User login
Tofacitinib improves disease activity in patients with polyarticular-course JIA
ATLANTA – Treatment of polyarticular-course juvenile idiopathic arthritis with tofacitinib led to significantly fewer disease flares and greater improvement in disease activity than with placebo in a phase 3, multinational, randomized, double-blind, controlled withdrawal study presented at the annual meeting of the American College of Rheumatology.
Hermine I. Brunner, MD, director of the division of rheumatology at Cincinnati Children’s Hospital Medical Center, and colleagues conducted the study in 225 patients between 2 and less than 18 years old with polyarticular-course juvenile idiopathic arthritis (pJIA; n = 184), psoriatic arthritis (PsA; n = 20), or enthesitis-related arthritis (ERA; n = 21). Patients were included if they had an inadequate response or intolerance to a disease-modifying antirheumatic drug and active disease with five or more active joints in the case of pJIA and three or more active joints in PsA or ERA.
Dr. Brunner presented results only for pJIA patients; the results for PsA and ERA patients will be assessed and presented separately.
The researchers divided their study into two sections. In the open-label portion of the study, patients received twice-daily tofacitinib (Xeljanz) at a dose of 5 mg or a weight-based lower dose in patients under 40 kg for 18 weeks. A total of 173 patients met JIA ACR30 response criteria, defined as 30% or greater improvement in three of six JIA core set variables and worsening in no more than one of the core set variables, and then were randomized in part 2 of the study to continue the same dose of tofacitinib or receive placebo until 44 weeks. Dr. Brunner noted that most patients who discontinued treatment in parts 1 and 2 did so because of insufficient clinical response rather than from adverse events.
Disease flare occurrence between 18 and 44 weeks was measured as a primary endpoint, and key secondary endpoints included JIA ACR30/50/70 response and change in Childhood Health Assessment Questionnaire Disability Index (CHAQ-DI) scores from part 2 baseline. The researchers used a “gatekeeping approach” that sequenced outcome measures in their statistical analysis to control for false positives in primary and secondary outcomes, where statistical significance could be achieved only if the previous outcome in the sequence was statistically significant.
Patients had a median age of 13 years, and most were female, white (about 87%), and between one-third and one-half of patients were based in North America. JIA disease duration was a median of about 2.5 years, C-reactive protein was about 0.3 mg/dL, and median CHAQ-DI scores were about 0.9 across tofacitinib and placebo groups. Other baseline characteristics were balanced between the two groups, Dr. Brunner said.
“Patients with polyarticular-course JIA in the open-label study experienced a rapid improvement of their disease activity from very high to moderate within 18 weeks,” Dr. Brunner said in her presentation. “[T]ofacitinib demonstrated significantly greater efficacy versus placebo in patients with polyarticular-course JIA based on occurrence of fewer flares in part 2.”
Specifically, disease flare occurred in 29.2% of patients by 44 weeks in the tofacitinib group, compared with 52.9% of patients in the placebo group (P = .0031), for an overall 54% lower risk of flare among patients receiving tofacitinib (hazard ratio, 0.459; 95% confidence interval, 0.268-0.785; P = .0037). The response rate was higher for patients receiving tofacitinib at 44 weeks when measured by JIA ACR30 (70.8% vs. 47.1% with placebo; P = .0031) or by JIA ACR50 (66.7% vs. 47.1%; P = .0166) and JIA ACR70 criteria (54.2% vs. 37.1%; P = .0387). The change in CHAQ-DI score also improved at 44 weeks to a significantly greater extent in the tofacitinib group than with placebo (–0.09 vs. 0.03; P = .0292).
“The safety profile of tofacitinib in children with JIA was comparable to what you have seen or known in the [rheumatoid arthritis] population, and no new safety risks were identified in this pediatric population,” Dr. Brunner said.
The researchers reported ties with Pfizer, which funded the study, and more than two dozen other pharmaceutical companies.
SOURCE: Brunner HI et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract L22.
ATLANTA – Treatment of polyarticular-course juvenile idiopathic arthritis with tofacitinib led to significantly fewer disease flares and greater improvement in disease activity than with placebo in a phase 3, multinational, randomized, double-blind, controlled withdrawal study presented at the annual meeting of the American College of Rheumatology.
Hermine I. Brunner, MD, director of the division of rheumatology at Cincinnati Children’s Hospital Medical Center, and colleagues conducted the study in 225 patients between 2 and less than 18 years old with polyarticular-course juvenile idiopathic arthritis (pJIA; n = 184), psoriatic arthritis (PsA; n = 20), or enthesitis-related arthritis (ERA; n = 21). Patients were included if they had an inadequate response or intolerance to a disease-modifying antirheumatic drug and active disease with five or more active joints in the case of pJIA and three or more active joints in PsA or ERA.
Dr. Brunner presented results only for pJIA patients; the results for PsA and ERA patients will be assessed and presented separately.
The researchers divided their study into two sections. In the open-label portion of the study, patients received twice-daily tofacitinib (Xeljanz) at a dose of 5 mg or a weight-based lower dose in patients under 40 kg for 18 weeks. A total of 173 patients met JIA ACR30 response criteria, defined as 30% or greater improvement in three of six JIA core set variables and worsening in no more than one of the core set variables, and then were randomized in part 2 of the study to continue the same dose of tofacitinib or receive placebo until 44 weeks. Dr. Brunner noted that most patients who discontinued treatment in parts 1 and 2 did so because of insufficient clinical response rather than from adverse events.
Disease flare occurrence between 18 and 44 weeks was measured as a primary endpoint, and key secondary endpoints included JIA ACR30/50/70 response and change in Childhood Health Assessment Questionnaire Disability Index (CHAQ-DI) scores from part 2 baseline. The researchers used a “gatekeeping approach” that sequenced outcome measures in their statistical analysis to control for false positives in primary and secondary outcomes, where statistical significance could be achieved only if the previous outcome in the sequence was statistically significant.
Patients had a median age of 13 years, and most were female, white (about 87%), and between one-third and one-half of patients were based in North America. JIA disease duration was a median of about 2.5 years, C-reactive protein was about 0.3 mg/dL, and median CHAQ-DI scores were about 0.9 across tofacitinib and placebo groups. Other baseline characteristics were balanced between the two groups, Dr. Brunner said.
“Patients with polyarticular-course JIA in the open-label study experienced a rapid improvement of their disease activity from very high to moderate within 18 weeks,” Dr. Brunner said in her presentation. “[T]ofacitinib demonstrated significantly greater efficacy versus placebo in patients with polyarticular-course JIA based on occurrence of fewer flares in part 2.”
Specifically, disease flare occurred in 29.2% of patients by 44 weeks in the tofacitinib group, compared with 52.9% of patients in the placebo group (P = .0031), for an overall 54% lower risk of flare among patients receiving tofacitinib (hazard ratio, 0.459; 95% confidence interval, 0.268-0.785; P = .0037). The response rate was higher for patients receiving tofacitinib at 44 weeks when measured by JIA ACR30 (70.8% vs. 47.1% with placebo; P = .0031) or by JIA ACR50 (66.7% vs. 47.1%; P = .0166) and JIA ACR70 criteria (54.2% vs. 37.1%; P = .0387). The change in CHAQ-DI score also improved at 44 weeks to a significantly greater extent in the tofacitinib group than with placebo (–0.09 vs. 0.03; P = .0292).
“The safety profile of tofacitinib in children with JIA was comparable to what you have seen or known in the [rheumatoid arthritis] population, and no new safety risks were identified in this pediatric population,” Dr. Brunner said.
The researchers reported ties with Pfizer, which funded the study, and more than two dozen other pharmaceutical companies.
SOURCE: Brunner HI et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract L22.
ATLANTA – Treatment of polyarticular-course juvenile idiopathic arthritis with tofacitinib led to significantly fewer disease flares and greater improvement in disease activity than with placebo in a phase 3, multinational, randomized, double-blind, controlled withdrawal study presented at the annual meeting of the American College of Rheumatology.
Hermine I. Brunner, MD, director of the division of rheumatology at Cincinnati Children’s Hospital Medical Center, and colleagues conducted the study in 225 patients between 2 and less than 18 years old with polyarticular-course juvenile idiopathic arthritis (pJIA; n = 184), psoriatic arthritis (PsA; n = 20), or enthesitis-related arthritis (ERA; n = 21). Patients were included if they had an inadequate response or intolerance to a disease-modifying antirheumatic drug and active disease with five or more active joints in the case of pJIA and three or more active joints in PsA or ERA.
Dr. Brunner presented results only for pJIA patients; the results for PsA and ERA patients will be assessed and presented separately.
The researchers divided their study into two sections. In the open-label portion of the study, patients received twice-daily tofacitinib (Xeljanz) at a dose of 5 mg or a weight-based lower dose in patients under 40 kg for 18 weeks. A total of 173 patients met JIA ACR30 response criteria, defined as 30% or greater improvement in three of six JIA core set variables and worsening in no more than one of the core set variables, and then were randomized in part 2 of the study to continue the same dose of tofacitinib or receive placebo until 44 weeks. Dr. Brunner noted that most patients who discontinued treatment in parts 1 and 2 did so because of insufficient clinical response rather than from adverse events.
Disease flare occurrence between 18 and 44 weeks was measured as a primary endpoint, and key secondary endpoints included JIA ACR30/50/70 response and change in Childhood Health Assessment Questionnaire Disability Index (CHAQ-DI) scores from part 2 baseline. The researchers used a “gatekeeping approach” that sequenced outcome measures in their statistical analysis to control for false positives in primary and secondary outcomes, where statistical significance could be achieved only if the previous outcome in the sequence was statistically significant.
Patients had a median age of 13 years, and most were female, white (about 87%), and between one-third and one-half of patients were based in North America. JIA disease duration was a median of about 2.5 years, C-reactive protein was about 0.3 mg/dL, and median CHAQ-DI scores were about 0.9 across tofacitinib and placebo groups. Other baseline characteristics were balanced between the two groups, Dr. Brunner said.
“Patients with polyarticular-course JIA in the open-label study experienced a rapid improvement of their disease activity from very high to moderate within 18 weeks,” Dr. Brunner said in her presentation. “[T]ofacitinib demonstrated significantly greater efficacy versus placebo in patients with polyarticular-course JIA based on occurrence of fewer flares in part 2.”
Specifically, disease flare occurred in 29.2% of patients by 44 weeks in the tofacitinib group, compared with 52.9% of patients in the placebo group (P = .0031), for an overall 54% lower risk of flare among patients receiving tofacitinib (hazard ratio, 0.459; 95% confidence interval, 0.268-0.785; P = .0037). The response rate was higher for patients receiving tofacitinib at 44 weeks when measured by JIA ACR30 (70.8% vs. 47.1% with placebo; P = .0031) or by JIA ACR50 (66.7% vs. 47.1%; P = .0166) and JIA ACR70 criteria (54.2% vs. 37.1%; P = .0387). The change in CHAQ-DI score also improved at 44 weeks to a significantly greater extent in the tofacitinib group than with placebo (–0.09 vs. 0.03; P = .0292).
“The safety profile of tofacitinib in children with JIA was comparable to what you have seen or known in the [rheumatoid arthritis] population, and no new safety risks were identified in this pediatric population,” Dr. Brunner said.
The researchers reported ties with Pfizer, which funded the study, and more than two dozen other pharmaceutical companies.
SOURCE: Brunner HI et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract L22.
REPORTING FROM ACR 2019
Brains of MDD patients show alterations in areas tied to positive emotions
The brains of medication-naive patients with major depressive disorder (MDD) exhibit interhemispheric structural imbalances in areas that regulate positive emotional processes, results of a small cross-sectional study suggest.
“To the best of our knowledge, asymmetric alterations in cortical thickness and subcortical volume in patients with MDD have not yet been reported,” wrote Zhiwei Zuo, of the department of radiology, Southwest Hospital, Army Medical University, Chongqing, China, and associates. “A comprehensive understanding of the cerebral pathophysiology changes in depression is essential and may lead to more targeted approaches for the prevention and treatment of MDD.”
The investigators enrolled 35 medication-naive, untreated patients with MDD from the hospital’s department of psychology, and 35 age-, gender-, and education-matched controls. Using whole-brain analysis, the investigators identified asymmetry in cortical thickness and subcortical volume that was mostly present in the cortical-striatal-pallidal-thalamic circuit. This part of the brain helps translate underlying positive affect processes into conscious feelings of pleasure, the authors reported. in recent years (Clin Psychol Psychother. 2012 Jul-Aug;19[4]:326-40). The current study results were published in NeuroImage: Clinical.
Some limitations of the study include its small sample size and its cross-sectional nature. Nevertheless, they said, the findings could provide possible targets for therapeutic monitoring of the illness.
“These alterations were independent of depressive symptom severity, suggesting that cerebral asymmetry could be an appropriate indicator of morphological variations in mental disease,” the investigators noted.
The study was funded by the National Nature Science Foundation of China, the National Key Research and Development Plan of China, and the Innovative Talents Project of Southwest Hospital. The authors had no conflicts of interest to disclose.
SOURCE: Zuo Z et al. Neuroimage Clin. 2019. doi: 10.1016/j.nicl.2018.101614.
The brains of medication-naive patients with major depressive disorder (MDD) exhibit interhemispheric structural imbalances in areas that regulate positive emotional processes, results of a small cross-sectional study suggest.
“To the best of our knowledge, asymmetric alterations in cortical thickness and subcortical volume in patients with MDD have not yet been reported,” wrote Zhiwei Zuo, of the department of radiology, Southwest Hospital, Army Medical University, Chongqing, China, and associates. “A comprehensive understanding of the cerebral pathophysiology changes in depression is essential and may lead to more targeted approaches for the prevention and treatment of MDD.”
The investigators enrolled 35 medication-naive, untreated patients with MDD from the hospital’s department of psychology, and 35 age-, gender-, and education-matched controls. Using whole-brain analysis, the investigators identified asymmetry in cortical thickness and subcortical volume that was mostly present in the cortical-striatal-pallidal-thalamic circuit. This part of the brain helps translate underlying positive affect processes into conscious feelings of pleasure, the authors reported. in recent years (Clin Psychol Psychother. 2012 Jul-Aug;19[4]:326-40). The current study results were published in NeuroImage: Clinical.
Some limitations of the study include its small sample size and its cross-sectional nature. Nevertheless, they said, the findings could provide possible targets for therapeutic monitoring of the illness.
“These alterations were independent of depressive symptom severity, suggesting that cerebral asymmetry could be an appropriate indicator of morphological variations in mental disease,” the investigators noted.
The study was funded by the National Nature Science Foundation of China, the National Key Research and Development Plan of China, and the Innovative Talents Project of Southwest Hospital. The authors had no conflicts of interest to disclose.
SOURCE: Zuo Z et al. Neuroimage Clin. 2019. doi: 10.1016/j.nicl.2018.101614.
The brains of medication-naive patients with major depressive disorder (MDD) exhibit interhemispheric structural imbalances in areas that regulate positive emotional processes, results of a small cross-sectional study suggest.
“To the best of our knowledge, asymmetric alterations in cortical thickness and subcortical volume in patients with MDD have not yet been reported,” wrote Zhiwei Zuo, of the department of radiology, Southwest Hospital, Army Medical University, Chongqing, China, and associates. “A comprehensive understanding of the cerebral pathophysiology changes in depression is essential and may lead to more targeted approaches for the prevention and treatment of MDD.”
The investigators enrolled 35 medication-naive, untreated patients with MDD from the hospital’s department of psychology, and 35 age-, gender-, and education-matched controls. Using whole-brain analysis, the investigators identified asymmetry in cortical thickness and subcortical volume that was mostly present in the cortical-striatal-pallidal-thalamic circuit. This part of the brain helps translate underlying positive affect processes into conscious feelings of pleasure, the authors reported. in recent years (Clin Psychol Psychother. 2012 Jul-Aug;19[4]:326-40). The current study results were published in NeuroImage: Clinical.
Some limitations of the study include its small sample size and its cross-sectional nature. Nevertheless, they said, the findings could provide possible targets for therapeutic monitoring of the illness.
“These alterations were independent of depressive symptom severity, suggesting that cerebral asymmetry could be an appropriate indicator of morphological variations in mental disease,” the investigators noted.
The study was funded by the National Nature Science Foundation of China, the National Key Research and Development Plan of China, and the Innovative Talents Project of Southwest Hospital. The authors had no conflicts of interest to disclose.
SOURCE: Zuo Z et al. Neuroimage Clin. 2019. doi: 10.1016/j.nicl.2018.101614.
FROM NEUROIMAGE: CLINICAL
FDA investigates NDMA contamination in metformin
This follows reports of low-level NDMA contamination of metformin in other countries and of a few regulatory agencies issuing recalls for the drug, according to a statement from Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research.
“There are no metformin recalls affecting the U.S. market at this time,” the agency emphasized in the statement. It said NDMA levels in affected medication have been low, at or even below the acceptable intake limit, and there is currently no evidence indicating that metformin drugs within the United States or European Union have been contaminated.
The FDA advised that patients should continue taking metformin alone or in combination with other drugs to control their diabetes and that it would be dangerous for them to stop taking the medication without first discussing it with their providers. It also recommended that providers continue to use metformin when “clinically appropriate” while the investigation is underway as there are no alternative therapies to treat the disease in the same way.
NDMA is a common contaminant that is found in water and some foods and has probable carcinogenic effects when exposure is too high. The acceptable daily intake for NDMA in the United States is 96 ng/day, according to the statement, though people who take in that amount or less every day for 70 years are not expected to have an increased risk of cancer.
Both the FDA and its counterpart, the European Medicines Agency, have recently investigated the presence of NDMA impurities in ranitidine, a drug used to reduce production of stomach acid, which led to several manufacturers issuing recalls for it.
The agencies have also investigated angiotensin II receptor blockers, which are used to treat hypertension, heart failure, and high blood pressure.
The presence of NDMA “can be related to the drug’s manufacturing process or its chemical structure or even the conditions in which they are stored or packaged. As food and drugs are processed in the body, nitrosamines, including NDMA, can be formed,” Dr. Woodcock noted in the statement.
“We are monitoring this issue closely to assess any potential impact on patients with diabetes,” said Robert W. Lash, MD, chief professional and clinical affairs officer of the Endocrine Society. “We have members around the world and are concerned about the possibility of carcinogenic impurities in medications, both in the United States and elsewhere.”
This follows reports of low-level NDMA contamination of metformin in other countries and of a few regulatory agencies issuing recalls for the drug, according to a statement from Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research.
“There are no metformin recalls affecting the U.S. market at this time,” the agency emphasized in the statement. It said NDMA levels in affected medication have been low, at or even below the acceptable intake limit, and there is currently no evidence indicating that metformin drugs within the United States or European Union have been contaminated.
The FDA advised that patients should continue taking metformin alone or in combination with other drugs to control their diabetes and that it would be dangerous for them to stop taking the medication without first discussing it with their providers. It also recommended that providers continue to use metformin when “clinically appropriate” while the investigation is underway as there are no alternative therapies to treat the disease in the same way.
NDMA is a common contaminant that is found in water and some foods and has probable carcinogenic effects when exposure is too high. The acceptable daily intake for NDMA in the United States is 96 ng/day, according to the statement, though people who take in that amount or less every day for 70 years are not expected to have an increased risk of cancer.
Both the FDA and its counterpart, the European Medicines Agency, have recently investigated the presence of NDMA impurities in ranitidine, a drug used to reduce production of stomach acid, which led to several manufacturers issuing recalls for it.
The agencies have also investigated angiotensin II receptor blockers, which are used to treat hypertension, heart failure, and high blood pressure.
The presence of NDMA “can be related to the drug’s manufacturing process or its chemical structure or even the conditions in which they are stored or packaged. As food and drugs are processed in the body, nitrosamines, including NDMA, can be formed,” Dr. Woodcock noted in the statement.
“We are monitoring this issue closely to assess any potential impact on patients with diabetes,” said Robert W. Lash, MD, chief professional and clinical affairs officer of the Endocrine Society. “We have members around the world and are concerned about the possibility of carcinogenic impurities in medications, both in the United States and elsewhere.”
This follows reports of low-level NDMA contamination of metformin in other countries and of a few regulatory agencies issuing recalls for the drug, according to a statement from Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research.
“There are no metformin recalls affecting the U.S. market at this time,” the agency emphasized in the statement. It said NDMA levels in affected medication have been low, at or even below the acceptable intake limit, and there is currently no evidence indicating that metformin drugs within the United States or European Union have been contaminated.
The FDA advised that patients should continue taking metformin alone or in combination with other drugs to control their diabetes and that it would be dangerous for them to stop taking the medication without first discussing it with their providers. It also recommended that providers continue to use metformin when “clinically appropriate” while the investigation is underway as there are no alternative therapies to treat the disease in the same way.
NDMA is a common contaminant that is found in water and some foods and has probable carcinogenic effects when exposure is too high. The acceptable daily intake for NDMA in the United States is 96 ng/day, according to the statement, though people who take in that amount or less every day for 70 years are not expected to have an increased risk of cancer.
Both the FDA and its counterpart, the European Medicines Agency, have recently investigated the presence of NDMA impurities in ranitidine, a drug used to reduce production of stomach acid, which led to several manufacturers issuing recalls for it.
The agencies have also investigated angiotensin II receptor blockers, which are used to treat hypertension, heart failure, and high blood pressure.
The presence of NDMA “can be related to the drug’s manufacturing process or its chemical structure or even the conditions in which they are stored or packaged. As food and drugs are processed in the body, nitrosamines, including NDMA, can be formed,” Dr. Woodcock noted in the statement.
“We are monitoring this issue closely to assess any potential impact on patients with diabetes,” said Robert W. Lash, MD, chief professional and clinical affairs officer of the Endocrine Society. “We have members around the world and are concerned about the possibility of carcinogenic impurities in medications, both in the United States and elsewhere.”
Bringing the HPV vaccination rate into line with other adolescent immunizations
Overall adolescent vaccination coverage is improving in the United States.1 But for adolescents up to 15 years of age, there’s a large gap between the rate of vaccination for human papillomavirus (HPV) and the higher rates of coverage for tetanus, diphtheria, and acellular pertussis (Tdap) and meningococcal conjugate (MenACWY) vaccines.1 Adopting or refining practice customs reviewed in this article can increase HPV vaccination rates and continue to improve coverage of all vaccines recommended by the Advisory Committee on Immunization Practices (ACIP) for adolescents between the ages of 11 and 12.
The evolution of ACIP’s HPV vaccine recommendations
Before December 2016, ACIP recommended a 3-dose HPV series for all adolescents between the ages of 11 and 12, given on a 0, 1-2, and 6-month schedule.2 The series could be started at 9 years of age. It could be administered to females as old as 26 years, and to males through 21 years (or ages 22-26 years for those who wish to be vaccinated, who have certain medical conditions, or who are included in special populations—ie, gay and bisexual men, men who have sex with men, immunocompromised men, men with human immunodeficiency virus [HIV], and transgender men).
In 2016, ACIP revised its recommendation for adolescents who initiate vaccination before their 15th birthday: a 2-dose schedule is adequate, with the second dose given 6 to 12 months after the first dose. For those who initiate vaccination on or after their 15th birthday, and for those with certain medical conditions, the recommendation remains 3 doses on a 0, 1-2, and 6-month schedule.3
As of August 2019,4 ACIP now recommends that all women and men receive catch-up HPV vaccination through age 26. For individuals 27 to 45 years of age who have not been adequately vaccinated, HPV vaccine may be given based on shared clinical decision making with their physician.
How are we doing?
Overall, adolescent vaccination coverage is improving in the United States (see “Vaccination goals from ACIP and Healthy People 2020”1,5,6), but the rate of improvement of HPV coverage is lower than that for Tdap and MenACWY coverage by age 15 years (although completion of the MenACWY vaccine series is low). From 2015 to 2016, coverage increased for 1 or more doses of Tdap, from 86.4% to 88% among 17-year olds (87.9% for 15-year olds), and coverage for 1 or more doses of MenACWY increased from 81.7% to 83.5% among 17-year olds (80.4% among 15-year olds).1 Both Tdap and MenACWY coverage rates have surpassed Healthy People 2020 goals of 80%, and the focus now is on maintenance of coverage. Data from the 2016 National Immunization Survey (NIS)-Teen show that completion of the HPV vaccine series (applying updated HPV vaccine recommendations retrospectively) increased to 45.4% for 15-year-olds,1 still far below the Healthy People 2020 goal of 80%. Completion rates for 2 or more doses of MenACWY also increased from 33.3% to 39.1%.1
SIDEBAR
Vaccination goals from ACIP and Healthy People 2020
The Advisory Committee on Immunization Practices (ACIP) recommends that adolescents routinely receive several vaccines between the ages of 11 and 12 years: an annual influenza vaccine, Tdap, the first dose of MenACWY, and initiation of the HPV series. ACIP also advises a booster dose of MenACWY at age 16 years, and teens and young adults (16-23 years) also may be vaccinated with a multidose serogroup B meningococcal vaccine, preferably before age 18. For those adolescents not up to date with their childhood vaccines, ACIP recommends the following catch-up vaccinations: measles, mumps, rubella (MMR, 2 doses); hepatitis B (HepB, 3 doses); and varicella (VAR, 2 doses).5
Healthy People 2020. In December 2010, the US Department of Health and Human Services released Healthy People 2020, a wide-ranging initiative on health promotion and disease prevention that includes 10-year objectives of increasing coverage with Tdap, at least one dose of MenACWY, and completion of the HPV series among 80% of those ages 13 to 15 years.6 This initiative reflects extensive feedback from more than 2000 organizations and authorities in public health and prevention at federal, state, and local levels—as well as from the public. Adolescent vaccination coverage is estimated by the Centers for Disease Control and Prevention using data from the National Immunization Survey (NIS)-Teen annual survey conducted among parents and guardians of adolescents ages 13 to 17 years.1
Common barriers to improved vaccine coverage
Barriers to improved vaccination rates include a lack of regular assessment of vaccine status; limited use of electronic records, tools, and immunization registries; lack of health care provider knowledge on current vaccine recommendations; vaccine costs; missed opportunities; and patient/parent refusals.7,8 The Community Preventive Services Task Force outlines several well-established evidence-based ways that administrators and physicians can counter these barriers:
- give a strong recommendation to vaccinate,9,10
- incorporate an audit/feedback mechanism for health care providers who vaccinate,9,11
- use electronic alerts to remind health care providers to vaccinate,9,12
- use your state’s electronic immunization information systems (IIS),7,13
- appoint a vaccine practice team/vaccine champion,9,14 and
- implement standing orders and reminder/recall systems.7,9,15
The passage of the Affordable Care Act (ACA)—which mandates that certain preventive services, including ACIP-recommended immunizations, be covered as part of basic care at no cost-sharing—reduces the once-common financial barrier to vaccine uptake.16 A key contributor to low uptake of HPV vaccination by adolescents is parental refusal.17
Continue to: The threats posed by HPV
The threats posed by HPV
HPV infections are the most commonly transmitted infections in the United States and nearly all men and women will be exposed to one or more types of HPV at some point in their lives. Current data show that 79 million Americans, most in their late teens and early 20s, are infected with HPV, and about 14 million people in the United States become newly infected each year.18 HPV is a DNA tumor virus that causes epithelial proliferation at cutaneous and mucosal surfaces.
There are more than 100 types of the virus,19 including more than 40 strains that infect the human genital tract. Of the latter 40 strains, there are oncogenic or high-risk types and non-oncogenic or low-risk types.20 HPV infection with high-risk types causes cervical, vaginal, and vulvar cancers in women; penile cancers in men; and oropharyngeal and anal cancers in both men and women. Low-risk HPV types cause genital warts in both men and women.21 The current available HPV vaccine in the United States is a 9-valent vaccine (9vHPV) that replaces the former 2- and 4-valent HPV vaccines and includes immunogenic coverage against high-risk HPV types 16, 18, 31, 33, 45, 52, and 58; and low-risk types 6 and 11.22
Centers for Disease Control and Prevention (CDC) data from 2010 to 2014 show that approximately 23,700 women and approximately 17,300 men in the United States developed HPV-associated cancer. Most common in women are cervical cancers and in men, oropharyngeal cancers (cancers of the back of the throat, base of the tongue, and tonsils). Using population-based data to genotype HPV types from cancer tissues, the CDC reports that HPV is responsible for about 90% of cervical and anal cancers, 70% of oropharyngeal, vaginal, and vulvar cancers, and 60% of penile cancers.23 A significant percentage of these cancers could potentially be prevented by receipt of 9vHPV.23,24
Make adolescent immunization a high priority
Anticipate opportunities to vaccinate and take steps to make your immunization and scheduling processes more prominent. With HPV specifically, you can strongly advocate for vaccination, address parental misgivings and educate them using clear communication styles, and acquire knowledge to answer concerns about potential vaccine adverse effects.
Every visit is an opportunity to vaccinate. The American Academy of Family Physicians and The American Academy of Pediatrics recommend that adolescents have annual preventive visits for screening, immunizations, and assessment and counseling for risky behaviors. However, many adolescents do not present annually for preventive visits, and fewer than half of adolescents receive regular preventive care.
Continue to: Missed opportunities for the HPV vaccine
Missed opportunities for the HPV vaccine. One study showed that at least 86% of unvaccinated adolescents had missed opportunities to receive HPV vaccine.29 A study of 14,588 adolescent girls from January 2010 through August 2015 showed that HPV vaccine was given at only 37.1% of visits in which MenACWY or Tdap vaccines were administered.30 The rate of HPV vaccination was just 26% during well adolescent visits, and 41.8% during all other primary care visits.30 Every adolescent health care visit—including visits for acute care, chronic care, follow-up, or office-based procedures—is an opportunity to review vaccination status.
Give vaccines concomitantly (simultaneously or same-day). ACIP counsels that minor illnesses, such as mild upper respiratory infections with or without low-grade fever, are not contraindications to routine vaccination.30 Also, the safety of simultaneous vaccine administration, often a concern of both parents and health care providers, has been well established. Each vaccine’s immunogenicity and safety profile are maintained when given concomitantly with other vaccines, and fewer visits are needed to complete an adolescent’s vaccination status.31,32
Immediately schedule follow up visits and use reminder/recall systems. Parents of adolescents who opt for HPV vaccination are not always aware of the timing of the 2- or 3-dose schedule and may not even be aware that more than 1 dose of vaccine is recommended.
A qualitative study of pediatric primary care providers and parents/guardians of adolescent patients showed that for HPV vaccination series completion, 65% of parents/guardians expected to be reminded of any needed doses, while 52% of the pediatric primary care providers relied on parents to schedule subsequent immunizations, and often the HPV series was not completed.33 Higher completion rates of the HPV vaccination series were achieved when follow-up appointments were scheduled at checkout for the 2nd or 3rd vaccine dose after initiation of HPV vaccination.33 The use of patient reminder/recall systems using telephone calls or mailings (phone usage is more effective than mailings) is also shown to improve vaccination completion rates.34
Recommend HPV vaccination clearly and resolutely
In a cross-sectional survey of 800 parents of adolescents ages 9 to 14 years, HPV vaccine was deemed the least likely vaccine to have been “very strongly” recommended by their health care provider, compared with the strength of recommendations for influenza, Tdap, and MenACWY vaccines.35 The strength of a health care provider’s recommendation to vaccinate is the single most influential factor in vaccine uptake.10,36,37 Most family physicians self-report “always recommending standard pediatric vaccines”; however, only a minority are following ACIP recommendations.38 A national study reported that only about two-thirds of parents who received HPV vaccine recommendations perceived a high level of health care provider endorsement.39 The takeaway point: Give a clear, unambiguous, strong recommendation to vaccinate with HPV to prevent infection; cervical, oropharyngeal, and other cancers; and genital warts.
Continue to: Tell parents why the timing is important
Tell parents why the timing is important. Inform parents that the HPV vaccine must be administered while their child is young (before the adolescent’s first sexual contact) to ensure the most robust immune response to the vaccine.40 Unsolicited explanations about sexual activity need not be offered when discussing HPV vaccination, as it is fair to assume that sexual contact is a reality for nearly all people in their adolescent or adult life; and by extension, most sexually active people will likely have exposure to HPV at some time in their lives. By adulthood, sexual activity is nearly universal: The National Longitudinal Study of Adolescent Health showed that only about 3% of participants tracked since adolescence reported no sexual experience by (average age) 28.5 years.41
How you say it matters. Many pediatricians and family physicians report recommending HPV vaccine inconsistently, behind schedule, or without urgency,42 sending mixed messages by failing to endorse HPV vaccination strongly, failing to differentiate it from other vaccines, and presenting it as an “optional” vaccine that could be delayed.43 Physicians and other health care providers who begin conversations about HPV vaccine by saying that the adolescent is “due” for the vaccine show higher vaccine recommendation quality scores than those who give unsolicited information about the vaccine, elicit questions before recommendation, or present the vaccine as an “option.”42 Parents who are “on the fence” may hesitate and decline HPV vaccination with a halfhearted recommendation.44
“Your child is due for his/her Tdap, HPV, influenza, and meningococcal vaccinations to prevent potentially devastating disease and several cancers. I highly recommend all 4 vaccinations today” is more persuasive than, “I recommend your child receive his/her Tdap, meningococcal, and influenza vaccines. And we can also discuss the HPV vaccine.”
Direct presumptive language that assumes vaccine delivery is associated with higher odds of HPV vaccine acceptance and same-day agreement to vaccination than is an open-ended participatory conversational style.45 Saying, “I believe in the importance of this cancer-preventing vaccine for your child” is more persuasive than saying, “What do you think about starting the HPV vaccination series today?”46
Don’t give up when parents initially refuse HPV vaccinations for their adolescents. Parents’ decisions about HPV vaccination may change over time. Repeated positive recommendations and counseling for HPV vaccination over multiple visits have been shown in a large multivariable analysis to increase parent acceptance of HPV vaccination: 45% of parents reported secondary acceptance of HPV vaccination, and an additional 24% intended to vaccinate in the next 12 months.47 Combining a presumptive communication style with motivational interviewing and a fact sheet has contributed to higher clinician-perceived levels of parental HPV vaccine acceptance and increased vaccination rates.48
Continue to: Know how to address parents' concerns about safety
Know how to address parents’ concerns about safety
Be prepared to discuss and answer parents’ questions or concerns regarding any vaccine, especially the HPV vaccine. Social networks are important in parents’ vaccination decision-making,49 and they may seek information from such sources as Twitter, Facebook, Google, and YouTube, where misinformation may be disseminated. A quantitative analysis of 560 YouTube videos relaying a false link between vaccines and autism or other serious adverse effects on children were uploaded between December 2007 and July 2017, with a peak of 224 videos uploaded in the first 7 months of 2017.50 Most were negative in tone and dispensed misinformation.50
The National Vaccine Information Center (NVIC) is an organization that takes a skeptical view of the US government and pharmaceutical companies. NVIC is widely criticized by scientists and leaders in vaccine science and public health as spreading false information on the risks of vaccines and, specifically, that HPV vaccination causes chronic disease. NVIC reports that receipt of HPV vaccine may increase the risk for cervical cancer and death.51 Pediatrician and vaccine researcher Dr. Paul Offit, interviewed by The Lancet in response to NVIC and other anti-vaccine groups’ messages, stated: “anti-vaccination organizations are unequivocally threatening public health.”52
Describe the robust safety-monitoring system. The CDC is aware of public concern about the safety of HPV vaccine. Ongoing monitoring of vaccine safety and studies conducted by the CDC, the Food and Drug Administration (FDA), and other organizations has documented a reassuring safety record since the vaccine’s introduction in 2006.53 Assure parents that the Vaccine Adverse Event Reporting System (VAERS) summary of 7244 reports following 9vHPV vaccination (December 1, 2014 – December 31, 2017) showed that most (97%) reports were nonserious: No new safety signals or unexpected patterns were observed, confirming consistency of the safety profile of 9vHPV with data from pre-licensure trials and post-licensure data on 4vHPV.54
Acknowledge the usually mild, transient potential risks of HPV vaccination as reported to VAERS: local injection site symptoms such as pain, redness, or swelling in the arm where the injection was given (most common adverse effect), dizziness, fainting, headache, nausea, and fever.53 Point out that fainting after vaccination is common in adolescents55 and that the CDC and ACIP recommend observation of adolescents for 15 minutes following HPV vaccination.56 Consider this 15-minute observation period after adolescent receipt of any vaccine to be part of standard practice in your vaccination setting.56
Contest unfounded views. Other common parental concerns about effects of HPV vaccine include supposed promotion of promiscuity, increased incidence of premature ovarian failure or insufficiency (POI), and increased risk of Guillain-Barré Syndrome (GBS), often propagated through published reports, media coverage, Web sites, and social media. Assure worried parents that many studies have shown that receipt of the vaccine is safe and does not lead to initiation of sexual activity or promiscuity, and, in fact, safer sexual health practices have been observed following vaccination.57-59
Continue to: A large longitudinal...
A large longitudinal adolescent health survey administered in British Columbia looked at sexual health behaviors and risk factors in adolescent girls before and after receipt of HPV vaccination (2003, 2008, 2013).59 Results showed no significant change in the reported number of sexual partners (2003-2013), increased reported use of contraception and condoms, and lower pregnancy rates.59 There is no evidence that HPV vaccines cause reproductive problems in women53; a review of VAERS reports from 2009 through 2015 did not detect any safety concerns for POI or other reproductive problems in females.60 A 2018 population-based study of nearly 200,000 women observed no increase of POI following receipt of HPV vaccination.61 In addition, several recent studies have shown no increased risk for GBS following receipt of HPV vaccine.62-64
CORRESPONDENCE
Pamela G. Rockwell, DO, FAAFP, 24 Frank Lloyd Wright Drive, SPC 5795, Room 2300, Lobby H, Ann Arbor, MI 48105; [email protected].
1. Walker TY, Elam-Evans LD, Singleton JA, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66:874-882.
2. Markowitz LE, Dunne EF, Saraiya M, et al. Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2014;63:1-30.
3. Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2016;65:1405-1408.
4. Meites E, Szilagyi PG, Chesson HW, et al. Human papillomavirus vaccination for adults: updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2019;68:698-702.
5. Robinson CL, Romero JR, Kempe A, et al. Advisory Committee on Immunization Practices (ACIP) Child/Adolescent Immunization Work Group. Advisory Committee on Immunization Practices recommended immunization schedules for persons aged 18 years or younger—United States, 2017. MMWR Morb Mortal Wkly Rep. 2017;66:134-135.
6. US Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2020. www.healthypeople.gov/node/4654/data_details. Accessed December 4, 2019.
7. Rockwell PG. What you can do to improve adult immunization rates. J Fam Pract. 2015;64:625-633.
8. Kimmel Sr, Burns IT, Wolfe RM, et al. Addressing immunization barriers, benefits, and risks. J Fam Pract. 2007;56:S61-S69.
9. Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based guide to community preventive services-methods. The Task Force on Community Preventive Services. Am J Prev Med. 2000;18:35-43.
10. Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the U.S. National Immunization Survey. Am J Public Health. 2013;103:164-169.
11. National Center for Immunization and Respiratory Diseases. General recommendations on immunization—recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 2011;60:1-64.
12. Klatt TE, Hopp E. Effect of a best-practice alert on the rate of influenza vaccination of pregnant women. Obstet Gynecol. 2012;119:301-305.
13. Jones KL, Hammer AL, Swenson C, et al. Improving adult immunization rates in primary care clinics. Nurs Econ. 2008;26:404-407.
14. Hainer BL. Vaccine administration: making the process more efficient in your practice. Fam Pract Manag. 2007;14:48-53.
15. Task Force on Community Preventive Services. Recommendations regarding interventions to improve vaccination coverage in children, adolescents, and adults. Am J Prev Med. 2000;18(suppl 1):92-96.
16. US Department of Health and Human Services. Preventive care. www.hhs.gov/healthcare/about-the-aca/preventive-care/index.html. Accessed December 4, 2019.
17. Gilkey MB, Calo WA, Marciniak, MW, et al. Parents who refuse or delay HPV vaccine: differences in vaccination behavior, beliefs, and clinical communication preferences. Hum Vaccin Immunother. 2017;13:680-686.
18. CDC. Genital HPV infection—fact sheet. www.cdc.gov/std/hpv/stdfact-hpv.htm. Accessed December 4, 2019.
19. WHO. Human papillomavirus (HPV) and cervical cancer. www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer. Accessed December 4, 2019.
20. Muñoz N, Bosch FX, de Sanjosé S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518-527.
21. Viens LJ, Henley SJ, Watson M, et al. Human papillomavirus-associated cancers—United States, 2008–2012. MMWR Morb Mortal Wkly Rep. 2016;65:661-666.
22. CDC. Luxembourg A. Program summary and new 9-valent HPV vaccine trial data. Presented at the Advisory Committee on Immunization Practices (ACIP), October 30, 2014. Atlanta, Ga. 2014. www.cdc.gov/vaccines/acip/meetings/downloads/min-archive/min-2014-10.pdf. Accessed December 4, 2019.
23. CDC. HPV and cancer. www.cdc.gov/cancer/hpv/statistics/cases.htm. Accessed December 4, 2019.
24. Lowy DR, Schiller JT. Reducing HPV-associated cancer globally. Cancer Prev Res (Phila). 2012;5:18-23.
25. Rand CM, Goldstein NPN. Patterns of primary care physician visits for US adolescents in 2014: implications for vaccination. Acad Pediatr. 2018;18:S72-S78.
26. Taylor JL, Aalsma MC, Gilbert AL, et al. Perspectives of family medicine physicians on the importance of adolescent preventive care: a multivariate analysis. BMC Fam Pract. 2016;17:4.
27. Harris SK, Aalsma MC, Weitzman ER, et al. Research on clinical preventive services for adolescents and young adults: Where are we and where do we need to go? J Adolesc Health. 2017;60:249-260.
28. Gilkey MB, Moss JL, McRee AL, et al. Do correlates of HPV vaccine initiation differ between adolescent boys and girls? Vaccine. 2012;30:5928-5934.
29. Espinosa CM, Marshall GS, Woods CR, et al. Missed opportunities for human papillomavirus vaccine initiation in an insured adolescent female population. J Pediatric Infect Dis Soc. 2017;6:360-365.
30. CDC. Update: Vaccine side effects, adverse reactions, contraindications, and precautions. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1996;45:1-35.
31. Moss JL, Reiter PL, Brewer NT. Concomitant adolescent vaccination in the U.S., 2007-2012. Am J Prev Med. 2016;51:693-705.
32. Noronha AS, Markowitz LE, Dunne EF. Systematic review of human papillomavirus vaccine coadministration. Vaccine. 2014;32:2670-2674.
33. Perkins RB, Chigurupati NL, Apte G, et al. Why don’t adolescents finish the HPV vaccine series? A qualitative study of parents and providers. Hum Vaccin Immunother. 2016;12:1528-1535.
34. Jacobson Vann JC, Szilagyi P. Patient reminder and patient recall systems to improve immunization rates. Cochrane Database Syst Rev. 2005;(3):CD003941.
35. Dempsey AF, O’Leary ST. Human papillomavirus vaccination: narrative review of studies on how providers’ vaccine communication affects attitudes and uptake. Acad Pediatr. 2018;18:S23-S27.
36. Rosenthal SL, Weiss TW, Zimet GD, et al. Predictors of HPV vaccine uptake among women aged 19–26: importance of a physician’s recommendation. Vaccine. 2011;29:890-895.
37. Gargano LM, Herbert NL, Painter JE, et al. Impact of a physician recommendation and parental immunization attitudes on receipt or intention to receive adolescent vaccines. Hum Vaccin Immunother. 2013;9:2627-2633.
38. Bonville CA, Domachowske JB, Cibula DA, et al. Immunization attitudes and practices among family medicine providers. Hum Vaccin Immunother. 2017;13:2646-2653.
39. Wilson R, Brown DR, Boothe MA, et al. Knowledge and acceptability of the HPV vaccine among ethnically diverse black women. J Immigr Minor Health. 2013;15:747-757.
40. Iversen O, Miranda MJ, Ulied A, et al. Immunogenicity of the 9-valent HPV vaccine using 2-dose regimens in girls and boys vs a 3-dose regimen in women. JAMA. 2016;316:2411–2421.
41. Haydon AA, Cheng MM, Herring AH, et al. Prevalence and predictors of sexual inexperience in adulthood. Arch Sex Behav. 2014;43:221-230.
42. Gilkey MB, Malo TL, Shah PD, et al. Quality of physician communication about human papillomavirus vaccine: findings from a national survey. Cancer Epidemiol Biomarkers Prev. 2015;24:1673-1679.
43. Gilkey MB, McRee AL. Provider communication about HPV vaccination: a systemic review. Hum Vaccin Immunother. 2016;12:1454-1468.
44. American Academy of Family Physicians. Strong recommendation to vaccinate against HPV is key to boosting uptake. www.aafp.org/news/health-of-the-public/20140212hpv-vaccltr.html. Accessed December 4, 2019.
45. Sturm L, Donahue K, Kasting M, et al. Pediatrician-parent conversations about human papillomavirus vaccination: an analysis of audio recordings. J Adolesc Health. 2017;61:246-251.
46. Malo TL, Gilkey MB, Hall ME, et al. Messages to motivate human papillomavirus vaccination: national studies of parents and physicians. Cancer Epidemiol Biomarkers Prev. 2016;25:1383-1391.
47. Kornides ML, McRee AL, Gilkey MB. Parents who decline HPV vaccination: Who later accepts and why? Acad Pediatr. 2018;18:S37-S43.
48. Reno JE, Thomas J, Pyrzanowski J, et al. Examining strategies for improving healthcare providers’ communication about adolescent HPV vaccination: evaluation of secondary outcomes in a randomized controlled trial. Hum Vaccin Immunother. 2018;15:1592-1598.
49. Brunson EK. The impact of social networks on parents’ vaccination decisions. Pediatrics. 2013;131:e1397-e1404.
50. Donzelli G, Palomba G, Federigi L, et al. Misinformation on vaccination: a quantitative analysis of YouTube videos. Hum Vaccin Immunother. 2018;14:1654-1659.
51. National Vaccine Information Center. Human papillomavirus (HPV) disease and vaccine information. www.nvic.org/Vaccines-and-Diseases/hpv.aspx. Accessed December 4, 2019.
52. Shetty P. Experts concerned about vaccination backlash. Lancet. 2010; 375:970-971.
53. CDC. Frequently asked questions about HPV vaccine safety. www.cdc.gov/vaccinesafety/vaccines/hpv/hpv-safety-faqs.html. Accessed December 4, 2019.
54. Arana J, Su J, Lewis P, et al. Post-licensure surveillance of 9-valent human papillomavirus vaccine (9vHPV) in the Vaccine Adverse Event Reporting System (VAERS), United States, 2014-2017. https://idsa.confex.com/idsa/2018/webprogram/Paper69618.html. Accessed December 4, 2019.
55. Braun MM, Patriarca PA, Ellenberg SS. Syncope after immunization. Arch Ped Adolesc Med. 1997;151:255-259.
56. Kroger AT, Duchin J, Vázquez M. General best practice guidelines for immunization. Best practices guidance of the Advisory Committee on Immunization Practices (ACIP). www.cdc.gov/vaccines/hcp/acip-recs/general-recs/index.html. Accessed December 4, 2019.
57. Hansen BT. No evidence that HPV vaccination leads to sexual risk compensation. Hum Vaccin Immunother. 2016;12:1451-1453.
58. Smith LM, Kaufman JS, Strumpf EC, et al. Effect of human papillomavirus (HPV) vaccination on clinical indicators of sexual behaviour among adolescent girls: the Ontario Grade 8 HPV Vaccine Cohort Study. CMAJ. 2015;187:E74-81.
59. Ogilvie GS, Phan F, Pederson HN, et al. Population-level sexual behaviours in adolescent girls before and after introduction of the human papillomavirus vaccine (2003-2013). CMAJ. 2018;190:E1221-E1226.
60. Arana JE, Harrington T, Cano M, et al. Post-licensure safety monitoring of quadrivalent human papillomavirus vaccine in the Vaccine Adverse Event Reporting System (VAERS), 2009-2015. Vaccine. 2018;36:1781-1788.
61. Naleway AL, Mittendorf KF, Irving SA, et al. Primary ovarian insufficiency and adolescent vaccination. Pediatrics. 2018;142. pii: e20190943.
62. Deceuninck G, Sauvageau C, Gilca V, et al. Absence of association between Guillain-Barré syndrome hospitalizations and HPV-vaccine. Expert Rev Vaccines. 2018;17:99-102.
63. Mouchet J, Salvo F, Raschi E, et al. Human papillomavirus vaccine and demyelinating diseases – a systematic review and meta-analysis. Pharmacol Res. 2018;132:108-118.
64. Gee J, Sukumaran L, Weinstraub E, et al. Risk of Guillain-Barre Syndrome following quadrivalent human papillomavirus vaccine in the Vaccine Safety Datalink. Vaccine. 2017;35:5756-5758.
Overall adolescent vaccination coverage is improving in the United States.1 But for adolescents up to 15 years of age, there’s a large gap between the rate of vaccination for human papillomavirus (HPV) and the higher rates of coverage for tetanus, diphtheria, and acellular pertussis (Tdap) and meningococcal conjugate (MenACWY) vaccines.1 Adopting or refining practice customs reviewed in this article can increase HPV vaccination rates and continue to improve coverage of all vaccines recommended by the Advisory Committee on Immunization Practices (ACIP) for adolescents between the ages of 11 and 12.
The evolution of ACIP’s HPV vaccine recommendations
Before December 2016, ACIP recommended a 3-dose HPV series for all adolescents between the ages of 11 and 12, given on a 0, 1-2, and 6-month schedule.2 The series could be started at 9 years of age. It could be administered to females as old as 26 years, and to males through 21 years (or ages 22-26 years for those who wish to be vaccinated, who have certain medical conditions, or who are included in special populations—ie, gay and bisexual men, men who have sex with men, immunocompromised men, men with human immunodeficiency virus [HIV], and transgender men).
In 2016, ACIP revised its recommendation for adolescents who initiate vaccination before their 15th birthday: a 2-dose schedule is adequate, with the second dose given 6 to 12 months after the first dose. For those who initiate vaccination on or after their 15th birthday, and for those with certain medical conditions, the recommendation remains 3 doses on a 0, 1-2, and 6-month schedule.3
As of August 2019,4 ACIP now recommends that all women and men receive catch-up HPV vaccination through age 26. For individuals 27 to 45 years of age who have not been adequately vaccinated, HPV vaccine may be given based on shared clinical decision making with their physician.
How are we doing?
Overall, adolescent vaccination coverage is improving in the United States (see “Vaccination goals from ACIP and Healthy People 2020”1,5,6), but the rate of improvement of HPV coverage is lower than that for Tdap and MenACWY coverage by age 15 years (although completion of the MenACWY vaccine series is low). From 2015 to 2016, coverage increased for 1 or more doses of Tdap, from 86.4% to 88% among 17-year olds (87.9% for 15-year olds), and coverage for 1 or more doses of MenACWY increased from 81.7% to 83.5% among 17-year olds (80.4% among 15-year olds).1 Both Tdap and MenACWY coverage rates have surpassed Healthy People 2020 goals of 80%, and the focus now is on maintenance of coverage. Data from the 2016 National Immunization Survey (NIS)-Teen show that completion of the HPV vaccine series (applying updated HPV vaccine recommendations retrospectively) increased to 45.4% for 15-year-olds,1 still far below the Healthy People 2020 goal of 80%. Completion rates for 2 or more doses of MenACWY also increased from 33.3% to 39.1%.1
SIDEBAR
Vaccination goals from ACIP and Healthy People 2020
The Advisory Committee on Immunization Practices (ACIP) recommends that adolescents routinely receive several vaccines between the ages of 11 and 12 years: an annual influenza vaccine, Tdap, the first dose of MenACWY, and initiation of the HPV series. ACIP also advises a booster dose of MenACWY at age 16 years, and teens and young adults (16-23 years) also may be vaccinated with a multidose serogroup B meningococcal vaccine, preferably before age 18. For those adolescents not up to date with their childhood vaccines, ACIP recommends the following catch-up vaccinations: measles, mumps, rubella (MMR, 2 doses); hepatitis B (HepB, 3 doses); and varicella (VAR, 2 doses).5
Healthy People 2020. In December 2010, the US Department of Health and Human Services released Healthy People 2020, a wide-ranging initiative on health promotion and disease prevention that includes 10-year objectives of increasing coverage with Tdap, at least one dose of MenACWY, and completion of the HPV series among 80% of those ages 13 to 15 years.6 This initiative reflects extensive feedback from more than 2000 organizations and authorities in public health and prevention at federal, state, and local levels—as well as from the public. Adolescent vaccination coverage is estimated by the Centers for Disease Control and Prevention using data from the National Immunization Survey (NIS)-Teen annual survey conducted among parents and guardians of adolescents ages 13 to 17 years.1
Common barriers to improved vaccine coverage
Barriers to improved vaccination rates include a lack of regular assessment of vaccine status; limited use of electronic records, tools, and immunization registries; lack of health care provider knowledge on current vaccine recommendations; vaccine costs; missed opportunities; and patient/parent refusals.7,8 The Community Preventive Services Task Force outlines several well-established evidence-based ways that administrators and physicians can counter these barriers:
- give a strong recommendation to vaccinate,9,10
- incorporate an audit/feedback mechanism for health care providers who vaccinate,9,11
- use electronic alerts to remind health care providers to vaccinate,9,12
- use your state’s electronic immunization information systems (IIS),7,13
- appoint a vaccine practice team/vaccine champion,9,14 and
- implement standing orders and reminder/recall systems.7,9,15
The passage of the Affordable Care Act (ACA)—which mandates that certain preventive services, including ACIP-recommended immunizations, be covered as part of basic care at no cost-sharing—reduces the once-common financial barrier to vaccine uptake.16 A key contributor to low uptake of HPV vaccination by adolescents is parental refusal.17
Continue to: The threats posed by HPV
The threats posed by HPV
HPV infections are the most commonly transmitted infections in the United States and nearly all men and women will be exposed to one or more types of HPV at some point in their lives. Current data show that 79 million Americans, most in their late teens and early 20s, are infected with HPV, and about 14 million people in the United States become newly infected each year.18 HPV is a DNA tumor virus that causes epithelial proliferation at cutaneous and mucosal surfaces.
There are more than 100 types of the virus,19 including more than 40 strains that infect the human genital tract. Of the latter 40 strains, there are oncogenic or high-risk types and non-oncogenic or low-risk types.20 HPV infection with high-risk types causes cervical, vaginal, and vulvar cancers in women; penile cancers in men; and oropharyngeal and anal cancers in both men and women. Low-risk HPV types cause genital warts in both men and women.21 The current available HPV vaccine in the United States is a 9-valent vaccine (9vHPV) that replaces the former 2- and 4-valent HPV vaccines and includes immunogenic coverage against high-risk HPV types 16, 18, 31, 33, 45, 52, and 58; and low-risk types 6 and 11.22
Centers for Disease Control and Prevention (CDC) data from 2010 to 2014 show that approximately 23,700 women and approximately 17,300 men in the United States developed HPV-associated cancer. Most common in women are cervical cancers and in men, oropharyngeal cancers (cancers of the back of the throat, base of the tongue, and tonsils). Using population-based data to genotype HPV types from cancer tissues, the CDC reports that HPV is responsible for about 90% of cervical and anal cancers, 70% of oropharyngeal, vaginal, and vulvar cancers, and 60% of penile cancers.23 A significant percentage of these cancers could potentially be prevented by receipt of 9vHPV.23,24
Make adolescent immunization a high priority
Anticipate opportunities to vaccinate and take steps to make your immunization and scheduling processes more prominent. With HPV specifically, you can strongly advocate for vaccination, address parental misgivings and educate them using clear communication styles, and acquire knowledge to answer concerns about potential vaccine adverse effects.
Every visit is an opportunity to vaccinate. The American Academy of Family Physicians and The American Academy of Pediatrics recommend that adolescents have annual preventive visits for screening, immunizations, and assessment and counseling for risky behaviors. However, many adolescents do not present annually for preventive visits, and fewer than half of adolescents receive regular preventive care.
Continue to: Missed opportunities for the HPV vaccine
Missed opportunities for the HPV vaccine. One study showed that at least 86% of unvaccinated adolescents had missed opportunities to receive HPV vaccine.29 A study of 14,588 adolescent girls from January 2010 through August 2015 showed that HPV vaccine was given at only 37.1% of visits in which MenACWY or Tdap vaccines were administered.30 The rate of HPV vaccination was just 26% during well adolescent visits, and 41.8% during all other primary care visits.30 Every adolescent health care visit—including visits for acute care, chronic care, follow-up, or office-based procedures—is an opportunity to review vaccination status.
Give vaccines concomitantly (simultaneously or same-day). ACIP counsels that minor illnesses, such as mild upper respiratory infections with or without low-grade fever, are not contraindications to routine vaccination.30 Also, the safety of simultaneous vaccine administration, often a concern of both parents and health care providers, has been well established. Each vaccine’s immunogenicity and safety profile are maintained when given concomitantly with other vaccines, and fewer visits are needed to complete an adolescent’s vaccination status.31,32
Immediately schedule follow up visits and use reminder/recall systems. Parents of adolescents who opt for HPV vaccination are not always aware of the timing of the 2- or 3-dose schedule and may not even be aware that more than 1 dose of vaccine is recommended.
A qualitative study of pediatric primary care providers and parents/guardians of adolescent patients showed that for HPV vaccination series completion, 65% of parents/guardians expected to be reminded of any needed doses, while 52% of the pediatric primary care providers relied on parents to schedule subsequent immunizations, and often the HPV series was not completed.33 Higher completion rates of the HPV vaccination series were achieved when follow-up appointments were scheduled at checkout for the 2nd or 3rd vaccine dose after initiation of HPV vaccination.33 The use of patient reminder/recall systems using telephone calls or mailings (phone usage is more effective than mailings) is also shown to improve vaccination completion rates.34
Recommend HPV vaccination clearly and resolutely
In a cross-sectional survey of 800 parents of adolescents ages 9 to 14 years, HPV vaccine was deemed the least likely vaccine to have been “very strongly” recommended by their health care provider, compared with the strength of recommendations for influenza, Tdap, and MenACWY vaccines.35 The strength of a health care provider’s recommendation to vaccinate is the single most influential factor in vaccine uptake.10,36,37 Most family physicians self-report “always recommending standard pediatric vaccines”; however, only a minority are following ACIP recommendations.38 A national study reported that only about two-thirds of parents who received HPV vaccine recommendations perceived a high level of health care provider endorsement.39 The takeaway point: Give a clear, unambiguous, strong recommendation to vaccinate with HPV to prevent infection; cervical, oropharyngeal, and other cancers; and genital warts.
Continue to: Tell parents why the timing is important
Tell parents why the timing is important. Inform parents that the HPV vaccine must be administered while their child is young (before the adolescent’s first sexual contact) to ensure the most robust immune response to the vaccine.40 Unsolicited explanations about sexual activity need not be offered when discussing HPV vaccination, as it is fair to assume that sexual contact is a reality for nearly all people in their adolescent or adult life; and by extension, most sexually active people will likely have exposure to HPV at some time in their lives. By adulthood, sexual activity is nearly universal: The National Longitudinal Study of Adolescent Health showed that only about 3% of participants tracked since adolescence reported no sexual experience by (average age) 28.5 years.41
How you say it matters. Many pediatricians and family physicians report recommending HPV vaccine inconsistently, behind schedule, or without urgency,42 sending mixed messages by failing to endorse HPV vaccination strongly, failing to differentiate it from other vaccines, and presenting it as an “optional” vaccine that could be delayed.43 Physicians and other health care providers who begin conversations about HPV vaccine by saying that the adolescent is “due” for the vaccine show higher vaccine recommendation quality scores than those who give unsolicited information about the vaccine, elicit questions before recommendation, or present the vaccine as an “option.”42 Parents who are “on the fence” may hesitate and decline HPV vaccination with a halfhearted recommendation.44
“Your child is due for his/her Tdap, HPV, influenza, and meningococcal vaccinations to prevent potentially devastating disease and several cancers. I highly recommend all 4 vaccinations today” is more persuasive than, “I recommend your child receive his/her Tdap, meningococcal, and influenza vaccines. And we can also discuss the HPV vaccine.”
Direct presumptive language that assumes vaccine delivery is associated with higher odds of HPV vaccine acceptance and same-day agreement to vaccination than is an open-ended participatory conversational style.45 Saying, “I believe in the importance of this cancer-preventing vaccine for your child” is more persuasive than saying, “What do you think about starting the HPV vaccination series today?”46
Don’t give up when parents initially refuse HPV vaccinations for their adolescents. Parents’ decisions about HPV vaccination may change over time. Repeated positive recommendations and counseling for HPV vaccination over multiple visits have been shown in a large multivariable analysis to increase parent acceptance of HPV vaccination: 45% of parents reported secondary acceptance of HPV vaccination, and an additional 24% intended to vaccinate in the next 12 months.47 Combining a presumptive communication style with motivational interviewing and a fact sheet has contributed to higher clinician-perceived levels of parental HPV vaccine acceptance and increased vaccination rates.48
Continue to: Know how to address parents' concerns about safety
Know how to address parents’ concerns about safety
Be prepared to discuss and answer parents’ questions or concerns regarding any vaccine, especially the HPV vaccine. Social networks are important in parents’ vaccination decision-making,49 and they may seek information from such sources as Twitter, Facebook, Google, and YouTube, where misinformation may be disseminated. A quantitative analysis of 560 YouTube videos relaying a false link between vaccines and autism or other serious adverse effects on children were uploaded between December 2007 and July 2017, with a peak of 224 videos uploaded in the first 7 months of 2017.50 Most were negative in tone and dispensed misinformation.50
The National Vaccine Information Center (NVIC) is an organization that takes a skeptical view of the US government and pharmaceutical companies. NVIC is widely criticized by scientists and leaders in vaccine science and public health as spreading false information on the risks of vaccines and, specifically, that HPV vaccination causes chronic disease. NVIC reports that receipt of HPV vaccine may increase the risk for cervical cancer and death.51 Pediatrician and vaccine researcher Dr. Paul Offit, interviewed by The Lancet in response to NVIC and other anti-vaccine groups’ messages, stated: “anti-vaccination organizations are unequivocally threatening public health.”52
Describe the robust safety-monitoring system. The CDC is aware of public concern about the safety of HPV vaccine. Ongoing monitoring of vaccine safety and studies conducted by the CDC, the Food and Drug Administration (FDA), and other organizations has documented a reassuring safety record since the vaccine’s introduction in 2006.53 Assure parents that the Vaccine Adverse Event Reporting System (VAERS) summary of 7244 reports following 9vHPV vaccination (December 1, 2014 – December 31, 2017) showed that most (97%) reports were nonserious: No new safety signals or unexpected patterns were observed, confirming consistency of the safety profile of 9vHPV with data from pre-licensure trials and post-licensure data on 4vHPV.54
Acknowledge the usually mild, transient potential risks of HPV vaccination as reported to VAERS: local injection site symptoms such as pain, redness, or swelling in the arm where the injection was given (most common adverse effect), dizziness, fainting, headache, nausea, and fever.53 Point out that fainting after vaccination is common in adolescents55 and that the CDC and ACIP recommend observation of adolescents for 15 minutes following HPV vaccination.56 Consider this 15-minute observation period after adolescent receipt of any vaccine to be part of standard practice in your vaccination setting.56
Contest unfounded views. Other common parental concerns about effects of HPV vaccine include supposed promotion of promiscuity, increased incidence of premature ovarian failure or insufficiency (POI), and increased risk of Guillain-Barré Syndrome (GBS), often propagated through published reports, media coverage, Web sites, and social media. Assure worried parents that many studies have shown that receipt of the vaccine is safe and does not lead to initiation of sexual activity or promiscuity, and, in fact, safer sexual health practices have been observed following vaccination.57-59
Continue to: A large longitudinal...
A large longitudinal adolescent health survey administered in British Columbia looked at sexual health behaviors and risk factors in adolescent girls before and after receipt of HPV vaccination (2003, 2008, 2013).59 Results showed no significant change in the reported number of sexual partners (2003-2013), increased reported use of contraception and condoms, and lower pregnancy rates.59 There is no evidence that HPV vaccines cause reproductive problems in women53; a review of VAERS reports from 2009 through 2015 did not detect any safety concerns for POI or other reproductive problems in females.60 A 2018 population-based study of nearly 200,000 women observed no increase of POI following receipt of HPV vaccination.61 In addition, several recent studies have shown no increased risk for GBS following receipt of HPV vaccine.62-64
CORRESPONDENCE
Pamela G. Rockwell, DO, FAAFP, 24 Frank Lloyd Wright Drive, SPC 5795, Room 2300, Lobby H, Ann Arbor, MI 48105; [email protected].
Overall adolescent vaccination coverage is improving in the United States.1 But for adolescents up to 15 years of age, there’s a large gap between the rate of vaccination for human papillomavirus (HPV) and the higher rates of coverage for tetanus, diphtheria, and acellular pertussis (Tdap) and meningococcal conjugate (MenACWY) vaccines.1 Adopting or refining practice customs reviewed in this article can increase HPV vaccination rates and continue to improve coverage of all vaccines recommended by the Advisory Committee on Immunization Practices (ACIP) for adolescents between the ages of 11 and 12.
The evolution of ACIP’s HPV vaccine recommendations
Before December 2016, ACIP recommended a 3-dose HPV series for all adolescents between the ages of 11 and 12, given on a 0, 1-2, and 6-month schedule.2 The series could be started at 9 years of age. It could be administered to females as old as 26 years, and to males through 21 years (or ages 22-26 years for those who wish to be vaccinated, who have certain medical conditions, or who are included in special populations—ie, gay and bisexual men, men who have sex with men, immunocompromised men, men with human immunodeficiency virus [HIV], and transgender men).
In 2016, ACIP revised its recommendation for adolescents who initiate vaccination before their 15th birthday: a 2-dose schedule is adequate, with the second dose given 6 to 12 months after the first dose. For those who initiate vaccination on or after their 15th birthday, and for those with certain medical conditions, the recommendation remains 3 doses on a 0, 1-2, and 6-month schedule.3
As of August 2019,4 ACIP now recommends that all women and men receive catch-up HPV vaccination through age 26. For individuals 27 to 45 years of age who have not been adequately vaccinated, HPV vaccine may be given based on shared clinical decision making with their physician.
How are we doing?
Overall, adolescent vaccination coverage is improving in the United States (see “Vaccination goals from ACIP and Healthy People 2020”1,5,6), but the rate of improvement of HPV coverage is lower than that for Tdap and MenACWY coverage by age 15 years (although completion of the MenACWY vaccine series is low). From 2015 to 2016, coverage increased for 1 or more doses of Tdap, from 86.4% to 88% among 17-year olds (87.9% for 15-year olds), and coverage for 1 or more doses of MenACWY increased from 81.7% to 83.5% among 17-year olds (80.4% among 15-year olds).1 Both Tdap and MenACWY coverage rates have surpassed Healthy People 2020 goals of 80%, and the focus now is on maintenance of coverage. Data from the 2016 National Immunization Survey (NIS)-Teen show that completion of the HPV vaccine series (applying updated HPV vaccine recommendations retrospectively) increased to 45.4% for 15-year-olds,1 still far below the Healthy People 2020 goal of 80%. Completion rates for 2 or more doses of MenACWY also increased from 33.3% to 39.1%.1
SIDEBAR
Vaccination goals from ACIP and Healthy People 2020
The Advisory Committee on Immunization Practices (ACIP) recommends that adolescents routinely receive several vaccines between the ages of 11 and 12 years: an annual influenza vaccine, Tdap, the first dose of MenACWY, and initiation of the HPV series. ACIP also advises a booster dose of MenACWY at age 16 years, and teens and young adults (16-23 years) also may be vaccinated with a multidose serogroup B meningococcal vaccine, preferably before age 18. For those adolescents not up to date with their childhood vaccines, ACIP recommends the following catch-up vaccinations: measles, mumps, rubella (MMR, 2 doses); hepatitis B (HepB, 3 doses); and varicella (VAR, 2 doses).5
Healthy People 2020. In December 2010, the US Department of Health and Human Services released Healthy People 2020, a wide-ranging initiative on health promotion and disease prevention that includes 10-year objectives of increasing coverage with Tdap, at least one dose of MenACWY, and completion of the HPV series among 80% of those ages 13 to 15 years.6 This initiative reflects extensive feedback from more than 2000 organizations and authorities in public health and prevention at federal, state, and local levels—as well as from the public. Adolescent vaccination coverage is estimated by the Centers for Disease Control and Prevention using data from the National Immunization Survey (NIS)-Teen annual survey conducted among parents and guardians of adolescents ages 13 to 17 years.1
Common barriers to improved vaccine coverage
Barriers to improved vaccination rates include a lack of regular assessment of vaccine status; limited use of electronic records, tools, and immunization registries; lack of health care provider knowledge on current vaccine recommendations; vaccine costs; missed opportunities; and patient/parent refusals.7,8 The Community Preventive Services Task Force outlines several well-established evidence-based ways that administrators and physicians can counter these barriers:
- give a strong recommendation to vaccinate,9,10
- incorporate an audit/feedback mechanism for health care providers who vaccinate,9,11
- use electronic alerts to remind health care providers to vaccinate,9,12
- use your state’s electronic immunization information systems (IIS),7,13
- appoint a vaccine practice team/vaccine champion,9,14 and
- implement standing orders and reminder/recall systems.7,9,15
The passage of the Affordable Care Act (ACA)—which mandates that certain preventive services, including ACIP-recommended immunizations, be covered as part of basic care at no cost-sharing—reduces the once-common financial barrier to vaccine uptake.16 A key contributor to low uptake of HPV vaccination by adolescents is parental refusal.17
Continue to: The threats posed by HPV
The threats posed by HPV
HPV infections are the most commonly transmitted infections in the United States and nearly all men and women will be exposed to one or more types of HPV at some point in their lives. Current data show that 79 million Americans, most in their late teens and early 20s, are infected with HPV, and about 14 million people in the United States become newly infected each year.18 HPV is a DNA tumor virus that causes epithelial proliferation at cutaneous and mucosal surfaces.
There are more than 100 types of the virus,19 including more than 40 strains that infect the human genital tract. Of the latter 40 strains, there are oncogenic or high-risk types and non-oncogenic or low-risk types.20 HPV infection with high-risk types causes cervical, vaginal, and vulvar cancers in women; penile cancers in men; and oropharyngeal and anal cancers in both men and women. Low-risk HPV types cause genital warts in both men and women.21 The current available HPV vaccine in the United States is a 9-valent vaccine (9vHPV) that replaces the former 2- and 4-valent HPV vaccines and includes immunogenic coverage against high-risk HPV types 16, 18, 31, 33, 45, 52, and 58; and low-risk types 6 and 11.22
Centers for Disease Control and Prevention (CDC) data from 2010 to 2014 show that approximately 23,700 women and approximately 17,300 men in the United States developed HPV-associated cancer. Most common in women are cervical cancers and in men, oropharyngeal cancers (cancers of the back of the throat, base of the tongue, and tonsils). Using population-based data to genotype HPV types from cancer tissues, the CDC reports that HPV is responsible for about 90% of cervical and anal cancers, 70% of oropharyngeal, vaginal, and vulvar cancers, and 60% of penile cancers.23 A significant percentage of these cancers could potentially be prevented by receipt of 9vHPV.23,24
Make adolescent immunization a high priority
Anticipate opportunities to vaccinate and take steps to make your immunization and scheduling processes more prominent. With HPV specifically, you can strongly advocate for vaccination, address parental misgivings and educate them using clear communication styles, and acquire knowledge to answer concerns about potential vaccine adverse effects.
Every visit is an opportunity to vaccinate. The American Academy of Family Physicians and The American Academy of Pediatrics recommend that adolescents have annual preventive visits for screening, immunizations, and assessment and counseling for risky behaviors. However, many adolescents do not present annually for preventive visits, and fewer than half of adolescents receive regular preventive care.
Continue to: Missed opportunities for the HPV vaccine
Missed opportunities for the HPV vaccine. One study showed that at least 86% of unvaccinated adolescents had missed opportunities to receive HPV vaccine.29 A study of 14,588 adolescent girls from January 2010 through August 2015 showed that HPV vaccine was given at only 37.1% of visits in which MenACWY or Tdap vaccines were administered.30 The rate of HPV vaccination was just 26% during well adolescent visits, and 41.8% during all other primary care visits.30 Every adolescent health care visit—including visits for acute care, chronic care, follow-up, or office-based procedures—is an opportunity to review vaccination status.
Give vaccines concomitantly (simultaneously or same-day). ACIP counsels that minor illnesses, such as mild upper respiratory infections with or without low-grade fever, are not contraindications to routine vaccination.30 Also, the safety of simultaneous vaccine administration, often a concern of both parents and health care providers, has been well established. Each vaccine’s immunogenicity and safety profile are maintained when given concomitantly with other vaccines, and fewer visits are needed to complete an adolescent’s vaccination status.31,32
Immediately schedule follow up visits and use reminder/recall systems. Parents of adolescents who opt for HPV vaccination are not always aware of the timing of the 2- or 3-dose schedule and may not even be aware that more than 1 dose of vaccine is recommended.
A qualitative study of pediatric primary care providers and parents/guardians of adolescent patients showed that for HPV vaccination series completion, 65% of parents/guardians expected to be reminded of any needed doses, while 52% of the pediatric primary care providers relied on parents to schedule subsequent immunizations, and often the HPV series was not completed.33 Higher completion rates of the HPV vaccination series were achieved when follow-up appointments were scheduled at checkout for the 2nd or 3rd vaccine dose after initiation of HPV vaccination.33 The use of patient reminder/recall systems using telephone calls or mailings (phone usage is more effective than mailings) is also shown to improve vaccination completion rates.34
Recommend HPV vaccination clearly and resolutely
In a cross-sectional survey of 800 parents of adolescents ages 9 to 14 years, HPV vaccine was deemed the least likely vaccine to have been “very strongly” recommended by their health care provider, compared with the strength of recommendations for influenza, Tdap, and MenACWY vaccines.35 The strength of a health care provider’s recommendation to vaccinate is the single most influential factor in vaccine uptake.10,36,37 Most family physicians self-report “always recommending standard pediatric vaccines”; however, only a minority are following ACIP recommendations.38 A national study reported that only about two-thirds of parents who received HPV vaccine recommendations perceived a high level of health care provider endorsement.39 The takeaway point: Give a clear, unambiguous, strong recommendation to vaccinate with HPV to prevent infection; cervical, oropharyngeal, and other cancers; and genital warts.
Continue to: Tell parents why the timing is important
Tell parents why the timing is important. Inform parents that the HPV vaccine must be administered while their child is young (before the adolescent’s first sexual contact) to ensure the most robust immune response to the vaccine.40 Unsolicited explanations about sexual activity need not be offered when discussing HPV vaccination, as it is fair to assume that sexual contact is a reality for nearly all people in their adolescent or adult life; and by extension, most sexually active people will likely have exposure to HPV at some time in their lives. By adulthood, sexual activity is nearly universal: The National Longitudinal Study of Adolescent Health showed that only about 3% of participants tracked since adolescence reported no sexual experience by (average age) 28.5 years.41
How you say it matters. Many pediatricians and family physicians report recommending HPV vaccine inconsistently, behind schedule, or without urgency,42 sending mixed messages by failing to endorse HPV vaccination strongly, failing to differentiate it from other vaccines, and presenting it as an “optional” vaccine that could be delayed.43 Physicians and other health care providers who begin conversations about HPV vaccine by saying that the adolescent is “due” for the vaccine show higher vaccine recommendation quality scores than those who give unsolicited information about the vaccine, elicit questions before recommendation, or present the vaccine as an “option.”42 Parents who are “on the fence” may hesitate and decline HPV vaccination with a halfhearted recommendation.44
“Your child is due for his/her Tdap, HPV, influenza, and meningococcal vaccinations to prevent potentially devastating disease and several cancers. I highly recommend all 4 vaccinations today” is more persuasive than, “I recommend your child receive his/her Tdap, meningococcal, and influenza vaccines. And we can also discuss the HPV vaccine.”
Direct presumptive language that assumes vaccine delivery is associated with higher odds of HPV vaccine acceptance and same-day agreement to vaccination than is an open-ended participatory conversational style.45 Saying, “I believe in the importance of this cancer-preventing vaccine for your child” is more persuasive than saying, “What do you think about starting the HPV vaccination series today?”46
Don’t give up when parents initially refuse HPV vaccinations for their adolescents. Parents’ decisions about HPV vaccination may change over time. Repeated positive recommendations and counseling for HPV vaccination over multiple visits have been shown in a large multivariable analysis to increase parent acceptance of HPV vaccination: 45% of parents reported secondary acceptance of HPV vaccination, and an additional 24% intended to vaccinate in the next 12 months.47 Combining a presumptive communication style with motivational interviewing and a fact sheet has contributed to higher clinician-perceived levels of parental HPV vaccine acceptance and increased vaccination rates.48
Continue to: Know how to address parents' concerns about safety
Know how to address parents’ concerns about safety
Be prepared to discuss and answer parents’ questions or concerns regarding any vaccine, especially the HPV vaccine. Social networks are important in parents’ vaccination decision-making,49 and they may seek information from such sources as Twitter, Facebook, Google, and YouTube, where misinformation may be disseminated. A quantitative analysis of 560 YouTube videos relaying a false link between vaccines and autism or other serious adverse effects on children were uploaded between December 2007 and July 2017, with a peak of 224 videos uploaded in the first 7 months of 2017.50 Most were negative in tone and dispensed misinformation.50
The National Vaccine Information Center (NVIC) is an organization that takes a skeptical view of the US government and pharmaceutical companies. NVIC is widely criticized by scientists and leaders in vaccine science and public health as spreading false information on the risks of vaccines and, specifically, that HPV vaccination causes chronic disease. NVIC reports that receipt of HPV vaccine may increase the risk for cervical cancer and death.51 Pediatrician and vaccine researcher Dr. Paul Offit, interviewed by The Lancet in response to NVIC and other anti-vaccine groups’ messages, stated: “anti-vaccination organizations are unequivocally threatening public health.”52
Describe the robust safety-monitoring system. The CDC is aware of public concern about the safety of HPV vaccine. Ongoing monitoring of vaccine safety and studies conducted by the CDC, the Food and Drug Administration (FDA), and other organizations has documented a reassuring safety record since the vaccine’s introduction in 2006.53 Assure parents that the Vaccine Adverse Event Reporting System (VAERS) summary of 7244 reports following 9vHPV vaccination (December 1, 2014 – December 31, 2017) showed that most (97%) reports were nonserious: No new safety signals or unexpected patterns were observed, confirming consistency of the safety profile of 9vHPV with data from pre-licensure trials and post-licensure data on 4vHPV.54
Acknowledge the usually mild, transient potential risks of HPV vaccination as reported to VAERS: local injection site symptoms such as pain, redness, or swelling in the arm where the injection was given (most common adverse effect), dizziness, fainting, headache, nausea, and fever.53 Point out that fainting after vaccination is common in adolescents55 and that the CDC and ACIP recommend observation of adolescents for 15 minutes following HPV vaccination.56 Consider this 15-minute observation period after adolescent receipt of any vaccine to be part of standard practice in your vaccination setting.56
Contest unfounded views. Other common parental concerns about effects of HPV vaccine include supposed promotion of promiscuity, increased incidence of premature ovarian failure or insufficiency (POI), and increased risk of Guillain-Barré Syndrome (GBS), often propagated through published reports, media coverage, Web sites, and social media. Assure worried parents that many studies have shown that receipt of the vaccine is safe and does not lead to initiation of sexual activity or promiscuity, and, in fact, safer sexual health practices have been observed following vaccination.57-59
Continue to: A large longitudinal...
A large longitudinal adolescent health survey administered in British Columbia looked at sexual health behaviors and risk factors in adolescent girls before and after receipt of HPV vaccination (2003, 2008, 2013).59 Results showed no significant change in the reported number of sexual partners (2003-2013), increased reported use of contraception and condoms, and lower pregnancy rates.59 There is no evidence that HPV vaccines cause reproductive problems in women53; a review of VAERS reports from 2009 through 2015 did not detect any safety concerns for POI or other reproductive problems in females.60 A 2018 population-based study of nearly 200,000 women observed no increase of POI following receipt of HPV vaccination.61 In addition, several recent studies have shown no increased risk for GBS following receipt of HPV vaccine.62-64
CORRESPONDENCE
Pamela G. Rockwell, DO, FAAFP, 24 Frank Lloyd Wright Drive, SPC 5795, Room 2300, Lobby H, Ann Arbor, MI 48105; [email protected].
1. Walker TY, Elam-Evans LD, Singleton JA, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66:874-882.
2. Markowitz LE, Dunne EF, Saraiya M, et al. Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2014;63:1-30.
3. Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2016;65:1405-1408.
4. Meites E, Szilagyi PG, Chesson HW, et al. Human papillomavirus vaccination for adults: updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2019;68:698-702.
5. Robinson CL, Romero JR, Kempe A, et al. Advisory Committee on Immunization Practices (ACIP) Child/Adolescent Immunization Work Group. Advisory Committee on Immunization Practices recommended immunization schedules for persons aged 18 years or younger—United States, 2017. MMWR Morb Mortal Wkly Rep. 2017;66:134-135.
6. US Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2020. www.healthypeople.gov/node/4654/data_details. Accessed December 4, 2019.
7. Rockwell PG. What you can do to improve adult immunization rates. J Fam Pract. 2015;64:625-633.
8. Kimmel Sr, Burns IT, Wolfe RM, et al. Addressing immunization barriers, benefits, and risks. J Fam Pract. 2007;56:S61-S69.
9. Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based guide to community preventive services-methods. The Task Force on Community Preventive Services. Am J Prev Med. 2000;18:35-43.
10. Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the U.S. National Immunization Survey. Am J Public Health. 2013;103:164-169.
11. National Center for Immunization and Respiratory Diseases. General recommendations on immunization—recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 2011;60:1-64.
12. Klatt TE, Hopp E. Effect of a best-practice alert on the rate of influenza vaccination of pregnant women. Obstet Gynecol. 2012;119:301-305.
13. Jones KL, Hammer AL, Swenson C, et al. Improving adult immunization rates in primary care clinics. Nurs Econ. 2008;26:404-407.
14. Hainer BL. Vaccine administration: making the process more efficient in your practice. Fam Pract Manag. 2007;14:48-53.
15. Task Force on Community Preventive Services. Recommendations regarding interventions to improve vaccination coverage in children, adolescents, and adults. Am J Prev Med. 2000;18(suppl 1):92-96.
16. US Department of Health and Human Services. Preventive care. www.hhs.gov/healthcare/about-the-aca/preventive-care/index.html. Accessed December 4, 2019.
17. Gilkey MB, Calo WA, Marciniak, MW, et al. Parents who refuse or delay HPV vaccine: differences in vaccination behavior, beliefs, and clinical communication preferences. Hum Vaccin Immunother. 2017;13:680-686.
18. CDC. Genital HPV infection—fact sheet. www.cdc.gov/std/hpv/stdfact-hpv.htm. Accessed December 4, 2019.
19. WHO. Human papillomavirus (HPV) and cervical cancer. www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer. Accessed December 4, 2019.
20. Muñoz N, Bosch FX, de Sanjosé S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518-527.
21. Viens LJ, Henley SJ, Watson M, et al. Human papillomavirus-associated cancers—United States, 2008–2012. MMWR Morb Mortal Wkly Rep. 2016;65:661-666.
22. CDC. Luxembourg A. Program summary and new 9-valent HPV vaccine trial data. Presented at the Advisory Committee on Immunization Practices (ACIP), October 30, 2014. Atlanta, Ga. 2014. www.cdc.gov/vaccines/acip/meetings/downloads/min-archive/min-2014-10.pdf. Accessed December 4, 2019.
23. CDC. HPV and cancer. www.cdc.gov/cancer/hpv/statistics/cases.htm. Accessed December 4, 2019.
24. Lowy DR, Schiller JT. Reducing HPV-associated cancer globally. Cancer Prev Res (Phila). 2012;5:18-23.
25. Rand CM, Goldstein NPN. Patterns of primary care physician visits for US adolescents in 2014: implications for vaccination. Acad Pediatr. 2018;18:S72-S78.
26. Taylor JL, Aalsma MC, Gilbert AL, et al. Perspectives of family medicine physicians on the importance of adolescent preventive care: a multivariate analysis. BMC Fam Pract. 2016;17:4.
27. Harris SK, Aalsma MC, Weitzman ER, et al. Research on clinical preventive services for adolescents and young adults: Where are we and where do we need to go? J Adolesc Health. 2017;60:249-260.
28. Gilkey MB, Moss JL, McRee AL, et al. Do correlates of HPV vaccine initiation differ between adolescent boys and girls? Vaccine. 2012;30:5928-5934.
29. Espinosa CM, Marshall GS, Woods CR, et al. Missed opportunities for human papillomavirus vaccine initiation in an insured adolescent female population. J Pediatric Infect Dis Soc. 2017;6:360-365.
30. CDC. Update: Vaccine side effects, adverse reactions, contraindications, and precautions. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1996;45:1-35.
31. Moss JL, Reiter PL, Brewer NT. Concomitant adolescent vaccination in the U.S., 2007-2012. Am J Prev Med. 2016;51:693-705.
32. Noronha AS, Markowitz LE, Dunne EF. Systematic review of human papillomavirus vaccine coadministration. Vaccine. 2014;32:2670-2674.
33. Perkins RB, Chigurupati NL, Apte G, et al. Why don’t adolescents finish the HPV vaccine series? A qualitative study of parents and providers. Hum Vaccin Immunother. 2016;12:1528-1535.
34. Jacobson Vann JC, Szilagyi P. Patient reminder and patient recall systems to improve immunization rates. Cochrane Database Syst Rev. 2005;(3):CD003941.
35. Dempsey AF, O’Leary ST. Human papillomavirus vaccination: narrative review of studies on how providers’ vaccine communication affects attitudes and uptake. Acad Pediatr. 2018;18:S23-S27.
36. Rosenthal SL, Weiss TW, Zimet GD, et al. Predictors of HPV vaccine uptake among women aged 19–26: importance of a physician’s recommendation. Vaccine. 2011;29:890-895.
37. Gargano LM, Herbert NL, Painter JE, et al. Impact of a physician recommendation and parental immunization attitudes on receipt or intention to receive adolescent vaccines. Hum Vaccin Immunother. 2013;9:2627-2633.
38. Bonville CA, Domachowske JB, Cibula DA, et al. Immunization attitudes and practices among family medicine providers. Hum Vaccin Immunother. 2017;13:2646-2653.
39. Wilson R, Brown DR, Boothe MA, et al. Knowledge and acceptability of the HPV vaccine among ethnically diverse black women. J Immigr Minor Health. 2013;15:747-757.
40. Iversen O, Miranda MJ, Ulied A, et al. Immunogenicity of the 9-valent HPV vaccine using 2-dose regimens in girls and boys vs a 3-dose regimen in women. JAMA. 2016;316:2411–2421.
41. Haydon AA, Cheng MM, Herring AH, et al. Prevalence and predictors of sexual inexperience in adulthood. Arch Sex Behav. 2014;43:221-230.
42. Gilkey MB, Malo TL, Shah PD, et al. Quality of physician communication about human papillomavirus vaccine: findings from a national survey. Cancer Epidemiol Biomarkers Prev. 2015;24:1673-1679.
43. Gilkey MB, McRee AL. Provider communication about HPV vaccination: a systemic review. Hum Vaccin Immunother. 2016;12:1454-1468.
44. American Academy of Family Physicians. Strong recommendation to vaccinate against HPV is key to boosting uptake. www.aafp.org/news/health-of-the-public/20140212hpv-vaccltr.html. Accessed December 4, 2019.
45. Sturm L, Donahue K, Kasting M, et al. Pediatrician-parent conversations about human papillomavirus vaccination: an analysis of audio recordings. J Adolesc Health. 2017;61:246-251.
46. Malo TL, Gilkey MB, Hall ME, et al. Messages to motivate human papillomavirus vaccination: national studies of parents and physicians. Cancer Epidemiol Biomarkers Prev. 2016;25:1383-1391.
47. Kornides ML, McRee AL, Gilkey MB. Parents who decline HPV vaccination: Who later accepts and why? Acad Pediatr. 2018;18:S37-S43.
48. Reno JE, Thomas J, Pyrzanowski J, et al. Examining strategies for improving healthcare providers’ communication about adolescent HPV vaccination: evaluation of secondary outcomes in a randomized controlled trial. Hum Vaccin Immunother. 2018;15:1592-1598.
49. Brunson EK. The impact of social networks on parents’ vaccination decisions. Pediatrics. 2013;131:e1397-e1404.
50. Donzelli G, Palomba G, Federigi L, et al. Misinformation on vaccination: a quantitative analysis of YouTube videos. Hum Vaccin Immunother. 2018;14:1654-1659.
51. National Vaccine Information Center. Human papillomavirus (HPV) disease and vaccine information. www.nvic.org/Vaccines-and-Diseases/hpv.aspx. Accessed December 4, 2019.
52. Shetty P. Experts concerned about vaccination backlash. Lancet. 2010; 375:970-971.
53. CDC. Frequently asked questions about HPV vaccine safety. www.cdc.gov/vaccinesafety/vaccines/hpv/hpv-safety-faqs.html. Accessed December 4, 2019.
54. Arana J, Su J, Lewis P, et al. Post-licensure surveillance of 9-valent human papillomavirus vaccine (9vHPV) in the Vaccine Adverse Event Reporting System (VAERS), United States, 2014-2017. https://idsa.confex.com/idsa/2018/webprogram/Paper69618.html. Accessed December 4, 2019.
55. Braun MM, Patriarca PA, Ellenberg SS. Syncope after immunization. Arch Ped Adolesc Med. 1997;151:255-259.
56. Kroger AT, Duchin J, Vázquez M. General best practice guidelines for immunization. Best practices guidance of the Advisory Committee on Immunization Practices (ACIP). www.cdc.gov/vaccines/hcp/acip-recs/general-recs/index.html. Accessed December 4, 2019.
57. Hansen BT. No evidence that HPV vaccination leads to sexual risk compensation. Hum Vaccin Immunother. 2016;12:1451-1453.
58. Smith LM, Kaufman JS, Strumpf EC, et al. Effect of human papillomavirus (HPV) vaccination on clinical indicators of sexual behaviour among adolescent girls: the Ontario Grade 8 HPV Vaccine Cohort Study. CMAJ. 2015;187:E74-81.
59. Ogilvie GS, Phan F, Pederson HN, et al. Population-level sexual behaviours in adolescent girls before and after introduction of the human papillomavirus vaccine (2003-2013). CMAJ. 2018;190:E1221-E1226.
60. Arana JE, Harrington T, Cano M, et al. Post-licensure safety monitoring of quadrivalent human papillomavirus vaccine in the Vaccine Adverse Event Reporting System (VAERS), 2009-2015. Vaccine. 2018;36:1781-1788.
61. Naleway AL, Mittendorf KF, Irving SA, et al. Primary ovarian insufficiency and adolescent vaccination. Pediatrics. 2018;142. pii: e20190943.
62. Deceuninck G, Sauvageau C, Gilca V, et al. Absence of association between Guillain-Barré syndrome hospitalizations and HPV-vaccine. Expert Rev Vaccines. 2018;17:99-102.
63. Mouchet J, Salvo F, Raschi E, et al. Human papillomavirus vaccine and demyelinating diseases – a systematic review and meta-analysis. Pharmacol Res. 2018;132:108-118.
64. Gee J, Sukumaran L, Weinstraub E, et al. Risk of Guillain-Barre Syndrome following quadrivalent human papillomavirus vaccine in the Vaccine Safety Datalink. Vaccine. 2017;35:5756-5758.
1. Walker TY, Elam-Evans LD, Singleton JA, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66:874-882.
2. Markowitz LE, Dunne EF, Saraiya M, et al. Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2014;63:1-30.
3. Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2016;65:1405-1408.
4. Meites E, Szilagyi PG, Chesson HW, et al. Human papillomavirus vaccination for adults: updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2019;68:698-702.
5. Robinson CL, Romero JR, Kempe A, et al. Advisory Committee on Immunization Practices (ACIP) Child/Adolescent Immunization Work Group. Advisory Committee on Immunization Practices recommended immunization schedules for persons aged 18 years or younger—United States, 2017. MMWR Morb Mortal Wkly Rep. 2017;66:134-135.
6. US Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2020. www.healthypeople.gov/node/4654/data_details. Accessed December 4, 2019.
7. Rockwell PG. What you can do to improve adult immunization rates. J Fam Pract. 2015;64:625-633.
8. Kimmel Sr, Burns IT, Wolfe RM, et al. Addressing immunization barriers, benefits, and risks. J Fam Pract. 2007;56:S61-S69.
9. Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based guide to community preventive services-methods. The Task Force on Community Preventive Services. Am J Prev Med. 2000;18:35-43.
10. Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the U.S. National Immunization Survey. Am J Public Health. 2013;103:164-169.
11. National Center for Immunization and Respiratory Diseases. General recommendations on immunization—recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 2011;60:1-64.
12. Klatt TE, Hopp E. Effect of a best-practice alert on the rate of influenza vaccination of pregnant women. Obstet Gynecol. 2012;119:301-305.
13. Jones KL, Hammer AL, Swenson C, et al. Improving adult immunization rates in primary care clinics. Nurs Econ. 2008;26:404-407.
14. Hainer BL. Vaccine administration: making the process more efficient in your practice. Fam Pract Manag. 2007;14:48-53.
15. Task Force on Community Preventive Services. Recommendations regarding interventions to improve vaccination coverage in children, adolescents, and adults. Am J Prev Med. 2000;18(suppl 1):92-96.
16. US Department of Health and Human Services. Preventive care. www.hhs.gov/healthcare/about-the-aca/preventive-care/index.html. Accessed December 4, 2019.
17. Gilkey MB, Calo WA, Marciniak, MW, et al. Parents who refuse or delay HPV vaccine: differences in vaccination behavior, beliefs, and clinical communication preferences. Hum Vaccin Immunother. 2017;13:680-686.
18. CDC. Genital HPV infection—fact sheet. www.cdc.gov/std/hpv/stdfact-hpv.htm. Accessed December 4, 2019.
19. WHO. Human papillomavirus (HPV) and cervical cancer. www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer. Accessed December 4, 2019.
20. Muñoz N, Bosch FX, de Sanjosé S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518-527.
21. Viens LJ, Henley SJ, Watson M, et al. Human papillomavirus-associated cancers—United States, 2008–2012. MMWR Morb Mortal Wkly Rep. 2016;65:661-666.
22. CDC. Luxembourg A. Program summary and new 9-valent HPV vaccine trial data. Presented at the Advisory Committee on Immunization Practices (ACIP), October 30, 2014. Atlanta, Ga. 2014. www.cdc.gov/vaccines/acip/meetings/downloads/min-archive/min-2014-10.pdf. Accessed December 4, 2019.
23. CDC. HPV and cancer. www.cdc.gov/cancer/hpv/statistics/cases.htm. Accessed December 4, 2019.
24. Lowy DR, Schiller JT. Reducing HPV-associated cancer globally. Cancer Prev Res (Phila). 2012;5:18-23.
25. Rand CM, Goldstein NPN. Patterns of primary care physician visits for US adolescents in 2014: implications for vaccination. Acad Pediatr. 2018;18:S72-S78.
26. Taylor JL, Aalsma MC, Gilbert AL, et al. Perspectives of family medicine physicians on the importance of adolescent preventive care: a multivariate analysis. BMC Fam Pract. 2016;17:4.
27. Harris SK, Aalsma MC, Weitzman ER, et al. Research on clinical preventive services for adolescents and young adults: Where are we and where do we need to go? J Adolesc Health. 2017;60:249-260.
28. Gilkey MB, Moss JL, McRee AL, et al. Do correlates of HPV vaccine initiation differ between adolescent boys and girls? Vaccine. 2012;30:5928-5934.
29. Espinosa CM, Marshall GS, Woods CR, et al. Missed opportunities for human papillomavirus vaccine initiation in an insured adolescent female population. J Pediatric Infect Dis Soc. 2017;6:360-365.
30. CDC. Update: Vaccine side effects, adverse reactions, contraindications, and precautions. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1996;45:1-35.
31. Moss JL, Reiter PL, Brewer NT. Concomitant adolescent vaccination in the U.S., 2007-2012. Am J Prev Med. 2016;51:693-705.
32. Noronha AS, Markowitz LE, Dunne EF. Systematic review of human papillomavirus vaccine coadministration. Vaccine. 2014;32:2670-2674.
33. Perkins RB, Chigurupati NL, Apte G, et al. Why don’t adolescents finish the HPV vaccine series? A qualitative study of parents and providers. Hum Vaccin Immunother. 2016;12:1528-1535.
34. Jacobson Vann JC, Szilagyi P. Patient reminder and patient recall systems to improve immunization rates. Cochrane Database Syst Rev. 2005;(3):CD003941.
35. Dempsey AF, O’Leary ST. Human papillomavirus vaccination: narrative review of studies on how providers’ vaccine communication affects attitudes and uptake. Acad Pediatr. 2018;18:S23-S27.
36. Rosenthal SL, Weiss TW, Zimet GD, et al. Predictors of HPV vaccine uptake among women aged 19–26: importance of a physician’s recommendation. Vaccine. 2011;29:890-895.
37. Gargano LM, Herbert NL, Painter JE, et al. Impact of a physician recommendation and parental immunization attitudes on receipt or intention to receive adolescent vaccines. Hum Vaccin Immunother. 2013;9:2627-2633.
38. Bonville CA, Domachowske JB, Cibula DA, et al. Immunization attitudes and practices among family medicine providers. Hum Vaccin Immunother. 2017;13:2646-2653.
39. Wilson R, Brown DR, Boothe MA, et al. Knowledge and acceptability of the HPV vaccine among ethnically diverse black women. J Immigr Minor Health. 2013;15:747-757.
40. Iversen O, Miranda MJ, Ulied A, et al. Immunogenicity of the 9-valent HPV vaccine using 2-dose regimens in girls and boys vs a 3-dose regimen in women. JAMA. 2016;316:2411–2421.
41. Haydon AA, Cheng MM, Herring AH, et al. Prevalence and predictors of sexual inexperience in adulthood. Arch Sex Behav. 2014;43:221-230.
42. Gilkey MB, Malo TL, Shah PD, et al. Quality of physician communication about human papillomavirus vaccine: findings from a national survey. Cancer Epidemiol Biomarkers Prev. 2015;24:1673-1679.
43. Gilkey MB, McRee AL. Provider communication about HPV vaccination: a systemic review. Hum Vaccin Immunother. 2016;12:1454-1468.
44. American Academy of Family Physicians. Strong recommendation to vaccinate against HPV is key to boosting uptake. www.aafp.org/news/health-of-the-public/20140212hpv-vaccltr.html. Accessed December 4, 2019.
45. Sturm L, Donahue K, Kasting M, et al. Pediatrician-parent conversations about human papillomavirus vaccination: an analysis of audio recordings. J Adolesc Health. 2017;61:246-251.
46. Malo TL, Gilkey MB, Hall ME, et al. Messages to motivate human papillomavirus vaccination: national studies of parents and physicians. Cancer Epidemiol Biomarkers Prev. 2016;25:1383-1391.
47. Kornides ML, McRee AL, Gilkey MB. Parents who decline HPV vaccination: Who later accepts and why? Acad Pediatr. 2018;18:S37-S43.
48. Reno JE, Thomas J, Pyrzanowski J, et al. Examining strategies for improving healthcare providers’ communication about adolescent HPV vaccination: evaluation of secondary outcomes in a randomized controlled trial. Hum Vaccin Immunother. 2018;15:1592-1598.
49. Brunson EK. The impact of social networks on parents’ vaccination decisions. Pediatrics. 2013;131:e1397-e1404.
50. Donzelli G, Palomba G, Federigi L, et al. Misinformation on vaccination: a quantitative analysis of YouTube videos. Hum Vaccin Immunother. 2018;14:1654-1659.
51. National Vaccine Information Center. Human papillomavirus (HPV) disease and vaccine information. www.nvic.org/Vaccines-and-Diseases/hpv.aspx. Accessed December 4, 2019.
52. Shetty P. Experts concerned about vaccination backlash. Lancet. 2010; 375:970-971.
53. CDC. Frequently asked questions about HPV vaccine safety. www.cdc.gov/vaccinesafety/vaccines/hpv/hpv-safety-faqs.html. Accessed December 4, 2019.
54. Arana J, Su J, Lewis P, et al. Post-licensure surveillance of 9-valent human papillomavirus vaccine (9vHPV) in the Vaccine Adverse Event Reporting System (VAERS), United States, 2014-2017. https://idsa.confex.com/idsa/2018/webprogram/Paper69618.html. Accessed December 4, 2019.
55. Braun MM, Patriarca PA, Ellenberg SS. Syncope after immunization. Arch Ped Adolesc Med. 1997;151:255-259.
56. Kroger AT, Duchin J, Vázquez M. General best practice guidelines for immunization. Best practices guidance of the Advisory Committee on Immunization Practices (ACIP). www.cdc.gov/vaccines/hcp/acip-recs/general-recs/index.html. Accessed December 4, 2019.
57. Hansen BT. No evidence that HPV vaccination leads to sexual risk compensation. Hum Vaccin Immunother. 2016;12:1451-1453.
58. Smith LM, Kaufman JS, Strumpf EC, et al. Effect of human papillomavirus (HPV) vaccination on clinical indicators of sexual behaviour among adolescent girls: the Ontario Grade 8 HPV Vaccine Cohort Study. CMAJ. 2015;187:E74-81.
59. Ogilvie GS, Phan F, Pederson HN, et al. Population-level sexual behaviours in adolescent girls before and after introduction of the human papillomavirus vaccine (2003-2013). CMAJ. 2018;190:E1221-E1226.
60. Arana JE, Harrington T, Cano M, et al. Post-licensure safety monitoring of quadrivalent human papillomavirus vaccine in the Vaccine Adverse Event Reporting System (VAERS), 2009-2015. Vaccine. 2018;36:1781-1788.
61. Naleway AL, Mittendorf KF, Irving SA, et al. Primary ovarian insufficiency and adolescent vaccination. Pediatrics. 2018;142. pii: e20190943.
62. Deceuninck G, Sauvageau C, Gilca V, et al. Absence of association between Guillain-Barré syndrome hospitalizations and HPV-vaccine. Expert Rev Vaccines. 2018;17:99-102.
63. Mouchet J, Salvo F, Raschi E, et al. Human papillomavirus vaccine and demyelinating diseases – a systematic review and meta-analysis. Pharmacol Res. 2018;132:108-118.
64. Gee J, Sukumaran L, Weinstraub E, et al. Risk of Guillain-Barre Syndrome following quadrivalent human papillomavirus vaccine in the Vaccine Safety Datalink. Vaccine. 2017;35:5756-5758.
From The Journal of Family Practice | 2019;68(10):E1-E7.
PRACTICE RECOMMENDATIONS
› Review vaccination status at every adolescent health care visit. C
› Give a clear, unambiguous, strong recommendation to vaccinate with human papillomavirus (HPV) to prevent infection; cervical, oropharyngeal, and other cancers; and genital warts. A
› Schedule follow-up appointments at checkout following initiation of HPV vaccination to help ensure completion of the series. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Docs push back on surprise billing compromise
Compromise bipartisan legislation to address surprise medical bills is getting push back from physician groups.
Leadership from the House Energy and Commerce Committee and the Senate Health, Education, Labor, and Pensions Committee on Dec. 9 unveiled a compromise bill that includes rate-setting for small surprise billing and arbitration for larger ones at a lower threshold than what was originally proposed.
The new bill, part of a broader Lower Health Care Costs Act, would protect patients from surprise medical bills related to emergency care, holding them responsible for in-network cost-sharing rates for out-of-network care provided at an in-network facility without their informed consent. Out-of-network surprise bills would be applied to the patient’s in-network deductible.
Under the legislation, providers would be paid at minimum the local, market-based median in-network negotiated rate for services, with a median rate under a $750 threshold. When the median exceeds $750, the provider or insurer would be allowed to choose arbitration process to resolve payment disputes.
The bill also protects patients by banning out-of-network facilities and providers from sending balance bills for more than in-network cost-sharing amounts.
Physician groups, however, see the legislation as a giveback to insurers that puts health care professionals at a disadvantage when negotiating to be included in insurer networks.
At issue is the $750 threshold for optional arbitration.
“If you set the arbitration system in such a way that limits the ability of a physician to go to arbitration to settle a dispute between a health plan and the doctor, and if you say that can only be done when there [are] bills that are greater than $750 for a particular service, then the vast majority of services provided by doctors will not be able to go to arbitration,” Christian Shalgian, director of advocacy and health policy at the American College of Surgeons, said in an interview.
Cynthia Moran, executive vice president of government relations and health policy at the American College of Radiology, agreed.
“This particular product is going in a direction that we’re not comfortable with so we can’t support it on the basis of the benchmarks and the independent dispute resolution (IDR) process with the $750 threshold,” she said in an interview. The services radiologists provide tend to be in the $100-200 range, she said, so that would automatically exclude them from accessing arbitration. She also said that it is her understanding that many physician services will fall under that $750 threshold.
“That $750 is really going to mean that the vast majority of this policy is a benchmark-driven policy,” she said. “It is not going to be an IDR-driven policy and that is the crux of our objection to it.”
And by taking arbitration off the table, insurers have no incentive to negotiate in good faith with doctors to ensure that doctors are getting paid for the services they perform.
“For those situations where there is an out-of-network physician at an in-network facility, we believe that the patient should not have to pay any more for those emergency situations where they patient doesn’t get to choose their doctor,” Mr. Shalgian said. “The dispute really comes down to how much does the health plan have to pay the doctor.”
He noted that the legislation ties the rate to median in-network rates “and that’s a problem for us as well because of the fact that [this is] going to allow the health plans to set median in-network rates as the rate that they can pay the doctors.”
If the bill becomes law, “when you have a situation where you have an in-network physician trying to negotiate with a health plan to stay in network, that health plan now has more power in that negotiation because if [the physician] is making more than median in-network rates, then the health plan can say, ‘go out of network because we will just pay you median in-network’ at that point. That is a significant concern to us as well.”
Mr. Shalgian said that the ideal solution would be to eliminate the threshold entirely and just send disputes to arbitration. Recognizing that it might not be practical, the $750 threshold should be lowered.
ACS supported a $300 threshold, he added.
The bill is expected to be tacked on to one of the mandatory spending bills that Congress needs to pass by the end of the year.
The $750 threshold would be a savings generator for the government and an important bill such as this should be passed on its own merits, Mr. Shalgian said.
Ms. Moran called for Congress to take its time with the legislation.
“We do think that this whole issue needs more time for everyone to understand what the impact is on this first run of the solution and we think it should be slowed down a bit,” she said. “It should not go to the floor until you hear more from the providers [after] the providers figure out what the impact will be.”
The American Medical Association also called for Congress to slow down.
“The current proposal relies on benchmark rate setting that would serve only to benefit the bottom line of insurance companies at the expense of patients seeking a robust network of physicians for their care,” AMA President Patrice Harris, MD, said in a statement. “Rather than rushing to meet arbitrary deadlines, it is important to get this legislation right.”
Compromise bipartisan legislation to address surprise medical bills is getting push back from physician groups.
Leadership from the House Energy and Commerce Committee and the Senate Health, Education, Labor, and Pensions Committee on Dec. 9 unveiled a compromise bill that includes rate-setting for small surprise billing and arbitration for larger ones at a lower threshold than what was originally proposed.
The new bill, part of a broader Lower Health Care Costs Act, would protect patients from surprise medical bills related to emergency care, holding them responsible for in-network cost-sharing rates for out-of-network care provided at an in-network facility without their informed consent. Out-of-network surprise bills would be applied to the patient’s in-network deductible.
Under the legislation, providers would be paid at minimum the local, market-based median in-network negotiated rate for services, with a median rate under a $750 threshold. When the median exceeds $750, the provider or insurer would be allowed to choose arbitration process to resolve payment disputes.
The bill also protects patients by banning out-of-network facilities and providers from sending balance bills for more than in-network cost-sharing amounts.
Physician groups, however, see the legislation as a giveback to insurers that puts health care professionals at a disadvantage when negotiating to be included in insurer networks.
At issue is the $750 threshold for optional arbitration.
“If you set the arbitration system in such a way that limits the ability of a physician to go to arbitration to settle a dispute between a health plan and the doctor, and if you say that can only be done when there [are] bills that are greater than $750 for a particular service, then the vast majority of services provided by doctors will not be able to go to arbitration,” Christian Shalgian, director of advocacy and health policy at the American College of Surgeons, said in an interview.
Cynthia Moran, executive vice president of government relations and health policy at the American College of Radiology, agreed.
“This particular product is going in a direction that we’re not comfortable with so we can’t support it on the basis of the benchmarks and the independent dispute resolution (IDR) process with the $750 threshold,” she said in an interview. The services radiologists provide tend to be in the $100-200 range, she said, so that would automatically exclude them from accessing arbitration. She also said that it is her understanding that many physician services will fall under that $750 threshold.
“That $750 is really going to mean that the vast majority of this policy is a benchmark-driven policy,” she said. “It is not going to be an IDR-driven policy and that is the crux of our objection to it.”
And by taking arbitration off the table, insurers have no incentive to negotiate in good faith with doctors to ensure that doctors are getting paid for the services they perform.
“For those situations where there is an out-of-network physician at an in-network facility, we believe that the patient should not have to pay any more for those emergency situations where they patient doesn’t get to choose their doctor,” Mr. Shalgian said. “The dispute really comes down to how much does the health plan have to pay the doctor.”
He noted that the legislation ties the rate to median in-network rates “and that’s a problem for us as well because of the fact that [this is] going to allow the health plans to set median in-network rates as the rate that they can pay the doctors.”
If the bill becomes law, “when you have a situation where you have an in-network physician trying to negotiate with a health plan to stay in network, that health plan now has more power in that negotiation because if [the physician] is making more than median in-network rates, then the health plan can say, ‘go out of network because we will just pay you median in-network’ at that point. That is a significant concern to us as well.”
Mr. Shalgian said that the ideal solution would be to eliminate the threshold entirely and just send disputes to arbitration. Recognizing that it might not be practical, the $750 threshold should be lowered.
ACS supported a $300 threshold, he added.
The bill is expected to be tacked on to one of the mandatory spending bills that Congress needs to pass by the end of the year.
The $750 threshold would be a savings generator for the government and an important bill such as this should be passed on its own merits, Mr. Shalgian said.
Ms. Moran called for Congress to take its time with the legislation.
“We do think that this whole issue needs more time for everyone to understand what the impact is on this first run of the solution and we think it should be slowed down a bit,” she said. “It should not go to the floor until you hear more from the providers [after] the providers figure out what the impact will be.”
The American Medical Association also called for Congress to slow down.
“The current proposal relies on benchmark rate setting that would serve only to benefit the bottom line of insurance companies at the expense of patients seeking a robust network of physicians for their care,” AMA President Patrice Harris, MD, said in a statement. “Rather than rushing to meet arbitrary deadlines, it is important to get this legislation right.”
Compromise bipartisan legislation to address surprise medical bills is getting push back from physician groups.
Leadership from the House Energy and Commerce Committee and the Senate Health, Education, Labor, and Pensions Committee on Dec. 9 unveiled a compromise bill that includes rate-setting for small surprise billing and arbitration for larger ones at a lower threshold than what was originally proposed.
The new bill, part of a broader Lower Health Care Costs Act, would protect patients from surprise medical bills related to emergency care, holding them responsible for in-network cost-sharing rates for out-of-network care provided at an in-network facility without their informed consent. Out-of-network surprise bills would be applied to the patient’s in-network deductible.
Under the legislation, providers would be paid at minimum the local, market-based median in-network negotiated rate for services, with a median rate under a $750 threshold. When the median exceeds $750, the provider or insurer would be allowed to choose arbitration process to resolve payment disputes.
The bill also protects patients by banning out-of-network facilities and providers from sending balance bills for more than in-network cost-sharing amounts.
Physician groups, however, see the legislation as a giveback to insurers that puts health care professionals at a disadvantage when negotiating to be included in insurer networks.
At issue is the $750 threshold for optional arbitration.
“If you set the arbitration system in such a way that limits the ability of a physician to go to arbitration to settle a dispute between a health plan and the doctor, and if you say that can only be done when there [are] bills that are greater than $750 for a particular service, then the vast majority of services provided by doctors will not be able to go to arbitration,” Christian Shalgian, director of advocacy and health policy at the American College of Surgeons, said in an interview.
Cynthia Moran, executive vice president of government relations and health policy at the American College of Radiology, agreed.
“This particular product is going in a direction that we’re not comfortable with so we can’t support it on the basis of the benchmarks and the independent dispute resolution (IDR) process with the $750 threshold,” she said in an interview. The services radiologists provide tend to be in the $100-200 range, she said, so that would automatically exclude them from accessing arbitration. She also said that it is her understanding that many physician services will fall under that $750 threshold.
“That $750 is really going to mean that the vast majority of this policy is a benchmark-driven policy,” she said. “It is not going to be an IDR-driven policy and that is the crux of our objection to it.”
And by taking arbitration off the table, insurers have no incentive to negotiate in good faith with doctors to ensure that doctors are getting paid for the services they perform.
“For those situations where there is an out-of-network physician at an in-network facility, we believe that the patient should not have to pay any more for those emergency situations where they patient doesn’t get to choose their doctor,” Mr. Shalgian said. “The dispute really comes down to how much does the health plan have to pay the doctor.”
He noted that the legislation ties the rate to median in-network rates “and that’s a problem for us as well because of the fact that [this is] going to allow the health plans to set median in-network rates as the rate that they can pay the doctors.”
If the bill becomes law, “when you have a situation where you have an in-network physician trying to negotiate with a health plan to stay in network, that health plan now has more power in that negotiation because if [the physician] is making more than median in-network rates, then the health plan can say, ‘go out of network because we will just pay you median in-network’ at that point. That is a significant concern to us as well.”
Mr. Shalgian said that the ideal solution would be to eliminate the threshold entirely and just send disputes to arbitration. Recognizing that it might not be practical, the $750 threshold should be lowered.
ACS supported a $300 threshold, he added.
The bill is expected to be tacked on to one of the mandatory spending bills that Congress needs to pass by the end of the year.
The $750 threshold would be a savings generator for the government and an important bill such as this should be passed on its own merits, Mr. Shalgian said.
Ms. Moran called for Congress to take its time with the legislation.
“We do think that this whole issue needs more time for everyone to understand what the impact is on this first run of the solution and we think it should be slowed down a bit,” she said. “It should not go to the floor until you hear more from the providers [after] the providers figure out what the impact will be.”
The American Medical Association also called for Congress to slow down.
“The current proposal relies on benchmark rate setting that would serve only to benefit the bottom line of insurance companies at the expense of patients seeking a robust network of physicians for their care,” AMA President Patrice Harris, MD, said in a statement. “Rather than rushing to meet arbitrary deadlines, it is important to get this legislation right.”
Do ObGyns think the EMR has improved patient care?
In the roundtable article, “The electronic medical record’s role in ObGyn burnout and patient care” (October 2019), Megan L. Evans, MD, MPH; John J. Dougherty, MD, MBA; and Mark B. Woodland, MS, MD, discussed burnout’s connection with the electronic medical record (EMR) and solutions implemented at their institutions to help cope with the problem. They highlighted changes they felt their EMR systems needed to undergo. In addition, they noted as a whole that the EMR has not improved patient care.
OBG Management polled readers to see their thoughts on this question: “Do you think that the EMR has improved patient care?”
A total of 123 readers cast their vote:
67.2% (84 readers)said no
31.2% (39 readers)said yes
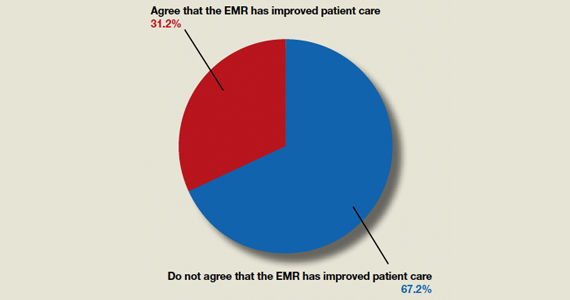
In the roundtable article, “The electronic medical record’s role in ObGyn burnout and patient care” (October 2019), Megan L. Evans, MD, MPH; John J. Dougherty, MD, MBA; and Mark B. Woodland, MS, MD, discussed burnout’s connection with the electronic medical record (EMR) and solutions implemented at their institutions to help cope with the problem. They highlighted changes they felt their EMR systems needed to undergo. In addition, they noted as a whole that the EMR has not improved patient care.
OBG Management polled readers to see their thoughts on this question: “Do you think that the EMR has improved patient care?”
A total of 123 readers cast their vote:
67.2% (84 readers)said no
31.2% (39 readers)said yes
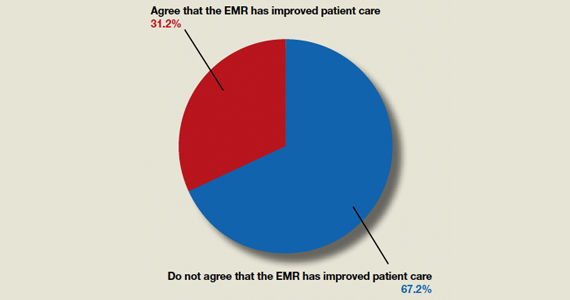
In the roundtable article, “The electronic medical record’s role in ObGyn burnout and patient care” (October 2019), Megan L. Evans, MD, MPH; John J. Dougherty, MD, MBA; and Mark B. Woodland, MS, MD, discussed burnout’s connection with the electronic medical record (EMR) and solutions implemented at their institutions to help cope with the problem. They highlighted changes they felt their EMR systems needed to undergo. In addition, they noted as a whole that the EMR has not improved patient care.
OBG Management polled readers to see their thoughts on this question: “Do you think that the EMR has improved patient care?”
A total of 123 readers cast their vote:
67.2% (84 readers)said no
31.2% (39 readers)said yes
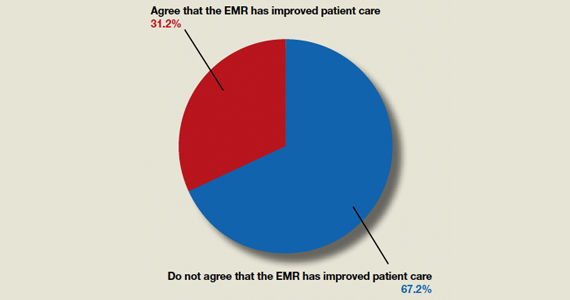
Study: More pediatricians participating in global health opportunities
A look across nearly 3 decades finds that
Lead author Kevin Chan, MD, MPH, of the University of Toronto, and colleagues analyzed the responses of 668 pediatricians from the 2017 American Academy of Pediatrics Periodic Survey and compared the data with responses from 638 pediatricians collected in the 1989 periodic survey about pediatricians’ global health experiences and interests. Findings showed that participation in global health activities rose from 2% in 1989 to 5% in 2017, while interest in future global health experiences grew from 25% in 1989 to 32% in 2017. The study was published in Pediatrics.
Notable increases in global health participation were found in women (1% in 1989 to 5% in 2017) and men (3% in 1989 to 6% in 2017), subspecialists (3% in 1989 to 9% in 2017), and pediatricians who worked in medical school, hospital, or clinic settings (3% in 1989 to 8% in 2017).
In terms of age, pediatricians 50 years or older had a higher rate of a recent global health experience, with the largest increase in global health participation occurring in pediatricians 60 years and older (2% in 1989 to 9% in 2017), the study found.
Similarly, interest in future global health activities increased during the same time period for male and female pediatricians, for generalists and subspecialists, and for those working in medical school, hospital, or clinic settings. Clinical care and teaching settings were the most common preferences for future global health experiences in both 1989 and 2017. Administration and research were the least likely selected preferences in both surveys. Pediatricians affiliated with an academic institution, hospital, or clinic were more likely to have recently engaged in a global health activity and also were more likely express interest in such an opportunity, compared with solo pediatricians or those in small practices.
In an editorial accompanying the article, Suzinne Pak-Gorstein, MD, MPH, PhD, of the University of Washington, Seattle, said that the study highlights the importance of preparation for pediatricians who seek global health opportunities, particularly experiences that are short term.
“Ethical approaches to international work should be thoughtful and intentional, such as deciding to work with organizations that offer short-term experiences only in the context of long-term partnerships, considering the burden on local partners for hosting visitors, and insisting on a commitment to equitable collaborations that are mutually beneficial,” she wrote.
Dr. Pak-Gorstein added that future innovations in global health education can inspire learning experiences for pediatricians that utilize their passion and enthusiasm, while also enabling them to become more globally minded.
“In this way, pediatricians can be empowered to understand the world’s daunting challenges; respect cultural, religious, and socioeconomic differences; and facilitate dialogue and solutions for improving child health worldwide,” she concluded.
The survey was funded by the American Academy of Pediatrics. The study authors had no relevant financial disclosures. Dr. Pak-Gorstein said she received no funding for the editorial and had no relevant financial disclosures.
SOURCE: Chan K et al. Pediatrics. 2019 Dec 10. doi: 10.1542/peds.2019-1655.
A look across nearly 3 decades finds that
Lead author Kevin Chan, MD, MPH, of the University of Toronto, and colleagues analyzed the responses of 668 pediatricians from the 2017 American Academy of Pediatrics Periodic Survey and compared the data with responses from 638 pediatricians collected in the 1989 periodic survey about pediatricians’ global health experiences and interests. Findings showed that participation in global health activities rose from 2% in 1989 to 5% in 2017, while interest in future global health experiences grew from 25% in 1989 to 32% in 2017. The study was published in Pediatrics.
Notable increases in global health participation were found in women (1% in 1989 to 5% in 2017) and men (3% in 1989 to 6% in 2017), subspecialists (3% in 1989 to 9% in 2017), and pediatricians who worked in medical school, hospital, or clinic settings (3% in 1989 to 8% in 2017).
In terms of age, pediatricians 50 years or older had a higher rate of a recent global health experience, with the largest increase in global health participation occurring in pediatricians 60 years and older (2% in 1989 to 9% in 2017), the study found.
Similarly, interest in future global health activities increased during the same time period for male and female pediatricians, for generalists and subspecialists, and for those working in medical school, hospital, or clinic settings. Clinical care and teaching settings were the most common preferences for future global health experiences in both 1989 and 2017. Administration and research were the least likely selected preferences in both surveys. Pediatricians affiliated with an academic institution, hospital, or clinic were more likely to have recently engaged in a global health activity and also were more likely express interest in such an opportunity, compared with solo pediatricians or those in small practices.
In an editorial accompanying the article, Suzinne Pak-Gorstein, MD, MPH, PhD, of the University of Washington, Seattle, said that the study highlights the importance of preparation for pediatricians who seek global health opportunities, particularly experiences that are short term.
“Ethical approaches to international work should be thoughtful and intentional, such as deciding to work with organizations that offer short-term experiences only in the context of long-term partnerships, considering the burden on local partners for hosting visitors, and insisting on a commitment to equitable collaborations that are mutually beneficial,” she wrote.
Dr. Pak-Gorstein added that future innovations in global health education can inspire learning experiences for pediatricians that utilize their passion and enthusiasm, while also enabling them to become more globally minded.
“In this way, pediatricians can be empowered to understand the world’s daunting challenges; respect cultural, religious, and socioeconomic differences; and facilitate dialogue and solutions for improving child health worldwide,” she concluded.
The survey was funded by the American Academy of Pediatrics. The study authors had no relevant financial disclosures. Dr. Pak-Gorstein said she received no funding for the editorial and had no relevant financial disclosures.
SOURCE: Chan K et al. Pediatrics. 2019 Dec 10. doi: 10.1542/peds.2019-1655.
A look across nearly 3 decades finds that
Lead author Kevin Chan, MD, MPH, of the University of Toronto, and colleagues analyzed the responses of 668 pediatricians from the 2017 American Academy of Pediatrics Periodic Survey and compared the data with responses from 638 pediatricians collected in the 1989 periodic survey about pediatricians’ global health experiences and interests. Findings showed that participation in global health activities rose from 2% in 1989 to 5% in 2017, while interest in future global health experiences grew from 25% in 1989 to 32% in 2017. The study was published in Pediatrics.
Notable increases in global health participation were found in women (1% in 1989 to 5% in 2017) and men (3% in 1989 to 6% in 2017), subspecialists (3% in 1989 to 9% in 2017), and pediatricians who worked in medical school, hospital, or clinic settings (3% in 1989 to 8% in 2017).
In terms of age, pediatricians 50 years or older had a higher rate of a recent global health experience, with the largest increase in global health participation occurring in pediatricians 60 years and older (2% in 1989 to 9% in 2017), the study found.
Similarly, interest in future global health activities increased during the same time period for male and female pediatricians, for generalists and subspecialists, and for those working in medical school, hospital, or clinic settings. Clinical care and teaching settings were the most common preferences for future global health experiences in both 1989 and 2017. Administration and research were the least likely selected preferences in both surveys. Pediatricians affiliated with an academic institution, hospital, or clinic were more likely to have recently engaged in a global health activity and also were more likely express interest in such an opportunity, compared with solo pediatricians or those in small practices.
In an editorial accompanying the article, Suzinne Pak-Gorstein, MD, MPH, PhD, of the University of Washington, Seattle, said that the study highlights the importance of preparation for pediatricians who seek global health opportunities, particularly experiences that are short term.
“Ethical approaches to international work should be thoughtful and intentional, such as deciding to work with organizations that offer short-term experiences only in the context of long-term partnerships, considering the burden on local partners for hosting visitors, and insisting on a commitment to equitable collaborations that are mutually beneficial,” she wrote.
Dr. Pak-Gorstein added that future innovations in global health education can inspire learning experiences for pediatricians that utilize their passion and enthusiasm, while also enabling them to become more globally minded.
“In this way, pediatricians can be empowered to understand the world’s daunting challenges; respect cultural, religious, and socioeconomic differences; and facilitate dialogue and solutions for improving child health worldwide,” she concluded.
The survey was funded by the American Academy of Pediatrics. The study authors had no relevant financial disclosures. Dr. Pak-Gorstein said she received no funding for the editorial and had no relevant financial disclosures.
SOURCE: Chan K et al. Pediatrics. 2019 Dec 10. doi: 10.1542/peds.2019-1655.
Some with mild Crohn’s disease need no treatment
Kim L. Isaacs, MD, PhD, said at the annual meeting of the American College of Gastroenterology.
First, it’s essential to establish that a patient truly falls into the mild disease category. And second, during that initial evaluation it’s important to look for the features that signal a high risk of subsequent disease progression.
“Patients with risk factors for disease progression should not be treated as mild Crohn’s disease. These are people that we need to treat perhaps more aggressively up front,” said Dr. Isaacs, professor of medicine and codirector of the Multidisciplinary Center for IBD Research and Treatment at the University of North Carolina, Chapel Hill.
Management of patients with severe Crohn’s disease can be challenging, but Dr. Isaacs finds patients with mild disease flat out “terrifying.”
“The reason I find this situation terrifying is we want to prevent the surgery, the progression from inflammatory disease to more stricturing and penetrating disease. And how can I know that my patient a year from now is not going to be very, very ill and I’ve lost my window to use some of our more potent therapies?” she explained.
Mild Crohn’s disease is characterized clinically by less than 10% weight loss; no fever, tachycardia, or other symptoms of systemic disease; lack of abdominal tenderness; and no signs or symptoms of obstruction. When reading the literature, mild disease is defined by a Crohn’s Disease Activity Index score of 150-220. However, nobody uses that metric outside of research studies; it’s just too cumbersome. More useful in routine clinical practice is the Harvey-Bradshaw Index, where a score of 5-7 indicates mild disease.
Many patients with mild Crohn’s disease will not progress over time. In a recent prospective 29-center European study, just 14% of patients progressed from mild to stricturing and/or penetrating disease within 5 years after diagnosis (Gut. 2018 Jan 23. doi: 10.1136/gutjnl-2017-315568).
Who is likely to progress
Risk factors for disease progression include patients with ileocolonic or perianal disease, smokers, those with inflammatory arthritis or other associated immune-mediated disease, and patients who require corticosteroids in order to maintain remission.
On the other hand, patients with mild Crohn’s disease at low risk for progression have no or only mild symptoms, a limited distribution of bowel inflammation, normal or merely slightly elevated C-reactive protein and/or fecal calprotectin levels, no or only superficial bowel ulceration on colonoscopy, and were diagnosed with inflammatory bowel disease after age 30.
Treatment options
“Our goal in a patient we think is low risk is symptomatic management while avoiding high therapeutic risks in someone we don’t think is going to be progressing,” according to the gastroenterologist.
In patients with mild disease who have symptoms in the ileum or right colon, a good strategy is to induce remission using controlled ileal-release budesonide at 9 mg/day, then follow up with colonoscopy 6-12 months later. The high-dose budesonide regimen has been shown in multiple studies to be more effective than placebo at inducing remission. It’s less effective than conventional oral corticosteroids, but it also causes fewer steroid-related side effects. In fact, the evidence shows that the side effect profile of controlled-release budesonide is no different from that of placebo.
In low-risk, mildly symptomatic patients with diffuse Crohn’s colitis, Dr. Isaacs recommends initial treatment with prednisone and/or sulfasalazine or 5-aminosalicylates. The 5-aminosalicylates aren’t part of most practice guidelines because of conflicting study results. However, a meta-analysis of 22 randomized controlled trials has shown that high-dose mesalamine was 2.29-fold more effective than placebo at inducing remission and is a good option for patients who would rather avoid corticosteroids (Inflamm Bowel Dis. 2017 Mar;23(3):461-72). Prednisone should be tapered after achieving clinical remission. Inability to stop steroids within 6 months after entering remission warrants a switch to maintenance therapy with a biologic or immunomodulatory agent.
Smoking cessation should be a top priority
“I spend a good portion of my time in clinic telling patients, ‘You can do more with stopping smoking than I can do with any of my medications,’ ” Dr. Isaacs said.
Another worthwhile intervention is to check for and correct low serum vitamin D levels. Vitamin D is a potent immunomodulator, and severely low levels below 15 ng/mL are associated with increased risk of Crohn’s disease relapse, more hospitalizations, more active disease activity, and heavier use of corticosteroids than in patients with moderate deficiency in the 15- to 30-ng/mL range (Nutrients. 2019 May 11;11[5]. doi: 10.3390/nu11051059).
Monitoring patients with mild Crohn’s disease
“Monitor closely for mucosal inflammation because if they start to progress, we want to get to them early so they get a good response to their first therapies. If the CRP starts moving up, consider doing something,” she advised.
A CRP above 5 mg/L is associated with a markedly increased risk of relapse. And Spanish investigators have shown in a prospective study of 95 patients in clinical remission for at least 6 months while on a tumor necrosis factor inhibitor that thereafter a fecal calprotein level greater than 300 mcg/g at any point was strongly predictive of relapse within the next 4 months (J Clin Gastroenterol. 2018 Mar;52[3]:229-34). Following a patient with mild Crohn’s disease over time endoscopically, it’s of value to utilize the Simple Endoscopic Score for Crohn’s Disease (SES-CD) to document that in fact the disease is mild. Dr. Isaacs recommended IG-IBD Scores – Calculators in Gastroenterology as “a great site” for assistance in calculating the SES-CD, the Harvey-Bradshaw Index, and a plethora of other inflammatory bowel disease scores.
She reported having no financial conflicts of interest.
Kim L. Isaacs, MD, PhD, said at the annual meeting of the American College of Gastroenterology.
First, it’s essential to establish that a patient truly falls into the mild disease category. And second, during that initial evaluation it’s important to look for the features that signal a high risk of subsequent disease progression.
“Patients with risk factors for disease progression should not be treated as mild Crohn’s disease. These are people that we need to treat perhaps more aggressively up front,” said Dr. Isaacs, professor of medicine and codirector of the Multidisciplinary Center for IBD Research and Treatment at the University of North Carolina, Chapel Hill.
Management of patients with severe Crohn’s disease can be challenging, but Dr. Isaacs finds patients with mild disease flat out “terrifying.”
“The reason I find this situation terrifying is we want to prevent the surgery, the progression from inflammatory disease to more stricturing and penetrating disease. And how can I know that my patient a year from now is not going to be very, very ill and I’ve lost my window to use some of our more potent therapies?” she explained.
Mild Crohn’s disease is characterized clinically by less than 10% weight loss; no fever, tachycardia, or other symptoms of systemic disease; lack of abdominal tenderness; and no signs or symptoms of obstruction. When reading the literature, mild disease is defined by a Crohn’s Disease Activity Index score of 150-220. However, nobody uses that metric outside of research studies; it’s just too cumbersome. More useful in routine clinical practice is the Harvey-Bradshaw Index, where a score of 5-7 indicates mild disease.
Many patients with mild Crohn’s disease will not progress over time. In a recent prospective 29-center European study, just 14% of patients progressed from mild to stricturing and/or penetrating disease within 5 years after diagnosis (Gut. 2018 Jan 23. doi: 10.1136/gutjnl-2017-315568).
Who is likely to progress
Risk factors for disease progression include patients with ileocolonic or perianal disease, smokers, those with inflammatory arthritis or other associated immune-mediated disease, and patients who require corticosteroids in order to maintain remission.
On the other hand, patients with mild Crohn’s disease at low risk for progression have no or only mild symptoms, a limited distribution of bowel inflammation, normal or merely slightly elevated C-reactive protein and/or fecal calprotectin levels, no or only superficial bowel ulceration on colonoscopy, and were diagnosed with inflammatory bowel disease after age 30.
Treatment options
“Our goal in a patient we think is low risk is symptomatic management while avoiding high therapeutic risks in someone we don’t think is going to be progressing,” according to the gastroenterologist.
In patients with mild disease who have symptoms in the ileum or right colon, a good strategy is to induce remission using controlled ileal-release budesonide at 9 mg/day, then follow up with colonoscopy 6-12 months later. The high-dose budesonide regimen has been shown in multiple studies to be more effective than placebo at inducing remission. It’s less effective than conventional oral corticosteroids, but it also causes fewer steroid-related side effects. In fact, the evidence shows that the side effect profile of controlled-release budesonide is no different from that of placebo.
In low-risk, mildly symptomatic patients with diffuse Crohn’s colitis, Dr. Isaacs recommends initial treatment with prednisone and/or sulfasalazine or 5-aminosalicylates. The 5-aminosalicylates aren’t part of most practice guidelines because of conflicting study results. However, a meta-analysis of 22 randomized controlled trials has shown that high-dose mesalamine was 2.29-fold more effective than placebo at inducing remission and is a good option for patients who would rather avoid corticosteroids (Inflamm Bowel Dis. 2017 Mar;23(3):461-72). Prednisone should be tapered after achieving clinical remission. Inability to stop steroids within 6 months after entering remission warrants a switch to maintenance therapy with a biologic or immunomodulatory agent.
Smoking cessation should be a top priority
“I spend a good portion of my time in clinic telling patients, ‘You can do more with stopping smoking than I can do with any of my medications,’ ” Dr. Isaacs said.
Another worthwhile intervention is to check for and correct low serum vitamin D levels. Vitamin D is a potent immunomodulator, and severely low levels below 15 ng/mL are associated with increased risk of Crohn’s disease relapse, more hospitalizations, more active disease activity, and heavier use of corticosteroids than in patients with moderate deficiency in the 15- to 30-ng/mL range (Nutrients. 2019 May 11;11[5]. doi: 10.3390/nu11051059).
Monitoring patients with mild Crohn’s disease
“Monitor closely for mucosal inflammation because if they start to progress, we want to get to them early so they get a good response to their first therapies. If the CRP starts moving up, consider doing something,” she advised.
A CRP above 5 mg/L is associated with a markedly increased risk of relapse. And Spanish investigators have shown in a prospective study of 95 patients in clinical remission for at least 6 months while on a tumor necrosis factor inhibitor that thereafter a fecal calprotein level greater than 300 mcg/g at any point was strongly predictive of relapse within the next 4 months (J Clin Gastroenterol. 2018 Mar;52[3]:229-34). Following a patient with mild Crohn’s disease over time endoscopically, it’s of value to utilize the Simple Endoscopic Score for Crohn’s Disease (SES-CD) to document that in fact the disease is mild. Dr. Isaacs recommended IG-IBD Scores – Calculators in Gastroenterology as “a great site” for assistance in calculating the SES-CD, the Harvey-Bradshaw Index, and a plethora of other inflammatory bowel disease scores.
She reported having no financial conflicts of interest.
Kim L. Isaacs, MD, PhD, said at the annual meeting of the American College of Gastroenterology.
First, it’s essential to establish that a patient truly falls into the mild disease category. And second, during that initial evaluation it’s important to look for the features that signal a high risk of subsequent disease progression.
“Patients with risk factors for disease progression should not be treated as mild Crohn’s disease. These are people that we need to treat perhaps more aggressively up front,” said Dr. Isaacs, professor of medicine and codirector of the Multidisciplinary Center for IBD Research and Treatment at the University of North Carolina, Chapel Hill.
Management of patients with severe Crohn’s disease can be challenging, but Dr. Isaacs finds patients with mild disease flat out “terrifying.”
“The reason I find this situation terrifying is we want to prevent the surgery, the progression from inflammatory disease to more stricturing and penetrating disease. And how can I know that my patient a year from now is not going to be very, very ill and I’ve lost my window to use some of our more potent therapies?” she explained.
Mild Crohn’s disease is characterized clinically by less than 10% weight loss; no fever, tachycardia, or other symptoms of systemic disease; lack of abdominal tenderness; and no signs or symptoms of obstruction. When reading the literature, mild disease is defined by a Crohn’s Disease Activity Index score of 150-220. However, nobody uses that metric outside of research studies; it’s just too cumbersome. More useful in routine clinical practice is the Harvey-Bradshaw Index, where a score of 5-7 indicates mild disease.
Many patients with mild Crohn’s disease will not progress over time. In a recent prospective 29-center European study, just 14% of patients progressed from mild to stricturing and/or penetrating disease within 5 years after diagnosis (Gut. 2018 Jan 23. doi: 10.1136/gutjnl-2017-315568).
Who is likely to progress
Risk factors for disease progression include patients with ileocolonic or perianal disease, smokers, those with inflammatory arthritis or other associated immune-mediated disease, and patients who require corticosteroids in order to maintain remission.
On the other hand, patients with mild Crohn’s disease at low risk for progression have no or only mild symptoms, a limited distribution of bowel inflammation, normal or merely slightly elevated C-reactive protein and/or fecal calprotectin levels, no or only superficial bowel ulceration on colonoscopy, and were diagnosed with inflammatory bowel disease after age 30.
Treatment options
“Our goal in a patient we think is low risk is symptomatic management while avoiding high therapeutic risks in someone we don’t think is going to be progressing,” according to the gastroenterologist.
In patients with mild disease who have symptoms in the ileum or right colon, a good strategy is to induce remission using controlled ileal-release budesonide at 9 mg/day, then follow up with colonoscopy 6-12 months later. The high-dose budesonide regimen has been shown in multiple studies to be more effective than placebo at inducing remission. It’s less effective than conventional oral corticosteroids, but it also causes fewer steroid-related side effects. In fact, the evidence shows that the side effect profile of controlled-release budesonide is no different from that of placebo.
In low-risk, mildly symptomatic patients with diffuse Crohn’s colitis, Dr. Isaacs recommends initial treatment with prednisone and/or sulfasalazine or 5-aminosalicylates. The 5-aminosalicylates aren’t part of most practice guidelines because of conflicting study results. However, a meta-analysis of 22 randomized controlled trials has shown that high-dose mesalamine was 2.29-fold more effective than placebo at inducing remission and is a good option for patients who would rather avoid corticosteroids (Inflamm Bowel Dis. 2017 Mar;23(3):461-72). Prednisone should be tapered after achieving clinical remission. Inability to stop steroids within 6 months after entering remission warrants a switch to maintenance therapy with a biologic or immunomodulatory agent.
Smoking cessation should be a top priority
“I spend a good portion of my time in clinic telling patients, ‘You can do more with stopping smoking than I can do with any of my medications,’ ” Dr. Isaacs said.
Another worthwhile intervention is to check for and correct low serum vitamin D levels. Vitamin D is a potent immunomodulator, and severely low levels below 15 ng/mL are associated with increased risk of Crohn’s disease relapse, more hospitalizations, more active disease activity, and heavier use of corticosteroids than in patients with moderate deficiency in the 15- to 30-ng/mL range (Nutrients. 2019 May 11;11[5]. doi: 10.3390/nu11051059).
Monitoring patients with mild Crohn’s disease
“Monitor closely for mucosal inflammation because if they start to progress, we want to get to them early so they get a good response to their first therapies. If the CRP starts moving up, consider doing something,” she advised.
A CRP above 5 mg/L is associated with a markedly increased risk of relapse. And Spanish investigators have shown in a prospective study of 95 patients in clinical remission for at least 6 months while on a tumor necrosis factor inhibitor that thereafter a fecal calprotein level greater than 300 mcg/g at any point was strongly predictive of relapse within the next 4 months (J Clin Gastroenterol. 2018 Mar;52[3]:229-34). Following a patient with mild Crohn’s disease over time endoscopically, it’s of value to utilize the Simple Endoscopic Score for Crohn’s Disease (SES-CD) to document that in fact the disease is mild. Dr. Isaacs recommended IG-IBD Scores – Calculators in Gastroenterology as “a great site” for assistance in calculating the SES-CD, the Harvey-Bradshaw Index, and a plethora of other inflammatory bowel disease scores.
She reported having no financial conflicts of interest.
REPORTING FROM ACG 2019
Consider Ovarian Cancer as a Differential Diagnosis
This year in the United States, there were an estimated 22,530 new cases of ovarian cancer and an estimated 13,980 ovarian cancer deaths.1 Ovarian cancer accounts for more deaths than any other female reproductive system cancer.2 The high mortality rate is attributed to the advanced stage of cancer at initial presentation: Women diagnosed with localized disease have an estimated 5-year survival rate of 92%, while those diagnosed with advanced disease have a 5-year survival rate of 29%.3 For this reason, early detection of ovarian cancer is paramount.
A Personal Story
I think about ovarian cancer every day, because I am a survivor of this deadly disease. In 2018, at age 53, I received the diagnosis of stage 1A high-grade serous carcinoma of the left ovary. My cancer was discovered incidentally: I presented to my health care provider with a 6-month history of metrorrhagia and a prior history of regular menstruation with dysmenorrhea controlled with ibuprofen. My family and personal history of cancer was negative, I had a normal BMI, I didn’t smoke and consumed alcohol only moderately, my lifestyle was active, and I had no chronic diseases and used no medications regularly. My clinician performed a pelvic exam and ordered sexually transmitted infection testing and blood work (complete blood count, metabolic panel, and TSH). The differential diagnosis at this point included
- Thyroid dysfunction
- Perimenopause
- Sexually transmitted infection
- Coagulation defect
- Foreign body
- Infection.
All testing yielded normal findings. At my follow-up appointment, we discussed perimenopause symptoms and agreed that I would continue monitoring the bleeding. If at a later date I wanted to pursue an ultrasound, I was instructed to call the office. It was not suggested that I schedule a follow-up office visit.
Several months later, persistent metrorrhagia prompted me to request a transvaginal ultrasound (TVU)—resulting in the discovery of a left adnexal solid mass and probable endometrial polyp. A referral to a gynecologic oncologist resulted in further imaging, which confirmed the TVU results. Surgical intervention was recommended.
One week later, I underwent robotic-assisted total laparoscopic hysterectomy, bilateral salpingo-oophorectomy, left pelvic and periaortic lymph node dissection, and omentectomy. The pathology report confirmed stage 1A high-grade serous carcinoma of the left ovary, as well as stage 1A grade 1 endometrioid adenocarcinoma of the uterus. I required 6 cycles of chemotherapy before follow-up imaging yielded negative results, with no evidence of metastatic disease.
A Call to Action
The recently updated US Preventive Services Task Force guidelines continue not to recommend annual screening with TVU and/or cancer antigen 125 (CA-125) blood testing for ovarian cancer in asymptomatic, average-risk women. A review of the evidence found no mortality benefit and high false-positive rates, which led to unnecessary surgeries and physiologic stress due to excess cancer worry.4 This (lack of) recommendation leaves the clinician in the position of not performing or ordering screening tests, except in cases in which the patient presents with symptoms or requests screening for ovarian cancer.
Yet it cannot be overstated: The clinician’s role in identifying risk factors for and recognizing symptoms of ovarian cancer is extremely important in the absence of routine screening recommendations. Risk factors include a positive family history of gynecologic, breast, or colon cancers; genetic predisposition; personal history of breast cancer; use of menopausal hormone therapy; excess body weight; smoking; and sedentary lifestyle.3 In my case, my risk for ovarian cancer was average.
Continue to: With regard to symptoms...
With regard to symptoms, most women do not report any until ovarian cancer has reached advanced stages—and even then, the symptoms are vague and nonspecific.5 They may include urinary urgency or frequency; change in bowel habit; difficulty eating or feeling full quickly; persistent back, pelvic, or abdominal pain; extreme tiredness; vaginal bleeding after menopause; increased abdominal size; or bloating on most days.5
So what can we as clinicians do? First, if I may offer a word of caution: When confronted with those vague and nonspecific symptoms, be careful not to dismiss them out of hand as a result of aging, stress, or menopause. As my case demonstrates, for example, metrorrhagia is not necessarily a benign condition for the premenopausal woman.
Furthermore, we can empower patients by educating them about ovarian cancer symptoms and risk factors, information that may promote help-seeking behaviors that aid in early detection. In my case, the continued symptom of abnormal uterine bleeding prompted me to seek further assessment, which led to the discovery of ovarian cancer. Had I not been an educated and empowered patient, I would be telling a completely different story today—most likely one that would include advanced staging. Partner with your patient to discuss available diagnostic testing options and schedule follow-up appointments to monitor presenting complaints.
We also need to partner with our oncology colleagues and researchers. A positive diagnostic test result for possible malignancy necessitates referral to a gynecologic oncologist. Treatment by specialists in high-volume hospitals results in improved ovarian cancer outcomes.6 And we should advocate for continued research to support the discovery of an efficient population screening protocol for this deadly disease.
Finally, and perhaps most radically, I encourage you not to take a watch-and-wait approach in these situations. Ultrasounds are inexpensive, have low mortality risk, and achieve high sensitivity and specificity in detecting and managing adnexal abnormalities.7 In my opinion, the endorsement of TVU testing in this clinical situation is a proactive, prudent, and reasonable action compared with watching and waiting, and it may result in early detection as opposed to advanced disease.
Continue to: I hope that...
I hope that sharing my personal experience with ovarian cancer will compel health care providers to consider this disease as a differential diagnosis and perform appropriate testing when average-risk patients present with nonspecific symptoms. Ultimately, our collective goal should be to increase the survival rate and reduce the suffering associated with ovarian cancer.
1. National Cancer Institute. Cancer Stat Facts: Ovarian Cancer. https://seer.cancer.gov/statfacts/html/ovary.html. Accessed December 3, 2019.
2. American Cancer Society. Key Statistics for Ovarian Cancer. Revised January 8, 2019. www.cancer.org/cancer/ovarian-cancer/about/key-statistics.html. Accessed December 3, 2019.
3. American Cancer Society. Cancer Facts & Figures 2019. www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf . Accessed December 4, 2019.
4. Grossman DC, Surry SJ, Owens DK, et al. Screening for ovarian cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319(6):588-594.
5. Smits S, Boivin J, Menon U, Brain K. Influences on anticipated time to ovarian cancer symptom presentation in women at increased risk compared to population risk of ovarian cancer. BMC Cancer. 2017;17(814):1-11.
6. Pavlik EJ. Ten important considerations for ovarian cancer screening. Diagnostics. 2017;7(22):1-11.
7. Ormsby EL, Pavlik EJ, McGahan JP. Ultrasound monitoring of extant adnexal masses in the era of type 1 and type 2 ovarian cancers: lessons learned from ovarian cancer screening trials. Diagnostics. 2017;7(25):1-19.
This year in the United States, there were an estimated 22,530 new cases of ovarian cancer and an estimated 13,980 ovarian cancer deaths.1 Ovarian cancer accounts for more deaths than any other female reproductive system cancer.2 The high mortality rate is attributed to the advanced stage of cancer at initial presentation: Women diagnosed with localized disease have an estimated 5-year survival rate of 92%, while those diagnosed with advanced disease have a 5-year survival rate of 29%.3 For this reason, early detection of ovarian cancer is paramount.
A Personal Story
I think about ovarian cancer every day, because I am a survivor of this deadly disease. In 2018, at age 53, I received the diagnosis of stage 1A high-grade serous carcinoma of the left ovary. My cancer was discovered incidentally: I presented to my health care provider with a 6-month history of metrorrhagia and a prior history of regular menstruation with dysmenorrhea controlled with ibuprofen. My family and personal history of cancer was negative, I had a normal BMI, I didn’t smoke and consumed alcohol only moderately, my lifestyle was active, and I had no chronic diseases and used no medications regularly. My clinician performed a pelvic exam and ordered sexually transmitted infection testing and blood work (complete blood count, metabolic panel, and TSH). The differential diagnosis at this point included
- Thyroid dysfunction
- Perimenopause
- Sexually transmitted infection
- Coagulation defect
- Foreign body
- Infection.
All testing yielded normal findings. At my follow-up appointment, we discussed perimenopause symptoms and agreed that I would continue monitoring the bleeding. If at a later date I wanted to pursue an ultrasound, I was instructed to call the office. It was not suggested that I schedule a follow-up office visit.
Several months later, persistent metrorrhagia prompted me to request a transvaginal ultrasound (TVU)—resulting in the discovery of a left adnexal solid mass and probable endometrial polyp. A referral to a gynecologic oncologist resulted in further imaging, which confirmed the TVU results. Surgical intervention was recommended.
One week later, I underwent robotic-assisted total laparoscopic hysterectomy, bilateral salpingo-oophorectomy, left pelvic and periaortic lymph node dissection, and omentectomy. The pathology report confirmed stage 1A high-grade serous carcinoma of the left ovary, as well as stage 1A grade 1 endometrioid adenocarcinoma of the uterus. I required 6 cycles of chemotherapy before follow-up imaging yielded negative results, with no evidence of metastatic disease.
A Call to Action
The recently updated US Preventive Services Task Force guidelines continue not to recommend annual screening with TVU and/or cancer antigen 125 (CA-125) blood testing for ovarian cancer in asymptomatic, average-risk women. A review of the evidence found no mortality benefit and high false-positive rates, which led to unnecessary surgeries and physiologic stress due to excess cancer worry.4 This (lack of) recommendation leaves the clinician in the position of not performing or ordering screening tests, except in cases in which the patient presents with symptoms or requests screening for ovarian cancer.
Yet it cannot be overstated: The clinician’s role in identifying risk factors for and recognizing symptoms of ovarian cancer is extremely important in the absence of routine screening recommendations. Risk factors include a positive family history of gynecologic, breast, or colon cancers; genetic predisposition; personal history of breast cancer; use of menopausal hormone therapy; excess body weight; smoking; and sedentary lifestyle.3 In my case, my risk for ovarian cancer was average.
Continue to: With regard to symptoms...
With regard to symptoms, most women do not report any until ovarian cancer has reached advanced stages—and even then, the symptoms are vague and nonspecific.5 They may include urinary urgency or frequency; change in bowel habit; difficulty eating or feeling full quickly; persistent back, pelvic, or abdominal pain; extreme tiredness; vaginal bleeding after menopause; increased abdominal size; or bloating on most days.5
So what can we as clinicians do? First, if I may offer a word of caution: When confronted with those vague and nonspecific symptoms, be careful not to dismiss them out of hand as a result of aging, stress, or menopause. As my case demonstrates, for example, metrorrhagia is not necessarily a benign condition for the premenopausal woman.
Furthermore, we can empower patients by educating them about ovarian cancer symptoms and risk factors, information that may promote help-seeking behaviors that aid in early detection. In my case, the continued symptom of abnormal uterine bleeding prompted me to seek further assessment, which led to the discovery of ovarian cancer. Had I not been an educated and empowered patient, I would be telling a completely different story today—most likely one that would include advanced staging. Partner with your patient to discuss available diagnostic testing options and schedule follow-up appointments to monitor presenting complaints.
We also need to partner with our oncology colleagues and researchers. A positive diagnostic test result for possible malignancy necessitates referral to a gynecologic oncologist. Treatment by specialists in high-volume hospitals results in improved ovarian cancer outcomes.6 And we should advocate for continued research to support the discovery of an efficient population screening protocol for this deadly disease.
Finally, and perhaps most radically, I encourage you not to take a watch-and-wait approach in these situations. Ultrasounds are inexpensive, have low mortality risk, and achieve high sensitivity and specificity in detecting and managing adnexal abnormalities.7 In my opinion, the endorsement of TVU testing in this clinical situation is a proactive, prudent, and reasonable action compared with watching and waiting, and it may result in early detection as opposed to advanced disease.
Continue to: I hope that...
I hope that sharing my personal experience with ovarian cancer will compel health care providers to consider this disease as a differential diagnosis and perform appropriate testing when average-risk patients present with nonspecific symptoms. Ultimately, our collective goal should be to increase the survival rate and reduce the suffering associated with ovarian cancer.
This year in the United States, there were an estimated 22,530 new cases of ovarian cancer and an estimated 13,980 ovarian cancer deaths.1 Ovarian cancer accounts for more deaths than any other female reproductive system cancer.2 The high mortality rate is attributed to the advanced stage of cancer at initial presentation: Women diagnosed with localized disease have an estimated 5-year survival rate of 92%, while those diagnosed with advanced disease have a 5-year survival rate of 29%.3 For this reason, early detection of ovarian cancer is paramount.
A Personal Story
I think about ovarian cancer every day, because I am a survivor of this deadly disease. In 2018, at age 53, I received the diagnosis of stage 1A high-grade serous carcinoma of the left ovary. My cancer was discovered incidentally: I presented to my health care provider with a 6-month history of metrorrhagia and a prior history of regular menstruation with dysmenorrhea controlled with ibuprofen. My family and personal history of cancer was negative, I had a normal BMI, I didn’t smoke and consumed alcohol only moderately, my lifestyle was active, and I had no chronic diseases and used no medications regularly. My clinician performed a pelvic exam and ordered sexually transmitted infection testing and blood work (complete blood count, metabolic panel, and TSH). The differential diagnosis at this point included
- Thyroid dysfunction
- Perimenopause
- Sexually transmitted infection
- Coagulation defect
- Foreign body
- Infection.
All testing yielded normal findings. At my follow-up appointment, we discussed perimenopause symptoms and agreed that I would continue monitoring the bleeding. If at a later date I wanted to pursue an ultrasound, I was instructed to call the office. It was not suggested that I schedule a follow-up office visit.
Several months later, persistent metrorrhagia prompted me to request a transvaginal ultrasound (TVU)—resulting in the discovery of a left adnexal solid mass and probable endometrial polyp. A referral to a gynecologic oncologist resulted in further imaging, which confirmed the TVU results. Surgical intervention was recommended.
One week later, I underwent robotic-assisted total laparoscopic hysterectomy, bilateral salpingo-oophorectomy, left pelvic and periaortic lymph node dissection, and omentectomy. The pathology report confirmed stage 1A high-grade serous carcinoma of the left ovary, as well as stage 1A grade 1 endometrioid adenocarcinoma of the uterus. I required 6 cycles of chemotherapy before follow-up imaging yielded negative results, with no evidence of metastatic disease.
A Call to Action
The recently updated US Preventive Services Task Force guidelines continue not to recommend annual screening with TVU and/or cancer antigen 125 (CA-125) blood testing for ovarian cancer in asymptomatic, average-risk women. A review of the evidence found no mortality benefit and high false-positive rates, which led to unnecessary surgeries and physiologic stress due to excess cancer worry.4 This (lack of) recommendation leaves the clinician in the position of not performing or ordering screening tests, except in cases in which the patient presents with symptoms or requests screening for ovarian cancer.
Yet it cannot be overstated: The clinician’s role in identifying risk factors for and recognizing symptoms of ovarian cancer is extremely important in the absence of routine screening recommendations. Risk factors include a positive family history of gynecologic, breast, or colon cancers; genetic predisposition; personal history of breast cancer; use of menopausal hormone therapy; excess body weight; smoking; and sedentary lifestyle.3 In my case, my risk for ovarian cancer was average.
Continue to: With regard to symptoms...
With regard to symptoms, most women do not report any until ovarian cancer has reached advanced stages—and even then, the symptoms are vague and nonspecific.5 They may include urinary urgency or frequency; change in bowel habit; difficulty eating or feeling full quickly; persistent back, pelvic, or abdominal pain; extreme tiredness; vaginal bleeding after menopause; increased abdominal size; or bloating on most days.5
So what can we as clinicians do? First, if I may offer a word of caution: When confronted with those vague and nonspecific symptoms, be careful not to dismiss them out of hand as a result of aging, stress, or menopause. As my case demonstrates, for example, metrorrhagia is not necessarily a benign condition for the premenopausal woman.
Furthermore, we can empower patients by educating them about ovarian cancer symptoms and risk factors, information that may promote help-seeking behaviors that aid in early detection. In my case, the continued symptom of abnormal uterine bleeding prompted me to seek further assessment, which led to the discovery of ovarian cancer. Had I not been an educated and empowered patient, I would be telling a completely different story today—most likely one that would include advanced staging. Partner with your patient to discuss available diagnostic testing options and schedule follow-up appointments to monitor presenting complaints.
We also need to partner with our oncology colleagues and researchers. A positive diagnostic test result for possible malignancy necessitates referral to a gynecologic oncologist. Treatment by specialists in high-volume hospitals results in improved ovarian cancer outcomes.6 And we should advocate for continued research to support the discovery of an efficient population screening protocol for this deadly disease.
Finally, and perhaps most radically, I encourage you not to take a watch-and-wait approach in these situations. Ultrasounds are inexpensive, have low mortality risk, and achieve high sensitivity and specificity in detecting and managing adnexal abnormalities.7 In my opinion, the endorsement of TVU testing in this clinical situation is a proactive, prudent, and reasonable action compared with watching and waiting, and it may result in early detection as opposed to advanced disease.
Continue to: I hope that...
I hope that sharing my personal experience with ovarian cancer will compel health care providers to consider this disease as a differential diagnosis and perform appropriate testing when average-risk patients present with nonspecific symptoms. Ultimately, our collective goal should be to increase the survival rate and reduce the suffering associated with ovarian cancer.
1. National Cancer Institute. Cancer Stat Facts: Ovarian Cancer. https://seer.cancer.gov/statfacts/html/ovary.html. Accessed December 3, 2019.
2. American Cancer Society. Key Statistics for Ovarian Cancer. Revised January 8, 2019. www.cancer.org/cancer/ovarian-cancer/about/key-statistics.html. Accessed December 3, 2019.
3. American Cancer Society. Cancer Facts & Figures 2019. www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf . Accessed December 4, 2019.
4. Grossman DC, Surry SJ, Owens DK, et al. Screening for ovarian cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319(6):588-594.
5. Smits S, Boivin J, Menon U, Brain K. Influences on anticipated time to ovarian cancer symptom presentation in women at increased risk compared to population risk of ovarian cancer. BMC Cancer. 2017;17(814):1-11.
6. Pavlik EJ. Ten important considerations for ovarian cancer screening. Diagnostics. 2017;7(22):1-11.
7. Ormsby EL, Pavlik EJ, McGahan JP. Ultrasound monitoring of extant adnexal masses in the era of type 1 and type 2 ovarian cancers: lessons learned from ovarian cancer screening trials. Diagnostics. 2017;7(25):1-19.
1. National Cancer Institute. Cancer Stat Facts: Ovarian Cancer. https://seer.cancer.gov/statfacts/html/ovary.html. Accessed December 3, 2019.
2. American Cancer Society. Key Statistics for Ovarian Cancer. Revised January 8, 2019. www.cancer.org/cancer/ovarian-cancer/about/key-statistics.html. Accessed December 3, 2019.
3. American Cancer Society. Cancer Facts & Figures 2019. www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf . Accessed December 4, 2019.
4. Grossman DC, Surry SJ, Owens DK, et al. Screening for ovarian cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319(6):588-594.
5. Smits S, Boivin J, Menon U, Brain K. Influences on anticipated time to ovarian cancer symptom presentation in women at increased risk compared to population risk of ovarian cancer. BMC Cancer. 2017;17(814):1-11.
6. Pavlik EJ. Ten important considerations for ovarian cancer screening. Diagnostics. 2017;7(22):1-11.
7. Ormsby EL, Pavlik EJ, McGahan JP. Ultrasound monitoring of extant adnexal masses in the era of type 1 and type 2 ovarian cancers: lessons learned from ovarian cancer screening trials. Diagnostics. 2017;7(25):1-19.
New evidence further supports starting CRC screening at age 45
SAN ANTONIO – The American Cancer Society’s 2018 qualified recommendation to lower the starting age for colorectal cancer screening from 50 to 45 years in average-risk individuals has picked up new support from a New Hampshire Colonoscopy Registry analysis.
Data from the population-based statewide colonoscopy registry demonstrated that the prevalence of both advanced adenomas and clinically significant serrated polyps was closely similar for average-risk New Hampshirites age 45-49 years and for those age 50-54, Lynn F. Butterly, MD, reported at the annual meeting of the American College of Gastroenterology.
“The clinical implication is that our data support the recommendation to begin average-risk colorectal cancer screening at age 45,” declared Dr. Butterly, a gastroenterologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
The American Cancer Society recommendation to lower the initial screening age was designed to address a disturbing national trend: the climbing incidence of colorectal cancer in young adults. Indeed, the incidence increased by 55% among 20- to 49-year-olds during 1995-2016, even while falling by 38% in individuals age 50 years and older. The 2018 recommendation was billed as “qualified” because it was based upon predictive modeling and National Cancer Institute Surveillance, Epidemiology, and End Results data which have been criticized as subject to potential bias. Several studies conducted in Korea and other Asian countries have reported a lower colorectal cancer risk in the younger adult population than in those age 50 or older, but questions have been raised about the applicability of such data to the U.S. population.
For Dr. Butterly and coinvestigators, the research imperative was clear: “We need to generate U.S. outcomes data for average-risk individuals age 45-49, versus those over age 50, for whom colorectal cancer screening is already strongly recommended.”
Toward that end, the investigators turned to the New Hampshire Colonoscopy Registry, which contains detailed data on 200,000 colonoscopies, with some 400 variables recorded per patient. To zero in on an average-risk population below age 50, they restricted the analysis to patients undergoing their first colonoscopy for evaluation of low-risk conditions including abdominal pain or constipation while excluding those with GI bleeding, iron-deficiency anemia, abnormal imaging, or a family history of colorectal cancer.
The final study population included 42,600 New Hampshire residents who underwent their first colonoscopy. The key outcomes were the prevalence of advanced adenomas, defined as adenomas more than 1 cm in size, or with high-grade dysplasia or villous elements, and the prevalence of clinically significant serrated polyps larger than 1 cm, or larger than 5 mm if proximally located, as well as traditional serrated adenomas and those with sessile features.
The prevalence of advanced adenomas in 1,870 average-risk patients aged 45-49 years was 3.7% and nearly identical at 3.6% in 22,160 individuals undergoing screening colonoscopy at age 50-54. The rate of clinically significant serrated polyps was 5.9% in the 45- to 49-year-olds, closely similar to the 6.1% rate in patients age 50-54.
Of note, the prevalence of advanced adenomas was just 1.1% in individuals younger than age 40 years, jumping to 3.0% among 40- to 44-year-olds, 5.1% in those age 55-59, and 6.9% at age 60 or more. Clinically significant serrated polyps followed a similar pattern, with rates of 3.0% before age 40, 5.1% in 40- to 44-year-olds, 6.6% in 55- to 59-year-olds, and 6.0% in those who were older.
In a multivariate logistic regression analysis adjusted for sex, body mass index, smoking, and other potential confounders, 45- to 49-year-olds were at a 243% increased risk of finding advanced adenomas on colonoscopy, compared with those less than 40 years old, while the 50- to 54-year-olds had a virtually identical 244% increased risk.
Dr. Butterly noted that there are now 15,000 cases of colorectal cancer occurring annually in individuals under age 50 in the United States, with 3,600 deaths.
“Prevention of colorectal cancer in young, productive individuals is an essential clinical imperative that must be addressed,” she concluded.
She reported having no financial conflicts regarding her study.
SAN ANTONIO – The American Cancer Society’s 2018 qualified recommendation to lower the starting age for colorectal cancer screening from 50 to 45 years in average-risk individuals has picked up new support from a New Hampshire Colonoscopy Registry analysis.
Data from the population-based statewide colonoscopy registry demonstrated that the prevalence of both advanced adenomas and clinically significant serrated polyps was closely similar for average-risk New Hampshirites age 45-49 years and for those age 50-54, Lynn F. Butterly, MD, reported at the annual meeting of the American College of Gastroenterology.
“The clinical implication is that our data support the recommendation to begin average-risk colorectal cancer screening at age 45,” declared Dr. Butterly, a gastroenterologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
The American Cancer Society recommendation to lower the initial screening age was designed to address a disturbing national trend: the climbing incidence of colorectal cancer in young adults. Indeed, the incidence increased by 55% among 20- to 49-year-olds during 1995-2016, even while falling by 38% in individuals age 50 years and older. The 2018 recommendation was billed as “qualified” because it was based upon predictive modeling and National Cancer Institute Surveillance, Epidemiology, and End Results data which have been criticized as subject to potential bias. Several studies conducted in Korea and other Asian countries have reported a lower colorectal cancer risk in the younger adult population than in those age 50 or older, but questions have been raised about the applicability of such data to the U.S. population.
For Dr. Butterly and coinvestigators, the research imperative was clear: “We need to generate U.S. outcomes data for average-risk individuals age 45-49, versus those over age 50, for whom colorectal cancer screening is already strongly recommended.”
Toward that end, the investigators turned to the New Hampshire Colonoscopy Registry, which contains detailed data on 200,000 colonoscopies, with some 400 variables recorded per patient. To zero in on an average-risk population below age 50, they restricted the analysis to patients undergoing their first colonoscopy for evaluation of low-risk conditions including abdominal pain or constipation while excluding those with GI bleeding, iron-deficiency anemia, abnormal imaging, or a family history of colorectal cancer.
The final study population included 42,600 New Hampshire residents who underwent their first colonoscopy. The key outcomes were the prevalence of advanced adenomas, defined as adenomas more than 1 cm in size, or with high-grade dysplasia or villous elements, and the prevalence of clinically significant serrated polyps larger than 1 cm, or larger than 5 mm if proximally located, as well as traditional serrated adenomas and those with sessile features.
The prevalence of advanced adenomas in 1,870 average-risk patients aged 45-49 years was 3.7% and nearly identical at 3.6% in 22,160 individuals undergoing screening colonoscopy at age 50-54. The rate of clinically significant serrated polyps was 5.9% in the 45- to 49-year-olds, closely similar to the 6.1% rate in patients age 50-54.
Of note, the prevalence of advanced adenomas was just 1.1% in individuals younger than age 40 years, jumping to 3.0% among 40- to 44-year-olds, 5.1% in those age 55-59, and 6.9% at age 60 or more. Clinically significant serrated polyps followed a similar pattern, with rates of 3.0% before age 40, 5.1% in 40- to 44-year-olds, 6.6% in 55- to 59-year-olds, and 6.0% in those who were older.
In a multivariate logistic regression analysis adjusted for sex, body mass index, smoking, and other potential confounders, 45- to 49-year-olds were at a 243% increased risk of finding advanced adenomas on colonoscopy, compared with those less than 40 years old, while the 50- to 54-year-olds had a virtually identical 244% increased risk.
Dr. Butterly noted that there are now 15,000 cases of colorectal cancer occurring annually in individuals under age 50 in the United States, with 3,600 deaths.
“Prevention of colorectal cancer in young, productive individuals is an essential clinical imperative that must be addressed,” she concluded.
She reported having no financial conflicts regarding her study.
SAN ANTONIO – The American Cancer Society’s 2018 qualified recommendation to lower the starting age for colorectal cancer screening from 50 to 45 years in average-risk individuals has picked up new support from a New Hampshire Colonoscopy Registry analysis.
Data from the population-based statewide colonoscopy registry demonstrated that the prevalence of both advanced adenomas and clinically significant serrated polyps was closely similar for average-risk New Hampshirites age 45-49 years and for those age 50-54, Lynn F. Butterly, MD, reported at the annual meeting of the American College of Gastroenterology.
“The clinical implication is that our data support the recommendation to begin average-risk colorectal cancer screening at age 45,” declared Dr. Butterly, a gastroenterologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
The American Cancer Society recommendation to lower the initial screening age was designed to address a disturbing national trend: the climbing incidence of colorectal cancer in young adults. Indeed, the incidence increased by 55% among 20- to 49-year-olds during 1995-2016, even while falling by 38% in individuals age 50 years and older. The 2018 recommendation was billed as “qualified” because it was based upon predictive modeling and National Cancer Institute Surveillance, Epidemiology, and End Results data which have been criticized as subject to potential bias. Several studies conducted in Korea and other Asian countries have reported a lower colorectal cancer risk in the younger adult population than in those age 50 or older, but questions have been raised about the applicability of such data to the U.S. population.
For Dr. Butterly and coinvestigators, the research imperative was clear: “We need to generate U.S. outcomes data for average-risk individuals age 45-49, versus those over age 50, for whom colorectal cancer screening is already strongly recommended.”
Toward that end, the investigators turned to the New Hampshire Colonoscopy Registry, which contains detailed data on 200,000 colonoscopies, with some 400 variables recorded per patient. To zero in on an average-risk population below age 50, they restricted the analysis to patients undergoing their first colonoscopy for evaluation of low-risk conditions including abdominal pain or constipation while excluding those with GI bleeding, iron-deficiency anemia, abnormal imaging, or a family history of colorectal cancer.
The final study population included 42,600 New Hampshire residents who underwent their first colonoscopy. The key outcomes were the prevalence of advanced adenomas, defined as adenomas more than 1 cm in size, or with high-grade dysplasia or villous elements, and the prevalence of clinically significant serrated polyps larger than 1 cm, or larger than 5 mm if proximally located, as well as traditional serrated adenomas and those with sessile features.
The prevalence of advanced adenomas in 1,870 average-risk patients aged 45-49 years was 3.7% and nearly identical at 3.6% in 22,160 individuals undergoing screening colonoscopy at age 50-54. The rate of clinically significant serrated polyps was 5.9% in the 45- to 49-year-olds, closely similar to the 6.1% rate in patients age 50-54.
Of note, the prevalence of advanced adenomas was just 1.1% in individuals younger than age 40 years, jumping to 3.0% among 40- to 44-year-olds, 5.1% in those age 55-59, and 6.9% at age 60 or more. Clinically significant serrated polyps followed a similar pattern, with rates of 3.0% before age 40, 5.1% in 40- to 44-year-olds, 6.6% in 55- to 59-year-olds, and 6.0% in those who were older.
In a multivariate logistic regression analysis adjusted for sex, body mass index, smoking, and other potential confounders, 45- to 49-year-olds were at a 243% increased risk of finding advanced adenomas on colonoscopy, compared with those less than 40 years old, while the 50- to 54-year-olds had a virtually identical 244% increased risk.
Dr. Butterly noted that there are now 15,000 cases of colorectal cancer occurring annually in individuals under age 50 in the United States, with 3,600 deaths.
“Prevention of colorectal cancer in young, productive individuals is an essential clinical imperative that must be addressed,” she concluded.
She reported having no financial conflicts regarding her study.
REPORTING FROM ACG 2019