User login
The future of pediatrics
Things will change. That is a constant. The practice of pediatrics will be different in the future. The pandemic has changed some things; mostly it has accelerated changes, advancements, improvements, and losses that were already occurring. Telemedicine will play a more prominent role in the future. The finances of solo and small-group practice have become more difficult.
As I wrote my prior column on the character traits/virtues of an admirable physician, I also began brainstorming this column on the traits of an admirable profession. Then the American Academy of Pediatrics’ virtual National Conference & Exhibition had many presentations encouraging pediatricians to adopt a conglomeration of activities in their offices. I became skeptical. Which should be selected? To make a wise choice, I review the major goals of medicine, which I have evolved to embrace as the quadruple aims.
First and hopefully always foremost, the health professions are dedicated to the health of their patients and, hopefully, the population at large. This trait dates to the Hippocratic Oath.
Second, physicians have a stewardship over a vast collection of knowledge, skills, resources, and funds. When I started my career, U.S. health care had increased from 6% of the gross domestic product to 9%, nearly twice that of other developed nations, and was expanding rapidly, contributing to widespread economic problems including the national debt. The health economists of the 1980’s made dire predictions that the nation was headed up to 12% of the GDP, which would cause the sky to start falling. Last I checked U.S. health care is approaching 18% of the GDP. The sky seems intact, although the oceans are rising and the hillsides are burning.
Managed care of the 1990s became focused on the consumer experience. Evaluations of physicians and nurses became dependent on consumer surveys. I recall one survey about the care I personally had received as day surgery. It was mostly about scheduling, being greeted on arrival, the waiting room, and other fluff. Only 1 of the over 20 questions had any bearing on whether I thought the diagnosis was correct, the treatment was effective, or my physician was competent. As a cancer patient, my priorities were not aligned with that survey’s concept of quality.
From 2008, I recall the Triple Aim: “Improving the U.S. health care system requires simultaneous pursuit of three aims: improving the experience of care, improving the health of populations, and reducing per capita costs of health care.”
Over the ensuing decade, physician wellness has been added to make a quadruple aim. If the system isn’t professionally rewarding, burnout occurs. Skills and experience are lost. The best and brightest are not attracted to the specialty. Quality goes down. So physicians must factor this into decisions about the future of pediatrics.
There are many social determinants of health that have large impacts on the population health of children, and it does not necessarily follow that I should spend my patient care time on those determinants. As a professional, I have a responsibility to ensure that I am treating important problems that match my extensive (and expensive) training, knowledge, skills, and experience.
I recently read a persuasive argument that caring for ADHD is an important and doable part of modern general pediatrics. I agree, but I agreed with the proponent’s idea 25 years ago when I joined a large group and saw my own ADHD patients. Change can be slow.
Pharmacology options for anxiety have become safer, more effective, and better understood in children. General pediatricians may now be able to provide important, earlier, and accessible intervention for pediatric anxiety and other mental health issues.
Food insecurity is a worsening issue during the pandemic, but not one which I have specialized abilities to address. A brochure listing available local resources could be posted in waiting rooms and exam rooms. Is spending time asking about it during a visit the best use of a pediatrician’s time? That is a choice a professional needs to make. It may depend on your patient panel and community resources. In the past, I was more inclined to focus on medical care and donate the extra income to my church’s food bank. But the world has changed. Perhaps the pediatrician’s office of the 2020s is a department store, with social workers, psychologists, and therapists located under the same roof. It reminds me of the Mayo model. Wealthy people would travel to Rochester for an executive physical. That physical would frequently recommend seeing a couple specialists before leaving town. It is an effective model but also luxurious.
Racism causes major harms, both to physical health and mental health. Is asking about it a wise use of limited time for well-child visits? What resources will you offer?
Climate change, hurricanes, and wildfires are harming children. Is debating the issue with your patient’s parents productive? I am zealous about the topic. I spend considerable time and money promoting the credibility of science within various religious organizations, but I try to avoid bringing politics into my interactions with patients.
As a professional, your choices may be different. Many people are telling you what you should care about. The executive well-child visit would be beneficial, but it would also take 2 hours. Don’t be misled into spending too much effort on issues not in your expertise. Choose wisely.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. He has no relevant financial disclosures. Email him at [email protected].
Things will change. That is a constant. The practice of pediatrics will be different in the future. The pandemic has changed some things; mostly it has accelerated changes, advancements, improvements, and losses that were already occurring. Telemedicine will play a more prominent role in the future. The finances of solo and small-group practice have become more difficult.
As I wrote my prior column on the character traits/virtues of an admirable physician, I also began brainstorming this column on the traits of an admirable profession. Then the American Academy of Pediatrics’ virtual National Conference & Exhibition had many presentations encouraging pediatricians to adopt a conglomeration of activities in their offices. I became skeptical. Which should be selected? To make a wise choice, I review the major goals of medicine, which I have evolved to embrace as the quadruple aims.
First and hopefully always foremost, the health professions are dedicated to the health of their patients and, hopefully, the population at large. This trait dates to the Hippocratic Oath.
Second, physicians have a stewardship over a vast collection of knowledge, skills, resources, and funds. When I started my career, U.S. health care had increased from 6% of the gross domestic product to 9%, nearly twice that of other developed nations, and was expanding rapidly, contributing to widespread economic problems including the national debt. The health economists of the 1980’s made dire predictions that the nation was headed up to 12% of the GDP, which would cause the sky to start falling. Last I checked U.S. health care is approaching 18% of the GDP. The sky seems intact, although the oceans are rising and the hillsides are burning.
Managed care of the 1990s became focused on the consumer experience. Evaluations of physicians and nurses became dependent on consumer surveys. I recall one survey about the care I personally had received as day surgery. It was mostly about scheduling, being greeted on arrival, the waiting room, and other fluff. Only 1 of the over 20 questions had any bearing on whether I thought the diagnosis was correct, the treatment was effective, or my physician was competent. As a cancer patient, my priorities were not aligned with that survey’s concept of quality.
From 2008, I recall the Triple Aim: “Improving the U.S. health care system requires simultaneous pursuit of three aims: improving the experience of care, improving the health of populations, and reducing per capita costs of health care.”
Over the ensuing decade, physician wellness has been added to make a quadruple aim. If the system isn’t professionally rewarding, burnout occurs. Skills and experience are lost. The best and brightest are not attracted to the specialty. Quality goes down. So physicians must factor this into decisions about the future of pediatrics.
There are many social determinants of health that have large impacts on the population health of children, and it does not necessarily follow that I should spend my patient care time on those determinants. As a professional, I have a responsibility to ensure that I am treating important problems that match my extensive (and expensive) training, knowledge, skills, and experience.
I recently read a persuasive argument that caring for ADHD is an important and doable part of modern general pediatrics. I agree, but I agreed with the proponent’s idea 25 years ago when I joined a large group and saw my own ADHD patients. Change can be slow.
Pharmacology options for anxiety have become safer, more effective, and better understood in children. General pediatricians may now be able to provide important, earlier, and accessible intervention for pediatric anxiety and other mental health issues.
Food insecurity is a worsening issue during the pandemic, but not one which I have specialized abilities to address. A brochure listing available local resources could be posted in waiting rooms and exam rooms. Is spending time asking about it during a visit the best use of a pediatrician’s time? That is a choice a professional needs to make. It may depend on your patient panel and community resources. In the past, I was more inclined to focus on medical care and donate the extra income to my church’s food bank. But the world has changed. Perhaps the pediatrician’s office of the 2020s is a department store, with social workers, psychologists, and therapists located under the same roof. It reminds me of the Mayo model. Wealthy people would travel to Rochester for an executive physical. That physical would frequently recommend seeing a couple specialists before leaving town. It is an effective model but also luxurious.
Racism causes major harms, both to physical health and mental health. Is asking about it a wise use of limited time for well-child visits? What resources will you offer?
Climate change, hurricanes, and wildfires are harming children. Is debating the issue with your patient’s parents productive? I am zealous about the topic. I spend considerable time and money promoting the credibility of science within various religious organizations, but I try to avoid bringing politics into my interactions with patients.
As a professional, your choices may be different. Many people are telling you what you should care about. The executive well-child visit would be beneficial, but it would also take 2 hours. Don’t be misled into spending too much effort on issues not in your expertise. Choose wisely.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. He has no relevant financial disclosures. Email him at [email protected].
Things will change. That is a constant. The practice of pediatrics will be different in the future. The pandemic has changed some things; mostly it has accelerated changes, advancements, improvements, and losses that were already occurring. Telemedicine will play a more prominent role in the future. The finances of solo and small-group practice have become more difficult.
As I wrote my prior column on the character traits/virtues of an admirable physician, I also began brainstorming this column on the traits of an admirable profession. Then the American Academy of Pediatrics’ virtual National Conference & Exhibition had many presentations encouraging pediatricians to adopt a conglomeration of activities in their offices. I became skeptical. Which should be selected? To make a wise choice, I review the major goals of medicine, which I have evolved to embrace as the quadruple aims.
First and hopefully always foremost, the health professions are dedicated to the health of their patients and, hopefully, the population at large. This trait dates to the Hippocratic Oath.
Second, physicians have a stewardship over a vast collection of knowledge, skills, resources, and funds. When I started my career, U.S. health care had increased from 6% of the gross domestic product to 9%, nearly twice that of other developed nations, and was expanding rapidly, contributing to widespread economic problems including the national debt. The health economists of the 1980’s made dire predictions that the nation was headed up to 12% of the GDP, which would cause the sky to start falling. Last I checked U.S. health care is approaching 18% of the GDP. The sky seems intact, although the oceans are rising and the hillsides are burning.
Managed care of the 1990s became focused on the consumer experience. Evaluations of physicians and nurses became dependent on consumer surveys. I recall one survey about the care I personally had received as day surgery. It was mostly about scheduling, being greeted on arrival, the waiting room, and other fluff. Only 1 of the over 20 questions had any bearing on whether I thought the diagnosis was correct, the treatment was effective, or my physician was competent. As a cancer patient, my priorities were not aligned with that survey’s concept of quality.
From 2008, I recall the Triple Aim: “Improving the U.S. health care system requires simultaneous pursuit of three aims: improving the experience of care, improving the health of populations, and reducing per capita costs of health care.”
Over the ensuing decade, physician wellness has been added to make a quadruple aim. If the system isn’t professionally rewarding, burnout occurs. Skills and experience are lost. The best and brightest are not attracted to the specialty. Quality goes down. So physicians must factor this into decisions about the future of pediatrics.
There are many social determinants of health that have large impacts on the population health of children, and it does not necessarily follow that I should spend my patient care time on those determinants. As a professional, I have a responsibility to ensure that I am treating important problems that match my extensive (and expensive) training, knowledge, skills, and experience.
I recently read a persuasive argument that caring for ADHD is an important and doable part of modern general pediatrics. I agree, but I agreed with the proponent’s idea 25 years ago when I joined a large group and saw my own ADHD patients. Change can be slow.
Pharmacology options for anxiety have become safer, more effective, and better understood in children. General pediatricians may now be able to provide important, earlier, and accessible intervention for pediatric anxiety and other mental health issues.
Food insecurity is a worsening issue during the pandemic, but not one which I have specialized abilities to address. A brochure listing available local resources could be posted in waiting rooms and exam rooms. Is spending time asking about it during a visit the best use of a pediatrician’s time? That is a choice a professional needs to make. It may depend on your patient panel and community resources. In the past, I was more inclined to focus on medical care and donate the extra income to my church’s food bank. But the world has changed. Perhaps the pediatrician’s office of the 2020s is a department store, with social workers, psychologists, and therapists located under the same roof. It reminds me of the Mayo model. Wealthy people would travel to Rochester for an executive physical. That physical would frequently recommend seeing a couple specialists before leaving town. It is an effective model but also luxurious.
Racism causes major harms, both to physical health and mental health. Is asking about it a wise use of limited time for well-child visits? What resources will you offer?
Climate change, hurricanes, and wildfires are harming children. Is debating the issue with your patient’s parents productive? I am zealous about the topic. I spend considerable time and money promoting the credibility of science within various religious organizations, but I try to avoid bringing politics into my interactions with patients.
As a professional, your choices may be different. Many people are telling you what you should care about. The executive well-child visit would be beneficial, but it would also take 2 hours. Don’t be misled into spending too much effort on issues not in your expertise. Choose wisely.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. He has no relevant financial disclosures. Email him at [email protected].
Fenway data, the final frontier
Data, as we all know, have taken over the world. ”
Statistical objectivity is in, individuality is out. You may have taught for 30 years and gained a sense for which child has a problem that needs intervention and which one just needs patience and time to develop. You may have managed patients for decades and have a hunch about who needs immediate help and who can be watched. But “senses” and “hunches” can’t be measured and therefore do not exist, or better, don’t count. Numbers count!
Data-obsession reflects what Germans call the Zeitgeist, the spirit of the age. But the Germans will have to come up with a different word for our age, won’t they? Nobody can measure a “spirit.”
Still, you know the spirit’s there, when it knocks you over and stomps on you.
The one sphere of life that has resisted being reduced to numbers is sports. In sports, you don’t need complex analysis to know who’s No. 1 and who’s number everything else. No. 1 crosses the finish line first, wins the most games, knocks out the opponent. The one lying on the mat is No. 2.
Of course, sports always had lots of numbers. Baseball fans have always known about batting averages, runs batted in, earned run averages. But there were always those individual intangibles that goggle the eyes of small boys and keep sportswriters in business: this athlete’s “ferocious drive,” that one’s “will to win,” the way a third “always comes through in the clutch.” Pitchers who couldn’t throw fast anymore were “crafty.” Grizzled, tobacco-chewing scouts could sense which youngster “looked like a ballplayer.”
As if you didn’t already know, you can tell how old I am to talk this way. Bill James and his statistical acolytes put paid to that old kind of thinking a long time ago. Read Moneyball or see the movie. In sports too, it’s now all about the stats.
To generate flagging interest among the young for America’s now-stodgy pastime, Major League Baseball has brought out Statcast 2.0., which adds, according to a recent news story, “Doppler-based tracking of pitch velocity, exit velocity, launch angles, and spin rates, and defensive tracking of players.” Multicamera arrays produce “biomechanical imaging and skeletal models that can help pitchers with delivery issues or batters with swing path quandaries.”
And so we have lots of new data to ponder: exit velocity – how fast a hit ball leaves the bat; launch angle – what angle it leaves at; spin rate – how fast a thrown curveball spins; and defensive tracking – how many feet this shortstop can move left to snag a ground ball, or a right-fielder to catch a fly. And there are new, composite stats, like OPS (on-base plus slugging). I will not try to explain OPS, because it is a mathematical abstraction that I cannot grasp. It signifies a blend of on-base percentage and slugging percentage, which to me is like what you get when you blend a tomato with a broccoli. Or something.
And, stats aside, you do still have to win. Not long ago the Boston Red Sox had a relief pitcher whose spin rate was splendid, but he couldn’t get anybody out.
The real aim of the new broadcast innovations noted above comes at the end of the report:
In an effort to at least reach, if not grow, a younger fan base, MLB from now on will focus on video engagement, gaming, and augmented reality on Snapchat.
You got it: the goal is to reduce baseball to a video game, and its players to gaming characters, perhaps with big contracts and marketing deals. Hey, check out that dude’s OPS!
You can’t measure a Zeitgeist, but you certainly know when it’s sitting on your chest. Your respirations get depressed. Measurably.
Yeah, I sound like every cranky old man in history. But hey – I’m Emeritus! See this column’s title!
In addition, the article has one more detail:
Curiosity about whether a fly ball to deep right field at Fenway Park would be a home run at Yankee Stadium can be satisfied by overlaying the Yankee Stadium footprint on top of Fenway.
Maybe it would satisfy you, buddy, but anything that superimposes Yankee Stadium on top of Fenway Park dissatisfies me by a factor of 6.7!
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Data, as we all know, have taken over the world. ”
Statistical objectivity is in, individuality is out. You may have taught for 30 years and gained a sense for which child has a problem that needs intervention and which one just needs patience and time to develop. You may have managed patients for decades and have a hunch about who needs immediate help and who can be watched. But “senses” and “hunches” can’t be measured and therefore do not exist, or better, don’t count. Numbers count!
Data-obsession reflects what Germans call the Zeitgeist, the spirit of the age. But the Germans will have to come up with a different word for our age, won’t they? Nobody can measure a “spirit.”
Still, you know the spirit’s there, when it knocks you over and stomps on you.
The one sphere of life that has resisted being reduced to numbers is sports. In sports, you don’t need complex analysis to know who’s No. 1 and who’s number everything else. No. 1 crosses the finish line first, wins the most games, knocks out the opponent. The one lying on the mat is No. 2.
Of course, sports always had lots of numbers. Baseball fans have always known about batting averages, runs batted in, earned run averages. But there were always those individual intangibles that goggle the eyes of small boys and keep sportswriters in business: this athlete’s “ferocious drive,” that one’s “will to win,” the way a third “always comes through in the clutch.” Pitchers who couldn’t throw fast anymore were “crafty.” Grizzled, tobacco-chewing scouts could sense which youngster “looked like a ballplayer.”
As if you didn’t already know, you can tell how old I am to talk this way. Bill James and his statistical acolytes put paid to that old kind of thinking a long time ago. Read Moneyball or see the movie. In sports too, it’s now all about the stats.
To generate flagging interest among the young for America’s now-stodgy pastime, Major League Baseball has brought out Statcast 2.0., which adds, according to a recent news story, “Doppler-based tracking of pitch velocity, exit velocity, launch angles, and spin rates, and defensive tracking of players.” Multicamera arrays produce “biomechanical imaging and skeletal models that can help pitchers with delivery issues or batters with swing path quandaries.”
And so we have lots of new data to ponder: exit velocity – how fast a hit ball leaves the bat; launch angle – what angle it leaves at; spin rate – how fast a thrown curveball spins; and defensive tracking – how many feet this shortstop can move left to snag a ground ball, or a right-fielder to catch a fly. And there are new, composite stats, like OPS (on-base plus slugging). I will not try to explain OPS, because it is a mathematical abstraction that I cannot grasp. It signifies a blend of on-base percentage and slugging percentage, which to me is like what you get when you blend a tomato with a broccoli. Or something.
And, stats aside, you do still have to win. Not long ago the Boston Red Sox had a relief pitcher whose spin rate was splendid, but he couldn’t get anybody out.
The real aim of the new broadcast innovations noted above comes at the end of the report:
In an effort to at least reach, if not grow, a younger fan base, MLB from now on will focus on video engagement, gaming, and augmented reality on Snapchat.
You got it: the goal is to reduce baseball to a video game, and its players to gaming characters, perhaps with big contracts and marketing deals. Hey, check out that dude’s OPS!
You can’t measure a Zeitgeist, but you certainly know when it’s sitting on your chest. Your respirations get depressed. Measurably.
Yeah, I sound like every cranky old man in history. But hey – I’m Emeritus! See this column’s title!
In addition, the article has one more detail:
Curiosity about whether a fly ball to deep right field at Fenway Park would be a home run at Yankee Stadium can be satisfied by overlaying the Yankee Stadium footprint on top of Fenway.
Maybe it would satisfy you, buddy, but anything that superimposes Yankee Stadium on top of Fenway Park dissatisfies me by a factor of 6.7!
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Data, as we all know, have taken over the world. ”
Statistical objectivity is in, individuality is out. You may have taught for 30 years and gained a sense for which child has a problem that needs intervention and which one just needs patience and time to develop. You may have managed patients for decades and have a hunch about who needs immediate help and who can be watched. But “senses” and “hunches” can’t be measured and therefore do not exist, or better, don’t count. Numbers count!
Data-obsession reflects what Germans call the Zeitgeist, the spirit of the age. But the Germans will have to come up with a different word for our age, won’t they? Nobody can measure a “spirit.”
Still, you know the spirit’s there, when it knocks you over and stomps on you.
The one sphere of life that has resisted being reduced to numbers is sports. In sports, you don’t need complex analysis to know who’s No. 1 and who’s number everything else. No. 1 crosses the finish line first, wins the most games, knocks out the opponent. The one lying on the mat is No. 2.
Of course, sports always had lots of numbers. Baseball fans have always known about batting averages, runs batted in, earned run averages. But there were always those individual intangibles that goggle the eyes of small boys and keep sportswriters in business: this athlete’s “ferocious drive,” that one’s “will to win,” the way a third “always comes through in the clutch.” Pitchers who couldn’t throw fast anymore were “crafty.” Grizzled, tobacco-chewing scouts could sense which youngster “looked like a ballplayer.”
As if you didn’t already know, you can tell how old I am to talk this way. Bill James and his statistical acolytes put paid to that old kind of thinking a long time ago. Read Moneyball or see the movie. In sports too, it’s now all about the stats.
To generate flagging interest among the young for America’s now-stodgy pastime, Major League Baseball has brought out Statcast 2.0., which adds, according to a recent news story, “Doppler-based tracking of pitch velocity, exit velocity, launch angles, and spin rates, and defensive tracking of players.” Multicamera arrays produce “biomechanical imaging and skeletal models that can help pitchers with delivery issues or batters with swing path quandaries.”
And so we have lots of new data to ponder: exit velocity – how fast a hit ball leaves the bat; launch angle – what angle it leaves at; spin rate – how fast a thrown curveball spins; and defensive tracking – how many feet this shortstop can move left to snag a ground ball, or a right-fielder to catch a fly. And there are new, composite stats, like OPS (on-base plus slugging). I will not try to explain OPS, because it is a mathematical abstraction that I cannot grasp. It signifies a blend of on-base percentage and slugging percentage, which to me is like what you get when you blend a tomato with a broccoli. Or something.
And, stats aside, you do still have to win. Not long ago the Boston Red Sox had a relief pitcher whose spin rate was splendid, but he couldn’t get anybody out.
The real aim of the new broadcast innovations noted above comes at the end of the report:
In an effort to at least reach, if not grow, a younger fan base, MLB from now on will focus on video engagement, gaming, and augmented reality on Snapchat.
You got it: the goal is to reduce baseball to a video game, and its players to gaming characters, perhaps with big contracts and marketing deals. Hey, check out that dude’s OPS!
You can’t measure a Zeitgeist, but you certainly know when it’s sitting on your chest. Your respirations get depressed. Measurably.
Yeah, I sound like every cranky old man in history. But hey – I’m Emeritus! See this column’s title!
In addition, the article has one more detail:
Curiosity about whether a fly ball to deep right field at Fenway Park would be a home run at Yankee Stadium can be satisfied by overlaying the Yankee Stadium footprint on top of Fenway.
Maybe it would satisfy you, buddy, but anything that superimposes Yankee Stadium on top of Fenway Park dissatisfies me by a factor of 6.7!
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Hospitalist Medicare payments are at risk for large cuts in 2021
Now is the time to act
From the beginning, SHM has consciously and consistently taken a unique approach to its advocacy efforts with the federal government. The advocacy priorities of SHM most often concern issues that we feel have an impact on our patients and the broader delivery system, as opposed to a focus on issues that have direct financial benefit to our members.
This strategy has served SHM well. It has earned respect among policymakers and we have seen significant success for a young and relatively small medical society. The issues where we spend the bulk of our time and effort include advocating for issues like alternative payment models (APMs), which reward care quality as opposed to volume, as well as issues related to data integrity that APMs require. We have advocated strongly for changes to dysfunctional observation status rules, for workforce adequacy and sustainability, and for recognition of the importance of hospital medicine’s contribution to the redesign of our nations delivery system. And SHM will continue to advocate for many other issues identified as being important to hospital medicine and our patients.
This year, for the first time in the two decades that I have served on the SHM Public Policy Committee, Medicare has proposed changes that would create unprecedented financial hardship for hospital medicine groups. Each year, as a part of its advocacy agenda, SHM reviews and comments on proposed changes to the Medicare Physician Fee Schedule (PFS). Among other things, the PFS adjusts payment rates to physicians for specific services. Changes under the PFS are required to be budget neutral. In effect, budget neutrality means that whenever certain services receive an increased payment rate, CMS is required to offset these changes by making cuts to other services. This year, in an effort to correct the long-standing underfunding of primary care services, CMS has increased payment for many Evaluation and Management (E&M) codes associated with outpatient primary care services. However, due to budget neutrality requirements, many inpatient E&M care services will be receiving significant cuts.
The goal of increasing payment rates for primary care services is laudable, as many of these cognitive services have been long underfunded. However, the proposed payment increases will only apply to outpatient E&M codes and not their corresponding inpatient codes. While our outpatient Internal Medicine and Family Practice colleagues will benefit from these changes, inpatient providers, including hospitalists, stand to lose a significant amount revenue. SHM and the hospitalists we represent estimate that the proposed budget neutrality adjustment will lead to an approximate 8 percent decrease in Medicare Fee for Services (FFS) revenue. Hospitalists are among the specialties that will be most impacted from these proposed changes. If put into effect, these proposals will leave hospital medicine behind.
These changes have been proposed at a time when hospitalists, along with their colleagues in critical care and emergency medicine, have been caring for patients on the frontlines of the COVID-19 pandemic at great risk to themselves at their families. While hospitalists are working tirelessly to provide lifesaving care to COVID-positive patients throughout the country, hospitalist groups have struggled financially as a result of the pandemic. Inpatient volumes, and therefore care reimbursement, has dropped significantly. Many hospitalists have already reported pay reductions of 20% or more. Others have seen their shifts reduced, resulting in understaffing, which may compromise the quality of care. For many groups, a Medicare reimbursement cut of this magnitude add fuel to an already strained revenue stream and will not be financially sustainable.
SHM is, of course, fighting back. We are not asking CMS to completely abandon the increases in reimbursement for primary care outpatient codes, and we support properly valuing outpatient care services. However, we are asking CMS to find a solution that does not come at the expense of hospital medicine and the other specialties that care for acutely ill hospitalized patients, including patients with COVID-19. If a better solution requires holding off on the proposal for another year, CMS should do so. Furthermore, SHM is asking Congress to abandon the statutory requirement for budget neutrality in these extraordinary times as CMS and Congress work to find towards a solution that properly values both inpatient and outpatient care services.
To send a message to your representatives urging them to stop these payment cuts, please visit SHM’s Legislative Action Center at www.votervoice.net/SHM/campaigns/77226/respond. You can read our full comments on the Medicare Physician Fee Schedule Proposed Rule at www.hospitalmedicine.org/policy--advocacy/letters/2021-physician-fee-schedule-proposed-rule/.
Now is the time to act
Now is the time to act
From the beginning, SHM has consciously and consistently taken a unique approach to its advocacy efforts with the federal government. The advocacy priorities of SHM most often concern issues that we feel have an impact on our patients and the broader delivery system, as opposed to a focus on issues that have direct financial benefit to our members.
This strategy has served SHM well. It has earned respect among policymakers and we have seen significant success for a young and relatively small medical society. The issues where we spend the bulk of our time and effort include advocating for issues like alternative payment models (APMs), which reward care quality as opposed to volume, as well as issues related to data integrity that APMs require. We have advocated strongly for changes to dysfunctional observation status rules, for workforce adequacy and sustainability, and for recognition of the importance of hospital medicine’s contribution to the redesign of our nations delivery system. And SHM will continue to advocate for many other issues identified as being important to hospital medicine and our patients.
This year, for the first time in the two decades that I have served on the SHM Public Policy Committee, Medicare has proposed changes that would create unprecedented financial hardship for hospital medicine groups. Each year, as a part of its advocacy agenda, SHM reviews and comments on proposed changes to the Medicare Physician Fee Schedule (PFS). Among other things, the PFS adjusts payment rates to physicians for specific services. Changes under the PFS are required to be budget neutral. In effect, budget neutrality means that whenever certain services receive an increased payment rate, CMS is required to offset these changes by making cuts to other services. This year, in an effort to correct the long-standing underfunding of primary care services, CMS has increased payment for many Evaluation and Management (E&M) codes associated with outpatient primary care services. However, due to budget neutrality requirements, many inpatient E&M care services will be receiving significant cuts.
The goal of increasing payment rates for primary care services is laudable, as many of these cognitive services have been long underfunded. However, the proposed payment increases will only apply to outpatient E&M codes and not their corresponding inpatient codes. While our outpatient Internal Medicine and Family Practice colleagues will benefit from these changes, inpatient providers, including hospitalists, stand to lose a significant amount revenue. SHM and the hospitalists we represent estimate that the proposed budget neutrality adjustment will lead to an approximate 8 percent decrease in Medicare Fee for Services (FFS) revenue. Hospitalists are among the specialties that will be most impacted from these proposed changes. If put into effect, these proposals will leave hospital medicine behind.
These changes have been proposed at a time when hospitalists, along with their colleagues in critical care and emergency medicine, have been caring for patients on the frontlines of the COVID-19 pandemic at great risk to themselves at their families. While hospitalists are working tirelessly to provide lifesaving care to COVID-positive patients throughout the country, hospitalist groups have struggled financially as a result of the pandemic. Inpatient volumes, and therefore care reimbursement, has dropped significantly. Many hospitalists have already reported pay reductions of 20% or more. Others have seen their shifts reduced, resulting in understaffing, which may compromise the quality of care. For many groups, a Medicare reimbursement cut of this magnitude add fuel to an already strained revenue stream and will not be financially sustainable.
SHM is, of course, fighting back. We are not asking CMS to completely abandon the increases in reimbursement for primary care outpatient codes, and we support properly valuing outpatient care services. However, we are asking CMS to find a solution that does not come at the expense of hospital medicine and the other specialties that care for acutely ill hospitalized patients, including patients with COVID-19. If a better solution requires holding off on the proposal for another year, CMS should do so. Furthermore, SHM is asking Congress to abandon the statutory requirement for budget neutrality in these extraordinary times as CMS and Congress work to find towards a solution that properly values both inpatient and outpatient care services.
To send a message to your representatives urging them to stop these payment cuts, please visit SHM’s Legislative Action Center at www.votervoice.net/SHM/campaigns/77226/respond. You can read our full comments on the Medicare Physician Fee Schedule Proposed Rule at www.hospitalmedicine.org/policy--advocacy/letters/2021-physician-fee-schedule-proposed-rule/.
From the beginning, SHM has consciously and consistently taken a unique approach to its advocacy efforts with the federal government. The advocacy priorities of SHM most often concern issues that we feel have an impact on our patients and the broader delivery system, as opposed to a focus on issues that have direct financial benefit to our members.
This strategy has served SHM well. It has earned respect among policymakers and we have seen significant success for a young and relatively small medical society. The issues where we spend the bulk of our time and effort include advocating for issues like alternative payment models (APMs), which reward care quality as opposed to volume, as well as issues related to data integrity that APMs require. We have advocated strongly for changes to dysfunctional observation status rules, for workforce adequacy and sustainability, and for recognition of the importance of hospital medicine’s contribution to the redesign of our nations delivery system. And SHM will continue to advocate for many other issues identified as being important to hospital medicine and our patients.
This year, for the first time in the two decades that I have served on the SHM Public Policy Committee, Medicare has proposed changes that would create unprecedented financial hardship for hospital medicine groups. Each year, as a part of its advocacy agenda, SHM reviews and comments on proposed changes to the Medicare Physician Fee Schedule (PFS). Among other things, the PFS adjusts payment rates to physicians for specific services. Changes under the PFS are required to be budget neutral. In effect, budget neutrality means that whenever certain services receive an increased payment rate, CMS is required to offset these changes by making cuts to other services. This year, in an effort to correct the long-standing underfunding of primary care services, CMS has increased payment for many Evaluation and Management (E&M) codes associated with outpatient primary care services. However, due to budget neutrality requirements, many inpatient E&M care services will be receiving significant cuts.
The goal of increasing payment rates for primary care services is laudable, as many of these cognitive services have been long underfunded. However, the proposed payment increases will only apply to outpatient E&M codes and not their corresponding inpatient codes. While our outpatient Internal Medicine and Family Practice colleagues will benefit from these changes, inpatient providers, including hospitalists, stand to lose a significant amount revenue. SHM and the hospitalists we represent estimate that the proposed budget neutrality adjustment will lead to an approximate 8 percent decrease in Medicare Fee for Services (FFS) revenue. Hospitalists are among the specialties that will be most impacted from these proposed changes. If put into effect, these proposals will leave hospital medicine behind.
These changes have been proposed at a time when hospitalists, along with their colleagues in critical care and emergency medicine, have been caring for patients on the frontlines of the COVID-19 pandemic at great risk to themselves at their families. While hospitalists are working tirelessly to provide lifesaving care to COVID-positive patients throughout the country, hospitalist groups have struggled financially as a result of the pandemic. Inpatient volumes, and therefore care reimbursement, has dropped significantly. Many hospitalists have already reported pay reductions of 20% or more. Others have seen their shifts reduced, resulting in understaffing, which may compromise the quality of care. For many groups, a Medicare reimbursement cut of this magnitude add fuel to an already strained revenue stream and will not be financially sustainable.
SHM is, of course, fighting back. We are not asking CMS to completely abandon the increases in reimbursement for primary care outpatient codes, and we support properly valuing outpatient care services. However, we are asking CMS to find a solution that does not come at the expense of hospital medicine and the other specialties that care for acutely ill hospitalized patients, including patients with COVID-19. If a better solution requires holding off on the proposal for another year, CMS should do so. Furthermore, SHM is asking Congress to abandon the statutory requirement for budget neutrality in these extraordinary times as CMS and Congress work to find towards a solution that properly values both inpatient and outpatient care services.
To send a message to your representatives urging them to stop these payment cuts, please visit SHM’s Legislative Action Center at www.votervoice.net/SHM/campaigns/77226/respond. You can read our full comments on the Medicare Physician Fee Schedule Proposed Rule at www.hospitalmedicine.org/policy--advocacy/letters/2021-physician-fee-schedule-proposed-rule/.
Case of the inappropriate endoscopy referral
A 53-year-old woman was referred for surveillance colonoscopy. She is a current smoker with a history of chronic kidney disease, chronic obstructive pulmonary disease, atrial fibrillation, and two diminutive hyperplastic polyps found on average-risk screening colonoscopy 3 years previously. Her prep at the time was excellent and she was advised to return in 10 years for follow-up. She has taken the day off work, arranged for a driver, is prepped, and is on your schedule for a colonoscopy for a “history of polyps.” Is this an appropriate referral and how should you handle it?
Most of us have had questionable referrals on our endoscopy schedules. While judgments can vary among providers about when a patient should undergo a procedure or what intervention is most needed, some direct-access referrals for endoscopy are considered inappropriate by most standards. In examining referrals for colonoscopy, studies have shown that as many as 23% of screening colonoscopies among Medicare beneficiaries and 14.2% of Veterans Affairs patients in a large colorectal cancer screening study are inappropriate.1,2 A prospective multicenter study found 29% of colonoscopies to be inappropriate, and surveillance studies were confirmed as the most frequent source of inappropriate procedures.3,4 Endoscopies are performed so frequently, effectively, and safely that they can be readily scheduled by gastroenterologists and nongastroenterologists alike. Open access has facilitated and expedited needed procedures, providing benefit to patient and provider and freeing clinic visit time for more complex consults. But while endoscopy is very safe, it is not without risk or cost. What should be the response when a patient in the endoscopy unit appears to be inappropriately referred?
The first step is to determine what is inappropriate. There are several situations when a procedure might be considered inappropriate, particularly when we try to apply ethical principles.
1. The performance of the procedure is contrary to society guidelines. The American Gastroenterological Association, American Society for Gastrointestinal Endoscopy, and American College of Gastroenterology publish clinical guidelines. These documents are drafted after rigorous research and literature review, and the strength of the recommendations is confirmed by incorporation of GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology. Such guidelines allow gastroenterologists across the country to practice confidently in a manner consistent with the current available data and the standards of care for the GI community. A patient who is referred for a procedure for an indication that does not adhere to – or contradicts – guidelines, may be at risk for substandard care and possibly at risk for harm. It is the physician’s ethical responsibility to provide the most “good” and the least harm for patients, consistent with the ethical principle of beneficence.
Guidelines, however, are not mandates, and an argument may be made that in order to provide the best care, alternatives may be offered to a patient. Some circumstances require clinical judgments based on unique patient characteristics and the need for individualized care. As a rule, however, the goal of guidelines is to assist doctors in providing the best care.
2. The procedure is not the correct test for the clinical question. While endoscopy can address many clinical queries, endoscopy is not always the right procedure for a specific medical question. A patient referred for an esophagogastroduodenoscopy (EGD) to rule out gastroparesis is being subjected to the wrong test to answer the clinical question. Some information may be obtained from an EGD (e.g., retained food may suggest dysmotility or the patient could have gastric outlet obstruction) but this is not the recommended initial management step. Is it reasonable to proceed with a test that cannot answer the question asked? Continuing with the endoscopy would not enhance beneficence and might be a futile service for the patient. Is this doing the best for the patient?
3. The risks of the procedure outweigh the benefits. Some procedures may be consistent with guidelines and able to answer the questions asked, but may present more risk than benefit. Should an elderly patient with multiple significant comorbidities and a likely limited life span undergo a follow-up colonoscopy even at an appropriate interval? The principle of nonmaleficence is the clear standard here.
4. The intent for doing the procedure has questionable merit. Some patients may request an EGD at the time of the screening colonoscopy just to “check,” regardless of symptoms or risk category. A patient has a right to make her/his own decisions but patient autonomy should not be an excuse for a nonindicated procedure.
In the case of the 53-year-old woman referred for surveillance colonoscopy, the physician needs to consider whether performing the test is inappropriate for any of the above reasons. First and foremost, is it doing the most good for the patient?
On the one hand, performing an inappropriately referred procedure contradicts guidelines and may present undue risk of complication from anesthesia or endoscopy. Would the physician be ethically compromised in this situation, or even legally liable should a complication arise during a procedure done for a questionable indication?
On the other hand, canceling such a procedure creates multiple dilemmas. The autonomy and the convenience of the patient need to be respected. The patient who has followed all the instructions, is prepped, has taken off work, arranged for transportation, and wants to have the procedure done may have difficulty accepting a cancellation. Colonoscopy is a safe test. Is it the right thing to cancel her procedure because of an imprudent referral? Would this undermine the patient’s confidence in her referring provider? Physicians may face other pressures to proceed, such as practice or institutional restraints that discourage same-day cancellations. Maintenance of robust financial practices, stable referral sources, and excellent patient satisfaction measures are critical to running an efficient endoscopy unit and maximizing patient service and care.
Is there a sensible way to address the dilemma? One approach is simply to move ahead with the procedure if the physician feels that the benefits outweigh the medical and ethical risks. Besides patient convenience, other “benefits” could be relevant: clinical value from an unexpected finding, affirmation of the patient’s invested time and effort, and avoidance of the apparent undermining of the authority of a referring colleague. Finally, maintaining productive and efficient practices or institutions ultimately allows for better patient care. The physician can explain the enhanced risks, present the alternatives, and – perhaps in less time than the ethical deliberations might take – complete the procedure and have the patient resting comfortably in the recovery unit.
An alternative approach is to cancel the procedure if the physician feels that the indication is not legitimate, or that the risks to the patient and the physician are significant. Explaining the cancellation can be difficult but may be the right decision if ethical principles of beneficence are upheld. It is understood that procedures consume health care resources and can present an undue expense to society if done for improper reasons. Unnecessary procedures clutter schedules for patients who truly need an endoscopy.
Neither approach is completely satisfying, although moving forward with a likely very safe procedure is often the easiest step and probably what many physicians do in this setting.
Is there a better way to approach this problem? Preventing the ethical dilemma is the ideal scenario, although not always feasible. Here are some suggestions to consider.
Reviewing referrals prior to the procedure day allows endoscopists to contact and cancel patients if needed, before the prep and travel begin. This addresses the convenience aspects but not the issue regarding the underlying indication.
The most important step toward avoiding inappropriate referrals is better education for referring providers. Even gastroenterologists, let alone primary care physicians, may struggle to stay current on changing clinical GI guidelines. Colorectal cancer screening, for example, is an area that gives gastroenterologists an opportunity to communicate with and educate colleagues about appropriate management. Keeping our referral base up to date about guidelines and prep and safety recommendations will likely reduce the number of inappropriate colonoscopy referrals and provide many of the benefits described above.
Providing the best care for patients by adhering to medical ethical principles is the goal of our work as physicians. Implementing this goal may demand tough decisions.
Dr. Fisher is professor of clinical medicine and director of small-bowel imaging, division of gastroenterology, University of Pennsylvania, Philadelphia.
References
1. Sheffield KM et al. JAMA Intern Med. 2013 Apr 8;173(7):542-50.
2. Powell AA et al. J Gen Intern Med. 2015 Jun;30(6):732-41.
3. Petruzziello L et al. J Clin Gastroenterol. 2012;46(7):590-4.
4. Kapila N et al. Dig Dis Sci. 2019;64(10):2798-805.
A 53-year-old woman was referred for surveillance colonoscopy. She is a current smoker with a history of chronic kidney disease, chronic obstructive pulmonary disease, atrial fibrillation, and two diminutive hyperplastic polyps found on average-risk screening colonoscopy 3 years previously. Her prep at the time was excellent and she was advised to return in 10 years for follow-up. She has taken the day off work, arranged for a driver, is prepped, and is on your schedule for a colonoscopy for a “history of polyps.” Is this an appropriate referral and how should you handle it?
Most of us have had questionable referrals on our endoscopy schedules. While judgments can vary among providers about when a patient should undergo a procedure or what intervention is most needed, some direct-access referrals for endoscopy are considered inappropriate by most standards. In examining referrals for colonoscopy, studies have shown that as many as 23% of screening colonoscopies among Medicare beneficiaries and 14.2% of Veterans Affairs patients in a large colorectal cancer screening study are inappropriate.1,2 A prospective multicenter study found 29% of colonoscopies to be inappropriate, and surveillance studies were confirmed as the most frequent source of inappropriate procedures.3,4 Endoscopies are performed so frequently, effectively, and safely that they can be readily scheduled by gastroenterologists and nongastroenterologists alike. Open access has facilitated and expedited needed procedures, providing benefit to patient and provider and freeing clinic visit time for more complex consults. But while endoscopy is very safe, it is not without risk or cost. What should be the response when a patient in the endoscopy unit appears to be inappropriately referred?
The first step is to determine what is inappropriate. There are several situations when a procedure might be considered inappropriate, particularly when we try to apply ethical principles.
1. The performance of the procedure is contrary to society guidelines. The American Gastroenterological Association, American Society for Gastrointestinal Endoscopy, and American College of Gastroenterology publish clinical guidelines. These documents are drafted after rigorous research and literature review, and the strength of the recommendations is confirmed by incorporation of GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology. Such guidelines allow gastroenterologists across the country to practice confidently in a manner consistent with the current available data and the standards of care for the GI community. A patient who is referred for a procedure for an indication that does not adhere to – or contradicts – guidelines, may be at risk for substandard care and possibly at risk for harm. It is the physician’s ethical responsibility to provide the most “good” and the least harm for patients, consistent with the ethical principle of beneficence.
Guidelines, however, are not mandates, and an argument may be made that in order to provide the best care, alternatives may be offered to a patient. Some circumstances require clinical judgments based on unique patient characteristics and the need for individualized care. As a rule, however, the goal of guidelines is to assist doctors in providing the best care.
2. The procedure is not the correct test for the clinical question. While endoscopy can address many clinical queries, endoscopy is not always the right procedure for a specific medical question. A patient referred for an esophagogastroduodenoscopy (EGD) to rule out gastroparesis is being subjected to the wrong test to answer the clinical question. Some information may be obtained from an EGD (e.g., retained food may suggest dysmotility or the patient could have gastric outlet obstruction) but this is not the recommended initial management step. Is it reasonable to proceed with a test that cannot answer the question asked? Continuing with the endoscopy would not enhance beneficence and might be a futile service for the patient. Is this doing the best for the patient?
3. The risks of the procedure outweigh the benefits. Some procedures may be consistent with guidelines and able to answer the questions asked, but may present more risk than benefit. Should an elderly patient with multiple significant comorbidities and a likely limited life span undergo a follow-up colonoscopy even at an appropriate interval? The principle of nonmaleficence is the clear standard here.
4. The intent for doing the procedure has questionable merit. Some patients may request an EGD at the time of the screening colonoscopy just to “check,” regardless of symptoms or risk category. A patient has a right to make her/his own decisions but patient autonomy should not be an excuse for a nonindicated procedure.
In the case of the 53-year-old woman referred for surveillance colonoscopy, the physician needs to consider whether performing the test is inappropriate for any of the above reasons. First and foremost, is it doing the most good for the patient?
On the one hand, performing an inappropriately referred procedure contradicts guidelines and may present undue risk of complication from anesthesia or endoscopy. Would the physician be ethically compromised in this situation, or even legally liable should a complication arise during a procedure done for a questionable indication?
On the other hand, canceling such a procedure creates multiple dilemmas. The autonomy and the convenience of the patient need to be respected. The patient who has followed all the instructions, is prepped, has taken off work, arranged for transportation, and wants to have the procedure done may have difficulty accepting a cancellation. Colonoscopy is a safe test. Is it the right thing to cancel her procedure because of an imprudent referral? Would this undermine the patient’s confidence in her referring provider? Physicians may face other pressures to proceed, such as practice or institutional restraints that discourage same-day cancellations. Maintenance of robust financial practices, stable referral sources, and excellent patient satisfaction measures are critical to running an efficient endoscopy unit and maximizing patient service and care.
Is there a sensible way to address the dilemma? One approach is simply to move ahead with the procedure if the physician feels that the benefits outweigh the medical and ethical risks. Besides patient convenience, other “benefits” could be relevant: clinical value from an unexpected finding, affirmation of the patient’s invested time and effort, and avoidance of the apparent undermining of the authority of a referring colleague. Finally, maintaining productive and efficient practices or institutions ultimately allows for better patient care. The physician can explain the enhanced risks, present the alternatives, and – perhaps in less time than the ethical deliberations might take – complete the procedure and have the patient resting comfortably in the recovery unit.
An alternative approach is to cancel the procedure if the physician feels that the indication is not legitimate, or that the risks to the patient and the physician are significant. Explaining the cancellation can be difficult but may be the right decision if ethical principles of beneficence are upheld. It is understood that procedures consume health care resources and can present an undue expense to society if done for improper reasons. Unnecessary procedures clutter schedules for patients who truly need an endoscopy.
Neither approach is completely satisfying, although moving forward with a likely very safe procedure is often the easiest step and probably what many physicians do in this setting.
Is there a better way to approach this problem? Preventing the ethical dilemma is the ideal scenario, although not always feasible. Here are some suggestions to consider.
Reviewing referrals prior to the procedure day allows endoscopists to contact and cancel patients if needed, before the prep and travel begin. This addresses the convenience aspects but not the issue regarding the underlying indication.
The most important step toward avoiding inappropriate referrals is better education for referring providers. Even gastroenterologists, let alone primary care physicians, may struggle to stay current on changing clinical GI guidelines. Colorectal cancer screening, for example, is an area that gives gastroenterologists an opportunity to communicate with and educate colleagues about appropriate management. Keeping our referral base up to date about guidelines and prep and safety recommendations will likely reduce the number of inappropriate colonoscopy referrals and provide many of the benefits described above.
Providing the best care for patients by adhering to medical ethical principles is the goal of our work as physicians. Implementing this goal may demand tough decisions.
Dr. Fisher is professor of clinical medicine and director of small-bowel imaging, division of gastroenterology, University of Pennsylvania, Philadelphia.
References
1. Sheffield KM et al. JAMA Intern Med. 2013 Apr 8;173(7):542-50.
2. Powell AA et al. J Gen Intern Med. 2015 Jun;30(6):732-41.
3. Petruzziello L et al. J Clin Gastroenterol. 2012;46(7):590-4.
4. Kapila N et al. Dig Dis Sci. 2019;64(10):2798-805.
A 53-year-old woman was referred for surveillance colonoscopy. She is a current smoker with a history of chronic kidney disease, chronic obstructive pulmonary disease, atrial fibrillation, and two diminutive hyperplastic polyps found on average-risk screening colonoscopy 3 years previously. Her prep at the time was excellent and she was advised to return in 10 years for follow-up. She has taken the day off work, arranged for a driver, is prepped, and is on your schedule for a colonoscopy for a “history of polyps.” Is this an appropriate referral and how should you handle it?
Most of us have had questionable referrals on our endoscopy schedules. While judgments can vary among providers about when a patient should undergo a procedure or what intervention is most needed, some direct-access referrals for endoscopy are considered inappropriate by most standards. In examining referrals for colonoscopy, studies have shown that as many as 23% of screening colonoscopies among Medicare beneficiaries and 14.2% of Veterans Affairs patients in a large colorectal cancer screening study are inappropriate.1,2 A prospective multicenter study found 29% of colonoscopies to be inappropriate, and surveillance studies were confirmed as the most frequent source of inappropriate procedures.3,4 Endoscopies are performed so frequently, effectively, and safely that they can be readily scheduled by gastroenterologists and nongastroenterologists alike. Open access has facilitated and expedited needed procedures, providing benefit to patient and provider and freeing clinic visit time for more complex consults. But while endoscopy is very safe, it is not without risk or cost. What should be the response when a patient in the endoscopy unit appears to be inappropriately referred?
The first step is to determine what is inappropriate. There are several situations when a procedure might be considered inappropriate, particularly when we try to apply ethical principles.
1. The performance of the procedure is contrary to society guidelines. The American Gastroenterological Association, American Society for Gastrointestinal Endoscopy, and American College of Gastroenterology publish clinical guidelines. These documents are drafted after rigorous research and literature review, and the strength of the recommendations is confirmed by incorporation of GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology. Such guidelines allow gastroenterologists across the country to practice confidently in a manner consistent with the current available data and the standards of care for the GI community. A patient who is referred for a procedure for an indication that does not adhere to – or contradicts – guidelines, may be at risk for substandard care and possibly at risk for harm. It is the physician’s ethical responsibility to provide the most “good” and the least harm for patients, consistent with the ethical principle of beneficence.
Guidelines, however, are not mandates, and an argument may be made that in order to provide the best care, alternatives may be offered to a patient. Some circumstances require clinical judgments based on unique patient characteristics and the need for individualized care. As a rule, however, the goal of guidelines is to assist doctors in providing the best care.
2. The procedure is not the correct test for the clinical question. While endoscopy can address many clinical queries, endoscopy is not always the right procedure for a specific medical question. A patient referred for an esophagogastroduodenoscopy (EGD) to rule out gastroparesis is being subjected to the wrong test to answer the clinical question. Some information may be obtained from an EGD (e.g., retained food may suggest dysmotility or the patient could have gastric outlet obstruction) but this is not the recommended initial management step. Is it reasonable to proceed with a test that cannot answer the question asked? Continuing with the endoscopy would not enhance beneficence and might be a futile service for the patient. Is this doing the best for the patient?
3. The risks of the procedure outweigh the benefits. Some procedures may be consistent with guidelines and able to answer the questions asked, but may present more risk than benefit. Should an elderly patient with multiple significant comorbidities and a likely limited life span undergo a follow-up colonoscopy even at an appropriate interval? The principle of nonmaleficence is the clear standard here.
4. The intent for doing the procedure has questionable merit. Some patients may request an EGD at the time of the screening colonoscopy just to “check,” regardless of symptoms or risk category. A patient has a right to make her/his own decisions but patient autonomy should not be an excuse for a nonindicated procedure.
In the case of the 53-year-old woman referred for surveillance colonoscopy, the physician needs to consider whether performing the test is inappropriate for any of the above reasons. First and foremost, is it doing the most good for the patient?
On the one hand, performing an inappropriately referred procedure contradicts guidelines and may present undue risk of complication from anesthesia or endoscopy. Would the physician be ethically compromised in this situation, or even legally liable should a complication arise during a procedure done for a questionable indication?
On the other hand, canceling such a procedure creates multiple dilemmas. The autonomy and the convenience of the patient need to be respected. The patient who has followed all the instructions, is prepped, has taken off work, arranged for transportation, and wants to have the procedure done may have difficulty accepting a cancellation. Colonoscopy is a safe test. Is it the right thing to cancel her procedure because of an imprudent referral? Would this undermine the patient’s confidence in her referring provider? Physicians may face other pressures to proceed, such as practice or institutional restraints that discourage same-day cancellations. Maintenance of robust financial practices, stable referral sources, and excellent patient satisfaction measures are critical to running an efficient endoscopy unit and maximizing patient service and care.
Is there a sensible way to address the dilemma? One approach is simply to move ahead with the procedure if the physician feels that the benefits outweigh the medical and ethical risks. Besides patient convenience, other “benefits” could be relevant: clinical value from an unexpected finding, affirmation of the patient’s invested time and effort, and avoidance of the apparent undermining of the authority of a referring colleague. Finally, maintaining productive and efficient practices or institutions ultimately allows for better patient care. The physician can explain the enhanced risks, present the alternatives, and – perhaps in less time than the ethical deliberations might take – complete the procedure and have the patient resting comfortably in the recovery unit.
An alternative approach is to cancel the procedure if the physician feels that the indication is not legitimate, or that the risks to the patient and the physician are significant. Explaining the cancellation can be difficult but may be the right decision if ethical principles of beneficence are upheld. It is understood that procedures consume health care resources and can present an undue expense to society if done for improper reasons. Unnecessary procedures clutter schedules for patients who truly need an endoscopy.
Neither approach is completely satisfying, although moving forward with a likely very safe procedure is often the easiest step and probably what many physicians do in this setting.
Is there a better way to approach this problem? Preventing the ethical dilemma is the ideal scenario, although not always feasible. Here are some suggestions to consider.
Reviewing referrals prior to the procedure day allows endoscopists to contact and cancel patients if needed, before the prep and travel begin. This addresses the convenience aspects but not the issue regarding the underlying indication.
The most important step toward avoiding inappropriate referrals is better education for referring providers. Even gastroenterologists, let alone primary care physicians, may struggle to stay current on changing clinical GI guidelines. Colorectal cancer screening, for example, is an area that gives gastroenterologists an opportunity to communicate with and educate colleagues about appropriate management. Keeping our referral base up to date about guidelines and prep and safety recommendations will likely reduce the number of inappropriate colonoscopy referrals and provide many of the benefits described above.
Providing the best care for patients by adhering to medical ethical principles is the goal of our work as physicians. Implementing this goal may demand tough decisions.
Dr. Fisher is professor of clinical medicine and director of small-bowel imaging, division of gastroenterology, University of Pennsylvania, Philadelphia.
References
1. Sheffield KM et al. JAMA Intern Med. 2013 Apr 8;173(7):542-50.
2. Powell AA et al. J Gen Intern Med. 2015 Jun;30(6):732-41.
3. Petruzziello L et al. J Clin Gastroenterol. 2012;46(7):590-4.
4. Kapila N et al. Dig Dis Sci. 2019;64(10):2798-805.
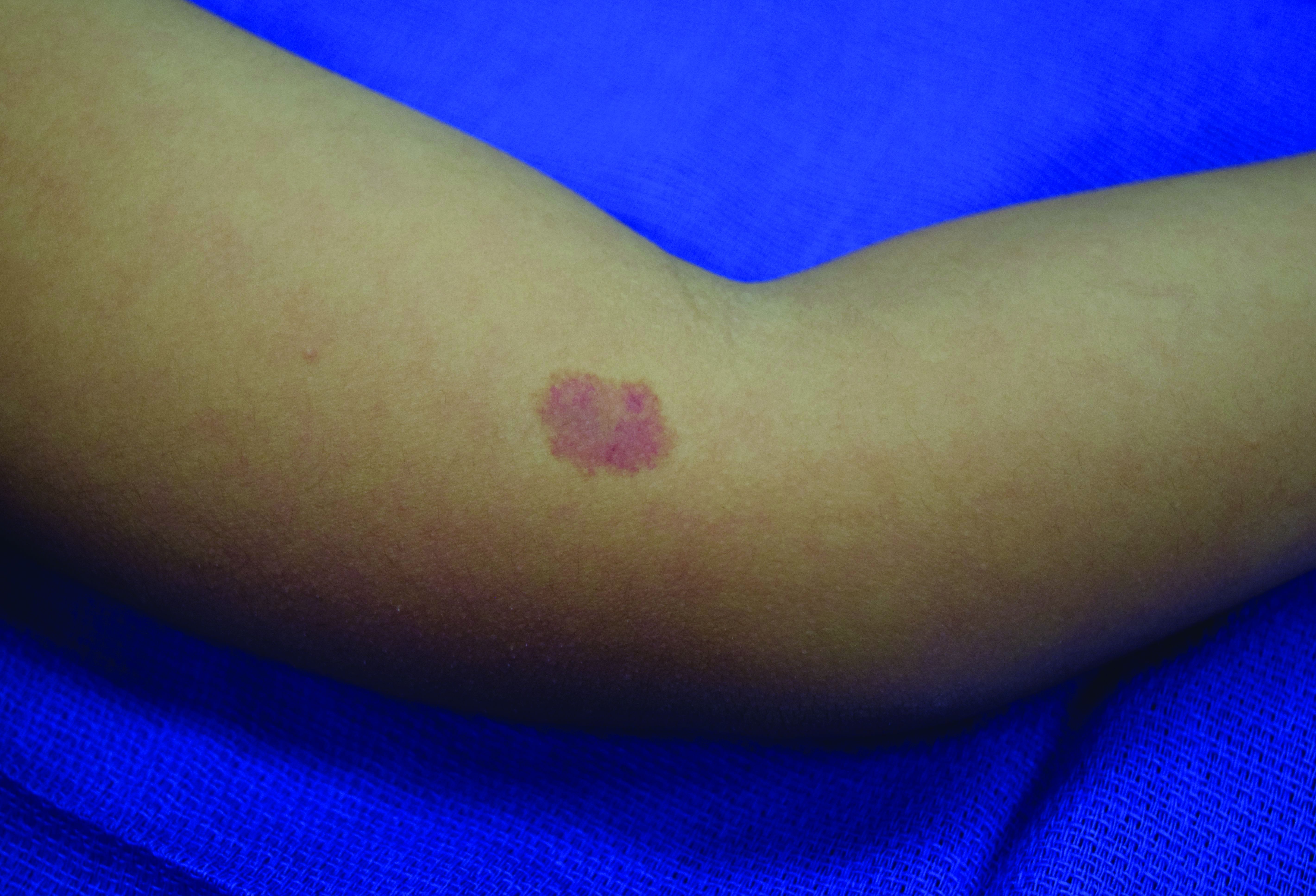
A 4-year-old presented to our pediatric dermatology clinic for evaluation of asymptomatic "brown spots."
Capillary malformation-arteriovenous malformation syndrome
with or without arteriovenous malformations, as well as arteriovenous fistulas (AVFs). CM-AVM is an autosomal dominant disorder.1 CM-AVM type 1 is caused by mutations in the RASA1 gene, and CM-AVM type 2 is caused by mutations in the EPHB4 gene.2 Approximately 70% of patients with RASA1-associated CM-AVM syndrome and 80% of patients with EPHB4-associated CM-AVM syndrome have an affected parent, while the remainder have de novo variants.1
In patients with CM-AVM syndrome, CMs are often present at birth and more are typically acquired over time. CMs are characteristically 1-3 cm in diameter, round or oval, dull red or red-brown macules and patches with a blanched halo.3 Some CMs may be warm to touch indicating a possible underlying AVM or AVF.4 This can be confirmed by Doppler ultrasound, which would demonstrate increased arterial flow.4 CMs are most commonly located on the face and limbs and may present in isolation, but approximately one-third of patients have associated AVMs and AVFs.1,5 These high-flow vascular malformations may be present in skin, muscle, bone, brain, and/or spine and may be asymptomatic or lead to serious sequelae, including bleeding, congestive heart failure, and neurologic complications, such as migraine headaches, seizures, or even stroke.5 Symptoms from intracranial and spinal high-flow lesions usually present in early childhood and affect approximately 7% of patients.3
The diagnosis of CM-AVM should be suspected in an individual with numerous characteristic CMs and may be supported by the presence of AVMs and AVFs, family history of CM-AVM, and/or identification of RASA1 or EPHB4 mutation by molecular genetic testing.1,3 Although there are no consensus protocols for imaging CM-AVM patients, MRI of the brain and spine is recommended at diagnosis to identify underlying high-flow lesions.1 This may allow for early treatment before the development of symptoms.1 Any lesions identified on screening imaging may require regular surveillance, which is best determined by discussion with the radiologist.1 Although there are no reports of patients with negative results on screening imaging who later develop AVMs or AVFs, there should be a low threshold for repeat imaging in patients who develop new symptoms or physical exam findings.3,4
It has previously been suggested that the CMs in CM-AVM may actually represent early or small AVMs and pulsed-dye laser (PDL) treatment was not recommended because of concern for potential progression of lesions.4 However, a recent study demonstrated good response to PDL in patients with CM-AVM with no evidence of worsening or recurrence of lesions with long-term follow-up.6 Treatment of CMs that cause cosmetic concerns may be considered following discussion of risks and benefits with a dermatologist. Management of AVMs and AVFs requires a multidisciplinary team that, depending on location and symptoms of these features, may require the expertise of specialists such as neurosurgery, surgery, orthopedics, cardiology, and/or interventional radiology.1
Given the suspicion for CM-AVM in our patient, further workup was completed. A skin biopsy was consistent with CM. Genetic testing with the Vascular Malformations Panel, Sequencing and Deletion/Duplication revealed a pathogenic variant in the RASA1 gene and a variant of unknown clinical significance in the TEK gene. Parental genetic testing for the RASA1 mutation was negative, supporting a de novo mutation in the patient. CNS imaging showed a small developmental venous malformation in the brain that neurosurgery did not think was clinically significant. At the most recent follow-up at age 8 years, our patient had developed a few new small CMs but was otherwise well.
Dr. Leszczynska is trained in pediatrics and is the current dermatology research fellow at the University of Texas at Austin. Ms. Croce is a dermatology-trained pediatric nurse practitioner and PhD student at the University of Texas at Austin School of Nursing. Dr. Diaz is chief of pediatric dermatology at Dell Children’s Medical Center, Austin, assistant professor of pediatrics and medicine (dermatology), and dermatology residency associate program director at University of Texas at Austin . The authors have no relevant conflicts of interest to disclose. Donna Bilu Martin, MD, is the editor of this column.
References
1. Bayrak-Toydemir P, Stevenson D. Capillary Malformation-Arteriovenous Malformation Syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al., eds. GeneReviews®. Seattle: University of Washington, Seattle; February 22, 2011.
2.Yu J et al. Pediatr Dermatol. 2017 Sep;34(5):e227-30.
3. Orme CM et al. Pediatr Dermatol. 2013 Jul-Aug;30(4):409-15.
4. Weitz NA et al. Pediatr Dermatol. 2015 Jan-Feb;32(1):76-84.
5. Revencu N et al. Hum Mutat. 2013 Dec;34(12):1632-41.
6. Iznardo H et al. Pediatr Dermatol. 2020 Mar;37(2):342-44.
Capillary malformation-arteriovenous malformation syndrome
with or without arteriovenous malformations, as well as arteriovenous fistulas (AVFs). CM-AVM is an autosomal dominant disorder.1 CM-AVM type 1 is caused by mutations in the RASA1 gene, and CM-AVM type 2 is caused by mutations in the EPHB4 gene.2 Approximately 70% of patients with RASA1-associated CM-AVM syndrome and 80% of patients with EPHB4-associated CM-AVM syndrome have an affected parent, while the remainder have de novo variants.1
In patients with CM-AVM syndrome, CMs are often present at birth and more are typically acquired over time. CMs are characteristically 1-3 cm in diameter, round or oval, dull red or red-brown macules and patches with a blanched halo.3 Some CMs may be warm to touch indicating a possible underlying AVM or AVF.4 This can be confirmed by Doppler ultrasound, which would demonstrate increased arterial flow.4 CMs are most commonly located on the face and limbs and may present in isolation, but approximately one-third of patients have associated AVMs and AVFs.1,5 These high-flow vascular malformations may be present in skin, muscle, bone, brain, and/or spine and may be asymptomatic or lead to serious sequelae, including bleeding, congestive heart failure, and neurologic complications, such as migraine headaches, seizures, or even stroke.5 Symptoms from intracranial and spinal high-flow lesions usually present in early childhood and affect approximately 7% of patients.3
The diagnosis of CM-AVM should be suspected in an individual with numerous characteristic CMs and may be supported by the presence of AVMs and AVFs, family history of CM-AVM, and/or identification of RASA1 or EPHB4 mutation by molecular genetic testing.1,3 Although there are no consensus protocols for imaging CM-AVM patients, MRI of the brain and spine is recommended at diagnosis to identify underlying high-flow lesions.1 This may allow for early treatment before the development of symptoms.1 Any lesions identified on screening imaging may require regular surveillance, which is best determined by discussion with the radiologist.1 Although there are no reports of patients with negative results on screening imaging who later develop AVMs or AVFs, there should be a low threshold for repeat imaging in patients who develop new symptoms or physical exam findings.3,4
It has previously been suggested that the CMs in CM-AVM may actually represent early or small AVMs and pulsed-dye laser (PDL) treatment was not recommended because of concern for potential progression of lesions.4 However, a recent study demonstrated good response to PDL in patients with CM-AVM with no evidence of worsening or recurrence of lesions with long-term follow-up.6 Treatment of CMs that cause cosmetic concerns may be considered following discussion of risks and benefits with a dermatologist. Management of AVMs and AVFs requires a multidisciplinary team that, depending on location and symptoms of these features, may require the expertise of specialists such as neurosurgery, surgery, orthopedics, cardiology, and/or interventional radiology.1
Given the suspicion for CM-AVM in our patient, further workup was completed. A skin biopsy was consistent with CM. Genetic testing with the Vascular Malformations Panel, Sequencing and Deletion/Duplication revealed a pathogenic variant in the RASA1 gene and a variant of unknown clinical significance in the TEK gene. Parental genetic testing for the RASA1 mutation was negative, supporting a de novo mutation in the patient. CNS imaging showed a small developmental venous malformation in the brain that neurosurgery did not think was clinically significant. At the most recent follow-up at age 8 years, our patient had developed a few new small CMs but was otherwise well.
Dr. Leszczynska is trained in pediatrics and is the current dermatology research fellow at the University of Texas at Austin. Ms. Croce is a dermatology-trained pediatric nurse practitioner and PhD student at the University of Texas at Austin School of Nursing. Dr. Diaz is chief of pediatric dermatology at Dell Children’s Medical Center, Austin, assistant professor of pediatrics and medicine (dermatology), and dermatology residency associate program director at University of Texas at Austin . The authors have no relevant conflicts of interest to disclose. Donna Bilu Martin, MD, is the editor of this column.
References
1. Bayrak-Toydemir P, Stevenson D. Capillary Malformation-Arteriovenous Malformation Syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al., eds. GeneReviews®. Seattle: University of Washington, Seattle; February 22, 2011.
2.Yu J et al. Pediatr Dermatol. 2017 Sep;34(5):e227-30.
3. Orme CM et al. Pediatr Dermatol. 2013 Jul-Aug;30(4):409-15.
4. Weitz NA et al. Pediatr Dermatol. 2015 Jan-Feb;32(1):76-84.
5. Revencu N et al. Hum Mutat. 2013 Dec;34(12):1632-41.
6. Iznardo H et al. Pediatr Dermatol. 2020 Mar;37(2):342-44.
Capillary malformation-arteriovenous malformation syndrome
with or without arteriovenous malformations, as well as arteriovenous fistulas (AVFs). CM-AVM is an autosomal dominant disorder.1 CM-AVM type 1 is caused by mutations in the RASA1 gene, and CM-AVM type 2 is caused by mutations in the EPHB4 gene.2 Approximately 70% of patients with RASA1-associated CM-AVM syndrome and 80% of patients with EPHB4-associated CM-AVM syndrome have an affected parent, while the remainder have de novo variants.1
In patients with CM-AVM syndrome, CMs are often present at birth and more are typically acquired over time. CMs are characteristically 1-3 cm in diameter, round or oval, dull red or red-brown macules and patches with a blanched halo.3 Some CMs may be warm to touch indicating a possible underlying AVM or AVF.4 This can be confirmed by Doppler ultrasound, which would demonstrate increased arterial flow.4 CMs are most commonly located on the face and limbs and may present in isolation, but approximately one-third of patients have associated AVMs and AVFs.1,5 These high-flow vascular malformations may be present in skin, muscle, bone, brain, and/or spine and may be asymptomatic or lead to serious sequelae, including bleeding, congestive heart failure, and neurologic complications, such as migraine headaches, seizures, or even stroke.5 Symptoms from intracranial and spinal high-flow lesions usually present in early childhood and affect approximately 7% of patients.3
The diagnosis of CM-AVM should be suspected in an individual with numerous characteristic CMs and may be supported by the presence of AVMs and AVFs, family history of CM-AVM, and/or identification of RASA1 or EPHB4 mutation by molecular genetic testing.1,3 Although there are no consensus protocols for imaging CM-AVM patients, MRI of the brain and spine is recommended at diagnosis to identify underlying high-flow lesions.1 This may allow for early treatment before the development of symptoms.1 Any lesions identified on screening imaging may require regular surveillance, which is best determined by discussion with the radiologist.1 Although there are no reports of patients with negative results on screening imaging who later develop AVMs or AVFs, there should be a low threshold for repeat imaging in patients who develop new symptoms or physical exam findings.3,4
It has previously been suggested that the CMs in CM-AVM may actually represent early or small AVMs and pulsed-dye laser (PDL) treatment was not recommended because of concern for potential progression of lesions.4 However, a recent study demonstrated good response to PDL in patients with CM-AVM with no evidence of worsening or recurrence of lesions with long-term follow-up.6 Treatment of CMs that cause cosmetic concerns may be considered following discussion of risks and benefits with a dermatologist. Management of AVMs and AVFs requires a multidisciplinary team that, depending on location and symptoms of these features, may require the expertise of specialists such as neurosurgery, surgery, orthopedics, cardiology, and/or interventional radiology.1
Given the suspicion for CM-AVM in our patient, further workup was completed. A skin biopsy was consistent with CM. Genetic testing with the Vascular Malformations Panel, Sequencing and Deletion/Duplication revealed a pathogenic variant in the RASA1 gene and a variant of unknown clinical significance in the TEK gene. Parental genetic testing for the RASA1 mutation was negative, supporting a de novo mutation in the patient. CNS imaging showed a small developmental venous malformation in the brain that neurosurgery did not think was clinically significant. At the most recent follow-up at age 8 years, our patient had developed a few new small CMs but was otherwise well.
Dr. Leszczynska is trained in pediatrics and is the current dermatology research fellow at the University of Texas at Austin. Ms. Croce is a dermatology-trained pediatric nurse practitioner and PhD student at the University of Texas at Austin School of Nursing. Dr. Diaz is chief of pediatric dermatology at Dell Children’s Medical Center, Austin, assistant professor of pediatrics and medicine (dermatology), and dermatology residency associate program director at University of Texas at Austin . The authors have no relevant conflicts of interest to disclose. Donna Bilu Martin, MD, is the editor of this column.
References
1. Bayrak-Toydemir P, Stevenson D. Capillary Malformation-Arteriovenous Malformation Syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al., eds. GeneReviews®. Seattle: University of Washington, Seattle; February 22, 2011.
2.Yu J et al. Pediatr Dermatol. 2017 Sep;34(5):e227-30.
3. Orme CM et al. Pediatr Dermatol. 2013 Jul-Aug;30(4):409-15.
4. Weitz NA et al. Pediatr Dermatol. 2015 Jan-Feb;32(1):76-84.
5. Revencu N et al. Hum Mutat. 2013 Dec;34(12):1632-41.
6. Iznardo H et al. Pediatr Dermatol. 2020 Mar;37(2):342-44.
Medication adherence challenges and helpers
For most chronic diseases, up to 20%-30% of the pills that are prescribed are not taken. In the case of inhalers for asthma and COPD, patients miss over half of the prescribed doses.
There are many things that contribute to the problem of poor adherence, but people often just simply forget. Thankfully, there are tools designed to help remind patients of what they need to take and when. A survey of apps developed to help patients remember to take their medicines found more than 700 available in Apple and Android app stores.1 Most apps focus on medication alerts, reminders, and medication logs.2 A recent review showed that apps have some – yet limited – effectiveness in increasing adherence, with patient self-reported improvements of 7%-40%.3
Another perhaps more promising area of improving adherence involves high-tech advances in the way medications can be taken. Inhalers are a primary target as they are complicated devices. A patient has to breathe in at the correct time after the inhaler is actuated, and the inhaler works optimally only if the rate of inhalation is sufficient to carry the medication into the lungs.
A number of companies have developed attachments for inhalers (and even inhalers themselves) that can record when the medication is taken through a Bluetooth connection to a patient’s smartphone. These can also assess inspiratory flow. Reminders to take the medication are built into the app, and those reminders disappear if the medication is taken. Patients can receive feedback about the quality of their timing and inspiratory rate to maximize medication delivery to the lungs.4
We learned long ago that it is difficult to take medications three to four times a day, so extended-release tablets were developed to reduce the frequency to once or twice a day. A great deal of work is now being done behind the scenes to develop medications that decrease the need for patients to remember to take their medications. The best examples of this are the long-acting reversible contraception (LARC) devices, specifically IUDs and Nexplanon. Compared with traditional oral contraceptives that need to be taken daily, LARCs reduce the rate of pregnancy by five- to tenfold.
We also now have medications for osteoporosis that can be taken monthly, or even annually. When bisphosphonates were first developed for osteoporosis prevention, they needed to be taken daily. Then a weekly bisphosphonate was developed. Now there is a once-monthly oral bisphosphonate, Ibandronate, and even a once yearly IV bisphosphonate.
Exciting developments have also occurred in the management of diabetes. We may be tempted to take for granted how once-daily long-acting insulin, which releases insulin slowly over the course of a day, has revolutionized the diabetic treatment since its Food and Drug Administration approval in 2000. Yet progress did not end there. The first GLP-1 receptor agonist for diabetes was approved in 2005 and was a twice-a-day medicine. Shortly afterward, a daily GLP-1 was approved, and now there are three once-weekly GLP-1 receptor agonists.
Several pharmaceutical manufacturers are now working on a once-weekly insulin,5 as well as an implantable GLP-1 receptor agonist that will need to be replaced every 6-12 months.6 Imagine your patient coming in once a year to replace his or her potent glucose lowering medication – one that offers a low incidence of hypoglycemia, maintains glucose control all year long, and requires no adherence to a complicated medication regimen.
Similar technology is being used to develop a once-yearly anti-HIV prophylactic medication delivery system.7 This could help prevent the spread of HIV in areas of the world where it may be difficult for people to take daily medications.7
The many technological advances we have described may help us reduce our likelihood of missing a dose of a medication. We are hopeful that progress in this area will continue, and that one day medication adherence will require even less effort from patients than it does today.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. Tabi K et al. Mobile apps for medication management: Review and analysis. JMIR Mhealth Uhealth. 2019 Sep 7(9):13608.
2. Park JYE et al. Mobile phone apps targeting medication adherence: Quality assessment and content analysis of user reviews. JMIR Mhealth Uhealth. 2019 Jan 31;7(1):e11919.
3. Pérez-Jover V et al. Mobile apps for increasing treatment adherence: Systematic review. J Med Internet Res. 2019;21(6):e12505. doi: 10.2196/12505.
4. 4 Smart inhalers that could be lifesaving for people living with asthma & COPD. MyTherapy, July 11, 2019.
5. Rosenstock J et al. Once-weekly insulin for type 2 diabetes without previous insulin treatment. N Engl J Med. 2020 Sep 22. doi: 10.1056/NEJMoa2022474.
6. GLP-1 agonists: From 2 daily injections to 1 per week and beyond. DiaTribe, Jan. 10, 2018.
7. Long-acting HIV prevention tools. Hiv.gov, July 20, 2019.
For most chronic diseases, up to 20%-30% of the pills that are prescribed are not taken. In the case of inhalers for asthma and COPD, patients miss over half of the prescribed doses.
There are many things that contribute to the problem of poor adherence, but people often just simply forget. Thankfully, there are tools designed to help remind patients of what they need to take and when. A survey of apps developed to help patients remember to take their medicines found more than 700 available in Apple and Android app stores.1 Most apps focus on medication alerts, reminders, and medication logs.2 A recent review showed that apps have some – yet limited – effectiveness in increasing adherence, with patient self-reported improvements of 7%-40%.3
Another perhaps more promising area of improving adherence involves high-tech advances in the way medications can be taken. Inhalers are a primary target as they are complicated devices. A patient has to breathe in at the correct time after the inhaler is actuated, and the inhaler works optimally only if the rate of inhalation is sufficient to carry the medication into the lungs.
A number of companies have developed attachments for inhalers (and even inhalers themselves) that can record when the medication is taken through a Bluetooth connection to a patient’s smartphone. These can also assess inspiratory flow. Reminders to take the medication are built into the app, and those reminders disappear if the medication is taken. Patients can receive feedback about the quality of their timing and inspiratory rate to maximize medication delivery to the lungs.4
We learned long ago that it is difficult to take medications three to four times a day, so extended-release tablets were developed to reduce the frequency to once or twice a day. A great deal of work is now being done behind the scenes to develop medications that decrease the need for patients to remember to take their medications. The best examples of this are the long-acting reversible contraception (LARC) devices, specifically IUDs and Nexplanon. Compared with traditional oral contraceptives that need to be taken daily, LARCs reduce the rate of pregnancy by five- to tenfold.
We also now have medications for osteoporosis that can be taken monthly, or even annually. When bisphosphonates were first developed for osteoporosis prevention, they needed to be taken daily. Then a weekly bisphosphonate was developed. Now there is a once-monthly oral bisphosphonate, Ibandronate, and even a once yearly IV bisphosphonate.
Exciting developments have also occurred in the management of diabetes. We may be tempted to take for granted how once-daily long-acting insulin, which releases insulin slowly over the course of a day, has revolutionized the diabetic treatment since its Food and Drug Administration approval in 2000. Yet progress did not end there. The first GLP-1 receptor agonist for diabetes was approved in 2005 and was a twice-a-day medicine. Shortly afterward, a daily GLP-1 was approved, and now there are three once-weekly GLP-1 receptor agonists.
Several pharmaceutical manufacturers are now working on a once-weekly insulin,5 as well as an implantable GLP-1 receptor agonist that will need to be replaced every 6-12 months.6 Imagine your patient coming in once a year to replace his or her potent glucose lowering medication – one that offers a low incidence of hypoglycemia, maintains glucose control all year long, and requires no adherence to a complicated medication regimen.
Similar technology is being used to develop a once-yearly anti-HIV prophylactic medication delivery system.7 This could help prevent the spread of HIV in areas of the world where it may be difficult for people to take daily medications.7
The many technological advances we have described may help us reduce our likelihood of missing a dose of a medication. We are hopeful that progress in this area will continue, and that one day medication adherence will require even less effort from patients than it does today.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. Tabi K et al. Mobile apps for medication management: Review and analysis. JMIR Mhealth Uhealth. 2019 Sep 7(9):13608.
2. Park JYE et al. Mobile phone apps targeting medication adherence: Quality assessment and content analysis of user reviews. JMIR Mhealth Uhealth. 2019 Jan 31;7(1):e11919.
3. Pérez-Jover V et al. Mobile apps for increasing treatment adherence: Systematic review. J Med Internet Res. 2019;21(6):e12505. doi: 10.2196/12505.
4. 4 Smart inhalers that could be lifesaving for people living with asthma & COPD. MyTherapy, July 11, 2019.
5. Rosenstock J et al. Once-weekly insulin for type 2 diabetes without previous insulin treatment. N Engl J Med. 2020 Sep 22. doi: 10.1056/NEJMoa2022474.
6. GLP-1 agonists: From 2 daily injections to 1 per week and beyond. DiaTribe, Jan. 10, 2018.
7. Long-acting HIV prevention tools. Hiv.gov, July 20, 2019.
For most chronic diseases, up to 20%-30% of the pills that are prescribed are not taken. In the case of inhalers for asthma and COPD, patients miss over half of the prescribed doses.
There are many things that contribute to the problem of poor adherence, but people often just simply forget. Thankfully, there are tools designed to help remind patients of what they need to take and when. A survey of apps developed to help patients remember to take their medicines found more than 700 available in Apple and Android app stores.1 Most apps focus on medication alerts, reminders, and medication logs.2 A recent review showed that apps have some – yet limited – effectiveness in increasing adherence, with patient self-reported improvements of 7%-40%.3
Another perhaps more promising area of improving adherence involves high-tech advances in the way medications can be taken. Inhalers are a primary target as they are complicated devices. A patient has to breathe in at the correct time after the inhaler is actuated, and the inhaler works optimally only if the rate of inhalation is sufficient to carry the medication into the lungs.
A number of companies have developed attachments for inhalers (and even inhalers themselves) that can record when the medication is taken through a Bluetooth connection to a patient’s smartphone. These can also assess inspiratory flow. Reminders to take the medication are built into the app, and those reminders disappear if the medication is taken. Patients can receive feedback about the quality of their timing and inspiratory rate to maximize medication delivery to the lungs.4
We learned long ago that it is difficult to take medications three to four times a day, so extended-release tablets were developed to reduce the frequency to once or twice a day. A great deal of work is now being done behind the scenes to develop medications that decrease the need for patients to remember to take their medications. The best examples of this are the long-acting reversible contraception (LARC) devices, specifically IUDs and Nexplanon. Compared with traditional oral contraceptives that need to be taken daily, LARCs reduce the rate of pregnancy by five- to tenfold.
We also now have medications for osteoporosis that can be taken monthly, or even annually. When bisphosphonates were first developed for osteoporosis prevention, they needed to be taken daily. Then a weekly bisphosphonate was developed. Now there is a once-monthly oral bisphosphonate, Ibandronate, and even a once yearly IV bisphosphonate.
Exciting developments have also occurred in the management of diabetes. We may be tempted to take for granted how once-daily long-acting insulin, which releases insulin slowly over the course of a day, has revolutionized the diabetic treatment since its Food and Drug Administration approval in 2000. Yet progress did not end there. The first GLP-1 receptor agonist for diabetes was approved in 2005 and was a twice-a-day medicine. Shortly afterward, a daily GLP-1 was approved, and now there are three once-weekly GLP-1 receptor agonists.
Several pharmaceutical manufacturers are now working on a once-weekly insulin,5 as well as an implantable GLP-1 receptor agonist that will need to be replaced every 6-12 months.6 Imagine your patient coming in once a year to replace his or her potent glucose lowering medication – one that offers a low incidence of hypoglycemia, maintains glucose control all year long, and requires no adherence to a complicated medication regimen.
Similar technology is being used to develop a once-yearly anti-HIV prophylactic medication delivery system.7 This could help prevent the spread of HIV in areas of the world where it may be difficult for people to take daily medications.7
The many technological advances we have described may help us reduce our likelihood of missing a dose of a medication. We are hopeful that progress in this area will continue, and that one day medication adherence will require even less effort from patients than it does today.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. Tabi K et al. Mobile apps for medication management: Review and analysis. JMIR Mhealth Uhealth. 2019 Sep 7(9):13608.
2. Park JYE et al. Mobile phone apps targeting medication adherence: Quality assessment and content analysis of user reviews. JMIR Mhealth Uhealth. 2019 Jan 31;7(1):e11919.
3. Pérez-Jover V et al. Mobile apps for increasing treatment adherence: Systematic review. J Med Internet Res. 2019;21(6):e12505. doi: 10.2196/12505.
4. 4 Smart inhalers that could be lifesaving for people living with asthma & COPD. MyTherapy, July 11, 2019.
5. Rosenstock J et al. Once-weekly insulin for type 2 diabetes without previous insulin treatment. N Engl J Med. 2020 Sep 22. doi: 10.1056/NEJMoa2022474.
6. GLP-1 agonists: From 2 daily injections to 1 per week and beyond. DiaTribe, Jan. 10, 2018.
7. Long-acting HIV prevention tools. Hiv.gov, July 20, 2019.
Coaching in medicine: A perspective
Coaching is a new topic in medicine. I first heard about coaching several years ago and met the term with skepticism. I was unsure how coaching was different than mentoring or advising and I wondered about its usefulness. However, the reason that I even started to learn about coaching was because I was struggling. I had finally arrived in my career, I had my dream job with two healthy kids, a perfect house, and good marriage. I kept hearing the refrain in my head: “Is this all there is?” I had this arrival fallacy that after all this striving and straining that I would finally be content. I felt unfulfilled and was dissatisfied with where I was that was affecting all parts of my life.
As I was wrestling with these thoughts, I had an opportunity to become a coach to residents around the country through the Association of Women Surgeons. I discussed with them what fills them up, what gets them down, how to set goals, and what their goals were for the year, as well as imposter syndrome. Impostor syndrome is defined as a pattern in which an individual doubts their accomplishments or talents and has a persistent internalized fear of being exposed as a “fraud.” Despite external evidence of their competence, those experiencing this phenomenon remain convinced that they are fooling everyone around them and do not deserve all they have achieved. Individuals incorrectly attribute their success to luck or interpret it as a result of deceiving others into thinking they are more intelligent than they perceive themselves to be. Imposter syndrome is prevalent and deep in medicine. As perfectionists, we are especially vulnerable to imposter syndrome as we set unrealistic ideals for ourselves. When we fail to reach these ideals, we feel like frauds, setting up this cycle of self-doubt that is toxic. When we feel that we can’t achieve the goals that we are striving for we will always find ourselves lacking. There is a slow, insidious erosion of self over the years. Imposter syndrome is well documented in medicine and is even felt as early as medical school.1,2
When I began coaching these residents the most profound thing that came out of these sessions was that my life was getting better – I knew what filled me up, what got me down, what my goals were for the year, and how I still deal with imposter syndrome. Coaching gave me a framework for helping determine what I wanted for the rest of my life. As I began coaching, I started learning all the ways in which I could figure out my values, my personal and professional goals, and perhaps most importantly, my relationships with myself and others.
Another perspective on coaching is to look at a professional athlete such as Tom Brady, one of the greatest quarterbacks of all time. He has a quarterback coach. No coach is going to be a better quarterback than Tom Brady. A coach for him is to be there as an advocate, break his fundamentals down technically, and help him improve upon what he already knows. A coach also identifies strengths and weaknesses, and helps him capitalize on both by bringing awareness, reflection, accountability, and support. If world-class athletes still want and benefit from coaching in a sport they have already mastered, coaching for physicians is just another tool to help us improve our abilities in and out of medicine.
Coaching is more encompassing than advising or mentoring. It is about examining deeply held beliefs to see if they are really serving us, if they are in line with our values and how we want to live our lives.
Coaching has also been validated in medicine in several papers. In an article by Dyrbye et al. in JAMA Internal Medicine, measures of emotional exhaustion and burnout decreased in physicians who were coached and increased in those who were not.3 In another study from this year by McGonagle et al., a randomized, controlled trial showed that primary care physicians who had sessions (as short as 6 weeks) to address burnout, psychological capital, and job satisfaction experienced an improvement in measures which persisted for 6 months after intervention.4 Numerous other articles in medicine also exist to demonstrate the effect of coaching on mitigating burnout at an institutional level.
Physicians are inherently driven by their love of learning. As physicians, we love getting to the root cause of any problem and coming up with creative solutions. Any challenge we have, or just wanting to improve the quality of our lives, can be addressed with coaching. As perpetual students we can use coaching to truly master ourselves.
Dr. Shah is associate professor of surgery, Rush University Medical Center, Chicago. Instagram: ami.shahmdcoaching.
References
1. Gottlieb M et al. Med Educ. 2020 Feb;54(2):116-24.
2. Villwock JA et al. Int J Med Educ. 2016 Oct 31;7:364-9.
3. Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5;179(10):1406-14.
4. McGonagle AK et al. J Occup Health Psychol. 2020 Apr 16. doi: 10.1037/ocp0000180.
Coaching is a new topic in medicine. I first heard about coaching several years ago and met the term with skepticism. I was unsure how coaching was different than mentoring or advising and I wondered about its usefulness. However, the reason that I even started to learn about coaching was because I was struggling. I had finally arrived in my career, I had my dream job with two healthy kids, a perfect house, and good marriage. I kept hearing the refrain in my head: “Is this all there is?” I had this arrival fallacy that after all this striving and straining that I would finally be content. I felt unfulfilled and was dissatisfied with where I was that was affecting all parts of my life.
As I was wrestling with these thoughts, I had an opportunity to become a coach to residents around the country through the Association of Women Surgeons. I discussed with them what fills them up, what gets them down, how to set goals, and what their goals were for the year, as well as imposter syndrome. Impostor syndrome is defined as a pattern in which an individual doubts their accomplishments or talents and has a persistent internalized fear of being exposed as a “fraud.” Despite external evidence of their competence, those experiencing this phenomenon remain convinced that they are fooling everyone around them and do not deserve all they have achieved. Individuals incorrectly attribute their success to luck or interpret it as a result of deceiving others into thinking they are more intelligent than they perceive themselves to be. Imposter syndrome is prevalent and deep in medicine. As perfectionists, we are especially vulnerable to imposter syndrome as we set unrealistic ideals for ourselves. When we fail to reach these ideals, we feel like frauds, setting up this cycle of self-doubt that is toxic. When we feel that we can’t achieve the goals that we are striving for we will always find ourselves lacking. There is a slow, insidious erosion of self over the years. Imposter syndrome is well documented in medicine and is even felt as early as medical school.1,2
When I began coaching these residents the most profound thing that came out of these sessions was that my life was getting better – I knew what filled me up, what got me down, what my goals were for the year, and how I still deal with imposter syndrome. Coaching gave me a framework for helping determine what I wanted for the rest of my life. As I began coaching, I started learning all the ways in which I could figure out my values, my personal and professional goals, and perhaps most importantly, my relationships with myself and others.
Another perspective on coaching is to look at a professional athlete such as Tom Brady, one of the greatest quarterbacks of all time. He has a quarterback coach. No coach is going to be a better quarterback than Tom Brady. A coach for him is to be there as an advocate, break his fundamentals down technically, and help him improve upon what he already knows. A coach also identifies strengths and weaknesses, and helps him capitalize on both by bringing awareness, reflection, accountability, and support. If world-class athletes still want and benefit from coaching in a sport they have already mastered, coaching for physicians is just another tool to help us improve our abilities in and out of medicine.
Coaching is more encompassing than advising or mentoring. It is about examining deeply held beliefs to see if they are really serving us, if they are in line with our values and how we want to live our lives.
Coaching has also been validated in medicine in several papers. In an article by Dyrbye et al. in JAMA Internal Medicine, measures of emotional exhaustion and burnout decreased in physicians who were coached and increased in those who were not.3 In another study from this year by McGonagle et al., a randomized, controlled trial showed that primary care physicians who had sessions (as short as 6 weeks) to address burnout, psychological capital, and job satisfaction experienced an improvement in measures which persisted for 6 months after intervention.4 Numerous other articles in medicine also exist to demonstrate the effect of coaching on mitigating burnout at an institutional level.
Physicians are inherently driven by their love of learning. As physicians, we love getting to the root cause of any problem and coming up with creative solutions. Any challenge we have, or just wanting to improve the quality of our lives, can be addressed with coaching. As perpetual students we can use coaching to truly master ourselves.
Dr. Shah is associate professor of surgery, Rush University Medical Center, Chicago. Instagram: ami.shahmdcoaching.
References
1. Gottlieb M et al. Med Educ. 2020 Feb;54(2):116-24.
2. Villwock JA et al. Int J Med Educ. 2016 Oct 31;7:364-9.
3. Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5;179(10):1406-14.
4. McGonagle AK et al. J Occup Health Psychol. 2020 Apr 16. doi: 10.1037/ocp0000180.
Coaching is a new topic in medicine. I first heard about coaching several years ago and met the term with skepticism. I was unsure how coaching was different than mentoring or advising and I wondered about its usefulness. However, the reason that I even started to learn about coaching was because I was struggling. I had finally arrived in my career, I had my dream job with two healthy kids, a perfect house, and good marriage. I kept hearing the refrain in my head: “Is this all there is?” I had this arrival fallacy that after all this striving and straining that I would finally be content. I felt unfulfilled and was dissatisfied with where I was that was affecting all parts of my life.
As I was wrestling with these thoughts, I had an opportunity to become a coach to residents around the country through the Association of Women Surgeons. I discussed with them what fills them up, what gets them down, how to set goals, and what their goals were for the year, as well as imposter syndrome. Impostor syndrome is defined as a pattern in which an individual doubts their accomplishments or talents and has a persistent internalized fear of being exposed as a “fraud.” Despite external evidence of their competence, those experiencing this phenomenon remain convinced that they are fooling everyone around them and do not deserve all they have achieved. Individuals incorrectly attribute their success to luck or interpret it as a result of deceiving others into thinking they are more intelligent than they perceive themselves to be. Imposter syndrome is prevalent and deep in medicine. As perfectionists, we are especially vulnerable to imposter syndrome as we set unrealistic ideals for ourselves. When we fail to reach these ideals, we feel like frauds, setting up this cycle of self-doubt that is toxic. When we feel that we can’t achieve the goals that we are striving for we will always find ourselves lacking. There is a slow, insidious erosion of self over the years. Imposter syndrome is well documented in medicine and is even felt as early as medical school.1,2
When I began coaching these residents the most profound thing that came out of these sessions was that my life was getting better – I knew what filled me up, what got me down, what my goals were for the year, and how I still deal with imposter syndrome. Coaching gave me a framework for helping determine what I wanted for the rest of my life. As I began coaching, I started learning all the ways in which I could figure out my values, my personal and professional goals, and perhaps most importantly, my relationships with myself and others.
Another perspective on coaching is to look at a professional athlete such as Tom Brady, one of the greatest quarterbacks of all time. He has a quarterback coach. No coach is going to be a better quarterback than Tom Brady. A coach for him is to be there as an advocate, break his fundamentals down technically, and help him improve upon what he already knows. A coach also identifies strengths and weaknesses, and helps him capitalize on both by bringing awareness, reflection, accountability, and support. If world-class athletes still want and benefit from coaching in a sport they have already mastered, coaching for physicians is just another tool to help us improve our abilities in and out of medicine.
Coaching is more encompassing than advising or mentoring. It is about examining deeply held beliefs to see if they are really serving us, if they are in line with our values and how we want to live our lives.
Coaching has also been validated in medicine in several papers. In an article by Dyrbye et al. in JAMA Internal Medicine, measures of emotional exhaustion and burnout decreased in physicians who were coached and increased in those who were not.3 In another study from this year by McGonagle et al., a randomized, controlled trial showed that primary care physicians who had sessions (as short as 6 weeks) to address burnout, psychological capital, and job satisfaction experienced an improvement in measures which persisted for 6 months after intervention.4 Numerous other articles in medicine also exist to demonstrate the effect of coaching on mitigating burnout at an institutional level.
Physicians are inherently driven by their love of learning. As physicians, we love getting to the root cause of any problem and coming up with creative solutions. Any challenge we have, or just wanting to improve the quality of our lives, can be addressed with coaching. As perpetual students we can use coaching to truly master ourselves.
Dr. Shah is associate professor of surgery, Rush University Medical Center, Chicago. Instagram: ami.shahmdcoaching.
References
1. Gottlieb M et al. Med Educ. 2020 Feb;54(2):116-24.
2. Villwock JA et al. Int J Med Educ. 2016 Oct 31;7:364-9.
3. Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5;179(10):1406-14.
4. McGonagle AK et al. J Occup Health Psychol. 2020 Apr 16. doi: 10.1037/ocp0000180.
Information blocking: Adolescent confidentiality is collateral damage
On April 4, 2021, a rule implementing the federal regulations of the Information Blocking 21st Century Cures Act will be enacted. This Act furthers the seamless release of medical records to promote improved outcomes, access to medical information, and transparency of costs. Each state will need to be thoughtful balancing the action or inaction of allowing access to confidential or sensitive progress notes, as interference with access may be considered information blocking and subject to penalties and fines.
With adolescent confidential notes, protection rules may not apply under the information blocking regulations. These regulations will release progress notes, imaging narratives, procedure notes, and labs to parents via their EHR portals. The release of information is not limited, and both inpatient and outpatient records will be released. These regulations are written for adults with the assumption that all information is released to the individual receiving the care and shared with outside providers.
Unfortunately, the rules do not take into consideration adolescent confidential care. There are eight rules for the exception of releasing information, but it may be a stretch to place adolescent confidential progress notes under any of these eight exceptions. These exceptions are ambiguous and open to interpretation yet require specific documentation as to the limitation of access. Exceptions are prevention of harm; privacy conflicts; the security of the electronic health information; infeasibility, which includes challenges limiting the ability to comply; Health IT performance; content and manner; fees; and licensing.
Ms. Thew is medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She is a member of the Pediatric News editorial advisory board. She had no relevant financial disclosures. Email Ms. Thew at [email protected].
On April 4, 2021, a rule implementing the federal regulations of the Information Blocking 21st Century Cures Act will be enacted. This Act furthers the seamless release of medical records to promote improved outcomes, access to medical information, and transparency of costs. Each state will need to be thoughtful balancing the action or inaction of allowing access to confidential or sensitive progress notes, as interference with access may be considered information blocking and subject to penalties and fines.
With adolescent confidential notes, protection rules may not apply under the information blocking regulations. These regulations will release progress notes, imaging narratives, procedure notes, and labs to parents via their EHR portals. The release of information is not limited, and both inpatient and outpatient records will be released. These regulations are written for adults with the assumption that all information is released to the individual receiving the care and shared with outside providers.
Unfortunately, the rules do not take into consideration adolescent confidential care. There are eight rules for the exception of releasing information, but it may be a stretch to place adolescent confidential progress notes under any of these eight exceptions. These exceptions are ambiguous and open to interpretation yet require specific documentation as to the limitation of access. Exceptions are prevention of harm; privacy conflicts; the security of the electronic health information; infeasibility, which includes challenges limiting the ability to comply; Health IT performance; content and manner; fees; and licensing.
Ms. Thew is medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She is a member of the Pediatric News editorial advisory board. She had no relevant financial disclosures. Email Ms. Thew at [email protected].
On April 4, 2021, a rule implementing the federal regulations of the Information Blocking 21st Century Cures Act will be enacted. This Act furthers the seamless release of medical records to promote improved outcomes, access to medical information, and transparency of costs. Each state will need to be thoughtful balancing the action or inaction of allowing access to confidential or sensitive progress notes, as interference with access may be considered information blocking and subject to penalties and fines.
With adolescent confidential notes, protection rules may not apply under the information blocking regulations. These regulations will release progress notes, imaging narratives, procedure notes, and labs to parents via their EHR portals. The release of information is not limited, and both inpatient and outpatient records will be released. These regulations are written for adults with the assumption that all information is released to the individual receiving the care and shared with outside providers.
Unfortunately, the rules do not take into consideration adolescent confidential care. There are eight rules for the exception of releasing information, but it may be a stretch to place adolescent confidential progress notes under any of these eight exceptions. These exceptions are ambiguous and open to interpretation yet require specific documentation as to the limitation of access. Exceptions are prevention of harm; privacy conflicts; the security of the electronic health information; infeasibility, which includes challenges limiting the ability to comply; Health IT performance; content and manner; fees; and licensing.
Ms. Thew is medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She is a member of the Pediatric News editorial advisory board. She had no relevant financial disclosures. Email Ms. Thew at [email protected].
How to help families get through climate-related disasters
Wildfires burned millions of acres in California, Oregon, and Washington this year. Record numbers of tropical storms and hurricanes formed in the Atlantic. “Climate change is here. Disasters are here. They are going to be increasing, which is why we want to talk about this and talk about how pediatricians can help and respond to these events,” Scott Needle, MD, said at the annual meeting American Academy of Pediatrics, held virtually this year.

said Dr. Needle, chief medical officer of Elica Health Centers in Sacramento, California. “We can be a positive influence in terms of getting out proactive messaging and keeping people informed.”
The Federal Emergency Management Agency (FEMA) 2019 National Household Survey found that about half of households had an emergency plan. A theme across surveys is that, although households take some steps to get ready for disasters, the public generally “is not as prepared for these events as they really need to be,” Dr. Needle said.
The AAP, the Red Cross, and FEMA are among the organizations that offer planning guides, most of which emphasize three simple things: have a kit, have a plan, and be informed, he said.
To prepare for a disaster, parents might refill a child’s medications ahead of time if possible, Dr. Needle suggested. And during the COVID-19 pandemic, families should add masks, sanitizers, and wipes to their go-bags.
Physicians also can help families by asking how they are coping.
Wildfire smoke
“Smoke from wildfires can blanket large, large areas,” Mark Miller, MD, MPH, said during the presentation at the AAP meeting. “This year, we have seen wildfire smoke from the western states reach all the way to the East Coast. So this impacts your patients and your own families sometimes, regardless of wherever you live.”
Children may be more vulnerable to wildfire smoke because they often spend more time outdoors and tend to be more active. In addition, their ongoing development means exposure to air pollutants could have lifelong consequences, said Dr. Miller, who recently reviewed the effects of wildfire smoke on children.
“Children with asthma should have some information about wildfires built into their asthma management plan,” said Dr. Miller, who is affiliated with Western States Pediatric Environmental Health Specialty Unit (PEHSU) and University of California, San Francisco. Pollutants are associated with respiratory visits and admissions, asthma exacerbations, decreased lung function, and neurocognitive effects. They also may be carcinogenic.
A study in monkeys found that smoke exposure during California wildfires in 2008 was associated with immune dysregulation and compromised lung function in adolescence.
Another study of three cohorts of children in southern California found that air pollutant levels were associated with children’s lung function.
Organizations have provided resources on creating cleaner air spaces during wildfires, including guides to build DIY air filter fans. AirNow.gov provides air quality and fire maps that can inform decisions about school closures and outdoor activities. Communities should prioritize establishing schools as clean air shelters, Dr. Miller suggested.
Studies have found that respirators and medical masks may decrease children’s exposure to smoke. Children should not use face coverings, however, if they are younger than 2 years, if they are not able to remove the face covering on their own or tell an adult that they need help, or if they have difficulty breathing with a face covering. Younger children should be observed by an adult.
During the pandemic, families should be aware that some types of masks are sold only for health care use, many foreign respirators are counterfeit, and cloth masks used for COVID-19 are not suitable for reducing wildfire smoke exposure, Dr. Miller said.
Hazards may linger
Long-term mental health issues may be the disaster consequence that pediatricians encounter most often, Dr. Needle said.
Eighteen months after a major wildfire in Canada, more than one-third of middle and high school students in one community had probable posttraumatic stress disorder (that is, intrusive thoughts, avoidance, and increased arousal). In addition, 31% of students had probable depression. Rates were elevated relative to a control group of students in another community that was not affected by the fire.
Findings indicate that a patient’s degree of exposure to a disaster affects the likelihood of adverse outcomes. On the other hand, resiliency may help mitigate adverse effects. “The hope is that if we can find ways to encourage resiliency before or in the aftermath of an event, we may be able to, in a sense, reduce some of these mental health sequelae,” Dr. Needle said.
Posttraumatic reactions in kids are likely after a disaster. “They may not rise to the level of a diagnosable condition, but they are very common in kids,” he said. “It is important to at least be able to counsel parents to recognize some of the common reactions,” such as acting withdrawn or aggressive, somatic complaints, and having trouble sleeping.
The AAP has a policy statement that encourages talking to children about their concerns with honest and age-appropriate responses, he noted.
When returning to an area after a disaster, many hazards may remain, such as floodwaters, ash pits, mold, and carbon monoxide from generators. “Generally speaking, you don’t want to have kids return to these areas until it is safe,” Dr. Needle said.
Exacerbation of existing conditions – perhaps because of lost medications, smoke exposure, or stress – may be another common problem. Other problems after a disaster could include domestic violence (direct or witnessed) and substance abuse.
“We have a responsibility to take care of our own health as well,” Dr. Needle added. “You can’t take care of others if you’re not taking care of yourself. It’s not being selfish. As a matter of fact, it’s being prudent. It’s survival.”
Dr. Needle and Dr. Miller had no relevant financial disclosures. Dr. Miller’s presentation was supported by the AAP and funded in part by the Agency for Toxic Substances and Disease Registry. The U.S. Environmental Protection Agency (EPA) provides funding support for the Pediatric Environmental Health Specialty Unit.
Wildfires burned millions of acres in California, Oregon, and Washington this year. Record numbers of tropical storms and hurricanes formed in the Atlantic. “Climate change is here. Disasters are here. They are going to be increasing, which is why we want to talk about this and talk about how pediatricians can help and respond to these events,” Scott Needle, MD, said at the annual meeting American Academy of Pediatrics, held virtually this year.

said Dr. Needle, chief medical officer of Elica Health Centers in Sacramento, California. “We can be a positive influence in terms of getting out proactive messaging and keeping people informed.”
The Federal Emergency Management Agency (FEMA) 2019 National Household Survey found that about half of households had an emergency plan. A theme across surveys is that, although households take some steps to get ready for disasters, the public generally “is not as prepared for these events as they really need to be,” Dr. Needle said.
The AAP, the Red Cross, and FEMA are among the organizations that offer planning guides, most of which emphasize three simple things: have a kit, have a plan, and be informed, he said.
To prepare for a disaster, parents might refill a child’s medications ahead of time if possible, Dr. Needle suggested. And during the COVID-19 pandemic, families should add masks, sanitizers, and wipes to their go-bags.
Physicians also can help families by asking how they are coping.
Wildfire smoke
“Smoke from wildfires can blanket large, large areas,” Mark Miller, MD, MPH, said during the presentation at the AAP meeting. “This year, we have seen wildfire smoke from the western states reach all the way to the East Coast. So this impacts your patients and your own families sometimes, regardless of wherever you live.”
Children may be more vulnerable to wildfire smoke because they often spend more time outdoors and tend to be more active. In addition, their ongoing development means exposure to air pollutants could have lifelong consequences, said Dr. Miller, who recently reviewed the effects of wildfire smoke on children.
“Children with asthma should have some information about wildfires built into their asthma management plan,” said Dr. Miller, who is affiliated with Western States Pediatric Environmental Health Specialty Unit (PEHSU) and University of California, San Francisco. Pollutants are associated with respiratory visits and admissions, asthma exacerbations, decreased lung function, and neurocognitive effects. They also may be carcinogenic.
A study in monkeys found that smoke exposure during California wildfires in 2008 was associated with immune dysregulation and compromised lung function in adolescence.
Another study of three cohorts of children in southern California found that air pollutant levels were associated with children’s lung function.
Organizations have provided resources on creating cleaner air spaces during wildfires, including guides to build DIY air filter fans. AirNow.gov provides air quality and fire maps that can inform decisions about school closures and outdoor activities. Communities should prioritize establishing schools as clean air shelters, Dr. Miller suggested.
Studies have found that respirators and medical masks may decrease children’s exposure to smoke. Children should not use face coverings, however, if they are younger than 2 years, if they are not able to remove the face covering on their own or tell an adult that they need help, or if they have difficulty breathing with a face covering. Younger children should be observed by an adult.
During the pandemic, families should be aware that some types of masks are sold only for health care use, many foreign respirators are counterfeit, and cloth masks used for COVID-19 are not suitable for reducing wildfire smoke exposure, Dr. Miller said.
Hazards may linger
Long-term mental health issues may be the disaster consequence that pediatricians encounter most often, Dr. Needle said.
Eighteen months after a major wildfire in Canada, more than one-third of middle and high school students in one community had probable posttraumatic stress disorder (that is, intrusive thoughts, avoidance, and increased arousal). In addition, 31% of students had probable depression. Rates were elevated relative to a control group of students in another community that was not affected by the fire.
Findings indicate that a patient’s degree of exposure to a disaster affects the likelihood of adverse outcomes. On the other hand, resiliency may help mitigate adverse effects. “The hope is that if we can find ways to encourage resiliency before or in the aftermath of an event, we may be able to, in a sense, reduce some of these mental health sequelae,” Dr. Needle said.
Posttraumatic reactions in kids are likely after a disaster. “They may not rise to the level of a diagnosable condition, but they are very common in kids,” he said. “It is important to at least be able to counsel parents to recognize some of the common reactions,” such as acting withdrawn or aggressive, somatic complaints, and having trouble sleeping.
The AAP has a policy statement that encourages talking to children about their concerns with honest and age-appropriate responses, he noted.
When returning to an area after a disaster, many hazards may remain, such as floodwaters, ash pits, mold, and carbon monoxide from generators. “Generally speaking, you don’t want to have kids return to these areas until it is safe,” Dr. Needle said.
Exacerbation of existing conditions – perhaps because of lost medications, smoke exposure, or stress – may be another common problem. Other problems after a disaster could include domestic violence (direct or witnessed) and substance abuse.
“We have a responsibility to take care of our own health as well,” Dr. Needle added. “You can’t take care of others if you’re not taking care of yourself. It’s not being selfish. As a matter of fact, it’s being prudent. It’s survival.”
Dr. Needle and Dr. Miller had no relevant financial disclosures. Dr. Miller’s presentation was supported by the AAP and funded in part by the Agency for Toxic Substances and Disease Registry. The U.S. Environmental Protection Agency (EPA) provides funding support for the Pediatric Environmental Health Specialty Unit.
Wildfires burned millions of acres in California, Oregon, and Washington this year. Record numbers of tropical storms and hurricanes formed in the Atlantic. “Climate change is here. Disasters are here. They are going to be increasing, which is why we want to talk about this and talk about how pediatricians can help and respond to these events,” Scott Needle, MD, said at the annual meeting American Academy of Pediatrics, held virtually this year.

said Dr. Needle, chief medical officer of Elica Health Centers in Sacramento, California. “We can be a positive influence in terms of getting out proactive messaging and keeping people informed.”
The Federal Emergency Management Agency (FEMA) 2019 National Household Survey found that about half of households had an emergency plan. A theme across surveys is that, although households take some steps to get ready for disasters, the public generally “is not as prepared for these events as they really need to be,” Dr. Needle said.
The AAP, the Red Cross, and FEMA are among the organizations that offer planning guides, most of which emphasize three simple things: have a kit, have a plan, and be informed, he said.
To prepare for a disaster, parents might refill a child’s medications ahead of time if possible, Dr. Needle suggested. And during the COVID-19 pandemic, families should add masks, sanitizers, and wipes to their go-bags.
Physicians also can help families by asking how they are coping.
Wildfire smoke
“Smoke from wildfires can blanket large, large areas,” Mark Miller, MD, MPH, said during the presentation at the AAP meeting. “This year, we have seen wildfire smoke from the western states reach all the way to the East Coast. So this impacts your patients and your own families sometimes, regardless of wherever you live.”
Children may be more vulnerable to wildfire smoke because they often spend more time outdoors and tend to be more active. In addition, their ongoing development means exposure to air pollutants could have lifelong consequences, said Dr. Miller, who recently reviewed the effects of wildfire smoke on children.
“Children with asthma should have some information about wildfires built into their asthma management plan,” said Dr. Miller, who is affiliated with Western States Pediatric Environmental Health Specialty Unit (PEHSU) and University of California, San Francisco. Pollutants are associated with respiratory visits and admissions, asthma exacerbations, decreased lung function, and neurocognitive effects. They also may be carcinogenic.
A study in monkeys found that smoke exposure during California wildfires in 2008 was associated with immune dysregulation and compromised lung function in adolescence.
Another study of three cohorts of children in southern California found that air pollutant levels were associated with children’s lung function.
Organizations have provided resources on creating cleaner air spaces during wildfires, including guides to build DIY air filter fans. AirNow.gov provides air quality and fire maps that can inform decisions about school closures and outdoor activities. Communities should prioritize establishing schools as clean air shelters, Dr. Miller suggested.
Studies have found that respirators and medical masks may decrease children’s exposure to smoke. Children should not use face coverings, however, if they are younger than 2 years, if they are not able to remove the face covering on their own or tell an adult that they need help, or if they have difficulty breathing with a face covering. Younger children should be observed by an adult.
During the pandemic, families should be aware that some types of masks are sold only for health care use, many foreign respirators are counterfeit, and cloth masks used for COVID-19 are not suitable for reducing wildfire smoke exposure, Dr. Miller said.
Hazards may linger
Long-term mental health issues may be the disaster consequence that pediatricians encounter most often, Dr. Needle said.
Eighteen months after a major wildfire in Canada, more than one-third of middle and high school students in one community had probable posttraumatic stress disorder (that is, intrusive thoughts, avoidance, and increased arousal). In addition, 31% of students had probable depression. Rates were elevated relative to a control group of students in another community that was not affected by the fire.
Findings indicate that a patient’s degree of exposure to a disaster affects the likelihood of adverse outcomes. On the other hand, resiliency may help mitigate adverse effects. “The hope is that if we can find ways to encourage resiliency before or in the aftermath of an event, we may be able to, in a sense, reduce some of these mental health sequelae,” Dr. Needle said.
Posttraumatic reactions in kids are likely after a disaster. “They may not rise to the level of a diagnosable condition, but they are very common in kids,” he said. “It is important to at least be able to counsel parents to recognize some of the common reactions,” such as acting withdrawn or aggressive, somatic complaints, and having trouble sleeping.
The AAP has a policy statement that encourages talking to children about their concerns with honest and age-appropriate responses, he noted.
When returning to an area after a disaster, many hazards may remain, such as floodwaters, ash pits, mold, and carbon monoxide from generators. “Generally speaking, you don’t want to have kids return to these areas until it is safe,” Dr. Needle said.
Exacerbation of existing conditions – perhaps because of lost medications, smoke exposure, or stress – may be another common problem. Other problems after a disaster could include domestic violence (direct or witnessed) and substance abuse.
“We have a responsibility to take care of our own health as well,” Dr. Needle added. “You can’t take care of others if you’re not taking care of yourself. It’s not being selfish. As a matter of fact, it’s being prudent. It’s survival.”
Dr. Needle and Dr. Miller had no relevant financial disclosures. Dr. Miller’s presentation was supported by the AAP and funded in part by the Agency for Toxic Substances and Disease Registry. The U.S. Environmental Protection Agency (EPA) provides funding support for the Pediatric Environmental Health Specialty Unit.
FROM AAP 2020
When Female Patients with MS Ask About Breastfeeding, Here’s What to Tell Them
Chances are your female patients of childbearing age with multiple sclerosis—particularly if they become pregnant—will ask about breastfeeding. What are they likely to ask, and how should you answer? Here’s a quick rundown.
What kind of impact will breastfeeding have on my child?
We know that MS is not a genetic disease per se-it is neither autosomal recessive nor dominant. But there is an increased risk among family members, particularly first-degree relatives. If a patient asks, you can tell them it appears that infants who are breastfed are less likely to develop pediatric-onset MS.
In 2017, Brenton and colleagues asked individuals who experienced pediatric-onset MS (n=36) and those in a control group (n=72) to complete a questionnaire that covered breastfeeding history and other birth and demographic features. While most demographic and birth features were similar, 36% of those in the pediatric-onset MS group reported being breastfed, compared with 71% of controls. Individuals who were not breastfed were nearly 4.5 times more likely to be diagnosed with pediatric-onset MS.
How will breastfeeding impact my risk of MS relapse after giving birth?
The issue of breastfeeding and MS relapses is somewhat controversial. In 1988, Nelson and colleagues found that among 191 women with MS who became pregnant, 10% relapsed during pregnancy, but relapse rate rose to 34% during the 9 months after birth. Moreover, nearly 4 in 10 of those who breastfed experienced exacerbations, versus 3 in 10 among those who did not.
However, more recent studies demonstrate no association with breastfeeding and relapse. Just this year, Gould and colleagues published a study showing that among 466 pregnancies, annualized relapse rates declined during pregnancy, and there was no increase seen in the postpartum period. Moreover, women who exclusively breastfed saw their risk of an early postpartum relapse lowered by 63%.
In late 2019, Krysko and colleagues published a meta-analysis of 24 studies involving nearly 3,000 women with MS which showed that breastfeeds were 43% less likely to experience postpartum relapse compared with their non-breastfeeding counterparts. The link was stronger in studies where women breastfed exclusively.
The bottom line: There is a plurality of physicians who believe that breastfeeding has a protective effect – and most will tell you that you should recommend exclusive breastfeeding.
What medicines can I take that will not adversely affect me and my baby?
Once a woman knows that breastfeeding could help her offspring avoid developing MS, and minimize her chance of a postpartum relapse, she will likely ask what to do about medications. You answer will depends on what she’s taking.
- Drugs she can take with relative peace of mind. Most experts believe it is safe to take corticosteroids and breastfeed. In fact, women who relapse while breastfeeding will in all likelihood be given intravenous corticosteroids, such as methylprednisolone. These medications are present in the blood at very low levels, peak an hour after infusion, and quickly dissipate. So, it’s important to tell your patients to delay breastfeeding by 2 to 4 hours after they receive the steroid.
- Drugs that are potentially concerning and require close monitoring. For the so-called platform therapies—such as interferon beta/glatiramer acetate, natalizumab, and their generic equivalents—there are no large studies that clearly demonstrate safety. Still, they are generally thought to be safe. Be sure to heed FDA labeling: weigh breastfeeding benefit against the potential risk
- Drug to avoid entirely. Under no circumstances should breastfeeding women receive teriflunomide, cladribine, alemtuzumab, or mitoxantrone. The jury is still out on rituximab—which is not yet approved for MS in the United States—and ocrelizumab. For now, err on the safe side and switch to another therapy.
Chances are your female patients of childbearing age with multiple sclerosis—particularly if they become pregnant—will ask about breastfeeding. What are they likely to ask, and how should you answer? Here’s a quick rundown.
What kind of impact will breastfeeding have on my child?
We know that MS is not a genetic disease per se-it is neither autosomal recessive nor dominant. But there is an increased risk among family members, particularly first-degree relatives. If a patient asks, you can tell them it appears that infants who are breastfed are less likely to develop pediatric-onset MS.
In 2017, Brenton and colleagues asked individuals who experienced pediatric-onset MS (n=36) and those in a control group (n=72) to complete a questionnaire that covered breastfeeding history and other birth and demographic features. While most demographic and birth features were similar, 36% of those in the pediatric-onset MS group reported being breastfed, compared with 71% of controls. Individuals who were not breastfed were nearly 4.5 times more likely to be diagnosed with pediatric-onset MS.
How will breastfeeding impact my risk of MS relapse after giving birth?
The issue of breastfeeding and MS relapses is somewhat controversial. In 1988, Nelson and colleagues found that among 191 women with MS who became pregnant, 10% relapsed during pregnancy, but relapse rate rose to 34% during the 9 months after birth. Moreover, nearly 4 in 10 of those who breastfed experienced exacerbations, versus 3 in 10 among those who did not.
However, more recent studies demonstrate no association with breastfeeding and relapse. Just this year, Gould and colleagues published a study showing that among 466 pregnancies, annualized relapse rates declined during pregnancy, and there was no increase seen in the postpartum period. Moreover, women who exclusively breastfed saw their risk of an early postpartum relapse lowered by 63%.
In late 2019, Krysko and colleagues published a meta-analysis of 24 studies involving nearly 3,000 women with MS which showed that breastfeeds were 43% less likely to experience postpartum relapse compared with their non-breastfeeding counterparts. The link was stronger in studies where women breastfed exclusively.
The bottom line: There is a plurality of physicians who believe that breastfeeding has a protective effect – and most will tell you that you should recommend exclusive breastfeeding.
What medicines can I take that will not adversely affect me and my baby?
Once a woman knows that breastfeeding could help her offspring avoid developing MS, and minimize her chance of a postpartum relapse, she will likely ask what to do about medications. You answer will depends on what she’s taking.
- Drugs she can take with relative peace of mind. Most experts believe it is safe to take corticosteroids and breastfeed. In fact, women who relapse while breastfeeding will in all likelihood be given intravenous corticosteroids, such as methylprednisolone. These medications are present in the blood at very low levels, peak an hour after infusion, and quickly dissipate. So, it’s important to tell your patients to delay breastfeeding by 2 to 4 hours after they receive the steroid.
- Drugs that are potentially concerning and require close monitoring. For the so-called platform therapies—such as interferon beta/glatiramer acetate, natalizumab, and their generic equivalents—there are no large studies that clearly demonstrate safety. Still, they are generally thought to be safe. Be sure to heed FDA labeling: weigh breastfeeding benefit against the potential risk
- Drug to avoid entirely. Under no circumstances should breastfeeding women receive teriflunomide, cladribine, alemtuzumab, or mitoxantrone. The jury is still out on rituximab—which is not yet approved for MS in the United States—and ocrelizumab. For now, err on the safe side and switch to another therapy.
Chances are your female patients of childbearing age with multiple sclerosis—particularly if they become pregnant—will ask about breastfeeding. What are they likely to ask, and how should you answer? Here’s a quick rundown.
What kind of impact will breastfeeding have on my child?
We know that MS is not a genetic disease per se-it is neither autosomal recessive nor dominant. But there is an increased risk among family members, particularly first-degree relatives. If a patient asks, you can tell them it appears that infants who are breastfed are less likely to develop pediatric-onset MS.
In 2017, Brenton and colleagues asked individuals who experienced pediatric-onset MS (n=36) and those in a control group (n=72) to complete a questionnaire that covered breastfeeding history and other birth and demographic features. While most demographic and birth features were similar, 36% of those in the pediatric-onset MS group reported being breastfed, compared with 71% of controls. Individuals who were not breastfed were nearly 4.5 times more likely to be diagnosed with pediatric-onset MS.
How will breastfeeding impact my risk of MS relapse after giving birth?
The issue of breastfeeding and MS relapses is somewhat controversial. In 1988, Nelson and colleagues found that among 191 women with MS who became pregnant, 10% relapsed during pregnancy, but relapse rate rose to 34% during the 9 months after birth. Moreover, nearly 4 in 10 of those who breastfed experienced exacerbations, versus 3 in 10 among those who did not.
However, more recent studies demonstrate no association with breastfeeding and relapse. Just this year, Gould and colleagues published a study showing that among 466 pregnancies, annualized relapse rates declined during pregnancy, and there was no increase seen in the postpartum period. Moreover, women who exclusively breastfed saw their risk of an early postpartum relapse lowered by 63%.
In late 2019, Krysko and colleagues published a meta-analysis of 24 studies involving nearly 3,000 women with MS which showed that breastfeeds were 43% less likely to experience postpartum relapse compared with their non-breastfeeding counterparts. The link was stronger in studies where women breastfed exclusively.
The bottom line: There is a plurality of physicians who believe that breastfeeding has a protective effect – and most will tell you that you should recommend exclusive breastfeeding.
What medicines can I take that will not adversely affect me and my baby?
Once a woman knows that breastfeeding could help her offspring avoid developing MS, and minimize her chance of a postpartum relapse, she will likely ask what to do about medications. You answer will depends on what she’s taking.
- Drugs she can take with relative peace of mind. Most experts believe it is safe to take corticosteroids and breastfeed. In fact, women who relapse while breastfeeding will in all likelihood be given intravenous corticosteroids, such as methylprednisolone. These medications are present in the blood at very low levels, peak an hour after infusion, and quickly dissipate. So, it’s important to tell your patients to delay breastfeeding by 2 to 4 hours after they receive the steroid.
- Drugs that are potentially concerning and require close monitoring. For the so-called platform therapies—such as interferon beta/glatiramer acetate, natalizumab, and their generic equivalents—there are no large studies that clearly demonstrate safety. Still, they are generally thought to be safe. Be sure to heed FDA labeling: weigh breastfeeding benefit against the potential risk
- Drug to avoid entirely. Under no circumstances should breastfeeding women receive teriflunomide, cladribine, alemtuzumab, or mitoxantrone. The jury is still out on rituximab—which is not yet approved for MS in the United States—and ocrelizumab. For now, err on the safe side and switch to another therapy.