User login
The fourth trimester: Achieving improved postpartum care
The field of ob.gyn. has long focused significantly more attention on the prenatal period – on determining the optimal frequency of ultrasound examinations, for instance, and on screening for diabetes and other conditions – than on women’s health and well-being after delivery.
The traditional 6-week postpartum visit has too often been a quick and cursory visit, with new mothers typically navigating the preceding postpartum transitions on their own.
The need to redefine postpartum care was a central message of Haywood Brown, MD, who in 2017 served as the president of the America College of Obstetricians and Gynecologists. Dr. Brown established a task force whose work resulted in important guidance for taking a more comprehensive and patient-centered approach to postpartum care.1
Improved care in the “fourth trimester,” as it has come to be known, is comprehensive and includes ensuring that our patients have a solid transition to health care beyond the pregnancy. We also hope that it will help us to reduce maternal mortality, given that more than half of pregnancy-related deaths occur after delivery.
Timing and frequency of contact
Historically, we’ve had a single 6-week postpartum visit, with little or no maternal support or patient contact before this visit unless the patient reported a complication. In the new paradigm, as described in the ACOG committee opinion on optimizing postpartum care, maternal care should be an ongoing process.1
so that any questions or concerns may be addressed and support can be provided.
This should be followed by individualized, ongoing care until a comprehensive postpartum visit covering physical, social, and psychological well-being is conducted by 12 weeks after birth – anytime between 4 and 12 weeks.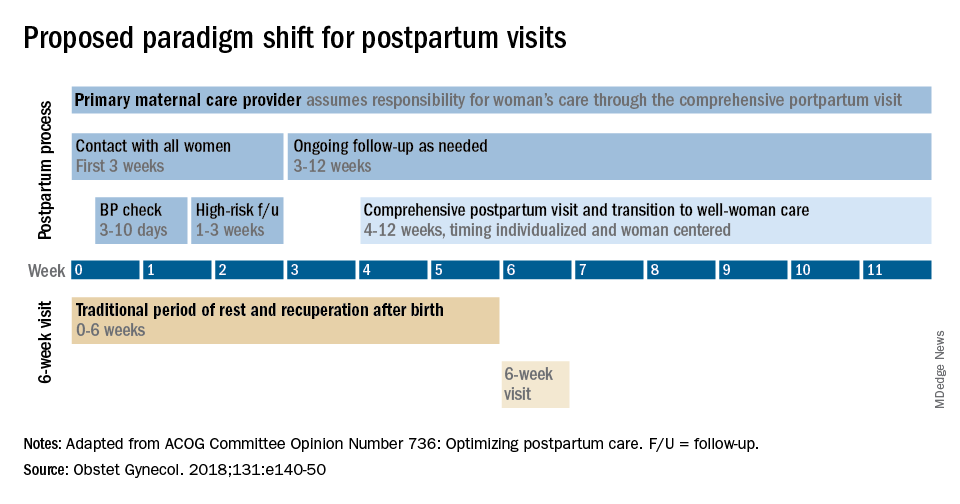
By stressing the importance of postpartum care during prenatal visits – and by talking about some of its key elements such as mental health, breastfeeding, and chronic disease management – we can let our patients know that postpartum care is not just an afterthought, but that it involves planning backed by evidence and expert opinion. Currently, as many as 40% of women do not attend a postpartum visit; early discussion, it is hoped, will increase attendance.
Certain high-risk groups should be seen or screened earlier than 3 weeks post partum. For instance, women who have hypertensive disorders of pregnancy should be evaluated no later than 7-10 days post partum, and women with severe hypertension should be seen within 72 hours, according to ACOG.
Early blood pressure checks – and follow-up as necessary – are critical for reducing the risk of postpartum stroke and other complications. I advocate uniformly checking blood pressure within several days after hospital discharge for all women who have hypertension at the end of their pregnancy.
Other high-risk conditions requiring early follow-up include diabetes and autoimmune conditions such as lupus, multiple sclerosis, and psoriasis that may flare in the postpartum period. Women with a history of postpartum depression similarly may benefit from early contact; they are at higher risk of having depression again, and there are clearly effective treatments, both medication and psychotherapy based.
In between the initial early contact (by 7-10 days post partum or by 3 weeks post partum) and the comprehensive visit between 4 and 12 weeks, the need for and timing of patient contact can be individualized. Some women will need only a brief contact and a visit at 8-10 weeks, while others will need much more. Our goal, as in all of medicine, is to provide individualized, patient-centered care.
Methods of contact
With the exception of the final comprehensive visit, postpartum care need not occur in person. Some conditions require an early office visit, but in general, as ACOG states, the usefulness of an in-person visit should be weighed against the burden of traveling to and attending that visit.
For many women, in-person visits are difficult, and we must be creative in utilizing telemedicine and phone support, text messaging, and app-based support. Having practiced during this pandemic, we are better positioned than ever before to make it relatively easy for new mothers to obtain ongoing postpartum care.
Notably, research is demonstrating that the use of technology may allow us to provide improved care and monitoring of hypertension in the postpartum period. For example, a randomized trial published in 2018 of over 200 women with a hypertensive disorder of pregnancy found that text-based surveillance with home blood pressure monitoring was more effective than usual in-person blood pressure checks in meeting clinical guidelines for postpartum monitoring.2
Women in the texting group were significantly more likely to have a single blood pressure obtained in the first 10 days post partum than women in the office group.
Postpartum care is also not a completely physician-driven endeavor. Much of what is needed to help women successfully navigate the fourth trimester can be provided by certified nurse midwives, advanced practice nurses, and other members of our maternal care teams.
Components of postpartum care
The postpartum care plan should be comprehensive, and having a checklist to guide one through initial and comprehensive visits may be helpful. The ACOG committee opinion categorizes the components of postpartum care into seven domains: mood and emotional well-being; infant care and feeding; sexuality, contraception, and birth spacing; sleep and fatigue; physical recovery from birth; chronic disease management; and health maintenance.1
The importance of screening for depression and anxiety cannot be emphasized enough. Perinatal depression is highly prevalent: It affects as many as one in seven women and can result in adverse short- and long-term effects on both the mother and child.
The U.S. Preventive Services Task Force has offered guidance for years, most recently in 2019 with its recommendations that clinicians refer pregnant and postpartum women who are at increased risk for depression to counseling interventions such as cognitive behavioral therapy and interpersonal therapy.3 There is evidence that some form of treatment for women who screen positive reduces the risk of perinatal depression.
Additionally, there is emerging evidence that postpartum PTSD may be as prevalent as postpartum depression.4 As ACOG points out, trauma is “in the eye of the beholder,” and an estimated 3%-16% of women have PTSD related to a traumatic birth experience. Complications like shoulder dystocia or postpartum hemorrhage, in which delivery processes rapidly change course, can be experienced as traumatic by women even though they and their infants are healthy. The risk of posttraumatic stress should be on our radar screen.
Interpregnancy intervals similarly are not discussed enough. We do not commonly talk to patients about how pregnancy and breastfeeding are nutritionally depleting and how it takes time to replenish these stores – yet birth spacing is so important.
Compared with interpregnancy intervals of at least 18 months, intervals shorter than 6 months were associated in a meta-analysis with increased risks of preterm birth, low birth weight, and small for gestational age.5 Optimal birth spacing is one of the few low-cost interventions available for reducing pregnancy complications in the future.
Finally, that chronic disease management is a domain of postpartum care warrants emphasis. We must work to ensure that patients have a solid plan of care in place for their diabetes, hypertension, lupus, or other chronic conditions. This includes who will provide that ongoing care, as well as when medical management should be restarted.
Some women are aware of the importance of timely care – of not waiting for 12 months, for instance, to see an internist or specialist – but others are not.
Again, certain health conditions such as multiple sclerosis and RA necessitate follow-up within a couple weeks after delivery so that medications can be restarted or dose adjustments made. The need for early postpartum follow-up can be discussed during prenatal visits, along with anticipatory guidance about breastfeeding, the signs and symptoms of perinatal depression and anxiety, and other components of the fourth trimester.
Dr. Macones has no relevant financial disclosures.
References
1. Obstet Gynecol. 2018 May;131(5):e140-50.
2. BMJ Qual Saf. 2018 Apr 27;27(11):871-7.
3. JAMA. 2019 Feb 12;321(6):580-7.
4. Clin Psychol Rev. 2014 Jul;34:389-401.JAMA. 2006 Apr 19;295(15):1809-23.
The field of ob.gyn. has long focused significantly more attention on the prenatal period – on determining the optimal frequency of ultrasound examinations, for instance, and on screening for diabetes and other conditions – than on women’s health and well-being after delivery.
The traditional 6-week postpartum visit has too often been a quick and cursory visit, with new mothers typically navigating the preceding postpartum transitions on their own.
The need to redefine postpartum care was a central message of Haywood Brown, MD, who in 2017 served as the president of the America College of Obstetricians and Gynecologists. Dr. Brown established a task force whose work resulted in important guidance for taking a more comprehensive and patient-centered approach to postpartum care.1
Improved care in the “fourth trimester,” as it has come to be known, is comprehensive and includes ensuring that our patients have a solid transition to health care beyond the pregnancy. We also hope that it will help us to reduce maternal mortality, given that more than half of pregnancy-related deaths occur after delivery.
Timing and frequency of contact
Historically, we’ve had a single 6-week postpartum visit, with little or no maternal support or patient contact before this visit unless the patient reported a complication. In the new paradigm, as described in the ACOG committee opinion on optimizing postpartum care, maternal care should be an ongoing process.1
so that any questions or concerns may be addressed and support can be provided.
This should be followed by individualized, ongoing care until a comprehensive postpartum visit covering physical, social, and psychological well-being is conducted by 12 weeks after birth – anytime between 4 and 12 weeks.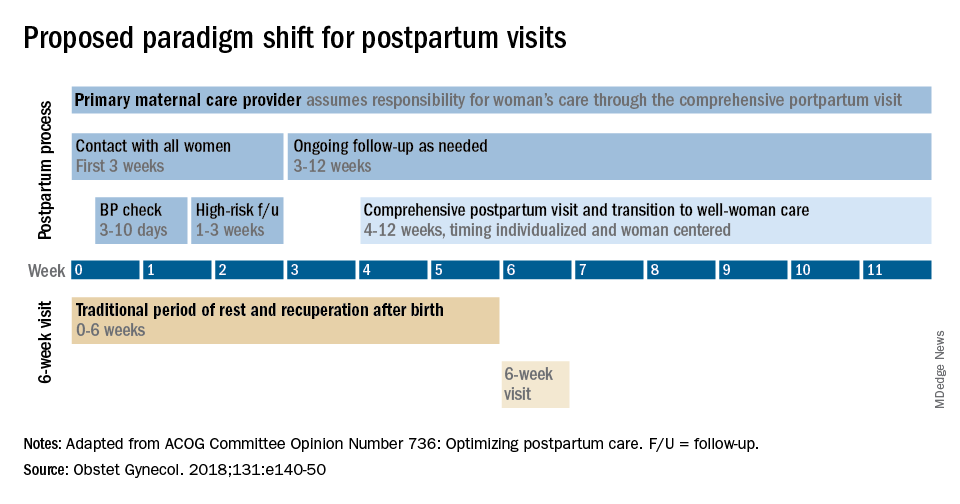
By stressing the importance of postpartum care during prenatal visits – and by talking about some of its key elements such as mental health, breastfeeding, and chronic disease management – we can let our patients know that postpartum care is not just an afterthought, but that it involves planning backed by evidence and expert opinion. Currently, as many as 40% of women do not attend a postpartum visit; early discussion, it is hoped, will increase attendance.
Certain high-risk groups should be seen or screened earlier than 3 weeks post partum. For instance, women who have hypertensive disorders of pregnancy should be evaluated no later than 7-10 days post partum, and women with severe hypertension should be seen within 72 hours, according to ACOG.
Early blood pressure checks – and follow-up as necessary – are critical for reducing the risk of postpartum stroke and other complications. I advocate uniformly checking blood pressure within several days after hospital discharge for all women who have hypertension at the end of their pregnancy.
Other high-risk conditions requiring early follow-up include diabetes and autoimmune conditions such as lupus, multiple sclerosis, and psoriasis that may flare in the postpartum period. Women with a history of postpartum depression similarly may benefit from early contact; they are at higher risk of having depression again, and there are clearly effective treatments, both medication and psychotherapy based.
In between the initial early contact (by 7-10 days post partum or by 3 weeks post partum) and the comprehensive visit between 4 and 12 weeks, the need for and timing of patient contact can be individualized. Some women will need only a brief contact and a visit at 8-10 weeks, while others will need much more. Our goal, as in all of medicine, is to provide individualized, patient-centered care.
Methods of contact
With the exception of the final comprehensive visit, postpartum care need not occur in person. Some conditions require an early office visit, but in general, as ACOG states, the usefulness of an in-person visit should be weighed against the burden of traveling to and attending that visit.
For many women, in-person visits are difficult, and we must be creative in utilizing telemedicine and phone support, text messaging, and app-based support. Having practiced during this pandemic, we are better positioned than ever before to make it relatively easy for new mothers to obtain ongoing postpartum care.
Notably, research is demonstrating that the use of technology may allow us to provide improved care and monitoring of hypertension in the postpartum period. For example, a randomized trial published in 2018 of over 200 women with a hypertensive disorder of pregnancy found that text-based surveillance with home blood pressure monitoring was more effective than usual in-person blood pressure checks in meeting clinical guidelines for postpartum monitoring.2
Women in the texting group were significantly more likely to have a single blood pressure obtained in the first 10 days post partum than women in the office group.
Postpartum care is also not a completely physician-driven endeavor. Much of what is needed to help women successfully navigate the fourth trimester can be provided by certified nurse midwives, advanced practice nurses, and other members of our maternal care teams.
Components of postpartum care
The postpartum care plan should be comprehensive, and having a checklist to guide one through initial and comprehensive visits may be helpful. The ACOG committee opinion categorizes the components of postpartum care into seven domains: mood and emotional well-being; infant care and feeding; sexuality, contraception, and birth spacing; sleep and fatigue; physical recovery from birth; chronic disease management; and health maintenance.1
The importance of screening for depression and anxiety cannot be emphasized enough. Perinatal depression is highly prevalent: It affects as many as one in seven women and can result in adverse short- and long-term effects on both the mother and child.
The U.S. Preventive Services Task Force has offered guidance for years, most recently in 2019 with its recommendations that clinicians refer pregnant and postpartum women who are at increased risk for depression to counseling interventions such as cognitive behavioral therapy and interpersonal therapy.3 There is evidence that some form of treatment for women who screen positive reduces the risk of perinatal depression.
Additionally, there is emerging evidence that postpartum PTSD may be as prevalent as postpartum depression.4 As ACOG points out, trauma is “in the eye of the beholder,” and an estimated 3%-16% of women have PTSD related to a traumatic birth experience. Complications like shoulder dystocia or postpartum hemorrhage, in which delivery processes rapidly change course, can be experienced as traumatic by women even though they and their infants are healthy. The risk of posttraumatic stress should be on our radar screen.
Interpregnancy intervals similarly are not discussed enough. We do not commonly talk to patients about how pregnancy and breastfeeding are nutritionally depleting and how it takes time to replenish these stores – yet birth spacing is so important.
Compared with interpregnancy intervals of at least 18 months, intervals shorter than 6 months were associated in a meta-analysis with increased risks of preterm birth, low birth weight, and small for gestational age.5 Optimal birth spacing is one of the few low-cost interventions available for reducing pregnancy complications in the future.
Finally, that chronic disease management is a domain of postpartum care warrants emphasis. We must work to ensure that patients have a solid plan of care in place for their diabetes, hypertension, lupus, or other chronic conditions. This includes who will provide that ongoing care, as well as when medical management should be restarted.
Some women are aware of the importance of timely care – of not waiting for 12 months, for instance, to see an internist or specialist – but others are not.
Again, certain health conditions such as multiple sclerosis and RA necessitate follow-up within a couple weeks after delivery so that medications can be restarted or dose adjustments made. The need for early postpartum follow-up can be discussed during prenatal visits, along with anticipatory guidance about breastfeeding, the signs and symptoms of perinatal depression and anxiety, and other components of the fourth trimester.
Dr. Macones has no relevant financial disclosures.
References
1. Obstet Gynecol. 2018 May;131(5):e140-50.
2. BMJ Qual Saf. 2018 Apr 27;27(11):871-7.
3. JAMA. 2019 Feb 12;321(6):580-7.
4. Clin Psychol Rev. 2014 Jul;34:389-401.JAMA. 2006 Apr 19;295(15):1809-23.
The field of ob.gyn. has long focused significantly more attention on the prenatal period – on determining the optimal frequency of ultrasound examinations, for instance, and on screening for diabetes and other conditions – than on women’s health and well-being after delivery.
The traditional 6-week postpartum visit has too often been a quick and cursory visit, with new mothers typically navigating the preceding postpartum transitions on their own.
The need to redefine postpartum care was a central message of Haywood Brown, MD, who in 2017 served as the president of the America College of Obstetricians and Gynecologists. Dr. Brown established a task force whose work resulted in important guidance for taking a more comprehensive and patient-centered approach to postpartum care.1
Improved care in the “fourth trimester,” as it has come to be known, is comprehensive and includes ensuring that our patients have a solid transition to health care beyond the pregnancy. We also hope that it will help us to reduce maternal mortality, given that more than half of pregnancy-related deaths occur after delivery.
Timing and frequency of contact
Historically, we’ve had a single 6-week postpartum visit, with little or no maternal support or patient contact before this visit unless the patient reported a complication. In the new paradigm, as described in the ACOG committee opinion on optimizing postpartum care, maternal care should be an ongoing process.1
so that any questions or concerns may be addressed and support can be provided.
This should be followed by individualized, ongoing care until a comprehensive postpartum visit covering physical, social, and psychological well-being is conducted by 12 weeks after birth – anytime between 4 and 12 weeks.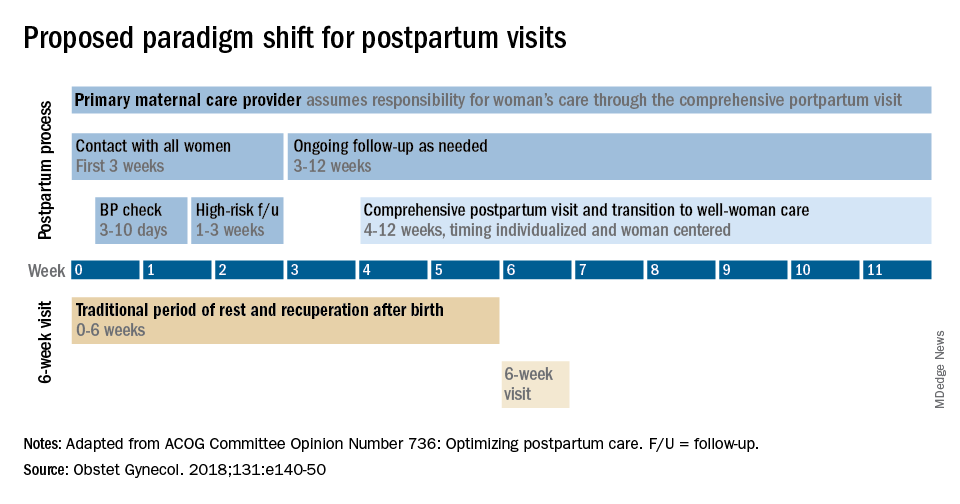
By stressing the importance of postpartum care during prenatal visits – and by talking about some of its key elements such as mental health, breastfeeding, and chronic disease management – we can let our patients know that postpartum care is not just an afterthought, but that it involves planning backed by evidence and expert opinion. Currently, as many as 40% of women do not attend a postpartum visit; early discussion, it is hoped, will increase attendance.
Certain high-risk groups should be seen or screened earlier than 3 weeks post partum. For instance, women who have hypertensive disorders of pregnancy should be evaluated no later than 7-10 days post partum, and women with severe hypertension should be seen within 72 hours, according to ACOG.
Early blood pressure checks – and follow-up as necessary – are critical for reducing the risk of postpartum stroke and other complications. I advocate uniformly checking blood pressure within several days after hospital discharge for all women who have hypertension at the end of their pregnancy.
Other high-risk conditions requiring early follow-up include diabetes and autoimmune conditions such as lupus, multiple sclerosis, and psoriasis that may flare in the postpartum period. Women with a history of postpartum depression similarly may benefit from early contact; they are at higher risk of having depression again, and there are clearly effective treatments, both medication and psychotherapy based.
In between the initial early contact (by 7-10 days post partum or by 3 weeks post partum) and the comprehensive visit between 4 and 12 weeks, the need for and timing of patient contact can be individualized. Some women will need only a brief contact and a visit at 8-10 weeks, while others will need much more. Our goal, as in all of medicine, is to provide individualized, patient-centered care.
Methods of contact
With the exception of the final comprehensive visit, postpartum care need not occur in person. Some conditions require an early office visit, but in general, as ACOG states, the usefulness of an in-person visit should be weighed against the burden of traveling to and attending that visit.
For many women, in-person visits are difficult, and we must be creative in utilizing telemedicine and phone support, text messaging, and app-based support. Having practiced during this pandemic, we are better positioned than ever before to make it relatively easy for new mothers to obtain ongoing postpartum care.
Notably, research is demonstrating that the use of technology may allow us to provide improved care and monitoring of hypertension in the postpartum period. For example, a randomized trial published in 2018 of over 200 women with a hypertensive disorder of pregnancy found that text-based surveillance with home blood pressure monitoring was more effective than usual in-person blood pressure checks in meeting clinical guidelines for postpartum monitoring.2
Women in the texting group were significantly more likely to have a single blood pressure obtained in the first 10 days post partum than women in the office group.
Postpartum care is also not a completely physician-driven endeavor. Much of what is needed to help women successfully navigate the fourth trimester can be provided by certified nurse midwives, advanced practice nurses, and other members of our maternal care teams.
Components of postpartum care
The postpartum care plan should be comprehensive, and having a checklist to guide one through initial and comprehensive visits may be helpful. The ACOG committee opinion categorizes the components of postpartum care into seven domains: mood and emotional well-being; infant care and feeding; sexuality, contraception, and birth spacing; sleep and fatigue; physical recovery from birth; chronic disease management; and health maintenance.1
The importance of screening for depression and anxiety cannot be emphasized enough. Perinatal depression is highly prevalent: It affects as many as one in seven women and can result in adverse short- and long-term effects on both the mother and child.
The U.S. Preventive Services Task Force has offered guidance for years, most recently in 2019 with its recommendations that clinicians refer pregnant and postpartum women who are at increased risk for depression to counseling interventions such as cognitive behavioral therapy and interpersonal therapy.3 There is evidence that some form of treatment for women who screen positive reduces the risk of perinatal depression.
Additionally, there is emerging evidence that postpartum PTSD may be as prevalent as postpartum depression.4 As ACOG points out, trauma is “in the eye of the beholder,” and an estimated 3%-16% of women have PTSD related to a traumatic birth experience. Complications like shoulder dystocia or postpartum hemorrhage, in which delivery processes rapidly change course, can be experienced as traumatic by women even though they and their infants are healthy. The risk of posttraumatic stress should be on our radar screen.
Interpregnancy intervals similarly are not discussed enough. We do not commonly talk to patients about how pregnancy and breastfeeding are nutritionally depleting and how it takes time to replenish these stores – yet birth spacing is so important.
Compared with interpregnancy intervals of at least 18 months, intervals shorter than 6 months were associated in a meta-analysis with increased risks of preterm birth, low birth weight, and small for gestational age.5 Optimal birth spacing is one of the few low-cost interventions available for reducing pregnancy complications in the future.
Finally, that chronic disease management is a domain of postpartum care warrants emphasis. We must work to ensure that patients have a solid plan of care in place for their diabetes, hypertension, lupus, or other chronic conditions. This includes who will provide that ongoing care, as well as when medical management should be restarted.
Some women are aware of the importance of timely care – of not waiting for 12 months, for instance, to see an internist or specialist – but others are not.
Again, certain health conditions such as multiple sclerosis and RA necessitate follow-up within a couple weeks after delivery so that medications can be restarted or dose adjustments made. The need for early postpartum follow-up can be discussed during prenatal visits, along with anticipatory guidance about breastfeeding, the signs and symptoms of perinatal depression and anxiety, and other components of the fourth trimester.
Dr. Macones has no relevant financial disclosures.
References
1. Obstet Gynecol. 2018 May;131(5):e140-50.
2. BMJ Qual Saf. 2018 Apr 27;27(11):871-7.
3. JAMA. 2019 Feb 12;321(6):580-7.
4. Clin Psychol Rev. 2014 Jul;34:389-401.JAMA. 2006 Apr 19;295(15):1809-23.
The fourth trimester
As we approach the end of this year, one of the most surreal times in human history, we will look back on the many things we taught ourselves, the many things we took for granted, the many things we were grateful for, the many things we missed, and the many things we plan to do once we can do things again. Among the many things 2020 taught us to appreciate was the very real manifestation of the old adage, “prevention is the best medicine.” To prevent transmission of SARS-CoV-2, we wore masks, we sanitized everything, we avoided crowds, we traded in-person meetings for virtual meetings, we learned how to homeschool our children, and we delayed seeing relatives and friends.
Ob.gyns. in small and large practices around the world had the tremendous challenge of balancing necessary in-person prenatal care services with keeping their patients and babies safe. Labor and delivery units had even greater demands to keep women and neonates free of SARS-CoV-2 infection. Practices quickly put into place new treatment protocols and new management strategies to maintain the health of their staff while ensuring a high quality of care.
While we have focused much of our attention on greater precautions during pregnancy and childbirth, an important component of care is the immediate postpartum period – colloquially referred to as the “fourth trimester” – which remains critical to maintaining physical and mental health and well-being.
Despite concerns regarding COVID-19 safety, we should continue monitoring our patients during these crucial first weeks after childbirth. This year of social isolation, financial strain, and incredible uncertainty has created additional stress in many women’s lives. The usual support that some women would receive from family members, friends, and other mothers in the early days post partum may not be available. The pandemic also has further highlighted inequities in access to health care for vulnerable groups. In addition, restrictions have increased the incidence of intimate partner violence as many women and children have needed to shelter with their abusers. Perhaps now more than any time previously, ob.gyns. must be attuned to their patients’ needs and be ready to provide compassionate and sensitive care.
In this final month of the year, we have invited George A. Macones, MD, professor and chair of the department of women’s health at the University of Texas, Austin, to address the importance of care in the final “trimester” of pregnancy – the first 3 months post partum.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
*This version has been updated to correct an erroneous byline, photo, and bio.
As we approach the end of this year, one of the most surreal times in human history, we will look back on the many things we taught ourselves, the many things we took for granted, the many things we were grateful for, the many things we missed, and the many things we plan to do once we can do things again. Among the many things 2020 taught us to appreciate was the very real manifestation of the old adage, “prevention is the best medicine.” To prevent transmission of SARS-CoV-2, we wore masks, we sanitized everything, we avoided crowds, we traded in-person meetings for virtual meetings, we learned how to homeschool our children, and we delayed seeing relatives and friends.
Ob.gyns. in small and large practices around the world had the tremendous challenge of balancing necessary in-person prenatal care services with keeping their patients and babies safe. Labor and delivery units had even greater demands to keep women and neonates free of SARS-CoV-2 infection. Practices quickly put into place new treatment protocols and new management strategies to maintain the health of their staff while ensuring a high quality of care.
While we have focused much of our attention on greater precautions during pregnancy and childbirth, an important component of care is the immediate postpartum period – colloquially referred to as the “fourth trimester” – which remains critical to maintaining physical and mental health and well-being.
Despite concerns regarding COVID-19 safety, we should continue monitoring our patients during these crucial first weeks after childbirth. This year of social isolation, financial strain, and incredible uncertainty has created additional stress in many women’s lives. The usual support that some women would receive from family members, friends, and other mothers in the early days post partum may not be available. The pandemic also has further highlighted inequities in access to health care for vulnerable groups. In addition, restrictions have increased the incidence of intimate partner violence as many women and children have needed to shelter with their abusers. Perhaps now more than any time previously, ob.gyns. must be attuned to their patients’ needs and be ready to provide compassionate and sensitive care.
In this final month of the year, we have invited George A. Macones, MD, professor and chair of the department of women’s health at the University of Texas, Austin, to address the importance of care in the final “trimester” of pregnancy – the first 3 months post partum.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
*This version has been updated to correct an erroneous byline, photo, and bio.
As we approach the end of this year, one of the most surreal times in human history, we will look back on the many things we taught ourselves, the many things we took for granted, the many things we were grateful for, the many things we missed, and the many things we plan to do once we can do things again. Among the many things 2020 taught us to appreciate was the very real manifestation of the old adage, “prevention is the best medicine.” To prevent transmission of SARS-CoV-2, we wore masks, we sanitized everything, we avoided crowds, we traded in-person meetings for virtual meetings, we learned how to homeschool our children, and we delayed seeing relatives and friends.
Ob.gyns. in small and large practices around the world had the tremendous challenge of balancing necessary in-person prenatal care services with keeping their patients and babies safe. Labor and delivery units had even greater demands to keep women and neonates free of SARS-CoV-2 infection. Practices quickly put into place new treatment protocols and new management strategies to maintain the health of their staff while ensuring a high quality of care.
While we have focused much of our attention on greater precautions during pregnancy and childbirth, an important component of care is the immediate postpartum period – colloquially referred to as the “fourth trimester” – which remains critical to maintaining physical and mental health and well-being.
Despite concerns regarding COVID-19 safety, we should continue monitoring our patients during these crucial first weeks after childbirth. This year of social isolation, financial strain, and incredible uncertainty has created additional stress in many women’s lives. The usual support that some women would receive from family members, friends, and other mothers in the early days post partum may not be available. The pandemic also has further highlighted inequities in access to health care for vulnerable groups. In addition, restrictions have increased the incidence of intimate partner violence as many women and children have needed to shelter with their abusers. Perhaps now more than any time previously, ob.gyns. must be attuned to their patients’ needs and be ready to provide compassionate and sensitive care.
In this final month of the year, we have invited George A. Macones, MD, professor and chair of the department of women’s health at the University of Texas, Austin, to address the importance of care in the final “trimester” of pregnancy – the first 3 months post partum.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
*This version has been updated to correct an erroneous byline, photo, and bio.
Scientific power will save us
COVID-19 numbers again are increasing dramatically. Community infection rates have nearly doubled, and hospitals and health care workers are stretched beyond their limits. It is difficult not to feel anger about how poorly this pandemic was managed (mismanaged) by so many officials in charge and by a large segment of our population who still refuse protective actions to limit spread. While politics and ideology continue to cost American lives, scientific firepower will emerge as our saving grace.
My editorial board and I are entering our final year at the helm of GI & Hepatology News. AGA issued a search for the next Editor in Chief (EIC), who will take over October 2021. I urge anyone interested to apply (https://gastro.org/news/prestigious-aga-publications-seek-new-editors-in-chief/). As EIC, you will choose the next editorial board and forge professional friendships that are gratifying. You will assume responsibility for the content, where you must balance your own views with those of both the AGA and our readership.
As EIC, each month I am given space for 300 words to communicate interesting ideas and opinions. The AGA gives the newspaper great editorial freedom, and I hope we have supported AGA’s mission and values when we publish its official newspaper. I always have next month’s editorial in mind, and I look for useful phrases, quotes, ideas, and opinions. If you are interested in becoming EIC, please email [email protected] for more information.
I would be remiss not to acknowledge the contribution that Lora McGlade has made to GI & Hepatology News. She has been my partner, as the Frontline Medical Communications Editor in charge of GI & Hepatology News. Next month, she will move on to assume a new role. I cannot thank her enough for helping make this newspaper work. As the months go on, I will highlight the contributions of others from the AGA, our Board, and Frontline.
Please stay safe and do not let your guard down. COVID-19 is merciless and relentless. “If you think research is expensive, try disease.” – Mary Lasker.
John I. Allen, MD, MBA, AGA
Editor in Chief
COVID-19 numbers again are increasing dramatically. Community infection rates have nearly doubled, and hospitals and health care workers are stretched beyond their limits. It is difficult not to feel anger about how poorly this pandemic was managed (mismanaged) by so many officials in charge and by a large segment of our population who still refuse protective actions to limit spread. While politics and ideology continue to cost American lives, scientific firepower will emerge as our saving grace.
My editorial board and I are entering our final year at the helm of GI & Hepatology News. AGA issued a search for the next Editor in Chief (EIC), who will take over October 2021. I urge anyone interested to apply (https://gastro.org/news/prestigious-aga-publications-seek-new-editors-in-chief/). As EIC, you will choose the next editorial board and forge professional friendships that are gratifying. You will assume responsibility for the content, where you must balance your own views with those of both the AGA and our readership.
As EIC, each month I am given space for 300 words to communicate interesting ideas and opinions. The AGA gives the newspaper great editorial freedom, and I hope we have supported AGA’s mission and values when we publish its official newspaper. I always have next month’s editorial in mind, and I look for useful phrases, quotes, ideas, and opinions. If you are interested in becoming EIC, please email [email protected] for more information.
I would be remiss not to acknowledge the contribution that Lora McGlade has made to GI & Hepatology News. She has been my partner, as the Frontline Medical Communications Editor in charge of GI & Hepatology News. Next month, she will move on to assume a new role. I cannot thank her enough for helping make this newspaper work. As the months go on, I will highlight the contributions of others from the AGA, our Board, and Frontline.
Please stay safe and do not let your guard down. COVID-19 is merciless and relentless. “If you think research is expensive, try disease.” – Mary Lasker.
John I. Allen, MD, MBA, AGA
Editor in Chief
COVID-19 numbers again are increasing dramatically. Community infection rates have nearly doubled, and hospitals and health care workers are stretched beyond their limits. It is difficult not to feel anger about how poorly this pandemic was managed (mismanaged) by so many officials in charge and by a large segment of our population who still refuse protective actions to limit spread. While politics and ideology continue to cost American lives, scientific firepower will emerge as our saving grace.
My editorial board and I are entering our final year at the helm of GI & Hepatology News. AGA issued a search for the next Editor in Chief (EIC), who will take over October 2021. I urge anyone interested to apply (https://gastro.org/news/prestigious-aga-publications-seek-new-editors-in-chief/). As EIC, you will choose the next editorial board and forge professional friendships that are gratifying. You will assume responsibility for the content, where you must balance your own views with those of both the AGA and our readership.
As EIC, each month I am given space for 300 words to communicate interesting ideas and opinions. The AGA gives the newspaper great editorial freedom, and I hope we have supported AGA’s mission and values when we publish its official newspaper. I always have next month’s editorial in mind, and I look for useful phrases, quotes, ideas, and opinions. If you are interested in becoming EIC, please email [email protected] for more information.
I would be remiss not to acknowledge the contribution that Lora McGlade has made to GI & Hepatology News. She has been my partner, as the Frontline Medical Communications Editor in charge of GI & Hepatology News. Next month, she will move on to assume a new role. I cannot thank her enough for helping make this newspaper work. As the months go on, I will highlight the contributions of others from the AGA, our Board, and Frontline.
Please stay safe and do not let your guard down. COVID-19 is merciless and relentless. “If you think research is expensive, try disease.” – Mary Lasker.
John I. Allen, MD, MBA, AGA
Editor in Chief
How much longer?
SHM has changed direction as needed during the pandemic
“How much longer?” As a kid, I can remember the long holiday car ride with my parents from my home in Annapolis, Md., to Upstate New York where my grandparents lived. At the time, the ride felt like an eternity: endless miles of frozen landscape, limited food, and a brother who constantly crossed over the invisible line that was my side of the car.
We made our parents crazy asking, “how much longer?” every few minutes. This was the late 1970s, with no GPS or Google Maps to give you arrival times to the minute, traffic warnings, or reroutes when the inevitable delays occurred. We just plowed ahead, and my parents’ answer was always something vague like, “in a few hours” or “we’re about halfway through.” They did not know when we’d arrive with certainty either.
We at SHM have that same feeling about the pandemic. How much longer? No one can tell us when the COVID-19 threat will abate. The experts’ answers are understandably vague, and the tools for forecasting are non-existent. Months? That is the best we know for now.
At SHM, we believe we will make it through this journey by adapting to roadblocks, providing tools for success to our professional community, and identifying opportunities for us to connect with each other, even if that means virtually.
Like the rest of the planet, the spring of 2020 hit SHM with a shock. Hospital Medicine 2020 (HM20) in San Diego was shaping up to be the largest Annual Conference SHM ever had, the Pediatric Hospital Medicine 2020 (PHM20) conference was well planned and expected to be a huge success, regional SHM chapters were meeting (and growing), and membership was thriving. I was transitioning out of my roles at Johns Hopkins and looking forward to my new role as CEO of SHM. All in all, March 2020 began with a fantastic outlook.
Wow, what a difference a few weeks made. We watched as the pandemic spread across regions of the country, concerned for the wellbeing of our patients and our hospitalists. We saw how our members were at the forefront of patient care during this crisis and understood that SHM had to adapt rapidly to meet their needs in real time.
By May, SHM had canceled HM20, Chapter activity was halted, PHM20 was on its way to being canceled, SHM committee work was put on hold, and I was spending my last few months at Hopkins as the chief medical officer at the Baltimore Convention Center Field Hospital (which we got up and running in less than a month)! Whew.
But just like my dad could pivot our 1970s Chevy station wagon around a traffic jam in a flash, so too did SHM leadership start navigating around the COVID-19 landscape. As soon as HM20 was canceled, SHM immediately began planning for a virtual offering in August. We had hoped to attract at least 100 attendees and we were thrilled to have more than 1,000! PHM20 was switched from an in-person to a virtual meeting with 634 attendees. We launched numerous COVID-19 webinars and made our clinical and educational offerings open access. Our Public Policy Committee was active around both COVID-19 and hospitalist-related topics – immigration, telehealth, wellbeing, and financial impacts, to name a few. (And I even met with the POTUS & advocated for PPE.) The Journal of Hospital Medicine worked with authors to get important publications out at record speed. And of course, The Hospitalist connected all of us to our professional leaders and experts.
By the fall of 2020, SHM had actively adjusted to the “new normal” of this pandemic: SHM staff have settled into their new “work from home” environments, SHM Chapters are connecting members in the virtual world, SHM’s 2021 Annual Conference will be all virtual – rebranded as “SHM Converge” – and the State of Hospital Medicine Report (our every-other-year source for trends in hospital medicine) now has a COVID-19 supplement, which was developed at lightning speed. Even our SHM Board of Directors is meeting virtually! All this while advancing the routine work at SHM, which never faltered. Our work on resources for quality improvement, the opioid epidemic, wellbeing, diversity, equity and inclusion (DEI), leadership, professional development, advocacy, and so much more is as active as ever.
I don’t know how much longer we have on this very long pandemic journey, so I’ll use my father’s answer of “we’re about halfway through.” We have been immersed in it for months already, with months still ahead. But regardless of the upcoming twists and turns COVID-19 forces you, our patients, and our larger society to take, SHM is ready to change direction faster than a 1970s Chevy. The SHM staff, leadership, and members will be sure that hospitalists receive the tools to navigate these unprecedented times. Our patients need our skills to get through this as safely as possible. While we may not be able to tell them “how much longer,” we can certainly be prepared for the long road ahead as we begin 2021.
Dr. Howell is CEO of the Society of Hospital Medicine.
SHM has changed direction as needed during the pandemic
SHM has changed direction as needed during the pandemic
“How much longer?” As a kid, I can remember the long holiday car ride with my parents from my home in Annapolis, Md., to Upstate New York where my grandparents lived. At the time, the ride felt like an eternity: endless miles of frozen landscape, limited food, and a brother who constantly crossed over the invisible line that was my side of the car.
We made our parents crazy asking, “how much longer?” every few minutes. This was the late 1970s, with no GPS or Google Maps to give you arrival times to the minute, traffic warnings, or reroutes when the inevitable delays occurred. We just plowed ahead, and my parents’ answer was always something vague like, “in a few hours” or “we’re about halfway through.” They did not know when we’d arrive with certainty either.
We at SHM have that same feeling about the pandemic. How much longer? No one can tell us when the COVID-19 threat will abate. The experts’ answers are understandably vague, and the tools for forecasting are non-existent. Months? That is the best we know for now.
At SHM, we believe we will make it through this journey by adapting to roadblocks, providing tools for success to our professional community, and identifying opportunities for us to connect with each other, even if that means virtually.
Like the rest of the planet, the spring of 2020 hit SHM with a shock. Hospital Medicine 2020 (HM20) in San Diego was shaping up to be the largest Annual Conference SHM ever had, the Pediatric Hospital Medicine 2020 (PHM20) conference was well planned and expected to be a huge success, regional SHM chapters were meeting (and growing), and membership was thriving. I was transitioning out of my roles at Johns Hopkins and looking forward to my new role as CEO of SHM. All in all, March 2020 began with a fantastic outlook.
Wow, what a difference a few weeks made. We watched as the pandemic spread across regions of the country, concerned for the wellbeing of our patients and our hospitalists. We saw how our members were at the forefront of patient care during this crisis and understood that SHM had to adapt rapidly to meet their needs in real time.
By May, SHM had canceled HM20, Chapter activity was halted, PHM20 was on its way to being canceled, SHM committee work was put on hold, and I was spending my last few months at Hopkins as the chief medical officer at the Baltimore Convention Center Field Hospital (which we got up and running in less than a month)! Whew.
But just like my dad could pivot our 1970s Chevy station wagon around a traffic jam in a flash, so too did SHM leadership start navigating around the COVID-19 landscape. As soon as HM20 was canceled, SHM immediately began planning for a virtual offering in August. We had hoped to attract at least 100 attendees and we were thrilled to have more than 1,000! PHM20 was switched from an in-person to a virtual meeting with 634 attendees. We launched numerous COVID-19 webinars and made our clinical and educational offerings open access. Our Public Policy Committee was active around both COVID-19 and hospitalist-related topics – immigration, telehealth, wellbeing, and financial impacts, to name a few. (And I even met with the POTUS & advocated for PPE.) The Journal of Hospital Medicine worked with authors to get important publications out at record speed. And of course, The Hospitalist connected all of us to our professional leaders and experts.
By the fall of 2020, SHM had actively adjusted to the “new normal” of this pandemic: SHM staff have settled into their new “work from home” environments, SHM Chapters are connecting members in the virtual world, SHM’s 2021 Annual Conference will be all virtual – rebranded as “SHM Converge” – and the State of Hospital Medicine Report (our every-other-year source for trends in hospital medicine) now has a COVID-19 supplement, which was developed at lightning speed. Even our SHM Board of Directors is meeting virtually! All this while advancing the routine work at SHM, which never faltered. Our work on resources for quality improvement, the opioid epidemic, wellbeing, diversity, equity and inclusion (DEI), leadership, professional development, advocacy, and so much more is as active as ever.
I don’t know how much longer we have on this very long pandemic journey, so I’ll use my father’s answer of “we’re about halfway through.” We have been immersed in it for months already, with months still ahead. But regardless of the upcoming twists and turns COVID-19 forces you, our patients, and our larger society to take, SHM is ready to change direction faster than a 1970s Chevy. The SHM staff, leadership, and members will be sure that hospitalists receive the tools to navigate these unprecedented times. Our patients need our skills to get through this as safely as possible. While we may not be able to tell them “how much longer,” we can certainly be prepared for the long road ahead as we begin 2021.
Dr. Howell is CEO of the Society of Hospital Medicine.
“How much longer?” As a kid, I can remember the long holiday car ride with my parents from my home in Annapolis, Md., to Upstate New York where my grandparents lived. At the time, the ride felt like an eternity: endless miles of frozen landscape, limited food, and a brother who constantly crossed over the invisible line that was my side of the car.
We made our parents crazy asking, “how much longer?” every few minutes. This was the late 1970s, with no GPS or Google Maps to give you arrival times to the minute, traffic warnings, or reroutes when the inevitable delays occurred. We just plowed ahead, and my parents’ answer was always something vague like, “in a few hours” or “we’re about halfway through.” They did not know when we’d arrive with certainty either.
We at SHM have that same feeling about the pandemic. How much longer? No one can tell us when the COVID-19 threat will abate. The experts’ answers are understandably vague, and the tools for forecasting are non-existent. Months? That is the best we know for now.
At SHM, we believe we will make it through this journey by adapting to roadblocks, providing tools for success to our professional community, and identifying opportunities for us to connect with each other, even if that means virtually.
Like the rest of the planet, the spring of 2020 hit SHM with a shock. Hospital Medicine 2020 (HM20) in San Diego was shaping up to be the largest Annual Conference SHM ever had, the Pediatric Hospital Medicine 2020 (PHM20) conference was well planned and expected to be a huge success, regional SHM chapters were meeting (and growing), and membership was thriving. I was transitioning out of my roles at Johns Hopkins and looking forward to my new role as CEO of SHM. All in all, March 2020 began with a fantastic outlook.
Wow, what a difference a few weeks made. We watched as the pandemic spread across regions of the country, concerned for the wellbeing of our patients and our hospitalists. We saw how our members were at the forefront of patient care during this crisis and understood that SHM had to adapt rapidly to meet their needs in real time.
By May, SHM had canceled HM20, Chapter activity was halted, PHM20 was on its way to being canceled, SHM committee work was put on hold, and I was spending my last few months at Hopkins as the chief medical officer at the Baltimore Convention Center Field Hospital (which we got up and running in less than a month)! Whew.
But just like my dad could pivot our 1970s Chevy station wagon around a traffic jam in a flash, so too did SHM leadership start navigating around the COVID-19 landscape. As soon as HM20 was canceled, SHM immediately began planning for a virtual offering in August. We had hoped to attract at least 100 attendees and we were thrilled to have more than 1,000! PHM20 was switched from an in-person to a virtual meeting with 634 attendees. We launched numerous COVID-19 webinars and made our clinical and educational offerings open access. Our Public Policy Committee was active around both COVID-19 and hospitalist-related topics – immigration, telehealth, wellbeing, and financial impacts, to name a few. (And I even met with the POTUS & advocated for PPE.) The Journal of Hospital Medicine worked with authors to get important publications out at record speed. And of course, The Hospitalist connected all of us to our professional leaders and experts.
By the fall of 2020, SHM had actively adjusted to the “new normal” of this pandemic: SHM staff have settled into their new “work from home” environments, SHM Chapters are connecting members in the virtual world, SHM’s 2021 Annual Conference will be all virtual – rebranded as “SHM Converge” – and the State of Hospital Medicine Report (our every-other-year source for trends in hospital medicine) now has a COVID-19 supplement, which was developed at lightning speed. Even our SHM Board of Directors is meeting virtually! All this while advancing the routine work at SHM, which never faltered. Our work on resources for quality improvement, the opioid epidemic, wellbeing, diversity, equity and inclusion (DEI), leadership, professional development, advocacy, and so much more is as active as ever.
I don’t know how much longer we have on this very long pandemic journey, so I’ll use my father’s answer of “we’re about halfway through.” We have been immersed in it for months already, with months still ahead. But regardless of the upcoming twists and turns COVID-19 forces you, our patients, and our larger society to take, SHM is ready to change direction faster than a 1970s Chevy. The SHM staff, leadership, and members will be sure that hospitalists receive the tools to navigate these unprecedented times. Our patients need our skills to get through this as safely as possible. While we may not be able to tell them “how much longer,” we can certainly be prepared for the long road ahead as we begin 2021.
Dr. Howell is CEO of the Society of Hospital Medicine.
What the Biden-Harris COVID-19 Advisory Board is missing
On Nov. 9, the Biden-Harris administration announced the members of its COVID-19 Advisory Board. Among them were many esteemed infectious disease and public health experts – encouraging, given that, for now, the COVID-19 pandemic shows no signs of slowing down. Not among them was a mental health professional.
As psychiatrists, we did not find this omission surprising, given the sidelined role our specialty too often plays among medical professionals. But we did find it disappointing. Not having a single behavioral health provider on the advisory board will prove to be a mistake that could affect millions of Americans.
Studies continue to roll in showing that patients with COVID-19 can present during and after infection with neuropsychiatric symptoms, including delirium, psychosis, and anxiety. In July, a meta-analysis published in The Lancet regarding the neuropsychological outcomes of earlier diseases caused by coronaviruses – severe acute respiratory syndrome and Middle East respiratory syndrome – suggested that, in the short term, close to one-quarter of patients experienced confusion representative of delirium. In the long term, following recovery, respondents frequently reported emotional lability, impaired concentration, and traumatic memories. Additionally, more recent research published in The Lancet suggests that rates of psychiatric disorders, dementia, and insomnia are significantly higher among survivors of COVID-19. This study echoes the findings of an article in JAMA from September that reported that, among patients who were hospitalized for COVID-19, mortality rates were higher for those who had previously been diagnosed with a psychiatric condition. And overall, the pandemic has been associated with significantly increased rates of anxiety and depression symptoms.
Although this research is preliminary,
This is especially true when you consider the following:
- It is very difficult to diagnose and treat mental health symptoms in a primary care setting that is already overburdened. Doing so results in delayed treatment and increased costs.
- In the long term, COVID-19 survivors will overburden the already underfunded mental healthcare system.
- Additional unforeseen psychological outcomes stem from the myriad traumas of events in 2020 (eg, racial unrest, children out of school, loss of jobs, the recent election).
Psychiatric disorders are notoriously difficult to diagnose and treat in the outpatient primary care setting, which is why mental health professionals will need to be a more integral part of the postpandemic treatment model and should be represented on the advisory board. Each year in the United States, there are more than 8 million doctors’ visits for depression, and more than half of these are in the primary care setting. Yet fewer than half of those patients leave with a diagnosis of depression or are treated for it.
Historically, screening for depression in the primary care setting is difficult given its broad presentation of symptoms, which include nonspecific physical complaints, such as digestive problems, headaches, insomnia, or general aches and pains. These shortcomings exist despite multiple changes in guidelines, such as regarding the use of self-screening tools and general screening for specific populations, such as postpartum women.
But screening alone has not been an effective strategy, especially when certain groups are less likely to be screened. These include older adults, Black persons, and men, all of whom are at higher risk for mortality after COVID-19. There is a failure to consistently apply standards of universal screening across all patient groups, and even if it occurs, there is a failure to establish reliable treatment and follow-up regimens. As clinicians, imagine how challenging diagnosis and treatment of more complicated psychiatric syndromes, such as somatoform disorder, will be in the primary care setting after the pandemic.
When almost two-thirds of symptoms in primary care are already “medically unexplained,” how do we expect primary care doctors to differentiate between those presenting with vague coronavirus-related “brain fog,” the run of the mill worrywart, and the 16%-34% with legitimate hypochondriasis of somatoform disorder who won’t improve without the involvement of a mental health provider?
A specialty in short supply
The mental health system we have now is inadequate for those who are currently diagnosed with mental disorders. Before the pandemic, emergency departments were boarding increasing numbers of patients with psychiatric illness because beds on inpatient units were unavailable. Individuals with insurance faced difficulty finding psychiatrists or psychotherapists who took insurance or who were availabile to accept new patients, given the growing shortage of providers in general. Community health centers continued to grapple with decreases in federal and state funding despite public political support for parity. Individuals with substance use faced few options for the outpatient, residential, or pharmacologic treatment that many needed to maintain sobriety.
Since the pandemic, we have seen rates of anxiety, depression, and suicidal thinking increase among adults and youth while many clinics have been forced to lay off employees, reduce services, or close their doors. As psychiatrists, we not only see the lack of treatment options for our patients but are forced to find creative solutions to meet their needs. How are we supposed to adapt (or feel confident) when individuals with or without previous mental illness face downstream consequences after COVID-19 when not one of our own is represented in the advisory board? How can we feel confident that downstream solutions acknowledge and address the intricacy of the behavioral health system that we, as mental health providers, know so intimately?
And what about the cumulative impact of everything else that has happened in 2020 in addition to the pandemic?! Although cataloging the various negative events that have happened this year is beyond the scope of this discussion, such lists have been compiled by the mainstream media and include the Australian brush fires, the crisis in Armenia, racial protests, economic uncertainties, and the run-up to and occurrence of the 2020 presidential election. Research is solid in its assertion that chronic stress can disturb our immune and cardiovascular systems, as well as mental health, leading to depression or anxiety. As a result of the pandemic itself, plus the events of this year, mental health providers are already warning not only of the current trauma underlying our day-to-day lives but also that of years to come.
More importantly, healthcare providers, both those represented by members of the advisory board and those who are not, are not immune to these issues. Before the pandemic, rates of suicide among doctors were already above average compared with other professions. After witnessing death repeatedly, self-isolation, the risk for infection to family, and dealing with the continued resistance to wearing masks, who knows what the eventual psychological toll our medical workforce will be?
Mental health providers have stepped up to the plate to provide care outside of traditional models to meet the needs that patients have now. One survey found that 81% of behavioral health providers began using telehealth for the first time in the past 6 months, owing to the COVID-19 pandemic. If not for the sake of the mental health of the Biden-Harris advisory board members themselves, who as doctors are likely to downplay the impact when struggling with mental health concerns in their own lives, a mental health provider deserves a seat at the table.
Plus, the outcomes speak for themselves when behavioral health providers collaborate with primary care providers to give treatment or when mental health experts are members of health crisis teams. Why wouldn’t the same be true for the Biden-Harris advisory board?
Kali Cyrus, MD, MPH, is an assistant professor of psychiatry and behavioral medicine at the Johns Hopkins School of Medicine, Baltimore, Maryland. She sees patients in private practice and offers consultation services in diversity strategy. Ranna Parekh, MD, MPH, is past deputy medical director and director of diversity and health equity for the American Psychiatric Association. She is currently a consultant psychiatrist at the Massachusetts General Hospital, Boston, and the chief diversity and inclusion officer at the American College of Cardiology.
A version of this article originally appeared on Medscape.com.
On Nov. 9, the Biden-Harris administration announced the members of its COVID-19 Advisory Board. Among them were many esteemed infectious disease and public health experts – encouraging, given that, for now, the COVID-19 pandemic shows no signs of slowing down. Not among them was a mental health professional.
As psychiatrists, we did not find this omission surprising, given the sidelined role our specialty too often plays among medical professionals. But we did find it disappointing. Not having a single behavioral health provider on the advisory board will prove to be a mistake that could affect millions of Americans.
Studies continue to roll in showing that patients with COVID-19 can present during and after infection with neuropsychiatric symptoms, including delirium, psychosis, and anxiety. In July, a meta-analysis published in The Lancet regarding the neuropsychological outcomes of earlier diseases caused by coronaviruses – severe acute respiratory syndrome and Middle East respiratory syndrome – suggested that, in the short term, close to one-quarter of patients experienced confusion representative of delirium. In the long term, following recovery, respondents frequently reported emotional lability, impaired concentration, and traumatic memories. Additionally, more recent research published in The Lancet suggests that rates of psychiatric disorders, dementia, and insomnia are significantly higher among survivors of COVID-19. This study echoes the findings of an article in JAMA from September that reported that, among patients who were hospitalized for COVID-19, mortality rates were higher for those who had previously been diagnosed with a psychiatric condition. And overall, the pandemic has been associated with significantly increased rates of anxiety and depression symptoms.
Although this research is preliminary,
This is especially true when you consider the following:
- It is very difficult to diagnose and treat mental health symptoms in a primary care setting that is already overburdened. Doing so results in delayed treatment and increased costs.
- In the long term, COVID-19 survivors will overburden the already underfunded mental healthcare system.
- Additional unforeseen psychological outcomes stem from the myriad traumas of events in 2020 (eg, racial unrest, children out of school, loss of jobs, the recent election).
Psychiatric disorders are notoriously difficult to diagnose and treat in the outpatient primary care setting, which is why mental health professionals will need to be a more integral part of the postpandemic treatment model and should be represented on the advisory board. Each year in the United States, there are more than 8 million doctors’ visits for depression, and more than half of these are in the primary care setting. Yet fewer than half of those patients leave with a diagnosis of depression or are treated for it.
Historically, screening for depression in the primary care setting is difficult given its broad presentation of symptoms, which include nonspecific physical complaints, such as digestive problems, headaches, insomnia, or general aches and pains. These shortcomings exist despite multiple changes in guidelines, such as regarding the use of self-screening tools and general screening for specific populations, such as postpartum women.
But screening alone has not been an effective strategy, especially when certain groups are less likely to be screened. These include older adults, Black persons, and men, all of whom are at higher risk for mortality after COVID-19. There is a failure to consistently apply standards of universal screening across all patient groups, and even if it occurs, there is a failure to establish reliable treatment and follow-up regimens. As clinicians, imagine how challenging diagnosis and treatment of more complicated psychiatric syndromes, such as somatoform disorder, will be in the primary care setting after the pandemic.
When almost two-thirds of symptoms in primary care are already “medically unexplained,” how do we expect primary care doctors to differentiate between those presenting with vague coronavirus-related “brain fog,” the run of the mill worrywart, and the 16%-34% with legitimate hypochondriasis of somatoform disorder who won’t improve without the involvement of a mental health provider?
A specialty in short supply
The mental health system we have now is inadequate for those who are currently diagnosed with mental disorders. Before the pandemic, emergency departments were boarding increasing numbers of patients with psychiatric illness because beds on inpatient units were unavailable. Individuals with insurance faced difficulty finding psychiatrists or psychotherapists who took insurance or who were availabile to accept new patients, given the growing shortage of providers in general. Community health centers continued to grapple with decreases in federal and state funding despite public political support for parity. Individuals with substance use faced few options for the outpatient, residential, or pharmacologic treatment that many needed to maintain sobriety.
Since the pandemic, we have seen rates of anxiety, depression, and suicidal thinking increase among adults and youth while many clinics have been forced to lay off employees, reduce services, or close their doors. As psychiatrists, we not only see the lack of treatment options for our patients but are forced to find creative solutions to meet their needs. How are we supposed to adapt (or feel confident) when individuals with or without previous mental illness face downstream consequences after COVID-19 when not one of our own is represented in the advisory board? How can we feel confident that downstream solutions acknowledge and address the intricacy of the behavioral health system that we, as mental health providers, know so intimately?
And what about the cumulative impact of everything else that has happened in 2020 in addition to the pandemic?! Although cataloging the various negative events that have happened this year is beyond the scope of this discussion, such lists have been compiled by the mainstream media and include the Australian brush fires, the crisis in Armenia, racial protests, economic uncertainties, and the run-up to and occurrence of the 2020 presidential election. Research is solid in its assertion that chronic stress can disturb our immune and cardiovascular systems, as well as mental health, leading to depression or anxiety. As a result of the pandemic itself, plus the events of this year, mental health providers are already warning not only of the current trauma underlying our day-to-day lives but also that of years to come.
More importantly, healthcare providers, both those represented by members of the advisory board and those who are not, are not immune to these issues. Before the pandemic, rates of suicide among doctors were already above average compared with other professions. After witnessing death repeatedly, self-isolation, the risk for infection to family, and dealing with the continued resistance to wearing masks, who knows what the eventual psychological toll our medical workforce will be?
Mental health providers have stepped up to the plate to provide care outside of traditional models to meet the needs that patients have now. One survey found that 81% of behavioral health providers began using telehealth for the first time in the past 6 months, owing to the COVID-19 pandemic. If not for the sake of the mental health of the Biden-Harris advisory board members themselves, who as doctors are likely to downplay the impact when struggling with mental health concerns in their own lives, a mental health provider deserves a seat at the table.
Plus, the outcomes speak for themselves when behavioral health providers collaborate with primary care providers to give treatment or when mental health experts are members of health crisis teams. Why wouldn’t the same be true for the Biden-Harris advisory board?
Kali Cyrus, MD, MPH, is an assistant professor of psychiatry and behavioral medicine at the Johns Hopkins School of Medicine, Baltimore, Maryland. She sees patients in private practice and offers consultation services in diversity strategy. Ranna Parekh, MD, MPH, is past deputy medical director and director of diversity and health equity for the American Psychiatric Association. She is currently a consultant psychiatrist at the Massachusetts General Hospital, Boston, and the chief diversity and inclusion officer at the American College of Cardiology.
A version of this article originally appeared on Medscape.com.
On Nov. 9, the Biden-Harris administration announced the members of its COVID-19 Advisory Board. Among them were many esteemed infectious disease and public health experts – encouraging, given that, for now, the COVID-19 pandemic shows no signs of slowing down. Not among them was a mental health professional.
As psychiatrists, we did not find this omission surprising, given the sidelined role our specialty too often plays among medical professionals. But we did find it disappointing. Not having a single behavioral health provider on the advisory board will prove to be a mistake that could affect millions of Americans.
Studies continue to roll in showing that patients with COVID-19 can present during and after infection with neuropsychiatric symptoms, including delirium, psychosis, and anxiety. In July, a meta-analysis published in The Lancet regarding the neuropsychological outcomes of earlier diseases caused by coronaviruses – severe acute respiratory syndrome and Middle East respiratory syndrome – suggested that, in the short term, close to one-quarter of patients experienced confusion representative of delirium. In the long term, following recovery, respondents frequently reported emotional lability, impaired concentration, and traumatic memories. Additionally, more recent research published in The Lancet suggests that rates of psychiatric disorders, dementia, and insomnia are significantly higher among survivors of COVID-19. This study echoes the findings of an article in JAMA from September that reported that, among patients who were hospitalized for COVID-19, mortality rates were higher for those who had previously been diagnosed with a psychiatric condition. And overall, the pandemic has been associated with significantly increased rates of anxiety and depression symptoms.
Although this research is preliminary,
This is especially true when you consider the following:
- It is very difficult to diagnose and treat mental health symptoms in a primary care setting that is already overburdened. Doing so results in delayed treatment and increased costs.
- In the long term, COVID-19 survivors will overburden the already underfunded mental healthcare system.
- Additional unforeseen psychological outcomes stem from the myriad traumas of events in 2020 (eg, racial unrest, children out of school, loss of jobs, the recent election).
Psychiatric disorders are notoriously difficult to diagnose and treat in the outpatient primary care setting, which is why mental health professionals will need to be a more integral part of the postpandemic treatment model and should be represented on the advisory board. Each year in the United States, there are more than 8 million doctors’ visits for depression, and more than half of these are in the primary care setting. Yet fewer than half of those patients leave with a diagnosis of depression or are treated for it.
Historically, screening for depression in the primary care setting is difficult given its broad presentation of symptoms, which include nonspecific physical complaints, such as digestive problems, headaches, insomnia, or general aches and pains. These shortcomings exist despite multiple changes in guidelines, such as regarding the use of self-screening tools and general screening for specific populations, such as postpartum women.
But screening alone has not been an effective strategy, especially when certain groups are less likely to be screened. These include older adults, Black persons, and men, all of whom are at higher risk for mortality after COVID-19. There is a failure to consistently apply standards of universal screening across all patient groups, and even if it occurs, there is a failure to establish reliable treatment and follow-up regimens. As clinicians, imagine how challenging diagnosis and treatment of more complicated psychiatric syndromes, such as somatoform disorder, will be in the primary care setting after the pandemic.
When almost two-thirds of symptoms in primary care are already “medically unexplained,” how do we expect primary care doctors to differentiate between those presenting with vague coronavirus-related “brain fog,” the run of the mill worrywart, and the 16%-34% with legitimate hypochondriasis of somatoform disorder who won’t improve without the involvement of a mental health provider?
A specialty in short supply
The mental health system we have now is inadequate for those who are currently diagnosed with mental disorders. Before the pandemic, emergency departments were boarding increasing numbers of patients with psychiatric illness because beds on inpatient units were unavailable. Individuals with insurance faced difficulty finding psychiatrists or psychotherapists who took insurance or who were availabile to accept new patients, given the growing shortage of providers in general. Community health centers continued to grapple with decreases in federal and state funding despite public political support for parity. Individuals with substance use faced few options for the outpatient, residential, or pharmacologic treatment that many needed to maintain sobriety.
Since the pandemic, we have seen rates of anxiety, depression, and suicidal thinking increase among adults and youth while many clinics have been forced to lay off employees, reduce services, or close their doors. As psychiatrists, we not only see the lack of treatment options for our patients but are forced to find creative solutions to meet their needs. How are we supposed to adapt (or feel confident) when individuals with or without previous mental illness face downstream consequences after COVID-19 when not one of our own is represented in the advisory board? How can we feel confident that downstream solutions acknowledge and address the intricacy of the behavioral health system that we, as mental health providers, know so intimately?
And what about the cumulative impact of everything else that has happened in 2020 in addition to the pandemic?! Although cataloging the various negative events that have happened this year is beyond the scope of this discussion, such lists have been compiled by the mainstream media and include the Australian brush fires, the crisis in Armenia, racial protests, economic uncertainties, and the run-up to and occurrence of the 2020 presidential election. Research is solid in its assertion that chronic stress can disturb our immune and cardiovascular systems, as well as mental health, leading to depression or anxiety. As a result of the pandemic itself, plus the events of this year, mental health providers are already warning not only of the current trauma underlying our day-to-day lives but also that of years to come.
More importantly, healthcare providers, both those represented by members of the advisory board and those who are not, are not immune to these issues. Before the pandemic, rates of suicide among doctors were already above average compared with other professions. After witnessing death repeatedly, self-isolation, the risk for infection to family, and dealing with the continued resistance to wearing masks, who knows what the eventual psychological toll our medical workforce will be?
Mental health providers have stepped up to the plate to provide care outside of traditional models to meet the needs that patients have now. One survey found that 81% of behavioral health providers began using telehealth for the first time in the past 6 months, owing to the COVID-19 pandemic. If not for the sake of the mental health of the Biden-Harris advisory board members themselves, who as doctors are likely to downplay the impact when struggling with mental health concerns in their own lives, a mental health provider deserves a seat at the table.
Plus, the outcomes speak for themselves when behavioral health providers collaborate with primary care providers to give treatment or when mental health experts are members of health crisis teams. Why wouldn’t the same be true for the Biden-Harris advisory board?
Kali Cyrus, MD, MPH, is an assistant professor of psychiatry and behavioral medicine at the Johns Hopkins School of Medicine, Baltimore, Maryland. She sees patients in private practice and offers consultation services in diversity strategy. Ranna Parekh, MD, MPH, is past deputy medical director and director of diversity and health equity for the American Psychiatric Association. She is currently a consultant psychiatrist at the Massachusetts General Hospital, Boston, and the chief diversity and inclusion officer at the American College of Cardiology.
A version of this article originally appeared on Medscape.com.
Twenty years later, two gambles that paid off
Amidst the pandemic and election, two anniversaries passed almost unnoticed in early November.
On Nov. 2, 2020, we reached 20 years since the first crew moved into the International Space Station (ISS). This may seem like a minor anniversary to some, but it means a lot if you think about it. From humble beginnings, and scattered launches in different craft between 1961 and 1999, it’s now been over a generation since people weren’t living in space. We certainly aren’t on the starship Enterprise yet, or even going to Mars, but today’s college kids have never known a world where people didn’t live and work in the void upstairs. That’s something to think about.
Equally important, but of significance to far fewer, is that on Nov. 6, 2020, my little solo practice also reached its 20-year anniversary.
To the central person involved, me, this is a pretty big deal. In early 2000, when I made the decision to leave a large practice, I was confident but still nervous. I’d developed a decent referral base while working for the other group, but still didn’t know what would happen. I was 33. My oldest kid was 1 and my wife and I had twins on the way.
Now, it’s 20 years later. All three kids grew up and went off to college, but in the strange circle of the pandemic, they are now back home. Granted they’re not waking us up at night when they’re hungry (they have microwave popcorn – lots of it – for that).
Some things have changed. I’m now across the street from the office I started in. My hospital work, which in 2000 was about 50% of my practice, is now down to 0% for the time being. My medical assistant is still the same one, and my secretary has been with me since 2004. I’m lucky to have such a long-lasting team. Even in 2020, when they’re working from home, we’re still doing a great job of keeping it running.
After 20 years I’m heavier and my hair is thinning and gray, but I still like this job. I still try to do the very best I can for my patients. I sometimes read the personal statement I wrote in the summer of 1987 for my medical school application, trying to keep in touch with who I was then when I started out.
Looking back after 20 years, going solo, like building the ISS, was a big gamble. But both have worked out. My job has allowed me to support and raise a family, to care for patients (contrary to the impression one gets from medical blogs, the vast majority of them are good, decent, people) and get to know them for who they are, and to work with my two terrific long-time office staff who, like my wife, kids, and dogs, still put up with me and my quirks. And all the while I am still doing something that I found I loved in my first week of residency.
Looking forward another 20 years, who knows where I (or the ISS) will be? I probably won’t want to be working full time then, but if I still enjoy medicine I doubt I’ll want to be completely retired, either. Looking back, I’ve been fortunate that I found this one.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Amidst the pandemic and election, two anniversaries passed almost unnoticed in early November.
On Nov. 2, 2020, we reached 20 years since the first crew moved into the International Space Station (ISS). This may seem like a minor anniversary to some, but it means a lot if you think about it. From humble beginnings, and scattered launches in different craft between 1961 and 1999, it’s now been over a generation since people weren’t living in space. We certainly aren’t on the starship Enterprise yet, or even going to Mars, but today’s college kids have never known a world where people didn’t live and work in the void upstairs. That’s something to think about.
Equally important, but of significance to far fewer, is that on Nov. 6, 2020, my little solo practice also reached its 20-year anniversary.
To the central person involved, me, this is a pretty big deal. In early 2000, when I made the decision to leave a large practice, I was confident but still nervous. I’d developed a decent referral base while working for the other group, but still didn’t know what would happen. I was 33. My oldest kid was 1 and my wife and I had twins on the way.
Now, it’s 20 years later. All three kids grew up and went off to college, but in the strange circle of the pandemic, they are now back home. Granted they’re not waking us up at night when they’re hungry (they have microwave popcorn – lots of it – for that).
Some things have changed. I’m now across the street from the office I started in. My hospital work, which in 2000 was about 50% of my practice, is now down to 0% for the time being. My medical assistant is still the same one, and my secretary has been with me since 2004. I’m lucky to have such a long-lasting team. Even in 2020, when they’re working from home, we’re still doing a great job of keeping it running.
After 20 years I’m heavier and my hair is thinning and gray, but I still like this job. I still try to do the very best I can for my patients. I sometimes read the personal statement I wrote in the summer of 1987 for my medical school application, trying to keep in touch with who I was then when I started out.
Looking back after 20 years, going solo, like building the ISS, was a big gamble. But both have worked out. My job has allowed me to support and raise a family, to care for patients (contrary to the impression one gets from medical blogs, the vast majority of them are good, decent, people) and get to know them for who they are, and to work with my two terrific long-time office staff who, like my wife, kids, and dogs, still put up with me and my quirks. And all the while I am still doing something that I found I loved in my first week of residency.
Looking forward another 20 years, who knows where I (or the ISS) will be? I probably won’t want to be working full time then, but if I still enjoy medicine I doubt I’ll want to be completely retired, either. Looking back, I’ve been fortunate that I found this one.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Amidst the pandemic and election, two anniversaries passed almost unnoticed in early November.
On Nov. 2, 2020, we reached 20 years since the first crew moved into the International Space Station (ISS). This may seem like a minor anniversary to some, but it means a lot if you think about it. From humble beginnings, and scattered launches in different craft between 1961 and 1999, it’s now been over a generation since people weren’t living in space. We certainly aren’t on the starship Enterprise yet, or even going to Mars, but today’s college kids have never known a world where people didn’t live and work in the void upstairs. That’s something to think about.
Equally important, but of significance to far fewer, is that on Nov. 6, 2020, my little solo practice also reached its 20-year anniversary.
To the central person involved, me, this is a pretty big deal. In early 2000, when I made the decision to leave a large practice, I was confident but still nervous. I’d developed a decent referral base while working for the other group, but still didn’t know what would happen. I was 33. My oldest kid was 1 and my wife and I had twins on the way.
Now, it’s 20 years later. All three kids grew up and went off to college, but in the strange circle of the pandemic, they are now back home. Granted they’re not waking us up at night when they’re hungry (they have microwave popcorn – lots of it – for that).
Some things have changed. I’m now across the street from the office I started in. My hospital work, which in 2000 was about 50% of my practice, is now down to 0% for the time being. My medical assistant is still the same one, and my secretary has been with me since 2004. I’m lucky to have such a long-lasting team. Even in 2020, when they’re working from home, we’re still doing a great job of keeping it running.
After 20 years I’m heavier and my hair is thinning and gray, but I still like this job. I still try to do the very best I can for my patients. I sometimes read the personal statement I wrote in the summer of 1987 for my medical school application, trying to keep in touch with who I was then when I started out.
Looking back after 20 years, going solo, like building the ISS, was a big gamble. But both have worked out. My job has allowed me to support and raise a family, to care for patients (contrary to the impression one gets from medical blogs, the vast majority of them are good, decent, people) and get to know them for who they are, and to work with my two terrific long-time office staff who, like my wife, kids, and dogs, still put up with me and my quirks. And all the while I am still doing something that I found I loved in my first week of residency.
Looking forward another 20 years, who knows where I (or the ISS) will be? I probably won’t want to be working full time then, but if I still enjoy medicine I doubt I’ll want to be completely retired, either. Looking back, I’ve been fortunate that I found this one.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Neoadjuvant chemotherapy for advanced ovarian cancer
Historically the standard treatment approach for advanced ovarian cancer has been to perform up-front primary cytoreduction surgery or primary “debulking” surgery (PDS) followed by adjuvant chemotherapy. The goal of surgery was to establish cytoreduction of the tumor to optimal (<1 cm3 disease) or, ideally, complete (no gross residual disease). While PDS has long been considered the default treatment approach, neoadjuvant chemotherapy (NACT) followed by interval cytoreductive surgery, typically after three or four cycles of chemotherapy, was the alternative strategy if it was anticipated or known that an “optimal” cytoreduction was not possible, feasible, or associated with acceptable morbidity. However, NACT was, and to some degree still is, widely considered the inferior strategy, reserved for patients with the worst prognosis. While mounting data challenges the inherent superiority of PDS, it still largely remains the default.
Why was PDS considered superior?
Why was PDS for advanced ovarian cancer considered a superior sequencing when it is so rarely considered appropriate for other disseminated cancers? This was born from the observation among retrospective data showing that survival was best when surgery was performed first, and when surgery was able to remove most or all visible disease (“complete” or “optimal” cytoreduction), NACT was performed.1 Several theories were proposed to explain the observations. These included the theory that bulky tumors contained avascular regions that would be less well accessed by chemotherapy, as well as the notion that chemotherapy exerts a constant fraction of kill on tumor cells, and if there is a lower burden of tumor cells to begin with, fewer cycles of chemotherapy will be necessary to eliminate all cells. Coupled with this was the notion that, if fewer cycles of chemotherapy are necessary, there would be less opportunity for development of drug resistance. Other theories such as the inflammatory effects of surgery impacting immune-mediated kill of malignant cells also are reported. These theories were largely found in the pages of textbooks, only supported by heavily biased observational series and not in the results of elegant translational studies. Of course, the observed superiority of PDS in these cohort studies was not surprising given that the patients who were historically selected for NACT had their treatment course chosen specifically for their poor prognostic factors (large volume, unresectable disease, poor performance status, and comorbidities). These “studies” were self-fulfilling prophecies.
Anecdotally I can attest that most patients are enthusiastic about a primary surgical approach to their advanced cancer. There is something concretely satisfying for patient and surgeon alike in the physical act of removing disease. As surgeons, if we believe that our added surgical effort will be rewarded with better outcomes for the patients, we will “try harder” in the operating room in order for them to do better. However, mounting data challenges whether it is our aggressive surgical effort as much as it is primary tumor biology that is the driver of prognosis in this disease. And aggressive primary surgery may add little other than perioperative morbidity.
Why that perspective may be changing
A culmination of many years of sophisticated translational research led by Anil Sood, MD, from the University of Texas MD Anderson Cancer Center, Houston, established there are fundamental biologic differences in the tumors of patients with ovarian cancer whose disease is amenable or not to a complete cytoreduction with PDS.2 In their work, the researchers sampled tumors from patients with advanced ovarian cancer who had been triaged either to PDS or NACT based on a standardized, validated laparoscopic algorithm that predicted a high probability of complete surgical resection. They performed pretreatment biopsies in both groups of patients and conducted a range of “omics” analyses to stratify these two subsets of patients – those who had a disease burden amenable to complete surgical resection versus those whose presenting disease burden exceeded an acceptable surgical effort). They identified several key molecular differences in the pretreatment biopsies of these two groups of patients, including alterations which might explain better or worse responses to therapy. These results suggest that the tumors of patients who go on to have successful PDS to no gross residual disease have different tumor biology to begin with. Otherwise said, perhaps it is favorable tumor biology that is associated with both a disease burden that is more amenable to both primary complete cytoreduction and better oncologic outcomes, rather than the surgical effort in and of itself.
This finding is supported by a study in which ovarian cancer survival outcomes were stratified by disease burden, surgical complexity scores, and postoperative residual disease among patients who were enrolled in GOG-182.3 Investigators led by Neil Horowitz, MD, created scores for surgical complexity, disease burden, and residual disease. They observed that the radicality of surgery (complexity score) was not an independent determinant of survival, but rather, patients who presented with a lower disease burden that required a less radical surgery had the best oncologic outcomes.
If the complexity of surgery does not influence outcomes as much as the predetermined, unmodifiable tumor biology, how should surgeons make decisions about the sequencing of treatment? Over the past 10 years, four randomized trials have been completed including more than 1,600 patients randomized to either PDS or NACT.4-7 All four have found no difference in the oncologic outcomes (progression-free or overall survival) between patients when randomized to PDS or NACT. While the statistical designs vary slightly, some being designed to look for noninferiority and others for superiority, they all showed that the sequence in which surgery and chemotherapy was performed mattered less than whether optimal cytoreduction was achieved when surgery was performed. As stated above, this phenomenon seems to be best determined by unmodifiable tumor biology. Unsurprisingly, these studies also have consistently found that perioperative outcomes (e.g., surgical complications, length of stay, death) were worse with PDS because of the higher surgical complexity that it demands. In the most recent SCORPION trial, rates of major postoperative complications in the PDS group were 25.9%, compared with only 7.6% in the NACT group (P < .0001) and all of the deaths from postoperative complications occurred in the PDS group at a rate of 8.3% (7 of 84 patients).7
Therefore, the wealth of data supports that oncologic outcomes are equivalent, and perioperative outcomes are improved for patients who undergo NACT for advanced, bulky ovarian cancer.
Why physicians still are questioning
Unfortunately, because ofthe nature of the disease, these prospective trials include heterogeneous populations of disease presentation, surgeon skill, and hospital settings. They have been criticized for achieving “low” rates of complete or optimal cytoreduction in the PDS arm. They also identified subgroups of patients who may do better with PDS (such as those with lower-volume stage IIIC disease) and those who have better outcomes with NACT (patients with stage IV disease). Therefore, not satisfied that we have definitively answered the question, a fifth randomized study, the TRUST trial, is underway.8 This study includes surgeons at high-volume institutions, purported to have the highest degree of skill and quality in executing radical debulking procedures. Perhaps this fifth trial will show that, if performed in the most skilled hands and quality settings, PDS is preferable to NACT. Perhaps. However, the generalizability of these results will be poor for all patients with advanced ovarian cancer, most of whom will have limited access to these highest-volume surgeons.
What can be agreed upon is that an individualized and nuanced approach is best for advanced ovarian cancer. There will be some patients who benefit from PDS (e.g., healthy, young patients with low-volume disease). However, for most patients, the bulk of prospective and translational research supports NACT as the default treatment course, associated with noninferior survival and superior perioperative outcomes (including postoperative death). While it may not be a one-size-fits-all approach, one could argue that NACT should be the default strategy, and surgeons should look for reasons to “opt in” to PDS in special circumstances guided by biomarkers such as imaging, tumor markers, clinical factors, and surgical findings.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Gynecol Oncol. 2006 Dec. doi: 10.1016/j.ygyno.2006.06.025.
2. Cell Rep. 2020 Apr 14. doi: 10.1016/j.celrep.2020.03.066.
3. J Clin Oncol. 2015 Mar 10. doi: 10.1200/JCO.2014.56.3106.
4. N Engl J Med. 2010 Sep 2. doi: 10.1056/NEJMoa0908806.
5. Lancet. 2015 Jul 18. doi: 10.1016/S0140-6736(14)62223-6.
6. Eur J Cancer. 2020. doi: 10.1016/j.ejca.2020.02.020.
7. Int J Gynecol Cancer. 2020. doi: 10.1136/ijgc-2020-001640.
8. Int J Gynecol Cancer. 2019. doi: 10.1136/ijgc-2019-000682.
Historically the standard treatment approach for advanced ovarian cancer has been to perform up-front primary cytoreduction surgery or primary “debulking” surgery (PDS) followed by adjuvant chemotherapy. The goal of surgery was to establish cytoreduction of the tumor to optimal (<1 cm3 disease) or, ideally, complete (no gross residual disease). While PDS has long been considered the default treatment approach, neoadjuvant chemotherapy (NACT) followed by interval cytoreductive surgery, typically after three or four cycles of chemotherapy, was the alternative strategy if it was anticipated or known that an “optimal” cytoreduction was not possible, feasible, or associated with acceptable morbidity. However, NACT was, and to some degree still is, widely considered the inferior strategy, reserved for patients with the worst prognosis. While mounting data challenges the inherent superiority of PDS, it still largely remains the default.
Why was PDS considered superior?
Why was PDS for advanced ovarian cancer considered a superior sequencing when it is so rarely considered appropriate for other disseminated cancers? This was born from the observation among retrospective data showing that survival was best when surgery was performed first, and when surgery was able to remove most or all visible disease (“complete” or “optimal” cytoreduction), NACT was performed.1 Several theories were proposed to explain the observations. These included the theory that bulky tumors contained avascular regions that would be less well accessed by chemotherapy, as well as the notion that chemotherapy exerts a constant fraction of kill on tumor cells, and if there is a lower burden of tumor cells to begin with, fewer cycles of chemotherapy will be necessary to eliminate all cells. Coupled with this was the notion that, if fewer cycles of chemotherapy are necessary, there would be less opportunity for development of drug resistance. Other theories such as the inflammatory effects of surgery impacting immune-mediated kill of malignant cells also are reported. These theories were largely found in the pages of textbooks, only supported by heavily biased observational series and not in the results of elegant translational studies. Of course, the observed superiority of PDS in these cohort studies was not surprising given that the patients who were historically selected for NACT had their treatment course chosen specifically for their poor prognostic factors (large volume, unresectable disease, poor performance status, and comorbidities). These “studies” were self-fulfilling prophecies.
Anecdotally I can attest that most patients are enthusiastic about a primary surgical approach to their advanced cancer. There is something concretely satisfying for patient and surgeon alike in the physical act of removing disease. As surgeons, if we believe that our added surgical effort will be rewarded with better outcomes for the patients, we will “try harder” in the operating room in order for them to do better. However, mounting data challenges whether it is our aggressive surgical effort as much as it is primary tumor biology that is the driver of prognosis in this disease. And aggressive primary surgery may add little other than perioperative morbidity.
Why that perspective may be changing
A culmination of many years of sophisticated translational research led by Anil Sood, MD, from the University of Texas MD Anderson Cancer Center, Houston, established there are fundamental biologic differences in the tumors of patients with ovarian cancer whose disease is amenable or not to a complete cytoreduction with PDS.2 In their work, the researchers sampled tumors from patients with advanced ovarian cancer who had been triaged either to PDS or NACT based on a standardized, validated laparoscopic algorithm that predicted a high probability of complete surgical resection. They performed pretreatment biopsies in both groups of patients and conducted a range of “omics” analyses to stratify these two subsets of patients – those who had a disease burden amenable to complete surgical resection versus those whose presenting disease burden exceeded an acceptable surgical effort). They identified several key molecular differences in the pretreatment biopsies of these two groups of patients, including alterations which might explain better or worse responses to therapy. These results suggest that the tumors of patients who go on to have successful PDS to no gross residual disease have different tumor biology to begin with. Otherwise said, perhaps it is favorable tumor biology that is associated with both a disease burden that is more amenable to both primary complete cytoreduction and better oncologic outcomes, rather than the surgical effort in and of itself.
This finding is supported by a study in which ovarian cancer survival outcomes were stratified by disease burden, surgical complexity scores, and postoperative residual disease among patients who were enrolled in GOG-182.3 Investigators led by Neil Horowitz, MD, created scores for surgical complexity, disease burden, and residual disease. They observed that the radicality of surgery (complexity score) was not an independent determinant of survival, but rather, patients who presented with a lower disease burden that required a less radical surgery had the best oncologic outcomes.
If the complexity of surgery does not influence outcomes as much as the predetermined, unmodifiable tumor biology, how should surgeons make decisions about the sequencing of treatment? Over the past 10 years, four randomized trials have been completed including more than 1,600 patients randomized to either PDS or NACT.4-7 All four have found no difference in the oncologic outcomes (progression-free or overall survival) between patients when randomized to PDS or NACT. While the statistical designs vary slightly, some being designed to look for noninferiority and others for superiority, they all showed that the sequence in which surgery and chemotherapy was performed mattered less than whether optimal cytoreduction was achieved when surgery was performed. As stated above, this phenomenon seems to be best determined by unmodifiable tumor biology. Unsurprisingly, these studies also have consistently found that perioperative outcomes (e.g., surgical complications, length of stay, death) were worse with PDS because of the higher surgical complexity that it demands. In the most recent SCORPION trial, rates of major postoperative complications in the PDS group were 25.9%, compared with only 7.6% in the NACT group (P < .0001) and all of the deaths from postoperative complications occurred in the PDS group at a rate of 8.3% (7 of 84 patients).7
Therefore, the wealth of data supports that oncologic outcomes are equivalent, and perioperative outcomes are improved for patients who undergo NACT for advanced, bulky ovarian cancer.
Why physicians still are questioning
Unfortunately, because ofthe nature of the disease, these prospective trials include heterogeneous populations of disease presentation, surgeon skill, and hospital settings. They have been criticized for achieving “low” rates of complete or optimal cytoreduction in the PDS arm. They also identified subgroups of patients who may do better with PDS (such as those with lower-volume stage IIIC disease) and those who have better outcomes with NACT (patients with stage IV disease). Therefore, not satisfied that we have definitively answered the question, a fifth randomized study, the TRUST trial, is underway.8 This study includes surgeons at high-volume institutions, purported to have the highest degree of skill and quality in executing radical debulking procedures. Perhaps this fifth trial will show that, if performed in the most skilled hands and quality settings, PDS is preferable to NACT. Perhaps. However, the generalizability of these results will be poor for all patients with advanced ovarian cancer, most of whom will have limited access to these highest-volume surgeons.
What can be agreed upon is that an individualized and nuanced approach is best for advanced ovarian cancer. There will be some patients who benefit from PDS (e.g., healthy, young patients with low-volume disease). However, for most patients, the bulk of prospective and translational research supports NACT as the default treatment course, associated with noninferior survival and superior perioperative outcomes (including postoperative death). While it may not be a one-size-fits-all approach, one could argue that NACT should be the default strategy, and surgeons should look for reasons to “opt in” to PDS in special circumstances guided by biomarkers such as imaging, tumor markers, clinical factors, and surgical findings.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Gynecol Oncol. 2006 Dec. doi: 10.1016/j.ygyno.2006.06.025.
2. Cell Rep. 2020 Apr 14. doi: 10.1016/j.celrep.2020.03.066.
3. J Clin Oncol. 2015 Mar 10. doi: 10.1200/JCO.2014.56.3106.
4. N Engl J Med. 2010 Sep 2. doi: 10.1056/NEJMoa0908806.
5. Lancet. 2015 Jul 18. doi: 10.1016/S0140-6736(14)62223-6.
6. Eur J Cancer. 2020. doi: 10.1016/j.ejca.2020.02.020.
7. Int J Gynecol Cancer. 2020. doi: 10.1136/ijgc-2020-001640.
8. Int J Gynecol Cancer. 2019. doi: 10.1136/ijgc-2019-000682.
Historically the standard treatment approach for advanced ovarian cancer has been to perform up-front primary cytoreduction surgery or primary “debulking” surgery (PDS) followed by adjuvant chemotherapy. The goal of surgery was to establish cytoreduction of the tumor to optimal (<1 cm3 disease) or, ideally, complete (no gross residual disease). While PDS has long been considered the default treatment approach, neoadjuvant chemotherapy (NACT) followed by interval cytoreductive surgery, typically after three or four cycles of chemotherapy, was the alternative strategy if it was anticipated or known that an “optimal” cytoreduction was not possible, feasible, or associated with acceptable morbidity. However, NACT was, and to some degree still is, widely considered the inferior strategy, reserved for patients with the worst prognosis. While mounting data challenges the inherent superiority of PDS, it still largely remains the default.
Why was PDS considered superior?
Why was PDS for advanced ovarian cancer considered a superior sequencing when it is so rarely considered appropriate for other disseminated cancers? This was born from the observation among retrospective data showing that survival was best when surgery was performed first, and when surgery was able to remove most or all visible disease (“complete” or “optimal” cytoreduction), NACT was performed.1 Several theories were proposed to explain the observations. These included the theory that bulky tumors contained avascular regions that would be less well accessed by chemotherapy, as well as the notion that chemotherapy exerts a constant fraction of kill on tumor cells, and if there is a lower burden of tumor cells to begin with, fewer cycles of chemotherapy will be necessary to eliminate all cells. Coupled with this was the notion that, if fewer cycles of chemotherapy are necessary, there would be less opportunity for development of drug resistance. Other theories such as the inflammatory effects of surgery impacting immune-mediated kill of malignant cells also are reported. These theories were largely found in the pages of textbooks, only supported by heavily biased observational series and not in the results of elegant translational studies. Of course, the observed superiority of PDS in these cohort studies was not surprising given that the patients who were historically selected for NACT had their treatment course chosen specifically for their poor prognostic factors (large volume, unresectable disease, poor performance status, and comorbidities). These “studies” were self-fulfilling prophecies.
Anecdotally I can attest that most patients are enthusiastic about a primary surgical approach to their advanced cancer. There is something concretely satisfying for patient and surgeon alike in the physical act of removing disease. As surgeons, if we believe that our added surgical effort will be rewarded with better outcomes for the patients, we will “try harder” in the operating room in order for them to do better. However, mounting data challenges whether it is our aggressive surgical effort as much as it is primary tumor biology that is the driver of prognosis in this disease. And aggressive primary surgery may add little other than perioperative morbidity.
Why that perspective may be changing
A culmination of many years of sophisticated translational research led by Anil Sood, MD, from the University of Texas MD Anderson Cancer Center, Houston, established there are fundamental biologic differences in the tumors of patients with ovarian cancer whose disease is amenable or not to a complete cytoreduction with PDS.2 In their work, the researchers sampled tumors from patients with advanced ovarian cancer who had been triaged either to PDS or NACT based on a standardized, validated laparoscopic algorithm that predicted a high probability of complete surgical resection. They performed pretreatment biopsies in both groups of patients and conducted a range of “omics” analyses to stratify these two subsets of patients – those who had a disease burden amenable to complete surgical resection versus those whose presenting disease burden exceeded an acceptable surgical effort). They identified several key molecular differences in the pretreatment biopsies of these two groups of patients, including alterations which might explain better or worse responses to therapy. These results suggest that the tumors of patients who go on to have successful PDS to no gross residual disease have different tumor biology to begin with. Otherwise said, perhaps it is favorable tumor biology that is associated with both a disease burden that is more amenable to both primary complete cytoreduction and better oncologic outcomes, rather than the surgical effort in and of itself.
This finding is supported by a study in which ovarian cancer survival outcomes were stratified by disease burden, surgical complexity scores, and postoperative residual disease among patients who were enrolled in GOG-182.3 Investigators led by Neil Horowitz, MD, created scores for surgical complexity, disease burden, and residual disease. They observed that the radicality of surgery (complexity score) was not an independent determinant of survival, but rather, patients who presented with a lower disease burden that required a less radical surgery had the best oncologic outcomes.
If the complexity of surgery does not influence outcomes as much as the predetermined, unmodifiable tumor biology, how should surgeons make decisions about the sequencing of treatment? Over the past 10 years, four randomized trials have been completed including more than 1,600 patients randomized to either PDS or NACT.4-7 All four have found no difference in the oncologic outcomes (progression-free or overall survival) between patients when randomized to PDS or NACT. While the statistical designs vary slightly, some being designed to look for noninferiority and others for superiority, they all showed that the sequence in which surgery and chemotherapy was performed mattered less than whether optimal cytoreduction was achieved when surgery was performed. As stated above, this phenomenon seems to be best determined by unmodifiable tumor biology. Unsurprisingly, these studies also have consistently found that perioperative outcomes (e.g., surgical complications, length of stay, death) were worse with PDS because of the higher surgical complexity that it demands. In the most recent SCORPION trial, rates of major postoperative complications in the PDS group were 25.9%, compared with only 7.6% in the NACT group (P < .0001) and all of the deaths from postoperative complications occurred in the PDS group at a rate of 8.3% (7 of 84 patients).7
Therefore, the wealth of data supports that oncologic outcomes are equivalent, and perioperative outcomes are improved for patients who undergo NACT for advanced, bulky ovarian cancer.
Why physicians still are questioning
Unfortunately, because ofthe nature of the disease, these prospective trials include heterogeneous populations of disease presentation, surgeon skill, and hospital settings. They have been criticized for achieving “low” rates of complete or optimal cytoreduction in the PDS arm. They also identified subgroups of patients who may do better with PDS (such as those with lower-volume stage IIIC disease) and those who have better outcomes with NACT (patients with stage IV disease). Therefore, not satisfied that we have definitively answered the question, a fifth randomized study, the TRUST trial, is underway.8 This study includes surgeons at high-volume institutions, purported to have the highest degree of skill and quality in executing radical debulking procedures. Perhaps this fifth trial will show that, if performed in the most skilled hands and quality settings, PDS is preferable to NACT. Perhaps. However, the generalizability of these results will be poor for all patients with advanced ovarian cancer, most of whom will have limited access to these highest-volume surgeons.
What can be agreed upon is that an individualized and nuanced approach is best for advanced ovarian cancer. There will be some patients who benefit from PDS (e.g., healthy, young patients with low-volume disease). However, for most patients, the bulk of prospective and translational research supports NACT as the default treatment course, associated with noninferior survival and superior perioperative outcomes (including postoperative death). While it may not be a one-size-fits-all approach, one could argue that NACT should be the default strategy, and surgeons should look for reasons to “opt in” to PDS in special circumstances guided by biomarkers such as imaging, tumor markers, clinical factors, and surgical findings.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Gynecol Oncol. 2006 Dec. doi: 10.1016/j.ygyno.2006.06.025.
2. Cell Rep. 2020 Apr 14. doi: 10.1016/j.celrep.2020.03.066.
3. J Clin Oncol. 2015 Mar 10. doi: 10.1200/JCO.2014.56.3106.
4. N Engl J Med. 2010 Sep 2. doi: 10.1056/NEJMoa0908806.
5. Lancet. 2015 Jul 18. doi: 10.1016/S0140-6736(14)62223-6.
6. Eur J Cancer. 2020. doi: 10.1016/j.ejca.2020.02.020.
7. Int J Gynecol Cancer. 2020. doi: 10.1136/ijgc-2020-001640.
8. Int J Gynecol Cancer. 2019. doi: 10.1136/ijgc-2019-000682.
Value-based care stunted from delayed Stark and anti-kickback statute reform
Anti-kickback statutes (AKSs) were originally enacted in 1931 to stop Great Depression–era employers from circumventing wage provisions in federal contracts. Since its enactment, AKSs’ main focus has changed and is currently aimed at the health care industry. In addition to AKSs, Stark laws were enacted over 30 years ago to address physician self-referral of Medicare patients. Both laws comprise the government’s main tools for fighting fraud, waste, and abuse.
However, AKSs and Stark laws have not been updated to keep pace with changes in how medical practices do business and care for patients.
Over the years, additional interpretation and clarification has been issued by the Department of Health and Human Services (DHHS) and the Office of Inspector General (OIG). In DHHSs’ June 1, 2012 Advisory Opinion No. 12-06 there is guidance regarding legality of anesthesia services providers’ contract with physician-owned professional corporations or limited liability companies to provide anesthesia services. Specifically, it focused on the “company model” where owners of an ambulatory surgery center (ASC) create a separate company for anesthesia services which directly contracts with anesthesia providers and charges for the anesthesia services while the ASC charges for facility fees. Anyone with specific questions may request an advisory opinion from the OIG about the application of OIG’s fraud and abuse authorities and existing or proposed business arrangements. An OIG advisory opinion is legally binding on the requesting party and DHHS, but not on any other governmental department or agency. While advisory opinions are specific to the entity that requested it and specifically states, “This opinion may not be relied on by any persons other than [name redacted], the requestor of this opinion....” It captured the attention of the medical community. The AGA has argued that this opinion should not be interpreted to mean that all company model frameworks necessarily violate the AKSs and the OIG’s Advisor Opinions FAQ states no person or entity can rely on an advisory opinion issued to someone else. However, Advisory Opinion No. 12-06 has been cited in AKS investigations ever since.
When Congress passed the Medicare Access and CHIP Reauthorization Act (MACRA) in 2015, it changed how physicians would be paid under Medicare and sought to transition physicians to a more value-based payment system. Physicians were incentivized to develop physician-driven payment models to improve efficiency and patient outcomes. However, existing Stark self-referral laws prohibit physicians from referring patients to an entity in which they have a financial interest. As a result, physician practices are unable to participate in many advanced alternative payment models. Stark laws, which have not been updated since their enactment 30 years ago, pose barriers to care coordination since they prohibit payment arrangements that consider volume or value of referrals or other business generated by the parties. These prohibitions stifle innovations in delivering care by inhibiting practices from incentivizing their physicians to deliver patient care more efficiently, because the practices cannot use resources from designated health services in rewarding or penalizing adherence to new clinical care pathways.
Congress recognized that the Stark law was a barrier to new health care delivery models. Congress, therefore, authorized the HHS Secretary to waive Stark self-referral and anti-kickback laws for accountable care organizations (ACOs). This waiver was not extended to physician-driven alternative payment models (APMs), that also need these exceptions to drive innovation in health care and to implement MACRA law as Congress intended.
AGA and the physician community have long sought to update Stark self-referral and AKSs. Last year, CMS proposed exceptions directed at value-based arrangements that would have allowed providers to participate in value-based arrangements while still protecting the Medicare program from potential abuses. Many of the changes that CMS proposed would have allowed physician practices to engage in value-based arrangements that would improve patient care and AGA provided comments on both the Stark and AKS proposed rules. However, CMS has not yet issued the final rules and has indicated that they will not issue a final rule on Stark which a lost opportunity to improve health care delivery.
On the legislative front, AGA supports S. 2051/H.R. 4206, the Medicare Care Coordination Improvement Act, which would provide CMS with the regulatory authority to create exceptions under the Stark law for APMs and to remove barriers in the current law to the development and operation of such arrangements. The legislation would allow CMS to waive the Stark laws for physicians seeking to develop and operate APMs similar to what Congress allowed for ACOs. The legislation would allow innovative payment models developed by gastroenterologists to be implemented in the Medicare program. Unfortunately, this legislation has received little traction in Congress.
Until meaningful regulatory and legislative reform updating both Stark and AKS occur, innovative payment models must wait and gastroenterologists and other providers will remain vulnerable to these outdated regulations. You can help us advance these issues by sharing how they impact your practice. Tell us what types of value-based arrangements you would participate in and how would they improve patient care and efficacy at [email protected].
Dr. Losurdo is the AGA’s Alternate Advisor to the American Medical Association’s CPT Editorial Panel, a member of the AGA Practice Management and Economics Committee’s Coverage and Reimbursement Subcommittee and is a partner with Elgin Gastro Endoscopy, who owns and ASC, and Managing Partner and Medical Director of Illinois Gastroenterology Group/GI Alliance, Elgin, Ill.
This story was updated on 12/11/2020.
Anti-kickback statutes (AKSs) were originally enacted in 1931 to stop Great Depression–era employers from circumventing wage provisions in federal contracts. Since its enactment, AKSs’ main focus has changed and is currently aimed at the health care industry. In addition to AKSs, Stark laws were enacted over 30 years ago to address physician self-referral of Medicare patients. Both laws comprise the government’s main tools for fighting fraud, waste, and abuse.
However, AKSs and Stark laws have not been updated to keep pace with changes in how medical practices do business and care for patients.
Over the years, additional interpretation and clarification has been issued by the Department of Health and Human Services (DHHS) and the Office of Inspector General (OIG). In DHHSs’ June 1, 2012 Advisory Opinion No. 12-06 there is guidance regarding legality of anesthesia services providers’ contract with physician-owned professional corporations or limited liability companies to provide anesthesia services. Specifically, it focused on the “company model” where owners of an ambulatory surgery center (ASC) create a separate company for anesthesia services which directly contracts with anesthesia providers and charges for the anesthesia services while the ASC charges for facility fees. Anyone with specific questions may request an advisory opinion from the OIG about the application of OIG’s fraud and abuse authorities and existing or proposed business arrangements. An OIG advisory opinion is legally binding on the requesting party and DHHS, but not on any other governmental department or agency. While advisory opinions are specific to the entity that requested it and specifically states, “This opinion may not be relied on by any persons other than [name redacted], the requestor of this opinion....” It captured the attention of the medical community. The AGA has argued that this opinion should not be interpreted to mean that all company model frameworks necessarily violate the AKSs and the OIG’s Advisor Opinions FAQ states no person or entity can rely on an advisory opinion issued to someone else. However, Advisory Opinion No. 12-06 has been cited in AKS investigations ever since.
When Congress passed the Medicare Access and CHIP Reauthorization Act (MACRA) in 2015, it changed how physicians would be paid under Medicare and sought to transition physicians to a more value-based payment system. Physicians were incentivized to develop physician-driven payment models to improve efficiency and patient outcomes. However, existing Stark self-referral laws prohibit physicians from referring patients to an entity in which they have a financial interest. As a result, physician practices are unable to participate in many advanced alternative payment models. Stark laws, which have not been updated since their enactment 30 years ago, pose barriers to care coordination since they prohibit payment arrangements that consider volume or value of referrals or other business generated by the parties. These prohibitions stifle innovations in delivering care by inhibiting practices from incentivizing their physicians to deliver patient care more efficiently, because the practices cannot use resources from designated health services in rewarding or penalizing adherence to new clinical care pathways.
Congress recognized that the Stark law was a barrier to new health care delivery models. Congress, therefore, authorized the HHS Secretary to waive Stark self-referral and anti-kickback laws for accountable care organizations (ACOs). This waiver was not extended to physician-driven alternative payment models (APMs), that also need these exceptions to drive innovation in health care and to implement MACRA law as Congress intended.
AGA and the physician community have long sought to update Stark self-referral and AKSs. Last year, CMS proposed exceptions directed at value-based arrangements that would have allowed providers to participate in value-based arrangements while still protecting the Medicare program from potential abuses. Many of the changes that CMS proposed would have allowed physician practices to engage in value-based arrangements that would improve patient care and AGA provided comments on both the Stark and AKS proposed rules. However, CMS has not yet issued the final rules and has indicated that they will not issue a final rule on Stark which a lost opportunity to improve health care delivery.
On the legislative front, AGA supports S. 2051/H.R. 4206, the Medicare Care Coordination Improvement Act, which would provide CMS with the regulatory authority to create exceptions under the Stark law for APMs and to remove barriers in the current law to the development and operation of such arrangements. The legislation would allow CMS to waive the Stark laws for physicians seeking to develop and operate APMs similar to what Congress allowed for ACOs. The legislation would allow innovative payment models developed by gastroenterologists to be implemented in the Medicare program. Unfortunately, this legislation has received little traction in Congress.
Until meaningful regulatory and legislative reform updating both Stark and AKS occur, innovative payment models must wait and gastroenterologists and other providers will remain vulnerable to these outdated regulations. You can help us advance these issues by sharing how they impact your practice. Tell us what types of value-based arrangements you would participate in and how would they improve patient care and efficacy at [email protected].
Dr. Losurdo is the AGA’s Alternate Advisor to the American Medical Association’s CPT Editorial Panel, a member of the AGA Practice Management and Economics Committee’s Coverage and Reimbursement Subcommittee and is a partner with Elgin Gastro Endoscopy, who owns and ASC, and Managing Partner and Medical Director of Illinois Gastroenterology Group/GI Alliance, Elgin, Ill.
This story was updated on 12/11/2020.
Anti-kickback statutes (AKSs) were originally enacted in 1931 to stop Great Depression–era employers from circumventing wage provisions in federal contracts. Since its enactment, AKSs’ main focus has changed and is currently aimed at the health care industry. In addition to AKSs, Stark laws were enacted over 30 years ago to address physician self-referral of Medicare patients. Both laws comprise the government’s main tools for fighting fraud, waste, and abuse.
However, AKSs and Stark laws have not been updated to keep pace with changes in how medical practices do business and care for patients.
Over the years, additional interpretation and clarification has been issued by the Department of Health and Human Services (DHHS) and the Office of Inspector General (OIG). In DHHSs’ June 1, 2012 Advisory Opinion No. 12-06 there is guidance regarding legality of anesthesia services providers’ contract with physician-owned professional corporations or limited liability companies to provide anesthesia services. Specifically, it focused on the “company model” where owners of an ambulatory surgery center (ASC) create a separate company for anesthesia services which directly contracts with anesthesia providers and charges for the anesthesia services while the ASC charges for facility fees. Anyone with specific questions may request an advisory opinion from the OIG about the application of OIG’s fraud and abuse authorities and existing or proposed business arrangements. An OIG advisory opinion is legally binding on the requesting party and DHHS, but not on any other governmental department or agency. While advisory opinions are specific to the entity that requested it and specifically states, “This opinion may not be relied on by any persons other than [name redacted], the requestor of this opinion....” It captured the attention of the medical community. The AGA has argued that this opinion should not be interpreted to mean that all company model frameworks necessarily violate the AKSs and the OIG’s Advisor Opinions FAQ states no person or entity can rely on an advisory opinion issued to someone else. However, Advisory Opinion No. 12-06 has been cited in AKS investigations ever since.
When Congress passed the Medicare Access and CHIP Reauthorization Act (MACRA) in 2015, it changed how physicians would be paid under Medicare and sought to transition physicians to a more value-based payment system. Physicians were incentivized to develop physician-driven payment models to improve efficiency and patient outcomes. However, existing Stark self-referral laws prohibit physicians from referring patients to an entity in which they have a financial interest. As a result, physician practices are unable to participate in many advanced alternative payment models. Stark laws, which have not been updated since their enactment 30 years ago, pose barriers to care coordination since they prohibit payment arrangements that consider volume or value of referrals or other business generated by the parties. These prohibitions stifle innovations in delivering care by inhibiting practices from incentivizing their physicians to deliver patient care more efficiently, because the practices cannot use resources from designated health services in rewarding or penalizing adherence to new clinical care pathways.
Congress recognized that the Stark law was a barrier to new health care delivery models. Congress, therefore, authorized the HHS Secretary to waive Stark self-referral and anti-kickback laws for accountable care organizations (ACOs). This waiver was not extended to physician-driven alternative payment models (APMs), that also need these exceptions to drive innovation in health care and to implement MACRA law as Congress intended.
AGA and the physician community have long sought to update Stark self-referral and AKSs. Last year, CMS proposed exceptions directed at value-based arrangements that would have allowed providers to participate in value-based arrangements while still protecting the Medicare program from potential abuses. Many of the changes that CMS proposed would have allowed physician practices to engage in value-based arrangements that would improve patient care and AGA provided comments on both the Stark and AKS proposed rules. However, CMS has not yet issued the final rules and has indicated that they will not issue a final rule on Stark which a lost opportunity to improve health care delivery.
On the legislative front, AGA supports S. 2051/H.R. 4206, the Medicare Care Coordination Improvement Act, which would provide CMS with the regulatory authority to create exceptions under the Stark law for APMs and to remove barriers in the current law to the development and operation of such arrangements. The legislation would allow CMS to waive the Stark laws for physicians seeking to develop and operate APMs similar to what Congress allowed for ACOs. The legislation would allow innovative payment models developed by gastroenterologists to be implemented in the Medicare program. Unfortunately, this legislation has received little traction in Congress.
Until meaningful regulatory and legislative reform updating both Stark and AKS occur, innovative payment models must wait and gastroenterologists and other providers will remain vulnerable to these outdated regulations. You can help us advance these issues by sharing how they impact your practice. Tell us what types of value-based arrangements you would participate in and how would they improve patient care and efficacy at [email protected].
Dr. Losurdo is the AGA’s Alternate Advisor to the American Medical Association’s CPT Editorial Panel, a member of the AGA Practice Management and Economics Committee’s Coverage and Reimbursement Subcommittee and is a partner with Elgin Gastro Endoscopy, who owns and ASC, and Managing Partner and Medical Director of Illinois Gastroenterology Group/GI Alliance, Elgin, Ill.
This story was updated on 12/11/2020.
Can mental health teams de-escalate crises in NYC?
“Defund the police”: It’s a slogan, or perhaps a battle cry, that has emerged from the Black Lives Matter movement as a response to race-related police brutality and concerns that people of color are profiled, targeted, arrested, charged, manhandled, and killed by law enforcement in a disproportionate and unjust manner. It crosses into our realm as psychiatrists as mental health emergency calls are handled by the police and not by mental health professionals. The result is sometimes tragic: As many as half of police shootings involve people with psychiatric disorders, and the hope is that many of the police shootings could be avoided if crises were handed by mental health clinicians instead of, or in cooperation with, the police.
At best, police officers receive a week of specialized, crisis intervention training about how to approach those with psychiatric disorders; most officers receive no training. This leaves psychiatry as the only field where medical crises are routinely handled by the police – it is demeaning and embarrassing for some of our patients and dangerous for others. The reality remains, however, that there are times when psychiatric disorders result in violent behavior, and patients being taken for involuntary treatment often resist transport, so either way there is risk, both to the patient and to anyone who responds to a call for assistance.
Early this month, the office of New York City Mayor Bill de Blasio announced that a major change would be made in how mental health calls to 911 are handled in two “high-need” areas. The mayor’s website states:
“Beginning in February 2021, new Mental Health Teams will use their physical and mental health expertise, and experience in crisis response to de-escalate emergency situations, will help reduce the number of times police will need to respond to 911 mental health calls in these precincts. These teams will have the expertise to respond to a range of behavioral health problems, such as suicide attempts, substance misuse, and serious mental illness, as well as physical health problems, which can be exacerbated by or mask mental health problems. NYC Health + Hospitals will train and provide ongoing technical assistance and support. In selecting team members for this program, FDNY will prioritize professionals with significant experience with mental health crises.”
The press release goes on to say that, in situations where there is a weapon or reason to believe there is a risk of violence, the police will be dispatched along with the new mental health team.
“This is the first time in our history that health professionals will be the default responders to mental health emergencies,” New York City First Lady Chirlane McCray said as she announced the new program. “Treating mental health crises as mental health challenges and not public safety ones is the modern and more appropriate approach.”
New York City is not the first city to employ this model. In the United States, the CAHOOTS (Crisis Assistance Helping Out on the Streets) program in Eugene, Ore., has been run by the White Bird Clinic since 1989 as part of a community policing initiative. Last year, the team responded to 24,000 calls and police backup was required on only 150 of those responses. The CAHOOTS website states:
“The CAHOOTS model has been in the spotlight recently as our nation struggles to reimagine public safety. The program mobilizes two-person teams consisting of a medic (a nurse, paramedic, or EMT) and a crisis worker who has substantial training and experience in the mental health field. The CAHOOTS teams deal with a wide range of mental health-related crises, including conflict resolution, welfare checks, substance abuse, suicide threats, and more, relying on trauma-informed de-escalation and harm reduction techniques. CAHOOTS staff are not law enforcement officers and do not carry weapons; their training and experience are the tools they use to ensure a non-violent resolution of crisis situations. They also handle non-emergent medical issues, avoiding costly ambulance transport and emergency room treatment.”
Other cities in the United States are also looking at implementing programs where mental health teams, and not the police, respond to emergency calls. Last year, Oakland, Calif.’s city council invested $40,000 in research to assess how they could best implement a program like the one in Eugene. They hope to begin the Mobile Assistance Community Responders of Oakland (MACROS) next year. Sigal Samuel writes in a Vox article, “The goal is to launch the pilot next year with funding from the city budget, and although supporters are not yet sure what its size and duration will be, they’re hopeful it’ll make a big difference to Oakland’s overpoliced community of people without homes. They were among those who first called for a non-policing approach.”
The model is not unique to the United States. In 2005, Stockholm started a program with a psychiatric ambulance – equipped with comfortable seating rather than a stretcher – to respond to mental health emergencies. The ambulance responds to 130 calls a month. It is staffed with a driver and two psychiatric nurses, and for half of the calls, the police also come. While the Swedish program was not about removing resources from the police, it has relieved the police of the responsibility for many psychiatric emergencies.
The New York City program will be modeled after the CAHOOTS initiative in Eugene. It differs from the mobile crisis response services in many other cities because CAHOOTS is hooked directly into the 911 emergency services system. Its website notes that the program has saved money:
“The cost savings are considerable. The CAHOOTS program budget is about $2.1 million annually, while the combined annual budgets for the Eugene and Springfield police departments are $90 million. In 2017, the CAHOOTS teams answered 17% of the Eugene Police Department’s overall call volume. The program saves the city of Eugene an estimated $8.5 million in public safety spending annually.”
Some worry there is an unpredictable aspect to calls for psychiatric emergencies, and the potential for mental health professions to be injured or killed. Annette Hanson, MD, a forensic psychiatrist at University of Maryland, Baltimore, voiced her concerns, “While multidisciplinary teams are useful, there have been rare cases of violence against responding mental health providers. People with serious mental illness are rarely violent but their dangerousness is unpredictable and cannot be predicted by case screening.”
Daniel Felts is a mental health crisis counselor who has worked at CAHOOTS for the past 4* years. He has responded to about 8,000 calls, and called for police backup only three times to request an immediate "Code 3 cover" when someone's safety has been in danger. Mr. Felts calls the police about once a month for concerns that do not require an immediate response for safety.* “Over the last 4 years, I am only aware of three instances when a team member’s safety was compromised because of a client’s violent behavior. No employee has been seriously physically harmed. In 30 years, with hundreds of thousands (millions?) of calls responded to, no CAHOOTS worker has ever been killed, shot, or stabbed in the line of duty,” Mr. Felts noted.
Emergency calls are screened. “It is not uncommon for CAHOOTS to be dispatched to ‘stage’ for calls involving active disputes or acutely suicidal individuals where means are present. “Staging” entails us parking roughly a mile away while police make first contact and advise whether it is safe for CAHOOTS to engage.”
Mr. Felts went on to discuss the program’s relationship with the community. “ and how we operate. Having operated in Eugene for 30 years, our service is well understood to be one that does not kill, harm, or violate personal boundaries or liberties.”
Would a program like the ones in Stockholm or in Eugene work in other places? Eugene is a city with a population of 172,000 with a low crime rate. Whether a program implemented in one city can be mimicked in another very different city is not clear.
Paul Appelbaum, MD, a forensic psychiatrist at Columbia University, New York, is optimistic about New York City’s forthcoming program.
“The proposed pilot project in NYC is a real step forward. Work that we’ve done looking at fatal encounters involving the police found that roughly 25% of all deaths at the hands of the police are of people with mental illness. In many of those cases, police were initially called to bring people who were clearly troubled for psychiatric evaluation, but as the situation escalated, the police turned to their weapons to control it, which led to a fatal outcome. Taking police out of the picture whenever possible in favor of trained mental health personnel is clearly a better approach. It will be important for the city to collect good outcome data to enable independent evaluation of the pilot project – not something that political entities are inclined toward, but a critical element in assessing the effectiveness of this approach.”
There are questions that remain about the new program. Mayor de Blasio’s office has not released information about which areas of the city are being chosen for the new program, how much the program will cost, or what the funding source will be. If it can be implemented safely and effectively, it has the potential to provide more sensitive care to patients in crisis, and to save lives.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
*Correction, 11/27/2020: An earlier version of this article misstated the number of years Daniel Felts has worked at CAHOOTS.
“Defund the police”: It’s a slogan, or perhaps a battle cry, that has emerged from the Black Lives Matter movement as a response to race-related police brutality and concerns that people of color are profiled, targeted, arrested, charged, manhandled, and killed by law enforcement in a disproportionate and unjust manner. It crosses into our realm as psychiatrists as mental health emergency calls are handled by the police and not by mental health professionals. The result is sometimes tragic: As many as half of police shootings involve people with psychiatric disorders, and the hope is that many of the police shootings could be avoided if crises were handed by mental health clinicians instead of, or in cooperation with, the police.
At best, police officers receive a week of specialized, crisis intervention training about how to approach those with psychiatric disorders; most officers receive no training. This leaves psychiatry as the only field where medical crises are routinely handled by the police – it is demeaning and embarrassing for some of our patients and dangerous for others. The reality remains, however, that there are times when psychiatric disorders result in violent behavior, and patients being taken for involuntary treatment often resist transport, so either way there is risk, both to the patient and to anyone who responds to a call for assistance.
Early this month, the office of New York City Mayor Bill de Blasio announced that a major change would be made in how mental health calls to 911 are handled in two “high-need” areas. The mayor’s website states:
“Beginning in February 2021, new Mental Health Teams will use their physical and mental health expertise, and experience in crisis response to de-escalate emergency situations, will help reduce the number of times police will need to respond to 911 mental health calls in these precincts. These teams will have the expertise to respond to a range of behavioral health problems, such as suicide attempts, substance misuse, and serious mental illness, as well as physical health problems, which can be exacerbated by or mask mental health problems. NYC Health + Hospitals will train and provide ongoing technical assistance and support. In selecting team members for this program, FDNY will prioritize professionals with significant experience with mental health crises.”
The press release goes on to say that, in situations where there is a weapon or reason to believe there is a risk of violence, the police will be dispatched along with the new mental health team.
“This is the first time in our history that health professionals will be the default responders to mental health emergencies,” New York City First Lady Chirlane McCray said as she announced the new program. “Treating mental health crises as mental health challenges and not public safety ones is the modern and more appropriate approach.”
New York City is not the first city to employ this model. In the United States, the CAHOOTS (Crisis Assistance Helping Out on the Streets) program in Eugene, Ore., has been run by the White Bird Clinic since 1989 as part of a community policing initiative. Last year, the team responded to 24,000 calls and police backup was required on only 150 of those responses. The CAHOOTS website states:
“The CAHOOTS model has been in the spotlight recently as our nation struggles to reimagine public safety. The program mobilizes two-person teams consisting of a medic (a nurse, paramedic, or EMT) and a crisis worker who has substantial training and experience in the mental health field. The CAHOOTS teams deal with a wide range of mental health-related crises, including conflict resolution, welfare checks, substance abuse, suicide threats, and more, relying on trauma-informed de-escalation and harm reduction techniques. CAHOOTS staff are not law enforcement officers and do not carry weapons; their training and experience are the tools they use to ensure a non-violent resolution of crisis situations. They also handle non-emergent medical issues, avoiding costly ambulance transport and emergency room treatment.”
Other cities in the United States are also looking at implementing programs where mental health teams, and not the police, respond to emergency calls. Last year, Oakland, Calif.’s city council invested $40,000 in research to assess how they could best implement a program like the one in Eugene. They hope to begin the Mobile Assistance Community Responders of Oakland (MACROS) next year. Sigal Samuel writes in a Vox article, “The goal is to launch the pilot next year with funding from the city budget, and although supporters are not yet sure what its size and duration will be, they’re hopeful it’ll make a big difference to Oakland’s overpoliced community of people without homes. They were among those who first called for a non-policing approach.”
The model is not unique to the United States. In 2005, Stockholm started a program with a psychiatric ambulance – equipped with comfortable seating rather than a stretcher – to respond to mental health emergencies. The ambulance responds to 130 calls a month. It is staffed with a driver and two psychiatric nurses, and for half of the calls, the police also come. While the Swedish program was not about removing resources from the police, it has relieved the police of the responsibility for many psychiatric emergencies.
The New York City program will be modeled after the CAHOOTS initiative in Eugene. It differs from the mobile crisis response services in many other cities because CAHOOTS is hooked directly into the 911 emergency services system. Its website notes that the program has saved money:
“The cost savings are considerable. The CAHOOTS program budget is about $2.1 million annually, while the combined annual budgets for the Eugene and Springfield police departments are $90 million. In 2017, the CAHOOTS teams answered 17% of the Eugene Police Department’s overall call volume. The program saves the city of Eugene an estimated $8.5 million in public safety spending annually.”
Some worry there is an unpredictable aspect to calls for psychiatric emergencies, and the potential for mental health professions to be injured or killed. Annette Hanson, MD, a forensic psychiatrist at University of Maryland, Baltimore, voiced her concerns, “While multidisciplinary teams are useful, there have been rare cases of violence against responding mental health providers. People with serious mental illness are rarely violent but their dangerousness is unpredictable and cannot be predicted by case screening.”
Daniel Felts is a mental health crisis counselor who has worked at CAHOOTS for the past 4* years. He has responded to about 8,000 calls, and called for police backup only three times to request an immediate "Code 3 cover" when someone's safety has been in danger. Mr. Felts calls the police about once a month for concerns that do not require an immediate response for safety.* “Over the last 4 years, I am only aware of three instances when a team member’s safety was compromised because of a client’s violent behavior. No employee has been seriously physically harmed. In 30 years, with hundreds of thousands (millions?) of calls responded to, no CAHOOTS worker has ever been killed, shot, or stabbed in the line of duty,” Mr. Felts noted.
Emergency calls are screened. “It is not uncommon for CAHOOTS to be dispatched to ‘stage’ for calls involving active disputes or acutely suicidal individuals where means are present. “Staging” entails us parking roughly a mile away while police make first contact and advise whether it is safe for CAHOOTS to engage.”
Mr. Felts went on to discuss the program’s relationship with the community. “ and how we operate. Having operated in Eugene for 30 years, our service is well understood to be one that does not kill, harm, or violate personal boundaries or liberties.”
Would a program like the ones in Stockholm or in Eugene work in other places? Eugene is a city with a population of 172,000 with a low crime rate. Whether a program implemented in one city can be mimicked in another very different city is not clear.
Paul Appelbaum, MD, a forensic psychiatrist at Columbia University, New York, is optimistic about New York City’s forthcoming program.
“The proposed pilot project in NYC is a real step forward. Work that we’ve done looking at fatal encounters involving the police found that roughly 25% of all deaths at the hands of the police are of people with mental illness. In many of those cases, police were initially called to bring people who were clearly troubled for psychiatric evaluation, but as the situation escalated, the police turned to their weapons to control it, which led to a fatal outcome. Taking police out of the picture whenever possible in favor of trained mental health personnel is clearly a better approach. It will be important for the city to collect good outcome data to enable independent evaluation of the pilot project – not something that political entities are inclined toward, but a critical element in assessing the effectiveness of this approach.”
There are questions that remain about the new program. Mayor de Blasio’s office has not released information about which areas of the city are being chosen for the new program, how much the program will cost, or what the funding source will be. If it can be implemented safely and effectively, it has the potential to provide more sensitive care to patients in crisis, and to save lives.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
*Correction, 11/27/2020: An earlier version of this article misstated the number of years Daniel Felts has worked at CAHOOTS.
“Defund the police”: It’s a slogan, or perhaps a battle cry, that has emerged from the Black Lives Matter movement as a response to race-related police brutality and concerns that people of color are profiled, targeted, arrested, charged, manhandled, and killed by law enforcement in a disproportionate and unjust manner. It crosses into our realm as psychiatrists as mental health emergency calls are handled by the police and not by mental health professionals. The result is sometimes tragic: As many as half of police shootings involve people with psychiatric disorders, and the hope is that many of the police shootings could be avoided if crises were handed by mental health clinicians instead of, or in cooperation with, the police.
At best, police officers receive a week of specialized, crisis intervention training about how to approach those with psychiatric disorders; most officers receive no training. This leaves psychiatry as the only field where medical crises are routinely handled by the police – it is demeaning and embarrassing for some of our patients and dangerous for others. The reality remains, however, that there are times when psychiatric disorders result in violent behavior, and patients being taken for involuntary treatment often resist transport, so either way there is risk, both to the patient and to anyone who responds to a call for assistance.
Early this month, the office of New York City Mayor Bill de Blasio announced that a major change would be made in how mental health calls to 911 are handled in two “high-need” areas. The mayor’s website states:
“Beginning in February 2021, new Mental Health Teams will use their physical and mental health expertise, and experience in crisis response to de-escalate emergency situations, will help reduce the number of times police will need to respond to 911 mental health calls in these precincts. These teams will have the expertise to respond to a range of behavioral health problems, such as suicide attempts, substance misuse, and serious mental illness, as well as physical health problems, which can be exacerbated by or mask mental health problems. NYC Health + Hospitals will train and provide ongoing technical assistance and support. In selecting team members for this program, FDNY will prioritize professionals with significant experience with mental health crises.”
The press release goes on to say that, in situations where there is a weapon or reason to believe there is a risk of violence, the police will be dispatched along with the new mental health team.
“This is the first time in our history that health professionals will be the default responders to mental health emergencies,” New York City First Lady Chirlane McCray said as she announced the new program. “Treating mental health crises as mental health challenges and not public safety ones is the modern and more appropriate approach.”
New York City is not the first city to employ this model. In the United States, the CAHOOTS (Crisis Assistance Helping Out on the Streets) program in Eugene, Ore., has been run by the White Bird Clinic since 1989 as part of a community policing initiative. Last year, the team responded to 24,000 calls and police backup was required on only 150 of those responses. The CAHOOTS website states:
“The CAHOOTS model has been in the spotlight recently as our nation struggles to reimagine public safety. The program mobilizes two-person teams consisting of a medic (a nurse, paramedic, or EMT) and a crisis worker who has substantial training and experience in the mental health field. The CAHOOTS teams deal with a wide range of mental health-related crises, including conflict resolution, welfare checks, substance abuse, suicide threats, and more, relying on trauma-informed de-escalation and harm reduction techniques. CAHOOTS staff are not law enforcement officers and do not carry weapons; their training and experience are the tools they use to ensure a non-violent resolution of crisis situations. They also handle non-emergent medical issues, avoiding costly ambulance transport and emergency room treatment.”
Other cities in the United States are also looking at implementing programs where mental health teams, and not the police, respond to emergency calls. Last year, Oakland, Calif.’s city council invested $40,000 in research to assess how they could best implement a program like the one in Eugene. They hope to begin the Mobile Assistance Community Responders of Oakland (MACROS) next year. Sigal Samuel writes in a Vox article, “The goal is to launch the pilot next year with funding from the city budget, and although supporters are not yet sure what its size and duration will be, they’re hopeful it’ll make a big difference to Oakland’s overpoliced community of people without homes. They were among those who first called for a non-policing approach.”
The model is not unique to the United States. In 2005, Stockholm started a program with a psychiatric ambulance – equipped with comfortable seating rather than a stretcher – to respond to mental health emergencies. The ambulance responds to 130 calls a month. It is staffed with a driver and two psychiatric nurses, and for half of the calls, the police also come. While the Swedish program was not about removing resources from the police, it has relieved the police of the responsibility for many psychiatric emergencies.
The New York City program will be modeled after the CAHOOTS initiative in Eugene. It differs from the mobile crisis response services in many other cities because CAHOOTS is hooked directly into the 911 emergency services system. Its website notes that the program has saved money:
“The cost savings are considerable. The CAHOOTS program budget is about $2.1 million annually, while the combined annual budgets for the Eugene and Springfield police departments are $90 million. In 2017, the CAHOOTS teams answered 17% of the Eugene Police Department’s overall call volume. The program saves the city of Eugene an estimated $8.5 million in public safety spending annually.”
Some worry there is an unpredictable aspect to calls for psychiatric emergencies, and the potential for mental health professions to be injured or killed. Annette Hanson, MD, a forensic psychiatrist at University of Maryland, Baltimore, voiced her concerns, “While multidisciplinary teams are useful, there have been rare cases of violence against responding mental health providers. People with serious mental illness are rarely violent but their dangerousness is unpredictable and cannot be predicted by case screening.”
Daniel Felts is a mental health crisis counselor who has worked at CAHOOTS for the past 4* years. He has responded to about 8,000 calls, and called for police backup only three times to request an immediate "Code 3 cover" when someone's safety has been in danger. Mr. Felts calls the police about once a month for concerns that do not require an immediate response for safety.* “Over the last 4 years, I am only aware of three instances when a team member’s safety was compromised because of a client’s violent behavior. No employee has been seriously physically harmed. In 30 years, with hundreds of thousands (millions?) of calls responded to, no CAHOOTS worker has ever been killed, shot, or stabbed in the line of duty,” Mr. Felts noted.
Emergency calls are screened. “It is not uncommon for CAHOOTS to be dispatched to ‘stage’ for calls involving active disputes or acutely suicidal individuals where means are present. “Staging” entails us parking roughly a mile away while police make first contact and advise whether it is safe for CAHOOTS to engage.”
Mr. Felts went on to discuss the program’s relationship with the community. “ and how we operate. Having operated in Eugene for 30 years, our service is well understood to be one that does not kill, harm, or violate personal boundaries or liberties.”
Would a program like the ones in Stockholm or in Eugene work in other places? Eugene is a city with a population of 172,000 with a low crime rate. Whether a program implemented in one city can be mimicked in another very different city is not clear.
Paul Appelbaum, MD, a forensic psychiatrist at Columbia University, New York, is optimistic about New York City’s forthcoming program.
“The proposed pilot project in NYC is a real step forward. Work that we’ve done looking at fatal encounters involving the police found that roughly 25% of all deaths at the hands of the police are of people with mental illness. In many of those cases, police were initially called to bring people who were clearly troubled for psychiatric evaluation, but as the situation escalated, the police turned to their weapons to control it, which led to a fatal outcome. Taking police out of the picture whenever possible in favor of trained mental health personnel is clearly a better approach. It will be important for the city to collect good outcome data to enable independent evaluation of the pilot project – not something that political entities are inclined toward, but a critical element in assessing the effectiveness of this approach.”
There are questions that remain about the new program. Mayor de Blasio’s office has not released information about which areas of the city are being chosen for the new program, how much the program will cost, or what the funding source will be. If it can be implemented safely and effectively, it has the potential to provide more sensitive care to patients in crisis, and to save lives.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
*Correction, 11/27/2020: An earlier version of this article misstated the number of years Daniel Felts has worked at CAHOOTS.
Excited delirium: Is it time to change the status quo?
Prior to George Floyd’s death, Officer Thomas Lane reportedly said, “I am worried about excited delirium or whatever” to his colleague, Officer Derek Chauvin.1 For those of us who frequently work with law enforcement and in correctional facilities, “excited delirium” is a common refrain. It would be too facile to dismiss the concept as an attempt by police officers to inappropriately use medically sounding jargon to justify violence. “Excited delirium” is a reminder of the complex situations faced by police officers and the need for better medical training, as well as the attention of research on this commonly used label.
Many law enforcement facilities, in particular jails that receive inmates directly from the community, will have large posters educating staff on the “signs of excited delirium.” The concept is not covered in residency training programs, or many of the leading textbooks of psychiatry. Yet, it has become common parlance in law enforcement. Officers in training receive education programs on excited delirium, although those are rarely conducted by clinicians.
In our practice and experience, “excited delirium” has been used by law enforcement officers to describe mood lability from the stress of arrest, acute agitation from stimulant or phencyclidine intoxication, actual delirium from a medical comorbidity, sociopathic aggression for the purpose of violence, and incoherence from psychosis, along with simply describing a person not following direction from a police officer.
Our differential diagnosis when informed that someone was described by a nonclinician as having so-called excited delirium is wider than the Diagnostic and Statistical Manual (DSM). In addition, the term comes at a cost. Its use has been implicated in police-related deaths and brutality.2 There is also concern of its disproportionate application to Black people.3,4
Nonetheless, the term “excited delirium” can sometimes accurately describe critical medical situations. We particularly remember a case of altered mental status from serotonin syndrome, a case of delirium tremens from alcohol withdrawal, and a case of life-threatening dehydration in the context of stimulant intoxication. Each of those cases was appropriately recognized as problematic by perceptive and caring police officers. It is important for police officers to recognize these life-threatening conditions, and they need the language to do so. Having a common label that can be used across professional fields and law enforcement departments to express medical concern in the context of aggressive behavior has value. The question is: can psychiatry help law enforcement describe situations more accurately?
As physicians, it would be overly simple to point out the limited understanding of medical information by police and correctional officers. Naming many behaviors poses significant challenges for psychiatrists and nonclinicians. Examples include the use of the word “agitation” to describe mild restlessness, “delusional” for uncooperative, and “irritable” for opinionated. We must also be cognizant of the infinite demands placed on police officers and that labels must be available to them to express complex situations without being forced to use medical diagnosis and terminology for which they do not have the license or expertise. It is possible that “excited delirium” serves an important role; the problem may not be as much “excited delirium,” the term itself, as the diversion of its use to justify poor policing.
It must be acknowledged that debates, concerns, poor nomenclature, confusing labels, and different interpretations of diagnoses and symptoms are not unusual things in psychiatry, even among professionals. In the 1970s, the famous American and British study of diagnostic criteria, showed that psychiatrists used the diagnosis of schizophrenia to describe vastly different patients.5 The findings of the study were a significant cause of the paradigm shift of the DSM in its 3rd edition. More recently, the DSM-5 field trials suggested that the field of psychiatry continues to struggle with this problem.6 Nonetheless, each edition of the DSM presents a new opportunity to discuss, refine, and improve our ability to communicate while emphasizing the importance of improving our common language.
Emergency physicians face delirious patients brought to them from the community on a regular basis. As such, it makes sense that they have been at the forefront of this issue and the American College of Emergency Physicians has recognized excited delirium as a condition since 2009.7 The emergency physician literature points out that death from excited delirium also happens in hospitals and is not a unique consequence of law enforcement. There is no accepted definition. Reported symptoms include agitation, bizarre behavior, tirelessness, unusual strength, pain tolerance, noncompliance, attraction to reflective surfaces, stupor, fear, panic, hyperthermia, inappropriate clothing, tachycardia, tachypnea, diaphoresis, seizure, and mydriasis. Etiology is suspected to be from catecholaminergic endogenous stress-related catecholamines and exogenous catecholaminergic drugs. In particular is the importance of dopamine through the use of stimulants, specifically cocaine. The literature makes some reference to management, including recommendations aimed at keeping patients on one of their sides, using de-escalation techniques, and performing evaluation in quiet rooms.
We certainly condone and commend efforts to understand and define this condition in the medical literature. The indiscriminate use of “excited delirium” to represent all sorts of behaviors by nonmedical personnel warrants intelligent, relevant, and researched commentary by physicians. There are several potentially appropriate ways forward. First, psychiatry may decide that excited delirium is not a useful diagnosis in the clinical setting and does not belong in the DSM. That distinction in itself would be potentially useful to law enforcement officers, who might welcome the opportunity to create their own nomenclature and classification. Second, psychiatry may decide that excited delirium is not a useful diagnosis in the clinical setting but warrants a definition nonetheless, akin to the ways homelessness and extreme poverty are defined in the DSM; this definition could take into account the wide use of the term by nonclinicians. Third, psychiatry may decide that excited delirium warrants a clinical diagnosis that warrants a distinction and clarification from the current delirium diagnosis with the hyperactive specifier.
At this time, the status quo doesn’t protect or help clinicians in their respective fields of work. “Excited delirium” is routinely used by law enforcement officers without clear meaning. Experts have difficulty pointing out the poor or ill-intended use of the term without a precise or accepted definition to rely on. Some of the proposed criteria, such as “unusual strength,” have unclear scientific legitimacy. Some, such as agitation or bizarre behavior, often have different meanings to nonphysicians. Some, such as poor clothing, may facilitate discrimination. The current state allows some professionals to hide their limited attempts at de-escalation by describing the person of interest as having excited delirium. On the other hand, the current state also prevents well-intended officers from using proper terminology that is understood by others as describing a concerning behavior reliably.
We wonder whether excited delirium is an important facet of the current dilemma of reconsidering the role of law enforcement in society. Frequent use of “excited delirium” by police officers is itself a testament to their desire to have assistance or delegation of certain duties to other social services, such as health care. In some ways, police officers face a difficult position: Admission that a behavior may be attributable to excited delirium should warrant a medical evaluation and, thus, render the person of interest a patient rather than a suspect. As such, this person interacting with police officers should be treated as someone in need of medical care, which makes many interventions – including neck compression – seemingly inappropriate. The frequent use of “excited delirium” suggests that law enforcement is ill-equipped in handling many situations and that an attempt to diversify the composition and funding of emergency response might be warranted. Psychiatry should be at the forefront of this research and effort.
References
1. State of Minnesota v. Derek Michael Chauvin (4th Judicial District, 2020 May 29).
2. J Forensic Leg Med. 2008 May 15(4):227-30.
3. “Excited delirium: Rare and deadly syndrome or a condition to excuse deaths by police?” Florida Today. 2020 Jan 20.
4. J Forensic Sci. 1997 Jan;42(1):25-31.
5. Arch Gen Psychiatry. 1971;25(2):123-30.
6. Am J Psychiatry. 2013 Jan;170(1):59-70.
7. White Paper Report on Excited Delirium Syndrome. ACEP Excited Delirium Task Force. 2009 Sep 10.
Dr. Amendolara is a first-year psychiatry resident at University of California, San Diego. He spent years advocating for survivors of rape and domestic violence at the Crime Victims Treatment Center in New York and conducted public health research at Lourdes Center for Public Health in Camden, N.J. Dr. Amendolara has no disclosures. Dr. Malik is a first-year psychiatry resident at the University of California, San Diego. She has a background in policy and grassroots organizing through her time working at the National Coalition for the Homeless and the Women’s Law Project. Dr. Malik has no disclosures. Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology, and correctional mental health. He holds teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures. Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings is chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Prior to George Floyd’s death, Officer Thomas Lane reportedly said, “I am worried about excited delirium or whatever” to his colleague, Officer Derek Chauvin.1 For those of us who frequently work with law enforcement and in correctional facilities, “excited delirium” is a common refrain. It would be too facile to dismiss the concept as an attempt by police officers to inappropriately use medically sounding jargon to justify violence. “Excited delirium” is a reminder of the complex situations faced by police officers and the need for better medical training, as well as the attention of research on this commonly used label.
Many law enforcement facilities, in particular jails that receive inmates directly from the community, will have large posters educating staff on the “signs of excited delirium.” The concept is not covered in residency training programs, or many of the leading textbooks of psychiatry. Yet, it has become common parlance in law enforcement. Officers in training receive education programs on excited delirium, although those are rarely conducted by clinicians.
In our practice and experience, “excited delirium” has been used by law enforcement officers to describe mood lability from the stress of arrest, acute agitation from stimulant or phencyclidine intoxication, actual delirium from a medical comorbidity, sociopathic aggression for the purpose of violence, and incoherence from psychosis, along with simply describing a person not following direction from a police officer.
Our differential diagnosis when informed that someone was described by a nonclinician as having so-called excited delirium is wider than the Diagnostic and Statistical Manual (DSM). In addition, the term comes at a cost. Its use has been implicated in police-related deaths and brutality.2 There is also concern of its disproportionate application to Black people.3,4
Nonetheless, the term “excited delirium” can sometimes accurately describe critical medical situations. We particularly remember a case of altered mental status from serotonin syndrome, a case of delirium tremens from alcohol withdrawal, and a case of life-threatening dehydration in the context of stimulant intoxication. Each of those cases was appropriately recognized as problematic by perceptive and caring police officers. It is important for police officers to recognize these life-threatening conditions, and they need the language to do so. Having a common label that can be used across professional fields and law enforcement departments to express medical concern in the context of aggressive behavior has value. The question is: can psychiatry help law enforcement describe situations more accurately?
As physicians, it would be overly simple to point out the limited understanding of medical information by police and correctional officers. Naming many behaviors poses significant challenges for psychiatrists and nonclinicians. Examples include the use of the word “agitation” to describe mild restlessness, “delusional” for uncooperative, and “irritable” for opinionated. We must also be cognizant of the infinite demands placed on police officers and that labels must be available to them to express complex situations without being forced to use medical diagnosis and terminology for which they do not have the license or expertise. It is possible that “excited delirium” serves an important role; the problem may not be as much “excited delirium,” the term itself, as the diversion of its use to justify poor policing.
It must be acknowledged that debates, concerns, poor nomenclature, confusing labels, and different interpretations of diagnoses and symptoms are not unusual things in psychiatry, even among professionals. In the 1970s, the famous American and British study of diagnostic criteria, showed that psychiatrists used the diagnosis of schizophrenia to describe vastly different patients.5 The findings of the study were a significant cause of the paradigm shift of the DSM in its 3rd edition. More recently, the DSM-5 field trials suggested that the field of psychiatry continues to struggle with this problem.6 Nonetheless, each edition of the DSM presents a new opportunity to discuss, refine, and improve our ability to communicate while emphasizing the importance of improving our common language.
Emergency physicians face delirious patients brought to them from the community on a regular basis. As such, it makes sense that they have been at the forefront of this issue and the American College of Emergency Physicians has recognized excited delirium as a condition since 2009.7 The emergency physician literature points out that death from excited delirium also happens in hospitals and is not a unique consequence of law enforcement. There is no accepted definition. Reported symptoms include agitation, bizarre behavior, tirelessness, unusual strength, pain tolerance, noncompliance, attraction to reflective surfaces, stupor, fear, panic, hyperthermia, inappropriate clothing, tachycardia, tachypnea, diaphoresis, seizure, and mydriasis. Etiology is suspected to be from catecholaminergic endogenous stress-related catecholamines and exogenous catecholaminergic drugs. In particular is the importance of dopamine through the use of stimulants, specifically cocaine. The literature makes some reference to management, including recommendations aimed at keeping patients on one of their sides, using de-escalation techniques, and performing evaluation in quiet rooms.
We certainly condone and commend efforts to understand and define this condition in the medical literature. The indiscriminate use of “excited delirium” to represent all sorts of behaviors by nonmedical personnel warrants intelligent, relevant, and researched commentary by physicians. There are several potentially appropriate ways forward. First, psychiatry may decide that excited delirium is not a useful diagnosis in the clinical setting and does not belong in the DSM. That distinction in itself would be potentially useful to law enforcement officers, who might welcome the opportunity to create their own nomenclature and classification. Second, psychiatry may decide that excited delirium is not a useful diagnosis in the clinical setting but warrants a definition nonetheless, akin to the ways homelessness and extreme poverty are defined in the DSM; this definition could take into account the wide use of the term by nonclinicians. Third, psychiatry may decide that excited delirium warrants a clinical diagnosis that warrants a distinction and clarification from the current delirium diagnosis with the hyperactive specifier.
At this time, the status quo doesn’t protect or help clinicians in their respective fields of work. “Excited delirium” is routinely used by law enforcement officers without clear meaning. Experts have difficulty pointing out the poor or ill-intended use of the term without a precise or accepted definition to rely on. Some of the proposed criteria, such as “unusual strength,” have unclear scientific legitimacy. Some, such as agitation or bizarre behavior, often have different meanings to nonphysicians. Some, such as poor clothing, may facilitate discrimination. The current state allows some professionals to hide their limited attempts at de-escalation by describing the person of interest as having excited delirium. On the other hand, the current state also prevents well-intended officers from using proper terminology that is understood by others as describing a concerning behavior reliably.
We wonder whether excited delirium is an important facet of the current dilemma of reconsidering the role of law enforcement in society. Frequent use of “excited delirium” by police officers is itself a testament to their desire to have assistance or delegation of certain duties to other social services, such as health care. In some ways, police officers face a difficult position: Admission that a behavior may be attributable to excited delirium should warrant a medical evaluation and, thus, render the person of interest a patient rather than a suspect. As such, this person interacting with police officers should be treated as someone in need of medical care, which makes many interventions – including neck compression – seemingly inappropriate. The frequent use of “excited delirium” suggests that law enforcement is ill-equipped in handling many situations and that an attempt to diversify the composition and funding of emergency response might be warranted. Psychiatry should be at the forefront of this research and effort.
References
1. State of Minnesota v. Derek Michael Chauvin (4th Judicial District, 2020 May 29).
2. J Forensic Leg Med. 2008 May 15(4):227-30.
3. “Excited delirium: Rare and deadly syndrome or a condition to excuse deaths by police?” Florida Today. 2020 Jan 20.
4. J Forensic Sci. 1997 Jan;42(1):25-31.
5. Arch Gen Psychiatry. 1971;25(2):123-30.
6. Am J Psychiatry. 2013 Jan;170(1):59-70.
7. White Paper Report on Excited Delirium Syndrome. ACEP Excited Delirium Task Force. 2009 Sep 10.
Dr. Amendolara is a first-year psychiatry resident at University of California, San Diego. He spent years advocating for survivors of rape and domestic violence at the Crime Victims Treatment Center in New York and conducted public health research at Lourdes Center for Public Health in Camden, N.J. Dr. Amendolara has no disclosures. Dr. Malik is a first-year psychiatry resident at the University of California, San Diego. She has a background in policy and grassroots organizing through her time working at the National Coalition for the Homeless and the Women’s Law Project. Dr. Malik has no disclosures. Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology, and correctional mental health. He holds teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures. Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings is chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Prior to George Floyd’s death, Officer Thomas Lane reportedly said, “I am worried about excited delirium or whatever” to his colleague, Officer Derek Chauvin.1 For those of us who frequently work with law enforcement and in correctional facilities, “excited delirium” is a common refrain. It would be too facile to dismiss the concept as an attempt by police officers to inappropriately use medically sounding jargon to justify violence. “Excited delirium” is a reminder of the complex situations faced by police officers and the need for better medical training, as well as the attention of research on this commonly used label.
Many law enforcement facilities, in particular jails that receive inmates directly from the community, will have large posters educating staff on the “signs of excited delirium.” The concept is not covered in residency training programs, or many of the leading textbooks of psychiatry. Yet, it has become common parlance in law enforcement. Officers in training receive education programs on excited delirium, although those are rarely conducted by clinicians.
In our practice and experience, “excited delirium” has been used by law enforcement officers to describe mood lability from the stress of arrest, acute agitation from stimulant or phencyclidine intoxication, actual delirium from a medical comorbidity, sociopathic aggression for the purpose of violence, and incoherence from psychosis, along with simply describing a person not following direction from a police officer.
Our differential diagnosis when informed that someone was described by a nonclinician as having so-called excited delirium is wider than the Diagnostic and Statistical Manual (DSM). In addition, the term comes at a cost. Its use has been implicated in police-related deaths and brutality.2 There is also concern of its disproportionate application to Black people.3,4
Nonetheless, the term “excited delirium” can sometimes accurately describe critical medical situations. We particularly remember a case of altered mental status from serotonin syndrome, a case of delirium tremens from alcohol withdrawal, and a case of life-threatening dehydration in the context of stimulant intoxication. Each of those cases was appropriately recognized as problematic by perceptive and caring police officers. It is important for police officers to recognize these life-threatening conditions, and they need the language to do so. Having a common label that can be used across professional fields and law enforcement departments to express medical concern in the context of aggressive behavior has value. The question is: can psychiatry help law enforcement describe situations more accurately?
As physicians, it would be overly simple to point out the limited understanding of medical information by police and correctional officers. Naming many behaviors poses significant challenges for psychiatrists and nonclinicians. Examples include the use of the word “agitation” to describe mild restlessness, “delusional” for uncooperative, and “irritable” for opinionated. We must also be cognizant of the infinite demands placed on police officers and that labels must be available to them to express complex situations without being forced to use medical diagnosis and terminology for which they do not have the license or expertise. It is possible that “excited delirium” serves an important role; the problem may not be as much “excited delirium,” the term itself, as the diversion of its use to justify poor policing.
It must be acknowledged that debates, concerns, poor nomenclature, confusing labels, and different interpretations of diagnoses and symptoms are not unusual things in psychiatry, even among professionals. In the 1970s, the famous American and British study of diagnostic criteria, showed that psychiatrists used the diagnosis of schizophrenia to describe vastly different patients.5 The findings of the study were a significant cause of the paradigm shift of the DSM in its 3rd edition. More recently, the DSM-5 field trials suggested that the field of psychiatry continues to struggle with this problem.6 Nonetheless, each edition of the DSM presents a new opportunity to discuss, refine, and improve our ability to communicate while emphasizing the importance of improving our common language.
Emergency physicians face delirious patients brought to them from the community on a regular basis. As such, it makes sense that they have been at the forefront of this issue and the American College of Emergency Physicians has recognized excited delirium as a condition since 2009.7 The emergency physician literature points out that death from excited delirium also happens in hospitals and is not a unique consequence of law enforcement. There is no accepted definition. Reported symptoms include agitation, bizarre behavior, tirelessness, unusual strength, pain tolerance, noncompliance, attraction to reflective surfaces, stupor, fear, panic, hyperthermia, inappropriate clothing, tachycardia, tachypnea, diaphoresis, seizure, and mydriasis. Etiology is suspected to be from catecholaminergic endogenous stress-related catecholamines and exogenous catecholaminergic drugs. In particular is the importance of dopamine through the use of stimulants, specifically cocaine. The literature makes some reference to management, including recommendations aimed at keeping patients on one of their sides, using de-escalation techniques, and performing evaluation in quiet rooms.
We certainly condone and commend efforts to understand and define this condition in the medical literature. The indiscriminate use of “excited delirium” to represent all sorts of behaviors by nonmedical personnel warrants intelligent, relevant, and researched commentary by physicians. There are several potentially appropriate ways forward. First, psychiatry may decide that excited delirium is not a useful diagnosis in the clinical setting and does not belong in the DSM. That distinction in itself would be potentially useful to law enforcement officers, who might welcome the opportunity to create their own nomenclature and classification. Second, psychiatry may decide that excited delirium is not a useful diagnosis in the clinical setting but warrants a definition nonetheless, akin to the ways homelessness and extreme poverty are defined in the DSM; this definition could take into account the wide use of the term by nonclinicians. Third, psychiatry may decide that excited delirium warrants a clinical diagnosis that warrants a distinction and clarification from the current delirium diagnosis with the hyperactive specifier.
At this time, the status quo doesn’t protect or help clinicians in their respective fields of work. “Excited delirium” is routinely used by law enforcement officers without clear meaning. Experts have difficulty pointing out the poor or ill-intended use of the term without a precise or accepted definition to rely on. Some of the proposed criteria, such as “unusual strength,” have unclear scientific legitimacy. Some, such as agitation or bizarre behavior, often have different meanings to nonphysicians. Some, such as poor clothing, may facilitate discrimination. The current state allows some professionals to hide their limited attempts at de-escalation by describing the person of interest as having excited delirium. On the other hand, the current state also prevents well-intended officers from using proper terminology that is understood by others as describing a concerning behavior reliably.
We wonder whether excited delirium is an important facet of the current dilemma of reconsidering the role of law enforcement in society. Frequent use of “excited delirium” by police officers is itself a testament to their desire to have assistance or delegation of certain duties to other social services, such as health care. In some ways, police officers face a difficult position: Admission that a behavior may be attributable to excited delirium should warrant a medical evaluation and, thus, render the person of interest a patient rather than a suspect. As such, this person interacting with police officers should be treated as someone in need of medical care, which makes many interventions – including neck compression – seemingly inappropriate. The frequent use of “excited delirium” suggests that law enforcement is ill-equipped in handling many situations and that an attempt to diversify the composition and funding of emergency response might be warranted. Psychiatry should be at the forefront of this research and effort.
References
1. State of Minnesota v. Derek Michael Chauvin (4th Judicial District, 2020 May 29).
2. J Forensic Leg Med. 2008 May 15(4):227-30.
3. “Excited delirium: Rare and deadly syndrome or a condition to excuse deaths by police?” Florida Today. 2020 Jan 20.
4. J Forensic Sci. 1997 Jan;42(1):25-31.
5. Arch Gen Psychiatry. 1971;25(2):123-30.
6. Am J Psychiatry. 2013 Jan;170(1):59-70.
7. White Paper Report on Excited Delirium Syndrome. ACEP Excited Delirium Task Force. 2009 Sep 10.
Dr. Amendolara is a first-year psychiatry resident at University of California, San Diego. He spent years advocating for survivors of rape and domestic violence at the Crime Victims Treatment Center in New York and conducted public health research at Lourdes Center for Public Health in Camden, N.J. Dr. Amendolara has no disclosures. Dr. Malik is a first-year psychiatry resident at the University of California, San Diego. She has a background in policy and grassroots organizing through her time working at the National Coalition for the Homeless and the Women’s Law Project. Dr. Malik has no disclosures. Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology, and correctional mental health. He holds teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures. Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings is chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.






















