User login
‘Update in HM’ highlights top research
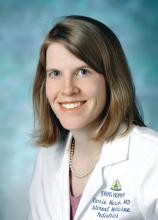
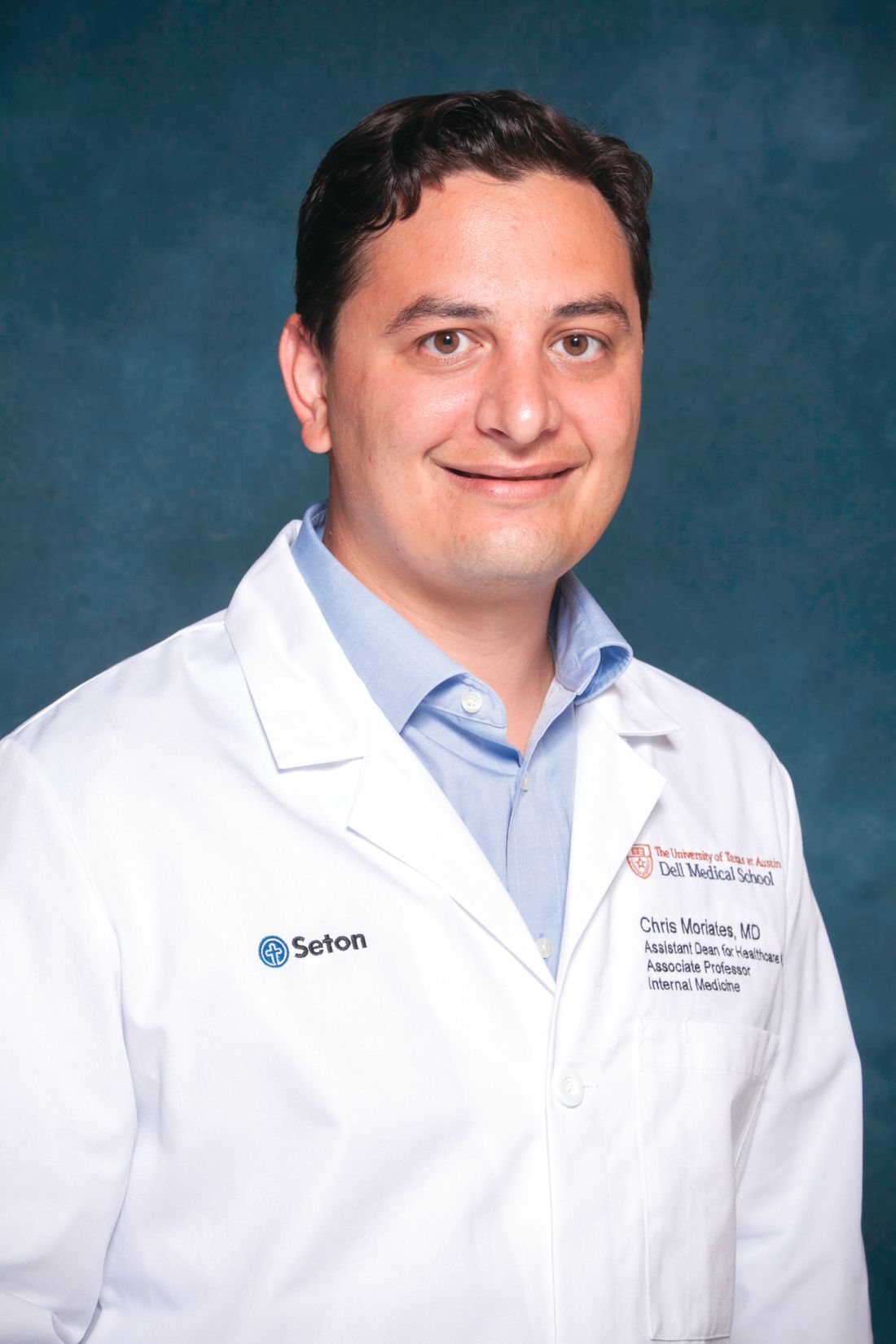
When Christopher Moriates, MD, SFHM, and Carrie Herzke, MD, SFHM, accepted the opportunity to present the “Update in Hospital Medicine” session at HM19, it was a big moment for both of them.
Not only will they headline one of the most popular sessions at the Annual Conference, but they also will be giving a talk on stage together for the first time. The possibility that it could all go wrong in front of more than 5,000 attendees at HM19 certainly crossed their minds.
“No matter what, it’ll be fun,” said Dr. Moriates, assistant dean for health care value at the University of Texas at Austin.
The aim of Tuesday afternoon’s session is to inform busy hospitalists of what they might have missed over the past year by highlighting the most important papers, from multiple specialties, that affect hospital medicine.
The two presenters may be familiar to hospitalists: Dr. Herzke, associate vice chair for clinical affairs in the department of medicine at Johns Hopkins Medicine in Baltimore, is a member of the SHM Academic Committee, the SHM Mentoring Subcommittee, and the Annual Conference Committee. Dr. Moriates is a regular contributor to The Hospital Leader, the official blog of SHM, and also has a personal connection to the “Update in Hospital Medicine” session.
“I watched with awe as my mentor, Michelle Mourad, MD, presented ‘Update in Hospital Medicine’ on the big stage at National Harbor in 2013,” Dr. Moriates said. “It is hard to imagine that I will be following her footsteps onto that same stage this year.”
Dr. Moriates and Dr. Herzke have spent months preparing for their presentation: Together, they have pored through a year’s worth of literature, narrowing down hundreds of studies to bring attendees the Top 20 papers with an impact on hospital medicine for the session. They each collected articles throughout the year, checking in regularly to outline the themes and rank papers for the session. In January, Dr. Moriates and Dr. Herzke reviewed all the articles they had collected, finalizing the major themes and highlights for the Update.
“The harder part was dropping a few of the articles we had selected in order to make it under an hour,” he said. “We tried to come up with the highlights that all hospitalists should know about, which are most likely to inform their practices over the coming year. And so, if you haven’t picked up a journal in a year, hopefully within an hour, Carrie and I can give you a quick download.”
Attendees familiar with “Update in Hospital Medicine” also will know that the exact details of what is being presented are secret. It is one of the few sessions at HM19 where slides are not published beforehand on the official Annual Conference app. The only way to know the details of the top studies is to attend the session.
“You have to be there to find out,” Dr. Moriates said.
But curiosity should not be the only reason for hospitalists to attend. Dr. Herzke said this year’s “Update in Hospital Medicine” session holds some practice pearls that may surprise attendees.
“We picked out some studies that we think should make people question common practices and consider making changes to how they practice medicine at their home institution, or their home hospital,” she said.
“It’s fair to say there were a number of studies this year that questioned conventional practices or put forth clear evidence that suggests we should be doing things differently in the hospital than the way we currently are doing them, across a number of scenarios,” Dr. Moriates said.
Attendees can expect studies in the fields of infectious disease, cardiology, and hematology to make the Top 20 list of best papers for the session. However, the challenge is always to present clinical pearls that apply to all hospitalists, regardless of where they practice.
“I think one thing about hospitalists is that our practices are very broad based, and we have to be up to date in lots of different fields,” Dr. Moriates said. “And so, we will cover the top literature across an array of fields matching the breadth and diversity of the patients that we take care of as hospitalists.”
Dr. Moriates and Dr. Herzke had no relevant financial conflicts.
Update in Hospital Medicine
Tuesday, 1:00 – 2:00 p.m.
Potomac ABCD
When Christopher Moriates, MD, SFHM, and Carrie Herzke, MD, SFHM, accepted the opportunity to present the “Update in Hospital Medicine” session at HM19, it was a big moment for both of them.
Not only will they headline one of the most popular sessions at the Annual Conference, but they also will be giving a talk on stage together for the first time. The possibility that it could all go wrong in front of more than 5,000 attendees at HM19 certainly crossed their minds.
“No matter what, it’ll be fun,” said Dr. Moriates, assistant dean for health care value at the University of Texas at Austin.
The aim of Tuesday afternoon’s session is to inform busy hospitalists of what they might have missed over the past year by highlighting the most important papers, from multiple specialties, that affect hospital medicine.
The two presenters may be familiar to hospitalists: Dr. Herzke, associate vice chair for clinical affairs in the department of medicine at Johns Hopkins Medicine in Baltimore, is a member of the SHM Academic Committee, the SHM Mentoring Subcommittee, and the Annual Conference Committee. Dr. Moriates is a regular contributor to The Hospital Leader, the official blog of SHM, and also has a personal connection to the “Update in Hospital Medicine” session.
“I watched with awe as my mentor, Michelle Mourad, MD, presented ‘Update in Hospital Medicine’ on the big stage at National Harbor in 2013,” Dr. Moriates said. “It is hard to imagine that I will be following her footsteps onto that same stage this year.”
Dr. Moriates and Dr. Herzke have spent months preparing for their presentation: Together, they have pored through a year’s worth of literature, narrowing down hundreds of studies to bring attendees the Top 20 papers with an impact on hospital medicine for the session. They each collected articles throughout the year, checking in regularly to outline the themes and rank papers for the session. In January, Dr. Moriates and Dr. Herzke reviewed all the articles they had collected, finalizing the major themes and highlights for the Update.
“The harder part was dropping a few of the articles we had selected in order to make it under an hour,” he said. “We tried to come up with the highlights that all hospitalists should know about, which are most likely to inform their practices over the coming year. And so, if you haven’t picked up a journal in a year, hopefully within an hour, Carrie and I can give you a quick download.”
Attendees familiar with “Update in Hospital Medicine” also will know that the exact details of what is being presented are secret. It is one of the few sessions at HM19 where slides are not published beforehand on the official Annual Conference app. The only way to know the details of the top studies is to attend the session.
“You have to be there to find out,” Dr. Moriates said.
But curiosity should not be the only reason for hospitalists to attend. Dr. Herzke said this year’s “Update in Hospital Medicine” session holds some practice pearls that may surprise attendees.
“We picked out some studies that we think should make people question common practices and consider making changes to how they practice medicine at their home institution, or their home hospital,” she said.
“It’s fair to say there were a number of studies this year that questioned conventional practices or put forth clear evidence that suggests we should be doing things differently in the hospital than the way we currently are doing them, across a number of scenarios,” Dr. Moriates said.
Attendees can expect studies in the fields of infectious disease, cardiology, and hematology to make the Top 20 list of best papers for the session. However, the challenge is always to present clinical pearls that apply to all hospitalists, regardless of where they practice.
“I think one thing about hospitalists is that our practices are very broad based, and we have to be up to date in lots of different fields,” Dr. Moriates said. “And so, we will cover the top literature across an array of fields matching the breadth and diversity of the patients that we take care of as hospitalists.”
Dr. Moriates and Dr. Herzke had no relevant financial conflicts.
Update in Hospital Medicine
Tuesday, 1:00 – 2:00 p.m.
Potomac ABCD
When Christopher Moriates, MD, SFHM, and Carrie Herzke, MD, SFHM, accepted the opportunity to present the “Update in Hospital Medicine” session at HM19, it was a big moment for both of them.
Not only will they headline one of the most popular sessions at the Annual Conference, but they also will be giving a talk on stage together for the first time. The possibility that it could all go wrong in front of more than 5,000 attendees at HM19 certainly crossed their minds.
“No matter what, it’ll be fun,” said Dr. Moriates, assistant dean for health care value at the University of Texas at Austin.
The aim of Tuesday afternoon’s session is to inform busy hospitalists of what they might have missed over the past year by highlighting the most important papers, from multiple specialties, that affect hospital medicine.
The two presenters may be familiar to hospitalists: Dr. Herzke, associate vice chair for clinical affairs in the department of medicine at Johns Hopkins Medicine in Baltimore, is a member of the SHM Academic Committee, the SHM Mentoring Subcommittee, and the Annual Conference Committee. Dr. Moriates is a regular contributor to The Hospital Leader, the official blog of SHM, and also has a personal connection to the “Update in Hospital Medicine” session.
“I watched with awe as my mentor, Michelle Mourad, MD, presented ‘Update in Hospital Medicine’ on the big stage at National Harbor in 2013,” Dr. Moriates said. “It is hard to imagine that I will be following her footsteps onto that same stage this year.”
Dr. Moriates and Dr. Herzke have spent months preparing for their presentation: Together, they have pored through a year’s worth of literature, narrowing down hundreds of studies to bring attendees the Top 20 papers with an impact on hospital medicine for the session. They each collected articles throughout the year, checking in regularly to outline the themes and rank papers for the session. In January, Dr. Moriates and Dr. Herzke reviewed all the articles they had collected, finalizing the major themes and highlights for the Update.
“The harder part was dropping a few of the articles we had selected in order to make it under an hour,” he said. “We tried to come up with the highlights that all hospitalists should know about, which are most likely to inform their practices over the coming year. And so, if you haven’t picked up a journal in a year, hopefully within an hour, Carrie and I can give you a quick download.”
Attendees familiar with “Update in Hospital Medicine” also will know that the exact details of what is being presented are secret. It is one of the few sessions at HM19 where slides are not published beforehand on the official Annual Conference app. The only way to know the details of the top studies is to attend the session.
“You have to be there to find out,” Dr. Moriates said.
But curiosity should not be the only reason for hospitalists to attend. Dr. Herzke said this year’s “Update in Hospital Medicine” session holds some practice pearls that may surprise attendees.
“We picked out some studies that we think should make people question common practices and consider making changes to how they practice medicine at their home institution, or their home hospital,” she said.
“It’s fair to say there were a number of studies this year that questioned conventional practices or put forth clear evidence that suggests we should be doing things differently in the hospital than the way we currently are doing them, across a number of scenarios,” Dr. Moriates said.
Attendees can expect studies in the fields of infectious disease, cardiology, and hematology to make the Top 20 list of best papers for the session. However, the challenge is always to present clinical pearls that apply to all hospitalists, regardless of where they practice.
“I think one thing about hospitalists is that our practices are very broad based, and we have to be up to date in lots of different fields,” Dr. Moriates said. “And so, we will cover the top literature across an array of fields matching the breadth and diversity of the patients that we take care of as hospitalists.”
Dr. Moriates and Dr. Herzke had no relevant financial conflicts.
Update in Hospital Medicine
Tuesday, 1:00 – 2:00 p.m.
Potomac ABCD
What’s your favorite aspect of HM19?
Attendees explain what they enjoy about the Annual Conference.

Attendees explain what they enjoy about the Annual Conference.

Attendees explain what they enjoy about the Annual Conference.

Female radiation oncologists taking in smaller Medicare payments
Female radiation oncologists are receiving less reimbursement from Medicare, compared with their male counterparts, according to a new study.
An examination of Medicare claims submitted by 4,393 radiation oncologists in 2016 (1,133 women) revealed that female physicians in the non–facility-based setting submitted a mean of 1,051 fewer charges, collected a mean of $143,610 less in revenue, and used a mean of 1.32 fewer billing codes. In the facility-based setting, female radiation oncologists submitted a mean of 423 fewer charges, collected a mean of $26,735 less in revenue, and submitted a mean of 1.28 fewer billing codes.
Additionally, the study noted that women accounted for 46 of the 397 most highly productive radiation oncologists in the facility-based setting and collected a mean of $33,206 less than men who were similarly productive. In the non–facility-based setting, women represented 54 of the 326 most highly productive radiation oncologists and collected $345,944 less than similarly productive men.
“Our study illustrates a gap between the sexes in Medicare charges and collection for radiation oncologists, the latter of which is possibly attributable to female physicians consistently submitting fewer charges and charging for services that are less well reimbursed,” Luca Valle, MD, of the University of California, Los Angeles, and colleagues wrote in JAMA Network Open.
The authors identified a number of factors that could be contributing to the discrepancy, the first of which could be traditional gender roles, particularly related to domestic responsibilities.
“A flexible work schedule and opportunities for part-time employment have been shown to be attractive options for female radiation oncologists; thus less clinical activity may be a natural consequence of the value-based labor choices that female practitioners make, particularly within a sex-structured society within which women continue to be expected to shoulder a greater share of domestic responsibilities,” Dr. Valle and colleagues wrote.
The authors also suggested that women “prioritize time spent with a given patient versus number of patients seen, and that extra time spent counseling patients is not reflected in HCPCS [Healthcare Common Procedure Coding System] code volume.”
Another possibility is the ongoing issues of gender discrimination, leaving female physicians to receive less referrals and fewer opportunities to care for patients, despite the authors noting that there is “no evidence to suggest that women are less competent and have more limited aspirations for their medical careers than men.”
Also contributing to the discrepancy is that women may have a greater portion of less well-reimbursed technologies (that is, three-dimensional conformal therapies used for treating breast cancer) rather than more favorably reimbursed technologies, such as intensity modulation radiation therapy, which is typically used for treating genitourinary malignant neoplasms.
“The sex-based distinctions in subspecialization may develop because men are more attuned to the possibility of differences in revenue generation, or because radiation oncology subspecialties that women choose [or are encouraged to choose] involve less revenue-generating ‘communal’ attributes rather than more favorably reimbursed ‘agentic’ attributes,” Dr. Valle and colleagues wrote.
The authors also suggest that it is possible that, when presented with multiple treatment options, female radiation oncologists are more likely to choose the more cost-effective option, “as women in other specialties have shown to adhere more closely to clinical guidelines, practice value-based care, forgo costly interventions, and engage in shared decision making with patients more frequently.”
The authors noted that the study was limited by using only Medicare payment data and it is not clear whether the same pattern occurs in different payer environments, such as Medicare Advantage or commercial insurance. It is also limited by the snapshot of a single year.
One coauthor reported receiving stock options from Equity Quotient; personal fees from Amgen and Vizient; and grants from the National Institutes of Health, the Doris Duke Foundation, the Greenwall Foundation, the Komen Foundation, and Blue Cross Blue Shield of Michigan; another reported receiving personal fees from ViewRay.
SOURCE: Valle L et al. JAMA Netw Open. 2019 Mar 22. doi: 10.1001/jamanetworkopen.2019.0932.
Female radiation oncologists are receiving less reimbursement from Medicare, compared with their male counterparts, according to a new study.
An examination of Medicare claims submitted by 4,393 radiation oncologists in 2016 (1,133 women) revealed that female physicians in the non–facility-based setting submitted a mean of 1,051 fewer charges, collected a mean of $143,610 less in revenue, and used a mean of 1.32 fewer billing codes. In the facility-based setting, female radiation oncologists submitted a mean of 423 fewer charges, collected a mean of $26,735 less in revenue, and submitted a mean of 1.28 fewer billing codes.
Additionally, the study noted that women accounted for 46 of the 397 most highly productive radiation oncologists in the facility-based setting and collected a mean of $33,206 less than men who were similarly productive. In the non–facility-based setting, women represented 54 of the 326 most highly productive radiation oncologists and collected $345,944 less than similarly productive men.
“Our study illustrates a gap between the sexes in Medicare charges and collection for radiation oncologists, the latter of which is possibly attributable to female physicians consistently submitting fewer charges and charging for services that are less well reimbursed,” Luca Valle, MD, of the University of California, Los Angeles, and colleagues wrote in JAMA Network Open.
The authors identified a number of factors that could be contributing to the discrepancy, the first of which could be traditional gender roles, particularly related to domestic responsibilities.
“A flexible work schedule and opportunities for part-time employment have been shown to be attractive options for female radiation oncologists; thus less clinical activity may be a natural consequence of the value-based labor choices that female practitioners make, particularly within a sex-structured society within which women continue to be expected to shoulder a greater share of domestic responsibilities,” Dr. Valle and colleagues wrote.
The authors also suggested that women “prioritize time spent with a given patient versus number of patients seen, and that extra time spent counseling patients is not reflected in HCPCS [Healthcare Common Procedure Coding System] code volume.”
Another possibility is the ongoing issues of gender discrimination, leaving female physicians to receive less referrals and fewer opportunities to care for patients, despite the authors noting that there is “no evidence to suggest that women are less competent and have more limited aspirations for their medical careers than men.”
Also contributing to the discrepancy is that women may have a greater portion of less well-reimbursed technologies (that is, three-dimensional conformal therapies used for treating breast cancer) rather than more favorably reimbursed technologies, such as intensity modulation radiation therapy, which is typically used for treating genitourinary malignant neoplasms.
“The sex-based distinctions in subspecialization may develop because men are more attuned to the possibility of differences in revenue generation, or because radiation oncology subspecialties that women choose [or are encouraged to choose] involve less revenue-generating ‘communal’ attributes rather than more favorably reimbursed ‘agentic’ attributes,” Dr. Valle and colleagues wrote.
The authors also suggest that it is possible that, when presented with multiple treatment options, female radiation oncologists are more likely to choose the more cost-effective option, “as women in other specialties have shown to adhere more closely to clinical guidelines, practice value-based care, forgo costly interventions, and engage in shared decision making with patients more frequently.”
The authors noted that the study was limited by using only Medicare payment data and it is not clear whether the same pattern occurs in different payer environments, such as Medicare Advantage or commercial insurance. It is also limited by the snapshot of a single year.
One coauthor reported receiving stock options from Equity Quotient; personal fees from Amgen and Vizient; and grants from the National Institutes of Health, the Doris Duke Foundation, the Greenwall Foundation, the Komen Foundation, and Blue Cross Blue Shield of Michigan; another reported receiving personal fees from ViewRay.
SOURCE: Valle L et al. JAMA Netw Open. 2019 Mar 22. doi: 10.1001/jamanetworkopen.2019.0932.
Female radiation oncologists are receiving less reimbursement from Medicare, compared with their male counterparts, according to a new study.
An examination of Medicare claims submitted by 4,393 radiation oncologists in 2016 (1,133 women) revealed that female physicians in the non–facility-based setting submitted a mean of 1,051 fewer charges, collected a mean of $143,610 less in revenue, and used a mean of 1.32 fewer billing codes. In the facility-based setting, female radiation oncologists submitted a mean of 423 fewer charges, collected a mean of $26,735 less in revenue, and submitted a mean of 1.28 fewer billing codes.
Additionally, the study noted that women accounted for 46 of the 397 most highly productive radiation oncologists in the facility-based setting and collected a mean of $33,206 less than men who were similarly productive. In the non–facility-based setting, women represented 54 of the 326 most highly productive radiation oncologists and collected $345,944 less than similarly productive men.
“Our study illustrates a gap between the sexes in Medicare charges and collection for radiation oncologists, the latter of which is possibly attributable to female physicians consistently submitting fewer charges and charging for services that are less well reimbursed,” Luca Valle, MD, of the University of California, Los Angeles, and colleagues wrote in JAMA Network Open.
The authors identified a number of factors that could be contributing to the discrepancy, the first of which could be traditional gender roles, particularly related to domestic responsibilities.
“A flexible work schedule and opportunities for part-time employment have been shown to be attractive options for female radiation oncologists; thus less clinical activity may be a natural consequence of the value-based labor choices that female practitioners make, particularly within a sex-structured society within which women continue to be expected to shoulder a greater share of domestic responsibilities,” Dr. Valle and colleagues wrote.
The authors also suggested that women “prioritize time spent with a given patient versus number of patients seen, and that extra time spent counseling patients is not reflected in HCPCS [Healthcare Common Procedure Coding System] code volume.”
Another possibility is the ongoing issues of gender discrimination, leaving female physicians to receive less referrals and fewer opportunities to care for patients, despite the authors noting that there is “no evidence to suggest that women are less competent and have more limited aspirations for their medical careers than men.”
Also contributing to the discrepancy is that women may have a greater portion of less well-reimbursed technologies (that is, three-dimensional conformal therapies used for treating breast cancer) rather than more favorably reimbursed technologies, such as intensity modulation radiation therapy, which is typically used for treating genitourinary malignant neoplasms.
“The sex-based distinctions in subspecialization may develop because men are more attuned to the possibility of differences in revenue generation, or because radiation oncology subspecialties that women choose [or are encouraged to choose] involve less revenue-generating ‘communal’ attributes rather than more favorably reimbursed ‘agentic’ attributes,” Dr. Valle and colleagues wrote.
The authors also suggest that it is possible that, when presented with multiple treatment options, female radiation oncologists are more likely to choose the more cost-effective option, “as women in other specialties have shown to adhere more closely to clinical guidelines, practice value-based care, forgo costly interventions, and engage in shared decision making with patients more frequently.”
The authors noted that the study was limited by using only Medicare payment data and it is not clear whether the same pattern occurs in different payer environments, such as Medicare Advantage or commercial insurance. It is also limited by the snapshot of a single year.
One coauthor reported receiving stock options from Equity Quotient; personal fees from Amgen and Vizient; and grants from the National Institutes of Health, the Doris Duke Foundation, the Greenwall Foundation, the Komen Foundation, and Blue Cross Blue Shield of Michigan; another reported receiving personal fees from ViewRay.
SOURCE: Valle L et al. JAMA Netw Open. 2019 Mar 22. doi: 10.1001/jamanetworkopen.2019.0932.
FROM JAMA NETWORK OPEN
Surge of gabapentinoids for pain lacks supporting evidence
Many clinicians are prescribing the gabapentinoid drugs pregabalin (Lyrica) and gabapentin (Neurontin) for off-label treatment of pain, despite a lack of supporting data or approval from the Food and Drug Administration, according to investigators.
Over the past 15 years, use of gabapentinoids has tripled, a level of growth that cannot be explained by prescriptions for approved indications, reported coauthors Christopher W. Goodman, MD, and Allan S. Brett, MD, of the University of South Carolina, Columbia. Instead, clinicians are turning to gabapentinoids, partly as an option to substitute for opioids, which now have greater prescribing restrictions as a result of the current opioid crisis.
Although clinicians may cite guidelines that support off-label use of gabapentinoids for pain, the investigators warned that many of these recommendations stand on shaky ground.
“Clinicians who prescribe gabapentinoids off-label for pain should be aware of the limited evidence and should acknowledge to patients that potential benefits are uncertain for most off-label uses,” the investigators wrote in a clinical review published online March 25 in JAMA Internal Medicine.
The investigators narrowed down 677 publications to 84 papers describing the use of gabapentinoids for outpatient noncancer pain syndromes for which they are not FDA approved; 54 for gabapentin and 30 for pregabalin. In the domain of analgesia, both agents are currently FDA-approved for postherpetic neuralgia, while pregabalin is additionally approved for pain associated with fibromyalgia and neuropathic pain from diabetic neuropathy and spinal cord injury. Indications in reviewed studies ranged broadly, from conditions somewhat related to those currently approved, such as unspecified neuropathy, to dissimilar conditions, such as chronic pancreatitis and burn injury.
The investigators summarized findings from randomized clinical trials while using case studies to illustrate potential problems with off-label use. In addition, they reviewed the history of gabapentinoids and sources of recommendations for off-label use, such as guidelines and previous review articles.
Six major findings were reported: (1) evidence supporting gabapentin for diabetic neuropathy pain is “mixed at best”; (2) evidence supporting gabapentin for nondiabetic neuropathies is very limited; (3) evidence does not support gabapentinoids for radiculopathy or low back pain; (4) gabapentin has minimal benefit for fibromyalgia pain, based on minimal evidence; (5) evidence does not support gabapentinoids for acute herpes zoster pain; and (6) in almost all studies for other painful indications, gabapentinoids were ineffective or “associated with small analgesic effects that were statistically significant but of questionable clinical importance.”
Case studies complemented this overview, highlighting related clinical dilemmas that the investigators encounter “repeatedly” during inpatient and outpatient care. Along with off-label use, such as gabapentinoid prescriptions for acute sciatica, the investigators reported cases in which neuropathy was diagnosed in place of nonspecific lower body pain to facilitate gabapentin prescription. They also described apparent disregard for risks of polypharmacy in prescriptions for elderly patients and rote use of gabapentinoids in patients with diabetic neuropathy who did not have sufficient discomfort to warrant prescription.
The investigators also cited a number of problems with the language of reviews and guidelines involving gabapentinoids.
“The wording in many guidelines and review articles reinforces an inflated view of gabapentinoid effectiveness or fails to distinguish carefully between evidence-based and non–evidence-based recommendations,” they wrote, adding that clinicians may have misconceptions about neuropathic pain. “One unintended effect of the broad definition [of neuropathic pain] might be to create a mistaken perception that an effective drug for one type of neuropathic pain is effective for all neuropathic pain, regardless of underlying etiology or mechanism,” the investigators suggested.
Another facet of prescribing behavior could be explained in economic terms. Pregabalin, sold under the brand name Lyrica, is considerably more expensive than gabapentin; however, the investigators warned that the similarity of these agents does not equate with interchangeability, noting differences in bioavailability and rate of absorption.
“Unfortunately, published direct comparisons between the 2 drugs in double-blind studies of patients with chronic noncancer pain are virtually nonexistent,” the investigators wrote.
In addition to questionable effectiveness of gabapentinoids for off-label chronic noncancer pain syndromes, Dr. Goodman and Dr. Brett noted that the drugs produce a “substantial incidence of dizziness, somnolence, and gait disturbance.”
They also described a new trend of gabapentinoid abuse and diversion, which may not be surprising, considering that gabapentinoids are reported to augment opioid-induced euphoria.
“Evidence of misuse of gabapentinoids is accumulating and likely related to the opioid epidemic. A recent review article reported an overall population prevalence of gabapentinoid ‘misuse and abuse’ as high as 1%, with substantially higher prevalence noted among patients with opioid use disorders,” the investigators wrote. “This trend is troubling, particularly because concomitant use of opioids and gabapentinoids is associated with increased odds of opioid-related death. Whether these concerns apply to patients receiving long-term prescribed opioid therapy is unclear.”
In the era of the opioid crisis, the investigators acknowledged that many clinicians have serious concerns about adequately treating chronic noncancer pain.
“Comprehensive management of pain in primary care settings is difficult. It requires time and resources that are frequently unavailable,” the investigators wrote. “Many patients with chronic pain have limited or no access to high-quality pain practices or to nonpharmacologic interventions, such as cognitive behavior therapy.”
The investigators reported no external funding or conflicts of interest.
SOURCE: Goodman CW et al. JAMA Intern Med. 2019 Mar 25. doi: 10.1001/jamainternmed.2019.0086
Many clinicians are prescribing the gabapentinoid drugs pregabalin (Lyrica) and gabapentin (Neurontin) for off-label treatment of pain, despite a lack of supporting data or approval from the Food and Drug Administration, according to investigators.
Over the past 15 years, use of gabapentinoids has tripled, a level of growth that cannot be explained by prescriptions for approved indications, reported coauthors Christopher W. Goodman, MD, and Allan S. Brett, MD, of the University of South Carolina, Columbia. Instead, clinicians are turning to gabapentinoids, partly as an option to substitute for opioids, which now have greater prescribing restrictions as a result of the current opioid crisis.
Although clinicians may cite guidelines that support off-label use of gabapentinoids for pain, the investigators warned that many of these recommendations stand on shaky ground.
“Clinicians who prescribe gabapentinoids off-label for pain should be aware of the limited evidence and should acknowledge to patients that potential benefits are uncertain for most off-label uses,” the investigators wrote in a clinical review published online March 25 in JAMA Internal Medicine.
The investigators narrowed down 677 publications to 84 papers describing the use of gabapentinoids for outpatient noncancer pain syndromes for which they are not FDA approved; 54 for gabapentin and 30 for pregabalin. In the domain of analgesia, both agents are currently FDA-approved for postherpetic neuralgia, while pregabalin is additionally approved for pain associated with fibromyalgia and neuropathic pain from diabetic neuropathy and spinal cord injury. Indications in reviewed studies ranged broadly, from conditions somewhat related to those currently approved, such as unspecified neuropathy, to dissimilar conditions, such as chronic pancreatitis and burn injury.
The investigators summarized findings from randomized clinical trials while using case studies to illustrate potential problems with off-label use. In addition, they reviewed the history of gabapentinoids and sources of recommendations for off-label use, such as guidelines and previous review articles.
Six major findings were reported: (1) evidence supporting gabapentin for diabetic neuropathy pain is “mixed at best”; (2) evidence supporting gabapentin for nondiabetic neuropathies is very limited; (3) evidence does not support gabapentinoids for radiculopathy or low back pain; (4) gabapentin has minimal benefit for fibromyalgia pain, based on minimal evidence; (5) evidence does not support gabapentinoids for acute herpes zoster pain; and (6) in almost all studies for other painful indications, gabapentinoids were ineffective or “associated with small analgesic effects that were statistically significant but of questionable clinical importance.”
Case studies complemented this overview, highlighting related clinical dilemmas that the investigators encounter “repeatedly” during inpatient and outpatient care. Along with off-label use, such as gabapentinoid prescriptions for acute sciatica, the investigators reported cases in which neuropathy was diagnosed in place of nonspecific lower body pain to facilitate gabapentin prescription. They also described apparent disregard for risks of polypharmacy in prescriptions for elderly patients and rote use of gabapentinoids in patients with diabetic neuropathy who did not have sufficient discomfort to warrant prescription.
The investigators also cited a number of problems with the language of reviews and guidelines involving gabapentinoids.
“The wording in many guidelines and review articles reinforces an inflated view of gabapentinoid effectiveness or fails to distinguish carefully between evidence-based and non–evidence-based recommendations,” they wrote, adding that clinicians may have misconceptions about neuropathic pain. “One unintended effect of the broad definition [of neuropathic pain] might be to create a mistaken perception that an effective drug for one type of neuropathic pain is effective for all neuropathic pain, regardless of underlying etiology or mechanism,” the investigators suggested.
Another facet of prescribing behavior could be explained in economic terms. Pregabalin, sold under the brand name Lyrica, is considerably more expensive than gabapentin; however, the investigators warned that the similarity of these agents does not equate with interchangeability, noting differences in bioavailability and rate of absorption.
“Unfortunately, published direct comparisons between the 2 drugs in double-blind studies of patients with chronic noncancer pain are virtually nonexistent,” the investigators wrote.
In addition to questionable effectiveness of gabapentinoids for off-label chronic noncancer pain syndromes, Dr. Goodman and Dr. Brett noted that the drugs produce a “substantial incidence of dizziness, somnolence, and gait disturbance.”
They also described a new trend of gabapentinoid abuse and diversion, which may not be surprising, considering that gabapentinoids are reported to augment opioid-induced euphoria.
“Evidence of misuse of gabapentinoids is accumulating and likely related to the opioid epidemic. A recent review article reported an overall population prevalence of gabapentinoid ‘misuse and abuse’ as high as 1%, with substantially higher prevalence noted among patients with opioid use disorders,” the investigators wrote. “This trend is troubling, particularly because concomitant use of opioids and gabapentinoids is associated with increased odds of opioid-related death. Whether these concerns apply to patients receiving long-term prescribed opioid therapy is unclear.”
In the era of the opioid crisis, the investigators acknowledged that many clinicians have serious concerns about adequately treating chronic noncancer pain.
“Comprehensive management of pain in primary care settings is difficult. It requires time and resources that are frequently unavailable,” the investigators wrote. “Many patients with chronic pain have limited or no access to high-quality pain practices or to nonpharmacologic interventions, such as cognitive behavior therapy.”
The investigators reported no external funding or conflicts of interest.
SOURCE: Goodman CW et al. JAMA Intern Med. 2019 Mar 25. doi: 10.1001/jamainternmed.2019.0086
Many clinicians are prescribing the gabapentinoid drugs pregabalin (Lyrica) and gabapentin (Neurontin) for off-label treatment of pain, despite a lack of supporting data or approval from the Food and Drug Administration, according to investigators.
Over the past 15 years, use of gabapentinoids has tripled, a level of growth that cannot be explained by prescriptions for approved indications, reported coauthors Christopher W. Goodman, MD, and Allan S. Brett, MD, of the University of South Carolina, Columbia. Instead, clinicians are turning to gabapentinoids, partly as an option to substitute for opioids, which now have greater prescribing restrictions as a result of the current opioid crisis.
Although clinicians may cite guidelines that support off-label use of gabapentinoids for pain, the investigators warned that many of these recommendations stand on shaky ground.
“Clinicians who prescribe gabapentinoids off-label for pain should be aware of the limited evidence and should acknowledge to patients that potential benefits are uncertain for most off-label uses,” the investigators wrote in a clinical review published online March 25 in JAMA Internal Medicine.
The investigators narrowed down 677 publications to 84 papers describing the use of gabapentinoids for outpatient noncancer pain syndromes for which they are not FDA approved; 54 for gabapentin and 30 for pregabalin. In the domain of analgesia, both agents are currently FDA-approved for postherpetic neuralgia, while pregabalin is additionally approved for pain associated with fibromyalgia and neuropathic pain from diabetic neuropathy and spinal cord injury. Indications in reviewed studies ranged broadly, from conditions somewhat related to those currently approved, such as unspecified neuropathy, to dissimilar conditions, such as chronic pancreatitis and burn injury.
The investigators summarized findings from randomized clinical trials while using case studies to illustrate potential problems with off-label use. In addition, they reviewed the history of gabapentinoids and sources of recommendations for off-label use, such as guidelines and previous review articles.
Six major findings were reported: (1) evidence supporting gabapentin for diabetic neuropathy pain is “mixed at best”; (2) evidence supporting gabapentin for nondiabetic neuropathies is very limited; (3) evidence does not support gabapentinoids for radiculopathy or low back pain; (4) gabapentin has minimal benefit for fibromyalgia pain, based on minimal evidence; (5) evidence does not support gabapentinoids for acute herpes zoster pain; and (6) in almost all studies for other painful indications, gabapentinoids were ineffective or “associated with small analgesic effects that were statistically significant but of questionable clinical importance.”
Case studies complemented this overview, highlighting related clinical dilemmas that the investigators encounter “repeatedly” during inpatient and outpatient care. Along with off-label use, such as gabapentinoid prescriptions for acute sciatica, the investigators reported cases in which neuropathy was diagnosed in place of nonspecific lower body pain to facilitate gabapentin prescription. They also described apparent disregard for risks of polypharmacy in prescriptions for elderly patients and rote use of gabapentinoids in patients with diabetic neuropathy who did not have sufficient discomfort to warrant prescription.
The investigators also cited a number of problems with the language of reviews and guidelines involving gabapentinoids.
“The wording in many guidelines and review articles reinforces an inflated view of gabapentinoid effectiveness or fails to distinguish carefully between evidence-based and non–evidence-based recommendations,” they wrote, adding that clinicians may have misconceptions about neuropathic pain. “One unintended effect of the broad definition [of neuropathic pain] might be to create a mistaken perception that an effective drug for one type of neuropathic pain is effective for all neuropathic pain, regardless of underlying etiology or mechanism,” the investigators suggested.
Another facet of prescribing behavior could be explained in economic terms. Pregabalin, sold under the brand name Lyrica, is considerably more expensive than gabapentin; however, the investigators warned that the similarity of these agents does not equate with interchangeability, noting differences in bioavailability and rate of absorption.
“Unfortunately, published direct comparisons between the 2 drugs in double-blind studies of patients with chronic noncancer pain are virtually nonexistent,” the investigators wrote.
In addition to questionable effectiveness of gabapentinoids for off-label chronic noncancer pain syndromes, Dr. Goodman and Dr. Brett noted that the drugs produce a “substantial incidence of dizziness, somnolence, and gait disturbance.”
They also described a new trend of gabapentinoid abuse and diversion, which may not be surprising, considering that gabapentinoids are reported to augment opioid-induced euphoria.
“Evidence of misuse of gabapentinoids is accumulating and likely related to the opioid epidemic. A recent review article reported an overall population prevalence of gabapentinoid ‘misuse and abuse’ as high as 1%, with substantially higher prevalence noted among patients with opioid use disorders,” the investigators wrote. “This trend is troubling, particularly because concomitant use of opioids and gabapentinoids is associated with increased odds of opioid-related death. Whether these concerns apply to patients receiving long-term prescribed opioid therapy is unclear.”
In the era of the opioid crisis, the investigators acknowledged that many clinicians have serious concerns about adequately treating chronic noncancer pain.
“Comprehensive management of pain in primary care settings is difficult. It requires time and resources that are frequently unavailable,” the investigators wrote. “Many patients with chronic pain have limited or no access to high-quality pain practices or to nonpharmacologic interventions, such as cognitive behavior therapy.”
The investigators reported no external funding or conflicts of interest.
SOURCE: Goodman CW et al. JAMA Intern Med. 2019 Mar 25. doi: 10.1001/jamainternmed.2019.0086
FROM JAMA INTERNAL MEDICINE
Long-acting injectables noninferior to tablet integrase for HIV
SEATTLE – A long-acting, injectable combination of the novel integrase inhibitor cabotegravir (CAB) and the second-generation nonnucleoside reverse transcriptase inhibitor rilpivirine (RPV) was noninferior to dolutegravir/abacavir/lamivudine (DTG/ABC/3TC) in one phase 3 study (FLAIR) and to three-drug oral antiretroviral therapy (ART) more broadly in the companion ATLAS phase 3 study. Patient acceptance of the injectable formulation was surprisingly high, although researchers admitted there was likely some selection bias because patients already interested in receiving an injection would have been predisposed to entering the trials.
Still, the numbers were impressive: 99% of patients who received the intramuscular injection expressed more satisfaction with it than with their previous oral regimen in the FLAIR study, and 98% expressed a similar opinion in the ATLAS study. Circumstantial evidence also suggests there may be some demand, according to Joseph Eron, MD, professor of medicine at the University of North Carolina at Chapel Hill, who commented during a press conference at the Conference on Retroviruses & Opportunistic Infections. “These studies didn’t take a long time to accrue. People were very interested, so it wasn’t as if people had to go around and beat the bushes to try to find people [to participate],” said Dr. Eron, who was not an author on either report.
“My patients tell me that they like not having to worry about taking their pills every day. There may be some relief from the stigma of HIV. You don’t have to think about it,” Susan Swindells, MBBS, medical director of the Specialty Care Clinic at the University of Nebraska Medical Center in Omaha and first author of the ATLAS trial, said during the press conference.
There were some injection site reactions, but they were generally mild and most resolved within 7 days. In the ATLAS study, 75% of participants reported injection site pain, and 1% discontinued as a result. In the FLAIR study, 82% in the CAB/RPV arm experienced an injection site reaction, with a median duration of 3 days; 99% of reactions were grade 1 or 2.
Should the combination achieve regulatory approval, it remains to be seen how challenging it will be to manage patients with monthly injections and ensure they stick to the schedule. The injections must be administered by a health care provider.
“In terms of generalizability outside of the study, it would be a paradigm shift in our therapy,” Chloe Orkin, MBBCh, said at a press conference. Dr. Orkin is the first author on the FLAIR trial report and a consultant in HIV Medicine at Barts Health National Health Service Trust. She pointed to the example of injectable contraception. “It can be done. It’s just that we haven’t done it. It will require some thought,” Dr. Orkin added.
In the ATLAS study, 616 participants taking two nucleoside reverse transcriptase inhibitor (NRTIs) and an integrase inhibitor, a non-NRTI, or a protease inhibitor, were randomized 1:1 to continue their regimen (CART arm) or switch to CAB/RPV, following a 4-week safety monitoring period of oral CAB/RPV. After 48 weeks, 1.6% in the CAB/RPV arm and 1.0% in the CART arm had HIV-1 RNA greater than or equal to 50 copies/mL, which met the prespecified noninferiority margin. Of patients in the CAB/RPV arm, 93% had HIV-1 RNA less than 50 copies/mL at week 48 versus 95% in the CART arm, and the difference was not statistically significant. Grade 3 or 4 events were seen in 11% of CAB/RPV and 7% of CART patients.
The FLAIR study randomized 566 ART-naive patients to receive either CAB/RPV or DTG/ABC/3TC after a 20-week induction phase, followed by a 4-week safety monitoring period for those going into the CAB/RPV arm. At week 48, 2.1% in the CAB/RPV arm and 2.5% in the DTG/ABC/3TC arm had HIV-1 RNA greater than or equal to 50 copies/mL, which met the prespecified noninferiority margin, while 94% in the CAB/RPV arm and 93% in the DTG/ABC/3TC arm had HIV-1 RNA less than 50 copies/mL. Confirmed virologic failure occurred in four patients (1.4%) in the CAB/RPV arm, and three of those patients had mutations in the NNRTI+INSTI domains, while the fourth patient was not tested. Three failures occurred in the DTG/ABC/3TC arm, and none of those patients had INSTI resistance mutations. A total of 82% of CAB/RPV patients had injection site reactions, 99% of which were grade 1 or 2, and the median duration was 3 days.
The ATLAS and FLAIR studies were sponsored by ViiV. Janssen and GlaxoSmithKline were collaborators.
SOURCES: Swindells S et al. CROI 2019, Abstract 139 LB. Orkin C et al. CROI 2019, Abstract 140.
SEATTLE – A long-acting, injectable combination of the novel integrase inhibitor cabotegravir (CAB) and the second-generation nonnucleoside reverse transcriptase inhibitor rilpivirine (RPV) was noninferior to dolutegravir/abacavir/lamivudine (DTG/ABC/3TC) in one phase 3 study (FLAIR) and to three-drug oral antiretroviral therapy (ART) more broadly in the companion ATLAS phase 3 study. Patient acceptance of the injectable formulation was surprisingly high, although researchers admitted there was likely some selection bias because patients already interested in receiving an injection would have been predisposed to entering the trials.
Still, the numbers were impressive: 99% of patients who received the intramuscular injection expressed more satisfaction with it than with their previous oral regimen in the FLAIR study, and 98% expressed a similar opinion in the ATLAS study. Circumstantial evidence also suggests there may be some demand, according to Joseph Eron, MD, professor of medicine at the University of North Carolina at Chapel Hill, who commented during a press conference at the Conference on Retroviruses & Opportunistic Infections. “These studies didn’t take a long time to accrue. People were very interested, so it wasn’t as if people had to go around and beat the bushes to try to find people [to participate],” said Dr. Eron, who was not an author on either report.
“My patients tell me that they like not having to worry about taking their pills every day. There may be some relief from the stigma of HIV. You don’t have to think about it,” Susan Swindells, MBBS, medical director of the Specialty Care Clinic at the University of Nebraska Medical Center in Omaha and first author of the ATLAS trial, said during the press conference.
There were some injection site reactions, but they were generally mild and most resolved within 7 days. In the ATLAS study, 75% of participants reported injection site pain, and 1% discontinued as a result. In the FLAIR study, 82% in the CAB/RPV arm experienced an injection site reaction, with a median duration of 3 days; 99% of reactions were grade 1 or 2.
Should the combination achieve regulatory approval, it remains to be seen how challenging it will be to manage patients with monthly injections and ensure they stick to the schedule. The injections must be administered by a health care provider.
“In terms of generalizability outside of the study, it would be a paradigm shift in our therapy,” Chloe Orkin, MBBCh, said at a press conference. Dr. Orkin is the first author on the FLAIR trial report and a consultant in HIV Medicine at Barts Health National Health Service Trust. She pointed to the example of injectable contraception. “It can be done. It’s just that we haven’t done it. It will require some thought,” Dr. Orkin added.
In the ATLAS study, 616 participants taking two nucleoside reverse transcriptase inhibitor (NRTIs) and an integrase inhibitor, a non-NRTI, or a protease inhibitor, were randomized 1:1 to continue their regimen (CART arm) or switch to CAB/RPV, following a 4-week safety monitoring period of oral CAB/RPV. After 48 weeks, 1.6% in the CAB/RPV arm and 1.0% in the CART arm had HIV-1 RNA greater than or equal to 50 copies/mL, which met the prespecified noninferiority margin. Of patients in the CAB/RPV arm, 93% had HIV-1 RNA less than 50 copies/mL at week 48 versus 95% in the CART arm, and the difference was not statistically significant. Grade 3 or 4 events were seen in 11% of CAB/RPV and 7% of CART patients.
The FLAIR study randomized 566 ART-naive patients to receive either CAB/RPV or DTG/ABC/3TC after a 20-week induction phase, followed by a 4-week safety monitoring period for those going into the CAB/RPV arm. At week 48, 2.1% in the CAB/RPV arm and 2.5% in the DTG/ABC/3TC arm had HIV-1 RNA greater than or equal to 50 copies/mL, which met the prespecified noninferiority margin, while 94% in the CAB/RPV arm and 93% in the DTG/ABC/3TC arm had HIV-1 RNA less than 50 copies/mL. Confirmed virologic failure occurred in four patients (1.4%) in the CAB/RPV arm, and three of those patients had mutations in the NNRTI+INSTI domains, while the fourth patient was not tested. Three failures occurred in the DTG/ABC/3TC arm, and none of those patients had INSTI resistance mutations. A total of 82% of CAB/RPV patients had injection site reactions, 99% of which were grade 1 or 2, and the median duration was 3 days.
The ATLAS and FLAIR studies were sponsored by ViiV. Janssen and GlaxoSmithKline were collaborators.
SOURCES: Swindells S et al. CROI 2019, Abstract 139 LB. Orkin C et al. CROI 2019, Abstract 140.
SEATTLE – A long-acting, injectable combination of the novel integrase inhibitor cabotegravir (CAB) and the second-generation nonnucleoside reverse transcriptase inhibitor rilpivirine (RPV) was noninferior to dolutegravir/abacavir/lamivudine (DTG/ABC/3TC) in one phase 3 study (FLAIR) and to three-drug oral antiretroviral therapy (ART) more broadly in the companion ATLAS phase 3 study. Patient acceptance of the injectable formulation was surprisingly high, although researchers admitted there was likely some selection bias because patients already interested in receiving an injection would have been predisposed to entering the trials.
Still, the numbers were impressive: 99% of patients who received the intramuscular injection expressed more satisfaction with it than with their previous oral regimen in the FLAIR study, and 98% expressed a similar opinion in the ATLAS study. Circumstantial evidence also suggests there may be some demand, according to Joseph Eron, MD, professor of medicine at the University of North Carolina at Chapel Hill, who commented during a press conference at the Conference on Retroviruses & Opportunistic Infections. “These studies didn’t take a long time to accrue. People were very interested, so it wasn’t as if people had to go around and beat the bushes to try to find people [to participate],” said Dr. Eron, who was not an author on either report.
“My patients tell me that they like not having to worry about taking their pills every day. There may be some relief from the stigma of HIV. You don’t have to think about it,” Susan Swindells, MBBS, medical director of the Specialty Care Clinic at the University of Nebraska Medical Center in Omaha and first author of the ATLAS trial, said during the press conference.
There were some injection site reactions, but they were generally mild and most resolved within 7 days. In the ATLAS study, 75% of participants reported injection site pain, and 1% discontinued as a result. In the FLAIR study, 82% in the CAB/RPV arm experienced an injection site reaction, with a median duration of 3 days; 99% of reactions were grade 1 or 2.
Should the combination achieve regulatory approval, it remains to be seen how challenging it will be to manage patients with monthly injections and ensure they stick to the schedule. The injections must be administered by a health care provider.
“In terms of generalizability outside of the study, it would be a paradigm shift in our therapy,” Chloe Orkin, MBBCh, said at a press conference. Dr. Orkin is the first author on the FLAIR trial report and a consultant in HIV Medicine at Barts Health National Health Service Trust. She pointed to the example of injectable contraception. “It can be done. It’s just that we haven’t done it. It will require some thought,” Dr. Orkin added.
In the ATLAS study, 616 participants taking two nucleoside reverse transcriptase inhibitor (NRTIs) and an integrase inhibitor, a non-NRTI, or a protease inhibitor, were randomized 1:1 to continue their regimen (CART arm) or switch to CAB/RPV, following a 4-week safety monitoring period of oral CAB/RPV. After 48 weeks, 1.6% in the CAB/RPV arm and 1.0% in the CART arm had HIV-1 RNA greater than or equal to 50 copies/mL, which met the prespecified noninferiority margin. Of patients in the CAB/RPV arm, 93% had HIV-1 RNA less than 50 copies/mL at week 48 versus 95% in the CART arm, and the difference was not statistically significant. Grade 3 or 4 events were seen in 11% of CAB/RPV and 7% of CART patients.
The FLAIR study randomized 566 ART-naive patients to receive either CAB/RPV or DTG/ABC/3TC after a 20-week induction phase, followed by a 4-week safety monitoring period for those going into the CAB/RPV arm. At week 48, 2.1% in the CAB/RPV arm and 2.5% in the DTG/ABC/3TC arm had HIV-1 RNA greater than or equal to 50 copies/mL, which met the prespecified noninferiority margin, while 94% in the CAB/RPV arm and 93% in the DTG/ABC/3TC arm had HIV-1 RNA less than 50 copies/mL. Confirmed virologic failure occurred in four patients (1.4%) in the CAB/RPV arm, and three of those patients had mutations in the NNRTI+INSTI domains, while the fourth patient was not tested. Three failures occurred in the DTG/ABC/3TC arm, and none of those patients had INSTI resistance mutations. A total of 82% of CAB/RPV patients had injection site reactions, 99% of which were grade 1 or 2, and the median duration was 3 days.
The ATLAS and FLAIR studies were sponsored by ViiV. Janssen and GlaxoSmithKline were collaborators.
SOURCES: Swindells S et al. CROI 2019, Abstract 139 LB. Orkin C et al. CROI 2019, Abstract 140.
REPORTING FROM CROI 2019
When Can You Stop Dialysis?
Q) When my patient was told that she needed dialysis, one of her first questions was, "For how long?" Which got me thinking: How often do dialysis patients regain kidney function? Are some more likely than others to be able to stop dialysis?
Diagnosis with end-stage renal disease (ESRD), which requires dialysis, is a life-changing event. Inevitably, patients ask about their chance of recovery and the likelihood of stopping dialysis. Studies have consistently demonstrated low rates of kidney recovery, ranging from 0.9% to 2.4%.1
According to the United States Renal Data System (USRDS), from 1995-2006 only 0.9% of ESRD patients regained kidney function resulting in the discontinuation of dialysis.2 In one study, Agraharkar and colleagues reviewed the medical records and lab results of patients discharged from a chronic dialysis unit and reported a 1% to 2% rate of kidney recovery. The researchers concluded that closer monitoring of residual kidney function was key to identification of patients with a greater chance of recovery.3 Chu and Folkert noted a recovery rate of 1.0% to 2.4% in a review of large observational studies, concluding that the underlying etiology of the kidney failure was the single most important predictor.4
Another study of approximately 194,000 patients who started dialysis between 2008-2009 demonstrated much higher rates of sustained recovery: up to 5%. This study showed that patients with kidney failure associated with acute kidney injury (AKI) were more likely to achieve recovery; patients with the AKI diagnosis of acute tubular necrosis had the highest rate of recovery.1
Similar studies of pediatric patients are rare. One European study followed 6,574 children who started dialysis before age 15. Within 2 years of dialysis initiation, just 2% showed kidney function recovery. This study also identified underlying etiology as an important predictor of recovery; ischemic kidney failure, hemolytic uremic syndrome, and vasculitis were associated with the greatest chance of recovery.5
Despite these recent findings, the prospect of discontinuation of dialysis with a diagnosis of ESRD remains very low. A patient's underlying etiology influences the possibility of recovery; those with AKI tend to have the greatest chance, making close monitoring of residual kidney function essential in this population.3 — MSG
Marlene Shaw-Gallagher, PA-C
Nephrology Division of Michigan Medicine
Assistant Professor at University of Detroit Mercy
1. Mohan S, Huff E, Wish J, et al. Recovery of renal function among ESRD patients in the US Medicare program. PLoS One. 2013;8(12):e83447.
2. United States Renal Data System. 2018 USRDS annual data report: epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018.
3. Agraharkar M, Nair V, Patlovany M. Recovery of renal function in dialysis patients. BMC Nephrol. 2003;4:9.
4. Chu JK, Folkert VW. Renal function recovery in chronic dialysis patients. Semin Dial. 2010;23(6):606-613.
5. Bonthius M, Harambat J, Berard E, et al. Recovery of kidney function in children treated with maintenance dialysis. Clin J Am Soc Nephrol. 2018;13(10):1510-1516.
Q) When my patient was told that she needed dialysis, one of her first questions was, "For how long?" Which got me thinking: How often do dialysis patients regain kidney function? Are some more likely than others to be able to stop dialysis?
Diagnosis with end-stage renal disease (ESRD), which requires dialysis, is a life-changing event. Inevitably, patients ask about their chance of recovery and the likelihood of stopping dialysis. Studies have consistently demonstrated low rates of kidney recovery, ranging from 0.9% to 2.4%.1
According to the United States Renal Data System (USRDS), from 1995-2006 only 0.9% of ESRD patients regained kidney function resulting in the discontinuation of dialysis.2 In one study, Agraharkar and colleagues reviewed the medical records and lab results of patients discharged from a chronic dialysis unit and reported a 1% to 2% rate of kidney recovery. The researchers concluded that closer monitoring of residual kidney function was key to identification of patients with a greater chance of recovery.3 Chu and Folkert noted a recovery rate of 1.0% to 2.4% in a review of large observational studies, concluding that the underlying etiology of the kidney failure was the single most important predictor.4
Another study of approximately 194,000 patients who started dialysis between 2008-2009 demonstrated much higher rates of sustained recovery: up to 5%. This study showed that patients with kidney failure associated with acute kidney injury (AKI) were more likely to achieve recovery; patients with the AKI diagnosis of acute tubular necrosis had the highest rate of recovery.1
Similar studies of pediatric patients are rare. One European study followed 6,574 children who started dialysis before age 15. Within 2 years of dialysis initiation, just 2% showed kidney function recovery. This study also identified underlying etiology as an important predictor of recovery; ischemic kidney failure, hemolytic uremic syndrome, and vasculitis were associated with the greatest chance of recovery.5
Despite these recent findings, the prospect of discontinuation of dialysis with a diagnosis of ESRD remains very low. A patient's underlying etiology influences the possibility of recovery; those with AKI tend to have the greatest chance, making close monitoring of residual kidney function essential in this population.3 — MSG
Marlene Shaw-Gallagher, PA-C
Nephrology Division of Michigan Medicine
Assistant Professor at University of Detroit Mercy
Q) When my patient was told that she needed dialysis, one of her first questions was, "For how long?" Which got me thinking: How often do dialysis patients regain kidney function? Are some more likely than others to be able to stop dialysis?
Diagnosis with end-stage renal disease (ESRD), which requires dialysis, is a life-changing event. Inevitably, patients ask about their chance of recovery and the likelihood of stopping dialysis. Studies have consistently demonstrated low rates of kidney recovery, ranging from 0.9% to 2.4%.1
According to the United States Renal Data System (USRDS), from 1995-2006 only 0.9% of ESRD patients regained kidney function resulting in the discontinuation of dialysis.2 In one study, Agraharkar and colleagues reviewed the medical records and lab results of patients discharged from a chronic dialysis unit and reported a 1% to 2% rate of kidney recovery. The researchers concluded that closer monitoring of residual kidney function was key to identification of patients with a greater chance of recovery.3 Chu and Folkert noted a recovery rate of 1.0% to 2.4% in a review of large observational studies, concluding that the underlying etiology of the kidney failure was the single most important predictor.4
Another study of approximately 194,000 patients who started dialysis between 2008-2009 demonstrated much higher rates of sustained recovery: up to 5%. This study showed that patients with kidney failure associated with acute kidney injury (AKI) were more likely to achieve recovery; patients with the AKI diagnosis of acute tubular necrosis had the highest rate of recovery.1
Similar studies of pediatric patients are rare. One European study followed 6,574 children who started dialysis before age 15. Within 2 years of dialysis initiation, just 2% showed kidney function recovery. This study also identified underlying etiology as an important predictor of recovery; ischemic kidney failure, hemolytic uremic syndrome, and vasculitis were associated with the greatest chance of recovery.5
Despite these recent findings, the prospect of discontinuation of dialysis with a diagnosis of ESRD remains very low. A patient's underlying etiology influences the possibility of recovery; those with AKI tend to have the greatest chance, making close monitoring of residual kidney function essential in this population.3 — MSG
Marlene Shaw-Gallagher, PA-C
Nephrology Division of Michigan Medicine
Assistant Professor at University of Detroit Mercy
1. Mohan S, Huff E, Wish J, et al. Recovery of renal function among ESRD patients in the US Medicare program. PLoS One. 2013;8(12):e83447.
2. United States Renal Data System. 2018 USRDS annual data report: epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018.
3. Agraharkar M, Nair V, Patlovany M. Recovery of renal function in dialysis patients. BMC Nephrol. 2003;4:9.
4. Chu JK, Folkert VW. Renal function recovery in chronic dialysis patients. Semin Dial. 2010;23(6):606-613.
5. Bonthius M, Harambat J, Berard E, et al. Recovery of kidney function in children treated with maintenance dialysis. Clin J Am Soc Nephrol. 2018;13(10):1510-1516.
1. Mohan S, Huff E, Wish J, et al. Recovery of renal function among ESRD patients in the US Medicare program. PLoS One. 2013;8(12):e83447.
2. United States Renal Data System. 2018 USRDS annual data report: epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018.
3. Agraharkar M, Nair V, Patlovany M. Recovery of renal function in dialysis patients. BMC Nephrol. 2003;4:9.
4. Chu JK, Folkert VW. Renal function recovery in chronic dialysis patients. Semin Dial. 2010;23(6):606-613.
5. Bonthius M, Harambat J, Berard E, et al. Recovery of kidney function in children treated with maintenance dialysis. Clin J Am Soc Nephrol. 2018;13(10):1510-1516.
Universal “Test-and-Treat” Strategy Cuts Down New HIV Infections
The findings suggest that a universal “test-and-treat” strategy could be “an important addition to our toolbox of proven HIV prevention modalities,” said Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases.
The National Institute of Allergy and Infectious Diseases (NIAID)-sponsored study, Population Effects of Antiretroviral Therapy to Reduce HIV Transmission (PopART), was conducted from 2013 to 2018 in 21 urban and peri-urban communities in Zambia and South Africa, each with about 50,000 residents.
The communities were grouped as 7 “triplets” matched by geographic location and estimated HIV prevalence. The first group received annual house-to-house voluntary HIV testing and counseling, linkage to care for those testing positive, and the offer of a suite of proven prevention measures for those who tested negative. The second group received the same services as the first except treatment was offered according to national guidelines. The third group served as a control and received HIV prevention and testing services according to the local standard of care and HIV treatment according to national guidelines.
At the start of the study, the national guidelines for HIV treatment in Zambia and South Africa specified starting ART when the CD4+ T-cell count had declined to 350 cells/µL. In 2014, that threshold was raised to 500 cells/µL. In 2016, both countries recommended that everyone diagnosed with HIV begin ART immediately regardless of CD4+ T-cell count. Consequently, the first and second groups received the same intervention during the last 2 years of the study.
The researchers also recruited a random sample of about 2,300 adults from each community and visited them once a year for 3 years to collect data and test blood.
In the first 3 years, during nearly 40,000 person-years of follow-up, 553 people developed HIV infection (1.4 infections per 100 person-years). HIV incidence was 7% lower in group 1 than in the control group, although the difference was not statistically significant. However, HIV incidence was 30% lower in group 2 compared with that in the control group—a highly statistically significant and consistent result. (The researchers can’t explain why new HIV infections didn’t decline in all the communities where people who tested positive were offered immediate treatment.)
Of participants who tested positive by year 2, 72% of group 1, 68% of group 2, and 60% of the control group had achieved viral suppression.
The findings suggest that a universal “test-and-treat” strategy could be “an important addition to our toolbox of proven HIV prevention modalities,” said Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases.
The National Institute of Allergy and Infectious Diseases (NIAID)-sponsored study, Population Effects of Antiretroviral Therapy to Reduce HIV Transmission (PopART), was conducted from 2013 to 2018 in 21 urban and peri-urban communities in Zambia and South Africa, each with about 50,000 residents.
The communities were grouped as 7 “triplets” matched by geographic location and estimated HIV prevalence. The first group received annual house-to-house voluntary HIV testing and counseling, linkage to care for those testing positive, and the offer of a suite of proven prevention measures for those who tested negative. The second group received the same services as the first except treatment was offered according to national guidelines. The third group served as a control and received HIV prevention and testing services according to the local standard of care and HIV treatment according to national guidelines.
At the start of the study, the national guidelines for HIV treatment in Zambia and South Africa specified starting ART when the CD4+ T-cell count had declined to 350 cells/µL. In 2014, that threshold was raised to 500 cells/µL. In 2016, both countries recommended that everyone diagnosed with HIV begin ART immediately regardless of CD4+ T-cell count. Consequently, the first and second groups received the same intervention during the last 2 years of the study.
The researchers also recruited a random sample of about 2,300 adults from each community and visited them once a year for 3 years to collect data and test blood.
In the first 3 years, during nearly 40,000 person-years of follow-up, 553 people developed HIV infection (1.4 infections per 100 person-years). HIV incidence was 7% lower in group 1 than in the control group, although the difference was not statistically significant. However, HIV incidence was 30% lower in group 2 compared with that in the control group—a highly statistically significant and consistent result. (The researchers can’t explain why new HIV infections didn’t decline in all the communities where people who tested positive were offered immediate treatment.)
Of participants who tested positive by year 2, 72% of group 1, 68% of group 2, and 60% of the control group had achieved viral suppression.
The findings suggest that a universal “test-and-treat” strategy could be “an important addition to our toolbox of proven HIV prevention modalities,” said Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases.
The National Institute of Allergy and Infectious Diseases (NIAID)-sponsored study, Population Effects of Antiretroviral Therapy to Reduce HIV Transmission (PopART), was conducted from 2013 to 2018 in 21 urban and peri-urban communities in Zambia and South Africa, each with about 50,000 residents.
The communities were grouped as 7 “triplets” matched by geographic location and estimated HIV prevalence. The first group received annual house-to-house voluntary HIV testing and counseling, linkage to care for those testing positive, and the offer of a suite of proven prevention measures for those who tested negative. The second group received the same services as the first except treatment was offered according to national guidelines. The third group served as a control and received HIV prevention and testing services according to the local standard of care and HIV treatment according to national guidelines.
At the start of the study, the national guidelines for HIV treatment in Zambia and South Africa specified starting ART when the CD4+ T-cell count had declined to 350 cells/µL. In 2014, that threshold was raised to 500 cells/µL. In 2016, both countries recommended that everyone diagnosed with HIV begin ART immediately regardless of CD4+ T-cell count. Consequently, the first and second groups received the same intervention during the last 2 years of the study.
The researchers also recruited a random sample of about 2,300 adults from each community and visited them once a year for 3 years to collect data and test blood.
In the first 3 years, during nearly 40,000 person-years of follow-up, 553 people developed HIV infection (1.4 infections per 100 person-years). HIV incidence was 7% lower in group 1 than in the control group, although the difference was not statistically significant. However, HIV incidence was 30% lower in group 2 compared with that in the control group—a highly statistically significant and consistent result. (The researchers can’t explain why new HIV infections didn’t decline in all the communities where people who tested positive were offered immediate treatment.)
Of participants who tested positive by year 2, 72% of group 1, 68% of group 2, and 60% of the control group had achieved viral suppression.
AAP, AHA push for policies limiting children’s sugary beverage consumption
Physicians should actively advocate for policies that will reduce children’s consumption of sugar-sweetened beverages and subsequently reduce their risk of obesity, type 2 diabetes and other chronic diseases, urges a new policy statement from the American Academy of Pediatrics and the American Heart Association.
As “the leading source of added sugars in the U.S. diet,” sugary drinks “provide little to no nutritional value, are high in energy density, and do little to increase feelings of satiety,” wrote Natalie D. Muth, MD, MPH, of the University of California, Los Angeles, and the Children’s Primary Care Medical Group in Carlsbad, Calif., and her associates from the AAP’s Section on Obesity, the AAP’s Committee on Nutrition, and the American Heart Association.
Added sugars include sucrose, glucose, high-fructose corn syrup and processed fruit juice (but not naturally occurring fructose or lactose) that are added as sweeteners to food and drink products. In addition to contributing to childhood obesity, consuming drinks with added sugars increases children’s risk for “dental decay, cardiovascular disease, hypertension, dyslipidemia, insulin resistance, type 2 diabetes mellitus, fatty liver disease and all-cause mortality,” the statement noted.
Although less than 10% of individuals’ total calories should come from added sugars, according to the 2015–2020 Dietary Guidelines for Americans, added sugars make up an estimated 17% of U.S. children’s and teens’ average total caloric intake, and sugary drinks comprise almost half of this excess sugar, the statement noted. Consumption is higher and therefore more harmful in several subgroups, particularly those from minority and economically disadvantaged communities.
Previous AAP policy statements have urged doctors to encourage children and teens to drink water instead of high-calorie drinks, such as fruit juice, energy drinks and high-carbohydrate “sports drinks.” But this statement takes a page from success with tobacco control measures and focuses on the need for policy changes at local, state, and federal levels to help to reduce children’s intake of sugary drinks.
The statement makes six major recommendations:
• Excise tax: The AAP and AHA support the use of excise taxes or other means of increasing the cost of sugar-sweetened beverages – alongside an educational campaign to explain the rationale – and apportioning some of the subsequent revenue to addressing health and socioeconomic disparities.
Evidence shows how tobacco and alcohol consumption declined as their prices rose from taxes, and several places that have already implemented a sugary beverage tax have seen similar declines in consumption. Research models suggest an excise tax would potentially prevent 575,000 cases of childhood obesity.
• Reducing advertising/marketing: Research shows that teens, especially low-income and minority teens, are exposed to high amounts of advertising for soft drinks, fruit drinks, energy drinks, and sports drinks. Though such advertising cannot be outright banned without violating free speech, policies can disincentivize such marketing, such as “eliminating the advertising subsidy for nutritionally poor foods and beverages marketed to children” and not allowing in-school marketing.
• Improve existing nutritional assistance programs: WIC, the Child and Adult Care Food Program, school breakfast and lunch programs, and the Supplemental Nutrition Assistance Program (SNAP) vary in how well they discourage sugary drink consumption and can be improved through legislative changes.
• Consumer risk information: The AAP and AHA promote use of clear nutrition labels and menu labeling that explain the sugar content and risks of products, “including warning labels of the health harms of consumption of added sugars” not unlike those on cigarette packages.
• Changing the default: Physicians should advocate for policies that reduce access to sugary drinks and prioritize access to water and similarly healthier options.
• Norm-changing medical industry: Hospitals should implement policies that reduce consumption and/or access to sugary beverages, such as higher prices, less availability and risk-related labeling.
Pediatricians should continue to advise families about the risks of consuming added sugars, the substantial contribution that sugary drinks make to excess sugars in one’s diet, and the need to replace sugar-sweetened beverages with drinking water. Yet pediatricians can go beyond individual recommendations by advocating “for policy change through school boards, school health councils, hospital and medical group boards and committees, outreach to elected representatives and public comment opportunities.”
The statement used no external funding, and the authors had no disclosures or conflicts of interest.
SOURCE: Muth ND et al. Pediatrics. 2019;143(4):e20190282. doi: 10.1542/peds.2019-0282
Make counseling on healthy eating and exercise a priority
Pediatricians daily bear witness to the impact of poor nutrition on the health and quality of life of children. Healthy eating and drinking has long been an expected domain of conversation with children, adolescents and their families. In recent years, counseling regarding the consumption of added sugars, especially those in sugar-sweetened beverages (SSB), has gained traction. Pediatricians are aware of the health risks associated with over-consumption of SSB and that these risks, and consumption of sugary drinks, are more prevalent among the most vulnerable of children, including minorities and those living in low-income communities.
Primary care pediatricians face many demands that compete for time and attention, and time spent counseling on healthy eating and exercise needs to continue to be a priority. AAP-supported initiatives, such as the 5-3-2-1-0 rule – five vegetables and fruits per day, three structured meals, 2 hours or less of screen time, 1 hour or more of physical activity and zero sugary drinks most days – provide simple, clear messaging about limiting of sugary drinks. We should promote drinking of water as first choice, including during sports activities.
Messaging with community partners and on social media maximizes the impact of these important messages. The new AAP guideline “Public Policies to Reduce Sugary Drink Consumption in Children and Adolescents” also advocates for decreasing sugary drink marketing to children and adolescents. Pediatricians are trusted, credible voices who are well-positioned to advocate for an ad-free childhood, including SSB ads.
Melinda Clark, MD, is an associate professor of pediatrics at the Albany (N.Y.) Medical Center, and a MDedge Pediatrics editorial advisory board member. Dr. Clark had no disclosures.
Make counseling on healthy eating and exercise a priority
Pediatricians daily bear witness to the impact of poor nutrition on the health and quality of life of children. Healthy eating and drinking has long been an expected domain of conversation with children, adolescents and their families. In recent years, counseling regarding the consumption of added sugars, especially those in sugar-sweetened beverages (SSB), has gained traction. Pediatricians are aware of the health risks associated with over-consumption of SSB and that these risks, and consumption of sugary drinks, are more prevalent among the most vulnerable of children, including minorities and those living in low-income communities.
Primary care pediatricians face many demands that compete for time and attention, and time spent counseling on healthy eating and exercise needs to continue to be a priority. AAP-supported initiatives, such as the 5-3-2-1-0 rule – five vegetables and fruits per day, three structured meals, 2 hours or less of screen time, 1 hour or more of physical activity and zero sugary drinks most days – provide simple, clear messaging about limiting of sugary drinks. We should promote drinking of water as first choice, including during sports activities.
Messaging with community partners and on social media maximizes the impact of these important messages. The new AAP guideline “Public Policies to Reduce Sugary Drink Consumption in Children and Adolescents” also advocates for decreasing sugary drink marketing to children and adolescents. Pediatricians are trusted, credible voices who are well-positioned to advocate for an ad-free childhood, including SSB ads.
Melinda Clark, MD, is an associate professor of pediatrics at the Albany (N.Y.) Medical Center, and a MDedge Pediatrics editorial advisory board member. Dr. Clark had no disclosures.
Make counseling on healthy eating and exercise a priority
Pediatricians daily bear witness to the impact of poor nutrition on the health and quality of life of children. Healthy eating and drinking has long been an expected domain of conversation with children, adolescents and their families. In recent years, counseling regarding the consumption of added sugars, especially those in sugar-sweetened beverages (SSB), has gained traction. Pediatricians are aware of the health risks associated with over-consumption of SSB and that these risks, and consumption of sugary drinks, are more prevalent among the most vulnerable of children, including minorities and those living in low-income communities.
Primary care pediatricians face many demands that compete for time and attention, and time spent counseling on healthy eating and exercise needs to continue to be a priority. AAP-supported initiatives, such as the 5-3-2-1-0 rule – five vegetables and fruits per day, three structured meals, 2 hours or less of screen time, 1 hour or more of physical activity and zero sugary drinks most days – provide simple, clear messaging about limiting of sugary drinks. We should promote drinking of water as first choice, including during sports activities.
Messaging with community partners and on social media maximizes the impact of these important messages. The new AAP guideline “Public Policies to Reduce Sugary Drink Consumption in Children and Adolescents” also advocates for decreasing sugary drink marketing to children and adolescents. Pediatricians are trusted, credible voices who are well-positioned to advocate for an ad-free childhood, including SSB ads.
Melinda Clark, MD, is an associate professor of pediatrics at the Albany (N.Y.) Medical Center, and a MDedge Pediatrics editorial advisory board member. Dr. Clark had no disclosures.
Physicians should actively advocate for policies that will reduce children’s consumption of sugar-sweetened beverages and subsequently reduce their risk of obesity, type 2 diabetes and other chronic diseases, urges a new policy statement from the American Academy of Pediatrics and the American Heart Association.
As “the leading source of added sugars in the U.S. diet,” sugary drinks “provide little to no nutritional value, are high in energy density, and do little to increase feelings of satiety,” wrote Natalie D. Muth, MD, MPH, of the University of California, Los Angeles, and the Children’s Primary Care Medical Group in Carlsbad, Calif., and her associates from the AAP’s Section on Obesity, the AAP’s Committee on Nutrition, and the American Heart Association.
Added sugars include sucrose, glucose, high-fructose corn syrup and processed fruit juice (but not naturally occurring fructose or lactose) that are added as sweeteners to food and drink products. In addition to contributing to childhood obesity, consuming drinks with added sugars increases children’s risk for “dental decay, cardiovascular disease, hypertension, dyslipidemia, insulin resistance, type 2 diabetes mellitus, fatty liver disease and all-cause mortality,” the statement noted.
Although less than 10% of individuals’ total calories should come from added sugars, according to the 2015–2020 Dietary Guidelines for Americans, added sugars make up an estimated 17% of U.S. children’s and teens’ average total caloric intake, and sugary drinks comprise almost half of this excess sugar, the statement noted. Consumption is higher and therefore more harmful in several subgroups, particularly those from minority and economically disadvantaged communities.
Previous AAP policy statements have urged doctors to encourage children and teens to drink water instead of high-calorie drinks, such as fruit juice, energy drinks and high-carbohydrate “sports drinks.” But this statement takes a page from success with tobacco control measures and focuses on the need for policy changes at local, state, and federal levels to help to reduce children’s intake of sugary drinks.
The statement makes six major recommendations:
• Excise tax: The AAP and AHA support the use of excise taxes or other means of increasing the cost of sugar-sweetened beverages – alongside an educational campaign to explain the rationale – and apportioning some of the subsequent revenue to addressing health and socioeconomic disparities.
Evidence shows how tobacco and alcohol consumption declined as their prices rose from taxes, and several places that have already implemented a sugary beverage tax have seen similar declines in consumption. Research models suggest an excise tax would potentially prevent 575,000 cases of childhood obesity.
• Reducing advertising/marketing: Research shows that teens, especially low-income and minority teens, are exposed to high amounts of advertising for soft drinks, fruit drinks, energy drinks, and sports drinks. Though such advertising cannot be outright banned without violating free speech, policies can disincentivize such marketing, such as “eliminating the advertising subsidy for nutritionally poor foods and beverages marketed to children” and not allowing in-school marketing.
• Improve existing nutritional assistance programs: WIC, the Child and Adult Care Food Program, school breakfast and lunch programs, and the Supplemental Nutrition Assistance Program (SNAP) vary in how well they discourage sugary drink consumption and can be improved through legislative changes.
• Consumer risk information: The AAP and AHA promote use of clear nutrition labels and menu labeling that explain the sugar content and risks of products, “including warning labels of the health harms of consumption of added sugars” not unlike those on cigarette packages.
• Changing the default: Physicians should advocate for policies that reduce access to sugary drinks and prioritize access to water and similarly healthier options.
• Norm-changing medical industry: Hospitals should implement policies that reduce consumption and/or access to sugary beverages, such as higher prices, less availability and risk-related labeling.
Pediatricians should continue to advise families about the risks of consuming added sugars, the substantial contribution that sugary drinks make to excess sugars in one’s diet, and the need to replace sugar-sweetened beverages with drinking water. Yet pediatricians can go beyond individual recommendations by advocating “for policy change through school boards, school health councils, hospital and medical group boards and committees, outreach to elected representatives and public comment opportunities.”
The statement used no external funding, and the authors had no disclosures or conflicts of interest.
SOURCE: Muth ND et al. Pediatrics. 2019;143(4):e20190282. doi: 10.1542/peds.2019-0282
Physicians should actively advocate for policies that will reduce children’s consumption of sugar-sweetened beverages and subsequently reduce their risk of obesity, type 2 diabetes and other chronic diseases, urges a new policy statement from the American Academy of Pediatrics and the American Heart Association.
As “the leading source of added sugars in the U.S. diet,” sugary drinks “provide little to no nutritional value, are high in energy density, and do little to increase feelings of satiety,” wrote Natalie D. Muth, MD, MPH, of the University of California, Los Angeles, and the Children’s Primary Care Medical Group in Carlsbad, Calif., and her associates from the AAP’s Section on Obesity, the AAP’s Committee on Nutrition, and the American Heart Association.
Added sugars include sucrose, glucose, high-fructose corn syrup and processed fruit juice (but not naturally occurring fructose or lactose) that are added as sweeteners to food and drink products. In addition to contributing to childhood obesity, consuming drinks with added sugars increases children’s risk for “dental decay, cardiovascular disease, hypertension, dyslipidemia, insulin resistance, type 2 diabetes mellitus, fatty liver disease and all-cause mortality,” the statement noted.
Although less than 10% of individuals’ total calories should come from added sugars, according to the 2015–2020 Dietary Guidelines for Americans, added sugars make up an estimated 17% of U.S. children’s and teens’ average total caloric intake, and sugary drinks comprise almost half of this excess sugar, the statement noted. Consumption is higher and therefore more harmful in several subgroups, particularly those from minority and economically disadvantaged communities.
Previous AAP policy statements have urged doctors to encourage children and teens to drink water instead of high-calorie drinks, such as fruit juice, energy drinks and high-carbohydrate “sports drinks.” But this statement takes a page from success with tobacco control measures and focuses on the need for policy changes at local, state, and federal levels to help to reduce children’s intake of sugary drinks.
The statement makes six major recommendations:
• Excise tax: The AAP and AHA support the use of excise taxes or other means of increasing the cost of sugar-sweetened beverages – alongside an educational campaign to explain the rationale – and apportioning some of the subsequent revenue to addressing health and socioeconomic disparities.
Evidence shows how tobacco and alcohol consumption declined as their prices rose from taxes, and several places that have already implemented a sugary beverage tax have seen similar declines in consumption. Research models suggest an excise tax would potentially prevent 575,000 cases of childhood obesity.
• Reducing advertising/marketing: Research shows that teens, especially low-income and minority teens, are exposed to high amounts of advertising for soft drinks, fruit drinks, energy drinks, and sports drinks. Though such advertising cannot be outright banned without violating free speech, policies can disincentivize such marketing, such as “eliminating the advertising subsidy for nutritionally poor foods and beverages marketed to children” and not allowing in-school marketing.
• Improve existing nutritional assistance programs: WIC, the Child and Adult Care Food Program, school breakfast and lunch programs, and the Supplemental Nutrition Assistance Program (SNAP) vary in how well they discourage sugary drink consumption and can be improved through legislative changes.
• Consumer risk information: The AAP and AHA promote use of clear nutrition labels and menu labeling that explain the sugar content and risks of products, “including warning labels of the health harms of consumption of added sugars” not unlike those on cigarette packages.
• Changing the default: Physicians should advocate for policies that reduce access to sugary drinks and prioritize access to water and similarly healthier options.
• Norm-changing medical industry: Hospitals should implement policies that reduce consumption and/or access to sugary beverages, such as higher prices, less availability and risk-related labeling.
Pediatricians should continue to advise families about the risks of consuming added sugars, the substantial contribution that sugary drinks make to excess sugars in one’s diet, and the need to replace sugar-sweetened beverages with drinking water. Yet pediatricians can go beyond individual recommendations by advocating “for policy change through school boards, school health councils, hospital and medical group boards and committees, outreach to elected representatives and public comment opportunities.”
The statement used no external funding, and the authors had no disclosures or conflicts of interest.
SOURCE: Muth ND et al. Pediatrics. 2019;143(4):e20190282. doi: 10.1542/peds.2019-0282
FROM PEDIATRICS
How to get involved in advocacy
Interested in advocacy but not sure how or whether you have time in your busy schedule? AGA has an array of options for how you can be active in advocacy. Some take as little as 5 minutes.
Letter writing. AGA uses GovPredict, an online advocacy platform that allows members to contact their member of Congress with just a few clicks. AGA develops messages on significant pieces of legislation, key efforts in Congress or on issues being advanced by federal agencies that have a great impact on gastroenterology. AGA’s ongoing letter writing campaigns can always be found on www.gastro.org/advocacy but be sure to keep an eye out for advocacy emails, AGA eDigest, and social media, so you do not miss your opportunity to take action on timely issues. AGA encourages its members to share letter writing campaigns with their colleagues, as well as posting them on social media.
Meetings with your member of Congress. In-person meetings are an excellent opportunity to share with your member of Congress, or their staff, how the issues that impact gastroenterology affect you, your patients, and your practice. AGA has a plethora of resources to help you set up a meeting with your member of Congress, including up-to-date issue briefs, tips and tricks for productive meetings, and webinars on how to host an on-site visit. AGA staff is always more than happy to help you arrange a meeting either in Washington, DC, or your home state. If you are interested in arranging a meeting with your member of Congress, please contact AGA Public Policy Coordinator, Jonathan Sollish, at [email protected] or 240-482-3228.
AGA PAC. AGA PAC is a voluntary, nonpartisan political organization affiliated with and supported by AGA. The only political action committee supported by a national gastroenterology society, its mission is to give gastroenterologists a greater presence on Capitol Hill and a more effective voice in policy discussions. AGA PAC supports candidates who support our policy priorities, such as fair reimbursement, cutting regulatory red tape, supporting patient protections, and access to specialty care, and sustained federal funding of digestive disease research. If you are interested in learning more, contact AGA Government and Political Affairs Manager, Navneet Buttar, at [email protected] or 240-482-3221.
Congressional Advocates Program. This grassroots program is aimed at establishing a stronger foundation for our current and future advocacy initiatives by creating state teams to work on advocacy on the local, state, and national levels. Participation can include a wide variety of activities, ranging from creating educational posts on social media to meeting with members of Congress. Members of the Congressional Advocates Program are mentored and receive advocacy training by AGA leadership and staff. Participating members receive an AGA Congressional Advocate Program Certificate, a Digestive Disease Week® (DDW) badge ribbon, policy badge on the AGA Community, and recognition on AGA’s website. Applications for the next cycle will be released in 2019.
[email protected]
Interested in advocacy but not sure how or whether you have time in your busy schedule? AGA has an array of options for how you can be active in advocacy. Some take as little as 5 minutes.
Letter writing. AGA uses GovPredict, an online advocacy platform that allows members to contact their member of Congress with just a few clicks. AGA develops messages on significant pieces of legislation, key efforts in Congress or on issues being advanced by federal agencies that have a great impact on gastroenterology. AGA’s ongoing letter writing campaigns can always be found on www.gastro.org/advocacy but be sure to keep an eye out for advocacy emails, AGA eDigest, and social media, so you do not miss your opportunity to take action on timely issues. AGA encourages its members to share letter writing campaigns with their colleagues, as well as posting them on social media.
Meetings with your member of Congress. In-person meetings are an excellent opportunity to share with your member of Congress, or their staff, how the issues that impact gastroenterology affect you, your patients, and your practice. AGA has a plethora of resources to help you set up a meeting with your member of Congress, including up-to-date issue briefs, tips and tricks for productive meetings, and webinars on how to host an on-site visit. AGA staff is always more than happy to help you arrange a meeting either in Washington, DC, or your home state. If you are interested in arranging a meeting with your member of Congress, please contact AGA Public Policy Coordinator, Jonathan Sollish, at [email protected] or 240-482-3228.
AGA PAC. AGA PAC is a voluntary, nonpartisan political organization affiliated with and supported by AGA. The only political action committee supported by a national gastroenterology society, its mission is to give gastroenterologists a greater presence on Capitol Hill and a more effective voice in policy discussions. AGA PAC supports candidates who support our policy priorities, such as fair reimbursement, cutting regulatory red tape, supporting patient protections, and access to specialty care, and sustained federal funding of digestive disease research. If you are interested in learning more, contact AGA Government and Political Affairs Manager, Navneet Buttar, at [email protected] or 240-482-3221.
Congressional Advocates Program. This grassroots program is aimed at establishing a stronger foundation for our current and future advocacy initiatives by creating state teams to work on advocacy on the local, state, and national levels. Participation can include a wide variety of activities, ranging from creating educational posts on social media to meeting with members of Congress. Members of the Congressional Advocates Program are mentored and receive advocacy training by AGA leadership and staff. Participating members receive an AGA Congressional Advocate Program Certificate, a Digestive Disease Week® (DDW) badge ribbon, policy badge on the AGA Community, and recognition on AGA’s website. Applications for the next cycle will be released in 2019.
[email protected]
Interested in advocacy but not sure how or whether you have time in your busy schedule? AGA has an array of options for how you can be active in advocacy. Some take as little as 5 minutes.
Letter writing. AGA uses GovPredict, an online advocacy platform that allows members to contact their member of Congress with just a few clicks. AGA develops messages on significant pieces of legislation, key efforts in Congress or on issues being advanced by federal agencies that have a great impact on gastroenterology. AGA’s ongoing letter writing campaigns can always be found on www.gastro.org/advocacy but be sure to keep an eye out for advocacy emails, AGA eDigest, and social media, so you do not miss your opportunity to take action on timely issues. AGA encourages its members to share letter writing campaigns with their colleagues, as well as posting them on social media.
Meetings with your member of Congress. In-person meetings are an excellent opportunity to share with your member of Congress, or their staff, how the issues that impact gastroenterology affect you, your patients, and your practice. AGA has a plethora of resources to help you set up a meeting with your member of Congress, including up-to-date issue briefs, tips and tricks for productive meetings, and webinars on how to host an on-site visit. AGA staff is always more than happy to help you arrange a meeting either in Washington, DC, or your home state. If you are interested in arranging a meeting with your member of Congress, please contact AGA Public Policy Coordinator, Jonathan Sollish, at [email protected] or 240-482-3228.
AGA PAC. AGA PAC is a voluntary, nonpartisan political organization affiliated with and supported by AGA. The only political action committee supported by a national gastroenterology society, its mission is to give gastroenterologists a greater presence on Capitol Hill and a more effective voice in policy discussions. AGA PAC supports candidates who support our policy priorities, such as fair reimbursement, cutting regulatory red tape, supporting patient protections, and access to specialty care, and sustained federal funding of digestive disease research. If you are interested in learning more, contact AGA Government and Political Affairs Manager, Navneet Buttar, at [email protected] or 240-482-3221.
Congressional Advocates Program. This grassroots program is aimed at establishing a stronger foundation for our current and future advocacy initiatives by creating state teams to work on advocacy on the local, state, and national levels. Participation can include a wide variety of activities, ranging from creating educational posts on social media to meeting with members of Congress. Members of the Congressional Advocates Program are mentored and receive advocacy training by AGA leadership and staff. Participating members receive an AGA Congressional Advocate Program Certificate, a Digestive Disease Week® (DDW) badge ribbon, policy badge on the AGA Community, and recognition on AGA’s website. Applications for the next cycle will be released in 2019.
[email protected]
AGA welcomes new governing board members
Sheila E. Crowe, MD, AGAF, chair of the nominating committee, is pleased to announce that John M. Inadomi, MD, AGAF, joins the presidential line up for AGA.
John M. Inadomi, MD, AGAF
Dr. Inadomi is a national expert in comparative effectiveness research and colorectal cancer who has lent his expertise to AGA in several capacities over the years, most recently as the clinical research councillor to the board. Dr. Inadomi will serve as vice president, then president elect and will become AGA president after Digestive Disease Week® (DDW) 2021.
The AGA Nominating Committee also appointed the following slate of councillors, which is subject to membership vote.
Maria T. Abreu, MD, AGAF
Councillor-At-Large: Maria T. Abreu, MD, AGAF, is former chair of the AGA Institute Council, which plans AGA’s programming for DDW, and a researcher and clinician focusing on inflammatory bowel disease (IBD), microbiome and colorectal cancer.
David A. Katzka, MD
Education and Training Councillor: David A. Katzka, MD, has been very active in AGA’s education and practice initiatives, including his recently completed service as the chair of the AGA Institute Clinical Practice Updates Committee. Dr. Katzka received AGA’s distinguished clinician award in 2010. His research and clinical work focus on esophageal disorders.
Michael L. Kochman, MD, AGAF
Councillor-at-Large, Growth and Development: Michael L. Kochman, MD, AGAF, takes on this newly created governing board position after successfully leading the AGA Center for GI Innovation and Technology. He is an interventional endoscopist at University of Pennsylvania.
Pending approval by the voting membership, all board members begin their terms after DDW 2019. The voting membership will be sent a ballot to approve the slate of officers on or before March 21, 2019, with a response date of no later than April 20, 2019.
Thank you to our nominating committee members, pictured here at a well-deserved dinner after their committee work was completed.
Sheila E. Crowe, MD, AGAF, chair of the nominating committee, is pleased to announce that John M. Inadomi, MD, AGAF, joins the presidential line up for AGA.
John M. Inadomi, MD, AGAF
Dr. Inadomi is a national expert in comparative effectiveness research and colorectal cancer who has lent his expertise to AGA in several capacities over the years, most recently as the clinical research councillor to the board. Dr. Inadomi will serve as vice president, then president elect and will become AGA president after Digestive Disease Week® (DDW) 2021.
The AGA Nominating Committee also appointed the following slate of councillors, which is subject to membership vote.
Maria T. Abreu, MD, AGAF
Councillor-At-Large: Maria T. Abreu, MD, AGAF, is former chair of the AGA Institute Council, which plans AGA’s programming for DDW, and a researcher and clinician focusing on inflammatory bowel disease (IBD), microbiome and colorectal cancer.
David A. Katzka, MD
Education and Training Councillor: David A. Katzka, MD, has been very active in AGA’s education and practice initiatives, including his recently completed service as the chair of the AGA Institute Clinical Practice Updates Committee. Dr. Katzka received AGA’s distinguished clinician award in 2010. His research and clinical work focus on esophageal disorders.
Michael L. Kochman, MD, AGAF
Councillor-at-Large, Growth and Development: Michael L. Kochman, MD, AGAF, takes on this newly created governing board position after successfully leading the AGA Center for GI Innovation and Technology. He is an interventional endoscopist at University of Pennsylvania.
Pending approval by the voting membership, all board members begin their terms after DDW 2019. The voting membership will be sent a ballot to approve the slate of officers on or before March 21, 2019, with a response date of no later than April 20, 2019.
Thank you to our nominating committee members, pictured here at a well-deserved dinner after their committee work was completed.
Sheila E. Crowe, MD, AGAF, chair of the nominating committee, is pleased to announce that John M. Inadomi, MD, AGAF, joins the presidential line up for AGA.
John M. Inadomi, MD, AGAF
Dr. Inadomi is a national expert in comparative effectiveness research and colorectal cancer who has lent his expertise to AGA in several capacities over the years, most recently as the clinical research councillor to the board. Dr. Inadomi will serve as vice president, then president elect and will become AGA president after Digestive Disease Week® (DDW) 2021.
The AGA Nominating Committee also appointed the following slate of councillors, which is subject to membership vote.
Maria T. Abreu, MD, AGAF
Councillor-At-Large: Maria T. Abreu, MD, AGAF, is former chair of the AGA Institute Council, which plans AGA’s programming for DDW, and a researcher and clinician focusing on inflammatory bowel disease (IBD), microbiome and colorectal cancer.
David A. Katzka, MD
Education and Training Councillor: David A. Katzka, MD, has been very active in AGA’s education and practice initiatives, including his recently completed service as the chair of the AGA Institute Clinical Practice Updates Committee. Dr. Katzka received AGA’s distinguished clinician award in 2010. His research and clinical work focus on esophageal disorders.
Michael L. Kochman, MD, AGAF
Councillor-at-Large, Growth and Development: Michael L. Kochman, MD, AGAF, takes on this newly created governing board position after successfully leading the AGA Center for GI Innovation and Technology. He is an interventional endoscopist at University of Pennsylvania.
Pending approval by the voting membership, all board members begin their terms after DDW 2019. The voting membership will be sent a ballot to approve the slate of officers on or before March 21, 2019, with a response date of no later than April 20, 2019.
Thank you to our nominating committee members, pictured here at a well-deserved dinner after their committee work was completed.