User login
Official Newspaper of the American College of Surgeons
The Right Choice? Paternalism, Autonomy, and the Incidental Finding
The case had been straightforward. My patient had primary hyperparathyroidism and her localization studies had shown a single parathyroid adenoma. In the operating room, with her under general anesthesia, I had found and removed the abnormal parathyroid gland. The intraoperative parathyroid hormone levels were being run outside the OR door. I was getting ready to close with my fellow when I happened to palpate the thyroid isthmus. There was a firm nodule right in the center of the isthmus. The thyroid looked fine, but the nodule was unmistakable.
This was a surprise. The patient had undergone an ultrasound in radiology the week before, and the study was notable for there being no thyroid nodules. We had performed our own ultrasound in the OR. We had confirmed the location of the parathyroid adenoma and saw no thyroid nodules. I was faced with the initial question of what to do with this incidental finding. Although I could not see the nodule, certainly by feel, it was suspicious, but it was also very small – several millimeters at most. One option was to simply ignore the finding – certainly a bad choice. I knew that the patient had come to the hospital with her sister and a close friend. They were both in the waiting room expecting my update as soon as we were finished. I could have discussed this unexpected finding with the sister and friend, but I felt certain that no one would object to me removing a small piece of thyroid when this added little or no risk. It seemed unnecessary to seek permission to do this small additional procedure.
We proceeded to resect the nodule within the thyroid gland, taking enough adjacent thyroid tissue that I never actually saw the nodule. Once it was removed, I faced another question: Should I send it for frozen section? This seemed to be an easy one to answer. If I was suspicious enough to remove it, I should also know what it is.
The frozen section report was called in a short time later. It was a 4-mm papillary thyroid cancer (PTC) that was within normal thyroid tissue. I had been expecting this possible result. Now I had more choices. I could talk with the family/friend in the waiting room and seek advice on what to do. Alternatively, I could simply say that the presence of PTC was enough of a reason to just take out the thyroid gland since I had not expected this finding and the negative preoperative ultrasound had certainly missed this small tumor (and there might even be others). Finally, I could simply close the patient based on the fact that a 4-mm PTC is of no real clinical significance. Certainly, if this small PTC had been removed with a thyroid lobe for other reasons, we would never go back to take out the rest of the thyroid gland.
As I considered these options, it seemed clear to me that if I went to talk with the family/friend with an unexpected diagnosis of cancer, it was very likely that the patient would wind up with a bigger operation than might be necessary. Ten or fifteen years ago, most surgeons would have removed the thyroid gland for almost any diagnosis of PTC so that patients could go on to receive radioactive iodine. However, today many patients with small incidental PTCs found on lobectomy are simply followed with surveillance ultrasounds because the risks of recurrence or spread are very low. It was clear that I had no basis to take out the whole thyroid gland for a small PTC that was already out. It also seemed unwise to ask what to do, when I felt certain that I knew what was best for the patient. Of course, the suggestion that “I knew what was best for the patient” is a very paternalistic thing to say. It suggests that the medical issues trump all others. It is also quite contrary to the movement of medical ethics in the last several decades that has emphasized shared decision making yet doing what is best for the patient is what surgical patients expect of their surgeons.
I decided to close the patient and then explain what I did and why I did it. She might have been angry with me that I had found a cancer and had not taken out her thyroid gland. However, I felt that the medical evidence supported a less-aggressive surgical approach. In addition, I could always take out her thyroid if she was too worried by the concept of surveillance but I could never put it back if I had removed it!
The patient was understandably surprised and concerned when talked to her. Her first response was one of concern about recurrence. She wanted to know how I knew that there was no more cancer in her thyroid gland. I explained that I actually could not know that, but based on the ultrasound, there was no evidence of any clinically significant thyroid cancer. Fortunately, she was ultimately relieved that the thyroid cancer had been found even though it raised concerns for the future that she had never considered previously.
Whenever surgeons operate on patients under general anesthesia, we are faced with the potential need to make decisions for our patients without the patient’s input. Sometimes it is appropriate to seek input from family when there are multiple good options. However, surgery requires surgeons to make many decisions on their patient’s behalf with no input from the patient – that is, surgeons are expected to act paternalistically in the OR. Rather than being detrimental to the ethical care of patients, such limited paternalism is sometimes the best that we can offer our patients and critical to our role as surgeon.
Dr. Angelos is an ACS Fellow; the Linda Kohler Anderson Professor of Surgery and Surgical Ethics; chief, endocrine surgery; and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
The case had been straightforward. My patient had primary hyperparathyroidism and her localization studies had shown a single parathyroid adenoma. In the operating room, with her under general anesthesia, I had found and removed the abnormal parathyroid gland. The intraoperative parathyroid hormone levels were being run outside the OR door. I was getting ready to close with my fellow when I happened to palpate the thyroid isthmus. There was a firm nodule right in the center of the isthmus. The thyroid looked fine, but the nodule was unmistakable.
This was a surprise. The patient had undergone an ultrasound in radiology the week before, and the study was notable for there being no thyroid nodules. We had performed our own ultrasound in the OR. We had confirmed the location of the parathyroid adenoma and saw no thyroid nodules. I was faced with the initial question of what to do with this incidental finding. Although I could not see the nodule, certainly by feel, it was suspicious, but it was also very small – several millimeters at most. One option was to simply ignore the finding – certainly a bad choice. I knew that the patient had come to the hospital with her sister and a close friend. They were both in the waiting room expecting my update as soon as we were finished. I could have discussed this unexpected finding with the sister and friend, but I felt certain that no one would object to me removing a small piece of thyroid when this added little or no risk. It seemed unnecessary to seek permission to do this small additional procedure.
We proceeded to resect the nodule within the thyroid gland, taking enough adjacent thyroid tissue that I never actually saw the nodule. Once it was removed, I faced another question: Should I send it for frozen section? This seemed to be an easy one to answer. If I was suspicious enough to remove it, I should also know what it is.
The frozen section report was called in a short time later. It was a 4-mm papillary thyroid cancer (PTC) that was within normal thyroid tissue. I had been expecting this possible result. Now I had more choices. I could talk with the family/friend in the waiting room and seek advice on what to do. Alternatively, I could simply say that the presence of PTC was enough of a reason to just take out the thyroid gland since I had not expected this finding and the negative preoperative ultrasound had certainly missed this small tumor (and there might even be others). Finally, I could simply close the patient based on the fact that a 4-mm PTC is of no real clinical significance. Certainly, if this small PTC had been removed with a thyroid lobe for other reasons, we would never go back to take out the rest of the thyroid gland.
As I considered these options, it seemed clear to me that if I went to talk with the family/friend with an unexpected diagnosis of cancer, it was very likely that the patient would wind up with a bigger operation than might be necessary. Ten or fifteen years ago, most surgeons would have removed the thyroid gland for almost any diagnosis of PTC so that patients could go on to receive radioactive iodine. However, today many patients with small incidental PTCs found on lobectomy are simply followed with surveillance ultrasounds because the risks of recurrence or spread are very low. It was clear that I had no basis to take out the whole thyroid gland for a small PTC that was already out. It also seemed unwise to ask what to do, when I felt certain that I knew what was best for the patient. Of course, the suggestion that “I knew what was best for the patient” is a very paternalistic thing to say. It suggests that the medical issues trump all others. It is also quite contrary to the movement of medical ethics in the last several decades that has emphasized shared decision making yet doing what is best for the patient is what surgical patients expect of their surgeons.
I decided to close the patient and then explain what I did and why I did it. She might have been angry with me that I had found a cancer and had not taken out her thyroid gland. However, I felt that the medical evidence supported a less-aggressive surgical approach. In addition, I could always take out her thyroid if she was too worried by the concept of surveillance but I could never put it back if I had removed it!
The patient was understandably surprised and concerned when talked to her. Her first response was one of concern about recurrence. She wanted to know how I knew that there was no more cancer in her thyroid gland. I explained that I actually could not know that, but based on the ultrasound, there was no evidence of any clinically significant thyroid cancer. Fortunately, she was ultimately relieved that the thyroid cancer had been found even though it raised concerns for the future that she had never considered previously.
Whenever surgeons operate on patients under general anesthesia, we are faced with the potential need to make decisions for our patients without the patient’s input. Sometimes it is appropriate to seek input from family when there are multiple good options. However, surgery requires surgeons to make many decisions on their patient’s behalf with no input from the patient – that is, surgeons are expected to act paternalistically in the OR. Rather than being detrimental to the ethical care of patients, such limited paternalism is sometimes the best that we can offer our patients and critical to our role as surgeon.
Dr. Angelos is an ACS Fellow; the Linda Kohler Anderson Professor of Surgery and Surgical Ethics; chief, endocrine surgery; and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
The case had been straightforward. My patient had primary hyperparathyroidism and her localization studies had shown a single parathyroid adenoma. In the operating room, with her under general anesthesia, I had found and removed the abnormal parathyroid gland. The intraoperative parathyroid hormone levels were being run outside the OR door. I was getting ready to close with my fellow when I happened to palpate the thyroid isthmus. There was a firm nodule right in the center of the isthmus. The thyroid looked fine, but the nodule was unmistakable.
This was a surprise. The patient had undergone an ultrasound in radiology the week before, and the study was notable for there being no thyroid nodules. We had performed our own ultrasound in the OR. We had confirmed the location of the parathyroid adenoma and saw no thyroid nodules. I was faced with the initial question of what to do with this incidental finding. Although I could not see the nodule, certainly by feel, it was suspicious, but it was also very small – several millimeters at most. One option was to simply ignore the finding – certainly a bad choice. I knew that the patient had come to the hospital with her sister and a close friend. They were both in the waiting room expecting my update as soon as we were finished. I could have discussed this unexpected finding with the sister and friend, but I felt certain that no one would object to me removing a small piece of thyroid when this added little or no risk. It seemed unnecessary to seek permission to do this small additional procedure.
We proceeded to resect the nodule within the thyroid gland, taking enough adjacent thyroid tissue that I never actually saw the nodule. Once it was removed, I faced another question: Should I send it for frozen section? This seemed to be an easy one to answer. If I was suspicious enough to remove it, I should also know what it is.
The frozen section report was called in a short time later. It was a 4-mm papillary thyroid cancer (PTC) that was within normal thyroid tissue. I had been expecting this possible result. Now I had more choices. I could talk with the family/friend in the waiting room and seek advice on what to do. Alternatively, I could simply say that the presence of PTC was enough of a reason to just take out the thyroid gland since I had not expected this finding and the negative preoperative ultrasound had certainly missed this small tumor (and there might even be others). Finally, I could simply close the patient based on the fact that a 4-mm PTC is of no real clinical significance. Certainly, if this small PTC had been removed with a thyroid lobe for other reasons, we would never go back to take out the rest of the thyroid gland.
As I considered these options, it seemed clear to me that if I went to talk with the family/friend with an unexpected diagnosis of cancer, it was very likely that the patient would wind up with a bigger operation than might be necessary. Ten or fifteen years ago, most surgeons would have removed the thyroid gland for almost any diagnosis of PTC so that patients could go on to receive radioactive iodine. However, today many patients with small incidental PTCs found on lobectomy are simply followed with surveillance ultrasounds because the risks of recurrence or spread are very low. It was clear that I had no basis to take out the whole thyroid gland for a small PTC that was already out. It also seemed unwise to ask what to do, when I felt certain that I knew what was best for the patient. Of course, the suggestion that “I knew what was best for the patient” is a very paternalistic thing to say. It suggests that the medical issues trump all others. It is also quite contrary to the movement of medical ethics in the last several decades that has emphasized shared decision making yet doing what is best for the patient is what surgical patients expect of their surgeons.
I decided to close the patient and then explain what I did and why I did it. She might have been angry with me that I had found a cancer and had not taken out her thyroid gland. However, I felt that the medical evidence supported a less-aggressive surgical approach. In addition, I could always take out her thyroid if she was too worried by the concept of surveillance but I could never put it back if I had removed it!
The patient was understandably surprised and concerned when talked to her. Her first response was one of concern about recurrence. She wanted to know how I knew that there was no more cancer in her thyroid gland. I explained that I actually could not know that, but based on the ultrasound, there was no evidence of any clinically significant thyroid cancer. Fortunately, she was ultimately relieved that the thyroid cancer had been found even though it raised concerns for the future that she had never considered previously.
Whenever surgeons operate on patients under general anesthesia, we are faced with the potential need to make decisions for our patients without the patient’s input. Sometimes it is appropriate to seek input from family when there are multiple good options. However, surgery requires surgeons to make many decisions on their patient’s behalf with no input from the patient – that is, surgeons are expected to act paternalistically in the OR. Rather than being detrimental to the ethical care of patients, such limited paternalism is sometimes the best that we can offer our patients and critical to our role as surgeon.
Dr. Angelos is an ACS Fellow; the Linda Kohler Anderson Professor of Surgery and Surgical Ethics; chief, endocrine surgery; and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
FDA approves simeprevir-sofosbuvir combo for hepatitis C
The Food and Drug Administration has approved the use of sofosbuvir in combination with simeprevir for treatment of patients with chronic hepatitis C virus. It is a ribavirin- and interferon-free regimen.
The approval is reflected in changes to the label of simeprevir (Olysio), an HCV NS3/4A protease inhibitor, which was approved in 2013 for chronic hepatitis C genotype 1 infection “as a component of a combination antiviral treatment regimen.”
The new label summarizes the results of COSMOS, an open label, randomized phase II trial of HCV genotype 1–infected prior null responders with a METAVIR fibrosis score of F0 F2 or treatment naive subjects and prior null responders with a METAVIR fibrosis score of F3 F4 and compensated liver disease. The sustained virologic response rates 12 weeks after planned end of treatment was 93% among those treated with the combination for 12 weeks, and 97% among those treated for 24 weeks. The study was published online (Lancet 2014 July [doi:10.1016/S0140-6736(14)61036-9]).
In COSMOS, the most common adverse reactions reported by more than 10% of treated patients during 12 weeks of combination treatment were fatigue in 25%, headache (21%), nausea (21%), insomnia (14%), pruritus (11%), rash (11%), and photosensitivity (7%). Among those treated for 24 weeks, dizziness (16%) and diarrhea (16%) were reported, according to the revised label.
When combined with sofosbuvir, treatment of treatment-naive and treatment-experienced patients is recommended for 12 weeks (for patients without cirrhosis) or 24 weeks (for patients with cirrhosis).
Simeprevir is marketed by Janssen Therapeutics. Sofosbuvir, an HCV nucleotide analog NS5B polymerase inhibitor approved in December 2013 for treatment of chronic hepatitis C as a component of a combination antiviral treatment regimen, is marketed as Sovaldi by Gilead Sciences. The combination was approved Nov. 5.
The Food and Drug Administration has approved the use of sofosbuvir in combination with simeprevir for treatment of patients with chronic hepatitis C virus. It is a ribavirin- and interferon-free regimen.
The approval is reflected in changes to the label of simeprevir (Olysio), an HCV NS3/4A protease inhibitor, which was approved in 2013 for chronic hepatitis C genotype 1 infection “as a component of a combination antiviral treatment regimen.”
The new label summarizes the results of COSMOS, an open label, randomized phase II trial of HCV genotype 1–infected prior null responders with a METAVIR fibrosis score of F0 F2 or treatment naive subjects and prior null responders with a METAVIR fibrosis score of F3 F4 and compensated liver disease. The sustained virologic response rates 12 weeks after planned end of treatment was 93% among those treated with the combination for 12 weeks, and 97% among those treated for 24 weeks. The study was published online (Lancet 2014 July [doi:10.1016/S0140-6736(14)61036-9]).
In COSMOS, the most common adverse reactions reported by more than 10% of treated patients during 12 weeks of combination treatment were fatigue in 25%, headache (21%), nausea (21%), insomnia (14%), pruritus (11%), rash (11%), and photosensitivity (7%). Among those treated for 24 weeks, dizziness (16%) and diarrhea (16%) were reported, according to the revised label.
When combined with sofosbuvir, treatment of treatment-naive and treatment-experienced patients is recommended for 12 weeks (for patients without cirrhosis) or 24 weeks (for patients with cirrhosis).
Simeprevir is marketed by Janssen Therapeutics. Sofosbuvir, an HCV nucleotide analog NS5B polymerase inhibitor approved in December 2013 for treatment of chronic hepatitis C as a component of a combination antiviral treatment regimen, is marketed as Sovaldi by Gilead Sciences. The combination was approved Nov. 5.
The Food and Drug Administration has approved the use of sofosbuvir in combination with simeprevir for treatment of patients with chronic hepatitis C virus. It is a ribavirin- and interferon-free regimen.
The approval is reflected in changes to the label of simeprevir (Olysio), an HCV NS3/4A protease inhibitor, which was approved in 2013 for chronic hepatitis C genotype 1 infection “as a component of a combination antiviral treatment regimen.”
The new label summarizes the results of COSMOS, an open label, randomized phase II trial of HCV genotype 1–infected prior null responders with a METAVIR fibrosis score of F0 F2 or treatment naive subjects and prior null responders with a METAVIR fibrosis score of F3 F4 and compensated liver disease. The sustained virologic response rates 12 weeks after planned end of treatment was 93% among those treated with the combination for 12 weeks, and 97% among those treated for 24 weeks. The study was published online (Lancet 2014 July [doi:10.1016/S0140-6736(14)61036-9]).
In COSMOS, the most common adverse reactions reported by more than 10% of treated patients during 12 weeks of combination treatment were fatigue in 25%, headache (21%), nausea (21%), insomnia (14%), pruritus (11%), rash (11%), and photosensitivity (7%). Among those treated for 24 weeks, dizziness (16%) and diarrhea (16%) were reported, according to the revised label.
When combined with sofosbuvir, treatment of treatment-naive and treatment-experienced patients is recommended for 12 weeks (for patients without cirrhosis) or 24 weeks (for patients with cirrhosis).
Simeprevir is marketed by Janssen Therapeutics. Sofosbuvir, an HCV nucleotide analog NS5B polymerase inhibitor approved in December 2013 for treatment of chronic hepatitis C as a component of a combination antiviral treatment regimen, is marketed as Sovaldi by Gilead Sciences. The combination was approved Nov. 5.
Midterm ballot initiatives mostly favor physicians
California voters rejected a ballot initiative that would have required doctors to submit to random drug and alcohol testing within 12 hours of when an adverse event has been identified, while voters in South Dakota approved a measure to loosen insurance companies’ provider panels.
With all precincts reporting, more than 67% of California voters (nearly 3.42 million) voted no on Proposition 46, a measure that doctors in the state said would unreasonably penalize doctors unable to meet testing rules and lead to excessive suspensions. The initiative applied only to doctors who practice in hospitals or have hospital privileges.
The ballot initiative also contained two other components – a requirement that doctors consult a statewide database before prescribing schedule II and schedule III drugs and a raising of the medical malpractice cap on noneconomic damages from $250,000 to $1.1 million. Doctors argued that the database lacked the funding and staff to be effective in identifying patients engaged in doctor-shopping or otherwise abusing prescription controlled substances.
In South Dakota, 61.8% of the voters (166,351, with all precincts reporting) approved Measure 17, which allows providers who are willing to meet a health insurer’s coverage terms to provide health care services to insured patients without having to join that patient’s insurance plan network, and protects patients from out-of-network costs if they use that physician.
Voters in Arizona approved Proposition 303, which allows eligible patients with a terminal illness that has no Food and Drug Administration–approved treatment option to have access to an investigational drug, provided the drug has successfully completed phase I testing and remains under clinical investigation. The pharmaceutical manufacturer would decide whether to provide access, and insurance companies are not required under the measure to provide coverage for it. The measure also offered some liability protection for physicians who recommend the investigational treatment. More than 78% of the votes (849,350, with 97% of the precincts reporting) supported the measure.
In Illinois, voters supported a ballot initiative that would require insurance plans in the state that have prescription drug coverage to “include prescription birth control as part of that coverage.” No details were included in the text of the initiative on the scope of what needs to be included, but its passage means the state legislature must enact a law to implement the will of the voters. Sixty-six percent of the votes (2.2 million, with 99 percent of precincts reporting) were in favor of this initiative.
Residents in three states acted on abortion-related measures. In North Dakota, a ballot initiative would have amended the state constitution to provide for the “inalienable right to life” beginning at conception. With all precincts reporting, the amendment failed, with more than 64% of votes against. In Colorado, a constitutional amendment to include the unborn in the definition of “person” and “child” in the state criminal code failed, with more than 64% of the votes (nearly 1.2 million, with 94% of precincts reporting) going against the amendment.
And in Tennessee, voters approved a constitutional amendment that empowers the state legislature “to enact, amend, or repeal statutes regarding abortion, including but not limited to, circumstances of pregnancy resulting from rape or incest, or when necessary to save the life of the mother.” It passed with more than 52% of the votes (728,751 with 99 percent of the precincts reporting). The amendment was in reaction to a 2000 state supreme court ruling that struck down a number of state laws that placed limits around abortions.
California voters rejected a ballot initiative that would have required doctors to submit to random drug and alcohol testing within 12 hours of when an adverse event has been identified, while voters in South Dakota approved a measure to loosen insurance companies’ provider panels.
With all precincts reporting, more than 67% of California voters (nearly 3.42 million) voted no on Proposition 46, a measure that doctors in the state said would unreasonably penalize doctors unable to meet testing rules and lead to excessive suspensions. The initiative applied only to doctors who practice in hospitals or have hospital privileges.
The ballot initiative also contained two other components – a requirement that doctors consult a statewide database before prescribing schedule II and schedule III drugs and a raising of the medical malpractice cap on noneconomic damages from $250,000 to $1.1 million. Doctors argued that the database lacked the funding and staff to be effective in identifying patients engaged in doctor-shopping or otherwise abusing prescription controlled substances.
In South Dakota, 61.8% of the voters (166,351, with all precincts reporting) approved Measure 17, which allows providers who are willing to meet a health insurer’s coverage terms to provide health care services to insured patients without having to join that patient’s insurance plan network, and protects patients from out-of-network costs if they use that physician.
Voters in Arizona approved Proposition 303, which allows eligible patients with a terminal illness that has no Food and Drug Administration–approved treatment option to have access to an investigational drug, provided the drug has successfully completed phase I testing and remains under clinical investigation. The pharmaceutical manufacturer would decide whether to provide access, and insurance companies are not required under the measure to provide coverage for it. The measure also offered some liability protection for physicians who recommend the investigational treatment. More than 78% of the votes (849,350, with 97% of the precincts reporting) supported the measure.
In Illinois, voters supported a ballot initiative that would require insurance plans in the state that have prescription drug coverage to “include prescription birth control as part of that coverage.” No details were included in the text of the initiative on the scope of what needs to be included, but its passage means the state legislature must enact a law to implement the will of the voters. Sixty-six percent of the votes (2.2 million, with 99 percent of precincts reporting) were in favor of this initiative.
Residents in three states acted on abortion-related measures. In North Dakota, a ballot initiative would have amended the state constitution to provide for the “inalienable right to life” beginning at conception. With all precincts reporting, the amendment failed, with more than 64% of votes against. In Colorado, a constitutional amendment to include the unborn in the definition of “person” and “child” in the state criminal code failed, with more than 64% of the votes (nearly 1.2 million, with 94% of precincts reporting) going against the amendment.
And in Tennessee, voters approved a constitutional amendment that empowers the state legislature “to enact, amend, or repeal statutes regarding abortion, including but not limited to, circumstances of pregnancy resulting from rape or incest, or when necessary to save the life of the mother.” It passed with more than 52% of the votes (728,751 with 99 percent of the precincts reporting). The amendment was in reaction to a 2000 state supreme court ruling that struck down a number of state laws that placed limits around abortions.
California voters rejected a ballot initiative that would have required doctors to submit to random drug and alcohol testing within 12 hours of when an adverse event has been identified, while voters in South Dakota approved a measure to loosen insurance companies’ provider panels.
With all precincts reporting, more than 67% of California voters (nearly 3.42 million) voted no on Proposition 46, a measure that doctors in the state said would unreasonably penalize doctors unable to meet testing rules and lead to excessive suspensions. The initiative applied only to doctors who practice in hospitals or have hospital privileges.
The ballot initiative also contained two other components – a requirement that doctors consult a statewide database before prescribing schedule II and schedule III drugs and a raising of the medical malpractice cap on noneconomic damages from $250,000 to $1.1 million. Doctors argued that the database lacked the funding and staff to be effective in identifying patients engaged in doctor-shopping or otherwise abusing prescription controlled substances.
In South Dakota, 61.8% of the voters (166,351, with all precincts reporting) approved Measure 17, which allows providers who are willing to meet a health insurer’s coverage terms to provide health care services to insured patients without having to join that patient’s insurance plan network, and protects patients from out-of-network costs if they use that physician.
Voters in Arizona approved Proposition 303, which allows eligible patients with a terminal illness that has no Food and Drug Administration–approved treatment option to have access to an investigational drug, provided the drug has successfully completed phase I testing and remains under clinical investigation. The pharmaceutical manufacturer would decide whether to provide access, and insurance companies are not required under the measure to provide coverage for it. The measure also offered some liability protection for physicians who recommend the investigational treatment. More than 78% of the votes (849,350, with 97% of the precincts reporting) supported the measure.
In Illinois, voters supported a ballot initiative that would require insurance plans in the state that have prescription drug coverage to “include prescription birth control as part of that coverage.” No details were included in the text of the initiative on the scope of what needs to be included, but its passage means the state legislature must enact a law to implement the will of the voters. Sixty-six percent of the votes (2.2 million, with 99 percent of precincts reporting) were in favor of this initiative.
Residents in three states acted on abortion-related measures. In North Dakota, a ballot initiative would have amended the state constitution to provide for the “inalienable right to life” beginning at conception. With all precincts reporting, the amendment failed, with more than 64% of votes against. In Colorado, a constitutional amendment to include the unborn in the definition of “person” and “child” in the state criminal code failed, with more than 64% of the votes (nearly 1.2 million, with 94% of precincts reporting) going against the amendment.
And in Tennessee, voters approved a constitutional amendment that empowers the state legislature “to enact, amend, or repeal statutes regarding abortion, including but not limited to, circumstances of pregnancy resulting from rape or incest, or when necessary to save the life of the mother.” It passed with more than 52% of the votes (728,751 with 99 percent of the precincts reporting). The amendment was in reaction to a 2000 state supreme court ruling that struck down a number of state laws that placed limits around abortions.
Inpatient handoff program reduced errors
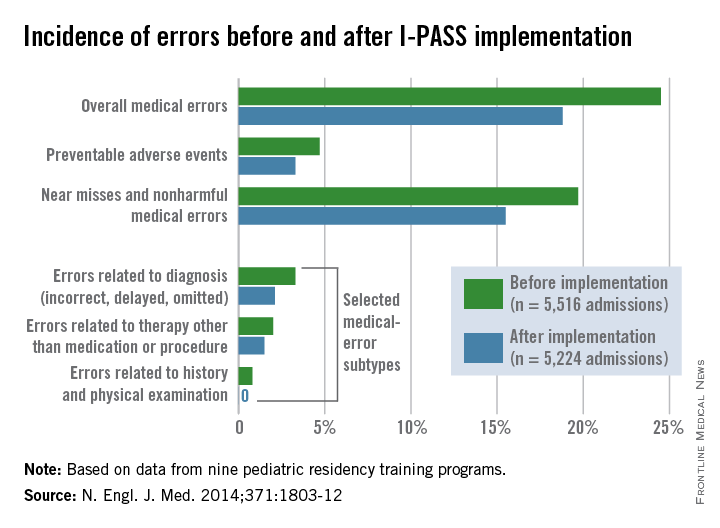
Implementation of a resident handoff program at nine hospitals reduced both medical errors and preventable adverse events, according to a study published Nov. 5 in the New England Journal of Medicine.
Dr. Amy J. Starmer of Boston Children’s Hospital and her coinvestigators at dozens of other institutions implemented an I-PASS-based program in nine pediatric residency training programs in the United States and Canada from 2011 through 2013. I-PASS, a mnemonic to standardize handoffs, stands for illness severity; patient summary; action list; situation awareness and contingency plans; and synthesis by receiver. Study sites ranged in size from 36 to 182 residents (N. Engl. J. Med. 2014;371:1803-12).
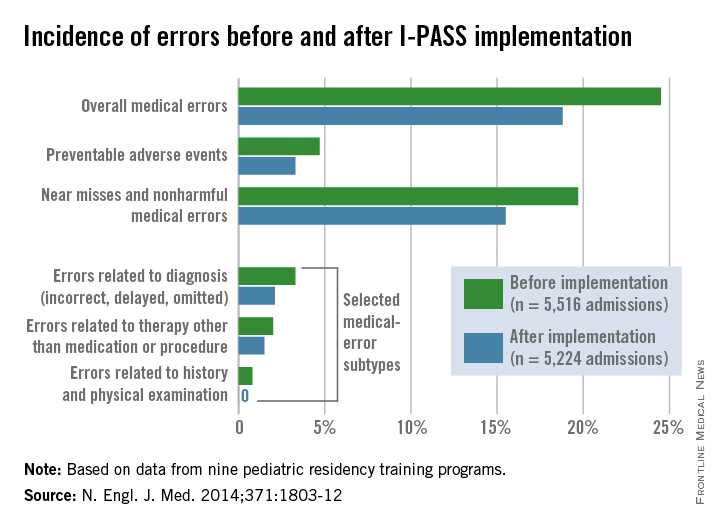
Of 10,740 patient admissions, the rate of medical errors decreased from 24.5 per 100 admissions preintervention to 18.8 per 100 admissions postintervention (23%), Dr. Starmer and her colleagues wrote. The rate of preventable adverse events fell from 4.7 events per 100 admissions to 3.3 events per 100 admissions (30%). Additionally, the rate of near misses and nonharmful medical errors went down by 21%. Investigators found no significant change in the rate of nonpreventable adverse events.
The I-PASS Handoff Bundle consisted of the I-PASS mnemonic; a 2-hour workshop on teamwork, communication skills, and I-PASS handoff techniques; a 1-hour role-playing session; a computer module; a faculty development program; direct-observation tools; and a process and culture-change campaign. Each site was assigned to one of three staggered intervention and data-collection waves from January 2011 through May 2013.
The hospitals integrated the I-PASS structure into both oral and written handoff processes. At seven sites, written handoff tools with a standardized I-PASS format were built into electronic medical record programs. The tools were built into word processing programs at two sites. Each hospital maintained an implementation log that was regularly reviewed to ensure adherence to program components.
Researchers found no significant time change in residents’ workflow after program implementation, including the time in a 24-hour period spent with patients and families.
Following the intervention period, the proportion of residents who rated the overall quality of their handoff training as very good or excellent rose from 28% to 72%.
“Implementing handoff improvement programs such as the I-PASS Handoff Bundle may potentiate the effectiveness of work-hour reductions, because doing both together may concurrently reduce both fatigue and handoff-related errors,” the study authors said.
The study was funded by the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services, and others. The investigators reported no relevant conflicts of interest. Boston Children’s Hospital and the main study investigators are exploring the potential licensing of I-PASS.
On Twitter @legal_med
Implementation of a resident handoff program at nine hospitals reduced both medical errors and preventable adverse events, according to a study published Nov. 5 in the New England Journal of Medicine.
Dr. Amy J. Starmer of Boston Children’s Hospital and her coinvestigators at dozens of other institutions implemented an I-PASS-based program in nine pediatric residency training programs in the United States and Canada from 2011 through 2013. I-PASS, a mnemonic to standardize handoffs, stands for illness severity; patient summary; action list; situation awareness and contingency plans; and synthesis by receiver. Study sites ranged in size from 36 to 182 residents (N. Engl. J. Med. 2014;371:1803-12).
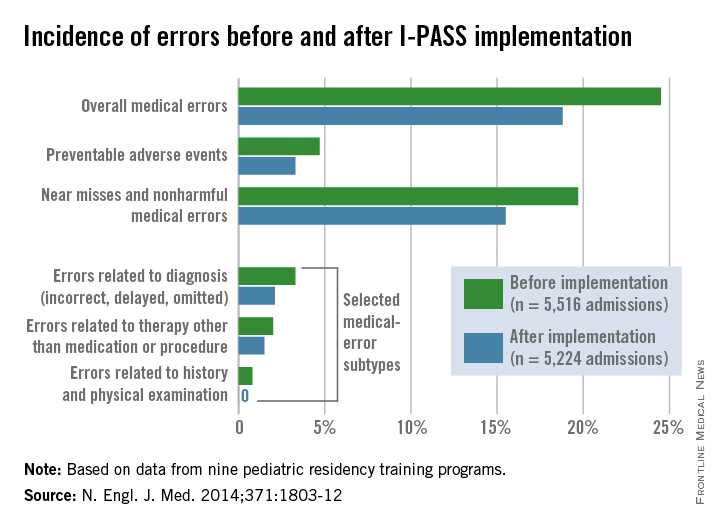
Of 10,740 patient admissions, the rate of medical errors decreased from 24.5 per 100 admissions preintervention to 18.8 per 100 admissions postintervention (23%), Dr. Starmer and her colleagues wrote. The rate of preventable adverse events fell from 4.7 events per 100 admissions to 3.3 events per 100 admissions (30%). Additionally, the rate of near misses and nonharmful medical errors went down by 21%. Investigators found no significant change in the rate of nonpreventable adverse events.
The I-PASS Handoff Bundle consisted of the I-PASS mnemonic; a 2-hour workshop on teamwork, communication skills, and I-PASS handoff techniques; a 1-hour role-playing session; a computer module; a faculty development program; direct-observation tools; and a process and culture-change campaign. Each site was assigned to one of three staggered intervention and data-collection waves from January 2011 through May 2013.
The hospitals integrated the I-PASS structure into both oral and written handoff processes. At seven sites, written handoff tools with a standardized I-PASS format were built into electronic medical record programs. The tools were built into word processing programs at two sites. Each hospital maintained an implementation log that was regularly reviewed to ensure adherence to program components.
Researchers found no significant time change in residents’ workflow after program implementation, including the time in a 24-hour period spent with patients and families.
Following the intervention period, the proportion of residents who rated the overall quality of their handoff training as very good or excellent rose from 28% to 72%.
“Implementing handoff improvement programs such as the I-PASS Handoff Bundle may potentiate the effectiveness of work-hour reductions, because doing both together may concurrently reduce both fatigue and handoff-related errors,” the study authors said.
The study was funded by the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services, and others. The investigators reported no relevant conflicts of interest. Boston Children’s Hospital and the main study investigators are exploring the potential licensing of I-PASS.
On Twitter @legal_med
Implementation of a resident handoff program at nine hospitals reduced both medical errors and preventable adverse events, according to a study published Nov. 5 in the New England Journal of Medicine.
Dr. Amy J. Starmer of Boston Children’s Hospital and her coinvestigators at dozens of other institutions implemented an I-PASS-based program in nine pediatric residency training programs in the United States and Canada from 2011 through 2013. I-PASS, a mnemonic to standardize handoffs, stands for illness severity; patient summary; action list; situation awareness and contingency plans; and synthesis by receiver. Study sites ranged in size from 36 to 182 residents (N. Engl. J. Med. 2014;371:1803-12).
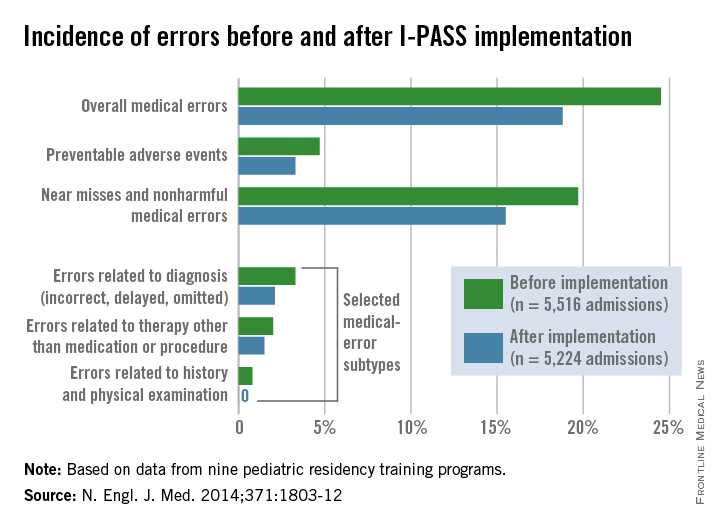
Of 10,740 patient admissions, the rate of medical errors decreased from 24.5 per 100 admissions preintervention to 18.8 per 100 admissions postintervention (23%), Dr. Starmer and her colleagues wrote. The rate of preventable adverse events fell from 4.7 events per 100 admissions to 3.3 events per 100 admissions (30%). Additionally, the rate of near misses and nonharmful medical errors went down by 21%. Investigators found no significant change in the rate of nonpreventable adverse events.
The I-PASS Handoff Bundle consisted of the I-PASS mnemonic; a 2-hour workshop on teamwork, communication skills, and I-PASS handoff techniques; a 1-hour role-playing session; a computer module; a faculty development program; direct-observation tools; and a process and culture-change campaign. Each site was assigned to one of three staggered intervention and data-collection waves from January 2011 through May 2013.
The hospitals integrated the I-PASS structure into both oral and written handoff processes. At seven sites, written handoff tools with a standardized I-PASS format were built into electronic medical record programs. The tools were built into word processing programs at two sites. Each hospital maintained an implementation log that was regularly reviewed to ensure adherence to program components.
Researchers found no significant time change in residents’ workflow after program implementation, including the time in a 24-hour period spent with patients and families.
Following the intervention period, the proportion of residents who rated the overall quality of their handoff training as very good or excellent rose from 28% to 72%.
“Implementing handoff improvement programs such as the I-PASS Handoff Bundle may potentiate the effectiveness of work-hour reductions, because doing both together may concurrently reduce both fatigue and handoff-related errors,” the study authors said.
The study was funded by the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services, and others. The investigators reported no relevant conflicts of interest. Boston Children’s Hospital and the main study investigators are exploring the potential licensing of I-PASS.
On Twitter @legal_med
Key clinical point: Medical errors and adverse events can be reduced through handoff programs that integrate oral and written tools.
Major finding: The rate of medical errors decreased by 23% and adverse events fell by 30% after implementation of the I-PASS Handoff Bundle.
Data source: A prospective study in nine hospitals that measured rates of medical errors, preventable adverse events, miscommunications, and workflow.
Disclosures: The study was funded by the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services, and others. The investigators reported no relevant conflicts of interest. Boston Children’s Hospital and the main study investigators are exploring the potential licensing of I-PASS.
Sharing is caring: A primer on EHR interoperability
The debate over the future of meaningful use seems to have found its bellwether issue: interoperability. For the uninitiated, this is the concept of sharing patient information across systems with the promise of improving the ease and quality of care. As you might expect, it is full of challenges, not the least of which is standardization. Competing vendors of electronic health record (EHR) software and technological hurdles have made the goal of true interoperability quite elusive, and there is no clear path to victory. Meaningful use and other incentive programs have set requirements for widespread rapid adoption of data sharing. Unfortunately, instead of encouraging innovation, they seem only to have created more stumbling blocks for physicians. Now providers are facing penalties for noncompliance, and national physician advocacy groups are taking notice.
On Oct. 15 of this year, a letter from key stakeholders including the American Medical Association (AMA), American Academy of Family Physicians (AAFP), and Medical Group Management Association (MGMA) to the Department of Health and Human Services laid out a “blueprint” for revamping the meaningful use program. The center point of this communication was a call for more emphasis on interoperability, as well as flexibility for both vendors and physicians. We tend to agree with these ideas, but wonder on a global scale what this interoperability should look like. In this column, we’ll address the essential pieces to making this a reality, and how physicians and patients can benefit from enhanced information exchange.
Information should be standardized
One of the fundamental challenges standing in the way of true interoperability is standardization: allowing data to be shared and viewed anywhere, independent of hardware or software. This is an idea that has allowed the World Wide Web to flourish; websites are readable by any computer or mobile device, using any operating system or browser. As of now, very little standardization exists in the world of medical data, in part because EHRs have been developed and promoted by private corporations, all competing for market share.
This evolution is quite unlike the history of the Internet, which was developed by government and educational institutions, with the express intent of connecting disparate computer systems. EHRs have essentially been developed in isolation, with much more emphasis placed on keeping information private than on making it shareable. Now meaningful use is forcing vendors to share data across systems, and – not surprisingly – each vendor is attempting to create their own method of doing so.
Some argue that EHR companies would prefer not to share, as this might threaten their hold on the market. In fact, Epic Health Systems, the world’s largest EHR vendor, has recently faced accusations of limiting interoperability to encourage physicians to use its software exclusively. Epic has fired back with statistics pointing to its accomplishments in data exchange. Both sides clearly disagree on what true interoperability should look like. This underscores a critical point: The concept of interoperability and what the standards should look like may mean different things to different parties.
One attempt at standardization that is commonly referenced is the continuity of care document (CCD), a key requirement for data exchange outlined in Stage 2 of meaningful use. This document, endorsed by the U.S. Healthcare Information Technology Standards Panel, has gained popularity as it can contain large amounts of data in one file. Unfortunately, it too is still limited and often isn’t user friendly at the point of care. It is in many ways merely a jumping-off point that will hopefully facilitate improved data accessibility and ease of sharing.
To improve usability and confidence in data exchange, many practices and health systems have joined together to create Regional Health Information Organizations and provide some governance structure to the process of data exchange. We strongly recommend getting involved in such an organization and engaging in the process of standardization. Regardless of your position on the usefulness or practicality of sharing patient records, a few notions are indisputable: Interoperability is coming, and point-of-care data availability – if accurate, secure, and useful – can ultimately usher in the promise of better patient care.
Information should be secure
In the process of seeking easier data exchange, we cannot lose sight of the importance of data security. Health care entities need to feel confident the information they are sending electronically will stay private until it reaches its ultimate destination. An attempt to address this issue led to the development of the “direct” encryption standard in 2010. Also known as Direct Exchange and Direct Secure Messaging, it specifies a secure method for the exchange of Protected Health Information. Providers can take advantage of the security offered through Direct by developing their own infrastructure or engaging the services of a Health Information Service Provider. These are private, HIPAA-compliant data exchange services that serve a health care community and facilitate direct messaging between health care settings. Ultimately, the goal is to create a robust Nationwide Health Information Network and achieve true widespread health information exchange. But before we actually achieve this, there is one more element essential to interoperability and improving patient care.
The information should be useful
In the preliminary stages of EHR interoperability, attempts at meaningful information exchange have led to only modest success. Outside of private health systems that have developed their own proprietary interfaces, data extraction and sharing between disparate electronic platforms have yet to have a meaningful impact on patient care. In part, this is because the information is not provided to clinicians in a useful format. Even the CCD described above is often confusing and replete with extraneous information – filtering through it during a patient encounter can be tedious and frustrating. Also, ensuring data integrity can be a real challenge, not only technically, but also practically. Questions occur regularly, such as “Did the data come through in the correct fields?” or “Did the medical resident remember to include all of the medications or allergies associated with the patient?” Ultimately, physicians need to decide whether or not to trust the information they receive before making it a permanent part of a patient’s health record.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
The debate over the future of meaningful use seems to have found its bellwether issue: interoperability. For the uninitiated, this is the concept of sharing patient information across systems with the promise of improving the ease and quality of care. As you might expect, it is full of challenges, not the least of which is standardization. Competing vendors of electronic health record (EHR) software and technological hurdles have made the goal of true interoperability quite elusive, and there is no clear path to victory. Meaningful use and other incentive programs have set requirements for widespread rapid adoption of data sharing. Unfortunately, instead of encouraging innovation, they seem only to have created more stumbling blocks for physicians. Now providers are facing penalties for noncompliance, and national physician advocacy groups are taking notice.
On Oct. 15 of this year, a letter from key stakeholders including the American Medical Association (AMA), American Academy of Family Physicians (AAFP), and Medical Group Management Association (MGMA) to the Department of Health and Human Services laid out a “blueprint” for revamping the meaningful use program. The center point of this communication was a call for more emphasis on interoperability, as well as flexibility for both vendors and physicians. We tend to agree with these ideas, but wonder on a global scale what this interoperability should look like. In this column, we’ll address the essential pieces to making this a reality, and how physicians and patients can benefit from enhanced information exchange.
Information should be standardized
One of the fundamental challenges standing in the way of true interoperability is standardization: allowing data to be shared and viewed anywhere, independent of hardware or software. This is an idea that has allowed the World Wide Web to flourish; websites are readable by any computer or mobile device, using any operating system or browser. As of now, very little standardization exists in the world of medical data, in part because EHRs have been developed and promoted by private corporations, all competing for market share.
This evolution is quite unlike the history of the Internet, which was developed by government and educational institutions, with the express intent of connecting disparate computer systems. EHRs have essentially been developed in isolation, with much more emphasis placed on keeping information private than on making it shareable. Now meaningful use is forcing vendors to share data across systems, and – not surprisingly – each vendor is attempting to create their own method of doing so.
Some argue that EHR companies would prefer not to share, as this might threaten their hold on the market. In fact, Epic Health Systems, the world’s largest EHR vendor, has recently faced accusations of limiting interoperability to encourage physicians to use its software exclusively. Epic has fired back with statistics pointing to its accomplishments in data exchange. Both sides clearly disagree on what true interoperability should look like. This underscores a critical point: The concept of interoperability and what the standards should look like may mean different things to different parties.
One attempt at standardization that is commonly referenced is the continuity of care document (CCD), a key requirement for data exchange outlined in Stage 2 of meaningful use. This document, endorsed by the U.S. Healthcare Information Technology Standards Panel, has gained popularity as it can contain large amounts of data in one file. Unfortunately, it too is still limited and often isn’t user friendly at the point of care. It is in many ways merely a jumping-off point that will hopefully facilitate improved data accessibility and ease of sharing.
To improve usability and confidence in data exchange, many practices and health systems have joined together to create Regional Health Information Organizations and provide some governance structure to the process of data exchange. We strongly recommend getting involved in such an organization and engaging in the process of standardization. Regardless of your position on the usefulness or practicality of sharing patient records, a few notions are indisputable: Interoperability is coming, and point-of-care data availability – if accurate, secure, and useful – can ultimately usher in the promise of better patient care.
Information should be secure
In the process of seeking easier data exchange, we cannot lose sight of the importance of data security. Health care entities need to feel confident the information they are sending electronically will stay private until it reaches its ultimate destination. An attempt to address this issue led to the development of the “direct” encryption standard in 2010. Also known as Direct Exchange and Direct Secure Messaging, it specifies a secure method for the exchange of Protected Health Information. Providers can take advantage of the security offered through Direct by developing their own infrastructure or engaging the services of a Health Information Service Provider. These are private, HIPAA-compliant data exchange services that serve a health care community and facilitate direct messaging between health care settings. Ultimately, the goal is to create a robust Nationwide Health Information Network and achieve true widespread health information exchange. But before we actually achieve this, there is one more element essential to interoperability and improving patient care.
The information should be useful
In the preliminary stages of EHR interoperability, attempts at meaningful information exchange have led to only modest success. Outside of private health systems that have developed their own proprietary interfaces, data extraction and sharing between disparate electronic platforms have yet to have a meaningful impact on patient care. In part, this is because the information is not provided to clinicians in a useful format. Even the CCD described above is often confusing and replete with extraneous information – filtering through it during a patient encounter can be tedious and frustrating. Also, ensuring data integrity can be a real challenge, not only technically, but also practically. Questions occur regularly, such as “Did the data come through in the correct fields?” or “Did the medical resident remember to include all of the medications or allergies associated with the patient?” Ultimately, physicians need to decide whether or not to trust the information they receive before making it a permanent part of a patient’s health record.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
The debate over the future of meaningful use seems to have found its bellwether issue: interoperability. For the uninitiated, this is the concept of sharing patient information across systems with the promise of improving the ease and quality of care. As you might expect, it is full of challenges, not the least of which is standardization. Competing vendors of electronic health record (EHR) software and technological hurdles have made the goal of true interoperability quite elusive, and there is no clear path to victory. Meaningful use and other incentive programs have set requirements for widespread rapid adoption of data sharing. Unfortunately, instead of encouraging innovation, they seem only to have created more stumbling blocks for physicians. Now providers are facing penalties for noncompliance, and national physician advocacy groups are taking notice.
On Oct. 15 of this year, a letter from key stakeholders including the American Medical Association (AMA), American Academy of Family Physicians (AAFP), and Medical Group Management Association (MGMA) to the Department of Health and Human Services laid out a “blueprint” for revamping the meaningful use program. The center point of this communication was a call for more emphasis on interoperability, as well as flexibility for both vendors and physicians. We tend to agree with these ideas, but wonder on a global scale what this interoperability should look like. In this column, we’ll address the essential pieces to making this a reality, and how physicians and patients can benefit from enhanced information exchange.
Information should be standardized
One of the fundamental challenges standing in the way of true interoperability is standardization: allowing data to be shared and viewed anywhere, independent of hardware or software. This is an idea that has allowed the World Wide Web to flourish; websites are readable by any computer or mobile device, using any operating system or browser. As of now, very little standardization exists in the world of medical data, in part because EHRs have been developed and promoted by private corporations, all competing for market share.
This evolution is quite unlike the history of the Internet, which was developed by government and educational institutions, with the express intent of connecting disparate computer systems. EHRs have essentially been developed in isolation, with much more emphasis placed on keeping information private than on making it shareable. Now meaningful use is forcing vendors to share data across systems, and – not surprisingly – each vendor is attempting to create their own method of doing so.
Some argue that EHR companies would prefer not to share, as this might threaten their hold on the market. In fact, Epic Health Systems, the world’s largest EHR vendor, has recently faced accusations of limiting interoperability to encourage physicians to use its software exclusively. Epic has fired back with statistics pointing to its accomplishments in data exchange. Both sides clearly disagree on what true interoperability should look like. This underscores a critical point: The concept of interoperability and what the standards should look like may mean different things to different parties.
One attempt at standardization that is commonly referenced is the continuity of care document (CCD), a key requirement for data exchange outlined in Stage 2 of meaningful use. This document, endorsed by the U.S. Healthcare Information Technology Standards Panel, has gained popularity as it can contain large amounts of data in one file. Unfortunately, it too is still limited and often isn’t user friendly at the point of care. It is in many ways merely a jumping-off point that will hopefully facilitate improved data accessibility and ease of sharing.
To improve usability and confidence in data exchange, many practices and health systems have joined together to create Regional Health Information Organizations and provide some governance structure to the process of data exchange. We strongly recommend getting involved in such an organization and engaging in the process of standardization. Regardless of your position on the usefulness or practicality of sharing patient records, a few notions are indisputable: Interoperability is coming, and point-of-care data availability – if accurate, secure, and useful – can ultimately usher in the promise of better patient care.
Information should be secure
In the process of seeking easier data exchange, we cannot lose sight of the importance of data security. Health care entities need to feel confident the information they are sending electronically will stay private until it reaches its ultimate destination. An attempt to address this issue led to the development of the “direct” encryption standard in 2010. Also known as Direct Exchange and Direct Secure Messaging, it specifies a secure method for the exchange of Protected Health Information. Providers can take advantage of the security offered through Direct by developing their own infrastructure or engaging the services of a Health Information Service Provider. These are private, HIPAA-compliant data exchange services that serve a health care community and facilitate direct messaging between health care settings. Ultimately, the goal is to create a robust Nationwide Health Information Network and achieve true widespread health information exchange. But before we actually achieve this, there is one more element essential to interoperability and improving patient care.
The information should be useful
In the preliminary stages of EHR interoperability, attempts at meaningful information exchange have led to only modest success. Outside of private health systems that have developed their own proprietary interfaces, data extraction and sharing between disparate electronic platforms have yet to have a meaningful impact on patient care. In part, this is because the information is not provided to clinicians in a useful format. Even the CCD described above is often confusing and replete with extraneous information – filtering through it during a patient encounter can be tedious and frustrating. Also, ensuring data integrity can be a real challenge, not only technically, but also practically. Questions occur regularly, such as “Did the data come through in the correct fields?” or “Did the medical resident remember to include all of the medications or allergies associated with the patient?” Ultimately, physicians need to decide whether or not to trust the information they receive before making it a permanent part of a patient’s health record.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
Colorectal cancer on the increase in young adults
Colorectal cancer rates have declined in both men and women since 1975, particularly in those over age 75 years, but there has also been a significant increase in the incidence among those aged 20-34 years, a retrospective cohort study shows.
Researchers analyzed data from 393,241 patients registered in the Surveillance, Epidemiology, and End Results (SEER) colorectal cancer registry from 1975 to 2010, finding the overall, age-adjusted incidence of colorectal cancer decreased by 0.92% during that time.
They observed a steady decline in the incidence of colorectal cancer in the over 50 age group, with a 1.15% decrease in those aged over 75 years, while in those aged 20-34 years, there was a nearly 2% increase, according to data published online November 5 in JAMA Surgery (doi:10.1001/jamasurg.2014.1756).
“At the present rate, the incidence rate for young patients with newly diagnosed colon or rectal cancer will nearly double by 2030, while it will similarly decline by more than one-third among patients older than the screening age of 50 years,” wrote Dr. Christina E. Bailey of the University of Texas M.D. Anderson Cancer Center, Houston, and colleagues.
The study was supported by grants from the National Institutes of Health and National Cancer Institute. There were no conflicts of interest declared.
Colorectal cancer rates have declined in both men and women since 1975, particularly in those over age 75 years, but there has also been a significant increase in the incidence among those aged 20-34 years, a retrospective cohort study shows.
Researchers analyzed data from 393,241 patients registered in the Surveillance, Epidemiology, and End Results (SEER) colorectal cancer registry from 1975 to 2010, finding the overall, age-adjusted incidence of colorectal cancer decreased by 0.92% during that time.
They observed a steady decline in the incidence of colorectal cancer in the over 50 age group, with a 1.15% decrease in those aged over 75 years, while in those aged 20-34 years, there was a nearly 2% increase, according to data published online November 5 in JAMA Surgery (doi:10.1001/jamasurg.2014.1756).
“At the present rate, the incidence rate for young patients with newly diagnosed colon or rectal cancer will nearly double by 2030, while it will similarly decline by more than one-third among patients older than the screening age of 50 years,” wrote Dr. Christina E. Bailey of the University of Texas M.D. Anderson Cancer Center, Houston, and colleagues.
The study was supported by grants from the National Institutes of Health and National Cancer Institute. There were no conflicts of interest declared.
Colorectal cancer rates have declined in both men and women since 1975, particularly in those over age 75 years, but there has also been a significant increase in the incidence among those aged 20-34 years, a retrospective cohort study shows.
Researchers analyzed data from 393,241 patients registered in the Surveillance, Epidemiology, and End Results (SEER) colorectal cancer registry from 1975 to 2010, finding the overall, age-adjusted incidence of colorectal cancer decreased by 0.92% during that time.
They observed a steady decline in the incidence of colorectal cancer in the over 50 age group, with a 1.15% decrease in those aged over 75 years, while in those aged 20-34 years, there was a nearly 2% increase, according to data published online November 5 in JAMA Surgery (doi:10.1001/jamasurg.2014.1756).
“At the present rate, the incidence rate for young patients with newly diagnosed colon or rectal cancer will nearly double by 2030, while it will similarly decline by more than one-third among patients older than the screening age of 50 years,” wrote Dr. Christina E. Bailey of the University of Texas M.D. Anderson Cancer Center, Houston, and colleagues.
The study was supported by grants from the National Institutes of Health and National Cancer Institute. There were no conflicts of interest declared.
FROM JAMA SURGERY
Key clinical point: Colorectal cancer rates have declined steadily since 1975 in those over 50, but have increased in the 20- to 34-year-old age group.
Major finding: Colorectal cancer incidence has increased nearly 2% in those aged 20-34 years.
Data source: Retrospective cohort study of data from 393,241 patients registered in the Surveillance, Epidemiology, and End Results (SEER) colorectal cancer registry.
Disclosures: The study was supported by grants from the National Institutes of Health and National Cancer Institute. There were no conflicts of interest declared.
Breast cancer margins, radiotherapy, axillary dissection evolve
SAN FRANCISCO – Recent research and guidelines have changed how surgeons should be thinking about some aspects of treating breast cancer, a panel of experts said in a press briefing at the annual clinical congress of the American College of Surgeons.
New guidelines on surgical margins, data supporting radiation rather than complete lymphadenectomy for patients with positive sentinel nodes, and other studies supporting targeted radiation therapy instead of whole-breast irradiation after lumpectomy should be on a surgeons’s radar, the speakers said.
The first U.S. guidelines on surgical margins for lumpectomy in women with breast cancer who are planning to undergo whole-breast radiation therapy adopted a standard of “no ink on tumor,” meaning no cancer at the edge of the tissue that was removed, Dr. Richard J. Gray said. The 2014 joint guidelines from the Society of Surgical Oncology and the American Society of Radiation Oncology based the recommendations on a meta-analysis of studies that found no advantage to wider excision margins for preventing in-breast recurrence (Ann. Surg. Oncol. 2014;21:717-730).
Previously, many surgeons sought to take 1, 2, or 3 mm of normal tissue around the cancer removed to reduce the risk of recurrence, he said.
“This guideline will become the standard throughout the United States. The evidence on which this is based is reasonable, but it will be important for individual institutions and national databases to track the rates of local recurrence over time as these guidelines are implemented,” said Dr. Gray of the Mayo Clinic, Scottsdale, Ariz. He confessed to being “a recovering addict” to margins of 2 mm or greater.
The guidelines apply only to patients with invasive cancer undergoing breast-conserving treatment, he noted. There are no guidelines yet specifically for surgical margins in women undergoing mastectomy for breast cancer, nor for women with ductal carcinoma in situ (DCIS).
While there is no evidence that a margin width wider than “no ink on tumor” is better for women undergoing mastectomy, Dr. Gray cautioned against extrapolating the guidelines to women having mastectomies “because they will generally not undergo adjuvant radiation therapy,” he said.
For women with DCIS, the available evidence suggests that a minimum 2-mm margin of excision is reasonable for those undergoing lumpectomy or at least negative margins (no ink on tumor) for those undergoing mastectomy, Dr. Gray said. Wider margins may help select patients with DCIS who undergo lumpectomy to avoid adjuvant radiation therapy, he added.
A separate recent study should change the way surgeons approach decisions about axillary surgery in patients with breast cancer, Dr. Roshni Rao said. She reported on a study that randomized women who had cancer in sentinel lymph nodes after mastectomy to further treatment by removing the rest of the lymph nodes under the arm, as is common practice, or to radiation of the lymph nodes area.
Rates of cancer recurrence did not differ between groups but the radiation approach significantly reduced the risk of lymphedema and other morbidity, said Dr. Rao of the University of Texas Southwestern Medical Center, Dallas.
“Going forward, we’re going to be performing less and less axillary lymph node dissections,” she said.
Also on the topic of radiation therapy, two recent studies of targeted breast irradiation rather than whole-breast radiotherapy suggest that the targeted approach may be beneficial, Dr. Courtney A. Vito said. Whole-breast radiation after lumpectomy reduces the risk of local recurrence by 50%, previous studies have shown, but it comes with potential side effects including burns, lymphedema, and damage to underlying structures like the heart and lungs. Patients who don’t live near specialized radiation centers may not be able to access the daily month-long treatments.
A randomized Italian trial of 1,305 patients found similar rates of overall survival or breast cancer–specific survival in patients treated with whole-breast radiation therapy or with intraoperative radiation therapy, in which a single, more intense dose of radiation is directed just at the site of lumpectomy during surgery. Survival rates were similar between groups but the rate of local recurrence after 5 years was 10 times higher in the intraoperative radiation group (4.4%), compared with the whole-breast radiation group (0.4%) (Lancet Oncol. 2013;14:1269-77).
Subset analyses showed, however, that most of the recurrences were in women who would not be considered ideal candidates for intraoperative radiotherapy in the United States because they had tumors larger than 2 cm, four or more positive lymph nodes, estrogen receptor–negative tumors, or other aggressive tumor biology, said Dr. Vito of the City of Hope National Medical Center, Duarte, Calif. Recurrence rates were more favorable in patients with lower-risk tumors.
“When you take out the high-risk group, the data actually look a lot better,” she said.
A separate randomized British trial of intraoperative radiation therapy produced similar overall results in 1,721 patients, but two-thirds of patients would be considered unsuitable or cautionary in the United States, Dr. Vito said (Lancet 2014;383:603-613).
Overall survival and breast cancer survival were similar in the intraoperative and whole-breast radiation groups except for worse outcomes in patients who had intraoperative radiation done as a second surgery after the operation to perform lumpectomy.
The rate of deaths from causes other than breast cancer was higher in the whole-breast radiation group, in many cases due to cardiac events, Dr. Vito noted. Whole-breast radiation on the left side of the chest has been shown to accelerate atherosclerosis of the vessels in the heart, and it may be that avoiding this through intraoperative targeted radiotherapy may provide a cardiovascular benefit, though this is yet to be proven, she added.
A separate presentation at the meeting explored the increasing rate of women with cancer in one breast who choose prophylactic mastectomy of the healthy contralateral breast. The rate of prophylactic contralateral mastectomy increased 150% between 1998 and 2003 in the United States, from 1.8% to 4.5%, Dr. Swati Kulkarni said.
She and her associates surveyed a diverse cohort of 150 women before surgery for cancer in one breast and again 6 months after surgery. Only 14% said that medical staff had provided information about removing the healthy breast along with the cancerous breast; 63% said they did not get that information, and 23% were unsure, reported Dr. Kulkarni of the University of Chicago.
Thirty-nine percent of patients had thought about their surgical choices before they were diagnosed with breast cancer, and 58% of the cohort wanted or considered contralateral prophylactic mastectomy.
Patients with a family history of breast cancer who had undergone genetic testing were significantly more likely to want or consider prophylactic contralateral mastectomy. Factors that were not significantly associated with prophylactic contralateral mastectomy were family history by itself, age, race, insurance status, cancer stage, use of breast MRI, or having one or more biopsies.
The findings suggest that education about prophylactic mastectomy is needed “inside and outside of the doctor’s office,” Dr. Kulkarni said.
The speakers reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Recent research and guidelines have changed how surgeons should be thinking about some aspects of treating breast cancer, a panel of experts said in a press briefing at the annual clinical congress of the American College of Surgeons.
New guidelines on surgical margins, data supporting radiation rather than complete lymphadenectomy for patients with positive sentinel nodes, and other studies supporting targeted radiation therapy instead of whole-breast irradiation after lumpectomy should be on a surgeons’s radar, the speakers said.
The first U.S. guidelines on surgical margins for lumpectomy in women with breast cancer who are planning to undergo whole-breast radiation therapy adopted a standard of “no ink on tumor,” meaning no cancer at the edge of the tissue that was removed, Dr. Richard J. Gray said. The 2014 joint guidelines from the Society of Surgical Oncology and the American Society of Radiation Oncology based the recommendations on a meta-analysis of studies that found no advantage to wider excision margins for preventing in-breast recurrence (Ann. Surg. Oncol. 2014;21:717-730).
Previously, many surgeons sought to take 1, 2, or 3 mm of normal tissue around the cancer removed to reduce the risk of recurrence, he said.
“This guideline will become the standard throughout the United States. The evidence on which this is based is reasonable, but it will be important for individual institutions and national databases to track the rates of local recurrence over time as these guidelines are implemented,” said Dr. Gray of the Mayo Clinic, Scottsdale, Ariz. He confessed to being “a recovering addict” to margins of 2 mm or greater.
The guidelines apply only to patients with invasive cancer undergoing breast-conserving treatment, he noted. There are no guidelines yet specifically for surgical margins in women undergoing mastectomy for breast cancer, nor for women with ductal carcinoma in situ (DCIS).
While there is no evidence that a margin width wider than “no ink on tumor” is better for women undergoing mastectomy, Dr. Gray cautioned against extrapolating the guidelines to women having mastectomies “because they will generally not undergo adjuvant radiation therapy,” he said.
For women with DCIS, the available evidence suggests that a minimum 2-mm margin of excision is reasonable for those undergoing lumpectomy or at least negative margins (no ink on tumor) for those undergoing mastectomy, Dr. Gray said. Wider margins may help select patients with DCIS who undergo lumpectomy to avoid adjuvant radiation therapy, he added.
A separate recent study should change the way surgeons approach decisions about axillary surgery in patients with breast cancer, Dr. Roshni Rao said. She reported on a study that randomized women who had cancer in sentinel lymph nodes after mastectomy to further treatment by removing the rest of the lymph nodes under the arm, as is common practice, or to radiation of the lymph nodes area.
Rates of cancer recurrence did not differ between groups but the radiation approach significantly reduced the risk of lymphedema and other morbidity, said Dr. Rao of the University of Texas Southwestern Medical Center, Dallas.
“Going forward, we’re going to be performing less and less axillary lymph node dissections,” she said.
Also on the topic of radiation therapy, two recent studies of targeted breast irradiation rather than whole-breast radiotherapy suggest that the targeted approach may be beneficial, Dr. Courtney A. Vito said. Whole-breast radiation after lumpectomy reduces the risk of local recurrence by 50%, previous studies have shown, but it comes with potential side effects including burns, lymphedema, and damage to underlying structures like the heart and lungs. Patients who don’t live near specialized radiation centers may not be able to access the daily month-long treatments.
A randomized Italian trial of 1,305 patients found similar rates of overall survival or breast cancer–specific survival in patients treated with whole-breast radiation therapy or with intraoperative radiation therapy, in which a single, more intense dose of radiation is directed just at the site of lumpectomy during surgery. Survival rates were similar between groups but the rate of local recurrence after 5 years was 10 times higher in the intraoperative radiation group (4.4%), compared with the whole-breast radiation group (0.4%) (Lancet Oncol. 2013;14:1269-77).
Subset analyses showed, however, that most of the recurrences were in women who would not be considered ideal candidates for intraoperative radiotherapy in the United States because they had tumors larger than 2 cm, four or more positive lymph nodes, estrogen receptor–negative tumors, or other aggressive tumor biology, said Dr. Vito of the City of Hope National Medical Center, Duarte, Calif. Recurrence rates were more favorable in patients with lower-risk tumors.
“When you take out the high-risk group, the data actually look a lot better,” she said.
A separate randomized British trial of intraoperative radiation therapy produced similar overall results in 1,721 patients, but two-thirds of patients would be considered unsuitable or cautionary in the United States, Dr. Vito said (Lancet 2014;383:603-613).
Overall survival and breast cancer survival were similar in the intraoperative and whole-breast radiation groups except for worse outcomes in patients who had intraoperative radiation done as a second surgery after the operation to perform lumpectomy.
The rate of deaths from causes other than breast cancer was higher in the whole-breast radiation group, in many cases due to cardiac events, Dr. Vito noted. Whole-breast radiation on the left side of the chest has been shown to accelerate atherosclerosis of the vessels in the heart, and it may be that avoiding this through intraoperative targeted radiotherapy may provide a cardiovascular benefit, though this is yet to be proven, she added.
A separate presentation at the meeting explored the increasing rate of women with cancer in one breast who choose prophylactic mastectomy of the healthy contralateral breast. The rate of prophylactic contralateral mastectomy increased 150% between 1998 and 2003 in the United States, from 1.8% to 4.5%, Dr. Swati Kulkarni said.
She and her associates surveyed a diverse cohort of 150 women before surgery for cancer in one breast and again 6 months after surgery. Only 14% said that medical staff had provided information about removing the healthy breast along with the cancerous breast; 63% said they did not get that information, and 23% were unsure, reported Dr. Kulkarni of the University of Chicago.
Thirty-nine percent of patients had thought about their surgical choices before they were diagnosed with breast cancer, and 58% of the cohort wanted or considered contralateral prophylactic mastectomy.
Patients with a family history of breast cancer who had undergone genetic testing were significantly more likely to want or consider prophylactic contralateral mastectomy. Factors that were not significantly associated with prophylactic contralateral mastectomy were family history by itself, age, race, insurance status, cancer stage, use of breast MRI, or having one or more biopsies.
The findings suggest that education about prophylactic mastectomy is needed “inside and outside of the doctor’s office,” Dr. Kulkarni said.
The speakers reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Recent research and guidelines have changed how surgeons should be thinking about some aspects of treating breast cancer, a panel of experts said in a press briefing at the annual clinical congress of the American College of Surgeons.
New guidelines on surgical margins, data supporting radiation rather than complete lymphadenectomy for patients with positive sentinel nodes, and other studies supporting targeted radiation therapy instead of whole-breast irradiation after lumpectomy should be on a surgeons’s radar, the speakers said.
The first U.S. guidelines on surgical margins for lumpectomy in women with breast cancer who are planning to undergo whole-breast radiation therapy adopted a standard of “no ink on tumor,” meaning no cancer at the edge of the tissue that was removed, Dr. Richard J. Gray said. The 2014 joint guidelines from the Society of Surgical Oncology and the American Society of Radiation Oncology based the recommendations on a meta-analysis of studies that found no advantage to wider excision margins for preventing in-breast recurrence (Ann. Surg. Oncol. 2014;21:717-730).
Previously, many surgeons sought to take 1, 2, or 3 mm of normal tissue around the cancer removed to reduce the risk of recurrence, he said.
“This guideline will become the standard throughout the United States. The evidence on which this is based is reasonable, but it will be important for individual institutions and national databases to track the rates of local recurrence over time as these guidelines are implemented,” said Dr. Gray of the Mayo Clinic, Scottsdale, Ariz. He confessed to being “a recovering addict” to margins of 2 mm or greater.
The guidelines apply only to patients with invasive cancer undergoing breast-conserving treatment, he noted. There are no guidelines yet specifically for surgical margins in women undergoing mastectomy for breast cancer, nor for women with ductal carcinoma in situ (DCIS).
While there is no evidence that a margin width wider than “no ink on tumor” is better for women undergoing mastectomy, Dr. Gray cautioned against extrapolating the guidelines to women having mastectomies “because they will generally not undergo adjuvant radiation therapy,” he said.
For women with DCIS, the available evidence suggests that a minimum 2-mm margin of excision is reasonable for those undergoing lumpectomy or at least negative margins (no ink on tumor) for those undergoing mastectomy, Dr. Gray said. Wider margins may help select patients with DCIS who undergo lumpectomy to avoid adjuvant radiation therapy, he added.
A separate recent study should change the way surgeons approach decisions about axillary surgery in patients with breast cancer, Dr. Roshni Rao said. She reported on a study that randomized women who had cancer in sentinel lymph nodes after mastectomy to further treatment by removing the rest of the lymph nodes under the arm, as is common practice, or to radiation of the lymph nodes area.
Rates of cancer recurrence did not differ between groups but the radiation approach significantly reduced the risk of lymphedema and other morbidity, said Dr. Rao of the University of Texas Southwestern Medical Center, Dallas.
“Going forward, we’re going to be performing less and less axillary lymph node dissections,” she said.
Also on the topic of radiation therapy, two recent studies of targeted breast irradiation rather than whole-breast radiotherapy suggest that the targeted approach may be beneficial, Dr. Courtney A. Vito said. Whole-breast radiation after lumpectomy reduces the risk of local recurrence by 50%, previous studies have shown, but it comes with potential side effects including burns, lymphedema, and damage to underlying structures like the heart and lungs. Patients who don’t live near specialized radiation centers may not be able to access the daily month-long treatments.
A randomized Italian trial of 1,305 patients found similar rates of overall survival or breast cancer–specific survival in patients treated with whole-breast radiation therapy or with intraoperative radiation therapy, in which a single, more intense dose of radiation is directed just at the site of lumpectomy during surgery. Survival rates were similar between groups but the rate of local recurrence after 5 years was 10 times higher in the intraoperative radiation group (4.4%), compared with the whole-breast radiation group (0.4%) (Lancet Oncol. 2013;14:1269-77).
Subset analyses showed, however, that most of the recurrences were in women who would not be considered ideal candidates for intraoperative radiotherapy in the United States because they had tumors larger than 2 cm, four or more positive lymph nodes, estrogen receptor–negative tumors, or other aggressive tumor biology, said Dr. Vito of the City of Hope National Medical Center, Duarte, Calif. Recurrence rates were more favorable in patients with lower-risk tumors.
“When you take out the high-risk group, the data actually look a lot better,” she said.
A separate randomized British trial of intraoperative radiation therapy produced similar overall results in 1,721 patients, but two-thirds of patients would be considered unsuitable or cautionary in the United States, Dr. Vito said (Lancet 2014;383:603-613).
Overall survival and breast cancer survival were similar in the intraoperative and whole-breast radiation groups except for worse outcomes in patients who had intraoperative radiation done as a second surgery after the operation to perform lumpectomy.
The rate of deaths from causes other than breast cancer was higher in the whole-breast radiation group, in many cases due to cardiac events, Dr. Vito noted. Whole-breast radiation on the left side of the chest has been shown to accelerate atherosclerosis of the vessels in the heart, and it may be that avoiding this through intraoperative targeted radiotherapy may provide a cardiovascular benefit, though this is yet to be proven, she added.
A separate presentation at the meeting explored the increasing rate of women with cancer in one breast who choose prophylactic mastectomy of the healthy contralateral breast. The rate of prophylactic contralateral mastectomy increased 150% between 1998 and 2003 in the United States, from 1.8% to 4.5%, Dr. Swati Kulkarni said.
She and her associates surveyed a diverse cohort of 150 women before surgery for cancer in one breast and again 6 months after surgery. Only 14% said that medical staff had provided information about removing the healthy breast along with the cancerous breast; 63% said they did not get that information, and 23% were unsure, reported Dr. Kulkarni of the University of Chicago.
Thirty-nine percent of patients had thought about their surgical choices before they were diagnosed with breast cancer, and 58% of the cohort wanted or considered contralateral prophylactic mastectomy.
Patients with a family history of breast cancer who had undergone genetic testing were significantly more likely to want or consider prophylactic contralateral mastectomy. Factors that were not significantly associated with prophylactic contralateral mastectomy were family history by itself, age, race, insurance status, cancer stage, use of breast MRI, or having one or more biopsies.
The findings suggest that education about prophylactic mastectomy is needed “inside and outside of the doctor’s office,” Dr. Kulkarni said.
The speakers reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ACS CLINICAL CONGRESS
Malpractice climate: ‘Stable, but still dysfunctional’
Fewer malpractice suits are resulting in paid claims against physicians while malpractice insurance premiums have remained stable or declined over the last 12 years, according to an analysis published Oct. 30 in JAMA.
Since 2002, the rate of paid malpractice claims against doctors of medicine has decreased by an estimated 6% annually; for doctors of osteopathy, the rate has declined about 5% annually, Michelle M. Mello of Stanford (Calif.) University and her colleagues reported (JAMA 2014 Oct. 30 [doi:10.1001/jama.2014.10705]).
Dr. Mello and her colleagues analyzed paid legal claims against MDs and DOs between 1994 and 2013 from the National Practitioner Data Bank and the American Medical Association’s Physician Masterfile. They also evaluated premium data from the Medical Liability Monitor’s Annual Rate Survey.
The rate of paid malpractice claims against MDs fell from 18.6 to 9.9 paid claims per 1,000 physicians between 2002 and 2013, they found. For DOs, rates dropped from about 19 in 2002 to about 12.2 paid claims per 1,000 physicians in 2013.
The median compensation paid to plaintiffs rose by 63% between 1994 and 2007, from $133,799 to $218,400, in adjusted 2013 dollars. However, since 2007, that number has declined, reaching $195,000 in 2013. Only 3.4% of payments made during the 20-year period resulted from jury verdicts; the others stemmed from settlements.
For the premiums review, Dr. Mello and colleagues analyzed insurance data from 2004 to 2013 from five geographical areas: Los Angeles, Orange, Kern, and Ventura counties in California; Nassau and Suffolk counties in New York; Cook, Madison, St. Clair, and Will counties in Illinois; and the states of Tennessee and Colorado. The locations were selected based on geographic diversity and because each had an insurer with a dominant market share.
In California, Illinois, and Tennessee, internists and ob.gyns. saw a 36% decrease in premiums charged by each state’s largest medical malpractice insurer from 2004 to 2013. Premiums charged to general surgeons fell by 30% in these states. In Colorado, internists saw a 20% decrease in premiums over the same time period, but general surgeons saw an increase of 13% and ob.gyns. experienced an 11% rise. In New York, rates charged by the largest insurer rose by 12% for ob.gyns, 16% for internists, and 35% for general surgeons.
It remains unclear why the rate of paid claims has decreased and why premiums have remained fairly stable, Dr. Mello and colleagues said. While medical organizations like to point to tort reform, traditional reforms such as award caps do not address problems within the malpractice system’s core functions – compensating negligently injured patients and deterring substandard care, they added.
“The weight of evidence suggests that the system’s effectiveness as both a compensation and a deterrence mechanism is mediocre at best, and there is little to suggest it has improved over the past decade,” they wrote. “Thus, ‘stable but still dysfunctional’ might describe today’s liability environment.”
The authors offered alternatives to traditional tort reform, such as communication and resolution programs, mandatory presuit notification laws, and judge-directed negotiation.
In communication and resolution programs, clinicians and institutions openly discuss adverse outcomes with patients and proactively seek resolution, including offering an apology, and, if the standard of care was not met, compensation. Mandatory presuit notification refers to requiring plaintiffs to give defendants advance notice that they intend to sue. Judge-directed negotiation centers on court policies in which malpractice litigants meet early and often with judges to discuss settlement. In such negotiations, the court employs an attorney with clinical training to help judges understand clinical issues.
The authors conclude that action to improve the medical liability system is necessary while the legal climate is stable, and not after a crisis.
“During malpractice crises, interest in liability reform intensifies, but one lesson of the last 40 years is that an atmosphere of crisis is not conducive to thoughtful and enduring solutions,” study authors said. “Action now to reduce the amplitude of the next medical liability cycle is both prudent and feasible. Further testing of nontraditional reforms, followed by wider implementation of those that work, holds the most promise.”
On Twitter @legal_med
Fewer malpractice suits are resulting in paid claims against physicians while malpractice insurance premiums have remained stable or declined over the last 12 years, according to an analysis published Oct. 30 in JAMA.
Since 2002, the rate of paid malpractice claims against doctors of medicine has decreased by an estimated 6% annually; for doctors of osteopathy, the rate has declined about 5% annually, Michelle M. Mello of Stanford (Calif.) University and her colleagues reported (JAMA 2014 Oct. 30 [doi:10.1001/jama.2014.10705]).
Dr. Mello and her colleagues analyzed paid legal claims against MDs and DOs between 1994 and 2013 from the National Practitioner Data Bank and the American Medical Association’s Physician Masterfile. They also evaluated premium data from the Medical Liability Monitor’s Annual Rate Survey.
The rate of paid malpractice claims against MDs fell from 18.6 to 9.9 paid claims per 1,000 physicians between 2002 and 2013, they found. For DOs, rates dropped from about 19 in 2002 to about 12.2 paid claims per 1,000 physicians in 2013.
The median compensation paid to plaintiffs rose by 63% between 1994 and 2007, from $133,799 to $218,400, in adjusted 2013 dollars. However, since 2007, that number has declined, reaching $195,000 in 2013. Only 3.4% of payments made during the 20-year period resulted from jury verdicts; the others stemmed from settlements.
For the premiums review, Dr. Mello and colleagues analyzed insurance data from 2004 to 2013 from five geographical areas: Los Angeles, Orange, Kern, and Ventura counties in California; Nassau and Suffolk counties in New York; Cook, Madison, St. Clair, and Will counties in Illinois; and the states of Tennessee and Colorado. The locations were selected based on geographic diversity and because each had an insurer with a dominant market share.
In California, Illinois, and Tennessee, internists and ob.gyns. saw a 36% decrease in premiums charged by each state’s largest medical malpractice insurer from 2004 to 2013. Premiums charged to general surgeons fell by 30% in these states. In Colorado, internists saw a 20% decrease in premiums over the same time period, but general surgeons saw an increase of 13% and ob.gyns. experienced an 11% rise. In New York, rates charged by the largest insurer rose by 12% for ob.gyns, 16% for internists, and 35% for general surgeons.
It remains unclear why the rate of paid claims has decreased and why premiums have remained fairly stable, Dr. Mello and colleagues said. While medical organizations like to point to tort reform, traditional reforms such as award caps do not address problems within the malpractice system’s core functions – compensating negligently injured patients and deterring substandard care, they added.
“The weight of evidence suggests that the system’s effectiveness as both a compensation and a deterrence mechanism is mediocre at best, and there is little to suggest it has improved over the past decade,” they wrote. “Thus, ‘stable but still dysfunctional’ might describe today’s liability environment.”
The authors offered alternatives to traditional tort reform, such as communication and resolution programs, mandatory presuit notification laws, and judge-directed negotiation.
In communication and resolution programs, clinicians and institutions openly discuss adverse outcomes with patients and proactively seek resolution, including offering an apology, and, if the standard of care was not met, compensation. Mandatory presuit notification refers to requiring plaintiffs to give defendants advance notice that they intend to sue. Judge-directed negotiation centers on court policies in which malpractice litigants meet early and often with judges to discuss settlement. In such negotiations, the court employs an attorney with clinical training to help judges understand clinical issues.
The authors conclude that action to improve the medical liability system is necessary while the legal climate is stable, and not after a crisis.
“During malpractice crises, interest in liability reform intensifies, but one lesson of the last 40 years is that an atmosphere of crisis is not conducive to thoughtful and enduring solutions,” study authors said. “Action now to reduce the amplitude of the next medical liability cycle is both prudent and feasible. Further testing of nontraditional reforms, followed by wider implementation of those that work, holds the most promise.”
On Twitter @legal_med
Fewer malpractice suits are resulting in paid claims against physicians while malpractice insurance premiums have remained stable or declined over the last 12 years, according to an analysis published Oct. 30 in JAMA.
Since 2002, the rate of paid malpractice claims against doctors of medicine has decreased by an estimated 6% annually; for doctors of osteopathy, the rate has declined about 5% annually, Michelle M. Mello of Stanford (Calif.) University and her colleagues reported (JAMA 2014 Oct. 30 [doi:10.1001/jama.2014.10705]).
Dr. Mello and her colleagues analyzed paid legal claims against MDs and DOs between 1994 and 2013 from the National Practitioner Data Bank and the American Medical Association’s Physician Masterfile. They also evaluated premium data from the Medical Liability Monitor’s Annual Rate Survey.
The rate of paid malpractice claims against MDs fell from 18.6 to 9.9 paid claims per 1,000 physicians between 2002 and 2013, they found. For DOs, rates dropped from about 19 in 2002 to about 12.2 paid claims per 1,000 physicians in 2013.
The median compensation paid to plaintiffs rose by 63% between 1994 and 2007, from $133,799 to $218,400, in adjusted 2013 dollars. However, since 2007, that number has declined, reaching $195,000 in 2013. Only 3.4% of payments made during the 20-year period resulted from jury verdicts; the others stemmed from settlements.
For the premiums review, Dr. Mello and colleagues analyzed insurance data from 2004 to 2013 from five geographical areas: Los Angeles, Orange, Kern, and Ventura counties in California; Nassau and Suffolk counties in New York; Cook, Madison, St. Clair, and Will counties in Illinois; and the states of Tennessee and Colorado. The locations were selected based on geographic diversity and because each had an insurer with a dominant market share.
In California, Illinois, and Tennessee, internists and ob.gyns. saw a 36% decrease in premiums charged by each state’s largest medical malpractice insurer from 2004 to 2013. Premiums charged to general surgeons fell by 30% in these states. In Colorado, internists saw a 20% decrease in premiums over the same time period, but general surgeons saw an increase of 13% and ob.gyns. experienced an 11% rise. In New York, rates charged by the largest insurer rose by 12% for ob.gyns, 16% for internists, and 35% for general surgeons.
It remains unclear why the rate of paid claims has decreased and why premiums have remained fairly stable, Dr. Mello and colleagues said. While medical organizations like to point to tort reform, traditional reforms such as award caps do not address problems within the malpractice system’s core functions – compensating negligently injured patients and deterring substandard care, they added.
“The weight of evidence suggests that the system’s effectiveness as both a compensation and a deterrence mechanism is mediocre at best, and there is little to suggest it has improved over the past decade,” they wrote. “Thus, ‘stable but still dysfunctional’ might describe today’s liability environment.”
The authors offered alternatives to traditional tort reform, such as communication and resolution programs, mandatory presuit notification laws, and judge-directed negotiation.
In communication and resolution programs, clinicians and institutions openly discuss adverse outcomes with patients and proactively seek resolution, including offering an apology, and, if the standard of care was not met, compensation. Mandatory presuit notification refers to requiring plaintiffs to give defendants advance notice that they intend to sue. Judge-directed negotiation centers on court policies in which malpractice litigants meet early and often with judges to discuss settlement. In such negotiations, the court employs an attorney with clinical training to help judges understand clinical issues.
The authors conclude that action to improve the medical liability system is necessary while the legal climate is stable, and not after a crisis.
“During malpractice crises, interest in liability reform intensifies, but one lesson of the last 40 years is that an atmosphere of crisis is not conducive to thoughtful and enduring solutions,” study authors said. “Action now to reduce the amplitude of the next medical liability cycle is both prudent and feasible. Further testing of nontraditional reforms, followed by wider implementation of those that work, holds the most promise.”
On Twitter @legal_med
Key clinical point: Doctors have experienced a steady decrease in paid malpractice claims since 2002.
Major finding: The rate of paid malpractice claims against MDs fell from 18.6 to 9.9 paid claims per 1,000 physicians between 2002 and 2013.
Data source: Data analysis of paid claims and insurance premiums
Disclosures: Michelle M. Mello, Ph.D., and Dr. Allen Kachalia report that they served as investigators on several of the demonstration projects described in the JAMA article. Dr Mello also reports that she is an investigator on the Agency for Healthcare Research and Quality’s toolkit project. Dr. Mello and Dr. Kachalia report that they have served as consultants to the state of Oregon on liability issues.
Bariatric surgery’s long-term durability, complications still unknown
The greatest research need regarding bariatric surgery is the critical lack of information about long-term durability and complications of the procedures, according to a report published online Nov. 4 in JAMA Surgery.
Bariatric surgery “results in greater weight loss than nonsurgical treatment,” but that crucial information about long-term outcomes – “at least 10 years’ worth” – is still missing, said Dr. Bruce M. Wolfe of Oregon Health and Science University, Portland, and Steven H. Belle, Ph.D., of the epidemiology department, University of Pittsburgh. They were speaking at a symposium sponsored by the National Institute of Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute to review the best available evidence on bariatric surgery outcomes from the most recent large observational studies and randomized clinical trials.
Very large multicenter, randomized, controlled trials are the best type of study to provide this information but are prohibitively expensive, especially given the difficulty retaining participants in weight-loss studies. Any such trial would require very large numbers of treatment centers and patients to generate results that were adequately powered and generalizable, they wrote (JAMA Surg. 2014 Nov. 4 [doi: 10.1001/jamasurg.2014.2440]).
Future research must address the substantial variability in weight loss after bariatric surgery, as well as the equally substantial variability in its effect on diabetes, hypertension, dyslipidemia, obstructive sleep apnea, and psychological and psychosocial issues. And long-term gastrointestinal complications must be a specific focus because these procedures alter the GI anatomy, and adverse effects may take many years to manifest.
“In summary, bariatric surgery offers the potential to address the morbidity and mortality of the obesity epidemic, but important research questions remain unresolved,” according to Dr. Wolfe and Dr. Belle.
The symposium was convened by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute’s division of cardiovascular sciences. Dr. Wolfe reported serving as a research consultant to EnteroMedics.
The greatest research need regarding bariatric surgery is the critical lack of information about long-term durability and complications of the procedures, according to a report published online Nov. 4 in JAMA Surgery.
Bariatric surgery “results in greater weight loss than nonsurgical treatment,” but that crucial information about long-term outcomes – “at least 10 years’ worth” – is still missing, said Dr. Bruce M. Wolfe of Oregon Health and Science University, Portland, and Steven H. Belle, Ph.D., of the epidemiology department, University of Pittsburgh. They were speaking at a symposium sponsored by the National Institute of Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute to review the best available evidence on bariatric surgery outcomes from the most recent large observational studies and randomized clinical trials.
Very large multicenter, randomized, controlled trials are the best type of study to provide this information but are prohibitively expensive, especially given the difficulty retaining participants in weight-loss studies. Any such trial would require very large numbers of treatment centers and patients to generate results that were adequately powered and generalizable, they wrote (JAMA Surg. 2014 Nov. 4 [doi: 10.1001/jamasurg.2014.2440]).
Future research must address the substantial variability in weight loss after bariatric surgery, as well as the equally substantial variability in its effect on diabetes, hypertension, dyslipidemia, obstructive sleep apnea, and psychological and psychosocial issues. And long-term gastrointestinal complications must be a specific focus because these procedures alter the GI anatomy, and adverse effects may take many years to manifest.
“In summary, bariatric surgery offers the potential to address the morbidity and mortality of the obesity epidemic, but important research questions remain unresolved,” according to Dr. Wolfe and Dr. Belle.
The symposium was convened by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute’s division of cardiovascular sciences. Dr. Wolfe reported serving as a research consultant to EnteroMedics.
The greatest research need regarding bariatric surgery is the critical lack of information about long-term durability and complications of the procedures, according to a report published online Nov. 4 in JAMA Surgery.
Bariatric surgery “results in greater weight loss than nonsurgical treatment,” but that crucial information about long-term outcomes – “at least 10 years’ worth” – is still missing, said Dr. Bruce M. Wolfe of Oregon Health and Science University, Portland, and Steven H. Belle, Ph.D., of the epidemiology department, University of Pittsburgh. They were speaking at a symposium sponsored by the National Institute of Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute to review the best available evidence on bariatric surgery outcomes from the most recent large observational studies and randomized clinical trials.
Very large multicenter, randomized, controlled trials are the best type of study to provide this information but are prohibitively expensive, especially given the difficulty retaining participants in weight-loss studies. Any such trial would require very large numbers of treatment centers and patients to generate results that were adequately powered and generalizable, they wrote (JAMA Surg. 2014 Nov. 4 [doi: 10.1001/jamasurg.2014.2440]).
Future research must address the substantial variability in weight loss after bariatric surgery, as well as the equally substantial variability in its effect on diabetes, hypertension, dyslipidemia, obstructive sleep apnea, and psychological and psychosocial issues. And long-term gastrointestinal complications must be a specific focus because these procedures alter the GI anatomy, and adverse effects may take many years to manifest.
“In summary, bariatric surgery offers the potential to address the morbidity and mortality of the obesity epidemic, but important research questions remain unresolved,” according to Dr. Wolfe and Dr. Belle.
The symposium was convened by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute’s division of cardiovascular sciences. Dr. Wolfe reported serving as a research consultant to EnteroMedics.
Key clinical point: The long-term durability and complications of bariatric surgery remain unknown because research is lacking.
Major finding: Crucial information about long-term outcomes – “at least 10 years’ worth” – is still missing.
Data source: A report from a National Institutes of Health symposium reviewing the best available evidence regarding bariatric surgery outcomes.
Disclosures: The symposium was convened by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute’s division of cardiovascular sciences. Dr. Wolfe reported serving as a research consultant to EnteroMedics.
Thumbs-up on laparoscopic splenectomy for malignancies
LAS VEGAS – Laparoscopic splenectomy for hematologic malignancies involving the spleen is an effective surgical strategy, although the operator must expect a higher rate of conversion to laparotomy than when laparoscopic splenectomy is performed for benign hematologic diseases, Dr. Roberta Gelmini said at the annual Minimally Invasive Surgery Week.
The rate of postoperative complications, including wound infection, abdominal abscess, hemiperitoneum, and splenic vein thrombosis, is low and similar to that associated with laparoscopic splenectomy for benign hematologic diseases. The one exception is the complication of pleural effusion, which is seven- to eightfold more frequent following laparoscopic splenectomy for malignancies, probably reflecting affected patients’ larger spleen size and higher conversion rate, observed Dr. Gelmini, professor of surgery at the University of Modena and Reggio Emilia (Italy).
She presented a retrospective analysis of a series of 126 consecutive elective laparoscopic splenectomies performed in adults. Fifty-five were performed for malignant diseases, 71 for benign hematologic conditions. The two groups were well matched except that the patients with benign hematologic diseases were younger and thinner, with a mean age of 39 and a body mass index of 24.4 kg/m2, as compared with 55 years and 25.9 kg/m2 in patients undergoing laparoscopic splenectomy for hematologic malignancies.
The No. 1 indication for splenectomy in patients with benign disease was idiopathic thrombocytopenic purpura, accounting for 61% of cases. In patients with malignancies, non-Hodgkin’s lymphoma was the indication for splenectomy in two-thirds of cases.
As part of their preoperative work-up, all patients underwent ultrasound to establish spleen size and vessel diameter. Bipolar splenic length was significantly greater in the group with malignancies: a mean of 17 cm, compared with 13.4 cm in patients with benign disease.
With regard to key intraoperative findings, the mean 148-minute operative time in patients with malignancies was 22 minutes longer than in patients with benign disease. The conversion rate was 18.2% in patients with malignancies, compared with 5.6% when laparoscopic splenectomy was undertaken for benign disease. But the incidence of intraoperative blood loss greater than 500 mL was similar in the two groups, as was the transfusion rate, Dr. Gelmini reported at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
Four patients underwent conversion to laparotomy or mini-laparotomy for malignancies because of a difficult splenic hilum dissection.
Pleural effusion occurred in 7% of patients operated upon for benign disease, compared with 56% of those with hematologic malignancies. Otherwise the complication rates in the two groups were similar.
Time to refeeding was similar in the two patient groups. Mean postoperative length of hospital stay was 5.3 days in patients who underwent laparoscopic splenectomy for benign disease and similar at 5.8 days for those with malignancies.
“Our data suggest that the nature of the disease does not significantly influence the postoperative outcome,” the surgeon observed.
She added that the results of her series were quite similar to those in an earlier report by surgeons at the University of Genoa (Italy) in terms of conversion rate and complications in 38 patients who underwent laparoscopic splenectomy for benign hematologic diseases and 25 with hematologic malignancies (Tumori 2004;90:229-32).
Dr. Gelmini reported having no financial conflicts regarding her presentation.
LAS VEGAS – Laparoscopic splenectomy for hematologic malignancies involving the spleen is an effective surgical strategy, although the operator must expect a higher rate of conversion to laparotomy than when laparoscopic splenectomy is performed for benign hematologic diseases, Dr. Roberta Gelmini said at the annual Minimally Invasive Surgery Week.
The rate of postoperative complications, including wound infection, abdominal abscess, hemiperitoneum, and splenic vein thrombosis, is low and similar to that associated with laparoscopic splenectomy for benign hematologic diseases. The one exception is the complication of pleural effusion, which is seven- to eightfold more frequent following laparoscopic splenectomy for malignancies, probably reflecting affected patients’ larger spleen size and higher conversion rate, observed Dr. Gelmini, professor of surgery at the University of Modena and Reggio Emilia (Italy).
She presented a retrospective analysis of a series of 126 consecutive elective laparoscopic splenectomies performed in adults. Fifty-five were performed for malignant diseases, 71 for benign hematologic conditions. The two groups were well matched except that the patients with benign hematologic diseases were younger and thinner, with a mean age of 39 and a body mass index of 24.4 kg/m2, as compared with 55 years and 25.9 kg/m2 in patients undergoing laparoscopic splenectomy for hematologic malignancies.
The No. 1 indication for splenectomy in patients with benign disease was idiopathic thrombocytopenic purpura, accounting for 61% of cases. In patients with malignancies, non-Hodgkin’s lymphoma was the indication for splenectomy in two-thirds of cases.
As part of their preoperative work-up, all patients underwent ultrasound to establish spleen size and vessel diameter. Bipolar splenic length was significantly greater in the group with malignancies: a mean of 17 cm, compared with 13.4 cm in patients with benign disease.
With regard to key intraoperative findings, the mean 148-minute operative time in patients with malignancies was 22 minutes longer than in patients with benign disease. The conversion rate was 18.2% in patients with malignancies, compared with 5.6% when laparoscopic splenectomy was undertaken for benign disease. But the incidence of intraoperative blood loss greater than 500 mL was similar in the two groups, as was the transfusion rate, Dr. Gelmini reported at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
Four patients underwent conversion to laparotomy or mini-laparotomy for malignancies because of a difficult splenic hilum dissection.
Pleural effusion occurred in 7% of patients operated upon for benign disease, compared with 56% of those with hematologic malignancies. Otherwise the complication rates in the two groups were similar.
Time to refeeding was similar in the two patient groups. Mean postoperative length of hospital stay was 5.3 days in patients who underwent laparoscopic splenectomy for benign disease and similar at 5.8 days for those with malignancies.
“Our data suggest that the nature of the disease does not significantly influence the postoperative outcome,” the surgeon observed.
She added that the results of her series were quite similar to those in an earlier report by surgeons at the University of Genoa (Italy) in terms of conversion rate and complications in 38 patients who underwent laparoscopic splenectomy for benign hematologic diseases and 25 with hematologic malignancies (Tumori 2004;90:229-32).
Dr. Gelmini reported having no financial conflicts regarding her presentation.
LAS VEGAS – Laparoscopic splenectomy for hematologic malignancies involving the spleen is an effective surgical strategy, although the operator must expect a higher rate of conversion to laparotomy than when laparoscopic splenectomy is performed for benign hematologic diseases, Dr. Roberta Gelmini said at the annual Minimally Invasive Surgery Week.
The rate of postoperative complications, including wound infection, abdominal abscess, hemiperitoneum, and splenic vein thrombosis, is low and similar to that associated with laparoscopic splenectomy for benign hematologic diseases. The one exception is the complication of pleural effusion, which is seven- to eightfold more frequent following laparoscopic splenectomy for malignancies, probably reflecting affected patients’ larger spleen size and higher conversion rate, observed Dr. Gelmini, professor of surgery at the University of Modena and Reggio Emilia (Italy).
She presented a retrospective analysis of a series of 126 consecutive elective laparoscopic splenectomies performed in adults. Fifty-five were performed for malignant diseases, 71 for benign hematologic conditions. The two groups were well matched except that the patients with benign hematologic diseases were younger and thinner, with a mean age of 39 and a body mass index of 24.4 kg/m2, as compared with 55 years and 25.9 kg/m2 in patients undergoing laparoscopic splenectomy for hematologic malignancies.
The No. 1 indication for splenectomy in patients with benign disease was idiopathic thrombocytopenic purpura, accounting for 61% of cases. In patients with malignancies, non-Hodgkin’s lymphoma was the indication for splenectomy in two-thirds of cases.
As part of their preoperative work-up, all patients underwent ultrasound to establish spleen size and vessel diameter. Bipolar splenic length was significantly greater in the group with malignancies: a mean of 17 cm, compared with 13.4 cm in patients with benign disease.
With regard to key intraoperative findings, the mean 148-minute operative time in patients with malignancies was 22 minutes longer than in patients with benign disease. The conversion rate was 18.2% in patients with malignancies, compared with 5.6% when laparoscopic splenectomy was undertaken for benign disease. But the incidence of intraoperative blood loss greater than 500 mL was similar in the two groups, as was the transfusion rate, Dr. Gelmini reported at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
Four patients underwent conversion to laparotomy or mini-laparotomy for malignancies because of a difficult splenic hilum dissection.
Pleural effusion occurred in 7% of patients operated upon for benign disease, compared with 56% of those with hematologic malignancies. Otherwise the complication rates in the two groups were similar.
Time to refeeding was similar in the two patient groups. Mean postoperative length of hospital stay was 5.3 days in patients who underwent laparoscopic splenectomy for benign disease and similar at 5.8 days for those with malignancies.
“Our data suggest that the nature of the disease does not significantly influence the postoperative outcome,” the surgeon observed.
She added that the results of her series were quite similar to those in an earlier report by surgeons at the University of Genoa (Italy) in terms of conversion rate and complications in 38 patients who underwent laparoscopic splenectomy for benign hematologic diseases and 25 with hematologic malignancies (Tumori 2004;90:229-32).
Dr. Gelmini reported having no financial conflicts regarding her presentation.
EXPERT ANALYSIS FROM MINIMALLY INVASIVE SURGERY WEEK