User login
Acne treatment may vary based on race, gender, insurance
based on findings from a retrospective, cohort study of 29,928 individuals with acne.
“Our findings suggest the presence of racial/ethnic, sex, and insurance-based disparities in health care use and treatment for acne and raise particular concern for undertreatment among racial/ethnic minority and female patients,” John S. Barbieri, MD, a dermatology research fellow at the University of Pennsylvania, Philadelphia, and colleagues wrote in a study published in JAMA Dermatology.
Data from previous studies have suggested racial disparities in the management of several dermatologic conditions, including atopic dermatitis and psoriasis, but associations between social demographics and prescribing patterns have not been well studied for acne treatment, the authors noted.
For the current study, the researchers used deidentified data from the Optum electronic health record from Jan. 1, 2007 to June 30, 2017. In all, 29,928 patients aged 15-35 years and who were being treated for acne were included in the study. Of that total, 64% were women, 8% were non-Hispanic black and 68% were white, with the remaining patients grouped as non-Hispanic Asian, Hispanic, or other.
Non-Hispanic black patients were significantly more likely to be seen by a dermatologist, compared with non-Hispanic white patients, who were designated as the reference (odds ratio, 1.20). However, the black patients were less likely to receive prescriptions for any acne medication (incidence rate ratio, 0.89).
Non-Hispanic black patients were more likely than non-Hispanic white patients to be prescribed topical retinoids or topical antibiotics (OR, 1.25 and 1.35, respectively). They were also were less likely than their white counterparts to be prescribed oral antibiotics, spironolactone, and isotretinoin (OR, 0.80, 0.68, and 0.39, respectively).
Overall, men were more than twice as likely as women to receive prescriptions for isotretinoin (OR, 2.44). They were also more likely to receive prescriptions for the other treatments, but the differences were not as high as those for isotretinoin.
In addition, patients with Medicaid insurance were significantly less likely than those with commercial insurance (the reference) to see a dermatologist (OR, 0.46). Medicaid patients also were less likely to be prescribed topical retinoids, oral antibiotics, spironolactone, or isotretinoin (OR, 0.82, 0.87, 0.50, and 0.43, respectively).
The study findings were limited by several factors, among them, the use of automated pharmacy data without confirmation that patients had picked up the medications they had been prescribed, the researchers said. The study also lacked data on acne severity, clinical outcomes, and the use of over-the-counter acne treatments.
“Further study is needed to confirm our findings, provide understanding of the reasons for these potential disparities, and develop strategies to ensure equitable care for patients with acne,” the researchers concluded.
The study was supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health, and by a Pfizer Fellowship in Dermatology Patient Oriented Research grant to the Trustees of the University of Pennsylvania. Dr. Barbieri had no financial conflicts to disclose. One of the study coauthors disclosed relationships with Pfizer, Eli Lilly, and Novartis.
SOURCE: Barbieri JS et al. JAMA Dermatol. 2020 Feb 5. doi: 10.1001/jamadermatol.2019.4818.
based on findings from a retrospective, cohort study of 29,928 individuals with acne.
“Our findings suggest the presence of racial/ethnic, sex, and insurance-based disparities in health care use and treatment for acne and raise particular concern for undertreatment among racial/ethnic minority and female patients,” John S. Barbieri, MD, a dermatology research fellow at the University of Pennsylvania, Philadelphia, and colleagues wrote in a study published in JAMA Dermatology.
Data from previous studies have suggested racial disparities in the management of several dermatologic conditions, including atopic dermatitis and psoriasis, but associations between social demographics and prescribing patterns have not been well studied for acne treatment, the authors noted.
For the current study, the researchers used deidentified data from the Optum electronic health record from Jan. 1, 2007 to June 30, 2017. In all, 29,928 patients aged 15-35 years and who were being treated for acne were included in the study. Of that total, 64% were women, 8% were non-Hispanic black and 68% were white, with the remaining patients grouped as non-Hispanic Asian, Hispanic, or other.
Non-Hispanic black patients were significantly more likely to be seen by a dermatologist, compared with non-Hispanic white patients, who were designated as the reference (odds ratio, 1.20). However, the black patients were less likely to receive prescriptions for any acne medication (incidence rate ratio, 0.89).
Non-Hispanic black patients were more likely than non-Hispanic white patients to be prescribed topical retinoids or topical antibiotics (OR, 1.25 and 1.35, respectively). They were also were less likely than their white counterparts to be prescribed oral antibiotics, spironolactone, and isotretinoin (OR, 0.80, 0.68, and 0.39, respectively).
Overall, men were more than twice as likely as women to receive prescriptions for isotretinoin (OR, 2.44). They were also more likely to receive prescriptions for the other treatments, but the differences were not as high as those for isotretinoin.
In addition, patients with Medicaid insurance were significantly less likely than those with commercial insurance (the reference) to see a dermatologist (OR, 0.46). Medicaid patients also were less likely to be prescribed topical retinoids, oral antibiotics, spironolactone, or isotretinoin (OR, 0.82, 0.87, 0.50, and 0.43, respectively).
The study findings were limited by several factors, among them, the use of automated pharmacy data without confirmation that patients had picked up the medications they had been prescribed, the researchers said. The study also lacked data on acne severity, clinical outcomes, and the use of over-the-counter acne treatments.
“Further study is needed to confirm our findings, provide understanding of the reasons for these potential disparities, and develop strategies to ensure equitable care for patients with acne,” the researchers concluded.
The study was supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health, and by a Pfizer Fellowship in Dermatology Patient Oriented Research grant to the Trustees of the University of Pennsylvania. Dr. Barbieri had no financial conflicts to disclose. One of the study coauthors disclosed relationships with Pfizer, Eli Lilly, and Novartis.
SOURCE: Barbieri JS et al. JAMA Dermatol. 2020 Feb 5. doi: 10.1001/jamadermatol.2019.4818.
based on findings from a retrospective, cohort study of 29,928 individuals with acne.
“Our findings suggest the presence of racial/ethnic, sex, and insurance-based disparities in health care use and treatment for acne and raise particular concern for undertreatment among racial/ethnic minority and female patients,” John S. Barbieri, MD, a dermatology research fellow at the University of Pennsylvania, Philadelphia, and colleagues wrote in a study published in JAMA Dermatology.
Data from previous studies have suggested racial disparities in the management of several dermatologic conditions, including atopic dermatitis and psoriasis, but associations between social demographics and prescribing patterns have not been well studied for acne treatment, the authors noted.
For the current study, the researchers used deidentified data from the Optum electronic health record from Jan. 1, 2007 to June 30, 2017. In all, 29,928 patients aged 15-35 years and who were being treated for acne were included in the study. Of that total, 64% were women, 8% were non-Hispanic black and 68% were white, with the remaining patients grouped as non-Hispanic Asian, Hispanic, or other.
Non-Hispanic black patients were significantly more likely to be seen by a dermatologist, compared with non-Hispanic white patients, who were designated as the reference (odds ratio, 1.20). However, the black patients were less likely to receive prescriptions for any acne medication (incidence rate ratio, 0.89).
Non-Hispanic black patients were more likely than non-Hispanic white patients to be prescribed topical retinoids or topical antibiotics (OR, 1.25 and 1.35, respectively). They were also were less likely than their white counterparts to be prescribed oral antibiotics, spironolactone, and isotretinoin (OR, 0.80, 0.68, and 0.39, respectively).
Overall, men were more than twice as likely as women to receive prescriptions for isotretinoin (OR, 2.44). They were also more likely to receive prescriptions for the other treatments, but the differences were not as high as those for isotretinoin.
In addition, patients with Medicaid insurance were significantly less likely than those with commercial insurance (the reference) to see a dermatologist (OR, 0.46). Medicaid patients also were less likely to be prescribed topical retinoids, oral antibiotics, spironolactone, or isotretinoin (OR, 0.82, 0.87, 0.50, and 0.43, respectively).
The study findings were limited by several factors, among them, the use of automated pharmacy data without confirmation that patients had picked up the medications they had been prescribed, the researchers said. The study also lacked data on acne severity, clinical outcomes, and the use of over-the-counter acne treatments.
“Further study is needed to confirm our findings, provide understanding of the reasons for these potential disparities, and develop strategies to ensure equitable care for patients with acne,” the researchers concluded.
The study was supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health, and by a Pfizer Fellowship in Dermatology Patient Oriented Research grant to the Trustees of the University of Pennsylvania. Dr. Barbieri had no financial conflicts to disclose. One of the study coauthors disclosed relationships with Pfizer, Eli Lilly, and Novartis.
SOURCE: Barbieri JS et al. JAMA Dermatol. 2020 Feb 5. doi: 10.1001/jamadermatol.2019.4818.
FROM JAMA DERMATOLOGY
Be alert for embezzlement
With myriad complex, high-tech problems facing private practice in this modern era, I am periodically reminded by long-time readers to revisit some of the low-tech issues that will always require our attention.
Few are lower tech (in most cases) and more easily overlooked than theft from within. Embezzlement remains far more common in medical offices than generally assumed – and it often occurs in full view of physicians who think everything is fine. Most embezzlers are not skillful or discreet; their transgressions may go undetected for years, simply because no one suspects it is happening.
Detecting fraud is an inexact science. There is no textbook approach that one can follow, but a few simple measures will prevent or expose the most common forms:
- Make it more difficult. Theft and embezzlement are usually products of opportunity, so minimize those opportunities. No one person should be in charge of the entire bookkeeping process: The person who enters charges should be different from the one who enters payments. The one who writes checks or makes electronic fund transfers should not balance the books, and so on. Internal audits should be done on a regular basis, and all employees should know that. Your accountant can help.
- Reconcile cash receipts daily. Embezzlement does not require sophisticated technology; the most common form is simply taking cash out of the till. In a typical scenario, a patient pays a copay of $15 in cash; the receptionist records the payment as $5, and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the charges, receipts, and cash totals daily.
- Inventory your stock. Cash isn’t the only susceptible commodity. If you sell cosmetics or other products, inventory your stock frequently. And office personnel are not the only potential thieves: Last year, a locum tenens physician down the street conspired with a receptionist to take cash transactions for cosmetic neurotoxins and fillers “off the books” and split the spoils. That office was being ripped off twice; first for the neurotoxin and filler materials themselves, and then for the cash proceeds.
- Separate all accounting duties. Another popular ploy is false invoicing for imaginary supplies. A friend’s experience provides a good example (retold with his permission): His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since the same employee also balanced the checkbook, she got away with it for years. “It wasn’t at all clever,” he told me, “and I’m embarrassed to admit that it happened to me.” Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
- Verify expense reports. False expense reporting is a subset of the fake invoice scam. When an employee asks for reimbursement of expenses, make sure those expenses are real.
- Consider computer safeguards. Computers facilitate a lot of financial chores, but they also consolidate financial data in one place, where it is potentially accessible to anybody, anywhere. Your computer vendor should be aware of this, and there should be safeguards built into your system. Ask about them. If they aren’t there, ask why.
- Hire honest employees. All applicants look great on paper, so check their references; and with their permission, you can run background checks for a few dollars on any of several public information web sites. My columns on hiring are available on the MDedge Dermatology website.
- Look for “red flags.” Examples include employees who refuse to take vacations, because someone else will have do their work or who insist on posting expenses that are a coworker’s responsibility, “just to be nice.” Anyone obviously living beyond his or her means merits suspicion as well.
- Consider bonding your employees. Dishonesty bonds are relatively inexpensive, and provide assurance of some measure of recovery if your safeguards fail. Also, just knowing that your staff is bonded will scare off most dishonest applicants. One effective screen is a question on your employment application: “Would you object to being bonded?”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
With myriad complex, high-tech problems facing private practice in this modern era, I am periodically reminded by long-time readers to revisit some of the low-tech issues that will always require our attention.
Few are lower tech (in most cases) and more easily overlooked than theft from within. Embezzlement remains far more common in medical offices than generally assumed – and it often occurs in full view of physicians who think everything is fine. Most embezzlers are not skillful or discreet; their transgressions may go undetected for years, simply because no one suspects it is happening.
Detecting fraud is an inexact science. There is no textbook approach that one can follow, but a few simple measures will prevent or expose the most common forms:
- Make it more difficult. Theft and embezzlement are usually products of opportunity, so minimize those opportunities. No one person should be in charge of the entire bookkeeping process: The person who enters charges should be different from the one who enters payments. The one who writes checks or makes electronic fund transfers should not balance the books, and so on. Internal audits should be done on a regular basis, and all employees should know that. Your accountant can help.
- Reconcile cash receipts daily. Embezzlement does not require sophisticated technology; the most common form is simply taking cash out of the till. In a typical scenario, a patient pays a copay of $15 in cash; the receptionist records the payment as $5, and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the charges, receipts, and cash totals daily.
- Inventory your stock. Cash isn’t the only susceptible commodity. If you sell cosmetics or other products, inventory your stock frequently. And office personnel are not the only potential thieves: Last year, a locum tenens physician down the street conspired with a receptionist to take cash transactions for cosmetic neurotoxins and fillers “off the books” and split the spoils. That office was being ripped off twice; first for the neurotoxin and filler materials themselves, and then for the cash proceeds.
- Separate all accounting duties. Another popular ploy is false invoicing for imaginary supplies. A friend’s experience provides a good example (retold with his permission): His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since the same employee also balanced the checkbook, she got away with it for years. “It wasn’t at all clever,” he told me, “and I’m embarrassed to admit that it happened to me.” Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
- Verify expense reports. False expense reporting is a subset of the fake invoice scam. When an employee asks for reimbursement of expenses, make sure those expenses are real.
- Consider computer safeguards. Computers facilitate a lot of financial chores, but they also consolidate financial data in one place, where it is potentially accessible to anybody, anywhere. Your computer vendor should be aware of this, and there should be safeguards built into your system. Ask about them. If they aren’t there, ask why.
- Hire honest employees. All applicants look great on paper, so check their references; and with their permission, you can run background checks for a few dollars on any of several public information web sites. My columns on hiring are available on the MDedge Dermatology website.
- Look for “red flags.” Examples include employees who refuse to take vacations, because someone else will have do their work or who insist on posting expenses that are a coworker’s responsibility, “just to be nice.” Anyone obviously living beyond his or her means merits suspicion as well.
- Consider bonding your employees. Dishonesty bonds are relatively inexpensive, and provide assurance of some measure of recovery if your safeguards fail. Also, just knowing that your staff is bonded will scare off most dishonest applicants. One effective screen is a question on your employment application: “Would you object to being bonded?”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
With myriad complex, high-tech problems facing private practice in this modern era, I am periodically reminded by long-time readers to revisit some of the low-tech issues that will always require our attention.
Few are lower tech (in most cases) and more easily overlooked than theft from within. Embezzlement remains far more common in medical offices than generally assumed – and it often occurs in full view of physicians who think everything is fine. Most embezzlers are not skillful or discreet; their transgressions may go undetected for years, simply because no one suspects it is happening.
Detecting fraud is an inexact science. There is no textbook approach that one can follow, but a few simple measures will prevent or expose the most common forms:
- Make it more difficult. Theft and embezzlement are usually products of opportunity, so minimize those opportunities. No one person should be in charge of the entire bookkeeping process: The person who enters charges should be different from the one who enters payments. The one who writes checks or makes electronic fund transfers should not balance the books, and so on. Internal audits should be done on a regular basis, and all employees should know that. Your accountant can help.
- Reconcile cash receipts daily. Embezzlement does not require sophisticated technology; the most common form is simply taking cash out of the till. In a typical scenario, a patient pays a copay of $15 in cash; the receptionist records the payment as $5, and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the charges, receipts, and cash totals daily.
- Inventory your stock. Cash isn’t the only susceptible commodity. If you sell cosmetics or other products, inventory your stock frequently. And office personnel are not the only potential thieves: Last year, a locum tenens physician down the street conspired with a receptionist to take cash transactions for cosmetic neurotoxins and fillers “off the books” and split the spoils. That office was being ripped off twice; first for the neurotoxin and filler materials themselves, and then for the cash proceeds.
- Separate all accounting duties. Another popular ploy is false invoicing for imaginary supplies. A friend’s experience provides a good example (retold with his permission): His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since the same employee also balanced the checkbook, she got away with it for years. “It wasn’t at all clever,” he told me, “and I’m embarrassed to admit that it happened to me.” Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
- Verify expense reports. False expense reporting is a subset of the fake invoice scam. When an employee asks for reimbursement of expenses, make sure those expenses are real.
- Consider computer safeguards. Computers facilitate a lot of financial chores, but they also consolidate financial data in one place, where it is potentially accessible to anybody, anywhere. Your computer vendor should be aware of this, and there should be safeguards built into your system. Ask about them. If they aren’t there, ask why.
- Hire honest employees. All applicants look great on paper, so check their references; and with their permission, you can run background checks for a few dollars on any of several public information web sites. My columns on hiring are available on the MDedge Dermatology website.
- Look for “red flags.” Examples include employees who refuse to take vacations, because someone else will have do their work or who insist on posting expenses that are a coworker’s responsibility, “just to be nice.” Anyone obviously living beyond his or her means merits suspicion as well.
- Consider bonding your employees. Dishonesty bonds are relatively inexpensive, and provide assurance of some measure of recovery if your safeguards fail. Also, just knowing that your staff is bonded will scare off most dishonest applicants. One effective screen is a question on your employment application: “Would you object to being bonded?”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Smartphone apps for suspicious skin lesions unreliable
Smartphone applications ( said U.K. researchers reporting a systematic review.
These apps are providing information that could lead to “potentially life-or-death decisions,” commented co-lead author Hywel C. Williams, MD, from the Centre of Evidence Based Dermatology, University of Nottingham (England).
“The one thing you mustn’t do in a situation where early diagnosis can make a difference between life and death is you mustn’t miss the melanoma,” he said in an interview.
“These apps were missing melanomas, and that’s very worrisome,” he commented.
The review included nine studies of skin cancer smartphone apps, including two apps, SkinScan and SkinVision, that have been given Conformit Europenne (CE) marks, allowing them to be marketed across Europe. These apps are also available in Australia and New Zealand, but not in the United States.
The review found that SkinScan was not able to identify any melanomas in the one study that assessed this app, while SkinVision had a relatively low sensitivity and specificity, with 12% of cancerous or precancerous lesions missed and 21% of benign lesions wrongly identified as cancerous.
This means that among 1,000 people with a melanoma prevalence of 3%, 4 of 30 melanomas would be missed, and 200 people would be incorrectly told that a mole was of high concern, the authors estimated.
The research was published by The BMJ on Feb. 10.
“Although I was broad minded on the potential benefit of apps for diagnosing skin cancer, I am now worried given the results of our study and the overall poor quality of studies used to test these apps,” Dr. Williams commented in a statement.
Coauthor Jac Dinnes, PhD, from the Institute of Applied Health Research at the University of Birmingham (England), added it is “really disappointing that there is not better quality evidence available to judge the efficacy of these apps.”
“It is vital that health care professionals are aware of the current limitations both in the technologies and in their evaluations,” she added.
The results also highlight the limitations of the regulatory system governing smartphone apps in that they are currently not subject to assessment by bodies such as the U.K.’s Medicines and Healthcare Products Regulatory Agency (MHRA), the authors commented.
“Regulators need to become alert to the potential harm that poorly performing algorithm-based diagnostic or risk monitoring apps create,” said co-lead author Jonathan J. Deeks, PhD, also at the Institute of Applied Health Research.
“We rely on the CE mark as a sign of quality, but the current CE mark assessment processes are not fit for protecting the public against the risks that these apps present.”
Speaking in an interview, Williams lamented the poor quality of the research that had been conducted. “These studies were not good enough,” he said, adding that “there’s no excuse for really poor study design and poor reporting.”
He would like to see the regulations tightened around AI apps purporting to inform decision making for the general public and suggests that these devices should be assessed by the MHRA. “I really do think a CE mark is not enough,” he said.
The team noted that the skin cancer apps “all include disclaimers that the results should only be used as a guide and cannot replace health care advice,” through which the manufacturers “attempt to evade any responsibility for negative outcomes experienced by users.”
Nevertheless, the “poor and variable performance” of the apps revealed by their review indicates that they “have not yet shown sufficient promise to recommend their use,” they concluded.
The “official approval” implied by a CE mark “will give consumers the impression that the apps have been assessed as effective and safe,” wrote Ben Goldacre, DataLab director, Nuffield Department of Primary Care, University of Oxford (England), and colleagues in an accompanying editorial.
“The implicit assumption is that apps are similarly low-risk technology” to devices such as sticking plasters and reading glasses, they comment.
“But shortcomings in diagnostic apps can have serious implications,” they warn. The “risks include psychological harm from health anxiety or ‘cyberchondria,’ and physical harm from misdiagnosis or overdiagnosis; for clinicians there is a risk of increased workload, and changes to ethical or legal responsibilities around triage, referral, diagnosis, and treatment.” There is also potential for “inappropriate resource use, and even loss of credibility for digital technology in general.”
Details of the review
For their review, the authors searched the Cochrane Central Register on Controlled Trials, the MEDLNE, Embase, Cumulative Index to Nursing and Allied Health Literature, Conference Proceedings Citation index, Zetoc, and Science Citation Index databases, and online trial registers for studies published between August 2016 and April 2019.
From 80 studies identified, 9 met the eligibility criteria.
Of those, six studies, evaluating a total of 725 skin lesions, determined the accuracy of smartphone apps in risk stratifying suspicious skin lesions by comparing them against a histopathological reference standard diagnosis or expert follow-up.
Five of these studies aimed to detect only melanoma, while one sought to differentiate between malignant or premalignant lesions (including melanoma, basal cell carcinoma, and squamous cell carcinoma) and benign lesions.
The three remaining studies, which evaluated 407 lesions in all, compared smartphone app recommendations against a reference standard of expert recommendations for further investigation or intervention.
The researchers found the studies had a string of potential biases and limitations.
For example, only four studies recruited a consecutive sample of study participants and lesions, and only two included lesions selected by study participants, whereas five studies used lesions that had been selected by a clinician.
Three studies reported that it took 5-10 attempts to obtain an adequate image. In seven studies, it was the researchers and not the patients who used the app to photograph the lesions, and two studies used images obtained from dermatology databases.
This “raised concerns that the results of the studies were unlikely to be representative of real life use,” the authors comment.
In addition, the exclusion of unevaluable images “might have systematically inflated the diagnostic performance of the tested apps,” they add.
The independent research was supported by the National Institute for Health Research (NIHR) Birmingham Biomedical Research Centre at the University Hospitals Birmingham NHS Foundation Trust and the University of Birmingham and is an update of one of a collection of reviews funded by the NIHR through its Cochrane Systematic Review Programme Grant.
This article first appeared on Medscape.com.
Smartphone applications ( said U.K. researchers reporting a systematic review.
These apps are providing information that could lead to “potentially life-or-death decisions,” commented co-lead author Hywel C. Williams, MD, from the Centre of Evidence Based Dermatology, University of Nottingham (England).
“The one thing you mustn’t do in a situation where early diagnosis can make a difference between life and death is you mustn’t miss the melanoma,” he said in an interview.
“These apps were missing melanomas, and that’s very worrisome,” he commented.
The review included nine studies of skin cancer smartphone apps, including two apps, SkinScan and SkinVision, that have been given Conformit Europenne (CE) marks, allowing them to be marketed across Europe. These apps are also available in Australia and New Zealand, but not in the United States.
The review found that SkinScan was not able to identify any melanomas in the one study that assessed this app, while SkinVision had a relatively low sensitivity and specificity, with 12% of cancerous or precancerous lesions missed and 21% of benign lesions wrongly identified as cancerous.
This means that among 1,000 people with a melanoma prevalence of 3%, 4 of 30 melanomas would be missed, and 200 people would be incorrectly told that a mole was of high concern, the authors estimated.
The research was published by The BMJ on Feb. 10.
“Although I was broad minded on the potential benefit of apps for diagnosing skin cancer, I am now worried given the results of our study and the overall poor quality of studies used to test these apps,” Dr. Williams commented in a statement.
Coauthor Jac Dinnes, PhD, from the Institute of Applied Health Research at the University of Birmingham (England), added it is “really disappointing that there is not better quality evidence available to judge the efficacy of these apps.”
“It is vital that health care professionals are aware of the current limitations both in the technologies and in their evaluations,” she added.
The results also highlight the limitations of the regulatory system governing smartphone apps in that they are currently not subject to assessment by bodies such as the U.K.’s Medicines and Healthcare Products Regulatory Agency (MHRA), the authors commented.
“Regulators need to become alert to the potential harm that poorly performing algorithm-based diagnostic or risk monitoring apps create,” said co-lead author Jonathan J. Deeks, PhD, also at the Institute of Applied Health Research.
“We rely on the CE mark as a sign of quality, but the current CE mark assessment processes are not fit for protecting the public against the risks that these apps present.”
Speaking in an interview, Williams lamented the poor quality of the research that had been conducted. “These studies were not good enough,” he said, adding that “there’s no excuse for really poor study design and poor reporting.”
He would like to see the regulations tightened around AI apps purporting to inform decision making for the general public and suggests that these devices should be assessed by the MHRA. “I really do think a CE mark is not enough,” he said.
The team noted that the skin cancer apps “all include disclaimers that the results should only be used as a guide and cannot replace health care advice,” through which the manufacturers “attempt to evade any responsibility for negative outcomes experienced by users.”
Nevertheless, the “poor and variable performance” of the apps revealed by their review indicates that they “have not yet shown sufficient promise to recommend their use,” they concluded.
The “official approval” implied by a CE mark “will give consumers the impression that the apps have been assessed as effective and safe,” wrote Ben Goldacre, DataLab director, Nuffield Department of Primary Care, University of Oxford (England), and colleagues in an accompanying editorial.
“The implicit assumption is that apps are similarly low-risk technology” to devices such as sticking plasters and reading glasses, they comment.
“But shortcomings in diagnostic apps can have serious implications,” they warn. The “risks include psychological harm from health anxiety or ‘cyberchondria,’ and physical harm from misdiagnosis or overdiagnosis; for clinicians there is a risk of increased workload, and changes to ethical or legal responsibilities around triage, referral, diagnosis, and treatment.” There is also potential for “inappropriate resource use, and even loss of credibility for digital technology in general.”
Details of the review
For their review, the authors searched the Cochrane Central Register on Controlled Trials, the MEDLNE, Embase, Cumulative Index to Nursing and Allied Health Literature, Conference Proceedings Citation index, Zetoc, and Science Citation Index databases, and online trial registers for studies published between August 2016 and April 2019.
From 80 studies identified, 9 met the eligibility criteria.
Of those, six studies, evaluating a total of 725 skin lesions, determined the accuracy of smartphone apps in risk stratifying suspicious skin lesions by comparing them against a histopathological reference standard diagnosis or expert follow-up.
Five of these studies aimed to detect only melanoma, while one sought to differentiate between malignant or premalignant lesions (including melanoma, basal cell carcinoma, and squamous cell carcinoma) and benign lesions.
The three remaining studies, which evaluated 407 lesions in all, compared smartphone app recommendations against a reference standard of expert recommendations for further investigation or intervention.
The researchers found the studies had a string of potential biases and limitations.
For example, only four studies recruited a consecutive sample of study participants and lesions, and only two included lesions selected by study participants, whereas five studies used lesions that had been selected by a clinician.
Three studies reported that it took 5-10 attempts to obtain an adequate image. In seven studies, it was the researchers and not the patients who used the app to photograph the lesions, and two studies used images obtained from dermatology databases.
This “raised concerns that the results of the studies were unlikely to be representative of real life use,” the authors comment.
In addition, the exclusion of unevaluable images “might have systematically inflated the diagnostic performance of the tested apps,” they add.
The independent research was supported by the National Institute for Health Research (NIHR) Birmingham Biomedical Research Centre at the University Hospitals Birmingham NHS Foundation Trust and the University of Birmingham and is an update of one of a collection of reviews funded by the NIHR through its Cochrane Systematic Review Programme Grant.
This article first appeared on Medscape.com.
Smartphone applications ( said U.K. researchers reporting a systematic review.
These apps are providing information that could lead to “potentially life-or-death decisions,” commented co-lead author Hywel C. Williams, MD, from the Centre of Evidence Based Dermatology, University of Nottingham (England).
“The one thing you mustn’t do in a situation where early diagnosis can make a difference between life and death is you mustn’t miss the melanoma,” he said in an interview.
“These apps were missing melanomas, and that’s very worrisome,” he commented.
The review included nine studies of skin cancer smartphone apps, including two apps, SkinScan and SkinVision, that have been given Conformit Europenne (CE) marks, allowing them to be marketed across Europe. These apps are also available in Australia and New Zealand, but not in the United States.
The review found that SkinScan was not able to identify any melanomas in the one study that assessed this app, while SkinVision had a relatively low sensitivity and specificity, with 12% of cancerous or precancerous lesions missed and 21% of benign lesions wrongly identified as cancerous.
This means that among 1,000 people with a melanoma prevalence of 3%, 4 of 30 melanomas would be missed, and 200 people would be incorrectly told that a mole was of high concern, the authors estimated.
The research was published by The BMJ on Feb. 10.
“Although I was broad minded on the potential benefit of apps for diagnosing skin cancer, I am now worried given the results of our study and the overall poor quality of studies used to test these apps,” Dr. Williams commented in a statement.
Coauthor Jac Dinnes, PhD, from the Institute of Applied Health Research at the University of Birmingham (England), added it is “really disappointing that there is not better quality evidence available to judge the efficacy of these apps.”
“It is vital that health care professionals are aware of the current limitations both in the technologies and in their evaluations,” she added.
The results also highlight the limitations of the regulatory system governing smartphone apps in that they are currently not subject to assessment by bodies such as the U.K.’s Medicines and Healthcare Products Regulatory Agency (MHRA), the authors commented.
“Regulators need to become alert to the potential harm that poorly performing algorithm-based diagnostic or risk monitoring apps create,” said co-lead author Jonathan J. Deeks, PhD, also at the Institute of Applied Health Research.
“We rely on the CE mark as a sign of quality, but the current CE mark assessment processes are not fit for protecting the public against the risks that these apps present.”
Speaking in an interview, Williams lamented the poor quality of the research that had been conducted. “These studies were not good enough,” he said, adding that “there’s no excuse for really poor study design and poor reporting.”
He would like to see the regulations tightened around AI apps purporting to inform decision making for the general public and suggests that these devices should be assessed by the MHRA. “I really do think a CE mark is not enough,” he said.
The team noted that the skin cancer apps “all include disclaimers that the results should only be used as a guide and cannot replace health care advice,” through which the manufacturers “attempt to evade any responsibility for negative outcomes experienced by users.”
Nevertheless, the “poor and variable performance” of the apps revealed by their review indicates that they “have not yet shown sufficient promise to recommend their use,” they concluded.
The “official approval” implied by a CE mark “will give consumers the impression that the apps have been assessed as effective and safe,” wrote Ben Goldacre, DataLab director, Nuffield Department of Primary Care, University of Oxford (England), and colleagues in an accompanying editorial.
“The implicit assumption is that apps are similarly low-risk technology” to devices such as sticking plasters and reading glasses, they comment.
“But shortcomings in diagnostic apps can have serious implications,” they warn. The “risks include psychological harm from health anxiety or ‘cyberchondria,’ and physical harm from misdiagnosis or overdiagnosis; for clinicians there is a risk of increased workload, and changes to ethical or legal responsibilities around triage, referral, diagnosis, and treatment.” There is also potential for “inappropriate resource use, and even loss of credibility for digital technology in general.”
Details of the review
For their review, the authors searched the Cochrane Central Register on Controlled Trials, the MEDLNE, Embase, Cumulative Index to Nursing and Allied Health Literature, Conference Proceedings Citation index, Zetoc, and Science Citation Index databases, and online trial registers for studies published between August 2016 and April 2019.
From 80 studies identified, 9 met the eligibility criteria.
Of those, six studies, evaluating a total of 725 skin lesions, determined the accuracy of smartphone apps in risk stratifying suspicious skin lesions by comparing them against a histopathological reference standard diagnosis or expert follow-up.
Five of these studies aimed to detect only melanoma, while one sought to differentiate between malignant or premalignant lesions (including melanoma, basal cell carcinoma, and squamous cell carcinoma) and benign lesions.
The three remaining studies, which evaluated 407 lesions in all, compared smartphone app recommendations against a reference standard of expert recommendations for further investigation or intervention.
The researchers found the studies had a string of potential biases and limitations.
For example, only four studies recruited a consecutive sample of study participants and lesions, and only two included lesions selected by study participants, whereas five studies used lesions that had been selected by a clinician.
Three studies reported that it took 5-10 attempts to obtain an adequate image. In seven studies, it was the researchers and not the patients who used the app to photograph the lesions, and two studies used images obtained from dermatology databases.
This “raised concerns that the results of the studies were unlikely to be representative of real life use,” the authors comment.
In addition, the exclusion of unevaluable images “might have systematically inflated the diagnostic performance of the tested apps,” they add.
The independent research was supported by the National Institute for Health Research (NIHR) Birmingham Biomedical Research Centre at the University Hospitals Birmingham NHS Foundation Trust and the University of Birmingham and is an update of one of a collection of reviews funded by the NIHR through its Cochrane Systematic Review Programme Grant.
This article first appeared on Medscape.com.
Phase 2 data: Inotuzumab, approved in adults with B-ALL, shows promise in kids, too
ORLANDO – Inotuzumab ozogamicin (InO), a CD22-targeted antibody approved for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL), showed promising safety and efficacy in children and young adults with R/R B-ALL in a phase 2 trial.
Of 48 patients aged 1-21 years enrolled in the Children’s Oncology Group (COG) Protocol AALL1621 and evaluable for response and toxicity after treatment with the approved adult InO dose, 19 achieved a complete response (CR) and 9 achieved a complete response with incomplete count recovery (CRi) after the first treatment cycle, for an overall CR/CRi rate of 58.3%, Maureen M. O’Brien, MD, reported at the annual meeting of the American Society of Hematology.
Of those with CR/CRi, 19 (65.5%) achieved minimal residual disease less than 0.01%, said Dr. O’Brien, a pediatric hematologist and medical director of the Leukemia/Lymphoma Program at the Cancer and Blood Diseases Institute, Cincinnati Children’s Hospital Medical Center.
Three patients had a partial response (PR), nine had stable disease (SD), and eight had progressive disease (PD), and one of each with PR and SD achieved CR/CRi after a second treatment cycle.
“Of note, two patients who were characterized as [having] progressive disease actually had marrow complete response with incomplete count recovery, but had progressive CNS disease,” she said.
Patients included in the single-arm trial had CD22-positive B-ALL, defined as B-ALL with greater than 20% of blasts expressing CD22, and were in at least their second relapse, were refractory to two prior induction regimens, or had a relapse after hematopoietic stem cell transplantation (HSCT). One exception was that patients with Down syndrome were allowed inclusion after a first relapse, she noted.
Median patient age was 9 years, four patients had CNS 3 status, three had Down syndrome, and most were heavily pretreated, with 32 in at least their second relapse.
“Most patients had significant marrow disease burden, with a median marrow blast percentage of 81%,” Dr. O’Brien said. “In terms of prior therapy, 23% had prior transplant, 23% had prior CD19 [chimeric antigen receptor (CAR)] T-cell therapy – including two patients with prior CD22 CAR T, and 29% of patients had received prior blinatumomab.”
All patients received one cycle of InO at a dose of 1.8mg/m2, with .8mg/m2 given on day 1 and 0.5mg/m2 given on days 8 and 15. Intrathecal therapy was determined based on CNS status.
Patients with at least stable disease at day 28 were eligible for a second cycle; those with CR or CRi received InO at a dose of 0.5 mg/m2 on days 1, 8, and 15 in cycle 2, and those without CR/CRi received the same fractionated dose as in cycle 1. Patients with CR/CRi after two cycles were eligible for up to six total cycles at investigator discretion, Dr. O’Brien explained, adding that 26 of 40 patients eligible for cycle 2 proceeded, including 13 of 18 with MRD less than .01%, 6 of 10 with MRD of 0.01% or greater, and 7 of 12 with PR/SD.
After cycle 2, all 13 with MRD less than .01% maintained that MRD level, 3 of 6 with MRD of .01% or greater achieved MRD less than .01%, 2 of 7 with PR/SD achieved CRi with MRD of .01% or greater – and one of those 2 was MRD negative after a third cycle.
Seven patients received three or more cycles.
“Therapy was extremely well tolerated,” Dr. O’Brien said, noting that the most common nonhematological grade 3 or higher adverse events occurring in at least 5% of patients in cycle 1 were febrile neutropenia and infection, occurring in 27.1% and 16.7% of patients, respectively. “But toxicity was quite minimal.”
Hepatic toxicity included four cases of grade 3 alanine transaminase and one grade 3 bilirubin toxicity in cycle 1, and one grade 3 ALT in cycle 2.
“Importantly, there were no inotuzumab dose modifications or delays due to hepatic toxicity,” she said.
Nine patients experienced 11 dose-limiting toxicities in cycle 1, including 7 involving prolonged count recovery beyond day 42, which was not attributable to disease, and 4 nonhematologic events, including drug reaction with eosinophilia and systemic symptoms, bronchopulmonary hemorrhage, respiratory distress, and a postintrathecal methotrexate stroke.
Sinusoidal obstruction syndrome (SOS) developed in 5 of the 48 patients, all in patients who underwent transplant after InO treatment. Only one of the five had undergone a prior transplant. All SOS cases were grade 3 and were treated with defibrotide; four cases resolved quickly, and one was resolving at the time of death from other causes, she said.
“We found no evidence of association with age, conditioning regimen, SOS prophylaxis, cumulative InO exposure, or time from InO to transplant, bearing in mind that it is a small number of cases, so analysis is limited,” she added.
Central CD22 evaluation in 27 patients with pre– and post–cycle 1 samples showed that 11 of those patients had residual disease at the end of cycle 1.
“There is clearly a subset of patients for whom the resistance mechanism does not seem to have any bearing on CD22, as it was still highly expressed at the time of relapse, but there are a significant number of patients who have downregulation of CD22 expression or a subset of blasts that were CD22 negative at the time of relapse,” she said. “Notably, two of three patients with baseline partial CD22 expression – so less than 90% ... did not achieve a morphologic complete response, and both of these patients had KMT2A rearrangements.”
The findings are important, because 10%-20% of children and young adults with B-ALL will relapse, and therapies that can bridge patients to HSCT or CAR T-cell therapy are critical for improving outcomes, Dr. O’Brien said, explaining that InO, a humanized CD22 IgG4 antibody conjugated to calicheamicin, was approved in adults based on “the impressive results from the INNOVATE trial, compared with chemotherapy,” but prospective data on its efficacy and safety in pediatric patients are lacking.
Retrospective data from a compassionate use program in children demonstrated a response rate of 67% in a heavily pretreated population, and phase 1 data from the ITCC-059 trial presented in a poster at the ASH meeting also showed “quite impressive results,” but a major concern has been hepatic toxicity, including SOS, she said.
Given the observed safety and efficacy in the current phase 2 trial, investigation in children will continue, she said, explaining that “COG is now undertaking a phase 3 trial – AALL1732 – which will randomize patients to chemotherapy [with or without] inotuzumab for patients aged 1-25 with newly diagnosed high-risk B-ALL.”
COG AALL1621 was funded by NCTN grants, St. Baldrick’s Foundation, and Pfizer. Dr. O’Brien reported research funding from Pfizer, Celgene, AbbVie, Amgen, Bristol-Myers Squibb, and BTG.
SOURCE: O’Brien M et al. ASH 2019, Abstract 741.
ORLANDO – Inotuzumab ozogamicin (InO), a CD22-targeted antibody approved for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL), showed promising safety and efficacy in children and young adults with R/R B-ALL in a phase 2 trial.
Of 48 patients aged 1-21 years enrolled in the Children’s Oncology Group (COG) Protocol AALL1621 and evaluable for response and toxicity after treatment with the approved adult InO dose, 19 achieved a complete response (CR) and 9 achieved a complete response with incomplete count recovery (CRi) after the first treatment cycle, for an overall CR/CRi rate of 58.3%, Maureen M. O’Brien, MD, reported at the annual meeting of the American Society of Hematology.
Of those with CR/CRi, 19 (65.5%) achieved minimal residual disease less than 0.01%, said Dr. O’Brien, a pediatric hematologist and medical director of the Leukemia/Lymphoma Program at the Cancer and Blood Diseases Institute, Cincinnati Children’s Hospital Medical Center.
Three patients had a partial response (PR), nine had stable disease (SD), and eight had progressive disease (PD), and one of each with PR and SD achieved CR/CRi after a second treatment cycle.
“Of note, two patients who were characterized as [having] progressive disease actually had marrow complete response with incomplete count recovery, but had progressive CNS disease,” she said.
Patients included in the single-arm trial had CD22-positive B-ALL, defined as B-ALL with greater than 20% of blasts expressing CD22, and were in at least their second relapse, were refractory to two prior induction regimens, or had a relapse after hematopoietic stem cell transplantation (HSCT). One exception was that patients with Down syndrome were allowed inclusion after a first relapse, she noted.
Median patient age was 9 years, four patients had CNS 3 status, three had Down syndrome, and most were heavily pretreated, with 32 in at least their second relapse.
“Most patients had significant marrow disease burden, with a median marrow blast percentage of 81%,” Dr. O’Brien said. “In terms of prior therapy, 23% had prior transplant, 23% had prior CD19 [chimeric antigen receptor (CAR)] T-cell therapy – including two patients with prior CD22 CAR T, and 29% of patients had received prior blinatumomab.”
All patients received one cycle of InO at a dose of 1.8mg/m2, with .8mg/m2 given on day 1 and 0.5mg/m2 given on days 8 and 15. Intrathecal therapy was determined based on CNS status.
Patients with at least stable disease at day 28 were eligible for a second cycle; those with CR or CRi received InO at a dose of 0.5 mg/m2 on days 1, 8, and 15 in cycle 2, and those without CR/CRi received the same fractionated dose as in cycle 1. Patients with CR/CRi after two cycles were eligible for up to six total cycles at investigator discretion, Dr. O’Brien explained, adding that 26 of 40 patients eligible for cycle 2 proceeded, including 13 of 18 with MRD less than .01%, 6 of 10 with MRD of 0.01% or greater, and 7 of 12 with PR/SD.
After cycle 2, all 13 with MRD less than .01% maintained that MRD level, 3 of 6 with MRD of .01% or greater achieved MRD less than .01%, 2 of 7 with PR/SD achieved CRi with MRD of .01% or greater – and one of those 2 was MRD negative after a third cycle.
Seven patients received three or more cycles.
“Therapy was extremely well tolerated,” Dr. O’Brien said, noting that the most common nonhematological grade 3 or higher adverse events occurring in at least 5% of patients in cycle 1 were febrile neutropenia and infection, occurring in 27.1% and 16.7% of patients, respectively. “But toxicity was quite minimal.”
Hepatic toxicity included four cases of grade 3 alanine transaminase and one grade 3 bilirubin toxicity in cycle 1, and one grade 3 ALT in cycle 2.
“Importantly, there were no inotuzumab dose modifications or delays due to hepatic toxicity,” she said.
Nine patients experienced 11 dose-limiting toxicities in cycle 1, including 7 involving prolonged count recovery beyond day 42, which was not attributable to disease, and 4 nonhematologic events, including drug reaction with eosinophilia and systemic symptoms, bronchopulmonary hemorrhage, respiratory distress, and a postintrathecal methotrexate stroke.
Sinusoidal obstruction syndrome (SOS) developed in 5 of the 48 patients, all in patients who underwent transplant after InO treatment. Only one of the five had undergone a prior transplant. All SOS cases were grade 3 and were treated with defibrotide; four cases resolved quickly, and one was resolving at the time of death from other causes, she said.
“We found no evidence of association with age, conditioning regimen, SOS prophylaxis, cumulative InO exposure, or time from InO to transplant, bearing in mind that it is a small number of cases, so analysis is limited,” she added.
Central CD22 evaluation in 27 patients with pre– and post–cycle 1 samples showed that 11 of those patients had residual disease at the end of cycle 1.
“There is clearly a subset of patients for whom the resistance mechanism does not seem to have any bearing on CD22, as it was still highly expressed at the time of relapse, but there are a significant number of patients who have downregulation of CD22 expression or a subset of blasts that were CD22 negative at the time of relapse,” she said. “Notably, two of three patients with baseline partial CD22 expression – so less than 90% ... did not achieve a morphologic complete response, and both of these patients had KMT2A rearrangements.”
The findings are important, because 10%-20% of children and young adults with B-ALL will relapse, and therapies that can bridge patients to HSCT or CAR T-cell therapy are critical for improving outcomes, Dr. O’Brien said, explaining that InO, a humanized CD22 IgG4 antibody conjugated to calicheamicin, was approved in adults based on “the impressive results from the INNOVATE trial, compared with chemotherapy,” but prospective data on its efficacy and safety in pediatric patients are lacking.
Retrospective data from a compassionate use program in children demonstrated a response rate of 67% in a heavily pretreated population, and phase 1 data from the ITCC-059 trial presented in a poster at the ASH meeting also showed “quite impressive results,” but a major concern has been hepatic toxicity, including SOS, she said.
Given the observed safety and efficacy in the current phase 2 trial, investigation in children will continue, she said, explaining that “COG is now undertaking a phase 3 trial – AALL1732 – which will randomize patients to chemotherapy [with or without] inotuzumab for patients aged 1-25 with newly diagnosed high-risk B-ALL.”
COG AALL1621 was funded by NCTN grants, St. Baldrick’s Foundation, and Pfizer. Dr. O’Brien reported research funding from Pfizer, Celgene, AbbVie, Amgen, Bristol-Myers Squibb, and BTG.
SOURCE: O’Brien M et al. ASH 2019, Abstract 741.
ORLANDO – Inotuzumab ozogamicin (InO), a CD22-targeted antibody approved for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL), showed promising safety and efficacy in children and young adults with R/R B-ALL in a phase 2 trial.
Of 48 patients aged 1-21 years enrolled in the Children’s Oncology Group (COG) Protocol AALL1621 and evaluable for response and toxicity after treatment with the approved adult InO dose, 19 achieved a complete response (CR) and 9 achieved a complete response with incomplete count recovery (CRi) after the first treatment cycle, for an overall CR/CRi rate of 58.3%, Maureen M. O’Brien, MD, reported at the annual meeting of the American Society of Hematology.
Of those with CR/CRi, 19 (65.5%) achieved minimal residual disease less than 0.01%, said Dr. O’Brien, a pediatric hematologist and medical director of the Leukemia/Lymphoma Program at the Cancer and Blood Diseases Institute, Cincinnati Children’s Hospital Medical Center.
Three patients had a partial response (PR), nine had stable disease (SD), and eight had progressive disease (PD), and one of each with PR and SD achieved CR/CRi after a second treatment cycle.
“Of note, two patients who were characterized as [having] progressive disease actually had marrow complete response with incomplete count recovery, but had progressive CNS disease,” she said.
Patients included in the single-arm trial had CD22-positive B-ALL, defined as B-ALL with greater than 20% of blasts expressing CD22, and were in at least their second relapse, were refractory to two prior induction regimens, or had a relapse after hematopoietic stem cell transplantation (HSCT). One exception was that patients with Down syndrome were allowed inclusion after a first relapse, she noted.
Median patient age was 9 years, four patients had CNS 3 status, three had Down syndrome, and most were heavily pretreated, with 32 in at least their second relapse.
“Most patients had significant marrow disease burden, with a median marrow blast percentage of 81%,” Dr. O’Brien said. “In terms of prior therapy, 23% had prior transplant, 23% had prior CD19 [chimeric antigen receptor (CAR)] T-cell therapy – including two patients with prior CD22 CAR T, and 29% of patients had received prior blinatumomab.”
All patients received one cycle of InO at a dose of 1.8mg/m2, with .8mg/m2 given on day 1 and 0.5mg/m2 given on days 8 and 15. Intrathecal therapy was determined based on CNS status.
Patients with at least stable disease at day 28 were eligible for a second cycle; those with CR or CRi received InO at a dose of 0.5 mg/m2 on days 1, 8, and 15 in cycle 2, and those without CR/CRi received the same fractionated dose as in cycle 1. Patients with CR/CRi after two cycles were eligible for up to six total cycles at investigator discretion, Dr. O’Brien explained, adding that 26 of 40 patients eligible for cycle 2 proceeded, including 13 of 18 with MRD less than .01%, 6 of 10 with MRD of 0.01% or greater, and 7 of 12 with PR/SD.
After cycle 2, all 13 with MRD less than .01% maintained that MRD level, 3 of 6 with MRD of .01% or greater achieved MRD less than .01%, 2 of 7 with PR/SD achieved CRi with MRD of .01% or greater – and one of those 2 was MRD negative after a third cycle.
Seven patients received three or more cycles.
“Therapy was extremely well tolerated,” Dr. O’Brien said, noting that the most common nonhematological grade 3 or higher adverse events occurring in at least 5% of patients in cycle 1 were febrile neutropenia and infection, occurring in 27.1% and 16.7% of patients, respectively. “But toxicity was quite minimal.”
Hepatic toxicity included four cases of grade 3 alanine transaminase and one grade 3 bilirubin toxicity in cycle 1, and one grade 3 ALT in cycle 2.
“Importantly, there were no inotuzumab dose modifications or delays due to hepatic toxicity,” she said.
Nine patients experienced 11 dose-limiting toxicities in cycle 1, including 7 involving prolonged count recovery beyond day 42, which was not attributable to disease, and 4 nonhematologic events, including drug reaction with eosinophilia and systemic symptoms, bronchopulmonary hemorrhage, respiratory distress, and a postintrathecal methotrexate stroke.
Sinusoidal obstruction syndrome (SOS) developed in 5 of the 48 patients, all in patients who underwent transplant after InO treatment. Only one of the five had undergone a prior transplant. All SOS cases were grade 3 and were treated with defibrotide; four cases resolved quickly, and one was resolving at the time of death from other causes, she said.
“We found no evidence of association with age, conditioning regimen, SOS prophylaxis, cumulative InO exposure, or time from InO to transplant, bearing in mind that it is a small number of cases, so analysis is limited,” she added.
Central CD22 evaluation in 27 patients with pre– and post–cycle 1 samples showed that 11 of those patients had residual disease at the end of cycle 1.
“There is clearly a subset of patients for whom the resistance mechanism does not seem to have any bearing on CD22, as it was still highly expressed at the time of relapse, but there are a significant number of patients who have downregulation of CD22 expression or a subset of blasts that were CD22 negative at the time of relapse,” she said. “Notably, two of three patients with baseline partial CD22 expression – so less than 90% ... did not achieve a morphologic complete response, and both of these patients had KMT2A rearrangements.”
The findings are important, because 10%-20% of children and young adults with B-ALL will relapse, and therapies that can bridge patients to HSCT or CAR T-cell therapy are critical for improving outcomes, Dr. O’Brien said, explaining that InO, a humanized CD22 IgG4 antibody conjugated to calicheamicin, was approved in adults based on “the impressive results from the INNOVATE trial, compared with chemotherapy,” but prospective data on its efficacy and safety in pediatric patients are lacking.
Retrospective data from a compassionate use program in children demonstrated a response rate of 67% in a heavily pretreated population, and phase 1 data from the ITCC-059 trial presented in a poster at the ASH meeting also showed “quite impressive results,” but a major concern has been hepatic toxicity, including SOS, she said.
Given the observed safety and efficacy in the current phase 2 trial, investigation in children will continue, she said, explaining that “COG is now undertaking a phase 3 trial – AALL1732 – which will randomize patients to chemotherapy [with or without] inotuzumab for patients aged 1-25 with newly diagnosed high-risk B-ALL.”
COG AALL1621 was funded by NCTN grants, St. Baldrick’s Foundation, and Pfizer. Dr. O’Brien reported research funding from Pfizer, Celgene, AbbVie, Amgen, Bristol-Myers Squibb, and BTG.
SOURCE: O’Brien M et al. ASH 2019, Abstract 741.
REPORTING FROM ASH 2019
CDC confirms 13th case of coronavirus in U.S.
The Centers for Disease Control and Prevention announced the number of confirmed cases of the 2019 Novel Coronavirus (2019-nCoV) in the United States has reached 13.
The latest case, announced Feb. 11, 2020, by the CDC, was in a person in California who was previously under federal quarantine because the patient had traveled to Wuhan, China.
The CDC is currently looking into who the patient may have come in contact with to understand the potential for further spread of the coronavirus.
“The contact investigation is ongoing,” CDC principal deputy director Anne Schuchat, MD, said during a Feb. 11 press conference to provide an update on coronavirus containment activities being taken by the CDC.
Dr. Schuchat also addressed issues related to the laboratory test, as the patient in California was initially thought to be negative for the coronavirus.
“With other cases around the country that we are evaluating, we have been doing serial tests to understand whether they are still infectious” and to gather other information about how results change over time, Dr. Schuchat said.
She noted that the CDC does not “have as much information as we would like on the severity of the virus,” noting that there are many cases in China with severe reactions, while the 13 cases in the United States represent a much more mild reaction to the virus so far.
With the latest case in California, she noted that there was “probably a mix-up and the original test wasn’t negative,” although she did not elaborate on what the nature of the mix-up was, stating that was all the information that she had.
In general, Dr. Schuchat touted the actions taken by the CDC and the federal government focused primarily on containing the spread of the virus in the United States, including the implementation of travel advisories, quarantining passengers returning from China, as well as the new test kits that are being distributed by the agency across the nation and around the world. She also mentioned CDC staff are being deployed around the world to monitor the spreading of the disease and highlighted the outreach efforts to keep the public informed.
Dr. Schuchat highlighted the fact that, of the 13 cases in the United States, 11 were with patients that were in Wuhan, and only 2 were because of close contact with a patient, something that she attributed to the actions being taken.
She also noted that cases in the United States have not been as severe as they have been in China, where deaths have been attributed to the coronavirus outbreak. She added that there have been only two deaths outside of mainland China attributed to the coronavirus.
“Some of the steps the CDC has taken have really put us in better shape should widespread transmission occur in the United States,” she said.
Dr. Schuchat also highlighted that the first charter flight of people quarantined after returning from Wuhan have reached the 14-day milestone and should be on their way home beginning today.
The Centers for Disease Control and Prevention announced the number of confirmed cases of the 2019 Novel Coronavirus (2019-nCoV) in the United States has reached 13.
The latest case, announced Feb. 11, 2020, by the CDC, was in a person in California who was previously under federal quarantine because the patient had traveled to Wuhan, China.
The CDC is currently looking into who the patient may have come in contact with to understand the potential for further spread of the coronavirus.
“The contact investigation is ongoing,” CDC principal deputy director Anne Schuchat, MD, said during a Feb. 11 press conference to provide an update on coronavirus containment activities being taken by the CDC.
Dr. Schuchat also addressed issues related to the laboratory test, as the patient in California was initially thought to be negative for the coronavirus.
“With other cases around the country that we are evaluating, we have been doing serial tests to understand whether they are still infectious” and to gather other information about how results change over time, Dr. Schuchat said.
She noted that the CDC does not “have as much information as we would like on the severity of the virus,” noting that there are many cases in China with severe reactions, while the 13 cases in the United States represent a much more mild reaction to the virus so far.
With the latest case in California, she noted that there was “probably a mix-up and the original test wasn’t negative,” although she did not elaborate on what the nature of the mix-up was, stating that was all the information that she had.
In general, Dr. Schuchat touted the actions taken by the CDC and the federal government focused primarily on containing the spread of the virus in the United States, including the implementation of travel advisories, quarantining passengers returning from China, as well as the new test kits that are being distributed by the agency across the nation and around the world. She also mentioned CDC staff are being deployed around the world to monitor the spreading of the disease and highlighted the outreach efforts to keep the public informed.
Dr. Schuchat highlighted the fact that, of the 13 cases in the United States, 11 were with patients that were in Wuhan, and only 2 were because of close contact with a patient, something that she attributed to the actions being taken.
She also noted that cases in the United States have not been as severe as they have been in China, where deaths have been attributed to the coronavirus outbreak. She added that there have been only two deaths outside of mainland China attributed to the coronavirus.
“Some of the steps the CDC has taken have really put us in better shape should widespread transmission occur in the United States,” she said.
Dr. Schuchat also highlighted that the first charter flight of people quarantined after returning from Wuhan have reached the 14-day milestone and should be on their way home beginning today.
The Centers for Disease Control and Prevention announced the number of confirmed cases of the 2019 Novel Coronavirus (2019-nCoV) in the United States has reached 13.
The latest case, announced Feb. 11, 2020, by the CDC, was in a person in California who was previously under federal quarantine because the patient had traveled to Wuhan, China.
The CDC is currently looking into who the patient may have come in contact with to understand the potential for further spread of the coronavirus.
“The contact investigation is ongoing,” CDC principal deputy director Anne Schuchat, MD, said during a Feb. 11 press conference to provide an update on coronavirus containment activities being taken by the CDC.
Dr. Schuchat also addressed issues related to the laboratory test, as the patient in California was initially thought to be negative for the coronavirus.
“With other cases around the country that we are evaluating, we have been doing serial tests to understand whether they are still infectious” and to gather other information about how results change over time, Dr. Schuchat said.
She noted that the CDC does not “have as much information as we would like on the severity of the virus,” noting that there are many cases in China with severe reactions, while the 13 cases in the United States represent a much more mild reaction to the virus so far.
With the latest case in California, she noted that there was “probably a mix-up and the original test wasn’t negative,” although she did not elaborate on what the nature of the mix-up was, stating that was all the information that she had.
In general, Dr. Schuchat touted the actions taken by the CDC and the federal government focused primarily on containing the spread of the virus in the United States, including the implementation of travel advisories, quarantining passengers returning from China, as well as the new test kits that are being distributed by the agency across the nation and around the world. She also mentioned CDC staff are being deployed around the world to monitor the spreading of the disease and highlighted the outreach efforts to keep the public informed.
Dr. Schuchat highlighted the fact that, of the 13 cases in the United States, 11 were with patients that were in Wuhan, and only 2 were because of close contact with a patient, something that she attributed to the actions being taken.
She also noted that cases in the United States have not been as severe as they have been in China, where deaths have been attributed to the coronavirus outbreak. She added that there have been only two deaths outside of mainland China attributed to the coronavirus.
“Some of the steps the CDC has taken have really put us in better shape should widespread transmission occur in the United States,” she said.
Dr. Schuchat also highlighted that the first charter flight of people quarantined after returning from Wuhan have reached the 14-day milestone and should be on their way home beginning today.
FDA: Cell phones still look safe
according to a review by the Food and Drug Administration.
The FDA reviewed the published literature from 2008 to 2018 and concluded that the data don’t support any quantifiable adverse health risks from RFR. However, the evidence is not without limitations.
The FDA’s evaluation included evidence from in vivo animal studies from Jan. 1, 2008, to Aug. 1, 2018, and epidemiologic studies in humans from Jan. 1, 2008, to May 8, 2018. Both kinds of evidence had limitations, but neither produced strong indications of any causal risks from cell phone use.
The FDA noted that in vivo animal studies are limited by variability of methods and RFR exposure, which make comparisons of results difficult. These studies are also impacted by the indirect effects of temperature increases (the only currently established biological effect of RFR) and stress experienced by the animals, which make teasing out the direct effects of RFR difficult.
The FDA noted that strong epidemiologic studies can provide more relevant and accurate information than in vivo studies, but epidemiologic studies are not without limitations. For example, most have participants track and self-report their cell phone use. There’s also no way to directly track certain factors of RFR exposure, such as frequency, duration, or intensity.
Even with those caveats in mind, the FDA wrote that, “based on the studies that are described in detail in this report, there is insufficient evidence to support a causal association between RFR exposure and tumorigenesis. There is a lack of clear dose-response relationship, a lack of consistent findings or specificity, and a lack of biological mechanistic plausibility.”
The full review is available on the FDA website.
according to a review by the Food and Drug Administration.
The FDA reviewed the published literature from 2008 to 2018 and concluded that the data don’t support any quantifiable adverse health risks from RFR. However, the evidence is not without limitations.
The FDA’s evaluation included evidence from in vivo animal studies from Jan. 1, 2008, to Aug. 1, 2018, and epidemiologic studies in humans from Jan. 1, 2008, to May 8, 2018. Both kinds of evidence had limitations, but neither produced strong indications of any causal risks from cell phone use.
The FDA noted that in vivo animal studies are limited by variability of methods and RFR exposure, which make comparisons of results difficult. These studies are also impacted by the indirect effects of temperature increases (the only currently established biological effect of RFR) and stress experienced by the animals, which make teasing out the direct effects of RFR difficult.
The FDA noted that strong epidemiologic studies can provide more relevant and accurate information than in vivo studies, but epidemiologic studies are not without limitations. For example, most have participants track and self-report their cell phone use. There’s also no way to directly track certain factors of RFR exposure, such as frequency, duration, or intensity.
Even with those caveats in mind, the FDA wrote that, “based on the studies that are described in detail in this report, there is insufficient evidence to support a causal association between RFR exposure and tumorigenesis. There is a lack of clear dose-response relationship, a lack of consistent findings or specificity, and a lack of biological mechanistic plausibility.”
The full review is available on the FDA website.
according to a review by the Food and Drug Administration.
The FDA reviewed the published literature from 2008 to 2018 and concluded that the data don’t support any quantifiable adverse health risks from RFR. However, the evidence is not without limitations.
The FDA’s evaluation included evidence from in vivo animal studies from Jan. 1, 2008, to Aug. 1, 2018, and epidemiologic studies in humans from Jan. 1, 2008, to May 8, 2018. Both kinds of evidence had limitations, but neither produced strong indications of any causal risks from cell phone use.
The FDA noted that in vivo animal studies are limited by variability of methods and RFR exposure, which make comparisons of results difficult. These studies are also impacted by the indirect effects of temperature increases (the only currently established biological effect of RFR) and stress experienced by the animals, which make teasing out the direct effects of RFR difficult.
The FDA noted that strong epidemiologic studies can provide more relevant and accurate information than in vivo studies, but epidemiologic studies are not without limitations. For example, most have participants track and self-report their cell phone use. There’s also no way to directly track certain factors of RFR exposure, such as frequency, duration, or intensity.
Even with those caveats in mind, the FDA wrote that, “based on the studies that are described in detail in this report, there is insufficient evidence to support a causal association between RFR exposure and tumorigenesis. There is a lack of clear dose-response relationship, a lack of consistent findings or specificity, and a lack of biological mechanistic plausibility.”
The full review is available on the FDA website.
U.S. Multi-Society Task Force publishes polypectomy guidance
The U.S. Multi-Society Task Force (USMSTF) on Colorectal Cancer recently published recommendations for endoscopic removal of precancerous colorectal lesions.
According to lead author Tonya Kaltenbach, MD, of the University of California, San Francisco, and fellow panelists, the publication aims to improve complete resection rates, which can vary widely between endoscopists; almost one out of four lesions (22.7%) may be incompletely removed by some practitioners, leading to higher rates of colorectal cancer.
“[A]lthough the majority (50%) of postcolonoscopy colon cancers [are] likely due to missed lesions, close to one-fifth of incident cancers [are] related to incomplete resection,” the panelists wrote in Gastroenterology, referring to a pooled analysis of eight surveillance studies.
The panelists’ recommendations, which were based on both evidence and clinical experience, range from specific polyp removal techniques to guidance for institution-wide quality assurance of polypectomies. Each statement is described by both strength of recommendation and level of evidence, the latter of which was determined by Grading of Recommendations, Assessment, Development, and Evaluation Ratings of Evidence (GRADE) criteria. Recommendations were written by a panel of nine experts and approved by the governing boards of the three societies they represented – the American College of Gastroenterology, the American Gastroenterological Association, and the American Society for Gastrointestinal Endoscopy. The recommendations were copublished in the March issues of the American Journal of Gastroenterology, Gastroenterology, and Gastrointestinal Endoscopy.
Central to the publication are recommended polypectomy techniques for specific types of lesions.
“Polypectomy techniques vary widely in clinical practice,” the panelists wrote. “They are often driven by physician preference based on how they were taught and on trial and error, due to the lack of standardized training and the paucity of published evidence. In the past decade, evidence has evolved on the superiority of specific methods.”
“Optimal techniques encompass effectiveness, safety, and efficiency,” they wrote. “Colorectal lesion characteristics, including location, size, morphology, and histology, influence the optimal removal method.”
For lesions up to 9 mm, the panelists recommended cold snare polypectomy “due to high complete resection rates and safety profile.” In contrast, they recommended against both cold and hot biopsy forceps, which have been associated with higher rates of incomplete resection. Furthermore, they cautioned that hot biopsy forceps may increase risks of complications and produce inadequate tissue samples for histopathology.
For nonpedunculated lesions between 10 and 19 mm, guidance is minimal. The panelists recommended cold or hot snare polypectomy, although this statement was conditional and based on low-quality evidence.
Recommendations were more extensive for large nonpedunculated lesions (at least 20 mm). For such lesions, the panelists strongly recommended endoscopic mucosal resection (EMR). They emphasized that large lesions should be removed in the fewest possible pieces by an appropriately experienced endoscopist during a single colonoscopy session. The panelists recommended the use of a viscous injection solution with a contrast agent and adjuvant thermal ablation of the post-EMR margin. They recommended against the use of tattoo as a submucosal injection solution, and ablation of residual lesion tissue that is endoscopically visible. Additional recommendations for large lesions, including prophylactic closure of resection defects and coagulation techniques, were based on low-quality evidence.
For pedunculated lesions greater than 10 mm, the panelists recommended hot snare polypectomy. For pedunculated lesions with a head greater than 20 mm or a stalk thickness greater than 5 mm, they recommended prophylactic mechanical ligation.
Beyond lesion assessment and removal, recommendations addressed lesion marking, equipment, surveillance, and quality of polypectomy.
Concerning quality, the panelists recommended that endoscopists participate in a quality assurance program that documents adverse events, and that institutions use standardized polypectomy competency assessments, such as Cold Snare Polypectomy Competency Assessment Tool and/or Direct Observation of Polypectomy Skills.
“Focused teaching is needed to ensure the optimal endoscopic management of colorectal lesions,” the panelists wrote. They went on to suggest that “development and implementation of polypectomy quality metrics may be necessary to optimize practice and outcomes.”
“For example, the type of resection method used for the colorectal lesion removal in the procedure report should be documented, and the inclusion of adequate resection technique as a quality indicator in colorectal cancer screening programs should be considered,” they wrote. “Adverse events, including bleeding, perforation, hospital admissions, and the number of benign colorectal lesions referred for surgical management, should be measured and reported. Finally, standards for pathology preparation and reporting of lesions suspicious for submucosal invasion should be in place to provide accurate staging and management.”
The investigators reported relationships with Covidien, Ironwood, Medtronic, and others.
SOURCE: Kaltenbach T et al. Gastroenterology. 2020 Jan 18. doi: 10.1053/j.gastro.2019.12.018.
The U.S. Multi-Society Task Force (USMSTF) on Colorectal Cancer recently published recommendations for endoscopic removal of precancerous colorectal lesions.
According to lead author Tonya Kaltenbach, MD, of the University of California, San Francisco, and fellow panelists, the publication aims to improve complete resection rates, which can vary widely between endoscopists; almost one out of four lesions (22.7%) may be incompletely removed by some practitioners, leading to higher rates of colorectal cancer.
“[A]lthough the majority (50%) of postcolonoscopy colon cancers [are] likely due to missed lesions, close to one-fifth of incident cancers [are] related to incomplete resection,” the panelists wrote in Gastroenterology, referring to a pooled analysis of eight surveillance studies.
The panelists’ recommendations, which were based on both evidence and clinical experience, range from specific polyp removal techniques to guidance for institution-wide quality assurance of polypectomies. Each statement is described by both strength of recommendation and level of evidence, the latter of which was determined by Grading of Recommendations, Assessment, Development, and Evaluation Ratings of Evidence (GRADE) criteria. Recommendations were written by a panel of nine experts and approved by the governing boards of the three societies they represented – the American College of Gastroenterology, the American Gastroenterological Association, and the American Society for Gastrointestinal Endoscopy. The recommendations were copublished in the March issues of the American Journal of Gastroenterology, Gastroenterology, and Gastrointestinal Endoscopy.
Central to the publication are recommended polypectomy techniques for specific types of lesions.
“Polypectomy techniques vary widely in clinical practice,” the panelists wrote. “They are often driven by physician preference based on how they were taught and on trial and error, due to the lack of standardized training and the paucity of published evidence. In the past decade, evidence has evolved on the superiority of specific methods.”
“Optimal techniques encompass effectiveness, safety, and efficiency,” they wrote. “Colorectal lesion characteristics, including location, size, morphology, and histology, influence the optimal removal method.”
For lesions up to 9 mm, the panelists recommended cold snare polypectomy “due to high complete resection rates and safety profile.” In contrast, they recommended against both cold and hot biopsy forceps, which have been associated with higher rates of incomplete resection. Furthermore, they cautioned that hot biopsy forceps may increase risks of complications and produce inadequate tissue samples for histopathology.
For nonpedunculated lesions between 10 and 19 mm, guidance is minimal. The panelists recommended cold or hot snare polypectomy, although this statement was conditional and based on low-quality evidence.
Recommendations were more extensive for large nonpedunculated lesions (at least 20 mm). For such lesions, the panelists strongly recommended endoscopic mucosal resection (EMR). They emphasized that large lesions should be removed in the fewest possible pieces by an appropriately experienced endoscopist during a single colonoscopy session. The panelists recommended the use of a viscous injection solution with a contrast agent and adjuvant thermal ablation of the post-EMR margin. They recommended against the use of tattoo as a submucosal injection solution, and ablation of residual lesion tissue that is endoscopically visible. Additional recommendations for large lesions, including prophylactic closure of resection defects and coagulation techniques, were based on low-quality evidence.
For pedunculated lesions greater than 10 mm, the panelists recommended hot snare polypectomy. For pedunculated lesions with a head greater than 20 mm or a stalk thickness greater than 5 mm, they recommended prophylactic mechanical ligation.
Beyond lesion assessment and removal, recommendations addressed lesion marking, equipment, surveillance, and quality of polypectomy.
Concerning quality, the panelists recommended that endoscopists participate in a quality assurance program that documents adverse events, and that institutions use standardized polypectomy competency assessments, such as Cold Snare Polypectomy Competency Assessment Tool and/or Direct Observation of Polypectomy Skills.
“Focused teaching is needed to ensure the optimal endoscopic management of colorectal lesions,” the panelists wrote. They went on to suggest that “development and implementation of polypectomy quality metrics may be necessary to optimize practice and outcomes.”
“For example, the type of resection method used for the colorectal lesion removal in the procedure report should be documented, and the inclusion of adequate resection technique as a quality indicator in colorectal cancer screening programs should be considered,” they wrote. “Adverse events, including bleeding, perforation, hospital admissions, and the number of benign colorectal lesions referred for surgical management, should be measured and reported. Finally, standards for pathology preparation and reporting of lesions suspicious for submucosal invasion should be in place to provide accurate staging and management.”
The investigators reported relationships with Covidien, Ironwood, Medtronic, and others.
SOURCE: Kaltenbach T et al. Gastroenterology. 2020 Jan 18. doi: 10.1053/j.gastro.2019.12.018.
The U.S. Multi-Society Task Force (USMSTF) on Colorectal Cancer recently published recommendations for endoscopic removal of precancerous colorectal lesions.
According to lead author Tonya Kaltenbach, MD, of the University of California, San Francisco, and fellow panelists, the publication aims to improve complete resection rates, which can vary widely between endoscopists; almost one out of four lesions (22.7%) may be incompletely removed by some practitioners, leading to higher rates of colorectal cancer.
“[A]lthough the majority (50%) of postcolonoscopy colon cancers [are] likely due to missed lesions, close to one-fifth of incident cancers [are] related to incomplete resection,” the panelists wrote in Gastroenterology, referring to a pooled analysis of eight surveillance studies.
The panelists’ recommendations, which were based on both evidence and clinical experience, range from specific polyp removal techniques to guidance for institution-wide quality assurance of polypectomies. Each statement is described by both strength of recommendation and level of evidence, the latter of which was determined by Grading of Recommendations, Assessment, Development, and Evaluation Ratings of Evidence (GRADE) criteria. Recommendations were written by a panel of nine experts and approved by the governing boards of the three societies they represented – the American College of Gastroenterology, the American Gastroenterological Association, and the American Society for Gastrointestinal Endoscopy. The recommendations were copublished in the March issues of the American Journal of Gastroenterology, Gastroenterology, and Gastrointestinal Endoscopy.
Central to the publication are recommended polypectomy techniques for specific types of lesions.
“Polypectomy techniques vary widely in clinical practice,” the panelists wrote. “They are often driven by physician preference based on how they were taught and on trial and error, due to the lack of standardized training and the paucity of published evidence. In the past decade, evidence has evolved on the superiority of specific methods.”
“Optimal techniques encompass effectiveness, safety, and efficiency,” they wrote. “Colorectal lesion characteristics, including location, size, morphology, and histology, influence the optimal removal method.”
For lesions up to 9 mm, the panelists recommended cold snare polypectomy “due to high complete resection rates and safety profile.” In contrast, they recommended against both cold and hot biopsy forceps, which have been associated with higher rates of incomplete resection. Furthermore, they cautioned that hot biopsy forceps may increase risks of complications and produce inadequate tissue samples for histopathology.
For nonpedunculated lesions between 10 and 19 mm, guidance is minimal. The panelists recommended cold or hot snare polypectomy, although this statement was conditional and based on low-quality evidence.
Recommendations were more extensive for large nonpedunculated lesions (at least 20 mm). For such lesions, the panelists strongly recommended endoscopic mucosal resection (EMR). They emphasized that large lesions should be removed in the fewest possible pieces by an appropriately experienced endoscopist during a single colonoscopy session. The panelists recommended the use of a viscous injection solution with a contrast agent and adjuvant thermal ablation of the post-EMR margin. They recommended against the use of tattoo as a submucosal injection solution, and ablation of residual lesion tissue that is endoscopically visible. Additional recommendations for large lesions, including prophylactic closure of resection defects and coagulation techniques, were based on low-quality evidence.
For pedunculated lesions greater than 10 mm, the panelists recommended hot snare polypectomy. For pedunculated lesions with a head greater than 20 mm or a stalk thickness greater than 5 mm, they recommended prophylactic mechanical ligation.
Beyond lesion assessment and removal, recommendations addressed lesion marking, equipment, surveillance, and quality of polypectomy.
Concerning quality, the panelists recommended that endoscopists participate in a quality assurance program that documents adverse events, and that institutions use standardized polypectomy competency assessments, such as Cold Snare Polypectomy Competency Assessment Tool and/or Direct Observation of Polypectomy Skills.
“Focused teaching is needed to ensure the optimal endoscopic management of colorectal lesions,” the panelists wrote. They went on to suggest that “development and implementation of polypectomy quality metrics may be necessary to optimize practice and outcomes.”
“For example, the type of resection method used for the colorectal lesion removal in the procedure report should be documented, and the inclusion of adequate resection technique as a quality indicator in colorectal cancer screening programs should be considered,” they wrote. “Adverse events, including bleeding, perforation, hospital admissions, and the number of benign colorectal lesions referred for surgical management, should be measured and reported. Finally, standards for pathology preparation and reporting of lesions suspicious for submucosal invasion should be in place to provide accurate staging and management.”
The investigators reported relationships with Covidien, Ironwood, Medtronic, and others.
SOURCE: Kaltenbach T et al. Gastroenterology. 2020 Jan 18. doi: 10.1053/j.gastro.2019.12.018.
FROM GASTROENTEROLOGY
Thank you to the CHEST 2020 Scientific Program Committee
The CHEST 2020 Scientific Program Committee has been working tirelessly to select the best and most clinically relevant sessions for the upcoming meeting. CHEST would like to extend a heartfelt thank you to all that actively participated in grading, curriculum group calls, the live meeting in February, and all the homework in between. We’re not done, but your work has been instrumental in making the CHEST Annual Meeting 2020 a success.
The CHEST 2020 Scientific Program Committee has been working tirelessly to select the best and most clinically relevant sessions for the upcoming meeting. CHEST would like to extend a heartfelt thank you to all that actively participated in grading, curriculum group calls, the live meeting in February, and all the homework in between. We’re not done, but your work has been instrumental in making the CHEST Annual Meeting 2020 a success.
The CHEST 2020 Scientific Program Committee has been working tirelessly to select the best and most clinically relevant sessions for the upcoming meeting. CHEST would like to extend a heartfelt thank you to all that actively participated in grading, curriculum group calls, the live meeting in February, and all the homework in between. We’re not done, but your work has been instrumental in making the CHEST Annual Meeting 2020 a success.
Antineutrophil Cytoplasmic Antibody Vasculitis Induced by Hydralazine
To the Editor:
Hydralazine-induced antineutrophil cytoplasmic antibody vasculitis (HIAV) is a rare side effect that may develop in patients treated with hydralazine. Without early recognition and hydralazine cessation, patients often develop acute renal failure and pulmonary hemorrhage that may result in death. We present a case of HIAV.
A 67-year-old woman presented with progressive, tense, hemorrhagic, and necrotic bullae on both sides of the face and neck as well as the extremities of 2 weeks’ duration. She had a history of hypertension and a thyroid nodule after unilateral thyroid lobectomy. A review of symptoms was positive for worsening dyspnea and progressive generalized weakness. Noteworthy medications included amlodipine, metoprolol, levothyroxine, and oral hydralazine 75 mg 3 times daily for 13 months.
Bullae first appeared on the patient’s scalp and quickly progressed with a cephalocaudal pattern with a propensity for the eyes, nostrils, and labial mucosa (Figure 1). The tongue was covered by an eschar, and she had diffuse periorbital edema. Additionally, concentric purpuric patches were noted on the thighs and lower legs (Figure 2).


Pertinent laboratory findings included a positive antinuclear antibody titer of 1:320 and perinuclear antineutrophil cytoplasmic antibody (ANCA) titer of 1:160, along with an elevated serum creatinine level (2.31 mg/dL [reference range, 0.6–1.2 mg/dL]). Bilateral perihilar infiltrates with bilateral pleural effusions were noted on a chest radiograph.
While hospitalized, she developed pulmonary hemorrhages and a progressive decline in respiratory status. She subsequently was admitted to the medical intensive care unit. Aggressive support was administered, and several skin biopsy specimens were obtained along with an endobronchial biopsy of the right middle lobe.
Skin histopathology revealed a necrotic vasculitis (Figure 3). Direct immunofluorescence was not performed. Lung histopathology showed fragments of bronchial tissue with acute and chronic inflammation, focal necrosis, granulation tissue formation, edema, and squamous metaplasia. Together with the clinical history, these findings were consistent with HIAV.

Hydralazine was immediately discontinued, and the patient was started on 65 mg daily of intravenous methylprednisolone; methylprednisolone was later changed to oral prednisone 30 mg daily. Due to multiple organ involvement—lung and kidney—intravenous rituximab 375 mg/m2 every week for 4 weeks, per lymphoma protocol, was started. Within 2 weeks of beginning therapy, her renal function and respiratory status improved, and by week 4, the skin lesions had completely resolved. Although initially she did well on immunosuppressive therapy with resolution of all symptoms, the patient contracted Clostridium difficile–induced systemic inflammatory response syndrome after 5 weeks of therapy and died.
Hydralazine was first introduced in 1951 for adjunctive hypertension therapy due to its vasodilation effects.1-3 Since its introduction, it has been implicated in 2 important disease processes: HIAV and hydralazine-induced lupus.
Hydralazine-induced ANCA vasculitis was first documented in 1980; by 2011, multiple cases had been reported.1-7 Hydralazine-induced ANCA vasculitis has occurred in patients aged 11 to 79 years taking 50 to 300 mg daily. Symptom onset varies from 6 months to 14 years, with a mean exposure duration of 4.7 years and mean daily dose of 142 mg.1-7
Clinical manifestations range from less specific, such as fever, malaise, arthralgia, myalgia, and weight loss, to single tissue or organ involvement that may be fatal. The most frequent clinical features include kidney involvement (81%), cutaneous vasculitis (25%), arthralgia (24%), and pleuropulmonary involvement (19%). Cutaneous manifestations include but are not limited to palpable lower extremity purpura; morbilliform eruptions; and hemorrhagic blisters on the lower legs, arms, trunk, nasal septum, and uvula.1-4,8
The most commonly affected organ is the kidney, which commonly presents as hematuria, proteinuria, and elevated serum creatinine level. Histopathologically, patients most likely will have necrotizing and crescentic glomerulonephritis that is pauci-immune by immunofluorescence.7,9 The lungs are the next most commonly affected organ, with a classic presentation of cough, dyspnea, and hemoptysis in the setting of intra-alveolar hemorrhage.6,8 When both the kidneys and lungs are involved, the patient is said to have pulmonary-renal syndrome that is characterized by lung infiltrates or nodules with or without hemorrhage, hemoptysis, and pleuritis in the setting of glomerulonephritis.1,6
Clear data on incidence and prevalence of HIAV does not exist due to the rarity of the disease and the lack of prospective studies. To identify a clear incidence and prevalence, prospective longitudinal studies with larger cohorts along with better recognition and diagnosis are needed.2,8,10 A few predisposing risk factors have been identified, including older age, a cumulative dose of 100 g at the time of presentation, female sex, a history of thyroid disease, HLA-DR4 genotypes, slow hepatic acetylation, and the null gene for C4.1,3,5,9-11 Our patient was an older woman with a history of thyroid disease who had been taking oral hydralazine 75 mg 3 times daily for 13 months. During this 13-month duration, she had no dose adjustments.
Currently, the pathomechanism for HIAV is unclear and may be multifactorial. There are 4 main theories2,8-10,12,13:
1. Hydralazine and its metabolites accumulate inside neutrophils, then subsequently bind and alter the configuration of myeloperoxidase (MPO). This alteration leads to spreading of the autoimmune response to other autoantigens, making neutrophil proteins (eg, elastase, lactoferrin, nuclear antigens) immunogenic.
2. Hydralazine binds MPO in neutrophils, creating cytotoxic products that induce neutrophil apoptosis. Neutrophil apoptosis without priming then results in ANCA antigen presence on the neutrophil cell membrane and the formation of MPO-ANCA. Myeloperoxidase-ANCA then binds to these membrane-bound antigens that cause self-perpetuating, constitutive activation through cross-linking with proteinase 3 or MPO and Fcγ receptors.
3. Activated neutrophils in the presence of hydrogen peroxidase release MPO that converts hydralazine into a cytotoxic product that is immunogenic for T cells that activate ANCA-producing B cells.
4. Histone H3 trimethyl Lys27 (H3K27me3) levels are perturbed in HIAV, which leads to aberrant gene silencing of proteinase 3 and MPO.In contrast, the demethylase Jumonji domain-containing protein 3 for the H3K27me3 histone is increased in patients without HIAV. Based on this data and the data showing a role for hydralazine in reversing epigenetic silencing of tumor suppressor genes in cancer cells,13 it has been proposed that hydralazine may reverse epigenetic silencing of proteinase 3 and MPO.
Diagnosing HIAV is still difficult because physicians do not recognize the drug as the etiologic agent, there is extensive variability in duration between starting the drug and onset of symptoms, and there often is a failure to order the appropriate laboratory and invasive tests needed for evaluation and diagnosis.3,5,8,10,12 Despite these difficulties, a set of criteria and practices for diagnosis are delineated in Table 1, with the key diagnostic feature being resolution with hydralazine cessation.1,5,7,8,12
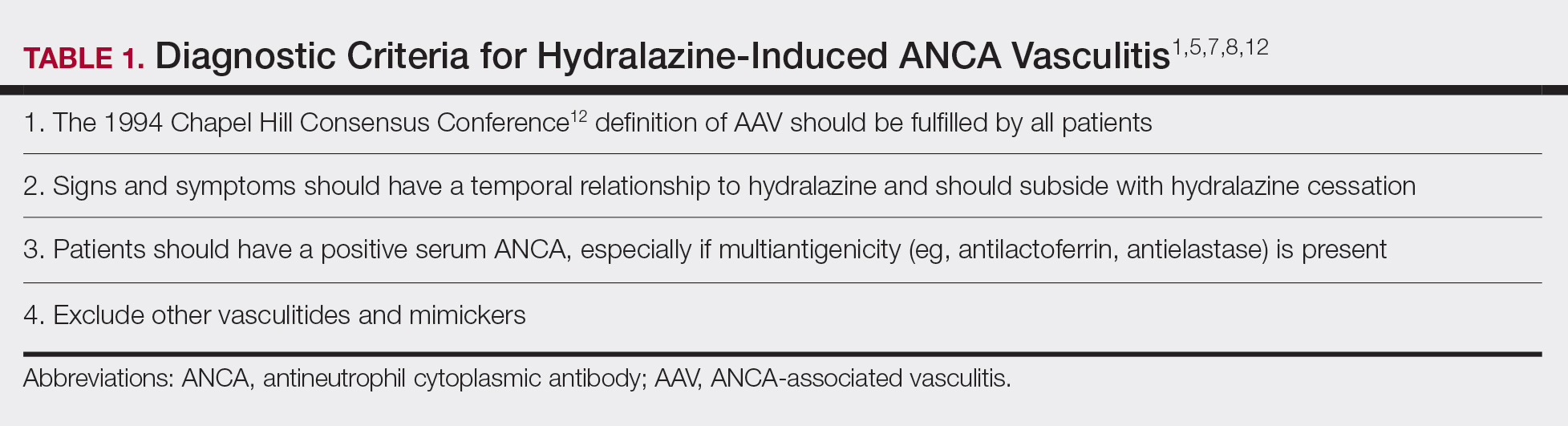
A comprehensive drug history from at least 6 months prior to presentation is essential. Biopsies also are strongly encouraged to confirm the presence of vasculitis and to determine its severity.8,12 If renal biopsies are performed, they typically show scant IgG, IgM, and C3 deposition that is characteristic of ANCA-positive pauci-immune glomerulonephritis. Compared to hydralazine-induced lupus, renal involvement in the setting of HIAV has a relative lack of immunoglobulin and complement deposition with histopathology and immunostaining.14
Laboratory test results including serum MPO-ANCA (perinuclear ANCA) with coexisting elastase and/or lactoferrin autoantibodies is characteristic of HIAV. Antinuclear antibody, antihistone, anti–double-stranded DNA, and antiphospholipid antibodies along with low complement levels also may be present.2,4,9,10,13,15 It is recommended that ANCA assays combine indirect immunofluorescence with antigen-specific enzyme-linked immunosorbent assay.8 With respect to its idiopathic counterpart, patients may only present with MPO-ANCA, while other aforementioned antibodies (eg, antihistone, anti–double-stranded DNA) are rarely found or are entirely absent.2,9 Patients with HIAV often have higher titers of MPO-ANCA.9,15 In hydralazine-induced lupus, patients rarely have MPO-ANCA.
When a diagnosis of HIAV is made, it cannot be confirmed until hydralazine is discontinued and the patient’s symptoms resolve. Therefore, it is both diagnostic and therapeutic to discontinue hydralazine when HIAV is suspected. If recognized when the patient is only presenting with nonspecific symptoms, simple hydralazine cessation may be all that is needed; however, because recognition and diagnosis of HIAV is difficult, most patients present when the disease is severe and has progressed to organ involvement.8-10
Treatment recommendations are highlighted in Table 2.8,9,12 Glucocorticoid therapy is believed to work by preventing T-cell and B-cell maturation needed to produce MPO-ANCA. Rituximab, on the other hand, is suspected to act by clearing the peripheral blood of MPO-ANCA B cells.12,16 Of note, patients with HIAV are different from their idiopathic counterparts because they usually need shorter courses of immunosuppressive therapy, long-term maintenance usually is unnecessary, and their prognosis generally is good if the offending agent is withdrawn.7-9,12 Once the appropriate therapy is instituted, vasculitic manifestations are expected to resolve 10 days to 8 months after hydralazine cessation; however, a response often is seen within 1 to 4 weeks after initiation of systemic treatment.4,8 Serum ANCA should be monitored, and there should be surveillance for the emergence of a chronic underlying vasculitis.8,12
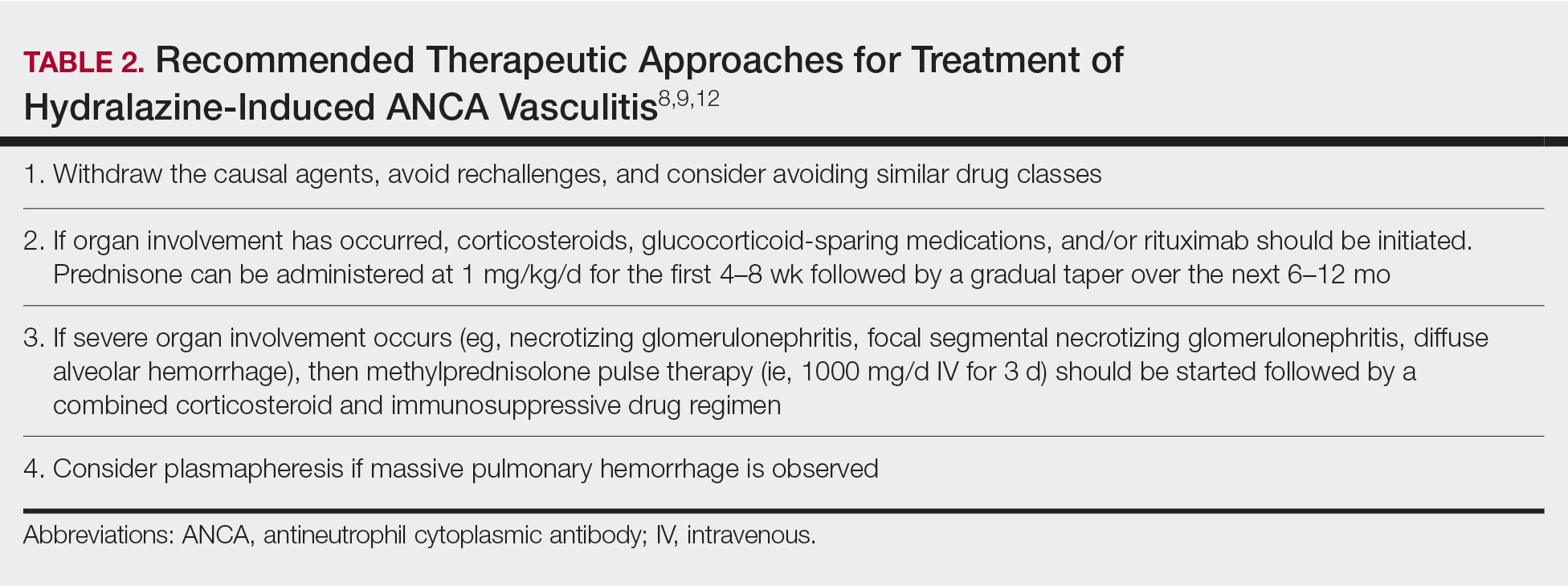
Our patient highlights the importance of identifying individuals at risk for HIAV. We seek to increase recognition of this entity, as it is not commonly seen in a dermatologic setting and is associated with high morbidity and mortality, as seen in our patient.
- Yokogawa N, Vivino FB. Hydralazine-induced autoimmune disease: comparison to idiopathic lupus and ANCA-positive vasculitis. Mod Rheumatol. 2009;19:338-347.
- Agarwal G, Sultan G, Werner SL, et al. Hydralazine induces myeloperoxidase and proteinase 3 anti-neutrophil cytoplasmic antibody vasculitis and leads to pulmonary renal syndrome. Case Rep Nephrol. 2014;2014:868590.
- Keasberry J, Frazier J, Isbel NM, et al. Hydralazine-induced anti-neutrophilic cytoplasmic antibody-positive renal vasculitis presenting with a vasculitic syndrome, acute nephritis and a puzzling skin rash: a case report. J Med Case Rep. 2013;7:20.
- ten Holder SM, Joy MS, Falk RJ. Cutaneous and systemic manifestations of drug-induced vasculitis. Ann Pharmacother. 2002;36:130-147.
- Namas R, Rubin B, Adwar W, et al. A challenging twist in pulmonary renal syndrome. Case Rep Rheumatol. 2014;2014:516362.
- Dobre M, Wish J, Negrea L. Hydralazine-induced ANCA-positive pauci-immune glomerulonephritis. Ren Fail. 2009;31:745-748.
- Hogan JJ, Markowitz GS, Radhakrishnan J. Drug-induced glomerular disease: immune-mediated injury. Clin J Am Soc Nephrol. 2015;10:1300-1310.
- Radic M, Martinovic Kaliterna D, Radic J. Drug-induced vasculitis: a clinical and pathological review. Neth J Med. 2012;70:12-17.
- Babar F, Posner JN, Obah EA. Hydralazine-induced pauci-immune glomerulonephritis: intriguing case series misleading diagnoses. J Community Hosp Intern Med Perspect. 2016;6:30632.
- Marina VP, Malhotra D, Kaw D. Hydralazine-induced ANCA vasculitis with pulmonary renal syndrome: a rare clinical presentation. Int Urol Nephrol. 2012;44:1907-1909.
- Magro CM. Associated ANCA positive vasculitis. The Dermatologist. 2015;23(7). http://www.the-dermatologist.com/content/associated-anca-positive-vasculitis. Accessed January 30, 2020.
- Gao Y, Zhao MH. Review article: Drug-induced anti-neutrophil cytoplasmic antibody-associated vasculitis. Nephrology (Carlton). 2009;14:33-41.
- Grau RG. Drug-induced vasculitis: new insights and a changing lineup of suspects. Curr Rheumatol Rep. 2015;17:71.
- Sangala N, Lee RW, Horsfield C, et al. Combined ANCA-associated vasculitis and lupus syndrome following prolonged use of hydralazine: a timely reminder of an old foe. Int Urol Nephrol. 2010;42:503-506.
- Choi HK, Merkel PA, Walker AM, et al. Drug-associated antineutrophil cytoplasmic antibody-positive vasculitis: prevalence among patients with high titers of antimyeloperoxidase antibodies. Arthritis Rheum. 2000;43:405-413.
- Coutinho AE, Chapman KE. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol. 2011;335:2-13.
To the Editor:
Hydralazine-induced antineutrophil cytoplasmic antibody vasculitis (HIAV) is a rare side effect that may develop in patients treated with hydralazine. Without early recognition and hydralazine cessation, patients often develop acute renal failure and pulmonary hemorrhage that may result in death. We present a case of HIAV.
A 67-year-old woman presented with progressive, tense, hemorrhagic, and necrotic bullae on both sides of the face and neck as well as the extremities of 2 weeks’ duration. She had a history of hypertension and a thyroid nodule after unilateral thyroid lobectomy. A review of symptoms was positive for worsening dyspnea and progressive generalized weakness. Noteworthy medications included amlodipine, metoprolol, levothyroxine, and oral hydralazine 75 mg 3 times daily for 13 months.
Bullae first appeared on the patient’s scalp and quickly progressed with a cephalocaudal pattern with a propensity for the eyes, nostrils, and labial mucosa (Figure 1). The tongue was covered by an eschar, and she had diffuse periorbital edema. Additionally, concentric purpuric patches were noted on the thighs and lower legs (Figure 2).


Pertinent laboratory findings included a positive antinuclear antibody titer of 1:320 and perinuclear antineutrophil cytoplasmic antibody (ANCA) titer of 1:160, along with an elevated serum creatinine level (2.31 mg/dL [reference range, 0.6–1.2 mg/dL]). Bilateral perihilar infiltrates with bilateral pleural effusions were noted on a chest radiograph.
While hospitalized, she developed pulmonary hemorrhages and a progressive decline in respiratory status. She subsequently was admitted to the medical intensive care unit. Aggressive support was administered, and several skin biopsy specimens were obtained along with an endobronchial biopsy of the right middle lobe.
Skin histopathology revealed a necrotic vasculitis (Figure 3). Direct immunofluorescence was not performed. Lung histopathology showed fragments of bronchial tissue with acute and chronic inflammation, focal necrosis, granulation tissue formation, edema, and squamous metaplasia. Together with the clinical history, these findings were consistent with HIAV.

Hydralazine was immediately discontinued, and the patient was started on 65 mg daily of intravenous methylprednisolone; methylprednisolone was later changed to oral prednisone 30 mg daily. Due to multiple organ involvement—lung and kidney—intravenous rituximab 375 mg/m2 every week for 4 weeks, per lymphoma protocol, was started. Within 2 weeks of beginning therapy, her renal function and respiratory status improved, and by week 4, the skin lesions had completely resolved. Although initially she did well on immunosuppressive therapy with resolution of all symptoms, the patient contracted Clostridium difficile–induced systemic inflammatory response syndrome after 5 weeks of therapy and died.
Hydralazine was first introduced in 1951 for adjunctive hypertension therapy due to its vasodilation effects.1-3 Since its introduction, it has been implicated in 2 important disease processes: HIAV and hydralazine-induced lupus.
Hydralazine-induced ANCA vasculitis was first documented in 1980; by 2011, multiple cases had been reported.1-7 Hydralazine-induced ANCA vasculitis has occurred in patients aged 11 to 79 years taking 50 to 300 mg daily. Symptom onset varies from 6 months to 14 years, with a mean exposure duration of 4.7 years and mean daily dose of 142 mg.1-7
Clinical manifestations range from less specific, such as fever, malaise, arthralgia, myalgia, and weight loss, to single tissue or organ involvement that may be fatal. The most frequent clinical features include kidney involvement (81%), cutaneous vasculitis (25%), arthralgia (24%), and pleuropulmonary involvement (19%). Cutaneous manifestations include but are not limited to palpable lower extremity purpura; morbilliform eruptions; and hemorrhagic blisters on the lower legs, arms, trunk, nasal septum, and uvula.1-4,8
The most commonly affected organ is the kidney, which commonly presents as hematuria, proteinuria, and elevated serum creatinine level. Histopathologically, patients most likely will have necrotizing and crescentic glomerulonephritis that is pauci-immune by immunofluorescence.7,9 The lungs are the next most commonly affected organ, with a classic presentation of cough, dyspnea, and hemoptysis in the setting of intra-alveolar hemorrhage.6,8 When both the kidneys and lungs are involved, the patient is said to have pulmonary-renal syndrome that is characterized by lung infiltrates or nodules with or without hemorrhage, hemoptysis, and pleuritis in the setting of glomerulonephritis.1,6
Clear data on incidence and prevalence of HIAV does not exist due to the rarity of the disease and the lack of prospective studies. To identify a clear incidence and prevalence, prospective longitudinal studies with larger cohorts along with better recognition and diagnosis are needed.2,8,10 A few predisposing risk factors have been identified, including older age, a cumulative dose of 100 g at the time of presentation, female sex, a history of thyroid disease, HLA-DR4 genotypes, slow hepatic acetylation, and the null gene for C4.1,3,5,9-11 Our patient was an older woman with a history of thyroid disease who had been taking oral hydralazine 75 mg 3 times daily for 13 months. During this 13-month duration, she had no dose adjustments.
Currently, the pathomechanism for HIAV is unclear and may be multifactorial. There are 4 main theories2,8-10,12,13:
1. Hydralazine and its metabolites accumulate inside neutrophils, then subsequently bind and alter the configuration of myeloperoxidase (MPO). This alteration leads to spreading of the autoimmune response to other autoantigens, making neutrophil proteins (eg, elastase, lactoferrin, nuclear antigens) immunogenic.
2. Hydralazine binds MPO in neutrophils, creating cytotoxic products that induce neutrophil apoptosis. Neutrophil apoptosis without priming then results in ANCA antigen presence on the neutrophil cell membrane and the formation of MPO-ANCA. Myeloperoxidase-ANCA then binds to these membrane-bound antigens that cause self-perpetuating, constitutive activation through cross-linking with proteinase 3 or MPO and Fcγ receptors.
3. Activated neutrophils in the presence of hydrogen peroxidase release MPO that converts hydralazine into a cytotoxic product that is immunogenic for T cells that activate ANCA-producing B cells.
4. Histone H3 trimethyl Lys27 (H3K27me3) levels are perturbed in HIAV, which leads to aberrant gene silencing of proteinase 3 and MPO.In contrast, the demethylase Jumonji domain-containing protein 3 for the H3K27me3 histone is increased in patients without HIAV. Based on this data and the data showing a role for hydralazine in reversing epigenetic silencing of tumor suppressor genes in cancer cells,13 it has been proposed that hydralazine may reverse epigenetic silencing of proteinase 3 and MPO.
Diagnosing HIAV is still difficult because physicians do not recognize the drug as the etiologic agent, there is extensive variability in duration between starting the drug and onset of symptoms, and there often is a failure to order the appropriate laboratory and invasive tests needed for evaluation and diagnosis.3,5,8,10,12 Despite these difficulties, a set of criteria and practices for diagnosis are delineated in Table 1, with the key diagnostic feature being resolution with hydralazine cessation.1,5,7,8,12
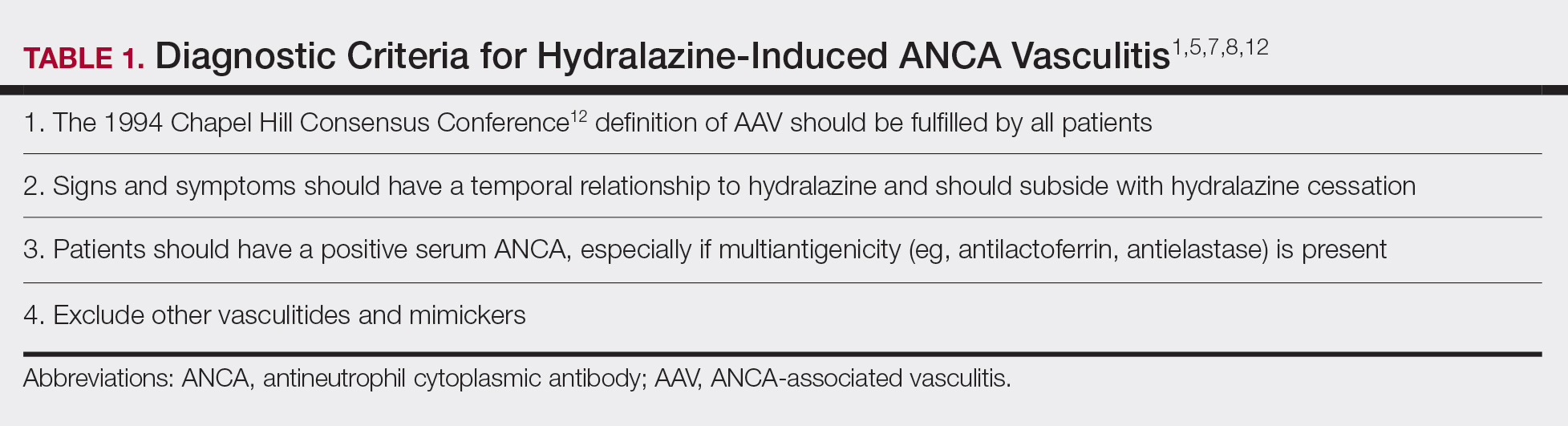
A comprehensive drug history from at least 6 months prior to presentation is essential. Biopsies also are strongly encouraged to confirm the presence of vasculitis and to determine its severity.8,12 If renal biopsies are performed, they typically show scant IgG, IgM, and C3 deposition that is characteristic of ANCA-positive pauci-immune glomerulonephritis. Compared to hydralazine-induced lupus, renal involvement in the setting of HIAV has a relative lack of immunoglobulin and complement deposition with histopathology and immunostaining.14
Laboratory test results including serum MPO-ANCA (perinuclear ANCA) with coexisting elastase and/or lactoferrin autoantibodies is characteristic of HIAV. Antinuclear antibody, antihistone, anti–double-stranded DNA, and antiphospholipid antibodies along with low complement levels also may be present.2,4,9,10,13,15 It is recommended that ANCA assays combine indirect immunofluorescence with antigen-specific enzyme-linked immunosorbent assay.8 With respect to its idiopathic counterpart, patients may only present with MPO-ANCA, while other aforementioned antibodies (eg, antihistone, anti–double-stranded DNA) are rarely found or are entirely absent.2,9 Patients with HIAV often have higher titers of MPO-ANCA.9,15 In hydralazine-induced lupus, patients rarely have MPO-ANCA.
When a diagnosis of HIAV is made, it cannot be confirmed until hydralazine is discontinued and the patient’s symptoms resolve. Therefore, it is both diagnostic and therapeutic to discontinue hydralazine when HIAV is suspected. If recognized when the patient is only presenting with nonspecific symptoms, simple hydralazine cessation may be all that is needed; however, because recognition and diagnosis of HIAV is difficult, most patients present when the disease is severe and has progressed to organ involvement.8-10
Treatment recommendations are highlighted in Table 2.8,9,12 Glucocorticoid therapy is believed to work by preventing T-cell and B-cell maturation needed to produce MPO-ANCA. Rituximab, on the other hand, is suspected to act by clearing the peripheral blood of MPO-ANCA B cells.12,16 Of note, patients with HIAV are different from their idiopathic counterparts because they usually need shorter courses of immunosuppressive therapy, long-term maintenance usually is unnecessary, and their prognosis generally is good if the offending agent is withdrawn.7-9,12 Once the appropriate therapy is instituted, vasculitic manifestations are expected to resolve 10 days to 8 months after hydralazine cessation; however, a response often is seen within 1 to 4 weeks after initiation of systemic treatment.4,8 Serum ANCA should be monitored, and there should be surveillance for the emergence of a chronic underlying vasculitis.8,12
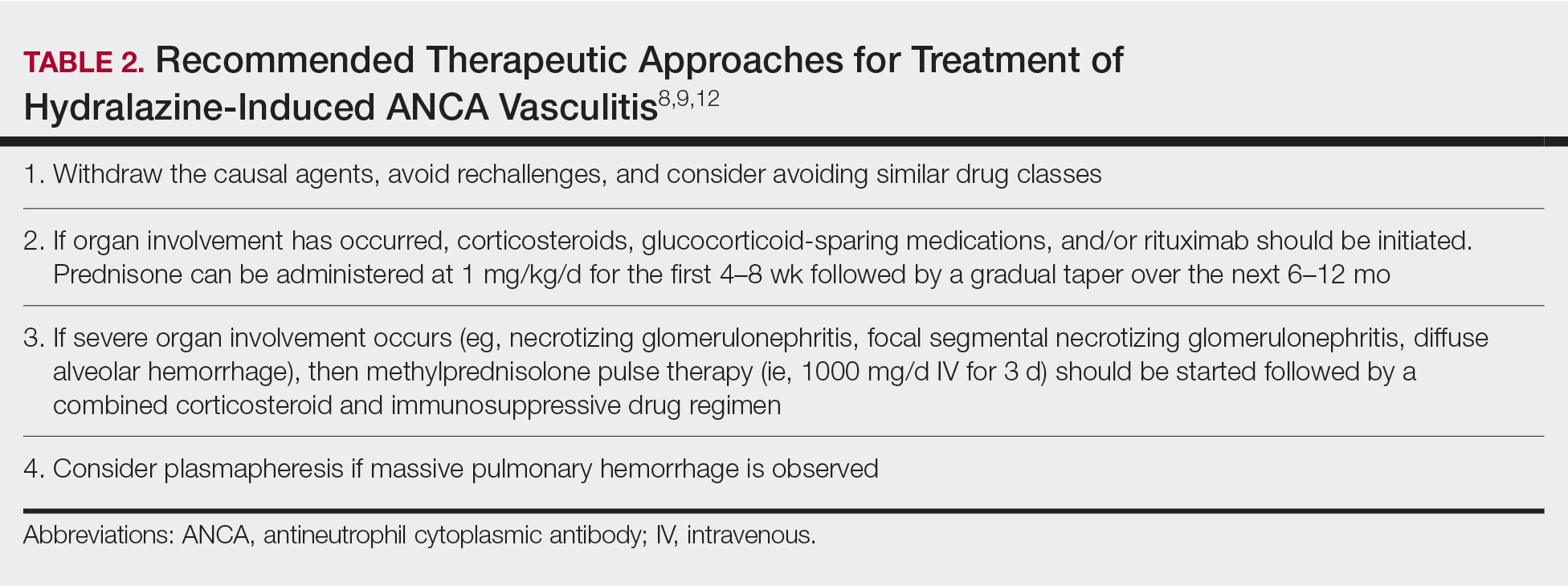
Our patient highlights the importance of identifying individuals at risk for HIAV. We seek to increase recognition of this entity, as it is not commonly seen in a dermatologic setting and is associated with high morbidity and mortality, as seen in our patient.
To the Editor:
Hydralazine-induced antineutrophil cytoplasmic antibody vasculitis (HIAV) is a rare side effect that may develop in patients treated with hydralazine. Without early recognition and hydralazine cessation, patients often develop acute renal failure and pulmonary hemorrhage that may result in death. We present a case of HIAV.
A 67-year-old woman presented with progressive, tense, hemorrhagic, and necrotic bullae on both sides of the face and neck as well as the extremities of 2 weeks’ duration. She had a history of hypertension and a thyroid nodule after unilateral thyroid lobectomy. A review of symptoms was positive for worsening dyspnea and progressive generalized weakness. Noteworthy medications included amlodipine, metoprolol, levothyroxine, and oral hydralazine 75 mg 3 times daily for 13 months.
Bullae first appeared on the patient’s scalp and quickly progressed with a cephalocaudal pattern with a propensity for the eyes, nostrils, and labial mucosa (Figure 1). The tongue was covered by an eschar, and she had diffuse periorbital edema. Additionally, concentric purpuric patches were noted on the thighs and lower legs (Figure 2).


Pertinent laboratory findings included a positive antinuclear antibody titer of 1:320 and perinuclear antineutrophil cytoplasmic antibody (ANCA) titer of 1:160, along with an elevated serum creatinine level (2.31 mg/dL [reference range, 0.6–1.2 mg/dL]). Bilateral perihilar infiltrates with bilateral pleural effusions were noted on a chest radiograph.
While hospitalized, she developed pulmonary hemorrhages and a progressive decline in respiratory status. She subsequently was admitted to the medical intensive care unit. Aggressive support was administered, and several skin biopsy specimens were obtained along with an endobronchial biopsy of the right middle lobe.
Skin histopathology revealed a necrotic vasculitis (Figure 3). Direct immunofluorescence was not performed. Lung histopathology showed fragments of bronchial tissue with acute and chronic inflammation, focal necrosis, granulation tissue formation, edema, and squamous metaplasia. Together with the clinical history, these findings were consistent with HIAV.

Hydralazine was immediately discontinued, and the patient was started on 65 mg daily of intravenous methylprednisolone; methylprednisolone was later changed to oral prednisone 30 mg daily. Due to multiple organ involvement—lung and kidney—intravenous rituximab 375 mg/m2 every week for 4 weeks, per lymphoma protocol, was started. Within 2 weeks of beginning therapy, her renal function and respiratory status improved, and by week 4, the skin lesions had completely resolved. Although initially she did well on immunosuppressive therapy with resolution of all symptoms, the patient contracted Clostridium difficile–induced systemic inflammatory response syndrome after 5 weeks of therapy and died.
Hydralazine was first introduced in 1951 for adjunctive hypertension therapy due to its vasodilation effects.1-3 Since its introduction, it has been implicated in 2 important disease processes: HIAV and hydralazine-induced lupus.
Hydralazine-induced ANCA vasculitis was first documented in 1980; by 2011, multiple cases had been reported.1-7 Hydralazine-induced ANCA vasculitis has occurred in patients aged 11 to 79 years taking 50 to 300 mg daily. Symptom onset varies from 6 months to 14 years, with a mean exposure duration of 4.7 years and mean daily dose of 142 mg.1-7
Clinical manifestations range from less specific, such as fever, malaise, arthralgia, myalgia, and weight loss, to single tissue or organ involvement that may be fatal. The most frequent clinical features include kidney involvement (81%), cutaneous vasculitis (25%), arthralgia (24%), and pleuropulmonary involvement (19%). Cutaneous manifestations include but are not limited to palpable lower extremity purpura; morbilliform eruptions; and hemorrhagic blisters on the lower legs, arms, trunk, nasal septum, and uvula.1-4,8
The most commonly affected organ is the kidney, which commonly presents as hematuria, proteinuria, and elevated serum creatinine level. Histopathologically, patients most likely will have necrotizing and crescentic glomerulonephritis that is pauci-immune by immunofluorescence.7,9 The lungs are the next most commonly affected organ, with a classic presentation of cough, dyspnea, and hemoptysis in the setting of intra-alveolar hemorrhage.6,8 When both the kidneys and lungs are involved, the patient is said to have pulmonary-renal syndrome that is characterized by lung infiltrates or nodules with or without hemorrhage, hemoptysis, and pleuritis in the setting of glomerulonephritis.1,6
Clear data on incidence and prevalence of HIAV does not exist due to the rarity of the disease and the lack of prospective studies. To identify a clear incidence and prevalence, prospective longitudinal studies with larger cohorts along with better recognition and diagnosis are needed.2,8,10 A few predisposing risk factors have been identified, including older age, a cumulative dose of 100 g at the time of presentation, female sex, a history of thyroid disease, HLA-DR4 genotypes, slow hepatic acetylation, and the null gene for C4.1,3,5,9-11 Our patient was an older woman with a history of thyroid disease who had been taking oral hydralazine 75 mg 3 times daily for 13 months. During this 13-month duration, she had no dose adjustments.
Currently, the pathomechanism for HIAV is unclear and may be multifactorial. There are 4 main theories2,8-10,12,13:
1. Hydralazine and its metabolites accumulate inside neutrophils, then subsequently bind and alter the configuration of myeloperoxidase (MPO). This alteration leads to spreading of the autoimmune response to other autoantigens, making neutrophil proteins (eg, elastase, lactoferrin, nuclear antigens) immunogenic.
2. Hydralazine binds MPO in neutrophils, creating cytotoxic products that induce neutrophil apoptosis. Neutrophil apoptosis without priming then results in ANCA antigen presence on the neutrophil cell membrane and the formation of MPO-ANCA. Myeloperoxidase-ANCA then binds to these membrane-bound antigens that cause self-perpetuating, constitutive activation through cross-linking with proteinase 3 or MPO and Fcγ receptors.
3. Activated neutrophils in the presence of hydrogen peroxidase release MPO that converts hydralazine into a cytotoxic product that is immunogenic for T cells that activate ANCA-producing B cells.
4. Histone H3 trimethyl Lys27 (H3K27me3) levels are perturbed in HIAV, which leads to aberrant gene silencing of proteinase 3 and MPO.In contrast, the demethylase Jumonji domain-containing protein 3 for the H3K27me3 histone is increased in patients without HIAV. Based on this data and the data showing a role for hydralazine in reversing epigenetic silencing of tumor suppressor genes in cancer cells,13 it has been proposed that hydralazine may reverse epigenetic silencing of proteinase 3 and MPO.
Diagnosing HIAV is still difficult because physicians do not recognize the drug as the etiologic agent, there is extensive variability in duration between starting the drug and onset of symptoms, and there often is a failure to order the appropriate laboratory and invasive tests needed for evaluation and diagnosis.3,5,8,10,12 Despite these difficulties, a set of criteria and practices for diagnosis are delineated in Table 1, with the key diagnostic feature being resolution with hydralazine cessation.1,5,7,8,12
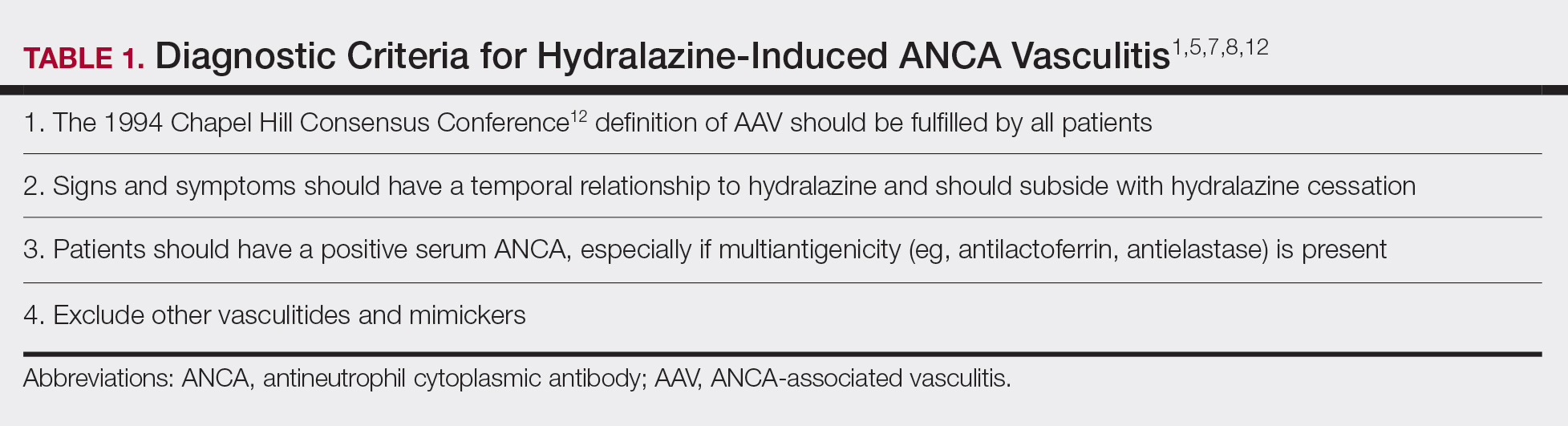
A comprehensive drug history from at least 6 months prior to presentation is essential. Biopsies also are strongly encouraged to confirm the presence of vasculitis and to determine its severity.8,12 If renal biopsies are performed, they typically show scant IgG, IgM, and C3 deposition that is characteristic of ANCA-positive pauci-immune glomerulonephritis. Compared to hydralazine-induced lupus, renal involvement in the setting of HIAV has a relative lack of immunoglobulin and complement deposition with histopathology and immunostaining.14
Laboratory test results including serum MPO-ANCA (perinuclear ANCA) with coexisting elastase and/or lactoferrin autoantibodies is characteristic of HIAV. Antinuclear antibody, antihistone, anti–double-stranded DNA, and antiphospholipid antibodies along with low complement levels also may be present.2,4,9,10,13,15 It is recommended that ANCA assays combine indirect immunofluorescence with antigen-specific enzyme-linked immunosorbent assay.8 With respect to its idiopathic counterpart, patients may only present with MPO-ANCA, while other aforementioned antibodies (eg, antihistone, anti–double-stranded DNA) are rarely found or are entirely absent.2,9 Patients with HIAV often have higher titers of MPO-ANCA.9,15 In hydralazine-induced lupus, patients rarely have MPO-ANCA.
When a diagnosis of HIAV is made, it cannot be confirmed until hydralazine is discontinued and the patient’s symptoms resolve. Therefore, it is both diagnostic and therapeutic to discontinue hydralazine when HIAV is suspected. If recognized when the patient is only presenting with nonspecific symptoms, simple hydralazine cessation may be all that is needed; however, because recognition and diagnosis of HIAV is difficult, most patients present when the disease is severe and has progressed to organ involvement.8-10
Treatment recommendations are highlighted in Table 2.8,9,12 Glucocorticoid therapy is believed to work by preventing T-cell and B-cell maturation needed to produce MPO-ANCA. Rituximab, on the other hand, is suspected to act by clearing the peripheral blood of MPO-ANCA B cells.12,16 Of note, patients with HIAV are different from their idiopathic counterparts because they usually need shorter courses of immunosuppressive therapy, long-term maintenance usually is unnecessary, and their prognosis generally is good if the offending agent is withdrawn.7-9,12 Once the appropriate therapy is instituted, vasculitic manifestations are expected to resolve 10 days to 8 months after hydralazine cessation; however, a response often is seen within 1 to 4 weeks after initiation of systemic treatment.4,8 Serum ANCA should be monitored, and there should be surveillance for the emergence of a chronic underlying vasculitis.8,12
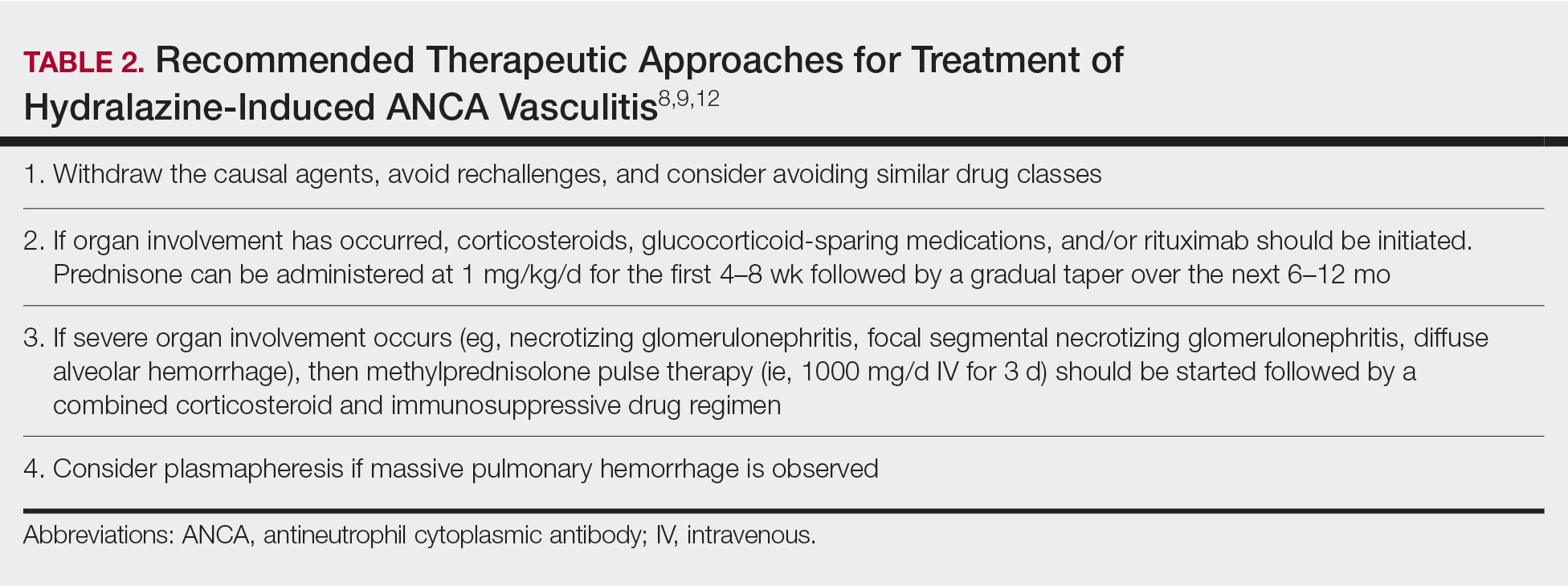
Our patient highlights the importance of identifying individuals at risk for HIAV. We seek to increase recognition of this entity, as it is not commonly seen in a dermatologic setting and is associated with high morbidity and mortality, as seen in our patient.
- Yokogawa N, Vivino FB. Hydralazine-induced autoimmune disease: comparison to idiopathic lupus and ANCA-positive vasculitis. Mod Rheumatol. 2009;19:338-347.
- Agarwal G, Sultan G, Werner SL, et al. Hydralazine induces myeloperoxidase and proteinase 3 anti-neutrophil cytoplasmic antibody vasculitis and leads to pulmonary renal syndrome. Case Rep Nephrol. 2014;2014:868590.
- Keasberry J, Frazier J, Isbel NM, et al. Hydralazine-induced anti-neutrophilic cytoplasmic antibody-positive renal vasculitis presenting with a vasculitic syndrome, acute nephritis and a puzzling skin rash: a case report. J Med Case Rep. 2013;7:20.
- ten Holder SM, Joy MS, Falk RJ. Cutaneous and systemic manifestations of drug-induced vasculitis. Ann Pharmacother. 2002;36:130-147.
- Namas R, Rubin B, Adwar W, et al. A challenging twist in pulmonary renal syndrome. Case Rep Rheumatol. 2014;2014:516362.
- Dobre M, Wish J, Negrea L. Hydralazine-induced ANCA-positive pauci-immune glomerulonephritis. Ren Fail. 2009;31:745-748.
- Hogan JJ, Markowitz GS, Radhakrishnan J. Drug-induced glomerular disease: immune-mediated injury. Clin J Am Soc Nephrol. 2015;10:1300-1310.
- Radic M, Martinovic Kaliterna D, Radic J. Drug-induced vasculitis: a clinical and pathological review. Neth J Med. 2012;70:12-17.
- Babar F, Posner JN, Obah EA. Hydralazine-induced pauci-immune glomerulonephritis: intriguing case series misleading diagnoses. J Community Hosp Intern Med Perspect. 2016;6:30632.
- Marina VP, Malhotra D, Kaw D. Hydralazine-induced ANCA vasculitis with pulmonary renal syndrome: a rare clinical presentation. Int Urol Nephrol. 2012;44:1907-1909.
- Magro CM. Associated ANCA positive vasculitis. The Dermatologist. 2015;23(7). http://www.the-dermatologist.com/content/associated-anca-positive-vasculitis. Accessed January 30, 2020.
- Gao Y, Zhao MH. Review article: Drug-induced anti-neutrophil cytoplasmic antibody-associated vasculitis. Nephrology (Carlton). 2009;14:33-41.
- Grau RG. Drug-induced vasculitis: new insights and a changing lineup of suspects. Curr Rheumatol Rep. 2015;17:71.
- Sangala N, Lee RW, Horsfield C, et al. Combined ANCA-associated vasculitis and lupus syndrome following prolonged use of hydralazine: a timely reminder of an old foe. Int Urol Nephrol. 2010;42:503-506.
- Choi HK, Merkel PA, Walker AM, et al. Drug-associated antineutrophil cytoplasmic antibody-positive vasculitis: prevalence among patients with high titers of antimyeloperoxidase antibodies. Arthritis Rheum. 2000;43:405-413.
- Coutinho AE, Chapman KE. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol. 2011;335:2-13.
- Yokogawa N, Vivino FB. Hydralazine-induced autoimmune disease: comparison to idiopathic lupus and ANCA-positive vasculitis. Mod Rheumatol. 2009;19:338-347.
- Agarwal G, Sultan G, Werner SL, et al. Hydralazine induces myeloperoxidase and proteinase 3 anti-neutrophil cytoplasmic antibody vasculitis and leads to pulmonary renal syndrome. Case Rep Nephrol. 2014;2014:868590.
- Keasberry J, Frazier J, Isbel NM, et al. Hydralazine-induced anti-neutrophilic cytoplasmic antibody-positive renal vasculitis presenting with a vasculitic syndrome, acute nephritis and a puzzling skin rash: a case report. J Med Case Rep. 2013;7:20.
- ten Holder SM, Joy MS, Falk RJ. Cutaneous and systemic manifestations of drug-induced vasculitis. Ann Pharmacother. 2002;36:130-147.
- Namas R, Rubin B, Adwar W, et al. A challenging twist in pulmonary renal syndrome. Case Rep Rheumatol. 2014;2014:516362.
- Dobre M, Wish J, Negrea L. Hydralazine-induced ANCA-positive pauci-immune glomerulonephritis. Ren Fail. 2009;31:745-748.
- Hogan JJ, Markowitz GS, Radhakrishnan J. Drug-induced glomerular disease: immune-mediated injury. Clin J Am Soc Nephrol. 2015;10:1300-1310.
- Radic M, Martinovic Kaliterna D, Radic J. Drug-induced vasculitis: a clinical and pathological review. Neth J Med. 2012;70:12-17.
- Babar F, Posner JN, Obah EA. Hydralazine-induced pauci-immune glomerulonephritis: intriguing case series misleading diagnoses. J Community Hosp Intern Med Perspect. 2016;6:30632.
- Marina VP, Malhotra D, Kaw D. Hydralazine-induced ANCA vasculitis with pulmonary renal syndrome: a rare clinical presentation. Int Urol Nephrol. 2012;44:1907-1909.
- Magro CM. Associated ANCA positive vasculitis. The Dermatologist. 2015;23(7). http://www.the-dermatologist.com/content/associated-anca-positive-vasculitis. Accessed January 30, 2020.
- Gao Y, Zhao MH. Review article: Drug-induced anti-neutrophil cytoplasmic antibody-associated vasculitis. Nephrology (Carlton). 2009;14:33-41.
- Grau RG. Drug-induced vasculitis: new insights and a changing lineup of suspects. Curr Rheumatol Rep. 2015;17:71.
- Sangala N, Lee RW, Horsfield C, et al. Combined ANCA-associated vasculitis and lupus syndrome following prolonged use of hydralazine: a timely reminder of an old foe. Int Urol Nephrol. 2010;42:503-506.
- Choi HK, Merkel PA, Walker AM, et al. Drug-associated antineutrophil cytoplasmic antibody-positive vasculitis: prevalence among patients with high titers of antimyeloperoxidase antibodies. Arthritis Rheum. 2000;43:405-413.
- Coutinho AE, Chapman KE. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol. 2011;335:2-13.
Practice Points
- Hydralazine-induced antineutrophil cytoplasmic antibody vasculitis (HIAV) is a rare side effect of hydralazine treatment and can have notable morbidity and mortality.
- Incidence and prevalence of HIAV is unclear due to its rarity, but risk factors that have been identified are older age, a cumulative dose of 100 g of hydralazine at the time of presentation, female sex, thyroid disease, HLA-DR4 genotypes, slow hepatic acetylation, and the null gene for C4.
- Symptoms of HIAV can include fever, malaise, arthralgia, weight loss, or even involvement of organs such as the kidneys and lungs.
- If recognized early, cessation of hydralazine and supportive therapy generally are sufficient; however, severe cases may need management with high-dose corticosteroids, rituximab, and even plasmapheresis.
Baby’s Got Back Rash
ANSWER
The correct answer is psoriasis vulgaris (choice “a”).
DISCUSSION
At least 30% of patients with psoriasis have a family history of the disease—a meaningful clue in developing a differential. Besides asking about the history, always look for corroborating signs in areas where the disease is commonly seen (eg, the fingernails). In this case, further corroboration was provided by the history of illness at the time of the rash’s onset; what was initially strep-driven guttate psoriasis morphed into full-blown psoriasis vulgaris.
The heavy scales, with their salmon-pink base, tipped the scales in favor of psoriasis as the diagnosis. The pinpoint bleeding (known as the Auspitz sign), although not pathognomic for psoriasis, is certainly suggestive of it.
In adults, these findings would probably have been sufficient to settle on psoriasis. But before labeling a young child with a serious, lifelong diagnosis, it was necessary to be sure. For one thing, advanced psoriasis is very unusual in children as young as this patient, and for another, treatment would likely be problematic. Fortunately for clarity’s sake, the biopsy was consistent with psoriasis and inconsistent with the other items in the differential.
TREATMENT
The patient was prescribed a topical steroid cream to apply every other day, alternating with vitamin D–derived ointment. In addition, he was advised to increase his exposure to natural sunlight. Phototherapy with narrow-band ultraviolet light B would be a superior option, but his family lives too far from the clinic to make 3 roundtrips per week for such treatment.
If these measures fail, a biologic agent may be appropriate. Unfortunately, the patient’s insurance carrier requires the failure of several other modalities before it will approve use of such therapy.
ANSWER
The correct answer is psoriasis vulgaris (choice “a”).
DISCUSSION
At least 30% of patients with psoriasis have a family history of the disease—a meaningful clue in developing a differential. Besides asking about the history, always look for corroborating signs in areas where the disease is commonly seen (eg, the fingernails). In this case, further corroboration was provided by the history of illness at the time of the rash’s onset; what was initially strep-driven guttate psoriasis morphed into full-blown psoriasis vulgaris.
The heavy scales, with their salmon-pink base, tipped the scales in favor of psoriasis as the diagnosis. The pinpoint bleeding (known as the Auspitz sign), although not pathognomic for psoriasis, is certainly suggestive of it.
In adults, these findings would probably have been sufficient to settle on psoriasis. But before labeling a young child with a serious, lifelong diagnosis, it was necessary to be sure. For one thing, advanced psoriasis is very unusual in children as young as this patient, and for another, treatment would likely be problematic. Fortunately for clarity’s sake, the biopsy was consistent with psoriasis and inconsistent with the other items in the differential.
TREATMENT
The patient was prescribed a topical steroid cream to apply every other day, alternating with vitamin D–derived ointment. In addition, he was advised to increase his exposure to natural sunlight. Phototherapy with narrow-band ultraviolet light B would be a superior option, but his family lives too far from the clinic to make 3 roundtrips per week for such treatment.
If these measures fail, a biologic agent may be appropriate. Unfortunately, the patient’s insurance carrier requires the failure of several other modalities before it will approve use of such therapy.
ANSWER
The correct answer is psoriasis vulgaris (choice “a”).
DISCUSSION
At least 30% of patients with psoriasis have a family history of the disease—a meaningful clue in developing a differential. Besides asking about the history, always look for corroborating signs in areas where the disease is commonly seen (eg, the fingernails). In this case, further corroboration was provided by the history of illness at the time of the rash’s onset; what was initially strep-driven guttate psoriasis morphed into full-blown psoriasis vulgaris.
The heavy scales, with their salmon-pink base, tipped the scales in favor of psoriasis as the diagnosis. The pinpoint bleeding (known as the Auspitz sign), although not pathognomic for psoriasis, is certainly suggestive of it.
In adults, these findings would probably have been sufficient to settle on psoriasis. But before labeling a young child with a serious, lifelong diagnosis, it was necessary to be sure. For one thing, advanced psoriasis is very unusual in children as young as this patient, and for another, treatment would likely be problematic. Fortunately for clarity’s sake, the biopsy was consistent with psoriasis and inconsistent with the other items in the differential.
TREATMENT
The patient was prescribed a topical steroid cream to apply every other day, alternating with vitamin D–derived ointment. In addition, he was advised to increase his exposure to natural sunlight. Phototherapy with narrow-band ultraviolet light B would be a superior option, but his family lives too far from the clinic to make 3 roundtrips per week for such treatment.
If these measures fail, a biologic agent may be appropriate. Unfortunately, the patient’s insurance carrier requires the failure of several other modalities before it will approve use of such therapy.

Several months ago, a rash of numerous small, red, scaly papules and patches manifested on this 3-year-old boy’s back and shoulders. At the time, he had been ill for about a week, and his primary care provider diagnosed chickenpox—even though the child had been immunized.
Although the patient’s health soon improved, the appearance of the rash worsened. Treatment with various products—including calamine lotion, OTC tolnaftate and miconazole, and a 2-week course of oral antibiotics—was of no help. Finally, the patient was referred to dermatology.
Family history is positive for psoriasis. However, the parents are quick to note that the boy’s rash appears far different from that of affected family members, and previous providers have dismissed this diagnosis from the differential. There is no family or personal history of atopy.
Examination reveals a dense papulosquamous rash mainly confined to the child’s back and posterior shoulders (the area over the scapula). No other areas are similarly affected, but 1 fingernail is mildly pitted.
A #10 blade lifts the edge of one of the scales gently (and painlessly) until there is pinpoint bleeding from 2 tiny foci. A 5-mm full-thickness punch biopsy with primary closure shows marked parakeratosis, collections of neutrophils on the crests of dermal papillae, and fusing of rete ridges, which effectively obscure the normal wave-like pattern of the dermoepidermal junction.





