User login
Researchers characterize novel subtype of endocervical adenocarcinoma
, including reduced survival and resistance to therapy, according to a retrospective histopathological study.
“[Gastric-type mucinous carcinoma] constitutes a unique tumor type with distinct etiologic, morphologic, and clinical features that set it apart from other mucinous carcinomas,” Shin Nishio, MD, PhD, of Kurume (Japan) University and his colleagues wrote in Gynecologic Oncology.
The researchers retrospectively analyzed 393 women with stage I or II endocervical adenocarcinoma who received surgical treatment without concomitant chemotherapy. Sample slides were collected from of all patients with endocervical adenocarcinoma and were compared for variations in clinicopathological features between disease subtypes.
Dr. Nishio and his colleagues performed histopathological analysis on both usual-type endocervical adenocarcinoma and gastric-type mucinous carcinoma.
“The outcomes in patients with each type of disease were statistically compared,” they wrote.
Multivariable analysis showed that, compared with usual-type endocervical adenocarcinoma, gastric-type mucinous carcinoma was associated with worse clinical outcomes, including more aggressive tumor behavior, resistance to radio- and chemotherapy, and reduced progression-free and overall survival.
“Our study clearly shows that recurrence was more common among patients with GAS [gastric-type endocervical adenocarcinoma],” they added.
The authors acknowledged that further research is needed to fully understand the molecular mechanisms of various forms of endocervical adenocarcinoma.
“The profiles of the genomic signatures of unusual cervical cancers are still limited, and definitive treatment guidelines for such cancers remain to be established,” they concluded.
The study was funded by the National Cancer Center Research and Development Fund of Japan. The authors reported no conflicts of interest.
SOURCE: Nishio S et al. Gynecol Oncol. 2019 Jan 29. doi: 10.1016/j.ygyno.2019.01.022.
, including reduced survival and resistance to therapy, according to a retrospective histopathological study.
“[Gastric-type mucinous carcinoma] constitutes a unique tumor type with distinct etiologic, morphologic, and clinical features that set it apart from other mucinous carcinomas,” Shin Nishio, MD, PhD, of Kurume (Japan) University and his colleagues wrote in Gynecologic Oncology.
The researchers retrospectively analyzed 393 women with stage I or II endocervical adenocarcinoma who received surgical treatment without concomitant chemotherapy. Sample slides were collected from of all patients with endocervical adenocarcinoma and were compared for variations in clinicopathological features between disease subtypes.
Dr. Nishio and his colleagues performed histopathological analysis on both usual-type endocervical adenocarcinoma and gastric-type mucinous carcinoma.
“The outcomes in patients with each type of disease were statistically compared,” they wrote.
Multivariable analysis showed that, compared with usual-type endocervical adenocarcinoma, gastric-type mucinous carcinoma was associated with worse clinical outcomes, including more aggressive tumor behavior, resistance to radio- and chemotherapy, and reduced progression-free and overall survival.
“Our study clearly shows that recurrence was more common among patients with GAS [gastric-type endocervical adenocarcinoma],” they added.
The authors acknowledged that further research is needed to fully understand the molecular mechanisms of various forms of endocervical adenocarcinoma.
“The profiles of the genomic signatures of unusual cervical cancers are still limited, and definitive treatment guidelines for such cancers remain to be established,” they concluded.
The study was funded by the National Cancer Center Research and Development Fund of Japan. The authors reported no conflicts of interest.
SOURCE: Nishio S et al. Gynecol Oncol. 2019 Jan 29. doi: 10.1016/j.ygyno.2019.01.022.
, including reduced survival and resistance to therapy, according to a retrospective histopathological study.
“[Gastric-type mucinous carcinoma] constitutes a unique tumor type with distinct etiologic, morphologic, and clinical features that set it apart from other mucinous carcinomas,” Shin Nishio, MD, PhD, of Kurume (Japan) University and his colleagues wrote in Gynecologic Oncology.
The researchers retrospectively analyzed 393 women with stage I or II endocervical adenocarcinoma who received surgical treatment without concomitant chemotherapy. Sample slides were collected from of all patients with endocervical adenocarcinoma and were compared for variations in clinicopathological features between disease subtypes.
Dr. Nishio and his colleagues performed histopathological analysis on both usual-type endocervical adenocarcinoma and gastric-type mucinous carcinoma.
“The outcomes in patients with each type of disease were statistically compared,” they wrote.
Multivariable analysis showed that, compared with usual-type endocervical adenocarcinoma, gastric-type mucinous carcinoma was associated with worse clinical outcomes, including more aggressive tumor behavior, resistance to radio- and chemotherapy, and reduced progression-free and overall survival.
“Our study clearly shows that recurrence was more common among patients with GAS [gastric-type endocervical adenocarcinoma],” they added.
The authors acknowledged that further research is needed to fully understand the molecular mechanisms of various forms of endocervical adenocarcinoma.
“The profiles of the genomic signatures of unusual cervical cancers are still limited, and definitive treatment guidelines for such cancers remain to be established,” they concluded.
The study was funded by the National Cancer Center Research and Development Fund of Japan. The authors reported no conflicts of interest.
SOURCE: Nishio S et al. Gynecol Oncol. 2019 Jan 29. doi: 10.1016/j.ygyno.2019.01.022.
FROM GYNECOLOGIC ONCOLOGY
March 2019 - Question 2
Correct Answer: E
Rationale
This patient has slow-transit constipation without concomitant defecatory disorder, which is unresponsive to newer pharmacologic agents. According to the recently published AGA medical position paper on constipation, the next step in this patient's evaluation should be to repeat colon transit testing on medications. If abnormal, the next step would be evaluation for possible upper GI motility disorder including a gastric-emptying scan. There is no role for repeat anorectal manometry, balloon expulsion testing, or a trial of biofeedback therapy in this patient.
References
1. Wald A, Bharucha AE, Cosman BC, Whitehead WE. ACG clinical guideline: management of benign anorectal disorders. Am J Gastroenterol. 2014;109(8):1141-57.
2. Bharucha AE, Pemberton JH, Locke GR 3rd. American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;144:218.
[email protected]
Correct Answer: E
Rationale
This patient has slow-transit constipation without concomitant defecatory disorder, which is unresponsive to newer pharmacologic agents. According to the recently published AGA medical position paper on constipation, the next step in this patient's evaluation should be to repeat colon transit testing on medications. If abnormal, the next step would be evaluation for possible upper GI motility disorder including a gastric-emptying scan. There is no role for repeat anorectal manometry, balloon expulsion testing, or a trial of biofeedback therapy in this patient.
References
1. Wald A, Bharucha AE, Cosman BC, Whitehead WE. ACG clinical guideline: management of benign anorectal disorders. Am J Gastroenterol. 2014;109(8):1141-57.
2. Bharucha AE, Pemberton JH, Locke GR 3rd. American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;144:218.
[email protected]
Correct Answer: E
Rationale
This patient has slow-transit constipation without concomitant defecatory disorder, which is unresponsive to newer pharmacologic agents. According to the recently published AGA medical position paper on constipation, the next step in this patient's evaluation should be to repeat colon transit testing on medications. If abnormal, the next step would be evaluation for possible upper GI motility disorder including a gastric-emptying scan. There is no role for repeat anorectal manometry, balloon expulsion testing, or a trial of biofeedback therapy in this patient.
References
1. Wald A, Bharucha AE, Cosman BC, Whitehead WE. ACG clinical guideline: management of benign anorectal disorders. Am J Gastroenterol. 2014;109(8):1141-57.
2. Bharucha AE, Pemberton JH, Locke GR 3rd. American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;144:218.
[email protected]
A 66-year-old woman presents for an evaluation of a 3-year history of constipation. She reports some mild abdominal pain, which is related to constipation. She denies GI bleeding and any relevant family history of colorectal neoplasia or IBD. A previous trial of fiber and polyethylene glycol was unsuccessful. Physical examination is normal, including the rectal examination. Evaluation including routine blood work and thyroid evaluation is normal. Her last colonoscopy was 1 year ago and was normal. She undergoes anorectal manometry, balloon expulsion testing and defecography, which do not reveal any significant abnormalities. Sitz marker test reveals 14 markers remaining in the colon on day 5. She is started on intestinal secretagogue therapy with no significant improvement in symptoms.
What is the next best step in the evaluation of this patient?
March 2019 - Question 1
Correct Answer: B
Rationale
The ultrasound finding of a hyperechoic protrusion is suggestive of a gallbladder polyp. These polyps can have malignant potential and should be monitored or referred for surgical management depending on their size. There is consensus that polyps larger than 10 mm should be referred for cholecystectomy. There is some debate about whether polyps greater than 6 mm should also be referred for surgery or whether they can be surveyed. For gallbladder polyps less than 6 mm, surveillance with ultrasound in 6-12 months is the recommended surveillance strategy.
Reference
1. Gallahan WC, Conway JD. Diagnosis and management of gallbladder polyps. Gastroenterol Clin North Am. 2010;39(2):359-67.
Correct Answer: B
Rationale
The ultrasound finding of a hyperechoic protrusion is suggestive of a gallbladder polyp. These polyps can have malignant potential and should be monitored or referred for surgical management depending on their size. There is consensus that polyps larger than 10 mm should be referred for cholecystectomy. There is some debate about whether polyps greater than 6 mm should also be referred for surgery or whether they can be surveyed. For gallbladder polyps less than 6 mm, surveillance with ultrasound in 6-12 months is the recommended surveillance strategy.
Reference
1. Gallahan WC, Conway JD. Diagnosis and management of gallbladder polyps. Gastroenterol Clin North Am. 2010;39(2):359-67.
Correct Answer: B
Rationale
The ultrasound finding of a hyperechoic protrusion is suggestive of a gallbladder polyp. These polyps can have malignant potential and should be monitored or referred for surgical management depending on their size. There is consensus that polyps larger than 10 mm should be referred for cholecystectomy. There is some debate about whether polyps greater than 6 mm should also be referred for surgery or whether they can be surveyed. For gallbladder polyps less than 6 mm, surveillance with ultrasound in 6-12 months is the recommended surveillance strategy.
Reference
1. Gallahan WC, Conway JD. Diagnosis and management of gallbladder polyps. Gastroenterol Clin North Am. 2010;39(2):359-67.
A 63-year-old woman undergoes a right upper quadrant ultrasound for intermittent epigastric pain. A 5-mm fixed hyperechoic protrusion in the gallbladder is identified, but there are no gallstones or wall thickening. Upper endoscopy shows moderate gastritis. Biopsies reveal active H. pylori gastritis. She is treated with triple therapy and reports complete resolution of her symptoms.
What is the best next step in management?
Cancer-battling breath, Zombie Bambi, and hops as health food
Does my breath smell like reduced cancer risk?
Cancer prevention just got a whole lot more ... fragrant. Allium vegetables – garlic, onions, leeks, chives, and shallots – have been found to decrease the risk of colorectal cancer (CRC), according to a Chinese study published last year. Very good news for Italians, but it looks like the risk of CRC in the vampire population might continue to rise.
The study authors reported that high allium intake correlated with lower CRC risk in both men and women, in the northeast Chinese population sampled. Bioactive compounds in these vegetables have anticarcinogenic properties, and researchers found that eating at least 35 pounds of allium vegetables per year could reduce cancer risk.
Unclear if this study was secretly funded by Big Onion, but as fans of delicious and anticancer flavor, we here at LOTME support these findings. However, we strongly advise against going the Tony Abbott route of chomping into whole onions.
An IPA a day keeps the doctor away
After you’re finished eating your annual 35 pounds of garlic and onions (sure, do it all in 1 day if you want), you might be a little thirsty. And we’ve got good news for you – have a brewski, it’s good for ya! Turns out, hops might have some health benefits, so drink up.
Hops contain a class of compound called isohumulones, which gives them that bitter taste. There have been multiple studies showing the metabolic effects of isohumulones, including cell inflammation suppression, reduced weight gain, reduced hyperglycemia, and increased glucose tolerance.
These isohumulones (try typing that 10 times in a row) interact with the bitter taste receptors in the gut, and researchers are hopeful that this could lead to isohumulone-esque drugs to treat metabolic disorders. In the meantime, maybe just chug a few IPAs a day.
My kingdom for a helmet
Most people like to root for the underdog. You know, the whole David vs. Goliath thing, the little guy who goes against overwhelming odds to take on some form of the Big Establishment.
But what if the little guy happens to be a fairly normal-sized lacrosse player with a very large head?
Alex Chu, a freshman at Division III Wheaton College in Norton, Mass., is just such a guy. “My head is wide,” he told WJAR TV. He wants to play goalie for the school’s lacrosse team, but he can’t because no current helmet will fit on the 25-inch-circumference head that sits atop his 6-foot-tall, 265-pound body.
He’s up against Big Sports Equipment in the form of Cascade-Maverik and Warrior, the two major manufacturers of lacrosse helmets, which won’t build him a custom helmet. It would be too expensive, they say – but the Boston Globe reported that there is a lacrosse player at a Division I school who wears a very large helmet “that was produced after [his] coaches and Cascade ‘huddled up.’ ”
We wish Mr. Chu well, and perhaps one day he will be mentioned with such large-skulled high achievers as Jay Leno, LeBron James, Jennifer Garner, Tyrannosaurus rex, Rihanna, Napoleon Bonaparte, SpongeBob SquarePants, and Simon Cowell.
We’ll just have the salad
Zombies, beware: You might want to eat us, but now, we can eat you.
Okay, “zombie” deer aren’t actually zombies, but they are infected with something almost as terrifying. Chronic wasting disease is a prion disorder similar to bovine spongiform encephalopathy, or mad cow disease, and has been found in deer across 24 U.S. states as of January 2019.
While venison is less commonly eaten than beef, if mad cow disease can make the jump to humans, can people who eat meat infected with chronic wasting disease also become infected?
Thanks to an Oneida County, N.Y., fire company and a 2005 Sportsmen’s feast we’re sure someone’s never heard the end of, we know the answer to be “no.”
The fire company accidentally served meat from a deer that was infected with chronic wasting disease, and more than 200 people were exposed. A group of about 80 of these individuals have been monitored since then by a research team from the Oneida County Health Department and the State University of New York at Binghamton. At the most recent follow-up, no individual had developed the disease.
Experts do caution that it’s entirely possible chronic wasting disease will make the jump to humans eventually, despite the species gap. But for now, you can enjoy without fear your sweet ironic revenge on those zombies.
Does my breath smell like reduced cancer risk?
Cancer prevention just got a whole lot more ... fragrant. Allium vegetables – garlic, onions, leeks, chives, and shallots – have been found to decrease the risk of colorectal cancer (CRC), according to a Chinese study published last year. Very good news for Italians, but it looks like the risk of CRC in the vampire population might continue to rise.
The study authors reported that high allium intake correlated with lower CRC risk in both men and women, in the northeast Chinese population sampled. Bioactive compounds in these vegetables have anticarcinogenic properties, and researchers found that eating at least 35 pounds of allium vegetables per year could reduce cancer risk.
Unclear if this study was secretly funded by Big Onion, but as fans of delicious and anticancer flavor, we here at LOTME support these findings. However, we strongly advise against going the Tony Abbott route of chomping into whole onions.
An IPA a day keeps the doctor away
After you’re finished eating your annual 35 pounds of garlic and onions (sure, do it all in 1 day if you want), you might be a little thirsty. And we’ve got good news for you – have a brewski, it’s good for ya! Turns out, hops might have some health benefits, so drink up.
Hops contain a class of compound called isohumulones, which gives them that bitter taste. There have been multiple studies showing the metabolic effects of isohumulones, including cell inflammation suppression, reduced weight gain, reduced hyperglycemia, and increased glucose tolerance.
These isohumulones (try typing that 10 times in a row) interact with the bitter taste receptors in the gut, and researchers are hopeful that this could lead to isohumulone-esque drugs to treat metabolic disorders. In the meantime, maybe just chug a few IPAs a day.
My kingdom for a helmet
Most people like to root for the underdog. You know, the whole David vs. Goliath thing, the little guy who goes against overwhelming odds to take on some form of the Big Establishment.
But what if the little guy happens to be a fairly normal-sized lacrosse player with a very large head?
Alex Chu, a freshman at Division III Wheaton College in Norton, Mass., is just such a guy. “My head is wide,” he told WJAR TV. He wants to play goalie for the school’s lacrosse team, but he can’t because no current helmet will fit on the 25-inch-circumference head that sits atop his 6-foot-tall, 265-pound body.
He’s up against Big Sports Equipment in the form of Cascade-Maverik and Warrior, the two major manufacturers of lacrosse helmets, which won’t build him a custom helmet. It would be too expensive, they say – but the Boston Globe reported that there is a lacrosse player at a Division I school who wears a very large helmet “that was produced after [his] coaches and Cascade ‘huddled up.’ ”
We wish Mr. Chu well, and perhaps one day he will be mentioned with such large-skulled high achievers as Jay Leno, LeBron James, Jennifer Garner, Tyrannosaurus rex, Rihanna, Napoleon Bonaparte, SpongeBob SquarePants, and Simon Cowell.
We’ll just have the salad
Zombies, beware: You might want to eat us, but now, we can eat you.
Okay, “zombie” deer aren’t actually zombies, but they are infected with something almost as terrifying. Chronic wasting disease is a prion disorder similar to bovine spongiform encephalopathy, or mad cow disease, and has been found in deer across 24 U.S. states as of January 2019.
While venison is less commonly eaten than beef, if mad cow disease can make the jump to humans, can people who eat meat infected with chronic wasting disease also become infected?
Thanks to an Oneida County, N.Y., fire company and a 2005 Sportsmen’s feast we’re sure someone’s never heard the end of, we know the answer to be “no.”
The fire company accidentally served meat from a deer that was infected with chronic wasting disease, and more than 200 people were exposed. A group of about 80 of these individuals have been monitored since then by a research team from the Oneida County Health Department and the State University of New York at Binghamton. At the most recent follow-up, no individual had developed the disease.
Experts do caution that it’s entirely possible chronic wasting disease will make the jump to humans eventually, despite the species gap. But for now, you can enjoy without fear your sweet ironic revenge on those zombies.
Does my breath smell like reduced cancer risk?
Cancer prevention just got a whole lot more ... fragrant. Allium vegetables – garlic, onions, leeks, chives, and shallots – have been found to decrease the risk of colorectal cancer (CRC), according to a Chinese study published last year. Very good news for Italians, but it looks like the risk of CRC in the vampire population might continue to rise.
The study authors reported that high allium intake correlated with lower CRC risk in both men and women, in the northeast Chinese population sampled. Bioactive compounds in these vegetables have anticarcinogenic properties, and researchers found that eating at least 35 pounds of allium vegetables per year could reduce cancer risk.
Unclear if this study was secretly funded by Big Onion, but as fans of delicious and anticancer flavor, we here at LOTME support these findings. However, we strongly advise against going the Tony Abbott route of chomping into whole onions.
An IPA a day keeps the doctor away
After you’re finished eating your annual 35 pounds of garlic and onions (sure, do it all in 1 day if you want), you might be a little thirsty. And we’ve got good news for you – have a brewski, it’s good for ya! Turns out, hops might have some health benefits, so drink up.
Hops contain a class of compound called isohumulones, which gives them that bitter taste. There have been multiple studies showing the metabolic effects of isohumulones, including cell inflammation suppression, reduced weight gain, reduced hyperglycemia, and increased glucose tolerance.
These isohumulones (try typing that 10 times in a row) interact with the bitter taste receptors in the gut, and researchers are hopeful that this could lead to isohumulone-esque drugs to treat metabolic disorders. In the meantime, maybe just chug a few IPAs a day.
My kingdom for a helmet
Most people like to root for the underdog. You know, the whole David vs. Goliath thing, the little guy who goes against overwhelming odds to take on some form of the Big Establishment.
But what if the little guy happens to be a fairly normal-sized lacrosse player with a very large head?
Alex Chu, a freshman at Division III Wheaton College in Norton, Mass., is just such a guy. “My head is wide,” he told WJAR TV. He wants to play goalie for the school’s lacrosse team, but he can’t because no current helmet will fit on the 25-inch-circumference head that sits atop his 6-foot-tall, 265-pound body.
He’s up against Big Sports Equipment in the form of Cascade-Maverik and Warrior, the two major manufacturers of lacrosse helmets, which won’t build him a custom helmet. It would be too expensive, they say – but the Boston Globe reported that there is a lacrosse player at a Division I school who wears a very large helmet “that was produced after [his] coaches and Cascade ‘huddled up.’ ”
We wish Mr. Chu well, and perhaps one day he will be mentioned with such large-skulled high achievers as Jay Leno, LeBron James, Jennifer Garner, Tyrannosaurus rex, Rihanna, Napoleon Bonaparte, SpongeBob SquarePants, and Simon Cowell.
We’ll just have the salad
Zombies, beware: You might want to eat us, but now, we can eat you.
Okay, “zombie” deer aren’t actually zombies, but they are infected with something almost as terrifying. Chronic wasting disease is a prion disorder similar to bovine spongiform encephalopathy, or mad cow disease, and has been found in deer across 24 U.S. states as of January 2019.
While venison is less commonly eaten than beef, if mad cow disease can make the jump to humans, can people who eat meat infected with chronic wasting disease also become infected?
Thanks to an Oneida County, N.Y., fire company and a 2005 Sportsmen’s feast we’re sure someone’s never heard the end of, we know the answer to be “no.”
The fire company accidentally served meat from a deer that was infected with chronic wasting disease, and more than 200 people were exposed. A group of about 80 of these individuals have been monitored since then by a research team from the Oneida County Health Department and the State University of New York at Binghamton. At the most recent follow-up, no individual had developed the disease.
Experts do caution that it’s entirely possible chronic wasting disease will make the jump to humans eventually, despite the species gap. But for now, you can enjoy without fear your sweet ironic revenge on those zombies.
New BinaxNOW influenza test gets CLIA waiver
The Food and Drug Administration has granted the reformulated BinaxNOW Influenza A & B Card 2 waived status under the Clinical Laboratory Improvements Amendments for use with Abbott’s DIGIVAL reader, which means the system is relatively simple and has a low risk of erroneous results.
According to Abbott’s press release, the DIGIVAL reader (formerly known as the Alere Reader) automatically interprets this rapid influenza diagnostic test’s results in seconds and is intended to remove subjectivity from the diagnostic process. The BinaxNOW Influenza Card A & B Card 2 is a Class II assay and complies with the FDA’s new reclassification requirements for rapid influenza diagnostic tests.
The Food and Drug Administration has granted the reformulated BinaxNOW Influenza A & B Card 2 waived status under the Clinical Laboratory Improvements Amendments for use with Abbott’s DIGIVAL reader, which means the system is relatively simple and has a low risk of erroneous results.
According to Abbott’s press release, the DIGIVAL reader (formerly known as the Alere Reader) automatically interprets this rapid influenza diagnostic test’s results in seconds and is intended to remove subjectivity from the diagnostic process. The BinaxNOW Influenza Card A & B Card 2 is a Class II assay and complies with the FDA’s new reclassification requirements for rapid influenza diagnostic tests.
The Food and Drug Administration has granted the reformulated BinaxNOW Influenza A & B Card 2 waived status under the Clinical Laboratory Improvements Amendments for use with Abbott’s DIGIVAL reader, which means the system is relatively simple and has a low risk of erroneous results.
According to Abbott’s press release, the DIGIVAL reader (formerly known as the Alere Reader) automatically interprets this rapid influenza diagnostic test’s results in seconds and is intended to remove subjectivity from the diagnostic process. The BinaxNOW Influenza Card A & B Card 2 is a Class II assay and complies with the FDA’s new reclassification requirements for rapid influenza diagnostic tests.
Joseph R. Berger, MD
Introducing the Multiple Sclerosis Resource Center Editor-in-Chief, Joseph R. Berger, M.D., FACP, FAAN, FANA.
Dr. Berger is Professor of Neurology and Associate Chief of the Multiple Sclerosis Division of the Department of Neurology at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia. He is a fellow of the American College of Physicians, American Academy of Neurology and the American Neurological Association. He has published more than 240 refereed papers, more than 100 chapters, and has co-edited three textbooks. Dr. Berger co-founded and chaired the first international conference on the neurological complications of HIV, the Neuroscience of HIV meeting. He also established the Commonwealth Neurological Society for neurologists in the state of Kentucky. Dr. Berger has a longstanding interest in international health and was one of the founding members of People-to-People, an organization for HIV/AIDS care and education in East Africa.
Introducing the Multiple Sclerosis Resource Center Editor-in-Chief, Joseph R. Berger, M.D., FACP, FAAN, FANA.
Dr. Berger is Professor of Neurology and Associate Chief of the Multiple Sclerosis Division of the Department of Neurology at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia. He is a fellow of the American College of Physicians, American Academy of Neurology and the American Neurological Association. He has published more than 240 refereed papers, more than 100 chapters, and has co-edited three textbooks. Dr. Berger co-founded and chaired the first international conference on the neurological complications of HIV, the Neuroscience of HIV meeting. He also established the Commonwealth Neurological Society for neurologists in the state of Kentucky. Dr. Berger has a longstanding interest in international health and was one of the founding members of People-to-People, an organization for HIV/AIDS care and education in East Africa.
Introducing the Multiple Sclerosis Resource Center Editor-in-Chief, Joseph R. Berger, M.D., FACP, FAAN, FANA.
Dr. Berger is Professor of Neurology and Associate Chief of the Multiple Sclerosis Division of the Department of Neurology at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia. He is a fellow of the American College of Physicians, American Academy of Neurology and the American Neurological Association. He has published more than 240 refereed papers, more than 100 chapters, and has co-edited three textbooks. Dr. Berger co-founded and chaired the first international conference on the neurological complications of HIV, the Neuroscience of HIV meeting. He also established the Commonwealth Neurological Society for neurologists in the state of Kentucky. Dr. Berger has a longstanding interest in international health and was one of the founding members of People-to-People, an organization for HIV/AIDS care and education in East Africa.
Fundamentals of Gene Therapy: Addressing Gaps in Physician Education
Click here to read supplement.
Gene therapy is a contemporary therapeutic intervention with recent positive results and regulatory approvals either completed or expected in the next several years for various conditions. In this supplement, learn more about:
- Basic principles of gene therapy
- In vivo vs ex vivo methods of gene transfer
- Vector types
- Clinical Considerations
About the Author
Click here to read supplement.
Click here to read supplement.
Gene therapy is a contemporary therapeutic intervention with recent positive results and regulatory approvals either completed or expected in the next several years for various conditions. In this supplement, learn more about:
- Basic principles of gene therapy
- In vivo vs ex vivo methods of gene transfer
- Vector types
- Clinical Considerations
About the Author
Click here to read supplement.
Click here to read supplement.
Gene therapy is a contemporary therapeutic intervention with recent positive results and regulatory approvals either completed or expected in the next several years for various conditions. In this supplement, learn more about:
- Basic principles of gene therapy
- In vivo vs ex vivo methods of gene transfer
- Vector types
- Clinical Considerations
About the Author
Click here to read supplement.
The Case of the Disappearing Eyebrows
When this 45-year-old man was in third grade, he began to notice areas of hair loss in his scalp. The affected area was always round and the hair loss complete—but it would grow back entirely within weeks to months. There was never any rash or discomfort associated with these changes.
Since then, he has experienced numerous similar episodes of focal hair loss, sometimes in the beard, sometimes on the arms or legs, and most recently, in his eyebrows. Again, no symptoms accompany the process.
Although his personal health history is relatively uneventful, his family has not been as fortunate. There are numerous cases of lupus, rheumatoid arthritis, diabetes, and thyroid disease.

EXAMINATION
There are sharply defined, crescent-shaped, 2.5-cm divots at the superior borders of both eyebrows in which every hair is gone. No redness, swelling, or scaling are seen or felt, and there is no detectable adenopathy in the region.
Examination of hair-bearing regions reveals no other areas of hair loss.
What’s the diagnosis?
DISCUSSION
This case illustrates several variants of an extremely common condition: alopecia areata (AA), literally translated as “hair loss confined to a particular localized area or areas.” Although AA is more common in adults, it often affects children. And though the scalp is by far the most commonly affected area, AA can cause hair loss anywhere on the body.
In general, the earlier the onset, the more likely the problem is to become recurrent or even progressive. In rare instances, a patient can develop alopecia totalis, in which there is permanent and total scalp hair loss, or even alopecia universalis, the permanent loss of every hair on the entire body. Other predictors of a poor prognosis include extensive involvement of the scalp, especially the periphery (termed ophiasis), and a history of atopy.
Much research has been done on the underlying pathology of AA, as well as potential remedies. This has proven, beyond any doubt, that the problem is autoimmune and tends to run in families (as with other autoimmune diseases), suggesting a hereditary basis. We also know that medications that dampen this autoimmune process, such as steroids and biologics, are useful but not always safe or practical.
What we don’t really know is what triggers an actual attack. My observation, based on 35 years of dermatology practice, is that stress often plays a part—but I’d be hard pressed to prove that, and it wouldn’t be very useful even if I could. This patient adamantly agreed that stress was the trigger for his AA.
The differential for AA includes tinea capitis, discoid lupus, and lichen planopilaris. This patient’s multiple episodes over decades made the correct diagnosis clear. However, when the diagnosis is in doubt—other items in the differential commonly affect the scalp, although they may also manifest with redness, scaling, or swelling—a punch biopsy may be necessary to sort through the possibilities. Care must be taken to enter the skin parallel to hair follicles when the sample is removed.
Many treatments have been tried for AA, but none are reliably effective. In the vast majority of patients, the problem resolves itself. Treatments to try when needed include topical steroids, intralesional steroids, and topical immune stimulators (eg, squaric acid or dinitrochlorobenzene)—all of which have their limitations.
TAKE-HOME LEARNING POINTS
- Alopecia areata (AA) is more common in adults but can affect children as well.
- In rare cases, the patient can experience permanent total hair loss on the scalp (alopecia totalis) or the entire body (alopecia universalis).
- Because AA is an autoimmune disease, steroids and biologics may be useful treatments—but they are not always safe or practical.
- In a majority of patients with AA, the problem will resolve on its own.
When this 45-year-old man was in third grade, he began to notice areas of hair loss in his scalp. The affected area was always round and the hair loss complete—but it would grow back entirely within weeks to months. There was never any rash or discomfort associated with these changes.
Since then, he has experienced numerous similar episodes of focal hair loss, sometimes in the beard, sometimes on the arms or legs, and most recently, in his eyebrows. Again, no symptoms accompany the process.
Although his personal health history is relatively uneventful, his family has not been as fortunate. There are numerous cases of lupus, rheumatoid arthritis, diabetes, and thyroid disease.

EXAMINATION
There are sharply defined, crescent-shaped, 2.5-cm divots at the superior borders of both eyebrows in which every hair is gone. No redness, swelling, or scaling are seen or felt, and there is no detectable adenopathy in the region.
Examination of hair-bearing regions reveals no other areas of hair loss.
What’s the diagnosis?
DISCUSSION
This case illustrates several variants of an extremely common condition: alopecia areata (AA), literally translated as “hair loss confined to a particular localized area or areas.” Although AA is more common in adults, it often affects children. And though the scalp is by far the most commonly affected area, AA can cause hair loss anywhere on the body.
In general, the earlier the onset, the more likely the problem is to become recurrent or even progressive. In rare instances, a patient can develop alopecia totalis, in which there is permanent and total scalp hair loss, or even alopecia universalis, the permanent loss of every hair on the entire body. Other predictors of a poor prognosis include extensive involvement of the scalp, especially the periphery (termed ophiasis), and a history of atopy.
Much research has been done on the underlying pathology of AA, as well as potential remedies. This has proven, beyond any doubt, that the problem is autoimmune and tends to run in families (as with other autoimmune diseases), suggesting a hereditary basis. We also know that medications that dampen this autoimmune process, such as steroids and biologics, are useful but not always safe or practical.
What we don’t really know is what triggers an actual attack. My observation, based on 35 years of dermatology practice, is that stress often plays a part—but I’d be hard pressed to prove that, and it wouldn’t be very useful even if I could. This patient adamantly agreed that stress was the trigger for his AA.
The differential for AA includes tinea capitis, discoid lupus, and lichen planopilaris. This patient’s multiple episodes over decades made the correct diagnosis clear. However, when the diagnosis is in doubt—other items in the differential commonly affect the scalp, although they may also manifest with redness, scaling, or swelling—a punch biopsy may be necessary to sort through the possibilities. Care must be taken to enter the skin parallel to hair follicles when the sample is removed.
Many treatments have been tried for AA, but none are reliably effective. In the vast majority of patients, the problem resolves itself. Treatments to try when needed include topical steroids, intralesional steroids, and topical immune stimulators (eg, squaric acid or dinitrochlorobenzene)—all of which have their limitations.
TAKE-HOME LEARNING POINTS
- Alopecia areata (AA) is more common in adults but can affect children as well.
- In rare cases, the patient can experience permanent total hair loss on the scalp (alopecia totalis) or the entire body (alopecia universalis).
- Because AA is an autoimmune disease, steroids and biologics may be useful treatments—but they are not always safe or practical.
- In a majority of patients with AA, the problem will resolve on its own.
When this 45-year-old man was in third grade, he began to notice areas of hair loss in his scalp. The affected area was always round and the hair loss complete—but it would grow back entirely within weeks to months. There was never any rash or discomfort associated with these changes.
Since then, he has experienced numerous similar episodes of focal hair loss, sometimes in the beard, sometimes on the arms or legs, and most recently, in his eyebrows. Again, no symptoms accompany the process.
Although his personal health history is relatively uneventful, his family has not been as fortunate. There are numerous cases of lupus, rheumatoid arthritis, diabetes, and thyroid disease.

EXAMINATION
There are sharply defined, crescent-shaped, 2.5-cm divots at the superior borders of both eyebrows in which every hair is gone. No redness, swelling, or scaling are seen or felt, and there is no detectable adenopathy in the region.
Examination of hair-bearing regions reveals no other areas of hair loss.
What’s the diagnosis?
DISCUSSION
This case illustrates several variants of an extremely common condition: alopecia areata (AA), literally translated as “hair loss confined to a particular localized area or areas.” Although AA is more common in adults, it often affects children. And though the scalp is by far the most commonly affected area, AA can cause hair loss anywhere on the body.
In general, the earlier the onset, the more likely the problem is to become recurrent or even progressive. In rare instances, a patient can develop alopecia totalis, in which there is permanent and total scalp hair loss, or even alopecia universalis, the permanent loss of every hair on the entire body. Other predictors of a poor prognosis include extensive involvement of the scalp, especially the periphery (termed ophiasis), and a history of atopy.
Much research has been done on the underlying pathology of AA, as well as potential remedies. This has proven, beyond any doubt, that the problem is autoimmune and tends to run in families (as with other autoimmune diseases), suggesting a hereditary basis. We also know that medications that dampen this autoimmune process, such as steroids and biologics, are useful but not always safe or practical.
What we don’t really know is what triggers an actual attack. My observation, based on 35 years of dermatology practice, is that stress often plays a part—but I’d be hard pressed to prove that, and it wouldn’t be very useful even if I could. This patient adamantly agreed that stress was the trigger for his AA.
The differential for AA includes tinea capitis, discoid lupus, and lichen planopilaris. This patient’s multiple episodes over decades made the correct diagnosis clear. However, when the diagnosis is in doubt—other items in the differential commonly affect the scalp, although they may also manifest with redness, scaling, or swelling—a punch biopsy may be necessary to sort through the possibilities. Care must be taken to enter the skin parallel to hair follicles when the sample is removed.
Many treatments have been tried for AA, but none are reliably effective. In the vast majority of patients, the problem resolves itself. Treatments to try when needed include topical steroids, intralesional steroids, and topical immune stimulators (eg, squaric acid or dinitrochlorobenzene)—all of which have their limitations.
TAKE-HOME LEARNING POINTS
- Alopecia areata (AA) is more common in adults but can affect children as well.
- In rare cases, the patient can experience permanent total hair loss on the scalp (alopecia totalis) or the entire body (alopecia universalis).
- Because AA is an autoimmune disease, steroids and biologics may be useful treatments—but they are not always safe or practical.
- In a majority of patients with AA, the problem will resolve on its own.
Barrett’s esophagus uncommon in patients with uncomplicated GERD
Uncomplicated gastroesophageal reflux disease (GERD) accounted for 13.5% of esophagogastroduodenoscopies, but 5.6% of these patients had suspected Barrett’s esophagus and only 1.4% had suspected long-segment Barrett’s esophagus, researchers reported. The study appears in the April issue of Clinical Gastroenterology and Hepatology.
“The prevalence of suspected Barrett’s esophagus is lower than in prior time periods. This raises questions about the utility of esophagogastroduodenoscopies to detect Barrett’s esophagus in patients with uncomplicated GERD,” wrote Emery C. Lin, MD, of Oregon Health and Science University, Portland, and his associates there and at Massachusetts General Hospital, Boston.
Symptoms of GERD affect more than one in four U.S. adults and are a risk factor for Barrett’s esophagus. However, the prevalence of Barrett’s esophagus is unclear in patients with dysphagia and in the era of proton pump inhibitors, the researchers said. The American Gastroenterological Association strongly discourages reflexively screening patients with GERD for Barrett’s esophagus, but “weakly recommends” screening GERD patients with multiple risk factors for Barrett’s esophagus, including chronic GERD, hiatal hernia, older age (50 years and up), white race, male sex, increased body mass index, and intra-abdominal adiposity.
To understand the prevalence and findings of esophagogastroduodenoscopy in patients with GERD without alarm symptoms (including weight loss, dysphagia, and bleeding), the investigators studied 543,103 of these procedures performed at 82 sites in the United States between 2003 and 2013. The data came from the National Endoscopic Database, which generates endoscopy reports using a structured computer form.
A total of 73,535 esophagogastroduodenoscopies (13.5%) were performed for GERD without alarm symptoms. Among these patients, 4,122 (5.6%) had suspected Barrett’s esophagus, of which 24.2% had suspected long-segment Barrett’s esophagus (3 cm or longer). Among patients with uncomplicated GERD, the prevalence of suspected Barrett’s esophagus was 5.6%, and the prevalence of long-segment disease was 1.4%.
Although male sex, older age, and white race were significant risk factors for suspected Barrett’s esophagus and suspected long-segment disease, 23.6% of esophagogastroduodenoscopies were performed in white men older than 50 years. “We find that low-risk populations with uncomplicated GERD make up a significant number of esophagogastroduodenoscopies done for uncomplicated GERD,” the investigators wrote. “If esophagogastroduodenoscopies were limited to patients that met the AGA criteria of being male, white, and age over 50, we would have detected 34 of 47 (72.3%) of esophageal tumors and found suspected Barrett’s esophagus in nearly 10%, while reducing the burden of endoscopy by more than 75%.”
Hiatal hernia was a significant correlate of suspected Barrett’s esophagus (odds ratio, 1.6), the researchers noted. Esophagitis was not associated with suspected Barrett’s esophagus overall but did correlate with long-segment disease. Esophagitis might mask underlying short-segment Barrett’s esophagus, and short-segment Barrett’s esophagus might be milder in nature and more responsive to antisecretory therapy, the researchers said. They noted that severe (grade C/D) esophagitis was strongly linked with both short-segment and long-segment Barrett’s esophagus.
The National Institute of Diabetes and Digestive and Kidney Diseases provided funding. The researchers reported having no conflicts of interest.
SOURCE: Lin EC et al. Clin Gastroenterol Hepatol. 2019 Apr. doi: 10.1016/j.cgh.2018.08.066.
The utility and cost-effectiveness of screening for Barrett’s esophagus with esophagogastroduodenoscopy (EGD) remain contentious issues. National GI societies currently recommend screening in only a limited high-risk population, mainly white men aged 50 or older with chronic GERD and one or more additional risk factors. It is unclear to what degree those guidelines are adhered to in clinical practice. This study by Lin et al. sheds further light on this issue. The investigators showed that a significant proportion (more than 10%) of EGDs were performed for uncomplicated GERD, with less than one-quarter of those patients meeting the minimal criteria for screening for Barrett’s esophagus. Among this group, the prevalence of Barrett’s esophagus was found to be lower than previously reported. The data offer compelling evidence that screening low-risk patients with uncomplicated GERD by using upper endoscopy is not cost effective, and is at best marginally cost effective if limited to the high-risk group identified by national GI societies. The question arises whether we should abandon screening for Barrett’s esophagus altogether.
The challenge, however, is that the incidence of esophageal adenocarcinoma continues to rise (albeit at a slower pace in recent years), and 5-year survival of patients diagnosed with esophageal adenocarcinoma remains extremely poor. Therefore, prevention remains the optimal strategy. The solution may lie in adopting a lower-cost screening modality that can replace endoscopy for this purpose, and while many such techniques are under investigation, further studies are required to find a widely applicable alternative to EGD.
Nabil M. Mansour, MD, is an assistant professor, department of medicine, section of gastroenterology and hepatology, Baylor College of Medicine, Houston. He has no conflicts of interest.
The utility and cost-effectiveness of screening for Barrett’s esophagus with esophagogastroduodenoscopy (EGD) remain contentious issues. National GI societies currently recommend screening in only a limited high-risk population, mainly white men aged 50 or older with chronic GERD and one or more additional risk factors. It is unclear to what degree those guidelines are adhered to in clinical practice. This study by Lin et al. sheds further light on this issue. The investigators showed that a significant proportion (more than 10%) of EGDs were performed for uncomplicated GERD, with less than one-quarter of those patients meeting the minimal criteria for screening for Barrett’s esophagus. Among this group, the prevalence of Barrett’s esophagus was found to be lower than previously reported. The data offer compelling evidence that screening low-risk patients with uncomplicated GERD by using upper endoscopy is not cost effective, and is at best marginally cost effective if limited to the high-risk group identified by national GI societies. The question arises whether we should abandon screening for Barrett’s esophagus altogether.
The challenge, however, is that the incidence of esophageal adenocarcinoma continues to rise (albeit at a slower pace in recent years), and 5-year survival of patients diagnosed with esophageal adenocarcinoma remains extremely poor. Therefore, prevention remains the optimal strategy. The solution may lie in adopting a lower-cost screening modality that can replace endoscopy for this purpose, and while many such techniques are under investigation, further studies are required to find a widely applicable alternative to EGD.
Nabil M. Mansour, MD, is an assistant professor, department of medicine, section of gastroenterology and hepatology, Baylor College of Medicine, Houston. He has no conflicts of interest.
The utility and cost-effectiveness of screening for Barrett’s esophagus with esophagogastroduodenoscopy (EGD) remain contentious issues. National GI societies currently recommend screening in only a limited high-risk population, mainly white men aged 50 or older with chronic GERD and one or more additional risk factors. It is unclear to what degree those guidelines are adhered to in clinical practice. This study by Lin et al. sheds further light on this issue. The investigators showed that a significant proportion (more than 10%) of EGDs were performed for uncomplicated GERD, with less than one-quarter of those patients meeting the minimal criteria for screening for Barrett’s esophagus. Among this group, the prevalence of Barrett’s esophagus was found to be lower than previously reported. The data offer compelling evidence that screening low-risk patients with uncomplicated GERD by using upper endoscopy is not cost effective, and is at best marginally cost effective if limited to the high-risk group identified by national GI societies. The question arises whether we should abandon screening for Barrett’s esophagus altogether.
The challenge, however, is that the incidence of esophageal adenocarcinoma continues to rise (albeit at a slower pace in recent years), and 5-year survival of patients diagnosed with esophageal adenocarcinoma remains extremely poor. Therefore, prevention remains the optimal strategy. The solution may lie in adopting a lower-cost screening modality that can replace endoscopy for this purpose, and while many such techniques are under investigation, further studies are required to find a widely applicable alternative to EGD.
Nabil M. Mansour, MD, is an assistant professor, department of medicine, section of gastroenterology and hepatology, Baylor College of Medicine, Houston. He has no conflicts of interest.
Uncomplicated gastroesophageal reflux disease (GERD) accounted for 13.5% of esophagogastroduodenoscopies, but 5.6% of these patients had suspected Barrett’s esophagus and only 1.4% had suspected long-segment Barrett’s esophagus, researchers reported. The study appears in the April issue of Clinical Gastroenterology and Hepatology.
“The prevalence of suspected Barrett’s esophagus is lower than in prior time periods. This raises questions about the utility of esophagogastroduodenoscopies to detect Barrett’s esophagus in patients with uncomplicated GERD,” wrote Emery C. Lin, MD, of Oregon Health and Science University, Portland, and his associates there and at Massachusetts General Hospital, Boston.
Symptoms of GERD affect more than one in four U.S. adults and are a risk factor for Barrett’s esophagus. However, the prevalence of Barrett’s esophagus is unclear in patients with dysphagia and in the era of proton pump inhibitors, the researchers said. The American Gastroenterological Association strongly discourages reflexively screening patients with GERD for Barrett’s esophagus, but “weakly recommends” screening GERD patients with multiple risk factors for Barrett’s esophagus, including chronic GERD, hiatal hernia, older age (50 years and up), white race, male sex, increased body mass index, and intra-abdominal adiposity.
To understand the prevalence and findings of esophagogastroduodenoscopy in patients with GERD without alarm symptoms (including weight loss, dysphagia, and bleeding), the investigators studied 543,103 of these procedures performed at 82 sites in the United States between 2003 and 2013. The data came from the National Endoscopic Database, which generates endoscopy reports using a structured computer form.
A total of 73,535 esophagogastroduodenoscopies (13.5%) were performed for GERD without alarm symptoms. Among these patients, 4,122 (5.6%) had suspected Barrett’s esophagus, of which 24.2% had suspected long-segment Barrett’s esophagus (3 cm or longer). Among patients with uncomplicated GERD, the prevalence of suspected Barrett’s esophagus was 5.6%, and the prevalence of long-segment disease was 1.4%.
Although male sex, older age, and white race were significant risk factors for suspected Barrett’s esophagus and suspected long-segment disease, 23.6% of esophagogastroduodenoscopies were performed in white men older than 50 years. “We find that low-risk populations with uncomplicated GERD make up a significant number of esophagogastroduodenoscopies done for uncomplicated GERD,” the investigators wrote. “If esophagogastroduodenoscopies were limited to patients that met the AGA criteria of being male, white, and age over 50, we would have detected 34 of 47 (72.3%) of esophageal tumors and found suspected Barrett’s esophagus in nearly 10%, while reducing the burden of endoscopy by more than 75%.”
Hiatal hernia was a significant correlate of suspected Barrett’s esophagus (odds ratio, 1.6), the researchers noted. Esophagitis was not associated with suspected Barrett’s esophagus overall but did correlate with long-segment disease. Esophagitis might mask underlying short-segment Barrett’s esophagus, and short-segment Barrett’s esophagus might be milder in nature and more responsive to antisecretory therapy, the researchers said. They noted that severe (grade C/D) esophagitis was strongly linked with both short-segment and long-segment Barrett’s esophagus.
The National Institute of Diabetes and Digestive and Kidney Diseases provided funding. The researchers reported having no conflicts of interest.
SOURCE: Lin EC et al. Clin Gastroenterol Hepatol. 2019 Apr. doi: 10.1016/j.cgh.2018.08.066.
Uncomplicated gastroesophageal reflux disease (GERD) accounted for 13.5% of esophagogastroduodenoscopies, but 5.6% of these patients had suspected Barrett’s esophagus and only 1.4% had suspected long-segment Barrett’s esophagus, researchers reported. The study appears in the April issue of Clinical Gastroenterology and Hepatology.
“The prevalence of suspected Barrett’s esophagus is lower than in prior time periods. This raises questions about the utility of esophagogastroduodenoscopies to detect Barrett’s esophagus in patients with uncomplicated GERD,” wrote Emery C. Lin, MD, of Oregon Health and Science University, Portland, and his associates there and at Massachusetts General Hospital, Boston.
Symptoms of GERD affect more than one in four U.S. adults and are a risk factor for Barrett’s esophagus. However, the prevalence of Barrett’s esophagus is unclear in patients with dysphagia and in the era of proton pump inhibitors, the researchers said. The American Gastroenterological Association strongly discourages reflexively screening patients with GERD for Barrett’s esophagus, but “weakly recommends” screening GERD patients with multiple risk factors for Barrett’s esophagus, including chronic GERD, hiatal hernia, older age (50 years and up), white race, male sex, increased body mass index, and intra-abdominal adiposity.
To understand the prevalence and findings of esophagogastroduodenoscopy in patients with GERD without alarm symptoms (including weight loss, dysphagia, and bleeding), the investigators studied 543,103 of these procedures performed at 82 sites in the United States between 2003 and 2013. The data came from the National Endoscopic Database, which generates endoscopy reports using a structured computer form.
A total of 73,535 esophagogastroduodenoscopies (13.5%) were performed for GERD without alarm symptoms. Among these patients, 4,122 (5.6%) had suspected Barrett’s esophagus, of which 24.2% had suspected long-segment Barrett’s esophagus (3 cm or longer). Among patients with uncomplicated GERD, the prevalence of suspected Barrett’s esophagus was 5.6%, and the prevalence of long-segment disease was 1.4%.
Although male sex, older age, and white race were significant risk factors for suspected Barrett’s esophagus and suspected long-segment disease, 23.6% of esophagogastroduodenoscopies were performed in white men older than 50 years. “We find that low-risk populations with uncomplicated GERD make up a significant number of esophagogastroduodenoscopies done for uncomplicated GERD,” the investigators wrote. “If esophagogastroduodenoscopies were limited to patients that met the AGA criteria of being male, white, and age over 50, we would have detected 34 of 47 (72.3%) of esophageal tumors and found suspected Barrett’s esophagus in nearly 10%, while reducing the burden of endoscopy by more than 75%.”
Hiatal hernia was a significant correlate of suspected Barrett’s esophagus (odds ratio, 1.6), the researchers noted. Esophagitis was not associated with suspected Barrett’s esophagus overall but did correlate with long-segment disease. Esophagitis might mask underlying short-segment Barrett’s esophagus, and short-segment Barrett’s esophagus might be milder in nature and more responsive to antisecretory therapy, the researchers said. They noted that severe (grade C/D) esophagitis was strongly linked with both short-segment and long-segment Barrett’s esophagus.
The National Institute of Diabetes and Digestive and Kidney Diseases provided funding. The researchers reported having no conflicts of interest.
SOURCE: Lin EC et al. Clin Gastroenterol Hepatol. 2019 Apr. doi: 10.1016/j.cgh.2018.08.066.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
CDC: United States has hit a plateau with HIV
The annual number of new HIV infections has remained stable in recent years, and the Centers for Disease Control and Prevention says that’s not good – but solutions are at hand.
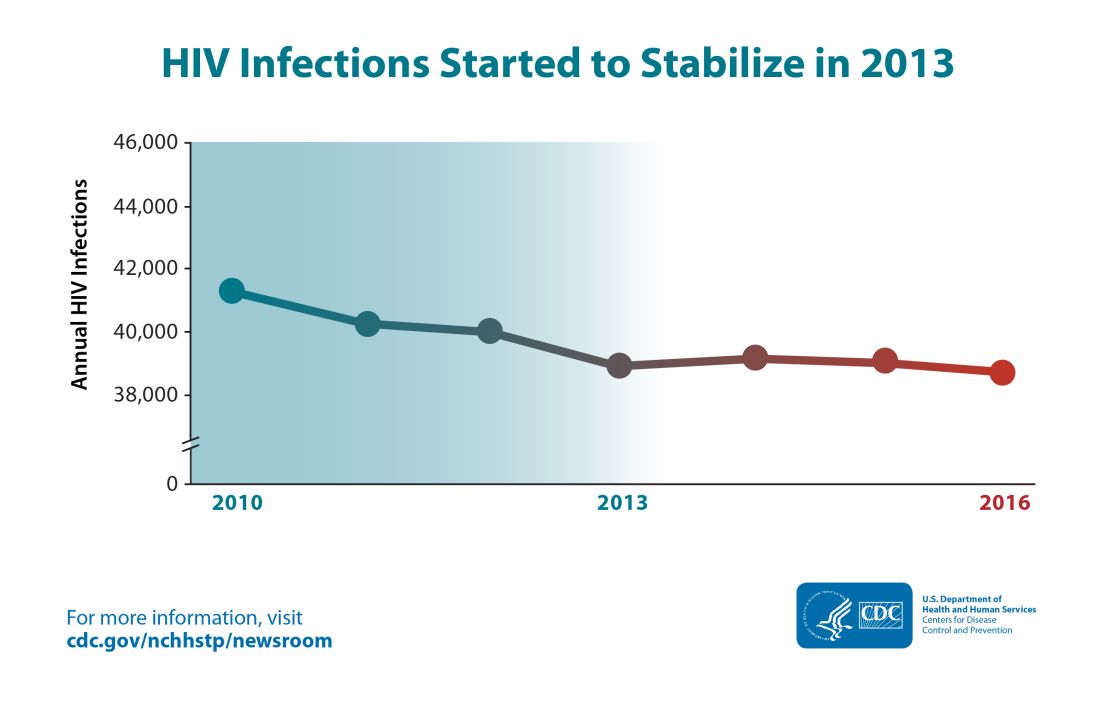
Though the estimated number of new HIV infections declined from just under 42,000 per year in 2010 to about 39,000 annually in 2013, that figure was essentially unchanged by 2016, with 38,700 new HIV infections seen that year.
“CDC estimates that the decline in HIV infections has plateaued because effective HIV prevention and treatment are not adequately reaching those who could most benefit from them. These gaps remain particularly troublesome in rural areas and in the South and among disproportionately affected populations like African Americans and Latinos,” said the CDC in a press release accompanying the report.
The report comes soon after President Trump’s State of the Union address, which announced a new multiagency initiative to eliminate the HIV epidemic in the United States, with the goal of reducing new HIV infections by 90% over the next 10 years. The multipronged initiative will implement geographically targeted HIV elimination teams in areas with high HIV prevalence, pulling together federal agencies, local and state governments, and community-level resources.
The initiative, called “Ending the Epidemic: A Plan for America” will combine an intensified approach to early diagnosis and treatment with efforts to boost uptake of pre-exposure prophylaxis for individuals at high risk for HIV infection.
The new CDC report used CD4 counts reported to the National HIV Surveillance System at the time of diagnosis to identify new (incident) cases and to track prevalence. Much of the report is devoted to finely detailed reporting of HIV incidence across sex, age, race/ethnicity, and transmission mode.
Though some groups, such as people who inject drugs, have seen a decrease of about 30% in the annual rate of new HIV cases, new cases have jumped for other groups. In particular, Latino gay and bisexual men saw new cases climb from 6,400 per year in 2010 to 8,300 in 2016. The incidence rate has stayed high and stable among African American gay and bisexual men, with 9,800 new cases reported in 2010; the same number was seen in 2016.
Among gay and bisexual men overall, the rate has also stayed stable, with about 26,000 new HIV infections reported at the beginning and end of the studied period. White heterosexual women saw about 1,000 new cases per year in 2010 and in 2016.
Some groups saw declines in new cases: African American and Latina heterosexual women each saw a falling incidence of new HIV cases. For the former group, new cases fell from 4,700 to 4,000, while the latter group of women saw new cases drop from 1,200 to 980 per year from 2010 to 2016.
Within these broad groups, HIV incidence also rose among some age groups and fell among others. Decreases were seen for younger African American gay and bisexual men (those aged 13-24 years), but rates increased by about two-thirds for men in this group aged 25-34 years. A similar increase was seen for Latino men in the 25-34 years age group, a change which drove the overall 30% increase in new infections for Latino gay and bisexual men.
White gay and bisexual men saw across-the-board decreases in new infections, though the overall decrease was less than 20%.
For heterosexual individuals as a group, new infections dropped by about 17%, from 10,900 to 9,100 annually. This change was driven mostly by decreases in women identifying as heterosexual.
“After a decades-long struggle, the path to eliminate America’s HIV epidemic is clear,” said Eugene McCray, MD, director of CDC’s Division of HIV/AIDS Prevention, in the press release. “Expanding efforts across the country will close gaps, overcome threats, and turn around troublesome trends.”
The press release cited local work in Washington and New York as evidence that targeted resources can make a difference in reducing new HIV cases. In these two areas, new infections dropped by 23% and 40% respectively from 2010 to 2016.
SOURCE: Centers for Disease Control. CDC Report: www.cdc.gov/hiv/library/reports/hiv-surveillance.html.
The annual number of new HIV infections has remained stable in recent years, and the Centers for Disease Control and Prevention says that’s not good – but solutions are at hand.
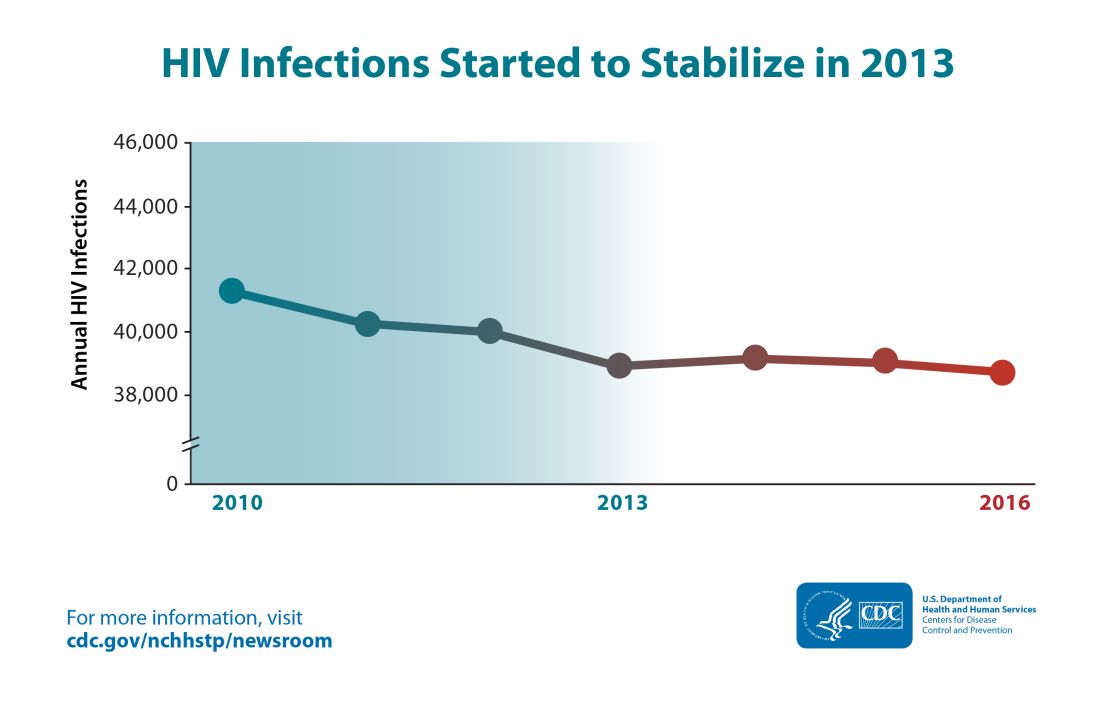
Though the estimated number of new HIV infections declined from just under 42,000 per year in 2010 to about 39,000 annually in 2013, that figure was essentially unchanged by 2016, with 38,700 new HIV infections seen that year.
“CDC estimates that the decline in HIV infections has plateaued because effective HIV prevention and treatment are not adequately reaching those who could most benefit from them. These gaps remain particularly troublesome in rural areas and in the South and among disproportionately affected populations like African Americans and Latinos,” said the CDC in a press release accompanying the report.
The report comes soon after President Trump’s State of the Union address, which announced a new multiagency initiative to eliminate the HIV epidemic in the United States, with the goal of reducing new HIV infections by 90% over the next 10 years. The multipronged initiative will implement geographically targeted HIV elimination teams in areas with high HIV prevalence, pulling together federal agencies, local and state governments, and community-level resources.
The initiative, called “Ending the Epidemic: A Plan for America” will combine an intensified approach to early diagnosis and treatment with efforts to boost uptake of pre-exposure prophylaxis for individuals at high risk for HIV infection.
The new CDC report used CD4 counts reported to the National HIV Surveillance System at the time of diagnosis to identify new (incident) cases and to track prevalence. Much of the report is devoted to finely detailed reporting of HIV incidence across sex, age, race/ethnicity, and transmission mode.
Though some groups, such as people who inject drugs, have seen a decrease of about 30% in the annual rate of new HIV cases, new cases have jumped for other groups. In particular, Latino gay and bisexual men saw new cases climb from 6,400 per year in 2010 to 8,300 in 2016. The incidence rate has stayed high and stable among African American gay and bisexual men, with 9,800 new cases reported in 2010; the same number was seen in 2016.
Among gay and bisexual men overall, the rate has also stayed stable, with about 26,000 new HIV infections reported at the beginning and end of the studied period. White heterosexual women saw about 1,000 new cases per year in 2010 and in 2016.
Some groups saw declines in new cases: African American and Latina heterosexual women each saw a falling incidence of new HIV cases. For the former group, new cases fell from 4,700 to 4,000, while the latter group of women saw new cases drop from 1,200 to 980 per year from 2010 to 2016.
Within these broad groups, HIV incidence also rose among some age groups and fell among others. Decreases were seen for younger African American gay and bisexual men (those aged 13-24 years), but rates increased by about two-thirds for men in this group aged 25-34 years. A similar increase was seen for Latino men in the 25-34 years age group, a change which drove the overall 30% increase in new infections for Latino gay and bisexual men.
White gay and bisexual men saw across-the-board decreases in new infections, though the overall decrease was less than 20%.
For heterosexual individuals as a group, new infections dropped by about 17%, from 10,900 to 9,100 annually. This change was driven mostly by decreases in women identifying as heterosexual.
“After a decades-long struggle, the path to eliminate America’s HIV epidemic is clear,” said Eugene McCray, MD, director of CDC’s Division of HIV/AIDS Prevention, in the press release. “Expanding efforts across the country will close gaps, overcome threats, and turn around troublesome trends.”
The press release cited local work in Washington and New York as evidence that targeted resources can make a difference in reducing new HIV cases. In these two areas, new infections dropped by 23% and 40% respectively from 2010 to 2016.
SOURCE: Centers for Disease Control. CDC Report: www.cdc.gov/hiv/library/reports/hiv-surveillance.html.
The annual number of new HIV infections has remained stable in recent years, and the Centers for Disease Control and Prevention says that’s not good – but solutions are at hand.
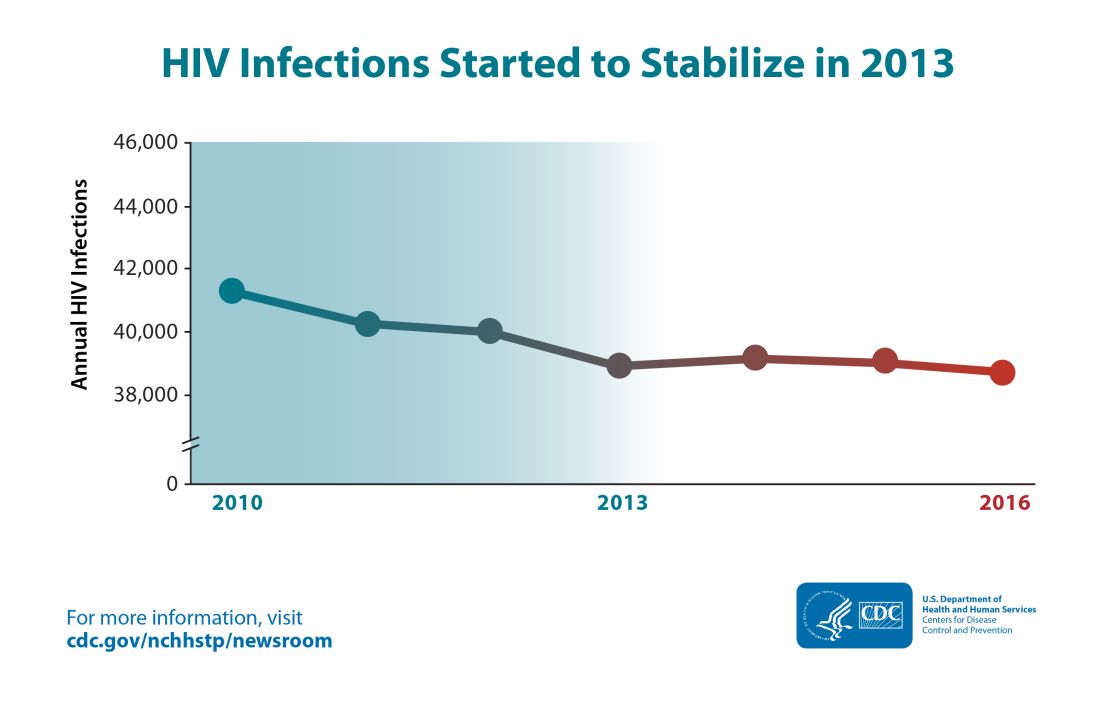
Though the estimated number of new HIV infections declined from just under 42,000 per year in 2010 to about 39,000 annually in 2013, that figure was essentially unchanged by 2016, with 38,700 new HIV infections seen that year.
“CDC estimates that the decline in HIV infections has plateaued because effective HIV prevention and treatment are not adequately reaching those who could most benefit from them. These gaps remain particularly troublesome in rural areas and in the South and among disproportionately affected populations like African Americans and Latinos,” said the CDC in a press release accompanying the report.
The report comes soon after President Trump’s State of the Union address, which announced a new multiagency initiative to eliminate the HIV epidemic in the United States, with the goal of reducing new HIV infections by 90% over the next 10 years. The multipronged initiative will implement geographically targeted HIV elimination teams in areas with high HIV prevalence, pulling together federal agencies, local and state governments, and community-level resources.
The initiative, called “Ending the Epidemic: A Plan for America” will combine an intensified approach to early diagnosis and treatment with efforts to boost uptake of pre-exposure prophylaxis for individuals at high risk for HIV infection.
The new CDC report used CD4 counts reported to the National HIV Surveillance System at the time of diagnosis to identify new (incident) cases and to track prevalence. Much of the report is devoted to finely detailed reporting of HIV incidence across sex, age, race/ethnicity, and transmission mode.
Though some groups, such as people who inject drugs, have seen a decrease of about 30% in the annual rate of new HIV cases, new cases have jumped for other groups. In particular, Latino gay and bisexual men saw new cases climb from 6,400 per year in 2010 to 8,300 in 2016. The incidence rate has stayed high and stable among African American gay and bisexual men, with 9,800 new cases reported in 2010; the same number was seen in 2016.
Among gay and bisexual men overall, the rate has also stayed stable, with about 26,000 new HIV infections reported at the beginning and end of the studied period. White heterosexual women saw about 1,000 new cases per year in 2010 and in 2016.
Some groups saw declines in new cases: African American and Latina heterosexual women each saw a falling incidence of new HIV cases. For the former group, new cases fell from 4,700 to 4,000, while the latter group of women saw new cases drop from 1,200 to 980 per year from 2010 to 2016.
Within these broad groups, HIV incidence also rose among some age groups and fell among others. Decreases were seen for younger African American gay and bisexual men (those aged 13-24 years), but rates increased by about two-thirds for men in this group aged 25-34 years. A similar increase was seen for Latino men in the 25-34 years age group, a change which drove the overall 30% increase in new infections for Latino gay and bisexual men.
White gay and bisexual men saw across-the-board decreases in new infections, though the overall decrease was less than 20%.
For heterosexual individuals as a group, new infections dropped by about 17%, from 10,900 to 9,100 annually. This change was driven mostly by decreases in women identifying as heterosexual.
“After a decades-long struggle, the path to eliminate America’s HIV epidemic is clear,” said Eugene McCray, MD, director of CDC’s Division of HIV/AIDS Prevention, in the press release. “Expanding efforts across the country will close gaps, overcome threats, and turn around troublesome trends.”
The press release cited local work in Washington and New York as evidence that targeted resources can make a difference in reducing new HIV cases. In these two areas, new infections dropped by 23% and 40% respectively from 2010 to 2016.
SOURCE: Centers for Disease Control. CDC Report: www.cdc.gov/hiv/library/reports/hiv-surveillance.html.