User login
Atypical used in Parkinson’s lifts hallucinations, delusions in refractory schizophrenia
Pimavanserin (Nuplazid), an atypical antipsychotic approved to treat hallucinations and delusions in Parkinson’s disease, shows promise as a treatment for patients with refractory schizophrenia who fail to respond to clozapine, a retrospective study suggests.
“Within a month, sometimes 2 months, hallucinations and delusions that have persisted for years were completely gone,” said lead author Henry A. Nasrallah, MD, in an interview. The study was published in Schizophrenia Research.
Dr. Nasrallah and his colleagues launched the study in a bid to help “the most desperate group of patients” with schizophrenia – the 60% of those with refractory psychosis who do not respond to clozapine.
“This group of patients is so desperate that psychiatrists have used everything in our pharmacopeia,” said Dr. Nasrallah, the Sydney W. Souers Endowed Chair and professor and chairman of the department of psychiatry and behavioral neuroscience at Saint Louis University. “Nothing has been shown to work. We decided to give them this medication [pimavanserin], which was approved by the FDA [Food and Drug Administration] 2 years ago for hallucinations and delusions for Parkinson’s disease.”
For the new study, Dr. Nasrallah and his coauthors gave 34 mg/day of pimavanserin to 10 patients, aged 21-77 years, with schizophrenia or schizoaffective disorder and refractory hallucinations and delusions. The subjects, all of whom live in a residential group home, had either failed clozapine (n = 6) or failed several antipsychotics but had not yet received clozapine (n = 4).
The results, Dr. Nasrallah said, were remarkable. “Not only did they get relief from their delusions and hallucinations, but nursing staff reported they were much more sociable and affable, getting out of their rooms, and mixing and mingling. It seems to help them beyond suppressing delusions and hallucinations. It made them more sociable and pleasant.”
Patients were able to avoid blood tests and the “sometimes life-threatening side effects of clozapine,” he said. According to the study, no patients needed to discontinue treatment because of safety or tolerability.
However, pimavanserin is expensive. According to GoodRx.com, monthly prices for 60 tablets of 17 mg pimavanserin – equal to the daily dose in this study – run from $2,759 to $2,907 with a free coupon.
Should psychiatrists prescribe the drug now for treatment-resistant schizophrenia? “We use drugs off label all the time for patients who do not have any FDA-approved medication,” Dr. Nasrallah said. “Sometimes, off-label use in psychiatry is a necessity, because around 80% of DSM-5 disorders do not have any approved drugs at this time.”
“It would also be interesting to test pimavanserin in first-episode psychosis to identify a ‘serotonergic subtype’ of the schizophrenia syndrome but also to completely avoid the extrapyramidal side effects of dopamine antagonists, to which first-episode psychosis patients are especially susceptible.”
No outside funding was reported. Dr. Nasrallah reported advisory board and consultant and speaker’s bureau relationships with Acadia, Alkermes, Allergan, Janssen, Lundbeck, Neurocrine Biosciences, Otsuka Pharmaceutical, Sunovion, and Teva. Another author reported no disclosures, and a third author reported numerous disclosures.
SOURCE: Nasrallah HA et al. Schizophr Res. 2019 Mar 2. doi: 10/1016/j.schres.2019.02.018.
Pimavanserin (Nuplazid), an atypical antipsychotic approved to treat hallucinations and delusions in Parkinson’s disease, shows promise as a treatment for patients with refractory schizophrenia who fail to respond to clozapine, a retrospective study suggests.
“Within a month, sometimes 2 months, hallucinations and delusions that have persisted for years were completely gone,” said lead author Henry A. Nasrallah, MD, in an interview. The study was published in Schizophrenia Research.
Dr. Nasrallah and his colleagues launched the study in a bid to help “the most desperate group of patients” with schizophrenia – the 60% of those with refractory psychosis who do not respond to clozapine.
“This group of patients is so desperate that psychiatrists have used everything in our pharmacopeia,” said Dr. Nasrallah, the Sydney W. Souers Endowed Chair and professor and chairman of the department of psychiatry and behavioral neuroscience at Saint Louis University. “Nothing has been shown to work. We decided to give them this medication [pimavanserin], which was approved by the FDA [Food and Drug Administration] 2 years ago for hallucinations and delusions for Parkinson’s disease.”
For the new study, Dr. Nasrallah and his coauthors gave 34 mg/day of pimavanserin to 10 patients, aged 21-77 years, with schizophrenia or schizoaffective disorder and refractory hallucinations and delusions. The subjects, all of whom live in a residential group home, had either failed clozapine (n = 6) or failed several antipsychotics but had not yet received clozapine (n = 4).
The results, Dr. Nasrallah said, were remarkable. “Not only did they get relief from their delusions and hallucinations, but nursing staff reported they were much more sociable and affable, getting out of their rooms, and mixing and mingling. It seems to help them beyond suppressing delusions and hallucinations. It made them more sociable and pleasant.”
Patients were able to avoid blood tests and the “sometimes life-threatening side effects of clozapine,” he said. According to the study, no patients needed to discontinue treatment because of safety or tolerability.
However, pimavanserin is expensive. According to GoodRx.com, monthly prices for 60 tablets of 17 mg pimavanserin – equal to the daily dose in this study – run from $2,759 to $2,907 with a free coupon.
Should psychiatrists prescribe the drug now for treatment-resistant schizophrenia? “We use drugs off label all the time for patients who do not have any FDA-approved medication,” Dr. Nasrallah said. “Sometimes, off-label use in psychiatry is a necessity, because around 80% of DSM-5 disorders do not have any approved drugs at this time.”
“It would also be interesting to test pimavanserin in first-episode psychosis to identify a ‘serotonergic subtype’ of the schizophrenia syndrome but also to completely avoid the extrapyramidal side effects of dopamine antagonists, to which first-episode psychosis patients are especially susceptible.”
No outside funding was reported. Dr. Nasrallah reported advisory board and consultant and speaker’s bureau relationships with Acadia, Alkermes, Allergan, Janssen, Lundbeck, Neurocrine Biosciences, Otsuka Pharmaceutical, Sunovion, and Teva. Another author reported no disclosures, and a third author reported numerous disclosures.
SOURCE: Nasrallah HA et al. Schizophr Res. 2019 Mar 2. doi: 10/1016/j.schres.2019.02.018.
Pimavanserin (Nuplazid), an atypical antipsychotic approved to treat hallucinations and delusions in Parkinson’s disease, shows promise as a treatment for patients with refractory schizophrenia who fail to respond to clozapine, a retrospective study suggests.
“Within a month, sometimes 2 months, hallucinations and delusions that have persisted for years were completely gone,” said lead author Henry A. Nasrallah, MD, in an interview. The study was published in Schizophrenia Research.
Dr. Nasrallah and his colleagues launched the study in a bid to help “the most desperate group of patients” with schizophrenia – the 60% of those with refractory psychosis who do not respond to clozapine.
“This group of patients is so desperate that psychiatrists have used everything in our pharmacopeia,” said Dr. Nasrallah, the Sydney W. Souers Endowed Chair and professor and chairman of the department of psychiatry and behavioral neuroscience at Saint Louis University. “Nothing has been shown to work. We decided to give them this medication [pimavanserin], which was approved by the FDA [Food and Drug Administration] 2 years ago for hallucinations and delusions for Parkinson’s disease.”
For the new study, Dr. Nasrallah and his coauthors gave 34 mg/day of pimavanserin to 10 patients, aged 21-77 years, with schizophrenia or schizoaffective disorder and refractory hallucinations and delusions. The subjects, all of whom live in a residential group home, had either failed clozapine (n = 6) or failed several antipsychotics but had not yet received clozapine (n = 4).
The results, Dr. Nasrallah said, were remarkable. “Not only did they get relief from their delusions and hallucinations, but nursing staff reported they were much more sociable and affable, getting out of their rooms, and mixing and mingling. It seems to help them beyond suppressing delusions and hallucinations. It made them more sociable and pleasant.”
Patients were able to avoid blood tests and the “sometimes life-threatening side effects of clozapine,” he said. According to the study, no patients needed to discontinue treatment because of safety or tolerability.
However, pimavanserin is expensive. According to GoodRx.com, monthly prices for 60 tablets of 17 mg pimavanserin – equal to the daily dose in this study – run from $2,759 to $2,907 with a free coupon.
Should psychiatrists prescribe the drug now for treatment-resistant schizophrenia? “We use drugs off label all the time for patients who do not have any FDA-approved medication,” Dr. Nasrallah said. “Sometimes, off-label use in psychiatry is a necessity, because around 80% of DSM-5 disorders do not have any approved drugs at this time.”
“It would also be interesting to test pimavanserin in first-episode psychosis to identify a ‘serotonergic subtype’ of the schizophrenia syndrome but also to completely avoid the extrapyramidal side effects of dopamine antagonists, to which first-episode psychosis patients are especially susceptible.”
No outside funding was reported. Dr. Nasrallah reported advisory board and consultant and speaker’s bureau relationships with Acadia, Alkermes, Allergan, Janssen, Lundbeck, Neurocrine Biosciences, Otsuka Pharmaceutical, Sunovion, and Teva. Another author reported no disclosures, and a third author reported numerous disclosures.
SOURCE: Nasrallah HA et al. Schizophr Res. 2019 Mar 2. doi: 10/1016/j.schres.2019.02.018.
FROM SCHIZOPHRENIA RESEARCH
Depression increasing among American teens, young adults
Time spent on social media is seen as partly to blame
Depression, suicidal thoughts, and mental distress appear to be on the rise among American teenagers and young adults, and a new study points to their use of social media as a cause. According to the study’s lead author, Jean M. Twenge, PhD, the findings might be evident of a generational shift in mental illness. The study looked at data from more than 200,000 adolescents aged 12-17 and nearly 400,000 young adults aged 18 and over from 2005 to 2017. During that time, reported symptoms consistent with major depression increased by 52% among the teens and 63% among the young adults. Girls were especially at risk, with one in five teenage girls having experienced major depression in 2017. In addition, by 2017, nearly three-quarters of young adults had experienced feelings of hopelessness about their lives. Meanwhile, the rate of suicide rose during that study period. Dr. Twenge said a major factor contributing to those trends is the plugged-in lifestyle of many teens and young adults. “Spending time on social media tends not to be in real time,” said Dr. Twenge, a psychologist at San Diego State University. “You’re not having a real-time conversation with someone – usually you’re not seeing their face, and you can’t give them a hug; it’s just not as emotionally fulfilling as seeing someone in person,” she said in an interview with National Public Radio. , according to Robert Crosnoe, PhD, a sociologist and adolescent health researcher from the University of Texas at Austin. “I think we are living in a time of great uncertainty, where people are unsure about the future of the country but also their own futures,” he said. “And that is anxiety provoking for anybody, but it’s especially true for young people whose whole future is ahead of them.” NPR.
Alexandra Valoras was a high school student who earned straight As and participated in extracurricular school activities like robotics and pastimes like snowboarding. On the outside, her future looked bright. But inside, Alexandra lived in a world of despair. Her journals revealed profound self-loathing and sadness. She repeatedly expressed a desire to end her own life, reported Jim Axelrod of CBS News. Alexandra is far from alone. The suicide rate for American teens her age is at a 40-year high. One reason is the pressure for perfection, with failure being viewed as catastrophic. “I don’t want this notebook to end, I love it more than myself (?) I need a place where there is no need for me to be perfect,” Alexandra wrote in one entry. “We have a culture that makes kids think that if they’re not perfect, they’re less than good,” said Scott White, a counselor at Alexandra’s high school. Not every person can reach them.” On March 18, 2018, Alexandra wrote her last entry. “What I will miss by dying tonight. The possibility of anything getting better.” She then tidied up her room, walked to an overpass, and jumped. She was 17 years old. Her parents, Dean and Alysia Valoras, shared their daughter’s journals with the hope of helping others. “The hurt, the sadness is evolving,” Mr. Valoras said in the report. “And now there is this thing called living, so that I am a good father, a good husband, a good person.” CBS Sunday Morning.
For college students, accessing mental health services can be a challenge – especially when cost is an issue. In an effort to address that problem Loyola University in New Orleans recently opened a clinic for low-income students in need of psychiatric services. The clinic, opened in February, hopes to serve about 50 patients each week and is open to students and community members. “I’m really stoked about working with this demographic. It’s a population that doesn’t make a lot of money. So you can go to this clinic, pay a small co-pay, and not have to rely on having health insurance,” said Sarah Zoghbi of the New Orleans Musicians’ Clinic & Assistance Foundation, one of the organizations providing support to the clinic. The clinic aims to address the gap in mental health services for the underinsured and uninsured in the area. And it’s sorely needed. Louisiana ranks 38th among the states for lower rates of access to care and higher prevalence of mental illness, according to the 2019 Mental Health America report. About 599,000 adults in Louisiana, about 17% of the population, have a mental illness. “It is our sincere hope to fill a gap in the community by providing high-quality services for those in need,” said the clinic’s director John Dewell, PhD. “No one will be turned away for lack of funds.” The Times-Picayune.
More and more video games are “tackling mental health issues,” Laura Parker wrote in the New York Times. “Mental health is becoming a more central narrative in our culture with efforts to normalize mental health challenges,” according to Eve Crevoshay, of Take This, a group that seeks to destigmatize mental illness within the video game industry. “With that trend comes response from creative industries, including games.” One of the games that Ms. Parker mentioned, called Sea of Solitude, is expected to publish this year. Another, called Celeste, examines depression and anxiety through a protagonist who tries to avoid obstacles. And yet another, called Hellblade, focuses on a warrior who deals with psychosis. Raffael Boccamazzo, PsyD, a psychotherapist who works as clinical director for Take This, said video games can be more effective at helping people bounce back “from negative moods than passive forms of media like TV or movies.” Take This provides resources, guidelines, and training about mental health on its website. The New York Times.
General offers of help to families in crisis are fine but might not get acted upon. It is better to offer something specific, and “the more specific, the better,” wrote Andrea Paterson in the Washington Post. “Not ‘Can I bring dinner sometime?’ Instead, something like, ‘I’d like to come over on Thursday and bring turkey chili.’ Ms. Paterson wrote that she came to that conclusion after her husband was diagnosed with stage 4 metastatic lung cancer in 2013. His death 4½ years later plunged Ms. Paterson and her sons “into crisis,” she wrote. Her tight network of friends and neighbors helped her cope, she said, and their concrete offers of help kept the family going. Such offers need not be earth shattering or monumental, she said. One of her “all-time favorites” was delightfully simple: “ ‘I’m having a cup of tea, watching Audrey learn to roller skate in the driveway. Come join me.’ Needless to say, I joined her.” Ms. Paterson shared several other specifics that might help families in crisis, such as getting a friend to set up a support network of helpers who can pick up prescriptions, meet repairmen, and so on. “Remember that what you offer doesn’t need to be expensive or extravagant,” Ms. Paterson wrote. “ ‘Tomorrow night we are watching the Super Bowl: Join us for tacos and ice cream.’ After all, no one can be in a crisis 24/7.” The Washington Post.
Time spent on social media is seen as partly to blame
Time spent on social media is seen as partly to blame
Depression, suicidal thoughts, and mental distress appear to be on the rise among American teenagers and young adults, and a new study points to their use of social media as a cause. According to the study’s lead author, Jean M. Twenge, PhD, the findings might be evident of a generational shift in mental illness. The study looked at data from more than 200,000 adolescents aged 12-17 and nearly 400,000 young adults aged 18 and over from 2005 to 2017. During that time, reported symptoms consistent with major depression increased by 52% among the teens and 63% among the young adults. Girls were especially at risk, with one in five teenage girls having experienced major depression in 2017. In addition, by 2017, nearly three-quarters of young adults had experienced feelings of hopelessness about their lives. Meanwhile, the rate of suicide rose during that study period. Dr. Twenge said a major factor contributing to those trends is the plugged-in lifestyle of many teens and young adults. “Spending time on social media tends not to be in real time,” said Dr. Twenge, a psychologist at San Diego State University. “You’re not having a real-time conversation with someone – usually you’re not seeing their face, and you can’t give them a hug; it’s just not as emotionally fulfilling as seeing someone in person,” she said in an interview with National Public Radio. , according to Robert Crosnoe, PhD, a sociologist and adolescent health researcher from the University of Texas at Austin. “I think we are living in a time of great uncertainty, where people are unsure about the future of the country but also their own futures,” he said. “And that is anxiety provoking for anybody, but it’s especially true for young people whose whole future is ahead of them.” NPR.
Alexandra Valoras was a high school student who earned straight As and participated in extracurricular school activities like robotics and pastimes like snowboarding. On the outside, her future looked bright. But inside, Alexandra lived in a world of despair. Her journals revealed profound self-loathing and sadness. She repeatedly expressed a desire to end her own life, reported Jim Axelrod of CBS News. Alexandra is far from alone. The suicide rate for American teens her age is at a 40-year high. One reason is the pressure for perfection, with failure being viewed as catastrophic. “I don’t want this notebook to end, I love it more than myself (?) I need a place where there is no need for me to be perfect,” Alexandra wrote in one entry. “We have a culture that makes kids think that if they’re not perfect, they’re less than good,” said Scott White, a counselor at Alexandra’s high school. Not every person can reach them.” On March 18, 2018, Alexandra wrote her last entry. “What I will miss by dying tonight. The possibility of anything getting better.” She then tidied up her room, walked to an overpass, and jumped. She was 17 years old. Her parents, Dean and Alysia Valoras, shared their daughter’s journals with the hope of helping others. “The hurt, the sadness is evolving,” Mr. Valoras said in the report. “And now there is this thing called living, so that I am a good father, a good husband, a good person.” CBS Sunday Morning.
For college students, accessing mental health services can be a challenge – especially when cost is an issue. In an effort to address that problem Loyola University in New Orleans recently opened a clinic for low-income students in need of psychiatric services. The clinic, opened in February, hopes to serve about 50 patients each week and is open to students and community members. “I’m really stoked about working with this demographic. It’s a population that doesn’t make a lot of money. So you can go to this clinic, pay a small co-pay, and not have to rely on having health insurance,” said Sarah Zoghbi of the New Orleans Musicians’ Clinic & Assistance Foundation, one of the organizations providing support to the clinic. The clinic aims to address the gap in mental health services for the underinsured and uninsured in the area. And it’s sorely needed. Louisiana ranks 38th among the states for lower rates of access to care and higher prevalence of mental illness, according to the 2019 Mental Health America report. About 599,000 adults in Louisiana, about 17% of the population, have a mental illness. “It is our sincere hope to fill a gap in the community by providing high-quality services for those in need,” said the clinic’s director John Dewell, PhD. “No one will be turned away for lack of funds.” The Times-Picayune.
More and more video games are “tackling mental health issues,” Laura Parker wrote in the New York Times. “Mental health is becoming a more central narrative in our culture with efforts to normalize mental health challenges,” according to Eve Crevoshay, of Take This, a group that seeks to destigmatize mental illness within the video game industry. “With that trend comes response from creative industries, including games.” One of the games that Ms. Parker mentioned, called Sea of Solitude, is expected to publish this year. Another, called Celeste, examines depression and anxiety through a protagonist who tries to avoid obstacles. And yet another, called Hellblade, focuses on a warrior who deals with psychosis. Raffael Boccamazzo, PsyD, a psychotherapist who works as clinical director for Take This, said video games can be more effective at helping people bounce back “from negative moods than passive forms of media like TV or movies.” Take This provides resources, guidelines, and training about mental health on its website. The New York Times.
General offers of help to families in crisis are fine but might not get acted upon. It is better to offer something specific, and “the more specific, the better,” wrote Andrea Paterson in the Washington Post. “Not ‘Can I bring dinner sometime?’ Instead, something like, ‘I’d like to come over on Thursday and bring turkey chili.’ Ms. Paterson wrote that she came to that conclusion after her husband was diagnosed with stage 4 metastatic lung cancer in 2013. His death 4½ years later plunged Ms. Paterson and her sons “into crisis,” she wrote. Her tight network of friends and neighbors helped her cope, she said, and their concrete offers of help kept the family going. Such offers need not be earth shattering or monumental, she said. One of her “all-time favorites” was delightfully simple: “ ‘I’m having a cup of tea, watching Audrey learn to roller skate in the driveway. Come join me.’ Needless to say, I joined her.” Ms. Paterson shared several other specifics that might help families in crisis, such as getting a friend to set up a support network of helpers who can pick up prescriptions, meet repairmen, and so on. “Remember that what you offer doesn’t need to be expensive or extravagant,” Ms. Paterson wrote. “ ‘Tomorrow night we are watching the Super Bowl: Join us for tacos and ice cream.’ After all, no one can be in a crisis 24/7.” The Washington Post.
Depression, suicidal thoughts, and mental distress appear to be on the rise among American teenagers and young adults, and a new study points to their use of social media as a cause. According to the study’s lead author, Jean M. Twenge, PhD, the findings might be evident of a generational shift in mental illness. The study looked at data from more than 200,000 adolescents aged 12-17 and nearly 400,000 young adults aged 18 and over from 2005 to 2017. During that time, reported symptoms consistent with major depression increased by 52% among the teens and 63% among the young adults. Girls were especially at risk, with one in five teenage girls having experienced major depression in 2017. In addition, by 2017, nearly three-quarters of young adults had experienced feelings of hopelessness about their lives. Meanwhile, the rate of suicide rose during that study period. Dr. Twenge said a major factor contributing to those trends is the plugged-in lifestyle of many teens and young adults. “Spending time on social media tends not to be in real time,” said Dr. Twenge, a psychologist at San Diego State University. “You’re not having a real-time conversation with someone – usually you’re not seeing their face, and you can’t give them a hug; it’s just not as emotionally fulfilling as seeing someone in person,” she said in an interview with National Public Radio. , according to Robert Crosnoe, PhD, a sociologist and adolescent health researcher from the University of Texas at Austin. “I think we are living in a time of great uncertainty, where people are unsure about the future of the country but also their own futures,” he said. “And that is anxiety provoking for anybody, but it’s especially true for young people whose whole future is ahead of them.” NPR.
Alexandra Valoras was a high school student who earned straight As and participated in extracurricular school activities like robotics and pastimes like snowboarding. On the outside, her future looked bright. But inside, Alexandra lived in a world of despair. Her journals revealed profound self-loathing and sadness. She repeatedly expressed a desire to end her own life, reported Jim Axelrod of CBS News. Alexandra is far from alone. The suicide rate for American teens her age is at a 40-year high. One reason is the pressure for perfection, with failure being viewed as catastrophic. “I don’t want this notebook to end, I love it more than myself (?) I need a place where there is no need for me to be perfect,” Alexandra wrote in one entry. “We have a culture that makes kids think that if they’re not perfect, they’re less than good,” said Scott White, a counselor at Alexandra’s high school. Not every person can reach them.” On March 18, 2018, Alexandra wrote her last entry. “What I will miss by dying tonight. The possibility of anything getting better.” She then tidied up her room, walked to an overpass, and jumped. She was 17 years old. Her parents, Dean and Alysia Valoras, shared their daughter’s journals with the hope of helping others. “The hurt, the sadness is evolving,” Mr. Valoras said in the report. “And now there is this thing called living, so that I am a good father, a good husband, a good person.” CBS Sunday Morning.
For college students, accessing mental health services can be a challenge – especially when cost is an issue. In an effort to address that problem Loyola University in New Orleans recently opened a clinic for low-income students in need of psychiatric services. The clinic, opened in February, hopes to serve about 50 patients each week and is open to students and community members. “I’m really stoked about working with this demographic. It’s a population that doesn’t make a lot of money. So you can go to this clinic, pay a small co-pay, and not have to rely on having health insurance,” said Sarah Zoghbi of the New Orleans Musicians’ Clinic & Assistance Foundation, one of the organizations providing support to the clinic. The clinic aims to address the gap in mental health services for the underinsured and uninsured in the area. And it’s sorely needed. Louisiana ranks 38th among the states for lower rates of access to care and higher prevalence of mental illness, according to the 2019 Mental Health America report. About 599,000 adults in Louisiana, about 17% of the population, have a mental illness. “It is our sincere hope to fill a gap in the community by providing high-quality services for those in need,” said the clinic’s director John Dewell, PhD. “No one will be turned away for lack of funds.” The Times-Picayune.
More and more video games are “tackling mental health issues,” Laura Parker wrote in the New York Times. “Mental health is becoming a more central narrative in our culture with efforts to normalize mental health challenges,” according to Eve Crevoshay, of Take This, a group that seeks to destigmatize mental illness within the video game industry. “With that trend comes response from creative industries, including games.” One of the games that Ms. Parker mentioned, called Sea of Solitude, is expected to publish this year. Another, called Celeste, examines depression and anxiety through a protagonist who tries to avoid obstacles. And yet another, called Hellblade, focuses on a warrior who deals with psychosis. Raffael Boccamazzo, PsyD, a psychotherapist who works as clinical director for Take This, said video games can be more effective at helping people bounce back “from negative moods than passive forms of media like TV or movies.” Take This provides resources, guidelines, and training about mental health on its website. The New York Times.
General offers of help to families in crisis are fine but might not get acted upon. It is better to offer something specific, and “the more specific, the better,” wrote Andrea Paterson in the Washington Post. “Not ‘Can I bring dinner sometime?’ Instead, something like, ‘I’d like to come over on Thursday and bring turkey chili.’ Ms. Paterson wrote that she came to that conclusion after her husband was diagnosed with stage 4 metastatic lung cancer in 2013. His death 4½ years later plunged Ms. Paterson and her sons “into crisis,” she wrote. Her tight network of friends and neighbors helped her cope, she said, and their concrete offers of help kept the family going. Such offers need not be earth shattering or monumental, she said. One of her “all-time favorites” was delightfully simple: “ ‘I’m having a cup of tea, watching Audrey learn to roller skate in the driveway. Come join me.’ Needless to say, I joined her.” Ms. Paterson shared several other specifics that might help families in crisis, such as getting a friend to set up a support network of helpers who can pick up prescriptions, meet repairmen, and so on. “Remember that what you offer doesn’t need to be expensive or extravagant,” Ms. Paterson wrote. “ ‘Tomorrow night we are watching the Super Bowl: Join us for tacos and ice cream.’ After all, no one can be in a crisis 24/7.” The Washington Post.
Gender wage gap varies by specialty
There is no specialty in which women physicians make as much as men, but hematology came the closest in 2018, according to a new survey by the medical social network Doximity.
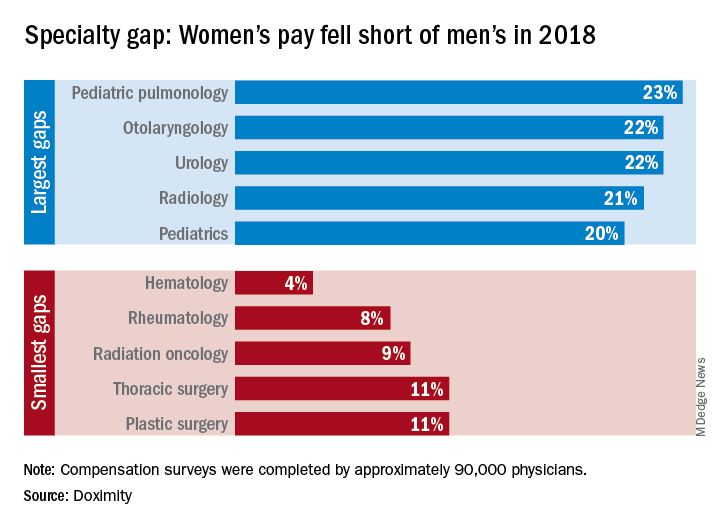
Female hematologists averaged $309,000 in earnings in 2018, just 4% less than their male counterparts, who brought in an average of $323,000. Rheumatology had the next-smallest gap, 8%, between women and men, followed by radiation oncology at 9% and thoracic surgery and plastic surgery at 11% each, Doximity reported March 26. All of the 90,000 physicians involved in the survey worked at least 40 hours per week.
At the other end of the scale is pediatric pulmonology, home of the largest gender wage gap. Average compensation for women in the specialty was $195,000, or 23% less than the $253,000 that men received. Women in otolaryngology and urology were next, earning 22% less than men in those specialties, while women in radiology and pediatrics averaged 21% and 20% less, respectively, than men, Doximity said in its report.
The gender wage gap has been persistent, but the latest data show that it is starting to close as the earnings curve for male physicians flattened in 2018 while pay increased for female physicians.
“Compensation transparency is a powerful force. As more data becomes available to us, exposing the pay gap between men and women, we see more movements to rectify this issue,” said Christopher Whaley, PhD, of the University of California, Berkeley, School of Public Health, who was lead author of the study.
To account for differences in specialty, geography, and physician-specific factors, the Doximity researchers used “a multivariate regression with fixed effects for provider specialty and [metropolitan statistical area].” They also controlled for how long each physician has been in practice and their self-reported average hours worked.
There is no specialty in which women physicians make as much as men, but hematology came the closest in 2018, according to a new survey by the medical social network Doximity.
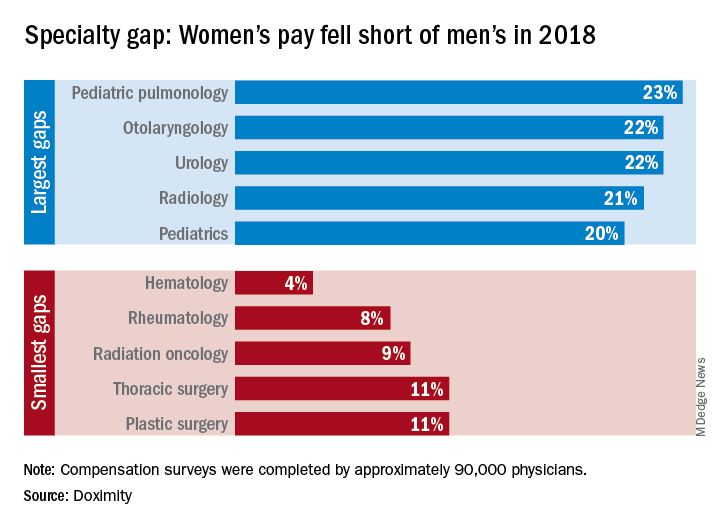
Female hematologists averaged $309,000 in earnings in 2018, just 4% less than their male counterparts, who brought in an average of $323,000. Rheumatology had the next-smallest gap, 8%, between women and men, followed by radiation oncology at 9% and thoracic surgery and plastic surgery at 11% each, Doximity reported March 26. All of the 90,000 physicians involved in the survey worked at least 40 hours per week.
At the other end of the scale is pediatric pulmonology, home of the largest gender wage gap. Average compensation for women in the specialty was $195,000, or 23% less than the $253,000 that men received. Women in otolaryngology and urology were next, earning 22% less than men in those specialties, while women in radiology and pediatrics averaged 21% and 20% less, respectively, than men, Doximity said in its report.
The gender wage gap has been persistent, but the latest data show that it is starting to close as the earnings curve for male physicians flattened in 2018 while pay increased for female physicians.
“Compensation transparency is a powerful force. As more data becomes available to us, exposing the pay gap between men and women, we see more movements to rectify this issue,” said Christopher Whaley, PhD, of the University of California, Berkeley, School of Public Health, who was lead author of the study.
To account for differences in specialty, geography, and physician-specific factors, the Doximity researchers used “a multivariate regression with fixed effects for provider specialty and [metropolitan statistical area].” They also controlled for how long each physician has been in practice and their self-reported average hours worked.
There is no specialty in which women physicians make as much as men, but hematology came the closest in 2018, according to a new survey by the medical social network Doximity.
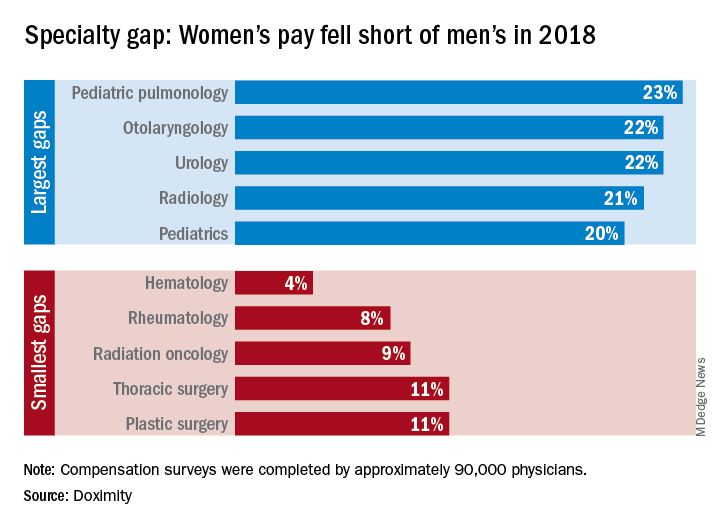
Female hematologists averaged $309,000 in earnings in 2018, just 4% less than their male counterparts, who brought in an average of $323,000. Rheumatology had the next-smallest gap, 8%, between women and men, followed by radiation oncology at 9% and thoracic surgery and plastic surgery at 11% each, Doximity reported March 26. All of the 90,000 physicians involved in the survey worked at least 40 hours per week.
At the other end of the scale is pediatric pulmonology, home of the largest gender wage gap. Average compensation for women in the specialty was $195,000, or 23% less than the $253,000 that men received. Women in otolaryngology and urology were next, earning 22% less than men in those specialties, while women in radiology and pediatrics averaged 21% and 20% less, respectively, than men, Doximity said in its report.
The gender wage gap has been persistent, but the latest data show that it is starting to close as the earnings curve for male physicians flattened in 2018 while pay increased for female physicians.
“Compensation transparency is a powerful force. As more data becomes available to us, exposing the pay gap between men and women, we see more movements to rectify this issue,” said Christopher Whaley, PhD, of the University of California, Berkeley, School of Public Health, who was lead author of the study.
To account for differences in specialty, geography, and physician-specific factors, the Doximity researchers used “a multivariate regression with fixed effects for provider specialty and [metropolitan statistical area].” They also controlled for how long each physician has been in practice and their self-reported average hours worked.
Presenting the 2019 SHM Award of Excellence winners
Award of Excellence in Outstanding Service in Hospital Medicine
Kendall Rogers, MD, CPE, SFHM, is chief of the division of hospital medicine at the University of New Mexico Health Sciences Center, Albuquerque, where he also serves as a professor. His numerous innovations have tremendously improved patient care and enhanced provider work flow. One of his most notable contributions was the hospital-wide intensive organized glycemic control program, which consists of a dedicated glycemic control advanced practice provider (APP) working closely with surgical and medical teams to ensure proper education and discharge planning for patients. He also helped to create an APP fellowship in hospital medicine at the UNM Health Sciences Center.
His innovations have been recognized on the national level, including with the 2011 John M. Eisenberg Award from the National Quality Forum and the Joint Commission in honor of his work as lead mentor in the SHM’s Glycemic Control Mentored Implementation program. Dr. Rogers also has served as chair of the SHM’s Information Technology Committee and has been a member of the society’s Public Policy Committee. He is also a senior fellow in hospital medicine.
Award of Excellence in Research
Tara Lagu, MD, MPH, is the associate director of the Institute for Healthcare Delivery and Population Science and an associate professor at the University of Massachusetts Medical School at Baystate Medical Center, Springfield.
Dr. Lagu has published 103 original peer-reviewed manuscripts in high-impact journals, including the New England Journal of Medicine, the Journal of Hospital Medicine, and JAMA. Her research primarily focuses on improving the quality and value of care for patients with acute illness. She has published papers examining hospital care quality for patients with sepsis, heart failure, acute coronary syndrome, pneumonia, and delirium, and has an R01 aimed at identifying strategies used by Medicare Accountable Care Organizations to reduce admission rates for patients with heart failure. Dr. Lagu also is very interested in improving access to care for patients with disabilities. In 2013, she conducted a “secret shopper” survey of physicians in a variety of practice settings nationwide and found that 20% of physicians would refuse to see a patient who uses a wheelchair. This work was published in the Annals of Internal Medicine and was profiled in the New York Times.
Dr. Lagu is a senior fellow in hospital medicine and also serves as a senior deputy editor for the Journal of Hospital Medicine.
Award of Clinical Leadership for Physicians
Hyung (Harry) Cho, MD, SFHM, is an academic hospitalist and the inaugural chief value officer for NYC Health + Hospitals health system, the largest public health system in the United States, serving more than 1.4 million people annually. In his previous role as the director of quality, safety and value at Mount Sinai Hospital, he founded and led the hospital high-value care committee, eventually leading more than 90 faculty, residents, and students in initiatives across the health system to improve costs and outcomes.
Nationally, he has demonstrated tremendous leadership as chair of the SHM High-Value Care Subcommittee and by leading the development of the next SHM Choosing Wisely list through collaboration with patient advocates and clinicians across the country. He is a former member of the SHM’s Chapter Support Committee and a current member of both the HQPS Committee and the editorial board for the Hospitalist.
For his work value and quality since he became a hospitalist in 2011, he has received more than 50 awards, spoken at more than 40 lectures and workshops in national venues, and been published widely in peer-reviewed journals, including the Journal of Hospital Medicine, Journal of General Internal Medicine, and JAMA Internal Medicine.
Award of Excellence in Teaching
Christopher J. Moreland, MD, MPH, FHM, is an associate professor of medicine and hospitalist at the University of Texas, San Antonio, where he also serves as the associate residency program director. He has established himself as an outstanding clinical educator, innovator, and administrator committed to seeing medical students and residents advance their abilities.
Dr. Moreland has been involved in several initiatives and innovations. In 2011, he collaborated with the UT Health faculty development specialist to develop and direct a month-long Resident as Teacher elective. In this extremely popular elective, participants learn evidence-based principles and build skills to become effective teachers, with an emphasis on bedside teaching.
Because he is deaf himself, Dr. Moreland has continuously mentored deaf residents and health care students across North America, while advising educators who work with deaf health trainees. He published the first formal study of a subpopulation of physicians and students with a disability – hearing loss – in 2013. Dr. Moreland also has worked with standardized patients, simulation experts, and community college educators to develop a simulated trilingual intervention, with documented improvement in students’ ability to work with interpreters. He is also a fellow in hospital medicine.
Award of Excellence in Clinical Leadership for NPs/PAs
Lorraine L. Britting, MS, CNP, SFHM, is the clinical director of advanced practice providers in cardiology medicine and a practicing acute care nurse practitioner at the Cardiovascular Institute at Beth Israel Deaconess Medical Center in Boston. She has overseen the growth of the program from 8 to 32 advanced practice providers in the last decade. Her efforts extend across the medical center, by creating and chairing multiple committees designed to address credentialing, billing, reimbursement, and recruitment issues specific to advanced practice providers.
Within SHM, she has served on the NP/PA Committee, the HQPS Committee, and Membership Committee and as a peer reviewer for the Journal of Hospital Medicine. She is a senior fellow in hospital medicine.
Award of Excellence in Humanitarian Service
Kristian Olson, MD, MPH, is an internist and pediatrician and has been an academic hospitalist member of the core educator faculty in the department of medicine at Massachusetts General Hospital in Boston since its founding in 2005. He is also the director of the Consortium for Affordable Medical Technologies, also known as CAMTech.
In 2005, he worked in Darfur, Sudan, before being contracted by the European Commission for Humanitarian Organizations to train birth attendants in rural Sumatra after the Asian tsunami. For the next 5 years, Dr. Olson’s work resulted in creating a network of more than 350 midwives who retrain each other in newborn resuscitation and postpartum hemorrhage three times per year. He is an inventor and developer of the Augmented Infant Resuscitator, a device that lets birth attendants achieve effective ventilation in less than half the time and maintain it for 50% longer. In 2009, he was instrumental in setting up Ethiopia’s first multidrug-resistant tuberculosis treatment program, where he developed care processes and attended to patients with active TB. By 2012, more than 1,000 patients had completed therapy with an unparalleled rate of success.
Work through Dr. Olson’s CAMTech open innovation platform has empowered people with the tools to solve their own medical challenges – principally in India, Uganda, and the United States. By reaching across disciplines, he has been able to align frontline health providers to work with patients, engineers, designers, policy makers, public health practitioners and more to make sustainable solutions to challenges in health care. This platform has attracted more than 4,300 innovators and resulted in the formation of some 30 companies and the filing of more than 40 patents.
Award of Excellence in Management of Hospital Medicine
Stephanie Perry, MA, SFHM, currently the Director of Hospital Medicine Services at Virginia Mason Medical Center in Seattle, is a leader in building sustainability into the work of hospitalists. While at Virginia Mason, she developed an internal auditing and education platform to improve revenue cycle opportunities, which brought more than $500,000 in additional gross revenue to the organization in 2018.
Ms. Perry also created a structured onboarding platform for hospitalists and created a new flexible scheduling method to improve the team’s work/life balance. In partnership with her leadership team, Ms. Perry has improved hospitalist engagement scores by 29 percent over a three-year period, with 86 percent of the physicians rating as engaged employees. This has resulted in zero attrition since July of 2017.
She is a Senior Fellow in Hospital Medicine and a true leader in her field.
Excellence in Teamwork in Quality Improvement
The Mount Sinai Hospital’s High-Value Care team is a multidisciplinary group focused on reducing overuse, decreasing costs throughout the institution, and allowing clinicians to focus on providing outstanding care and developing relationships with their patients.
Founded by Dr. Harry Cho, the High-Value Care team has chosen projects that have meaningfully affected waste reduction and patient care. They have created a sustainable structure engaging multiple members of the care team, including staff, trainees, and students. Its collaborative environment demonstrates high value, as it helps improve staff satisfaction and retention.
The team has focused on areas identified as wasteful by SHM as part of ABIM’s Choosing Wisely initiative. Projects have decreased lab testing – including amylase, folate, and “routine” daily labs – as well as medications such antihypertensives and docusate. Additionally, teams have tackled telemetry and urinary catheters, and improved patient mobility and inpatient sleep. Their innovative work can help spark similar programs nationally. As a result, the team has greatly reduced wasteful practices, decreased costs, and allowed clinicians to focus on providing outstanding care and developing relationships with patients.
In addition to many hospitalists, the High-Value Care team consists of members of Mount Sinai’s Nursing, Medicine, Pharmacy, Laboratory and IT Departments, including Andrew Dunn, MD; Beth Raucher, MD; John McClaskey, MD; Nicole Wells; Suzanne Cushnie; Surafel Tsega; and Gina Caliendo.
Junior Investigator Award
Oanh Nguyen, MD, MAS, is an assistant professor in the division of hospital medicine at the University of California, San Francisco.
Dr. Nguyen’s research is focused on the optimization of hospital care in safety-net settings and pragmatic approaches to addressing social determinants of health and transitional care strategies that address coexisting social vulnerabilities.
Her current work, funded through a K23 award, seeks to develop a strategy to predict, understand, and address coexisting social vulnerabilities among adults hospitalized with heart failure or ischemic heart disease who are at high risk for readmission.
While she is early in her investigative career, she already has 32 peer-reviewed publications, with another four first-authored manuscripts under review or in preparation.
She is an associate editor of the Journal of Hospital Medicine.
This article was updated 3/26/19.
Award of Excellence in Outstanding Service in Hospital Medicine
Kendall Rogers, MD, CPE, SFHM, is chief of the division of hospital medicine at the University of New Mexico Health Sciences Center, Albuquerque, where he also serves as a professor. His numerous innovations have tremendously improved patient care and enhanced provider work flow. One of his most notable contributions was the hospital-wide intensive organized glycemic control program, which consists of a dedicated glycemic control advanced practice provider (APP) working closely with surgical and medical teams to ensure proper education and discharge planning for patients. He also helped to create an APP fellowship in hospital medicine at the UNM Health Sciences Center.
His innovations have been recognized on the national level, including with the 2011 John M. Eisenberg Award from the National Quality Forum and the Joint Commission in honor of his work as lead mentor in the SHM’s Glycemic Control Mentored Implementation program. Dr. Rogers also has served as chair of the SHM’s Information Technology Committee and has been a member of the society’s Public Policy Committee. He is also a senior fellow in hospital medicine.
Award of Excellence in Research
Tara Lagu, MD, MPH, is the associate director of the Institute for Healthcare Delivery and Population Science and an associate professor at the University of Massachusetts Medical School at Baystate Medical Center, Springfield.
Dr. Lagu has published 103 original peer-reviewed manuscripts in high-impact journals, including the New England Journal of Medicine, the Journal of Hospital Medicine, and JAMA. Her research primarily focuses on improving the quality and value of care for patients with acute illness. She has published papers examining hospital care quality for patients with sepsis, heart failure, acute coronary syndrome, pneumonia, and delirium, and has an R01 aimed at identifying strategies used by Medicare Accountable Care Organizations to reduce admission rates for patients with heart failure. Dr. Lagu also is very interested in improving access to care for patients with disabilities. In 2013, she conducted a “secret shopper” survey of physicians in a variety of practice settings nationwide and found that 20% of physicians would refuse to see a patient who uses a wheelchair. This work was published in the Annals of Internal Medicine and was profiled in the New York Times.
Dr. Lagu is a senior fellow in hospital medicine and also serves as a senior deputy editor for the Journal of Hospital Medicine.
Award of Clinical Leadership for Physicians
Hyung (Harry) Cho, MD, SFHM, is an academic hospitalist and the inaugural chief value officer for NYC Health + Hospitals health system, the largest public health system in the United States, serving more than 1.4 million people annually. In his previous role as the director of quality, safety and value at Mount Sinai Hospital, he founded and led the hospital high-value care committee, eventually leading more than 90 faculty, residents, and students in initiatives across the health system to improve costs and outcomes.
Nationally, he has demonstrated tremendous leadership as chair of the SHM High-Value Care Subcommittee and by leading the development of the next SHM Choosing Wisely list through collaboration with patient advocates and clinicians across the country. He is a former member of the SHM’s Chapter Support Committee and a current member of both the HQPS Committee and the editorial board for the Hospitalist.
For his work value and quality since he became a hospitalist in 2011, he has received more than 50 awards, spoken at more than 40 lectures and workshops in national venues, and been published widely in peer-reviewed journals, including the Journal of Hospital Medicine, Journal of General Internal Medicine, and JAMA Internal Medicine.
Award of Excellence in Teaching
Christopher J. Moreland, MD, MPH, FHM, is an associate professor of medicine and hospitalist at the University of Texas, San Antonio, where he also serves as the associate residency program director. He has established himself as an outstanding clinical educator, innovator, and administrator committed to seeing medical students and residents advance their abilities.
Dr. Moreland has been involved in several initiatives and innovations. In 2011, he collaborated with the UT Health faculty development specialist to develop and direct a month-long Resident as Teacher elective. In this extremely popular elective, participants learn evidence-based principles and build skills to become effective teachers, with an emphasis on bedside teaching.
Because he is deaf himself, Dr. Moreland has continuously mentored deaf residents and health care students across North America, while advising educators who work with deaf health trainees. He published the first formal study of a subpopulation of physicians and students with a disability – hearing loss – in 2013. Dr. Moreland also has worked with standardized patients, simulation experts, and community college educators to develop a simulated trilingual intervention, with documented improvement in students’ ability to work with interpreters. He is also a fellow in hospital medicine.
Award of Excellence in Clinical Leadership for NPs/PAs
Lorraine L. Britting, MS, CNP, SFHM, is the clinical director of advanced practice providers in cardiology medicine and a practicing acute care nurse practitioner at the Cardiovascular Institute at Beth Israel Deaconess Medical Center in Boston. She has overseen the growth of the program from 8 to 32 advanced practice providers in the last decade. Her efforts extend across the medical center, by creating and chairing multiple committees designed to address credentialing, billing, reimbursement, and recruitment issues specific to advanced practice providers.
Within SHM, she has served on the NP/PA Committee, the HQPS Committee, and Membership Committee and as a peer reviewer for the Journal of Hospital Medicine. She is a senior fellow in hospital medicine.
Award of Excellence in Humanitarian Service
Kristian Olson, MD, MPH, is an internist and pediatrician and has been an academic hospitalist member of the core educator faculty in the department of medicine at Massachusetts General Hospital in Boston since its founding in 2005. He is also the director of the Consortium for Affordable Medical Technologies, also known as CAMTech.
In 2005, he worked in Darfur, Sudan, before being contracted by the European Commission for Humanitarian Organizations to train birth attendants in rural Sumatra after the Asian tsunami. For the next 5 years, Dr. Olson’s work resulted in creating a network of more than 350 midwives who retrain each other in newborn resuscitation and postpartum hemorrhage three times per year. He is an inventor and developer of the Augmented Infant Resuscitator, a device that lets birth attendants achieve effective ventilation in less than half the time and maintain it for 50% longer. In 2009, he was instrumental in setting up Ethiopia’s first multidrug-resistant tuberculosis treatment program, where he developed care processes and attended to patients with active TB. By 2012, more than 1,000 patients had completed therapy with an unparalleled rate of success.
Work through Dr. Olson’s CAMTech open innovation platform has empowered people with the tools to solve their own medical challenges – principally in India, Uganda, and the United States. By reaching across disciplines, he has been able to align frontline health providers to work with patients, engineers, designers, policy makers, public health practitioners and more to make sustainable solutions to challenges in health care. This platform has attracted more than 4,300 innovators and resulted in the formation of some 30 companies and the filing of more than 40 patents.
Award of Excellence in Management of Hospital Medicine
Stephanie Perry, MA, SFHM, currently the Director of Hospital Medicine Services at Virginia Mason Medical Center in Seattle, is a leader in building sustainability into the work of hospitalists. While at Virginia Mason, she developed an internal auditing and education platform to improve revenue cycle opportunities, which brought more than $500,000 in additional gross revenue to the organization in 2018.
Ms. Perry also created a structured onboarding platform for hospitalists and created a new flexible scheduling method to improve the team’s work/life balance. In partnership with her leadership team, Ms. Perry has improved hospitalist engagement scores by 29 percent over a three-year period, with 86 percent of the physicians rating as engaged employees. This has resulted in zero attrition since July of 2017.
She is a Senior Fellow in Hospital Medicine and a true leader in her field.
Excellence in Teamwork in Quality Improvement
The Mount Sinai Hospital’s High-Value Care team is a multidisciplinary group focused on reducing overuse, decreasing costs throughout the institution, and allowing clinicians to focus on providing outstanding care and developing relationships with their patients.
Founded by Dr. Harry Cho, the High-Value Care team has chosen projects that have meaningfully affected waste reduction and patient care. They have created a sustainable structure engaging multiple members of the care team, including staff, trainees, and students. Its collaborative environment demonstrates high value, as it helps improve staff satisfaction and retention.
The team has focused on areas identified as wasteful by SHM as part of ABIM’s Choosing Wisely initiative. Projects have decreased lab testing – including amylase, folate, and “routine” daily labs – as well as medications such antihypertensives and docusate. Additionally, teams have tackled telemetry and urinary catheters, and improved patient mobility and inpatient sleep. Their innovative work can help spark similar programs nationally. As a result, the team has greatly reduced wasteful practices, decreased costs, and allowed clinicians to focus on providing outstanding care and developing relationships with patients.
In addition to many hospitalists, the High-Value Care team consists of members of Mount Sinai’s Nursing, Medicine, Pharmacy, Laboratory and IT Departments, including Andrew Dunn, MD; Beth Raucher, MD; John McClaskey, MD; Nicole Wells; Suzanne Cushnie; Surafel Tsega; and Gina Caliendo.
Junior Investigator Award
Oanh Nguyen, MD, MAS, is an assistant professor in the division of hospital medicine at the University of California, San Francisco.
Dr. Nguyen’s research is focused on the optimization of hospital care in safety-net settings and pragmatic approaches to addressing social determinants of health and transitional care strategies that address coexisting social vulnerabilities.
Her current work, funded through a K23 award, seeks to develop a strategy to predict, understand, and address coexisting social vulnerabilities among adults hospitalized with heart failure or ischemic heart disease who are at high risk for readmission.
While she is early in her investigative career, she already has 32 peer-reviewed publications, with another four first-authored manuscripts under review or in preparation.
She is an associate editor of the Journal of Hospital Medicine.
This article was updated 3/26/19.
Award of Excellence in Outstanding Service in Hospital Medicine
Kendall Rogers, MD, CPE, SFHM, is chief of the division of hospital medicine at the University of New Mexico Health Sciences Center, Albuquerque, where he also serves as a professor. His numerous innovations have tremendously improved patient care and enhanced provider work flow. One of his most notable contributions was the hospital-wide intensive organized glycemic control program, which consists of a dedicated glycemic control advanced practice provider (APP) working closely with surgical and medical teams to ensure proper education and discharge planning for patients. He also helped to create an APP fellowship in hospital medicine at the UNM Health Sciences Center.
His innovations have been recognized on the national level, including with the 2011 John M. Eisenberg Award from the National Quality Forum and the Joint Commission in honor of his work as lead mentor in the SHM’s Glycemic Control Mentored Implementation program. Dr. Rogers also has served as chair of the SHM’s Information Technology Committee and has been a member of the society’s Public Policy Committee. He is also a senior fellow in hospital medicine.
Award of Excellence in Research
Tara Lagu, MD, MPH, is the associate director of the Institute for Healthcare Delivery and Population Science and an associate professor at the University of Massachusetts Medical School at Baystate Medical Center, Springfield.
Dr. Lagu has published 103 original peer-reviewed manuscripts in high-impact journals, including the New England Journal of Medicine, the Journal of Hospital Medicine, and JAMA. Her research primarily focuses on improving the quality and value of care for patients with acute illness. She has published papers examining hospital care quality for patients with sepsis, heart failure, acute coronary syndrome, pneumonia, and delirium, and has an R01 aimed at identifying strategies used by Medicare Accountable Care Organizations to reduce admission rates for patients with heart failure. Dr. Lagu also is very interested in improving access to care for patients with disabilities. In 2013, she conducted a “secret shopper” survey of physicians in a variety of practice settings nationwide and found that 20% of physicians would refuse to see a patient who uses a wheelchair. This work was published in the Annals of Internal Medicine and was profiled in the New York Times.
Dr. Lagu is a senior fellow in hospital medicine and also serves as a senior deputy editor for the Journal of Hospital Medicine.
Award of Clinical Leadership for Physicians
Hyung (Harry) Cho, MD, SFHM, is an academic hospitalist and the inaugural chief value officer for NYC Health + Hospitals health system, the largest public health system in the United States, serving more than 1.4 million people annually. In his previous role as the director of quality, safety and value at Mount Sinai Hospital, he founded and led the hospital high-value care committee, eventually leading more than 90 faculty, residents, and students in initiatives across the health system to improve costs and outcomes.
Nationally, he has demonstrated tremendous leadership as chair of the SHM High-Value Care Subcommittee and by leading the development of the next SHM Choosing Wisely list through collaboration with patient advocates and clinicians across the country. He is a former member of the SHM’s Chapter Support Committee and a current member of both the HQPS Committee and the editorial board for the Hospitalist.
For his work value and quality since he became a hospitalist in 2011, he has received more than 50 awards, spoken at more than 40 lectures and workshops in national venues, and been published widely in peer-reviewed journals, including the Journal of Hospital Medicine, Journal of General Internal Medicine, and JAMA Internal Medicine.
Award of Excellence in Teaching
Christopher J. Moreland, MD, MPH, FHM, is an associate professor of medicine and hospitalist at the University of Texas, San Antonio, where he also serves as the associate residency program director. He has established himself as an outstanding clinical educator, innovator, and administrator committed to seeing medical students and residents advance their abilities.
Dr. Moreland has been involved in several initiatives and innovations. In 2011, he collaborated with the UT Health faculty development specialist to develop and direct a month-long Resident as Teacher elective. In this extremely popular elective, participants learn evidence-based principles and build skills to become effective teachers, with an emphasis on bedside teaching.
Because he is deaf himself, Dr. Moreland has continuously mentored deaf residents and health care students across North America, while advising educators who work with deaf health trainees. He published the first formal study of a subpopulation of physicians and students with a disability – hearing loss – in 2013. Dr. Moreland also has worked with standardized patients, simulation experts, and community college educators to develop a simulated trilingual intervention, with documented improvement in students’ ability to work with interpreters. He is also a fellow in hospital medicine.
Award of Excellence in Clinical Leadership for NPs/PAs
Lorraine L. Britting, MS, CNP, SFHM, is the clinical director of advanced practice providers in cardiology medicine and a practicing acute care nurse practitioner at the Cardiovascular Institute at Beth Israel Deaconess Medical Center in Boston. She has overseen the growth of the program from 8 to 32 advanced practice providers in the last decade. Her efforts extend across the medical center, by creating and chairing multiple committees designed to address credentialing, billing, reimbursement, and recruitment issues specific to advanced practice providers.
Within SHM, she has served on the NP/PA Committee, the HQPS Committee, and Membership Committee and as a peer reviewer for the Journal of Hospital Medicine. She is a senior fellow in hospital medicine.
Award of Excellence in Humanitarian Service
Kristian Olson, MD, MPH, is an internist and pediatrician and has been an academic hospitalist member of the core educator faculty in the department of medicine at Massachusetts General Hospital in Boston since its founding in 2005. He is also the director of the Consortium for Affordable Medical Technologies, also known as CAMTech.
In 2005, he worked in Darfur, Sudan, before being contracted by the European Commission for Humanitarian Organizations to train birth attendants in rural Sumatra after the Asian tsunami. For the next 5 years, Dr. Olson’s work resulted in creating a network of more than 350 midwives who retrain each other in newborn resuscitation and postpartum hemorrhage three times per year. He is an inventor and developer of the Augmented Infant Resuscitator, a device that lets birth attendants achieve effective ventilation in less than half the time and maintain it for 50% longer. In 2009, he was instrumental in setting up Ethiopia’s first multidrug-resistant tuberculosis treatment program, where he developed care processes and attended to patients with active TB. By 2012, more than 1,000 patients had completed therapy with an unparalleled rate of success.
Work through Dr. Olson’s CAMTech open innovation platform has empowered people with the tools to solve their own medical challenges – principally in India, Uganda, and the United States. By reaching across disciplines, he has been able to align frontline health providers to work with patients, engineers, designers, policy makers, public health practitioners and more to make sustainable solutions to challenges in health care. This platform has attracted more than 4,300 innovators and resulted in the formation of some 30 companies and the filing of more than 40 patents.
Award of Excellence in Management of Hospital Medicine
Stephanie Perry, MA, SFHM, currently the Director of Hospital Medicine Services at Virginia Mason Medical Center in Seattle, is a leader in building sustainability into the work of hospitalists. While at Virginia Mason, she developed an internal auditing and education platform to improve revenue cycle opportunities, which brought more than $500,000 in additional gross revenue to the organization in 2018.
Ms. Perry also created a structured onboarding platform for hospitalists and created a new flexible scheduling method to improve the team’s work/life balance. In partnership with her leadership team, Ms. Perry has improved hospitalist engagement scores by 29 percent over a three-year period, with 86 percent of the physicians rating as engaged employees. This has resulted in zero attrition since July of 2017.
She is a Senior Fellow in Hospital Medicine and a true leader in her field.
Excellence in Teamwork in Quality Improvement
The Mount Sinai Hospital’s High-Value Care team is a multidisciplinary group focused on reducing overuse, decreasing costs throughout the institution, and allowing clinicians to focus on providing outstanding care and developing relationships with their patients.
Founded by Dr. Harry Cho, the High-Value Care team has chosen projects that have meaningfully affected waste reduction and patient care. They have created a sustainable structure engaging multiple members of the care team, including staff, trainees, and students. Its collaborative environment demonstrates high value, as it helps improve staff satisfaction and retention.
The team has focused on areas identified as wasteful by SHM as part of ABIM’s Choosing Wisely initiative. Projects have decreased lab testing – including amylase, folate, and “routine” daily labs – as well as medications such antihypertensives and docusate. Additionally, teams have tackled telemetry and urinary catheters, and improved patient mobility and inpatient sleep. Their innovative work can help spark similar programs nationally. As a result, the team has greatly reduced wasteful practices, decreased costs, and allowed clinicians to focus on providing outstanding care and developing relationships with patients.
In addition to many hospitalists, the High-Value Care team consists of members of Mount Sinai’s Nursing, Medicine, Pharmacy, Laboratory and IT Departments, including Andrew Dunn, MD; Beth Raucher, MD; John McClaskey, MD; Nicole Wells; Suzanne Cushnie; Surafel Tsega; and Gina Caliendo.
Junior Investigator Award
Oanh Nguyen, MD, MAS, is an assistant professor in the division of hospital medicine at the University of California, San Francisco.
Dr. Nguyen’s research is focused on the optimization of hospital care in safety-net settings and pragmatic approaches to addressing social determinants of health and transitional care strategies that address coexisting social vulnerabilities.
Her current work, funded through a K23 award, seeks to develop a strategy to predict, understand, and address coexisting social vulnerabilities among adults hospitalized with heart failure or ischemic heart disease who are at high risk for readmission.
While she is early in her investigative career, she already has 32 peer-reviewed publications, with another four first-authored manuscripts under review or in preparation.
She is an associate editor of the Journal of Hospital Medicine.
This article was updated 3/26/19.
Hospitalist, care for thyself
Tuesday keynote addresses “well-being”
You won’t want to miss Tuesday’s keynote speaker at HM19. Tait Shanafelt, MD, a hematologist, oncologist, and translational researcher of chronic lymphocytic leukemia, will discuss “clinician well-being” – a research interest of his for almost 20 years.
“A small study that I led as a resident was one of the first to look at the relationship between clinicians’ own well-being and how it impacted the care they provide patients,” he said in an interview. “That study was a real lightning rod; it got coverage everywhere – the cover of USA Today, Paul Harvey’s show. It was done by this junior person with great mentorship, and here it was galvanizing a national conversation, and I remember wondering, ‘Why is it the case? We’ve known about this in an anecdotal way for a long time.’ But we had studied it in a methodologically rigorous way, using good scientific practices, and that had allowed this to change the conversation.”
At HM19, Dr. Shanafelt will share his thoughts about where we are today with our understanding of the clinician’s experience: What are the main drivers of both distress and professional fulfillment for clinicians? “I’ll really focus on the organizational and system-level approaches that we need to be improving to make meaningful progress in reducing burnout and distress and cultivating professional fulfillment,” he said.
For too long, Dr. Shanafelt added, we’ve approached this as a problem of personal resilience, which has implied to clinicians that they just need to take better care of themselves – sleep more, exercise, do yoga. “There’s nothing wrong with those things, but they don’t address the root cause of this problem, and they will not make a meaningful dent in burnout,” he said.
Instead, we should look at the characteristics of the practice environment – whether the environment makes it easy to do the right things and provide the care patients need or whether it erects barriers to those things, barriers clinicians then have to overcome. “Can we design work flows, processes, and so forth that reduce low-value work and allow clinicians to spend more of their professional effort on the piece that only they can do: making key medical decisions, counseling patients, supporting patients?”
We know now that the well-being and professional fulfillment of clinicians is a fundamental driver of quality of care and has profound financial implications for our organizations, Dr. Shanafelt affirmed.
“This isn’t just that we want happy people here; this is fundamental if we want to achieve our mission as health care organizations,” he said. “We can’t have quality of care if we have a burned-out clinician work force. We also know now, with data from Stanford [(Calif.) University] and the Cleveland Clinic, that there is a strong relationship between burnout, turnover, and productivity and that there is a clear financial cost to the health care organization such that it merits investment of resources to bend that curve. As we start to make those investments, how do we deploy that resource to do the most good within our organizations and really transform our organizational environment and culture?”
The High Cost of Clinician Burnout: Organizational Approaches to Clinician Well-Being
Tait Shanafelt, MD
Tuesday, 9:10 – 10:00 a.m.
Potomac ABCD
Tuesday keynote addresses “well-being”
Tuesday keynote addresses “well-being”
You won’t want to miss Tuesday’s keynote speaker at HM19. Tait Shanafelt, MD, a hematologist, oncologist, and translational researcher of chronic lymphocytic leukemia, will discuss “clinician well-being” – a research interest of his for almost 20 years.
“A small study that I led as a resident was one of the first to look at the relationship between clinicians’ own well-being and how it impacted the care they provide patients,” he said in an interview. “That study was a real lightning rod; it got coverage everywhere – the cover of USA Today, Paul Harvey’s show. It was done by this junior person with great mentorship, and here it was galvanizing a national conversation, and I remember wondering, ‘Why is it the case? We’ve known about this in an anecdotal way for a long time.’ But we had studied it in a methodologically rigorous way, using good scientific practices, and that had allowed this to change the conversation.”
At HM19, Dr. Shanafelt will share his thoughts about where we are today with our understanding of the clinician’s experience: What are the main drivers of both distress and professional fulfillment for clinicians? “I’ll really focus on the organizational and system-level approaches that we need to be improving to make meaningful progress in reducing burnout and distress and cultivating professional fulfillment,” he said.
For too long, Dr. Shanafelt added, we’ve approached this as a problem of personal resilience, which has implied to clinicians that they just need to take better care of themselves – sleep more, exercise, do yoga. “There’s nothing wrong with those things, but they don’t address the root cause of this problem, and they will not make a meaningful dent in burnout,” he said.
Instead, we should look at the characteristics of the practice environment – whether the environment makes it easy to do the right things and provide the care patients need or whether it erects barriers to those things, barriers clinicians then have to overcome. “Can we design work flows, processes, and so forth that reduce low-value work and allow clinicians to spend more of their professional effort on the piece that only they can do: making key medical decisions, counseling patients, supporting patients?”
We know now that the well-being and professional fulfillment of clinicians is a fundamental driver of quality of care and has profound financial implications for our organizations, Dr. Shanafelt affirmed.
“This isn’t just that we want happy people here; this is fundamental if we want to achieve our mission as health care organizations,” he said. “We can’t have quality of care if we have a burned-out clinician work force. We also know now, with data from Stanford [(Calif.) University] and the Cleveland Clinic, that there is a strong relationship between burnout, turnover, and productivity and that there is a clear financial cost to the health care organization such that it merits investment of resources to bend that curve. As we start to make those investments, how do we deploy that resource to do the most good within our organizations and really transform our organizational environment and culture?”
The High Cost of Clinician Burnout: Organizational Approaches to Clinician Well-Being
Tait Shanafelt, MD
Tuesday, 9:10 – 10:00 a.m.
Potomac ABCD
You won’t want to miss Tuesday’s keynote speaker at HM19. Tait Shanafelt, MD, a hematologist, oncologist, and translational researcher of chronic lymphocytic leukemia, will discuss “clinician well-being” – a research interest of his for almost 20 years.
“A small study that I led as a resident was one of the first to look at the relationship between clinicians’ own well-being and how it impacted the care they provide patients,” he said in an interview. “That study was a real lightning rod; it got coverage everywhere – the cover of USA Today, Paul Harvey’s show. It was done by this junior person with great mentorship, and here it was galvanizing a national conversation, and I remember wondering, ‘Why is it the case? We’ve known about this in an anecdotal way for a long time.’ But we had studied it in a methodologically rigorous way, using good scientific practices, and that had allowed this to change the conversation.”
At HM19, Dr. Shanafelt will share his thoughts about where we are today with our understanding of the clinician’s experience: What are the main drivers of both distress and professional fulfillment for clinicians? “I’ll really focus on the organizational and system-level approaches that we need to be improving to make meaningful progress in reducing burnout and distress and cultivating professional fulfillment,” he said.
For too long, Dr. Shanafelt added, we’ve approached this as a problem of personal resilience, which has implied to clinicians that they just need to take better care of themselves – sleep more, exercise, do yoga. “There’s nothing wrong with those things, but they don’t address the root cause of this problem, and they will not make a meaningful dent in burnout,” he said.
Instead, we should look at the characteristics of the practice environment – whether the environment makes it easy to do the right things and provide the care patients need or whether it erects barriers to those things, barriers clinicians then have to overcome. “Can we design work flows, processes, and so forth that reduce low-value work and allow clinicians to spend more of their professional effort on the piece that only they can do: making key medical decisions, counseling patients, supporting patients?”
We know now that the well-being and professional fulfillment of clinicians is a fundamental driver of quality of care and has profound financial implications for our organizations, Dr. Shanafelt affirmed.
“This isn’t just that we want happy people here; this is fundamental if we want to achieve our mission as health care organizations,” he said. “We can’t have quality of care if we have a burned-out clinician work force. We also know now, with data from Stanford [(Calif.) University] and the Cleveland Clinic, that there is a strong relationship between burnout, turnover, and productivity and that there is a clear financial cost to the health care organization such that it merits investment of resources to bend that curve. As we start to make those investments, how do we deploy that resource to do the most good within our organizations and really transform our organizational environment and culture?”
The High Cost of Clinician Burnout: Organizational Approaches to Clinician Well-Being
Tait Shanafelt, MD
Tuesday, 9:10 – 10:00 a.m.
Potomac ABCD
Use time-appropriate scar improvement sequencing
WAIKOLOA, HAWAII – , according to American Academy of Dermatology President-elect George J. Hruza, MD – and he’s got a raft of them.
“There are going to be situations where your scars aren’t going to be as wonderful as you’d like, or even if they’re pretty good, you might improve them further if you do some modifications,” he observed at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
He became convinced of the importance of having a large toolbox for scar improvement in part as a result of an Australian prospective study of 576 patients surveyed 6-9 months following skin cancer surgery. Far and away the most important factor influencing patients’ overall perception of their experience wasn’t the cost, pain, quality of nursing care, complications, wait time prior to surgery, or gratitude that they’d successfully had a cancer removed. It was their perception of the scar (J Am Acad Dermatol. 2007 Sep;57[3]:445-53).
To be effective, interventions for scar improvement need to be timed in sync with the three phases of cellular activity involved in wound healing. For example, neurotoxin injections are effective during the first few days of the initial acute inflammation period, when cellular migration is active. Silicone and taping are of value when employed long term, starting at about 1 month and continuing for 3-6 months, throughout the neovascularization/granulation phase, then the time of fibroblast proliferation and matrix formation that follows, and even beyond. Pulsed dye and fractionated ablative lasers are best utilized to reshape matrix formation, starting at about 2 weeks. Intervention using dermabrasion or fillers has to wait for the scar to be a bit more mature, at about 2 months; utilized earlier these can cause dehiscence, explained Dr. Hruza of St. Louis University.
He shared what he called his “scar improvement hierarchy,” the sequence of interventions he turns to from the most to least often. But he began with prevention, noting that more than 2 decades ago, he and his coinvestigators demonstrated that running horizontal mattress sutures for primary closures of facial wounds provide better cosmetic results, with a final scar that’s smoother and flatter than the more commonly used simple running sutures (Dermatol Surg. 2005 Oct;31[10]:1313-6).
Scar improvement sequence
Massage. “I recommend this to almost every patient. I have them start at about 6 weeks and do it for several months. It’s really more like kneading dough, not rubbing. You want the skin pressing on the bone underneath,” according to Dr. Hruza. Various investigators have suggested that scar massage works by increasing hydration and capillary proliferation, while promoting desensitization, but the evidence is really anecdotal.
“I think it’s mainly tincture of time. Scars get better on their own,” he observed. Regardless, massage allows patients the satisfaction of actively participating in their own recovery.
Intralesional triamcinolone. Dr. Hruza calls this “our big friend.”
“I find that 90% of the time when you look at a thickened scar and you think, ‘Oh gee, I’m going to have to do some scar revision, the intralesional triamcinolone takes care of the problem,” he said. He usually injects the site at about 6 weeks post surgery using 10 mg/mL. If the response is inadequate he reinjects about a month later using 20 mg/mL. He generally avoids going to 40 mg/mL for facial scars. The goal is to make therapeutic use of the steroid’s major side effect – atrophy – to shrink the thickened scar. But because this can be a tricky business, of late he has turned increasingly to intralesional triamcinolone and 5-fluorouracil (5-FU).
Intralesional triamcinolone plus 5-FU. This combination causes less atrophy, hypopigmentation, and telangiectasias than full-on triamcinolone. He injects 0.9 mL of 5-FU at 50 mg/mL and 0.1 mL of triamcinolone at 40 mg/mL into and under the scar. The 5-FU inhibits fibroblast proliferation. It is rated pregnancy category D, so he avoids using it in women of childbearing age.
Spot dermabrasion. “To me, this is the go-to. After my intralesional steroids, if the scar hasn’t fully smoothed out, then I go to dermabrasion or the spot CO2 laser,” Dr. Hruza said.
“Dermabrasion is an old technology, but it’s actually still very useful,” he continued. “Do it at 6-10 weeks; that’s the sweet spot. Do it sooner and you can get into problems with dehiscence. And if you do it later than 10 weeks the improvement is much less because everything is stabilized and the collagen is set.” He uses a diamond fraise to abrade and sculpt, rather than sandpaper, which doesn’t allow him to go sufficiently deep once bleeding starts and the sandpaper gets wet.
Spot conventional CO2 or Er:YAG laser resurfacing. “I really find in my hands these ablative techniques are much more effective than using a fractionated laser, which only gives you a little bit of improvement,” he said.
Pulsed dye laser. Very effective for red, thickened scars. Dr. Hruza does two to four treatments at 4-week intervals. At wavelengths of 585-595 nm, a pulse of 0.5-1.5 millisecs, and 4-5 Joules/cm2, there is only minimal purpura.
The pulsed dye laser can also be employed preventively starting at the time of suture removal and then again at 4-6 weeks in order to reduce hypertrophy. “It’s something to consider in areas like the chest, upper back, and shoulders, where you’re trying to prevent problems. The only danger is occasionally patients have dehiscence,” according to the dermatologic surgeon.
Fractionated nonablative laser. Four or five treatments are typically required in order to achieve significant resurfacing.
Micropore tape. Dr. Hruza finds this works just as well as topical silicone gel sheets, rolls, and gels, all of which are quite expensive. A roll of micropore tape costs only a few dollars and will last a patient for a couple months. Patients are taught to apply the tape at the time of suture removal in a line parallel to the suture line, replacing the tape when it begins to peel off. As with the vastly more expensive silicone products, the tape needs to be left on 12-24 hours per day for 3-6 months in order to achieve a flat white scar. The benefit is thought to come from relief of mechanical stress coupled with occlusion.
Botulinum toxin A and other neurotoxins. Inject into muscle near the wound edges right after closing the wound, using 1-3 units at 1- to 3-cm intervals in order to prevent scar formation, Dr. Hruza advised. If the wound is on one side of the face, the other side needs to receive injections as well in order to spare the patient from several months of cosmetically undesirable asymmetry. However, Dr. Hruza rarely utilizes neurotoxin injections. “It’s a cost issue. I’m in the Midwest, where a lot of insurers are unwilling to pay for it,” he explained.
Flap defatting. Here the surgeon opens the flap and keeps digging with scalpel and scissors until the scar is slightly depressed, since there is likely to be some recurrence. Then it’s time to resuture the flap.
Technical scar revision procedures. The simplest of these is Z-plasty, which entails making two skin incisions to create a Z-shaped incision, then flipping the two sides to reorient the scar. The Z-plasty has two major uses: correction of a retracted lip or medial canthus webbing. “If you get either of these, Z-plasty is the way to go,” Dr. Hruza said.
Fillers for atrophic scars. “To me, this is the last thing to go to. The reason is that, if a patient has skin cancer surgery, they don’t expect to pay extra to improve that scar. And I can do dermabrasion with no incremental product cost to the practice,” he commented. The technique entails making a subcision to create a pocket for the filler. The products marketed as Restylane Silk, Belotero, and Radiesse all yield good results, he said.
Dr. Hruza reported having no financial conflicts of interest regarding his presentation.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – , according to American Academy of Dermatology President-elect George J. Hruza, MD – and he’s got a raft of them.
“There are going to be situations where your scars aren’t going to be as wonderful as you’d like, or even if they’re pretty good, you might improve them further if you do some modifications,” he observed at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
He became convinced of the importance of having a large toolbox for scar improvement in part as a result of an Australian prospective study of 576 patients surveyed 6-9 months following skin cancer surgery. Far and away the most important factor influencing patients’ overall perception of their experience wasn’t the cost, pain, quality of nursing care, complications, wait time prior to surgery, or gratitude that they’d successfully had a cancer removed. It was their perception of the scar (J Am Acad Dermatol. 2007 Sep;57[3]:445-53).
To be effective, interventions for scar improvement need to be timed in sync with the three phases of cellular activity involved in wound healing. For example, neurotoxin injections are effective during the first few days of the initial acute inflammation period, when cellular migration is active. Silicone and taping are of value when employed long term, starting at about 1 month and continuing for 3-6 months, throughout the neovascularization/granulation phase, then the time of fibroblast proliferation and matrix formation that follows, and even beyond. Pulsed dye and fractionated ablative lasers are best utilized to reshape matrix formation, starting at about 2 weeks. Intervention using dermabrasion or fillers has to wait for the scar to be a bit more mature, at about 2 months; utilized earlier these can cause dehiscence, explained Dr. Hruza of St. Louis University.
He shared what he called his “scar improvement hierarchy,” the sequence of interventions he turns to from the most to least often. But he began with prevention, noting that more than 2 decades ago, he and his coinvestigators demonstrated that running horizontal mattress sutures for primary closures of facial wounds provide better cosmetic results, with a final scar that’s smoother and flatter than the more commonly used simple running sutures (Dermatol Surg. 2005 Oct;31[10]:1313-6).
Scar improvement sequence
Massage. “I recommend this to almost every patient. I have them start at about 6 weeks and do it for several months. It’s really more like kneading dough, not rubbing. You want the skin pressing on the bone underneath,” according to Dr. Hruza. Various investigators have suggested that scar massage works by increasing hydration and capillary proliferation, while promoting desensitization, but the evidence is really anecdotal.
“I think it’s mainly tincture of time. Scars get better on their own,” he observed. Regardless, massage allows patients the satisfaction of actively participating in their own recovery.
Intralesional triamcinolone. Dr. Hruza calls this “our big friend.”
“I find that 90% of the time when you look at a thickened scar and you think, ‘Oh gee, I’m going to have to do some scar revision, the intralesional triamcinolone takes care of the problem,” he said. He usually injects the site at about 6 weeks post surgery using 10 mg/mL. If the response is inadequate he reinjects about a month later using 20 mg/mL. He generally avoids going to 40 mg/mL for facial scars. The goal is to make therapeutic use of the steroid’s major side effect – atrophy – to shrink the thickened scar. But because this can be a tricky business, of late he has turned increasingly to intralesional triamcinolone and 5-fluorouracil (5-FU).
Intralesional triamcinolone plus 5-FU. This combination causes less atrophy, hypopigmentation, and telangiectasias than full-on triamcinolone. He injects 0.9 mL of 5-FU at 50 mg/mL and 0.1 mL of triamcinolone at 40 mg/mL into and under the scar. The 5-FU inhibits fibroblast proliferation. It is rated pregnancy category D, so he avoids using it in women of childbearing age.
Spot dermabrasion. “To me, this is the go-to. After my intralesional steroids, if the scar hasn’t fully smoothed out, then I go to dermabrasion or the spot CO2 laser,” Dr. Hruza said.
“Dermabrasion is an old technology, but it’s actually still very useful,” he continued. “Do it at 6-10 weeks; that’s the sweet spot. Do it sooner and you can get into problems with dehiscence. And if you do it later than 10 weeks the improvement is much less because everything is stabilized and the collagen is set.” He uses a diamond fraise to abrade and sculpt, rather than sandpaper, which doesn’t allow him to go sufficiently deep once bleeding starts and the sandpaper gets wet.
Spot conventional CO2 or Er:YAG laser resurfacing. “I really find in my hands these ablative techniques are much more effective than using a fractionated laser, which only gives you a little bit of improvement,” he said.
Pulsed dye laser. Very effective for red, thickened scars. Dr. Hruza does two to four treatments at 4-week intervals. At wavelengths of 585-595 nm, a pulse of 0.5-1.5 millisecs, and 4-5 Joules/cm2, there is only minimal purpura.
The pulsed dye laser can also be employed preventively starting at the time of suture removal and then again at 4-6 weeks in order to reduce hypertrophy. “It’s something to consider in areas like the chest, upper back, and shoulders, where you’re trying to prevent problems. The only danger is occasionally patients have dehiscence,” according to the dermatologic surgeon.
Fractionated nonablative laser. Four or five treatments are typically required in order to achieve significant resurfacing.
Micropore tape. Dr. Hruza finds this works just as well as topical silicone gel sheets, rolls, and gels, all of which are quite expensive. A roll of micropore tape costs only a few dollars and will last a patient for a couple months. Patients are taught to apply the tape at the time of suture removal in a line parallel to the suture line, replacing the tape when it begins to peel off. As with the vastly more expensive silicone products, the tape needs to be left on 12-24 hours per day for 3-6 months in order to achieve a flat white scar. The benefit is thought to come from relief of mechanical stress coupled with occlusion.
Botulinum toxin A and other neurotoxins. Inject into muscle near the wound edges right after closing the wound, using 1-3 units at 1- to 3-cm intervals in order to prevent scar formation, Dr. Hruza advised. If the wound is on one side of the face, the other side needs to receive injections as well in order to spare the patient from several months of cosmetically undesirable asymmetry. However, Dr. Hruza rarely utilizes neurotoxin injections. “It’s a cost issue. I’m in the Midwest, where a lot of insurers are unwilling to pay for it,” he explained.
Flap defatting. Here the surgeon opens the flap and keeps digging with scalpel and scissors until the scar is slightly depressed, since there is likely to be some recurrence. Then it’s time to resuture the flap.
Technical scar revision procedures. The simplest of these is Z-plasty, which entails making two skin incisions to create a Z-shaped incision, then flipping the two sides to reorient the scar. The Z-plasty has two major uses: correction of a retracted lip or medial canthus webbing. “If you get either of these, Z-plasty is the way to go,” Dr. Hruza said.
Fillers for atrophic scars. “To me, this is the last thing to go to. The reason is that, if a patient has skin cancer surgery, they don’t expect to pay extra to improve that scar. And I can do dermabrasion with no incremental product cost to the practice,” he commented. The technique entails making a subcision to create a pocket for the filler. The products marketed as Restylane Silk, Belotero, and Radiesse all yield good results, he said.
Dr. Hruza reported having no financial conflicts of interest regarding his presentation.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – , according to American Academy of Dermatology President-elect George J. Hruza, MD – and he’s got a raft of them.
“There are going to be situations where your scars aren’t going to be as wonderful as you’d like, or even if they’re pretty good, you might improve them further if you do some modifications,” he observed at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
He became convinced of the importance of having a large toolbox for scar improvement in part as a result of an Australian prospective study of 576 patients surveyed 6-9 months following skin cancer surgery. Far and away the most important factor influencing patients’ overall perception of their experience wasn’t the cost, pain, quality of nursing care, complications, wait time prior to surgery, or gratitude that they’d successfully had a cancer removed. It was their perception of the scar (J Am Acad Dermatol. 2007 Sep;57[3]:445-53).
To be effective, interventions for scar improvement need to be timed in sync with the three phases of cellular activity involved in wound healing. For example, neurotoxin injections are effective during the first few days of the initial acute inflammation period, when cellular migration is active. Silicone and taping are of value when employed long term, starting at about 1 month and continuing for 3-6 months, throughout the neovascularization/granulation phase, then the time of fibroblast proliferation and matrix formation that follows, and even beyond. Pulsed dye and fractionated ablative lasers are best utilized to reshape matrix formation, starting at about 2 weeks. Intervention using dermabrasion or fillers has to wait for the scar to be a bit more mature, at about 2 months; utilized earlier these can cause dehiscence, explained Dr. Hruza of St. Louis University.
He shared what he called his “scar improvement hierarchy,” the sequence of interventions he turns to from the most to least often. But he began with prevention, noting that more than 2 decades ago, he and his coinvestigators demonstrated that running horizontal mattress sutures for primary closures of facial wounds provide better cosmetic results, with a final scar that’s smoother and flatter than the more commonly used simple running sutures (Dermatol Surg. 2005 Oct;31[10]:1313-6).
Scar improvement sequence
Massage. “I recommend this to almost every patient. I have them start at about 6 weeks and do it for several months. It’s really more like kneading dough, not rubbing. You want the skin pressing on the bone underneath,” according to Dr. Hruza. Various investigators have suggested that scar massage works by increasing hydration and capillary proliferation, while promoting desensitization, but the evidence is really anecdotal.
“I think it’s mainly tincture of time. Scars get better on their own,” he observed. Regardless, massage allows patients the satisfaction of actively participating in their own recovery.
Intralesional triamcinolone. Dr. Hruza calls this “our big friend.”
“I find that 90% of the time when you look at a thickened scar and you think, ‘Oh gee, I’m going to have to do some scar revision, the intralesional triamcinolone takes care of the problem,” he said. He usually injects the site at about 6 weeks post surgery using 10 mg/mL. If the response is inadequate he reinjects about a month later using 20 mg/mL. He generally avoids going to 40 mg/mL for facial scars. The goal is to make therapeutic use of the steroid’s major side effect – atrophy – to shrink the thickened scar. But because this can be a tricky business, of late he has turned increasingly to intralesional triamcinolone and 5-fluorouracil (5-FU).
Intralesional triamcinolone plus 5-FU. This combination causes less atrophy, hypopigmentation, and telangiectasias than full-on triamcinolone. He injects 0.9 mL of 5-FU at 50 mg/mL and 0.1 mL of triamcinolone at 40 mg/mL into and under the scar. The 5-FU inhibits fibroblast proliferation. It is rated pregnancy category D, so he avoids using it in women of childbearing age.
Spot dermabrasion. “To me, this is the go-to. After my intralesional steroids, if the scar hasn’t fully smoothed out, then I go to dermabrasion or the spot CO2 laser,” Dr. Hruza said.
“Dermabrasion is an old technology, but it’s actually still very useful,” he continued. “Do it at 6-10 weeks; that’s the sweet spot. Do it sooner and you can get into problems with dehiscence. And if you do it later than 10 weeks the improvement is much less because everything is stabilized and the collagen is set.” He uses a diamond fraise to abrade and sculpt, rather than sandpaper, which doesn’t allow him to go sufficiently deep once bleeding starts and the sandpaper gets wet.
Spot conventional CO2 or Er:YAG laser resurfacing. “I really find in my hands these ablative techniques are much more effective than using a fractionated laser, which only gives you a little bit of improvement,” he said.
Pulsed dye laser. Very effective for red, thickened scars. Dr. Hruza does two to four treatments at 4-week intervals. At wavelengths of 585-595 nm, a pulse of 0.5-1.5 millisecs, and 4-5 Joules/cm2, there is only minimal purpura.
The pulsed dye laser can also be employed preventively starting at the time of suture removal and then again at 4-6 weeks in order to reduce hypertrophy. “It’s something to consider in areas like the chest, upper back, and shoulders, where you’re trying to prevent problems. The only danger is occasionally patients have dehiscence,” according to the dermatologic surgeon.
Fractionated nonablative laser. Four or five treatments are typically required in order to achieve significant resurfacing.
Micropore tape. Dr. Hruza finds this works just as well as topical silicone gel sheets, rolls, and gels, all of which are quite expensive. A roll of micropore tape costs only a few dollars and will last a patient for a couple months. Patients are taught to apply the tape at the time of suture removal in a line parallel to the suture line, replacing the tape when it begins to peel off. As with the vastly more expensive silicone products, the tape needs to be left on 12-24 hours per day for 3-6 months in order to achieve a flat white scar. The benefit is thought to come from relief of mechanical stress coupled with occlusion.
Botulinum toxin A and other neurotoxins. Inject into muscle near the wound edges right after closing the wound, using 1-3 units at 1- to 3-cm intervals in order to prevent scar formation, Dr. Hruza advised. If the wound is on one side of the face, the other side needs to receive injections as well in order to spare the patient from several months of cosmetically undesirable asymmetry. However, Dr. Hruza rarely utilizes neurotoxin injections. “It’s a cost issue. I’m in the Midwest, where a lot of insurers are unwilling to pay for it,” he explained.
Flap defatting. Here the surgeon opens the flap and keeps digging with scalpel and scissors until the scar is slightly depressed, since there is likely to be some recurrence. Then it’s time to resuture the flap.
Technical scar revision procedures. The simplest of these is Z-plasty, which entails making two skin incisions to create a Z-shaped incision, then flipping the two sides to reorient the scar. The Z-plasty has two major uses: correction of a retracted lip or medial canthus webbing. “If you get either of these, Z-plasty is the way to go,” Dr. Hruza said.
Fillers for atrophic scars. “To me, this is the last thing to go to. The reason is that, if a patient has skin cancer surgery, they don’t expect to pay extra to improve that scar. And I can do dermabrasion with no incremental product cost to the practice,” he commented. The technique entails making a subcision to create a pocket for the filler. The products marketed as Restylane Silk, Belotero, and Radiesse all yield good results, he said.
Dr. Hruza reported having no financial conflicts of interest regarding his presentation.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
REPORTING FROM SDEF HAWAII DERMATOLOGY SEMINAR
For patients with HBV, daily aspirin may reduce risk of liver cancer
Sixteen years of data showed that daily aspirin therapy reduced the risk of HBV-related HCC by 29%, reported lead author Teng-Yu Lee, MD, PhD, of Taichung (Taiwan) Veterans General Hospital and his colleagues. Analysis also showed that antiviral nucleos(t)ide analogue therapy and statin use were independently associated with reduced risk of HCC, whereas older age, cirrhosis, and male sex increased risk.
“Therapy with [nucleos(t)ide analogues] is associated with reductions in HCC risk, but the risk is not erased,” the investigators wrote in JAMA Internal Medicine. “Therefore, using only [nucleos(t)ide analogue] therapy may not be enough for HCC prevention. Antiviral therapy is not indicated in most HBV carriers, so another effective way of reducing HCC risk needs to be developed.”
Previous studies have shown that aspirin can reduce the risk of colorectal cancer; however, data supporting aspirin for HCC prevention are limited to a few animal models and human studies, the latter of which are statistically unreliable.
“Therefore, we conducted a nationwide cohort study to evaluate the association of daily aspirin therapy with HBV-related HCC,” the investigators wrote.
They screened 204,507 patients with HBV included in the Taiwanese National Health Insurance Research Database (NHIRD) between 1997 and 2012, first excluding any with confounding conditions, such as hepatitis C infection or alcoholic liver disease. Next, 2,123 patients were identified who had taken aspirin for 90 days or longer. Finally, these cases were randomly matched with 8,492 control patients with HBV who had never received antiplatelet therapy. The main measured outcome was diagnosis with HCC. Patients were followed until this diagnosis was made, death occurred, or the end of the study period.
Analysis showed that most patients were male (72.4%) and took aspirin for about 4 years, usually prescribed for cardiovascular disease risk factors. Almost all patients in the treatment group (98%) received an aspirin dose of 100 mg or less.
After 5 years, the cumulative incidence of HCC in the aspirin group was 5.20% versus 7.87% in the control group (P less than .001). Multivariable analysis revealed that daily aspirin was associated with a significant risk reduction of 29% (HR 0.71; P less than .001), as were nucleos(t)ide analogues and statins, which lowered risk by 46% and 38%, respectively. In contrast, risk increased with older age at the rate of 1% per year, male sex carried an additional risk of 75%, and liver cirrhosis was associated with a 2.89-fold risk increase.
“In the present study, we report that daily aspirin therapy was associated with a reduced incidence of HCC in patients with [chronic hepatitis B],” the investigators wrote. “Our findings may be of help in future efforts to further improve the chemoprevention of HBV-related HCC, and a proof-of-concept study is thus warranted.”
The investigators described several mechanisms that may have contribute to the possible risk reduction provided by aspirin. For one, aspirin inhibits platelet activation, which is associated with development of HBV-related liver disease. Additional benefit may come from induction of HCC cell apoptosis, control of tumor growth, reduced liver fibrosis, and increased liver regeneration, all of which have been associated with aspirin in rodent models.
“Hepatitis B virus–related HCC is generally a consequence of chronic inflammation due to hepatitis, fibrosis, dysplasia, and tumor growth,” the investigators wrote, suggesting that aspirin-related reductions in inflammation could also explain reduced neoplastic activity.
To assess for increased risk of peptic ulcers secondary to aspirin, the investigators performed a subanalysis of peptic ulcer bleeding. These results showed that rates of peptic ulcer bleeding, at around 5%-6%, were similar between the aspirin group and the control group. Among other variables, cirrhosis didn’t significantly affect rates of peptic ulcer bleeding, and aspirin users had similar rates of peptic ulcer bleeding regardless of HBV status. Because of the study design, however, the investigators cautioned that these analyses could underestimate ulcer risk because patients who could not tolerate aspirin for at least 90 days were excluded from the study.
Although statins stood out as another possible risk reducer, the investigators noted that “randomized clinical trials are required to confirm the chemopreventive effect of statins.”
Similarly, the investigators suggested that a prospective trial is needed before aspirin can be adopted as an HCC preventive.
The study was funded by the Ministry of Science and Technology, National Health Research Institutes, and Taichung (Taiwan) Veterans General Hospital, Taiwan. One author reported financial compensation from Gilead and Bristol-Myers Squibb.
SOURCE: Lee T-Y et al. JAMA Intern Med. 2019 Mar 18. doi:10.1001/jamainternmed.2018.8342.
Sixteen years of data showed that daily aspirin therapy reduced the risk of HBV-related HCC by 29%, reported lead author Teng-Yu Lee, MD, PhD, of Taichung (Taiwan) Veterans General Hospital and his colleagues. Analysis also showed that antiviral nucleos(t)ide analogue therapy and statin use were independently associated with reduced risk of HCC, whereas older age, cirrhosis, and male sex increased risk.
“Therapy with [nucleos(t)ide analogues] is associated with reductions in HCC risk, but the risk is not erased,” the investigators wrote in JAMA Internal Medicine. “Therefore, using only [nucleos(t)ide analogue] therapy may not be enough for HCC prevention. Antiviral therapy is not indicated in most HBV carriers, so another effective way of reducing HCC risk needs to be developed.”
Previous studies have shown that aspirin can reduce the risk of colorectal cancer; however, data supporting aspirin for HCC prevention are limited to a few animal models and human studies, the latter of which are statistically unreliable.
“Therefore, we conducted a nationwide cohort study to evaluate the association of daily aspirin therapy with HBV-related HCC,” the investigators wrote.
They screened 204,507 patients with HBV included in the Taiwanese National Health Insurance Research Database (NHIRD) between 1997 and 2012, first excluding any with confounding conditions, such as hepatitis C infection or alcoholic liver disease. Next, 2,123 patients were identified who had taken aspirin for 90 days or longer. Finally, these cases were randomly matched with 8,492 control patients with HBV who had never received antiplatelet therapy. The main measured outcome was diagnosis with HCC. Patients were followed until this diagnosis was made, death occurred, or the end of the study period.
Analysis showed that most patients were male (72.4%) and took aspirin for about 4 years, usually prescribed for cardiovascular disease risk factors. Almost all patients in the treatment group (98%) received an aspirin dose of 100 mg or less.
After 5 years, the cumulative incidence of HCC in the aspirin group was 5.20% versus 7.87% in the control group (P less than .001). Multivariable analysis revealed that daily aspirin was associated with a significant risk reduction of 29% (HR 0.71; P less than .001), as were nucleos(t)ide analogues and statins, which lowered risk by 46% and 38%, respectively. In contrast, risk increased with older age at the rate of 1% per year, male sex carried an additional risk of 75%, and liver cirrhosis was associated with a 2.89-fold risk increase.
“In the present study, we report that daily aspirin therapy was associated with a reduced incidence of HCC in patients with [chronic hepatitis B],” the investigators wrote. “Our findings may be of help in future efforts to further improve the chemoprevention of HBV-related HCC, and a proof-of-concept study is thus warranted.”
The investigators described several mechanisms that may have contribute to the possible risk reduction provided by aspirin. For one, aspirin inhibits platelet activation, which is associated with development of HBV-related liver disease. Additional benefit may come from induction of HCC cell apoptosis, control of tumor growth, reduced liver fibrosis, and increased liver regeneration, all of which have been associated with aspirin in rodent models.
“Hepatitis B virus–related HCC is generally a consequence of chronic inflammation due to hepatitis, fibrosis, dysplasia, and tumor growth,” the investigators wrote, suggesting that aspirin-related reductions in inflammation could also explain reduced neoplastic activity.
To assess for increased risk of peptic ulcers secondary to aspirin, the investigators performed a subanalysis of peptic ulcer bleeding. These results showed that rates of peptic ulcer bleeding, at around 5%-6%, were similar between the aspirin group and the control group. Among other variables, cirrhosis didn’t significantly affect rates of peptic ulcer bleeding, and aspirin users had similar rates of peptic ulcer bleeding regardless of HBV status. Because of the study design, however, the investigators cautioned that these analyses could underestimate ulcer risk because patients who could not tolerate aspirin for at least 90 days were excluded from the study.
Although statins stood out as another possible risk reducer, the investigators noted that “randomized clinical trials are required to confirm the chemopreventive effect of statins.”
Similarly, the investigators suggested that a prospective trial is needed before aspirin can be adopted as an HCC preventive.
The study was funded by the Ministry of Science and Technology, National Health Research Institutes, and Taichung (Taiwan) Veterans General Hospital, Taiwan. One author reported financial compensation from Gilead and Bristol-Myers Squibb.
SOURCE: Lee T-Y et al. JAMA Intern Med. 2019 Mar 18. doi:10.1001/jamainternmed.2018.8342.
Sixteen years of data showed that daily aspirin therapy reduced the risk of HBV-related HCC by 29%, reported lead author Teng-Yu Lee, MD, PhD, of Taichung (Taiwan) Veterans General Hospital and his colleagues. Analysis also showed that antiviral nucleos(t)ide analogue therapy and statin use were independently associated with reduced risk of HCC, whereas older age, cirrhosis, and male sex increased risk.
“Therapy with [nucleos(t)ide analogues] is associated with reductions in HCC risk, but the risk is not erased,” the investigators wrote in JAMA Internal Medicine. “Therefore, using only [nucleos(t)ide analogue] therapy may not be enough for HCC prevention. Antiviral therapy is not indicated in most HBV carriers, so another effective way of reducing HCC risk needs to be developed.”
Previous studies have shown that aspirin can reduce the risk of colorectal cancer; however, data supporting aspirin for HCC prevention are limited to a few animal models and human studies, the latter of which are statistically unreliable.
“Therefore, we conducted a nationwide cohort study to evaluate the association of daily aspirin therapy with HBV-related HCC,” the investigators wrote.
They screened 204,507 patients with HBV included in the Taiwanese National Health Insurance Research Database (NHIRD) between 1997 and 2012, first excluding any with confounding conditions, such as hepatitis C infection or alcoholic liver disease. Next, 2,123 patients were identified who had taken aspirin for 90 days or longer. Finally, these cases were randomly matched with 8,492 control patients with HBV who had never received antiplatelet therapy. The main measured outcome was diagnosis with HCC. Patients were followed until this diagnosis was made, death occurred, or the end of the study period.
Analysis showed that most patients were male (72.4%) and took aspirin for about 4 years, usually prescribed for cardiovascular disease risk factors. Almost all patients in the treatment group (98%) received an aspirin dose of 100 mg or less.
After 5 years, the cumulative incidence of HCC in the aspirin group was 5.20% versus 7.87% in the control group (P less than .001). Multivariable analysis revealed that daily aspirin was associated with a significant risk reduction of 29% (HR 0.71; P less than .001), as were nucleos(t)ide analogues and statins, which lowered risk by 46% and 38%, respectively. In contrast, risk increased with older age at the rate of 1% per year, male sex carried an additional risk of 75%, and liver cirrhosis was associated with a 2.89-fold risk increase.
“In the present study, we report that daily aspirin therapy was associated with a reduced incidence of HCC in patients with [chronic hepatitis B],” the investigators wrote. “Our findings may be of help in future efforts to further improve the chemoprevention of HBV-related HCC, and a proof-of-concept study is thus warranted.”
The investigators described several mechanisms that may have contribute to the possible risk reduction provided by aspirin. For one, aspirin inhibits platelet activation, which is associated with development of HBV-related liver disease. Additional benefit may come from induction of HCC cell apoptosis, control of tumor growth, reduced liver fibrosis, and increased liver regeneration, all of which have been associated with aspirin in rodent models.
“Hepatitis B virus–related HCC is generally a consequence of chronic inflammation due to hepatitis, fibrosis, dysplasia, and tumor growth,” the investigators wrote, suggesting that aspirin-related reductions in inflammation could also explain reduced neoplastic activity.
To assess for increased risk of peptic ulcers secondary to aspirin, the investigators performed a subanalysis of peptic ulcer bleeding. These results showed that rates of peptic ulcer bleeding, at around 5%-6%, were similar between the aspirin group and the control group. Among other variables, cirrhosis didn’t significantly affect rates of peptic ulcer bleeding, and aspirin users had similar rates of peptic ulcer bleeding regardless of HBV status. Because of the study design, however, the investigators cautioned that these analyses could underestimate ulcer risk because patients who could not tolerate aspirin for at least 90 days were excluded from the study.
Although statins stood out as another possible risk reducer, the investigators noted that “randomized clinical trials are required to confirm the chemopreventive effect of statins.”
Similarly, the investigators suggested that a prospective trial is needed before aspirin can be adopted as an HCC preventive.
The study was funded by the Ministry of Science and Technology, National Health Research Institutes, and Taichung (Taiwan) Veterans General Hospital, Taiwan. One author reported financial compensation from Gilead and Bristol-Myers Squibb.
SOURCE: Lee T-Y et al. JAMA Intern Med. 2019 Mar 18. doi:10.1001/jamainternmed.2018.8342.
FROM JAMA INTERNAL MEDICINE
Tuesday’s Product Theaters
12:30 - 1:30 p.m., Product Theater 1
Reduction in the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation (NVAF)
Speaker: Charles J. Dow, MD, FACC, cardiologist, Harvard Medical School, Boston
Sponsored by Pfizer
12:30 - 1:30 p.m., Product Theater 2
Improving Outcomes for Hospitalized Patients with HFrEF: Looking Beyond Stabilization
Speaker: Jennifer Brown, MD
Medstar Cardiology Associates
Annapolis, MD
Sponsored by Novartis Pharmaceuticals Corp.
12:30 - 1:30 p.m., Product Theater 3
The Role of the Hospital Medicine Specialist in Managing Transitions of Care in Acute Coronary Syndrome
Speaker: John Venditto, MD, MBA, senior medical director, cardiovascular metabolic disease,
U.S. Medical Affairs – AstraZeneca
Sponsored by AstraZeneca Pharmaceuticals LP
12:30 - 1:30 p.m., Product Theater 1
Reduction in the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation (NVAF)
Speaker: Charles J. Dow, MD, FACC, cardiologist, Harvard Medical School, Boston
Sponsored by Pfizer
12:30 - 1:30 p.m., Product Theater 2
Improving Outcomes for Hospitalized Patients with HFrEF: Looking Beyond Stabilization
Speaker: Jennifer Brown, MD
Medstar Cardiology Associates
Annapolis, MD
Sponsored by Novartis Pharmaceuticals Corp.
12:30 - 1:30 p.m., Product Theater 3
The Role of the Hospital Medicine Specialist in Managing Transitions of Care in Acute Coronary Syndrome
Speaker: John Venditto, MD, MBA, senior medical director, cardiovascular metabolic disease,
U.S. Medical Affairs – AstraZeneca
Sponsored by AstraZeneca Pharmaceuticals LP
12:30 - 1:30 p.m., Product Theater 1
Reduction in the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation (NVAF)
Speaker: Charles J. Dow, MD, FACC, cardiologist, Harvard Medical School, Boston
Sponsored by Pfizer
12:30 - 1:30 p.m., Product Theater 2
Improving Outcomes for Hospitalized Patients with HFrEF: Looking Beyond Stabilization
Speaker: Jennifer Brown, MD
Medstar Cardiology Associates
Annapolis, MD
Sponsored by Novartis Pharmaceuticals Corp.
12:30 - 1:30 p.m., Product Theater 3
The Role of the Hospital Medicine Specialist in Managing Transitions of Care in Acute Coronary Syndrome
Speaker: John Venditto, MD, MBA, senior medical director, cardiovascular metabolic disease,
U.S. Medical Affairs – AstraZeneca
Sponsored by AstraZeneca Pharmaceuticals LP
Hospitalists get emergency airway management training
A patient is having a medical emergency and is having difficulty breathing. If the airway isn’t managed well, the consequences could be tragic. If asked to step in, would you? Could you?
More hospitalists are being faced with this situation, said Joshua Lenchus, DO, RPh, SFHM, chief medical officer at the Broward Health Medical Center in South Florida. But when they are, they tend to be hesitant – usually with good reason, since training is frequently lacking.
Dr. Lenchus and a group of five other physicians who are experienced in airway management led 25 hospitalists in emergent airway management training on Monday at HM19, a first-of-its-kind session at the annual conference.
“Not all facilities that hospitalists practice at would require or even ask a hospitalist to step into a situation like this,” said Dr. Lenchus, who oversaw the training. “But as you walk around the exhibit hall at SHM, you find that of the locum tenens companies that ask for hospitalists to perform procedures, airway management is very high on the list.”
The trainers were Armando Ariza Giammaria, MD, an anesthesiologist and clinical assistant professor at Tulane University, New Orleans; Jorge Cabrera, DO, an intensivist and assistant professor of medicine at the University of Miami; Alice Gallo de Moraes, MD, a pulmonary critical care doctor at Mayo Clinic, Rochester, Minn.; Fernando Caceres, MD, a pulmonary critical care specialist at the Billings (Mont.) Clinic; and Aldo Pavon Canseco, MD, a hospitalist and assistant professor of medicine at the University of Miami who was trained as a pediatric anesthesiologist.
Over 3 hours, hospitalists first heard tips for airway management, with words of caution, and then did hands-on work using manikins under the guidance of the faculty members with a low trainee-to-instructor ratio.
“Do the basics well and the scary things will become manageable,” Dr. Cabrera said in the session.
Instructors said it was vital to have a checklist in the form of a mnemonic device, and to have not just Plan A for clearing an airway, but Plans B and C, too.
Dr. Ariza told the learners not to focus too much on intubation — it’s not always necessary. In fact, he said he couldn’t over-emphasize the importance of mastering bag-mask ventilation, a go-to method when other approaches fail.
Participants learned about devices that can be deployed through the nose to keep the airway clear, those that can be used in the mouth but that might not go down quite as far as the lung, an inflatable bag that can be placed over patients’ mouths and squeezed to help with their breathing, and endotracheal tubes.
Dr. Lenchus said that more training would likely be needed for most clinicians – perhaps with other faculty at their own institutions – before they could be expected to employ these techniques in a real-life emergency situation.
A patient is having a medical emergency and is having difficulty breathing. If the airway isn’t managed well, the consequences could be tragic. If asked to step in, would you? Could you?
More hospitalists are being faced with this situation, said Joshua Lenchus, DO, RPh, SFHM, chief medical officer at the Broward Health Medical Center in South Florida. But when they are, they tend to be hesitant – usually with good reason, since training is frequently lacking.
Dr. Lenchus and a group of five other physicians who are experienced in airway management led 25 hospitalists in emergent airway management training on Monday at HM19, a first-of-its-kind session at the annual conference.
“Not all facilities that hospitalists practice at would require or even ask a hospitalist to step into a situation like this,” said Dr. Lenchus, who oversaw the training. “But as you walk around the exhibit hall at SHM, you find that of the locum tenens companies that ask for hospitalists to perform procedures, airway management is very high on the list.”
The trainers were Armando Ariza Giammaria, MD, an anesthesiologist and clinical assistant professor at Tulane University, New Orleans; Jorge Cabrera, DO, an intensivist and assistant professor of medicine at the University of Miami; Alice Gallo de Moraes, MD, a pulmonary critical care doctor at Mayo Clinic, Rochester, Minn.; Fernando Caceres, MD, a pulmonary critical care specialist at the Billings (Mont.) Clinic; and Aldo Pavon Canseco, MD, a hospitalist and assistant professor of medicine at the University of Miami who was trained as a pediatric anesthesiologist.
Over 3 hours, hospitalists first heard tips for airway management, with words of caution, and then did hands-on work using manikins under the guidance of the faculty members with a low trainee-to-instructor ratio.
“Do the basics well and the scary things will become manageable,” Dr. Cabrera said in the session.
Instructors said it was vital to have a checklist in the form of a mnemonic device, and to have not just Plan A for clearing an airway, but Plans B and C, too.
Dr. Ariza told the learners not to focus too much on intubation — it’s not always necessary. In fact, he said he couldn’t over-emphasize the importance of mastering bag-mask ventilation, a go-to method when other approaches fail.
Participants learned about devices that can be deployed through the nose to keep the airway clear, those that can be used in the mouth but that might not go down quite as far as the lung, an inflatable bag that can be placed over patients’ mouths and squeezed to help with their breathing, and endotracheal tubes.
Dr. Lenchus said that more training would likely be needed for most clinicians – perhaps with other faculty at their own institutions – before they could be expected to employ these techniques in a real-life emergency situation.
A patient is having a medical emergency and is having difficulty breathing. If the airway isn’t managed well, the consequences could be tragic. If asked to step in, would you? Could you?
More hospitalists are being faced with this situation, said Joshua Lenchus, DO, RPh, SFHM, chief medical officer at the Broward Health Medical Center in South Florida. But when they are, they tend to be hesitant – usually with good reason, since training is frequently lacking.
Dr. Lenchus and a group of five other physicians who are experienced in airway management led 25 hospitalists in emergent airway management training on Monday at HM19, a first-of-its-kind session at the annual conference.
“Not all facilities that hospitalists practice at would require or even ask a hospitalist to step into a situation like this,” said Dr. Lenchus, who oversaw the training. “But as you walk around the exhibit hall at SHM, you find that of the locum tenens companies that ask for hospitalists to perform procedures, airway management is very high on the list.”
The trainers were Armando Ariza Giammaria, MD, an anesthesiologist and clinical assistant professor at Tulane University, New Orleans; Jorge Cabrera, DO, an intensivist and assistant professor of medicine at the University of Miami; Alice Gallo de Moraes, MD, a pulmonary critical care doctor at Mayo Clinic, Rochester, Minn.; Fernando Caceres, MD, a pulmonary critical care specialist at the Billings (Mont.) Clinic; and Aldo Pavon Canseco, MD, a hospitalist and assistant professor of medicine at the University of Miami who was trained as a pediatric anesthesiologist.
Over 3 hours, hospitalists first heard tips for airway management, with words of caution, and then did hands-on work using manikins under the guidance of the faculty members with a low trainee-to-instructor ratio.
“Do the basics well and the scary things will become manageable,” Dr. Cabrera said in the session.
Instructors said it was vital to have a checklist in the form of a mnemonic device, and to have not just Plan A for clearing an airway, but Plans B and C, too.
Dr. Ariza told the learners not to focus too much on intubation — it’s not always necessary. In fact, he said he couldn’t over-emphasize the importance of mastering bag-mask ventilation, a go-to method when other approaches fail.
Participants learned about devices that can be deployed through the nose to keep the airway clear, those that can be used in the mouth but that might not go down quite as far as the lung, an inflatable bag that can be placed over patients’ mouths and squeezed to help with their breathing, and endotracheal tubes.
Dr. Lenchus said that more training would likely be needed for most clinicians – perhaps with other faculty at their own institutions – before they could be expected to employ these techniques in a real-life emergency situation.
Welcome to Day 2 of HM19!
Hospitalists, welcome to Day 2 of HM19 – the only meeting solely dedicated to the training and advancement of hospitalists.
What an exciting start to the meeting. Pre-Course Day on Sunday focused on some key skills essential to hospitalists – from ultrasound to practice management and palliative care, hospitalists mastered new expertise and forged new collaborations with colleagues. On Monday, Dr. Marc Harrison’s keynote address kicked us off, reminding us of the critical role we all play in population health management. I was thrilled to see the recognition of our new class of SHM Fellows, Senior Fellows, and Masters – a testament to the hard work and dedication of many providers who bear the name “hospitalist.”
Today, we have yet another energizing day of thought-provoking plenaries and educational sessions. Starting off with the Best of Research and Innovations in 2019, come and learn from our colleagues about advancements in hospital medicine. Next, we celebrate our hospitalists who have demonstrated exemplary contributions in teaching, clinical excellence, and service in our Awards of Excellence. The plenary will be led by Tait Shanafelt, MD, who will discuss “The High Cost of Clinician Burnout” and how we can ensure wellness and wellbeing in a dynamic health care environment with competing priorities and an ever-increasing demand for quality, volume, and patient satisfaction. Don’t miss out on the sessions and workshops scheduled at 11:00 a.m. to 12:30 p.m., on topics from nutritional counseling to “Things We Do for No Reason,” updates in acute coronary syndrome and heart failure, and telemedicine – you’re sure to find an engaging topic of interest.
After lunch, we have the highly anticipated and always entertaining “Update in Hospital Medicine” by Carrie Herzke, MD, SFHM, and Chris Moriates, MD, SFHM. Learn the latest and most high-impact published research influencing our practice. You can attend several sessions this afternoon, from a review of medical marijuana, being fe(male) in hospital medicine, dermatologic exam pearls, top new guidelines in hospital medicine, and understanding and addressing the educational needs of millennium learners.
Plan your evening around SHM’s exciting offerings and opportunities:
- Special Interest Forums: Connects hospitalists with a variety of interests from across the country and the globe.
- Top Pediatric Articles in 2018: Leverages the expertise of our leaders to highlight key areas of research advancement for the care of our pediatric patients.
- Solving Clinical and Cultural Conundrums in the Rubik’s Cube of NP/PA/MD/DO HM Practice: Discusses the key challenges we face in the day-to-day practice of hospital medicine and practice management.
- Mastering the Job Interview: Builds skills for our student and resident attendees.
Our heartfelt thank you to the amazing SHM staff who have worked tirelessly on HM19 – our gratitude to the Annual Conference Committee and all our faculty who have made this meeting a tremendous success. Enjoy Day 2!
Dr. Afsar is president of the Society of Hospital Medicine, and chief ambulatory officer and chief medical officer for accountable care organizations at UC Irvine Health.
Hospitalists, welcome to Day 2 of HM19 – the only meeting solely dedicated to the training and advancement of hospitalists.
What an exciting start to the meeting. Pre-Course Day on Sunday focused on some key skills essential to hospitalists – from ultrasound to practice management and palliative care, hospitalists mastered new expertise and forged new collaborations with colleagues. On Monday, Dr. Marc Harrison’s keynote address kicked us off, reminding us of the critical role we all play in population health management. I was thrilled to see the recognition of our new class of SHM Fellows, Senior Fellows, and Masters – a testament to the hard work and dedication of many providers who bear the name “hospitalist.”
Today, we have yet another energizing day of thought-provoking plenaries and educational sessions. Starting off with the Best of Research and Innovations in 2019, come and learn from our colleagues about advancements in hospital medicine. Next, we celebrate our hospitalists who have demonstrated exemplary contributions in teaching, clinical excellence, and service in our Awards of Excellence. The plenary will be led by Tait Shanafelt, MD, who will discuss “The High Cost of Clinician Burnout” and how we can ensure wellness and wellbeing in a dynamic health care environment with competing priorities and an ever-increasing demand for quality, volume, and patient satisfaction. Don’t miss out on the sessions and workshops scheduled at 11:00 a.m. to 12:30 p.m., on topics from nutritional counseling to “Things We Do for No Reason,” updates in acute coronary syndrome and heart failure, and telemedicine – you’re sure to find an engaging topic of interest.
After lunch, we have the highly anticipated and always entertaining “Update in Hospital Medicine” by Carrie Herzke, MD, SFHM, and Chris Moriates, MD, SFHM. Learn the latest and most high-impact published research influencing our practice. You can attend several sessions this afternoon, from a review of medical marijuana, being fe(male) in hospital medicine, dermatologic exam pearls, top new guidelines in hospital medicine, and understanding and addressing the educational needs of millennium learners.
Plan your evening around SHM’s exciting offerings and opportunities:
- Special Interest Forums: Connects hospitalists with a variety of interests from across the country and the globe.
- Top Pediatric Articles in 2018: Leverages the expertise of our leaders to highlight key areas of research advancement for the care of our pediatric patients.
- Solving Clinical and Cultural Conundrums in the Rubik’s Cube of NP/PA/MD/DO HM Practice: Discusses the key challenges we face in the day-to-day practice of hospital medicine and practice management.
- Mastering the Job Interview: Builds skills for our student and resident attendees.
Our heartfelt thank you to the amazing SHM staff who have worked tirelessly on HM19 – our gratitude to the Annual Conference Committee and all our faculty who have made this meeting a tremendous success. Enjoy Day 2!
Dr. Afsar is president of the Society of Hospital Medicine, and chief ambulatory officer and chief medical officer for accountable care organizations at UC Irvine Health.
Hospitalists, welcome to Day 2 of HM19 – the only meeting solely dedicated to the training and advancement of hospitalists.
What an exciting start to the meeting. Pre-Course Day on Sunday focused on some key skills essential to hospitalists – from ultrasound to practice management and palliative care, hospitalists mastered new expertise and forged new collaborations with colleagues. On Monday, Dr. Marc Harrison’s keynote address kicked us off, reminding us of the critical role we all play in population health management. I was thrilled to see the recognition of our new class of SHM Fellows, Senior Fellows, and Masters – a testament to the hard work and dedication of many providers who bear the name “hospitalist.”
Today, we have yet another energizing day of thought-provoking plenaries and educational sessions. Starting off with the Best of Research and Innovations in 2019, come and learn from our colleagues about advancements in hospital medicine. Next, we celebrate our hospitalists who have demonstrated exemplary contributions in teaching, clinical excellence, and service in our Awards of Excellence. The plenary will be led by Tait Shanafelt, MD, who will discuss “The High Cost of Clinician Burnout” and how we can ensure wellness and wellbeing in a dynamic health care environment with competing priorities and an ever-increasing demand for quality, volume, and patient satisfaction. Don’t miss out on the sessions and workshops scheduled at 11:00 a.m. to 12:30 p.m., on topics from nutritional counseling to “Things We Do for No Reason,” updates in acute coronary syndrome and heart failure, and telemedicine – you’re sure to find an engaging topic of interest.
After lunch, we have the highly anticipated and always entertaining “Update in Hospital Medicine” by Carrie Herzke, MD, SFHM, and Chris Moriates, MD, SFHM. Learn the latest and most high-impact published research influencing our practice. You can attend several sessions this afternoon, from a review of medical marijuana, being fe(male) in hospital medicine, dermatologic exam pearls, top new guidelines in hospital medicine, and understanding and addressing the educational needs of millennium learners.
Plan your evening around SHM’s exciting offerings and opportunities:
- Special Interest Forums: Connects hospitalists with a variety of interests from across the country and the globe.
- Top Pediatric Articles in 2018: Leverages the expertise of our leaders to highlight key areas of research advancement for the care of our pediatric patients.
- Solving Clinical and Cultural Conundrums in the Rubik’s Cube of NP/PA/MD/DO HM Practice: Discusses the key challenges we face in the day-to-day practice of hospital medicine and practice management.
- Mastering the Job Interview: Builds skills for our student and resident attendees.
Our heartfelt thank you to the amazing SHM staff who have worked tirelessly on HM19 – our gratitude to the Annual Conference Committee and all our faculty who have made this meeting a tremendous success. Enjoy Day 2!
Dr. Afsar is president of the Society of Hospital Medicine, and chief ambulatory officer and chief medical officer for accountable care organizations at UC Irvine Health.