User login
Migraine Linked to Adverse Pregnancy Outcomes
Key clinical point: Pregnant women with a history of migraine are at an increased risk of adverse outcomes, including preeclampsia (PE) and low birth weight (LBW).
Major finding: Women with migraine had a higher risk for PE (odds ratio, 2.07; 95% confidence interval, 1.51-2.85) and LBW (odds ratio, 1.18; 95% confidence interval, 1.03-1.34) compared with women without migraine. No significant association was observed between the history of migraine and preterm birth or small for gestational age.
Study details: A systematic review and meta-analysis of 14 studies.
Disclosures: Authors declared no conflict of interest.
Citation: Aukes AM et al. Obstet Gynecol Surv. 2019 Dec. doi: 10.1097/OGX.0000000000000738.
Key clinical point: Pregnant women with a history of migraine are at an increased risk of adverse outcomes, including preeclampsia (PE) and low birth weight (LBW).
Major finding: Women with migraine had a higher risk for PE (odds ratio, 2.07; 95% confidence interval, 1.51-2.85) and LBW (odds ratio, 1.18; 95% confidence interval, 1.03-1.34) compared with women without migraine. No significant association was observed between the history of migraine and preterm birth or small for gestational age.
Study details: A systematic review and meta-analysis of 14 studies.
Disclosures: Authors declared no conflict of interest.
Citation: Aukes AM et al. Obstet Gynecol Surv. 2019 Dec. doi: 10.1097/OGX.0000000000000738.
Key clinical point: Pregnant women with a history of migraine are at an increased risk of adverse outcomes, including preeclampsia (PE) and low birth weight (LBW).
Major finding: Women with migraine had a higher risk for PE (odds ratio, 2.07; 95% confidence interval, 1.51-2.85) and LBW (odds ratio, 1.18; 95% confidence interval, 1.03-1.34) compared with women without migraine. No significant association was observed between the history of migraine and preterm birth or small for gestational age.
Study details: A systematic review and meta-analysis of 14 studies.
Disclosures: Authors declared no conflict of interest.
Citation: Aukes AM et al. Obstet Gynecol Surv. 2019 Dec. doi: 10.1097/OGX.0000000000000738.
HBV: Surface antigen titer and ALT predict seroconversion
Among patients with hepatitis B virus (HBV) infection who are not receiving antiviral therapy, surface antigen titers and alanine aminotransferase (ALT) levels may independently predict spontaneous seroconversion, based on a recent case-control study.
, reported principal author Sammy Saab, MD, of the University of California, Los Angeles, and colleagues.
While the predictive value of HBsAg titers has been demonstrated for patients undergoing antiviral therapy, data are limited for spontaneous seroconversion, the investigators wrote in Journal of Clinical Gastroenterology.
To learn more about this scenario, the investigators reviewed medical records from 2,126 patients who visited a large community practice in the Los Angeles area between 2014 and 2019. Cases were defined by HBV infection with seroconversion, whereas matched controls were defined by HBV without seroconversion. A variety of demographic and clinical data were also evaluated, including age, ethnicity, sex, HBsAg titer, ALT, HBV DNA, total cholesterol, presence of fatty liver, and other factors.
The investigators identified 167 patients with HBV who were not on antiviral therapy. Of these, 14 underwent seroconversion, and were matched with 70 patients who did not seroconvert. All patients were of Asian descent, most were women, and none had cirrhosis.
Across all demographic and clinical parameters, the two factors that significantly differed between cases and controls were ALT and HBsAg titer. The mean ALT for patients who seroconverted was 17.6 U/L, versus 25.1 U/L in those who did not undergo seroconversion (P less than .01). Similarly, mean titer was lower in the seroconversion group (459.8 vs. 782.0 IU/mL; P = .01).
The investigators noted that seroconversion was more common among patients with an HBsAg titer level less than 1,000 IU/mL. Specifically, 79% of patients who seroconverted had a titer less than 1,000 IU/mL, compared with just 16% of patients who did not seroconvert (P = .001).
HBV DNA levels were not predictive of seroconversion, the investigators noted, which aligns with most, but not all, previous research.
The investigators reported no disclosures.
SOURCE: Wu CF et al. J Clin Gastroenterol. 2020 Feb 11. doi: 10.1097/MCG.0000000000001324.
Among patients with hepatitis B virus (HBV) infection who are not receiving antiviral therapy, surface antigen titers and alanine aminotransferase (ALT) levels may independently predict spontaneous seroconversion, based on a recent case-control study.
, reported principal author Sammy Saab, MD, of the University of California, Los Angeles, and colleagues.
While the predictive value of HBsAg titers has been demonstrated for patients undergoing antiviral therapy, data are limited for spontaneous seroconversion, the investigators wrote in Journal of Clinical Gastroenterology.
To learn more about this scenario, the investigators reviewed medical records from 2,126 patients who visited a large community practice in the Los Angeles area between 2014 and 2019. Cases were defined by HBV infection with seroconversion, whereas matched controls were defined by HBV without seroconversion. A variety of demographic and clinical data were also evaluated, including age, ethnicity, sex, HBsAg titer, ALT, HBV DNA, total cholesterol, presence of fatty liver, and other factors.
The investigators identified 167 patients with HBV who were not on antiviral therapy. Of these, 14 underwent seroconversion, and were matched with 70 patients who did not seroconvert. All patients were of Asian descent, most were women, and none had cirrhosis.
Across all demographic and clinical parameters, the two factors that significantly differed between cases and controls were ALT and HBsAg titer. The mean ALT for patients who seroconverted was 17.6 U/L, versus 25.1 U/L in those who did not undergo seroconversion (P less than .01). Similarly, mean titer was lower in the seroconversion group (459.8 vs. 782.0 IU/mL; P = .01).
The investigators noted that seroconversion was more common among patients with an HBsAg titer level less than 1,000 IU/mL. Specifically, 79% of patients who seroconverted had a titer less than 1,000 IU/mL, compared with just 16% of patients who did not seroconvert (P = .001).
HBV DNA levels were not predictive of seroconversion, the investigators noted, which aligns with most, but not all, previous research.
The investigators reported no disclosures.
SOURCE: Wu CF et al. J Clin Gastroenterol. 2020 Feb 11. doi: 10.1097/MCG.0000000000001324.
Among patients with hepatitis B virus (HBV) infection who are not receiving antiviral therapy, surface antigen titers and alanine aminotransferase (ALT) levels may independently predict spontaneous seroconversion, based on a recent case-control study.
, reported principal author Sammy Saab, MD, of the University of California, Los Angeles, and colleagues.
While the predictive value of HBsAg titers has been demonstrated for patients undergoing antiviral therapy, data are limited for spontaneous seroconversion, the investigators wrote in Journal of Clinical Gastroenterology.
To learn more about this scenario, the investigators reviewed medical records from 2,126 patients who visited a large community practice in the Los Angeles area between 2014 and 2019. Cases were defined by HBV infection with seroconversion, whereas matched controls were defined by HBV without seroconversion. A variety of demographic and clinical data were also evaluated, including age, ethnicity, sex, HBsAg titer, ALT, HBV DNA, total cholesterol, presence of fatty liver, and other factors.
The investigators identified 167 patients with HBV who were not on antiviral therapy. Of these, 14 underwent seroconversion, and were matched with 70 patients who did not seroconvert. All patients were of Asian descent, most were women, and none had cirrhosis.
Across all demographic and clinical parameters, the two factors that significantly differed between cases and controls were ALT and HBsAg titer. The mean ALT for patients who seroconverted was 17.6 U/L, versus 25.1 U/L in those who did not undergo seroconversion (P less than .01). Similarly, mean titer was lower in the seroconversion group (459.8 vs. 782.0 IU/mL; P = .01).
The investigators noted that seroconversion was more common among patients with an HBsAg titer level less than 1,000 IU/mL. Specifically, 79% of patients who seroconverted had a titer less than 1,000 IU/mL, compared with just 16% of patients who did not seroconvert (P = .001).
HBV DNA levels were not predictive of seroconversion, the investigators noted, which aligns with most, but not all, previous research.
The investigators reported no disclosures.
SOURCE: Wu CF et al. J Clin Gastroenterol. 2020 Feb 11. doi: 10.1097/MCG.0000000000001324.
FROM JOURNAL OF CLINICAL GASTROENTEROLOGY
Migraineurs Likely to Exhibit Metacognitive Deficits
Key clinical point: Patients with migraine are likely to have metacognitive deficits.
Major finding: Patients with migraine performed worse on measures of metacognitive functions, including accuracy score (P = .012), global monitoring (P = .015), monetary gains (P = .022), and control sensitivity (P = .027) compared with control participants.
Study details: An Italian study evaluated the metacognitive abilities of 64 patients with chronic and episodic migraine and 29 healthy control participants.
Disclosures: The authors declared no conflicts of interest.
Citation: Zucca M et al. J Clin Neurosci. 2020 Jan 5. doi: 10.1016/j.jocn.2019.12.048.
Key clinical point: Patients with migraine are likely to have metacognitive deficits.
Major finding: Patients with migraine performed worse on measures of metacognitive functions, including accuracy score (P = .012), global monitoring (P = .015), monetary gains (P = .022), and control sensitivity (P = .027) compared with control participants.
Study details: An Italian study evaluated the metacognitive abilities of 64 patients with chronic and episodic migraine and 29 healthy control participants.
Disclosures: The authors declared no conflicts of interest.
Citation: Zucca M et al. J Clin Neurosci. 2020 Jan 5. doi: 10.1016/j.jocn.2019.12.048.
Key clinical point: Patients with migraine are likely to have metacognitive deficits.
Major finding: Patients with migraine performed worse on measures of metacognitive functions, including accuracy score (P = .012), global monitoring (P = .015), monetary gains (P = .022), and control sensitivity (P = .027) compared with control participants.
Study details: An Italian study evaluated the metacognitive abilities of 64 patients with chronic and episodic migraine and 29 healthy control participants.
Disclosures: The authors declared no conflicts of interest.
Citation: Zucca M et al. J Clin Neurosci. 2020 Jan 5. doi: 10.1016/j.jocn.2019.12.048.
ID physicians twice as happy outside work than at work
Infectious disease physicians are more than twice as likely to be happy outside of work than in the office, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

About 25% of infectious disease physicians reported that they were very happy in the office, compared with dermatologists, who had the highest rate of in-office happiness at 41%, according to the Medscape report. The out-of-office happiness rate rose to 52% for ID physicians, compared with the top spot of rheumatologists, who reported a 60% happiness rate.
The burnout rate for ID physicians was 46%, compared with 41% for physicians overall, with 12% of ID physicians reporting that they were both burned out and depressed. Having too many bureaucratic tasks was the most commonly reported reason for ID physician burnout at 49%, followed by a lack of respect from colleagues at 46% and spending too much time at work at 43%.
ID physicians most commonly dealt with burnout by talking with friends/family (49%), exercising (48%), and isolating themselves from others (43%). In addition, 52% of ID physicians reported taking 3-4 weeks of vacation, compared with 44% of all physicians, with 33% of ID physicians saying that they took less than 3 weeks’ vacation.
About 14% of ID physicians reported that they’d contemplated suicide, with 0% reporting that they’d attempted it; 80% reported that they’d never thought about it. About 54% said they weren’t considering seeking professional help for symptoms of burnout or depression, 13% said they’d used therapy in the past but weren’t currently looking, 7% said they were planning on seeking help, and 17% said they were currently seeking help.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.
Infectious disease physicians are more than twice as likely to be happy outside of work than in the office, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

About 25% of infectious disease physicians reported that they were very happy in the office, compared with dermatologists, who had the highest rate of in-office happiness at 41%, according to the Medscape report. The out-of-office happiness rate rose to 52% for ID physicians, compared with the top spot of rheumatologists, who reported a 60% happiness rate.
The burnout rate for ID physicians was 46%, compared with 41% for physicians overall, with 12% of ID physicians reporting that they were both burned out and depressed. Having too many bureaucratic tasks was the most commonly reported reason for ID physician burnout at 49%, followed by a lack of respect from colleagues at 46% and spending too much time at work at 43%.
ID physicians most commonly dealt with burnout by talking with friends/family (49%), exercising (48%), and isolating themselves from others (43%). In addition, 52% of ID physicians reported taking 3-4 weeks of vacation, compared with 44% of all physicians, with 33% of ID physicians saying that they took less than 3 weeks’ vacation.
About 14% of ID physicians reported that they’d contemplated suicide, with 0% reporting that they’d attempted it; 80% reported that they’d never thought about it. About 54% said they weren’t considering seeking professional help for symptoms of burnout or depression, 13% said they’d used therapy in the past but weren’t currently looking, 7% said they were planning on seeking help, and 17% said they were currently seeking help.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.
Infectious disease physicians are more than twice as likely to be happy outside of work than in the office, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

About 25% of infectious disease physicians reported that they were very happy in the office, compared with dermatologists, who had the highest rate of in-office happiness at 41%, according to the Medscape report. The out-of-office happiness rate rose to 52% for ID physicians, compared with the top spot of rheumatologists, who reported a 60% happiness rate.
The burnout rate for ID physicians was 46%, compared with 41% for physicians overall, with 12% of ID physicians reporting that they were both burned out and depressed. Having too many bureaucratic tasks was the most commonly reported reason for ID physician burnout at 49%, followed by a lack of respect from colleagues at 46% and spending too much time at work at 43%.
ID physicians most commonly dealt with burnout by talking with friends/family (49%), exercising (48%), and isolating themselves from others (43%). In addition, 52% of ID physicians reported taking 3-4 weeks of vacation, compared with 44% of all physicians, with 33% of ID physicians saying that they took less than 3 weeks’ vacation.
About 14% of ID physicians reported that they’d contemplated suicide, with 0% reporting that they’d attempted it; 80% reported that they’d never thought about it. About 54% said they weren’t considering seeking professional help for symptoms of burnout or depression, 13% said they’d used therapy in the past but weren’t currently looking, 7% said they were planning on seeking help, and 17% said they were currently seeking help.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.
Number of sexual partners linked to cancer risk
A higher lifetime number of sexual partners was associated with a greater risk of being diagnosed with cancer in older adults, according to a recent study.
Additionally, among women, having had more lifetime partners was linked to higher odds of reporting a limiting long-standing condition.
Igor Grabovac, MD, of the Medical University of Vienna, and colleagues reported these results in BMJ Sexual & Reproductive Health.
The exploratory analysis included 2,537 men and 3,185 women, aged 50 years and older, who were a part of the English Longitudinal Study of Ageing. The mean age of study subjects was 64 years in men and 65 years in women, and most were either married or cohabitating.
Researchers collected data on sexual history using a self-administered questionnaire, which privately recorded the lifetime number of sexual partners among study participants. Data on other health outcomes, such as limiting long-standing illness and cancer diagnoses, were also self-reported.
Among male participants, 28.5% reported a history of 0-1 lifetime sexual partners, 29.0% had 2-4 partners, 20.2% had 5-9 partners, and 22.2% had 10 or more partners. The respective measures in women were 40.8%, 35.5%, 15.8%, and 7.8%.
Among all participants, a greater number of sexual partners was associated with being single, younger age, and being in the least or greatest brackets of household income.
The researchers found that, compared with having 0-1 sexual partners, a lifetime history of 10 or more sexual partners was associated with a greater risk of reported cancer in both men (odds ratio, 1.69; P = .047) and women (OR, 1.91; P = .038).
In addition, women with a lifetime history of 10 or more sexual partners had greater odds of reporting a limiting long-standing condition (OR, 1.64; P = .007).
“We observed no statistically significant association between number of lifetime sexual partners and self-rated health, CHD [coronary heart disease], or stroke in either sex, or with limiting long-standing illness in men,” the researchers explained.
They acknowledged that a key limitation of the study was the self-reported nature of the data. As a result, further studies are required to establish causality.
“Sexual history may be a relevant clinical indicator for cancer risk in older patients,” they concluded.
No funding sources were reported. The authors reported having no conflicts of interest.
SOURCE: Grabovac I et al. BMJ Sex Reprod Health. 2020 Feb 13. doi: 10.1136/bmjsrh-2019-200352.
A higher lifetime number of sexual partners was associated with a greater risk of being diagnosed with cancer in older adults, according to a recent study.
Additionally, among women, having had more lifetime partners was linked to higher odds of reporting a limiting long-standing condition.
Igor Grabovac, MD, of the Medical University of Vienna, and colleagues reported these results in BMJ Sexual & Reproductive Health.
The exploratory analysis included 2,537 men and 3,185 women, aged 50 years and older, who were a part of the English Longitudinal Study of Ageing. The mean age of study subjects was 64 years in men and 65 years in women, and most were either married or cohabitating.
Researchers collected data on sexual history using a self-administered questionnaire, which privately recorded the lifetime number of sexual partners among study participants. Data on other health outcomes, such as limiting long-standing illness and cancer diagnoses, were also self-reported.
Among male participants, 28.5% reported a history of 0-1 lifetime sexual partners, 29.0% had 2-4 partners, 20.2% had 5-9 partners, and 22.2% had 10 or more partners. The respective measures in women were 40.8%, 35.5%, 15.8%, and 7.8%.
Among all participants, a greater number of sexual partners was associated with being single, younger age, and being in the least or greatest brackets of household income.
The researchers found that, compared with having 0-1 sexual partners, a lifetime history of 10 or more sexual partners was associated with a greater risk of reported cancer in both men (odds ratio, 1.69; P = .047) and women (OR, 1.91; P = .038).
In addition, women with a lifetime history of 10 or more sexual partners had greater odds of reporting a limiting long-standing condition (OR, 1.64; P = .007).
“We observed no statistically significant association between number of lifetime sexual partners and self-rated health, CHD [coronary heart disease], or stroke in either sex, or with limiting long-standing illness in men,” the researchers explained.
They acknowledged that a key limitation of the study was the self-reported nature of the data. As a result, further studies are required to establish causality.
“Sexual history may be a relevant clinical indicator for cancer risk in older patients,” they concluded.
No funding sources were reported. The authors reported having no conflicts of interest.
SOURCE: Grabovac I et al. BMJ Sex Reprod Health. 2020 Feb 13. doi: 10.1136/bmjsrh-2019-200352.
A higher lifetime number of sexual partners was associated with a greater risk of being diagnosed with cancer in older adults, according to a recent study.
Additionally, among women, having had more lifetime partners was linked to higher odds of reporting a limiting long-standing condition.
Igor Grabovac, MD, of the Medical University of Vienna, and colleagues reported these results in BMJ Sexual & Reproductive Health.
The exploratory analysis included 2,537 men and 3,185 women, aged 50 years and older, who were a part of the English Longitudinal Study of Ageing. The mean age of study subjects was 64 years in men and 65 years in women, and most were either married or cohabitating.
Researchers collected data on sexual history using a self-administered questionnaire, which privately recorded the lifetime number of sexual partners among study participants. Data on other health outcomes, such as limiting long-standing illness and cancer diagnoses, were also self-reported.
Among male participants, 28.5% reported a history of 0-1 lifetime sexual partners, 29.0% had 2-4 partners, 20.2% had 5-9 partners, and 22.2% had 10 or more partners. The respective measures in women were 40.8%, 35.5%, 15.8%, and 7.8%.
Among all participants, a greater number of sexual partners was associated with being single, younger age, and being in the least or greatest brackets of household income.
The researchers found that, compared with having 0-1 sexual partners, a lifetime history of 10 or more sexual partners was associated with a greater risk of reported cancer in both men (odds ratio, 1.69; P = .047) and women (OR, 1.91; P = .038).
In addition, women with a lifetime history of 10 or more sexual partners had greater odds of reporting a limiting long-standing condition (OR, 1.64; P = .007).
“We observed no statistically significant association between number of lifetime sexual partners and self-rated health, CHD [coronary heart disease], or stroke in either sex, or with limiting long-standing illness in men,” the researchers explained.
They acknowledged that a key limitation of the study was the self-reported nature of the data. As a result, further studies are required to establish causality.
“Sexual history may be a relevant clinical indicator for cancer risk in older patients,” they concluded.
No funding sources were reported. The authors reported having no conflicts of interest.
SOURCE: Grabovac I et al. BMJ Sex Reprod Health. 2020 Feb 13. doi: 10.1136/bmjsrh-2019-200352.
FROM BMJ SEXUAL AND REPRODUCTIVE HEALTH
After gestational diabetes, longer lactation tied to lower risk for type 2
Among women with a history of gestational diabetes, a longer period of breastfeeding was associated with a lower probability of going on to develop type 2 diabetes, as well as a more favorable glucose metabolic biomarker profile. Women who breastfed for 2 years or longer had a 27% lower risk than that of those who did not breastfeed at all, even after adjustment for age, ethnicity, family history of diabetes, parity, age at first birth, smoking, diet quality, physical activity, and prepregnancy body mass index, according to findings published in Diabetes Care.
It remains to be seen if the association is causal, and if so, what mechanisms might connect breastfeeding duration to risk for type 2 diabetes, wrote study leaders Sylvia Ley, PhD, of Tulane University School of Public Health and Tropical Medicine, New Orleans, and the Harvard T.H. Chan School of Public Health, Boston, and Cuilin Zhang, MD, PhD, of the Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md., and colleagues.
“It’s really nice to see this consistency and the long-term association being borne out in a very large sample of women with gestational diabetes,” Erica P. Gunderson, PhD, said in an interview about the study. Dr. Gunderson has conducted similar studies of her own, including one published in 2018 that showed an independent association between lactation and reduced diabetes risk in women (JAMA Intern Med. 2018;178:328-37). That analysis showed no sign that the presence of gestational diabetes affected the reduction of diabetes risk associated with lactation.
Dr. Gunderson noted that pregnancy is a hyperlipidemic state, with triglyceride levels sometimes doubling, likely in response to the need to support the placenta and the growing fetus. Lactation may help restore lipid levels to the prepregnancy state by redirecting lipids to breast milk. She and others are working to produce more direct evidence of metabolic changes in the postpartum period associated with lactation. “That’s where we don’t have much mechanistic evidence right now,” said Dr. Gunderson, a senior research scientist and epidemiologist at Kaiser Permanente Northern California, Oakland.
Gestational diabetes occurs in an estimated 5%-9% of pregnancies in the United States, and women who experience this complication are at greater risk of developing type 2 diabetes in the future. Findings from other studies have shown that longer lactation periods are associated with lowered risk of future type 2 disease (JAMA. 2005;294:2601-10).
In the latest study, the researchers included 4,372 women with a history of gestational diabetes, identified through the Nurses’ Health Study II. Participants were excluded if they had a history of cancer, cardiovascular disease, or multiple-birth pregnancy before the pregnancy during which they were diagnosed with gestational diabetes. In all, 873 women developed type 2 diabetes over 87,411 person-years of follow-up. The median age at gestational diabetes diagnosis was 31.8 years, and 49.8 years for diagnoses of type 2 diabetes.
After adjustment, the researchers found a steadying decline of risk for type 2 diabetes with increasing length of lactation: for up to 6 months of lactation, the hazard ratio was 1.05 (95% confidence interval, 0.82-1.34); for 6-12 months, the HR was 0.91 (95% CI, 0.71-1.15); 12-24 months, 0.84 (95% CI, 0.67-1.06); more than 24 months, 0.73 (95% CI, 0.57-0.93; P for trend = .004). Age, parity, primipara, prepregnancy body mass index, and age had no statistically significant effect modification on the association.
At a follow-up blood collection taken at median age of 58.2 years and 26.3 years after the gestational-diabetes index pregnancy, the researchers found associations between longer breastfeeding (greater than 24 months vs. 0 months) and lower hemoglobin A1c percentage (5.58 vs. 5.68; P for trend = .04), lower insulin levels (53.1 vs. 64.7 pmol/L; P for trend = .02), and lower C-peptide levels (3.42 vs. 3.88 ng/mL; P for trend = .02).
The study was supported by the National Institutes of Health. Dr. Ley was supported by a National Institute of General Medical Sciences grant from the NIH. None of the study authors reported any conflicts of interest, and neither did Dr. Gunderson.
SOURCE: Ley S et al. Diabetes Care. 2020 Feb 10. doi: 10.2337/dc19-2237.
Among women with a history of gestational diabetes, a longer period of breastfeeding was associated with a lower probability of going on to develop type 2 diabetes, as well as a more favorable glucose metabolic biomarker profile. Women who breastfed for 2 years or longer had a 27% lower risk than that of those who did not breastfeed at all, even after adjustment for age, ethnicity, family history of diabetes, parity, age at first birth, smoking, diet quality, physical activity, and prepregnancy body mass index, according to findings published in Diabetes Care.
It remains to be seen if the association is causal, and if so, what mechanisms might connect breastfeeding duration to risk for type 2 diabetes, wrote study leaders Sylvia Ley, PhD, of Tulane University School of Public Health and Tropical Medicine, New Orleans, and the Harvard T.H. Chan School of Public Health, Boston, and Cuilin Zhang, MD, PhD, of the Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md., and colleagues.
“It’s really nice to see this consistency and the long-term association being borne out in a very large sample of women with gestational diabetes,” Erica P. Gunderson, PhD, said in an interview about the study. Dr. Gunderson has conducted similar studies of her own, including one published in 2018 that showed an independent association between lactation and reduced diabetes risk in women (JAMA Intern Med. 2018;178:328-37). That analysis showed no sign that the presence of gestational diabetes affected the reduction of diabetes risk associated with lactation.
Dr. Gunderson noted that pregnancy is a hyperlipidemic state, with triglyceride levels sometimes doubling, likely in response to the need to support the placenta and the growing fetus. Lactation may help restore lipid levels to the prepregnancy state by redirecting lipids to breast milk. She and others are working to produce more direct evidence of metabolic changes in the postpartum period associated with lactation. “That’s where we don’t have much mechanistic evidence right now,” said Dr. Gunderson, a senior research scientist and epidemiologist at Kaiser Permanente Northern California, Oakland.
Gestational diabetes occurs in an estimated 5%-9% of pregnancies in the United States, and women who experience this complication are at greater risk of developing type 2 diabetes in the future. Findings from other studies have shown that longer lactation periods are associated with lowered risk of future type 2 disease (JAMA. 2005;294:2601-10).
In the latest study, the researchers included 4,372 women with a history of gestational diabetes, identified through the Nurses’ Health Study II. Participants were excluded if they had a history of cancer, cardiovascular disease, or multiple-birth pregnancy before the pregnancy during which they were diagnosed with gestational diabetes. In all, 873 women developed type 2 diabetes over 87,411 person-years of follow-up. The median age at gestational diabetes diagnosis was 31.8 years, and 49.8 years for diagnoses of type 2 diabetes.
After adjustment, the researchers found a steadying decline of risk for type 2 diabetes with increasing length of lactation: for up to 6 months of lactation, the hazard ratio was 1.05 (95% confidence interval, 0.82-1.34); for 6-12 months, the HR was 0.91 (95% CI, 0.71-1.15); 12-24 months, 0.84 (95% CI, 0.67-1.06); more than 24 months, 0.73 (95% CI, 0.57-0.93; P for trend = .004). Age, parity, primipara, prepregnancy body mass index, and age had no statistically significant effect modification on the association.
At a follow-up blood collection taken at median age of 58.2 years and 26.3 years after the gestational-diabetes index pregnancy, the researchers found associations between longer breastfeeding (greater than 24 months vs. 0 months) and lower hemoglobin A1c percentage (5.58 vs. 5.68; P for trend = .04), lower insulin levels (53.1 vs. 64.7 pmol/L; P for trend = .02), and lower C-peptide levels (3.42 vs. 3.88 ng/mL; P for trend = .02).
The study was supported by the National Institutes of Health. Dr. Ley was supported by a National Institute of General Medical Sciences grant from the NIH. None of the study authors reported any conflicts of interest, and neither did Dr. Gunderson.
SOURCE: Ley S et al. Diabetes Care. 2020 Feb 10. doi: 10.2337/dc19-2237.
Among women with a history of gestational diabetes, a longer period of breastfeeding was associated with a lower probability of going on to develop type 2 diabetes, as well as a more favorable glucose metabolic biomarker profile. Women who breastfed for 2 years or longer had a 27% lower risk than that of those who did not breastfeed at all, even after adjustment for age, ethnicity, family history of diabetes, parity, age at first birth, smoking, diet quality, physical activity, and prepregnancy body mass index, according to findings published in Diabetes Care.
It remains to be seen if the association is causal, and if so, what mechanisms might connect breastfeeding duration to risk for type 2 diabetes, wrote study leaders Sylvia Ley, PhD, of Tulane University School of Public Health and Tropical Medicine, New Orleans, and the Harvard T.H. Chan School of Public Health, Boston, and Cuilin Zhang, MD, PhD, of the Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md., and colleagues.
“It’s really nice to see this consistency and the long-term association being borne out in a very large sample of women with gestational diabetes,” Erica P. Gunderson, PhD, said in an interview about the study. Dr. Gunderson has conducted similar studies of her own, including one published in 2018 that showed an independent association between lactation and reduced diabetes risk in women (JAMA Intern Med. 2018;178:328-37). That analysis showed no sign that the presence of gestational diabetes affected the reduction of diabetes risk associated with lactation.
Dr. Gunderson noted that pregnancy is a hyperlipidemic state, with triglyceride levels sometimes doubling, likely in response to the need to support the placenta and the growing fetus. Lactation may help restore lipid levels to the prepregnancy state by redirecting lipids to breast milk. She and others are working to produce more direct evidence of metabolic changes in the postpartum period associated with lactation. “That’s where we don’t have much mechanistic evidence right now,” said Dr. Gunderson, a senior research scientist and epidemiologist at Kaiser Permanente Northern California, Oakland.
Gestational diabetes occurs in an estimated 5%-9% of pregnancies in the United States, and women who experience this complication are at greater risk of developing type 2 diabetes in the future. Findings from other studies have shown that longer lactation periods are associated with lowered risk of future type 2 disease (JAMA. 2005;294:2601-10).
In the latest study, the researchers included 4,372 women with a history of gestational diabetes, identified through the Nurses’ Health Study II. Participants were excluded if they had a history of cancer, cardiovascular disease, or multiple-birth pregnancy before the pregnancy during which they were diagnosed with gestational diabetes. In all, 873 women developed type 2 diabetes over 87,411 person-years of follow-up. The median age at gestational diabetes diagnosis was 31.8 years, and 49.8 years for diagnoses of type 2 diabetes.
After adjustment, the researchers found a steadying decline of risk for type 2 diabetes with increasing length of lactation: for up to 6 months of lactation, the hazard ratio was 1.05 (95% confidence interval, 0.82-1.34); for 6-12 months, the HR was 0.91 (95% CI, 0.71-1.15); 12-24 months, 0.84 (95% CI, 0.67-1.06); more than 24 months, 0.73 (95% CI, 0.57-0.93; P for trend = .004). Age, parity, primipara, prepregnancy body mass index, and age had no statistically significant effect modification on the association.
At a follow-up blood collection taken at median age of 58.2 years and 26.3 years after the gestational-diabetes index pregnancy, the researchers found associations between longer breastfeeding (greater than 24 months vs. 0 months) and lower hemoglobin A1c percentage (5.58 vs. 5.68; P for trend = .04), lower insulin levels (53.1 vs. 64.7 pmol/L; P for trend = .02), and lower C-peptide levels (3.42 vs. 3.88 ng/mL; P for trend = .02).
The study was supported by the National Institutes of Health. Dr. Ley was supported by a National Institute of General Medical Sciences grant from the NIH. None of the study authors reported any conflicts of interest, and neither did Dr. Gunderson.
SOURCE: Ley S et al. Diabetes Care. 2020 Feb 10. doi: 10.2337/dc19-2237.
FROM DIABETES CARE
‘Momentous’ USMLE change: New pass/fail format stuns medicine
News that the United States Medical Licensing Examination (USMLE) program will change its Step 1 scoring from a 3-digit number to pass/fail starting Jan. 1, 2022, has set off a flurry of shocked responses from students and physicians.
J. Bryan Carmody, MD, MPH, an assistant professor at Eastern Virginia Medical School in Norfolk, said in an interview that he was “stunned” when he heard the news on Wednesday and said the switch presents “the single biggest opportunity for medical school education reform since the Flexner Report,” which in 1910 established standards for modern medical education.
Numbers will continue for some tests
The USMLE cosponsors – the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) – said that the Step 2 Clinical Knowledge (CK) exam and Step 3 will continue to be scored numerically. Step 2 Clinical Skills (CS) will continue its pass/fail system.
The change was made after Step 1 had been roundly criticized as playing too big a role in the process of becoming a physician and for causing students to study for the test instead of engaging fully in their medical education.
Ramie Fathy, a third-year medical student at the University of Pennsylvania, Philadelphia, currently studying for Step 1, said in an interview that it would have been nice personally to have the pass/fail choice, but he predicts both good and unintended consequences in the change.
The positive news, Mr. Fathy said, is that less emphasis will be put on the Step 1 test, which includes memorizing basic science details that may or not be relevant depending on later specialty choice.
“It’s not necessarily measuring what the test makers intended, which was whether or not a student can understand and apply basic science concepts to the practice of medicine,” he said.
“The current system encourages students to get as high a score as possible, which – after a certain point – translates to memorizing many little details that become increasingly less practically relevant,” Mr. Fathy said.
Pressure may move elsewhere?
However, Mr. Fathy worries that, without a scoring system to help decide who stands out in Step 1, residency program directors will depend more on the reputation of candidates’ medical school and the clout of the person writing a letter of recommendation – factors that are often influenced by family resources and social standing. That could wedge a further economic divide into the path to becoming a physician.
Mr. Fathy said he and fellow students are watching for information on what the passing bar will be and what happens with Step 2 Clinical Knowledge exam. USMLE has promised more information as soon as it is available.
“The question is whether that test will replace Step 1 as the standardized metric of student competency,” Mr. Fathy said, which would put more pressure on students further down the medical path.
Will Step 2 anxiety increase?
Dr. Carmody agreed that there is the danger that students now will spend their time studying for Step 2 CK at the expense of other parts of their education.
Meaningful reform will depend on the pass/fail move being coupled with other reforms, most importantly application caps, said Dr. Carmody, who teaches preclinical medical students and works with the residency program.
He has been blogging about Step 1 pass/fail for the past year.
Currently students can apply for as many residencies as they can pay for and Carmody said the number of applications per student has been rising over the past decade.
“That puts program directors under an impossible burden,” he said. “With our Step 1-based system, there’s significant inequality in the number of interviews people get. Programs end up overinviting the same group of people who look good on paper.”
People outside that group respond by sending more applications than they need to just to get a few interviews, Dr. Carmody added.
With caps, students would have an incentive to apply to only those programs in which they had a sincere interest, he said. Program directors also would then be better able to evaluate each application.
Switching Step 1 to pass/fail may have some effect on medical school burnout, Dr. Carmody said.
“It’s one thing to work hard when you’re on call and your patients depend on it,” he said. “But I would have a hard time staying up late every night studying something that I know in my heart is not going to help my patients, but I have to do it because I have to do better than the person who’s studying in the apartment next to me.”
Test has strayed from original purpose
Joseph Safdieh, MD, an assistant dean for clinical curriculum and director of the medical student neurology clerkship for the Weill Cornell Medicine, New York, sees the move as positive overall.
“We should not be using any single metric to define or describe our students’ overall profile,” he said in an interview.
“This has been a very significant anxiety point for our medical students for quite a number of years,” Dr. Safdieh said. “They were frustrated that their entire 4 years of medical school seemingly came down to one number.”
The test was created originally as one of three parts of licensure, he pointed out.
“Over the past 10 or 15 years, the exam has morphed to become a litmus test for very specific residency programs,” he said.
However, Dr. Safdieh has concerns that Step 2 will cultivate the same anxiety and may get too big a spotlight without the Step 1 metric, “although one could argue that test does more accurately reflect clinical material,” he said.
He also worries that students who have selected a specialty by the time they take Step 2 may find late in the game that they are less competitive in their field than they thought they were and may have to make a last-minute switch.
Dr. Safdieh said he thinks Step 2 will be next to go the pass/fail route. In reading between the lines of the announcement, he believes the test cosponsors didn’t make both pass/fail at once because it would have been “a nuclear bomb to the system.”
He credited the cosponsors with making what he called a “bold and momentous decision to initiate radical change in the overall transition between undergraduate and graduate medical education.”
Dr. Safdieh added that few in medicine were expecting Wednesday’s announcement.
“I think many of us were expecting them to go to quartile grading, not to go this far,” he said.
Dr. Safdieh suggested that, among those who may see downstream effects from the pass/fail move are offshore schools, such as those in the Caribbean. “Those schools rely on Step 1 to demonstrate that their students are meeting the rigor,” he said. But he hopes that this will lead to more holistic review.
“We’re hoping that this will force change in the system so that residency directors will look at more than just test-taking ability. They’ll look at publications and scholarship, community service and advocacy and performance in medical school,” Dr. Safdieh said.
Alison J. Whelan, MD, chief medical education officer of the Association of American Medical Colleges said in a statement, “The transition from medical school to residency training is a matter of great concern throughout academic medicine.
“The decision by the NBME and FSMB to change USMLE Step 1 score reporting to pass/fail was very carefully considered to balance student learning and student well-being,” she said. “The medical education community must now work together to identify and implement additional changes to improve the overall UME-GME [undergraduate and graduate medical education] transition system for all stakeholders and the AAMC is committed to helping lead this work.”
Dr. Fathy, Dr. Carmody, and Dr. Safdieh have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
News that the United States Medical Licensing Examination (USMLE) program will change its Step 1 scoring from a 3-digit number to pass/fail starting Jan. 1, 2022, has set off a flurry of shocked responses from students and physicians.
J. Bryan Carmody, MD, MPH, an assistant professor at Eastern Virginia Medical School in Norfolk, said in an interview that he was “stunned” when he heard the news on Wednesday and said the switch presents “the single biggest opportunity for medical school education reform since the Flexner Report,” which in 1910 established standards for modern medical education.
Numbers will continue for some tests
The USMLE cosponsors – the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) – said that the Step 2 Clinical Knowledge (CK) exam and Step 3 will continue to be scored numerically. Step 2 Clinical Skills (CS) will continue its pass/fail system.
The change was made after Step 1 had been roundly criticized as playing too big a role in the process of becoming a physician and for causing students to study for the test instead of engaging fully in their medical education.
Ramie Fathy, a third-year medical student at the University of Pennsylvania, Philadelphia, currently studying for Step 1, said in an interview that it would have been nice personally to have the pass/fail choice, but he predicts both good and unintended consequences in the change.
The positive news, Mr. Fathy said, is that less emphasis will be put on the Step 1 test, which includes memorizing basic science details that may or not be relevant depending on later specialty choice.
“It’s not necessarily measuring what the test makers intended, which was whether or not a student can understand and apply basic science concepts to the practice of medicine,” he said.
“The current system encourages students to get as high a score as possible, which – after a certain point – translates to memorizing many little details that become increasingly less practically relevant,” Mr. Fathy said.
Pressure may move elsewhere?
However, Mr. Fathy worries that, without a scoring system to help decide who stands out in Step 1, residency program directors will depend more on the reputation of candidates’ medical school and the clout of the person writing a letter of recommendation – factors that are often influenced by family resources and social standing. That could wedge a further economic divide into the path to becoming a physician.
Mr. Fathy said he and fellow students are watching for information on what the passing bar will be and what happens with Step 2 Clinical Knowledge exam. USMLE has promised more information as soon as it is available.
“The question is whether that test will replace Step 1 as the standardized metric of student competency,” Mr. Fathy said, which would put more pressure on students further down the medical path.
Will Step 2 anxiety increase?
Dr. Carmody agreed that there is the danger that students now will spend their time studying for Step 2 CK at the expense of other parts of their education.
Meaningful reform will depend on the pass/fail move being coupled with other reforms, most importantly application caps, said Dr. Carmody, who teaches preclinical medical students and works with the residency program.
He has been blogging about Step 1 pass/fail for the past year.
Currently students can apply for as many residencies as they can pay for and Carmody said the number of applications per student has been rising over the past decade.
“That puts program directors under an impossible burden,” he said. “With our Step 1-based system, there’s significant inequality in the number of interviews people get. Programs end up overinviting the same group of people who look good on paper.”
People outside that group respond by sending more applications than they need to just to get a few interviews, Dr. Carmody added.
With caps, students would have an incentive to apply to only those programs in which they had a sincere interest, he said. Program directors also would then be better able to evaluate each application.
Switching Step 1 to pass/fail may have some effect on medical school burnout, Dr. Carmody said.
“It’s one thing to work hard when you’re on call and your patients depend on it,” he said. “But I would have a hard time staying up late every night studying something that I know in my heart is not going to help my patients, but I have to do it because I have to do better than the person who’s studying in the apartment next to me.”
Test has strayed from original purpose
Joseph Safdieh, MD, an assistant dean for clinical curriculum and director of the medical student neurology clerkship for the Weill Cornell Medicine, New York, sees the move as positive overall.
“We should not be using any single metric to define or describe our students’ overall profile,” he said in an interview.
“This has been a very significant anxiety point for our medical students for quite a number of years,” Dr. Safdieh said. “They were frustrated that their entire 4 years of medical school seemingly came down to one number.”
The test was created originally as one of three parts of licensure, he pointed out.
“Over the past 10 or 15 years, the exam has morphed to become a litmus test for very specific residency programs,” he said.
However, Dr. Safdieh has concerns that Step 2 will cultivate the same anxiety and may get too big a spotlight without the Step 1 metric, “although one could argue that test does more accurately reflect clinical material,” he said.
He also worries that students who have selected a specialty by the time they take Step 2 may find late in the game that they are less competitive in their field than they thought they were and may have to make a last-minute switch.
Dr. Safdieh said he thinks Step 2 will be next to go the pass/fail route. In reading between the lines of the announcement, he believes the test cosponsors didn’t make both pass/fail at once because it would have been “a nuclear bomb to the system.”
He credited the cosponsors with making what he called a “bold and momentous decision to initiate radical change in the overall transition between undergraduate and graduate medical education.”
Dr. Safdieh added that few in medicine were expecting Wednesday’s announcement.
“I think many of us were expecting them to go to quartile grading, not to go this far,” he said.
Dr. Safdieh suggested that, among those who may see downstream effects from the pass/fail move are offshore schools, such as those in the Caribbean. “Those schools rely on Step 1 to demonstrate that their students are meeting the rigor,” he said. But he hopes that this will lead to more holistic review.
“We’re hoping that this will force change in the system so that residency directors will look at more than just test-taking ability. They’ll look at publications and scholarship, community service and advocacy and performance in medical school,” Dr. Safdieh said.
Alison J. Whelan, MD, chief medical education officer of the Association of American Medical Colleges said in a statement, “The transition from medical school to residency training is a matter of great concern throughout academic medicine.
“The decision by the NBME and FSMB to change USMLE Step 1 score reporting to pass/fail was very carefully considered to balance student learning and student well-being,” she said. “The medical education community must now work together to identify and implement additional changes to improve the overall UME-GME [undergraduate and graduate medical education] transition system for all stakeholders and the AAMC is committed to helping lead this work.”
Dr. Fathy, Dr. Carmody, and Dr. Safdieh have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
News that the United States Medical Licensing Examination (USMLE) program will change its Step 1 scoring from a 3-digit number to pass/fail starting Jan. 1, 2022, has set off a flurry of shocked responses from students and physicians.
J. Bryan Carmody, MD, MPH, an assistant professor at Eastern Virginia Medical School in Norfolk, said in an interview that he was “stunned” when he heard the news on Wednesday and said the switch presents “the single biggest opportunity for medical school education reform since the Flexner Report,” which in 1910 established standards for modern medical education.
Numbers will continue for some tests
The USMLE cosponsors – the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) – said that the Step 2 Clinical Knowledge (CK) exam and Step 3 will continue to be scored numerically. Step 2 Clinical Skills (CS) will continue its pass/fail system.
The change was made after Step 1 had been roundly criticized as playing too big a role in the process of becoming a physician and for causing students to study for the test instead of engaging fully in their medical education.
Ramie Fathy, a third-year medical student at the University of Pennsylvania, Philadelphia, currently studying for Step 1, said in an interview that it would have been nice personally to have the pass/fail choice, but he predicts both good and unintended consequences in the change.
The positive news, Mr. Fathy said, is that less emphasis will be put on the Step 1 test, which includes memorizing basic science details that may or not be relevant depending on later specialty choice.
“It’s not necessarily measuring what the test makers intended, which was whether or not a student can understand and apply basic science concepts to the practice of medicine,” he said.
“The current system encourages students to get as high a score as possible, which – after a certain point – translates to memorizing many little details that become increasingly less practically relevant,” Mr. Fathy said.
Pressure may move elsewhere?
However, Mr. Fathy worries that, without a scoring system to help decide who stands out in Step 1, residency program directors will depend more on the reputation of candidates’ medical school and the clout of the person writing a letter of recommendation – factors that are often influenced by family resources and social standing. That could wedge a further economic divide into the path to becoming a physician.
Mr. Fathy said he and fellow students are watching for information on what the passing bar will be and what happens with Step 2 Clinical Knowledge exam. USMLE has promised more information as soon as it is available.
“The question is whether that test will replace Step 1 as the standardized metric of student competency,” Mr. Fathy said, which would put more pressure on students further down the medical path.
Will Step 2 anxiety increase?
Dr. Carmody agreed that there is the danger that students now will spend their time studying for Step 2 CK at the expense of other parts of their education.
Meaningful reform will depend on the pass/fail move being coupled with other reforms, most importantly application caps, said Dr. Carmody, who teaches preclinical medical students and works with the residency program.
He has been blogging about Step 1 pass/fail for the past year.
Currently students can apply for as many residencies as they can pay for and Carmody said the number of applications per student has been rising over the past decade.
“That puts program directors under an impossible burden,” he said. “With our Step 1-based system, there’s significant inequality in the number of interviews people get. Programs end up overinviting the same group of people who look good on paper.”
People outside that group respond by sending more applications than they need to just to get a few interviews, Dr. Carmody added.
With caps, students would have an incentive to apply to only those programs in which they had a sincere interest, he said. Program directors also would then be better able to evaluate each application.
Switching Step 1 to pass/fail may have some effect on medical school burnout, Dr. Carmody said.
“It’s one thing to work hard when you’re on call and your patients depend on it,” he said. “But I would have a hard time staying up late every night studying something that I know in my heart is not going to help my patients, but I have to do it because I have to do better than the person who’s studying in the apartment next to me.”
Test has strayed from original purpose
Joseph Safdieh, MD, an assistant dean for clinical curriculum and director of the medical student neurology clerkship for the Weill Cornell Medicine, New York, sees the move as positive overall.
“We should not be using any single metric to define or describe our students’ overall profile,” he said in an interview.
“This has been a very significant anxiety point for our medical students for quite a number of years,” Dr. Safdieh said. “They were frustrated that their entire 4 years of medical school seemingly came down to one number.”
The test was created originally as one of three parts of licensure, he pointed out.
“Over the past 10 or 15 years, the exam has morphed to become a litmus test for very specific residency programs,” he said.
However, Dr. Safdieh has concerns that Step 2 will cultivate the same anxiety and may get too big a spotlight without the Step 1 metric, “although one could argue that test does more accurately reflect clinical material,” he said.
He also worries that students who have selected a specialty by the time they take Step 2 may find late in the game that they are less competitive in their field than they thought they were and may have to make a last-minute switch.
Dr. Safdieh said he thinks Step 2 will be next to go the pass/fail route. In reading between the lines of the announcement, he believes the test cosponsors didn’t make both pass/fail at once because it would have been “a nuclear bomb to the system.”
He credited the cosponsors with making what he called a “bold and momentous decision to initiate radical change in the overall transition between undergraduate and graduate medical education.”
Dr. Safdieh added that few in medicine were expecting Wednesday’s announcement.
“I think many of us were expecting them to go to quartile grading, not to go this far,” he said.
Dr. Safdieh suggested that, among those who may see downstream effects from the pass/fail move are offshore schools, such as those in the Caribbean. “Those schools rely on Step 1 to demonstrate that their students are meeting the rigor,” he said. But he hopes that this will lead to more holistic review.
“We’re hoping that this will force change in the system so that residency directors will look at more than just test-taking ability. They’ll look at publications and scholarship, community service and advocacy and performance in medical school,” Dr. Safdieh said.
Alison J. Whelan, MD, chief medical education officer of the Association of American Medical Colleges said in a statement, “The transition from medical school to residency training is a matter of great concern throughout academic medicine.
“The decision by the NBME and FSMB to change USMLE Step 1 score reporting to pass/fail was very carefully considered to balance student learning and student well-being,” she said. “The medical education community must now work together to identify and implement additional changes to improve the overall UME-GME [undergraduate and graduate medical education] transition system for all stakeholders and the AAMC is committed to helping lead this work.”
Dr. Fathy, Dr. Carmody, and Dr. Safdieh have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Avoid ‘mutant selection window’ when prescribing antibiotics for acne
LAHAINA, HAWAII – Consider the “mutant selection window” to reduce antibiotic resistance when treating acne, Hilary E. Baldwin, MD, advised at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Dermatologists continue to write a disproportionate number of prescriptions for antibiotics, particularly tetracyclines, noted Dr. Baldwin, medical director of the Acne Treatment and Research Center in New York. In addition to limiting unnecessary use of antimicrobials, strategies for slowing antimicrobial resistance include using anti-inflammatory doses of doxycycline; using more retinoids, isotretinoin, spironolactone, and oral contraceptives; and improving patient compliance with treatment.
Dermatologists can also “pay attention to the bug we are treating and ... make sure the concentration of the drug that we are using is appropriate to the bug we’re trying to kill,” while also targeting resistant organisms. Dr. Baldwin referred to a paper in the infectious disease literature titled: “The mutant selection window and antimicrobial resistance,” which points out that a drug concentration range exists for which mutant strains of bacteria are selected most frequently (J Antimicrob Chemother. 2003 Jul;52[1]:11-7). The dimensions of this range, or “window,” are characteristic of each pathogen-antimicrobial combination. A high enough drug concentration will eliminate both resistant and sensitive strains of the pathogen.
The paper notes that the minimum inhibitory concentration (MIC) is the lowest concentration that will inhibit the visible growth of a microorganism. The mutant prevention concentration (MPC) is the minimum drug concentration needed to prevent the growth of resistant strains, Dr. Baldwin said. The mutant selection window is the concentration range that extends from the MIC up to the MPC, the range “within which resistant mutants are likely to emerge.” If the antimicrobial concentration falls within this window, a mutant strain is likely to develop and “you’re going to add to the problem of antibiotic resistance,” she explained. “So the goal is to treat low or to treat high, but not right in the middle.”
“This is not theoretical,” and has been shown over and over again, with, for example, Streptococcus pneumonia and moxifloxacin, she said (J Antimicrob Chemother. 2003 Oct;52[4]:616-22.).
When the therapeutic window does not extend all the way to the MPC, “toxicity starts to kick in before you can get high enough to kill off the whole group of organisms,” in which case a low-dose strategy would reduce the development of resistant organisms, she noted.
“We’re doing this already,” with topical antifungals, Dr. Baldwin pointed out, asking when the last time anyone heard that a fungus developed resistance to topical antifungal therapy. “Never, because we use our antifungals in such a high dose, that we’re 500 times the MPC.”
Using an anti-inflammatory dose of doxycycline for treating acne or rosacea is a low-dose strategy, and the 40-mg delayed-release dose stays “way below” the antimicrobial threshold, she said, but the 50-mg dose falls “right in the middle of that mutant selection window.”
As more treatments become available, it will be important to determine how to dose topical antibiotics so that they do not fall within the mutant selection window and avoid what happened with clindamycin and erythromycin, “where the topical use of these medications led to the development of resistance such that they no longer work for the treatment” of Cutibacterium acnes.
Dr. Baldwin disclosures included being on the speakers bureau, serving as an advisor, and/or an investigator for companies that include Almirall, BioPharmx, Foamix, Galderma, Ortho Dermatologics, Sun Pharmaceuticals, Johnson & Johnson, and La Roche–Posay.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – Consider the “mutant selection window” to reduce antibiotic resistance when treating acne, Hilary E. Baldwin, MD, advised at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Dermatologists continue to write a disproportionate number of prescriptions for antibiotics, particularly tetracyclines, noted Dr. Baldwin, medical director of the Acne Treatment and Research Center in New York. In addition to limiting unnecessary use of antimicrobials, strategies for slowing antimicrobial resistance include using anti-inflammatory doses of doxycycline; using more retinoids, isotretinoin, spironolactone, and oral contraceptives; and improving patient compliance with treatment.
Dermatologists can also “pay attention to the bug we are treating and ... make sure the concentration of the drug that we are using is appropriate to the bug we’re trying to kill,” while also targeting resistant organisms. Dr. Baldwin referred to a paper in the infectious disease literature titled: “The mutant selection window and antimicrobial resistance,” which points out that a drug concentration range exists for which mutant strains of bacteria are selected most frequently (J Antimicrob Chemother. 2003 Jul;52[1]:11-7). The dimensions of this range, or “window,” are characteristic of each pathogen-antimicrobial combination. A high enough drug concentration will eliminate both resistant and sensitive strains of the pathogen.
The paper notes that the minimum inhibitory concentration (MIC) is the lowest concentration that will inhibit the visible growth of a microorganism. The mutant prevention concentration (MPC) is the minimum drug concentration needed to prevent the growth of resistant strains, Dr. Baldwin said. The mutant selection window is the concentration range that extends from the MIC up to the MPC, the range “within which resistant mutants are likely to emerge.” If the antimicrobial concentration falls within this window, a mutant strain is likely to develop and “you’re going to add to the problem of antibiotic resistance,” she explained. “So the goal is to treat low or to treat high, but not right in the middle.”
“This is not theoretical,” and has been shown over and over again, with, for example, Streptococcus pneumonia and moxifloxacin, she said (J Antimicrob Chemother. 2003 Oct;52[4]:616-22.).
When the therapeutic window does not extend all the way to the MPC, “toxicity starts to kick in before you can get high enough to kill off the whole group of organisms,” in which case a low-dose strategy would reduce the development of resistant organisms, she noted.
“We’re doing this already,” with topical antifungals, Dr. Baldwin pointed out, asking when the last time anyone heard that a fungus developed resistance to topical antifungal therapy. “Never, because we use our antifungals in such a high dose, that we’re 500 times the MPC.”
Using an anti-inflammatory dose of doxycycline for treating acne or rosacea is a low-dose strategy, and the 40-mg delayed-release dose stays “way below” the antimicrobial threshold, she said, but the 50-mg dose falls “right in the middle of that mutant selection window.”
As more treatments become available, it will be important to determine how to dose topical antibiotics so that they do not fall within the mutant selection window and avoid what happened with clindamycin and erythromycin, “where the topical use of these medications led to the development of resistance such that they no longer work for the treatment” of Cutibacterium acnes.
Dr. Baldwin disclosures included being on the speakers bureau, serving as an advisor, and/or an investigator for companies that include Almirall, BioPharmx, Foamix, Galderma, Ortho Dermatologics, Sun Pharmaceuticals, Johnson & Johnson, and La Roche–Posay.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – Consider the “mutant selection window” to reduce antibiotic resistance when treating acne, Hilary E. Baldwin, MD, advised at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Dermatologists continue to write a disproportionate number of prescriptions for antibiotics, particularly tetracyclines, noted Dr. Baldwin, medical director of the Acne Treatment and Research Center in New York. In addition to limiting unnecessary use of antimicrobials, strategies for slowing antimicrobial resistance include using anti-inflammatory doses of doxycycline; using more retinoids, isotretinoin, spironolactone, and oral contraceptives; and improving patient compliance with treatment.
Dermatologists can also “pay attention to the bug we are treating and ... make sure the concentration of the drug that we are using is appropriate to the bug we’re trying to kill,” while also targeting resistant organisms. Dr. Baldwin referred to a paper in the infectious disease literature titled: “The mutant selection window and antimicrobial resistance,” which points out that a drug concentration range exists for which mutant strains of bacteria are selected most frequently (J Antimicrob Chemother. 2003 Jul;52[1]:11-7). The dimensions of this range, or “window,” are characteristic of each pathogen-antimicrobial combination. A high enough drug concentration will eliminate both resistant and sensitive strains of the pathogen.
The paper notes that the minimum inhibitory concentration (MIC) is the lowest concentration that will inhibit the visible growth of a microorganism. The mutant prevention concentration (MPC) is the minimum drug concentration needed to prevent the growth of resistant strains, Dr. Baldwin said. The mutant selection window is the concentration range that extends from the MIC up to the MPC, the range “within which resistant mutants are likely to emerge.” If the antimicrobial concentration falls within this window, a mutant strain is likely to develop and “you’re going to add to the problem of antibiotic resistance,” she explained. “So the goal is to treat low or to treat high, but not right in the middle.”
“This is not theoretical,” and has been shown over and over again, with, for example, Streptococcus pneumonia and moxifloxacin, she said (J Antimicrob Chemother. 2003 Oct;52[4]:616-22.).
When the therapeutic window does not extend all the way to the MPC, “toxicity starts to kick in before you can get high enough to kill off the whole group of organisms,” in which case a low-dose strategy would reduce the development of resistant organisms, she noted.
“We’re doing this already,” with topical antifungals, Dr. Baldwin pointed out, asking when the last time anyone heard that a fungus developed resistance to topical antifungal therapy. “Never, because we use our antifungals in such a high dose, that we’re 500 times the MPC.”
Using an anti-inflammatory dose of doxycycline for treating acne or rosacea is a low-dose strategy, and the 40-mg delayed-release dose stays “way below” the antimicrobial threshold, she said, but the 50-mg dose falls “right in the middle of that mutant selection window.”
As more treatments become available, it will be important to determine how to dose topical antibiotics so that they do not fall within the mutant selection window and avoid what happened with clindamycin and erythromycin, “where the topical use of these medications led to the development of resistance such that they no longer work for the treatment” of Cutibacterium acnes.
Dr. Baldwin disclosures included being on the speakers bureau, serving as an advisor, and/or an investigator for companies that include Almirall, BioPharmx, Foamix, Galderma, Ortho Dermatologics, Sun Pharmaceuticals, Johnson & Johnson, and La Roche–Posay.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
REPORTING FROM SDEF HAWAII DERMATOLOGY SEMINAR
Vascular occlusion management
The time course and proper management of vascular occlusion attributable to interarterial hyaluronic acid fillers is critical. Albeit a rare complication, off-label uses of HA fillers, lack of proper training of injectors, and lack of clear appropriate guidelines in the management of these complications are some of the causes of delayed treatment and necrotic complications.
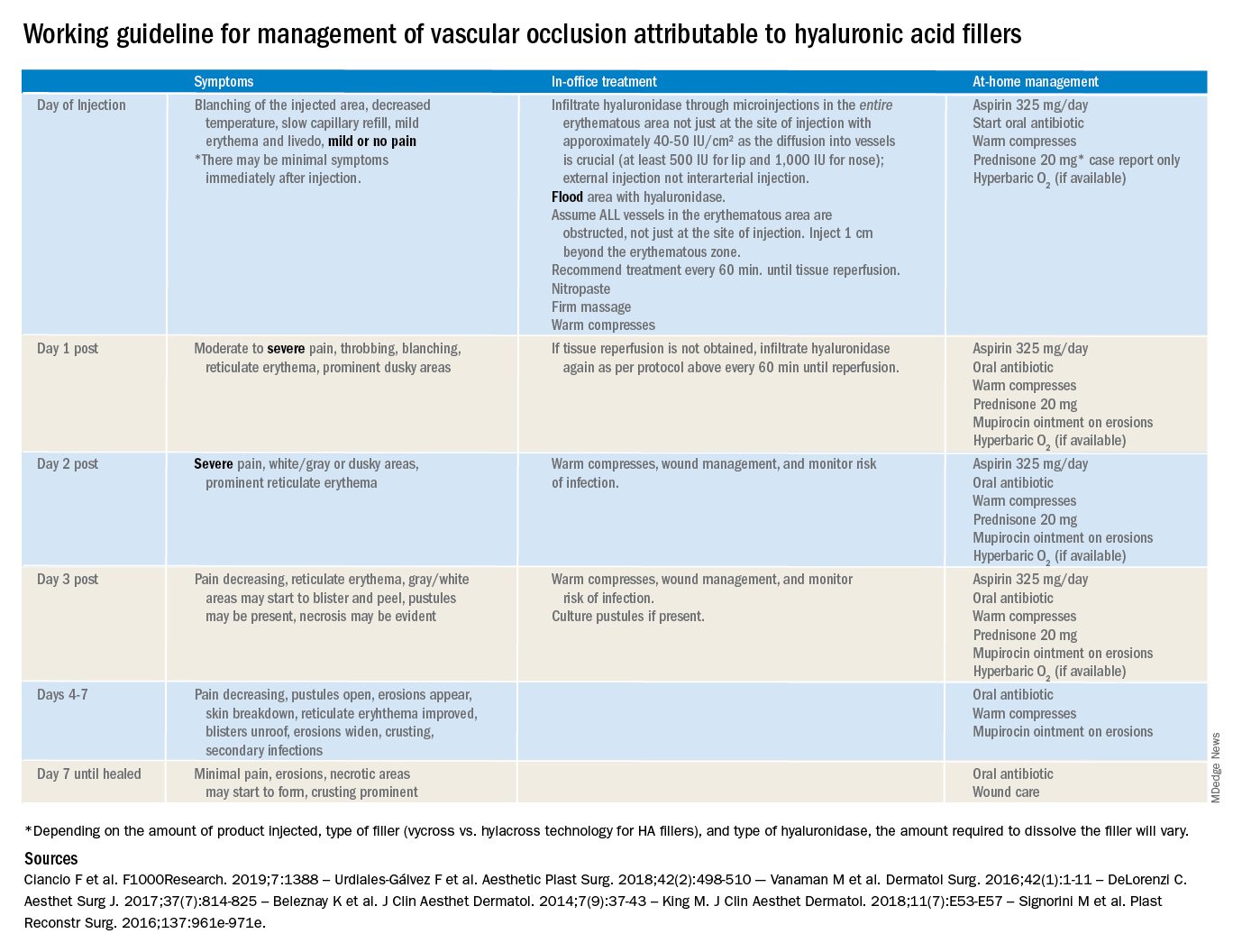
There are currently no definitive guidelines for the management of filler-associated cutaneous necrosis as experience with its treatment continues to evolve and be reported. In an attempt to consolidate the published data, as well as to give somewhat of a clear guideline of expectations, a time course and treatment guide has been outlined. The following is a working guideline for management of vascular occlusion attributable to HA fillers based on reports in the literature. This is not a consensus statement, rather it is a consolidation of the anecdotal reports and case studies outlined to help practitioners. It is also not inclusive of all the presentations of vascular occlusion. There are delayed cases of vascular occlusion beginning several days after injection, as well as alternative treatment options that may be considered.
These guidelines also are not for the devastating complication of blindness because of vascular occlusion secondary to fillers. Blindness is beyond the scope of the current article; however, we believe all experienced injectors should have emergency preparations in place and a relationship with an ophthalmologist or other trained surgeons experienced in performing retrobulbar hyaluronidase injections who can be reached in the event of a suspected occlusion. Any symptoms of eye pain, headache, or visual changes need to be immediately treated. Vascular occlusion is an emergency and timing is critical to prevent permanent blindness and facial deformities.
As with all filler injections, risks and complications can happen, and we cannot stress enough the appropriate level of training, as well as expert understanding of anatomy and injection technique, in minimizing potential risks. We encourage regulations and a required level of training to perform these procedures.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
The time course and proper management of vascular occlusion attributable to interarterial hyaluronic acid fillers is critical. Albeit a rare complication, off-label uses of HA fillers, lack of proper training of injectors, and lack of clear appropriate guidelines in the management of these complications are some of the causes of delayed treatment and necrotic complications.
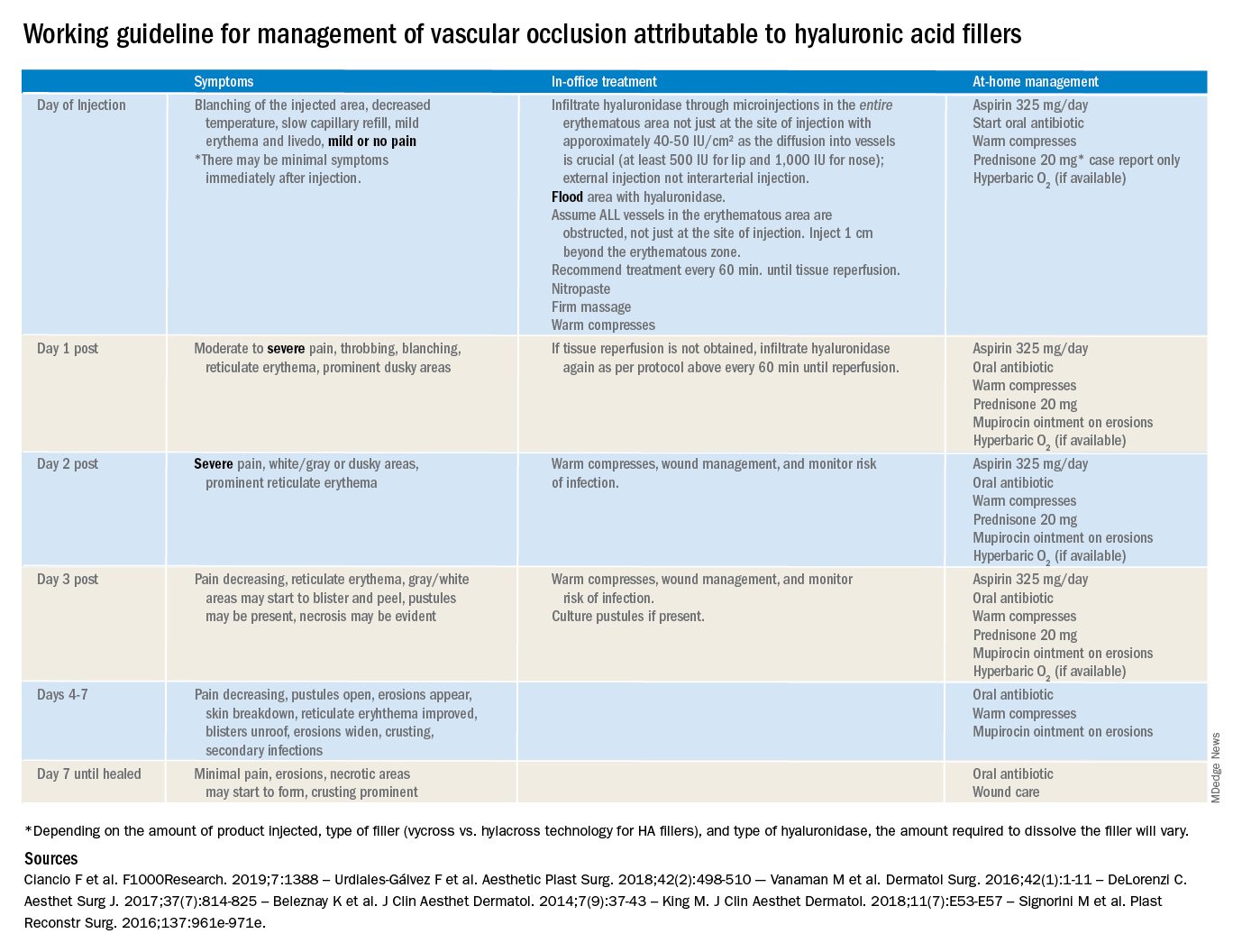
There are currently no definitive guidelines for the management of filler-associated cutaneous necrosis as experience with its treatment continues to evolve and be reported. In an attempt to consolidate the published data, as well as to give somewhat of a clear guideline of expectations, a time course and treatment guide has been outlined. The following is a working guideline for management of vascular occlusion attributable to HA fillers based on reports in the literature. This is not a consensus statement, rather it is a consolidation of the anecdotal reports and case studies outlined to help practitioners. It is also not inclusive of all the presentations of vascular occlusion. There are delayed cases of vascular occlusion beginning several days after injection, as well as alternative treatment options that may be considered.
These guidelines also are not for the devastating complication of blindness because of vascular occlusion secondary to fillers. Blindness is beyond the scope of the current article; however, we believe all experienced injectors should have emergency preparations in place and a relationship with an ophthalmologist or other trained surgeons experienced in performing retrobulbar hyaluronidase injections who can be reached in the event of a suspected occlusion. Any symptoms of eye pain, headache, or visual changes need to be immediately treated. Vascular occlusion is an emergency and timing is critical to prevent permanent blindness and facial deformities.
As with all filler injections, risks and complications can happen, and we cannot stress enough the appropriate level of training, as well as expert understanding of anatomy and injection technique, in minimizing potential risks. We encourage regulations and a required level of training to perform these procedures.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
The time course and proper management of vascular occlusion attributable to interarterial hyaluronic acid fillers is critical. Albeit a rare complication, off-label uses of HA fillers, lack of proper training of injectors, and lack of clear appropriate guidelines in the management of these complications are some of the causes of delayed treatment and necrotic complications.
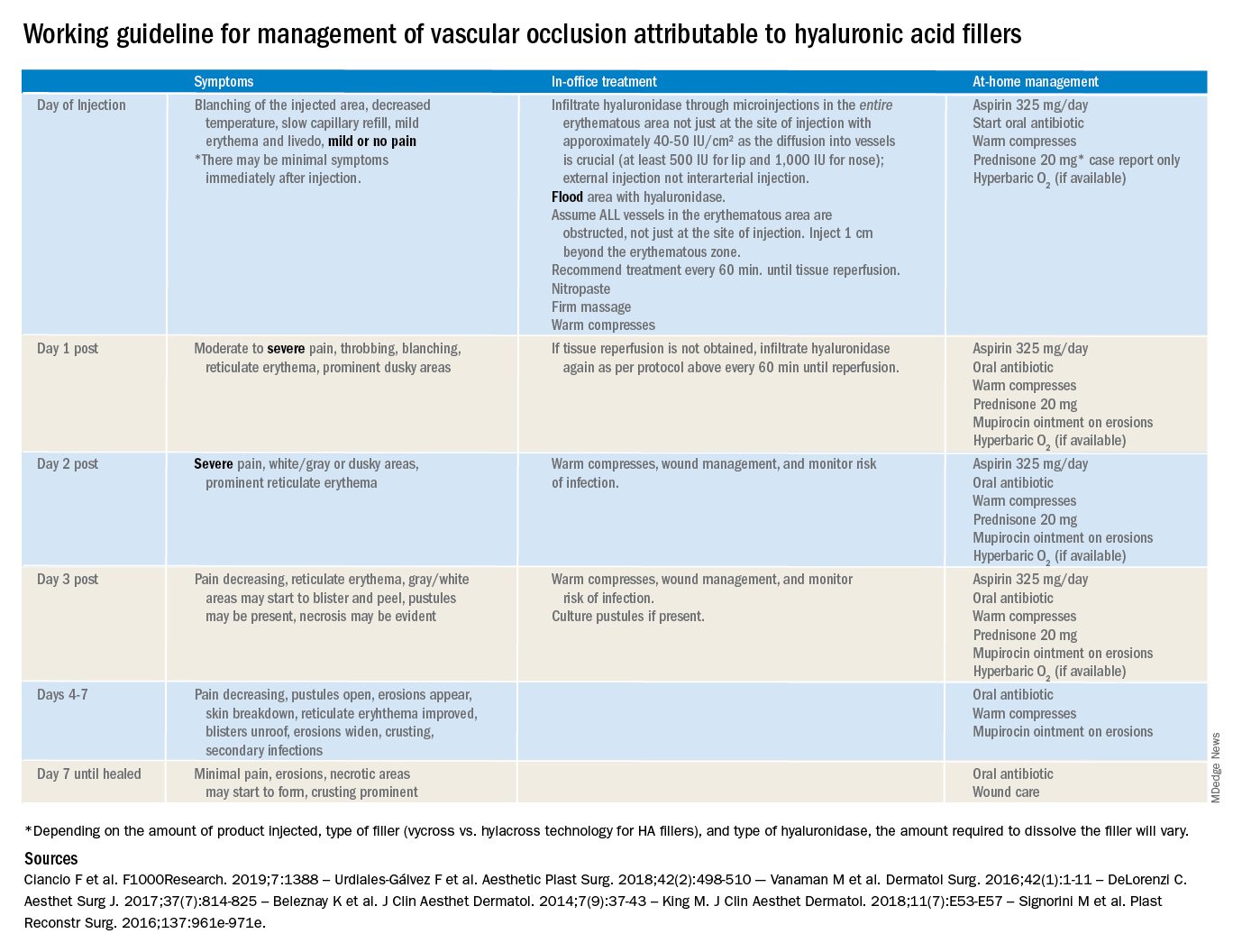
There are currently no definitive guidelines for the management of filler-associated cutaneous necrosis as experience with its treatment continues to evolve and be reported. In an attempt to consolidate the published data, as well as to give somewhat of a clear guideline of expectations, a time course and treatment guide has been outlined. The following is a working guideline for management of vascular occlusion attributable to HA fillers based on reports in the literature. This is not a consensus statement, rather it is a consolidation of the anecdotal reports and case studies outlined to help practitioners. It is also not inclusive of all the presentations of vascular occlusion. There are delayed cases of vascular occlusion beginning several days after injection, as well as alternative treatment options that may be considered.
These guidelines also are not for the devastating complication of blindness because of vascular occlusion secondary to fillers. Blindness is beyond the scope of the current article; however, we believe all experienced injectors should have emergency preparations in place and a relationship with an ophthalmologist or other trained surgeons experienced in performing retrobulbar hyaluronidase injections who can be reached in the event of a suspected occlusion. Any symptoms of eye pain, headache, or visual changes need to be immediately treated. Vascular occlusion is an emergency and timing is critical to prevent permanent blindness and facial deformities.
As with all filler injections, risks and complications can happen, and we cannot stress enough the appropriate level of training, as well as expert understanding of anatomy and injection technique, in minimizing potential risks. We encourage regulations and a required level of training to perform these procedures.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
Proteogenomics provides molecular insights into endometrial carcinoma
according to a proteogenomic study.
Further insights into the regulatory mechanisms of the disease were also identified, based on findings from genome-wide phosphoproteome and acetylome surveys.
“This study provides a comprehensive overview of the molecular systems of endometrial carcinoma at the genomic, transcriptomic, and proteomic levels,” wrote Yongchao Dou, PhD, of Baylor College of Medicine, Houston, and colleagues. The findings were published in Cell.
The researchers prospectively analyzed proteogenomic data from 95 endometrial carcinoma tumors, including 83 endometrioid and 12 serous samples, and 49 nonmalignant tissue samples. Whole genome and exome, DNA methylation, and total and microRNA sequencing analyses were performed for each sample.
An integrated evaluation of proteins, posttranslational modifications (phosphorylation and acetylation), DNA, and RNA were used to detect novel regulatory mechanisms and potential therapeutic targets.
The researchers confirmed previous data on the impact of gain-of-function TP53 mutations on the Aurora kinase pathway, notably the relationship between AURKA expression and negative outcomes in endometrial carcinoma.
“[These findings] provide a theoretical basis for the use of AURKA inhibitors in these tumors,” the researchers wrote.
In addition, the team found evidence of a new regulatory pathway involving ESRP2, circular RNA (circRNA), and QKI, each of which plays a key role in regulatory function.
“Through its known function in isoform regulation, ESRP2 could also directly regulate circRNA levels, and, if so, it could compete with QKI in circRNA-mediated gene regulation,” the researchers wrote.
Furthermore, they identified several gene products that could play a role in optimizing selection of patients for checkpoint blockade immunotherapy. One product in particular, CDK12, may better clinical response rates to immune checkpoint blockade.
The researchers also found evidence to suggest that measuring tumor antigen presentation defects could be more effective than measuring tumor mutation burden when selecting immunotherapy for patients with endometrial carcinoma.
“Although the results presented herein are predominantly observational, they provide the basis for multiple hypotheses of clinical relevance that can and should be further explored,” the researchers concluded.
The study was funded by the National Cancer Institute, the Cancer Prevention & Research Institutes of Texas, and the Robert and Janice McNair Foundation. The authors reported having no conflicts of interest.
SOURCE: Dou Y et al. Cell. 2020 Feb 13. doi: 10.1016/j.cell.2020.01.026.
according to a proteogenomic study.
Further insights into the regulatory mechanisms of the disease were also identified, based on findings from genome-wide phosphoproteome and acetylome surveys.
“This study provides a comprehensive overview of the molecular systems of endometrial carcinoma at the genomic, transcriptomic, and proteomic levels,” wrote Yongchao Dou, PhD, of Baylor College of Medicine, Houston, and colleagues. The findings were published in Cell.
The researchers prospectively analyzed proteogenomic data from 95 endometrial carcinoma tumors, including 83 endometrioid and 12 serous samples, and 49 nonmalignant tissue samples. Whole genome and exome, DNA methylation, and total and microRNA sequencing analyses were performed for each sample.
An integrated evaluation of proteins, posttranslational modifications (phosphorylation and acetylation), DNA, and RNA were used to detect novel regulatory mechanisms and potential therapeutic targets.
The researchers confirmed previous data on the impact of gain-of-function TP53 mutations on the Aurora kinase pathway, notably the relationship between AURKA expression and negative outcomes in endometrial carcinoma.
“[These findings] provide a theoretical basis for the use of AURKA inhibitors in these tumors,” the researchers wrote.
In addition, the team found evidence of a new regulatory pathway involving ESRP2, circular RNA (circRNA), and QKI, each of which plays a key role in regulatory function.
“Through its known function in isoform regulation, ESRP2 could also directly regulate circRNA levels, and, if so, it could compete with QKI in circRNA-mediated gene regulation,” the researchers wrote.
Furthermore, they identified several gene products that could play a role in optimizing selection of patients for checkpoint blockade immunotherapy. One product in particular, CDK12, may better clinical response rates to immune checkpoint blockade.
The researchers also found evidence to suggest that measuring tumor antigen presentation defects could be more effective than measuring tumor mutation burden when selecting immunotherapy for patients with endometrial carcinoma.
“Although the results presented herein are predominantly observational, they provide the basis for multiple hypotheses of clinical relevance that can and should be further explored,” the researchers concluded.
The study was funded by the National Cancer Institute, the Cancer Prevention & Research Institutes of Texas, and the Robert and Janice McNair Foundation. The authors reported having no conflicts of interest.
SOURCE: Dou Y et al. Cell. 2020 Feb 13. doi: 10.1016/j.cell.2020.01.026.
according to a proteogenomic study.
Further insights into the regulatory mechanisms of the disease were also identified, based on findings from genome-wide phosphoproteome and acetylome surveys.
“This study provides a comprehensive overview of the molecular systems of endometrial carcinoma at the genomic, transcriptomic, and proteomic levels,” wrote Yongchao Dou, PhD, of Baylor College of Medicine, Houston, and colleagues. The findings were published in Cell.
The researchers prospectively analyzed proteogenomic data from 95 endometrial carcinoma tumors, including 83 endometrioid and 12 serous samples, and 49 nonmalignant tissue samples. Whole genome and exome, DNA methylation, and total and microRNA sequencing analyses were performed for each sample.
An integrated evaluation of proteins, posttranslational modifications (phosphorylation and acetylation), DNA, and RNA were used to detect novel regulatory mechanisms and potential therapeutic targets.
The researchers confirmed previous data on the impact of gain-of-function TP53 mutations on the Aurora kinase pathway, notably the relationship between AURKA expression and negative outcomes in endometrial carcinoma.
“[These findings] provide a theoretical basis for the use of AURKA inhibitors in these tumors,” the researchers wrote.
In addition, the team found evidence of a new regulatory pathway involving ESRP2, circular RNA (circRNA), and QKI, each of which plays a key role in regulatory function.
“Through its known function in isoform regulation, ESRP2 could also directly regulate circRNA levels, and, if so, it could compete with QKI in circRNA-mediated gene regulation,” the researchers wrote.
Furthermore, they identified several gene products that could play a role in optimizing selection of patients for checkpoint blockade immunotherapy. One product in particular, CDK12, may better clinical response rates to immune checkpoint blockade.
The researchers also found evidence to suggest that measuring tumor antigen presentation defects could be more effective than measuring tumor mutation burden when selecting immunotherapy for patients with endometrial carcinoma.
“Although the results presented herein are predominantly observational, they provide the basis for multiple hypotheses of clinical relevance that can and should be further explored,” the researchers concluded.
The study was funded by the National Cancer Institute, the Cancer Prevention & Research Institutes of Texas, and the Robert and Janice McNair Foundation. The authors reported having no conflicts of interest.
SOURCE: Dou Y et al. Cell. 2020 Feb 13. doi: 10.1016/j.cell.2020.01.026.
FROM CELL


