User login
Official Newspaper of the American College of Surgeons
VIDEO: EMR reminder reduces unnecessary transfusions
SAN FRANCISCO – To reduce unnecessary transfusions, all it takes is a reminder in the electronic medical record system that they aren’t generally necessary if surgery patients have hemoglobins greater than 10 g/dL, according to investigators from Emory University in Atlanta.
A reminder in Emory’s EMR dropped transfusion rates in cardiothoracic patients without increasing negative outcomes. It also saved money and reduced the number of surgical site infections. Emory is now rolling it out systemwide (J. Am. Coll. Surg. 2014 June 25 [doi: 10.1016/j.jamcollsurg.2014.06.012]). Lead investigator Dr. Seyed Razavi explained the initiative in a video interview at the annual clinical congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Hossein Almassi, FCCP, comments: By their nature, cardiac operations are associated with higher transfusion rates than other surgical procedures. The negative impact of blood transfusion on short term hospital outcomes and mortality is well known. Any effort in reducing the adverse outcomes is a step in the right direction, especially in this era of 'pay per performance". A "reminder in the EMR" is but one such step.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: By their nature, cardiac operations are associated with higher transfusion rates than other surgical procedures. The negative impact of blood transfusion on short term hospital outcomes and mortality is well known. Any effort in reducing the adverse outcomes is a step in the right direction, especially in this era of 'pay per performance". A "reminder in the EMR" is but one such step.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: By their nature, cardiac operations are associated with higher transfusion rates than other surgical procedures. The negative impact of blood transfusion on short term hospital outcomes and mortality is well known. Any effort in reducing the adverse outcomes is a step in the right direction, especially in this era of 'pay per performance". A "reminder in the EMR" is but one such step.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
SAN FRANCISCO – To reduce unnecessary transfusions, all it takes is a reminder in the electronic medical record system that they aren’t generally necessary if surgery patients have hemoglobins greater than 10 g/dL, according to investigators from Emory University in Atlanta.
A reminder in Emory’s EMR dropped transfusion rates in cardiothoracic patients without increasing negative outcomes. It also saved money and reduced the number of surgical site infections. Emory is now rolling it out systemwide (J. Am. Coll. Surg. 2014 June 25 [doi: 10.1016/j.jamcollsurg.2014.06.012]). Lead investigator Dr. Seyed Razavi explained the initiative in a video interview at the annual clinical congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – To reduce unnecessary transfusions, all it takes is a reminder in the electronic medical record system that they aren’t generally necessary if surgery patients have hemoglobins greater than 10 g/dL, according to investigators from Emory University in Atlanta.
A reminder in Emory’s EMR dropped transfusion rates in cardiothoracic patients without increasing negative outcomes. It also saved money and reduced the number of surgical site infections. Emory is now rolling it out systemwide (J. Am. Coll. Surg. 2014 June 25 [doi: 10.1016/j.jamcollsurg.2014.06.012]). Lead investigator Dr. Seyed Razavi explained the initiative in a video interview at the annual clinical congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACS CLINICAL CONGRESS
No survival benefit of RAI seen in early-stage thyroid cancer
CORONADO, CALIF. – In a large cohort of patients with differentiated thyroid cancer, the use of radioactive iodine was associated with improved disease-specific survival in those with advanced disease but not in those with papillary thyroid microcarcinoma.
“Everything in medicine is a risk-benefit balance,” lead author Dr. Ryan K. Orosco said in an interview in advance of the annual meeting of the American Thyroid Association, where the work was presented. “Any two patients that receive radioactive iodine (RAI) for differentiated thyroid cancer are likely to have different survival benefit from that therapy. This study provides a quantitative comparison of the impact of RAI in various patient subgroups.”
In one of the largest studies of its kind, Dr. Orosco of the division of head and neck surgery at the University of California, San Diego, and his associates identified 85,740 patients with differentiated thyroid carcinoma from the Surveillance, Epidemiology, and End Results database from 1973 through 2009. They used multivariate analyses to explore the association between RAI and cancer-specific survival in 149 population subgroups, controlling for age, decade of diagnosis, race, gender, tumor type, nodal involvement, metastasis stage, and RAI therapy.
More than three-quarters of the patients (78%) were female, 68% were white, their mean age at diagnosis was 46 years, and the median follow-up time was 85 months. The researchers found that nearly half of patients (43%) received RAI. By American Joint Committee on Cancer stage, RAI was used in 55% of stage I patients, 41% of stage II patients, 94% of stage III patients, and 85% of stage IV patients. In addition, 42% of patients with T1a disease and 88% of those with T4 disease received RAI.
Use of RAI was positively associated with survival in the overall cohort (hazard ratio 1.3; P = .002), while statistically significant HRs for RAI were observed in 49 population subgroups. In patients with metastatic disease, use of RAI was associated with a decreased risk for disease-specific mortality (HR range of 2.28-3.82). Protective effects of RAI were also observed in patients with regional metastases (HR 1.4-1.9), those with T3-positive tumors (HR 1.36-1.39), those with T4 tumors (HR 1.85), and in those with stage IV disease (HR 1.47-1.73).
Dr. Orosco and his associates observed a negative effect of RAI in patients with macropapillary carcinoma. Specifically, those with T1a disease had an increased likelihood of thyroid cancer–specific mortality (HR .13; P less than .001), while similar associations were seen in multiple subgroups of patients with T1a disease (HR 0.04-0.25). No statistically significant effects of RAI were observed in patients with T1b or T2 tumors.
“RAI appears to offer the best survival impact in patients with advanced differentiated thyroid carcinoma,” Dr. Orosco said. “Its use in early-stage patients should be carefully considered.”
In their abstract, the researchers noted that the findings “might help clinicians personalize RAI therapy to specific differentiated thyroid cancer populations – offering treatment in patients most likely to benefit, and sparing others unnecessary costs and potential side effects.”
Dr. Orosco acknowledged certain limitations of the study, including the fact that the SEER database does not contain details about each patient’s surgery, the dose of RAI used, other comorbidities, or data on cancer recurrence. “This study does not attempt to explore the reasons behind the apparent survival disadvantage seen in patients with T1a disease,” he said. “We don’t know exactly why early-stage patients have an increased risk of disease-specific mortality when RAI is used. Additional work is needed to explore this further.”
Dr. Orosco reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – In a large cohort of patients with differentiated thyroid cancer, the use of radioactive iodine was associated with improved disease-specific survival in those with advanced disease but not in those with papillary thyroid microcarcinoma.
“Everything in medicine is a risk-benefit balance,” lead author Dr. Ryan K. Orosco said in an interview in advance of the annual meeting of the American Thyroid Association, where the work was presented. “Any two patients that receive radioactive iodine (RAI) for differentiated thyroid cancer are likely to have different survival benefit from that therapy. This study provides a quantitative comparison of the impact of RAI in various patient subgroups.”
In one of the largest studies of its kind, Dr. Orosco of the division of head and neck surgery at the University of California, San Diego, and his associates identified 85,740 patients with differentiated thyroid carcinoma from the Surveillance, Epidemiology, and End Results database from 1973 through 2009. They used multivariate analyses to explore the association between RAI and cancer-specific survival in 149 population subgroups, controlling for age, decade of diagnosis, race, gender, tumor type, nodal involvement, metastasis stage, and RAI therapy.
More than three-quarters of the patients (78%) were female, 68% were white, their mean age at diagnosis was 46 years, and the median follow-up time was 85 months. The researchers found that nearly half of patients (43%) received RAI. By American Joint Committee on Cancer stage, RAI was used in 55% of stage I patients, 41% of stage II patients, 94% of stage III patients, and 85% of stage IV patients. In addition, 42% of patients with T1a disease and 88% of those with T4 disease received RAI.
Use of RAI was positively associated with survival in the overall cohort (hazard ratio 1.3; P = .002), while statistically significant HRs for RAI were observed in 49 population subgroups. In patients with metastatic disease, use of RAI was associated with a decreased risk for disease-specific mortality (HR range of 2.28-3.82). Protective effects of RAI were also observed in patients with regional metastases (HR 1.4-1.9), those with T3-positive tumors (HR 1.36-1.39), those with T4 tumors (HR 1.85), and in those with stage IV disease (HR 1.47-1.73).
Dr. Orosco and his associates observed a negative effect of RAI in patients with macropapillary carcinoma. Specifically, those with T1a disease had an increased likelihood of thyroid cancer–specific mortality (HR .13; P less than .001), while similar associations were seen in multiple subgroups of patients with T1a disease (HR 0.04-0.25). No statistically significant effects of RAI were observed in patients with T1b or T2 tumors.
“RAI appears to offer the best survival impact in patients with advanced differentiated thyroid carcinoma,” Dr. Orosco said. “Its use in early-stage patients should be carefully considered.”
In their abstract, the researchers noted that the findings “might help clinicians personalize RAI therapy to specific differentiated thyroid cancer populations – offering treatment in patients most likely to benefit, and sparing others unnecessary costs and potential side effects.”
Dr. Orosco acknowledged certain limitations of the study, including the fact that the SEER database does not contain details about each patient’s surgery, the dose of RAI used, other comorbidities, or data on cancer recurrence. “This study does not attempt to explore the reasons behind the apparent survival disadvantage seen in patients with T1a disease,” he said. “We don’t know exactly why early-stage patients have an increased risk of disease-specific mortality when RAI is used. Additional work is needed to explore this further.”
Dr. Orosco reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – In a large cohort of patients with differentiated thyroid cancer, the use of radioactive iodine was associated with improved disease-specific survival in those with advanced disease but not in those with papillary thyroid microcarcinoma.
“Everything in medicine is a risk-benefit balance,” lead author Dr. Ryan K. Orosco said in an interview in advance of the annual meeting of the American Thyroid Association, where the work was presented. “Any two patients that receive radioactive iodine (RAI) for differentiated thyroid cancer are likely to have different survival benefit from that therapy. This study provides a quantitative comparison of the impact of RAI in various patient subgroups.”
In one of the largest studies of its kind, Dr. Orosco of the division of head and neck surgery at the University of California, San Diego, and his associates identified 85,740 patients with differentiated thyroid carcinoma from the Surveillance, Epidemiology, and End Results database from 1973 through 2009. They used multivariate analyses to explore the association between RAI and cancer-specific survival in 149 population subgroups, controlling for age, decade of diagnosis, race, gender, tumor type, nodal involvement, metastasis stage, and RAI therapy.
More than three-quarters of the patients (78%) were female, 68% were white, their mean age at diagnosis was 46 years, and the median follow-up time was 85 months. The researchers found that nearly half of patients (43%) received RAI. By American Joint Committee on Cancer stage, RAI was used in 55% of stage I patients, 41% of stage II patients, 94% of stage III patients, and 85% of stage IV patients. In addition, 42% of patients with T1a disease and 88% of those with T4 disease received RAI.
Use of RAI was positively associated with survival in the overall cohort (hazard ratio 1.3; P = .002), while statistically significant HRs for RAI were observed in 49 population subgroups. In patients with metastatic disease, use of RAI was associated with a decreased risk for disease-specific mortality (HR range of 2.28-3.82). Protective effects of RAI were also observed in patients with regional metastases (HR 1.4-1.9), those with T3-positive tumors (HR 1.36-1.39), those with T4 tumors (HR 1.85), and in those with stage IV disease (HR 1.47-1.73).
Dr. Orosco and his associates observed a negative effect of RAI in patients with macropapillary carcinoma. Specifically, those with T1a disease had an increased likelihood of thyroid cancer–specific mortality (HR .13; P less than .001), while similar associations were seen in multiple subgroups of patients with T1a disease (HR 0.04-0.25). No statistically significant effects of RAI were observed in patients with T1b or T2 tumors.
“RAI appears to offer the best survival impact in patients with advanced differentiated thyroid carcinoma,” Dr. Orosco said. “Its use in early-stage patients should be carefully considered.”
In their abstract, the researchers noted that the findings “might help clinicians personalize RAI therapy to specific differentiated thyroid cancer populations – offering treatment in patients most likely to benefit, and sparing others unnecessary costs and potential side effects.”
Dr. Orosco acknowledged certain limitations of the study, including the fact that the SEER database does not contain details about each patient’s surgery, the dose of RAI used, other comorbidities, or data on cancer recurrence. “This study does not attempt to explore the reasons behind the apparent survival disadvantage seen in patients with T1a disease,” he said. “We don’t know exactly why early-stage patients have an increased risk of disease-specific mortality when RAI is used. Additional work is needed to explore this further.”
Dr. Orosco reported having no financial disclosures.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: Radioactive iodine appears to offer the best survival impact in patients with advanced differentiated thyroid carcinoma.
Major finding: In patients with metastatic disease, use of RAI was associated with a decreased risk for disease-specific mortality (HR range of 2.28-3.82). However, those with T1a disease had an increased likelihood of thyroid cancer-specific mortality (HR .13; P less than .001), while similar associations were seen in multiple subgroups of patients with T1a disease (HR .04-.25).
Data source: An analysis of 85,740 patients with differentiated thyroid carcinoma from the Surveillance, Epidemiology, and End Results database from 1973 through 2009.
Disclosures: Dr. Orosco reported having no financial disclosures.
Supreme Court to hear ACA subsidy challenge
The U.S. Supreme Court has agreed to review a case challenging the legality of federal subsidies provided under the Affordable Care Act.
The Court issued the order Nov. 7, granting the plaintiffs in King v. Burwell a review of the case. The plaintiffs assert that under the ACA, only state marketplaces can issue subsidies to eligible patients.
In July, the Fourth Circuit Court of Appeals ruled against the plaintiffs, upholding the government’s ability to provide subsidies to eligible patients who purchase insurance through the 36 federally facilitated health care marketplaces.
On the same day, a limited panel of judges on the District of Columbia Circuit of the U.S. Court of Appeals ruled that the federal marketplace subsidies were not legal in a similar challenge, Halbig v. Burwell.
The government appealed, seeking a full review, which was granted in September. All 17 D.C. Circuit judges will review the case on Dec. 17.
The Supreme Court is not likely to hear King v. Burwell before that date.
On Twitter @aliciaault
The U.S. Supreme Court has agreed to review a case challenging the legality of federal subsidies provided under the Affordable Care Act.
The Court issued the order Nov. 7, granting the plaintiffs in King v. Burwell a review of the case. The plaintiffs assert that under the ACA, only state marketplaces can issue subsidies to eligible patients.
In July, the Fourth Circuit Court of Appeals ruled against the plaintiffs, upholding the government’s ability to provide subsidies to eligible patients who purchase insurance through the 36 federally facilitated health care marketplaces.
On the same day, a limited panel of judges on the District of Columbia Circuit of the U.S. Court of Appeals ruled that the federal marketplace subsidies were not legal in a similar challenge, Halbig v. Burwell.
The government appealed, seeking a full review, which was granted in September. All 17 D.C. Circuit judges will review the case on Dec. 17.
The Supreme Court is not likely to hear King v. Burwell before that date.
On Twitter @aliciaault
The U.S. Supreme Court has agreed to review a case challenging the legality of federal subsidies provided under the Affordable Care Act.
The Court issued the order Nov. 7, granting the plaintiffs in King v. Burwell a review of the case. The plaintiffs assert that under the ACA, only state marketplaces can issue subsidies to eligible patients.
In July, the Fourth Circuit Court of Appeals ruled against the plaintiffs, upholding the government’s ability to provide subsidies to eligible patients who purchase insurance through the 36 federally facilitated health care marketplaces.
On the same day, a limited panel of judges on the District of Columbia Circuit of the U.S. Court of Appeals ruled that the federal marketplace subsidies were not legal in a similar challenge, Halbig v. Burwell.
The government appealed, seeking a full review, which was granted in September. All 17 D.C. Circuit judges will review the case on Dec. 17.
The Supreme Court is not likely to hear King v. Burwell before that date.
On Twitter @aliciaault
Medicare inches closer to advance care planning payment
Medicare won’t pay physicians for counseling their patients on advance care directives in 2015, but they are open to doing it sometime in the future.
In the 2015 Medicare Physician Fee Schedule, federal officials said they “will consider” whether to pay for codes related to advance care planning services after they have had the opportunity to go through notice and comment rulemaking.
The final physician payment rule, which was released on Oct. 31, highlights two codes recently created by the American Medical Association’s Relative Value Update Committee. The CPT code 99497 covers the first 30 minutes of a face-to-face discussion with the patient, family member, or surrogate about advance directives, as well as the completion of forms. The add-on CPT code 99498 covers each additional 30 minutes.
Physicians can use the new codes, but Medicare will not pay for them in 2015, according to the rule.
Dr. Diane E. Meier, director of the Center to Advance Palliative Care, said the agency’s decision not to move forward immediately with payment is not a surprise. “I think it’s promising,” she said. “I think it’s not surprising that they are being extremely cautious and hesitant given the political firestorm that an effort to do this created in 2009.”
Public opinion on end-of-life care is beginning to shift, Dr. Meier said, which could bode well for future Medicare payment. But payment is only one barrier to making counseling available to all patients. Training physicians and other health care providers in how to have conversations about the end of life is a far bigger hurdle, she said.
“If the clinician is afraid, uncomfortable, doesn’t even know how to begin, it doesn’t matter if there’s a payment,” she said. “They’re not going to do it.”
There has been some momentum building for Medicare payment for end-of-life counseling, including pressure from Congress. In September, 34 members of the U.S. House of Representatives wrote to CMS urging them to begin paying for the newly created codes 99497 and 99498.
The Institute of Medicine in its September report, Dying in America, also recommended that physicians be compensated for counseling patients on end-of-life planning.
On Twitter @maryellenny
Dr. Michael Nelson, FCCP, comments: Pulmonary and critical care physicians counsel patients and offer advance directives as part of routine care, as do many other physicians. It is appropriate to expect reimbursement for providing this often time-consuming process. However, CMS occasionally chooses not to reimburse for CPT codes until it has an opportunity to study the financial implications of this decision. While CMS cannot be compelled to decide in favor of physicians, contacting your senators and representatives at the federal level and requesting their support for payment is a good way to help CMS decide to "do the right thing."
Dr. Nelson is a physician with Shawnee Mission Pulmonary Consultants in Shawnee Mission, Kansas.
Dr. Michael Nelson, FCCP, comments: Pulmonary and critical care physicians counsel patients and offer advance directives as part of routine care, as do many other physicians. It is appropriate to expect reimbursement for providing this often time-consuming process. However, CMS occasionally chooses not to reimburse for CPT codes until it has an opportunity to study the financial implications of this decision. While CMS cannot be compelled to decide in favor of physicians, contacting your senators and representatives at the federal level and requesting their support for payment is a good way to help CMS decide to "do the right thing."
Dr. Nelson is a physician with Shawnee Mission Pulmonary Consultants in Shawnee Mission, Kansas.
Dr. Michael Nelson, FCCP, comments: Pulmonary and critical care physicians counsel patients and offer advance directives as part of routine care, as do many other physicians. It is appropriate to expect reimbursement for providing this often time-consuming process. However, CMS occasionally chooses not to reimburse for CPT codes until it has an opportunity to study the financial implications of this decision. While CMS cannot be compelled to decide in favor of physicians, contacting your senators and representatives at the federal level and requesting their support for payment is a good way to help CMS decide to "do the right thing."
Dr. Nelson is a physician with Shawnee Mission Pulmonary Consultants in Shawnee Mission, Kansas.
Medicare won’t pay physicians for counseling their patients on advance care directives in 2015, but they are open to doing it sometime in the future.
In the 2015 Medicare Physician Fee Schedule, federal officials said they “will consider” whether to pay for codes related to advance care planning services after they have had the opportunity to go through notice and comment rulemaking.
The final physician payment rule, which was released on Oct. 31, highlights two codes recently created by the American Medical Association’s Relative Value Update Committee. The CPT code 99497 covers the first 30 minutes of a face-to-face discussion with the patient, family member, or surrogate about advance directives, as well as the completion of forms. The add-on CPT code 99498 covers each additional 30 minutes.
Physicians can use the new codes, but Medicare will not pay for them in 2015, according to the rule.
Dr. Diane E. Meier, director of the Center to Advance Palliative Care, said the agency’s decision not to move forward immediately with payment is not a surprise. “I think it’s promising,” she said. “I think it’s not surprising that they are being extremely cautious and hesitant given the political firestorm that an effort to do this created in 2009.”
Public opinion on end-of-life care is beginning to shift, Dr. Meier said, which could bode well for future Medicare payment. But payment is only one barrier to making counseling available to all patients. Training physicians and other health care providers in how to have conversations about the end of life is a far bigger hurdle, she said.
“If the clinician is afraid, uncomfortable, doesn’t even know how to begin, it doesn’t matter if there’s a payment,” she said. “They’re not going to do it.”
There has been some momentum building for Medicare payment for end-of-life counseling, including pressure from Congress. In September, 34 members of the U.S. House of Representatives wrote to CMS urging them to begin paying for the newly created codes 99497 and 99498.
The Institute of Medicine in its September report, Dying in America, also recommended that physicians be compensated for counseling patients on end-of-life planning.
On Twitter @maryellenny
Medicare won’t pay physicians for counseling their patients on advance care directives in 2015, but they are open to doing it sometime in the future.
In the 2015 Medicare Physician Fee Schedule, federal officials said they “will consider” whether to pay for codes related to advance care planning services after they have had the opportunity to go through notice and comment rulemaking.
The final physician payment rule, which was released on Oct. 31, highlights two codes recently created by the American Medical Association’s Relative Value Update Committee. The CPT code 99497 covers the first 30 minutes of a face-to-face discussion with the patient, family member, or surrogate about advance directives, as well as the completion of forms. The add-on CPT code 99498 covers each additional 30 minutes.
Physicians can use the new codes, but Medicare will not pay for them in 2015, according to the rule.
Dr. Diane E. Meier, director of the Center to Advance Palliative Care, said the agency’s decision not to move forward immediately with payment is not a surprise. “I think it’s promising,” she said. “I think it’s not surprising that they are being extremely cautious and hesitant given the political firestorm that an effort to do this created in 2009.”
Public opinion on end-of-life care is beginning to shift, Dr. Meier said, which could bode well for future Medicare payment. But payment is only one barrier to making counseling available to all patients. Training physicians and other health care providers in how to have conversations about the end of life is a far bigger hurdle, she said.
“If the clinician is afraid, uncomfortable, doesn’t even know how to begin, it doesn’t matter if there’s a payment,” she said. “They’re not going to do it.”
There has been some momentum building for Medicare payment for end-of-life counseling, including pressure from Congress. In September, 34 members of the U.S. House of Representatives wrote to CMS urging them to begin paying for the newly created codes 99497 and 99498.
The Institute of Medicine in its September report, Dying in America, also recommended that physicians be compensated for counseling patients on end-of-life planning.
On Twitter @maryellenny
VIDEO: Risks for anastomotic leak after colectomy identified
SAN FRANCISCO– A large retrospective study identified risk factors for anastomotic leak within 30 days of colectomy.
The analysis of data on 13,684 patients looked at a multicenter cohort, compared with previous smaller studies that generally focused on single institutions, Dr. Emily F. Midura and her associates reported at the annual clinical congress of the American College of Surgeons.
In a video interview at the meeting, Dr. Midura described the risk factors identified in the study.
The 4% of patients who developed a leak averaged 13 days in the hospital, compared with 8 days for patients with no leak, said Dr. Midura of the University of Cincinnati. A total of 6% of patients who developed an anastomotic leak died, compared with a 2% mortality rate in patients without a leak.
Indications for colectomy included cancer in 42% of patients, diverticulitis in 23%, inflammatory bowel disease in 6%, and other reasons in the rest of the cohort.
Dr. Midura reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO– A large retrospective study identified risk factors for anastomotic leak within 30 days of colectomy.
The analysis of data on 13,684 patients looked at a multicenter cohort, compared with previous smaller studies that generally focused on single institutions, Dr. Emily F. Midura and her associates reported at the annual clinical congress of the American College of Surgeons.
In a video interview at the meeting, Dr. Midura described the risk factors identified in the study.
The 4% of patients who developed a leak averaged 13 days in the hospital, compared with 8 days for patients with no leak, said Dr. Midura of the University of Cincinnati. A total of 6% of patients who developed an anastomotic leak died, compared with a 2% mortality rate in patients without a leak.
Indications for colectomy included cancer in 42% of patients, diverticulitis in 23%, inflammatory bowel disease in 6%, and other reasons in the rest of the cohort.
Dr. Midura reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO– A large retrospective study identified risk factors for anastomotic leak within 30 days of colectomy.
The analysis of data on 13,684 patients looked at a multicenter cohort, compared with previous smaller studies that generally focused on single institutions, Dr. Emily F. Midura and her associates reported at the annual clinical congress of the American College of Surgeons.
In a video interview at the meeting, Dr. Midura described the risk factors identified in the study.
The 4% of patients who developed a leak averaged 13 days in the hospital, compared with 8 days for patients with no leak, said Dr. Midura of the University of Cincinnati. A total of 6% of patients who developed an anastomotic leak died, compared with a 2% mortality rate in patients without a leak.
Indications for colectomy included cancer in 42% of patients, diverticulitis in 23%, inflammatory bowel disease in 6%, and other reasons in the rest of the cohort.
Dr. Midura reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE ACS CLINICAL CONGRESS
Anticoagulants sharply increase hematoma risk after thyroid, parathyroid surgery
SAN FRANCISCO – Patients undergoing thyroid or parathyroid surgery have a sharply higher risk of postoperative hematoma if they are on clopidogrel or anticoagulants – even if these agents are stopped in advance – researchers reported at the annual clinical congress of the American College of Surgeons.
“Patients with multiple factors considered high risk for postoperative hematoma formation after parathyroid or thyroid surgery should probably undergo a period of observation,” recommended lead investigator Dr. Sarah C. Oltmann, who at the time of the study was the director of endocrine surgery at Parkland Memorial Hospital, University of Texas Southwestern Medical Center, Dallas.
“The need specifically for anticoagulation in the perioperative period should really be carefully assessed, and decisions regarding their use in the perioperative period need to be made very cautiously,” she added. “This is particularly important when considering the need for an injectable bridge [anticoagulant], and discussions with the patient’s primary care provider or cardiologist should be prompted because obviously a hematoma risk of 11% [seen with injectable anticoagulants] is not insignificant.”
The researchers retrospectively studied 4,514 patients who underwent thyroid or parathyroid surgery at the center between 1994 and 2013. Most of the operations were performed by high-volume surgeons.
Overall, 25% of patients were using an antiplatelet agent and 3% were using an anticoagulant agent, defined in the study as current use or use up to 5-7 days before surgery. “We felt that there may be some alteration of hemostasis both at the time of surgery and in the days following surgery if they were resumed on their home meds,” explained Dr. Oltmann, who is now a clinical instructor of surgery at the University of Wisconsin–Madison.
Overall, 0.5% of patients developed a postoperative hematoma, with the majority of these events occurring in the first 24 hours. Three-fourths of the affected patients had to undergo repeat surgery.
In multivariate analyses, clopidogrel (Plavix) users had 5.6 times the odds of developing a hematoma. But neither lower-dose aspirin (less than 325 mg daily) alone nor higher-dose aspirin alone was associated with this complication.
Hematoma odds were elevated by an even greater extent, 7.5 and 29.5 times, for patients using oral and injectable anticoagulants, respectively. (Subcutaneous heparin was not included among injectable anticoagulants because surgeons at the center seldom use it in this setting, according to Dr. Oltmann.)
Patients also had increased odds of hematoma if they underwent thyroid surgery as compared with parathyroid surgery (odds ratio, 7.9), and had a bilateral procedure as compared with a unilateral one (OR, 4.9).
“Additional studies are needed to better clarify both the risk-benefit ratio of injectable anticoagulation in this patient population and potentially being able to better risk-stratify which patients would be better served with a period of overnight observation,” Dr. Oltmann concluded.
Invited discussant Dr. Raymon H. Grogan, director of the endocrine surgery research program at University of Chicago Medicine, commented, “I think this work represents a level of detail and granularity in regard to anticoagulants that we haven’t seen before in this literature, so it’s really important for us to see these data.
“We tend to get lulled into a false sense of security when we talk about complications related to thyroidectomy because they are so rare. But the truth of the matter is that this is a complication that causes deaths. A recent Nationwide Inpatient Sample study showed that about 1.3% of people who developed a hematoma will actually die in the United States, which is not an insignificant number of people who will die from a complication that’s directly caused by something we’ve done as surgeons,” he said.
Patients often have other risk factors for hematoma, Dr. Grogan noted. Therefore, he wondered, “Who can actually be sent home as a same-day patient after thyroidectomy? … When you combine your … people on these medications, along with all these other risk factors, as well as the risk of significant hypocalcemia postop, it starts to get to the point where, is it really safe to send anyone home the same day after thyroidectomy, given this overwhelming number of different factors that could cause problems?”
“That’s something we all struggle with to a certain degree, trying to be able to best determine who is safe to go home at night and who is not,” Dr. Oltmann replied, noting that risk in the study was greatest for the small proportion of patients on anticoagulants. “So I think a patient who is on some form of anticoagulant, I would definitely have significant reservations about sending home on the same day. They would be somebody I would at least want to keep overnight.”
“As far as the other variables – Graves disease, the size of the tumor, some people would also argue smoking and poorly controlled hypertension – it really becomes a conversation between the surgeon and the patient to know how reliable is the patient, how do you feel the operation went. … Hopefully, the next step is being able to find a way to weigh these different factors to be able to figure out, well, if my patient has A, B, and C, I must observe versus if they don’t, this might be somebody I can send home.”
Another attendee asked, “How do you [handle] aspirin use, given that it’s low risk as seen in your data set? How do you preop the patients, [do you] ask them to stop any low-risk agents, such as aspirin, or if they take the combination of aspirin and Plavix, which one do you hold and which do you continue in your practice?”
“After kind of combing through this data and becoming very familiar with it, I feel very comfortable with continuing aspirin use through the perioperative period,” Dr. Oltmann commented.
“For Plavix, obviously, you just have to juggle the risk-benefit ratio of why they are on that medication,” she said. “I think the most compelling situation is for our patients with atrial fibrillation, with the primary care provider wanting to … have them done on a Lovenox [enoxaparin] bridge, and now having some sort of objective data to get back with them and say, ‘Listen, they have an 11% risk of this really bad complication. Do you really think their risk of stroke trumps that?’ In most patients, that’s not the case, and I think [these data are] finally going to be able to give us some ammunition in that particular battle.”
Dr. Oltmann disclosed that she had no relevant conflicts of interest.
SAN FRANCISCO – Patients undergoing thyroid or parathyroid surgery have a sharply higher risk of postoperative hematoma if they are on clopidogrel or anticoagulants – even if these agents are stopped in advance – researchers reported at the annual clinical congress of the American College of Surgeons.
“Patients with multiple factors considered high risk for postoperative hematoma formation after parathyroid or thyroid surgery should probably undergo a period of observation,” recommended lead investigator Dr. Sarah C. Oltmann, who at the time of the study was the director of endocrine surgery at Parkland Memorial Hospital, University of Texas Southwestern Medical Center, Dallas.
“The need specifically for anticoagulation in the perioperative period should really be carefully assessed, and decisions regarding their use in the perioperative period need to be made very cautiously,” she added. “This is particularly important when considering the need for an injectable bridge [anticoagulant], and discussions with the patient’s primary care provider or cardiologist should be prompted because obviously a hematoma risk of 11% [seen with injectable anticoagulants] is not insignificant.”
The researchers retrospectively studied 4,514 patients who underwent thyroid or parathyroid surgery at the center between 1994 and 2013. Most of the operations were performed by high-volume surgeons.
Overall, 25% of patients were using an antiplatelet agent and 3% were using an anticoagulant agent, defined in the study as current use or use up to 5-7 days before surgery. “We felt that there may be some alteration of hemostasis both at the time of surgery and in the days following surgery if they were resumed on their home meds,” explained Dr. Oltmann, who is now a clinical instructor of surgery at the University of Wisconsin–Madison.
Overall, 0.5% of patients developed a postoperative hematoma, with the majority of these events occurring in the first 24 hours. Three-fourths of the affected patients had to undergo repeat surgery.
In multivariate analyses, clopidogrel (Plavix) users had 5.6 times the odds of developing a hematoma. But neither lower-dose aspirin (less than 325 mg daily) alone nor higher-dose aspirin alone was associated with this complication.
Hematoma odds were elevated by an even greater extent, 7.5 and 29.5 times, for patients using oral and injectable anticoagulants, respectively. (Subcutaneous heparin was not included among injectable anticoagulants because surgeons at the center seldom use it in this setting, according to Dr. Oltmann.)
Patients also had increased odds of hematoma if they underwent thyroid surgery as compared with parathyroid surgery (odds ratio, 7.9), and had a bilateral procedure as compared with a unilateral one (OR, 4.9).
“Additional studies are needed to better clarify both the risk-benefit ratio of injectable anticoagulation in this patient population and potentially being able to better risk-stratify which patients would be better served with a period of overnight observation,” Dr. Oltmann concluded.
Invited discussant Dr. Raymon H. Grogan, director of the endocrine surgery research program at University of Chicago Medicine, commented, “I think this work represents a level of detail and granularity in regard to anticoagulants that we haven’t seen before in this literature, so it’s really important for us to see these data.
“We tend to get lulled into a false sense of security when we talk about complications related to thyroidectomy because they are so rare. But the truth of the matter is that this is a complication that causes deaths. A recent Nationwide Inpatient Sample study showed that about 1.3% of people who developed a hematoma will actually die in the United States, which is not an insignificant number of people who will die from a complication that’s directly caused by something we’ve done as surgeons,” he said.
Patients often have other risk factors for hematoma, Dr. Grogan noted. Therefore, he wondered, “Who can actually be sent home as a same-day patient after thyroidectomy? … When you combine your … people on these medications, along with all these other risk factors, as well as the risk of significant hypocalcemia postop, it starts to get to the point where, is it really safe to send anyone home the same day after thyroidectomy, given this overwhelming number of different factors that could cause problems?”
“That’s something we all struggle with to a certain degree, trying to be able to best determine who is safe to go home at night and who is not,” Dr. Oltmann replied, noting that risk in the study was greatest for the small proportion of patients on anticoagulants. “So I think a patient who is on some form of anticoagulant, I would definitely have significant reservations about sending home on the same day. They would be somebody I would at least want to keep overnight.”
“As far as the other variables – Graves disease, the size of the tumor, some people would also argue smoking and poorly controlled hypertension – it really becomes a conversation between the surgeon and the patient to know how reliable is the patient, how do you feel the operation went. … Hopefully, the next step is being able to find a way to weigh these different factors to be able to figure out, well, if my patient has A, B, and C, I must observe versus if they don’t, this might be somebody I can send home.”
Another attendee asked, “How do you [handle] aspirin use, given that it’s low risk as seen in your data set? How do you preop the patients, [do you] ask them to stop any low-risk agents, such as aspirin, or if they take the combination of aspirin and Plavix, which one do you hold and which do you continue in your practice?”
“After kind of combing through this data and becoming very familiar with it, I feel very comfortable with continuing aspirin use through the perioperative period,” Dr. Oltmann commented.
“For Plavix, obviously, you just have to juggle the risk-benefit ratio of why they are on that medication,” she said. “I think the most compelling situation is for our patients with atrial fibrillation, with the primary care provider wanting to … have them done on a Lovenox [enoxaparin] bridge, and now having some sort of objective data to get back with them and say, ‘Listen, they have an 11% risk of this really bad complication. Do you really think their risk of stroke trumps that?’ In most patients, that’s not the case, and I think [these data are] finally going to be able to give us some ammunition in that particular battle.”
Dr. Oltmann disclosed that she had no relevant conflicts of interest.
SAN FRANCISCO – Patients undergoing thyroid or parathyroid surgery have a sharply higher risk of postoperative hematoma if they are on clopidogrel or anticoagulants – even if these agents are stopped in advance – researchers reported at the annual clinical congress of the American College of Surgeons.
“Patients with multiple factors considered high risk for postoperative hematoma formation after parathyroid or thyroid surgery should probably undergo a period of observation,” recommended lead investigator Dr. Sarah C. Oltmann, who at the time of the study was the director of endocrine surgery at Parkland Memorial Hospital, University of Texas Southwestern Medical Center, Dallas.
“The need specifically for anticoagulation in the perioperative period should really be carefully assessed, and decisions regarding their use in the perioperative period need to be made very cautiously,” she added. “This is particularly important when considering the need for an injectable bridge [anticoagulant], and discussions with the patient’s primary care provider or cardiologist should be prompted because obviously a hematoma risk of 11% [seen with injectable anticoagulants] is not insignificant.”
The researchers retrospectively studied 4,514 patients who underwent thyroid or parathyroid surgery at the center between 1994 and 2013. Most of the operations were performed by high-volume surgeons.
Overall, 25% of patients were using an antiplatelet agent and 3% were using an anticoagulant agent, defined in the study as current use or use up to 5-7 days before surgery. “We felt that there may be some alteration of hemostasis both at the time of surgery and in the days following surgery if they were resumed on their home meds,” explained Dr. Oltmann, who is now a clinical instructor of surgery at the University of Wisconsin–Madison.
Overall, 0.5% of patients developed a postoperative hematoma, with the majority of these events occurring in the first 24 hours. Three-fourths of the affected patients had to undergo repeat surgery.
In multivariate analyses, clopidogrel (Plavix) users had 5.6 times the odds of developing a hematoma. But neither lower-dose aspirin (less than 325 mg daily) alone nor higher-dose aspirin alone was associated with this complication.
Hematoma odds were elevated by an even greater extent, 7.5 and 29.5 times, for patients using oral and injectable anticoagulants, respectively. (Subcutaneous heparin was not included among injectable anticoagulants because surgeons at the center seldom use it in this setting, according to Dr. Oltmann.)
Patients also had increased odds of hematoma if they underwent thyroid surgery as compared with parathyroid surgery (odds ratio, 7.9), and had a bilateral procedure as compared with a unilateral one (OR, 4.9).
“Additional studies are needed to better clarify both the risk-benefit ratio of injectable anticoagulation in this patient population and potentially being able to better risk-stratify which patients would be better served with a period of overnight observation,” Dr. Oltmann concluded.
Invited discussant Dr. Raymon H. Grogan, director of the endocrine surgery research program at University of Chicago Medicine, commented, “I think this work represents a level of detail and granularity in regard to anticoagulants that we haven’t seen before in this literature, so it’s really important for us to see these data.
“We tend to get lulled into a false sense of security when we talk about complications related to thyroidectomy because they are so rare. But the truth of the matter is that this is a complication that causes deaths. A recent Nationwide Inpatient Sample study showed that about 1.3% of people who developed a hematoma will actually die in the United States, which is not an insignificant number of people who will die from a complication that’s directly caused by something we’ve done as surgeons,” he said.
Patients often have other risk factors for hematoma, Dr. Grogan noted. Therefore, he wondered, “Who can actually be sent home as a same-day patient after thyroidectomy? … When you combine your … people on these medications, along with all these other risk factors, as well as the risk of significant hypocalcemia postop, it starts to get to the point where, is it really safe to send anyone home the same day after thyroidectomy, given this overwhelming number of different factors that could cause problems?”
“That’s something we all struggle with to a certain degree, trying to be able to best determine who is safe to go home at night and who is not,” Dr. Oltmann replied, noting that risk in the study was greatest for the small proportion of patients on anticoagulants. “So I think a patient who is on some form of anticoagulant, I would definitely have significant reservations about sending home on the same day. They would be somebody I would at least want to keep overnight.”
“As far as the other variables – Graves disease, the size of the tumor, some people would also argue smoking and poorly controlled hypertension – it really becomes a conversation between the surgeon and the patient to know how reliable is the patient, how do you feel the operation went. … Hopefully, the next step is being able to find a way to weigh these different factors to be able to figure out, well, if my patient has A, B, and C, I must observe versus if they don’t, this might be somebody I can send home.”
Another attendee asked, “How do you [handle] aspirin use, given that it’s low risk as seen in your data set? How do you preop the patients, [do you] ask them to stop any low-risk agents, such as aspirin, or if they take the combination of aspirin and Plavix, which one do you hold and which do you continue in your practice?”
“After kind of combing through this data and becoming very familiar with it, I feel very comfortable with continuing aspirin use through the perioperative period,” Dr. Oltmann commented.
“For Plavix, obviously, you just have to juggle the risk-benefit ratio of why they are on that medication,” she said. “I think the most compelling situation is for our patients with atrial fibrillation, with the primary care provider wanting to … have them done on a Lovenox [enoxaparin] bridge, and now having some sort of objective data to get back with them and say, ‘Listen, they have an 11% risk of this really bad complication. Do you really think their risk of stroke trumps that?’ In most patients, that’s not the case, and I think [these data are] finally going to be able to give us some ammunition in that particular battle.”
Dr. Oltmann disclosed that she had no relevant conflicts of interest.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Clopidogrel and anticoagulants are risk factors for hematoma after thyroid or parathyroid surgery.
Major finding: The odds of hematoma were 5.6 times higher with clopidogrel use and 7.5 and 29.5 times higher with oral and injectable anticoagulant use, respectively.
Data source: A retrospective study of 4,514 patients undergoing thyroid or parathyroid surgery.
Disclosures: Dr. Oltmann disclosed that she had no relevant conflicts of interest.
Larger plasma volumes increase transfusion thrombosis risk
SAN FRANCISCO – Venous thromboembolism is about 50% more likely when trauma patients are transfused with more than 1 unit of fresh frozen plasma for every 2 units of red blood cells, according to a retrospective review of 139,842 adult patients in the National Trauma Data Bank, all of whom received at least 1 unit of red blood cells from 2007 to 2012.
The risk quadrupled when patients received 6 or more red blood cell (RBC) units; for those patients, the only independent risk factor for venous thromboembolism (VTE) was transfusion with more than 1 unit of fresh frozen plasma (FFP) per 2 units of RBCs (odds ratio, 4.12; P = .011).
When patients get that much plasma, they “should be monitored closely for deep vein thrombosis [DVT] and pulmonary embolism [PE], and started on VTE prophylaxis as soon as possible,” said lead investigator Dr. Gregory Magee, a trauma and critical care fellow at the University of Southern California, Los Angeles. The findings complicate an emerging idea of how best to transfuse trauma patients. A 2013 investigation found that 6-hour survival is significantly higher when patients get more plasma with their RBCs than they might have in the past, at least 1 FFP unit for every 2 RBC units. Some research suggests that a 1:1 ratio might be even better (JAMA Surg. 2013;148:127-36). “You need to do what you need to do to help your patients survive,” but there should be a “balancing act to make sure they have enough clotting factors [onboard] to stop the bleeding, but not enough to cause thrombosis,” Dr. Magee said at the annual clinical congress of the American College of Surgeons.
The rate of transfusion-associated PEs in his study was 0.4%, and the rate of DVTs 0.8%. How serious they were is not known; the information was unavailable in the database review. Though low, the incidence of thrombosis increased with increasing volumes of transfused RBCs.
In addition to the 50% increased risk of VTE with higher volumes of transfused plasma (OR 1.47, P < .001), VTE was independently associated with transfusions of 6 or more RBC units (OR 2.10, P = .001); blunt trauma (OR 1.49, P = .001); male gender (OR 1.29, P < .001); and Abbreviated Injury Scale (AIS) scores of 3 or higher for chest injuries (OR 1.30, P < .001), head injuries (OR 1.18, P = .032), and lower extremity injuries (OR 1.16, P = .034).
Several of Dr. Magee’s colleagues are coinvestigators on a recently concluded randomized transfusion trial that pitted plasma, platelet, and RBC ratios of 1:1:1 and 1:1:2 against each other, looking for survival and complication differences. They hope to publish their results soon, he said. The randomized study was the only way to counter the survival bias that might have been at work in the 2013 investigation, which was a prospective cohort study. Higher volumes of plasma might have improved survival, but it’s possible that patients who lived longer were more likely to get FFP, since it’s often administered well after RBC transfusions are underway.
For now, “we don’t know which one is best or if it makes a difference,” Dr. Magee said.
Dr. Magee had no disclosures. The work was funded in part by the National Institutes of Health.
SAN FRANCISCO – Venous thromboembolism is about 50% more likely when trauma patients are transfused with more than 1 unit of fresh frozen plasma for every 2 units of red blood cells, according to a retrospective review of 139,842 adult patients in the National Trauma Data Bank, all of whom received at least 1 unit of red blood cells from 2007 to 2012.
The risk quadrupled when patients received 6 or more red blood cell (RBC) units; for those patients, the only independent risk factor for venous thromboembolism (VTE) was transfusion with more than 1 unit of fresh frozen plasma (FFP) per 2 units of RBCs (odds ratio, 4.12; P = .011).
When patients get that much plasma, they “should be monitored closely for deep vein thrombosis [DVT] and pulmonary embolism [PE], and started on VTE prophylaxis as soon as possible,” said lead investigator Dr. Gregory Magee, a trauma and critical care fellow at the University of Southern California, Los Angeles. The findings complicate an emerging idea of how best to transfuse trauma patients. A 2013 investigation found that 6-hour survival is significantly higher when patients get more plasma with their RBCs than they might have in the past, at least 1 FFP unit for every 2 RBC units. Some research suggests that a 1:1 ratio might be even better (JAMA Surg. 2013;148:127-36). “You need to do what you need to do to help your patients survive,” but there should be a “balancing act to make sure they have enough clotting factors [onboard] to stop the bleeding, but not enough to cause thrombosis,” Dr. Magee said at the annual clinical congress of the American College of Surgeons.
The rate of transfusion-associated PEs in his study was 0.4%, and the rate of DVTs 0.8%. How serious they were is not known; the information was unavailable in the database review. Though low, the incidence of thrombosis increased with increasing volumes of transfused RBCs.
In addition to the 50% increased risk of VTE with higher volumes of transfused plasma (OR 1.47, P < .001), VTE was independently associated with transfusions of 6 or more RBC units (OR 2.10, P = .001); blunt trauma (OR 1.49, P = .001); male gender (OR 1.29, P < .001); and Abbreviated Injury Scale (AIS) scores of 3 or higher for chest injuries (OR 1.30, P < .001), head injuries (OR 1.18, P = .032), and lower extremity injuries (OR 1.16, P = .034).
Several of Dr. Magee’s colleagues are coinvestigators on a recently concluded randomized transfusion trial that pitted plasma, platelet, and RBC ratios of 1:1:1 and 1:1:2 against each other, looking for survival and complication differences. They hope to publish their results soon, he said. The randomized study was the only way to counter the survival bias that might have been at work in the 2013 investigation, which was a prospective cohort study. Higher volumes of plasma might have improved survival, but it’s possible that patients who lived longer were more likely to get FFP, since it’s often administered well after RBC transfusions are underway.
For now, “we don’t know which one is best or if it makes a difference,” Dr. Magee said.
Dr. Magee had no disclosures. The work was funded in part by the National Institutes of Health.
SAN FRANCISCO – Venous thromboembolism is about 50% more likely when trauma patients are transfused with more than 1 unit of fresh frozen plasma for every 2 units of red blood cells, according to a retrospective review of 139,842 adult patients in the National Trauma Data Bank, all of whom received at least 1 unit of red blood cells from 2007 to 2012.
The risk quadrupled when patients received 6 or more red blood cell (RBC) units; for those patients, the only independent risk factor for venous thromboembolism (VTE) was transfusion with more than 1 unit of fresh frozen plasma (FFP) per 2 units of RBCs (odds ratio, 4.12; P = .011).
When patients get that much plasma, they “should be monitored closely for deep vein thrombosis [DVT] and pulmonary embolism [PE], and started on VTE prophylaxis as soon as possible,” said lead investigator Dr. Gregory Magee, a trauma and critical care fellow at the University of Southern California, Los Angeles. The findings complicate an emerging idea of how best to transfuse trauma patients. A 2013 investigation found that 6-hour survival is significantly higher when patients get more plasma with their RBCs than they might have in the past, at least 1 FFP unit for every 2 RBC units. Some research suggests that a 1:1 ratio might be even better (JAMA Surg. 2013;148:127-36). “You need to do what you need to do to help your patients survive,” but there should be a “balancing act to make sure they have enough clotting factors [onboard] to stop the bleeding, but not enough to cause thrombosis,” Dr. Magee said at the annual clinical congress of the American College of Surgeons.
The rate of transfusion-associated PEs in his study was 0.4%, and the rate of DVTs 0.8%. How serious they were is not known; the information was unavailable in the database review. Though low, the incidence of thrombosis increased with increasing volumes of transfused RBCs.
In addition to the 50% increased risk of VTE with higher volumes of transfused plasma (OR 1.47, P < .001), VTE was independently associated with transfusions of 6 or more RBC units (OR 2.10, P = .001); blunt trauma (OR 1.49, P = .001); male gender (OR 1.29, P < .001); and Abbreviated Injury Scale (AIS) scores of 3 or higher for chest injuries (OR 1.30, P < .001), head injuries (OR 1.18, P = .032), and lower extremity injuries (OR 1.16, P = .034).
Several of Dr. Magee’s colleagues are coinvestigators on a recently concluded randomized transfusion trial that pitted plasma, platelet, and RBC ratios of 1:1:1 and 1:1:2 against each other, looking for survival and complication differences. They hope to publish their results soon, he said. The randomized study was the only way to counter the survival bias that might have been at work in the 2013 investigation, which was a prospective cohort study. Higher volumes of plasma might have improved survival, but it’s possible that patients who lived longer were more likely to get FFP, since it’s often administered well after RBC transfusions are underway.
For now, “we don’t know which one is best or if it makes a difference,” Dr. Magee said.
Dr. Magee had no disclosures. The work was funded in part by the National Institutes of Health.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Keep an eye out for VTEs when transfusion ratios go above 1:2 plasma to RBC units, and start prophylaxis against VTEs when it becomes safe to do so.
Major finding: Venous thromboembolism is about 50% more likely when trauma patients are transfused with more than 1 unit of fresh frozen plasma for every 2 units of red blood cells (odds ratio,1.47; P < .001).
Data source: Retrospective review of 139,842 adult patients in the National Trauma Data Bank.
Disclosures: The lead investigator has no disclosures. The work was funded in part by the National Institutes of Health.
Spotlight falls on rising levels of tricuspid valve surgery
CHICAGO – Ten times as many papers were published on the mitral valve as were published on the tricuspid valve during the 1990s, based on a literature review.
Things have picked up over the past decade, however, for the “forgotten,” little-respected “Rodney Dangerfield” valve, with surgeons writing more about tricuspid regurgitation and doing more tricuspid surgery than ever before, Dr. Patrick McCarthy said at Heart Valve Summit 2014.
Tricuspid interventions more than doubled from 1999 to 2008, although overall hospital mortality was substantial at 10.6%. (J. Thorac. Cardiovasc. Surg. 2012;143:1043-9).
A Society of Thoracic Surgeons risk model containing intraoperative variables showed that multiple-valve surgery mortality is more than twice that of single-valve surgery, but that performance of arrhythmia ablation and atrioventricular valve repair are protective for mortality (Ann. Thorac. Surg. 2013;95:1484-90).
“There isn’t any data that the tricuspid per se is actually the reason that the operation is higher risk,” said Dr. McCarthy, director of the Bluhm Cardiovascular Institute and chief of cardiac surgery, Northwestern University in Chicago.
The new American Heart Association/American College of Cardiology (AHA/ACC) guideline on valvular heart disease, published earlier this year, reflects the changing attitudes about mitral valve surgery and the need for earlier intervention.
A class I indication for surgery remains in place for severe tricuspid regurgitation (TR) with mitral valve disease. However, what had been a class IIb indication in the 2006 guidelines for primary TR with symptoms is now a class I indication in the 2014 guidelines.
“Don’t wait for right ventricular failure in primary TR. Plan for earlier intervention, and think of it more like we do mitral regurgitation,” Dr. McCarthy said.
The recommendation for more moderate TR has also changed. The class IIb recommendation for patients with less than severe TR during mitral valve repair with pulmonary hypertension, right heart failure, or tricuspid dilation is now class IIa, indicating a lower threshold for surgery for these patients, he said.
Asymptomatic primary TR with right ventricle dilation or reoperations for TR with symptoms and prior left heart surgery had been a class III indication against surgery in 2006, but are now in sync with the European valvular guidelines with a class IIb indication, suggesting surgery may be considered.
The move toward earlier surgery is supported by results showing that TR only gets worse if left untreated, Dr. McCarthy said. Among patients with annular dilation greater than 70 mm as the only criterion for tricuspid valve repair (TVR), TR was shown to increase by more than 2 grades after 2 years in just 2% of patients who underwent TVR during mitral valve repair (MVR), versus 48% without TVR (Ann. Thorac. Surg. 2005;79:127-32).
Another study showed that prophylactic tricuspid annuloplasty in patients with dilated tricuspid annulus undergoing MVR reduces the rate of TR progression, improves right ventricular remodeling, and improves functional outcomes on the 6-minute walk test (J. Thorac. Cardiovasc. Surg. 2012;143:632-8).
Not all data, however, have been viewed through the same lens, with the “Mayo Clinic and Cleveland Clinic finding the same thing but drawing different conclusions,” Dr. McCarthy observed.
A Cleveland Clinic analysis involving 1,833 patients with degenerative mitral valve disease reported that MVR alone improved TR and right ventricular function in patients with severe TR (grade 3+/4+), but that improvements were incomplete and temporary. In contrast, MVR with concomitant TVR eliminated severe TR and improved RV function toward normal, “supporting an aggressive approach to important functional tricuspid regurgitation” (J. Cardiovasc Surg. 2013;146:1126-32).
An 11-year review by the Mayo Clinic in Rochester, Minn., involving 699 patients with functional TR and degenerative mitral valve leaflet prolapse also showed that MVR alone significantly reduced TR within the first year in all patients and produced significant decreases until the third year in those with severe regurgitation. Only one patient required tricuspid reoperation 4.5 years after mitral repair. The authors argued for a selective approach to TR, concluding that “tricuspid valve surgery is rarely necessary for most patients undergoing repair of isolated mitral valve prolapse.”
“While both Cleveland and Mayo Clinic found that untreated TR persisted, Mayo interpreted the rare need for reoperation and no decrease in 5-year survival as evidence that it need not be repaired, while Cleveland suggested with the evidence of improved RV function that it should be repaired,” Dr. McCarthy said in an interview. “The European Society of Cardiology and AHA/ACC guidelines would support the approach from the Cleveland Clinic.”
Dr. McCarthy disclosed inventing the Edwards MC3 tricuspid valve repair ring.
Dr. Hossein Almassi, FCCP,comments: Historically, cardiac surgeons have been reluctant to operate on the tricuspid valve, mainly because of poor outcome and a high mortality rate. The excellent results with mitral valve repair and the emerging experience on tricuspid valve surgery have led to a welcome shift in the attitude of cardiac surgeons and cardiologists in adopting an earlier and more proactive approach in treating patients with significant tricuspid valve regurgitation, either alone or in conjunction with other valvular operations, as evidenced by changes in the 2014 AHA/ACC guidelines.
Dr. Almassi is with the Cardiothoracic Surgery Division at the Medical College of Wisconsin in Milwaukee, WI.
Dr. Hossein Almassi, FCCP,comments: Historically, cardiac surgeons have been reluctant to operate on the tricuspid valve, mainly because of poor outcome and a high mortality rate. The excellent results with mitral valve repair and the emerging experience on tricuspid valve surgery have led to a welcome shift in the attitude of cardiac surgeons and cardiologists in adopting an earlier and more proactive approach in treating patients with significant tricuspid valve regurgitation, either alone or in conjunction with other valvular operations, as evidenced by changes in the 2014 AHA/ACC guidelines.
Dr. Almassi is with the Cardiothoracic Surgery Division at the Medical College of Wisconsin in Milwaukee, WI.
Dr. Hossein Almassi, FCCP,comments: Historically, cardiac surgeons have been reluctant to operate on the tricuspid valve, mainly because of poor outcome and a high mortality rate. The excellent results with mitral valve repair and the emerging experience on tricuspid valve surgery have led to a welcome shift in the attitude of cardiac surgeons and cardiologists in adopting an earlier and more proactive approach in treating patients with significant tricuspid valve regurgitation, either alone or in conjunction with other valvular operations, as evidenced by changes in the 2014 AHA/ACC guidelines.
Dr. Almassi is with the Cardiothoracic Surgery Division at the Medical College of Wisconsin in Milwaukee, WI.
CHICAGO – Ten times as many papers were published on the mitral valve as were published on the tricuspid valve during the 1990s, based on a literature review.
Things have picked up over the past decade, however, for the “forgotten,” little-respected “Rodney Dangerfield” valve, with surgeons writing more about tricuspid regurgitation and doing more tricuspid surgery than ever before, Dr. Patrick McCarthy said at Heart Valve Summit 2014.
Tricuspid interventions more than doubled from 1999 to 2008, although overall hospital mortality was substantial at 10.6%. (J. Thorac. Cardiovasc. Surg. 2012;143:1043-9).
A Society of Thoracic Surgeons risk model containing intraoperative variables showed that multiple-valve surgery mortality is more than twice that of single-valve surgery, but that performance of arrhythmia ablation and atrioventricular valve repair are protective for mortality (Ann. Thorac. Surg. 2013;95:1484-90).
“There isn’t any data that the tricuspid per se is actually the reason that the operation is higher risk,” said Dr. McCarthy, director of the Bluhm Cardiovascular Institute and chief of cardiac surgery, Northwestern University in Chicago.
The new American Heart Association/American College of Cardiology (AHA/ACC) guideline on valvular heart disease, published earlier this year, reflects the changing attitudes about mitral valve surgery and the need for earlier intervention.
A class I indication for surgery remains in place for severe tricuspid regurgitation (TR) with mitral valve disease. However, what had been a class IIb indication in the 2006 guidelines for primary TR with symptoms is now a class I indication in the 2014 guidelines.
“Don’t wait for right ventricular failure in primary TR. Plan for earlier intervention, and think of it more like we do mitral regurgitation,” Dr. McCarthy said.
The recommendation for more moderate TR has also changed. The class IIb recommendation for patients with less than severe TR during mitral valve repair with pulmonary hypertension, right heart failure, or tricuspid dilation is now class IIa, indicating a lower threshold for surgery for these patients, he said.
Asymptomatic primary TR with right ventricle dilation or reoperations for TR with symptoms and prior left heart surgery had been a class III indication against surgery in 2006, but are now in sync with the European valvular guidelines with a class IIb indication, suggesting surgery may be considered.
The move toward earlier surgery is supported by results showing that TR only gets worse if left untreated, Dr. McCarthy said. Among patients with annular dilation greater than 70 mm as the only criterion for tricuspid valve repair (TVR), TR was shown to increase by more than 2 grades after 2 years in just 2% of patients who underwent TVR during mitral valve repair (MVR), versus 48% without TVR (Ann. Thorac. Surg. 2005;79:127-32).
Another study showed that prophylactic tricuspid annuloplasty in patients with dilated tricuspid annulus undergoing MVR reduces the rate of TR progression, improves right ventricular remodeling, and improves functional outcomes on the 6-minute walk test (J. Thorac. Cardiovasc. Surg. 2012;143:632-8).
Not all data, however, have been viewed through the same lens, with the “Mayo Clinic and Cleveland Clinic finding the same thing but drawing different conclusions,” Dr. McCarthy observed.
A Cleveland Clinic analysis involving 1,833 patients with degenerative mitral valve disease reported that MVR alone improved TR and right ventricular function in patients with severe TR (grade 3+/4+), but that improvements were incomplete and temporary. In contrast, MVR with concomitant TVR eliminated severe TR and improved RV function toward normal, “supporting an aggressive approach to important functional tricuspid regurgitation” (J. Cardiovasc Surg. 2013;146:1126-32).
An 11-year review by the Mayo Clinic in Rochester, Minn., involving 699 patients with functional TR and degenerative mitral valve leaflet prolapse also showed that MVR alone significantly reduced TR within the first year in all patients and produced significant decreases until the third year in those with severe regurgitation. Only one patient required tricuspid reoperation 4.5 years after mitral repair. The authors argued for a selective approach to TR, concluding that “tricuspid valve surgery is rarely necessary for most patients undergoing repair of isolated mitral valve prolapse.”
“While both Cleveland and Mayo Clinic found that untreated TR persisted, Mayo interpreted the rare need for reoperation and no decrease in 5-year survival as evidence that it need not be repaired, while Cleveland suggested with the evidence of improved RV function that it should be repaired,” Dr. McCarthy said in an interview. “The European Society of Cardiology and AHA/ACC guidelines would support the approach from the Cleveland Clinic.”
Dr. McCarthy disclosed inventing the Edwards MC3 tricuspid valve repair ring.
CHICAGO – Ten times as many papers were published on the mitral valve as were published on the tricuspid valve during the 1990s, based on a literature review.
Things have picked up over the past decade, however, for the “forgotten,” little-respected “Rodney Dangerfield” valve, with surgeons writing more about tricuspid regurgitation and doing more tricuspid surgery than ever before, Dr. Patrick McCarthy said at Heart Valve Summit 2014.
Tricuspid interventions more than doubled from 1999 to 2008, although overall hospital mortality was substantial at 10.6%. (J. Thorac. Cardiovasc. Surg. 2012;143:1043-9).
A Society of Thoracic Surgeons risk model containing intraoperative variables showed that multiple-valve surgery mortality is more than twice that of single-valve surgery, but that performance of arrhythmia ablation and atrioventricular valve repair are protective for mortality (Ann. Thorac. Surg. 2013;95:1484-90).
“There isn’t any data that the tricuspid per se is actually the reason that the operation is higher risk,” said Dr. McCarthy, director of the Bluhm Cardiovascular Institute and chief of cardiac surgery, Northwestern University in Chicago.
The new American Heart Association/American College of Cardiology (AHA/ACC) guideline on valvular heart disease, published earlier this year, reflects the changing attitudes about mitral valve surgery and the need for earlier intervention.
A class I indication for surgery remains in place for severe tricuspid regurgitation (TR) with mitral valve disease. However, what had been a class IIb indication in the 2006 guidelines for primary TR with symptoms is now a class I indication in the 2014 guidelines.
“Don’t wait for right ventricular failure in primary TR. Plan for earlier intervention, and think of it more like we do mitral regurgitation,” Dr. McCarthy said.
The recommendation for more moderate TR has also changed. The class IIb recommendation for patients with less than severe TR during mitral valve repair with pulmonary hypertension, right heart failure, or tricuspid dilation is now class IIa, indicating a lower threshold for surgery for these patients, he said.
Asymptomatic primary TR with right ventricle dilation or reoperations for TR with symptoms and prior left heart surgery had been a class III indication against surgery in 2006, but are now in sync with the European valvular guidelines with a class IIb indication, suggesting surgery may be considered.
The move toward earlier surgery is supported by results showing that TR only gets worse if left untreated, Dr. McCarthy said. Among patients with annular dilation greater than 70 mm as the only criterion for tricuspid valve repair (TVR), TR was shown to increase by more than 2 grades after 2 years in just 2% of patients who underwent TVR during mitral valve repair (MVR), versus 48% without TVR (Ann. Thorac. Surg. 2005;79:127-32).
Another study showed that prophylactic tricuspid annuloplasty in patients with dilated tricuspid annulus undergoing MVR reduces the rate of TR progression, improves right ventricular remodeling, and improves functional outcomes on the 6-minute walk test (J. Thorac. Cardiovasc. Surg. 2012;143:632-8).
Not all data, however, have been viewed through the same lens, with the “Mayo Clinic and Cleveland Clinic finding the same thing but drawing different conclusions,” Dr. McCarthy observed.
A Cleveland Clinic analysis involving 1,833 patients with degenerative mitral valve disease reported that MVR alone improved TR and right ventricular function in patients with severe TR (grade 3+/4+), but that improvements were incomplete and temporary. In contrast, MVR with concomitant TVR eliminated severe TR and improved RV function toward normal, “supporting an aggressive approach to important functional tricuspid regurgitation” (J. Cardiovasc Surg. 2013;146:1126-32).
An 11-year review by the Mayo Clinic in Rochester, Minn., involving 699 patients with functional TR and degenerative mitral valve leaflet prolapse also showed that MVR alone significantly reduced TR within the first year in all patients and produced significant decreases until the third year in those with severe regurgitation. Only one patient required tricuspid reoperation 4.5 years after mitral repair. The authors argued for a selective approach to TR, concluding that “tricuspid valve surgery is rarely necessary for most patients undergoing repair of isolated mitral valve prolapse.”
“While both Cleveland and Mayo Clinic found that untreated TR persisted, Mayo interpreted the rare need for reoperation and no decrease in 5-year survival as evidence that it need not be repaired, while Cleveland suggested with the evidence of improved RV function that it should be repaired,” Dr. McCarthy said in an interview. “The European Society of Cardiology and AHA/ACC guidelines would support the approach from the Cleveland Clinic.”
Dr. McCarthy disclosed inventing the Edwards MC3 tricuspid valve repair ring.
EXPERT ANALYSIS FROM HEART VALVE SUMMIT 2014
Annual echo an option for cardiac allograft vasculopathy screening
LAS VEGAS – The experience at one major heart transplantation center indicates that annual screening dobutamine stress echocardiography to detect cardiac allograft vasculopathy renders annual coronary angiography unnecessary.
“This noninvasive method has very good specificity and is associated with a negative predictive value of 94%-97%. It can be used in our experience in lieu of annual invasive coronary angiography,” Dr. Jerry D. Estep declared at the annual meeting of the Heart Failure Society of America.
Cardiac allograft vasculopathy (CAV) is a unique, highly aggressive form of CAD. After 3 years post transplant it becomes the No. 1 cause of cardiac retransplantation and mortality. Guidelines recommend consideration of annual screening coronary angiography to detect it early to institute aggressive countermeasures. That’s the practice at most transplant centers.
However, at Houston Methodist Hospital, where Dr. Estep is medical director of the heart transplant and LVAD program, annual dobutamine stress echocardiography (DSE) is used instead. Because there is a scarcity of published data on this noninvasive alternative approach, he presented a retrospective study of the Houston transplant center’s experience over a recent 5-year period.
The study included 144 heart transplant recipients who underwent screening DSE for CAV annually for the first 4 years post transplant and coronary angiography at year 5.
During years 1-4, DSE detected CAV in 19% of patients. They didn’t differ in terms of baseline characteristics from those who remained free of this serious complication.
The good news: Ninety-four percent of patients with normal DSEs during years 1-4 had no CAV upon angiography at year 5. Moreover, the 5% who did have CAV at year 5 after earlier negative DSEs had mild to moderate disease.
The investigators documented the performance of annual screening DSE in predicting the development of major adverse cardiac events, defined as readmission for acute coronary syndrome, heart failure, revascularization, repeat heart transplantation, or cardiac death.
Dr. Estep reported having no financial conflicts regarding this study.
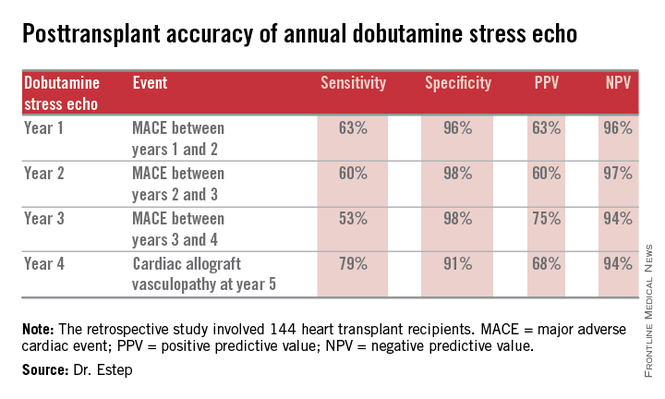
Dr. Hossein Almassi, FCCP, comments: Among solid organ transplants, cardiac transplant is rather unique in its need for invasive biopsy and angiography in following up the cardiac allograft. The search for noninvasive monitoring tools has been ongoing for a number of years. The report by the Houston group is a positive development in the right direction awaiting further confirmation by other cardiac transplant centers.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: Among solid organ transplants, cardiac transplant is rather unique in its need for invasive biopsy and angiography in following up the cardiac allograft. The search for noninvasive monitoring tools has been ongoing for a number of years. The report by the Houston group is a positive development in the right direction awaiting further confirmation by other cardiac transplant centers.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: Among solid organ transplants, cardiac transplant is rather unique in its need for invasive biopsy and angiography in following up the cardiac allograft. The search for noninvasive monitoring tools has been ongoing for a number of years. The report by the Houston group is a positive development in the right direction awaiting further confirmation by other cardiac transplant centers.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
LAS VEGAS – The experience at one major heart transplantation center indicates that annual screening dobutamine stress echocardiography to detect cardiac allograft vasculopathy renders annual coronary angiography unnecessary.
“This noninvasive method has very good specificity and is associated with a negative predictive value of 94%-97%. It can be used in our experience in lieu of annual invasive coronary angiography,” Dr. Jerry D. Estep declared at the annual meeting of the Heart Failure Society of America.
Cardiac allograft vasculopathy (CAV) is a unique, highly aggressive form of CAD. After 3 years post transplant it becomes the No. 1 cause of cardiac retransplantation and mortality. Guidelines recommend consideration of annual screening coronary angiography to detect it early to institute aggressive countermeasures. That’s the practice at most transplant centers.
However, at Houston Methodist Hospital, where Dr. Estep is medical director of the heart transplant and LVAD program, annual dobutamine stress echocardiography (DSE) is used instead. Because there is a scarcity of published data on this noninvasive alternative approach, he presented a retrospective study of the Houston transplant center’s experience over a recent 5-year period.
The study included 144 heart transplant recipients who underwent screening DSE for CAV annually for the first 4 years post transplant and coronary angiography at year 5.
During years 1-4, DSE detected CAV in 19% of patients. They didn’t differ in terms of baseline characteristics from those who remained free of this serious complication.
The good news: Ninety-four percent of patients with normal DSEs during years 1-4 had no CAV upon angiography at year 5. Moreover, the 5% who did have CAV at year 5 after earlier negative DSEs had mild to moderate disease.
The investigators documented the performance of annual screening DSE in predicting the development of major adverse cardiac events, defined as readmission for acute coronary syndrome, heart failure, revascularization, repeat heart transplantation, or cardiac death.
Dr. Estep reported having no financial conflicts regarding this study.
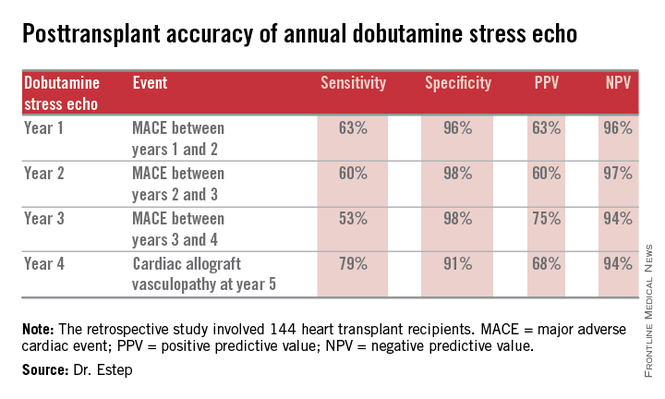
LAS VEGAS – The experience at one major heart transplantation center indicates that annual screening dobutamine stress echocardiography to detect cardiac allograft vasculopathy renders annual coronary angiography unnecessary.
“This noninvasive method has very good specificity and is associated with a negative predictive value of 94%-97%. It can be used in our experience in lieu of annual invasive coronary angiography,” Dr. Jerry D. Estep declared at the annual meeting of the Heart Failure Society of America.
Cardiac allograft vasculopathy (CAV) is a unique, highly aggressive form of CAD. After 3 years post transplant it becomes the No. 1 cause of cardiac retransplantation and mortality. Guidelines recommend consideration of annual screening coronary angiography to detect it early to institute aggressive countermeasures. That’s the practice at most transplant centers.
However, at Houston Methodist Hospital, where Dr. Estep is medical director of the heart transplant and LVAD program, annual dobutamine stress echocardiography (DSE) is used instead. Because there is a scarcity of published data on this noninvasive alternative approach, he presented a retrospective study of the Houston transplant center’s experience over a recent 5-year period.
The study included 144 heart transplant recipients who underwent screening DSE for CAV annually for the first 4 years post transplant and coronary angiography at year 5.
During years 1-4, DSE detected CAV in 19% of patients. They didn’t differ in terms of baseline characteristics from those who remained free of this serious complication.
The good news: Ninety-four percent of patients with normal DSEs during years 1-4 had no CAV upon angiography at year 5. Moreover, the 5% who did have CAV at year 5 after earlier negative DSEs had mild to moderate disease.
The investigators documented the performance of annual screening DSE in predicting the development of major adverse cardiac events, defined as readmission for acute coronary syndrome, heart failure, revascularization, repeat heart transplantation, or cardiac death.
Dr. Estep reported having no financial conflicts regarding this study.
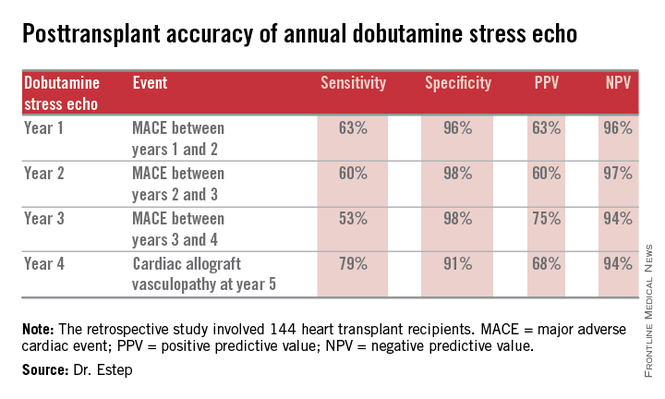
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point: Annual dobutamine stress echocardiography to screen heart transplant recipients for cardiac allograft vasculopathy is an excellent noninvasive alternative to the widely used practice of annual screening coronary angiography.
Major finding: Annual screening dobutamine stress echo during years 1-4 after heart transplant had a 94% negative predictive value for cardiac allograft vasculopathy at year 5.
Data source: A retrospective study of 144 heart transplant recipients at a major transplant center where screening for cardiac allograft vasculopathy is done noninvasively by annual dobutamine stress echocardiography rather than angiography, which is widely used elsewhere.
Disclosures: The presenter reported having no conflicts relevant to the study, which was free of commercial support.
Obesity, diabetes spur on group A strep infections
PHILADELPHIA – Obesity and diabetes are independent risk factors for invasive group A Streptococcus infections, with the highest risk among those with diabetes and morbid obesity.
The relative risk of invasive group A Streptococcus (iGAS) infection was 15 times higher in adults with diabetes and grade 3 morbid obesity (body mass index ≥ 40 kg/m2) than in those of normal weight, Dr. Gayle Langley reported at Infectious Diseases Week 2014.
Moreover, grades 1-2 obesity and morbid obesity increased the odds of ICU admission and death from an iGAS infection in multivariable logistic regression.
The adjusted odds ratios for ICU admission and death were 1.46 and 1.55 for patients with grades 1-2 obesity (BMI 30 < 40 kg/m2) and 2.07 and 1.62 for those with morbid obesity, she said.
Diabetes was not associated with an increased risk for either ICU admission (odds ratio, 1.06) or death (OR, 0.77) in the analysis.
Skin and soft tissue infections, which were significantly more common in obese and diabetic patients, appear to be driving the increased risk for iGAS in these groups, Dr. Langley of the Centers for Disease Control and Prevention said in an interview.
“Based on the literature, I’m not all that surprised because we definitely know that they are at increased risk for these skin and soft tissue infections, and that is a common manifestation of strep,” she said. “The mortality is slightly increased, but not to the extent of the incidence.”
The study was prompted by the limited number of prevention strategies for what Langley described as a “really serious infection” and by the rise in obesity and diabetes in the United States.
Data from select counties in 10 of the CDC’s Active Bacterial Core surveillance sites were used to identify 2,927 cases of 2010-2012 community onset iGAS. Cases were defined by isolation of GAS from a normally sterile site or from a wound in a patient with necrotizing fasciitis or streptococcal toxic shock syndrome in a resident in the surveillance area. Clinical data were obtained from medical records, with height and weight used to calculate BMI.
Diabetes was present in 859 patients (29.3%), grades 1-2 obesity in 743 (25.4%), grade 3 obesity in 399 patients (13.6%), and skin/soft tissue infections in 976 (33.3%). Most patients were aged 18-49 years (37.6%) and male (55%).
Among diabetic patients, the relative risk of an iGAS infection was 4.09 for those who were underweight (BMI < 18.5), 1.23 for the overweight (BMI 25 < 30), 3.14 for those with grade 1-2 obesity, and 15.6 for the morbidly obese. Among nondiabetics, the corresponding relative risks were 3.29, 0.87, 1.15, and 2.95, the authors reported in the poster presentation.
Dr. Langley said the next step is to look at treatment options and whether antibiotic dosing is important and “Long term, if we have a vaccine, this might be a group that needs to be targeted for vaccination.”
ID Week is a joint meeting of the Infectious Diseases Society of America, Society for Healthcare Epidemiology of America, HIV Medicine Association, and Pediatric Infectious Diseases Society.
PHILADELPHIA – Obesity and diabetes are independent risk factors for invasive group A Streptococcus infections, with the highest risk among those with diabetes and morbid obesity.
The relative risk of invasive group A Streptococcus (iGAS) infection was 15 times higher in adults with diabetes and grade 3 morbid obesity (body mass index ≥ 40 kg/m2) than in those of normal weight, Dr. Gayle Langley reported at Infectious Diseases Week 2014.
Moreover, grades 1-2 obesity and morbid obesity increased the odds of ICU admission and death from an iGAS infection in multivariable logistic regression.
The adjusted odds ratios for ICU admission and death were 1.46 and 1.55 for patients with grades 1-2 obesity (BMI 30 < 40 kg/m2) and 2.07 and 1.62 for those with morbid obesity, she said.
Diabetes was not associated with an increased risk for either ICU admission (odds ratio, 1.06) or death (OR, 0.77) in the analysis.
Skin and soft tissue infections, which were significantly more common in obese and diabetic patients, appear to be driving the increased risk for iGAS in these groups, Dr. Langley of the Centers for Disease Control and Prevention said in an interview.
“Based on the literature, I’m not all that surprised because we definitely know that they are at increased risk for these skin and soft tissue infections, and that is a common manifestation of strep,” she said. “The mortality is slightly increased, but not to the extent of the incidence.”
The study was prompted by the limited number of prevention strategies for what Langley described as a “really serious infection” and by the rise in obesity and diabetes in the United States.
Data from select counties in 10 of the CDC’s Active Bacterial Core surveillance sites were used to identify 2,927 cases of 2010-2012 community onset iGAS. Cases were defined by isolation of GAS from a normally sterile site or from a wound in a patient with necrotizing fasciitis or streptococcal toxic shock syndrome in a resident in the surveillance area. Clinical data were obtained from medical records, with height and weight used to calculate BMI.
Diabetes was present in 859 patients (29.3%), grades 1-2 obesity in 743 (25.4%), grade 3 obesity in 399 patients (13.6%), and skin/soft tissue infections in 976 (33.3%). Most patients were aged 18-49 years (37.6%) and male (55%).
Among diabetic patients, the relative risk of an iGAS infection was 4.09 for those who were underweight (BMI < 18.5), 1.23 for the overweight (BMI 25 < 30), 3.14 for those with grade 1-2 obesity, and 15.6 for the morbidly obese. Among nondiabetics, the corresponding relative risks were 3.29, 0.87, 1.15, and 2.95, the authors reported in the poster presentation.
Dr. Langley said the next step is to look at treatment options and whether antibiotic dosing is important and “Long term, if we have a vaccine, this might be a group that needs to be targeted for vaccination.”
ID Week is a joint meeting of the Infectious Diseases Society of America, Society for Healthcare Epidemiology of America, HIV Medicine Association, and Pediatric Infectious Diseases Society.
PHILADELPHIA – Obesity and diabetes are independent risk factors for invasive group A Streptococcus infections, with the highest risk among those with diabetes and morbid obesity.
The relative risk of invasive group A Streptococcus (iGAS) infection was 15 times higher in adults with diabetes and grade 3 morbid obesity (body mass index ≥ 40 kg/m2) than in those of normal weight, Dr. Gayle Langley reported at Infectious Diseases Week 2014.
Moreover, grades 1-2 obesity and morbid obesity increased the odds of ICU admission and death from an iGAS infection in multivariable logistic regression.
The adjusted odds ratios for ICU admission and death were 1.46 and 1.55 for patients with grades 1-2 obesity (BMI 30 < 40 kg/m2) and 2.07 and 1.62 for those with morbid obesity, she said.
Diabetes was not associated with an increased risk for either ICU admission (odds ratio, 1.06) or death (OR, 0.77) in the analysis.
Skin and soft tissue infections, which were significantly more common in obese and diabetic patients, appear to be driving the increased risk for iGAS in these groups, Dr. Langley of the Centers for Disease Control and Prevention said in an interview.
“Based on the literature, I’m not all that surprised because we definitely know that they are at increased risk for these skin and soft tissue infections, and that is a common manifestation of strep,” she said. “The mortality is slightly increased, but not to the extent of the incidence.”
The study was prompted by the limited number of prevention strategies for what Langley described as a “really serious infection” and by the rise in obesity and diabetes in the United States.
Data from select counties in 10 of the CDC’s Active Bacterial Core surveillance sites were used to identify 2,927 cases of 2010-2012 community onset iGAS. Cases were defined by isolation of GAS from a normally sterile site or from a wound in a patient with necrotizing fasciitis or streptococcal toxic shock syndrome in a resident in the surveillance area. Clinical data were obtained from medical records, with height and weight used to calculate BMI.
Diabetes was present in 859 patients (29.3%), grades 1-2 obesity in 743 (25.4%), grade 3 obesity in 399 patients (13.6%), and skin/soft tissue infections in 976 (33.3%). Most patients were aged 18-49 years (37.6%) and male (55%).
Among diabetic patients, the relative risk of an iGAS infection was 4.09 for those who were underweight (BMI < 18.5), 1.23 for the overweight (BMI 25 < 30), 3.14 for those with grade 1-2 obesity, and 15.6 for the morbidly obese. Among nondiabetics, the corresponding relative risks were 3.29, 0.87, 1.15, and 2.95, the authors reported in the poster presentation.
Dr. Langley said the next step is to look at treatment options and whether antibiotic dosing is important and “Long term, if we have a vaccine, this might be a group that needs to be targeted for vaccination.”
ID Week is a joint meeting of the Infectious Diseases Society of America, Society for Healthcare Epidemiology of America, HIV Medicine Association, and Pediatric Infectious Diseases Society.
AT ID WEEK 2014
Key clinical point: Patients with diabetes and obesity are at increased risk for invasive group A Streptococcus infection.
Major finding: The relative risk of invasive group A Streptococcus (iGAS) infection was 15.6 in diabetics with grade 3 morbid obesity vs. normal-weight diabetics.
Data source: Active surveillance data from 2,927 cases of iGAS.
Disclosures: Dr. Langley reported having no financial disclosures. The CDC funds the ABC surveillance sites.