User login
Delaying antibiotics in elderly with UTI linked to higher sepsis, death rates
results of a large, population-based study suggest.
The risk of bloodstream infection was more than seven times greater in patients who did not receive antibiotics immediately after seeing a general practitioner for a UTI versus those who did, according to results of the study based on primary care records and other data for nearly 160,000 U.K. patients aged 65 years or older. Death rates and hospital admissions were significantly higher for these patients, according to the study published in The BMJ by Myriam Gharbi, PharmD, Phd, Imperial College London, and her colleagues.
The publication of these findings coincides with an increase in Escherichia coli bloodstream infections in England.
“Our study suggests the early initiation of antibiotics for UTI in older high risk adult populations (especially men aged [older than] 85 years) should be recommended to prevent serious complications,” Dr. Gharbi and her coauthors said in their report.
The population-based cohort study comprised 157,264 adult primary care patients at least 65 years of age who had one or more suspected or confirmed lower UTIs from November 2007 to May 2015. The researchers found that health care providers had diagnosed a total of 312,896 UTI episodes in these patients during the period they studied. In 7.2% (22,534) of the UTI episodes, the researchers were unable to find records of the patients having been prescribed antibiotics by a general practitioner within 7 days of the UTI diagnosis. These 22,534 episodes included those that occurred in patients who had a complication before an antibiotic was prescribed. An additional 6.2% (19,292) of the episodes occurred in patients who were prescribed antibiotics, but not during their first UTI-related visit to a general practitioner or on the same day of such a visit. The researchers classified this group of patients as having been prescribed antibiotics on a deferred or delayed basis, as they were not prescribed such drugs within 7 days of their visit.
Overall, there were 1,539 cases (0.5% of the total number of UTIs) of bloodstream infection within 60 days of the initial urinary tract infection diagnosis, the researchers reported.
The bloodstream infection rate was 2.9% for patients who were not prescribed antibiotics ever or prior to an infection occurring, 2.2% in those who were prescribed antibiotics on a deferred basis, and 0.2% in those who were prescribed antibiotics immediately, meaning during their first visit to a general practitioner for a UTI or on the same day of such a visit (P less than .001). After adjustment for potential confounding variables such as age, sex, and region, the patients classified as having not been prescribed antibiotics or having been prescribed antibiotics on a deferred basis were significantly more likely to have a bloodstream infection within 60 days of their visit to a health care provider, compared with those who received antibiotics immediately, with odds ratios of 8.08 (95% confidence interval, 7.12-9.16) and 7.12 (95% CI, 6.22-8.14), respectively.
Hospital admissions after a UTI episode were nearly twice as high in the no- or deferred-antibiotics groups (27.0% and 26.8%, respectively), compared with the group that received antibiotics right away (14.8%), the investigators reported. The lengths of hospital stays were 12.1 days for the group classified as having not been prescribed antibiotics, 7.7 days for the group subject to delayed antibiotic prescribing, and 6.3 days for the group who received antibiotics immediately.
Deaths within 60 days of experiencing a urinary tract infection occurred in 5.4% of patients in the no-antibiotics group, 2.8% of the deferred-antibiotics group, and 1.6% of the immediate-antibiotics group. After adjustment for covariates, a regression analysis showed the risks for all-cause mortality were 1.16 and 2.18 times higher in the deferred-antibiotics group and the no-antibiotics group, respectively, according to the paper.
In the immediate-antibiotics group, those patients who received nitrofurantoin had a “small but significant increase” in 60-day survival versus those who received trimethoprim, the investigators noted in the discussion section of their report.
“This increase could reflect either higher levels of resistance to trimethoprim or a healthier population treated with nitrofurantoin, the latest being not recommended for patients with poor kidney function,” the researchers wrote.
This study was supported by the National Institute for Health Research and other U.K. sources. One study coauthor reported working as an epidemiologist with GSK in areas not related to the study.
SOURCE: Gharbi M et al. BMJ. 2019 Feb 27. doi: 10.1136/bmj.l525.
This study linking primary care prescribing to serious infections in elderly patients with urinary tract infections is timely, as rates of bloodstream infection and mortality are increasing in this age group, according to Alastair D. Hay, MB.ChB, a professor at University of Bristol, England.
“Prompt treatment should be offered to older patients, men (who are at higher risk than women), and those living in areas of greater socioeconomic deprivation who are at the highest risk of bloodstream infections,” Dr. Hay said in an editorial accompanying the report by Gharbi et al.
That said, the link between prescribing and infection in this particular study may not be causal: “The implications are likely to be more nuanced than primary care doctors risking the health of older adults to meet targets for antimicrobial stewardship,” Dr. Hay noted.
Doctors are cautious when managing infections in vulnerable groups, evidence shows, and the deferred prescribing reported in this study is likely not the same as the delayed prescribing seen in primary care, he explained.
“Most clinicians issue a prescription on the day of presentation, with verbal advice to delay treatment, rather than waiting for a patient to return or issuing a postdated prescription,” he said. “The group given immediate antibiotics in the study by Gharbi and colleagues likely contained some patients managed in this way.”
Patients who apparently had no prescription in this retrospective analysis may have had a same-day admission with a bloodstream infection; moreover, a number of bloodstream infections in older people are due to urinary tract bacteria, and so would not be prevented by treatment for urinary tract infection, Dr. Hay said.
“Further research is needed to establish whether treatment should be initiated with a broad or a narrow spectrum antibiotic and to identify those in whom delaying treatment (while awaiting investigation) is safe,” he concluded.
Dr. Hay is a professor in the Centre for Academic Primary Care, University of Bristol, England. His editorial appears in The BMJ (2019 Feb 27. doi: 10.1136/bmj.l780). Dr. Hay declared that he is a member of the managing common infections guideline committee for the National Institute for Health and Care Excellence (NICE).
This study linking primary care prescribing to serious infections in elderly patients with urinary tract infections is timely, as rates of bloodstream infection and mortality are increasing in this age group, according to Alastair D. Hay, MB.ChB, a professor at University of Bristol, England.
“Prompt treatment should be offered to older patients, men (who are at higher risk than women), and those living in areas of greater socioeconomic deprivation who are at the highest risk of bloodstream infections,” Dr. Hay said in an editorial accompanying the report by Gharbi et al.
That said, the link between prescribing and infection in this particular study may not be causal: “The implications are likely to be more nuanced than primary care doctors risking the health of older adults to meet targets for antimicrobial stewardship,” Dr. Hay noted.
Doctors are cautious when managing infections in vulnerable groups, evidence shows, and the deferred prescribing reported in this study is likely not the same as the delayed prescribing seen in primary care, he explained.
“Most clinicians issue a prescription on the day of presentation, with verbal advice to delay treatment, rather than waiting for a patient to return or issuing a postdated prescription,” he said. “The group given immediate antibiotics in the study by Gharbi and colleagues likely contained some patients managed in this way.”
Patients who apparently had no prescription in this retrospective analysis may have had a same-day admission with a bloodstream infection; moreover, a number of bloodstream infections in older people are due to urinary tract bacteria, and so would not be prevented by treatment for urinary tract infection, Dr. Hay said.
“Further research is needed to establish whether treatment should be initiated with a broad or a narrow spectrum antibiotic and to identify those in whom delaying treatment (while awaiting investigation) is safe,” he concluded.
Dr. Hay is a professor in the Centre for Academic Primary Care, University of Bristol, England. His editorial appears in The BMJ (2019 Feb 27. doi: 10.1136/bmj.l780). Dr. Hay declared that he is a member of the managing common infections guideline committee for the National Institute for Health and Care Excellence (NICE).
This study linking primary care prescribing to serious infections in elderly patients with urinary tract infections is timely, as rates of bloodstream infection and mortality are increasing in this age group, according to Alastair D. Hay, MB.ChB, a professor at University of Bristol, England.
“Prompt treatment should be offered to older patients, men (who are at higher risk than women), and those living in areas of greater socioeconomic deprivation who are at the highest risk of bloodstream infections,” Dr. Hay said in an editorial accompanying the report by Gharbi et al.
That said, the link between prescribing and infection in this particular study may not be causal: “The implications are likely to be more nuanced than primary care doctors risking the health of older adults to meet targets for antimicrobial stewardship,” Dr. Hay noted.
Doctors are cautious when managing infections in vulnerable groups, evidence shows, and the deferred prescribing reported in this study is likely not the same as the delayed prescribing seen in primary care, he explained.
“Most clinicians issue a prescription on the day of presentation, with verbal advice to delay treatment, rather than waiting for a patient to return or issuing a postdated prescription,” he said. “The group given immediate antibiotics in the study by Gharbi and colleagues likely contained some patients managed in this way.”
Patients who apparently had no prescription in this retrospective analysis may have had a same-day admission with a bloodstream infection; moreover, a number of bloodstream infections in older people are due to urinary tract bacteria, and so would not be prevented by treatment for urinary tract infection, Dr. Hay said.
“Further research is needed to establish whether treatment should be initiated with a broad or a narrow spectrum antibiotic and to identify those in whom delaying treatment (while awaiting investigation) is safe,” he concluded.
Dr. Hay is a professor in the Centre for Academic Primary Care, University of Bristol, England. His editorial appears in The BMJ (2019 Feb 27. doi: 10.1136/bmj.l780). Dr. Hay declared that he is a member of the managing common infections guideline committee for the National Institute for Health and Care Excellence (NICE).
results of a large, population-based study suggest.
The risk of bloodstream infection was more than seven times greater in patients who did not receive antibiotics immediately after seeing a general practitioner for a UTI versus those who did, according to results of the study based on primary care records and other data for nearly 160,000 U.K. patients aged 65 years or older. Death rates and hospital admissions were significantly higher for these patients, according to the study published in The BMJ by Myriam Gharbi, PharmD, Phd, Imperial College London, and her colleagues.
The publication of these findings coincides with an increase in Escherichia coli bloodstream infections in England.
“Our study suggests the early initiation of antibiotics for UTI in older high risk adult populations (especially men aged [older than] 85 years) should be recommended to prevent serious complications,” Dr. Gharbi and her coauthors said in their report.
The population-based cohort study comprised 157,264 adult primary care patients at least 65 years of age who had one or more suspected or confirmed lower UTIs from November 2007 to May 2015. The researchers found that health care providers had diagnosed a total of 312,896 UTI episodes in these patients during the period they studied. In 7.2% (22,534) of the UTI episodes, the researchers were unable to find records of the patients having been prescribed antibiotics by a general practitioner within 7 days of the UTI diagnosis. These 22,534 episodes included those that occurred in patients who had a complication before an antibiotic was prescribed. An additional 6.2% (19,292) of the episodes occurred in patients who were prescribed antibiotics, but not during their first UTI-related visit to a general practitioner or on the same day of such a visit. The researchers classified this group of patients as having been prescribed antibiotics on a deferred or delayed basis, as they were not prescribed such drugs within 7 days of their visit.
Overall, there were 1,539 cases (0.5% of the total number of UTIs) of bloodstream infection within 60 days of the initial urinary tract infection diagnosis, the researchers reported.
The bloodstream infection rate was 2.9% for patients who were not prescribed antibiotics ever or prior to an infection occurring, 2.2% in those who were prescribed antibiotics on a deferred basis, and 0.2% in those who were prescribed antibiotics immediately, meaning during their first visit to a general practitioner for a UTI or on the same day of such a visit (P less than .001). After adjustment for potential confounding variables such as age, sex, and region, the patients classified as having not been prescribed antibiotics or having been prescribed antibiotics on a deferred basis were significantly more likely to have a bloodstream infection within 60 days of their visit to a health care provider, compared with those who received antibiotics immediately, with odds ratios of 8.08 (95% confidence interval, 7.12-9.16) and 7.12 (95% CI, 6.22-8.14), respectively.
Hospital admissions after a UTI episode were nearly twice as high in the no- or deferred-antibiotics groups (27.0% and 26.8%, respectively), compared with the group that received antibiotics right away (14.8%), the investigators reported. The lengths of hospital stays were 12.1 days for the group classified as having not been prescribed antibiotics, 7.7 days for the group subject to delayed antibiotic prescribing, and 6.3 days for the group who received antibiotics immediately.
Deaths within 60 days of experiencing a urinary tract infection occurred in 5.4% of patients in the no-antibiotics group, 2.8% of the deferred-antibiotics group, and 1.6% of the immediate-antibiotics group. After adjustment for covariates, a regression analysis showed the risks for all-cause mortality were 1.16 and 2.18 times higher in the deferred-antibiotics group and the no-antibiotics group, respectively, according to the paper.
In the immediate-antibiotics group, those patients who received nitrofurantoin had a “small but significant increase” in 60-day survival versus those who received trimethoprim, the investigators noted in the discussion section of their report.
“This increase could reflect either higher levels of resistance to trimethoprim or a healthier population treated with nitrofurantoin, the latest being not recommended for patients with poor kidney function,” the researchers wrote.
This study was supported by the National Institute for Health Research and other U.K. sources. One study coauthor reported working as an epidemiologist with GSK in areas not related to the study.
SOURCE: Gharbi M et al. BMJ. 2019 Feb 27. doi: 10.1136/bmj.l525.
results of a large, population-based study suggest.
The risk of bloodstream infection was more than seven times greater in patients who did not receive antibiotics immediately after seeing a general practitioner for a UTI versus those who did, according to results of the study based on primary care records and other data for nearly 160,000 U.K. patients aged 65 years or older. Death rates and hospital admissions were significantly higher for these patients, according to the study published in The BMJ by Myriam Gharbi, PharmD, Phd, Imperial College London, and her colleagues.
The publication of these findings coincides with an increase in Escherichia coli bloodstream infections in England.
“Our study suggests the early initiation of antibiotics for UTI in older high risk adult populations (especially men aged [older than] 85 years) should be recommended to prevent serious complications,” Dr. Gharbi and her coauthors said in their report.
The population-based cohort study comprised 157,264 adult primary care patients at least 65 years of age who had one or more suspected or confirmed lower UTIs from November 2007 to May 2015. The researchers found that health care providers had diagnosed a total of 312,896 UTI episodes in these patients during the period they studied. In 7.2% (22,534) of the UTI episodes, the researchers were unable to find records of the patients having been prescribed antibiotics by a general practitioner within 7 days of the UTI diagnosis. These 22,534 episodes included those that occurred in patients who had a complication before an antibiotic was prescribed. An additional 6.2% (19,292) of the episodes occurred in patients who were prescribed antibiotics, but not during their first UTI-related visit to a general practitioner or on the same day of such a visit. The researchers classified this group of patients as having been prescribed antibiotics on a deferred or delayed basis, as they were not prescribed such drugs within 7 days of their visit.
Overall, there were 1,539 cases (0.5% of the total number of UTIs) of bloodstream infection within 60 days of the initial urinary tract infection diagnosis, the researchers reported.
The bloodstream infection rate was 2.9% for patients who were not prescribed antibiotics ever or prior to an infection occurring, 2.2% in those who were prescribed antibiotics on a deferred basis, and 0.2% in those who were prescribed antibiotics immediately, meaning during their first visit to a general practitioner for a UTI or on the same day of such a visit (P less than .001). After adjustment for potential confounding variables such as age, sex, and region, the patients classified as having not been prescribed antibiotics or having been prescribed antibiotics on a deferred basis were significantly more likely to have a bloodstream infection within 60 days of their visit to a health care provider, compared with those who received antibiotics immediately, with odds ratios of 8.08 (95% confidence interval, 7.12-9.16) and 7.12 (95% CI, 6.22-8.14), respectively.
Hospital admissions after a UTI episode were nearly twice as high in the no- or deferred-antibiotics groups (27.0% and 26.8%, respectively), compared with the group that received antibiotics right away (14.8%), the investigators reported. The lengths of hospital stays were 12.1 days for the group classified as having not been prescribed antibiotics, 7.7 days for the group subject to delayed antibiotic prescribing, and 6.3 days for the group who received antibiotics immediately.
Deaths within 60 days of experiencing a urinary tract infection occurred in 5.4% of patients in the no-antibiotics group, 2.8% of the deferred-antibiotics group, and 1.6% of the immediate-antibiotics group. After adjustment for covariates, a regression analysis showed the risks for all-cause mortality were 1.16 and 2.18 times higher in the deferred-antibiotics group and the no-antibiotics group, respectively, according to the paper.
In the immediate-antibiotics group, those patients who received nitrofurantoin had a “small but significant increase” in 60-day survival versus those who received trimethoprim, the investigators noted in the discussion section of their report.
“This increase could reflect either higher levels of resistance to trimethoprim or a healthier population treated with nitrofurantoin, the latest being not recommended for patients with poor kidney function,” the researchers wrote.
This study was supported by the National Institute for Health Research and other U.K. sources. One study coauthor reported working as an epidemiologist with GSK in areas not related to the study.
SOURCE: Gharbi M et al. BMJ. 2019 Feb 27. doi: 10.1136/bmj.l525.
FROM THE BMJ
AHA drills into CV risk factors in children
the FDA says a popular gout drug raises cardiovascular risk, an AHA statement targets CV risk factors in children, and a class action suit against the American Board of Internal Medicine over MOC gets financial support from doctors.
the FDA says a popular gout drug raises cardiovascular risk, an AHA statement targets CV risk factors in children, and a class action suit against the American Board of Internal Medicine over MOC gets financial support from doctors.
the FDA says a popular gout drug raises cardiovascular risk, an AHA statement targets CV risk factors in children, and a class action suit against the American Board of Internal Medicine over MOC gets financial support from doctors.
New noninvasive wireless devices aim to more gently monitor neonatal vital signs
and lowering the risk of iatrogenic injuries, according to a series of tests on neonates in two level III NICUs.
“By eliminating wired connections, these platforms also facilitate therapeutic skin-to-skin contact between neonates and parents, which is known to stabilize vital signs, reduce morbidity, and promote parental bonding,” lead author Ha Uk Chung of the University of Illinois at Urbana-Champaign and coauthors wrote in Science.
In an effort to replace current wired systems that rigidly attach to fragile neonate skin, the investigators created a pair of ultrathin, noninvasive devices that can capture and transmit full vital signs with clinical-grade precision. One of the devices is mounted on the chest and captures ECGs; the other records photoplethysmograms from the base of the foot. That data plus skin temperature is wirelessly transmitted and used to measure heart rate, respiration rate, blood oxygenation, and systolic blood pressure via pulse arrival time.
The devices were tested on neonates in two level III NICUs; the infants had gestational ages ranging from 28 weeks to full term, and the results “demonstrate[d] the full range of functions,” the investigators noted. Because the devices are smaller and lighter, they interface with infant skin with forces that are “nearly an order of magnitude smaller” than adhesives used with conventional NICU measuring systems. The coauthors also noted that these cost-effective systems have potential uses beyond typical hospital settings, including “potential relevance to global health.”
No conflicts of interest were reported.
SOURCE: Chung HU et al. Science. 2019 Mar 1. doi: 10.1126/science.aau0780.
and lowering the risk of iatrogenic injuries, according to a series of tests on neonates in two level III NICUs.
“By eliminating wired connections, these platforms also facilitate therapeutic skin-to-skin contact between neonates and parents, which is known to stabilize vital signs, reduce morbidity, and promote parental bonding,” lead author Ha Uk Chung of the University of Illinois at Urbana-Champaign and coauthors wrote in Science.
In an effort to replace current wired systems that rigidly attach to fragile neonate skin, the investigators created a pair of ultrathin, noninvasive devices that can capture and transmit full vital signs with clinical-grade precision. One of the devices is mounted on the chest and captures ECGs; the other records photoplethysmograms from the base of the foot. That data plus skin temperature is wirelessly transmitted and used to measure heart rate, respiration rate, blood oxygenation, and systolic blood pressure via pulse arrival time.
The devices were tested on neonates in two level III NICUs; the infants had gestational ages ranging from 28 weeks to full term, and the results “demonstrate[d] the full range of functions,” the investigators noted. Because the devices are smaller and lighter, they interface with infant skin with forces that are “nearly an order of magnitude smaller” than adhesives used with conventional NICU measuring systems. The coauthors also noted that these cost-effective systems have potential uses beyond typical hospital settings, including “potential relevance to global health.”
No conflicts of interest were reported.
SOURCE: Chung HU et al. Science. 2019 Mar 1. doi: 10.1126/science.aau0780.
and lowering the risk of iatrogenic injuries, according to a series of tests on neonates in two level III NICUs.
“By eliminating wired connections, these platforms also facilitate therapeutic skin-to-skin contact between neonates and parents, which is known to stabilize vital signs, reduce morbidity, and promote parental bonding,” lead author Ha Uk Chung of the University of Illinois at Urbana-Champaign and coauthors wrote in Science.
In an effort to replace current wired systems that rigidly attach to fragile neonate skin, the investigators created a pair of ultrathin, noninvasive devices that can capture and transmit full vital signs with clinical-grade precision. One of the devices is mounted on the chest and captures ECGs; the other records photoplethysmograms from the base of the foot. That data plus skin temperature is wirelessly transmitted and used to measure heart rate, respiration rate, blood oxygenation, and systolic blood pressure via pulse arrival time.
The devices were tested on neonates in two level III NICUs; the infants had gestational ages ranging from 28 weeks to full term, and the results “demonstrate[d] the full range of functions,” the investigators noted. Because the devices are smaller and lighter, they interface with infant skin with forces that are “nearly an order of magnitude smaller” than adhesives used with conventional NICU measuring systems. The coauthors also noted that these cost-effective systems have potential uses beyond typical hospital settings, including “potential relevance to global health.”
No conflicts of interest were reported.
SOURCE: Chung HU et al. Science. 2019 Mar 1. doi: 10.1126/science.aau0780.
FROM SCIENCE
Dietary, Lifestyle Factors Add to MS Progression
Lifestyle risk factors contribute to accelerated central brain atrophy in patients with multiple sclerosis (MS), whereas unhealthier diet is associated with MS lesion accrual, a recent study found. 175 MS or clinically isolated syndrome (CIS) patients and 42 age- and sex-matched healthy controls (HCs) were enrolled and longitudinally followed for 5.5 years. The 20-year cardiovascular disease risk was calculated by Healthy Heart Score (HHS) prediction model, which includes age, smoking, body mass index, dietary intake, exercise, and alcohol consumption. Baseline and follow-up MRI scans were obtained and cross-sectional and longitudinal changes of T2-lesion volume (LV), whole brain volume (WBV), white matter volume (WMV), gray matter volume (GMV), and lateral ventricular volume (LVV) were calculated. Researchers found:
- After correcting for disease duration, the baseline HHS values of the MS group were associated with baseline GMV, and longitudinal LVV change.
- The association with LVV remained significant after adjusting for baseline LVV volumes in MS patients.
- The diet component of the HHS was associated with the 5-year T2-LV accrual in MS.
- In the HC group, the HHS was associated with LVV, GMV, WBV, T2-LV, and WMV.
Jakimovski D, Weinstock-Guttman B, Gandhi S, et al. Dietary and lifestyle factors in multiple sclerosis progression: Results from a 5-year longitudinal MRI study. [Published online ahead of print February 13, 2019]. J Neurol. doi:10.1007/s00415-019-09208-0.
Lifestyle risk factors contribute to accelerated central brain atrophy in patients with multiple sclerosis (MS), whereas unhealthier diet is associated with MS lesion accrual, a recent study found. 175 MS or clinically isolated syndrome (CIS) patients and 42 age- and sex-matched healthy controls (HCs) were enrolled and longitudinally followed for 5.5 years. The 20-year cardiovascular disease risk was calculated by Healthy Heart Score (HHS) prediction model, which includes age, smoking, body mass index, dietary intake, exercise, and alcohol consumption. Baseline and follow-up MRI scans were obtained and cross-sectional and longitudinal changes of T2-lesion volume (LV), whole brain volume (WBV), white matter volume (WMV), gray matter volume (GMV), and lateral ventricular volume (LVV) were calculated. Researchers found:
- After correcting for disease duration, the baseline HHS values of the MS group were associated with baseline GMV, and longitudinal LVV change.
- The association with LVV remained significant after adjusting for baseline LVV volumes in MS patients.
- The diet component of the HHS was associated with the 5-year T2-LV accrual in MS.
- In the HC group, the HHS was associated with LVV, GMV, WBV, T2-LV, and WMV.
Jakimovski D, Weinstock-Guttman B, Gandhi S, et al. Dietary and lifestyle factors in multiple sclerosis progression: Results from a 5-year longitudinal MRI study. [Published online ahead of print February 13, 2019]. J Neurol. doi:10.1007/s00415-019-09208-0.
Lifestyle risk factors contribute to accelerated central brain atrophy in patients with multiple sclerosis (MS), whereas unhealthier diet is associated with MS lesion accrual, a recent study found. 175 MS or clinically isolated syndrome (CIS) patients and 42 age- and sex-matched healthy controls (HCs) were enrolled and longitudinally followed for 5.5 years. The 20-year cardiovascular disease risk was calculated by Healthy Heart Score (HHS) prediction model, which includes age, smoking, body mass index, dietary intake, exercise, and alcohol consumption. Baseline and follow-up MRI scans were obtained and cross-sectional and longitudinal changes of T2-lesion volume (LV), whole brain volume (WBV), white matter volume (WMV), gray matter volume (GMV), and lateral ventricular volume (LVV) were calculated. Researchers found:
- After correcting for disease duration, the baseline HHS values of the MS group were associated with baseline GMV, and longitudinal LVV change.
- The association with LVV remained significant after adjusting for baseline LVV volumes in MS patients.
- The diet component of the HHS was associated with the 5-year T2-LV accrual in MS.
- In the HC group, the HHS was associated with LVV, GMV, WBV, T2-LV, and WMV.
Jakimovski D, Weinstock-Guttman B, Gandhi S, et al. Dietary and lifestyle factors in multiple sclerosis progression: Results from a 5-year longitudinal MRI study. [Published online ahead of print February 13, 2019]. J Neurol. doi:10.1007/s00415-019-09208-0.
Validity of Cognitive Assessment Battery for MS
The specific computerized assessment battery (CAB) evaluated is valid for cognitive screening of people with multiple sclerosis (MS) and may be more likely to detect prolonged response times and impaired executive function, according to a recent study. 81 people with MS (PwMS) and 15 healthy controls (HC) completed the CAB and a set of traditional neuropsychological tests recommended for MS on the same day. Principal component factor analysis was used to assess construct validity. For criterion validity, the gold standard definition of cognitive impairment was a score of ≥1.5SD below average on at least 1 cognitive domain, based upon traditional test normative data. Researchers found:
- Traditional and computerized tests of memory, processing speed, visuospatial, and executive function converged by factor analysis.
- Computerized tests detected cognitive impairment with 85% sensitivity and 70% specificity.
- PwMS classified as impaired on only the computerized battery had significantly prolonged response times and a higher rate of unemployment compared with PwMS classified as unimpaired on both batteries.
- Poor executive function was more likely to be revealed by the CAB.
Golan D, Wilken J, Doniger GM, et al. Validity of a multi-domain computerized cognitive assessment battery for patients with multiple sclerosis. Mult Scler Relat Disord. 2019(30):154–162. doi:10.1016/j.msard.2019.01.051.
The specific computerized assessment battery (CAB) evaluated is valid for cognitive screening of people with multiple sclerosis (MS) and may be more likely to detect prolonged response times and impaired executive function, according to a recent study. 81 people with MS (PwMS) and 15 healthy controls (HC) completed the CAB and a set of traditional neuropsychological tests recommended for MS on the same day. Principal component factor analysis was used to assess construct validity. For criterion validity, the gold standard definition of cognitive impairment was a score of ≥1.5SD below average on at least 1 cognitive domain, based upon traditional test normative data. Researchers found:
- Traditional and computerized tests of memory, processing speed, visuospatial, and executive function converged by factor analysis.
- Computerized tests detected cognitive impairment with 85% sensitivity and 70% specificity.
- PwMS classified as impaired on only the computerized battery had significantly prolonged response times and a higher rate of unemployment compared with PwMS classified as unimpaired on both batteries.
- Poor executive function was more likely to be revealed by the CAB.
Golan D, Wilken J, Doniger GM, et al. Validity of a multi-domain computerized cognitive assessment battery for patients with multiple sclerosis. Mult Scler Relat Disord. 2019(30):154–162. doi:10.1016/j.msard.2019.01.051.
The specific computerized assessment battery (CAB) evaluated is valid for cognitive screening of people with multiple sclerosis (MS) and may be more likely to detect prolonged response times and impaired executive function, according to a recent study. 81 people with MS (PwMS) and 15 healthy controls (HC) completed the CAB and a set of traditional neuropsychological tests recommended for MS on the same day. Principal component factor analysis was used to assess construct validity. For criterion validity, the gold standard definition of cognitive impairment was a score of ≥1.5SD below average on at least 1 cognitive domain, based upon traditional test normative data. Researchers found:
- Traditional and computerized tests of memory, processing speed, visuospatial, and executive function converged by factor analysis.
- Computerized tests detected cognitive impairment with 85% sensitivity and 70% specificity.
- PwMS classified as impaired on only the computerized battery had significantly prolonged response times and a higher rate of unemployment compared with PwMS classified as unimpaired on both batteries.
- Poor executive function was more likely to be revealed by the CAB.
Golan D, Wilken J, Doniger GM, et al. Validity of a multi-domain computerized cognitive assessment battery for patients with multiple sclerosis. Mult Scler Relat Disord. 2019(30):154–162. doi:10.1016/j.msard.2019.01.051.
2010 MS Prevalence in the US Highest Ever to Date
The estimated US national multiple sclerosis (MS) prevalence for 2010 is the highest reported to date and provides evidence that the north-south gradient persists, according to a recent study. A validated algorithm was applied to private, military, and public agglomerative hierarchical clustering (AHC) datasets to identify adult cases of MS between 2008 and 2010. In each dataset, researchers determined the 3-year cumulative prevalence overall and stratified by age, sex, and census region. They applied insurance-specific and stratum-specific estimates to the 2010 US Census data and pooled the findings to calculate the 2010 prevalence of MS in the US cumulated over 3 years. They also estimated the 2010 prevalence cumulated over 10 years using 2 models and extrapolated their estimate to 2017. They found:
- The estimated 2010 prevalence of MS in the US adult population cumulated over 10 years was 309.2 per 100,000, representing 727,344 cases.
- During the same time period, the MS prevalence was 450.1 per 100,000 for women and 159.7 for men (female:male ratio 2:8).
- The estimated 2010 prevalence of MS was highest in the 55- to 64-year age group.
- A US north-south decreasing prevalence gradient was identified.
Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States. A population-based estimate using health claims data. [Published online ahead of print February 15, 2019]. Neurology. doi:10.1212/WNL.0000000000007035.
The estimated US national multiple sclerosis (MS) prevalence for 2010 is the highest reported to date and provides evidence that the north-south gradient persists, according to a recent study. A validated algorithm was applied to private, military, and public agglomerative hierarchical clustering (AHC) datasets to identify adult cases of MS between 2008 and 2010. In each dataset, researchers determined the 3-year cumulative prevalence overall and stratified by age, sex, and census region. They applied insurance-specific and stratum-specific estimates to the 2010 US Census data and pooled the findings to calculate the 2010 prevalence of MS in the US cumulated over 3 years. They also estimated the 2010 prevalence cumulated over 10 years using 2 models and extrapolated their estimate to 2017. They found:
- The estimated 2010 prevalence of MS in the US adult population cumulated over 10 years was 309.2 per 100,000, representing 727,344 cases.
- During the same time period, the MS prevalence was 450.1 per 100,000 for women and 159.7 for men (female:male ratio 2:8).
- The estimated 2010 prevalence of MS was highest in the 55- to 64-year age group.
- A US north-south decreasing prevalence gradient was identified.
Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States. A population-based estimate using health claims data. [Published online ahead of print February 15, 2019]. Neurology. doi:10.1212/WNL.0000000000007035.
The estimated US national multiple sclerosis (MS) prevalence for 2010 is the highest reported to date and provides evidence that the north-south gradient persists, according to a recent study. A validated algorithm was applied to private, military, and public agglomerative hierarchical clustering (AHC) datasets to identify adult cases of MS between 2008 and 2010. In each dataset, researchers determined the 3-year cumulative prevalence overall and stratified by age, sex, and census region. They applied insurance-specific and stratum-specific estimates to the 2010 US Census data and pooled the findings to calculate the 2010 prevalence of MS in the US cumulated over 3 years. They also estimated the 2010 prevalence cumulated over 10 years using 2 models and extrapolated their estimate to 2017. They found:
- The estimated 2010 prevalence of MS in the US adult population cumulated over 10 years was 309.2 per 100,000, representing 727,344 cases.
- During the same time period, the MS prevalence was 450.1 per 100,000 for women and 159.7 for men (female:male ratio 2:8).
- The estimated 2010 prevalence of MS was highest in the 55- to 64-year age group.
- A US north-south decreasing prevalence gradient was identified.
Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States. A population-based estimate using health claims data. [Published online ahead of print February 15, 2019]. Neurology. doi:10.1212/WNL.0000000000007035.
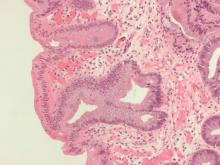
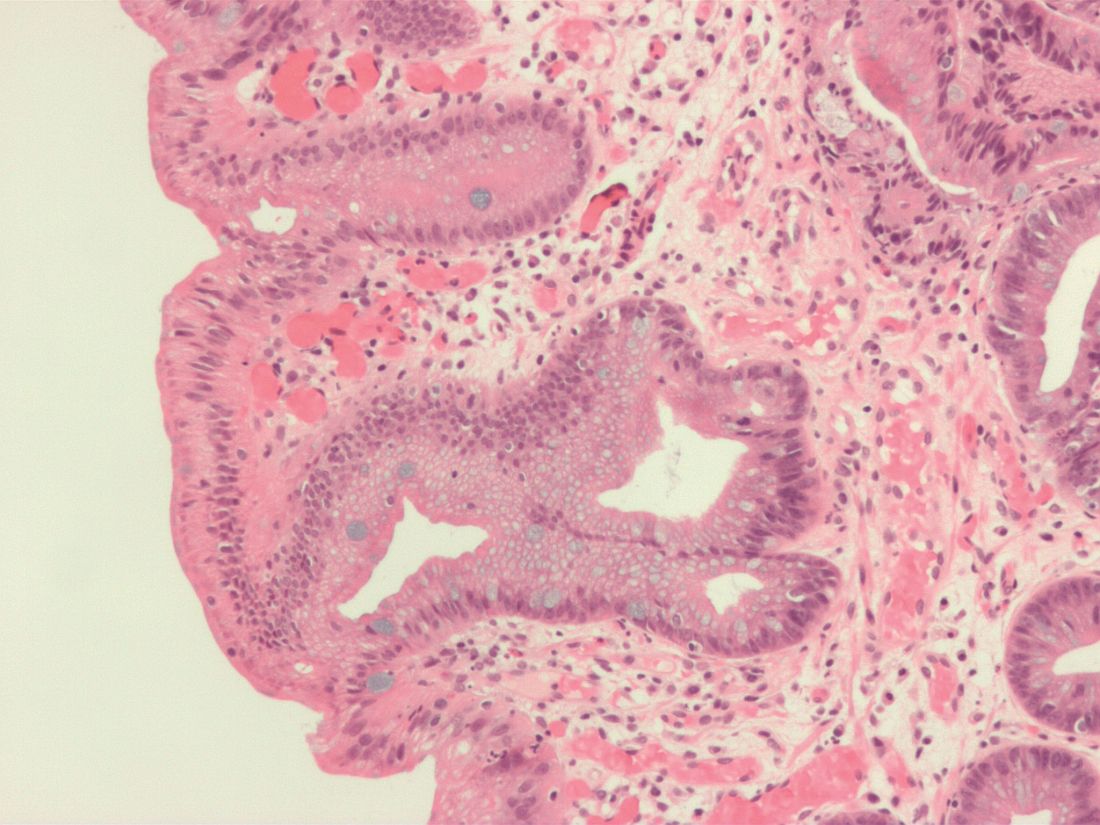
Interactive online module improved detection of Barrett’s esophagus neoplasia
An online educational tool for endoscopists helped improve their detection of Barrett’s esophagus–related neoplasia (BORN), researchers reported in the April issue of Gastroenterology.
In tests administered before and after training, endoscopists increased their rates of BORN detection by a median of 30% (P less than .001), reported J.J. Bergman, MD, PhD, of the University of Amsterdam, together with his associates. “To our knowledge, this is the first validated online, interactive endoscopic training program in our field,” they wrote. “Widespread use of this tool might improve management of Barrett’s esophagus by general endoscopists.”
To develop the program, the investigators recorded high-definition videos of upper endoscopies of patients with either BORN or nondysplastic Barrett’s esophagus. They sent these videos to three experts, who used special tools to superimpose their delineations of lesions.
Next, 68 general endoscopists (fellows, early-career general gastroenterologists, and senior general gastroenterologists) watched four batches of 20 videos each. The researchers compared the assessors’ interpretations with the experts’ to identify the 25 videos with the most educational impact. These were then shown in four batches of five to 121 new assessors (five videos were reserved for pre- and post testing).
From the first to the fourth batch of training videos, assessors sequentially improved their scores for detection, delineation, agreement delineation, and relative delineation of BORN, the researchers said. Among the 121 assessors in the second phase of development, median rates of detection of BORN rose by 30% after training. Furthermore, from baseline to the end of the study, scores rose by 46% for detection, 129% for delineation, 105% for agreement delineation, and 106% for relative delineation (all P less than .001). These improvements did not depend on the country of origin of the assessors or their level of endoscopic experience.
This module requires the use of high-definition videos whose resolution is not lost during replay or when viewed on the web, the researchers emphasized. They noted that the module is active, not passive – learners select the video frame to position a biopsy mark and delineate the lesion, and the software then gives them tailored feedback on their choice. Learners also can add and remove the experts’ delineations as well as their own during feedback sessions at the end of each batch of videos. This enables them to “fully appreciate the subtle appearance of the lesion on the selected time frame,” the investigators wrote.
By completing the training module, “general endoscopists with a wide range of experience and from different countries of origin can substantially and conveniently increase their skills for detection and delineation of early BORN lesions,” they concluded. “Therefore, the module could provide training in an essential upper gastrointestinal endoscopic skill that is not otherwise readily available.”
The investigators disclosed no external funding sources. They reported having no conflicts of interest.
SOURCE: Bergman JJ et al. Gastroenterology. 2019 Jan 2. doi: 10.1053/j.gastro.2018.12.021.
Endoscopic mucosal resection and ablation strategies offer the potential for minimally invasive, curative treatment for patients with Barrett’s esophagus–associated intramucosal neoplasia. For the gastroenterologist interested in endoscopic prevention and management of esophageal cancer, however, achieving proficiency in performance of these endoscopic techniques represents only part of the requisite preparatory experience. Acquisition of cognitive skills in lesion recognition is a fundamental and underappreciated component to a successful endoscopic treatment paradigm.
General endoscopist assessors were grouped into three groups based on level of experience. Following completion of the training module, scores in lesion detection and delineation increased irrespective of level of endoscopist experience.
The module is free, CME-accredited, and available for online use. Any endoscopist who performs Barrett’s screening, surveillance, and therapy should be motivated and incentivized to engage with this important educational tool.
Patrick Yachimski, MD, MPH, AGAF, is associate professor of medicine, director of pancreatobiliary endoscopy, division of gastroenterology, hepatology & nutrition, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
Endoscopic mucosal resection and ablation strategies offer the potential for minimally invasive, curative treatment for patients with Barrett’s esophagus–associated intramucosal neoplasia. For the gastroenterologist interested in endoscopic prevention and management of esophageal cancer, however, achieving proficiency in performance of these endoscopic techniques represents only part of the requisite preparatory experience. Acquisition of cognitive skills in lesion recognition is a fundamental and underappreciated component to a successful endoscopic treatment paradigm.
General endoscopist assessors were grouped into three groups based on level of experience. Following completion of the training module, scores in lesion detection and delineation increased irrespective of level of endoscopist experience.
The module is free, CME-accredited, and available for online use. Any endoscopist who performs Barrett’s screening, surveillance, and therapy should be motivated and incentivized to engage with this important educational tool.
Patrick Yachimski, MD, MPH, AGAF, is associate professor of medicine, director of pancreatobiliary endoscopy, division of gastroenterology, hepatology & nutrition, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
Endoscopic mucosal resection and ablation strategies offer the potential for minimally invasive, curative treatment for patients with Barrett’s esophagus–associated intramucosal neoplasia. For the gastroenterologist interested in endoscopic prevention and management of esophageal cancer, however, achieving proficiency in performance of these endoscopic techniques represents only part of the requisite preparatory experience. Acquisition of cognitive skills in lesion recognition is a fundamental and underappreciated component to a successful endoscopic treatment paradigm.
General endoscopist assessors were grouped into three groups based on level of experience. Following completion of the training module, scores in lesion detection and delineation increased irrespective of level of endoscopist experience.
The module is free, CME-accredited, and available for online use. Any endoscopist who performs Barrett’s screening, surveillance, and therapy should be motivated and incentivized to engage with this important educational tool.
Patrick Yachimski, MD, MPH, AGAF, is associate professor of medicine, director of pancreatobiliary endoscopy, division of gastroenterology, hepatology & nutrition, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
An online educational tool for endoscopists helped improve their detection of Barrett’s esophagus–related neoplasia (BORN), researchers reported in the April issue of Gastroenterology.
In tests administered before and after training, endoscopists increased their rates of BORN detection by a median of 30% (P less than .001), reported J.J. Bergman, MD, PhD, of the University of Amsterdam, together with his associates. “To our knowledge, this is the first validated online, interactive endoscopic training program in our field,” they wrote. “Widespread use of this tool might improve management of Barrett’s esophagus by general endoscopists.”
To develop the program, the investigators recorded high-definition videos of upper endoscopies of patients with either BORN or nondysplastic Barrett’s esophagus. They sent these videos to three experts, who used special tools to superimpose their delineations of lesions.
Next, 68 general endoscopists (fellows, early-career general gastroenterologists, and senior general gastroenterologists) watched four batches of 20 videos each. The researchers compared the assessors’ interpretations with the experts’ to identify the 25 videos with the most educational impact. These were then shown in four batches of five to 121 new assessors (five videos were reserved for pre- and post testing).
From the first to the fourth batch of training videos, assessors sequentially improved their scores for detection, delineation, agreement delineation, and relative delineation of BORN, the researchers said. Among the 121 assessors in the second phase of development, median rates of detection of BORN rose by 30% after training. Furthermore, from baseline to the end of the study, scores rose by 46% for detection, 129% for delineation, 105% for agreement delineation, and 106% for relative delineation (all P less than .001). These improvements did not depend on the country of origin of the assessors or their level of endoscopic experience.
This module requires the use of high-definition videos whose resolution is not lost during replay or when viewed on the web, the researchers emphasized. They noted that the module is active, not passive – learners select the video frame to position a biopsy mark and delineate the lesion, and the software then gives them tailored feedback on their choice. Learners also can add and remove the experts’ delineations as well as their own during feedback sessions at the end of each batch of videos. This enables them to “fully appreciate the subtle appearance of the lesion on the selected time frame,” the investigators wrote.
By completing the training module, “general endoscopists with a wide range of experience and from different countries of origin can substantially and conveniently increase their skills for detection and delineation of early BORN lesions,” they concluded. “Therefore, the module could provide training in an essential upper gastrointestinal endoscopic skill that is not otherwise readily available.”
The investigators disclosed no external funding sources. They reported having no conflicts of interest.
SOURCE: Bergman JJ et al. Gastroenterology. 2019 Jan 2. doi: 10.1053/j.gastro.2018.12.021.
An online educational tool for endoscopists helped improve their detection of Barrett’s esophagus–related neoplasia (BORN), researchers reported in the April issue of Gastroenterology.
In tests administered before and after training, endoscopists increased their rates of BORN detection by a median of 30% (P less than .001), reported J.J. Bergman, MD, PhD, of the University of Amsterdam, together with his associates. “To our knowledge, this is the first validated online, interactive endoscopic training program in our field,” they wrote. “Widespread use of this tool might improve management of Barrett’s esophagus by general endoscopists.”
To develop the program, the investigators recorded high-definition videos of upper endoscopies of patients with either BORN or nondysplastic Barrett’s esophagus. They sent these videos to three experts, who used special tools to superimpose their delineations of lesions.
Next, 68 general endoscopists (fellows, early-career general gastroenterologists, and senior general gastroenterologists) watched four batches of 20 videos each. The researchers compared the assessors’ interpretations with the experts’ to identify the 25 videos with the most educational impact. These were then shown in four batches of five to 121 new assessors (five videos were reserved for pre- and post testing).
From the first to the fourth batch of training videos, assessors sequentially improved their scores for detection, delineation, agreement delineation, and relative delineation of BORN, the researchers said. Among the 121 assessors in the second phase of development, median rates of detection of BORN rose by 30% after training. Furthermore, from baseline to the end of the study, scores rose by 46% for detection, 129% for delineation, 105% for agreement delineation, and 106% for relative delineation (all P less than .001). These improvements did not depend on the country of origin of the assessors or their level of endoscopic experience.
This module requires the use of high-definition videos whose resolution is not lost during replay or when viewed on the web, the researchers emphasized. They noted that the module is active, not passive – learners select the video frame to position a biopsy mark and delineate the lesion, and the software then gives them tailored feedback on their choice. Learners also can add and remove the experts’ delineations as well as their own during feedback sessions at the end of each batch of videos. This enables them to “fully appreciate the subtle appearance of the lesion on the selected time frame,” the investigators wrote.
By completing the training module, “general endoscopists with a wide range of experience and from different countries of origin can substantially and conveniently increase their skills for detection and delineation of early BORN lesions,” they concluded. “Therefore, the module could provide training in an essential upper gastrointestinal endoscopic skill that is not otherwise readily available.”
The investigators disclosed no external funding sources. They reported having no conflicts of interest.
SOURCE: Bergman JJ et al. Gastroenterology. 2019 Jan 2. doi: 10.1053/j.gastro.2018.12.021.
FROM GASTROENTEROLOGY
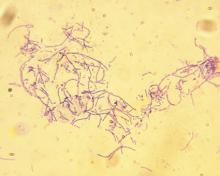
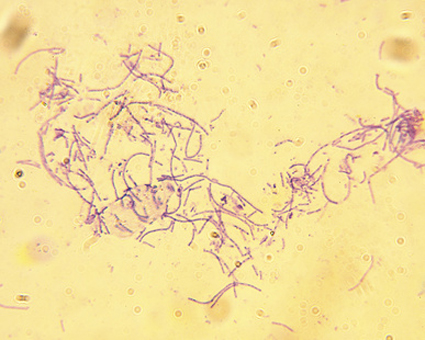
Anthrax booster expanded to 3 years for moderate-risk groups
A booster dose for pre-exposure prophylaxis with an anthrax vaccine may be given at 3 years after an initial series for individuals not currently at risk who wish to maintain protection, according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
In a unanimous 15-0 vote at the February meeting, ACIP committee members agreed on the recommendation after adjusting the wording to reflect a permissive, rather than mandated, guidance.
William Bower, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), presented data on Anthrax Vaccine Adsorbed (AVA) to support its protective effects over a longer booster dose interval.
The recommendations apply to persons aged 18 years or older who are not currently at high risk of exposure to Bacillus anthracis, but who might need to deploy to a high-risk area quickly, such as military personnel, Dr. Bower said.
In addition, data suggest that adults who have started, but not completed the pre-exposure priming series, can transition to the postexposure schedule prior to entering a high-risk area, he noted.
The previous pre-exposure anthrax vaccination schedule was a three-dose priming series at 0, 1, and 3 months, followed by a booster at 12 months and 18 months, then annually.
with “sustained immunological memory to at least month 42,” and suggested that even longer intervals between boosters may be possible, Dr. Bower said.
A dosing schedule of intramuscular injections at 0 and at 1 month and 6 months, with a booster at 42 months yielded survival estimates of approximately 84%-93%.
Dr. Bower noted that a new vaccine, AV7909, has demonstrated safety and effectiveness similar to AVA and could be used for pre-exposure prophylaxis if AVA is not available. AVA remains the preferred option, but ultimately will be replaced by AV7909, when the current AVA stockpile is exhausted.
Additional safety data on AV7909 will be reviewed by ACIP as they become available, and future guidance from the CDC will include statements on dosing for special populations including pregnant and breastfeeding women, said Dr. Bower.
“We anticipate that this [anthrax vaccine] work group will reconvene in 2021 to review data from pending studies” of AV7909, he said.
The ACIP members had no financial conflicts to disclose.
A booster dose for pre-exposure prophylaxis with an anthrax vaccine may be given at 3 years after an initial series for individuals not currently at risk who wish to maintain protection, according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
In a unanimous 15-0 vote at the February meeting, ACIP committee members agreed on the recommendation after adjusting the wording to reflect a permissive, rather than mandated, guidance.
William Bower, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), presented data on Anthrax Vaccine Adsorbed (AVA) to support its protective effects over a longer booster dose interval.
The recommendations apply to persons aged 18 years or older who are not currently at high risk of exposure to Bacillus anthracis, but who might need to deploy to a high-risk area quickly, such as military personnel, Dr. Bower said.
In addition, data suggest that adults who have started, but not completed the pre-exposure priming series, can transition to the postexposure schedule prior to entering a high-risk area, he noted.
The previous pre-exposure anthrax vaccination schedule was a three-dose priming series at 0, 1, and 3 months, followed by a booster at 12 months and 18 months, then annually.
with “sustained immunological memory to at least month 42,” and suggested that even longer intervals between boosters may be possible, Dr. Bower said.
A dosing schedule of intramuscular injections at 0 and at 1 month and 6 months, with a booster at 42 months yielded survival estimates of approximately 84%-93%.
Dr. Bower noted that a new vaccine, AV7909, has demonstrated safety and effectiveness similar to AVA and could be used for pre-exposure prophylaxis if AVA is not available. AVA remains the preferred option, but ultimately will be replaced by AV7909, when the current AVA stockpile is exhausted.
Additional safety data on AV7909 will be reviewed by ACIP as they become available, and future guidance from the CDC will include statements on dosing for special populations including pregnant and breastfeeding women, said Dr. Bower.
“We anticipate that this [anthrax vaccine] work group will reconvene in 2021 to review data from pending studies” of AV7909, he said.
The ACIP members had no financial conflicts to disclose.
A booster dose for pre-exposure prophylaxis with an anthrax vaccine may be given at 3 years after an initial series for individuals not currently at risk who wish to maintain protection, according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
In a unanimous 15-0 vote at the February meeting, ACIP committee members agreed on the recommendation after adjusting the wording to reflect a permissive, rather than mandated, guidance.
William Bower, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), presented data on Anthrax Vaccine Adsorbed (AVA) to support its protective effects over a longer booster dose interval.
The recommendations apply to persons aged 18 years or older who are not currently at high risk of exposure to Bacillus anthracis, but who might need to deploy to a high-risk area quickly, such as military personnel, Dr. Bower said.
In addition, data suggest that adults who have started, but not completed the pre-exposure priming series, can transition to the postexposure schedule prior to entering a high-risk area, he noted.
The previous pre-exposure anthrax vaccination schedule was a three-dose priming series at 0, 1, and 3 months, followed by a booster at 12 months and 18 months, then annually.
with “sustained immunological memory to at least month 42,” and suggested that even longer intervals between boosters may be possible, Dr. Bower said.
A dosing schedule of intramuscular injections at 0 and at 1 month and 6 months, with a booster at 42 months yielded survival estimates of approximately 84%-93%.
Dr. Bower noted that a new vaccine, AV7909, has demonstrated safety and effectiveness similar to AVA and could be used for pre-exposure prophylaxis if AVA is not available. AVA remains the preferred option, but ultimately will be replaced by AV7909, when the current AVA stockpile is exhausted.
Additional safety data on AV7909 will be reviewed by ACIP as they become available, and future guidance from the CDC will include statements on dosing for special populations including pregnant and breastfeeding women, said Dr. Bower.
“We anticipate that this [anthrax vaccine] work group will reconvene in 2021 to review data from pending studies” of AV7909, he said.
The ACIP members had no financial conflicts to disclose.
FROM AN ACIP MEETING
ACIP unanimously supports updates to Japanese encephalitis vaccination
according to a vote at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
Japanese encephalitis (JE) virus is a mosquito-borne flavivirus and those at risk for infection include travelers to countries where JE is endemic, as well as laboratory personnel who work with the virus.
The committee voted unanimously 15-0 in favor of the recommendations, which also advised vaccination for those whose travels in endemic areas are uncertain, but not for travelers with low-risk itineraries “such as shorter term travel limited to urban areas or travel that occurs outside of a well-defined JE virus transmission season.”
Susan Hills, MD, of the of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, presented data in support of the recommendations.
A second unanimous vote confirmed recommendations for a primary series schedule for JE vaccination for adults aged 18-65 years as “two doses of vaccine administered on days 0 and 7-28.”
The third vote, also a unanimous 15-0, updated recommendations for a JE booster dose. The new recommendation is that adults and children receive a booster dose (a third dose) at least a year after completion of the primary JE vaccine series “if ongoing exposure or re-exposure to JE virus is expected.”
The currently available Japanese encephalitis vaccine in the United States is an inactivated Vero cell culture-derived vaccine marketed as IXIARO that was approved in March 2009 for individuals aged 17 years and older and approved in May 2013 for children aged 2 months through 16 years.
The ACIP members had no financial conflicts to disclose.
according to a vote at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
Japanese encephalitis (JE) virus is a mosquito-borne flavivirus and those at risk for infection include travelers to countries where JE is endemic, as well as laboratory personnel who work with the virus.
The committee voted unanimously 15-0 in favor of the recommendations, which also advised vaccination for those whose travels in endemic areas are uncertain, but not for travelers with low-risk itineraries “such as shorter term travel limited to urban areas or travel that occurs outside of a well-defined JE virus transmission season.”
Susan Hills, MD, of the of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, presented data in support of the recommendations.
A second unanimous vote confirmed recommendations for a primary series schedule for JE vaccination for adults aged 18-65 years as “two doses of vaccine administered on days 0 and 7-28.”
The third vote, also a unanimous 15-0, updated recommendations for a JE booster dose. The new recommendation is that adults and children receive a booster dose (a third dose) at least a year after completion of the primary JE vaccine series “if ongoing exposure or re-exposure to JE virus is expected.”
The currently available Japanese encephalitis vaccine in the United States is an inactivated Vero cell culture-derived vaccine marketed as IXIARO that was approved in March 2009 for individuals aged 17 years and older and approved in May 2013 for children aged 2 months through 16 years.
The ACIP members had no financial conflicts to disclose.
according to a vote at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
Japanese encephalitis (JE) virus is a mosquito-borne flavivirus and those at risk for infection include travelers to countries where JE is endemic, as well as laboratory personnel who work with the virus.
The committee voted unanimously 15-0 in favor of the recommendations, which also advised vaccination for those whose travels in endemic areas are uncertain, but not for travelers with low-risk itineraries “such as shorter term travel limited to urban areas or travel that occurs outside of a well-defined JE virus transmission season.”
Susan Hills, MD, of the of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, presented data in support of the recommendations.
A second unanimous vote confirmed recommendations for a primary series schedule for JE vaccination for adults aged 18-65 years as “two doses of vaccine administered on days 0 and 7-28.”
The third vote, also a unanimous 15-0, updated recommendations for a JE booster dose. The new recommendation is that adults and children receive a booster dose (a third dose) at least a year after completion of the primary JE vaccine series “if ongoing exposure or re-exposure to JE virus is expected.”
The currently available Japanese encephalitis vaccine in the United States is an inactivated Vero cell culture-derived vaccine marketed as IXIARO that was approved in March 2009 for individuals aged 17 years and older and approved in May 2013 for children aged 2 months through 16 years.
The ACIP members had no financial conflicts to disclose.
FROM AN ACIP MEETING
App, role-playing used as interventions
Help for people with mental health and substance use issues has become more accessible now that the Georgia Crisis & Access Line launched a mobile app. The aim of the My GCAL app is to guide people to free and confidential access, and the targets are those who would rather send a text message than speak to someone over the phone. In Georgia and elsewhere, this tends to be younger people. “We are trying to be proactive,” said Georgia Gov. Brian Kemp. Atlanta Journal-Constitution.
Ninth-grade students at the Uplift Hampton Preparatory school in Dallas have been taking part in classroom sessions where role-playing activities are helping them spot the signs of depression in themselves and others. “It’s kind of like ‘Mental Health 101,’ ” said Tony Walker, senior director of student support services at Uplift Education, in an Associated Press article published in the National Post. “So they talk about depression and anxiety and just common mental health issues, and then I think the most important thing is they talk about what to do if you feel that way.” The Youth Aware of Mental Health (YAM) program, administered by Madhukar H. Trivedi, MD, of the University of Texas Southwestern Medical Center is offered to all 9th-graders in the 20-school Uplift Education network in the Dallas area. The program, consisting of five 45-minute sessions, originally was developed at the Karolinska Institute in Stockholm and Columbia University in New York. A similar initiative offered by the National Alliance on Mental Illness (NAMI) teaches students the warning signs of mental health problems. Since the NAMI program launched in 2014, it has reached almost 450,000 youth in 41 states. National Post.
Identifying the source of students’ frustration and anger can prevent them from lashing out, according to a National Public Radio report. But responses rooted in compassion can help diffuse potentially tragic outcomes. The report describes the story of a young man whose struggles started in middle school. An encounter with bullies left him with severe damage in his right eye, and he spent his high school years getting into fights. After school officials stepped in, acknowledged that he had reasons to be angry, and connected him with a mentor who was able to talk and reason with him, the young man graduated on time. He’s now 25 and works full time for a security firm. “Moving kids from despair to hope. That’s the bumper sticker for what we do,” said school psychologist John Van Dreal. The approach “really works,” he added. NPR.
An exhibition now running at the Science Center of Iowa in Des Moines is helping patrons explore the reality of mental illness. The Mental Health: Mind Matters exhibition is intended to show the real lives of people with mental illness, with the hope of inspiring better appreciation and empathy. It features audio renderings of what the world can sound like to someone with psychosis, walk-through rooms that take patrons inside the homes of people with depression, and exercises that inspire worry or fear, as well as photography. The aim is to take the patron inside the heads of those with mental illnesses. “A possibility now exists to utilize a constellation of exhibits like Mind Matters to revolutionize understanding, prevention, and wellness nationally, all while unlocking economic benefits and advancing human dignity,” wrote Paul Piwko, the author of an article describing the exhibit. Des Moines Register.
Students are creating a dialogue about suicide awareness and prevention at Gardner (Kansas) Edgerton High School. At a recent basketball game with Shawnee Mission West High School, Gardner Edgerton team members, students, cheerleaders, and fans donned T-shirts emblazoned with “#ZeroReasonsWhy.” The student-led campaign is aimed at encouraging students to seek help rather than consider suicide. At the game, T-shirts and bracelets also were handed out to Shawnee Mission West players in an effort to spread the message. The Kansas City Star.
Help for people with mental health and substance use issues has become more accessible now that the Georgia Crisis & Access Line launched a mobile app. The aim of the My GCAL app is to guide people to free and confidential access, and the targets are those who would rather send a text message than speak to someone over the phone. In Georgia and elsewhere, this tends to be younger people. “We are trying to be proactive,” said Georgia Gov. Brian Kemp. Atlanta Journal-Constitution.
Ninth-grade students at the Uplift Hampton Preparatory school in Dallas have been taking part in classroom sessions where role-playing activities are helping them spot the signs of depression in themselves and others. “It’s kind of like ‘Mental Health 101,’ ” said Tony Walker, senior director of student support services at Uplift Education, in an Associated Press article published in the National Post. “So they talk about depression and anxiety and just common mental health issues, and then I think the most important thing is they talk about what to do if you feel that way.” The Youth Aware of Mental Health (YAM) program, administered by Madhukar H. Trivedi, MD, of the University of Texas Southwestern Medical Center is offered to all 9th-graders in the 20-school Uplift Education network in the Dallas area. The program, consisting of five 45-minute sessions, originally was developed at the Karolinska Institute in Stockholm and Columbia University in New York. A similar initiative offered by the National Alliance on Mental Illness (NAMI) teaches students the warning signs of mental health problems. Since the NAMI program launched in 2014, it has reached almost 450,000 youth in 41 states. National Post.
Identifying the source of students’ frustration and anger can prevent them from lashing out, according to a National Public Radio report. But responses rooted in compassion can help diffuse potentially tragic outcomes. The report describes the story of a young man whose struggles started in middle school. An encounter with bullies left him with severe damage in his right eye, and he spent his high school years getting into fights. After school officials stepped in, acknowledged that he had reasons to be angry, and connected him with a mentor who was able to talk and reason with him, the young man graduated on time. He’s now 25 and works full time for a security firm. “Moving kids from despair to hope. That’s the bumper sticker for what we do,” said school psychologist John Van Dreal. The approach “really works,” he added. NPR.
An exhibition now running at the Science Center of Iowa in Des Moines is helping patrons explore the reality of mental illness. The Mental Health: Mind Matters exhibition is intended to show the real lives of people with mental illness, with the hope of inspiring better appreciation and empathy. It features audio renderings of what the world can sound like to someone with psychosis, walk-through rooms that take patrons inside the homes of people with depression, and exercises that inspire worry or fear, as well as photography. The aim is to take the patron inside the heads of those with mental illnesses. “A possibility now exists to utilize a constellation of exhibits like Mind Matters to revolutionize understanding, prevention, and wellness nationally, all while unlocking economic benefits and advancing human dignity,” wrote Paul Piwko, the author of an article describing the exhibit. Des Moines Register.
Students are creating a dialogue about suicide awareness and prevention at Gardner (Kansas) Edgerton High School. At a recent basketball game with Shawnee Mission West High School, Gardner Edgerton team members, students, cheerleaders, and fans donned T-shirts emblazoned with “#ZeroReasonsWhy.” The student-led campaign is aimed at encouraging students to seek help rather than consider suicide. At the game, T-shirts and bracelets also were handed out to Shawnee Mission West players in an effort to spread the message. The Kansas City Star.
Help for people with mental health and substance use issues has become more accessible now that the Georgia Crisis & Access Line launched a mobile app. The aim of the My GCAL app is to guide people to free and confidential access, and the targets are those who would rather send a text message than speak to someone over the phone. In Georgia and elsewhere, this tends to be younger people. “We are trying to be proactive,” said Georgia Gov. Brian Kemp. Atlanta Journal-Constitution.
Ninth-grade students at the Uplift Hampton Preparatory school in Dallas have been taking part in classroom sessions where role-playing activities are helping them spot the signs of depression in themselves and others. “It’s kind of like ‘Mental Health 101,’ ” said Tony Walker, senior director of student support services at Uplift Education, in an Associated Press article published in the National Post. “So they talk about depression and anxiety and just common mental health issues, and then I think the most important thing is they talk about what to do if you feel that way.” The Youth Aware of Mental Health (YAM) program, administered by Madhukar H. Trivedi, MD, of the University of Texas Southwestern Medical Center is offered to all 9th-graders in the 20-school Uplift Education network in the Dallas area. The program, consisting of five 45-minute sessions, originally was developed at the Karolinska Institute in Stockholm and Columbia University in New York. A similar initiative offered by the National Alliance on Mental Illness (NAMI) teaches students the warning signs of mental health problems. Since the NAMI program launched in 2014, it has reached almost 450,000 youth in 41 states. National Post.
Identifying the source of students’ frustration and anger can prevent them from lashing out, according to a National Public Radio report. But responses rooted in compassion can help diffuse potentially tragic outcomes. The report describes the story of a young man whose struggles started in middle school. An encounter with bullies left him with severe damage in his right eye, and he spent his high school years getting into fights. After school officials stepped in, acknowledged that he had reasons to be angry, and connected him with a mentor who was able to talk and reason with him, the young man graduated on time. He’s now 25 and works full time for a security firm. “Moving kids from despair to hope. That’s the bumper sticker for what we do,” said school psychologist John Van Dreal. The approach “really works,” he added. NPR.
An exhibition now running at the Science Center of Iowa in Des Moines is helping patrons explore the reality of mental illness. The Mental Health: Mind Matters exhibition is intended to show the real lives of people with mental illness, with the hope of inspiring better appreciation and empathy. It features audio renderings of what the world can sound like to someone with psychosis, walk-through rooms that take patrons inside the homes of people with depression, and exercises that inspire worry or fear, as well as photography. The aim is to take the patron inside the heads of those with mental illnesses. “A possibility now exists to utilize a constellation of exhibits like Mind Matters to revolutionize understanding, prevention, and wellness nationally, all while unlocking economic benefits and advancing human dignity,” wrote Paul Piwko, the author of an article describing the exhibit. Des Moines Register.
Students are creating a dialogue about suicide awareness and prevention at Gardner (Kansas) Edgerton High School. At a recent basketball game with Shawnee Mission West High School, Gardner Edgerton team members, students, cheerleaders, and fans donned T-shirts emblazoned with “#ZeroReasonsWhy.” The student-led campaign is aimed at encouraging students to seek help rather than consider suicide. At the game, T-shirts and bracelets also were handed out to Shawnee Mission West players in an effort to spread the message. The Kansas City Star.