User login
Circulating tumor DNA identified by fragment size
Circulating tumor DNA could be effectively isolated from plasma by focusing on a particular range of fragment sizes, which paves the way for noninvasive genomic analysis of tumor DNA, new research suggests.
In a study of 344 plasma samples from 200 patients with 18 cancer types and 65 samples from healthy controls, DNA fragment length could be used to distinguish circulating tumor DNA (ctDNA) from other cell-free DNA (cfDNA), investigators reported in Science Translational Medicine.
“We hypothesized that we could improve the sensitivity for noninvasive cancer genomics by selective sequencing of ctDNA fragments and by leveraging differences in the biology that determine DNA fragmentation,” wrote Florent Mouliere, PhD, from the Cancer Research UK Cambridge Institute, and coauthors.
Cell-free plasma fragments are often cleaved at around 167 base pairs in length and differences in length between circulating fetal and maternal DNA are already used for noninvasive prenatal diagnosis. However, the authors said that only a few studies, with conflicting results, have looked at the size distribution of tumor-derived cfDNA.
The study used two approaches to determining the size profile of mutant ctDNA. The first looked at tumor and nontumor cfDNA in mice with human ovarian cancer xenografts and the second approach used deep sequencing in 19 cancer patients. This revealed that tumor-derived cfDNA was most commonly found in fragments between 90-150 base pairs or 250-320 base pairs in size.
The researchers also noted that mutant circulating tumor DNA was generally more fragmented than nonmutant cfDNA and that patients with untreated advanced cancer showed consistently shorter lengths of mutant DNA.
The next question was whether size selection and other biological properties – such as somatic alterations – of the cfDNA could be used to enhance detection of ctDNA via machine learning technology.
Two models, designed to distinguish between healthy and cancerous samples, were developed using 153 samples, then validated on two datasets of 94 and 83 samples.
One of these models correctly classified cancerous samples in 94% of samples from patients with cancers known to have high levels of ctDNA – colorectal, cholangiocarcinoma, ovarian, breast, and melanoma – and in 65% of samples from low-ctDNA cancers – pancreatic, renal, and glioma.
Another model focused just on fragmentation patterns and was still able to distinguish cancer samples from those of healthy controls, although with slightly reduced area under the curve.
“Our results indicate that exploiting fundamental properties of cfDNA with fragment-specific analyses can allow more sensitive evaluation of ctDNA,” the authors wrote. “We identified features that could determine the presence and amount of ctDNA in plasma samples, without a prior knowledge of somatic aberrations.”
The authors pointed out that size selection of DNA fragments was relatively simple and cheap, and was also compatible with other genome-wide and targeted genomic analyses, “greatly increasing the potential value and utility of liquid biopsies as well as the cost-effectiveness of cfDNA sequencing.”
However, they cautioned that their catalogue had focused solely on double-stranded DNA and was subject to potential biases from the DNA extraction and sequencing methods they used in the study. They also commented that other biological effects could help refine the analysis of ctDNA.
“Other bodily fluids [urine, cerebrospinal fluid, and saliva], different nucleic acids and structures, altered mechanisms of release into circulation, or sample processing methods could exhibit varying fragment size signatures and could offer additional exploitable biological patterns for selective sequencing,” they wrote.
The study was supported by the University of Cambridge, Cancer Research UK, and the Engineering and Physical Sciences Research Council. Research supporting the study was also funded by the European Research Council, the National Institute for Health Research Cambridge, National Cancer Research Network, Cambridge Experimental Cancer Medicine Centre, Hutchison Whampoa, Target Ovarian Cancer, the Medical Research Council, and AstraZeneca. Three authors are cofounders, shareholders, and officers/consultants in a company specializing in ctDNA analysis. One author declared research funding and advisory board fees from private industry. Seven authors are listed on related patents.
SOURCE: Mouliere F et al. Sci Transl Med. 2018 Nov 7. doi: 10.1126/scitranslmed.aat4921.
Cell-free DNA analysis has tremendous diagnostic potential and so is a very active area of research. In this study, researchers were able to identify five variables and develop models for the detection of cancer following analysis of circulating tumor DNA. One of these models based on DNA fragmentation pattern performed very well, and so fragment length analyses could develop into a general test for the presence of cancer.
However confirmation of these findings in large, multicenter clinical trials is still needed. There is also the problem that size selection can result in a loss of circulating tumor DNA for analysis or may introduce biases. We also need to understand the mechanisms underpinning the different fragment size patterns seen in the study. But this study still substantially extends the potential of cell-free, DNA-based diagnostic tests.
Ellen Heitzer, PhD, and Michael R. Speicher, MD, are from the Medical University of Graz (Austria). These comments are taken from an accompanying editorial (Sci Transl Med. 2018 Nov 7. doi: 10.1126/scitranslmed.aav3873). Both authors declared research funding from Servier and Dr. Heitzer declared laboratory research funding from Freenome and PreAnalytiX.
Cell-free DNA analysis has tremendous diagnostic potential and so is a very active area of research. In this study, researchers were able to identify five variables and develop models for the detection of cancer following analysis of circulating tumor DNA. One of these models based on DNA fragmentation pattern performed very well, and so fragment length analyses could develop into a general test for the presence of cancer.
However confirmation of these findings in large, multicenter clinical trials is still needed. There is also the problem that size selection can result in a loss of circulating tumor DNA for analysis or may introduce biases. We also need to understand the mechanisms underpinning the different fragment size patterns seen in the study. But this study still substantially extends the potential of cell-free, DNA-based diagnostic tests.
Ellen Heitzer, PhD, and Michael R. Speicher, MD, are from the Medical University of Graz (Austria). These comments are taken from an accompanying editorial (Sci Transl Med. 2018 Nov 7. doi: 10.1126/scitranslmed.aav3873). Both authors declared research funding from Servier and Dr. Heitzer declared laboratory research funding from Freenome and PreAnalytiX.
Cell-free DNA analysis has tremendous diagnostic potential and so is a very active area of research. In this study, researchers were able to identify five variables and develop models for the detection of cancer following analysis of circulating tumor DNA. One of these models based on DNA fragmentation pattern performed very well, and so fragment length analyses could develop into a general test for the presence of cancer.
However confirmation of these findings in large, multicenter clinical trials is still needed. There is also the problem that size selection can result in a loss of circulating tumor DNA for analysis or may introduce biases. We also need to understand the mechanisms underpinning the different fragment size patterns seen in the study. But this study still substantially extends the potential of cell-free, DNA-based diagnostic tests.
Ellen Heitzer, PhD, and Michael R. Speicher, MD, are from the Medical University of Graz (Austria). These comments are taken from an accompanying editorial (Sci Transl Med. 2018 Nov 7. doi: 10.1126/scitranslmed.aav3873). Both authors declared research funding from Servier and Dr. Heitzer declared laboratory research funding from Freenome and PreAnalytiX.
Circulating tumor DNA could be effectively isolated from plasma by focusing on a particular range of fragment sizes, which paves the way for noninvasive genomic analysis of tumor DNA, new research suggests.
In a study of 344 plasma samples from 200 patients with 18 cancer types and 65 samples from healthy controls, DNA fragment length could be used to distinguish circulating tumor DNA (ctDNA) from other cell-free DNA (cfDNA), investigators reported in Science Translational Medicine.
“We hypothesized that we could improve the sensitivity for noninvasive cancer genomics by selective sequencing of ctDNA fragments and by leveraging differences in the biology that determine DNA fragmentation,” wrote Florent Mouliere, PhD, from the Cancer Research UK Cambridge Institute, and coauthors.
Cell-free plasma fragments are often cleaved at around 167 base pairs in length and differences in length between circulating fetal and maternal DNA are already used for noninvasive prenatal diagnosis. However, the authors said that only a few studies, with conflicting results, have looked at the size distribution of tumor-derived cfDNA.
The study used two approaches to determining the size profile of mutant ctDNA. The first looked at tumor and nontumor cfDNA in mice with human ovarian cancer xenografts and the second approach used deep sequencing in 19 cancer patients. This revealed that tumor-derived cfDNA was most commonly found in fragments between 90-150 base pairs or 250-320 base pairs in size.
The researchers also noted that mutant circulating tumor DNA was generally more fragmented than nonmutant cfDNA and that patients with untreated advanced cancer showed consistently shorter lengths of mutant DNA.
The next question was whether size selection and other biological properties – such as somatic alterations – of the cfDNA could be used to enhance detection of ctDNA via machine learning technology.
Two models, designed to distinguish between healthy and cancerous samples, were developed using 153 samples, then validated on two datasets of 94 and 83 samples.
One of these models correctly classified cancerous samples in 94% of samples from patients with cancers known to have high levels of ctDNA – colorectal, cholangiocarcinoma, ovarian, breast, and melanoma – and in 65% of samples from low-ctDNA cancers – pancreatic, renal, and glioma.
Another model focused just on fragmentation patterns and was still able to distinguish cancer samples from those of healthy controls, although with slightly reduced area under the curve.
“Our results indicate that exploiting fundamental properties of cfDNA with fragment-specific analyses can allow more sensitive evaluation of ctDNA,” the authors wrote. “We identified features that could determine the presence and amount of ctDNA in plasma samples, without a prior knowledge of somatic aberrations.”
The authors pointed out that size selection of DNA fragments was relatively simple and cheap, and was also compatible with other genome-wide and targeted genomic analyses, “greatly increasing the potential value and utility of liquid biopsies as well as the cost-effectiveness of cfDNA sequencing.”
However, they cautioned that their catalogue had focused solely on double-stranded DNA and was subject to potential biases from the DNA extraction and sequencing methods they used in the study. They also commented that other biological effects could help refine the analysis of ctDNA.
“Other bodily fluids [urine, cerebrospinal fluid, and saliva], different nucleic acids and structures, altered mechanisms of release into circulation, or sample processing methods could exhibit varying fragment size signatures and could offer additional exploitable biological patterns for selective sequencing,” they wrote.
The study was supported by the University of Cambridge, Cancer Research UK, and the Engineering and Physical Sciences Research Council. Research supporting the study was also funded by the European Research Council, the National Institute for Health Research Cambridge, National Cancer Research Network, Cambridge Experimental Cancer Medicine Centre, Hutchison Whampoa, Target Ovarian Cancer, the Medical Research Council, and AstraZeneca. Three authors are cofounders, shareholders, and officers/consultants in a company specializing in ctDNA analysis. One author declared research funding and advisory board fees from private industry. Seven authors are listed on related patents.
SOURCE: Mouliere F et al. Sci Transl Med. 2018 Nov 7. doi: 10.1126/scitranslmed.aat4921.
Circulating tumor DNA could be effectively isolated from plasma by focusing on a particular range of fragment sizes, which paves the way for noninvasive genomic analysis of tumor DNA, new research suggests.
In a study of 344 plasma samples from 200 patients with 18 cancer types and 65 samples from healthy controls, DNA fragment length could be used to distinguish circulating tumor DNA (ctDNA) from other cell-free DNA (cfDNA), investigators reported in Science Translational Medicine.
“We hypothesized that we could improve the sensitivity for noninvasive cancer genomics by selective sequencing of ctDNA fragments and by leveraging differences in the biology that determine DNA fragmentation,” wrote Florent Mouliere, PhD, from the Cancer Research UK Cambridge Institute, and coauthors.
Cell-free plasma fragments are often cleaved at around 167 base pairs in length and differences in length between circulating fetal and maternal DNA are already used for noninvasive prenatal diagnosis. However, the authors said that only a few studies, with conflicting results, have looked at the size distribution of tumor-derived cfDNA.
The study used two approaches to determining the size profile of mutant ctDNA. The first looked at tumor and nontumor cfDNA in mice with human ovarian cancer xenografts and the second approach used deep sequencing in 19 cancer patients. This revealed that tumor-derived cfDNA was most commonly found in fragments between 90-150 base pairs or 250-320 base pairs in size.
The researchers also noted that mutant circulating tumor DNA was generally more fragmented than nonmutant cfDNA and that patients with untreated advanced cancer showed consistently shorter lengths of mutant DNA.
The next question was whether size selection and other biological properties – such as somatic alterations – of the cfDNA could be used to enhance detection of ctDNA via machine learning technology.
Two models, designed to distinguish between healthy and cancerous samples, were developed using 153 samples, then validated on two datasets of 94 and 83 samples.
One of these models correctly classified cancerous samples in 94% of samples from patients with cancers known to have high levels of ctDNA – colorectal, cholangiocarcinoma, ovarian, breast, and melanoma – and in 65% of samples from low-ctDNA cancers – pancreatic, renal, and glioma.
Another model focused just on fragmentation patterns and was still able to distinguish cancer samples from those of healthy controls, although with slightly reduced area under the curve.
“Our results indicate that exploiting fundamental properties of cfDNA with fragment-specific analyses can allow more sensitive evaluation of ctDNA,” the authors wrote. “We identified features that could determine the presence and amount of ctDNA in plasma samples, without a prior knowledge of somatic aberrations.”
The authors pointed out that size selection of DNA fragments was relatively simple and cheap, and was also compatible with other genome-wide and targeted genomic analyses, “greatly increasing the potential value and utility of liquid biopsies as well as the cost-effectiveness of cfDNA sequencing.”
However, they cautioned that their catalogue had focused solely on double-stranded DNA and was subject to potential biases from the DNA extraction and sequencing methods they used in the study. They also commented that other biological effects could help refine the analysis of ctDNA.
“Other bodily fluids [urine, cerebrospinal fluid, and saliva], different nucleic acids and structures, altered mechanisms of release into circulation, or sample processing methods could exhibit varying fragment size signatures and could offer additional exploitable biological patterns for selective sequencing,” they wrote.
The study was supported by the University of Cambridge, Cancer Research UK, and the Engineering and Physical Sciences Research Council. Research supporting the study was also funded by the European Research Council, the National Institute for Health Research Cambridge, National Cancer Research Network, Cambridge Experimental Cancer Medicine Centre, Hutchison Whampoa, Target Ovarian Cancer, the Medical Research Council, and AstraZeneca. Three authors are cofounders, shareholders, and officers/consultants in a company specializing in ctDNA analysis. One author declared research funding and advisory board fees from private industry. Seven authors are listed on related patents.
SOURCE: Mouliere F et al. Sci Transl Med. 2018 Nov 7. doi: 10.1126/scitranslmed.aat4921.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point: The size of cell-free DNA could be used to single out circulating tumor DNA.
Major finding: Circulating tumor DNA fragments are more commonly found in the 90-150 base pair range.
Study details: A study of 344 plasma samples from 200 patients with 18 cancer types and 65 samples from healthy controls.
Disclosures: The study was supported by the University of Cambridge, Cancer Research UK, and the Engineering and Physical Sciences Research Council. Research supporting the study was also funded by the European Research Council, the National Institute for Health Research Cambridge, National Cancer Research Network, Cambridge Experimental Cancer Medicine Centre, Hutchison Whampoa, Target Ovarian Cancer, the Medical Research Council, and AstraZeneca. Three authors are cofounders, shareholders, and officers/consultants in a company specializing in circulating tumor DNA analysis. One author declared research funding and advisory board fees from private industry. Seven authors are listed on related patents.
Source: Mouliere F et al. Sci Transl Med. 2018 Nov 7. doi: 10.1126/scitranslmed.aat4921.
Innovations in Dermatology: Sarecycline Approved for Acne



Novel theory explains SSRIs’ variable efficacy
BARCELONA – New evidence from the landmark 12-year-old STAR*D clinical trial provides fresh support for a novel Italian hypothesis that the efficacy of selective serotonin reuptake inhibitors in major depressive disorder results from their capacity to amplify the influence of living conditions upon mood.
“This hypothesis claims that SSRIs do not affect mood by themselves, but by increasing brain plasticity to render an individual more susceptible to the influence of living conditions. So in a positive environment, treatment leads to a beneficial outcome, and in a stressful environment it may lead to a worse prognosis,” Aurelia Viglione explained at the annual congress of the European College of Neuropsychopharmacology.
This originally was demonstrated by her senior coinvestigators in mouse studies, which showed increased brain plasticity and responsiveness of mood to living conditions in the presence of the serotonin boost provided by SSRIs. Now this animal research has been confirmed in a more clinically relevant fashion via a secondary analysis of the venerable National Institute of Mental Health–funded STAR*D (Sequenced Treatment Alternatives to Relieve Depression) data set, which Ms. Viglione presented at the ECNP congress.
This hypothesis, which she and her colleagues have dubbed the “undirected susceptibility to change” hypothesis of the mechanism of action of SSRIs, attempts to account for the drugs’ highly variable efficacy. As prescribing physicians and their often-frustrated patients with major depression are all too aware, the SSRIs – the most widely prescribed treatment for the disorder – induce remission in only 30%-40% of patients, while an additional 30%-40% fail to experience even a significant response. And despite much research effort, to date there is no reliable way to match the best antidepressant to a given individual in accord with the current priority to develop a personalized medicine approach.
The undirected susceptibility to change hypothesis provides a plausible explanation for these mixed clinical outcomes. The hypothesis posits that high serotonin levels lead to increased brain plasticity and consequent openness to change in mood, which can be for the better or worse – depending upon the quality of the surrounding environment.
Ms. Viglione, a PhD student in neuroscience at the University of Pisa (Italy), presented a study of a 591-patient subset of patients with major depression in STAR*D who received citalopram at 20 mg/day for 4 weeks, at which point the 40% of participants who weren’t showing a sufficiently favorable response trend had their citalopram increased to 40 mg/day. Patients’ living conditions were categorized as favorable or adverse based upon an amalgam of sociodemographic characteristics, including employment status, education, marital status, income, insurance status, ethnicity, drug abuse, and history of traumatic events. Treatment response was measured using the 16-item Quick Inventory of Depressive Symptomatology (QIDS-SR16) score.
. Patients were more likely to achieve remission as defined by a QIDS-SR16 score of 5 or less at week 6 if they had a college education, a job, higher income, and/or private health insurance than if those proxies for favorable living conditions were not present.
The impact of sociodemographic factors on change in mood was much larger in patients on citalopram at 40 mg/day than 20 mg/day. For example, having a college education rather than a high school education was independently associated with up to a 37-fold greater remission rate among patients on the higher dose of the SSRI, depending upon their sociodemographic status, compared with a 2-fold greater likelihood of remission in patients on citalopram at 20 mg/day.
“The correlation is very high. It’s a very huge effect,” Ms. Viglione commented.
On the other hand, the 40-mg dose also was associated with an increased likelihood of worsening in patients living in an unfavorable environment. For example, 35% of patients in the 40-mg group with only a high school degree showed worsening depression, compared with 21% on citalopram at 20 mg/day. And 40% of low-income patients on citalopram at 40 mg/day showed worsening depression, compared with 35% of low-income patients on 20 mg. These figures probably underestimate the true downside of higher-dose treatment in patients living in an adverse environment, because STAR*D guidelines called for treatment discontinuation in the setting of worsening depression, she noted.
The correlation between higher-dose SSRI therapy, sociodemographic environment, and change in depressive symptoms was not uniform across all symptom categories. Ms. Viglione and her colleagues grouped the elements of the QIDS-SR16 rating scale into three domains: core emotional symptoms, sleep/insomnia symptoms, and weight/appetite. They found that the impact of higher-dose therapy in combination with favorable living conditions was greatest on sleep/insomnia symptoms.
The next step for the Italian investigators will be to determine in a prospective study whether the undirected susceptibility to change hypothesis can predict which patients will benefit from SSRI therapy.
Ms. Viglione reported having no financial conflicts regarding her study, which was funded by the Italian Ministry of Health.
BARCELONA – New evidence from the landmark 12-year-old STAR*D clinical trial provides fresh support for a novel Italian hypothesis that the efficacy of selective serotonin reuptake inhibitors in major depressive disorder results from their capacity to amplify the influence of living conditions upon mood.
“This hypothesis claims that SSRIs do not affect mood by themselves, but by increasing brain plasticity to render an individual more susceptible to the influence of living conditions. So in a positive environment, treatment leads to a beneficial outcome, and in a stressful environment it may lead to a worse prognosis,” Aurelia Viglione explained at the annual congress of the European College of Neuropsychopharmacology.
This originally was demonstrated by her senior coinvestigators in mouse studies, which showed increased brain plasticity and responsiveness of mood to living conditions in the presence of the serotonin boost provided by SSRIs. Now this animal research has been confirmed in a more clinically relevant fashion via a secondary analysis of the venerable National Institute of Mental Health–funded STAR*D (Sequenced Treatment Alternatives to Relieve Depression) data set, which Ms. Viglione presented at the ECNP congress.
This hypothesis, which she and her colleagues have dubbed the “undirected susceptibility to change” hypothesis of the mechanism of action of SSRIs, attempts to account for the drugs’ highly variable efficacy. As prescribing physicians and their often-frustrated patients with major depression are all too aware, the SSRIs – the most widely prescribed treatment for the disorder – induce remission in only 30%-40% of patients, while an additional 30%-40% fail to experience even a significant response. And despite much research effort, to date there is no reliable way to match the best antidepressant to a given individual in accord with the current priority to develop a personalized medicine approach.
The undirected susceptibility to change hypothesis provides a plausible explanation for these mixed clinical outcomes. The hypothesis posits that high serotonin levels lead to increased brain plasticity and consequent openness to change in mood, which can be for the better or worse – depending upon the quality of the surrounding environment.
Ms. Viglione, a PhD student in neuroscience at the University of Pisa (Italy), presented a study of a 591-patient subset of patients with major depression in STAR*D who received citalopram at 20 mg/day for 4 weeks, at which point the 40% of participants who weren’t showing a sufficiently favorable response trend had their citalopram increased to 40 mg/day. Patients’ living conditions were categorized as favorable or adverse based upon an amalgam of sociodemographic characteristics, including employment status, education, marital status, income, insurance status, ethnicity, drug abuse, and history of traumatic events. Treatment response was measured using the 16-item Quick Inventory of Depressive Symptomatology (QIDS-SR16) score.
. Patients were more likely to achieve remission as defined by a QIDS-SR16 score of 5 or less at week 6 if they had a college education, a job, higher income, and/or private health insurance than if those proxies for favorable living conditions were not present.
The impact of sociodemographic factors on change in mood was much larger in patients on citalopram at 40 mg/day than 20 mg/day. For example, having a college education rather than a high school education was independently associated with up to a 37-fold greater remission rate among patients on the higher dose of the SSRI, depending upon their sociodemographic status, compared with a 2-fold greater likelihood of remission in patients on citalopram at 20 mg/day.
“The correlation is very high. It’s a very huge effect,” Ms. Viglione commented.
On the other hand, the 40-mg dose also was associated with an increased likelihood of worsening in patients living in an unfavorable environment. For example, 35% of patients in the 40-mg group with only a high school degree showed worsening depression, compared with 21% on citalopram at 20 mg/day. And 40% of low-income patients on citalopram at 40 mg/day showed worsening depression, compared with 35% of low-income patients on 20 mg. These figures probably underestimate the true downside of higher-dose treatment in patients living in an adverse environment, because STAR*D guidelines called for treatment discontinuation in the setting of worsening depression, she noted.
The correlation between higher-dose SSRI therapy, sociodemographic environment, and change in depressive symptoms was not uniform across all symptom categories. Ms. Viglione and her colleagues grouped the elements of the QIDS-SR16 rating scale into three domains: core emotional symptoms, sleep/insomnia symptoms, and weight/appetite. They found that the impact of higher-dose therapy in combination with favorable living conditions was greatest on sleep/insomnia symptoms.
The next step for the Italian investigators will be to determine in a prospective study whether the undirected susceptibility to change hypothesis can predict which patients will benefit from SSRI therapy.
Ms. Viglione reported having no financial conflicts regarding her study, which was funded by the Italian Ministry of Health.
BARCELONA – New evidence from the landmark 12-year-old STAR*D clinical trial provides fresh support for a novel Italian hypothesis that the efficacy of selective serotonin reuptake inhibitors in major depressive disorder results from their capacity to amplify the influence of living conditions upon mood.
“This hypothesis claims that SSRIs do not affect mood by themselves, but by increasing brain plasticity to render an individual more susceptible to the influence of living conditions. So in a positive environment, treatment leads to a beneficial outcome, and in a stressful environment it may lead to a worse prognosis,” Aurelia Viglione explained at the annual congress of the European College of Neuropsychopharmacology.
This originally was demonstrated by her senior coinvestigators in mouse studies, which showed increased brain plasticity and responsiveness of mood to living conditions in the presence of the serotonin boost provided by SSRIs. Now this animal research has been confirmed in a more clinically relevant fashion via a secondary analysis of the venerable National Institute of Mental Health–funded STAR*D (Sequenced Treatment Alternatives to Relieve Depression) data set, which Ms. Viglione presented at the ECNP congress.
This hypothesis, which she and her colleagues have dubbed the “undirected susceptibility to change” hypothesis of the mechanism of action of SSRIs, attempts to account for the drugs’ highly variable efficacy. As prescribing physicians and their often-frustrated patients with major depression are all too aware, the SSRIs – the most widely prescribed treatment for the disorder – induce remission in only 30%-40% of patients, while an additional 30%-40% fail to experience even a significant response. And despite much research effort, to date there is no reliable way to match the best antidepressant to a given individual in accord with the current priority to develop a personalized medicine approach.
The undirected susceptibility to change hypothesis provides a plausible explanation for these mixed clinical outcomes. The hypothesis posits that high serotonin levels lead to increased brain plasticity and consequent openness to change in mood, which can be for the better or worse – depending upon the quality of the surrounding environment.
Ms. Viglione, a PhD student in neuroscience at the University of Pisa (Italy), presented a study of a 591-patient subset of patients with major depression in STAR*D who received citalopram at 20 mg/day for 4 weeks, at which point the 40% of participants who weren’t showing a sufficiently favorable response trend had their citalopram increased to 40 mg/day. Patients’ living conditions were categorized as favorable or adverse based upon an amalgam of sociodemographic characteristics, including employment status, education, marital status, income, insurance status, ethnicity, drug abuse, and history of traumatic events. Treatment response was measured using the 16-item Quick Inventory of Depressive Symptomatology (QIDS-SR16) score.
. Patients were more likely to achieve remission as defined by a QIDS-SR16 score of 5 or less at week 6 if they had a college education, a job, higher income, and/or private health insurance than if those proxies for favorable living conditions were not present.
The impact of sociodemographic factors on change in mood was much larger in patients on citalopram at 40 mg/day than 20 mg/day. For example, having a college education rather than a high school education was independently associated with up to a 37-fold greater remission rate among patients on the higher dose of the SSRI, depending upon their sociodemographic status, compared with a 2-fold greater likelihood of remission in patients on citalopram at 20 mg/day.
“The correlation is very high. It’s a very huge effect,” Ms. Viglione commented.
On the other hand, the 40-mg dose also was associated with an increased likelihood of worsening in patients living in an unfavorable environment. For example, 35% of patients in the 40-mg group with only a high school degree showed worsening depression, compared with 21% on citalopram at 20 mg/day. And 40% of low-income patients on citalopram at 40 mg/day showed worsening depression, compared with 35% of low-income patients on 20 mg. These figures probably underestimate the true downside of higher-dose treatment in patients living in an adverse environment, because STAR*D guidelines called for treatment discontinuation in the setting of worsening depression, she noted.
The correlation between higher-dose SSRI therapy, sociodemographic environment, and change in depressive symptoms was not uniform across all symptom categories. Ms. Viglione and her colleagues grouped the elements of the QIDS-SR16 rating scale into three domains: core emotional symptoms, sleep/insomnia symptoms, and weight/appetite. They found that the impact of higher-dose therapy in combination with favorable living conditions was greatest on sleep/insomnia symptoms.
The next step for the Italian investigators will be to determine in a prospective study whether the undirected susceptibility to change hypothesis can predict which patients will benefit from SSRI therapy.
Ms. Viglione reported having no financial conflicts regarding her study, which was funded by the Italian Ministry of Health.
REPORTING FROM THE ECNP CONGRESS
Key clinical point: There’s a new hypothesis to explain the mixed results of selective serotonin reuptake inhibitors for major depression.
Major finding: Improvement in symptoms of major depression was strongly correlated with SSRI dose and patients’ living conditions.
Study details: This secondary analysis of the STAR*D data set included 591 patients who received citalopram for major depression.
Disclosures: The presenter reported having no financial conflicts regarding the study, funded by the Italian Ministry of Health.
Draft JIA recommendations from ACR seek inactive disease
CHICAGO – New draft guidelines for treating juvenile idiopathic arthritis (JIA) written by experts assembled by the American College of Rheumatology “formalize inactive disease as the goal of treatment,” Timothy G. Beukelman, MD, said at the annual meeting of the American College of Rheumatology.
“We defined low disease activity as patients with a single active joint, and the goal is to have zero active joints. Low disease activity should not be tolerated” in patients with JIA, said Dr. Beukelman, a pediatric rheumatologist at the University of Alabama at Birmingham and a member of the guideline-writing committee. “Until now, treating these patients to zero active joints has not been recommended. But clinically inactive disease is a realistic target for a majority of JIA patients,” he said in an interview.
Despite this shift in the recommended treatment goal, the writing panel was forced to rely largely on their expertise rather than reported evidence. The recommendation by the committee to escalate therapy in patients with low disease activity was “conditional,” with a level of evidence deemed “very low,” Dr. Beukelman said during a talk in which he cited selected highlights from the committee’s full list of 39 recommendations.
The paucity of evidence reflected the status of many of the recommendations: 31 of the 39 recommendations were conditional, which means that the desirable effects from treatment “probably” outweigh the undesirable effects, and they may not apply to some patients. The writing panel pegged 22 of their recommendations as having a very low evidence backing and another 13 recommendations had low evidence. The JIA committee believed that none of its recommendations had strong evidence to back them up.
Dr. Beukelman defended writing recommendations despite this absence of evidence. “We should continue to write conditional recommendations when we don’t have the evidence. These recommendations had approval from at least 70% of the writing group, a diverse committee of experts. They should not be taken lightly just because they are conditional.”
Dr. Beukelman also stressed that he was presenting draft recommendations that still awaited approval from the ACR and the Arthritis Foundation, which collaborated with the ACR on this project. Once adopted, the new document would revise the existing management recommendations that the ACR approved in 2011 (Arthritis Rheum. 2011 Apr;63[4]:465-82).
The recommendations Dr. Beukelman outlined focused on treatment of polyarthritis, sacroiliitis, and enthesitis, and Dr. Beukelman devoted the most time to detailing some of the statements on polyarthritis. The panel conditionally recommended methotrexate over leflunomide (Arava) or sulfasalazine with moderate or very low evidence and said that subcutaneous methotrexate was conditionally preferred over oral dosing for reasons of both better efficacy and tolerability. Combination of a biologic agent with a nonbiologic received a conditional recommendation over biologic monotherapy, with moderate to very low evidence, but with a strong recommendation for this combined approach when using infliximab (Remicade), based on moderate evidence.
Another strong recommendation was to avoid treating patients with a chronic course of a low-dose, systemic glucocorticoid, based on a very low level of evidence. A brief course, less than 3 months, of an oral glucocorticoid received conditional recommendation for patients with moderate or high disease activity, based on very low evidence, but also received a conditional negative recommendation for patients with low disease activity, also based on very low evidence.
Initial therapy with a disease-modifying antirheumatic drug (DMARD) instead of monotherapy with an NSAID received a strong recommendation, based on a moderate level of evidence, while initial therapy with a DMARD received conditional support over initial therapy with a biologic agent, based on low evidence.
The panel gave a conditional endorsement to the idea of switching from a tumor necrosis factor inhibitor (TNFi) to a different biologic drug class when patients remained with moderate or high disease activity, based on a very low level of evidence.
Regarding sacroiliitis, the panel strongly recommended starting a TNFi in patients with active sacroiliitis despite NSAID treatment, based on low evidence, and the committee strongly recommended against starting methotrexate treatment in these patients, based on very low evidence. For treating active enthesitis despite NSAID treatment, the panel conditionally recommended adding a TNFi over treatment with methotrexate or sulfasalazine, based on a low level of evidence. Dr. Beukelman highlighted that the new recommendations placed increased emphasis on treating sacroiliitis, compared with the 2011 statement, and that the new recommendations dealt with treating enthesitis for the first time.
Dr. Beukelman has been a consultant to Bristol-Myers Squibb, Novartis, Sobi, and UCB.
CHICAGO – New draft guidelines for treating juvenile idiopathic arthritis (JIA) written by experts assembled by the American College of Rheumatology “formalize inactive disease as the goal of treatment,” Timothy G. Beukelman, MD, said at the annual meeting of the American College of Rheumatology.
“We defined low disease activity as patients with a single active joint, and the goal is to have zero active joints. Low disease activity should not be tolerated” in patients with JIA, said Dr. Beukelman, a pediatric rheumatologist at the University of Alabama at Birmingham and a member of the guideline-writing committee. “Until now, treating these patients to zero active joints has not been recommended. But clinically inactive disease is a realistic target for a majority of JIA patients,” he said in an interview.
Despite this shift in the recommended treatment goal, the writing panel was forced to rely largely on their expertise rather than reported evidence. The recommendation by the committee to escalate therapy in patients with low disease activity was “conditional,” with a level of evidence deemed “very low,” Dr. Beukelman said during a talk in which he cited selected highlights from the committee’s full list of 39 recommendations.
The paucity of evidence reflected the status of many of the recommendations: 31 of the 39 recommendations were conditional, which means that the desirable effects from treatment “probably” outweigh the undesirable effects, and they may not apply to some patients. The writing panel pegged 22 of their recommendations as having a very low evidence backing and another 13 recommendations had low evidence. The JIA committee believed that none of its recommendations had strong evidence to back them up.
Dr. Beukelman defended writing recommendations despite this absence of evidence. “We should continue to write conditional recommendations when we don’t have the evidence. These recommendations had approval from at least 70% of the writing group, a diverse committee of experts. They should not be taken lightly just because they are conditional.”
Dr. Beukelman also stressed that he was presenting draft recommendations that still awaited approval from the ACR and the Arthritis Foundation, which collaborated with the ACR on this project. Once adopted, the new document would revise the existing management recommendations that the ACR approved in 2011 (Arthritis Rheum. 2011 Apr;63[4]:465-82).
The recommendations Dr. Beukelman outlined focused on treatment of polyarthritis, sacroiliitis, and enthesitis, and Dr. Beukelman devoted the most time to detailing some of the statements on polyarthritis. The panel conditionally recommended methotrexate over leflunomide (Arava) or sulfasalazine with moderate or very low evidence and said that subcutaneous methotrexate was conditionally preferred over oral dosing for reasons of both better efficacy and tolerability. Combination of a biologic agent with a nonbiologic received a conditional recommendation over biologic monotherapy, with moderate to very low evidence, but with a strong recommendation for this combined approach when using infliximab (Remicade), based on moderate evidence.
Another strong recommendation was to avoid treating patients with a chronic course of a low-dose, systemic glucocorticoid, based on a very low level of evidence. A brief course, less than 3 months, of an oral glucocorticoid received conditional recommendation for patients with moderate or high disease activity, based on very low evidence, but also received a conditional negative recommendation for patients with low disease activity, also based on very low evidence.
Initial therapy with a disease-modifying antirheumatic drug (DMARD) instead of monotherapy with an NSAID received a strong recommendation, based on a moderate level of evidence, while initial therapy with a DMARD received conditional support over initial therapy with a biologic agent, based on low evidence.
The panel gave a conditional endorsement to the idea of switching from a tumor necrosis factor inhibitor (TNFi) to a different biologic drug class when patients remained with moderate or high disease activity, based on a very low level of evidence.
Regarding sacroiliitis, the panel strongly recommended starting a TNFi in patients with active sacroiliitis despite NSAID treatment, based on low evidence, and the committee strongly recommended against starting methotrexate treatment in these patients, based on very low evidence. For treating active enthesitis despite NSAID treatment, the panel conditionally recommended adding a TNFi over treatment with methotrexate or sulfasalazine, based on a low level of evidence. Dr. Beukelman highlighted that the new recommendations placed increased emphasis on treating sacroiliitis, compared with the 2011 statement, and that the new recommendations dealt with treating enthesitis for the first time.
Dr. Beukelman has been a consultant to Bristol-Myers Squibb, Novartis, Sobi, and UCB.
CHICAGO – New draft guidelines for treating juvenile idiopathic arthritis (JIA) written by experts assembled by the American College of Rheumatology “formalize inactive disease as the goal of treatment,” Timothy G. Beukelman, MD, said at the annual meeting of the American College of Rheumatology.
“We defined low disease activity as patients with a single active joint, and the goal is to have zero active joints. Low disease activity should not be tolerated” in patients with JIA, said Dr. Beukelman, a pediatric rheumatologist at the University of Alabama at Birmingham and a member of the guideline-writing committee. “Until now, treating these patients to zero active joints has not been recommended. But clinically inactive disease is a realistic target for a majority of JIA patients,” he said in an interview.
Despite this shift in the recommended treatment goal, the writing panel was forced to rely largely on their expertise rather than reported evidence. The recommendation by the committee to escalate therapy in patients with low disease activity was “conditional,” with a level of evidence deemed “very low,” Dr. Beukelman said during a talk in which he cited selected highlights from the committee’s full list of 39 recommendations.
The paucity of evidence reflected the status of many of the recommendations: 31 of the 39 recommendations were conditional, which means that the desirable effects from treatment “probably” outweigh the undesirable effects, and they may not apply to some patients. The writing panel pegged 22 of their recommendations as having a very low evidence backing and another 13 recommendations had low evidence. The JIA committee believed that none of its recommendations had strong evidence to back them up.
Dr. Beukelman defended writing recommendations despite this absence of evidence. “We should continue to write conditional recommendations when we don’t have the evidence. These recommendations had approval from at least 70% of the writing group, a diverse committee of experts. They should not be taken lightly just because they are conditional.”
Dr. Beukelman also stressed that he was presenting draft recommendations that still awaited approval from the ACR and the Arthritis Foundation, which collaborated with the ACR on this project. Once adopted, the new document would revise the existing management recommendations that the ACR approved in 2011 (Arthritis Rheum. 2011 Apr;63[4]:465-82).
The recommendations Dr. Beukelman outlined focused on treatment of polyarthritis, sacroiliitis, and enthesitis, and Dr. Beukelman devoted the most time to detailing some of the statements on polyarthritis. The panel conditionally recommended methotrexate over leflunomide (Arava) or sulfasalazine with moderate or very low evidence and said that subcutaneous methotrexate was conditionally preferred over oral dosing for reasons of both better efficacy and tolerability. Combination of a biologic agent with a nonbiologic received a conditional recommendation over biologic monotherapy, with moderate to very low evidence, but with a strong recommendation for this combined approach when using infliximab (Remicade), based on moderate evidence.
Another strong recommendation was to avoid treating patients with a chronic course of a low-dose, systemic glucocorticoid, based on a very low level of evidence. A brief course, less than 3 months, of an oral glucocorticoid received conditional recommendation for patients with moderate or high disease activity, based on very low evidence, but also received a conditional negative recommendation for patients with low disease activity, also based on very low evidence.
Initial therapy with a disease-modifying antirheumatic drug (DMARD) instead of monotherapy with an NSAID received a strong recommendation, based on a moderate level of evidence, while initial therapy with a DMARD received conditional support over initial therapy with a biologic agent, based on low evidence.
The panel gave a conditional endorsement to the idea of switching from a tumor necrosis factor inhibitor (TNFi) to a different biologic drug class when patients remained with moderate or high disease activity, based on a very low level of evidence.
Regarding sacroiliitis, the panel strongly recommended starting a TNFi in patients with active sacroiliitis despite NSAID treatment, based on low evidence, and the committee strongly recommended against starting methotrexate treatment in these patients, based on very low evidence. For treating active enthesitis despite NSAID treatment, the panel conditionally recommended adding a TNFi over treatment with methotrexate or sulfasalazine, based on a low level of evidence. Dr. Beukelman highlighted that the new recommendations placed increased emphasis on treating sacroiliitis, compared with the 2011 statement, and that the new recommendations dealt with treating enthesitis for the first time.
Dr. Beukelman has been a consultant to Bristol-Myers Squibb, Novartis, Sobi, and UCB.
EXPERT ANALYSIS FROM THE ACR ANNUAL MEETING
Ob.Gyn. News welcomes Dr. Trolice to the board
Dr. Trolice is director of Fertility CARE: The IVF Center in Winter Park, Fla., and associate professor of obstetrics and gynecology at the University of Central Florida, Orlando, responsible for the medical education of ob.gyn. residents and medical students, as well as medical endocrinology fellows. He is past president of the Florida Society of Reproductive Endocrinology & Infertility (REI) and past division director of REI at Winnie Palmer Hospital, part of Orlando Health.
He is double board-certified in REI and ob.gyn., maintains annual recertification, and has been awarded the American Medical Association’s “Physicians’ Recognition Award” annually. He holds the unique distinction of being a fellow in all three American colleges: ob.gyn., surgeons, and endocrinology. His colleagues select him as a “Top Doctor in America” annually, one among the top 5% of doctors in the United States. In 2018, he was awarded the “Social Responsibility Award” by the National Polycystic Ovary Syndrome Association. For 10 years, his foundation, Fertile Dreams, organized seminars to increase fertility awareness and granted national scholarships for those unable to afford in vitro fertilization (IVF) treatment.
Dr. Trolice serves on committees for the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. He has conducted scientific studies with resultant numerous publications and been appointed a reviewer in many leading medical journals and textbooks. He has lectured at numerous physician and patient seminars around the country. In addition, he is interviewed regularly on TV news/talk shows, radio, podcasts, print/online magazines, and newspapers on reproductive health topics. In the fall of 2018, he launched a podcast entitled “Fertility Health” featuring discussions with national experts on pertinent infertility and reproductive medicine topics. His current book is on the infertility journey, to be published by Harvard Common Press in mid 2019.
Dr. Trolice is director of Fertility CARE: The IVF Center in Winter Park, Fla., and associate professor of obstetrics and gynecology at the University of Central Florida, Orlando, responsible for the medical education of ob.gyn. residents and medical students, as well as medical endocrinology fellows. He is past president of the Florida Society of Reproductive Endocrinology & Infertility (REI) and past division director of REI at Winnie Palmer Hospital, part of Orlando Health.
He is double board-certified in REI and ob.gyn., maintains annual recertification, and has been awarded the American Medical Association’s “Physicians’ Recognition Award” annually. He holds the unique distinction of being a fellow in all three American colleges: ob.gyn., surgeons, and endocrinology. His colleagues select him as a “Top Doctor in America” annually, one among the top 5% of doctors in the United States. In 2018, he was awarded the “Social Responsibility Award” by the National Polycystic Ovary Syndrome Association. For 10 years, his foundation, Fertile Dreams, organized seminars to increase fertility awareness and granted national scholarships for those unable to afford in vitro fertilization (IVF) treatment.
Dr. Trolice serves on committees for the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. He has conducted scientific studies with resultant numerous publications and been appointed a reviewer in many leading medical journals and textbooks. He has lectured at numerous physician and patient seminars around the country. In addition, he is interviewed regularly on TV news/talk shows, radio, podcasts, print/online magazines, and newspapers on reproductive health topics. In the fall of 2018, he launched a podcast entitled “Fertility Health” featuring discussions with national experts on pertinent infertility and reproductive medicine topics. His current book is on the infertility journey, to be published by Harvard Common Press in mid 2019.
Dr. Trolice is director of Fertility CARE: The IVF Center in Winter Park, Fla., and associate professor of obstetrics and gynecology at the University of Central Florida, Orlando, responsible for the medical education of ob.gyn. residents and medical students, as well as medical endocrinology fellows. He is past president of the Florida Society of Reproductive Endocrinology & Infertility (REI) and past division director of REI at Winnie Palmer Hospital, part of Orlando Health.
He is double board-certified in REI and ob.gyn., maintains annual recertification, and has been awarded the American Medical Association’s “Physicians’ Recognition Award” annually. He holds the unique distinction of being a fellow in all three American colleges: ob.gyn., surgeons, and endocrinology. His colleagues select him as a “Top Doctor in America” annually, one among the top 5% of doctors in the United States. In 2018, he was awarded the “Social Responsibility Award” by the National Polycystic Ovary Syndrome Association. For 10 years, his foundation, Fertile Dreams, organized seminars to increase fertility awareness and granted national scholarships for those unable to afford in vitro fertilization (IVF) treatment.
Dr. Trolice serves on committees for the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. He has conducted scientific studies with resultant numerous publications and been appointed a reviewer in many leading medical journals and textbooks. He has lectured at numerous physician and patient seminars around the country. In addition, he is interviewed regularly on TV news/talk shows, radio, podcasts, print/online magazines, and newspapers on reproductive health topics. In the fall of 2018, he launched a podcast entitled “Fertility Health” featuring discussions with national experts on pertinent infertility and reproductive medicine topics. His current book is on the infertility journey, to be published by Harvard Common Press in mid 2019.
Caffeinated coffee intake linked to lower rosacea risk
Caffeinated coffee intake is linked to a decreased incidence of rosacea, results of a large, observational study suggest.
Increased levels of caffeinated coffee consumption were associated with progressively lower levels of incident rosacea in a study of more than 82,000 participants representing more than 1.1 million person-years of follow-up.
By contrast, caffeine from other foods was not associated with rosacea incidence, reported Wen-Qing Li, PhD, of the department of dermatology at Brown University, Providence, R.I., and his coinvestigators. Those findings may have implications for the “causes and clinical approach” to rosacea.
“Our findings do not support limiting caffeine intake as a preventive strategy for rosacea,” they concluded in the study, published in JAMA Dermatology.
This is not the first study looking for potential links between rosacea and caffeine or coffee intake. However, previous studies didn’t distinguish between caffeinated coffee versus other beverages, and only one previous study made a distinction between the amounts of caffeine and coffee consumed, according to the authors.
Their research was based on data from the Nurses’ Health Study II, a prospective cohort study started in 1989. They looked specifically at 82,737 women who, in 2005, responded to the question about whether they had been diagnosed with rosacea. They identified 4,945 incident rosacea cases over the 1,120,051 person-years of follow-up.
A significant inverse association was found between caffeinated coffee intake and rosacea: Individuals who consumed four or more servings a day had a significantly lower risk of rosacea, compared with those who consumed one or fewer servings per month (hazard ratio, 0.77; 95% confidence interval, 0.69-0.87; P less than .001). They also found a dose-dependent effect, with the absolute risk of rosacea decreased by 131 per 100,000 person-years with at least four daily servings of caffeinated coffee, compared with under one serving a month.
By contrast, decaffeinated coffee was not associated with a reduced risk of rosacea, and in further analysis, the investigators found that there was no significant inverse association when they looked just at caffeine intake from sources other than coffee, such as chocolate, tea, and soda.
Caffeine could influence rosacea incidence by one of several mechanisms, including its effect on vascular contractility, the investigators hypothesized. “Increased caffeine intake may decrease vasodilation and consequently lead to diminution of rosacea symptoms.”
However, caffeine also has documented immunosuppressant effects that could possibly decrease rosacea-associated inflammation and has been shown to modulate hormone levels. “Hormonal factors have been implicated in the development of rosacea, and caffeine can modulate hormone levels,” they wrote.
Two study authors reported disclosures related to AbbVie, Amgen, Astellas Pharma, Janssen, Merck, Novartis, and Pfizer, among others. Funding for the study came from several sources, including National Institutes of Health grants for the Nurses’ Health Study II.
SOURCE: Li W-Q et al. JAMA Dermatol. 2018 Oct 17. doi: 10.1001/jamadermatol.2018.3301.
This study shows an inverse association between caffeine intake and incidence rosacea, which suggests that patients with rosacea need not avoid coffee, according to Mackenzie R. Wehner, MD, and Eleni Linos, MD, MPH.
For everyone else, the findings offer yet another reason to keep indulging in one of “life’s habitual pleasures,” they wrote. “We will raise an insulated travel mug to that.”
This latest study fits in with numerous studies suggesting coffee may be protective against a number of maladies, including cancer, cardiovascular disease, type 2 diabetes, and Parkinson’s disease, they wrote in their editorial published in JAMA Dermatology.
However, this is an observational study, not a rigorous, randomized trial that could more conclusively prove coffee actually provides an antirosacea benefit that cannot be explained by other factors, such as systematic differences between people who do and do not drink coffee. Enrollment of all women, mostly white, in the Nurses’ Health Study II is another limitation, they added.
Nevertheless, studies like this are the “next-best option” in lieu of randomized, controlled trials to evaluate these relationships, they wrote. “Importantly, the strength of the protective effect noted and the dose-response relationship with increasing coffee and caffeine intake are convincing.”
Dr. Wehner , is with the department of dermatology at the University of Pennsylvania, Philadelphia. Dr. Linos is with the department of dermatology at the University of California, San Francisco. Dr. Wehner reported support from a National Institute of Arthritis and Musculoskeletal and Skin Diseases/National Institutes of Health Dermatology Research Training grant. Dr. Linos reported support from the National Cancer Institute and the National Institute of Aging.
This study shows an inverse association between caffeine intake and incidence rosacea, which suggests that patients with rosacea need not avoid coffee, according to Mackenzie R. Wehner, MD, and Eleni Linos, MD, MPH.
For everyone else, the findings offer yet another reason to keep indulging in one of “life’s habitual pleasures,” they wrote. “We will raise an insulated travel mug to that.”
This latest study fits in with numerous studies suggesting coffee may be protective against a number of maladies, including cancer, cardiovascular disease, type 2 diabetes, and Parkinson’s disease, they wrote in their editorial published in JAMA Dermatology.
However, this is an observational study, not a rigorous, randomized trial that could more conclusively prove coffee actually provides an antirosacea benefit that cannot be explained by other factors, such as systematic differences between people who do and do not drink coffee. Enrollment of all women, mostly white, in the Nurses’ Health Study II is another limitation, they added.
Nevertheless, studies like this are the “next-best option” in lieu of randomized, controlled trials to evaluate these relationships, they wrote. “Importantly, the strength of the protective effect noted and the dose-response relationship with increasing coffee and caffeine intake are convincing.”
Dr. Wehner , is with the department of dermatology at the University of Pennsylvania, Philadelphia. Dr. Linos is with the department of dermatology at the University of California, San Francisco. Dr. Wehner reported support from a National Institute of Arthritis and Musculoskeletal and Skin Diseases/National Institutes of Health Dermatology Research Training grant. Dr. Linos reported support from the National Cancer Institute and the National Institute of Aging.
This study shows an inverse association between caffeine intake and incidence rosacea, which suggests that patients with rosacea need not avoid coffee, according to Mackenzie R. Wehner, MD, and Eleni Linos, MD, MPH.
For everyone else, the findings offer yet another reason to keep indulging in one of “life’s habitual pleasures,” they wrote. “We will raise an insulated travel mug to that.”
This latest study fits in with numerous studies suggesting coffee may be protective against a number of maladies, including cancer, cardiovascular disease, type 2 diabetes, and Parkinson’s disease, they wrote in their editorial published in JAMA Dermatology.
However, this is an observational study, not a rigorous, randomized trial that could more conclusively prove coffee actually provides an antirosacea benefit that cannot be explained by other factors, such as systematic differences between people who do and do not drink coffee. Enrollment of all women, mostly white, in the Nurses’ Health Study II is another limitation, they added.
Nevertheless, studies like this are the “next-best option” in lieu of randomized, controlled trials to evaluate these relationships, they wrote. “Importantly, the strength of the protective effect noted and the dose-response relationship with increasing coffee and caffeine intake are convincing.”
Dr. Wehner , is with the department of dermatology at the University of Pennsylvania, Philadelphia. Dr. Linos is with the department of dermatology at the University of California, San Francisco. Dr. Wehner reported support from a National Institute of Arthritis and Musculoskeletal and Skin Diseases/National Institutes of Health Dermatology Research Training grant. Dr. Linos reported support from the National Cancer Institute and the National Institute of Aging.
Caffeinated coffee intake is linked to a decreased incidence of rosacea, results of a large, observational study suggest.
Increased levels of caffeinated coffee consumption were associated with progressively lower levels of incident rosacea in a study of more than 82,000 participants representing more than 1.1 million person-years of follow-up.
By contrast, caffeine from other foods was not associated with rosacea incidence, reported Wen-Qing Li, PhD, of the department of dermatology at Brown University, Providence, R.I., and his coinvestigators. Those findings may have implications for the “causes and clinical approach” to rosacea.
“Our findings do not support limiting caffeine intake as a preventive strategy for rosacea,” they concluded in the study, published in JAMA Dermatology.
This is not the first study looking for potential links between rosacea and caffeine or coffee intake. However, previous studies didn’t distinguish between caffeinated coffee versus other beverages, and only one previous study made a distinction between the amounts of caffeine and coffee consumed, according to the authors.
Their research was based on data from the Nurses’ Health Study II, a prospective cohort study started in 1989. They looked specifically at 82,737 women who, in 2005, responded to the question about whether they had been diagnosed with rosacea. They identified 4,945 incident rosacea cases over the 1,120,051 person-years of follow-up.
A significant inverse association was found between caffeinated coffee intake and rosacea: Individuals who consumed four or more servings a day had a significantly lower risk of rosacea, compared with those who consumed one or fewer servings per month (hazard ratio, 0.77; 95% confidence interval, 0.69-0.87; P less than .001). They also found a dose-dependent effect, with the absolute risk of rosacea decreased by 131 per 100,000 person-years with at least four daily servings of caffeinated coffee, compared with under one serving a month.
By contrast, decaffeinated coffee was not associated with a reduced risk of rosacea, and in further analysis, the investigators found that there was no significant inverse association when they looked just at caffeine intake from sources other than coffee, such as chocolate, tea, and soda.
Caffeine could influence rosacea incidence by one of several mechanisms, including its effect on vascular contractility, the investigators hypothesized. “Increased caffeine intake may decrease vasodilation and consequently lead to diminution of rosacea symptoms.”
However, caffeine also has documented immunosuppressant effects that could possibly decrease rosacea-associated inflammation and has been shown to modulate hormone levels. “Hormonal factors have been implicated in the development of rosacea, and caffeine can modulate hormone levels,” they wrote.
Two study authors reported disclosures related to AbbVie, Amgen, Astellas Pharma, Janssen, Merck, Novartis, and Pfizer, among others. Funding for the study came from several sources, including National Institutes of Health grants for the Nurses’ Health Study II.
SOURCE: Li W-Q et al. JAMA Dermatol. 2018 Oct 17. doi: 10.1001/jamadermatol.2018.3301.
Caffeinated coffee intake is linked to a decreased incidence of rosacea, results of a large, observational study suggest.
Increased levels of caffeinated coffee consumption were associated with progressively lower levels of incident rosacea in a study of more than 82,000 participants representing more than 1.1 million person-years of follow-up.
By contrast, caffeine from other foods was not associated with rosacea incidence, reported Wen-Qing Li, PhD, of the department of dermatology at Brown University, Providence, R.I., and his coinvestigators. Those findings may have implications for the “causes and clinical approach” to rosacea.
“Our findings do not support limiting caffeine intake as a preventive strategy for rosacea,” they concluded in the study, published in JAMA Dermatology.
This is not the first study looking for potential links between rosacea and caffeine or coffee intake. However, previous studies didn’t distinguish between caffeinated coffee versus other beverages, and only one previous study made a distinction between the amounts of caffeine and coffee consumed, according to the authors.
Their research was based on data from the Nurses’ Health Study II, a prospective cohort study started in 1989. They looked specifically at 82,737 women who, in 2005, responded to the question about whether they had been diagnosed with rosacea. They identified 4,945 incident rosacea cases over the 1,120,051 person-years of follow-up.
A significant inverse association was found between caffeinated coffee intake and rosacea: Individuals who consumed four or more servings a day had a significantly lower risk of rosacea, compared with those who consumed one or fewer servings per month (hazard ratio, 0.77; 95% confidence interval, 0.69-0.87; P less than .001). They also found a dose-dependent effect, with the absolute risk of rosacea decreased by 131 per 100,000 person-years with at least four daily servings of caffeinated coffee, compared with under one serving a month.
By contrast, decaffeinated coffee was not associated with a reduced risk of rosacea, and in further analysis, the investigators found that there was no significant inverse association when they looked just at caffeine intake from sources other than coffee, such as chocolate, tea, and soda.
Caffeine could influence rosacea incidence by one of several mechanisms, including its effect on vascular contractility, the investigators hypothesized. “Increased caffeine intake may decrease vasodilation and consequently lead to diminution of rosacea symptoms.”
However, caffeine also has documented immunosuppressant effects that could possibly decrease rosacea-associated inflammation and has been shown to modulate hormone levels. “Hormonal factors have been implicated in the development of rosacea, and caffeine can modulate hormone levels,” they wrote.
Two study authors reported disclosures related to AbbVie, Amgen, Astellas Pharma, Janssen, Merck, Novartis, and Pfizer, among others. Funding for the study came from several sources, including National Institutes of Health grants for the Nurses’ Health Study II.
SOURCE: Li W-Q et al. JAMA Dermatol. 2018 Oct 17. doi: 10.1001/jamadermatol.2018.3301.
FROM JAMA DERMATOLOGY
Key clinical point: Caffeinated coffee intake was linked to decreased incidence of rosacea, while decaffeinated coffee and noncoffee sources of caffeine had no such effect.
Major finding: Consuming four or more servings of caffeinated coffee was associated with lower risk of rosacea versus one or fewer servings per month (hazard ratio, 0.77; P less than .001).
Study details: An analysis based on 82,737 participants in the Nurses’ Health Study II who responded to a question about rosacea.
Disclosures: Two study authors reported disclosures related to AbbVie, Amgen, Astellas Pharma, Janssen, Merck, Novartis, and Pfizer, among others. Funding for the study came from National Institutes of Health grants for the Nurses’ Health Study II and other sources.
Source: Li W-Q et al. JAMA Dermatol. 2018 Oct 17. doi: 10.1001/jamadermatol.2018.3301.
Dulaglutide meets primary endpoint in REWIND
Eli Lilly has announced top line results from REWIND, a multicenter, randomized, double-blind, placebo-controlled trial designed to study dulaglutide (Trulicity). The cardiovascular outcomes trial, which had a median follow-up period of more than 5 years, evaluated cardiovascular outcomes in nearly 10,000 patients with type 2 diabetes.
The primary endpoint of REWIND was time until the first occurrence of a major adverse cardiovascular event. Patients who received dulaglutide had a significantly reduced incidence of these events, compared with placebo, meeting the primary trial endpoint. No specific results were announced.
REWIND was distinct in that it had limited participation from people with established cardiovascular disease, which allowed dulaglutide’s effect to be measured in a broad population of people with type 2 diabetes, Eli Lilly said in their press release.
Dulaglutide is a GLP-1 receptor agonist, and trial participants received a 1.5-mg dose once a week.
Full results of the REWIND trial will be presented at the annual scientific sessions of the American Diabetes Association in June 2019.
Eli Lilly has announced top line results from REWIND, a multicenter, randomized, double-blind, placebo-controlled trial designed to study dulaglutide (Trulicity). The cardiovascular outcomes trial, which had a median follow-up period of more than 5 years, evaluated cardiovascular outcomes in nearly 10,000 patients with type 2 diabetes.
The primary endpoint of REWIND was time until the first occurrence of a major adverse cardiovascular event. Patients who received dulaglutide had a significantly reduced incidence of these events, compared with placebo, meeting the primary trial endpoint. No specific results were announced.
REWIND was distinct in that it had limited participation from people with established cardiovascular disease, which allowed dulaglutide’s effect to be measured in a broad population of people with type 2 diabetes, Eli Lilly said in their press release.
Dulaglutide is a GLP-1 receptor agonist, and trial participants received a 1.5-mg dose once a week.
Full results of the REWIND trial will be presented at the annual scientific sessions of the American Diabetes Association in June 2019.
Eli Lilly has announced top line results from REWIND, a multicenter, randomized, double-blind, placebo-controlled trial designed to study dulaglutide (Trulicity). The cardiovascular outcomes trial, which had a median follow-up period of more than 5 years, evaluated cardiovascular outcomes in nearly 10,000 patients with type 2 diabetes.
The primary endpoint of REWIND was time until the first occurrence of a major adverse cardiovascular event. Patients who received dulaglutide had a significantly reduced incidence of these events, compared with placebo, meeting the primary trial endpoint. No specific results were announced.
REWIND was distinct in that it had limited participation from people with established cardiovascular disease, which allowed dulaglutide’s effect to be measured in a broad population of people with type 2 diabetes, Eli Lilly said in their press release.
Dulaglutide is a GLP-1 receptor agonist, and trial participants received a 1.5-mg dose once a week.
Full results of the REWIND trial will be presented at the annual scientific sessions of the American Diabetes Association in June 2019.
Mood stabilizers protect bipolar patients from suicide
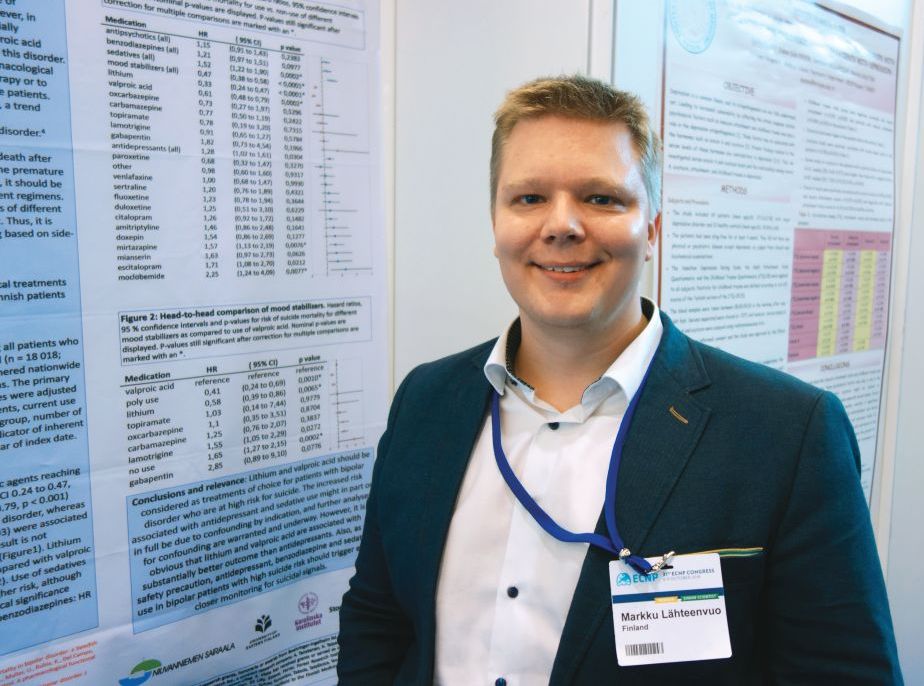
BARCELONA – Lithium and valproic acid are the treatments of choice for patients with bipolar disorder at increased risk for suicide, according to the findings of a large Finnish national study.
“We found that – surprise, surprise – lithium and valproic acid had the lowest risk of anyone committing suicide on them. And funnily enough, some antidepressants seemed to be correlated with a higher risk of committing suicide,” Markku Lähteenvuo, MD, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
However, he suspects that the correlation between antidepressant therapy and suicide in bipolar patients probably was caused by confounding by indication.
“I wouldn’t have as a take-home message that SSRI [selective serotonin reuptake inhibitor] antidepressants are bad for you; it’s probably rather that these are really bad cases, treatment gets initiated when someone gets worse, and the antidepressants just aren’t quick enough to really give an effect. It takes 3-4 weeks for an SSRI to really kick in, whereas mood stabilizers like lithium and valproic acid usually kick in almost immediately, within a couple of days to a week,” explained Dr. Lähteenvuo, a forensic psychiatrist at Niuvanniemi Hospital and the University of Eastern Finland, in Kuopio.
He presented a study of all suicides among the 18,018 Finnish patients hospitalized for bipolar disorder nationwide during 1996-2012. Using prospective national databases to follow patients for a mean of 7.2 years, he and his coinvestigators were able to determine what medications they were on when they committed suicide and the likelihood they were actually taking their prescribed medications at the time.
In a multivariate proportional hazards analysis adjusted for concomitant psychotropic medications, duration of bipolar illness, intervals of drug exposure and nonexposure, age, sex, and number of hospitalizations for suicidality within the prior 2 years, bipolar patients on lithium had a 67% lower risk of suicide than did those not on the drug. Those on valproic acid were 39% less likely to commit suicide than those not on that mood stabilizer. And bipolar patients on lithium were 42% less likely to die from suicide than those on valproic acid.
At the other extreme, patients on antidepressants were in aggregate 28% more likely to commit suicide than those who were not. This risk varied considerably according to the specific antidepressant: for example, escitalopram and mirtazapine were associated with 71% and 57% greater risks of suicide, respectively, than in patients not on those antidepressants, while patients on paroxetine, venlafaxine, or sertraline were not at increased risk.
Also, the use of sedatives was associated with a 52% greater likelihood of suicide, and benzodiazepines were linked to a 21% increase in risk. Again, as with antidepressants, these associations with increased risk of completed suicide could be attributable in part or in whole to confounding by indication, the psychiatrist noted. He and his colleagues are conducting further analyses examining that possibility.
Pending the outcome of that closer look, however, Dr. Lähteenvuo believes the study’s message to clinicians is clear: “The use of lithium is getting less and less common all the time because of side effects. That’s also true for valproic acid. Many bipolar patients are now prescribed only antidepressants, even though all the guidelines advise against it due to the risk of hypomania. We think that this is a bad trend and that lithium and valproic acid should be prescribed more. Also, as a safety precaution, anyone with bipolar disorder on antidepressants or benzodiazepines or sedatives should be followed especially closely for suicidal signals, because they could carry a really highly increased risk – up to 50% – due to the medication as well.”
He reported having no financial conflicts regarding the study, funded by the Finnish government.
Dr. Lähteenvuo also was first author of a recent study showing that among the various drugs prescribed for treatment of bipolar disorder, lithium was the clear winner for prevention of rehospitalization in the same national Finnish population of more than 18,000 bipolar patients (JAMA Psychiatry. 2018;75[4]:347-55). One expert named this among the top four studies of the year in the field of mood disorders.
BARCELONA – Lithium and valproic acid are the treatments of choice for patients with bipolar disorder at increased risk for suicide, according to the findings of a large Finnish national study.
“We found that – surprise, surprise – lithium and valproic acid had the lowest risk of anyone committing suicide on them. And funnily enough, some antidepressants seemed to be correlated with a higher risk of committing suicide,” Markku Lähteenvuo, MD, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
However, he suspects that the correlation between antidepressant therapy and suicide in bipolar patients probably was caused by confounding by indication.
“I wouldn’t have as a take-home message that SSRI [selective serotonin reuptake inhibitor] antidepressants are bad for you; it’s probably rather that these are really bad cases, treatment gets initiated when someone gets worse, and the antidepressants just aren’t quick enough to really give an effect. It takes 3-4 weeks for an SSRI to really kick in, whereas mood stabilizers like lithium and valproic acid usually kick in almost immediately, within a couple of days to a week,” explained Dr. Lähteenvuo, a forensic psychiatrist at Niuvanniemi Hospital and the University of Eastern Finland, in Kuopio.
He presented a study of all suicides among the 18,018 Finnish patients hospitalized for bipolar disorder nationwide during 1996-2012. Using prospective national databases to follow patients for a mean of 7.2 years, he and his coinvestigators were able to determine what medications they were on when they committed suicide and the likelihood they were actually taking their prescribed medications at the time.
In a multivariate proportional hazards analysis adjusted for concomitant psychotropic medications, duration of bipolar illness, intervals of drug exposure and nonexposure, age, sex, and number of hospitalizations for suicidality within the prior 2 years, bipolar patients on lithium had a 67% lower risk of suicide than did those not on the drug. Those on valproic acid were 39% less likely to commit suicide than those not on that mood stabilizer. And bipolar patients on lithium were 42% less likely to die from suicide than those on valproic acid.
At the other extreme, patients on antidepressants were in aggregate 28% more likely to commit suicide than those who were not. This risk varied considerably according to the specific antidepressant: for example, escitalopram and mirtazapine were associated with 71% and 57% greater risks of suicide, respectively, than in patients not on those antidepressants, while patients on paroxetine, venlafaxine, or sertraline were not at increased risk.
Also, the use of sedatives was associated with a 52% greater likelihood of suicide, and benzodiazepines were linked to a 21% increase in risk. Again, as with antidepressants, these associations with increased risk of completed suicide could be attributable in part or in whole to confounding by indication, the psychiatrist noted. He and his colleagues are conducting further analyses examining that possibility.
Pending the outcome of that closer look, however, Dr. Lähteenvuo believes the study’s message to clinicians is clear: “The use of lithium is getting less and less common all the time because of side effects. That’s also true for valproic acid. Many bipolar patients are now prescribed only antidepressants, even though all the guidelines advise against it due to the risk of hypomania. We think that this is a bad trend and that lithium and valproic acid should be prescribed more. Also, as a safety precaution, anyone with bipolar disorder on antidepressants or benzodiazepines or sedatives should be followed especially closely for suicidal signals, because they could carry a really highly increased risk – up to 50% – due to the medication as well.”
He reported having no financial conflicts regarding the study, funded by the Finnish government.
Dr. Lähteenvuo also was first author of a recent study showing that among the various drugs prescribed for treatment of bipolar disorder, lithium was the clear winner for prevention of rehospitalization in the same national Finnish population of more than 18,000 bipolar patients (JAMA Psychiatry. 2018;75[4]:347-55). One expert named this among the top four studies of the year in the field of mood disorders.
BARCELONA – Lithium and valproic acid are the treatments of choice for patients with bipolar disorder at increased risk for suicide, according to the findings of a large Finnish national study.
“We found that – surprise, surprise – lithium and valproic acid had the lowest risk of anyone committing suicide on them. And funnily enough, some antidepressants seemed to be correlated with a higher risk of committing suicide,” Markku Lähteenvuo, MD, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
However, he suspects that the correlation between antidepressant therapy and suicide in bipolar patients probably was caused by confounding by indication.
“I wouldn’t have as a take-home message that SSRI [selective serotonin reuptake inhibitor] antidepressants are bad for you; it’s probably rather that these are really bad cases, treatment gets initiated when someone gets worse, and the antidepressants just aren’t quick enough to really give an effect. It takes 3-4 weeks for an SSRI to really kick in, whereas mood stabilizers like lithium and valproic acid usually kick in almost immediately, within a couple of days to a week,” explained Dr. Lähteenvuo, a forensic psychiatrist at Niuvanniemi Hospital and the University of Eastern Finland, in Kuopio.
He presented a study of all suicides among the 18,018 Finnish patients hospitalized for bipolar disorder nationwide during 1996-2012. Using prospective national databases to follow patients for a mean of 7.2 years, he and his coinvestigators were able to determine what medications they were on when they committed suicide and the likelihood they were actually taking their prescribed medications at the time.
In a multivariate proportional hazards analysis adjusted for concomitant psychotropic medications, duration of bipolar illness, intervals of drug exposure and nonexposure, age, sex, and number of hospitalizations for suicidality within the prior 2 years, bipolar patients on lithium had a 67% lower risk of suicide than did those not on the drug. Those on valproic acid were 39% less likely to commit suicide than those not on that mood stabilizer. And bipolar patients on lithium were 42% less likely to die from suicide than those on valproic acid.
At the other extreme, patients on antidepressants were in aggregate 28% more likely to commit suicide than those who were not. This risk varied considerably according to the specific antidepressant: for example, escitalopram and mirtazapine were associated with 71% and 57% greater risks of suicide, respectively, than in patients not on those antidepressants, while patients on paroxetine, venlafaxine, or sertraline were not at increased risk.
Also, the use of sedatives was associated with a 52% greater likelihood of suicide, and benzodiazepines were linked to a 21% increase in risk. Again, as with antidepressants, these associations with increased risk of completed suicide could be attributable in part or in whole to confounding by indication, the psychiatrist noted. He and his colleagues are conducting further analyses examining that possibility.
Pending the outcome of that closer look, however, Dr. Lähteenvuo believes the study’s message to clinicians is clear: “The use of lithium is getting less and less common all the time because of side effects. That’s also true for valproic acid. Many bipolar patients are now prescribed only antidepressants, even though all the guidelines advise against it due to the risk of hypomania. We think that this is a bad trend and that lithium and valproic acid should be prescribed more. Also, as a safety precaution, anyone with bipolar disorder on antidepressants or benzodiazepines or sedatives should be followed especially closely for suicidal signals, because they could carry a really highly increased risk – up to 50% – due to the medication as well.”
He reported having no financial conflicts regarding the study, funded by the Finnish government.
Dr. Lähteenvuo also was first author of a recent study showing that among the various drugs prescribed for treatment of bipolar disorder, lithium was the clear winner for prevention of rehospitalization in the same national Finnish population of more than 18,000 bipolar patients (JAMA Psychiatry. 2018;75[4]:347-55). One expert named this among the top four studies of the year in the field of mood disorders.
REPORTING FROM THE ECNP CONGRESS
Key clinical point: Lithium and valproic acid protect patients with bipolar disorder from suicide.
Major finding: The likelihood of suicide was reduced by two-thirds in bipolar patients on lithium, compared with that of patients not on the mood stabilizer.
Study details: This was a retrospective study of more than 18,000 Finnish patients hospitalized at some point for bipolar disorder and the medications they were on when a subset of them committed suicide.
Disclosures: The presenter reported having no financial conflicts regarding the study, funded by the Finnish government.
Conference News Roundup—American Association of Neuromuscular & Electrodiagnostic Medicine
Does Thymectomy Benefit Patients With Anti-MuSK Myasthenia Gravis?
Among patients with anti-muscle-specific kinase (MuSK) myasthenia gravis, thymectomy is not associated with greater likelihood of clinical improvement, according to an analysis of data from a multicenter cohort study.
Although a randomized trial has demonstrated benefit from thymectomy in nonthymomatous antiacetylcholine receptor (AChR) antibody positive generalized myasthenia gravis, observational studies suggest that thymectomy may not be efficacious in anti-MuSK myasthenia gravis. Histologic studies have found that patients with anti-MuSK myasthenia gravis have less hyperplastic thymic tissue, compared with patients with anti-AChR myasthenia gravis.
To evaluate the therapeutic impact of thymectomy in patients with anti-MuSK myasthenia gravis, Katherine Clifford, a medical student at the University of Vermont Larner College of Medicine in Burlington, and colleagues analyzed data from a multicenter, retrospective, blinded review of rituximab treatment in patients with anti-MuSK myasthenia gravis. The primary outcome was favorable outcome on the Myasthenia Gravis Foundation of America (MGFA) Post-Intervention Status (PIS). The researchers defined a favorable outcome as an MGFA PIS score of minimal manifestations or better.
Secondary outcomes included prednisone dose; use of other immunosuppressant medications, IV immunoglobulin (IVIG), or plasma exchange (PLEX) treatment; and Myasthenia Gravis Status and Treatment Intensity (MGSTI).
Baseline characteristics were similar between patients with anti-MuSK myasthenia gravis who received thymectomy (n = 26) and those who did not (n = 29), including treatment with rituximab (42% vs 45%). Median follow-up was more than three years.
At last visit, 35% (nine of 26) of patients who received thymectomy had a favorable outcome, compared with 55% (16 of 29) of patients who did not receive thymectomy. In addition, 69% of patients who received thymectomy were taking prednisone, compared with 41% of patients who did not receive thymectomy (median dose, 10 mg/day vs 0 mg/day).
“After controlling for rituximab, baseline prednisone, and final IVIG/PLEX treatment, thymectomy was not associated with greater likelihood of favorable clinical outcome, but broad confidence intervals cannot exclude therapeutic effect (odds ratio, 0.43),” the investigators reported.
“The recent MGTX trial clearly demonstrated the benefit of thymectomy for patients with AChR antibody positive myasthenia gravis,” said A. Gordon Smith, MD, Cochair of the AANEM Annual Meeting Program Committee. “Ms. Clifford and her colleagues now provide compelling data suggesting thymectomy may not be effective in MuSK-positive myasthenia gravis.”
The study’s follow-up is long enough for the findings to be clinically “relevant to all physicians treating myasthenia gravis,” said Robert W. Irwin, MD, Cochair of the AANEM Annual Meeting Program Committee.
What Are the Clinical, Laboratory, and Electrodiagnostic Features of Zinc Deficiency-InducedPeripheral Neuropathy?
Patients with zinc deficiency-induced peripheral neuropathy may present with paresthesia, gait abnormalities, sensory deficits, reduced tendon reflexes, an abnormal Romberg test, and increased CSF protein, according to a study.
Recognition of the features of zinc deficiency-induced peripheral neuropathy may help neurologists diagnose the disorder and manage patients, researchers said.
“Zinc, an essential trace element, plays a critical role in maintaining normal structural and functional conditions in the body,” said lead author Favio C. Bumanlag, Chief Technologist in the Department of Neurology at the Lewis Katz School of Medicine at Temple University in Philadelphia. “Peripheral nerves are susceptible to damage when zinc deficiency occurs.... Recognition of [zinc deficiency-induced peripheral neuropathy] will help physicians and technologists effectively manage patients.”
To study the clinical and electrophysiologic features of zinc deficiency-induced peripheral neuropathy, Mr. Bumanlag and Jin Luo, MD, PhD, Professor of Neurology and Pharmacology at Temple University, retrospectively reviewed charts in their neuromuscular clinic and EMG laboratory database to identify patients with peripheral neuropathy and zinc deficiency. They included charts from between January 1, 2015, and December 31, 2017, in their review. They excluded patients with abnormal copper levels.
Mr. Bumanlag and Dr. Luo obtained information about patients’ clinical presentations, past medical histories, BMI, neurologic examinations, and laboratory results. They also examined patients’ needle electromyograms and nerve conduction studies.
In all, they identified 12 patients with peripheral neuropathy and zinc deficiency. Patients had a mean age of 55.1. Six were female. Patients’ mean zinc level was 52.5 μg/dL, with a range of 37 μg/dL to 58 μg/dL (reference, 56–134 μg/dL). Mean copper level was 107.6 μg/dL, with a range of 84 μg/dL to 173 μg/dL (reference, 72–166
Notable findings in presentation included paresthesia in 75 and gait abnormalities in 42%. One patient was obese (8%), and three patients had diarrhea (25%). Neurologic examination showed sensory deficits in 83%, reduced tendon reflexes in 67%, and an abnormal Romberg test in 67%. Four of five patients had increased CSF protein. Electrophysiologic evaluations showed features of demyelinating peripheral neuropathy (28%) and distally active denervation in the lower extremities.
“Zinc participates in more than 200 enzymatic reactions,” said the researchers. “Unfortunately, zinc deficiency-induced peripheral neuropathy is often misdiagnosed or delayed in diagnosis. Literature on zinc deficiency-induced peripheral neuropathy is sparse.”
Disability in Patients With Stiff Person Syndrome May Progress Faster Than Thought
Stiff person syndrome leads to disability if therapy is not initiated early in the disease course, according to a prospective study. In addition, patients with stiff person syndrome may have “faster progression of disablement than originally reported and believed,” said lead study author Goran Rakocevic, MD. Dr. Rakocevic is Associate Professor of Neurology, Director of the Neuromuscular Electrodiagnostic Laboratory, Clinical Director of the Jefferson Weinberg ALS Center, and Director of the Neuromuscular Medicine Fellowship Program at Thomas Jefferson University in Philadelphia.
Stiff person syndrome is a disorder characterized by muscle rigidity and episodic spasms in axial and limb musculature, as well as heightened sensitivity to external stimuli. To describe the natural history of stiff person syndrome, the extent of accumulated disability, and associated clinical features, Dr. Rakocevic and his research colleagues conducted a prospective cohort study in patients followed for up to eight years in a single center.
The cohort included 57 patients with mean age at disease onset of 42 (range, 22 to 60). Of these, 32 patients were examined every six months for two years without receiving immune therapies. The investigators assessed disease progression using quantitative scales of stiffness and heightened sensitivity.
Patients’ most frequent initial symptoms were leg stiffness, paraspinal muscle rigidity, and painful spasms. Although no patients required assistance for ambulation during the first two years of the disease, 46 patients (80%) lost the ability to walk independently during follow-up, despite symptomatic medications. In the longitudinal cohort, the number of stiff areas increased, which was consistent with worsening functional status and quality of life. The researchers confirmed a strong association between stiff person syndrome and the HLA-DR and DQ haplotypes.
The study is the largest prospective study of patients with stiff person syndrome and the first to provide longitudinal data on the natural course of the disorder in a large patient subgroup using objective clinical measures, Dr. Rakocevic and colleagues said. “The study shows that stiff person syndrome is a progressive autoimmune disease that leads to disability if ... immunotherapy is not applied,” said the investigators.
“Early diagnosis and management of stiff person syndrome can be challenging,” said A. Gordon Smith, MD, Cochair of the AANEM Annual Meeting Program Committee. The study by Dr. Rakocevic’s team demonstrates “that stiff person syndrome causes progressive stiffness and functional decline, with 80% [of patients] becoming unable to walk independently,” he said. “Their research emphasizes the need to treat early and will help clinicians recognize stiff person syndrome earlier in its course.”
The study adds to neurologists’ understanding of the rare disorder, and its strengths include the length of follow-up and the number of patients, said Robert W. Irwin, MD, Cochair of the AANEM Annual Meeting Program Committee.
Does Thymectomy Benefit Patients With Anti-MuSK Myasthenia Gravis?
Among patients with anti-muscle-specific kinase (MuSK) myasthenia gravis, thymectomy is not associated with greater likelihood of clinical improvement, according to an analysis of data from a multicenter cohort study.
Although a randomized trial has demonstrated benefit from thymectomy in nonthymomatous antiacetylcholine receptor (AChR) antibody positive generalized myasthenia gravis, observational studies suggest that thymectomy may not be efficacious in anti-MuSK myasthenia gravis. Histologic studies have found that patients with anti-MuSK myasthenia gravis have less hyperplastic thymic tissue, compared with patients with anti-AChR myasthenia gravis.
To evaluate the therapeutic impact of thymectomy in patients with anti-MuSK myasthenia gravis, Katherine Clifford, a medical student at the University of Vermont Larner College of Medicine in Burlington, and colleagues analyzed data from a multicenter, retrospective, blinded review of rituximab treatment in patients with anti-MuSK myasthenia gravis. The primary outcome was favorable outcome on the Myasthenia Gravis Foundation of America (MGFA) Post-Intervention Status (PIS). The researchers defined a favorable outcome as an MGFA PIS score of minimal manifestations or better.
Secondary outcomes included prednisone dose; use of other immunosuppressant medications, IV immunoglobulin (IVIG), or plasma exchange (PLEX) treatment; and Myasthenia Gravis Status and Treatment Intensity (MGSTI).
Baseline characteristics were similar between patients with anti-MuSK myasthenia gravis who received thymectomy (n = 26) and those who did not (n = 29), including treatment with rituximab (42% vs 45%). Median follow-up was more than three years.
At last visit, 35% (nine of 26) of patients who received thymectomy had a favorable outcome, compared with 55% (16 of 29) of patients who did not receive thymectomy. In addition, 69% of patients who received thymectomy were taking prednisone, compared with 41% of patients who did not receive thymectomy (median dose, 10 mg/day vs 0 mg/day).
“After controlling for rituximab, baseline prednisone, and final IVIG/PLEX treatment, thymectomy was not associated with greater likelihood of favorable clinical outcome, but broad confidence intervals cannot exclude therapeutic effect (odds ratio, 0.43),” the investigators reported.
“The recent MGTX trial clearly demonstrated the benefit of thymectomy for patients with AChR antibody positive myasthenia gravis,” said A. Gordon Smith, MD, Cochair of the AANEM Annual Meeting Program Committee. “Ms. Clifford and her colleagues now provide compelling data suggesting thymectomy may not be effective in MuSK-positive myasthenia gravis.”
The study’s follow-up is long enough for the findings to be clinically “relevant to all physicians treating myasthenia gravis,” said Robert W. Irwin, MD, Cochair of the AANEM Annual Meeting Program Committee.
What Are the Clinical, Laboratory, and Electrodiagnostic Features of Zinc Deficiency-InducedPeripheral Neuropathy?
Patients with zinc deficiency-induced peripheral neuropathy may present with paresthesia, gait abnormalities, sensory deficits, reduced tendon reflexes, an abnormal Romberg test, and increased CSF protein, according to a study.
Recognition of the features of zinc deficiency-induced peripheral neuropathy may help neurologists diagnose the disorder and manage patients, researchers said.
“Zinc, an essential trace element, plays a critical role in maintaining normal structural and functional conditions in the body,” said lead author Favio C. Bumanlag, Chief Technologist in the Department of Neurology at the Lewis Katz School of Medicine at Temple University in Philadelphia. “Peripheral nerves are susceptible to damage when zinc deficiency occurs.... Recognition of [zinc deficiency-induced peripheral neuropathy] will help physicians and technologists effectively manage patients.”
To study the clinical and electrophysiologic features of zinc deficiency-induced peripheral neuropathy, Mr. Bumanlag and Jin Luo, MD, PhD, Professor of Neurology and Pharmacology at Temple University, retrospectively reviewed charts in their neuromuscular clinic and EMG laboratory database to identify patients with peripheral neuropathy and zinc deficiency. They included charts from between January 1, 2015, and December 31, 2017, in their review. They excluded patients with abnormal copper levels.
Mr. Bumanlag and Dr. Luo obtained information about patients’ clinical presentations, past medical histories, BMI, neurologic examinations, and laboratory results. They also examined patients’ needle electromyograms and nerve conduction studies.
In all, they identified 12 patients with peripheral neuropathy and zinc deficiency. Patients had a mean age of 55.1. Six were female. Patients’ mean zinc level was 52.5 μg/dL, with a range of 37 μg/dL to 58 μg/dL (reference, 56–134 μg/dL). Mean copper level was 107.6 μg/dL, with a range of 84 μg/dL to 173 μg/dL (reference, 72–166
Notable findings in presentation included paresthesia in 75 and gait abnormalities in 42%. One patient was obese (8%), and three patients had diarrhea (25%). Neurologic examination showed sensory deficits in 83%, reduced tendon reflexes in 67%, and an abnormal Romberg test in 67%. Four of five patients had increased CSF protein. Electrophysiologic evaluations showed features of demyelinating peripheral neuropathy (28%) and distally active denervation in the lower extremities.
“Zinc participates in more than 200 enzymatic reactions,” said the researchers. “Unfortunately, zinc deficiency-induced peripheral neuropathy is often misdiagnosed or delayed in diagnosis. Literature on zinc deficiency-induced peripheral neuropathy is sparse.”
Disability in Patients With Stiff Person Syndrome May Progress Faster Than Thought
Stiff person syndrome leads to disability if therapy is not initiated early in the disease course, according to a prospective study. In addition, patients with stiff person syndrome may have “faster progression of disablement than originally reported and believed,” said lead study author Goran Rakocevic, MD. Dr. Rakocevic is Associate Professor of Neurology, Director of the Neuromuscular Electrodiagnostic Laboratory, Clinical Director of the Jefferson Weinberg ALS Center, and Director of the Neuromuscular Medicine Fellowship Program at Thomas Jefferson University in Philadelphia.
Stiff person syndrome is a disorder characterized by muscle rigidity and episodic spasms in axial and limb musculature, as well as heightened sensitivity to external stimuli. To describe the natural history of stiff person syndrome, the extent of accumulated disability, and associated clinical features, Dr. Rakocevic and his research colleagues conducted a prospective cohort study in patients followed for up to eight years in a single center.
The cohort included 57 patients with mean age at disease onset of 42 (range, 22 to 60). Of these, 32 patients were examined every six months for two years without receiving immune therapies. The investigators assessed disease progression using quantitative scales of stiffness and heightened sensitivity.
Patients’ most frequent initial symptoms were leg stiffness, paraspinal muscle rigidity, and painful spasms. Although no patients required assistance for ambulation during the first two years of the disease, 46 patients (80%) lost the ability to walk independently during follow-up, despite symptomatic medications. In the longitudinal cohort, the number of stiff areas increased, which was consistent with worsening functional status and quality of life. The researchers confirmed a strong association between stiff person syndrome and the HLA-DR and DQ haplotypes.
The study is the largest prospective study of patients with stiff person syndrome and the first to provide longitudinal data on the natural course of the disorder in a large patient subgroup using objective clinical measures, Dr. Rakocevic and colleagues said. “The study shows that stiff person syndrome is a progressive autoimmune disease that leads to disability if ... immunotherapy is not applied,” said the investigators.
“Early diagnosis and management of stiff person syndrome can be challenging,” said A. Gordon Smith, MD, Cochair of the AANEM Annual Meeting Program Committee. The study by Dr. Rakocevic’s team demonstrates “that stiff person syndrome causes progressive stiffness and functional decline, with 80% [of patients] becoming unable to walk independently,” he said. “Their research emphasizes the need to treat early and will help clinicians recognize stiff person syndrome earlier in its course.”
The study adds to neurologists’ understanding of the rare disorder, and its strengths include the length of follow-up and the number of patients, said Robert W. Irwin, MD, Cochair of the AANEM Annual Meeting Program Committee.
Does Thymectomy Benefit Patients With Anti-MuSK Myasthenia Gravis?
Among patients with anti-muscle-specific kinase (MuSK) myasthenia gravis, thymectomy is not associated with greater likelihood of clinical improvement, according to an analysis of data from a multicenter cohort study.
Although a randomized trial has demonstrated benefit from thymectomy in nonthymomatous antiacetylcholine receptor (AChR) antibody positive generalized myasthenia gravis, observational studies suggest that thymectomy may not be efficacious in anti-MuSK myasthenia gravis. Histologic studies have found that patients with anti-MuSK myasthenia gravis have less hyperplastic thymic tissue, compared with patients with anti-AChR myasthenia gravis.
To evaluate the therapeutic impact of thymectomy in patients with anti-MuSK myasthenia gravis, Katherine Clifford, a medical student at the University of Vermont Larner College of Medicine in Burlington, and colleagues analyzed data from a multicenter, retrospective, blinded review of rituximab treatment in patients with anti-MuSK myasthenia gravis. The primary outcome was favorable outcome on the Myasthenia Gravis Foundation of America (MGFA) Post-Intervention Status (PIS). The researchers defined a favorable outcome as an MGFA PIS score of minimal manifestations or better.
Secondary outcomes included prednisone dose; use of other immunosuppressant medications, IV immunoglobulin (IVIG), or plasma exchange (PLEX) treatment; and Myasthenia Gravis Status and Treatment Intensity (MGSTI).
Baseline characteristics were similar between patients with anti-MuSK myasthenia gravis who received thymectomy (n = 26) and those who did not (n = 29), including treatment with rituximab (42% vs 45%). Median follow-up was more than three years.
At last visit, 35% (nine of 26) of patients who received thymectomy had a favorable outcome, compared with 55% (16 of 29) of patients who did not receive thymectomy. In addition, 69% of patients who received thymectomy were taking prednisone, compared with 41% of patients who did not receive thymectomy (median dose, 10 mg/day vs 0 mg/day).
“After controlling for rituximab, baseline prednisone, and final IVIG/PLEX treatment, thymectomy was not associated with greater likelihood of favorable clinical outcome, but broad confidence intervals cannot exclude therapeutic effect (odds ratio, 0.43),” the investigators reported.
“The recent MGTX trial clearly demonstrated the benefit of thymectomy for patients with AChR antibody positive myasthenia gravis,” said A. Gordon Smith, MD, Cochair of the AANEM Annual Meeting Program Committee. “Ms. Clifford and her colleagues now provide compelling data suggesting thymectomy may not be effective in MuSK-positive myasthenia gravis.”
The study’s follow-up is long enough for the findings to be clinically “relevant to all physicians treating myasthenia gravis,” said Robert W. Irwin, MD, Cochair of the AANEM Annual Meeting Program Committee.
What Are the Clinical, Laboratory, and Electrodiagnostic Features of Zinc Deficiency-InducedPeripheral Neuropathy?
Patients with zinc deficiency-induced peripheral neuropathy may present with paresthesia, gait abnormalities, sensory deficits, reduced tendon reflexes, an abnormal Romberg test, and increased CSF protein, according to a study.
Recognition of the features of zinc deficiency-induced peripheral neuropathy may help neurologists diagnose the disorder and manage patients, researchers said.
“Zinc, an essential trace element, plays a critical role in maintaining normal structural and functional conditions in the body,” said lead author Favio C. Bumanlag, Chief Technologist in the Department of Neurology at the Lewis Katz School of Medicine at Temple University in Philadelphia. “Peripheral nerves are susceptible to damage when zinc deficiency occurs.... Recognition of [zinc deficiency-induced peripheral neuropathy] will help physicians and technologists effectively manage patients.”
To study the clinical and electrophysiologic features of zinc deficiency-induced peripheral neuropathy, Mr. Bumanlag and Jin Luo, MD, PhD, Professor of Neurology and Pharmacology at Temple University, retrospectively reviewed charts in their neuromuscular clinic and EMG laboratory database to identify patients with peripheral neuropathy and zinc deficiency. They included charts from between January 1, 2015, and December 31, 2017, in their review. They excluded patients with abnormal copper levels.
Mr. Bumanlag and Dr. Luo obtained information about patients’ clinical presentations, past medical histories, BMI, neurologic examinations, and laboratory results. They also examined patients’ needle electromyograms and nerve conduction studies.
In all, they identified 12 patients with peripheral neuropathy and zinc deficiency. Patients had a mean age of 55.1. Six were female. Patients’ mean zinc level was 52.5 μg/dL, with a range of 37 μg/dL to 58 μg/dL (reference, 56–134 μg/dL). Mean copper level was 107.6 μg/dL, with a range of 84 μg/dL to 173 μg/dL (reference, 72–166
Notable findings in presentation included paresthesia in 75 and gait abnormalities in 42%. One patient was obese (8%), and three patients had diarrhea (25%). Neurologic examination showed sensory deficits in 83%, reduced tendon reflexes in 67%, and an abnormal Romberg test in 67%. Four of five patients had increased CSF protein. Electrophysiologic evaluations showed features of demyelinating peripheral neuropathy (28%) and distally active denervation in the lower extremities.
“Zinc participates in more than 200 enzymatic reactions,” said the researchers. “Unfortunately, zinc deficiency-induced peripheral neuropathy is often misdiagnosed or delayed in diagnosis. Literature on zinc deficiency-induced peripheral neuropathy is sparse.”
Disability in Patients With Stiff Person Syndrome May Progress Faster Than Thought
Stiff person syndrome leads to disability if therapy is not initiated early in the disease course, according to a prospective study. In addition, patients with stiff person syndrome may have “faster progression of disablement than originally reported and believed,” said lead study author Goran Rakocevic, MD. Dr. Rakocevic is Associate Professor of Neurology, Director of the Neuromuscular Electrodiagnostic Laboratory, Clinical Director of the Jefferson Weinberg ALS Center, and Director of the Neuromuscular Medicine Fellowship Program at Thomas Jefferson University in Philadelphia.
Stiff person syndrome is a disorder characterized by muscle rigidity and episodic spasms in axial and limb musculature, as well as heightened sensitivity to external stimuli. To describe the natural history of stiff person syndrome, the extent of accumulated disability, and associated clinical features, Dr. Rakocevic and his research colleagues conducted a prospective cohort study in patients followed for up to eight years in a single center.
The cohort included 57 patients with mean age at disease onset of 42 (range, 22 to 60). Of these, 32 patients were examined every six months for two years without receiving immune therapies. The investigators assessed disease progression using quantitative scales of stiffness and heightened sensitivity.
Patients’ most frequent initial symptoms were leg stiffness, paraspinal muscle rigidity, and painful spasms. Although no patients required assistance for ambulation during the first two years of the disease, 46 patients (80%) lost the ability to walk independently during follow-up, despite symptomatic medications. In the longitudinal cohort, the number of stiff areas increased, which was consistent with worsening functional status and quality of life. The researchers confirmed a strong association between stiff person syndrome and the HLA-DR and DQ haplotypes.
The study is the largest prospective study of patients with stiff person syndrome and the first to provide longitudinal data on the natural course of the disorder in a large patient subgroup using objective clinical measures, Dr. Rakocevic and colleagues said. “The study shows that stiff person syndrome is a progressive autoimmune disease that leads to disability if ... immunotherapy is not applied,” said the investigators.
“Early diagnosis and management of stiff person syndrome can be challenging,” said A. Gordon Smith, MD, Cochair of the AANEM Annual Meeting Program Committee. The study by Dr. Rakocevic’s team demonstrates “that stiff person syndrome causes progressive stiffness and functional decline, with 80% [of patients] becoming unable to walk independently,” he said. “Their research emphasizes the need to treat early and will help clinicians recognize stiff person syndrome earlier in its course.”
The study adds to neurologists’ understanding of the rare disorder, and its strengths include the length of follow-up and the number of patients, said Robert W. Irwin, MD, Cochair of the AANEM Annual Meeting Program Committee.