User login
Official Newspaper of the American College of Surgeons
Better thromboprophylaxis didn’t reduce emboli after trauma
SAN FRANCISCO – Delivering prophylactic therapies against venous thromboembolism sooner and to more patients admitted for trauma failed to reduce the risk of pulmonary embolism in a 6-year study of data on 23,863 patients.
Dr. Matthew J. Pommerening and his associates at the University of Texas, Houston, retrospectively studied data on the management and outcomes of 11,292 adults admitted to their level 1 trauma center in 2006-2008 before implementation of a performance-improvement program, and 12,571 patients admitted in 2009-2011, after the program was in place.
The performance-improvement program included sequential interventions such as audits for missed doses of thromboprophylactic medications, goals for earlier and more aggressive chemical prophylaxis, and placing prophylactic filters in the inferior vena cava (IVC) in high-risk patients.
Overall, 1% of patients developed a pulmonary embolism. Comparing rates of pulmonary emboli, deaths from pulmonary embolism, or mortality in the preprogram and postprogram time periods, however, showed no significant differences, he said at the annual clinical congress of the American College of Surgeons.
One percent of patients in both time periods developed a pulmonary embolism. The rate of death from pulmonary embolism was 7% in the earlier period and 8% in the later period. Mortality rates were 4.5% in both periods.
That’s despite great improvements in reducing the proportion of patients who got no prophylaxis from 45% in the earlier period to 11% under the improvement program. The use of prophylactic IVC filters increased from 3% in the earlier period to nearly 8% under the program. The time to initiation of prophylaxis decreased from 57 hours to 32 hours, on average.
The proportion of patients who missed a dose of thromboprophylaxis did not change significantly, from 39% in the earlier period to 36% under the program.
“Current prophylactic strategies and therapies for pulmonary embolism may be inadequate,” Dr. Pommerening said, perhaps due to inadequate dosing or inadequate therapies. The utility or potential thrombogenicity of IVC filters is a topic of “serious discussion” at his institution, he said.
“There’s still room for improvement,” he added, by eliminating missed doses and reducing the 11% of patients who got no prophylaxis, he added.
The time to diagnosis of pulmonary embolism and the proportion of emboli located in the main pulmonary artery did not differ significantly by time period.
The size of the study may not have provided enough power to detect differences in rates of emboli between time periods with such a low overall rate of pulmonary emboli to begin with, he said.
The investigators have started to look at whether the performance improvement program made any difference in the rate of deep-vein thrombosis.
Dr. Pommerening reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Delivering prophylactic therapies against venous thromboembolism sooner and to more patients admitted for trauma failed to reduce the risk of pulmonary embolism in a 6-year study of data on 23,863 patients.
Dr. Matthew J. Pommerening and his associates at the University of Texas, Houston, retrospectively studied data on the management and outcomes of 11,292 adults admitted to their level 1 trauma center in 2006-2008 before implementation of a performance-improvement program, and 12,571 patients admitted in 2009-2011, after the program was in place.
The performance-improvement program included sequential interventions such as audits for missed doses of thromboprophylactic medications, goals for earlier and more aggressive chemical prophylaxis, and placing prophylactic filters in the inferior vena cava (IVC) in high-risk patients.
Overall, 1% of patients developed a pulmonary embolism. Comparing rates of pulmonary emboli, deaths from pulmonary embolism, or mortality in the preprogram and postprogram time periods, however, showed no significant differences, he said at the annual clinical congress of the American College of Surgeons.
One percent of patients in both time periods developed a pulmonary embolism. The rate of death from pulmonary embolism was 7% in the earlier period and 8% in the later period. Mortality rates were 4.5% in both periods.
That’s despite great improvements in reducing the proportion of patients who got no prophylaxis from 45% in the earlier period to 11% under the improvement program. The use of prophylactic IVC filters increased from 3% in the earlier period to nearly 8% under the program. The time to initiation of prophylaxis decreased from 57 hours to 32 hours, on average.
The proportion of patients who missed a dose of thromboprophylaxis did not change significantly, from 39% in the earlier period to 36% under the program.
“Current prophylactic strategies and therapies for pulmonary embolism may be inadequate,” Dr. Pommerening said, perhaps due to inadequate dosing or inadequate therapies. The utility or potential thrombogenicity of IVC filters is a topic of “serious discussion” at his institution, he said.
“There’s still room for improvement,” he added, by eliminating missed doses and reducing the 11% of patients who got no prophylaxis, he added.
The time to diagnosis of pulmonary embolism and the proportion of emboli located in the main pulmonary artery did not differ significantly by time period.
The size of the study may not have provided enough power to detect differences in rates of emboli between time periods with such a low overall rate of pulmonary emboli to begin with, he said.
The investigators have started to look at whether the performance improvement program made any difference in the rate of deep-vein thrombosis.
Dr. Pommerening reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Delivering prophylactic therapies against venous thromboembolism sooner and to more patients admitted for trauma failed to reduce the risk of pulmonary embolism in a 6-year study of data on 23,863 patients.
Dr. Matthew J. Pommerening and his associates at the University of Texas, Houston, retrospectively studied data on the management and outcomes of 11,292 adults admitted to their level 1 trauma center in 2006-2008 before implementation of a performance-improvement program, and 12,571 patients admitted in 2009-2011, after the program was in place.
The performance-improvement program included sequential interventions such as audits for missed doses of thromboprophylactic medications, goals for earlier and more aggressive chemical prophylaxis, and placing prophylactic filters in the inferior vena cava (IVC) in high-risk patients.
Overall, 1% of patients developed a pulmonary embolism. Comparing rates of pulmonary emboli, deaths from pulmonary embolism, or mortality in the preprogram and postprogram time periods, however, showed no significant differences, he said at the annual clinical congress of the American College of Surgeons.
One percent of patients in both time periods developed a pulmonary embolism. The rate of death from pulmonary embolism was 7% in the earlier period and 8% in the later period. Mortality rates were 4.5% in both periods.
That’s despite great improvements in reducing the proportion of patients who got no prophylaxis from 45% in the earlier period to 11% under the improvement program. The use of prophylactic IVC filters increased from 3% in the earlier period to nearly 8% under the program. The time to initiation of prophylaxis decreased from 57 hours to 32 hours, on average.
The proportion of patients who missed a dose of thromboprophylaxis did not change significantly, from 39% in the earlier period to 36% under the program.
“Current prophylactic strategies and therapies for pulmonary embolism may be inadequate,” Dr. Pommerening said, perhaps due to inadequate dosing or inadequate therapies. The utility or potential thrombogenicity of IVC filters is a topic of “serious discussion” at his institution, he said.
“There’s still room for improvement,” he added, by eliminating missed doses and reducing the 11% of patients who got no prophylaxis, he added.
The time to diagnosis of pulmonary embolism and the proportion of emboli located in the main pulmonary artery did not differ significantly by time period.
The size of the study may not have provided enough power to detect differences in rates of emboli between time periods with such a low overall rate of pulmonary emboli to begin with, he said.
The investigators have started to look at whether the performance improvement program made any difference in the rate of deep-vein thrombosis.
Dr. Pommerening reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ACS CLINICAL CONGRESS
Key clinical point: Current thromboprophylaxis strategies may not reduce pulmonary emboli after trauma.
Major finding: Pulmonary embolism occurred in 1% of trauma patients in each time period.
Data source: Retrospective study of 23,863 patients admitted before or after initiation of a thromboprophylaxis improvement program.
Disclosures: Dr. Pommerening reported having no financial disclosures.
Hospital charges not a marker for bariatric surgery outcomes
SAN FRANCISCO – Hospital charges are not a reliable indicator of quality of care for patients undergoing bariatric surgery, according to results from a cohort study reported at the annual clinical congress of the American College of Surgeons.
Researchers queried the SPARCS (New York Statewide Planning and Research Cooperative System) administrative database and identified 46,180 adult patients who underwent primary bariatric surgery between 2004 and 2010.
Charges for this same surgery differed by more than $10,000 between hospitals with low, bottom-tertile charges (less than $25,027) and hospitals with high, top-tertile charges (more than $35,449), reported Dr. Aurora D. Pryor, chief of the general surgery division and director of the Bariatric and Metabolic Weight Loss Center at the State University of New York at Stony Brook Medical Center.
High-charge hospitals were more often located in New York City or on Long Island. Low-charge hospitals more commonly performed a Roux-en-Y gastric bypass surgical procedure and had proportionately more patients with diabetes and liver disease.
Overall, 24% of the patients were operated on in hospitals with low charges, 26% in those with medium charges, and 50% in those with high charges.
In univariate analysis, the rate of major perioperative complications differed significantly, at 4.1%, 4.8%, and 3.75% for patients undergoing surgery in low-, medium-, and high-charge hospitals, respectively. But in multivariate analysis that controlled for patient demographics, comorbidities, insurance provider, and operative procedure, differences were no longer significant.
Additionally, the hospitals were statistically indistinguishable with respect to rates of 30-day mortality and mortality beyond that time point.
“Hospital charge does not correlate with outcomes following bariatric surgery. The initial differences we think are really based on the higher-risk patients and higher-risk operations performed at the lower-cost centers,” Dr. Pryor proposed.
“I think we should be paying attention to the charges. They vary by geographic location, and I think it’s the higher-cost areas that have the higher charges,” she commented.
Session attendee Dr. Mark Ott, a surgeon with Intermountain Healthcare in Murray, Utah, asked, “So do you think if the patients had that information that they would travel outside New York City to go to a lower-cost center?”
“I think they might actually do that,” Dr. Pryor replied. “In particular, some of the self-pay patients are driving into New York City because they think they’ll have a better outcome, and maybe they should actually pay attention to the outcomes at their local places more.”
Dr. Benedict C. Nwomeh, one of the session’s comoderators and a pediatric surgeon at Nationwide Children’s Hospital, Columbus, Ohio, asked, “So what do you think is responsible for this disparity in charges?”
“I honestly think it’s the city effect and the cost of living in those places, that they are able to charge more for their patients,” Dr. Pryor replied.
In an interview, Dr. Maureen A. Killackey, the other comoderator and clinical director of the New York-Presbyterian/Lawrence Hospital Cancer Center in Bronxville, N.Y., commented, “This study is quite provocative, and it also adds to the body of evidence that we already have, like in colonoscopy, on the variation in charges. This information probably needs to get to the attention of both the private payers as well as the governmental payers, because it really does show a tremendous discrepancy.”
“New York is a highly regulated state, and I think this would be perhaps very interesting to the governmental payers of the state to see these differences in both charges as well as practices, as well as the case-mix index and the geographic access and utilization of these services,” she added.
Dr. Pryor disclosed that she had no relevant conflicts of interest.
SAN FRANCISCO – Hospital charges are not a reliable indicator of quality of care for patients undergoing bariatric surgery, according to results from a cohort study reported at the annual clinical congress of the American College of Surgeons.
Researchers queried the SPARCS (New York Statewide Planning and Research Cooperative System) administrative database and identified 46,180 adult patients who underwent primary bariatric surgery between 2004 and 2010.
Charges for this same surgery differed by more than $10,000 between hospitals with low, bottom-tertile charges (less than $25,027) and hospitals with high, top-tertile charges (more than $35,449), reported Dr. Aurora D. Pryor, chief of the general surgery division and director of the Bariatric and Metabolic Weight Loss Center at the State University of New York at Stony Brook Medical Center.
High-charge hospitals were more often located in New York City or on Long Island. Low-charge hospitals more commonly performed a Roux-en-Y gastric bypass surgical procedure and had proportionately more patients with diabetes and liver disease.
Overall, 24% of the patients were operated on in hospitals with low charges, 26% in those with medium charges, and 50% in those with high charges.
In univariate analysis, the rate of major perioperative complications differed significantly, at 4.1%, 4.8%, and 3.75% for patients undergoing surgery in low-, medium-, and high-charge hospitals, respectively. But in multivariate analysis that controlled for patient demographics, comorbidities, insurance provider, and operative procedure, differences were no longer significant.
Additionally, the hospitals were statistically indistinguishable with respect to rates of 30-day mortality and mortality beyond that time point.
“Hospital charge does not correlate with outcomes following bariatric surgery. The initial differences we think are really based on the higher-risk patients and higher-risk operations performed at the lower-cost centers,” Dr. Pryor proposed.
“I think we should be paying attention to the charges. They vary by geographic location, and I think it’s the higher-cost areas that have the higher charges,” she commented.
Session attendee Dr. Mark Ott, a surgeon with Intermountain Healthcare in Murray, Utah, asked, “So do you think if the patients had that information that they would travel outside New York City to go to a lower-cost center?”
“I think they might actually do that,” Dr. Pryor replied. “In particular, some of the self-pay patients are driving into New York City because they think they’ll have a better outcome, and maybe they should actually pay attention to the outcomes at their local places more.”
Dr. Benedict C. Nwomeh, one of the session’s comoderators and a pediatric surgeon at Nationwide Children’s Hospital, Columbus, Ohio, asked, “So what do you think is responsible for this disparity in charges?”
“I honestly think it’s the city effect and the cost of living in those places, that they are able to charge more for their patients,” Dr. Pryor replied.
In an interview, Dr. Maureen A. Killackey, the other comoderator and clinical director of the New York-Presbyterian/Lawrence Hospital Cancer Center in Bronxville, N.Y., commented, “This study is quite provocative, and it also adds to the body of evidence that we already have, like in colonoscopy, on the variation in charges. This information probably needs to get to the attention of both the private payers as well as the governmental payers, because it really does show a tremendous discrepancy.”
“New York is a highly regulated state, and I think this would be perhaps very interesting to the governmental payers of the state to see these differences in both charges as well as practices, as well as the case-mix index and the geographic access and utilization of these services,” she added.
Dr. Pryor disclosed that she had no relevant conflicts of interest.
SAN FRANCISCO – Hospital charges are not a reliable indicator of quality of care for patients undergoing bariatric surgery, according to results from a cohort study reported at the annual clinical congress of the American College of Surgeons.
Researchers queried the SPARCS (New York Statewide Planning and Research Cooperative System) administrative database and identified 46,180 adult patients who underwent primary bariatric surgery between 2004 and 2010.
Charges for this same surgery differed by more than $10,000 between hospitals with low, bottom-tertile charges (less than $25,027) and hospitals with high, top-tertile charges (more than $35,449), reported Dr. Aurora D. Pryor, chief of the general surgery division and director of the Bariatric and Metabolic Weight Loss Center at the State University of New York at Stony Brook Medical Center.
High-charge hospitals were more often located in New York City or on Long Island. Low-charge hospitals more commonly performed a Roux-en-Y gastric bypass surgical procedure and had proportionately more patients with diabetes and liver disease.
Overall, 24% of the patients were operated on in hospitals with low charges, 26% in those with medium charges, and 50% in those with high charges.
In univariate analysis, the rate of major perioperative complications differed significantly, at 4.1%, 4.8%, and 3.75% for patients undergoing surgery in low-, medium-, and high-charge hospitals, respectively. But in multivariate analysis that controlled for patient demographics, comorbidities, insurance provider, and operative procedure, differences were no longer significant.
Additionally, the hospitals were statistically indistinguishable with respect to rates of 30-day mortality and mortality beyond that time point.
“Hospital charge does not correlate with outcomes following bariatric surgery. The initial differences we think are really based on the higher-risk patients and higher-risk operations performed at the lower-cost centers,” Dr. Pryor proposed.
“I think we should be paying attention to the charges. They vary by geographic location, and I think it’s the higher-cost areas that have the higher charges,” she commented.
Session attendee Dr. Mark Ott, a surgeon with Intermountain Healthcare in Murray, Utah, asked, “So do you think if the patients had that information that they would travel outside New York City to go to a lower-cost center?”
“I think they might actually do that,” Dr. Pryor replied. “In particular, some of the self-pay patients are driving into New York City because they think they’ll have a better outcome, and maybe they should actually pay attention to the outcomes at their local places more.”
Dr. Benedict C. Nwomeh, one of the session’s comoderators and a pediatric surgeon at Nationwide Children’s Hospital, Columbus, Ohio, asked, “So what do you think is responsible for this disparity in charges?”
“I honestly think it’s the city effect and the cost of living in those places, that they are able to charge more for their patients,” Dr. Pryor replied.
In an interview, Dr. Maureen A. Killackey, the other comoderator and clinical director of the New York-Presbyterian/Lawrence Hospital Cancer Center in Bronxville, N.Y., commented, “This study is quite provocative, and it also adds to the body of evidence that we already have, like in colonoscopy, on the variation in charges. This information probably needs to get to the attention of both the private payers as well as the governmental payers, because it really does show a tremendous discrepancy.”
“New York is a highly regulated state, and I think this would be perhaps very interesting to the governmental payers of the state to see these differences in both charges as well as practices, as well as the case-mix index and the geographic access and utilization of these services,” she added.
Dr. Pryor disclosed that she had no relevant conflicts of interest.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Hospitals charging more do not have lower adjusted morbidity or mortality.
Major finding: Patients undergoing surgery at hospitals with higher and lower charges had similar risks of complications and death.
Data source: A cohort study of 46,180 patients in New York who underwent bariatric surgery.
Disclosures: Dr. Pryor disclosed that she had no relevant conflicts of interest.
Fellow involvement is linked to better outcomes of colorectal surgery
SAN FRANCISCO – Patients undergoing colorectal surgery have lower rates of complications and are 20% less likely to die if a fellow is involved in the surgery as compared with a senior resident, new data show.
“Advanced trainee level was associated with improved outcomes in colorectal surgery,” first author Dr. Lilian Chen concluded at the annual clinical congress of the American College of Surgeons, where she presented the data.
“Future studies should attempt to delineate the relative contributions of trainees on intraoperative and postoperative patient care and effects on outcome, and perhaps emphasis on appropriate case selection and resident involvement to optimize patient outcomes,” she recommended.
Using data from the National Surgical Quality Improvement Program (NSQIP), the investigators analyzed outcomes of 68,327 common open and laparoscopic abdominal colorectal operations done during 2005-2012 in which trainees participated.
Outcomes were compared for junior residents in postgraduate years 1 through 3 (involved in 23% of surgeries), senior residents in postgraduate years 4 and 5 (61%), and fellows in postgraduate years beyond year 5 (16%).
The prevalence of many surgical risk factors differed significantly across the three groups of trainees, but most differences were not considered clinically important, according to Dr. Chen, who is a fellow at the Lahey Hospital and Medical Center in Burlington, Mass. “The exceptions were systemic sepsis and emergency cases, where it appears that the fellows are doing proportionately less of these cases,” she noted.
Rates of several 30-day outcomes – septic shock, stroke, unplanned intubation, postoperative pneumonia, wound disruption, acute renal failure, deep incisional surgical site infection, and return to the operating room – differed significantly across groups, being less common for fellows than for either resident group.
The rate of mortality also differed significantly, at 2% for fellows but 4% each for junior and senior residents. In multivariate analysis, patients were significantly less likely to die if a fellow was involved in their surgery as compared with a senior resident (odds ratio, 0.80), but there was no significant difference between junior and senior residents.
“Our limitations include the retrospective analysis, and our inability to adjust for the type of hospital and training program, attending surgeon experience, the presence of subspecialty training in those programs, and the actual level of involvement of the trainee in intraoperative as well as postoperative care of patients,” acknowledged Dr. Chen, who disclosed that she had no relevant conflicts of interest.
Indeed, several session attendees took issue with potential confounders. Dr. Mary T. Hawn, chief of Gastrointestinal Surgery at the University of Alabama at Birmingham, commented, “I think you have to be really careful about understanding the data that you are working with. The first thing is that you can’t adjust for hospital characteristics, so you don’t know that a patient didn’t get transferred to a higher level of care, where there are residents available. ...
“So, I would say you should exclude all emergency cases, you should exclude all patients who are transferred, and things like that, and really try to do propensity adjustment or [seek] some reason that might explain what level of trainee is involved,” she recommended, noting that adjustment does not rule out a role for that factor. “I think this is really concerning because it’s harmful to our community programs to publish data like these, where we don’t really understand the true involvement or the mechanisms of why having the trainee there might be associated with higher mortality.”
Another attendee agreed, saying, “If I’m doing a case with a fellow, I’m going to let the fellow do it, and perhaps assisting, sometimes watching, while I let the fellow do it with the junior resident. If I’m in there with the junior resident, I’m doing the case while the junior resident is assisting me. So I think you need to take things like that into account when you think about what your data actually mean.”
Residents are commonly involved in nighttime emergency cases because the fellow is not at the hospital, a third attendee noted. Additionally, “the fellows will tend to cherry-pick the cases they want to do. The fellow is going to be involved in the cases that are more likely to be quality elective cases. So the diabetic on oxygen who’s coming in for the right colon is potentially going to get handed over to someone else to pick it up. So I would agree, I think that just publishing this and having that as your statement can be very harmful. You really need to be very objective and truthful about owning up to these confounding factors that you can’t really measure.”
“I have to completely agree with that, there are certainly things that we can’t prove. All we can say is that fellows are associated with this reduction in mortality, but we can’t say why ... ” Dr. Chen concurred. “I can’t say the fellow is the reason. There are too many variables involved, one of those being that if you have a colorectal fellow, you are probably at a specialty center with a colorectal fellowship or oncology fellowship and that could be the reason why you have lower mortality, better outcomes. It is just because of the staff and the facility that’s equipped to take those complex cases. So it could have nothing to do with the fellows at all.”
SAN FRANCISCO – Patients undergoing colorectal surgery have lower rates of complications and are 20% less likely to die if a fellow is involved in the surgery as compared with a senior resident, new data show.
“Advanced trainee level was associated with improved outcomes in colorectal surgery,” first author Dr. Lilian Chen concluded at the annual clinical congress of the American College of Surgeons, where she presented the data.
“Future studies should attempt to delineate the relative contributions of trainees on intraoperative and postoperative patient care and effects on outcome, and perhaps emphasis on appropriate case selection and resident involvement to optimize patient outcomes,” she recommended.
Using data from the National Surgical Quality Improvement Program (NSQIP), the investigators analyzed outcomes of 68,327 common open and laparoscopic abdominal colorectal operations done during 2005-2012 in which trainees participated.
Outcomes were compared for junior residents in postgraduate years 1 through 3 (involved in 23% of surgeries), senior residents in postgraduate years 4 and 5 (61%), and fellows in postgraduate years beyond year 5 (16%).
The prevalence of many surgical risk factors differed significantly across the three groups of trainees, but most differences were not considered clinically important, according to Dr. Chen, who is a fellow at the Lahey Hospital and Medical Center in Burlington, Mass. “The exceptions were systemic sepsis and emergency cases, where it appears that the fellows are doing proportionately less of these cases,” she noted.
Rates of several 30-day outcomes – septic shock, stroke, unplanned intubation, postoperative pneumonia, wound disruption, acute renal failure, deep incisional surgical site infection, and return to the operating room – differed significantly across groups, being less common for fellows than for either resident group.
The rate of mortality also differed significantly, at 2% for fellows but 4% each for junior and senior residents. In multivariate analysis, patients were significantly less likely to die if a fellow was involved in their surgery as compared with a senior resident (odds ratio, 0.80), but there was no significant difference between junior and senior residents.
“Our limitations include the retrospective analysis, and our inability to adjust for the type of hospital and training program, attending surgeon experience, the presence of subspecialty training in those programs, and the actual level of involvement of the trainee in intraoperative as well as postoperative care of patients,” acknowledged Dr. Chen, who disclosed that she had no relevant conflicts of interest.
Indeed, several session attendees took issue with potential confounders. Dr. Mary T. Hawn, chief of Gastrointestinal Surgery at the University of Alabama at Birmingham, commented, “I think you have to be really careful about understanding the data that you are working with. The first thing is that you can’t adjust for hospital characteristics, so you don’t know that a patient didn’t get transferred to a higher level of care, where there are residents available. ...
“So, I would say you should exclude all emergency cases, you should exclude all patients who are transferred, and things like that, and really try to do propensity adjustment or [seek] some reason that might explain what level of trainee is involved,” she recommended, noting that adjustment does not rule out a role for that factor. “I think this is really concerning because it’s harmful to our community programs to publish data like these, where we don’t really understand the true involvement or the mechanisms of why having the trainee there might be associated with higher mortality.”
Another attendee agreed, saying, “If I’m doing a case with a fellow, I’m going to let the fellow do it, and perhaps assisting, sometimes watching, while I let the fellow do it with the junior resident. If I’m in there with the junior resident, I’m doing the case while the junior resident is assisting me. So I think you need to take things like that into account when you think about what your data actually mean.”
Residents are commonly involved in nighttime emergency cases because the fellow is not at the hospital, a third attendee noted. Additionally, “the fellows will tend to cherry-pick the cases they want to do. The fellow is going to be involved in the cases that are more likely to be quality elective cases. So the diabetic on oxygen who’s coming in for the right colon is potentially going to get handed over to someone else to pick it up. So I would agree, I think that just publishing this and having that as your statement can be very harmful. You really need to be very objective and truthful about owning up to these confounding factors that you can’t really measure.”
“I have to completely agree with that, there are certainly things that we can’t prove. All we can say is that fellows are associated with this reduction in mortality, but we can’t say why ... ” Dr. Chen concurred. “I can’t say the fellow is the reason. There are too many variables involved, one of those being that if you have a colorectal fellow, you are probably at a specialty center with a colorectal fellowship or oncology fellowship and that could be the reason why you have lower mortality, better outcomes. It is just because of the staff and the facility that’s equipped to take those complex cases. So it could have nothing to do with the fellows at all.”
SAN FRANCISCO – Patients undergoing colorectal surgery have lower rates of complications and are 20% less likely to die if a fellow is involved in the surgery as compared with a senior resident, new data show.
“Advanced trainee level was associated with improved outcomes in colorectal surgery,” first author Dr. Lilian Chen concluded at the annual clinical congress of the American College of Surgeons, where she presented the data.
“Future studies should attempt to delineate the relative contributions of trainees on intraoperative and postoperative patient care and effects on outcome, and perhaps emphasis on appropriate case selection and resident involvement to optimize patient outcomes,” she recommended.
Using data from the National Surgical Quality Improvement Program (NSQIP), the investigators analyzed outcomes of 68,327 common open and laparoscopic abdominal colorectal operations done during 2005-2012 in which trainees participated.
Outcomes were compared for junior residents in postgraduate years 1 through 3 (involved in 23% of surgeries), senior residents in postgraduate years 4 and 5 (61%), and fellows in postgraduate years beyond year 5 (16%).
The prevalence of many surgical risk factors differed significantly across the three groups of trainees, but most differences were not considered clinically important, according to Dr. Chen, who is a fellow at the Lahey Hospital and Medical Center in Burlington, Mass. “The exceptions were systemic sepsis and emergency cases, where it appears that the fellows are doing proportionately less of these cases,” she noted.
Rates of several 30-day outcomes – septic shock, stroke, unplanned intubation, postoperative pneumonia, wound disruption, acute renal failure, deep incisional surgical site infection, and return to the operating room – differed significantly across groups, being less common for fellows than for either resident group.
The rate of mortality also differed significantly, at 2% for fellows but 4% each for junior and senior residents. In multivariate analysis, patients were significantly less likely to die if a fellow was involved in their surgery as compared with a senior resident (odds ratio, 0.80), but there was no significant difference between junior and senior residents.
“Our limitations include the retrospective analysis, and our inability to adjust for the type of hospital and training program, attending surgeon experience, the presence of subspecialty training in those programs, and the actual level of involvement of the trainee in intraoperative as well as postoperative care of patients,” acknowledged Dr. Chen, who disclosed that she had no relevant conflicts of interest.
Indeed, several session attendees took issue with potential confounders. Dr. Mary T. Hawn, chief of Gastrointestinal Surgery at the University of Alabama at Birmingham, commented, “I think you have to be really careful about understanding the data that you are working with. The first thing is that you can’t adjust for hospital characteristics, so you don’t know that a patient didn’t get transferred to a higher level of care, where there are residents available. ...
“So, I would say you should exclude all emergency cases, you should exclude all patients who are transferred, and things like that, and really try to do propensity adjustment or [seek] some reason that might explain what level of trainee is involved,” she recommended, noting that adjustment does not rule out a role for that factor. “I think this is really concerning because it’s harmful to our community programs to publish data like these, where we don’t really understand the true involvement or the mechanisms of why having the trainee there might be associated with higher mortality.”
Another attendee agreed, saying, “If I’m doing a case with a fellow, I’m going to let the fellow do it, and perhaps assisting, sometimes watching, while I let the fellow do it with the junior resident. If I’m in there with the junior resident, I’m doing the case while the junior resident is assisting me. So I think you need to take things like that into account when you think about what your data actually mean.”
Residents are commonly involved in nighttime emergency cases because the fellow is not at the hospital, a third attendee noted. Additionally, “the fellows will tend to cherry-pick the cases they want to do. The fellow is going to be involved in the cases that are more likely to be quality elective cases. So the diabetic on oxygen who’s coming in for the right colon is potentially going to get handed over to someone else to pick it up. So I would agree, I think that just publishing this and having that as your statement can be very harmful. You really need to be very objective and truthful about owning up to these confounding factors that you can’t really measure.”
“I have to completely agree with that, there are certainly things that we can’t prove. All we can say is that fellows are associated with this reduction in mortality, but we can’t say why ... ” Dr. Chen concurred. “I can’t say the fellow is the reason. There are too many variables involved, one of those being that if you have a colorectal fellow, you are probably at a specialty center with a colorectal fellowship or oncology fellowship and that could be the reason why you have lower mortality, better outcomes. It is just because of the staff and the facility that’s equipped to take those complex cases. So it could have nothing to do with the fellows at all.”
AT THE ACS CLINICAL CONGRESS
Key clinical point: Morbidity and mortality were lower with fellows involved than with residents involved.
Major finding: Patients were less likely to have complications and 20% less likely to die when a fellow was involved with the surgery as compared with a senior resident.
Data source: A retrospective cohort study of 68,327 colorectal surgeries from the NSQIP database.
Disclosures: Dr. Chen disclosed that she had no relevant conflicts of interest.
Medicare expanding coverage of telehealth services
Medicare will begin paying for more care delivered by telehealth next year, but restrictions could limit the growth in these virtual or remote visits.
The program pays for telehealth services only when provided in designated Health Professional Shortage Areas; additionally, patients must receive the remote care at a hospital, doctor’s office, or another approved ambulatory care site.
Physician organizations say it’s important that Medicare continues to add services that are covered when delivered via telehealth, but that greater adoption will not happen until payment and licensure issues are addressed.
According to the 2015 Medicare physician fee schedule, doctors can be paid for providing annual wellness visits, psychoanalysis, psychotherapy, and prolonged evaluation and management via telehealth.
Currently, about 10 million patients have received some form of telehealth services, according to the American Telemedicine Association. More than half (55%) of that is the remote reading of imaging by a radiologist, 24% is remote consultations, and 15% is remote monitoring. The remainder (6%) is comprised of miscellaneous and pharmacy services.
A recent survey of hospital, group practice, and home health executives found that most (84%) said that it was important or very important to develop their telehealth capability, but that reimbursement uncertainty was holding them back. Forty-one percent said they were not being reimbursed at all for telehealth, and 21% said that the rates were lower than for in-person services.
Only 6% said their programs were “mature,” according to the survey, which was conducted by Foley & Lardner, a law firm.
The American Medical Association has made expanded coverage of telehealth a priority. “We need coverage and reimbursement of telemedicine services and fewer restrictions in Medicare,” Dr. Robert Wah, the AMA president, said at the group’s interim policy meeting. “We want patients to use it if they need it. Lift geographic restrictions. Free up its use in alternative payment models.”
Telemedicine can increase access to care, especially in rural and underserved areas, according to Dr. Reid Blackwelder, board chair of the American Academy of Family Physicians. Currently, many family physicians are delivering health care remotely – by smartphone or Skype, for instance – but they often don’t get paid, he said.
Medicare requires that physicians use a G code to bill for health care provided remotely, and that additional documentation burden may mean that physicians don’t bill for it, even if they’ve delivered the care, Dr. Blackwelder said in an interview.
The AAFP would like to see a move away from those G codes, substituting a per member per month fee instead, he said.
Although Medicare pays the same amount for telehealth services as it would for the same services delivered in a face-to-face visit, not all private payers do so, which also dampens enthusiasm for telehealth, said Dr. Blackwelder.
According to the ATA, 22 states and Washington, D.C. require telehealth coverage to be on par with in-person visits.
Licensure is also an issue. Both the AAFP and the AMA support a model license plan developed by the Federation of State Medical Boards that would allow physicians to deliver services across state lines.
The Interstate Medical Licensure Compact was issued in September. According to the FSMB, 11 state medical boards have formally endorsed it: Texas, South Dakota, Wisconsin, Washington, Maine, Nevada, Alabama, Utah, Vermont, and Wyoming.
However, for licensure requirements to change, the compact must be enacted in every state.
Physician groups also want to ensure that telehealth services are given by “providers that have ongoing and established relationship with the patient,” said Dr. Blackwelder.
Medicare will begin paying for more care delivered by telehealth next year, but restrictions could limit the growth in these virtual or remote visits.
The program pays for telehealth services only when provided in designated Health Professional Shortage Areas; additionally, patients must receive the remote care at a hospital, doctor’s office, or another approved ambulatory care site.
Physician organizations say it’s important that Medicare continues to add services that are covered when delivered via telehealth, but that greater adoption will not happen until payment and licensure issues are addressed.
According to the 2015 Medicare physician fee schedule, doctors can be paid for providing annual wellness visits, psychoanalysis, psychotherapy, and prolonged evaluation and management via telehealth.
Currently, about 10 million patients have received some form of telehealth services, according to the American Telemedicine Association. More than half (55%) of that is the remote reading of imaging by a radiologist, 24% is remote consultations, and 15% is remote monitoring. The remainder (6%) is comprised of miscellaneous and pharmacy services.
A recent survey of hospital, group practice, and home health executives found that most (84%) said that it was important or very important to develop their telehealth capability, but that reimbursement uncertainty was holding them back. Forty-one percent said they were not being reimbursed at all for telehealth, and 21% said that the rates were lower than for in-person services.
Only 6% said their programs were “mature,” according to the survey, which was conducted by Foley & Lardner, a law firm.
The American Medical Association has made expanded coverage of telehealth a priority. “We need coverage and reimbursement of telemedicine services and fewer restrictions in Medicare,” Dr. Robert Wah, the AMA president, said at the group’s interim policy meeting. “We want patients to use it if they need it. Lift geographic restrictions. Free up its use in alternative payment models.”
Telemedicine can increase access to care, especially in rural and underserved areas, according to Dr. Reid Blackwelder, board chair of the American Academy of Family Physicians. Currently, many family physicians are delivering health care remotely – by smartphone or Skype, for instance – but they often don’t get paid, he said.
Medicare requires that physicians use a G code to bill for health care provided remotely, and that additional documentation burden may mean that physicians don’t bill for it, even if they’ve delivered the care, Dr. Blackwelder said in an interview.
The AAFP would like to see a move away from those G codes, substituting a per member per month fee instead, he said.
Although Medicare pays the same amount for telehealth services as it would for the same services delivered in a face-to-face visit, not all private payers do so, which also dampens enthusiasm for telehealth, said Dr. Blackwelder.
According to the ATA, 22 states and Washington, D.C. require telehealth coverage to be on par with in-person visits.
Licensure is also an issue. Both the AAFP and the AMA support a model license plan developed by the Federation of State Medical Boards that would allow physicians to deliver services across state lines.
The Interstate Medical Licensure Compact was issued in September. According to the FSMB, 11 state medical boards have formally endorsed it: Texas, South Dakota, Wisconsin, Washington, Maine, Nevada, Alabama, Utah, Vermont, and Wyoming.
However, for licensure requirements to change, the compact must be enacted in every state.
Physician groups also want to ensure that telehealth services are given by “providers that have ongoing and established relationship with the patient,” said Dr. Blackwelder.
Medicare will begin paying for more care delivered by telehealth next year, but restrictions could limit the growth in these virtual or remote visits.
The program pays for telehealth services only when provided in designated Health Professional Shortage Areas; additionally, patients must receive the remote care at a hospital, doctor’s office, or another approved ambulatory care site.
Physician organizations say it’s important that Medicare continues to add services that are covered when delivered via telehealth, but that greater adoption will not happen until payment and licensure issues are addressed.
According to the 2015 Medicare physician fee schedule, doctors can be paid for providing annual wellness visits, psychoanalysis, psychotherapy, and prolonged evaluation and management via telehealth.
Currently, about 10 million patients have received some form of telehealth services, according to the American Telemedicine Association. More than half (55%) of that is the remote reading of imaging by a radiologist, 24% is remote consultations, and 15% is remote monitoring. The remainder (6%) is comprised of miscellaneous and pharmacy services.
A recent survey of hospital, group practice, and home health executives found that most (84%) said that it was important or very important to develop their telehealth capability, but that reimbursement uncertainty was holding them back. Forty-one percent said they were not being reimbursed at all for telehealth, and 21% said that the rates were lower than for in-person services.
Only 6% said their programs were “mature,” according to the survey, which was conducted by Foley & Lardner, a law firm.
The American Medical Association has made expanded coverage of telehealth a priority. “We need coverage and reimbursement of telemedicine services and fewer restrictions in Medicare,” Dr. Robert Wah, the AMA president, said at the group’s interim policy meeting. “We want patients to use it if they need it. Lift geographic restrictions. Free up its use in alternative payment models.”
Telemedicine can increase access to care, especially in rural and underserved areas, according to Dr. Reid Blackwelder, board chair of the American Academy of Family Physicians. Currently, many family physicians are delivering health care remotely – by smartphone or Skype, for instance – but they often don’t get paid, he said.
Medicare requires that physicians use a G code to bill for health care provided remotely, and that additional documentation burden may mean that physicians don’t bill for it, even if they’ve delivered the care, Dr. Blackwelder said in an interview.
The AAFP would like to see a move away from those G codes, substituting a per member per month fee instead, he said.
Although Medicare pays the same amount for telehealth services as it would for the same services delivered in a face-to-face visit, not all private payers do so, which also dampens enthusiasm for telehealth, said Dr. Blackwelder.
According to the ATA, 22 states and Washington, D.C. require telehealth coverage to be on par with in-person visits.
Licensure is also an issue. Both the AAFP and the AMA support a model license plan developed by the Federation of State Medical Boards that would allow physicians to deliver services across state lines.
The Interstate Medical Licensure Compact was issued in September. According to the FSMB, 11 state medical boards have formally endorsed it: Texas, South Dakota, Wisconsin, Washington, Maine, Nevada, Alabama, Utah, Vermont, and Wyoming.
However, for licensure requirements to change, the compact must be enacted in every state.
Physician groups also want to ensure that telehealth services are given by “providers that have ongoing and established relationship with the patient,” said Dr. Blackwelder.
VIDEO: How to halve serious reportable events in the OR
SAN FRANCISCO– Little steps, when added together, lead to big reductions in serious reportable events in the operating room, according to investigators from the Phoenix-based Banner Health system.
After slight modifications to the count, timeout, and other OR procedures, Banner saw a 52% reduction in serious reportable events (SREs), including a 70% reduction in wrong-site surgeries, across its 22 hospitals and 8 ambulatory surgery centers (J. Am. Coll. Surg. 2014 Oct. 4 [doi:http://dx.doi.org/10.1016/j.jamcollsurg.2014.09.018]).
In an interview at the annual clinical congress of the American College of Surgeons, lead investigator Dr. Terrence Loftus, the health system’s medical director of surgery services and clinical resources, explained how they did it. He also explained why surgical SREs are seven times more common in the system’s robotic surgery program, despite overall improvements, and what Banner is planning to do about it.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO– Little steps, when added together, lead to big reductions in serious reportable events in the operating room, according to investigators from the Phoenix-based Banner Health system.
After slight modifications to the count, timeout, and other OR procedures, Banner saw a 52% reduction in serious reportable events (SREs), including a 70% reduction in wrong-site surgeries, across its 22 hospitals and 8 ambulatory surgery centers (J. Am. Coll. Surg. 2014 Oct. 4 [doi:http://dx.doi.org/10.1016/j.jamcollsurg.2014.09.018]).
In an interview at the annual clinical congress of the American College of Surgeons, lead investigator Dr. Terrence Loftus, the health system’s medical director of surgery services and clinical resources, explained how they did it. He also explained why surgical SREs are seven times more common in the system’s robotic surgery program, despite overall improvements, and what Banner is planning to do about it.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO– Little steps, when added together, lead to big reductions in serious reportable events in the operating room, according to investigators from the Phoenix-based Banner Health system.
After slight modifications to the count, timeout, and other OR procedures, Banner saw a 52% reduction in serious reportable events (SREs), including a 70% reduction in wrong-site surgeries, across its 22 hospitals and 8 ambulatory surgery centers (J. Am. Coll. Surg. 2014 Oct. 4 [doi:http://dx.doi.org/10.1016/j.jamcollsurg.2014.09.018]).
In an interview at the annual clinical congress of the American College of Surgeons, lead investigator Dr. Terrence Loftus, the health system’s medical director of surgery services and clinical resources, explained how they did it. He also explained why surgical SREs are seven times more common in the system’s robotic surgery program, despite overall improvements, and what Banner is planning to do about it.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACS CLINICAL CONGRESS
No recurrence of cervical cancer seen with simple trachelectomy
MELBOURNE – Simple trachelectomy can achieve fertility-sparing outcomes similar to those obtained from radical trachelectomy in women with early-stage cervical cancer without any increased risk of recurrence, according to a poster presented at the biennial meeting of the International Gynecologic Cancer Society.
A retrospective cohort study of 25 patients who underwent a simple vaginal trachelectomy to remove the cervix after a diagnosis of cervical cancer found that 6 of the 10 patients who declared an intention to conceive were successful in doing so.
“The radical trachelectomy procedures [resulted in] a pregnancy rate between 70% and 80%, so we think the simple trachelectomy will do quite well,” said lead author Dr. Shamitha Kathurusinghe, an obstetrics/gynecology trainee at Royal Women’s Hospital, Melbourne.“We had 10 people with the intention to conceive, and we had 10 pregnancies in 6 patients, and our intention to conceive was about 50%,” she said in an interview.
While the majority of patients in the study sought assisted reproductive technologies, some also conceived naturally.
All pregnancies were treated as high risk, and all patients delivered via cesarean section. Two pregnancies were achieved via a surrogate; there was one first-trimester miscarriage; one ectopic pregnancy; and one second-trimester miscarriage, but the cause was unknown.”
Researchers found no incidence of cancer recurrence during the median 54-month follow-up period, among a group of patients which included 7 with stage IA1 disease, 5 with stage IA2, 11 with stage IB1 disease, and 2 with stage IB2 disease.
The study group included 7 cases of squamous cell carcinoma, 10 adenocarcinomas, 4 adenosquamous tumors, 2 adenosarcomas, and 2 neuroendocrine tumors. In all, 48% of patients were nulliparous prior to the procedure.
Dr. Kathurusinghe said surgical treatments for cervical cancer seemed to be shifting away from more radical toward more conservative approaches.
“What we’ve noticed over time is that the gold standard management is a radical hysterectomy, but we’ve gone back from that and said, maybe we can get away without that, let’s do a radical trachelectomy,” Dr. Kathurusinghe said.
“Now we’re slowly going back and saying we can be a little bit less radical and leave a bit more behind.”
While the study included women with stage IB2 tumors, Dr. Kathurusinghe said the general advice would be to use the more conservative procedure up to stage IB1 tumors only.
“Every patient should be considered on an individual basis by a specialist that’s in that area. Sit down with the patient and decide, does this patient need radical therapy? Is this woman still of a childbearing age, [who] would want to preserve their fertility; and can this be an option for that patient?”
Researchers also found that 15 patients actually had no residual disease on the final histopathology, echoing similar findings from an earlier study.
There were no conflicts of interest declared.
MELBOURNE – Simple trachelectomy can achieve fertility-sparing outcomes similar to those obtained from radical trachelectomy in women with early-stage cervical cancer without any increased risk of recurrence, according to a poster presented at the biennial meeting of the International Gynecologic Cancer Society.
A retrospective cohort study of 25 patients who underwent a simple vaginal trachelectomy to remove the cervix after a diagnosis of cervical cancer found that 6 of the 10 patients who declared an intention to conceive were successful in doing so.
“The radical trachelectomy procedures [resulted in] a pregnancy rate between 70% and 80%, so we think the simple trachelectomy will do quite well,” said lead author Dr. Shamitha Kathurusinghe, an obstetrics/gynecology trainee at Royal Women’s Hospital, Melbourne.“We had 10 people with the intention to conceive, and we had 10 pregnancies in 6 patients, and our intention to conceive was about 50%,” she said in an interview.
While the majority of patients in the study sought assisted reproductive technologies, some also conceived naturally.
All pregnancies were treated as high risk, and all patients delivered via cesarean section. Two pregnancies were achieved via a surrogate; there was one first-trimester miscarriage; one ectopic pregnancy; and one second-trimester miscarriage, but the cause was unknown.”
Researchers found no incidence of cancer recurrence during the median 54-month follow-up period, among a group of patients which included 7 with stage IA1 disease, 5 with stage IA2, 11 with stage IB1 disease, and 2 with stage IB2 disease.
The study group included 7 cases of squamous cell carcinoma, 10 adenocarcinomas, 4 adenosquamous tumors, 2 adenosarcomas, and 2 neuroendocrine tumors. In all, 48% of patients were nulliparous prior to the procedure.
Dr. Kathurusinghe said surgical treatments for cervical cancer seemed to be shifting away from more radical toward more conservative approaches.
“What we’ve noticed over time is that the gold standard management is a radical hysterectomy, but we’ve gone back from that and said, maybe we can get away without that, let’s do a radical trachelectomy,” Dr. Kathurusinghe said.
“Now we’re slowly going back and saying we can be a little bit less radical and leave a bit more behind.”
While the study included women with stage IB2 tumors, Dr. Kathurusinghe said the general advice would be to use the more conservative procedure up to stage IB1 tumors only.
“Every patient should be considered on an individual basis by a specialist that’s in that area. Sit down with the patient and decide, does this patient need radical therapy? Is this woman still of a childbearing age, [who] would want to preserve their fertility; and can this be an option for that patient?”
Researchers also found that 15 patients actually had no residual disease on the final histopathology, echoing similar findings from an earlier study.
There were no conflicts of interest declared.
MELBOURNE – Simple trachelectomy can achieve fertility-sparing outcomes similar to those obtained from radical trachelectomy in women with early-stage cervical cancer without any increased risk of recurrence, according to a poster presented at the biennial meeting of the International Gynecologic Cancer Society.
A retrospective cohort study of 25 patients who underwent a simple vaginal trachelectomy to remove the cervix after a diagnosis of cervical cancer found that 6 of the 10 patients who declared an intention to conceive were successful in doing so.
“The radical trachelectomy procedures [resulted in] a pregnancy rate between 70% and 80%, so we think the simple trachelectomy will do quite well,” said lead author Dr. Shamitha Kathurusinghe, an obstetrics/gynecology trainee at Royal Women’s Hospital, Melbourne.“We had 10 people with the intention to conceive, and we had 10 pregnancies in 6 patients, and our intention to conceive was about 50%,” she said in an interview.
While the majority of patients in the study sought assisted reproductive technologies, some also conceived naturally.
All pregnancies were treated as high risk, and all patients delivered via cesarean section. Two pregnancies were achieved via a surrogate; there was one first-trimester miscarriage; one ectopic pregnancy; and one second-trimester miscarriage, but the cause was unknown.”
Researchers found no incidence of cancer recurrence during the median 54-month follow-up period, among a group of patients which included 7 with stage IA1 disease, 5 with stage IA2, 11 with stage IB1 disease, and 2 with stage IB2 disease.
The study group included 7 cases of squamous cell carcinoma, 10 adenocarcinomas, 4 adenosquamous tumors, 2 adenosarcomas, and 2 neuroendocrine tumors. In all, 48% of patients were nulliparous prior to the procedure.
Dr. Kathurusinghe said surgical treatments for cervical cancer seemed to be shifting away from more radical toward more conservative approaches.
“What we’ve noticed over time is that the gold standard management is a radical hysterectomy, but we’ve gone back from that and said, maybe we can get away without that, let’s do a radical trachelectomy,” Dr. Kathurusinghe said.
“Now we’re slowly going back and saying we can be a little bit less radical and leave a bit more behind.”
While the study included women with stage IB2 tumors, Dr. Kathurusinghe said the general advice would be to use the more conservative procedure up to stage IB1 tumors only.
“Every patient should be considered on an individual basis by a specialist that’s in that area. Sit down with the patient and decide, does this patient need radical therapy? Is this woman still of a childbearing age, [who] would want to preserve their fertility; and can this be an option for that patient?”
Researchers also found that 15 patients actually had no residual disease on the final histopathology, echoing similar findings from an earlier study.
There were no conflicts of interest declared.
AT IGCS 2014
Key clinical point: Simple trachelectomy can achieve fertility-sparing outcomes similar to outcomes obtained from radical trachelectomy, with no increase in recurrence of cervical cancer.
Major finding: Half of women undergoing simple trachelectomy were able to conceive, and without cancer recurrence.
Data source: Retrospective cohort study of 25 patients undergoing simple vaginal trachelectomy for cervical cancer.
Disclosures: There were no conflicts of interest declared.
VIDEO: Less trauma, more success with bleeding peptic ulcer management
SAN FRANCISCO – If current trends continue, vagotomy and gastrectomy for bleeding peptic ulcers will be mostly a thing of the past, according to Dr. Mikhail Kryzhanouski, a surgery resident at the University of Illinois, Chicago.
Their use is quickly fading, eclipsed by better techniques and a steady drop in adverse outcomes, even though patients are presenting with more comorbidities, Dr. Kryzhanouski found in a review of patients in the U.S. Nationwide Inpatient Sample who were hospitalized for peptic ulcers from 1998 to 2011 (J. Am. Coll. Surg. 2014;219:e142).
Dr. Kryzhanouski shared the results of his study – and the reasons for his prediction – at the American College of Surgeons Clinical Congress.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – If current trends continue, vagotomy and gastrectomy for bleeding peptic ulcers will be mostly a thing of the past, according to Dr. Mikhail Kryzhanouski, a surgery resident at the University of Illinois, Chicago.
Their use is quickly fading, eclipsed by better techniques and a steady drop in adverse outcomes, even though patients are presenting with more comorbidities, Dr. Kryzhanouski found in a review of patients in the U.S. Nationwide Inpatient Sample who were hospitalized for peptic ulcers from 1998 to 2011 (J. Am. Coll. Surg. 2014;219:e142).
Dr. Kryzhanouski shared the results of his study – and the reasons for his prediction – at the American College of Surgeons Clinical Congress.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – If current trends continue, vagotomy and gastrectomy for bleeding peptic ulcers will be mostly a thing of the past, according to Dr. Mikhail Kryzhanouski, a surgery resident at the University of Illinois, Chicago.
Their use is quickly fading, eclipsed by better techniques and a steady drop in adverse outcomes, even though patients are presenting with more comorbidities, Dr. Kryzhanouski found in a review of patients in the U.S. Nationwide Inpatient Sample who were hospitalized for peptic ulcers from 1998 to 2011 (J. Am. Coll. Surg. 2014;219:e142).
Dr. Kryzhanouski shared the results of his study – and the reasons for his prediction – at the American College of Surgeons Clinical Congress.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AMERICAN COLLEGE OF SURGEONS CLINICAL CONGRESS
VIDEO: An easy way to improve breast biopsy practices
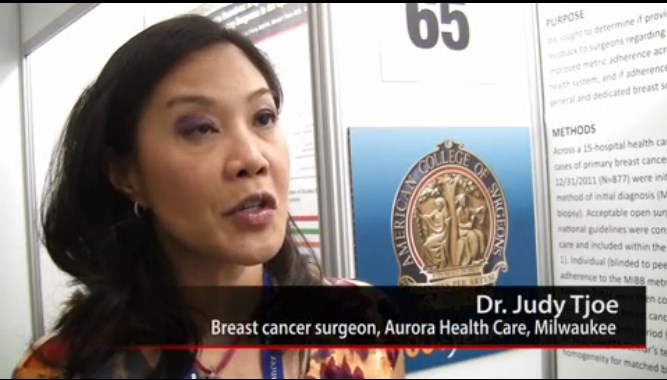
SAN FRANCISCO – Surgeons improve if they know they are behind the curve, according to Dr. Judy A. Tjoe, a breast cancer surgeon with Milwaukee-based Aurora Health Care.
She and her colleagues used that principle to significantly increase Aurora’s use of minimally invasive breast biopsies, the gold standard to diagnose breast cancer.
Although Dr. Tjoe and the system’s other three dedicated breast surgeons were using MIBB as appropriate, they found that 9 of 42 general surgeons (21%) were not, opting instead for open biopsies.
All it took to fix the problem was letting those surgeons know that minimally invasive breast biopsies was the preferred method, and that most of their peers were using it.
In a video interview at the American College of Surgeons Clinical Congress, Dr. Tjoe, also chair of Aurora’s quality committee for breast cancer care, explained why that message was so powerful, and how, in an era of pay for performance, the project is a model for improving health care without punitive measures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – Surgeons improve if they know they are behind the curve, according to Dr. Judy A. Tjoe, a breast cancer surgeon with Milwaukee-based Aurora Health Care.
She and her colleagues used that principle to significantly increase Aurora’s use of minimally invasive breast biopsies, the gold standard to diagnose breast cancer.
Although Dr. Tjoe and the system’s other three dedicated breast surgeons were using MIBB as appropriate, they found that 9 of 42 general surgeons (21%) were not, opting instead for open biopsies.
All it took to fix the problem was letting those surgeons know that minimally invasive breast biopsies was the preferred method, and that most of their peers were using it.
In a video interview at the American College of Surgeons Clinical Congress, Dr. Tjoe, also chair of Aurora’s quality committee for breast cancer care, explained why that message was so powerful, and how, in an era of pay for performance, the project is a model for improving health care without punitive measures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – Surgeons improve if they know they are behind the curve, according to Dr. Judy A. Tjoe, a breast cancer surgeon with Milwaukee-based Aurora Health Care.
She and her colleagues used that principle to significantly increase Aurora’s use of minimally invasive breast biopsies, the gold standard to diagnose breast cancer.
Although Dr. Tjoe and the system’s other three dedicated breast surgeons were using MIBB as appropriate, they found that 9 of 42 general surgeons (21%) were not, opting instead for open biopsies.
All it took to fix the problem was letting those surgeons know that minimally invasive breast biopsies was the preferred method, and that most of their peers were using it.
In a video interview at the American College of Surgeons Clinical Congress, Dr. Tjoe, also chair of Aurora’s quality committee for breast cancer care, explained why that message was so powerful, and how, in an era of pay for performance, the project is a model for improving health care without punitive measures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AMERICAN COLLEGE OF SURGEONS CLINICAL CONGRESS
Interferon-free regimen benefits HCV-infected liver transplant recipients
An oral, interferon-free drug regimen produced a 97% rate of sustained virologic response in liver transplant recipients who had recurrent hepatitis C viral infection – “an historically difficult-to-treat population” at high risk of death who have extremely limited treatment options, according to a study reported at the annual meeting of the American Association for the Study of Liver Diseases.
In an industry-sponsored, open-label phase II trial involving 34 adults with recurrent HCV infection following liver transplantation, 24 weeks of daily ombitasvir plus the ritonavir-boosted protease inhibitor ABT-450 (ABT-50/r), added to dasabuvir and ribavirin, eradicated every patient’s HCV RNA levels within 4 months. Only one patient had a relapse during a further 24 weeks of follow-up, said Dr. Parvez Mantry of the Liver Institute at Methodist Dallas, who presented the data at the meeting.*
Results of the study, which was conducted at 10 transplant centers in the United States and Spain, were presented at the meeting and simultaneously published online Nov. 11 in the New England Journal of Medicine (N. Engl. J. Med. 2014 Nov. 11 [doi: 10.1056/NEJMoa1408921]).
The standard of care for treating recurrent HCV infection after liver transplantation has been 48 weeks of peginterferon with ribavirin, but response rates are relatively low (13%-43%) because of interferon’s toxic effects. Moreover, the agent is known to induce graft injury, reducing both graft and patient survival.
The investigators assessed the safety and efficacy of a tablet formulation combining ombitasvir, a potent NS5A inhibitor, with ABT-50/r, a protease inhibitor that increases peak, trough, and overall drug exposure and allows once-daily dosing. To this was added standard dasabuvir and ribavirin, with ribavirin dosing adjusted according to the treating physician’s discretion to avert adverse hematologic effects in these immunosuppressed transplant recipients. Modified doses of standard calcineurin inhibitors (cyclosporine or tacrolimus) also were recommended for all patients, and low-dose glucocorticoids were permitted as needed.
The study participants were 18-70 years of age (mean age, 59.6 years) and had received liver transplants because of chronic HCV infection a minimum of 1 year previously. They had no or only mild liver fibrosis, were receiving stable cyclosporine- or tacrolimus-based immunosuppression, and were not coinfected with HIV or hepatitis B.
The primary efficacy endpoint was a sustained virologic response (SVR) 12 weeks after treatment was completed. All the study participants achieved an SVR by week 4 of treatment, which persisted in all of them until treatment was completed. At that time, 1 patient relapsed, so the overall SVR rate was 97%. This same SVR rate was sustained through final follow-up at post-treatment week 24.
In the patient who relapsed, HCV DNA showed resistance-associated genetic variants that had not been present at baseline. This patient also had been unresponsive to previous peginterferon-ribavirin therapy.
Adverse events were common, although the majority were mild or moderate in severity. Fatigue, headache, and cough were the most frequent adverse events. Grade 2 elevations in total bilirubin developed in two patients (6%), with no jaundice or scleral icterus. Nine patients showed grade 2 decreases in hemoglobin; none required a blood transfusion, and five required erythropoietin. There were no deaths and no cases of graft rejection.
One patient discontinued the study drug at week 18 after developing moderate rash, memory impairment, and anxiety deemed to be possibly drug related. However, that patient had already achieved an SVR before discontinuing treatment, and that SVR persisted at final follow-up 12 weeks later.
However, this study was not large enough to allow adequate assessment of adverse event rates or comparison of them with rates for other treatments, the investigators noted.
The researchers also noted that these study participants were easier to treat than the general population of liver transplant recipients with recurrent HCV, because they did not have advanced fibrosis or comorbid infections. In addition, patients with early, aggressive forms of recurrent HCV, such as fibrosing cholestatic hepatitis, were excluded from this study, as were patients maintained on immunosuppressive agents other than cyclosporine or tacrolimus.
This trial was sponsored by AbbVie, whose employees also designed the study, gathered and analyzed the data, and wrote the report. Study investigator Dr. Paul Y. Kwo reported receiving personal fees and grants from, and serving on advisory boards for, AbbVie, Bristol-Myers Squibb, and other companies. His associates reported ties to numerous industry sources.
*Clarification, 11/11/14: A previous version of this story did not state that the data were presented by Dr. Mantry
An oral, interferon-free drug regimen produced a 97% rate of sustained virologic response in liver transplant recipients who had recurrent hepatitis C viral infection – “an historically difficult-to-treat population” at high risk of death who have extremely limited treatment options, according to a study reported at the annual meeting of the American Association for the Study of Liver Diseases.
In an industry-sponsored, open-label phase II trial involving 34 adults with recurrent HCV infection following liver transplantation, 24 weeks of daily ombitasvir plus the ritonavir-boosted protease inhibitor ABT-450 (ABT-50/r), added to dasabuvir and ribavirin, eradicated every patient’s HCV RNA levels within 4 months. Only one patient had a relapse during a further 24 weeks of follow-up, said Dr. Parvez Mantry of the Liver Institute at Methodist Dallas, who presented the data at the meeting.*
Results of the study, which was conducted at 10 transplant centers in the United States and Spain, were presented at the meeting and simultaneously published online Nov. 11 in the New England Journal of Medicine (N. Engl. J. Med. 2014 Nov. 11 [doi: 10.1056/NEJMoa1408921]).
The standard of care for treating recurrent HCV infection after liver transplantation has been 48 weeks of peginterferon with ribavirin, but response rates are relatively low (13%-43%) because of interferon’s toxic effects. Moreover, the agent is known to induce graft injury, reducing both graft and patient survival.
The investigators assessed the safety and efficacy of a tablet formulation combining ombitasvir, a potent NS5A inhibitor, with ABT-50/r, a protease inhibitor that increases peak, trough, and overall drug exposure and allows once-daily dosing. To this was added standard dasabuvir and ribavirin, with ribavirin dosing adjusted according to the treating physician’s discretion to avert adverse hematologic effects in these immunosuppressed transplant recipients. Modified doses of standard calcineurin inhibitors (cyclosporine or tacrolimus) also were recommended for all patients, and low-dose glucocorticoids were permitted as needed.
The study participants were 18-70 years of age (mean age, 59.6 years) and had received liver transplants because of chronic HCV infection a minimum of 1 year previously. They had no or only mild liver fibrosis, were receiving stable cyclosporine- or tacrolimus-based immunosuppression, and were not coinfected with HIV or hepatitis B.
The primary efficacy endpoint was a sustained virologic response (SVR) 12 weeks after treatment was completed. All the study participants achieved an SVR by week 4 of treatment, which persisted in all of them until treatment was completed. At that time, 1 patient relapsed, so the overall SVR rate was 97%. This same SVR rate was sustained through final follow-up at post-treatment week 24.
In the patient who relapsed, HCV DNA showed resistance-associated genetic variants that had not been present at baseline. This patient also had been unresponsive to previous peginterferon-ribavirin therapy.
Adverse events were common, although the majority were mild or moderate in severity. Fatigue, headache, and cough were the most frequent adverse events. Grade 2 elevations in total bilirubin developed in two patients (6%), with no jaundice or scleral icterus. Nine patients showed grade 2 decreases in hemoglobin; none required a blood transfusion, and five required erythropoietin. There were no deaths and no cases of graft rejection.
One patient discontinued the study drug at week 18 after developing moderate rash, memory impairment, and anxiety deemed to be possibly drug related. However, that patient had already achieved an SVR before discontinuing treatment, and that SVR persisted at final follow-up 12 weeks later.
However, this study was not large enough to allow adequate assessment of adverse event rates or comparison of them with rates for other treatments, the investigators noted.
The researchers also noted that these study participants were easier to treat than the general population of liver transplant recipients with recurrent HCV, because they did not have advanced fibrosis or comorbid infections. In addition, patients with early, aggressive forms of recurrent HCV, such as fibrosing cholestatic hepatitis, were excluded from this study, as were patients maintained on immunosuppressive agents other than cyclosporine or tacrolimus.
This trial was sponsored by AbbVie, whose employees also designed the study, gathered and analyzed the data, and wrote the report. Study investigator Dr. Paul Y. Kwo reported receiving personal fees and grants from, and serving on advisory boards for, AbbVie, Bristol-Myers Squibb, and other companies. His associates reported ties to numerous industry sources.
*Clarification, 11/11/14: A previous version of this story did not state that the data were presented by Dr. Mantry
An oral, interferon-free drug regimen produced a 97% rate of sustained virologic response in liver transplant recipients who had recurrent hepatitis C viral infection – “an historically difficult-to-treat population” at high risk of death who have extremely limited treatment options, according to a study reported at the annual meeting of the American Association for the Study of Liver Diseases.
In an industry-sponsored, open-label phase II trial involving 34 adults with recurrent HCV infection following liver transplantation, 24 weeks of daily ombitasvir plus the ritonavir-boosted protease inhibitor ABT-450 (ABT-50/r), added to dasabuvir and ribavirin, eradicated every patient’s HCV RNA levels within 4 months. Only one patient had a relapse during a further 24 weeks of follow-up, said Dr. Parvez Mantry of the Liver Institute at Methodist Dallas, who presented the data at the meeting.*
Results of the study, which was conducted at 10 transplant centers in the United States and Spain, were presented at the meeting and simultaneously published online Nov. 11 in the New England Journal of Medicine (N. Engl. J. Med. 2014 Nov. 11 [doi: 10.1056/NEJMoa1408921]).
The standard of care for treating recurrent HCV infection after liver transplantation has been 48 weeks of peginterferon with ribavirin, but response rates are relatively low (13%-43%) because of interferon’s toxic effects. Moreover, the agent is known to induce graft injury, reducing both graft and patient survival.
The investigators assessed the safety and efficacy of a tablet formulation combining ombitasvir, a potent NS5A inhibitor, with ABT-50/r, a protease inhibitor that increases peak, trough, and overall drug exposure and allows once-daily dosing. To this was added standard dasabuvir and ribavirin, with ribavirin dosing adjusted according to the treating physician’s discretion to avert adverse hematologic effects in these immunosuppressed transplant recipients. Modified doses of standard calcineurin inhibitors (cyclosporine or tacrolimus) also were recommended for all patients, and low-dose glucocorticoids were permitted as needed.
The study participants were 18-70 years of age (mean age, 59.6 years) and had received liver transplants because of chronic HCV infection a minimum of 1 year previously. They had no or only mild liver fibrosis, were receiving stable cyclosporine- or tacrolimus-based immunosuppression, and were not coinfected with HIV or hepatitis B.
The primary efficacy endpoint was a sustained virologic response (SVR) 12 weeks after treatment was completed. All the study participants achieved an SVR by week 4 of treatment, which persisted in all of them until treatment was completed. At that time, 1 patient relapsed, so the overall SVR rate was 97%. This same SVR rate was sustained through final follow-up at post-treatment week 24.
In the patient who relapsed, HCV DNA showed resistance-associated genetic variants that had not been present at baseline. This patient also had been unresponsive to previous peginterferon-ribavirin therapy.
Adverse events were common, although the majority were mild or moderate in severity. Fatigue, headache, and cough were the most frequent adverse events. Grade 2 elevations in total bilirubin developed in two patients (6%), with no jaundice or scleral icterus. Nine patients showed grade 2 decreases in hemoglobin; none required a blood transfusion, and five required erythropoietin. There were no deaths and no cases of graft rejection.
One patient discontinued the study drug at week 18 after developing moderate rash, memory impairment, and anxiety deemed to be possibly drug related. However, that patient had already achieved an SVR before discontinuing treatment, and that SVR persisted at final follow-up 12 weeks later.
However, this study was not large enough to allow adequate assessment of adverse event rates or comparison of them with rates for other treatments, the investigators noted.
The researchers also noted that these study participants were easier to treat than the general population of liver transplant recipients with recurrent HCV, because they did not have advanced fibrosis or comorbid infections. In addition, patients with early, aggressive forms of recurrent HCV, such as fibrosing cholestatic hepatitis, were excluded from this study, as were patients maintained on immunosuppressive agents other than cyclosporine or tacrolimus.
This trial was sponsored by AbbVie, whose employees also designed the study, gathered and analyzed the data, and wrote the report. Study investigator Dr. Paul Y. Kwo reported receiving personal fees and grants from, and serving on advisory boards for, AbbVie, Bristol-Myers Squibb, and other companies. His associates reported ties to numerous industry sources.
*Clarification, 11/11/14: A previous version of this story did not state that the data were presented by Dr. Mantry
Key clinical point: An oral, interferon-free drug combination produced a 97% sustained virologic response rate in liver transplant recipients with recurrent HCV infection.
Major finding: The primary efficacy endpoint, an SVR 12 weeks after completion of treatment, was 97% (33 of 34 patients).
Data source: An industry-sponsored, multicenter, open-label phase II trial involving 34 adults with chronic HCV infection despite liver transplantation.
Disclosures: This trial was sponsored by AbbVie, whose employees also designed the study, gathered and analyzed the data, and wrote the report. Dr. Kwo reported receiving personal fees and grants from, and serving on advisory boards for, AbbVie, Bristol-Myers Squibb, and other companies. His associates reported ties to numerous industry sources.
HHS cuts 2015 ACA enrollment estimates by a quarter
Federal health officials expect that somewhere between 9 million and 9.9 million individuals will have obtained health insurance through the Affordable Care Act marketplaces by the end of the 2015 open enrollment period, down from a previous government estimate of 13 million.
The 9 million to 9.9 million estimate from the Health and Human Services department assumes that about 83% of individuals who purchased insurance through the marketplaces during 2014 will renew their coverage, with most of the new enrollment coming from previously uninsured individuals.
HHS released the figures just days ahead of the start of the Affordable Care Act’s (ACA’s) second open enrollment period, which runs from Nov. 15 through Feb. 15, 2015.
The Congressional Budget Office, which provides nonpartisan budget analysis for Congress, had projected in April 2014 that 13 million Americans would be insured through the ACA marketplaces by the end of the second enrollment period in February 2015.
The HHS projection is lower, according to the agency, because it assumes that fewer people who have employer-sponsored insurance will jump to the ACA marketplaces in 2015. Fewer individuals who purchased individual market insurance on their own are expected to shop on the ACA marketplaces right away, according to HHS.
Another factor is that the Congressional Budget Office made its projections in April, before the final 2014 enrollment figures were available. In the spring, HHS had said that more than 8 million people had selected plans through the ACA marketplaces, but as of October 2014, 7.1 million individuals had enrolled and were paying for coverage.
The new enrollment estimates were criticized by Republicans on Capitol Hill.
“The administration is again trying to rewrite its definition of success for the president’s signature law on the eve of Saturday’s second enrollment,” Rep. Marsha Blackburn (R-Tenn.), House Energy and Commerce Committee Vice Chairman, said in a statement. “There are still a number of important, unanswered questions, including whether or not the back end is built and if the millions of inconsistencies have been resolved.”
On Twitter @maryellenny
Federal health officials expect that somewhere between 9 million and 9.9 million individuals will have obtained health insurance through the Affordable Care Act marketplaces by the end of the 2015 open enrollment period, down from a previous government estimate of 13 million.
The 9 million to 9.9 million estimate from the Health and Human Services department assumes that about 83% of individuals who purchased insurance through the marketplaces during 2014 will renew their coverage, with most of the new enrollment coming from previously uninsured individuals.
HHS released the figures just days ahead of the start of the Affordable Care Act’s (ACA’s) second open enrollment period, which runs from Nov. 15 through Feb. 15, 2015.
The Congressional Budget Office, which provides nonpartisan budget analysis for Congress, had projected in April 2014 that 13 million Americans would be insured through the ACA marketplaces by the end of the second enrollment period in February 2015.
The HHS projection is lower, according to the agency, because it assumes that fewer people who have employer-sponsored insurance will jump to the ACA marketplaces in 2015. Fewer individuals who purchased individual market insurance on their own are expected to shop on the ACA marketplaces right away, according to HHS.
Another factor is that the Congressional Budget Office made its projections in April, before the final 2014 enrollment figures were available. In the spring, HHS had said that more than 8 million people had selected plans through the ACA marketplaces, but as of October 2014, 7.1 million individuals had enrolled and were paying for coverage.
The new enrollment estimates were criticized by Republicans on Capitol Hill.
“The administration is again trying to rewrite its definition of success for the president’s signature law on the eve of Saturday’s second enrollment,” Rep. Marsha Blackburn (R-Tenn.), House Energy and Commerce Committee Vice Chairman, said in a statement. “There are still a number of important, unanswered questions, including whether or not the back end is built and if the millions of inconsistencies have been resolved.”
On Twitter @maryellenny
Federal health officials expect that somewhere between 9 million and 9.9 million individuals will have obtained health insurance through the Affordable Care Act marketplaces by the end of the 2015 open enrollment period, down from a previous government estimate of 13 million.
The 9 million to 9.9 million estimate from the Health and Human Services department assumes that about 83% of individuals who purchased insurance through the marketplaces during 2014 will renew their coverage, with most of the new enrollment coming from previously uninsured individuals.
HHS released the figures just days ahead of the start of the Affordable Care Act’s (ACA’s) second open enrollment period, which runs from Nov. 15 through Feb. 15, 2015.
The Congressional Budget Office, which provides nonpartisan budget analysis for Congress, had projected in April 2014 that 13 million Americans would be insured through the ACA marketplaces by the end of the second enrollment period in February 2015.
The HHS projection is lower, according to the agency, because it assumes that fewer people who have employer-sponsored insurance will jump to the ACA marketplaces in 2015. Fewer individuals who purchased individual market insurance on their own are expected to shop on the ACA marketplaces right away, according to HHS.
Another factor is that the Congressional Budget Office made its projections in April, before the final 2014 enrollment figures were available. In the spring, HHS had said that more than 8 million people had selected plans through the ACA marketplaces, but as of October 2014, 7.1 million individuals had enrolled and were paying for coverage.
The new enrollment estimates were criticized by Republicans on Capitol Hill.
“The administration is again trying to rewrite its definition of success for the president’s signature law on the eve of Saturday’s second enrollment,” Rep. Marsha Blackburn (R-Tenn.), House Energy and Commerce Committee Vice Chairman, said in a statement. “There are still a number of important, unanswered questions, including whether or not the back end is built and if the millions of inconsistencies have been resolved.”
On Twitter @maryellenny