User login
Experts offer insight on embracing diversity in the profession
Physicians have had diverse patients as long as there have been physicians (and patients). But diversity among health professionals remains elusive.
Can we do better? Absolutely, says a team of experts who will offer perspective to colleagues in a Wednesday morning session titled, “Best Practices and Tips for Developing Diversity in a Hospitalist Group.”
“The goals of our session are to review best practices for recruiting and retaining a diverse health care workforce, discuss strategies for dealing with implicit and explicit bias, and identify ways in which we can achieve common goals when working across cultures,” said hospitalist Amira del Pino-Jones, MD, assistant professor of medicine at the University of Colorado at Denver, Aurora, and director of the CU Hospitalist Scholars Program.
“Those who are interested in achieving excellence in hospital medicine through prioritizing diversity and equity efforts within their divisions, departments, and groups should attend,” said Dr. del Pino-Jones, who will be one of the speakers at the session.
Why is diversity important in hospital medicine? “Studies have shown that diversity enhances learning and work environments, promotes innovation, broadens research agendas, and improves the quality of care we provide for patients,” Dr. del Pino-Jones said. “In short, it is central to achieving excellence in hospital medicine.”
The session will focus on diverse groups, which have been historically underrepresented or discriminated against in medicine, including racial and ethnic minorities, women, LGBTQ+ individuals, and those with disabilities.
All speakers at the session are physicians, and each has seen or experienced challenges in diversifying their groups and divisions. “We hope to share our experiences, what we have learned, and ways to approach each of these issues. We also are hoping to hear from others and come up with new ways to approach these issues as a collective,” Dr. del Pino-Jones said.
Women and members of minority groups often have small numbers in their hospital medicine workplaces, especially in higher-level positions, and have trouble developing the critical mass to make progress on the diversity front, she said. Even when leaders recognize the importance of a diverse workforce, she said, “there is often a disconnect between motivation for increasing diversity and the ability to develop tangible, evidence-based methods that can be used to increase diversity.”
The session will tackle more than diversity at the workplace. Speakers also will discuss the relationship between medical professionals and patients.
“We will focus on the importance of inclusion and belonging, both of which are essential for creating a positive climate for all individuals,” Dr. del Pino-Jones said. “We will also discuss ways in which to cultivate cultural intelligence and enhance cross-cultural interactions between patients and providers. And we’ll look at ways to reduce and/or mitigate implicit and explicit bias in medicine.”
Dr. del Pino-Jones has no relevant disclosures.
Best Practices and Tips
for Developing Diversity in a Hospitalist Group
Wednesday, 10 - 11:30 a.m.
Potomac 4-6
Physicians have had diverse patients as long as there have been physicians (and patients). But diversity among health professionals remains elusive.
Can we do better? Absolutely, says a team of experts who will offer perspective to colleagues in a Wednesday morning session titled, “Best Practices and Tips for Developing Diversity in a Hospitalist Group.”
“The goals of our session are to review best practices for recruiting and retaining a diverse health care workforce, discuss strategies for dealing with implicit and explicit bias, and identify ways in which we can achieve common goals when working across cultures,” said hospitalist Amira del Pino-Jones, MD, assistant professor of medicine at the University of Colorado at Denver, Aurora, and director of the CU Hospitalist Scholars Program.
“Those who are interested in achieving excellence in hospital medicine through prioritizing diversity and equity efforts within their divisions, departments, and groups should attend,” said Dr. del Pino-Jones, who will be one of the speakers at the session.
Why is diversity important in hospital medicine? “Studies have shown that diversity enhances learning and work environments, promotes innovation, broadens research agendas, and improves the quality of care we provide for patients,” Dr. del Pino-Jones said. “In short, it is central to achieving excellence in hospital medicine.”
The session will focus on diverse groups, which have been historically underrepresented or discriminated against in medicine, including racial and ethnic minorities, women, LGBTQ+ individuals, and those with disabilities.
All speakers at the session are physicians, and each has seen or experienced challenges in diversifying their groups and divisions. “We hope to share our experiences, what we have learned, and ways to approach each of these issues. We also are hoping to hear from others and come up with new ways to approach these issues as a collective,” Dr. del Pino-Jones said.
Women and members of minority groups often have small numbers in their hospital medicine workplaces, especially in higher-level positions, and have trouble developing the critical mass to make progress on the diversity front, she said. Even when leaders recognize the importance of a diverse workforce, she said, “there is often a disconnect between motivation for increasing diversity and the ability to develop tangible, evidence-based methods that can be used to increase diversity.”
The session will tackle more than diversity at the workplace. Speakers also will discuss the relationship between medical professionals and patients.
“We will focus on the importance of inclusion and belonging, both of which are essential for creating a positive climate for all individuals,” Dr. del Pino-Jones said. “We will also discuss ways in which to cultivate cultural intelligence and enhance cross-cultural interactions between patients and providers. And we’ll look at ways to reduce and/or mitigate implicit and explicit bias in medicine.”
Dr. del Pino-Jones has no relevant disclosures.
Best Practices and Tips
for Developing Diversity in a Hospitalist Group
Wednesday, 10 - 11:30 a.m.
Potomac 4-6
Physicians have had diverse patients as long as there have been physicians (and patients). But diversity among health professionals remains elusive.
Can we do better? Absolutely, says a team of experts who will offer perspective to colleagues in a Wednesday morning session titled, “Best Practices and Tips for Developing Diversity in a Hospitalist Group.”
“The goals of our session are to review best practices for recruiting and retaining a diverse health care workforce, discuss strategies for dealing with implicit and explicit bias, and identify ways in which we can achieve common goals when working across cultures,” said hospitalist Amira del Pino-Jones, MD, assistant professor of medicine at the University of Colorado at Denver, Aurora, and director of the CU Hospitalist Scholars Program.
“Those who are interested in achieving excellence in hospital medicine through prioritizing diversity and equity efforts within their divisions, departments, and groups should attend,” said Dr. del Pino-Jones, who will be one of the speakers at the session.
Why is diversity important in hospital medicine? “Studies have shown that diversity enhances learning and work environments, promotes innovation, broadens research agendas, and improves the quality of care we provide for patients,” Dr. del Pino-Jones said. “In short, it is central to achieving excellence in hospital medicine.”
The session will focus on diverse groups, which have been historically underrepresented or discriminated against in medicine, including racial and ethnic minorities, women, LGBTQ+ individuals, and those with disabilities.
All speakers at the session are physicians, and each has seen or experienced challenges in diversifying their groups and divisions. “We hope to share our experiences, what we have learned, and ways to approach each of these issues. We also are hoping to hear from others and come up with new ways to approach these issues as a collective,” Dr. del Pino-Jones said.
Women and members of minority groups often have small numbers in their hospital medicine workplaces, especially in higher-level positions, and have trouble developing the critical mass to make progress on the diversity front, she said. Even when leaders recognize the importance of a diverse workforce, she said, “there is often a disconnect between motivation for increasing diversity and the ability to develop tangible, evidence-based methods that can be used to increase diversity.”
The session will tackle more than diversity at the workplace. Speakers also will discuss the relationship between medical professionals and patients.
“We will focus on the importance of inclusion and belonging, both of which are essential for creating a positive climate for all individuals,” Dr. del Pino-Jones said. “We will also discuss ways in which to cultivate cultural intelligence and enhance cross-cultural interactions between patients and providers. And we’ll look at ways to reduce and/or mitigate implicit and explicit bias in medicine.”
Dr. del Pino-Jones has no relevant disclosures.
Best Practices and Tips
for Developing Diversity in a Hospitalist Group
Wednesday, 10 - 11:30 a.m.
Potomac 4-6
How has hospital medicine changed? (VIDEO)

HM19 attendees describe how hospital medicine has changed over the years.

HM19 attendees describe how hospital medicine has changed over the years.

HM19 attendees describe how hospital medicine has changed over the years.
SHM’s Research Shark Tank a resounding success
A few lucky hospitalists had the chance to compete for dedicated consultation time from experienced hospital medicine mentors during the SHM Annual Conference’s first Research Shark Tank.

During the Monday afternoon session, four hospitalist projects were each presented in a 5-minute “pitch” to three senior quality and research leaders in hospital medicine who served as the “sharks.” These pitches were followed by 7 minutes of moderated questions and feedback from the sharks and the audience. Sharks then “bid” on the projects, offering up to 2 hours of one-on-one consultation during the conference or as needed.
The four projects included a study of the use of off-site scribes listening in to patient/hospitalist interactions to eliminate the need for the doctor to be glued to the computer screen, which was presented by Thea Dalfino, MD, chief of hospital medicine at Albany (N.Y.) Memorial Hospital; a rethinking of medical education to emphasize the role of hospitalists as mentors to individual student “apprentices,” presented by Amulya Nagarur, MD, of the department of medicine at Massachusetts General Hospital, Boston, and Christiana Renner, MD, of University of Texas Southwestern Medical Center, Dallas; and a redesign of patient hospital gowns to optimize, comfort, morale, and functionality, presented by Cheryl Dellasega, PhD, professor of medicine and humanities at Penn State University, Hershey.
The winning project was presented by Meera Udayakumar, MD, medical director at the University of North Carolina REX Healthcare in Raleigh. She discussed “The Equalizer,” a computerized tool to optimize patient distribution among hospitalists in order to balance workflow in a practice.
In discussing the thinking behind this unique session, Luci Leykum, MD, SFHM, chief of the division of general and hospital medicine at the University of Texas, San Antonio, who served as one of the sharks, stated that: “We’ve always tried to do things to promote the pipeline of research in hospital medicine and to raise the visibility of research activities at the annual conference. In the past, we have done one-on-one ‘speed dating’ with mentors, but the research committee thought this format would be more interactive and that audience members could benefit from hearing the discussion.”
The other participating sharks were Andrew Auerbach, MD, MPH, MHM, professor of medicine at the University of California, San Francisco, and former editor of the Journal of Hospital Medicine, and Hardeep Singh, MD, MPH, chief of the health policy, quality, and informatics program at the Center for Innovations in Quality, Effectiveness, and Safety at the Michael E. DeBakey Veterans Affairs Medical Center in Houston.
The selection process for those looking to pitch was rigorous. Projects submitted to the research committee had to focus on research, quality improvement, or medical education and be very specific to the practice of hospital medicine. In addition, the ideas needed to be relatively well developed, ideally with some pilot data. Applicants also needed to address a significant problem in hospital medicine, showcase an innovative approach, and make the case for how their solution would have short- and long-term effects.
Dr. Leykum said she was looking to see whether the pitched projects have clearly articulated questions that are important and interesting and whether the proposed methods would sufficiently answer those questions. She also considered what the implications were if the work was done.
Audience members had a chance to ask questions and, if they were interested, to potentially partner with presenters or adopt similar ideas at their own institutions. Attendees were exposed to innovative ways of solving problems that are common and ideas that have a big impact on the way problems are approached in hospital medicine.
“I think it was a fun, fast, interactive session, and it was interesting to see,” said Dr. Leykum. “Those of us who were the sharks know each other and each other’s work, so that was a fun dynamic.”
A few lucky hospitalists had the chance to compete for dedicated consultation time from experienced hospital medicine mentors during the SHM Annual Conference’s first Research Shark Tank.

During the Monday afternoon session, four hospitalist projects were each presented in a 5-minute “pitch” to three senior quality and research leaders in hospital medicine who served as the “sharks.” These pitches were followed by 7 minutes of moderated questions and feedback from the sharks and the audience. Sharks then “bid” on the projects, offering up to 2 hours of one-on-one consultation during the conference or as needed.
The four projects included a study of the use of off-site scribes listening in to patient/hospitalist interactions to eliminate the need for the doctor to be glued to the computer screen, which was presented by Thea Dalfino, MD, chief of hospital medicine at Albany (N.Y.) Memorial Hospital; a rethinking of medical education to emphasize the role of hospitalists as mentors to individual student “apprentices,” presented by Amulya Nagarur, MD, of the department of medicine at Massachusetts General Hospital, Boston, and Christiana Renner, MD, of University of Texas Southwestern Medical Center, Dallas; and a redesign of patient hospital gowns to optimize, comfort, morale, and functionality, presented by Cheryl Dellasega, PhD, professor of medicine and humanities at Penn State University, Hershey.
The winning project was presented by Meera Udayakumar, MD, medical director at the University of North Carolina REX Healthcare in Raleigh. She discussed “The Equalizer,” a computerized tool to optimize patient distribution among hospitalists in order to balance workflow in a practice.
In discussing the thinking behind this unique session, Luci Leykum, MD, SFHM, chief of the division of general and hospital medicine at the University of Texas, San Antonio, who served as one of the sharks, stated that: “We’ve always tried to do things to promote the pipeline of research in hospital medicine and to raise the visibility of research activities at the annual conference. In the past, we have done one-on-one ‘speed dating’ with mentors, but the research committee thought this format would be more interactive and that audience members could benefit from hearing the discussion.”
The other participating sharks were Andrew Auerbach, MD, MPH, MHM, professor of medicine at the University of California, San Francisco, and former editor of the Journal of Hospital Medicine, and Hardeep Singh, MD, MPH, chief of the health policy, quality, and informatics program at the Center for Innovations in Quality, Effectiveness, and Safety at the Michael E. DeBakey Veterans Affairs Medical Center in Houston.
The selection process for those looking to pitch was rigorous. Projects submitted to the research committee had to focus on research, quality improvement, or medical education and be very specific to the practice of hospital medicine. In addition, the ideas needed to be relatively well developed, ideally with some pilot data. Applicants also needed to address a significant problem in hospital medicine, showcase an innovative approach, and make the case for how their solution would have short- and long-term effects.
Dr. Leykum said she was looking to see whether the pitched projects have clearly articulated questions that are important and interesting and whether the proposed methods would sufficiently answer those questions. She also considered what the implications were if the work was done.
Audience members had a chance to ask questions and, if they were interested, to potentially partner with presenters or adopt similar ideas at their own institutions. Attendees were exposed to innovative ways of solving problems that are common and ideas that have a big impact on the way problems are approached in hospital medicine.
“I think it was a fun, fast, interactive session, and it was interesting to see,” said Dr. Leykum. “Those of us who were the sharks know each other and each other’s work, so that was a fun dynamic.”
A few lucky hospitalists had the chance to compete for dedicated consultation time from experienced hospital medicine mentors during the SHM Annual Conference’s first Research Shark Tank.

During the Monday afternoon session, four hospitalist projects were each presented in a 5-minute “pitch” to three senior quality and research leaders in hospital medicine who served as the “sharks.” These pitches were followed by 7 minutes of moderated questions and feedback from the sharks and the audience. Sharks then “bid” on the projects, offering up to 2 hours of one-on-one consultation during the conference or as needed.
The four projects included a study of the use of off-site scribes listening in to patient/hospitalist interactions to eliminate the need for the doctor to be glued to the computer screen, which was presented by Thea Dalfino, MD, chief of hospital medicine at Albany (N.Y.) Memorial Hospital; a rethinking of medical education to emphasize the role of hospitalists as mentors to individual student “apprentices,” presented by Amulya Nagarur, MD, of the department of medicine at Massachusetts General Hospital, Boston, and Christiana Renner, MD, of University of Texas Southwestern Medical Center, Dallas; and a redesign of patient hospital gowns to optimize, comfort, morale, and functionality, presented by Cheryl Dellasega, PhD, professor of medicine and humanities at Penn State University, Hershey.
The winning project was presented by Meera Udayakumar, MD, medical director at the University of North Carolina REX Healthcare in Raleigh. She discussed “The Equalizer,” a computerized tool to optimize patient distribution among hospitalists in order to balance workflow in a practice.
In discussing the thinking behind this unique session, Luci Leykum, MD, SFHM, chief of the division of general and hospital medicine at the University of Texas, San Antonio, who served as one of the sharks, stated that: “We’ve always tried to do things to promote the pipeline of research in hospital medicine and to raise the visibility of research activities at the annual conference. In the past, we have done one-on-one ‘speed dating’ with mentors, but the research committee thought this format would be more interactive and that audience members could benefit from hearing the discussion.”
The other participating sharks were Andrew Auerbach, MD, MPH, MHM, professor of medicine at the University of California, San Francisco, and former editor of the Journal of Hospital Medicine, and Hardeep Singh, MD, MPH, chief of the health policy, quality, and informatics program at the Center for Innovations in Quality, Effectiveness, and Safety at the Michael E. DeBakey Veterans Affairs Medical Center in Houston.
The selection process for those looking to pitch was rigorous. Projects submitted to the research committee had to focus on research, quality improvement, or medical education and be very specific to the practice of hospital medicine. In addition, the ideas needed to be relatively well developed, ideally with some pilot data. Applicants also needed to address a significant problem in hospital medicine, showcase an innovative approach, and make the case for how their solution would have short- and long-term effects.
Dr. Leykum said she was looking to see whether the pitched projects have clearly articulated questions that are important and interesting and whether the proposed methods would sufficiently answer those questions. She also considered what the implications were if the work was done.
Audience members had a chance to ask questions and, if they were interested, to potentially partner with presenters or adopt similar ideas at their own institutions. Attendees were exposed to innovative ways of solving problems that are common and ideas that have a big impact on the way problems are approached in hospital medicine.
“I think it was a fun, fast, interactive session, and it was interesting to see,” said Dr. Leykum. “Those of us who were the sharks know each other and each other’s work, so that was a fun dynamic.”
Antibiotic Overprescribing
Proinflammatory microbiome tied to colorectal adenoma
MIAMI – The fecal presence of least two genes harbored by toxin-producing or proinflammatory bacteria conferred a nearly 200% rise in the odds of colorectal adenoma, investigators reported.
Moreover, the fecal presence of usp (uropathogenic-specific protein), a bacterial gene encoding a genotoxin that damages DNA, correlated with nearly 1,200% greater odds of colorectal adenoma (P =.08), said senior investigator María González-Pons, PhD, of the University of Puerto Rico Comprehensive Cancer Center in San Juan.
“We are continuing to enlarge this study. We need more power to assess statistical significance and look at associations for individual combinations of bacterial genes,” Dr. Pons said in an interview. “Our ultimate goal is to risk-stratify patients so that we know whom to target for [colorectal cancer] prevention.”
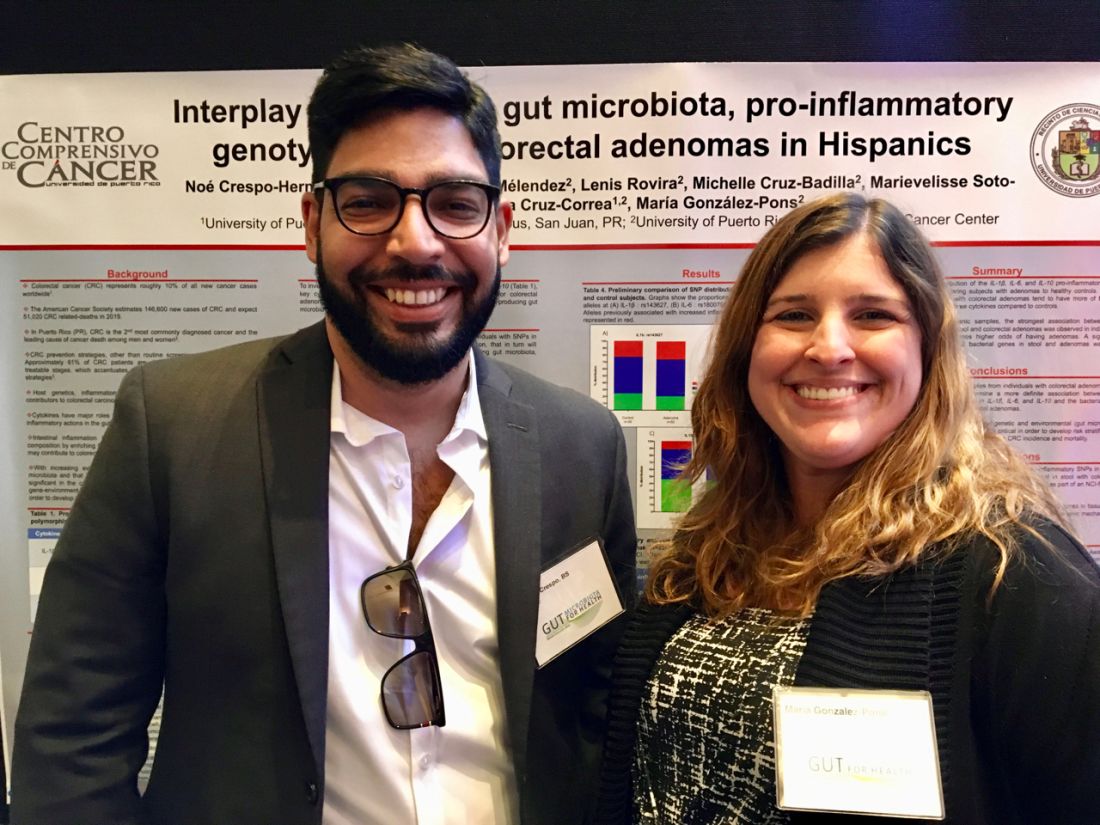
Dr. Pons and the study’s lead author, Noe Crespo-Hernandez, of the University of Puerto Rico, presented the findings with their associates in a poster at the the annual Gut Microbiota for Health World Summit.
Colorectal cancer is the most lethal cancer and the second-most common malignancy in Puerto Rico. Despite recommendations for screening colonoscopy, many patients are diagnosed in late-stage disease, when treatment options are limited. Intestinal inflammation is itself key to colorectal carcinogenesis and also promotes the enteric proliferation of gram-negative bacteria that produce potentially carcinogenic toxins. Thus, gut inflammation and the microbiome are of great interest to researchers who are working to develop reliable, minimally invasive tests that assess future colorectal cancer risk.
For their study presented at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, Dr. Pons and her coinvestigators compared stool samples from 67 adults with colonoscopically confirmed colorectal adenomas and 39 controls with negative screening colonoscopies. Both groups were captured in the Puerto Rico Familial Colorectal Cancer Registry. The researchers used TaqMan SNP Genotyping to look for single-nucleotide polymorphisms (SNPs) from promoter regions of genes encoding interleukin-1 beta, IL-6, and IL-10, cytokines that regulate gut inflammation. They found nonsignificant associations between colorectal adenoma and two of the three SNPs: rs143627 (encoding IL-1B) and rs1800795 (IL-6).
The real-time polymerase chain reaction results were even more striking. Using SYBR Green, the researchers tested stool for six genotoxic or proinflammatory bacterial genes and identified five, each of which correlated with colorectal adenoma. Colorectal adenoma also was linked with the fecal presence of a nonpathogenic housekeeping gene that is a surrogate for a mucolytic bacterium abundant in the stool of colorectal cancer patients.
Odds ratios for these associations ranged from 1.17 (for cnf, or cytotoxic necrotizing factor) to 12.83 (for usp), the researchers reported. Dr. Pons commented that Hurricane Maria greatly delayed this study and thus the cohort was underpowered to test for statistical significance. Nonetheless, P values approached significance for the usp gene (OR, 12.83; 95% confidence interval, 0.73-226.8; P = .08) and the fecal presence of at least two genes in combination (OR, 2.84; 95% CI, 1.01-8.90; P = .05).
Next, Dr. Pons and her team will expand the study to assess links between colorectal adenoma and these pathogenic bacterial genes, individually and in various combinations. They also plan to compare genes in normal and adenomatous colon tissue and to use enteroid (small intestinal organoid) models to tease out the carcinogenic mechanisms of these bacterial toxins.
The National Institutes of Health provided funding. The researchers disclosed no competing interests.
MIAMI – The fecal presence of least two genes harbored by toxin-producing or proinflammatory bacteria conferred a nearly 200% rise in the odds of colorectal adenoma, investigators reported.
Moreover, the fecal presence of usp (uropathogenic-specific protein), a bacterial gene encoding a genotoxin that damages DNA, correlated with nearly 1,200% greater odds of colorectal adenoma (P =.08), said senior investigator María González-Pons, PhD, of the University of Puerto Rico Comprehensive Cancer Center in San Juan.
“We are continuing to enlarge this study. We need more power to assess statistical significance and look at associations for individual combinations of bacterial genes,” Dr. Pons said in an interview. “Our ultimate goal is to risk-stratify patients so that we know whom to target for [colorectal cancer] prevention.”
Dr. Pons and the study’s lead author, Noe Crespo-Hernandez, of the University of Puerto Rico, presented the findings with their associates in a poster at the the annual Gut Microbiota for Health World Summit.
Colorectal cancer is the most lethal cancer and the second-most common malignancy in Puerto Rico. Despite recommendations for screening colonoscopy, many patients are diagnosed in late-stage disease, when treatment options are limited. Intestinal inflammation is itself key to colorectal carcinogenesis and also promotes the enteric proliferation of gram-negative bacteria that produce potentially carcinogenic toxins. Thus, gut inflammation and the microbiome are of great interest to researchers who are working to develop reliable, minimally invasive tests that assess future colorectal cancer risk.
For their study presented at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, Dr. Pons and her coinvestigators compared stool samples from 67 adults with colonoscopically confirmed colorectal adenomas and 39 controls with negative screening colonoscopies. Both groups were captured in the Puerto Rico Familial Colorectal Cancer Registry. The researchers used TaqMan SNP Genotyping to look for single-nucleotide polymorphisms (SNPs) from promoter regions of genes encoding interleukin-1 beta, IL-6, and IL-10, cytokines that regulate gut inflammation. They found nonsignificant associations between colorectal adenoma and two of the three SNPs: rs143627 (encoding IL-1B) and rs1800795 (IL-6).
The real-time polymerase chain reaction results were even more striking. Using SYBR Green, the researchers tested stool for six genotoxic or proinflammatory bacterial genes and identified five, each of which correlated with colorectal adenoma. Colorectal adenoma also was linked with the fecal presence of a nonpathogenic housekeeping gene that is a surrogate for a mucolytic bacterium abundant in the stool of colorectal cancer patients.
Odds ratios for these associations ranged from 1.17 (for cnf, or cytotoxic necrotizing factor) to 12.83 (for usp), the researchers reported. Dr. Pons commented that Hurricane Maria greatly delayed this study and thus the cohort was underpowered to test for statistical significance. Nonetheless, P values approached significance for the usp gene (OR, 12.83; 95% confidence interval, 0.73-226.8; P = .08) and the fecal presence of at least two genes in combination (OR, 2.84; 95% CI, 1.01-8.90; P = .05).
Next, Dr. Pons and her team will expand the study to assess links between colorectal adenoma and these pathogenic bacterial genes, individually and in various combinations. They also plan to compare genes in normal and adenomatous colon tissue and to use enteroid (small intestinal organoid) models to tease out the carcinogenic mechanisms of these bacterial toxins.
The National Institutes of Health provided funding. The researchers disclosed no competing interests.
MIAMI – The fecal presence of least two genes harbored by toxin-producing or proinflammatory bacteria conferred a nearly 200% rise in the odds of colorectal adenoma, investigators reported.
Moreover, the fecal presence of usp (uropathogenic-specific protein), a bacterial gene encoding a genotoxin that damages DNA, correlated with nearly 1,200% greater odds of colorectal adenoma (P =.08), said senior investigator María González-Pons, PhD, of the University of Puerto Rico Comprehensive Cancer Center in San Juan.
“We are continuing to enlarge this study. We need more power to assess statistical significance and look at associations for individual combinations of bacterial genes,” Dr. Pons said in an interview. “Our ultimate goal is to risk-stratify patients so that we know whom to target for [colorectal cancer] prevention.”
Dr. Pons and the study’s lead author, Noe Crespo-Hernandez, of the University of Puerto Rico, presented the findings with their associates in a poster at the the annual Gut Microbiota for Health World Summit.
Colorectal cancer is the most lethal cancer and the second-most common malignancy in Puerto Rico. Despite recommendations for screening colonoscopy, many patients are diagnosed in late-stage disease, when treatment options are limited. Intestinal inflammation is itself key to colorectal carcinogenesis and also promotes the enteric proliferation of gram-negative bacteria that produce potentially carcinogenic toxins. Thus, gut inflammation and the microbiome are of great interest to researchers who are working to develop reliable, minimally invasive tests that assess future colorectal cancer risk.
For their study presented at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, Dr. Pons and her coinvestigators compared stool samples from 67 adults with colonoscopically confirmed colorectal adenomas and 39 controls with negative screening colonoscopies. Both groups were captured in the Puerto Rico Familial Colorectal Cancer Registry. The researchers used TaqMan SNP Genotyping to look for single-nucleotide polymorphisms (SNPs) from promoter regions of genes encoding interleukin-1 beta, IL-6, and IL-10, cytokines that regulate gut inflammation. They found nonsignificant associations between colorectal adenoma and two of the three SNPs: rs143627 (encoding IL-1B) and rs1800795 (IL-6).
The real-time polymerase chain reaction results were even more striking. Using SYBR Green, the researchers tested stool for six genotoxic or proinflammatory bacterial genes and identified five, each of which correlated with colorectal adenoma. Colorectal adenoma also was linked with the fecal presence of a nonpathogenic housekeeping gene that is a surrogate for a mucolytic bacterium abundant in the stool of colorectal cancer patients.
Odds ratios for these associations ranged from 1.17 (for cnf, or cytotoxic necrotizing factor) to 12.83 (for usp), the researchers reported. Dr. Pons commented that Hurricane Maria greatly delayed this study and thus the cohort was underpowered to test for statistical significance. Nonetheless, P values approached significance for the usp gene (OR, 12.83; 95% confidence interval, 0.73-226.8; P = .08) and the fecal presence of at least two genes in combination (OR, 2.84; 95% CI, 1.01-8.90; P = .05).
Next, Dr. Pons and her team will expand the study to assess links between colorectal adenoma and these pathogenic bacterial genes, individually and in various combinations. They also plan to compare genes in normal and adenomatous colon tissue and to use enteroid (small intestinal organoid) models to tease out the carcinogenic mechanisms of these bacterial toxins.
The National Institutes of Health provided funding. The researchers disclosed no competing interests.
REPORTING FROM GUT 2019
Plasma genotyping yields actionable mutation in advanced NSCLC
Taking a deep dive into plasma cell-free DNA in patients with advanced non–small cell lung cancer may reveal targetable mutations and cancer resistance mechanisms in tumors, even when tissue biopsy samples are not adequate for genotyping, investigators say,
Noninvasive tumor genotyping of plasma cell-free DNA (cfDNA) with ultra-deep next generation sequencing (NGS) in plasma samples from 127 patients identified known oncogenic drivers with a sensitivity of 75% and ruled out the presence of driver mutations with a specificity of 100% in patients with tissue samples indicating no mutations, reported Bob T. Li, MD, MPH, of Memorial Sloan Kettering Cancer Center (MSKCC) in New York, and his colleagues.
“These results reveal the potential utility of NGS assays that use cfDNA as input for detecting actionable driver alterations and both de novo and emergent resistance mechanisms in the clinical setting,” they wrote. The report is in Annals of Oncology.
Although the researchers did not directly assess clinical utility, the results suggest that NGS-based analysis of cfDNA may help guide treatment selection, they added.
Ultra-deep NGS is a kind of obsessive-compulsive form of sequencing in which the same genomic region is read repeatedly – in this study, 50,000 times over – with filtering of somatic mutations attributable to clonal hematopoiesis. The technique allows for detection of rare genetic alterations that can be missed by other methods.
“More recent studies employing plasma cfDNA NGS have shown promise in detecting a broader variety of genetic alterations with similar sensitivity to that of digital PCR, with potential to change clinical practice,” Dr. Li and his colleagues wrote.
They conducted a systematic study of a novel cfDNA assay in patients whose cancers had oncogenic driver mutations, those who were driver negative on tissue-based NGS, and those whose tumors had unknown mutational status.
A total of 127 patients from three centers (MSKCC, the Dana-Farber Cancer Center in Boston, and the University of Texas MD Anderson Cancer Center in Houston) were available for assessment.
Ultra-deep NGS was performed on cfDNA and matched white blood cells using a hybrid capture panel covering 37 lung cancer-related genes sequenced to 50,000 times raw-target coverage filtering somatic mutations attributable to clonal hematopoiesis.
Plasma NGS was able to detect driver mutations with variant allele frequencies ranging from as low as 0.14% to as high as 52%.
In 21 of 22 patients, plasma digital drop polymerase chain reaction (ddPCR) results for EGFR or KRAS mutations were nearly identical to those of NGS, with high concordance for variant allele frequencies (r = .98).
In analyses blinded to tissue genotyping results in 91 patients, plasma NGS detected de novo known oncogenic driver alterations in 68 samples, for a sensitivity of 75%, and in 19 of 19 patients who were driver negative by tissue sequencing, plasma NGS also showed an absence of mutations, for a specificity of 100%.
Furthermore, plasma NGS identified four KRAS mutations in plasma from 17 patients for whom tissues samples were not adequate for genotyping, and the plasma-based technique was able to identify potential resistance mutations in samples from 23 patients with EGFR mutations whose tumors had required resistance to targeted therapy.
“The sensitivity of detection by NGS was comparable to that of established ddPCR methods. Its high concordance with tissue genotyping and the detection of drivers in settings where tissue biopsy had failed or was not feasible lend credence to the potential clinical use of plasma cfDNA NGS and the development of cfDNA-guided intervention studies,” the investigators wrote.
The study was supported by Illumina. Authors from MSKCC and MD Anderson were supported by National Institutes of Health grants. Dr. Li received consulting/advisory board fees from Genentech, Thermo-Fisher Scientific, and Guardant Health outside of the submitted work. Multiple coauthors reported similar relationships, and eight coauthors were current or former employees of Illumina.
SOURCE: Source: Li BT et al. Ann Oncol. doi: 10.1093/annonc/mdz046.
Taking a deep dive into plasma cell-free DNA in patients with advanced non–small cell lung cancer may reveal targetable mutations and cancer resistance mechanisms in tumors, even when tissue biopsy samples are not adequate for genotyping, investigators say,
Noninvasive tumor genotyping of plasma cell-free DNA (cfDNA) with ultra-deep next generation sequencing (NGS) in plasma samples from 127 patients identified known oncogenic drivers with a sensitivity of 75% and ruled out the presence of driver mutations with a specificity of 100% in patients with tissue samples indicating no mutations, reported Bob T. Li, MD, MPH, of Memorial Sloan Kettering Cancer Center (MSKCC) in New York, and his colleagues.
“These results reveal the potential utility of NGS assays that use cfDNA as input for detecting actionable driver alterations and both de novo and emergent resistance mechanisms in the clinical setting,” they wrote. The report is in Annals of Oncology.
Although the researchers did not directly assess clinical utility, the results suggest that NGS-based analysis of cfDNA may help guide treatment selection, they added.
Ultra-deep NGS is a kind of obsessive-compulsive form of sequencing in which the same genomic region is read repeatedly – in this study, 50,000 times over – with filtering of somatic mutations attributable to clonal hematopoiesis. The technique allows for detection of rare genetic alterations that can be missed by other methods.
“More recent studies employing plasma cfDNA NGS have shown promise in detecting a broader variety of genetic alterations with similar sensitivity to that of digital PCR, with potential to change clinical practice,” Dr. Li and his colleagues wrote.
They conducted a systematic study of a novel cfDNA assay in patients whose cancers had oncogenic driver mutations, those who were driver negative on tissue-based NGS, and those whose tumors had unknown mutational status.
A total of 127 patients from three centers (MSKCC, the Dana-Farber Cancer Center in Boston, and the University of Texas MD Anderson Cancer Center in Houston) were available for assessment.
Ultra-deep NGS was performed on cfDNA and matched white blood cells using a hybrid capture panel covering 37 lung cancer-related genes sequenced to 50,000 times raw-target coverage filtering somatic mutations attributable to clonal hematopoiesis.
Plasma NGS was able to detect driver mutations with variant allele frequencies ranging from as low as 0.14% to as high as 52%.
In 21 of 22 patients, plasma digital drop polymerase chain reaction (ddPCR) results for EGFR or KRAS mutations were nearly identical to those of NGS, with high concordance for variant allele frequencies (r = .98).
In analyses blinded to tissue genotyping results in 91 patients, plasma NGS detected de novo known oncogenic driver alterations in 68 samples, for a sensitivity of 75%, and in 19 of 19 patients who were driver negative by tissue sequencing, plasma NGS also showed an absence of mutations, for a specificity of 100%.
Furthermore, plasma NGS identified four KRAS mutations in plasma from 17 patients for whom tissues samples were not adequate for genotyping, and the plasma-based technique was able to identify potential resistance mutations in samples from 23 patients with EGFR mutations whose tumors had required resistance to targeted therapy.
“The sensitivity of detection by NGS was comparable to that of established ddPCR methods. Its high concordance with tissue genotyping and the detection of drivers in settings where tissue biopsy had failed or was not feasible lend credence to the potential clinical use of plasma cfDNA NGS and the development of cfDNA-guided intervention studies,” the investigators wrote.
The study was supported by Illumina. Authors from MSKCC and MD Anderson were supported by National Institutes of Health grants. Dr. Li received consulting/advisory board fees from Genentech, Thermo-Fisher Scientific, and Guardant Health outside of the submitted work. Multiple coauthors reported similar relationships, and eight coauthors were current or former employees of Illumina.
SOURCE: Source: Li BT et al. Ann Oncol. doi: 10.1093/annonc/mdz046.
Taking a deep dive into plasma cell-free DNA in patients with advanced non–small cell lung cancer may reveal targetable mutations and cancer resistance mechanisms in tumors, even when tissue biopsy samples are not adequate for genotyping, investigators say,
Noninvasive tumor genotyping of plasma cell-free DNA (cfDNA) with ultra-deep next generation sequencing (NGS) in plasma samples from 127 patients identified known oncogenic drivers with a sensitivity of 75% and ruled out the presence of driver mutations with a specificity of 100% in patients with tissue samples indicating no mutations, reported Bob T. Li, MD, MPH, of Memorial Sloan Kettering Cancer Center (MSKCC) in New York, and his colleagues.
“These results reveal the potential utility of NGS assays that use cfDNA as input for detecting actionable driver alterations and both de novo and emergent resistance mechanisms in the clinical setting,” they wrote. The report is in Annals of Oncology.
Although the researchers did not directly assess clinical utility, the results suggest that NGS-based analysis of cfDNA may help guide treatment selection, they added.
Ultra-deep NGS is a kind of obsessive-compulsive form of sequencing in which the same genomic region is read repeatedly – in this study, 50,000 times over – with filtering of somatic mutations attributable to clonal hematopoiesis. The technique allows for detection of rare genetic alterations that can be missed by other methods.
“More recent studies employing plasma cfDNA NGS have shown promise in detecting a broader variety of genetic alterations with similar sensitivity to that of digital PCR, with potential to change clinical practice,” Dr. Li and his colleagues wrote.
They conducted a systematic study of a novel cfDNA assay in patients whose cancers had oncogenic driver mutations, those who were driver negative on tissue-based NGS, and those whose tumors had unknown mutational status.
A total of 127 patients from three centers (MSKCC, the Dana-Farber Cancer Center in Boston, and the University of Texas MD Anderson Cancer Center in Houston) were available for assessment.
Ultra-deep NGS was performed on cfDNA and matched white blood cells using a hybrid capture panel covering 37 lung cancer-related genes sequenced to 50,000 times raw-target coverage filtering somatic mutations attributable to clonal hematopoiesis.
Plasma NGS was able to detect driver mutations with variant allele frequencies ranging from as low as 0.14% to as high as 52%.
In 21 of 22 patients, plasma digital drop polymerase chain reaction (ddPCR) results for EGFR or KRAS mutations were nearly identical to those of NGS, with high concordance for variant allele frequencies (r = .98).
In analyses blinded to tissue genotyping results in 91 patients, plasma NGS detected de novo known oncogenic driver alterations in 68 samples, for a sensitivity of 75%, and in 19 of 19 patients who were driver negative by tissue sequencing, plasma NGS also showed an absence of mutations, for a specificity of 100%.
Furthermore, plasma NGS identified four KRAS mutations in plasma from 17 patients for whom tissues samples were not adequate for genotyping, and the plasma-based technique was able to identify potential resistance mutations in samples from 23 patients with EGFR mutations whose tumors had required resistance to targeted therapy.
“The sensitivity of detection by NGS was comparable to that of established ddPCR methods. Its high concordance with tissue genotyping and the detection of drivers in settings where tissue biopsy had failed or was not feasible lend credence to the potential clinical use of plasma cfDNA NGS and the development of cfDNA-guided intervention studies,” the investigators wrote.
The study was supported by Illumina. Authors from MSKCC and MD Anderson were supported by National Institutes of Health grants. Dr. Li received consulting/advisory board fees from Genentech, Thermo-Fisher Scientific, and Guardant Health outside of the submitted work. Multiple coauthors reported similar relationships, and eight coauthors were current or former employees of Illumina.
SOURCE: Source: Li BT et al. Ann Oncol. doi: 10.1093/annonc/mdz046.
FROM ANNALS OF ONCOLOGY
Announcing the 2019 chapter awards and grant recipients
Chapter Excellence Awards
The Society of Hospital Medicine is proud to recognize its chapters for their hard work and dedication through Chapter Excellence Awards. Each year, chapters strive to demonstrate growth, sustainability, and innovation within their activities, which are then recognized at SHM’s annual conference.
Please join SHM in congratulating the following chapters on their year of success in 2018!
Platinum Chapters: Iowa; Knoxville; Maryland; Michigan; Minnesota; New Mexico; North Carolina Triangle; Pacific Northwest; Southwest Florida; Wiregrass.
Gold Chapters: Houston; NYC/Westchester; Piedmont Triad; San Francisco Bay Area
Silver Chapters: Boston/Eastern Massachusetts; Charlotte Metro Area; Gulf States; Hampton Roads; Kentucky; Maine; Nebraska; North Jersey; Rocky Mountain; South Central Pennsylvania; South Texas; St. Louis.
Outstanding Chapter of the Year
Michigan. The Outstanding Chapter of the Year Award goes to one chapter that exemplifies high performance, going above and beyond the basic chapter requirements. The recipient of the Outstanding Chapter of the Year Award for 2018 is the Michigan chapter of SHM.
The Michigan chapter continues to embrace the mission of our society and nurtures a vibrant, multidisciplinary membership. It is currently the largest chapter in the program, representing more than 750 SHM members.
Using a technology-enabled platform, the Michigan chapter has expanded its meetings to four different sites, leveraging expertise from across the state. The chapter recently held its largest meeting focused on provider burnout, with more than 100 attendees across four different sites. It featured a main speaker as well as a multidisciplinary panel of leaders from eight different health systems.
The chapter has successfully incorporated advocacy into its annual planning and actively responds to new legislation affecting hospital medicine. It continues to be an active and valued member of the Michigan medical community and the SHM chapter community at large.
In addition to the service to members, the chapter strives to serve the SHM chapter community at large by collaborating and sharing best practices.
The chapter’s level of originality is not only a benefit to the chapter, but also to SHM’s Chapter program as a whole. Congratulations to the Michigan chapter on being named the Outstanding Chapter of 2018.
Rising Star Chapter
Knoxville. The Rising Star Chapter Award goes to one chapter that has been active for 2 years or less and in the past 12 months has made improvements to its leadership, stability and growth, and membership.
The recipient of the Rising Star Chapter Award for 2018 is the Knoxville (Tenn.) Chapter of SHM, which has made significant strides since its launch in the spring of 2017. The chapter assembled a group of local hospitalists from Knoxville and the surrounding region to encourage participation and drive quality initiatives in area hospitals.
The Knoxville chapter developed a leadership framework, including officers and board members, and just completed its first formal chapter leadership election. In 2018, the chapter held four meetings, including an event steered toward residents and students. Membership in the chapter has grown by more than 20% since inception. The chapter has engaged in statewide quality initiatives with the Tennessee Hospital Association and has engaged with other chapters across the state.
The Knoxville’s Chapter is an active, enthusiastic organization that is rapidly growing and thriving. Congratulations to the Knoxville chapter on being named the Rising Star Chapter for 2018.
Student Hospitalist Scholar Grant recipients
SHM is proud to acknowledge the latest winners of its Student Hospitalist Scholar Grant. These medical students were awarded grants to complete scholarly work with an active SHM mentor in a project related to patient safety, quality improvement, or other areas relevant to the field of hospital medicine.
Sandeep Bala
University of Chicago Pritzker School of Medicine
Poster 382 – The impact of plain language open medical notes on patient activation
Location: Denver (Colo.) Health Hospital
Monisha Bhatia
Vanderbilt University School of Medicine
Poster 23 – Using electronic medical record phenotypic data to predict discharge destination
Location: Vanderbilt University Medical Center, Nashville, Tenn.
Maximilian Hemmrich
University of Chicago Pritzker School of Medicine
Oral presentation, 11:45 a.m. – Noon, Tuesday, March 26
Project: Derivation and validation of a COPD readmission risk prediction tool
Location: University of Chicago
Ilana Scandariato Lavina
Weill Cornell Medical College
Poster 424 – Understanding the experience of the long-term hospitalized patient with provider fragmentation: A qualitative study
Yun Li
Geisel School of Medicine at Dartmouth
Poster 320 – Developing and implementing clinical pathway(s) for hospitalized injection drug users due to injection-related infection sequelae
Location: Dartmouth-Hitchcock Medical Center, Lebanon, N.H.
Resident Travel Grant recipients
We would like to congratulate the latest winners of SHM’s Resident Travel Grant. To qualify for this award, residents submitted an abstract for consideration in the RIV session at HM19 as first authors. Each of them produced outstanding work worthy of recognition:
Daniel Choi, MD – New York Presbyterian Hospital–Weill Cornell
Poster 277 – Improving rates of appropriate ICD deactivation discussions in admitted patients made DNR and/or comfort care
Armond Esmaili, MD – University of California, San Francisco, and the San Francisco VA Medical Center
Poster 649 – Early isolated hypotension, a sepsis “Canary in the Coal Mine”: Timing of antibiotics according to hypotension identifies different sepsis subtypes at differing risks of treatment delay
Poster 8 – Who’s waiting? Predictors of antibiotic delays in hypotensive patients with sepsis
Geoffroy Fauchet, MD – University of Colorado at Denver, Aurora – Rocky Mountain Regional VA Medical Center
Poster 288 – Tackling opioid prescriptions through resident engagement
Nick Zessis, MD – Washington University School of Medicine, St. Louis Children’s Hospital
Poster 101 – Smartphone-based teaching app increases frequency of residents teaching medical students
David Sterken, MD – University of California, San Francisco
Poster 230 – Safety of antimotility agent use during treatment for Clostridioides difficile infection in malignant hepatology patients
James Anstey, MD – University of California, San Francisco
Poster 57 – The POCUS supervision safety gap: Attending physician knowledge in point-of-care ultrasound lags behind that of internal medicine residents
Poster 147 – Association of post paracentesis albumin dosage and acute kidney injury in hospitalized patients
Nicholas Iverson, MD – University of California, San Francisco
Poster 408 – Implications of using an alternative measure to assess opiate days supplied at discharge
Marwah Shahid, MD – Baylor College of Medicine, Houston
Poster 22 – Topic modeling to evaluate hospital Google reviews
Abhishek Chaturvedi, MD – Allegheny Health Network, Pittsburgh
Poster 152 – Association of socioeconomic and racial disparities with health care utilization and outcomes in opioid overdose–related hospitalizations in the United States: Insights from National Inpatient Sample from 2012 through 2014
Pratyusha Tirumanisetty, MD – Unity Hospital, Rochester (N.Y.) Regional Health
Poster 9 – Does hospital-onset Clostridium difficile infection increase the risk of hospital discharge to skilled nursing facilities? A retrospective case-control study from a community hospital.
Chapter Excellence Awards
The Society of Hospital Medicine is proud to recognize its chapters for their hard work and dedication through Chapter Excellence Awards. Each year, chapters strive to demonstrate growth, sustainability, and innovation within their activities, which are then recognized at SHM’s annual conference.
Please join SHM in congratulating the following chapters on their year of success in 2018!
Platinum Chapters: Iowa; Knoxville; Maryland; Michigan; Minnesota; New Mexico; North Carolina Triangle; Pacific Northwest; Southwest Florida; Wiregrass.
Gold Chapters: Houston; NYC/Westchester; Piedmont Triad; San Francisco Bay Area
Silver Chapters: Boston/Eastern Massachusetts; Charlotte Metro Area; Gulf States; Hampton Roads; Kentucky; Maine; Nebraska; North Jersey; Rocky Mountain; South Central Pennsylvania; South Texas; St. Louis.
Outstanding Chapter of the Year
Michigan. The Outstanding Chapter of the Year Award goes to one chapter that exemplifies high performance, going above and beyond the basic chapter requirements. The recipient of the Outstanding Chapter of the Year Award for 2018 is the Michigan chapter of SHM.
The Michigan chapter continues to embrace the mission of our society and nurtures a vibrant, multidisciplinary membership. It is currently the largest chapter in the program, representing more than 750 SHM members.
Using a technology-enabled platform, the Michigan chapter has expanded its meetings to four different sites, leveraging expertise from across the state. The chapter recently held its largest meeting focused on provider burnout, with more than 100 attendees across four different sites. It featured a main speaker as well as a multidisciplinary panel of leaders from eight different health systems.
The chapter has successfully incorporated advocacy into its annual planning and actively responds to new legislation affecting hospital medicine. It continues to be an active and valued member of the Michigan medical community and the SHM chapter community at large.
In addition to the service to members, the chapter strives to serve the SHM chapter community at large by collaborating and sharing best practices.
The chapter’s level of originality is not only a benefit to the chapter, but also to SHM’s Chapter program as a whole. Congratulations to the Michigan chapter on being named the Outstanding Chapter of 2018.
Rising Star Chapter
Knoxville. The Rising Star Chapter Award goes to one chapter that has been active for 2 years or less and in the past 12 months has made improvements to its leadership, stability and growth, and membership.
The recipient of the Rising Star Chapter Award for 2018 is the Knoxville (Tenn.) Chapter of SHM, which has made significant strides since its launch in the spring of 2017. The chapter assembled a group of local hospitalists from Knoxville and the surrounding region to encourage participation and drive quality initiatives in area hospitals.
The Knoxville chapter developed a leadership framework, including officers and board members, and just completed its first formal chapter leadership election. In 2018, the chapter held four meetings, including an event steered toward residents and students. Membership in the chapter has grown by more than 20% since inception. The chapter has engaged in statewide quality initiatives with the Tennessee Hospital Association and has engaged with other chapters across the state.
The Knoxville’s Chapter is an active, enthusiastic organization that is rapidly growing and thriving. Congratulations to the Knoxville chapter on being named the Rising Star Chapter for 2018.
Student Hospitalist Scholar Grant recipients
SHM is proud to acknowledge the latest winners of its Student Hospitalist Scholar Grant. These medical students were awarded grants to complete scholarly work with an active SHM mentor in a project related to patient safety, quality improvement, or other areas relevant to the field of hospital medicine.
Sandeep Bala
University of Chicago Pritzker School of Medicine
Poster 382 – The impact of plain language open medical notes on patient activation
Location: Denver (Colo.) Health Hospital
Monisha Bhatia
Vanderbilt University School of Medicine
Poster 23 – Using electronic medical record phenotypic data to predict discharge destination
Location: Vanderbilt University Medical Center, Nashville, Tenn.
Maximilian Hemmrich
University of Chicago Pritzker School of Medicine
Oral presentation, 11:45 a.m. – Noon, Tuesday, March 26
Project: Derivation and validation of a COPD readmission risk prediction tool
Location: University of Chicago
Ilana Scandariato Lavina
Weill Cornell Medical College
Poster 424 – Understanding the experience of the long-term hospitalized patient with provider fragmentation: A qualitative study
Yun Li
Geisel School of Medicine at Dartmouth
Poster 320 – Developing and implementing clinical pathway(s) for hospitalized injection drug users due to injection-related infection sequelae
Location: Dartmouth-Hitchcock Medical Center, Lebanon, N.H.
Resident Travel Grant recipients
We would like to congratulate the latest winners of SHM’s Resident Travel Grant. To qualify for this award, residents submitted an abstract for consideration in the RIV session at HM19 as first authors. Each of them produced outstanding work worthy of recognition:
Daniel Choi, MD – New York Presbyterian Hospital–Weill Cornell
Poster 277 – Improving rates of appropriate ICD deactivation discussions in admitted patients made DNR and/or comfort care
Armond Esmaili, MD – University of California, San Francisco, and the San Francisco VA Medical Center
Poster 649 – Early isolated hypotension, a sepsis “Canary in the Coal Mine”: Timing of antibiotics according to hypotension identifies different sepsis subtypes at differing risks of treatment delay
Poster 8 – Who’s waiting? Predictors of antibiotic delays in hypotensive patients with sepsis
Geoffroy Fauchet, MD – University of Colorado at Denver, Aurora – Rocky Mountain Regional VA Medical Center
Poster 288 – Tackling opioid prescriptions through resident engagement
Nick Zessis, MD – Washington University School of Medicine, St. Louis Children’s Hospital
Poster 101 – Smartphone-based teaching app increases frequency of residents teaching medical students
David Sterken, MD – University of California, San Francisco
Poster 230 – Safety of antimotility agent use during treatment for Clostridioides difficile infection in malignant hepatology patients
James Anstey, MD – University of California, San Francisco
Poster 57 – The POCUS supervision safety gap: Attending physician knowledge in point-of-care ultrasound lags behind that of internal medicine residents
Poster 147 – Association of post paracentesis albumin dosage and acute kidney injury in hospitalized patients
Nicholas Iverson, MD – University of California, San Francisco
Poster 408 – Implications of using an alternative measure to assess opiate days supplied at discharge
Marwah Shahid, MD – Baylor College of Medicine, Houston
Poster 22 – Topic modeling to evaluate hospital Google reviews
Abhishek Chaturvedi, MD – Allegheny Health Network, Pittsburgh
Poster 152 – Association of socioeconomic and racial disparities with health care utilization and outcomes in opioid overdose–related hospitalizations in the United States: Insights from National Inpatient Sample from 2012 through 2014
Pratyusha Tirumanisetty, MD – Unity Hospital, Rochester (N.Y.) Regional Health
Poster 9 – Does hospital-onset Clostridium difficile infection increase the risk of hospital discharge to skilled nursing facilities? A retrospective case-control study from a community hospital.
Chapter Excellence Awards
The Society of Hospital Medicine is proud to recognize its chapters for their hard work and dedication through Chapter Excellence Awards. Each year, chapters strive to demonstrate growth, sustainability, and innovation within their activities, which are then recognized at SHM’s annual conference.
Please join SHM in congratulating the following chapters on their year of success in 2018!
Platinum Chapters: Iowa; Knoxville; Maryland; Michigan; Minnesota; New Mexico; North Carolina Triangle; Pacific Northwest; Southwest Florida; Wiregrass.
Gold Chapters: Houston; NYC/Westchester; Piedmont Triad; San Francisco Bay Area
Silver Chapters: Boston/Eastern Massachusetts; Charlotte Metro Area; Gulf States; Hampton Roads; Kentucky; Maine; Nebraska; North Jersey; Rocky Mountain; South Central Pennsylvania; South Texas; St. Louis.
Outstanding Chapter of the Year
Michigan. The Outstanding Chapter of the Year Award goes to one chapter that exemplifies high performance, going above and beyond the basic chapter requirements. The recipient of the Outstanding Chapter of the Year Award for 2018 is the Michigan chapter of SHM.
The Michigan chapter continues to embrace the mission of our society and nurtures a vibrant, multidisciplinary membership. It is currently the largest chapter in the program, representing more than 750 SHM members.
Using a technology-enabled platform, the Michigan chapter has expanded its meetings to four different sites, leveraging expertise from across the state. The chapter recently held its largest meeting focused on provider burnout, with more than 100 attendees across four different sites. It featured a main speaker as well as a multidisciplinary panel of leaders from eight different health systems.
The chapter has successfully incorporated advocacy into its annual planning and actively responds to new legislation affecting hospital medicine. It continues to be an active and valued member of the Michigan medical community and the SHM chapter community at large.
In addition to the service to members, the chapter strives to serve the SHM chapter community at large by collaborating and sharing best practices.
The chapter’s level of originality is not only a benefit to the chapter, but also to SHM’s Chapter program as a whole. Congratulations to the Michigan chapter on being named the Outstanding Chapter of 2018.
Rising Star Chapter
Knoxville. The Rising Star Chapter Award goes to one chapter that has been active for 2 years or less and in the past 12 months has made improvements to its leadership, stability and growth, and membership.
The recipient of the Rising Star Chapter Award for 2018 is the Knoxville (Tenn.) Chapter of SHM, which has made significant strides since its launch in the spring of 2017. The chapter assembled a group of local hospitalists from Knoxville and the surrounding region to encourage participation and drive quality initiatives in area hospitals.
The Knoxville chapter developed a leadership framework, including officers and board members, and just completed its first formal chapter leadership election. In 2018, the chapter held four meetings, including an event steered toward residents and students. Membership in the chapter has grown by more than 20% since inception. The chapter has engaged in statewide quality initiatives with the Tennessee Hospital Association and has engaged with other chapters across the state.
The Knoxville’s Chapter is an active, enthusiastic organization that is rapidly growing and thriving. Congratulations to the Knoxville chapter on being named the Rising Star Chapter for 2018.
Student Hospitalist Scholar Grant recipients
SHM is proud to acknowledge the latest winners of its Student Hospitalist Scholar Grant. These medical students were awarded grants to complete scholarly work with an active SHM mentor in a project related to patient safety, quality improvement, or other areas relevant to the field of hospital medicine.
Sandeep Bala
University of Chicago Pritzker School of Medicine
Poster 382 – The impact of plain language open medical notes on patient activation
Location: Denver (Colo.) Health Hospital
Monisha Bhatia
Vanderbilt University School of Medicine
Poster 23 – Using electronic medical record phenotypic data to predict discharge destination
Location: Vanderbilt University Medical Center, Nashville, Tenn.
Maximilian Hemmrich
University of Chicago Pritzker School of Medicine
Oral presentation, 11:45 a.m. – Noon, Tuesday, March 26
Project: Derivation and validation of a COPD readmission risk prediction tool
Location: University of Chicago
Ilana Scandariato Lavina
Weill Cornell Medical College
Poster 424 – Understanding the experience of the long-term hospitalized patient with provider fragmentation: A qualitative study
Yun Li
Geisel School of Medicine at Dartmouth
Poster 320 – Developing and implementing clinical pathway(s) for hospitalized injection drug users due to injection-related infection sequelae
Location: Dartmouth-Hitchcock Medical Center, Lebanon, N.H.
Resident Travel Grant recipients
We would like to congratulate the latest winners of SHM’s Resident Travel Grant. To qualify for this award, residents submitted an abstract for consideration in the RIV session at HM19 as first authors. Each of them produced outstanding work worthy of recognition:
Daniel Choi, MD – New York Presbyterian Hospital–Weill Cornell
Poster 277 – Improving rates of appropriate ICD deactivation discussions in admitted patients made DNR and/or comfort care
Armond Esmaili, MD – University of California, San Francisco, and the San Francisco VA Medical Center
Poster 649 – Early isolated hypotension, a sepsis “Canary in the Coal Mine”: Timing of antibiotics according to hypotension identifies different sepsis subtypes at differing risks of treatment delay
Poster 8 – Who’s waiting? Predictors of antibiotic delays in hypotensive patients with sepsis
Geoffroy Fauchet, MD – University of Colorado at Denver, Aurora – Rocky Mountain Regional VA Medical Center
Poster 288 – Tackling opioid prescriptions through resident engagement
Nick Zessis, MD – Washington University School of Medicine, St. Louis Children’s Hospital
Poster 101 – Smartphone-based teaching app increases frequency of residents teaching medical students
David Sterken, MD – University of California, San Francisco
Poster 230 – Safety of antimotility agent use during treatment for Clostridioides difficile infection in malignant hepatology patients
James Anstey, MD – University of California, San Francisco
Poster 57 – The POCUS supervision safety gap: Attending physician knowledge in point-of-care ultrasound lags behind that of internal medicine residents
Poster 147 – Association of post paracentesis albumin dosage and acute kidney injury in hospitalized patients
Nicholas Iverson, MD – University of California, San Francisco
Poster 408 – Implications of using an alternative measure to assess opiate days supplied at discharge
Marwah Shahid, MD – Baylor College of Medicine, Houston
Poster 22 – Topic modeling to evaluate hospital Google reviews
Abhishek Chaturvedi, MD – Allegheny Health Network, Pittsburgh
Poster 152 – Association of socioeconomic and racial disparities with health care utilization and outcomes in opioid overdose–related hospitalizations in the United States: Insights from National Inpatient Sample from 2012 through 2014
Pratyusha Tirumanisetty, MD – Unity Hospital, Rochester (N.Y.) Regional Health
Poster 9 – Does hospital-onset Clostridium difficile infection increase the risk of hospital discharge to skilled nursing facilities? A retrospective case-control study from a community hospital.
Many EMS protocols for status epilepticus do not follow evidence-based guidelines
“Many protocols did not follow evidence-based guidelines and did not accurately define generalized convulsive status epilepticus,” said John P. Betjemann, MD, associate professor of neurology at the University of California, San Francisco, and his colleagues. They reported their findings in the March 26 issue of JAMA.
Generalized convulsive status epilepticus is a neurologic emergency, and trials published in 2001 and 2012 found that benzodiazepines are effective prehospital treatments for patients with generalized convulsive status epilepticus. These trials informed a 2016 evidence-based guideline that cites level A evidence for intramuscular midazolam, IV lorazepam, and IV diazepam as initial treatment options for adults.
To determine whether EMS system protocols follow these recommendations, the investigators reviewed treatment protocols from 33 EMS systems that cover the 58 counties in California. The researchers reviewed EMS system protocols between May and June 2018 to determine when they were last updated and whether they defined generalized convulsive status epilepticus according to the guideline (namely, 5 or more minutes of continuous seizure or two or more discrete seizures between which a patient has incomplete recovery of consciousness). They also determined whether the protocols included any of the three benzodiazepines in the guideline and, if so, at what dose and using which route of administration.
Protocols’ most recent revision dates ranged between 2007 and 2018. Twenty-seven protocols (81.8%) were revised after the second clinical trial was published in 2012, and 17 (51.5%) were revised after the 2016 guideline. Seven EMS system protocols (21.2%) defined generalized convulsive status epilepticus according to the guideline. Thirty-two protocols (97.0%) included intramuscular midazolam, 2 (6.1%) included IV lorazepam, and 5 (15.2%) included IV diazepam.
Although the protocols “appropriately emphasized” intramuscular midazolam, the protocol doses often were lower than those used in the trials or recommended in the guideline. In addition, most protocols listed IV and intraosseous midazolam as options, although these treatments were not studied in the trials nor recommended in the guideline. In all, six of the protocols (18.2%) recommended at least one medication by the route and dose suggested in the trials or in the guideline.
“Why EMS system protocols deviate from the evidence and how this affects patient outcomes deserves further study,” the authors said.
The researchers noted that they examined EMS protocols in only one state and that “protocols may not necessarily reflect what emergency medical technicians actually do in practice.” In addition, the researchers accessed the most recent protocols by consulting EMS system websites rather than by contacting each EMS system for its most up-to-date protocol.
The authors reported personal compensation from JAMA Neurology and from Continuum Audio unrelated to the present study, as well as grants from the National Institutes of Health.
SOURCE: Betjemann JP et al. JAMA. 2019 Mar 26.
“Many protocols did not follow evidence-based guidelines and did not accurately define generalized convulsive status epilepticus,” said John P. Betjemann, MD, associate professor of neurology at the University of California, San Francisco, and his colleagues. They reported their findings in the March 26 issue of JAMA.
Generalized convulsive status epilepticus is a neurologic emergency, and trials published in 2001 and 2012 found that benzodiazepines are effective prehospital treatments for patients with generalized convulsive status epilepticus. These trials informed a 2016 evidence-based guideline that cites level A evidence for intramuscular midazolam, IV lorazepam, and IV diazepam as initial treatment options for adults.
To determine whether EMS system protocols follow these recommendations, the investigators reviewed treatment protocols from 33 EMS systems that cover the 58 counties in California. The researchers reviewed EMS system protocols between May and June 2018 to determine when they were last updated and whether they defined generalized convulsive status epilepticus according to the guideline (namely, 5 or more minutes of continuous seizure or two or more discrete seizures between which a patient has incomplete recovery of consciousness). They also determined whether the protocols included any of the three benzodiazepines in the guideline and, if so, at what dose and using which route of administration.
Protocols’ most recent revision dates ranged between 2007 and 2018. Twenty-seven protocols (81.8%) were revised after the second clinical trial was published in 2012, and 17 (51.5%) were revised after the 2016 guideline. Seven EMS system protocols (21.2%) defined generalized convulsive status epilepticus according to the guideline. Thirty-two protocols (97.0%) included intramuscular midazolam, 2 (6.1%) included IV lorazepam, and 5 (15.2%) included IV diazepam.
Although the protocols “appropriately emphasized” intramuscular midazolam, the protocol doses often were lower than those used in the trials or recommended in the guideline. In addition, most protocols listed IV and intraosseous midazolam as options, although these treatments were not studied in the trials nor recommended in the guideline. In all, six of the protocols (18.2%) recommended at least one medication by the route and dose suggested in the trials or in the guideline.
“Why EMS system protocols deviate from the evidence and how this affects patient outcomes deserves further study,” the authors said.
The researchers noted that they examined EMS protocols in only one state and that “protocols may not necessarily reflect what emergency medical technicians actually do in practice.” In addition, the researchers accessed the most recent protocols by consulting EMS system websites rather than by contacting each EMS system for its most up-to-date protocol.
The authors reported personal compensation from JAMA Neurology and from Continuum Audio unrelated to the present study, as well as grants from the National Institutes of Health.
SOURCE: Betjemann JP et al. JAMA. 2019 Mar 26.
“Many protocols did not follow evidence-based guidelines and did not accurately define generalized convulsive status epilepticus,” said John P. Betjemann, MD, associate professor of neurology at the University of California, San Francisco, and his colleagues. They reported their findings in the March 26 issue of JAMA.
Generalized convulsive status epilepticus is a neurologic emergency, and trials published in 2001 and 2012 found that benzodiazepines are effective prehospital treatments for patients with generalized convulsive status epilepticus. These trials informed a 2016 evidence-based guideline that cites level A evidence for intramuscular midazolam, IV lorazepam, and IV diazepam as initial treatment options for adults.
To determine whether EMS system protocols follow these recommendations, the investigators reviewed treatment protocols from 33 EMS systems that cover the 58 counties in California. The researchers reviewed EMS system protocols between May and June 2018 to determine when they were last updated and whether they defined generalized convulsive status epilepticus according to the guideline (namely, 5 or more minutes of continuous seizure or two or more discrete seizures between which a patient has incomplete recovery of consciousness). They also determined whether the protocols included any of the three benzodiazepines in the guideline and, if so, at what dose and using which route of administration.
Protocols’ most recent revision dates ranged between 2007 and 2018. Twenty-seven protocols (81.8%) were revised after the second clinical trial was published in 2012, and 17 (51.5%) were revised after the 2016 guideline. Seven EMS system protocols (21.2%) defined generalized convulsive status epilepticus according to the guideline. Thirty-two protocols (97.0%) included intramuscular midazolam, 2 (6.1%) included IV lorazepam, and 5 (15.2%) included IV diazepam.
Although the protocols “appropriately emphasized” intramuscular midazolam, the protocol doses often were lower than those used in the trials or recommended in the guideline. In addition, most protocols listed IV and intraosseous midazolam as options, although these treatments were not studied in the trials nor recommended in the guideline. In all, six of the protocols (18.2%) recommended at least one medication by the route and dose suggested in the trials or in the guideline.
“Why EMS system protocols deviate from the evidence and how this affects patient outcomes deserves further study,” the authors said.
The researchers noted that they examined EMS protocols in only one state and that “protocols may not necessarily reflect what emergency medical technicians actually do in practice.” In addition, the researchers accessed the most recent protocols by consulting EMS system websites rather than by contacting each EMS system for its most up-to-date protocol.
The authors reported personal compensation from JAMA Neurology and from Continuum Audio unrelated to the present study, as well as grants from the National Institutes of Health.
SOURCE: Betjemann JP et al. JAMA. 2019 Mar 26.
FROM JAMA
Key clinical point: Many emergency medical services (EMS) system protocols may not follow evidence-based guidelines or accurately define generalized convulsive status epilepticus.
Major finding: In all, 18.2% of the protocols recommended at least one medication by the route and at the dose suggested in clinical trials or in an evidence-based guideline.
Study details: A review of treatment protocols from 33 EMS systems that cover the 58 counties in California.
Disclosures: The authors reported personal compensation from JAMA Neurology and Continuum Audio unrelated to the present study and grants from the National Institutes of Health.
Source: Betjemann JP et al. JAMA. 2019 March 26.
Swedish strategies improve survival for premature infants
based on data from a study of two cohorts including 2,205 births at 22-26 weeks’ gestational age.
The impact of the recommendations has not been well studied, wrote Mikael Norman, MD, PhD, of the Karolinska Institutet, Stockholm, and his colleagues in JAMA. To determine the impact, the researchers compared data from 1,009 births at 22-26 weeks’ gestational age during 2004-2007 with 1,196 births at 22-26 weeks’ gestational age during 2014-2016, after the implementation of guidelines on “centralization of care, antenatal corticosteroid treatment, mode of delivery, a neonatologist attending at the birth, and resuscitation of infants delivered at 22, 23, and 24 weeks’ gestational age.”
The 1-year survival increased from 70% during 2004-2007 to 77% during 2014-2016; a significant improvement (P = .003).
In addition, 1-year survival with no major morbidity improved significantly between the two time periods, from 32% to 38%, respectively (P = .008).
The mothers and infants were part of EXPRESS (Extremely Preterm Infants in Sweden Study), a national, population-based, prospective cohort study. In most cases, gestational age was determined by routine antenatal ultrasound early in the second trimester, or by date of embryo transfer in cases of in vitro fertilization. The primary outcome was survival at the age of 1 year; the secondary outcome was survival at 1 year with no major neonatal comorbidity.
Among premature infants who survived at 1 year, some conditions were significantly more prevalent in the earlier birth cohort, compared with the later cohort, notably cystic periventricular leukomalacia (6% vs. 2%), any bronchopulmonary dysplasia (73% vs. 62%), and severe bronchopulmonary dysplasia (25% vs. 14%).
Although the proportion of premature births with a neonatologist attending was similar between the two cohorts, significantly more premature infants were born outside of university hospitals and transported to a level III neonatal ICU after birth during 2004-2007, compared with 2014-2016, the researchers noted.
The study findings were limited by several factors including the retrospective design of the second cohort, inability to account for fetal losses prior to 22 weeks’ gestational age, lack of data on the causes of fetal and infant deaths, potentially unknown confounding variables that impacted infant survival, and the small sample size of some gestational age groups, the researchers noted. However, the results show improvements in 1-year survival in the wake of specific guidelines on perinatal management.
Dr. Norman reported receiving grants from the Swedish Heart Lung Foundation and the H2020/European Union, as well as personal fees from a Swedish medical journal, the Swedish patient insurance, Liber, Studentlitteratur, and AbbVie. The study was funded by the Swedish Order of Freemasons’ Foundation for Children’s Welfare.
SOURCE: Norman M et al. JAMA. 2019;321:1188-99.
The wide variation in outcomes for preterm birth worldwide raise questions as to whether the success seen in Sweden is possible in other countries, Matthew A. Rysavy, MD, PhD, and Danielle E. Y. Ehret, MD, MPH, wrote in an accompanying editorial. Considerations include population demographics, current guidelines, gestational age at which intensive care is offered, and the nature of follow-up care.
Sweden already has low rates of perinatal mortality, and current guidelines call for use of antenatal corticosteroids for births at 22 weeks’ gestation. By contrast, in the United States, antenatal corticosteroids are not recommended until 23-24 weeks’ gestation, they noted.
The editorialists called particular attention to the improvements in survival at 1 year and survival without major morbidity at 22-23 weeks’ gestation. “At 22 weeks’ gestation, the stillbirth rate decreased from 65% of all births during 2004-2007 to 35% during 2014-2016, with a reciprocal increase in live births.”
Although the results are promising, and show the possibilities for improving survival, the editorialists wrote that ongoing follow up of children born prematurely is essential to inform future research, as “much remains unknown about the later-life effects of being born so early and of the therapies used to sustain life after birth.”
Dr. Rysavy is affiliated with the department of pediatrics at the University of Iowa, Iowa City; Dr. Ehret is affiliated with the department of pediatrics at the University of Vermont, Burlington. This is a summary of their editorial accompanying the article by Norman et al. (JAMA. 2019 Mar 26;321:1163-64). They reported no financial conflicts.
The wide variation in outcomes for preterm birth worldwide raise questions as to whether the success seen in Sweden is possible in other countries, Matthew A. Rysavy, MD, PhD, and Danielle E. Y. Ehret, MD, MPH, wrote in an accompanying editorial. Considerations include population demographics, current guidelines, gestational age at which intensive care is offered, and the nature of follow-up care.
Sweden already has low rates of perinatal mortality, and current guidelines call for use of antenatal corticosteroids for births at 22 weeks’ gestation. By contrast, in the United States, antenatal corticosteroids are not recommended until 23-24 weeks’ gestation, they noted.
The editorialists called particular attention to the improvements in survival at 1 year and survival without major morbidity at 22-23 weeks’ gestation. “At 22 weeks’ gestation, the stillbirth rate decreased from 65% of all births during 2004-2007 to 35% during 2014-2016, with a reciprocal increase in live births.”
Although the results are promising, and show the possibilities for improving survival, the editorialists wrote that ongoing follow up of children born prematurely is essential to inform future research, as “much remains unknown about the later-life effects of being born so early and of the therapies used to sustain life after birth.”
Dr. Rysavy is affiliated with the department of pediatrics at the University of Iowa, Iowa City; Dr. Ehret is affiliated with the department of pediatrics at the University of Vermont, Burlington. This is a summary of their editorial accompanying the article by Norman et al. (JAMA. 2019 Mar 26;321:1163-64). They reported no financial conflicts.
The wide variation in outcomes for preterm birth worldwide raise questions as to whether the success seen in Sweden is possible in other countries, Matthew A. Rysavy, MD, PhD, and Danielle E. Y. Ehret, MD, MPH, wrote in an accompanying editorial. Considerations include population demographics, current guidelines, gestational age at which intensive care is offered, and the nature of follow-up care.
Sweden already has low rates of perinatal mortality, and current guidelines call for use of antenatal corticosteroids for births at 22 weeks’ gestation. By contrast, in the United States, antenatal corticosteroids are not recommended until 23-24 weeks’ gestation, they noted.
The editorialists called particular attention to the improvements in survival at 1 year and survival without major morbidity at 22-23 weeks’ gestation. “At 22 weeks’ gestation, the stillbirth rate decreased from 65% of all births during 2004-2007 to 35% during 2014-2016, with a reciprocal increase in live births.”
Although the results are promising, and show the possibilities for improving survival, the editorialists wrote that ongoing follow up of children born prematurely is essential to inform future research, as “much remains unknown about the later-life effects of being born so early and of the therapies used to sustain life after birth.”
Dr. Rysavy is affiliated with the department of pediatrics at the University of Iowa, Iowa City; Dr. Ehret is affiliated with the department of pediatrics at the University of Vermont, Burlington. This is a summary of their editorial accompanying the article by Norman et al. (JAMA. 2019 Mar 26;321:1163-64). They reported no financial conflicts.
based on data from a study of two cohorts including 2,205 births at 22-26 weeks’ gestational age.
The impact of the recommendations has not been well studied, wrote Mikael Norman, MD, PhD, of the Karolinska Institutet, Stockholm, and his colleagues in JAMA. To determine the impact, the researchers compared data from 1,009 births at 22-26 weeks’ gestational age during 2004-2007 with 1,196 births at 22-26 weeks’ gestational age during 2014-2016, after the implementation of guidelines on “centralization of care, antenatal corticosteroid treatment, mode of delivery, a neonatologist attending at the birth, and resuscitation of infants delivered at 22, 23, and 24 weeks’ gestational age.”
The 1-year survival increased from 70% during 2004-2007 to 77% during 2014-2016; a significant improvement (P = .003).
In addition, 1-year survival with no major morbidity improved significantly between the two time periods, from 32% to 38%, respectively (P = .008).
The mothers and infants were part of EXPRESS (Extremely Preterm Infants in Sweden Study), a national, population-based, prospective cohort study. In most cases, gestational age was determined by routine antenatal ultrasound early in the second trimester, or by date of embryo transfer in cases of in vitro fertilization. The primary outcome was survival at the age of 1 year; the secondary outcome was survival at 1 year with no major neonatal comorbidity.
Among premature infants who survived at 1 year, some conditions were significantly more prevalent in the earlier birth cohort, compared with the later cohort, notably cystic periventricular leukomalacia (6% vs. 2%), any bronchopulmonary dysplasia (73% vs. 62%), and severe bronchopulmonary dysplasia (25% vs. 14%).
Although the proportion of premature births with a neonatologist attending was similar between the two cohorts, significantly more premature infants were born outside of university hospitals and transported to a level III neonatal ICU after birth during 2004-2007, compared with 2014-2016, the researchers noted.
The study findings were limited by several factors including the retrospective design of the second cohort, inability to account for fetal losses prior to 22 weeks’ gestational age, lack of data on the causes of fetal and infant deaths, potentially unknown confounding variables that impacted infant survival, and the small sample size of some gestational age groups, the researchers noted. However, the results show improvements in 1-year survival in the wake of specific guidelines on perinatal management.
Dr. Norman reported receiving grants from the Swedish Heart Lung Foundation and the H2020/European Union, as well as personal fees from a Swedish medical journal, the Swedish patient insurance, Liber, Studentlitteratur, and AbbVie. The study was funded by the Swedish Order of Freemasons’ Foundation for Children’s Welfare.
SOURCE: Norman M et al. JAMA. 2019;321:1188-99.
based on data from a study of two cohorts including 2,205 births at 22-26 weeks’ gestational age.
The impact of the recommendations has not been well studied, wrote Mikael Norman, MD, PhD, of the Karolinska Institutet, Stockholm, and his colleagues in JAMA. To determine the impact, the researchers compared data from 1,009 births at 22-26 weeks’ gestational age during 2004-2007 with 1,196 births at 22-26 weeks’ gestational age during 2014-2016, after the implementation of guidelines on “centralization of care, antenatal corticosteroid treatment, mode of delivery, a neonatologist attending at the birth, and resuscitation of infants delivered at 22, 23, and 24 weeks’ gestational age.”
The 1-year survival increased from 70% during 2004-2007 to 77% during 2014-2016; a significant improvement (P = .003).
In addition, 1-year survival with no major morbidity improved significantly between the two time periods, from 32% to 38%, respectively (P = .008).
The mothers and infants were part of EXPRESS (Extremely Preterm Infants in Sweden Study), a national, population-based, prospective cohort study. In most cases, gestational age was determined by routine antenatal ultrasound early in the second trimester, or by date of embryo transfer in cases of in vitro fertilization. The primary outcome was survival at the age of 1 year; the secondary outcome was survival at 1 year with no major neonatal comorbidity.
Among premature infants who survived at 1 year, some conditions were significantly more prevalent in the earlier birth cohort, compared with the later cohort, notably cystic periventricular leukomalacia (6% vs. 2%), any bronchopulmonary dysplasia (73% vs. 62%), and severe bronchopulmonary dysplasia (25% vs. 14%).
Although the proportion of premature births with a neonatologist attending was similar between the two cohorts, significantly more premature infants were born outside of university hospitals and transported to a level III neonatal ICU after birth during 2004-2007, compared with 2014-2016, the researchers noted.
The study findings were limited by several factors including the retrospective design of the second cohort, inability to account for fetal losses prior to 22 weeks’ gestational age, lack of data on the causes of fetal and infant deaths, potentially unknown confounding variables that impacted infant survival, and the small sample size of some gestational age groups, the researchers noted. However, the results show improvements in 1-year survival in the wake of specific guidelines on perinatal management.
Dr. Norman reported receiving grants from the Swedish Heart Lung Foundation and the H2020/European Union, as well as personal fees from a Swedish medical journal, the Swedish patient insurance, Liber, Studentlitteratur, and AbbVie. The study was funded by the Swedish Order of Freemasons’ Foundation for Children’s Welfare.
SOURCE: Norman M et al. JAMA. 2019;321:1188-99.
FROM JAMA
Erythematous and Necrotic Papules in an Immunosuppressed Woman
The Diagnosis: Disseminated Fusariosis
Histologic evaluation of the punch biopsy demonstrated thrombosed vessels in the deep dermis and along fibrous septae of subcutaneous tissue, as well as delicate, thin-walled, branching hyphae with vesicular swellings (Figure). The hyphae were present within the vascular thrombi and extended into surrounding tissue. The fungal tissue culture eventually grew scant Fusarium. At the time of biopsy, there was a high index of suspicion for fungal infection, which supported the decision to empirically treat with anidulafungin and voriconazole.
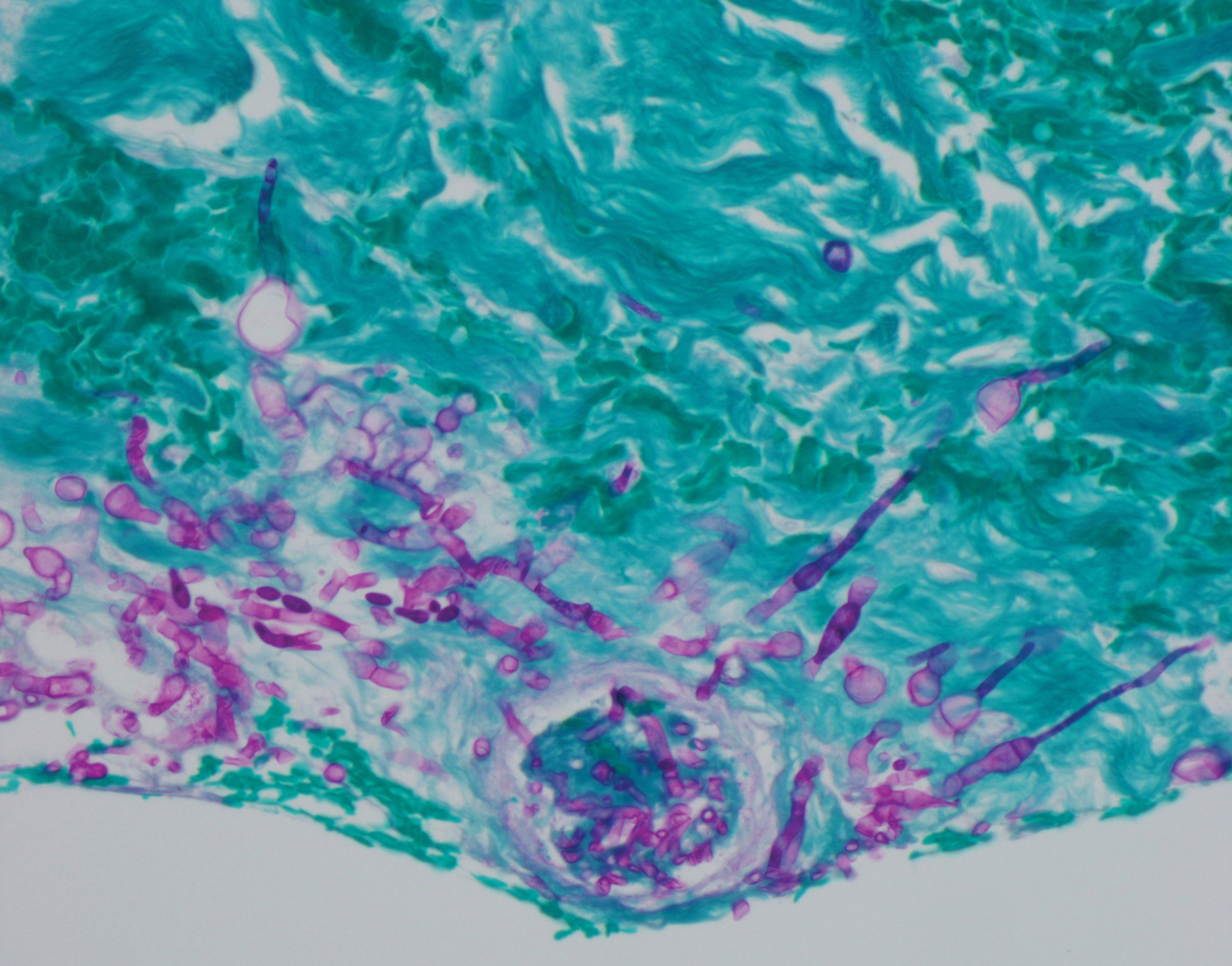
Differentiating the diagnosis in this case was done primarily with histopathology. Although Aspergillus also has slender hyphae, it lacks the vesicular swellings characteristic of fusariosis. Disseminated candidiasis would demonstrate budding yeast and pseudohyphae in the dermis. Ecthyma gangrenosum histologically presents as necrotizing hemorrhagic vasculitis with gram-negative rods in the walls of deeper vessels, characteristically sparing the intima. Leukemia cutis histologically varies but would display a neoplastic infiltrate of atypical monocytoid cells with nuclear pleomorphism.
Our patient had been treated with palliative chemotherapy as a salvage regimen with idarubicin and cytarabine. She had persistent pancytopenia despite granulocyte-macrophage colony-stimulating factor therapy. The mortality rate for disseminated Fusarium infection approaches 100% when risk factors such as angiotropism and prolonged neutropenia are present.1,2 Additionally, our patient's susceptibility profile subsequently demonstrated an elevated minimum inhibitory concentration to amphotericin B, itraconazole, voriconazole, and posaconazole. The neutropenia and Fusarium infection were not responsive to treatment. She was discharged on palliative voriconazole with home hospice care.
Fusarium species are soil-dwelling saprophytes and important plant pathogens that have increasingly emerged as rare but notable causes of morbidity and mortality in immunocompromised patients.1-3 More specifically, Fusarium infection is most commonly observed in patients with hematologic malignancy complicated by persistent neutropenia. The 3 most frequently encountered Fusarium species in human disease are Fusarium solani, Fusarium oxysporum, and Fusarium moniliforme, with F solani being the most virulent.1,2 Infection with Fusarium may manifest as a broad range of presentations depending on the route of entry, such as endophthalmitis, sinusitis, pneumonia, and cutaneous lesions.1 Disseminated infection is marked by skin lesions or positive blood cultures for Fusarium.3 This fungus is notorious for its limited susceptibility profile.1 It requires systemic antifungal medications such as triazoles and amphotericin B. Fusarium is most susceptible in vitro to amphotericin B but often requires toxic dosages to be effective in decreasing fungal load.2,3 The high mortality rate of disseminated fusariosis further emphasizes that prevention is an important component to protecting high-risk patients. Keeping patients in rooms with high-efficiency particulate arresting filters and limiting exposure to unsanitized tap water faucets can help decrease exposure; however, reducing immunosuppression and improving neutropenia are the most effective ways to prevent fusariosis.1 Although skin breakdown can facilitate the spread of infection, it has been observed that immunosuppressed individuals do not necessarily have this finding.4
This case emphasizes the importance of considering disseminated fusariosis in patients with hematologic malignancy or other immunosuppressed conditions. The most important factors that should raise clinical suspicion are persistent neutropenia and recent corticosteroid therapy.1 A clinical picture that suggests fungal infection should warrant consideration of prophylactic treatment as well as tissue and blood cultures to determine species and susceptibility.
- Nucci M, Anaissie E. Fusarium infections in immunocompromised patients. Clin Microbiol Rev. 2007;20:695-704.
- Jossi M, Ambrosioni J, Macedo-Vinas M, et al. Invasive fusariosis with prolonged fungemia in a patient with acute lymphoblastic leukemia: case report and review of the literature. Int J Infect Dis. 2010;14:E354-E356.
- Tan R, Ng KP, Gan GG, et al. Fusarium sp. infection in a patient with Acute Lymphoblastic Leukaemia. Med J Malaysia. 2013;68:479-480.
- Nucci M, Anaissie E. Cutaneous infection by Fusarium species in healthy and immunocompromised hosts: implications for diagnosis and management. Clin Infect Dis. 2002;35:909-920.
The Diagnosis: Disseminated Fusariosis
Histologic evaluation of the punch biopsy demonstrated thrombosed vessels in the deep dermis and along fibrous septae of subcutaneous tissue, as well as delicate, thin-walled, branching hyphae with vesicular swellings (Figure). The hyphae were present within the vascular thrombi and extended into surrounding tissue. The fungal tissue culture eventually grew scant Fusarium. At the time of biopsy, there was a high index of suspicion for fungal infection, which supported the decision to empirically treat with anidulafungin and voriconazole.
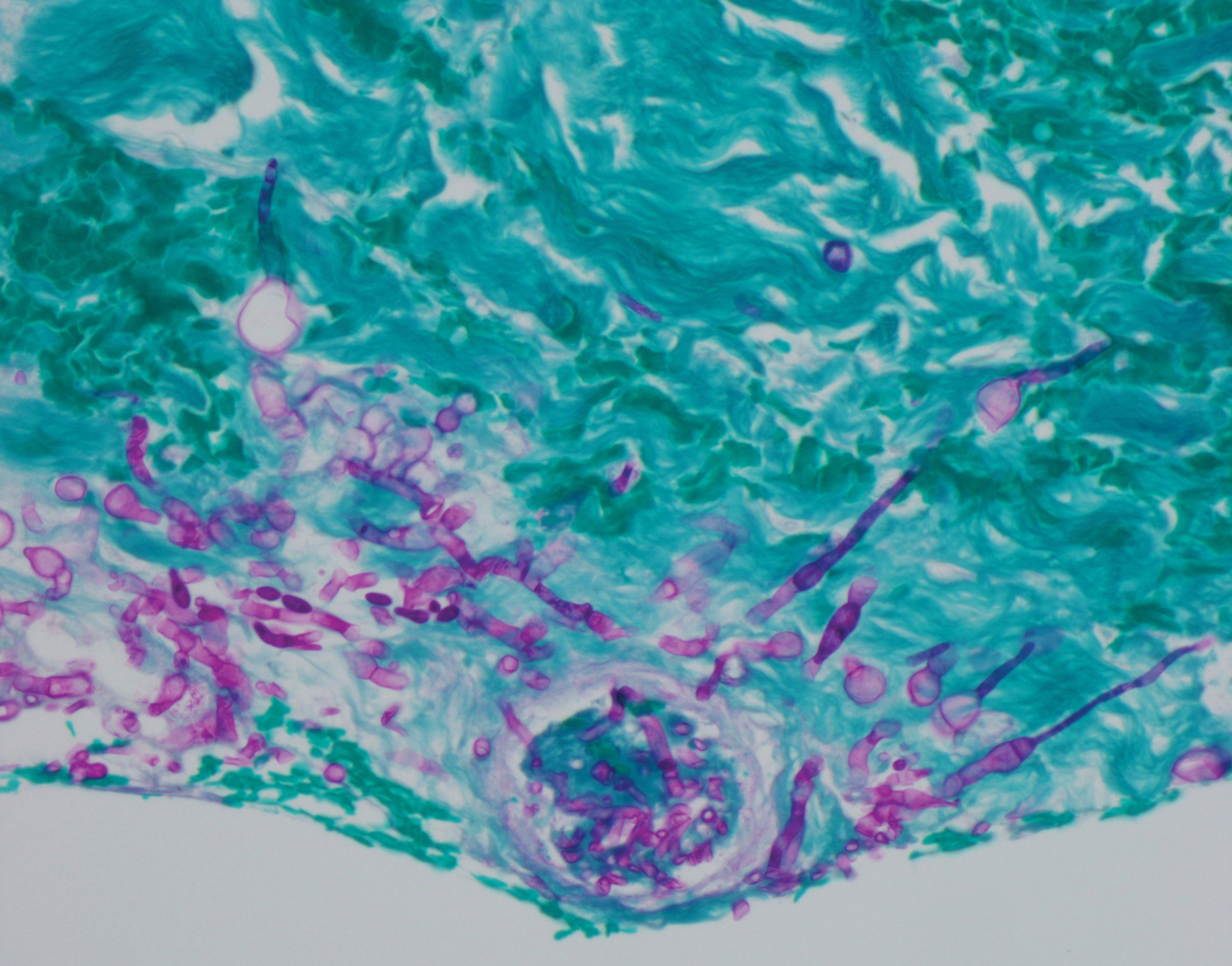
Differentiating the diagnosis in this case was done primarily with histopathology. Although Aspergillus also has slender hyphae, it lacks the vesicular swellings characteristic of fusariosis. Disseminated candidiasis would demonstrate budding yeast and pseudohyphae in the dermis. Ecthyma gangrenosum histologically presents as necrotizing hemorrhagic vasculitis with gram-negative rods in the walls of deeper vessels, characteristically sparing the intima. Leukemia cutis histologically varies but would display a neoplastic infiltrate of atypical monocytoid cells with nuclear pleomorphism.
Our patient had been treated with palliative chemotherapy as a salvage regimen with idarubicin and cytarabine. She had persistent pancytopenia despite granulocyte-macrophage colony-stimulating factor therapy. The mortality rate for disseminated Fusarium infection approaches 100% when risk factors such as angiotropism and prolonged neutropenia are present.1,2 Additionally, our patient's susceptibility profile subsequently demonstrated an elevated minimum inhibitory concentration to amphotericin B, itraconazole, voriconazole, and posaconazole. The neutropenia and Fusarium infection were not responsive to treatment. She was discharged on palliative voriconazole with home hospice care.
Fusarium species are soil-dwelling saprophytes and important plant pathogens that have increasingly emerged as rare but notable causes of morbidity and mortality in immunocompromised patients.1-3 More specifically, Fusarium infection is most commonly observed in patients with hematologic malignancy complicated by persistent neutropenia. The 3 most frequently encountered Fusarium species in human disease are Fusarium solani, Fusarium oxysporum, and Fusarium moniliforme, with F solani being the most virulent.1,2 Infection with Fusarium may manifest as a broad range of presentations depending on the route of entry, such as endophthalmitis, sinusitis, pneumonia, and cutaneous lesions.1 Disseminated infection is marked by skin lesions or positive blood cultures for Fusarium.3 This fungus is notorious for its limited susceptibility profile.1 It requires systemic antifungal medications such as triazoles and amphotericin B. Fusarium is most susceptible in vitro to amphotericin B but often requires toxic dosages to be effective in decreasing fungal load.2,3 The high mortality rate of disseminated fusariosis further emphasizes that prevention is an important component to protecting high-risk patients. Keeping patients in rooms with high-efficiency particulate arresting filters and limiting exposure to unsanitized tap water faucets can help decrease exposure; however, reducing immunosuppression and improving neutropenia are the most effective ways to prevent fusariosis.1 Although skin breakdown can facilitate the spread of infection, it has been observed that immunosuppressed individuals do not necessarily have this finding.4
This case emphasizes the importance of considering disseminated fusariosis in patients with hematologic malignancy or other immunosuppressed conditions. The most important factors that should raise clinical suspicion are persistent neutropenia and recent corticosteroid therapy.1 A clinical picture that suggests fungal infection should warrant consideration of prophylactic treatment as well as tissue and blood cultures to determine species and susceptibility.
The Diagnosis: Disseminated Fusariosis
Histologic evaluation of the punch biopsy demonstrated thrombosed vessels in the deep dermis and along fibrous septae of subcutaneous tissue, as well as delicate, thin-walled, branching hyphae with vesicular swellings (Figure). The hyphae were present within the vascular thrombi and extended into surrounding tissue. The fungal tissue culture eventually grew scant Fusarium. At the time of biopsy, there was a high index of suspicion for fungal infection, which supported the decision to empirically treat with anidulafungin and voriconazole.
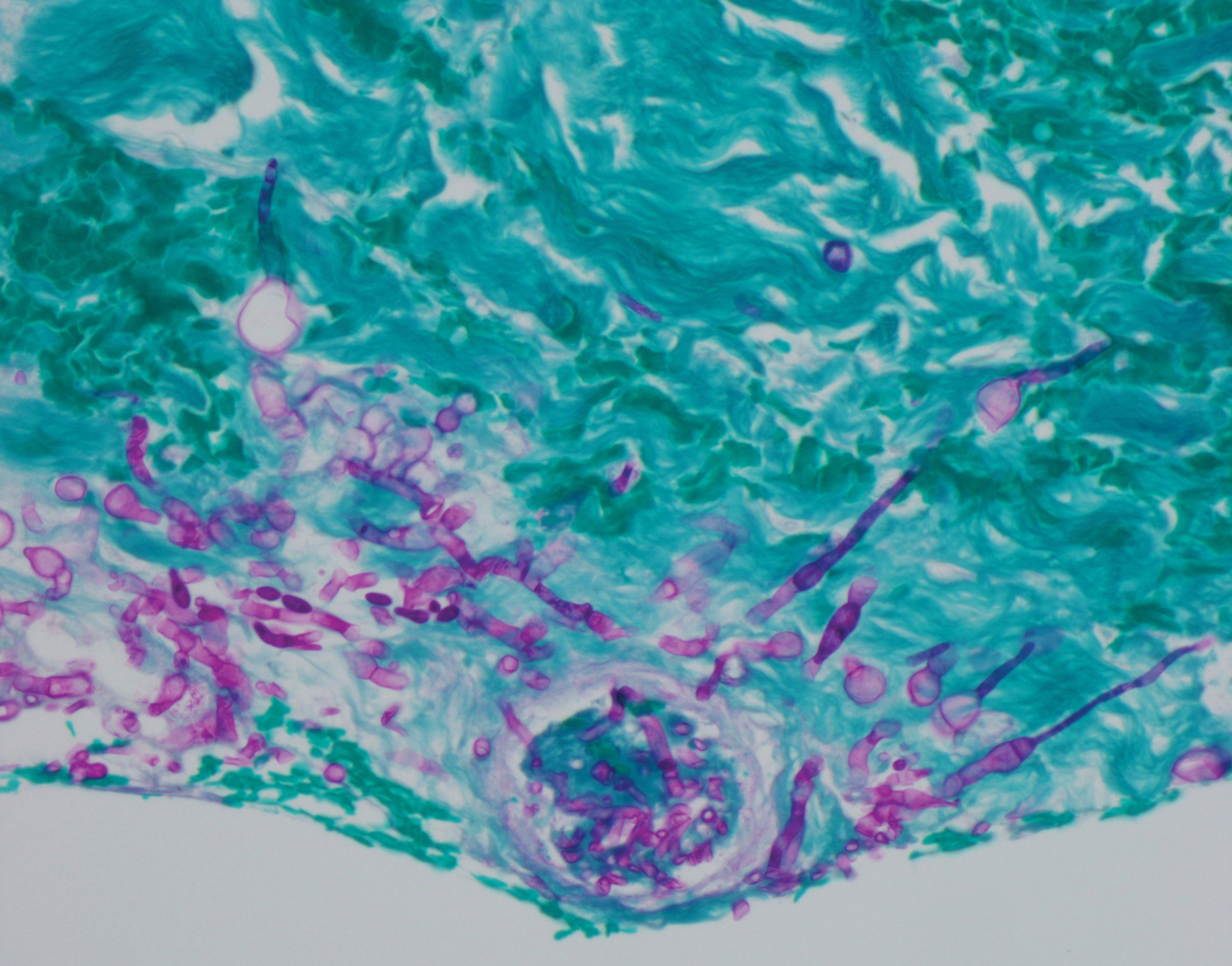
Differentiating the diagnosis in this case was done primarily with histopathology. Although Aspergillus also has slender hyphae, it lacks the vesicular swellings characteristic of fusariosis. Disseminated candidiasis would demonstrate budding yeast and pseudohyphae in the dermis. Ecthyma gangrenosum histologically presents as necrotizing hemorrhagic vasculitis with gram-negative rods in the walls of deeper vessels, characteristically sparing the intima. Leukemia cutis histologically varies but would display a neoplastic infiltrate of atypical monocytoid cells with nuclear pleomorphism.
Our patient had been treated with palliative chemotherapy as a salvage regimen with idarubicin and cytarabine. She had persistent pancytopenia despite granulocyte-macrophage colony-stimulating factor therapy. The mortality rate for disseminated Fusarium infection approaches 100% when risk factors such as angiotropism and prolonged neutropenia are present.1,2 Additionally, our patient's susceptibility profile subsequently demonstrated an elevated minimum inhibitory concentration to amphotericin B, itraconazole, voriconazole, and posaconazole. The neutropenia and Fusarium infection were not responsive to treatment. She was discharged on palliative voriconazole with home hospice care.
Fusarium species are soil-dwelling saprophytes and important plant pathogens that have increasingly emerged as rare but notable causes of morbidity and mortality in immunocompromised patients.1-3 More specifically, Fusarium infection is most commonly observed in patients with hematologic malignancy complicated by persistent neutropenia. The 3 most frequently encountered Fusarium species in human disease are Fusarium solani, Fusarium oxysporum, and Fusarium moniliforme, with F solani being the most virulent.1,2 Infection with Fusarium may manifest as a broad range of presentations depending on the route of entry, such as endophthalmitis, sinusitis, pneumonia, and cutaneous lesions.1 Disseminated infection is marked by skin lesions or positive blood cultures for Fusarium.3 This fungus is notorious for its limited susceptibility profile.1 It requires systemic antifungal medications such as triazoles and amphotericin B. Fusarium is most susceptible in vitro to amphotericin B but often requires toxic dosages to be effective in decreasing fungal load.2,3 The high mortality rate of disseminated fusariosis further emphasizes that prevention is an important component to protecting high-risk patients. Keeping patients in rooms with high-efficiency particulate arresting filters and limiting exposure to unsanitized tap water faucets can help decrease exposure; however, reducing immunosuppression and improving neutropenia are the most effective ways to prevent fusariosis.1 Although skin breakdown can facilitate the spread of infection, it has been observed that immunosuppressed individuals do not necessarily have this finding.4
This case emphasizes the importance of considering disseminated fusariosis in patients with hematologic malignancy or other immunosuppressed conditions. The most important factors that should raise clinical suspicion are persistent neutropenia and recent corticosteroid therapy.1 A clinical picture that suggests fungal infection should warrant consideration of prophylactic treatment as well as tissue and blood cultures to determine species and susceptibility.
- Nucci M, Anaissie E. Fusarium infections in immunocompromised patients. Clin Microbiol Rev. 2007;20:695-704.
- Jossi M, Ambrosioni J, Macedo-Vinas M, et al. Invasive fusariosis with prolonged fungemia in a patient with acute lymphoblastic leukemia: case report and review of the literature. Int J Infect Dis. 2010;14:E354-E356.
- Tan R, Ng KP, Gan GG, et al. Fusarium sp. infection in a patient with Acute Lymphoblastic Leukaemia. Med J Malaysia. 2013;68:479-480.
- Nucci M, Anaissie E. Cutaneous infection by Fusarium species in healthy and immunocompromised hosts: implications for diagnosis and management. Clin Infect Dis. 2002;35:909-920.
- Nucci M, Anaissie E. Fusarium infections in immunocompromised patients. Clin Microbiol Rev. 2007;20:695-704.
- Jossi M, Ambrosioni J, Macedo-Vinas M, et al. Invasive fusariosis with prolonged fungemia in a patient with acute lymphoblastic leukemia: case report and review of the literature. Int J Infect Dis. 2010;14:E354-E356.
- Tan R, Ng KP, Gan GG, et al. Fusarium sp. infection in a patient with Acute Lymphoblastic Leukaemia. Med J Malaysia. 2013;68:479-480.
- Nucci M, Anaissie E. Cutaneous infection by Fusarium species in healthy and immunocompromised hosts: implications for diagnosis and management. Clin Infect Dis. 2002;35:909-920.