User login
Are microRNAs the key to an endometriosis biomarker?
SAN ANTONIO – The results of a prospective study showed that, in patients without a surgical endometriosis diagnosis, a serum test of microRNA (miRNA) levels yielded a very high predictive value when endometriosis was later surgically confirmed.
“This is the first prospective study performed within a diverse population that identifies miRNAs can reliably be used to differentiate between endometriosis and other gynecologic pathologies,” Sarah Moustafa, MD, said at the annual meeting of the American Society for Reproductive Medicine.
Dr. Moustafa and her collaborators found that the area under the receiver operating characteristic curve (AUC) for the combination of miRNAs 125, 451, and 3613 was 0.917. The AUC of another combination was even higher: the miRNAs let-7b, 150, 342, and 451 yielded an AUC of 0.977 for endometriosis. These figures support that the miRNA combinations give “an excellent diagnostic potential for endometriosis,” Dr. Moustafa said.
The study enrolled 86 women of reproductive age who were scheduled to have a laparotomy or laparoscopy for benign gynecologic reasons. Pregnant patients and those with malignancy were excluded. Patients had blood drawn before their surgeries to have blinded miRNA analysis via quantitative reverse transcriptase polymerase chain reaction.
Dr. Moustafa and her colleagues looked at the diagnostic value of individual miRNAs and also examined combinations of promising miRNAs by seeing which levels were elevated or depressed in patients who were later found to have surgically diagnosed endometriosis. The study built on previous retrospective work that had identified some candidate miRNAs.
In this prospective study, women with endometriosis had significantly lower serum levels of miRNAs 3613 and let-7b and significantly higher serum levels of miRNAs 150, 125b, 451, and 342. The investigators also analyzed the data to see if there were miRNA level differences between women who were on hormones and those who were not, and also to see if cycle timing affected results; neither of these factors affected miRNA levels, Dr. Moustafa reported.
When the enrolled patients had surgery, 36 were found to have endometriosis and 50 had a variety of other diagnoses, with uterine fibroids (48%) and no abnormal pathology (28%) predominating.
“A noninvasive diagnostic test does not currently exist” but is sorely needed, Dr. Moustafa said.
There’s a long gap from the onset of endometriosis symptoms to diagnosis, with one study showing that symptoms can be present for an average of 6.7-11 years before surgical diagnosis occurs. In one survey of more than 7,000 women, nearly half (46%) saw more than five physicians before they got the correct diagnosis, said Dr. Moustafa, a resident in the obstetrics, gynecology, and reproductive sciences department at Yale University, New Haven, Conn.
In a discussion following the presentation, attendee Steve Young, MD, PhD, professor of reproductive endocrinology and fertility at the University of North Carolina, Chapel Hill, said it would be useful to have a biomarker that could be a surrogate for disease burden. “You could look at miRNAs after surgery. Do you see changes back toward normal?” Dr. Young said.
Dr. Moustafa responded that the research team is in the process of collecting postoperative data to see whether levels change when the disease burden is diminished by surgery.
Next steps, she said, include looking for miRNAs in saliva to explore whether an even less invasive test might be possible. Also, there are suggestions that miRNA 125 might be a marker for more severe disease, so the team is investigating this association as well.
Whether the combination miRNA screen is ready for prime time is still an open question, she said. “Any time a new screening test is developed we have to have caution.” Current thinking, she said, points toward the utility of miRNA screening for patients with unexplained fertility, for example.
“At this point, the pendulum is so far on the side of underdiagnosis that we think patients would benefit from a screening test,” Dr. Moustafa added.
The study was supported by OvaScience. Dr. Moustafa reported having no relevant financial disclosures.
[email protected]
On Twitter @karioakes
SAN ANTONIO – The results of a prospective study showed that, in patients without a surgical endometriosis diagnosis, a serum test of microRNA (miRNA) levels yielded a very high predictive value when endometriosis was later surgically confirmed.
“This is the first prospective study performed within a diverse population that identifies miRNAs can reliably be used to differentiate between endometriosis and other gynecologic pathologies,” Sarah Moustafa, MD, said at the annual meeting of the American Society for Reproductive Medicine.
Dr. Moustafa and her collaborators found that the area under the receiver operating characteristic curve (AUC) for the combination of miRNAs 125, 451, and 3613 was 0.917. The AUC of another combination was even higher: the miRNAs let-7b, 150, 342, and 451 yielded an AUC of 0.977 for endometriosis. These figures support that the miRNA combinations give “an excellent diagnostic potential for endometriosis,” Dr. Moustafa said.
The study enrolled 86 women of reproductive age who were scheduled to have a laparotomy or laparoscopy for benign gynecologic reasons. Pregnant patients and those with malignancy were excluded. Patients had blood drawn before their surgeries to have blinded miRNA analysis via quantitative reverse transcriptase polymerase chain reaction.
Dr. Moustafa and her colleagues looked at the diagnostic value of individual miRNAs and also examined combinations of promising miRNAs by seeing which levels were elevated or depressed in patients who were later found to have surgically diagnosed endometriosis. The study built on previous retrospective work that had identified some candidate miRNAs.
In this prospective study, women with endometriosis had significantly lower serum levels of miRNAs 3613 and let-7b and significantly higher serum levels of miRNAs 150, 125b, 451, and 342. The investigators also analyzed the data to see if there were miRNA level differences between women who were on hormones and those who were not, and also to see if cycle timing affected results; neither of these factors affected miRNA levels, Dr. Moustafa reported.
When the enrolled patients had surgery, 36 were found to have endometriosis and 50 had a variety of other diagnoses, with uterine fibroids (48%) and no abnormal pathology (28%) predominating.
“A noninvasive diagnostic test does not currently exist” but is sorely needed, Dr. Moustafa said.
There’s a long gap from the onset of endometriosis symptoms to diagnosis, with one study showing that symptoms can be present for an average of 6.7-11 years before surgical diagnosis occurs. In one survey of more than 7,000 women, nearly half (46%) saw more than five physicians before they got the correct diagnosis, said Dr. Moustafa, a resident in the obstetrics, gynecology, and reproductive sciences department at Yale University, New Haven, Conn.
In a discussion following the presentation, attendee Steve Young, MD, PhD, professor of reproductive endocrinology and fertility at the University of North Carolina, Chapel Hill, said it would be useful to have a biomarker that could be a surrogate for disease burden. “You could look at miRNAs after surgery. Do you see changes back toward normal?” Dr. Young said.
Dr. Moustafa responded that the research team is in the process of collecting postoperative data to see whether levels change when the disease burden is diminished by surgery.
Next steps, she said, include looking for miRNAs in saliva to explore whether an even less invasive test might be possible. Also, there are suggestions that miRNA 125 might be a marker for more severe disease, so the team is investigating this association as well.
Whether the combination miRNA screen is ready for prime time is still an open question, she said. “Any time a new screening test is developed we have to have caution.” Current thinking, she said, points toward the utility of miRNA screening for patients with unexplained fertility, for example.
“At this point, the pendulum is so far on the side of underdiagnosis that we think patients would benefit from a screening test,” Dr. Moustafa added.
The study was supported by OvaScience. Dr. Moustafa reported having no relevant financial disclosures.
[email protected]
On Twitter @karioakes
SAN ANTONIO – The results of a prospective study showed that, in patients without a surgical endometriosis diagnosis, a serum test of microRNA (miRNA) levels yielded a very high predictive value when endometriosis was later surgically confirmed.
“This is the first prospective study performed within a diverse population that identifies miRNAs can reliably be used to differentiate between endometriosis and other gynecologic pathologies,” Sarah Moustafa, MD, said at the annual meeting of the American Society for Reproductive Medicine.
Dr. Moustafa and her collaborators found that the area under the receiver operating characteristic curve (AUC) for the combination of miRNAs 125, 451, and 3613 was 0.917. The AUC of another combination was even higher: the miRNAs let-7b, 150, 342, and 451 yielded an AUC of 0.977 for endometriosis. These figures support that the miRNA combinations give “an excellent diagnostic potential for endometriosis,” Dr. Moustafa said.
The study enrolled 86 women of reproductive age who were scheduled to have a laparotomy or laparoscopy for benign gynecologic reasons. Pregnant patients and those with malignancy were excluded. Patients had blood drawn before their surgeries to have blinded miRNA analysis via quantitative reverse transcriptase polymerase chain reaction.
Dr. Moustafa and her colleagues looked at the diagnostic value of individual miRNAs and also examined combinations of promising miRNAs by seeing which levels were elevated or depressed in patients who were later found to have surgically diagnosed endometriosis. The study built on previous retrospective work that had identified some candidate miRNAs.
In this prospective study, women with endometriosis had significantly lower serum levels of miRNAs 3613 and let-7b and significantly higher serum levels of miRNAs 150, 125b, 451, and 342. The investigators also analyzed the data to see if there were miRNA level differences between women who were on hormones and those who were not, and also to see if cycle timing affected results; neither of these factors affected miRNA levels, Dr. Moustafa reported.
When the enrolled patients had surgery, 36 were found to have endometriosis and 50 had a variety of other diagnoses, with uterine fibroids (48%) and no abnormal pathology (28%) predominating.
“A noninvasive diagnostic test does not currently exist” but is sorely needed, Dr. Moustafa said.
There’s a long gap from the onset of endometriosis symptoms to diagnosis, with one study showing that symptoms can be present for an average of 6.7-11 years before surgical diagnosis occurs. In one survey of more than 7,000 women, nearly half (46%) saw more than five physicians before they got the correct diagnosis, said Dr. Moustafa, a resident in the obstetrics, gynecology, and reproductive sciences department at Yale University, New Haven, Conn.
In a discussion following the presentation, attendee Steve Young, MD, PhD, professor of reproductive endocrinology and fertility at the University of North Carolina, Chapel Hill, said it would be useful to have a biomarker that could be a surrogate for disease burden. “You could look at miRNAs after surgery. Do you see changes back toward normal?” Dr. Young said.
Dr. Moustafa responded that the research team is in the process of collecting postoperative data to see whether levels change when the disease burden is diminished by surgery.
Next steps, she said, include looking for miRNAs in saliva to explore whether an even less invasive test might be possible. Also, there are suggestions that miRNA 125 might be a marker for more severe disease, so the team is investigating this association as well.
Whether the combination miRNA screen is ready for prime time is still an open question, she said. “Any time a new screening test is developed we have to have caution.” Current thinking, she said, points toward the utility of miRNA screening for patients with unexplained fertility, for example.
“At this point, the pendulum is so far on the side of underdiagnosis that we think patients would benefit from a screening test,” Dr. Moustafa added.
The study was supported by OvaScience. Dr. Moustafa reported having no relevant financial disclosures.
[email protected]
On Twitter @karioakes
AT ASRM 2017
Key clinical point:
Major finding: The areas under the receiver operating curve for the most promising miRNA combinations were 0.917 and 0.977.
Data source: Blinded, prospective study of 86 women slated to have diagnostic pelvic laparoscopy or laparotomy.
Disclosures: Dr. Moustafa reported no relevant disclosures. OvaScience supported the study.
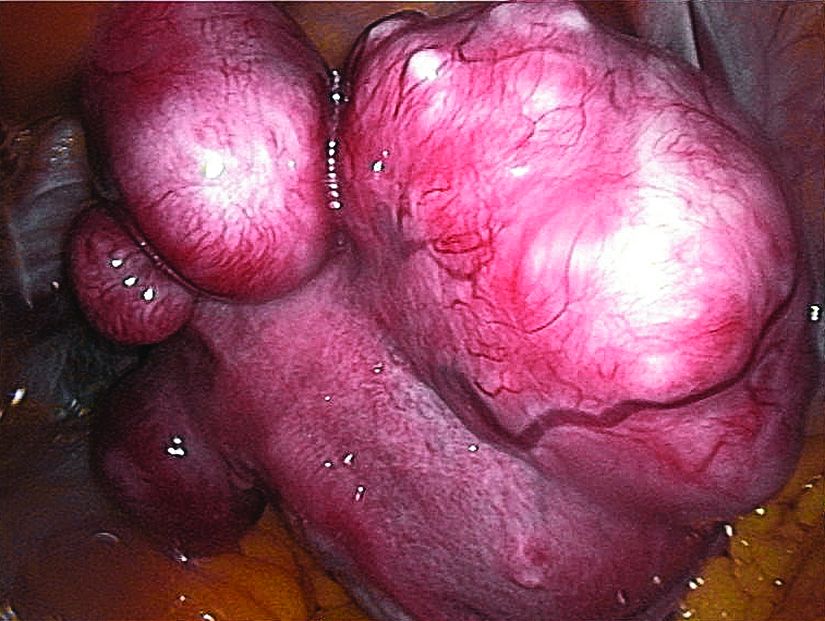
Ulipristal acetate reduced bleeding for women with fibroids
SAN ANTONIO – About half of women with uterine fibroids became amenorrheic when taking the selective progesterone receptor modulator ulipristal acetate (UPA) during a 12-week study cycle, and women taking UPA experienced significant improvement of quality of life, compared with those taking placebo.
Of those women taking 5 mg of UPA, 40.5%-42% became amenorrheic; of those taking 10 mg, 54.8%-57.3% became amenorrheic, James Liu, MD, reported at the annual meeting of the American Society for Reproductive Medicine. These results compared to amenorrhea rates of 0%-8% for women on placebo (P less than .0001 for all values).
The primary aim of VENUS II was to evaluate UPA’s efficacy and safety as intermittent treatment of abnormal uterine bleeding associated with uterine fibroids. Patients received UPA at either 5 mg or 10 mg orally. Secondary efficacy measures included the maintenance effect of UPA at both doses when compared to placebo, by assessing the rate of amenorrhea and the time to amenorrhea. Another secondary measure assessed uterine fibroid–related quality of life.
Safety was assessed by tracking adverse events through both courses of treatment. The study was not powered to compare the two doses against each other, but rather compared each against placebo.
Altogether, 432 patients were randomized to one of the treatment arms, which was begun after an initial screening period of about 10-12 weeks. The first treatment course lasted 12 weeks, after which patients went off treatment for two menstrual cycles. They then began another treatment course for 12 weeks and were followed for an additional 12 weeks after treatment was stopped.
Patients were included if they were premenopausal, aged 18-50 years old, had prolonged bleeding in at least 4 of the last 6 menstrual periods, had menstrual blood loss of at least 80 mL by cycle by the alkaline hematin method, and had at least one discrete leiomyoma without a uterine size greater than 20 weeks. About two-thirds of patients were black, reflecting the higher prevalence of uterine fibroids in this population, said Dr. Liu, professor of medicine and reproductive biology at Case Western Reserve University, Cleveland.
Most patients (60%-80%) had their bleeding controlled on either dose of UPA, compared with fewer than 10% of women taking placebo.
Quality of life data, presented separately at ASRM by Lee Shulman, MD, examined the impact of treatment on patients’ physical and social activities, and also on the severity of symptoms and health-related quality of life.
“The majority of patients on UPA versus a minority of patients on placebo described their menstrual/vaginal bleeding at the end of treatment course 1 as ‘much better’ or ‘very much better,’ ” said Dr. Shulman, chief of clinical genetics in the department of ob.gyn. at Northwestern University in Evanston, Ill.
Of patients taking 5 mg UPA, 75% reported that degree of improvement, as did 87% of those on 10 mg UPA, compared with 17.9% of those taking placebo. .
Adverse events were rare, with hot flashes occurring in about 10% of women taking UPA, compared with less than 2% of those taking placebo. Headaches, fatigue, and nausea were also reported, but rates were not significantly different from rates for those taking placebo. One serious adverse event that was deemed treatment related was a uterine hemorrhage experienced by a woman taking UPA.
“Even in treatment course 1 we already had profound and statistically significant effects in symptoms across the board,” Dr. Shulman said. “How long will they last? We obviously need more data. But the study suggests that the benefits last significantly longer than that associated with leuprolide acetate.”
Ulipristal acetate is already approved by the Food and Drug Administration at a different dosage as emergency contraception. The VENUS II data support its use for women with uterine fibroids, the researchers said. “Our results provide reassurance,” Dr. Liu said. “We can conclude that UPA is effective and safe in the management of uterine fibroids in the U.S. population.”
Dr. Liu reported that he had no relevant disclosures. Dr. Shulman reported relationships with multiple pharmaceutical companies, including Allergan, which funded the VENUS II study.
[email protected]
On Twitter @karioakes
SAN ANTONIO – About half of women with uterine fibroids became amenorrheic when taking the selective progesterone receptor modulator ulipristal acetate (UPA) during a 12-week study cycle, and women taking UPA experienced significant improvement of quality of life, compared with those taking placebo.
Of those women taking 5 mg of UPA, 40.5%-42% became amenorrheic; of those taking 10 mg, 54.8%-57.3% became amenorrheic, James Liu, MD, reported at the annual meeting of the American Society for Reproductive Medicine. These results compared to amenorrhea rates of 0%-8% for women on placebo (P less than .0001 for all values).
The primary aim of VENUS II was to evaluate UPA’s efficacy and safety as intermittent treatment of abnormal uterine bleeding associated with uterine fibroids. Patients received UPA at either 5 mg or 10 mg orally. Secondary efficacy measures included the maintenance effect of UPA at both doses when compared to placebo, by assessing the rate of amenorrhea and the time to amenorrhea. Another secondary measure assessed uterine fibroid–related quality of life.
Safety was assessed by tracking adverse events through both courses of treatment. The study was not powered to compare the two doses against each other, but rather compared each against placebo.
Altogether, 432 patients were randomized to one of the treatment arms, which was begun after an initial screening period of about 10-12 weeks. The first treatment course lasted 12 weeks, after which patients went off treatment for two menstrual cycles. They then began another treatment course for 12 weeks and were followed for an additional 12 weeks after treatment was stopped.
Patients were included if they were premenopausal, aged 18-50 years old, had prolonged bleeding in at least 4 of the last 6 menstrual periods, had menstrual blood loss of at least 80 mL by cycle by the alkaline hematin method, and had at least one discrete leiomyoma without a uterine size greater than 20 weeks. About two-thirds of patients were black, reflecting the higher prevalence of uterine fibroids in this population, said Dr. Liu, professor of medicine and reproductive biology at Case Western Reserve University, Cleveland.
Most patients (60%-80%) had their bleeding controlled on either dose of UPA, compared with fewer than 10% of women taking placebo.
Quality of life data, presented separately at ASRM by Lee Shulman, MD, examined the impact of treatment on patients’ physical and social activities, and also on the severity of symptoms and health-related quality of life.
“The majority of patients on UPA versus a minority of patients on placebo described their menstrual/vaginal bleeding at the end of treatment course 1 as ‘much better’ or ‘very much better,’ ” said Dr. Shulman, chief of clinical genetics in the department of ob.gyn. at Northwestern University in Evanston, Ill.
Of patients taking 5 mg UPA, 75% reported that degree of improvement, as did 87% of those on 10 mg UPA, compared with 17.9% of those taking placebo. .
Adverse events were rare, with hot flashes occurring in about 10% of women taking UPA, compared with less than 2% of those taking placebo. Headaches, fatigue, and nausea were also reported, but rates were not significantly different from rates for those taking placebo. One serious adverse event that was deemed treatment related was a uterine hemorrhage experienced by a woman taking UPA.
“Even in treatment course 1 we already had profound and statistically significant effects in symptoms across the board,” Dr. Shulman said. “How long will they last? We obviously need more data. But the study suggests that the benefits last significantly longer than that associated with leuprolide acetate.”
Ulipristal acetate is already approved by the Food and Drug Administration at a different dosage as emergency contraception. The VENUS II data support its use for women with uterine fibroids, the researchers said. “Our results provide reassurance,” Dr. Liu said. “We can conclude that UPA is effective and safe in the management of uterine fibroids in the U.S. population.”
Dr. Liu reported that he had no relevant disclosures. Dr. Shulman reported relationships with multiple pharmaceutical companies, including Allergan, which funded the VENUS II study.
[email protected]
On Twitter @karioakes
SAN ANTONIO – About half of women with uterine fibroids became amenorrheic when taking the selective progesterone receptor modulator ulipristal acetate (UPA) during a 12-week study cycle, and women taking UPA experienced significant improvement of quality of life, compared with those taking placebo.
Of those women taking 5 mg of UPA, 40.5%-42% became amenorrheic; of those taking 10 mg, 54.8%-57.3% became amenorrheic, James Liu, MD, reported at the annual meeting of the American Society for Reproductive Medicine. These results compared to amenorrhea rates of 0%-8% for women on placebo (P less than .0001 for all values).
The primary aim of VENUS II was to evaluate UPA’s efficacy and safety as intermittent treatment of abnormal uterine bleeding associated with uterine fibroids. Patients received UPA at either 5 mg or 10 mg orally. Secondary efficacy measures included the maintenance effect of UPA at both doses when compared to placebo, by assessing the rate of amenorrhea and the time to amenorrhea. Another secondary measure assessed uterine fibroid–related quality of life.
Safety was assessed by tracking adverse events through both courses of treatment. The study was not powered to compare the two doses against each other, but rather compared each against placebo.
Altogether, 432 patients were randomized to one of the treatment arms, which was begun after an initial screening period of about 10-12 weeks. The first treatment course lasted 12 weeks, after which patients went off treatment for two menstrual cycles. They then began another treatment course for 12 weeks and were followed for an additional 12 weeks after treatment was stopped.
Patients were included if they were premenopausal, aged 18-50 years old, had prolonged bleeding in at least 4 of the last 6 menstrual periods, had menstrual blood loss of at least 80 mL by cycle by the alkaline hematin method, and had at least one discrete leiomyoma without a uterine size greater than 20 weeks. About two-thirds of patients were black, reflecting the higher prevalence of uterine fibroids in this population, said Dr. Liu, professor of medicine and reproductive biology at Case Western Reserve University, Cleveland.
Most patients (60%-80%) had their bleeding controlled on either dose of UPA, compared with fewer than 10% of women taking placebo.
Quality of life data, presented separately at ASRM by Lee Shulman, MD, examined the impact of treatment on patients’ physical and social activities, and also on the severity of symptoms and health-related quality of life.
“The majority of patients on UPA versus a minority of patients on placebo described their menstrual/vaginal bleeding at the end of treatment course 1 as ‘much better’ or ‘very much better,’ ” said Dr. Shulman, chief of clinical genetics in the department of ob.gyn. at Northwestern University in Evanston, Ill.
Of patients taking 5 mg UPA, 75% reported that degree of improvement, as did 87% of those on 10 mg UPA, compared with 17.9% of those taking placebo. .
Adverse events were rare, with hot flashes occurring in about 10% of women taking UPA, compared with less than 2% of those taking placebo. Headaches, fatigue, and nausea were also reported, but rates were not significantly different from rates for those taking placebo. One serious adverse event that was deemed treatment related was a uterine hemorrhage experienced by a woman taking UPA.
“Even in treatment course 1 we already had profound and statistically significant effects in symptoms across the board,” Dr. Shulman said. “How long will they last? We obviously need more data. But the study suggests that the benefits last significantly longer than that associated with leuprolide acetate.”
Ulipristal acetate is already approved by the Food and Drug Administration at a different dosage as emergency contraception. The VENUS II data support its use for women with uterine fibroids, the researchers said. “Our results provide reassurance,” Dr. Liu said. “We can conclude that UPA is effective and safe in the management of uterine fibroids in the U.S. population.”
Dr. Liu reported that he had no relevant disclosures. Dr. Shulman reported relationships with multiple pharmaceutical companies, including Allergan, which funded the VENUS II study.
[email protected]
On Twitter @karioakes
AT ASRM 2017
Key clinical point:
Major finding: Between 40.5% and 57.3% of women taking ulipristal acetate (UPA) achieved amenorrhea, compared with 0%-8% of women on placebo (P less than .0001).
Data source: Venus II, a phase 3 prospective, randomized, double-blind, double-dummy, placebo-controlled study that was partially parallel and partially crossover, with 432 patients.
Disclosures: Dr. Liu reported no relevant disclosures; Dr. Shulman reported financial relationships with multiple pharmaceutical companies, including Allergan, which funded the trial.
Nail biopsies made simple
CHICAGO – Maral Skelsey, MD, doesn’t get flowers from her patients very often. But, she said, a big bouquet recently landed on her desk after she had performed a nail biopsy on a patient. The note from the patient read, “That wasn’t as bad as I thought it would be!”
The patient’s relief after the procedure highlights the apprehension that both patients and dermatologists can feel when a nail biopsy becomes necessary, said Dr. Skelsey, director of dermatologic surgery at Georgetown University, Washington, D.C.
Speaking at the summer meeting of the American Academy of Dermatology, Dr. Skelsey said that the most important advice she can give about the nail biopsy is, “Do it early and often.”
Dr. Skelsey reminded the audience that the musician Bob Marley died of malignant melanoma; the first sign of his cancer was a longitudinal melanonychia that went unbiopsied. “The biggest mistake we make is not doing it,” she said.
In performing a nail biopsy, said Dr. Skelsey, the goals are, first and foremost, to optimize the pathologic diagnosis. Correct technique can help avoid complications such as bleeding, infection, and nail dystrophy; the right approach can minimize pain and anxiety, she added.
In preparing for a biopsy for melanonychia, “dermoscopy can be very helpful” in assessing the location of the pigment and fine-tuning planning for the biopsy, said Dr. Skelsey. Also, if the streak of melanonychia has reached the distal nail, sending the clipping for pathology can be useful as well.
For dorsal pigmentation, the proximal nail matrix should be biopsied.
“Do not use a punch biopsy on the nail fold to diagnose melanoma – you will get a false negative,” Dr. Skelsey said. It’s not possible to get an accurate diagnosis going through the nail plate to the nail bed, she said.
The preoperative assessment is usually straightforward. Pertinent items in the patient’s history include any medication allergies, current anticoagulation, and any history of prior trauma to the digit to be biopsied. Occasionally, imaging may be helpful, and patients should always be assessed for vascular insufficiency, she noted.
Preoperatively, she asks her patients to remove nail polish and pretreat the area with povidone iodine for 2 days prior to the procedure. Patients need to have a ride home after the procedure, and should be prepared to elevate the affected extremity for 48 hours post procedure. If a toenail is biopsied, they’re advised to come with a postop shoe.
Her patients receive a 5-minute isopropyl alcohol wash of the area to be biopsied just before the procedure, followed by air drying and a 5-minute scrub with 7.5% povidone iodine, which then is wiped off preprocedure.
For hemostasis, a tourniquet can be improvised with a sterile glove finger and a hemostat; there are also dedicated finger cots available that work well for this purpose, she said. In addition to nail nippers and a nail elevator, an English nail splitter can be helpful, said Dr. Skelsey.
For anesthesia, she said she ordinarily uses a 30 gauge needle with buffered lidocaine and epinephrine at room temperature to deliver a wing block. Beginning about 1 cm proximal and lateral to the junction of the proximal and lateral nail fold, the dermatologist can slowly inject about 1.5 cc per side. As the block takes effect, the lateral nail fold will blanch distally in a wing-shaped pattern. This technique, she said, also has the benefit of acting as a volumetric tourniquet.
“To avulse or not to avulse?” asked Dr. Skelsey. “I used to avulse almost everything,” she said, but noted that a complete avulsion is a “pretty traumatic” procedure. Now, unless a full avulsion is required for complete and accurate pathology, she will usually perform a partial nail plate avulsion.
A partial avulsion can reduce pain and morbidity, and can be done by two different methods: the partial proximal avulsion, and the “trap door” avulsion. In a trap door avulsion, she said, the distal matrix is primarily visualized, so this may be a good option for a longitudinal melanonychia arising from the distal matrix. A Freer elevator is used to detach the nail plate from the bed and the matrix, after which the nail plate can be lifted with a hemostat.
In a partial proximal avulsion, the proximal nail fold is reflected, so it’s a better option when the proximal nail matrix needs evaluation, she said.
After the avulsion has been done, “the matrix has been exposed. Now what? Punch or shave?” asked Dr. Skelsey. She noted that she used to perform punch biopsies on “everything,” and that it’s a good option if the pigmented area spans 3 mm or less. One issue, though, is that the specimen can get stuck in the puncher, and extraction can make it difficult to deliver an intact specimen.
Shave biopsies, Dr. Skelsey said, are effective in dealing with nail matrix lesions. They can yield an accurate pathologic diagnosis, and the biopsied digits healed without nail dystrophy in about three quarters of the cases in one study, she said. Potential recurrence of pigmentation is one drawback of the shave technique, she said.
With a shave biopsy, she performs tangential incisions of the proximal and lateral nail folds, and scores and reflects the nail. Then, the band of pigment is shaved tangentially. She cauterizes the area, and sometimes will use a bit of an absorbable gelatin sponge (Gelfoam) as well. Then the proximal nail fold and nail plate are sutured.
Replacing the nail plate results in better cosmesis and is much more comfortable for the patient, she said. An 18-gauge needle can be used to bore a hole through the avulsed nail plate, which may be held in an antiseptic solution soak during the biopsy. The sutures should then be placed from skin to nail plate, so nail fragments aren’t driven into the skin during the suturing process. Finally, specimen margins should be inked, and separate labeled formalin jars are needed for the nail plate, nail bed, and the matrix.
Dr. Skelsey reported that she had no conflicts of interest.
[email protected]
On Twitter @karioakes
CHICAGO – Maral Skelsey, MD, doesn’t get flowers from her patients very often. But, she said, a big bouquet recently landed on her desk after she had performed a nail biopsy on a patient. The note from the patient read, “That wasn’t as bad as I thought it would be!”
The patient’s relief after the procedure highlights the apprehension that both patients and dermatologists can feel when a nail biopsy becomes necessary, said Dr. Skelsey, director of dermatologic surgery at Georgetown University, Washington, D.C.
Speaking at the summer meeting of the American Academy of Dermatology, Dr. Skelsey said that the most important advice she can give about the nail biopsy is, “Do it early and often.”
Dr. Skelsey reminded the audience that the musician Bob Marley died of malignant melanoma; the first sign of his cancer was a longitudinal melanonychia that went unbiopsied. “The biggest mistake we make is not doing it,” she said.
In performing a nail biopsy, said Dr. Skelsey, the goals are, first and foremost, to optimize the pathologic diagnosis. Correct technique can help avoid complications such as bleeding, infection, and nail dystrophy; the right approach can minimize pain and anxiety, she added.
In preparing for a biopsy for melanonychia, “dermoscopy can be very helpful” in assessing the location of the pigment and fine-tuning planning for the biopsy, said Dr. Skelsey. Also, if the streak of melanonychia has reached the distal nail, sending the clipping for pathology can be useful as well.
For dorsal pigmentation, the proximal nail matrix should be biopsied.
“Do not use a punch biopsy on the nail fold to diagnose melanoma – you will get a false negative,” Dr. Skelsey said. It’s not possible to get an accurate diagnosis going through the nail plate to the nail bed, she said.
The preoperative assessment is usually straightforward. Pertinent items in the patient’s history include any medication allergies, current anticoagulation, and any history of prior trauma to the digit to be biopsied. Occasionally, imaging may be helpful, and patients should always be assessed for vascular insufficiency, she noted.
Preoperatively, she asks her patients to remove nail polish and pretreat the area with povidone iodine for 2 days prior to the procedure. Patients need to have a ride home after the procedure, and should be prepared to elevate the affected extremity for 48 hours post procedure. If a toenail is biopsied, they’re advised to come with a postop shoe.
Her patients receive a 5-minute isopropyl alcohol wash of the area to be biopsied just before the procedure, followed by air drying and a 5-minute scrub with 7.5% povidone iodine, which then is wiped off preprocedure.
For hemostasis, a tourniquet can be improvised with a sterile glove finger and a hemostat; there are also dedicated finger cots available that work well for this purpose, she said. In addition to nail nippers and a nail elevator, an English nail splitter can be helpful, said Dr. Skelsey.
For anesthesia, she said she ordinarily uses a 30 gauge needle with buffered lidocaine and epinephrine at room temperature to deliver a wing block. Beginning about 1 cm proximal and lateral to the junction of the proximal and lateral nail fold, the dermatologist can slowly inject about 1.5 cc per side. As the block takes effect, the lateral nail fold will blanch distally in a wing-shaped pattern. This technique, she said, also has the benefit of acting as a volumetric tourniquet.
“To avulse or not to avulse?” asked Dr. Skelsey. “I used to avulse almost everything,” she said, but noted that a complete avulsion is a “pretty traumatic” procedure. Now, unless a full avulsion is required for complete and accurate pathology, she will usually perform a partial nail plate avulsion.
A partial avulsion can reduce pain and morbidity, and can be done by two different methods: the partial proximal avulsion, and the “trap door” avulsion. In a trap door avulsion, she said, the distal matrix is primarily visualized, so this may be a good option for a longitudinal melanonychia arising from the distal matrix. A Freer elevator is used to detach the nail plate from the bed and the matrix, after which the nail plate can be lifted with a hemostat.
In a partial proximal avulsion, the proximal nail fold is reflected, so it’s a better option when the proximal nail matrix needs evaluation, she said.
After the avulsion has been done, “the matrix has been exposed. Now what? Punch or shave?” asked Dr. Skelsey. She noted that she used to perform punch biopsies on “everything,” and that it’s a good option if the pigmented area spans 3 mm or less. One issue, though, is that the specimen can get stuck in the puncher, and extraction can make it difficult to deliver an intact specimen.
Shave biopsies, Dr. Skelsey said, are effective in dealing with nail matrix lesions. They can yield an accurate pathologic diagnosis, and the biopsied digits healed without nail dystrophy in about three quarters of the cases in one study, she said. Potential recurrence of pigmentation is one drawback of the shave technique, she said.
With a shave biopsy, she performs tangential incisions of the proximal and lateral nail folds, and scores and reflects the nail. Then, the band of pigment is shaved tangentially. She cauterizes the area, and sometimes will use a bit of an absorbable gelatin sponge (Gelfoam) as well. Then the proximal nail fold and nail plate are sutured.
Replacing the nail plate results in better cosmesis and is much more comfortable for the patient, she said. An 18-gauge needle can be used to bore a hole through the avulsed nail plate, which may be held in an antiseptic solution soak during the biopsy. The sutures should then be placed from skin to nail plate, so nail fragments aren’t driven into the skin during the suturing process. Finally, specimen margins should be inked, and separate labeled formalin jars are needed for the nail plate, nail bed, and the matrix.
Dr. Skelsey reported that she had no conflicts of interest.
[email protected]
On Twitter @karioakes
CHICAGO – Maral Skelsey, MD, doesn’t get flowers from her patients very often. But, she said, a big bouquet recently landed on her desk after she had performed a nail biopsy on a patient. The note from the patient read, “That wasn’t as bad as I thought it would be!”
The patient’s relief after the procedure highlights the apprehension that both patients and dermatologists can feel when a nail biopsy becomes necessary, said Dr. Skelsey, director of dermatologic surgery at Georgetown University, Washington, D.C.
Speaking at the summer meeting of the American Academy of Dermatology, Dr. Skelsey said that the most important advice she can give about the nail biopsy is, “Do it early and often.”
Dr. Skelsey reminded the audience that the musician Bob Marley died of malignant melanoma; the first sign of his cancer was a longitudinal melanonychia that went unbiopsied. “The biggest mistake we make is not doing it,” she said.
In performing a nail biopsy, said Dr. Skelsey, the goals are, first and foremost, to optimize the pathologic diagnosis. Correct technique can help avoid complications such as bleeding, infection, and nail dystrophy; the right approach can minimize pain and anxiety, she added.
In preparing for a biopsy for melanonychia, “dermoscopy can be very helpful” in assessing the location of the pigment and fine-tuning planning for the biopsy, said Dr. Skelsey. Also, if the streak of melanonychia has reached the distal nail, sending the clipping for pathology can be useful as well.
For dorsal pigmentation, the proximal nail matrix should be biopsied.
“Do not use a punch biopsy on the nail fold to diagnose melanoma – you will get a false negative,” Dr. Skelsey said. It’s not possible to get an accurate diagnosis going through the nail plate to the nail bed, she said.
The preoperative assessment is usually straightforward. Pertinent items in the patient’s history include any medication allergies, current anticoagulation, and any history of prior trauma to the digit to be biopsied. Occasionally, imaging may be helpful, and patients should always be assessed for vascular insufficiency, she noted.
Preoperatively, she asks her patients to remove nail polish and pretreat the area with povidone iodine for 2 days prior to the procedure. Patients need to have a ride home after the procedure, and should be prepared to elevate the affected extremity for 48 hours post procedure. If a toenail is biopsied, they’re advised to come with a postop shoe.
Her patients receive a 5-minute isopropyl alcohol wash of the area to be biopsied just before the procedure, followed by air drying and a 5-minute scrub with 7.5% povidone iodine, which then is wiped off preprocedure.
For hemostasis, a tourniquet can be improvised with a sterile glove finger and a hemostat; there are also dedicated finger cots available that work well for this purpose, she said. In addition to nail nippers and a nail elevator, an English nail splitter can be helpful, said Dr. Skelsey.
For anesthesia, she said she ordinarily uses a 30 gauge needle with buffered lidocaine and epinephrine at room temperature to deliver a wing block. Beginning about 1 cm proximal and lateral to the junction of the proximal and lateral nail fold, the dermatologist can slowly inject about 1.5 cc per side. As the block takes effect, the lateral nail fold will blanch distally in a wing-shaped pattern. This technique, she said, also has the benefit of acting as a volumetric tourniquet.
“To avulse or not to avulse?” asked Dr. Skelsey. “I used to avulse almost everything,” she said, but noted that a complete avulsion is a “pretty traumatic” procedure. Now, unless a full avulsion is required for complete and accurate pathology, she will usually perform a partial nail plate avulsion.
A partial avulsion can reduce pain and morbidity, and can be done by two different methods: the partial proximal avulsion, and the “trap door” avulsion. In a trap door avulsion, she said, the distal matrix is primarily visualized, so this may be a good option for a longitudinal melanonychia arising from the distal matrix. A Freer elevator is used to detach the nail plate from the bed and the matrix, after which the nail plate can be lifted with a hemostat.
In a partial proximal avulsion, the proximal nail fold is reflected, so it’s a better option when the proximal nail matrix needs evaluation, she said.
After the avulsion has been done, “the matrix has been exposed. Now what? Punch or shave?” asked Dr. Skelsey. She noted that she used to perform punch biopsies on “everything,” and that it’s a good option if the pigmented area spans 3 mm or less. One issue, though, is that the specimen can get stuck in the puncher, and extraction can make it difficult to deliver an intact specimen.
Shave biopsies, Dr. Skelsey said, are effective in dealing with nail matrix lesions. They can yield an accurate pathologic diagnosis, and the biopsied digits healed without nail dystrophy in about three quarters of the cases in one study, she said. Potential recurrence of pigmentation is one drawback of the shave technique, she said.
With a shave biopsy, she performs tangential incisions of the proximal and lateral nail folds, and scores and reflects the nail. Then, the band of pigment is shaved tangentially. She cauterizes the area, and sometimes will use a bit of an absorbable gelatin sponge (Gelfoam) as well. Then the proximal nail fold and nail plate are sutured.
Replacing the nail plate results in better cosmesis and is much more comfortable for the patient, she said. An 18-gauge needle can be used to bore a hole through the avulsed nail plate, which may be held in an antiseptic solution soak during the biopsy. The sutures should then be placed from skin to nail plate, so nail fragments aren’t driven into the skin during the suturing process. Finally, specimen margins should be inked, and separate labeled formalin jars are needed for the nail plate, nail bed, and the matrix.
Dr. Skelsey reported that she had no conflicts of interest.
[email protected]
On Twitter @karioakes
AT THE 2017 AAD SUMMER MEETING
Beyond the Kegel: the who, why, and how of pelvic floor PT
PHILADELPHIA – When a woman is referred for pelvic floor physical therapy, what’s involved? Is there evidence behind the treatments, and what exactly does pelvic floor therapy look like?
Denise Hartzell Leggin, a physical therapist who specializes in pelvic floor dysfunction, reviewed how the female pelvic floor can change with age, and provided the rationale for pelvic floor physical therapy (PT) at the annual meeting of the North American Menopause Society.
“Physical therapists treat musculoskeletal and neuromuscular dysfunctions,” said Ms. Hartzell Leggin. So, when a physician suspects a musculoskeletal cause for pelvic floor dysfunction, a PT referral may be appropriate, she said.
Why refer for PT?
As part of the aging process, pelvic floor dysfunction can coexist with the genitourinary syndrome of menopause (GSM), said Ms. Hartzell. Though the pathophysiology is not always clear, aging does have some effect on the pelvic floor musculature and, together with GSM, can contribute to women’s urogenital symptoms in later life.
These symptoms, she said, can be the harbingers of “a host of clinical conditions,” including urinary incontinence and fecal incontinence, constipation, and bladder-emptying problems. Also, changes in the pelvic musculature from childbirth, surgeries, and hypotonicity or hypertonicity can contribute to sexual dysfunction in later life, said Ms. Hartzell Leggin, who is affiliated with Good Shepherd Penn Partners and in private practice in the Philadelphia area.
The musculature of the pelvic floor functions as more than a bowl for carrying the pelvic organs, Ms. Hartzell Leggin said. The collective muscles and fascia form a sling that fills in the pelvic ring and functions as an integrated system with constant resting tone. But the musculature is also active and interactive.
“The diaphragm and the pelvic floor move in symmetry during respiration,” and pelvic floor tone tightens in anticipation of increased intra-abdominal pressure from a cough, a sneeze, or even a laugh. “These are active structures – the brain can talk to the pelvic floor and make it do something,” she said.
Who’s a good candidate?
Looking at risk factors for pelvic organ prolapse alone, Ms. Hartzell Leggin said these can include age, body mass index, a history of occupational or recreational heavy lifting, chronic cough, and even genetics.
However, one of the most significant risk factors for prolapse of pelvic organs is simply having had a vaginal delivery. Up to 50% of women who have delivered a child vaginally may eventually have some degree of pelvic organ prolapse, though not all women will be symptomatic, Ms. Hartzell Leggin said.
Since postsurgical pelvic organ prolapse rates may top 30% within 2 years, an initial referral for pelvic floor PT is a rational conservative approach, she said. And even if a patient progresses to surgery, PT may be a useful adjunct.
Pelvic floor dysfunction may also be considered if a diastasis recti is discovered on physical exam, or if the patient reports a linear abdominal bulge. Patients with diastasis recti are more likely to have pelvic floor dysfunction than the general population, she said, so it’s worth asking about any related symptoms.
For voiding issues, “conservative treatment is first-line,” said Ms. Hartzell Leggin, so a PT referral for pelvic floor therapy and, in some cases, some behavioral retraining can help with issues of urinary frequency and urgency. These are options that may be considered before prescribing anticholinergic medication, she said.
How does pelvic floor PT work?
When a physician refers a patient for pelvic floor PT, what’s the process? The physical therapy evaluation will begin with history taking, including the chief complaint, past medical and surgical history, and an obstetric/gynecologic/sexual history, said Ms. Hartzell Leggin. Medications are also reviewed.
The physical therapist’s examination should encompass a thorough orthopedic examination, with attention to the lumbar spine and hips, and posture and gait. An external and internal examination of the pelvic floor will look for muscle tone at rest and with strain, and for any defects or prolapse.
Pelvic floor strength is assessed according to ability to contract, with some assessment of strength available through palpation. More quantitative means may include manometry, dynamometry, or the use of progressive weighted vaginal cones.
There’s no single standardized measurement tool to assess pelvic floor strength. Palpation is a valuable tool for an experienced clinician, and it also can provide real-time feedback to the patient as she becomes more aware of her pelvic floor. The discipline is moving toward more standardized terminology, with several reporting scales now available to report pelvic floor strength, said Ms. Hartzell Leggin.
The Pelvic Floor Distress Inventory is a validated tool that captures information about the impact of pelvic floor dysfunction on a patient’s daily functioning. “I think I capture a lot when my patient comes in and completes that form,” said Ms. Hartzell Leggin. The Genitourinary Pain Index is another validated tool that measures urinary symptoms, pain, and associated quality of life impacts. Patients may be asked to keep a home therapy and symptom or voiding diary for additional information.
The pelvic floor PT treatment algorithm will vary, depending on whether there’s underlying hypertonicity or hypotonicity, but will involve pelvic floor exercises, soft tissue mobilization, and consideration of a variety of modalities including electrical stimulation and ultrasound. For hypertonicity, vaginal dilators may be used, while weighted vaginal cones may be used for hypotonicity.
Physical therapists should know when to refer a patient back to a physician and should always work as part of an interdisciplinary team, she said.
Ms. Hartzell Leggin reported that she is the president of Elite Rehabilitation Services in Audubon, Pa.
[email protected]
On Twitter @karioakes
PHILADELPHIA – When a woman is referred for pelvic floor physical therapy, what’s involved? Is there evidence behind the treatments, and what exactly does pelvic floor therapy look like?
Denise Hartzell Leggin, a physical therapist who specializes in pelvic floor dysfunction, reviewed how the female pelvic floor can change with age, and provided the rationale for pelvic floor physical therapy (PT) at the annual meeting of the North American Menopause Society.
“Physical therapists treat musculoskeletal and neuromuscular dysfunctions,” said Ms. Hartzell Leggin. So, when a physician suspects a musculoskeletal cause for pelvic floor dysfunction, a PT referral may be appropriate, she said.
Why refer for PT?
As part of the aging process, pelvic floor dysfunction can coexist with the genitourinary syndrome of menopause (GSM), said Ms. Hartzell. Though the pathophysiology is not always clear, aging does have some effect on the pelvic floor musculature and, together with GSM, can contribute to women’s urogenital symptoms in later life.
These symptoms, she said, can be the harbingers of “a host of clinical conditions,” including urinary incontinence and fecal incontinence, constipation, and bladder-emptying problems. Also, changes in the pelvic musculature from childbirth, surgeries, and hypotonicity or hypertonicity can contribute to sexual dysfunction in later life, said Ms. Hartzell Leggin, who is affiliated with Good Shepherd Penn Partners and in private practice in the Philadelphia area.
The musculature of the pelvic floor functions as more than a bowl for carrying the pelvic organs, Ms. Hartzell Leggin said. The collective muscles and fascia form a sling that fills in the pelvic ring and functions as an integrated system with constant resting tone. But the musculature is also active and interactive.
“The diaphragm and the pelvic floor move in symmetry during respiration,” and pelvic floor tone tightens in anticipation of increased intra-abdominal pressure from a cough, a sneeze, or even a laugh. “These are active structures – the brain can talk to the pelvic floor and make it do something,” she said.
Who’s a good candidate?
Looking at risk factors for pelvic organ prolapse alone, Ms. Hartzell Leggin said these can include age, body mass index, a history of occupational or recreational heavy lifting, chronic cough, and even genetics.
However, one of the most significant risk factors for prolapse of pelvic organs is simply having had a vaginal delivery. Up to 50% of women who have delivered a child vaginally may eventually have some degree of pelvic organ prolapse, though not all women will be symptomatic, Ms. Hartzell Leggin said.
Since postsurgical pelvic organ prolapse rates may top 30% within 2 years, an initial referral for pelvic floor PT is a rational conservative approach, she said. And even if a patient progresses to surgery, PT may be a useful adjunct.
Pelvic floor dysfunction may also be considered if a diastasis recti is discovered on physical exam, or if the patient reports a linear abdominal bulge. Patients with diastasis recti are more likely to have pelvic floor dysfunction than the general population, she said, so it’s worth asking about any related symptoms.
For voiding issues, “conservative treatment is first-line,” said Ms. Hartzell Leggin, so a PT referral for pelvic floor therapy and, in some cases, some behavioral retraining can help with issues of urinary frequency and urgency. These are options that may be considered before prescribing anticholinergic medication, she said.
How does pelvic floor PT work?
When a physician refers a patient for pelvic floor PT, what’s the process? The physical therapy evaluation will begin with history taking, including the chief complaint, past medical and surgical history, and an obstetric/gynecologic/sexual history, said Ms. Hartzell Leggin. Medications are also reviewed.
The physical therapist’s examination should encompass a thorough orthopedic examination, with attention to the lumbar spine and hips, and posture and gait. An external and internal examination of the pelvic floor will look for muscle tone at rest and with strain, and for any defects or prolapse.
Pelvic floor strength is assessed according to ability to contract, with some assessment of strength available through palpation. More quantitative means may include manometry, dynamometry, or the use of progressive weighted vaginal cones.
There’s no single standardized measurement tool to assess pelvic floor strength. Palpation is a valuable tool for an experienced clinician, and it also can provide real-time feedback to the patient as she becomes more aware of her pelvic floor. The discipline is moving toward more standardized terminology, with several reporting scales now available to report pelvic floor strength, said Ms. Hartzell Leggin.
The Pelvic Floor Distress Inventory is a validated tool that captures information about the impact of pelvic floor dysfunction on a patient’s daily functioning. “I think I capture a lot when my patient comes in and completes that form,” said Ms. Hartzell Leggin. The Genitourinary Pain Index is another validated tool that measures urinary symptoms, pain, and associated quality of life impacts. Patients may be asked to keep a home therapy and symptom or voiding diary for additional information.
The pelvic floor PT treatment algorithm will vary, depending on whether there’s underlying hypertonicity or hypotonicity, but will involve pelvic floor exercises, soft tissue mobilization, and consideration of a variety of modalities including electrical stimulation and ultrasound. For hypertonicity, vaginal dilators may be used, while weighted vaginal cones may be used for hypotonicity.
Physical therapists should know when to refer a patient back to a physician and should always work as part of an interdisciplinary team, she said.
Ms. Hartzell Leggin reported that she is the president of Elite Rehabilitation Services in Audubon, Pa.
[email protected]
On Twitter @karioakes
PHILADELPHIA – When a woman is referred for pelvic floor physical therapy, what’s involved? Is there evidence behind the treatments, and what exactly does pelvic floor therapy look like?
Denise Hartzell Leggin, a physical therapist who specializes in pelvic floor dysfunction, reviewed how the female pelvic floor can change with age, and provided the rationale for pelvic floor physical therapy (PT) at the annual meeting of the North American Menopause Society.
“Physical therapists treat musculoskeletal and neuromuscular dysfunctions,” said Ms. Hartzell Leggin. So, when a physician suspects a musculoskeletal cause for pelvic floor dysfunction, a PT referral may be appropriate, she said.
Why refer for PT?
As part of the aging process, pelvic floor dysfunction can coexist with the genitourinary syndrome of menopause (GSM), said Ms. Hartzell. Though the pathophysiology is not always clear, aging does have some effect on the pelvic floor musculature and, together with GSM, can contribute to women’s urogenital symptoms in later life.
These symptoms, she said, can be the harbingers of “a host of clinical conditions,” including urinary incontinence and fecal incontinence, constipation, and bladder-emptying problems. Also, changes in the pelvic musculature from childbirth, surgeries, and hypotonicity or hypertonicity can contribute to sexual dysfunction in later life, said Ms. Hartzell Leggin, who is affiliated with Good Shepherd Penn Partners and in private practice in the Philadelphia area.
The musculature of the pelvic floor functions as more than a bowl for carrying the pelvic organs, Ms. Hartzell Leggin said. The collective muscles and fascia form a sling that fills in the pelvic ring and functions as an integrated system with constant resting tone. But the musculature is also active and interactive.
“The diaphragm and the pelvic floor move in symmetry during respiration,” and pelvic floor tone tightens in anticipation of increased intra-abdominal pressure from a cough, a sneeze, or even a laugh. “These are active structures – the brain can talk to the pelvic floor and make it do something,” she said.
Who’s a good candidate?
Looking at risk factors for pelvic organ prolapse alone, Ms. Hartzell Leggin said these can include age, body mass index, a history of occupational or recreational heavy lifting, chronic cough, and even genetics.
However, one of the most significant risk factors for prolapse of pelvic organs is simply having had a vaginal delivery. Up to 50% of women who have delivered a child vaginally may eventually have some degree of pelvic organ prolapse, though not all women will be symptomatic, Ms. Hartzell Leggin said.
Since postsurgical pelvic organ prolapse rates may top 30% within 2 years, an initial referral for pelvic floor PT is a rational conservative approach, she said. And even if a patient progresses to surgery, PT may be a useful adjunct.
Pelvic floor dysfunction may also be considered if a diastasis recti is discovered on physical exam, or if the patient reports a linear abdominal bulge. Patients with diastasis recti are more likely to have pelvic floor dysfunction than the general population, she said, so it’s worth asking about any related symptoms.
For voiding issues, “conservative treatment is first-line,” said Ms. Hartzell Leggin, so a PT referral for pelvic floor therapy and, in some cases, some behavioral retraining can help with issues of urinary frequency and urgency. These are options that may be considered before prescribing anticholinergic medication, she said.
How does pelvic floor PT work?
When a physician refers a patient for pelvic floor PT, what’s the process? The physical therapy evaluation will begin with history taking, including the chief complaint, past medical and surgical history, and an obstetric/gynecologic/sexual history, said Ms. Hartzell Leggin. Medications are also reviewed.
The physical therapist’s examination should encompass a thorough orthopedic examination, with attention to the lumbar spine and hips, and posture and gait. An external and internal examination of the pelvic floor will look for muscle tone at rest and with strain, and for any defects or prolapse.
Pelvic floor strength is assessed according to ability to contract, with some assessment of strength available through palpation. More quantitative means may include manometry, dynamometry, or the use of progressive weighted vaginal cones.
There’s no single standardized measurement tool to assess pelvic floor strength. Palpation is a valuable tool for an experienced clinician, and it also can provide real-time feedback to the patient as she becomes more aware of her pelvic floor. The discipline is moving toward more standardized terminology, with several reporting scales now available to report pelvic floor strength, said Ms. Hartzell Leggin.
The Pelvic Floor Distress Inventory is a validated tool that captures information about the impact of pelvic floor dysfunction on a patient’s daily functioning. “I think I capture a lot when my patient comes in and completes that form,” said Ms. Hartzell Leggin. The Genitourinary Pain Index is another validated tool that measures urinary symptoms, pain, and associated quality of life impacts. Patients may be asked to keep a home therapy and symptom or voiding diary for additional information.
The pelvic floor PT treatment algorithm will vary, depending on whether there’s underlying hypertonicity or hypotonicity, but will involve pelvic floor exercises, soft tissue mobilization, and consideration of a variety of modalities including electrical stimulation and ultrasound. For hypertonicity, vaginal dilators may be used, while weighted vaginal cones may be used for hypotonicity.
Physical therapists should know when to refer a patient back to a physician and should always work as part of an interdisciplinary team, she said.
Ms. Hartzell Leggin reported that she is the president of Elite Rehabilitation Services in Audubon, Pa.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM NAMS 2017
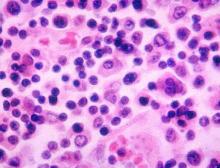
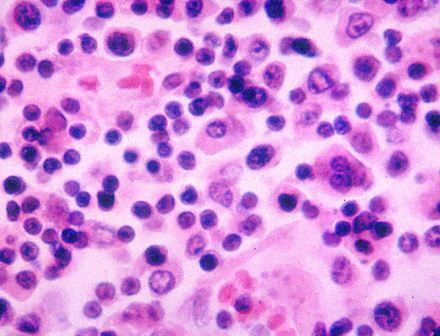
Morphology index guides adnexal mass workup in postmenopausal women
PHILADELPHIA – The report provides guidelines for risk stratification and diagnostic evaluation when an ovarian mass is found.
Accurate and thorough evaluation of an adnexal mass in a menopausal woman must respect cancer prevalence data, Frederick Ueland, MD, one of the report’s coauthors, said at the annual meeting of the North American Menopause Society. In premenopausal women, there are “many tumors, but few cancers,” he said. Only about 15% of ovarian tumors are malignant when found before menopause.
But after menopause, there are “few tumors, but many cancers,” Dr. Ueland said. Up to 50% of tumors in postmenopausal women are malignant, with epithelial ovarian cancer, metastatic cancer, and granulosa cell tumors predominating.
Multiple clinical trials have taught physicians that “tumor morphology helps stratify cancer risk,” he noted.
Ultrasound is the best imaging modality to evaluate adnexal masses, he said. At his institution, the use of a morphology index to guide management of adnexal masses has reduced the number of surgeries performed to remove one cancer over the years, said Dr. Ueland, chief of the division of gynecologic oncology at the University of Kentucky, Lexington.
During the 1990s, when the Morphology Index was first used at the University of Kentucky, surgeons performed 12.5 surgeries per cancer. In the 2000s, that number fell to 5.2, and during the present decade, one cancer is detected in every 4 surgeries, he reported.
Limiting subjectivity is a key to accurate cancer detection when evaluating adnexal masses, so that the dual goals of accurate cancer detection and avoidance of unnecessary surgeries can be met, Dr. Ueland said. To address these dual needs, the first international consensus report on adnexal masses was issued in May 2017 (J Ultrasound Med. 2017 May;36[5]:849-863).
The report noted the sharp discrepancy between surgery rates in the United States and Europe. “In the United States, there are approximately 9.1 surgeries per malignancy, compared with the European International Ovarian Tumor Analysis center trials, with only 2.3 (oncology centers) and 5.9 (other centers) reported surgeries per malignancy, suggesting that there is room to improve our preoperative assessments,” the investigators wrote.
In reviewing management guidelines, Dr. Ueland said that, when the risk of malignancy is low, as with smooth-walled, unilocular or septate cysts, the mass can be monitored without surgery, with ultrasound reevaluation at the 6-month mark. If there are no concerning changes, the mass can then be imaged annually for 5 years. No further follow-up is needed at the 5-year mark, barring growth or other changes of the mass.
If the ultrasound evaluation of the mass shows intermediate risk, then secondary testing is needed. Masses that show as partly solid or that have small, irregular wall abnormalities, or atypical nonpapillary projections on ultrasound fall into this category. Secondary testing may be accomplished either by serial ultrasound or by using biomarker testing.
Commercially available triage biomarker tests such as OVA1, ROMA, and Overa may offer higher detection rates than cancer antigen 125 (CA 125) testing alone, Dr. Ueland said. For instance, OVA1, a multivariate index assay, detected 76% of malignancies missed by CA 125 (Am J Obstet Gynecol. 2016 Jul;215[1]:82.e1-11).
If the mass has high-risk characteristics, then a prompt surgical referral to a gynecologic oncologist is a must. Included in this category are mostly solid masses and those with papillary projections, as well as those associated with any ascites. No secondary testing or watchful waiting is recommended in these cases, said Dr. Ueland, since they carry a greater than 25% risk of malignancy.
Dr. Ueland is currently enrolling patients in a clinical trial to assess whether serial transvaginal ultrasonography with Morphology Index can reduce false-positive results by more accurately distinguishing benign from malignant ovarian tumors. He reported having no financial disclosures.
[email protected]
On Twitter @karioakes
PHILADELPHIA – The report provides guidelines for risk stratification and diagnostic evaluation when an ovarian mass is found.
Accurate and thorough evaluation of an adnexal mass in a menopausal woman must respect cancer prevalence data, Frederick Ueland, MD, one of the report’s coauthors, said at the annual meeting of the North American Menopause Society. In premenopausal women, there are “many tumors, but few cancers,” he said. Only about 15% of ovarian tumors are malignant when found before menopause.
But after menopause, there are “few tumors, but many cancers,” Dr. Ueland said. Up to 50% of tumors in postmenopausal women are malignant, with epithelial ovarian cancer, metastatic cancer, and granulosa cell tumors predominating.
Multiple clinical trials have taught physicians that “tumor morphology helps stratify cancer risk,” he noted.
Ultrasound is the best imaging modality to evaluate adnexal masses, he said. At his institution, the use of a morphology index to guide management of adnexal masses has reduced the number of surgeries performed to remove one cancer over the years, said Dr. Ueland, chief of the division of gynecologic oncology at the University of Kentucky, Lexington.
During the 1990s, when the Morphology Index was first used at the University of Kentucky, surgeons performed 12.5 surgeries per cancer. In the 2000s, that number fell to 5.2, and during the present decade, one cancer is detected in every 4 surgeries, he reported.
Limiting subjectivity is a key to accurate cancer detection when evaluating adnexal masses, so that the dual goals of accurate cancer detection and avoidance of unnecessary surgeries can be met, Dr. Ueland said. To address these dual needs, the first international consensus report on adnexal masses was issued in May 2017 (J Ultrasound Med. 2017 May;36[5]:849-863).
The report noted the sharp discrepancy between surgery rates in the United States and Europe. “In the United States, there are approximately 9.1 surgeries per malignancy, compared with the European International Ovarian Tumor Analysis center trials, with only 2.3 (oncology centers) and 5.9 (other centers) reported surgeries per malignancy, suggesting that there is room to improve our preoperative assessments,” the investigators wrote.
In reviewing management guidelines, Dr. Ueland said that, when the risk of malignancy is low, as with smooth-walled, unilocular or septate cysts, the mass can be monitored without surgery, with ultrasound reevaluation at the 6-month mark. If there are no concerning changes, the mass can then be imaged annually for 5 years. No further follow-up is needed at the 5-year mark, barring growth or other changes of the mass.
If the ultrasound evaluation of the mass shows intermediate risk, then secondary testing is needed. Masses that show as partly solid or that have small, irregular wall abnormalities, or atypical nonpapillary projections on ultrasound fall into this category. Secondary testing may be accomplished either by serial ultrasound or by using biomarker testing.
Commercially available triage biomarker tests such as OVA1, ROMA, and Overa may offer higher detection rates than cancer antigen 125 (CA 125) testing alone, Dr. Ueland said. For instance, OVA1, a multivariate index assay, detected 76% of malignancies missed by CA 125 (Am J Obstet Gynecol. 2016 Jul;215[1]:82.e1-11).
If the mass has high-risk characteristics, then a prompt surgical referral to a gynecologic oncologist is a must. Included in this category are mostly solid masses and those with papillary projections, as well as those associated with any ascites. No secondary testing or watchful waiting is recommended in these cases, said Dr. Ueland, since they carry a greater than 25% risk of malignancy.
Dr. Ueland is currently enrolling patients in a clinical trial to assess whether serial transvaginal ultrasonography with Morphology Index can reduce false-positive results by more accurately distinguishing benign from malignant ovarian tumors. He reported having no financial disclosures.
[email protected]
On Twitter @karioakes
PHILADELPHIA – The report provides guidelines for risk stratification and diagnostic evaluation when an ovarian mass is found.
Accurate and thorough evaluation of an adnexal mass in a menopausal woman must respect cancer prevalence data, Frederick Ueland, MD, one of the report’s coauthors, said at the annual meeting of the North American Menopause Society. In premenopausal women, there are “many tumors, but few cancers,” he said. Only about 15% of ovarian tumors are malignant when found before menopause.
But after menopause, there are “few tumors, but many cancers,” Dr. Ueland said. Up to 50% of tumors in postmenopausal women are malignant, with epithelial ovarian cancer, metastatic cancer, and granulosa cell tumors predominating.
Multiple clinical trials have taught physicians that “tumor morphology helps stratify cancer risk,” he noted.
Ultrasound is the best imaging modality to evaluate adnexal masses, he said. At his institution, the use of a morphology index to guide management of adnexal masses has reduced the number of surgeries performed to remove one cancer over the years, said Dr. Ueland, chief of the division of gynecologic oncology at the University of Kentucky, Lexington.
During the 1990s, when the Morphology Index was first used at the University of Kentucky, surgeons performed 12.5 surgeries per cancer. In the 2000s, that number fell to 5.2, and during the present decade, one cancer is detected in every 4 surgeries, he reported.
Limiting subjectivity is a key to accurate cancer detection when evaluating adnexal masses, so that the dual goals of accurate cancer detection and avoidance of unnecessary surgeries can be met, Dr. Ueland said. To address these dual needs, the first international consensus report on adnexal masses was issued in May 2017 (J Ultrasound Med. 2017 May;36[5]:849-863).
The report noted the sharp discrepancy between surgery rates in the United States and Europe. “In the United States, there are approximately 9.1 surgeries per malignancy, compared with the European International Ovarian Tumor Analysis center trials, with only 2.3 (oncology centers) and 5.9 (other centers) reported surgeries per malignancy, suggesting that there is room to improve our preoperative assessments,” the investigators wrote.
In reviewing management guidelines, Dr. Ueland said that, when the risk of malignancy is low, as with smooth-walled, unilocular or septate cysts, the mass can be monitored without surgery, with ultrasound reevaluation at the 6-month mark. If there are no concerning changes, the mass can then be imaged annually for 5 years. No further follow-up is needed at the 5-year mark, barring growth or other changes of the mass.
If the ultrasound evaluation of the mass shows intermediate risk, then secondary testing is needed. Masses that show as partly solid or that have small, irregular wall abnormalities, or atypical nonpapillary projections on ultrasound fall into this category. Secondary testing may be accomplished either by serial ultrasound or by using biomarker testing.
Commercially available triage biomarker tests such as OVA1, ROMA, and Overa may offer higher detection rates than cancer antigen 125 (CA 125) testing alone, Dr. Ueland said. For instance, OVA1, a multivariate index assay, detected 76% of malignancies missed by CA 125 (Am J Obstet Gynecol. 2016 Jul;215[1]:82.e1-11).
If the mass has high-risk characteristics, then a prompt surgical referral to a gynecologic oncologist is a must. Included in this category are mostly solid masses and those with papillary projections, as well as those associated with any ascites. No secondary testing or watchful waiting is recommended in these cases, said Dr. Ueland, since they carry a greater than 25% risk of malignancy.
Dr. Ueland is currently enrolling patients in a clinical trial to assess whether serial transvaginal ultrasonography with Morphology Index can reduce false-positive results by more accurately distinguishing benign from malignant ovarian tumors. He reported having no financial disclosures.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM NAMS 2017
Conjugate typhoid vaccine safe and effective in phase 2 trials
A new conjugate typhoid vaccine suitable for administration to infants and young children was efficacious, highly immunogenic, and well tolerated, compared with placebo, in a phase 2 study that tested the vaccine using a human typhoid infection model.
In a study that compared two formulations of typhoid vaccine to a control meningococcal vaccine, the new Vi-conjugate (Vi-TT) vaccine had an efficacy of 54.6% (95% confidence interval, 26.8-71.8) and a 100% seroconversion rate.
The study was not powered for a direct comparison of the efficacy of the Vi-TT with the efficacy of the Vi-polysaccharide (Vi-PS), the other vaccine used in the study. The Vi-PS vaccine had an efficacy of 52.0% (95% CI, 23.2-70.0), and 88.6% of the Vi-PS recipients had seroconversion.
However, “clinical manifestations of typhoid fever seemed less severe among diagnosed participants following Vi-TT vaccination,” Celina Jin, MD, and her colleagues wrote (Lancet. 2017 Sep 28: doi: 10.1016/S0140-6736[17]32149-9). Fever, defined as an oral temperature of 38° C or higher, was seen in 6 of 37 (16%) Vi-TT recipients, 17 of 31 (55%) receiving control, and 11 of 35 (31%) receiving Vi-PS.
Geometric mean titers also were significantly higher in the Vi-TT group than in the Vi-PS group, with an adjusted geometric mean titer of 562.9 EU/mL for Vi-TT and 140.5 EU/mL for Vi-PS (P less than .0001).
The study enrolled 112 healthy adult volunteers who were randomized 1:1:1 to receive Vi-PS, Vi-TT, or control meningococcal vaccine. A total of 103 of the participants eventually received one of the two study vaccines or the control vaccines, and that group was included in the per-protocol analysis.
After vaccination (recipients and investigators were masked as to which formulation participants received), study participants kept an online diary to report any vaccination-related symptoms for 7 days, and also had clinic visits scheduled at days 1, 3, 7, and 10.
Participants received one oral dose of wild-type Salmonella enterica serovar Typhi Quailes strain bacteria about 1 month after vaccination. The dose was 1-5x104 colony forming units, and was administered immediately following a 120-mL oral bolus of sodium bicarbonate (to neutralize stomach acid).
Participants then were seen daily in an outpatient clinic for 2 weeks. At each visit, investigators monitored vital signs, performed a general assessment, and drew blood to assess for typhoid bacteremia. Participants also kept an online diary for 21 days, reporting twice-daily self-measured temperatures as well. No antipyretics were allowed before typhoid diagnosis.
Participants who met the study’s criteria for typhoid diagnosis were treated with a 2-week course of ciprofloxacin or azithromycin; patients who did not become ill were treated 14 days after the oral typhoid challenge. None of the four serious adverse events reported during the study was deemed to be related to vaccination.
That broad definition of typhoid infection was used to determine attack rates for the study’s primary outcome measure. However, Dr. Jin and her colleagues also looked at a less stringent – and perhaps more clinically pertinent – definition of 12 hours of fever of 38° C or higher followed by S. Typhi bacteremia. Using those criteria, the Vi-TT vaccine prevented up to 87% of infections.
Salmonella Typhi is the world’s leading cause of enteric fever, said Dr. Jin, of the Oxford Vaccine Group at the University of Oxford (England). Up to 20.6 million people per year are affected, with children most commonly infected and low-resource populations in Asia and Africa hardest hit.
Both prescription and over-the-counter antibiotics are used worldwide to combat typhoid fever, and S. Typhi strains are becoming increasingly antibiotic resistant in South Asia and Africa, Dr. Jin and her coauthors said.
The typhoid vaccines that are currently licensed are either not suitable for administration to infants and young children, or are insufficiently immunogenic in younger populations.
The typhoid conjugate vaccine used in the study combines the Vi-polysaccharide capsule with a protein carrier, increasing host immunologic response and making the vaccine effective in infancy.
“This human challenge study provides further evidence to support the deployment of Vi-conjugate vaccines as a control measure to reduce the burden of typhoid fever, because those individuals living in endemic regions should not be made to wait another 60 years,” wrote Dr. Jin and her coauthors.
The study was funded by the Bill & Melinda Gates Foundation and the European commission FP7 grant, Advanced Immunization Technologies.
The Oxford Vaccine Group has developed a typhoid challenge model that provides an important bridge in clinical testing and affords the possibility of significant acceleration of the vaccine development process. Despite the controversy human challenge models sometimes engender, previous human typhoid challenge studies contributed to the development of the live attenuated typhoid vaccine Ty21a.
The conjugate vaccine tested by Dr. Jin and her colleagues is a much-needed weapon in the public health armamentarium of typhoid control. Treatment options are limited in regions of South Asia and Africa where endemic typhoid shows increasing antibiotic resistance.
This human challenge study provides the first evidence that the conjugate vaccine reduces the attack rate of typhoid fever, though its use in India has shown it to be safe and immunogenic, even in children as young as 6 months of age.
The stringent definition of typhoid fever attack used in this study may result in a finding of lower efficacy than would be seen in a field trial, and a National Institutes of Health–sponsored study of another conjugate vaccine found efficacy rates of 89% among Vietnamese preschoolers followed for nearly 4 years after vaccination. When the present study’s data were reanalyzed with use of the less stringent case definition of fever followed by typhoid bacteremia, a similar efficacy of 87.1% was seen for the conjugate vaccine. A larger sample size would be needed in a challenge study that included the less stringent definition as a coprimary endpoint, but results might better correlate with real-world field trials.
Phase 3 and 4 trials for the typhoid conjugate vaccine are forthcoming, but final results will not be tallied for many years. The typhoid challenge study reported by Dr. Jin and her colleagues bolsters hopes that the candidate vaccine will help with typhoid control where it’s most needed.
Nicholas A. Feasey, MD , is at the Liverpool (England) School of Tropical Medicine. Myron M. Levine, MD , is at the University of Maryland, Baltimore. Their comments were drawn from an editorial accompanying the study (Lancet. 2017 Sep 28. doi: 10.1016/S0140-6736[17]32407-8 ).
The Oxford Vaccine Group has developed a typhoid challenge model that provides an important bridge in clinical testing and affords the possibility of significant acceleration of the vaccine development process. Despite the controversy human challenge models sometimes engender, previous human typhoid challenge studies contributed to the development of the live attenuated typhoid vaccine Ty21a.
The conjugate vaccine tested by Dr. Jin and her colleagues is a much-needed weapon in the public health armamentarium of typhoid control. Treatment options are limited in regions of South Asia and Africa where endemic typhoid shows increasing antibiotic resistance.
This human challenge study provides the first evidence that the conjugate vaccine reduces the attack rate of typhoid fever, though its use in India has shown it to be safe and immunogenic, even in children as young as 6 months of age.
The stringent definition of typhoid fever attack used in this study may result in a finding of lower efficacy than would be seen in a field trial, and a National Institutes of Health–sponsored study of another conjugate vaccine found efficacy rates of 89% among Vietnamese preschoolers followed for nearly 4 years after vaccination. When the present study’s data were reanalyzed with use of the less stringent case definition of fever followed by typhoid bacteremia, a similar efficacy of 87.1% was seen for the conjugate vaccine. A larger sample size would be needed in a challenge study that included the less stringent definition as a coprimary endpoint, but results might better correlate with real-world field trials.
Phase 3 and 4 trials for the typhoid conjugate vaccine are forthcoming, but final results will not be tallied for many years. The typhoid challenge study reported by Dr. Jin and her colleagues bolsters hopes that the candidate vaccine will help with typhoid control where it’s most needed.
Nicholas A. Feasey, MD , is at the Liverpool (England) School of Tropical Medicine. Myron M. Levine, MD , is at the University of Maryland, Baltimore. Their comments were drawn from an editorial accompanying the study (Lancet. 2017 Sep 28. doi: 10.1016/S0140-6736[17]32407-8 ).
The Oxford Vaccine Group has developed a typhoid challenge model that provides an important bridge in clinical testing and affords the possibility of significant acceleration of the vaccine development process. Despite the controversy human challenge models sometimes engender, previous human typhoid challenge studies contributed to the development of the live attenuated typhoid vaccine Ty21a.
The conjugate vaccine tested by Dr. Jin and her colleagues is a much-needed weapon in the public health armamentarium of typhoid control. Treatment options are limited in regions of South Asia and Africa where endemic typhoid shows increasing antibiotic resistance.
This human challenge study provides the first evidence that the conjugate vaccine reduces the attack rate of typhoid fever, though its use in India has shown it to be safe and immunogenic, even in children as young as 6 months of age.
The stringent definition of typhoid fever attack used in this study may result in a finding of lower efficacy than would be seen in a field trial, and a National Institutes of Health–sponsored study of another conjugate vaccine found efficacy rates of 89% among Vietnamese preschoolers followed for nearly 4 years after vaccination. When the present study’s data were reanalyzed with use of the less stringent case definition of fever followed by typhoid bacteremia, a similar efficacy of 87.1% was seen for the conjugate vaccine. A larger sample size would be needed in a challenge study that included the less stringent definition as a coprimary endpoint, but results might better correlate with real-world field trials.
Phase 3 and 4 trials for the typhoid conjugate vaccine are forthcoming, but final results will not be tallied for many years. The typhoid challenge study reported by Dr. Jin and her colleagues bolsters hopes that the candidate vaccine will help with typhoid control where it’s most needed.
Nicholas A. Feasey, MD , is at the Liverpool (England) School of Tropical Medicine. Myron M. Levine, MD , is at the University of Maryland, Baltimore. Their comments were drawn from an editorial accompanying the study (Lancet. 2017 Sep 28. doi: 10.1016/S0140-6736[17]32407-8 ).
A new conjugate typhoid vaccine suitable for administration to infants and young children was efficacious, highly immunogenic, and well tolerated, compared with placebo, in a phase 2 study that tested the vaccine using a human typhoid infection model.
In a study that compared two formulations of typhoid vaccine to a control meningococcal vaccine, the new Vi-conjugate (Vi-TT) vaccine had an efficacy of 54.6% (95% confidence interval, 26.8-71.8) and a 100% seroconversion rate.
The study was not powered for a direct comparison of the efficacy of the Vi-TT with the efficacy of the Vi-polysaccharide (Vi-PS), the other vaccine used in the study. The Vi-PS vaccine had an efficacy of 52.0% (95% CI, 23.2-70.0), and 88.6% of the Vi-PS recipients had seroconversion.
However, “clinical manifestations of typhoid fever seemed less severe among diagnosed participants following Vi-TT vaccination,” Celina Jin, MD, and her colleagues wrote (Lancet. 2017 Sep 28: doi: 10.1016/S0140-6736[17]32149-9). Fever, defined as an oral temperature of 38° C or higher, was seen in 6 of 37 (16%) Vi-TT recipients, 17 of 31 (55%) receiving control, and 11 of 35 (31%) receiving Vi-PS.
Geometric mean titers also were significantly higher in the Vi-TT group than in the Vi-PS group, with an adjusted geometric mean titer of 562.9 EU/mL for Vi-TT and 140.5 EU/mL for Vi-PS (P less than .0001).
The study enrolled 112 healthy adult volunteers who were randomized 1:1:1 to receive Vi-PS, Vi-TT, or control meningococcal vaccine. A total of 103 of the participants eventually received one of the two study vaccines or the control vaccines, and that group was included in the per-protocol analysis.
After vaccination (recipients and investigators were masked as to which formulation participants received), study participants kept an online diary to report any vaccination-related symptoms for 7 days, and also had clinic visits scheduled at days 1, 3, 7, and 10.
Participants received one oral dose of wild-type Salmonella enterica serovar Typhi Quailes strain bacteria about 1 month after vaccination. The dose was 1-5x104 colony forming units, and was administered immediately following a 120-mL oral bolus of sodium bicarbonate (to neutralize stomach acid).
Participants then were seen daily in an outpatient clinic for 2 weeks. At each visit, investigators monitored vital signs, performed a general assessment, and drew blood to assess for typhoid bacteremia. Participants also kept an online diary for 21 days, reporting twice-daily self-measured temperatures as well. No antipyretics were allowed before typhoid diagnosis.
Participants who met the study’s criteria for typhoid diagnosis were treated with a 2-week course of ciprofloxacin or azithromycin; patients who did not become ill were treated 14 days after the oral typhoid challenge. None of the four serious adverse events reported during the study was deemed to be related to vaccination.
That broad definition of typhoid infection was used to determine attack rates for the study’s primary outcome measure. However, Dr. Jin and her colleagues also looked at a less stringent – and perhaps more clinically pertinent – definition of 12 hours of fever of 38° C or higher followed by S. Typhi bacteremia. Using those criteria, the Vi-TT vaccine prevented up to 87% of infections.
Salmonella Typhi is the world’s leading cause of enteric fever, said Dr. Jin, of the Oxford Vaccine Group at the University of Oxford (England). Up to 20.6 million people per year are affected, with children most commonly infected and low-resource populations in Asia and Africa hardest hit.
Both prescription and over-the-counter antibiotics are used worldwide to combat typhoid fever, and S. Typhi strains are becoming increasingly antibiotic resistant in South Asia and Africa, Dr. Jin and her coauthors said.
The typhoid vaccines that are currently licensed are either not suitable for administration to infants and young children, or are insufficiently immunogenic in younger populations.
The typhoid conjugate vaccine used in the study combines the Vi-polysaccharide capsule with a protein carrier, increasing host immunologic response and making the vaccine effective in infancy.
“This human challenge study provides further evidence to support the deployment of Vi-conjugate vaccines as a control measure to reduce the burden of typhoid fever, because those individuals living in endemic regions should not be made to wait another 60 years,” wrote Dr. Jin and her coauthors.
The study was funded by the Bill & Melinda Gates Foundation and the European commission FP7 grant, Advanced Immunization Technologies.
A new conjugate typhoid vaccine suitable for administration to infants and young children was efficacious, highly immunogenic, and well tolerated, compared with placebo, in a phase 2 study that tested the vaccine using a human typhoid infection model.
In a study that compared two formulations of typhoid vaccine to a control meningococcal vaccine, the new Vi-conjugate (Vi-TT) vaccine had an efficacy of 54.6% (95% confidence interval, 26.8-71.8) and a 100% seroconversion rate.
The study was not powered for a direct comparison of the efficacy of the Vi-TT with the efficacy of the Vi-polysaccharide (Vi-PS), the other vaccine used in the study. The Vi-PS vaccine had an efficacy of 52.0% (95% CI, 23.2-70.0), and 88.6% of the Vi-PS recipients had seroconversion.
However, “clinical manifestations of typhoid fever seemed less severe among diagnosed participants following Vi-TT vaccination,” Celina Jin, MD, and her colleagues wrote (Lancet. 2017 Sep 28: doi: 10.1016/S0140-6736[17]32149-9). Fever, defined as an oral temperature of 38° C or higher, was seen in 6 of 37 (16%) Vi-TT recipients, 17 of 31 (55%) receiving control, and 11 of 35 (31%) receiving Vi-PS.
Geometric mean titers also were significantly higher in the Vi-TT group than in the Vi-PS group, with an adjusted geometric mean titer of 562.9 EU/mL for Vi-TT and 140.5 EU/mL for Vi-PS (P less than .0001).
The study enrolled 112 healthy adult volunteers who were randomized 1:1:1 to receive Vi-PS, Vi-TT, or control meningococcal vaccine. A total of 103 of the participants eventually received one of the two study vaccines or the control vaccines, and that group was included in the per-protocol analysis.
After vaccination (recipients and investigators were masked as to which formulation participants received), study participants kept an online diary to report any vaccination-related symptoms for 7 days, and also had clinic visits scheduled at days 1, 3, 7, and 10.
Participants received one oral dose of wild-type Salmonella enterica serovar Typhi Quailes strain bacteria about 1 month after vaccination. The dose was 1-5x104 colony forming units, and was administered immediately following a 120-mL oral bolus of sodium bicarbonate (to neutralize stomach acid).
Participants then were seen daily in an outpatient clinic for 2 weeks. At each visit, investigators monitored vital signs, performed a general assessment, and drew blood to assess for typhoid bacteremia. Participants also kept an online diary for 21 days, reporting twice-daily self-measured temperatures as well. No antipyretics were allowed before typhoid diagnosis.
Participants who met the study’s criteria for typhoid diagnosis were treated with a 2-week course of ciprofloxacin or azithromycin; patients who did not become ill were treated 14 days after the oral typhoid challenge. None of the four serious adverse events reported during the study was deemed to be related to vaccination.
That broad definition of typhoid infection was used to determine attack rates for the study’s primary outcome measure. However, Dr. Jin and her colleagues also looked at a less stringent – and perhaps more clinically pertinent – definition of 12 hours of fever of 38° C or higher followed by S. Typhi bacteremia. Using those criteria, the Vi-TT vaccine prevented up to 87% of infections.
Salmonella Typhi is the world’s leading cause of enteric fever, said Dr. Jin, of the Oxford Vaccine Group at the University of Oxford (England). Up to 20.6 million people per year are affected, with children most commonly infected and low-resource populations in Asia and Africa hardest hit.
Both prescription and over-the-counter antibiotics are used worldwide to combat typhoid fever, and S. Typhi strains are becoming increasingly antibiotic resistant in South Asia and Africa, Dr. Jin and her coauthors said.
The typhoid vaccines that are currently licensed are either not suitable for administration to infants and young children, or are insufficiently immunogenic in younger populations.
The typhoid conjugate vaccine used in the study combines the Vi-polysaccharide capsule with a protein carrier, increasing host immunologic response and making the vaccine effective in infancy.
“This human challenge study provides further evidence to support the deployment of Vi-conjugate vaccines as a control measure to reduce the burden of typhoid fever, because those individuals living in endemic regions should not be made to wait another 60 years,” wrote Dr. Jin and her coauthors.
The study was funded by the Bill & Melinda Gates Foundation and the European commission FP7 grant, Advanced Immunization Technologies.
FROM THE LANCET
Key clinical point: A conjugate typhoid vaccine significantly reduced typhoid fever rates under a stringent case definition.
Major finding: Efficacy was 54.6% for the Vi-conjugate vaccine, with 100% seroconversion.
Study details: Randomized, controlled phase 2b trial of 112 participants receiving one of two typhoid vaccines, or control meningococcal vaccine.
Disclosures: The study was funded by the Bill & Melinda Gates Foundation and the European Commission FP7 grant, Advanced Immunization Technologies.
Dermatologists, rheumatologists differ in management of pediatric discoid lupus erythematosus
CHICAGO – With no consensus guidelines, rheumatologists and dermatologists have significant practice-based differences in their treatment of children with discoid lupus erythematosus, according to a survey of the two specialties.
The survey’s results from 57 pediatric dermatologists and 47 pediatric rheumatologists showed a lack of consensus between the two specialties in how to screen for systemic lupus erythematosus (SLE). The two specialties also differed in identification of which features of discoid lupus erythematosus (DLE) might predispose children to developing SLE, and in some therapy choices for DLE.
Although rare in children, DLE may develop into systemic lupus erythematosus in about 25%-30% of pediatric patients, according to Lisa Arkin, MD, who shared the survey results during a poster presentation at the World Congress of Pediatric Dermatology.
Dr. Arkin and her colleagues conducted a Web-based survey to examine differences in DLE treatment practice patterns between pediatric dermatologists and pediatric rheumatologists. They sent the survey to 292 members of the Childhood Arthritis and Rheumatology Research Alliance (CARRA), and to 200 members of the Pediatric Dermatology Research Alliance (PeDRA), and received responses from 44% of the rheumatologists and 56% of the dermatologists. Of those, 57 dermatologists and 47 rheumatologists met inclusion criteria for the study.
More than half of the respondents in each specialty had seen fewer than 10 patients with skin-limited DLE, and fewer than 10 patients with SLE and DLE, over the course of their careers, said Dr. Arkin, director of pediatric dermatology at the University of Wisconsin, Madison.
Consensus was defined by Dr. Arkin and her colleagues as greater than 70% agreement from both specialties, and 2-sided P values less than .05 showed practice differences between rheumatologists and dermatologists.
Clinicians reached a consensus that the presence of either arthritis or nephritis in a pediatric patient with DLE put the patient at high risk for SLE. Arthritis was identified as a high-risk feature by 41 of 57 dermatologists (72%) and 36 of 47 rheumatologists (77%), while nephritis was seen as a high-risk feature by 39 dermatologists (68%) and 37 rheumatologists (79%). However, said Dr. Arkin, “no other features from a list of 30 risk factors including demographics, clinical, or laboratory features achieved consensus.”
In deciding which laboratory studies to order to screen for SLE upon DLE diagnosis, 26 dermatologists (46%) and 38 rheumatologists (81%) choose a full screening panel, according to the survey results. That was a significant between-specialty difference (P less than .001). The full panel consisted of obtaining a complete blood count with differential, testing for renal and hepatic function, obtaining the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level, and doing urine studies. The panel also included testing for complements, autoantibodies including anti–double-stranded DNA, single-stranded A and B, ribonucleoprotein, anti-Smith, and antiphospholipid antibodies.
However, when individual laboratory studies were examined, several did achieve consensus for baseline screening. Those included the CBC with differential; urinalysis (but not urine protein creatinine), ESR (but not CRP); complement, renal, and hepatic function testing; and most autoantibody testing (but not antiphospholipid antibody testing). Where there were differences in likelihood to order a test, rheumatologists were more likely to order the test than dermatologists.
In deciding on initial treatment, “rheumatologists were more likely to always initiate hydroxychloroquine than dermatologists,” said Dr. Arkin. Of the rheumatologists, 49% always initiated hydroxychloroquine, compared with 14% of the dermatologists (P less than .001).
In contrast, “dermatologists were more likely to always initiate topical therapy than the rheumatologists,” said Dr. Arkin. Topical therapy was always started by 81% of the dermatologists and 33% of the rheumatologists (P less than .001).
Although the specialties differed in whether they always initiated a certain treatment, “hydroxychloroquine achieved consensus as first-line therapy,” Dr. Arkin noted, with 81% of dermatologists and 87% of rheumatologists choosing hydroxychloroquine when the survey asked for a first-line systemic therapy.
There was no consensus about which agents were best for add-on therapy. Of the dermatologists, 32% would sometimes use methotrexate, which was used by 21% of rheumatologists for refractory skin disease. Quinacrine was used as add-on therapy by 21% of dermatologists and 15% of rheumatologists. Rheumatologists were significantly more likely to add dapsone than dermatologists (28% vs. 5%, P = .002).
The survey points to the need to develop consensus guidelines in the treatment of pediatric DLE, said Dr. Arkin. “Knowledge gaps include risk factors for SLE, optimal screening, and therapy,” she explained. “Collection of robust longitudinal data will aid in developing pediatric consensus guidelines for DLE.”
Dr. Arkin had no conflicts of interest.
[email protected]
On Twitter @karioakes
CHICAGO – With no consensus guidelines, rheumatologists and dermatologists have significant practice-based differences in their treatment of children with discoid lupus erythematosus, according to a survey of the two specialties.
The survey’s results from 57 pediatric dermatologists and 47 pediatric rheumatologists showed a lack of consensus between the two specialties in how to screen for systemic lupus erythematosus (SLE). The two specialties also differed in identification of which features of discoid lupus erythematosus (DLE) might predispose children to developing SLE, and in some therapy choices for DLE.
Although rare in children, DLE may develop into systemic lupus erythematosus in about 25%-30% of pediatric patients, according to Lisa Arkin, MD, who shared the survey results during a poster presentation at the World Congress of Pediatric Dermatology.
Dr. Arkin and her colleagues conducted a Web-based survey to examine differences in DLE treatment practice patterns between pediatric dermatologists and pediatric rheumatologists. They sent the survey to 292 members of the Childhood Arthritis and Rheumatology Research Alliance (CARRA), and to 200 members of the Pediatric Dermatology Research Alliance (PeDRA), and received responses from 44% of the rheumatologists and 56% of the dermatologists. Of those, 57 dermatologists and 47 rheumatologists met inclusion criteria for the study.
More than half of the respondents in each specialty had seen fewer than 10 patients with skin-limited DLE, and fewer than 10 patients with SLE and DLE, over the course of their careers, said Dr. Arkin, director of pediatric dermatology at the University of Wisconsin, Madison.
Consensus was defined by Dr. Arkin and her colleagues as greater than 70% agreement from both specialties, and 2-sided P values less than .05 showed practice differences between rheumatologists and dermatologists.
Clinicians reached a consensus that the presence of either arthritis or nephritis in a pediatric patient with DLE put the patient at high risk for SLE. Arthritis was identified as a high-risk feature by 41 of 57 dermatologists (72%) and 36 of 47 rheumatologists (77%), while nephritis was seen as a high-risk feature by 39 dermatologists (68%) and 37 rheumatologists (79%). However, said Dr. Arkin, “no other features from a list of 30 risk factors including demographics, clinical, or laboratory features achieved consensus.”
In deciding which laboratory studies to order to screen for SLE upon DLE diagnosis, 26 dermatologists (46%) and 38 rheumatologists (81%) choose a full screening panel, according to the survey results. That was a significant between-specialty difference (P less than .001). The full panel consisted of obtaining a complete blood count with differential, testing for renal and hepatic function, obtaining the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level, and doing urine studies. The panel also included testing for complements, autoantibodies including anti–double-stranded DNA, single-stranded A and B, ribonucleoprotein, anti-Smith, and antiphospholipid antibodies.
However, when individual laboratory studies were examined, several did achieve consensus for baseline screening. Those included the CBC with differential; urinalysis (but not urine protein creatinine), ESR (but not CRP); complement, renal, and hepatic function testing; and most autoantibody testing (but not antiphospholipid antibody testing). Where there were differences in likelihood to order a test, rheumatologists were more likely to order the test than dermatologists.
In deciding on initial treatment, “rheumatologists were more likely to always initiate hydroxychloroquine than dermatologists,” said Dr. Arkin. Of the rheumatologists, 49% always initiated hydroxychloroquine, compared with 14% of the dermatologists (P less than .001).
In contrast, “dermatologists were more likely to always initiate topical therapy than the rheumatologists,” said Dr. Arkin. Topical therapy was always started by 81% of the dermatologists and 33% of the rheumatologists (P less than .001).
Although the specialties differed in whether they always initiated a certain treatment, “hydroxychloroquine achieved consensus as first-line therapy,” Dr. Arkin noted, with 81% of dermatologists and 87% of rheumatologists choosing hydroxychloroquine when the survey asked for a first-line systemic therapy.
There was no consensus about which agents were best for add-on therapy. Of the dermatologists, 32% would sometimes use methotrexate, which was used by 21% of rheumatologists for refractory skin disease. Quinacrine was used as add-on therapy by 21% of dermatologists and 15% of rheumatologists. Rheumatologists were significantly more likely to add dapsone than dermatologists (28% vs. 5%, P = .002).
The survey points to the need to develop consensus guidelines in the treatment of pediatric DLE, said Dr. Arkin. “Knowledge gaps include risk factors for SLE, optimal screening, and therapy,” she explained. “Collection of robust longitudinal data will aid in developing pediatric consensus guidelines for DLE.”
Dr. Arkin had no conflicts of interest.
[email protected]
On Twitter @karioakes
CHICAGO – With no consensus guidelines, rheumatologists and dermatologists have significant practice-based differences in their treatment of children with discoid lupus erythematosus, according to a survey of the two specialties.
The survey’s results from 57 pediatric dermatologists and 47 pediatric rheumatologists showed a lack of consensus between the two specialties in how to screen for systemic lupus erythematosus (SLE). The two specialties also differed in identification of which features of discoid lupus erythematosus (DLE) might predispose children to developing SLE, and in some therapy choices for DLE.
Although rare in children, DLE may develop into systemic lupus erythematosus in about 25%-30% of pediatric patients, according to Lisa Arkin, MD, who shared the survey results during a poster presentation at the World Congress of Pediatric Dermatology.
Dr. Arkin and her colleagues conducted a Web-based survey to examine differences in DLE treatment practice patterns between pediatric dermatologists and pediatric rheumatologists. They sent the survey to 292 members of the Childhood Arthritis and Rheumatology Research Alliance (CARRA), and to 200 members of the Pediatric Dermatology Research Alliance (PeDRA), and received responses from 44% of the rheumatologists and 56% of the dermatologists. Of those, 57 dermatologists and 47 rheumatologists met inclusion criteria for the study.
More than half of the respondents in each specialty had seen fewer than 10 patients with skin-limited DLE, and fewer than 10 patients with SLE and DLE, over the course of their careers, said Dr. Arkin, director of pediatric dermatology at the University of Wisconsin, Madison.
Consensus was defined by Dr. Arkin and her colleagues as greater than 70% agreement from both specialties, and 2-sided P values less than .05 showed practice differences between rheumatologists and dermatologists.
Clinicians reached a consensus that the presence of either arthritis or nephritis in a pediatric patient with DLE put the patient at high risk for SLE. Arthritis was identified as a high-risk feature by 41 of 57 dermatologists (72%) and 36 of 47 rheumatologists (77%), while nephritis was seen as a high-risk feature by 39 dermatologists (68%) and 37 rheumatologists (79%). However, said Dr. Arkin, “no other features from a list of 30 risk factors including demographics, clinical, or laboratory features achieved consensus.”
In deciding which laboratory studies to order to screen for SLE upon DLE diagnosis, 26 dermatologists (46%) and 38 rheumatologists (81%) choose a full screening panel, according to the survey results. That was a significant between-specialty difference (P less than .001). The full panel consisted of obtaining a complete blood count with differential, testing for renal and hepatic function, obtaining the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level, and doing urine studies. The panel also included testing for complements, autoantibodies including anti–double-stranded DNA, single-stranded A and B, ribonucleoprotein, anti-Smith, and antiphospholipid antibodies.
However, when individual laboratory studies were examined, several did achieve consensus for baseline screening. Those included the CBC with differential; urinalysis (but not urine protein creatinine), ESR (but not CRP); complement, renal, and hepatic function testing; and most autoantibody testing (but not antiphospholipid antibody testing). Where there were differences in likelihood to order a test, rheumatologists were more likely to order the test than dermatologists.
In deciding on initial treatment, “rheumatologists were more likely to always initiate hydroxychloroquine than dermatologists,” said Dr. Arkin. Of the rheumatologists, 49% always initiated hydroxychloroquine, compared with 14% of the dermatologists (P less than .001).
In contrast, “dermatologists were more likely to always initiate topical therapy than the rheumatologists,” said Dr. Arkin. Topical therapy was always started by 81% of the dermatologists and 33% of the rheumatologists (P less than .001).
Although the specialties differed in whether they always initiated a certain treatment, “hydroxychloroquine achieved consensus as first-line therapy,” Dr. Arkin noted, with 81% of dermatologists and 87% of rheumatologists choosing hydroxychloroquine when the survey asked for a first-line systemic therapy.
There was no consensus about which agents were best for add-on therapy. Of the dermatologists, 32% would sometimes use methotrexate, which was used by 21% of rheumatologists for refractory skin disease. Quinacrine was used as add-on therapy by 21% of dermatologists and 15% of rheumatologists. Rheumatologists were significantly more likely to add dapsone than dermatologists (28% vs. 5%, P = .002).
The survey points to the need to develop consensus guidelines in the treatment of pediatric DLE, said Dr. Arkin. “Knowledge gaps include risk factors for SLE, optimal screening, and therapy,” she explained. “Collection of robust longitudinal data will aid in developing pediatric consensus guidelines for DLE.”
Dr. Arkin had no conflicts of interest.
[email protected]
On Twitter @karioakes
AT WCPD 2017
Key clinical point:
Major finding: The two specialties reached a consensus in identifying 2 of 30 potential high-risk features for the development of systemic lupus erythematosus.
Data source: Survey results from 57 pediatric dermatologists and 47 pediatric rheumatologists who treat children with DLE.Disclosures: Dr. Arkin had no relevant financial conflicts.
CBT for insomnia and hot flashes lifts mood in midlife
PHILADELPHIA – Cognitive-behavioral therapy tailored to perimenopausal and postmenopausal women who were experiencing both insomnia and vasomotor symptoms effectively improved both sleep and mood, according to a small controlled study.
When 40 women were randomized to receive either cognitive-behavioral therapy for menopausal insomnia (CBTMI) or education about menopause and sleep, those who received CBTMI had significantly reduced scores on both objective and subjective scales of depression, and their sleep also improved.
The CBTMI intervention was effective even for women with high scores on the depression scales at baseline, Sara Nowakowski, PhD, said at a top abstracts session at the annual meeting of the North American Menopause Society.
Over the 8 weeks of the study intervention, women in the CBTMI arm received four 50-minute individual sessions with either a social worker or a psychologist in a gynecology clinic outpatient setting. Counseling during the sessions focused both on hot flashes and insomnia, using evidence-based CBT techniques to address both. These included sleep restriction, changing behaviors to strengthen the association of the bed with sleep, cognitive therapy to address maladaptive beliefs about both sleep and host flashes, general sleep hygiene, hot flash coping mechanisms, and relaxation training.
Those in the menopause education control arm had a 1-hour educational session about menopausal symptoms and sleep hygiene, received written material, and were told they could make any changes desired.
Participants, whose mean age was 55 years, were included if they reported at least one nocturnal hot flash per night and met criteria for the sleep disorder of insomnia. Although patients who met criteria for major depression were not excluded, women with surgical menopause or cancer treatment–related menopause were excluded, as were those with substance use disorder, significant other psychiatric comorbidities, and those with obstructive sleep apnea or periodic limb movements/restless leg syndrome.
Dr. Nowakowski, a clinical psychologist in the department of obstetrics and gynecology, University of Texas, Galveston, and her colleagues administered the Insomnia Severity Index (ISI), the Center for Epidemiologic Studies Depression Scale (CES-D), and the Hamilton Depression Rating Scale (HDRS) both before and after the 8-week intervention.
The investigators used a mixed-models statistical analysis, finding a significant improvement over time during the study period in both patient-reported (P = .001) and clinician-assessed (P = .001) ratings of depression for the CBTMI group.
When the effect of the treatment arm was analyzed, CBTMI also offered significantly greater improvement in patient-reported (P = .009) and clinician-assessed (P = .022) depression ratings.
Patients were divided into high and low depression severity, with a score over 8 on the CES-D and 16 on the HDRS putting the participant into the high-severity category. Both groups had significant improvement on the ISI from baseline. “Treatment response for insomnia severity did not differ based on baseline depression severity,” Dr. Nowakowski said.
The efficacy of the relatively brief intervention has clinical relevance to those caring for the 39%-60% of women in midlife who have symptoms of insomnia and the 8%-40% of midlife women who report elevated depression symptoms. “Comprehensive interventions that simultaneously improve sleep and mood in midlife women are greatly needed,” she said.
The National Institutes of Health and the Hogg Foundation for Mental Health funded the study. Dr. Nowakowski reported no conflicts of interest.
[email protected]
On Twitter @karioakes
PHILADELPHIA – Cognitive-behavioral therapy tailored to perimenopausal and postmenopausal women who were experiencing both insomnia and vasomotor symptoms effectively improved both sleep and mood, according to a small controlled study.
When 40 women were randomized to receive either cognitive-behavioral therapy for menopausal insomnia (CBTMI) or education about menopause and sleep, those who received CBTMI had significantly reduced scores on both objective and subjective scales of depression, and their sleep also improved.
The CBTMI intervention was effective even for women with high scores on the depression scales at baseline, Sara Nowakowski, PhD, said at a top abstracts session at the annual meeting of the North American Menopause Society.
Over the 8 weeks of the study intervention, women in the CBTMI arm received four 50-minute individual sessions with either a social worker or a psychologist in a gynecology clinic outpatient setting. Counseling during the sessions focused both on hot flashes and insomnia, using evidence-based CBT techniques to address both. These included sleep restriction, changing behaviors to strengthen the association of the bed with sleep, cognitive therapy to address maladaptive beliefs about both sleep and host flashes, general sleep hygiene, hot flash coping mechanisms, and relaxation training.
Those in the menopause education control arm had a 1-hour educational session about menopausal symptoms and sleep hygiene, received written material, and were told they could make any changes desired.
Participants, whose mean age was 55 years, were included if they reported at least one nocturnal hot flash per night and met criteria for the sleep disorder of insomnia. Although patients who met criteria for major depression were not excluded, women with surgical menopause or cancer treatment–related menopause were excluded, as were those with substance use disorder, significant other psychiatric comorbidities, and those with obstructive sleep apnea or periodic limb movements/restless leg syndrome.
Dr. Nowakowski, a clinical psychologist in the department of obstetrics and gynecology, University of Texas, Galveston, and her colleagues administered the Insomnia Severity Index (ISI), the Center for Epidemiologic Studies Depression Scale (CES-D), and the Hamilton Depression Rating Scale (HDRS) both before and after the 8-week intervention.
The investigators used a mixed-models statistical analysis, finding a significant improvement over time during the study period in both patient-reported (P = .001) and clinician-assessed (P = .001) ratings of depression for the CBTMI group.
When the effect of the treatment arm was analyzed, CBTMI also offered significantly greater improvement in patient-reported (P = .009) and clinician-assessed (P = .022) depression ratings.
Patients were divided into high and low depression severity, with a score over 8 on the CES-D and 16 on the HDRS putting the participant into the high-severity category. Both groups had significant improvement on the ISI from baseline. “Treatment response for insomnia severity did not differ based on baseline depression severity,” Dr. Nowakowski said.
The efficacy of the relatively brief intervention has clinical relevance to those caring for the 39%-60% of women in midlife who have symptoms of insomnia and the 8%-40% of midlife women who report elevated depression symptoms. “Comprehensive interventions that simultaneously improve sleep and mood in midlife women are greatly needed,” she said.
The National Institutes of Health and the Hogg Foundation for Mental Health funded the study. Dr. Nowakowski reported no conflicts of interest.
[email protected]
On Twitter @karioakes
PHILADELPHIA – Cognitive-behavioral therapy tailored to perimenopausal and postmenopausal women who were experiencing both insomnia and vasomotor symptoms effectively improved both sleep and mood, according to a small controlled study.
When 40 women were randomized to receive either cognitive-behavioral therapy for menopausal insomnia (CBTMI) or education about menopause and sleep, those who received CBTMI had significantly reduced scores on both objective and subjective scales of depression, and their sleep also improved.
The CBTMI intervention was effective even for women with high scores on the depression scales at baseline, Sara Nowakowski, PhD, said at a top abstracts session at the annual meeting of the North American Menopause Society.
Over the 8 weeks of the study intervention, women in the CBTMI arm received four 50-minute individual sessions with either a social worker or a psychologist in a gynecology clinic outpatient setting. Counseling during the sessions focused both on hot flashes and insomnia, using evidence-based CBT techniques to address both. These included sleep restriction, changing behaviors to strengthen the association of the bed with sleep, cognitive therapy to address maladaptive beliefs about both sleep and host flashes, general sleep hygiene, hot flash coping mechanisms, and relaxation training.
Those in the menopause education control arm had a 1-hour educational session about menopausal symptoms and sleep hygiene, received written material, and were told they could make any changes desired.
Participants, whose mean age was 55 years, were included if they reported at least one nocturnal hot flash per night and met criteria for the sleep disorder of insomnia. Although patients who met criteria for major depression were not excluded, women with surgical menopause or cancer treatment–related menopause were excluded, as were those with substance use disorder, significant other psychiatric comorbidities, and those with obstructive sleep apnea or periodic limb movements/restless leg syndrome.
Dr. Nowakowski, a clinical psychologist in the department of obstetrics and gynecology, University of Texas, Galveston, and her colleagues administered the Insomnia Severity Index (ISI), the Center for Epidemiologic Studies Depression Scale (CES-D), and the Hamilton Depression Rating Scale (HDRS) both before and after the 8-week intervention.
The investigators used a mixed-models statistical analysis, finding a significant improvement over time during the study period in both patient-reported (P = .001) and clinician-assessed (P = .001) ratings of depression for the CBTMI group.
When the effect of the treatment arm was analyzed, CBTMI also offered significantly greater improvement in patient-reported (P = .009) and clinician-assessed (P = .022) depression ratings.
Patients were divided into high and low depression severity, with a score over 8 on the CES-D and 16 on the HDRS putting the participant into the high-severity category. Both groups had significant improvement on the ISI from baseline. “Treatment response for insomnia severity did not differ based on baseline depression severity,” Dr. Nowakowski said.
The efficacy of the relatively brief intervention has clinical relevance to those caring for the 39%-60% of women in midlife who have symptoms of insomnia and the 8%-40% of midlife women who report elevated depression symptoms. “Comprehensive interventions that simultaneously improve sleep and mood in midlife women are greatly needed,” she said.
The National Institutes of Health and the Hogg Foundation for Mental Health funded the study. Dr. Nowakowski reported no conflicts of interest.
[email protected]
On Twitter @karioakes
AT NAMS 2017
Key clinical point:
Major finding: Patient-reported and clinician-assessed depression scores dropped after the intervention (P = .001 for both).
Data source: Randomized controlled trial of 40 midlife women with insomnia and hot flashes.
Disclosures: The National Institutes of Health and the Hogg Foundation for Mental Health funded the study. Dr. Nowakowski reported no conflicts of interest.
Oral bioidentical combo improves quality of life, vasomotor symptoms
PHILADELPHIA – An oral estradiol/progesterone formulation significantly improved menopause-related quality of life, compared with placebo, for up to 1 year after beginning treatment, according to a new study.
If approved, the new formulation “may be an option for the estimated millions of women currently using less-regulated and unapproved compounded bioidentical hormone therapy,” said James Simon, MD, the study’s senior author.
Patients receiving the combination therapy, termed TX-001HR, experienced a significant improvement in quality of life, compared with placebo and compared with baseline, at all study points, said Dr. Simon of George Washington University, Washington.
Using the Menopause-Specific Quality of Life questionnaire (MENQOL), Dr. Simon and his coinvestigators found that women taking the combination therapy saw reductions in the vasomotor domain of MENQOL within 12 weeks of beginning the study. The significant symptomatic improvement persisted for the full year that patients were followed.
For patients with particularly bothersome vasomotor symptoms, vasomotor domain scores ranged from 6.9 to 7.2 at baseline and were 2.8-3.6 with TX-001HR and 4.4 with placebo at month 12, according to Dr. Simon.
Speaking during a top abstracts session at the annual meeting of the North American Menopause Society, Dr. Simon said that TX-001HR combines the physiologic sex hormones 17-beta estradiol and progesterone (E2/P4) into a single oral soft-gel.
The phase 3 randomized, double blind, placebo-controlled REPLENISH trial explored the safety and efficacy of one of four dose combinations of E2/P4. A total of 1,833 patients were randomized to receive E2/P4 in doses of 1.0/100 mg, 0.5/100 mg, 0.5/50 mg, or 0.25/50 mg, or to receive placebo. An approximately equal number of patients were allocated to each study arm, except that 151 patients were allocated to receive placebo.
The MENQOL is structured so that the 29 items in the symptom inventory are grouped into four domains: vasomotor, psychosocial, physical, and sexual. Significant reductions were seen at 12 weeks for all patients in overall MENQOL scores and for the four domains.
The REPLENISH investigators also performed a separate analysis of data from the subset of patients who had moderate to severe vasomotor symptoms (VMS). At the 6- and 12-month assessment points, the VMS patients on all but the lowest dose of TX-001HR had significant improvement over placebo.
“Independent of treatment, the largest correlation observed was between changes in moderate to severe VMS frequency and changes in the MENQOL vasomotor symptom domain score at 12 weeks,” said Dr. Simon. The quality of life and moderate to severe VMS frequency were highly correlated, he added (rho = 0.561, P less than .0001). Improvements in the other MENQOL domains were also highly correlated with reduction in moderate to severe frequency (P less than .0001 for all).
Among patients who reported significant improvement on the MENQOL, said Dr. Simon, more of the TX-001HR patients had improvements that were judged to be clinically significant compared to those taking placebo. Women who experienced a minimal clinically important difference in their symptoms had a weekly improvement of 34 fewer VMS events. Those who had a stronger response, which was judged to be clinically important, had a weekly improvement of 44 fewer VMS events.
Dr. Simon reported financial relationships with several pharmaceutical companies, including TherapeuticsMD, the sponsor of the THX-001HR clinical trials.
[email protected]
On Twitter @karioakes
PHILADELPHIA – An oral estradiol/progesterone formulation significantly improved menopause-related quality of life, compared with placebo, for up to 1 year after beginning treatment, according to a new study.
If approved, the new formulation “may be an option for the estimated millions of women currently using less-regulated and unapproved compounded bioidentical hormone therapy,” said James Simon, MD, the study’s senior author.
Patients receiving the combination therapy, termed TX-001HR, experienced a significant improvement in quality of life, compared with placebo and compared with baseline, at all study points, said Dr. Simon of George Washington University, Washington.
Using the Menopause-Specific Quality of Life questionnaire (MENQOL), Dr. Simon and his coinvestigators found that women taking the combination therapy saw reductions in the vasomotor domain of MENQOL within 12 weeks of beginning the study. The significant symptomatic improvement persisted for the full year that patients were followed.
For patients with particularly bothersome vasomotor symptoms, vasomotor domain scores ranged from 6.9 to 7.2 at baseline and were 2.8-3.6 with TX-001HR and 4.4 with placebo at month 12, according to Dr. Simon.
Speaking during a top abstracts session at the annual meeting of the North American Menopause Society, Dr. Simon said that TX-001HR combines the physiologic sex hormones 17-beta estradiol and progesterone (E2/P4) into a single oral soft-gel.
The phase 3 randomized, double blind, placebo-controlled REPLENISH trial explored the safety and efficacy of one of four dose combinations of E2/P4. A total of 1,833 patients were randomized to receive E2/P4 in doses of 1.0/100 mg, 0.5/100 mg, 0.5/50 mg, or 0.25/50 mg, or to receive placebo. An approximately equal number of patients were allocated to each study arm, except that 151 patients were allocated to receive placebo.
The MENQOL is structured so that the 29 items in the symptom inventory are grouped into four domains: vasomotor, psychosocial, physical, and sexual. Significant reductions were seen at 12 weeks for all patients in overall MENQOL scores and for the four domains.
The REPLENISH investigators also performed a separate analysis of data from the subset of patients who had moderate to severe vasomotor symptoms (VMS). At the 6- and 12-month assessment points, the VMS patients on all but the lowest dose of TX-001HR had significant improvement over placebo.
“Independent of treatment, the largest correlation observed was between changes in moderate to severe VMS frequency and changes in the MENQOL vasomotor symptom domain score at 12 weeks,” said Dr. Simon. The quality of life and moderate to severe VMS frequency were highly correlated, he added (rho = 0.561, P less than .0001). Improvements in the other MENQOL domains were also highly correlated with reduction in moderate to severe frequency (P less than .0001 for all).
Among patients who reported significant improvement on the MENQOL, said Dr. Simon, more of the TX-001HR patients had improvements that were judged to be clinically significant compared to those taking placebo. Women who experienced a minimal clinically important difference in their symptoms had a weekly improvement of 34 fewer VMS events. Those who had a stronger response, which was judged to be clinically important, had a weekly improvement of 44 fewer VMS events.
Dr. Simon reported financial relationships with several pharmaceutical companies, including TherapeuticsMD, the sponsor of the THX-001HR clinical trials.
[email protected]
On Twitter @karioakes
PHILADELPHIA – An oral estradiol/progesterone formulation significantly improved menopause-related quality of life, compared with placebo, for up to 1 year after beginning treatment, according to a new study.
If approved, the new formulation “may be an option for the estimated millions of women currently using less-regulated and unapproved compounded bioidentical hormone therapy,” said James Simon, MD, the study’s senior author.
Patients receiving the combination therapy, termed TX-001HR, experienced a significant improvement in quality of life, compared with placebo and compared with baseline, at all study points, said Dr. Simon of George Washington University, Washington.
Using the Menopause-Specific Quality of Life questionnaire (MENQOL), Dr. Simon and his coinvestigators found that women taking the combination therapy saw reductions in the vasomotor domain of MENQOL within 12 weeks of beginning the study. The significant symptomatic improvement persisted for the full year that patients were followed.
For patients with particularly bothersome vasomotor symptoms, vasomotor domain scores ranged from 6.9 to 7.2 at baseline and were 2.8-3.6 with TX-001HR and 4.4 with placebo at month 12, according to Dr. Simon.
Speaking during a top abstracts session at the annual meeting of the North American Menopause Society, Dr. Simon said that TX-001HR combines the physiologic sex hormones 17-beta estradiol and progesterone (E2/P4) into a single oral soft-gel.
The phase 3 randomized, double blind, placebo-controlled REPLENISH trial explored the safety and efficacy of one of four dose combinations of E2/P4. A total of 1,833 patients were randomized to receive E2/P4 in doses of 1.0/100 mg, 0.5/100 mg, 0.5/50 mg, or 0.25/50 mg, or to receive placebo. An approximately equal number of patients were allocated to each study arm, except that 151 patients were allocated to receive placebo.
The MENQOL is structured so that the 29 items in the symptom inventory are grouped into four domains: vasomotor, psychosocial, physical, and sexual. Significant reductions were seen at 12 weeks for all patients in overall MENQOL scores and for the four domains.
The REPLENISH investigators also performed a separate analysis of data from the subset of patients who had moderate to severe vasomotor symptoms (VMS). At the 6- and 12-month assessment points, the VMS patients on all but the lowest dose of TX-001HR had significant improvement over placebo.
“Independent of treatment, the largest correlation observed was between changes in moderate to severe VMS frequency and changes in the MENQOL vasomotor symptom domain score at 12 weeks,” said Dr. Simon. The quality of life and moderate to severe VMS frequency were highly correlated, he added (rho = 0.561, P less than .0001). Improvements in the other MENQOL domains were also highly correlated with reduction in moderate to severe frequency (P less than .0001 for all).
Among patients who reported significant improvement on the MENQOL, said Dr. Simon, more of the TX-001HR patients had improvements that were judged to be clinically significant compared to those taking placebo. Women who experienced a minimal clinically important difference in their symptoms had a weekly improvement of 34 fewer VMS events. Those who had a stronger response, which was judged to be clinically important, had a weekly improvement of 44 fewer VMS events.
Dr. Simon reported financial relationships with several pharmaceutical companies, including TherapeuticsMD, the sponsor of the THX-001HR clinical trials.
[email protected]
On Twitter @karioakes
AT NAMS 2017
Key clinical point:
Major finding: Patients taking TX-100HR had significant improvements in a menopause-related quality of life scale at all study time points.
Data source: REPLENISH, a phase 3, randomized, double blind, placebo-controlled study of 1,833 postmenopausal women.
Disclosures: Dr. Simon reported financial relationships with multiple pharmaceutical companies, including TherapeuticsMD, sponsor of the REPLENISH trial.
Time to take the fear out of the hormone therapy conversation
PHILADELPHIA – It’s time to be clear about the benefits of hormone therapy for many women in midlife, JoAnn Pinkerton, MD, executive director of the North American Menopause Society, said during the keynote address at the group’s annual meeting.
“I want to take fear out of the conversation. Hormone therapy remains the most effective treatment for vasomotor symptoms and the genitourinary syndrome of menopause and has been shown to prevent bone loss and fracture,” said Dr. Pinkerton, who also chaired the advisory panel that penned the 2017 NAMS position statement on hormone therapy.

Hormone therapy is currently approved by the Food and Drug Administration as first-line therapy to relieve vasomotor symptoms (VMS). Low-dose vaginal estrogen therapy is also a first-line treatment for the genitourinary syndrome of menopause, since it can directly address vulvovaginal atrophy.
An additional approved indication for systemic hormone therapy (HT) is the prevention of bone loss and fracture reduction in postmenopausal women who have increased risk of osteoporosis or fractures. It’s also FDA approved for women who had hypogonadism, primary ovarian insufficiency, or premature surgical menopause, who may use HT until the average age of menopause – about 52 years.
Unopposed systemic estrogen should not be used as HT in women with an intact uterus because of the elevated risk of endometrial cancer, and all indications assume there are no contraindications to HT use.
The position statement was developed by an expert panel, and has been endorsed by a number of international menopause societies, other American women’s health societies, and the American Association of Clinical Endocrinologists.
Cardiovascular risks
Early analysis of cardiovascular health data from the large, prospective Women’s Health Initiative trial raised significant concerns about increased risk. But further study of data from the Women’s Health Initiative, as well as meta-analyses of randomized controlled trials, have yielded a more nuanced view of the relationship between HT and cardiovascular disease, she said.
“Age matters,” Dr. Pinkerton said. “Data show that there is reduced heart disease in women who start [hormone replacement] early.” There is increasing data, she said, to support the “timing hypothesis.”
“Women who start HT before the age of 60 years, or within 10 years of menopause, may have a reduced risk of coronary heart disease,” Dr. Pinkerton said. “There is concern of increased risk of [coronary heart disease] in women who initiate hormone therapy more than 10 or 20 years from menopause.”
Use of HT is associated with a significantly increased risk of venous thromboembolism, a risk that increases with time, as does the risk of stroke and pulmonary embolism. Using lower doses or transdermal HT may reduce this risk, but “the lack of comparative randomized controlled trial data limit recommendations,” she said.
Transdermal therapy can also be considered for women with metabolic syndrome, hypertriglyceridemia, and fatty liver, since this route avoids first-pass hepatic metabolism.
Breast cancer
“The effect of hormone therapy on breast cancer risk is complex and conflicting,” said Dr Pinkerton, noting that breast cancer risk from HT may depend on many factors, including whether progestins are added to estrogen, the dose and duration of HT use, and how HT is administered.
Regarding the use of vaginal estrogen for women who have had breast cancer, Dr. Pinkerton said, “It’s a data-free zone.” Systemic absorption of vaginally-dosed estrogen is minimal, but the decision to use vaginal estrogen for a breast cancer survivor who is experiencing genitourinary syndrome of menopause symptoms should always be made in consultation with the woman’s oncologist and in shared decision-making with the patient herself, Dr. Pinkerton added.
Bioidentical HT
“Unique concerns about safety surround the use of compounded bioidentical hormone therapy,” Dr. Pinkerton said.
The lack of regulation and monitoring, together with lax labeling requirements, are areas of concern. Accurate dosing may not be occurring, and data are lacking to support safety and efficacy of compounded bioidentical products, she said. Neither is there evidence to support routine testing of serum or salivary hormone levels, she added.
Symptom relief
For isolated symptoms of genitourinary syndrome of menopause, low-dose vaginal preparations are safe and effective, Dr. Pinkerton said. For women who are symptomatic, use of either low-dose vaginal estrogen or systemic HT increases sexual function scores; however, she said, “hormone therapy is not recommended as the sole treatment of other sexual function problems,” such as diminished libido, though it can be a useful adjunct.
“Hormone therapy is the most effective treatment for hot flashes,” said Dr. Pinkerton, and using HT improves sleep quality and duration in women with bothersome nighttime hot flashes.
Fracture prevention
Data from the Women’s Health Initiative showed a highly significant 33% reduction in hip fractures for women using both estrogen alone and estrogen with progestogen. “That seems to get forgotten,” Dr. Pinkerton said. Though HT’s osteoporosis and fracture prevention effects stop when HT is discontinued, there’s no evidence of elevated fracture risk above baseline in women who have used HT and then stopped.
“Younger women may need higher doses to protect bone, but make sure you get adequate endometrial protection if you do that,” said Dr. Pinkerton, professor of obstetrics and gynecology at the University of Virginia.
Unapproved uses
“Hormone therapy is not recommended at any age to prevent or treat cognition or dementia,” said Dr. Pinkerton, citing a lack of data to support its use for these reasons. Observational data may show some reduction in risk of Alzheimer’s disease in women who use HT at younger ages or soon after menopause, she said.
Though HT users have a reduced risk of developing type 2 diabetes, diabetes prevention is not a Food and Drug Administration–approved indication for HT. Abdominal fat accumulation and weight gain may be reduced by HT as well, Dr. Pinkerton said.
Similarly, there are no data to support the use of HT for the treatment of clinical depression. Perimenopausal – but not postmenopausal – women may see some benefit from estrogen therapy; progestins may actually contribute to mood disturbance, she said.
Special populations
“Systemic hormone therapy is not recommended for survivors of breast cancer,” Dr. Pinkerton said. Any consideration for systemic HT in this population should include the oncologist, and only be entertained after other nonhormonal options have been tried, she said.
Women with a family history of breast or ovarian cancer, or with the BRCA mutation, do not appear to have their risk increased by the use of HT, though the ovarian cancer data are limited and observational, Dr. Pinkerton said.
The NAMS position statement also addresses the use of HT in other special populations, including survivors of other cancers and women who have primary ovarian insufficiency or early menopause, BRCA-positive women who have undergone oophorectomy, and those over age 65 years.
“The recommendation to routinely discontinue systemic hormone therapy after age 65 is not supported by data,” Dr. Pinkerton said. “I would tell you that there’s a lack of good data about prolonged duration. What I tell patients is, we really are in another data-free zone.” She recommends an individualized approach that balances benefits and risks and includes ongoing surveillance.
New message
“So what do I want us to do? I want us to change the message,” she said. Rather than advocating for HT to be used in “the lowest dose, for the shortest period of time,” she said the new message should be for women to use “appropriate hormone therapy to meet their treatment goals.”
The bottom line? After accounting for women who should avoid HT for specific contraindications, “benefits are likely to outweigh risks for symptomatic women who initiate hormone therapy when aged younger than 60 years and within 10 years of menopause,” Dr. Pinkerton said.
Dr. Pinkerton reported that she has received grant or research support from TherapeuticsMD.
[email protected]
On Twitter @karioakes
PHILADELPHIA – It’s time to be clear about the benefits of hormone therapy for many women in midlife, JoAnn Pinkerton, MD, executive director of the North American Menopause Society, said during the keynote address at the group’s annual meeting.
“I want to take fear out of the conversation. Hormone therapy remains the most effective treatment for vasomotor symptoms and the genitourinary syndrome of menopause and has been shown to prevent bone loss and fracture,” said Dr. Pinkerton, who also chaired the advisory panel that penned the 2017 NAMS position statement on hormone therapy.

Hormone therapy is currently approved by the Food and Drug Administration as first-line therapy to relieve vasomotor symptoms (VMS). Low-dose vaginal estrogen therapy is also a first-line treatment for the genitourinary syndrome of menopause, since it can directly address vulvovaginal atrophy.
An additional approved indication for systemic hormone therapy (HT) is the prevention of bone loss and fracture reduction in postmenopausal women who have increased risk of osteoporosis or fractures. It’s also FDA approved for women who had hypogonadism, primary ovarian insufficiency, or premature surgical menopause, who may use HT until the average age of menopause – about 52 years.
Unopposed systemic estrogen should not be used as HT in women with an intact uterus because of the elevated risk of endometrial cancer, and all indications assume there are no contraindications to HT use.
The position statement was developed by an expert panel, and has been endorsed by a number of international menopause societies, other American women’s health societies, and the American Association of Clinical Endocrinologists.
Cardiovascular risks
Early analysis of cardiovascular health data from the large, prospective Women’s Health Initiative trial raised significant concerns about increased risk. But further study of data from the Women’s Health Initiative, as well as meta-analyses of randomized controlled trials, have yielded a more nuanced view of the relationship between HT and cardiovascular disease, she said.
“Age matters,” Dr. Pinkerton said. “Data show that there is reduced heart disease in women who start [hormone replacement] early.” There is increasing data, she said, to support the “timing hypothesis.”
“Women who start HT before the age of 60 years, or within 10 years of menopause, may have a reduced risk of coronary heart disease,” Dr. Pinkerton said. “There is concern of increased risk of [coronary heart disease] in women who initiate hormone therapy more than 10 or 20 years from menopause.”
Use of HT is associated with a significantly increased risk of venous thromboembolism, a risk that increases with time, as does the risk of stroke and pulmonary embolism. Using lower doses or transdermal HT may reduce this risk, but “the lack of comparative randomized controlled trial data limit recommendations,” she said.
Transdermal therapy can also be considered for women with metabolic syndrome, hypertriglyceridemia, and fatty liver, since this route avoids first-pass hepatic metabolism.
Breast cancer
“The effect of hormone therapy on breast cancer risk is complex and conflicting,” said Dr Pinkerton, noting that breast cancer risk from HT may depend on many factors, including whether progestins are added to estrogen, the dose and duration of HT use, and how HT is administered.
Regarding the use of vaginal estrogen for women who have had breast cancer, Dr. Pinkerton said, “It’s a data-free zone.” Systemic absorption of vaginally-dosed estrogen is minimal, but the decision to use vaginal estrogen for a breast cancer survivor who is experiencing genitourinary syndrome of menopause symptoms should always be made in consultation with the woman’s oncologist and in shared decision-making with the patient herself, Dr. Pinkerton added.
Bioidentical HT
“Unique concerns about safety surround the use of compounded bioidentical hormone therapy,” Dr. Pinkerton said.
The lack of regulation and monitoring, together with lax labeling requirements, are areas of concern. Accurate dosing may not be occurring, and data are lacking to support safety and efficacy of compounded bioidentical products, she said. Neither is there evidence to support routine testing of serum or salivary hormone levels, she added.
Symptom relief
For isolated symptoms of genitourinary syndrome of menopause, low-dose vaginal preparations are safe and effective, Dr. Pinkerton said. For women who are symptomatic, use of either low-dose vaginal estrogen or systemic HT increases sexual function scores; however, she said, “hormone therapy is not recommended as the sole treatment of other sexual function problems,” such as diminished libido, though it can be a useful adjunct.
“Hormone therapy is the most effective treatment for hot flashes,” said Dr. Pinkerton, and using HT improves sleep quality and duration in women with bothersome nighttime hot flashes.
Fracture prevention
Data from the Women’s Health Initiative showed a highly significant 33% reduction in hip fractures for women using both estrogen alone and estrogen with progestogen. “That seems to get forgotten,” Dr. Pinkerton said. Though HT’s osteoporosis and fracture prevention effects stop when HT is discontinued, there’s no evidence of elevated fracture risk above baseline in women who have used HT and then stopped.
“Younger women may need higher doses to protect bone, but make sure you get adequate endometrial protection if you do that,” said Dr. Pinkerton, professor of obstetrics and gynecology at the University of Virginia.
Unapproved uses
“Hormone therapy is not recommended at any age to prevent or treat cognition or dementia,” said Dr. Pinkerton, citing a lack of data to support its use for these reasons. Observational data may show some reduction in risk of Alzheimer’s disease in women who use HT at younger ages or soon after menopause, she said.
Though HT users have a reduced risk of developing type 2 diabetes, diabetes prevention is not a Food and Drug Administration–approved indication for HT. Abdominal fat accumulation and weight gain may be reduced by HT as well, Dr. Pinkerton said.
Similarly, there are no data to support the use of HT for the treatment of clinical depression. Perimenopausal – but not postmenopausal – women may see some benefit from estrogen therapy; progestins may actually contribute to mood disturbance, she said.
Special populations
“Systemic hormone therapy is not recommended for survivors of breast cancer,” Dr. Pinkerton said. Any consideration for systemic HT in this population should include the oncologist, and only be entertained after other nonhormonal options have been tried, she said.
Women with a family history of breast or ovarian cancer, or with the BRCA mutation, do not appear to have their risk increased by the use of HT, though the ovarian cancer data are limited and observational, Dr. Pinkerton said.
The NAMS position statement also addresses the use of HT in other special populations, including survivors of other cancers and women who have primary ovarian insufficiency or early menopause, BRCA-positive women who have undergone oophorectomy, and those over age 65 years.
“The recommendation to routinely discontinue systemic hormone therapy after age 65 is not supported by data,” Dr. Pinkerton said. “I would tell you that there’s a lack of good data about prolonged duration. What I tell patients is, we really are in another data-free zone.” She recommends an individualized approach that balances benefits and risks and includes ongoing surveillance.
New message
“So what do I want us to do? I want us to change the message,” she said. Rather than advocating for HT to be used in “the lowest dose, for the shortest period of time,” she said the new message should be for women to use “appropriate hormone therapy to meet their treatment goals.”
The bottom line? After accounting for women who should avoid HT for specific contraindications, “benefits are likely to outweigh risks for symptomatic women who initiate hormone therapy when aged younger than 60 years and within 10 years of menopause,” Dr. Pinkerton said.
Dr. Pinkerton reported that she has received grant or research support from TherapeuticsMD.
[email protected]
On Twitter @karioakes
PHILADELPHIA – It’s time to be clear about the benefits of hormone therapy for many women in midlife, JoAnn Pinkerton, MD, executive director of the North American Menopause Society, said during the keynote address at the group’s annual meeting.
“I want to take fear out of the conversation. Hormone therapy remains the most effective treatment for vasomotor symptoms and the genitourinary syndrome of menopause and has been shown to prevent bone loss and fracture,” said Dr. Pinkerton, who also chaired the advisory panel that penned the 2017 NAMS position statement on hormone therapy.

Hormone therapy is currently approved by the Food and Drug Administration as first-line therapy to relieve vasomotor symptoms (VMS). Low-dose vaginal estrogen therapy is also a first-line treatment for the genitourinary syndrome of menopause, since it can directly address vulvovaginal atrophy.
An additional approved indication for systemic hormone therapy (HT) is the prevention of bone loss and fracture reduction in postmenopausal women who have increased risk of osteoporosis or fractures. It’s also FDA approved for women who had hypogonadism, primary ovarian insufficiency, or premature surgical menopause, who may use HT until the average age of menopause – about 52 years.
Unopposed systemic estrogen should not be used as HT in women with an intact uterus because of the elevated risk of endometrial cancer, and all indications assume there are no contraindications to HT use.
The position statement was developed by an expert panel, and has been endorsed by a number of international menopause societies, other American women’s health societies, and the American Association of Clinical Endocrinologists.
Cardiovascular risks
Early analysis of cardiovascular health data from the large, prospective Women’s Health Initiative trial raised significant concerns about increased risk. But further study of data from the Women’s Health Initiative, as well as meta-analyses of randomized controlled trials, have yielded a more nuanced view of the relationship between HT and cardiovascular disease, she said.
“Age matters,” Dr. Pinkerton said. “Data show that there is reduced heart disease in women who start [hormone replacement] early.” There is increasing data, she said, to support the “timing hypothesis.”
“Women who start HT before the age of 60 years, or within 10 years of menopause, may have a reduced risk of coronary heart disease,” Dr. Pinkerton said. “There is concern of increased risk of [coronary heart disease] in women who initiate hormone therapy more than 10 or 20 years from menopause.”
Use of HT is associated with a significantly increased risk of venous thromboembolism, a risk that increases with time, as does the risk of stroke and pulmonary embolism. Using lower doses or transdermal HT may reduce this risk, but “the lack of comparative randomized controlled trial data limit recommendations,” she said.
Transdermal therapy can also be considered for women with metabolic syndrome, hypertriglyceridemia, and fatty liver, since this route avoids first-pass hepatic metabolism.
Breast cancer
“The effect of hormone therapy on breast cancer risk is complex and conflicting,” said Dr Pinkerton, noting that breast cancer risk from HT may depend on many factors, including whether progestins are added to estrogen, the dose and duration of HT use, and how HT is administered.
Regarding the use of vaginal estrogen for women who have had breast cancer, Dr. Pinkerton said, “It’s a data-free zone.” Systemic absorption of vaginally-dosed estrogen is minimal, but the decision to use vaginal estrogen for a breast cancer survivor who is experiencing genitourinary syndrome of menopause symptoms should always be made in consultation with the woman’s oncologist and in shared decision-making with the patient herself, Dr. Pinkerton added.
Bioidentical HT
“Unique concerns about safety surround the use of compounded bioidentical hormone therapy,” Dr. Pinkerton said.
The lack of regulation and monitoring, together with lax labeling requirements, are areas of concern. Accurate dosing may not be occurring, and data are lacking to support safety and efficacy of compounded bioidentical products, she said. Neither is there evidence to support routine testing of serum or salivary hormone levels, she added.
Symptom relief
For isolated symptoms of genitourinary syndrome of menopause, low-dose vaginal preparations are safe and effective, Dr. Pinkerton said. For women who are symptomatic, use of either low-dose vaginal estrogen or systemic HT increases sexual function scores; however, she said, “hormone therapy is not recommended as the sole treatment of other sexual function problems,” such as diminished libido, though it can be a useful adjunct.
“Hormone therapy is the most effective treatment for hot flashes,” said Dr. Pinkerton, and using HT improves sleep quality and duration in women with bothersome nighttime hot flashes.
Fracture prevention
Data from the Women’s Health Initiative showed a highly significant 33% reduction in hip fractures for women using both estrogen alone and estrogen with progestogen. “That seems to get forgotten,” Dr. Pinkerton said. Though HT’s osteoporosis and fracture prevention effects stop when HT is discontinued, there’s no evidence of elevated fracture risk above baseline in women who have used HT and then stopped.
“Younger women may need higher doses to protect bone, but make sure you get adequate endometrial protection if you do that,” said Dr. Pinkerton, professor of obstetrics and gynecology at the University of Virginia.
Unapproved uses
“Hormone therapy is not recommended at any age to prevent or treat cognition or dementia,” said Dr. Pinkerton, citing a lack of data to support its use for these reasons. Observational data may show some reduction in risk of Alzheimer’s disease in women who use HT at younger ages or soon after menopause, she said.
Though HT users have a reduced risk of developing type 2 diabetes, diabetes prevention is not a Food and Drug Administration–approved indication for HT. Abdominal fat accumulation and weight gain may be reduced by HT as well, Dr. Pinkerton said.
Similarly, there are no data to support the use of HT for the treatment of clinical depression. Perimenopausal – but not postmenopausal – women may see some benefit from estrogen therapy; progestins may actually contribute to mood disturbance, she said.
Special populations
“Systemic hormone therapy is not recommended for survivors of breast cancer,” Dr. Pinkerton said. Any consideration for systemic HT in this population should include the oncologist, and only be entertained after other nonhormonal options have been tried, she said.
Women with a family history of breast or ovarian cancer, or with the BRCA mutation, do not appear to have their risk increased by the use of HT, though the ovarian cancer data are limited and observational, Dr. Pinkerton said.
The NAMS position statement also addresses the use of HT in other special populations, including survivors of other cancers and women who have primary ovarian insufficiency or early menopause, BRCA-positive women who have undergone oophorectomy, and those over age 65 years.
“The recommendation to routinely discontinue systemic hormone therapy after age 65 is not supported by data,” Dr. Pinkerton said. “I would tell you that there’s a lack of good data about prolonged duration. What I tell patients is, we really are in another data-free zone.” She recommends an individualized approach that balances benefits and risks and includes ongoing surveillance.
New message
“So what do I want us to do? I want us to change the message,” she said. Rather than advocating for HT to be used in “the lowest dose, for the shortest period of time,” she said the new message should be for women to use “appropriate hormone therapy to meet their treatment goals.”
The bottom line? After accounting for women who should avoid HT for specific contraindications, “benefits are likely to outweigh risks for symptomatic women who initiate hormone therapy when aged younger than 60 years and within 10 years of menopause,” Dr. Pinkerton said.
Dr. Pinkerton reported that she has received grant or research support from TherapeuticsMD.
[email protected]
On Twitter @karioakes
AT NAMS 2017