User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
ACST-2: Carotid stenting, surgery on par in asymptomatic patients
Carotid artery stenting (CAS) and carotid endarterectomy (CEA) provided comparable outcomes over time in asymptomatic patients receiving good medical therapy in the largest trial to date of what to do with severe carotid artery narrowing that is yet to cause a stroke.
Among more than 3,600 patients, stenting and surgery performed by experienced physicians involved a 1.0% risk for causing disabling stroke or death within 30 days.
The annual rate of fatal or disabling strokes was about 0.5% with either procedure over an average 5 years’ follow-up – essentially halving the annual stroke risk had neither procedure been performed, according to Alison Halliday, MD, principal investigator of the Asymptomatic Carotid Surgery Trial-2 (ACST-2).
The results were reported Aug. 29 in a Hot Line session at the virtual annual congress of the European Society of Cardiology and published simultaneously online in The Lancet.
Session chair Gilles Montalescot, MD, Sorbonne University, Paris, noted that ACST-2 doubled the number of randomly assigned patients with asymptomatic carotid stenosis studied in previous trials, “so, a huge contribution to the evidence base in this field and apparently good news for both revascularization techniques.”
Thirty-day and 5-year outcomes
The trial was conducted in 33 countries between January 2008 and December 2020, enrolling 3,625 patients (70% were male; mean age, 70 years) with carotid stenosis of at least 60% on ultrasonography, in whom stenting or surgery was suitable but both the doctor and patient were “substantially uncertain” which procedure to prefer.
Among the 1,811 patients assigned to stenting, 87% underwent the procedure at a median of 14 days; 6% crossed over to surgery, typically because of a highly calcified lesion or a more tortuous carotid than anticipated; and 6% had no intervention.
Among the 1,814 patients assigned to surgery, 92% had the procedure at a median of 14 days; 3% crossed over to stenting, typically because of patient or doctor preference or reluctance to undergo general anesthesia; and 4% had no intervention.
Patients without complications who had stenting stayed on average 1 day less than did those undergoing surgery.
During an earlier press briefing, Dr. Halliday highlighted the need for procedural competency and said doctors had to submit a record of their CEA or CAS experience and, consistent with current guidelines, had to demonstrate an independently verified stroke or death rate of 6% or less for symptomatic patients and 3% or lower for asymptomatic patients.
The results showed the 30-day risk for death, myocardial infarction (MI), or any stroke was 3.9% with carotid stenting and 3.2% with surgery (P = .26).
But with stenting, there was a slightly higher risk for procedural nondisabling strokes (48 vs. 29; P = .03), including 15 strokes vs. 5 strokes, respectively, that left patients with no residual symptoms. This is “consistent with large, recent nationally representative registry data,” observed Dr. Halliday, of the University of Oxford (England).
For those undergoing surgery, cranial nerve palsies were reported in 5.4% vs. no patients undergoing stenting.
At 5 years, the nonprocedural fatal or disabling stroke rate was 2.5% in each group (rate ratio [RR], 0.98; P = .91), with any nonprocedural stroke occurring in 5.3% of patients with stenting vs. 4.5% with surgery (RR, 1.16; P = .33).
The investigators performed a meta-analysis combining the ACST-2 results with those of eight prior trials (four in asymptomatic and four in symptomatic patients) that yielded a similar nonsignificant result for any nonprocedural stroke (RR, 1.11; P = .21).
Based on the results from ACST-2 plus the major trials, stenting and surgery involve “similar risks and similar benefits,” Dr. Halliday concluded.
Discussant Marco Roffi, MD, University Hospital of Geneva, said, “In centers with documented expertise, carotid artery stenting should be offered as an alternative to carotid endarterectomy in patients with asymptomatic stenosis and suitable anatomy.”
While the trial provides “good news” for patients, he pointed out that a reduction in the sample size from 5,000 to 3,625 limited the statistical power and that enrollment over a long period of time may have introduced confounders, such as changes in equipment technique, and medical therapy.
Also, many centers enrolled few patients, raising the concern over low-volume centers and operators, Dr. Roffi said. “We know that 8% of the centers enrolled 39% of the patients,” and “information on the credentialing and experience of the interventionalists was limited.”
Further, a lack of systematic MI assessment may have favored the surgery group, and more recent developments in stenting with the potential of reducing periprocedural stroke were rarely used, such as proximal emboli protection in only 15% and double-layer stents in 11%.
Friedhelm Beyersdorf, MD, University Hospital of Freiburg, Germany, said that, as a vascular surgeon, he finds it understandable that there might be a higher incidence of nonfatal strokes when treating carotid stenosis with stents, given the vulnerability of these lesions.
“Nevertheless, the main conclusion from the entire study is that carotid artery treatment is extremely safe, it has to be done in order to avoid strokes, and, obviously, there seems to be an advantage for surgery in terms of nondisabling stroke,” he said.
Session chair Dr. Montalescot, however, said that what the study cannot address – and what was the subject of many online audience comments – is whether either intervention should be performed in these patients.
Unlike earlier trials comparing interventions to medical therapy, Dr. Halliday said ACST-2 enrolled patients for whom the decision had been made that revascularization was needed. In addition, 99%-100% were receiving antithrombotic therapy at baseline, 85%-90% were receiving antihypertensives, and about 85% were taking statins.
Longer-term follow-up should provide a better picture of the nonprocedural stroke risk, with patients asked annually about exactly what medications and doses they are taking, she said.
“We will have an enormous list of exactly what’s gone on and the intensity of that therapy, which is, of course, much more intense than when we carried out our first trial. But these were people in whom a procedure was thought to be necessary,” she noted.
When asked during the press conference which procedure she would choose, Dr. Halliday, a surgeon, observed that patient preference is important but that the nature of the lesion itself often determines the optimal choice.
“If you know the competence of the people doing it is equal, then the less invasive procedure – providing it has good long-term viability, and that’s why we’re following for 10 years – is the more important,” she added.
The study was funded by the UK Medical Research Council and Health Technology Assessment Programme. Dr. Halliday reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Carotid artery stenting (CAS) and carotid endarterectomy (CEA) provided comparable outcomes over time in asymptomatic patients receiving good medical therapy in the largest trial to date of what to do with severe carotid artery narrowing that is yet to cause a stroke.
Among more than 3,600 patients, stenting and surgery performed by experienced physicians involved a 1.0% risk for causing disabling stroke or death within 30 days.
The annual rate of fatal or disabling strokes was about 0.5% with either procedure over an average 5 years’ follow-up – essentially halving the annual stroke risk had neither procedure been performed, according to Alison Halliday, MD, principal investigator of the Asymptomatic Carotid Surgery Trial-2 (ACST-2).
The results were reported Aug. 29 in a Hot Line session at the virtual annual congress of the European Society of Cardiology and published simultaneously online in The Lancet.
Session chair Gilles Montalescot, MD, Sorbonne University, Paris, noted that ACST-2 doubled the number of randomly assigned patients with asymptomatic carotid stenosis studied in previous trials, “so, a huge contribution to the evidence base in this field and apparently good news for both revascularization techniques.”
Thirty-day and 5-year outcomes
The trial was conducted in 33 countries between January 2008 and December 2020, enrolling 3,625 patients (70% were male; mean age, 70 years) with carotid stenosis of at least 60% on ultrasonography, in whom stenting or surgery was suitable but both the doctor and patient were “substantially uncertain” which procedure to prefer.
Among the 1,811 patients assigned to stenting, 87% underwent the procedure at a median of 14 days; 6% crossed over to surgery, typically because of a highly calcified lesion or a more tortuous carotid than anticipated; and 6% had no intervention.
Among the 1,814 patients assigned to surgery, 92% had the procedure at a median of 14 days; 3% crossed over to stenting, typically because of patient or doctor preference or reluctance to undergo general anesthesia; and 4% had no intervention.
Patients without complications who had stenting stayed on average 1 day less than did those undergoing surgery.
During an earlier press briefing, Dr. Halliday highlighted the need for procedural competency and said doctors had to submit a record of their CEA or CAS experience and, consistent with current guidelines, had to demonstrate an independently verified stroke or death rate of 6% or less for symptomatic patients and 3% or lower for asymptomatic patients.
The results showed the 30-day risk for death, myocardial infarction (MI), or any stroke was 3.9% with carotid stenting and 3.2% with surgery (P = .26).
But with stenting, there was a slightly higher risk for procedural nondisabling strokes (48 vs. 29; P = .03), including 15 strokes vs. 5 strokes, respectively, that left patients with no residual symptoms. This is “consistent with large, recent nationally representative registry data,” observed Dr. Halliday, of the University of Oxford (England).
For those undergoing surgery, cranial nerve palsies were reported in 5.4% vs. no patients undergoing stenting.
At 5 years, the nonprocedural fatal or disabling stroke rate was 2.5% in each group (rate ratio [RR], 0.98; P = .91), with any nonprocedural stroke occurring in 5.3% of patients with stenting vs. 4.5% with surgery (RR, 1.16; P = .33).
The investigators performed a meta-analysis combining the ACST-2 results with those of eight prior trials (four in asymptomatic and four in symptomatic patients) that yielded a similar nonsignificant result for any nonprocedural stroke (RR, 1.11; P = .21).
Based on the results from ACST-2 plus the major trials, stenting and surgery involve “similar risks and similar benefits,” Dr. Halliday concluded.
Discussant Marco Roffi, MD, University Hospital of Geneva, said, “In centers with documented expertise, carotid artery stenting should be offered as an alternative to carotid endarterectomy in patients with asymptomatic stenosis and suitable anatomy.”
While the trial provides “good news” for patients, he pointed out that a reduction in the sample size from 5,000 to 3,625 limited the statistical power and that enrollment over a long period of time may have introduced confounders, such as changes in equipment technique, and medical therapy.
Also, many centers enrolled few patients, raising the concern over low-volume centers and operators, Dr. Roffi said. “We know that 8% of the centers enrolled 39% of the patients,” and “information on the credentialing and experience of the interventionalists was limited.”
Further, a lack of systematic MI assessment may have favored the surgery group, and more recent developments in stenting with the potential of reducing periprocedural stroke were rarely used, such as proximal emboli protection in only 15% and double-layer stents in 11%.
Friedhelm Beyersdorf, MD, University Hospital of Freiburg, Germany, said that, as a vascular surgeon, he finds it understandable that there might be a higher incidence of nonfatal strokes when treating carotid stenosis with stents, given the vulnerability of these lesions.
“Nevertheless, the main conclusion from the entire study is that carotid artery treatment is extremely safe, it has to be done in order to avoid strokes, and, obviously, there seems to be an advantage for surgery in terms of nondisabling stroke,” he said.
Session chair Dr. Montalescot, however, said that what the study cannot address – and what was the subject of many online audience comments – is whether either intervention should be performed in these patients.
Unlike earlier trials comparing interventions to medical therapy, Dr. Halliday said ACST-2 enrolled patients for whom the decision had been made that revascularization was needed. In addition, 99%-100% were receiving antithrombotic therapy at baseline, 85%-90% were receiving antihypertensives, and about 85% were taking statins.
Longer-term follow-up should provide a better picture of the nonprocedural stroke risk, with patients asked annually about exactly what medications and doses they are taking, she said.
“We will have an enormous list of exactly what’s gone on and the intensity of that therapy, which is, of course, much more intense than when we carried out our first trial. But these were people in whom a procedure was thought to be necessary,” she noted.
When asked during the press conference which procedure she would choose, Dr. Halliday, a surgeon, observed that patient preference is important but that the nature of the lesion itself often determines the optimal choice.
“If you know the competence of the people doing it is equal, then the less invasive procedure – providing it has good long-term viability, and that’s why we’re following for 10 years – is the more important,” she added.
The study was funded by the UK Medical Research Council and Health Technology Assessment Programme. Dr. Halliday reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Carotid artery stenting (CAS) and carotid endarterectomy (CEA) provided comparable outcomes over time in asymptomatic patients receiving good medical therapy in the largest trial to date of what to do with severe carotid artery narrowing that is yet to cause a stroke.
Among more than 3,600 patients, stenting and surgery performed by experienced physicians involved a 1.0% risk for causing disabling stroke or death within 30 days.
The annual rate of fatal or disabling strokes was about 0.5% with either procedure over an average 5 years’ follow-up – essentially halving the annual stroke risk had neither procedure been performed, according to Alison Halliday, MD, principal investigator of the Asymptomatic Carotid Surgery Trial-2 (ACST-2).
The results were reported Aug. 29 in a Hot Line session at the virtual annual congress of the European Society of Cardiology and published simultaneously online in The Lancet.
Session chair Gilles Montalescot, MD, Sorbonne University, Paris, noted that ACST-2 doubled the number of randomly assigned patients with asymptomatic carotid stenosis studied in previous trials, “so, a huge contribution to the evidence base in this field and apparently good news for both revascularization techniques.”
Thirty-day and 5-year outcomes
The trial was conducted in 33 countries between January 2008 and December 2020, enrolling 3,625 patients (70% were male; mean age, 70 years) with carotid stenosis of at least 60% on ultrasonography, in whom stenting or surgery was suitable but both the doctor and patient were “substantially uncertain” which procedure to prefer.
Among the 1,811 patients assigned to stenting, 87% underwent the procedure at a median of 14 days; 6% crossed over to surgery, typically because of a highly calcified lesion or a more tortuous carotid than anticipated; and 6% had no intervention.
Among the 1,814 patients assigned to surgery, 92% had the procedure at a median of 14 days; 3% crossed over to stenting, typically because of patient or doctor preference or reluctance to undergo general anesthesia; and 4% had no intervention.
Patients without complications who had stenting stayed on average 1 day less than did those undergoing surgery.
During an earlier press briefing, Dr. Halliday highlighted the need for procedural competency and said doctors had to submit a record of their CEA or CAS experience and, consistent with current guidelines, had to demonstrate an independently verified stroke or death rate of 6% or less for symptomatic patients and 3% or lower for asymptomatic patients.
The results showed the 30-day risk for death, myocardial infarction (MI), or any stroke was 3.9% with carotid stenting and 3.2% with surgery (P = .26).
But with stenting, there was a slightly higher risk for procedural nondisabling strokes (48 vs. 29; P = .03), including 15 strokes vs. 5 strokes, respectively, that left patients with no residual symptoms. This is “consistent with large, recent nationally representative registry data,” observed Dr. Halliday, of the University of Oxford (England).
For those undergoing surgery, cranial nerve palsies were reported in 5.4% vs. no patients undergoing stenting.
At 5 years, the nonprocedural fatal or disabling stroke rate was 2.5% in each group (rate ratio [RR], 0.98; P = .91), with any nonprocedural stroke occurring in 5.3% of patients with stenting vs. 4.5% with surgery (RR, 1.16; P = .33).
The investigators performed a meta-analysis combining the ACST-2 results with those of eight prior trials (four in asymptomatic and four in symptomatic patients) that yielded a similar nonsignificant result for any nonprocedural stroke (RR, 1.11; P = .21).
Based on the results from ACST-2 plus the major trials, stenting and surgery involve “similar risks and similar benefits,” Dr. Halliday concluded.
Discussant Marco Roffi, MD, University Hospital of Geneva, said, “In centers with documented expertise, carotid artery stenting should be offered as an alternative to carotid endarterectomy in patients with asymptomatic stenosis and suitable anatomy.”
While the trial provides “good news” for patients, he pointed out that a reduction in the sample size from 5,000 to 3,625 limited the statistical power and that enrollment over a long period of time may have introduced confounders, such as changes in equipment technique, and medical therapy.
Also, many centers enrolled few patients, raising the concern over low-volume centers and operators, Dr. Roffi said. “We know that 8% of the centers enrolled 39% of the patients,” and “information on the credentialing and experience of the interventionalists was limited.”
Further, a lack of systematic MI assessment may have favored the surgery group, and more recent developments in stenting with the potential of reducing periprocedural stroke were rarely used, such as proximal emboli protection in only 15% and double-layer stents in 11%.
Friedhelm Beyersdorf, MD, University Hospital of Freiburg, Germany, said that, as a vascular surgeon, he finds it understandable that there might be a higher incidence of nonfatal strokes when treating carotid stenosis with stents, given the vulnerability of these lesions.
“Nevertheless, the main conclusion from the entire study is that carotid artery treatment is extremely safe, it has to be done in order to avoid strokes, and, obviously, there seems to be an advantage for surgery in terms of nondisabling stroke,” he said.
Session chair Dr. Montalescot, however, said that what the study cannot address – and what was the subject of many online audience comments – is whether either intervention should be performed in these patients.
Unlike earlier trials comparing interventions to medical therapy, Dr. Halliday said ACST-2 enrolled patients for whom the decision had been made that revascularization was needed. In addition, 99%-100% were receiving antithrombotic therapy at baseline, 85%-90% were receiving antihypertensives, and about 85% were taking statins.
Longer-term follow-up should provide a better picture of the nonprocedural stroke risk, with patients asked annually about exactly what medications and doses they are taking, she said.
“We will have an enormous list of exactly what’s gone on and the intensity of that therapy, which is, of course, much more intense than when we carried out our first trial. But these were people in whom a procedure was thought to be necessary,” she noted.
When asked during the press conference which procedure she would choose, Dr. Halliday, a surgeon, observed that patient preference is important but that the nature of the lesion itself often determines the optimal choice.
“If you know the competence of the people doing it is equal, then the less invasive procedure – providing it has good long-term viability, and that’s why we’re following for 10 years – is the more important,” she added.
The study was funded by the UK Medical Research Council and Health Technology Assessment Programme. Dr. Halliday reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Angiography can wait for cardiac arrest without ST-elevation
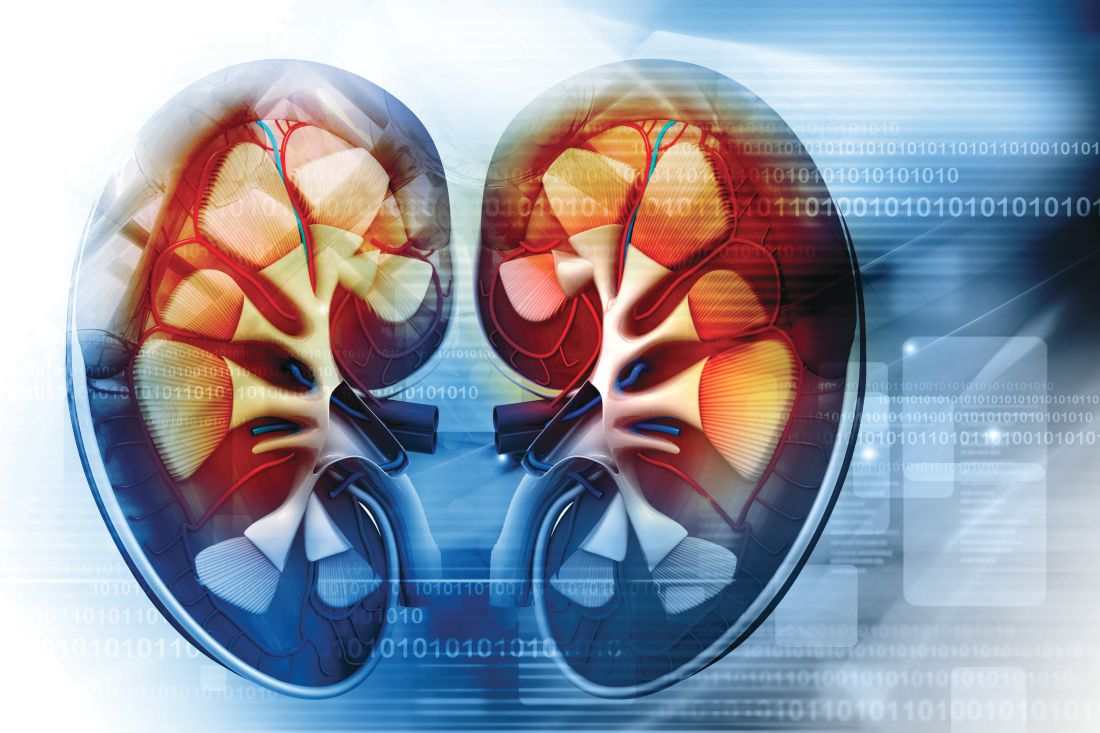
A protocol of immediate angiography provided no mortality benefit over a strategy or delayed or more selective angiography among patients resuscitated from out-of-hospital cardiac arrest and without ST-segment elevation, new randomized results show.
“Among patients with resuscitated out-of-hospital cardiac arrest of possible cardiac origin, with shockable and nonshockable arrest rhythm and no ST-elevation, a strategy of immediate, unselected coronary angiography was not found to be beneficial over a delayed and selective approach with regard to the 30-day risk of all-cause death,” concluded principal investigator Steffen Desch, MD, University of Leipzig (Germany) Heart Center.
The results support previous results of the Coronary Angiography after Cardiac Arrest (COACT) trial, in patients with shockable rhythms, which also showed no differences in clinical outcomes between immediate and delayed coronary angiography at both 90 days and 1 year, he noted.
“What the clinicians wanted to know is, is it really necessary to get up at 3 a.m. in the morning to perform a coronary angiography on these patients, and that’s certainly out,” Dr. Desch said in an interview. “So, there’s really no room for this strategy anymore. You can take your time and wait a day or 2.”
These findings, from the TOMAHAWK trial, were presented Aug. 29 at the annual congress of the European Society of Cardiology and simultaneously published online in the New England Journal of Medicine.
Larger group without ST-segment elevation
Prognosis after out-of-hospital cardiac arrest is extremely poor, with an overall survival rate of less than 10%, Dr. Desch noted. “Actually, only 20% make it to the hospital; the vast majority of these patients die out in the field, so there’s really a great need in improving treatment.”
Acute coronary syndrome accounts for up to 60% of out-of-hospital arrests in which a cardiac cause has been identified, the authors wrote in their report. ST-segment elevation on postresuscitation electrocardiography “has good positive predictive value” for acute coronary lesions triggering the arrest, but in the far larger subgroup of patients without ST-segment elevation, “the spectrum of underlying causes is considerably broader and includes both cardiac and noncardiac causes.”
In patients with myocardial infarction, early revascularization would prevent negative consequences of myocardial injury, but unselected early coronary angiography would put patients not having an MI at unnecessary risk for procedural complications or delay in the diagnosis of the actual cause of their arrest, they noted.
In this trial, the researchers randomly assigned 554 patients from 31 sites in Germany and Denmark who were successfully resuscitated after cardiac arrest of possible cardiac origin to immediate transfer for coronary angiography or to initial intensive care assessment with delayed or selective angiography after a minimum delay of at least 1 day.
In the end, the average delay in this arm was 2 days, Dr. Desch noted. If the clinical course indicated that a coronary cause was unlikely, angiography might not be performed at all in this group.
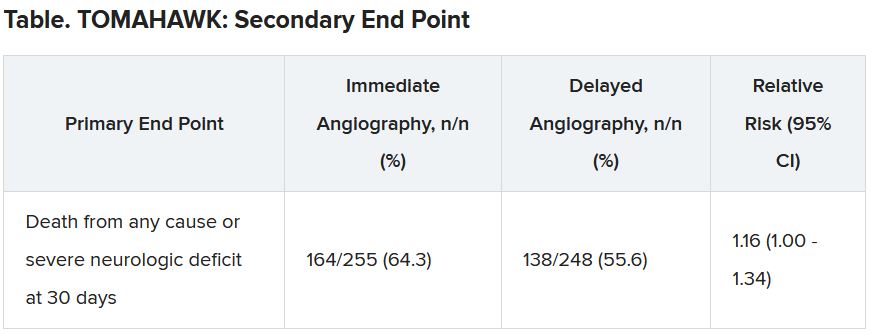
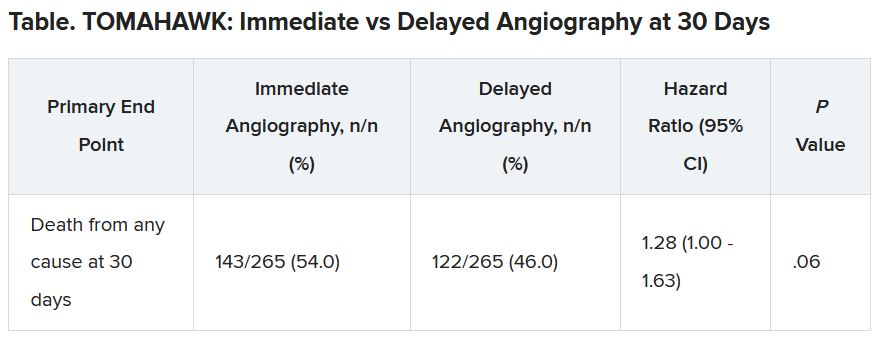
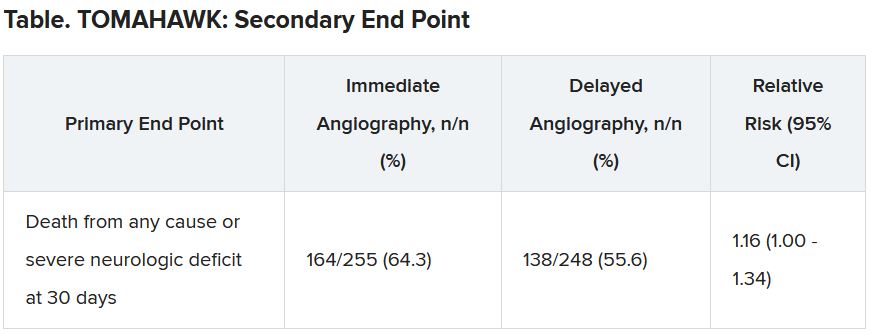
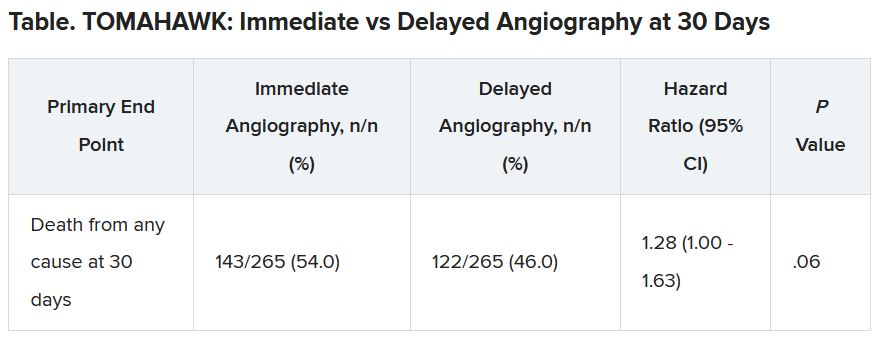
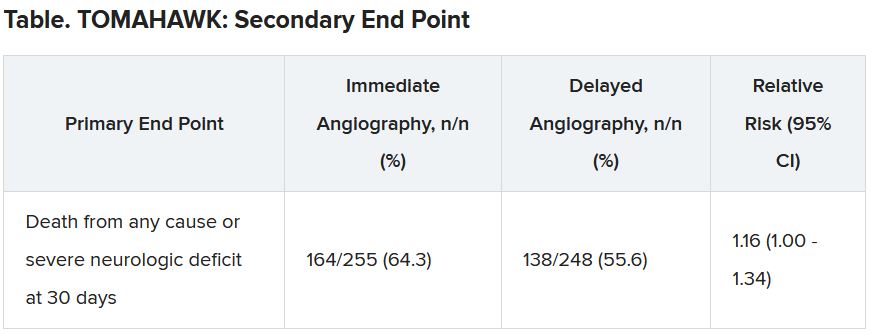
No patient had ST-segment elevation on postresuscitation electrocardiography. The primary endpoint was death from any cause at 30 days; secondary end points were death from any cause or severe neurologic deficit at 30 days.
Results showed that 95% of patients in the immediate angiography group actually underwent the procedure, compared with 62% of those in the delayed group, a finding that was “logical” given the study design, he said.
At 30 days, 54% of patients in the immediate angiography group and 46% in the delayed group had died, a nonsignificant difference (P = .06). Because the researchers had performed an interim analysis, Dr. Desch explained, the final P value for significance in this trial was not .05, but rather .034, to account for multiple comparisons.
The secondary end point of death from any cause or severe neurologic deficit at 30 days “was actually nominally significant in favor of the delayed group,” he said. “So, this is not corrected for multiple testing, it’s just a hypothesis that’s in the room, but it’s certainly worthy of discussion that the immediate strategy might actually cause harm.”
There was no difference between the groups in peak release of myocardial enzymes, or any other safety end points, including bleeding, stroke, or renal failure, Dr. Desch said.
Further analyses showed no large differences between subgroups, including age, diabetes, first monitored rhythm, confirmed MI as the trigger of the arrest, sex, and the time from cardiac arrest to the return of spontaneous circulation, he noted.
Opportunity to minimize harm
Discussant for the results during the presentation was Susanna Price, MBBS, PhD, Royal Brompton Hospital, London.
Dr. Price concluded: “What this means for me, is it gives me information that’s useful regarding the opportunity to minimize harm, which is a lot of what critical care is about, so we don’t necessarily now have to move these patients very acutely when they’ve just come in through the ED [emergency department]. It has implications for resource utilization, but also implications for mobilizing patients around the hospital during COVID-19.”
It’s also important to note that coronary angiography was still carried out in certain patients, “so we still have to have that dialogue with our interventional cardiologists for certain patients who may need to go to the cath lab, and what it should now allow us to do is give appropriate focus to how to manage these patients when they come in to the ED or to our ICUs [intensive care units],” she said.
Dr. Price added, though, that perhaps “the most important slide” in the presentation was that showing 90% of these patients had a witnessed cardiac arrest, “and yet a third of these patients, 168 of them, had no bystander CPR at all.”
She pointed to the “chain of survival” after cardiac arrest, of which Charles D. Deakin, MD, University Hospital Southampton (England), wrote that “not all links are equal.”
“Early recognition and calling for help, early CPR, early defibrillation where appropriate are very, very important, and we need to be addressing all of these, as well as what happens in the cath lab and after admission,” Dr. Price said.
This research was funded by the German Center for Cardiovascular Research. Dr. Desch and Dr. Price reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
A protocol of immediate angiography provided no mortality benefit over a strategy or delayed or more selective angiography among patients resuscitated from out-of-hospital cardiac arrest and without ST-segment elevation, new randomized results show.
“Among patients with resuscitated out-of-hospital cardiac arrest of possible cardiac origin, with shockable and nonshockable arrest rhythm and no ST-elevation, a strategy of immediate, unselected coronary angiography was not found to be beneficial over a delayed and selective approach with regard to the 30-day risk of all-cause death,” concluded principal investigator Steffen Desch, MD, University of Leipzig (Germany) Heart Center.
The results support previous results of the Coronary Angiography after Cardiac Arrest (COACT) trial, in patients with shockable rhythms, which also showed no differences in clinical outcomes between immediate and delayed coronary angiography at both 90 days and 1 year, he noted.
“What the clinicians wanted to know is, is it really necessary to get up at 3 a.m. in the morning to perform a coronary angiography on these patients, and that’s certainly out,” Dr. Desch said in an interview. “So, there’s really no room for this strategy anymore. You can take your time and wait a day or 2.”
These findings, from the TOMAHAWK trial, were presented Aug. 29 at the annual congress of the European Society of Cardiology and simultaneously published online in the New England Journal of Medicine.
Larger group without ST-segment elevation
Prognosis after out-of-hospital cardiac arrest is extremely poor, with an overall survival rate of less than 10%, Dr. Desch noted. “Actually, only 20% make it to the hospital; the vast majority of these patients die out in the field, so there’s really a great need in improving treatment.”
Acute coronary syndrome accounts for up to 60% of out-of-hospital arrests in which a cardiac cause has been identified, the authors wrote in their report. ST-segment elevation on postresuscitation electrocardiography “has good positive predictive value” for acute coronary lesions triggering the arrest, but in the far larger subgroup of patients without ST-segment elevation, “the spectrum of underlying causes is considerably broader and includes both cardiac and noncardiac causes.”
In patients with myocardial infarction, early revascularization would prevent negative consequences of myocardial injury, but unselected early coronary angiography would put patients not having an MI at unnecessary risk for procedural complications or delay in the diagnosis of the actual cause of their arrest, they noted.
In this trial, the researchers randomly assigned 554 patients from 31 sites in Germany and Denmark who were successfully resuscitated after cardiac arrest of possible cardiac origin to immediate transfer for coronary angiography or to initial intensive care assessment with delayed or selective angiography after a minimum delay of at least 1 day.
In the end, the average delay in this arm was 2 days, Dr. Desch noted. If the clinical course indicated that a coronary cause was unlikely, angiography might not be performed at all in this group.
No patient had ST-segment elevation on postresuscitation electrocardiography. The primary endpoint was death from any cause at 30 days; secondary end points were death from any cause or severe neurologic deficit at 30 days.
Results showed that 95% of patients in the immediate angiography group actually underwent the procedure, compared with 62% of those in the delayed group, a finding that was “logical” given the study design, he said.
At 30 days, 54% of patients in the immediate angiography group and 46% in the delayed group had died, a nonsignificant difference (P = .06). Because the researchers had performed an interim analysis, Dr. Desch explained, the final P value for significance in this trial was not .05, but rather .034, to account for multiple comparisons.
The secondary end point of death from any cause or severe neurologic deficit at 30 days “was actually nominally significant in favor of the delayed group,” he said. “So, this is not corrected for multiple testing, it’s just a hypothesis that’s in the room, but it’s certainly worthy of discussion that the immediate strategy might actually cause harm.”
There was no difference between the groups in peak release of myocardial enzymes, or any other safety end points, including bleeding, stroke, or renal failure, Dr. Desch said.
Further analyses showed no large differences between subgroups, including age, diabetes, first monitored rhythm, confirmed MI as the trigger of the arrest, sex, and the time from cardiac arrest to the return of spontaneous circulation, he noted.
Opportunity to minimize harm
Discussant for the results during the presentation was Susanna Price, MBBS, PhD, Royal Brompton Hospital, London.
Dr. Price concluded: “What this means for me, is it gives me information that’s useful regarding the opportunity to minimize harm, which is a lot of what critical care is about, so we don’t necessarily now have to move these patients very acutely when they’ve just come in through the ED [emergency department]. It has implications for resource utilization, but also implications for mobilizing patients around the hospital during COVID-19.”
It’s also important to note that coronary angiography was still carried out in certain patients, “so we still have to have that dialogue with our interventional cardiologists for certain patients who may need to go to the cath lab, and what it should now allow us to do is give appropriate focus to how to manage these patients when they come in to the ED or to our ICUs [intensive care units],” she said.
Dr. Price added, though, that perhaps “the most important slide” in the presentation was that showing 90% of these patients had a witnessed cardiac arrest, “and yet a third of these patients, 168 of them, had no bystander CPR at all.”
She pointed to the “chain of survival” after cardiac arrest, of which Charles D. Deakin, MD, University Hospital Southampton (England), wrote that “not all links are equal.”
“Early recognition and calling for help, early CPR, early defibrillation where appropriate are very, very important, and we need to be addressing all of these, as well as what happens in the cath lab and after admission,” Dr. Price said.
This research was funded by the German Center for Cardiovascular Research. Dr. Desch and Dr. Price reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
A protocol of immediate angiography provided no mortality benefit over a strategy or delayed or more selective angiography among patients resuscitated from out-of-hospital cardiac arrest and without ST-segment elevation, new randomized results show.
“Among patients with resuscitated out-of-hospital cardiac arrest of possible cardiac origin, with shockable and nonshockable arrest rhythm and no ST-elevation, a strategy of immediate, unselected coronary angiography was not found to be beneficial over a delayed and selective approach with regard to the 30-day risk of all-cause death,” concluded principal investigator Steffen Desch, MD, University of Leipzig (Germany) Heart Center.
The results support previous results of the Coronary Angiography after Cardiac Arrest (COACT) trial, in patients with shockable rhythms, which also showed no differences in clinical outcomes between immediate and delayed coronary angiography at both 90 days and 1 year, he noted.
“What the clinicians wanted to know is, is it really necessary to get up at 3 a.m. in the morning to perform a coronary angiography on these patients, and that’s certainly out,” Dr. Desch said in an interview. “So, there’s really no room for this strategy anymore. You can take your time and wait a day or 2.”
These findings, from the TOMAHAWK trial, were presented Aug. 29 at the annual congress of the European Society of Cardiology and simultaneously published online in the New England Journal of Medicine.
Larger group without ST-segment elevation
Prognosis after out-of-hospital cardiac arrest is extremely poor, with an overall survival rate of less than 10%, Dr. Desch noted. “Actually, only 20% make it to the hospital; the vast majority of these patients die out in the field, so there’s really a great need in improving treatment.”
Acute coronary syndrome accounts for up to 60% of out-of-hospital arrests in which a cardiac cause has been identified, the authors wrote in their report. ST-segment elevation on postresuscitation electrocardiography “has good positive predictive value” for acute coronary lesions triggering the arrest, but in the far larger subgroup of patients without ST-segment elevation, “the spectrum of underlying causes is considerably broader and includes both cardiac and noncardiac causes.”
In patients with myocardial infarction, early revascularization would prevent negative consequences of myocardial injury, but unselected early coronary angiography would put patients not having an MI at unnecessary risk for procedural complications or delay in the diagnosis of the actual cause of their arrest, they noted.
In this trial, the researchers randomly assigned 554 patients from 31 sites in Germany and Denmark who were successfully resuscitated after cardiac arrest of possible cardiac origin to immediate transfer for coronary angiography or to initial intensive care assessment with delayed or selective angiography after a minimum delay of at least 1 day.
In the end, the average delay in this arm was 2 days, Dr. Desch noted. If the clinical course indicated that a coronary cause was unlikely, angiography might not be performed at all in this group.
No patient had ST-segment elevation on postresuscitation electrocardiography. The primary endpoint was death from any cause at 30 days; secondary end points were death from any cause or severe neurologic deficit at 30 days.
Results showed that 95% of patients in the immediate angiography group actually underwent the procedure, compared with 62% of those in the delayed group, a finding that was “logical” given the study design, he said.
At 30 days, 54% of patients in the immediate angiography group and 46% in the delayed group had died, a nonsignificant difference (P = .06). Because the researchers had performed an interim analysis, Dr. Desch explained, the final P value for significance in this trial was not .05, but rather .034, to account for multiple comparisons.
The secondary end point of death from any cause or severe neurologic deficit at 30 days “was actually nominally significant in favor of the delayed group,” he said. “So, this is not corrected for multiple testing, it’s just a hypothesis that’s in the room, but it’s certainly worthy of discussion that the immediate strategy might actually cause harm.”
There was no difference between the groups in peak release of myocardial enzymes, or any other safety end points, including bleeding, stroke, or renal failure, Dr. Desch said.
Further analyses showed no large differences between subgroups, including age, diabetes, first monitored rhythm, confirmed MI as the trigger of the arrest, sex, and the time from cardiac arrest to the return of spontaneous circulation, he noted.
Opportunity to minimize harm
Discussant for the results during the presentation was Susanna Price, MBBS, PhD, Royal Brompton Hospital, London.
Dr. Price concluded: “What this means for me, is it gives me information that’s useful regarding the opportunity to minimize harm, which is a lot of what critical care is about, so we don’t necessarily now have to move these patients very acutely when they’ve just come in through the ED [emergency department]. It has implications for resource utilization, but also implications for mobilizing patients around the hospital during COVID-19.”
It’s also important to note that coronary angiography was still carried out in certain patients, “so we still have to have that dialogue with our interventional cardiologists for certain patients who may need to go to the cath lab, and what it should now allow us to do is give appropriate focus to how to manage these patients when they come in to the ED or to our ICUs [intensive care units],” she said.
Dr. Price added, though, that perhaps “the most important slide” in the presentation was that showing 90% of these patients had a witnessed cardiac arrest, “and yet a third of these patients, 168 of them, had no bystander CPR at all.”
She pointed to the “chain of survival” after cardiac arrest, of which Charles D. Deakin, MD, University Hospital Southampton (England), wrote that “not all links are equal.”
“Early recognition and calling for help, early CPR, early defibrillation where appropriate are very, very important, and we need to be addressing all of these, as well as what happens in the cath lab and after admission,” Dr. Price said.
This research was funded by the German Center for Cardiovascular Research. Dr. Desch and Dr. Price reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
A hot dog a day takes 36 minutes away
The death ‘dog’
Imagine you’re out in your backyard managing the grill for a big family barbecue. You’ve got a dazzling assortment of meat assorted on your fancy new propane grill, all charring nicely. Naturally, the hot dogs finish first, and as you pull them off, you figure you’ll help yourself to one now. After all, you are the chef, you deserve a reward. But, as you bite into your smoking hot sandwich, a cold, bony finger taps you on the shoulder. You turn and come face to face with the Grim Reaper. “YOU JUST LOST 36 MINUTES,” Death says. “ALSO, MAY I HAVE ONE OF THOSE? THEY LOOK DELICIOUS.”
Nonplussed and moving automatically, you scoop up another hot dog and place it in a bun. “WITH KETCHUP PLEASE,” Death says. “I NEVER CARED FOR MUSTARD.”
“I don’t understand,” you say. “Surely I won’t die at a family barbecue.”
“DO NOT CALL ME SHIRLEY,” Death says. “AND YOU WILL NOT. IT’S PART OF MY NEW CONTRACT.”
A new study, published in Nature Food, found that a person may lose up to 36 minutes for every hot dog consumed. Researchers from the University of Michigan analyzed nearly 6,000 different foods using a new nutritional index to quantify their health effects in minutes of healthy life lost or gained. Eating a serving of nuts adds an extra 26 minutes of life. The researchers determined that replacing just 10% of daily caloric intake from beef and processed foods with fruits, vegetables, and nuts can add 48 minutes per day. It would also reduce the daily carbon footprint by 33%.
“So you go around to everyone eating bad food and tell them how much life they’ve lost?” you ask when the Grim Reaper finishes his story. “Sounds like a drag.”
“IT IS. WE’VE HAD TO HIRE NEW BLOOD.” Death chuckles at its own bad pun. “NOW IF YOU’LL EXCUSE ME, I MUST CHASTISE A MAN IN FLORIDA FOR EATING A WELL-DONE STEAK.”
More stress, less sex
As the world becomes a more stressful place, the human population could face a 50% drop by the end of the century.
Think of stress as a one-two punch to the libido and human fertility. The more people are stressed out, the less likely they are to have quality interactions with others. Many of us would rather be alone with our wine and cheese to watch our favorite show.
Researchers have found that high stress levels have been known to drop sperm count, ovulation, and sexual activity. Guess what? There has been a 50% decrease in sperm counts over the last 50 years. That’s the second punch. But let’s not forget, the times are changing.
“Changes in reproductive behavior that contribute to the population drop include more young couples choosing to be ‘child-free,’ people having fewer children, and couples waiting longer to start families,” said Alexander Suvorov, PhD, of the University of Massachusetts, the paper’s author.
Let’s summarize: The more stress we’re dealing with, the less people want to deal with each other.
Who would have thought the future would be less fun?
‘You are not a horse. You are not a cow. Seriously, y’all. Stop it.’
WARNING: The following descriptions of COVID-19–related insanity may be offensive to some readers.
Greetings, ladies and gentlemen! Welcome to the first round of Pandemic Pandemonium. Let’s get right to the action.
This week’s preshow match-off involves face mask woes. The first comes to us from Alabama, where a woman wore a space helmet to a school board meeting to protest mask mandates. The second comes from Australia, in the form of mischievous magpies. We will explain.
It is not uncommon for magpies to attack those who come too close to their nests in the spring, or “swooping season,” as it’s affectionately called. The magpies are smart enough to recognize the faces of people they see regularly and not attack; however, it’s feared that mask wearing will change this.
While you’re chewing on that exciting appetizer, let’s take a look at our main course, which has a distinct governmental flavor. Jeff Landry is the attorney general of Louisiana, and, like our space-helmet wearer, he’s not a fan of mask mandates. According to Business Insider, Mr. Landry “drafted and distributed sample letters intended to help parents evade mask-wearing ordinances and COVID-19 vaccination requirements for their children in schools.”
Up against him is the Food and Drug Administration’s Twitter account. In an unrelated matter, the agency tweeted, “You are not a horse. You are not a cow. Seriously, y’all. Stop it.” This was in response to people using the nonhuman forms of ivermectin to treat very human COVID-19.
Well, there you have it. Who will win tonight’s exciting edition of Pandemic Pandemonium? The first reader to contact us gets to decide the fate of these worthy contestants.
From venomous poison to heart drug
It’s not likely that anyone who sees a giant, venomous spider is thinking, “Hey! That thing could save my life!” It’s usually quite the opposite. Honestly, we would run away from just about any spider. But what if one of the deadliest spiders in the world could also save you from dying of a heart attack?
You probably don’t believe us, right? That’s fair, but the deadly Fraser Island (K’gari) funnel web spider, might also be the most helpful. Investigators from the University of Queensland in Australia have found a way to extract a molecule from the spider’s venom that might help stop damage from heart attacks and may even preserve hearts being used for transplants. “The Hi1a protein from spider venom blocks acid-sensing ion channels in the heart, so the death message is blocked, cell death is reduced, and we see improved heart cell survival,” Nathan Palpant, PhD, of the university, noted in a written statement.
No one has ever developed a drug to stop the “death signal,” so maybe it’s time to befriend spiders instead of running away from them in horror. Just leave the venom extraction to the professionals.
The death ‘dog’
Imagine you’re out in your backyard managing the grill for a big family barbecue. You’ve got a dazzling assortment of meat assorted on your fancy new propane grill, all charring nicely. Naturally, the hot dogs finish first, and as you pull them off, you figure you’ll help yourself to one now. After all, you are the chef, you deserve a reward. But, as you bite into your smoking hot sandwich, a cold, bony finger taps you on the shoulder. You turn and come face to face with the Grim Reaper. “YOU JUST LOST 36 MINUTES,” Death says. “ALSO, MAY I HAVE ONE OF THOSE? THEY LOOK DELICIOUS.”
Nonplussed and moving automatically, you scoop up another hot dog and place it in a bun. “WITH KETCHUP PLEASE,” Death says. “I NEVER CARED FOR MUSTARD.”
“I don’t understand,” you say. “Surely I won’t die at a family barbecue.”
“DO NOT CALL ME SHIRLEY,” Death says. “AND YOU WILL NOT. IT’S PART OF MY NEW CONTRACT.”
A new study, published in Nature Food, found that a person may lose up to 36 minutes for every hot dog consumed. Researchers from the University of Michigan analyzed nearly 6,000 different foods using a new nutritional index to quantify their health effects in minutes of healthy life lost or gained. Eating a serving of nuts adds an extra 26 minutes of life. The researchers determined that replacing just 10% of daily caloric intake from beef and processed foods with fruits, vegetables, and nuts can add 48 minutes per day. It would also reduce the daily carbon footprint by 33%.
“So you go around to everyone eating bad food and tell them how much life they’ve lost?” you ask when the Grim Reaper finishes his story. “Sounds like a drag.”
“IT IS. WE’VE HAD TO HIRE NEW BLOOD.” Death chuckles at its own bad pun. “NOW IF YOU’LL EXCUSE ME, I MUST CHASTISE A MAN IN FLORIDA FOR EATING A WELL-DONE STEAK.”
More stress, less sex
As the world becomes a more stressful place, the human population could face a 50% drop by the end of the century.
Think of stress as a one-two punch to the libido and human fertility. The more people are stressed out, the less likely they are to have quality interactions with others. Many of us would rather be alone with our wine and cheese to watch our favorite show.
Researchers have found that high stress levels have been known to drop sperm count, ovulation, and sexual activity. Guess what? There has been a 50% decrease in sperm counts over the last 50 years. That’s the second punch. But let’s not forget, the times are changing.
“Changes in reproductive behavior that contribute to the population drop include more young couples choosing to be ‘child-free,’ people having fewer children, and couples waiting longer to start families,” said Alexander Suvorov, PhD, of the University of Massachusetts, the paper’s author.
Let’s summarize: The more stress we’re dealing with, the less people want to deal with each other.
Who would have thought the future would be less fun?
‘You are not a horse. You are not a cow. Seriously, y’all. Stop it.’
WARNING: The following descriptions of COVID-19–related insanity may be offensive to some readers.
Greetings, ladies and gentlemen! Welcome to the first round of Pandemic Pandemonium. Let’s get right to the action.
This week’s preshow match-off involves face mask woes. The first comes to us from Alabama, where a woman wore a space helmet to a school board meeting to protest mask mandates. The second comes from Australia, in the form of mischievous magpies. We will explain.
It is not uncommon for magpies to attack those who come too close to their nests in the spring, or “swooping season,” as it’s affectionately called. The magpies are smart enough to recognize the faces of people they see regularly and not attack; however, it’s feared that mask wearing will change this.
While you’re chewing on that exciting appetizer, let’s take a look at our main course, which has a distinct governmental flavor. Jeff Landry is the attorney general of Louisiana, and, like our space-helmet wearer, he’s not a fan of mask mandates. According to Business Insider, Mr. Landry “drafted and distributed sample letters intended to help parents evade mask-wearing ordinances and COVID-19 vaccination requirements for their children in schools.”
Up against him is the Food and Drug Administration’s Twitter account. In an unrelated matter, the agency tweeted, “You are not a horse. You are not a cow. Seriously, y’all. Stop it.” This was in response to people using the nonhuman forms of ivermectin to treat very human COVID-19.
Well, there you have it. Who will win tonight’s exciting edition of Pandemic Pandemonium? The first reader to contact us gets to decide the fate of these worthy contestants.
From venomous poison to heart drug
It’s not likely that anyone who sees a giant, venomous spider is thinking, “Hey! That thing could save my life!” It’s usually quite the opposite. Honestly, we would run away from just about any spider. But what if one of the deadliest spiders in the world could also save you from dying of a heart attack?
You probably don’t believe us, right? That’s fair, but the deadly Fraser Island (K’gari) funnel web spider, might also be the most helpful. Investigators from the University of Queensland in Australia have found a way to extract a molecule from the spider’s venom that might help stop damage from heart attacks and may even preserve hearts being used for transplants. “The Hi1a protein from spider venom blocks acid-sensing ion channels in the heart, so the death message is blocked, cell death is reduced, and we see improved heart cell survival,” Nathan Palpant, PhD, of the university, noted in a written statement.
No one has ever developed a drug to stop the “death signal,” so maybe it’s time to befriend spiders instead of running away from them in horror. Just leave the venom extraction to the professionals.
The death ‘dog’
Imagine you’re out in your backyard managing the grill for a big family barbecue. You’ve got a dazzling assortment of meat assorted on your fancy new propane grill, all charring nicely. Naturally, the hot dogs finish first, and as you pull them off, you figure you’ll help yourself to one now. After all, you are the chef, you deserve a reward. But, as you bite into your smoking hot sandwich, a cold, bony finger taps you on the shoulder. You turn and come face to face with the Grim Reaper. “YOU JUST LOST 36 MINUTES,” Death says. “ALSO, MAY I HAVE ONE OF THOSE? THEY LOOK DELICIOUS.”
Nonplussed and moving automatically, you scoop up another hot dog and place it in a bun. “WITH KETCHUP PLEASE,” Death says. “I NEVER CARED FOR MUSTARD.”
“I don’t understand,” you say. “Surely I won’t die at a family barbecue.”
“DO NOT CALL ME SHIRLEY,” Death says. “AND YOU WILL NOT. IT’S PART OF MY NEW CONTRACT.”
A new study, published in Nature Food, found that a person may lose up to 36 minutes for every hot dog consumed. Researchers from the University of Michigan analyzed nearly 6,000 different foods using a new nutritional index to quantify their health effects in minutes of healthy life lost or gained. Eating a serving of nuts adds an extra 26 minutes of life. The researchers determined that replacing just 10% of daily caloric intake from beef and processed foods with fruits, vegetables, and nuts can add 48 minutes per day. It would also reduce the daily carbon footprint by 33%.
“So you go around to everyone eating bad food and tell them how much life they’ve lost?” you ask when the Grim Reaper finishes his story. “Sounds like a drag.”
“IT IS. WE’VE HAD TO HIRE NEW BLOOD.” Death chuckles at its own bad pun. “NOW IF YOU’LL EXCUSE ME, I MUST CHASTISE A MAN IN FLORIDA FOR EATING A WELL-DONE STEAK.”
More stress, less sex
As the world becomes a more stressful place, the human population could face a 50% drop by the end of the century.
Think of stress as a one-two punch to the libido and human fertility. The more people are stressed out, the less likely they are to have quality interactions with others. Many of us would rather be alone with our wine and cheese to watch our favorite show.
Researchers have found that high stress levels have been known to drop sperm count, ovulation, and sexual activity. Guess what? There has been a 50% decrease in sperm counts over the last 50 years. That’s the second punch. But let’s not forget, the times are changing.
“Changes in reproductive behavior that contribute to the population drop include more young couples choosing to be ‘child-free,’ people having fewer children, and couples waiting longer to start families,” said Alexander Suvorov, PhD, of the University of Massachusetts, the paper’s author.
Let’s summarize: The more stress we’re dealing with, the less people want to deal with each other.
Who would have thought the future would be less fun?
‘You are not a horse. You are not a cow. Seriously, y’all. Stop it.’
WARNING: The following descriptions of COVID-19–related insanity may be offensive to some readers.
Greetings, ladies and gentlemen! Welcome to the first round of Pandemic Pandemonium. Let’s get right to the action.
This week’s preshow match-off involves face mask woes. The first comes to us from Alabama, where a woman wore a space helmet to a school board meeting to protest mask mandates. The second comes from Australia, in the form of mischievous magpies. We will explain.
It is not uncommon for magpies to attack those who come too close to their nests in the spring, or “swooping season,” as it’s affectionately called. The magpies are smart enough to recognize the faces of people they see regularly and not attack; however, it’s feared that mask wearing will change this.
While you’re chewing on that exciting appetizer, let’s take a look at our main course, which has a distinct governmental flavor. Jeff Landry is the attorney general of Louisiana, and, like our space-helmet wearer, he’s not a fan of mask mandates. According to Business Insider, Mr. Landry “drafted and distributed sample letters intended to help parents evade mask-wearing ordinances and COVID-19 vaccination requirements for their children in schools.”
Up against him is the Food and Drug Administration’s Twitter account. In an unrelated matter, the agency tweeted, “You are not a horse. You are not a cow. Seriously, y’all. Stop it.” This was in response to people using the nonhuman forms of ivermectin to treat very human COVID-19.
Well, there you have it. Who will win tonight’s exciting edition of Pandemic Pandemonium? The first reader to contact us gets to decide the fate of these worthy contestants.
From venomous poison to heart drug
It’s not likely that anyone who sees a giant, venomous spider is thinking, “Hey! That thing could save my life!” It’s usually quite the opposite. Honestly, we would run away from just about any spider. But what if one of the deadliest spiders in the world could also save you from dying of a heart attack?
You probably don’t believe us, right? That’s fair, but the deadly Fraser Island (K’gari) funnel web spider, might also be the most helpful. Investigators from the University of Queensland in Australia have found a way to extract a molecule from the spider’s venom that might help stop damage from heart attacks and may even preserve hearts being used for transplants. “The Hi1a protein from spider venom blocks acid-sensing ion channels in the heart, so the death message is blocked, cell death is reduced, and we see improved heart cell survival,” Nathan Palpant, PhD, of the university, noted in a written statement.
No one has ever developed a drug to stop the “death signal,” so maybe it’s time to befriend spiders instead of running away from them in horror. Just leave the venom extraction to the professionals.
U.S. kidney transplants grow in number and success
During 2016-2019, U.S. centers performed kidney transplants in nearly 77,000 patients, a jump of almost 25% compared with 4-year averages of about 62,000 patients throughout 2004-2015. That works out to about 15,000 more patients receiving donor kidneys, Sundaram Hariharan, MD, and associates reported in the New England Journal of Medicine in a review of all U.S. renal transplantations performed during 1996-2019.
Coupled with the volume uptick during this 24-year period were new lows in graft losses and patient deaths. By 2018, mortality during the first year following transplantation occurred at about a 1% rate among patients who had received a kidney from a living donor, and at about a 3% rate when the organ came from a deceased donor, nearly half the rate of 2 decades earlier, in 1996. Rates of first-year graft loss during 2017 were also about half of what they had been in 1996, occurring in about 2% of patients who received a living donor organ and in about 6% of those who got a kidney from a deceased donor during 2017.
“Twenty years ago, kidney transplantation was the preferred option compared with dialysis, and even more so now,” summed up Dr. Hariharan, a senior transplant nephrologist and professor of medicine and surgery at the University of Pittsburgh Medical Center and first author of the report. Kidney transplantation survival at U.S. centers “improved steadily over the past 24 years, despite patient variables becoming worse,” he said in an interview.
Kidney recipients are older, more obese, and have more prevalent diabetes
During the period studied, kidney transplant recipients became on average older and more obese, and had a higher prevalence of diabetes; the age of organ donors grew as well. The prevalence of diabetes among patients who received a kidney from a deceased donor increased from 24% during 1996-1999 to 36% during 2016-2019, while diabetes prevalence among recipients of an organ from a living donor rose from 25% in 1996-1999 to 29% during 2016-2019.
The improved graft and patient survival numbers “are very encouraging trends,” said Michelle A. Josephson, MD, professor and medical director of kidney transplantation at the University of Chicago, who was not involved with the report. “We have been hearing for a number of years that short-term graft survival had improved, but I’m thrilled to learn that long-term survival has also improved.”
The report documented 10-year survival of graft recipients during 2008-2011 of 67%, up from 61% during 1996-1999, and a 10-year overall graft survival rate of 54% in the 2008-2011 cohort, an improvement from the 42% rate in patients who received their organs in 1996-1999, changes Dr. Hariharan characterized as “modest.”
These improvements in long-term graft and patient survival are “meaningful, and particularly notable that outcomes improved despite increased complexity of the transplant population,” said Krista L. Lentine, MD, PhD, professor and medical director of living donation at Saint Louis University. But “despite these improvements, long-term graft survival remains limited,” she cautioned, especially because of risks for substantial complications from chronic immunosuppressive treatment including infection, cancer, glucose intolerance, and dyslipidemia.
The analysis reported by Dr. Hariharan and his associates used data collected by the Scientific Registry of Transplant Patients, run under contract with the U.S. Department of Health and Human Services, which has tracked all patients who have had kidney transplants at U.S. centers since the late 1980s, said Dr. Hariharan. The database included just over 362,000 total transplants during the 24-year period studied, with 36% of all transplants involving organs from living donors with the remaining patients receiving kidneys from deceased donors.
Living donations still stagnant; deceased-donor kidneys rise
The data showed that the rate of transplants from living donors was stagnant for 2 decades, with 22,525 patients transplanted during 2000-2003, and 23,746 transplanted during 2016-2019, with very similar rates during the intervening years. The recent spurt in transplants during 2016-2019 compared with the preceding decade depended almost entirely on kidneys from deceased donors. This rate jumped from the steady, slow rise it showed during 1996-2015, when deceased-donor transplants rose from about 30,000 during 1996-1999 to about 41,000 during 2012-2015, to a more dramatic increase of about 12,000 additional transplants during the most recent period, adding up to a total of more than 53,000 transplants from deceased donors during 2016-2019.
“I strongly recommend organs from living donors” when feasible, said Dr. Hariharan. “At some centers, a high proportion of transplants use living donors, but not at other centers,” he said.
It’s unknown why transplants using organs from deceased donors has shown this growth, but Dr. Hariharan suggested a multifactorial explanation. Those factors include growth in the number of patients with end-stage renal disease who require dialysis, increased numbers of patients listed for kidney transplant, new approaches that allow organs from older donors and those infected with pathogens such as hepatitis C virus or HIV, greater numbers of people and families agreeing to donate organs, and possibly the opioid crisis that may have led to increased organ donation. The number of U.S. centers performing kidney transplants rose from fewer than 200 about a quarter of a century ago to about 250 today, he added.
‘Immuno Bill’ guarantees Medicare coverage for immunosuppression
Dr. Hariharan voiced optimism that graft and patient survival rates will continue to improve going forward. One factor will likely be the passage in late 2020 of the “Immuno Bill” by the U.S. Congress, which among other things mandated ongoing coverage starting in 2023 for immunosuppressive drugs for all Medicare beneficiaries with a kidney transplant. Until then, Medicare provides coverage for only 36 months, a time limit that has resulted in nearly 400 kidney recipients annually losing coverage of their immunosuppression medications.
Dr. Hariharan and coauthors called the existing potential for discontinuation of immunosuppressive drug an “unnecessary impediment to long-term survival for which patients and society paid a heavy price.”
“Kidney transplantation, especially from living donors, offers patients with kidney failure the best chance for long-term survival and improved quality of life, with lower cost to the health care system,” Dr. Lentine said in an interview. Despite the many positive trends detailed in the report from Dr. Hariharan and coauthors, “the vast majority of the more than 700,000 people in the United States with kidney failure will not have an opportunity to receive a transplant due to limitations in organ supply.” And many patients who receive a kidney transplant eventually must resume dialysis because of “limited long-term graft survival resulting from allograft nephropathy, recurrent native disease, medication nonadherence, or other causes.” Plus many potentially transplantable organs go unused.
Dr. Lentine cited a position statement issued in July 2021 by the National Kidney Foundation that made several recommendations on how to improve access to kidney transplants and improve outcomes. “Expanding opportunities for safe living donation, eliminating racial disparities in living-donor access, improving wait-list access and transport readiness, maximizing use of deceased-donor organs, and extending graft longevity are critical priorities,” said Dr. Lentine, lead author on the statement.
“For many or even most patients with kidney failure transplantation is the optimal form of renal replacement. The better recent outcomes and evolving management strategies make transplantation an even more attractive option,” said Dr. Josephson. Improved outcomes among U.S. transplant patients also highlights the “importance of increasing access to kidney transplantation” for all people with kidney failure who could benefit from this treatment, she added.
Dr. Hariharan and Dr. Lentine had no relevant disclosures. Dr. Josephson has been a consultant to UCB and has an ownership interest in Seagen.
During 2016-2019, U.S. centers performed kidney transplants in nearly 77,000 patients, a jump of almost 25% compared with 4-year averages of about 62,000 patients throughout 2004-2015. That works out to about 15,000 more patients receiving donor kidneys, Sundaram Hariharan, MD, and associates reported in the New England Journal of Medicine in a review of all U.S. renal transplantations performed during 1996-2019.
Coupled with the volume uptick during this 24-year period were new lows in graft losses and patient deaths. By 2018, mortality during the first year following transplantation occurred at about a 1% rate among patients who had received a kidney from a living donor, and at about a 3% rate when the organ came from a deceased donor, nearly half the rate of 2 decades earlier, in 1996. Rates of first-year graft loss during 2017 were also about half of what they had been in 1996, occurring in about 2% of patients who received a living donor organ and in about 6% of those who got a kidney from a deceased donor during 2017.
“Twenty years ago, kidney transplantation was the preferred option compared with dialysis, and even more so now,” summed up Dr. Hariharan, a senior transplant nephrologist and professor of medicine and surgery at the University of Pittsburgh Medical Center and first author of the report. Kidney transplantation survival at U.S. centers “improved steadily over the past 24 years, despite patient variables becoming worse,” he said in an interview.
Kidney recipients are older, more obese, and have more prevalent diabetes
During the period studied, kidney transplant recipients became on average older and more obese, and had a higher prevalence of diabetes; the age of organ donors grew as well. The prevalence of diabetes among patients who received a kidney from a deceased donor increased from 24% during 1996-1999 to 36% during 2016-2019, while diabetes prevalence among recipients of an organ from a living donor rose from 25% in 1996-1999 to 29% during 2016-2019.
The improved graft and patient survival numbers “are very encouraging trends,” said Michelle A. Josephson, MD, professor and medical director of kidney transplantation at the University of Chicago, who was not involved with the report. “We have been hearing for a number of years that short-term graft survival had improved, but I’m thrilled to learn that long-term survival has also improved.”
The report documented 10-year survival of graft recipients during 2008-2011 of 67%, up from 61% during 1996-1999, and a 10-year overall graft survival rate of 54% in the 2008-2011 cohort, an improvement from the 42% rate in patients who received their organs in 1996-1999, changes Dr. Hariharan characterized as “modest.”
These improvements in long-term graft and patient survival are “meaningful, and particularly notable that outcomes improved despite increased complexity of the transplant population,” said Krista L. Lentine, MD, PhD, professor and medical director of living donation at Saint Louis University. But “despite these improvements, long-term graft survival remains limited,” she cautioned, especially because of risks for substantial complications from chronic immunosuppressive treatment including infection, cancer, glucose intolerance, and dyslipidemia.
The analysis reported by Dr. Hariharan and his associates used data collected by the Scientific Registry of Transplant Patients, run under contract with the U.S. Department of Health and Human Services, which has tracked all patients who have had kidney transplants at U.S. centers since the late 1980s, said Dr. Hariharan. The database included just over 362,000 total transplants during the 24-year period studied, with 36% of all transplants involving organs from living donors with the remaining patients receiving kidneys from deceased donors.
Living donations still stagnant; deceased-donor kidneys rise
The data showed that the rate of transplants from living donors was stagnant for 2 decades, with 22,525 patients transplanted during 2000-2003, and 23,746 transplanted during 2016-2019, with very similar rates during the intervening years. The recent spurt in transplants during 2016-2019 compared with the preceding decade depended almost entirely on kidneys from deceased donors. This rate jumped from the steady, slow rise it showed during 1996-2015, when deceased-donor transplants rose from about 30,000 during 1996-1999 to about 41,000 during 2012-2015, to a more dramatic increase of about 12,000 additional transplants during the most recent period, adding up to a total of more than 53,000 transplants from deceased donors during 2016-2019.
“I strongly recommend organs from living donors” when feasible, said Dr. Hariharan. “At some centers, a high proportion of transplants use living donors, but not at other centers,” he said.
It’s unknown why transplants using organs from deceased donors has shown this growth, but Dr. Hariharan suggested a multifactorial explanation. Those factors include growth in the number of patients with end-stage renal disease who require dialysis, increased numbers of patients listed for kidney transplant, new approaches that allow organs from older donors and those infected with pathogens such as hepatitis C virus or HIV, greater numbers of people and families agreeing to donate organs, and possibly the opioid crisis that may have led to increased organ donation. The number of U.S. centers performing kidney transplants rose from fewer than 200 about a quarter of a century ago to about 250 today, he added.
‘Immuno Bill’ guarantees Medicare coverage for immunosuppression
Dr. Hariharan voiced optimism that graft and patient survival rates will continue to improve going forward. One factor will likely be the passage in late 2020 of the “Immuno Bill” by the U.S. Congress, which among other things mandated ongoing coverage starting in 2023 for immunosuppressive drugs for all Medicare beneficiaries with a kidney transplant. Until then, Medicare provides coverage for only 36 months, a time limit that has resulted in nearly 400 kidney recipients annually losing coverage of their immunosuppression medications.
Dr. Hariharan and coauthors called the existing potential for discontinuation of immunosuppressive drug an “unnecessary impediment to long-term survival for which patients and society paid a heavy price.”
“Kidney transplantation, especially from living donors, offers patients with kidney failure the best chance for long-term survival and improved quality of life, with lower cost to the health care system,” Dr. Lentine said in an interview. Despite the many positive trends detailed in the report from Dr. Hariharan and coauthors, “the vast majority of the more than 700,000 people in the United States with kidney failure will not have an opportunity to receive a transplant due to limitations in organ supply.” And many patients who receive a kidney transplant eventually must resume dialysis because of “limited long-term graft survival resulting from allograft nephropathy, recurrent native disease, medication nonadherence, or other causes.” Plus many potentially transplantable organs go unused.
Dr. Lentine cited a position statement issued in July 2021 by the National Kidney Foundation that made several recommendations on how to improve access to kidney transplants and improve outcomes. “Expanding opportunities for safe living donation, eliminating racial disparities in living-donor access, improving wait-list access and transport readiness, maximizing use of deceased-donor organs, and extending graft longevity are critical priorities,” said Dr. Lentine, lead author on the statement.
“For many or even most patients with kidney failure transplantation is the optimal form of renal replacement. The better recent outcomes and evolving management strategies make transplantation an even more attractive option,” said Dr. Josephson. Improved outcomes among U.S. transplant patients also highlights the “importance of increasing access to kidney transplantation” for all people with kidney failure who could benefit from this treatment, she added.
Dr. Hariharan and Dr. Lentine had no relevant disclosures. Dr. Josephson has been a consultant to UCB and has an ownership interest in Seagen.
During 2016-2019, U.S. centers performed kidney transplants in nearly 77,000 patients, a jump of almost 25% compared with 4-year averages of about 62,000 patients throughout 2004-2015. That works out to about 15,000 more patients receiving donor kidneys, Sundaram Hariharan, MD, and associates reported in the New England Journal of Medicine in a review of all U.S. renal transplantations performed during 1996-2019.
Coupled with the volume uptick during this 24-year period were new lows in graft losses and patient deaths. By 2018, mortality during the first year following transplantation occurred at about a 1% rate among patients who had received a kidney from a living donor, and at about a 3% rate when the organ came from a deceased donor, nearly half the rate of 2 decades earlier, in 1996. Rates of first-year graft loss during 2017 were also about half of what they had been in 1996, occurring in about 2% of patients who received a living donor organ and in about 6% of those who got a kidney from a deceased donor during 2017.
“Twenty years ago, kidney transplantation was the preferred option compared with dialysis, and even more so now,” summed up Dr. Hariharan, a senior transplant nephrologist and professor of medicine and surgery at the University of Pittsburgh Medical Center and first author of the report. Kidney transplantation survival at U.S. centers “improved steadily over the past 24 years, despite patient variables becoming worse,” he said in an interview.
Kidney recipients are older, more obese, and have more prevalent diabetes
During the period studied, kidney transplant recipients became on average older and more obese, and had a higher prevalence of diabetes; the age of organ donors grew as well. The prevalence of diabetes among patients who received a kidney from a deceased donor increased from 24% during 1996-1999 to 36% during 2016-2019, while diabetes prevalence among recipients of an organ from a living donor rose from 25% in 1996-1999 to 29% during 2016-2019.
The improved graft and patient survival numbers “are very encouraging trends,” said Michelle A. Josephson, MD, professor and medical director of kidney transplantation at the University of Chicago, who was not involved with the report. “We have been hearing for a number of years that short-term graft survival had improved, but I’m thrilled to learn that long-term survival has also improved.”
The report documented 10-year survival of graft recipients during 2008-2011 of 67%, up from 61% during 1996-1999, and a 10-year overall graft survival rate of 54% in the 2008-2011 cohort, an improvement from the 42% rate in patients who received their organs in 1996-1999, changes Dr. Hariharan characterized as “modest.”
These improvements in long-term graft and patient survival are “meaningful, and particularly notable that outcomes improved despite increased complexity of the transplant population,” said Krista L. Lentine, MD, PhD, professor and medical director of living donation at Saint Louis University. But “despite these improvements, long-term graft survival remains limited,” she cautioned, especially because of risks for substantial complications from chronic immunosuppressive treatment including infection, cancer, glucose intolerance, and dyslipidemia.
The analysis reported by Dr. Hariharan and his associates used data collected by the Scientific Registry of Transplant Patients, run under contract with the U.S. Department of Health and Human Services, which has tracked all patients who have had kidney transplants at U.S. centers since the late 1980s, said Dr. Hariharan. The database included just over 362,000 total transplants during the 24-year period studied, with 36% of all transplants involving organs from living donors with the remaining patients receiving kidneys from deceased donors.
Living donations still stagnant; deceased-donor kidneys rise
The data showed that the rate of transplants from living donors was stagnant for 2 decades, with 22,525 patients transplanted during 2000-2003, and 23,746 transplanted during 2016-2019, with very similar rates during the intervening years. The recent spurt in transplants during 2016-2019 compared with the preceding decade depended almost entirely on kidneys from deceased donors. This rate jumped from the steady, slow rise it showed during 1996-2015, when deceased-donor transplants rose from about 30,000 during 1996-1999 to about 41,000 during 2012-2015, to a more dramatic increase of about 12,000 additional transplants during the most recent period, adding up to a total of more than 53,000 transplants from deceased donors during 2016-2019.
“I strongly recommend organs from living donors” when feasible, said Dr. Hariharan. “At some centers, a high proportion of transplants use living donors, but not at other centers,” he said.
It’s unknown why transplants using organs from deceased donors has shown this growth, but Dr. Hariharan suggested a multifactorial explanation. Those factors include growth in the number of patients with end-stage renal disease who require dialysis, increased numbers of patients listed for kidney transplant, new approaches that allow organs from older donors and those infected with pathogens such as hepatitis C virus or HIV, greater numbers of people and families agreeing to donate organs, and possibly the opioid crisis that may have led to increased organ donation. The number of U.S. centers performing kidney transplants rose from fewer than 200 about a quarter of a century ago to about 250 today, he added.
‘Immuno Bill’ guarantees Medicare coverage for immunosuppression
Dr. Hariharan voiced optimism that graft and patient survival rates will continue to improve going forward. One factor will likely be the passage in late 2020 of the “Immuno Bill” by the U.S. Congress, which among other things mandated ongoing coverage starting in 2023 for immunosuppressive drugs for all Medicare beneficiaries with a kidney transplant. Until then, Medicare provides coverage for only 36 months, a time limit that has resulted in nearly 400 kidney recipients annually losing coverage of their immunosuppression medications.
Dr. Hariharan and coauthors called the existing potential for discontinuation of immunosuppressive drug an “unnecessary impediment to long-term survival for which patients and society paid a heavy price.”
“Kidney transplantation, especially from living donors, offers patients with kidney failure the best chance for long-term survival and improved quality of life, with lower cost to the health care system,” Dr. Lentine said in an interview. Despite the many positive trends detailed in the report from Dr. Hariharan and coauthors, “the vast majority of the more than 700,000 people in the United States with kidney failure will not have an opportunity to receive a transplant due to limitations in organ supply.” And many patients who receive a kidney transplant eventually must resume dialysis because of “limited long-term graft survival resulting from allograft nephropathy, recurrent native disease, medication nonadherence, or other causes.” Plus many potentially transplantable organs go unused.
Dr. Lentine cited a position statement issued in July 2021 by the National Kidney Foundation that made several recommendations on how to improve access to kidney transplants and improve outcomes. “Expanding opportunities for safe living donation, eliminating racial disparities in living-donor access, improving wait-list access and transport readiness, maximizing use of deceased-donor organs, and extending graft longevity are critical priorities,” said Dr. Lentine, lead author on the statement.
“For many or even most patients with kidney failure transplantation is the optimal form of renal replacement. The better recent outcomes and evolving management strategies make transplantation an even more attractive option,” said Dr. Josephson. Improved outcomes among U.S. transplant patients also highlights the “importance of increasing access to kidney transplantation” for all people with kidney failure who could benefit from this treatment, she added.
Dr. Hariharan and Dr. Lentine had no relevant disclosures. Dr. Josephson has been a consultant to UCB and has an ownership interest in Seagen.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
FDA fully approves Pfizer COVID-19 vaccine
The Food and Drug Administration has granted a biological license application, more commonly known as “full approval,” to the Pfizer-BioNTech COVID-19 vaccine.
It is the first COVID-19 vaccine to be fully licensed in the United States. It will be marketed under the trade name Comirnaty.
The approval applies to individuals ages 16 years and older. The vaccine is still available for emergency use for those ages 12-15.
The FDA’s stamp of approval is somewhat anticlimactic, following months of real-world use and millions of doses doled out to the general population. It comes after months of scrutiny by the agency of the clinical trial data.
Still, the approval puts the vaccines on firmer legal footing and is expected to spur a raft of new vaccination requirements by employers, schools, and universities.
“The FDA approval is the gold standard,” President Joe Biden said from the White House. “Those who have been waiting for full approval should go and get your shot now.”
“It could save your life or the lives of those you love,” he said.
Biden also called on businesses to mandate COVID vaccines for their employees.
Indeed, soon after the approval was announced, Defense Secretary Lloyd Austin said the vaccines would be required for all 1.4 million active duty service members.
Public health advocates have seen full approval as an important tool to increase U.S. vaccination rates and had criticized the FDA for taking so long to grant the license.
In a news briefing on the approval, Peter Marks, MD, director of the FDA’s Center for Biologics Evaluation and Research, said the agency had not dragged its feet.
Marks noted that his team had reviewed tens of thousands of pages of clinical trial data -- down to the level of individual patients. They also inspected clinical trial sites and manufacturing facilities, and reviewed information gathered after the vaccines were authorized for use.
“It’s been 97 days since Pfizer completed the role of its [application for approval] and the clock started, which means that we completed this in about 40% of the normal clock time for a submission of this magnitude,” he said. “People worked day and night.”
The agency resisted pressure to speed up its process, saying a thorough review was necessary to ensure public confidence.
“While millions of people have already safely received COVID-19 vaccines, we recognize that for some, the FDA approval of a vaccine may now instill additional confidence to get vaccinated. Today’s milestone puts us one step closer to altering the course of this pandemic in the U.S.,” acting FDA Commissioner Janet Woodcock said in a FDA news release.
Experts agreed the move would increase public confidence.
“I don't expect a big line outside of vaccination sites this afternoon or tomorrow morning, but it will persuade some,” said William Schaffner, MD, a professor of infectious diseases at Vanderbilt University in Nashville.
A recent Kaiser Family Foundation poll found that 3 in 10 unvaccinated adults said they would be more likely to get vaccinated if the vaccines were given full approval.
More importantly, Schaffner said, the FDA’s approval would lay the groundwork for vaccine mandates. “I think those kinds of mandates are going to be necessary to get us up over 80% vaccinated.”
In granting the approval, the agency reviewed a record amount of data from more than 40,000 people who took part in clinical trials. About 12,000 recipients have been followed for at least 6 months, the agency said.
The FDA also reviewed safety data collected since it issued its emergency use authorization for the shots in December.
Based on the results from the clinical trials, the vaccine was 91% effective at preventing COVID-19 disease. But that estimate came from data collected before the Delta variant became widespread.
The most commonly reported side effects in the clinical trials were pain, redness and swelling at the injection site, fatigue, headache, muscle or joint pain, chills, and fever.
The FDA said the vaccine is effective in preventing COVID-19 and potentially serious outcomes, including hospitalization and death.
Based on safety data reviewed since the two-dose vaccine was approved, the FDA said the data demonstrates a higher risk for heart inflammation -- clinically known as myocarditis or pericarditis -- especially within 7 days after the second dose of the shots. The risk is highest for men under age 40, compared to women and older men.
The prescription information includes warnings about these risks. The FDA said the drugmakers must continue to study the risks and long-term effects on people who have myocarditis after vaccination.
A version of this article first appeared on Medscape.com.
This article was updated on 8/24/21.
The Food and Drug Administration has granted a biological license application, more commonly known as “full approval,” to the Pfizer-BioNTech COVID-19 vaccine.
It is the first COVID-19 vaccine to be fully licensed in the United States. It will be marketed under the trade name Comirnaty.
The approval applies to individuals ages 16 years and older. The vaccine is still available for emergency use for those ages 12-15.
The FDA’s stamp of approval is somewhat anticlimactic, following months of real-world use and millions of doses doled out to the general population. It comes after months of scrutiny by the agency of the clinical trial data.
Still, the approval puts the vaccines on firmer legal footing and is expected to spur a raft of new vaccination requirements by employers, schools, and universities.
“The FDA approval is the gold standard,” President Joe Biden said from the White House. “Those who have been waiting for full approval should go and get your shot now.”
“It could save your life or the lives of those you love,” he said.
Biden also called on businesses to mandate COVID vaccines for their employees.
Indeed, soon after the approval was announced, Defense Secretary Lloyd Austin said the vaccines would be required for all 1.4 million active duty service members.
Public health advocates have seen full approval as an important tool to increase U.S. vaccination rates and had criticized the FDA for taking so long to grant the license.
In a news briefing on the approval, Peter Marks, MD, director of the FDA’s Center for Biologics Evaluation and Research, said the agency had not dragged its feet.
Marks noted that his team had reviewed tens of thousands of pages of clinical trial data -- down to the level of individual patients. They also inspected clinical trial sites and manufacturing facilities, and reviewed information gathered after the vaccines were authorized for use.
“It’s been 97 days since Pfizer completed the role of its [application for approval] and the clock started, which means that we completed this in about 40% of the normal clock time for a submission of this magnitude,” he said. “People worked day and night.”
The agency resisted pressure to speed up its process, saying a thorough review was necessary to ensure public confidence.
“While millions of people have already safely received COVID-19 vaccines, we recognize that for some, the FDA approval of a vaccine may now instill additional confidence to get vaccinated. Today’s milestone puts us one step closer to altering the course of this pandemic in the U.S.,” acting FDA Commissioner Janet Woodcock said in a FDA news release.
Experts agreed the move would increase public confidence.
“I don't expect a big line outside of vaccination sites this afternoon or tomorrow morning, but it will persuade some,” said William Schaffner, MD, a professor of infectious diseases at Vanderbilt University in Nashville.
A recent Kaiser Family Foundation poll found that 3 in 10 unvaccinated adults said they would be more likely to get vaccinated if the vaccines were given full approval.
More importantly, Schaffner said, the FDA’s approval would lay the groundwork for vaccine mandates. “I think those kinds of mandates are going to be necessary to get us up over 80% vaccinated.”
In granting the approval, the agency reviewed a record amount of data from more than 40,000 people who took part in clinical trials. About 12,000 recipients have been followed for at least 6 months, the agency said.
The FDA also reviewed safety data collected since it issued its emergency use authorization for the shots in December.
Based on the results from the clinical trials, the vaccine was 91% effective at preventing COVID-19 disease. But that estimate came from data collected before the Delta variant became widespread.
The most commonly reported side effects in the clinical trials were pain, redness and swelling at the injection site, fatigue, headache, muscle or joint pain, chills, and fever.
The FDA said the vaccine is effective in preventing COVID-19 and potentially serious outcomes, including hospitalization and death.
Based on safety data reviewed since the two-dose vaccine was approved, the FDA said the data demonstrates a higher risk for heart inflammation -- clinically known as myocarditis or pericarditis -- especially within 7 days after the second dose of the shots. The risk is highest for men under age 40, compared to women and older men.
The prescription information includes warnings about these risks. The FDA said the drugmakers must continue to study the risks and long-term effects on people who have myocarditis after vaccination.
A version of this article first appeared on Medscape.com.
This article was updated on 8/24/21.
The Food and Drug Administration has granted a biological license application, more commonly known as “full approval,” to the Pfizer-BioNTech COVID-19 vaccine.
It is the first COVID-19 vaccine to be fully licensed in the United States. It will be marketed under the trade name Comirnaty.
The approval applies to individuals ages 16 years and older. The vaccine is still available for emergency use for those ages 12-15.
The FDA’s stamp of approval is somewhat anticlimactic, following months of real-world use and millions of doses doled out to the general population. It comes after months of scrutiny by the agency of the clinical trial data.
Still, the approval puts the vaccines on firmer legal footing and is expected to spur a raft of new vaccination requirements by employers, schools, and universities.
“The FDA approval is the gold standard,” President Joe Biden said from the White House. “Those who have been waiting for full approval should go and get your shot now.”
“It could save your life or the lives of those you love,” he said.
Biden also called on businesses to mandate COVID vaccines for their employees.
Indeed, soon after the approval was announced, Defense Secretary Lloyd Austin said the vaccines would be required for all 1.4 million active duty service members.
Public health advocates have seen full approval as an important tool to increase U.S. vaccination rates and had criticized the FDA for taking so long to grant the license.
In a news briefing on the approval, Peter Marks, MD, director of the FDA’s Center for Biologics Evaluation and Research, said the agency had not dragged its feet.
Marks noted that his team had reviewed tens of thousands of pages of clinical trial data -- down to the level of individual patients. They also inspected clinical trial sites and manufacturing facilities, and reviewed information gathered after the vaccines were authorized for use.
“It’s been 97 days since Pfizer completed the role of its [application for approval] and the clock started, which means that we completed this in about 40% of the normal clock time for a submission of this magnitude,” he said. “People worked day and night.”
The agency resisted pressure to speed up its process, saying a thorough review was necessary to ensure public confidence.
“While millions of people have already safely received COVID-19 vaccines, we recognize that for some, the FDA approval of a vaccine may now instill additional confidence to get vaccinated. Today’s milestone puts us one step closer to altering the course of this pandemic in the U.S.,” acting FDA Commissioner Janet Woodcock said in a FDA news release.
Experts agreed the move would increase public confidence.
“I don't expect a big line outside of vaccination sites this afternoon or tomorrow morning, but it will persuade some,” said William Schaffner, MD, a professor of infectious diseases at Vanderbilt University in Nashville.
A recent Kaiser Family Foundation poll found that 3 in 10 unvaccinated adults said they would be more likely to get vaccinated if the vaccines were given full approval.
More importantly, Schaffner said, the FDA’s approval would lay the groundwork for vaccine mandates. “I think those kinds of mandates are going to be necessary to get us up over 80% vaccinated.”
In granting the approval, the agency reviewed a record amount of data from more than 40,000 people who took part in clinical trials. About 12,000 recipients have been followed for at least 6 months, the agency said.
The FDA also reviewed safety data collected since it issued its emergency use authorization for the shots in December.
Based on the results from the clinical trials, the vaccine was 91% effective at preventing COVID-19 disease. But that estimate came from data collected before the Delta variant became widespread.
The most commonly reported side effects in the clinical trials were pain, redness and swelling at the injection site, fatigue, headache, muscle or joint pain, chills, and fever.
The FDA said the vaccine is effective in preventing COVID-19 and potentially serious outcomes, including hospitalization and death.
Based on safety data reviewed since the two-dose vaccine was approved, the FDA said the data demonstrates a higher risk for heart inflammation -- clinically known as myocarditis or pericarditis -- especially within 7 days after the second dose of the shots. The risk is highest for men under age 40, compared to women and older men.
The prescription information includes warnings about these risks. The FDA said the drugmakers must continue to study the risks and long-term effects on people who have myocarditis after vaccination.
A version of this article first appeared on Medscape.com.
This article was updated on 8/24/21.
What is the most likely cause of this patient’s fever?
A 63-year-old man undergoes cardiac bypass surgery. He is able to be extubated at 8 hours. The next morning he has a fever to 38.5° C His exam shows no redness at the surgical site, or at his IV sites. His lung exam is unremarkable. His urinalysis is without white blood cells. His white blood cell count is 8,500, and his chest x-ray shows atelectasis without other abnormalities.
One of the earliest things I was taught in my clinical years were the causes of postoperative fever, or the 5Ws, which are wind, water, wound, walk, and wonder drug.
Atelectasis was touted as the cause of early postoperative fever. This became clear fact in my medical student mind, not something that I had ever questioned. But investigation into whether there is evidence of this shows it is only a myth. In actuality, there is scant evidence, if any, for atelectasis causing fever. Frequently, no cause of postoperative fever has been found, despite aggressive attempts to look for one.
What the research says
Fanning and colleagues prospectively looked at 537 women who were undergoing major gynecologic surgery.1 Postoperative fever occurred in 211 of them. In 92% of these patients, no cause for fever was found.
Atelectasis is frequently seen postoperatively. Schlenker and colleagues reported that, in patients with postoperative atelectasis, temperature elevation on the first postoperative day was directly related to the degree of atelectasis, but the white blood cell count elevation was inversely related.2
In this study, atelectasis was diagnosed by auscultation, with chest x-rays ordered at the discretion of the physician. There was little correlation with the auscultatory findings and presence or absence of atelectasis in the patients who did receive chest x-rays.
Engoren did a study to prospectively evaluate 100 postoperative patients with daily chest x-rays and continuous temperature monitoring.3 Results from the day of surgery (day 0) to the second postoperative day showed an increase in presence of atelectasis from 43% on the day of surgery to 79% by day 2.
Fever, defined as temperature greater than 38° C, fell from 37% on the day of surgery to 17% by day 2. Engoren found no association between fever and degree of atelectasis.
Mavros and colleagues did a comprehensive review to determine whether there was evidence to support atelectasis causing fever.4 They concluded that there was no clinical evidence supporting the concept that atelectasis is associated with early postoperative fever.
A possible cause of fever
Mavros and colleagues’ paper suggested that early postoperative fever was caused by stress derived by surgery, which can increase the patient’s interleukin-6 levels and thermostatic set point. This was demonstrated in a small study by Wortel and colleagues, who measured IL-6 levels in the portal and peripheral blood of patients following pancreaticoduodenectomy.5 They found IL-6 levels correlated strongly with peak body temperature.
In conclusion, atelectasis is not a well-established cause of postoperative fever.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Fanning J et al. Infect Dis Obstet Gynecol. 1998; 6(6):252-5 .
2. Schlenker JD and Hubay CA. Arch Surg 1973;107:846-50
3. Engoren M. Chest. 1995;107(1):81-4 .
4. Michael N et al. Chest. 2011;140(2):418-24
5. Wortel CH et al. Surgery. 1993;114(3):564-70 .
A 63-year-old man undergoes cardiac bypass surgery. He is able to be extubated at 8 hours. The next morning he has a fever to 38.5° C His exam shows no redness at the surgical site, or at his IV sites. His lung exam is unremarkable. His urinalysis is without white blood cells. His white blood cell count is 8,500, and his chest x-ray shows atelectasis without other abnormalities.
One of the earliest things I was taught in my clinical years were the causes of postoperative fever, or the 5Ws, which are wind, water, wound, walk, and wonder drug.
Atelectasis was touted as the cause of early postoperative fever. This became clear fact in my medical student mind, not something that I had ever questioned. But investigation into whether there is evidence of this shows it is only a myth. In actuality, there is scant evidence, if any, for atelectasis causing fever. Frequently, no cause of postoperative fever has been found, despite aggressive attempts to look for one.
What the research says
Fanning and colleagues prospectively looked at 537 women who were undergoing major gynecologic surgery.1 Postoperative fever occurred in 211 of them. In 92% of these patients, no cause for fever was found.
Atelectasis is frequently seen postoperatively. Schlenker and colleagues reported that, in patients with postoperative atelectasis, temperature elevation on the first postoperative day was directly related to the degree of atelectasis, but the white blood cell count elevation was inversely related.2
In this study, atelectasis was diagnosed by auscultation, with chest x-rays ordered at the discretion of the physician. There was little correlation with the auscultatory findings and presence or absence of atelectasis in the patients who did receive chest x-rays.
Engoren did a study to prospectively evaluate 100 postoperative patients with daily chest x-rays and continuous temperature monitoring.3 Results from the day of surgery (day 0) to the second postoperative day showed an increase in presence of atelectasis from 43% on the day of surgery to 79% by day 2.
Fever, defined as temperature greater than 38° C, fell from 37% on the day of surgery to 17% by day 2. Engoren found no association between fever and degree of atelectasis.
Mavros and colleagues did a comprehensive review to determine whether there was evidence to support atelectasis causing fever.4 They concluded that there was no clinical evidence supporting the concept that atelectasis is associated with early postoperative fever.
A possible cause of fever
Mavros and colleagues’ paper suggested that early postoperative fever was caused by stress derived by surgery, which can increase the patient’s interleukin-6 levels and thermostatic set point. This was demonstrated in a small study by Wortel and colleagues, who measured IL-6 levels in the portal and peripheral blood of patients following pancreaticoduodenectomy.5 They found IL-6 levels correlated strongly with peak body temperature.
In conclusion, atelectasis is not a well-established cause of postoperative fever.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Fanning J et al. Infect Dis Obstet Gynecol. 1998; 6(6):252-5 .
2. Schlenker JD and Hubay CA. Arch Surg 1973;107:846-50
3. Engoren M. Chest. 1995;107(1):81-4 .
4. Michael N et al. Chest. 2011;140(2):418-24
5. Wortel CH et al. Surgery. 1993;114(3):564-70 .
A 63-year-old man undergoes cardiac bypass surgery. He is able to be extubated at 8 hours. The next morning he has a fever to 38.5° C His exam shows no redness at the surgical site, or at his IV sites. His lung exam is unremarkable. His urinalysis is without white blood cells. His white blood cell count is 8,500, and his chest x-ray shows atelectasis without other abnormalities.
One of the earliest things I was taught in my clinical years were the causes of postoperative fever, or the 5Ws, which are wind, water, wound, walk, and wonder drug.
Atelectasis was touted as the cause of early postoperative fever. This became clear fact in my medical student mind, not something that I had ever questioned. But investigation into whether there is evidence of this shows it is only a myth. In actuality, there is scant evidence, if any, for atelectasis causing fever. Frequently, no cause of postoperative fever has been found, despite aggressive attempts to look for one.
What the research says
Fanning and colleagues prospectively looked at 537 women who were undergoing major gynecologic surgery.1 Postoperative fever occurred in 211 of them. In 92% of these patients, no cause for fever was found.
Atelectasis is frequently seen postoperatively. Schlenker and colleagues reported that, in patients with postoperative atelectasis, temperature elevation on the first postoperative day was directly related to the degree of atelectasis, but the white blood cell count elevation was inversely related.2
In this study, atelectasis was diagnosed by auscultation, with chest x-rays ordered at the discretion of the physician. There was little correlation with the auscultatory findings and presence or absence of atelectasis in the patients who did receive chest x-rays.
Engoren did a study to prospectively evaluate 100 postoperative patients with daily chest x-rays and continuous temperature monitoring.3 Results from the day of surgery (day 0) to the second postoperative day showed an increase in presence of atelectasis from 43% on the day of surgery to 79% by day 2.
Fever, defined as temperature greater than 38° C, fell from 37% on the day of surgery to 17% by day 2. Engoren found no association between fever and degree of atelectasis.
Mavros and colleagues did a comprehensive review to determine whether there was evidence to support atelectasis causing fever.4 They concluded that there was no clinical evidence supporting the concept that atelectasis is associated with early postoperative fever.
A possible cause of fever
Mavros and colleagues’ paper suggested that early postoperative fever was caused by stress derived by surgery, which can increase the patient’s interleukin-6 levels and thermostatic set point. This was demonstrated in a small study by Wortel and colleagues, who measured IL-6 levels in the portal and peripheral blood of patients following pancreaticoduodenectomy.5 They found IL-6 levels correlated strongly with peak body temperature.
In conclusion, atelectasis is not a well-established cause of postoperative fever.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Fanning J et al. Infect Dis Obstet Gynecol. 1998; 6(6):252-5 .
2. Schlenker JD and Hubay CA. Arch Surg 1973;107:846-50
3. Engoren M. Chest. 1995;107(1):81-4 .
4. Michael N et al. Chest. 2011;140(2):418-24
5. Wortel CH et al. Surgery. 1993;114(3):564-70 .
Pandemic derails small success in lowering diabetes-related amputations
Rates of minor diabetes-related lower extremity amputations (LEAs) in hospitalized patients increased between 2009 and 2017 in all racial and ethnic groups, in both rural and urban areas, and in all geographic regions across the United States, a new retrospective, observational study indicates.
In contrast, major lower extremity amputation rates held steady during the study period with a few exceptions.
There was also a decline in major-to-minor amputation ratios, especially among Native Americans – a sign that diabetes was being better managed and foot ulcers were being caught earlier, preventing the need for a major amputation above the foot or below or above the knee.
Minor LEAs include the loss of a toe, toes, or a foot.
“While I know an amputation is devastating either way, having a minor amputation is better than having a major amputation, and trends [at least to 2017] show that comprehensive foot examinations are paying off,” lead author Marvellous Akinlotan, PhD, MPH, a research associate at the Southwest Rural Health Research Center in Bryan, Texas, said in an interview.
Asked to comment, Marcia Ory, PhD, MPH, director of the Center for Population Health & Aging, Texas A&M School of Public Health, College Station, who was not involved in the study, said: “It points to some successes, but it also points to the need for continued education and preventive care to reduce all types of amputations.”
The study was published online in Diabetes Care.
Amputations increased during COVID-19
However, the study was conducted prior to the COVID-19 pandemic, and amputation rates appear to have significantly worsened during the past 18 months.
In a summary of recent evidence collated by the Amputee Coalition, the authors point out that not only does COVID-19 itself put patients at higher risk for limb loss because severe infection increases the risk of blood clots, but patients with diabetes appear to have been far more likely to undergo any level of amputation during the pandemic than before it began.
In a study of patients with diabetes attending a foot and ankle surgery service in Ohio, the risk of having any level of amputation was 10.8 times higher during compared with before the pandemic. And of patients undergoing any amputation, the odds for receiving a major amputation was 3.1 times higher than before the pandemic.
Telehealth and web-based options for diabetes care and education could help improve health outcomes, particularly during lockdowns.
“Having a diabetes-related amputation is life-changing – it brings disability and functional limitations to the individual – and within the health care system, it reflects the failure of secondary prevention efforts, which ideally should slow the progression of diabetic complications,” noted Dr. Akinlotan.
Race and geography affect risk of amputation
In their study, Dr. Akinlotan and colleagues used data from the National Inpatient Sample to identify trends in LEAs among patients primarily hospitalized for diabetes in the United States between 2009 and 2017.
“The primary outcome variable was documentation of either minor or major LEA during a diabetes-related admission,” they explain.
Minor LEAs increased significantly across all ethnic groups.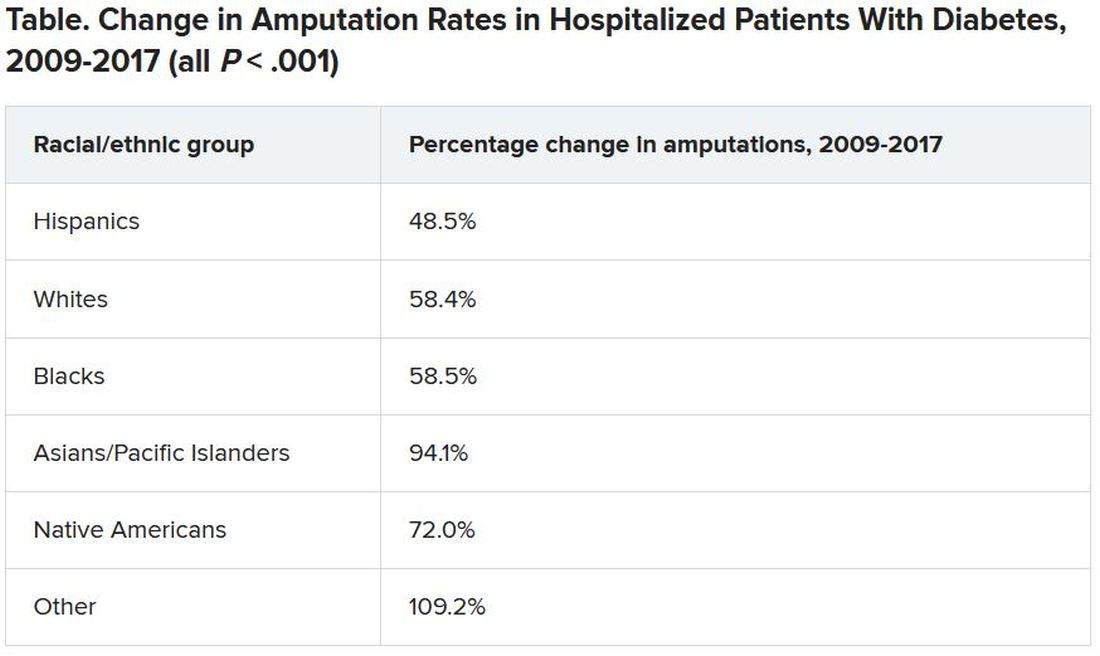
Although major amputation rates remained steady, “we did find that some groups remained at risk for having a major amputation,” Dr. Akinlotan noted.
White populations, people in the Midwest, and rural areas saw notable increases in major LEAs, as did “... Blacks, Hispanics, [and] those living in the South,” she said.
Patients need to be encouraged to monitor and control their blood glucose, to offset modifiable risk factors, and to seek regular medical attention to prevent an insidious diabetic complication from developing further, she said.
“It’s important for patients to know that continuing care is necessary,” Dr. Akinlotan stressed. “Diabetes is chronic and complex, but it can be managed, so that’s the good news.”
Dr. Ory agrees: “Effective management will require an all-in approach, with doctors and patients working together.
“Given the limited time in doctor-patient encounters, physicians can benefit patients by referring them to evidence-based, self-management education programs, which are proliferating around in the county,” she added.
The authors and Dr. Ory have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rates of minor diabetes-related lower extremity amputations (LEAs) in hospitalized patients increased between 2009 and 2017 in all racial and ethnic groups, in both rural and urban areas, and in all geographic regions across the United States, a new retrospective, observational study indicates.
In contrast, major lower extremity amputation rates held steady during the study period with a few exceptions.
There was also a decline in major-to-minor amputation ratios, especially among Native Americans – a sign that diabetes was being better managed and foot ulcers were being caught earlier, preventing the need for a major amputation above the foot or below or above the knee.
Minor LEAs include the loss of a toe, toes, or a foot.
“While I know an amputation is devastating either way, having a minor amputation is better than having a major amputation, and trends [at least to 2017] show that comprehensive foot examinations are paying off,” lead author Marvellous Akinlotan, PhD, MPH, a research associate at the Southwest Rural Health Research Center in Bryan, Texas, said in an interview.
Asked to comment, Marcia Ory, PhD, MPH, director of the Center for Population Health & Aging, Texas A&M School of Public Health, College Station, who was not involved in the study, said: “It points to some successes, but it also points to the need for continued education and preventive care to reduce all types of amputations.”
The study was published online in Diabetes Care.
Amputations increased during COVID-19
However, the study was conducted prior to the COVID-19 pandemic, and amputation rates appear to have significantly worsened during the past 18 months.
In a summary of recent evidence collated by the Amputee Coalition, the authors point out that not only does COVID-19 itself put patients at higher risk for limb loss because severe infection increases the risk of blood clots, but patients with diabetes appear to have been far more likely to undergo any level of amputation during the pandemic than before it began.
In a study of patients with diabetes attending a foot and ankle surgery service in Ohio, the risk of having any level of amputation was 10.8 times higher during compared with before the pandemic. And of patients undergoing any amputation, the odds for receiving a major amputation was 3.1 times higher than before the pandemic.
Telehealth and web-based options for diabetes care and education could help improve health outcomes, particularly during lockdowns.
“Having a diabetes-related amputation is life-changing – it brings disability and functional limitations to the individual – and within the health care system, it reflects the failure of secondary prevention efforts, which ideally should slow the progression of diabetic complications,” noted Dr. Akinlotan.
Race and geography affect risk of amputation
In their study, Dr. Akinlotan and colleagues used data from the National Inpatient Sample to identify trends in LEAs among patients primarily hospitalized for diabetes in the United States between 2009 and 2017.
“The primary outcome variable was documentation of either minor or major LEA during a diabetes-related admission,” they explain.
Minor LEAs increased significantly across all ethnic groups.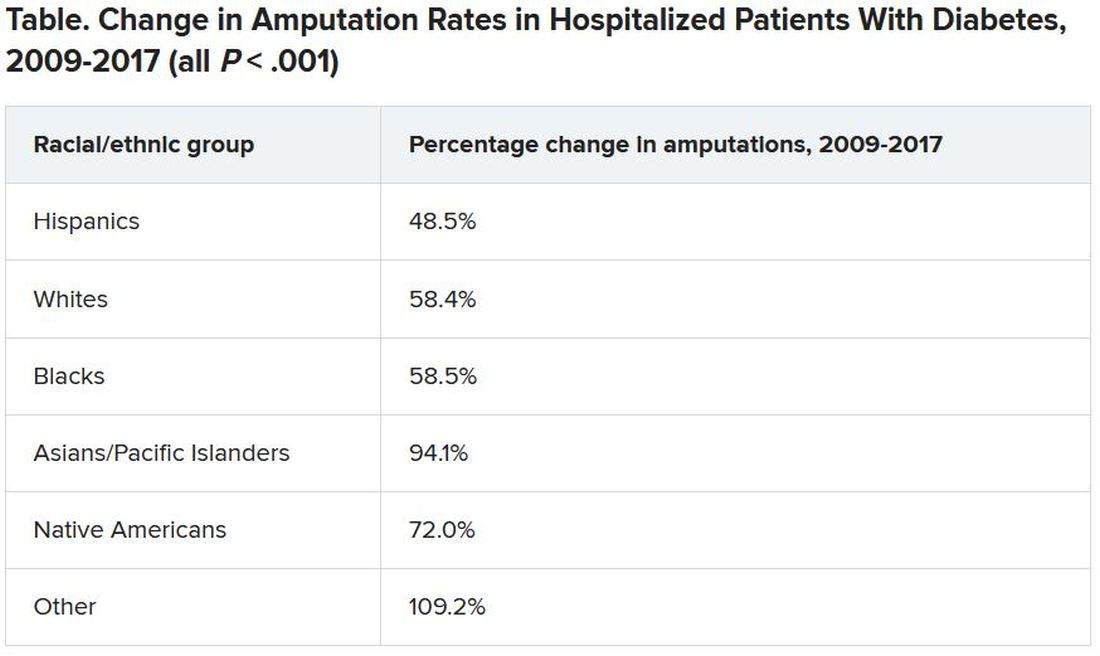
Although major amputation rates remained steady, “we did find that some groups remained at risk for having a major amputation,” Dr. Akinlotan noted.
White populations, people in the Midwest, and rural areas saw notable increases in major LEAs, as did “... Blacks, Hispanics, [and] those living in the South,” she said.
Patients need to be encouraged to monitor and control their blood glucose, to offset modifiable risk factors, and to seek regular medical attention to prevent an insidious diabetic complication from developing further, she said.
“It’s important for patients to know that continuing care is necessary,” Dr. Akinlotan stressed. “Diabetes is chronic and complex, but it can be managed, so that’s the good news.”
Dr. Ory agrees: “Effective management will require an all-in approach, with doctors and patients working together.
“Given the limited time in doctor-patient encounters, physicians can benefit patients by referring them to evidence-based, self-management education programs, which are proliferating around in the county,” she added.
The authors and Dr. Ory have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rates of minor diabetes-related lower extremity amputations (LEAs) in hospitalized patients increased between 2009 and 2017 in all racial and ethnic groups, in both rural and urban areas, and in all geographic regions across the United States, a new retrospective, observational study indicates.
In contrast, major lower extremity amputation rates held steady during the study period with a few exceptions.
There was also a decline in major-to-minor amputation ratios, especially among Native Americans – a sign that diabetes was being better managed and foot ulcers were being caught earlier, preventing the need for a major amputation above the foot or below or above the knee.
Minor LEAs include the loss of a toe, toes, or a foot.
“While I know an amputation is devastating either way, having a minor amputation is better than having a major amputation, and trends [at least to 2017] show that comprehensive foot examinations are paying off,” lead author Marvellous Akinlotan, PhD, MPH, a research associate at the Southwest Rural Health Research Center in Bryan, Texas, said in an interview.
Asked to comment, Marcia Ory, PhD, MPH, director of the Center for Population Health & Aging, Texas A&M School of Public Health, College Station, who was not involved in the study, said: “It points to some successes, but it also points to the need for continued education and preventive care to reduce all types of amputations.”
The study was published online in Diabetes Care.
Amputations increased during COVID-19
However, the study was conducted prior to the COVID-19 pandemic, and amputation rates appear to have significantly worsened during the past 18 months.
In a summary of recent evidence collated by the Amputee Coalition, the authors point out that not only does COVID-19 itself put patients at higher risk for limb loss because severe infection increases the risk of blood clots, but patients with diabetes appear to have been far more likely to undergo any level of amputation during the pandemic than before it began.
In a study of patients with diabetes attending a foot and ankle surgery service in Ohio, the risk of having any level of amputation was 10.8 times higher during compared with before the pandemic. And of patients undergoing any amputation, the odds for receiving a major amputation was 3.1 times higher than before the pandemic.
Telehealth and web-based options for diabetes care and education could help improve health outcomes, particularly during lockdowns.
“Having a diabetes-related amputation is life-changing – it brings disability and functional limitations to the individual – and within the health care system, it reflects the failure of secondary prevention efforts, which ideally should slow the progression of diabetic complications,” noted Dr. Akinlotan.
Race and geography affect risk of amputation
In their study, Dr. Akinlotan and colleagues used data from the National Inpatient Sample to identify trends in LEAs among patients primarily hospitalized for diabetes in the United States between 2009 and 2017.
“The primary outcome variable was documentation of either minor or major LEA during a diabetes-related admission,” they explain.
Minor LEAs increased significantly across all ethnic groups.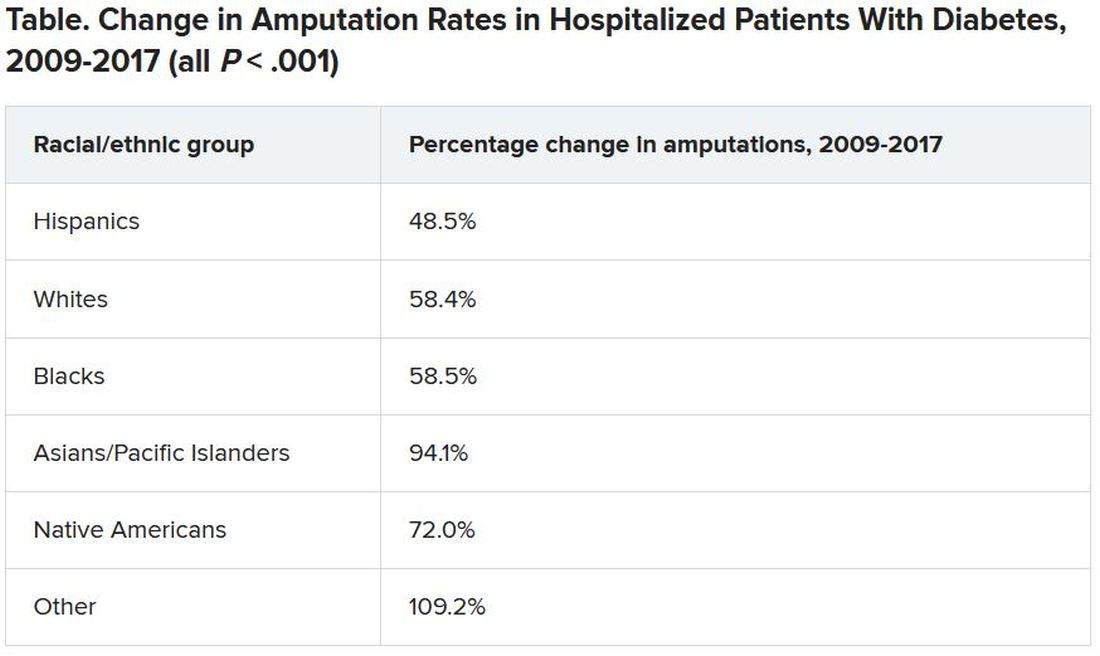
Although major amputation rates remained steady, “we did find that some groups remained at risk for having a major amputation,” Dr. Akinlotan noted.
White populations, people in the Midwest, and rural areas saw notable increases in major LEAs, as did “... Blacks, Hispanics, [and] those living in the South,” she said.
Patients need to be encouraged to monitor and control their blood glucose, to offset modifiable risk factors, and to seek regular medical attention to prevent an insidious diabetic complication from developing further, she said.
“It’s important for patients to know that continuing care is necessary,” Dr. Akinlotan stressed. “Diabetes is chronic and complex, but it can be managed, so that’s the good news.”
Dr. Ory agrees: “Effective management will require an all-in approach, with doctors and patients working together.
“Given the limited time in doctor-patient encounters, physicians can benefit patients by referring them to evidence-based, self-management education programs, which are proliferating around in the county,” she added.
The authors and Dr. Ory have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ED docs are cleaning up the messes of medical tourism
It was a typical, busy evening shift in the emergency department (ED) when Steve Carroll, DO, an emergency medicine physician in the Philadelphia area, noticed an odd listing on the tracking board. In the waiting room, there was someone whose chief complaint was that she needed to have surgical drains pulled.
According to the woman’s chart, she’d undergone liposuction in Miami a week before. The surgeon had effectively relinquished all follow-up care to the woman’s local ED.
Dr. Carroll searched the name of her surgeon and found that his site “specifically advertised medical tourism,” Dr. Carroll said. The site lured patients with the idea of recovering by the beach and that a local nurse would come to their room every day.
But when Dr. Carroll told the patient that her surgeon should be the one who removes the drains, she became concerned. She didn’t know that her surgeon wasn’t providing the standard of care, he said. Somewhat appalled that a board-certified plastic surgeon would place the burden of follow-up care on an ED doctor hundreds of miles away, Dr. Carroll posted the case to Twitter and several Facebook groups.
“Yes I could refuse to take [the drains] out but that’s not patient-centered care,” Dr. Carroll wrote in a Twitter thread. “It’s unfairly shifting routine outpatient surgical followup (and liability) onto me and extra cost to [the patient].” Comments from ED physicians and sympathetic surgeons across the country flowed in. Dr. Carroll quickly realized his situation was part of a much larger problem than he’d thought.
Dr. Carroll’s patient told him that the Miami surgery cost less than undergoing the surgery locally; that’s why she’d made the trip. She’s not alone. Traveling to get the lowest price for a plastic surgery procedure has been a rising phenomenon since the early 2000s, according to the American Society of Plastic Surgeons (ASPS). Many countries are actively fostering their medical tourism industries, as are states such as Florida.
People have long traveled to get the best medical care. But “medical tourism is completely different,” said Alan Matarasso, MD, FACS, a Manhattan-based plastic surgeon and member of the ASPS Executive Committee. “People [are] traveling to get a simultaneous vacation or lower cost,” he said.
Choosing facilities on the basis of these criteria comes with myriad problems, and the quality of medical care may be lower. It’s difficult to verify the credentials of the surgeons, anesthesiologists, and facilities involved. Medical records can be in a different language, and traveling immediately after surgery increases the risk for pulmonary embolism and death, not to mention the added complications of traveling and being a surgical patient during the COVID-19 pandemic, he said.
Typically, surgeons are protective of their patients. But Murtaza Akhter, MD, an emergency medicine physician based in Miami, says it’s the opposite with the medical tourism surgeons whose patients regularly end up in his ED. “There’s almost no ownership,” he said. “Every time, [the patients] say, ‘My doctor isn’t responding,’ or they said go to the ER.” And that’s before they’ve even made it out of Miami.
The most common cosmetic surgery complications Dr. Akhter sees occur in patients who’ve undergone so-called Brazilian butt lifts. They show up in his ED face down, suffering from severe blood loss. He has them undergo a transfusion and maybe some imaging, but if they need a higher degree of care, they have to be transferred. “There’s a reason it’s cheaper,” he said.
Medical tourism mishaps are such a regular occurrence in Miami that no one flinches when the patients show up in the ED, Dr. Akhter said. He had begun to think he was overreacting to the problem until he saw Dr. Carroll’s Twitter thread.
“Since it’s daily, I just thought maybe I had gone crazy and that it’s considered normal for plastic surgeons to do this. Thanks for making me feel sane again,” Dr. Akhter tweeted in a reply to Dr. Carroll.
There are no reliable data as to of how often or where such surgeries are occurring or of patients’ outcomes. But Nicholas Genes, MD, an ED physician in Manhattan, says he sees far more postsurgical patients who traveled for their procedures than ones who underwent surgery locally. He can’t say for certain whether that’s because procedures performed by doctors in New York City have fewer complications or the physicians just handle postprocedure problems themselves.
In a 2021 systematic review of aesthetic breast surgeries performed through medical tourism, researchers found that of 171 patients who traveled for surgery, 88 (51%) had a total of 106 complications that required returning to the operating room and undergoing general anesthesia. They also found that 39% of breast augmentation implant surgeries required either a unilateral or bilateral explantation procedure after patients returned home.
The rate of complications was higher than the study authors had expected. “These are totally elective procedures,” Dr. Matarasso said. “They should be optimized.” And high rates of complications come with hefty price tags.
The cost of managing these complications, which falls to the home healthcare system or the patient themselves, can range from $5,500 (determined on the basis of data from a 2019 study in the United Kingdom) to as much as $123,000, researchers in New York City calculated, if the patient develops a complicated mycobacterium infection.
“In your effort to get a good deal or around the system, you could still end up with a lot of extensive medical bills if something goes wrong,” Dr. Genes said.
The liability dilemma
Many of the ED physicians Dr. Carroll heard from said that they wouldn’t have treated the woman who needed to have drains removed. Unlike the Brazilian-butt-lifts-gone-wrong in Miami or the complications Dr. Genes sees in New York City, Dr. Carroll’s patient wasn’t in a state of emergency. Most ED physicians said they would have sent her on her way to find a surgeon.
“In general, we shouldn’t be doing things we aren’t trained to do. It’s sort of a slippery slope,” Dr. Genes said. He’s comfortable with removing stitches, but for surgical drains and plastic apparatuses, “I don’t feel particularly well trained. I’d have to consult a colleague in general surgery,” he said. When he does get one of these patients, he works the phones to find a plastic surgeon who will see the patient, something he says their original plastic surgeon should have done.
“Sitting there with the patient, I felt a little bad for her,” Dr. Carroll said. “I knew if I didn’t do it, it would be weeks while she bounced around to urgent care, primary care, and finally found a surgeon.” But by removing the drains, he did shift some of the liability to himself. “If she developed a wound infection, then I’m on the hook for [that],” he said. “If I send her away, I have less liability but didn’t quite do the right thing for the patient.”
In replies to Dr. Carroll’s thread, some doctors debated whether these types of cases, particularly those in which surgeons forgo follow-up care, could be considered medical abandonment. Legal experts say that’s not exactly the case, at least it would not be the case with Dr. Carroll’s patient.
“I don’t think they’ve abandoned the patient; I think they’ve abandoned care,” said Michael Flynn, JD, professor of personal injury law at Nova Southeastern University, in Fort Lauderdale–Davie, Fla. “And that abandonment of follow-up care, if it falls below the standard of what medical professionals should do, then it’s malpractice.”
“The doctor didn’t just walk away and become unreachable,” said Bernard Black, JD, a medical malpractice attorney and law professor at Northwestern University, in Evanston, Ill. Technically, the surgeon referred the patient to the ED. Mr. Black agreed that it sounds more like a question of malpractice, “but without real damages, there’s no claim.”
Even if not illegal, sending these patients to the ED is still highly unethical, Dr. Carroll said. The authors of a 2014 article in Aesthetic Plastic Surgery concur: “It is the duty and ethical responsibility of plastic surgeons to prevent unnecessary complications following tourism medicine by adequately counseling patients, defining perioperative treatment protocols, and reporting complications to regional and specialty-specific governing bodies,” they write.
Sometimes patients need to travel, Dr. Matarasso said. Recently, three out-of-state patients came to him for procedures. Two stayed in Manhattan until their follow-up care was finished; he arranged care elsewhere for the third. It’s the operating surgeon’s job to connect patients with someone who can provide follow-up care when they go home, Dr. Matarasso said. If a surgeon doesn’t have a connection in a patient’s home city, the ASPS has a referral service to help, he said.
“My frustration was never with the patient,” Dr. Carroll said. “No one should feel bad about coming to an ED for literally anything, and I mean that. My frustration is with the surgeon who didn’t go the one extra step to arrange her follow-up.”
A version of this article first appeared on Medscape.com.
It was a typical, busy evening shift in the emergency department (ED) when Steve Carroll, DO, an emergency medicine physician in the Philadelphia area, noticed an odd listing on the tracking board. In the waiting room, there was someone whose chief complaint was that she needed to have surgical drains pulled.
According to the woman’s chart, she’d undergone liposuction in Miami a week before. The surgeon had effectively relinquished all follow-up care to the woman’s local ED.
Dr. Carroll searched the name of her surgeon and found that his site “specifically advertised medical tourism,” Dr. Carroll said. The site lured patients with the idea of recovering by the beach and that a local nurse would come to their room every day.
But when Dr. Carroll told the patient that her surgeon should be the one who removes the drains, she became concerned. She didn’t know that her surgeon wasn’t providing the standard of care, he said. Somewhat appalled that a board-certified plastic surgeon would place the burden of follow-up care on an ED doctor hundreds of miles away, Dr. Carroll posted the case to Twitter and several Facebook groups.
“Yes I could refuse to take [the drains] out but that’s not patient-centered care,” Dr. Carroll wrote in a Twitter thread. “It’s unfairly shifting routine outpatient surgical followup (and liability) onto me and extra cost to [the patient].” Comments from ED physicians and sympathetic surgeons across the country flowed in. Dr. Carroll quickly realized his situation was part of a much larger problem than he’d thought.
Dr. Carroll’s patient told him that the Miami surgery cost less than undergoing the surgery locally; that’s why she’d made the trip. She’s not alone. Traveling to get the lowest price for a plastic surgery procedure has been a rising phenomenon since the early 2000s, according to the American Society of Plastic Surgeons (ASPS). Many countries are actively fostering their medical tourism industries, as are states such as Florida.
People have long traveled to get the best medical care. But “medical tourism is completely different,” said Alan Matarasso, MD, FACS, a Manhattan-based plastic surgeon and member of the ASPS Executive Committee. “People [are] traveling to get a simultaneous vacation or lower cost,” he said.
Choosing facilities on the basis of these criteria comes with myriad problems, and the quality of medical care may be lower. It’s difficult to verify the credentials of the surgeons, anesthesiologists, and facilities involved. Medical records can be in a different language, and traveling immediately after surgery increases the risk for pulmonary embolism and death, not to mention the added complications of traveling and being a surgical patient during the COVID-19 pandemic, he said.
Typically, surgeons are protective of their patients. But Murtaza Akhter, MD, an emergency medicine physician based in Miami, says it’s the opposite with the medical tourism surgeons whose patients regularly end up in his ED. “There’s almost no ownership,” he said. “Every time, [the patients] say, ‘My doctor isn’t responding,’ or they said go to the ER.” And that’s before they’ve even made it out of Miami.
The most common cosmetic surgery complications Dr. Akhter sees occur in patients who’ve undergone so-called Brazilian butt lifts. They show up in his ED face down, suffering from severe blood loss. He has them undergo a transfusion and maybe some imaging, but if they need a higher degree of care, they have to be transferred. “There’s a reason it’s cheaper,” he said.
Medical tourism mishaps are such a regular occurrence in Miami that no one flinches when the patients show up in the ED, Dr. Akhter said. He had begun to think he was overreacting to the problem until he saw Dr. Carroll’s Twitter thread.
“Since it’s daily, I just thought maybe I had gone crazy and that it’s considered normal for plastic surgeons to do this. Thanks for making me feel sane again,” Dr. Akhter tweeted in a reply to Dr. Carroll.
There are no reliable data as to of how often or where such surgeries are occurring or of patients’ outcomes. But Nicholas Genes, MD, an ED physician in Manhattan, says he sees far more postsurgical patients who traveled for their procedures than ones who underwent surgery locally. He can’t say for certain whether that’s because procedures performed by doctors in New York City have fewer complications or the physicians just handle postprocedure problems themselves.
In a 2021 systematic review of aesthetic breast surgeries performed through medical tourism, researchers found that of 171 patients who traveled for surgery, 88 (51%) had a total of 106 complications that required returning to the operating room and undergoing general anesthesia. They also found that 39% of breast augmentation implant surgeries required either a unilateral or bilateral explantation procedure after patients returned home.
The rate of complications was higher than the study authors had expected. “These are totally elective procedures,” Dr. Matarasso said. “They should be optimized.” And high rates of complications come with hefty price tags.
The cost of managing these complications, which falls to the home healthcare system or the patient themselves, can range from $5,500 (determined on the basis of data from a 2019 study in the United Kingdom) to as much as $123,000, researchers in New York City calculated, if the patient develops a complicated mycobacterium infection.
“In your effort to get a good deal or around the system, you could still end up with a lot of extensive medical bills if something goes wrong,” Dr. Genes said.
The liability dilemma
Many of the ED physicians Dr. Carroll heard from said that they wouldn’t have treated the woman who needed to have drains removed. Unlike the Brazilian-butt-lifts-gone-wrong in Miami or the complications Dr. Genes sees in New York City, Dr. Carroll’s patient wasn’t in a state of emergency. Most ED physicians said they would have sent her on her way to find a surgeon.
“In general, we shouldn’t be doing things we aren’t trained to do. It’s sort of a slippery slope,” Dr. Genes said. He’s comfortable with removing stitches, but for surgical drains and plastic apparatuses, “I don’t feel particularly well trained. I’d have to consult a colleague in general surgery,” he said. When he does get one of these patients, he works the phones to find a plastic surgeon who will see the patient, something he says their original plastic surgeon should have done.
“Sitting there with the patient, I felt a little bad for her,” Dr. Carroll said. “I knew if I didn’t do it, it would be weeks while she bounced around to urgent care, primary care, and finally found a surgeon.” But by removing the drains, he did shift some of the liability to himself. “If she developed a wound infection, then I’m on the hook for [that],” he said. “If I send her away, I have less liability but didn’t quite do the right thing for the patient.”
In replies to Dr. Carroll’s thread, some doctors debated whether these types of cases, particularly those in which surgeons forgo follow-up care, could be considered medical abandonment. Legal experts say that’s not exactly the case, at least it would not be the case with Dr. Carroll’s patient.
“I don’t think they’ve abandoned the patient; I think they’ve abandoned care,” said Michael Flynn, JD, professor of personal injury law at Nova Southeastern University, in Fort Lauderdale–Davie, Fla. “And that abandonment of follow-up care, if it falls below the standard of what medical professionals should do, then it’s malpractice.”
“The doctor didn’t just walk away and become unreachable,” said Bernard Black, JD, a medical malpractice attorney and law professor at Northwestern University, in Evanston, Ill. Technically, the surgeon referred the patient to the ED. Mr. Black agreed that it sounds more like a question of malpractice, “but without real damages, there’s no claim.”
Even if not illegal, sending these patients to the ED is still highly unethical, Dr. Carroll said. The authors of a 2014 article in Aesthetic Plastic Surgery concur: “It is the duty and ethical responsibility of plastic surgeons to prevent unnecessary complications following tourism medicine by adequately counseling patients, defining perioperative treatment protocols, and reporting complications to regional and specialty-specific governing bodies,” they write.
Sometimes patients need to travel, Dr. Matarasso said. Recently, three out-of-state patients came to him for procedures. Two stayed in Manhattan until their follow-up care was finished; he arranged care elsewhere for the third. It’s the operating surgeon’s job to connect patients with someone who can provide follow-up care when they go home, Dr. Matarasso said. If a surgeon doesn’t have a connection in a patient’s home city, the ASPS has a referral service to help, he said.
“My frustration was never with the patient,” Dr. Carroll said. “No one should feel bad about coming to an ED for literally anything, and I mean that. My frustration is with the surgeon who didn’t go the one extra step to arrange her follow-up.”
A version of this article first appeared on Medscape.com.
It was a typical, busy evening shift in the emergency department (ED) when Steve Carroll, DO, an emergency medicine physician in the Philadelphia area, noticed an odd listing on the tracking board. In the waiting room, there was someone whose chief complaint was that she needed to have surgical drains pulled.
According to the woman’s chart, she’d undergone liposuction in Miami a week before. The surgeon had effectively relinquished all follow-up care to the woman’s local ED.
Dr. Carroll searched the name of her surgeon and found that his site “specifically advertised medical tourism,” Dr. Carroll said. The site lured patients with the idea of recovering by the beach and that a local nurse would come to their room every day.
But when Dr. Carroll told the patient that her surgeon should be the one who removes the drains, she became concerned. She didn’t know that her surgeon wasn’t providing the standard of care, he said. Somewhat appalled that a board-certified plastic surgeon would place the burden of follow-up care on an ED doctor hundreds of miles away, Dr. Carroll posted the case to Twitter and several Facebook groups.
“Yes I could refuse to take [the drains] out but that’s not patient-centered care,” Dr. Carroll wrote in a Twitter thread. “It’s unfairly shifting routine outpatient surgical followup (and liability) onto me and extra cost to [the patient].” Comments from ED physicians and sympathetic surgeons across the country flowed in. Dr. Carroll quickly realized his situation was part of a much larger problem than he’d thought.
Dr. Carroll’s patient told him that the Miami surgery cost less than undergoing the surgery locally; that’s why she’d made the trip. She’s not alone. Traveling to get the lowest price for a plastic surgery procedure has been a rising phenomenon since the early 2000s, according to the American Society of Plastic Surgeons (ASPS). Many countries are actively fostering their medical tourism industries, as are states such as Florida.
People have long traveled to get the best medical care. But “medical tourism is completely different,” said Alan Matarasso, MD, FACS, a Manhattan-based plastic surgeon and member of the ASPS Executive Committee. “People [are] traveling to get a simultaneous vacation or lower cost,” he said.
Choosing facilities on the basis of these criteria comes with myriad problems, and the quality of medical care may be lower. It’s difficult to verify the credentials of the surgeons, anesthesiologists, and facilities involved. Medical records can be in a different language, and traveling immediately after surgery increases the risk for pulmonary embolism and death, not to mention the added complications of traveling and being a surgical patient during the COVID-19 pandemic, he said.
Typically, surgeons are protective of their patients. But Murtaza Akhter, MD, an emergency medicine physician based in Miami, says it’s the opposite with the medical tourism surgeons whose patients regularly end up in his ED. “There’s almost no ownership,” he said. “Every time, [the patients] say, ‘My doctor isn’t responding,’ or they said go to the ER.” And that’s before they’ve even made it out of Miami.
The most common cosmetic surgery complications Dr. Akhter sees occur in patients who’ve undergone so-called Brazilian butt lifts. They show up in his ED face down, suffering from severe blood loss. He has them undergo a transfusion and maybe some imaging, but if they need a higher degree of care, they have to be transferred. “There’s a reason it’s cheaper,” he said.
Medical tourism mishaps are such a regular occurrence in Miami that no one flinches when the patients show up in the ED, Dr. Akhter said. He had begun to think he was overreacting to the problem until he saw Dr. Carroll’s Twitter thread.
“Since it’s daily, I just thought maybe I had gone crazy and that it’s considered normal for plastic surgeons to do this. Thanks for making me feel sane again,” Dr. Akhter tweeted in a reply to Dr. Carroll.
There are no reliable data as to of how often or where such surgeries are occurring or of patients’ outcomes. But Nicholas Genes, MD, an ED physician in Manhattan, says he sees far more postsurgical patients who traveled for their procedures than ones who underwent surgery locally. He can’t say for certain whether that’s because procedures performed by doctors in New York City have fewer complications or the physicians just handle postprocedure problems themselves.
In a 2021 systematic review of aesthetic breast surgeries performed through medical tourism, researchers found that of 171 patients who traveled for surgery, 88 (51%) had a total of 106 complications that required returning to the operating room and undergoing general anesthesia. They also found that 39% of breast augmentation implant surgeries required either a unilateral or bilateral explantation procedure after patients returned home.
The rate of complications was higher than the study authors had expected. “These are totally elective procedures,” Dr. Matarasso said. “They should be optimized.” And high rates of complications come with hefty price tags.
The cost of managing these complications, which falls to the home healthcare system or the patient themselves, can range from $5,500 (determined on the basis of data from a 2019 study in the United Kingdom) to as much as $123,000, researchers in New York City calculated, if the patient develops a complicated mycobacterium infection.
“In your effort to get a good deal or around the system, you could still end up with a lot of extensive medical bills if something goes wrong,” Dr. Genes said.
The liability dilemma
Many of the ED physicians Dr. Carroll heard from said that they wouldn’t have treated the woman who needed to have drains removed. Unlike the Brazilian-butt-lifts-gone-wrong in Miami or the complications Dr. Genes sees in New York City, Dr. Carroll’s patient wasn’t in a state of emergency. Most ED physicians said they would have sent her on her way to find a surgeon.
“In general, we shouldn’t be doing things we aren’t trained to do. It’s sort of a slippery slope,” Dr. Genes said. He’s comfortable with removing stitches, but for surgical drains and plastic apparatuses, “I don’t feel particularly well trained. I’d have to consult a colleague in general surgery,” he said. When he does get one of these patients, he works the phones to find a plastic surgeon who will see the patient, something he says their original plastic surgeon should have done.
“Sitting there with the patient, I felt a little bad for her,” Dr. Carroll said. “I knew if I didn’t do it, it would be weeks while she bounced around to urgent care, primary care, and finally found a surgeon.” But by removing the drains, he did shift some of the liability to himself. “If she developed a wound infection, then I’m on the hook for [that],” he said. “If I send her away, I have less liability but didn’t quite do the right thing for the patient.”
In replies to Dr. Carroll’s thread, some doctors debated whether these types of cases, particularly those in which surgeons forgo follow-up care, could be considered medical abandonment. Legal experts say that’s not exactly the case, at least it would not be the case with Dr. Carroll’s patient.
“I don’t think they’ve abandoned the patient; I think they’ve abandoned care,” said Michael Flynn, JD, professor of personal injury law at Nova Southeastern University, in Fort Lauderdale–Davie, Fla. “And that abandonment of follow-up care, if it falls below the standard of what medical professionals should do, then it’s malpractice.”
“The doctor didn’t just walk away and become unreachable,” said Bernard Black, JD, a medical malpractice attorney and law professor at Northwestern University, in Evanston, Ill. Technically, the surgeon referred the patient to the ED. Mr. Black agreed that it sounds more like a question of malpractice, “but without real damages, there’s no claim.”
Even if not illegal, sending these patients to the ED is still highly unethical, Dr. Carroll said. The authors of a 2014 article in Aesthetic Plastic Surgery concur: “It is the duty and ethical responsibility of plastic surgeons to prevent unnecessary complications following tourism medicine by adequately counseling patients, defining perioperative treatment protocols, and reporting complications to regional and specialty-specific governing bodies,” they write.
Sometimes patients need to travel, Dr. Matarasso said. Recently, three out-of-state patients came to him for procedures. Two stayed in Manhattan until their follow-up care was finished; he arranged care elsewhere for the third. It’s the operating surgeon’s job to connect patients with someone who can provide follow-up care when they go home, Dr. Matarasso said. If a surgeon doesn’t have a connection in a patient’s home city, the ASPS has a referral service to help, he said.
“My frustration was never with the patient,” Dr. Carroll said. “No one should feel bad about coming to an ED for literally anything, and I mean that. My frustration is with the surgeon who didn’t go the one extra step to arrange her follow-up.”
A version of this article first appeared on Medscape.com.
Medicinal liquor and edited mosquitoes
Drink to your health?
Whether you drink or not, most of us can agree that liquor is not the first thing that comes to mind when looking to make health improvements. But researchers have found a small exception in something traditional.
We’ve added buckwheat to pancakes, bread, and other baked goodies we made during the height of quarantine, but it’s also used to create a traditional liquor in some East Asian countries, where it is used medicinally.
Investigators have found that extracts in the Tartary buckwheat used to make the liquor induce autophagy, a process cells go through to remove proteins that are damaged or not needed anymore – sort of like a cellular spring cleaning.
To test this, the researchers treated liver and skin cells with Tartary buckwheat extract and looked to see how the cells responded with fluorescent markers. The results were clear.
“Treating cells with the extract stimulated the formation of autophagosomes, specialized cellular structures that carry out autophagy, and altered the location of proteins involved in regulating autophagy,” said senior author Takeshi Noda of Osaka (Japan) University.
Looking deeper, the researchers found that quercetin, a component of the buckwheat extract, had the same autophagic effect. And both the buckwheat and the quercetin gave the green light for liver cells to induce aggrephagy, the process of cleaning up protein aggregates.
Those protein aggregates in liver cells are closely linked to alcoholic liver disease, suggesting that quercetin could be a game changer in its treatment. In other words, liquor could help fix the problem that liquor started. Go figure.
From hospital bills to X-rated
Ralph Puglisi was an accounting manager for the University Medical Service Association (UMSA), a nonprofit that supports the massive University of South Florida health system. The association took in over $300 million in revenue in the 2019-2020 fiscal year, which is a rather large sum of money, but we’ll glide over the ethics of a “nonprofit” making a few hundred million for now.
Mr. Puglisi was in very close proximity to the money, generated from patient care, and he pled guilty to stealing it using UMSA credit cards. Now, that wouldn’t be LOTME worthy on its own, but what elevates this above garden-variety embezzlement is how the intrepid Mr. Puglisi chose to spend the millions he stole from the university health system: Adult entertainment.
And before you ask, he didn’t spend $11.5 million on something most people so inclined can find for free with judicious Google searches. What Mr. Puglisi actually did was invest in a website providing adult content through individual user profiles, one of which is believed to belong to his stepson’s fiancée, which brings a whole new level of sleaze to this enterprise. Over the course of 2 years, he visited her profile 2,800 times, an amount some might view as excessive.
While the vast majority of the embezzled money went to the adult website, Mr. Puglisi also used thousands of UMSA dollars to pay for travel, household improvements, rent, the works. Almost $44,000 was spent at a resort sometimes known as the happiest place on earth.
Then there’s Mr. Puglisi’s wife. Oh yes, this guy is married. He poured over $600,000 into a company he and his wife owned, which is a lot, but how much do you think went to the woman he married? Probably quite a bit. Go ahead, try to think of a number. It’s not like it was his money.
Did you guess $100 went into his wife’s PayPal account? No? Clearly you don’t understand the criminal mind. His stepson’s fiancée got millions, and his wife got a hundred. Now there are some priorities.
Step 1: Sit at desk. Step 2: Get in shape
Being a physician is not really a desk job, but doctors must spend a fair share of their time sitting, yes? Dealing with recalcitrant EHRs or talking on the phone to insurers or PBMs? If you are one of these physicians, or if you have patients who spend a lot of time sitting at their desks and might need to get a bit of exercise, then we’ve got a multitasking tip for you.
It came to us via one of our favorite websites, Sad and Useless. It’s the site that declares itself “the most depressive humor site on the Internet” and they’re offering up the “12 Best Exercises To Do At Your Desk.” It may not sound like much, but we think that the gang at Dunder-Mifflin would approve. And besides, who couldn’t stand to burn a few calories without having to leave the chair?
We won’t spoil your fun by going through all 12 – each one comes with step-by-step instructions and a helpful illustration or GIF – but here are just a few:
- Bending over backwards: “Agree to do something you don’t want to do. Spend twice as long as expected doing that thing. Hate yourself.”
- Fake laughter: “Hear a joke that isn’t even remotely funny. Open your mouth and make laughing sounds.”
- Bang your head: Feel the “pointlessness of your job overwhelm you” and then “bring your head forcefully down to your desk.”
Now, we here at LOTME are, of course [Bang!], highly skilled, professional wordsmithing humorists [Bang!], so when we tell you that this is a great workout [Bang!] … that this is a great workout [Bang!] … it’s great … uggh.
Wooooo. Feel the burn.
One order of mosquitoes, extra Crispr
What would it be like to have a barbecue in your backyard on a humid summer night and not get eaten alive by mosquitoes? If you’re like us, you probably thought you’d never see that day.
Mosquitoes cause itchy bites, but, more importantly, they can carry dengue, malaria, yellow fever, and Zika virus. New research shows that protection from these diseases may be possible with use of the Crispr-Cas9 gene-editing tool, which could make humans invisible to mosquitoes by taking away their light-sensing abilities and, thus, their ability to find us.
“The better we understand how they sense the human, the better we can control the mosquito in an eco-friendly manner,” Yinpeng Zhan, a postdoctoral researcher at the University of California, Santa Barbara, and the study’s lead author, told the New York Times.
After studying the mosquitoes and figuring out their hunting patterns, the researchers found that mosquitoes are attracted to dark spots more than white spots and used this to their advantage. After knocking out two of the proteins that mosquitoes need for vision – via Crispr – the little suckers could not distinguish the difference between the white and dark spots.
We’re sure mosquitoes don’t mean any harm – they’re just trying to survive and reproduce like any other species – but thanks to this new tool, gone might be the days of having to douse yourself in bug spray that smells like a mix of chemicals and melon.
Drink to your health?
Whether you drink or not, most of us can agree that liquor is not the first thing that comes to mind when looking to make health improvements. But researchers have found a small exception in something traditional.
We’ve added buckwheat to pancakes, bread, and other baked goodies we made during the height of quarantine, but it’s also used to create a traditional liquor in some East Asian countries, where it is used medicinally.
Investigators have found that extracts in the Tartary buckwheat used to make the liquor induce autophagy, a process cells go through to remove proteins that are damaged or not needed anymore – sort of like a cellular spring cleaning.
To test this, the researchers treated liver and skin cells with Tartary buckwheat extract and looked to see how the cells responded with fluorescent markers. The results were clear.
“Treating cells with the extract stimulated the formation of autophagosomes, specialized cellular structures that carry out autophagy, and altered the location of proteins involved in regulating autophagy,” said senior author Takeshi Noda of Osaka (Japan) University.
Looking deeper, the researchers found that quercetin, a component of the buckwheat extract, had the same autophagic effect. And both the buckwheat and the quercetin gave the green light for liver cells to induce aggrephagy, the process of cleaning up protein aggregates.
Those protein aggregates in liver cells are closely linked to alcoholic liver disease, suggesting that quercetin could be a game changer in its treatment. In other words, liquor could help fix the problem that liquor started. Go figure.
From hospital bills to X-rated
Ralph Puglisi was an accounting manager for the University Medical Service Association (UMSA), a nonprofit that supports the massive University of South Florida health system. The association took in over $300 million in revenue in the 2019-2020 fiscal year, which is a rather large sum of money, but we’ll glide over the ethics of a “nonprofit” making a few hundred million for now.
Mr. Puglisi was in very close proximity to the money, generated from patient care, and he pled guilty to stealing it using UMSA credit cards. Now, that wouldn’t be LOTME worthy on its own, but what elevates this above garden-variety embezzlement is how the intrepid Mr. Puglisi chose to spend the millions he stole from the university health system: Adult entertainment.
And before you ask, he didn’t spend $11.5 million on something most people so inclined can find for free with judicious Google searches. What Mr. Puglisi actually did was invest in a website providing adult content through individual user profiles, one of which is believed to belong to his stepson’s fiancée, which brings a whole new level of sleaze to this enterprise. Over the course of 2 years, he visited her profile 2,800 times, an amount some might view as excessive.
While the vast majority of the embezzled money went to the adult website, Mr. Puglisi also used thousands of UMSA dollars to pay for travel, household improvements, rent, the works. Almost $44,000 was spent at a resort sometimes known as the happiest place on earth.
Then there’s Mr. Puglisi’s wife. Oh yes, this guy is married. He poured over $600,000 into a company he and his wife owned, which is a lot, but how much do you think went to the woman he married? Probably quite a bit. Go ahead, try to think of a number. It’s not like it was his money.
Did you guess $100 went into his wife’s PayPal account? No? Clearly you don’t understand the criminal mind. His stepson’s fiancée got millions, and his wife got a hundred. Now there are some priorities.
Step 1: Sit at desk. Step 2: Get in shape
Being a physician is not really a desk job, but doctors must spend a fair share of their time sitting, yes? Dealing with recalcitrant EHRs or talking on the phone to insurers or PBMs? If you are one of these physicians, or if you have patients who spend a lot of time sitting at their desks and might need to get a bit of exercise, then we’ve got a multitasking tip for you.
It came to us via one of our favorite websites, Sad and Useless. It’s the site that declares itself “the most depressive humor site on the Internet” and they’re offering up the “12 Best Exercises To Do At Your Desk.” It may not sound like much, but we think that the gang at Dunder-Mifflin would approve. And besides, who couldn’t stand to burn a few calories without having to leave the chair?
We won’t spoil your fun by going through all 12 – each one comes with step-by-step instructions and a helpful illustration or GIF – but here are just a few:
- Bending over backwards: “Agree to do something you don’t want to do. Spend twice as long as expected doing that thing. Hate yourself.”
- Fake laughter: “Hear a joke that isn’t even remotely funny. Open your mouth and make laughing sounds.”
- Bang your head: Feel the “pointlessness of your job overwhelm you” and then “bring your head forcefully down to your desk.”
Now, we here at LOTME are, of course [Bang!], highly skilled, professional wordsmithing humorists [Bang!], so when we tell you that this is a great workout [Bang!] … that this is a great workout [Bang!] … it’s great … uggh.
Wooooo. Feel the burn.
One order of mosquitoes, extra Crispr
What would it be like to have a barbecue in your backyard on a humid summer night and not get eaten alive by mosquitoes? If you’re like us, you probably thought you’d never see that day.
Mosquitoes cause itchy bites, but, more importantly, they can carry dengue, malaria, yellow fever, and Zika virus. New research shows that protection from these diseases may be possible with use of the Crispr-Cas9 gene-editing tool, which could make humans invisible to mosquitoes by taking away their light-sensing abilities and, thus, their ability to find us.
“The better we understand how they sense the human, the better we can control the mosquito in an eco-friendly manner,” Yinpeng Zhan, a postdoctoral researcher at the University of California, Santa Barbara, and the study’s lead author, told the New York Times.
After studying the mosquitoes and figuring out their hunting patterns, the researchers found that mosquitoes are attracted to dark spots more than white spots and used this to their advantage. After knocking out two of the proteins that mosquitoes need for vision – via Crispr – the little suckers could not distinguish the difference between the white and dark spots.
We’re sure mosquitoes don’t mean any harm – they’re just trying to survive and reproduce like any other species – but thanks to this new tool, gone might be the days of having to douse yourself in bug spray that smells like a mix of chemicals and melon.
Drink to your health?
Whether you drink or not, most of us can agree that liquor is not the first thing that comes to mind when looking to make health improvements. But researchers have found a small exception in something traditional.
We’ve added buckwheat to pancakes, bread, and other baked goodies we made during the height of quarantine, but it’s also used to create a traditional liquor in some East Asian countries, where it is used medicinally.
Investigators have found that extracts in the Tartary buckwheat used to make the liquor induce autophagy, a process cells go through to remove proteins that are damaged or not needed anymore – sort of like a cellular spring cleaning.
To test this, the researchers treated liver and skin cells with Tartary buckwheat extract and looked to see how the cells responded with fluorescent markers. The results were clear.
“Treating cells with the extract stimulated the formation of autophagosomes, specialized cellular structures that carry out autophagy, and altered the location of proteins involved in regulating autophagy,” said senior author Takeshi Noda of Osaka (Japan) University.
Looking deeper, the researchers found that quercetin, a component of the buckwheat extract, had the same autophagic effect. And both the buckwheat and the quercetin gave the green light for liver cells to induce aggrephagy, the process of cleaning up protein aggregates.
Those protein aggregates in liver cells are closely linked to alcoholic liver disease, suggesting that quercetin could be a game changer in its treatment. In other words, liquor could help fix the problem that liquor started. Go figure.
From hospital bills to X-rated
Ralph Puglisi was an accounting manager for the University Medical Service Association (UMSA), a nonprofit that supports the massive University of South Florida health system. The association took in over $300 million in revenue in the 2019-2020 fiscal year, which is a rather large sum of money, but we’ll glide over the ethics of a “nonprofit” making a few hundred million for now.
Mr. Puglisi was in very close proximity to the money, generated from patient care, and he pled guilty to stealing it using UMSA credit cards. Now, that wouldn’t be LOTME worthy on its own, but what elevates this above garden-variety embezzlement is how the intrepid Mr. Puglisi chose to spend the millions he stole from the university health system: Adult entertainment.
And before you ask, he didn’t spend $11.5 million on something most people so inclined can find for free with judicious Google searches. What Mr. Puglisi actually did was invest in a website providing adult content through individual user profiles, one of which is believed to belong to his stepson’s fiancée, which brings a whole new level of sleaze to this enterprise. Over the course of 2 years, he visited her profile 2,800 times, an amount some might view as excessive.
While the vast majority of the embezzled money went to the adult website, Mr. Puglisi also used thousands of UMSA dollars to pay for travel, household improvements, rent, the works. Almost $44,000 was spent at a resort sometimes known as the happiest place on earth.
Then there’s Mr. Puglisi’s wife. Oh yes, this guy is married. He poured over $600,000 into a company he and his wife owned, which is a lot, but how much do you think went to the woman he married? Probably quite a bit. Go ahead, try to think of a number. It’s not like it was his money.
Did you guess $100 went into his wife’s PayPal account? No? Clearly you don’t understand the criminal mind. His stepson’s fiancée got millions, and his wife got a hundred. Now there are some priorities.
Step 1: Sit at desk. Step 2: Get in shape
Being a physician is not really a desk job, but doctors must spend a fair share of their time sitting, yes? Dealing with recalcitrant EHRs or talking on the phone to insurers or PBMs? If you are one of these physicians, or if you have patients who spend a lot of time sitting at their desks and might need to get a bit of exercise, then we’ve got a multitasking tip for you.
It came to us via one of our favorite websites, Sad and Useless. It’s the site that declares itself “the most depressive humor site on the Internet” and they’re offering up the “12 Best Exercises To Do At Your Desk.” It may not sound like much, but we think that the gang at Dunder-Mifflin would approve. And besides, who couldn’t stand to burn a few calories without having to leave the chair?
We won’t spoil your fun by going through all 12 – each one comes with step-by-step instructions and a helpful illustration or GIF – but here are just a few:
- Bending over backwards: “Agree to do something you don’t want to do. Spend twice as long as expected doing that thing. Hate yourself.”
- Fake laughter: “Hear a joke that isn’t even remotely funny. Open your mouth and make laughing sounds.”
- Bang your head: Feel the “pointlessness of your job overwhelm you” and then “bring your head forcefully down to your desk.”
Now, we here at LOTME are, of course [Bang!], highly skilled, professional wordsmithing humorists [Bang!], so when we tell you that this is a great workout [Bang!] … that this is a great workout [Bang!] … it’s great … uggh.
Wooooo. Feel the burn.
One order of mosquitoes, extra Crispr
What would it be like to have a barbecue in your backyard on a humid summer night and not get eaten alive by mosquitoes? If you’re like us, you probably thought you’d never see that day.
Mosquitoes cause itchy bites, but, more importantly, they can carry dengue, malaria, yellow fever, and Zika virus. New research shows that protection from these diseases may be possible with use of the Crispr-Cas9 gene-editing tool, which could make humans invisible to mosquitoes by taking away their light-sensing abilities and, thus, their ability to find us.
“The better we understand how they sense the human, the better we can control the mosquito in an eco-friendly manner,” Yinpeng Zhan, a postdoctoral researcher at the University of California, Santa Barbara, and the study’s lead author, told the New York Times.
After studying the mosquitoes and figuring out their hunting patterns, the researchers found that mosquitoes are attracted to dark spots more than white spots and used this to their advantage. After knocking out two of the proteins that mosquitoes need for vision – via Crispr – the little suckers could not distinguish the difference between the white and dark spots.
We’re sure mosquitoes don’t mean any harm – they’re just trying to survive and reproduce like any other species – but thanks to this new tool, gone might be the days of having to douse yourself in bug spray that smells like a mix of chemicals and melon.
The hateful patient
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].