User login
Insomnia + COPD linked to more outpatient, ED visits
Insomnia is “highly prevalent” in veterans with chronic pulmonary obstructive disease and is significantly associated with greater COPD-related health care utilization, according to an analysis of national Veterans Health Administration data.
“The study highlights the importance of exploring potential sleep disturbances and disorders in this population and suggests that a targeted treatment for insomnia may help to improve COPD outcomes in veterans with COPD and insomnia,” said Faith Luyster, PhD, assistant professor at the University of Pittsburgh, in an interview after the virtual annual meeting of the Associated Professional Sleep Societies, where she presented the findings.
Dr. Luyster and coinvestigators used an administrative database from the Veterans Affairs Corporate Data Warehouse to identify more than 1.5 million patients with COPD who used VHA services over a 6-year period (fiscal years 2011-2017). Insomnia was defined by ICD-9/10 diagnostic codes and/or a sedative-hypnotic prescription for at least 30 doses during any of these years.
Insomnia with COPD was prevalent in this sample of veterans at 37.3%. Compared with veterans without comorbid insomnia, those who had both COPD and insomnia (575,539 of the total 1,542,642) were older (69 vs. 64 years), more likely to be female (6.3% vs. 3.7%), more likely to be Black (14% vs. 11%) and more likely to be a current smoker (46.1% vs. 35.5%).
Those with both COPD and insomnia were also more likely to have a service-connected disability rating of 50% of greater; use supplemental oxygen; be divorced, widowed, or separated; have a higher body mass index; or have other medical or psychiatric conditions – in particular obstructive sleep apnea (39% vs. 7%), depression (21% vs. 5%), and PTSD (33% vs. 3%).
P values were < .001 for all of these demographic and clinical variables, Dr. Luyster reported at the meeting.
Comorbid insomnia clearly impacted health care utilization, she said. Veterans with insomnia in addition to COPD had more outpatient and ED visits (10.5 vs 6.9, and 1.6 vs. 1.4, respectively) and more hospitalizations (2.2 vs. 1.8) with a primary diagnostic code for COPD or COPD exacerbation (P < .001).
A negative binomial regression analysis (P < .001) showed that “even after controlling for demographic and other medical conditions, COPD patients with insomnia had greater rates of health care utilization relative to COPD patients without insomnia,” Dr. Luyster said in the interview.
Prior studies have suggested that disturbed sleep is a predictor of poorer longitudinal outcomes in COPD, even after controlling for COPD severity, but have not looked specifically at insomnia, she said.
Commenting on the study Octavian C. Ioachimescu, MD, PhD, of Emory University, Atlanta, and the Atlanta VA Medical Center in Decatur, said the criteria used to define insomnia – unadjudicated ICD diagnoses as well as sedative-hypnotic prescriptions – may explain part of the reported prevalence of insomnia. Even so, the findings add to existing literature demonstrating that COPD and insomnia are both common disorders among VHA patients, and that their frequent coexistence “could have adverse consequences on the overall health, functional status, long-term outcomes, and quality of life of these patients.”
Questions of causation are yet to be answered, he said. “Is it that uncontrolled or severe airflow obstruction causing frequent nocturnal arousals, dyspnea, orthopnea, overuse of inhaled sympathomimetics and heightened anxiety leads to insomnia? Or is it that insomnia – possibly in a cluster with other affective disorders such as depression, anxiety disorders, or PTSD – elicits more frequent or more severe symptoms of shortness of breath in those with smoking-induced airway and parenchymal lung disease, making the latter diagnosis more overt than in others?
“My bet is on a bidirectional causal relationship,” said Dr. Ioachimescu, an editorial board advisor of CHEST Physician.
“Regardless of the etiology [of insomnia in veterans with COPD],” Dr. Luyster said, “it’s important that [insomnia] be addressed and treated appropriately, whether that be through pharmacological treatment, or probably more ideally through [cognitive behavioral therapy] for insomnia.”
The study did not control for COPD severity, she said, because of the difficulty of extracting this data from the VA Corporate Data Warehouse. The study was funded by the VA Competitive Career Development Fund.Dr. Luyster reported that she had no disclosures. Dr. Ioachimescu also said he had no relevant disclosures.
Insomnia is “highly prevalent” in veterans with chronic pulmonary obstructive disease and is significantly associated with greater COPD-related health care utilization, according to an analysis of national Veterans Health Administration data.
“The study highlights the importance of exploring potential sleep disturbances and disorders in this population and suggests that a targeted treatment for insomnia may help to improve COPD outcomes in veterans with COPD and insomnia,” said Faith Luyster, PhD, assistant professor at the University of Pittsburgh, in an interview after the virtual annual meeting of the Associated Professional Sleep Societies, where she presented the findings.
Dr. Luyster and coinvestigators used an administrative database from the Veterans Affairs Corporate Data Warehouse to identify more than 1.5 million patients with COPD who used VHA services over a 6-year period (fiscal years 2011-2017). Insomnia was defined by ICD-9/10 diagnostic codes and/or a sedative-hypnotic prescription for at least 30 doses during any of these years.
Insomnia with COPD was prevalent in this sample of veterans at 37.3%. Compared with veterans without comorbid insomnia, those who had both COPD and insomnia (575,539 of the total 1,542,642) were older (69 vs. 64 years), more likely to be female (6.3% vs. 3.7%), more likely to be Black (14% vs. 11%) and more likely to be a current smoker (46.1% vs. 35.5%).
Those with both COPD and insomnia were also more likely to have a service-connected disability rating of 50% of greater; use supplemental oxygen; be divorced, widowed, or separated; have a higher body mass index; or have other medical or psychiatric conditions – in particular obstructive sleep apnea (39% vs. 7%), depression (21% vs. 5%), and PTSD (33% vs. 3%).
P values were < .001 for all of these demographic and clinical variables, Dr. Luyster reported at the meeting.
Comorbid insomnia clearly impacted health care utilization, she said. Veterans with insomnia in addition to COPD had more outpatient and ED visits (10.5 vs 6.9, and 1.6 vs. 1.4, respectively) and more hospitalizations (2.2 vs. 1.8) with a primary diagnostic code for COPD or COPD exacerbation (P < .001).
A negative binomial regression analysis (P < .001) showed that “even after controlling for demographic and other medical conditions, COPD patients with insomnia had greater rates of health care utilization relative to COPD patients without insomnia,” Dr. Luyster said in the interview.
Prior studies have suggested that disturbed sleep is a predictor of poorer longitudinal outcomes in COPD, even after controlling for COPD severity, but have not looked specifically at insomnia, she said.
Commenting on the study Octavian C. Ioachimescu, MD, PhD, of Emory University, Atlanta, and the Atlanta VA Medical Center in Decatur, said the criteria used to define insomnia – unadjudicated ICD diagnoses as well as sedative-hypnotic prescriptions – may explain part of the reported prevalence of insomnia. Even so, the findings add to existing literature demonstrating that COPD and insomnia are both common disorders among VHA patients, and that their frequent coexistence “could have adverse consequences on the overall health, functional status, long-term outcomes, and quality of life of these patients.”
Questions of causation are yet to be answered, he said. “Is it that uncontrolled or severe airflow obstruction causing frequent nocturnal arousals, dyspnea, orthopnea, overuse of inhaled sympathomimetics and heightened anxiety leads to insomnia? Or is it that insomnia – possibly in a cluster with other affective disorders such as depression, anxiety disorders, or PTSD – elicits more frequent or more severe symptoms of shortness of breath in those with smoking-induced airway and parenchymal lung disease, making the latter diagnosis more overt than in others?
“My bet is on a bidirectional causal relationship,” said Dr. Ioachimescu, an editorial board advisor of CHEST Physician.
“Regardless of the etiology [of insomnia in veterans with COPD],” Dr. Luyster said, “it’s important that [insomnia] be addressed and treated appropriately, whether that be through pharmacological treatment, or probably more ideally through [cognitive behavioral therapy] for insomnia.”
The study did not control for COPD severity, she said, because of the difficulty of extracting this data from the VA Corporate Data Warehouse. The study was funded by the VA Competitive Career Development Fund.Dr. Luyster reported that she had no disclosures. Dr. Ioachimescu also said he had no relevant disclosures.
Insomnia is “highly prevalent” in veterans with chronic pulmonary obstructive disease and is significantly associated with greater COPD-related health care utilization, according to an analysis of national Veterans Health Administration data.
“The study highlights the importance of exploring potential sleep disturbances and disorders in this population and suggests that a targeted treatment for insomnia may help to improve COPD outcomes in veterans with COPD and insomnia,” said Faith Luyster, PhD, assistant professor at the University of Pittsburgh, in an interview after the virtual annual meeting of the Associated Professional Sleep Societies, where she presented the findings.
Dr. Luyster and coinvestigators used an administrative database from the Veterans Affairs Corporate Data Warehouse to identify more than 1.5 million patients with COPD who used VHA services over a 6-year period (fiscal years 2011-2017). Insomnia was defined by ICD-9/10 diagnostic codes and/or a sedative-hypnotic prescription for at least 30 doses during any of these years.
Insomnia with COPD was prevalent in this sample of veterans at 37.3%. Compared with veterans without comorbid insomnia, those who had both COPD and insomnia (575,539 of the total 1,542,642) were older (69 vs. 64 years), more likely to be female (6.3% vs. 3.7%), more likely to be Black (14% vs. 11%) and more likely to be a current smoker (46.1% vs. 35.5%).
Those with both COPD and insomnia were also more likely to have a service-connected disability rating of 50% of greater; use supplemental oxygen; be divorced, widowed, or separated; have a higher body mass index; or have other medical or psychiatric conditions – in particular obstructive sleep apnea (39% vs. 7%), depression (21% vs. 5%), and PTSD (33% vs. 3%).
P values were < .001 for all of these demographic and clinical variables, Dr. Luyster reported at the meeting.
Comorbid insomnia clearly impacted health care utilization, she said. Veterans with insomnia in addition to COPD had more outpatient and ED visits (10.5 vs 6.9, and 1.6 vs. 1.4, respectively) and more hospitalizations (2.2 vs. 1.8) with a primary diagnostic code for COPD or COPD exacerbation (P < .001).
A negative binomial regression analysis (P < .001) showed that “even after controlling for demographic and other medical conditions, COPD patients with insomnia had greater rates of health care utilization relative to COPD patients without insomnia,” Dr. Luyster said in the interview.
Prior studies have suggested that disturbed sleep is a predictor of poorer longitudinal outcomes in COPD, even after controlling for COPD severity, but have not looked specifically at insomnia, she said.
Commenting on the study Octavian C. Ioachimescu, MD, PhD, of Emory University, Atlanta, and the Atlanta VA Medical Center in Decatur, said the criteria used to define insomnia – unadjudicated ICD diagnoses as well as sedative-hypnotic prescriptions – may explain part of the reported prevalence of insomnia. Even so, the findings add to existing literature demonstrating that COPD and insomnia are both common disorders among VHA patients, and that their frequent coexistence “could have adverse consequences on the overall health, functional status, long-term outcomes, and quality of life of these patients.”
Questions of causation are yet to be answered, he said. “Is it that uncontrolled or severe airflow obstruction causing frequent nocturnal arousals, dyspnea, orthopnea, overuse of inhaled sympathomimetics and heightened anxiety leads to insomnia? Or is it that insomnia – possibly in a cluster with other affective disorders such as depression, anxiety disorders, or PTSD – elicits more frequent or more severe symptoms of shortness of breath in those with smoking-induced airway and parenchymal lung disease, making the latter diagnosis more overt than in others?
“My bet is on a bidirectional causal relationship,” said Dr. Ioachimescu, an editorial board advisor of CHEST Physician.
“Regardless of the etiology [of insomnia in veterans with COPD],” Dr. Luyster said, “it’s important that [insomnia] be addressed and treated appropriately, whether that be through pharmacological treatment, or probably more ideally through [cognitive behavioral therapy] for insomnia.”
The study did not control for COPD severity, she said, because of the difficulty of extracting this data from the VA Corporate Data Warehouse. The study was funded by the VA Competitive Career Development Fund.Dr. Luyster reported that she had no disclosures. Dr. Ioachimescu also said he had no relevant disclosures.
FROM SLEEP 2020
Should beta-blockers be used in portal hypertension?
Dear colleagues and friends,
Thank you for your continued support of the Perspectives debates. In this edition, Dr. Guadalupe Garcia-Tsao and Dr. Marwan Ghabril discuss the rationale for and against beta-blocker therapy in portal hypertension, and ultimately highlight the nuances required for appropriate decision-making. This topic invariably generates controversy and debate, and is broadly relevant to general GI and hepatology practices. I hope you will find it as informative as I did, and I welcome your comments and suggestions for future topics at [email protected].
Charles J. Kahi, MD, MS, AGAF, professor of medicine, Indiana University, Indianapolis. He is also an associate editor for GI & Hepatology News.
Beta-blockers in portal hypertension – Yes!
BY GUADALUPE GARCIA-TSAO, MD
Portal hypertension is the main consequence of cirrhosis and is responsible for most of its complications. In compensated cirrhosis, a threshold portal pressure gradient, as determined by the hepatic venous pressure gradient (HVPG), of at least 10 mm Hg is the strongest predictor of clinical decompensation (ascites, variceal hemorrhage, or encephalopathy) which is, in turn, the main determinant of death in cirrhosis.
Portal hypertension is initially caused by an increase in intrahepatic resistance that leads to mild portal hypertension (HVPG, 5-10 mm Hg) but is then enhanced and maintained by an increase in portal venous inflow that leads to clinically significant portal hypertension (HVPG, at least 10 mm Hg).
Portal pressure can be reduced by either ameliorating intrahepatic resistance (which is mostly caused by structural changes that are difficult to reverse) and/or by decreasing portal vein blood inflow (the most modifiable pathogenic mechanism). For over 30 years, treatment of portal hypertension has been based on the use of nonselective beta-blockers (NSBB), drugs that decrease portal pressure through a reduction in splanchnic blood flow. Reduction in portal pressure is greater with NSBB (propranolol, nadolol) than with selective beta-blockers because, as demonstrated experimentally, the main portal pressure–reducing effect stems from splanchnic vasoconstriction because of beta2-adrenergic blockade. This has been confirmed in patients with cirrhosis, in whom the reduction in HVPG is greater with NSBB than with selective BB. On the other hand, carvedilol, an NSBB that also has a vasodilatory alpha1 adrenergic blocking effect, has a greater effect in reducing HVPG, compared with traditional NSBB.
A significant decrease in portal pressure has been associated with better outcomes in cirrhosis. A favorable portal pressure reduction (“response”) has been traditionally defined as a decrease in HVPG below 12 mm Hg or greater than 20% from baseline, although even decreases of 10% are associated with better outcomes. Initial studies had been focused on variceal hemorrhage, a complication that is clearly related to portal hypertension. In this setting, reducing portal pressure clearly leads to a decreased in the incidence of variceal hemorrhage and a decrease in mortality.1 More recently, the focus has been on preventing decompensation (in compensated cirrhosis) and preventing further decompensation/death (in decompensated cirrhosis).
In compensated cirrhosis, a recent meta-analysis of clinical trials of prevention of variceal hemorrhage showed that patients with varices (therefore with clinically significant portal hypertension) without ascites who were NSBB hemodynamic responders, had a reduced risk of developing not only variceal hemorrhage but also ascites and/or encephalopathy, and had lower mortality.2 More importantly, a recent seminal randomized, double-blind, placebo-controlled trial performed in patients with compensated cirrhosis and clinically significant portal hypertension with no or small varices, showed that NSBB (propranolol or carvedilol) led to a significantly lower incidence of decompensation, with ascites being the single event that was significantly lower in the NSBB group.3 This study thereby demonstrates that NSBBs not only reduce the risk of variceal hemorrhage, as previously demonstrated, but also significantly reduces the probability of developing ascites, the most common complication of cirrhosis.
In decompensated cirrhosis, a recent meta-analysis of clinical trials of prevention of variceal hemorrhage showed that patients with varices and ascites (decompensated) who were NSBB responders, had a reduced risk of developing not only variceal hemorrhage but also refractory ascites, spontaneous bacterial peritonitis and/or hepatorenal syndrome, and also had a lower mortality.2 In patients with variceal hemorrhage, the recommended therapy to prevent recurrent variceal hemorrhage is the combination of NSBB plus variceal ligation but this is based on trials that combined compensated and decompensated patients. An individual patient data meta-analysis of these trials showed that, in the group of patients with decompensated Child-Pugh class B/C cirrhosis, rebleeding and mortality were higher with ligation alone, compared with combined therapy with NSBBs and ligation, underlining that NSBB is the key element of combination therapy in these patients.4
There is a fading controversy regarding the potential for increased mortality with the use of NSBBs in patients with refractory ascites and SBP, reported in two retrospective studies.5 These studies lacked information regarding the number of patients in whom NSBBs were withdrawn before the last observation and number of patients in whom NSBBs were started in the course of follow-up. Notably, a recent meta-analysis that included these and subsequent retrospective studies, encompassing a collective of over 1,300 patients, demonstrated that NSBB use in patients with ascites is not related to increased mortality.1,4
Nevertheless, NSBBs should be used cautiously in patients with cirrhosis and ascites. Hemodynamic alterations typical of decompensated cirrhosis are maximal in patients with refractory ascites and spontaneous bacterial peritonitis and the use of NSBB in this setting could lead to worsening hemodynamics, with decreased mean arterial pressure and renal perfusion that could in turn lead to acute kidney injury and death. In studies showing a deleterious effect of NSBB, the mean arterial pressure was significantly lower in patients in the NSBB group.5 In a recent retrospective study, the beneficial effect of NSBBs in patients with refractory ascites, spontaneous bacterial peritonitis, and acute-on-chronic liver failure appeared to apply only to those with a mean arterial pressure of at least 65 mm Hg.6 This evidence has led to guideline recommendations that limit the dose of NSBB to a maximum of 160 mg/day for propranolol or 80 mg/day for nadolol in patients with ascites with close follow-up of arterial blood pressure. Carvedilol should preferably not be used. In the presence of a systolic blood pressure <90 mm Hg or acute kidney injury, NSBBs should be dose-reduced or discontinued. If a precipitant for hypotension is identified (e.g., spontaneous bacterial peritonitis), NSBB can be reinitiated once the precipitating event is resolved and hypotension/acute kidney injury has resolved.
In conclusion, NSBBs are a definite “yes” in the management of cirrhosis and portal hypertension as they prevent poor outcomes (including death) in patients with both compensated and decompensated cirrhosis. In patients with ascites and spontaneous bacterial peritonitis, NSBBs could have deleterious effects but these can be prevented by careful monitoring of blood pressure.
References
1. D’Amico G et al. Gastroenterology. 2006;131:1611-24.
2. Turco L et al. Clin Gastroenterol Hepatol. 2020;18:313-27.
3. Villanueva C et al. Lancet. 2019;393:1597-608.
4. Albillos A et al. Hepatology. 2017;66:1219-31.
5. Garcia-Tsao G. J Hepatol. 2016 Mar;64(3):532-4.
6. Tergast TL et al. Aliment Pharmacol. Ther 2019;50:696-706.
Dr. Garcia-Tsao is professor of medicine, digestive diseases; chief, digestive diseases, Veterans Affairs Connecticut Healthcare System; director, clinical and translational core, Yale Liver Center; program director, VA Connecticut Hepatitis C Resource Center, New Haven. She has no conflicts.
Can be a double-edged blade too dangerous to wield
BY MARWAN S. GHABRIL, MD, AGAF
Nonselective beta-blockers (NSBB) are a cornerstone in the primary and secondary prophylaxis of variceal bleeding in patients with cirrhosis and clinically significant portal hypertension (CSPH), defined as a hepatic venous pressure gradient (HVPG) of at least 10 mm Hg. In the absence of routine HVPG measurement in most clinical practices, NSBB therapy is targeted to a 25% heart rate reduction or target heart rate of 55-60 beats per minute. There is ample evidence supporting this indication for NSBB as summarized in the Baveno VI consensus recommendations in a wide range of liver disease severity, encompassing patients with low-risk small esophageal varices to those with large varices, stigmata, and advanced Child-Pugh class. Tasked with the contrarian perspective on NSBB use, the argument for caution hinges on observations that disease progression can shift the balance of risk and reward to NSBB minimization or avoidance. Understanding the hyperdynamic circulation in worsening portal hypertension of cirrhosis is paramount to these considerations.
The pathophysiology of portal hypertension
Portal hypertension arises as a result of both increased portal venous inflow and increased hepatic sinusoidal resistance and is characterized by splanchnic and systemic vasodilation and reduced effective systemic arterial volume. Compensatory mechanisms include systemic neurohormonal activation, increased heart rate and cardiac output, sodium and water retention (increased plasma volume), and vasoconstrictor system activation. These mechanisms suffice in restoring effective arterial volume initially but also contribute to increased splanchnic/portal inflow and portal hypertension. In advanced decompensation the cardiovascular reserve is overwhelmed with progressive systemic vasodilation, worsening sodium and water retention, vasoconstriction of vital organ vascular beds and an ineffective hyperdynamic state (tachycardia, inadequate cardiac output, and systemic hypotension). This pathophysiological state is heralded clinically by the development of worsening or refractory ascites, and belies the development of other complications of advanced cirrhosis including hyponatremia and hepatorenal syndrome.
The beneficial effects of NSBB in decreasing portal hypertension are mediated by inhibition of splanchnic vasodilation and cardiac effects (reduced heart rate and cardiac output) leading to reduced portal inflow. However, these cardiac effects can be deleterious to systemic hemodynamics in more advanced disease, particularly with acute insults that exacerbate arterial hypovolemia such as bleeding or infection. As such, blunting of sympathetic drive by NSBB carries different degrees of tolerance and risk depending on the hemodynamic reserve in the hyperdynamic state.
Reported clinical experiences
The controversy over NSBB use in advanced cirrhosis arises out of heterogeneous, commonly retrospective datasets and nonrandomized cohorts, with conflicting reports of positive, negative, or neutral effects on mortality and acute kidney injury. Not surprisingly, studies describing detrimental effects of NSBB are based on patients with strictly defined refractory ascites or those with spontaneous bacterial peritonitis.1,2 Importantly, these studies also describe significantly lower blood pressure in at-risk NSBB treated patients, This baseline hemodynamic difference is either not observed,or not explicitly compared in studies/subcohorts with decreased or unaffected mortality with NSBB use in advanced cirrhosis.2
In the largest prospective study of NSBB in cirrhosis with ascites (which used data from three randomized satavaptan trials), NSBB users and nonusers were more closely matched for baseline mean arterial pressure.3 There was no effect of NSBB on mortality but there was a 29% rate of NSBB discontinuation (i.e., intolerance) during the year of follow-up. Predictors of NSBB discontinuation were hospitalization, variceal bleeding, infection, hepatorenal syndrome, Child-Pugh class C, and refractory ascites. Furthermore, NSBB discontinuation was associated with a notable increase in mortality. Similarly, clinically driven discontinuation of NSBB was observed in half of hospitalized patients with acute-on-chronic liver failure in the prospective CANONIC study, and was also associated with significantly higher short-term mortality.
It is possible that NSBB tolerance may select patients with adequate hemodynamic reserve despite the severity of other liver decompensations. Conversely, intolerance of therapeutic NSBB may signify evolving inadequacy of hemodynamic reserve, giving rise to two distinctly different risk/benefit profiles. This double-edged blade perspective is supported by findings of impaired cardiac output in patients with refractory ascites with impaired renal perfusion, and increased wait-list mortality with NSBB use in patients with compromised global cardiac function.4,5
When is caution due?
Rather than a “therapeutic window” that is either wide open or suddenly shut, in nonhospitalized patients risk is on a continuum and there are no agreed upon liver-specific parameters that define strict barriers to NSBB treatment. Refractory ascites may not absolutely define the closure of this window but should put clinicians on notice for a patient’s vulnerability. The Baveno VI recommendations echo the need for caution, with NSBB in refractory ascites with close monitoring of blood pressure, serum sodium, and creatinine. Treatment cessation, reduction or temporary withholding, and careful reintroduction (with reversible insults) are advised in patients with systolic blood pressure <90 mm Hg, serum Na <130 mEq/L, or those with acute kidney injury.
In the absence of randomized trials that account for cirrhotic cardiomyopathy and cardiac reserve, the risks and putative nonvariceal benefits of NSBB (e.g., reducing gut bacterial translocation) are not truly defined in this patient population. We lack HVPG-based or surrogate assessments in routine practice to determine which patients are hemodynamically benefiting from NSBB therapy, or reliable indicators of imminent NSBB intolerance or risk. While the indications for NSBB may expand to prevention of decompensation, serious questions about their safety are being asked in advanced decompensation. Poor tolerance of therapeutic NSBB dosing and unquantified, but likely negative, impact on quality of life raise additional questions. In a shared decision-making partnership, the patient’s perspective on the utility, tolerance, and monitoring of NSBB therapy in preventing variceal bleeding is vital, particularly when there are endoscopic or earlier shunting alternatives. “Primum non nocere” is not a gladiatorial cry, and in the wrong patients NSBB can be a double-edged blade too dangerous to wield.
References
1. Serste T et al. Hepatology. 2010;52:1017-22.
2. Mandorfer M et al. Gastroenterology. 2014;146:1680-90 e1.
3. Bossen L et al. Hepatology. 2016;63:1968-76.
4. Giannelli V et al. J Hepatol. 2020;72:463-71.
5. Tellez L et al. J Hepatol. 2020 May 20. doi: 10.1016/j.jhep.2020.05.011.
Dr. Ghabril is a gastroenterologist with the Indiana University, Indianapolis. He has no conflicts.
Dear colleagues and friends,
Thank you for your continued support of the Perspectives debates. In this edition, Dr. Guadalupe Garcia-Tsao and Dr. Marwan Ghabril discuss the rationale for and against beta-blocker therapy in portal hypertension, and ultimately highlight the nuances required for appropriate decision-making. This topic invariably generates controversy and debate, and is broadly relevant to general GI and hepatology practices. I hope you will find it as informative as I did, and I welcome your comments and suggestions for future topics at [email protected].
Charles J. Kahi, MD, MS, AGAF, professor of medicine, Indiana University, Indianapolis. He is also an associate editor for GI & Hepatology News.
Beta-blockers in portal hypertension – Yes!
BY GUADALUPE GARCIA-TSAO, MD
Portal hypertension is the main consequence of cirrhosis and is responsible for most of its complications. In compensated cirrhosis, a threshold portal pressure gradient, as determined by the hepatic venous pressure gradient (HVPG), of at least 10 mm Hg is the strongest predictor of clinical decompensation (ascites, variceal hemorrhage, or encephalopathy) which is, in turn, the main determinant of death in cirrhosis.
Portal hypertension is initially caused by an increase in intrahepatic resistance that leads to mild portal hypertension (HVPG, 5-10 mm Hg) but is then enhanced and maintained by an increase in portal venous inflow that leads to clinically significant portal hypertension (HVPG, at least 10 mm Hg).
Portal pressure can be reduced by either ameliorating intrahepatic resistance (which is mostly caused by structural changes that are difficult to reverse) and/or by decreasing portal vein blood inflow (the most modifiable pathogenic mechanism). For over 30 years, treatment of portal hypertension has been based on the use of nonselective beta-blockers (NSBB), drugs that decrease portal pressure through a reduction in splanchnic blood flow. Reduction in portal pressure is greater with NSBB (propranolol, nadolol) than with selective beta-blockers because, as demonstrated experimentally, the main portal pressure–reducing effect stems from splanchnic vasoconstriction because of beta2-adrenergic blockade. This has been confirmed in patients with cirrhosis, in whom the reduction in HVPG is greater with NSBB than with selective BB. On the other hand, carvedilol, an NSBB that also has a vasodilatory alpha1 adrenergic blocking effect, has a greater effect in reducing HVPG, compared with traditional NSBB.
A significant decrease in portal pressure has been associated with better outcomes in cirrhosis. A favorable portal pressure reduction (“response”) has been traditionally defined as a decrease in HVPG below 12 mm Hg or greater than 20% from baseline, although even decreases of 10% are associated with better outcomes. Initial studies had been focused on variceal hemorrhage, a complication that is clearly related to portal hypertension. In this setting, reducing portal pressure clearly leads to a decreased in the incidence of variceal hemorrhage and a decrease in mortality.1 More recently, the focus has been on preventing decompensation (in compensated cirrhosis) and preventing further decompensation/death (in decompensated cirrhosis).
In compensated cirrhosis, a recent meta-analysis of clinical trials of prevention of variceal hemorrhage showed that patients with varices (therefore with clinically significant portal hypertension) without ascites who were NSBB hemodynamic responders, had a reduced risk of developing not only variceal hemorrhage but also ascites and/or encephalopathy, and had lower mortality.2 More importantly, a recent seminal randomized, double-blind, placebo-controlled trial performed in patients with compensated cirrhosis and clinically significant portal hypertension with no or small varices, showed that NSBB (propranolol or carvedilol) led to a significantly lower incidence of decompensation, with ascites being the single event that was significantly lower in the NSBB group.3 This study thereby demonstrates that NSBBs not only reduce the risk of variceal hemorrhage, as previously demonstrated, but also significantly reduces the probability of developing ascites, the most common complication of cirrhosis.
In decompensated cirrhosis, a recent meta-analysis of clinical trials of prevention of variceal hemorrhage showed that patients with varices and ascites (decompensated) who were NSBB responders, had a reduced risk of developing not only variceal hemorrhage but also refractory ascites, spontaneous bacterial peritonitis and/or hepatorenal syndrome, and also had a lower mortality.2 In patients with variceal hemorrhage, the recommended therapy to prevent recurrent variceal hemorrhage is the combination of NSBB plus variceal ligation but this is based on trials that combined compensated and decompensated patients. An individual patient data meta-analysis of these trials showed that, in the group of patients with decompensated Child-Pugh class B/C cirrhosis, rebleeding and mortality were higher with ligation alone, compared with combined therapy with NSBBs and ligation, underlining that NSBB is the key element of combination therapy in these patients.4
There is a fading controversy regarding the potential for increased mortality with the use of NSBBs in patients with refractory ascites and SBP, reported in two retrospective studies.5 These studies lacked information regarding the number of patients in whom NSBBs were withdrawn before the last observation and number of patients in whom NSBBs were started in the course of follow-up. Notably, a recent meta-analysis that included these and subsequent retrospective studies, encompassing a collective of over 1,300 patients, demonstrated that NSBB use in patients with ascites is not related to increased mortality.1,4
Nevertheless, NSBBs should be used cautiously in patients with cirrhosis and ascites. Hemodynamic alterations typical of decompensated cirrhosis are maximal in patients with refractory ascites and spontaneous bacterial peritonitis and the use of NSBB in this setting could lead to worsening hemodynamics, with decreased mean arterial pressure and renal perfusion that could in turn lead to acute kidney injury and death. In studies showing a deleterious effect of NSBB, the mean arterial pressure was significantly lower in patients in the NSBB group.5 In a recent retrospective study, the beneficial effect of NSBBs in patients with refractory ascites, spontaneous bacterial peritonitis, and acute-on-chronic liver failure appeared to apply only to those with a mean arterial pressure of at least 65 mm Hg.6 This evidence has led to guideline recommendations that limit the dose of NSBB to a maximum of 160 mg/day for propranolol or 80 mg/day for nadolol in patients with ascites with close follow-up of arterial blood pressure. Carvedilol should preferably not be used. In the presence of a systolic blood pressure <90 mm Hg or acute kidney injury, NSBBs should be dose-reduced or discontinued. If a precipitant for hypotension is identified (e.g., spontaneous bacterial peritonitis), NSBB can be reinitiated once the precipitating event is resolved and hypotension/acute kidney injury has resolved.
In conclusion, NSBBs are a definite “yes” in the management of cirrhosis and portal hypertension as they prevent poor outcomes (including death) in patients with both compensated and decompensated cirrhosis. In patients with ascites and spontaneous bacterial peritonitis, NSBBs could have deleterious effects but these can be prevented by careful monitoring of blood pressure.
References
1. D’Amico G et al. Gastroenterology. 2006;131:1611-24.
2. Turco L et al. Clin Gastroenterol Hepatol. 2020;18:313-27.
3. Villanueva C et al. Lancet. 2019;393:1597-608.
4. Albillos A et al. Hepatology. 2017;66:1219-31.
5. Garcia-Tsao G. J Hepatol. 2016 Mar;64(3):532-4.
6. Tergast TL et al. Aliment Pharmacol. Ther 2019;50:696-706.
Dr. Garcia-Tsao is professor of medicine, digestive diseases; chief, digestive diseases, Veterans Affairs Connecticut Healthcare System; director, clinical and translational core, Yale Liver Center; program director, VA Connecticut Hepatitis C Resource Center, New Haven. She has no conflicts.
Can be a double-edged blade too dangerous to wield
BY MARWAN S. GHABRIL, MD, AGAF
Nonselective beta-blockers (NSBB) are a cornerstone in the primary and secondary prophylaxis of variceal bleeding in patients with cirrhosis and clinically significant portal hypertension (CSPH), defined as a hepatic venous pressure gradient (HVPG) of at least 10 mm Hg. In the absence of routine HVPG measurement in most clinical practices, NSBB therapy is targeted to a 25% heart rate reduction or target heart rate of 55-60 beats per minute. There is ample evidence supporting this indication for NSBB as summarized in the Baveno VI consensus recommendations in a wide range of liver disease severity, encompassing patients with low-risk small esophageal varices to those with large varices, stigmata, and advanced Child-Pugh class. Tasked with the contrarian perspective on NSBB use, the argument for caution hinges on observations that disease progression can shift the balance of risk and reward to NSBB minimization or avoidance. Understanding the hyperdynamic circulation in worsening portal hypertension of cirrhosis is paramount to these considerations.
The pathophysiology of portal hypertension
Portal hypertension arises as a result of both increased portal venous inflow and increased hepatic sinusoidal resistance and is characterized by splanchnic and systemic vasodilation and reduced effective systemic arterial volume. Compensatory mechanisms include systemic neurohormonal activation, increased heart rate and cardiac output, sodium and water retention (increased plasma volume), and vasoconstrictor system activation. These mechanisms suffice in restoring effective arterial volume initially but also contribute to increased splanchnic/portal inflow and portal hypertension. In advanced decompensation the cardiovascular reserve is overwhelmed with progressive systemic vasodilation, worsening sodium and water retention, vasoconstriction of vital organ vascular beds and an ineffective hyperdynamic state (tachycardia, inadequate cardiac output, and systemic hypotension). This pathophysiological state is heralded clinically by the development of worsening or refractory ascites, and belies the development of other complications of advanced cirrhosis including hyponatremia and hepatorenal syndrome.
The beneficial effects of NSBB in decreasing portal hypertension are mediated by inhibition of splanchnic vasodilation and cardiac effects (reduced heart rate and cardiac output) leading to reduced portal inflow. However, these cardiac effects can be deleterious to systemic hemodynamics in more advanced disease, particularly with acute insults that exacerbate arterial hypovolemia such as bleeding or infection. As such, blunting of sympathetic drive by NSBB carries different degrees of tolerance and risk depending on the hemodynamic reserve in the hyperdynamic state.
Reported clinical experiences
The controversy over NSBB use in advanced cirrhosis arises out of heterogeneous, commonly retrospective datasets and nonrandomized cohorts, with conflicting reports of positive, negative, or neutral effects on mortality and acute kidney injury. Not surprisingly, studies describing detrimental effects of NSBB are based on patients with strictly defined refractory ascites or those with spontaneous bacterial peritonitis.1,2 Importantly, these studies also describe significantly lower blood pressure in at-risk NSBB treated patients, This baseline hemodynamic difference is either not observed,or not explicitly compared in studies/subcohorts with decreased or unaffected mortality with NSBB use in advanced cirrhosis.2
In the largest prospective study of NSBB in cirrhosis with ascites (which used data from three randomized satavaptan trials), NSBB users and nonusers were more closely matched for baseline mean arterial pressure.3 There was no effect of NSBB on mortality but there was a 29% rate of NSBB discontinuation (i.e., intolerance) during the year of follow-up. Predictors of NSBB discontinuation were hospitalization, variceal bleeding, infection, hepatorenal syndrome, Child-Pugh class C, and refractory ascites. Furthermore, NSBB discontinuation was associated with a notable increase in mortality. Similarly, clinically driven discontinuation of NSBB was observed in half of hospitalized patients with acute-on-chronic liver failure in the prospective CANONIC study, and was also associated with significantly higher short-term mortality.
It is possible that NSBB tolerance may select patients with adequate hemodynamic reserve despite the severity of other liver decompensations. Conversely, intolerance of therapeutic NSBB may signify evolving inadequacy of hemodynamic reserve, giving rise to two distinctly different risk/benefit profiles. This double-edged blade perspective is supported by findings of impaired cardiac output in patients with refractory ascites with impaired renal perfusion, and increased wait-list mortality with NSBB use in patients with compromised global cardiac function.4,5
When is caution due?
Rather than a “therapeutic window” that is either wide open or suddenly shut, in nonhospitalized patients risk is on a continuum and there are no agreed upon liver-specific parameters that define strict barriers to NSBB treatment. Refractory ascites may not absolutely define the closure of this window but should put clinicians on notice for a patient’s vulnerability. The Baveno VI recommendations echo the need for caution, with NSBB in refractory ascites with close monitoring of blood pressure, serum sodium, and creatinine. Treatment cessation, reduction or temporary withholding, and careful reintroduction (with reversible insults) are advised in patients with systolic blood pressure <90 mm Hg, serum Na <130 mEq/L, or those with acute kidney injury.
In the absence of randomized trials that account for cirrhotic cardiomyopathy and cardiac reserve, the risks and putative nonvariceal benefits of NSBB (e.g., reducing gut bacterial translocation) are not truly defined in this patient population. We lack HVPG-based or surrogate assessments in routine practice to determine which patients are hemodynamically benefiting from NSBB therapy, or reliable indicators of imminent NSBB intolerance or risk. While the indications for NSBB may expand to prevention of decompensation, serious questions about their safety are being asked in advanced decompensation. Poor tolerance of therapeutic NSBB dosing and unquantified, but likely negative, impact on quality of life raise additional questions. In a shared decision-making partnership, the patient’s perspective on the utility, tolerance, and monitoring of NSBB therapy in preventing variceal bleeding is vital, particularly when there are endoscopic or earlier shunting alternatives. “Primum non nocere” is not a gladiatorial cry, and in the wrong patients NSBB can be a double-edged blade too dangerous to wield.
References
1. Serste T et al. Hepatology. 2010;52:1017-22.
2. Mandorfer M et al. Gastroenterology. 2014;146:1680-90 e1.
3. Bossen L et al. Hepatology. 2016;63:1968-76.
4. Giannelli V et al. J Hepatol. 2020;72:463-71.
5. Tellez L et al. J Hepatol. 2020 May 20. doi: 10.1016/j.jhep.2020.05.011.
Dr. Ghabril is a gastroenterologist with the Indiana University, Indianapolis. He has no conflicts.
Dear colleagues and friends,
Thank you for your continued support of the Perspectives debates. In this edition, Dr. Guadalupe Garcia-Tsao and Dr. Marwan Ghabril discuss the rationale for and against beta-blocker therapy in portal hypertension, and ultimately highlight the nuances required for appropriate decision-making. This topic invariably generates controversy and debate, and is broadly relevant to general GI and hepatology practices. I hope you will find it as informative as I did, and I welcome your comments and suggestions for future topics at [email protected].
Charles J. Kahi, MD, MS, AGAF, professor of medicine, Indiana University, Indianapolis. He is also an associate editor for GI & Hepatology News.
Beta-blockers in portal hypertension – Yes!
BY GUADALUPE GARCIA-TSAO, MD
Portal hypertension is the main consequence of cirrhosis and is responsible for most of its complications. In compensated cirrhosis, a threshold portal pressure gradient, as determined by the hepatic venous pressure gradient (HVPG), of at least 10 mm Hg is the strongest predictor of clinical decompensation (ascites, variceal hemorrhage, or encephalopathy) which is, in turn, the main determinant of death in cirrhosis.
Portal hypertension is initially caused by an increase in intrahepatic resistance that leads to mild portal hypertension (HVPG, 5-10 mm Hg) but is then enhanced and maintained by an increase in portal venous inflow that leads to clinically significant portal hypertension (HVPG, at least 10 mm Hg).
Portal pressure can be reduced by either ameliorating intrahepatic resistance (which is mostly caused by structural changes that are difficult to reverse) and/or by decreasing portal vein blood inflow (the most modifiable pathogenic mechanism). For over 30 years, treatment of portal hypertension has been based on the use of nonselective beta-blockers (NSBB), drugs that decrease portal pressure through a reduction in splanchnic blood flow. Reduction in portal pressure is greater with NSBB (propranolol, nadolol) than with selective beta-blockers because, as demonstrated experimentally, the main portal pressure–reducing effect stems from splanchnic vasoconstriction because of beta2-adrenergic blockade. This has been confirmed in patients with cirrhosis, in whom the reduction in HVPG is greater with NSBB than with selective BB. On the other hand, carvedilol, an NSBB that also has a vasodilatory alpha1 adrenergic blocking effect, has a greater effect in reducing HVPG, compared with traditional NSBB.
A significant decrease in portal pressure has been associated with better outcomes in cirrhosis. A favorable portal pressure reduction (“response”) has been traditionally defined as a decrease in HVPG below 12 mm Hg or greater than 20% from baseline, although even decreases of 10% are associated with better outcomes. Initial studies had been focused on variceal hemorrhage, a complication that is clearly related to portal hypertension. In this setting, reducing portal pressure clearly leads to a decreased in the incidence of variceal hemorrhage and a decrease in mortality.1 More recently, the focus has been on preventing decompensation (in compensated cirrhosis) and preventing further decompensation/death (in decompensated cirrhosis).
In compensated cirrhosis, a recent meta-analysis of clinical trials of prevention of variceal hemorrhage showed that patients with varices (therefore with clinically significant portal hypertension) without ascites who were NSBB hemodynamic responders, had a reduced risk of developing not only variceal hemorrhage but also ascites and/or encephalopathy, and had lower mortality.2 More importantly, a recent seminal randomized, double-blind, placebo-controlled trial performed in patients with compensated cirrhosis and clinically significant portal hypertension with no or small varices, showed that NSBB (propranolol or carvedilol) led to a significantly lower incidence of decompensation, with ascites being the single event that was significantly lower in the NSBB group.3 This study thereby demonstrates that NSBBs not only reduce the risk of variceal hemorrhage, as previously demonstrated, but also significantly reduces the probability of developing ascites, the most common complication of cirrhosis.
In decompensated cirrhosis, a recent meta-analysis of clinical trials of prevention of variceal hemorrhage showed that patients with varices and ascites (decompensated) who were NSBB responders, had a reduced risk of developing not only variceal hemorrhage but also refractory ascites, spontaneous bacterial peritonitis and/or hepatorenal syndrome, and also had a lower mortality.2 In patients with variceal hemorrhage, the recommended therapy to prevent recurrent variceal hemorrhage is the combination of NSBB plus variceal ligation but this is based on trials that combined compensated and decompensated patients. An individual patient data meta-analysis of these trials showed that, in the group of patients with decompensated Child-Pugh class B/C cirrhosis, rebleeding and mortality were higher with ligation alone, compared with combined therapy with NSBBs and ligation, underlining that NSBB is the key element of combination therapy in these patients.4
There is a fading controversy regarding the potential for increased mortality with the use of NSBBs in patients with refractory ascites and SBP, reported in two retrospective studies.5 These studies lacked information regarding the number of patients in whom NSBBs were withdrawn before the last observation and number of patients in whom NSBBs were started in the course of follow-up. Notably, a recent meta-analysis that included these and subsequent retrospective studies, encompassing a collective of over 1,300 patients, demonstrated that NSBB use in patients with ascites is not related to increased mortality.1,4
Nevertheless, NSBBs should be used cautiously in patients with cirrhosis and ascites. Hemodynamic alterations typical of decompensated cirrhosis are maximal in patients with refractory ascites and spontaneous bacterial peritonitis and the use of NSBB in this setting could lead to worsening hemodynamics, with decreased mean arterial pressure and renal perfusion that could in turn lead to acute kidney injury and death. In studies showing a deleterious effect of NSBB, the mean arterial pressure was significantly lower in patients in the NSBB group.5 In a recent retrospective study, the beneficial effect of NSBBs in patients with refractory ascites, spontaneous bacterial peritonitis, and acute-on-chronic liver failure appeared to apply only to those with a mean arterial pressure of at least 65 mm Hg.6 This evidence has led to guideline recommendations that limit the dose of NSBB to a maximum of 160 mg/day for propranolol or 80 mg/day for nadolol in patients with ascites with close follow-up of arterial blood pressure. Carvedilol should preferably not be used. In the presence of a systolic blood pressure <90 mm Hg or acute kidney injury, NSBBs should be dose-reduced or discontinued. If a precipitant for hypotension is identified (e.g., spontaneous bacterial peritonitis), NSBB can be reinitiated once the precipitating event is resolved and hypotension/acute kidney injury has resolved.
In conclusion, NSBBs are a definite “yes” in the management of cirrhosis and portal hypertension as they prevent poor outcomes (including death) in patients with both compensated and decompensated cirrhosis. In patients with ascites and spontaneous bacterial peritonitis, NSBBs could have deleterious effects but these can be prevented by careful monitoring of blood pressure.
References
1. D’Amico G et al. Gastroenterology. 2006;131:1611-24.
2. Turco L et al. Clin Gastroenterol Hepatol. 2020;18:313-27.
3. Villanueva C et al. Lancet. 2019;393:1597-608.
4. Albillos A et al. Hepatology. 2017;66:1219-31.
5. Garcia-Tsao G. J Hepatol. 2016 Mar;64(3):532-4.
6. Tergast TL et al. Aliment Pharmacol. Ther 2019;50:696-706.
Dr. Garcia-Tsao is professor of medicine, digestive diseases; chief, digestive diseases, Veterans Affairs Connecticut Healthcare System; director, clinical and translational core, Yale Liver Center; program director, VA Connecticut Hepatitis C Resource Center, New Haven. She has no conflicts.
Can be a double-edged blade too dangerous to wield
BY MARWAN S. GHABRIL, MD, AGAF
Nonselective beta-blockers (NSBB) are a cornerstone in the primary and secondary prophylaxis of variceal bleeding in patients with cirrhosis and clinically significant portal hypertension (CSPH), defined as a hepatic venous pressure gradient (HVPG) of at least 10 mm Hg. In the absence of routine HVPG measurement in most clinical practices, NSBB therapy is targeted to a 25% heart rate reduction or target heart rate of 55-60 beats per minute. There is ample evidence supporting this indication for NSBB as summarized in the Baveno VI consensus recommendations in a wide range of liver disease severity, encompassing patients with low-risk small esophageal varices to those with large varices, stigmata, and advanced Child-Pugh class. Tasked with the contrarian perspective on NSBB use, the argument for caution hinges on observations that disease progression can shift the balance of risk and reward to NSBB minimization or avoidance. Understanding the hyperdynamic circulation in worsening portal hypertension of cirrhosis is paramount to these considerations.
The pathophysiology of portal hypertension
Portal hypertension arises as a result of both increased portal venous inflow and increased hepatic sinusoidal resistance and is characterized by splanchnic and systemic vasodilation and reduced effective systemic arterial volume. Compensatory mechanisms include systemic neurohormonal activation, increased heart rate and cardiac output, sodium and water retention (increased plasma volume), and vasoconstrictor system activation. These mechanisms suffice in restoring effective arterial volume initially but also contribute to increased splanchnic/portal inflow and portal hypertension. In advanced decompensation the cardiovascular reserve is overwhelmed with progressive systemic vasodilation, worsening sodium and water retention, vasoconstriction of vital organ vascular beds and an ineffective hyperdynamic state (tachycardia, inadequate cardiac output, and systemic hypotension). This pathophysiological state is heralded clinically by the development of worsening or refractory ascites, and belies the development of other complications of advanced cirrhosis including hyponatremia and hepatorenal syndrome.
The beneficial effects of NSBB in decreasing portal hypertension are mediated by inhibition of splanchnic vasodilation and cardiac effects (reduced heart rate and cardiac output) leading to reduced portal inflow. However, these cardiac effects can be deleterious to systemic hemodynamics in more advanced disease, particularly with acute insults that exacerbate arterial hypovolemia such as bleeding or infection. As such, blunting of sympathetic drive by NSBB carries different degrees of tolerance and risk depending on the hemodynamic reserve in the hyperdynamic state.
Reported clinical experiences
The controversy over NSBB use in advanced cirrhosis arises out of heterogeneous, commonly retrospective datasets and nonrandomized cohorts, with conflicting reports of positive, negative, or neutral effects on mortality and acute kidney injury. Not surprisingly, studies describing detrimental effects of NSBB are based on patients with strictly defined refractory ascites or those with spontaneous bacterial peritonitis.1,2 Importantly, these studies also describe significantly lower blood pressure in at-risk NSBB treated patients, This baseline hemodynamic difference is either not observed,or not explicitly compared in studies/subcohorts with decreased or unaffected mortality with NSBB use in advanced cirrhosis.2
In the largest prospective study of NSBB in cirrhosis with ascites (which used data from three randomized satavaptan trials), NSBB users and nonusers were more closely matched for baseline mean arterial pressure.3 There was no effect of NSBB on mortality but there was a 29% rate of NSBB discontinuation (i.e., intolerance) during the year of follow-up. Predictors of NSBB discontinuation were hospitalization, variceal bleeding, infection, hepatorenal syndrome, Child-Pugh class C, and refractory ascites. Furthermore, NSBB discontinuation was associated with a notable increase in mortality. Similarly, clinically driven discontinuation of NSBB was observed in half of hospitalized patients with acute-on-chronic liver failure in the prospective CANONIC study, and was also associated with significantly higher short-term mortality.
It is possible that NSBB tolerance may select patients with adequate hemodynamic reserve despite the severity of other liver decompensations. Conversely, intolerance of therapeutic NSBB may signify evolving inadequacy of hemodynamic reserve, giving rise to two distinctly different risk/benefit profiles. This double-edged blade perspective is supported by findings of impaired cardiac output in patients with refractory ascites with impaired renal perfusion, and increased wait-list mortality with NSBB use in patients with compromised global cardiac function.4,5
When is caution due?
Rather than a “therapeutic window” that is either wide open or suddenly shut, in nonhospitalized patients risk is on a continuum and there are no agreed upon liver-specific parameters that define strict barriers to NSBB treatment. Refractory ascites may not absolutely define the closure of this window but should put clinicians on notice for a patient’s vulnerability. The Baveno VI recommendations echo the need for caution, with NSBB in refractory ascites with close monitoring of blood pressure, serum sodium, and creatinine. Treatment cessation, reduction or temporary withholding, and careful reintroduction (with reversible insults) are advised in patients with systolic blood pressure <90 mm Hg, serum Na <130 mEq/L, or those with acute kidney injury.
In the absence of randomized trials that account for cirrhotic cardiomyopathy and cardiac reserve, the risks and putative nonvariceal benefits of NSBB (e.g., reducing gut bacterial translocation) are not truly defined in this patient population. We lack HVPG-based or surrogate assessments in routine practice to determine which patients are hemodynamically benefiting from NSBB therapy, or reliable indicators of imminent NSBB intolerance or risk. While the indications for NSBB may expand to prevention of decompensation, serious questions about their safety are being asked in advanced decompensation. Poor tolerance of therapeutic NSBB dosing and unquantified, but likely negative, impact on quality of life raise additional questions. In a shared decision-making partnership, the patient’s perspective on the utility, tolerance, and monitoring of NSBB therapy in preventing variceal bleeding is vital, particularly when there are endoscopic or earlier shunting alternatives. “Primum non nocere” is not a gladiatorial cry, and in the wrong patients NSBB can be a double-edged blade too dangerous to wield.
References
1. Serste T et al. Hepatology. 2010;52:1017-22.
2. Mandorfer M et al. Gastroenterology. 2014;146:1680-90 e1.
3. Bossen L et al. Hepatology. 2016;63:1968-76.
4. Giannelli V et al. J Hepatol. 2020;72:463-71.
5. Tellez L et al. J Hepatol. 2020 May 20. doi: 10.1016/j.jhep.2020.05.011.
Dr. Ghabril is a gastroenterologist with the Indiana University, Indianapolis. He has no conflicts.
Combination approach to melasma treatment yields best results
When establishing a treatment plan for patients with melasma, counseling them about realistic expectations is key.
“It’s important that they understand that this is a chronic condition, so it does require long-term maintenance therapy,” Arisa E. Ortiz, MD, said at the virtual annual Masters of Aesthetics Symposium. “We can improve melasma, but it’s difficult to cure melasma.”
While hydroquinone and other bleaching agents are typical treatment mainstays, chemical peels with glycolic acid, trichloroacetic acid, and salicylic acid can benefit some individuals. “For chemical peels, I really like glycolic acid peels because there is no downtime; it peels at the microscopic level,” said Dr. Ortiz, who is director of laser and cosmetic dermatology at the University of California, San Diego. “This is something they may need to repeat monthly, and having a week of peeling may be difficult to go through every month.”
Other common melasma treatments include lasers, intense pulsed light (IPL), and oral medications. “I personally am not impressed with microdermabrasion for melasma, so I don’t use that very much,” she said. “With laser treatment, you want to make sure you’re using low-energy lasers so that it doesn’t exacerbate or make them relapse or rebound.”
While hydroquinone is a mainstay of therapy, “you can’t use it chronically because of the risk of ochronosis (permanent darkening), so you do need to take drug holidays,” Dr. Ortiz said. “During those drug holidays, you want to make sure patients have a nonhydroquinone bleaching agent so that they don’t flare.” Options include lignin peroxidase, oligopeptide, Lytera, Melaplex, 4-n-butylresorcinol, Cysteamine cream, tranexamic acid, and oral antioxidants.
In a study sponsored by SkinMedica, investigators conducted a randomized, double-blind, half-face study in females with moderate to severe facial hyperpigmentation to assess the efficacy and tolerability of three new skin brightener formulations containing SMA-432, a prostaglandin E2 inhibitor, compared with topical 4% hydroquinone (J Drugs Dermatol 2012 Dec;11[12]:1478-82). They found that the nonhydroquinone skin formulations were better tolerated and were just as effective as 4% hydroquinone.
In a separate unpublished study of 22 females, investigators assessed the efficacy of the U.SK Advanced Defense Booster, which contains ferulic acid, maslinic acid, peptides, and olive leaf extract. They observed that 98% of patients saw improvement after 28 days of treatment.
When it comes to using lasers for melasma treatment, low-energy devices provide the best outcomes. “I prefer using something like the 1927-nm fractional diode lasers at 3.75% density, really low densities because there’s less risk for rebound,” Dr. Ortiz said. “They also enhance skin permeability for the use of topicals.”
In an observational study of 27 female patients with refractory melasma, Arielle Kauvar, MD, director of New York Laser & Skin Care, combined microdermabrasion with the Q-switched Nd:YAG (Lasers in Surgery and Medicine 2012; 44:117-24). “The settings she used were very low fluence, so there was no clinical endpoint or no whitening,” Dr. Ortiz said. Specifically, she used a laser at 1.6-2 J/cm2 with a 5- or 6-mm spot size immediately following microdermabrasion for 4 weeks. “She got a good improvement using a skin care regimen of sunscreen, hydroquinone, and tretinoin or vitamin C,” she said. “Remission lasted at least 6 months.”
In a study presented at the 2019 annual meeting of the America Society for Laser Medicine and Surgery, Dr. Ortiz and Tanya Greywal, MD, of the University of California, San Diego, used three passes of the 10764-nm Nd:YAG laser to treat 10 subjects with melasma skin types 2-5. The device has a 650-microsecond pulse duration, a 6-mm spot size, and an energy mode of 11-14 J/cm3. “There was no downtime with these patients, and they saw a mean improvement of 26%-50% as early as 3 weeks,” she said. “Patients did require multiple treatments to see adequate resolution, but no anesthesia or numbing cream was required. This is a good option for patients who need chronic maintenance treatment.”
Topicals also play a key role following the laser treatment of melasma. Dr. Ortiz characterized clobetasol as “kind of like the magic ointment.” She uses one application immediately post procedure “whenever I’m worried about a patient having postinflammatory hyperpigmentation or if I don’t want melasma patients to rebound. It can help reduce swelling and inflammation to decrease the risk of postinflammatory hyperpigmentation.”
Researchers have discovered that there is a vascular component to melasma. Paul M. Friedman, MD, of the Dermatology and Laser Surgery Center, Houston, and his colleagues used spectrocolorimetry to detect an underlying prominent vascular component in 11 patients with melasma (Lasers Surg Med 2017 Jan;49[1]:20-6). They determined that melasma lesions exhibiting subtle or subclinical telangiectatic erythema may be improved by combined vascular-targeted laser therapy together with fractional low-powered diode laser therapy. “A parallel improvement in telangiectatic erythema suggests a relationship between the underlying vasculature and hyperpigmentation,” said Dr. Ortiz, who was not affiliated with the study. “So, patients who have a vascular component to their melasma actually can get improved efficacy.”
Another strategy for melasma patients involves oral treatment with Polypodium leucotomos extract (PLE), a fern from the Polypodiaceae family with antioxidant properties that has been shown to be photoprotective against UVA and UVB radiation. “I like to think of it as an internal sunscreen,” Dr. Ortiz said. “It does not replace your external sunscreen, but it adds extra protection. It has been shown to significantly reduce the severity of sunburn and decrease the risk of UV radiation–induced skin cancer, as well as prevent skin aging.” The purported mechanism of action includes decreasing UV-mediated oxidative damage to DNA, enhancing the activity of endogenous antioxidant systems, increasing the minimal erythema dose, blocking UV radiation–induced cyclooxygenase-2 expression, reducing UV-induced immune suppression, and promoting p53 suppressor gene expression.
In a pilot placebo-controlled study of melasma patients on their normal regimen of hydroquinone and sunscreen, 40 Asian patients with melasma were randomized to receive either oral PLE supplementation or placebo for 12 weeks (J Clin Aesthet Dermatol 2018 Mar;11[3]:14-9). They found that PLE significantly improved and accelerated the outcome reached with hydroquinone and sunscreen from the first month of treatment, compared with placebo.
Dr. Ortiz next discussed the role of oral tranexamic acid, an antifibrinolytic, procoagulant agent that is approved by the Food and Drug Administration for the treatment of menorrhagia and for prevention of hemorrhage in patients with hemophilia undergoing tooth extractions. “It is a synthetic lysine derivative that inhibits plasminogen activation by blocking lysine-binding sites on the plasminogen molecule, and it’s a game changer for melasma treatment,” she said. “One of the side effects is that it inhibits melanogenesis and neovascularization. It’s been effective for melasma, but its use is limited by the risk for thromboembolism. It’s a slight increased risk, something patients should be aware of, but not something that should scare us away from prescribing it.”
In a study of 561 patients with melasma, 90% improved after a median treatment duration of 4 months, and only 7% had side effects (J Am Acad Dermatol 2016;75:385-92). The most common side effects were abdominal bloating and pain. One patient developed a DVT during treatment, but that person was found to have a protein S deficiency.
The daily dosing of tranexamic acid for menorrhagia is 3,900 mg daily, while the dose for melasma has ranged from 500 mg-1,500 mg per day, Dr. Ortiz said. It’s available as a 650-mg pill in the United States. “I prescribe 325 mg twice a day, but studies have shown that 650 mg once a day is just as effective,” she said.
Prior to prescribing tranexamic acid, Dr. Ortiz does not order labs, but she performs an extensive history of present illness. She does not prescribe it in patients with an increased risk of clotting, including people who smoke and those who take oral contraceptives or are on hormone supplementation. Use is also contraindicated in people with a current malignancy, those with a history of stroke or DVT, and those who have any clotting disorder.
She concluded her presentation by noting that she favors a combination approach to treating melasma patients that starts with a broad spectrum sunscreen and PLE. “For bleaching, I like to use 12% hydroquinone with 6% kojic acid in VersaBase,” she said. “Once I get them in better control, then I switch them to 4% hydroquinone for maintenance. I use glycolic peels, low-energy lasers, and tranexamic acid if the melasma is severe, and they have no contraindications. A combination approach really achieves the best results, and counseling is key.”
Dr. Ortiz disclosed having financial relationships with numerous pharmaceutical and device companies. She is also cochair of MOA.
When establishing a treatment plan for patients with melasma, counseling them about realistic expectations is key.
“It’s important that they understand that this is a chronic condition, so it does require long-term maintenance therapy,” Arisa E. Ortiz, MD, said at the virtual annual Masters of Aesthetics Symposium. “We can improve melasma, but it’s difficult to cure melasma.”
While hydroquinone and other bleaching agents are typical treatment mainstays, chemical peels with glycolic acid, trichloroacetic acid, and salicylic acid can benefit some individuals. “For chemical peels, I really like glycolic acid peels because there is no downtime; it peels at the microscopic level,” said Dr. Ortiz, who is director of laser and cosmetic dermatology at the University of California, San Diego. “This is something they may need to repeat monthly, and having a week of peeling may be difficult to go through every month.”
Other common melasma treatments include lasers, intense pulsed light (IPL), and oral medications. “I personally am not impressed with microdermabrasion for melasma, so I don’t use that very much,” she said. “With laser treatment, you want to make sure you’re using low-energy lasers so that it doesn’t exacerbate or make them relapse or rebound.”
While hydroquinone is a mainstay of therapy, “you can’t use it chronically because of the risk of ochronosis (permanent darkening), so you do need to take drug holidays,” Dr. Ortiz said. “During those drug holidays, you want to make sure patients have a nonhydroquinone bleaching agent so that they don’t flare.” Options include lignin peroxidase, oligopeptide, Lytera, Melaplex, 4-n-butylresorcinol, Cysteamine cream, tranexamic acid, and oral antioxidants.
In a study sponsored by SkinMedica, investigators conducted a randomized, double-blind, half-face study in females with moderate to severe facial hyperpigmentation to assess the efficacy and tolerability of three new skin brightener formulations containing SMA-432, a prostaglandin E2 inhibitor, compared with topical 4% hydroquinone (J Drugs Dermatol 2012 Dec;11[12]:1478-82). They found that the nonhydroquinone skin formulations were better tolerated and were just as effective as 4% hydroquinone.
In a separate unpublished study of 22 females, investigators assessed the efficacy of the U.SK Advanced Defense Booster, which contains ferulic acid, maslinic acid, peptides, and olive leaf extract. They observed that 98% of patients saw improvement after 28 days of treatment.
When it comes to using lasers for melasma treatment, low-energy devices provide the best outcomes. “I prefer using something like the 1927-nm fractional diode lasers at 3.75% density, really low densities because there’s less risk for rebound,” Dr. Ortiz said. “They also enhance skin permeability for the use of topicals.”
In an observational study of 27 female patients with refractory melasma, Arielle Kauvar, MD, director of New York Laser & Skin Care, combined microdermabrasion with the Q-switched Nd:YAG (Lasers in Surgery and Medicine 2012; 44:117-24). “The settings she used were very low fluence, so there was no clinical endpoint or no whitening,” Dr. Ortiz said. Specifically, she used a laser at 1.6-2 J/cm2 with a 5- or 6-mm spot size immediately following microdermabrasion for 4 weeks. “She got a good improvement using a skin care regimen of sunscreen, hydroquinone, and tretinoin or vitamin C,” she said. “Remission lasted at least 6 months.”
In a study presented at the 2019 annual meeting of the America Society for Laser Medicine and Surgery, Dr. Ortiz and Tanya Greywal, MD, of the University of California, San Diego, used three passes of the 10764-nm Nd:YAG laser to treat 10 subjects with melasma skin types 2-5. The device has a 650-microsecond pulse duration, a 6-mm spot size, and an energy mode of 11-14 J/cm3. “There was no downtime with these patients, and they saw a mean improvement of 26%-50% as early as 3 weeks,” she said. “Patients did require multiple treatments to see adequate resolution, but no anesthesia or numbing cream was required. This is a good option for patients who need chronic maintenance treatment.”
Topicals also play a key role following the laser treatment of melasma. Dr. Ortiz characterized clobetasol as “kind of like the magic ointment.” She uses one application immediately post procedure “whenever I’m worried about a patient having postinflammatory hyperpigmentation or if I don’t want melasma patients to rebound. It can help reduce swelling and inflammation to decrease the risk of postinflammatory hyperpigmentation.”
Researchers have discovered that there is a vascular component to melasma. Paul M. Friedman, MD, of the Dermatology and Laser Surgery Center, Houston, and his colleagues used spectrocolorimetry to detect an underlying prominent vascular component in 11 patients with melasma (Lasers Surg Med 2017 Jan;49[1]:20-6). They determined that melasma lesions exhibiting subtle or subclinical telangiectatic erythema may be improved by combined vascular-targeted laser therapy together with fractional low-powered diode laser therapy. “A parallel improvement in telangiectatic erythema suggests a relationship between the underlying vasculature and hyperpigmentation,” said Dr. Ortiz, who was not affiliated with the study. “So, patients who have a vascular component to their melasma actually can get improved efficacy.”
Another strategy for melasma patients involves oral treatment with Polypodium leucotomos extract (PLE), a fern from the Polypodiaceae family with antioxidant properties that has been shown to be photoprotective against UVA and UVB radiation. “I like to think of it as an internal sunscreen,” Dr. Ortiz said. “It does not replace your external sunscreen, but it adds extra protection. It has been shown to significantly reduce the severity of sunburn and decrease the risk of UV radiation–induced skin cancer, as well as prevent skin aging.” The purported mechanism of action includes decreasing UV-mediated oxidative damage to DNA, enhancing the activity of endogenous antioxidant systems, increasing the minimal erythema dose, blocking UV radiation–induced cyclooxygenase-2 expression, reducing UV-induced immune suppression, and promoting p53 suppressor gene expression.
In a pilot placebo-controlled study of melasma patients on their normal regimen of hydroquinone and sunscreen, 40 Asian patients with melasma were randomized to receive either oral PLE supplementation or placebo for 12 weeks (J Clin Aesthet Dermatol 2018 Mar;11[3]:14-9). They found that PLE significantly improved and accelerated the outcome reached with hydroquinone and sunscreen from the first month of treatment, compared with placebo.
Dr. Ortiz next discussed the role of oral tranexamic acid, an antifibrinolytic, procoagulant agent that is approved by the Food and Drug Administration for the treatment of menorrhagia and for prevention of hemorrhage in patients with hemophilia undergoing tooth extractions. “It is a synthetic lysine derivative that inhibits plasminogen activation by blocking lysine-binding sites on the plasminogen molecule, and it’s a game changer for melasma treatment,” she said. “One of the side effects is that it inhibits melanogenesis and neovascularization. It’s been effective for melasma, but its use is limited by the risk for thromboembolism. It’s a slight increased risk, something patients should be aware of, but not something that should scare us away from prescribing it.”
In a study of 561 patients with melasma, 90% improved after a median treatment duration of 4 months, and only 7% had side effects (J Am Acad Dermatol 2016;75:385-92). The most common side effects were abdominal bloating and pain. One patient developed a DVT during treatment, but that person was found to have a protein S deficiency.
The daily dosing of tranexamic acid for menorrhagia is 3,900 mg daily, while the dose for melasma has ranged from 500 mg-1,500 mg per day, Dr. Ortiz said. It’s available as a 650-mg pill in the United States. “I prescribe 325 mg twice a day, but studies have shown that 650 mg once a day is just as effective,” she said.
Prior to prescribing tranexamic acid, Dr. Ortiz does not order labs, but she performs an extensive history of present illness. She does not prescribe it in patients with an increased risk of clotting, including people who smoke and those who take oral contraceptives or are on hormone supplementation. Use is also contraindicated in people with a current malignancy, those with a history of stroke or DVT, and those who have any clotting disorder.
She concluded her presentation by noting that she favors a combination approach to treating melasma patients that starts with a broad spectrum sunscreen and PLE. “For bleaching, I like to use 12% hydroquinone with 6% kojic acid in VersaBase,” she said. “Once I get them in better control, then I switch them to 4% hydroquinone for maintenance. I use glycolic peels, low-energy lasers, and tranexamic acid if the melasma is severe, and they have no contraindications. A combination approach really achieves the best results, and counseling is key.”
Dr. Ortiz disclosed having financial relationships with numerous pharmaceutical and device companies. She is also cochair of MOA.
When establishing a treatment plan for patients with melasma, counseling them about realistic expectations is key.
“It’s important that they understand that this is a chronic condition, so it does require long-term maintenance therapy,” Arisa E. Ortiz, MD, said at the virtual annual Masters of Aesthetics Symposium. “We can improve melasma, but it’s difficult to cure melasma.”
While hydroquinone and other bleaching agents are typical treatment mainstays, chemical peels with glycolic acid, trichloroacetic acid, and salicylic acid can benefit some individuals. “For chemical peels, I really like glycolic acid peels because there is no downtime; it peels at the microscopic level,” said Dr. Ortiz, who is director of laser and cosmetic dermatology at the University of California, San Diego. “This is something they may need to repeat monthly, and having a week of peeling may be difficult to go through every month.”
Other common melasma treatments include lasers, intense pulsed light (IPL), and oral medications. “I personally am not impressed with microdermabrasion for melasma, so I don’t use that very much,” she said. “With laser treatment, you want to make sure you’re using low-energy lasers so that it doesn’t exacerbate or make them relapse or rebound.”
While hydroquinone is a mainstay of therapy, “you can’t use it chronically because of the risk of ochronosis (permanent darkening), so you do need to take drug holidays,” Dr. Ortiz said. “During those drug holidays, you want to make sure patients have a nonhydroquinone bleaching agent so that they don’t flare.” Options include lignin peroxidase, oligopeptide, Lytera, Melaplex, 4-n-butylresorcinol, Cysteamine cream, tranexamic acid, and oral antioxidants.
In a study sponsored by SkinMedica, investigators conducted a randomized, double-blind, half-face study in females with moderate to severe facial hyperpigmentation to assess the efficacy and tolerability of three new skin brightener formulations containing SMA-432, a prostaglandin E2 inhibitor, compared with topical 4% hydroquinone (J Drugs Dermatol 2012 Dec;11[12]:1478-82). They found that the nonhydroquinone skin formulations were better tolerated and were just as effective as 4% hydroquinone.
In a separate unpublished study of 22 females, investigators assessed the efficacy of the U.SK Advanced Defense Booster, which contains ferulic acid, maslinic acid, peptides, and olive leaf extract. They observed that 98% of patients saw improvement after 28 days of treatment.
When it comes to using lasers for melasma treatment, low-energy devices provide the best outcomes. “I prefer using something like the 1927-nm fractional diode lasers at 3.75% density, really low densities because there’s less risk for rebound,” Dr. Ortiz said. “They also enhance skin permeability for the use of topicals.”
In an observational study of 27 female patients with refractory melasma, Arielle Kauvar, MD, director of New York Laser & Skin Care, combined microdermabrasion with the Q-switched Nd:YAG (Lasers in Surgery and Medicine 2012; 44:117-24). “The settings she used were very low fluence, so there was no clinical endpoint or no whitening,” Dr. Ortiz said. Specifically, she used a laser at 1.6-2 J/cm2 with a 5- or 6-mm spot size immediately following microdermabrasion for 4 weeks. “She got a good improvement using a skin care regimen of sunscreen, hydroquinone, and tretinoin or vitamin C,” she said. “Remission lasted at least 6 months.”
In a study presented at the 2019 annual meeting of the America Society for Laser Medicine and Surgery, Dr. Ortiz and Tanya Greywal, MD, of the University of California, San Diego, used three passes of the 10764-nm Nd:YAG laser to treat 10 subjects with melasma skin types 2-5. The device has a 650-microsecond pulse duration, a 6-mm spot size, and an energy mode of 11-14 J/cm3. “There was no downtime with these patients, and they saw a mean improvement of 26%-50% as early as 3 weeks,” she said. “Patients did require multiple treatments to see adequate resolution, but no anesthesia or numbing cream was required. This is a good option for patients who need chronic maintenance treatment.”
Topicals also play a key role following the laser treatment of melasma. Dr. Ortiz characterized clobetasol as “kind of like the magic ointment.” She uses one application immediately post procedure “whenever I’m worried about a patient having postinflammatory hyperpigmentation or if I don’t want melasma patients to rebound. It can help reduce swelling and inflammation to decrease the risk of postinflammatory hyperpigmentation.”
Researchers have discovered that there is a vascular component to melasma. Paul M. Friedman, MD, of the Dermatology and Laser Surgery Center, Houston, and his colleagues used spectrocolorimetry to detect an underlying prominent vascular component in 11 patients with melasma (Lasers Surg Med 2017 Jan;49[1]:20-6). They determined that melasma lesions exhibiting subtle or subclinical telangiectatic erythema may be improved by combined vascular-targeted laser therapy together with fractional low-powered diode laser therapy. “A parallel improvement in telangiectatic erythema suggests a relationship between the underlying vasculature and hyperpigmentation,” said Dr. Ortiz, who was not affiliated with the study. “So, patients who have a vascular component to their melasma actually can get improved efficacy.”
Another strategy for melasma patients involves oral treatment with Polypodium leucotomos extract (PLE), a fern from the Polypodiaceae family with antioxidant properties that has been shown to be photoprotective against UVA and UVB radiation. “I like to think of it as an internal sunscreen,” Dr. Ortiz said. “It does not replace your external sunscreen, but it adds extra protection. It has been shown to significantly reduce the severity of sunburn and decrease the risk of UV radiation–induced skin cancer, as well as prevent skin aging.” The purported mechanism of action includes decreasing UV-mediated oxidative damage to DNA, enhancing the activity of endogenous antioxidant systems, increasing the minimal erythema dose, blocking UV radiation–induced cyclooxygenase-2 expression, reducing UV-induced immune suppression, and promoting p53 suppressor gene expression.
In a pilot placebo-controlled study of melasma patients on their normal regimen of hydroquinone and sunscreen, 40 Asian patients with melasma were randomized to receive either oral PLE supplementation or placebo for 12 weeks (J Clin Aesthet Dermatol 2018 Mar;11[3]:14-9). They found that PLE significantly improved and accelerated the outcome reached with hydroquinone and sunscreen from the first month of treatment, compared with placebo.
Dr. Ortiz next discussed the role of oral tranexamic acid, an antifibrinolytic, procoagulant agent that is approved by the Food and Drug Administration for the treatment of menorrhagia and for prevention of hemorrhage in patients with hemophilia undergoing tooth extractions. “It is a synthetic lysine derivative that inhibits plasminogen activation by blocking lysine-binding sites on the plasminogen molecule, and it’s a game changer for melasma treatment,” she said. “One of the side effects is that it inhibits melanogenesis and neovascularization. It’s been effective for melasma, but its use is limited by the risk for thromboembolism. It’s a slight increased risk, something patients should be aware of, but not something that should scare us away from prescribing it.”
In a study of 561 patients with melasma, 90% improved after a median treatment duration of 4 months, and only 7% had side effects (J Am Acad Dermatol 2016;75:385-92). The most common side effects were abdominal bloating and pain. One patient developed a DVT during treatment, but that person was found to have a protein S deficiency.
The daily dosing of tranexamic acid for menorrhagia is 3,900 mg daily, while the dose for melasma has ranged from 500 mg-1,500 mg per day, Dr. Ortiz said. It’s available as a 650-mg pill in the United States. “I prescribe 325 mg twice a day, but studies have shown that 650 mg once a day is just as effective,” she said.
Prior to prescribing tranexamic acid, Dr. Ortiz does not order labs, but she performs an extensive history of present illness. She does not prescribe it in patients with an increased risk of clotting, including people who smoke and those who take oral contraceptives or are on hormone supplementation. Use is also contraindicated in people with a current malignancy, those with a history of stroke or DVT, and those who have any clotting disorder.
She concluded her presentation by noting that she favors a combination approach to treating melasma patients that starts with a broad spectrum sunscreen and PLE. “For bleaching, I like to use 12% hydroquinone with 6% kojic acid in VersaBase,” she said. “Once I get them in better control, then I switch them to 4% hydroquinone for maintenance. I use glycolic peels, low-energy lasers, and tranexamic acid if the melasma is severe, and they have no contraindications. A combination approach really achieves the best results, and counseling is key.”
Dr. Ortiz disclosed having financial relationships with numerous pharmaceutical and device companies. She is also cochair of MOA.
EXPERT ANALYSIS FROM MOA 2020
A woman with an asymptomatic eruption on her palms after exposure to water
This eruption can be accompanied by a mild burning or tingling sensation, which will subside with the rest of the symptoms in minutes to hours after drying.1
AWP is most frequently associated with cystic fibrosis (CF).2 It can be observed in up to 80% of CF patients and is considered a clinical sign of the disease. AWP can be present in CF carriers to a lesser extent,2,4 and has also been associated with focal hyperhidrosis, atopic dermatitis, Raynaud phenomenon, and COX-2 inhibitor use.5
While a definitive cause is unknown, it is thought that AWP is caused by dysregulation of sweat glands in the palms through increased expression of aquaporin, a protein crucial in the transport of water between cells.3
AWP is quite rare and benign in nature. However, because of its strong association with CF, genetic screening should be considered in asymptomatic patients. Our patient had been screened in the past and is not a CF carrier. Often, the itching or burning associated with CF is mild and easily controlled. The patient was placed on low dose isotretinoin for treatment of her acne. Interestingly, the patient claimed her eruption no longer appeared after starting isotretinoin therapy. To our knowledge, this is the first reported case of AWP resolving with isotretinoin use.
This case and photo were submitted by Mr. Birk, University of Texas, Austin, Texas; and Dr. Mamelak, Sanova Dermatology, in Austin. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at MDedge.com/Dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Katz M, Ramot Y. CMAJ. 2015 Dec 8;187(18):E515.
2. Tolland JP et al. Dermatology. 2010;221(4):326-30.
3. Kabashima K et al. J Am Acad Dermatol. 2008 Aug;59(2 Suppl 1):S28-32.
4. Gild R et al. Br J Dermatol. 2010 Nov;163(5):1082-4.
5. Glatz M and Muellegger RR. BMJ Case Rep. 2014. doi: 10.1136/bcr-2014-203929.
This eruption can be accompanied by a mild burning or tingling sensation, which will subside with the rest of the symptoms in minutes to hours after drying.1
AWP is most frequently associated with cystic fibrosis (CF).2 It can be observed in up to 80% of CF patients and is considered a clinical sign of the disease. AWP can be present in CF carriers to a lesser extent,2,4 and has also been associated with focal hyperhidrosis, atopic dermatitis, Raynaud phenomenon, and COX-2 inhibitor use.5
While a definitive cause is unknown, it is thought that AWP is caused by dysregulation of sweat glands in the palms through increased expression of aquaporin, a protein crucial in the transport of water between cells.3
AWP is quite rare and benign in nature. However, because of its strong association with CF, genetic screening should be considered in asymptomatic patients. Our patient had been screened in the past and is not a CF carrier. Often, the itching or burning associated with CF is mild and easily controlled. The patient was placed on low dose isotretinoin for treatment of her acne. Interestingly, the patient claimed her eruption no longer appeared after starting isotretinoin therapy. To our knowledge, this is the first reported case of AWP resolving with isotretinoin use.
This case and photo were submitted by Mr. Birk, University of Texas, Austin, Texas; and Dr. Mamelak, Sanova Dermatology, in Austin. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at MDedge.com/Dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Katz M, Ramot Y. CMAJ. 2015 Dec 8;187(18):E515.
2. Tolland JP et al. Dermatology. 2010;221(4):326-30.
3. Kabashima K et al. J Am Acad Dermatol. 2008 Aug;59(2 Suppl 1):S28-32.
4. Gild R et al. Br J Dermatol. 2010 Nov;163(5):1082-4.
5. Glatz M and Muellegger RR. BMJ Case Rep. 2014. doi: 10.1136/bcr-2014-203929.
This eruption can be accompanied by a mild burning or tingling sensation, which will subside with the rest of the symptoms in minutes to hours after drying.1
AWP is most frequently associated with cystic fibrosis (CF).2 It can be observed in up to 80% of CF patients and is considered a clinical sign of the disease. AWP can be present in CF carriers to a lesser extent,2,4 and has also been associated with focal hyperhidrosis, atopic dermatitis, Raynaud phenomenon, and COX-2 inhibitor use.5
While a definitive cause is unknown, it is thought that AWP is caused by dysregulation of sweat glands in the palms through increased expression of aquaporin, a protein crucial in the transport of water between cells.3
AWP is quite rare and benign in nature. However, because of its strong association with CF, genetic screening should be considered in asymptomatic patients. Our patient had been screened in the past and is not a CF carrier. Often, the itching or burning associated with CF is mild and easily controlled. The patient was placed on low dose isotretinoin for treatment of her acne. Interestingly, the patient claimed her eruption no longer appeared after starting isotretinoin therapy. To our knowledge, this is the first reported case of AWP resolving with isotretinoin use.
This case and photo were submitted by Mr. Birk, University of Texas, Austin, Texas; and Dr. Mamelak, Sanova Dermatology, in Austin. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at MDedge.com/Dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Katz M, Ramot Y. CMAJ. 2015 Dec 8;187(18):E515.
2. Tolland JP et al. Dermatology. 2010;221(4):326-30.
3. Kabashima K et al. J Am Acad Dermatol. 2008 Aug;59(2 Suppl 1):S28-32.
4. Gild R et al. Br J Dermatol. 2010 Nov;163(5):1082-4.
5. Glatz M and Muellegger RR. BMJ Case Rep. 2014. doi: 10.1136/bcr-2014-203929.
Rash, muscle weakness, and confusion

The constellation of symptoms was suggestive of Lyme disease, although connective tissue disease and syphilis were also considered. Two punch biopsies were performed in the office, and erythrocyte sedimentation rate (ESR), complete blood cell count (CBC), international normalized ratio (INR), comprehensive metabolic panel (CMP), Lyme enzyme-linked immunosorbent assay (ELISA) antibody panel, and rapid plasma reagin (RPR) laboratory tests were ordered.
Immediately available laboratory results included ESR, CBC, INR, and CMP. Findings were notable for elevated INR, as well as elevated alanine aminotransferase and aspartate transaminase. The transaminitis suggested myopathy and was consistent with clinical muscle weakness. RPR testing was negative.
Because of the confusion, severity of muscle weakness, and plausibility of early encephalopathy with Lyme disease, the patient was admitted to the hospital for further work-up. Lumbar puncture was delayed until his INR was reduced, but subsequently was found to be normal. He received intravenous (IV) ceftriaxone (2 g/d) empirically for possible early disseminated disease with neurologic complications. His confusion, muscle weakness, and transaminitis rapidly improved.
His Lyme antibody panel was positive for IgM after his third day of hospitalization. A reflexive confirmatory western blot for IgG was not positive on the initial set of labs but was positive when redrawn 4 weeks after this hospitalization, confirming Lyme disease.
Lyme disease is a vector-borne disease caused by the Borrelia genus of spirochete bacteria, most commonly Borrelia burgdorferi in North America. Transmission occurs through prolonged (typically 36-48 hours) attachment of a blacklegged tick.
The disease can be divided into 3 stages:
- localized (3-30 days): erythema migrans rash and flulike illness
- early disseminated (days to weeks; seen in this patient): multiple erythema migrans rashes, early neuroborreliosis, arthritis, carditis, and rarely hepatitis and uveitis
- late disseminated (months to years): chronic Lyme arthritis, chronic neurological disorders (eg, encephalopathy, radicular pain, and chronic neuropathy).
The initial erythema migrans rash is classically red and targetoid; it expands from the site of attachment. Early disseminated patches tend to be smaller and can occur on any body part. The rash is rarely itchy or painful but may be warm to the touch or sensitive. The rash resolves spontaneously within 3 to 4 weeks of onset.
Treatment of all early and early disseminated Lyme disease typically involves a 14- to 28-day course of doxycycline (100 mg bid for adults, 2.2 mg/kg bid [maximum 100 mg bid] for children). Patients with acute neurologic disease often can be treated with doxycycline, but patients who cannot tolerate doxycycline and those with parenchymal disease such as encephalitis should receive IV therapy with ceftriaxone 2 g/d.
In this case, the patient was discharged home on a 3-week course of doxycycline 100 mg bid and cleared without further symptoms.
Text courtesy of Tristan Reynolds, DO, Maine Dartmouth Family Medicine Residency, and Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
Lyme disease. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/lyme/healthcare/index.html. Accessed September 1, 2020.

The constellation of symptoms was suggestive of Lyme disease, although connective tissue disease and syphilis were also considered. Two punch biopsies were performed in the office, and erythrocyte sedimentation rate (ESR), complete blood cell count (CBC), international normalized ratio (INR), comprehensive metabolic panel (CMP), Lyme enzyme-linked immunosorbent assay (ELISA) antibody panel, and rapid plasma reagin (RPR) laboratory tests were ordered.
Immediately available laboratory results included ESR, CBC, INR, and CMP. Findings were notable for elevated INR, as well as elevated alanine aminotransferase and aspartate transaminase. The transaminitis suggested myopathy and was consistent with clinical muscle weakness. RPR testing was negative.
Because of the confusion, severity of muscle weakness, and plausibility of early encephalopathy with Lyme disease, the patient was admitted to the hospital for further work-up. Lumbar puncture was delayed until his INR was reduced, but subsequently was found to be normal. He received intravenous (IV) ceftriaxone (2 g/d) empirically for possible early disseminated disease with neurologic complications. His confusion, muscle weakness, and transaminitis rapidly improved.
His Lyme antibody panel was positive for IgM after his third day of hospitalization. A reflexive confirmatory western blot for IgG was not positive on the initial set of labs but was positive when redrawn 4 weeks after this hospitalization, confirming Lyme disease.
Lyme disease is a vector-borne disease caused by the Borrelia genus of spirochete bacteria, most commonly Borrelia burgdorferi in North America. Transmission occurs through prolonged (typically 36-48 hours) attachment of a blacklegged tick.
The disease can be divided into 3 stages:
- localized (3-30 days): erythema migrans rash and flulike illness
- early disseminated (days to weeks; seen in this patient): multiple erythema migrans rashes, early neuroborreliosis, arthritis, carditis, and rarely hepatitis and uveitis
- late disseminated (months to years): chronic Lyme arthritis, chronic neurological disorders (eg, encephalopathy, radicular pain, and chronic neuropathy).
The initial erythema migrans rash is classically red and targetoid; it expands from the site of attachment. Early disseminated patches tend to be smaller and can occur on any body part. The rash is rarely itchy or painful but may be warm to the touch or sensitive. The rash resolves spontaneously within 3 to 4 weeks of onset.
Treatment of all early and early disseminated Lyme disease typically involves a 14- to 28-day course of doxycycline (100 mg bid for adults, 2.2 mg/kg bid [maximum 100 mg bid] for children). Patients with acute neurologic disease often can be treated with doxycycline, but patients who cannot tolerate doxycycline and those with parenchymal disease such as encephalitis should receive IV therapy with ceftriaxone 2 g/d.
In this case, the patient was discharged home on a 3-week course of doxycycline 100 mg bid and cleared without further symptoms.
Text courtesy of Tristan Reynolds, DO, Maine Dartmouth Family Medicine Residency, and Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).

The constellation of symptoms was suggestive of Lyme disease, although connective tissue disease and syphilis were also considered. Two punch biopsies were performed in the office, and erythrocyte sedimentation rate (ESR), complete blood cell count (CBC), international normalized ratio (INR), comprehensive metabolic panel (CMP), Lyme enzyme-linked immunosorbent assay (ELISA) antibody panel, and rapid plasma reagin (RPR) laboratory tests were ordered.
Immediately available laboratory results included ESR, CBC, INR, and CMP. Findings were notable for elevated INR, as well as elevated alanine aminotransferase and aspartate transaminase. The transaminitis suggested myopathy and was consistent with clinical muscle weakness. RPR testing was negative.
Because of the confusion, severity of muscle weakness, and plausibility of early encephalopathy with Lyme disease, the patient was admitted to the hospital for further work-up. Lumbar puncture was delayed until his INR was reduced, but subsequently was found to be normal. He received intravenous (IV) ceftriaxone (2 g/d) empirically for possible early disseminated disease with neurologic complications. His confusion, muscle weakness, and transaminitis rapidly improved.
His Lyme antibody panel was positive for IgM after his third day of hospitalization. A reflexive confirmatory western blot for IgG was not positive on the initial set of labs but was positive when redrawn 4 weeks after this hospitalization, confirming Lyme disease.
Lyme disease is a vector-borne disease caused by the Borrelia genus of spirochete bacteria, most commonly Borrelia burgdorferi in North America. Transmission occurs through prolonged (typically 36-48 hours) attachment of a blacklegged tick.
The disease can be divided into 3 stages:
- localized (3-30 days): erythema migrans rash and flulike illness
- early disseminated (days to weeks; seen in this patient): multiple erythema migrans rashes, early neuroborreliosis, arthritis, carditis, and rarely hepatitis and uveitis
- late disseminated (months to years): chronic Lyme arthritis, chronic neurological disorders (eg, encephalopathy, radicular pain, and chronic neuropathy).
The initial erythema migrans rash is classically red and targetoid; it expands from the site of attachment. Early disseminated patches tend to be smaller and can occur on any body part. The rash is rarely itchy or painful but may be warm to the touch or sensitive. The rash resolves spontaneously within 3 to 4 weeks of onset.
Treatment of all early and early disseminated Lyme disease typically involves a 14- to 28-day course of doxycycline (100 mg bid for adults, 2.2 mg/kg bid [maximum 100 mg bid] for children). Patients with acute neurologic disease often can be treated with doxycycline, but patients who cannot tolerate doxycycline and those with parenchymal disease such as encephalitis should receive IV therapy with ceftriaxone 2 g/d.
In this case, the patient was discharged home on a 3-week course of doxycycline 100 mg bid and cleared without further symptoms.
Text courtesy of Tristan Reynolds, DO, Maine Dartmouth Family Medicine Residency, and Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
Lyme disease. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/lyme/healthcare/index.html. Accessed September 1, 2020.
Lyme disease. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/lyme/healthcare/index.html. Accessed September 1, 2020.
Study supports multigene panel testing for all breast cancer patients with second primary cancers
according to a paper published in JCO Precision Oncology.
The authors noted that women with breast cancer have a 4%-16% lifetime risk of a second primary cancer. However, it hasn’t been clear if mutations in genes other than BRCA1/2 are enriched in patients with multiple primary cancers.
“Surprisingly few papers have focused on genetic evaluation of patients with multiple primary cancers,” senior author Katherine L. Nathanson, MD, of the University of Pennsylvania in Philadelphia, said in an interview.
“Ours is one of the first studies to look closely at this issue. We know from clinical experience that these patients are more likely to have more than one genetic mutation,” she added.
For their study, Dr. Nathanson and colleagues identified pathogenic germline mutations in 17 cancer susceptibility genes in patients with BRCA1/2-negative breast cancer in two cohorts.
Cohort 1 consisted of 1,000 high-risk breast cancer patients – 551 with multiple primary cancers and 449 with a single breast cancer.
Cohort 2 included 1,804 familial breast cancer patients – 340 with multiple primaries and 1,464 with a single breast cancer.
The researchers assessed mutations in these cohorts and compared them with mutations in a control data set.
Mutation rates and age
Pathogenic mutation rates were higher in both cohorts in patients with multiple primaries as compared with patients with single primaries.
In cohort 1, the overall panel positive rate was 8.53% in the multiple-primaries group and 4.90% in the single-primary group (P = .024).
In cohort 2, the overall panel positive rate was 7.06% in the multiple-primaries group and 4.23% in the single-primary group (P = .034).
In both cohorts, younger age at first breast cancer was associated with higher mutation rates. However, the age at onset of cancers other than breast cancer was not related to mutation rate.
“Regardless of age, mutations in genes other than BRCA1/2 are found in at least 5% of patients with breast cancer and another primary cancer, with up to 25% in patients with their first breast cancer at age 30 years,” Dr. Nathanson said. “This supports the need for multigene panel testing in all patients with breast cancer and another primary cancer.”
“Once a woman has multiple primaries with breast cancer, it doesn’t matter what her family history is, she is more likely to be at risk,” Dr. Nathanson added.
Genetic susceptibility
The researchers also identified genes associated with multiple primary cancers. TP53 and MSH6 mutations were significantly enriched in patients with multiple primaries but not single primaries. ATM and PALB2 mutations were significantly enriched in both groups when compared with controls.
The researchers noted that high-penetrance cancer genes were responsible for higher mutation rates in the cohort enriched for early-onset breast cancer and non–breast cancer second primaries. Moderate-penetrance cancer genes were responsible for the higher mutation rates in the cohort enriched for familial breast cancer and second breast cancer primaries.
“In multiple primary cancers, we found additional genes with moderate penetrance and some genes with high penetrance associated with TP53 and Lynch syndrome,” Dr. Nathanson said.
Cancer prevention and screening
The results of this study could lead to better implementation of cancer prevention and screening strategies, according to the researchers.
“As we look at guidelines in development and NCCN recommendations, our data suggest that age should not be part of the criteria for genetic testing in patients who have more than one primary cancer. These patients are at high risk and should be recommended for screening,” Dr. Nathanson said.
“If you see a patient with multiple primary cancers, refer for genetic testing. Age does not matter,” she reiterated.
Future research will look at potentially missing mutations.
“With targeted sequencing, structurally rearranged genes might be missed for those at risk. We will try to identify cancer susceptibility genes and define the true risk of penetrance of these genes in the general population,” Dr. Nathanson said.
This research was supported by grants from government agencies and foundations as well as the University of Pennsylvania. Dr. Nathanson disclosed no conflicts of interest. Other authors disclosed relationships with a range of companies, all listed in the paper.
SOURCE: Maxwell KN et al. JCO Precis Oncol. 2020. doi: 10.1200/PO.19.00301.
according to a paper published in JCO Precision Oncology.
The authors noted that women with breast cancer have a 4%-16% lifetime risk of a second primary cancer. However, it hasn’t been clear if mutations in genes other than BRCA1/2 are enriched in patients with multiple primary cancers.
“Surprisingly few papers have focused on genetic evaluation of patients with multiple primary cancers,” senior author Katherine L. Nathanson, MD, of the University of Pennsylvania in Philadelphia, said in an interview.
“Ours is one of the first studies to look closely at this issue. We know from clinical experience that these patients are more likely to have more than one genetic mutation,” she added.
For their study, Dr. Nathanson and colleagues identified pathogenic germline mutations in 17 cancer susceptibility genes in patients with BRCA1/2-negative breast cancer in two cohorts.
Cohort 1 consisted of 1,000 high-risk breast cancer patients – 551 with multiple primary cancers and 449 with a single breast cancer.
Cohort 2 included 1,804 familial breast cancer patients – 340 with multiple primaries and 1,464 with a single breast cancer.
The researchers assessed mutations in these cohorts and compared them with mutations in a control data set.
Mutation rates and age
Pathogenic mutation rates were higher in both cohorts in patients with multiple primaries as compared with patients with single primaries.
In cohort 1, the overall panel positive rate was 8.53% in the multiple-primaries group and 4.90% in the single-primary group (P = .024).
In cohort 2, the overall panel positive rate was 7.06% in the multiple-primaries group and 4.23% in the single-primary group (P = .034).
In both cohorts, younger age at first breast cancer was associated with higher mutation rates. However, the age at onset of cancers other than breast cancer was not related to mutation rate.
“Regardless of age, mutations in genes other than BRCA1/2 are found in at least 5% of patients with breast cancer and another primary cancer, with up to 25% in patients with their first breast cancer at age 30 years,” Dr. Nathanson said. “This supports the need for multigene panel testing in all patients with breast cancer and another primary cancer.”
“Once a woman has multiple primaries with breast cancer, it doesn’t matter what her family history is, she is more likely to be at risk,” Dr. Nathanson added.
Genetic susceptibility
The researchers also identified genes associated with multiple primary cancers. TP53 and MSH6 mutations were significantly enriched in patients with multiple primaries but not single primaries. ATM and PALB2 mutations were significantly enriched in both groups when compared with controls.
The researchers noted that high-penetrance cancer genes were responsible for higher mutation rates in the cohort enriched for early-onset breast cancer and non–breast cancer second primaries. Moderate-penetrance cancer genes were responsible for the higher mutation rates in the cohort enriched for familial breast cancer and second breast cancer primaries.
“In multiple primary cancers, we found additional genes with moderate penetrance and some genes with high penetrance associated with TP53 and Lynch syndrome,” Dr. Nathanson said.
Cancer prevention and screening
The results of this study could lead to better implementation of cancer prevention and screening strategies, according to the researchers.
“As we look at guidelines in development and NCCN recommendations, our data suggest that age should not be part of the criteria for genetic testing in patients who have more than one primary cancer. These patients are at high risk and should be recommended for screening,” Dr. Nathanson said.
“If you see a patient with multiple primary cancers, refer for genetic testing. Age does not matter,” she reiterated.
Future research will look at potentially missing mutations.
“With targeted sequencing, structurally rearranged genes might be missed for those at risk. We will try to identify cancer susceptibility genes and define the true risk of penetrance of these genes in the general population,” Dr. Nathanson said.
This research was supported by grants from government agencies and foundations as well as the University of Pennsylvania. Dr. Nathanson disclosed no conflicts of interest. Other authors disclosed relationships with a range of companies, all listed in the paper.
SOURCE: Maxwell KN et al. JCO Precis Oncol. 2020. doi: 10.1200/PO.19.00301.
according to a paper published in JCO Precision Oncology.
The authors noted that women with breast cancer have a 4%-16% lifetime risk of a second primary cancer. However, it hasn’t been clear if mutations in genes other than BRCA1/2 are enriched in patients with multiple primary cancers.
“Surprisingly few papers have focused on genetic evaluation of patients with multiple primary cancers,” senior author Katherine L. Nathanson, MD, of the University of Pennsylvania in Philadelphia, said in an interview.
“Ours is one of the first studies to look closely at this issue. We know from clinical experience that these patients are more likely to have more than one genetic mutation,” she added.
For their study, Dr. Nathanson and colleagues identified pathogenic germline mutations in 17 cancer susceptibility genes in patients with BRCA1/2-negative breast cancer in two cohorts.
Cohort 1 consisted of 1,000 high-risk breast cancer patients – 551 with multiple primary cancers and 449 with a single breast cancer.
Cohort 2 included 1,804 familial breast cancer patients – 340 with multiple primaries and 1,464 with a single breast cancer.
The researchers assessed mutations in these cohorts and compared them with mutations in a control data set.
Mutation rates and age
Pathogenic mutation rates were higher in both cohorts in patients with multiple primaries as compared with patients with single primaries.
In cohort 1, the overall panel positive rate was 8.53% in the multiple-primaries group and 4.90% in the single-primary group (P = .024).
In cohort 2, the overall panel positive rate was 7.06% in the multiple-primaries group and 4.23% in the single-primary group (P = .034).
In both cohorts, younger age at first breast cancer was associated with higher mutation rates. However, the age at onset of cancers other than breast cancer was not related to mutation rate.
“Regardless of age, mutations in genes other than BRCA1/2 are found in at least 5% of patients with breast cancer and another primary cancer, with up to 25% in patients with their first breast cancer at age 30 years,” Dr. Nathanson said. “This supports the need for multigene panel testing in all patients with breast cancer and another primary cancer.”
“Once a woman has multiple primaries with breast cancer, it doesn’t matter what her family history is, she is more likely to be at risk,” Dr. Nathanson added.
Genetic susceptibility
The researchers also identified genes associated with multiple primary cancers. TP53 and MSH6 mutations were significantly enriched in patients with multiple primaries but not single primaries. ATM and PALB2 mutations were significantly enriched in both groups when compared with controls.
The researchers noted that high-penetrance cancer genes were responsible for higher mutation rates in the cohort enriched for early-onset breast cancer and non–breast cancer second primaries. Moderate-penetrance cancer genes were responsible for the higher mutation rates in the cohort enriched for familial breast cancer and second breast cancer primaries.
“In multiple primary cancers, we found additional genes with moderate penetrance and some genes with high penetrance associated with TP53 and Lynch syndrome,” Dr. Nathanson said.
Cancer prevention and screening
The results of this study could lead to better implementation of cancer prevention and screening strategies, according to the researchers.
“As we look at guidelines in development and NCCN recommendations, our data suggest that age should not be part of the criteria for genetic testing in patients who have more than one primary cancer. These patients are at high risk and should be recommended for screening,” Dr. Nathanson said.
“If you see a patient with multiple primary cancers, refer for genetic testing. Age does not matter,” she reiterated.
Future research will look at potentially missing mutations.
“With targeted sequencing, structurally rearranged genes might be missed for those at risk. We will try to identify cancer susceptibility genes and define the true risk of penetrance of these genes in the general population,” Dr. Nathanson said.
This research was supported by grants from government agencies and foundations as well as the University of Pennsylvania. Dr. Nathanson disclosed no conflicts of interest. Other authors disclosed relationships with a range of companies, all listed in the paper.
SOURCE: Maxwell KN et al. JCO Precis Oncol. 2020. doi: 10.1200/PO.19.00301.
FROM JCO PRECISION ONCOLOGY
U.S. tops 500,000 COVID-19 cases in children
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
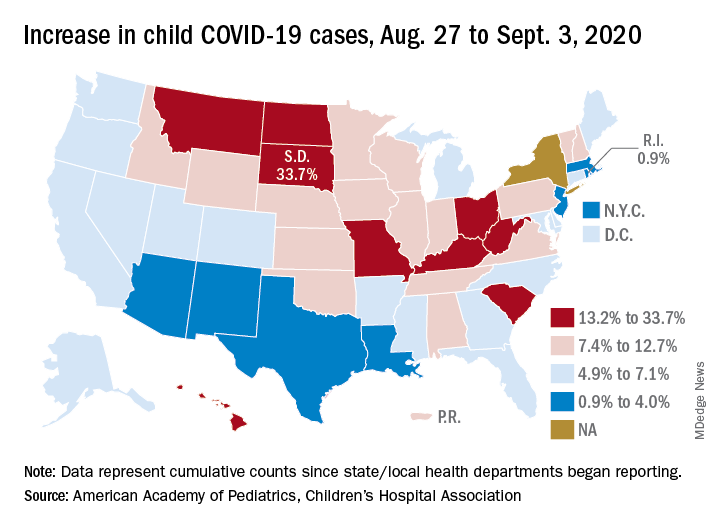
States have reported 513,415 cases of COVID-19 in children since the beginning of the pandemic, with almost 37,000 coming in the last week, the AAP and the CHA said Sept. 8 in the weekly report. That figure includes New York City – the rest of New York State is not reporting ages for COVID-19 patients – as well as Puerto Rico, the District of Columbia, and Guam.
“These numbers are a chilling reminder of why we need to take this virus seriously,” AAP President Sara Goza, MD, said in a written statement.
Children now represent 9.8% of the almost 5.3 million cases that have been reported in Americans of all ages. The proportion of child cases has continued to increase as the pandemic has progressed – it was 8.0% as of mid-July and 5.2% in early June, the data show.
“Throughout the summer, surges in the virus have occurred in Southern, Western, and Midwestern states,” the AAP statement said.
The latest AAP/CHA report shows that, from Aug. 27 to Sept. 3, the total number of child cases jumped by 33.7% in South Dakota, more than any other state. North Dakota was next at 22.7%, followed by Hawaii (18.1%), Missouri (16.8%), and Kentucky (16.4%).
“This rapid rise in positive cases occurred over the summer, and as the weather cools, we know people will spend more time indoors,” said Sean O’Leary, MD, MPH, vice chair of the AAP Committee on Infectious Diseases. “The goal is to get children back into schools for in-person learning, but in many communities, this is not possible as the virus spreads unchecked.”
The smallest increase over the last week, just 0.9%, came in Rhode Island, with Massachusetts just a bit higher at 1.0%. Also at the low end of the increase scale are Arizona (3.3%) and Louisiana (4.0%), two states that have very high rates of cumulative cases: 1,380 per 100,000 children for Arizona and 1,234 per 100,000 for Louisiana, the report said.
To give those figures some context, Tennessee has the highest cumulative count of any state at 1,553 cases per 100,000 children and Vermont has the lowest at 151, based on the data gathered by the AAP and CHA.
“While much remains unknown about COVID-19, we do know that the spread among children reflects what is happening in the broader communities. A disproportionate number of cases are reported in Black and Hispanic children and in places where there is high poverty. We must work harder to address societal inequities that contribute to these disparities,” Dr. Goza said.
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
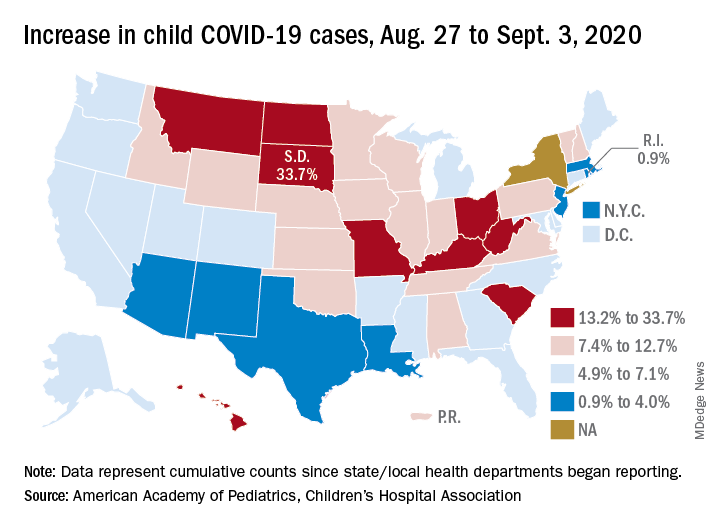
States have reported 513,415 cases of COVID-19 in children since the beginning of the pandemic, with almost 37,000 coming in the last week, the AAP and the CHA said Sept. 8 in the weekly report. That figure includes New York City – the rest of New York State is not reporting ages for COVID-19 patients – as well as Puerto Rico, the District of Columbia, and Guam.
“These numbers are a chilling reminder of why we need to take this virus seriously,” AAP President Sara Goza, MD, said in a written statement.
Children now represent 9.8% of the almost 5.3 million cases that have been reported in Americans of all ages. The proportion of child cases has continued to increase as the pandemic has progressed – it was 8.0% as of mid-July and 5.2% in early June, the data show.
“Throughout the summer, surges in the virus have occurred in Southern, Western, and Midwestern states,” the AAP statement said.
The latest AAP/CHA report shows that, from Aug. 27 to Sept. 3, the total number of child cases jumped by 33.7% in South Dakota, more than any other state. North Dakota was next at 22.7%, followed by Hawaii (18.1%), Missouri (16.8%), and Kentucky (16.4%).
“This rapid rise in positive cases occurred over the summer, and as the weather cools, we know people will spend more time indoors,” said Sean O’Leary, MD, MPH, vice chair of the AAP Committee on Infectious Diseases. “The goal is to get children back into schools for in-person learning, but in many communities, this is not possible as the virus spreads unchecked.”
The smallest increase over the last week, just 0.9%, came in Rhode Island, with Massachusetts just a bit higher at 1.0%. Also at the low end of the increase scale are Arizona (3.3%) and Louisiana (4.0%), two states that have very high rates of cumulative cases: 1,380 per 100,000 children for Arizona and 1,234 per 100,000 for Louisiana, the report said.
To give those figures some context, Tennessee has the highest cumulative count of any state at 1,553 cases per 100,000 children and Vermont has the lowest at 151, based on the data gathered by the AAP and CHA.
“While much remains unknown about COVID-19, we do know that the spread among children reflects what is happening in the broader communities. A disproportionate number of cases are reported in Black and Hispanic children and in places where there is high poverty. We must work harder to address societal inequities that contribute to these disparities,” Dr. Goza said.
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
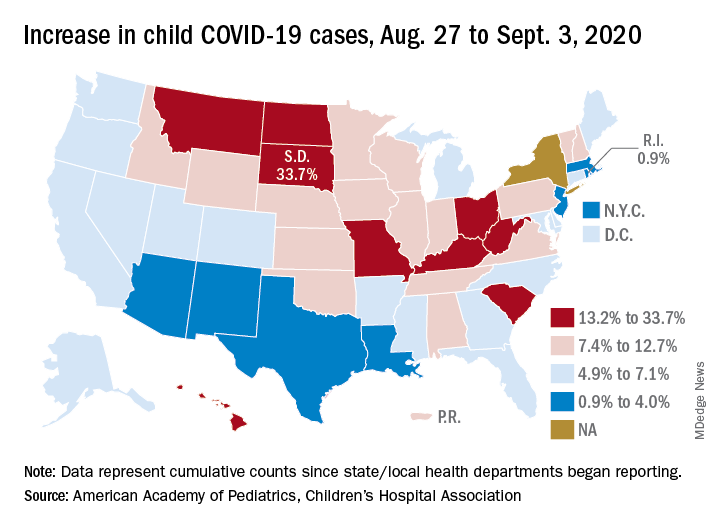
States have reported 513,415 cases of COVID-19 in children since the beginning of the pandemic, with almost 37,000 coming in the last week, the AAP and the CHA said Sept. 8 in the weekly report. That figure includes New York City – the rest of New York State is not reporting ages for COVID-19 patients – as well as Puerto Rico, the District of Columbia, and Guam.
“These numbers are a chilling reminder of why we need to take this virus seriously,” AAP President Sara Goza, MD, said in a written statement.
Children now represent 9.8% of the almost 5.3 million cases that have been reported in Americans of all ages. The proportion of child cases has continued to increase as the pandemic has progressed – it was 8.0% as of mid-July and 5.2% in early June, the data show.
“Throughout the summer, surges in the virus have occurred in Southern, Western, and Midwestern states,” the AAP statement said.
The latest AAP/CHA report shows that, from Aug. 27 to Sept. 3, the total number of child cases jumped by 33.7% in South Dakota, more than any other state. North Dakota was next at 22.7%, followed by Hawaii (18.1%), Missouri (16.8%), and Kentucky (16.4%).
“This rapid rise in positive cases occurred over the summer, and as the weather cools, we know people will spend more time indoors,” said Sean O’Leary, MD, MPH, vice chair of the AAP Committee on Infectious Diseases. “The goal is to get children back into schools for in-person learning, but in many communities, this is not possible as the virus spreads unchecked.”
The smallest increase over the last week, just 0.9%, came in Rhode Island, with Massachusetts just a bit higher at 1.0%. Also at the low end of the increase scale are Arizona (3.3%) and Louisiana (4.0%), two states that have very high rates of cumulative cases: 1,380 per 100,000 children for Arizona and 1,234 per 100,000 for Louisiana, the report said.
To give those figures some context, Tennessee has the highest cumulative count of any state at 1,553 cases per 100,000 children and Vermont has the lowest at 151, based on the data gathered by the AAP and CHA.
“While much remains unknown about COVID-19, we do know that the spread among children reflects what is happening in the broader communities. A disproportionate number of cases are reported in Black and Hispanic children and in places where there is high poverty. We must work harder to address societal inequities that contribute to these disparities,” Dr. Goza said.
Mounting data support COVID-19 acute pancreatitis
Mounting data support acute pancreatitis as one possible GI manifestation of COVID-19, according to investigators.
While previous case reports suggested that infection with SARS-CoV2 may lead to pancreatitis, this retrospective analysis, which is the largest to date, is the first to offer substantial evidence for this claim, reported lead author Sumant Inamdar, MBBS, of the University of Arkansas, Little Rock, and colleagues.
“It has become increasingly clear that COVID-19 has systemic effects that also includes the gastrointestinal and pancreaticobiliary systems,” the investigators wrote in Gastroenterology. “As islet cells of the pancreas contain ACE2 receptor proteins, SARS-CoV2 can bind to these receptors and cause pancreatic injury.”
For the present analysis, Dr. Inamdar and colleagues reviewed charts from 48,012 patients who were hospitalized in New York between March and June of this year. While pancreatitis is usually diagnosed based on two out of three criteria, disease classification in the study required all three: characteristic upper abdominal pain upon admission, lipase greater than three times the upper limit of normal, and evidence of pancreatitis on cross-sectional imaging.
“[B]y including all three criteria for pancreatitis in our definition, we may be underestimating the rate of pancreatitis,” the investigators wrote. “However, we felt including diagnostic lipase levels and imaging was important for the accuracy of the diagnosis.”
Primary outcomes included mechanical ventilation, length of stay, development of pancreatic necrosis, and mortality. Outcomes were compared between patients with and without COVID-19.
Out of 48,012 hospitalized patients, 11,883 (24.75%) tested positive for SARS-CoV2. Across the entire population, 189 patients had pancreatitis (0.39%), and of these, 32 (17%) also had COVID-19. This translates to a point prevalence for pancreatitis of 0.27% for patients hospitalized with COVID-19.
Among patients with pancreatitis who did not have COVID-19, the most common etiologies for pancreatitis were gallstones (34%) and alcohol (37%), compared with just 16% and 6% of SARS-CoV2-positive cases of pancreatitis, respectively. Idiopathic pancreatitis was significantly more common among patients with COVID-19 than those without (69% vs 21%; P less than .0001).
Black or Hispanic patients with pancreatitis were 4-5 times more likely to have COVID-19 than patients with pancreatitis who were white. Across all races/ethnicities, patients with pancreatitis and COVID-19 more often required mechanical ventilation (odds ratio [OR], 5.65) and longer hospital stays (OR, 3.22), compared with those who had pancreatitis alone. While rates of mortality and pancreatic necrosis showed similar trends, associations with COVID-19 were not statistically significant.
“These findings support the notion that pancreatitis should be included in the list of GI manifestations of COVID-19,” the investigators wrote.
When caring for patients with COVID-19, Dr. Inamdar and colleagues recommended that clinicians pay close attention to any history of abdominal pain, and consider testing serum lipase levels.
“Further large studies are needed to confirm our findings,” they concluded.
Gyanprakash Avinash Ketwaroo, MD, of Baylor College of Medicine in Houston, agreed that more work is needed; in the meantime, he suggested that evidence is now strong enough for clinicians to take notice.
“Overall, this study adds further weight to COVID-19 acute pancreatitis,” he said. “Larger studies, and convincing pathophysiologic data, will be needed to confirm COVID-19 as a cause of acute pancreatitis. However, there appears to be enough circumstantial evidence to consider a COVID-19 diagnosis in patients presenting with acute pancreatitis.”
He noted that the new clinical evidence also stands on a solid theoretical foundation.
“Viruses, especially mumps and measles, have long been known to cause acute pancreatitis,” he said. “Additionally, the ACE2 receptor is present on pancreatic beta-cells and may mediate COVID-19 induced pancreatitis.”
Along with larger observational studies, Dr. Ketwaroo suggested that a number of interventional questions remain unanswered.
“While most acute pancreatitis is treated with supportive care, could proven therapies for COVID-19, such as steroids, also mitigate COVID-19 acute pancreatitis?” he asked. “Is COVID-19 a cofactor for acute pancreatitis caused by alcohol or endoscopic retrograde cholangiopancreatography? We await further information from an active area of research.”
The investigators disclosed relationships with Boston Scientific, Olympus, Fujifilm, and others.
SOURCE: Inamdar S et al. Gastroenterology. 2020 Aug 26. doi: 10.1053/j.gastro.2020.08.044.
Mounting data support acute pancreatitis as one possible GI manifestation of COVID-19, according to investigators.
While previous case reports suggested that infection with SARS-CoV2 may lead to pancreatitis, this retrospective analysis, which is the largest to date, is the first to offer substantial evidence for this claim, reported lead author Sumant Inamdar, MBBS, of the University of Arkansas, Little Rock, and colleagues.
“It has become increasingly clear that COVID-19 has systemic effects that also includes the gastrointestinal and pancreaticobiliary systems,” the investigators wrote in Gastroenterology. “As islet cells of the pancreas contain ACE2 receptor proteins, SARS-CoV2 can bind to these receptors and cause pancreatic injury.”
For the present analysis, Dr. Inamdar and colleagues reviewed charts from 48,012 patients who were hospitalized in New York between March and June of this year. While pancreatitis is usually diagnosed based on two out of three criteria, disease classification in the study required all three: characteristic upper abdominal pain upon admission, lipase greater than three times the upper limit of normal, and evidence of pancreatitis on cross-sectional imaging.
“[B]y including all three criteria for pancreatitis in our definition, we may be underestimating the rate of pancreatitis,” the investigators wrote. “However, we felt including diagnostic lipase levels and imaging was important for the accuracy of the diagnosis.”
Primary outcomes included mechanical ventilation, length of stay, development of pancreatic necrosis, and mortality. Outcomes were compared between patients with and without COVID-19.
Out of 48,012 hospitalized patients, 11,883 (24.75%) tested positive for SARS-CoV2. Across the entire population, 189 patients had pancreatitis (0.39%), and of these, 32 (17%) also had COVID-19. This translates to a point prevalence for pancreatitis of 0.27% for patients hospitalized with COVID-19.
Among patients with pancreatitis who did not have COVID-19, the most common etiologies for pancreatitis were gallstones (34%) and alcohol (37%), compared with just 16% and 6% of SARS-CoV2-positive cases of pancreatitis, respectively. Idiopathic pancreatitis was significantly more common among patients with COVID-19 than those without (69% vs 21%; P less than .0001).
Black or Hispanic patients with pancreatitis were 4-5 times more likely to have COVID-19 than patients with pancreatitis who were white. Across all races/ethnicities, patients with pancreatitis and COVID-19 more often required mechanical ventilation (odds ratio [OR], 5.65) and longer hospital stays (OR, 3.22), compared with those who had pancreatitis alone. While rates of mortality and pancreatic necrosis showed similar trends, associations with COVID-19 were not statistically significant.
“These findings support the notion that pancreatitis should be included in the list of GI manifestations of COVID-19,” the investigators wrote.
When caring for patients with COVID-19, Dr. Inamdar and colleagues recommended that clinicians pay close attention to any history of abdominal pain, and consider testing serum lipase levels.
“Further large studies are needed to confirm our findings,” they concluded.
Gyanprakash Avinash Ketwaroo, MD, of Baylor College of Medicine in Houston, agreed that more work is needed; in the meantime, he suggested that evidence is now strong enough for clinicians to take notice.
“Overall, this study adds further weight to COVID-19 acute pancreatitis,” he said. “Larger studies, and convincing pathophysiologic data, will be needed to confirm COVID-19 as a cause of acute pancreatitis. However, there appears to be enough circumstantial evidence to consider a COVID-19 diagnosis in patients presenting with acute pancreatitis.”
He noted that the new clinical evidence also stands on a solid theoretical foundation.
“Viruses, especially mumps and measles, have long been known to cause acute pancreatitis,” he said. “Additionally, the ACE2 receptor is present on pancreatic beta-cells and may mediate COVID-19 induced pancreatitis.”
Along with larger observational studies, Dr. Ketwaroo suggested that a number of interventional questions remain unanswered.
“While most acute pancreatitis is treated with supportive care, could proven therapies for COVID-19, such as steroids, also mitigate COVID-19 acute pancreatitis?” he asked. “Is COVID-19 a cofactor for acute pancreatitis caused by alcohol or endoscopic retrograde cholangiopancreatography? We await further information from an active area of research.”
The investigators disclosed relationships with Boston Scientific, Olympus, Fujifilm, and others.
SOURCE: Inamdar S et al. Gastroenterology. 2020 Aug 26. doi: 10.1053/j.gastro.2020.08.044.
Mounting data support acute pancreatitis as one possible GI manifestation of COVID-19, according to investigators.
While previous case reports suggested that infection with SARS-CoV2 may lead to pancreatitis, this retrospective analysis, which is the largest to date, is the first to offer substantial evidence for this claim, reported lead author Sumant Inamdar, MBBS, of the University of Arkansas, Little Rock, and colleagues.
“It has become increasingly clear that COVID-19 has systemic effects that also includes the gastrointestinal and pancreaticobiliary systems,” the investigators wrote in Gastroenterology. “As islet cells of the pancreas contain ACE2 receptor proteins, SARS-CoV2 can bind to these receptors and cause pancreatic injury.”
For the present analysis, Dr. Inamdar and colleagues reviewed charts from 48,012 patients who were hospitalized in New York between March and June of this year. While pancreatitis is usually diagnosed based on two out of three criteria, disease classification in the study required all three: characteristic upper abdominal pain upon admission, lipase greater than three times the upper limit of normal, and evidence of pancreatitis on cross-sectional imaging.
“[B]y including all three criteria for pancreatitis in our definition, we may be underestimating the rate of pancreatitis,” the investigators wrote. “However, we felt including diagnostic lipase levels and imaging was important for the accuracy of the diagnosis.”
Primary outcomes included mechanical ventilation, length of stay, development of pancreatic necrosis, and mortality. Outcomes were compared between patients with and without COVID-19.
Out of 48,012 hospitalized patients, 11,883 (24.75%) tested positive for SARS-CoV2. Across the entire population, 189 patients had pancreatitis (0.39%), and of these, 32 (17%) also had COVID-19. This translates to a point prevalence for pancreatitis of 0.27% for patients hospitalized with COVID-19.
Among patients with pancreatitis who did not have COVID-19, the most common etiologies for pancreatitis were gallstones (34%) and alcohol (37%), compared with just 16% and 6% of SARS-CoV2-positive cases of pancreatitis, respectively. Idiopathic pancreatitis was significantly more common among patients with COVID-19 than those without (69% vs 21%; P less than .0001).
Black or Hispanic patients with pancreatitis were 4-5 times more likely to have COVID-19 than patients with pancreatitis who were white. Across all races/ethnicities, patients with pancreatitis and COVID-19 more often required mechanical ventilation (odds ratio [OR], 5.65) and longer hospital stays (OR, 3.22), compared with those who had pancreatitis alone. While rates of mortality and pancreatic necrosis showed similar trends, associations with COVID-19 were not statistically significant.
“These findings support the notion that pancreatitis should be included in the list of GI manifestations of COVID-19,” the investigators wrote.
When caring for patients with COVID-19, Dr. Inamdar and colleagues recommended that clinicians pay close attention to any history of abdominal pain, and consider testing serum lipase levels.
“Further large studies are needed to confirm our findings,” they concluded.
Gyanprakash Avinash Ketwaroo, MD, of Baylor College of Medicine in Houston, agreed that more work is needed; in the meantime, he suggested that evidence is now strong enough for clinicians to take notice.
“Overall, this study adds further weight to COVID-19 acute pancreatitis,” he said. “Larger studies, and convincing pathophysiologic data, will be needed to confirm COVID-19 as a cause of acute pancreatitis. However, there appears to be enough circumstantial evidence to consider a COVID-19 diagnosis in patients presenting with acute pancreatitis.”
He noted that the new clinical evidence also stands on a solid theoretical foundation.
“Viruses, especially mumps and measles, have long been known to cause acute pancreatitis,” he said. “Additionally, the ACE2 receptor is present on pancreatic beta-cells and may mediate COVID-19 induced pancreatitis.”
Along with larger observational studies, Dr. Ketwaroo suggested that a number of interventional questions remain unanswered.
“While most acute pancreatitis is treated with supportive care, could proven therapies for COVID-19, such as steroids, also mitigate COVID-19 acute pancreatitis?” he asked. “Is COVID-19 a cofactor for acute pancreatitis caused by alcohol or endoscopic retrograde cholangiopancreatography? We await further information from an active area of research.”
The investigators disclosed relationships with Boston Scientific, Olympus, Fujifilm, and others.
SOURCE: Inamdar S et al. Gastroenterology. 2020 Aug 26. doi: 10.1053/j.gastro.2020.08.044.
FROM GASTROENTEROLOGY
Five reasons why medical meetings will never be the same
In the wake of the COVID-19 pandemic, the virtual medical meeting is now the norm. And while it’s admirable that key data are being disseminated (often for free), there is no escaping the fact that it is a fundamentally different and lesser experience.
Watching from home, most of us split our attention between live streams of the meeting and work and family obligations. There is far less urgency when early live presentations are recorded and can be viewed later.
In terms of discussing the data, Twitter may offer broader participation than a live meeting, yet only a small number of attendees actively engage online.
And the exhibit halls for these online meetings? With neither free coffee nor company-branded tchotchkes, I expect that they have virtual tumbleweeds blowing through and crickets chirping.
Even still, the virtual meeting experience, while inferior to the live one, is a tremendous advance. It should never be banished as a historical footnote but rather should remain an option. It’s analogous to watching the Super Bowl at home: Obviously, it’s not the same as being there, but it’s a terrific alternative. Like telemedicine, this pandemic has provided a critical proof of concept that there is a better model.
Reshaping the medical meeting
Let’s consider five reasons why medical meetings should be permanently reshaped by this pandemic.
This pandemic isn’t going away in 2020. While nearly every country has done a far better job than the United States of containing COVID-19 thus far, outbreaks remain a problem wherever crowds assemble. You’d be hard-pressed to devise a setting more conducive to mass spread than a conference of 20,000 attendees from all over the world sitting alongside each other cheek to jowl for 5 days. Worse yet is the thought of them returning home and infecting their patients, families, and friends. What medical society wants to be remembered for creating a COVID-19 superspreader event? Professional medical societies will need to offer this option as the safest alternative moving forward.
Virtual learning still conveys the most important content. Despite the many social benefits of a live meeting, its core purpose is to disseminate new research and current and emerging treatment options. Virtual meetings have proven that this format can effectively deliver the content, and not as a secondary offering but as the sole platform in real time.
Virtual learning levels the playing field. Traveling to attend conferences typically costs thousands of dollars, accounting for the registration fees, inflated hotel rates, ground transportation, and meals out for days on end. Most meetings also demand several days away from our work and families, forcing many of us to work extra in the days before we leave and upon our return. Parents and those with commitments at home also face special challenges. For international participants, the financial and time costs are even greater. A virtual meeting helps overcome these hurdles and erases barriers that have long precluded many from attending a conference.
Virtual learning is efficient and comfortable. Virtual meetings over the past 6 months have given us a glimpse of an astonishingly more efficient form. If the content seems of a lower magnitude without the fanfare of a live conference, it is in part because so much of a live meeting is spent walking a mile between session rooms, waiting in concession or taxi lines, sitting in traffic between venues, or simply waiting for a session to begin. All of that has been replaced with time that you can use productively in between video sessions viewed either live or on demand. And with a virtual meeting, you can comfortably watch the sessions. There’s no need to stand along the back wall of an overcrowded room or step over 10 people to squeeze into an open middle seat. You can be focused, rather than having an end-of-day presentation wash over you as your eyes cross because you’ve been running around for the past 12 hours.
Virtual learning and social media will only improve. While virtual meetings unquestionably have limitations, it’s important to acknowledge that the successes thus far still represent only the earliest forays into this endeavor. In-person meetings evolved to their present form over centuries. In contrast, virtual meetings are being cobbled together within a few weeks or months. They can only be expected to improve as presenters adapt their skills to the online audience and new tools improve virtual discussions.
I am not implying that live meetings will or should be replaced by virtual ones. We still need that experience of trainees and experts presenting to a live audience and discussing the results together, all while sharing the energy of the moment. But there should be room for both a live conference and a virtual version.
Practically speaking, it is unclear whether professional societies could forgo the revenue they receive from registration fees, meeting sponsorships, and corporate exhibits. Yet, there are certainly ways to obtain sponsorship revenue for a virtual program. Even if the virtual version of a conference costs far less than attending in person, there is plenty of room between that number and free. It costs remarkably little for a professional society to share its content, and virtual offerings further the mission of distributing this content broadly.
We should not rush to return to the previous status quo. Despite their limitations, virtual meetings have brought a new, higher standard of access and efficiency for sharing important new data and treatment options in medicine.
H. Jack West, MD, associate clinical professor and executive director of employer services at City of Hope Comprehensive Cancer Center in Duarte, Calif., regularly comments on lung cancer for Medscape. West serves as web editor for JAMA Oncology, edits and writes several sections on lung cancer for UpToDate, and leads a wide range of continuing education programs and other educational programs, including hosting the audio podcast West Wind.
This article first appeared on Medscape.com.
In the wake of the COVID-19 pandemic, the virtual medical meeting is now the norm. And while it’s admirable that key data are being disseminated (often for free), there is no escaping the fact that it is a fundamentally different and lesser experience.
Watching from home, most of us split our attention between live streams of the meeting and work and family obligations. There is far less urgency when early live presentations are recorded and can be viewed later.
In terms of discussing the data, Twitter may offer broader participation than a live meeting, yet only a small number of attendees actively engage online.
And the exhibit halls for these online meetings? With neither free coffee nor company-branded tchotchkes, I expect that they have virtual tumbleweeds blowing through and crickets chirping.
Even still, the virtual meeting experience, while inferior to the live one, is a tremendous advance. It should never be banished as a historical footnote but rather should remain an option. It’s analogous to watching the Super Bowl at home: Obviously, it’s not the same as being there, but it’s a terrific alternative. Like telemedicine, this pandemic has provided a critical proof of concept that there is a better model.
Reshaping the medical meeting
Let’s consider five reasons why medical meetings should be permanently reshaped by this pandemic.
This pandemic isn’t going away in 2020. While nearly every country has done a far better job than the United States of containing COVID-19 thus far, outbreaks remain a problem wherever crowds assemble. You’d be hard-pressed to devise a setting more conducive to mass spread than a conference of 20,000 attendees from all over the world sitting alongside each other cheek to jowl for 5 days. Worse yet is the thought of them returning home and infecting their patients, families, and friends. What medical society wants to be remembered for creating a COVID-19 superspreader event? Professional medical societies will need to offer this option as the safest alternative moving forward.
Virtual learning still conveys the most important content. Despite the many social benefits of a live meeting, its core purpose is to disseminate new research and current and emerging treatment options. Virtual meetings have proven that this format can effectively deliver the content, and not as a secondary offering but as the sole platform in real time.
Virtual learning levels the playing field. Traveling to attend conferences typically costs thousands of dollars, accounting for the registration fees, inflated hotel rates, ground transportation, and meals out for days on end. Most meetings also demand several days away from our work and families, forcing many of us to work extra in the days before we leave and upon our return. Parents and those with commitments at home also face special challenges. For international participants, the financial and time costs are even greater. A virtual meeting helps overcome these hurdles and erases barriers that have long precluded many from attending a conference.
Virtual learning is efficient and comfortable. Virtual meetings over the past 6 months have given us a glimpse of an astonishingly more efficient form. If the content seems of a lower magnitude without the fanfare of a live conference, it is in part because so much of a live meeting is spent walking a mile between session rooms, waiting in concession or taxi lines, sitting in traffic between venues, or simply waiting for a session to begin. All of that has been replaced with time that you can use productively in between video sessions viewed either live or on demand. And with a virtual meeting, you can comfortably watch the sessions. There’s no need to stand along the back wall of an overcrowded room or step over 10 people to squeeze into an open middle seat. You can be focused, rather than having an end-of-day presentation wash over you as your eyes cross because you’ve been running around for the past 12 hours.
Virtual learning and social media will only improve. While virtual meetings unquestionably have limitations, it’s important to acknowledge that the successes thus far still represent only the earliest forays into this endeavor. In-person meetings evolved to their present form over centuries. In contrast, virtual meetings are being cobbled together within a few weeks or months. They can only be expected to improve as presenters adapt their skills to the online audience and new tools improve virtual discussions.
I am not implying that live meetings will or should be replaced by virtual ones. We still need that experience of trainees and experts presenting to a live audience and discussing the results together, all while sharing the energy of the moment. But there should be room for both a live conference and a virtual version.
Practically speaking, it is unclear whether professional societies could forgo the revenue they receive from registration fees, meeting sponsorships, and corporate exhibits. Yet, there are certainly ways to obtain sponsorship revenue for a virtual program. Even if the virtual version of a conference costs far less than attending in person, there is plenty of room between that number and free. It costs remarkably little for a professional society to share its content, and virtual offerings further the mission of distributing this content broadly.
We should not rush to return to the previous status quo. Despite their limitations, virtual meetings have brought a new, higher standard of access and efficiency for sharing important new data and treatment options in medicine.
H. Jack West, MD, associate clinical professor and executive director of employer services at City of Hope Comprehensive Cancer Center in Duarte, Calif., regularly comments on lung cancer for Medscape. West serves as web editor for JAMA Oncology, edits and writes several sections on lung cancer for UpToDate, and leads a wide range of continuing education programs and other educational programs, including hosting the audio podcast West Wind.
This article first appeared on Medscape.com.
In the wake of the COVID-19 pandemic, the virtual medical meeting is now the norm. And while it’s admirable that key data are being disseminated (often for free), there is no escaping the fact that it is a fundamentally different and lesser experience.
Watching from home, most of us split our attention between live streams of the meeting and work and family obligations. There is far less urgency when early live presentations are recorded and can be viewed later.
In terms of discussing the data, Twitter may offer broader participation than a live meeting, yet only a small number of attendees actively engage online.
And the exhibit halls for these online meetings? With neither free coffee nor company-branded tchotchkes, I expect that they have virtual tumbleweeds blowing through and crickets chirping.
Even still, the virtual meeting experience, while inferior to the live one, is a tremendous advance. It should never be banished as a historical footnote but rather should remain an option. It’s analogous to watching the Super Bowl at home: Obviously, it’s not the same as being there, but it’s a terrific alternative. Like telemedicine, this pandemic has provided a critical proof of concept that there is a better model.
Reshaping the medical meeting
Let’s consider five reasons why medical meetings should be permanently reshaped by this pandemic.
This pandemic isn’t going away in 2020. While nearly every country has done a far better job than the United States of containing COVID-19 thus far, outbreaks remain a problem wherever crowds assemble. You’d be hard-pressed to devise a setting more conducive to mass spread than a conference of 20,000 attendees from all over the world sitting alongside each other cheek to jowl for 5 days. Worse yet is the thought of them returning home and infecting their patients, families, and friends. What medical society wants to be remembered for creating a COVID-19 superspreader event? Professional medical societies will need to offer this option as the safest alternative moving forward.
Virtual learning still conveys the most important content. Despite the many social benefits of a live meeting, its core purpose is to disseminate new research and current and emerging treatment options. Virtual meetings have proven that this format can effectively deliver the content, and not as a secondary offering but as the sole platform in real time.
Virtual learning levels the playing field. Traveling to attend conferences typically costs thousands of dollars, accounting for the registration fees, inflated hotel rates, ground transportation, and meals out for days on end. Most meetings also demand several days away from our work and families, forcing many of us to work extra in the days before we leave and upon our return. Parents and those with commitments at home also face special challenges. For international participants, the financial and time costs are even greater. A virtual meeting helps overcome these hurdles and erases barriers that have long precluded many from attending a conference.
Virtual learning is efficient and comfortable. Virtual meetings over the past 6 months have given us a glimpse of an astonishingly more efficient form. If the content seems of a lower magnitude without the fanfare of a live conference, it is in part because so much of a live meeting is spent walking a mile between session rooms, waiting in concession or taxi lines, sitting in traffic between venues, or simply waiting for a session to begin. All of that has been replaced with time that you can use productively in between video sessions viewed either live or on demand. And with a virtual meeting, you can comfortably watch the sessions. There’s no need to stand along the back wall of an overcrowded room or step over 10 people to squeeze into an open middle seat. You can be focused, rather than having an end-of-day presentation wash over you as your eyes cross because you’ve been running around for the past 12 hours.
Virtual learning and social media will only improve. While virtual meetings unquestionably have limitations, it’s important to acknowledge that the successes thus far still represent only the earliest forays into this endeavor. In-person meetings evolved to their present form over centuries. In contrast, virtual meetings are being cobbled together within a few weeks or months. They can only be expected to improve as presenters adapt their skills to the online audience and new tools improve virtual discussions.
I am not implying that live meetings will or should be replaced by virtual ones. We still need that experience of trainees and experts presenting to a live audience and discussing the results together, all while sharing the energy of the moment. But there should be room for both a live conference and a virtual version.
Practically speaking, it is unclear whether professional societies could forgo the revenue they receive from registration fees, meeting sponsorships, and corporate exhibits. Yet, there are certainly ways to obtain sponsorship revenue for a virtual program. Even if the virtual version of a conference costs far less than attending in person, there is plenty of room between that number and free. It costs remarkably little for a professional society to share its content, and virtual offerings further the mission of distributing this content broadly.
We should not rush to return to the previous status quo. Despite their limitations, virtual meetings have brought a new, higher standard of access and efficiency for sharing important new data and treatment options in medicine.
H. Jack West, MD, associate clinical professor and executive director of employer services at City of Hope Comprehensive Cancer Center in Duarte, Calif., regularly comments on lung cancer for Medscape. West serves as web editor for JAMA Oncology, edits and writes several sections on lung cancer for UpToDate, and leads a wide range of continuing education programs and other educational programs, including hosting the audio podcast West Wind.
This article first appeared on Medscape.com.
Lowering rituximab dose in patients with MS proves safe and effective
“Given its favorable cost-effectiveness profile, [rituximab] remains a valuable treatment option in the current landscape of MS treatments, even at the reduced dose,” wrote Giulio Disanto, MD, PhD, of the Neurocenter of Southern Switzerland in Lugano, and coauthors. The study was published in Multiple Sclerosis Journal.
To determine the clinical and radiologic effectiveness of deescalating rituximab dosage – along with assessing any adverse outcomes – this observational, single-center study examined 59 patients with MS who had been treated with rituximab at 1,000 mg for at least 1 year before the study began. Roughly 63% (n = 37) of the patients had relapsing remitting MS (RRMS), while the rest (n = 22) had secondary progressive disease (SPD). Their median age was 51, and nearly 75% were women.
All patients underwent neurologic examinations at baseline and then every 3 months for 1 year, with new symptoms, infections, or adverse events being assessed via the Expanded Disability Status Scale (EDSS). They also underwent brain and spinal MRI at baseline and at 12 months while blood samples were taken at baseline and then every 3 months for 1 year, with previous data for both collected when available.
Study results
All 59 patients completed 12-month follow-up, and no relapses occurred in the year after lowering rituximab dosage to 500 mg. No significant differences were observed when comparing EDSS scores at the start of the 1,000-mg dose with the start of the 500-mg dose (Wilcoxon P = .131) as well as from the start of the 500-mg dose to the end of follow-up (Wilcoxon P = .284). Analyzing RRMS and SPD patients separately also led to no differences in EDSS scores from the start of the 500-mg dose to the end of follow-up (Wilcoxon P = .531; Wilcoxon P = .408).
During the 1,000-mg treatment period the number of patients who developed at least one new T2 lesion on their brain or spine was 9 and 4, respectively. During the 500-mg period, just one patient developed a new T2 brain lesion and two patients developed new T2 spine lesions. IgG and IgM levels did not change from the start of 500-mg treatment, although total dose of rituximab was inversely associated with IgG concentrations when previous treatment with 1,000 mg was factored in (coefficient, −0.439; P = 0.041).
A total of 33 patients reported at least one adverse event during the 500-mg treatment period, with only three events being classified as serious: one pancreatitis, one coronary stenting, and one neutropenia.
Validating clinical experience
“This randomized trial is an important step,” said Timothy Vollmer, MD, of the Rocky Mountain MS Center in Westminster, Colo., in an interview. “It clearly supports that you can lessen the dose, which will allow us to use this revolutionary drug for a longer period of time in patients.”
Dr. Vollmer noted that, at his center, they have been using 500 mg of rituximab over a 6-month period since 2010 without a formal clinical trial and with no notable difference in adverse outcomes on MRIs or disability scales. “This validates what we’ve been doing, which we appreciate,” he said.
“The next thing you have to do is determine whether you really have to give it every 6 months,” he added, “because the treatment effect in most patients will last, in terms of B-cell depletion, about a year or more. What we should be testing next is giving the 500 mg and waiting until patients begin to recover B cells before we give them the next cycle, to see if that helps decrease the major side effect, which is a drop in IgG levels.”
The authors acknowledged their study’s limitations, including a moderate sample size, a short follow-up period after 500-mg dosage, and an inability to confirm consistency among 1,000-mg dose administration among all patients, which “may well influence efficacy and safety measures.”
The study was supported by the Neurocenter of Southern Switzerland. One author declared numerous potential conflicts of interest, including receiving speaker fees, research fees, and travel support, and serving on advisory boards for various foundations, universities, and pharmaceutical companies.
SOURCE: Disanto G et al. Mult Scler J. 2020 Aug 25. doi: 10.1177/1352458520952036.
“Given its favorable cost-effectiveness profile, [rituximab] remains a valuable treatment option in the current landscape of MS treatments, even at the reduced dose,” wrote Giulio Disanto, MD, PhD, of the Neurocenter of Southern Switzerland in Lugano, and coauthors. The study was published in Multiple Sclerosis Journal.
To determine the clinical and radiologic effectiveness of deescalating rituximab dosage – along with assessing any adverse outcomes – this observational, single-center study examined 59 patients with MS who had been treated with rituximab at 1,000 mg for at least 1 year before the study began. Roughly 63% (n = 37) of the patients had relapsing remitting MS (RRMS), while the rest (n = 22) had secondary progressive disease (SPD). Their median age was 51, and nearly 75% were women.
All patients underwent neurologic examinations at baseline and then every 3 months for 1 year, with new symptoms, infections, or adverse events being assessed via the Expanded Disability Status Scale (EDSS). They also underwent brain and spinal MRI at baseline and at 12 months while blood samples were taken at baseline and then every 3 months for 1 year, with previous data for both collected when available.
Study results
All 59 patients completed 12-month follow-up, and no relapses occurred in the year after lowering rituximab dosage to 500 mg. No significant differences were observed when comparing EDSS scores at the start of the 1,000-mg dose with the start of the 500-mg dose (Wilcoxon P = .131) as well as from the start of the 500-mg dose to the end of follow-up (Wilcoxon P = .284). Analyzing RRMS and SPD patients separately also led to no differences in EDSS scores from the start of the 500-mg dose to the end of follow-up (Wilcoxon P = .531; Wilcoxon P = .408).
During the 1,000-mg treatment period the number of patients who developed at least one new T2 lesion on their brain or spine was 9 and 4, respectively. During the 500-mg period, just one patient developed a new T2 brain lesion and two patients developed new T2 spine lesions. IgG and IgM levels did not change from the start of 500-mg treatment, although total dose of rituximab was inversely associated with IgG concentrations when previous treatment with 1,000 mg was factored in (coefficient, −0.439; P = 0.041).
A total of 33 patients reported at least one adverse event during the 500-mg treatment period, with only three events being classified as serious: one pancreatitis, one coronary stenting, and one neutropenia.
Validating clinical experience
“This randomized trial is an important step,” said Timothy Vollmer, MD, of the Rocky Mountain MS Center in Westminster, Colo., in an interview. “It clearly supports that you can lessen the dose, which will allow us to use this revolutionary drug for a longer period of time in patients.”
Dr. Vollmer noted that, at his center, they have been using 500 mg of rituximab over a 6-month period since 2010 without a formal clinical trial and with no notable difference in adverse outcomes on MRIs or disability scales. “This validates what we’ve been doing, which we appreciate,” he said.
“The next thing you have to do is determine whether you really have to give it every 6 months,” he added, “because the treatment effect in most patients will last, in terms of B-cell depletion, about a year or more. What we should be testing next is giving the 500 mg and waiting until patients begin to recover B cells before we give them the next cycle, to see if that helps decrease the major side effect, which is a drop in IgG levels.”
The authors acknowledged their study’s limitations, including a moderate sample size, a short follow-up period after 500-mg dosage, and an inability to confirm consistency among 1,000-mg dose administration among all patients, which “may well influence efficacy and safety measures.”
The study was supported by the Neurocenter of Southern Switzerland. One author declared numerous potential conflicts of interest, including receiving speaker fees, research fees, and travel support, and serving on advisory boards for various foundations, universities, and pharmaceutical companies.
SOURCE: Disanto G et al. Mult Scler J. 2020 Aug 25. doi: 10.1177/1352458520952036.
“Given its favorable cost-effectiveness profile, [rituximab] remains a valuable treatment option in the current landscape of MS treatments, even at the reduced dose,” wrote Giulio Disanto, MD, PhD, of the Neurocenter of Southern Switzerland in Lugano, and coauthors. The study was published in Multiple Sclerosis Journal.
To determine the clinical and radiologic effectiveness of deescalating rituximab dosage – along with assessing any adverse outcomes – this observational, single-center study examined 59 patients with MS who had been treated with rituximab at 1,000 mg for at least 1 year before the study began. Roughly 63% (n = 37) of the patients had relapsing remitting MS (RRMS), while the rest (n = 22) had secondary progressive disease (SPD). Their median age was 51, and nearly 75% were women.
All patients underwent neurologic examinations at baseline and then every 3 months for 1 year, with new symptoms, infections, or adverse events being assessed via the Expanded Disability Status Scale (EDSS). They also underwent brain and spinal MRI at baseline and at 12 months while blood samples were taken at baseline and then every 3 months for 1 year, with previous data for both collected when available.
Study results
All 59 patients completed 12-month follow-up, and no relapses occurred in the year after lowering rituximab dosage to 500 mg. No significant differences were observed when comparing EDSS scores at the start of the 1,000-mg dose with the start of the 500-mg dose (Wilcoxon P = .131) as well as from the start of the 500-mg dose to the end of follow-up (Wilcoxon P = .284). Analyzing RRMS and SPD patients separately also led to no differences in EDSS scores from the start of the 500-mg dose to the end of follow-up (Wilcoxon P = .531; Wilcoxon P = .408).
During the 1,000-mg treatment period the number of patients who developed at least one new T2 lesion on their brain or spine was 9 and 4, respectively. During the 500-mg period, just one patient developed a new T2 brain lesion and two patients developed new T2 spine lesions. IgG and IgM levels did not change from the start of 500-mg treatment, although total dose of rituximab was inversely associated with IgG concentrations when previous treatment with 1,000 mg was factored in (coefficient, −0.439; P = 0.041).
A total of 33 patients reported at least one adverse event during the 500-mg treatment period, with only three events being classified as serious: one pancreatitis, one coronary stenting, and one neutropenia.
Validating clinical experience
“This randomized trial is an important step,” said Timothy Vollmer, MD, of the Rocky Mountain MS Center in Westminster, Colo., in an interview. “It clearly supports that you can lessen the dose, which will allow us to use this revolutionary drug for a longer period of time in patients.”
Dr. Vollmer noted that, at his center, they have been using 500 mg of rituximab over a 6-month period since 2010 without a formal clinical trial and with no notable difference in adverse outcomes on MRIs or disability scales. “This validates what we’ve been doing, which we appreciate,” he said.
“The next thing you have to do is determine whether you really have to give it every 6 months,” he added, “because the treatment effect in most patients will last, in terms of B-cell depletion, about a year or more. What we should be testing next is giving the 500 mg and waiting until patients begin to recover B cells before we give them the next cycle, to see if that helps decrease the major side effect, which is a drop in IgG levels.”
The authors acknowledged their study’s limitations, including a moderate sample size, a short follow-up period after 500-mg dosage, and an inability to confirm consistency among 1,000-mg dose administration among all patients, which “may well influence efficacy and safety measures.”
The study was supported by the Neurocenter of Southern Switzerland. One author declared numerous potential conflicts of interest, including receiving speaker fees, research fees, and travel support, and serving on advisory boards for various foundations, universities, and pharmaceutical companies.
SOURCE: Disanto G et al. Mult Scler J. 2020 Aug 25. doi: 10.1177/1352458520952036.
FROM MULTIPLE SCLEROSIS JOURNAL













