User login
‘Like a coin flip’: Assay denies some cancer patients new drug
In December, at a major breast cancer conference, some attendees couldn’t find a seat and were told to leave an overcrowded session on immunotherapy for metastatic triple-negative breast cancer (TNBC). They refused, and pushed in to hear what was being said.
The crowd might have been surprised to learn that the main draw of the event, a successful new drug, was not all it might have been for women with the disease, being handicapped by a test that determines who is eligible for it.
“That room was overpacked ― there were five people deep against the wall. ... It was amazing,” said Janice Cowden of Bradenton, Florida. She attended the meeting, the San Antonio Breast Cancer Symposium, as a patient advocate.
Cowden lives with metastatic TNBC, which is known for poor prognoses, aggressiveness, and a lack of targeted treatment options. “Stage IV is a state of desperation. We just want something to work,” she said.
That’s why the conference room was packed – the session was focused on something that had been found to work – the immunotherapy atezolizumab (Tecentriq, Genentech/Roche).
Atezolizumab had recently been conditionally approved for first-line use in advanced TNBC, having been shown to significantly slow disease progression and, in some patients, to possibly improve survival. A pair of medical oncologists reviewed the clinical trial data during the session.
One important point from the trial data was that the benefit was greater in patients whose tumors had the biomarker PD-L1, and so the Food and Drug Administration approval of the drug specified that it should be used only in those patients.
The drug approval was accompanied by approval of a companion diagnostic test used to identify this PD-L1-positive subgroup of patients, the Ventana SP142 Assay (Roche Diagnostics).
At the meeting, pathologist David Rimm, MD, of Yale University, New Haven, Connecticut, discussed the biomarker PD-L1 and the test. Rimm had a subtle but unsettling message about the crucial test: that the SP142 diagnostic assay, when used by increasing numbers of pathologists, resulted in increasing rates of PD-L1 scores that were not concordant.
A related meeting poster, presented the next day with Rimm as senior author, was more explicit and concluded that “more than half of the pathologists in real-world situations may mis- assign” patient scores with SP142 (and another Roche assay) because of wide variability in readouts.
“They’ve made a test that is inadequate – it just doesn’t work. It’s like flipping a coin,” he told Medscape Medical News about Roche’s SP142 assay in everyday practice.
The general problem is not a new one – for some years there have been problems with the use of PD-L1 as a biomarker for immunotherapy and with assays for that biomarker, with many groups questioning both accuracy and reproducibility. But the problems with SP142 are “the most egregious,” said Rimm, who has served as a paid consultant to Roche Diagnostics in the past.
In clinical practice, Rimm’s overall message is that because of the difficulty of reading SP142 assay results, some TNBC patients who were PD-L1-positive would not get the drug, and some who were not positive would get the drug.
Patient advocate Cowden was not worried about overtreatment. She was concerned about patients who “might die without receiving a potentially life-extending treatment.”
In an essay in the Pathologist, Rimm echoed that sentiment about undertreatment (as well as overtreatment) with atezolizumab for breast cancer: “In all cases, the patients are the potential victims, but this appears to be completely under the radar of the hype surrounding this new drug.”
Roche Disputes Problems With Assay
Roche, manufacturer of both atezolizumab and the companion diagnostic test, disputes that there is a problem.
The FDA and multiple health authorities worldwide have approved atezolizumab and the companion diagnostic SP142 assay for use in TNBC, points out Eslie Dennis, MD, vice president of medical affairs at Roche Tissue Diagnostics.
“The role of a companion diagnostic assay is to discriminate between responders and non-responders for a specific therapeutic product in a specific indication, with a cut-off based on clinical outcomes,” she wrote in an email to Medscape Medical News.
Data from the pivotal IMpassion130 trial show that the assay was effective at that task. Among the 369 patients in the 902-patient trial whose tumors were ≥1% positive for PD-L1, those treated with atezolizumab (and nab-paclitaxel; n = 185) had a median progression-free survival (PFS) of 7.4 months, vs. 4.8 months among those treated with placebo (and nab-paclitaxel; n = 184) (P < .0001).
“Exploratory analysis showed no [PFS] benefit in PD-L1-negative patients as tested by the SP142 assay [in IMpassion130],” Dennis and three other physicians write in a reply to Rimm in a letter published in July 2019 in the Pathologist.
The same held true for overall survival in exploratory analysis – there was no benefit with atezolizumab among the PD-L1-negative patients, they write.
Notably, overall survival benefit for patients who were PD-L1 positive was about 10 months (at the first interim analysis; at the second analysis, the benefit dropped to 7 months and was not statistically significant).
But Rimm points out that the pivotal trial used only one pathologist in a central lab to determine PD-L1 status, who was undoubtedly an expert with the SP142 assay.
Further, Rimm observes that additional data submitted to the FDA to show that SP142 test results are reproducible outside of the pivotal trial setting were performed with only three pathologists and thus unsurprisingly yielded high rates of agreement – all above 90%.
The data from both of these circumstances are problematic, Rimm said, because in the real world, hundreds of pathologists will score the SP142 assay – all in the context of a busy day reading a variety of other tests for other diseases.
It’s one thing to get an FDA approval for an assay, and it’s another thing to be a reliable, well-functioning assay in the real world, he summarized.
Last year, Roberto Salgado, MD, PhD, a pathologist at the Université Libre de Bruxelles, Belgium, commented that “a positive phase III trial should not be taken as a guarantee that the assay used in the trial can be implemented in daily practice” in an opinion piece in the Pathologist.
SP142 Identifies the “Fewest Possible Patients”
The SP142 assay has been shown in multiple studies to have lower sensitivity for PD-L1 than other competing PD-L1 assays, said Rimm, citing examples such as a 2017 study and a 2018 study.
Angela DeMichele, MD, a medical oncologist at the University of Pennsylvania in Philadelphia, agreed and explained what that meant in practical terms for women whose tumors are tested with SP142. “It means that the test is going to identify the fewest possible PD-L1-positive patients [relative to the other available assays],” she said. “It [the SP142 assay] is far from a perfect test for this situation,” added DeMichele, an expert on biomarkers in breast cancer clinical trials.
She said that biomarker tests, like many products of science, tend to become dated with the passage of time, as more is learned about the target and new assays are developed. “Unfortunately, you can’t change assays midstream,” said DeMichele. She has received a grant from Roche and Stand Up to Cancer to study atezolizumab and another drug in a clinical trial among patients with metastatic TNBC who have minimal residual disease.
DeMichele also said that “David Rimm is one of the most knowledgeable people in the world about this issue.”
But DeMichelle also points out the practical: “We’re stuck as clinicians” because regulatory bodies and insurance companies only pay for atezolizumab when the SP142 assay indicates PD-L1 positivity. That’s not the case in Europe, where health authorities do not specify which PD-L1 assay is to be used with atezolizumab for breast cancer, pointed out Belgium’s Salgado last year.
Another Level of Complexity
At the immunotherapy session in San Antonio, Rimm discussed the results of a study of 68 TNBC archived cases in which specimens were stained with the SP142 assay at Yale and were distributed via electronic images to 19 pathologists at 14 institutions across the United States for PD-L1 scoring.
The study, coauthored by academics from Iowa, Texas A&M, UC San Diego, Mayo Clinic, Memorial Sloan Kettering, and others, used a novel method to determine the minimum number of evaluators needed to estimate “concordance” or agreement about a test result among large numbers of readers. The consensus/agreement was as high as 80% when eight or fewer pathologists’ scores were compared, but was as low as 40% when results from more than eight pathologists were included, said Rimm.
These are some of the data that led him to declare that using the assay is no better than flipping a coin.
Yes, PD-L1 testing is a challenge, and it has “introduced another level of complexity” for pathologists in reading assays, write experts Emina Torlakovic, MD, University of Saskatchewan, Canada, and Allen Gown, MD, PhenoPath Laboratories, Seattle, in response to Rimm last year.
But there is “poor” consensus among pathologists, they point out, “for many scoring systems that are still clinically applied (such as Gleason grading).” Consensus “improves with education and training,” the pair add. To that end, Roche has initiated a global training program for pathologists using the SP142 assay for TNBC. At San Antonio, Roche’s Dennis reported that among 432 pathologists from 58 countries, there was overall agreement of 98.2% in scoring assays.
Rimm commented that such high agreement would not be a surprise if testing took place soon after any such training program.
In an email to Medscape Medical News, Torlakovic encouraged pathologists who wish to practice their skill in interpreting assays, including SP142, to visit CBQAReadout.ca, a testing site. The site, which was founded by Torlakovic and may be one of a kind, offers CME credits and is sponsored by independent pathology organizations, such as CAP-ACP and the Saskatchewan Health Authority, as well as pharmaceutical companies, including Roche.
No Clue
Patient advocate Cowden believes the controversy about PD-L1 testing for atezolizumab is largely unknown among breast cancer patients. She learned about SP142 assay ambiguities in San Antonio, when the Florida Breast Cancer Foundation funded her trip to the meeting and the Alamo Breast Cancer Foundation asked her to write a report on Rimm’s presentation.
Cowden is a member of a Facebook group for stage IV TNBC, which has about 1500 members. She estimates that 75%-80% would be willing to try atezolizumab “no matter what,” meaning they don’t care about PD-L1 positivity being associated with efficacy.
The Facebook group members “know there is a test and if you are positive, there is an immunotherapy for their breast cancer,” said Cowden.
None know that women may be excluded from treatment because of shortcomings with the SP142 test. “They have no clue,” she said.
Rimm and DeMichele have financial ties to Roche and other companies. Dennis is an employee of Roche. Torlakovic has ties to multiple companies, including Roche, for whom she has acted as a paid consultant, grant recipient, and paid lecturer. Gown did not respond to a request for financial disclosures. Cowden reports no relevant financial relationships.
This article first appeared on Medscape.com.
In December, at a major breast cancer conference, some attendees couldn’t find a seat and were told to leave an overcrowded session on immunotherapy for metastatic triple-negative breast cancer (TNBC). They refused, and pushed in to hear what was being said.
The crowd might have been surprised to learn that the main draw of the event, a successful new drug, was not all it might have been for women with the disease, being handicapped by a test that determines who is eligible for it.
“That room was overpacked ― there were five people deep against the wall. ... It was amazing,” said Janice Cowden of Bradenton, Florida. She attended the meeting, the San Antonio Breast Cancer Symposium, as a patient advocate.
Cowden lives with metastatic TNBC, which is known for poor prognoses, aggressiveness, and a lack of targeted treatment options. “Stage IV is a state of desperation. We just want something to work,” she said.
That’s why the conference room was packed – the session was focused on something that had been found to work – the immunotherapy atezolizumab (Tecentriq, Genentech/Roche).
Atezolizumab had recently been conditionally approved for first-line use in advanced TNBC, having been shown to significantly slow disease progression and, in some patients, to possibly improve survival. A pair of medical oncologists reviewed the clinical trial data during the session.
One important point from the trial data was that the benefit was greater in patients whose tumors had the biomarker PD-L1, and so the Food and Drug Administration approval of the drug specified that it should be used only in those patients.
The drug approval was accompanied by approval of a companion diagnostic test used to identify this PD-L1-positive subgroup of patients, the Ventana SP142 Assay (Roche Diagnostics).
At the meeting, pathologist David Rimm, MD, of Yale University, New Haven, Connecticut, discussed the biomarker PD-L1 and the test. Rimm had a subtle but unsettling message about the crucial test: that the SP142 diagnostic assay, when used by increasing numbers of pathologists, resulted in increasing rates of PD-L1 scores that were not concordant.
A related meeting poster, presented the next day with Rimm as senior author, was more explicit and concluded that “more than half of the pathologists in real-world situations may mis- assign” patient scores with SP142 (and another Roche assay) because of wide variability in readouts.
“They’ve made a test that is inadequate – it just doesn’t work. It’s like flipping a coin,” he told Medscape Medical News about Roche’s SP142 assay in everyday practice.
The general problem is not a new one – for some years there have been problems with the use of PD-L1 as a biomarker for immunotherapy and with assays for that biomarker, with many groups questioning both accuracy and reproducibility. But the problems with SP142 are “the most egregious,” said Rimm, who has served as a paid consultant to Roche Diagnostics in the past.
In clinical practice, Rimm’s overall message is that because of the difficulty of reading SP142 assay results, some TNBC patients who were PD-L1-positive would not get the drug, and some who were not positive would get the drug.
Patient advocate Cowden was not worried about overtreatment. She was concerned about patients who “might die without receiving a potentially life-extending treatment.”
In an essay in the Pathologist, Rimm echoed that sentiment about undertreatment (as well as overtreatment) with atezolizumab for breast cancer: “In all cases, the patients are the potential victims, but this appears to be completely under the radar of the hype surrounding this new drug.”
Roche Disputes Problems With Assay
Roche, manufacturer of both atezolizumab and the companion diagnostic test, disputes that there is a problem.
The FDA and multiple health authorities worldwide have approved atezolizumab and the companion diagnostic SP142 assay for use in TNBC, points out Eslie Dennis, MD, vice president of medical affairs at Roche Tissue Diagnostics.
“The role of a companion diagnostic assay is to discriminate between responders and non-responders for a specific therapeutic product in a specific indication, with a cut-off based on clinical outcomes,” she wrote in an email to Medscape Medical News.
Data from the pivotal IMpassion130 trial show that the assay was effective at that task. Among the 369 patients in the 902-patient trial whose tumors were ≥1% positive for PD-L1, those treated with atezolizumab (and nab-paclitaxel; n = 185) had a median progression-free survival (PFS) of 7.4 months, vs. 4.8 months among those treated with placebo (and nab-paclitaxel; n = 184) (P < .0001).
“Exploratory analysis showed no [PFS] benefit in PD-L1-negative patients as tested by the SP142 assay [in IMpassion130],” Dennis and three other physicians write in a reply to Rimm in a letter published in July 2019 in the Pathologist.
The same held true for overall survival in exploratory analysis – there was no benefit with atezolizumab among the PD-L1-negative patients, they write.
Notably, overall survival benefit for patients who were PD-L1 positive was about 10 months (at the first interim analysis; at the second analysis, the benefit dropped to 7 months and was not statistically significant).
But Rimm points out that the pivotal trial used only one pathologist in a central lab to determine PD-L1 status, who was undoubtedly an expert with the SP142 assay.
Further, Rimm observes that additional data submitted to the FDA to show that SP142 test results are reproducible outside of the pivotal trial setting were performed with only three pathologists and thus unsurprisingly yielded high rates of agreement – all above 90%.
The data from both of these circumstances are problematic, Rimm said, because in the real world, hundreds of pathologists will score the SP142 assay – all in the context of a busy day reading a variety of other tests for other diseases.
It’s one thing to get an FDA approval for an assay, and it’s another thing to be a reliable, well-functioning assay in the real world, he summarized.
Last year, Roberto Salgado, MD, PhD, a pathologist at the Université Libre de Bruxelles, Belgium, commented that “a positive phase III trial should not be taken as a guarantee that the assay used in the trial can be implemented in daily practice” in an opinion piece in the Pathologist.
SP142 Identifies the “Fewest Possible Patients”
The SP142 assay has been shown in multiple studies to have lower sensitivity for PD-L1 than other competing PD-L1 assays, said Rimm, citing examples such as a 2017 study and a 2018 study.
Angela DeMichele, MD, a medical oncologist at the University of Pennsylvania in Philadelphia, agreed and explained what that meant in practical terms for women whose tumors are tested with SP142. “It means that the test is going to identify the fewest possible PD-L1-positive patients [relative to the other available assays],” she said. “It [the SP142 assay] is far from a perfect test for this situation,” added DeMichele, an expert on biomarkers in breast cancer clinical trials.
She said that biomarker tests, like many products of science, tend to become dated with the passage of time, as more is learned about the target and new assays are developed. “Unfortunately, you can’t change assays midstream,” said DeMichele. She has received a grant from Roche and Stand Up to Cancer to study atezolizumab and another drug in a clinical trial among patients with metastatic TNBC who have minimal residual disease.
DeMichele also said that “David Rimm is one of the most knowledgeable people in the world about this issue.”
But DeMichelle also points out the practical: “We’re stuck as clinicians” because regulatory bodies and insurance companies only pay for atezolizumab when the SP142 assay indicates PD-L1 positivity. That’s not the case in Europe, where health authorities do not specify which PD-L1 assay is to be used with atezolizumab for breast cancer, pointed out Belgium’s Salgado last year.
Another Level of Complexity
At the immunotherapy session in San Antonio, Rimm discussed the results of a study of 68 TNBC archived cases in which specimens were stained with the SP142 assay at Yale and were distributed via electronic images to 19 pathologists at 14 institutions across the United States for PD-L1 scoring.
The study, coauthored by academics from Iowa, Texas A&M, UC San Diego, Mayo Clinic, Memorial Sloan Kettering, and others, used a novel method to determine the minimum number of evaluators needed to estimate “concordance” or agreement about a test result among large numbers of readers. The consensus/agreement was as high as 80% when eight or fewer pathologists’ scores were compared, but was as low as 40% when results from more than eight pathologists were included, said Rimm.
These are some of the data that led him to declare that using the assay is no better than flipping a coin.
Yes, PD-L1 testing is a challenge, and it has “introduced another level of complexity” for pathologists in reading assays, write experts Emina Torlakovic, MD, University of Saskatchewan, Canada, and Allen Gown, MD, PhenoPath Laboratories, Seattle, in response to Rimm last year.
But there is “poor” consensus among pathologists, they point out, “for many scoring systems that are still clinically applied (such as Gleason grading).” Consensus “improves with education and training,” the pair add. To that end, Roche has initiated a global training program for pathologists using the SP142 assay for TNBC. At San Antonio, Roche’s Dennis reported that among 432 pathologists from 58 countries, there was overall agreement of 98.2% in scoring assays.
Rimm commented that such high agreement would not be a surprise if testing took place soon after any such training program.
In an email to Medscape Medical News, Torlakovic encouraged pathologists who wish to practice their skill in interpreting assays, including SP142, to visit CBQAReadout.ca, a testing site. The site, which was founded by Torlakovic and may be one of a kind, offers CME credits and is sponsored by independent pathology organizations, such as CAP-ACP and the Saskatchewan Health Authority, as well as pharmaceutical companies, including Roche.
No Clue
Patient advocate Cowden believes the controversy about PD-L1 testing for atezolizumab is largely unknown among breast cancer patients. She learned about SP142 assay ambiguities in San Antonio, when the Florida Breast Cancer Foundation funded her trip to the meeting and the Alamo Breast Cancer Foundation asked her to write a report on Rimm’s presentation.
Cowden is a member of a Facebook group for stage IV TNBC, which has about 1500 members. She estimates that 75%-80% would be willing to try atezolizumab “no matter what,” meaning they don’t care about PD-L1 positivity being associated with efficacy.
The Facebook group members “know there is a test and if you are positive, there is an immunotherapy for their breast cancer,” said Cowden.
None know that women may be excluded from treatment because of shortcomings with the SP142 test. “They have no clue,” she said.
Rimm and DeMichele have financial ties to Roche and other companies. Dennis is an employee of Roche. Torlakovic has ties to multiple companies, including Roche, for whom she has acted as a paid consultant, grant recipient, and paid lecturer. Gown did not respond to a request for financial disclosures. Cowden reports no relevant financial relationships.
This article first appeared on Medscape.com.
In December, at a major breast cancer conference, some attendees couldn’t find a seat and were told to leave an overcrowded session on immunotherapy for metastatic triple-negative breast cancer (TNBC). They refused, and pushed in to hear what was being said.
The crowd might have been surprised to learn that the main draw of the event, a successful new drug, was not all it might have been for women with the disease, being handicapped by a test that determines who is eligible for it.
“That room was overpacked ― there were five people deep against the wall. ... It was amazing,” said Janice Cowden of Bradenton, Florida. She attended the meeting, the San Antonio Breast Cancer Symposium, as a patient advocate.
Cowden lives with metastatic TNBC, which is known for poor prognoses, aggressiveness, and a lack of targeted treatment options. “Stage IV is a state of desperation. We just want something to work,” she said.
That’s why the conference room was packed – the session was focused on something that had been found to work – the immunotherapy atezolizumab (Tecentriq, Genentech/Roche).
Atezolizumab had recently been conditionally approved for first-line use in advanced TNBC, having been shown to significantly slow disease progression and, in some patients, to possibly improve survival. A pair of medical oncologists reviewed the clinical trial data during the session.
One important point from the trial data was that the benefit was greater in patients whose tumors had the biomarker PD-L1, and so the Food and Drug Administration approval of the drug specified that it should be used only in those patients.
The drug approval was accompanied by approval of a companion diagnostic test used to identify this PD-L1-positive subgroup of patients, the Ventana SP142 Assay (Roche Diagnostics).
At the meeting, pathologist David Rimm, MD, of Yale University, New Haven, Connecticut, discussed the biomarker PD-L1 and the test. Rimm had a subtle but unsettling message about the crucial test: that the SP142 diagnostic assay, when used by increasing numbers of pathologists, resulted in increasing rates of PD-L1 scores that were not concordant.
A related meeting poster, presented the next day with Rimm as senior author, was more explicit and concluded that “more than half of the pathologists in real-world situations may mis- assign” patient scores with SP142 (and another Roche assay) because of wide variability in readouts.
“They’ve made a test that is inadequate – it just doesn’t work. It’s like flipping a coin,” he told Medscape Medical News about Roche’s SP142 assay in everyday practice.
The general problem is not a new one – for some years there have been problems with the use of PD-L1 as a biomarker for immunotherapy and with assays for that biomarker, with many groups questioning both accuracy and reproducibility. But the problems with SP142 are “the most egregious,” said Rimm, who has served as a paid consultant to Roche Diagnostics in the past.
In clinical practice, Rimm’s overall message is that because of the difficulty of reading SP142 assay results, some TNBC patients who were PD-L1-positive would not get the drug, and some who were not positive would get the drug.
Patient advocate Cowden was not worried about overtreatment. She was concerned about patients who “might die without receiving a potentially life-extending treatment.”
In an essay in the Pathologist, Rimm echoed that sentiment about undertreatment (as well as overtreatment) with atezolizumab for breast cancer: “In all cases, the patients are the potential victims, but this appears to be completely under the radar of the hype surrounding this new drug.”
Roche Disputes Problems With Assay
Roche, manufacturer of both atezolizumab and the companion diagnostic test, disputes that there is a problem.
The FDA and multiple health authorities worldwide have approved atezolizumab and the companion diagnostic SP142 assay for use in TNBC, points out Eslie Dennis, MD, vice president of medical affairs at Roche Tissue Diagnostics.
“The role of a companion diagnostic assay is to discriminate between responders and non-responders for a specific therapeutic product in a specific indication, with a cut-off based on clinical outcomes,” she wrote in an email to Medscape Medical News.
Data from the pivotal IMpassion130 trial show that the assay was effective at that task. Among the 369 patients in the 902-patient trial whose tumors were ≥1% positive for PD-L1, those treated with atezolizumab (and nab-paclitaxel; n = 185) had a median progression-free survival (PFS) of 7.4 months, vs. 4.8 months among those treated with placebo (and nab-paclitaxel; n = 184) (P < .0001).
“Exploratory analysis showed no [PFS] benefit in PD-L1-negative patients as tested by the SP142 assay [in IMpassion130],” Dennis and three other physicians write in a reply to Rimm in a letter published in July 2019 in the Pathologist.
The same held true for overall survival in exploratory analysis – there was no benefit with atezolizumab among the PD-L1-negative patients, they write.
Notably, overall survival benefit for patients who were PD-L1 positive was about 10 months (at the first interim analysis; at the second analysis, the benefit dropped to 7 months and was not statistically significant).
But Rimm points out that the pivotal trial used only one pathologist in a central lab to determine PD-L1 status, who was undoubtedly an expert with the SP142 assay.
Further, Rimm observes that additional data submitted to the FDA to show that SP142 test results are reproducible outside of the pivotal trial setting were performed with only three pathologists and thus unsurprisingly yielded high rates of agreement – all above 90%.
The data from both of these circumstances are problematic, Rimm said, because in the real world, hundreds of pathologists will score the SP142 assay – all in the context of a busy day reading a variety of other tests for other diseases.
It’s one thing to get an FDA approval for an assay, and it’s another thing to be a reliable, well-functioning assay in the real world, he summarized.
Last year, Roberto Salgado, MD, PhD, a pathologist at the Université Libre de Bruxelles, Belgium, commented that “a positive phase III trial should not be taken as a guarantee that the assay used in the trial can be implemented in daily practice” in an opinion piece in the Pathologist.
SP142 Identifies the “Fewest Possible Patients”
The SP142 assay has been shown in multiple studies to have lower sensitivity for PD-L1 than other competing PD-L1 assays, said Rimm, citing examples such as a 2017 study and a 2018 study.
Angela DeMichele, MD, a medical oncologist at the University of Pennsylvania in Philadelphia, agreed and explained what that meant in practical terms for women whose tumors are tested with SP142. “It means that the test is going to identify the fewest possible PD-L1-positive patients [relative to the other available assays],” she said. “It [the SP142 assay] is far from a perfect test for this situation,” added DeMichele, an expert on biomarkers in breast cancer clinical trials.
She said that biomarker tests, like many products of science, tend to become dated with the passage of time, as more is learned about the target and new assays are developed. “Unfortunately, you can’t change assays midstream,” said DeMichele. She has received a grant from Roche and Stand Up to Cancer to study atezolizumab and another drug in a clinical trial among patients with metastatic TNBC who have minimal residual disease.
DeMichele also said that “David Rimm is one of the most knowledgeable people in the world about this issue.”
But DeMichelle also points out the practical: “We’re stuck as clinicians” because regulatory bodies and insurance companies only pay for atezolizumab when the SP142 assay indicates PD-L1 positivity. That’s not the case in Europe, where health authorities do not specify which PD-L1 assay is to be used with atezolizumab for breast cancer, pointed out Belgium’s Salgado last year.
Another Level of Complexity
At the immunotherapy session in San Antonio, Rimm discussed the results of a study of 68 TNBC archived cases in which specimens were stained with the SP142 assay at Yale and were distributed via electronic images to 19 pathologists at 14 institutions across the United States for PD-L1 scoring.
The study, coauthored by academics from Iowa, Texas A&M, UC San Diego, Mayo Clinic, Memorial Sloan Kettering, and others, used a novel method to determine the minimum number of evaluators needed to estimate “concordance” or agreement about a test result among large numbers of readers. The consensus/agreement was as high as 80% when eight or fewer pathologists’ scores were compared, but was as low as 40% when results from more than eight pathologists were included, said Rimm.
These are some of the data that led him to declare that using the assay is no better than flipping a coin.
Yes, PD-L1 testing is a challenge, and it has “introduced another level of complexity” for pathologists in reading assays, write experts Emina Torlakovic, MD, University of Saskatchewan, Canada, and Allen Gown, MD, PhenoPath Laboratories, Seattle, in response to Rimm last year.
But there is “poor” consensus among pathologists, they point out, “for many scoring systems that are still clinically applied (such as Gleason grading).” Consensus “improves with education and training,” the pair add. To that end, Roche has initiated a global training program for pathologists using the SP142 assay for TNBC. At San Antonio, Roche’s Dennis reported that among 432 pathologists from 58 countries, there was overall agreement of 98.2% in scoring assays.
Rimm commented that such high agreement would not be a surprise if testing took place soon after any such training program.
In an email to Medscape Medical News, Torlakovic encouraged pathologists who wish to practice their skill in interpreting assays, including SP142, to visit CBQAReadout.ca, a testing site. The site, which was founded by Torlakovic and may be one of a kind, offers CME credits and is sponsored by independent pathology organizations, such as CAP-ACP and the Saskatchewan Health Authority, as well as pharmaceutical companies, including Roche.
No Clue
Patient advocate Cowden believes the controversy about PD-L1 testing for atezolizumab is largely unknown among breast cancer patients. She learned about SP142 assay ambiguities in San Antonio, when the Florida Breast Cancer Foundation funded her trip to the meeting and the Alamo Breast Cancer Foundation asked her to write a report on Rimm’s presentation.
Cowden is a member of a Facebook group for stage IV TNBC, which has about 1500 members. She estimates that 75%-80% would be willing to try atezolizumab “no matter what,” meaning they don’t care about PD-L1 positivity being associated with efficacy.
The Facebook group members “know there is a test and if you are positive, there is an immunotherapy for their breast cancer,” said Cowden.
None know that women may be excluded from treatment because of shortcomings with the SP142 test. “They have no clue,” she said.
Rimm and DeMichele have financial ties to Roche and other companies. Dennis is an employee of Roche. Torlakovic has ties to multiple companies, including Roche, for whom she has acted as a paid consultant, grant recipient, and paid lecturer. Gown did not respond to a request for financial disclosures. Cowden reports no relevant financial relationships.
This article first appeared on Medscape.com.
TAVR device orientation may reduce coronary overlap
For patients undergoing transcatheter aortic valve replacement, using a specific orientation at deployment may optimize valve alignment and potentially preserve coronary access, at least for some devices, results of a pilot imaging study suggest.
In particular, positioning the Evolut THV (Medtronic) at a certain way at deployment led to an improvement in commissural alignment and a significant reduction in coronary artery overlap, according to authors of the study, led by Gilbert H. L. Tang, MD, MSc, MBA, surgical director of the structural heart program at Mount Sinai Health System, and associate professor of cardiovascular surgery, Mount Sinai Medical Center, New York.
Likewise, a specific positioning of the commissural post at deployment appeared to improve alignment and reduce coronary overlap when using the ACURATE-neo (Boston Scientific), though results with this transcatheter heart valve need to be considered preliminary because of the smaller number of cases, Dr. Tang said in an interview.
By contrast, initial deployment orientation of the SAPIEN 3 (Edwards Lifesciences) did not seem to have an impact on final orientation or neocommissural overlap with arteries in this study by Dr. Tang and colleagues, which was published in JACC: Cardiovascular Interventions and had been planned for presentation at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
Improved positioning may have important future implications for patients undergoing transcatheter aortic valve replacement (TAVR), particularly if they are younger and therefore perhaps more likely than older patients to undergo a procedure requiring coronary access at some point in the future, according to Dr. Tang.
“Right now, device design does not permit us to have consistent commissural alignment,” said Dr. Tang in the interview. “What this study shows is that, with modification of delivery catheter insertion technique, at least for the EVOLUT valve, we can improve commissural alignment and hypothetically speaking, improve the likelihood of coronary access.”
While the technique modifications described by Dr. Tang and colleagues are commendable, the overall impact on commissural alignment and coronary overlap are “modest” and do not solve the problem, according to Hasan Jilaihawi, MD, associate professor of medicine and cardiothoracic surgery at NYU Langone Health, New York.
Instead, the onus should be on the device manufacturers to develop solutions that allow for better alignment between their devices and patients’ commissures, said Dr. Jilaihawi.
“We need really industry to focus wholeheartedly on this,” Dr. Jilaihawi said in an interview. “I think they will, and there will be some discussions about focusing on [commissural alignment], but I think it’s coming really very late.”
Dr. Tang agreed on the need for increased focus on achieving commissural alignment. Of note, he said, there are newer transcatheter heart valves under study that may be more likely to achieve alignment and reduce the possibility of severe coronary overlap, including the JenaValve (JenaValve Technology) and the J-Valve (JC Medical).
“We hope that manufacturers can design valves that would improve commissural alignment for these patients, so that in 10 or even 20 years’ time, when these patients require reintervention, we won’t have to do surgery because the valves are not aligned,” said Dr. Tang. “Ideally, we might have to do one surgical intervention in their lifetime, but really what we are talking about now is the lifetime management of these patients as the coronary artery disease progresses, and also the aortic valve disease returns with the prosthetic valve.”
The pilot imaging study by Dr. Tang and colleagues included a total of 828 patients undergoing TAVR, including 483 treated with SAPIEN 3, 245 with Evolut, and 100 with ACURATE-neo.
To track deployment orientation, the SAPIEN 3 cases had a commissure crimped at 3, 6, 9, or 12 o’clock orientation relative to the delivery catheter. However, crimping orientation at initial deployment did not appear to have an impact on the final orientation, with overall incidence of severe coronary overlap of 36.6% for the left main coronary artery (LMCA), 23.6% for the right coronary artery (RCA), and 51.3% for one or both, according to the report.
For 107 cases treated with Evolut, the investigators sought to have a marker on the device (known as the “hat” marker) oriented to the outer curve of the descending aorta; to do that, they inserted the delivery catheter with the flush port at the 3 o’clock position. Those cases with the hat marker at the outer curve or the center front had improved commissural alignment as compared to those with the hat at the inner curve or center back, according to investigators. The incidence of coronary overlap with the LMCA was 15.7% for those with the hat at the outer curve or center front, compared to 66.0% for those with the hat at the inner curve or center back (P < .001), and the differences in coronary overlap were likewise significantly different in favor of the outer curve/center front for the RCA or both coronaries.
Finally, the incidence of coronary overlap with the ACURATE-neo was much lower when the commissural post at initial deployment was at the center back or inner curve, and in a few cases where the operators tried to torque the delivery catheter to position the commissural post to the inner curve, commissural alignment was achieved in about three-quarters of the patients (five of seven cases).
This is believed to be the first study to systematically characterize how the initial orientation of different transcatheter heart valves impact commissural alignment and coronary overlap, according to Dr. Tang and coinvestigators.
Dr. Jilaihawi, who was not involved in the study, said the investigators studied this phenomenon in a “very detailed, methodical fashion,” but emphasized the need for new device innovations to improve alignment and overlap.
“Their efforts weren’t completely in vain, but they really made a small difference in something that is too important to be [addressed] in a kind of ‘MacGyver’ approach to this problem,” he said in the interview.
Disclosures reported by Dr. Tang were related to Edwards Lifesciences (physician proctor) and Medtronic (physician proctor, consultant). Coauthors reported disclosures related to Edwards, Medtronic, and Boston Scientific, among others.
SOURCE: ACC 20. Tang GHL et al. JACC Cardiovasc Interv. 2020 Mar 16. doi: 10.1016/j.jcin.2020.02.005.
For patients undergoing transcatheter aortic valve replacement, using a specific orientation at deployment may optimize valve alignment and potentially preserve coronary access, at least for some devices, results of a pilot imaging study suggest.
In particular, positioning the Evolut THV (Medtronic) at a certain way at deployment led to an improvement in commissural alignment and a significant reduction in coronary artery overlap, according to authors of the study, led by Gilbert H. L. Tang, MD, MSc, MBA, surgical director of the structural heart program at Mount Sinai Health System, and associate professor of cardiovascular surgery, Mount Sinai Medical Center, New York.
Likewise, a specific positioning of the commissural post at deployment appeared to improve alignment and reduce coronary overlap when using the ACURATE-neo (Boston Scientific), though results with this transcatheter heart valve need to be considered preliminary because of the smaller number of cases, Dr. Tang said in an interview.
By contrast, initial deployment orientation of the SAPIEN 3 (Edwards Lifesciences) did not seem to have an impact on final orientation or neocommissural overlap with arteries in this study by Dr. Tang and colleagues, which was published in JACC: Cardiovascular Interventions and had been planned for presentation at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
Improved positioning may have important future implications for patients undergoing transcatheter aortic valve replacement (TAVR), particularly if they are younger and therefore perhaps more likely than older patients to undergo a procedure requiring coronary access at some point in the future, according to Dr. Tang.
“Right now, device design does not permit us to have consistent commissural alignment,” said Dr. Tang in the interview. “What this study shows is that, with modification of delivery catheter insertion technique, at least for the EVOLUT valve, we can improve commissural alignment and hypothetically speaking, improve the likelihood of coronary access.”
While the technique modifications described by Dr. Tang and colleagues are commendable, the overall impact on commissural alignment and coronary overlap are “modest” and do not solve the problem, according to Hasan Jilaihawi, MD, associate professor of medicine and cardiothoracic surgery at NYU Langone Health, New York.
Instead, the onus should be on the device manufacturers to develop solutions that allow for better alignment between their devices and patients’ commissures, said Dr. Jilaihawi.
“We need really industry to focus wholeheartedly on this,” Dr. Jilaihawi said in an interview. “I think they will, and there will be some discussions about focusing on [commissural alignment], but I think it’s coming really very late.”
Dr. Tang agreed on the need for increased focus on achieving commissural alignment. Of note, he said, there are newer transcatheter heart valves under study that may be more likely to achieve alignment and reduce the possibility of severe coronary overlap, including the JenaValve (JenaValve Technology) and the J-Valve (JC Medical).
“We hope that manufacturers can design valves that would improve commissural alignment for these patients, so that in 10 or even 20 years’ time, when these patients require reintervention, we won’t have to do surgery because the valves are not aligned,” said Dr. Tang. “Ideally, we might have to do one surgical intervention in their lifetime, but really what we are talking about now is the lifetime management of these patients as the coronary artery disease progresses, and also the aortic valve disease returns with the prosthetic valve.”
The pilot imaging study by Dr. Tang and colleagues included a total of 828 patients undergoing TAVR, including 483 treated with SAPIEN 3, 245 with Evolut, and 100 with ACURATE-neo.
To track deployment orientation, the SAPIEN 3 cases had a commissure crimped at 3, 6, 9, or 12 o’clock orientation relative to the delivery catheter. However, crimping orientation at initial deployment did not appear to have an impact on the final orientation, with overall incidence of severe coronary overlap of 36.6% for the left main coronary artery (LMCA), 23.6% for the right coronary artery (RCA), and 51.3% for one or both, according to the report.
For 107 cases treated with Evolut, the investigators sought to have a marker on the device (known as the “hat” marker) oriented to the outer curve of the descending aorta; to do that, they inserted the delivery catheter with the flush port at the 3 o’clock position. Those cases with the hat marker at the outer curve or the center front had improved commissural alignment as compared to those with the hat at the inner curve or center back, according to investigators. The incidence of coronary overlap with the LMCA was 15.7% for those with the hat at the outer curve or center front, compared to 66.0% for those with the hat at the inner curve or center back (P < .001), and the differences in coronary overlap were likewise significantly different in favor of the outer curve/center front for the RCA or both coronaries.
Finally, the incidence of coronary overlap with the ACURATE-neo was much lower when the commissural post at initial deployment was at the center back or inner curve, and in a few cases where the operators tried to torque the delivery catheter to position the commissural post to the inner curve, commissural alignment was achieved in about three-quarters of the patients (five of seven cases).
This is believed to be the first study to systematically characterize how the initial orientation of different transcatheter heart valves impact commissural alignment and coronary overlap, according to Dr. Tang and coinvestigators.
Dr. Jilaihawi, who was not involved in the study, said the investigators studied this phenomenon in a “very detailed, methodical fashion,” but emphasized the need for new device innovations to improve alignment and overlap.
“Their efforts weren’t completely in vain, but they really made a small difference in something that is too important to be [addressed] in a kind of ‘MacGyver’ approach to this problem,” he said in the interview.
Disclosures reported by Dr. Tang were related to Edwards Lifesciences (physician proctor) and Medtronic (physician proctor, consultant). Coauthors reported disclosures related to Edwards, Medtronic, and Boston Scientific, among others.
SOURCE: ACC 20. Tang GHL et al. JACC Cardiovasc Interv. 2020 Mar 16. doi: 10.1016/j.jcin.2020.02.005.
For patients undergoing transcatheter aortic valve replacement, using a specific orientation at deployment may optimize valve alignment and potentially preserve coronary access, at least for some devices, results of a pilot imaging study suggest.
In particular, positioning the Evolut THV (Medtronic) at a certain way at deployment led to an improvement in commissural alignment and a significant reduction in coronary artery overlap, according to authors of the study, led by Gilbert H. L. Tang, MD, MSc, MBA, surgical director of the structural heart program at Mount Sinai Health System, and associate professor of cardiovascular surgery, Mount Sinai Medical Center, New York.
Likewise, a specific positioning of the commissural post at deployment appeared to improve alignment and reduce coronary overlap when using the ACURATE-neo (Boston Scientific), though results with this transcatheter heart valve need to be considered preliminary because of the smaller number of cases, Dr. Tang said in an interview.
By contrast, initial deployment orientation of the SAPIEN 3 (Edwards Lifesciences) did not seem to have an impact on final orientation or neocommissural overlap with arteries in this study by Dr. Tang and colleagues, which was published in JACC: Cardiovascular Interventions and had been planned for presentation at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
Improved positioning may have important future implications for patients undergoing transcatheter aortic valve replacement (TAVR), particularly if they are younger and therefore perhaps more likely than older patients to undergo a procedure requiring coronary access at some point in the future, according to Dr. Tang.
“Right now, device design does not permit us to have consistent commissural alignment,” said Dr. Tang in the interview. “What this study shows is that, with modification of delivery catheter insertion technique, at least for the EVOLUT valve, we can improve commissural alignment and hypothetically speaking, improve the likelihood of coronary access.”
While the technique modifications described by Dr. Tang and colleagues are commendable, the overall impact on commissural alignment and coronary overlap are “modest” and do not solve the problem, according to Hasan Jilaihawi, MD, associate professor of medicine and cardiothoracic surgery at NYU Langone Health, New York.
Instead, the onus should be on the device manufacturers to develop solutions that allow for better alignment between their devices and patients’ commissures, said Dr. Jilaihawi.
“We need really industry to focus wholeheartedly on this,” Dr. Jilaihawi said in an interview. “I think they will, and there will be some discussions about focusing on [commissural alignment], but I think it’s coming really very late.”
Dr. Tang agreed on the need for increased focus on achieving commissural alignment. Of note, he said, there are newer transcatheter heart valves under study that may be more likely to achieve alignment and reduce the possibility of severe coronary overlap, including the JenaValve (JenaValve Technology) and the J-Valve (JC Medical).
“We hope that manufacturers can design valves that would improve commissural alignment for these patients, so that in 10 or even 20 years’ time, when these patients require reintervention, we won’t have to do surgery because the valves are not aligned,” said Dr. Tang. “Ideally, we might have to do one surgical intervention in their lifetime, but really what we are talking about now is the lifetime management of these patients as the coronary artery disease progresses, and also the aortic valve disease returns with the prosthetic valve.”
The pilot imaging study by Dr. Tang and colleagues included a total of 828 patients undergoing TAVR, including 483 treated with SAPIEN 3, 245 with Evolut, and 100 with ACURATE-neo.
To track deployment orientation, the SAPIEN 3 cases had a commissure crimped at 3, 6, 9, or 12 o’clock orientation relative to the delivery catheter. However, crimping orientation at initial deployment did not appear to have an impact on the final orientation, with overall incidence of severe coronary overlap of 36.6% for the left main coronary artery (LMCA), 23.6% for the right coronary artery (RCA), and 51.3% for one or both, according to the report.
For 107 cases treated with Evolut, the investigators sought to have a marker on the device (known as the “hat” marker) oriented to the outer curve of the descending aorta; to do that, they inserted the delivery catheter with the flush port at the 3 o’clock position. Those cases with the hat marker at the outer curve or the center front had improved commissural alignment as compared to those with the hat at the inner curve or center back, according to investigators. The incidence of coronary overlap with the LMCA was 15.7% for those with the hat at the outer curve or center front, compared to 66.0% for those with the hat at the inner curve or center back (P < .001), and the differences in coronary overlap were likewise significantly different in favor of the outer curve/center front for the RCA or both coronaries.
Finally, the incidence of coronary overlap with the ACURATE-neo was much lower when the commissural post at initial deployment was at the center back or inner curve, and in a few cases where the operators tried to torque the delivery catheter to position the commissural post to the inner curve, commissural alignment was achieved in about three-quarters of the patients (five of seven cases).
This is believed to be the first study to systematically characterize how the initial orientation of different transcatheter heart valves impact commissural alignment and coronary overlap, according to Dr. Tang and coinvestigators.
Dr. Jilaihawi, who was not involved in the study, said the investigators studied this phenomenon in a “very detailed, methodical fashion,” but emphasized the need for new device innovations to improve alignment and overlap.
“Their efforts weren’t completely in vain, but they really made a small difference in something that is too important to be [addressed] in a kind of ‘MacGyver’ approach to this problem,” he said in the interview.
Disclosures reported by Dr. Tang were related to Edwards Lifesciences (physician proctor) and Medtronic (physician proctor, consultant). Coauthors reported disclosures related to Edwards, Medtronic, and Boston Scientific, among others.
SOURCE: ACC 20. Tang GHL et al. JACC Cardiovasc Interv. 2020 Mar 16. doi: 10.1016/j.jcin.2020.02.005.
REPORTING FROM ACC 20
Coronavirus stays in aerosols for hours, on surfaces for days
according to a new study.
The data indicate that the stability of the new virus is similar to that of SARS-CoV-1, which caused the SARS epidemic, researchers report in an article published on the medRxivpreprint server. (The posted article has been submitted for journal publication but has not been peer reviewed.)
Transmission of SARS-CoV-2, which causes COVID-19, has quickly outstripped the pace of the 2003 SARS epidemic. “Superspread” of the earlier disease arose from infection during medical procedures, in which a single infected individual seeded many secondary cases. In contrast, the novel coronavirus appears to be spread more through human-to-human transmission in a variety of settings.
However, it’s not yet known the extent to which asymptomatic or presymptomatic individuals spread the new virus through daily routine.
To investigate how long SARS-CoV-2 remains infective in the environment, Neeltje van Doremalen, PhD, of the Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, in Hamilton, Montana, and colleagues conducted simulation experiments in which they compared the viability of SARS-CoV-2 with that of SARS-CoV-1 in aerosols and on surfaces.
Among patients infected with SARS-CoV-2, viral loads in the upper respiratory tract are high; as a consequence, respiratory secretion in the form of aerosols (<5 μm) or droplets (>5 mcm) is likely, the authors note.
van Doremalen and colleagues used nebulizers to generate aerosols. Samples of SARS-CoV-1 and SARS-CoV-2 were collecting at 0, 30, 60, 120, and 180 minutes on a gelatin filter. The researchers then tested the infectivity of the viruses on Vero cells grown in culture.
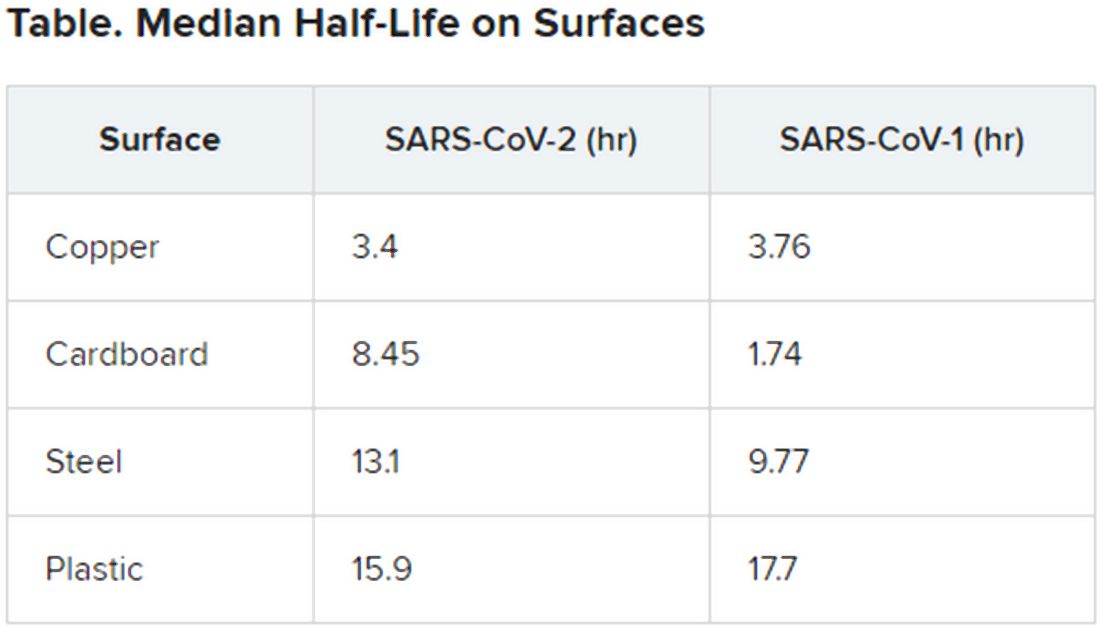
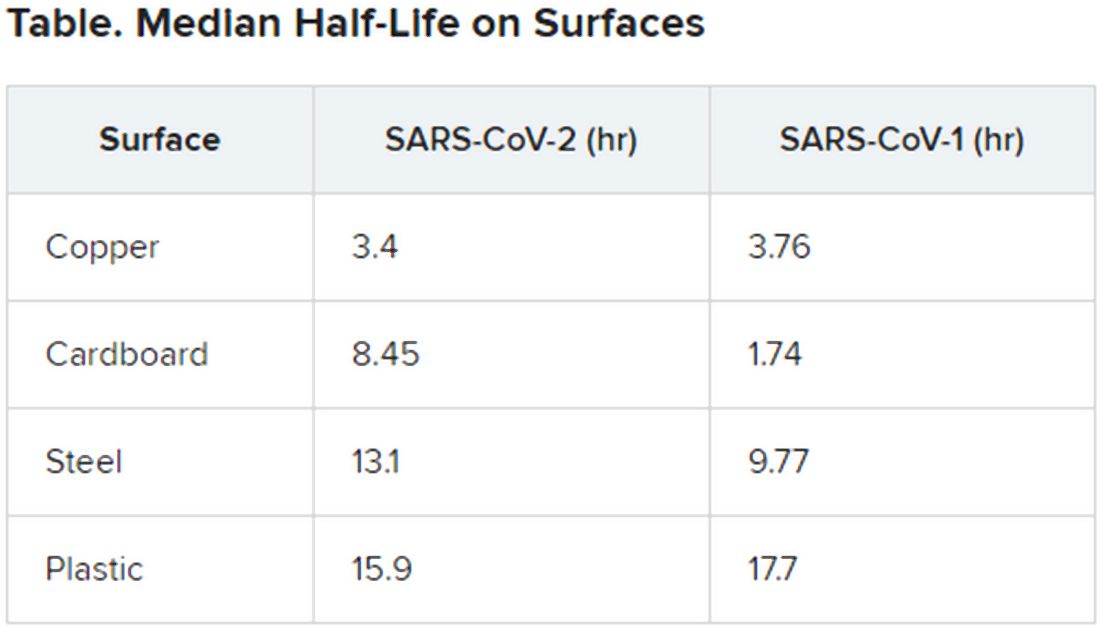
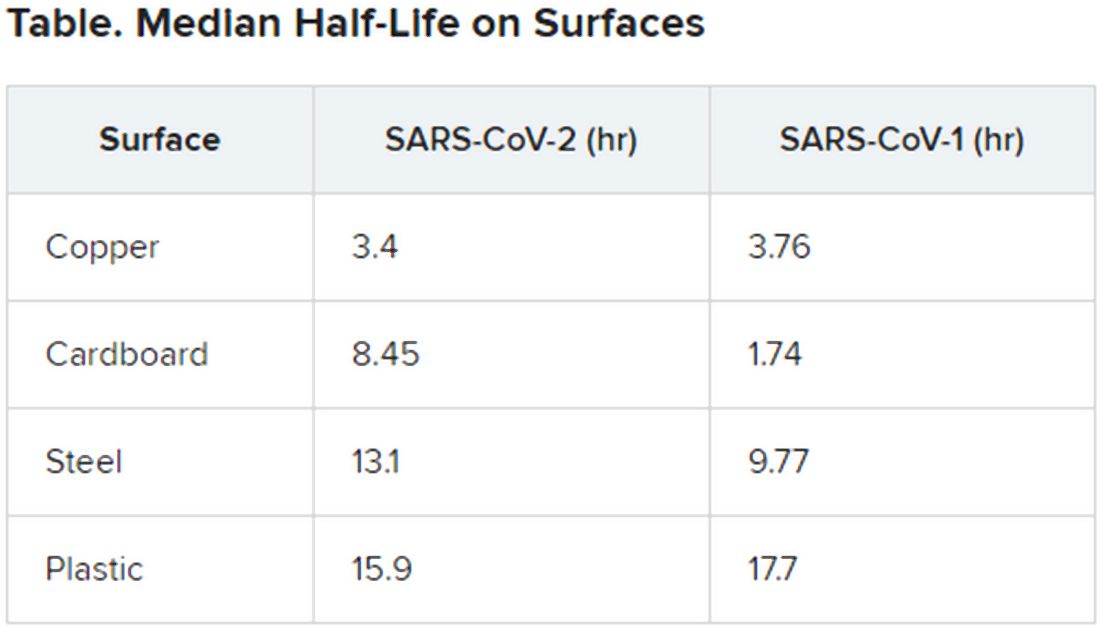
They found that SARS-CoV-2 was largely stable through the full 180-minute test, with only a slight decline at 3 hours. This time course is similar to that of SARS-CoV-1; both viruses have a median half-life in aerosols of 2.7 hours (range, 1.65 hr for SARS-CoV-1, vs 7.24 hr for SARS-CoV-2).
The researchers then tested the viruses on a variety of surfaces for up to 7 days, using humidity values and temperatures designed to mimic “a variety of household and hospital situations.” The volumes of viral exposures that the team used were consistent with amounts found in the human upper and lower respiratory tracts.
For example, they applied 50 mcL of virus-containing solution to a piece of cardboard and then swabbed the surface, at different times, with an additional 1 mcL of medium. Each surface assay was replicated three times.
The novel coronavirus was most stable on plastic and stainless steel, with some virus remaining viable up to 72 hours. However, by that time the viral load had fallen by about three orders of magnitude, indicating exponential decay. This profile was remarkably similar to that of SARS-CoV-1, according to the authors.
However, the two viruses differed in staying power on copper and cardboard. No viable SARS-CoV-2 was detectable on copper after 4 hours or on cardboard after 24 hours. In contrast, SARS-CoV-1 was not viable beyond 8 hours for either copper or cardboard.
“Taken together, our results indicate that aerosol and fomite transmission of HCoV-19 [SARS-CoV-2] are plausible, as the virus can remain viable in aerosols for multiple hours and on surfaces up to days,” the authors conclude.
Andrew Pekosz, PhD, codirector of the Center of Excellence in Influenza Research and Surveillance and director of the Center for Emerging Viruses and Infectious Diseases at the Johns Hopkins Center for Global Health, Baltimore, Maryland, applauds the real-world value of the experiments.
“The PCR [polymerase chain reaction] test used [in other studies] to detect SARS-CoV-2 just detects the virus genome. It doesn’t tell you if the virus was still infectious, or ‘viable.’ That’s why this study is interesting,” Pekosz said. “It focuses on infectious virus, which is the virus that has the potential to transmit and infect another person. What we don’t know yet is how much infectious (viable) virus is needed to initiate infection in another person.”
He suggests that further investigations evaluate other types of environmental surfaces, including lacquered wood that is made into desks and ceramic tiles found in bathrooms and kitchens.
One limitation of the study is that the data for experiments on cardboard were more variable than the data for other surfaces tested.
The investigators and Pekosz have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
according to a new study.
The data indicate that the stability of the new virus is similar to that of SARS-CoV-1, which caused the SARS epidemic, researchers report in an article published on the medRxivpreprint server. (The posted article has been submitted for journal publication but has not been peer reviewed.)
Transmission of SARS-CoV-2, which causes COVID-19, has quickly outstripped the pace of the 2003 SARS epidemic. “Superspread” of the earlier disease arose from infection during medical procedures, in which a single infected individual seeded many secondary cases. In contrast, the novel coronavirus appears to be spread more through human-to-human transmission in a variety of settings.
However, it’s not yet known the extent to which asymptomatic or presymptomatic individuals spread the new virus through daily routine.
To investigate how long SARS-CoV-2 remains infective in the environment, Neeltje van Doremalen, PhD, of the Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, in Hamilton, Montana, and colleagues conducted simulation experiments in which they compared the viability of SARS-CoV-2 with that of SARS-CoV-1 in aerosols and on surfaces.
Among patients infected with SARS-CoV-2, viral loads in the upper respiratory tract are high; as a consequence, respiratory secretion in the form of aerosols (<5 μm) or droplets (>5 mcm) is likely, the authors note.
van Doremalen and colleagues used nebulizers to generate aerosols. Samples of SARS-CoV-1 and SARS-CoV-2 were collecting at 0, 30, 60, 120, and 180 minutes on a gelatin filter. The researchers then tested the infectivity of the viruses on Vero cells grown in culture.
They found that SARS-CoV-2 was largely stable through the full 180-minute test, with only a slight decline at 3 hours. This time course is similar to that of SARS-CoV-1; both viruses have a median half-life in aerosols of 2.7 hours (range, 1.65 hr for SARS-CoV-1, vs 7.24 hr for SARS-CoV-2).
The researchers then tested the viruses on a variety of surfaces for up to 7 days, using humidity values and temperatures designed to mimic “a variety of household and hospital situations.” The volumes of viral exposures that the team used were consistent with amounts found in the human upper and lower respiratory tracts.
For example, they applied 50 mcL of virus-containing solution to a piece of cardboard and then swabbed the surface, at different times, with an additional 1 mcL of medium. Each surface assay was replicated three times.
The novel coronavirus was most stable on plastic and stainless steel, with some virus remaining viable up to 72 hours. However, by that time the viral load had fallen by about three orders of magnitude, indicating exponential decay. This profile was remarkably similar to that of SARS-CoV-1, according to the authors.
However, the two viruses differed in staying power on copper and cardboard. No viable SARS-CoV-2 was detectable on copper after 4 hours or on cardboard after 24 hours. In contrast, SARS-CoV-1 was not viable beyond 8 hours for either copper or cardboard.
“Taken together, our results indicate that aerosol and fomite transmission of HCoV-19 [SARS-CoV-2] are plausible, as the virus can remain viable in aerosols for multiple hours and on surfaces up to days,” the authors conclude.
Andrew Pekosz, PhD, codirector of the Center of Excellence in Influenza Research and Surveillance and director of the Center for Emerging Viruses and Infectious Diseases at the Johns Hopkins Center for Global Health, Baltimore, Maryland, applauds the real-world value of the experiments.
“The PCR [polymerase chain reaction] test used [in other studies] to detect SARS-CoV-2 just detects the virus genome. It doesn’t tell you if the virus was still infectious, or ‘viable.’ That’s why this study is interesting,” Pekosz said. “It focuses on infectious virus, which is the virus that has the potential to transmit and infect another person. What we don’t know yet is how much infectious (viable) virus is needed to initiate infection in another person.”
He suggests that further investigations evaluate other types of environmental surfaces, including lacquered wood that is made into desks and ceramic tiles found in bathrooms and kitchens.
One limitation of the study is that the data for experiments on cardboard were more variable than the data for other surfaces tested.
The investigators and Pekosz have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
according to a new study.
The data indicate that the stability of the new virus is similar to that of SARS-CoV-1, which caused the SARS epidemic, researchers report in an article published on the medRxivpreprint server. (The posted article has been submitted for journal publication but has not been peer reviewed.)
Transmission of SARS-CoV-2, which causes COVID-19, has quickly outstripped the pace of the 2003 SARS epidemic. “Superspread” of the earlier disease arose from infection during medical procedures, in which a single infected individual seeded many secondary cases. In contrast, the novel coronavirus appears to be spread more through human-to-human transmission in a variety of settings.
However, it’s not yet known the extent to which asymptomatic or presymptomatic individuals spread the new virus through daily routine.
To investigate how long SARS-CoV-2 remains infective in the environment, Neeltje van Doremalen, PhD, of the Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, in Hamilton, Montana, and colleagues conducted simulation experiments in which they compared the viability of SARS-CoV-2 with that of SARS-CoV-1 in aerosols and on surfaces.
Among patients infected with SARS-CoV-2, viral loads in the upper respiratory tract are high; as a consequence, respiratory secretion in the form of aerosols (<5 μm) or droplets (>5 mcm) is likely, the authors note.
van Doremalen and colleagues used nebulizers to generate aerosols. Samples of SARS-CoV-1 and SARS-CoV-2 were collecting at 0, 30, 60, 120, and 180 minutes on a gelatin filter. The researchers then tested the infectivity of the viruses on Vero cells grown in culture.
They found that SARS-CoV-2 was largely stable through the full 180-minute test, with only a slight decline at 3 hours. This time course is similar to that of SARS-CoV-1; both viruses have a median half-life in aerosols of 2.7 hours (range, 1.65 hr for SARS-CoV-1, vs 7.24 hr for SARS-CoV-2).
The researchers then tested the viruses on a variety of surfaces for up to 7 days, using humidity values and temperatures designed to mimic “a variety of household and hospital situations.” The volumes of viral exposures that the team used were consistent with amounts found in the human upper and lower respiratory tracts.
For example, they applied 50 mcL of virus-containing solution to a piece of cardboard and then swabbed the surface, at different times, with an additional 1 mcL of medium. Each surface assay was replicated three times.
The novel coronavirus was most stable on plastic and stainless steel, with some virus remaining viable up to 72 hours. However, by that time the viral load had fallen by about three orders of magnitude, indicating exponential decay. This profile was remarkably similar to that of SARS-CoV-1, according to the authors.
However, the two viruses differed in staying power on copper and cardboard. No viable SARS-CoV-2 was detectable on copper after 4 hours or on cardboard after 24 hours. In contrast, SARS-CoV-1 was not viable beyond 8 hours for either copper or cardboard.
“Taken together, our results indicate that aerosol and fomite transmission of HCoV-19 [SARS-CoV-2] are plausible, as the virus can remain viable in aerosols for multiple hours and on surfaces up to days,” the authors conclude.
Andrew Pekosz, PhD, codirector of the Center of Excellence in Influenza Research and Surveillance and director of the Center for Emerging Viruses and Infectious Diseases at the Johns Hopkins Center for Global Health, Baltimore, Maryland, applauds the real-world value of the experiments.
“The PCR [polymerase chain reaction] test used [in other studies] to detect SARS-CoV-2 just detects the virus genome. It doesn’t tell you if the virus was still infectious, or ‘viable.’ That’s why this study is interesting,” Pekosz said. “It focuses on infectious virus, which is the virus that has the potential to transmit and infect another person. What we don’t know yet is how much infectious (viable) virus is needed to initiate infection in another person.”
He suggests that further investigations evaluate other types of environmental surfaces, including lacquered wood that is made into desks and ceramic tiles found in bathrooms and kitchens.
One limitation of the study is that the data for experiments on cardboard were more variable than the data for other surfaces tested.
The investigators and Pekosz have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Potential GI manifestation, transmission of coronavirus
The novel coronavirus (2019-nCoV) shows evidence of causing gastrointestinal symptoms and has the potential to be transmitted by the fecal-oral route, according to a new report from physicians at Shanghai Jiao Tong University, published online (Gastroenterology. 2020 March 3. doi: 10.1053/j.gastro.2020.02.054).
The virus’s respiratory symptoms are well documented and suggest primary transmission by droplet or contact, while other symptoms such as diarrhea, nausea, vomiting, and abdominal discomfort are less common and appear to vary between populations. The SARS coronavirus showed up in stool, even sometimes in patients discharged from the hospital. In a study of hospitalized patients in Wuhan, China, 10.1% of coronavirus patients had diarrhea and nausea in the 1-2 days before onset of fever and dyspnea. The first U.S. patient to be diagnosed had a 2-day history of nausea and vomiting, and had a loose bowel movement on the second day in the hospital. Clinicians later confirmed the presence of viral RNA in both the patient’s stool and airway.
The authors say that researchers in China have isolated viral RNA from the stool of two patients (unpublished), and it has been found in saliva, suggesting the possibility of the salivary gland as an infection or transmission route.
The authors maintain that previous studies likely overlooked or neglected patients who had mild intestinal symptoms. “Many efforts should be made to be alert on the initial digestive symptoms of COVID-19 for early detection, early diagnosis, early isolation and early intervention,” the authors wrote.
Like other coronaviruses, it appears that 2019-nCoV infects cells through an interaction between viral transmembrane spike glycoprotein (S-protein) receptor-binding domain, and the cell receptors angiotensin-converting enzyme 2 (ACE-2) and host cellular transmembrane serine protease (TMPRSS). Transcriptome analysis has shown that human lung AT2 cells express ACE-2 and TMPRSS, but esophagus upper and stratified epithelial cells also express both factors, as do stratified epithelial cells and absorptive enterocytes in the ileum and colon.
The researchers call for investigation into ACE-2 fusion proteins and TMPRSS inhibitors for diagnosis, prophylaxis, or treatment of COVID-19.
The authors also noted that COVID-19 has been linked to mild to moderate liver injury as revealed by elevated aminotransferases, hypoproteinemia and prothrombin time prolongation. This also has precedent in that the SARS coronavirus can infect the liver, and biopsies revealed mitoses and apoptosis, along with other abnormalities. SARS-associated hepatitis may be the result of viral hepatitis, immune overreaction, or a secondary effect of antiviral medications or other drugs. Little is known to date about the ability of 2019-nCoV to infect the liver, but single-cell RNA sequencing data from two distinct cohorts showed more ACE-2 expression in cholangiocytes (59.7%) than hepatocytes (2.6%), which indicates that the virus might directly affect intrahepatic bile ducts.
The authors had no sources of funding or financial conflicts.
SOURCE: GU J et al. Gastroenterology. 2020 March 3. doi: 10.1053/j.gastro.2020.02.054.
*This story was updated on 4/10.2020.
The novel coronavirus (2019-nCoV) shows evidence of causing gastrointestinal symptoms and has the potential to be transmitted by the fecal-oral route, according to a new report from physicians at Shanghai Jiao Tong University, published online (Gastroenterology. 2020 March 3. doi: 10.1053/j.gastro.2020.02.054).
The virus’s respiratory symptoms are well documented and suggest primary transmission by droplet or contact, while other symptoms such as diarrhea, nausea, vomiting, and abdominal discomfort are less common and appear to vary between populations. The SARS coronavirus showed up in stool, even sometimes in patients discharged from the hospital. In a study of hospitalized patients in Wuhan, China, 10.1% of coronavirus patients had diarrhea and nausea in the 1-2 days before onset of fever and dyspnea. The first U.S. patient to be diagnosed had a 2-day history of nausea and vomiting, and had a loose bowel movement on the second day in the hospital. Clinicians later confirmed the presence of viral RNA in both the patient’s stool and airway.
The authors say that researchers in China have isolated viral RNA from the stool of two patients (unpublished), and it has been found in saliva, suggesting the possibility of the salivary gland as an infection or transmission route.
The authors maintain that previous studies likely overlooked or neglected patients who had mild intestinal symptoms. “Many efforts should be made to be alert on the initial digestive symptoms of COVID-19 for early detection, early diagnosis, early isolation and early intervention,” the authors wrote.
Like other coronaviruses, it appears that 2019-nCoV infects cells through an interaction between viral transmembrane spike glycoprotein (S-protein) receptor-binding domain, and the cell receptors angiotensin-converting enzyme 2 (ACE-2) and host cellular transmembrane serine protease (TMPRSS). Transcriptome analysis has shown that human lung AT2 cells express ACE-2 and TMPRSS, but esophagus upper and stratified epithelial cells also express both factors, as do stratified epithelial cells and absorptive enterocytes in the ileum and colon.
The researchers call for investigation into ACE-2 fusion proteins and TMPRSS inhibitors for diagnosis, prophylaxis, or treatment of COVID-19.
The authors also noted that COVID-19 has been linked to mild to moderate liver injury as revealed by elevated aminotransferases, hypoproteinemia and prothrombin time prolongation. This also has precedent in that the SARS coronavirus can infect the liver, and biopsies revealed mitoses and apoptosis, along with other abnormalities. SARS-associated hepatitis may be the result of viral hepatitis, immune overreaction, or a secondary effect of antiviral medications or other drugs. Little is known to date about the ability of 2019-nCoV to infect the liver, but single-cell RNA sequencing data from two distinct cohorts showed more ACE-2 expression in cholangiocytes (59.7%) than hepatocytes (2.6%), which indicates that the virus might directly affect intrahepatic bile ducts.
The authors had no sources of funding or financial conflicts.
SOURCE: GU J et al. Gastroenterology. 2020 March 3. doi: 10.1053/j.gastro.2020.02.054.
*This story was updated on 4/10.2020.
The novel coronavirus (2019-nCoV) shows evidence of causing gastrointestinal symptoms and has the potential to be transmitted by the fecal-oral route, according to a new report from physicians at Shanghai Jiao Tong University, published online (Gastroenterology. 2020 March 3. doi: 10.1053/j.gastro.2020.02.054).
The virus’s respiratory symptoms are well documented and suggest primary transmission by droplet or contact, while other symptoms such as diarrhea, nausea, vomiting, and abdominal discomfort are less common and appear to vary between populations. The SARS coronavirus showed up in stool, even sometimes in patients discharged from the hospital. In a study of hospitalized patients in Wuhan, China, 10.1% of coronavirus patients had diarrhea and nausea in the 1-2 days before onset of fever and dyspnea. The first U.S. patient to be diagnosed had a 2-day history of nausea and vomiting, and had a loose bowel movement on the second day in the hospital. Clinicians later confirmed the presence of viral RNA in both the patient’s stool and airway.
The authors say that researchers in China have isolated viral RNA from the stool of two patients (unpublished), and it has been found in saliva, suggesting the possibility of the salivary gland as an infection or transmission route.
The authors maintain that previous studies likely overlooked or neglected patients who had mild intestinal symptoms. “Many efforts should be made to be alert on the initial digestive symptoms of COVID-19 for early detection, early diagnosis, early isolation and early intervention,” the authors wrote.
Like other coronaviruses, it appears that 2019-nCoV infects cells through an interaction between viral transmembrane spike glycoprotein (S-protein) receptor-binding domain, and the cell receptors angiotensin-converting enzyme 2 (ACE-2) and host cellular transmembrane serine protease (TMPRSS). Transcriptome analysis has shown that human lung AT2 cells express ACE-2 and TMPRSS, but esophagus upper and stratified epithelial cells also express both factors, as do stratified epithelial cells and absorptive enterocytes in the ileum and colon.
The researchers call for investigation into ACE-2 fusion proteins and TMPRSS inhibitors for diagnosis, prophylaxis, or treatment of COVID-19.
The authors also noted that COVID-19 has been linked to mild to moderate liver injury as revealed by elevated aminotransferases, hypoproteinemia and prothrombin time prolongation. This also has precedent in that the SARS coronavirus can infect the liver, and biopsies revealed mitoses and apoptosis, along with other abnormalities. SARS-associated hepatitis may be the result of viral hepatitis, immune overreaction, or a secondary effect of antiviral medications or other drugs. Little is known to date about the ability of 2019-nCoV to infect the liver, but single-cell RNA sequencing data from two distinct cohorts showed more ACE-2 expression in cholangiocytes (59.7%) than hepatocytes (2.6%), which indicates that the virus might directly affect intrahepatic bile ducts.
The authors had no sources of funding or financial conflicts.
SOURCE: GU J et al. Gastroenterology. 2020 March 3. doi: 10.1053/j.gastro.2020.02.054.
*This story was updated on 4/10.2020.
FROM GASTROENTEROLOGY
ICH survival lags in the community setting
LOS ANGELES – Although recent findings from circumscribed patient populations enrolled in intervention studies have shown improved survival rates in patients with a recent intracerebral hemorrhagic stroke, data from a large, observational study in the Netherlands suggested a much darker real-world picture, with a 6-month mortality of 64% identified in a total cohort of nearly 15,000 people followed prospectively starting in 1990.
In striking contrast to the survival pattern over time of patients in the same Dutch study who had a first acute ischemic stroke, which showed a statistically significant and meaningful cut in mortality for ischemic stroke patients during the 25-year period examined, survival rates for patients during the first months following a first intracerebral hemorrhage (ICH) stayed flat during 1991-2015, Reem Waziry, MD, said at the International Stroke Conference sponsored by the American Heart Association.
“The promising treatment advances [applied to patients] in the recent ICH trials may not be reflected in community-based treatment,” suggested Dr. Waziry, a research and teaching fellow in clinical epidemiology at the Harvard School of Public Health in Boston.
The data she reported came from the Rotterdam Study, which followed unselected, older people in the Rotterdam community with no stroke history, and during 25 years of monitoring identified 162 incident ICH strokes and 988 acute ischemic strokes. Concurrently with Dr. Waziry’s talk at the conference, the data she reported were published in Stroke. The data she reported also showed that, during the 25 years studied, mortality at 3 years following a first ICH stroke rose to 73% on average.
During her talk, Dr. Waziry also presented an unpublished comparison of the 64% 6-month mortality in the Rotterdam Study with the 3- to 6-month mortality reported in the control arms of four recent, randomized intervention trials, including the MISTIE III trial. Among the four randomized trials Dr. Waziry selected to make this post-hoc comparison, the study with the highest mortality among control patients was MISTIE III, which showed about 25% mortality after 6 months. In contrast, the 19% 6-month mortality among ischemic stroke patients in the Rotterdam Study was roughly similar to the mortality seem in the control arms of some recent studies of interventions for patients with acute ischemic stroke.
The Rotterdam Study receives no commercial funding. Dr. Waziry had no disclosures.
SOURCE: Waziry R et al. ISC 2020, Abstract LB14.
LOS ANGELES – Although recent findings from circumscribed patient populations enrolled in intervention studies have shown improved survival rates in patients with a recent intracerebral hemorrhagic stroke, data from a large, observational study in the Netherlands suggested a much darker real-world picture, with a 6-month mortality of 64% identified in a total cohort of nearly 15,000 people followed prospectively starting in 1990.
In striking contrast to the survival pattern over time of patients in the same Dutch study who had a first acute ischemic stroke, which showed a statistically significant and meaningful cut in mortality for ischemic stroke patients during the 25-year period examined, survival rates for patients during the first months following a first intracerebral hemorrhage (ICH) stayed flat during 1991-2015, Reem Waziry, MD, said at the International Stroke Conference sponsored by the American Heart Association.
“The promising treatment advances [applied to patients] in the recent ICH trials may not be reflected in community-based treatment,” suggested Dr. Waziry, a research and teaching fellow in clinical epidemiology at the Harvard School of Public Health in Boston.
The data she reported came from the Rotterdam Study, which followed unselected, older people in the Rotterdam community with no stroke history, and during 25 years of monitoring identified 162 incident ICH strokes and 988 acute ischemic strokes. Concurrently with Dr. Waziry’s talk at the conference, the data she reported were published in Stroke. The data she reported also showed that, during the 25 years studied, mortality at 3 years following a first ICH stroke rose to 73% on average.
During her talk, Dr. Waziry also presented an unpublished comparison of the 64% 6-month mortality in the Rotterdam Study with the 3- to 6-month mortality reported in the control arms of four recent, randomized intervention trials, including the MISTIE III trial. Among the four randomized trials Dr. Waziry selected to make this post-hoc comparison, the study with the highest mortality among control patients was MISTIE III, which showed about 25% mortality after 6 months. In contrast, the 19% 6-month mortality among ischemic stroke patients in the Rotterdam Study was roughly similar to the mortality seem in the control arms of some recent studies of interventions for patients with acute ischemic stroke.
The Rotterdam Study receives no commercial funding. Dr. Waziry had no disclosures.
SOURCE: Waziry R et al. ISC 2020, Abstract LB14.
LOS ANGELES – Although recent findings from circumscribed patient populations enrolled in intervention studies have shown improved survival rates in patients with a recent intracerebral hemorrhagic stroke, data from a large, observational study in the Netherlands suggested a much darker real-world picture, with a 6-month mortality of 64% identified in a total cohort of nearly 15,000 people followed prospectively starting in 1990.
In striking contrast to the survival pattern over time of patients in the same Dutch study who had a first acute ischemic stroke, which showed a statistically significant and meaningful cut in mortality for ischemic stroke patients during the 25-year period examined, survival rates for patients during the first months following a first intracerebral hemorrhage (ICH) stayed flat during 1991-2015, Reem Waziry, MD, said at the International Stroke Conference sponsored by the American Heart Association.
“The promising treatment advances [applied to patients] in the recent ICH trials may not be reflected in community-based treatment,” suggested Dr. Waziry, a research and teaching fellow in clinical epidemiology at the Harvard School of Public Health in Boston.
The data she reported came from the Rotterdam Study, which followed unselected, older people in the Rotterdam community with no stroke history, and during 25 years of monitoring identified 162 incident ICH strokes and 988 acute ischemic strokes. Concurrently with Dr. Waziry’s talk at the conference, the data she reported were published in Stroke. The data she reported also showed that, during the 25 years studied, mortality at 3 years following a first ICH stroke rose to 73% on average.
During her talk, Dr. Waziry also presented an unpublished comparison of the 64% 6-month mortality in the Rotterdam Study with the 3- to 6-month mortality reported in the control arms of four recent, randomized intervention trials, including the MISTIE III trial. Among the four randomized trials Dr. Waziry selected to make this post-hoc comparison, the study with the highest mortality among control patients was MISTIE III, which showed about 25% mortality after 6 months. In contrast, the 19% 6-month mortality among ischemic stroke patients in the Rotterdam Study was roughly similar to the mortality seem in the control arms of some recent studies of interventions for patients with acute ischemic stroke.
The Rotterdam Study receives no commercial funding. Dr. Waziry had no disclosures.
SOURCE: Waziry R et al. ISC 2020, Abstract LB14.
REPORTING FROM ISC 2020
Get With the Guidelines – Stroke targets ICH
The Get With the Guidelines – Stroke program is finally turning its attention to hemorrhagic strokes after having spurred improved patient management performance from participating U.S. stroke centers since its start in 2003 with a focus on acute ischemic stroke.
The advisers who craft policy for Get With the Guidelines – Stroke (GWTG–S) are planning to launch a pilot program later in 2020 that will initiate data monitoring and quality improvement aimed at optimizing care for patients following an intracerebral hemorrhage (ICH) starting at 15 U.S. stroke centers, with announcement of these 15 participating centers expected later in 2020. The program will start by targeting nine specific, evidence-based, key aspects of the acute management of ICH patients, said Kevin N. Sheth, MD, professor of neurology and neurosurgery, and chief of neurocritical care and emergency neurology at Yale University in New Haven, Conn, and a volunteer expert who is part of the team developing the ICH initiative.
According to Dr. Sheth, the nine imperatives of acute ICH care that the program plans to monitor at participating centers are:
- Obtain a baseline severity score.
- Identify etiology as spontaneous or treatment related.
- Perform coagulopathy reversal or anticoagulant reversal.
- Administer venous thromboembolism prophylaxis.
- Apply dysphagia screening within 24 hours, and delay oral intake until patient passes dysphagia screen.
- Provide patient management in a multidisciplinary stroke or ICU unit.
- Prescribe appropriate blood pressure treatment at discharge.
- Perform assessment for rehabilitation.
- Avoid prescribing corticosteroids and other contraindicated drugs.
GWTG–S is adopting these metrics for assessing the acute care of ICH patients based largely on the recommendations of an expert 2018 panel organized by the American Heart Association and American Stroke. Association that proposed a set of performance measures for the care of ICH patients. This set of performance measures served as the primary basis for designing the new GWTG–S program, along with considerations of feasibility for collecting data on these measures, Dr. Sheth said in an interview. “We hope to make it easy” for centers to collect the data needed to participate.
The existing GWTG–S program is now 17-years old, and has spread to nearly 2,400 U.S. stroke centers as of early 2020, but the time has come to broaden its reach to patients with ICH and the programs that treat these patients, Dr. Sheth said. After years of nihilism about the prospects for patients following an ICH stroke, survival rates have increased, presenting “an opportunity to optimize care, for quality improvement,” he explained. “It’s a huge shift.” ICH patients “do better than we used to think.”
The Get With the Guidelines – Stroke program is finally turning its attention to hemorrhagic strokes after having spurred improved patient management performance from participating U.S. stroke centers since its start in 2003 with a focus on acute ischemic stroke.
The advisers who craft policy for Get With the Guidelines – Stroke (GWTG–S) are planning to launch a pilot program later in 2020 that will initiate data monitoring and quality improvement aimed at optimizing care for patients following an intracerebral hemorrhage (ICH) starting at 15 U.S. stroke centers, with announcement of these 15 participating centers expected later in 2020. The program will start by targeting nine specific, evidence-based, key aspects of the acute management of ICH patients, said Kevin N. Sheth, MD, professor of neurology and neurosurgery, and chief of neurocritical care and emergency neurology at Yale University in New Haven, Conn, and a volunteer expert who is part of the team developing the ICH initiative.
According to Dr. Sheth, the nine imperatives of acute ICH care that the program plans to monitor at participating centers are:
- Obtain a baseline severity score.
- Identify etiology as spontaneous or treatment related.
- Perform coagulopathy reversal or anticoagulant reversal.
- Administer venous thromboembolism prophylaxis.
- Apply dysphagia screening within 24 hours, and delay oral intake until patient passes dysphagia screen.
- Provide patient management in a multidisciplinary stroke or ICU unit.
- Prescribe appropriate blood pressure treatment at discharge.
- Perform assessment for rehabilitation.
- Avoid prescribing corticosteroids and other contraindicated drugs.
GWTG–S is adopting these metrics for assessing the acute care of ICH patients based largely on the recommendations of an expert 2018 panel organized by the American Heart Association and American Stroke. Association that proposed a set of performance measures for the care of ICH patients. This set of performance measures served as the primary basis for designing the new GWTG–S program, along with considerations of feasibility for collecting data on these measures, Dr. Sheth said in an interview. “We hope to make it easy” for centers to collect the data needed to participate.
The existing GWTG–S program is now 17-years old, and has spread to nearly 2,400 U.S. stroke centers as of early 2020, but the time has come to broaden its reach to patients with ICH and the programs that treat these patients, Dr. Sheth said. After years of nihilism about the prospects for patients following an ICH stroke, survival rates have increased, presenting “an opportunity to optimize care, for quality improvement,” he explained. “It’s a huge shift.” ICH patients “do better than we used to think.”
The Get With the Guidelines – Stroke program is finally turning its attention to hemorrhagic strokes after having spurred improved patient management performance from participating U.S. stroke centers since its start in 2003 with a focus on acute ischemic stroke.
The advisers who craft policy for Get With the Guidelines – Stroke (GWTG–S) are planning to launch a pilot program later in 2020 that will initiate data monitoring and quality improvement aimed at optimizing care for patients following an intracerebral hemorrhage (ICH) starting at 15 U.S. stroke centers, with announcement of these 15 participating centers expected later in 2020. The program will start by targeting nine specific, evidence-based, key aspects of the acute management of ICH patients, said Kevin N. Sheth, MD, professor of neurology and neurosurgery, and chief of neurocritical care and emergency neurology at Yale University in New Haven, Conn, and a volunteer expert who is part of the team developing the ICH initiative.
According to Dr. Sheth, the nine imperatives of acute ICH care that the program plans to monitor at participating centers are:
- Obtain a baseline severity score.
- Identify etiology as spontaneous or treatment related.
- Perform coagulopathy reversal or anticoagulant reversal.
- Administer venous thromboembolism prophylaxis.
- Apply dysphagia screening within 24 hours, and delay oral intake until patient passes dysphagia screen.
- Provide patient management in a multidisciplinary stroke or ICU unit.
- Prescribe appropriate blood pressure treatment at discharge.
- Perform assessment for rehabilitation.
- Avoid prescribing corticosteroids and other contraindicated drugs.
GWTG–S is adopting these metrics for assessing the acute care of ICH patients based largely on the recommendations of an expert 2018 panel organized by the American Heart Association and American Stroke. Association that proposed a set of performance measures for the care of ICH patients. This set of performance measures served as the primary basis for designing the new GWTG–S program, along with considerations of feasibility for collecting data on these measures, Dr. Sheth said in an interview. “We hope to make it easy” for centers to collect the data needed to participate.
The existing GWTG–S program is now 17-years old, and has spread to nearly 2,400 U.S. stroke centers as of early 2020, but the time has come to broaden its reach to patients with ICH and the programs that treat these patients, Dr. Sheth said. After years of nihilism about the prospects for patients following an ICH stroke, survival rates have increased, presenting “an opportunity to optimize care, for quality improvement,” he explained. “It’s a huge shift.” ICH patients “do better than we used to think.”
Recent treatment advances brighten prospects for intracerebral hemorrhage patients
LOS ANGELES – Intracerebral hemorrhage (ICH) appears to be not nearly as uniformly devastating to patients as its reputation suggests. Recent study results documented unexpectedly decent recovery prospects for hemorrhagic stroke patients assessed after 1 year who were earlier considered moderately severe or severely disabled based on their 30-day status. And these data provide further support for the growing impression among clinicians that a way forward for improving outcomes even more is with a “gentle” surgical intervention designed to substantially reduce ICH clot volume.
“Historically, there’s been a lot of nihilism around these patients. Intracerebral hemorrhage has always been the deadliest stroke type, but one of the great advances of the past 10-20 years is that ICH survival has improved. Patients do better than we used to think,” said Kevin N. Sheth, MD, professor of neurology and neurosurgery, and chief of neurocritical care and emergency neurology at Yale University in New Haven, Conn. “Even though ICH remains a difficult disease, this change has two big implications,” Dr. Sheth said in an interview during the International Stroke Conference sponsored by the American Heart Association. First, increased ICH survival offers an opportunity to expand the reach of recent management advances through quality improvement programs that emphasize new strategies that work better and incentivize delivery of these successful strategies to more patients.
The second implication is simply a growing number of ICH survivors, expanding the population of patients who stand to gain from these new management strategies. Dr. Sheth is working with the Get With the Guidelines – Stroke program, a quality-improvement program begun in 2003 and until now aimed at patients with acute ischemic stroke, to develop a 15-site pilot program planned to start in 2020 that will begin implementing and studying a Get With the Guidelines – Stroke quality-improvement program focused on patients with an ICH. The current conception of a quality measurement and improvement program like Get with the Guidelines – Stroke for patients with ICH stems from an important, earlier milestone in the emergence of effective ICH treatments, the 2018 publication of performance measures for ICH care that identified nine key management steps for assessing quality of care and documented the evidence behind them.
“Evidence for optimal treatment of ICH has lagged behind that for ischemic stroke, and consequently, metrics specific to ICH care have not been widely promulgated,” said the authors of the 2018 ICH performance measures, a panel that included Dr. Sheth. “However, numerous more recent studies and clinical trials of various medical and surgical interventions for ICH have been published and form the basis of evidence-based guidelines for the management of ICH,” they explained.
MISTIE III showcases better ICH outcomes
Perhaps the most dramatic recent evidence of brighter prospects for ICH patients came in data collected during the MISTIE III (Minimally Invasive Surgery with Thrombolysis in Intracerebral Hemorrhage Evacuation III) trial, which randomized 506 ICH patients with a hematoma of at least 30 mL to standard care or to a “gentle” clot-reduction protocol using a small-bore catheter placed with stereotactic guidance to both evacuate clot and introduce a serial infusion of alteplase into the clot to try to shrink its volume to less than 15 mL. The study’s results showed a neutral effect for the primary outcome, the incidence of recovery to a modified Rankin Scale (mRS) score of 0-3 at 1 year after entry, which occurred in 45% of the surgically treated patients and 41% of the controls in a modified intention-to-treat analysis that included 499 of the randomized patients, a difference that did not reach statistical significance.
However, when the analysis focused on the 146 of 247 patients (59%) randomized to surgical plus lytic intervention who underwent the procedure and actually had their clot volume reduced to 15 mL or less per protocol, the adjusted incidence of the primary endpoint was double that of patients who underwent the procedure but failed to have their residual clot reduced to this size. A similar doubling of good outcomes occurred when MISTIE patients had their residual clot cut to 20 mL or less, compared with those who didn’t reach this, with the differences in both analyses statistically significant. The actual rates showed patients with clot cut to 15 mL or less having a 53% rate of a mRS score of 0-3 after 1 year, compared with 33% of patients who received the intervention but had their residual clot remain above 15 mL.
The MISTIE III investigators looked at their data to try to get better insight into the outcome of all “poor prognosis” patients in the study regardless of their treatment arm assignment, and how patients and their family members made decisions for withdrawal of life-sustaining therapy. In MISTIE III, 61 patients had withdrawal of life-sustaining treatment (WoLST), with more than 40% of the WoLST occurring with patients randomized to the intervention arm including 10 patients treated to a residual clot volume of 15 mL or less. To quantify the disease severity in these 61 patients, the researchers applied a six-item formula at 30 days after the stroke, a metric their 2019 report described in detail. They then used these severity scores to identify 104 matched patients who were alive at 30 days and remained on life-sustaining treatment to see their 1-year outcomes. At 30 days, the 104 matched patients included 82 (79%) with a mRS score of 5 (severe disability) and 22 patients (21%) with a mRS score of 4 (moderately severe disability). Overall, an mRS score of 4 or 5 was quite prevalent 30 days after the stroke, with 87% of the patients treated with the MISTIE intervention and 90% of the control patients having this degree of disability at 30 days.
When the MISTIE III investigators followed these patients for a year, they made an unexpected finding: A substantial incidence of patients whose condition had improved since day 30. One year out, 40 (39%) of these 104 patients had improved to a mRS score of 1-3, including 10 (10%) with a mRS score of 1 or 2. Another indicator of the reasonable outcome many of these patients achieved was that after 1 year 69% were living at home.
“Our data show that many ICH subjects with clinical factors that suggest ‘poor prognosis,’ when given time, can achieve a favorable outcome and return home,” concluded Noeleen Ostapkovich, who presented these results at the Stroke Conference.
She cited these findings as potentially helpful for refining the information given to patients and families on the prognosis for ICH patients at about 30 days after their event, the usual time for assessment. “These patients looked like they weren’t going to do well after 30 days, but by 365 days they had improved physically and in their ability to care for themselves at home,” noted Ms. Ostapkovich, a researcher in the Brain Injury Outcomes Clinical Trial Coordinating Center of Johns Hopkins University in Baltimore.
A message for acute-care clinicians
She and her colleagues highlighted the implications these new findings have for clinical decision making in the first weeks after an ICH.
“Acute-care physicians see these patients at day 30, not at day 365, so it’s important that they have a clear picture of what these patients could look like a year later. It’s an important message,” Ms. Ostapkovich said in an interview.
In fact, a colleague of hers at Johns Hopkins ran an analysis that looked at factors that contributed to families opting for WoLST for 61 of the MISTIE III patients, and found that 38 family groups (62%) cited the anticipated outcome of the patient in a dependent state as their primary reason for opting for WoLST, Lourdes J. Carhuapoma reported in a separate talk at the conference.
“The main message is that many patients with significant ICH did well and recovered despite having very poor prognostic factors at 30 days, but it took more time. A concern is that the [prognostic] information families receive may be wrong. There is a disconnect,” between what families get told to expect and what actually happens, said Ms. Carhuapoma, an acute care nurse practitioner at Johns Hopkins.
“When physicians, nurses, and family members get together” to discuss ICH patients like these after 30 days, “they see the glass as empty. But the real message is that the glass is half full,” summed up Daniel F. Hanley, MD, lead investigator of MISTIE III and professor of neurology at Johns Hopkins. “These data show a large amount of improvement between 30 and 180 days.” The 104 patients with exclusively mRS scores of 4 or 5 at day 30 had a 30% incidence of improvement to an mRS score of 2 or 3 after 180 days, on their way to a 39% rate of mRS scores of 1-3 at 1 year.
An additional analysis that has not yet been presented showed that the “strongest predictor” of whether or not patients who presented with a mRS score of 4 or 5 after 30 days improved their status at 1 year was if their residual hematoma volume shrank to 15 mL or less, Dr. Hanley said in an interview. “It’s not rocket science. If you had to choose between a 45-mL hematoma and less than 15 mL, which would you choose? What’s new here is how this recovery can play out,” taking 180 days or longer in some patients to become apparent.
More evidence needed to prove MISTIE’s hypothesis
According to Dr. Hanley, the MISTIE III findings have begun to influence practice despite its neutral primary finding, with more attention being paid to reducing residual clot volume following an ICH. And evidence continues to mount that more aggressive minimization of hematoma size can have an important effect on outcomes. For example, another study presented at the conference assessed the incremental change in prognostic accuracy when the ICH score, a five-item formula for estimating the prognosis of an ICH patient, substituted a precise quantification of residual hematoma volume rather than the original, dichotomous entry for either a hematoma volume of 30 mL or greater, or less than 30 mL, and when the severity score also quantified intraventricular hemorrhage (IVH) volume rather than simply designating IVH as present or absent.
Using data from 933 patients who had been enrolled in either MISTIE III or in another study of hematoma volume reduction, CLEAR III, the analysis showed that including specific quantification of both residual ICH volume as well as residual IVH volume improved the area under the receiver operating characteristic curve of the ICH score as a prognostic assessment from 0.70 to 0.75 in the intervention arms of the two trials, and from 0.60 to 0.68 in the two combined control arms, Adam de Havenon, MD, reported in a talk at the conference. “These data show that quantifying ICH and IVH volume improves mortality prognostication,” concluded Dr. de Havenon, a vascular and stroke neurologist at the University of Utah in Salt Lake City.
Furthermore, it’s “certainly evidence for the importance of volume reduction,” he said during discussion of his talk. “The MISTIE procedure can reset patients” so that their outcomes become more like patients with much smaller clot volumes even if they start with large hematomas. “In our experience, if the volume is reduced to 5 mL, there is real benefit regardless of how big the clot was initially,” Dr. de Havenon said.
But the neutral result for the MISTIE III primary endpoint will, for the time being, hobble application of this concept and keep the MISTIE intervention from rising to a level I recommendation until greater evidence for its efficacy comes out.
“It’s been known for many years that clot size matters when it comes to ICH. The MISTIE team has made a very compelling case that [reducing clot volume] is a very reasonable hypothesis, but we must continue to acquire data that can confirm it,” Dr. Sheth commented.
Dr. Sheth’s institution receives research funding from Novartis and Bard for studies that Dr. Sheth helps run. The MISTIE III study received the alteplase used in the study at no cost from Genentech. Ms. Ostapkovich and Ms. Carhuapoma had no disclosures. Dr. Hanley has received personal fees from BrainScope, Medtronic, Neurotrope, Op2Lysis, and Portola. Dr. de Havenon has received research funding from Regeneron.
LOS ANGELES – Intracerebral hemorrhage (ICH) appears to be not nearly as uniformly devastating to patients as its reputation suggests. Recent study results documented unexpectedly decent recovery prospects for hemorrhagic stroke patients assessed after 1 year who were earlier considered moderately severe or severely disabled based on their 30-day status. And these data provide further support for the growing impression among clinicians that a way forward for improving outcomes even more is with a “gentle” surgical intervention designed to substantially reduce ICH clot volume.
“Historically, there’s been a lot of nihilism around these patients. Intracerebral hemorrhage has always been the deadliest stroke type, but one of the great advances of the past 10-20 years is that ICH survival has improved. Patients do better than we used to think,” said Kevin N. Sheth, MD, professor of neurology and neurosurgery, and chief of neurocritical care and emergency neurology at Yale University in New Haven, Conn. “Even though ICH remains a difficult disease, this change has two big implications,” Dr. Sheth said in an interview during the International Stroke Conference sponsored by the American Heart Association. First, increased ICH survival offers an opportunity to expand the reach of recent management advances through quality improvement programs that emphasize new strategies that work better and incentivize delivery of these successful strategies to more patients.
The second implication is simply a growing number of ICH survivors, expanding the population of patients who stand to gain from these new management strategies. Dr. Sheth is working with the Get With the Guidelines – Stroke program, a quality-improvement program begun in 2003 and until now aimed at patients with acute ischemic stroke, to develop a 15-site pilot program planned to start in 2020 that will begin implementing and studying a Get With the Guidelines – Stroke quality-improvement program focused on patients with an ICH. The current conception of a quality measurement and improvement program like Get with the Guidelines – Stroke for patients with ICH stems from an important, earlier milestone in the emergence of effective ICH treatments, the 2018 publication of performance measures for ICH care that identified nine key management steps for assessing quality of care and documented the evidence behind them.
“Evidence for optimal treatment of ICH has lagged behind that for ischemic stroke, and consequently, metrics specific to ICH care have not been widely promulgated,” said the authors of the 2018 ICH performance measures, a panel that included Dr. Sheth. “However, numerous more recent studies and clinical trials of various medical and surgical interventions for ICH have been published and form the basis of evidence-based guidelines for the management of ICH,” they explained.
MISTIE III showcases better ICH outcomes
Perhaps the most dramatic recent evidence of brighter prospects for ICH patients came in data collected during the MISTIE III (Minimally Invasive Surgery with Thrombolysis in Intracerebral Hemorrhage Evacuation III) trial, which randomized 506 ICH patients with a hematoma of at least 30 mL to standard care or to a “gentle” clot-reduction protocol using a small-bore catheter placed with stereotactic guidance to both evacuate clot and introduce a serial infusion of alteplase into the clot to try to shrink its volume to less than 15 mL. The study’s results showed a neutral effect for the primary outcome, the incidence of recovery to a modified Rankin Scale (mRS) score of 0-3 at 1 year after entry, which occurred in 45% of the surgically treated patients and 41% of the controls in a modified intention-to-treat analysis that included 499 of the randomized patients, a difference that did not reach statistical significance.
However, when the analysis focused on the 146 of 247 patients (59%) randomized to surgical plus lytic intervention who underwent the procedure and actually had their clot volume reduced to 15 mL or less per protocol, the adjusted incidence of the primary endpoint was double that of patients who underwent the procedure but failed to have their residual clot reduced to this size. A similar doubling of good outcomes occurred when MISTIE patients had their residual clot cut to 20 mL or less, compared with those who didn’t reach this, with the differences in both analyses statistically significant. The actual rates showed patients with clot cut to 15 mL or less having a 53% rate of a mRS score of 0-3 after 1 year, compared with 33% of patients who received the intervention but had their residual clot remain above 15 mL.
The MISTIE III investigators looked at their data to try to get better insight into the outcome of all “poor prognosis” patients in the study regardless of their treatment arm assignment, and how patients and their family members made decisions for withdrawal of life-sustaining therapy. In MISTIE III, 61 patients had withdrawal of life-sustaining treatment (WoLST), with more than 40% of the WoLST occurring with patients randomized to the intervention arm including 10 patients treated to a residual clot volume of 15 mL or less. To quantify the disease severity in these 61 patients, the researchers applied a six-item formula at 30 days after the stroke, a metric their 2019 report described in detail. They then used these severity scores to identify 104 matched patients who were alive at 30 days and remained on life-sustaining treatment to see their 1-year outcomes. At 30 days, the 104 matched patients included 82 (79%) with a mRS score of 5 (severe disability) and 22 patients (21%) with a mRS score of 4 (moderately severe disability). Overall, an mRS score of 4 or 5 was quite prevalent 30 days after the stroke, with 87% of the patients treated with the MISTIE intervention and 90% of the control patients having this degree of disability at 30 days.
When the MISTIE III investigators followed these patients for a year, they made an unexpected finding: A substantial incidence of patients whose condition had improved since day 30. One year out, 40 (39%) of these 104 patients had improved to a mRS score of 1-3, including 10 (10%) with a mRS score of 1 or 2. Another indicator of the reasonable outcome many of these patients achieved was that after 1 year 69% were living at home.
“Our data show that many ICH subjects with clinical factors that suggest ‘poor prognosis,’ when given time, can achieve a favorable outcome and return home,” concluded Noeleen Ostapkovich, who presented these results at the Stroke Conference.
She cited these findings as potentially helpful for refining the information given to patients and families on the prognosis for ICH patients at about 30 days after their event, the usual time for assessment. “These patients looked like they weren’t going to do well after 30 days, but by 365 days they had improved physically and in their ability to care for themselves at home,” noted Ms. Ostapkovich, a researcher in the Brain Injury Outcomes Clinical Trial Coordinating Center of Johns Hopkins University in Baltimore.
A message for acute-care clinicians
She and her colleagues highlighted the implications these new findings have for clinical decision making in the first weeks after an ICH.
“Acute-care physicians see these patients at day 30, not at day 365, so it’s important that they have a clear picture of what these patients could look like a year later. It’s an important message,” Ms. Ostapkovich said in an interview.
In fact, a colleague of hers at Johns Hopkins ran an analysis that looked at factors that contributed to families opting for WoLST for 61 of the MISTIE III patients, and found that 38 family groups (62%) cited the anticipated outcome of the patient in a dependent state as their primary reason for opting for WoLST, Lourdes J. Carhuapoma reported in a separate talk at the conference.
“The main message is that many patients with significant ICH did well and recovered despite having very poor prognostic factors at 30 days, but it took more time. A concern is that the [prognostic] information families receive may be wrong. There is a disconnect,” between what families get told to expect and what actually happens, said Ms. Carhuapoma, an acute care nurse practitioner at Johns Hopkins.
“When physicians, nurses, and family members get together” to discuss ICH patients like these after 30 days, “they see the glass as empty. But the real message is that the glass is half full,” summed up Daniel F. Hanley, MD, lead investigator of MISTIE III and professor of neurology at Johns Hopkins. “These data show a large amount of improvement between 30 and 180 days.” The 104 patients with exclusively mRS scores of 4 or 5 at day 30 had a 30% incidence of improvement to an mRS score of 2 or 3 after 180 days, on their way to a 39% rate of mRS scores of 1-3 at 1 year.
An additional analysis that has not yet been presented showed that the “strongest predictor” of whether or not patients who presented with a mRS score of 4 or 5 after 30 days improved their status at 1 year was if their residual hematoma volume shrank to 15 mL or less, Dr. Hanley said in an interview. “It’s not rocket science. If you had to choose between a 45-mL hematoma and less than 15 mL, which would you choose? What’s new here is how this recovery can play out,” taking 180 days or longer in some patients to become apparent.
More evidence needed to prove MISTIE’s hypothesis
According to Dr. Hanley, the MISTIE III findings have begun to influence practice despite its neutral primary finding, with more attention being paid to reducing residual clot volume following an ICH. And evidence continues to mount that more aggressive minimization of hematoma size can have an important effect on outcomes. For example, another study presented at the conference assessed the incremental change in prognostic accuracy when the ICH score, a five-item formula for estimating the prognosis of an ICH patient, substituted a precise quantification of residual hematoma volume rather than the original, dichotomous entry for either a hematoma volume of 30 mL or greater, or less than 30 mL, and when the severity score also quantified intraventricular hemorrhage (IVH) volume rather than simply designating IVH as present or absent.
Using data from 933 patients who had been enrolled in either MISTIE III or in another study of hematoma volume reduction, CLEAR III, the analysis showed that including specific quantification of both residual ICH volume as well as residual IVH volume improved the area under the receiver operating characteristic curve of the ICH score as a prognostic assessment from 0.70 to 0.75 in the intervention arms of the two trials, and from 0.60 to 0.68 in the two combined control arms, Adam de Havenon, MD, reported in a talk at the conference. “These data show that quantifying ICH and IVH volume improves mortality prognostication,” concluded Dr. de Havenon, a vascular and stroke neurologist at the University of Utah in Salt Lake City.
Furthermore, it’s “certainly evidence for the importance of volume reduction,” he said during discussion of his talk. “The MISTIE procedure can reset patients” so that their outcomes become more like patients with much smaller clot volumes even if they start with large hematomas. “In our experience, if the volume is reduced to 5 mL, there is real benefit regardless of how big the clot was initially,” Dr. de Havenon said.
But the neutral result for the MISTIE III primary endpoint will, for the time being, hobble application of this concept and keep the MISTIE intervention from rising to a level I recommendation until greater evidence for its efficacy comes out.
“It’s been known for many years that clot size matters when it comes to ICH. The MISTIE team has made a very compelling case that [reducing clot volume] is a very reasonable hypothesis, but we must continue to acquire data that can confirm it,” Dr. Sheth commented.
Dr. Sheth’s institution receives research funding from Novartis and Bard for studies that Dr. Sheth helps run. The MISTIE III study received the alteplase used in the study at no cost from Genentech. Ms. Ostapkovich and Ms. Carhuapoma had no disclosures. Dr. Hanley has received personal fees from BrainScope, Medtronic, Neurotrope, Op2Lysis, and Portola. Dr. de Havenon has received research funding from Regeneron.
LOS ANGELES – Intracerebral hemorrhage (ICH) appears to be not nearly as uniformly devastating to patients as its reputation suggests. Recent study results documented unexpectedly decent recovery prospects for hemorrhagic stroke patients assessed after 1 year who were earlier considered moderately severe or severely disabled based on their 30-day status. And these data provide further support for the growing impression among clinicians that a way forward for improving outcomes even more is with a “gentle” surgical intervention designed to substantially reduce ICH clot volume.
“Historically, there’s been a lot of nihilism around these patients. Intracerebral hemorrhage has always been the deadliest stroke type, but one of the great advances of the past 10-20 years is that ICH survival has improved. Patients do better than we used to think,” said Kevin N. Sheth, MD, professor of neurology and neurosurgery, and chief of neurocritical care and emergency neurology at Yale University in New Haven, Conn. “Even though ICH remains a difficult disease, this change has two big implications,” Dr. Sheth said in an interview during the International Stroke Conference sponsored by the American Heart Association. First, increased ICH survival offers an opportunity to expand the reach of recent management advances through quality improvement programs that emphasize new strategies that work better and incentivize delivery of these successful strategies to more patients.
The second implication is simply a growing number of ICH survivors, expanding the population of patients who stand to gain from these new management strategies. Dr. Sheth is working with the Get With the Guidelines – Stroke program, a quality-improvement program begun in 2003 and until now aimed at patients with acute ischemic stroke, to develop a 15-site pilot program planned to start in 2020 that will begin implementing and studying a Get With the Guidelines – Stroke quality-improvement program focused on patients with an ICH. The current conception of a quality measurement and improvement program like Get with the Guidelines – Stroke for patients with ICH stems from an important, earlier milestone in the emergence of effective ICH treatments, the 2018 publication of performance measures for ICH care that identified nine key management steps for assessing quality of care and documented the evidence behind them.
“Evidence for optimal treatment of ICH has lagged behind that for ischemic stroke, and consequently, metrics specific to ICH care have not been widely promulgated,” said the authors of the 2018 ICH performance measures, a panel that included Dr. Sheth. “However, numerous more recent studies and clinical trials of various medical and surgical interventions for ICH have been published and form the basis of evidence-based guidelines for the management of ICH,” they explained.
MISTIE III showcases better ICH outcomes
Perhaps the most dramatic recent evidence of brighter prospects for ICH patients came in data collected during the MISTIE III (Minimally Invasive Surgery with Thrombolysis in Intracerebral Hemorrhage Evacuation III) trial, which randomized 506 ICH patients with a hematoma of at least 30 mL to standard care or to a “gentle” clot-reduction protocol using a small-bore catheter placed with stereotactic guidance to both evacuate clot and introduce a serial infusion of alteplase into the clot to try to shrink its volume to less than 15 mL. The study’s results showed a neutral effect for the primary outcome, the incidence of recovery to a modified Rankin Scale (mRS) score of 0-3 at 1 year after entry, which occurred in 45% of the surgically treated patients and 41% of the controls in a modified intention-to-treat analysis that included 499 of the randomized patients, a difference that did not reach statistical significance.
However, when the analysis focused on the 146 of 247 patients (59%) randomized to surgical plus lytic intervention who underwent the procedure and actually had their clot volume reduced to 15 mL or less per protocol, the adjusted incidence of the primary endpoint was double that of patients who underwent the procedure but failed to have their residual clot reduced to this size. A similar doubling of good outcomes occurred when MISTIE patients had their residual clot cut to 20 mL or less, compared with those who didn’t reach this, with the differences in both analyses statistically significant. The actual rates showed patients with clot cut to 15 mL or less having a 53% rate of a mRS score of 0-3 after 1 year, compared with 33% of patients who received the intervention but had their residual clot remain above 15 mL.
The MISTIE III investigators looked at their data to try to get better insight into the outcome of all “poor prognosis” patients in the study regardless of their treatment arm assignment, and how patients and their family members made decisions for withdrawal of life-sustaining therapy. In MISTIE III, 61 patients had withdrawal of life-sustaining treatment (WoLST), with more than 40% of the WoLST occurring with patients randomized to the intervention arm including 10 patients treated to a residual clot volume of 15 mL or less. To quantify the disease severity in these 61 patients, the researchers applied a six-item formula at 30 days after the stroke, a metric their 2019 report described in detail. They then used these severity scores to identify 104 matched patients who were alive at 30 days and remained on life-sustaining treatment to see their 1-year outcomes. At 30 days, the 104 matched patients included 82 (79%) with a mRS score of 5 (severe disability) and 22 patients (21%) with a mRS score of 4 (moderately severe disability). Overall, an mRS score of 4 or 5 was quite prevalent 30 days after the stroke, with 87% of the patients treated with the MISTIE intervention and 90% of the control patients having this degree of disability at 30 days.
When the MISTIE III investigators followed these patients for a year, they made an unexpected finding: A substantial incidence of patients whose condition had improved since day 30. One year out, 40 (39%) of these 104 patients had improved to a mRS score of 1-3, including 10 (10%) with a mRS score of 1 or 2. Another indicator of the reasonable outcome many of these patients achieved was that after 1 year 69% were living at home.
“Our data show that many ICH subjects with clinical factors that suggest ‘poor prognosis,’ when given time, can achieve a favorable outcome and return home,” concluded Noeleen Ostapkovich, who presented these results at the Stroke Conference.
She cited these findings as potentially helpful for refining the information given to patients and families on the prognosis for ICH patients at about 30 days after their event, the usual time for assessment. “These patients looked like they weren’t going to do well after 30 days, but by 365 days they had improved physically and in their ability to care for themselves at home,” noted Ms. Ostapkovich, a researcher in the Brain Injury Outcomes Clinical Trial Coordinating Center of Johns Hopkins University in Baltimore.
A message for acute-care clinicians
She and her colleagues highlighted the implications these new findings have for clinical decision making in the first weeks after an ICH.
“Acute-care physicians see these patients at day 30, not at day 365, so it’s important that they have a clear picture of what these patients could look like a year later. It’s an important message,” Ms. Ostapkovich said in an interview.
In fact, a colleague of hers at Johns Hopkins ran an analysis that looked at factors that contributed to families opting for WoLST for 61 of the MISTIE III patients, and found that 38 family groups (62%) cited the anticipated outcome of the patient in a dependent state as their primary reason for opting for WoLST, Lourdes J. Carhuapoma reported in a separate talk at the conference.
“The main message is that many patients with significant ICH did well and recovered despite having very poor prognostic factors at 30 days, but it took more time. A concern is that the [prognostic] information families receive may be wrong. There is a disconnect,” between what families get told to expect and what actually happens, said Ms. Carhuapoma, an acute care nurse practitioner at Johns Hopkins.
“When physicians, nurses, and family members get together” to discuss ICH patients like these after 30 days, “they see the glass as empty. But the real message is that the glass is half full,” summed up Daniel F. Hanley, MD, lead investigator of MISTIE III and professor of neurology at Johns Hopkins. “These data show a large amount of improvement between 30 and 180 days.” The 104 patients with exclusively mRS scores of 4 or 5 at day 30 had a 30% incidence of improvement to an mRS score of 2 or 3 after 180 days, on their way to a 39% rate of mRS scores of 1-3 at 1 year.
An additional analysis that has not yet been presented showed that the “strongest predictor” of whether or not patients who presented with a mRS score of 4 or 5 after 30 days improved their status at 1 year was if their residual hematoma volume shrank to 15 mL or less, Dr. Hanley said in an interview. “It’s not rocket science. If you had to choose between a 45-mL hematoma and less than 15 mL, which would you choose? What’s new here is how this recovery can play out,” taking 180 days or longer in some patients to become apparent.
More evidence needed to prove MISTIE’s hypothesis
According to Dr. Hanley, the MISTIE III findings have begun to influence practice despite its neutral primary finding, with more attention being paid to reducing residual clot volume following an ICH. And evidence continues to mount that more aggressive minimization of hematoma size can have an important effect on outcomes. For example, another study presented at the conference assessed the incremental change in prognostic accuracy when the ICH score, a five-item formula for estimating the prognosis of an ICH patient, substituted a precise quantification of residual hematoma volume rather than the original, dichotomous entry for either a hematoma volume of 30 mL or greater, or less than 30 mL, and when the severity score also quantified intraventricular hemorrhage (IVH) volume rather than simply designating IVH as present or absent.
Using data from 933 patients who had been enrolled in either MISTIE III or in another study of hematoma volume reduction, CLEAR III, the analysis showed that including specific quantification of both residual ICH volume as well as residual IVH volume improved the area under the receiver operating characteristic curve of the ICH score as a prognostic assessment from 0.70 to 0.75 in the intervention arms of the two trials, and from 0.60 to 0.68 in the two combined control arms, Adam de Havenon, MD, reported in a talk at the conference. “These data show that quantifying ICH and IVH volume improves mortality prognostication,” concluded Dr. de Havenon, a vascular and stroke neurologist at the University of Utah in Salt Lake City.
Furthermore, it’s “certainly evidence for the importance of volume reduction,” he said during discussion of his talk. “The MISTIE procedure can reset patients” so that their outcomes become more like patients with much smaller clot volumes even if they start with large hematomas. “In our experience, if the volume is reduced to 5 mL, there is real benefit regardless of how big the clot was initially,” Dr. de Havenon said.
But the neutral result for the MISTIE III primary endpoint will, for the time being, hobble application of this concept and keep the MISTIE intervention from rising to a level I recommendation until greater evidence for its efficacy comes out.
“It’s been known for many years that clot size matters when it comes to ICH. The MISTIE team has made a very compelling case that [reducing clot volume] is a very reasonable hypothesis, but we must continue to acquire data that can confirm it,” Dr. Sheth commented.
Dr. Sheth’s institution receives research funding from Novartis and Bard for studies that Dr. Sheth helps run. The MISTIE III study received the alteplase used in the study at no cost from Genentech. Ms. Ostapkovich and Ms. Carhuapoma had no disclosures. Dr. Hanley has received personal fees from BrainScope, Medtronic, Neurotrope, Op2Lysis, and Portola. Dr. de Havenon has received research funding from Regeneron.
REPORTING FROM ISC 2020
Do urgent care centers use optimal medications for acute migraine?
according to a study published in the March issue of Headache. Pain and nausea or vomiting associated with migraine may go undertreated, and treatment may not be consistent with American Headache Society (AHS) guidelines for EDs, said Mia T. Minen, MD, of the department of neurology and population health at NYU Langone Health in New York and colleagues.
“Our study findings raise the question as to whether the patients with migraine in the urgent care setting should be managed similarly to the ED, and whether the AHS guidelines for the ED should be revisited and applied to urgent care,” the researchers noted.
Relative to the ED, urgent care centers may provide cost savings and emerge “as a preferred place for treatment for people with migraine, perhaps as they are potentially more quiet medical settings where people with migraine might expeditiously receive care,” the authors said.
Dr. Minen and colleagues conducted a retrospective chart review to assess migraine management at two urgent care centers in New York. They examined the number of urgent care visits for migraine, treatments used, and how closely clinicians followed the AHS recommendations for administration of antiemetic medication and triptans, among other outcomes.
The study population included adults diagnosed with migraine at the NYU Langone Medhattan Urgent Care center between Dec. 1, 2015, and Dec. 1, 2018, or at the NYU Langone Ambulatory Care Urgent Care West Side center between May 1, 2017, and Dec. 1, 2018. Of more than 32,000 urgent care visits during the study period, 78 patients received a migraine diagnosis. Patients with migraine had an average age of 32.5 years, and 79.5% were female. More than half had a documented history of migraine. Two of the patients (2.6%) had been to an emergency department for headache or migraine.
Less than half of the patients who presented with pain (46.6%) were given medication, most commonly ketorolac injection. Most patients (78.2%) received prescriptions, and 25.6% received a triptan prescription. About 60% of patients were told to follow up with a neurologist. In addition, 11.5% revisited urgent care with a migraine or headache or to request a prescription refill.
“Patients in this study appeared to be using the urgent care centers specifically for acute care,” the researchers said. “The patients generally had infrequent headaches and the majority would not have qualified for migraine preventive treatment.”
Although AHS guidelines include three “should offer” medications for acute management of migraine in the ED – intravenous metoclopramide, intravenous prochlorperazine, and subcutaneous sumatriptan – two of the medications, subcutaneous sumatriptan and intravenous prochlorperazine, were not available in the urgent care pharmacy. “Of the level B migraine medications, only metoclopramide IV was in the pharmacy, and only 12.3% was given this at their urgent care visit,” the researchers said. “There was also likely undertreatment of nausea/vomiting; despite 39 patients with recorded nausea or vomiting with their migraine, less than half (46.2%) received an antiemetic at the visit,” including metoclopramide or ondansetron through oral or intravenous administration.
Future studies should look at headache and migraine visits at urgent care centers across the United States, the investigators suggested.
One of the authors of the study (Leslie Miller, MD) is the head of the NYU Langone Health Urgent Care Centers. Dr. Minen has received grant support, honoraria, or travel funds from the National Institutes of Health, the American Academy of Neurology, the American Brain Foundation, the National Multiple Sclerosis Society, the National Headache Foundation, the American Headache Society, Barnard College, and NYU. Dr. Minen is associate editor of Headache.
SOURCE: Minen MT et al. Headache. 2020;60(3):542-52.
according to a study published in the March issue of Headache. Pain and nausea or vomiting associated with migraine may go undertreated, and treatment may not be consistent with American Headache Society (AHS) guidelines for EDs, said Mia T. Minen, MD, of the department of neurology and population health at NYU Langone Health in New York and colleagues.
“Our study findings raise the question as to whether the patients with migraine in the urgent care setting should be managed similarly to the ED, and whether the AHS guidelines for the ED should be revisited and applied to urgent care,” the researchers noted.
Relative to the ED, urgent care centers may provide cost savings and emerge “as a preferred place for treatment for people with migraine, perhaps as they are potentially more quiet medical settings where people with migraine might expeditiously receive care,” the authors said.
Dr. Minen and colleagues conducted a retrospective chart review to assess migraine management at two urgent care centers in New York. They examined the number of urgent care visits for migraine, treatments used, and how closely clinicians followed the AHS recommendations for administration of antiemetic medication and triptans, among other outcomes.
The study population included adults diagnosed with migraine at the NYU Langone Medhattan Urgent Care center between Dec. 1, 2015, and Dec. 1, 2018, or at the NYU Langone Ambulatory Care Urgent Care West Side center between May 1, 2017, and Dec. 1, 2018. Of more than 32,000 urgent care visits during the study period, 78 patients received a migraine diagnosis. Patients with migraine had an average age of 32.5 years, and 79.5% were female. More than half had a documented history of migraine. Two of the patients (2.6%) had been to an emergency department for headache or migraine.
Less than half of the patients who presented with pain (46.6%) were given medication, most commonly ketorolac injection. Most patients (78.2%) received prescriptions, and 25.6% received a triptan prescription. About 60% of patients were told to follow up with a neurologist. In addition, 11.5% revisited urgent care with a migraine or headache or to request a prescription refill.
“Patients in this study appeared to be using the urgent care centers specifically for acute care,” the researchers said. “The patients generally had infrequent headaches and the majority would not have qualified for migraine preventive treatment.”
Although AHS guidelines include three “should offer” medications for acute management of migraine in the ED – intravenous metoclopramide, intravenous prochlorperazine, and subcutaneous sumatriptan – two of the medications, subcutaneous sumatriptan and intravenous prochlorperazine, were not available in the urgent care pharmacy. “Of the level B migraine medications, only metoclopramide IV was in the pharmacy, and only 12.3% was given this at their urgent care visit,” the researchers said. “There was also likely undertreatment of nausea/vomiting; despite 39 patients with recorded nausea or vomiting with their migraine, less than half (46.2%) received an antiemetic at the visit,” including metoclopramide or ondansetron through oral or intravenous administration.
Future studies should look at headache and migraine visits at urgent care centers across the United States, the investigators suggested.
One of the authors of the study (Leslie Miller, MD) is the head of the NYU Langone Health Urgent Care Centers. Dr. Minen has received grant support, honoraria, or travel funds from the National Institutes of Health, the American Academy of Neurology, the American Brain Foundation, the National Multiple Sclerosis Society, the National Headache Foundation, the American Headache Society, Barnard College, and NYU. Dr. Minen is associate editor of Headache.
SOURCE: Minen MT et al. Headache. 2020;60(3):542-52.
according to a study published in the March issue of Headache. Pain and nausea or vomiting associated with migraine may go undertreated, and treatment may not be consistent with American Headache Society (AHS) guidelines for EDs, said Mia T. Minen, MD, of the department of neurology and population health at NYU Langone Health in New York and colleagues.
“Our study findings raise the question as to whether the patients with migraine in the urgent care setting should be managed similarly to the ED, and whether the AHS guidelines for the ED should be revisited and applied to urgent care,” the researchers noted.
Relative to the ED, urgent care centers may provide cost savings and emerge “as a preferred place for treatment for people with migraine, perhaps as they are potentially more quiet medical settings where people with migraine might expeditiously receive care,” the authors said.
Dr. Minen and colleagues conducted a retrospective chart review to assess migraine management at two urgent care centers in New York. They examined the number of urgent care visits for migraine, treatments used, and how closely clinicians followed the AHS recommendations for administration of antiemetic medication and triptans, among other outcomes.
The study population included adults diagnosed with migraine at the NYU Langone Medhattan Urgent Care center between Dec. 1, 2015, and Dec. 1, 2018, or at the NYU Langone Ambulatory Care Urgent Care West Side center between May 1, 2017, and Dec. 1, 2018. Of more than 32,000 urgent care visits during the study period, 78 patients received a migraine diagnosis. Patients with migraine had an average age of 32.5 years, and 79.5% were female. More than half had a documented history of migraine. Two of the patients (2.6%) had been to an emergency department for headache or migraine.
Less than half of the patients who presented with pain (46.6%) were given medication, most commonly ketorolac injection. Most patients (78.2%) received prescriptions, and 25.6% received a triptan prescription. About 60% of patients were told to follow up with a neurologist. In addition, 11.5% revisited urgent care with a migraine or headache or to request a prescription refill.
“Patients in this study appeared to be using the urgent care centers specifically for acute care,” the researchers said. “The patients generally had infrequent headaches and the majority would not have qualified for migraine preventive treatment.”
Although AHS guidelines include three “should offer” medications for acute management of migraine in the ED – intravenous metoclopramide, intravenous prochlorperazine, and subcutaneous sumatriptan – two of the medications, subcutaneous sumatriptan and intravenous prochlorperazine, were not available in the urgent care pharmacy. “Of the level B migraine medications, only metoclopramide IV was in the pharmacy, and only 12.3% was given this at their urgent care visit,” the researchers said. “There was also likely undertreatment of nausea/vomiting; despite 39 patients with recorded nausea or vomiting with their migraine, less than half (46.2%) received an antiemetic at the visit,” including metoclopramide or ondansetron through oral or intravenous administration.
Future studies should look at headache and migraine visits at urgent care centers across the United States, the investigators suggested.
One of the authors of the study (Leslie Miller, MD) is the head of the NYU Langone Health Urgent Care Centers. Dr. Minen has received grant support, honoraria, or travel funds from the National Institutes of Health, the American Academy of Neurology, the American Brain Foundation, the National Multiple Sclerosis Society, the National Headache Foundation, the American Headache Society, Barnard College, and NYU. Dr. Minen is associate editor of Headache.
SOURCE: Minen MT et al. Headache. 2020;60(3):542-52.
FROM HEADACHE
ASCO guidelines take global view of late-stage colorectal cancer
Ideally, all cases of colorectal cancer would be detected at an early and curable stage, but, as new guidelines for late-stage colorectal cancer suggest, the world is far from perfect.
“Different regions of the world, both among and within countries, differ with respect to access to early detection,” the guideline authors wrote in JCO Global Oncology. “Many regions do not have mass or even opportunistic screening, and even within regions with mass screening, subpopulations may not have access to screening.”
The guidelines were developed by the American Society of Clinical Oncology’s Resource-Stratified Guidelines Advisory Group. Based on and adapted from existing guidelines developed by four international agencies, the ASCO guidelines take into account economic and social realities and offer recommendations for diagnosis, staging, and treatment by resource level: basic, limited, enhanced, or maximal.
“We made these guidelines to apply to countries or regions that have basic resources,” lead author E. Gabriela Chiorean, MD, of the University of Washington, Seattle, and the Seattle Cancer Care Alliance, said in an interview.
“We decided what should be the most basic resources – diagnostics, imaging, and treatment – that should be available to patients, and we make recommendations for the use of limited resources and supplies,” she added.
The guidelines pose and answer seven questions about optimal initial symptom management, diagnosis, and staging; optimal first and later lines of therapy; liver-directed therapy options for patients with late-stage colorectal cancer and liver metastases; and optimal on-treatment surveillance and follow-up strategies for patients treated for metastatic colorectal cancer.
For each question, the document offers guidance based on the availability of resources. As defined by the authors, the recommendations are stratified according to the following categories:
- Basic resources – “Core resources or fundamental services that are absolutely necessary for any cancer health care system to function.”
- Limited resources – “Second-tier resources or services that are intended to produce major improvements in outcome, such as increased survival and cost effectiveness, and are attainable with limited financial means and modest infrastructure.”
- Enhanced resources – “Third-tier resources or services that are optional but important; enhanced-level resources should produce further improvements in outcome and increase the number and quality of options and patient choice.”
- Maximal resources – “High-level/state-of-the art resources or services that may be used/available in some high-resource regions and/or may be recommended by high-resource setting guidelines that do not adapt to resource constraints but that nonetheless should be considered a lower priority than those resources or services listed in the other categories on the basis of extreme cost and/or impracticality for broad use in a resource-limited environment.”
The guidelines address common elements of symptom management for patients with acute disease, such as diagnosis involving the primary tumor, endoscopy when possible, and staging to include digital rectal exam and/or imaging when possible. The guidelines also include information tailored to resource level about chemotherapy and surgical resection.
“If, for example, a patient presents with bleeding and you suspect it to be of colorectal origin, we make recommendations that if the patient has symptoms of obstruction and bleeding and is resectable, they should undergo surgery, which should be available in countries of all resource levels,” Dr. Chiorean said.
The guidelines also recommend following the ASCO palliative care guidelines (J Clin Oncol. 2017 Jan;35[1]:96-112) for those patients who present with clinically unstable disease because of bowel obstruction, uncontrolled bleeding, or uncontrolled pain. Patients with clinically stable disease and ongoing bleeding from the primary tumor site are recommended to undergo transfusion and primary-site resection if only basic resources are available or transfusion plus multidisciplinary specialized evaluation when higher-level resources are available.
The ASCO guidelines are adapted from guidelines developed by Cancer Council Australia; the European Society for Medical Oncology; the National Institute for Health and Care Excellence, including separate recommendation for therapy combinations (https://www.nice.org.uk/guidance/ta212, https://www.nice.org.uk/guidance/ta439); and the National Comprehensive Cancer Network. Some of these guidelines have been updated since the creation of the ASCO guidelines.
ASCO funds the guideline development process. Dr. Chiorean and other authors disclosed relationships with multiple companies.
SOURCE: Chiorean EG et al. JCO Glob Oncol. 2020 Mar;6:414-38.
Ideally, all cases of colorectal cancer would be detected at an early and curable stage, but, as new guidelines for late-stage colorectal cancer suggest, the world is far from perfect.
“Different regions of the world, both among and within countries, differ with respect to access to early detection,” the guideline authors wrote in JCO Global Oncology. “Many regions do not have mass or even opportunistic screening, and even within regions with mass screening, subpopulations may not have access to screening.”
The guidelines were developed by the American Society of Clinical Oncology’s Resource-Stratified Guidelines Advisory Group. Based on and adapted from existing guidelines developed by four international agencies, the ASCO guidelines take into account economic and social realities and offer recommendations for diagnosis, staging, and treatment by resource level: basic, limited, enhanced, or maximal.
“We made these guidelines to apply to countries or regions that have basic resources,” lead author E. Gabriela Chiorean, MD, of the University of Washington, Seattle, and the Seattle Cancer Care Alliance, said in an interview.
“We decided what should be the most basic resources – diagnostics, imaging, and treatment – that should be available to patients, and we make recommendations for the use of limited resources and supplies,” she added.
The guidelines pose and answer seven questions about optimal initial symptom management, diagnosis, and staging; optimal first and later lines of therapy; liver-directed therapy options for patients with late-stage colorectal cancer and liver metastases; and optimal on-treatment surveillance and follow-up strategies for patients treated for metastatic colorectal cancer.
For each question, the document offers guidance based on the availability of resources. As defined by the authors, the recommendations are stratified according to the following categories:
- Basic resources – “Core resources or fundamental services that are absolutely necessary for any cancer health care system to function.”
- Limited resources – “Second-tier resources or services that are intended to produce major improvements in outcome, such as increased survival and cost effectiveness, and are attainable with limited financial means and modest infrastructure.”
- Enhanced resources – “Third-tier resources or services that are optional but important; enhanced-level resources should produce further improvements in outcome and increase the number and quality of options and patient choice.”
- Maximal resources – “High-level/state-of-the art resources or services that may be used/available in some high-resource regions and/or may be recommended by high-resource setting guidelines that do not adapt to resource constraints but that nonetheless should be considered a lower priority than those resources or services listed in the other categories on the basis of extreme cost and/or impracticality for broad use in a resource-limited environment.”
The guidelines address common elements of symptom management for patients with acute disease, such as diagnosis involving the primary tumor, endoscopy when possible, and staging to include digital rectal exam and/or imaging when possible. The guidelines also include information tailored to resource level about chemotherapy and surgical resection.
“If, for example, a patient presents with bleeding and you suspect it to be of colorectal origin, we make recommendations that if the patient has symptoms of obstruction and bleeding and is resectable, they should undergo surgery, which should be available in countries of all resource levels,” Dr. Chiorean said.
The guidelines also recommend following the ASCO palliative care guidelines (J Clin Oncol. 2017 Jan;35[1]:96-112) for those patients who present with clinically unstable disease because of bowel obstruction, uncontrolled bleeding, or uncontrolled pain. Patients with clinically stable disease and ongoing bleeding from the primary tumor site are recommended to undergo transfusion and primary-site resection if only basic resources are available or transfusion plus multidisciplinary specialized evaluation when higher-level resources are available.
The ASCO guidelines are adapted from guidelines developed by Cancer Council Australia; the European Society for Medical Oncology; the National Institute for Health and Care Excellence, including separate recommendation for therapy combinations (https://www.nice.org.uk/guidance/ta212, https://www.nice.org.uk/guidance/ta439); and the National Comprehensive Cancer Network. Some of these guidelines have been updated since the creation of the ASCO guidelines.
ASCO funds the guideline development process. Dr. Chiorean and other authors disclosed relationships with multiple companies.
SOURCE: Chiorean EG et al. JCO Glob Oncol. 2020 Mar;6:414-38.
Ideally, all cases of colorectal cancer would be detected at an early and curable stage, but, as new guidelines for late-stage colorectal cancer suggest, the world is far from perfect.
“Different regions of the world, both among and within countries, differ with respect to access to early detection,” the guideline authors wrote in JCO Global Oncology. “Many regions do not have mass or even opportunistic screening, and even within regions with mass screening, subpopulations may not have access to screening.”
The guidelines were developed by the American Society of Clinical Oncology’s Resource-Stratified Guidelines Advisory Group. Based on and adapted from existing guidelines developed by four international agencies, the ASCO guidelines take into account economic and social realities and offer recommendations for diagnosis, staging, and treatment by resource level: basic, limited, enhanced, or maximal.
“We made these guidelines to apply to countries or regions that have basic resources,” lead author E. Gabriela Chiorean, MD, of the University of Washington, Seattle, and the Seattle Cancer Care Alliance, said in an interview.
“We decided what should be the most basic resources – diagnostics, imaging, and treatment – that should be available to patients, and we make recommendations for the use of limited resources and supplies,” she added.
The guidelines pose and answer seven questions about optimal initial symptom management, diagnosis, and staging; optimal first and later lines of therapy; liver-directed therapy options for patients with late-stage colorectal cancer and liver metastases; and optimal on-treatment surveillance and follow-up strategies for patients treated for metastatic colorectal cancer.
For each question, the document offers guidance based on the availability of resources. As defined by the authors, the recommendations are stratified according to the following categories:
- Basic resources – “Core resources or fundamental services that are absolutely necessary for any cancer health care system to function.”
- Limited resources – “Second-tier resources or services that are intended to produce major improvements in outcome, such as increased survival and cost effectiveness, and are attainable with limited financial means and modest infrastructure.”
- Enhanced resources – “Third-tier resources or services that are optional but important; enhanced-level resources should produce further improvements in outcome and increase the number and quality of options and patient choice.”
- Maximal resources – “High-level/state-of-the art resources or services that may be used/available in some high-resource regions and/or may be recommended by high-resource setting guidelines that do not adapt to resource constraints but that nonetheless should be considered a lower priority than those resources or services listed in the other categories on the basis of extreme cost and/or impracticality for broad use in a resource-limited environment.”
The guidelines address common elements of symptom management for patients with acute disease, such as diagnosis involving the primary tumor, endoscopy when possible, and staging to include digital rectal exam and/or imaging when possible. The guidelines also include information tailored to resource level about chemotherapy and surgical resection.
“If, for example, a patient presents with bleeding and you suspect it to be of colorectal origin, we make recommendations that if the patient has symptoms of obstruction and bleeding and is resectable, they should undergo surgery, which should be available in countries of all resource levels,” Dr. Chiorean said.
The guidelines also recommend following the ASCO palliative care guidelines (J Clin Oncol. 2017 Jan;35[1]:96-112) for those patients who present with clinically unstable disease because of bowel obstruction, uncontrolled bleeding, or uncontrolled pain. Patients with clinically stable disease and ongoing bleeding from the primary tumor site are recommended to undergo transfusion and primary-site resection if only basic resources are available or transfusion plus multidisciplinary specialized evaluation when higher-level resources are available.
The ASCO guidelines are adapted from guidelines developed by Cancer Council Australia; the European Society for Medical Oncology; the National Institute for Health and Care Excellence, including separate recommendation for therapy combinations (https://www.nice.org.uk/guidance/ta212, https://www.nice.org.uk/guidance/ta439); and the National Comprehensive Cancer Network. Some of these guidelines have been updated since the creation of the ASCO guidelines.
ASCO funds the guideline development process. Dr. Chiorean and other authors disclosed relationships with multiple companies.
SOURCE: Chiorean EG et al. JCO Glob Oncol. 2020 Mar;6:414-38.
FROM JCO GLOBAL ONCOLOGY
Treating COVID-19 in patients with diabetes
Patients with diabetes may be at extra risk for coronavirus disease (COVID-19) mortality, and doctors treating them need to keep up with the latest guidelines and expert advice.
Most health advisories about COVID-19 mention diabetes as one of the high-risk categories for the disease, likely because early data coming out of China, where the disease was first reported, indicated an elevated case-fatality rate for COVID-19 patients who also had diabetes.
In an article published in JAMA, Zunyou Wu, MD, and Jennifer M. McGoogan, PhD, summarized the findings from a February report on 44,672 confirmed cases of the disease from the Chinese Center for Disease Control and Prevention. The overall case-fatality rate (CFR) at that stage was 2.3% (1,023 deaths of the 44,672 confirmed cases). The data indicated that the CFR was elevated among COVID-19 patients with preexisting comorbid conditions, specifically, cardiovascular disease (CFR, 10.5%), diabetes (7.3%), chronic respiratory disease (6.3%), hypertension (6%), and cancer (5.6%).
The data also showed an aged-related trend in the CFR, with patients aged 80 years or older having a CFR of 14.8% and those aged 70-79 years, a rate of 8.0%, while there were no fatal cases reported in patients aged 9 years or younger (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
Those findings have been echoed by the U.S. Centers of Disease Control and Prevention. The American Diabetes Association and the American Association of Clinical Endocrinologists have in turn referenced the CDC in their COVID-19 guidance recommendations for patients with diabetes.
Guidelines were already in place for treatment of infections in patients with diabetes, and
In general, patients with diabetes – especially those whose disease is not controlled, or not well controlled – can be more susceptible to more common infections, such as influenza and pneumonia, possibly because hyperglycemia can subdue immunity by disrupting function of the white blood cells.
Glucose control is key
An important factor in any form of infection control in patients with diabetes seems to be whether or not a patient’s glucose levels are well controlled, according to comments from members of the editorial advisory board for Clinical Endocrinology News. Good glucose control, therefore, could be instrumental in reducing both the risk for and severity of infection.
Paul Jellinger, MD, of the Center for Diabetes & Endocrine Care, Hollywood, Fla., said that, over the years, he had not observed higher infection rates in general in patients with hemoglobin A1c levels below 7, or even higher. However, “a bigger question for me, given the broad category of ‘diabetes’ listed as a risk for serious coronavirus complications by the CDC, has been: Just which individuals with diabetes are really at risk? Are patients with well-controlled diabetes at increased risk as much as those with significant hyperglycemia and uncontrolled diabetes? In my view, not likely.”
Alan Jay Cohen, MD, agreed with Dr. Jellinger. “Many patients have called the office in the last 10 days to ask if there are special precautions they should take because they are reading that they are in the high-risk group because they have diabetes. Many of them are in superb, or at least pretty good, control. I have not seen where they have had a higher incidence of infection than the general population, and I have not seen data with COVID-19 that specifically demonstrates that a person with diabetes in good control has an increased risk,” he said.
“My recommendations to these patients have been the same as those given to the general population,” added Dr. Cohen, medical director at Baptist Medical Group: The Endocrine Clinic, Memphis.
Herbert I. Rettinger, MD, also conceded that poorly controlled blood sugars and confounding illnesses, such as renal and cardiac conditions, are common in patients with long-standing diabetes, but “there is a huge population of patients with type 1 diabetes, and very few seem to be more susceptible to infection. Perhaps I am missing those with poor diet and glucose control.”
Philip Levy, MD, picked up on that latter point, emphasizing that “endocrinologists take care of fewer patients with diabetes than do primary care physicians. Most patients with type 2 diabetes are not seen by us unless the PCP has problems [treating them],” so it could be that PCPs may see a higher number of patients who are at a greater risk for infections.
Ultimately, “good glucose control is very helpful in avoiding infections,” said Dr. Levy, of the Banner University Medical Group Endocrinology & Diabetes, Phoenix.
For sick patients
Guidelines for patients at the Joslin Diabetes Center in Boston advise patients who are feeling sick to continue taking their diabetes medications, unless instructed otherwise by their providers, and to monitor their glucose more frequently because it can spike suddenly.
Patients with type 1 diabetes should check for ketones if their glucose passes 250 mg/dL, according to the guidelines, and patients should remain hydrated at all times and get plenty of rest.
“Sick-day guidelines definitely apply, but patients should be advised to get tested if they have any symptoms they are concerned about,” said Dr. Rettinger, of the Endocrinology Medical Group of Orange County, Orange, Calif.
If patients with diabetes develop COVID-19, then home management may still be possible, according to Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues (Diabetes Metab Syndr. 2020 Mar 10;14[3]:211-2. doi: 10.1016/j.dsx.2020.03.002).
Dr. Rettinger agreed, noting that home management would be feasible as long as “everything is going well, that is, the patient is not experiencing respiratory problems or difficulties in controlling glucose levels. Consider patients with type 1 diabetes who have COVID-19 as you would a nursing home patient – ever vigilant.”
Dr. Gupta and coauthors also recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve. However, the ADA warns in its guidelines that patients should “be aware that some constant glucose monitoring sensors (Dexcom G5, Medtronic Enlite, and Guardian) are impacted by acetaminophen (Tylenol), and that patients should check with finger sticks to ensure accuracy [if they are taking acetaminophen].”
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often, the authors wrote, cautioning that “frequent changes in dosage and correctional bolus may be required to maintain normoglycemia.” Dr Rettinger emphasized that “hyperglycemia, as always, is best treated with fluids and insulin and frequent checks of sugars to be sure the treatment regimen is successful.”
In regard to diabetic drug regimens, patients with type 1 or 2 disease should continue on their current medications, advised Yehuda Handelsman, MD. “Some, especially those on insulin, may require more of it. And the patient should increase fluid intake to prevent fluid depletion. We do not reduce antihyperglycemic medication to preserve fluids.
“As for hypoglycemia, we always aim for less to no hypoglycemia,” he continued. “Monitoring glucose and appropriate dosage is the way to go. In other words, do not reduce medications in sick patients who typically need more medication.”
Dr. Handelsman, medical director and principal investigator at Metabolic Institute of America, Tarzana, Calif., added that very sick patients who are hospitalized should be managed with insulin and that oral agents – particularly metformin and sodium-glucose transporter 2 inhibitors – should be stopped.
“Once the patient has recovered and stabilized, you can return to the prior regimen, and, even if the patient is still in hospital, noninsulin therapy can be reintroduced,” he said.
“This is standard procedure in very sick patients, especially those in critical care. Metformin may raise lactic acid levels, and the SGLT2 inhibitors cause volume contraction, fat metabolism, and acidosis,” he explained. “We also stop the glucagon-like peptide receptor–1 analogues, which can cause nausea and vomiting, and pioglitazone because it causes fluid overload.
“Only insulin can be used for acutely sick patients – those with sepsis, for example. The same would apply if they have severe breathing disorders, and definitely, if they are on a ventilator. This is also the time we stop aromatase inhibitor orals and we use insulin.”
Preventive measures
In the interest of maintaining good glucose control, patients also should monitor their glucose levels more frequently so that fluctuations can be detected early and quickly addressed with the appropriate medication adjustments, according to guidelines from the ADA and AACE. They should continue to follow a healthy diet that includes adequate protein and they should exercise regularly.
Patients should ensure that they have enough medication and testing supplies – for at least 14 days, and longer, if costs permit – in case they have to go into quarantine.
General preventive measures, such as frequent hand washing with soap and water, practicing good respiratory hygiene by sneezing or coughing into a facial tissue or bent elbow, also apply for reducing the risk of infection. Touching of the face should be avoided, as should nonessential travel and contact with infected individuals.
Patients with diabetes should always be current with their influenza and pneumonia shots.
Dr. Rettinger said that he always recommends the following preventative measures to his patients and he is using the current health crisis to reinforce them:
- Eat lots of multicolored fruits and vegetables.
- Eat yogurt and take probiotics to keep the intestinal biome strong and functional.
- Be extra vigilant regarding sugars and sugar control to avoid peaks and valleys wherever possible.
- Keep the immune system strong with at least 7-8 hours sleep and reduce stress levels whenever possible.
- Avoid crowds and handshaking.
- Wash hands regularly.
Possible therapies
There are currently no drugs that have been approved specifically for the treatment of COVID-19, although a vaccine against the disease is currently under development.
Dr. Gupta and his colleagues noted in their article that there have been reports of the anecdotal use of antiviral drugs such as lopinavir, ritonavir, interferon-beta, the RNA polymerase inhibitor remdesivir, and chloroquine.
However, Dr. Handelsman said that, as far as he knows, none of these drugs has been shown to be beneficial for COVID-19. “Some [providers] have tried Tamiflu, but with no clear outcomes, and for severely sick patients, they tried medications for anti-HIV, hepatitis C, and malaria, but so far, there has been no breakthrough.”
Dr. Cohen, Dr. Handelsman, Dr. Jellinger, Dr. Levy, and Dr. Rettinger are members of the editorial advisory board of Clinical Endocrinology News. Dr. Gupta and Dr. Wu, and their colleagues, reported no conflicts of interest.
Patients with diabetes may be at extra risk for coronavirus disease (COVID-19) mortality, and doctors treating them need to keep up with the latest guidelines and expert advice.
Most health advisories about COVID-19 mention diabetes as one of the high-risk categories for the disease, likely because early data coming out of China, where the disease was first reported, indicated an elevated case-fatality rate for COVID-19 patients who also had diabetes.
In an article published in JAMA, Zunyou Wu, MD, and Jennifer M. McGoogan, PhD, summarized the findings from a February report on 44,672 confirmed cases of the disease from the Chinese Center for Disease Control and Prevention. The overall case-fatality rate (CFR) at that stage was 2.3% (1,023 deaths of the 44,672 confirmed cases). The data indicated that the CFR was elevated among COVID-19 patients with preexisting comorbid conditions, specifically, cardiovascular disease (CFR, 10.5%), diabetes (7.3%), chronic respiratory disease (6.3%), hypertension (6%), and cancer (5.6%).
The data also showed an aged-related trend in the CFR, with patients aged 80 years or older having a CFR of 14.8% and those aged 70-79 years, a rate of 8.0%, while there were no fatal cases reported in patients aged 9 years or younger (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
Those findings have been echoed by the U.S. Centers of Disease Control and Prevention. The American Diabetes Association and the American Association of Clinical Endocrinologists have in turn referenced the CDC in their COVID-19 guidance recommendations for patients with diabetes.
Guidelines were already in place for treatment of infections in patients with diabetes, and
In general, patients with diabetes – especially those whose disease is not controlled, or not well controlled – can be more susceptible to more common infections, such as influenza and pneumonia, possibly because hyperglycemia can subdue immunity by disrupting function of the white blood cells.
Glucose control is key
An important factor in any form of infection control in patients with diabetes seems to be whether or not a patient’s glucose levels are well controlled, according to comments from members of the editorial advisory board for Clinical Endocrinology News. Good glucose control, therefore, could be instrumental in reducing both the risk for and severity of infection.
Paul Jellinger, MD, of the Center for Diabetes & Endocrine Care, Hollywood, Fla., said that, over the years, he had not observed higher infection rates in general in patients with hemoglobin A1c levels below 7, or even higher. However, “a bigger question for me, given the broad category of ‘diabetes’ listed as a risk for serious coronavirus complications by the CDC, has been: Just which individuals with diabetes are really at risk? Are patients with well-controlled diabetes at increased risk as much as those with significant hyperglycemia and uncontrolled diabetes? In my view, not likely.”
Alan Jay Cohen, MD, agreed with Dr. Jellinger. “Many patients have called the office in the last 10 days to ask if there are special precautions they should take because they are reading that they are in the high-risk group because they have diabetes. Many of them are in superb, or at least pretty good, control. I have not seen where they have had a higher incidence of infection than the general population, and I have not seen data with COVID-19 that specifically demonstrates that a person with diabetes in good control has an increased risk,” he said.
“My recommendations to these patients have been the same as those given to the general population,” added Dr. Cohen, medical director at Baptist Medical Group: The Endocrine Clinic, Memphis.
Herbert I. Rettinger, MD, also conceded that poorly controlled blood sugars and confounding illnesses, such as renal and cardiac conditions, are common in patients with long-standing diabetes, but “there is a huge population of patients with type 1 diabetes, and very few seem to be more susceptible to infection. Perhaps I am missing those with poor diet and glucose control.”
Philip Levy, MD, picked up on that latter point, emphasizing that “endocrinologists take care of fewer patients with diabetes than do primary care physicians. Most patients with type 2 diabetes are not seen by us unless the PCP has problems [treating them],” so it could be that PCPs may see a higher number of patients who are at a greater risk for infections.
Ultimately, “good glucose control is very helpful in avoiding infections,” said Dr. Levy, of the Banner University Medical Group Endocrinology & Diabetes, Phoenix.
For sick patients
Guidelines for patients at the Joslin Diabetes Center in Boston advise patients who are feeling sick to continue taking their diabetes medications, unless instructed otherwise by their providers, and to monitor their glucose more frequently because it can spike suddenly.
Patients with type 1 diabetes should check for ketones if their glucose passes 250 mg/dL, according to the guidelines, and patients should remain hydrated at all times and get plenty of rest.
“Sick-day guidelines definitely apply, but patients should be advised to get tested if they have any symptoms they are concerned about,” said Dr. Rettinger, of the Endocrinology Medical Group of Orange County, Orange, Calif.
If patients with diabetes develop COVID-19, then home management may still be possible, according to Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues (Diabetes Metab Syndr. 2020 Mar 10;14[3]:211-2. doi: 10.1016/j.dsx.2020.03.002).
Dr. Rettinger agreed, noting that home management would be feasible as long as “everything is going well, that is, the patient is not experiencing respiratory problems or difficulties in controlling glucose levels. Consider patients with type 1 diabetes who have COVID-19 as you would a nursing home patient – ever vigilant.”
Dr. Gupta and coauthors also recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve. However, the ADA warns in its guidelines that patients should “be aware that some constant glucose monitoring sensors (Dexcom G5, Medtronic Enlite, and Guardian) are impacted by acetaminophen (Tylenol), and that patients should check with finger sticks to ensure accuracy [if they are taking acetaminophen].”
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often, the authors wrote, cautioning that “frequent changes in dosage and correctional bolus may be required to maintain normoglycemia.” Dr Rettinger emphasized that “hyperglycemia, as always, is best treated with fluids and insulin and frequent checks of sugars to be sure the treatment regimen is successful.”
In regard to diabetic drug regimens, patients with type 1 or 2 disease should continue on their current medications, advised Yehuda Handelsman, MD. “Some, especially those on insulin, may require more of it. And the patient should increase fluid intake to prevent fluid depletion. We do not reduce antihyperglycemic medication to preserve fluids.
“As for hypoglycemia, we always aim for less to no hypoglycemia,” he continued. “Monitoring glucose and appropriate dosage is the way to go. In other words, do not reduce medications in sick patients who typically need more medication.”
Dr. Handelsman, medical director and principal investigator at Metabolic Institute of America, Tarzana, Calif., added that very sick patients who are hospitalized should be managed with insulin and that oral agents – particularly metformin and sodium-glucose transporter 2 inhibitors – should be stopped.
“Once the patient has recovered and stabilized, you can return to the prior regimen, and, even if the patient is still in hospital, noninsulin therapy can be reintroduced,” he said.
“This is standard procedure in very sick patients, especially those in critical care. Metformin may raise lactic acid levels, and the SGLT2 inhibitors cause volume contraction, fat metabolism, and acidosis,” he explained. “We also stop the glucagon-like peptide receptor–1 analogues, which can cause nausea and vomiting, and pioglitazone because it causes fluid overload.
“Only insulin can be used for acutely sick patients – those with sepsis, for example. The same would apply if they have severe breathing disorders, and definitely, if they are on a ventilator. This is also the time we stop aromatase inhibitor orals and we use insulin.”
Preventive measures
In the interest of maintaining good glucose control, patients also should monitor their glucose levels more frequently so that fluctuations can be detected early and quickly addressed with the appropriate medication adjustments, according to guidelines from the ADA and AACE. They should continue to follow a healthy diet that includes adequate protein and they should exercise regularly.
Patients should ensure that they have enough medication and testing supplies – for at least 14 days, and longer, if costs permit – in case they have to go into quarantine.
General preventive measures, such as frequent hand washing with soap and water, practicing good respiratory hygiene by sneezing or coughing into a facial tissue or bent elbow, also apply for reducing the risk of infection. Touching of the face should be avoided, as should nonessential travel and contact with infected individuals.
Patients with diabetes should always be current with their influenza and pneumonia shots.
Dr. Rettinger said that he always recommends the following preventative measures to his patients and he is using the current health crisis to reinforce them:
- Eat lots of multicolored fruits and vegetables.
- Eat yogurt and take probiotics to keep the intestinal biome strong and functional.
- Be extra vigilant regarding sugars and sugar control to avoid peaks and valleys wherever possible.
- Keep the immune system strong with at least 7-8 hours sleep and reduce stress levels whenever possible.
- Avoid crowds and handshaking.
- Wash hands regularly.
Possible therapies
There are currently no drugs that have been approved specifically for the treatment of COVID-19, although a vaccine against the disease is currently under development.
Dr. Gupta and his colleagues noted in their article that there have been reports of the anecdotal use of antiviral drugs such as lopinavir, ritonavir, interferon-beta, the RNA polymerase inhibitor remdesivir, and chloroquine.
However, Dr. Handelsman said that, as far as he knows, none of these drugs has been shown to be beneficial for COVID-19. “Some [providers] have tried Tamiflu, but with no clear outcomes, and for severely sick patients, they tried medications for anti-HIV, hepatitis C, and malaria, but so far, there has been no breakthrough.”
Dr. Cohen, Dr. Handelsman, Dr. Jellinger, Dr. Levy, and Dr. Rettinger are members of the editorial advisory board of Clinical Endocrinology News. Dr. Gupta and Dr. Wu, and their colleagues, reported no conflicts of interest.
Patients with diabetes may be at extra risk for coronavirus disease (COVID-19) mortality, and doctors treating them need to keep up with the latest guidelines and expert advice.
Most health advisories about COVID-19 mention diabetes as one of the high-risk categories for the disease, likely because early data coming out of China, where the disease was first reported, indicated an elevated case-fatality rate for COVID-19 patients who also had diabetes.
In an article published in JAMA, Zunyou Wu, MD, and Jennifer M. McGoogan, PhD, summarized the findings from a February report on 44,672 confirmed cases of the disease from the Chinese Center for Disease Control and Prevention. The overall case-fatality rate (CFR) at that stage was 2.3% (1,023 deaths of the 44,672 confirmed cases). The data indicated that the CFR was elevated among COVID-19 patients with preexisting comorbid conditions, specifically, cardiovascular disease (CFR, 10.5%), diabetes (7.3%), chronic respiratory disease (6.3%), hypertension (6%), and cancer (5.6%).
The data also showed an aged-related trend in the CFR, with patients aged 80 years or older having a CFR of 14.8% and those aged 70-79 years, a rate of 8.0%, while there were no fatal cases reported in patients aged 9 years or younger (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
Those findings have been echoed by the U.S. Centers of Disease Control and Prevention. The American Diabetes Association and the American Association of Clinical Endocrinologists have in turn referenced the CDC in their COVID-19 guidance recommendations for patients with diabetes.
Guidelines were already in place for treatment of infections in patients with diabetes, and
In general, patients with diabetes – especially those whose disease is not controlled, or not well controlled – can be more susceptible to more common infections, such as influenza and pneumonia, possibly because hyperglycemia can subdue immunity by disrupting function of the white blood cells.
Glucose control is key
An important factor in any form of infection control in patients with diabetes seems to be whether or not a patient’s glucose levels are well controlled, according to comments from members of the editorial advisory board for Clinical Endocrinology News. Good glucose control, therefore, could be instrumental in reducing both the risk for and severity of infection.
Paul Jellinger, MD, of the Center for Diabetes & Endocrine Care, Hollywood, Fla., said that, over the years, he had not observed higher infection rates in general in patients with hemoglobin A1c levels below 7, or even higher. However, “a bigger question for me, given the broad category of ‘diabetes’ listed as a risk for serious coronavirus complications by the CDC, has been: Just which individuals with diabetes are really at risk? Are patients with well-controlled diabetes at increased risk as much as those with significant hyperglycemia and uncontrolled diabetes? In my view, not likely.”
Alan Jay Cohen, MD, agreed with Dr. Jellinger. “Many patients have called the office in the last 10 days to ask if there are special precautions they should take because they are reading that they are in the high-risk group because they have diabetes. Many of them are in superb, or at least pretty good, control. I have not seen where they have had a higher incidence of infection than the general population, and I have not seen data with COVID-19 that specifically demonstrates that a person with diabetes in good control has an increased risk,” he said.
“My recommendations to these patients have been the same as those given to the general population,” added Dr. Cohen, medical director at Baptist Medical Group: The Endocrine Clinic, Memphis.
Herbert I. Rettinger, MD, also conceded that poorly controlled blood sugars and confounding illnesses, such as renal and cardiac conditions, are common in patients with long-standing diabetes, but “there is a huge population of patients with type 1 diabetes, and very few seem to be more susceptible to infection. Perhaps I am missing those with poor diet and glucose control.”
Philip Levy, MD, picked up on that latter point, emphasizing that “endocrinologists take care of fewer patients with diabetes than do primary care physicians. Most patients with type 2 diabetes are not seen by us unless the PCP has problems [treating them],” so it could be that PCPs may see a higher number of patients who are at a greater risk for infections.
Ultimately, “good glucose control is very helpful in avoiding infections,” said Dr. Levy, of the Banner University Medical Group Endocrinology & Diabetes, Phoenix.
For sick patients
Guidelines for patients at the Joslin Diabetes Center in Boston advise patients who are feeling sick to continue taking their diabetes medications, unless instructed otherwise by their providers, and to monitor their glucose more frequently because it can spike suddenly.
Patients with type 1 diabetes should check for ketones if their glucose passes 250 mg/dL, according to the guidelines, and patients should remain hydrated at all times and get plenty of rest.
“Sick-day guidelines definitely apply, but patients should be advised to get tested if they have any symptoms they are concerned about,” said Dr. Rettinger, of the Endocrinology Medical Group of Orange County, Orange, Calif.
If patients with diabetes develop COVID-19, then home management may still be possible, according to Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues (Diabetes Metab Syndr. 2020 Mar 10;14[3]:211-2. doi: 10.1016/j.dsx.2020.03.002).
Dr. Rettinger agreed, noting that home management would be feasible as long as “everything is going well, that is, the patient is not experiencing respiratory problems or difficulties in controlling glucose levels. Consider patients with type 1 diabetes who have COVID-19 as you would a nursing home patient – ever vigilant.”
Dr. Gupta and coauthors also recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve. However, the ADA warns in its guidelines that patients should “be aware that some constant glucose monitoring sensors (Dexcom G5, Medtronic Enlite, and Guardian) are impacted by acetaminophen (Tylenol), and that patients should check with finger sticks to ensure accuracy [if they are taking acetaminophen].”
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often, the authors wrote, cautioning that “frequent changes in dosage and correctional bolus may be required to maintain normoglycemia.” Dr Rettinger emphasized that “hyperglycemia, as always, is best treated with fluids and insulin and frequent checks of sugars to be sure the treatment regimen is successful.”
In regard to diabetic drug regimens, patients with type 1 or 2 disease should continue on their current medications, advised Yehuda Handelsman, MD. “Some, especially those on insulin, may require more of it. And the patient should increase fluid intake to prevent fluid depletion. We do not reduce antihyperglycemic medication to preserve fluids.
“As for hypoglycemia, we always aim for less to no hypoglycemia,” he continued. “Monitoring glucose and appropriate dosage is the way to go. In other words, do not reduce medications in sick patients who typically need more medication.”
Dr. Handelsman, medical director and principal investigator at Metabolic Institute of America, Tarzana, Calif., added that very sick patients who are hospitalized should be managed with insulin and that oral agents – particularly metformin and sodium-glucose transporter 2 inhibitors – should be stopped.
“Once the patient has recovered and stabilized, you can return to the prior regimen, and, even if the patient is still in hospital, noninsulin therapy can be reintroduced,” he said.
“This is standard procedure in very sick patients, especially those in critical care. Metformin may raise lactic acid levels, and the SGLT2 inhibitors cause volume contraction, fat metabolism, and acidosis,” he explained. “We also stop the glucagon-like peptide receptor–1 analogues, which can cause nausea and vomiting, and pioglitazone because it causes fluid overload.
“Only insulin can be used for acutely sick patients – those with sepsis, for example. The same would apply if they have severe breathing disorders, and definitely, if they are on a ventilator. This is also the time we stop aromatase inhibitor orals and we use insulin.”
Preventive measures
In the interest of maintaining good glucose control, patients also should monitor their glucose levels more frequently so that fluctuations can be detected early and quickly addressed with the appropriate medication adjustments, according to guidelines from the ADA and AACE. They should continue to follow a healthy diet that includes adequate protein and they should exercise regularly.
Patients should ensure that they have enough medication and testing supplies – for at least 14 days, and longer, if costs permit – in case they have to go into quarantine.
General preventive measures, such as frequent hand washing with soap and water, practicing good respiratory hygiene by sneezing or coughing into a facial tissue or bent elbow, also apply for reducing the risk of infection. Touching of the face should be avoided, as should nonessential travel and contact with infected individuals.
Patients with diabetes should always be current with their influenza and pneumonia shots.
Dr. Rettinger said that he always recommends the following preventative measures to his patients and he is using the current health crisis to reinforce them:
- Eat lots of multicolored fruits and vegetables.
- Eat yogurt and take probiotics to keep the intestinal biome strong and functional.
- Be extra vigilant regarding sugars and sugar control to avoid peaks and valleys wherever possible.
- Keep the immune system strong with at least 7-8 hours sleep and reduce stress levels whenever possible.
- Avoid crowds and handshaking.
- Wash hands regularly.
Possible therapies
There are currently no drugs that have been approved specifically for the treatment of COVID-19, although a vaccine against the disease is currently under development.
Dr. Gupta and his colleagues noted in their article that there have been reports of the anecdotal use of antiviral drugs such as lopinavir, ritonavir, interferon-beta, the RNA polymerase inhibitor remdesivir, and chloroquine.
However, Dr. Handelsman said that, as far as he knows, none of these drugs has been shown to be beneficial for COVID-19. “Some [providers] have tried Tamiflu, but with no clear outcomes, and for severely sick patients, they tried medications for anti-HIV, hepatitis C, and malaria, but so far, there has been no breakthrough.”
Dr. Cohen, Dr. Handelsman, Dr. Jellinger, Dr. Levy, and Dr. Rettinger are members of the editorial advisory board of Clinical Endocrinology News. Dr. Gupta and Dr. Wu, and their colleagues, reported no conflicts of interest.