User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Feds slap UPMC, lead cardiothoracic surgeon with fraud lawsuit
Following a 2-year investigation, the U.S. government has filed suit against the University of Pittsburgh Medical Center (UPMC), University of Pittsburgh Physicians (UPP), and James Luketich, MD, for billing related to concurrent surgeries performed by the long-time chair of cardiothoracic surgery.
The lawsuit alleges that UPMC “knowingly allowed” Dr. Luketich to “book and perform three surgeries at the same time, to miss the surgical time outs at the outset of those procedures, to go back-and-forth between operating rooms and even hospital facilities while his surgical patients remain under general anesthesia...”
UPMC, the lawsuit claims, also allowed Dr. Luketich to falsely attest that “he was with his patients throughout the entirety of their surgical procedures or during all ‘key and critical’ portions of those procedures and to unlawfully bill Government Health Benefit Programs for those procedures, all in order to increase surgical volume, maximize UPMC and UPP’s revenue, and/or appease Dr. Luketich.”
These practices violate the statutes and regulations governing the defendants, including those that prohibit “teaching physicians” like Dr. Luketich from performing and billing the U.S. for concurrent surgeries, the Department of Justice said in news release.
The Justice Department contends the defendants “knowingly submitted hundreds of materially false claims for payment” to Medicare, Medicaid, and other government programs over the past 6 years.
“The laws prohibiting ‘concurrent surgeries’ are in place for a reason: To protect patients and ensure they receive appropriate and focused medical care,” Stephen R. Kaufman, Acting U.S. Attorney for the Western District of Pennsylvania, said in the release.
According to the lawsuit, “some of Dr. Luketich’s patients were forced to endure additional surgical procedures and/or extended hospital stays as a result of his unlawful conduct. Numerous patients developed painful pressure ulcers. A few were diagnosed with compartment syndrome. And at least two had to undergo amputations.”
The allegations were originally brought forward under the federal False Claims Act’s whistleblower provisions by Jonathan D’Cunha, MD, PhD, who worked closely with Dr. Luketich from 2012 to 2019 and now chairs the department of cardiothoracic surgery at the Mayo Clinic, Phoenix.
The charges cited in the lawsuit include three counts of violating the False Claims Act, one count of unjust enrichment, and one count of payment by mistake.
The 56-page lawsuit includes numerous case examples and cites an October 2015 Boston Globe Spotlight Team report on the safety of running concurrent operations, which reportedly prompted UPMC to reevaluate its policies and identify physicians or departments in potential violation.
Hospital officials met with Dr. Luketich in March 2016 and devised a “plan” to ensure his availability and “compliance with concurrency rules,” it alleges, but also highlights an email that notes “continued problems” with Dr. Luketich’s schedule.
“UPMC has persistently ignored or minimized complaints by employees and staff regarding Dr. Luketich, his hyper-busy schedule, his refusal to delegate surgeries and surgical tasks” and “protected him from meaningful sanction; refused to curtail his surgical practice; and continued to allow Dr. Luketich to skirt the rules and endanger his patients,” according to the lawsuit.
The suit notes that Dr. Luketich is one of UPMC and UPP’s highest sources of revenue and that UPMC advertises him as a “life-saving pioneer” who routinely performs dramatic, last-ditch procedures on patients who are otherwise hopeless.
In response to an interview request from this news organization, a UPMC spokesperson wrote: “As the government itself concedes in its complaint, many of Dr. Luketich’s surgical patients are elderly, frail, and/or very ill. They include the ‘hopeless’ patients ... who suffer from chronic illness or metastatic cancer, and/or have extensive surgical histories and choose UPMC and Dr. Luketich when other physicians and health care providers have turned them down.”
“Dr. Luketich always performs the most critical portions of every operation he undertakes,” the spokesperson said, adding that no law or regulation prohibits overlapping surgeries or billing for those surgeries, “let alone surgeries conducted by teams of surgeons like those led by Dr. Luketich.”
“The government’s claims are, rather, based on a misapplication or misinterpretation of UPMC’s internal policies and [Centers for Medicare & Medicaid Services] guidance, neither of which can support a claim for fraudulent billing. UPMC and Dr. Luketich plan to vigorously defend against the government’s claims,” the spokesperson concluded.
The claims asserted against the defendants are allegations only; there has been no determination of liability. The government is seeking three times the amount of actual damages suffered as a result of the alleged false claims and/or fraud; a sum of $23,331 (or the maximum penalty, whichever is greater) for each false claim submitted by UPMC, UPP, and/or Dr. Luketich; and costs and expenses associated with the civil suit.
A version of this article first appeared on Medscape.com.
Following a 2-year investigation, the U.S. government has filed suit against the University of Pittsburgh Medical Center (UPMC), University of Pittsburgh Physicians (UPP), and James Luketich, MD, for billing related to concurrent surgeries performed by the long-time chair of cardiothoracic surgery.
The lawsuit alleges that UPMC “knowingly allowed” Dr. Luketich to “book and perform three surgeries at the same time, to miss the surgical time outs at the outset of those procedures, to go back-and-forth between operating rooms and even hospital facilities while his surgical patients remain under general anesthesia...”
UPMC, the lawsuit claims, also allowed Dr. Luketich to falsely attest that “he was with his patients throughout the entirety of their surgical procedures or during all ‘key and critical’ portions of those procedures and to unlawfully bill Government Health Benefit Programs for those procedures, all in order to increase surgical volume, maximize UPMC and UPP’s revenue, and/or appease Dr. Luketich.”
These practices violate the statutes and regulations governing the defendants, including those that prohibit “teaching physicians” like Dr. Luketich from performing and billing the U.S. for concurrent surgeries, the Department of Justice said in news release.
The Justice Department contends the defendants “knowingly submitted hundreds of materially false claims for payment” to Medicare, Medicaid, and other government programs over the past 6 years.
“The laws prohibiting ‘concurrent surgeries’ are in place for a reason: To protect patients and ensure they receive appropriate and focused medical care,” Stephen R. Kaufman, Acting U.S. Attorney for the Western District of Pennsylvania, said in the release.
According to the lawsuit, “some of Dr. Luketich’s patients were forced to endure additional surgical procedures and/or extended hospital stays as a result of his unlawful conduct. Numerous patients developed painful pressure ulcers. A few were diagnosed with compartment syndrome. And at least two had to undergo amputations.”
The allegations were originally brought forward under the federal False Claims Act’s whistleblower provisions by Jonathan D’Cunha, MD, PhD, who worked closely with Dr. Luketich from 2012 to 2019 and now chairs the department of cardiothoracic surgery at the Mayo Clinic, Phoenix.
The charges cited in the lawsuit include three counts of violating the False Claims Act, one count of unjust enrichment, and one count of payment by mistake.
The 56-page lawsuit includes numerous case examples and cites an October 2015 Boston Globe Spotlight Team report on the safety of running concurrent operations, which reportedly prompted UPMC to reevaluate its policies and identify physicians or departments in potential violation.
Hospital officials met with Dr. Luketich in March 2016 and devised a “plan” to ensure his availability and “compliance with concurrency rules,” it alleges, but also highlights an email that notes “continued problems” with Dr. Luketich’s schedule.
“UPMC has persistently ignored or minimized complaints by employees and staff regarding Dr. Luketich, his hyper-busy schedule, his refusal to delegate surgeries and surgical tasks” and “protected him from meaningful sanction; refused to curtail his surgical practice; and continued to allow Dr. Luketich to skirt the rules and endanger his patients,” according to the lawsuit.
The suit notes that Dr. Luketich is one of UPMC and UPP’s highest sources of revenue and that UPMC advertises him as a “life-saving pioneer” who routinely performs dramatic, last-ditch procedures on patients who are otherwise hopeless.
In response to an interview request from this news organization, a UPMC spokesperson wrote: “As the government itself concedes in its complaint, many of Dr. Luketich’s surgical patients are elderly, frail, and/or very ill. They include the ‘hopeless’ patients ... who suffer from chronic illness or metastatic cancer, and/or have extensive surgical histories and choose UPMC and Dr. Luketich when other physicians and health care providers have turned them down.”
“Dr. Luketich always performs the most critical portions of every operation he undertakes,” the spokesperson said, adding that no law or regulation prohibits overlapping surgeries or billing for those surgeries, “let alone surgeries conducted by teams of surgeons like those led by Dr. Luketich.”
“The government’s claims are, rather, based on a misapplication or misinterpretation of UPMC’s internal policies and [Centers for Medicare & Medicaid Services] guidance, neither of which can support a claim for fraudulent billing. UPMC and Dr. Luketich plan to vigorously defend against the government’s claims,” the spokesperson concluded.
The claims asserted against the defendants are allegations only; there has been no determination of liability. The government is seeking three times the amount of actual damages suffered as a result of the alleged false claims and/or fraud; a sum of $23,331 (or the maximum penalty, whichever is greater) for each false claim submitted by UPMC, UPP, and/or Dr. Luketich; and costs and expenses associated with the civil suit.
A version of this article first appeared on Medscape.com.
Following a 2-year investigation, the U.S. government has filed suit against the University of Pittsburgh Medical Center (UPMC), University of Pittsburgh Physicians (UPP), and James Luketich, MD, for billing related to concurrent surgeries performed by the long-time chair of cardiothoracic surgery.
The lawsuit alleges that UPMC “knowingly allowed” Dr. Luketich to “book and perform three surgeries at the same time, to miss the surgical time outs at the outset of those procedures, to go back-and-forth between operating rooms and even hospital facilities while his surgical patients remain under general anesthesia...”
UPMC, the lawsuit claims, also allowed Dr. Luketich to falsely attest that “he was with his patients throughout the entirety of their surgical procedures or during all ‘key and critical’ portions of those procedures and to unlawfully bill Government Health Benefit Programs for those procedures, all in order to increase surgical volume, maximize UPMC and UPP’s revenue, and/or appease Dr. Luketich.”
These practices violate the statutes and regulations governing the defendants, including those that prohibit “teaching physicians” like Dr. Luketich from performing and billing the U.S. for concurrent surgeries, the Department of Justice said in news release.
The Justice Department contends the defendants “knowingly submitted hundreds of materially false claims for payment” to Medicare, Medicaid, and other government programs over the past 6 years.
“The laws prohibiting ‘concurrent surgeries’ are in place for a reason: To protect patients and ensure they receive appropriate and focused medical care,” Stephen R. Kaufman, Acting U.S. Attorney for the Western District of Pennsylvania, said in the release.
According to the lawsuit, “some of Dr. Luketich’s patients were forced to endure additional surgical procedures and/or extended hospital stays as a result of his unlawful conduct. Numerous patients developed painful pressure ulcers. A few were diagnosed with compartment syndrome. And at least two had to undergo amputations.”
The allegations were originally brought forward under the federal False Claims Act’s whistleblower provisions by Jonathan D’Cunha, MD, PhD, who worked closely with Dr. Luketich from 2012 to 2019 and now chairs the department of cardiothoracic surgery at the Mayo Clinic, Phoenix.
The charges cited in the lawsuit include three counts of violating the False Claims Act, one count of unjust enrichment, and one count of payment by mistake.
The 56-page lawsuit includes numerous case examples and cites an October 2015 Boston Globe Spotlight Team report on the safety of running concurrent operations, which reportedly prompted UPMC to reevaluate its policies and identify physicians or departments in potential violation.
Hospital officials met with Dr. Luketich in March 2016 and devised a “plan” to ensure his availability and “compliance with concurrency rules,” it alleges, but also highlights an email that notes “continued problems” with Dr. Luketich’s schedule.
“UPMC has persistently ignored or minimized complaints by employees and staff regarding Dr. Luketich, his hyper-busy schedule, his refusal to delegate surgeries and surgical tasks” and “protected him from meaningful sanction; refused to curtail his surgical practice; and continued to allow Dr. Luketich to skirt the rules and endanger his patients,” according to the lawsuit.
The suit notes that Dr. Luketich is one of UPMC and UPP’s highest sources of revenue and that UPMC advertises him as a “life-saving pioneer” who routinely performs dramatic, last-ditch procedures on patients who are otherwise hopeless.
In response to an interview request from this news organization, a UPMC spokesperson wrote: “As the government itself concedes in its complaint, many of Dr. Luketich’s surgical patients are elderly, frail, and/or very ill. They include the ‘hopeless’ patients ... who suffer from chronic illness or metastatic cancer, and/or have extensive surgical histories and choose UPMC and Dr. Luketich when other physicians and health care providers have turned them down.”
“Dr. Luketich always performs the most critical portions of every operation he undertakes,” the spokesperson said, adding that no law or regulation prohibits overlapping surgeries or billing for those surgeries, “let alone surgeries conducted by teams of surgeons like those led by Dr. Luketich.”
“The government’s claims are, rather, based on a misapplication or misinterpretation of UPMC’s internal policies and [Centers for Medicare & Medicaid Services] guidance, neither of which can support a claim for fraudulent billing. UPMC and Dr. Luketich plan to vigorously defend against the government’s claims,” the spokesperson concluded.
The claims asserted against the defendants are allegations only; there has been no determination of liability. The government is seeking three times the amount of actual damages suffered as a result of the alleged false claims and/or fraud; a sum of $23,331 (or the maximum penalty, whichever is greater) for each false claim submitted by UPMC, UPP, and/or Dr. Luketich; and costs and expenses associated with the civil suit.
A version of this article first appeared on Medscape.com.
New guidance on preventing cutaneous SCC in solid organ transplant patients
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.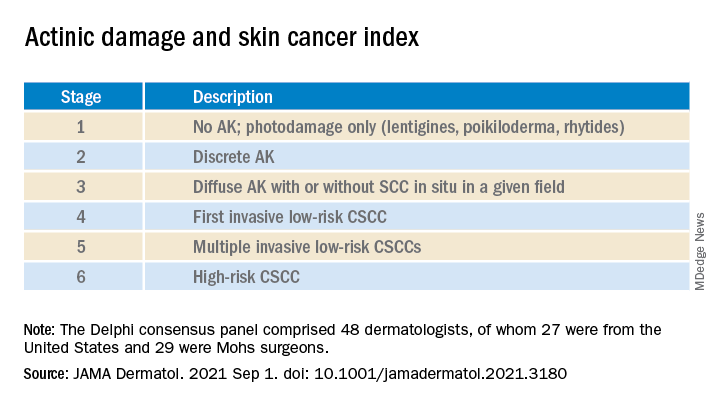
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.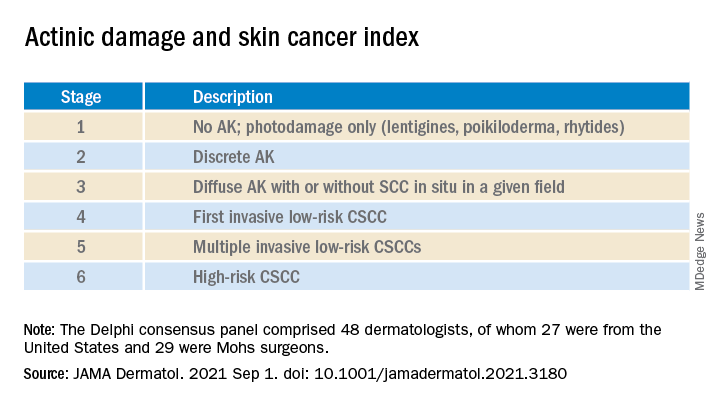
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.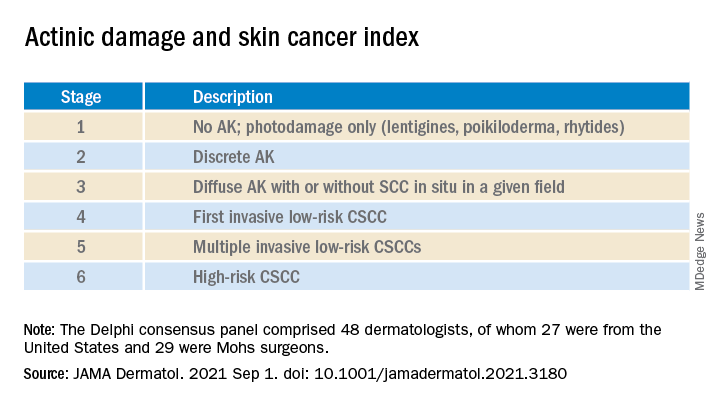
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
Sweeping new vaccine mandates will impact most U.S. workers
, including sweeping vaccine mandates that will affect 100 million American workers, nearly two-thirds of the country’s workforce.
“As your president, I’m announcing tonight a new plan to get more Americans vaccinated to combat those blocking public health,” he said Sept. 9.
As part of a six-part plan unveiled in a speech from the State Dining Room of the White House, President Biden said he would require vaccinations for nearly 4 million federal workers and the employees of companies that contract with the federal government.
He has also directed the Occupational Safety and Health Administration to develop a rule that will require large employers -- those with at least 100 employees -- to ensure their workers are vaccinated or tested weekly.
Nearly 17 million health care workers will face new vaccine mandates as part of the conditions of participation in the Medicare and Medicaid programs.
President Biden said the federal government will require staff at federally funded Head Start programs and schools to be vaccinated. He’s also calling on all states to mandate vaccines for teachers.
“A distinct minority of Americans, supported by a distinct minority of elected officials, are keeping us from turning the corner,” PresidentBiden said. “These pandemic politics, as I refer to them, are making people sick, causing unvaccinated people to die.”
One public health official said he was glad to see the president’s bold action.
“What I saw today was the federal government trying to use its powers to create greater safety in the American population,” said Ashish K. Jha, MD, dean of the school of public health at Brown University, Providence, R.I., in a call with reporters after the speech.
National Nurses United, the largest union of registered nurses in the United States, issued a statement in support of President Biden’s new vaccination requirements, but pushed back on his language.
“…as advocates for public health, registered nurses want to be extremely clear: There is no such thing as a pandemic of only the unvaccinated. The science of epidemiology tells us there is just one deadly, global pandemic that has not yet ended, and we are all in it together. To get out of it, we must act together. All of us,” the statement says.
A host of other professional groups, including the American Medical Association and the Association of State and Territorial Health Officials, also issued statements of support for President Biden’s plan.
But the plan was not well received by all.
“I will pursue every legal option available to the state of Georgia to stop this blatantly unlawful overreach by the Biden Administration,” said Georgia Governor Brian Kemp, a Republican, in a Tweet.
The National Council for Occupational Safety and Health called the plan “a missed opportunity” because it failed to include workplace protections for essential workers such as grocery, postal, and transit workers.
“Social distancing, improved ventilation, shift rotation, and protective equipment to reduce exposure are important components of an overall plan to reduce risk and stop the virus. These tools are missing from the new steps President Biden announced today,” said Jessica Martinez, co-executive director of the group.
In addition to the new vaccination requirements, President Biden said extra doses would be on the way for people who have already been fully vaccinated in order to protect against waning immunity, starting on Sept. 20. But he noted that those plans would be contingent on the Food and Drug Administration’s approval for third doses and the Centers for Disease Control and Prevention’s recommendation of the shots.
President Biden pledged to use the Defense Production Act to ramp up production of at-home tests, which have been selling out across the nation as the Delta variant spreads.
He also announced plans to expand access to COVID-19 testing, including offering testing for free at thousands of pharmacies nationwide and getting major retailers to sell at-home COVID-19 tests at cost.
The BinaxNow test kit, which currently retails for $23.99, will now cost about $15 for two tests at Kroger, Amazon, and Walmart, according to the White House. Food banks and community health centers will get free tests, too.
He called on states to set up COVID-19 testing programs at all schools.
Jha said that in his view, the big, game-changing news out of the president’s speech was the expansion of testing.
“Our country has failed to deploy tests in a way that can really bring this pandemic under control,” Jha said. “There are plenty of reasons, data, experience to indicate that if these were widely available, it would make a dramatic difference in reducing infection numbers across our country.”.
Dr. Jha said the private market had not worked effectively to make testing more widely available, so it was “absolutely a requirement of the federal government to step in and make testing more widely available,” he said.
President Biden also announced new economic stimulus programs, saying he’s expanding loan programs to small businesses and streamlining the loan forgiveness process.
President Biden said he’s boosting help for overburdened hospitals, doubling the number of federal surge response teams sent to hard-hit areas to reduce the strain on local health care workers. He said he would increase the pace of antibody treatments to states by 50%.
“We made so much progress during the past 7 months of this pandemic. Even so, we remain at a critical moment, a critical time,” he said. “We have the tools. Now, we just have to finish the job with truth, with science, with confidence and together as one nation.”
A version of this article first appeared on WebMD.com.
, including sweeping vaccine mandates that will affect 100 million American workers, nearly two-thirds of the country’s workforce.
“As your president, I’m announcing tonight a new plan to get more Americans vaccinated to combat those blocking public health,” he said Sept. 9.
As part of a six-part plan unveiled in a speech from the State Dining Room of the White House, President Biden said he would require vaccinations for nearly 4 million federal workers and the employees of companies that contract with the federal government.
He has also directed the Occupational Safety and Health Administration to develop a rule that will require large employers -- those with at least 100 employees -- to ensure their workers are vaccinated or tested weekly.
Nearly 17 million health care workers will face new vaccine mandates as part of the conditions of participation in the Medicare and Medicaid programs.
President Biden said the federal government will require staff at federally funded Head Start programs and schools to be vaccinated. He’s also calling on all states to mandate vaccines for teachers.
“A distinct minority of Americans, supported by a distinct minority of elected officials, are keeping us from turning the corner,” PresidentBiden said. “These pandemic politics, as I refer to them, are making people sick, causing unvaccinated people to die.”
One public health official said he was glad to see the president’s bold action.
“What I saw today was the federal government trying to use its powers to create greater safety in the American population,” said Ashish K. Jha, MD, dean of the school of public health at Brown University, Providence, R.I., in a call with reporters after the speech.
National Nurses United, the largest union of registered nurses in the United States, issued a statement in support of President Biden’s new vaccination requirements, but pushed back on his language.
“…as advocates for public health, registered nurses want to be extremely clear: There is no such thing as a pandemic of only the unvaccinated. The science of epidemiology tells us there is just one deadly, global pandemic that has not yet ended, and we are all in it together. To get out of it, we must act together. All of us,” the statement says.
A host of other professional groups, including the American Medical Association and the Association of State and Territorial Health Officials, also issued statements of support for President Biden’s plan.
But the plan was not well received by all.
“I will pursue every legal option available to the state of Georgia to stop this blatantly unlawful overreach by the Biden Administration,” said Georgia Governor Brian Kemp, a Republican, in a Tweet.
The National Council for Occupational Safety and Health called the plan “a missed opportunity” because it failed to include workplace protections for essential workers such as grocery, postal, and transit workers.
“Social distancing, improved ventilation, shift rotation, and protective equipment to reduce exposure are important components of an overall plan to reduce risk and stop the virus. These tools are missing from the new steps President Biden announced today,” said Jessica Martinez, co-executive director of the group.
In addition to the new vaccination requirements, President Biden said extra doses would be on the way for people who have already been fully vaccinated in order to protect against waning immunity, starting on Sept. 20. But he noted that those plans would be contingent on the Food and Drug Administration’s approval for third doses and the Centers for Disease Control and Prevention’s recommendation of the shots.
President Biden pledged to use the Defense Production Act to ramp up production of at-home tests, which have been selling out across the nation as the Delta variant spreads.
He also announced plans to expand access to COVID-19 testing, including offering testing for free at thousands of pharmacies nationwide and getting major retailers to sell at-home COVID-19 tests at cost.
The BinaxNow test kit, which currently retails for $23.99, will now cost about $15 for two tests at Kroger, Amazon, and Walmart, according to the White House. Food banks and community health centers will get free tests, too.
He called on states to set up COVID-19 testing programs at all schools.
Jha said that in his view, the big, game-changing news out of the president’s speech was the expansion of testing.
“Our country has failed to deploy tests in a way that can really bring this pandemic under control,” Jha said. “There are plenty of reasons, data, experience to indicate that if these were widely available, it would make a dramatic difference in reducing infection numbers across our country.”.
Dr. Jha said the private market had not worked effectively to make testing more widely available, so it was “absolutely a requirement of the federal government to step in and make testing more widely available,” he said.
President Biden also announced new economic stimulus programs, saying he’s expanding loan programs to small businesses and streamlining the loan forgiveness process.
President Biden said he’s boosting help for overburdened hospitals, doubling the number of federal surge response teams sent to hard-hit areas to reduce the strain on local health care workers. He said he would increase the pace of antibody treatments to states by 50%.
“We made so much progress during the past 7 months of this pandemic. Even so, we remain at a critical moment, a critical time,” he said. “We have the tools. Now, we just have to finish the job with truth, with science, with confidence and together as one nation.”
A version of this article first appeared on WebMD.com.
, including sweeping vaccine mandates that will affect 100 million American workers, nearly two-thirds of the country’s workforce.
“As your president, I’m announcing tonight a new plan to get more Americans vaccinated to combat those blocking public health,” he said Sept. 9.
As part of a six-part plan unveiled in a speech from the State Dining Room of the White House, President Biden said he would require vaccinations for nearly 4 million federal workers and the employees of companies that contract with the federal government.
He has also directed the Occupational Safety and Health Administration to develop a rule that will require large employers -- those with at least 100 employees -- to ensure their workers are vaccinated or tested weekly.
Nearly 17 million health care workers will face new vaccine mandates as part of the conditions of participation in the Medicare and Medicaid programs.
President Biden said the federal government will require staff at federally funded Head Start programs and schools to be vaccinated. He’s also calling on all states to mandate vaccines for teachers.
“A distinct minority of Americans, supported by a distinct minority of elected officials, are keeping us from turning the corner,” PresidentBiden said. “These pandemic politics, as I refer to them, are making people sick, causing unvaccinated people to die.”
One public health official said he was glad to see the president’s bold action.
“What I saw today was the federal government trying to use its powers to create greater safety in the American population,” said Ashish K. Jha, MD, dean of the school of public health at Brown University, Providence, R.I., in a call with reporters after the speech.
National Nurses United, the largest union of registered nurses in the United States, issued a statement in support of President Biden’s new vaccination requirements, but pushed back on his language.
“…as advocates for public health, registered nurses want to be extremely clear: There is no such thing as a pandemic of only the unvaccinated. The science of epidemiology tells us there is just one deadly, global pandemic that has not yet ended, and we are all in it together. To get out of it, we must act together. All of us,” the statement says.
A host of other professional groups, including the American Medical Association and the Association of State and Territorial Health Officials, also issued statements of support for President Biden’s plan.
But the plan was not well received by all.
“I will pursue every legal option available to the state of Georgia to stop this blatantly unlawful overreach by the Biden Administration,” said Georgia Governor Brian Kemp, a Republican, in a Tweet.
The National Council for Occupational Safety and Health called the plan “a missed opportunity” because it failed to include workplace protections for essential workers such as grocery, postal, and transit workers.
“Social distancing, improved ventilation, shift rotation, and protective equipment to reduce exposure are important components of an overall plan to reduce risk and stop the virus. These tools are missing from the new steps President Biden announced today,” said Jessica Martinez, co-executive director of the group.
In addition to the new vaccination requirements, President Biden said extra doses would be on the way for people who have already been fully vaccinated in order to protect against waning immunity, starting on Sept. 20. But he noted that those plans would be contingent on the Food and Drug Administration’s approval for third doses and the Centers for Disease Control and Prevention’s recommendation of the shots.
President Biden pledged to use the Defense Production Act to ramp up production of at-home tests, which have been selling out across the nation as the Delta variant spreads.
He also announced plans to expand access to COVID-19 testing, including offering testing for free at thousands of pharmacies nationwide and getting major retailers to sell at-home COVID-19 tests at cost.
The BinaxNow test kit, which currently retails for $23.99, will now cost about $15 for two tests at Kroger, Amazon, and Walmart, according to the White House. Food banks and community health centers will get free tests, too.
He called on states to set up COVID-19 testing programs at all schools.
Jha said that in his view, the big, game-changing news out of the president’s speech was the expansion of testing.
“Our country has failed to deploy tests in a way that can really bring this pandemic under control,” Jha said. “There are plenty of reasons, data, experience to indicate that if these were widely available, it would make a dramatic difference in reducing infection numbers across our country.”.
Dr. Jha said the private market had not worked effectively to make testing more widely available, so it was “absolutely a requirement of the federal government to step in and make testing more widely available,” he said.
President Biden also announced new economic stimulus programs, saying he’s expanding loan programs to small businesses and streamlining the loan forgiveness process.
President Biden said he’s boosting help for overburdened hospitals, doubling the number of federal surge response teams sent to hard-hit areas to reduce the strain on local health care workers. He said he would increase the pace of antibody treatments to states by 50%.
“We made so much progress during the past 7 months of this pandemic. Even so, we remain at a critical moment, a critical time,” he said. “We have the tools. Now, we just have to finish the job with truth, with science, with confidence and together as one nation.”
A version of this article first appeared on WebMD.com.
Elderly mice receive the gift of warmth
Steal from the warm, give to the cold
If there’s one constant in life other than taxes, it’s elderly people moving to Florida. The Sunshine State’s reputation as a giant retirement home needs no elaboration, but why do senior citizens gravitate there? Well, many reasons, but a big one is that, the older you get, the more susceptible and sensitive you are to the cold. And now, according to a new study, we may have identified a culprit.
Researchers from Yale University examined a group of mice and found that the older ones lacked ICL2 cells in their fatty tissue. These cells, at least in younger mice, help restore body heat when exposed to cold temperatures. Lacking these cells meant that older mice had a limited ability to burn their fat and raise their temperature in response to cold.
Well, job done, all we need to do now is stimulate production of ICL2 cells in elderly people, and they’ll be able to go outside in 80-degree weather without a sweater again. Except there’s a problem. In a cruel twist of fate, when the elderly mice were given a molecule to boost ICL2 cell production, they actually became less tolerant of the cold than at baseline. Oops.
The scientists didn’t give up though, and gave their elderly mice ICL2 cells from young mice. This finally did the trick, though we have to admit, if that treatment does eventually scale up to humans, the prospect of a bunch of senior citizens taking ICL2 cells from young people to stay warm does sound a bit like a bad vampire movie premise. “I vant to suck your immune cell group 2 innate lymphoid cells!” Not the most pithy catch phrase in the world.
Grocery store tapping your subconscious? It’s a good thing
We all know there’s marketing and functionality elements to grocery stores and how they’re set up for your shopping pleasure. But what if I told you that the good old supermarket subconscious trick works on how healthy food decisions are?
In a recent study, researchers at the University of Southampton in England found that if you placed a wider selection of fruits and vegetables near the entrances and more nonfood items near checkouts, sales decreased on the sweets and increased on the produce. “The findings of our study suggest that a healthier store layout could lead to nearly 10,000 extra portions of fruit and vegetables and approximately 1,500 fewer portions of confectionery being sold on a weekly basis in each store,” lead author Dr. Christina Vogel explained.
You’re probably thinking that food placement studies aren’t new. That’s true, but this one went above and beyond. Instead of just looking at the influence placement has on purchase, this one took it further by trying to reduce the consumers’ “calorie opportunities” and examining the effect on sales. Also, customer loyalty, patterns, and diets were taken into account across multiple household members.
The researchers think shifting the layouts in grocery stores could shift people’s food choices, producing a domino effect on the population’s overall diet. With obesity, diabetes, and cardiology concerns always looming, swaying consumers toward healthier food choices makes for better public health overall.
So if you feel like you’re being subconsciously assaulted by veggies every time you walk into Trader Joe’s, just know it’s for your own good.
TikTokers take on tics
We know TikTok is what makes a lot of teens and young adults tick, but what if TikTokers are actually catching tic disorders from other TikTokers?
TikTok blew up during the pandemic. Many people were stuck at home and had nothing better to do than make and watch TikTok videos. The pandemic brought isolation, uncertainty, and anxiety. The stress that followed may have caused many people, mostly women and young girls, to develop tic disorders.
There’s a TikTok for everything, whether it’s a new dance or a recipe. Many people even use TikTok to speak out about their illnesses. Several TikTokers have Tourette’s syndrome and show their tics on their videos. It appears that some audience members actually “catch” the tics from watching the videos and are then unable to stop certain jerking movements or saying specific words.
Neurologists at the University of Calgary (Alta.), who were hearing from colleagues and getting referrals of such patients, called it “an epidemic within the pandemic.” The behavior is not actually Tourette’s, they told Vice, but the patients “cannot stop, and we have absolutely witnessed that.”
There is, of course, controversy over the issue. One individual with the condition said, “I feel like there’s a lot of really weird, backwards stigma on TikTok about tic disorders. Like, you aren’t allowed to have one unless it’s this one.”
Who would have guessed that people would disagree over stuff on the Internet?
Look on the bright side: Obesity edition
The pandemic may have postponed “Top Gun: Maverick” and “The Marvelous Mrs. Maisel” until who-knows-when, but we here at LOTME are happy to announce the nearly-as-anticipated return of Bacteria vs. the World.
As you may recall from our last edition of BVTW, bacteria battled the ghost of Charles Darwin, who had taken the earthly form of antibiotics capable of stopping bacterial evolution. Tonight, our prokaryotic protagonists take on an equally relentless and ubiquitous challenger: obesity.
Specifically, we’re putting bacteria up against the obesity survival paradox, that phenomenon in which obesity and overweight seem to protect against – yes, you guessed it – bacterial infections.
A Swedish research team observed a group of 2,196 individual adults who received care for suspected severe bacterial infection at Skaraborg Hospital in Skövde. One year after hospitalization, 26% of normal-weight (body mass index, 18.5-24.99) patients were dead, compared with 17% of overweight (BMI, 25.0-29.99), 16% of obese (BMI, 30.0-34.99), and 9% of very obese (BMI >35) patients.
These results confirm the obesity survival paradox, but “what we don’t know is how being overweight can benefit the patient with a bacterial infection, or whether it’s connected with functions in the immune system and how they’re regulated,” lead author Dr. Åsa Alsiö said in a written statement.
A spokes-cell for the bacteria disputed the results and challenged the legitimacy of the investigators. When asked if there should be some sort of reexamination of the findings, he/she/it replied: “You bet your flagella.” We then pointed out that humans don’t have flagellum, and the representative raised his/her/its flagella in what could only be considered an obscene gesture.
Steal from the warm, give to the cold
If there’s one constant in life other than taxes, it’s elderly people moving to Florida. The Sunshine State’s reputation as a giant retirement home needs no elaboration, but why do senior citizens gravitate there? Well, many reasons, but a big one is that, the older you get, the more susceptible and sensitive you are to the cold. And now, according to a new study, we may have identified a culprit.
Researchers from Yale University examined a group of mice and found that the older ones lacked ICL2 cells in their fatty tissue. These cells, at least in younger mice, help restore body heat when exposed to cold temperatures. Lacking these cells meant that older mice had a limited ability to burn their fat and raise their temperature in response to cold.
Well, job done, all we need to do now is stimulate production of ICL2 cells in elderly people, and they’ll be able to go outside in 80-degree weather without a sweater again. Except there’s a problem. In a cruel twist of fate, when the elderly mice were given a molecule to boost ICL2 cell production, they actually became less tolerant of the cold than at baseline. Oops.
The scientists didn’t give up though, and gave their elderly mice ICL2 cells from young mice. This finally did the trick, though we have to admit, if that treatment does eventually scale up to humans, the prospect of a bunch of senior citizens taking ICL2 cells from young people to stay warm does sound a bit like a bad vampire movie premise. “I vant to suck your immune cell group 2 innate lymphoid cells!” Not the most pithy catch phrase in the world.
Grocery store tapping your subconscious? It’s a good thing
We all know there’s marketing and functionality elements to grocery stores and how they’re set up for your shopping pleasure. But what if I told you that the good old supermarket subconscious trick works on how healthy food decisions are?
In a recent study, researchers at the University of Southampton in England found that if you placed a wider selection of fruits and vegetables near the entrances and more nonfood items near checkouts, sales decreased on the sweets and increased on the produce. “The findings of our study suggest that a healthier store layout could lead to nearly 10,000 extra portions of fruit and vegetables and approximately 1,500 fewer portions of confectionery being sold on a weekly basis in each store,” lead author Dr. Christina Vogel explained.
You’re probably thinking that food placement studies aren’t new. That’s true, but this one went above and beyond. Instead of just looking at the influence placement has on purchase, this one took it further by trying to reduce the consumers’ “calorie opportunities” and examining the effect on sales. Also, customer loyalty, patterns, and diets were taken into account across multiple household members.
The researchers think shifting the layouts in grocery stores could shift people’s food choices, producing a domino effect on the population’s overall diet. With obesity, diabetes, and cardiology concerns always looming, swaying consumers toward healthier food choices makes for better public health overall.
So if you feel like you’re being subconsciously assaulted by veggies every time you walk into Trader Joe’s, just know it’s for your own good.
TikTokers take on tics
We know TikTok is what makes a lot of teens and young adults tick, but what if TikTokers are actually catching tic disorders from other TikTokers?
TikTok blew up during the pandemic. Many people were stuck at home and had nothing better to do than make and watch TikTok videos. The pandemic brought isolation, uncertainty, and anxiety. The stress that followed may have caused many people, mostly women and young girls, to develop tic disorders.
There’s a TikTok for everything, whether it’s a new dance or a recipe. Many people even use TikTok to speak out about their illnesses. Several TikTokers have Tourette’s syndrome and show their tics on their videos. It appears that some audience members actually “catch” the tics from watching the videos and are then unable to stop certain jerking movements or saying specific words.
Neurologists at the University of Calgary (Alta.), who were hearing from colleagues and getting referrals of such patients, called it “an epidemic within the pandemic.” The behavior is not actually Tourette’s, they told Vice, but the patients “cannot stop, and we have absolutely witnessed that.”
There is, of course, controversy over the issue. One individual with the condition said, “I feel like there’s a lot of really weird, backwards stigma on TikTok about tic disorders. Like, you aren’t allowed to have one unless it’s this one.”
Who would have guessed that people would disagree over stuff on the Internet?
Look on the bright side: Obesity edition
The pandemic may have postponed “Top Gun: Maverick” and “The Marvelous Mrs. Maisel” until who-knows-when, but we here at LOTME are happy to announce the nearly-as-anticipated return of Bacteria vs. the World.
As you may recall from our last edition of BVTW, bacteria battled the ghost of Charles Darwin, who had taken the earthly form of antibiotics capable of stopping bacterial evolution. Tonight, our prokaryotic protagonists take on an equally relentless and ubiquitous challenger: obesity.
Specifically, we’re putting bacteria up against the obesity survival paradox, that phenomenon in which obesity and overweight seem to protect against – yes, you guessed it – bacterial infections.
A Swedish research team observed a group of 2,196 individual adults who received care for suspected severe bacterial infection at Skaraborg Hospital in Skövde. One year after hospitalization, 26% of normal-weight (body mass index, 18.5-24.99) patients were dead, compared with 17% of overweight (BMI, 25.0-29.99), 16% of obese (BMI, 30.0-34.99), and 9% of very obese (BMI >35) patients.
These results confirm the obesity survival paradox, but “what we don’t know is how being overweight can benefit the patient with a bacterial infection, or whether it’s connected with functions in the immune system and how they’re regulated,” lead author Dr. Åsa Alsiö said in a written statement.
A spokes-cell for the bacteria disputed the results and challenged the legitimacy of the investigators. When asked if there should be some sort of reexamination of the findings, he/she/it replied: “You bet your flagella.” We then pointed out that humans don’t have flagellum, and the representative raised his/her/its flagella in what could only be considered an obscene gesture.
Steal from the warm, give to the cold
If there’s one constant in life other than taxes, it’s elderly people moving to Florida. The Sunshine State’s reputation as a giant retirement home needs no elaboration, but why do senior citizens gravitate there? Well, many reasons, but a big one is that, the older you get, the more susceptible and sensitive you are to the cold. And now, according to a new study, we may have identified a culprit.
Researchers from Yale University examined a group of mice and found that the older ones lacked ICL2 cells in their fatty tissue. These cells, at least in younger mice, help restore body heat when exposed to cold temperatures. Lacking these cells meant that older mice had a limited ability to burn their fat and raise their temperature in response to cold.
Well, job done, all we need to do now is stimulate production of ICL2 cells in elderly people, and they’ll be able to go outside in 80-degree weather without a sweater again. Except there’s a problem. In a cruel twist of fate, when the elderly mice were given a molecule to boost ICL2 cell production, they actually became less tolerant of the cold than at baseline. Oops.
The scientists didn’t give up though, and gave their elderly mice ICL2 cells from young mice. This finally did the trick, though we have to admit, if that treatment does eventually scale up to humans, the prospect of a bunch of senior citizens taking ICL2 cells from young people to stay warm does sound a bit like a bad vampire movie premise. “I vant to suck your immune cell group 2 innate lymphoid cells!” Not the most pithy catch phrase in the world.
Grocery store tapping your subconscious? It’s a good thing
We all know there’s marketing and functionality elements to grocery stores and how they’re set up for your shopping pleasure. But what if I told you that the good old supermarket subconscious trick works on how healthy food decisions are?
In a recent study, researchers at the University of Southampton in England found that if you placed a wider selection of fruits and vegetables near the entrances and more nonfood items near checkouts, sales decreased on the sweets and increased on the produce. “The findings of our study suggest that a healthier store layout could lead to nearly 10,000 extra portions of fruit and vegetables and approximately 1,500 fewer portions of confectionery being sold on a weekly basis in each store,” lead author Dr. Christina Vogel explained.
You’re probably thinking that food placement studies aren’t new. That’s true, but this one went above and beyond. Instead of just looking at the influence placement has on purchase, this one took it further by trying to reduce the consumers’ “calorie opportunities” and examining the effect on sales. Also, customer loyalty, patterns, and diets were taken into account across multiple household members.
The researchers think shifting the layouts in grocery stores could shift people’s food choices, producing a domino effect on the population’s overall diet. With obesity, diabetes, and cardiology concerns always looming, swaying consumers toward healthier food choices makes for better public health overall.
So if you feel like you’re being subconsciously assaulted by veggies every time you walk into Trader Joe’s, just know it’s for your own good.
TikTokers take on tics
We know TikTok is what makes a lot of teens and young adults tick, but what if TikTokers are actually catching tic disorders from other TikTokers?
TikTok blew up during the pandemic. Many people were stuck at home and had nothing better to do than make and watch TikTok videos. The pandemic brought isolation, uncertainty, and anxiety. The stress that followed may have caused many people, mostly women and young girls, to develop tic disorders.
There’s a TikTok for everything, whether it’s a new dance or a recipe. Many people even use TikTok to speak out about their illnesses. Several TikTokers have Tourette’s syndrome and show their tics on their videos. It appears that some audience members actually “catch” the tics from watching the videos and are then unable to stop certain jerking movements or saying specific words.
Neurologists at the University of Calgary (Alta.), who were hearing from colleagues and getting referrals of such patients, called it “an epidemic within the pandemic.” The behavior is not actually Tourette’s, they told Vice, but the patients “cannot stop, and we have absolutely witnessed that.”
There is, of course, controversy over the issue. One individual with the condition said, “I feel like there’s a lot of really weird, backwards stigma on TikTok about tic disorders. Like, you aren’t allowed to have one unless it’s this one.”
Who would have guessed that people would disagree over stuff on the Internet?
Look on the bright side: Obesity edition
The pandemic may have postponed “Top Gun: Maverick” and “The Marvelous Mrs. Maisel” until who-knows-when, but we here at LOTME are happy to announce the nearly-as-anticipated return of Bacteria vs. the World.
As you may recall from our last edition of BVTW, bacteria battled the ghost of Charles Darwin, who had taken the earthly form of antibiotics capable of stopping bacterial evolution. Tonight, our prokaryotic protagonists take on an equally relentless and ubiquitous challenger: obesity.
Specifically, we’re putting bacteria up against the obesity survival paradox, that phenomenon in which obesity and overweight seem to protect against – yes, you guessed it – bacterial infections.
A Swedish research team observed a group of 2,196 individual adults who received care for suspected severe bacterial infection at Skaraborg Hospital in Skövde. One year after hospitalization, 26% of normal-weight (body mass index, 18.5-24.99) patients were dead, compared with 17% of overweight (BMI, 25.0-29.99), 16% of obese (BMI, 30.0-34.99), and 9% of very obese (BMI >35) patients.
These results confirm the obesity survival paradox, but “what we don’t know is how being overweight can benefit the patient with a bacterial infection, or whether it’s connected with functions in the immune system and how they’re regulated,” lead author Dr. Åsa Alsiö said in a written statement.
A spokes-cell for the bacteria disputed the results and challenged the legitimacy of the investigators. When asked if there should be some sort of reexamination of the findings, he/she/it replied: “You bet your flagella.” We then pointed out that humans don’t have flagellum, and the representative raised his/her/its flagella in what could only be considered an obscene gesture.
I did peer review: I saw turf wars, ego, and unfairness
After making an insulting comment to a surgery scheduler, a surgeon become the subject of a peer review investigation.
The surgeon had been called in on a Saturday morning for surgery, but when he arrived at the hospital, staff informed him that the operating room had been incorrectly booked and asked him to come back that afternoon. When the surgeon returned, the room still wasn’t ready, recounted David Beran, DO, a peer reviewer and medical director for the emergency department at University Medical Center New Orleans, in Louisiana. After more waiting and staff uncertainty about which operating room was going to open, the surgeon became frustrated and said to the scheduler: “Any idiot could figure this out!”
During his peer review, the surgeon acknowledged that he shouldn’t have made the rude remark to the scheduler, Dr. Beran said. His exasperation stemmed from an ongoing problem – operating rooms at the hospital were being inefficiently managed.
“The surgeon acknowledged that even though there was a systems issue at the root, that’s not justification to speak to people unprofessionally,” Dr. Beran said. “So, there was education for the surgeon, but the surgeon was also able to explain the frustration that led to that point.”
System problems are commonly encountered by peer reviewers, said Dr. Beran.
“There’s a huge gap between administration and clinical professionals when it comes to peer review,” he said. “So many times, bad situations, whether they’re clinical or behavioral, often boil down to systems issues or some inadequacy, whether it’s an EMR [electronic medical record] problem, an inefficacy, or how complicated a process is for an end user. But having a peer review situation that then leads to a system-level change that prevents that problem from happening again is really unlikely. There’s a huge disconnect between those two.”
Peer review is generally a process that goes on behind closed doors. Although structures may differ, peer review is generally described as the process by which physicians assess the quality of their peers’ work to ensure that standards of care are being met. The process is often used to evaluate issues regarding clinical care as well as behavioral complaints against physicians.
Doctors who undergo peer review frequently share their experiences, but reviewers themselves rarely speak out. For this story,
“Peer review processes are in place to build stronger institutions and stronger practices, and they’re supposed to be helpful,” Dr. Beran said. “But because of how opaque they are, it immediately puts physicians on the defensive, and it doesn’t always succeed in what it’s trying to do. I think that’s one of the biggest challenges.”
Biased reviewers taint evaluations
A peer reviewer on and off throughout her career, Indiana family physician Lana Patch, MD, said she always strived to be fair when evaluating fellow physicians. But not every reviewer she encountered operated the same way, she said. Some were biased.
In one case, Dr. Patch peer reviewed a general surgeon who had performed a hysterectomy on a 16-year-old girl. The surgeon believed the teenager likely had an acute appendicitis, but it turned out she had a uterine pathology, Dr. Patch said. The surgeon saved the girl’s life, but the case came under review because of the patient’s age and the fact that her uterus was removed. A local obstetrician-gynecologist weighed in on the case.
“The local ob.gyn. saw it as a turf battle,” recalled Dr. Patch, who is now retired after 30 years of practice in eastern Indiana. “The doctor had nothing but bad to say about the surgeon. He was a competitor.”
Because it was a small hospital, the committee sometimes had trouble finding a specialist who was qualified to give an opinion and who wasn’t in competition with the physician in question, said Dr. Patch. Eventually they found an outside pediatric gynecologist who reviewed the case and concluded that the surgeon had followed the standard of care.
Personal agendas in can come from different directions, said Robert Marder, MD, the author of several books on peer review. Dr. Marder is a consultant who assists with peer review redesign. He has worked with hundreds of medical staff leaders and is a former vice president at the Greeley Company, a consulting firm in Danvers, Mass., that performs peer review redesign. Dr. Marder is president of Robert J. Marder Consulting.
“It goes both ways,” Dr. Marder said. “I’ve seen where somebody with a personal view decides to bring things to the peer review committee specifically because they want the peer review committee to have an adverse view of this person and get them off the medical staff. And I’ve seen hospitals that are uncomfortable with a certain person for whatever reason and want the peer review committee to address it, as opposed to addressing it from a human resource standpoint.”
Dr. Patch recalled a case in which reviewers and hospital leaders were at odds over the credentialing of a physician. Fifteen years earlier, while driving in California, the psychiatrist had been pulled over and was found with an ounce of marijuana, she said.
“We wanted to privilege him,” Dr. Patch said. “As staff physicians, we felt that was 15 years ago, people change over time. Doctors are human beings, too. He seemed to have good credentials and good training. The hospital said, ‘Oh no, we can’t have somebody like this.’ “
The psychiatrist was placed on probation and had to undergo a review every 90 days for about 3 years. Eventually, he was privileged, Dr. Patch said.
Bias among reviewers, including unintentional bias, is also a challenge, Dr. Marder noted. Some initial reviewers score a physician too harshly, he said, whereas others underscore.
“Underscoring is more insidious and more difficult to deal with,” Dr. Marder said. “Underscoring is where the reviewer is too nice. They tend to dismiss things from their colleagues rather than recognize them as an opportunity to help them improve. With underscoring, a lot of committees, if the initial reviewer says the care was appropriate, they don’t even look at the case. They just take that one person’s word for it.”
Reviewers: Looks can be deceiving
When first examining the documented details of a case, it can be easy for peer reviewers to make a quick judgment about what happened, Dr. Beran said.
“You get these complaints, and you read through it, and you think, ‘Oh man, this person really messed up,’ “ he said. “Then you hear the doctor’s side of it, and you realize, ‘No, there’s a much bigger picture at play.’ You realize both sides have valid perspectives on it.”
In one case, for example, Dr. Beran recalled a complaint against a physician who made a snarky remark to a nurse. The doctor had asked the nurse for a piece of equipment, and the nurse said she was busy preparing the room for a patient. The doctor made a comment along the lines of, “Well, would you like me to do that for you and also intubate the patient while you do some charting?!”
At first glance, it appeared that the physician lashed out inappropriately at the nurse. But when reviewers heard from the doctor, they learned that the nurses knew that a trauma patient was coming by ambulance and that he would likely require a ventilator, Dr. Beran said. As the minutes ticked by, however, the nurses were seen in the break room chatting. Nothing had been prepared in the room, including any airway supply.
“The patient had a prolonged course and a very difficult intubation and could have very easily wound up with a much worse outcome for something the nurses had been warned about prior to the patient’s arrival,” he said. “I can see anybody getting upset in that situation if I warned them 5 or 10 minutes beforehand, ‘Get this stuff ready,’ and then nothing was done.”
There was no direct penalty for the physician.
Just as some complaints can be misleading, the clinical record in some peer review cases can also lead reviewers astray.
Physicians frequently include too much irrelevant information in the record, which can cloud a peer review, said Hans Duvefelt, MD, a family physician at Pines Health Services, in Van Buren, Maine. Dr. Duvefelt is a former medical director at Bucksport Regional Health Center, in Ellsworth, Maine. Both facilities are federally qualified health centers where continuous, random peer reviews are required.
In one case, Dr. Duvefelt was peer reviewing a physician’s office note regarding an elderly patient with a low-grade fever. The final diagnosis was urinary tract infection. Dr. Duvefelt said he had trouble following the doctor’s line of thinking because of a plethora of unnecessary data in the 10-page document. The office note included past medical history, prior lab and imaging test results, and an extensive narrative section that included a mixture of active medical problems and ongoing relationships with specialists, he said.
After reading through the printout three times, Dr. Duvefelt said he finally found mention of increased urinary dribbling and details about an enlarged prostate. He also spotted a same-day urinalysis among nearly a dozen other previous lab tests that had no connection to body temperature. Dr. Duvefelt gave the physician a passing grade but also left a scathing note about all the irrelevant information.
“It’s very common,” Dr. Duvefelt said. “It’s a disaster. Other doctors can’t follow your thinking. A reviewer has a hard time determining whether the doctor acted reasonably.”
Slackers make bad reviewers
Although dedicated reviewers work hard to get to the bottom of cases, it’s not uncommon for some committee members to hardly work at all, according to experts.
Dr. Marder said he’s seen many instances in which reviewers were assigned a review but did not complete it for months. Most committees have set time frames in which reviewers must complete their review.
“That delays that review, and by that time, the review is older and it’s harder to remember things,” he said. “It’s not fair to the physician. If there was a problem the physician could fix and you don’t tell him for 3 or 4 months what it is, he may do the same thing again. The case might come before the committee again and it looks like he’s repeated something, but you never gave him the opportunity to improve.”
Other reviewers fail to attend meetings regularly. Peer review committee members are generally volunteers, and meetings are usually held in the early mornings or late evenings.
“There are reasons for not attending occasionally, but some people put on a committee just don’t take it seriously,” Dr. Marder said. “They don’t fulfill their responsibilities as well as they should. If you accept the job, do the job.”
For physicians considering becoming a peer reviewer, Dr. Beran offers these tips: Be transparent, help physicians understand next steps, and make yourself as available as allowed to answer questions.
Know your committee’s policies and procedures, and follow them, added Dr. Marder. It’s also a good idea to work with your hospital’s quality staff, he said.
Reviewers should keep in mind that they may not always be the one assessing someone else, Dr. Beran said.
“Realize very easily you could be on the other side of that table for things that are outside your control,” he said. “How would you want to be treated?”
A version of this article first appeared on Medscape.com.
After making an insulting comment to a surgery scheduler, a surgeon become the subject of a peer review investigation.
The surgeon had been called in on a Saturday morning for surgery, but when he arrived at the hospital, staff informed him that the operating room had been incorrectly booked and asked him to come back that afternoon. When the surgeon returned, the room still wasn’t ready, recounted David Beran, DO, a peer reviewer and medical director for the emergency department at University Medical Center New Orleans, in Louisiana. After more waiting and staff uncertainty about which operating room was going to open, the surgeon became frustrated and said to the scheduler: “Any idiot could figure this out!”
During his peer review, the surgeon acknowledged that he shouldn’t have made the rude remark to the scheduler, Dr. Beran said. His exasperation stemmed from an ongoing problem – operating rooms at the hospital were being inefficiently managed.
“The surgeon acknowledged that even though there was a systems issue at the root, that’s not justification to speak to people unprofessionally,” Dr. Beran said. “So, there was education for the surgeon, but the surgeon was also able to explain the frustration that led to that point.”
System problems are commonly encountered by peer reviewers, said Dr. Beran.
“There’s a huge gap between administration and clinical professionals when it comes to peer review,” he said. “So many times, bad situations, whether they’re clinical or behavioral, often boil down to systems issues or some inadequacy, whether it’s an EMR [electronic medical record] problem, an inefficacy, or how complicated a process is for an end user. But having a peer review situation that then leads to a system-level change that prevents that problem from happening again is really unlikely. There’s a huge disconnect between those two.”
Peer review is generally a process that goes on behind closed doors. Although structures may differ, peer review is generally described as the process by which physicians assess the quality of their peers’ work to ensure that standards of care are being met. The process is often used to evaluate issues regarding clinical care as well as behavioral complaints against physicians.
Doctors who undergo peer review frequently share their experiences, but reviewers themselves rarely speak out. For this story,
“Peer review processes are in place to build stronger institutions and stronger practices, and they’re supposed to be helpful,” Dr. Beran said. “But because of how opaque they are, it immediately puts physicians on the defensive, and it doesn’t always succeed in what it’s trying to do. I think that’s one of the biggest challenges.”
Biased reviewers taint evaluations
A peer reviewer on and off throughout her career, Indiana family physician Lana Patch, MD, said she always strived to be fair when evaluating fellow physicians. But not every reviewer she encountered operated the same way, she said. Some were biased.
In one case, Dr. Patch peer reviewed a general surgeon who had performed a hysterectomy on a 16-year-old girl. The surgeon believed the teenager likely had an acute appendicitis, but it turned out she had a uterine pathology, Dr. Patch said. The surgeon saved the girl’s life, but the case came under review because of the patient’s age and the fact that her uterus was removed. A local obstetrician-gynecologist weighed in on the case.
“The local ob.gyn. saw it as a turf battle,” recalled Dr. Patch, who is now retired after 30 years of practice in eastern Indiana. “The doctor had nothing but bad to say about the surgeon. He was a competitor.”
Because it was a small hospital, the committee sometimes had trouble finding a specialist who was qualified to give an opinion and who wasn’t in competition with the physician in question, said Dr. Patch. Eventually they found an outside pediatric gynecologist who reviewed the case and concluded that the surgeon had followed the standard of care.
Personal agendas in can come from different directions, said Robert Marder, MD, the author of several books on peer review. Dr. Marder is a consultant who assists with peer review redesign. He has worked with hundreds of medical staff leaders and is a former vice president at the Greeley Company, a consulting firm in Danvers, Mass., that performs peer review redesign. Dr. Marder is president of Robert J. Marder Consulting.
“It goes both ways,” Dr. Marder said. “I’ve seen where somebody with a personal view decides to bring things to the peer review committee specifically because they want the peer review committee to have an adverse view of this person and get them off the medical staff. And I’ve seen hospitals that are uncomfortable with a certain person for whatever reason and want the peer review committee to address it, as opposed to addressing it from a human resource standpoint.”
Dr. Patch recalled a case in which reviewers and hospital leaders were at odds over the credentialing of a physician. Fifteen years earlier, while driving in California, the psychiatrist had been pulled over and was found with an ounce of marijuana, she said.
“We wanted to privilege him,” Dr. Patch said. “As staff physicians, we felt that was 15 years ago, people change over time. Doctors are human beings, too. He seemed to have good credentials and good training. The hospital said, ‘Oh no, we can’t have somebody like this.’ “
The psychiatrist was placed on probation and had to undergo a review every 90 days for about 3 years. Eventually, he was privileged, Dr. Patch said.
Bias among reviewers, including unintentional bias, is also a challenge, Dr. Marder noted. Some initial reviewers score a physician too harshly, he said, whereas others underscore.
“Underscoring is more insidious and more difficult to deal with,” Dr. Marder said. “Underscoring is where the reviewer is too nice. They tend to dismiss things from their colleagues rather than recognize them as an opportunity to help them improve. With underscoring, a lot of committees, if the initial reviewer says the care was appropriate, they don’t even look at the case. They just take that one person’s word for it.”
Reviewers: Looks can be deceiving
When first examining the documented details of a case, it can be easy for peer reviewers to make a quick judgment about what happened, Dr. Beran said.
“You get these complaints, and you read through it, and you think, ‘Oh man, this person really messed up,’ “ he said. “Then you hear the doctor’s side of it, and you realize, ‘No, there’s a much bigger picture at play.’ You realize both sides have valid perspectives on it.”
In one case, for example, Dr. Beran recalled a complaint against a physician who made a snarky remark to a nurse. The doctor had asked the nurse for a piece of equipment, and the nurse said she was busy preparing the room for a patient. The doctor made a comment along the lines of, “Well, would you like me to do that for you and also intubate the patient while you do some charting?!”
At first glance, it appeared that the physician lashed out inappropriately at the nurse. But when reviewers heard from the doctor, they learned that the nurses knew that a trauma patient was coming by ambulance and that he would likely require a ventilator, Dr. Beran said. As the minutes ticked by, however, the nurses were seen in the break room chatting. Nothing had been prepared in the room, including any airway supply.
“The patient had a prolonged course and a very difficult intubation and could have very easily wound up with a much worse outcome for something the nurses had been warned about prior to the patient’s arrival,” he said. “I can see anybody getting upset in that situation if I warned them 5 or 10 minutes beforehand, ‘Get this stuff ready,’ and then nothing was done.”
There was no direct penalty for the physician.
Just as some complaints can be misleading, the clinical record in some peer review cases can also lead reviewers astray.
Physicians frequently include too much irrelevant information in the record, which can cloud a peer review, said Hans Duvefelt, MD, a family physician at Pines Health Services, in Van Buren, Maine. Dr. Duvefelt is a former medical director at Bucksport Regional Health Center, in Ellsworth, Maine. Both facilities are federally qualified health centers where continuous, random peer reviews are required.
In one case, Dr. Duvefelt was peer reviewing a physician’s office note regarding an elderly patient with a low-grade fever. The final diagnosis was urinary tract infection. Dr. Duvefelt said he had trouble following the doctor’s line of thinking because of a plethora of unnecessary data in the 10-page document. The office note included past medical history, prior lab and imaging test results, and an extensive narrative section that included a mixture of active medical problems and ongoing relationships with specialists, he said.
After reading through the printout three times, Dr. Duvefelt said he finally found mention of increased urinary dribbling and details about an enlarged prostate. He also spotted a same-day urinalysis among nearly a dozen other previous lab tests that had no connection to body temperature. Dr. Duvefelt gave the physician a passing grade but also left a scathing note about all the irrelevant information.
“It’s very common,” Dr. Duvefelt said. “It’s a disaster. Other doctors can’t follow your thinking. A reviewer has a hard time determining whether the doctor acted reasonably.”
Slackers make bad reviewers
Although dedicated reviewers work hard to get to the bottom of cases, it’s not uncommon for some committee members to hardly work at all, according to experts.
Dr. Marder said he’s seen many instances in which reviewers were assigned a review but did not complete it for months. Most committees have set time frames in which reviewers must complete their review.
“That delays that review, and by that time, the review is older and it’s harder to remember things,” he said. “It’s not fair to the physician. If there was a problem the physician could fix and you don’t tell him for 3 or 4 months what it is, he may do the same thing again. The case might come before the committee again and it looks like he’s repeated something, but you never gave him the opportunity to improve.”
Other reviewers fail to attend meetings regularly. Peer review committee members are generally volunteers, and meetings are usually held in the early mornings or late evenings.
“There are reasons for not attending occasionally, but some people put on a committee just don’t take it seriously,” Dr. Marder said. “They don’t fulfill their responsibilities as well as they should. If you accept the job, do the job.”
For physicians considering becoming a peer reviewer, Dr. Beran offers these tips: Be transparent, help physicians understand next steps, and make yourself as available as allowed to answer questions.
Know your committee’s policies and procedures, and follow them, added Dr. Marder. It’s also a good idea to work with your hospital’s quality staff, he said.
Reviewers should keep in mind that they may not always be the one assessing someone else, Dr. Beran said.
“Realize very easily you could be on the other side of that table for things that are outside your control,” he said. “How would you want to be treated?”
A version of this article first appeared on Medscape.com.
After making an insulting comment to a surgery scheduler, a surgeon become the subject of a peer review investigation.
The surgeon had been called in on a Saturday morning for surgery, but when he arrived at the hospital, staff informed him that the operating room had been incorrectly booked and asked him to come back that afternoon. When the surgeon returned, the room still wasn’t ready, recounted David Beran, DO, a peer reviewer and medical director for the emergency department at University Medical Center New Orleans, in Louisiana. After more waiting and staff uncertainty about which operating room was going to open, the surgeon became frustrated and said to the scheduler: “Any idiot could figure this out!”
During his peer review, the surgeon acknowledged that he shouldn’t have made the rude remark to the scheduler, Dr. Beran said. His exasperation stemmed from an ongoing problem – operating rooms at the hospital were being inefficiently managed.
“The surgeon acknowledged that even though there was a systems issue at the root, that’s not justification to speak to people unprofessionally,” Dr. Beran said. “So, there was education for the surgeon, but the surgeon was also able to explain the frustration that led to that point.”
System problems are commonly encountered by peer reviewers, said Dr. Beran.
“There’s a huge gap between administration and clinical professionals when it comes to peer review,” he said. “So many times, bad situations, whether they’re clinical or behavioral, often boil down to systems issues or some inadequacy, whether it’s an EMR [electronic medical record] problem, an inefficacy, or how complicated a process is for an end user. But having a peer review situation that then leads to a system-level change that prevents that problem from happening again is really unlikely. There’s a huge disconnect between those two.”
Peer review is generally a process that goes on behind closed doors. Although structures may differ, peer review is generally described as the process by which physicians assess the quality of their peers’ work to ensure that standards of care are being met. The process is often used to evaluate issues regarding clinical care as well as behavioral complaints against physicians.
Doctors who undergo peer review frequently share their experiences, but reviewers themselves rarely speak out. For this story,
“Peer review processes are in place to build stronger institutions and stronger practices, and they’re supposed to be helpful,” Dr. Beran said. “But because of how opaque they are, it immediately puts physicians on the defensive, and it doesn’t always succeed in what it’s trying to do. I think that’s one of the biggest challenges.”
Biased reviewers taint evaluations
A peer reviewer on and off throughout her career, Indiana family physician Lana Patch, MD, said she always strived to be fair when evaluating fellow physicians. But not every reviewer she encountered operated the same way, she said. Some were biased.
In one case, Dr. Patch peer reviewed a general surgeon who had performed a hysterectomy on a 16-year-old girl. The surgeon believed the teenager likely had an acute appendicitis, but it turned out she had a uterine pathology, Dr. Patch said. The surgeon saved the girl’s life, but the case came under review because of the patient’s age and the fact that her uterus was removed. A local obstetrician-gynecologist weighed in on the case.
“The local ob.gyn. saw it as a turf battle,” recalled Dr. Patch, who is now retired after 30 years of practice in eastern Indiana. “The doctor had nothing but bad to say about the surgeon. He was a competitor.”
Because it was a small hospital, the committee sometimes had trouble finding a specialist who was qualified to give an opinion and who wasn’t in competition with the physician in question, said Dr. Patch. Eventually they found an outside pediatric gynecologist who reviewed the case and concluded that the surgeon had followed the standard of care.
Personal agendas in can come from different directions, said Robert Marder, MD, the author of several books on peer review. Dr. Marder is a consultant who assists with peer review redesign. He has worked with hundreds of medical staff leaders and is a former vice president at the Greeley Company, a consulting firm in Danvers, Mass., that performs peer review redesign. Dr. Marder is president of Robert J. Marder Consulting.
“It goes both ways,” Dr. Marder said. “I’ve seen where somebody with a personal view decides to bring things to the peer review committee specifically because they want the peer review committee to have an adverse view of this person and get them off the medical staff. And I’ve seen hospitals that are uncomfortable with a certain person for whatever reason and want the peer review committee to address it, as opposed to addressing it from a human resource standpoint.”
Dr. Patch recalled a case in which reviewers and hospital leaders were at odds over the credentialing of a physician. Fifteen years earlier, while driving in California, the psychiatrist had been pulled over and was found with an ounce of marijuana, she said.
“We wanted to privilege him,” Dr. Patch said. “As staff physicians, we felt that was 15 years ago, people change over time. Doctors are human beings, too. He seemed to have good credentials and good training. The hospital said, ‘Oh no, we can’t have somebody like this.’ “
The psychiatrist was placed on probation and had to undergo a review every 90 days for about 3 years. Eventually, he was privileged, Dr. Patch said.
Bias among reviewers, including unintentional bias, is also a challenge, Dr. Marder noted. Some initial reviewers score a physician too harshly, he said, whereas others underscore.
“Underscoring is more insidious and more difficult to deal with,” Dr. Marder said. “Underscoring is where the reviewer is too nice. They tend to dismiss things from their colleagues rather than recognize them as an opportunity to help them improve. With underscoring, a lot of committees, if the initial reviewer says the care was appropriate, they don’t even look at the case. They just take that one person’s word for it.”
Reviewers: Looks can be deceiving
When first examining the documented details of a case, it can be easy for peer reviewers to make a quick judgment about what happened, Dr. Beran said.
“You get these complaints, and you read through it, and you think, ‘Oh man, this person really messed up,’ “ he said. “Then you hear the doctor’s side of it, and you realize, ‘No, there’s a much bigger picture at play.’ You realize both sides have valid perspectives on it.”
In one case, for example, Dr. Beran recalled a complaint against a physician who made a snarky remark to a nurse. The doctor had asked the nurse for a piece of equipment, and the nurse said she was busy preparing the room for a patient. The doctor made a comment along the lines of, “Well, would you like me to do that for you and also intubate the patient while you do some charting?!”
At first glance, it appeared that the physician lashed out inappropriately at the nurse. But when reviewers heard from the doctor, they learned that the nurses knew that a trauma patient was coming by ambulance and that he would likely require a ventilator, Dr. Beran said. As the minutes ticked by, however, the nurses were seen in the break room chatting. Nothing had been prepared in the room, including any airway supply.
“The patient had a prolonged course and a very difficult intubation and could have very easily wound up with a much worse outcome for something the nurses had been warned about prior to the patient’s arrival,” he said. “I can see anybody getting upset in that situation if I warned them 5 or 10 minutes beforehand, ‘Get this stuff ready,’ and then nothing was done.”
There was no direct penalty for the physician.
Just as some complaints can be misleading, the clinical record in some peer review cases can also lead reviewers astray.
Physicians frequently include too much irrelevant information in the record, which can cloud a peer review, said Hans Duvefelt, MD, a family physician at Pines Health Services, in Van Buren, Maine. Dr. Duvefelt is a former medical director at Bucksport Regional Health Center, in Ellsworth, Maine. Both facilities are federally qualified health centers where continuous, random peer reviews are required.
In one case, Dr. Duvefelt was peer reviewing a physician’s office note regarding an elderly patient with a low-grade fever. The final diagnosis was urinary tract infection. Dr. Duvefelt said he had trouble following the doctor’s line of thinking because of a plethora of unnecessary data in the 10-page document. The office note included past medical history, prior lab and imaging test results, and an extensive narrative section that included a mixture of active medical problems and ongoing relationships with specialists, he said.
After reading through the printout three times, Dr. Duvefelt said he finally found mention of increased urinary dribbling and details about an enlarged prostate. He also spotted a same-day urinalysis among nearly a dozen other previous lab tests that had no connection to body temperature. Dr. Duvefelt gave the physician a passing grade but also left a scathing note about all the irrelevant information.
“It’s very common,” Dr. Duvefelt said. “It’s a disaster. Other doctors can’t follow your thinking. A reviewer has a hard time determining whether the doctor acted reasonably.”
Slackers make bad reviewers
Although dedicated reviewers work hard to get to the bottom of cases, it’s not uncommon for some committee members to hardly work at all, according to experts.
Dr. Marder said he’s seen many instances in which reviewers were assigned a review but did not complete it for months. Most committees have set time frames in which reviewers must complete their review.
“That delays that review, and by that time, the review is older and it’s harder to remember things,” he said. “It’s not fair to the physician. If there was a problem the physician could fix and you don’t tell him for 3 or 4 months what it is, he may do the same thing again. The case might come before the committee again and it looks like he’s repeated something, but you never gave him the opportunity to improve.”
Other reviewers fail to attend meetings regularly. Peer review committee members are generally volunteers, and meetings are usually held in the early mornings or late evenings.
“There are reasons for not attending occasionally, but some people put on a committee just don’t take it seriously,” Dr. Marder said. “They don’t fulfill their responsibilities as well as they should. If you accept the job, do the job.”
For physicians considering becoming a peer reviewer, Dr. Beran offers these tips: Be transparent, help physicians understand next steps, and make yourself as available as allowed to answer questions.
Know your committee’s policies and procedures, and follow them, added Dr. Marder. It’s also a good idea to work with your hospital’s quality staff, he said.
Reviewers should keep in mind that they may not always be the one assessing someone else, Dr. Beran said.
“Realize very easily you could be on the other side of that table for things that are outside your control,” he said. “How would you want to be treated?”
A version of this article first appeared on Medscape.com.
‘Lopioid protocol’ – low-dose opioids – proposed for fracture surgery
In a paper presented at the annual meeting of the American Academy of Orthopaedic Surgeons, researchers from NYU reported on the implementation of their multimodal strategy, dubbed the “lopioid protocol.”
According to the 2019 National Survey on Drug Use and Health, orthopedic surgeons are the third-highest opioid prescribers in the United States.
Kennneth A. Egol, MD, vice chair of the department of orthopedic surgery at NYU, who is the first author of the study, was motivated to help create the protocol following misconceptions that orthopedic surgeons were helping to fuel the opioid epidemic.
Dr. Egol pointed to the year 1995, when pain became the fifth vital sign after body temperature, pulse rate, respiratory rate, and blood pressure.
Since then, in light of the opioid epidemic, the focus of physicians has shifted away from prescribing strong pain medication and reducing pain scores to zero to instead reducing pain to a manageable level.
Reducing opioid prescriptions can be challenging when patients are prescribed an anti-inflammatory and they subsequently ask their physician for a “pain pill.” Patients sometimes don’t understand that inflammation is what causes pain.
It can also be difficult to convince patients that medications that they can buy over the counter can adequately control their pain, as confirmed in numerous studies.
Multimodal pain therapy aims to reduce the need for opioids by supplementing their use with other oral medications and, at times, long-lasting regional nerve blocks.
Anti-inflammatories act at the site of injury or surgery where inflammation is occurring. Nerves then carry the pain signal to the brain. These signals can be dampened by medications such as gabapentin that act on the nerves themselves. The pain signal is received in the brain, where opioids act by binding to receptors in the brain.
The so-called lopioid protocol does not eliminate opioids completely but rather uses “safer” opioids, such as tramadol, in lieu of stronger narcotics.
The protocol began at NYU on Jan. 1, 2019. It consists in the prescribing of tramadol, meloxicam, gabapentin, and acetaminophen.
The study presented at the AAOS meeting demonstrated statistically significant reductions in visual analogue pain scores at discharge and subsequent medication refills for the 931 patients in the lopioid group, compared with a group of 848 patients who received narcotic prescriptions containing oxycodone from the year prior to the protocol initiation.
Educating patients on the rationale for the prescription combination can help to allay their fears. Dr. Egol thinks it’s important for physicians to explain the dangers of opioids to patients. He said in an interview that he also believes surgeons need to “give [patients] an understanding of why we are pursuing these protocols. They also need to know we will not ignore their pain and concerns.”
Brannon Orton, MD, is an orthopedic surgeon at Confluence Health, in Moses Lake, Wash. He sees a large number of trauma patients and thinks NYU is doing a good job of addressing a difficult problem in orthopedics – especially in the field of trauma.
He said in an interview: “Managing narcotics postoperatively can be challenging due to the fact that many people come into these fractures with a history of narcotic use.” Not only are they used to turning to opioids for pain relief, but they also may have built up a tolerance to them.
Although he hasn’t been using the lopioid protocol specifically, he has been following a multimodal approach regarding the postoperative use of narcotics. Of the study by Dr. Egol and colleagues, he said, “I think their paper presents an effective way of decreasing use of oral narcotics and still adequately managing patients’ pain postoperatively.” Dr. Orton’s own practice utilizes tramadol, acetaminophen, and ibuprofen after fracture surgery.
From Dr. Orton’s perspective, a significant challenge in implementing the lopioid protocol in practice is simply sticking to the plan. “It can become difficult when patients are pressuring staff or physicians for more narcotics. However, I feel that if everybody is on the same page with the plan, then it can be very doable.”
Dr. Egol and NYU try to limit narcotic prescriptions beginning with the patient’s initial visit to the ED. The ED physicians at his institution only “prescribe small amounts of narcotics. Our ED people really limit the amount of opioids prescribed.”
Dr. Egol recommends that all practitioners begin with nonnarcotic medication, even if treating a fracture nonoperatively. “Start low and go higher. I always try to start with NSAIDs and Tylenol,” he said.
Dr. Egol and Dr. Orton reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
In a paper presented at the annual meeting of the American Academy of Orthopaedic Surgeons, researchers from NYU reported on the implementation of their multimodal strategy, dubbed the “lopioid protocol.”
According to the 2019 National Survey on Drug Use and Health, orthopedic surgeons are the third-highest opioid prescribers in the United States.
Kennneth A. Egol, MD, vice chair of the department of orthopedic surgery at NYU, who is the first author of the study, was motivated to help create the protocol following misconceptions that orthopedic surgeons were helping to fuel the opioid epidemic.
Dr. Egol pointed to the year 1995, when pain became the fifth vital sign after body temperature, pulse rate, respiratory rate, and blood pressure.
Since then, in light of the opioid epidemic, the focus of physicians has shifted away from prescribing strong pain medication and reducing pain scores to zero to instead reducing pain to a manageable level.
Reducing opioid prescriptions can be challenging when patients are prescribed an anti-inflammatory and they subsequently ask their physician for a “pain pill.” Patients sometimes don’t understand that inflammation is what causes pain.
It can also be difficult to convince patients that medications that they can buy over the counter can adequately control their pain, as confirmed in numerous studies.
Multimodal pain therapy aims to reduce the need for opioids by supplementing their use with other oral medications and, at times, long-lasting regional nerve blocks.
Anti-inflammatories act at the site of injury or surgery where inflammation is occurring. Nerves then carry the pain signal to the brain. These signals can be dampened by medications such as gabapentin that act on the nerves themselves. The pain signal is received in the brain, where opioids act by binding to receptors in the brain.
The so-called lopioid protocol does not eliminate opioids completely but rather uses “safer” opioids, such as tramadol, in lieu of stronger narcotics.
The protocol began at NYU on Jan. 1, 2019. It consists in the prescribing of tramadol, meloxicam, gabapentin, and acetaminophen.
The study presented at the AAOS meeting demonstrated statistically significant reductions in visual analogue pain scores at discharge and subsequent medication refills for the 931 patients in the lopioid group, compared with a group of 848 patients who received narcotic prescriptions containing oxycodone from the year prior to the protocol initiation.
Educating patients on the rationale for the prescription combination can help to allay their fears. Dr. Egol thinks it’s important for physicians to explain the dangers of opioids to patients. He said in an interview that he also believes surgeons need to “give [patients] an understanding of why we are pursuing these protocols. They also need to know we will not ignore their pain and concerns.”
Brannon Orton, MD, is an orthopedic surgeon at Confluence Health, in Moses Lake, Wash. He sees a large number of trauma patients and thinks NYU is doing a good job of addressing a difficult problem in orthopedics – especially in the field of trauma.
He said in an interview: “Managing narcotics postoperatively can be challenging due to the fact that many people come into these fractures with a history of narcotic use.” Not only are they used to turning to opioids for pain relief, but they also may have built up a tolerance to them.
Although he hasn’t been using the lopioid protocol specifically, he has been following a multimodal approach regarding the postoperative use of narcotics. Of the study by Dr. Egol and colleagues, he said, “I think their paper presents an effective way of decreasing use of oral narcotics and still adequately managing patients’ pain postoperatively.” Dr. Orton’s own practice utilizes tramadol, acetaminophen, and ibuprofen after fracture surgery.
From Dr. Orton’s perspective, a significant challenge in implementing the lopioid protocol in practice is simply sticking to the plan. “It can become difficult when patients are pressuring staff or physicians for more narcotics. However, I feel that if everybody is on the same page with the plan, then it can be very doable.”
Dr. Egol and NYU try to limit narcotic prescriptions beginning with the patient’s initial visit to the ED. The ED physicians at his institution only “prescribe small amounts of narcotics. Our ED people really limit the amount of opioids prescribed.”
Dr. Egol recommends that all practitioners begin with nonnarcotic medication, even if treating a fracture nonoperatively. “Start low and go higher. I always try to start with NSAIDs and Tylenol,” he said.
Dr. Egol and Dr. Orton reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
In a paper presented at the annual meeting of the American Academy of Orthopaedic Surgeons, researchers from NYU reported on the implementation of their multimodal strategy, dubbed the “lopioid protocol.”
According to the 2019 National Survey on Drug Use and Health, orthopedic surgeons are the third-highest opioid prescribers in the United States.
Kennneth A. Egol, MD, vice chair of the department of orthopedic surgery at NYU, who is the first author of the study, was motivated to help create the protocol following misconceptions that orthopedic surgeons were helping to fuel the opioid epidemic.
Dr. Egol pointed to the year 1995, when pain became the fifth vital sign after body temperature, pulse rate, respiratory rate, and blood pressure.
Since then, in light of the opioid epidemic, the focus of physicians has shifted away from prescribing strong pain medication and reducing pain scores to zero to instead reducing pain to a manageable level.
Reducing opioid prescriptions can be challenging when patients are prescribed an anti-inflammatory and they subsequently ask their physician for a “pain pill.” Patients sometimes don’t understand that inflammation is what causes pain.
It can also be difficult to convince patients that medications that they can buy over the counter can adequately control their pain, as confirmed in numerous studies.
Multimodal pain therapy aims to reduce the need for opioids by supplementing their use with other oral medications and, at times, long-lasting regional nerve blocks.
Anti-inflammatories act at the site of injury or surgery where inflammation is occurring. Nerves then carry the pain signal to the brain. These signals can be dampened by medications such as gabapentin that act on the nerves themselves. The pain signal is received in the brain, where opioids act by binding to receptors in the brain.
The so-called lopioid protocol does not eliminate opioids completely but rather uses “safer” opioids, such as tramadol, in lieu of stronger narcotics.
The protocol began at NYU on Jan. 1, 2019. It consists in the prescribing of tramadol, meloxicam, gabapentin, and acetaminophen.
The study presented at the AAOS meeting demonstrated statistically significant reductions in visual analogue pain scores at discharge and subsequent medication refills for the 931 patients in the lopioid group, compared with a group of 848 patients who received narcotic prescriptions containing oxycodone from the year prior to the protocol initiation.
Educating patients on the rationale for the prescription combination can help to allay their fears. Dr. Egol thinks it’s important for physicians to explain the dangers of opioids to patients. He said in an interview that he also believes surgeons need to “give [patients] an understanding of why we are pursuing these protocols. They also need to know we will not ignore their pain and concerns.”
Brannon Orton, MD, is an orthopedic surgeon at Confluence Health, in Moses Lake, Wash. He sees a large number of trauma patients and thinks NYU is doing a good job of addressing a difficult problem in orthopedics – especially in the field of trauma.
He said in an interview: “Managing narcotics postoperatively can be challenging due to the fact that many people come into these fractures with a history of narcotic use.” Not only are they used to turning to opioids for pain relief, but they also may have built up a tolerance to them.
Although he hasn’t been using the lopioid protocol specifically, he has been following a multimodal approach regarding the postoperative use of narcotics. Of the study by Dr. Egol and colleagues, he said, “I think their paper presents an effective way of decreasing use of oral narcotics and still adequately managing patients’ pain postoperatively.” Dr. Orton’s own practice utilizes tramadol, acetaminophen, and ibuprofen after fracture surgery.
From Dr. Orton’s perspective, a significant challenge in implementing the lopioid protocol in practice is simply sticking to the plan. “It can become difficult when patients are pressuring staff or physicians for more narcotics. However, I feel that if everybody is on the same page with the plan, then it can be very doable.”
Dr. Egol and NYU try to limit narcotic prescriptions beginning with the patient’s initial visit to the ED. The ED physicians at his institution only “prescribe small amounts of narcotics. Our ED people really limit the amount of opioids prescribed.”
Dr. Egol recommends that all practitioners begin with nonnarcotic medication, even if treating a fracture nonoperatively. “Start low and go higher. I always try to start with NSAIDs and Tylenol,” he said.
Dr. Egol and Dr. Orton reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
COVID-19 linked to baby bust in high-income countries
In an assessment of the pandemic’s early effects, Arnstein Aassve, PhD, and colleagues found a significant COVID-19–related decline in crude birth rates (CBRs) in 7 of 22 high-income countries, particularly in Southwestern Europe.
Dr. Aassve, an economist at the Carlo F. Dondena Center for Research on Social Dynamics and Public Policy at the Università Commerciale Luigi Bocconi, Milan, and colleagues report the results in an article published online August 30 in the Proceedings of the National Academy of Sciences.
Defining the start of the COVID-19 pandemic as February 2020, the study identifies strong declines in Italy (-9.1%), Hungary (-8.5%), Spain (-8.4%), and Portugal (-6.6%) beyond those predicted by past trends. In the United States, CBRs fell by 7.1% relative to 2019 for births occurring in Nov. and Dec. 2020 following conceptions in February and March of that year.
Significant declines in CBR also occurred in Belgium, Austria, and Singapore.
A year-to-year comparison of the mean for monthly CBRs per 1,000 population before and during the pandemic suggests a negative difference for all countries studied except for Denmark, Finland, Germany, and the Netherlands, Dr. Aassve and colleagues write. These findings may have policy implications for childcare, housing, and the labor market.
The Milan researchers compared monthly vital statistics data on live births from the international Human Fertility Database for the period of Jan. 2016 to March 2021. These figures reflect conceptions carried to term between April 2015 and June 2020. The 22 countries in the analysis represent 37% of the total reported COVID-19 cases and 34% of deaths worldwide.
The study findings align with surveys on “fertility intentions” collected early in the first COVID-19 wave in Germany, France, Spain, and the United Kingdom. These surveys indicated that 73% of people who were planning pregnancies in 2020 either decided to delay the pregnancy or they abandoned their plans.
“The popular media speculated that the lockdown would lead to a baby boom, as couples spent more time together,” Dr. Aassve told this news organization. “There’s very little evidence of this when you look to previous disasters and shocks, and the first data suggest more of an immediate collapse than a boom. But as you also see from the paper, the collapse is not seen everywhere.” Other current studies suggest the fertility drop is immediate but temporary, says Dr. Aassve, who is also a professor of demography.
Interestingly, Dr. Aassve and colleagues found that CBRs were relatively stable in Northern Europe. The authors point to supportive social and family policies in that region that might have reduced the effect of the pandemic on births. “These factors are likely to affect CBRs in the subsequent pandemic waves,” they write. They call for future studies to assess the full population implications of the pandemic, the moderating impact of policy interventions, and the nexus between short- and long-run effects in relation to the various waves of the COVID-19 pandemic.
Rebounds
Some regions have already reported a rebound from the COVID-19 fertility trough. Molly J. Stout, MD, director of maternal fetal medicine at the University of Michigan, Ann Arbor, and colleagues used electronic medical records to predict a surge in births after the initial decline.
“The surge we’ve seen at the end of this summer is exceeding the usual annual birth rate, as predicted,” she said in an interview. “But I think there’ll be a return to normal after this transient escalation. I don’t think birth rates will stay elevated above the normal because the birth surge is a temporary response to an event, although there will likely be regional differences.”
Looking ahead, Dr. Stout, who was not involved in Dr. Aassve’s analysis, is not certain how a fourth pandemic wave might ultimately modify a couple’s overall family size. But the toll the health crisis has taken on working women who have been forced to withdraw from the economy because of a lack of childcare points to a societal need that should be addressed.
According to Philip N. Cohen, PhD, a professor of sociology at the University of Maryland, College Park, who’s been tracking fertility trends since the onset of the COVID-19 emergency, the pandemic has combined a health crisis with an economic crisis, along with “the additional factor of social distancing and isolation, which all contributed to the decline in birth rates. Some people changed their plans to hold off on having children, while others didn’t get pregnant because they weren’t socializing and meeting people as much.”
Dr. Cohen, who was not involved in the study by Dr. Aassve and associates, said his provisional data show that although in many places, birth rates have rebounded more or less to prepandemic levels after a nadir around Jan. 2021, some areas of the United States still show substantially lower rates, including California, Hawaii, and Oregon.
As to the duration of the pandemic effect, Dr. Aassve cautions that his group’s estimates refer to the first wave only. “We then have the second, third, and currently the fourth wave. We can’t be sure about the impact of these waves on fertility since the data are not there yet, but I’d be surprised if they didn’t continue to have an impact on fertility rates,” he said.
Dr. Cohen agreed: “Some people who delayed childbearing will make up the delay. However, whenever there’s a delay, there’s inevitably some portion of the decline that’s not recouped.”
As for the wider effect across the world, Dr. Aassve said his team’s figures derive from high-income countries where data are readily available. For middle- and low-income countries, fewer data exist, and the quality of those data is not as good.
The lessons from this and other upheavals teach us that unforeseen shocks almost always have a negative impact on fertility, says Dr. Aassve. “[B]ut these effects may be separate from existing declining trends. The issue here is that those overall declining trends may be driven by other factors. In contrast, the shock of the pandemic is short-lived, and we may return to normal rather quickly. But if the pandemic also impacts other societal structures, such as the occupational and industrial sectors, then the pandemic might exacerbate the negative trend.”
The study was supported by funding from the European Research Council for funding under the European Union’s Horizon 2020 Research and Innovation Programme. The study authors, Dr. Stout, and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In an assessment of the pandemic’s early effects, Arnstein Aassve, PhD, and colleagues found a significant COVID-19–related decline in crude birth rates (CBRs) in 7 of 22 high-income countries, particularly in Southwestern Europe.
Dr. Aassve, an economist at the Carlo F. Dondena Center for Research on Social Dynamics and Public Policy at the Università Commerciale Luigi Bocconi, Milan, and colleagues report the results in an article published online August 30 in the Proceedings of the National Academy of Sciences.
Defining the start of the COVID-19 pandemic as February 2020, the study identifies strong declines in Italy (-9.1%), Hungary (-8.5%), Spain (-8.4%), and Portugal (-6.6%) beyond those predicted by past trends. In the United States, CBRs fell by 7.1% relative to 2019 for births occurring in Nov. and Dec. 2020 following conceptions in February and March of that year.
Significant declines in CBR also occurred in Belgium, Austria, and Singapore.
A year-to-year comparison of the mean for monthly CBRs per 1,000 population before and during the pandemic suggests a negative difference for all countries studied except for Denmark, Finland, Germany, and the Netherlands, Dr. Aassve and colleagues write. These findings may have policy implications for childcare, housing, and the labor market.
The Milan researchers compared monthly vital statistics data on live births from the international Human Fertility Database for the period of Jan. 2016 to March 2021. These figures reflect conceptions carried to term between April 2015 and June 2020. The 22 countries in the analysis represent 37% of the total reported COVID-19 cases and 34% of deaths worldwide.
The study findings align with surveys on “fertility intentions” collected early in the first COVID-19 wave in Germany, France, Spain, and the United Kingdom. These surveys indicated that 73% of people who were planning pregnancies in 2020 either decided to delay the pregnancy or they abandoned their plans.
“The popular media speculated that the lockdown would lead to a baby boom, as couples spent more time together,” Dr. Aassve told this news organization. “There’s very little evidence of this when you look to previous disasters and shocks, and the first data suggest more of an immediate collapse than a boom. But as you also see from the paper, the collapse is not seen everywhere.” Other current studies suggest the fertility drop is immediate but temporary, says Dr. Aassve, who is also a professor of demography.
Interestingly, Dr. Aassve and colleagues found that CBRs were relatively stable in Northern Europe. The authors point to supportive social and family policies in that region that might have reduced the effect of the pandemic on births. “These factors are likely to affect CBRs in the subsequent pandemic waves,” they write. They call for future studies to assess the full population implications of the pandemic, the moderating impact of policy interventions, and the nexus between short- and long-run effects in relation to the various waves of the COVID-19 pandemic.
Rebounds
Some regions have already reported a rebound from the COVID-19 fertility trough. Molly J. Stout, MD, director of maternal fetal medicine at the University of Michigan, Ann Arbor, and colleagues used electronic medical records to predict a surge in births after the initial decline.
“The surge we’ve seen at the end of this summer is exceeding the usual annual birth rate, as predicted,” she said in an interview. “But I think there’ll be a return to normal after this transient escalation. I don’t think birth rates will stay elevated above the normal because the birth surge is a temporary response to an event, although there will likely be regional differences.”
Looking ahead, Dr. Stout, who was not involved in Dr. Aassve’s analysis, is not certain how a fourth pandemic wave might ultimately modify a couple’s overall family size. But the toll the health crisis has taken on working women who have been forced to withdraw from the economy because of a lack of childcare points to a societal need that should be addressed.
According to Philip N. Cohen, PhD, a professor of sociology at the University of Maryland, College Park, who’s been tracking fertility trends since the onset of the COVID-19 emergency, the pandemic has combined a health crisis with an economic crisis, along with “the additional factor of social distancing and isolation, which all contributed to the decline in birth rates. Some people changed their plans to hold off on having children, while others didn’t get pregnant because they weren’t socializing and meeting people as much.”
Dr. Cohen, who was not involved in the study by Dr. Aassve and associates, said his provisional data show that although in many places, birth rates have rebounded more or less to prepandemic levels after a nadir around Jan. 2021, some areas of the United States still show substantially lower rates, including California, Hawaii, and Oregon.
As to the duration of the pandemic effect, Dr. Aassve cautions that his group’s estimates refer to the first wave only. “We then have the second, third, and currently the fourth wave. We can’t be sure about the impact of these waves on fertility since the data are not there yet, but I’d be surprised if they didn’t continue to have an impact on fertility rates,” he said.
Dr. Cohen agreed: “Some people who delayed childbearing will make up the delay. However, whenever there’s a delay, there’s inevitably some portion of the decline that’s not recouped.”
As for the wider effect across the world, Dr. Aassve said his team’s figures derive from high-income countries where data are readily available. For middle- and low-income countries, fewer data exist, and the quality of those data is not as good.
The lessons from this and other upheavals teach us that unforeseen shocks almost always have a negative impact on fertility, says Dr. Aassve. “[B]ut these effects may be separate from existing declining trends. The issue here is that those overall declining trends may be driven by other factors. In contrast, the shock of the pandemic is short-lived, and we may return to normal rather quickly. But if the pandemic also impacts other societal structures, such as the occupational and industrial sectors, then the pandemic might exacerbate the negative trend.”
The study was supported by funding from the European Research Council for funding under the European Union’s Horizon 2020 Research and Innovation Programme. The study authors, Dr. Stout, and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In an assessment of the pandemic’s early effects, Arnstein Aassve, PhD, and colleagues found a significant COVID-19–related decline in crude birth rates (CBRs) in 7 of 22 high-income countries, particularly in Southwestern Europe.
Dr. Aassve, an economist at the Carlo F. Dondena Center for Research on Social Dynamics and Public Policy at the Università Commerciale Luigi Bocconi, Milan, and colleagues report the results in an article published online August 30 in the Proceedings of the National Academy of Sciences.
Defining the start of the COVID-19 pandemic as February 2020, the study identifies strong declines in Italy (-9.1%), Hungary (-8.5%), Spain (-8.4%), and Portugal (-6.6%) beyond those predicted by past trends. In the United States, CBRs fell by 7.1% relative to 2019 for births occurring in Nov. and Dec. 2020 following conceptions in February and March of that year.
Significant declines in CBR also occurred in Belgium, Austria, and Singapore.
A year-to-year comparison of the mean for monthly CBRs per 1,000 population before and during the pandemic suggests a negative difference for all countries studied except for Denmark, Finland, Germany, and the Netherlands, Dr. Aassve and colleagues write. These findings may have policy implications for childcare, housing, and the labor market.
The Milan researchers compared monthly vital statistics data on live births from the international Human Fertility Database for the period of Jan. 2016 to March 2021. These figures reflect conceptions carried to term between April 2015 and June 2020. The 22 countries in the analysis represent 37% of the total reported COVID-19 cases and 34% of deaths worldwide.
The study findings align with surveys on “fertility intentions” collected early in the first COVID-19 wave in Germany, France, Spain, and the United Kingdom. These surveys indicated that 73% of people who were planning pregnancies in 2020 either decided to delay the pregnancy or they abandoned their plans.
“The popular media speculated that the lockdown would lead to a baby boom, as couples spent more time together,” Dr. Aassve told this news organization. “There’s very little evidence of this when you look to previous disasters and shocks, and the first data suggest more of an immediate collapse than a boom. But as you also see from the paper, the collapse is not seen everywhere.” Other current studies suggest the fertility drop is immediate but temporary, says Dr. Aassve, who is also a professor of demography.
Interestingly, Dr. Aassve and colleagues found that CBRs were relatively stable in Northern Europe. The authors point to supportive social and family policies in that region that might have reduced the effect of the pandemic on births. “These factors are likely to affect CBRs in the subsequent pandemic waves,” they write. They call for future studies to assess the full population implications of the pandemic, the moderating impact of policy interventions, and the nexus between short- and long-run effects in relation to the various waves of the COVID-19 pandemic.
Rebounds
Some regions have already reported a rebound from the COVID-19 fertility trough. Molly J. Stout, MD, director of maternal fetal medicine at the University of Michigan, Ann Arbor, and colleagues used electronic medical records to predict a surge in births after the initial decline.
“The surge we’ve seen at the end of this summer is exceeding the usual annual birth rate, as predicted,” she said in an interview. “But I think there’ll be a return to normal after this transient escalation. I don’t think birth rates will stay elevated above the normal because the birth surge is a temporary response to an event, although there will likely be regional differences.”
Looking ahead, Dr. Stout, who was not involved in Dr. Aassve’s analysis, is not certain how a fourth pandemic wave might ultimately modify a couple’s overall family size. But the toll the health crisis has taken on working women who have been forced to withdraw from the economy because of a lack of childcare points to a societal need that should be addressed.
According to Philip N. Cohen, PhD, a professor of sociology at the University of Maryland, College Park, who’s been tracking fertility trends since the onset of the COVID-19 emergency, the pandemic has combined a health crisis with an economic crisis, along with “the additional factor of social distancing and isolation, which all contributed to the decline in birth rates. Some people changed their plans to hold off on having children, while others didn’t get pregnant because they weren’t socializing and meeting people as much.”
Dr. Cohen, who was not involved in the study by Dr. Aassve and associates, said his provisional data show that although in many places, birth rates have rebounded more or less to prepandemic levels after a nadir around Jan. 2021, some areas of the United States still show substantially lower rates, including California, Hawaii, and Oregon.
As to the duration of the pandemic effect, Dr. Aassve cautions that his group’s estimates refer to the first wave only. “We then have the second, third, and currently the fourth wave. We can’t be sure about the impact of these waves on fertility since the data are not there yet, but I’d be surprised if they didn’t continue to have an impact on fertility rates,” he said.
Dr. Cohen agreed: “Some people who delayed childbearing will make up the delay. However, whenever there’s a delay, there’s inevitably some portion of the decline that’s not recouped.”
As for the wider effect across the world, Dr. Aassve said his team’s figures derive from high-income countries where data are readily available. For middle- and low-income countries, fewer data exist, and the quality of those data is not as good.
The lessons from this and other upheavals teach us that unforeseen shocks almost always have a negative impact on fertility, says Dr. Aassve. “[B]ut these effects may be separate from existing declining trends. The issue here is that those overall declining trends may be driven by other factors. In contrast, the shock of the pandemic is short-lived, and we may return to normal rather quickly. But if the pandemic also impacts other societal structures, such as the occupational and industrial sectors, then the pandemic might exacerbate the negative trend.”
The study was supported by funding from the European Research Council for funding under the European Union’s Horizon 2020 Research and Innovation Programme. The study authors, Dr. Stout, and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Exercising to lose weight is not for every ‘body’
Exercising to lose weight is not for every ‘body’
This first item comes from the “You’ve got to be kidding” section of LOTME’s supersecret topics-of-interest file.
Investigators at the Shenzhen Institute of Advanced Technology of the Chinese Academy of Sciences and the University of Roehampton noticed that some people who enrolled in exercise programs to lose weight did just the opposite: they gained weight.
Being scientists, they decided to look at the effects of energy expenditure and how those effects varied among individuals. The likely culprit in this case, they determined, is something called compensatory mechanisms. One such mechanism involves eating more food because exercise stimulates appetite, and another might reduce energy expenditure on other components like resting metabolism so that the exercise is, in effect, less costly.
A look at the numbers shows how compensatory mechanisms worked in the study population of 1,750 adults. Among individuals with the highest BMI, 51% of the calories burned during activity translated into calories burned at the end of the day. For those with normal BMI, however, 72% of calories burned during activity were reflected in total expenditure.
“People living with obesity cut back their resting metabolism when they are more active. The result is that for every calorie they spend on exercise they save about half a calorie on resting,” the investigators explained.
In other words, some bodies will, unconsciously, work against the conscious effort of exercising to lose weight. Thank you very much, compensatory mechanisms, for the boundarylessness exhibited in exceeding your job description.
When it comes to the mix, walnuts go nuts
When it comes to mixed nuts, walnuts get no love. But we may be able to give you a reason to not pick them out: Your arteries.
Participants in a recent study who ate about a half-cup of walnuts every day for 2 years saw a drop in their low-density lipoprotein (LDL) cholesterol. The number and quality of LDL particles in healthy older adults also improved. How? Good ol’ omega-3 fatty acids.
Omega-3 is found in many foods linked to lower risks of heart disease, lower cholesterol levels, and lower blood sugar levels, but the one thing that makes the walnut a front runner for Miss Super Food 2021 is their ability to improve the quality of LDL particles.
“LDL particles come in various sizes [and] research has shown that small, dense LDL particles are more often associated with atherosclerosis, the plaque or fatty deposits that build up in the arteries,” Emilio Ros, MD, PhD, of the Hospital Clínic of Barcelona and the study’s senior investigator, said in a written statement.
The 708 participants, aged 63-79 years and mostly women, were divided into two groups: One received the walnut diet and the other did not. After 2 years, the walnut group had lower LDL levels by an average of 4.3 mg/dL. Total cholesterol was reduced by an average of 8.5 mg/dL. Also, their total LDL particle count was 4.3% lower and small LDL particles were down by 6.1%.
So instead of picking the walnuts out of the mix, try to find it in your heart to appreciate them. Your body already does.
Begun, the clone war has
Well, not quite yet, Master Yoda, but perhaps one day soon, if a study from Japan into the uncanny valley of the usage of cloned humanlike faces in robotics and artificial intelligence, published in PLOS One, is to be believed.
The study consisted of a number of six smaller experiments in which participants judged a series of images based on subjective eeriness, emotional valence, and realism. The images included people with the same cloned face; people with different faces; dogs; identical twins, triplets, quadruplets, etc.; and cloned animated characters. In the sixth experiment, the photos were the same as in the second (six cloned faces, six different faces, and a single face) but participants also answered the Disgust Scale–Revised to accurately analyze disgust sensitivity.
The results of all these experiments were quite clear: People found the cloned faces far creepier than the varied or single face, an effect the researchers called clone devaluation. Notably, this effect only applied to realistic human faces; most people didn’t find the cloned dogs or cloned animated characters creepy. However, those who did were more likely to find the human clones eerie on the Disgust Scale.
The authors noted that future robotics technology needs to be carefully considered to avoid the uncanny valley and this clone devaluation effect, which is a very good point. The last thing we need is a few million robots with identical faces getting angry at us and pulling a Terminator/Order 66 combo. We’re already in a viral apocalypse; we don’t need a robot one on top of that.
Congratulations to our new favorite reader
The winner of last week’s inaugural Pandemic Pandemonium comes to us from Tiffanie Roe. By getting her entry in first, just ahead of the flood of responses we received – and by flood we mean a very slow and very quickly repaired drip – Ms. Roe puts the gold medal for COVID-related insanity around the necks of Australian magpies, who may start attacking people wearing face masks during “swooping season” because the birds don’t recognize them.
Exercising to lose weight is not for every ‘body’
This first item comes from the “You’ve got to be kidding” section of LOTME’s supersecret topics-of-interest file.
Investigators at the Shenzhen Institute of Advanced Technology of the Chinese Academy of Sciences and the University of Roehampton noticed that some people who enrolled in exercise programs to lose weight did just the opposite: they gained weight.
Being scientists, they decided to look at the effects of energy expenditure and how those effects varied among individuals. The likely culprit in this case, they determined, is something called compensatory mechanisms. One such mechanism involves eating more food because exercise stimulates appetite, and another might reduce energy expenditure on other components like resting metabolism so that the exercise is, in effect, less costly.
A look at the numbers shows how compensatory mechanisms worked in the study population of 1,750 adults. Among individuals with the highest BMI, 51% of the calories burned during activity translated into calories burned at the end of the day. For those with normal BMI, however, 72% of calories burned during activity were reflected in total expenditure.
“People living with obesity cut back their resting metabolism when they are more active. The result is that for every calorie they spend on exercise they save about half a calorie on resting,” the investigators explained.
In other words, some bodies will, unconsciously, work against the conscious effort of exercising to lose weight. Thank you very much, compensatory mechanisms, for the boundarylessness exhibited in exceeding your job description.
When it comes to the mix, walnuts go nuts
When it comes to mixed nuts, walnuts get no love. But we may be able to give you a reason to not pick them out: Your arteries.
Participants in a recent study who ate about a half-cup of walnuts every day for 2 years saw a drop in their low-density lipoprotein (LDL) cholesterol. The number and quality of LDL particles in healthy older adults also improved. How? Good ol’ omega-3 fatty acids.
Omega-3 is found in many foods linked to lower risks of heart disease, lower cholesterol levels, and lower blood sugar levels, but the one thing that makes the walnut a front runner for Miss Super Food 2021 is their ability to improve the quality of LDL particles.
“LDL particles come in various sizes [and] research has shown that small, dense LDL particles are more often associated with atherosclerosis, the plaque or fatty deposits that build up in the arteries,” Emilio Ros, MD, PhD, of the Hospital Clínic of Barcelona and the study’s senior investigator, said in a written statement.
The 708 participants, aged 63-79 years and mostly women, were divided into two groups: One received the walnut diet and the other did not. After 2 years, the walnut group had lower LDL levels by an average of 4.3 mg/dL. Total cholesterol was reduced by an average of 8.5 mg/dL. Also, their total LDL particle count was 4.3% lower and small LDL particles were down by 6.1%.
So instead of picking the walnuts out of the mix, try to find it in your heart to appreciate them. Your body already does.
Begun, the clone war has
Well, not quite yet, Master Yoda, but perhaps one day soon, if a study from Japan into the uncanny valley of the usage of cloned humanlike faces in robotics and artificial intelligence, published in PLOS One, is to be believed.
The study consisted of a number of six smaller experiments in which participants judged a series of images based on subjective eeriness, emotional valence, and realism. The images included people with the same cloned face; people with different faces; dogs; identical twins, triplets, quadruplets, etc.; and cloned animated characters. In the sixth experiment, the photos were the same as in the second (six cloned faces, six different faces, and a single face) but participants also answered the Disgust Scale–Revised to accurately analyze disgust sensitivity.
The results of all these experiments were quite clear: People found the cloned faces far creepier than the varied or single face, an effect the researchers called clone devaluation. Notably, this effect only applied to realistic human faces; most people didn’t find the cloned dogs or cloned animated characters creepy. However, those who did were more likely to find the human clones eerie on the Disgust Scale.
The authors noted that future robotics technology needs to be carefully considered to avoid the uncanny valley and this clone devaluation effect, which is a very good point. The last thing we need is a few million robots with identical faces getting angry at us and pulling a Terminator/Order 66 combo. We’re already in a viral apocalypse; we don’t need a robot one on top of that.
Congratulations to our new favorite reader
The winner of last week’s inaugural Pandemic Pandemonium comes to us from Tiffanie Roe. By getting her entry in first, just ahead of the flood of responses we received – and by flood we mean a very slow and very quickly repaired drip – Ms. Roe puts the gold medal for COVID-related insanity around the necks of Australian magpies, who may start attacking people wearing face masks during “swooping season” because the birds don’t recognize them.
Exercising to lose weight is not for every ‘body’
This first item comes from the “You’ve got to be kidding” section of LOTME’s supersecret topics-of-interest file.
Investigators at the Shenzhen Institute of Advanced Technology of the Chinese Academy of Sciences and the University of Roehampton noticed that some people who enrolled in exercise programs to lose weight did just the opposite: they gained weight.
Being scientists, they decided to look at the effects of energy expenditure and how those effects varied among individuals. The likely culprit in this case, they determined, is something called compensatory mechanisms. One such mechanism involves eating more food because exercise stimulates appetite, and another might reduce energy expenditure on other components like resting metabolism so that the exercise is, in effect, less costly.
A look at the numbers shows how compensatory mechanisms worked in the study population of 1,750 adults. Among individuals with the highest BMI, 51% of the calories burned during activity translated into calories burned at the end of the day. For those with normal BMI, however, 72% of calories burned during activity were reflected in total expenditure.
“People living with obesity cut back their resting metabolism when they are more active. The result is that for every calorie they spend on exercise they save about half a calorie on resting,” the investigators explained.
In other words, some bodies will, unconsciously, work against the conscious effort of exercising to lose weight. Thank you very much, compensatory mechanisms, for the boundarylessness exhibited in exceeding your job description.
When it comes to the mix, walnuts go nuts
When it comes to mixed nuts, walnuts get no love. But we may be able to give you a reason to not pick them out: Your arteries.
Participants in a recent study who ate about a half-cup of walnuts every day for 2 years saw a drop in their low-density lipoprotein (LDL) cholesterol. The number and quality of LDL particles in healthy older adults also improved. How? Good ol’ omega-3 fatty acids.
Omega-3 is found in many foods linked to lower risks of heart disease, lower cholesterol levels, and lower blood sugar levels, but the one thing that makes the walnut a front runner for Miss Super Food 2021 is their ability to improve the quality of LDL particles.
“LDL particles come in various sizes [and] research has shown that small, dense LDL particles are more often associated with atherosclerosis, the plaque or fatty deposits that build up in the arteries,” Emilio Ros, MD, PhD, of the Hospital Clínic of Barcelona and the study’s senior investigator, said in a written statement.
The 708 participants, aged 63-79 years and mostly women, were divided into two groups: One received the walnut diet and the other did not. After 2 years, the walnut group had lower LDL levels by an average of 4.3 mg/dL. Total cholesterol was reduced by an average of 8.5 mg/dL. Also, their total LDL particle count was 4.3% lower and small LDL particles were down by 6.1%.
So instead of picking the walnuts out of the mix, try to find it in your heart to appreciate them. Your body already does.
Begun, the clone war has
Well, not quite yet, Master Yoda, but perhaps one day soon, if a study from Japan into the uncanny valley of the usage of cloned humanlike faces in robotics and artificial intelligence, published in PLOS One, is to be believed.
The study consisted of a number of six smaller experiments in which participants judged a series of images based on subjective eeriness, emotional valence, and realism. The images included people with the same cloned face; people with different faces; dogs; identical twins, triplets, quadruplets, etc.; and cloned animated characters. In the sixth experiment, the photos were the same as in the second (six cloned faces, six different faces, and a single face) but participants also answered the Disgust Scale–Revised to accurately analyze disgust sensitivity.
The results of all these experiments were quite clear: People found the cloned faces far creepier than the varied or single face, an effect the researchers called clone devaluation. Notably, this effect only applied to realistic human faces; most people didn’t find the cloned dogs or cloned animated characters creepy. However, those who did were more likely to find the human clones eerie on the Disgust Scale.
The authors noted that future robotics technology needs to be carefully considered to avoid the uncanny valley and this clone devaluation effect, which is a very good point. The last thing we need is a few million robots with identical faces getting angry at us and pulling a Terminator/Order 66 combo. We’re already in a viral apocalypse; we don’t need a robot one on top of that.
Congratulations to our new favorite reader
The winner of last week’s inaugural Pandemic Pandemonium comes to us from Tiffanie Roe. By getting her entry in first, just ahead of the flood of responses we received – and by flood we mean a very slow and very quickly repaired drip – Ms. Roe puts the gold medal for COVID-related insanity around the necks of Australian magpies, who may start attacking people wearing face masks during “swooping season” because the birds don’t recognize them.
Study calls higher surgery costs at NCI centers into question
according to a recent report in JAMA Network Open.
“While acceptable to pay higher prices for care that is expected to be of higher quality, we found no differences in short-term postsurgical outcomes,” said authors led by Samuel Takvorian, MD, a medical oncologist at the University of Pennsylvania, Philadelphia.
The team looked at what insurance companies paid for incident breast, colon, and lung cancer surgeries, which together account for most cancer surgeries, among 66,878 patients treated from 2011 to 2014 at almost 3,000 U.S. hospitals.
Three-quarters had surgery at a community hospital, and 8.3% were treated at one of the nation’s 71 NCI centers, which are recognized by the NCI as meeting rigorous standards in cancer care. The remaining patients were treated at non-NCI academic hospitals.
The mean surgery-specific insurer prices paid at NCI centers was $18,526 versus $14,772 at community hospitals, a difference of $3,755 (P < .001) that was driven primarily by higher facility payments at NCI centers, a mean of $17,704 versus $14,120 at community hospitals.
Mean 90-day postdischarge payments were also $5,744 higher at NCI centers, $47,035 versus $41,291 at community hospitals (P = .006).
The team used postsurgical acute care utilization as a marker of quality but found no differences between the two settings. Mean length of stay was 5.1 days and the probability of ED utilization just over 13% in both, and both had a 90-day readmission rate of just over 10%.
Who should be treated at an NCI center?
The data didn’t allow for direct comparison of surgical quality, such as margin status, number of lymph nodes assessed, or postoperative complications, but the postsurgery utilization outcomes “suggest that quality may have been similar,” said Nancy Keating, MD, a health care policy and medicine professor at Harvard Medical School, Boston, in an invited commentary.
The price differences are probably because NCI centers, with their comprehensive offerings, market share, and prestige, can negotiate higher reimbursement rates from insurers, the researchers said.
There is also evidence of better outcomes at NCI centers, particularly for more advanced and complex cases. However, “this study focused on common cancer surgical procedures ... revealing that there is a premium associated with receipt of surgical cancer care at NCI centers.” Further research “is necessary to judge whether and under what circumstances the premium price of NCI centers is justified,” the investigators said.
Dr. Keating noted that “it is likely that some patients benefit from the highly specialized care available at NCI-designated cancer centers ... but it is also likely that many other patients will do equally well regardless of where they receive their care.”
Amid ever-increasing cancer care costs and the need to strategically allocate financial resources, more research is needed to “identify subgroups of patients for whom highly specialized care is particularly necessary to achieve better outcomes. Such data could also be used by payers considering tiered networks and by physician organizations participating in risk contracts for decisions about where to refer patients with cancer for treatment,” she said.
Rectifying a ‘misalignment’
The researchers also said the findings reveal competing incentives, with commercial payers wanting to steer patients away from high-cost hospitals but health systems hoping to maximize surgical volume at lucrative referral centers.
“Value-based or bundled payment reimbursement for surgical episodes, particularly when paired with mandatory reporting on surgical outcomes, could help to rectify this misalignment,” they said.
Out-of-pocket spending wasn’t analyzed in the study, so it’s unknown how the higher prices at NCI centers hit patients in the pocketbook.
Meanwhile, non-NCI academic hospitals also had higher insurer prices paid than community hospitals, but the differences were not statistically significant, nor were differences in the study’s utilization outcomes.
Over half the patients had breast cancer, about one-third had colon cancer, and the rest had lung tumors. Patients treated at NCI centers tended to be younger than those treated at community hospitals and more likely to be women, but comorbidity scores were similar between the groups.
NCI centers, compared with community hospitals, were larger with higher surgical volumes and in more populated areas. They also had higher rates of laparoscopic partial colectomies and pneumonectomies.
Data came from the Health Care Cost Institute’s national commercial claims data set, which includes claims from three of the country’s five largest commercial insurers: Aetna, Humana, and UnitedHealthcare.
The work was funded by the Commonwealth of Pennsylvania and the National Cancer Institute. Dr. Takvorian and Dr. Keating didn’t have any disclosures. One of Dr. Takvorian’s coauthors reported grants and/or personal fees from several sources, including Pfizer, UnitedHealthcare, and Blue Cross Blue Shield of North Carolina.
according to a recent report in JAMA Network Open.
“While acceptable to pay higher prices for care that is expected to be of higher quality, we found no differences in short-term postsurgical outcomes,” said authors led by Samuel Takvorian, MD, a medical oncologist at the University of Pennsylvania, Philadelphia.
The team looked at what insurance companies paid for incident breast, colon, and lung cancer surgeries, which together account for most cancer surgeries, among 66,878 patients treated from 2011 to 2014 at almost 3,000 U.S. hospitals.
Three-quarters had surgery at a community hospital, and 8.3% were treated at one of the nation’s 71 NCI centers, which are recognized by the NCI as meeting rigorous standards in cancer care. The remaining patients were treated at non-NCI academic hospitals.
The mean surgery-specific insurer prices paid at NCI centers was $18,526 versus $14,772 at community hospitals, a difference of $3,755 (P < .001) that was driven primarily by higher facility payments at NCI centers, a mean of $17,704 versus $14,120 at community hospitals.
Mean 90-day postdischarge payments were also $5,744 higher at NCI centers, $47,035 versus $41,291 at community hospitals (P = .006).
The team used postsurgical acute care utilization as a marker of quality but found no differences between the two settings. Mean length of stay was 5.1 days and the probability of ED utilization just over 13% in both, and both had a 90-day readmission rate of just over 10%.
Who should be treated at an NCI center?
The data didn’t allow for direct comparison of surgical quality, such as margin status, number of lymph nodes assessed, or postoperative complications, but the postsurgery utilization outcomes “suggest that quality may have been similar,” said Nancy Keating, MD, a health care policy and medicine professor at Harvard Medical School, Boston, in an invited commentary.
The price differences are probably because NCI centers, with their comprehensive offerings, market share, and prestige, can negotiate higher reimbursement rates from insurers, the researchers said.
There is also evidence of better outcomes at NCI centers, particularly for more advanced and complex cases. However, “this study focused on common cancer surgical procedures ... revealing that there is a premium associated with receipt of surgical cancer care at NCI centers.” Further research “is necessary to judge whether and under what circumstances the premium price of NCI centers is justified,” the investigators said.
Dr. Keating noted that “it is likely that some patients benefit from the highly specialized care available at NCI-designated cancer centers ... but it is also likely that many other patients will do equally well regardless of where they receive their care.”
Amid ever-increasing cancer care costs and the need to strategically allocate financial resources, more research is needed to “identify subgroups of patients for whom highly specialized care is particularly necessary to achieve better outcomes. Such data could also be used by payers considering tiered networks and by physician organizations participating in risk contracts for decisions about where to refer patients with cancer for treatment,” she said.
Rectifying a ‘misalignment’
The researchers also said the findings reveal competing incentives, with commercial payers wanting to steer patients away from high-cost hospitals but health systems hoping to maximize surgical volume at lucrative referral centers.
“Value-based or bundled payment reimbursement for surgical episodes, particularly when paired with mandatory reporting on surgical outcomes, could help to rectify this misalignment,” they said.
Out-of-pocket spending wasn’t analyzed in the study, so it’s unknown how the higher prices at NCI centers hit patients in the pocketbook.
Meanwhile, non-NCI academic hospitals also had higher insurer prices paid than community hospitals, but the differences were not statistically significant, nor were differences in the study’s utilization outcomes.
Over half the patients had breast cancer, about one-third had colon cancer, and the rest had lung tumors. Patients treated at NCI centers tended to be younger than those treated at community hospitals and more likely to be women, but comorbidity scores were similar between the groups.
NCI centers, compared with community hospitals, were larger with higher surgical volumes and in more populated areas. They also had higher rates of laparoscopic partial colectomies and pneumonectomies.
Data came from the Health Care Cost Institute’s national commercial claims data set, which includes claims from three of the country’s five largest commercial insurers: Aetna, Humana, and UnitedHealthcare.
The work was funded by the Commonwealth of Pennsylvania and the National Cancer Institute. Dr. Takvorian and Dr. Keating didn’t have any disclosures. One of Dr. Takvorian’s coauthors reported grants and/or personal fees from several sources, including Pfizer, UnitedHealthcare, and Blue Cross Blue Shield of North Carolina.
according to a recent report in JAMA Network Open.
“While acceptable to pay higher prices for care that is expected to be of higher quality, we found no differences in short-term postsurgical outcomes,” said authors led by Samuel Takvorian, MD, a medical oncologist at the University of Pennsylvania, Philadelphia.
The team looked at what insurance companies paid for incident breast, colon, and lung cancer surgeries, which together account for most cancer surgeries, among 66,878 patients treated from 2011 to 2014 at almost 3,000 U.S. hospitals.
Three-quarters had surgery at a community hospital, and 8.3% were treated at one of the nation’s 71 NCI centers, which are recognized by the NCI as meeting rigorous standards in cancer care. The remaining patients were treated at non-NCI academic hospitals.
The mean surgery-specific insurer prices paid at NCI centers was $18,526 versus $14,772 at community hospitals, a difference of $3,755 (P < .001) that was driven primarily by higher facility payments at NCI centers, a mean of $17,704 versus $14,120 at community hospitals.
Mean 90-day postdischarge payments were also $5,744 higher at NCI centers, $47,035 versus $41,291 at community hospitals (P = .006).
The team used postsurgical acute care utilization as a marker of quality but found no differences between the two settings. Mean length of stay was 5.1 days and the probability of ED utilization just over 13% in both, and both had a 90-day readmission rate of just over 10%.
Who should be treated at an NCI center?
The data didn’t allow for direct comparison of surgical quality, such as margin status, number of lymph nodes assessed, or postoperative complications, but the postsurgery utilization outcomes “suggest that quality may have been similar,” said Nancy Keating, MD, a health care policy and medicine professor at Harvard Medical School, Boston, in an invited commentary.
The price differences are probably because NCI centers, with their comprehensive offerings, market share, and prestige, can negotiate higher reimbursement rates from insurers, the researchers said.
There is also evidence of better outcomes at NCI centers, particularly for more advanced and complex cases. However, “this study focused on common cancer surgical procedures ... revealing that there is a premium associated with receipt of surgical cancer care at NCI centers.” Further research “is necessary to judge whether and under what circumstances the premium price of NCI centers is justified,” the investigators said.
Dr. Keating noted that “it is likely that some patients benefit from the highly specialized care available at NCI-designated cancer centers ... but it is also likely that many other patients will do equally well regardless of where they receive their care.”
Amid ever-increasing cancer care costs and the need to strategically allocate financial resources, more research is needed to “identify subgroups of patients for whom highly specialized care is particularly necessary to achieve better outcomes. Such data could also be used by payers considering tiered networks and by physician organizations participating in risk contracts for decisions about where to refer patients with cancer for treatment,” she said.
Rectifying a ‘misalignment’
The researchers also said the findings reveal competing incentives, with commercial payers wanting to steer patients away from high-cost hospitals but health systems hoping to maximize surgical volume at lucrative referral centers.
“Value-based or bundled payment reimbursement for surgical episodes, particularly when paired with mandatory reporting on surgical outcomes, could help to rectify this misalignment,” they said.
Out-of-pocket spending wasn’t analyzed in the study, so it’s unknown how the higher prices at NCI centers hit patients in the pocketbook.
Meanwhile, non-NCI academic hospitals also had higher insurer prices paid than community hospitals, but the differences were not statistically significant, nor were differences in the study’s utilization outcomes.
Over half the patients had breast cancer, about one-third had colon cancer, and the rest had lung tumors. Patients treated at NCI centers tended to be younger than those treated at community hospitals and more likely to be women, but comorbidity scores were similar between the groups.
NCI centers, compared with community hospitals, were larger with higher surgical volumes and in more populated areas. They also had higher rates of laparoscopic partial colectomies and pneumonectomies.
Data came from the Health Care Cost Institute’s national commercial claims data set, which includes claims from three of the country’s five largest commercial insurers: Aetna, Humana, and UnitedHealthcare.
The work was funded by the Commonwealth of Pennsylvania and the National Cancer Institute. Dr. Takvorian and Dr. Keating didn’t have any disclosures. One of Dr. Takvorian’s coauthors reported grants and/or personal fees from several sources, including Pfizer, UnitedHealthcare, and Blue Cross Blue Shield of North Carolina.
FROM JAMA NETWORK OPEN
Report urges complete residency overhaul
from the Graduate Medical Education Review Committee (UGRC) of the Coalition for Physician Accountability.
The 275-page report presents preliminary findings that were released in April 2021 and a long list of stakeholder comments. According to the report, the coalition will meet soon to discuss the final recommendations and consider next steps toward implementation.
The UGRC includes representatives of national medical organizations, medical schools, and residency programs. Among the organizations that participated in the report’s creation are the American Medical Association, the National Board of Medical Examiners, the American Osteopathic Association, the National Board of Osteopathic Medical Examiners, the Educational Commission for Foreign Medical Graduates, and the Association of American Medical Colleges.
The report identifies a list of challenges that affect the transition of medical students into residency programs and beyond. They include:
- Too much focus on finding and filling residency positions instead of “assuring learner competence and readiness for residency training”
- Inattention to assuring congruence between applicant goals and program missions
- Overreliance on licensure exam scores rather than “valid, trustworthy measures of students’ competence and clinical abilities”
- Increasing financial costs to students
- Individual and systemic biases in the UME-GME transition, as well as inequities related to international medical graduates
Seeking a common framework for competence
Overall, the report calls for increased standardization of how students are evaluated in medical school and how residency programs evaluate students. Less reliance should be placed on the numerical scores of the U.S. Medical Licensing Examination (USMLE), the report says, and more attention should be paid to the direct observation of student performance in clinical situations. In addition, the various organizations involved in the UME-GME transition process are asked to work better together.
To develop better methods of evaluating medical students and residents, UME and GME educators should jointly define and implement a common framework and set of competencies to apply to learners across the UME-GME transition, the report suggests.
While emphasizing the need for a broader student assessment framework, the report says, USMLE scores should also continue to be used in judging residency applicants. “Assessment information should be shared in residency applications and a postmatch learner handover. Licensing examinations should be used for their intended purpose to ensure requisite competence.”
Among the committee’s three dozen recommendations are the following:
- The Centers for Medicare & Medicaid Services should change the GME funding structure so that the initial residency period is calculated starting with the second year of postgraduate training. This change would allow residents to reconsider their career choices. Currently, if a resident decides to switch to another program or specialty after beginning training, the hospital may not receive full GME funding, so may be less likely to approve the change.
- Residency programs should improve recruitment practices to increase specialty-specific diversity of residents. Medical educators should also receive additional training regarding antiracism, avoiding bias, and ensuring equity.
- The self-reported demographic information of applicants to residency programs should be measured and shared with stakeholders, including the programs and medical schools, to promote equity. “A residency program that finds bias in its selection process could go back in real time to find qualified applicants who may have been missed, potentially improving outcomes,” the report notes.
- An interactive database of GME program and specialty track information should be created and made available to all applicants, medical schools, and residency programs at no cost to applicants. “Applicants and their advisors should be able to sort the information according to demographic and educational features that may significantly impact the likelihood of matching at a program.”
Less than half of applicants get in-depth reviews
The 2020 National Resident Matching Program Program Director Survey found that only 49% of applications received in-depth review. In light of this, the report suggests that the application system be updated to use modern information technology, including discrete fields for key data to expedite application reviews.
Many applications have been discarded because of various filters used to block consideration of certain applications. The report suggests that new filters be designed to ensure that each detects meaningful differences among applicants and promotes review based on mission alignment and likelihood of success in a program. Filters should be improved to decrease the likelihood of random exclusions of qualified applicants.
Specialty-specific, just-in-time training for all incoming first-year residents is also suggested to support the transition from the role of student to a physician ready to assume increased responsibility for patient care. In addition, the report urges adequate time be allowed between medical school graduation and residency to enable new residents to relocate and find homes.
The report also calls for a standardized process in the United States for initial licensing of doctors at entrance to residency in order to streamline the process of credentialing for both residency training and continuing practice.
Osteopathic students’ dilemma
To promote equitable treatment of applicants regardless of licensure examination requirements, comparable exams with different scales (COMLEX-USA and USMLE) should be reported within the electronic application system in a single field, the report said.
Osteopathic students, who make up 25% of U.S. medical students, must take the COMLEX-USA exam, but residency programs may filter them out if they don’t also take the USMLE exam. Thus, many osteopathic students take both exams, incurring extra time, cost, and stress.
The UGRC recommends creating a combined field in the electronic residency application service that normalizes the scores between the two exams. Residency programs could then filter applications based only on the single normalized score.
This approach makes sense from the viewpoint that it would reduce the pressure on osteopathic students to take the USMLE, Bryan Carmody, MD, an outspoken critic of various current training policies, said in an interview. But it could also have serious disadvantages.
For one thing, only osteopathic students can take the COMLEX-USA exam, he noted. If they don’t like their score, they can then take the USMLE test to get a higher score – an option that allopathic students don’t have. It’s not clear that they’d be prevented from doing this under the UGRC recommendation.
Second, he said, osteopathic students, on average, don’t do as well as allopathic students on the UMSLE exam. If they only take the COMLEX-USA test, they’re competing against other students who don’t do as well on tests as allopathic students do. If their scores were normalized with those of the USMLE test takers, they’d gain an unfair advantage against students who can only take the USMLE, including international medical graduates.
Although Dr. Carmody admitted that osteopathic students face a harder challenge than allopathic students in matching to residency programs, he said that the UGRC approach to the licensing exams might actually penalize them further. As a result of the scores of the two exams being averaged, residency program directors might discount the scores of all osteopathic students.
A version of this article first appeared on Medscape.com.
from the Graduate Medical Education Review Committee (UGRC) of the Coalition for Physician Accountability.
The 275-page report presents preliminary findings that were released in April 2021 and a long list of stakeholder comments. According to the report, the coalition will meet soon to discuss the final recommendations and consider next steps toward implementation.
The UGRC includes representatives of national medical organizations, medical schools, and residency programs. Among the organizations that participated in the report’s creation are the American Medical Association, the National Board of Medical Examiners, the American Osteopathic Association, the National Board of Osteopathic Medical Examiners, the Educational Commission for Foreign Medical Graduates, and the Association of American Medical Colleges.
The report identifies a list of challenges that affect the transition of medical students into residency programs and beyond. They include:
- Too much focus on finding and filling residency positions instead of “assuring learner competence and readiness for residency training”
- Inattention to assuring congruence between applicant goals and program missions
- Overreliance on licensure exam scores rather than “valid, trustworthy measures of students’ competence and clinical abilities”
- Increasing financial costs to students
- Individual and systemic biases in the UME-GME transition, as well as inequities related to international medical graduates
Seeking a common framework for competence
Overall, the report calls for increased standardization of how students are evaluated in medical school and how residency programs evaluate students. Less reliance should be placed on the numerical scores of the U.S. Medical Licensing Examination (USMLE), the report says, and more attention should be paid to the direct observation of student performance in clinical situations. In addition, the various organizations involved in the UME-GME transition process are asked to work better together.
To develop better methods of evaluating medical students and residents, UME and GME educators should jointly define and implement a common framework and set of competencies to apply to learners across the UME-GME transition, the report suggests.
While emphasizing the need for a broader student assessment framework, the report says, USMLE scores should also continue to be used in judging residency applicants. “Assessment information should be shared in residency applications and a postmatch learner handover. Licensing examinations should be used for their intended purpose to ensure requisite competence.”
Among the committee’s three dozen recommendations are the following:
- The Centers for Medicare & Medicaid Services should change the GME funding structure so that the initial residency period is calculated starting with the second year of postgraduate training. This change would allow residents to reconsider their career choices. Currently, if a resident decides to switch to another program or specialty after beginning training, the hospital may not receive full GME funding, so may be less likely to approve the change.
- Residency programs should improve recruitment practices to increase specialty-specific diversity of residents. Medical educators should also receive additional training regarding antiracism, avoiding bias, and ensuring equity.
- The self-reported demographic information of applicants to residency programs should be measured and shared with stakeholders, including the programs and medical schools, to promote equity. “A residency program that finds bias in its selection process could go back in real time to find qualified applicants who may have been missed, potentially improving outcomes,” the report notes.
- An interactive database of GME program and specialty track information should be created and made available to all applicants, medical schools, and residency programs at no cost to applicants. “Applicants and their advisors should be able to sort the information according to demographic and educational features that may significantly impact the likelihood of matching at a program.”
Less than half of applicants get in-depth reviews
The 2020 National Resident Matching Program Program Director Survey found that only 49% of applications received in-depth review. In light of this, the report suggests that the application system be updated to use modern information technology, including discrete fields for key data to expedite application reviews.
Many applications have been discarded because of various filters used to block consideration of certain applications. The report suggests that new filters be designed to ensure that each detects meaningful differences among applicants and promotes review based on mission alignment and likelihood of success in a program. Filters should be improved to decrease the likelihood of random exclusions of qualified applicants.
Specialty-specific, just-in-time training for all incoming first-year residents is also suggested to support the transition from the role of student to a physician ready to assume increased responsibility for patient care. In addition, the report urges adequate time be allowed between medical school graduation and residency to enable new residents to relocate and find homes.
The report also calls for a standardized process in the United States for initial licensing of doctors at entrance to residency in order to streamline the process of credentialing for both residency training and continuing practice.
Osteopathic students’ dilemma
To promote equitable treatment of applicants regardless of licensure examination requirements, comparable exams with different scales (COMLEX-USA and USMLE) should be reported within the electronic application system in a single field, the report said.
Osteopathic students, who make up 25% of U.S. medical students, must take the COMLEX-USA exam, but residency programs may filter them out if they don’t also take the USMLE exam. Thus, many osteopathic students take both exams, incurring extra time, cost, and stress.
The UGRC recommends creating a combined field in the electronic residency application service that normalizes the scores between the two exams. Residency programs could then filter applications based only on the single normalized score.
This approach makes sense from the viewpoint that it would reduce the pressure on osteopathic students to take the USMLE, Bryan Carmody, MD, an outspoken critic of various current training policies, said in an interview. But it could also have serious disadvantages.
For one thing, only osteopathic students can take the COMLEX-USA exam, he noted. If they don’t like their score, they can then take the USMLE test to get a higher score – an option that allopathic students don’t have. It’s not clear that they’d be prevented from doing this under the UGRC recommendation.
Second, he said, osteopathic students, on average, don’t do as well as allopathic students on the UMSLE exam. If they only take the COMLEX-USA test, they’re competing against other students who don’t do as well on tests as allopathic students do. If their scores were normalized with those of the USMLE test takers, they’d gain an unfair advantage against students who can only take the USMLE, including international medical graduates.
Although Dr. Carmody admitted that osteopathic students face a harder challenge than allopathic students in matching to residency programs, he said that the UGRC approach to the licensing exams might actually penalize them further. As a result of the scores of the two exams being averaged, residency program directors might discount the scores of all osteopathic students.
A version of this article first appeared on Medscape.com.
from the Graduate Medical Education Review Committee (UGRC) of the Coalition for Physician Accountability.
The 275-page report presents preliminary findings that were released in April 2021 and a long list of stakeholder comments. According to the report, the coalition will meet soon to discuss the final recommendations and consider next steps toward implementation.
The UGRC includes representatives of national medical organizations, medical schools, and residency programs. Among the organizations that participated in the report’s creation are the American Medical Association, the National Board of Medical Examiners, the American Osteopathic Association, the National Board of Osteopathic Medical Examiners, the Educational Commission for Foreign Medical Graduates, and the Association of American Medical Colleges.
The report identifies a list of challenges that affect the transition of medical students into residency programs and beyond. They include:
- Too much focus on finding and filling residency positions instead of “assuring learner competence and readiness for residency training”
- Inattention to assuring congruence between applicant goals and program missions
- Overreliance on licensure exam scores rather than “valid, trustworthy measures of students’ competence and clinical abilities”
- Increasing financial costs to students
- Individual and systemic biases in the UME-GME transition, as well as inequities related to international medical graduates
Seeking a common framework for competence
Overall, the report calls for increased standardization of how students are evaluated in medical school and how residency programs evaluate students. Less reliance should be placed on the numerical scores of the U.S. Medical Licensing Examination (USMLE), the report says, and more attention should be paid to the direct observation of student performance in clinical situations. In addition, the various organizations involved in the UME-GME transition process are asked to work better together.
To develop better methods of evaluating medical students and residents, UME and GME educators should jointly define and implement a common framework and set of competencies to apply to learners across the UME-GME transition, the report suggests.
While emphasizing the need for a broader student assessment framework, the report says, USMLE scores should also continue to be used in judging residency applicants. “Assessment information should be shared in residency applications and a postmatch learner handover. Licensing examinations should be used for their intended purpose to ensure requisite competence.”
Among the committee’s three dozen recommendations are the following:
- The Centers for Medicare & Medicaid Services should change the GME funding structure so that the initial residency period is calculated starting with the second year of postgraduate training. This change would allow residents to reconsider their career choices. Currently, if a resident decides to switch to another program or specialty after beginning training, the hospital may not receive full GME funding, so may be less likely to approve the change.
- Residency programs should improve recruitment practices to increase specialty-specific diversity of residents. Medical educators should also receive additional training regarding antiracism, avoiding bias, and ensuring equity.
- The self-reported demographic information of applicants to residency programs should be measured and shared with stakeholders, including the programs and medical schools, to promote equity. “A residency program that finds bias in its selection process could go back in real time to find qualified applicants who may have been missed, potentially improving outcomes,” the report notes.
- An interactive database of GME program and specialty track information should be created and made available to all applicants, medical schools, and residency programs at no cost to applicants. “Applicants and their advisors should be able to sort the information according to demographic and educational features that may significantly impact the likelihood of matching at a program.”
Less than half of applicants get in-depth reviews
The 2020 National Resident Matching Program Program Director Survey found that only 49% of applications received in-depth review. In light of this, the report suggests that the application system be updated to use modern information technology, including discrete fields for key data to expedite application reviews.
Many applications have been discarded because of various filters used to block consideration of certain applications. The report suggests that new filters be designed to ensure that each detects meaningful differences among applicants and promotes review based on mission alignment and likelihood of success in a program. Filters should be improved to decrease the likelihood of random exclusions of qualified applicants.
Specialty-specific, just-in-time training for all incoming first-year residents is also suggested to support the transition from the role of student to a physician ready to assume increased responsibility for patient care. In addition, the report urges adequate time be allowed between medical school graduation and residency to enable new residents to relocate and find homes.
The report also calls for a standardized process in the United States for initial licensing of doctors at entrance to residency in order to streamline the process of credentialing for both residency training and continuing practice.
Osteopathic students’ dilemma
To promote equitable treatment of applicants regardless of licensure examination requirements, comparable exams with different scales (COMLEX-USA and USMLE) should be reported within the electronic application system in a single field, the report said.
Osteopathic students, who make up 25% of U.S. medical students, must take the COMLEX-USA exam, but residency programs may filter them out if they don’t also take the USMLE exam. Thus, many osteopathic students take both exams, incurring extra time, cost, and stress.
The UGRC recommends creating a combined field in the electronic residency application service that normalizes the scores between the two exams. Residency programs could then filter applications based only on the single normalized score.
This approach makes sense from the viewpoint that it would reduce the pressure on osteopathic students to take the USMLE, Bryan Carmody, MD, an outspoken critic of various current training policies, said in an interview. But it could also have serious disadvantages.
For one thing, only osteopathic students can take the COMLEX-USA exam, he noted. If they don’t like their score, they can then take the USMLE test to get a higher score – an option that allopathic students don’t have. It’s not clear that they’d be prevented from doing this under the UGRC recommendation.
Second, he said, osteopathic students, on average, don’t do as well as allopathic students on the UMSLE exam. If they only take the COMLEX-USA test, they’re competing against other students who don’t do as well on tests as allopathic students do. If their scores were normalized with those of the USMLE test takers, they’d gain an unfair advantage against students who can only take the USMLE, including international medical graduates.
Although Dr. Carmody admitted that osteopathic students face a harder challenge than allopathic students in matching to residency programs, he said that the UGRC approach to the licensing exams might actually penalize them further. As a result of the scores of the two exams being averaged, residency program directors might discount the scores of all osteopathic students.
A version of this article first appeared on Medscape.com.










