User login
COAPT 5-year results ‘remarkable,’ but patient selection issues remain
It remained an open question in 2018, on the unveiling of the COAPT trial’s 2-year primary results, whether the striking reductions in mortality and heart-failure (HF) hospitalization observed for transcatheter edge-to-edge repair (TEER) with the MitraClip (Abbott) would be durable with longer follow-up.
The trial had enrolled an especially sick population of symptomatic patients with mitral regurgitation (MR) secondary to HF.
As it turns out, the therapy’s benefits at 2 years were indeed durable, at least out to 5 years, investigators reported March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The results were simultaneously published in the New England Journal of Medicine.
Patients who received the MitraClip on top of intensive medical therapy, compared with a group assigned to medical management alone, benefited significantly at 5 years with risk reductions of 51% for HF hospitalization, 28% for death from any cause, and 47% for the composite of the two events.
Still, mortality at 5 years among the 614 randomized patients was steep at 57.3% in the MitraClip group and 67.2% for those assigned to meds only, underscoring the need for early identification of patients appropriate for the device therapy, Gregg W. Stone, MD, said during his presentation.
Dr. Stone, of the Icahn School of Medicine at Mount Sinai, New York, is a COAPT co-principal investigator and lead author of the 5-year outcomes publication.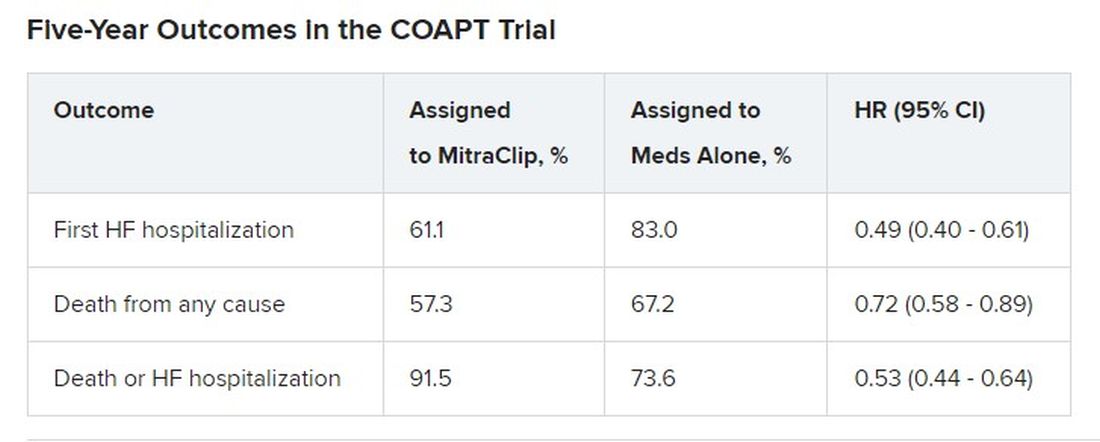
Outcomes were consistent across all prespecified patient subgroups, including by age, sex, MR, left ventricular (LV) function and volume, cardiomyopathy etiology, and degree of surgical risk, the researchers reported.
Symptom status, as measured by New York Heart Association (NYHA) functional class, improved throughout the 5-year follow-up for patients assigned to the MitraClip group, compared with the control group, and the intervention group was significantly more likely to be in NYHA class 1 or 2, the authors noted.
The relative benefits in terms of clinical outcomes of MitraClip therapy narrowed after 2-3 years, Dr. Stone said, primarily because at 2 years, patients who had been assigned to meds only were eligible to undergo TEER. Indeed, he noted, 45% of the 138 patients in the control group who were eligible for TEER at 2 years “crossed over” to receive a MitraClip. Those patients benefited despite their delay in undergoing the procedure, he observed.
However, nearly half of the control patients died before becoming eligible for crossover at 2 years. “We have to identify the appropriate patients for treatment and treat them early because the mortality is very high in this population,” Dr. Stone said.
“We need to do more because the MitraClip doesn’t do anything directly to the underlying left ventricular dysfunction, which is the cause of the patient’s disease,” he said. “We need advanced therapies to address the underlying left ventricular dysfunction” in this high-risk population.
Exclusions based on LV dimension
The COAPT trial included 614 patients with HF and symptomatic MR despite guideline-directed medical therapy. They were required to have moderate to severe (3+) or severe (4+) MR confirmed by an echocardiographic core laboratory and a left ventricular ejection fraction (LVEF) of 20%-50%.
Among the exclusion criteria were an LV end-systolic diameter greater than 70 mm, severe pulmonary hypertension, and moderate to severe symptomatic right ventricular failure.
The systolic LV dimension exclusion helped address the persistent question of whether “severe mitral regurgitation is a marker of a bad left ventricle or ... contributes to the pathophysiology” of MR and its poor outcomes, Dr. Stone said.
The 51% reduction in risk for time-to-first HF hospitalization among patients assigned to TEER “accrued very early,” Dr. Stone pointed out. “You can see the curves start to separate almost immediately after you reduce left atrial pressure and volume overload with the MitraClip.”
The curves stopped diverging after about 3 years because of crossover from the control group, he said. Still, “we had shown a substantial absolute 17% reduction in mortality at 2 years” with MitraClip. “That has continued out to 5 years, with a statistically significant 28% relative reduction,” he continued, and the absolute risk reduction reaching 10%.
Patients in the control group who crossed over “basically assumed the death and heart failure hospitalization rate of the MitraClip group,” Dr. Stone said. That wasn’t surprising “because most of the patients enrolled in the trial originally had chronic heart failure.” It’s “confirmation of the principal results of the trial.”
Comparison With MITRA-FR
“We know that MITRA-FR was a negative trial,” observed Wayne B. Batchelor, MD, an invited discussant following Dr. Stone’s presentation, referring to an earlier similar trial that showed no advantage for MitraClip. Compared with MITRA-FR, COAPT “has created an entirely different story.”
The marked reductions in mortality and risk for adverse events and low number-needed-to-treat with MitraClip are “really remarkable,” said Dr. Batchelor, who is with the Inova Heart and Vascular Institute, Falls Church, Va.
But the high absolute mortality for patients in the COAPT control group “speaks volumes to me and tells us that we’ve got to identify our patients well early,” he agreed, and to “implement transcatheter edge-to-edge therapy in properly selected patients on guideline-directed medical therapy in order to avoid that.”
The trial findings “suggest that we’re reducing HF hospitalization,” he said, “so this is an extremely potent therapy, potentially.
“The dramatic difference between the treated arm and the medical therapy arm in this trial makes me feel that this therapy is here to stay,” Dr. Batchelor concluded. “We just have to figure out how to deploy it properly in the right patients.”
The COAPT trial presents “a practice-changing paradigm,” said Suzanne J. Baron, MD, of Lahey Hospital & Medical Center, Burlington, Mass., another invited discussant.
The crossover data “really jumped out,” she added. “Waiting to treat patients with TEER may be harmful, so if we’re going to consider treating earlier, how do we identify the right patient?” Dr. Baron asked, especially given the negative MITRA-FR results.
MITRA-FR didn’t follow patients beyond 2 years, Dr. Stone noted. Still, “we do think that the main difference was that COAPT enrolled a patient population with more severe MR and slightly less LV dysfunction, at least in terms of the LV not being as dilated, so they didn’t have end-stage LV disease. Whereas in MITRA-FR, more of the patients had only moderate mitral regurgitation.” And big dilated left ventricles “are less likely to benefit.”
There were also differences between the studies in technique and background medical therapies, he added.
The Food and Drug Administration has approved – and payers are paying – for the treatment of patients who meet the COAPT criteria, “in whom we can be very confident they have a benefit,” Dr. Stone said.
“The real question is: Where are the edges where we should consider this? LVEF slightly less than 20% or slightly greater than 50%? Or primary atrial functional mitral regurgitation? There are registry data to suggest that they would benefit,” he said, but “we need more data.”
COAPT was supported by Abbott. Dr. Stone disclosed receiving speaker honoraria from Abbott and consulting fees or equity from Neovasc, Ancora, Valfix, and Cardiac Success; and that Mount Sinai receives research funding from Abbott. Disclosures for the other authors are available at nejm.org. Dr. Batchelor has disclosed receiving consultant fees or honoraria from Abbott, Boston Scientific, Idorsia, and V-Wave Medical, and having other ties with Medtronic. Dr. Baron has disclosed receiving consultant fees or honoraria from Abiomed, Biotronik, Boston Scientific, Edwards Lifesciences, Medtronic, Shockwave, and Zoll Medical, and conducting research or receiving research grants from Abiomed and Boston Scientific.
A version of this article originally appeared on Medscape.com.
It remained an open question in 2018, on the unveiling of the COAPT trial’s 2-year primary results, whether the striking reductions in mortality and heart-failure (HF) hospitalization observed for transcatheter edge-to-edge repair (TEER) with the MitraClip (Abbott) would be durable with longer follow-up.
The trial had enrolled an especially sick population of symptomatic patients with mitral regurgitation (MR) secondary to HF.
As it turns out, the therapy’s benefits at 2 years were indeed durable, at least out to 5 years, investigators reported March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The results were simultaneously published in the New England Journal of Medicine.
Patients who received the MitraClip on top of intensive medical therapy, compared with a group assigned to medical management alone, benefited significantly at 5 years with risk reductions of 51% for HF hospitalization, 28% for death from any cause, and 47% for the composite of the two events.
Still, mortality at 5 years among the 614 randomized patients was steep at 57.3% in the MitraClip group and 67.2% for those assigned to meds only, underscoring the need for early identification of patients appropriate for the device therapy, Gregg W. Stone, MD, said during his presentation.
Dr. Stone, of the Icahn School of Medicine at Mount Sinai, New York, is a COAPT co-principal investigator and lead author of the 5-year outcomes publication.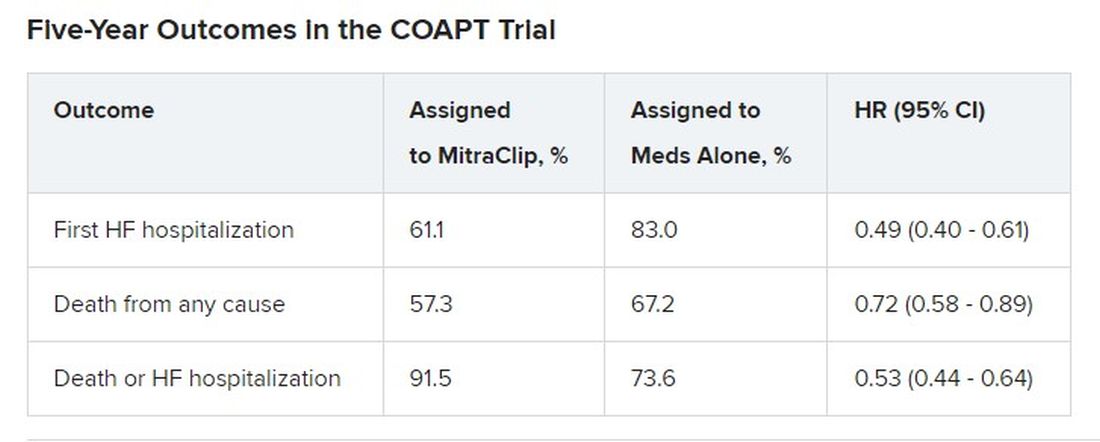
Outcomes were consistent across all prespecified patient subgroups, including by age, sex, MR, left ventricular (LV) function and volume, cardiomyopathy etiology, and degree of surgical risk, the researchers reported.
Symptom status, as measured by New York Heart Association (NYHA) functional class, improved throughout the 5-year follow-up for patients assigned to the MitraClip group, compared with the control group, and the intervention group was significantly more likely to be in NYHA class 1 or 2, the authors noted.
The relative benefits in terms of clinical outcomes of MitraClip therapy narrowed after 2-3 years, Dr. Stone said, primarily because at 2 years, patients who had been assigned to meds only were eligible to undergo TEER. Indeed, he noted, 45% of the 138 patients in the control group who were eligible for TEER at 2 years “crossed over” to receive a MitraClip. Those patients benefited despite their delay in undergoing the procedure, he observed.
However, nearly half of the control patients died before becoming eligible for crossover at 2 years. “We have to identify the appropriate patients for treatment and treat them early because the mortality is very high in this population,” Dr. Stone said.
“We need to do more because the MitraClip doesn’t do anything directly to the underlying left ventricular dysfunction, which is the cause of the patient’s disease,” he said. “We need advanced therapies to address the underlying left ventricular dysfunction” in this high-risk population.
Exclusions based on LV dimension
The COAPT trial included 614 patients with HF and symptomatic MR despite guideline-directed medical therapy. They were required to have moderate to severe (3+) or severe (4+) MR confirmed by an echocardiographic core laboratory and a left ventricular ejection fraction (LVEF) of 20%-50%.
Among the exclusion criteria were an LV end-systolic diameter greater than 70 mm, severe pulmonary hypertension, and moderate to severe symptomatic right ventricular failure.
The systolic LV dimension exclusion helped address the persistent question of whether “severe mitral regurgitation is a marker of a bad left ventricle or ... contributes to the pathophysiology” of MR and its poor outcomes, Dr. Stone said.
The 51% reduction in risk for time-to-first HF hospitalization among patients assigned to TEER “accrued very early,” Dr. Stone pointed out. “You can see the curves start to separate almost immediately after you reduce left atrial pressure and volume overload with the MitraClip.”
The curves stopped diverging after about 3 years because of crossover from the control group, he said. Still, “we had shown a substantial absolute 17% reduction in mortality at 2 years” with MitraClip. “That has continued out to 5 years, with a statistically significant 28% relative reduction,” he continued, and the absolute risk reduction reaching 10%.
Patients in the control group who crossed over “basically assumed the death and heart failure hospitalization rate of the MitraClip group,” Dr. Stone said. That wasn’t surprising “because most of the patients enrolled in the trial originally had chronic heart failure.” It’s “confirmation of the principal results of the trial.”
Comparison With MITRA-FR
“We know that MITRA-FR was a negative trial,” observed Wayne B. Batchelor, MD, an invited discussant following Dr. Stone’s presentation, referring to an earlier similar trial that showed no advantage for MitraClip. Compared with MITRA-FR, COAPT “has created an entirely different story.”
The marked reductions in mortality and risk for adverse events and low number-needed-to-treat with MitraClip are “really remarkable,” said Dr. Batchelor, who is with the Inova Heart and Vascular Institute, Falls Church, Va.
But the high absolute mortality for patients in the COAPT control group “speaks volumes to me and tells us that we’ve got to identify our patients well early,” he agreed, and to “implement transcatheter edge-to-edge therapy in properly selected patients on guideline-directed medical therapy in order to avoid that.”
The trial findings “suggest that we’re reducing HF hospitalization,” he said, “so this is an extremely potent therapy, potentially.
“The dramatic difference between the treated arm and the medical therapy arm in this trial makes me feel that this therapy is here to stay,” Dr. Batchelor concluded. “We just have to figure out how to deploy it properly in the right patients.”
The COAPT trial presents “a practice-changing paradigm,” said Suzanne J. Baron, MD, of Lahey Hospital & Medical Center, Burlington, Mass., another invited discussant.
The crossover data “really jumped out,” she added. “Waiting to treat patients with TEER may be harmful, so if we’re going to consider treating earlier, how do we identify the right patient?” Dr. Baron asked, especially given the negative MITRA-FR results.
MITRA-FR didn’t follow patients beyond 2 years, Dr. Stone noted. Still, “we do think that the main difference was that COAPT enrolled a patient population with more severe MR and slightly less LV dysfunction, at least in terms of the LV not being as dilated, so they didn’t have end-stage LV disease. Whereas in MITRA-FR, more of the patients had only moderate mitral regurgitation.” And big dilated left ventricles “are less likely to benefit.”
There were also differences between the studies in technique and background medical therapies, he added.
The Food and Drug Administration has approved – and payers are paying – for the treatment of patients who meet the COAPT criteria, “in whom we can be very confident they have a benefit,” Dr. Stone said.
“The real question is: Where are the edges where we should consider this? LVEF slightly less than 20% or slightly greater than 50%? Or primary atrial functional mitral regurgitation? There are registry data to suggest that they would benefit,” he said, but “we need more data.”
COAPT was supported by Abbott. Dr. Stone disclosed receiving speaker honoraria from Abbott and consulting fees or equity from Neovasc, Ancora, Valfix, and Cardiac Success; and that Mount Sinai receives research funding from Abbott. Disclosures for the other authors are available at nejm.org. Dr. Batchelor has disclosed receiving consultant fees or honoraria from Abbott, Boston Scientific, Idorsia, and V-Wave Medical, and having other ties with Medtronic. Dr. Baron has disclosed receiving consultant fees or honoraria from Abiomed, Biotronik, Boston Scientific, Edwards Lifesciences, Medtronic, Shockwave, and Zoll Medical, and conducting research or receiving research grants from Abiomed and Boston Scientific.
A version of this article originally appeared on Medscape.com.
It remained an open question in 2018, on the unveiling of the COAPT trial’s 2-year primary results, whether the striking reductions in mortality and heart-failure (HF) hospitalization observed for transcatheter edge-to-edge repair (TEER) with the MitraClip (Abbott) would be durable with longer follow-up.
The trial had enrolled an especially sick population of symptomatic patients with mitral regurgitation (MR) secondary to HF.
As it turns out, the therapy’s benefits at 2 years were indeed durable, at least out to 5 years, investigators reported March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The results were simultaneously published in the New England Journal of Medicine.
Patients who received the MitraClip on top of intensive medical therapy, compared with a group assigned to medical management alone, benefited significantly at 5 years with risk reductions of 51% for HF hospitalization, 28% for death from any cause, and 47% for the composite of the two events.
Still, mortality at 5 years among the 614 randomized patients was steep at 57.3% in the MitraClip group and 67.2% for those assigned to meds only, underscoring the need for early identification of patients appropriate for the device therapy, Gregg W. Stone, MD, said during his presentation.
Dr. Stone, of the Icahn School of Medicine at Mount Sinai, New York, is a COAPT co-principal investigator and lead author of the 5-year outcomes publication.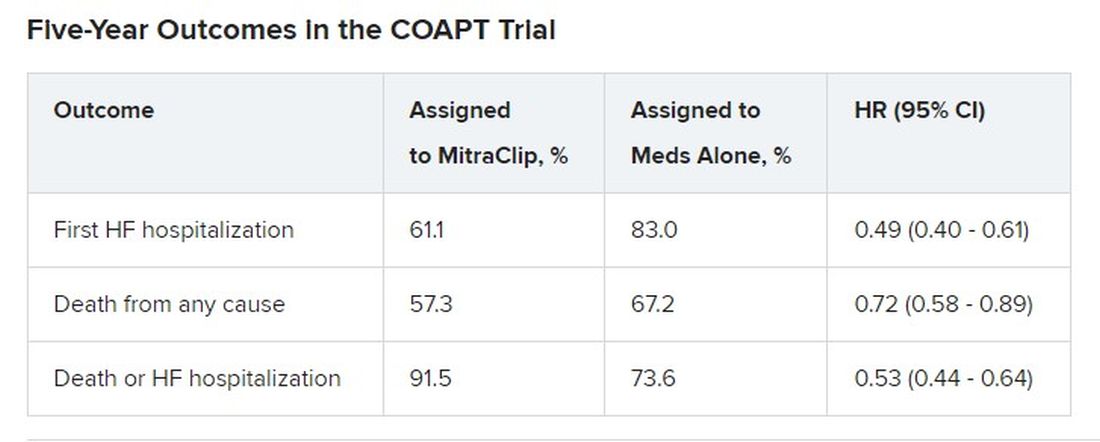
Outcomes were consistent across all prespecified patient subgroups, including by age, sex, MR, left ventricular (LV) function and volume, cardiomyopathy etiology, and degree of surgical risk, the researchers reported.
Symptom status, as measured by New York Heart Association (NYHA) functional class, improved throughout the 5-year follow-up for patients assigned to the MitraClip group, compared with the control group, and the intervention group was significantly more likely to be in NYHA class 1 or 2, the authors noted.
The relative benefits in terms of clinical outcomes of MitraClip therapy narrowed after 2-3 years, Dr. Stone said, primarily because at 2 years, patients who had been assigned to meds only were eligible to undergo TEER. Indeed, he noted, 45% of the 138 patients in the control group who were eligible for TEER at 2 years “crossed over” to receive a MitraClip. Those patients benefited despite their delay in undergoing the procedure, he observed.
However, nearly half of the control patients died before becoming eligible for crossover at 2 years. “We have to identify the appropriate patients for treatment and treat them early because the mortality is very high in this population,” Dr. Stone said.
“We need to do more because the MitraClip doesn’t do anything directly to the underlying left ventricular dysfunction, which is the cause of the patient’s disease,” he said. “We need advanced therapies to address the underlying left ventricular dysfunction” in this high-risk population.
Exclusions based on LV dimension
The COAPT trial included 614 patients with HF and symptomatic MR despite guideline-directed medical therapy. They were required to have moderate to severe (3+) or severe (4+) MR confirmed by an echocardiographic core laboratory and a left ventricular ejection fraction (LVEF) of 20%-50%.
Among the exclusion criteria were an LV end-systolic diameter greater than 70 mm, severe pulmonary hypertension, and moderate to severe symptomatic right ventricular failure.
The systolic LV dimension exclusion helped address the persistent question of whether “severe mitral regurgitation is a marker of a bad left ventricle or ... contributes to the pathophysiology” of MR and its poor outcomes, Dr. Stone said.
The 51% reduction in risk for time-to-first HF hospitalization among patients assigned to TEER “accrued very early,” Dr. Stone pointed out. “You can see the curves start to separate almost immediately after you reduce left atrial pressure and volume overload with the MitraClip.”
The curves stopped diverging after about 3 years because of crossover from the control group, he said. Still, “we had shown a substantial absolute 17% reduction in mortality at 2 years” with MitraClip. “That has continued out to 5 years, with a statistically significant 28% relative reduction,” he continued, and the absolute risk reduction reaching 10%.
Patients in the control group who crossed over “basically assumed the death and heart failure hospitalization rate of the MitraClip group,” Dr. Stone said. That wasn’t surprising “because most of the patients enrolled in the trial originally had chronic heart failure.” It’s “confirmation of the principal results of the trial.”
Comparison With MITRA-FR
“We know that MITRA-FR was a negative trial,” observed Wayne B. Batchelor, MD, an invited discussant following Dr. Stone’s presentation, referring to an earlier similar trial that showed no advantage for MitraClip. Compared with MITRA-FR, COAPT “has created an entirely different story.”
The marked reductions in mortality and risk for adverse events and low number-needed-to-treat with MitraClip are “really remarkable,” said Dr. Batchelor, who is with the Inova Heart and Vascular Institute, Falls Church, Va.
But the high absolute mortality for patients in the COAPT control group “speaks volumes to me and tells us that we’ve got to identify our patients well early,” he agreed, and to “implement transcatheter edge-to-edge therapy in properly selected patients on guideline-directed medical therapy in order to avoid that.”
The trial findings “suggest that we’re reducing HF hospitalization,” he said, “so this is an extremely potent therapy, potentially.
“The dramatic difference between the treated arm and the medical therapy arm in this trial makes me feel that this therapy is here to stay,” Dr. Batchelor concluded. “We just have to figure out how to deploy it properly in the right patients.”
The COAPT trial presents “a practice-changing paradigm,” said Suzanne J. Baron, MD, of Lahey Hospital & Medical Center, Burlington, Mass., another invited discussant.
The crossover data “really jumped out,” she added. “Waiting to treat patients with TEER may be harmful, so if we’re going to consider treating earlier, how do we identify the right patient?” Dr. Baron asked, especially given the negative MITRA-FR results.
MITRA-FR didn’t follow patients beyond 2 years, Dr. Stone noted. Still, “we do think that the main difference was that COAPT enrolled a patient population with more severe MR and slightly less LV dysfunction, at least in terms of the LV not being as dilated, so they didn’t have end-stage LV disease. Whereas in MITRA-FR, more of the patients had only moderate mitral regurgitation.” And big dilated left ventricles “are less likely to benefit.”
There were also differences between the studies in technique and background medical therapies, he added.
The Food and Drug Administration has approved – and payers are paying – for the treatment of patients who meet the COAPT criteria, “in whom we can be very confident they have a benefit,” Dr. Stone said.
“The real question is: Where are the edges where we should consider this? LVEF slightly less than 20% or slightly greater than 50%? Or primary atrial functional mitral regurgitation? There are registry data to suggest that they would benefit,” he said, but “we need more data.”
COAPT was supported by Abbott. Dr. Stone disclosed receiving speaker honoraria from Abbott and consulting fees or equity from Neovasc, Ancora, Valfix, and Cardiac Success; and that Mount Sinai receives research funding from Abbott. Disclosures for the other authors are available at nejm.org. Dr. Batchelor has disclosed receiving consultant fees or honoraria from Abbott, Boston Scientific, Idorsia, and V-Wave Medical, and having other ties with Medtronic. Dr. Baron has disclosed receiving consultant fees or honoraria from Abiomed, Biotronik, Boston Scientific, Edwards Lifesciences, Medtronic, Shockwave, and Zoll Medical, and conducting research or receiving research grants from Abiomed and Boston Scientific.
A version of this article originally appeared on Medscape.com.
FROM ACC 2023
Like mother, like daughter? Moms pass obesity risk to girls
Girls between 4 and 9 years old were more likely to have high fat mass and a high body mass index if their mothers had excess adiposity – but this relationship was not seen between mothers and sons, or between fathers and sons or daughters, in a new study.
The researchers measured fat mass, lean mass, and BMI in the sons and daughters when they were age 4 (before a phenomenon known as “adiposity rebound”), ages 6-7 (around the adiposity rebound), and ages 8-9 (before or at the onset of puberty).
They also obtained measurements from the mothers and fathers when the offspring were ages 8-9.
The group found “a strong association between the fat mass of mothers and their daughters but not their sons,” Rebecca J. Moon, BM, PhD, and colleagues report.
“It would be important to establish persistence through puberty,” according to the researchers, “but nonetheless, these findings are clinically important, highlighting girls who are born to mothers with high BMI and excess adiposity are at high risk of themselves of becoming overweight/obese or having unfavorable body composition early in childhood.”
The mother-daughter relationship for fat mass appears to be established by age 4 years, note Dr. Moon, of the MRC Lifecourse Epidemiology Centre, University of Southampton (England), and colleagues.
Therefore, “early awareness and intervention is needed in mothers with excess adiposity, and potentially beginning even in the periconception and in utero period.”
Because 97% of the mothers and fathers were White, the findings may not be generalizable to other populations, they caution.
The results, from the Southampton Women’s Survey prospective cohort study, were published online in the Journal of Clinical Endocrinology & Metabolism.
One of the first studies to look at fat mass, not just BMI
Children with overweight or obesity are more likely to have excess weight in adulthood that puts them at risk of developing type 2 diabetes, cardiovascular disease, cancer, and osteoarthritis. Previous research has reported that children with overweight or obesity were more likely to have mothers with adiposity.
However, most prior studies have looked at BMI alone and did not measure fat mass, and it was not known how a father’s obesity might affect offspring or how risk may differ in boy versus girl children.
Researchers analyzed data from a subset of participants in the Southampton Women’s Survey of 3,158 women who were aged 20-34 in 1998-2002 and delivered a liveborn infant.
The current study included 240 mother-father-offspring trios who had data for BMI and dual-energy X-ray absorptiometry (DXA) scans (whole body less head).
Mothers were a mean age of 31 years at delivery and had a median pre-pregnancy BMI of 23.7 kg/m2.
The offspring were 129 boys (54%) and 111 girls.
The offspring had DXA scans at ages 4, 6-7, and 8-9 years, and the mothers and fathers had a DXA scan at the last time point.
At ages 6-7 and ages 8-9, BMI and fat mass of the girls reflected that of their mothers (a significant association).
At age 4, BMI and fat mass of the daughters tended to be associated with that of their mothers, but the 95% confidence interval crossed zero.
There were no significant mother-son, father-son, or father-daughter associations for BMI or fat mass at each of the three studied ages.
The study received funding from the Medical Research Council, the British Heart Foundation, the National Institute for Health and Care Research Southampton Biomedical Research Centre, the NIHR Oxford Biomedical Research Centre, the Seventh Framework Program, the Biotechnology and Biological Sciences Research Council, the Horizon 2020 Framework Program, and the National Institute on Aging. Dr. Moon has reported receiving travel bursaries from Kyowa Kirin unrelated to the current study. Disclosures for the other authors are listed with the article.
A version of this article originally appeared on Medscape.com.
Girls between 4 and 9 years old were more likely to have high fat mass and a high body mass index if their mothers had excess adiposity – but this relationship was not seen between mothers and sons, or between fathers and sons or daughters, in a new study.
The researchers measured fat mass, lean mass, and BMI in the sons and daughters when they were age 4 (before a phenomenon known as “adiposity rebound”), ages 6-7 (around the adiposity rebound), and ages 8-9 (before or at the onset of puberty).
They also obtained measurements from the mothers and fathers when the offspring were ages 8-9.
The group found “a strong association between the fat mass of mothers and their daughters but not their sons,” Rebecca J. Moon, BM, PhD, and colleagues report.
“It would be important to establish persistence through puberty,” according to the researchers, “but nonetheless, these findings are clinically important, highlighting girls who are born to mothers with high BMI and excess adiposity are at high risk of themselves of becoming overweight/obese or having unfavorable body composition early in childhood.”
The mother-daughter relationship for fat mass appears to be established by age 4 years, note Dr. Moon, of the MRC Lifecourse Epidemiology Centre, University of Southampton (England), and colleagues.
Therefore, “early awareness and intervention is needed in mothers with excess adiposity, and potentially beginning even in the periconception and in utero period.”
Because 97% of the mothers and fathers were White, the findings may not be generalizable to other populations, they caution.
The results, from the Southampton Women’s Survey prospective cohort study, were published online in the Journal of Clinical Endocrinology & Metabolism.
One of the first studies to look at fat mass, not just BMI
Children with overweight or obesity are more likely to have excess weight in adulthood that puts them at risk of developing type 2 diabetes, cardiovascular disease, cancer, and osteoarthritis. Previous research has reported that children with overweight or obesity were more likely to have mothers with adiposity.
However, most prior studies have looked at BMI alone and did not measure fat mass, and it was not known how a father’s obesity might affect offspring or how risk may differ in boy versus girl children.
Researchers analyzed data from a subset of participants in the Southampton Women’s Survey of 3,158 women who were aged 20-34 in 1998-2002 and delivered a liveborn infant.
The current study included 240 mother-father-offspring trios who had data for BMI and dual-energy X-ray absorptiometry (DXA) scans (whole body less head).
Mothers were a mean age of 31 years at delivery and had a median pre-pregnancy BMI of 23.7 kg/m2.
The offspring were 129 boys (54%) and 111 girls.
The offspring had DXA scans at ages 4, 6-7, and 8-9 years, and the mothers and fathers had a DXA scan at the last time point.
At ages 6-7 and ages 8-9, BMI and fat mass of the girls reflected that of their mothers (a significant association).
At age 4, BMI and fat mass of the daughters tended to be associated with that of their mothers, but the 95% confidence interval crossed zero.
There were no significant mother-son, father-son, or father-daughter associations for BMI or fat mass at each of the three studied ages.
The study received funding from the Medical Research Council, the British Heart Foundation, the National Institute for Health and Care Research Southampton Biomedical Research Centre, the NIHR Oxford Biomedical Research Centre, the Seventh Framework Program, the Biotechnology and Biological Sciences Research Council, the Horizon 2020 Framework Program, and the National Institute on Aging. Dr. Moon has reported receiving travel bursaries from Kyowa Kirin unrelated to the current study. Disclosures for the other authors are listed with the article.
A version of this article originally appeared on Medscape.com.
Girls between 4 and 9 years old were more likely to have high fat mass and a high body mass index if their mothers had excess adiposity – but this relationship was not seen between mothers and sons, or between fathers and sons or daughters, in a new study.
The researchers measured fat mass, lean mass, and BMI in the sons and daughters when they were age 4 (before a phenomenon known as “adiposity rebound”), ages 6-7 (around the adiposity rebound), and ages 8-9 (before or at the onset of puberty).
They also obtained measurements from the mothers and fathers when the offspring were ages 8-9.
The group found “a strong association between the fat mass of mothers and their daughters but not their sons,” Rebecca J. Moon, BM, PhD, and colleagues report.
“It would be important to establish persistence through puberty,” according to the researchers, “but nonetheless, these findings are clinically important, highlighting girls who are born to mothers with high BMI and excess adiposity are at high risk of themselves of becoming overweight/obese or having unfavorable body composition early in childhood.”
The mother-daughter relationship for fat mass appears to be established by age 4 years, note Dr. Moon, of the MRC Lifecourse Epidemiology Centre, University of Southampton (England), and colleagues.
Therefore, “early awareness and intervention is needed in mothers with excess adiposity, and potentially beginning even in the periconception and in utero period.”
Because 97% of the mothers and fathers were White, the findings may not be generalizable to other populations, they caution.
The results, from the Southampton Women’s Survey prospective cohort study, were published online in the Journal of Clinical Endocrinology & Metabolism.
One of the first studies to look at fat mass, not just BMI
Children with overweight or obesity are more likely to have excess weight in adulthood that puts them at risk of developing type 2 diabetes, cardiovascular disease, cancer, and osteoarthritis. Previous research has reported that children with overweight or obesity were more likely to have mothers with adiposity.
However, most prior studies have looked at BMI alone and did not measure fat mass, and it was not known how a father’s obesity might affect offspring or how risk may differ in boy versus girl children.
Researchers analyzed data from a subset of participants in the Southampton Women’s Survey of 3,158 women who were aged 20-34 in 1998-2002 and delivered a liveborn infant.
The current study included 240 mother-father-offspring trios who had data for BMI and dual-energy X-ray absorptiometry (DXA) scans (whole body less head).
Mothers were a mean age of 31 years at delivery and had a median pre-pregnancy BMI of 23.7 kg/m2.
The offspring were 129 boys (54%) and 111 girls.
The offspring had DXA scans at ages 4, 6-7, and 8-9 years, and the mothers and fathers had a DXA scan at the last time point.
At ages 6-7 and ages 8-9, BMI and fat mass of the girls reflected that of their mothers (a significant association).
At age 4, BMI and fat mass of the daughters tended to be associated with that of their mothers, but the 95% confidence interval crossed zero.
There were no significant mother-son, father-son, or father-daughter associations for BMI or fat mass at each of the three studied ages.
The study received funding from the Medical Research Council, the British Heart Foundation, the National Institute for Health and Care Research Southampton Biomedical Research Centre, the NIHR Oxford Biomedical Research Centre, the Seventh Framework Program, the Biotechnology and Biological Sciences Research Council, the Horizon 2020 Framework Program, and the National Institute on Aging. Dr. Moon has reported receiving travel bursaries from Kyowa Kirin unrelated to the current study. Disclosures for the other authors are listed with the article.
A version of this article originally appeared on Medscape.com.
Do artificial sweeteners alter postmeal glucose, hunger hormones?
Drinking a sugar-sweetened beverage (SSB), however, had a different effect on postprandial levels of glucose and the hormones insulin, glucagonlike peptide–1 (GLP-1), gastric inhibitory polypeptide (GIP), peptide YY (PYY), ghrelin, leptin, and glucagon.
These findings are from a new meta-analysis by Roselyn Zhang and colleagues, supported by the nonprofit organization Institute for the Advancement of Food and Nutrition Sciences. The study was published recently in Nutrients.
“Nonnutritive sweeteners have no acute metabolic or endocrine effects and they are similar to water in that respect, and they show a different response from caloric sweeteners,” study author Tauseef Khan, MBBS, PhD, summarized in an interview following a press briefing from the IAFNS.
“Our study supports that nonnutritive sweeteners are a healthier alternative to sugar-sweetened beverages or caloric beverages,” said Dr. Khan, an epidemiologist in the department of nutritional sciences, University of Toronto.
Most participants in the 36 trials included in the meta-analysis were healthy, he noted. However, for certain types of NNS beverages, “we had enough studies for type 2 diabetes to also assess that separately, and the results were the same: Nonnutritive sweeteners were no different from water; however, they were different from caloric sweeteners.”
Of note, none of the studies included erythritol – a sugar alcohol (polyol) increasingly used as an artificial sweetener in keto and other types of foods – which was associated with a risk for adverse cardiac events in a paper in Nature Medicine.
Are these NNS drinks largely inert?
“This [meta-analysis] implies that sweeteners are largely inert,” in terms of acute postprandial glucose and hormone response, but the review did not include newer reports that differ, Duane Mellor, PhD, RD, RNutr, who was not involved with the research, noted in an email.
“This is possibly,” he said, because the study “only reviewed the literature up until January 2022 and therefore it missed the World Health Organization review ‘Health Effects of the Use of Non-Sugar Sweeteners’ published in April [2022], and a study published in August 2022 in the journal Cell suggesting that some nonnutritive sweeteners may have a minor effect on gut microbiome and glucose response.
“Although there is a place of nonnutritive sweeteners as a way to reduce sugar intake, they are a small part of dietary pattern and lifestyle which can help reduce risk of disease,” said Dr. Mellor, a registered dietitian and senior teaching fellow at Aston University, Birmingham, England.
“So, although we are clear we need to reduce our intake of sugar-sweetened beverages, switching to non-nutritive sweetened beverages (such as diet sodas) is not necessarily the healthiest option, as unlike water, it seems that some nonnutritive sweeteners may influence glucose responses and levels of related hormones in more recent studies.”
NNS beverages ‘are similar to water’
Dr. Khan pointed out that the meta-analysis addressed two major concerns about NNS beverages.
First, the “sweet uncoupling hypothesis” proposes that low-calorie sweeteners affect sweet taste by separating sweet taste from calories. “The body is confused, and then there is hormonal change. Our study shows that actually that’s not true, and [NNS beverages] are similar to water.”
Second, when no-calorie or low-calorie sweeteners are taken with calories (coupling), a concern is that “then you eat more somehow, or your response is different. However, the results [in this meta-analysis] also show that that is not the case for glucose response, insulin response, and other hormonal markers.”
“The strength is not that low-calorie sweeteners have some benefit per se,” he elaborated. “The advantage is that they replace caloric beverages.
“We are not saying that anybody who is not taking low-calorie sweeteners should start taking [them],” he continued. “What we are saying is somebody who is taking sugar-sweetened beverages and has a problem of taking excess calories, if you replace those calories with low-calorie sweetener, replacement of calories itself may be beneficial, and also they should not be concerned of any [acute] issues with a moderate amount of low-calorie sweeteners.”
Postprandial effect of NNS beverages, SSBs, water
Eight NNS are currently approved by the Food and Drug Administration: aspartame, acesulfame potassium (ace-K), luo han guo (monkfruit) extract, neotame, saccharin, stevia, sucralose, and advantame, the researchers noted.
Ms. Zhang and colleagues searched the literature up until Jan. 15, 2022, for studies of NNS beverages and acute postprandial glycemic and endocrine responses.
Trials were excluded if they involved sugar alcohols (eg, erythritol) or rare sugars (eg, allulose), or if they were shorter than 2 hours, lacked a comparator arm, or did not provide suitable endpoint data.
They identified 36 randomized and nonrandomized clinical trials of 472 predominantly healthy participants: 21 trials (15 reports, n = 266) with NNS consumed alone (uncoupled), 3 trials (3 reports, n = 27) with NNS consumed in a solution containing a carbohydrate (coupled), and 12 trials (7 reports, n = 179) with NNS consumed up to 15 minutes before oral glucose carbohydrate load (delayed coupling).
The four types of beverages were single NNS (ace-K, aspartame, cyclamate, saccharin, stevia, and sucralose), NNS blends (ace-K + aspartame; ace-K + sucralose; ace-K + aspartame + cyclamate; and ace-K + aspartame + sucralose), SSBs (glucose, sucrose, and fructose), and water (control).
In the uncoupled interventions, NNS beverages (single or blends) had no effect on postprandial glucose, insulin, GLP-1, GIP, PYY, ghrelin, and glucagon, with responses similar to water.
In the uncoupled interventions, SSBs sweetened with caloric sugars (glucose and sucrose) increased postprandial glucose, insulin, GLP-1, and GIP responses, with no differences in postprandial ghrelin and glucagon responses.
In the coupled and delayed coupling interventions, NNS beverages had no postprandial glucose and endocrine effects, with responses similar to water.
The studies generally had low to moderate confidence.
The study was supported by an unrestricted grant from IAFNS. Dr. Khan has received research support from the Canadian Institutes of Health Research, the International Life Sciences Institute, and the National Honey Board. He has received honorariums for lectures from the International Food Information Council and the IAFNS. Dr. Mellor has no disclosures.
A version of this article first appeared on Medscape.com.
Drinking a sugar-sweetened beverage (SSB), however, had a different effect on postprandial levels of glucose and the hormones insulin, glucagonlike peptide–1 (GLP-1), gastric inhibitory polypeptide (GIP), peptide YY (PYY), ghrelin, leptin, and glucagon.
These findings are from a new meta-analysis by Roselyn Zhang and colleagues, supported by the nonprofit organization Institute for the Advancement of Food and Nutrition Sciences. The study was published recently in Nutrients.
“Nonnutritive sweeteners have no acute metabolic or endocrine effects and they are similar to water in that respect, and they show a different response from caloric sweeteners,” study author Tauseef Khan, MBBS, PhD, summarized in an interview following a press briefing from the IAFNS.
“Our study supports that nonnutritive sweeteners are a healthier alternative to sugar-sweetened beverages or caloric beverages,” said Dr. Khan, an epidemiologist in the department of nutritional sciences, University of Toronto.
Most participants in the 36 trials included in the meta-analysis were healthy, he noted. However, for certain types of NNS beverages, “we had enough studies for type 2 diabetes to also assess that separately, and the results were the same: Nonnutritive sweeteners were no different from water; however, they were different from caloric sweeteners.”
Of note, none of the studies included erythritol – a sugar alcohol (polyol) increasingly used as an artificial sweetener in keto and other types of foods – which was associated with a risk for adverse cardiac events in a paper in Nature Medicine.
Are these NNS drinks largely inert?
“This [meta-analysis] implies that sweeteners are largely inert,” in terms of acute postprandial glucose and hormone response, but the review did not include newer reports that differ, Duane Mellor, PhD, RD, RNutr, who was not involved with the research, noted in an email.
“This is possibly,” he said, because the study “only reviewed the literature up until January 2022 and therefore it missed the World Health Organization review ‘Health Effects of the Use of Non-Sugar Sweeteners’ published in April [2022], and a study published in August 2022 in the journal Cell suggesting that some nonnutritive sweeteners may have a minor effect on gut microbiome and glucose response.
“Although there is a place of nonnutritive sweeteners as a way to reduce sugar intake, they are a small part of dietary pattern and lifestyle which can help reduce risk of disease,” said Dr. Mellor, a registered dietitian and senior teaching fellow at Aston University, Birmingham, England.
“So, although we are clear we need to reduce our intake of sugar-sweetened beverages, switching to non-nutritive sweetened beverages (such as diet sodas) is not necessarily the healthiest option, as unlike water, it seems that some nonnutritive sweeteners may influence glucose responses and levels of related hormones in more recent studies.”
NNS beverages ‘are similar to water’
Dr. Khan pointed out that the meta-analysis addressed two major concerns about NNS beverages.
First, the “sweet uncoupling hypothesis” proposes that low-calorie sweeteners affect sweet taste by separating sweet taste from calories. “The body is confused, and then there is hormonal change. Our study shows that actually that’s not true, and [NNS beverages] are similar to water.”
Second, when no-calorie or low-calorie sweeteners are taken with calories (coupling), a concern is that “then you eat more somehow, or your response is different. However, the results [in this meta-analysis] also show that that is not the case for glucose response, insulin response, and other hormonal markers.”
“The strength is not that low-calorie sweeteners have some benefit per se,” he elaborated. “The advantage is that they replace caloric beverages.
“We are not saying that anybody who is not taking low-calorie sweeteners should start taking [them],” he continued. “What we are saying is somebody who is taking sugar-sweetened beverages and has a problem of taking excess calories, if you replace those calories with low-calorie sweetener, replacement of calories itself may be beneficial, and also they should not be concerned of any [acute] issues with a moderate amount of low-calorie sweeteners.”
Postprandial effect of NNS beverages, SSBs, water
Eight NNS are currently approved by the Food and Drug Administration: aspartame, acesulfame potassium (ace-K), luo han guo (monkfruit) extract, neotame, saccharin, stevia, sucralose, and advantame, the researchers noted.
Ms. Zhang and colleagues searched the literature up until Jan. 15, 2022, for studies of NNS beverages and acute postprandial glycemic and endocrine responses.
Trials were excluded if they involved sugar alcohols (eg, erythritol) or rare sugars (eg, allulose), or if they were shorter than 2 hours, lacked a comparator arm, or did not provide suitable endpoint data.
They identified 36 randomized and nonrandomized clinical trials of 472 predominantly healthy participants: 21 trials (15 reports, n = 266) with NNS consumed alone (uncoupled), 3 trials (3 reports, n = 27) with NNS consumed in a solution containing a carbohydrate (coupled), and 12 trials (7 reports, n = 179) with NNS consumed up to 15 minutes before oral glucose carbohydrate load (delayed coupling).
The four types of beverages were single NNS (ace-K, aspartame, cyclamate, saccharin, stevia, and sucralose), NNS blends (ace-K + aspartame; ace-K + sucralose; ace-K + aspartame + cyclamate; and ace-K + aspartame + sucralose), SSBs (glucose, sucrose, and fructose), and water (control).
In the uncoupled interventions, NNS beverages (single or blends) had no effect on postprandial glucose, insulin, GLP-1, GIP, PYY, ghrelin, and glucagon, with responses similar to water.
In the uncoupled interventions, SSBs sweetened with caloric sugars (glucose and sucrose) increased postprandial glucose, insulin, GLP-1, and GIP responses, with no differences in postprandial ghrelin and glucagon responses.
In the coupled and delayed coupling interventions, NNS beverages had no postprandial glucose and endocrine effects, with responses similar to water.
The studies generally had low to moderate confidence.
The study was supported by an unrestricted grant from IAFNS. Dr. Khan has received research support from the Canadian Institutes of Health Research, the International Life Sciences Institute, and the National Honey Board. He has received honorariums for lectures from the International Food Information Council and the IAFNS. Dr. Mellor has no disclosures.
A version of this article first appeared on Medscape.com.
Drinking a sugar-sweetened beverage (SSB), however, had a different effect on postprandial levels of glucose and the hormones insulin, glucagonlike peptide–1 (GLP-1), gastric inhibitory polypeptide (GIP), peptide YY (PYY), ghrelin, leptin, and glucagon.
These findings are from a new meta-analysis by Roselyn Zhang and colleagues, supported by the nonprofit organization Institute for the Advancement of Food and Nutrition Sciences. The study was published recently in Nutrients.
“Nonnutritive sweeteners have no acute metabolic or endocrine effects and they are similar to water in that respect, and they show a different response from caloric sweeteners,” study author Tauseef Khan, MBBS, PhD, summarized in an interview following a press briefing from the IAFNS.
“Our study supports that nonnutritive sweeteners are a healthier alternative to sugar-sweetened beverages or caloric beverages,” said Dr. Khan, an epidemiologist in the department of nutritional sciences, University of Toronto.
Most participants in the 36 trials included in the meta-analysis were healthy, he noted. However, for certain types of NNS beverages, “we had enough studies for type 2 diabetes to also assess that separately, and the results were the same: Nonnutritive sweeteners were no different from water; however, they were different from caloric sweeteners.”
Of note, none of the studies included erythritol – a sugar alcohol (polyol) increasingly used as an artificial sweetener in keto and other types of foods – which was associated with a risk for adverse cardiac events in a paper in Nature Medicine.
Are these NNS drinks largely inert?
“This [meta-analysis] implies that sweeteners are largely inert,” in terms of acute postprandial glucose and hormone response, but the review did not include newer reports that differ, Duane Mellor, PhD, RD, RNutr, who was not involved with the research, noted in an email.
“This is possibly,” he said, because the study “only reviewed the literature up until January 2022 and therefore it missed the World Health Organization review ‘Health Effects of the Use of Non-Sugar Sweeteners’ published in April [2022], and a study published in August 2022 in the journal Cell suggesting that some nonnutritive sweeteners may have a minor effect on gut microbiome and glucose response.
“Although there is a place of nonnutritive sweeteners as a way to reduce sugar intake, they are a small part of dietary pattern and lifestyle which can help reduce risk of disease,” said Dr. Mellor, a registered dietitian and senior teaching fellow at Aston University, Birmingham, England.
“So, although we are clear we need to reduce our intake of sugar-sweetened beverages, switching to non-nutritive sweetened beverages (such as diet sodas) is not necessarily the healthiest option, as unlike water, it seems that some nonnutritive sweeteners may influence glucose responses and levels of related hormones in more recent studies.”
NNS beverages ‘are similar to water’
Dr. Khan pointed out that the meta-analysis addressed two major concerns about NNS beverages.
First, the “sweet uncoupling hypothesis” proposes that low-calorie sweeteners affect sweet taste by separating sweet taste from calories. “The body is confused, and then there is hormonal change. Our study shows that actually that’s not true, and [NNS beverages] are similar to water.”
Second, when no-calorie or low-calorie sweeteners are taken with calories (coupling), a concern is that “then you eat more somehow, or your response is different. However, the results [in this meta-analysis] also show that that is not the case for glucose response, insulin response, and other hormonal markers.”
“The strength is not that low-calorie sweeteners have some benefit per se,” he elaborated. “The advantage is that they replace caloric beverages.
“We are not saying that anybody who is not taking low-calorie sweeteners should start taking [them],” he continued. “What we are saying is somebody who is taking sugar-sweetened beverages and has a problem of taking excess calories, if you replace those calories with low-calorie sweetener, replacement of calories itself may be beneficial, and also they should not be concerned of any [acute] issues with a moderate amount of low-calorie sweeteners.”
Postprandial effect of NNS beverages, SSBs, water
Eight NNS are currently approved by the Food and Drug Administration: aspartame, acesulfame potassium (ace-K), luo han guo (monkfruit) extract, neotame, saccharin, stevia, sucralose, and advantame, the researchers noted.
Ms. Zhang and colleagues searched the literature up until Jan. 15, 2022, for studies of NNS beverages and acute postprandial glycemic and endocrine responses.
Trials were excluded if they involved sugar alcohols (eg, erythritol) or rare sugars (eg, allulose), or if they were shorter than 2 hours, lacked a comparator arm, or did not provide suitable endpoint data.
They identified 36 randomized and nonrandomized clinical trials of 472 predominantly healthy participants: 21 trials (15 reports, n = 266) with NNS consumed alone (uncoupled), 3 trials (3 reports, n = 27) with NNS consumed in a solution containing a carbohydrate (coupled), and 12 trials (7 reports, n = 179) with NNS consumed up to 15 minutes before oral glucose carbohydrate load (delayed coupling).
The four types of beverages were single NNS (ace-K, aspartame, cyclamate, saccharin, stevia, and sucralose), NNS blends (ace-K + aspartame; ace-K + sucralose; ace-K + aspartame + cyclamate; and ace-K + aspartame + sucralose), SSBs (glucose, sucrose, and fructose), and water (control).
In the uncoupled interventions, NNS beverages (single or blends) had no effect on postprandial glucose, insulin, GLP-1, GIP, PYY, ghrelin, and glucagon, with responses similar to water.
In the uncoupled interventions, SSBs sweetened with caloric sugars (glucose and sucrose) increased postprandial glucose, insulin, GLP-1, and GIP responses, with no differences in postprandial ghrelin and glucagon responses.
In the coupled and delayed coupling interventions, NNS beverages had no postprandial glucose and endocrine effects, with responses similar to water.
The studies generally had low to moderate confidence.
The study was supported by an unrestricted grant from IAFNS. Dr. Khan has received research support from the Canadian Institutes of Health Research, the International Life Sciences Institute, and the National Honey Board. He has received honorariums for lectures from the International Food Information Council and the IAFNS. Dr. Mellor has no disclosures.
A version of this article first appeared on Medscape.com.
FROM NUTRIENTS
NUDGE-FLU: Electronic ‘nudges’ boost flu shot uptake in seniors
Two types of electronically delivered letter strategies – a letter highlighting potential cardiovascular benefits of influenza vaccination and a repeat reminder letter – increased flu shot uptake, compared with usual care alone, in a national study of seniors in Denmark.
And in a prespecified subanalysis focusing on older adults with cardiovascular disease, these two strategies were also effective in boosting vaccine uptake in those with or without CVD.
The findings are from the Nationwide Utilization of Danish Government Electronic Letter System for Increasing Influenza Vaccine Uptake (NUDGE-FLU) trial, which compared usual care alone with one of nine different electronic letter “behavioral nudge” strategies during the 2022-2023 flu season in people aged 65 years and older.
Niklas Dyrby Johansen, MD, Hospital–Herlev and Gentofte and Copenhagen University, presented the main study findings in a late-breaking clinical trial session at the joint scientific sessions of the American College of Cardiology and the World Heart Federation, and the article was simultaneously published in The Lancet
The subanalysis in patients with CVD was published online March 5 in Circulation.
“Despite modest effect sizes, the results may have important implications when translated to a population level,” Dr. Dyrby Johansen concluded during his presentation. Still, the authors write, “the low-touch (no person-to-person interaction), inexpensive, and highly scalable nature of these electronic letters might have important population-level public health implications.”
They note that, among approximately 63 million Medicare beneficiaries in the United States, a 0.89–percentage point absolute increase in vaccination rate achieved through the most successful electronic letter in NUDGE-FLU, the one highlighting cardiovascular gain, would be expected to lead to 500,000 additional vaccinations and potentially prevent 7,849 illnesses, 4,395 medical visits, 714 hospitalizations, and 66 deaths each year.
Electronic letter systems similar to the one used in this trial are already in place in several European countries, including Sweden, Norway, and Ireland, the researchers note.
In countries such as the United States, where implementing a nationwide government electronic letter system might not be feasible, nudges could be done via email, text message, or other systems, but whether this would be as effective remains to be seen.
Commenting on the findings, David Cho, MD, UCLA Health and chair of the ACC Health Care Innovation Council, commended the researchers on engaging patients with more than a million separate nudges sent out during one flu season, and randomly assigning participants to 10 different types of nudges, calling it “impressive.”
“I think the concept that the nudge is to plant an idea that leads to an action is pretty much the basis of a lot of these health care interventions, which seems like a small way to have a big impact at outcome,” Dr. Cho noted. “The behavioral science aspects of the nudges are also fascinating to me personally, and I think to a lot of the cardiologists in the audience – about how you actually get people to act. I think it’s been a lifelong question for people in general, how do you get people to follow through on an action?”
“So I found the fact that secondary gain from a cardiovascular health standpoint, but also the repeated nudges were sort of simple ways that you could have people take ownership and get their flu vaccination,” he said.
“This is ACC, this is a cardiovascular conference, but the influence of vaccine is not just a primary care problem, it is also directly affecting cardiovascular disease,” Dr. Cho concluded.
‘Small but important effect’
In an accompanying editorial (Lancet. 2023 Mar 5. doi: 10.1016/S0140-6736(23)00453-1), Melissa Stockwell, MD, Columbia University, New York, writes, “The study by Johansen and colleagues highlights the small but still important effect of scalable, digital interventions across an entire at-risk population.”
A difference of 0.89% in the entire study population of over 960,000 adults age 65 years or older would be more than 8,500 additional adults protected, she notes. “That increase is important for a scalable intervention that has a low cost per letter.”
Moreover, “that the cardiovascular gain–framed messages worked best in those who had not been vaccinated in the previous season further highlights the potential impact on a more vaccine-hesitant population,” Dr. Stockwell notes.
However, with the mandatory government electronic notification system in Denmark, “notifications are sent via regular email and SMS message, and recipients log in through a portal or smartphone app to view the letter.” Similar studies in the United States that included this extra step of needing to sign in online have not been effective in older populations.
Another limitation is that the intervention may have a different effect in populations for which there is a digital divide between people with or without Internet access of sufficient data on their mobile phones.
First-of-its kind, nationwide pragmatic trial
The NUDGE-FLU protocol was previously published in the American Heart Journal. NUDGE-FLU is a first-of-its kind nationwide, pragmatic, registry-based, cluster-randomized implementation trial of electronically delivered nudges to increase influenza vaccination uptake, the researchers note.
They identified 964,870 individuals who were 65 years or older (or would turn 65 by Jan. 15, 2023) who lived in one of 691,820 households in Denmark.
This excluded individuals who lived in a nursing home or were exempt from the government’s mandatory electronic letter system that is used for official communications.
Households were randomly assigned 9:1:1:1:1:1:1:1:1:1 to receive usual care alone or to one of nine electronic letter strategies based on different behavioral science approaches to encourage influenza vaccination uptake:
- Standard electronic letter
- Standard electronic letter sent at randomization and again 14 days later (repeated letter)
- Depersonalized letter without the recipient’s name
- Gain-framing nudge (“Vaccinations help end pandemics, like COVID-19 and the flu. Protect yourself and your loved ones.”)
- Loss-framing nudge (“When too few people get vaccinated, pandemics from diseases like COVID-19 and the flu can spread and place you and your loved ones at risk.”)
- Collective-goal nudge (“78% of Danes 65 and above were vaccinated against influenza last year. Help us achieve an even higher goal this year.”)
- Active choice or implementation-intention prompt (“We encourage you to record your appointment time here.”)
- Cardiovascular gain–framing nudge (“In addition to its protection against influenza infection, influenza vaccination also seems to protect against cardiovascular disease such as heart attacks and heart failure.”)
- Expert-authority statement (“I recommend everyone over the age of 65 years to get vaccinated against influenza – Tyra Grove Krause, Executive Vice President, Statens Serum Institut.”)
The electronic letters were sent out Sept. 16, 2022, and the primary endpoint was vaccine receipt on or before Jan. 1, 2023.
All individuals received an informative vaccination encouragement letter from the Danish Health Authority (usual care) delivered via the same electronic letter system during Sept. 17 through Sept. 21, 2022.
The individuals had a mean age of 73.8 years, 51.5% were women, and 27.4% had chronic cardiovascular disease.
The analyses were done in one randomly selected individual per household.
Influenza vaccination rates were significantly higher in the cardiovascular gain–framing nudge group vs. usual care (81.00% vs. 80.12%; difference, 0.89 percentage points; P < .0001) and in the repeat-letter group vs. usual care (80.85% vs 80.12%; difference, 0.73 percentage points; P = .0006).
These two strategies also improved vaccination rates across major subgroups.
The cardiovascular gain–framed letter was particularly effective among participants who had not been vaccinated for influenza in the previous season.
The seven other letter strategies did not increase flu shot uptake.
Subanalysis in CVD
In the prespecified subanalysis of the NUDGE-FLU trial of patients aged 65 and older that focused on patients with CVD, Daniel Modin, MB, and colleagues report that 83.1% of patients with CVD vs. 79.2% of patients without CVD received influenza vaccination within the requested time (P < .0001).
The two nudging strategies – a letter highlighting potential cardiovascular benefits of influenza vaccination or a repeat letter – that were effective in boosting flu shot rates in the main analysis were also effective in all major CVD subgroups (ischemic heart disease, pulmonary heart disease, heart failure, atrial fibrillation, cerebrovascular disease, atherosclerotic CVD, embolic or thrombotic disease, and congenital heart disease).
Despite strong guideline endorsement, “influenza vaccination rates remain suboptimal in patients with high-risk cardiovascular disease,” Dr. Morin and colleagues write, possibly because of “insufficient knowledge among patients and providers of potential clinical benefits, concerns about vaccine safety, and other forms of vaccine hesitancy.”
Their findings suggest that “select digital behaviorally informed nudges delivered in advance of vaccine availability might be utilized to increase influenza vaccinate uptake in individuals with cardiovascular disease.”
NUDGE-HF was funded by Sanofi. Dr. Johansen and Dr. Modin have no disclosures. The disclosures of the other authors are listed with the articles. Dr. Stockwell has no disclosures.
A version of this article first appeared on Medscape.com.
Two types of electronically delivered letter strategies – a letter highlighting potential cardiovascular benefits of influenza vaccination and a repeat reminder letter – increased flu shot uptake, compared with usual care alone, in a national study of seniors in Denmark.
And in a prespecified subanalysis focusing on older adults with cardiovascular disease, these two strategies were also effective in boosting vaccine uptake in those with or without CVD.
The findings are from the Nationwide Utilization of Danish Government Electronic Letter System for Increasing Influenza Vaccine Uptake (NUDGE-FLU) trial, which compared usual care alone with one of nine different electronic letter “behavioral nudge” strategies during the 2022-2023 flu season in people aged 65 years and older.
Niklas Dyrby Johansen, MD, Hospital–Herlev and Gentofte and Copenhagen University, presented the main study findings in a late-breaking clinical trial session at the joint scientific sessions of the American College of Cardiology and the World Heart Federation, and the article was simultaneously published in The Lancet
The subanalysis in patients with CVD was published online March 5 in Circulation.
“Despite modest effect sizes, the results may have important implications when translated to a population level,” Dr. Dyrby Johansen concluded during his presentation. Still, the authors write, “the low-touch (no person-to-person interaction), inexpensive, and highly scalable nature of these electronic letters might have important population-level public health implications.”
They note that, among approximately 63 million Medicare beneficiaries in the United States, a 0.89–percentage point absolute increase in vaccination rate achieved through the most successful electronic letter in NUDGE-FLU, the one highlighting cardiovascular gain, would be expected to lead to 500,000 additional vaccinations and potentially prevent 7,849 illnesses, 4,395 medical visits, 714 hospitalizations, and 66 deaths each year.
Electronic letter systems similar to the one used in this trial are already in place in several European countries, including Sweden, Norway, and Ireland, the researchers note.
In countries such as the United States, where implementing a nationwide government electronic letter system might not be feasible, nudges could be done via email, text message, or other systems, but whether this would be as effective remains to be seen.
Commenting on the findings, David Cho, MD, UCLA Health and chair of the ACC Health Care Innovation Council, commended the researchers on engaging patients with more than a million separate nudges sent out during one flu season, and randomly assigning participants to 10 different types of nudges, calling it “impressive.”
“I think the concept that the nudge is to plant an idea that leads to an action is pretty much the basis of a lot of these health care interventions, which seems like a small way to have a big impact at outcome,” Dr. Cho noted. “The behavioral science aspects of the nudges are also fascinating to me personally, and I think to a lot of the cardiologists in the audience – about how you actually get people to act. I think it’s been a lifelong question for people in general, how do you get people to follow through on an action?”
“So I found the fact that secondary gain from a cardiovascular health standpoint, but also the repeated nudges were sort of simple ways that you could have people take ownership and get their flu vaccination,” he said.
“This is ACC, this is a cardiovascular conference, but the influence of vaccine is not just a primary care problem, it is also directly affecting cardiovascular disease,” Dr. Cho concluded.
‘Small but important effect’
In an accompanying editorial (Lancet. 2023 Mar 5. doi: 10.1016/S0140-6736(23)00453-1), Melissa Stockwell, MD, Columbia University, New York, writes, “The study by Johansen and colleagues highlights the small but still important effect of scalable, digital interventions across an entire at-risk population.”
A difference of 0.89% in the entire study population of over 960,000 adults age 65 years or older would be more than 8,500 additional adults protected, she notes. “That increase is important for a scalable intervention that has a low cost per letter.”
Moreover, “that the cardiovascular gain–framed messages worked best in those who had not been vaccinated in the previous season further highlights the potential impact on a more vaccine-hesitant population,” Dr. Stockwell notes.
However, with the mandatory government electronic notification system in Denmark, “notifications are sent via regular email and SMS message, and recipients log in through a portal or smartphone app to view the letter.” Similar studies in the United States that included this extra step of needing to sign in online have not been effective in older populations.
Another limitation is that the intervention may have a different effect in populations for which there is a digital divide between people with or without Internet access of sufficient data on their mobile phones.
First-of-its kind, nationwide pragmatic trial
The NUDGE-FLU protocol was previously published in the American Heart Journal. NUDGE-FLU is a first-of-its kind nationwide, pragmatic, registry-based, cluster-randomized implementation trial of electronically delivered nudges to increase influenza vaccination uptake, the researchers note.
They identified 964,870 individuals who were 65 years or older (or would turn 65 by Jan. 15, 2023) who lived in one of 691,820 households in Denmark.
This excluded individuals who lived in a nursing home or were exempt from the government’s mandatory electronic letter system that is used for official communications.
Households were randomly assigned 9:1:1:1:1:1:1:1:1:1 to receive usual care alone or to one of nine electronic letter strategies based on different behavioral science approaches to encourage influenza vaccination uptake:
- Standard electronic letter
- Standard electronic letter sent at randomization and again 14 days later (repeated letter)
- Depersonalized letter without the recipient’s name
- Gain-framing nudge (“Vaccinations help end pandemics, like COVID-19 and the flu. Protect yourself and your loved ones.”)
- Loss-framing nudge (“When too few people get vaccinated, pandemics from diseases like COVID-19 and the flu can spread and place you and your loved ones at risk.”)
- Collective-goal nudge (“78% of Danes 65 and above were vaccinated against influenza last year. Help us achieve an even higher goal this year.”)
- Active choice or implementation-intention prompt (“We encourage you to record your appointment time here.”)
- Cardiovascular gain–framing nudge (“In addition to its protection against influenza infection, influenza vaccination also seems to protect against cardiovascular disease such as heart attacks and heart failure.”)
- Expert-authority statement (“I recommend everyone over the age of 65 years to get vaccinated against influenza – Tyra Grove Krause, Executive Vice President, Statens Serum Institut.”)
The electronic letters were sent out Sept. 16, 2022, and the primary endpoint was vaccine receipt on or before Jan. 1, 2023.
All individuals received an informative vaccination encouragement letter from the Danish Health Authority (usual care) delivered via the same electronic letter system during Sept. 17 through Sept. 21, 2022.
The individuals had a mean age of 73.8 years, 51.5% were women, and 27.4% had chronic cardiovascular disease.
The analyses were done in one randomly selected individual per household.
Influenza vaccination rates were significantly higher in the cardiovascular gain–framing nudge group vs. usual care (81.00% vs. 80.12%; difference, 0.89 percentage points; P < .0001) and in the repeat-letter group vs. usual care (80.85% vs 80.12%; difference, 0.73 percentage points; P = .0006).
These two strategies also improved vaccination rates across major subgroups.
The cardiovascular gain–framed letter was particularly effective among participants who had not been vaccinated for influenza in the previous season.
The seven other letter strategies did not increase flu shot uptake.
Subanalysis in CVD
In the prespecified subanalysis of the NUDGE-FLU trial of patients aged 65 and older that focused on patients with CVD, Daniel Modin, MB, and colleagues report that 83.1% of patients with CVD vs. 79.2% of patients without CVD received influenza vaccination within the requested time (P < .0001).
The two nudging strategies – a letter highlighting potential cardiovascular benefits of influenza vaccination or a repeat letter – that were effective in boosting flu shot rates in the main analysis were also effective in all major CVD subgroups (ischemic heart disease, pulmonary heart disease, heart failure, atrial fibrillation, cerebrovascular disease, atherosclerotic CVD, embolic or thrombotic disease, and congenital heart disease).
Despite strong guideline endorsement, “influenza vaccination rates remain suboptimal in patients with high-risk cardiovascular disease,” Dr. Morin and colleagues write, possibly because of “insufficient knowledge among patients and providers of potential clinical benefits, concerns about vaccine safety, and other forms of vaccine hesitancy.”
Their findings suggest that “select digital behaviorally informed nudges delivered in advance of vaccine availability might be utilized to increase influenza vaccinate uptake in individuals with cardiovascular disease.”
NUDGE-HF was funded by Sanofi. Dr. Johansen and Dr. Modin have no disclosures. The disclosures of the other authors are listed with the articles. Dr. Stockwell has no disclosures.
A version of this article first appeared on Medscape.com.
Two types of electronically delivered letter strategies – a letter highlighting potential cardiovascular benefits of influenza vaccination and a repeat reminder letter – increased flu shot uptake, compared with usual care alone, in a national study of seniors in Denmark.
And in a prespecified subanalysis focusing on older adults with cardiovascular disease, these two strategies were also effective in boosting vaccine uptake in those with or without CVD.
The findings are from the Nationwide Utilization of Danish Government Electronic Letter System for Increasing Influenza Vaccine Uptake (NUDGE-FLU) trial, which compared usual care alone with one of nine different electronic letter “behavioral nudge” strategies during the 2022-2023 flu season in people aged 65 years and older.
Niklas Dyrby Johansen, MD, Hospital–Herlev and Gentofte and Copenhagen University, presented the main study findings in a late-breaking clinical trial session at the joint scientific sessions of the American College of Cardiology and the World Heart Federation, and the article was simultaneously published in The Lancet
The subanalysis in patients with CVD was published online March 5 in Circulation.
“Despite modest effect sizes, the results may have important implications when translated to a population level,” Dr. Dyrby Johansen concluded during his presentation. Still, the authors write, “the low-touch (no person-to-person interaction), inexpensive, and highly scalable nature of these electronic letters might have important population-level public health implications.”
They note that, among approximately 63 million Medicare beneficiaries in the United States, a 0.89–percentage point absolute increase in vaccination rate achieved through the most successful electronic letter in NUDGE-FLU, the one highlighting cardiovascular gain, would be expected to lead to 500,000 additional vaccinations and potentially prevent 7,849 illnesses, 4,395 medical visits, 714 hospitalizations, and 66 deaths each year.
Electronic letter systems similar to the one used in this trial are already in place in several European countries, including Sweden, Norway, and Ireland, the researchers note.
In countries such as the United States, where implementing a nationwide government electronic letter system might not be feasible, nudges could be done via email, text message, or other systems, but whether this would be as effective remains to be seen.
Commenting on the findings, David Cho, MD, UCLA Health and chair of the ACC Health Care Innovation Council, commended the researchers on engaging patients with more than a million separate nudges sent out during one flu season, and randomly assigning participants to 10 different types of nudges, calling it “impressive.”
“I think the concept that the nudge is to plant an idea that leads to an action is pretty much the basis of a lot of these health care interventions, which seems like a small way to have a big impact at outcome,” Dr. Cho noted. “The behavioral science aspects of the nudges are also fascinating to me personally, and I think to a lot of the cardiologists in the audience – about how you actually get people to act. I think it’s been a lifelong question for people in general, how do you get people to follow through on an action?”
“So I found the fact that secondary gain from a cardiovascular health standpoint, but also the repeated nudges were sort of simple ways that you could have people take ownership and get their flu vaccination,” he said.
“This is ACC, this is a cardiovascular conference, but the influence of vaccine is not just a primary care problem, it is also directly affecting cardiovascular disease,” Dr. Cho concluded.
‘Small but important effect’
In an accompanying editorial (Lancet. 2023 Mar 5. doi: 10.1016/S0140-6736(23)00453-1), Melissa Stockwell, MD, Columbia University, New York, writes, “The study by Johansen and colleagues highlights the small but still important effect of scalable, digital interventions across an entire at-risk population.”
A difference of 0.89% in the entire study population of over 960,000 adults age 65 years or older would be more than 8,500 additional adults protected, she notes. “That increase is important for a scalable intervention that has a low cost per letter.”
Moreover, “that the cardiovascular gain–framed messages worked best in those who had not been vaccinated in the previous season further highlights the potential impact on a more vaccine-hesitant population,” Dr. Stockwell notes.
However, with the mandatory government electronic notification system in Denmark, “notifications are sent via regular email and SMS message, and recipients log in through a portal or smartphone app to view the letter.” Similar studies in the United States that included this extra step of needing to sign in online have not been effective in older populations.
Another limitation is that the intervention may have a different effect in populations for which there is a digital divide between people with or without Internet access of sufficient data on their mobile phones.
First-of-its kind, nationwide pragmatic trial
The NUDGE-FLU protocol was previously published in the American Heart Journal. NUDGE-FLU is a first-of-its kind nationwide, pragmatic, registry-based, cluster-randomized implementation trial of electronically delivered nudges to increase influenza vaccination uptake, the researchers note.
They identified 964,870 individuals who were 65 years or older (or would turn 65 by Jan. 15, 2023) who lived in one of 691,820 households in Denmark.
This excluded individuals who lived in a nursing home or were exempt from the government’s mandatory electronic letter system that is used for official communications.
Households were randomly assigned 9:1:1:1:1:1:1:1:1:1 to receive usual care alone or to one of nine electronic letter strategies based on different behavioral science approaches to encourage influenza vaccination uptake:
- Standard electronic letter
- Standard electronic letter sent at randomization and again 14 days later (repeated letter)
- Depersonalized letter without the recipient’s name
- Gain-framing nudge (“Vaccinations help end pandemics, like COVID-19 and the flu. Protect yourself and your loved ones.”)
- Loss-framing nudge (“When too few people get vaccinated, pandemics from diseases like COVID-19 and the flu can spread and place you and your loved ones at risk.”)
- Collective-goal nudge (“78% of Danes 65 and above were vaccinated against influenza last year. Help us achieve an even higher goal this year.”)
- Active choice or implementation-intention prompt (“We encourage you to record your appointment time here.”)
- Cardiovascular gain–framing nudge (“In addition to its protection against influenza infection, influenza vaccination also seems to protect against cardiovascular disease such as heart attacks and heart failure.”)
- Expert-authority statement (“I recommend everyone over the age of 65 years to get vaccinated against influenza – Tyra Grove Krause, Executive Vice President, Statens Serum Institut.”)
The electronic letters were sent out Sept. 16, 2022, and the primary endpoint was vaccine receipt on or before Jan. 1, 2023.
All individuals received an informative vaccination encouragement letter from the Danish Health Authority (usual care) delivered via the same electronic letter system during Sept. 17 through Sept. 21, 2022.
The individuals had a mean age of 73.8 years, 51.5% were women, and 27.4% had chronic cardiovascular disease.
The analyses were done in one randomly selected individual per household.
Influenza vaccination rates were significantly higher in the cardiovascular gain–framing nudge group vs. usual care (81.00% vs. 80.12%; difference, 0.89 percentage points; P < .0001) and in the repeat-letter group vs. usual care (80.85% vs 80.12%; difference, 0.73 percentage points; P = .0006).
These two strategies also improved vaccination rates across major subgroups.
The cardiovascular gain–framed letter was particularly effective among participants who had not been vaccinated for influenza in the previous season.
The seven other letter strategies did not increase flu shot uptake.
Subanalysis in CVD
In the prespecified subanalysis of the NUDGE-FLU trial of patients aged 65 and older that focused on patients with CVD, Daniel Modin, MB, and colleagues report that 83.1% of patients with CVD vs. 79.2% of patients without CVD received influenza vaccination within the requested time (P < .0001).
The two nudging strategies – a letter highlighting potential cardiovascular benefits of influenza vaccination or a repeat letter – that were effective in boosting flu shot rates in the main analysis were also effective in all major CVD subgroups (ischemic heart disease, pulmonary heart disease, heart failure, atrial fibrillation, cerebrovascular disease, atherosclerotic CVD, embolic or thrombotic disease, and congenital heart disease).
Despite strong guideline endorsement, “influenza vaccination rates remain suboptimal in patients with high-risk cardiovascular disease,” Dr. Morin and colleagues write, possibly because of “insufficient knowledge among patients and providers of potential clinical benefits, concerns about vaccine safety, and other forms of vaccine hesitancy.”
Their findings suggest that “select digital behaviorally informed nudges delivered in advance of vaccine availability might be utilized to increase influenza vaccinate uptake in individuals with cardiovascular disease.”
NUDGE-HF was funded by Sanofi. Dr. Johansen and Dr. Modin have no disclosures. The disclosures of the other authors are listed with the articles. Dr. Stockwell has no disclosures.
A version of this article first appeared on Medscape.com.
FROM ACC 2023
Frequent cannabis use tied to coronary artery disease
In the first part, in an observational study, daily cannabis use was associated with 34% higher odds for CAD, compared with never-users, in a large population-based U.S. cohort. Less frequent use was not associated with increased odds for CAD.
In the second part, people with a genetic susceptibility to cannabis use disorder or severe cannabis dependency had an increased risk for CAD, compared with other people.
Ishan Paranjpe, MD, the study’s lead author, reported these results in a press briefing and will present the study at the upcoming joint scientific sessions of the American College of Cardiology and the World Heart Federation 2023.
“A couple of takeaway points are that daily cannabis use, but not less frequent cannabis use, was associated with CAD” in the large population-based cohort, said Dr. Paranjpe, a resident physician at Stanford (Calif.) University, during the press conference.
“This analysis was adjusted for several possible confounders including age, sex at birth, [body mass index (BMI)], race, education, cigarette use, hypertension, high cholesterol, and diabetes,” he noted, and even after accounting for these risk factors, the association with heart disease remained.
“And the next thing, using Mendelian randomization, we sort of implied that there might be a causal relationship between cannabis and heart disease. Importantly this effect is independent of alcohol and cigarette use.
“The notion that cannabis is completely benign is probably wrong, and there might be certain risk of certain cardiovascular effects of cannabis we should be more on the lookout for,” Dr. Paranjpe said in an interview.
“Our main conclusion was that prevalent CAD is associated with cannabis consumption,” he added. “Other mechanistic work published in Cell has also shown that cannabis causes vascular inflammation that may lead to CAD.
“Thus, there is growing evidence from both laboratory and population studies that cannabis consumption may be harmful for cardiovascular health,” he said. “However, we still need more work on whether it affects the risk of incident cardiovascular events (i.e., stroke, heart attack) in patient[s] with existing CAD.”
ASCVD risk
Invited to comment, Robert L. Page II, PharmD, chair of the writing group for the American Heart Association’s scientific statement Medical Marijuana, Recreational Cannabis, and Cardiovascular Health, published in 2020, said, “This adds to our hypothesis that if you are using marijuana over a longer period, greater exposure, you’re going to see an increase in the risk” for atherosclerotic cardiovascular disease (ASCVD).
“We’re seeing this increased risk for ASCVD in young adults between ages 18 to 40 – people who think that they’re invincible,” Dr. Page, a professor at the University of Colorado at Denver, Aurora, who was not involved with this research, told this news organization in an interview.
“The bottom line is that the risk that they are seeing is what has also been documented in other observational studies, and it adds fuel to the fire. We need to be paying close attention to this,” he said.
“Primary care [clinicians], cardiologists, need to address this, particularly in younger adults – because that’s where you’re seeing the highest amount of use.”
‘All of Us’ observational study
In the first part of the study, the researchers analyzed data from the “All of Us” cohort comprising adults age 18 and older from 340 inpatient and outpatient sites across the United States.
They identified 57,958 individuals who replied to a questionnaire asking about cannabis use (medicinal or recreational and whether it was edible or used by smoking or vaping) over the past 3 months.
There were 39,678 never-users, 8,749 who used it once or twice, 2,075 who used it monthly, 2,720 who used it weekly, and 4,736 who used it daily.
Of these, 3,506 individuals had CAD, based on medical records.
Only daily users had a significantly higher risk for CAD, compared with never-users (odds ratio, 1.34; P = .001) after adjusting for age, sex, hypertension, hyperlipidemia, type 2 diabetes, BMI, education, insurance status, and cigarette use.
The median age for daily users was 41, whereas the median age for never-users was 59.
GWAS analyses
The researchers then performed a Mendelian randomization analysis based on genome-wide association studies (GWAS) of cannabis use disorder and of CAD.
“Cannabis use disorder is a psychiatric diagnosis of severe cannabis dependency, equivalent to ‘alcohol use disorder’ for alcohol consumption,” Dr. Paranjpe explained. “The exact definition involves frequent use leading to significant dependence (but does not specify how often it is used).”
The GWAS data for cannabis use disorder came from a recent meta-analysis of three cohorts: the Psychiatric Genomics Consortium Substance Use Disorders working group, iPSYCH, and deCODE.
The GWAS statistics for CAD were obtained from the CARDIoGRAMplusC4D Consortium.
Cannabis use disorder was associated with significantly increased odds for CAD (OR, 1.05; P = .001), which remained after adjusting for both cigarette and alcohol use (OR, 1.04).
A version of this article first appeared on Medscape.com.
In the first part, in an observational study, daily cannabis use was associated with 34% higher odds for CAD, compared with never-users, in a large population-based U.S. cohort. Less frequent use was not associated with increased odds for CAD.
In the second part, people with a genetic susceptibility to cannabis use disorder or severe cannabis dependency had an increased risk for CAD, compared with other people.
Ishan Paranjpe, MD, the study’s lead author, reported these results in a press briefing and will present the study at the upcoming joint scientific sessions of the American College of Cardiology and the World Heart Federation 2023.
“A couple of takeaway points are that daily cannabis use, but not less frequent cannabis use, was associated with CAD” in the large population-based cohort, said Dr. Paranjpe, a resident physician at Stanford (Calif.) University, during the press conference.
“This analysis was adjusted for several possible confounders including age, sex at birth, [body mass index (BMI)], race, education, cigarette use, hypertension, high cholesterol, and diabetes,” he noted, and even after accounting for these risk factors, the association with heart disease remained.
“And the next thing, using Mendelian randomization, we sort of implied that there might be a causal relationship between cannabis and heart disease. Importantly this effect is independent of alcohol and cigarette use.
“The notion that cannabis is completely benign is probably wrong, and there might be certain risk of certain cardiovascular effects of cannabis we should be more on the lookout for,” Dr. Paranjpe said in an interview.
“Our main conclusion was that prevalent CAD is associated with cannabis consumption,” he added. “Other mechanistic work published in Cell has also shown that cannabis causes vascular inflammation that may lead to CAD.
“Thus, there is growing evidence from both laboratory and population studies that cannabis consumption may be harmful for cardiovascular health,” he said. “However, we still need more work on whether it affects the risk of incident cardiovascular events (i.e., stroke, heart attack) in patient[s] with existing CAD.”
ASCVD risk
Invited to comment, Robert L. Page II, PharmD, chair of the writing group for the American Heart Association’s scientific statement Medical Marijuana, Recreational Cannabis, and Cardiovascular Health, published in 2020, said, “This adds to our hypothesis that if you are using marijuana over a longer period, greater exposure, you’re going to see an increase in the risk” for atherosclerotic cardiovascular disease (ASCVD).
“We’re seeing this increased risk for ASCVD in young adults between ages 18 to 40 – people who think that they’re invincible,” Dr. Page, a professor at the University of Colorado at Denver, Aurora, who was not involved with this research, told this news organization in an interview.
“The bottom line is that the risk that they are seeing is what has also been documented in other observational studies, and it adds fuel to the fire. We need to be paying close attention to this,” he said.
“Primary care [clinicians], cardiologists, need to address this, particularly in younger adults – because that’s where you’re seeing the highest amount of use.”
‘All of Us’ observational study
In the first part of the study, the researchers analyzed data from the “All of Us” cohort comprising adults age 18 and older from 340 inpatient and outpatient sites across the United States.
They identified 57,958 individuals who replied to a questionnaire asking about cannabis use (medicinal or recreational and whether it was edible or used by smoking or vaping) over the past 3 months.
There were 39,678 never-users, 8,749 who used it once or twice, 2,075 who used it monthly, 2,720 who used it weekly, and 4,736 who used it daily.
Of these, 3,506 individuals had CAD, based on medical records.
Only daily users had a significantly higher risk for CAD, compared with never-users (odds ratio, 1.34; P = .001) after adjusting for age, sex, hypertension, hyperlipidemia, type 2 diabetes, BMI, education, insurance status, and cigarette use.
The median age for daily users was 41, whereas the median age for never-users was 59.
GWAS analyses
The researchers then performed a Mendelian randomization analysis based on genome-wide association studies (GWAS) of cannabis use disorder and of CAD.
“Cannabis use disorder is a psychiatric diagnosis of severe cannabis dependency, equivalent to ‘alcohol use disorder’ for alcohol consumption,” Dr. Paranjpe explained. “The exact definition involves frequent use leading to significant dependence (but does not specify how often it is used).”
The GWAS data for cannabis use disorder came from a recent meta-analysis of three cohorts: the Psychiatric Genomics Consortium Substance Use Disorders working group, iPSYCH, and deCODE.
The GWAS statistics for CAD were obtained from the CARDIoGRAMplusC4D Consortium.
Cannabis use disorder was associated with significantly increased odds for CAD (OR, 1.05; P = .001), which remained after adjusting for both cigarette and alcohol use (OR, 1.04).
A version of this article first appeared on Medscape.com.
In the first part, in an observational study, daily cannabis use was associated with 34% higher odds for CAD, compared with never-users, in a large population-based U.S. cohort. Less frequent use was not associated with increased odds for CAD.
In the second part, people with a genetic susceptibility to cannabis use disorder or severe cannabis dependency had an increased risk for CAD, compared with other people.
Ishan Paranjpe, MD, the study’s lead author, reported these results in a press briefing and will present the study at the upcoming joint scientific sessions of the American College of Cardiology and the World Heart Federation 2023.
“A couple of takeaway points are that daily cannabis use, but not less frequent cannabis use, was associated with CAD” in the large population-based cohort, said Dr. Paranjpe, a resident physician at Stanford (Calif.) University, during the press conference.
“This analysis was adjusted for several possible confounders including age, sex at birth, [body mass index (BMI)], race, education, cigarette use, hypertension, high cholesterol, and diabetes,” he noted, and even after accounting for these risk factors, the association with heart disease remained.
“And the next thing, using Mendelian randomization, we sort of implied that there might be a causal relationship between cannabis and heart disease. Importantly this effect is independent of alcohol and cigarette use.
“The notion that cannabis is completely benign is probably wrong, and there might be certain risk of certain cardiovascular effects of cannabis we should be more on the lookout for,” Dr. Paranjpe said in an interview.
“Our main conclusion was that prevalent CAD is associated with cannabis consumption,” he added. “Other mechanistic work published in Cell has also shown that cannabis causes vascular inflammation that may lead to CAD.
“Thus, there is growing evidence from both laboratory and population studies that cannabis consumption may be harmful for cardiovascular health,” he said. “However, we still need more work on whether it affects the risk of incident cardiovascular events (i.e., stroke, heart attack) in patient[s] with existing CAD.”
ASCVD risk
Invited to comment, Robert L. Page II, PharmD, chair of the writing group for the American Heart Association’s scientific statement Medical Marijuana, Recreational Cannabis, and Cardiovascular Health, published in 2020, said, “This adds to our hypothesis that if you are using marijuana over a longer period, greater exposure, you’re going to see an increase in the risk” for atherosclerotic cardiovascular disease (ASCVD).
“We’re seeing this increased risk for ASCVD in young adults between ages 18 to 40 – people who think that they’re invincible,” Dr. Page, a professor at the University of Colorado at Denver, Aurora, who was not involved with this research, told this news organization in an interview.
“The bottom line is that the risk that they are seeing is what has also been documented in other observational studies, and it adds fuel to the fire. We need to be paying close attention to this,” he said.
“Primary care [clinicians], cardiologists, need to address this, particularly in younger adults – because that’s where you’re seeing the highest amount of use.”
‘All of Us’ observational study
In the first part of the study, the researchers analyzed data from the “All of Us” cohort comprising adults age 18 and older from 340 inpatient and outpatient sites across the United States.
They identified 57,958 individuals who replied to a questionnaire asking about cannabis use (medicinal or recreational and whether it was edible or used by smoking or vaping) over the past 3 months.
There were 39,678 never-users, 8,749 who used it once or twice, 2,075 who used it monthly, 2,720 who used it weekly, and 4,736 who used it daily.
Of these, 3,506 individuals had CAD, based on medical records.
Only daily users had a significantly higher risk for CAD, compared with never-users (odds ratio, 1.34; P = .001) after adjusting for age, sex, hypertension, hyperlipidemia, type 2 diabetes, BMI, education, insurance status, and cigarette use.
The median age for daily users was 41, whereas the median age for never-users was 59.
GWAS analyses
The researchers then performed a Mendelian randomization analysis based on genome-wide association studies (GWAS) of cannabis use disorder and of CAD.
“Cannabis use disorder is a psychiatric diagnosis of severe cannabis dependency, equivalent to ‘alcohol use disorder’ for alcohol consumption,” Dr. Paranjpe explained. “The exact definition involves frequent use leading to significant dependence (but does not specify how often it is used).”
The GWAS data for cannabis use disorder came from a recent meta-analysis of three cohorts: the Psychiatric Genomics Consortium Substance Use Disorders working group, iPSYCH, and deCODE.
The GWAS statistics for CAD were obtained from the CARDIoGRAMplusC4D Consortium.
Cannabis use disorder was associated with significantly increased odds for CAD (OR, 1.05; P = .001), which remained after adjusting for both cigarette and alcohol use (OR, 1.04).
A version of this article first appeared on Medscape.com.
FROM ACC 2023
Insomnia, short sleep linked to greater risk for MI
Insomnia – difficulty falling or staying asleep – was associated with a 69% greater risk of having a myocardial infarction than among adults without insomnia, according to new research.
Those who slept 5 or fewer hours per night had the highest risk for MI, and those with both diabetes and insomnia had double the risk for MI, compared with patients without these comorbidities.
The findings are from a meta-analysis of studies in more than 1 million patients, almost all without prior MI who were, on average, in their early 50s and followed for 9 years.
Yomna E. Dean, a medical student at Alexandria (Egypt) University, reported these results in a press briefing, and the study was simultaneously published in Clinical Cardiology. It will be presented at the upcoming at the annual scientific sessions of the American College of Cardiology.
“Insomnia and ]at least] 5 hours of sleep are highly associated with increased incidence of MI, an association comparable to that of other MI risk factors and as such, it should be considered as a risk factor for MI and to be incorporated into MI prevention guidelines,” the researchers concluded.
“We believe that [insomnia] should be screened and patients should be educated about the importance of sleep because nowadays insomnia is no longer a disease – sleep deprivation could also be a life choice,” Ms, Dean told a press conference prior to the meeting.
“Clinicians must educate the patients about the importance of sleep in maintaining a healthy heart and encourage proper sleep hygiene,” Ms. Dean reiterated in an email. “And if a patient still has insomnia, other methods should be considered such as cognitive-behavior[al] therapy for insomnia [CBT-I].”
Adds to growing evidence
This study does not allow any conclusion about whether treating insomnia will reduce heart attack risk, Jennifer L. Martin, PhD, president of the American Academy of Sleep Medicine, noted in a comment. Nor does it report the diversity of study participants, since insomnia is also a health equity issue, she noted, and insomnia symptoms and comorbidities were self-reported.
However, this analysis “adds to the growing evidence that poor quality or insufficient sleep is associated with poor health,” said Dr. Martin, professor of medicine at the University of California, Los Angeles, who was not involved with this research.
The study reinforces the recommendation from the American Heart Association, which includes “Get Healthy Sleep” as one of “Life’s Essential 8” for heart health, Dr. Martin noted.
“Particularly in primary care where disease prevention and health promotion are important, clinicians should be asking all patients about their sleep – just like they ask about diet and exercise – as a key aspect of maintaining heart health,” she said.
Advice about basic sleep hygiene advice is a first step, she noted.
When improved sleep hygiene is not enough to address chronic insomnia, the AASM’s clinical practice guidelines and the guidelines of the Department of Veterans Affairs/Department of Defense, recommend first-line treatment with CBT-I, typically offered by a sleep specialist or mental health clinician.
Similarly, the American College of Physicians suggests that sleeping pills should be reserved for short-term use in patients who may not benefit sufficiently from CBT-I.
Sleeping too little, too much, equally harmful
“Studies have found that insomnia and subsequent sleep deprivation puts the body under stress,” Ms. Dean said. “This triggers cortisol release which could accelerate atherosclerosis,” and increase risk of MI.
For this analysis, the researchers identified nine observational studies, published from 1998 to 2019, with data on incident MI in adults who had insomnia.
The diagnosis of insomnia was based on ICD diagnostic codes or on the DSM‐5, which defines insomnia as the presence of any of the following three symptoms: difficulty initiating sleep, difficulty maintaining sleep, or early morning awakening with inability to return to sleep. Patients with sleep apnea were excluded.
The studies were in populations in China, Germany, Norway, Taiwan, United Kingdom, and United States, in 1.1 million adults aged 18 and older. The patients had a mean age of 52 years and 13% had insomnia.
During follow-up, 2,406 of 153,881 patients with insomnia, and 12,398 of 1,030,375 patients without insomnia had an MI.
In the pooled analysis, patients with insomnia had a significantly increased risk of MI (relative risk, 1.69; P < .00001), after adjusting for age, gender, diabetes, hypertension, high cholesterol, and smoking.
Sleeping 5 hours or less was associated with a greater risk for MI than sleeping 6 hours, or 7-8 hours, but sleeping 9 hours or more was just as harmful.
Patients who had difficulty initiating and maintaining sleep – two symptoms of insomnia – had a 13% increased risk for MI compared with other patients (RR, 1.13; P = .003).
However, patients who had nonrestorative sleep and daytime dysfunction despite adequate sleep – which is common – did not have an increased risk of MI, compared with other patients (RR, 1.06; P = .46).
Women with insomnia had a 2.24-fold greater risk for MI than other women, whereas men with insomnia had a 2.03-fold greater risk for MI than other men.
Patients with insomnia had a greater risk for MI than those without insomnia in subgroups based on patients’ age (< 65 and > 65), follow up duration (≤ 5 years and > 5 years), and comorbidities (diabetes, hypertension, and hyperlipidemia).
The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Insomnia – difficulty falling or staying asleep – was associated with a 69% greater risk of having a myocardial infarction than among adults without insomnia, according to new research.
Those who slept 5 or fewer hours per night had the highest risk for MI, and those with both diabetes and insomnia had double the risk for MI, compared with patients without these comorbidities.
The findings are from a meta-analysis of studies in more than 1 million patients, almost all without prior MI who were, on average, in their early 50s and followed for 9 years.
Yomna E. Dean, a medical student at Alexandria (Egypt) University, reported these results in a press briefing, and the study was simultaneously published in Clinical Cardiology. It will be presented at the upcoming at the annual scientific sessions of the American College of Cardiology.
“Insomnia and ]at least] 5 hours of sleep are highly associated with increased incidence of MI, an association comparable to that of other MI risk factors and as such, it should be considered as a risk factor for MI and to be incorporated into MI prevention guidelines,” the researchers concluded.
“We believe that [insomnia] should be screened and patients should be educated about the importance of sleep because nowadays insomnia is no longer a disease – sleep deprivation could also be a life choice,” Ms, Dean told a press conference prior to the meeting.
“Clinicians must educate the patients about the importance of sleep in maintaining a healthy heart and encourage proper sleep hygiene,” Ms. Dean reiterated in an email. “And if a patient still has insomnia, other methods should be considered such as cognitive-behavior[al] therapy for insomnia [CBT-I].”
Adds to growing evidence
This study does not allow any conclusion about whether treating insomnia will reduce heart attack risk, Jennifer L. Martin, PhD, president of the American Academy of Sleep Medicine, noted in a comment. Nor does it report the diversity of study participants, since insomnia is also a health equity issue, she noted, and insomnia symptoms and comorbidities were self-reported.
However, this analysis “adds to the growing evidence that poor quality or insufficient sleep is associated with poor health,” said Dr. Martin, professor of medicine at the University of California, Los Angeles, who was not involved with this research.
The study reinforces the recommendation from the American Heart Association, which includes “Get Healthy Sleep” as one of “Life’s Essential 8” for heart health, Dr. Martin noted.
“Particularly in primary care where disease prevention and health promotion are important, clinicians should be asking all patients about their sleep – just like they ask about diet and exercise – as a key aspect of maintaining heart health,” she said.
Advice about basic sleep hygiene advice is a first step, she noted.
When improved sleep hygiene is not enough to address chronic insomnia, the AASM’s clinical practice guidelines and the guidelines of the Department of Veterans Affairs/Department of Defense, recommend first-line treatment with CBT-I, typically offered by a sleep specialist or mental health clinician.
Similarly, the American College of Physicians suggests that sleeping pills should be reserved for short-term use in patients who may not benefit sufficiently from CBT-I.
Sleeping too little, too much, equally harmful
“Studies have found that insomnia and subsequent sleep deprivation puts the body under stress,” Ms. Dean said. “This triggers cortisol release which could accelerate atherosclerosis,” and increase risk of MI.
For this analysis, the researchers identified nine observational studies, published from 1998 to 2019, with data on incident MI in adults who had insomnia.
The diagnosis of insomnia was based on ICD diagnostic codes or on the DSM‐5, which defines insomnia as the presence of any of the following three symptoms: difficulty initiating sleep, difficulty maintaining sleep, or early morning awakening with inability to return to sleep. Patients with sleep apnea were excluded.
The studies were in populations in China, Germany, Norway, Taiwan, United Kingdom, and United States, in 1.1 million adults aged 18 and older. The patients had a mean age of 52 years and 13% had insomnia.
During follow-up, 2,406 of 153,881 patients with insomnia, and 12,398 of 1,030,375 patients without insomnia had an MI.
In the pooled analysis, patients with insomnia had a significantly increased risk of MI (relative risk, 1.69; P < .00001), after adjusting for age, gender, diabetes, hypertension, high cholesterol, and smoking.
Sleeping 5 hours or less was associated with a greater risk for MI than sleeping 6 hours, or 7-8 hours, but sleeping 9 hours or more was just as harmful.
Patients who had difficulty initiating and maintaining sleep – two symptoms of insomnia – had a 13% increased risk for MI compared with other patients (RR, 1.13; P = .003).
However, patients who had nonrestorative sleep and daytime dysfunction despite adequate sleep – which is common – did not have an increased risk of MI, compared with other patients (RR, 1.06; P = .46).
Women with insomnia had a 2.24-fold greater risk for MI than other women, whereas men with insomnia had a 2.03-fold greater risk for MI than other men.
Patients with insomnia had a greater risk for MI than those without insomnia in subgroups based on patients’ age (< 65 and > 65), follow up duration (≤ 5 years and > 5 years), and comorbidities (diabetes, hypertension, and hyperlipidemia).
The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Insomnia – difficulty falling or staying asleep – was associated with a 69% greater risk of having a myocardial infarction than among adults without insomnia, according to new research.
Those who slept 5 or fewer hours per night had the highest risk for MI, and those with both diabetes and insomnia had double the risk for MI, compared with patients without these comorbidities.
The findings are from a meta-analysis of studies in more than 1 million patients, almost all without prior MI who were, on average, in their early 50s and followed for 9 years.
Yomna E. Dean, a medical student at Alexandria (Egypt) University, reported these results in a press briefing, and the study was simultaneously published in Clinical Cardiology. It will be presented at the upcoming at the annual scientific sessions of the American College of Cardiology.
“Insomnia and ]at least] 5 hours of sleep are highly associated with increased incidence of MI, an association comparable to that of other MI risk factors and as such, it should be considered as a risk factor for MI and to be incorporated into MI prevention guidelines,” the researchers concluded.
“We believe that [insomnia] should be screened and patients should be educated about the importance of sleep because nowadays insomnia is no longer a disease – sleep deprivation could also be a life choice,” Ms, Dean told a press conference prior to the meeting.
“Clinicians must educate the patients about the importance of sleep in maintaining a healthy heart and encourage proper sleep hygiene,” Ms. Dean reiterated in an email. “And if a patient still has insomnia, other methods should be considered such as cognitive-behavior[al] therapy for insomnia [CBT-I].”
Adds to growing evidence
This study does not allow any conclusion about whether treating insomnia will reduce heart attack risk, Jennifer L. Martin, PhD, president of the American Academy of Sleep Medicine, noted in a comment. Nor does it report the diversity of study participants, since insomnia is also a health equity issue, she noted, and insomnia symptoms and comorbidities were self-reported.
However, this analysis “adds to the growing evidence that poor quality or insufficient sleep is associated with poor health,” said Dr. Martin, professor of medicine at the University of California, Los Angeles, who was not involved with this research.
The study reinforces the recommendation from the American Heart Association, which includes “Get Healthy Sleep” as one of “Life’s Essential 8” for heart health, Dr. Martin noted.
“Particularly in primary care where disease prevention and health promotion are important, clinicians should be asking all patients about their sleep – just like they ask about diet and exercise – as a key aspect of maintaining heart health,” she said.
Advice about basic sleep hygiene advice is a first step, she noted.
When improved sleep hygiene is not enough to address chronic insomnia, the AASM’s clinical practice guidelines and the guidelines of the Department of Veterans Affairs/Department of Defense, recommend first-line treatment with CBT-I, typically offered by a sleep specialist or mental health clinician.
Similarly, the American College of Physicians suggests that sleeping pills should be reserved for short-term use in patients who may not benefit sufficiently from CBT-I.
Sleeping too little, too much, equally harmful
“Studies have found that insomnia and subsequent sleep deprivation puts the body under stress,” Ms. Dean said. “This triggers cortisol release which could accelerate atherosclerosis,” and increase risk of MI.
For this analysis, the researchers identified nine observational studies, published from 1998 to 2019, with data on incident MI in adults who had insomnia.
The diagnosis of insomnia was based on ICD diagnostic codes or on the DSM‐5, which defines insomnia as the presence of any of the following three symptoms: difficulty initiating sleep, difficulty maintaining sleep, or early morning awakening with inability to return to sleep. Patients with sleep apnea were excluded.
The studies were in populations in China, Germany, Norway, Taiwan, United Kingdom, and United States, in 1.1 million adults aged 18 and older. The patients had a mean age of 52 years and 13% had insomnia.
During follow-up, 2,406 of 153,881 patients with insomnia, and 12,398 of 1,030,375 patients without insomnia had an MI.
In the pooled analysis, patients with insomnia had a significantly increased risk of MI (relative risk, 1.69; P < .00001), after adjusting for age, gender, diabetes, hypertension, high cholesterol, and smoking.
Sleeping 5 hours or less was associated with a greater risk for MI than sleeping 6 hours, or 7-8 hours, but sleeping 9 hours or more was just as harmful.
Patients who had difficulty initiating and maintaining sleep – two symptoms of insomnia – had a 13% increased risk for MI compared with other patients (RR, 1.13; P = .003).
However, patients who had nonrestorative sleep and daytime dysfunction despite adequate sleep – which is common – did not have an increased risk of MI, compared with other patients (RR, 1.06; P = .46).
Women with insomnia had a 2.24-fold greater risk for MI than other women, whereas men with insomnia had a 2.03-fold greater risk for MI than other men.
Patients with insomnia had a greater risk for MI than those without insomnia in subgroups based on patients’ age (< 65 and > 65), follow up duration (≤ 5 years and > 5 years), and comorbidities (diabetes, hypertension, and hyperlipidemia).
The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACC 2023
Artificial sweetener in ‘keto foods’ tied to cardiovascular risk
Erythritol is one of the most widely used artificial sweeteners with rapidly increasing prevalence in processed and “keto-related” foods. Artificial sweeteners are “generally recognized as safe” (GRAS) by the U.S. Food and Drug Administration, so there is no requirement for long-term safety studies, and little is known about the long-term health effects.
The current research, published online in Nature Medicine by Marco Witkowski, MD, of the Lerner Research Institute at Cleveland Clinic and colleagues, had multiple parts.
First, in a group of patients undergoing cardiac risk assessment, the researchers found that high levels of polyols, especially erythritol, were associated with increased 3-year risk of MACE, defined as cardiovascular death or nonfatal myocardial infarction or stroke.
Next, the association of erythritol with this outcome was reproduced in two large U.S. and European groups of stable patients undergoing elective cardiac evaluation.
Next, adding erythritol to whole blood or platelets led to clot activation. And lastly, in eight healthy volunteers, ingesting 30 g of an erythritol-sweetened drink – comparable to a single can of commercially available beverage or a pint of keto ice cream – induced marked and sustained (> 2 day) increases in levels of plasma erythritol.
“Our study shows that when participants consumed an artificially sweetened beverage with an amount of erythritol found in many processed foods, markedly elevated levels in the blood are observed for days – levels well above those observed to enhance clotting risks,” said senior author Stanley L. Hazen, MD, PhD.
“It is important that further safety studies are conducted to examine the long-term effects of artificial sweeteners in general, and erythritol specifically, on risks for heart attack and stroke, particularly in people at higher risk for cardiovascular disease,” Dr. Hazen, co–section head of preventive cardiology at Cleveland Clinic, said in a press release from his institution.
“Sweeteners like erythritol have rapidly increased in popularity in recent years, but there needs to be more in-depth research into their long-term effects. Cardiovascular disease builds over time, and heart disease is the leading cause of death globally. We need to make sure the foods we eat aren’t hidden contributors,” Dr. Hazen urged.
The topic remains controversial.
Duane Mellor, PhD, a registered dietitian and senior teaching fellow at Aston University, Birmingham, England, told the U.K. Science Media Centre: “This paper effectively shows multiple pieces of a jigsaw exploring the effects of erythritol – although it claims to show an associated risk with the use of erythritol as an artificial sweetener and cardiovascular disease, I believe it fails to do so, as ultimately, erythritol can be made inside our bodies and the intake in most people’s diet is much lower than the amount given in this study.”
Dr. Hazen countered that data from the 2013-2014 National Health and Nutrition Examination Survey (NHANES) in the United States show that, in some individuals, daily intake of erythritol is estimated to reach 30 g/day.
“Many try and reduce sugar intake by taking many teaspoons of erythritol in their tea, coffee, etc., instead of sugar,” Dr. Hazen added. “Or they eat keto processed foods that have significant quantities of erythritol within it.”
“These studies are a warning for how our processed food (keto and zero sugar, especially) may inadvertently be causing risk/harm. … in the very subset of subjects who are most vulnerable,” according to Dr. Hazen.
Erythritol marketed as ‘zero calorie’, ‘non-nutritive’, or ‘natural’
Patients with type 2 diabetes and obesity are often advised to replace sugar with artificial sweeteners for better glucose control and weight loss, but growing epidemiologic evidence links artificial sweetener consumption with weight gain, insulin resistance, type 2 diabetes, and cardiovascular disease, the researchers write.
Erythritol is naturally present in low amounts in fruits and vegetables; the artificial sweetener erythritol that is produced from corn is only 70% as sweet as sugar.
Upon ingestion it is poorly metabolized, and most is excreted in the urine, so it is characterized as a “zero-calorie,” “non-nutritive,” or “natural sweetener.” It is predicted to double in marketshare in the sweetener sector in the next 5 years.
Multipart study
In the first part of their study, in a discovery cohort in 1,157 patients undergoing cardiovascular assessment with 3-year outcomes, the researchers identified polyols that were associated with MACE, and erythritol was among the top MACE-associated molecules.
Next, in a U.S. validation cohort of 2,149 patients, over a 3-year follow-up, patients with plasma levels of erythritol in the highest quartile had a 1.8-fold higher risk of MACE than patients in the lowest quartile (P = .007), after adjusting for cardiovascular risk factors.
In a European validation cohort of 833 patients, over a 3-year follow-up, patients with plasma levels of erythritol in the highest quartile had a 2.21-fold higher risk of MACE than patients in the lowest quartile (P = .010, after adjustment).
At physiologic levels, erythritol enhanced platelet reactivity in vitro and thrombosis formation in vivo.
Finally, in a prospective pilot intervention study, erythritol ingestion in healthy volunteers induced marked and sustained increases in plasma erythritol levels well above thresholds associated with heightened platelet reactivity and thrombosis potential in in vitro and in vivo studies.
Others weigh in
“While I think the finding certainly warrants further investigation, don’t throw out your sweeteners just yet,” commented Oliver Jones, PhD, professor of chemistry at the Royal Melbourne Institute of Technology.
“This study only looks at erythritol, and artificial sweeteners are generally considered safe. Any possible (and, as yet unproven) risks of excess erythritol would also need to be balanced against the very real health risks of excess glucose consumption,” he said.
Dr. Hazen responded: “True enough. Erythritol is but one of many artificial sweeteners. That is why it is important to read labels. This study can make patients be informed about how to potentially avoid something that might cause them inadvertent harm.”
“The key findings of this study are that high blood levels of erythritol are strongly associated with cardiovascular outcomes in high-risk patients, which has been replicated in separate validation studies,” said Tom Sanders, DSc, PhD, professor emeritus of nutrition and dietetics, King’s College London.
“Diabetes UK currently advises diabetes patients not to use polyols,” he added.
Dr. Hazen noted that “About three-quarters of the participants had coronary disease, high blood pressure, and about a fifth had diabetes.”
The researchers acknowledge, however, that the observational studies cannot show cause and effect.
The study was supported by the Office of Dietary Supplements at the National Institutes of Health, the Leducq Foundation, and the German Research Foundation (Deutsche Forschungsgemeinschaft). Dr. Mellor, Dr. Jones, and Dr. Sanders have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Erythritol is one of the most widely used artificial sweeteners with rapidly increasing prevalence in processed and “keto-related” foods. Artificial sweeteners are “generally recognized as safe” (GRAS) by the U.S. Food and Drug Administration, so there is no requirement for long-term safety studies, and little is known about the long-term health effects.
The current research, published online in Nature Medicine by Marco Witkowski, MD, of the Lerner Research Institute at Cleveland Clinic and colleagues, had multiple parts.
First, in a group of patients undergoing cardiac risk assessment, the researchers found that high levels of polyols, especially erythritol, were associated with increased 3-year risk of MACE, defined as cardiovascular death or nonfatal myocardial infarction or stroke.
Next, the association of erythritol with this outcome was reproduced in two large U.S. and European groups of stable patients undergoing elective cardiac evaluation.
Next, adding erythritol to whole blood or platelets led to clot activation. And lastly, in eight healthy volunteers, ingesting 30 g of an erythritol-sweetened drink – comparable to a single can of commercially available beverage or a pint of keto ice cream – induced marked and sustained (> 2 day) increases in levels of plasma erythritol.
“Our study shows that when participants consumed an artificially sweetened beverage with an amount of erythritol found in many processed foods, markedly elevated levels in the blood are observed for days – levels well above those observed to enhance clotting risks,” said senior author Stanley L. Hazen, MD, PhD.
“It is important that further safety studies are conducted to examine the long-term effects of artificial sweeteners in general, and erythritol specifically, on risks for heart attack and stroke, particularly in people at higher risk for cardiovascular disease,” Dr. Hazen, co–section head of preventive cardiology at Cleveland Clinic, said in a press release from his institution.
“Sweeteners like erythritol have rapidly increased in popularity in recent years, but there needs to be more in-depth research into their long-term effects. Cardiovascular disease builds over time, and heart disease is the leading cause of death globally. We need to make sure the foods we eat aren’t hidden contributors,” Dr. Hazen urged.
The topic remains controversial.
Duane Mellor, PhD, a registered dietitian and senior teaching fellow at Aston University, Birmingham, England, told the U.K. Science Media Centre: “This paper effectively shows multiple pieces of a jigsaw exploring the effects of erythritol – although it claims to show an associated risk with the use of erythritol as an artificial sweetener and cardiovascular disease, I believe it fails to do so, as ultimately, erythritol can be made inside our bodies and the intake in most people’s diet is much lower than the amount given in this study.”
Dr. Hazen countered that data from the 2013-2014 National Health and Nutrition Examination Survey (NHANES) in the United States show that, in some individuals, daily intake of erythritol is estimated to reach 30 g/day.
“Many try and reduce sugar intake by taking many teaspoons of erythritol in their tea, coffee, etc., instead of sugar,” Dr. Hazen added. “Or they eat keto processed foods that have significant quantities of erythritol within it.”
“These studies are a warning for how our processed food (keto and zero sugar, especially) may inadvertently be causing risk/harm. … in the very subset of subjects who are most vulnerable,” according to Dr. Hazen.
Erythritol marketed as ‘zero calorie’, ‘non-nutritive’, or ‘natural’
Patients with type 2 diabetes and obesity are often advised to replace sugar with artificial sweeteners for better glucose control and weight loss, but growing epidemiologic evidence links artificial sweetener consumption with weight gain, insulin resistance, type 2 diabetes, and cardiovascular disease, the researchers write.
Erythritol is naturally present in low amounts in fruits and vegetables; the artificial sweetener erythritol that is produced from corn is only 70% as sweet as sugar.
Upon ingestion it is poorly metabolized, and most is excreted in the urine, so it is characterized as a “zero-calorie,” “non-nutritive,” or “natural sweetener.” It is predicted to double in marketshare in the sweetener sector in the next 5 years.
Multipart study
In the first part of their study, in a discovery cohort in 1,157 patients undergoing cardiovascular assessment with 3-year outcomes, the researchers identified polyols that were associated with MACE, and erythritol was among the top MACE-associated molecules.
Next, in a U.S. validation cohort of 2,149 patients, over a 3-year follow-up, patients with plasma levels of erythritol in the highest quartile had a 1.8-fold higher risk of MACE than patients in the lowest quartile (P = .007), after adjusting for cardiovascular risk factors.
In a European validation cohort of 833 patients, over a 3-year follow-up, patients with plasma levels of erythritol in the highest quartile had a 2.21-fold higher risk of MACE than patients in the lowest quartile (P = .010, after adjustment).
At physiologic levels, erythritol enhanced platelet reactivity in vitro and thrombosis formation in vivo.
Finally, in a prospective pilot intervention study, erythritol ingestion in healthy volunteers induced marked and sustained increases in plasma erythritol levels well above thresholds associated with heightened platelet reactivity and thrombosis potential in in vitro and in vivo studies.
Others weigh in
“While I think the finding certainly warrants further investigation, don’t throw out your sweeteners just yet,” commented Oliver Jones, PhD, professor of chemistry at the Royal Melbourne Institute of Technology.
“This study only looks at erythritol, and artificial sweeteners are generally considered safe. Any possible (and, as yet unproven) risks of excess erythritol would also need to be balanced against the very real health risks of excess glucose consumption,” he said.
Dr. Hazen responded: “True enough. Erythritol is but one of many artificial sweeteners. That is why it is important to read labels. This study can make patients be informed about how to potentially avoid something that might cause them inadvertent harm.”
“The key findings of this study are that high blood levels of erythritol are strongly associated with cardiovascular outcomes in high-risk patients, which has been replicated in separate validation studies,” said Tom Sanders, DSc, PhD, professor emeritus of nutrition and dietetics, King’s College London.
“Diabetes UK currently advises diabetes patients not to use polyols,” he added.
Dr. Hazen noted that “About three-quarters of the participants had coronary disease, high blood pressure, and about a fifth had diabetes.”
The researchers acknowledge, however, that the observational studies cannot show cause and effect.
The study was supported by the Office of Dietary Supplements at the National Institutes of Health, the Leducq Foundation, and the German Research Foundation (Deutsche Forschungsgemeinschaft). Dr. Mellor, Dr. Jones, and Dr. Sanders have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Erythritol is one of the most widely used artificial sweeteners with rapidly increasing prevalence in processed and “keto-related” foods. Artificial sweeteners are “generally recognized as safe” (GRAS) by the U.S. Food and Drug Administration, so there is no requirement for long-term safety studies, and little is known about the long-term health effects.
The current research, published online in Nature Medicine by Marco Witkowski, MD, of the Lerner Research Institute at Cleveland Clinic and colleagues, had multiple parts.
First, in a group of patients undergoing cardiac risk assessment, the researchers found that high levels of polyols, especially erythritol, were associated with increased 3-year risk of MACE, defined as cardiovascular death or nonfatal myocardial infarction or stroke.
Next, the association of erythritol with this outcome was reproduced in two large U.S. and European groups of stable patients undergoing elective cardiac evaluation.
Next, adding erythritol to whole blood or platelets led to clot activation. And lastly, in eight healthy volunteers, ingesting 30 g of an erythritol-sweetened drink – comparable to a single can of commercially available beverage or a pint of keto ice cream – induced marked and sustained (> 2 day) increases in levels of plasma erythritol.
“Our study shows that when participants consumed an artificially sweetened beverage with an amount of erythritol found in many processed foods, markedly elevated levels in the blood are observed for days – levels well above those observed to enhance clotting risks,” said senior author Stanley L. Hazen, MD, PhD.
“It is important that further safety studies are conducted to examine the long-term effects of artificial sweeteners in general, and erythritol specifically, on risks for heart attack and stroke, particularly in people at higher risk for cardiovascular disease,” Dr. Hazen, co–section head of preventive cardiology at Cleveland Clinic, said in a press release from his institution.
“Sweeteners like erythritol have rapidly increased in popularity in recent years, but there needs to be more in-depth research into their long-term effects. Cardiovascular disease builds over time, and heart disease is the leading cause of death globally. We need to make sure the foods we eat aren’t hidden contributors,” Dr. Hazen urged.
The topic remains controversial.
Duane Mellor, PhD, a registered dietitian and senior teaching fellow at Aston University, Birmingham, England, told the U.K. Science Media Centre: “This paper effectively shows multiple pieces of a jigsaw exploring the effects of erythritol – although it claims to show an associated risk with the use of erythritol as an artificial sweetener and cardiovascular disease, I believe it fails to do so, as ultimately, erythritol can be made inside our bodies and the intake in most people’s diet is much lower than the amount given in this study.”
Dr. Hazen countered that data from the 2013-2014 National Health and Nutrition Examination Survey (NHANES) in the United States show that, in some individuals, daily intake of erythritol is estimated to reach 30 g/day.
“Many try and reduce sugar intake by taking many teaspoons of erythritol in their tea, coffee, etc., instead of sugar,” Dr. Hazen added. “Or they eat keto processed foods that have significant quantities of erythritol within it.”
“These studies are a warning for how our processed food (keto and zero sugar, especially) may inadvertently be causing risk/harm. … in the very subset of subjects who are most vulnerable,” according to Dr. Hazen.
Erythritol marketed as ‘zero calorie’, ‘non-nutritive’, or ‘natural’
Patients with type 2 diabetes and obesity are often advised to replace sugar with artificial sweeteners for better glucose control and weight loss, but growing epidemiologic evidence links artificial sweetener consumption with weight gain, insulin resistance, type 2 diabetes, and cardiovascular disease, the researchers write.
Erythritol is naturally present in low amounts in fruits and vegetables; the artificial sweetener erythritol that is produced from corn is only 70% as sweet as sugar.
Upon ingestion it is poorly metabolized, and most is excreted in the urine, so it is characterized as a “zero-calorie,” “non-nutritive,” or “natural sweetener.” It is predicted to double in marketshare in the sweetener sector in the next 5 years.
Multipart study
In the first part of their study, in a discovery cohort in 1,157 patients undergoing cardiovascular assessment with 3-year outcomes, the researchers identified polyols that were associated with MACE, and erythritol was among the top MACE-associated molecules.
Next, in a U.S. validation cohort of 2,149 patients, over a 3-year follow-up, patients with plasma levels of erythritol in the highest quartile had a 1.8-fold higher risk of MACE than patients in the lowest quartile (P = .007), after adjusting for cardiovascular risk factors.
In a European validation cohort of 833 patients, over a 3-year follow-up, patients with plasma levels of erythritol in the highest quartile had a 2.21-fold higher risk of MACE than patients in the lowest quartile (P = .010, after adjustment).
At physiologic levels, erythritol enhanced platelet reactivity in vitro and thrombosis formation in vivo.
Finally, in a prospective pilot intervention study, erythritol ingestion in healthy volunteers induced marked and sustained increases in plasma erythritol levels well above thresholds associated with heightened platelet reactivity and thrombosis potential in in vitro and in vivo studies.
Others weigh in
“While I think the finding certainly warrants further investigation, don’t throw out your sweeteners just yet,” commented Oliver Jones, PhD, professor of chemistry at the Royal Melbourne Institute of Technology.
“This study only looks at erythritol, and artificial sweeteners are generally considered safe. Any possible (and, as yet unproven) risks of excess erythritol would also need to be balanced against the very real health risks of excess glucose consumption,” he said.
Dr. Hazen responded: “True enough. Erythritol is but one of many artificial sweeteners. That is why it is important to read labels. This study can make patients be informed about how to potentially avoid something that might cause them inadvertent harm.”
“The key findings of this study are that high blood levels of erythritol are strongly associated with cardiovascular outcomes in high-risk patients, which has been replicated in separate validation studies,” said Tom Sanders, DSc, PhD, professor emeritus of nutrition and dietetics, King’s College London.
“Diabetes UK currently advises diabetes patients not to use polyols,” he added.
Dr. Hazen noted that “About three-quarters of the participants had coronary disease, high blood pressure, and about a fifth had diabetes.”
The researchers acknowledge, however, that the observational studies cannot show cause and effect.
The study was supported by the Office of Dietary Supplements at the National Institutes of Health, the Leducq Foundation, and the German Research Foundation (Deutsche Forschungsgemeinschaft). Dr. Mellor, Dr. Jones, and Dr. Sanders have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NATURE MEDICINE
Zero tolerance for patient bias: Too harsh? Clinicians respond
If a patient refuses care from a health care practitioner because of their race or sex, should their request be accommodated?
In a recent blog on Medscape titled “No, You Can’t See a Different Doctor: We Need Zero Tolerance of Patient Bias,” Cleveland Francis Jr., MD, argued no.
Dr. Francis, who is Black, is a recently retired cardiologist who practiced for 50 years. He is currently Diversity, Equity, and Inclusion Advisor at Inova Heart and Vascular Institute in Falls Church, Va.
When Francis was a medical student and was preparing to take a patient’s history and perform a medical exam, the patient refused and requested a “White doctor,” he recounted.
“I can remember the hurt and embarrassment as if it were yesterday,” he wrote.
The blog, especially the title, drew strong reactions. Close to 500 readers weighed in.
“The title of my blog sounds harsh,” Dr. Francis said, “but in reality, a simple conversation with the patient usually resolves these issues. The difference is that in the old days, there was utter silence, and the wishes of the patient would be granted”
Health care practitioners “should expect to be treated with respect,” he concluded his blog.
Readers agreed on that point, but they debated whether being uncomfortable with a health care practitioner of a different sex or race always constituted “patient bias.”
Some noted that difficulty understanding a practitioner’s accent, for example, is a legitimate reason for asking for another clinician.
Accents and understanding
“If I am struggling to understand you because your accent is too thick or ... because hearing aids can only do so much, I need to ask for someone else,” a reader commented.
Another chimed in: “My elderly parents changed PCPs frequently during the final years of their lives, mainly due to language barriers encountered with foreign-born providers. Due to progressive hearing loss, they simply couldn’t understand them.”
“It is important to remember that there is a Patient Bill of Rights,” she noted, “the first part of which states, ‘You have the right to safe, considerate, and respectful care, provided in a manner consistent with your beliefs.’ ”
A former charge nurse added: “If a request for change was substantive (poor communication, perceived incompetence, trauma history, etc.), I would move mountains to accommodate it, but IMHO [in my humble opinion], the belief in honoring patient preference doesn’t necessarily need to include rearranging the world in order to accommodate racism, sexism, etc.”
Bias against female doctors, male nurses
Many commenters described how they gladly traded when a patient requested a practitioner of the opposite sex.
A female hospitalist related how she contacted the senior male doctor working with her to arrange a patient trade, adding, “I do agree that racial discrimination ought to be discouraged.”
Similarly, a male ICU RN commented: “Over 13 years, I have had a handful of female (usually older) patients request a female nurse. I have always strived to make this happen.”
However, an older woman related how at first she “had some bias against a male nurse touching me and also felt self-conscious,” she said. “So, I tried to relax ... and let him do his job. He was one of the most compassionate, kind, and sensitive nurses I’ve ever had.”
“I think in some cases,” she noted, “some women have had a history of some sort of abuse by a male, whether it’s sexual or psychological,” but in other cases, “it’s often just a personal preference, not a bias.”
A physician assistant (PA) who worked in a rural ED recounted how “there was only one physician and one PA on at any given evening/night shift, both usually White males.”
“Sometimes, you just have to cope as best you can with whomever is available, and in doing so,” he said, “they might just end up being pleasantly surprised.”
Don’t take it personally, move on
“If a patient doesn’t want to see me for whatever reason, then I would rather not treat them,” was a common sentiment.
Patients “should feel comfortable with their provider even if it’s with someone other than myself,” a reader wrote.
A female physician chimed in: “I frequently have older male patients refuse to see me. ... While this is irritating on several levels, I recognize that it is the patient’s choice, sigh, and move on to the next patient.”
“There are many more patients who specifically ask to see me, so I don’t waste my time and energy on being bothered by those who refuse.”
Similarly, a female mental health provider and sometimes patient wrote: “If any patient tells me that they prefer a male ... or someone of a particular race or religion or whatever, I don’t take it personally.”
A female Hispanic doctor chimed in: “Honestly, if a patient does not want to see me due to my race, I’m OK with that. Patients need to feel comfortable with me for the relationship to be therapeutic and effective,” she said.
“Forcing the patient to see me is adding injury to insult to ME! Not to mention increase[d] workload since that patient will take [so] much more time.”
Similarly, an Asian American doctor commented: “There are people who choose not to see me because of my ethnicity. However, I strongly believe that it should always be the patient’s preference. Whatever the reason, do not force the patient to see you in the name of Diversity, Equity, Inclusion, or whatever hurts your feeling. Let the patient go.”
Patient bias vs. patient preference
A physician referring to Dr. Francis’s experience suggested that “perhaps there was an opportunity to explore this misconception directly with the patient. If not, your supervising senior resident or attending should have been informed and brought into the process and conversation.”
“If/when I were rejected by a patient for whatever reason,” another physician commented, “I would gracefully accede, and hope that my colleague would tactfully point out to the patient their error.”
“Having a nurse ask the patient ... what they need style-wise (keeping race, gender, etc., out of it) might help identify whether or not the underlying issue(s) are based on style/needs mismatch match rather than bias,” a reader suggested.
A health care worker commented: “We generally assure patients that we are professionals and think nothing of situations that they might find uncomfortable, but don’t realize that our comfort does not translate to theirs.”
Maybe a different strategy is needed
“Having been the target of bias many times,” a reader said, “I understand the pain that is inflicted. Unfortunately, a patient bias policy, while a good idea, will not prevent patient bias. This is a much larger societal problem. But we can at least tell patients that it is not okay. On the other hand, I would not want to be the provider for a patient who was biased against me and held me in disdain.”
“I do not like Zero Tolerance policies ever. They are too absolute,” another reader commented. “Sometimes, there are reasons and we do have to listen to our patients for why. ... I do not think a policy of zero tolerance will fix the problem of racism.”
“Instead of trying to educate the general public about how not to be jerks,” another reader suggested, “perhaps it would be easier to provide elective classes for doctors and employees who believe themselves to be at-risk for discrimination, providing them with a ‘toolkit’ of strategies for responding to discrimination in the moment, processing it emotionally later on, and reporting the most egregious events through designated channels.”
Another commenter agreed and wrote that, “While we as doctors need and deserve protection, we are also called to act with compassion. So, rather than ask the system for ‘zero-tolerance’ in either direction, we could encourage our health systems to provide education, support, and mediation to any party who feels or fears that they are not being well served. Such a model would include support for physicians who have been the victims of bias and hurt.”
A version of this article originally appeared on Medscape.com.
If a patient refuses care from a health care practitioner because of their race or sex, should their request be accommodated?
In a recent blog on Medscape titled “No, You Can’t See a Different Doctor: We Need Zero Tolerance of Patient Bias,” Cleveland Francis Jr., MD, argued no.
Dr. Francis, who is Black, is a recently retired cardiologist who practiced for 50 years. He is currently Diversity, Equity, and Inclusion Advisor at Inova Heart and Vascular Institute in Falls Church, Va.
When Francis was a medical student and was preparing to take a patient’s history and perform a medical exam, the patient refused and requested a “White doctor,” he recounted.
“I can remember the hurt and embarrassment as if it were yesterday,” he wrote.
The blog, especially the title, drew strong reactions. Close to 500 readers weighed in.
“The title of my blog sounds harsh,” Dr. Francis said, “but in reality, a simple conversation with the patient usually resolves these issues. The difference is that in the old days, there was utter silence, and the wishes of the patient would be granted”
Health care practitioners “should expect to be treated with respect,” he concluded his blog.
Readers agreed on that point, but they debated whether being uncomfortable with a health care practitioner of a different sex or race always constituted “patient bias.”
Some noted that difficulty understanding a practitioner’s accent, for example, is a legitimate reason for asking for another clinician.
Accents and understanding
“If I am struggling to understand you because your accent is too thick or ... because hearing aids can only do so much, I need to ask for someone else,” a reader commented.
Another chimed in: “My elderly parents changed PCPs frequently during the final years of their lives, mainly due to language barriers encountered with foreign-born providers. Due to progressive hearing loss, they simply couldn’t understand them.”
“It is important to remember that there is a Patient Bill of Rights,” she noted, “the first part of which states, ‘You have the right to safe, considerate, and respectful care, provided in a manner consistent with your beliefs.’ ”
A former charge nurse added: “If a request for change was substantive (poor communication, perceived incompetence, trauma history, etc.), I would move mountains to accommodate it, but IMHO [in my humble opinion], the belief in honoring patient preference doesn’t necessarily need to include rearranging the world in order to accommodate racism, sexism, etc.”
Bias against female doctors, male nurses
Many commenters described how they gladly traded when a patient requested a practitioner of the opposite sex.
A female hospitalist related how she contacted the senior male doctor working with her to arrange a patient trade, adding, “I do agree that racial discrimination ought to be discouraged.”
Similarly, a male ICU RN commented: “Over 13 years, I have had a handful of female (usually older) patients request a female nurse. I have always strived to make this happen.”
However, an older woman related how at first she “had some bias against a male nurse touching me and also felt self-conscious,” she said. “So, I tried to relax ... and let him do his job. He was one of the most compassionate, kind, and sensitive nurses I’ve ever had.”
“I think in some cases,” she noted, “some women have had a history of some sort of abuse by a male, whether it’s sexual or psychological,” but in other cases, “it’s often just a personal preference, not a bias.”
A physician assistant (PA) who worked in a rural ED recounted how “there was only one physician and one PA on at any given evening/night shift, both usually White males.”
“Sometimes, you just have to cope as best you can with whomever is available, and in doing so,” he said, “they might just end up being pleasantly surprised.”
Don’t take it personally, move on
“If a patient doesn’t want to see me for whatever reason, then I would rather not treat them,” was a common sentiment.
Patients “should feel comfortable with their provider even if it’s with someone other than myself,” a reader wrote.
A female physician chimed in: “I frequently have older male patients refuse to see me. ... While this is irritating on several levels, I recognize that it is the patient’s choice, sigh, and move on to the next patient.”
“There are many more patients who specifically ask to see me, so I don’t waste my time and energy on being bothered by those who refuse.”
Similarly, a female mental health provider and sometimes patient wrote: “If any patient tells me that they prefer a male ... or someone of a particular race or religion or whatever, I don’t take it personally.”
A female Hispanic doctor chimed in: “Honestly, if a patient does not want to see me due to my race, I’m OK with that. Patients need to feel comfortable with me for the relationship to be therapeutic and effective,” she said.
“Forcing the patient to see me is adding injury to insult to ME! Not to mention increase[d] workload since that patient will take [so] much more time.”
Similarly, an Asian American doctor commented: “There are people who choose not to see me because of my ethnicity. However, I strongly believe that it should always be the patient’s preference. Whatever the reason, do not force the patient to see you in the name of Diversity, Equity, Inclusion, or whatever hurts your feeling. Let the patient go.”
Patient bias vs. patient preference
A physician referring to Dr. Francis’s experience suggested that “perhaps there was an opportunity to explore this misconception directly with the patient. If not, your supervising senior resident or attending should have been informed and brought into the process and conversation.”
“If/when I were rejected by a patient for whatever reason,” another physician commented, “I would gracefully accede, and hope that my colleague would tactfully point out to the patient their error.”
“Having a nurse ask the patient ... what they need style-wise (keeping race, gender, etc., out of it) might help identify whether or not the underlying issue(s) are based on style/needs mismatch match rather than bias,” a reader suggested.
A health care worker commented: “We generally assure patients that we are professionals and think nothing of situations that they might find uncomfortable, but don’t realize that our comfort does not translate to theirs.”
Maybe a different strategy is needed
“Having been the target of bias many times,” a reader said, “I understand the pain that is inflicted. Unfortunately, a patient bias policy, while a good idea, will not prevent patient bias. This is a much larger societal problem. But we can at least tell patients that it is not okay. On the other hand, I would not want to be the provider for a patient who was biased against me and held me in disdain.”
“I do not like Zero Tolerance policies ever. They are too absolute,” another reader commented. “Sometimes, there are reasons and we do have to listen to our patients for why. ... I do not think a policy of zero tolerance will fix the problem of racism.”
“Instead of trying to educate the general public about how not to be jerks,” another reader suggested, “perhaps it would be easier to provide elective classes for doctors and employees who believe themselves to be at-risk for discrimination, providing them with a ‘toolkit’ of strategies for responding to discrimination in the moment, processing it emotionally later on, and reporting the most egregious events through designated channels.”
Another commenter agreed and wrote that, “While we as doctors need and deserve protection, we are also called to act with compassion. So, rather than ask the system for ‘zero-tolerance’ in either direction, we could encourage our health systems to provide education, support, and mediation to any party who feels or fears that they are not being well served. Such a model would include support for physicians who have been the victims of bias and hurt.”
A version of this article originally appeared on Medscape.com.
If a patient refuses care from a health care practitioner because of their race or sex, should their request be accommodated?
In a recent blog on Medscape titled “No, You Can’t See a Different Doctor: We Need Zero Tolerance of Patient Bias,” Cleveland Francis Jr., MD, argued no.
Dr. Francis, who is Black, is a recently retired cardiologist who practiced for 50 years. He is currently Diversity, Equity, and Inclusion Advisor at Inova Heart and Vascular Institute in Falls Church, Va.
When Francis was a medical student and was preparing to take a patient’s history and perform a medical exam, the patient refused and requested a “White doctor,” he recounted.
“I can remember the hurt and embarrassment as if it were yesterday,” he wrote.
The blog, especially the title, drew strong reactions. Close to 500 readers weighed in.
“The title of my blog sounds harsh,” Dr. Francis said, “but in reality, a simple conversation with the patient usually resolves these issues. The difference is that in the old days, there was utter silence, and the wishes of the patient would be granted”
Health care practitioners “should expect to be treated with respect,” he concluded his blog.
Readers agreed on that point, but they debated whether being uncomfortable with a health care practitioner of a different sex or race always constituted “patient bias.”
Some noted that difficulty understanding a practitioner’s accent, for example, is a legitimate reason for asking for another clinician.
Accents and understanding
“If I am struggling to understand you because your accent is too thick or ... because hearing aids can only do so much, I need to ask for someone else,” a reader commented.
Another chimed in: “My elderly parents changed PCPs frequently during the final years of their lives, mainly due to language barriers encountered with foreign-born providers. Due to progressive hearing loss, they simply couldn’t understand them.”
“It is important to remember that there is a Patient Bill of Rights,” she noted, “the first part of which states, ‘You have the right to safe, considerate, and respectful care, provided in a manner consistent with your beliefs.’ ”
A former charge nurse added: “If a request for change was substantive (poor communication, perceived incompetence, trauma history, etc.), I would move mountains to accommodate it, but IMHO [in my humble opinion], the belief in honoring patient preference doesn’t necessarily need to include rearranging the world in order to accommodate racism, sexism, etc.”
Bias against female doctors, male nurses
Many commenters described how they gladly traded when a patient requested a practitioner of the opposite sex.
A female hospitalist related how she contacted the senior male doctor working with her to arrange a patient trade, adding, “I do agree that racial discrimination ought to be discouraged.”
Similarly, a male ICU RN commented: “Over 13 years, I have had a handful of female (usually older) patients request a female nurse. I have always strived to make this happen.”
However, an older woman related how at first she “had some bias against a male nurse touching me and also felt self-conscious,” she said. “So, I tried to relax ... and let him do his job. He was one of the most compassionate, kind, and sensitive nurses I’ve ever had.”
“I think in some cases,” she noted, “some women have had a history of some sort of abuse by a male, whether it’s sexual or psychological,” but in other cases, “it’s often just a personal preference, not a bias.”
A physician assistant (PA) who worked in a rural ED recounted how “there was only one physician and one PA on at any given evening/night shift, both usually White males.”
“Sometimes, you just have to cope as best you can with whomever is available, and in doing so,” he said, “they might just end up being pleasantly surprised.”
Don’t take it personally, move on
“If a patient doesn’t want to see me for whatever reason, then I would rather not treat them,” was a common sentiment.
Patients “should feel comfortable with their provider even if it’s with someone other than myself,” a reader wrote.
A female physician chimed in: “I frequently have older male patients refuse to see me. ... While this is irritating on several levels, I recognize that it is the patient’s choice, sigh, and move on to the next patient.”
“There are many more patients who specifically ask to see me, so I don’t waste my time and energy on being bothered by those who refuse.”
Similarly, a female mental health provider and sometimes patient wrote: “If any patient tells me that they prefer a male ... or someone of a particular race or religion or whatever, I don’t take it personally.”
A female Hispanic doctor chimed in: “Honestly, if a patient does not want to see me due to my race, I’m OK with that. Patients need to feel comfortable with me for the relationship to be therapeutic and effective,” she said.
“Forcing the patient to see me is adding injury to insult to ME! Not to mention increase[d] workload since that patient will take [so] much more time.”
Similarly, an Asian American doctor commented: “There are people who choose not to see me because of my ethnicity. However, I strongly believe that it should always be the patient’s preference. Whatever the reason, do not force the patient to see you in the name of Diversity, Equity, Inclusion, or whatever hurts your feeling. Let the patient go.”
Patient bias vs. patient preference
A physician referring to Dr. Francis’s experience suggested that “perhaps there was an opportunity to explore this misconception directly with the patient. If not, your supervising senior resident or attending should have been informed and brought into the process and conversation.”
“If/when I were rejected by a patient for whatever reason,” another physician commented, “I would gracefully accede, and hope that my colleague would tactfully point out to the patient their error.”
“Having a nurse ask the patient ... what they need style-wise (keeping race, gender, etc., out of it) might help identify whether or not the underlying issue(s) are based on style/needs mismatch match rather than bias,” a reader suggested.
A health care worker commented: “We generally assure patients that we are professionals and think nothing of situations that they might find uncomfortable, but don’t realize that our comfort does not translate to theirs.”
Maybe a different strategy is needed
“Having been the target of bias many times,” a reader said, “I understand the pain that is inflicted. Unfortunately, a patient bias policy, while a good idea, will not prevent patient bias. This is a much larger societal problem. But we can at least tell patients that it is not okay. On the other hand, I would not want to be the provider for a patient who was biased against me and held me in disdain.”
“I do not like Zero Tolerance policies ever. They are too absolute,” another reader commented. “Sometimes, there are reasons and we do have to listen to our patients for why. ... I do not think a policy of zero tolerance will fix the problem of racism.”
“Instead of trying to educate the general public about how not to be jerks,” another reader suggested, “perhaps it would be easier to provide elective classes for doctors and employees who believe themselves to be at-risk for discrimination, providing them with a ‘toolkit’ of strategies for responding to discrimination in the moment, processing it emotionally later on, and reporting the most egregious events through designated channels.”
Another commenter agreed and wrote that, “While we as doctors need and deserve protection, we are also called to act with compassion. So, rather than ask the system for ‘zero-tolerance’ in either direction, we could encourage our health systems to provide education, support, and mediation to any party who feels or fears that they are not being well served. Such a model would include support for physicians who have been the victims of bias and hurt.”
A version of this article originally appeared on Medscape.com.
Intermittent fasting plus exercise a good option for fatty liver
However, the combined approach did not give significantly added benefit, compared with fasting alone, the researchers report.
Eighty patients with NAFLD were randomized to one of four lifestyle strategies (alternate-day fasting, aerobic exercise, both, or neither) for 3 months.
The primary outcome was change in intrahepatic triglyceride (IHTG) content from baseline to study end, measured by magnetic resonance imaging proton density fat fraction.
The results suggest that “combining intermittent fasting with exercise is effective for reducing hepatic steatosis [fatty liver] in patients with NAFLD but may offer no additional benefit versus fasting alone,” Mark Ezpeleta, PhD, formerly at the University of Illinois, Chicago, and now at the University of Colorado Anschutz Medical Campus, and colleagues conclude.
“Our findings also indicate that the combination intervention was effective for reducing body weight, fat mass, waist circumference, [the liver enzyme alanine transaminase (ALT)], fasting insulin, [and] insulin resistance and increasing insulin sensitivity, among patients with obesity and NAFLD versus controls,” the group reports.
“When we compared the results of our study groups, we saw clearly that the most improved patients were in the group that followed the alternate-day fasting diet and exercised 5 days a week,” senior author Krista A. Varady, PhD, professor of nutrition, University of Illinois, said in a press release from the university.
“The people who only dieted or only exercised did not see the same improvements,” she added, “which reinforces the importance of these two relatively inexpensive lifestyle modifications on overall health and on combating chronic diseases like fatty liver disease.”
Moreover, “alternate-day fasting and exercise interventions can be difficult for people to stick to, and in prior studies we have seen significant dropout,” she noted. “It was very interesting to see that in this trial we had very high adherence to the interventions.”
The study was recently published in Cell Metabolism.
An estimated 65% of people with obesity have NAFLD, or fat in the liver that is not the result of excessive alcohol consumption, which is strongly related to the development of insulin resistance and type 2 diabetes, the group writes.
Thiazolidinediones such as pioglitazone reduce hepatic steatosis, but there is mounting concern about the weight-gaining effect of these compounds.
Recent attention has focused on lifestyle interventions to resolve hepatic steatosis, and previous trials showed that alternate-day fasting was effective for certain outcomes in NAFLD, but those studies did not measure changes in IHTG content or include an exercise intervention.
The researchers enrolled 80 adults with obesity and NAFLD and randomized them to one of four groups for 3 months:
- Alternate day fasting group: Participants were instructed to consume 600 kcal at dinner between 5 PM and 8 PM on a fasting day alternating with food as desired on a feasting day.
- Exercise group: A 60-minute moderate-intensity aerobic exercise session 5 times a week.
- Fasting plus exercise group.
- Control group (no intervention).
Participants were age 23-65 (mean age, 44) and 81% were women.
Half were Hispanic, and the rest were Black (30%), White (11%), or Asian (9%).
They had a mean weight of 99 kg (218 lb) and a mean body mass index of 36 kg/m2.
Dropout rates were minimal in the combination group (0%) and fasting groups (5%) and moderately high in the exercise group (25%).
IHTG content was reduced by a significantly greater amount in the combination group (–5.48%) than in the exercise alone group (–1.30%; P = .02) or in the control group (–0.17%; P < .01) and by a greater amount than in the fasting alone group, although this was not significant (–2.25%; P = .05).
Lean mass, aspartate transaminase (AST), A1c, blood pressure, plasma lipids, liver fibrosis score, and hepatokines (fetuin-A, FGF-21, and selenoprotein P) did not differ between groups.
Researchers acknowledge that although the combination intervention resulted in improved NAFLD parameters, IHTG and ALT did not reach the normal range.
Participants likely had early stage NAFLD (their baseline IHTG was in the 16% to 18% range, where 5% to 33% is mild steatosis) and they were likely highly motivated (indicated by the low dropout rate), so the findings may not be generalizable.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. Dr. Varady has reported receiving author fees from the Hachette Book Group for the book entitled “The Every Other Day Diet.” The other authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
However, the combined approach did not give significantly added benefit, compared with fasting alone, the researchers report.
Eighty patients with NAFLD were randomized to one of four lifestyle strategies (alternate-day fasting, aerobic exercise, both, or neither) for 3 months.
The primary outcome was change in intrahepatic triglyceride (IHTG) content from baseline to study end, measured by magnetic resonance imaging proton density fat fraction.
The results suggest that “combining intermittent fasting with exercise is effective for reducing hepatic steatosis [fatty liver] in patients with NAFLD but may offer no additional benefit versus fasting alone,” Mark Ezpeleta, PhD, formerly at the University of Illinois, Chicago, and now at the University of Colorado Anschutz Medical Campus, and colleagues conclude.
“Our findings also indicate that the combination intervention was effective for reducing body weight, fat mass, waist circumference, [the liver enzyme alanine transaminase (ALT)], fasting insulin, [and] insulin resistance and increasing insulin sensitivity, among patients with obesity and NAFLD versus controls,” the group reports.
“When we compared the results of our study groups, we saw clearly that the most improved patients were in the group that followed the alternate-day fasting diet and exercised 5 days a week,” senior author Krista A. Varady, PhD, professor of nutrition, University of Illinois, said in a press release from the university.
“The people who only dieted or only exercised did not see the same improvements,” she added, “which reinforces the importance of these two relatively inexpensive lifestyle modifications on overall health and on combating chronic diseases like fatty liver disease.”
Moreover, “alternate-day fasting and exercise interventions can be difficult for people to stick to, and in prior studies we have seen significant dropout,” she noted. “It was very interesting to see that in this trial we had very high adherence to the interventions.”
The study was recently published in Cell Metabolism.
An estimated 65% of people with obesity have NAFLD, or fat in the liver that is not the result of excessive alcohol consumption, which is strongly related to the development of insulin resistance and type 2 diabetes, the group writes.
Thiazolidinediones such as pioglitazone reduce hepatic steatosis, but there is mounting concern about the weight-gaining effect of these compounds.
Recent attention has focused on lifestyle interventions to resolve hepatic steatosis, and previous trials showed that alternate-day fasting was effective for certain outcomes in NAFLD, but those studies did not measure changes in IHTG content or include an exercise intervention.
The researchers enrolled 80 adults with obesity and NAFLD and randomized them to one of four groups for 3 months:
- Alternate day fasting group: Participants were instructed to consume 600 kcal at dinner between 5 PM and 8 PM on a fasting day alternating with food as desired on a feasting day.
- Exercise group: A 60-minute moderate-intensity aerobic exercise session 5 times a week.
- Fasting plus exercise group.
- Control group (no intervention).
Participants were age 23-65 (mean age, 44) and 81% were women.
Half were Hispanic, and the rest were Black (30%), White (11%), or Asian (9%).
They had a mean weight of 99 kg (218 lb) and a mean body mass index of 36 kg/m2.
Dropout rates were minimal in the combination group (0%) and fasting groups (5%) and moderately high in the exercise group (25%).
IHTG content was reduced by a significantly greater amount in the combination group (–5.48%) than in the exercise alone group (–1.30%; P = .02) or in the control group (–0.17%; P < .01) and by a greater amount than in the fasting alone group, although this was not significant (–2.25%; P = .05).
Lean mass, aspartate transaminase (AST), A1c, blood pressure, plasma lipids, liver fibrosis score, and hepatokines (fetuin-A, FGF-21, and selenoprotein P) did not differ between groups.
Researchers acknowledge that although the combination intervention resulted in improved NAFLD parameters, IHTG and ALT did not reach the normal range.
Participants likely had early stage NAFLD (their baseline IHTG was in the 16% to 18% range, where 5% to 33% is mild steatosis) and they were likely highly motivated (indicated by the low dropout rate), so the findings may not be generalizable.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. Dr. Varady has reported receiving author fees from the Hachette Book Group for the book entitled “The Every Other Day Diet.” The other authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
However, the combined approach did not give significantly added benefit, compared with fasting alone, the researchers report.
Eighty patients with NAFLD were randomized to one of four lifestyle strategies (alternate-day fasting, aerobic exercise, both, or neither) for 3 months.
The primary outcome was change in intrahepatic triglyceride (IHTG) content from baseline to study end, measured by magnetic resonance imaging proton density fat fraction.
The results suggest that “combining intermittent fasting with exercise is effective for reducing hepatic steatosis [fatty liver] in patients with NAFLD but may offer no additional benefit versus fasting alone,” Mark Ezpeleta, PhD, formerly at the University of Illinois, Chicago, and now at the University of Colorado Anschutz Medical Campus, and colleagues conclude.
“Our findings also indicate that the combination intervention was effective for reducing body weight, fat mass, waist circumference, [the liver enzyme alanine transaminase (ALT)], fasting insulin, [and] insulin resistance and increasing insulin sensitivity, among patients with obesity and NAFLD versus controls,” the group reports.
“When we compared the results of our study groups, we saw clearly that the most improved patients were in the group that followed the alternate-day fasting diet and exercised 5 days a week,” senior author Krista A. Varady, PhD, professor of nutrition, University of Illinois, said in a press release from the university.
“The people who only dieted or only exercised did not see the same improvements,” she added, “which reinforces the importance of these two relatively inexpensive lifestyle modifications on overall health and on combating chronic diseases like fatty liver disease.”
Moreover, “alternate-day fasting and exercise interventions can be difficult for people to stick to, and in prior studies we have seen significant dropout,” she noted. “It was very interesting to see that in this trial we had very high adherence to the interventions.”
The study was recently published in Cell Metabolism.
An estimated 65% of people with obesity have NAFLD, or fat in the liver that is not the result of excessive alcohol consumption, which is strongly related to the development of insulin resistance and type 2 diabetes, the group writes.
Thiazolidinediones such as pioglitazone reduce hepatic steatosis, but there is mounting concern about the weight-gaining effect of these compounds.
Recent attention has focused on lifestyle interventions to resolve hepatic steatosis, and previous trials showed that alternate-day fasting was effective for certain outcomes in NAFLD, but those studies did not measure changes in IHTG content or include an exercise intervention.
The researchers enrolled 80 adults with obesity and NAFLD and randomized them to one of four groups for 3 months:
- Alternate day fasting group: Participants were instructed to consume 600 kcal at dinner between 5 PM and 8 PM on a fasting day alternating with food as desired on a feasting day.
- Exercise group: A 60-minute moderate-intensity aerobic exercise session 5 times a week.
- Fasting plus exercise group.
- Control group (no intervention).
Participants were age 23-65 (mean age, 44) and 81% were women.
Half were Hispanic, and the rest were Black (30%), White (11%), or Asian (9%).
They had a mean weight of 99 kg (218 lb) and a mean body mass index of 36 kg/m2.
Dropout rates were minimal in the combination group (0%) and fasting groups (5%) and moderately high in the exercise group (25%).
IHTG content was reduced by a significantly greater amount in the combination group (–5.48%) than in the exercise alone group (–1.30%; P = .02) or in the control group (–0.17%; P < .01) and by a greater amount than in the fasting alone group, although this was not significant (–2.25%; P = .05).
Lean mass, aspartate transaminase (AST), A1c, blood pressure, plasma lipids, liver fibrosis score, and hepatokines (fetuin-A, FGF-21, and selenoprotein P) did not differ between groups.
Researchers acknowledge that although the combination intervention resulted in improved NAFLD parameters, IHTG and ALT did not reach the normal range.
Participants likely had early stage NAFLD (their baseline IHTG was in the 16% to 18% range, where 5% to 33% is mild steatosis) and they were likely highly motivated (indicated by the low dropout rate), so the findings may not be generalizable.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. Dr. Varady has reported receiving author fees from the Hachette Book Group for the book entitled “The Every Other Day Diet.” The other authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CELL METABOLISM
‘Forever chemicals’ up type 2 diabetes risk in midlife White women
Middle-aged White women who had higher levels of some breakdown products of phthalates – a class of endocrine disrupting chemicals (EDCs), or “forever chemicals,” that act as plasticizers – had a significantly greater risk of developing type 2 diabetes over a 6-year period compared with other similar women.
However, this association was not seen among Black or Asian middle-aged women.
These findings from the Study of Women’s Health Across the Nation – Multipollutant Study (SWAN-MPS), by Mia Q. Peng, PhD, MPH, and colleagues, have been published online in the Journal of Clinical Endocrinology & Metabolism.
“Overall, our study has added some evidence to support the potential diabetogenic effects of phthalates, but it also highlights that much is still unknown about the metabolic effects of these chemicals,” the group noted.
“The apparent racial/ethnic differences in the associations between phthalates and incident diabetes should be investigated in future studies,” they cautioned.
Recruiting younger participants and observing them longer, they suggested, “will also help us understand the effects of phthalates on different stages of the diabetogenic process, including whether body fat gain is an important mediator.”
Phthalates are all around us
Low-molecular-weight phthalates are frequently added to personal care products, such as fragrance, nail polish, and some feminine hygiene products, as solvents, plasticizers, and fixatives, the researchers explained.
And high-molecular-weight phthalates are frequently added to polyvinyl chloride plastic products, such as plastic food packaging, clothing, and vinyl flooring, as plasticizers.
Phthalates have been hypothesized to contribute to the development of diabetes, but longitudinal evidence in humans was limited.
“Given widespread exposure to phthalates and the enormous costs of diabetes to individuals and societies, ongoing investments in the research on phthalates’ metabolic effects are warranted,” the researchers concluded.
Racial differences in phthalates and incident diabetes
“A new finding is that we observed some phthalates are associated with a higher risk of diabetes development, especially in White women [that] were not seen in Black or Asian women,” senior author Sung Kyun Park, ScD, MPH, of the University of Michigan, Ann Arbor, told this news organization.
“We were surprised to see the racial/ethnic differences,” added Dr. Peng, formerly of the University of Michigan and now at Lifecourse Epidemiology of Adiposity and Diabetes Center, University of Colorado Anschutz Medical Campus.
A possible explanation is that “compared to White women, Black women develop diabetes at a younger age and are exposed to higher levels of several phthalates,” and this study excluded women who already had diabetes by midlife, she noted.
“Although our study was conducted in a cohort of women,” Dr. Park stressed, “we hope that our findings are not interpreted that only women should be concerned of phthalates. Our findings add to the current literature that phthalates may be a potential risk factor for type 2 diabetes.
“Certain phthalates are prohibited in children’s toys and child care articles,” Dr. Peng noted, as explained by the U.S. Consumer Product Safety Commission. In addition, a bill has been introduced in Congress to ban phthalates in food contact substances.
“If phthalates are removed from plastics and other consumer products,” she cautioned, “we do have to be careful in the process to avoid replacing them with some other potentially harmful chemicals.”
A well-known example of this type of “regrettable substitution,” Dr. Park added, “is ‘BPA-free’ plastics that replaced bisphenol A with other bisphenols such as bisphenol-F (BPF) or bisphenol-S (BPS). The product has a label of ‘BPA-free’, but those replaced chemicals turned out to be equally toxic. Science is slow to determine if a new chemical introduced to the market is safe and can replace a regulated chemical.”
And studies have shown that a diet rich in meat, fat, and ultraprocessed foods is associated with increased exposures to some phthalates, especially when the foods are obtained away from home, such as fast foods, Dr. Peng observed. In addition, some phthalates are added to personal care products such as fragrance.
“As a first step,” she said, “I think reducing consumption of ultraprocessed foods packaged in plastics may help reduce phthalate exposure.”
A 2020 report from the Endocrine Society and the International Pollutants Elimination Network (IPEN), titled, “Plastics, EDCs, and Health,” summarizes research on bisphenol A, per- and polyfluoroalkyl substances (PFAS), phthalates, and other EDCs that leach from plastics. The Endocrine Society website also has a link to a 2-page summary.
Levels of 12 phthalate metabolites
Previously, the researchers reported how another class of “forever chemicals,” PFAS, were associated with risk of hypertension in a 17-year follow-up of middle-aged women in the SWAN study.
In the current study, they analyzed data from 1,308 women in SWAN-MPS who had been recruited at five study sites (Oakland, Calif; Los Angeles; Detroit; Pittsburgh; and Boston).
The women were between ages 42 and 52 years in 1996-1997 and self-identified as White, Black, Chinese, or Japanese.
They did not have diabetes in 1999-2000 and had sufficient urine samples for phthalate assessment then and midway through a 6-year follow-up.
The women were a median age of 49 years in 1999-2000. About half were White, 20% were Black, 13% were Chinese, and 15% were Japanese.
Researchers analyzed levels of 12 metabolites, chosen because their parent phthalates have been widely used in industry and commerce, and exposure to these phthalates is a national biomonitoring priority.
The measured phthalates were:
Three metabolites of low-molecular-weight phthalates:
- mono-ethyl phthalate (MEP)
- mono-n-butyl phthalate (MnBP)
- mono-isobutyl phthalate (MiBP)
Four metabolites of the high-molecular-weight phthalate di(2-ethylhexyl) phthalate (DEHP), which is of particular public health interest:
- mono(2-ethylhexyl) phthalate (MEHP)
- mono(2-ethyl-5-hydroxyhexyl) phthalate (MEHHP)
- mono(2-ethyl-5-oxohexyl) phthalate (MEOHP)
- mono(2-ethyl-5-carboxypentyl) phthalate (MECPP)
Five metabolites of other high-molecular-weight phthalates:
- monobenzyl phthalate (MBzP)
- monoisononyl phthalate (MiNP)
- mono-carboxyoctyl phthalate (MCOP)
- mono-carboxy-isononyl phthalate (MCNP)
- mono(3-carboxypropyl) phthalate (MCPP)
The researchers excluded MiNP from all analyses because it was detected in less than 1% of urine samples.
The different phthalate metabolites were detected in 84.8% of samples (MEHP) to 100% of samples (MnBP and MECPP).
Women who were younger, Black, current smokers, or obese generally had higher concentrations of phthalate metabolites.
Over 6 years, 61 women developed diabetes (an incidence rate of 8.1 per 1000 person-years).
Compared with other women, those with incident diabetes had significantly higher concentrations of all phthalate metabolites except DEHP metabolites and MCPP.
Phthalates were not associated with incident diabetes in Black or Asian women.
However, among White women, each doubling of the concentrations of MiBP, MBzP, MCOP, MCNP, and MCCP was associated with a 30% to 63% higher incidence of diabetes (HR 1.30 for MCNP; HR 1.63 for MiBP).
The SWAN study was supported by the National Institutes of Health, Department of Health & Human Services, National Institute on Aging, National Institute of Nursing Research, NIH Office of Research on Women’s Health, and SWAN Repository. The current study was supported by the National Center for Research Resources, National Center for Advancing Translational Sciences, NIH, National Institute of Environmental Health, and Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. Dr. Peng was supported by an Interdisciplinary Research Training on Health and Aging grant from the NIA. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Middle-aged White women who had higher levels of some breakdown products of phthalates – a class of endocrine disrupting chemicals (EDCs), or “forever chemicals,” that act as plasticizers – had a significantly greater risk of developing type 2 diabetes over a 6-year period compared with other similar women.
However, this association was not seen among Black or Asian middle-aged women.
These findings from the Study of Women’s Health Across the Nation – Multipollutant Study (SWAN-MPS), by Mia Q. Peng, PhD, MPH, and colleagues, have been published online in the Journal of Clinical Endocrinology & Metabolism.
“Overall, our study has added some evidence to support the potential diabetogenic effects of phthalates, but it also highlights that much is still unknown about the metabolic effects of these chemicals,” the group noted.
“The apparent racial/ethnic differences in the associations between phthalates and incident diabetes should be investigated in future studies,” they cautioned.
Recruiting younger participants and observing them longer, they suggested, “will also help us understand the effects of phthalates on different stages of the diabetogenic process, including whether body fat gain is an important mediator.”
Phthalates are all around us
Low-molecular-weight phthalates are frequently added to personal care products, such as fragrance, nail polish, and some feminine hygiene products, as solvents, plasticizers, and fixatives, the researchers explained.
And high-molecular-weight phthalates are frequently added to polyvinyl chloride plastic products, such as plastic food packaging, clothing, and vinyl flooring, as plasticizers.
Phthalates have been hypothesized to contribute to the development of diabetes, but longitudinal evidence in humans was limited.
“Given widespread exposure to phthalates and the enormous costs of diabetes to individuals and societies, ongoing investments in the research on phthalates’ metabolic effects are warranted,” the researchers concluded.
Racial differences in phthalates and incident diabetes
“A new finding is that we observed some phthalates are associated with a higher risk of diabetes development, especially in White women [that] were not seen in Black or Asian women,” senior author Sung Kyun Park, ScD, MPH, of the University of Michigan, Ann Arbor, told this news organization.
“We were surprised to see the racial/ethnic differences,” added Dr. Peng, formerly of the University of Michigan and now at Lifecourse Epidemiology of Adiposity and Diabetes Center, University of Colorado Anschutz Medical Campus.
A possible explanation is that “compared to White women, Black women develop diabetes at a younger age and are exposed to higher levels of several phthalates,” and this study excluded women who already had diabetes by midlife, she noted.
“Although our study was conducted in a cohort of women,” Dr. Park stressed, “we hope that our findings are not interpreted that only women should be concerned of phthalates. Our findings add to the current literature that phthalates may be a potential risk factor for type 2 diabetes.
“Certain phthalates are prohibited in children’s toys and child care articles,” Dr. Peng noted, as explained by the U.S. Consumer Product Safety Commission. In addition, a bill has been introduced in Congress to ban phthalates in food contact substances.
“If phthalates are removed from plastics and other consumer products,” she cautioned, “we do have to be careful in the process to avoid replacing them with some other potentially harmful chemicals.”
A well-known example of this type of “regrettable substitution,” Dr. Park added, “is ‘BPA-free’ plastics that replaced bisphenol A with other bisphenols such as bisphenol-F (BPF) or bisphenol-S (BPS). The product has a label of ‘BPA-free’, but those replaced chemicals turned out to be equally toxic. Science is slow to determine if a new chemical introduced to the market is safe and can replace a regulated chemical.”
And studies have shown that a diet rich in meat, fat, and ultraprocessed foods is associated with increased exposures to some phthalates, especially when the foods are obtained away from home, such as fast foods, Dr. Peng observed. In addition, some phthalates are added to personal care products such as fragrance.
“As a first step,” she said, “I think reducing consumption of ultraprocessed foods packaged in plastics may help reduce phthalate exposure.”
A 2020 report from the Endocrine Society and the International Pollutants Elimination Network (IPEN), titled, “Plastics, EDCs, and Health,” summarizes research on bisphenol A, per- and polyfluoroalkyl substances (PFAS), phthalates, and other EDCs that leach from plastics. The Endocrine Society website also has a link to a 2-page summary.
Levels of 12 phthalate metabolites
Previously, the researchers reported how another class of “forever chemicals,” PFAS, were associated with risk of hypertension in a 17-year follow-up of middle-aged women in the SWAN study.
In the current study, they analyzed data from 1,308 women in SWAN-MPS who had been recruited at five study sites (Oakland, Calif; Los Angeles; Detroit; Pittsburgh; and Boston).
The women were between ages 42 and 52 years in 1996-1997 and self-identified as White, Black, Chinese, or Japanese.
They did not have diabetes in 1999-2000 and had sufficient urine samples for phthalate assessment then and midway through a 6-year follow-up.
The women were a median age of 49 years in 1999-2000. About half were White, 20% were Black, 13% were Chinese, and 15% were Japanese.
Researchers analyzed levels of 12 metabolites, chosen because their parent phthalates have been widely used in industry and commerce, and exposure to these phthalates is a national biomonitoring priority.
The measured phthalates were:
Three metabolites of low-molecular-weight phthalates:
- mono-ethyl phthalate (MEP)
- mono-n-butyl phthalate (MnBP)
- mono-isobutyl phthalate (MiBP)
Four metabolites of the high-molecular-weight phthalate di(2-ethylhexyl) phthalate (DEHP), which is of particular public health interest:
- mono(2-ethylhexyl) phthalate (MEHP)
- mono(2-ethyl-5-hydroxyhexyl) phthalate (MEHHP)
- mono(2-ethyl-5-oxohexyl) phthalate (MEOHP)
- mono(2-ethyl-5-carboxypentyl) phthalate (MECPP)
Five metabolites of other high-molecular-weight phthalates:
- monobenzyl phthalate (MBzP)
- monoisononyl phthalate (MiNP)
- mono-carboxyoctyl phthalate (MCOP)
- mono-carboxy-isononyl phthalate (MCNP)
- mono(3-carboxypropyl) phthalate (MCPP)
The researchers excluded MiNP from all analyses because it was detected in less than 1% of urine samples.
The different phthalate metabolites were detected in 84.8% of samples (MEHP) to 100% of samples (MnBP and MECPP).
Women who were younger, Black, current smokers, or obese generally had higher concentrations of phthalate metabolites.
Over 6 years, 61 women developed diabetes (an incidence rate of 8.1 per 1000 person-years).
Compared with other women, those with incident diabetes had significantly higher concentrations of all phthalate metabolites except DEHP metabolites and MCPP.
Phthalates were not associated with incident diabetes in Black or Asian women.
However, among White women, each doubling of the concentrations of MiBP, MBzP, MCOP, MCNP, and MCCP was associated with a 30% to 63% higher incidence of diabetes (HR 1.30 for MCNP; HR 1.63 for MiBP).
The SWAN study was supported by the National Institutes of Health, Department of Health & Human Services, National Institute on Aging, National Institute of Nursing Research, NIH Office of Research on Women’s Health, and SWAN Repository. The current study was supported by the National Center for Research Resources, National Center for Advancing Translational Sciences, NIH, National Institute of Environmental Health, and Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. Dr. Peng was supported by an Interdisciplinary Research Training on Health and Aging grant from the NIA. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Middle-aged White women who had higher levels of some breakdown products of phthalates – a class of endocrine disrupting chemicals (EDCs), or “forever chemicals,” that act as plasticizers – had a significantly greater risk of developing type 2 diabetes over a 6-year period compared with other similar women.
However, this association was not seen among Black or Asian middle-aged women.
These findings from the Study of Women’s Health Across the Nation – Multipollutant Study (SWAN-MPS), by Mia Q. Peng, PhD, MPH, and colleagues, have been published online in the Journal of Clinical Endocrinology & Metabolism.
“Overall, our study has added some evidence to support the potential diabetogenic effects of phthalates, but it also highlights that much is still unknown about the metabolic effects of these chemicals,” the group noted.
“The apparent racial/ethnic differences in the associations between phthalates and incident diabetes should be investigated in future studies,” they cautioned.
Recruiting younger participants and observing them longer, they suggested, “will also help us understand the effects of phthalates on different stages of the diabetogenic process, including whether body fat gain is an important mediator.”
Phthalates are all around us
Low-molecular-weight phthalates are frequently added to personal care products, such as fragrance, nail polish, and some feminine hygiene products, as solvents, plasticizers, and fixatives, the researchers explained.
And high-molecular-weight phthalates are frequently added to polyvinyl chloride plastic products, such as plastic food packaging, clothing, and vinyl flooring, as plasticizers.
Phthalates have been hypothesized to contribute to the development of diabetes, but longitudinal evidence in humans was limited.
“Given widespread exposure to phthalates and the enormous costs of diabetes to individuals and societies, ongoing investments in the research on phthalates’ metabolic effects are warranted,” the researchers concluded.
Racial differences in phthalates and incident diabetes
“A new finding is that we observed some phthalates are associated with a higher risk of diabetes development, especially in White women [that] were not seen in Black or Asian women,” senior author Sung Kyun Park, ScD, MPH, of the University of Michigan, Ann Arbor, told this news organization.
“We were surprised to see the racial/ethnic differences,” added Dr. Peng, formerly of the University of Michigan and now at Lifecourse Epidemiology of Adiposity and Diabetes Center, University of Colorado Anschutz Medical Campus.
A possible explanation is that “compared to White women, Black women develop diabetes at a younger age and are exposed to higher levels of several phthalates,” and this study excluded women who already had diabetes by midlife, she noted.
“Although our study was conducted in a cohort of women,” Dr. Park stressed, “we hope that our findings are not interpreted that only women should be concerned of phthalates. Our findings add to the current literature that phthalates may be a potential risk factor for type 2 diabetes.
“Certain phthalates are prohibited in children’s toys and child care articles,” Dr. Peng noted, as explained by the U.S. Consumer Product Safety Commission. In addition, a bill has been introduced in Congress to ban phthalates in food contact substances.
“If phthalates are removed from plastics and other consumer products,” she cautioned, “we do have to be careful in the process to avoid replacing them with some other potentially harmful chemicals.”
A well-known example of this type of “regrettable substitution,” Dr. Park added, “is ‘BPA-free’ plastics that replaced bisphenol A with other bisphenols such as bisphenol-F (BPF) or bisphenol-S (BPS). The product has a label of ‘BPA-free’, but those replaced chemicals turned out to be equally toxic. Science is slow to determine if a new chemical introduced to the market is safe and can replace a regulated chemical.”
And studies have shown that a diet rich in meat, fat, and ultraprocessed foods is associated with increased exposures to some phthalates, especially when the foods are obtained away from home, such as fast foods, Dr. Peng observed. In addition, some phthalates are added to personal care products such as fragrance.
“As a first step,” she said, “I think reducing consumption of ultraprocessed foods packaged in plastics may help reduce phthalate exposure.”
A 2020 report from the Endocrine Society and the International Pollutants Elimination Network (IPEN), titled, “Plastics, EDCs, and Health,” summarizes research on bisphenol A, per- and polyfluoroalkyl substances (PFAS), phthalates, and other EDCs that leach from plastics. The Endocrine Society website also has a link to a 2-page summary.
Levels of 12 phthalate metabolites
Previously, the researchers reported how another class of “forever chemicals,” PFAS, were associated with risk of hypertension in a 17-year follow-up of middle-aged women in the SWAN study.
In the current study, they analyzed data from 1,308 women in SWAN-MPS who had been recruited at five study sites (Oakland, Calif; Los Angeles; Detroit; Pittsburgh; and Boston).
The women were between ages 42 and 52 years in 1996-1997 and self-identified as White, Black, Chinese, or Japanese.
They did not have diabetes in 1999-2000 and had sufficient urine samples for phthalate assessment then and midway through a 6-year follow-up.
The women were a median age of 49 years in 1999-2000. About half were White, 20% were Black, 13% were Chinese, and 15% were Japanese.
Researchers analyzed levels of 12 metabolites, chosen because their parent phthalates have been widely used in industry and commerce, and exposure to these phthalates is a national biomonitoring priority.
The measured phthalates were:
Three metabolites of low-molecular-weight phthalates:
- mono-ethyl phthalate (MEP)
- mono-n-butyl phthalate (MnBP)
- mono-isobutyl phthalate (MiBP)
Four metabolites of the high-molecular-weight phthalate di(2-ethylhexyl) phthalate (DEHP), which is of particular public health interest:
- mono(2-ethylhexyl) phthalate (MEHP)
- mono(2-ethyl-5-hydroxyhexyl) phthalate (MEHHP)
- mono(2-ethyl-5-oxohexyl) phthalate (MEOHP)
- mono(2-ethyl-5-carboxypentyl) phthalate (MECPP)
Five metabolites of other high-molecular-weight phthalates:
- monobenzyl phthalate (MBzP)
- monoisononyl phthalate (MiNP)
- mono-carboxyoctyl phthalate (MCOP)
- mono-carboxy-isononyl phthalate (MCNP)
- mono(3-carboxypropyl) phthalate (MCPP)
The researchers excluded MiNP from all analyses because it was detected in less than 1% of urine samples.
The different phthalate metabolites were detected in 84.8% of samples (MEHP) to 100% of samples (MnBP and MECPP).
Women who were younger, Black, current smokers, or obese generally had higher concentrations of phthalate metabolites.
Over 6 years, 61 women developed diabetes (an incidence rate of 8.1 per 1000 person-years).
Compared with other women, those with incident diabetes had significantly higher concentrations of all phthalate metabolites except DEHP metabolites and MCPP.
Phthalates were not associated with incident diabetes in Black or Asian women.
However, among White women, each doubling of the concentrations of MiBP, MBzP, MCOP, MCNP, and MCCP was associated with a 30% to 63% higher incidence of diabetes (HR 1.30 for MCNP; HR 1.63 for MiBP).
The SWAN study was supported by the National Institutes of Health, Department of Health & Human Services, National Institute on Aging, National Institute of Nursing Research, NIH Office of Research on Women’s Health, and SWAN Repository. The current study was supported by the National Center for Research Resources, National Center for Advancing Translational Sciences, NIH, National Institute of Environmental Health, and Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. Dr. Peng was supported by an Interdisciplinary Research Training on Health and Aging grant from the NIA. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.