User login
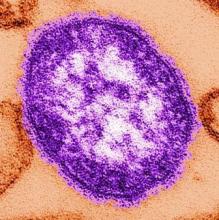
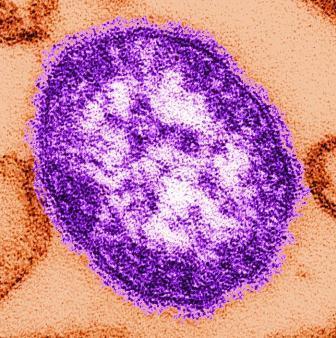
Measles cases now at highest level since 1992
With 971 cases of measles reported after just 5 months of 2019, the United States has hit another dubious milestone by surpassing the 963 cases reported in the preelimination year of 1994, according to the Centers for Disease Control and Prevention.
That leaves 1992, when there were 2,237 cases reported, as the next big obstacle on measles’ current path of distinction, the CDC data show. Only 312 cases were reported in 1993.
“Outbreaks in New York City and Rockland County, New York have continued for nearly 8 months. That loss would be a huge blow for the nation and erase the hard work done by all levels of public health,” the CDC said May 30.
The CDC defines measles elimination as “the absence of continuous disease transmission for 12 months or more in a specific geographic area” and notes that “measles is no longer endemic [constantly present] in the United States.”
“Measles is preventable and the way to end this outbreak is to ensure that all children and adults who can get vaccinated, do get vaccinated. Again, I want to reassure parents that vaccines are safe, they do not cause autism. The greater danger is the disease that vaccination prevents,” CDC director Robert Redfield, MD, said in a statement.
With 971 cases of measles reported after just 5 months of 2019, the United States has hit another dubious milestone by surpassing the 963 cases reported in the preelimination year of 1994, according to the Centers for Disease Control and Prevention.
That leaves 1992, when there were 2,237 cases reported, as the next big obstacle on measles’ current path of distinction, the CDC data show. Only 312 cases were reported in 1993.
“Outbreaks in New York City and Rockland County, New York have continued for nearly 8 months. That loss would be a huge blow for the nation and erase the hard work done by all levels of public health,” the CDC said May 30.
The CDC defines measles elimination as “the absence of continuous disease transmission for 12 months or more in a specific geographic area” and notes that “measles is no longer endemic [constantly present] in the United States.”
“Measles is preventable and the way to end this outbreak is to ensure that all children and adults who can get vaccinated, do get vaccinated. Again, I want to reassure parents that vaccines are safe, they do not cause autism. The greater danger is the disease that vaccination prevents,” CDC director Robert Redfield, MD, said in a statement.
With 971 cases of measles reported after just 5 months of 2019, the United States has hit another dubious milestone by surpassing the 963 cases reported in the preelimination year of 1994, according to the Centers for Disease Control and Prevention.
That leaves 1992, when there were 2,237 cases reported, as the next big obstacle on measles’ current path of distinction, the CDC data show. Only 312 cases were reported in 1993.
“Outbreaks in New York City and Rockland County, New York have continued for nearly 8 months. That loss would be a huge blow for the nation and erase the hard work done by all levels of public health,” the CDC said May 30.
The CDC defines measles elimination as “the absence of continuous disease transmission for 12 months or more in a specific geographic area” and notes that “measles is no longer endemic [constantly present] in the United States.”
“Measles is preventable and the way to end this outbreak is to ensure that all children and adults who can get vaccinated, do get vaccinated. Again, I want to reassure parents that vaccines are safe, they do not cause autism. The greater danger is the disease that vaccination prevents,” CDC director Robert Redfield, MD, said in a statement.
Artificial intelligence advances optical biopsy
SAN DIEGO – Artificial intelligence is improving the accuracy of optical biopsies, a development that may ultimately avoid the need for tissue biopsies of many low-risk colonic polyps, Michael Byrne, MD, said at the annual Digestive Disease Week.

Dr. Byrne, chief executive officer of Satisfai Health, founder of ai4gi, and gastroenterologist at Vancouver General Hospital; Nicolas Guizard, medical imaging researcher at Imagia; and their colleagues at ai4gi developed a “full clinical workflow” for detecting colonic polyps and performing optical biopsies of the polyps.”
Using narrow band imaging (NBI) enhanced with artificial intelligence, the system was used to review 21,804 colonoscopy frames and it achieved a “near-perfect” diagnostic accuracy of 99.9%. In an assessment of colonoscopy videos that included 125 polyps, the system had 95.9% sensitivity, with a specificity of 91.6% and a negative predictive value of 93.6%, Dr. Byrne said.
The speed of the system’s decision-making is rapid, with a typical reaction time of 360 milliseconds. The system was able to make diagnostic inferences at a rate of 26 milliseconds per frame.
With exposure to more learning experiences, the artificial intelligence system improved and committed to a prediction for 97.6% of the polyps it visualized. Dr. Byrne said this result represented a 12.8% improvement from previously published data on the model’s performance.
Dr. Byrne and his colleagues found the system had a tracking accuracy of 92.8%, meaning that this percentage of polyps was both correctly detected and assigned to a unique identifier for follow-up of the site of each excised polyp over time. The interface worked even when multiple polyps were seen on the same screen.
In a video interview, Dr. Byrne discussed the implications for gastroenterology and plans for a clinical trial for rigorous testing of the model.
ai4gi is developing the AI colonoscopy technology. Dr. Byrne is founder of the ai4gi joint venture, which holds a technology codevelopment agreement with Olympus US.
SAN DIEGO – Artificial intelligence is improving the accuracy of optical biopsies, a development that may ultimately avoid the need for tissue biopsies of many low-risk colonic polyps, Michael Byrne, MD, said at the annual Digestive Disease Week.

Dr. Byrne, chief executive officer of Satisfai Health, founder of ai4gi, and gastroenterologist at Vancouver General Hospital; Nicolas Guizard, medical imaging researcher at Imagia; and their colleagues at ai4gi developed a “full clinical workflow” for detecting colonic polyps and performing optical biopsies of the polyps.”
Using narrow band imaging (NBI) enhanced with artificial intelligence, the system was used to review 21,804 colonoscopy frames and it achieved a “near-perfect” diagnostic accuracy of 99.9%. In an assessment of colonoscopy videos that included 125 polyps, the system had 95.9% sensitivity, with a specificity of 91.6% and a negative predictive value of 93.6%, Dr. Byrne said.
The speed of the system’s decision-making is rapid, with a typical reaction time of 360 milliseconds. The system was able to make diagnostic inferences at a rate of 26 milliseconds per frame.
With exposure to more learning experiences, the artificial intelligence system improved and committed to a prediction for 97.6% of the polyps it visualized. Dr. Byrne said this result represented a 12.8% improvement from previously published data on the model’s performance.
Dr. Byrne and his colleagues found the system had a tracking accuracy of 92.8%, meaning that this percentage of polyps was both correctly detected and assigned to a unique identifier for follow-up of the site of each excised polyp over time. The interface worked even when multiple polyps were seen on the same screen.
In a video interview, Dr. Byrne discussed the implications for gastroenterology and plans for a clinical trial for rigorous testing of the model.
ai4gi is developing the AI colonoscopy technology. Dr. Byrne is founder of the ai4gi joint venture, which holds a technology codevelopment agreement with Olympus US.
SAN DIEGO – Artificial intelligence is improving the accuracy of optical biopsies, a development that may ultimately avoid the need for tissue biopsies of many low-risk colonic polyps, Michael Byrne, MD, said at the annual Digestive Disease Week.

Dr. Byrne, chief executive officer of Satisfai Health, founder of ai4gi, and gastroenterologist at Vancouver General Hospital; Nicolas Guizard, medical imaging researcher at Imagia; and their colleagues at ai4gi developed a “full clinical workflow” for detecting colonic polyps and performing optical biopsies of the polyps.”
Using narrow band imaging (NBI) enhanced with artificial intelligence, the system was used to review 21,804 colonoscopy frames and it achieved a “near-perfect” diagnostic accuracy of 99.9%. In an assessment of colonoscopy videos that included 125 polyps, the system had 95.9% sensitivity, with a specificity of 91.6% and a negative predictive value of 93.6%, Dr. Byrne said.
The speed of the system’s decision-making is rapid, with a typical reaction time of 360 milliseconds. The system was able to make diagnostic inferences at a rate of 26 milliseconds per frame.
With exposure to more learning experiences, the artificial intelligence system improved and committed to a prediction for 97.6% of the polyps it visualized. Dr. Byrne said this result represented a 12.8% improvement from previously published data on the model’s performance.
Dr. Byrne and his colleagues found the system had a tracking accuracy of 92.8%, meaning that this percentage of polyps was both correctly detected and assigned to a unique identifier for follow-up of the site of each excised polyp over time. The interface worked even when multiple polyps were seen on the same screen.
In a video interview, Dr. Byrne discussed the implications for gastroenterology and plans for a clinical trial for rigorous testing of the model.
ai4gi is developing the AI colonoscopy technology. Dr. Byrne is founder of the ai4gi joint venture, which holds a technology codevelopment agreement with Olympus US.
REPORTING FROM DDW 2019
Psoriasis Journal Scan: May 2019
The Broad-Spectrum Impact of Hidradenitis Suppurativa on Quality of Life: A Comparison with Psoriasis.
Sampogna F, Fania L, Mazzanti C, et al. Dermatology. 2019 May 23:1-7.
The aim of this study was to evaluate in detail the QoL impact of HS comparing it with other skin conditions, and in particular with psoriasis. HS had the worst QoL among several skin conditions. Compared to psoriasis the mean symptom score was 69.4 versus 53.7, and the mean psychosocial score was 56.1 versus 32.7. Overall, the scores of patients with HS were higher than those of psoriasis patients on 16 of the 17 items of the Skindex-17.
Suicidality and risk of suicidality in psoriasis: A critical appraisal of two systematic reviews and meta-analyses.
Matterne U, Baumeister SE, Apfelbacher C. Br J Dermatol. 2019 May 10.
Chi et al. and Singh et al each conducted a systematic review and meta-analysis of observational studies examining the relationship between suicidality and psoriasis. Singh et al. concluded that patients with psoriasis have a significantly higher risk of suicidal ideation, suicide attempts, and completed suicides, while Chi et al concluded that the available limited, very low-quality evidence does not support the notion of an association between psoriasis on the one hand, and suicide, suicidal ideation and attempts on the other.
Psoriasis and Inflammatory Bowel Disease.
Cottone M, Sapienza C, Macaluso FS, Cannizzaro M. Dig Dis. 2019 May 10:1-7.
Inflammatory bowel disease (IBD) and psoriasis (PS) are associated conditions. The reason for this association lies in the sharing of predisposition genes and common immunological mechanisms. This review will focus on the interplay between IBD and PS, with details on prevalence and phenotype of PS in IBD, genetics, pathogenetic pathways, and therapy.
Psoriasis in HIV infection: an update.
Alpalhão M, Borges-Costa J, Filipe P. Int J STD AIDS. 2019 May;30(6):596-604.
A review of the available literature to highlight the updated evidence on psoriasis in HIV-infected individuals, particularly in regards to its epidemiology, proposed pathophysiology, clinical presentation, currently available therapeutic options, and future perspectives.
All-cause and cause-specific mortality in psoriasis: A systematic review and meta-analysis.
Dhana A, Yen H, Yen H, Cho E. J Am Acad Dermatol. 2019 May;80(5):1332-1343.
A systematic review and meta-analysis of mortality risk in psoriasis that included studies reporting all-cause or cause-specific mortality risk estimates in psoriasis patients compared with general population or subjects free of psoriasis. The pooled RRs for cardiovascular mortality were 1.15 (95% CI 1.09-1.21) in psoriasis, 1.05 (95% CI 0.92-1.20) in mild psoriasis, and 1.38 (95% CI 1.09-1.74) in severe psoriasis. For noncardiovascular causes, mortality risk from liver disease, kidney disease, and infection was significantly increased in psoriasis, regardless of disease severity.
The Broad-Spectrum Impact of Hidradenitis Suppurativa on Quality of Life: A Comparison with Psoriasis.
Sampogna F, Fania L, Mazzanti C, et al. Dermatology. 2019 May 23:1-7.
The aim of this study was to evaluate in detail the QoL impact of HS comparing it with other skin conditions, and in particular with psoriasis. HS had the worst QoL among several skin conditions. Compared to psoriasis the mean symptom score was 69.4 versus 53.7, and the mean psychosocial score was 56.1 versus 32.7. Overall, the scores of patients with HS were higher than those of psoriasis patients on 16 of the 17 items of the Skindex-17.
Suicidality and risk of suicidality in psoriasis: A critical appraisal of two systematic reviews and meta-analyses.
Matterne U, Baumeister SE, Apfelbacher C. Br J Dermatol. 2019 May 10.
Chi et al. and Singh et al each conducted a systematic review and meta-analysis of observational studies examining the relationship between suicidality and psoriasis. Singh et al. concluded that patients with psoriasis have a significantly higher risk of suicidal ideation, suicide attempts, and completed suicides, while Chi et al concluded that the available limited, very low-quality evidence does not support the notion of an association between psoriasis on the one hand, and suicide, suicidal ideation and attempts on the other.
Psoriasis and Inflammatory Bowel Disease.
Cottone M, Sapienza C, Macaluso FS, Cannizzaro M. Dig Dis. 2019 May 10:1-7.
Inflammatory bowel disease (IBD) and psoriasis (PS) are associated conditions. The reason for this association lies in the sharing of predisposition genes and common immunological mechanisms. This review will focus on the interplay between IBD and PS, with details on prevalence and phenotype of PS in IBD, genetics, pathogenetic pathways, and therapy.
Psoriasis in HIV infection: an update.
Alpalhão M, Borges-Costa J, Filipe P. Int J STD AIDS. 2019 May;30(6):596-604.
A review of the available literature to highlight the updated evidence on psoriasis in HIV-infected individuals, particularly in regards to its epidemiology, proposed pathophysiology, clinical presentation, currently available therapeutic options, and future perspectives.
All-cause and cause-specific mortality in psoriasis: A systematic review and meta-analysis.
Dhana A, Yen H, Yen H, Cho E. J Am Acad Dermatol. 2019 May;80(5):1332-1343.
A systematic review and meta-analysis of mortality risk in psoriasis that included studies reporting all-cause or cause-specific mortality risk estimates in psoriasis patients compared with general population or subjects free of psoriasis. The pooled RRs for cardiovascular mortality were 1.15 (95% CI 1.09-1.21) in psoriasis, 1.05 (95% CI 0.92-1.20) in mild psoriasis, and 1.38 (95% CI 1.09-1.74) in severe psoriasis. For noncardiovascular causes, mortality risk from liver disease, kidney disease, and infection was significantly increased in psoriasis, regardless of disease severity.
The Broad-Spectrum Impact of Hidradenitis Suppurativa on Quality of Life: A Comparison with Psoriasis.
Sampogna F, Fania L, Mazzanti C, et al. Dermatology. 2019 May 23:1-7.
The aim of this study was to evaluate in detail the QoL impact of HS comparing it with other skin conditions, and in particular with psoriasis. HS had the worst QoL among several skin conditions. Compared to psoriasis the mean symptom score was 69.4 versus 53.7, and the mean psychosocial score was 56.1 versus 32.7. Overall, the scores of patients with HS were higher than those of psoriasis patients on 16 of the 17 items of the Skindex-17.
Suicidality and risk of suicidality in psoriasis: A critical appraisal of two systematic reviews and meta-analyses.
Matterne U, Baumeister SE, Apfelbacher C. Br J Dermatol. 2019 May 10.
Chi et al. and Singh et al each conducted a systematic review and meta-analysis of observational studies examining the relationship between suicidality and psoriasis. Singh et al. concluded that patients with psoriasis have a significantly higher risk of suicidal ideation, suicide attempts, and completed suicides, while Chi et al concluded that the available limited, very low-quality evidence does not support the notion of an association between psoriasis on the one hand, and suicide, suicidal ideation and attempts on the other.
Psoriasis and Inflammatory Bowel Disease.
Cottone M, Sapienza C, Macaluso FS, Cannizzaro M. Dig Dis. 2019 May 10:1-7.
Inflammatory bowel disease (IBD) and psoriasis (PS) are associated conditions. The reason for this association lies in the sharing of predisposition genes and common immunological mechanisms. This review will focus on the interplay between IBD and PS, with details on prevalence and phenotype of PS in IBD, genetics, pathogenetic pathways, and therapy.
Psoriasis in HIV infection: an update.
Alpalhão M, Borges-Costa J, Filipe P. Int J STD AIDS. 2019 May;30(6):596-604.
A review of the available literature to highlight the updated evidence on psoriasis in HIV-infected individuals, particularly in regards to its epidemiology, proposed pathophysiology, clinical presentation, currently available therapeutic options, and future perspectives.
All-cause and cause-specific mortality in psoriasis: A systematic review and meta-analysis.
Dhana A, Yen H, Yen H, Cho E. J Am Acad Dermatol. 2019 May;80(5):1332-1343.
A systematic review and meta-analysis of mortality risk in psoriasis that included studies reporting all-cause or cause-specific mortality risk estimates in psoriasis patients compared with general population or subjects free of psoriasis. The pooled RRs for cardiovascular mortality were 1.15 (95% CI 1.09-1.21) in psoriasis, 1.05 (95% CI 0.92-1.20) in mild psoriasis, and 1.38 (95% CI 1.09-1.74) in severe psoriasis. For noncardiovascular causes, mortality risk from liver disease, kidney disease, and infection was significantly increased in psoriasis, regardless of disease severity.
Studies cast doubt on FDA’s accelerated cancer drug pathway
In the first study, lead investigator Emerson Y. Chen, MD, of Oregon Health & Science University, Portland, and colleagues conducted a retrospective analysis of all drugs approved by the FDA on the basis of response rate – the percentage of patients who experience tumor shrinkage – from Jan. 1, 2006, to Sept. 30, 2018. The data set consisted of 59 oncology drugs with 85 unique indications approved by the FDA for advanced-stage metastatic cancer on the basis of a response rate (RR) endpoint during the study period.
Of the 85 indications, 32 were granted regular approval immediately with limited postmarketing efficacy requirements and 53 (62%) were granted accelerated approval. Of the accelerated approvals, 29 (55%) were later converted to regular approval.
The median RR for the 85 indications was 41%, and the median sample size of such RR trials was 117 patients, according to the analysis published in JAMA Internal Medicine.
Among all approvals, 14 of 85 (16%) had an RR less than 20%, 28 of 85 (33%) had an RR less than 30%, and 40 of 85 (47%) had an RR less than 40%.
Most approved drugs had an RR ranging from 20% to 59%, the study found. Of 81 available indications, the median complete response rate – defined as the percentage of patients with no visible disease and normalization of lymph nodes – was 6%. (Complete response data were not reported for four drug indications.)
The investigators found that many of the drugs studied have remained on the market for years without subsequent confirmatory data. For example, when the accelerated approvals based on RR were converted to full approval, 23 of 29 were made on the basis of surrogate endpoints (progression-free survival or RR), 7 of 29 were made on the basis of RR, and just 6 of 29 were made on the basis of overall survival (OS).
The findings suggest that most cancer drugs approved by the FDA based on RR have less than transformational response rates, and that such indications do not have confirmed clinical benefit, the study authors wrote.
While in some settings, a response can equal prognostic value regarding overall survival, the authors wrote that “the ability of RR to serve as a validated surrogate for OS varies among cancer types and is generally poor.”
In the second study, researchers found that confirmatory trials for only one-fifth of cancer drug indications approved via the FDA’s accelerated approval route demonstrated improvements in overall patient survival.
Lead investigator Bishal Gyawali, MD, PhD, of Queen’s University, Kingston, Ont., and colleagues examined FDA data on recent drugs and indications that received accelerated approval and were later granted full approval.
For their analysis, the investigators reviewed the FDA’s database of postmarketing requirements and commitments, as well as PubMed, to determine the current status of postmarket trials for indications labeled as “ongoing” in the original FDA data.
Of 93 cancer drug indications for which accelerated approval was granted from Dec. 11, 1992, to May 31, 2017, the FDA reported clinical benefit was adequately confirmed in 51 indications. Of these confirmations, 15 demonstrated improvement in overall survival.
In their updated analysis, the investigators determined that confirmatory trials for 19 of the 93 (20%) cancer drug approvals reported an improvement in OS, 19 trials (20%) reported improvement in the same surrogate used in the preapproval trial, and 20 trials (21%) reported improvement in a different surrogate, according to the study, also published in JAMA Internal Medicine.
Additionally, results showed that 5 confirmatory trials were delayed, 10 trials were pending, and 9 trials were ongoing.
For three recent accelerated approvals, the primary endpoints were not met in the confirmatory trials, but one of the indications still received full approval.
The findings raise several concerns about the accelerated cancer drug pathway, including whether the same surrogate efficacy measure should be used as verification of drug benefit, according to the investigators. Conversely, using a different surrogate endpoint than the original measure can cause confusion among physicians and patients about whether the cancer drug improves survival or quality of life, information that is essential in the benefit-risk evaluation for clinical decision making.
That a number of the confirmatory trials examined were delayed or pending emphasize the considerable time that can elapse between drug approval and confirmatory trial completion, they added.
“Timely planning and completion of postmarketing trials is necessary for proper implementation of the accelerated approval pathway, and the FDA should minimize the period during which patients and physicians are using drugs approved through accelerated pathways without rigorous data on their ultimate clinical benefit,” the authors wrote in the analysis.
Dr. Chen, lead author of the RR study, said both studies call into question what criteria is optimal when assessing cancer drug value, while ensuring such measurements are not too high to achieve – preventing useful drugs to market – but also not too low – allowing drugs with marginal benefit into the market.
“There has been tremendous drug development within the oncology space, and it is always important to look back to reassess and see if the process [matches] the original vision so that we can correct any misuse or concerns,” Dr. Chen said in an interview.
Dr. Chen said his study indicates the RR endpoint has been misused in scenarios with low response rate, common cancer, and/or situations with already available therapies. In the study by Dr. Gyawali, the results suggest many drugs approved on the basis of a surrogate endpoint (RR or progression-free survival) ultimately do not demonstrate survival benefit confirmation or patient-reported benefit, Dr. Chen said.
“We hope that readers of these JAMA IM studies and the accompanying commentaries will recognize that there could be a set of guidance criteria from regulatory agencies or oncology organizations to recommend use of surrogate endpoints in special situations: high response rate of the drug, very rare cancer, or highly innovative therapy not yet seen before,” he said. “The use of surrogate endpoints to justify these therapies must also have postmarketing confirmation of survival or patient-reported benefit.”
The study led by Dr. Chen was supported by the Laura and John Arnold Foundation. Dr Chen reported receiving lecture honorarium from Horizon CME; another coauthor reported receiving honorarium from universities, medical centers, and publishers. The study led by Dr. Gyawali was supported by the Arnold Ventures; one of the coauthors reported receiving grant support from the Harvard-MIT Center for Regulatory Science and the Engelberg Foundation, as well as unrelated research funding from the FDA.
SOURCES: Chen EY et al. JAMA Intern Med. 2019 May 28. doi: 10.1001/jamainternmed.2019.0583; Gyawali B et al. JAMA Intern Med. 2019 May 28. doi: 10.1001/jamainternmed.2019.0462.
In the first study, lead investigator Emerson Y. Chen, MD, of Oregon Health & Science University, Portland, and colleagues conducted a retrospective analysis of all drugs approved by the FDA on the basis of response rate – the percentage of patients who experience tumor shrinkage – from Jan. 1, 2006, to Sept. 30, 2018. The data set consisted of 59 oncology drugs with 85 unique indications approved by the FDA for advanced-stage metastatic cancer on the basis of a response rate (RR) endpoint during the study period.
Of the 85 indications, 32 were granted regular approval immediately with limited postmarketing efficacy requirements and 53 (62%) were granted accelerated approval. Of the accelerated approvals, 29 (55%) were later converted to regular approval.
The median RR for the 85 indications was 41%, and the median sample size of such RR trials was 117 patients, according to the analysis published in JAMA Internal Medicine.
Among all approvals, 14 of 85 (16%) had an RR less than 20%, 28 of 85 (33%) had an RR less than 30%, and 40 of 85 (47%) had an RR less than 40%.
Most approved drugs had an RR ranging from 20% to 59%, the study found. Of 81 available indications, the median complete response rate – defined as the percentage of patients with no visible disease and normalization of lymph nodes – was 6%. (Complete response data were not reported for four drug indications.)
The investigators found that many of the drugs studied have remained on the market for years without subsequent confirmatory data. For example, when the accelerated approvals based on RR were converted to full approval, 23 of 29 were made on the basis of surrogate endpoints (progression-free survival or RR), 7 of 29 were made on the basis of RR, and just 6 of 29 were made on the basis of overall survival (OS).
The findings suggest that most cancer drugs approved by the FDA based on RR have less than transformational response rates, and that such indications do not have confirmed clinical benefit, the study authors wrote.
While in some settings, a response can equal prognostic value regarding overall survival, the authors wrote that “the ability of RR to serve as a validated surrogate for OS varies among cancer types and is generally poor.”
In the second study, researchers found that confirmatory trials for only one-fifth of cancer drug indications approved via the FDA’s accelerated approval route demonstrated improvements in overall patient survival.
Lead investigator Bishal Gyawali, MD, PhD, of Queen’s University, Kingston, Ont., and colleagues examined FDA data on recent drugs and indications that received accelerated approval and were later granted full approval.
For their analysis, the investigators reviewed the FDA’s database of postmarketing requirements and commitments, as well as PubMed, to determine the current status of postmarket trials for indications labeled as “ongoing” in the original FDA data.
Of 93 cancer drug indications for which accelerated approval was granted from Dec. 11, 1992, to May 31, 2017, the FDA reported clinical benefit was adequately confirmed in 51 indications. Of these confirmations, 15 demonstrated improvement in overall survival.
In their updated analysis, the investigators determined that confirmatory trials for 19 of the 93 (20%) cancer drug approvals reported an improvement in OS, 19 trials (20%) reported improvement in the same surrogate used in the preapproval trial, and 20 trials (21%) reported improvement in a different surrogate, according to the study, also published in JAMA Internal Medicine.
Additionally, results showed that 5 confirmatory trials were delayed, 10 trials were pending, and 9 trials were ongoing.
For three recent accelerated approvals, the primary endpoints were not met in the confirmatory trials, but one of the indications still received full approval.
The findings raise several concerns about the accelerated cancer drug pathway, including whether the same surrogate efficacy measure should be used as verification of drug benefit, according to the investigators. Conversely, using a different surrogate endpoint than the original measure can cause confusion among physicians and patients about whether the cancer drug improves survival or quality of life, information that is essential in the benefit-risk evaluation for clinical decision making.
That a number of the confirmatory trials examined were delayed or pending emphasize the considerable time that can elapse between drug approval and confirmatory trial completion, they added.
“Timely planning and completion of postmarketing trials is necessary for proper implementation of the accelerated approval pathway, and the FDA should minimize the period during which patients and physicians are using drugs approved through accelerated pathways without rigorous data on their ultimate clinical benefit,” the authors wrote in the analysis.
Dr. Chen, lead author of the RR study, said both studies call into question what criteria is optimal when assessing cancer drug value, while ensuring such measurements are not too high to achieve – preventing useful drugs to market – but also not too low – allowing drugs with marginal benefit into the market.
“There has been tremendous drug development within the oncology space, and it is always important to look back to reassess and see if the process [matches] the original vision so that we can correct any misuse or concerns,” Dr. Chen said in an interview.
Dr. Chen said his study indicates the RR endpoint has been misused in scenarios with low response rate, common cancer, and/or situations with already available therapies. In the study by Dr. Gyawali, the results suggest many drugs approved on the basis of a surrogate endpoint (RR or progression-free survival) ultimately do not demonstrate survival benefit confirmation or patient-reported benefit, Dr. Chen said.
“We hope that readers of these JAMA IM studies and the accompanying commentaries will recognize that there could be a set of guidance criteria from regulatory agencies or oncology organizations to recommend use of surrogate endpoints in special situations: high response rate of the drug, very rare cancer, or highly innovative therapy not yet seen before,” he said. “The use of surrogate endpoints to justify these therapies must also have postmarketing confirmation of survival or patient-reported benefit.”
The study led by Dr. Chen was supported by the Laura and John Arnold Foundation. Dr Chen reported receiving lecture honorarium from Horizon CME; another coauthor reported receiving honorarium from universities, medical centers, and publishers. The study led by Dr. Gyawali was supported by the Arnold Ventures; one of the coauthors reported receiving grant support from the Harvard-MIT Center for Regulatory Science and the Engelberg Foundation, as well as unrelated research funding from the FDA.
SOURCES: Chen EY et al. JAMA Intern Med. 2019 May 28. doi: 10.1001/jamainternmed.2019.0583; Gyawali B et al. JAMA Intern Med. 2019 May 28. doi: 10.1001/jamainternmed.2019.0462.
In the first study, lead investigator Emerson Y. Chen, MD, of Oregon Health & Science University, Portland, and colleagues conducted a retrospective analysis of all drugs approved by the FDA on the basis of response rate – the percentage of patients who experience tumor shrinkage – from Jan. 1, 2006, to Sept. 30, 2018. The data set consisted of 59 oncology drugs with 85 unique indications approved by the FDA for advanced-stage metastatic cancer on the basis of a response rate (RR) endpoint during the study period.
Of the 85 indications, 32 were granted regular approval immediately with limited postmarketing efficacy requirements and 53 (62%) were granted accelerated approval. Of the accelerated approvals, 29 (55%) were later converted to regular approval.
The median RR for the 85 indications was 41%, and the median sample size of such RR trials was 117 patients, according to the analysis published in JAMA Internal Medicine.
Among all approvals, 14 of 85 (16%) had an RR less than 20%, 28 of 85 (33%) had an RR less than 30%, and 40 of 85 (47%) had an RR less than 40%.
Most approved drugs had an RR ranging from 20% to 59%, the study found. Of 81 available indications, the median complete response rate – defined as the percentage of patients with no visible disease and normalization of lymph nodes – was 6%. (Complete response data were not reported for four drug indications.)
The investigators found that many of the drugs studied have remained on the market for years without subsequent confirmatory data. For example, when the accelerated approvals based on RR were converted to full approval, 23 of 29 were made on the basis of surrogate endpoints (progression-free survival or RR), 7 of 29 were made on the basis of RR, and just 6 of 29 were made on the basis of overall survival (OS).
The findings suggest that most cancer drugs approved by the FDA based on RR have less than transformational response rates, and that such indications do not have confirmed clinical benefit, the study authors wrote.
While in some settings, a response can equal prognostic value regarding overall survival, the authors wrote that “the ability of RR to serve as a validated surrogate for OS varies among cancer types and is generally poor.”
In the second study, researchers found that confirmatory trials for only one-fifth of cancer drug indications approved via the FDA’s accelerated approval route demonstrated improvements in overall patient survival.
Lead investigator Bishal Gyawali, MD, PhD, of Queen’s University, Kingston, Ont., and colleagues examined FDA data on recent drugs and indications that received accelerated approval and were later granted full approval.
For their analysis, the investigators reviewed the FDA’s database of postmarketing requirements and commitments, as well as PubMed, to determine the current status of postmarket trials for indications labeled as “ongoing” in the original FDA data.
Of 93 cancer drug indications for which accelerated approval was granted from Dec. 11, 1992, to May 31, 2017, the FDA reported clinical benefit was adequately confirmed in 51 indications. Of these confirmations, 15 demonstrated improvement in overall survival.
In their updated analysis, the investigators determined that confirmatory trials for 19 of the 93 (20%) cancer drug approvals reported an improvement in OS, 19 trials (20%) reported improvement in the same surrogate used in the preapproval trial, and 20 trials (21%) reported improvement in a different surrogate, according to the study, also published in JAMA Internal Medicine.
Additionally, results showed that 5 confirmatory trials were delayed, 10 trials were pending, and 9 trials were ongoing.
For three recent accelerated approvals, the primary endpoints were not met in the confirmatory trials, but one of the indications still received full approval.
The findings raise several concerns about the accelerated cancer drug pathway, including whether the same surrogate efficacy measure should be used as verification of drug benefit, according to the investigators. Conversely, using a different surrogate endpoint than the original measure can cause confusion among physicians and patients about whether the cancer drug improves survival or quality of life, information that is essential in the benefit-risk evaluation for clinical decision making.
That a number of the confirmatory trials examined were delayed or pending emphasize the considerable time that can elapse between drug approval and confirmatory trial completion, they added.
“Timely planning and completion of postmarketing trials is necessary for proper implementation of the accelerated approval pathway, and the FDA should minimize the period during which patients and physicians are using drugs approved through accelerated pathways without rigorous data on their ultimate clinical benefit,” the authors wrote in the analysis.
Dr. Chen, lead author of the RR study, said both studies call into question what criteria is optimal when assessing cancer drug value, while ensuring such measurements are not too high to achieve – preventing useful drugs to market – but also not too low – allowing drugs with marginal benefit into the market.
“There has been tremendous drug development within the oncology space, and it is always important to look back to reassess and see if the process [matches] the original vision so that we can correct any misuse or concerns,” Dr. Chen said in an interview.
Dr. Chen said his study indicates the RR endpoint has been misused in scenarios with low response rate, common cancer, and/or situations with already available therapies. In the study by Dr. Gyawali, the results suggest many drugs approved on the basis of a surrogate endpoint (RR or progression-free survival) ultimately do not demonstrate survival benefit confirmation or patient-reported benefit, Dr. Chen said.
“We hope that readers of these JAMA IM studies and the accompanying commentaries will recognize that there could be a set of guidance criteria from regulatory agencies or oncology organizations to recommend use of surrogate endpoints in special situations: high response rate of the drug, very rare cancer, or highly innovative therapy not yet seen before,” he said. “The use of surrogate endpoints to justify these therapies must also have postmarketing confirmation of survival or patient-reported benefit.”
The study led by Dr. Chen was supported by the Laura and John Arnold Foundation. Dr Chen reported receiving lecture honorarium from Horizon CME; another coauthor reported receiving honorarium from universities, medical centers, and publishers. The study led by Dr. Gyawali was supported by the Arnold Ventures; one of the coauthors reported receiving grant support from the Harvard-MIT Center for Regulatory Science and the Engelberg Foundation, as well as unrelated research funding from the FDA.
SOURCES: Chen EY et al. JAMA Intern Med. 2019 May 28. doi: 10.1001/jamainternmed.2019.0583; Gyawali B et al. JAMA Intern Med. 2019 May 28. doi: 10.1001/jamainternmed.2019.0462.
FROM JAMA INTERNAL MEDICINE
Tofacitinib upped herpes zoster risk in ulcerative colitis
Among patients with moderate to severe ulcerative colitis, a median of 1.4 years and up to 4.4 years of tofacitinib therapy was safe apart from a dose-related increase in risk of herpes zoster infection, according to an integrated analysis of data from five clinical trials.
Compared with placebo, a 5-mg twice-daily maintenance dose of tofacitinib (Xeljanz) produced a 2.1-fold greater risk of herpes zoster infection (95% confidence interval, 0.4-6.0), while a 10-mg, twice-daily dose produced a statistically significant 6.6-fold increase in incidence (95% CI, 3.2-12.2).
With the exception of the higher incidence rate of herpes zoster, “in the overall cohort, the safety profile of tofacitinib was generally similar to that of tumor necrosis factor inhibitor therapies,” wrote William J. Sandborn, MD, director of the inflammatory bowel disease center and professor of medicine, at the University of California, San Diego, and associates. The findings were published in Clinical Gastroenterology and Hepatology.
Tofacitinib is an oral, small-molecular Janus kinase inhibitor approved in the United States for treating moderate to severe ulcerative colitis, as well as rheumatoid and psoriatic arthritis. The recommended ulcerative colitis dose is 10 mg twice daily for at least 8 weeks (induction therapy) followed by 5 or 10 mg twice daily (maintenance). The safety of tofacitinib has been studied in patients with rheumatoid arthritis through 9 years of treatment. To begin a similar undertaking in ulcerative colitis, Dr. Sandborn and associates pooled data from three 8-week, double-blind, placebo-controlled induction trials, as well as one 52-week, double-blind, placebo-controlled maintenance trial and one ongoing open-label trial. All patients received twice-daily tofacitinib (5 mg or 10 mg) or placebo.
Among 1,157 tofacitinib recipients in the pooled analysis, 84% received an average of 10 mg twice daily. For every 100 person-years of tofacitinib exposure, there were an estimated 2.0 serious infections, 1.3 opportunistic infections, 4.1 herpes zoster infections, 1.4 malignancies (including nonmelanoma skin cancer, which had an incidence of 0.7), 0.2 major adverse cardiovascular events, and 0.2 gastrointestinal perforations. The likelihood of these events did not increase with time on tofacitinib, the researchers said.
Worsening ulcerative colitis was the most common serious adverse event for patients who received both induction and maintenance therapy. For patients on maintenance therapy, only herpes zoster infection had a higher incidence than placebo, which reached statistical significance at the 10-mg dose. These safety findings resemble those in rheumatoid arthritis trials of tofacitinib, and apart from herpes zoster, they also resemble safety data for vedolizumab (an integrin receptor antagonist), and anti-tumor necrosis factor agents in ulcerative colitis, the researchers wrote.
There were four deaths during the entire tofacitinib ulcerative colitis program, for an incidence rate of 0.2 per 100 person-years of exposure. All occurred in patients receiving 10 mg twice daily. Causes of death were dissecting aortic aneurysm, hepatic angiosarcoma, acute myeloid leukemia, and pulmonary embolism in a patient with cholangiocarcinoma that had metastasized to the peritoneum. Recently, concerns about pulmonary embolism have led the European Medicines Agency (EMA) to recommend against the use of 10-mg twice daily tofacitinib dose in patients at increased risk for pulmonary embolism.
“Compared with prior experience with tofacitinib in rheumatoid arthritis, no new or unexpected safety signals were identified,” the researchers concluded. “These
Pfizer makes tofacitinib, funded the individual trials, and paid for medical writing. Dr. Sandborn disclosed grants, personal fees, and nonfinancial support from Pfizer and many other pharmaceutical companies.
SOURCE: Sandborn WJ et al. Clin Gastroenterol Hepatol. 2018 Nov 23. doi: 10.1016/j.cgh.2018.11.035.
Among patients with moderate to severe ulcerative colitis, a median of 1.4 years and up to 4.4 years of tofacitinib therapy was safe apart from a dose-related increase in risk of herpes zoster infection, according to an integrated analysis of data from five clinical trials.
Compared with placebo, a 5-mg twice-daily maintenance dose of tofacitinib (Xeljanz) produced a 2.1-fold greater risk of herpes zoster infection (95% confidence interval, 0.4-6.0), while a 10-mg, twice-daily dose produced a statistically significant 6.6-fold increase in incidence (95% CI, 3.2-12.2).
With the exception of the higher incidence rate of herpes zoster, “in the overall cohort, the safety profile of tofacitinib was generally similar to that of tumor necrosis factor inhibitor therapies,” wrote William J. Sandborn, MD, director of the inflammatory bowel disease center and professor of medicine, at the University of California, San Diego, and associates. The findings were published in Clinical Gastroenterology and Hepatology.
Tofacitinib is an oral, small-molecular Janus kinase inhibitor approved in the United States for treating moderate to severe ulcerative colitis, as well as rheumatoid and psoriatic arthritis. The recommended ulcerative colitis dose is 10 mg twice daily for at least 8 weeks (induction therapy) followed by 5 or 10 mg twice daily (maintenance). The safety of tofacitinib has been studied in patients with rheumatoid arthritis through 9 years of treatment. To begin a similar undertaking in ulcerative colitis, Dr. Sandborn and associates pooled data from three 8-week, double-blind, placebo-controlled induction trials, as well as one 52-week, double-blind, placebo-controlled maintenance trial and one ongoing open-label trial. All patients received twice-daily tofacitinib (5 mg or 10 mg) or placebo.
Among 1,157 tofacitinib recipients in the pooled analysis, 84% received an average of 10 mg twice daily. For every 100 person-years of tofacitinib exposure, there were an estimated 2.0 serious infections, 1.3 opportunistic infections, 4.1 herpes zoster infections, 1.4 malignancies (including nonmelanoma skin cancer, which had an incidence of 0.7), 0.2 major adverse cardiovascular events, and 0.2 gastrointestinal perforations. The likelihood of these events did not increase with time on tofacitinib, the researchers said.
Worsening ulcerative colitis was the most common serious adverse event for patients who received both induction and maintenance therapy. For patients on maintenance therapy, only herpes zoster infection had a higher incidence than placebo, which reached statistical significance at the 10-mg dose. These safety findings resemble those in rheumatoid arthritis trials of tofacitinib, and apart from herpes zoster, they also resemble safety data for vedolizumab (an integrin receptor antagonist), and anti-tumor necrosis factor agents in ulcerative colitis, the researchers wrote.
There were four deaths during the entire tofacitinib ulcerative colitis program, for an incidence rate of 0.2 per 100 person-years of exposure. All occurred in patients receiving 10 mg twice daily. Causes of death were dissecting aortic aneurysm, hepatic angiosarcoma, acute myeloid leukemia, and pulmonary embolism in a patient with cholangiocarcinoma that had metastasized to the peritoneum. Recently, concerns about pulmonary embolism have led the European Medicines Agency (EMA) to recommend against the use of 10-mg twice daily tofacitinib dose in patients at increased risk for pulmonary embolism.
“Compared with prior experience with tofacitinib in rheumatoid arthritis, no new or unexpected safety signals were identified,” the researchers concluded. “These
Pfizer makes tofacitinib, funded the individual trials, and paid for medical writing. Dr. Sandborn disclosed grants, personal fees, and nonfinancial support from Pfizer and many other pharmaceutical companies.
SOURCE: Sandborn WJ et al. Clin Gastroenterol Hepatol. 2018 Nov 23. doi: 10.1016/j.cgh.2018.11.035.
Among patients with moderate to severe ulcerative colitis, a median of 1.4 years and up to 4.4 years of tofacitinib therapy was safe apart from a dose-related increase in risk of herpes zoster infection, according to an integrated analysis of data from five clinical trials.
Compared with placebo, a 5-mg twice-daily maintenance dose of tofacitinib (Xeljanz) produced a 2.1-fold greater risk of herpes zoster infection (95% confidence interval, 0.4-6.0), while a 10-mg, twice-daily dose produced a statistically significant 6.6-fold increase in incidence (95% CI, 3.2-12.2).
With the exception of the higher incidence rate of herpes zoster, “in the overall cohort, the safety profile of tofacitinib was generally similar to that of tumor necrosis factor inhibitor therapies,” wrote William J. Sandborn, MD, director of the inflammatory bowel disease center and professor of medicine, at the University of California, San Diego, and associates. The findings were published in Clinical Gastroenterology and Hepatology.
Tofacitinib is an oral, small-molecular Janus kinase inhibitor approved in the United States for treating moderate to severe ulcerative colitis, as well as rheumatoid and psoriatic arthritis. The recommended ulcerative colitis dose is 10 mg twice daily for at least 8 weeks (induction therapy) followed by 5 or 10 mg twice daily (maintenance). The safety of tofacitinib has been studied in patients with rheumatoid arthritis through 9 years of treatment. To begin a similar undertaking in ulcerative colitis, Dr. Sandborn and associates pooled data from three 8-week, double-blind, placebo-controlled induction trials, as well as one 52-week, double-blind, placebo-controlled maintenance trial and one ongoing open-label trial. All patients received twice-daily tofacitinib (5 mg or 10 mg) or placebo.
Among 1,157 tofacitinib recipients in the pooled analysis, 84% received an average of 10 mg twice daily. For every 100 person-years of tofacitinib exposure, there were an estimated 2.0 serious infections, 1.3 opportunistic infections, 4.1 herpes zoster infections, 1.4 malignancies (including nonmelanoma skin cancer, which had an incidence of 0.7), 0.2 major adverse cardiovascular events, and 0.2 gastrointestinal perforations. The likelihood of these events did not increase with time on tofacitinib, the researchers said.
Worsening ulcerative colitis was the most common serious adverse event for patients who received both induction and maintenance therapy. For patients on maintenance therapy, only herpes zoster infection had a higher incidence than placebo, which reached statistical significance at the 10-mg dose. These safety findings resemble those in rheumatoid arthritis trials of tofacitinib, and apart from herpes zoster, they also resemble safety data for vedolizumab (an integrin receptor antagonist), and anti-tumor necrosis factor agents in ulcerative colitis, the researchers wrote.
There were four deaths during the entire tofacitinib ulcerative colitis program, for an incidence rate of 0.2 per 100 person-years of exposure. All occurred in patients receiving 10 mg twice daily. Causes of death were dissecting aortic aneurysm, hepatic angiosarcoma, acute myeloid leukemia, and pulmonary embolism in a patient with cholangiocarcinoma that had metastasized to the peritoneum. Recently, concerns about pulmonary embolism have led the European Medicines Agency (EMA) to recommend against the use of 10-mg twice daily tofacitinib dose in patients at increased risk for pulmonary embolism.
“Compared with prior experience with tofacitinib in rheumatoid arthritis, no new or unexpected safety signals were identified,” the researchers concluded. “These
Pfizer makes tofacitinib, funded the individual trials, and paid for medical writing. Dr. Sandborn disclosed grants, personal fees, and nonfinancial support from Pfizer and many other pharmaceutical companies.
SOURCE: Sandborn WJ et al. Clin Gastroenterol Hepatol. 2018 Nov 23. doi: 10.1016/j.cgh.2018.11.035.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Pharmacist-prescribed hormonal contraception safe, effective
Pharmacists in Oregon with the authority to prescribe hormonal contraceptive therapy have improved access to and continuation of contraceptive therapy, based on two retrospective studies of Medicaid patients published in Obstetrics & Gynecology.
Additionally, the safety profile associated with pharmacist prescribing of hormonal contraceptive therapy was on par with that of other prescribing clinicians.
“In the first 2 years of program implementation, we found evidence that pharmacists were safely reaching new contraceptive users and [helping to meet national goals in reducing unwanted pregnancy],” Lorinda Anderson, PharmD, and colleagues, the authors of one of the studies, wrote.
In 2016, Oregon became the first state to grant pharmacists authority to prescribe hormonal contraception without requiring consultation. The findings suggest that expanding prescribing authority for contraceptive therapy to pharmacists in other states could limit barriers to access, as 90% of United States residents live within 5 miles of a pharmacy.
In one of the two studies, Maria I. Rodriguez, MD, MPH, and colleagues conducted a claims-based review of the primary outcomes of pharmacist-initiated and non-pharmacist-initiated prescriptions on unintended pregnancies in Oregon’s Medicaid program. They also evaluated secondary outcomes, such as costs and quality-adjusted life years (QALYs).
In the first 2 years after the Oregon law went into effect, 248 pharmacists wrote 1,313, or 10%, of all hormonal contraception prescriptions for women who were Medicaid recipients and were prescribed hormonal contraception by any legally allowed healthcare provider. Pharmacists prescribed hormonal contraception for 367 of the 3,614 women studied.
Based on an economic model, pharmacist-initiated hormonal contraceptive therapy prevented an estimated 51 unintended pregnancies and saved $1.6 million in the first two years following the program’s inception in Oregon. Quality of life improved with 158 QALYs per 198,100 women.
Additionally, pharmacist-provided services cost less per patient than non pharmacist health care provider-services, $28 vs. $81.
“We believe our findings to be conservative given that our model was based on use 24 months after implementation. We expect over time that knowledge of and use of contraceptive access from pharmacists will increase,” Dr. Rodriguez, of Oregon Health & Science University, Portland, and colleagues wrote.
In the second study, Dr. Anderson, of the Oregon State University, Corvallis, and colleagues pooled Oregon Medicaid pharmacy claims, eligibility, medical, diagnostic, and demographic data over the 2-year period for the 3,614 patients who received new prescriptions for transdermal and oral contraception, and the 1,313 claims filed for 367 women prescribed contraception by 162 pharmacists.
Within the first 4 months following the program’s inception in Oregon, pharmacists averaged 40 contraceptive claims per month. Over the next 7 months, claims increased to 61 and peaked at 80 claims after 18 months. Chain community pharmacies accounted for 94% of the claims; 71% of claims were in metropolitan areas.
Based on demographics, 73.8% of the women who were prescribed contraception by a pharmacist were first-time recipients. Combined oral contraception was prescribed for 90.5% of the women, and 82% of the women were 18-35 years of age. In the 180-day period prior to receiving pharmacist-prescribed contraception, 61.5% of patients were not using contraception but were attempting to engage in pharmacy-provided hormonal contraceptive care.
The researchers also examined contraceptive safety by looking at whether patients with medical contraindications (Medical Eligibility Criteria Category 3 or 4) were receiving contraindicated methods. “We found that overall adherence to the clinical algorithm for prescribing pharmacists was high. Only 12 (5%) patients were identified as having Medical Eligibility Criteria Category 3 or 4 medical conditions, and two (less than 1%) patients with medications contraindicating OC use received a prescription,” Dr. Anderson and her colleagues wrote.
They noted that the initial legislation passed in Oregon only included oral and transdermal hormonal contraception as methods pharmacists could prescribe. In 2017, with implementation in 2018, this was amended to include the vaginal ring and injection. “As the program matures, and contracts with additional insurers are implemented at pharmacies, we expect the number of pharmacist prescriptions to increase,” the authors wrote.
Dr. Rodriguez reported financial compensation from Merck, the World Health Organization, CooperSurgical, and a previous relationship with Merck. Dr. Anderson reports no conflicts of interest.
SOURCES: Rodriguez M et al. Obstet Gynecol. 2019 Jun;133(6):1238-46; Anderson A et al. Obstet Gynecol. 2019 Jun;133(6):1231-7.
Pharmacists in Oregon with the authority to prescribe hormonal contraceptive therapy have improved access to and continuation of contraceptive therapy, based on two retrospective studies of Medicaid patients published in Obstetrics & Gynecology.
Additionally, the safety profile associated with pharmacist prescribing of hormonal contraceptive therapy was on par with that of other prescribing clinicians.
“In the first 2 years of program implementation, we found evidence that pharmacists were safely reaching new contraceptive users and [helping to meet national goals in reducing unwanted pregnancy],” Lorinda Anderson, PharmD, and colleagues, the authors of one of the studies, wrote.
In 2016, Oregon became the first state to grant pharmacists authority to prescribe hormonal contraception without requiring consultation. The findings suggest that expanding prescribing authority for contraceptive therapy to pharmacists in other states could limit barriers to access, as 90% of United States residents live within 5 miles of a pharmacy.
In one of the two studies, Maria I. Rodriguez, MD, MPH, and colleagues conducted a claims-based review of the primary outcomes of pharmacist-initiated and non-pharmacist-initiated prescriptions on unintended pregnancies in Oregon’s Medicaid program. They also evaluated secondary outcomes, such as costs and quality-adjusted life years (QALYs).
In the first 2 years after the Oregon law went into effect, 248 pharmacists wrote 1,313, or 10%, of all hormonal contraception prescriptions for women who were Medicaid recipients and were prescribed hormonal contraception by any legally allowed healthcare provider. Pharmacists prescribed hormonal contraception for 367 of the 3,614 women studied.
Based on an economic model, pharmacist-initiated hormonal contraceptive therapy prevented an estimated 51 unintended pregnancies and saved $1.6 million in the first two years following the program’s inception in Oregon. Quality of life improved with 158 QALYs per 198,100 women.
Additionally, pharmacist-provided services cost less per patient than non pharmacist health care provider-services, $28 vs. $81.
“We believe our findings to be conservative given that our model was based on use 24 months after implementation. We expect over time that knowledge of and use of contraceptive access from pharmacists will increase,” Dr. Rodriguez, of Oregon Health & Science University, Portland, and colleagues wrote.
In the second study, Dr. Anderson, of the Oregon State University, Corvallis, and colleagues pooled Oregon Medicaid pharmacy claims, eligibility, medical, diagnostic, and demographic data over the 2-year period for the 3,614 patients who received new prescriptions for transdermal and oral contraception, and the 1,313 claims filed for 367 women prescribed contraception by 162 pharmacists.
Within the first 4 months following the program’s inception in Oregon, pharmacists averaged 40 contraceptive claims per month. Over the next 7 months, claims increased to 61 and peaked at 80 claims after 18 months. Chain community pharmacies accounted for 94% of the claims; 71% of claims were in metropolitan areas.
Based on demographics, 73.8% of the women who were prescribed contraception by a pharmacist were first-time recipients. Combined oral contraception was prescribed for 90.5% of the women, and 82% of the women were 18-35 years of age. In the 180-day period prior to receiving pharmacist-prescribed contraception, 61.5% of patients were not using contraception but were attempting to engage in pharmacy-provided hormonal contraceptive care.
The researchers also examined contraceptive safety by looking at whether patients with medical contraindications (Medical Eligibility Criteria Category 3 or 4) were receiving contraindicated methods. “We found that overall adherence to the clinical algorithm for prescribing pharmacists was high. Only 12 (5%) patients were identified as having Medical Eligibility Criteria Category 3 or 4 medical conditions, and two (less than 1%) patients with medications contraindicating OC use received a prescription,” Dr. Anderson and her colleagues wrote.
They noted that the initial legislation passed in Oregon only included oral and transdermal hormonal contraception as methods pharmacists could prescribe. In 2017, with implementation in 2018, this was amended to include the vaginal ring and injection. “As the program matures, and contracts with additional insurers are implemented at pharmacies, we expect the number of pharmacist prescriptions to increase,” the authors wrote.
Dr. Rodriguez reported financial compensation from Merck, the World Health Organization, CooperSurgical, and a previous relationship with Merck. Dr. Anderson reports no conflicts of interest.
SOURCES: Rodriguez M et al. Obstet Gynecol. 2019 Jun;133(6):1238-46; Anderson A et al. Obstet Gynecol. 2019 Jun;133(6):1231-7.
Pharmacists in Oregon with the authority to prescribe hormonal contraceptive therapy have improved access to and continuation of contraceptive therapy, based on two retrospective studies of Medicaid patients published in Obstetrics & Gynecology.
Additionally, the safety profile associated with pharmacist prescribing of hormonal contraceptive therapy was on par with that of other prescribing clinicians.
“In the first 2 years of program implementation, we found evidence that pharmacists were safely reaching new contraceptive users and [helping to meet national goals in reducing unwanted pregnancy],” Lorinda Anderson, PharmD, and colleagues, the authors of one of the studies, wrote.
In 2016, Oregon became the first state to grant pharmacists authority to prescribe hormonal contraception without requiring consultation. The findings suggest that expanding prescribing authority for contraceptive therapy to pharmacists in other states could limit barriers to access, as 90% of United States residents live within 5 miles of a pharmacy.
In one of the two studies, Maria I. Rodriguez, MD, MPH, and colleagues conducted a claims-based review of the primary outcomes of pharmacist-initiated and non-pharmacist-initiated prescriptions on unintended pregnancies in Oregon’s Medicaid program. They also evaluated secondary outcomes, such as costs and quality-adjusted life years (QALYs).
In the first 2 years after the Oregon law went into effect, 248 pharmacists wrote 1,313, or 10%, of all hormonal contraception prescriptions for women who were Medicaid recipients and were prescribed hormonal contraception by any legally allowed healthcare provider. Pharmacists prescribed hormonal contraception for 367 of the 3,614 women studied.
Based on an economic model, pharmacist-initiated hormonal contraceptive therapy prevented an estimated 51 unintended pregnancies and saved $1.6 million in the first two years following the program’s inception in Oregon. Quality of life improved with 158 QALYs per 198,100 women.
Additionally, pharmacist-provided services cost less per patient than non pharmacist health care provider-services, $28 vs. $81.
“We believe our findings to be conservative given that our model was based on use 24 months after implementation. We expect over time that knowledge of and use of contraceptive access from pharmacists will increase,” Dr. Rodriguez, of Oregon Health & Science University, Portland, and colleagues wrote.
In the second study, Dr. Anderson, of the Oregon State University, Corvallis, and colleagues pooled Oregon Medicaid pharmacy claims, eligibility, medical, diagnostic, and demographic data over the 2-year period for the 3,614 patients who received new prescriptions for transdermal and oral contraception, and the 1,313 claims filed for 367 women prescribed contraception by 162 pharmacists.
Within the first 4 months following the program’s inception in Oregon, pharmacists averaged 40 contraceptive claims per month. Over the next 7 months, claims increased to 61 and peaked at 80 claims after 18 months. Chain community pharmacies accounted for 94% of the claims; 71% of claims were in metropolitan areas.
Based on demographics, 73.8% of the women who were prescribed contraception by a pharmacist were first-time recipients. Combined oral contraception was prescribed for 90.5% of the women, and 82% of the women were 18-35 years of age. In the 180-day period prior to receiving pharmacist-prescribed contraception, 61.5% of patients were not using contraception but were attempting to engage in pharmacy-provided hormonal contraceptive care.
The researchers also examined contraceptive safety by looking at whether patients with medical contraindications (Medical Eligibility Criteria Category 3 or 4) were receiving contraindicated methods. “We found that overall adherence to the clinical algorithm for prescribing pharmacists was high. Only 12 (5%) patients were identified as having Medical Eligibility Criteria Category 3 or 4 medical conditions, and two (less than 1%) patients with medications contraindicating OC use received a prescription,” Dr. Anderson and her colleagues wrote.
They noted that the initial legislation passed in Oregon only included oral and transdermal hormonal contraception as methods pharmacists could prescribe. In 2017, with implementation in 2018, this was amended to include the vaginal ring and injection. “As the program matures, and contracts with additional insurers are implemented at pharmacies, we expect the number of pharmacist prescriptions to increase,” the authors wrote.
Dr. Rodriguez reported financial compensation from Merck, the World Health Organization, CooperSurgical, and a previous relationship with Merck. Dr. Anderson reports no conflicts of interest.
SOURCES: Rodriguez M et al. Obstet Gynecol. 2019 Jun;133(6):1238-46; Anderson A et al. Obstet Gynecol. 2019 Jun;133(6):1231-7.
FROM OBSTETRICS & GYNECOLOGY
C-section linked to serious infection in preschoolers
LJUBLJANA, SLOVENIA – Delivery by C-section – especially when elective – carries a significantly higher hospitalization risk for severe infection in the first 5 years of life than vaginal delivery in a study of nearly 7.3 million singleton deliveries in four asset-rich countries, David Burgner, MD, PhD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“This is something that obstetricians might need to consider when discussing with the family the pros and cons for an elective C-section, particularly one that isn’t otherwise indicated for the baby or the mother,” said Dr. Burgner of the Murdoch Children’s Research Institute in Melbourne.
He presented an observational study of 7.29 million singleton births in Denmark, Great Britain, Scotland, and two Australian states during 1996-2015. C-section rates ranged from a low of 17.5% in Denmark to 29.4% in Western Australia, all of which are greater than the 10%-15% rate endorsed by the World Health Organization. Elective C-section rates varied by country from 39% to 57%. Of note, pediatric hospital care in all four countries is free, so economic considerations didn’t drive admission.
The impetus for this international collaboration was to gain new insight into the differential susceptibility to childhood infection, he explained.
“We know from our clinical practice that pretty much all of the children are exposed to pretty much all potentially serious pathogens during early life. And yet it’s only a minority that develop severe infection. It’s an extremely interesting scientific question and an extremely important clinical question as to what’s driving that differential susceptibility,” according to the pediatric infectious disease specialist.
There are a number of established risk factors for infection-related hospitalization in children, including parental smoking, maternal antibiotic exposure during pregnancy, and growth measurements at birth. Dr. Burgner and coinvestigators hypothesized that another important risk factor is the nature of the microbiome transmitted from mother to baby during delivery. This postnatal microbiome varies depending upon mode of delivery: Vaginal delivery transmits the maternal enteric microbiome, which they reasoned might be through direct immunomodulation that sets up protective immune responses early in life, especially against respiratory and gastrointestinal tract infections. In contrast, delivery by C-section causes the baby to pick up the maternal skin and hospital environment microbiomes, but not the maternal enteric microbiome.
Thus, the investigators hypothesized that C-section poses a greater risk of infection-related hospitalization during the first 5 years of life than does vaginal delivery, and that elective C-section poses a higher risk than does emergency C-section because it is more likely to involve rupture of membranes.
The center-specific rates of C-section and infection-related pediatric infection, when combined into a meta-analysis, bore out the study hypothesis. Emergency C-section was associated with a 9% greater risk of infection-related hospitalization through 5 years of age than was vaginal delivery, while elective C-section was associated with a 13% increased risk, both of which were statistically significant and clinically important.
“We were quite taken with these results. We think they provide evidence that C-section is consistently associated with infection-related hospitalization. It’s an association study that can’t prove causality, but the results implicate the postnatal microbiome as the most plausible explanation in terms of what’s driving this association,” according to Dr. Burgner.
The association between C-section and infection-related hospitalization was persistent throughout the preschool years. For example, the increased risk associated with elective C-section was 16% during age 0-3 months, 20% during months 4-6, 14% in months 7-12, 13% during ages 1-2 years, and 11% among 2- to 5-year-olds, he continued.
The increased risk of severe preschool infection was highest for upper and lower respiratory tract and gastrointestinal infections, which involve the organ systems most likely to experience direct inoculation of the maternal microbiome, he noted.
Because the investigators recognized that the study results were potentially vulnerable to confounding by indication – that is, that the reason for doing a C-section might itself confer increased risk of subsequent preschool infection-related hospitalization – they repeated their analysis in a predefined low-risk subpopulation. The results closely mirrored those in the overall study population: an 8% increased risk in the emergency C-section group and a 14% increased risk with elective C-section.
Results of this large multinational study should provide further support for ongoing research aimed at supporting the infant microbiome after delivery by C-section via vaginal microbial transfer and other methods, he observed.
Dr. Burgner reported having no financial conflicts regarding the study, which was cosponsored by the National Health and Medical Research Council of Australia, the Danish Council for Independent Research, and nonprofit foundations.
LJUBLJANA, SLOVENIA – Delivery by C-section – especially when elective – carries a significantly higher hospitalization risk for severe infection in the first 5 years of life than vaginal delivery in a study of nearly 7.3 million singleton deliveries in four asset-rich countries, David Burgner, MD, PhD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“This is something that obstetricians might need to consider when discussing with the family the pros and cons for an elective C-section, particularly one that isn’t otherwise indicated for the baby or the mother,” said Dr. Burgner of the Murdoch Children’s Research Institute in Melbourne.
He presented an observational study of 7.29 million singleton births in Denmark, Great Britain, Scotland, and two Australian states during 1996-2015. C-section rates ranged from a low of 17.5% in Denmark to 29.4% in Western Australia, all of which are greater than the 10%-15% rate endorsed by the World Health Organization. Elective C-section rates varied by country from 39% to 57%. Of note, pediatric hospital care in all four countries is free, so economic considerations didn’t drive admission.
The impetus for this international collaboration was to gain new insight into the differential susceptibility to childhood infection, he explained.
“We know from our clinical practice that pretty much all of the children are exposed to pretty much all potentially serious pathogens during early life. And yet it’s only a minority that develop severe infection. It’s an extremely interesting scientific question and an extremely important clinical question as to what’s driving that differential susceptibility,” according to the pediatric infectious disease specialist.
There are a number of established risk factors for infection-related hospitalization in children, including parental smoking, maternal antibiotic exposure during pregnancy, and growth measurements at birth. Dr. Burgner and coinvestigators hypothesized that another important risk factor is the nature of the microbiome transmitted from mother to baby during delivery. This postnatal microbiome varies depending upon mode of delivery: Vaginal delivery transmits the maternal enteric microbiome, which they reasoned might be through direct immunomodulation that sets up protective immune responses early in life, especially against respiratory and gastrointestinal tract infections. In contrast, delivery by C-section causes the baby to pick up the maternal skin and hospital environment microbiomes, but not the maternal enteric microbiome.
Thus, the investigators hypothesized that C-section poses a greater risk of infection-related hospitalization during the first 5 years of life than does vaginal delivery, and that elective C-section poses a higher risk than does emergency C-section because it is more likely to involve rupture of membranes.
The center-specific rates of C-section and infection-related pediatric infection, when combined into a meta-analysis, bore out the study hypothesis. Emergency C-section was associated with a 9% greater risk of infection-related hospitalization through 5 years of age than was vaginal delivery, while elective C-section was associated with a 13% increased risk, both of which were statistically significant and clinically important.
“We were quite taken with these results. We think they provide evidence that C-section is consistently associated with infection-related hospitalization. It’s an association study that can’t prove causality, but the results implicate the postnatal microbiome as the most plausible explanation in terms of what’s driving this association,” according to Dr. Burgner.
The association between C-section and infection-related hospitalization was persistent throughout the preschool years. For example, the increased risk associated with elective C-section was 16% during age 0-3 months, 20% during months 4-6, 14% in months 7-12, 13% during ages 1-2 years, and 11% among 2- to 5-year-olds, he continued.
The increased risk of severe preschool infection was highest for upper and lower respiratory tract and gastrointestinal infections, which involve the organ systems most likely to experience direct inoculation of the maternal microbiome, he noted.
Because the investigators recognized that the study results were potentially vulnerable to confounding by indication – that is, that the reason for doing a C-section might itself confer increased risk of subsequent preschool infection-related hospitalization – they repeated their analysis in a predefined low-risk subpopulation. The results closely mirrored those in the overall study population: an 8% increased risk in the emergency C-section group and a 14% increased risk with elective C-section.
Results of this large multinational study should provide further support for ongoing research aimed at supporting the infant microbiome after delivery by C-section via vaginal microbial transfer and other methods, he observed.
Dr. Burgner reported having no financial conflicts regarding the study, which was cosponsored by the National Health and Medical Research Council of Australia, the Danish Council for Independent Research, and nonprofit foundations.
LJUBLJANA, SLOVENIA – Delivery by C-section – especially when elective – carries a significantly higher hospitalization risk for severe infection in the first 5 years of life than vaginal delivery in a study of nearly 7.3 million singleton deliveries in four asset-rich countries, David Burgner, MD, PhD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“This is something that obstetricians might need to consider when discussing with the family the pros and cons for an elective C-section, particularly one that isn’t otherwise indicated for the baby or the mother,” said Dr. Burgner of the Murdoch Children’s Research Institute in Melbourne.
He presented an observational study of 7.29 million singleton births in Denmark, Great Britain, Scotland, and two Australian states during 1996-2015. C-section rates ranged from a low of 17.5% in Denmark to 29.4% in Western Australia, all of which are greater than the 10%-15% rate endorsed by the World Health Organization. Elective C-section rates varied by country from 39% to 57%. Of note, pediatric hospital care in all four countries is free, so economic considerations didn’t drive admission.
The impetus for this international collaboration was to gain new insight into the differential susceptibility to childhood infection, he explained.
“We know from our clinical practice that pretty much all of the children are exposed to pretty much all potentially serious pathogens during early life. And yet it’s only a minority that develop severe infection. It’s an extremely interesting scientific question and an extremely important clinical question as to what’s driving that differential susceptibility,” according to the pediatric infectious disease specialist.
There are a number of established risk factors for infection-related hospitalization in children, including parental smoking, maternal antibiotic exposure during pregnancy, and growth measurements at birth. Dr. Burgner and coinvestigators hypothesized that another important risk factor is the nature of the microbiome transmitted from mother to baby during delivery. This postnatal microbiome varies depending upon mode of delivery: Vaginal delivery transmits the maternal enteric microbiome, which they reasoned might be through direct immunomodulation that sets up protective immune responses early in life, especially against respiratory and gastrointestinal tract infections. In contrast, delivery by C-section causes the baby to pick up the maternal skin and hospital environment microbiomes, but not the maternal enteric microbiome.
Thus, the investigators hypothesized that C-section poses a greater risk of infection-related hospitalization during the first 5 years of life than does vaginal delivery, and that elective C-section poses a higher risk than does emergency C-section because it is more likely to involve rupture of membranes.
The center-specific rates of C-section and infection-related pediatric infection, when combined into a meta-analysis, bore out the study hypothesis. Emergency C-section was associated with a 9% greater risk of infection-related hospitalization through 5 years of age than was vaginal delivery, while elective C-section was associated with a 13% increased risk, both of which were statistically significant and clinically important.
“We were quite taken with these results. We think they provide evidence that C-section is consistently associated with infection-related hospitalization. It’s an association study that can’t prove causality, but the results implicate the postnatal microbiome as the most plausible explanation in terms of what’s driving this association,” according to Dr. Burgner.
The association between C-section and infection-related hospitalization was persistent throughout the preschool years. For example, the increased risk associated with elective C-section was 16% during age 0-3 months, 20% during months 4-6, 14% in months 7-12, 13% during ages 1-2 years, and 11% among 2- to 5-year-olds, he continued.
The increased risk of severe preschool infection was highest for upper and lower respiratory tract and gastrointestinal infections, which involve the organ systems most likely to experience direct inoculation of the maternal microbiome, he noted.
Because the investigators recognized that the study results were potentially vulnerable to confounding by indication – that is, that the reason for doing a C-section might itself confer increased risk of subsequent preschool infection-related hospitalization – they repeated their analysis in a predefined low-risk subpopulation. The results closely mirrored those in the overall study population: an 8% increased risk in the emergency C-section group and a 14% increased risk with elective C-section.
Results of this large multinational study should provide further support for ongoing research aimed at supporting the infant microbiome after delivery by C-section via vaginal microbial transfer and other methods, he observed.
Dr. Burgner reported having no financial conflicts regarding the study, which was cosponsored by the National Health and Medical Research Council of Australia, the Danish Council for Independent Research, and nonprofit foundations.
REPORTING FROM ESPID 2019
CPAP for infants with OSA is effective with high adherence
DALLAS – ), according to a study.
“Positive airway pressure is a common treatment for OSA in children,” wrote Christopher Cielo, DO, of Children’s Hospital of Philadelphia Sleep Center, and his colleagues. But the authors note that treating infants with CPAP can be more challenging because infants have less consolidated sleep, may have greater medical complexity, and have smaller faces that make mask fit, titration, and adherence difficult.
The researchers therefore compared use of CPAP for OSA on 32 infants who began the therapy before age 6 months and 102 school-age children who began the therapy between ages 5 and 10 years, all treated at a single sleep center between March 2013 and September 2018.
Only one of the infants (mean age 3 months) had obesity, compared with 37.3% of the school-age children (mean age 7.7 years), but more of the infants (50%) had a craniofacial abnormality compared with the older children (8.9%) (P less than .001).
None of the infants had had an adenotonsillectomy, whereas the majority of the older children (80.4%) had (P less than .001). Rates of neurological abnormality and genetic syndromes (including Down syndrome) were similar between the groups.
In baseline polysomnograms, infants had a higher mean obstructive apnea-hypopnea index (AHI) compared with older children (22.6 vs. 12; P less than .001) and a slightly, but significantly, lower oxygen saturation nadir (81% vs. 87%; P = .002).
Only 9.8% of the children and none of the infants used autotitrating. Similar proportions of both groups – 90.6% of infants and 93.1% of children – achieved a mean AHI below 5 with CPAP treatment, and both CPAP pressure and mean oxygen saturation nadir at final pressure were similar in both groups.
Adherence was higher in infants than in children: Infants used CPAP for at least some time for 93.3% of nights compared with children (83.4%) (P = .009), and infants used CPAP for more than 4 hours for 78.4% of nights, compared with 59.5% of nights among children (P = .04).
Barriers to adherence reported by caregivers were similar between both groups. The most common barrier was child behavior, such as crying or refusing the CPAP, which 25% of infant caregivers and 35.3% of child caregivers reported. While a higher proportion of caregivers reported a poor mask fit for infants (15.6%) than for children (10.8%), the difference was not significant (P = .47). Rates of skin irritation also did not significantly differ between the groups.
In addition to the limitations accompanying any retrospective analysis from a single center, another study limitation was the inability to account for differences in total sleep time between infants and school-age children in comparing CPAP usage.
The National Institutes of Health and the Francis Family Foundation funded the research. The authors had no disclosures.
DALLAS – ), according to a study.
“Positive airway pressure is a common treatment for OSA in children,” wrote Christopher Cielo, DO, of Children’s Hospital of Philadelphia Sleep Center, and his colleagues. But the authors note that treating infants with CPAP can be more challenging because infants have less consolidated sleep, may have greater medical complexity, and have smaller faces that make mask fit, titration, and adherence difficult.
The researchers therefore compared use of CPAP for OSA on 32 infants who began the therapy before age 6 months and 102 school-age children who began the therapy between ages 5 and 10 years, all treated at a single sleep center between March 2013 and September 2018.
Only one of the infants (mean age 3 months) had obesity, compared with 37.3% of the school-age children (mean age 7.7 years), but more of the infants (50%) had a craniofacial abnormality compared with the older children (8.9%) (P less than .001).
None of the infants had had an adenotonsillectomy, whereas the majority of the older children (80.4%) had (P less than .001). Rates of neurological abnormality and genetic syndromes (including Down syndrome) were similar between the groups.
In baseline polysomnograms, infants had a higher mean obstructive apnea-hypopnea index (AHI) compared with older children (22.6 vs. 12; P less than .001) and a slightly, but significantly, lower oxygen saturation nadir (81% vs. 87%; P = .002).
Only 9.8% of the children and none of the infants used autotitrating. Similar proportions of both groups – 90.6% of infants and 93.1% of children – achieved a mean AHI below 5 with CPAP treatment, and both CPAP pressure and mean oxygen saturation nadir at final pressure were similar in both groups.
Adherence was higher in infants than in children: Infants used CPAP for at least some time for 93.3% of nights compared with children (83.4%) (P = .009), and infants used CPAP for more than 4 hours for 78.4% of nights, compared with 59.5% of nights among children (P = .04).
Barriers to adherence reported by caregivers were similar between both groups. The most common barrier was child behavior, such as crying or refusing the CPAP, which 25% of infant caregivers and 35.3% of child caregivers reported. While a higher proportion of caregivers reported a poor mask fit for infants (15.6%) than for children (10.8%), the difference was not significant (P = .47). Rates of skin irritation also did not significantly differ between the groups.
In addition to the limitations accompanying any retrospective analysis from a single center, another study limitation was the inability to account for differences in total sleep time between infants and school-age children in comparing CPAP usage.
The National Institutes of Health and the Francis Family Foundation funded the research. The authors had no disclosures.
DALLAS – ), according to a study.
“Positive airway pressure is a common treatment for OSA in children,” wrote Christopher Cielo, DO, of Children’s Hospital of Philadelphia Sleep Center, and his colleagues. But the authors note that treating infants with CPAP can be more challenging because infants have less consolidated sleep, may have greater medical complexity, and have smaller faces that make mask fit, titration, and adherence difficult.
The researchers therefore compared use of CPAP for OSA on 32 infants who began the therapy before age 6 months and 102 school-age children who began the therapy between ages 5 and 10 years, all treated at a single sleep center between March 2013 and September 2018.
Only one of the infants (mean age 3 months) had obesity, compared with 37.3% of the school-age children (mean age 7.7 years), but more of the infants (50%) had a craniofacial abnormality compared with the older children (8.9%) (P less than .001).
None of the infants had had an adenotonsillectomy, whereas the majority of the older children (80.4%) had (P less than .001). Rates of neurological abnormality and genetic syndromes (including Down syndrome) were similar between the groups.
In baseline polysomnograms, infants had a higher mean obstructive apnea-hypopnea index (AHI) compared with older children (22.6 vs. 12; P less than .001) and a slightly, but significantly, lower oxygen saturation nadir (81% vs. 87%; P = .002).
Only 9.8% of the children and none of the infants used autotitrating. Similar proportions of both groups – 90.6% of infants and 93.1% of children – achieved a mean AHI below 5 with CPAP treatment, and both CPAP pressure and mean oxygen saturation nadir at final pressure were similar in both groups.
Adherence was higher in infants than in children: Infants used CPAP for at least some time for 93.3% of nights compared with children (83.4%) (P = .009), and infants used CPAP for more than 4 hours for 78.4% of nights, compared with 59.5% of nights among children (P = .04).
Barriers to adherence reported by caregivers were similar between both groups. The most common barrier was child behavior, such as crying or refusing the CPAP, which 25% of infant caregivers and 35.3% of child caregivers reported. While a higher proportion of caregivers reported a poor mask fit for infants (15.6%) than for children (10.8%), the difference was not significant (P = .47). Rates of skin irritation also did not significantly differ between the groups.
In addition to the limitations accompanying any retrospective analysis from a single center, another study limitation was the inability to account for differences in total sleep time between infants and school-age children in comparing CPAP usage.
The National Institutes of Health and the Francis Family Foundation funded the research. The authors had no disclosures.
REPORTING FROM ATS 2019
Fear
Fear annoys. Fear mystifies. Fear masquerades. Fear can be trivial or terrifying. But fear is always there.
Boris has a spot on his nose. I call with test results.
“Boris, I got back your biopsy report. As expected, it did show a basal cell skin cancer.”
“Skin cancer?”
“Yes. As we discussed, basal cells are not serious and don’t spread, but you have to get it taken off.”
“Will I have to stay in the hospital?”
“No, it’s done under local anesthesia. You get it done and go home.”
“Is it urgent?”
“It can wait a few weeks. Just call for an appointment.”
“Will it be done in the hospital itself, or in another building?”
One question succeeds another. Each answer prompts another question. Sometimes the queries circle back and threaten to start the interrogation over. Children use the same tactic before you freeze their wart. “Wait! Will it hurt?” “Wait, wait, how many times will you freeze it?” “Wait, wait, how many seconds will it take?”
It takes patience, but Boris’s tone finally softens, and the questions stop. The queries are less requests for information than stalling tactics. Maybe if I keep asking, the problem will go away.
Stella is more perplexing than Boris, not to mention more challenging.
“I had a melanoma on my forehead, Doctor. But it’s all taken care of.”
“Taken care of?”
“Yes. The dermatologist in Clarksville did a biopsy, which showed melanoma, but I had a healer take care of it.”
“A healer?”
“Yes. I tell the healer my problem. She doesn’t even have to be there. She can heal from anywhere. She took care of it.”
“With due respect, I don’t think she did.”
“Why do you say that?”
“Because it’s still there on your forehead. I can see it.”
Stella and I negotiate. I will perform another biopsy, but only after she promises me that if the biopsy confirms the presence of melanoma, she’ll see a surgeon.
The biopsy shows melanoma in situ. Two weeks later the surgeon’s office calls to say that Stella has canceled her appointment.
I call Stella.
“I decided to cancel my appointment,” she says. “I asked the surgeon to perform another biopsy, but she refused. I found another dermatologist who will do it.”
“Just curious,” I say. “If two previous biopsies didn’t convince you that you have melanoma, why would a third?”
“Because I thought the healer had finished taking care of it, but she hadn’t,” Stella says. “Now she has.”
Stella pauses. “I know I’m on shaky ground here,” she says. “Maybe I don’t have a leg to stand on. But I just need to be sure.”
“You know,” I say, “if you don’t remove a melanoma, it can spread and cause death.”
Stella does know this. But she still isn’t sure it hasn’t already been taken care of. She has to be sure. Wait, wait ...
“You understand,” I say, “that I can’t be your doctor anymore, since you aren’t willing to follow my advice.”
“Of course,” says Stella, “that goes without saying.”
“Actually, it doesn’t,” I say. “If I can’t be responsible for your health, I have to make sure you know that, that you know why, and that you pick someone else to take care of you. It seems you have chosen someone.”
We all see many Borises. There are plenty of Stellas, too, though we don’t often see them. People who think as she does, who put their trust in strange treatments and sundry healers, don’t often show up in our offices. How they can think the way they do passes my understanding. But then much that I read or hear in the news about what people think passes my understanding. They are not my responsibility, though; Stella is, or at least she was.
Stella’s faith in her remote healer seems like one way of abetting denial and addressing fear, one step beyond just pretending the symptom or sign simply isn’t there. How much more obvious can a problem be than a black spot on your forehead?
Dealing with it may be wearying, or impossible. But it’s part of our job, because it’s always there.
Besides, we should be able to relate. Doctors know fear too, don’t we?
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
Fear annoys. Fear mystifies. Fear masquerades. Fear can be trivial or terrifying. But fear is always there.
Boris has a spot on his nose. I call with test results.
“Boris, I got back your biopsy report. As expected, it did show a basal cell skin cancer.”
“Skin cancer?”
“Yes. As we discussed, basal cells are not serious and don’t spread, but you have to get it taken off.”
“Will I have to stay in the hospital?”
“No, it’s done under local anesthesia. You get it done and go home.”
“Is it urgent?”
“It can wait a few weeks. Just call for an appointment.”
“Will it be done in the hospital itself, or in another building?”
One question succeeds another. Each answer prompts another question. Sometimes the queries circle back and threaten to start the interrogation over. Children use the same tactic before you freeze their wart. “Wait! Will it hurt?” “Wait, wait, how many times will you freeze it?” “Wait, wait, how many seconds will it take?”
It takes patience, but Boris’s tone finally softens, and the questions stop. The queries are less requests for information than stalling tactics. Maybe if I keep asking, the problem will go away.
Stella is more perplexing than Boris, not to mention more challenging.
“I had a melanoma on my forehead, Doctor. But it’s all taken care of.”
“Taken care of?”
“Yes. The dermatologist in Clarksville did a biopsy, which showed melanoma, but I had a healer take care of it.”
“A healer?”
“Yes. I tell the healer my problem. She doesn’t even have to be there. She can heal from anywhere. She took care of it.”
“With due respect, I don’t think she did.”
“Why do you say that?”
“Because it’s still there on your forehead. I can see it.”
Stella and I negotiate. I will perform another biopsy, but only after she promises me that if the biopsy confirms the presence of melanoma, she’ll see a surgeon.
The biopsy shows melanoma in situ. Two weeks later the surgeon’s office calls to say that Stella has canceled her appointment.
I call Stella.
“I decided to cancel my appointment,” she says. “I asked the surgeon to perform another biopsy, but she refused. I found another dermatologist who will do it.”
“Just curious,” I say. “If two previous biopsies didn’t convince you that you have melanoma, why would a third?”
“Because I thought the healer had finished taking care of it, but she hadn’t,” Stella says. “Now she has.”
Stella pauses. “I know I’m on shaky ground here,” she says. “Maybe I don’t have a leg to stand on. But I just need to be sure.”
“You know,” I say, “if you don’t remove a melanoma, it can spread and cause death.”
Stella does know this. But she still isn’t sure it hasn’t already been taken care of. She has to be sure. Wait, wait ...
“You understand,” I say, “that I can’t be your doctor anymore, since you aren’t willing to follow my advice.”
“Of course,” says Stella, “that goes without saying.”
“Actually, it doesn’t,” I say. “If I can’t be responsible for your health, I have to make sure you know that, that you know why, and that you pick someone else to take care of you. It seems you have chosen someone.”
We all see many Borises. There are plenty of Stellas, too, though we don’t often see them. People who think as she does, who put their trust in strange treatments and sundry healers, don’t often show up in our offices. How they can think the way they do passes my understanding. But then much that I read or hear in the news about what people think passes my understanding. They are not my responsibility, though; Stella is, or at least she was.
Stella’s faith in her remote healer seems like one way of abetting denial and addressing fear, one step beyond just pretending the symptom or sign simply isn’t there. How much more obvious can a problem be than a black spot on your forehead?
Dealing with it may be wearying, or impossible. But it’s part of our job, because it’s always there.
Besides, we should be able to relate. Doctors know fear too, don’t we?
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
Fear annoys. Fear mystifies. Fear masquerades. Fear can be trivial or terrifying. But fear is always there.
Boris has a spot on his nose. I call with test results.
“Boris, I got back your biopsy report. As expected, it did show a basal cell skin cancer.”
“Skin cancer?”
“Yes. As we discussed, basal cells are not serious and don’t spread, but you have to get it taken off.”
“Will I have to stay in the hospital?”
“No, it’s done under local anesthesia. You get it done and go home.”
“Is it urgent?”
“It can wait a few weeks. Just call for an appointment.”
“Will it be done in the hospital itself, or in another building?”
One question succeeds another. Each answer prompts another question. Sometimes the queries circle back and threaten to start the interrogation over. Children use the same tactic before you freeze their wart. “Wait! Will it hurt?” “Wait, wait, how many times will you freeze it?” “Wait, wait, how many seconds will it take?”
It takes patience, but Boris’s tone finally softens, and the questions stop. The queries are less requests for information than stalling tactics. Maybe if I keep asking, the problem will go away.
Stella is more perplexing than Boris, not to mention more challenging.
“I had a melanoma on my forehead, Doctor. But it’s all taken care of.”
“Taken care of?”
“Yes. The dermatologist in Clarksville did a biopsy, which showed melanoma, but I had a healer take care of it.”
“A healer?”
“Yes. I tell the healer my problem. She doesn’t even have to be there. She can heal from anywhere. She took care of it.”
“With due respect, I don’t think she did.”
“Why do you say that?”
“Because it’s still there on your forehead. I can see it.”
Stella and I negotiate. I will perform another biopsy, but only after she promises me that if the biopsy confirms the presence of melanoma, she’ll see a surgeon.
The biopsy shows melanoma in situ. Two weeks later the surgeon’s office calls to say that Stella has canceled her appointment.
I call Stella.
“I decided to cancel my appointment,” she says. “I asked the surgeon to perform another biopsy, but she refused. I found another dermatologist who will do it.”
“Just curious,” I say. “If two previous biopsies didn’t convince you that you have melanoma, why would a third?”
“Because I thought the healer had finished taking care of it, but she hadn’t,” Stella says. “Now she has.”
Stella pauses. “I know I’m on shaky ground here,” she says. “Maybe I don’t have a leg to stand on. But I just need to be sure.”
“You know,” I say, “if you don’t remove a melanoma, it can spread and cause death.”
Stella does know this. But she still isn’t sure it hasn’t already been taken care of. She has to be sure. Wait, wait ...
“You understand,” I say, “that I can’t be your doctor anymore, since you aren’t willing to follow my advice.”
“Of course,” says Stella, “that goes without saying.”
“Actually, it doesn’t,” I say. “If I can’t be responsible for your health, I have to make sure you know that, that you know why, and that you pick someone else to take care of you. It seems you have chosen someone.”
We all see many Borises. There are plenty of Stellas, too, though we don’t often see them. People who think as she does, who put their trust in strange treatments and sundry healers, don’t often show up in our offices. How they can think the way they do passes my understanding. But then much that I read or hear in the news about what people think passes my understanding. They are not my responsibility, though; Stella is, or at least she was.
Stella’s faith in her remote healer seems like one way of abetting denial and addressing fear, one step beyond just pretending the symptom or sign simply isn’t there. How much more obvious can a problem be than a black spot on your forehead?
Dealing with it may be wearying, or impossible. But it’s part of our job, because it’s always there.
Besides, we should be able to relate. Doctors know fear too, don’t we?
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
Antimalarials in pregnancy and lactation
According to the World Health Organization, there were about 219 million cases of malaria and an estimated 660,000 deaths in 2010. Although huge, this was a 26% decrease from the rates in 2000. Six countries in Africa account for 47% of malaria cases: Cote d’Ivoire, Democratic Republic of the Congo, Mozambique, Nigeria, Uganda, and the United Republic of Tanzania. The second-most affected region in the world is Southeast Asia, which includes Myanmar, India, and Indonesia. In comparison, about 1,500 malaria cases and 5 deaths are reported annually in the United States, mostly from returned travelers.
if they will be traveling in any of the above regions. Malaria during pregnancy increases the risk for adverse pregnancy outcomes, including maternal anemia, prematurity, spontaneous abortion, and stillbirth.
As stated by the Centers for Disease Control and Prevention, no antimalarial agent is 100% protective. Therefore, whatever agent is used must be combined with personal protective measures such as wearing insect repellent, long sleeves, and long pants; sleeping in a mosquito-free setting; or using an insecticide-treated bed net.
There are nine antimalarial drugs available in the United States.
Atovaquone/Proguanil Hcl (Malarone and as generic)
This agent is good for last-minute travelers because the drug is started 1-2 days before traveling to areas where malaria transmission occurs. The combination can be classified as compatible in pregnancy. No reports in breastfeeding with atovaquone or the combination have been found. Proguanil is not available in the United States as a single agent.
Chloroquine (generic)
This is the drug of choice to prevent and treat sensitive malaria species during pregnancy. The drug crosses the placenta producing fetal concentrations that are similar to those in the mother. The drug appears to be low risk for embryo-fetal harm.
It is compatible in breastfeeding.
Dapsone (generic)
This agent does not appear to represent a major risk of harm to the fetus. Although it has been used in combination with pyrimethamine (an antiparasitic) or trimethoprim (an antibiotic) to prevent malaria, the efficacy of the combination has not been confirmed.
In breastfeeding, there is one case of mild hemolytic anemia in the mother and her breastfeeding infant that may have been caused by the drug.
Hydroxychloroquine (generic)
This agent is used for the treatment of malaria, systemic erythematosus, and rheumatoid arthritis. For antimalarial prophylaxis, 400 mg/week appears to be low risk for embryo-fetal harm. Doses used to treat malaria have been 200-400 mg/day.
Because very low concentrations of the drug have been found in breast milk, breastfeeding is probably compatible.
Mefloquine (generic)
This agent is a quinoline-methanol agent that does not appear to cause embryo-fetal harm based on a large number of pregnancy exposures.
There are no reports of its use while breastfeeding.
Primaquine (generic)
This agent is best avoided in pregnancy. There is no human pregnancy data, but it may cause hemolytic anemia in patients with glucose-6-phosphate dehydrogenase deficiency (G6PD). Because the fetus is relatively G6PD deficient, it is best avoided in pregnancy regardless of the mother’s status.
There are no reports describing the use of the drug during lactation. Both the mother and baby should be tested for G6PD deficiency before the drug is used during breastfeeding.
Pyrimethamine (generic)
This agent has been used for the treatment or prophylaxis of malaria. Most studies have found this agent to be relatively safe and effective.
It is excreted into breast milk and has been effective in eliminating malaria parasites from breastfeeding infants.
Quinidine (generic)
Reports linking the use of this agent with congenital defects have not been found. Although the drug has data on its use as an antiarrhythmic, its published use to treat malaria is limited.
The drug is excreted into breast milk, but there are no reports of its during breastfeeding.
Quinine (generic)
This agent has a large amount of human pregnancy data (more than 1,000 exposures) that found no increased risk of birth defects. The drug has been replaced by newer agents but still may be used for chloroquine-resistant malaria.
The drug appears to be compatible during breastfeeding.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
According to the World Health Organization, there were about 219 million cases of malaria and an estimated 660,000 deaths in 2010. Although huge, this was a 26% decrease from the rates in 2000. Six countries in Africa account for 47% of malaria cases: Cote d’Ivoire, Democratic Republic of the Congo, Mozambique, Nigeria, Uganda, and the United Republic of Tanzania. The second-most affected region in the world is Southeast Asia, which includes Myanmar, India, and Indonesia. In comparison, about 1,500 malaria cases and 5 deaths are reported annually in the United States, mostly from returned travelers.
if they will be traveling in any of the above regions. Malaria during pregnancy increases the risk for adverse pregnancy outcomes, including maternal anemia, prematurity, spontaneous abortion, and stillbirth.
As stated by the Centers for Disease Control and Prevention, no antimalarial agent is 100% protective. Therefore, whatever agent is used must be combined with personal protective measures such as wearing insect repellent, long sleeves, and long pants; sleeping in a mosquito-free setting; or using an insecticide-treated bed net.
There are nine antimalarial drugs available in the United States.
Atovaquone/Proguanil Hcl (Malarone and as generic)
This agent is good for last-minute travelers because the drug is started 1-2 days before traveling to areas where malaria transmission occurs. The combination can be classified as compatible in pregnancy. No reports in breastfeeding with atovaquone or the combination have been found. Proguanil is not available in the United States as a single agent.
Chloroquine (generic)
This is the drug of choice to prevent and treat sensitive malaria species during pregnancy. The drug crosses the placenta producing fetal concentrations that are similar to those in the mother. The drug appears to be low risk for embryo-fetal harm.
It is compatible in breastfeeding.
Dapsone (generic)
This agent does not appear to represent a major risk of harm to the fetus. Although it has been used in combination with pyrimethamine (an antiparasitic) or trimethoprim (an antibiotic) to prevent malaria, the efficacy of the combination has not been confirmed.
In breastfeeding, there is one case of mild hemolytic anemia in the mother and her breastfeeding infant that may have been caused by the drug.
Hydroxychloroquine (generic)
This agent is used for the treatment of malaria, systemic erythematosus, and rheumatoid arthritis. For antimalarial prophylaxis, 400 mg/week appears to be low risk for embryo-fetal harm. Doses used to treat malaria have been 200-400 mg/day.
Because very low concentrations of the drug have been found in breast milk, breastfeeding is probably compatible.
Mefloquine (generic)
This agent is a quinoline-methanol agent that does not appear to cause embryo-fetal harm based on a large number of pregnancy exposures.
There are no reports of its use while breastfeeding.
Primaquine (generic)
This agent is best avoided in pregnancy. There is no human pregnancy data, but it may cause hemolytic anemia in patients with glucose-6-phosphate dehydrogenase deficiency (G6PD). Because the fetus is relatively G6PD deficient, it is best avoided in pregnancy regardless of the mother’s status.
There are no reports describing the use of the drug during lactation. Both the mother and baby should be tested for G6PD deficiency before the drug is used during breastfeeding.
Pyrimethamine (generic)
This agent has been used for the treatment or prophylaxis of malaria. Most studies have found this agent to be relatively safe and effective.
It is excreted into breast milk and has been effective in eliminating malaria parasites from breastfeeding infants.
Quinidine (generic)
Reports linking the use of this agent with congenital defects have not been found. Although the drug has data on its use as an antiarrhythmic, its published use to treat malaria is limited.
The drug is excreted into breast milk, but there are no reports of its during breastfeeding.
Quinine (generic)
This agent has a large amount of human pregnancy data (more than 1,000 exposures) that found no increased risk of birth defects. The drug has been replaced by newer agents but still may be used for chloroquine-resistant malaria.
The drug appears to be compatible during breastfeeding.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
According to the World Health Organization, there were about 219 million cases of malaria and an estimated 660,000 deaths in 2010. Although huge, this was a 26% decrease from the rates in 2000. Six countries in Africa account for 47% of malaria cases: Cote d’Ivoire, Democratic Republic of the Congo, Mozambique, Nigeria, Uganda, and the United Republic of Tanzania. The second-most affected region in the world is Southeast Asia, which includes Myanmar, India, and Indonesia. In comparison, about 1,500 malaria cases and 5 deaths are reported annually in the United States, mostly from returned travelers.
if they will be traveling in any of the above regions. Malaria during pregnancy increases the risk for adverse pregnancy outcomes, including maternal anemia, prematurity, spontaneous abortion, and stillbirth.
As stated by the Centers for Disease Control and Prevention, no antimalarial agent is 100% protective. Therefore, whatever agent is used must be combined with personal protective measures such as wearing insect repellent, long sleeves, and long pants; sleeping in a mosquito-free setting; or using an insecticide-treated bed net.
There are nine antimalarial drugs available in the United States.
Atovaquone/Proguanil Hcl (Malarone and as generic)
This agent is good for last-minute travelers because the drug is started 1-2 days before traveling to areas where malaria transmission occurs. The combination can be classified as compatible in pregnancy. No reports in breastfeeding with atovaquone or the combination have been found. Proguanil is not available in the United States as a single agent.
Chloroquine (generic)
This is the drug of choice to prevent and treat sensitive malaria species during pregnancy. The drug crosses the placenta producing fetal concentrations that are similar to those in the mother. The drug appears to be low risk for embryo-fetal harm.
It is compatible in breastfeeding.
Dapsone (generic)
This agent does not appear to represent a major risk of harm to the fetus. Although it has been used in combination with pyrimethamine (an antiparasitic) or trimethoprim (an antibiotic) to prevent malaria, the efficacy of the combination has not been confirmed.
In breastfeeding, there is one case of mild hemolytic anemia in the mother and her breastfeeding infant that may have been caused by the drug.
Hydroxychloroquine (generic)
This agent is used for the treatment of malaria, systemic erythematosus, and rheumatoid arthritis. For antimalarial prophylaxis, 400 mg/week appears to be low risk for embryo-fetal harm. Doses used to treat malaria have been 200-400 mg/day.
Because very low concentrations of the drug have been found in breast milk, breastfeeding is probably compatible.
Mefloquine (generic)
This agent is a quinoline-methanol agent that does not appear to cause embryo-fetal harm based on a large number of pregnancy exposures.
There are no reports of its use while breastfeeding.
Primaquine (generic)
This agent is best avoided in pregnancy. There is no human pregnancy data, but it may cause hemolytic anemia in patients with glucose-6-phosphate dehydrogenase deficiency (G6PD). Because the fetus is relatively G6PD deficient, it is best avoided in pregnancy regardless of the mother’s status.
There are no reports describing the use of the drug during lactation. Both the mother and baby should be tested for G6PD deficiency before the drug is used during breastfeeding.
Pyrimethamine (generic)
This agent has been used for the treatment or prophylaxis of malaria. Most studies have found this agent to be relatively safe and effective.
It is excreted into breast milk and has been effective in eliminating malaria parasites from breastfeeding infants.
Quinidine (generic)
Reports linking the use of this agent with congenital defects have not been found. Although the drug has data on its use as an antiarrhythmic, its published use to treat malaria is limited.
The drug is excreted into breast milk, but there are no reports of its during breastfeeding.
Quinine (generic)
This agent has a large amount of human pregnancy data (more than 1,000 exposures) that found no increased risk of birth defects. The drug has been replaced by newer agents but still may be used for chloroquine-resistant malaria.
The drug appears to be compatible during breastfeeding.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].