User login
Recommendations from a gynecologic oncologist to a general ob.gyn., part 2
In this month’s column we continue to discuss recommendations from the gynecologic oncologist to the general gynecologist.
Don’t screen average-risk women for ovarian cancer.
Ovarian cancer is most often diagnosed at an advanced stage, which limits the curability of the disease. Consequently, there is a strong focus on attempting to diagnose the disease at earlier, more curable stages. This leads to the impulse by some well-intentioned providers to implement screening tests, such as ultrasounds and tumor markers, for all women. Unfortunately, the screening of “average risk” women for ovarian cancer is not recommended. Randomized controlled trials of tens of thousands of women have not observed a clinically significant decrease in ovarian cancer mortality with the addition of screening with tumor markers and ultrasound.1 These studies did observe a false-positive rate of 5%. While that may seem like a low rate of false-positive testing, the definitive diagnostic test which follows is a major abdominal surgery (oophorectomy) and serious complications are encountered in 15% of patients undergoing surgery for false-positive ovarian cancer screening.1 Therefore, quite simply, the harms are not balanced by benefits.
The key to offering patients appropriate and effective screening is case selection. It is important to identify which patients are at higher risk for ovarian cancer and offer those women testing for germline mutations and screening strategies. An important component of a well-woman visit is to take a thorough family history of cancer. Women are considered at high risk for having hereditary predisposition to ovarian cancer if they have a first- or second-degree relative with breast cancer younger than 45-50 years, or any age if Ashkenazi Jewish, triple-negative breast cancer younger than 60 years of age, two or more primary breast cancers with the first diagnosed at less than 50 years of age, male breast cancer, ovarian cancer, pancreatic cancer, a known BRCA 1/2 mutation, or a personal history of those same conditions. These women should be recommended to undergo genetic testing for BRCA 1, 2, and Lynch syndrome. They should not automatically be offered ovarian cancer screening. If a patient has a more remote family history for ovarian cancer, their personal risk may be somewhat elevated above the baseline population risk, however, not substantially enough to justify implementing screening in the absence of a confirmed genetic mutation.
While screening tests may not be appropriate for all patients, all patients should be asked about the early symptoms of ovarian cancer because these are consistently present, and frequently overlooked, prior to the eventual diagnosis of advanced disease. Those symptoms include abdominal discomfort, abdominal swelling and bloating, and urinary urgency.2 Consider offering all patients a dedicated ovarian cancer specific review of systems that includes inquiries about these symptoms at their annual wellness visits.
Opt for vertical midline incisions when surgery is anticipated to be complex
What is the first thing gynecologic oncologists do when called in to assist in a difficult gynecologic procedure? Get better exposure. Exposure is the cornerstone of safe, effective surgery. Sometimes this simply means placing a more effective retractor. In other cases, it might mean extending the incision. However, if the incision is a low transverse incision (the go-to for many gynecologists because of its favorable cosmetic and pain-producing profile) this proves to be difficult. Attempting to assist in a complicated case, such as a frozen pelvis, severed ureter or rectal injury, through a pfannensteil incision can be extraordinarily difficult, and while these incisions can be extended by incising the rectus muscle bellies, upper abdominal visualization remains elusive in most patients. This is particularly problematic if the ureter or splenic flexure need to be mobilized, or if extensive lysis of adhesions is necessary to ensure there is no occult enterotomy. As my mentor Dr. John Soper once described to me: “It’s like trying to scratch your armpit by reaching through your fly.”
While pfannensteil incisions come naturally, and comfortably, to most gynecologists, likely because of their frequent application during cesarean section, all gynecologists should be confident in the steps and anatomy for vertical midline, or paramedian incisions. This is not only beneficial for complex gynecologic cases, but also in the event of vascular emergency. In the hands of an experienced abdominal/pelvic surgeon, the vertical midline incision is the quickest way to safely enter the abdomen, and provides the kind of exposure that may be critical in safely repairing or controlling hemorrhage from a major vessel.
While low transverse incisions may be more cosmetic, less painful, and associated with fewer wound complications, our first concern as surgeons should be mitigating complications. In situations where risks of complications are high, it is best to not handicap ourselves with the incision location. And always remember, wound complications are highest when a transverse incision needs to be converted to a vertical one with a “T.”
It’s not just about diagnosis of cancer, it’s also prevention
Detection of cancer is an important role of the obstetrician gynecologist. However, equally important is being able to seize opportunities for cancer prevention. Cervical, vulvar, endometrial and ovarian cancer are all known to have preventative strategies.
All patients up to the age of 45 should be offered vaccination against HPV. Initial indications for HPV vaccination were for women up to age 26; however, recent data support the safety and efficacy of the vaccine in older women.3 HPV vaccination is most effective at preventing cancer when administered prior to exposure (ideally age 9-11), leaving this in the hands of our pediatrician colleagues. However, we must be vigilant to inquire about vaccination status for all our patients and encourage vaccines for those who were missed earlier in their life.
Patients should be counseled regarding the significant risk reduction for cancer that is gained from use of oral hormonal contraceptives and progestin-releasing IUDs (especially for endometrial and ovarian cancers). Providing them with knowledge of this information when considering options for contraception or menstrual cycle management is important in their decision-making process.
Endometrial cancer incidence is sadly on the rise in the United States, likely secondary to increasing rates of obesity. Pregnancy is a time when many women begin to gain, and accumulate, weight and therefore obstetric providers have a unique opportunity to assist patients in strategies to normalize their weight after pregnancy. Many of my patients with endometrial cancer state that they have never heard that it is associated with obesity. This suggests that more can be done to educate patients on the carcinogenic effect of obesity (for both endometrial and breast cancer), which may aid in motivating change of modifiable behaviors.
The fallopian tubes are the source of many ovarian cancers and knowledge of this has led to the recommendation to perform opportunistic salpingectomy as a cancer risk-reducing strategy. Hysterectomy and sterilization procedures are most apropos for this modification. While prospective data to confirm a reduced risk of ovarian cancer with opportunistic salpingectomy are lacking, a reduced incidence of cancer has been observed when the tubes have been removed for indicated surgeries; there appear to be no significant deleterious sequelae.4,5 A focus should be made on removal of the entire distal third of the tube, particularly the fimbriated ends, as this is the portion most implicated in malignancy.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant disclosures. Contact her at [email protected].
References
1. Buys SS et al. JAMA. 2011;305(22):2295.
2. Goff BA et al. JAMA. 2004;291(22):2705.
3. Castellsagué X et al. Br J Cancer. 2011;105(1):28.
4. Yoon SH et al. Eur J Cancer. 2016 Mar;55:38-46.
5. Hanley GE et al. Am J Obstet Gynecol. 2018;219(2):172.
In this month’s column we continue to discuss recommendations from the gynecologic oncologist to the general gynecologist.
Don’t screen average-risk women for ovarian cancer.
Ovarian cancer is most often diagnosed at an advanced stage, which limits the curability of the disease. Consequently, there is a strong focus on attempting to diagnose the disease at earlier, more curable stages. This leads to the impulse by some well-intentioned providers to implement screening tests, such as ultrasounds and tumor markers, for all women. Unfortunately, the screening of “average risk” women for ovarian cancer is not recommended. Randomized controlled trials of tens of thousands of women have not observed a clinically significant decrease in ovarian cancer mortality with the addition of screening with tumor markers and ultrasound.1 These studies did observe a false-positive rate of 5%. While that may seem like a low rate of false-positive testing, the definitive diagnostic test which follows is a major abdominal surgery (oophorectomy) and serious complications are encountered in 15% of patients undergoing surgery for false-positive ovarian cancer screening.1 Therefore, quite simply, the harms are not balanced by benefits.
The key to offering patients appropriate and effective screening is case selection. It is important to identify which patients are at higher risk for ovarian cancer and offer those women testing for germline mutations and screening strategies. An important component of a well-woman visit is to take a thorough family history of cancer. Women are considered at high risk for having hereditary predisposition to ovarian cancer if they have a first- or second-degree relative with breast cancer younger than 45-50 years, or any age if Ashkenazi Jewish, triple-negative breast cancer younger than 60 years of age, two or more primary breast cancers with the first diagnosed at less than 50 years of age, male breast cancer, ovarian cancer, pancreatic cancer, a known BRCA 1/2 mutation, or a personal history of those same conditions. These women should be recommended to undergo genetic testing for BRCA 1, 2, and Lynch syndrome. They should not automatically be offered ovarian cancer screening. If a patient has a more remote family history for ovarian cancer, their personal risk may be somewhat elevated above the baseline population risk, however, not substantially enough to justify implementing screening in the absence of a confirmed genetic mutation.
While screening tests may not be appropriate for all patients, all patients should be asked about the early symptoms of ovarian cancer because these are consistently present, and frequently overlooked, prior to the eventual diagnosis of advanced disease. Those symptoms include abdominal discomfort, abdominal swelling and bloating, and urinary urgency.2 Consider offering all patients a dedicated ovarian cancer specific review of systems that includes inquiries about these symptoms at their annual wellness visits.
Opt for vertical midline incisions when surgery is anticipated to be complex
What is the first thing gynecologic oncologists do when called in to assist in a difficult gynecologic procedure? Get better exposure. Exposure is the cornerstone of safe, effective surgery. Sometimes this simply means placing a more effective retractor. In other cases, it might mean extending the incision. However, if the incision is a low transverse incision (the go-to for many gynecologists because of its favorable cosmetic and pain-producing profile) this proves to be difficult. Attempting to assist in a complicated case, such as a frozen pelvis, severed ureter or rectal injury, through a pfannensteil incision can be extraordinarily difficult, and while these incisions can be extended by incising the rectus muscle bellies, upper abdominal visualization remains elusive in most patients. This is particularly problematic if the ureter or splenic flexure need to be mobilized, or if extensive lysis of adhesions is necessary to ensure there is no occult enterotomy. As my mentor Dr. John Soper once described to me: “It’s like trying to scratch your armpit by reaching through your fly.”
While pfannensteil incisions come naturally, and comfortably, to most gynecologists, likely because of their frequent application during cesarean section, all gynecologists should be confident in the steps and anatomy for vertical midline, or paramedian incisions. This is not only beneficial for complex gynecologic cases, but also in the event of vascular emergency. In the hands of an experienced abdominal/pelvic surgeon, the vertical midline incision is the quickest way to safely enter the abdomen, and provides the kind of exposure that may be critical in safely repairing or controlling hemorrhage from a major vessel.
While low transverse incisions may be more cosmetic, less painful, and associated with fewer wound complications, our first concern as surgeons should be mitigating complications. In situations where risks of complications are high, it is best to not handicap ourselves with the incision location. And always remember, wound complications are highest when a transverse incision needs to be converted to a vertical one with a “T.”
It’s not just about diagnosis of cancer, it’s also prevention
Detection of cancer is an important role of the obstetrician gynecologist. However, equally important is being able to seize opportunities for cancer prevention. Cervical, vulvar, endometrial and ovarian cancer are all known to have preventative strategies.
All patients up to the age of 45 should be offered vaccination against HPV. Initial indications for HPV vaccination were for women up to age 26; however, recent data support the safety and efficacy of the vaccine in older women.3 HPV vaccination is most effective at preventing cancer when administered prior to exposure (ideally age 9-11), leaving this in the hands of our pediatrician colleagues. However, we must be vigilant to inquire about vaccination status for all our patients and encourage vaccines for those who were missed earlier in their life.
Patients should be counseled regarding the significant risk reduction for cancer that is gained from use of oral hormonal contraceptives and progestin-releasing IUDs (especially for endometrial and ovarian cancers). Providing them with knowledge of this information when considering options for contraception or menstrual cycle management is important in their decision-making process.
Endometrial cancer incidence is sadly on the rise in the United States, likely secondary to increasing rates of obesity. Pregnancy is a time when many women begin to gain, and accumulate, weight and therefore obstetric providers have a unique opportunity to assist patients in strategies to normalize their weight after pregnancy. Many of my patients with endometrial cancer state that they have never heard that it is associated with obesity. This suggests that more can be done to educate patients on the carcinogenic effect of obesity (for both endometrial and breast cancer), which may aid in motivating change of modifiable behaviors.
The fallopian tubes are the source of many ovarian cancers and knowledge of this has led to the recommendation to perform opportunistic salpingectomy as a cancer risk-reducing strategy. Hysterectomy and sterilization procedures are most apropos for this modification. While prospective data to confirm a reduced risk of ovarian cancer with opportunistic salpingectomy are lacking, a reduced incidence of cancer has been observed when the tubes have been removed for indicated surgeries; there appear to be no significant deleterious sequelae.4,5 A focus should be made on removal of the entire distal third of the tube, particularly the fimbriated ends, as this is the portion most implicated in malignancy.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant disclosures. Contact her at [email protected].
References
1. Buys SS et al. JAMA. 2011;305(22):2295.
2. Goff BA et al. JAMA. 2004;291(22):2705.
3. Castellsagué X et al. Br J Cancer. 2011;105(1):28.
4. Yoon SH et al. Eur J Cancer. 2016 Mar;55:38-46.
5. Hanley GE et al. Am J Obstet Gynecol. 2018;219(2):172.
In this month’s column we continue to discuss recommendations from the gynecologic oncologist to the general gynecologist.
Don’t screen average-risk women for ovarian cancer.
Ovarian cancer is most often diagnosed at an advanced stage, which limits the curability of the disease. Consequently, there is a strong focus on attempting to diagnose the disease at earlier, more curable stages. This leads to the impulse by some well-intentioned providers to implement screening tests, such as ultrasounds and tumor markers, for all women. Unfortunately, the screening of “average risk” women for ovarian cancer is not recommended. Randomized controlled trials of tens of thousands of women have not observed a clinically significant decrease in ovarian cancer mortality with the addition of screening with tumor markers and ultrasound.1 These studies did observe a false-positive rate of 5%. While that may seem like a low rate of false-positive testing, the definitive diagnostic test which follows is a major abdominal surgery (oophorectomy) and serious complications are encountered in 15% of patients undergoing surgery for false-positive ovarian cancer screening.1 Therefore, quite simply, the harms are not balanced by benefits.
The key to offering patients appropriate and effective screening is case selection. It is important to identify which patients are at higher risk for ovarian cancer and offer those women testing for germline mutations and screening strategies. An important component of a well-woman visit is to take a thorough family history of cancer. Women are considered at high risk for having hereditary predisposition to ovarian cancer if they have a first- or second-degree relative with breast cancer younger than 45-50 years, or any age if Ashkenazi Jewish, triple-negative breast cancer younger than 60 years of age, two or more primary breast cancers with the first diagnosed at less than 50 years of age, male breast cancer, ovarian cancer, pancreatic cancer, a known BRCA 1/2 mutation, or a personal history of those same conditions. These women should be recommended to undergo genetic testing for BRCA 1, 2, and Lynch syndrome. They should not automatically be offered ovarian cancer screening. If a patient has a more remote family history for ovarian cancer, their personal risk may be somewhat elevated above the baseline population risk, however, not substantially enough to justify implementing screening in the absence of a confirmed genetic mutation.
While screening tests may not be appropriate for all patients, all patients should be asked about the early symptoms of ovarian cancer because these are consistently present, and frequently overlooked, prior to the eventual diagnosis of advanced disease. Those symptoms include abdominal discomfort, abdominal swelling and bloating, and urinary urgency.2 Consider offering all patients a dedicated ovarian cancer specific review of systems that includes inquiries about these symptoms at their annual wellness visits.
Opt for vertical midline incisions when surgery is anticipated to be complex
What is the first thing gynecologic oncologists do when called in to assist in a difficult gynecologic procedure? Get better exposure. Exposure is the cornerstone of safe, effective surgery. Sometimes this simply means placing a more effective retractor. In other cases, it might mean extending the incision. However, if the incision is a low transverse incision (the go-to for many gynecologists because of its favorable cosmetic and pain-producing profile) this proves to be difficult. Attempting to assist in a complicated case, such as a frozen pelvis, severed ureter or rectal injury, through a pfannensteil incision can be extraordinarily difficult, and while these incisions can be extended by incising the rectus muscle bellies, upper abdominal visualization remains elusive in most patients. This is particularly problematic if the ureter or splenic flexure need to be mobilized, or if extensive lysis of adhesions is necessary to ensure there is no occult enterotomy. As my mentor Dr. John Soper once described to me: “It’s like trying to scratch your armpit by reaching through your fly.”
While pfannensteil incisions come naturally, and comfortably, to most gynecologists, likely because of their frequent application during cesarean section, all gynecologists should be confident in the steps and anatomy for vertical midline, or paramedian incisions. This is not only beneficial for complex gynecologic cases, but also in the event of vascular emergency. In the hands of an experienced abdominal/pelvic surgeon, the vertical midline incision is the quickest way to safely enter the abdomen, and provides the kind of exposure that may be critical in safely repairing or controlling hemorrhage from a major vessel.
While low transverse incisions may be more cosmetic, less painful, and associated with fewer wound complications, our first concern as surgeons should be mitigating complications. In situations where risks of complications are high, it is best to not handicap ourselves with the incision location. And always remember, wound complications are highest when a transverse incision needs to be converted to a vertical one with a “T.”
It’s not just about diagnosis of cancer, it’s also prevention
Detection of cancer is an important role of the obstetrician gynecologist. However, equally important is being able to seize opportunities for cancer prevention. Cervical, vulvar, endometrial and ovarian cancer are all known to have preventative strategies.
All patients up to the age of 45 should be offered vaccination against HPV. Initial indications for HPV vaccination were for women up to age 26; however, recent data support the safety and efficacy of the vaccine in older women.3 HPV vaccination is most effective at preventing cancer when administered prior to exposure (ideally age 9-11), leaving this in the hands of our pediatrician colleagues. However, we must be vigilant to inquire about vaccination status for all our patients and encourage vaccines for those who were missed earlier in their life.
Patients should be counseled regarding the significant risk reduction for cancer that is gained from use of oral hormonal contraceptives and progestin-releasing IUDs (especially for endometrial and ovarian cancers). Providing them with knowledge of this information when considering options for contraception or menstrual cycle management is important in their decision-making process.
Endometrial cancer incidence is sadly on the rise in the United States, likely secondary to increasing rates of obesity. Pregnancy is a time when many women begin to gain, and accumulate, weight and therefore obstetric providers have a unique opportunity to assist patients in strategies to normalize their weight after pregnancy. Many of my patients with endometrial cancer state that they have never heard that it is associated with obesity. This suggests that more can be done to educate patients on the carcinogenic effect of obesity (for both endometrial and breast cancer), which may aid in motivating change of modifiable behaviors.
The fallopian tubes are the source of many ovarian cancers and knowledge of this has led to the recommendation to perform opportunistic salpingectomy as a cancer risk-reducing strategy. Hysterectomy and sterilization procedures are most apropos for this modification. While prospective data to confirm a reduced risk of ovarian cancer with opportunistic salpingectomy are lacking, a reduced incidence of cancer has been observed when the tubes have been removed for indicated surgeries; there appear to be no significant deleterious sequelae.4,5 A focus should be made on removal of the entire distal third of the tube, particularly the fimbriated ends, as this is the portion most implicated in malignancy.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant disclosures. Contact her at [email protected].
References
1. Buys SS et al. JAMA. 2011;305(22):2295.
2. Goff BA et al. JAMA. 2004;291(22):2705.
3. Castellsagué X et al. Br J Cancer. 2011;105(1):28.
4. Yoon SH et al. Eur J Cancer. 2016 Mar;55:38-46.
5. Hanley GE et al. Am J Obstet Gynecol. 2018;219(2):172.
AHA targets rising prevalence of obstructive sleep apnea in children
Obstructive sleep apnea is becoming more common in children and adolescents as the prevalence of obesity increases, but it may also be a preventable risk factor for cardiovascular disease, according to a new scientific statement from the American Heart Association.
The statement focuses on the links between OSA and CVD risk factors in children and adolescents, and reviews diagnostic strategies and treatments. The writing committee reported that 1%-6% of children and adolescents have OSA, as do up to 60% of adolescents considered obese.
The statement was created by the AHA’s Atherosclerosis, Hypertension, and Obesity in the Young subcommittee of the Council on Cardiovascular Disease in the Young and was published online in the Journal of the American Heart Association.
Carissa M. Baker-Smith, MD, chair of the writing group chair and director of pediatric preventive cardiology at Nemours Cardiac Center, Alfred I. duPont Hospital for Children, Wilmington, Del., explained the rationale for issuing the statement at this time, noting that the relationship between OSA and CVD in adults is well documented.
“There has been less focus on the importance of recognizing and treating sleep apnea in youth,” she said in an interview. “Thus, we felt that it was vitally important to get the word out to parents and to providers that paying attention to the quality and duration of your child’s sleep is vitally important to a child’s long-term heart health. Risk factors for heart disease, when present in childhood, can persist into adulthood.”
Clarity on polysomnography
For making the diagnosis of OSA in children, the statement provides clarity on the use of polysomnography and the role of the apnea-hypopnea index, which is lower in children with OSA than in adults. “One controversy, or at least as I saw it, was whether or not polysomnography testing is always required to make the diagnosis of OSA and before proceeding with tonsil and adenoid removal among children for whom enlarged tonsils and adenoids are present,” Dr. Baker-Smith said. “Polysomnography testing is not always needed before an ear, nose, and throat surgeon may recommend surgery.”
The statement also noted that history and physical examination may not yield enough reliable information to distinguish OSA from snoring.
In areas where sleep laboratories that work with children aren’t available, alternative tests such as daytime nap polysomnography, nocturnal oximetry, and nocturnal video recording may be used – with a caveat. “These alternative tests have weaker positive and negative predictive values when compared with polysomnography,” the writing committee noted. Home sleep apnea tests aren’t recommended in children. Questionnaires “are useful as screening, but not as diagnostic tools.”
Pediatric patients being evaluated for OSA should also be screened for hypertension and metabolic syndrome, as well as central nervous system and behavioral disorders. Diagnosing OSA in children and adolescents requires “a high index of suspicion,” the committee wrote.
Pediatricians and pediatric cardiologists should exercise that high index of suspicion when receiving referrals for cardiac evaluations for attention deficit hyperactivity disorder medication, Dr. Baker-Smith said. “Take the time to ask about a child’s sleep – snoring, apnea, etc. – especially if the child has obesity, difficulty focusing during the day, and if there is evidence of systemic hypertension or other signs of metabolic syndrome,” she said.
Risk factors for OSA in children
The statement also reviewed risk factors for OSA, among them obesity, particularly among children younger than 6 years. Other risk factors include upper and lower airway disease, hypotonia, parental history of hyperplasia of the adenoids and tonsils, craniofacial malformations, and neuromuscular disorders. However, the committee cited “limited data” to support that children with congenital heart disease may be at greater risk for OSA and sleep-disordered breathing (SDB).
Black children are at significantly greater risk, and socioeconomic factors “may be potential confounders,” the committee stated. Other risk factors include allergic rhinitis and sickle cell disease.
But the statement underscores that “obesity is the main risk factor” for OSA in children and adolescents, and that the presence of increased inflammation may explain this relationship. Steroids may alleviate these symptoms, even in nonobese children, and removal of the adenoids or tonsils is an option to reduce inflammation in children with OSA.
“Obesity is a significant risk factor for sleep disturbances and obstructive sleep apnea, and the severity of sleep apnea may be improved by weight-loss interventions, which then improves metabolic syndrome factors such as insulin sensitivity,” Dr. Baker-Smith said. “We need to increase awareness about how the rising prevalence of obesity may be impacting sleep quality in kids and recognize sleep-disordered breathing as something that could contribute to risks for hypertension and later cardiovascular disease.”
Children in whom OSA is suspected should also undergo screening for metabolic syndrome, and central nervous system and behavioral disorders.
Cardiovascular risks
The statement explores the connection between cardiovascular complications and SDB and OSA in depth.
“Inadequate sleep duration of < 5 hours per night in children and adolescents has been linked to an increased risk of hypertension and is also associated with an increased prevalence of obesity,” the committee wrote.
However, the statement left one question hanging: whether OSA alone or obesity cause higher BP in younger patients with OSA. But the committee concluded that BP levels increase with the severity of OSA, although the effects can vary with age. OSA in children peaks between ages 2 and 8, corresponding to the peak prevalence of hypertrophy of the tonsils and adenoids. Children aged 10-11 with more severe OSA may have BP dysregulation, while older adolescents develop higher sustained BP. Obesity may be a confounder for daytime BP elevations, while nighttime hypertension depends less on obesity and more on OSA severity.
“OSA is associated with abnormal BP in youth and, in particular, higher nighttime blood pressures and loss of the normal decline in BP that should occur during sleep,” Dr. Baker-Smith said. “Children with OSA appear to have higher BP than controls during both sleep and wake times, and BP levels increase with increasing severity of OSA.”
Nonetheless, children with OSA are at greater risk for other cardiovascular problems. Left ventricular hypertrophy may be a secondary outcome. “The presence of obstructive sleep apnea in children is associated with an 11-fold increased risk for LVH in children, a relationship not seen in the presence of primary snoring alone,” Dr. Baker-Smith said.
Dr. Baker-Smith had no relevant disclosures. Coauthor Amal Isaiah, MD, is coinventor of an imaging system for sleep apnea and receives royalties from the University of Maryland. The other coauthors have no relevant financial relationships to disclose.
Obstructive sleep apnea is becoming more common in children and adolescents as the prevalence of obesity increases, but it may also be a preventable risk factor for cardiovascular disease, according to a new scientific statement from the American Heart Association.
The statement focuses on the links between OSA and CVD risk factors in children and adolescents, and reviews diagnostic strategies and treatments. The writing committee reported that 1%-6% of children and adolescents have OSA, as do up to 60% of adolescents considered obese.
The statement was created by the AHA’s Atherosclerosis, Hypertension, and Obesity in the Young subcommittee of the Council on Cardiovascular Disease in the Young and was published online in the Journal of the American Heart Association.
Carissa M. Baker-Smith, MD, chair of the writing group chair and director of pediatric preventive cardiology at Nemours Cardiac Center, Alfred I. duPont Hospital for Children, Wilmington, Del., explained the rationale for issuing the statement at this time, noting that the relationship between OSA and CVD in adults is well documented.
“There has been less focus on the importance of recognizing and treating sleep apnea in youth,” she said in an interview. “Thus, we felt that it was vitally important to get the word out to parents and to providers that paying attention to the quality and duration of your child’s sleep is vitally important to a child’s long-term heart health. Risk factors for heart disease, when present in childhood, can persist into adulthood.”
Clarity on polysomnography
For making the diagnosis of OSA in children, the statement provides clarity on the use of polysomnography and the role of the apnea-hypopnea index, which is lower in children with OSA than in adults. “One controversy, or at least as I saw it, was whether or not polysomnography testing is always required to make the diagnosis of OSA and before proceeding with tonsil and adenoid removal among children for whom enlarged tonsils and adenoids are present,” Dr. Baker-Smith said. “Polysomnography testing is not always needed before an ear, nose, and throat surgeon may recommend surgery.”
The statement also noted that history and physical examination may not yield enough reliable information to distinguish OSA from snoring.
In areas where sleep laboratories that work with children aren’t available, alternative tests such as daytime nap polysomnography, nocturnal oximetry, and nocturnal video recording may be used – with a caveat. “These alternative tests have weaker positive and negative predictive values when compared with polysomnography,” the writing committee noted. Home sleep apnea tests aren’t recommended in children. Questionnaires “are useful as screening, but not as diagnostic tools.”
Pediatric patients being evaluated for OSA should also be screened for hypertension and metabolic syndrome, as well as central nervous system and behavioral disorders. Diagnosing OSA in children and adolescents requires “a high index of suspicion,” the committee wrote.
Pediatricians and pediatric cardiologists should exercise that high index of suspicion when receiving referrals for cardiac evaluations for attention deficit hyperactivity disorder medication, Dr. Baker-Smith said. “Take the time to ask about a child’s sleep – snoring, apnea, etc. – especially if the child has obesity, difficulty focusing during the day, and if there is evidence of systemic hypertension or other signs of metabolic syndrome,” she said.
Risk factors for OSA in children
The statement also reviewed risk factors for OSA, among them obesity, particularly among children younger than 6 years. Other risk factors include upper and lower airway disease, hypotonia, parental history of hyperplasia of the adenoids and tonsils, craniofacial malformations, and neuromuscular disorders. However, the committee cited “limited data” to support that children with congenital heart disease may be at greater risk for OSA and sleep-disordered breathing (SDB).
Black children are at significantly greater risk, and socioeconomic factors “may be potential confounders,” the committee stated. Other risk factors include allergic rhinitis and sickle cell disease.
But the statement underscores that “obesity is the main risk factor” for OSA in children and adolescents, and that the presence of increased inflammation may explain this relationship. Steroids may alleviate these symptoms, even in nonobese children, and removal of the adenoids or tonsils is an option to reduce inflammation in children with OSA.
“Obesity is a significant risk factor for sleep disturbances and obstructive sleep apnea, and the severity of sleep apnea may be improved by weight-loss interventions, which then improves metabolic syndrome factors such as insulin sensitivity,” Dr. Baker-Smith said. “We need to increase awareness about how the rising prevalence of obesity may be impacting sleep quality in kids and recognize sleep-disordered breathing as something that could contribute to risks for hypertension and later cardiovascular disease.”
Children in whom OSA is suspected should also undergo screening for metabolic syndrome, and central nervous system and behavioral disorders.
Cardiovascular risks
The statement explores the connection between cardiovascular complications and SDB and OSA in depth.
“Inadequate sleep duration of < 5 hours per night in children and adolescents has been linked to an increased risk of hypertension and is also associated with an increased prevalence of obesity,” the committee wrote.
However, the statement left one question hanging: whether OSA alone or obesity cause higher BP in younger patients with OSA. But the committee concluded that BP levels increase with the severity of OSA, although the effects can vary with age. OSA in children peaks between ages 2 and 8, corresponding to the peak prevalence of hypertrophy of the tonsils and adenoids. Children aged 10-11 with more severe OSA may have BP dysregulation, while older adolescents develop higher sustained BP. Obesity may be a confounder for daytime BP elevations, while nighttime hypertension depends less on obesity and more on OSA severity.
“OSA is associated with abnormal BP in youth and, in particular, higher nighttime blood pressures and loss of the normal decline in BP that should occur during sleep,” Dr. Baker-Smith said. “Children with OSA appear to have higher BP than controls during both sleep and wake times, and BP levels increase with increasing severity of OSA.”
Nonetheless, children with OSA are at greater risk for other cardiovascular problems. Left ventricular hypertrophy may be a secondary outcome. “The presence of obstructive sleep apnea in children is associated with an 11-fold increased risk for LVH in children, a relationship not seen in the presence of primary snoring alone,” Dr. Baker-Smith said.
Dr. Baker-Smith had no relevant disclosures. Coauthor Amal Isaiah, MD, is coinventor of an imaging system for sleep apnea and receives royalties from the University of Maryland. The other coauthors have no relevant financial relationships to disclose.
Obstructive sleep apnea is becoming more common in children and adolescents as the prevalence of obesity increases, but it may also be a preventable risk factor for cardiovascular disease, according to a new scientific statement from the American Heart Association.
The statement focuses on the links between OSA and CVD risk factors in children and adolescents, and reviews diagnostic strategies and treatments. The writing committee reported that 1%-6% of children and adolescents have OSA, as do up to 60% of adolescents considered obese.
The statement was created by the AHA’s Atherosclerosis, Hypertension, and Obesity in the Young subcommittee of the Council on Cardiovascular Disease in the Young and was published online in the Journal of the American Heart Association.
Carissa M. Baker-Smith, MD, chair of the writing group chair and director of pediatric preventive cardiology at Nemours Cardiac Center, Alfred I. duPont Hospital for Children, Wilmington, Del., explained the rationale for issuing the statement at this time, noting that the relationship between OSA and CVD in adults is well documented.
“There has been less focus on the importance of recognizing and treating sleep apnea in youth,” she said in an interview. “Thus, we felt that it was vitally important to get the word out to parents and to providers that paying attention to the quality and duration of your child’s sleep is vitally important to a child’s long-term heart health. Risk factors for heart disease, when present in childhood, can persist into adulthood.”
Clarity on polysomnography
For making the diagnosis of OSA in children, the statement provides clarity on the use of polysomnography and the role of the apnea-hypopnea index, which is lower in children with OSA than in adults. “One controversy, or at least as I saw it, was whether or not polysomnography testing is always required to make the diagnosis of OSA and before proceeding with tonsil and adenoid removal among children for whom enlarged tonsils and adenoids are present,” Dr. Baker-Smith said. “Polysomnography testing is not always needed before an ear, nose, and throat surgeon may recommend surgery.”
The statement also noted that history and physical examination may not yield enough reliable information to distinguish OSA from snoring.
In areas where sleep laboratories that work with children aren’t available, alternative tests such as daytime nap polysomnography, nocturnal oximetry, and nocturnal video recording may be used – with a caveat. “These alternative tests have weaker positive and negative predictive values when compared with polysomnography,” the writing committee noted. Home sleep apnea tests aren’t recommended in children. Questionnaires “are useful as screening, but not as diagnostic tools.”
Pediatric patients being evaluated for OSA should also be screened for hypertension and metabolic syndrome, as well as central nervous system and behavioral disorders. Diagnosing OSA in children and adolescents requires “a high index of suspicion,” the committee wrote.
Pediatricians and pediatric cardiologists should exercise that high index of suspicion when receiving referrals for cardiac evaluations for attention deficit hyperactivity disorder medication, Dr. Baker-Smith said. “Take the time to ask about a child’s sleep – snoring, apnea, etc. – especially if the child has obesity, difficulty focusing during the day, and if there is evidence of systemic hypertension or other signs of metabolic syndrome,” she said.
Risk factors for OSA in children
The statement also reviewed risk factors for OSA, among them obesity, particularly among children younger than 6 years. Other risk factors include upper and lower airway disease, hypotonia, parental history of hyperplasia of the adenoids and tonsils, craniofacial malformations, and neuromuscular disorders. However, the committee cited “limited data” to support that children with congenital heart disease may be at greater risk for OSA and sleep-disordered breathing (SDB).
Black children are at significantly greater risk, and socioeconomic factors “may be potential confounders,” the committee stated. Other risk factors include allergic rhinitis and sickle cell disease.
But the statement underscores that “obesity is the main risk factor” for OSA in children and adolescents, and that the presence of increased inflammation may explain this relationship. Steroids may alleviate these symptoms, even in nonobese children, and removal of the adenoids or tonsils is an option to reduce inflammation in children with OSA.
“Obesity is a significant risk factor for sleep disturbances and obstructive sleep apnea, and the severity of sleep apnea may be improved by weight-loss interventions, which then improves metabolic syndrome factors such as insulin sensitivity,” Dr. Baker-Smith said. “We need to increase awareness about how the rising prevalence of obesity may be impacting sleep quality in kids and recognize sleep-disordered breathing as something that could contribute to risks for hypertension and later cardiovascular disease.”
Children in whom OSA is suspected should also undergo screening for metabolic syndrome, and central nervous system and behavioral disorders.
Cardiovascular risks
The statement explores the connection between cardiovascular complications and SDB and OSA in depth.
“Inadequate sleep duration of < 5 hours per night in children and adolescents has been linked to an increased risk of hypertension and is also associated with an increased prevalence of obesity,” the committee wrote.
However, the statement left one question hanging: whether OSA alone or obesity cause higher BP in younger patients with OSA. But the committee concluded that BP levels increase with the severity of OSA, although the effects can vary with age. OSA in children peaks between ages 2 and 8, corresponding to the peak prevalence of hypertrophy of the tonsils and adenoids. Children aged 10-11 with more severe OSA may have BP dysregulation, while older adolescents develop higher sustained BP. Obesity may be a confounder for daytime BP elevations, while nighttime hypertension depends less on obesity and more on OSA severity.
“OSA is associated with abnormal BP in youth and, in particular, higher nighttime blood pressures and loss of the normal decline in BP that should occur during sleep,” Dr. Baker-Smith said. “Children with OSA appear to have higher BP than controls during both sleep and wake times, and BP levels increase with increasing severity of OSA.”
Nonetheless, children with OSA are at greater risk for other cardiovascular problems. Left ventricular hypertrophy may be a secondary outcome. “The presence of obstructive sleep apnea in children is associated with an 11-fold increased risk for LVH in children, a relationship not seen in the presence of primary snoring alone,” Dr. Baker-Smith said.
Dr. Baker-Smith had no relevant disclosures. Coauthor Amal Isaiah, MD, is coinventor of an imaging system for sleep apnea and receives royalties from the University of Maryland. The other coauthors have no relevant financial relationships to disclose.
FROM JOURNAL OF THE AMERICAN HEART ASSOCIATION
COVID booster may benefit active-treatment cancer patients
A COVID-19 booster shot may be beneficial for patients with cancer who are undergoing treatment, according to new findings from an Israeli case-control study.
The seropositivity rate among the patients with cancer remained high (87%) about 4 months after the patients had received the second BNT162b2 (Pfizer/BioNTech) vaccination. However, the median IgG titer in the patients and the control persons who were without cancer decreased over time. Notably, in a previous analysis that the authors conducted and in the current one, the IgG titers were statistically significantly lower in the patients with cancer as compared to control persons.
The correlation between antibody levels following vaccination and clinical protection has yet to be proven, but the accumulating evidence supports antibody response as a possible correlate of disease protection.
“Our data can’t predict if a third booster dose is necessary,” said study author Salomon M. Stemmer, MD, professor at the Institute of Oncology of Rabin Medical Center, Petah Tikva, Israel. “It does seem quite logical that a booster dose will cause an increase in IgG levels.”
The findings were published Aug. 11, 2021, in a research letter in JAMA Oncology.
In their previous study, Dr. Stemmer and colleagues compared the rates of anti–spike antibody response to the initial shot of the BNT162b2 vaccine among 102 adults with solid-tumor cancers who were undergoing treatment with that of 78 healthy control persons. They found that a high percentage of patients undergoing treatment for cancer (90%) achieved a sufficient antibody response to the BNT162b2 vaccine.
Booster endorsed
Responses to COVID-19 vaccination have varied among patients with cancer. For patients with solid tumors, responses have been good even while the patients were receiving systemic therapy. However, among patients with blood cancers, particularly those receiving immunosuppressive therapies, responses have been poor. Studies have identified factors associated with a poor response, but it has been unclear whether to recommend booster shots.
In August the Food and Drug Administration authorized a third dose of either the Pfizer or the Moderna COVID-19 vaccine for all individuals with compromised immune systems. Those eligible for a third dose include solid-organ transplant recipients, those undergoing cancer treatments, and people with autoimmune diseases that suppress their immune systems.
IgG titers lower in cancer patients
In the current analysis, the authors evaluated the anti-S response in the patients with cancer approximately 4 months after they had received the second vaccine dose. They compared the responses in those patients with the responses in a control group.
The cohort included 95 patients from the prior study and 66 control persons. The most common malignancies were gastrointestinal (26%), lung (25%), and breast (18%).
All patients were receiving systemic therapy. Chemotherapy was the most common (28%), followed by immunotherapy (21%) and combination chemotherapy/biological therapy (20%).
At a median of 123 days after the second vaccination, 83 patients with cancer (87%) and all of the control patients (100%) were seropositive for anti-S IgG antibodies. The median titer levels were significantly lower among case patients as compared with control patients (417 AU/mL [interquartile range, 136-895] vs. 1,220 AU/mL [IQR, 588-1,987]; P < .001)
There was a 3.6-fold range in median titer values across tumor types and an even wider range (8.8-fold) across the different types of treatment. The lowest titers were observed among patients who had received immunotherapy plus chemotherapy/biological therapy (median [IQR], 94.4 [49.4-191] AU/mL vs. 147 [62.8-339] AU/mL).
In an exploratory multivariable analysis, treatments with chemotherapy plus immunotherapy and immunotherapy plus biological therapy were significantly associated with lower IgG titers.
No downside for cancer patients
The Biden administration announced a plan to begin booster COVID-19 vaccinations for all American adults in September, with recommendations that the third vaccine be given at least 8 months after the second mRNA vaccine dose.
Jeremy M. Levin, DPhil, the chairman and CEO of Ovid Therapeutics, explained that, concerning boosters, “it is inconceivable that we will have all data at this stage.
“Knowledge about how boosters work and don’t work and when you should ideally have them is imperfect,” he told this news organization. “However, we can have a lot of confidence in the fact that hundreds of millions of people have received the vaccine, so we know a lot about the safety and efficacy.”
Immunocompromised adults represent less than 5% of the total population, and most of the available data on vaccination are from patients who have undergone solid-organ transplant, Dr. Levin explained. Studies have shown that their response is less robust to vaccination in comparison with adults in the general population.
“Although it is still preliminary, the strongest data come from Israel,” he said, “where they found that the booster was highly effective and doubled the number of transplant patients who developed antibodies.”
But data are not yet available in the setting of cancer. “But even though we don’t have the data yet, the answer is that no matter, the booster process is essential,” he said. “The evidence we have is that boosters raise the immune response, and it is the best data we have now.”
Martin J. Edelman, MD, chair, department of hematology/oncology, Fox Chase Cancer Center, Philadelphia, noted that the current recommendation is that patients who are immunocompromised receive a booster immediately.
At his health system, this is interpreted to include patients who have undergone the following treatments: Transplant (solid-organ and bone marrow transplant), hemodialysis, hematologic malignancy treatment, active immunosuppressive (chemotherapy, chemoimmunotherapy, and nonhormonal or single-agent immunotherapy) treatment, rheumatology treatments, and high-dose steroids.
“As for cancer patients, we are making arrangements to vaccinate patients who meet the above criteria now,” he said. “There is no known downside to receiving booster immediately. While there may be less of a response than waiting for completion of treatment, we know that patients on active therapy are frequently able to mount a response, and any response is better than none.”
Dr. Edelman added that this area is changing very rapidly. “We will modify our approach as information and guidance from appropriate organizations, such as the FDA and CDC, become available.”
Dr. Stemmer has received institutional research grants from CAN-FITE, AstraZeneca, Bioline RX, BMS, Halozyme, Clovis Oncology, CTG Pharma, Exelixis, Geicam, Incyte, Lilly, Moderna, Teva Pharmaceuticals, and Roche, and owns stocks and options in CTG Pharma, DocBoxMD, Tyrnovo, VYPE, Cytora, and CAN-FITE. Dr. Edelman has received personal fees and other compensation from Windmil, Biomarker Strategies, AstraZeneca, Takeda, GlaxoSmithKline, Apexigen, Nektar, Bristol-Myers Squibb, Armo, Bergen Bio, and Apexigen outside the submitted work. He has submitted a patent for epigenetic modifications to increase susceptibility to radiopharmaceuticals and is a paid adviser for Kanaph and Flame. Dr. Levin is chairman and CEO of Ovid Therapeutics.
A version of this article first appeared on Medscape.com.
A COVID-19 booster shot may be beneficial for patients with cancer who are undergoing treatment, according to new findings from an Israeli case-control study.
The seropositivity rate among the patients with cancer remained high (87%) about 4 months after the patients had received the second BNT162b2 (Pfizer/BioNTech) vaccination. However, the median IgG titer in the patients and the control persons who were without cancer decreased over time. Notably, in a previous analysis that the authors conducted and in the current one, the IgG titers were statistically significantly lower in the patients with cancer as compared to control persons.
The correlation between antibody levels following vaccination and clinical protection has yet to be proven, but the accumulating evidence supports antibody response as a possible correlate of disease protection.
“Our data can’t predict if a third booster dose is necessary,” said study author Salomon M. Stemmer, MD, professor at the Institute of Oncology of Rabin Medical Center, Petah Tikva, Israel. “It does seem quite logical that a booster dose will cause an increase in IgG levels.”
The findings were published Aug. 11, 2021, in a research letter in JAMA Oncology.
In their previous study, Dr. Stemmer and colleagues compared the rates of anti–spike antibody response to the initial shot of the BNT162b2 vaccine among 102 adults with solid-tumor cancers who were undergoing treatment with that of 78 healthy control persons. They found that a high percentage of patients undergoing treatment for cancer (90%) achieved a sufficient antibody response to the BNT162b2 vaccine.
Booster endorsed
Responses to COVID-19 vaccination have varied among patients with cancer. For patients with solid tumors, responses have been good even while the patients were receiving systemic therapy. However, among patients with blood cancers, particularly those receiving immunosuppressive therapies, responses have been poor. Studies have identified factors associated with a poor response, but it has been unclear whether to recommend booster shots.
In August the Food and Drug Administration authorized a third dose of either the Pfizer or the Moderna COVID-19 vaccine for all individuals with compromised immune systems. Those eligible for a third dose include solid-organ transplant recipients, those undergoing cancer treatments, and people with autoimmune diseases that suppress their immune systems.
IgG titers lower in cancer patients
In the current analysis, the authors evaluated the anti-S response in the patients with cancer approximately 4 months after they had received the second vaccine dose. They compared the responses in those patients with the responses in a control group.
The cohort included 95 patients from the prior study and 66 control persons. The most common malignancies were gastrointestinal (26%), lung (25%), and breast (18%).
All patients were receiving systemic therapy. Chemotherapy was the most common (28%), followed by immunotherapy (21%) and combination chemotherapy/biological therapy (20%).
At a median of 123 days after the second vaccination, 83 patients with cancer (87%) and all of the control patients (100%) were seropositive for anti-S IgG antibodies. The median titer levels were significantly lower among case patients as compared with control patients (417 AU/mL [interquartile range, 136-895] vs. 1,220 AU/mL [IQR, 588-1,987]; P < .001)
There was a 3.6-fold range in median titer values across tumor types and an even wider range (8.8-fold) across the different types of treatment. The lowest titers were observed among patients who had received immunotherapy plus chemotherapy/biological therapy (median [IQR], 94.4 [49.4-191] AU/mL vs. 147 [62.8-339] AU/mL).
In an exploratory multivariable analysis, treatments with chemotherapy plus immunotherapy and immunotherapy plus biological therapy were significantly associated with lower IgG titers.
No downside for cancer patients
The Biden administration announced a plan to begin booster COVID-19 vaccinations for all American adults in September, with recommendations that the third vaccine be given at least 8 months after the second mRNA vaccine dose.
Jeremy M. Levin, DPhil, the chairman and CEO of Ovid Therapeutics, explained that, concerning boosters, “it is inconceivable that we will have all data at this stage.
“Knowledge about how boosters work and don’t work and when you should ideally have them is imperfect,” he told this news organization. “However, we can have a lot of confidence in the fact that hundreds of millions of people have received the vaccine, so we know a lot about the safety and efficacy.”
Immunocompromised adults represent less than 5% of the total population, and most of the available data on vaccination are from patients who have undergone solid-organ transplant, Dr. Levin explained. Studies have shown that their response is less robust to vaccination in comparison with adults in the general population.
“Although it is still preliminary, the strongest data come from Israel,” he said, “where they found that the booster was highly effective and doubled the number of transplant patients who developed antibodies.”
But data are not yet available in the setting of cancer. “But even though we don’t have the data yet, the answer is that no matter, the booster process is essential,” he said. “The evidence we have is that boosters raise the immune response, and it is the best data we have now.”
Martin J. Edelman, MD, chair, department of hematology/oncology, Fox Chase Cancer Center, Philadelphia, noted that the current recommendation is that patients who are immunocompromised receive a booster immediately.
At his health system, this is interpreted to include patients who have undergone the following treatments: Transplant (solid-organ and bone marrow transplant), hemodialysis, hematologic malignancy treatment, active immunosuppressive (chemotherapy, chemoimmunotherapy, and nonhormonal or single-agent immunotherapy) treatment, rheumatology treatments, and high-dose steroids.
“As for cancer patients, we are making arrangements to vaccinate patients who meet the above criteria now,” he said. “There is no known downside to receiving booster immediately. While there may be less of a response than waiting for completion of treatment, we know that patients on active therapy are frequently able to mount a response, and any response is better than none.”
Dr. Edelman added that this area is changing very rapidly. “We will modify our approach as information and guidance from appropriate organizations, such as the FDA and CDC, become available.”
Dr. Stemmer has received institutional research grants from CAN-FITE, AstraZeneca, Bioline RX, BMS, Halozyme, Clovis Oncology, CTG Pharma, Exelixis, Geicam, Incyte, Lilly, Moderna, Teva Pharmaceuticals, and Roche, and owns stocks and options in CTG Pharma, DocBoxMD, Tyrnovo, VYPE, Cytora, and CAN-FITE. Dr. Edelman has received personal fees and other compensation from Windmil, Biomarker Strategies, AstraZeneca, Takeda, GlaxoSmithKline, Apexigen, Nektar, Bristol-Myers Squibb, Armo, Bergen Bio, and Apexigen outside the submitted work. He has submitted a patent for epigenetic modifications to increase susceptibility to radiopharmaceuticals and is a paid adviser for Kanaph and Flame. Dr. Levin is chairman and CEO of Ovid Therapeutics.
A version of this article first appeared on Medscape.com.
A COVID-19 booster shot may be beneficial for patients with cancer who are undergoing treatment, according to new findings from an Israeli case-control study.
The seropositivity rate among the patients with cancer remained high (87%) about 4 months after the patients had received the second BNT162b2 (Pfizer/BioNTech) vaccination. However, the median IgG titer in the patients and the control persons who were without cancer decreased over time. Notably, in a previous analysis that the authors conducted and in the current one, the IgG titers were statistically significantly lower in the patients with cancer as compared to control persons.
The correlation between antibody levels following vaccination and clinical protection has yet to be proven, but the accumulating evidence supports antibody response as a possible correlate of disease protection.
“Our data can’t predict if a third booster dose is necessary,” said study author Salomon M. Stemmer, MD, professor at the Institute of Oncology of Rabin Medical Center, Petah Tikva, Israel. “It does seem quite logical that a booster dose will cause an increase in IgG levels.”
The findings were published Aug. 11, 2021, in a research letter in JAMA Oncology.
In their previous study, Dr. Stemmer and colleagues compared the rates of anti–spike antibody response to the initial shot of the BNT162b2 vaccine among 102 adults with solid-tumor cancers who were undergoing treatment with that of 78 healthy control persons. They found that a high percentage of patients undergoing treatment for cancer (90%) achieved a sufficient antibody response to the BNT162b2 vaccine.
Booster endorsed
Responses to COVID-19 vaccination have varied among patients with cancer. For patients with solid tumors, responses have been good even while the patients were receiving systemic therapy. However, among patients with blood cancers, particularly those receiving immunosuppressive therapies, responses have been poor. Studies have identified factors associated with a poor response, but it has been unclear whether to recommend booster shots.
In August the Food and Drug Administration authorized a third dose of either the Pfizer or the Moderna COVID-19 vaccine for all individuals with compromised immune systems. Those eligible for a third dose include solid-organ transplant recipients, those undergoing cancer treatments, and people with autoimmune diseases that suppress their immune systems.
IgG titers lower in cancer patients
In the current analysis, the authors evaluated the anti-S response in the patients with cancer approximately 4 months after they had received the second vaccine dose. They compared the responses in those patients with the responses in a control group.
The cohort included 95 patients from the prior study and 66 control persons. The most common malignancies were gastrointestinal (26%), lung (25%), and breast (18%).
All patients were receiving systemic therapy. Chemotherapy was the most common (28%), followed by immunotherapy (21%) and combination chemotherapy/biological therapy (20%).
At a median of 123 days after the second vaccination, 83 patients with cancer (87%) and all of the control patients (100%) were seropositive for anti-S IgG antibodies. The median titer levels were significantly lower among case patients as compared with control patients (417 AU/mL [interquartile range, 136-895] vs. 1,220 AU/mL [IQR, 588-1,987]; P < .001)
There was a 3.6-fold range in median titer values across tumor types and an even wider range (8.8-fold) across the different types of treatment. The lowest titers were observed among patients who had received immunotherapy plus chemotherapy/biological therapy (median [IQR], 94.4 [49.4-191] AU/mL vs. 147 [62.8-339] AU/mL).
In an exploratory multivariable analysis, treatments with chemotherapy plus immunotherapy and immunotherapy plus biological therapy were significantly associated with lower IgG titers.
No downside for cancer patients
The Biden administration announced a plan to begin booster COVID-19 vaccinations for all American adults in September, with recommendations that the third vaccine be given at least 8 months after the second mRNA vaccine dose.
Jeremy M. Levin, DPhil, the chairman and CEO of Ovid Therapeutics, explained that, concerning boosters, “it is inconceivable that we will have all data at this stage.
“Knowledge about how boosters work and don’t work and when you should ideally have them is imperfect,” he told this news organization. “However, we can have a lot of confidence in the fact that hundreds of millions of people have received the vaccine, so we know a lot about the safety and efficacy.”
Immunocompromised adults represent less than 5% of the total population, and most of the available data on vaccination are from patients who have undergone solid-organ transplant, Dr. Levin explained. Studies have shown that their response is less robust to vaccination in comparison with adults in the general population.
“Although it is still preliminary, the strongest data come from Israel,” he said, “where they found that the booster was highly effective and doubled the number of transplant patients who developed antibodies.”
But data are not yet available in the setting of cancer. “But even though we don’t have the data yet, the answer is that no matter, the booster process is essential,” he said. “The evidence we have is that boosters raise the immune response, and it is the best data we have now.”
Martin J. Edelman, MD, chair, department of hematology/oncology, Fox Chase Cancer Center, Philadelphia, noted that the current recommendation is that patients who are immunocompromised receive a booster immediately.
At his health system, this is interpreted to include patients who have undergone the following treatments: Transplant (solid-organ and bone marrow transplant), hemodialysis, hematologic malignancy treatment, active immunosuppressive (chemotherapy, chemoimmunotherapy, and nonhormonal or single-agent immunotherapy) treatment, rheumatology treatments, and high-dose steroids.
“As for cancer patients, we are making arrangements to vaccinate patients who meet the above criteria now,” he said. “There is no known downside to receiving booster immediately. While there may be less of a response than waiting for completion of treatment, we know that patients on active therapy are frequently able to mount a response, and any response is better than none.”
Dr. Edelman added that this area is changing very rapidly. “We will modify our approach as information and guidance from appropriate organizations, such as the FDA and CDC, become available.”
Dr. Stemmer has received institutional research grants from CAN-FITE, AstraZeneca, Bioline RX, BMS, Halozyme, Clovis Oncology, CTG Pharma, Exelixis, Geicam, Incyte, Lilly, Moderna, Teva Pharmaceuticals, and Roche, and owns stocks and options in CTG Pharma, DocBoxMD, Tyrnovo, VYPE, Cytora, and CAN-FITE. Dr. Edelman has received personal fees and other compensation from Windmil, Biomarker Strategies, AstraZeneca, Takeda, GlaxoSmithKline, Apexigen, Nektar, Bristol-Myers Squibb, Armo, Bergen Bio, and Apexigen outside the submitted work. He has submitted a patent for epigenetic modifications to increase susceptibility to radiopharmaceuticals and is a paid adviser for Kanaph and Flame. Dr. Levin is chairman and CEO of Ovid Therapeutics.
A version of this article first appeared on Medscape.com.
Psoriatic arthritis health care costs continue to rise over time
Annual health care costs for patients with psoriatic arthritis rose over recent 5-year periods across all categories of resource use to a significantly greater extent than among patients with psoriasis only or those without any psoriatic disease diagnoses, according to commercial insurance claims data.
Using an IBM MarketScan Commercial Database, researchers examined claims data for 208,434 patients with psoriasis, 47,274 with PsA, and 255,708 controls who had neither psoriasis nor PsA. Controls were matched for age and sex. Those with RA, ankylosing spondylitis, Crohn’s disease, or ulcerative colitis were excluded.
The investigators examined data for 2009-2020, following patients for 5 years within that period. They looked at hospitalizations, outpatient and pharmacy services, lab services, and office visits, Steven Peterson, director of market access for rheumatology at Janssen Pharmaceuticals, said in his presentation of the data at the Pan American League of Associations for Rheumatology 2021 annual meeting, held recently as a virtual event.
The research was also published online May 2, 2021, in Clinical Rheumatology.
Big differences between the groups were seen in the first year, when the average health care costs for the PsA group were $28,322, about half of which was outpatient drug costs. That compared with $12,039 for the psoriasis group and $6,672 for the control group.
The differences tended to widen over time. By the fifth year, average costs for the PsA group were $34,290, nearly 60% of which were drug costs. That compared with $12,877 for the psoriasis group and $8,569 for the control group. In each year examined, outpatient drug costs accounted for less than half of the expenses for the psoriasis group and about a quarter for the control group.
Researchers found that the PsA group needed 28.7 prescriptions per person per year, compared with 17.0 and 12.7 in the psoriasis and control groups, respectively, Mr. Peterson said. He also noted that patients with PsA and psoriasis tended to have higher rates of hypertension, depression, and anxiety.
“The cost and resource utilization disparity between these patient groups demonstrates the high remaining unmet medical need for patients with psoriasis and psoriatic arthritis,” Mr. Peterson said during the virtual proceedings.
Do findings reflect treatment advances?
Elaine Husni, MD, MPH, director of the Arthritis and Musculoskeletal Center at the Cleveland Clinic, where she studies health outcomes in PsA, said the findings are helpful in pointing to a trend across a large sample. But she added it’s important to remember that the increasing costs could reflect recent advances in PsA treatment, which include costly biologic drugs.
“There’s a ton more treatments for psoriasis and psoriatic arthritis than there were even just 5 years ago,” she said in an interview. She was not involved in the research.
Dr. Husni would like to see a more detailed look at the costs, from the categories of expenses to the patients who are incurring the highest costs.
“Is it just a couple of percent of really sick patients that are driving the psoriatic arthritis group?” she wondered.
She also pointed out that PsA is going to be more expensive by its very nature. PsA tends to develop 3-10 years after psoriasis, adding to the costs for someone who already has psoriasis and at a time when they are older and likely have higher health care costs because of comorbidities that develop with age.
Dr. Husni said she does think about treatment costs, in that a less expensive first-line drug might be more appropriate than going straight to a more expensive biologic, especially because they also tend to be safer. She said it’s not just a simple question of curbing costs.
“Is there a way that we can personalize medicine?” she asked. “Is there a way that we can be more accurate about which people may need the more expensive drugs, and which patients may need the less expensive drugs? Are we getting better at monitoring so we can avoid high-cost events?”
Mr. Peterson is an employee of Janssen Pharmaceuticals. Dr. Husni reported serving as a consultant to AbbVie, Amgen, Bristol-Myers Squibb, UCB, Novartis, Lilly, and Pfizer.
* Update, 9/28/21: The headline and parts of this story were updated to better reflect the study on which it reports.
A version of this article first appeared on Medscape.com.
Annual health care costs for patients with psoriatic arthritis rose over recent 5-year periods across all categories of resource use to a significantly greater extent than among patients with psoriasis only or those without any psoriatic disease diagnoses, according to commercial insurance claims data.
Using an IBM MarketScan Commercial Database, researchers examined claims data for 208,434 patients with psoriasis, 47,274 with PsA, and 255,708 controls who had neither psoriasis nor PsA. Controls were matched for age and sex. Those with RA, ankylosing spondylitis, Crohn’s disease, or ulcerative colitis were excluded.
The investigators examined data for 2009-2020, following patients for 5 years within that period. They looked at hospitalizations, outpatient and pharmacy services, lab services, and office visits, Steven Peterson, director of market access for rheumatology at Janssen Pharmaceuticals, said in his presentation of the data at the Pan American League of Associations for Rheumatology 2021 annual meeting, held recently as a virtual event.
The research was also published online May 2, 2021, in Clinical Rheumatology.
Big differences between the groups were seen in the first year, when the average health care costs for the PsA group were $28,322, about half of which was outpatient drug costs. That compared with $12,039 for the psoriasis group and $6,672 for the control group.
The differences tended to widen over time. By the fifth year, average costs for the PsA group were $34,290, nearly 60% of which were drug costs. That compared with $12,877 for the psoriasis group and $8,569 for the control group. In each year examined, outpatient drug costs accounted for less than half of the expenses for the psoriasis group and about a quarter for the control group.
Researchers found that the PsA group needed 28.7 prescriptions per person per year, compared with 17.0 and 12.7 in the psoriasis and control groups, respectively, Mr. Peterson said. He also noted that patients with PsA and psoriasis tended to have higher rates of hypertension, depression, and anxiety.
“The cost and resource utilization disparity between these patient groups demonstrates the high remaining unmet medical need for patients with psoriasis and psoriatic arthritis,” Mr. Peterson said during the virtual proceedings.
Do findings reflect treatment advances?
Elaine Husni, MD, MPH, director of the Arthritis and Musculoskeletal Center at the Cleveland Clinic, where she studies health outcomes in PsA, said the findings are helpful in pointing to a trend across a large sample. But she added it’s important to remember that the increasing costs could reflect recent advances in PsA treatment, which include costly biologic drugs.
“There’s a ton more treatments for psoriasis and psoriatic arthritis than there were even just 5 years ago,” she said in an interview. She was not involved in the research.
Dr. Husni would like to see a more detailed look at the costs, from the categories of expenses to the patients who are incurring the highest costs.
“Is it just a couple of percent of really sick patients that are driving the psoriatic arthritis group?” she wondered.
She also pointed out that PsA is going to be more expensive by its very nature. PsA tends to develop 3-10 years after psoriasis, adding to the costs for someone who already has psoriasis and at a time when they are older and likely have higher health care costs because of comorbidities that develop with age.
Dr. Husni said she does think about treatment costs, in that a less expensive first-line drug might be more appropriate than going straight to a more expensive biologic, especially because they also tend to be safer. She said it’s not just a simple question of curbing costs.
“Is there a way that we can personalize medicine?” she asked. “Is there a way that we can be more accurate about which people may need the more expensive drugs, and which patients may need the less expensive drugs? Are we getting better at monitoring so we can avoid high-cost events?”
Mr. Peterson is an employee of Janssen Pharmaceuticals. Dr. Husni reported serving as a consultant to AbbVie, Amgen, Bristol-Myers Squibb, UCB, Novartis, Lilly, and Pfizer.
* Update, 9/28/21: The headline and parts of this story were updated to better reflect the study on which it reports.
A version of this article first appeared on Medscape.com.
Annual health care costs for patients with psoriatic arthritis rose over recent 5-year periods across all categories of resource use to a significantly greater extent than among patients with psoriasis only or those without any psoriatic disease diagnoses, according to commercial insurance claims data.
Using an IBM MarketScan Commercial Database, researchers examined claims data for 208,434 patients with psoriasis, 47,274 with PsA, and 255,708 controls who had neither psoriasis nor PsA. Controls were matched for age and sex. Those with RA, ankylosing spondylitis, Crohn’s disease, or ulcerative colitis were excluded.
The investigators examined data for 2009-2020, following patients for 5 years within that period. They looked at hospitalizations, outpatient and pharmacy services, lab services, and office visits, Steven Peterson, director of market access for rheumatology at Janssen Pharmaceuticals, said in his presentation of the data at the Pan American League of Associations for Rheumatology 2021 annual meeting, held recently as a virtual event.
The research was also published online May 2, 2021, in Clinical Rheumatology.
Big differences between the groups were seen in the first year, when the average health care costs for the PsA group were $28,322, about half of which was outpatient drug costs. That compared with $12,039 for the psoriasis group and $6,672 for the control group.
The differences tended to widen over time. By the fifth year, average costs for the PsA group were $34,290, nearly 60% of which were drug costs. That compared with $12,877 for the psoriasis group and $8,569 for the control group. In each year examined, outpatient drug costs accounted for less than half of the expenses for the psoriasis group and about a quarter for the control group.
Researchers found that the PsA group needed 28.7 prescriptions per person per year, compared with 17.0 and 12.7 in the psoriasis and control groups, respectively, Mr. Peterson said. He also noted that patients with PsA and psoriasis tended to have higher rates of hypertension, depression, and anxiety.
“The cost and resource utilization disparity between these patient groups demonstrates the high remaining unmet medical need for patients with psoriasis and psoriatic arthritis,” Mr. Peterson said during the virtual proceedings.
Do findings reflect treatment advances?
Elaine Husni, MD, MPH, director of the Arthritis and Musculoskeletal Center at the Cleveland Clinic, where she studies health outcomes in PsA, said the findings are helpful in pointing to a trend across a large sample. But she added it’s important to remember that the increasing costs could reflect recent advances in PsA treatment, which include costly biologic drugs.
“There’s a ton more treatments for psoriasis and psoriatic arthritis than there were even just 5 years ago,” she said in an interview. She was not involved in the research.
Dr. Husni would like to see a more detailed look at the costs, from the categories of expenses to the patients who are incurring the highest costs.
“Is it just a couple of percent of really sick patients that are driving the psoriatic arthritis group?” she wondered.
She also pointed out that PsA is going to be more expensive by its very nature. PsA tends to develop 3-10 years after psoriasis, adding to the costs for someone who already has psoriasis and at a time when they are older and likely have higher health care costs because of comorbidities that develop with age.
Dr. Husni said she does think about treatment costs, in that a less expensive first-line drug might be more appropriate than going straight to a more expensive biologic, especially because they also tend to be safer. She said it’s not just a simple question of curbing costs.
“Is there a way that we can personalize medicine?” she asked. “Is there a way that we can be more accurate about which people may need the more expensive drugs, and which patients may need the less expensive drugs? Are we getting better at monitoring so we can avoid high-cost events?”
Mr. Peterson is an employee of Janssen Pharmaceuticals. Dr. Husni reported serving as a consultant to AbbVie, Amgen, Bristol-Myers Squibb, UCB, Novartis, Lilly, and Pfizer.
* Update, 9/28/21: The headline and parts of this story were updated to better reflect the study on which it reports.
A version of this article first appeared on Medscape.com.
Military Medical Teams Deploy to Relieve COVID-Battered Hospitals
Last summer, a team of US Department of Veterans Affairs (VA) health care professionals deployed to Alabama’s Bill Nichols State Veterans Home to help during the COVID-19 crisis. They were there as part of the “Fourth Mission”—supporting national, state, and local emergency management, public health, safety and homeland security efforts. “It was a really humbling experience,” said Mary Holloway, an RN with the Birmingham VA Health Care System. “Seeing the dedication of the staff there, some coming back to work after recovering from COVID themselves, was inspiring.”
But that turned out to be only one battle in a sadly long and drawn-out war. Since March 2020, more than 5,000 military medical personnel have deployed to 14 states and the Navajo Nation, 51 cities, 71 hospitals, all struggling to keep their heads above a cresting tsunami of new COVID patients.
Last year, the crisis spots for deployments included major metropolitan areas in coastal states: New York, California, and New Jersey. The urgency now is in the Southern states. Those tend to be reporting the highest numbers of new cases and deaths. Alabama, Arkansas, Florida, Louisiana, and Mississippi, for example, have all ranked among the highest rates of cases and hospitalizations per 100,000 people across the country in the last seven days.
This year, military teams have also deployed to support vaccination centers in 25 states and 42 cities. Nearly all—97%—of the new COVID patients in recent months are unvaccinated. And, again, they predominate in Southern states. In Alabama, for instance, only 37% of the population are fully vaccinated. In Louisiana, that number is 40%.
The at-risk states also tend to be the ones that are rapidly running out of space to put the patients in, ICU or otherwise. Where patients who might have been in the intensive care unit (ICU) are housed in the emergency department and in hallways, and where patients without COVID-19 who might have been hospitalized are being turned away. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
These states are at a breaking point. Take Alabama. On August 18, it was “negative 11.” It had 1,568 patients with COVID-19 who needed ICU beds. Only 1,557 beds were available. Patients “may even stay on the regular floor where you’re already stretched for capacity to take care of these people because so many of our staff are out with COVID,” Jeanne Marrazzo, director, Division of Infectious Diseases at the University of Alabama at Birmingham, told a CNN reporter. “It’s really just a domino effect that then clogs up our ERs, clogs up everything else. … It’s a very very tenuous situation.”
The state reported more than 4,000 new cases of COVID-19—“a new high for us,” Marrazzo said. “If you project these numbers out, you can expect that we will at some point, probably around Sept. 1, have at least 5,000 people in our hospitals. If the ratio of people who have to go to the ICU remains stable. That means that probably a third of those people are going to require ICU beds,” she continued. “That is frankly untenable, given the infrastructure, the resources, and really importantly, the staff that we have. I think it is basically apocalyptic. I do not use that word lightly.”
Thus, the US Defense Department (DoD) must once again rise to a sad and desperate occasion. At the request of Federal Emergency Management Agency and the state of Louisiana, the first of five teams of Navy doctors, nurses, and respiratory therapists were sent last week to Ochsner Lafayette General Medical Center in Lafayette, Louisiana.
The teams, consisting of approximately 20 members each, are coming from throughout the DoD’s universe, including the National Guard. US Army North, under US Northern Command’s oversight, is providing operational command of the active-duty military COVID-19 response. Lt. Gen. Laura J. Richardson, ARNORTH commander, noting that “[t]his is the second time Department of Defense medical assets have deployed to support Louisiana during the pandemic,” calls it a “whole-of-government fight against COVID-19.”
Why Louisiana and Mississippi, with so many states in dire need? “Our joint forces go where FEMA needs us,” Richardson says. “[R]ight now FEMA has determined the military’s unique surge capabilities are most needed in these two states.”
In a press briefing at the time, Pentagon Press Secretary Rear Adm. John Kirby said, “We expect that there could be additional requests from other states for other teams, so that’s why we’re being prepared to stand up five teams.” He was right: An Air Force team has now headed to Our Lady of the Lake Regional Medical Center in Baton Rouge. Mississippi also asked for assistance; an Air Force team will be supporting at University of Mississippi Medical Center in Jackson, and an Army team at North Mississippi Medical Center-Tupelo.
The support will likely include bolstering and extending the infrastructure. From July to December 2020, the Veterans Health Administration (VHA) Emergency Management Coordination Cell delivered Fold-Out Rigid Temporary Shelters (FORTS), C-FORTS (clinics), mobile ICUs and isolation units to locations across the US, such as North Chicago, El Paso, and Oklahoma City. In 2021, they’ll be needed in more hospitals unprepared to house the spiking numbers of patients. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
The first go-round with COVID taught hard lessons that can help hone the Fourth Mission responses. One lesson, according to the VHA COVID-19 Response Report- Annex A, published this May, was the need to conduct due diligence, to be both efficient and effective. VHA, it says, now works to determine actual need before deploying resources. “For example, VHA might receive a request from a [State Veterans Home] for 50 RNs. But once VHA delved into the request and worked with the associated VISNs, it would find that 20 RNs or 10 LPNs could meet the needs of the request.”
Meeting the requests is, for the beleaguered hospitals, like answering letters to Santa. When the team of doctors, nurses, and respiratory therapists arrived at Ochsner Lafayette General Medical Center (OLGMC) last week the hospital staff greeted them with cheers and applause.
OLGMC CEO Al Patin said, "We're already in a nursing shortage, coupled with high numbers of this pandemic [which] creates a situation where we need additional support. We have patients boarding in our emergency rooms, patients in our ICU setting that can't transition out. That creates a bottleneck and does not allow us to continue to take in patients from our community."
That day, OLG posted on Twitter:
“Today, we received some much-needed assistance in the fight against COVID-19. Our team at Ochsner Lafayette General Medical Center is being expanded by four doctors, 14 nurses and two respiratory therapists – all highly trained personnel on loan from the U.S. Navy.
“These healthcare professionals are being onboarded in our facility today and are specially trained for the emergency department, ICU and Med Surg. Because of them, we’ll be able to staff an additional 16-18 beds – beds sorely needed as cases continue to rise in our area.
“We requested support from the Federal Emergency Management Agency and we were one of five U.S. cities to receive it.. We are most grateful and humbled.”
Last summer, a team of US Department of Veterans Affairs (VA) health care professionals deployed to Alabama’s Bill Nichols State Veterans Home to help during the COVID-19 crisis. They were there as part of the “Fourth Mission”—supporting national, state, and local emergency management, public health, safety and homeland security efforts. “It was a really humbling experience,” said Mary Holloway, an RN with the Birmingham VA Health Care System. “Seeing the dedication of the staff there, some coming back to work after recovering from COVID themselves, was inspiring.”
But that turned out to be only one battle in a sadly long and drawn-out war. Since March 2020, more than 5,000 military medical personnel have deployed to 14 states and the Navajo Nation, 51 cities, 71 hospitals, all struggling to keep their heads above a cresting tsunami of new COVID patients.
Last year, the crisis spots for deployments included major metropolitan areas in coastal states: New York, California, and New Jersey. The urgency now is in the Southern states. Those tend to be reporting the highest numbers of new cases and deaths. Alabama, Arkansas, Florida, Louisiana, and Mississippi, for example, have all ranked among the highest rates of cases and hospitalizations per 100,000 people across the country in the last seven days.
This year, military teams have also deployed to support vaccination centers in 25 states and 42 cities. Nearly all—97%—of the new COVID patients in recent months are unvaccinated. And, again, they predominate in Southern states. In Alabama, for instance, only 37% of the population are fully vaccinated. In Louisiana, that number is 40%.
The at-risk states also tend to be the ones that are rapidly running out of space to put the patients in, ICU or otherwise. Where patients who might have been in the intensive care unit (ICU) are housed in the emergency department and in hallways, and where patients without COVID-19 who might have been hospitalized are being turned away. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
These states are at a breaking point. Take Alabama. On August 18, it was “negative 11.” It had 1,568 patients with COVID-19 who needed ICU beds. Only 1,557 beds were available. Patients “may even stay on the regular floor where you’re already stretched for capacity to take care of these people because so many of our staff are out with COVID,” Jeanne Marrazzo, director, Division of Infectious Diseases at the University of Alabama at Birmingham, told a CNN reporter. “It’s really just a domino effect that then clogs up our ERs, clogs up everything else. … It’s a very very tenuous situation.”
The state reported more than 4,000 new cases of COVID-19—“a new high for us,” Marrazzo said. “If you project these numbers out, you can expect that we will at some point, probably around Sept. 1, have at least 5,000 people in our hospitals. If the ratio of people who have to go to the ICU remains stable. That means that probably a third of those people are going to require ICU beds,” she continued. “That is frankly untenable, given the infrastructure, the resources, and really importantly, the staff that we have. I think it is basically apocalyptic. I do not use that word lightly.”
Thus, the US Defense Department (DoD) must once again rise to a sad and desperate occasion. At the request of Federal Emergency Management Agency and the state of Louisiana, the first of five teams of Navy doctors, nurses, and respiratory therapists were sent last week to Ochsner Lafayette General Medical Center in Lafayette, Louisiana.
The teams, consisting of approximately 20 members each, are coming from throughout the DoD’s universe, including the National Guard. US Army North, under US Northern Command’s oversight, is providing operational command of the active-duty military COVID-19 response. Lt. Gen. Laura J. Richardson, ARNORTH commander, noting that “[t]his is the second time Department of Defense medical assets have deployed to support Louisiana during the pandemic,” calls it a “whole-of-government fight against COVID-19.”
Why Louisiana and Mississippi, with so many states in dire need? “Our joint forces go where FEMA needs us,” Richardson says. “[R]ight now FEMA has determined the military’s unique surge capabilities are most needed in these two states.”
In a press briefing at the time, Pentagon Press Secretary Rear Adm. John Kirby said, “We expect that there could be additional requests from other states for other teams, so that’s why we’re being prepared to stand up five teams.” He was right: An Air Force team has now headed to Our Lady of the Lake Regional Medical Center in Baton Rouge. Mississippi also asked for assistance; an Air Force team will be supporting at University of Mississippi Medical Center in Jackson, and an Army team at North Mississippi Medical Center-Tupelo.
The support will likely include bolstering and extending the infrastructure. From July to December 2020, the Veterans Health Administration (VHA) Emergency Management Coordination Cell delivered Fold-Out Rigid Temporary Shelters (FORTS), C-FORTS (clinics), mobile ICUs and isolation units to locations across the US, such as North Chicago, El Paso, and Oklahoma City. In 2021, they’ll be needed in more hospitals unprepared to house the spiking numbers of patients. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
The first go-round with COVID taught hard lessons that can help hone the Fourth Mission responses. One lesson, according to the VHA COVID-19 Response Report- Annex A, published this May, was the need to conduct due diligence, to be both efficient and effective. VHA, it says, now works to determine actual need before deploying resources. “For example, VHA might receive a request from a [State Veterans Home] for 50 RNs. But once VHA delved into the request and worked with the associated VISNs, it would find that 20 RNs or 10 LPNs could meet the needs of the request.”
Meeting the requests is, for the beleaguered hospitals, like answering letters to Santa. When the team of doctors, nurses, and respiratory therapists arrived at Ochsner Lafayette General Medical Center (OLGMC) last week the hospital staff greeted them with cheers and applause.
OLGMC CEO Al Patin said, "We're already in a nursing shortage, coupled with high numbers of this pandemic [which] creates a situation where we need additional support. We have patients boarding in our emergency rooms, patients in our ICU setting that can't transition out. That creates a bottleneck and does not allow us to continue to take in patients from our community."
That day, OLG posted on Twitter:
“Today, we received some much-needed assistance in the fight against COVID-19. Our team at Ochsner Lafayette General Medical Center is being expanded by four doctors, 14 nurses and two respiratory therapists – all highly trained personnel on loan from the U.S. Navy.
“These healthcare professionals are being onboarded in our facility today and are specially trained for the emergency department, ICU and Med Surg. Because of them, we’ll be able to staff an additional 16-18 beds – beds sorely needed as cases continue to rise in our area.
“We requested support from the Federal Emergency Management Agency and we were one of five U.S. cities to receive it.. We are most grateful and humbled.”
Last summer, a team of US Department of Veterans Affairs (VA) health care professionals deployed to Alabama’s Bill Nichols State Veterans Home to help during the COVID-19 crisis. They were there as part of the “Fourth Mission”—supporting national, state, and local emergency management, public health, safety and homeland security efforts. “It was a really humbling experience,” said Mary Holloway, an RN with the Birmingham VA Health Care System. “Seeing the dedication of the staff there, some coming back to work after recovering from COVID themselves, was inspiring.”
But that turned out to be only one battle in a sadly long and drawn-out war. Since March 2020, more than 5,000 military medical personnel have deployed to 14 states and the Navajo Nation, 51 cities, 71 hospitals, all struggling to keep their heads above a cresting tsunami of new COVID patients.
Last year, the crisis spots for deployments included major metropolitan areas in coastal states: New York, California, and New Jersey. The urgency now is in the Southern states. Those tend to be reporting the highest numbers of new cases and deaths. Alabama, Arkansas, Florida, Louisiana, and Mississippi, for example, have all ranked among the highest rates of cases and hospitalizations per 100,000 people across the country in the last seven days.
This year, military teams have also deployed to support vaccination centers in 25 states and 42 cities. Nearly all—97%—of the new COVID patients in recent months are unvaccinated. And, again, they predominate in Southern states. In Alabama, for instance, only 37% of the population are fully vaccinated. In Louisiana, that number is 40%.
The at-risk states also tend to be the ones that are rapidly running out of space to put the patients in, ICU or otherwise. Where patients who might have been in the intensive care unit (ICU) are housed in the emergency department and in hallways, and where patients without COVID-19 who might have been hospitalized are being turned away. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
These states are at a breaking point. Take Alabama. On August 18, it was “negative 11.” It had 1,568 patients with COVID-19 who needed ICU beds. Only 1,557 beds were available. Patients “may even stay on the regular floor where you’re already stretched for capacity to take care of these people because so many of our staff are out with COVID,” Jeanne Marrazzo, director, Division of Infectious Diseases at the University of Alabama at Birmingham, told a CNN reporter. “It’s really just a domino effect that then clogs up our ERs, clogs up everything else. … It’s a very very tenuous situation.”
The state reported more than 4,000 new cases of COVID-19—“a new high for us,” Marrazzo said. “If you project these numbers out, you can expect that we will at some point, probably around Sept. 1, have at least 5,000 people in our hospitals. If the ratio of people who have to go to the ICU remains stable. That means that probably a third of those people are going to require ICU beds,” she continued. “That is frankly untenable, given the infrastructure, the resources, and really importantly, the staff that we have. I think it is basically apocalyptic. I do not use that word lightly.”
Thus, the US Defense Department (DoD) must once again rise to a sad and desperate occasion. At the request of Federal Emergency Management Agency and the state of Louisiana, the first of five teams of Navy doctors, nurses, and respiratory therapists were sent last week to Ochsner Lafayette General Medical Center in Lafayette, Louisiana.
The teams, consisting of approximately 20 members each, are coming from throughout the DoD’s universe, including the National Guard. US Army North, under US Northern Command’s oversight, is providing operational command of the active-duty military COVID-19 response. Lt. Gen. Laura J. Richardson, ARNORTH commander, noting that “[t]his is the second time Department of Defense medical assets have deployed to support Louisiana during the pandemic,” calls it a “whole-of-government fight against COVID-19.”
Why Louisiana and Mississippi, with so many states in dire need? “Our joint forces go where FEMA needs us,” Richardson says. “[R]ight now FEMA has determined the military’s unique surge capabilities are most needed in these two states.”
In a press briefing at the time, Pentagon Press Secretary Rear Adm. John Kirby said, “We expect that there could be additional requests from other states for other teams, so that’s why we’re being prepared to stand up five teams.” He was right: An Air Force team has now headed to Our Lady of the Lake Regional Medical Center in Baton Rouge. Mississippi also asked for assistance; an Air Force team will be supporting at University of Mississippi Medical Center in Jackson, and an Army team at North Mississippi Medical Center-Tupelo.
The support will likely include bolstering and extending the infrastructure. From July to December 2020, the Veterans Health Administration (VHA) Emergency Management Coordination Cell delivered Fold-Out Rigid Temporary Shelters (FORTS), C-FORTS (clinics), mobile ICUs and isolation units to locations across the US, such as North Chicago, El Paso, and Oklahoma City. In 2021, they’ll be needed in more hospitals unprepared to house the spiking numbers of patients. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
The first go-round with COVID taught hard lessons that can help hone the Fourth Mission responses. One lesson, according to the VHA COVID-19 Response Report- Annex A, published this May, was the need to conduct due diligence, to be both efficient and effective. VHA, it says, now works to determine actual need before deploying resources. “For example, VHA might receive a request from a [State Veterans Home] for 50 RNs. But once VHA delved into the request and worked with the associated VISNs, it would find that 20 RNs or 10 LPNs could meet the needs of the request.”
Meeting the requests is, for the beleaguered hospitals, like answering letters to Santa. When the team of doctors, nurses, and respiratory therapists arrived at Ochsner Lafayette General Medical Center (OLGMC) last week the hospital staff greeted them with cheers and applause.
OLGMC CEO Al Patin said, "We're already in a nursing shortage, coupled with high numbers of this pandemic [which] creates a situation where we need additional support. We have patients boarding in our emergency rooms, patients in our ICU setting that can't transition out. That creates a bottleneck and does not allow us to continue to take in patients from our community."
That day, OLG posted on Twitter:
“Today, we received some much-needed assistance in the fight against COVID-19. Our team at Ochsner Lafayette General Medical Center is being expanded by four doctors, 14 nurses and two respiratory therapists – all highly trained personnel on loan from the U.S. Navy.
“These healthcare professionals are being onboarded in our facility today and are specially trained for the emergency department, ICU and Med Surg. Because of them, we’ll be able to staff an additional 16-18 beds – beds sorely needed as cases continue to rise in our area.
“We requested support from the Federal Emergency Management Agency and we were one of five U.S. cities to receive it.. We are most grateful and humbled.”
Military Medical Teams Deploy to Relieve COVID-Battered Hospitals
Last summer, a team of US Department of Veterans Affairs (VA) health care professionals deployed to Alabama’s Bill Nichols State Veterans Home to help during the COVID-19 crisis. They were there as part of the “Fourth Mission”—supporting national, state, and local emergency management, public health, safety and homeland security efforts. “It was a really humbling experience,” said Mary Holloway, an RN with the Birmingham VA Health Care System. “Seeing the dedication of the staff there, some coming back to work after recovering from COVID themselves, was inspiring.”
But that turned out to be only one battle in a sadly long and drawn-out war. Since March 2020, more than 5,000 military medical personnel have deployed to 14 states and the Navajo Nation, 51 cities, 71 hospitals, all struggling to keep their heads above a cresting tsunami of new COVID patients.
Last year, the crisis spots for deployments included major metropolitan areas in coastal states: New York, California, and New Jersey. The urgency now is in the Southern states. Those tend to be reporting the highest numbers of new cases and deaths. Alabama, Arkansas, Florida, Louisiana, and Mississippi, for example, have all ranked among the highest rates of cases and hospitalizations per 100,000 people across the country in the last seven days.
This year, military teams have also deployed to support vaccination centers in 25 states and 42 cities. Nearly all—97%—of the new COVID patients in recent months are unvaccinated. And, again, they predominate in Southern states. In Alabama, for instance, only 37% of the population are fully vaccinated. In Louisiana, that number is 40%.
The at-risk states also tend to be the ones that are rapidly running out of space to put the patients in, ICU or otherwise. Where patients who might have been in the intensive care unit (ICU) are housed in the emergency department and in hallways, and where patients without COVID-19 who might have been hospitalized are being turned away. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
These states are at a breaking point. Take Alabama. On August 18, it was “negative 11.” It had 1,568 patients with COVID-19 who needed ICU beds. Only 1,557 beds were available. Patients “may even stay on the regular floor where you’re already stretched for capacity to take care of these people because so many of our staff are out with COVID,” Jeanne Marrazzo, director, Division of Infectious Diseases at the University of Alabama at Birmingham, told a CNN reporter. “It’s really just a domino effect that then clogs up our ERs, clogs up everything else. … It’s a very very tenuous situation.”
The state reported more than 4,000 new cases of COVID-19—“a new high for us,” Marrazzo said. “If you project these numbers out, you can expect that we will at some point, probably around Sept. 1, have at least 5,000 people in our hospitals. If the ratio of people who have to go to the ICU remains stable. That means that probably a third of those people are going to require ICU beds,” she continued. “That is frankly untenable, given the infrastructure, the resources, and really importantly, the staff that we have. I think it is basically apocalyptic. I do not use that word lightly.”
Thus, the US Defense Department (DoD) must once again rise to a sad and desperate occasion. At the request of Federal Emergency Management Agency and the state of Louisiana, the first of five teams of Navy doctors, nurses, and respiratory therapists were sent last week to Ochsner Lafayette General Medical Center in Lafayette, Louisiana.
The teams, consisting of approximately 20 members each, are coming from throughout the DoD’s universe, including the National Guard. US Army North, under US Northern Command’s oversight, is providing operational command of the active-duty military COVID-19 response. Lt. Gen. Laura J. Richardson, ARNORTH commander, noting that “[t]his is the second time Department of Defense medical assets have deployed to support Louisiana during the pandemic,” calls it a “whole-of-government fight against COVID-19.”
Why Louisiana and Mississippi, with so many states in dire need? “Our joint forces go where FEMA needs us,” Richardson says. “[R]ight now FEMA has determined the military’s unique surge capabilities are most needed in these two states.”
In a press briefing at the time, Pentagon Press Secretary Rear Adm. John Kirby said, “We expect that there could be additional requests from other states for other teams, so that’s why we’re being prepared to stand up five teams.” He was right: An Air Force team has now headed to Our Lady of the Lake Regional Medical Center in Baton Rouge. Mississippi also asked for assistance; an Air Force team will be supporting at University of Mississippi Medical Center in Jackson, and an Army team at North Mississippi Medical Center-Tupelo.
The support will likely include bolstering and extending the infrastructure. From July to December 2020, the Veterans Health Administration (VHA) Emergency Management Coordination Cell delivered Fold-Out Rigid Temporary Shelters (FORTS), C-FORTS (clinics), mobile ICUs and isolation units to locations across the US, such as North Chicago, El Paso, and Oklahoma City. In 2021, they’ll be needed in more hospitals unprepared to house the spiking numbers of patients. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
The first go-round with COVID taught hard lessons that can help hone the Fourth Mission responses. One lesson, according to the VHA COVID-19 Response Report- Annex A, published this May, was the need to conduct due diligence, to be both efficient and effective. VHA, it says, now works to determine actual need before deploying resources. “For example, VHA might receive a request from a [State Veterans Home] for 50 RNs. But once VHA delved into the request and worked with the associated VISNs, it would find that 20 RNs or 10 LPNs could meet the needs of the request.”
Meeting the requests is, for the beleaguered hospitals, like answering letters to Santa. When the team of doctors, nurses, and respiratory therapists arrived at Ochsner Lafayette General Medical Center (OLGMC) last week the hospital staff greeted them with cheers and applause.
OLGMC CEO Al Patin said, "We're already in a nursing shortage, coupled with high numbers of this pandemic [which] creates a situation where we need additional support. We have patients boarding in our emergency rooms, patients in our ICU setting that can't transition out. That creates a bottleneck and does not allow us to continue to take in patients from our community."
That day, OLG posted on Twitter:
“Today, we received some much-needed assistance in the fight against COVID-19. Our team at Ochsner Lafayette General Medical Center is being expanded by four doctors, 14 nurses and two respiratory therapists – all highly trained personnel on loan from the U.S. Navy.
“These healthcare professionals are being onboarded in our facility today and are specially trained for the emergency department, ICU and Med Surg. Because of them, we’ll be able to staff an additional 16-18 beds – beds sorely needed as cases continue to rise in our area.
“We requested support from the Federal Emergency Management Agency and we were one of five U.S. cities to receive it.. We are most grateful and humbled.”
Last summer, a team of US Department of Veterans Affairs (VA) health care professionals deployed to Alabama’s Bill Nichols State Veterans Home to help during the COVID-19 crisis. They were there as part of the “Fourth Mission”—supporting national, state, and local emergency management, public health, safety and homeland security efforts. “It was a really humbling experience,” said Mary Holloway, an RN with the Birmingham VA Health Care System. “Seeing the dedication of the staff there, some coming back to work after recovering from COVID themselves, was inspiring.”
But that turned out to be only one battle in a sadly long and drawn-out war. Since March 2020, more than 5,000 military medical personnel have deployed to 14 states and the Navajo Nation, 51 cities, 71 hospitals, all struggling to keep their heads above a cresting tsunami of new COVID patients.
Last year, the crisis spots for deployments included major metropolitan areas in coastal states: New York, California, and New Jersey. The urgency now is in the Southern states. Those tend to be reporting the highest numbers of new cases and deaths. Alabama, Arkansas, Florida, Louisiana, and Mississippi, for example, have all ranked among the highest rates of cases and hospitalizations per 100,000 people across the country in the last seven days.
This year, military teams have also deployed to support vaccination centers in 25 states and 42 cities. Nearly all—97%—of the new COVID patients in recent months are unvaccinated. And, again, they predominate in Southern states. In Alabama, for instance, only 37% of the population are fully vaccinated. In Louisiana, that number is 40%.
The at-risk states also tend to be the ones that are rapidly running out of space to put the patients in, ICU or otherwise. Where patients who might have been in the intensive care unit (ICU) are housed in the emergency department and in hallways, and where patients without COVID-19 who might have been hospitalized are being turned away. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
These states are at a breaking point. Take Alabama. On August 18, it was “negative 11.” It had 1,568 patients with COVID-19 who needed ICU beds. Only 1,557 beds were available. Patients “may even stay on the regular floor where you’re already stretched for capacity to take care of these people because so many of our staff are out with COVID,” Jeanne Marrazzo, director, Division of Infectious Diseases at the University of Alabama at Birmingham, told a CNN reporter. “It’s really just a domino effect that then clogs up our ERs, clogs up everything else. … It’s a very very tenuous situation.”
The state reported more than 4,000 new cases of COVID-19—“a new high for us,” Marrazzo said. “If you project these numbers out, you can expect that we will at some point, probably around Sept. 1, have at least 5,000 people in our hospitals. If the ratio of people who have to go to the ICU remains stable. That means that probably a third of those people are going to require ICU beds,” she continued. “That is frankly untenable, given the infrastructure, the resources, and really importantly, the staff that we have. I think it is basically apocalyptic. I do not use that word lightly.”
Thus, the US Defense Department (DoD) must once again rise to a sad and desperate occasion. At the request of Federal Emergency Management Agency and the state of Louisiana, the first of five teams of Navy doctors, nurses, and respiratory therapists were sent last week to Ochsner Lafayette General Medical Center in Lafayette, Louisiana.
The teams, consisting of approximately 20 members each, are coming from throughout the DoD’s universe, including the National Guard. US Army North, under US Northern Command’s oversight, is providing operational command of the active-duty military COVID-19 response. Lt. Gen. Laura J. Richardson, ARNORTH commander, noting that “[t]his is the second time Department of Defense medical assets have deployed to support Louisiana during the pandemic,” calls it a “whole-of-government fight against COVID-19.”
Why Louisiana and Mississippi, with so many states in dire need? “Our joint forces go where FEMA needs us,” Richardson says. “[R]ight now FEMA has determined the military’s unique surge capabilities are most needed in these two states.”
In a press briefing at the time, Pentagon Press Secretary Rear Adm. John Kirby said, “We expect that there could be additional requests from other states for other teams, so that’s why we’re being prepared to stand up five teams.” He was right: An Air Force team has now headed to Our Lady of the Lake Regional Medical Center in Baton Rouge. Mississippi also asked for assistance; an Air Force team will be supporting at University of Mississippi Medical Center in Jackson, and an Army team at North Mississippi Medical Center-Tupelo.
The support will likely include bolstering and extending the infrastructure. From July to December 2020, the Veterans Health Administration (VHA) Emergency Management Coordination Cell delivered Fold-Out Rigid Temporary Shelters (FORTS), C-FORTS (clinics), mobile ICUs and isolation units to locations across the US, such as North Chicago, El Paso, and Oklahoma City. In 2021, they’ll be needed in more hospitals unprepared to house the spiking numbers of patients. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
The first go-round with COVID taught hard lessons that can help hone the Fourth Mission responses. One lesson, according to the VHA COVID-19 Response Report- Annex A, published this May, was the need to conduct due diligence, to be both efficient and effective. VHA, it says, now works to determine actual need before deploying resources. “For example, VHA might receive a request from a [State Veterans Home] for 50 RNs. But once VHA delved into the request and worked with the associated VISNs, it would find that 20 RNs or 10 LPNs could meet the needs of the request.”
Meeting the requests is, for the beleaguered hospitals, like answering letters to Santa. When the team of doctors, nurses, and respiratory therapists arrived at Ochsner Lafayette General Medical Center (OLGMC) last week the hospital staff greeted them with cheers and applause.
OLGMC CEO Al Patin said, "We're already in a nursing shortage, coupled with high numbers of this pandemic [which] creates a situation where we need additional support. We have patients boarding in our emergency rooms, patients in our ICU setting that can't transition out. That creates a bottleneck and does not allow us to continue to take in patients from our community."
That day, OLG posted on Twitter:
“Today, we received some much-needed assistance in the fight against COVID-19. Our team at Ochsner Lafayette General Medical Center is being expanded by four doctors, 14 nurses and two respiratory therapists – all highly trained personnel on loan from the U.S. Navy.
“These healthcare professionals are being onboarded in our facility today and are specially trained for the emergency department, ICU and Med Surg. Because of them, we’ll be able to staff an additional 16-18 beds – beds sorely needed as cases continue to rise in our area.
“We requested support from the Federal Emergency Management Agency and we were one of five U.S. cities to receive it.. We are most grateful and humbled.”
Last summer, a team of US Department of Veterans Affairs (VA) health care professionals deployed to Alabama’s Bill Nichols State Veterans Home to help during the COVID-19 crisis. They were there as part of the “Fourth Mission”—supporting national, state, and local emergency management, public health, safety and homeland security efforts. “It was a really humbling experience,” said Mary Holloway, an RN with the Birmingham VA Health Care System. “Seeing the dedication of the staff there, some coming back to work after recovering from COVID themselves, was inspiring.”
But that turned out to be only one battle in a sadly long and drawn-out war. Since March 2020, more than 5,000 military medical personnel have deployed to 14 states and the Navajo Nation, 51 cities, 71 hospitals, all struggling to keep their heads above a cresting tsunami of new COVID patients.
Last year, the crisis spots for deployments included major metropolitan areas in coastal states: New York, California, and New Jersey. The urgency now is in the Southern states. Those tend to be reporting the highest numbers of new cases and deaths. Alabama, Arkansas, Florida, Louisiana, and Mississippi, for example, have all ranked among the highest rates of cases and hospitalizations per 100,000 people across the country in the last seven days.
This year, military teams have also deployed to support vaccination centers in 25 states and 42 cities. Nearly all—97%—of the new COVID patients in recent months are unvaccinated. And, again, they predominate in Southern states. In Alabama, for instance, only 37% of the population are fully vaccinated. In Louisiana, that number is 40%.
The at-risk states also tend to be the ones that are rapidly running out of space to put the patients in, ICU or otherwise. Where patients who might have been in the intensive care unit (ICU) are housed in the emergency department and in hallways, and where patients without COVID-19 who might have been hospitalized are being turned away. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
These states are at a breaking point. Take Alabama. On August 18, it was “negative 11.” It had 1,568 patients with COVID-19 who needed ICU beds. Only 1,557 beds were available. Patients “may even stay on the regular floor where you’re already stretched for capacity to take care of these people because so many of our staff are out with COVID,” Jeanne Marrazzo, director, Division of Infectious Diseases at the University of Alabama at Birmingham, told a CNN reporter. “It’s really just a domino effect that then clogs up our ERs, clogs up everything else. … It’s a very very tenuous situation.”
The state reported more than 4,000 new cases of COVID-19—“a new high for us,” Marrazzo said. “If you project these numbers out, you can expect that we will at some point, probably around Sept. 1, have at least 5,000 people in our hospitals. If the ratio of people who have to go to the ICU remains stable. That means that probably a third of those people are going to require ICU beds,” she continued. “That is frankly untenable, given the infrastructure, the resources, and really importantly, the staff that we have. I think it is basically apocalyptic. I do not use that word lightly.”
Thus, the US Defense Department (DoD) must once again rise to a sad and desperate occasion. At the request of Federal Emergency Management Agency and the state of Louisiana, the first of five teams of Navy doctors, nurses, and respiratory therapists were sent last week to Ochsner Lafayette General Medical Center in Lafayette, Louisiana.
The teams, consisting of approximately 20 members each, are coming from throughout the DoD’s universe, including the National Guard. US Army North, under US Northern Command’s oversight, is providing operational command of the active-duty military COVID-19 response. Lt. Gen. Laura J. Richardson, ARNORTH commander, noting that “[t]his is the second time Department of Defense medical assets have deployed to support Louisiana during the pandemic,” calls it a “whole-of-government fight against COVID-19.”
Why Louisiana and Mississippi, with so many states in dire need? “Our joint forces go where FEMA needs us,” Richardson says. “[R]ight now FEMA has determined the military’s unique surge capabilities are most needed in these two states.”
In a press briefing at the time, Pentagon Press Secretary Rear Adm. John Kirby said, “We expect that there could be additional requests from other states for other teams, so that’s why we’re being prepared to stand up five teams.” He was right: An Air Force team has now headed to Our Lady of the Lake Regional Medical Center in Baton Rouge. Mississippi also asked for assistance; an Air Force team will be supporting at University of Mississippi Medical Center in Jackson, and an Army team at North Mississippi Medical Center-Tupelo.
The support will likely include bolstering and extending the infrastructure. From July to December 2020, the Veterans Health Administration (VHA) Emergency Management Coordination Cell delivered Fold-Out Rigid Temporary Shelters (FORTS), C-FORTS (clinics), mobile ICUs and isolation units to locations across the US, such as North Chicago, El Paso, and Oklahoma City. In 2021, they’ll be needed in more hospitals unprepared to house the spiking numbers of patients. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
The first go-round with COVID taught hard lessons that can help hone the Fourth Mission responses. One lesson, according to the VHA COVID-19 Response Report- Annex A, published this May, was the need to conduct due diligence, to be both efficient and effective. VHA, it says, now works to determine actual need before deploying resources. “For example, VHA might receive a request from a [State Veterans Home] for 50 RNs. But once VHA delved into the request and worked with the associated VISNs, it would find that 20 RNs or 10 LPNs could meet the needs of the request.”
Meeting the requests is, for the beleaguered hospitals, like answering letters to Santa. When the team of doctors, nurses, and respiratory therapists arrived at Ochsner Lafayette General Medical Center (OLGMC) last week the hospital staff greeted them with cheers and applause.
OLGMC CEO Al Patin said, "We're already in a nursing shortage, coupled with high numbers of this pandemic [which] creates a situation where we need additional support. We have patients boarding in our emergency rooms, patients in our ICU setting that can't transition out. That creates a bottleneck and does not allow us to continue to take in patients from our community."
That day, OLG posted on Twitter:
“Today, we received some much-needed assistance in the fight against COVID-19. Our team at Ochsner Lafayette General Medical Center is being expanded by four doctors, 14 nurses and two respiratory therapists – all highly trained personnel on loan from the U.S. Navy.
“These healthcare professionals are being onboarded in our facility today and are specially trained for the emergency department, ICU and Med Surg. Because of them, we’ll be able to staff an additional 16-18 beds – beds sorely needed as cases continue to rise in our area.
“We requested support from the Federal Emergency Management Agency and we were one of five U.S. cities to receive it.. We are most grateful and humbled.”
Military Medical Teams Deploy to Relieve COVID-Battered Hospitals
Last summer, a team of US Department of Veterans Affairs (VA) health care professionals deployed to Alabama’s Bill Nichols State Veterans Home to help during the COVID-19 crisis. They were there as part of the “Fourth Mission”—supporting national, state, and local emergency management, public health, safety and homeland security efforts. “It was a really humbling experience,” said Mary Holloway, an RN with the Birmingham VA Health Care System. “Seeing the dedication of the staff there, some coming back to work after recovering from COVID themselves, was inspiring.”
But that turned out to be only one battle in a sadly long and drawn-out war. Since March 2020, more than 5,000 military medical personnel have deployed to 14 states and the Navajo Nation, 51 cities, 71 hospitals, all struggling to keep their heads above a cresting tsunami of new COVID patients.
Last year, the crisis spots for deployments included major metropolitan areas in coastal states: New York, California, and New Jersey. The urgency now is in the Southern states. Those tend to be reporting the highest numbers of new cases and deaths. Alabama, Arkansas, Florida, Louisiana, and Mississippi, for example, have all ranked among the highest rates of cases and hospitalizations per 100,000 people across the country in the last seven days.
This year, military teams have also deployed to support vaccination centers in 25 states and 42 cities. Nearly all—97%—of the new COVID patients in recent months are unvaccinated. And, again, they predominate in Southern states. In Alabama, for instance, only 37% of the population are fully vaccinated. In Louisiana, that number is 40%.
The at-risk states also tend to be the ones that are rapidly running out of space to put the patients in, ICU or otherwise. Where patients who might have been in the intensive care unit (ICU) are housed in the emergency department and in hallways, and where patients without COVID-19 who might have been hospitalized are being turned away. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
These states are at a breaking point. Take Alabama. On August 18, it was “negative 11.” It had 1,568 patients with COVID-19 who needed ICU beds. Only 1,557 beds were available. Patients “may even stay on the regular floor where you’re already stretched for capacity to take care of these people because so many of our staff are out with COVID,” Jeanne Marrazzo, director, Division of Infectious Diseases at the University of Alabama at Birmingham, told a CNN reporter. “It’s really just a domino effect that then clogs up our ERs, clogs up everything else. … It’s a very very tenuous situation.”
The state reported more than 4,000 new cases of COVID-19—“a new high for us,” Marrazzo said. “If you project these numbers out, you can expect that we will at some point, probably around Sept. 1, have at least 5,000 people in our hospitals. If the ratio of people who have to go to the ICU remains stable. That means that probably a third of those people are going to require ICU beds,” she continued. “That is frankly untenable, given the infrastructure, the resources, and really importantly, the staff that we have. I think it is basically apocalyptic. I do not use that word lightly.”
Thus, the US Defense Department (DoD) must once again rise to a sad and desperate occasion. At the request of Federal Emergency Management Agency and the state of Louisiana, the first of five teams of Navy doctors, nurses, and respiratory therapists were sent last week to Ochsner Lafayette General Medical Center in Lafayette, Louisiana.
The teams, consisting of approximately 20 members each, are coming from throughout the DoD’s universe, including the National Guard. US Army North, under US Northern Command’s oversight, is providing operational command of the active-duty military COVID-19 response. Lt. Gen. Laura J. Richardson, ARNORTH commander, noting that “[t]his is the second time Department of Defense medical assets have deployed to support Louisiana during the pandemic,” calls it a “whole-of-government fight against COVID-19.”
Why Louisiana and Mississippi, with so many states in dire need? “Our joint forces go where FEMA needs us,” Richardson says. “[R]ight now FEMA has determined the military’s unique surge capabilities are most needed in these two states.”
In a press briefing at the time, Pentagon Press Secretary Rear Adm. John Kirby said, “We expect that there could be additional requests from other states for other teams, so that’s why we’re being prepared to stand up five teams.” He was right: An Air Force team has now headed to Our Lady of the Lake Regional Medical Center in Baton Rouge. Mississippi also asked for assistance; an Air Force team will be supporting at University of Mississippi Medical Center in Jackson, and an Army team at North Mississippi Medical Center-Tupelo.
The support will likely include bolstering and extending the infrastructure. From July to December 2020, the Veterans Health Administration (VHA) Emergency Management Coordination Cell delivered Fold-Out Rigid Temporary Shelters (FORTS), C-FORTS (clinics), mobile ICUs and isolation units to locations across the US, such as North Chicago, El Paso, and Oklahoma City. In 2021, they’ll be needed in more hospitals unprepared to house the spiking numbers of patients. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
The first go-round with COVID taught hard lessons that can help hone the Fourth Mission responses. One lesson, according to the VHA COVID-19 Response Report- Annex A, published this May, was the need to conduct due diligence, to be both efficient and effective. VHA, it says, now works to determine actual need before deploying resources. “For example, VHA might receive a request from a [State Veterans Home] for 50 RNs. But once VHA delved into the request and worked with the associated VISNs, it would find that 20 RNs or 10 LPNs could meet the needs of the request.”
Meeting the requests is, for the beleaguered hospitals, like answering letters to Santa. When the team of doctors, nurses, and respiratory therapists arrived at Ochsner Lafayette General Medical Center (OLGMC) last week the hospital staff greeted them with cheers and applause.
OLGMC CEO Al Patin said, "We're already in a nursing shortage, coupled with high numbers of this pandemic [which] creates a situation where we need additional support. We have patients boarding in our emergency rooms, patients in our ICU setting that can't transition out. That creates a bottleneck and does not allow us to continue to take in patients from our community."
That day, OLG posted on Twitter:
“Today, we received some much-needed assistance in the fight against COVID-19. Our team at Ochsner Lafayette General Medical Center is being expanded by four doctors, 14 nurses and two respiratory therapists – all highly trained personnel on loan from the U.S. Navy.
“These healthcare professionals are being onboarded in our facility today and are specially trained for the emergency department, ICU and Med Surg. Because of them, we’ll be able to staff an additional 16-18 beds – beds sorely needed as cases continue to rise in our area.
“We requested support from the Federal Emergency Management Agency and we were one of five U.S. cities to receive it.. We are most grateful and humbled.”
Last summer, a team of US Department of Veterans Affairs (VA) health care professionals deployed to Alabama’s Bill Nichols State Veterans Home to help during the COVID-19 crisis. They were there as part of the “Fourth Mission”—supporting national, state, and local emergency management, public health, safety and homeland security efforts. “It was a really humbling experience,” said Mary Holloway, an RN with the Birmingham VA Health Care System. “Seeing the dedication of the staff there, some coming back to work after recovering from COVID themselves, was inspiring.”
But that turned out to be only one battle in a sadly long and drawn-out war. Since March 2020, more than 5,000 military medical personnel have deployed to 14 states and the Navajo Nation, 51 cities, 71 hospitals, all struggling to keep their heads above a cresting tsunami of new COVID patients.
Last year, the crisis spots for deployments included major metropolitan areas in coastal states: New York, California, and New Jersey. The urgency now is in the Southern states. Those tend to be reporting the highest numbers of new cases and deaths. Alabama, Arkansas, Florida, Louisiana, and Mississippi, for example, have all ranked among the highest rates of cases and hospitalizations per 100,000 people across the country in the last seven days.
This year, military teams have also deployed to support vaccination centers in 25 states and 42 cities. Nearly all—97%—of the new COVID patients in recent months are unvaccinated. And, again, they predominate in Southern states. In Alabama, for instance, only 37% of the population are fully vaccinated. In Louisiana, that number is 40%.
The at-risk states also tend to be the ones that are rapidly running out of space to put the patients in, ICU or otherwise. Where patients who might have been in the intensive care unit (ICU) are housed in the emergency department and in hallways, and where patients without COVID-19 who might have been hospitalized are being turned away. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
These states are at a breaking point. Take Alabama. On August 18, it was “negative 11.” It had 1,568 patients with COVID-19 who needed ICU beds. Only 1,557 beds were available. Patients “may even stay on the regular floor where you’re already stretched for capacity to take care of these people because so many of our staff are out with COVID,” Jeanne Marrazzo, director, Division of Infectious Diseases at the University of Alabama at Birmingham, told a CNN reporter. “It’s really just a domino effect that then clogs up our ERs, clogs up everything else. … It’s a very very tenuous situation.”
The state reported more than 4,000 new cases of COVID-19—“a new high for us,” Marrazzo said. “If you project these numbers out, you can expect that we will at some point, probably around Sept. 1, have at least 5,000 people in our hospitals. If the ratio of people who have to go to the ICU remains stable. That means that probably a third of those people are going to require ICU beds,” she continued. “That is frankly untenable, given the infrastructure, the resources, and really importantly, the staff that we have. I think it is basically apocalyptic. I do not use that word lightly.”
Thus, the US Defense Department (DoD) must once again rise to a sad and desperate occasion. At the request of Federal Emergency Management Agency and the state of Louisiana, the first of five teams of Navy doctors, nurses, and respiratory therapists were sent last week to Ochsner Lafayette General Medical Center in Lafayette, Louisiana.
The teams, consisting of approximately 20 members each, are coming from throughout the DoD’s universe, including the National Guard. US Army North, under US Northern Command’s oversight, is providing operational command of the active-duty military COVID-19 response. Lt. Gen. Laura J. Richardson, ARNORTH commander, noting that “[t]his is the second time Department of Defense medical assets have deployed to support Louisiana during the pandemic,” calls it a “whole-of-government fight against COVID-19.”
Why Louisiana and Mississippi, with so many states in dire need? “Our joint forces go where FEMA needs us,” Richardson says. “[R]ight now FEMA has determined the military’s unique surge capabilities are most needed in these two states.”
In a press briefing at the time, Pentagon Press Secretary Rear Adm. John Kirby said, “We expect that there could be additional requests from other states for other teams, so that’s why we’re being prepared to stand up five teams.” He was right: An Air Force team has now headed to Our Lady of the Lake Regional Medical Center in Baton Rouge. Mississippi also asked for assistance; an Air Force team will be supporting at University of Mississippi Medical Center in Jackson, and an Army team at North Mississippi Medical Center-Tupelo.
The support will likely include bolstering and extending the infrastructure. From July to December 2020, the Veterans Health Administration (VHA) Emergency Management Coordination Cell delivered Fold-Out Rigid Temporary Shelters (FORTS), C-FORTS (clinics), mobile ICUs and isolation units to locations across the US, such as North Chicago, El Paso, and Oklahoma City. In 2021, they’ll be needed in more hospitals unprepared to house the spiking numbers of patients. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
The first go-round with COVID taught hard lessons that can help hone the Fourth Mission responses. One lesson, according to the VHA COVID-19 Response Report- Annex A, published this May, was the need to conduct due diligence, to be both efficient and effective. VHA, it says, now works to determine actual need before deploying resources. “For example, VHA might receive a request from a [State Veterans Home] for 50 RNs. But once VHA delved into the request and worked with the associated VISNs, it would find that 20 RNs or 10 LPNs could meet the needs of the request.”
Meeting the requests is, for the beleaguered hospitals, like answering letters to Santa. When the team of doctors, nurses, and respiratory therapists arrived at Ochsner Lafayette General Medical Center (OLGMC) last week the hospital staff greeted them with cheers and applause.
OLGMC CEO Al Patin said, "We're already in a nursing shortage, coupled with high numbers of this pandemic [which] creates a situation where we need additional support. We have patients boarding in our emergency rooms, patients in our ICU setting that can't transition out. That creates a bottleneck and does not allow us to continue to take in patients from our community."
That day, OLG posted on Twitter:
“Today, we received some much-needed assistance in the fight against COVID-19. Our team at Ochsner Lafayette General Medical Center is being expanded by four doctors, 14 nurses and two respiratory therapists – all highly trained personnel on loan from the U.S. Navy.
“These healthcare professionals are being onboarded in our facility today and are specially trained for the emergency department, ICU and Med Surg. Because of them, we’ll be able to staff an additional 16-18 beds – beds sorely needed as cases continue to rise in our area.
“We requested support from the Federal Emergency Management Agency and we were one of five U.S. cities to receive it.. We are most grateful and humbled.”
Last summer, a team of US Department of Veterans Affairs (VA) health care professionals deployed to Alabama’s Bill Nichols State Veterans Home to help during the COVID-19 crisis. They were there as part of the “Fourth Mission”—supporting national, state, and local emergency management, public health, safety and homeland security efforts. “It was a really humbling experience,” said Mary Holloway, an RN with the Birmingham VA Health Care System. “Seeing the dedication of the staff there, some coming back to work after recovering from COVID themselves, was inspiring.”
But that turned out to be only one battle in a sadly long and drawn-out war. Since March 2020, more than 5,000 military medical personnel have deployed to 14 states and the Navajo Nation, 51 cities, 71 hospitals, all struggling to keep their heads above a cresting tsunami of new COVID patients.
Last year, the crisis spots for deployments included major metropolitan areas in coastal states: New York, California, and New Jersey. The urgency now is in the Southern states. Those tend to be reporting the highest numbers of new cases and deaths. Alabama, Arkansas, Florida, Louisiana, and Mississippi, for example, have all ranked among the highest rates of cases and hospitalizations per 100,000 people across the country in the last seven days.
This year, military teams have also deployed to support vaccination centers in 25 states and 42 cities. Nearly all—97%—of the new COVID patients in recent months are unvaccinated. And, again, they predominate in Southern states. In Alabama, for instance, only 37% of the population are fully vaccinated. In Louisiana, that number is 40%.
The at-risk states also tend to be the ones that are rapidly running out of space to put the patients in, ICU or otherwise. Where patients who might have been in the intensive care unit (ICU) are housed in the emergency department and in hallways, and where patients without COVID-19 who might have been hospitalized are being turned away. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
These states are at a breaking point. Take Alabama. On August 18, it was “negative 11.” It had 1,568 patients with COVID-19 who needed ICU beds. Only 1,557 beds were available. Patients “may even stay on the regular floor where you’re already stretched for capacity to take care of these people because so many of our staff are out with COVID,” Jeanne Marrazzo, director, Division of Infectious Diseases at the University of Alabama at Birmingham, told a CNN reporter. “It’s really just a domino effect that then clogs up our ERs, clogs up everything else. … It’s a very very tenuous situation.”
The state reported more than 4,000 new cases of COVID-19—“a new high for us,” Marrazzo said. “If you project these numbers out, you can expect that we will at some point, probably around Sept. 1, have at least 5,000 people in our hospitals. If the ratio of people who have to go to the ICU remains stable. That means that probably a third of those people are going to require ICU beds,” she continued. “That is frankly untenable, given the infrastructure, the resources, and really importantly, the staff that we have. I think it is basically apocalyptic. I do not use that word lightly.”
Thus, the US Defense Department (DoD) must once again rise to a sad and desperate occasion. At the request of Federal Emergency Management Agency and the state of Louisiana, the first of five teams of Navy doctors, nurses, and respiratory therapists were sent last week to Ochsner Lafayette General Medical Center in Lafayette, Louisiana.
The teams, consisting of approximately 20 members each, are coming from throughout the DoD’s universe, including the National Guard. US Army North, under US Northern Command’s oversight, is providing operational command of the active-duty military COVID-19 response. Lt. Gen. Laura J. Richardson, ARNORTH commander, noting that “[t]his is the second time Department of Defense medical assets have deployed to support Louisiana during the pandemic,” calls it a “whole-of-government fight against COVID-19.”
Why Louisiana and Mississippi, with so many states in dire need? “Our joint forces go where FEMA needs us,” Richardson says. “[R]ight now FEMA has determined the military’s unique surge capabilities are most needed in these two states.”
In a press briefing at the time, Pentagon Press Secretary Rear Adm. John Kirby said, “We expect that there could be additional requests from other states for other teams, so that’s why we’re being prepared to stand up five teams.” He was right: An Air Force team has now headed to Our Lady of the Lake Regional Medical Center in Baton Rouge. Mississippi also asked for assistance; an Air Force team will be supporting at University of Mississippi Medical Center in Jackson, and an Army team at North Mississippi Medical Center-Tupelo.
The support will likely include bolstering and extending the infrastructure. From July to December 2020, the Veterans Health Administration (VHA) Emergency Management Coordination Cell delivered Fold-Out Rigid Temporary Shelters (FORTS), C-FORTS (clinics), mobile ICUs and isolation units to locations across the US, such as North Chicago, El Paso, and Oklahoma City. In 2021, they’ll be needed in more hospitals unprepared to house the spiking numbers of patients. Some Louisiana hospitals, for instance, have been sending patients in ambulances to Texas for care.
The first go-round with COVID taught hard lessons that can help hone the Fourth Mission responses. One lesson, according to the VHA COVID-19 Response Report- Annex A, published this May, was the need to conduct due diligence, to be both efficient and effective. VHA, it says, now works to determine actual need before deploying resources. “For example, VHA might receive a request from a [State Veterans Home] for 50 RNs. But once VHA delved into the request and worked with the associated VISNs, it would find that 20 RNs or 10 LPNs could meet the needs of the request.”
Meeting the requests is, for the beleaguered hospitals, like answering letters to Santa. When the team of doctors, nurses, and respiratory therapists arrived at Ochsner Lafayette General Medical Center (OLGMC) last week the hospital staff greeted them with cheers and applause.
OLGMC CEO Al Patin said, "We're already in a nursing shortage, coupled with high numbers of this pandemic [which] creates a situation where we need additional support. We have patients boarding in our emergency rooms, patients in our ICU setting that can't transition out. That creates a bottleneck and does not allow us to continue to take in patients from our community."
That day, OLG posted on Twitter:
“Today, we received some much-needed assistance in the fight against COVID-19. Our team at Ochsner Lafayette General Medical Center is being expanded by four doctors, 14 nurses and two respiratory therapists – all highly trained personnel on loan from the U.S. Navy.
“These healthcare professionals are being onboarded in our facility today and are specially trained for the emergency department, ICU and Med Surg. Because of them, we’ll be able to staff an additional 16-18 beds – beds sorely needed as cases continue to rise in our area.
“We requested support from the Federal Emergency Management Agency and we were one of five U.S. cities to receive it.. We are most grateful and humbled.”
Not so fast food
As long as I can remember, children have been notoriously wasteful when dining in school cafeterias. Even those children who bring their own food often return home in the afternoon with their lunches half eaten. Not surprisingly, the food tossed out is often the healthier portion of the meal. Schools have tried a variety of strategies to curb this wastage, including using volunteer student monitors to police and encourage ecologically based recycling.
The authors of a recent study published on JAMA Network Open observed that when elementary and middle-school students were allowed a 20-minute seated lunch period they consumed more food and there was significantly less waste of fruits and vegetable compared with when the students’ lunch period was limited to 10 minutes. Interestingly, there was no difference in the beverage and entrée consumption when the lunch period was doubled.
The authors postulate that younger children may not have acquired the dexterity to feed themselves optimally in the shorter lunch period. I’m not sure I buy that argument. It may be simply that the children ate and drank their favorites first and needed a bit more time to allow their little guts to move things along. But, regardless of the explanation, the investigators’ observations deserve further study.
When I was in high school our lunch period was a full hour, which allowed me to make the half mile walk to home and back to eat a home-prepared meal. The noon hour was when school clubs and committees met and there was a full schedule of diversions to fill out the hour. I don’t recall the seated portion of the lunch period having any time restriction.
By the time my own children were in middle school, lunch periods lasted no longer than 20 minutes. I was not surprised to learn from this recent study that in some schools the seated lunch period has been shortened to 10 minutes. In some cases the truncated lunch periods are a response to space and time limitations. I fear that occasionally, educators and administrators have found it so difficult to keep young children who are accustomed to watching television while they eat engaged that the periods have been shortened to minimize the chaos.
Here in Maine, the governor has just announced plans to offer free breakfast and lunch to every student in response to a federal initiative. If we intend to make nutrition a cornerstone of the educational process this study from the University of Illinois at Urbana-Champaign suggests that we must do more than simply provide the food at no cost. We must somehow carve out more time in the day for the children to eat a healthy diet.
But, where is this time going to come from? Many school systems have already cannibalized physical education to the point that most children are not getting a healthy amount of exercise. It is unfortunate that we have come to expect public school systems to solve all of our societal ills and compensate for less-than-healthy home environments. But that is the reality. If we think nutrition and physical activity are important components of our children’s educations then we must make the time necessary to provide them.
Will this mean longer school days? And will those longer days cost money? You bet they will, but that may be the price we have to pay for healthier, better educated children.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
As long as I can remember, children have been notoriously wasteful when dining in school cafeterias. Even those children who bring their own food often return home in the afternoon with their lunches half eaten. Not surprisingly, the food tossed out is often the healthier portion of the meal. Schools have tried a variety of strategies to curb this wastage, including using volunteer student monitors to police and encourage ecologically based recycling.
The authors of a recent study published on JAMA Network Open observed that when elementary and middle-school students were allowed a 20-minute seated lunch period they consumed more food and there was significantly less waste of fruits and vegetable compared with when the students’ lunch period was limited to 10 minutes. Interestingly, there was no difference in the beverage and entrée consumption when the lunch period was doubled.
The authors postulate that younger children may not have acquired the dexterity to feed themselves optimally in the shorter lunch period. I’m not sure I buy that argument. It may be simply that the children ate and drank their favorites first and needed a bit more time to allow their little guts to move things along. But, regardless of the explanation, the investigators’ observations deserve further study.
When I was in high school our lunch period was a full hour, which allowed me to make the half mile walk to home and back to eat a home-prepared meal. The noon hour was when school clubs and committees met and there was a full schedule of diversions to fill out the hour. I don’t recall the seated portion of the lunch period having any time restriction.
By the time my own children were in middle school, lunch periods lasted no longer than 20 minutes. I was not surprised to learn from this recent study that in some schools the seated lunch period has been shortened to 10 minutes. In some cases the truncated lunch periods are a response to space and time limitations. I fear that occasionally, educators and administrators have found it so difficult to keep young children who are accustomed to watching television while they eat engaged that the periods have been shortened to minimize the chaos.
Here in Maine, the governor has just announced plans to offer free breakfast and lunch to every student in response to a federal initiative. If we intend to make nutrition a cornerstone of the educational process this study from the University of Illinois at Urbana-Champaign suggests that we must do more than simply provide the food at no cost. We must somehow carve out more time in the day for the children to eat a healthy diet.
But, where is this time going to come from? Many school systems have already cannibalized physical education to the point that most children are not getting a healthy amount of exercise. It is unfortunate that we have come to expect public school systems to solve all of our societal ills and compensate for less-than-healthy home environments. But that is the reality. If we think nutrition and physical activity are important components of our children’s educations then we must make the time necessary to provide them.
Will this mean longer school days? And will those longer days cost money? You bet they will, but that may be the price we have to pay for healthier, better educated children.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
As long as I can remember, children have been notoriously wasteful when dining in school cafeterias. Even those children who bring their own food often return home in the afternoon with their lunches half eaten. Not surprisingly, the food tossed out is often the healthier portion of the meal. Schools have tried a variety of strategies to curb this wastage, including using volunteer student monitors to police and encourage ecologically based recycling.
The authors of a recent study published on JAMA Network Open observed that when elementary and middle-school students were allowed a 20-minute seated lunch period they consumed more food and there was significantly less waste of fruits and vegetable compared with when the students’ lunch period was limited to 10 minutes. Interestingly, there was no difference in the beverage and entrée consumption when the lunch period was doubled.
The authors postulate that younger children may not have acquired the dexterity to feed themselves optimally in the shorter lunch period. I’m not sure I buy that argument. It may be simply that the children ate and drank their favorites first and needed a bit more time to allow their little guts to move things along. But, regardless of the explanation, the investigators’ observations deserve further study.
When I was in high school our lunch period was a full hour, which allowed me to make the half mile walk to home and back to eat a home-prepared meal. The noon hour was when school clubs and committees met and there was a full schedule of diversions to fill out the hour. I don’t recall the seated portion of the lunch period having any time restriction.
By the time my own children were in middle school, lunch periods lasted no longer than 20 minutes. I was not surprised to learn from this recent study that in some schools the seated lunch period has been shortened to 10 minutes. In some cases the truncated lunch periods are a response to space and time limitations. I fear that occasionally, educators and administrators have found it so difficult to keep young children who are accustomed to watching television while they eat engaged that the periods have been shortened to minimize the chaos.
Here in Maine, the governor has just announced plans to offer free breakfast and lunch to every student in response to a federal initiative. If we intend to make nutrition a cornerstone of the educational process this study from the University of Illinois at Urbana-Champaign suggests that we must do more than simply provide the food at no cost. We must somehow carve out more time in the day for the children to eat a healthy diet.
But, where is this time going to come from? Many school systems have already cannibalized physical education to the point that most children are not getting a healthy amount of exercise. It is unfortunate that we have come to expect public school systems to solve all of our societal ills and compensate for less-than-healthy home environments. But that is the reality. If we think nutrition and physical activity are important components of our children’s educations then we must make the time necessary to provide them.
Will this mean longer school days? And will those longer days cost money? You bet they will, but that may be the price we have to pay for healthier, better educated children.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Children and COVID: New cases soar to near-record level
Weekly cases of COVID-19 in children jumped by nearly 50% in the United States, posting the highest count since hitting a pandemic high back in mid-January, a new report shows.
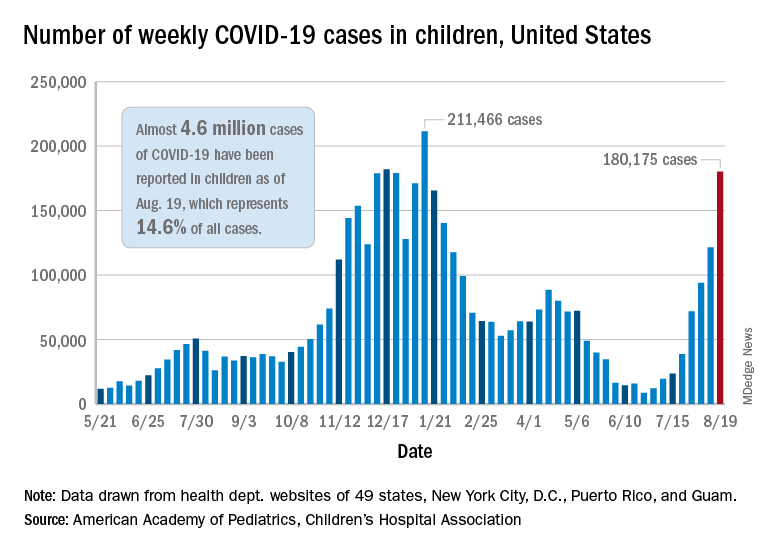
The latest weekly figure represents a 48% increase over the previous week and an increase of over 2,000% in the 8 weeks since the national count dropped to a low of 8,500 cases for the week of June 18-24, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
Vaccinations, in the meantime, appear to be headed in the opposite direction. Vaccine initiations were down for the second consecutive week, falling by 18% among 12- to 15-year-olds and by 15% in those aged 16-17 years, according to data from the Centers for Disease Control and Prevention.
Nationally, about 47% of children aged 12-15 and 56% of those aged 16-17 have received at least one dose of COVID vaccine as of Aug. 23, with 34% and 44%, respectively, reaching full vaccination. The total number of children with at least one dose is 11.6 million, including a relatively small number (about 200,000) of children under age 12 years, the CDC said on its COVID Data Tracker.
At the state level, vaccination is a source of considerable disparity. In Vermont, 73% of children aged 12-17 had received at least one dose by Aug. 18, and 63% were fully vaccinated. In Wyoming, however, just 25% of children had received at least one dose (17% are fully vaccinated), while Alabama has a lowest-in-the-nation full vaccination rate of 14%, based on a separate AAP analysis of CDC data.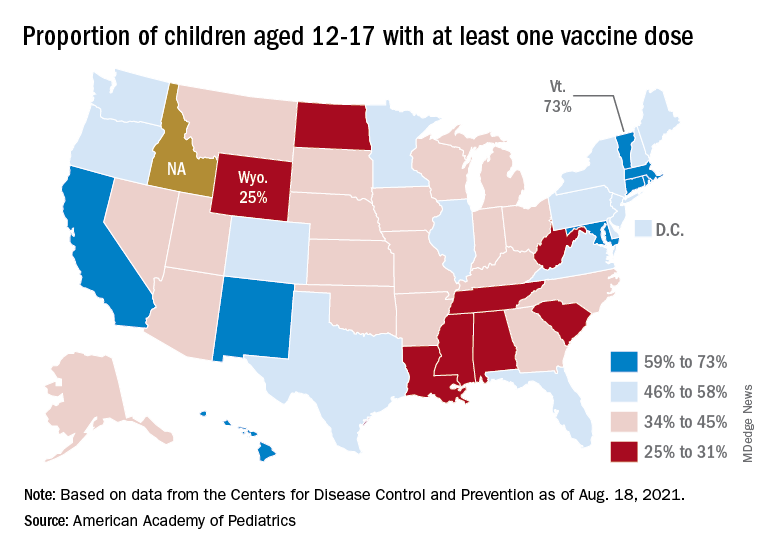
There are seven states in which over 60% of 12- to 17-year-olds have at least started the vaccine regimen and five states where less than 30% have received at least one dose, the AAP noted.
Back on the incidence side of the pandemic, Mississippi and Hawaii had the largest increases in new cases over the past 2 weeks, followed by Florida and West Virginia. Cumulative figures show that California has had the most cases overall in children (550,337), Vermont has the highest proportion of all cases in children (22.9%), and Rhode Island has the highest rate of cases per 100,000 (10,636), the AAP and CHA said in the joint report based on data from 49 states, the District of Columbia, New York City, Puerto Rico, and Guam.
Add up all those jurisdictions, and it works out to 4.6 million children infected with SARS-CoV-2 as of Aug. 19, with children representing 14.6% of all cases since the start of the pandemic. There have been over 18,000 hospitalizations so far, which is just 2.3% of the total for all ages in the 23 states (and New York City) that are reporting such data on their health department websites, the AAP and CHA said.
The number of COVID-related deaths in children is now 402 after the largest 1-week increase (24) since late May of 2020, when the AAP/CHA coverage began. Mortality data by age are available from 44 states, New York City, Puerto Rico, and Guam.
Weekly cases of COVID-19 in children jumped by nearly 50% in the United States, posting the highest count since hitting a pandemic high back in mid-January, a new report shows.
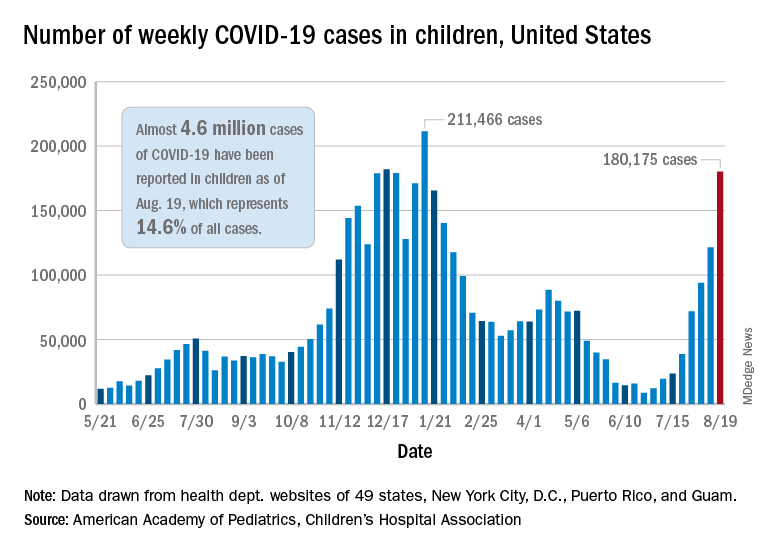
The latest weekly figure represents a 48% increase over the previous week and an increase of over 2,000% in the 8 weeks since the national count dropped to a low of 8,500 cases for the week of June 18-24, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
Vaccinations, in the meantime, appear to be headed in the opposite direction. Vaccine initiations were down for the second consecutive week, falling by 18% among 12- to 15-year-olds and by 15% in those aged 16-17 years, according to data from the Centers for Disease Control and Prevention.
Nationally, about 47% of children aged 12-15 and 56% of those aged 16-17 have received at least one dose of COVID vaccine as of Aug. 23, with 34% and 44%, respectively, reaching full vaccination. The total number of children with at least one dose is 11.6 million, including a relatively small number (about 200,000) of children under age 12 years, the CDC said on its COVID Data Tracker.
At the state level, vaccination is a source of considerable disparity. In Vermont, 73% of children aged 12-17 had received at least one dose by Aug. 18, and 63% were fully vaccinated. In Wyoming, however, just 25% of children had received at least one dose (17% are fully vaccinated), while Alabama has a lowest-in-the-nation full vaccination rate of 14%, based on a separate AAP analysis of CDC data.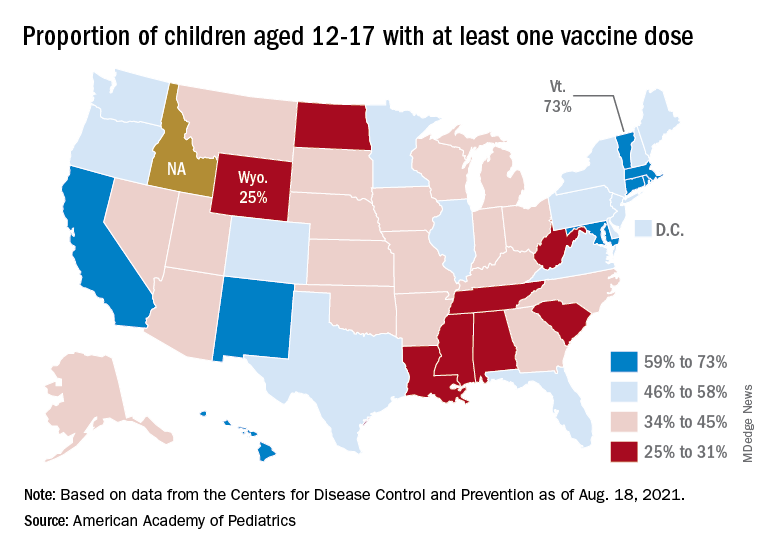
There are seven states in which over 60% of 12- to 17-year-olds have at least started the vaccine regimen and five states where less than 30% have received at least one dose, the AAP noted.
Back on the incidence side of the pandemic, Mississippi and Hawaii had the largest increases in new cases over the past 2 weeks, followed by Florida and West Virginia. Cumulative figures show that California has had the most cases overall in children (550,337), Vermont has the highest proportion of all cases in children (22.9%), and Rhode Island has the highest rate of cases per 100,000 (10,636), the AAP and CHA said in the joint report based on data from 49 states, the District of Columbia, New York City, Puerto Rico, and Guam.
Add up all those jurisdictions, and it works out to 4.6 million children infected with SARS-CoV-2 as of Aug. 19, with children representing 14.6% of all cases since the start of the pandemic. There have been over 18,000 hospitalizations so far, which is just 2.3% of the total for all ages in the 23 states (and New York City) that are reporting such data on their health department websites, the AAP and CHA said.
The number of COVID-related deaths in children is now 402 after the largest 1-week increase (24) since late May of 2020, when the AAP/CHA coverage began. Mortality data by age are available from 44 states, New York City, Puerto Rico, and Guam.
Weekly cases of COVID-19 in children jumped by nearly 50% in the United States, posting the highest count since hitting a pandemic high back in mid-January, a new report shows.
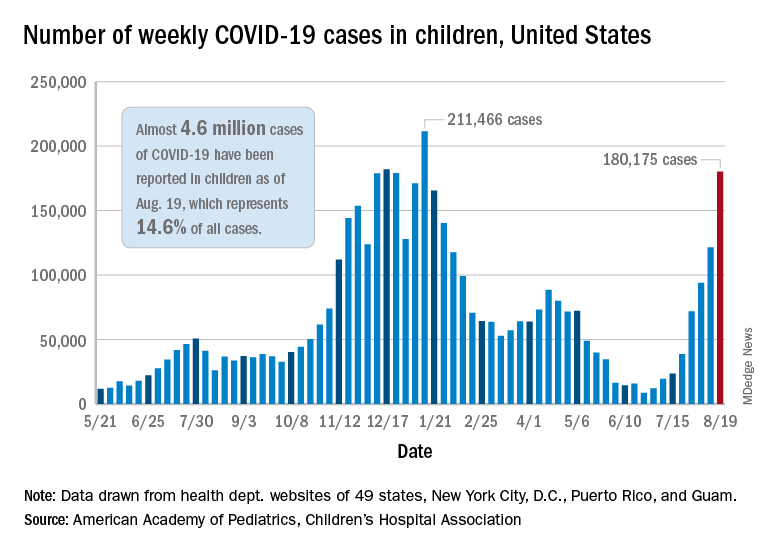
The latest weekly figure represents a 48% increase over the previous week and an increase of over 2,000% in the 8 weeks since the national count dropped to a low of 8,500 cases for the week of June 18-24, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
Vaccinations, in the meantime, appear to be headed in the opposite direction. Vaccine initiations were down for the second consecutive week, falling by 18% among 12- to 15-year-olds and by 15% in those aged 16-17 years, according to data from the Centers for Disease Control and Prevention.
Nationally, about 47% of children aged 12-15 and 56% of those aged 16-17 have received at least one dose of COVID vaccine as of Aug. 23, with 34% and 44%, respectively, reaching full vaccination. The total number of children with at least one dose is 11.6 million, including a relatively small number (about 200,000) of children under age 12 years, the CDC said on its COVID Data Tracker.
At the state level, vaccination is a source of considerable disparity. In Vermont, 73% of children aged 12-17 had received at least one dose by Aug. 18, and 63% were fully vaccinated. In Wyoming, however, just 25% of children had received at least one dose (17% are fully vaccinated), while Alabama has a lowest-in-the-nation full vaccination rate of 14%, based on a separate AAP analysis of CDC data.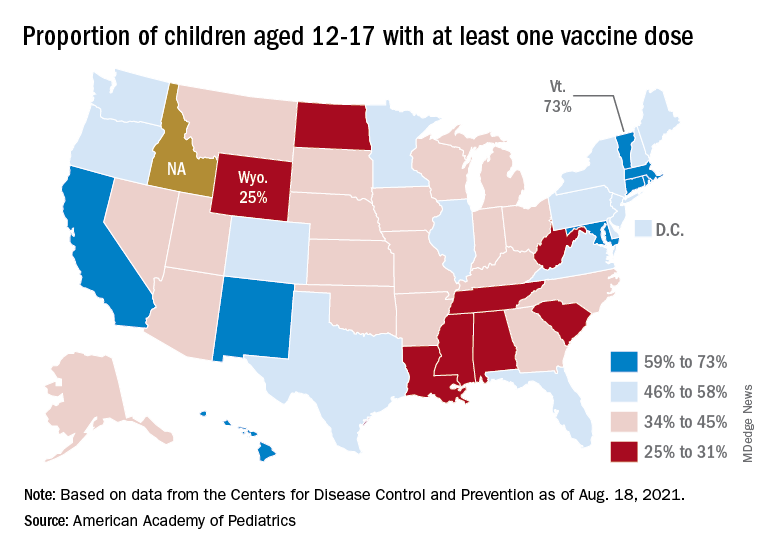
There are seven states in which over 60% of 12- to 17-year-olds have at least started the vaccine regimen and five states where less than 30% have received at least one dose, the AAP noted.
Back on the incidence side of the pandemic, Mississippi and Hawaii had the largest increases in new cases over the past 2 weeks, followed by Florida and West Virginia. Cumulative figures show that California has had the most cases overall in children (550,337), Vermont has the highest proportion of all cases in children (22.9%), and Rhode Island has the highest rate of cases per 100,000 (10,636), the AAP and CHA said in the joint report based on data from 49 states, the District of Columbia, New York City, Puerto Rico, and Guam.
Add up all those jurisdictions, and it works out to 4.6 million children infected with SARS-CoV-2 as of Aug. 19, with children representing 14.6% of all cases since the start of the pandemic. There have been over 18,000 hospitalizations so far, which is just 2.3% of the total for all ages in the 23 states (and New York City) that are reporting such data on their health department websites, the AAP and CHA said.
The number of COVID-related deaths in children is now 402 after the largest 1-week increase (24) since late May of 2020, when the AAP/CHA coverage began. Mortality data by age are available from 44 states, New York City, Puerto Rico, and Guam.
U.S. kidney transplants grow in number and success
During 2016-2019, U.S. centers performed kidney transplants in nearly 77,000 patients, a jump of almost 25% compared with 4-year averages of about 62,000 patients throughout 2004-2015. That works out to about 15,000 more patients receiving donor kidneys, Sundaram Hariharan, MD, and associates reported in the New England Journal of Medicine in a review of all U.S. renal transplantations performed during 1996-2019.
Coupled with the volume uptick during this 24-year period were new lows in graft losses and patient deaths. By 2018, mortality during the first year following transplantation occurred at about a 1% rate among patients who had received a kidney from a living donor, and at about a 3% rate when the organ came from a deceased donor, nearly half the rate of 2 decades earlier, in 1996. Rates of first-year graft loss during 2017 were also about half of what they had been in 1996, occurring in about 2% of patients who received a living donor organ and in about 6% of those who got a kidney from a deceased donor during 2017.
“Twenty years ago, kidney transplantation was the preferred option compared with dialysis, and even more so now,” summed up Dr. Hariharan, a senior transplant nephrologist and professor of medicine and surgery at the University of Pittsburgh Medical Center and first author of the report. Kidney transplantation survival at U.S. centers “improved steadily over the past 24 years, despite patient variables becoming worse,” he said in an interview.
Kidney recipients are older, more obese, and have more prevalent diabetes
During the period studied, kidney transplant recipients became on average older and more obese, and had a higher prevalence of diabetes; the age of organ donors grew as well. The prevalence of diabetes among patients who received a kidney from a deceased donor increased from 24% during 1996-1999 to 36% during 2016-2019, while diabetes prevalence among recipients of an organ from a living donor rose from 25% in 1996-1999 to 29% during 2016-2019.
The improved graft and patient survival numbers “are very encouraging trends,” said Michelle A. Josephson, MD, professor and medical director of kidney transplantation at the University of Chicago, who was not involved with the report. “We have been hearing for a number of years that short-term graft survival had improved, but I’m thrilled to learn that long-term survival has also improved.”
The report documented 10-year survival of graft recipients during 2008-2011 of 67%, up from 61% during 1996-1999, and a 10-year overall graft survival rate of 54% in the 2008-2011 cohort, an improvement from the 42% rate in patients who received their organs in 1996-1999, changes Dr. Hariharan characterized as “modest.”
These improvements in long-term graft and patient survival are “meaningful, and particularly notable that outcomes improved despite increased complexity of the transplant population,” said Krista L. Lentine, MD, PhD, professor and medical director of living donation at Saint Louis University. But “despite these improvements, long-term graft survival remains limited,” she cautioned, especially because of risks for substantial complications from chronic immunosuppressive treatment including infection, cancer, glucose intolerance, and dyslipidemia.
The analysis reported by Dr. Hariharan and his associates used data collected by the Scientific Registry of Transplant Patients, run under contract with the U.S. Department of Health and Human Services, which has tracked all patients who have had kidney transplants at U.S. centers since the late 1980s, said Dr. Hariharan. The database included just over 362,000 total transplants during the 24-year period studied, with 36% of all transplants involving organs from living donors with the remaining patients receiving kidneys from deceased donors.
Living donations still stagnant; deceased-donor kidneys rise
The data showed that the rate of transplants from living donors was stagnant for 2 decades, with 22,525 patients transplanted during 2000-2003, and 23,746 transplanted during 2016-2019, with very similar rates during the intervening years. The recent spurt in transplants during 2016-2019 compared with the preceding decade depended almost entirely on kidneys from deceased donors. This rate jumped from the steady, slow rise it showed during 1996-2015, when deceased-donor transplants rose from about 30,000 during 1996-1999 to about 41,000 during 2012-2015, to a more dramatic increase of about 12,000 additional transplants during the most recent period, adding up to a total of more than 53,000 transplants from deceased donors during 2016-2019.
“I strongly recommend organs from living donors” when feasible, said Dr. Hariharan. “At some centers, a high proportion of transplants use living donors, but not at other centers,” he said.
It’s unknown why transplants using organs from deceased donors has shown this growth, but Dr. Hariharan suggested a multifactorial explanation. Those factors include growth in the number of patients with end-stage renal disease who require dialysis, increased numbers of patients listed for kidney transplant, new approaches that allow organs from older donors and those infected with pathogens such as hepatitis C virus or HIV, greater numbers of people and families agreeing to donate organs, and possibly the opioid crisis that may have led to increased organ donation. The number of U.S. centers performing kidney transplants rose from fewer than 200 about a quarter of a century ago to about 250 today, he added.
‘Immuno Bill’ guarantees Medicare coverage for immunosuppression
Dr. Hariharan voiced optimism that graft and patient survival rates will continue to improve going forward. One factor will likely be the passage in late 2020 of the “Immuno Bill” by the U.S. Congress, which among other things mandated ongoing coverage starting in 2023 for immunosuppressive drugs for all Medicare beneficiaries with a kidney transplant. Until then, Medicare provides coverage for only 36 months, a time limit that has resulted in nearly 400 kidney recipients annually losing coverage of their immunosuppression medications.
Dr. Hariharan and coauthors called the existing potential for discontinuation of immunosuppressive drug an “unnecessary impediment to long-term survival for which patients and society paid a heavy price.”
“Kidney transplantation, especially from living donors, offers patients with kidney failure the best chance for long-term survival and improved quality of life, with lower cost to the health care system,” Dr. Lentine said in an interview. Despite the many positive trends detailed in the report from Dr. Hariharan and coauthors, “the vast majority of the more than 700,000 people in the United States with kidney failure will not have an opportunity to receive a transplant due to limitations in organ supply.” And many patients who receive a kidney transplant eventually must resume dialysis because of “limited long-term graft survival resulting from allograft nephropathy, recurrent native disease, medication nonadherence, or other causes.” Plus many potentially transplantable organs go unused.
Dr. Lentine cited a position statement issued in July 2021 by the National Kidney Foundation that made several recommendations on how to improve access to kidney transplants and improve outcomes. “Expanding opportunities for safe living donation, eliminating racial disparities in living-donor access, improving wait-list access and transport readiness, maximizing use of deceased-donor organs, and extending graft longevity are critical priorities,” said Dr. Lentine, lead author on the statement.
“For many or even most patients with kidney failure transplantation is the optimal form of renal replacement. The better recent outcomes and evolving management strategies make transplantation an even more attractive option,” said Dr. Josephson. Improved outcomes among U.S. transplant patients also highlights the “importance of increasing access to kidney transplantation” for all people with kidney failure who could benefit from this treatment, she added.
Dr. Hariharan and Dr. Lentine had no relevant disclosures. Dr. Josephson has been a consultant to UCB and has an ownership interest in Seagen.
During 2016-2019, U.S. centers performed kidney transplants in nearly 77,000 patients, a jump of almost 25% compared with 4-year averages of about 62,000 patients throughout 2004-2015. That works out to about 15,000 more patients receiving donor kidneys, Sundaram Hariharan, MD, and associates reported in the New England Journal of Medicine in a review of all U.S. renal transplantations performed during 1996-2019.
Coupled with the volume uptick during this 24-year period were new lows in graft losses and patient deaths. By 2018, mortality during the first year following transplantation occurred at about a 1% rate among patients who had received a kidney from a living donor, and at about a 3% rate when the organ came from a deceased donor, nearly half the rate of 2 decades earlier, in 1996. Rates of first-year graft loss during 2017 were also about half of what they had been in 1996, occurring in about 2% of patients who received a living donor organ and in about 6% of those who got a kidney from a deceased donor during 2017.
“Twenty years ago, kidney transplantation was the preferred option compared with dialysis, and even more so now,” summed up Dr. Hariharan, a senior transplant nephrologist and professor of medicine and surgery at the University of Pittsburgh Medical Center and first author of the report. Kidney transplantation survival at U.S. centers “improved steadily over the past 24 years, despite patient variables becoming worse,” he said in an interview.
Kidney recipients are older, more obese, and have more prevalent diabetes
During the period studied, kidney transplant recipients became on average older and more obese, and had a higher prevalence of diabetes; the age of organ donors grew as well. The prevalence of diabetes among patients who received a kidney from a deceased donor increased from 24% during 1996-1999 to 36% during 2016-2019, while diabetes prevalence among recipients of an organ from a living donor rose from 25% in 1996-1999 to 29% during 2016-2019.
The improved graft and patient survival numbers “are very encouraging trends,” said Michelle A. Josephson, MD, professor and medical director of kidney transplantation at the University of Chicago, who was not involved with the report. “We have been hearing for a number of years that short-term graft survival had improved, but I’m thrilled to learn that long-term survival has also improved.”
The report documented 10-year survival of graft recipients during 2008-2011 of 67%, up from 61% during 1996-1999, and a 10-year overall graft survival rate of 54% in the 2008-2011 cohort, an improvement from the 42% rate in patients who received their organs in 1996-1999, changes Dr. Hariharan characterized as “modest.”
These improvements in long-term graft and patient survival are “meaningful, and particularly notable that outcomes improved despite increased complexity of the transplant population,” said Krista L. Lentine, MD, PhD, professor and medical director of living donation at Saint Louis University. But “despite these improvements, long-term graft survival remains limited,” she cautioned, especially because of risks for substantial complications from chronic immunosuppressive treatment including infection, cancer, glucose intolerance, and dyslipidemia.
The analysis reported by Dr. Hariharan and his associates used data collected by the Scientific Registry of Transplant Patients, run under contract with the U.S. Department of Health and Human Services, which has tracked all patients who have had kidney transplants at U.S. centers since the late 1980s, said Dr. Hariharan. The database included just over 362,000 total transplants during the 24-year period studied, with 36% of all transplants involving organs from living donors with the remaining patients receiving kidneys from deceased donors.
Living donations still stagnant; deceased-donor kidneys rise
The data showed that the rate of transplants from living donors was stagnant for 2 decades, with 22,525 patients transplanted during 2000-2003, and 23,746 transplanted during 2016-2019, with very similar rates during the intervening years. The recent spurt in transplants during 2016-2019 compared with the preceding decade depended almost entirely on kidneys from deceased donors. This rate jumped from the steady, slow rise it showed during 1996-2015, when deceased-donor transplants rose from about 30,000 during 1996-1999 to about 41,000 during 2012-2015, to a more dramatic increase of about 12,000 additional transplants during the most recent period, adding up to a total of more than 53,000 transplants from deceased donors during 2016-2019.
“I strongly recommend organs from living donors” when feasible, said Dr. Hariharan. “At some centers, a high proportion of transplants use living donors, but not at other centers,” he said.
It’s unknown why transplants using organs from deceased donors has shown this growth, but Dr. Hariharan suggested a multifactorial explanation. Those factors include growth in the number of patients with end-stage renal disease who require dialysis, increased numbers of patients listed for kidney transplant, new approaches that allow organs from older donors and those infected with pathogens such as hepatitis C virus or HIV, greater numbers of people and families agreeing to donate organs, and possibly the opioid crisis that may have led to increased organ donation. The number of U.S. centers performing kidney transplants rose from fewer than 200 about a quarter of a century ago to about 250 today, he added.
‘Immuno Bill’ guarantees Medicare coverage for immunosuppression
Dr. Hariharan voiced optimism that graft and patient survival rates will continue to improve going forward. One factor will likely be the passage in late 2020 of the “Immuno Bill” by the U.S. Congress, which among other things mandated ongoing coverage starting in 2023 for immunosuppressive drugs for all Medicare beneficiaries with a kidney transplant. Until then, Medicare provides coverage for only 36 months, a time limit that has resulted in nearly 400 kidney recipients annually losing coverage of their immunosuppression medications.
Dr. Hariharan and coauthors called the existing potential for discontinuation of immunosuppressive drug an “unnecessary impediment to long-term survival for which patients and society paid a heavy price.”
“Kidney transplantation, especially from living donors, offers patients with kidney failure the best chance for long-term survival and improved quality of life, with lower cost to the health care system,” Dr. Lentine said in an interview. Despite the many positive trends detailed in the report from Dr. Hariharan and coauthors, “the vast majority of the more than 700,000 people in the United States with kidney failure will not have an opportunity to receive a transplant due to limitations in organ supply.” And many patients who receive a kidney transplant eventually must resume dialysis because of “limited long-term graft survival resulting from allograft nephropathy, recurrent native disease, medication nonadherence, or other causes.” Plus many potentially transplantable organs go unused.
Dr. Lentine cited a position statement issued in July 2021 by the National Kidney Foundation that made several recommendations on how to improve access to kidney transplants and improve outcomes. “Expanding opportunities for safe living donation, eliminating racial disparities in living-donor access, improving wait-list access and transport readiness, maximizing use of deceased-donor organs, and extending graft longevity are critical priorities,” said Dr. Lentine, lead author on the statement.
“For many or even most patients with kidney failure transplantation is the optimal form of renal replacement. The better recent outcomes and evolving management strategies make transplantation an even more attractive option,” said Dr. Josephson. Improved outcomes among U.S. transplant patients also highlights the “importance of increasing access to kidney transplantation” for all people with kidney failure who could benefit from this treatment, she added.
Dr. Hariharan and Dr. Lentine had no relevant disclosures. Dr. Josephson has been a consultant to UCB and has an ownership interest in Seagen.
During 2016-2019, U.S. centers performed kidney transplants in nearly 77,000 patients, a jump of almost 25% compared with 4-year averages of about 62,000 patients throughout 2004-2015. That works out to about 15,000 more patients receiving donor kidneys, Sundaram Hariharan, MD, and associates reported in the New England Journal of Medicine in a review of all U.S. renal transplantations performed during 1996-2019.
Coupled with the volume uptick during this 24-year period were new lows in graft losses and patient deaths. By 2018, mortality during the first year following transplantation occurred at about a 1% rate among patients who had received a kidney from a living donor, and at about a 3% rate when the organ came from a deceased donor, nearly half the rate of 2 decades earlier, in 1996. Rates of first-year graft loss during 2017 were also about half of what they had been in 1996, occurring in about 2% of patients who received a living donor organ and in about 6% of those who got a kidney from a deceased donor during 2017.
“Twenty years ago, kidney transplantation was the preferred option compared with dialysis, and even more so now,” summed up Dr. Hariharan, a senior transplant nephrologist and professor of medicine and surgery at the University of Pittsburgh Medical Center and first author of the report. Kidney transplantation survival at U.S. centers “improved steadily over the past 24 years, despite patient variables becoming worse,” he said in an interview.
Kidney recipients are older, more obese, and have more prevalent diabetes
During the period studied, kidney transplant recipients became on average older and more obese, and had a higher prevalence of diabetes; the age of organ donors grew as well. The prevalence of diabetes among patients who received a kidney from a deceased donor increased from 24% during 1996-1999 to 36% during 2016-2019, while diabetes prevalence among recipients of an organ from a living donor rose from 25% in 1996-1999 to 29% during 2016-2019.
The improved graft and patient survival numbers “are very encouraging trends,” said Michelle A. Josephson, MD, professor and medical director of kidney transplantation at the University of Chicago, who was not involved with the report. “We have been hearing for a number of years that short-term graft survival had improved, but I’m thrilled to learn that long-term survival has also improved.”
The report documented 10-year survival of graft recipients during 2008-2011 of 67%, up from 61% during 1996-1999, and a 10-year overall graft survival rate of 54% in the 2008-2011 cohort, an improvement from the 42% rate in patients who received their organs in 1996-1999, changes Dr. Hariharan characterized as “modest.”
These improvements in long-term graft and patient survival are “meaningful, and particularly notable that outcomes improved despite increased complexity of the transplant population,” said Krista L. Lentine, MD, PhD, professor and medical director of living donation at Saint Louis University. But “despite these improvements, long-term graft survival remains limited,” she cautioned, especially because of risks for substantial complications from chronic immunosuppressive treatment including infection, cancer, glucose intolerance, and dyslipidemia.
The analysis reported by Dr. Hariharan and his associates used data collected by the Scientific Registry of Transplant Patients, run under contract with the U.S. Department of Health and Human Services, which has tracked all patients who have had kidney transplants at U.S. centers since the late 1980s, said Dr. Hariharan. The database included just over 362,000 total transplants during the 24-year period studied, with 36% of all transplants involving organs from living donors with the remaining patients receiving kidneys from deceased donors.
Living donations still stagnant; deceased-donor kidneys rise
The data showed that the rate of transplants from living donors was stagnant for 2 decades, with 22,525 patients transplanted during 2000-2003, and 23,746 transplanted during 2016-2019, with very similar rates during the intervening years. The recent spurt in transplants during 2016-2019 compared with the preceding decade depended almost entirely on kidneys from deceased donors. This rate jumped from the steady, slow rise it showed during 1996-2015, when deceased-donor transplants rose from about 30,000 during 1996-1999 to about 41,000 during 2012-2015, to a more dramatic increase of about 12,000 additional transplants during the most recent period, adding up to a total of more than 53,000 transplants from deceased donors during 2016-2019.
“I strongly recommend organs from living donors” when feasible, said Dr. Hariharan. “At some centers, a high proportion of transplants use living donors, but not at other centers,” he said.
It’s unknown why transplants using organs from deceased donors has shown this growth, but Dr. Hariharan suggested a multifactorial explanation. Those factors include growth in the number of patients with end-stage renal disease who require dialysis, increased numbers of patients listed for kidney transplant, new approaches that allow organs from older donors and those infected with pathogens such as hepatitis C virus or HIV, greater numbers of people and families agreeing to donate organs, and possibly the opioid crisis that may have led to increased organ donation. The number of U.S. centers performing kidney transplants rose from fewer than 200 about a quarter of a century ago to about 250 today, he added.
‘Immuno Bill’ guarantees Medicare coverage for immunosuppression
Dr. Hariharan voiced optimism that graft and patient survival rates will continue to improve going forward. One factor will likely be the passage in late 2020 of the “Immuno Bill” by the U.S. Congress, which among other things mandated ongoing coverage starting in 2023 for immunosuppressive drugs for all Medicare beneficiaries with a kidney transplant. Until then, Medicare provides coverage for only 36 months, a time limit that has resulted in nearly 400 kidney recipients annually losing coverage of their immunosuppression medications.
Dr. Hariharan and coauthors called the existing potential for discontinuation of immunosuppressive drug an “unnecessary impediment to long-term survival for which patients and society paid a heavy price.”
“Kidney transplantation, especially from living donors, offers patients with kidney failure the best chance for long-term survival and improved quality of life, with lower cost to the health care system,” Dr. Lentine said in an interview. Despite the many positive trends detailed in the report from Dr. Hariharan and coauthors, “the vast majority of the more than 700,000 people in the United States with kidney failure will not have an opportunity to receive a transplant due to limitations in organ supply.” And many patients who receive a kidney transplant eventually must resume dialysis because of “limited long-term graft survival resulting from allograft nephropathy, recurrent native disease, medication nonadherence, or other causes.” Plus many potentially transplantable organs go unused.
Dr. Lentine cited a position statement issued in July 2021 by the National Kidney Foundation that made several recommendations on how to improve access to kidney transplants and improve outcomes. “Expanding opportunities for safe living donation, eliminating racial disparities in living-donor access, improving wait-list access and transport readiness, maximizing use of deceased-donor organs, and extending graft longevity are critical priorities,” said Dr. Lentine, lead author on the statement.
“For many or even most patients with kidney failure transplantation is the optimal form of renal replacement. The better recent outcomes and evolving management strategies make transplantation an even more attractive option,” said Dr. Josephson. Improved outcomes among U.S. transplant patients also highlights the “importance of increasing access to kidney transplantation” for all people with kidney failure who could benefit from this treatment, she added.
Dr. Hariharan and Dr. Lentine had no relevant disclosures. Dr. Josephson has been a consultant to UCB and has an ownership interest in Seagen.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE