User login
Sharing mental health notes with patients: Differentiating between access and accessibility
As a result of technology, data to which individuals have long had a legal right of access are now easily accessible. The advent of secure online portals has converted what was once largely a hypothetical proposition – i.e., ready patient access to clinical records – into the increasing reality of open notes. Unsurprisingly, this movement toward greater transparency carries special implications and complexities for mental health professionals concerned with balancing patient autonomy and safety.1
In setting clinician expectations for incorporating clinical note-sharing into patient care, it is important to clarify the already robust legal rights of patients to obtain copies of their treatment records, including in the mental health context. For example, the provision of access to one’s own health information is one of the rare circumstances in which the HIPAA Privacy Rule compels, rather than merely permits, health care organizations to disclose records to external parties.2 This requirement accords with a prevailing principle of medical ethics that records should be furnished to patients or their designees upon request.3
While HIPAA provides mechanisms for denying individuals access to their health records when a licensed health care professional determines that such access is “reasonably likely” to jeopardize someone’s life or physical safety, this standard sets a high bar of physical endangerment. A psychiatrist or other physician’s concern that sharing clinical notes would be therapeutically suboptimal, discomforting, emotionally harmful, confusing, or deleterious to the doctor-patient relationship would not constitute sufficient legal grounds for denial of access.4
Moreover, because access is framed as a patient right, denial on the aforementioned safety grounds implicates due process requirements to include a written explanation and appellate review by a designated disinterested official. Importantly, this federally mandated right of access would preempt or override any contrary state law classified as less protective of patient prerogatives.
Contrary to popular misconception, mental health notes are not necessarily entitled to a greater degree of secrecy vis-à-vis patients than records pertaining to physical health. The HIPAA Privacy Rule, for example, generally does not distinguish between medical and mental health information, nor does it provide special rules for the latter.5 Specifically, patients’ access rights remain unchanged regardless of whether the requested record is classified as medical or psychiatric.
One narrow exception involves “psychotherapy notes,” but the legal definition of this term is considerably more restrictive than in common psychiatric usage. Psychotherapy notes under health privacy law include therapists’ private, desk-drawer notes on counseling sessions intended for personal use as memory joggers. They explicitly exclude any discussion of treatment modalities, diagnosis, or clinical progress. To retain their protected status, psychotherapy notes must be kept separate and apart from the patient chart. Indeed, a primary reason why such notes are exempted from patient access is because they have so little legitimate use other than to their creator.
Integrating the proliferation of open notes into practice regimens will likely pose a continuing and growing challenge for mental health professionals. From a medicolegal perspective, however, even psychiatrists who are understandably hesitant about widespread note-sharing would do well to remember that patients’ underlying right of access is generally well established, and is merely being operationalized and automated via web portals. Ultimately, adapting clinical record-keeping to both anticipate patient access – and, where possible, leverage it to improve care – may prove the most effective path forward for practicing psychiatry in the digital age.
Lt. Col. Kels teaches at the U.S. Army Medical Center of Excellence, and Dr. Kels teaches and practices psychiatry at the University of the Incarnate Word School of Osteopathic Medicine, both in San Antonio, Tex. Neither Lt. Col. Kels nor Dr. Kels have any conflicts of interest to disclose. Opinions expressed in this article are those of the authors alone and do not necessarily reflect those of any government agency.
References
1. Lancet Psychiatry. 2020;7(11):924-5.
2. 45 CFR Parts 160 and 164, subparts A and E.
3. American Medical Association. Code of medical ethics, opinion 3.3.1: management of medical records.
4. Department of Health & Human Services. Individuals’ right under HIPAA to access their health information.
5. Department of Health & Human Services. HIPAA privacy rule and sharing information related to mental health.
As a result of technology, data to which individuals have long had a legal right of access are now easily accessible. The advent of secure online portals has converted what was once largely a hypothetical proposition – i.e., ready patient access to clinical records – into the increasing reality of open notes. Unsurprisingly, this movement toward greater transparency carries special implications and complexities for mental health professionals concerned with balancing patient autonomy and safety.1
In setting clinician expectations for incorporating clinical note-sharing into patient care, it is important to clarify the already robust legal rights of patients to obtain copies of their treatment records, including in the mental health context. For example, the provision of access to one’s own health information is one of the rare circumstances in which the HIPAA Privacy Rule compels, rather than merely permits, health care organizations to disclose records to external parties.2 This requirement accords with a prevailing principle of medical ethics that records should be furnished to patients or their designees upon request.3
While HIPAA provides mechanisms for denying individuals access to their health records when a licensed health care professional determines that such access is “reasonably likely” to jeopardize someone’s life or physical safety, this standard sets a high bar of physical endangerment. A psychiatrist or other physician’s concern that sharing clinical notes would be therapeutically suboptimal, discomforting, emotionally harmful, confusing, or deleterious to the doctor-patient relationship would not constitute sufficient legal grounds for denial of access.4
Moreover, because access is framed as a patient right, denial on the aforementioned safety grounds implicates due process requirements to include a written explanation and appellate review by a designated disinterested official. Importantly, this federally mandated right of access would preempt or override any contrary state law classified as less protective of patient prerogatives.
Contrary to popular misconception, mental health notes are not necessarily entitled to a greater degree of secrecy vis-à-vis patients than records pertaining to physical health. The HIPAA Privacy Rule, for example, generally does not distinguish between medical and mental health information, nor does it provide special rules for the latter.5 Specifically, patients’ access rights remain unchanged regardless of whether the requested record is classified as medical or psychiatric.
One narrow exception involves “psychotherapy notes,” but the legal definition of this term is considerably more restrictive than in common psychiatric usage. Psychotherapy notes under health privacy law include therapists’ private, desk-drawer notes on counseling sessions intended for personal use as memory joggers. They explicitly exclude any discussion of treatment modalities, diagnosis, or clinical progress. To retain their protected status, psychotherapy notes must be kept separate and apart from the patient chart. Indeed, a primary reason why such notes are exempted from patient access is because they have so little legitimate use other than to their creator.
Integrating the proliferation of open notes into practice regimens will likely pose a continuing and growing challenge for mental health professionals. From a medicolegal perspective, however, even psychiatrists who are understandably hesitant about widespread note-sharing would do well to remember that patients’ underlying right of access is generally well established, and is merely being operationalized and automated via web portals. Ultimately, adapting clinical record-keeping to both anticipate patient access – and, where possible, leverage it to improve care – may prove the most effective path forward for practicing psychiatry in the digital age.
Lt. Col. Kels teaches at the U.S. Army Medical Center of Excellence, and Dr. Kels teaches and practices psychiatry at the University of the Incarnate Word School of Osteopathic Medicine, both in San Antonio, Tex. Neither Lt. Col. Kels nor Dr. Kels have any conflicts of interest to disclose. Opinions expressed in this article are those of the authors alone and do not necessarily reflect those of any government agency.
References
1. Lancet Psychiatry. 2020;7(11):924-5.
2. 45 CFR Parts 160 and 164, subparts A and E.
3. American Medical Association. Code of medical ethics, opinion 3.3.1: management of medical records.
4. Department of Health & Human Services. Individuals’ right under HIPAA to access their health information.
5. Department of Health & Human Services. HIPAA privacy rule and sharing information related to mental health.
As a result of technology, data to which individuals have long had a legal right of access are now easily accessible. The advent of secure online portals has converted what was once largely a hypothetical proposition – i.e., ready patient access to clinical records – into the increasing reality of open notes. Unsurprisingly, this movement toward greater transparency carries special implications and complexities for mental health professionals concerned with balancing patient autonomy and safety.1
In setting clinician expectations for incorporating clinical note-sharing into patient care, it is important to clarify the already robust legal rights of patients to obtain copies of their treatment records, including in the mental health context. For example, the provision of access to one’s own health information is one of the rare circumstances in which the HIPAA Privacy Rule compels, rather than merely permits, health care organizations to disclose records to external parties.2 This requirement accords with a prevailing principle of medical ethics that records should be furnished to patients or their designees upon request.3
While HIPAA provides mechanisms for denying individuals access to their health records when a licensed health care professional determines that such access is “reasonably likely” to jeopardize someone’s life or physical safety, this standard sets a high bar of physical endangerment. A psychiatrist or other physician’s concern that sharing clinical notes would be therapeutically suboptimal, discomforting, emotionally harmful, confusing, or deleterious to the doctor-patient relationship would not constitute sufficient legal grounds for denial of access.4
Moreover, because access is framed as a patient right, denial on the aforementioned safety grounds implicates due process requirements to include a written explanation and appellate review by a designated disinterested official. Importantly, this federally mandated right of access would preempt or override any contrary state law classified as less protective of patient prerogatives.
Contrary to popular misconception, mental health notes are not necessarily entitled to a greater degree of secrecy vis-à-vis patients than records pertaining to physical health. The HIPAA Privacy Rule, for example, generally does not distinguish between medical and mental health information, nor does it provide special rules for the latter.5 Specifically, patients’ access rights remain unchanged regardless of whether the requested record is classified as medical or psychiatric.
One narrow exception involves “psychotherapy notes,” but the legal definition of this term is considerably more restrictive than in common psychiatric usage. Psychotherapy notes under health privacy law include therapists’ private, desk-drawer notes on counseling sessions intended for personal use as memory joggers. They explicitly exclude any discussion of treatment modalities, diagnosis, or clinical progress. To retain their protected status, psychotherapy notes must be kept separate and apart from the patient chart. Indeed, a primary reason why such notes are exempted from patient access is because they have so little legitimate use other than to their creator.
Integrating the proliferation of open notes into practice regimens will likely pose a continuing and growing challenge for mental health professionals. From a medicolegal perspective, however, even psychiatrists who are understandably hesitant about widespread note-sharing would do well to remember that patients’ underlying right of access is generally well established, and is merely being operationalized and automated via web portals. Ultimately, adapting clinical record-keeping to both anticipate patient access – and, where possible, leverage it to improve care – may prove the most effective path forward for practicing psychiatry in the digital age.
Lt. Col. Kels teaches at the U.S. Army Medical Center of Excellence, and Dr. Kels teaches and practices psychiatry at the University of the Incarnate Word School of Osteopathic Medicine, both in San Antonio, Tex. Neither Lt. Col. Kels nor Dr. Kels have any conflicts of interest to disclose. Opinions expressed in this article are those of the authors alone and do not necessarily reflect those of any government agency.
References
1. Lancet Psychiatry. 2020;7(11):924-5.
2. 45 CFR Parts 160 and 164, subparts A and E.
3. American Medical Association. Code of medical ethics, opinion 3.3.1: management of medical records.
4. Department of Health & Human Services. Individuals’ right under HIPAA to access their health information.
5. Department of Health & Human Services. HIPAA privacy rule and sharing information related to mental health.
Tips for physicians, patients to make the most of the holidays amid COVID
“We must accept finite disappointment, but never lose infinite hope,” Martin Luther King, Jr.
This holiday season will be like no other. We will remember it for the rest of our lives, and we will look back to see how we faced the holidays during a pandemic.
Like the rest of 2020, the holidays will need to be reimagined. Years and even decades of tradition will be broken as we place health above merriment.
Here are a few tips to help all of us and our patients make the most of this holiday season.
- Reprioritize: This holiday season will be about depth not breadth, quality not quantity, and less not more. Trips are canceled and gatherings have shrunk. We are not running from store to store or party to party. Instead, you will find yourself surrounded by fewer friends and family. Some will be alone to optimally protect their health and the health of others. Do your best to focus on the half-full portion.
- Embrace change: Don’t compare or try to make this year like previous years. Be creative and try to find ways to make a new format fun. Meeting during the day and limiting alcohol intake can assist in making sure everyone stays safe. It has been interesting to see how many of my patients have decreased their alcohol use during quarantine. I hope this pattern will continue over the next weeks and months.
- Practice self-care: As health care professionals, we must remember the old adage “physician, heal thyself.” This year has been so difficult for almost all of us. It was filled with unprecedented levels of personal and professional stress. Holidays are often about what we can do for others, but this year we may need to place self-care first. Do what brings you happiness.
Even though you aren’t traveling, you can still disconnect from work. Set up a schedule and stick to it making sure you take plenty of time to rest and enjoy. Many of us have been working extremely long hours and a break is so needed. Take it if you possibly can. Detox from your screen! Limit the news. Creativity and productivity will be enhanced in 2021 if we can come in recharged.
For those remaining on the front lines, be patient; the end is nearing. Take care of yourself when you are not working. We are all so grateful to those in our field who have sacrificed so much to care for others. Eat, drink, and rest well to keep your immune system strong.
- Acknowledge your negative emotions: As we all know, if you try to deny negative emotions, they continue to pop up. If we give them time and space to be felt, we will find they diminish in intensity. Long work hours may have prevented us from feeling our emotions, so don’t be surprised if they surface when we take a break.
Let yourself feel the sadness for what you have experienced this year. Be open about missing those who can’t be with you because of travel or other restrictions. Let yourself feel the disappointment about your holiday travel plans that you can’t embark upon.
You may elect to share these emotions with someone close to you or with a professional. To paraphrase Carl Jung, “what we resist, persists,” so don’t try to hide from your negative emotions. Most of us had lots of them in 2020, so don’t be shy about admitting it.
- Focus on growth: What have we learned from 2020 and how can we be better equipped in 2021 and beyond?
Trauma can bring growth not just disorder. This year has returned well-deserved prestige to our fields. We are being lauded as heroes as we have scarified our health and the health of our loved ones to serve others. Can we choose to celebrate our accomplishments?
We have become more resilient and learned to continue on in the face of great hardship. Many of us have gained confidence as we confronted this historic challenge. As we have been reminded of death daily, we learn to appreciate life more fully and not take any day for granted.
I am proud to be a physician during this pandemic, and I hope you are, too!
- Find joy: Often times, we find real happiness in smaller moments and experiences. For many, this time of year is filled with so much stress that it can be hard to carve out moments of joy. As we may be less busy socially this holiday season, might we find even more joy?
Joy can only be experienced in the present moment. Tap into all your senses. Eat slowly making sure to smell and taste every bite. Cherish those who can still gather at your table. If you find yourself alone, embrace that experience. Safety must continue to come first, and we can’t let down our guard now.
- Reflect: New Year’s Eve is always a time for reflection and hope for the future. Most of us will be glad to see 2020 in the rearview mirror. With multiple and very promising vaccines on the horizon, we can anticipate a brighter future. We must continue to work hard; remain patient; and be creative, resilient, and optimistic. Let’s try to fill our days with hope and purpose and work together to achieve a brighter future for all.
“Learn from yesterday, live for today, hope for tomorrow,” Albert Einstein
Wishing you health and happiness in this holiday season and beyond.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). She also is founder of the Bekindr Global Initiative, a movement aimed at cultivating kindness in the world.
“We must accept finite disappointment, but never lose infinite hope,” Martin Luther King, Jr.
This holiday season will be like no other. We will remember it for the rest of our lives, and we will look back to see how we faced the holidays during a pandemic.
Like the rest of 2020, the holidays will need to be reimagined. Years and even decades of tradition will be broken as we place health above merriment.
Here are a few tips to help all of us and our patients make the most of this holiday season.
- Reprioritize: This holiday season will be about depth not breadth, quality not quantity, and less not more. Trips are canceled and gatherings have shrunk. We are not running from store to store or party to party. Instead, you will find yourself surrounded by fewer friends and family. Some will be alone to optimally protect their health and the health of others. Do your best to focus on the half-full portion.
- Embrace change: Don’t compare or try to make this year like previous years. Be creative and try to find ways to make a new format fun. Meeting during the day and limiting alcohol intake can assist in making sure everyone stays safe. It has been interesting to see how many of my patients have decreased their alcohol use during quarantine. I hope this pattern will continue over the next weeks and months.
- Practice self-care: As health care professionals, we must remember the old adage “physician, heal thyself.” This year has been so difficult for almost all of us. It was filled with unprecedented levels of personal and professional stress. Holidays are often about what we can do for others, but this year we may need to place self-care first. Do what brings you happiness.
Even though you aren’t traveling, you can still disconnect from work. Set up a schedule and stick to it making sure you take plenty of time to rest and enjoy. Many of us have been working extremely long hours and a break is so needed. Take it if you possibly can. Detox from your screen! Limit the news. Creativity and productivity will be enhanced in 2021 if we can come in recharged.
For those remaining on the front lines, be patient; the end is nearing. Take care of yourself when you are not working. We are all so grateful to those in our field who have sacrificed so much to care for others. Eat, drink, and rest well to keep your immune system strong.
- Acknowledge your negative emotions: As we all know, if you try to deny negative emotions, they continue to pop up. If we give them time and space to be felt, we will find they diminish in intensity. Long work hours may have prevented us from feeling our emotions, so don’t be surprised if they surface when we take a break.
Let yourself feel the sadness for what you have experienced this year. Be open about missing those who can’t be with you because of travel or other restrictions. Let yourself feel the disappointment about your holiday travel plans that you can’t embark upon.
You may elect to share these emotions with someone close to you or with a professional. To paraphrase Carl Jung, “what we resist, persists,” so don’t try to hide from your negative emotions. Most of us had lots of them in 2020, so don’t be shy about admitting it.
- Focus on growth: What have we learned from 2020 and how can we be better equipped in 2021 and beyond?
Trauma can bring growth not just disorder. This year has returned well-deserved prestige to our fields. We are being lauded as heroes as we have scarified our health and the health of our loved ones to serve others. Can we choose to celebrate our accomplishments?
We have become more resilient and learned to continue on in the face of great hardship. Many of us have gained confidence as we confronted this historic challenge. As we have been reminded of death daily, we learn to appreciate life more fully and not take any day for granted.
I am proud to be a physician during this pandemic, and I hope you are, too!
- Find joy: Often times, we find real happiness in smaller moments and experiences. For many, this time of year is filled with so much stress that it can be hard to carve out moments of joy. As we may be less busy socially this holiday season, might we find even more joy?
Joy can only be experienced in the present moment. Tap into all your senses. Eat slowly making sure to smell and taste every bite. Cherish those who can still gather at your table. If you find yourself alone, embrace that experience. Safety must continue to come first, and we can’t let down our guard now.
- Reflect: New Year’s Eve is always a time for reflection and hope for the future. Most of us will be glad to see 2020 in the rearview mirror. With multiple and very promising vaccines on the horizon, we can anticipate a brighter future. We must continue to work hard; remain patient; and be creative, resilient, and optimistic. Let’s try to fill our days with hope and purpose and work together to achieve a brighter future for all.
“Learn from yesterday, live for today, hope for tomorrow,” Albert Einstein
Wishing you health and happiness in this holiday season and beyond.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). She also is founder of the Bekindr Global Initiative, a movement aimed at cultivating kindness in the world.
“We must accept finite disappointment, but never lose infinite hope,” Martin Luther King, Jr.
This holiday season will be like no other. We will remember it for the rest of our lives, and we will look back to see how we faced the holidays during a pandemic.
Like the rest of 2020, the holidays will need to be reimagined. Years and even decades of tradition will be broken as we place health above merriment.
Here are a few tips to help all of us and our patients make the most of this holiday season.
- Reprioritize: This holiday season will be about depth not breadth, quality not quantity, and less not more. Trips are canceled and gatherings have shrunk. We are not running from store to store or party to party. Instead, you will find yourself surrounded by fewer friends and family. Some will be alone to optimally protect their health and the health of others. Do your best to focus on the half-full portion.
- Embrace change: Don’t compare or try to make this year like previous years. Be creative and try to find ways to make a new format fun. Meeting during the day and limiting alcohol intake can assist in making sure everyone stays safe. It has been interesting to see how many of my patients have decreased their alcohol use during quarantine. I hope this pattern will continue over the next weeks and months.
- Practice self-care: As health care professionals, we must remember the old adage “physician, heal thyself.” This year has been so difficult for almost all of us. It was filled with unprecedented levels of personal and professional stress. Holidays are often about what we can do for others, but this year we may need to place self-care first. Do what brings you happiness.
Even though you aren’t traveling, you can still disconnect from work. Set up a schedule and stick to it making sure you take plenty of time to rest and enjoy. Many of us have been working extremely long hours and a break is so needed. Take it if you possibly can. Detox from your screen! Limit the news. Creativity and productivity will be enhanced in 2021 if we can come in recharged.
For those remaining on the front lines, be patient; the end is nearing. Take care of yourself when you are not working. We are all so grateful to those in our field who have sacrificed so much to care for others. Eat, drink, and rest well to keep your immune system strong.
- Acknowledge your negative emotions: As we all know, if you try to deny negative emotions, they continue to pop up. If we give them time and space to be felt, we will find they diminish in intensity. Long work hours may have prevented us from feeling our emotions, so don’t be surprised if they surface when we take a break.
Let yourself feel the sadness for what you have experienced this year. Be open about missing those who can’t be with you because of travel or other restrictions. Let yourself feel the disappointment about your holiday travel plans that you can’t embark upon.
You may elect to share these emotions with someone close to you or with a professional. To paraphrase Carl Jung, “what we resist, persists,” so don’t try to hide from your negative emotions. Most of us had lots of them in 2020, so don’t be shy about admitting it.
- Focus on growth: What have we learned from 2020 and how can we be better equipped in 2021 and beyond?
Trauma can bring growth not just disorder. This year has returned well-deserved prestige to our fields. We are being lauded as heroes as we have scarified our health and the health of our loved ones to serve others. Can we choose to celebrate our accomplishments?
We have become more resilient and learned to continue on in the face of great hardship. Many of us have gained confidence as we confronted this historic challenge. As we have been reminded of death daily, we learn to appreciate life more fully and not take any day for granted.
I am proud to be a physician during this pandemic, and I hope you are, too!
- Find joy: Often times, we find real happiness in smaller moments and experiences. For many, this time of year is filled with so much stress that it can be hard to carve out moments of joy. As we may be less busy socially this holiday season, might we find even more joy?
Joy can only be experienced in the present moment. Tap into all your senses. Eat slowly making sure to smell and taste every bite. Cherish those who can still gather at your table. If you find yourself alone, embrace that experience. Safety must continue to come first, and we can’t let down our guard now.
- Reflect: New Year’s Eve is always a time for reflection and hope for the future. Most of us will be glad to see 2020 in the rearview mirror. With multiple and very promising vaccines on the horizon, we can anticipate a brighter future. We must continue to work hard; remain patient; and be creative, resilient, and optimistic. Let’s try to fill our days with hope and purpose and work together to achieve a brighter future for all.
“Learn from yesterday, live for today, hope for tomorrow,” Albert Einstein
Wishing you health and happiness in this holiday season and beyond.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). She also is founder of the Bekindr Global Initiative, a movement aimed at cultivating kindness in the world.
Vanquishing hepatitis C: A remarkable success story
One of the most remarkable stories in medicine must be the relatively brief 25 years between the discovery of the hepatitis C virus (HCV) in 1989 to its eventual cure in 2014.
HCV afflicted over 5 million Americans and was the cause of death in approximately 10,000 patients annually, the leading indication for liver transplantation, and the leading risk factor for hepatocellular carcinoma, clearly signaling it as one of the era’s major public health villains. Within that span of time, it is the work beginning in the mid-1990s until today that perhaps best defines the race for the HCV “cure.”
In the early to mid-1990s, polymerase chain reaction techniques were just becoming commonplace for HCV diagnosis, whereas HCV genotypes were emerging as major factors determining response to interferon therapy. The sustained viral response (SVR) rates were mired at around 6%-12% for a 24- to 48-week course of three-times-weekly injection therapy. Severe side effects were common and there was a relatively high relapse rate, even in patients who responded to treatment.
By 1996, the addition of ribavirin to the interferon treatment was associated with a modest but significant improvement in SVR rates to above 20%. And by 2000, the use of pegylated interferon – allowing once-weekly injection therapy – along with ribavirin, improved SVR rates to above 50% for the first time. The therapy was still poorly tolerated but was associated with better compliance.
The real breakthrough in therapy came in the early 2000s with the discovery and availability of HCV protease inhibitors: telaprevir and boceprevir. These agents could induce a more rapid decline in viral replication than interferon but could not be administered alone owing to the rapid emergence of resistant HCV variants. Therefore, these agents were administered with interferon and ribavirin as a three-drug cocktail to take advantage of interferon to prevent emergence of resistant variants. Although SVR rates improved substantially to around 75%, adverse events also increased and limited its usefulness in patients with more advanced liver disease, precisely those who were most in need of better therapies.
Nonetheless, the incredible advances in understanding the replication machinery of HCV that led to the discovery of the protease inhibitors in turn led to further elucidation and unlocking of three additional classes of HCV protein targets and inhibitors: NS5A complex inhibitors (e.g., ledipasvir), the NS5B nonnucleoside inhibitors (e.g., dasabuvir), and NS5B nucleoside inhibitors (e.g., sofosbuvir). It quickly became apparent that the use of combinations of these direct-acting antivirals (DAAs) could limit emergence of resistant variants while also providing rapid and profound viral suppression. Because HCV required viral replication to persist in the hepatocyte, it became possible to induce HCV eradication, and thus cure, with combinations of DAAs.
In addition, investigators soon learned that the duration of therapy no longer needed to be the generally accepted 24-48 weeks for SVR, but instead could be reduced eventually to 8-12 weeks. This shortened treatment duration allowed for more rapid testing of new agents and combinations, and the field took a rapid step forward between 2011 and 2017. HCV cure rates rose to 90%-95%.
The competition for Food and Drug Administration approval of new agents among several pharmaceutical companies also meant that the time-honored process of issuing treatment guidelines every 3-5 years by societies would not be adequate. Therefore, in 2013, the American Association for the Study of Liver Diseases and the Infectious Diseases Society of America joined forces to establish more nimble and responsive online HCV guidance. This important resource debuted in January 2014 just as the FDA approved the first DAA therapies.
The high cost initially associated with many of these new therapies (up to $1,000 per pill) significantly limited uptake owing to insurance and health plan cost factors. Early on, the cost was also analyzed by price per cure, seemingly to justify the high cost by the high cure rate. However, advocacy and negotiations ultimately led to marked reductions in the cost of a course of therapy (with some therapies at $225 per pill), thus making these treatments now widely available.
By 2020, the HCV field has shifted from therapeutic development to improving the care cascade by enhanced identification and testing of unsuspected but HCV infected individuals. This is our current challenge.
Moving toward noninvasive tests
While curative therapy has revolutionized HCV management, innovation in diagnostics eliminated a significant barrier in access to therapy: the liver biopsy.
Staging, or accurately identifying advanced fibrosis in persons infected with HCV, is essential for long-term follow-up. The presence of advanced disease affects drug choices, especially before the approval of all-oral therapy. Historically, a liver biopsy was obligatory before treatment. Invasive with a significant risk for complications, this requirement effectively prevented treatment in those who were unwilling to undergo the procedure and deterred those at risk from even being tested.
Over the past 25 years, numerous methods to noninvasively assess for liver fibrosis have been used. Serum biomarkers can be either indirect (based on routine tests) or direct (reflecting components of the extracellular matrix). Although highly available, they are only moderately useful for identifying advanced fibrosis and thus cannot replace liver biopsy in the care cascade. The technique of elastography dates back to the 1980s, though the role of vibration-controlled transient liver elastography in the assessment of hepatic fibrosis in patients with HCV was not recognized until around 2005 and it was not commonly used for nearly another decade.
Yet, a paradigm shift in the care cascade occurred with the release of the AASLD/IDSA guidance document in 2014. For the first time in the United States, noninvasive tests were recommended as first-line testing for the assessment of advanced fibrosis. Prior guidelines specifically stated that although noninvasive tests might be useful, they “should not replace the liver biopsy in routine clinical practice.” Current guidelines recommend combining elastography with serum biomarkers and considering biopsy only in patients with discordant results if the biopsy would affect clinical decision-making.
The last frontier
Curative therapy has also allowed the unthinkable: willingly exposing patients to the virus through donor-positive/recipient-negative solid organ transplant. Traditionally, an HCV-infected donor would be considered only for an HCV-positive recipient; however, with effective DAA therapy, the number of HCV actively infected patients in need of transplant has dwindled.
Unfortunately as a consequence of the opioid epidemic, the HCV-exposed donor population has blossomed. Given that HCV therapy is near universally curative, using organs from HCV-viremic donors can greatly expand the organ transplantation pool. Small studies[1-5] have demonstrated the safety and efficacy of this approach, both in HCV-positive liver donors as well as in other solid organs.
A disease pegged for elimination
In the past 25 years, HCV has evolved from non-A, non-B hepatitis into a disease pegged for elimination. This is a direct reflection of improved therapeutics with highly effective DAAs. Yet, without improved diagnostics, we would be unable to navigate patients through the clinical care cascade. These incredible strides in diagnostics and therapeutics allow us to push the cutting edge through iatrogenic infection of organ recipients, while recognizing that the largest hurdle to elimination remains in finding those who are chronically infected. Ultimately, the crux of elimination remains unchanged over the past 25 years and resides in screening and diagnosis with effective linkage to care.
Donald M. Jensen, MD, is a professor of medicine at Rush University Medical Center, Chicago. He was previously the director of the Center for Liver Disease at the University of Chicago until 2015. His research interest has been in newer HCV therapies. He recently received the Distinguished Service Award from the AASLD for his many contributions to the field.
Nancy S. Reau, MD, is chief of the hepatology section at Rush University Medical Center and a regular contributor to Medscape. She serves as editor of Clinical Liver Disease, a multimedia review journal, and recently as a member of HCVGuidelines.org, a web-based resource from the AASLD and the IDSA, as well as educational chair for the AASLD hepatitis C special interest group. She continues to have an active role in the hepatology interest group of the World Gastroenterology Organisation and the American Liver Foundation at the regional and national levels.
References
Woolley AE et al. Heart and lung transplants from HCV-infected donors to uninfected recipients. N Engl J Med. 2019;380:1606-17.
Franco A et al. Renal transplantation from seropositive hepatitis C virus donors to seronegative recipients in Spain: A prospective study. Transpl Int. 2019;32:710-6.
Goldberg DS et al. Transplanting HCV-infected kidneys into uninfected recipients. N Engl J Med. 2017;377:1105.
Kwong AJ et al. Liver transplantation for hepatitis C virus (HCV) nonviremic recipients with HCV viremic donors. Am J Transplant. 2019;19:1380-7.
Bethea E et al. Immediate administration of antiviral therapy after transplantation of hepatitis C–infected livers into uninfected recipients: Implications for therapeutic planning. Am J Transplant. 2020;20:1619-28.
This article first appeared on Medscape.com.
One of the most remarkable stories in medicine must be the relatively brief 25 years between the discovery of the hepatitis C virus (HCV) in 1989 to its eventual cure in 2014.
HCV afflicted over 5 million Americans and was the cause of death in approximately 10,000 patients annually, the leading indication for liver transplantation, and the leading risk factor for hepatocellular carcinoma, clearly signaling it as one of the era’s major public health villains. Within that span of time, it is the work beginning in the mid-1990s until today that perhaps best defines the race for the HCV “cure.”
In the early to mid-1990s, polymerase chain reaction techniques were just becoming commonplace for HCV diagnosis, whereas HCV genotypes were emerging as major factors determining response to interferon therapy. The sustained viral response (SVR) rates were mired at around 6%-12% for a 24- to 48-week course of three-times-weekly injection therapy. Severe side effects were common and there was a relatively high relapse rate, even in patients who responded to treatment.
By 1996, the addition of ribavirin to the interferon treatment was associated with a modest but significant improvement in SVR rates to above 20%. And by 2000, the use of pegylated interferon – allowing once-weekly injection therapy – along with ribavirin, improved SVR rates to above 50% for the first time. The therapy was still poorly tolerated but was associated with better compliance.
The real breakthrough in therapy came in the early 2000s with the discovery and availability of HCV protease inhibitors: telaprevir and boceprevir. These agents could induce a more rapid decline in viral replication than interferon but could not be administered alone owing to the rapid emergence of resistant HCV variants. Therefore, these agents were administered with interferon and ribavirin as a three-drug cocktail to take advantage of interferon to prevent emergence of resistant variants. Although SVR rates improved substantially to around 75%, adverse events also increased and limited its usefulness in patients with more advanced liver disease, precisely those who were most in need of better therapies.
Nonetheless, the incredible advances in understanding the replication machinery of HCV that led to the discovery of the protease inhibitors in turn led to further elucidation and unlocking of three additional classes of HCV protein targets and inhibitors: NS5A complex inhibitors (e.g., ledipasvir), the NS5B nonnucleoside inhibitors (e.g., dasabuvir), and NS5B nucleoside inhibitors (e.g., sofosbuvir). It quickly became apparent that the use of combinations of these direct-acting antivirals (DAAs) could limit emergence of resistant variants while also providing rapid and profound viral suppression. Because HCV required viral replication to persist in the hepatocyte, it became possible to induce HCV eradication, and thus cure, with combinations of DAAs.
In addition, investigators soon learned that the duration of therapy no longer needed to be the generally accepted 24-48 weeks for SVR, but instead could be reduced eventually to 8-12 weeks. This shortened treatment duration allowed for more rapid testing of new agents and combinations, and the field took a rapid step forward between 2011 and 2017. HCV cure rates rose to 90%-95%.
The competition for Food and Drug Administration approval of new agents among several pharmaceutical companies also meant that the time-honored process of issuing treatment guidelines every 3-5 years by societies would not be adequate. Therefore, in 2013, the American Association for the Study of Liver Diseases and the Infectious Diseases Society of America joined forces to establish more nimble and responsive online HCV guidance. This important resource debuted in January 2014 just as the FDA approved the first DAA therapies.
The high cost initially associated with many of these new therapies (up to $1,000 per pill) significantly limited uptake owing to insurance and health plan cost factors. Early on, the cost was also analyzed by price per cure, seemingly to justify the high cost by the high cure rate. However, advocacy and negotiations ultimately led to marked reductions in the cost of a course of therapy (with some therapies at $225 per pill), thus making these treatments now widely available.
By 2020, the HCV field has shifted from therapeutic development to improving the care cascade by enhanced identification and testing of unsuspected but HCV infected individuals. This is our current challenge.
Moving toward noninvasive tests
While curative therapy has revolutionized HCV management, innovation in diagnostics eliminated a significant barrier in access to therapy: the liver biopsy.
Staging, or accurately identifying advanced fibrosis in persons infected with HCV, is essential for long-term follow-up. The presence of advanced disease affects drug choices, especially before the approval of all-oral therapy. Historically, a liver biopsy was obligatory before treatment. Invasive with a significant risk for complications, this requirement effectively prevented treatment in those who were unwilling to undergo the procedure and deterred those at risk from even being tested.
Over the past 25 years, numerous methods to noninvasively assess for liver fibrosis have been used. Serum biomarkers can be either indirect (based on routine tests) or direct (reflecting components of the extracellular matrix). Although highly available, they are only moderately useful for identifying advanced fibrosis and thus cannot replace liver biopsy in the care cascade. The technique of elastography dates back to the 1980s, though the role of vibration-controlled transient liver elastography in the assessment of hepatic fibrosis in patients with HCV was not recognized until around 2005 and it was not commonly used for nearly another decade.
Yet, a paradigm shift in the care cascade occurred with the release of the AASLD/IDSA guidance document in 2014. For the first time in the United States, noninvasive tests were recommended as first-line testing for the assessment of advanced fibrosis. Prior guidelines specifically stated that although noninvasive tests might be useful, they “should not replace the liver biopsy in routine clinical practice.” Current guidelines recommend combining elastography with serum biomarkers and considering biopsy only in patients with discordant results if the biopsy would affect clinical decision-making.
The last frontier
Curative therapy has also allowed the unthinkable: willingly exposing patients to the virus through donor-positive/recipient-negative solid organ transplant. Traditionally, an HCV-infected donor would be considered only for an HCV-positive recipient; however, with effective DAA therapy, the number of HCV actively infected patients in need of transplant has dwindled.
Unfortunately as a consequence of the opioid epidemic, the HCV-exposed donor population has blossomed. Given that HCV therapy is near universally curative, using organs from HCV-viremic donors can greatly expand the organ transplantation pool. Small studies[1-5] have demonstrated the safety and efficacy of this approach, both in HCV-positive liver donors as well as in other solid organs.
A disease pegged for elimination
In the past 25 years, HCV has evolved from non-A, non-B hepatitis into a disease pegged for elimination. This is a direct reflection of improved therapeutics with highly effective DAAs. Yet, without improved diagnostics, we would be unable to navigate patients through the clinical care cascade. These incredible strides in diagnostics and therapeutics allow us to push the cutting edge through iatrogenic infection of organ recipients, while recognizing that the largest hurdle to elimination remains in finding those who are chronically infected. Ultimately, the crux of elimination remains unchanged over the past 25 years and resides in screening and diagnosis with effective linkage to care.
Donald M. Jensen, MD, is a professor of medicine at Rush University Medical Center, Chicago. He was previously the director of the Center for Liver Disease at the University of Chicago until 2015. His research interest has been in newer HCV therapies. He recently received the Distinguished Service Award from the AASLD for his many contributions to the field.
Nancy S. Reau, MD, is chief of the hepatology section at Rush University Medical Center and a regular contributor to Medscape. She serves as editor of Clinical Liver Disease, a multimedia review journal, and recently as a member of HCVGuidelines.org, a web-based resource from the AASLD and the IDSA, as well as educational chair for the AASLD hepatitis C special interest group. She continues to have an active role in the hepatology interest group of the World Gastroenterology Organisation and the American Liver Foundation at the regional and national levels.
References
Woolley AE et al. Heart and lung transplants from HCV-infected donors to uninfected recipients. N Engl J Med. 2019;380:1606-17.
Franco A et al. Renal transplantation from seropositive hepatitis C virus donors to seronegative recipients in Spain: A prospective study. Transpl Int. 2019;32:710-6.
Goldberg DS et al. Transplanting HCV-infected kidneys into uninfected recipients. N Engl J Med. 2017;377:1105.
Kwong AJ et al. Liver transplantation for hepatitis C virus (HCV) nonviremic recipients with HCV viremic donors. Am J Transplant. 2019;19:1380-7.
Bethea E et al. Immediate administration of antiviral therapy after transplantation of hepatitis C–infected livers into uninfected recipients: Implications for therapeutic planning. Am J Transplant. 2020;20:1619-28.
This article first appeared on Medscape.com.
One of the most remarkable stories in medicine must be the relatively brief 25 years between the discovery of the hepatitis C virus (HCV) in 1989 to its eventual cure in 2014.
HCV afflicted over 5 million Americans and was the cause of death in approximately 10,000 patients annually, the leading indication for liver transplantation, and the leading risk factor for hepatocellular carcinoma, clearly signaling it as one of the era’s major public health villains. Within that span of time, it is the work beginning in the mid-1990s until today that perhaps best defines the race for the HCV “cure.”
In the early to mid-1990s, polymerase chain reaction techniques were just becoming commonplace for HCV diagnosis, whereas HCV genotypes were emerging as major factors determining response to interferon therapy. The sustained viral response (SVR) rates were mired at around 6%-12% for a 24- to 48-week course of three-times-weekly injection therapy. Severe side effects were common and there was a relatively high relapse rate, even in patients who responded to treatment.
By 1996, the addition of ribavirin to the interferon treatment was associated with a modest but significant improvement in SVR rates to above 20%. And by 2000, the use of pegylated interferon – allowing once-weekly injection therapy – along with ribavirin, improved SVR rates to above 50% for the first time. The therapy was still poorly tolerated but was associated with better compliance.
The real breakthrough in therapy came in the early 2000s with the discovery and availability of HCV protease inhibitors: telaprevir and boceprevir. These agents could induce a more rapid decline in viral replication than interferon but could not be administered alone owing to the rapid emergence of resistant HCV variants. Therefore, these agents were administered with interferon and ribavirin as a three-drug cocktail to take advantage of interferon to prevent emergence of resistant variants. Although SVR rates improved substantially to around 75%, adverse events also increased and limited its usefulness in patients with more advanced liver disease, precisely those who were most in need of better therapies.
Nonetheless, the incredible advances in understanding the replication machinery of HCV that led to the discovery of the protease inhibitors in turn led to further elucidation and unlocking of three additional classes of HCV protein targets and inhibitors: NS5A complex inhibitors (e.g., ledipasvir), the NS5B nonnucleoside inhibitors (e.g., dasabuvir), and NS5B nucleoside inhibitors (e.g., sofosbuvir). It quickly became apparent that the use of combinations of these direct-acting antivirals (DAAs) could limit emergence of resistant variants while also providing rapid and profound viral suppression. Because HCV required viral replication to persist in the hepatocyte, it became possible to induce HCV eradication, and thus cure, with combinations of DAAs.
In addition, investigators soon learned that the duration of therapy no longer needed to be the generally accepted 24-48 weeks for SVR, but instead could be reduced eventually to 8-12 weeks. This shortened treatment duration allowed for more rapid testing of new agents and combinations, and the field took a rapid step forward between 2011 and 2017. HCV cure rates rose to 90%-95%.
The competition for Food and Drug Administration approval of new agents among several pharmaceutical companies also meant that the time-honored process of issuing treatment guidelines every 3-5 years by societies would not be adequate. Therefore, in 2013, the American Association for the Study of Liver Diseases and the Infectious Diseases Society of America joined forces to establish more nimble and responsive online HCV guidance. This important resource debuted in January 2014 just as the FDA approved the first DAA therapies.
The high cost initially associated with many of these new therapies (up to $1,000 per pill) significantly limited uptake owing to insurance and health plan cost factors. Early on, the cost was also analyzed by price per cure, seemingly to justify the high cost by the high cure rate. However, advocacy and negotiations ultimately led to marked reductions in the cost of a course of therapy (with some therapies at $225 per pill), thus making these treatments now widely available.
By 2020, the HCV field has shifted from therapeutic development to improving the care cascade by enhanced identification and testing of unsuspected but HCV infected individuals. This is our current challenge.
Moving toward noninvasive tests
While curative therapy has revolutionized HCV management, innovation in diagnostics eliminated a significant barrier in access to therapy: the liver biopsy.
Staging, or accurately identifying advanced fibrosis in persons infected with HCV, is essential for long-term follow-up. The presence of advanced disease affects drug choices, especially before the approval of all-oral therapy. Historically, a liver biopsy was obligatory before treatment. Invasive with a significant risk for complications, this requirement effectively prevented treatment in those who were unwilling to undergo the procedure and deterred those at risk from even being tested.
Over the past 25 years, numerous methods to noninvasively assess for liver fibrosis have been used. Serum biomarkers can be either indirect (based on routine tests) or direct (reflecting components of the extracellular matrix). Although highly available, they are only moderately useful for identifying advanced fibrosis and thus cannot replace liver biopsy in the care cascade. The technique of elastography dates back to the 1980s, though the role of vibration-controlled transient liver elastography in the assessment of hepatic fibrosis in patients with HCV was not recognized until around 2005 and it was not commonly used for nearly another decade.
Yet, a paradigm shift in the care cascade occurred with the release of the AASLD/IDSA guidance document in 2014. For the first time in the United States, noninvasive tests were recommended as first-line testing for the assessment of advanced fibrosis. Prior guidelines specifically stated that although noninvasive tests might be useful, they “should not replace the liver biopsy in routine clinical practice.” Current guidelines recommend combining elastography with serum biomarkers and considering biopsy only in patients with discordant results if the biopsy would affect clinical decision-making.
The last frontier
Curative therapy has also allowed the unthinkable: willingly exposing patients to the virus through donor-positive/recipient-negative solid organ transplant. Traditionally, an HCV-infected donor would be considered only for an HCV-positive recipient; however, with effective DAA therapy, the number of HCV actively infected patients in need of transplant has dwindled.
Unfortunately as a consequence of the opioid epidemic, the HCV-exposed donor population has blossomed. Given that HCV therapy is near universally curative, using organs from HCV-viremic donors can greatly expand the organ transplantation pool. Small studies[1-5] have demonstrated the safety and efficacy of this approach, both in HCV-positive liver donors as well as in other solid organs.
A disease pegged for elimination
In the past 25 years, HCV has evolved from non-A, non-B hepatitis into a disease pegged for elimination. This is a direct reflection of improved therapeutics with highly effective DAAs. Yet, without improved diagnostics, we would be unable to navigate patients through the clinical care cascade. These incredible strides in diagnostics and therapeutics allow us to push the cutting edge through iatrogenic infection of organ recipients, while recognizing that the largest hurdle to elimination remains in finding those who are chronically infected. Ultimately, the crux of elimination remains unchanged over the past 25 years and resides in screening and diagnosis with effective linkage to care.
Donald M. Jensen, MD, is a professor of medicine at Rush University Medical Center, Chicago. He was previously the director of the Center for Liver Disease at the University of Chicago until 2015. His research interest has been in newer HCV therapies. He recently received the Distinguished Service Award from the AASLD for his many contributions to the field.
Nancy S. Reau, MD, is chief of the hepatology section at Rush University Medical Center and a regular contributor to Medscape. She serves as editor of Clinical Liver Disease, a multimedia review journal, and recently as a member of HCVGuidelines.org, a web-based resource from the AASLD and the IDSA, as well as educational chair for the AASLD hepatitis C special interest group. She continues to have an active role in the hepatology interest group of the World Gastroenterology Organisation and the American Liver Foundation at the regional and national levels.
References
Woolley AE et al. Heart and lung transplants from HCV-infected donors to uninfected recipients. N Engl J Med. 2019;380:1606-17.
Franco A et al. Renal transplantation from seropositive hepatitis C virus donors to seronegative recipients in Spain: A prospective study. Transpl Int. 2019;32:710-6.
Goldberg DS et al. Transplanting HCV-infected kidneys into uninfected recipients. N Engl J Med. 2017;377:1105.
Kwong AJ et al. Liver transplantation for hepatitis C virus (HCV) nonviremic recipients with HCV viremic donors. Am J Transplant. 2019;19:1380-7.
Bethea E et al. Immediate administration of antiviral therapy after transplantation of hepatitis C–infected livers into uninfected recipients: Implications for therapeutic planning. Am J Transplant. 2020;20:1619-28.
This article first appeared on Medscape.com.
Do general neurologists fall victim to a plethora of treatment options?
In 1993 I graduated from medical school. That same year Betaseron (interferon beta-1b) came to market as the first treatment specifically approved for multiple sclerosis (MS). This was a groundbreaker at the time, as there’d been little besides steroids and other potent immunosuppressants to try. Now we had a real drug to offer patients.
The demand for Betaseron was huge, so much so that a lottery system was used to determine which patients would get it first, as there simply wasn’t enough to go around. In the next several years a few more agents jumped into the ring – Avonex (interferon beta-1a), Copaxone (glatiramer acetate), Novantrone (mitoxantrone), and Rebif (interferon beta-1a) – before things went quiet for a while.
In 2006 the first monoclonal antibody for MS – Tysabri (natalizumab) – came out, then almost just as quickly vanished again, not returning until 2009.
Since then we’ve had a gradual explosion of new treatments for MS – like watching kernels become popcorn – first one, then two, then a deluge filling up the basket.
So here we are, approaching the end of 2020, with a remarkable collection of monoclonal antibodies, S1P modulators, fumarates, immunosuppressants, and one symptomatic treatment, many of which weren’t even imagined in 1993. Not to mention the original ABCR (Avonex, Betaseron, Copaxone, Rebif) agents, though they’re riding into the sunset.
A friend and I were talking about this remarkable success story. MS certainly hasn’t been cured, but its treatments have had a dramatic improvement in efficacy over the last quarter century.
He made a point though: that this selection of treatments may be relegating MS from the province of a general neurologist to that of the fellowship-trained MS subspecialist.
Not that that is such a bad thing, as MS is a very challenging disease. But the point is well taken. As treatments become increasingly complicated, and numerous, it becomes harder to know which one is best. Most of us likely choose orals first and monoclonal antibodies second, but the question of “which one?” arises for each category. They each have their own risks, side effects, initiation protocols, and peculiarities. In a disease of heterogeneous presentations and courses, there are no clear data on which agent to start first for what patient type. To a general neurologist, also juggling migraines, strokes, Parkinson’s disease, dementia, and neuropathy (and many other disorders) in the course of a day, it becomes tricky to keep up on such.
At some point do general neurologists become a victim of this success? Maybe, but probably not. Just as there are more general practitioners than neurologists, there are more general neurologists than MS subspecialists. Their knowledge and training should be reserved for those patients not responding to our first- (and second-) line treatments, presentations that are atypical, and more complex issues outside the scope of those of us practicing whatever-comes-to-the-door neurology.
It would, however, be nice to have a good consensus on how to best use this array of treatments. Solid guidelines, breaking disease subtypes and treatments down by patient types, drugs, and mechanisms of action, would help those of us on the neurology frontlines to better care for those who need us.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In 1993 I graduated from medical school. That same year Betaseron (interferon beta-1b) came to market as the first treatment specifically approved for multiple sclerosis (MS). This was a groundbreaker at the time, as there’d been little besides steroids and other potent immunosuppressants to try. Now we had a real drug to offer patients.
The demand for Betaseron was huge, so much so that a lottery system was used to determine which patients would get it first, as there simply wasn’t enough to go around. In the next several years a few more agents jumped into the ring – Avonex (interferon beta-1a), Copaxone (glatiramer acetate), Novantrone (mitoxantrone), and Rebif (interferon beta-1a) – before things went quiet for a while.
In 2006 the first monoclonal antibody for MS – Tysabri (natalizumab) – came out, then almost just as quickly vanished again, not returning until 2009.
Since then we’ve had a gradual explosion of new treatments for MS – like watching kernels become popcorn – first one, then two, then a deluge filling up the basket.
So here we are, approaching the end of 2020, with a remarkable collection of monoclonal antibodies, S1P modulators, fumarates, immunosuppressants, and one symptomatic treatment, many of which weren’t even imagined in 1993. Not to mention the original ABCR (Avonex, Betaseron, Copaxone, Rebif) agents, though they’re riding into the sunset.
A friend and I were talking about this remarkable success story. MS certainly hasn’t been cured, but its treatments have had a dramatic improvement in efficacy over the last quarter century.
He made a point though: that this selection of treatments may be relegating MS from the province of a general neurologist to that of the fellowship-trained MS subspecialist.
Not that that is such a bad thing, as MS is a very challenging disease. But the point is well taken. As treatments become increasingly complicated, and numerous, it becomes harder to know which one is best. Most of us likely choose orals first and monoclonal antibodies second, but the question of “which one?” arises for each category. They each have their own risks, side effects, initiation protocols, and peculiarities. In a disease of heterogeneous presentations and courses, there are no clear data on which agent to start first for what patient type. To a general neurologist, also juggling migraines, strokes, Parkinson’s disease, dementia, and neuropathy (and many other disorders) in the course of a day, it becomes tricky to keep up on such.
At some point do general neurologists become a victim of this success? Maybe, but probably not. Just as there are more general practitioners than neurologists, there are more general neurologists than MS subspecialists. Their knowledge and training should be reserved for those patients not responding to our first- (and second-) line treatments, presentations that are atypical, and more complex issues outside the scope of those of us practicing whatever-comes-to-the-door neurology.
It would, however, be nice to have a good consensus on how to best use this array of treatments. Solid guidelines, breaking disease subtypes and treatments down by patient types, drugs, and mechanisms of action, would help those of us on the neurology frontlines to better care for those who need us.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In 1993 I graduated from medical school. That same year Betaseron (interferon beta-1b) came to market as the first treatment specifically approved for multiple sclerosis (MS). This was a groundbreaker at the time, as there’d been little besides steroids and other potent immunosuppressants to try. Now we had a real drug to offer patients.
The demand for Betaseron was huge, so much so that a lottery system was used to determine which patients would get it first, as there simply wasn’t enough to go around. In the next several years a few more agents jumped into the ring – Avonex (interferon beta-1a), Copaxone (glatiramer acetate), Novantrone (mitoxantrone), and Rebif (interferon beta-1a) – before things went quiet for a while.
In 2006 the first monoclonal antibody for MS – Tysabri (natalizumab) – came out, then almost just as quickly vanished again, not returning until 2009.
Since then we’ve had a gradual explosion of new treatments for MS – like watching kernels become popcorn – first one, then two, then a deluge filling up the basket.
So here we are, approaching the end of 2020, with a remarkable collection of monoclonal antibodies, S1P modulators, fumarates, immunosuppressants, and one symptomatic treatment, many of which weren’t even imagined in 1993. Not to mention the original ABCR (Avonex, Betaseron, Copaxone, Rebif) agents, though they’re riding into the sunset.
A friend and I were talking about this remarkable success story. MS certainly hasn’t been cured, but its treatments have had a dramatic improvement in efficacy over the last quarter century.
He made a point though: that this selection of treatments may be relegating MS from the province of a general neurologist to that of the fellowship-trained MS subspecialist.
Not that that is such a bad thing, as MS is a very challenging disease. But the point is well taken. As treatments become increasingly complicated, and numerous, it becomes harder to know which one is best. Most of us likely choose orals first and monoclonal antibodies second, but the question of “which one?” arises for each category. They each have their own risks, side effects, initiation protocols, and peculiarities. In a disease of heterogeneous presentations and courses, there are no clear data on which agent to start first for what patient type. To a general neurologist, also juggling migraines, strokes, Parkinson’s disease, dementia, and neuropathy (and many other disorders) in the course of a day, it becomes tricky to keep up on such.
At some point do general neurologists become a victim of this success? Maybe, but probably not. Just as there are more general practitioners than neurologists, there are more general neurologists than MS subspecialists. Their knowledge and training should be reserved for those patients not responding to our first- (and second-) line treatments, presentations that are atypical, and more complex issues outside the scope of those of us practicing whatever-comes-to-the-door neurology.
It would, however, be nice to have a good consensus on how to best use this array of treatments. Solid guidelines, breaking disease subtypes and treatments down by patient types, drugs, and mechanisms of action, would help those of us on the neurology frontlines to better care for those who need us.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Dermatologists and the history of skin care and beauty devices: Part 4
In this series on the role dermatologists have played in the history of skin care, I have covered dermatologists who developed cosmeceutical ingredients, dermatologists who consulted for the skin care industry, and those who developed a novel and successful skin care line. In this column, part 4 of the series, I will continue to discuss .
Dermatologists and Stiefel Laboratories
The Stiefel Medicinal Soap Company, founded in 1847, later became Stiefel Laboratories and was sold to GlaxoSmithKline in 2009. Stiefel Laboratories made many contributions over the years to the field of dermatology as chronicled in the excellent book, “Skin Saga” written by Charles Stiefel and published in 2018. The company was first known for soaps and groundbreaking products, such as “Freckle Soap” that sped epidermal turnover, resulting in a more even toned complexion.
Many dermatologists were involved in developing products and providing advice to the company. Herman Sharlit, MD, in New York, had the idea for a moisturizing soap (Oilatum), a detergent soap (Acne Aid detergent soap), and a coal tar soap (Polytar). Eugene Farber, MD, who was professor and chairman of the department of dermatology at Stanford (Calif.) University, consulted for Stiefel Laboratories and helped them identify and develop many products over the years.1 Stiefel Labs came out with the first facial scrub called Brasivol, an abrasive cream with aluminum oxide particles – the predecessor to modern day microdermabrasion. This facial scrub was conceived by dermatologist Rose Saperstein, MD, Los Angeles, who published a report2 on this in 1960 and also received a patent for it in 1963.3 Brasivol became the company’s first million dollar product.1
Stiefel Laboratories worked with many dermatologists to help them develop their ideas. They included Cleveland White, MD, who patented a highly absorbent foot and body powder known as Zeasorb powder. William Pace, MD, was a Canadian dermatologist who patented an acne treatment containing benzoyl peroxide and sulfur that Stiefel Labs marketed as Sulfoxyl Lotion. Dr. Pace is lovingly referred to as “the father of benzoyl peroxide” because his idea led Stiefel Labs to develop more benzoyl peroxide products. Benzoyl peroxide remains the most popular OTC ingredient to treat acne.
Comedone extractors
Many dermatologists have developed ways to extract comedones. There are publications on using paper clips,4,5safety pins,6 and medicine droppers,7 but some dermatologists have developed special comedone extractors, which include the following: Jay Schamberg, MD, developed a comedone extractor with a loop at each end. He disapproved of cutting a comedone, so did not include a needle or scalpel in his extractor.8
- Leonard Savitt, MD,9 attached a scalpel to one end of the Schamberg extractor.
- Alan Shalita, MD, developed a comedone extractor with a large, keyhole-shaped extracting orifice that made the tool easier to clean.10
The Saalfield comedone extractor combines a fixed pointed blade at one end and a small spoon-shaped expressor foot at the other end. (However, I have not been able to determine if Saalfield was a dermatologist.)
Dermatologist who developed methods for lesion excisions
Robert Segal, MD, a dermatologist at the University of Arizona, Tucson, invented the Dermablade. Although this is technically not a beauty device, I am including it because it has made the removal of unsightly moles and lesions much easier. He holds six patents on this device.
Dermatologists developed dermabrasion and microneedling
Ernst Kromayer, MD,11 a dermatologist in Germany, first described microneedling in 1905 when he mounted dental burrs on motor-driven flexible cord equipment to treat scars. Abner Kurtin, MD, a New York dermatologist, learned about Dr. Kromayer’s technique and modified it using stainless wireless brushes. Dr. Kurtin is known as the “father of dermabrasion.” His work was noted by Nobel Laureate Alexis Carrel, MD, who moved to New York City and began using the technique. Dr. Carrel’s protege, New York dermatologist, Norman Orentreich, MD, began using hypodermic needles instead of wire brushes. Microneedling has gained much popularity over the last decade and has been combined with platelet rich plasma injections.
Dermatologist-developed injection to shrink fat
Adam Rotunda, MD, was a dermatology resident at the University of California, Los Angeles, when he and his professor Michael Kolodney, MD, PhD, had the idea to develop deoxycholate as an injectable to reduce fat deposits. They filed a patent in 2004, conducted clinical trials, and it worked! In 2009, the patent for deoxycholic acid (ATX-10), marketed as Kybella, was granted. The rights to the drug were purchased by Aestherx, which later became Kythera Biopharmaceuticals. Kybella received Food and Drug Administration approval in 2015, and 6 months later, Kythera was acquired by Allergan.
Development of FDA-approved drugs to improve skin appearance
In 2004, dermatologists Stuart Shanler, MD, and Andrew Ondo, MD, filed a patent for the use of topical oxymetazoline for the treatment of the erythema of rosacea. They published their observations in 2007, noting that oxymetazoline improved facial flushing and erythema.11 Dr. Shanler then teamed up with dermatologist Neal Walker, MD, to form a start-up pharmaceutical company, Vicept Therapeutics, and took this compound through phase 2 clinical trials, while Dr. Shanler filed additional patents on oxymetazoline compositions and their uses. Once they successfully demonstrated the efficacy of topical oxymetazoline for rosacea, Allergan acquired the rights of the drug, successfully completed the phase 3 clinical trials, and Rhofade was approved by the FDA in 2017. It is the only topical drug invented and developed by a dermatologist to receive FDA approval since tretinoin (Renova) was developed by Albert Kligman, MD, and approved by the FDA for the improvement in appearance of fine wrinkling, mottled hyperpigmentation and roughness associated with photodamage in 1992.
The development of lasers
The last dermatologist I will discuss in this history series is R. Rox Anderson, MD, professor of dermatology at Harvard University, and director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston. It is impossible to list all his contributions in such a limited space. It would take a book. Building on efforts pioneered by Leon Goldman, MD, Dr. Anderson and his associates pioneered the use of lasers in dermatology and invented the idea of photothermolysis when they filed a patent on using light to remove hair in 1995.Dieter Manstein, MD, PhD,Dr. Anderson and others filed many patents that led to devices such as hair removal lasers, resurfacing lasers, and Fraxel lasers. They also made discoveries related to using cold to shrink fat. One of their inventions is known as CoolSculpting. They were so influential in the development of cosmetic dermatology that it is hard to imagine the field without their contributions.
This concludes my four-part series on the history of dermatologists’ role in the development of the skin care industry. I hope I have not forgotten anyone; if I did, I apologize. I have asked for ideas on Dermchat, Facebook and LinkedIn. Feel free to reach out if I missed one of your contributions. I will be giving lectures on this topic in the future and would be happy to include anyone I missed.
As the year 2020 ends, I want to say, Happy 50th Anniversary Dermatology News! I hope you enjoyed this historical series in honor of this anniversary.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Stiefel, CW. (n.d.). Skin Saga: How a Tiny Family Soap Business Evolved Over Six Generations Into the #1 Dermatology Company in the World. United States: Smart Business Network.
2. Saperstein, RB. Arch Dermatol. 1960 Apr;81:601.
3. Saperstein, RB, and Stiefel, WK (1963). U.S. Patent No. 3,092,111. Washington, DC: U.S. Patent and Trademark Office.
4. George DE et al. J Am Acad Dermatol. 2006 Feb;54(2):326.
5. Cvancara JL, Meffert JJ. J Am Acad Dermatol. 1999 Mar;40(3):477-8.
6. Mukhtar M., Sharma R. Int J Dermatol. 2004 Dec;43(12):967-8.
7. Shellow, H. JAMA. 1951;147(18):1777.
8. Wright CS. Arch Dermatol. 1961;84(3):515.
9. Savitt LE. Arch Dermatol. 1961 Apr;83:660-1.
10. Shalita AR, Harris H. Arch Dermatol. 1972 May;105(5):759-60.
11. Shanler SD, Ondo AL. Arch Dermatol. 2007 Nov;143(11):1369-71.
In this series on the role dermatologists have played in the history of skin care, I have covered dermatologists who developed cosmeceutical ingredients, dermatologists who consulted for the skin care industry, and those who developed a novel and successful skin care line. In this column, part 4 of the series, I will continue to discuss .
Dermatologists and Stiefel Laboratories
The Stiefel Medicinal Soap Company, founded in 1847, later became Stiefel Laboratories and was sold to GlaxoSmithKline in 2009. Stiefel Laboratories made many contributions over the years to the field of dermatology as chronicled in the excellent book, “Skin Saga” written by Charles Stiefel and published in 2018. The company was first known for soaps and groundbreaking products, such as “Freckle Soap” that sped epidermal turnover, resulting in a more even toned complexion.
Many dermatologists were involved in developing products and providing advice to the company. Herman Sharlit, MD, in New York, had the idea for a moisturizing soap (Oilatum), a detergent soap (Acne Aid detergent soap), and a coal tar soap (Polytar). Eugene Farber, MD, who was professor and chairman of the department of dermatology at Stanford (Calif.) University, consulted for Stiefel Laboratories and helped them identify and develop many products over the years.1 Stiefel Labs came out with the first facial scrub called Brasivol, an abrasive cream with aluminum oxide particles – the predecessor to modern day microdermabrasion. This facial scrub was conceived by dermatologist Rose Saperstein, MD, Los Angeles, who published a report2 on this in 1960 and also received a patent for it in 1963.3 Brasivol became the company’s first million dollar product.1
Stiefel Laboratories worked with many dermatologists to help them develop their ideas. They included Cleveland White, MD, who patented a highly absorbent foot and body powder known as Zeasorb powder. William Pace, MD, was a Canadian dermatologist who patented an acne treatment containing benzoyl peroxide and sulfur that Stiefel Labs marketed as Sulfoxyl Lotion. Dr. Pace is lovingly referred to as “the father of benzoyl peroxide” because his idea led Stiefel Labs to develop more benzoyl peroxide products. Benzoyl peroxide remains the most popular OTC ingredient to treat acne.
Comedone extractors
Many dermatologists have developed ways to extract comedones. There are publications on using paper clips,4,5safety pins,6 and medicine droppers,7 but some dermatologists have developed special comedone extractors, which include the following: Jay Schamberg, MD, developed a comedone extractor with a loop at each end. He disapproved of cutting a comedone, so did not include a needle or scalpel in his extractor.8
- Leonard Savitt, MD,9 attached a scalpel to one end of the Schamberg extractor.
- Alan Shalita, MD, developed a comedone extractor with a large, keyhole-shaped extracting orifice that made the tool easier to clean.10
The Saalfield comedone extractor combines a fixed pointed blade at one end and a small spoon-shaped expressor foot at the other end. (However, I have not been able to determine if Saalfield was a dermatologist.)
Dermatologist who developed methods for lesion excisions
Robert Segal, MD, a dermatologist at the University of Arizona, Tucson, invented the Dermablade. Although this is technically not a beauty device, I am including it because it has made the removal of unsightly moles and lesions much easier. He holds six patents on this device.
Dermatologists developed dermabrasion and microneedling
Ernst Kromayer, MD,11 a dermatologist in Germany, first described microneedling in 1905 when he mounted dental burrs on motor-driven flexible cord equipment to treat scars. Abner Kurtin, MD, a New York dermatologist, learned about Dr. Kromayer’s technique and modified it using stainless wireless brushes. Dr. Kurtin is known as the “father of dermabrasion.” His work was noted by Nobel Laureate Alexis Carrel, MD, who moved to New York City and began using the technique. Dr. Carrel’s protege, New York dermatologist, Norman Orentreich, MD, began using hypodermic needles instead of wire brushes. Microneedling has gained much popularity over the last decade and has been combined with platelet rich plasma injections.
Dermatologist-developed injection to shrink fat
Adam Rotunda, MD, was a dermatology resident at the University of California, Los Angeles, when he and his professor Michael Kolodney, MD, PhD, had the idea to develop deoxycholate as an injectable to reduce fat deposits. They filed a patent in 2004, conducted clinical trials, and it worked! In 2009, the patent for deoxycholic acid (ATX-10), marketed as Kybella, was granted. The rights to the drug were purchased by Aestherx, which later became Kythera Biopharmaceuticals. Kybella received Food and Drug Administration approval in 2015, and 6 months later, Kythera was acquired by Allergan.
Development of FDA-approved drugs to improve skin appearance
In 2004, dermatologists Stuart Shanler, MD, and Andrew Ondo, MD, filed a patent for the use of topical oxymetazoline for the treatment of the erythema of rosacea. They published their observations in 2007, noting that oxymetazoline improved facial flushing and erythema.11 Dr. Shanler then teamed up with dermatologist Neal Walker, MD, to form a start-up pharmaceutical company, Vicept Therapeutics, and took this compound through phase 2 clinical trials, while Dr. Shanler filed additional patents on oxymetazoline compositions and their uses. Once they successfully demonstrated the efficacy of topical oxymetazoline for rosacea, Allergan acquired the rights of the drug, successfully completed the phase 3 clinical trials, and Rhofade was approved by the FDA in 2017. It is the only topical drug invented and developed by a dermatologist to receive FDA approval since tretinoin (Renova) was developed by Albert Kligman, MD, and approved by the FDA for the improvement in appearance of fine wrinkling, mottled hyperpigmentation and roughness associated with photodamage in 1992.
The development of lasers
The last dermatologist I will discuss in this history series is R. Rox Anderson, MD, professor of dermatology at Harvard University, and director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston. It is impossible to list all his contributions in such a limited space. It would take a book. Building on efforts pioneered by Leon Goldman, MD, Dr. Anderson and his associates pioneered the use of lasers in dermatology and invented the idea of photothermolysis when they filed a patent on using light to remove hair in 1995.Dieter Manstein, MD, PhD,Dr. Anderson and others filed many patents that led to devices such as hair removal lasers, resurfacing lasers, and Fraxel lasers. They also made discoveries related to using cold to shrink fat. One of their inventions is known as CoolSculpting. They were so influential in the development of cosmetic dermatology that it is hard to imagine the field without their contributions.
This concludes my four-part series on the history of dermatologists’ role in the development of the skin care industry. I hope I have not forgotten anyone; if I did, I apologize. I have asked for ideas on Dermchat, Facebook and LinkedIn. Feel free to reach out if I missed one of your contributions. I will be giving lectures on this topic in the future and would be happy to include anyone I missed.
As the year 2020 ends, I want to say, Happy 50th Anniversary Dermatology News! I hope you enjoyed this historical series in honor of this anniversary.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Stiefel, CW. (n.d.). Skin Saga: How a Tiny Family Soap Business Evolved Over Six Generations Into the #1 Dermatology Company in the World. United States: Smart Business Network.
2. Saperstein, RB. Arch Dermatol. 1960 Apr;81:601.
3. Saperstein, RB, and Stiefel, WK (1963). U.S. Patent No. 3,092,111. Washington, DC: U.S. Patent and Trademark Office.
4. George DE et al. J Am Acad Dermatol. 2006 Feb;54(2):326.
5. Cvancara JL, Meffert JJ. J Am Acad Dermatol. 1999 Mar;40(3):477-8.
6. Mukhtar M., Sharma R. Int J Dermatol. 2004 Dec;43(12):967-8.
7. Shellow, H. JAMA. 1951;147(18):1777.
8. Wright CS. Arch Dermatol. 1961;84(3):515.
9. Savitt LE. Arch Dermatol. 1961 Apr;83:660-1.
10. Shalita AR, Harris H. Arch Dermatol. 1972 May;105(5):759-60.
11. Shanler SD, Ondo AL. Arch Dermatol. 2007 Nov;143(11):1369-71.
In this series on the role dermatologists have played in the history of skin care, I have covered dermatologists who developed cosmeceutical ingredients, dermatologists who consulted for the skin care industry, and those who developed a novel and successful skin care line. In this column, part 4 of the series, I will continue to discuss .
Dermatologists and Stiefel Laboratories
The Stiefel Medicinal Soap Company, founded in 1847, later became Stiefel Laboratories and was sold to GlaxoSmithKline in 2009. Stiefel Laboratories made many contributions over the years to the field of dermatology as chronicled in the excellent book, “Skin Saga” written by Charles Stiefel and published in 2018. The company was first known for soaps and groundbreaking products, such as “Freckle Soap” that sped epidermal turnover, resulting in a more even toned complexion.
Many dermatologists were involved in developing products and providing advice to the company. Herman Sharlit, MD, in New York, had the idea for a moisturizing soap (Oilatum), a detergent soap (Acne Aid detergent soap), and a coal tar soap (Polytar). Eugene Farber, MD, who was professor and chairman of the department of dermatology at Stanford (Calif.) University, consulted for Stiefel Laboratories and helped them identify and develop many products over the years.1 Stiefel Labs came out with the first facial scrub called Brasivol, an abrasive cream with aluminum oxide particles – the predecessor to modern day microdermabrasion. This facial scrub was conceived by dermatologist Rose Saperstein, MD, Los Angeles, who published a report2 on this in 1960 and also received a patent for it in 1963.3 Brasivol became the company’s first million dollar product.1
Stiefel Laboratories worked with many dermatologists to help them develop their ideas. They included Cleveland White, MD, who patented a highly absorbent foot and body powder known as Zeasorb powder. William Pace, MD, was a Canadian dermatologist who patented an acne treatment containing benzoyl peroxide and sulfur that Stiefel Labs marketed as Sulfoxyl Lotion. Dr. Pace is lovingly referred to as “the father of benzoyl peroxide” because his idea led Stiefel Labs to develop more benzoyl peroxide products. Benzoyl peroxide remains the most popular OTC ingredient to treat acne.
Comedone extractors
Many dermatologists have developed ways to extract comedones. There are publications on using paper clips,4,5safety pins,6 and medicine droppers,7 but some dermatologists have developed special comedone extractors, which include the following: Jay Schamberg, MD, developed a comedone extractor with a loop at each end. He disapproved of cutting a comedone, so did not include a needle or scalpel in his extractor.8
- Leonard Savitt, MD,9 attached a scalpel to one end of the Schamberg extractor.
- Alan Shalita, MD, developed a comedone extractor with a large, keyhole-shaped extracting orifice that made the tool easier to clean.10
The Saalfield comedone extractor combines a fixed pointed blade at one end and a small spoon-shaped expressor foot at the other end. (However, I have not been able to determine if Saalfield was a dermatologist.)
Dermatologist who developed methods for lesion excisions
Robert Segal, MD, a dermatologist at the University of Arizona, Tucson, invented the Dermablade. Although this is technically not a beauty device, I am including it because it has made the removal of unsightly moles and lesions much easier. He holds six patents on this device.
Dermatologists developed dermabrasion and microneedling
Ernst Kromayer, MD,11 a dermatologist in Germany, first described microneedling in 1905 when he mounted dental burrs on motor-driven flexible cord equipment to treat scars. Abner Kurtin, MD, a New York dermatologist, learned about Dr. Kromayer’s technique and modified it using stainless wireless brushes. Dr. Kurtin is known as the “father of dermabrasion.” His work was noted by Nobel Laureate Alexis Carrel, MD, who moved to New York City and began using the technique. Dr. Carrel’s protege, New York dermatologist, Norman Orentreich, MD, began using hypodermic needles instead of wire brushes. Microneedling has gained much popularity over the last decade and has been combined with platelet rich plasma injections.
Dermatologist-developed injection to shrink fat
Adam Rotunda, MD, was a dermatology resident at the University of California, Los Angeles, when he and his professor Michael Kolodney, MD, PhD, had the idea to develop deoxycholate as an injectable to reduce fat deposits. They filed a patent in 2004, conducted clinical trials, and it worked! In 2009, the patent for deoxycholic acid (ATX-10), marketed as Kybella, was granted. The rights to the drug were purchased by Aestherx, which later became Kythera Biopharmaceuticals. Kybella received Food and Drug Administration approval in 2015, and 6 months later, Kythera was acquired by Allergan.
Development of FDA-approved drugs to improve skin appearance
In 2004, dermatologists Stuart Shanler, MD, and Andrew Ondo, MD, filed a patent for the use of topical oxymetazoline for the treatment of the erythema of rosacea. They published their observations in 2007, noting that oxymetazoline improved facial flushing and erythema.11 Dr. Shanler then teamed up with dermatologist Neal Walker, MD, to form a start-up pharmaceutical company, Vicept Therapeutics, and took this compound through phase 2 clinical trials, while Dr. Shanler filed additional patents on oxymetazoline compositions and their uses. Once they successfully demonstrated the efficacy of topical oxymetazoline for rosacea, Allergan acquired the rights of the drug, successfully completed the phase 3 clinical trials, and Rhofade was approved by the FDA in 2017. It is the only topical drug invented and developed by a dermatologist to receive FDA approval since tretinoin (Renova) was developed by Albert Kligman, MD, and approved by the FDA for the improvement in appearance of fine wrinkling, mottled hyperpigmentation and roughness associated with photodamage in 1992.
The development of lasers
The last dermatologist I will discuss in this history series is R. Rox Anderson, MD, professor of dermatology at Harvard University, and director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston. It is impossible to list all his contributions in such a limited space. It would take a book. Building on efforts pioneered by Leon Goldman, MD, Dr. Anderson and his associates pioneered the use of lasers in dermatology and invented the idea of photothermolysis when they filed a patent on using light to remove hair in 1995.Dieter Manstein, MD, PhD,Dr. Anderson and others filed many patents that led to devices such as hair removal lasers, resurfacing lasers, and Fraxel lasers. They also made discoveries related to using cold to shrink fat. One of their inventions is known as CoolSculpting. They were so influential in the development of cosmetic dermatology that it is hard to imagine the field without their contributions.
This concludes my four-part series on the history of dermatologists’ role in the development of the skin care industry. I hope I have not forgotten anyone; if I did, I apologize. I have asked for ideas on Dermchat, Facebook and LinkedIn. Feel free to reach out if I missed one of your contributions. I will be giving lectures on this topic in the future and would be happy to include anyone I missed.
As the year 2020 ends, I want to say, Happy 50th Anniversary Dermatology News! I hope you enjoyed this historical series in honor of this anniversary.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Stiefel, CW. (n.d.). Skin Saga: How a Tiny Family Soap Business Evolved Over Six Generations Into the #1 Dermatology Company in the World. United States: Smart Business Network.
2. Saperstein, RB. Arch Dermatol. 1960 Apr;81:601.
3. Saperstein, RB, and Stiefel, WK (1963). U.S. Patent No. 3,092,111. Washington, DC: U.S. Patent and Trademark Office.
4. George DE et al. J Am Acad Dermatol. 2006 Feb;54(2):326.
5. Cvancara JL, Meffert JJ. J Am Acad Dermatol. 1999 Mar;40(3):477-8.
6. Mukhtar M., Sharma R. Int J Dermatol. 2004 Dec;43(12):967-8.
7. Shellow, H. JAMA. 1951;147(18):1777.
8. Wright CS. Arch Dermatol. 1961;84(3):515.
9. Savitt LE. Arch Dermatol. 1961 Apr;83:660-1.
10. Shalita AR, Harris H. Arch Dermatol. 1972 May;105(5):759-60.
11. Shanler SD, Ondo AL. Arch Dermatol. 2007 Nov;143(11):1369-71.
Escaping the daily grind
Few films have universal appeal these days, but one that comes close is the 1993 classic Groundhog Day, in which the protagonist is trapped in a time loop, doomed to living the same day over and over for many years.
One reason that this story resonates with so many, I think, is that we are all living a similar life. Not as a same-day loop, of course; but each week seems eerily similar to the last, as does each month, each year – on and on, ad infinitum. That’s why it is so important, every so often, to step out of the “loop” and reassess the bigger picture.
I write this reminder every couple of years because it’s so easy to lose sight of the overall landscape among the pressures of our daily routines. . And we are too busy to sit down and think about what we might do to break that vicious cycle. This is detrimental to our own well being, as well as that of our patients.
There are many ways to maintain your intellectual and emotional health, but here’s how I do it: I take individual days off (average of one a month) to catch up on journals or taking a CME course; or to try something new – something I’ve been thinking about doing “someday, when there is time” – such as a guitar, bass, or sailing lessons; or a long weekend away with my wife.
And until COVID-19 put a temporary stop to them earlier this year, we have embarked on at least one longer adventure each year, some of which have been shared in these pages. Our 2019 expedition to Easter Island remains among the most memorable, and fulfilled a dream I’ve had since I read Thor Heyerdahl’s Aku Aku in grade school. As we explored the giant stone moai – which are found nowhere else in the world – I didn’t have the time – or the slightest inclination – to worry about the office. But I did accumulate some great ideas – practical, medical, and literary. Original thoughts are hard to chase down during the daily grind; but in a refreshing environment, they will seek you out. When our trip was over, I returned ready to take on the world, and my practice, anew.
I know how some of you feel about “wasting” a day – or, God forbid, a week. Patients might go elsewhere while you’re gone, and every day the office is idle you “lose money.” That whole paradigm is wrong. You bring in a given amount of revenue per year – more on some days, less on other days, none on weekends and vacations; it all averages out in the end.
Besides, this is much more important than money; this is breaking the routine, clearing the cobwebs, living your life. Trust me, your practice will still be there when you return. And while COVID-19 will not last forever, there are plenty of other “sharpeners” while we wait.
More than once I’ve recounted the story of Alex Müller and J. Georg Bednorz, the Swiss Nobel Laureates whose superconductivity research ground to a halt in 1986. The harder they pressed, the more elusive progress became. So Müller decided to take a break to read a new book on ceramics – a subject that had always interested him.
Nothing could have been less relevant to his work, of course; ceramics are among the poorest conductors known. But in that lower-pressure environment, Müller realized that a unique property of ceramics might apply to their project.
Back in the lab, the team created a ceramic compound that became the first successful “high-temperature” superconductor, which in turn triggered an explosion of research leading to breakthroughs in computing, electricity transmission, magnetically-elevated trains, and many applications yet to be realized.
Sharpening your saw may not change the world, but it will change you; any nudge out of your comfort zone will give you fresh ideas and help you look at seemingly insoluble problems in completely new ways.
And to those who still can’t bear the thought of taking time off, remember the dying words that no one has spoken, ever: “I wish I had spent more time in my office!”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Few films have universal appeal these days, but one that comes close is the 1993 classic Groundhog Day, in which the protagonist is trapped in a time loop, doomed to living the same day over and over for many years.
One reason that this story resonates with so many, I think, is that we are all living a similar life. Not as a same-day loop, of course; but each week seems eerily similar to the last, as does each month, each year – on and on, ad infinitum. That’s why it is so important, every so often, to step out of the “loop” and reassess the bigger picture.
I write this reminder every couple of years because it’s so easy to lose sight of the overall landscape among the pressures of our daily routines. . And we are too busy to sit down and think about what we might do to break that vicious cycle. This is detrimental to our own well being, as well as that of our patients.
There are many ways to maintain your intellectual and emotional health, but here’s how I do it: I take individual days off (average of one a month) to catch up on journals or taking a CME course; or to try something new – something I’ve been thinking about doing “someday, when there is time” – such as a guitar, bass, or sailing lessons; or a long weekend away with my wife.
And until COVID-19 put a temporary stop to them earlier this year, we have embarked on at least one longer adventure each year, some of which have been shared in these pages. Our 2019 expedition to Easter Island remains among the most memorable, and fulfilled a dream I’ve had since I read Thor Heyerdahl’s Aku Aku in grade school. As we explored the giant stone moai – which are found nowhere else in the world – I didn’t have the time – or the slightest inclination – to worry about the office. But I did accumulate some great ideas – practical, medical, and literary. Original thoughts are hard to chase down during the daily grind; but in a refreshing environment, they will seek you out. When our trip was over, I returned ready to take on the world, and my practice, anew.
I know how some of you feel about “wasting” a day – or, God forbid, a week. Patients might go elsewhere while you’re gone, and every day the office is idle you “lose money.” That whole paradigm is wrong. You bring in a given amount of revenue per year – more on some days, less on other days, none on weekends and vacations; it all averages out in the end.
Besides, this is much more important than money; this is breaking the routine, clearing the cobwebs, living your life. Trust me, your practice will still be there when you return. And while COVID-19 will not last forever, there are plenty of other “sharpeners” while we wait.
More than once I’ve recounted the story of Alex Müller and J. Georg Bednorz, the Swiss Nobel Laureates whose superconductivity research ground to a halt in 1986. The harder they pressed, the more elusive progress became. So Müller decided to take a break to read a new book on ceramics – a subject that had always interested him.
Nothing could have been less relevant to his work, of course; ceramics are among the poorest conductors known. But in that lower-pressure environment, Müller realized that a unique property of ceramics might apply to their project.
Back in the lab, the team created a ceramic compound that became the first successful “high-temperature” superconductor, which in turn triggered an explosion of research leading to breakthroughs in computing, electricity transmission, magnetically-elevated trains, and many applications yet to be realized.
Sharpening your saw may not change the world, but it will change you; any nudge out of your comfort zone will give you fresh ideas and help you look at seemingly insoluble problems in completely new ways.
And to those who still can’t bear the thought of taking time off, remember the dying words that no one has spoken, ever: “I wish I had spent more time in my office!”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Few films have universal appeal these days, but one that comes close is the 1993 classic Groundhog Day, in which the protagonist is trapped in a time loop, doomed to living the same day over and over for many years.
One reason that this story resonates with so many, I think, is that we are all living a similar life. Not as a same-day loop, of course; but each week seems eerily similar to the last, as does each month, each year – on and on, ad infinitum. That’s why it is so important, every so often, to step out of the “loop” and reassess the bigger picture.
I write this reminder every couple of years because it’s so easy to lose sight of the overall landscape among the pressures of our daily routines. . And we are too busy to sit down and think about what we might do to break that vicious cycle. This is detrimental to our own well being, as well as that of our patients.
There are many ways to maintain your intellectual and emotional health, but here’s how I do it: I take individual days off (average of one a month) to catch up on journals or taking a CME course; or to try something new – something I’ve been thinking about doing “someday, when there is time” – such as a guitar, bass, or sailing lessons; or a long weekend away with my wife.
And until COVID-19 put a temporary stop to them earlier this year, we have embarked on at least one longer adventure each year, some of which have been shared in these pages. Our 2019 expedition to Easter Island remains among the most memorable, and fulfilled a dream I’ve had since I read Thor Heyerdahl’s Aku Aku in grade school. As we explored the giant stone moai – which are found nowhere else in the world – I didn’t have the time – or the slightest inclination – to worry about the office. But I did accumulate some great ideas – practical, medical, and literary. Original thoughts are hard to chase down during the daily grind; but in a refreshing environment, they will seek you out. When our trip was over, I returned ready to take on the world, and my practice, anew.
I know how some of you feel about “wasting” a day – or, God forbid, a week. Patients might go elsewhere while you’re gone, and every day the office is idle you “lose money.” That whole paradigm is wrong. You bring in a given amount of revenue per year – more on some days, less on other days, none on weekends and vacations; it all averages out in the end.
Besides, this is much more important than money; this is breaking the routine, clearing the cobwebs, living your life. Trust me, your practice will still be there when you return. And while COVID-19 will not last forever, there are plenty of other “sharpeners” while we wait.
More than once I’ve recounted the story of Alex Müller and J. Georg Bednorz, the Swiss Nobel Laureates whose superconductivity research ground to a halt in 1986. The harder they pressed, the more elusive progress became. So Müller decided to take a break to read a new book on ceramics – a subject that had always interested him.
Nothing could have been less relevant to his work, of course; ceramics are among the poorest conductors known. But in that lower-pressure environment, Müller realized that a unique property of ceramics might apply to their project.
Back in the lab, the team created a ceramic compound that became the first successful “high-temperature” superconductor, which in turn triggered an explosion of research leading to breakthroughs in computing, electricity transmission, magnetically-elevated trains, and many applications yet to be realized.
Sharpening your saw may not change the world, but it will change you; any nudge out of your comfort zone will give you fresh ideas and help you look at seemingly insoluble problems in completely new ways.
And to those who still can’t bear the thought of taking time off, remember the dying words that no one has spoken, ever: “I wish I had spent more time in my office!”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Practicing medicine without judgment
“What do you think of all this election stuff?” I froze. Sitting on the exam table was a 50-something-year-old woman. Her hair was long, but not gray. She was wearing a mask without distinctive markings, such as Trump lips or #BLM to identify the political leanings of the owner. She had a subtle New York accent, perhaps dating back to the Giuliani years. It was hard to know her intention. “It’s a trap!” I could hear Admiral Ackbar’s voice in my head. “Don’t engage.” We all know nothing erodes trust faster than showing your blue or red colors before you know which your patient identifies.
Instead, I replied that indeed it has been a stressful year for us all. Then I paused. She shifted a bit and tugged at the gown sleeves and admitted this was the most stress she felt in years. She was seeing me for lichen sclerosus et atrophicus, a terribly itchy, sometimes-disfiguring eruption that can occur in the vulva. She was dealing with COVID-19, kids, divorce, a new partner, working from home, parents, and now the election drama.
At this point in the visit, I knew I could help her. First, the treatment for lichen sclerosus is straightforward and mostly effective. Second, I knew I’d have 7 minutes to spare to just listen. It was a lucky break, as often no such gift of time presents itself while seeing patients in a busy clinic. We take vitals, history (typing), do an exam, make a diagnosis (more typing), and maybe a procedure (yet more typing). All of this is necessary, but sometimes not what our patient needs. Some really need just to connect and share their burden with someone who isn’t a friend or family. As physicians, we have a unique opportunity to see and hear people without judgment.
This reminds me of a recent episode from Sam Harris’s podcast, “Making Sense.” Mr. Harris, a philosopher (and “blue” all the way through) revealed his insight into Presidents Trump’s appeal. Leaving policy aside, Mr. Harris notes that people are drawn to the President because he never judges you. He is incapable of being sanctimonious, Mr. Harris argues, and therefore creates a safe space for people to continue their lives, however flawed, without expectation that they improve.
I’m unsure just how much of this theory explains the devotion of his supporters, but it resonated with me. We doctors are sanctimonious by nature. The better part of my day is spent prodding people to be better: Wear more sunscreen, exercise more, stop believing in conspiracy theories, get your flu shot, and above all, stop scratching! In doing so, I’m in a way judging them. Finger wagging: You’re lazy or poor or dumb or stubborn. “You aren’t as good as me,” is what they might feel after 15 minutes of my pep talk.
But what if that’s wrong? What if they are just fine exactly the way they are? Perhaps what my lichen sclerosis patient needs more than anything is unconditional attention? She, like most of our patients, is well aware of how her shortcomings might contribute to her own anxiety or difficulties. And now she has this rash and that’s probably somehow her fault too, she thinks.
How can I best help her? Betamethasone dipropionate b.i.d. for 2 weeks and spend the last 7 minutes just sitting and listening without judgment or advice. I don’t know who she wanted to win the election. It didn’t matter, she was exactly right to believe what she believed, either way.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
“What do you think of all this election stuff?” I froze. Sitting on the exam table was a 50-something-year-old woman. Her hair was long, but not gray. She was wearing a mask without distinctive markings, such as Trump lips or #BLM to identify the political leanings of the owner. She had a subtle New York accent, perhaps dating back to the Giuliani years. It was hard to know her intention. “It’s a trap!” I could hear Admiral Ackbar’s voice in my head. “Don’t engage.” We all know nothing erodes trust faster than showing your blue or red colors before you know which your patient identifies.
Instead, I replied that indeed it has been a stressful year for us all. Then I paused. She shifted a bit and tugged at the gown sleeves and admitted this was the most stress she felt in years. She was seeing me for lichen sclerosus et atrophicus, a terribly itchy, sometimes-disfiguring eruption that can occur in the vulva. She was dealing with COVID-19, kids, divorce, a new partner, working from home, parents, and now the election drama.
At this point in the visit, I knew I could help her. First, the treatment for lichen sclerosus is straightforward and mostly effective. Second, I knew I’d have 7 minutes to spare to just listen. It was a lucky break, as often no such gift of time presents itself while seeing patients in a busy clinic. We take vitals, history (typing), do an exam, make a diagnosis (more typing), and maybe a procedure (yet more typing). All of this is necessary, but sometimes not what our patient needs. Some really need just to connect and share their burden with someone who isn’t a friend or family. As physicians, we have a unique opportunity to see and hear people without judgment.
This reminds me of a recent episode from Sam Harris’s podcast, “Making Sense.” Mr. Harris, a philosopher (and “blue” all the way through) revealed his insight into Presidents Trump’s appeal. Leaving policy aside, Mr. Harris notes that people are drawn to the President because he never judges you. He is incapable of being sanctimonious, Mr. Harris argues, and therefore creates a safe space for people to continue their lives, however flawed, without expectation that they improve.
I’m unsure just how much of this theory explains the devotion of his supporters, but it resonated with me. We doctors are sanctimonious by nature. The better part of my day is spent prodding people to be better: Wear more sunscreen, exercise more, stop believing in conspiracy theories, get your flu shot, and above all, stop scratching! In doing so, I’m in a way judging them. Finger wagging: You’re lazy or poor or dumb or stubborn. “You aren’t as good as me,” is what they might feel after 15 minutes of my pep talk.
But what if that’s wrong? What if they are just fine exactly the way they are? Perhaps what my lichen sclerosis patient needs more than anything is unconditional attention? She, like most of our patients, is well aware of how her shortcomings might contribute to her own anxiety or difficulties. And now she has this rash and that’s probably somehow her fault too, she thinks.
How can I best help her? Betamethasone dipropionate b.i.d. for 2 weeks and spend the last 7 minutes just sitting and listening without judgment or advice. I don’t know who she wanted to win the election. It didn’t matter, she was exactly right to believe what she believed, either way.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
“What do you think of all this election stuff?” I froze. Sitting on the exam table was a 50-something-year-old woman. Her hair was long, but not gray. She was wearing a mask without distinctive markings, such as Trump lips or #BLM to identify the political leanings of the owner. She had a subtle New York accent, perhaps dating back to the Giuliani years. It was hard to know her intention. “It’s a trap!” I could hear Admiral Ackbar’s voice in my head. “Don’t engage.” We all know nothing erodes trust faster than showing your blue or red colors before you know which your patient identifies.
Instead, I replied that indeed it has been a stressful year for us all. Then I paused. She shifted a bit and tugged at the gown sleeves and admitted this was the most stress she felt in years. She was seeing me for lichen sclerosus et atrophicus, a terribly itchy, sometimes-disfiguring eruption that can occur in the vulva. She was dealing with COVID-19, kids, divorce, a new partner, working from home, parents, and now the election drama.
At this point in the visit, I knew I could help her. First, the treatment for lichen sclerosus is straightforward and mostly effective. Second, I knew I’d have 7 minutes to spare to just listen. It was a lucky break, as often no such gift of time presents itself while seeing patients in a busy clinic. We take vitals, history (typing), do an exam, make a diagnosis (more typing), and maybe a procedure (yet more typing). All of this is necessary, but sometimes not what our patient needs. Some really need just to connect and share their burden with someone who isn’t a friend or family. As physicians, we have a unique opportunity to see and hear people without judgment.
This reminds me of a recent episode from Sam Harris’s podcast, “Making Sense.” Mr. Harris, a philosopher (and “blue” all the way through) revealed his insight into Presidents Trump’s appeal. Leaving policy aside, Mr. Harris notes that people are drawn to the President because he never judges you. He is incapable of being sanctimonious, Mr. Harris argues, and therefore creates a safe space for people to continue their lives, however flawed, without expectation that they improve.
I’m unsure just how much of this theory explains the devotion of his supporters, but it resonated with me. We doctors are sanctimonious by nature. The better part of my day is spent prodding people to be better: Wear more sunscreen, exercise more, stop believing in conspiracy theories, get your flu shot, and above all, stop scratching! In doing so, I’m in a way judging them. Finger wagging: You’re lazy or poor or dumb or stubborn. “You aren’t as good as me,” is what they might feel after 15 minutes of my pep talk.
But what if that’s wrong? What if they are just fine exactly the way they are? Perhaps what my lichen sclerosis patient needs more than anything is unconditional attention? She, like most of our patients, is well aware of how her shortcomings might contribute to her own anxiety or difficulties. And now she has this rash and that’s probably somehow her fault too, she thinks.
How can I best help her? Betamethasone dipropionate b.i.d. for 2 weeks and spend the last 7 minutes just sitting and listening without judgment or advice. I don’t know who she wanted to win the election. It didn’t matter, she was exactly right to believe what she believed, either way.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A novel method for assessing attractiveness and beauty
While Phi (or the Golden Ratio) and Leonardo da Vinci’s neoclassical canons have been used as traditional mathematical approaches to assess and calculate beauty, there may be more than meets the eye.
This model was created to denote “natural beauty,” both at baseline and after cosmetic procedures, which is what many physicians and patients ideally want to achieve after any aesthetic procedure.
In this model, when all three variables are at a maximum, a desirable attractive appearance is achieved that can be interpreted as “natural.” In his paper introducing this novel model, Dr. Dayan wrote that similar to the time-space dilemma, attractiveness “is relative, dynamic, and highly dependent on the position of the projector and the interpreter.” The 3-D cube of attractiveness “is therefore contained within a fourth dimension that takes into account the perspective of the judger.”
Similarly, in a pilot study,2 Dr. Dayan and colleagues also demonstrated that visually blind individuals can detect beauty. “This study further isolates the nature of beauty as a primal form of messaging that is subconsciously appreciated via embodied senses other than vision,” he and his coauthors wrote.
This observational study consisted of 8 blind and 10 nonblind test subjects and 6 models who were categorized into predetermined beauty categories. Test subjects were blindfolded and unblindfolded during their assessments. All groups rated those models, who were preselected as more beautiful, higher, except for the blindfolded, nonblind group – demonstrating a primal or neural pathway ability to perceive attractiveness in blind individuals. The study, “revealed that beauty is not only detected by visual sense but also through embodied senses other than sight,” the authors commented.
It should be noted that sometimes ethnic features and features that are unique outside of the neoclassical canons or golden ratio can also uniquely make people look more attractive. Ethnic variations in beauty standards exist and need to be further studied and celebrated. There is certainly high expertise and an art required to perceiving aesthetics and performing aesthetic procedures, further exemplified by the complex nature of the different models and mathematical approaches of assessing it. These newer models account for attractiveness that may also start on the inside or beyond purely visual perception.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
References:
1. Dayan S, Romero DH. J Cosmet Dermatol. 2018 Oct;17(5):925-30.
2. Dayan SH et al. Dermatol Surg. 2020 Oct;46(10):1317-22.
While Phi (or the Golden Ratio) and Leonardo da Vinci’s neoclassical canons have been used as traditional mathematical approaches to assess and calculate beauty, there may be more than meets the eye.
This model was created to denote “natural beauty,” both at baseline and after cosmetic procedures, which is what many physicians and patients ideally want to achieve after any aesthetic procedure.
In this model, when all three variables are at a maximum, a desirable attractive appearance is achieved that can be interpreted as “natural.” In his paper introducing this novel model, Dr. Dayan wrote that similar to the time-space dilemma, attractiveness “is relative, dynamic, and highly dependent on the position of the projector and the interpreter.” The 3-D cube of attractiveness “is therefore contained within a fourth dimension that takes into account the perspective of the judger.”
Similarly, in a pilot study,2 Dr. Dayan and colleagues also demonstrated that visually blind individuals can detect beauty. “This study further isolates the nature of beauty as a primal form of messaging that is subconsciously appreciated via embodied senses other than vision,” he and his coauthors wrote.
This observational study consisted of 8 blind and 10 nonblind test subjects and 6 models who were categorized into predetermined beauty categories. Test subjects were blindfolded and unblindfolded during their assessments. All groups rated those models, who were preselected as more beautiful, higher, except for the blindfolded, nonblind group – demonstrating a primal or neural pathway ability to perceive attractiveness in blind individuals. The study, “revealed that beauty is not only detected by visual sense but also through embodied senses other than sight,” the authors commented.
It should be noted that sometimes ethnic features and features that are unique outside of the neoclassical canons or golden ratio can also uniquely make people look more attractive. Ethnic variations in beauty standards exist and need to be further studied and celebrated. There is certainly high expertise and an art required to perceiving aesthetics and performing aesthetic procedures, further exemplified by the complex nature of the different models and mathematical approaches of assessing it. These newer models account for attractiveness that may also start on the inside or beyond purely visual perception.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
References:
1. Dayan S, Romero DH. J Cosmet Dermatol. 2018 Oct;17(5):925-30.
2. Dayan SH et al. Dermatol Surg. 2020 Oct;46(10):1317-22.
While Phi (or the Golden Ratio) and Leonardo da Vinci’s neoclassical canons have been used as traditional mathematical approaches to assess and calculate beauty, there may be more than meets the eye.
This model was created to denote “natural beauty,” both at baseline and after cosmetic procedures, which is what many physicians and patients ideally want to achieve after any aesthetic procedure.
In this model, when all three variables are at a maximum, a desirable attractive appearance is achieved that can be interpreted as “natural.” In his paper introducing this novel model, Dr. Dayan wrote that similar to the time-space dilemma, attractiveness “is relative, dynamic, and highly dependent on the position of the projector and the interpreter.” The 3-D cube of attractiveness “is therefore contained within a fourth dimension that takes into account the perspective of the judger.”
Similarly, in a pilot study,2 Dr. Dayan and colleagues also demonstrated that visually blind individuals can detect beauty. “This study further isolates the nature of beauty as a primal form of messaging that is subconsciously appreciated via embodied senses other than vision,” he and his coauthors wrote.
This observational study consisted of 8 blind and 10 nonblind test subjects and 6 models who were categorized into predetermined beauty categories. Test subjects were blindfolded and unblindfolded during their assessments. All groups rated those models, who were preselected as more beautiful, higher, except for the blindfolded, nonblind group – demonstrating a primal or neural pathway ability to perceive attractiveness in blind individuals. The study, “revealed that beauty is not only detected by visual sense but also through embodied senses other than sight,” the authors commented.
It should be noted that sometimes ethnic features and features that are unique outside of the neoclassical canons or golden ratio can also uniquely make people look more attractive. Ethnic variations in beauty standards exist and need to be further studied and celebrated. There is certainly high expertise and an art required to perceiving aesthetics and performing aesthetic procedures, further exemplified by the complex nature of the different models and mathematical approaches of assessing it. These newer models account for attractiveness that may also start on the inside or beyond purely visual perception.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
References:
1. Dayan S, Romero DH. J Cosmet Dermatol. 2018 Oct;17(5):925-30.
2. Dayan SH et al. Dermatol Surg. 2020 Oct;46(10):1317-22.
An 11-year-old female with a 3-year history of alopecia
Given the longstanding scarring alopecia, with negative fungal cultures and with perifollicular erythema and scaling, this diagnosis is most consistent with lichen planopilaris.
Lichen planopilaris (LPP) is considered one of the primary scarring alopecias, a group of diseases characterized by inflammation and subsequent irreversible hair loss.1 LPP specifically is believed to be caused by dysfunction of cell-mediated immunity, resulting in T lymphocytes attacking follicular hair stem cells.2 It typically presents with hair loss, pruritus, scaling, burning pain, and tenderness of the scalp when active,1,3 with exam showing perifollicular scale and erythema on the borders of the patches of alopecia.4,5 Over time, scarring of the scalp develops with loss of follicular ostia.1 Definitive diagnosis typically requires punch biopsy of the affected scalp, as such can determine the presence or absence of inflammation in affected areas of the scalp.1
What’s the treatment plan?
Given that LPP is an autoimmune inflammatory disease process, the goal of treatment is to calm down the inflammation of the scalp to prevent further progression of a patient’s hair loss. This is typically achieved with superpotent topical corticosteroids, such as clobetasol applied directly to the scalp, and/or intralesional corticosteroids, such as triamcinolone acetonide suspension injected directly to the affected scalp.3,6,7 Other treatment options include systemic agents, such as hydroxychloroquine, methotrexate, mycophenolate mofetil, pioglitazone, and doxycycline.3,6 Hair loss is not reversible as loss of follicular ostia and hair stem cells results in permanent scarring.1 Management often requires a referral to dermatology for aggressive treatment to prevent further hair loss.
What’s the differential diagnosis?
The differential diagnosis of lichen planopilaris includes other scarring alopecias, including central centrifugal cicatricial alopecia, discoid lupus erythematosus, folliculitis decalvans. While nonscarring, alopecia areata, trichotillomania, and telogen effluvium are discussed below as well.
Central centrifugal cicatricial alopecia is very rare in pediatrics, and is a type of asymptomatic scarring alopecia that begins at the vertex of the scalp, spreading centrifugally and resulting in shiny plaque development. Treatment involves reduction of hair grooming as well as topical and intralesional steroids.
Discoid lupus erythematosus presents as scaling erythematous plaques on the face and scalp that result in skin pigment changes and atrophy over time. Scalp involvement results in scarring alopecia. Treatment includes the use of high-potency topical corticosteroids, topical calcineurin inhibitors, and hydroxychloroquine.
Folliculitis decalvans is another form of scarring alopecia believed to be caused by an inflammatory response to Staphylococcus aureus in the scalp, resulting in the formation of scarring of the scalp and perifollicular pustules. Treatment is topical antibiotics and intralesional steroids.
Alopecia areata is a form of nonscarring alopecia resulting in small round patches of partially reversible hair loss characterized by the pathognomonic finding of so-called exclamation point hairs that are broader distally and taper toward the scalp on physical exam. Considered an autoimmune disorder, it varies greatly in extent and course. While focal hair loss is the hallmark of this disease, usually hair follicles are present.
Trichotillosis, also known as trichotillomania (hair pulling), results in alopecia with irregular borders and broken hairs of different lengths secondary to the urge to remove or pull one’s own hair, resulting in nonscarring alopecia. It may be associated with stress or anxiety, obsessive-compulsive disorders, or other repetitive body-altering behaviors. Treatments include reassurance and education as it can be self-limited in some, behavior modification, or systemic therapy including tricyclic antidepressants or SSRIs.
Our patient underwent scalp punch biopsy to confirm the diagnosis and was started on potent topical corticosteroids with good disease control.
Dr. Haft is a pediatric dermatology research associate in the division of pediatric and adolescent dermatology, University of California, San Diego, and Rady Children’s Hospital, San Diego. Dr. Eichenfield is the vice chair of the department of dermatology and a professor of dermatology and pediatrics at the university, and he is chief of pediatric and adolescent dermatology at the hospital. Neither of the doctors had any relevant financial disclosures. Email them at [email protected].
References
1. J Am Acad Dermatol. 2005 Jul. doi: 10.1016/j.jaad.2004.06.015.
2. J Pathol. 2013 Oct. doi: 10.1002/path.4233.
3. Pediatr Dermatol. 2015 Sep-Oct. doi: 10.1111/pde.12624.
4. J Am Acad Dermatol. 2004 Jan. doi: 10.1016/j.jaad.2003.04.001.
5. J Am Acad Dermatol. 1992 Dec. doi: 10.1016/0190-9622(92)70290-v.
6. Clin Cosmet Investig Dermatol. 2018 Feb 27. doi: 10.2147/CCID.S137870.
7. Semin Cutan Med Surg. 2009 Mar. doi: 10.1016/j.sder.2008.12.006.
Given the longstanding scarring alopecia, with negative fungal cultures and with perifollicular erythema and scaling, this diagnosis is most consistent with lichen planopilaris.
Lichen planopilaris (LPP) is considered one of the primary scarring alopecias, a group of diseases characterized by inflammation and subsequent irreversible hair loss.1 LPP specifically is believed to be caused by dysfunction of cell-mediated immunity, resulting in T lymphocytes attacking follicular hair stem cells.2 It typically presents with hair loss, pruritus, scaling, burning pain, and tenderness of the scalp when active,1,3 with exam showing perifollicular scale and erythema on the borders of the patches of alopecia.4,5 Over time, scarring of the scalp develops with loss of follicular ostia.1 Definitive diagnosis typically requires punch biopsy of the affected scalp, as such can determine the presence or absence of inflammation in affected areas of the scalp.1
What’s the treatment plan?
Given that LPP is an autoimmune inflammatory disease process, the goal of treatment is to calm down the inflammation of the scalp to prevent further progression of a patient’s hair loss. This is typically achieved with superpotent topical corticosteroids, such as clobetasol applied directly to the scalp, and/or intralesional corticosteroids, such as triamcinolone acetonide suspension injected directly to the affected scalp.3,6,7 Other treatment options include systemic agents, such as hydroxychloroquine, methotrexate, mycophenolate mofetil, pioglitazone, and doxycycline.3,6 Hair loss is not reversible as loss of follicular ostia and hair stem cells results in permanent scarring.1 Management often requires a referral to dermatology for aggressive treatment to prevent further hair loss.
What’s the differential diagnosis?
The differential diagnosis of lichen planopilaris includes other scarring alopecias, including central centrifugal cicatricial alopecia, discoid lupus erythematosus, folliculitis decalvans. While nonscarring, alopecia areata, trichotillomania, and telogen effluvium are discussed below as well.
Central centrifugal cicatricial alopecia is very rare in pediatrics, and is a type of asymptomatic scarring alopecia that begins at the vertex of the scalp, spreading centrifugally and resulting in shiny plaque development. Treatment involves reduction of hair grooming as well as topical and intralesional steroids.
Discoid lupus erythematosus presents as scaling erythematous plaques on the face and scalp that result in skin pigment changes and atrophy over time. Scalp involvement results in scarring alopecia. Treatment includes the use of high-potency topical corticosteroids, topical calcineurin inhibitors, and hydroxychloroquine.
Folliculitis decalvans is another form of scarring alopecia believed to be caused by an inflammatory response to Staphylococcus aureus in the scalp, resulting in the formation of scarring of the scalp and perifollicular pustules. Treatment is topical antibiotics and intralesional steroids.
Alopecia areata is a form of nonscarring alopecia resulting in small round patches of partially reversible hair loss characterized by the pathognomonic finding of so-called exclamation point hairs that are broader distally and taper toward the scalp on physical exam. Considered an autoimmune disorder, it varies greatly in extent and course. While focal hair loss is the hallmark of this disease, usually hair follicles are present.
Trichotillosis, also known as trichotillomania (hair pulling), results in alopecia with irregular borders and broken hairs of different lengths secondary to the urge to remove or pull one’s own hair, resulting in nonscarring alopecia. It may be associated with stress or anxiety, obsessive-compulsive disorders, or other repetitive body-altering behaviors. Treatments include reassurance and education as it can be self-limited in some, behavior modification, or systemic therapy including tricyclic antidepressants or SSRIs.
Our patient underwent scalp punch biopsy to confirm the diagnosis and was started on potent topical corticosteroids with good disease control.
Dr. Haft is a pediatric dermatology research associate in the division of pediatric and adolescent dermatology, University of California, San Diego, and Rady Children’s Hospital, San Diego. Dr. Eichenfield is the vice chair of the department of dermatology and a professor of dermatology and pediatrics at the university, and he is chief of pediatric and adolescent dermatology at the hospital. Neither of the doctors had any relevant financial disclosures. Email them at [email protected].
References
1. J Am Acad Dermatol. 2005 Jul. doi: 10.1016/j.jaad.2004.06.015.
2. J Pathol. 2013 Oct. doi: 10.1002/path.4233.
3. Pediatr Dermatol. 2015 Sep-Oct. doi: 10.1111/pde.12624.
4. J Am Acad Dermatol. 2004 Jan. doi: 10.1016/j.jaad.2003.04.001.
5. J Am Acad Dermatol. 1992 Dec. doi: 10.1016/0190-9622(92)70290-v.
6. Clin Cosmet Investig Dermatol. 2018 Feb 27. doi: 10.2147/CCID.S137870.
7. Semin Cutan Med Surg. 2009 Mar. doi: 10.1016/j.sder.2008.12.006.
Given the longstanding scarring alopecia, with negative fungal cultures and with perifollicular erythema and scaling, this diagnosis is most consistent with lichen planopilaris.
Lichen planopilaris (LPP) is considered one of the primary scarring alopecias, a group of diseases characterized by inflammation and subsequent irreversible hair loss.1 LPP specifically is believed to be caused by dysfunction of cell-mediated immunity, resulting in T lymphocytes attacking follicular hair stem cells.2 It typically presents with hair loss, pruritus, scaling, burning pain, and tenderness of the scalp when active,1,3 with exam showing perifollicular scale and erythema on the borders of the patches of alopecia.4,5 Over time, scarring of the scalp develops with loss of follicular ostia.1 Definitive diagnosis typically requires punch biopsy of the affected scalp, as such can determine the presence or absence of inflammation in affected areas of the scalp.1
What’s the treatment plan?
Given that LPP is an autoimmune inflammatory disease process, the goal of treatment is to calm down the inflammation of the scalp to prevent further progression of a patient’s hair loss. This is typically achieved with superpotent topical corticosteroids, such as clobetasol applied directly to the scalp, and/or intralesional corticosteroids, such as triamcinolone acetonide suspension injected directly to the affected scalp.3,6,7 Other treatment options include systemic agents, such as hydroxychloroquine, methotrexate, mycophenolate mofetil, pioglitazone, and doxycycline.3,6 Hair loss is not reversible as loss of follicular ostia and hair stem cells results in permanent scarring.1 Management often requires a referral to dermatology for aggressive treatment to prevent further hair loss.
What’s the differential diagnosis?
The differential diagnosis of lichen planopilaris includes other scarring alopecias, including central centrifugal cicatricial alopecia, discoid lupus erythematosus, folliculitis decalvans. While nonscarring, alopecia areata, trichotillomania, and telogen effluvium are discussed below as well.
Central centrifugal cicatricial alopecia is very rare in pediatrics, and is a type of asymptomatic scarring alopecia that begins at the vertex of the scalp, spreading centrifugally and resulting in shiny plaque development. Treatment involves reduction of hair grooming as well as topical and intralesional steroids.
Discoid lupus erythematosus presents as scaling erythematous plaques on the face and scalp that result in skin pigment changes and atrophy over time. Scalp involvement results in scarring alopecia. Treatment includes the use of high-potency topical corticosteroids, topical calcineurin inhibitors, and hydroxychloroquine.
Folliculitis decalvans is another form of scarring alopecia believed to be caused by an inflammatory response to Staphylococcus aureus in the scalp, resulting in the formation of scarring of the scalp and perifollicular pustules. Treatment is topical antibiotics and intralesional steroids.
Alopecia areata is a form of nonscarring alopecia resulting in small round patches of partially reversible hair loss characterized by the pathognomonic finding of so-called exclamation point hairs that are broader distally and taper toward the scalp on physical exam. Considered an autoimmune disorder, it varies greatly in extent and course. While focal hair loss is the hallmark of this disease, usually hair follicles are present.
Trichotillosis, also known as trichotillomania (hair pulling), results in alopecia with irregular borders and broken hairs of different lengths secondary to the urge to remove or pull one’s own hair, resulting in nonscarring alopecia. It may be associated with stress or anxiety, obsessive-compulsive disorders, or other repetitive body-altering behaviors. Treatments include reassurance and education as it can be self-limited in some, behavior modification, or systemic therapy including tricyclic antidepressants or SSRIs.
Our patient underwent scalp punch biopsy to confirm the diagnosis and was started on potent topical corticosteroids with good disease control.
Dr. Haft is a pediatric dermatology research associate in the division of pediatric and adolescent dermatology, University of California, San Diego, and Rady Children’s Hospital, San Diego. Dr. Eichenfield is the vice chair of the department of dermatology and a professor of dermatology and pediatrics at the university, and he is chief of pediatric and adolescent dermatology at the hospital. Neither of the doctors had any relevant financial disclosures. Email them at [email protected].
References
1. J Am Acad Dermatol. 2005 Jul. doi: 10.1016/j.jaad.2004.06.015.
2. J Pathol. 2013 Oct. doi: 10.1002/path.4233.
3. Pediatr Dermatol. 2015 Sep-Oct. doi: 10.1111/pde.12624.
4. J Am Acad Dermatol. 2004 Jan. doi: 10.1016/j.jaad.2003.04.001.
5. J Am Acad Dermatol. 1992 Dec. doi: 10.1016/0190-9622(92)70290-v.
6. Clin Cosmet Investig Dermatol. 2018 Feb 27. doi: 10.2147/CCID.S137870.
7. Semin Cutan Med Surg. 2009 Mar. doi: 10.1016/j.sder.2008.12.006.
An 11-year-old female is seen in clinic with a 3-year history of alopecia. The patient recently immigrated to the United States from Afghanistan. Prior to immigrating, she was evaluated for "scarring alopecia" and had been treated with oral and topical steroids as well as oral and topical antifungals. When active, she had itching and tenderness. She is not actively losing any hair at this time, but she has not regrown any of her hair. The patient has no family members with alopecia. She reports some burning pain and itching of her scalp, and denies any muscle pain or weakness or sun sensitivity.
On physical exam, you see 50% loss of hair on the superior scalp with preservation of the anterior hair line. Patches of hair can be seen throughout, with segments of smooth-skinned alopecia, without pustules. There is a loss of the follicle pattern in scarred areas, and magnification or "dermoscopy" shows perifollicular erythema and scaling at the border of the affected scalp. Labs are all within normal limits. Bacterial and fungal cultures of the scalp do not grow organisms.
Should our patients really go home for the holidays?
As an East Coast transplant residing in Texas, I look forward to the annual sojourn home to celebrate the holidays with family and friends – as do many of our patients and their families. But this is 2020. SARS-CoV-2, the causative agent of COVID-19, is still circulating. To make matters worse, cases are rising in 45 states and internationally. The day of this writing 102,831 new cases were reported in the United States. 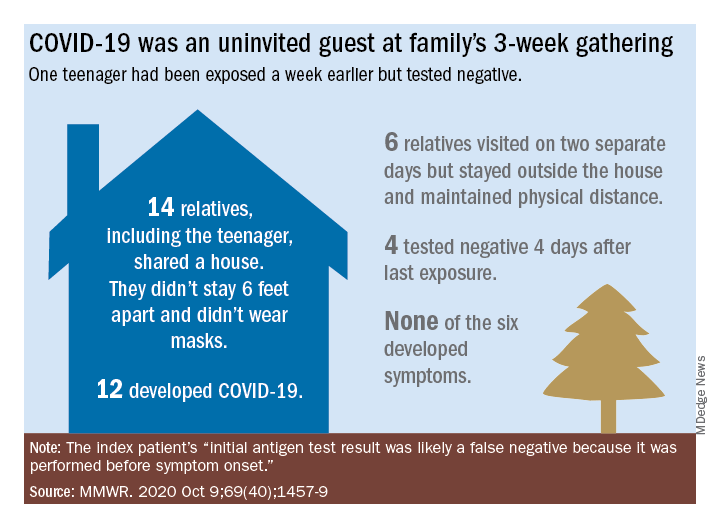
Social distancing, wearing masks, and hand washing have been strategies recommended to help mitigate the spread of the virus. We know adherence is not always 100%. The reality is that several families will consider traveling and gathering with others over the holidays. Their actions may lead to increased infections, hospitalizations, and even deaths. It behooves us to at least remind them of the potential consequences of the activity, and if travel and/or holiday gatherings are inevitable, to provide some guidance to help them look at both the risks and benefits and offer strategies to minimize infection and spread.
What should be considered prior to travel?
Here is a list of points to ponder:
- Is your patient is in a high-risk group for developing severe disease or visiting someone who is in a high-risk group?
- What is their mode of transportation?
- What is their destination?
- How prevalent is the disease at their destination, compared with their community?
- What will be their accommodations?
- How will attendees prepare for the gathering, if at all?
- Will multiple families congregate after quarantining for 2 weeks or simply arrive?
- At the destination, will people wear masks and socially distance?
- Is an outdoor venue an option?
All of these questions should be considered by patients.
Review high-risk groups
In terms of high-risk groups, we usually focus on underlying medical conditions or extremes of age, but Black and LatinX children and their families have been diagnosed with COVID-19 and hospitalized more frequently than other racial/ ethnic groups in the United States. Of 277,285 school-aged children infected between March 1 and Sept. 19, 2020, 42% were LatinX, 32% White, and 17% Black, yet they comprise 18%, 60%, and 11% of the U.S. population, respectively. Of those hospitalized, 45% were LatinX, 22% White, and 24% Black. LatinX and Black children also have disproportionately higher mortality rates.
Think about transmission and how to mitigate it
Many patients erroneously think combining multiple households for small group gatherings is inconsequential. These types of gatherings serve as a continued source of SARS-CoV-2 spread. For example, a person in Illinois with mild upper respiratory infection symptoms attended a funeral; he reported embracing the family members after the funeral. He dined with two people the evening prior to the funeral, sharing the meal using common serving dishes. Four days later, he attended a birthday party with nine family members. Some of the family members with symptoms subsequently attended church, infecting another church attendee. A cluster of 16 cases of COVID-19 was subsequently identified, including three deaths likely resulting from this one introduction of COVID-19 at these two family gatherings.
In Tennessee and Wisconsin, household transmission of SARS-CoV-2 was studied prospectively. A total of 101 index cases and 191 asymptomatic household contacts were enrolled between April and Sept. 2020; 102 of 191 (53%) had SARS-CoV-2 detected during the 14-day follow-up. Most infections (75%) were identified within 5 days and occurred whether the index case was an adult or child.
Lastly, one adolescent was identified as the source for an outbreak at a family gathering where 15 persons from five households and four states shared a house between 8 and 25 days in July 2020. Six additional members visited the house. The index case had an exposure to COVID-19 and had a negative antigen test 4 days after exposure. She was asymptomatic when tested. She developed nasal congestion 2 days later, the same day she and her family departed for the gathering. A total of 11 household contacts developed confirmed, suspected, or probable COVID-19, and the teen developed symptoms. This report illustrates how easily SARS-CoV-2 is transmitted, and how when implemented, mitigation strategies work because none of the six who only visited the house was infected. It also serves as a reminder that antigen testing is indicated only for use within the first 5-12 days of onset of symptoms. In this case, the adolescent was asymptomatic when tested and had a false-negative test result.
Ponder modes of transportation
How will your patient arrive to their holiday destination? Nonstop travel by car with household members is probably the safest way. However, for many families, buses and trains are the only options, and social distancing may be challenging. Air travel is a must for others. Acquisition of COVID-19 during air travel appears to be low, but not absent based on how air enters and leaves the cabin. The challenge is socially distancing throughout the check in and boarding processes, as well as minimizing contact with common surfaces. There also is loss of social distancing once on board. Ideally, masks should be worn during the flight. Additionally, for those with international destinations, most countries now require a negative polymerase chain reaction COVID-19 test within a specified time frame for entry.
Essentially the safest place for your patients during the holidays is celebrating at home with their household contacts. The risk for disease acquisition increases with travel. You will not have the opportunity to discuss holiday plans with most parents. However, you can encourage them to consider the pros and cons of travel with reminders via telephone, e-mail, and /or social messaging directly from your practices similar to those sent for other medically necessary interventions. As for me, I will be celebrating virtually this year. There is a first time for everything.
For additional information that also is patient friendly, the Centers for Disease Control and Prevention offers information about travel within the United States and international travel.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
As an East Coast transplant residing in Texas, I look forward to the annual sojourn home to celebrate the holidays with family and friends – as do many of our patients and their families. But this is 2020. SARS-CoV-2, the causative agent of COVID-19, is still circulating. To make matters worse, cases are rising in 45 states and internationally. The day of this writing 102,831 new cases were reported in the United States. 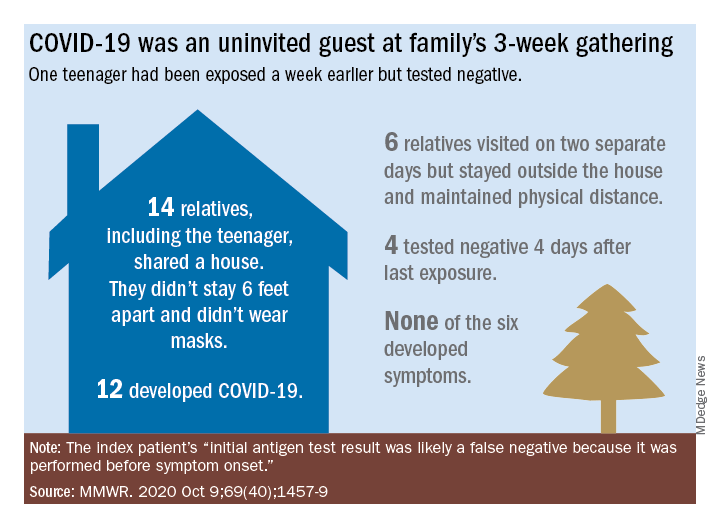
Social distancing, wearing masks, and hand washing have been strategies recommended to help mitigate the spread of the virus. We know adherence is not always 100%. The reality is that several families will consider traveling and gathering with others over the holidays. Their actions may lead to increased infections, hospitalizations, and even deaths. It behooves us to at least remind them of the potential consequences of the activity, and if travel and/or holiday gatherings are inevitable, to provide some guidance to help them look at both the risks and benefits and offer strategies to minimize infection and spread.
What should be considered prior to travel?
Here is a list of points to ponder:
- Is your patient is in a high-risk group for developing severe disease or visiting someone who is in a high-risk group?
- What is their mode of transportation?
- What is their destination?
- How prevalent is the disease at their destination, compared with their community?
- What will be their accommodations?
- How will attendees prepare for the gathering, if at all?
- Will multiple families congregate after quarantining for 2 weeks or simply arrive?
- At the destination, will people wear masks and socially distance?
- Is an outdoor venue an option?
All of these questions should be considered by patients.
Review high-risk groups
In terms of high-risk groups, we usually focus on underlying medical conditions or extremes of age, but Black and LatinX children and their families have been diagnosed with COVID-19 and hospitalized more frequently than other racial/ ethnic groups in the United States. Of 277,285 school-aged children infected between March 1 and Sept. 19, 2020, 42% were LatinX, 32% White, and 17% Black, yet they comprise 18%, 60%, and 11% of the U.S. population, respectively. Of those hospitalized, 45% were LatinX, 22% White, and 24% Black. LatinX and Black children also have disproportionately higher mortality rates.
Think about transmission and how to mitigate it
Many patients erroneously think combining multiple households for small group gatherings is inconsequential. These types of gatherings serve as a continued source of SARS-CoV-2 spread. For example, a person in Illinois with mild upper respiratory infection symptoms attended a funeral; he reported embracing the family members after the funeral. He dined with two people the evening prior to the funeral, sharing the meal using common serving dishes. Four days later, he attended a birthday party with nine family members. Some of the family members with symptoms subsequently attended church, infecting another church attendee. A cluster of 16 cases of COVID-19 was subsequently identified, including three deaths likely resulting from this one introduction of COVID-19 at these two family gatherings.
In Tennessee and Wisconsin, household transmission of SARS-CoV-2 was studied prospectively. A total of 101 index cases and 191 asymptomatic household contacts were enrolled between April and Sept. 2020; 102 of 191 (53%) had SARS-CoV-2 detected during the 14-day follow-up. Most infections (75%) were identified within 5 days and occurred whether the index case was an adult or child.
Lastly, one adolescent was identified as the source for an outbreak at a family gathering where 15 persons from five households and four states shared a house between 8 and 25 days in July 2020. Six additional members visited the house. The index case had an exposure to COVID-19 and had a negative antigen test 4 days after exposure. She was asymptomatic when tested. She developed nasal congestion 2 days later, the same day she and her family departed for the gathering. A total of 11 household contacts developed confirmed, suspected, or probable COVID-19, and the teen developed symptoms. This report illustrates how easily SARS-CoV-2 is transmitted, and how when implemented, mitigation strategies work because none of the six who only visited the house was infected. It also serves as a reminder that antigen testing is indicated only for use within the first 5-12 days of onset of symptoms. In this case, the adolescent was asymptomatic when tested and had a false-negative test result.
Ponder modes of transportation
How will your patient arrive to their holiday destination? Nonstop travel by car with household members is probably the safest way. However, for many families, buses and trains are the only options, and social distancing may be challenging. Air travel is a must for others. Acquisition of COVID-19 during air travel appears to be low, but not absent based on how air enters and leaves the cabin. The challenge is socially distancing throughout the check in and boarding processes, as well as minimizing contact with common surfaces. There also is loss of social distancing once on board. Ideally, masks should be worn during the flight. Additionally, for those with international destinations, most countries now require a negative polymerase chain reaction COVID-19 test within a specified time frame for entry.
Essentially the safest place for your patients during the holidays is celebrating at home with their household contacts. The risk for disease acquisition increases with travel. You will not have the opportunity to discuss holiday plans with most parents. However, you can encourage them to consider the pros and cons of travel with reminders via telephone, e-mail, and /or social messaging directly from your practices similar to those sent for other medically necessary interventions. As for me, I will be celebrating virtually this year. There is a first time for everything.
For additional information that also is patient friendly, the Centers for Disease Control and Prevention offers information about travel within the United States and international travel.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
As an East Coast transplant residing in Texas, I look forward to the annual sojourn home to celebrate the holidays with family and friends – as do many of our patients and their families. But this is 2020. SARS-CoV-2, the causative agent of COVID-19, is still circulating. To make matters worse, cases are rising in 45 states and internationally. The day of this writing 102,831 new cases were reported in the United States. 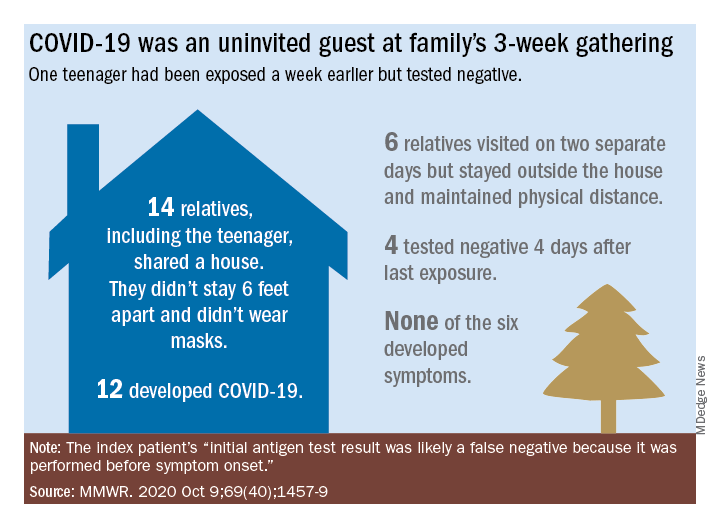
Social distancing, wearing masks, and hand washing have been strategies recommended to help mitigate the spread of the virus. We know adherence is not always 100%. The reality is that several families will consider traveling and gathering with others over the holidays. Their actions may lead to increased infections, hospitalizations, and even deaths. It behooves us to at least remind them of the potential consequences of the activity, and if travel and/or holiday gatherings are inevitable, to provide some guidance to help them look at both the risks and benefits and offer strategies to minimize infection and spread.
What should be considered prior to travel?
Here is a list of points to ponder:
- Is your patient is in a high-risk group for developing severe disease or visiting someone who is in a high-risk group?
- What is their mode of transportation?
- What is their destination?
- How prevalent is the disease at their destination, compared with their community?
- What will be their accommodations?
- How will attendees prepare for the gathering, if at all?
- Will multiple families congregate after quarantining for 2 weeks or simply arrive?
- At the destination, will people wear masks and socially distance?
- Is an outdoor venue an option?
All of these questions should be considered by patients.
Review high-risk groups
In terms of high-risk groups, we usually focus on underlying medical conditions or extremes of age, but Black and LatinX children and their families have been diagnosed with COVID-19 and hospitalized more frequently than other racial/ ethnic groups in the United States. Of 277,285 school-aged children infected between March 1 and Sept. 19, 2020, 42% were LatinX, 32% White, and 17% Black, yet they comprise 18%, 60%, and 11% of the U.S. population, respectively. Of those hospitalized, 45% were LatinX, 22% White, and 24% Black. LatinX and Black children also have disproportionately higher mortality rates.
Think about transmission and how to mitigate it
Many patients erroneously think combining multiple households for small group gatherings is inconsequential. These types of gatherings serve as a continued source of SARS-CoV-2 spread. For example, a person in Illinois with mild upper respiratory infection symptoms attended a funeral; he reported embracing the family members after the funeral. He dined with two people the evening prior to the funeral, sharing the meal using common serving dishes. Four days later, he attended a birthday party with nine family members. Some of the family members with symptoms subsequently attended church, infecting another church attendee. A cluster of 16 cases of COVID-19 was subsequently identified, including three deaths likely resulting from this one introduction of COVID-19 at these two family gatherings.
In Tennessee and Wisconsin, household transmission of SARS-CoV-2 was studied prospectively. A total of 101 index cases and 191 asymptomatic household contacts were enrolled between April and Sept. 2020; 102 of 191 (53%) had SARS-CoV-2 detected during the 14-day follow-up. Most infections (75%) were identified within 5 days and occurred whether the index case was an adult or child.
Lastly, one adolescent was identified as the source for an outbreak at a family gathering where 15 persons from five households and four states shared a house between 8 and 25 days in July 2020. Six additional members visited the house. The index case had an exposure to COVID-19 and had a negative antigen test 4 days after exposure. She was asymptomatic when tested. She developed nasal congestion 2 days later, the same day she and her family departed for the gathering. A total of 11 household contacts developed confirmed, suspected, or probable COVID-19, and the teen developed symptoms. This report illustrates how easily SARS-CoV-2 is transmitted, and how when implemented, mitigation strategies work because none of the six who only visited the house was infected. It also serves as a reminder that antigen testing is indicated only for use within the first 5-12 days of onset of symptoms. In this case, the adolescent was asymptomatic when tested and had a false-negative test result.
Ponder modes of transportation
How will your patient arrive to their holiday destination? Nonstop travel by car with household members is probably the safest way. However, for many families, buses and trains are the only options, and social distancing may be challenging. Air travel is a must for others. Acquisition of COVID-19 during air travel appears to be low, but not absent based on how air enters and leaves the cabin. The challenge is socially distancing throughout the check in and boarding processes, as well as minimizing contact with common surfaces. There also is loss of social distancing once on board. Ideally, masks should be worn during the flight. Additionally, for those with international destinations, most countries now require a negative polymerase chain reaction COVID-19 test within a specified time frame for entry.
Essentially the safest place for your patients during the holidays is celebrating at home with their household contacts. The risk for disease acquisition increases with travel. You will not have the opportunity to discuss holiday plans with most parents. However, you can encourage them to consider the pros and cons of travel with reminders via telephone, e-mail, and /or social messaging directly from your practices similar to those sent for other medically necessary interventions. As for me, I will be celebrating virtually this year. There is a first time for everything.
For additional information that also is patient friendly, the Centers for Disease Control and Prevention offers information about travel within the United States and international travel.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].























