative regimen to decrease the risk of VOD.”
CAR T-cell therapy
As for CAR T-cell therapy in the relapsed/refractory ALL setting, tisagenlecleucel was approved in 2017 for those up to age 25 years with B-cell precursor ALL that is refractory or in second or later relapse.
Approval was based on a single-arm trial of 63 patients with relapsed or refractory pediatric precursor B-cell ALL, including 35 patients who had prior transplant. The confirmed overall remission rate was 82%, with a 63% CR rate and 19% CRi rate.
“This is a very exciting area,” Dr. Advani said. “There are multiple trials being done in adults with ALL to really look at the older subgroup of patients.”
Overall outcomes
“These treatments we have now really seem to be effective in the relapse setting, but the problem is that once patients relapse and then go to transplant, their overall survival is still poor,” Dr. Advani said. “So the question is how can we improve the up-front treatment of patients so that hopefully they don’t relapse, and hopefully we also can send a smaller number of patients to transplant.”
Two trials seek to address this, she said.
The A041501 study (NCT03150693) is comparing C10403 chemotherapy with C10403 induction followed by two cycles of inotuzumab before continuing with chemotherapy in adults under age 40 years with previously untreated B ALL.
The primary objective is improved 3-year event-free survival, she said, adding that minimal residual disease (MRD) testing will be used and that CD20-positive patients will receive rituximab, as is now standard.
The phase 3 E1910 study (NCT02003222) is evaluating up-front blinatumomab in patients aged 30-70 years with newly diagnosed BCR-ABL–negative B-lineage ALL. This trial was complicated by the recent approval of blinatumomab for MRD-positive disease, which rendered randomization of MRD-positive patients unethical. MRD-negative patients will be randomized, however.
“The hope is that, by incorporating blinatumomab up front, this will again improve outcomes for patients,” she said.
Dr. Advani reported consultancy for Pfizer; research funding from Genzyme, Novartis, Pfizer, and Sigma Tau; and honoraria from Genzyme, Pfizer, and Sigma Tau. She is also on the speakers bureau for Sigma Tau.
CHICAGO – Novel antibodies are improving outcomes in relapsed and refractory acute lymphoblastic leukemia (ALL), and the hope is that they will also show benefit in the up-front treatment setting and thereby improve overall outcomes, according to Anjali Advani, MD.
“It has been a really exciting time in ALL because several drugs have now been FDA approved: blinatumomab, inotuzumab, and now – for patients who are less than 26 years of age – we actually have CAR [chimeric antigen receptor] T cells that have been approved,” Dr. Advani, a hematologist and director of the inpatient leukemia program at the Cleveland Clinic said at the American Society of Hematology Meeting on Hematologic Malignancies.
At the time of relapse, however, the only known cure is allogeneic bone marrow transplant. That may change as more data regarding CAR T cells become available, but the typical goal at this time is to get patients into remission and then to transplant, she said.
Blinatumomab
“Blinatumomab is a very interesting antibody,” Dr. Advani said, explaining that it is a bispecific, T cell–engaging antibody with an anti-CD3 arm that engages the T cell and an anti-CD19 antibody that engages the B lymphoblast.
“Basically this drug then acts as a bridge between the lymphoblast and the T cell to lead to proliferation of the cytotoxic T cell and apoptosis of the lymphoblast,” she said. “It’s interesting because it’s an antibody but it actually works through the immune system through the T cells.”
The largest study to date of blinatumomab in the relapsed/refractory ALL setting showed a 43% complete remission (CR) or CR with partial hematological recovery of peripheral blood counts (CRi) in 189 treated patients with Philadelphia chromosome–negative ALL. It also demonstrated and a 39% rate of salvage status 2 or higher, she said, noting that the response was impressive given that about 30% of participants had a prior transplant (Lancet. 2015 Jan 1;16[1]:57-66).
Of the responders, 40% went on to allogeneic transplant. This was a “fairly impressive” rate given the 30% prior-transplant rate, Dr. Advani said.
“There also was a high minimal residual disease response in those patients achieving CR,” she said, adding that the only significant predictor of response was bone marrow blast count; patients with 50% or more blasts in the bone marrow had a reduced likelihood of responding to blinatumomab.
The agent was approved by the Food and Drug Administration in December 2014 based on these phase 2 findings.
Adverse events mainly included toxicities that are expected in leukemia patients; the most frequent were febrile neutropenia, neutropenia, and anemia. Two patients developed cytokine release syndrome, and about half of the blinatumomab-treated patients experienced neurological events, although the majority of those were grade 1 or 2 and were easily manageable, she noted.
Blinatumomab was further evaluated in the phase 3 TOWER study (NCT02013167), which compared it with standard-of-care chemotherapy regimens. This study showed much higher response rates with blinatumomab than with the chemotherapy regimens (CR with full, partial, or incomplete hematologic recovery, 44% vs. 25%, respectively), Dr. Advani said (N Engl J Med. 2017 Mar 2;376[9]:836-47).
“The main things to remember [are that blinatumomab is] generally very well tolerated and it has been shown to be superior over standard chemotherapy,” she said. “I think it’s a very good drug to use as a bridge to transplant.”
One setting where blinatumomab perhaps should not be used is in patients with central nervous system disease, she noted.
“There is some concern, at least theoretically, that if you have to use concurrent intrathecal chemo along with blinatumomab, there could be some neurotoxicity,” Dr. Advani said, adding that there are no clear data in that setting because patients with CNS disease were not included in the trials.
Patients with high tumor burden may also be poor candidates for blinatumomab because they tend to have lower response rates.
“That doesn’t mean you can’t use it, but you have to kind of think about what the best option would be,” she said.
Additionally, patients treated with CAR T-cell therapy may develop CD19 loss or CD19-negative disease, and blinatumomab should be avoided in these patients.
“The nice thing ... is you don’t have to worry about veno-occlusive disease [VOD] in patients who are proceeding to transplant,” she said, explaining that no increased risk of VOD was seen in these trials.
Inotuzumab
Inotuzumab, which was approved in 2017, differs from blinatumomab in that it is an anti-CD22-calicheamicin conjugate; however, it also showed high response rates in the initial phase 2 trial in relapsed/refractory ALL. The overall response rate was 57%, with 18% achieving a complete response and 63% achieving complete molecular remission.
Of 49 treated patients, 22 patients proceeded to allogeneic transplant, and 5 of those developed VOD.
“Interestingly, four out of five of these patients had received a clofarabine-based preparative regimen, and this likely explains why there was a higher risk of VOD in this study,” she said, noting that the VOD risk has been lower in subsequent studies of inotuzumab.
The international INO-VATE ALL study (NCT01564784) that led to FDA approval was similar in design to the TOWER study in that it compared inotuzumab with standard chemotherapy regimens, and response rates were clearly higher (81% vs. 33%) with inotuzumab (N Engl J Med. 2016 Aug 25;375[8]:740-53).
The VOD risk in the INO-VATE trial was 11%, and it seemed to be higher in those who received dual alkylator–conditioning regimens, which are commonly used in Europe.
Longer-term outcomes after transplant in INO-VATE participants show that median survival has not been reached.
“It’s encouraging that with longer follow-up these patients actually look like they’re doing well,” Dr. Advani said, adding that inotuzumab is a good treatment option for relapsed patients with high disease burden or with CNS disease.
The continuous hookup required for this treatment may be problematic for some younger and older patients, but it is generally not an issue, she noted.
It is important, though, to give as few cycles prior to transplant as possible and to “really think about the preparative regimen to decrease the risk of VOD.”
CAR T-cell therapy
As for CAR T-cell therapy in the relapsed/refractory ALL setting, tisagenlecleucel was approved in 2017 for those up to age 25 years with B-cell precursor ALL that is refractory or in second or later relapse.
Approval was based on a single-arm trial of 63 patients with relapsed or refractory pediatric precursor B-cell ALL, including 35 patients who had prior transplant. The confirmed overall remission rate was 82%, with a 63% CR rate and 19% CRi rate.
“This is a very exciting area,” Dr. Advani said. “There are multiple trials being done in adults with ALL to really look at the older subgroup of patients.”
Overall outcomes
“These treatments we have now really seem to be effective in the relapse setting, but the problem is that once patients relapse and then go to transplant, their overall survival is still poor,” Dr. Advani said. “So the question is how can we improve the up-front treatment of patients so that hopefully they don’t relapse, and hopefully we also can send a smaller number of patients to transplant.”
Two trials seek to address this, she said.
The A041501 study (NCT03150693) is comparing C10403 chemotherapy with C10403 induction followed by two cycles of inotuzumab before continuing with chemotherapy in adults under age 40 years with previously untreated B ALL.
The primary objective is improved 3-year event-free survival, she said, adding that minimal residual disease (MRD) testing will be used and that CD20-positive patients will receive rituximab, as is now standard.
The phase 3 E1910 study (NCT02003222) is evaluating up-front blinatumomab in patients aged 30-70 years with newly diagnosed BCR-ABL–negative B-lineage ALL. This trial was complicated by the recent approval of blinatumomab for MRD-positive disease, which rendered randomization of MRD-positive patients unethical. MRD-negative patients will be randomized, however.
“The hope is that, by incorporating blinatumomab up front, this will again improve outcomes for patients,” she said.
Dr. Advani reported consultancy for Pfizer; research funding from Genzyme, Novartis, Pfizer, and Sigma Tau; and honoraria from Genzyme, Pfizer, and Sigma Tau. She is also on the speakers bureau for Sigma Tau.
CHICAGO – Novel antibodies are improving outcomes in relapsed and refractory acute lymphoblastic leukemia (ALL), and the hope is that they will also show benefit in the up-front treatment setting and thereby improve overall outcomes, according to Anjali Advani, MD.
“It has been a really exciting time in ALL because several drugs have now been FDA approved: blinatumomab, inotuzumab, and now – for patients who are less than 26 years of age – we actually have CAR [chimeric antigen receptor] T cells that have been approved,” Dr. Advani, a hematologist and director of the inpatient leukemia program at the Cleveland Clinic said at the American Society of Hematology Meeting on Hematologic Malignancies.
At the time of relapse, however, the only known cure is allogeneic bone marrow transplant. That may change as more data regarding CAR T cells become available, but the typical goal at this time is to get patients into remission and then to transplant, she said.
Blinatumomab
“Blinatumomab is a very interesting antibody,” Dr. Advani said, explaining that it is a bispecific, T cell–engaging antibody with an anti-CD3 arm that engages the T cell and an anti-CD19 antibody that engages the B lymphoblast.
“Basically this drug then acts as a bridge between the lymphoblast and the T cell to lead to proliferation of the cytotoxic T cell and apoptosis of the lymphoblast,” she said. “It’s interesting because it’s an antibody but it actually works through the immune system through the T cells.”
The largest study to date of blinatumomab in the relapsed/refractory ALL setting showed a 43% complete remission (CR) or CR with partial hematological recovery of peripheral blood counts (CRi) in 189 treated patients with Philadelphia chromosome–negative ALL. It also demonstrated and a 39% rate of salvage status 2 or higher, she said, noting that the response was impressive given that about 30% of participants had a prior transplant (Lancet. 2015 Jan 1;16[1]:57-66).
Of the responders, 40% went on to allogeneic transplant. This was a “fairly impressive” rate given the 30% prior-transplant rate, Dr. Advani said.
“There also was a high minimal residual disease response in those patients achieving CR,” she said, adding that the only significant predictor of response was bone marrow blast count; patients with 50% or more blasts in the bone marrow had a reduced likelihood of responding to blinatumomab.
The agent was approved by the Food and Drug Administration in December 2014 based on these phase 2 findings.
Adverse events mainly included toxicities that are expected in leukemia patients; the most frequent were febrile neutropenia, neutropenia, and anemia. Two patients developed cytokine release syndrome, and about half of the blinatumomab-treated patients experienced neurological events, although the majority of those were grade 1 or 2 and were easily manageable, she noted.
Blinatumomab was further evaluated in the phase 3 TOWER study (NCT02013167), which compared it with standard-of-care chemotherapy regimens. This study showed much higher response rates with blinatumomab than with the chemotherapy regimens (CR with full, partial, or incomplete hematologic recovery, 44% vs. 25%, respectively), Dr. Advani said (N Engl J Med. 2017 Mar 2;376[9]:836-47).
“The main things to remember [are that blinatumomab is] generally very well tolerated and it has been shown to be superior over standard chemotherapy,” she said. “I think it’s a very good drug to use as a bridge to transplant.”
One setting where blinatumomab perhaps should not be used is in patients with central nervous system disease, she noted.
“There is some concern, at least theoretically, that if you have to use concurrent intrathecal chemo along with blinatumomab, there could be some neurotoxicity,” Dr. Advani said, adding that there are no clear data in that setting because patients with CNS disease were not included in the trials.
Patients with high tumor burden may also be poor candidates for blinatumomab because they tend to have lower response rates.
“That doesn’t mean you can’t use it, but you have to kind of think about what the best option would be,” she said.
Additionally, patients treated with CAR T-cell therapy may develop CD19 loss or CD19-negative disease, and blinatumomab should be avoided in these patients.
“The nice thing ... is you don’t have to worry about veno-occlusive disease [VOD] in patients who are proceeding to transplant,” she said, explaining that no increased risk of VOD was seen in these trials.
Inotuzumab
Inotuzumab, which was approved in 2017, differs from blinatumomab in that it is an anti-CD22-calicheamicin conjugate; however, it also showed high response rates in the initial phase 2 trial in relapsed/refractory ALL. The overall response rate was 57%, with 18% achieving a complete response and 63% achieving complete molecular remission.
Of 49 treated patients, 22 patients proceeded to allogeneic transplant, and 5 of those developed VOD.
“Interestingly, four out of five of these patients had received a clofarabine-based preparative regimen, and this likely explains why there was a higher risk of VOD in this study,” she said, noting that the VOD risk has been lower in subsequent studies of inotuzumab.
The international INO-VATE ALL study (NCT01564784) that led to FDA approval was similar in design to the TOWER study in that it compared inotuzumab with standard chemotherapy regimens, and response rates were clearly higher (81% vs. 33%) with inotuzumab (N Engl J Med. 2016 Aug 25;375[8]:740-53).
The VOD risk in the INO-VATE trial was 11%, and it seemed to be higher in those who received dual alkylator–conditioning regimens, which are commonly used in Europe.
Longer-term outcomes after transplant in INO-VATE participants show that median survival has not been reached.
“It’s encouraging that with longer follow-up these patients actually look like they’re doing well,” Dr. Advani said, adding that inotuzumab is a good treatment option for relapsed patients with high disease burden or with CNS disease.
The continuous hookup required for this treatment may be problematic for some younger and older patients, but it is generally not an issue, she noted.
It is important, though, to give as few cycles prior to transplant as possible and to “really think about the preparative regimen to decrease the risk of VOD.”
CAR T-cell therapy
As for CAR T-cell therapy in the relapsed/refractory ALL setting, tisagenlecleucel was approved in 2017 for those up to age 25 years with B-cell precursor ALL that is refractory or in second or later relapse.
Approval was based on a single-arm trial of 63 patients with relapsed or refractory pediatric precursor B-cell ALL, including 35 patients who had prior transplant. The confirmed overall remission rate was 82%, with a 63% CR rate and 19% CRi rate.
“This is a very exciting area,” Dr. Advani said. “There are multiple trials being done in adults with ALL to really look at the older subgroup of patients.”
Overall outcomes
“These treatments we have now really seem to be effective in the relapse setting, but the problem is that once patients relapse and then go to transplant, their overall survival is still poor,” Dr. Advani said. “So the question is how can we improve the up-front treatment of patients so that hopefully they don’t relapse, and hopefully we also can send a smaller number of patients to transplant.”
Two trials seek to address this, she said.
The A041501 study (NCT03150693) is comparing C10403 chemotherapy with C10403 induction followed by two cycles of inotuzumab before continuing with chemotherapy in adults under age 40 years with previously untreated B ALL.
The primary objective is improved 3-year event-free survival, she said, adding that minimal residual disease (MRD) testing will be used and that CD20-positive patients will receive rituximab, as is now standard.
The phase 3 E1910 study (NCT02003222) is evaluating up-front blinatumomab in patients aged 30-70 years with newly diagnosed BCR-ABL–negative B-lineage ALL. This trial was complicated by the recent approval of blinatumomab for MRD-positive disease, which rendered randomization of MRD-positive patients unethical. MRD-negative patients will be randomized, however.
“The hope is that, by incorporating blinatumomab up front, this will again improve outcomes for patients,” she said.
Dr. Advani reported consultancy for Pfizer; research funding from Genzyme, Novartis, Pfizer, and Sigma Tau; and honoraria from Genzyme, Pfizer, and Sigma Tau. She is also on the speakers bureau for Sigma Tau.
EXPERT ANALYSIS FROM MHM 2018
Ibrutinib plus obinutuzumab gets priority review in CLL/SLL
The Food and Drug Administration has granted priority review to an anti-CD20, chemotherapy-free combination – ibrutinib plus obinutuzumab – for the frontline treatment of chronic lymphocytic leukemia or small lymphocytic lymphoma (CLL/SLL).
The agency will review the combination in previously untreated adults.
Ibrutinib (Imbruvica) is already approved as a single agent for adults with CLL/SLL for all lines of therapy and in combination with bendamustine and rituximab. Obinutuzumab (Gazyva) has been approved for patients with previously untreated CLL, in combination with chlorambucil.
The current application, which is sponsored by Janssen and Pharmacyclics, is based on results from the phase 3 iLLUMINATE trial. Preliminary results announced by Janssen and Pharmacyclics showed that ibrutinib plus obinutuzumab had statistically significant better progression-free survival, compared with chlorambucil plus obinutuzumab, as assessed by an independent review committee.
Complete results from the trial will be presented at an upcoming medical meeting, according to the sponsors.
The Food and Drug Administration has granted priority review to an anti-CD20, chemotherapy-free combination – ibrutinib plus obinutuzumab – for the frontline treatment of chronic lymphocytic leukemia or small lymphocytic lymphoma (CLL/SLL).
The agency will review the combination in previously untreated adults.
Ibrutinib (Imbruvica) is already approved as a single agent for adults with CLL/SLL for all lines of therapy and in combination with bendamustine and rituximab. Obinutuzumab (Gazyva) has been approved for patients with previously untreated CLL, in combination with chlorambucil.
The current application, which is sponsored by Janssen and Pharmacyclics, is based on results from the phase 3 iLLUMINATE trial. Preliminary results announced by Janssen and Pharmacyclics showed that ibrutinib plus obinutuzumab had statistically significant better progression-free survival, compared with chlorambucil plus obinutuzumab, as assessed by an independent review committee.
Complete results from the trial will be presented at an upcoming medical meeting, according to the sponsors.
The Food and Drug Administration has granted priority review to an anti-CD20, chemotherapy-free combination – ibrutinib plus obinutuzumab – for the frontline treatment of chronic lymphocytic leukemia or small lymphocytic lymphoma (CLL/SLL).
The agency will review the combination in previously untreated adults.
Ibrutinib (Imbruvica) is already approved as a single agent for adults with CLL/SLL for all lines of therapy and in combination with bendamustine and rituximab. Obinutuzumab (Gazyva) has been approved for patients with previously untreated CLL, in combination with chlorambucil.
The current application, which is sponsored by Janssen and Pharmacyclics, is based on results from the phase 3 iLLUMINATE trial. Preliminary results announced by Janssen and Pharmacyclics showed that ibrutinib plus obinutuzumab had statistically significant better progression-free survival, compared with chlorambucil plus obinutuzumab, as assessed by an independent review committee.
Complete results from the trial will be presented at an upcoming medical meeting, according to the sponsors.
Mysterious polio-like illness baffles medical experts while frightening parents
A spike in the number of children with a rare neurological disease that causes polio-like symptoms has health officials across the country scrambling to understand the illness. Yet, more than 4 years after health officials first recorded the most recent uptick in cases, much about the national outbreak remains a mystery.
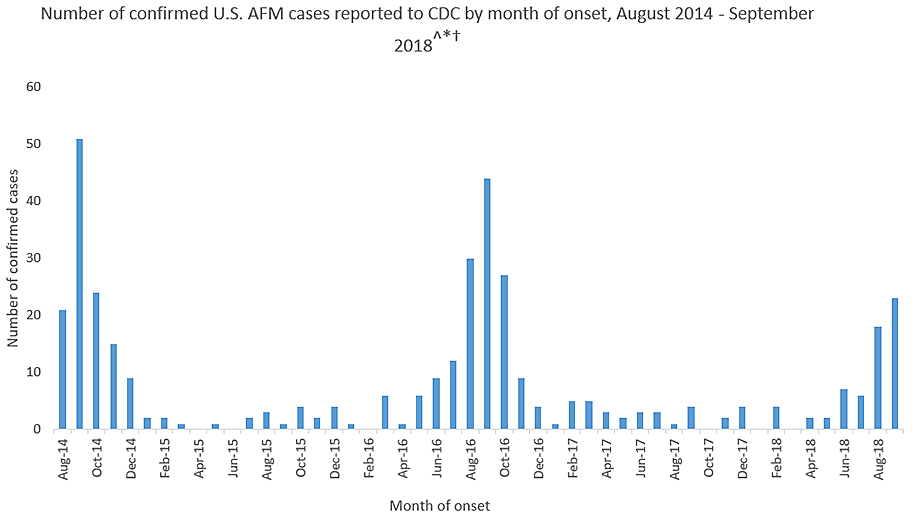
Acute flaccid myelitis (AFM) affects the gray matter in the spinal cord, causing sudden muscle weakness and a loss of reflexes. The illness can lead to serious complications – including paralysis or respiratory failure – and requires immediate medical attention.
The Centers for Disease Control and Prevention is investigating 127 cases of possible AFM, including 62 that have been confirmed in 22 states this year. At least 90% of the cases are among patients 18 years old and younger. The average age of a patient is 4 years old.
AFM remains extremely rare, even with the recent increase. The CDC estimates fewer than 1 in a million Americans will get the disease. Officials advised parents not to panic but remain vigilant for any sudden onset of symptoms. They also suggested that children stay up to date with their vaccines and practice good hand washing habits.
This year’s outbreak marks the third spike of AFM in 4 years. From August 2014 to September 2018, 386 cases have been confirmed. Yet, experts still do not understand crucial aspects of the disease, including its origins and who is most at risk.
“There is a lot we don’t know about AFM,” said Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases. Here’s what puzzles health officials about AFM:
The cause is still unknown
Acute flaccid myelitis can be caused by viruses, such as polio or West Nile. But federal officials said that those viruses have not been linked to the U.S. outbreak over the past 4 years. They have not isolated the cause of these cases.
Despite symptoms reminiscent of polio, no AFM cases have tested positive for that virus, according to the CDC. Investigators have also ruled out a variety of germs. Environmental agents, viruses, and other pathogens are still being considered.
The 2014 outbreak of AFM coincided with a surge of another virus that caused severe respiratory problems, called EV-D68. However, the CDC could not establish a causal link between AFM and the virus. Since then, no large outbreaks of the virus have occurred, according to the CDC.
Carlos Pardo-Villamizar, MD, a neurologist and director of the Johns Hopkins Transverse Myelitis Center, said that the mystery lies in whether the damage seen in AFM is caused by an external agent or the body’s own defenses.
“At this moment, we don’t know if it’s a virus that is coming and producing direct damage of the gray matter in the spinal cord,” he said, “or if a virus is triggering immunological responses that produce a secondary damage in the spinal cord.”
It’s not clear who is at risk
Although the disease appears to target a certain age group, federal disease experts do not know who is likely to get acute flaccid myelitis.
Dr. Pardo-Villamizar said identifying vulnerable populations is “a work in progress.”
Mary Anne Jackson, MD, a pediatric infectious disease specialist and interim dean of the school of medicine at the University of Missouri–Kansas City, said many of the patients she saw were healthy children before falling ill with the disease. She suspects that a host of factors play a role in the likelihood of getting AFM, but more cases must be reviewed in order to find an answer.
The long-term effects are unknown
The CDC said it doesn’t know how long symptoms of the disease will last for patients. However, experts say that initial indications from a small number of cases suggest a grim outlook.
A study published last year found six of eight children in Colorado with acute flaccid myelitis still struggled with motor skills 1 year after their diagnosis. Nonetheless, the researchers found that the patients and families “demonstrated a high degree of resilience and recovery.”
“The majority of these patients are left with extensive problems,” said Dr. Pardo-Villamizar, who was not involved in the study.
Dr. Jackson, who also saw persistent muscle weakness in her patients, said she believes the CDC may be hesitant to specify the long-term effects of the disease because existing studies have included only small numbers of patients. More studies that include a larger proportion of confirmed cases are needed to better understand long-term outcomes, she said.
KHN’s coverage of children’s health care issues is supported in part by the Heising-Simons Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
A spike in the number of children with a rare neurological disease that causes polio-like symptoms has health officials across the country scrambling to understand the illness. Yet, more than 4 years after health officials first recorded the most recent uptick in cases, much about the national outbreak remains a mystery.
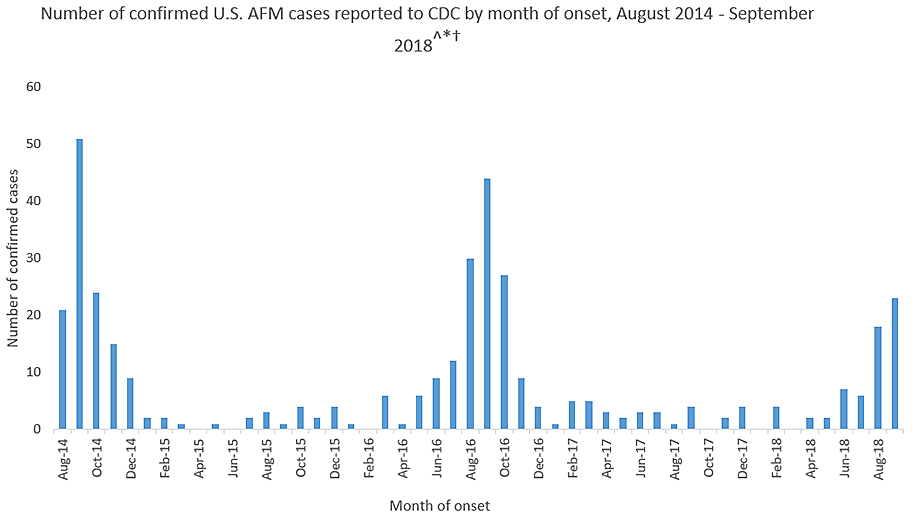
Acute flaccid myelitis (AFM) affects the gray matter in the spinal cord, causing sudden muscle weakness and a loss of reflexes. The illness can lead to serious complications – including paralysis or respiratory failure – and requires immediate medical attention.
The Centers for Disease Control and Prevention is investigating 127 cases of possible AFM, including 62 that have been confirmed in 22 states this year. At least 90% of the cases are among patients 18 years old and younger. The average age of a patient is 4 years old.
AFM remains extremely rare, even with the recent increase. The CDC estimates fewer than 1 in a million Americans will get the disease. Officials advised parents not to panic but remain vigilant for any sudden onset of symptoms. They also suggested that children stay up to date with their vaccines and practice good hand washing habits.
This year’s outbreak marks the third spike of AFM in 4 years. From August 2014 to September 2018, 386 cases have been confirmed. Yet, experts still do not understand crucial aspects of the disease, including its origins and who is most at risk.
“There is a lot we don’t know about AFM,” said Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases. Here’s what puzzles health officials about AFM:
The cause is still unknown
Acute flaccid myelitis can be caused by viruses, such as polio or West Nile. But federal officials said that those viruses have not been linked to the U.S. outbreak over the past 4 years. They have not isolated the cause of these cases.
Despite symptoms reminiscent of polio, no AFM cases have tested positive for that virus, according to the CDC. Investigators have also ruled out a variety of germs. Environmental agents, viruses, and other pathogens are still being considered.
The 2014 outbreak of AFM coincided with a surge of another virus that caused severe respiratory problems, called EV-D68. However, the CDC could not establish a causal link between AFM and the virus. Since then, no large outbreaks of the virus have occurred, according to the CDC.
Carlos Pardo-Villamizar, MD, a neurologist and director of the Johns Hopkins Transverse Myelitis Center, said that the mystery lies in whether the damage seen in AFM is caused by an external agent or the body’s own defenses.
“At this moment, we don’t know if it’s a virus that is coming and producing direct damage of the gray matter in the spinal cord,” he said, “or if a virus is triggering immunological responses that produce a secondary damage in the spinal cord.”
It’s not clear who is at risk
Although the disease appears to target a certain age group, federal disease experts do not know who is likely to get acute flaccid myelitis.
Dr. Pardo-Villamizar said identifying vulnerable populations is “a work in progress.”
Mary Anne Jackson, MD, a pediatric infectious disease specialist and interim dean of the school of medicine at the University of Missouri–Kansas City, said many of the patients she saw were healthy children before falling ill with the disease. She suspects that a host of factors play a role in the likelihood of getting AFM, but more cases must be reviewed in order to find an answer.
The long-term effects are unknown
The CDC said it doesn’t know how long symptoms of the disease will last for patients. However, experts say that initial indications from a small number of cases suggest a grim outlook.
A study published last year found six of eight children in Colorado with acute flaccid myelitis still struggled with motor skills 1 year after their diagnosis. Nonetheless, the researchers found that the patients and families “demonstrated a high degree of resilience and recovery.”
“The majority of these patients are left with extensive problems,” said Dr. Pardo-Villamizar, who was not involved in the study.
Dr. Jackson, who also saw persistent muscle weakness in her patients, said she believes the CDC may be hesitant to specify the long-term effects of the disease because existing studies have included only small numbers of patients. More studies that include a larger proportion of confirmed cases are needed to better understand long-term outcomes, she said.
KHN’s coverage of children’s health care issues is supported in part by the Heising-Simons Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
A spike in the number of children with a rare neurological disease that causes polio-like symptoms has health officials across the country scrambling to understand the illness. Yet, more than 4 years after health officials first recorded the most recent uptick in cases, much about the national outbreak remains a mystery.
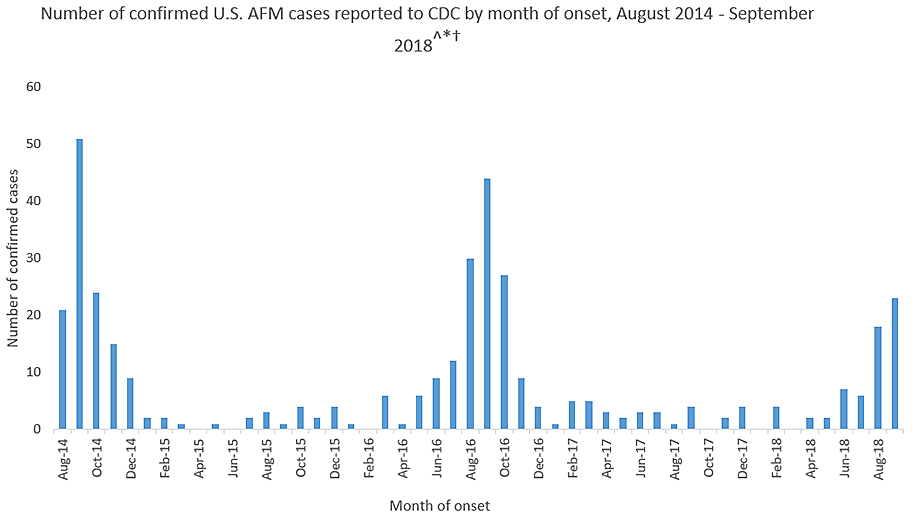
Acute flaccid myelitis (AFM) affects the gray matter in the spinal cord, causing sudden muscle weakness and a loss of reflexes. The illness can lead to serious complications – including paralysis or respiratory failure – and requires immediate medical attention.
The Centers for Disease Control and Prevention is investigating 127 cases of possible AFM, including 62 that have been confirmed in 22 states this year. At least 90% of the cases are among patients 18 years old and younger. The average age of a patient is 4 years old.
AFM remains extremely rare, even with the recent increase. The CDC estimates fewer than 1 in a million Americans will get the disease. Officials advised parents not to panic but remain vigilant for any sudden onset of symptoms. They also suggested that children stay up to date with their vaccines and practice good hand washing habits.
This year’s outbreak marks the third spike of AFM in 4 years. From August 2014 to September 2018, 386 cases have been confirmed. Yet, experts still do not understand crucial aspects of the disease, including its origins and who is most at risk.
“There is a lot we don’t know about AFM,” said Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases. Here’s what puzzles health officials about AFM:
The cause is still unknown
Acute flaccid myelitis can be caused by viruses, such as polio or West Nile. But federal officials said that those viruses have not been linked to the U.S. outbreak over the past 4 years. They have not isolated the cause of these cases.
Despite symptoms reminiscent of polio, no AFM cases have tested positive for that virus, according to the CDC. Investigators have also ruled out a variety of germs. Environmental agents, viruses, and other pathogens are still being considered.
The 2014 outbreak of AFM coincided with a surge of another virus that caused severe respiratory problems, called EV-D68. However, the CDC could not establish a causal link between AFM and the virus. Since then, no large outbreaks of the virus have occurred, according to the CDC.
Carlos Pardo-Villamizar, MD, a neurologist and director of the Johns Hopkins Transverse Myelitis Center, said that the mystery lies in whether the damage seen in AFM is caused by an external agent or the body’s own defenses.
“At this moment, we don’t know if it’s a virus that is coming and producing direct damage of the gray matter in the spinal cord,” he said, “or if a virus is triggering immunological responses that produce a secondary damage in the spinal cord.”
It’s not clear who is at risk
Although the disease appears to target a certain age group, federal disease experts do not know who is likely to get acute flaccid myelitis.
Dr. Pardo-Villamizar said identifying vulnerable populations is “a work in progress.”
Mary Anne Jackson, MD, a pediatric infectious disease specialist and interim dean of the school of medicine at the University of Missouri–Kansas City, said many of the patients she saw were healthy children before falling ill with the disease. She suspects that a host of factors play a role in the likelihood of getting AFM, but more cases must be reviewed in order to find an answer.
The long-term effects are unknown
The CDC said it doesn’t know how long symptoms of the disease will last for patients. However, experts say that initial indications from a small number of cases suggest a grim outlook.
A study published last year found six of eight children in Colorado with acute flaccid myelitis still struggled with motor skills 1 year after their diagnosis. Nonetheless, the researchers found that the patients and families “demonstrated a high degree of resilience and recovery.”
“The majority of these patients are left with extensive problems,” said Dr. Pardo-Villamizar, who was not involved in the study.
Dr. Jackson, who also saw persistent muscle weakness in her patients, said she believes the CDC may be hesitant to specify the long-term effects of the disease because existing studies have included only small numbers of patients. More studies that include a larger proportion of confirmed cases are needed to better understand long-term outcomes, she said.
KHN’s coverage of children’s health care issues is supported in part by the Heising-Simons Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.