User login
Commentary: Genetic Components of NSCLC, June 2022
Real-World Retrospective Study Suggests Inferior Outcomes to First-Line Systemic Treatment in Advanced NFE2L2 and KEAP1 Mutant Squamous NSCLC
Targeted therapies against oncogene-driven lung cancer, such as epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK), in lung adenocarcinoma have revolutionized lung cancer treatment. However, there are no US Food and Drug Administration–approved targeted therapies for commonly occurring mutations in advanced squamous non–small cell lung cancer (NSCLC).
NFE2L2 and KEAP1 mutations are molecular alterations that occur in about 25%-30% of squamous NSCLC. NFE2L2 encodes for the NRF2 transcription factor that is involved in the oxidative stress pathway and KEAP1 encodes for the KEAP1 protein, which is the negative regulator of NFE2L2.1 When the NRF2-KEAP1 signaling pathway is disrupted, there is persistent activation of NRF2, which promotes cell proliferation and carcinogenesis and may contribute to resistance to cancer-directed treatments. Previous retrospective studies suggest that patients with lung cancers harboring NFE2L2 and KEAP1 mutations have a poorer prognosis and do worse with both systemic anticancer treatments and radiation.2-5
Wu and colleagues, in a retrospective cohort study, identified 703 patients with squamous NSCLC from 2011 to 2018 who had NFE2L2 or KEAP1 mutations identified by comprehensive genomic profiling in the Flatiron Health-Foundation Medicine Clinico-Genomic Database. Real-world progression-free survival (PFS), defined as a distinct episode where the clinician concluded that there was growth or worsening of disease, was assessed by line and type of treatment, as was overall survival (OS). Patients with squamous NSCLC with NFE2L2/KEAP1 mutations had shorter real-world PFS to first-line treatment compared with patients whose tumors were wild-type for these mutations (4.54 months vs 6.25 months; P = .0027). Median OS was numerically shorter in patients with NFE2L2/KEAP1 mutations, but this was not statistically significant (13.59 vs 17.37 months; P = .41). This retrospective real-world analysis suggests that patients with squamous NSCLC and NFE2L2/KEAP1 mutations have inferior outcomes with systemic treatments and may have worsened OS; however, this was not statistically significant. Many of these patients were treated before the approval of the KEYNOTE-407 chemo-immunotherapy regimen in squamous NSCLC, so they did not have what we would consider contemporary standard treatment. Further studies are needed to evaluate the role of NRF2 activation in resistance to NSCLC treatments, and there is a need for therapeutics to target these common mutations in squamous NSCLC. Fortunately, there are current ongoing clinical trials.[6]
Segmentectomy Is Noninferior to and Improves Overall Survival Compared With Lobectomy in Selected Cases of Small Peripheral Early-Stage NSCLC
Lobectomy has been the standard of care for surgical treatment of early-stage NSCLC. Saji and colleagues investigated whether segmentectomy was noninferior to lobectomy in selected cases of small-sized peripheral NSCLC. This randomized, controlled, noninferiority trial was conducted at 70 institutions in Japan.
Patients with selected stage IA (American Joint Committee on Cancer [AJCC], seventh edition) NSCLC (peripheral tumors, £ 2 cm diameter, consolidation-to-tumor ratio > 0.5) were randomly assigned to undergo segmentectomy or lobectomy. The primary endpoint was OS. Pertinent secondary endpoints included postoperative respiratory function, relapse-free survival, and adverse events.
A total of 1106 patients were enrolled: 554 in the lobectomy group and 552 in the segmentectomy group. The 5-year OS was 94.3% for segmentectomy and 91.1% for lobectomy (hazard ratio 0.663; one-sided P < .001 for noninferiority; P = .0082 for superiority). In addition to the modestly improved OS observed, 5-year relapse-free survival was comparable between the groups (88% for segmentectomy and 87.9% for lobectomy). However, more local relapse was observed for segmentectomy (10.5%) than for lobectomy (5.4%) (P = .0018). Despite significantly more locoregional recurrences with segmentectomy compared with lobectomy, rates of combined distant and locoregional relapses were similar. Slightly more patients died in the lobectomy group than the segmentectomy group, and the rate of cancer-related deaths, including second primary lung cancers, was higher in the lobectomy group. Interestingly, although segmentectomy had better OS, the survival advantage was not cancer-specific.
The mechanism by which segmentectomy improved survival over lobectomy in these selected patients with small, peripheral stage IA NSCLC is still unclear. Limitations of the study included that all patients were from one geographic region (Japan) and that the study was unblinded, which can introduce bias. We await the results of CALGB 140503: A Randomized Phase III Trial of Lobectomy versus Sublobar Resection for Small (< 2cm) Peripheral Non-Small Cell Lung Cancer (NCT00499330). This study is being done in a US population and includes nonanatomic wedge in its sublobar resection cohort.
The study by Saji and colleagues suggests that surgeons should consider segmentectomy in appropriate patients (select small stage IA NSCLC [peripheral tumors, £ 2 cm diameter, consolidation-to-tumor ratio > 0.5]), based on the modest improvement in OS compared with lobectomy.
Immunotherapy Activity in Cachexic and Noncachexic Patients With Advanced NSCLC and Clinical Outcomes, by Adipose Tissue Loss on Treatment
There are emerging data that body mass index (BMI) and the presence or absence of cachexia in cancers, including NSCLC, may change the efficacy of programmed cell death-ligand 1 (PD-L1) immune checkpoint inhibitors. Nishioka and colleagues, in a single-center retrospective cohort, examined patients with advanced NSCLC (40 with cachexia and 34 without cachexia) who received PD-L1 inhibitors (pembrolizumab, nivolumab, or atezolizumab). Patients were excluded if they had poor performance status, EGFR/ALK/ROS1 oncogene drivers, unknown PD-L1 expression status, and unknown weight loss in the 6 months before immunotherapy administration. In addition to BMI, measurements of adipose tissue quantity and muscle mass were used.
The overall response rate was 28.4% in the 74 patients analyzed. Patients with cachexia had a lower overall response rate than those without cachexia (15.0% vs 44.1%; P < .05). Among the patients without cachexia, those with total adipose tissue loss had a significantly longer PFS than those with total adipose tissue maintenance (18.5 months vs 2.86 months; P = .037), including in a multivariate analyses (hazard ratio 0.34; P < .05), after adjustment for PD-L1 expression and performance status (Eastern Cooperative Oncology Group [ECOG] 0 vs. 1).
Mechanistically, a paradoxical effect of obesity on T-cell function that relates to leptin, which is secreted by adipose tissue, has been observed in preclinical studies.7 In a previously published study, obesity resulted in tumor progression and PD-1–mediated T-cell dysfunction, which can be overcome by PD-L1 blockade with improved clinical outcomes to these therapies in patients with obesity and cancer, including NSCLC.7 This "obesity paradox" may underlie some of the findings observed in Nishioka and colleagues' study. More research needs to be done regarding the activity of immune checkpoint inhibition in NSCLC as it relates to BMI, cachexia, and amount of adipose tissue.
Additional References
1. Shibata T, Ohta T, Tong KI, et al. Cancer related mutations in NRF2 impair its recognition by Keap1-Cul3 E3 ligase and promote malignancy. Proc Natl Acad Sci U S A. 2008;105(36):13568-13573. doi: 10.1073/pnas.0806268105
2. Frank R, Scheffler M, Merkelbach-Bruse S, et al. Clinical and pathological characteristics of KEAP1- and NFE2L2-mutated non-small cell lung carcinoma (NSCLC). Clin Cancer Res. 2018;24:3087-3096. doi: 10.1158/1078-0432.CCR-17-3416
3. Binkley MS, Jeon YJ, Nesselbush M, et al. KEAP1/NFE2L2 mutations predict lung cancer radiation resistance that can be targeted by glutaminase inhibition. Cancer Discov. 2020;10(12):1826-1841. doi: 10.1158/2159-8290.CD-20-0282
4. Hellyer JA, Padda SK, Diehn M, et al. Clinical implications of KEAP1-NFE2L2 mutations in NSCLC. J Thorac Oncol. 2021;16(3):395-403. doi: 10.1016/j.jtho.2020.11.015
5. Jeong Y, Hellyer JA, Stehr H, et al. Role of KEAP1/NFE2L2 mutations in the chemotherapeutic response of patients with non-small cell lung cancer. Clin Cancer Res. 2020;26(1):274-281. doi: 10.1158/1078-0432.CCR-19-1237
6. Riess JW, Frankel P, Shackelford D, et al. Phase 1 trial of MLN0128 (sapanisertib) and CB-839 HCl (telaglenastat) in patients with advanced NSCLC (NCI 10327): Rationale and study design. Clin Lung Cancer. 2021;22:67-70. doi: 10.1016/j.cllc.2020.10.006
Real-World Retrospective Study Suggests Inferior Outcomes to First-Line Systemic Treatment in Advanced NFE2L2 and KEAP1 Mutant Squamous NSCLC
Targeted therapies against oncogene-driven lung cancer, such as epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK), in lung adenocarcinoma have revolutionized lung cancer treatment. However, there are no US Food and Drug Administration–approved targeted therapies for commonly occurring mutations in advanced squamous non–small cell lung cancer (NSCLC).
NFE2L2 and KEAP1 mutations are molecular alterations that occur in about 25%-30% of squamous NSCLC. NFE2L2 encodes for the NRF2 transcription factor that is involved in the oxidative stress pathway and KEAP1 encodes for the KEAP1 protein, which is the negative regulator of NFE2L2.1 When the NRF2-KEAP1 signaling pathway is disrupted, there is persistent activation of NRF2, which promotes cell proliferation and carcinogenesis and may contribute to resistance to cancer-directed treatments. Previous retrospective studies suggest that patients with lung cancers harboring NFE2L2 and KEAP1 mutations have a poorer prognosis and do worse with both systemic anticancer treatments and radiation.2-5
Wu and colleagues, in a retrospective cohort study, identified 703 patients with squamous NSCLC from 2011 to 2018 who had NFE2L2 or KEAP1 mutations identified by comprehensive genomic profiling in the Flatiron Health-Foundation Medicine Clinico-Genomic Database. Real-world progression-free survival (PFS), defined as a distinct episode where the clinician concluded that there was growth or worsening of disease, was assessed by line and type of treatment, as was overall survival (OS). Patients with squamous NSCLC with NFE2L2/KEAP1 mutations had shorter real-world PFS to first-line treatment compared with patients whose tumors were wild-type for these mutations (4.54 months vs 6.25 months; P = .0027). Median OS was numerically shorter in patients with NFE2L2/KEAP1 mutations, but this was not statistically significant (13.59 vs 17.37 months; P = .41). This retrospective real-world analysis suggests that patients with squamous NSCLC and NFE2L2/KEAP1 mutations have inferior outcomes with systemic treatments and may have worsened OS; however, this was not statistically significant. Many of these patients were treated before the approval of the KEYNOTE-407 chemo-immunotherapy regimen in squamous NSCLC, so they did not have what we would consider contemporary standard treatment. Further studies are needed to evaluate the role of NRF2 activation in resistance to NSCLC treatments, and there is a need for therapeutics to target these common mutations in squamous NSCLC. Fortunately, there are current ongoing clinical trials.[6]
Segmentectomy Is Noninferior to and Improves Overall Survival Compared With Lobectomy in Selected Cases of Small Peripheral Early-Stage NSCLC
Lobectomy has been the standard of care for surgical treatment of early-stage NSCLC. Saji and colleagues investigated whether segmentectomy was noninferior to lobectomy in selected cases of small-sized peripheral NSCLC. This randomized, controlled, noninferiority trial was conducted at 70 institutions in Japan.
Patients with selected stage IA (American Joint Committee on Cancer [AJCC], seventh edition) NSCLC (peripheral tumors, £ 2 cm diameter, consolidation-to-tumor ratio > 0.5) were randomly assigned to undergo segmentectomy or lobectomy. The primary endpoint was OS. Pertinent secondary endpoints included postoperative respiratory function, relapse-free survival, and adverse events.
A total of 1106 patients were enrolled: 554 in the lobectomy group and 552 in the segmentectomy group. The 5-year OS was 94.3% for segmentectomy and 91.1% for lobectomy (hazard ratio 0.663; one-sided P < .001 for noninferiority; P = .0082 for superiority). In addition to the modestly improved OS observed, 5-year relapse-free survival was comparable between the groups (88% for segmentectomy and 87.9% for lobectomy). However, more local relapse was observed for segmentectomy (10.5%) than for lobectomy (5.4%) (P = .0018). Despite significantly more locoregional recurrences with segmentectomy compared with lobectomy, rates of combined distant and locoregional relapses were similar. Slightly more patients died in the lobectomy group than the segmentectomy group, and the rate of cancer-related deaths, including second primary lung cancers, was higher in the lobectomy group. Interestingly, although segmentectomy had better OS, the survival advantage was not cancer-specific.
The mechanism by which segmentectomy improved survival over lobectomy in these selected patients with small, peripheral stage IA NSCLC is still unclear. Limitations of the study included that all patients were from one geographic region (Japan) and that the study was unblinded, which can introduce bias. We await the results of CALGB 140503: A Randomized Phase III Trial of Lobectomy versus Sublobar Resection for Small (< 2cm) Peripheral Non-Small Cell Lung Cancer (NCT00499330). This study is being done in a US population and includes nonanatomic wedge in its sublobar resection cohort.
The study by Saji and colleagues suggests that surgeons should consider segmentectomy in appropriate patients (select small stage IA NSCLC [peripheral tumors, £ 2 cm diameter, consolidation-to-tumor ratio > 0.5]), based on the modest improvement in OS compared with lobectomy.
Immunotherapy Activity in Cachexic and Noncachexic Patients With Advanced NSCLC and Clinical Outcomes, by Adipose Tissue Loss on Treatment
There are emerging data that body mass index (BMI) and the presence or absence of cachexia in cancers, including NSCLC, may change the efficacy of programmed cell death-ligand 1 (PD-L1) immune checkpoint inhibitors. Nishioka and colleagues, in a single-center retrospective cohort, examined patients with advanced NSCLC (40 with cachexia and 34 without cachexia) who received PD-L1 inhibitors (pembrolizumab, nivolumab, or atezolizumab). Patients were excluded if they had poor performance status, EGFR/ALK/ROS1 oncogene drivers, unknown PD-L1 expression status, and unknown weight loss in the 6 months before immunotherapy administration. In addition to BMI, measurements of adipose tissue quantity and muscle mass were used.
The overall response rate was 28.4% in the 74 patients analyzed. Patients with cachexia had a lower overall response rate than those without cachexia (15.0% vs 44.1%; P < .05). Among the patients without cachexia, those with total adipose tissue loss had a significantly longer PFS than those with total adipose tissue maintenance (18.5 months vs 2.86 months; P = .037), including in a multivariate analyses (hazard ratio 0.34; P < .05), after adjustment for PD-L1 expression and performance status (Eastern Cooperative Oncology Group [ECOG] 0 vs. 1).
Mechanistically, a paradoxical effect of obesity on T-cell function that relates to leptin, which is secreted by adipose tissue, has been observed in preclinical studies.7 In a previously published study, obesity resulted in tumor progression and PD-1–mediated T-cell dysfunction, which can be overcome by PD-L1 blockade with improved clinical outcomes to these therapies in patients with obesity and cancer, including NSCLC.7 This "obesity paradox" may underlie some of the findings observed in Nishioka and colleagues' study. More research needs to be done regarding the activity of immune checkpoint inhibition in NSCLC as it relates to BMI, cachexia, and amount of adipose tissue.
Additional References
1. Shibata T, Ohta T, Tong KI, et al. Cancer related mutations in NRF2 impair its recognition by Keap1-Cul3 E3 ligase and promote malignancy. Proc Natl Acad Sci U S A. 2008;105(36):13568-13573. doi: 10.1073/pnas.0806268105
2. Frank R, Scheffler M, Merkelbach-Bruse S, et al. Clinical and pathological characteristics of KEAP1- and NFE2L2-mutated non-small cell lung carcinoma (NSCLC). Clin Cancer Res. 2018;24:3087-3096. doi: 10.1158/1078-0432.CCR-17-3416
3. Binkley MS, Jeon YJ, Nesselbush M, et al. KEAP1/NFE2L2 mutations predict lung cancer radiation resistance that can be targeted by glutaminase inhibition. Cancer Discov. 2020;10(12):1826-1841. doi: 10.1158/2159-8290.CD-20-0282
4. Hellyer JA, Padda SK, Diehn M, et al. Clinical implications of KEAP1-NFE2L2 mutations in NSCLC. J Thorac Oncol. 2021;16(3):395-403. doi: 10.1016/j.jtho.2020.11.015
5. Jeong Y, Hellyer JA, Stehr H, et al. Role of KEAP1/NFE2L2 mutations in the chemotherapeutic response of patients with non-small cell lung cancer. Clin Cancer Res. 2020;26(1):274-281. doi: 10.1158/1078-0432.CCR-19-1237
6. Riess JW, Frankel P, Shackelford D, et al. Phase 1 trial of MLN0128 (sapanisertib) and CB-839 HCl (telaglenastat) in patients with advanced NSCLC (NCI 10327): Rationale and study design. Clin Lung Cancer. 2021;22:67-70. doi: 10.1016/j.cllc.2020.10.006
Real-World Retrospective Study Suggests Inferior Outcomes to First-Line Systemic Treatment in Advanced NFE2L2 and KEAP1 Mutant Squamous NSCLC
Targeted therapies against oncogene-driven lung cancer, such as epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK), in lung adenocarcinoma have revolutionized lung cancer treatment. However, there are no US Food and Drug Administration–approved targeted therapies for commonly occurring mutations in advanced squamous non–small cell lung cancer (NSCLC).
NFE2L2 and KEAP1 mutations are molecular alterations that occur in about 25%-30% of squamous NSCLC. NFE2L2 encodes for the NRF2 transcription factor that is involved in the oxidative stress pathway and KEAP1 encodes for the KEAP1 protein, which is the negative regulator of NFE2L2.1 When the NRF2-KEAP1 signaling pathway is disrupted, there is persistent activation of NRF2, which promotes cell proliferation and carcinogenesis and may contribute to resistance to cancer-directed treatments. Previous retrospective studies suggest that patients with lung cancers harboring NFE2L2 and KEAP1 mutations have a poorer prognosis and do worse with both systemic anticancer treatments and radiation.2-5
Wu and colleagues, in a retrospective cohort study, identified 703 patients with squamous NSCLC from 2011 to 2018 who had NFE2L2 or KEAP1 mutations identified by comprehensive genomic profiling in the Flatiron Health-Foundation Medicine Clinico-Genomic Database. Real-world progression-free survival (PFS), defined as a distinct episode where the clinician concluded that there was growth or worsening of disease, was assessed by line and type of treatment, as was overall survival (OS). Patients with squamous NSCLC with NFE2L2/KEAP1 mutations had shorter real-world PFS to first-line treatment compared with patients whose tumors were wild-type for these mutations (4.54 months vs 6.25 months; P = .0027). Median OS was numerically shorter in patients with NFE2L2/KEAP1 mutations, but this was not statistically significant (13.59 vs 17.37 months; P = .41). This retrospective real-world analysis suggests that patients with squamous NSCLC and NFE2L2/KEAP1 mutations have inferior outcomes with systemic treatments and may have worsened OS; however, this was not statistically significant. Many of these patients were treated before the approval of the KEYNOTE-407 chemo-immunotherapy regimen in squamous NSCLC, so they did not have what we would consider contemporary standard treatment. Further studies are needed to evaluate the role of NRF2 activation in resistance to NSCLC treatments, and there is a need for therapeutics to target these common mutations in squamous NSCLC. Fortunately, there are current ongoing clinical trials.[6]
Segmentectomy Is Noninferior to and Improves Overall Survival Compared With Lobectomy in Selected Cases of Small Peripheral Early-Stage NSCLC
Lobectomy has been the standard of care for surgical treatment of early-stage NSCLC. Saji and colleagues investigated whether segmentectomy was noninferior to lobectomy in selected cases of small-sized peripheral NSCLC. This randomized, controlled, noninferiority trial was conducted at 70 institutions in Japan.
Patients with selected stage IA (American Joint Committee on Cancer [AJCC], seventh edition) NSCLC (peripheral tumors, £ 2 cm diameter, consolidation-to-tumor ratio > 0.5) were randomly assigned to undergo segmentectomy or lobectomy. The primary endpoint was OS. Pertinent secondary endpoints included postoperative respiratory function, relapse-free survival, and adverse events.
A total of 1106 patients were enrolled: 554 in the lobectomy group and 552 in the segmentectomy group. The 5-year OS was 94.3% for segmentectomy and 91.1% for lobectomy (hazard ratio 0.663; one-sided P < .001 for noninferiority; P = .0082 for superiority). In addition to the modestly improved OS observed, 5-year relapse-free survival was comparable between the groups (88% for segmentectomy and 87.9% for lobectomy). However, more local relapse was observed for segmentectomy (10.5%) than for lobectomy (5.4%) (P = .0018). Despite significantly more locoregional recurrences with segmentectomy compared with lobectomy, rates of combined distant and locoregional relapses were similar. Slightly more patients died in the lobectomy group than the segmentectomy group, and the rate of cancer-related deaths, including second primary lung cancers, was higher in the lobectomy group. Interestingly, although segmentectomy had better OS, the survival advantage was not cancer-specific.
The mechanism by which segmentectomy improved survival over lobectomy in these selected patients with small, peripheral stage IA NSCLC is still unclear. Limitations of the study included that all patients were from one geographic region (Japan) and that the study was unblinded, which can introduce bias. We await the results of CALGB 140503: A Randomized Phase III Trial of Lobectomy versus Sublobar Resection for Small (< 2cm) Peripheral Non-Small Cell Lung Cancer (NCT00499330). This study is being done in a US population and includes nonanatomic wedge in its sublobar resection cohort.
The study by Saji and colleagues suggests that surgeons should consider segmentectomy in appropriate patients (select small stage IA NSCLC [peripheral tumors, £ 2 cm diameter, consolidation-to-tumor ratio > 0.5]), based on the modest improvement in OS compared with lobectomy.
Immunotherapy Activity in Cachexic and Noncachexic Patients With Advanced NSCLC and Clinical Outcomes, by Adipose Tissue Loss on Treatment
There are emerging data that body mass index (BMI) and the presence or absence of cachexia in cancers, including NSCLC, may change the efficacy of programmed cell death-ligand 1 (PD-L1) immune checkpoint inhibitors. Nishioka and colleagues, in a single-center retrospective cohort, examined patients with advanced NSCLC (40 with cachexia and 34 without cachexia) who received PD-L1 inhibitors (pembrolizumab, nivolumab, or atezolizumab). Patients were excluded if they had poor performance status, EGFR/ALK/ROS1 oncogene drivers, unknown PD-L1 expression status, and unknown weight loss in the 6 months before immunotherapy administration. In addition to BMI, measurements of adipose tissue quantity and muscle mass were used.
The overall response rate was 28.4% in the 74 patients analyzed. Patients with cachexia had a lower overall response rate than those without cachexia (15.0% vs 44.1%; P < .05). Among the patients without cachexia, those with total adipose tissue loss had a significantly longer PFS than those with total adipose tissue maintenance (18.5 months vs 2.86 months; P = .037), including in a multivariate analyses (hazard ratio 0.34; P < .05), after adjustment for PD-L1 expression and performance status (Eastern Cooperative Oncology Group [ECOG] 0 vs. 1).
Mechanistically, a paradoxical effect of obesity on T-cell function that relates to leptin, which is secreted by adipose tissue, has been observed in preclinical studies.7 In a previously published study, obesity resulted in tumor progression and PD-1–mediated T-cell dysfunction, which can be overcome by PD-L1 blockade with improved clinical outcomes to these therapies in patients with obesity and cancer, including NSCLC.7 This "obesity paradox" may underlie some of the findings observed in Nishioka and colleagues' study. More research needs to be done regarding the activity of immune checkpoint inhibition in NSCLC as it relates to BMI, cachexia, and amount of adipose tissue.
Additional References
1. Shibata T, Ohta T, Tong KI, et al. Cancer related mutations in NRF2 impair its recognition by Keap1-Cul3 E3 ligase and promote malignancy. Proc Natl Acad Sci U S A. 2008;105(36):13568-13573. doi: 10.1073/pnas.0806268105
2. Frank R, Scheffler M, Merkelbach-Bruse S, et al. Clinical and pathological characteristics of KEAP1- and NFE2L2-mutated non-small cell lung carcinoma (NSCLC). Clin Cancer Res. 2018;24:3087-3096. doi: 10.1158/1078-0432.CCR-17-3416
3. Binkley MS, Jeon YJ, Nesselbush M, et al. KEAP1/NFE2L2 mutations predict lung cancer radiation resistance that can be targeted by glutaminase inhibition. Cancer Discov. 2020;10(12):1826-1841. doi: 10.1158/2159-8290.CD-20-0282
4. Hellyer JA, Padda SK, Diehn M, et al. Clinical implications of KEAP1-NFE2L2 mutations in NSCLC. J Thorac Oncol. 2021;16(3):395-403. doi: 10.1016/j.jtho.2020.11.015
5. Jeong Y, Hellyer JA, Stehr H, et al. Role of KEAP1/NFE2L2 mutations in the chemotherapeutic response of patients with non-small cell lung cancer. Clin Cancer Res. 2020;26(1):274-281. doi: 10.1158/1078-0432.CCR-19-1237
6. Riess JW, Frankel P, Shackelford D, et al. Phase 1 trial of MLN0128 (sapanisertib) and CB-839 HCl (telaglenastat) in patients with advanced NSCLC (NCI 10327): Rationale and study design. Clin Lung Cancer. 2021;22:67-70. doi: 10.1016/j.cllc.2020.10.006
Commentary: Factors in Psoriatic Arthritis Development and Treatment Response, June 2022
Infections have long been identified as possible triggers for psoriasis and psoriatic arthritis (PsA) onset. Thrastardottir and colleagues evaluated the association between sites where the culture sample was obtained, the culture result, and pathogens and incident PsA and psoriasis. They obtained data on all samples sent for bacterial culture in the Stockholm region of Sweden (313,235 bacterial cultures from 128,982 individuals) from January 1, 2004, to December 31, 2006. Among all samples sent for culture, a pharyngeal sample was associated with a higher risk for PsA onset within the next 50 days compared with urine (hazard ratio [HR] 8.78; 95% CI 3.23-23.91), nasopharyngeal (HR 8.26; 95% CI 2.23-30.63), or blood (HR 25.22; 95% CI 3.12-204.13) samples. Streptococcal infections in the pharynx or at any other site were not associated with an increased risk for PsA. Similar associations were found for psoriasis, but not for rheumatoid arthritis. These results indicate that having sent a pharyngeal sample for culture was associated with an increased risk for psoriatic disease onset, suggesting that the site of infection—rather than the pathogen—is associated with the increased risk. These intriguing results support the need to further study the role of site and type of infection and antibiotic use on psoriatic disease onset.
With regard to other risk factors for PsA, a meta-analysis by Pouw and colleagues looked at 29 studies including adult patients with psoriasis with or without concurrent PsA or adult patients with psoriasis who developed PsA. The analysis showed that the body surface area affected by psoriasis was significantly higher in patients with psoriasis and concurrent PsA vs patients with only psoriasis (mean difference 5.31; 95% CI 1.78-8.83). Severe psoriasis was a significant predictor of concurrent PsA (odds ratio 3.34; P < .001). Thus, optimum care of patients with PsA requires excellent collaboration between rheumatologists and dermatologists.
Factors such as sex and body mass index (BMI) are likely to have a role in PsA treatment response but have not been extensively evaluated. To address this issue, Mease and colleagues conducted a post hoc analysis of the phase 3 SEAM-PsA trial including 851 patients who were methotrexate (MTX)/biologics naive and had early PsA. They were randomly assigned to receive MTX + placebo, etanercept + placebo, or MTX + etanercept. The study demonstrated that at week 24 a higher proportion of men vs women receiving MTX + etanercept achieved the American College of Rheumatology 20% criteria (ACR20) (71.5% vs 58.3%; P = .0194) and minimal disease activity (MDA) (45.8% vs 25.2%; P = .0003). A higher proportion of patients with a BMI ≤ 30 vs > 30 in all treatment groups achieved MDA (all P < .05), and those in the MTX + etanercept group achieved ACR20 (P = .0241). Thus, men (vs women) and those with lower BMI experience significantly better outcomes with treatment. When counseling patients about response to treatment, sex and BMI need to be taken into consideration. Moreover, further research is required to confirm and identify the reasons underlying these findings and to optimize treatment outcomes.
Another post hoc study explored the association between baseline disease activity and achieving the treatment target in PsA. Mease and colleagues analysed data from the phase 3 PALACE 4 study including 175 patients who were disease-modifying antirheumatic drug (DMARD)–naive and had active PsA. They received 30 mg apremilast twice daily. The study found that at week 52, remission or low disease activity according to the Clinical Disease Activity Index for Psoriatic Arthritis was achieved in 61.7% of patients with moderate disease activity vs 28.2% of these with high disease activity at baseline. Thus, DMARD-naive patients with moderate (vs high) disease activity at baseline are more likely to achieve low disease activity after apremilast therapy.
Infections have long been identified as possible triggers for psoriasis and psoriatic arthritis (PsA) onset. Thrastardottir and colleagues evaluated the association between sites where the culture sample was obtained, the culture result, and pathogens and incident PsA and psoriasis. They obtained data on all samples sent for bacterial culture in the Stockholm region of Sweden (313,235 bacterial cultures from 128,982 individuals) from January 1, 2004, to December 31, 2006. Among all samples sent for culture, a pharyngeal sample was associated with a higher risk for PsA onset within the next 50 days compared with urine (hazard ratio [HR] 8.78; 95% CI 3.23-23.91), nasopharyngeal (HR 8.26; 95% CI 2.23-30.63), or blood (HR 25.22; 95% CI 3.12-204.13) samples. Streptococcal infections in the pharynx or at any other site were not associated with an increased risk for PsA. Similar associations were found for psoriasis, but not for rheumatoid arthritis. These results indicate that having sent a pharyngeal sample for culture was associated with an increased risk for psoriatic disease onset, suggesting that the site of infection—rather than the pathogen—is associated with the increased risk. These intriguing results support the need to further study the role of site and type of infection and antibiotic use on psoriatic disease onset.
With regard to other risk factors for PsA, a meta-analysis by Pouw and colleagues looked at 29 studies including adult patients with psoriasis with or without concurrent PsA or adult patients with psoriasis who developed PsA. The analysis showed that the body surface area affected by psoriasis was significantly higher in patients with psoriasis and concurrent PsA vs patients with only psoriasis (mean difference 5.31; 95% CI 1.78-8.83). Severe psoriasis was a significant predictor of concurrent PsA (odds ratio 3.34; P < .001). Thus, optimum care of patients with PsA requires excellent collaboration between rheumatologists and dermatologists.
Factors such as sex and body mass index (BMI) are likely to have a role in PsA treatment response but have not been extensively evaluated. To address this issue, Mease and colleagues conducted a post hoc analysis of the phase 3 SEAM-PsA trial including 851 patients who were methotrexate (MTX)/biologics naive and had early PsA. They were randomly assigned to receive MTX + placebo, etanercept + placebo, or MTX + etanercept. The study demonstrated that at week 24 a higher proportion of men vs women receiving MTX + etanercept achieved the American College of Rheumatology 20% criteria (ACR20) (71.5% vs 58.3%; P = .0194) and minimal disease activity (MDA) (45.8% vs 25.2%; P = .0003). A higher proportion of patients with a BMI ≤ 30 vs > 30 in all treatment groups achieved MDA (all P < .05), and those in the MTX + etanercept group achieved ACR20 (P = .0241). Thus, men (vs women) and those with lower BMI experience significantly better outcomes with treatment. When counseling patients about response to treatment, sex and BMI need to be taken into consideration. Moreover, further research is required to confirm and identify the reasons underlying these findings and to optimize treatment outcomes.
Another post hoc study explored the association between baseline disease activity and achieving the treatment target in PsA. Mease and colleagues analysed data from the phase 3 PALACE 4 study including 175 patients who were disease-modifying antirheumatic drug (DMARD)–naive and had active PsA. They received 30 mg apremilast twice daily. The study found that at week 52, remission or low disease activity according to the Clinical Disease Activity Index for Psoriatic Arthritis was achieved in 61.7% of patients with moderate disease activity vs 28.2% of these with high disease activity at baseline. Thus, DMARD-naive patients with moderate (vs high) disease activity at baseline are more likely to achieve low disease activity after apremilast therapy.
Infections have long been identified as possible triggers for psoriasis and psoriatic arthritis (PsA) onset. Thrastardottir and colleagues evaluated the association between sites where the culture sample was obtained, the culture result, and pathogens and incident PsA and psoriasis. They obtained data on all samples sent for bacterial culture in the Stockholm region of Sweden (313,235 bacterial cultures from 128,982 individuals) from January 1, 2004, to December 31, 2006. Among all samples sent for culture, a pharyngeal sample was associated with a higher risk for PsA onset within the next 50 days compared with urine (hazard ratio [HR] 8.78; 95% CI 3.23-23.91), nasopharyngeal (HR 8.26; 95% CI 2.23-30.63), or blood (HR 25.22; 95% CI 3.12-204.13) samples. Streptococcal infections in the pharynx or at any other site were not associated with an increased risk for PsA. Similar associations were found for psoriasis, but not for rheumatoid arthritis. These results indicate that having sent a pharyngeal sample for culture was associated with an increased risk for psoriatic disease onset, suggesting that the site of infection—rather than the pathogen—is associated with the increased risk. These intriguing results support the need to further study the role of site and type of infection and antibiotic use on psoriatic disease onset.
With regard to other risk factors for PsA, a meta-analysis by Pouw and colleagues looked at 29 studies including adult patients with psoriasis with or without concurrent PsA or adult patients with psoriasis who developed PsA. The analysis showed that the body surface area affected by psoriasis was significantly higher in patients with psoriasis and concurrent PsA vs patients with only psoriasis (mean difference 5.31; 95% CI 1.78-8.83). Severe psoriasis was a significant predictor of concurrent PsA (odds ratio 3.34; P < .001). Thus, optimum care of patients with PsA requires excellent collaboration between rheumatologists and dermatologists.
Factors such as sex and body mass index (BMI) are likely to have a role in PsA treatment response but have not been extensively evaluated. To address this issue, Mease and colleagues conducted a post hoc analysis of the phase 3 SEAM-PsA trial including 851 patients who were methotrexate (MTX)/biologics naive and had early PsA. They were randomly assigned to receive MTX + placebo, etanercept + placebo, or MTX + etanercept. The study demonstrated that at week 24 a higher proportion of men vs women receiving MTX + etanercept achieved the American College of Rheumatology 20% criteria (ACR20) (71.5% vs 58.3%; P = .0194) and minimal disease activity (MDA) (45.8% vs 25.2%; P = .0003). A higher proportion of patients with a BMI ≤ 30 vs > 30 in all treatment groups achieved MDA (all P < .05), and those in the MTX + etanercept group achieved ACR20 (P = .0241). Thus, men (vs women) and those with lower BMI experience significantly better outcomes with treatment. When counseling patients about response to treatment, sex and BMI need to be taken into consideration. Moreover, further research is required to confirm and identify the reasons underlying these findings and to optimize treatment outcomes.
Another post hoc study explored the association between baseline disease activity and achieving the treatment target in PsA. Mease and colleagues analysed data from the phase 3 PALACE 4 study including 175 patients who were disease-modifying antirheumatic drug (DMARD)–naive and had active PsA. They received 30 mg apremilast twice daily. The study found that at week 52, remission or low disease activity according to the Clinical Disease Activity Index for Psoriatic Arthritis was achieved in 61.7% of patients with moderate disease activity vs 28.2% of these with high disease activity at baseline. Thus, DMARD-naive patients with moderate (vs high) disease activity at baseline are more likely to achieve low disease activity after apremilast therapy.
Commentary: Gastric Cancer Chemotherapy in Select Populations, June 2022
Chemotherapy plays a critical role in the management of patients with advanced gastroesophageal adenocarcinoma, and a fluoropyrimidine and platinum doublet (either oxaliplatin or cisplatin) is the standard regimen used. Chemotherapy is associated with toxicity, which is particularly concerning in frail and older adult patients.1 A study by Chinen and colleagues specifically looked at the use of platinum chemotherapy agents in the older adult patient population. This retrospective cohort study analyzed survival outcomes and granulocyte colony–stimulating factor (G-CSF) use in 242 patients with advanced gastric cancer who were at least 70 years old and who were treated with either an oxaliplatin- or cisplatin-containing regimen. After propensity score weighting, the study demonstrated that treatment with these agents resulted in similar overall survival, but G-CSF use was more frequent with oxaliplatin use. These results are in line with previous data regarding these agents. In a prospective noninferiority study with a two-by-two design (REAL-2), an oxaliplatin-containing regimen had similar activity to a cisplatin-containing regimen.2 However, oxaliplatin use was associated with less neutropenia. Going forward, the use of oxaliplatin should be preferred over cisplatin in older adult patients given its more favorable toxicity profile.
A study by Sotelo and colleagues looked at the presence of gastric preneoplastic lesions in the first-degree relatives of patients with gastric cancer. In this cross-sectional study conducted in Chile, endoscopic evaluation was performed in 110 people eligible for evaluation. Among the participants, 95 cases (86.4%) of preneoplastic lesions were identified, most commonly atrophic gastritis (86.4%) and intestinal metaplasia (82.7%). There was no association with sex, age, or Helicobacter pylori infection. The high rates of these lesions in the study are probably reflective of a high prevalence of gastric cancer in this geographic area. Although the data interpretation is limited by the small study size, these results suggest that endoscopic surveillance of first-degree relatives is warranted in areas of high gastric cancer incidence, and that optimal surveillance protocols, as well as management of these precancerous conditions, should be defined further.
The role of hyperthermic intraperitoneal chemotherapy (HIPEC) has been controversial in the management of gastric cancer. Thus far, there has not been a definitive study demonstrating a positive impact of HIPEC on survival in patients with this disease. A study by Lee and colleagues looked at the role of prophylactic HIPEC in patients with clinical stage T4 gastric cancer who do not have evidence of distant metastasis. Retrospective analysis included 132 patients with clinical stage T4 gastric cancer who underwent gastrectomy and D2 lymphadenectomy. After propensity score matching to reduce selection bias, the outcomes of 35 patients per cohort (gastrectomy vs gastrectomy plus prophylactic HIPEC) were analyzed. The two groups were well matched in regard to histology, pathologic T and N stage, perioperative therapy, and the type of resection. There was no difference in the incidence of postoperative complications. While the rate of peritoneal recurrences was lower in the HIPEC cohort, there was no difference in the rate of distant metastasis between the two groups. In terms of survival outcomes, the study demonstrated that disease-free survival and overall survival were improved with prophylactic HIPEC. Although firm conclusions cannot be drawn from this small retrospective study, these results suggest that it may be worth further investigating the role of prophylactic HIPEC in a subset of patients with high-risk early-stage disease.
Additional References
1. Hwang IG, Ji JH, Kang JH, et al. A multi-center, open-label, randomized phase III trial of first-line chemotherapy with capecitabine monotherapy versus capecitabine plus oxaliplatin in elderly patients with advanced gastric cancer. J Geriatr Oncol. 2017;8(3):170-175. Doi: 10.1016/j.jgo.2017.01.002
2. Cunningham D, Starling N, Rao S, et al. Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med. 2008;358:36-46. Doi: 10.1056/NEJMoa073149
Chemotherapy plays a critical role in the management of patients with advanced gastroesophageal adenocarcinoma, and a fluoropyrimidine and platinum doublet (either oxaliplatin or cisplatin) is the standard regimen used. Chemotherapy is associated with toxicity, which is particularly concerning in frail and older adult patients.1 A study by Chinen and colleagues specifically looked at the use of platinum chemotherapy agents in the older adult patient population. This retrospective cohort study analyzed survival outcomes and granulocyte colony–stimulating factor (G-CSF) use in 242 patients with advanced gastric cancer who were at least 70 years old and who were treated with either an oxaliplatin- or cisplatin-containing regimen. After propensity score weighting, the study demonstrated that treatment with these agents resulted in similar overall survival, but G-CSF use was more frequent with oxaliplatin use. These results are in line with previous data regarding these agents. In a prospective noninferiority study with a two-by-two design (REAL-2), an oxaliplatin-containing regimen had similar activity to a cisplatin-containing regimen.2 However, oxaliplatin use was associated with less neutropenia. Going forward, the use of oxaliplatin should be preferred over cisplatin in older adult patients given its more favorable toxicity profile.
A study by Sotelo and colleagues looked at the presence of gastric preneoplastic lesions in the first-degree relatives of patients with gastric cancer. In this cross-sectional study conducted in Chile, endoscopic evaluation was performed in 110 people eligible for evaluation. Among the participants, 95 cases (86.4%) of preneoplastic lesions were identified, most commonly atrophic gastritis (86.4%) and intestinal metaplasia (82.7%). There was no association with sex, age, or Helicobacter pylori infection. The high rates of these lesions in the study are probably reflective of a high prevalence of gastric cancer in this geographic area. Although the data interpretation is limited by the small study size, these results suggest that endoscopic surveillance of first-degree relatives is warranted in areas of high gastric cancer incidence, and that optimal surveillance protocols, as well as management of these precancerous conditions, should be defined further.
The role of hyperthermic intraperitoneal chemotherapy (HIPEC) has been controversial in the management of gastric cancer. Thus far, there has not been a definitive study demonstrating a positive impact of HIPEC on survival in patients with this disease. A study by Lee and colleagues looked at the role of prophylactic HIPEC in patients with clinical stage T4 gastric cancer who do not have evidence of distant metastasis. Retrospective analysis included 132 patients with clinical stage T4 gastric cancer who underwent gastrectomy and D2 lymphadenectomy. After propensity score matching to reduce selection bias, the outcomes of 35 patients per cohort (gastrectomy vs gastrectomy plus prophylactic HIPEC) were analyzed. The two groups were well matched in regard to histology, pathologic T and N stage, perioperative therapy, and the type of resection. There was no difference in the incidence of postoperative complications. While the rate of peritoneal recurrences was lower in the HIPEC cohort, there was no difference in the rate of distant metastasis between the two groups. In terms of survival outcomes, the study demonstrated that disease-free survival and overall survival were improved with prophylactic HIPEC. Although firm conclusions cannot be drawn from this small retrospective study, these results suggest that it may be worth further investigating the role of prophylactic HIPEC in a subset of patients with high-risk early-stage disease.
Additional References
1. Hwang IG, Ji JH, Kang JH, et al. A multi-center, open-label, randomized phase III trial of first-line chemotherapy with capecitabine monotherapy versus capecitabine plus oxaliplatin in elderly patients with advanced gastric cancer. J Geriatr Oncol. 2017;8(3):170-175. Doi: 10.1016/j.jgo.2017.01.002
2. Cunningham D, Starling N, Rao S, et al. Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med. 2008;358:36-46. Doi: 10.1056/NEJMoa073149
Chemotherapy plays a critical role in the management of patients with advanced gastroesophageal adenocarcinoma, and a fluoropyrimidine and platinum doublet (either oxaliplatin or cisplatin) is the standard regimen used. Chemotherapy is associated with toxicity, which is particularly concerning in frail and older adult patients.1 A study by Chinen and colleagues specifically looked at the use of platinum chemotherapy agents in the older adult patient population. This retrospective cohort study analyzed survival outcomes and granulocyte colony–stimulating factor (G-CSF) use in 242 patients with advanced gastric cancer who were at least 70 years old and who were treated with either an oxaliplatin- or cisplatin-containing regimen. After propensity score weighting, the study demonstrated that treatment with these agents resulted in similar overall survival, but G-CSF use was more frequent with oxaliplatin use. These results are in line with previous data regarding these agents. In a prospective noninferiority study with a two-by-two design (REAL-2), an oxaliplatin-containing regimen had similar activity to a cisplatin-containing regimen.2 However, oxaliplatin use was associated with less neutropenia. Going forward, the use of oxaliplatin should be preferred over cisplatin in older adult patients given its more favorable toxicity profile.
A study by Sotelo and colleagues looked at the presence of gastric preneoplastic lesions in the first-degree relatives of patients with gastric cancer. In this cross-sectional study conducted in Chile, endoscopic evaluation was performed in 110 people eligible for evaluation. Among the participants, 95 cases (86.4%) of preneoplastic lesions were identified, most commonly atrophic gastritis (86.4%) and intestinal metaplasia (82.7%). There was no association with sex, age, or Helicobacter pylori infection. The high rates of these lesions in the study are probably reflective of a high prevalence of gastric cancer in this geographic area. Although the data interpretation is limited by the small study size, these results suggest that endoscopic surveillance of first-degree relatives is warranted in areas of high gastric cancer incidence, and that optimal surveillance protocols, as well as management of these precancerous conditions, should be defined further.
The role of hyperthermic intraperitoneal chemotherapy (HIPEC) has been controversial in the management of gastric cancer. Thus far, there has not been a definitive study demonstrating a positive impact of HIPEC on survival in patients with this disease. A study by Lee and colleagues looked at the role of prophylactic HIPEC in patients with clinical stage T4 gastric cancer who do not have evidence of distant metastasis. Retrospective analysis included 132 patients with clinical stage T4 gastric cancer who underwent gastrectomy and D2 lymphadenectomy. After propensity score matching to reduce selection bias, the outcomes of 35 patients per cohort (gastrectomy vs gastrectomy plus prophylactic HIPEC) were analyzed. The two groups were well matched in regard to histology, pathologic T and N stage, perioperative therapy, and the type of resection. There was no difference in the incidence of postoperative complications. While the rate of peritoneal recurrences was lower in the HIPEC cohort, there was no difference in the rate of distant metastasis between the two groups. In terms of survival outcomes, the study demonstrated that disease-free survival and overall survival were improved with prophylactic HIPEC. Although firm conclusions cannot be drawn from this small retrospective study, these results suggest that it may be worth further investigating the role of prophylactic HIPEC in a subset of patients with high-risk early-stage disease.
Additional References
1. Hwang IG, Ji JH, Kang JH, et al. A multi-center, open-label, randomized phase III trial of first-line chemotherapy with capecitabine monotherapy versus capecitabine plus oxaliplatin in elderly patients with advanced gastric cancer. J Geriatr Oncol. 2017;8(3):170-175. Doi: 10.1016/j.jgo.2017.01.002
2. Cunningham D, Starling N, Rao S, et al. Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med. 2008;358:36-46. Doi: 10.1056/NEJMoa073149
Commentary: New Treatments in T2D and Potential New Benefits From Metformin, June 2022
Tirzepatide, recently approved by the US Food and Drug Administration, is a unique dual gastric inhibitory peptide/glucagon-like peptide 1 (GLP-1) receptor agonist that has been formulated as a once-weekly injection. The results from the phase 3 SURPASS program demonstrated its efficacy for type 2 diabetes management. Glycosylated hemoglobin reduction ranged from 1.9%-2.6%; up to 97% of participants achieved an A1c < 7% and up to 62% achieved an A1c < 5.7%, and weight loss ranged from 6 to 13 kg. Tirzepatide was superior to 1 mg semaglutide, insulin degludec, and insulin glargine for A1c lowering and weight loss.
In a subgroup of SURPASS-3, Battelino and colleagues compared tirzepatide to insulin degludec using continuous glucose monitoring. Patients treated with tirzepatide at doses of 5 mg and 10 mg achieved a mean time in tight range (71-140 mg/dL) of 72.4% and 72.6%, respectively, which was significantly better than the 48.0% for patients treated with insulin degludec. Remarkably, time in range (71-180 mg/dL) was 91% for the 10- and 15-mg doses of tirzepatide compared with 75% for insulin degludec. Time spent in hypoglycemia and glycemic variability were lower with tirzepatide vs insulin degludec. This analysis shows the superiority of tirzepatide in achieving clinically meaningful improvements in the percentage of time spent within a tight target range and target range for tirzepatide compared with insulin degludec, further supporting the use of this dual Incretin before starting basal insulin.
Cotadutide is a GLP-1 receptor/glucagon dual agonist currently in phase 2b/3 trials in patients with either nonalcoholic steatohepatitis (NASH) or type 2 diabetes with chronic kidney disease. In a recent meta-analysis of early cotadutide trials vs placebo, Ali and colleagues reported a significant 3.3 kg weight loss and a 0.68% reduction in A1c, as well as reductions in glucose area under the plasma concentration curve and fasting plasma glucose. Although we will have to await the results of further studies, these and other early data with cotadutide suggests that this GLP-1 receptor/glucagon co-agonist may offer benefits in patients with type 2 diabetes or NASH.
It has been over 60 years since the first clinical use of metformin, yet we continue to learn about potential uses beyond just glycemic control in type 2 diabetes. In a Chinese prospective cohort study of 7587 patients with type 2 diabetes who were hospitalized with a first stroke, Tu and colleagues found lower rates of in-hospital mortality, 12-month mortality, and disability in those treated with metformin vs those not treated with metformin. The authors speculate that metformin has antioxidant, anti-inflammatory, and neuroprotective effects that may lead to better stroke outcomes. Of course, this study is limited by its observational design, and randomized controlled studies are required to determine whether metformin use may have a protective effect against the poor functional outcome in first-ever stroke patients with type 2 diabetes.
In another study of metformin, Jiang and colleagues reported that among patients with long-standing type 2 diabetes, metformin users were 83% less likely than metformin nonusers to develop early age-related macular degeneration (AMD). This was a small retrospective study from which conclusions cannot be made. Given that AMD is a leading cause of vision loss for older adults, future prospective studies of metformin in the treatment of AMD would be helpful in determining the impact of metformin in this common eye condition.
Tirzepatide, recently approved by the US Food and Drug Administration, is a unique dual gastric inhibitory peptide/glucagon-like peptide 1 (GLP-1) receptor agonist that has been formulated as a once-weekly injection. The results from the phase 3 SURPASS program demonstrated its efficacy for type 2 diabetes management. Glycosylated hemoglobin reduction ranged from 1.9%-2.6%; up to 97% of participants achieved an A1c < 7% and up to 62% achieved an A1c < 5.7%, and weight loss ranged from 6 to 13 kg. Tirzepatide was superior to 1 mg semaglutide, insulin degludec, and insulin glargine for A1c lowering and weight loss.
In a subgroup of SURPASS-3, Battelino and colleagues compared tirzepatide to insulin degludec using continuous glucose monitoring. Patients treated with tirzepatide at doses of 5 mg and 10 mg achieved a mean time in tight range (71-140 mg/dL) of 72.4% and 72.6%, respectively, which was significantly better than the 48.0% for patients treated with insulin degludec. Remarkably, time in range (71-180 mg/dL) was 91% for the 10- and 15-mg doses of tirzepatide compared with 75% for insulin degludec. Time spent in hypoglycemia and glycemic variability were lower with tirzepatide vs insulin degludec. This analysis shows the superiority of tirzepatide in achieving clinically meaningful improvements in the percentage of time spent within a tight target range and target range for tirzepatide compared with insulin degludec, further supporting the use of this dual Incretin before starting basal insulin.
Cotadutide is a GLP-1 receptor/glucagon dual agonist currently in phase 2b/3 trials in patients with either nonalcoholic steatohepatitis (NASH) or type 2 diabetes with chronic kidney disease. In a recent meta-analysis of early cotadutide trials vs placebo, Ali and colleagues reported a significant 3.3 kg weight loss and a 0.68% reduction in A1c, as well as reductions in glucose area under the plasma concentration curve and fasting plasma glucose. Although we will have to await the results of further studies, these and other early data with cotadutide suggests that this GLP-1 receptor/glucagon co-agonist may offer benefits in patients with type 2 diabetes or NASH.
It has been over 60 years since the first clinical use of metformin, yet we continue to learn about potential uses beyond just glycemic control in type 2 diabetes. In a Chinese prospective cohort study of 7587 patients with type 2 diabetes who were hospitalized with a first stroke, Tu and colleagues found lower rates of in-hospital mortality, 12-month mortality, and disability in those treated with metformin vs those not treated with metformin. The authors speculate that metformin has antioxidant, anti-inflammatory, and neuroprotective effects that may lead to better stroke outcomes. Of course, this study is limited by its observational design, and randomized controlled studies are required to determine whether metformin use may have a protective effect against the poor functional outcome in first-ever stroke patients with type 2 diabetes.
In another study of metformin, Jiang and colleagues reported that among patients with long-standing type 2 diabetes, metformin users were 83% less likely than metformin nonusers to develop early age-related macular degeneration (AMD). This was a small retrospective study from which conclusions cannot be made. Given that AMD is a leading cause of vision loss for older adults, future prospective studies of metformin in the treatment of AMD would be helpful in determining the impact of metformin in this common eye condition.
Tirzepatide, recently approved by the US Food and Drug Administration, is a unique dual gastric inhibitory peptide/glucagon-like peptide 1 (GLP-1) receptor agonist that has been formulated as a once-weekly injection. The results from the phase 3 SURPASS program demonstrated its efficacy for type 2 diabetes management. Glycosylated hemoglobin reduction ranged from 1.9%-2.6%; up to 97% of participants achieved an A1c < 7% and up to 62% achieved an A1c < 5.7%, and weight loss ranged from 6 to 13 kg. Tirzepatide was superior to 1 mg semaglutide, insulin degludec, and insulin glargine for A1c lowering and weight loss.
In a subgroup of SURPASS-3, Battelino and colleagues compared tirzepatide to insulin degludec using continuous glucose monitoring. Patients treated with tirzepatide at doses of 5 mg and 10 mg achieved a mean time in tight range (71-140 mg/dL) of 72.4% and 72.6%, respectively, which was significantly better than the 48.0% for patients treated with insulin degludec. Remarkably, time in range (71-180 mg/dL) was 91% for the 10- and 15-mg doses of tirzepatide compared with 75% for insulin degludec. Time spent in hypoglycemia and glycemic variability were lower with tirzepatide vs insulin degludec. This analysis shows the superiority of tirzepatide in achieving clinically meaningful improvements in the percentage of time spent within a tight target range and target range for tirzepatide compared with insulin degludec, further supporting the use of this dual Incretin before starting basal insulin.
Cotadutide is a GLP-1 receptor/glucagon dual agonist currently in phase 2b/3 trials in patients with either nonalcoholic steatohepatitis (NASH) or type 2 diabetes with chronic kidney disease. In a recent meta-analysis of early cotadutide trials vs placebo, Ali and colleagues reported a significant 3.3 kg weight loss and a 0.68% reduction in A1c, as well as reductions in glucose area under the plasma concentration curve and fasting plasma glucose. Although we will have to await the results of further studies, these and other early data with cotadutide suggests that this GLP-1 receptor/glucagon co-agonist may offer benefits in patients with type 2 diabetes or NASH.
It has been over 60 years since the first clinical use of metformin, yet we continue to learn about potential uses beyond just glycemic control in type 2 diabetes. In a Chinese prospective cohort study of 7587 patients with type 2 diabetes who were hospitalized with a first stroke, Tu and colleagues found lower rates of in-hospital mortality, 12-month mortality, and disability in those treated with metformin vs those not treated with metformin. The authors speculate that metformin has antioxidant, anti-inflammatory, and neuroprotective effects that may lead to better stroke outcomes. Of course, this study is limited by its observational design, and randomized controlled studies are required to determine whether metformin use may have a protective effect against the poor functional outcome in first-ever stroke patients with type 2 diabetes.
In another study of metformin, Jiang and colleagues reported that among patients with long-standing type 2 diabetes, metformin users were 83% less likely than metformin nonusers to develop early age-related macular degeneration (AMD). This was a small retrospective study from which conclusions cannot be made. Given that AMD is a leading cause of vision loss for older adults, future prospective studies of metformin in the treatment of AMD would be helpful in determining the impact of metformin in this common eye condition.
Psilocybin benefits in severe depression observed up to 12 weeks
NEW ORLEANS –
“This is easily the largest study of a psychedelic drug employing modern randomized controlled trial methodology [with] 22 sites and 10 countries, so it’s not your typical phase 2 trial,” the study’s lead author, Guy M. Goodwin, MD, emeritus professor of psychiatry at the University of Oxford, England, said in an interview.
“Importantly, 94% of the patients in the study were psilocybin naive, which is very important for generalizability,” Dr. Goodwin noted.
Long used as psychedelic ‘magic mushrooms,’ psilocybin has gained increased interest in psychiatry in recent years as a potential treatment for severe depression after showing benefits in patients with life-threatening cancers and others with major depressive disorder (MDD).
To put the therapy to test in a more rigorous, randomized trial, Dr. Goodwin and colleagues conducted the phase 2b study of a proprietary synthetic formulation of psilocybin, COMP360 (COMPASS Pathways), recruiting 233 patients with treatment-resistant depression at 22 centers.
The study was presented at the annual meeting of the American Psychiatric Association.
After a 2-week washout period following the discontinuation of antidepressants, the patients were randomized to one of three groups: A single dose of 25 mg (n = 79), 10 mg (n = 75), or a subtherapeutic comparison of 1 mg (n = 79).
The psilocybin was administered in the presence of specially trained therapists who provided psychological support before, during, and after the 6- to 8-hour session.
Patients were then asked to refrain from antidepressant use for at least 3 weeks following the session, and had periodic follow-up for 12 weeks.
For the primary endpoint, those in the 25-mg group, but not the 10-mg dose, showed a significantly greater reduction in depression from baseline versus the 1-mg group on the Montgomery-Åsberg Depression Rating Scale at week 3 (MADRS; -6.6; P < .001).
The benefit was observed at day 2 and week 1 following administration, “confirming the rapid-acting character of the effect,” the investigators reported.
Sustained responses, defined as at least a 50% change from baseline in MADRS total score, were further observed up to week 12 among 20.3% in the 25-mg group and among 5.3% in the 10-mg groups versus 10.1% in the 1-mg group.
On the day of psilocybin treatment, the treatment-emergent side effects that were reported were headache, nausea, and dizziness, with event rates of 83.5% in the 25-mg group, 74.7% in the 10-mg group, and 72.2% in the 1-mg group.
One participant in the 25-mg group experienced acute anxiety and was treated with lorazepam.
The incidence of treatment-emergent serious adverse events from day 2 to week 3 was 6.3% (five patients) in the 25-mg group, 8.0% (six patients) in the 10-mg group, and 1.3% (one patient) in the 1-mg group.
Serious AEs included suicidal ideation and intentional self-injury among two patients each in the 25-mg group, while in the 10-mg group, two had suicidal ideation and one had hospitalization for severe depression.
There were no significant differences between the groups in terms of vital signs or clinical laboratory tests.
Of note, two patients in the 25-mg group had a change from baseline in QTcF >60 msec on day 2. For one patient, the increase was within normal range, and the other had a QTcF interval duration >500 msec on day 2, but levels returned to normal by day 9.
Improvements in context
Dr. Goodwin noted that the improvements were swift and impressive when compared with those of the STAR*D trial, which is the largest prospective study of treatment outcomes in patients with MDD.
“In the STAR*D trial, third- and fourth-step treatments showed low response rates of under 15% and high relapse rates,” Dr. Goodwin said. “By comparison, our response rates at 12 weeks were 20%-25%, so almost double that seen for probably equivalent treatment steps in STAR*D, with a single treatment with 25 mg, and no additional antidepressant, so no side effect burden.
“We hope to follow up enough of these patients [in the new study] to get some idea of relapse rates,” Dr. Goodwin added. “These have been low in comparable studies with MDD patients: We will see.”
Commenting on the research, Balwinder Singh, MD, of the department of psychiatry and psychology, Mayo Clinic, Rochester, Minn., said the study represents a valuable addition to needed evidence on psilocybin – with some caveats.
“This study adds to the emerging evidence base of psilocybin for treatment-resistant depression, at least in the short term,” he said in an interview. “I think the challenge in the real world would be to have access to 6-8 hours of therapy with psilocybin when patients struggle to find good therapists who could provide even weekly therapy for an hour.”
In addition, Dr. Singh questioned the durability of a single dose of psilocybin in the long term, noting a recent study (N Engl J Med. 2021 Apr 15. doi: 10.1056/NEJMoa2032994) that evaluated two doses of psilocybin (25 mg) 3 weeks apart, and failed to show any significant difference compared with the serotonergic antidepressant escitalopram at 6 weeks.
He further expressed concern about the emergence of suicidal behaviors in some patients, as well as the prolongation of QTc > 60 msec reported in the two patients.
“This is something to be carefully assessed in future studies, due to the risk of arrhythmias,” Dr. Singh said.
The study was sponsored by COMPASS Pathfinder Limited. Dr. Goodwin is chief medical officer for COMPASS Pathways. Dr. Singh had no disclosures to report.
NEW ORLEANS –
“This is easily the largest study of a psychedelic drug employing modern randomized controlled trial methodology [with] 22 sites and 10 countries, so it’s not your typical phase 2 trial,” the study’s lead author, Guy M. Goodwin, MD, emeritus professor of psychiatry at the University of Oxford, England, said in an interview.
“Importantly, 94% of the patients in the study were psilocybin naive, which is very important for generalizability,” Dr. Goodwin noted.
Long used as psychedelic ‘magic mushrooms,’ psilocybin has gained increased interest in psychiatry in recent years as a potential treatment for severe depression after showing benefits in patients with life-threatening cancers and others with major depressive disorder (MDD).
To put the therapy to test in a more rigorous, randomized trial, Dr. Goodwin and colleagues conducted the phase 2b study of a proprietary synthetic formulation of psilocybin, COMP360 (COMPASS Pathways), recruiting 233 patients with treatment-resistant depression at 22 centers.
The study was presented at the annual meeting of the American Psychiatric Association.
After a 2-week washout period following the discontinuation of antidepressants, the patients were randomized to one of three groups: A single dose of 25 mg (n = 79), 10 mg (n = 75), or a subtherapeutic comparison of 1 mg (n = 79).
The psilocybin was administered in the presence of specially trained therapists who provided psychological support before, during, and after the 6- to 8-hour session.
Patients were then asked to refrain from antidepressant use for at least 3 weeks following the session, and had periodic follow-up for 12 weeks.
For the primary endpoint, those in the 25-mg group, but not the 10-mg dose, showed a significantly greater reduction in depression from baseline versus the 1-mg group on the Montgomery-Åsberg Depression Rating Scale at week 3 (MADRS; -6.6; P < .001).
The benefit was observed at day 2 and week 1 following administration, “confirming the rapid-acting character of the effect,” the investigators reported.
Sustained responses, defined as at least a 50% change from baseline in MADRS total score, were further observed up to week 12 among 20.3% in the 25-mg group and among 5.3% in the 10-mg groups versus 10.1% in the 1-mg group.
On the day of psilocybin treatment, the treatment-emergent side effects that were reported were headache, nausea, and dizziness, with event rates of 83.5% in the 25-mg group, 74.7% in the 10-mg group, and 72.2% in the 1-mg group.
One participant in the 25-mg group experienced acute anxiety and was treated with lorazepam.
The incidence of treatment-emergent serious adverse events from day 2 to week 3 was 6.3% (five patients) in the 25-mg group, 8.0% (six patients) in the 10-mg group, and 1.3% (one patient) in the 1-mg group.
Serious AEs included suicidal ideation and intentional self-injury among two patients each in the 25-mg group, while in the 10-mg group, two had suicidal ideation and one had hospitalization for severe depression.
There were no significant differences between the groups in terms of vital signs or clinical laboratory tests.
Of note, two patients in the 25-mg group had a change from baseline in QTcF >60 msec on day 2. For one patient, the increase was within normal range, and the other had a QTcF interval duration >500 msec on day 2, but levels returned to normal by day 9.
Improvements in context
Dr. Goodwin noted that the improvements were swift and impressive when compared with those of the STAR*D trial, which is the largest prospective study of treatment outcomes in patients with MDD.
“In the STAR*D trial, third- and fourth-step treatments showed low response rates of under 15% and high relapse rates,” Dr. Goodwin said. “By comparison, our response rates at 12 weeks were 20%-25%, so almost double that seen for probably equivalent treatment steps in STAR*D, with a single treatment with 25 mg, and no additional antidepressant, so no side effect burden.
“We hope to follow up enough of these patients [in the new study] to get some idea of relapse rates,” Dr. Goodwin added. “These have been low in comparable studies with MDD patients: We will see.”
Commenting on the research, Balwinder Singh, MD, of the department of psychiatry and psychology, Mayo Clinic, Rochester, Minn., said the study represents a valuable addition to needed evidence on psilocybin – with some caveats.
“This study adds to the emerging evidence base of psilocybin for treatment-resistant depression, at least in the short term,” he said in an interview. “I think the challenge in the real world would be to have access to 6-8 hours of therapy with psilocybin when patients struggle to find good therapists who could provide even weekly therapy for an hour.”
In addition, Dr. Singh questioned the durability of a single dose of psilocybin in the long term, noting a recent study (N Engl J Med. 2021 Apr 15. doi: 10.1056/NEJMoa2032994) that evaluated two doses of psilocybin (25 mg) 3 weeks apart, and failed to show any significant difference compared with the serotonergic antidepressant escitalopram at 6 weeks.
He further expressed concern about the emergence of suicidal behaviors in some patients, as well as the prolongation of QTc > 60 msec reported in the two patients.
“This is something to be carefully assessed in future studies, due to the risk of arrhythmias,” Dr. Singh said.
The study was sponsored by COMPASS Pathfinder Limited. Dr. Goodwin is chief medical officer for COMPASS Pathways. Dr. Singh had no disclosures to report.
NEW ORLEANS –
“This is easily the largest study of a psychedelic drug employing modern randomized controlled trial methodology [with] 22 sites and 10 countries, so it’s not your typical phase 2 trial,” the study’s lead author, Guy M. Goodwin, MD, emeritus professor of psychiatry at the University of Oxford, England, said in an interview.
“Importantly, 94% of the patients in the study were psilocybin naive, which is very important for generalizability,” Dr. Goodwin noted.
Long used as psychedelic ‘magic mushrooms,’ psilocybin has gained increased interest in psychiatry in recent years as a potential treatment for severe depression after showing benefits in patients with life-threatening cancers and others with major depressive disorder (MDD).
To put the therapy to test in a more rigorous, randomized trial, Dr. Goodwin and colleagues conducted the phase 2b study of a proprietary synthetic formulation of psilocybin, COMP360 (COMPASS Pathways), recruiting 233 patients with treatment-resistant depression at 22 centers.
The study was presented at the annual meeting of the American Psychiatric Association.
After a 2-week washout period following the discontinuation of antidepressants, the patients were randomized to one of three groups: A single dose of 25 mg (n = 79), 10 mg (n = 75), or a subtherapeutic comparison of 1 mg (n = 79).
The psilocybin was administered in the presence of specially trained therapists who provided psychological support before, during, and after the 6- to 8-hour session.
Patients were then asked to refrain from antidepressant use for at least 3 weeks following the session, and had periodic follow-up for 12 weeks.
For the primary endpoint, those in the 25-mg group, but not the 10-mg dose, showed a significantly greater reduction in depression from baseline versus the 1-mg group on the Montgomery-Åsberg Depression Rating Scale at week 3 (MADRS; -6.6; P < .001).
The benefit was observed at day 2 and week 1 following administration, “confirming the rapid-acting character of the effect,” the investigators reported.
Sustained responses, defined as at least a 50% change from baseline in MADRS total score, were further observed up to week 12 among 20.3% in the 25-mg group and among 5.3% in the 10-mg groups versus 10.1% in the 1-mg group.
On the day of psilocybin treatment, the treatment-emergent side effects that were reported were headache, nausea, and dizziness, with event rates of 83.5% in the 25-mg group, 74.7% in the 10-mg group, and 72.2% in the 1-mg group.
One participant in the 25-mg group experienced acute anxiety and was treated with lorazepam.
The incidence of treatment-emergent serious adverse events from day 2 to week 3 was 6.3% (five patients) in the 25-mg group, 8.0% (six patients) in the 10-mg group, and 1.3% (one patient) in the 1-mg group.
Serious AEs included suicidal ideation and intentional self-injury among two patients each in the 25-mg group, while in the 10-mg group, two had suicidal ideation and one had hospitalization for severe depression.
There were no significant differences between the groups in terms of vital signs or clinical laboratory tests.
Of note, two patients in the 25-mg group had a change from baseline in QTcF >60 msec on day 2. For one patient, the increase was within normal range, and the other had a QTcF interval duration >500 msec on day 2, but levels returned to normal by day 9.
Improvements in context
Dr. Goodwin noted that the improvements were swift and impressive when compared with those of the STAR*D trial, which is the largest prospective study of treatment outcomes in patients with MDD.
“In the STAR*D trial, third- and fourth-step treatments showed low response rates of under 15% and high relapse rates,” Dr. Goodwin said. “By comparison, our response rates at 12 weeks were 20%-25%, so almost double that seen for probably equivalent treatment steps in STAR*D, with a single treatment with 25 mg, and no additional antidepressant, so no side effect burden.
“We hope to follow up enough of these patients [in the new study] to get some idea of relapse rates,” Dr. Goodwin added. “These have been low in comparable studies with MDD patients: We will see.”
Commenting on the research, Balwinder Singh, MD, of the department of psychiatry and psychology, Mayo Clinic, Rochester, Minn., said the study represents a valuable addition to needed evidence on psilocybin – with some caveats.
“This study adds to the emerging evidence base of psilocybin for treatment-resistant depression, at least in the short term,” he said in an interview. “I think the challenge in the real world would be to have access to 6-8 hours of therapy with psilocybin when patients struggle to find good therapists who could provide even weekly therapy for an hour.”
In addition, Dr. Singh questioned the durability of a single dose of psilocybin in the long term, noting a recent study (N Engl J Med. 2021 Apr 15. doi: 10.1056/NEJMoa2032994) that evaluated two doses of psilocybin (25 mg) 3 weeks apart, and failed to show any significant difference compared with the serotonergic antidepressant escitalopram at 6 weeks.
He further expressed concern about the emergence of suicidal behaviors in some patients, as well as the prolongation of QTc > 60 msec reported in the two patients.
“This is something to be carefully assessed in future studies, due to the risk of arrhythmias,” Dr. Singh said.
The study was sponsored by COMPASS Pathfinder Limited. Dr. Goodwin is chief medical officer for COMPASS Pathways. Dr. Singh had no disclosures to report.
AT APA 2022
‘Smart inhalers’ may help diagnose and treat asthma – if used
After years going on and off medications for occasional asthma symptoms, things went downhill for Brian Blome in November 2020. The retired carpenter started feeling short of breath and wheezing during bike rides. At home, he struggled with chores.
“I was having a hard time climbing a flight of stairs, just doing laundry,” said Mr. Blome, who lives in the Chicago suburb of Palatine.
To get things under control, he saw an allergist and started regular medications – two tablets, two nasal sprays, and inhaled corticosteroids each day, plus an albuterol inhaler for flare-ups.
The inhalers have an extra feature: an electronic monitor that attaches to the device and automatically tracks where and when the medication is used. Bluetooth sends this information to an app on the patient’s mobile phone and to a dashboard where the medical team can see, at a glance, when symptoms are popping up and how regularly medications are taken – leading to the devices often being called “smart inhalers.”
At the 2022 American Academy of Allergy, Asthma, and Immunology conference in Phoenix, researchers explained how digital monitoring devices can help diagnose and treat hard-to-control asthma, potentially reducing the need for oral steroids or biologic therapies.
Even though electric monitors have been on the market for years, their use has been slow to catch on because of uncertainties around insurance coverage, liability, and how to manage and best use the data. One recent study said these devices cost $100-$500, but that price depends on many things, such as insurance.
About 17% of adult asthma patients have “difficult-to-control” asthma, meaning they limit their activity because of breathing symptoms and use reliever medications multiple times a week.
But research suggests that correcting inhaling technique and sticking to the use of the medications can cut that 17% down to just 3.7%, said Mr. Blome’s allergist, Giselle Mosnaim, MD, of NorthShore University HealthSystem in Glenview, Ill. Dr. Mosnaim spoke about digital monitoring at a conference session on digital technologies for asthma management.
A study of more than 5,000 asthma patients “showed that, if you have critical errors in inhaler technique, this leads to worse asthma outcomes and increased asthma exacerbations,” she said. It also shows that, despite new devices and new technologies, “we still have poor inhaler technique.”
Yet adherence is poorly gauged by doctors and patient self-reporting. “The ideal measure of adherence should be objective, accurate, and unobtrusive to minimize impact on patient behavior and allow reliable data collection in real-world settings,” Dr. Mosnaim said. “So electronic medication monitors are the gold standard.”
Improving use
Patients not following instructions or guidelines “is something we saw nonstop with kids,” said Caroline Moassessi, founder of the allergy and asthma blog Gratefulfoodie.com who formerly served on a regional board of the American Lung Association. She’s also the mother of two asthmatic children, now in college, who years ago used electronic medication monitors as part of a research trial.
They were “unimpressed – mostly since I think they thought their asthma was controlled,” she said. “When patients are not in crisis, they don’t manage their asthma well.”
Even in research studies such as the one Rachelle Ramsey, PhD, presented at the conference, it’s not only hard to determine if better adherence leads to improved health, but when.
“For example, does your adherence this week impact your asthma control this week, or does it impact your asthma control next week? Or is it even further out? Do you need to have some level of adherence over the course of a month in order to have better outcomes at the end of that month?” said Dr. Ramsey, a pediatric research psychologist at Cincinnati Children’s Hospital Medical Center. “I think it’s a little complicated.”
That said, results from several small studies do show a connection between remote monitoring and better clinical outcomes. One study enrolled asthma patients in the United Kingdom, and another was done by Dr. Mosnaim with Chicago-area patients.
In the U.K. quality improvement project, nurses asked patients with difficult-to-control asthma if they knew how to use their inhalers and were following treatment guidelines.
Those who said “yes” were invited to swap their steroid/inhalers for a controller fitted with a device that tracks use and measures acoustics to test inhaler technique. After 28 days of monitoring, many people in the study had better clinical outcomes.
And after 3 months of digital monitoring, patients didn’t use their rescue medication quite as often.
Mr. Blome has seen a marked improvement in his asthma since starting regular appointments and getting back on daily medications a year and a half ago. He says that now and then, he has wheezing and shortness of breath, usually while biking or exercising. But those symptoms aren’t as severe or frequent as before.
From a doctor’s perspective, “digital inhaler systems allow me to discern patterns in order to determine what triggers his asthma symptoms and to adjust medications at different times of the year,” Dr. Mosnaim said.
Electronic systems can monitor pollen counts and air quality as well as how often a patient uses a quick reliever medication. Thus, she said, tracking these measures year-round could raise attention to impending asthma attacks and suggest when to increase the dose of controller medications or add other treatments.
A version of this article first appeared on WebMD.com.
After years going on and off medications for occasional asthma symptoms, things went downhill for Brian Blome in November 2020. The retired carpenter started feeling short of breath and wheezing during bike rides. At home, he struggled with chores.
“I was having a hard time climbing a flight of stairs, just doing laundry,” said Mr. Blome, who lives in the Chicago suburb of Palatine.
To get things under control, he saw an allergist and started regular medications – two tablets, two nasal sprays, and inhaled corticosteroids each day, plus an albuterol inhaler for flare-ups.
The inhalers have an extra feature: an electronic monitor that attaches to the device and automatically tracks where and when the medication is used. Bluetooth sends this information to an app on the patient’s mobile phone and to a dashboard where the medical team can see, at a glance, when symptoms are popping up and how regularly medications are taken – leading to the devices often being called “smart inhalers.”
At the 2022 American Academy of Allergy, Asthma, and Immunology conference in Phoenix, researchers explained how digital monitoring devices can help diagnose and treat hard-to-control asthma, potentially reducing the need for oral steroids or biologic therapies.
Even though electric monitors have been on the market for years, their use has been slow to catch on because of uncertainties around insurance coverage, liability, and how to manage and best use the data. One recent study said these devices cost $100-$500, but that price depends on many things, such as insurance.
About 17% of adult asthma patients have “difficult-to-control” asthma, meaning they limit their activity because of breathing symptoms and use reliever medications multiple times a week.
But research suggests that correcting inhaling technique and sticking to the use of the medications can cut that 17% down to just 3.7%, said Mr. Blome’s allergist, Giselle Mosnaim, MD, of NorthShore University HealthSystem in Glenview, Ill. Dr. Mosnaim spoke about digital monitoring at a conference session on digital technologies for asthma management.
A study of more than 5,000 asthma patients “showed that, if you have critical errors in inhaler technique, this leads to worse asthma outcomes and increased asthma exacerbations,” she said. It also shows that, despite new devices and new technologies, “we still have poor inhaler technique.”
Yet adherence is poorly gauged by doctors and patient self-reporting. “The ideal measure of adherence should be objective, accurate, and unobtrusive to minimize impact on patient behavior and allow reliable data collection in real-world settings,” Dr. Mosnaim said. “So electronic medication monitors are the gold standard.”
Improving use
Patients not following instructions or guidelines “is something we saw nonstop with kids,” said Caroline Moassessi, founder of the allergy and asthma blog Gratefulfoodie.com who formerly served on a regional board of the American Lung Association. She’s also the mother of two asthmatic children, now in college, who years ago used electronic medication monitors as part of a research trial.
They were “unimpressed – mostly since I think they thought their asthma was controlled,” she said. “When patients are not in crisis, they don’t manage their asthma well.”
Even in research studies such as the one Rachelle Ramsey, PhD, presented at the conference, it’s not only hard to determine if better adherence leads to improved health, but when.
“For example, does your adherence this week impact your asthma control this week, or does it impact your asthma control next week? Or is it even further out? Do you need to have some level of adherence over the course of a month in order to have better outcomes at the end of that month?” said Dr. Ramsey, a pediatric research psychologist at Cincinnati Children’s Hospital Medical Center. “I think it’s a little complicated.”
That said, results from several small studies do show a connection between remote monitoring and better clinical outcomes. One study enrolled asthma patients in the United Kingdom, and another was done by Dr. Mosnaim with Chicago-area patients.
In the U.K. quality improvement project, nurses asked patients with difficult-to-control asthma if they knew how to use their inhalers and were following treatment guidelines.
Those who said “yes” were invited to swap their steroid/inhalers for a controller fitted with a device that tracks use and measures acoustics to test inhaler technique. After 28 days of monitoring, many people in the study had better clinical outcomes.
And after 3 months of digital monitoring, patients didn’t use their rescue medication quite as often.
Mr. Blome has seen a marked improvement in his asthma since starting regular appointments and getting back on daily medications a year and a half ago. He says that now and then, he has wheezing and shortness of breath, usually while biking or exercising. But those symptoms aren’t as severe or frequent as before.
From a doctor’s perspective, “digital inhaler systems allow me to discern patterns in order to determine what triggers his asthma symptoms and to adjust medications at different times of the year,” Dr. Mosnaim said.
Electronic systems can monitor pollen counts and air quality as well as how often a patient uses a quick reliever medication. Thus, she said, tracking these measures year-round could raise attention to impending asthma attacks and suggest when to increase the dose of controller medications or add other treatments.
A version of this article first appeared on WebMD.com.
After years going on and off medications for occasional asthma symptoms, things went downhill for Brian Blome in November 2020. The retired carpenter started feeling short of breath and wheezing during bike rides. At home, he struggled with chores.
“I was having a hard time climbing a flight of stairs, just doing laundry,” said Mr. Blome, who lives in the Chicago suburb of Palatine.
To get things under control, he saw an allergist and started regular medications – two tablets, two nasal sprays, and inhaled corticosteroids each day, plus an albuterol inhaler for flare-ups.
The inhalers have an extra feature: an electronic monitor that attaches to the device and automatically tracks where and when the medication is used. Bluetooth sends this information to an app on the patient’s mobile phone and to a dashboard where the medical team can see, at a glance, when symptoms are popping up and how regularly medications are taken – leading to the devices often being called “smart inhalers.”
At the 2022 American Academy of Allergy, Asthma, and Immunology conference in Phoenix, researchers explained how digital monitoring devices can help diagnose and treat hard-to-control asthma, potentially reducing the need for oral steroids or biologic therapies.
Even though electric monitors have been on the market for years, their use has been slow to catch on because of uncertainties around insurance coverage, liability, and how to manage and best use the data. One recent study said these devices cost $100-$500, but that price depends on many things, such as insurance.
About 17% of adult asthma patients have “difficult-to-control” asthma, meaning they limit their activity because of breathing symptoms and use reliever medications multiple times a week.
But research suggests that correcting inhaling technique and sticking to the use of the medications can cut that 17% down to just 3.7%, said Mr. Blome’s allergist, Giselle Mosnaim, MD, of NorthShore University HealthSystem in Glenview, Ill. Dr. Mosnaim spoke about digital monitoring at a conference session on digital technologies for asthma management.
A study of more than 5,000 asthma patients “showed that, if you have critical errors in inhaler technique, this leads to worse asthma outcomes and increased asthma exacerbations,” she said. It also shows that, despite new devices and new technologies, “we still have poor inhaler technique.”
Yet adherence is poorly gauged by doctors and patient self-reporting. “The ideal measure of adherence should be objective, accurate, and unobtrusive to minimize impact on patient behavior and allow reliable data collection in real-world settings,” Dr. Mosnaim said. “So electronic medication monitors are the gold standard.”
Improving use
Patients not following instructions or guidelines “is something we saw nonstop with kids,” said Caroline Moassessi, founder of the allergy and asthma blog Gratefulfoodie.com who formerly served on a regional board of the American Lung Association. She’s also the mother of two asthmatic children, now in college, who years ago used electronic medication monitors as part of a research trial.
They were “unimpressed – mostly since I think they thought their asthma was controlled,” she said. “When patients are not in crisis, they don’t manage their asthma well.”
Even in research studies such as the one Rachelle Ramsey, PhD, presented at the conference, it’s not only hard to determine if better adherence leads to improved health, but when.
“For example, does your adherence this week impact your asthma control this week, or does it impact your asthma control next week? Or is it even further out? Do you need to have some level of adherence over the course of a month in order to have better outcomes at the end of that month?” said Dr. Ramsey, a pediatric research psychologist at Cincinnati Children’s Hospital Medical Center. “I think it’s a little complicated.”
That said, results from several small studies do show a connection between remote monitoring and better clinical outcomes. One study enrolled asthma patients in the United Kingdom, and another was done by Dr. Mosnaim with Chicago-area patients.
In the U.K. quality improvement project, nurses asked patients with difficult-to-control asthma if they knew how to use their inhalers and were following treatment guidelines.
Those who said “yes” were invited to swap their steroid/inhalers for a controller fitted with a device that tracks use and measures acoustics to test inhaler technique. After 28 days of monitoring, many people in the study had better clinical outcomes.
And after 3 months of digital monitoring, patients didn’t use their rescue medication quite as often.
Mr. Blome has seen a marked improvement in his asthma since starting regular appointments and getting back on daily medications a year and a half ago. He says that now and then, he has wheezing and shortness of breath, usually while biking or exercising. But those symptoms aren’t as severe or frequent as before.
From a doctor’s perspective, “digital inhaler systems allow me to discern patterns in order to determine what triggers his asthma symptoms and to adjust medications at different times of the year,” Dr. Mosnaim said.
Electronic systems can monitor pollen counts and air quality as well as how often a patient uses a quick reliever medication. Thus, she said, tracking these measures year-round could raise attention to impending asthma attacks and suggest when to increase the dose of controller medications or add other treatments.
A version of this article first appeared on WebMD.com.
Adjunctive confocal microscopy found to reduce unnecessary skin excisions
results from a large randomized clinical trial showed.
“Skin cancer management exerts a sizable burden on health systems,” researchers led by Giovanni Pellacani, MD, wrote in an article published in JAMA Dermatology. “The systematic application of RCM in the triage of high-risk patients should improve diagnostic accuracy and reduce unnecessary excisions for histopathological diagnostic confirmation, thereby reducing costs, surgical waiting lists, and delayed diagnoses.”
However, they added, “the clinical application of RCM has mainly been limited to retrospective and prospective observational studies producing hypothetical estimates of clinical applicability without intention to affect clinical and therapeutic patient pathways.”
For the current study, Dr. Pellacani, who chairs the department of dermatology at Sapienza University, Rome, and colleagues hypothesized that RCM would reduce unnecessary excisions by more than 30% and would identify all melanoma lesions 0.5 mm or thinner at baseline. They enrolled 3,165 patients with suspect lesions from three dermatology referral centers between January 2017 and December 2019, with a mean follow-up of 9.6 months in the study. Participants were randomly assigned 1:1 to standard therapeutic care, which consisted of clinical and dermoscopy evaluation with or without adjunctive RCM, a novel noninvasive technology that provides in vivo imaging of the skin, with a high diagnostic accuracy.
Histopathologic examination of all excised lesions was performed at the pathology department of the referral center. Resulting information guided prospective clinical decision-making (excision or follow-up). The mean age of patients was 49 years, 49% were women, 21% had a personal history of melanoma, and 51% had Fitzpatrick phototype 2 skin.
When compared with standard therapeutic care only, adjunctive RCM was associated with a higher positive predictive value (18.9 vs. 33.3, respectively), lower benign to malignant ratio (3.7:1.0 vs. 1.8:1.0), and a reduction in the number needed to excise of 43.4% (5.3 vs. 3.0). In addition, all 15 lesions with delayed melanoma diagnoses were thinner than 0.5 mm. Of these, eight were diagnosed as melanoma in situ.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., who was asked to comment on the study, said that a strength of the analysis was its follow-up and histopathologic evaluation, “which are both essentially forms of feedback. Good, relevant feedback is necessary for all of us to improve.”
She pointed out that, while RCM does appear to reduce the number of benign lesions unnecessarily removed and increase the number of skin cancers appropriately excised, the authors acknowledged that they had at least 4 years of experience with RCM. “The study also does not address the time factor (the procedure takes about 7 minutes per lesion) and the financial cost of reflectance confocal microscopy, as compared to the cost of standard follow-up alone with an increased number of excisions.”
She added that the findings “are not yet applicable to general dermatology across the world, as the authors comment, given that reflectance confocal microscopy is not yet widely available.”
The Italian Ministry of Health supported the study. Neither the researchers nor Dr. Ko reported having relevant financial conflicts.
results from a large randomized clinical trial showed.
“Skin cancer management exerts a sizable burden on health systems,” researchers led by Giovanni Pellacani, MD, wrote in an article published in JAMA Dermatology. “The systematic application of RCM in the triage of high-risk patients should improve diagnostic accuracy and reduce unnecessary excisions for histopathological diagnostic confirmation, thereby reducing costs, surgical waiting lists, and delayed diagnoses.”
However, they added, “the clinical application of RCM has mainly been limited to retrospective and prospective observational studies producing hypothetical estimates of clinical applicability without intention to affect clinical and therapeutic patient pathways.”
For the current study, Dr. Pellacani, who chairs the department of dermatology at Sapienza University, Rome, and colleagues hypothesized that RCM would reduce unnecessary excisions by more than 30% and would identify all melanoma lesions 0.5 mm or thinner at baseline. They enrolled 3,165 patients with suspect lesions from three dermatology referral centers between January 2017 and December 2019, with a mean follow-up of 9.6 months in the study. Participants were randomly assigned 1:1 to standard therapeutic care, which consisted of clinical and dermoscopy evaluation with or without adjunctive RCM, a novel noninvasive technology that provides in vivo imaging of the skin, with a high diagnostic accuracy.
Histopathologic examination of all excised lesions was performed at the pathology department of the referral center. Resulting information guided prospective clinical decision-making (excision or follow-up). The mean age of patients was 49 years, 49% were women, 21% had a personal history of melanoma, and 51% had Fitzpatrick phototype 2 skin.
When compared with standard therapeutic care only, adjunctive RCM was associated with a higher positive predictive value (18.9 vs. 33.3, respectively), lower benign to malignant ratio (3.7:1.0 vs. 1.8:1.0), and a reduction in the number needed to excise of 43.4% (5.3 vs. 3.0). In addition, all 15 lesions with delayed melanoma diagnoses were thinner than 0.5 mm. Of these, eight were diagnosed as melanoma in situ.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., who was asked to comment on the study, said that a strength of the analysis was its follow-up and histopathologic evaluation, “which are both essentially forms of feedback. Good, relevant feedback is necessary for all of us to improve.”
She pointed out that, while RCM does appear to reduce the number of benign lesions unnecessarily removed and increase the number of skin cancers appropriately excised, the authors acknowledged that they had at least 4 years of experience with RCM. “The study also does not address the time factor (the procedure takes about 7 minutes per lesion) and the financial cost of reflectance confocal microscopy, as compared to the cost of standard follow-up alone with an increased number of excisions.”
She added that the findings “are not yet applicable to general dermatology across the world, as the authors comment, given that reflectance confocal microscopy is not yet widely available.”
The Italian Ministry of Health supported the study. Neither the researchers nor Dr. Ko reported having relevant financial conflicts.
results from a large randomized clinical trial showed.
“Skin cancer management exerts a sizable burden on health systems,” researchers led by Giovanni Pellacani, MD, wrote in an article published in JAMA Dermatology. “The systematic application of RCM in the triage of high-risk patients should improve diagnostic accuracy and reduce unnecessary excisions for histopathological diagnostic confirmation, thereby reducing costs, surgical waiting lists, and delayed diagnoses.”
However, they added, “the clinical application of RCM has mainly been limited to retrospective and prospective observational studies producing hypothetical estimates of clinical applicability without intention to affect clinical and therapeutic patient pathways.”
For the current study, Dr. Pellacani, who chairs the department of dermatology at Sapienza University, Rome, and colleagues hypothesized that RCM would reduce unnecessary excisions by more than 30% and would identify all melanoma lesions 0.5 mm or thinner at baseline. They enrolled 3,165 patients with suspect lesions from three dermatology referral centers between January 2017 and December 2019, with a mean follow-up of 9.6 months in the study. Participants were randomly assigned 1:1 to standard therapeutic care, which consisted of clinical and dermoscopy evaluation with or without adjunctive RCM, a novel noninvasive technology that provides in vivo imaging of the skin, with a high diagnostic accuracy.
Histopathologic examination of all excised lesions was performed at the pathology department of the referral center. Resulting information guided prospective clinical decision-making (excision or follow-up). The mean age of patients was 49 years, 49% were women, 21% had a personal history of melanoma, and 51% had Fitzpatrick phototype 2 skin.
When compared with standard therapeutic care only, adjunctive RCM was associated with a higher positive predictive value (18.9 vs. 33.3, respectively), lower benign to malignant ratio (3.7:1.0 vs. 1.8:1.0), and a reduction in the number needed to excise of 43.4% (5.3 vs. 3.0). In addition, all 15 lesions with delayed melanoma diagnoses were thinner than 0.5 mm. Of these, eight were diagnosed as melanoma in situ.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., who was asked to comment on the study, said that a strength of the analysis was its follow-up and histopathologic evaluation, “which are both essentially forms of feedback. Good, relevant feedback is necessary for all of us to improve.”
She pointed out that, while RCM does appear to reduce the number of benign lesions unnecessarily removed and increase the number of skin cancers appropriately excised, the authors acknowledged that they had at least 4 years of experience with RCM. “The study also does not address the time factor (the procedure takes about 7 minutes per lesion) and the financial cost of reflectance confocal microscopy, as compared to the cost of standard follow-up alone with an increased number of excisions.”
She added that the findings “are not yet applicable to general dermatology across the world, as the authors comment, given that reflectance confocal microscopy is not yet widely available.”
The Italian Ministry of Health supported the study. Neither the researchers nor Dr. Ko reported having relevant financial conflicts.
FROM JAMA DERMATOLOGY
Tin in permanent contraception implants causes toxicity
Essure implants arrived on the market in 2002 as permanent contraception for women older than age 45 years with children. They were recalled in 2017. Presented as an alternative to laparoscopic tubal ligation, this medical device resulted in rare side effects affecting thousands of women, most notably the nervous system, cardiovascular system, endocrine system, and musculoskeletal system.
Implant analysis protocol
“My research focuses on a variety of medical devices, mostly joint replacements, and more specifically, hip replacements. I look at how these materials behave in humans and how the wear debris affects the body,” explained Ana Maria Trunfio-Sfarghiu, bioengineering expert and research associate with the French National Center for Scientific Research at the Lyon National Institute of Applied Sciences’ Contact and Structure Mechanics Laboratory.
“The problems with Essure implants started with a woman who had been using one for about 10 years and was experiencing side effects such as trouble concentrating and focusing, significant vaginal bleeding, extreme tiredness, hair loss, etc. She had the implant removed, and we retrieved it from her gynecologist and analyzed it alongside other implants,” said Ms. Trunfio-Sfarghiu.
“Together with the hospital, we set up an implant analysis protocol. We visited hospital teams to demonstrate how to prepare the biopsies, embedded in paraffin blocks, before sending them to us for analysis. We gave the same specimen preparation instructions for all subjects,” Ms. Trunfio-Sfarghiu explained.
After a year of clinical analysis, the Journal of Trace Elements in Medicine and Biology published an article about 18 cases.
Implant weld corrosion
The Essure implant measures a few centimeters long and resembles a small spring. Once it is released inside the fallopian tube, its goal is to create inflammation and block the tube. It triggers fibrosis, which prevents the sperm from reaching the egg. Premarketing tests had shown that the fibrosis surrounding the implant would keep it from moving. However, the pharmaceutical company hadn’t assessed the mechanical integrity of the spring weld, which was made of silver-tin.
During their analysis in collaboration with the Minapath laboratory, Ms. Trunfio-Sfarghiu’s team found that the weld had corroded and that tin particles had been released into the subjects’ bodies. “The study included about 40 women, and we found tin in all of them,” said Ms. Trunfio-Sfarghiu.
This weld corrosion has several possible consequences. “When the implant degrades, it can travel anywhere in the pelvis, like a needle moving through the body with no apparent destination. The surgeons who operate to remove it describe similar surgeries in military medicine when the patient has been hit by a bullet!”
Organotin toxicity
Although tin is not especially toxic for the body when ingested, it can bind to organic compounds if it passes through to the blood. “When tin binds to a carbon atom, it becomes organotin, a neurotoxin,” said Ms. Trunfio-Sfarghiu.
She said that this organotin can travel to the brain and trigger symptoms like those found in patients with Essure implants. “For the time being, there is insufficient data to assert that we found organotin in all subjects. Another more in-depth study would be needed to assess migration to the brain. For the past 2 years, we have tried to obtain academic funding to continue our research, so far without success. Academic and political authorities seem to be a bit scared of what we’ve found,” said Ms. Trunfio-Sfarghiu.
For her, “it’s how the implant was marketed that is problematic. The implant was designed to create local inflammation, inflammation in itself being difficult to control. Some women need to have their entire uterus and ovaries removed to resolve problems caused by the implant.”
Harm in the United States
Ms. Trunfio-Sfarghiu’s research has helped American victims obtain acknowledgment of their suffering in the United States. “But the harm caused to women by defective implants has yet to be acknowledged in France,” she added.
She explained that Essure was recalled in 2017 because sales were poor, not because it was deemed dangerous. Her conclusion? “No implant that creates inflammation should be authorized, especially if there is a surgical alternative, which there is here: tubal ligation.”
A version of this article appeared on Medscape.com. This article was translated from the Medscape French edition.
Essure implants arrived on the market in 2002 as permanent contraception for women older than age 45 years with children. They were recalled in 2017. Presented as an alternative to laparoscopic tubal ligation, this medical device resulted in rare side effects affecting thousands of women, most notably the nervous system, cardiovascular system, endocrine system, and musculoskeletal system.
Implant analysis protocol
“My research focuses on a variety of medical devices, mostly joint replacements, and more specifically, hip replacements. I look at how these materials behave in humans and how the wear debris affects the body,” explained Ana Maria Trunfio-Sfarghiu, bioengineering expert and research associate with the French National Center for Scientific Research at the Lyon National Institute of Applied Sciences’ Contact and Structure Mechanics Laboratory.
“The problems with Essure implants started with a woman who had been using one for about 10 years and was experiencing side effects such as trouble concentrating and focusing, significant vaginal bleeding, extreme tiredness, hair loss, etc. She had the implant removed, and we retrieved it from her gynecologist and analyzed it alongside other implants,” said Ms. Trunfio-Sfarghiu.
“Together with the hospital, we set up an implant analysis protocol. We visited hospital teams to demonstrate how to prepare the biopsies, embedded in paraffin blocks, before sending them to us for analysis. We gave the same specimen preparation instructions for all subjects,” Ms. Trunfio-Sfarghiu explained.
After a year of clinical analysis, the Journal of Trace Elements in Medicine and Biology published an article about 18 cases.
Implant weld corrosion
The Essure implant measures a few centimeters long and resembles a small spring. Once it is released inside the fallopian tube, its goal is to create inflammation and block the tube. It triggers fibrosis, which prevents the sperm from reaching the egg. Premarketing tests had shown that the fibrosis surrounding the implant would keep it from moving. However, the pharmaceutical company hadn’t assessed the mechanical integrity of the spring weld, which was made of silver-tin.
During their analysis in collaboration with the Minapath laboratory, Ms. Trunfio-Sfarghiu’s team found that the weld had corroded and that tin particles had been released into the subjects’ bodies. “The study included about 40 women, and we found tin in all of them,” said Ms. Trunfio-Sfarghiu.
This weld corrosion has several possible consequences. “When the implant degrades, it can travel anywhere in the pelvis, like a needle moving through the body with no apparent destination. The surgeons who operate to remove it describe similar surgeries in military medicine when the patient has been hit by a bullet!”
Organotin toxicity
Although tin is not especially toxic for the body when ingested, it can bind to organic compounds if it passes through to the blood. “When tin binds to a carbon atom, it becomes organotin, a neurotoxin,” said Ms. Trunfio-Sfarghiu.
She said that this organotin can travel to the brain and trigger symptoms like those found in patients with Essure implants. “For the time being, there is insufficient data to assert that we found organotin in all subjects. Another more in-depth study would be needed to assess migration to the brain. For the past 2 years, we have tried to obtain academic funding to continue our research, so far without success. Academic and political authorities seem to be a bit scared of what we’ve found,” said Ms. Trunfio-Sfarghiu.
For her, “it’s how the implant was marketed that is problematic. The implant was designed to create local inflammation, inflammation in itself being difficult to control. Some women need to have their entire uterus and ovaries removed to resolve problems caused by the implant.”
Harm in the United States
Ms. Trunfio-Sfarghiu’s research has helped American victims obtain acknowledgment of their suffering in the United States. “But the harm caused to women by defective implants has yet to be acknowledged in France,” she added.
She explained that Essure was recalled in 2017 because sales were poor, not because it was deemed dangerous. Her conclusion? “No implant that creates inflammation should be authorized, especially if there is a surgical alternative, which there is here: tubal ligation.”
A version of this article appeared on Medscape.com. This article was translated from the Medscape French edition.
Essure implants arrived on the market in 2002 as permanent contraception for women older than age 45 years with children. They were recalled in 2017. Presented as an alternative to laparoscopic tubal ligation, this medical device resulted in rare side effects affecting thousands of women, most notably the nervous system, cardiovascular system, endocrine system, and musculoskeletal system.
Implant analysis protocol
“My research focuses on a variety of medical devices, mostly joint replacements, and more specifically, hip replacements. I look at how these materials behave in humans and how the wear debris affects the body,” explained Ana Maria Trunfio-Sfarghiu, bioengineering expert and research associate with the French National Center for Scientific Research at the Lyon National Institute of Applied Sciences’ Contact and Structure Mechanics Laboratory.
“The problems with Essure implants started with a woman who had been using one for about 10 years and was experiencing side effects such as trouble concentrating and focusing, significant vaginal bleeding, extreme tiredness, hair loss, etc. She had the implant removed, and we retrieved it from her gynecologist and analyzed it alongside other implants,” said Ms. Trunfio-Sfarghiu.
“Together with the hospital, we set up an implant analysis protocol. We visited hospital teams to demonstrate how to prepare the biopsies, embedded in paraffin blocks, before sending them to us for analysis. We gave the same specimen preparation instructions for all subjects,” Ms. Trunfio-Sfarghiu explained.
After a year of clinical analysis, the Journal of Trace Elements in Medicine and Biology published an article about 18 cases.
Implant weld corrosion
The Essure implant measures a few centimeters long and resembles a small spring. Once it is released inside the fallopian tube, its goal is to create inflammation and block the tube. It triggers fibrosis, which prevents the sperm from reaching the egg. Premarketing tests had shown that the fibrosis surrounding the implant would keep it from moving. However, the pharmaceutical company hadn’t assessed the mechanical integrity of the spring weld, which was made of silver-tin.
During their analysis in collaboration with the Minapath laboratory, Ms. Trunfio-Sfarghiu’s team found that the weld had corroded and that tin particles had been released into the subjects’ bodies. “The study included about 40 women, and we found tin in all of them,” said Ms. Trunfio-Sfarghiu.
This weld corrosion has several possible consequences. “When the implant degrades, it can travel anywhere in the pelvis, like a needle moving through the body with no apparent destination. The surgeons who operate to remove it describe similar surgeries in military medicine when the patient has been hit by a bullet!”
Organotin toxicity
Although tin is not especially toxic for the body when ingested, it can bind to organic compounds if it passes through to the blood. “When tin binds to a carbon atom, it becomes organotin, a neurotoxin,” said Ms. Trunfio-Sfarghiu.
She said that this organotin can travel to the brain and trigger symptoms like those found in patients with Essure implants. “For the time being, there is insufficient data to assert that we found organotin in all subjects. Another more in-depth study would be needed to assess migration to the brain. For the past 2 years, we have tried to obtain academic funding to continue our research, so far without success. Academic and political authorities seem to be a bit scared of what we’ve found,” said Ms. Trunfio-Sfarghiu.
For her, “it’s how the implant was marketed that is problematic. The implant was designed to create local inflammation, inflammation in itself being difficult to control. Some women need to have their entire uterus and ovaries removed to resolve problems caused by the implant.”
Harm in the United States
Ms. Trunfio-Sfarghiu’s research has helped American victims obtain acknowledgment of their suffering in the United States. “But the harm caused to women by defective implants has yet to be acknowledged in France,” she added.
She explained that Essure was recalled in 2017 because sales were poor, not because it was deemed dangerous. Her conclusion? “No implant that creates inflammation should be authorized, especially if there is a surgical alternative, which there is here: tubal ligation.”
A version of this article appeared on Medscape.com. This article was translated from the Medscape French edition.
Journalism or medicine: Why not both?
I had an early attraction to newspapers. As a child growing up in Jersey City, N.J., I delivered them door-to-door. I was editor-in-chief of my high school newspaper and worked as a copy boy and sports reporter on the daily Jersey Journal. At Princeton, I joined the University Press Club, working as a string reporter for the New York Herald Tribune, Philadelphia Inquirer, and Associated Press.
I thought I might become a journalist, but medicine was too strong a calling. During my GI elective as a senior medical resident at New York Hospital, I was able to work with some of the first commercial fiberoptic instruments, which presaged my academic career in endoscopic innovation. I was editor-in-chief of Gastrointestinal Endoscopy from 1988 to 1996, and have been the consulting editor for GI Endoscopy Clinics of North America since 1997.
As the first editor-in-chief of GI & Hepatology News, I had the opportunity to combine a background in peer review with my early newspaper experience. My vision for the new publication was to provide information curated and vetted by experts, in contrast to the torrent pouring down from the Internet that was (pertinent to our specialty) “indigestible.” I put in much effort selecting stories provided by Elsevier Global Medical News, especially in constructing the front page. AGA Institute provided strong support, allowing me to choose an editorial board covering all subspecialties. I wanted to highlight the excitement of researchers balanced by expert review and commentary. The digital version added search features, and I tried to promote the “browse factor” that would also encourage advertising, critical to the success of any newspaper. At the end of my term, I felt I had laid a strong foundation, and have been delighted to see the publication continue to thrive.
Charles Lightdale, MD, is professor of medicine at Columbia University Medical Center in New York. He disclosed having no conflicts of interest.
I had an early attraction to newspapers. As a child growing up in Jersey City, N.J., I delivered them door-to-door. I was editor-in-chief of my high school newspaper and worked as a copy boy and sports reporter on the daily Jersey Journal. At Princeton, I joined the University Press Club, working as a string reporter for the New York Herald Tribune, Philadelphia Inquirer, and Associated Press.
I thought I might become a journalist, but medicine was too strong a calling. During my GI elective as a senior medical resident at New York Hospital, I was able to work with some of the first commercial fiberoptic instruments, which presaged my academic career in endoscopic innovation. I was editor-in-chief of Gastrointestinal Endoscopy from 1988 to 1996, and have been the consulting editor for GI Endoscopy Clinics of North America since 1997.
As the first editor-in-chief of GI & Hepatology News, I had the opportunity to combine a background in peer review with my early newspaper experience. My vision for the new publication was to provide information curated and vetted by experts, in contrast to the torrent pouring down from the Internet that was (pertinent to our specialty) “indigestible.” I put in much effort selecting stories provided by Elsevier Global Medical News, especially in constructing the front page. AGA Institute provided strong support, allowing me to choose an editorial board covering all subspecialties. I wanted to highlight the excitement of researchers balanced by expert review and commentary. The digital version added search features, and I tried to promote the “browse factor” that would also encourage advertising, critical to the success of any newspaper. At the end of my term, I felt I had laid a strong foundation, and have been delighted to see the publication continue to thrive.
Charles Lightdale, MD, is professor of medicine at Columbia University Medical Center in New York. He disclosed having no conflicts of interest.
I had an early attraction to newspapers. As a child growing up in Jersey City, N.J., I delivered them door-to-door. I was editor-in-chief of my high school newspaper and worked as a copy boy and sports reporter on the daily Jersey Journal. At Princeton, I joined the University Press Club, working as a string reporter for the New York Herald Tribune, Philadelphia Inquirer, and Associated Press.
I thought I might become a journalist, but medicine was too strong a calling. During my GI elective as a senior medical resident at New York Hospital, I was able to work with some of the first commercial fiberoptic instruments, which presaged my academic career in endoscopic innovation. I was editor-in-chief of Gastrointestinal Endoscopy from 1988 to 1996, and have been the consulting editor for GI Endoscopy Clinics of North America since 1997.
As the first editor-in-chief of GI & Hepatology News, I had the opportunity to combine a background in peer review with my early newspaper experience. My vision for the new publication was to provide information curated and vetted by experts, in contrast to the torrent pouring down from the Internet that was (pertinent to our specialty) “indigestible.” I put in much effort selecting stories provided by Elsevier Global Medical News, especially in constructing the front page. AGA Institute provided strong support, allowing me to choose an editorial board covering all subspecialties. I wanted to highlight the excitement of researchers balanced by expert review and commentary. The digital version added search features, and I tried to promote the “browse factor” that would also encourage advertising, critical to the success of any newspaper. At the end of my term, I felt I had laid a strong foundation, and have been delighted to see the publication continue to thrive.
Charles Lightdale, MD, is professor of medicine at Columbia University Medical Center in New York. He disclosed having no conflicts of interest.
Vascular Plaque in a Pregnant Patient With a History of Breast Cancer
The Diagnosis: Tufted Angioma
Histopathology revealed discrete lobules of closely packed capillaries with bland endothelial cells throughout the upper and lower dermis (Figure 1). The surrounding crescentlike vessels and lymphatics stained with D2-40 (Figure 2). These histologic findings were consistent with tufted angioma, and the patient elected for observation.
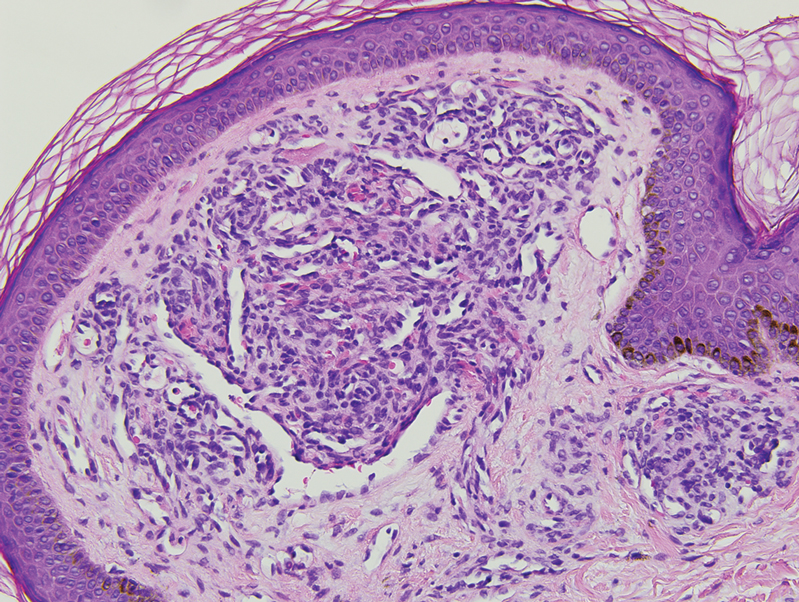
Tufted angiomas are benign vascular lesions named for the tufted appearance of capillaries on histology.1 They commonly present in children, with a lower incidence in adults and rare cases in pregnancy.2 Tufted angiomas typically present as solitary, slowly expanding, erythematous macules, plaques, or nodules on the neck or trunk ranging in size from less than 1 to 10 cm.2-4 They can be histologically distinguished from other vascular tumors, including aggressive malignant neoplasms.1
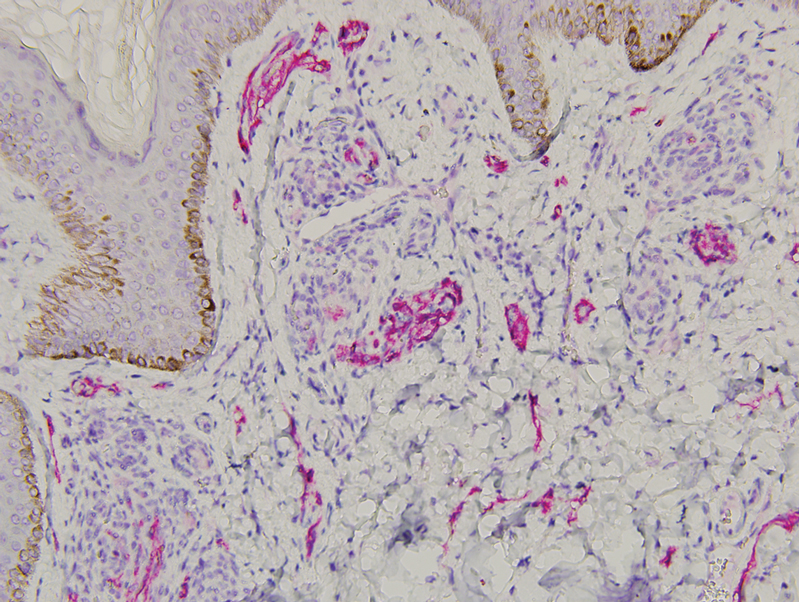
Tufted angiomas are identified by characteristic “cannon ball tufts” of capillaries in the dermis and subcutis at low power.3,5 Distinct cellular lobules may be found bulging into thin-walled vascular channels at the margins of the lobules in the dermis and subcutis (Figure 3).4 The lobules are formed by cells with spindle-shaped nuclei.6 Some mitotic figures may be present, but no cellular atypia is seen.2 The capillaries at the periphery appear as dilated semilunar vessels.4 Dilated lymphatics, which stain with D2-40, can be found at the periphery of the tufted capillaries and throughout the remaining dermis.3,4
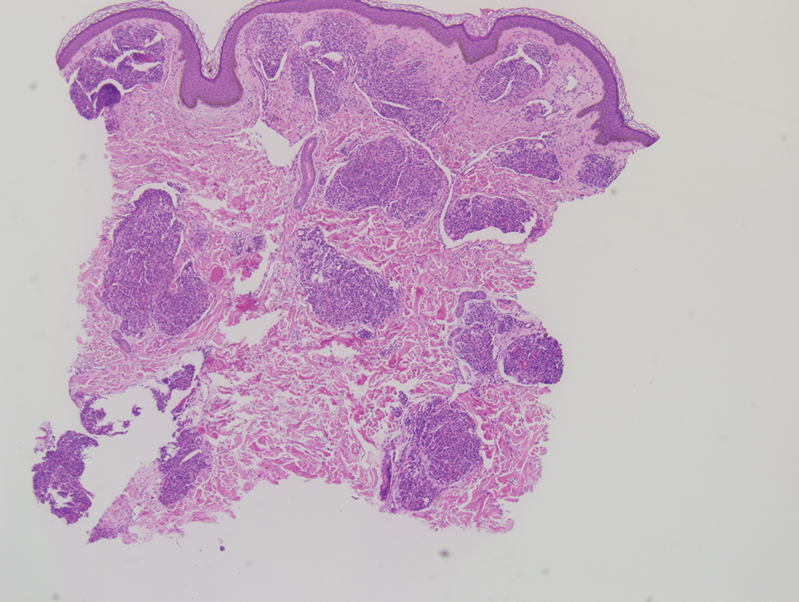
Tufted angiomas may arise independently in adults but also have been associated with conditions such as pregnancy. Omori et al7 identified an acquired tufted angioma in pregnancy that was positive for estrogen and progesterone receptors. Reports of tufted angiomas in pregnancy vary; some are multiple lesions, some regress postpartum, and some undergo successful surgical treatment.3,5
Vascular lesions such as tufted angiomas specifically may appear in pregnancy due to a high-volume state with vasodilation and increased vascular proliferation. Although tumor angiogenesis has been linked to specific growth factors and cytokines, it has been hypothesized that the systemic hormones of pregnancy such as human chorionic gonadotropin, estradiol, and progesterone also shift the body to a more angiogenic state.8 In a study of cutaneous changes in pregnant women (N=905), 41% developed a vascular skin change, including spider veins, varicosities, hemangiomas, and granulomas.9 The most common vascular tumor in pregnancy is pyogenic granuloma. Pyogenic granulomas are small, solitary, friable papules that commonly are found on the hands, forearms, face, or in the mouth; histologically they demonstrate dilated capillaries in lobular structures accompanied by larger thick-walled vessels.3,10,11
Tufted angiomas may mimic a variety of other conditions. Epithelioid hemangioma, considered by some to be on the same morphologic spectrum as angiolymphoid hyperplasia with eosinophilia, classically occurs in young adults on the head and in the neck region. It histologically demonstrates a lobular appearance at low power; however, these lobules are made up of vessels with histiocytoid to epithelioid endothelial cells surrounded by a prominent inflammatory infiltrate consisting of lymphocytes and eosinophils.12
Kaposi sarcoma may appear on the neck but most often presents as macules and patches on the extremities that may form nodules with a rubbery consistency. In tufted angiomas, the cellular nodules with dilated channels at the margins bear a resemblance to Kaposi sarcoma or kaposiform hemangioendothelioma; however, in tufted angiomas the lobules are composed of bland spindle cells and slitlike vessels at the periphery.3,13,14 Tufted angiomas are negative for human herpesvirus 8 and typically do not have an associated inflammatory infiltrate with plasma cells.11,15
Moreover, it is important to differentiate tufted angioma from a cutaneous manifestation of an underlying malignancy, which has been described previously in cases of breast cancer.16,17 Our case illustrates a rare vascular tumor arising in the novel context of a pregnant patient with breast cancer. Distinguishing tufted angioma from other benign or malignant vascular tumors is necessary to avoid inappropriate therapeutic interventions.
- Jones EW, Orkin M. Tufted angioma (angioblastoma). a benign progressive angioma, not to be confused with Kaposi’s sarcoma or low-grade angiosarcoma. J Am Acad Dermatol. 1989;20(2 pt 1):214-225.
- Lee B, Chiu M, Soriano T, et al. Adult-onset tufted angioma: a case report and review of the literature. Cutis. 2006;78:341-345.
- Kim YK, Kim HJ, Lee KG. Acquired tufted angioma associated with pregnancy. Clin Exp Dermatol. 1992;17:458-459.
- Feito-Rodriguez M, Sanchez-Orta A, De Lucas R, et al. Congenital tufted angioma: a multicenter retrospective study of 30 cases. Pediatr Dermatol. 2018;35:808-816.
- Pietroletti R, Leardi S, Simi M. Perianal acquired tufted angioma associated with pregnancy: case report. Tech Coloproctol. 2002;6:117-119.
- Osio A, Fraitag S, Hadj-Rabia S, et al. Clinical spectrum of tufted angiomas in childhood: a report of 13 cases and a review of the literature. Arch Dermatol. 2010;146:758-763.
- Omori M, Bito T, Nishigori C. Acquired tufted angioma in pregnancy showing expression of estrogen and progesterone receptors. Eur J Dermatol. 2013;23:898-899.
- Boeldt DS, Bird IM. Vascular adaptation in pregnancy and endothelial dysfunction in preeclampsia. J Endocrinol. 2017;232:R27-R44.
- Fernandes LB, Amaral W. Clinical study of skin changes in low and high risk pregnant women. An Bras Dermatol. 2015;90:822-826.
- Walker JL, Wang AR, Kroumpouzos G, et al. Cutaneous tumors in pregnancy. Clin Dermatol. 2016;34:359-367.
- Sarwal P, Lapumnuaypol K. Pyogenic granuloma. In: StatPearls. StatPearls Publishing; 2021.
- Ortins-Pina A, Llamas-Velasco M, Turpin S, et al. FOSB immunoreactivity in endothelia of epithelioid hemangioma (angiolymphoid hyperplasia with eosinophilia). J Cutan Pathol. 2018;45:395-402.
- Arai E, Kuramochi A, Tsuchida T, et al. Usefulness of D2-40 immunohistochemistry for differentiation between kaposiform hemangioendothelioma and tufted angioma. J Cutan Pathol. 2006;33:492-497.
- Grassi S, Carugno A, Vignini M, et al. Adult-onset tufted angiomas associated with an arteriovenous malformation in a renal transplant recipient: case report and review of the literature. Am J Dermatopathol. 2015;37:162-165.
- Lyons LL, North PE, Mac-Moune Lai F, et al. Kaposiform hemangioendothelioma: a study of 33 cases emphasizing its pathologic, immunophenotypic, and biologic uniqueness from juvenile hemangioma. Am J Surg Pathol. 2004;28:559-568.
- Putra HP, Djawad K, Nurdin AR. Cutaneous lesions as the first manifestation of breast cancer: a rare case. Pan Afr Med J. 2020;37:383.
- Thiers BH, Sahn RE, Callen JP. Cutaneous manifestations of internal malignancy. CA Cancer J Clin. 2009;59:73-98.
The Diagnosis: Tufted Angioma
Histopathology revealed discrete lobules of closely packed capillaries with bland endothelial cells throughout the upper and lower dermis (Figure 1). The surrounding crescentlike vessels and lymphatics stained with D2-40 (Figure 2). These histologic findings were consistent with tufted angioma, and the patient elected for observation.
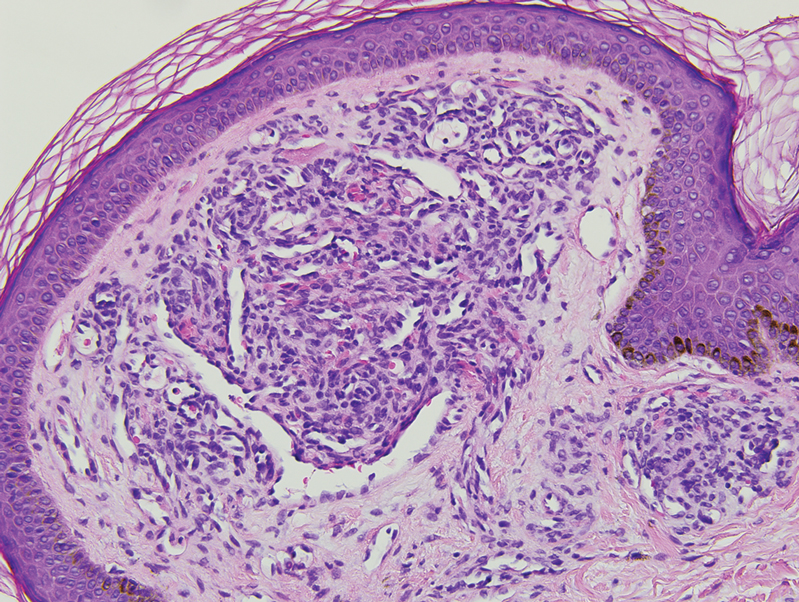
Tufted angiomas are benign vascular lesions named for the tufted appearance of capillaries on histology.1 They commonly present in children, with a lower incidence in adults and rare cases in pregnancy.2 Tufted angiomas typically present as solitary, slowly expanding, erythematous macules, plaques, or nodules on the neck or trunk ranging in size from less than 1 to 10 cm.2-4 They can be histologically distinguished from other vascular tumors, including aggressive malignant neoplasms.1
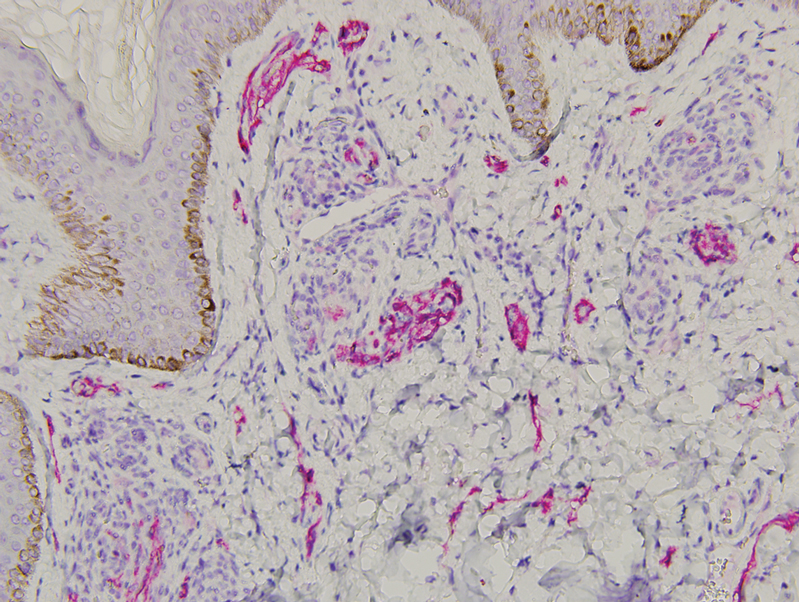
Tufted angiomas are identified by characteristic “cannon ball tufts” of capillaries in the dermis and subcutis at low power.3,5 Distinct cellular lobules may be found bulging into thin-walled vascular channels at the margins of the lobules in the dermis and subcutis (Figure 3).4 The lobules are formed by cells with spindle-shaped nuclei.6 Some mitotic figures may be present, but no cellular atypia is seen.2 The capillaries at the periphery appear as dilated semilunar vessels.4 Dilated lymphatics, which stain with D2-40, can be found at the periphery of the tufted capillaries and throughout the remaining dermis.3,4
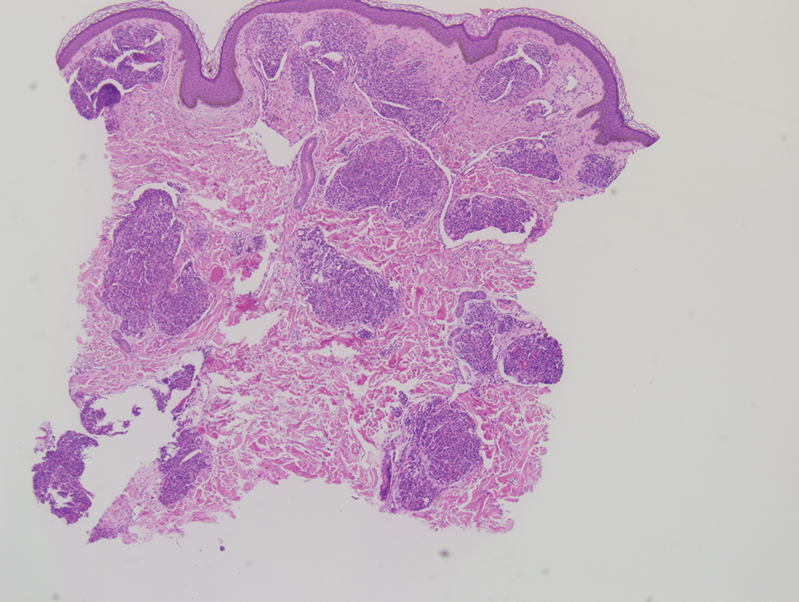
Tufted angiomas may arise independently in adults but also have been associated with conditions such as pregnancy. Omori et al7 identified an acquired tufted angioma in pregnancy that was positive for estrogen and progesterone receptors. Reports of tufted angiomas in pregnancy vary; some are multiple lesions, some regress postpartum, and some undergo successful surgical treatment.3,5
Vascular lesions such as tufted angiomas specifically may appear in pregnancy due to a high-volume state with vasodilation and increased vascular proliferation. Although tumor angiogenesis has been linked to specific growth factors and cytokines, it has been hypothesized that the systemic hormones of pregnancy such as human chorionic gonadotropin, estradiol, and progesterone also shift the body to a more angiogenic state.8 In a study of cutaneous changes in pregnant women (N=905), 41% developed a vascular skin change, including spider veins, varicosities, hemangiomas, and granulomas.9 The most common vascular tumor in pregnancy is pyogenic granuloma. Pyogenic granulomas are small, solitary, friable papules that commonly are found on the hands, forearms, face, or in the mouth; histologically they demonstrate dilated capillaries in lobular structures accompanied by larger thick-walled vessels.3,10,11
Tufted angiomas may mimic a variety of other conditions. Epithelioid hemangioma, considered by some to be on the same morphologic spectrum as angiolymphoid hyperplasia with eosinophilia, classically occurs in young adults on the head and in the neck region. It histologically demonstrates a lobular appearance at low power; however, these lobules are made up of vessels with histiocytoid to epithelioid endothelial cells surrounded by a prominent inflammatory infiltrate consisting of lymphocytes and eosinophils.12
Kaposi sarcoma may appear on the neck but most often presents as macules and patches on the extremities that may form nodules with a rubbery consistency. In tufted angiomas, the cellular nodules with dilated channels at the margins bear a resemblance to Kaposi sarcoma or kaposiform hemangioendothelioma; however, in tufted angiomas the lobules are composed of bland spindle cells and slitlike vessels at the periphery.3,13,14 Tufted angiomas are negative for human herpesvirus 8 and typically do not have an associated inflammatory infiltrate with plasma cells.11,15
Moreover, it is important to differentiate tufted angioma from a cutaneous manifestation of an underlying malignancy, which has been described previously in cases of breast cancer.16,17 Our case illustrates a rare vascular tumor arising in the novel context of a pregnant patient with breast cancer. Distinguishing tufted angioma from other benign or malignant vascular tumors is necessary to avoid inappropriate therapeutic interventions.
The Diagnosis: Tufted Angioma
Histopathology revealed discrete lobules of closely packed capillaries with bland endothelial cells throughout the upper and lower dermis (Figure 1). The surrounding crescentlike vessels and lymphatics stained with D2-40 (Figure 2). These histologic findings were consistent with tufted angioma, and the patient elected for observation.
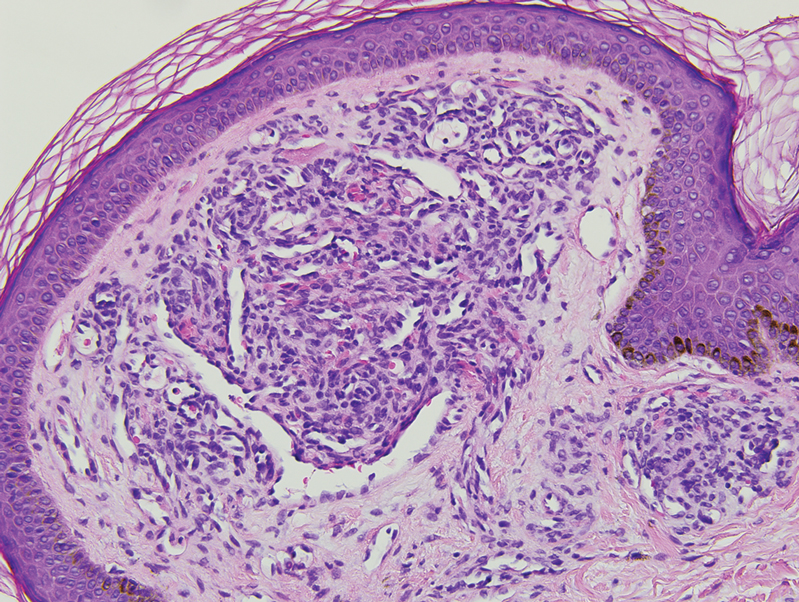
Tufted angiomas are benign vascular lesions named for the tufted appearance of capillaries on histology.1 They commonly present in children, with a lower incidence in adults and rare cases in pregnancy.2 Tufted angiomas typically present as solitary, slowly expanding, erythematous macules, plaques, or nodules on the neck or trunk ranging in size from less than 1 to 10 cm.2-4 They can be histologically distinguished from other vascular tumors, including aggressive malignant neoplasms.1
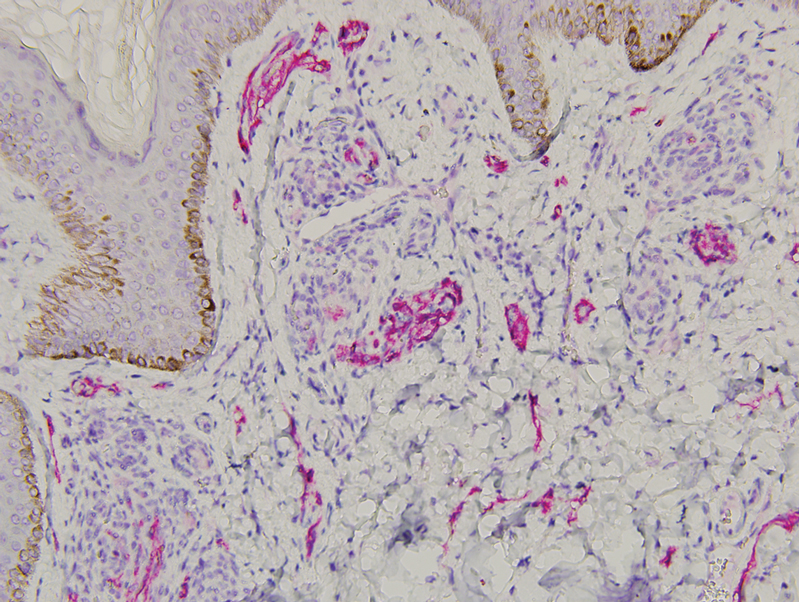
Tufted angiomas are identified by characteristic “cannon ball tufts” of capillaries in the dermis and subcutis at low power.3,5 Distinct cellular lobules may be found bulging into thin-walled vascular channels at the margins of the lobules in the dermis and subcutis (Figure 3).4 The lobules are formed by cells with spindle-shaped nuclei.6 Some mitotic figures may be present, but no cellular atypia is seen.2 The capillaries at the periphery appear as dilated semilunar vessels.4 Dilated lymphatics, which stain with D2-40, can be found at the periphery of the tufted capillaries and throughout the remaining dermis.3,4
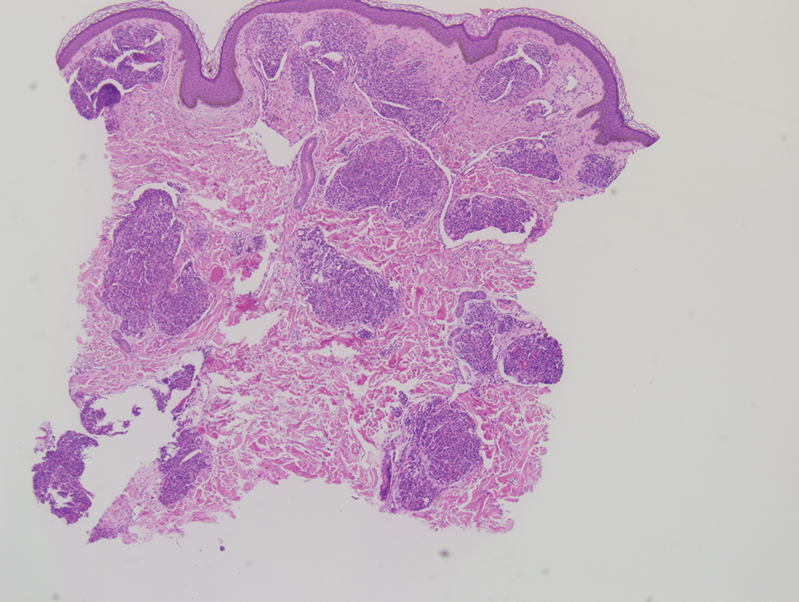
Tufted angiomas may arise independently in adults but also have been associated with conditions such as pregnancy. Omori et al7 identified an acquired tufted angioma in pregnancy that was positive for estrogen and progesterone receptors. Reports of tufted angiomas in pregnancy vary; some are multiple lesions, some regress postpartum, and some undergo successful surgical treatment.3,5
Vascular lesions such as tufted angiomas specifically may appear in pregnancy due to a high-volume state with vasodilation and increased vascular proliferation. Although tumor angiogenesis has been linked to specific growth factors and cytokines, it has been hypothesized that the systemic hormones of pregnancy such as human chorionic gonadotropin, estradiol, and progesterone also shift the body to a more angiogenic state.8 In a study of cutaneous changes in pregnant women (N=905), 41% developed a vascular skin change, including spider veins, varicosities, hemangiomas, and granulomas.9 The most common vascular tumor in pregnancy is pyogenic granuloma. Pyogenic granulomas are small, solitary, friable papules that commonly are found on the hands, forearms, face, or in the mouth; histologically they demonstrate dilated capillaries in lobular structures accompanied by larger thick-walled vessels.3,10,11
Tufted angiomas may mimic a variety of other conditions. Epithelioid hemangioma, considered by some to be on the same morphologic spectrum as angiolymphoid hyperplasia with eosinophilia, classically occurs in young adults on the head and in the neck region. It histologically demonstrates a lobular appearance at low power; however, these lobules are made up of vessels with histiocytoid to epithelioid endothelial cells surrounded by a prominent inflammatory infiltrate consisting of lymphocytes and eosinophils.12
Kaposi sarcoma may appear on the neck but most often presents as macules and patches on the extremities that may form nodules with a rubbery consistency. In tufted angiomas, the cellular nodules with dilated channels at the margins bear a resemblance to Kaposi sarcoma or kaposiform hemangioendothelioma; however, in tufted angiomas the lobules are composed of bland spindle cells and slitlike vessels at the periphery.3,13,14 Tufted angiomas are negative for human herpesvirus 8 and typically do not have an associated inflammatory infiltrate with plasma cells.11,15
Moreover, it is important to differentiate tufted angioma from a cutaneous manifestation of an underlying malignancy, which has been described previously in cases of breast cancer.16,17 Our case illustrates a rare vascular tumor arising in the novel context of a pregnant patient with breast cancer. Distinguishing tufted angioma from other benign or malignant vascular tumors is necessary to avoid inappropriate therapeutic interventions.
- Jones EW, Orkin M. Tufted angioma (angioblastoma). a benign progressive angioma, not to be confused with Kaposi’s sarcoma or low-grade angiosarcoma. J Am Acad Dermatol. 1989;20(2 pt 1):214-225.
- Lee B, Chiu M, Soriano T, et al. Adult-onset tufted angioma: a case report and review of the literature. Cutis. 2006;78:341-345.
- Kim YK, Kim HJ, Lee KG. Acquired tufted angioma associated with pregnancy. Clin Exp Dermatol. 1992;17:458-459.
- Feito-Rodriguez M, Sanchez-Orta A, De Lucas R, et al. Congenital tufted angioma: a multicenter retrospective study of 30 cases. Pediatr Dermatol. 2018;35:808-816.
- Pietroletti R, Leardi S, Simi M. Perianal acquired tufted angioma associated with pregnancy: case report. Tech Coloproctol. 2002;6:117-119.
- Osio A, Fraitag S, Hadj-Rabia S, et al. Clinical spectrum of tufted angiomas in childhood: a report of 13 cases and a review of the literature. Arch Dermatol. 2010;146:758-763.
- Omori M, Bito T, Nishigori C. Acquired tufted angioma in pregnancy showing expression of estrogen and progesterone receptors. Eur J Dermatol. 2013;23:898-899.
- Boeldt DS, Bird IM. Vascular adaptation in pregnancy and endothelial dysfunction in preeclampsia. J Endocrinol. 2017;232:R27-R44.
- Fernandes LB, Amaral W. Clinical study of skin changes in low and high risk pregnant women. An Bras Dermatol. 2015;90:822-826.
- Walker JL, Wang AR, Kroumpouzos G, et al. Cutaneous tumors in pregnancy. Clin Dermatol. 2016;34:359-367.
- Sarwal P, Lapumnuaypol K. Pyogenic granuloma. In: StatPearls. StatPearls Publishing; 2021.
- Ortins-Pina A, Llamas-Velasco M, Turpin S, et al. FOSB immunoreactivity in endothelia of epithelioid hemangioma (angiolymphoid hyperplasia with eosinophilia). J Cutan Pathol. 2018;45:395-402.
- Arai E, Kuramochi A, Tsuchida T, et al. Usefulness of D2-40 immunohistochemistry for differentiation between kaposiform hemangioendothelioma and tufted angioma. J Cutan Pathol. 2006;33:492-497.
- Grassi S, Carugno A, Vignini M, et al. Adult-onset tufted angiomas associated with an arteriovenous malformation in a renal transplant recipient: case report and review of the literature. Am J Dermatopathol. 2015;37:162-165.
- Lyons LL, North PE, Mac-Moune Lai F, et al. Kaposiform hemangioendothelioma: a study of 33 cases emphasizing its pathologic, immunophenotypic, and biologic uniqueness from juvenile hemangioma. Am J Surg Pathol. 2004;28:559-568.
- Putra HP, Djawad K, Nurdin AR. Cutaneous lesions as the first manifestation of breast cancer: a rare case. Pan Afr Med J. 2020;37:383.
- Thiers BH, Sahn RE, Callen JP. Cutaneous manifestations of internal malignancy. CA Cancer J Clin. 2009;59:73-98.
- Jones EW, Orkin M. Tufted angioma (angioblastoma). a benign progressive angioma, not to be confused with Kaposi’s sarcoma or low-grade angiosarcoma. J Am Acad Dermatol. 1989;20(2 pt 1):214-225.
- Lee B, Chiu M, Soriano T, et al. Adult-onset tufted angioma: a case report and review of the literature. Cutis. 2006;78:341-345.
- Kim YK, Kim HJ, Lee KG. Acquired tufted angioma associated with pregnancy. Clin Exp Dermatol. 1992;17:458-459.
- Feito-Rodriguez M, Sanchez-Orta A, De Lucas R, et al. Congenital tufted angioma: a multicenter retrospective study of 30 cases. Pediatr Dermatol. 2018;35:808-816.
- Pietroletti R, Leardi S, Simi M. Perianal acquired tufted angioma associated with pregnancy: case report. Tech Coloproctol. 2002;6:117-119.
- Osio A, Fraitag S, Hadj-Rabia S, et al. Clinical spectrum of tufted angiomas in childhood: a report of 13 cases and a review of the literature. Arch Dermatol. 2010;146:758-763.
- Omori M, Bito T, Nishigori C. Acquired tufted angioma in pregnancy showing expression of estrogen and progesterone receptors. Eur J Dermatol. 2013;23:898-899.
- Boeldt DS, Bird IM. Vascular adaptation in pregnancy and endothelial dysfunction in preeclampsia. J Endocrinol. 2017;232:R27-R44.
- Fernandes LB, Amaral W. Clinical study of skin changes in low and high risk pregnant women. An Bras Dermatol. 2015;90:822-826.
- Walker JL, Wang AR, Kroumpouzos G, et al. Cutaneous tumors in pregnancy. Clin Dermatol. 2016;34:359-367.
- Sarwal P, Lapumnuaypol K. Pyogenic granuloma. In: StatPearls. StatPearls Publishing; 2021.
- Ortins-Pina A, Llamas-Velasco M, Turpin S, et al. FOSB immunoreactivity in endothelia of epithelioid hemangioma (angiolymphoid hyperplasia with eosinophilia). J Cutan Pathol. 2018;45:395-402.
- Arai E, Kuramochi A, Tsuchida T, et al. Usefulness of D2-40 immunohistochemistry for differentiation between kaposiform hemangioendothelioma and tufted angioma. J Cutan Pathol. 2006;33:492-497.
- Grassi S, Carugno A, Vignini M, et al. Adult-onset tufted angiomas associated with an arteriovenous malformation in a renal transplant recipient: case report and review of the literature. Am J Dermatopathol. 2015;37:162-165.
- Lyons LL, North PE, Mac-Moune Lai F, et al. Kaposiform hemangioendothelioma: a study of 33 cases emphasizing its pathologic, immunophenotypic, and biologic uniqueness from juvenile hemangioma. Am J Surg Pathol. 2004;28:559-568.
- Putra HP, Djawad K, Nurdin AR. Cutaneous lesions as the first manifestation of breast cancer: a rare case. Pan Afr Med J. 2020;37:383.
- Thiers BH, Sahn RE, Callen JP. Cutaneous manifestations of internal malignancy. CA Cancer J Clin. 2009;59:73-98.
A 31-year-old woman at 34 weeks’ gestation presented with skin discoloration of the anterior neck of 7 months’ duration. Her pregnancy had been complicated by a diagnosis of invasive papillary carcinoma of the breast with unilateral complete mastectomy and negative sentinel lymph node biopsy in the first trimester. The lesion was tender, darkening, and rapidly enlarging. Physical examination demonstrated a linear, violaceous, vascular, and indurated plaque with microvesiculation that was 3.5 cm in width. She had no history of blistering sunburns, frequent UV exposure, or skin cancer.