User login
Official Newspaper of the American College of Surgeons
Attorney: Be prepared for next round of HIPAA audits
With the next round of HIPAA compliance audits on the horizon, physicians should ensure they are prepared for both on-site and off-site privacy investigations.
The Office for Civil Rights (OCR) concluded its first pilot of HIPAA audits in 2012 after reviewing the practices and compliance of 115 health care entities. The assessments included health care providers, health plans, and clearing houses. Round two of the audits, originally scheduled for 2014, is expected to begin in early 2015. The next phase will be based on preaudit surveys of 800 covered entities and 400 business associates of covered entities, according to a May announcement in the Federal Register.
The first wave of HIPAA audits revealed weaknesses in the internal controls and compliance programs of many health care entities, particularly small group practices, said Anna C. Watterson, a Washington-based health information privacy and securities attorney and a former OCR policy analyst. Practices of 10-50 providers (Level 4) made up 41% of findings by the OCR and “struggled” with all three focus areas – breach notification, privacy, and security, according to audit results. Findings were generated only for entities that did not meet audit criteria or had potential compliance violations.
“Small providers generally have struggled more with compliance than other organizations,” Ms. Watterson said in an interview. “It’s largely a resource issue. Having a full HIPAA security program is very resource-intensive.”
Understanding the differences between on and off-site audits and what may be required is key to preparing for inquires, said Ms. Watterson, who spoke about HIPAA audits at the American Health Lawyers Association’s health fraud and compliance forum. Off-site audits refer to documentation requests by phone or electronic means. These audits often are limited in scope and pertain to one or two provisions under HIPAA. On-site audits are frequently more intensive and include visits by federal investigators to the provider’s premises.
It is essential to make certain that all compliance and sanction policies are well documented and to reply to requests in a timely manner, Ms. Watterson said. All documentation must be current as of the request date and cannot be created after the inquiry.
During on-site audits, doctors should be prepared to answer questions and have inquires directed at their staff. For example, HIPAA investigators may ask employees about their HIPAA privacy officer, whether they can bring work laptops home and if so, what privacy safeguards are in place.
“Be prepared for OCR to ask employees about actual practices,” Ms. Watterson said. “It’s something organizations want to think about.”
For the first time, phase 2 of the audits will include business associates. Under the omnibus rule, a business associate is defined as any person or entity that creates, receives, maintains, or transmits protected health information (PHI) on behalf of a covered entity. The regulation includes patient safety organizations, data transmission organizations, personal health record vendors, entities that transmit and need routine access to PHI, and data storage vendors – paper based and cloud based.
“OCR will be asking all covered entities for a list of their business associates,” Ms. Watterson said. “Vendor management is something organizations should be [considering]. Have they identified all their vendors? Do they have agreements?”
Business-associate agreements should confirm that associates comply with all measures of the Security Rule for electronic PHI and that business associates report any breach of unsecured PHI.
Having an IT consultant or third-party company perform a security risk analysis is one way to address security weaknesses before an audit, Ms. Watterson said. For doctors in smaller practices with fewer resources, the Office of the National Coordinator for Health Information Technology provides a free, downloadable security risk assessment tool. The National Institute of Standards and Technology also has a free HIPAA Security Rule toolkit for health care organizations.
While preparing for a HIPAA audit may seem daunting, physicians within all practice sizes can plan by reviewing and improving compliance one step at a time, Ms. Watterson stressed. “For a lot of organizations, it’s difficult to set aside the time and resources to just look at all of the compliance. Providers need to prioritize and take a few things that they can tackle” at a time.
On Twitter @legal_med
With the next round of HIPAA compliance audits on the horizon, physicians should ensure they are prepared for both on-site and off-site privacy investigations.
The Office for Civil Rights (OCR) concluded its first pilot of HIPAA audits in 2012 after reviewing the practices and compliance of 115 health care entities. The assessments included health care providers, health plans, and clearing houses. Round two of the audits, originally scheduled for 2014, is expected to begin in early 2015. The next phase will be based on preaudit surveys of 800 covered entities and 400 business associates of covered entities, according to a May announcement in the Federal Register.
The first wave of HIPAA audits revealed weaknesses in the internal controls and compliance programs of many health care entities, particularly small group practices, said Anna C. Watterson, a Washington-based health information privacy and securities attorney and a former OCR policy analyst. Practices of 10-50 providers (Level 4) made up 41% of findings by the OCR and “struggled” with all three focus areas – breach notification, privacy, and security, according to audit results. Findings were generated only for entities that did not meet audit criteria or had potential compliance violations.
“Small providers generally have struggled more with compliance than other organizations,” Ms. Watterson said in an interview. “It’s largely a resource issue. Having a full HIPAA security program is very resource-intensive.”
Understanding the differences between on and off-site audits and what may be required is key to preparing for inquires, said Ms. Watterson, who spoke about HIPAA audits at the American Health Lawyers Association’s health fraud and compliance forum. Off-site audits refer to documentation requests by phone or electronic means. These audits often are limited in scope and pertain to one or two provisions under HIPAA. On-site audits are frequently more intensive and include visits by federal investigators to the provider’s premises.
It is essential to make certain that all compliance and sanction policies are well documented and to reply to requests in a timely manner, Ms. Watterson said. All documentation must be current as of the request date and cannot be created after the inquiry.
During on-site audits, doctors should be prepared to answer questions and have inquires directed at their staff. For example, HIPAA investigators may ask employees about their HIPAA privacy officer, whether they can bring work laptops home and if so, what privacy safeguards are in place.
“Be prepared for OCR to ask employees about actual practices,” Ms. Watterson said. “It’s something organizations want to think about.”
For the first time, phase 2 of the audits will include business associates. Under the omnibus rule, a business associate is defined as any person or entity that creates, receives, maintains, or transmits protected health information (PHI) on behalf of a covered entity. The regulation includes patient safety organizations, data transmission organizations, personal health record vendors, entities that transmit and need routine access to PHI, and data storage vendors – paper based and cloud based.
“OCR will be asking all covered entities for a list of their business associates,” Ms. Watterson said. “Vendor management is something organizations should be [considering]. Have they identified all their vendors? Do they have agreements?”
Business-associate agreements should confirm that associates comply with all measures of the Security Rule for electronic PHI and that business associates report any breach of unsecured PHI.
Having an IT consultant or third-party company perform a security risk analysis is one way to address security weaknesses before an audit, Ms. Watterson said. For doctors in smaller practices with fewer resources, the Office of the National Coordinator for Health Information Technology provides a free, downloadable security risk assessment tool. The National Institute of Standards and Technology also has a free HIPAA Security Rule toolkit for health care organizations.
While preparing for a HIPAA audit may seem daunting, physicians within all practice sizes can plan by reviewing and improving compliance one step at a time, Ms. Watterson stressed. “For a lot of organizations, it’s difficult to set aside the time and resources to just look at all of the compliance. Providers need to prioritize and take a few things that they can tackle” at a time.
On Twitter @legal_med
With the next round of HIPAA compliance audits on the horizon, physicians should ensure they are prepared for both on-site and off-site privacy investigations.
The Office for Civil Rights (OCR) concluded its first pilot of HIPAA audits in 2012 after reviewing the practices and compliance of 115 health care entities. The assessments included health care providers, health plans, and clearing houses. Round two of the audits, originally scheduled for 2014, is expected to begin in early 2015. The next phase will be based on preaudit surveys of 800 covered entities and 400 business associates of covered entities, according to a May announcement in the Federal Register.
The first wave of HIPAA audits revealed weaknesses in the internal controls and compliance programs of many health care entities, particularly small group practices, said Anna C. Watterson, a Washington-based health information privacy and securities attorney and a former OCR policy analyst. Practices of 10-50 providers (Level 4) made up 41% of findings by the OCR and “struggled” with all three focus areas – breach notification, privacy, and security, according to audit results. Findings were generated only for entities that did not meet audit criteria or had potential compliance violations.
“Small providers generally have struggled more with compliance than other organizations,” Ms. Watterson said in an interview. “It’s largely a resource issue. Having a full HIPAA security program is very resource-intensive.”
Understanding the differences between on and off-site audits and what may be required is key to preparing for inquires, said Ms. Watterson, who spoke about HIPAA audits at the American Health Lawyers Association’s health fraud and compliance forum. Off-site audits refer to documentation requests by phone or electronic means. These audits often are limited in scope and pertain to one or two provisions under HIPAA. On-site audits are frequently more intensive and include visits by federal investigators to the provider’s premises.
It is essential to make certain that all compliance and sanction policies are well documented and to reply to requests in a timely manner, Ms. Watterson said. All documentation must be current as of the request date and cannot be created after the inquiry.
During on-site audits, doctors should be prepared to answer questions and have inquires directed at their staff. For example, HIPAA investigators may ask employees about their HIPAA privacy officer, whether they can bring work laptops home and if so, what privacy safeguards are in place.
“Be prepared for OCR to ask employees about actual practices,” Ms. Watterson said. “It’s something organizations want to think about.”
For the first time, phase 2 of the audits will include business associates. Under the omnibus rule, a business associate is defined as any person or entity that creates, receives, maintains, or transmits protected health information (PHI) on behalf of a covered entity. The regulation includes patient safety organizations, data transmission organizations, personal health record vendors, entities that transmit and need routine access to PHI, and data storage vendors – paper based and cloud based.
“OCR will be asking all covered entities for a list of their business associates,” Ms. Watterson said. “Vendor management is something organizations should be [considering]. Have they identified all their vendors? Do they have agreements?”
Business-associate agreements should confirm that associates comply with all measures of the Security Rule for electronic PHI and that business associates report any breach of unsecured PHI.
Having an IT consultant or third-party company perform a security risk analysis is one way to address security weaknesses before an audit, Ms. Watterson said. For doctors in smaller practices with fewer resources, the Office of the National Coordinator for Health Information Technology provides a free, downloadable security risk assessment tool. The National Institute of Standards and Technology also has a free HIPAA Security Rule toolkit for health care organizations.
While preparing for a HIPAA audit may seem daunting, physicians within all practice sizes can plan by reviewing and improving compliance one step at a time, Ms. Watterson stressed. “For a lot of organizations, it’s difficult to set aside the time and resources to just look at all of the compliance. Providers need to prioritize and take a few things that they can tackle” at a time.
On Twitter @legal_med
Patient-led follow-up safe and cost effective
MELBOURNE – Patient-initiated follow-up is a safe, cost-effective alternative to conventional follow-ups every 3 months in patients with gynecological cancer, according to data from a prospective trial presented at the biennial meeting of the International Gynecologic Cancer Society.
Researchers found a much longer time to follow-up among patients who chose patient-initiated follow-up compared with those who elected to remain with conventional follow-up (718 days vs. 386 days), but the median time to death also was longer: 1,035 days in the patient-initiated follow-up group compared with 795 days in the conventional follow-up group.
“What is very clear is that many of our patients want an alternative to conventional follow up,” said Dr. Peter Larsen-Disney of the department of gynecology at Brighton and Sussex University Hospital NHS Trust, Brighton, England.
Dr Larsen-Disney told the conference that he realized patients with a good prognosis after treatment for their gynecological cancers were being given mixed messages by being asked to return for regular follow-up.
“We were saying, ‘there’s every reason to believe you’re cured, you have an excellent prognosis, and we’ll see you every 3 months,’ ” he said.
“The other realization I had was, with the exception of ovarian cancer patients, who we were following up for tumor markers, I believe that I make very few diagnoses of recurrence that the patient didn’t tell me was there.”
After realizing there was little evidence to support follow-up every 3 months in these patients, Dr. Larsen-Disney and his colleagues conducted a prospective study of 997 patients who were offered the choice of conventional follow-up or patient-initiated follow-up.
Patients who chose patient-initiated follow-up were registered in a database, and were provided with disease-specific booklets that outlined the follow-up system, listed details on what symptoms to look out for, and gave information on how to access review if needed.
Patients were able to access a nurse specialist by phone for advice and referrals for other services such as counseling.
Of the 568 patients who registered for patient-initiated follow-up, 71 later switched back to conventional follow-up, mostly at the time of recurrence.
More than half of the patients who registered for patient-initiated follow-up had endometrial cancer, while there were significantly more patients with cervical and vulvar cancer in the conventional follow-up arm than in the patient-initiated follow-up arm, which Dr. Larsen-Disney said partly reflected physician bias.
“We were a little bit reluctant to release the [patients with] very early cervix cancers back into the community because we wanted to follow them up with smears, and ... we weren’t confident that they would get the appropriate smears in the community,” he said.
He said there was no doubt in his mind of the importance of patient-led follow-up to the patients themselves, as well as the fact that it appeared to be a safe, acceptable, and cost-effective alternative to conventional follow-up.
“I think the concerns are that people are nervous that they’re going to miss recurrences and, to be honest, there will be a tiny minority of patients where you will, who won’t present with classical signs of recurrence but I’m not convinced you’d pick them up anyway,” Dr. Larsen-Disney said in an interview.
There were no conflicts of interest declared.
MELBOURNE – Patient-initiated follow-up is a safe, cost-effective alternative to conventional follow-ups every 3 months in patients with gynecological cancer, according to data from a prospective trial presented at the biennial meeting of the International Gynecologic Cancer Society.
Researchers found a much longer time to follow-up among patients who chose patient-initiated follow-up compared with those who elected to remain with conventional follow-up (718 days vs. 386 days), but the median time to death also was longer: 1,035 days in the patient-initiated follow-up group compared with 795 days in the conventional follow-up group.
“What is very clear is that many of our patients want an alternative to conventional follow up,” said Dr. Peter Larsen-Disney of the department of gynecology at Brighton and Sussex University Hospital NHS Trust, Brighton, England.
Dr Larsen-Disney told the conference that he realized patients with a good prognosis after treatment for their gynecological cancers were being given mixed messages by being asked to return for regular follow-up.
“We were saying, ‘there’s every reason to believe you’re cured, you have an excellent prognosis, and we’ll see you every 3 months,’ ” he said.
“The other realization I had was, with the exception of ovarian cancer patients, who we were following up for tumor markers, I believe that I make very few diagnoses of recurrence that the patient didn’t tell me was there.”
After realizing there was little evidence to support follow-up every 3 months in these patients, Dr. Larsen-Disney and his colleagues conducted a prospective study of 997 patients who were offered the choice of conventional follow-up or patient-initiated follow-up.
Patients who chose patient-initiated follow-up were registered in a database, and were provided with disease-specific booklets that outlined the follow-up system, listed details on what symptoms to look out for, and gave information on how to access review if needed.
Patients were able to access a nurse specialist by phone for advice and referrals for other services such as counseling.
Of the 568 patients who registered for patient-initiated follow-up, 71 later switched back to conventional follow-up, mostly at the time of recurrence.
More than half of the patients who registered for patient-initiated follow-up had endometrial cancer, while there were significantly more patients with cervical and vulvar cancer in the conventional follow-up arm than in the patient-initiated follow-up arm, which Dr. Larsen-Disney said partly reflected physician bias.
“We were a little bit reluctant to release the [patients with] very early cervix cancers back into the community because we wanted to follow them up with smears, and ... we weren’t confident that they would get the appropriate smears in the community,” he said.
He said there was no doubt in his mind of the importance of patient-led follow-up to the patients themselves, as well as the fact that it appeared to be a safe, acceptable, and cost-effective alternative to conventional follow-up.
“I think the concerns are that people are nervous that they’re going to miss recurrences and, to be honest, there will be a tiny minority of patients where you will, who won’t present with classical signs of recurrence but I’m not convinced you’d pick them up anyway,” Dr. Larsen-Disney said in an interview.
There were no conflicts of interest declared.
MELBOURNE – Patient-initiated follow-up is a safe, cost-effective alternative to conventional follow-ups every 3 months in patients with gynecological cancer, according to data from a prospective trial presented at the biennial meeting of the International Gynecologic Cancer Society.
Researchers found a much longer time to follow-up among patients who chose patient-initiated follow-up compared with those who elected to remain with conventional follow-up (718 days vs. 386 days), but the median time to death also was longer: 1,035 days in the patient-initiated follow-up group compared with 795 days in the conventional follow-up group.
“What is very clear is that many of our patients want an alternative to conventional follow up,” said Dr. Peter Larsen-Disney of the department of gynecology at Brighton and Sussex University Hospital NHS Trust, Brighton, England.
Dr Larsen-Disney told the conference that he realized patients with a good prognosis after treatment for their gynecological cancers were being given mixed messages by being asked to return for regular follow-up.
“We were saying, ‘there’s every reason to believe you’re cured, you have an excellent prognosis, and we’ll see you every 3 months,’ ” he said.
“The other realization I had was, with the exception of ovarian cancer patients, who we were following up for tumor markers, I believe that I make very few diagnoses of recurrence that the patient didn’t tell me was there.”
After realizing there was little evidence to support follow-up every 3 months in these patients, Dr. Larsen-Disney and his colleagues conducted a prospective study of 997 patients who were offered the choice of conventional follow-up or patient-initiated follow-up.
Patients who chose patient-initiated follow-up were registered in a database, and were provided with disease-specific booklets that outlined the follow-up system, listed details on what symptoms to look out for, and gave information on how to access review if needed.
Patients were able to access a nurse specialist by phone for advice and referrals for other services such as counseling.
Of the 568 patients who registered for patient-initiated follow-up, 71 later switched back to conventional follow-up, mostly at the time of recurrence.
More than half of the patients who registered for patient-initiated follow-up had endometrial cancer, while there were significantly more patients with cervical and vulvar cancer in the conventional follow-up arm than in the patient-initiated follow-up arm, which Dr. Larsen-Disney said partly reflected physician bias.
“We were a little bit reluctant to release the [patients with] very early cervix cancers back into the community because we wanted to follow them up with smears, and ... we weren’t confident that they would get the appropriate smears in the community,” he said.
He said there was no doubt in his mind of the importance of patient-led follow-up to the patients themselves, as well as the fact that it appeared to be a safe, acceptable, and cost-effective alternative to conventional follow-up.
“I think the concerns are that people are nervous that they’re going to miss recurrences and, to be honest, there will be a tiny minority of patients where you will, who won’t present with classical signs of recurrence but I’m not convinced you’d pick them up anyway,” Dr. Larsen-Disney said in an interview.
There were no conflicts of interest declared.
AT IGCS 2014
Key clinical point: Patient-initiated follow-up is a safe, cost-effective alternative to conventional follow-up every 3 months in patients with gynecological cancer.
Major finding: Patient-led follow-up was associated with a median follow-up of 742 days compared to 386 days with conventional follow-up.
Data source: Prospective study of 997 women with gynecological cancer.
Disclosures: No conflicts of interest declared.
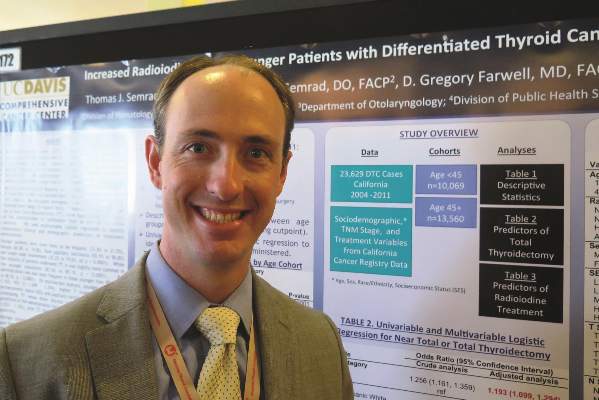
Total thyroidectomy more likely with younger thyroid cancer patients
CORONADO, CALIF. – Patients with differentiated thyroid cancer who were younger than age 45 years were more likely to undergo total or near-total thyroidectomy and to receive radioactive iodine, compared with their older counterparts, a large registry analysis demonstrated.
In addition, younger patients were more likely to be Hispanic and female and to have papillary carcinoma, lead study author Dr. Thomas J. Semrad reported during the annual meeting of the American Thyroid Association.
“Not much is known about how treatment administration differs between younger and older patients with thyroid cancer,” Dr. Semrad of the division of hematology/oncology at the University of California, Davis, Comprehensive Cancer Center, Sacramento, said in an interview. “Some data suggest that perhaps patients younger than age 15 years may respond better to radioactive iodine and may present with more advanced disease. But not much is known about how they’re treated.”
To find out, Dr. Semrad and his associates used the California Cancer Registry to identify 23,629 patients who were diagnosed with differentiated thyroid cancer between 2004 and 2011. They divided the patients into two cohorts: younger (defined as those younger than 45 years) and older (those 45 years or older). Treatment variables of interest included total or near-total thyroidectomy, other types of thyroid surgery, and the administration of radioactive iodine (RAI). The researchers compared the descriptive statistics between the two groups and used univariate and multivariate logistic regression to identify predictors of the treatment administered.
Compared with older patients, younger patients were significantly more likely to be Hispanic (33% vs. 22%), to be female (83% vs. 75%), to have papillary carcinoma (93% vs. 91%), and to have lymph node involvement (32% vs. 20%, all P < .0001).
Overall, the majority of patients (86%) underwent total or near-total thyroidectomy, but the surgery was slightly and significantly more common in younger patients, compared with their older counterparts (88% vs. 85%, P < .0001). Younger patients also were significantly more likely to receive RAI (55% vs. 49%, P < .0001).
On multivariate analysis, statistically significant predictors of total thyroidectomy, compared with other thyroid surgery, included younger age (odds ratio, 1.193); higher socioeconomic status (OR, 1.263, for higher-middle SES and OR, 1.325, for highest SES); higher T stage (OR, 1.848, for T2; OR, 2.473, for T3; and OR, 2.908, for T4); and papillary histology (OR, 0.349).
At the same time, statistically significant predictors of RAI administration included younger age (OR, 1.116); higher SES (OR, 1.410, for higher-middle SES and OR, 1.307, for highest SES); more advanced T stage (OR, 2.194 for T2; OR, 2.084, for T3; and OR, 1.527, for T4); node positivity (OR, 0.481), and total thyroidectomy (OR, 3.76).
“As we expected, the younger population was more likely to be female, but we did find that the younger population was also more likely to be Hispanic,” Dr. Semrad said. “We don’t know if they were native Hispanics or if it has something to do with immigration rates.”
Dr. Semrad acknowledged certain limitations of the study, including the risk of misclassification bias in registry data, the lack of details about surgical procedures performed, and the fact that the radioiodine dose was not captured.
“We have data regarding the T stage, the nodal stage, and the number of lymph nodes examined, but we don’t have some of the finer histology data,” he said.
Even so, he characterized the findings as “provocative in suggesting that perhaps our treatment patterns in younger patients are different. With more aggressive surgery and more use of radioactive iodine, that can have potential implications in terms of long-term side effects and follow-up.”
The researchers said they plan to use linked administrative data to analyze initial and subsequent thyroid surgical procedures in this patient population.
The study was supported by a grant from the National Institutes of Health. Dr. Semrad reported having no relevant financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – Patients with differentiated thyroid cancer who were younger than age 45 years were more likely to undergo total or near-total thyroidectomy and to receive radioactive iodine, compared with their older counterparts, a large registry analysis demonstrated.
In addition, younger patients were more likely to be Hispanic and female and to have papillary carcinoma, lead study author Dr. Thomas J. Semrad reported during the annual meeting of the American Thyroid Association.
“Not much is known about how treatment administration differs between younger and older patients with thyroid cancer,” Dr. Semrad of the division of hematology/oncology at the University of California, Davis, Comprehensive Cancer Center, Sacramento, said in an interview. “Some data suggest that perhaps patients younger than age 15 years may respond better to radioactive iodine and may present with more advanced disease. But not much is known about how they’re treated.”
To find out, Dr. Semrad and his associates used the California Cancer Registry to identify 23,629 patients who were diagnosed with differentiated thyroid cancer between 2004 and 2011. They divided the patients into two cohorts: younger (defined as those younger than 45 years) and older (those 45 years or older). Treatment variables of interest included total or near-total thyroidectomy, other types of thyroid surgery, and the administration of radioactive iodine (RAI). The researchers compared the descriptive statistics between the two groups and used univariate and multivariate logistic regression to identify predictors of the treatment administered.
Compared with older patients, younger patients were significantly more likely to be Hispanic (33% vs. 22%), to be female (83% vs. 75%), to have papillary carcinoma (93% vs. 91%), and to have lymph node involvement (32% vs. 20%, all P < .0001).
Overall, the majority of patients (86%) underwent total or near-total thyroidectomy, but the surgery was slightly and significantly more common in younger patients, compared with their older counterparts (88% vs. 85%, P < .0001). Younger patients also were significantly more likely to receive RAI (55% vs. 49%, P < .0001).
On multivariate analysis, statistically significant predictors of total thyroidectomy, compared with other thyroid surgery, included younger age (odds ratio, 1.193); higher socioeconomic status (OR, 1.263, for higher-middle SES and OR, 1.325, for highest SES); higher T stage (OR, 1.848, for T2; OR, 2.473, for T3; and OR, 2.908, for T4); and papillary histology (OR, 0.349).
At the same time, statistically significant predictors of RAI administration included younger age (OR, 1.116); higher SES (OR, 1.410, for higher-middle SES and OR, 1.307, for highest SES); more advanced T stage (OR, 2.194 for T2; OR, 2.084, for T3; and OR, 1.527, for T4); node positivity (OR, 0.481), and total thyroidectomy (OR, 3.76).
“As we expected, the younger population was more likely to be female, but we did find that the younger population was also more likely to be Hispanic,” Dr. Semrad said. “We don’t know if they were native Hispanics or if it has something to do with immigration rates.”
Dr. Semrad acknowledged certain limitations of the study, including the risk of misclassification bias in registry data, the lack of details about surgical procedures performed, and the fact that the radioiodine dose was not captured.
“We have data regarding the T stage, the nodal stage, and the number of lymph nodes examined, but we don’t have some of the finer histology data,” he said.
Even so, he characterized the findings as “provocative in suggesting that perhaps our treatment patterns in younger patients are different. With more aggressive surgery and more use of radioactive iodine, that can have potential implications in terms of long-term side effects and follow-up.”
The researchers said they plan to use linked administrative data to analyze initial and subsequent thyroid surgical procedures in this patient population.
The study was supported by a grant from the National Institutes of Health. Dr. Semrad reported having no relevant financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – Patients with differentiated thyroid cancer who were younger than age 45 years were more likely to undergo total or near-total thyroidectomy and to receive radioactive iodine, compared with their older counterparts, a large registry analysis demonstrated.
In addition, younger patients were more likely to be Hispanic and female and to have papillary carcinoma, lead study author Dr. Thomas J. Semrad reported during the annual meeting of the American Thyroid Association.
“Not much is known about how treatment administration differs between younger and older patients with thyroid cancer,” Dr. Semrad of the division of hematology/oncology at the University of California, Davis, Comprehensive Cancer Center, Sacramento, said in an interview. “Some data suggest that perhaps patients younger than age 15 years may respond better to radioactive iodine and may present with more advanced disease. But not much is known about how they’re treated.”
To find out, Dr. Semrad and his associates used the California Cancer Registry to identify 23,629 patients who were diagnosed with differentiated thyroid cancer between 2004 and 2011. They divided the patients into two cohorts: younger (defined as those younger than 45 years) and older (those 45 years or older). Treatment variables of interest included total or near-total thyroidectomy, other types of thyroid surgery, and the administration of radioactive iodine (RAI). The researchers compared the descriptive statistics between the two groups and used univariate and multivariate logistic regression to identify predictors of the treatment administered.
Compared with older patients, younger patients were significantly more likely to be Hispanic (33% vs. 22%), to be female (83% vs. 75%), to have papillary carcinoma (93% vs. 91%), and to have lymph node involvement (32% vs. 20%, all P < .0001).
Overall, the majority of patients (86%) underwent total or near-total thyroidectomy, but the surgery was slightly and significantly more common in younger patients, compared with their older counterparts (88% vs. 85%, P < .0001). Younger patients also were significantly more likely to receive RAI (55% vs. 49%, P < .0001).
On multivariate analysis, statistically significant predictors of total thyroidectomy, compared with other thyroid surgery, included younger age (odds ratio, 1.193); higher socioeconomic status (OR, 1.263, for higher-middle SES and OR, 1.325, for highest SES); higher T stage (OR, 1.848, for T2; OR, 2.473, for T3; and OR, 2.908, for T4); and papillary histology (OR, 0.349).
At the same time, statistically significant predictors of RAI administration included younger age (OR, 1.116); higher SES (OR, 1.410, for higher-middle SES and OR, 1.307, for highest SES); more advanced T stage (OR, 2.194 for T2; OR, 2.084, for T3; and OR, 1.527, for T4); node positivity (OR, 0.481), and total thyroidectomy (OR, 3.76).
“As we expected, the younger population was more likely to be female, but we did find that the younger population was also more likely to be Hispanic,” Dr. Semrad said. “We don’t know if they were native Hispanics or if it has something to do with immigration rates.”
Dr. Semrad acknowledged certain limitations of the study, including the risk of misclassification bias in registry data, the lack of details about surgical procedures performed, and the fact that the radioiodine dose was not captured.
“We have data regarding the T stage, the nodal stage, and the number of lymph nodes examined, but we don’t have some of the finer histology data,” he said.
Even so, he characterized the findings as “provocative in suggesting that perhaps our treatment patterns in younger patients are different. With more aggressive surgery and more use of radioactive iodine, that can have potential implications in terms of long-term side effects and follow-up.”
The researchers said they plan to use linked administrative data to analyze initial and subsequent thyroid surgical procedures in this patient population.
The study was supported by a grant from the National Institutes of Health. Dr. Semrad reported having no relevant financial disclosures.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: Younger patients with differentiated thyroid cancer were more likely to undergo total thyroidectomy and receive radioactive iodine.
Major finding: Total or near-total thyroidectomy was slightly more common in patients younger than age 45 years, compared with their older counterparts (88% vs. 85%, P < .0001). Younger patients were also more likely to receive RAI (55% vs. 49%, P < .0001).
Data source: A study of 23,629 patients from the California Cancer Registry who were diagnosed with differentiated thyroid cancer between 2004 and 2011.
Disclosures: The study was supported by a grant from the National Institutes of Health. Dr. Semrad reported having no relevant financial disclosures.
Levofloxacin didn’t prevent BK virus after kidney transplant, increased quinolone resistance
PHILADELPHIA – A 3-month course of levofloxacin after kidney transplant didn’t prevent BK virus from colonizing the urine, setting the stage for viremia in these immunosuppressed patients.
However, the antibiotic was associated with a significant 75% increase in the risk of developing a quinolone-resistant infection, compared with placebo, Dr. Greg A. Knoll and his colleagues reported in the Nov. 15 issue of JAMA (2014 [doi:10.1001/jama.2014.14721]).In a randomized trial of 154 kidney transplant patients, BK virus developed in 29% of those taking levofloxacin and in 33% of those taking placebo, a nonsignificant difference, coauthor Greg Knoll said at a late-breaking poster session during Kidney Week 2014, where the study was simultaneously presented.Levofloxacin, a quinolone antibiotic, has been shown to have some antiviral properties, especially against polyomaviruses – including BK virus, said Dr. Knoll of the University of Ottawa and the Ottawa Hospital.
Almost everyone harbors latent BK virus, Dr. Knoll said in an interview. It sometimes causes mild cold symptoms when first contracted, but often there’s no indication of illness at all. “If you’re otherwise healthy, it goes dormant and stays that way,” he noted.
But it can cause serious problems in immunocompromised patients, especially those with a kidney transplant. “BK virus tends to live in the bladder and urinary tract,” Dr. Knoll said, “So, when it reactivates, that’s the site where it does its damage.”
The virus will first appear in the urine, and then follow a logical progression through the ureters and into the kidney. If it remains unchecked, it causes very severe kidney inflammation. That inflammation “looks a lot like rejection,” Dr. Knoll said. “In fact, for years, we were very confused about this and ended up giving patients with BK viremia more immunosuppressants – when we actually should have been giving them less.”
It’s been tough to find the right balance of treatment to combat BK infections and immunosuppressants to maintain the allograft, he said.
Some retrospective studies suggested that quinolone antibiotics – including levofloxacin – could help fight cytomegalovirus infections and viral pneumonia, and decrease inflammatory markers in the urine of kidney transplant patients. “This was the little bit of evidence we needed to launch this study,” Dr. Knoll said.
The study investigators examined the time to first occurrence of BK viruria within the first year of transplant. Secondary outcomes included BK viremia, peak viral load, rejection, and patient and allograft survival.
Patients’ mean age was 48 years. They had undergone kidney transplant for a variety of reasons, including glomerulonephritis, polycystic kidney disease, diabetes, and hypertension. Comorbidities were common and included diabetes, history of cancer, cardiovascular disease, and hepatitis C and B infections. Most had received a living donor transplant (60%); the rest had kidneys from deceased donors.
Treatment began soon after transplantation. Patients were randomized to a target dose of 500 mg/day levofloxacin for 3 months. The mean length of follow-up was 46 weeks.
The primary outcome of BK viruria occurred in 46 patients – 29% of those in the levofloxacin group and 33.3% of those in the placebo group. That translated to a nonsignificant increased viruria risk of about 4%.
The time to viruria was not significantly different between the groups, with nearly 25% of each group developing it by 25 weeks. Nor was there a between-group difference in the occurrence of sustained viruria.
The secondary endpoint of BK viremia occurred in 7.9% of the levofloxacin group and 11.5% of the placebo group, also a nonsignificant finding. Infections were similar in both group, occurring in 59% of those taking levofloxacin and 45% of those taking placebo. The types of infections were similar: urinary tract/pyelonephritis (37% active vs. 38% placebo); cytomegalovirus (35% vs. 33%); pneumonia (3.5% vs. 1.7%); cellulitis (2.7% vs. 0.8%); and line infections and bacteremias, which were less than 1% in each group. No patient developed a Clostridium difficile infection.
However, patients taking levofloxacin developed significantly more quinolone-resistant infections (46.7% vs. 32.6%). Among isolates that are usually sensitive to quinolones, those patients taking the study drug were 75% more likely than were placebo patients to have a resistant strain (58.3% vs. 33.3%).
Because quinolones are an important part of infection prophylaxis in kidney transplant patients, “This would have significant implications for the management of common infections after transplantation,” Dr. Knoll said. “Our results don’t support the use of levofloxacin for preventing infections in patients with kidney transplants.”
The researchers were disappointed in the outcomes, “but there were people doing this already, and now we have the evidence to tell them to stop,” Dr. Knoll explained. “Of course, we are back to square one, with no proven treatment.”
He added that the quinolones remain critical antibiotics for kidney transplant patients – and that the study in no way suggests that should change.
“We were using these daily for 3 months, and that’s where we got into the resistance trouble,” he said. “That’s not anything like a 7- to 10-day course for a urinary tract infection.”
Dr. Knoll reported receiving investigator-initiated research grants from Astellas Canada and Pfizer Canada. The other coauthors had a number of financial relationships with pharmaceutical companies.
On Twitter @alz_gal
PHILADELPHIA – A 3-month course of levofloxacin after kidney transplant didn’t prevent BK virus from colonizing the urine, setting the stage for viremia in these immunosuppressed patients.
However, the antibiotic was associated with a significant 75% increase in the risk of developing a quinolone-resistant infection, compared with placebo, Dr. Greg A. Knoll and his colleagues reported in the Nov. 15 issue of JAMA (2014 [doi:10.1001/jama.2014.14721]).In a randomized trial of 154 kidney transplant patients, BK virus developed in 29% of those taking levofloxacin and in 33% of those taking placebo, a nonsignificant difference, coauthor Greg Knoll said at a late-breaking poster session during Kidney Week 2014, where the study was simultaneously presented.Levofloxacin, a quinolone antibiotic, has been shown to have some antiviral properties, especially against polyomaviruses – including BK virus, said Dr. Knoll of the University of Ottawa and the Ottawa Hospital.
Almost everyone harbors latent BK virus, Dr. Knoll said in an interview. It sometimes causes mild cold symptoms when first contracted, but often there’s no indication of illness at all. “If you’re otherwise healthy, it goes dormant and stays that way,” he noted.
But it can cause serious problems in immunocompromised patients, especially those with a kidney transplant. “BK virus tends to live in the bladder and urinary tract,” Dr. Knoll said, “So, when it reactivates, that’s the site where it does its damage.”
The virus will first appear in the urine, and then follow a logical progression through the ureters and into the kidney. If it remains unchecked, it causes very severe kidney inflammation. That inflammation “looks a lot like rejection,” Dr. Knoll said. “In fact, for years, we were very confused about this and ended up giving patients with BK viremia more immunosuppressants – when we actually should have been giving them less.”
It’s been tough to find the right balance of treatment to combat BK infections and immunosuppressants to maintain the allograft, he said.
Some retrospective studies suggested that quinolone antibiotics – including levofloxacin – could help fight cytomegalovirus infections and viral pneumonia, and decrease inflammatory markers in the urine of kidney transplant patients. “This was the little bit of evidence we needed to launch this study,” Dr. Knoll said.
The study investigators examined the time to first occurrence of BK viruria within the first year of transplant. Secondary outcomes included BK viremia, peak viral load, rejection, and patient and allograft survival.
Patients’ mean age was 48 years. They had undergone kidney transplant for a variety of reasons, including glomerulonephritis, polycystic kidney disease, diabetes, and hypertension. Comorbidities were common and included diabetes, history of cancer, cardiovascular disease, and hepatitis C and B infections. Most had received a living donor transplant (60%); the rest had kidneys from deceased donors.
Treatment began soon after transplantation. Patients were randomized to a target dose of 500 mg/day levofloxacin for 3 months. The mean length of follow-up was 46 weeks.
The primary outcome of BK viruria occurred in 46 patients – 29% of those in the levofloxacin group and 33.3% of those in the placebo group. That translated to a nonsignificant increased viruria risk of about 4%.
The time to viruria was not significantly different between the groups, with nearly 25% of each group developing it by 25 weeks. Nor was there a between-group difference in the occurrence of sustained viruria.
The secondary endpoint of BK viremia occurred in 7.9% of the levofloxacin group and 11.5% of the placebo group, also a nonsignificant finding. Infections were similar in both group, occurring in 59% of those taking levofloxacin and 45% of those taking placebo. The types of infections were similar: urinary tract/pyelonephritis (37% active vs. 38% placebo); cytomegalovirus (35% vs. 33%); pneumonia (3.5% vs. 1.7%); cellulitis (2.7% vs. 0.8%); and line infections and bacteremias, which were less than 1% in each group. No patient developed a Clostridium difficile infection.
However, patients taking levofloxacin developed significantly more quinolone-resistant infections (46.7% vs. 32.6%). Among isolates that are usually sensitive to quinolones, those patients taking the study drug were 75% more likely than were placebo patients to have a resistant strain (58.3% vs. 33.3%).
Because quinolones are an important part of infection prophylaxis in kidney transplant patients, “This would have significant implications for the management of common infections after transplantation,” Dr. Knoll said. “Our results don’t support the use of levofloxacin for preventing infections in patients with kidney transplants.”
The researchers were disappointed in the outcomes, “but there were people doing this already, and now we have the evidence to tell them to stop,” Dr. Knoll explained. “Of course, we are back to square one, with no proven treatment.”
He added that the quinolones remain critical antibiotics for kidney transplant patients – and that the study in no way suggests that should change.
“We were using these daily for 3 months, and that’s where we got into the resistance trouble,” he said. “That’s not anything like a 7- to 10-day course for a urinary tract infection.”
Dr. Knoll reported receiving investigator-initiated research grants from Astellas Canada and Pfizer Canada. The other coauthors had a number of financial relationships with pharmaceutical companies.
On Twitter @alz_gal
PHILADELPHIA – A 3-month course of levofloxacin after kidney transplant didn’t prevent BK virus from colonizing the urine, setting the stage for viremia in these immunosuppressed patients.
However, the antibiotic was associated with a significant 75% increase in the risk of developing a quinolone-resistant infection, compared with placebo, Dr. Greg A. Knoll and his colleagues reported in the Nov. 15 issue of JAMA (2014 [doi:10.1001/jama.2014.14721]).In a randomized trial of 154 kidney transplant patients, BK virus developed in 29% of those taking levofloxacin and in 33% of those taking placebo, a nonsignificant difference, coauthor Greg Knoll said at a late-breaking poster session during Kidney Week 2014, where the study was simultaneously presented.Levofloxacin, a quinolone antibiotic, has been shown to have some antiviral properties, especially against polyomaviruses – including BK virus, said Dr. Knoll of the University of Ottawa and the Ottawa Hospital.
Almost everyone harbors latent BK virus, Dr. Knoll said in an interview. It sometimes causes mild cold symptoms when first contracted, but often there’s no indication of illness at all. “If you’re otherwise healthy, it goes dormant and stays that way,” he noted.
But it can cause serious problems in immunocompromised patients, especially those with a kidney transplant. “BK virus tends to live in the bladder and urinary tract,” Dr. Knoll said, “So, when it reactivates, that’s the site where it does its damage.”
The virus will first appear in the urine, and then follow a logical progression through the ureters and into the kidney. If it remains unchecked, it causes very severe kidney inflammation. That inflammation “looks a lot like rejection,” Dr. Knoll said. “In fact, for years, we were very confused about this and ended up giving patients with BK viremia more immunosuppressants – when we actually should have been giving them less.”
It’s been tough to find the right balance of treatment to combat BK infections and immunosuppressants to maintain the allograft, he said.
Some retrospective studies suggested that quinolone antibiotics – including levofloxacin – could help fight cytomegalovirus infections and viral pneumonia, and decrease inflammatory markers in the urine of kidney transplant patients. “This was the little bit of evidence we needed to launch this study,” Dr. Knoll said.
The study investigators examined the time to first occurrence of BK viruria within the first year of transplant. Secondary outcomes included BK viremia, peak viral load, rejection, and patient and allograft survival.
Patients’ mean age was 48 years. They had undergone kidney transplant for a variety of reasons, including glomerulonephritis, polycystic kidney disease, diabetes, and hypertension. Comorbidities were common and included diabetes, history of cancer, cardiovascular disease, and hepatitis C and B infections. Most had received a living donor transplant (60%); the rest had kidneys from deceased donors.
Treatment began soon after transplantation. Patients were randomized to a target dose of 500 mg/day levofloxacin for 3 months. The mean length of follow-up was 46 weeks.
The primary outcome of BK viruria occurred in 46 patients – 29% of those in the levofloxacin group and 33.3% of those in the placebo group. That translated to a nonsignificant increased viruria risk of about 4%.
The time to viruria was not significantly different between the groups, with nearly 25% of each group developing it by 25 weeks. Nor was there a between-group difference in the occurrence of sustained viruria.
The secondary endpoint of BK viremia occurred in 7.9% of the levofloxacin group and 11.5% of the placebo group, also a nonsignificant finding. Infections were similar in both group, occurring in 59% of those taking levofloxacin and 45% of those taking placebo. The types of infections were similar: urinary tract/pyelonephritis (37% active vs. 38% placebo); cytomegalovirus (35% vs. 33%); pneumonia (3.5% vs. 1.7%); cellulitis (2.7% vs. 0.8%); and line infections and bacteremias, which were less than 1% in each group. No patient developed a Clostridium difficile infection.
However, patients taking levofloxacin developed significantly more quinolone-resistant infections (46.7% vs. 32.6%). Among isolates that are usually sensitive to quinolones, those patients taking the study drug were 75% more likely than were placebo patients to have a resistant strain (58.3% vs. 33.3%).
Because quinolones are an important part of infection prophylaxis in kidney transplant patients, “This would have significant implications for the management of common infections after transplantation,” Dr. Knoll said. “Our results don’t support the use of levofloxacin for preventing infections in patients with kidney transplants.”
The researchers were disappointed in the outcomes, “but there were people doing this already, and now we have the evidence to tell them to stop,” Dr. Knoll explained. “Of course, we are back to square one, with no proven treatment.”
He added that the quinolones remain critical antibiotics for kidney transplant patients – and that the study in no way suggests that should change.
“We were using these daily for 3 months, and that’s where we got into the resistance trouble,” he said. “That’s not anything like a 7- to 10-day course for a urinary tract infection.”
Dr. Knoll reported receiving investigator-initiated research grants from Astellas Canada and Pfizer Canada. The other coauthors had a number of financial relationships with pharmaceutical companies.
On Twitter @alz_gal
FROM KIDNEY WEEK 2014
Key clinical point: Levofloxacin prophylaxis isn’t recommended after kidney transplant, because it failed to prevent BK viruria and was associated with an increase in quinolone-resistant bacterial isolates.
Major finding: Levofloxacin 500 mg daily for 3 months did not reduce the risk of BK viruria in patients who had a kidney transplant.
Data source: The randomized trial comprised 154 patients.
Disclosures: Dr. Knoll reported receiving investigator-initiated research grants from Astellas Canada and Pfizer Canada. The other coauthors had a number of financial relationships with pharmaceutical companies
Feds try to clarify meaningful use attestation, hardship rules
WASHINGTON – Feeling confused about how to attest to meaningful use or how to claim a hardship exemption in 2014?
You’re not alone. Federal officials say they’ve gotten lots of questions and comments in the wake of allowing flexibility on the version of certified electronic health record that can be used and on hardship exemptions for a subset of meaningful users.
Elizabeth Myers, Policy and Outreach Lead for the Centers for Medicare & Medicaid Services’ Office of E-Health Standards and Services, tried to provide some clarity to what those rules mean for practicing physicians at the annual symposium of the American Medical Informatics Association.
On the first rule on certified EHRs, “all we did is delay the expiration of 2011 edition software,” Ms. Myers said.
Physicians who have used the 2011 edition all year will be attesting to the 2013 definition of meaningful use, using those specific objectives and clinical quality measures. Those using the 2014 edition will be attesting to the 2014 definition.
The rule was “pretty vague” on what was expected for those using a combination of the 2011 and 2014 editions, Ms. Myers said. “That’s not trying to be confusing or difficult, much as it may seem that way sometimes,” she said. “It’s really on purpose, because we recognize it will be different for every provider.”
The first step for any meaningful user seeking to attest is to visit the Office of the National Coordinator’s Certified Health IT Product website. Once there, enter in all the product names used. The system will determine whether you are using the 2011 or 2014 version, or a combination.
Users of the 2011 version are taken directly to the 2013 definitions and measures, and can follow through on attestation. Those using the 2014 version are taken to the 2014 definitions and measures for attestation.
Combination users are given a unique identifier. Once that’s entered, the system asks whether the user wants to use the 2013 or 2014 measures for attestation. The meaningful user is then walked through one of those two paths, Ms. Myers said.
Hospitals have until Nov. 30 to attest. Physicians and other eligible health care providers can start attesting now. They have the option of attesting all the way through end of February, Ms. Myers said.
She also sought to clear up confusion about the hardship exemptions. For first-time participants in 2014, applying for a hardship this year was necessary to avoid a penalty in 2015.
“The reopened, extended period for hardship applications ... is for those new participants who are still struggling to get their 2014 software in place,” Ms. Myers said. “If you are unable to fully implement 2014 edition software in 2014 and you have participated in the program in the past, your application for your hardship is due in 2015 to avoid the 2016 payment adjustment.”
Those hardship applications are due April 1 for hospitals and July 1 for eligible professionals, Ms. Myers said.
In terms of what can be claimed as a hardship, the reason has to be related to the functioning of the software – not that “I didn’t feel like paying for it,” or “I was on vacation,” she said. It has to be that you were unable to implement the software to fully meet meaningful use.
Be ready to document the request, but certified letters from vendors saying it was their fault aren’t necessary. “You need the documentation that demonstrates your circumstances,” she said. That means being able to show the certified software used, your approach for meeting objectives and measures, and how the system may have failed you.
“Keep those records,” Ms. Myers said.
On Twitter @aliciaault
WASHINGTON – Feeling confused about how to attest to meaningful use or how to claim a hardship exemption in 2014?
You’re not alone. Federal officials say they’ve gotten lots of questions and comments in the wake of allowing flexibility on the version of certified electronic health record that can be used and on hardship exemptions for a subset of meaningful users.
Elizabeth Myers, Policy and Outreach Lead for the Centers for Medicare & Medicaid Services’ Office of E-Health Standards and Services, tried to provide some clarity to what those rules mean for practicing physicians at the annual symposium of the American Medical Informatics Association.
On the first rule on certified EHRs, “all we did is delay the expiration of 2011 edition software,” Ms. Myers said.
Physicians who have used the 2011 edition all year will be attesting to the 2013 definition of meaningful use, using those specific objectives and clinical quality measures. Those using the 2014 edition will be attesting to the 2014 definition.
The rule was “pretty vague” on what was expected for those using a combination of the 2011 and 2014 editions, Ms. Myers said. “That’s not trying to be confusing or difficult, much as it may seem that way sometimes,” she said. “It’s really on purpose, because we recognize it will be different for every provider.”
The first step for any meaningful user seeking to attest is to visit the Office of the National Coordinator’s Certified Health IT Product website. Once there, enter in all the product names used. The system will determine whether you are using the 2011 or 2014 version, or a combination.
Users of the 2011 version are taken directly to the 2013 definitions and measures, and can follow through on attestation. Those using the 2014 version are taken to the 2014 definitions and measures for attestation.
Combination users are given a unique identifier. Once that’s entered, the system asks whether the user wants to use the 2013 or 2014 measures for attestation. The meaningful user is then walked through one of those two paths, Ms. Myers said.
Hospitals have until Nov. 30 to attest. Physicians and other eligible health care providers can start attesting now. They have the option of attesting all the way through end of February, Ms. Myers said.
She also sought to clear up confusion about the hardship exemptions. For first-time participants in 2014, applying for a hardship this year was necessary to avoid a penalty in 2015.
“The reopened, extended period for hardship applications ... is for those new participants who are still struggling to get their 2014 software in place,” Ms. Myers said. “If you are unable to fully implement 2014 edition software in 2014 and you have participated in the program in the past, your application for your hardship is due in 2015 to avoid the 2016 payment adjustment.”
Those hardship applications are due April 1 for hospitals and July 1 for eligible professionals, Ms. Myers said.
In terms of what can be claimed as a hardship, the reason has to be related to the functioning of the software – not that “I didn’t feel like paying for it,” or “I was on vacation,” she said. It has to be that you were unable to implement the software to fully meet meaningful use.
Be ready to document the request, but certified letters from vendors saying it was their fault aren’t necessary. “You need the documentation that demonstrates your circumstances,” she said. That means being able to show the certified software used, your approach for meeting objectives and measures, and how the system may have failed you.
“Keep those records,” Ms. Myers said.
On Twitter @aliciaault
WASHINGTON – Feeling confused about how to attest to meaningful use or how to claim a hardship exemption in 2014?
You’re not alone. Federal officials say they’ve gotten lots of questions and comments in the wake of allowing flexibility on the version of certified electronic health record that can be used and on hardship exemptions for a subset of meaningful users.
Elizabeth Myers, Policy and Outreach Lead for the Centers for Medicare & Medicaid Services’ Office of E-Health Standards and Services, tried to provide some clarity to what those rules mean for practicing physicians at the annual symposium of the American Medical Informatics Association.
On the first rule on certified EHRs, “all we did is delay the expiration of 2011 edition software,” Ms. Myers said.
Physicians who have used the 2011 edition all year will be attesting to the 2013 definition of meaningful use, using those specific objectives and clinical quality measures. Those using the 2014 edition will be attesting to the 2014 definition.
The rule was “pretty vague” on what was expected for those using a combination of the 2011 and 2014 editions, Ms. Myers said. “That’s not trying to be confusing or difficult, much as it may seem that way sometimes,” she said. “It’s really on purpose, because we recognize it will be different for every provider.”
The first step for any meaningful user seeking to attest is to visit the Office of the National Coordinator’s Certified Health IT Product website. Once there, enter in all the product names used. The system will determine whether you are using the 2011 or 2014 version, or a combination.
Users of the 2011 version are taken directly to the 2013 definitions and measures, and can follow through on attestation. Those using the 2014 version are taken to the 2014 definitions and measures for attestation.
Combination users are given a unique identifier. Once that’s entered, the system asks whether the user wants to use the 2013 or 2014 measures for attestation. The meaningful user is then walked through one of those two paths, Ms. Myers said.
Hospitals have until Nov. 30 to attest. Physicians and other eligible health care providers can start attesting now. They have the option of attesting all the way through end of February, Ms. Myers said.
She also sought to clear up confusion about the hardship exemptions. For first-time participants in 2014, applying for a hardship this year was necessary to avoid a penalty in 2015.
“The reopened, extended period for hardship applications ... is for those new participants who are still struggling to get their 2014 software in place,” Ms. Myers said. “If you are unable to fully implement 2014 edition software in 2014 and you have participated in the program in the past, your application for your hardship is due in 2015 to avoid the 2016 payment adjustment.”
Those hardship applications are due April 1 for hospitals and July 1 for eligible professionals, Ms. Myers said.
In terms of what can be claimed as a hardship, the reason has to be related to the functioning of the software – not that “I didn’t feel like paying for it,” or “I was on vacation,” she said. It has to be that you were unable to implement the software to fully meet meaningful use.
Be ready to document the request, but certified letters from vendors saying it was their fault aren’t necessary. “You need the documentation that demonstrates your circumstances,” she said. That means being able to show the certified software used, your approach for meeting objectives and measures, and how the system may have failed you.
“Keep those records,” Ms. Myers said.
On Twitter @aliciaault
AT THE AMIA 2014 ANNUAL SYMPOSIUM
Antibiotic bowel prep significantly reduces colon surgery infections
SAN FRANCISCO – Oral antibiotics with mechanical bowel preparation significantly reduce surgical site infections, length of hospital stay, and readmissions in both open and laparoscopic elective colorectal surgery, according to a review of 8,415 cases in the National Surgery Quality Improvement Program.
It “should be adopted for elective colorectal surgery,” concluded the investigators, led by colorectal surgeon Melanie Morris of the University of Alabama at Birmingham.
A quarter of the patients had no bowel prep, 45% had mechanical prep alone – GoLytely or another laxative, and 30% received both oral antibiotics and mechanical prep. Partial colectomy and sigmoid resections were the most common procedures, generally for neoplasms or diverticulitis.
Overall, 15% of the no-prep group, 12% of the mechanical prep group, and 6.5% of the oral antibiotic plus mechanical prep group developed subsequent surgical site infections (SSIs), a statistically significant difference. Results were similar when broken down into superficial, deep wound, and organ space infections (J. Am. Coll. Surg. 2014:219;S18-19).
On multivariate analysis and after adjusting for diabetes, smoking, age, and other potential confounders, the antibiotic group was 54% less likely than the no-prep group to develop an SSI (odds ratio 0.46), 26% less likely to be readmitted (OR 0.74), and more likely to leave the hospital earlier, at about 4 days instead of 5 (OR 0.90). SSIs and readmissions were only slightly less likely in the mechanical prep–only group, compared with the no-prep group, and there was no difference in length of stay.
There were fewer anastomotic leaks, fewer cases of sepsis, less significant bleeding, and other benefits for oral antibiotics with mechanical preparation. In addition, there was a protective effect against 30-day mortality in open procedures.
“Even in the minimally invasive group,” about two-thirds of patients, “oral antibiotic prep … was protective for surgical site infections,” Dr. Morris said at the annual clinical congress of the American College of Surgeons.
Still, bowel prep remains “a very controversial topic.” Nationwide some surgeons prep, some don’t. “People have very strong beliefs that may or may not be rooted in the data,” she said.
There are concerns about fluid and electrolyte disturbances, Clostridium difficile overgrowth, and other potential problems. Plus, mechanical preparation hasn’t worked any better than placebo in recent studies, but many of those studies didn’t include oral antibiotics. Effective bowel prep includes both, Dr. Morris said.
It’s possible that confounders might have been at work in the Alabama study. Perhaps surgeons shied away from bowel prep in older, sicker patients, but the rate of acute renal injury was the same in all three study groups at about 0.9%, suggesting similar background comorbidities.
“I don’t think confounding issues” explain the findings. Previously, “we’ve shown the benefit of oral antibiotic bowel prep in a [Veterans Affairs] cohort, and now we’ve shown it in this national cohort,” Dr. Morris said (Dis. Colon. Rectum 2012;55:1160-6).
After a marked reduction in surgical site infections in the VA study, “we changed our practices. We now do mechanical and oral antibiotic preps and have seen a 50% reduction in our SSI rate. We don’t feel like we are doing anything else differently,” she said.
Dr. Morris has no disclosures.
SAN FRANCISCO – Oral antibiotics with mechanical bowel preparation significantly reduce surgical site infections, length of hospital stay, and readmissions in both open and laparoscopic elective colorectal surgery, according to a review of 8,415 cases in the National Surgery Quality Improvement Program.
It “should be adopted for elective colorectal surgery,” concluded the investigators, led by colorectal surgeon Melanie Morris of the University of Alabama at Birmingham.
A quarter of the patients had no bowel prep, 45% had mechanical prep alone – GoLytely or another laxative, and 30% received both oral antibiotics and mechanical prep. Partial colectomy and sigmoid resections were the most common procedures, generally for neoplasms or diverticulitis.
Overall, 15% of the no-prep group, 12% of the mechanical prep group, and 6.5% of the oral antibiotic plus mechanical prep group developed subsequent surgical site infections (SSIs), a statistically significant difference. Results were similar when broken down into superficial, deep wound, and organ space infections (J. Am. Coll. Surg. 2014:219;S18-19).
On multivariate analysis and after adjusting for diabetes, smoking, age, and other potential confounders, the antibiotic group was 54% less likely than the no-prep group to develop an SSI (odds ratio 0.46), 26% less likely to be readmitted (OR 0.74), and more likely to leave the hospital earlier, at about 4 days instead of 5 (OR 0.90). SSIs and readmissions were only slightly less likely in the mechanical prep–only group, compared with the no-prep group, and there was no difference in length of stay.
There were fewer anastomotic leaks, fewer cases of sepsis, less significant bleeding, and other benefits for oral antibiotics with mechanical preparation. In addition, there was a protective effect against 30-day mortality in open procedures.
“Even in the minimally invasive group,” about two-thirds of patients, “oral antibiotic prep … was protective for surgical site infections,” Dr. Morris said at the annual clinical congress of the American College of Surgeons.
Still, bowel prep remains “a very controversial topic.” Nationwide some surgeons prep, some don’t. “People have very strong beliefs that may or may not be rooted in the data,” she said.
There are concerns about fluid and electrolyte disturbances, Clostridium difficile overgrowth, and other potential problems. Plus, mechanical preparation hasn’t worked any better than placebo in recent studies, but many of those studies didn’t include oral antibiotics. Effective bowel prep includes both, Dr. Morris said.
It’s possible that confounders might have been at work in the Alabama study. Perhaps surgeons shied away from bowel prep in older, sicker patients, but the rate of acute renal injury was the same in all three study groups at about 0.9%, suggesting similar background comorbidities.
“I don’t think confounding issues” explain the findings. Previously, “we’ve shown the benefit of oral antibiotic bowel prep in a [Veterans Affairs] cohort, and now we’ve shown it in this national cohort,” Dr. Morris said (Dis. Colon. Rectum 2012;55:1160-6).
After a marked reduction in surgical site infections in the VA study, “we changed our practices. We now do mechanical and oral antibiotic preps and have seen a 50% reduction in our SSI rate. We don’t feel like we are doing anything else differently,” she said.
Dr. Morris has no disclosures.
SAN FRANCISCO – Oral antibiotics with mechanical bowel preparation significantly reduce surgical site infections, length of hospital stay, and readmissions in both open and laparoscopic elective colorectal surgery, according to a review of 8,415 cases in the National Surgery Quality Improvement Program.
It “should be adopted for elective colorectal surgery,” concluded the investigators, led by colorectal surgeon Melanie Morris of the University of Alabama at Birmingham.
A quarter of the patients had no bowel prep, 45% had mechanical prep alone – GoLytely or another laxative, and 30% received both oral antibiotics and mechanical prep. Partial colectomy and sigmoid resections were the most common procedures, generally for neoplasms or diverticulitis.
Overall, 15% of the no-prep group, 12% of the mechanical prep group, and 6.5% of the oral antibiotic plus mechanical prep group developed subsequent surgical site infections (SSIs), a statistically significant difference. Results were similar when broken down into superficial, deep wound, and organ space infections (J. Am. Coll. Surg. 2014:219;S18-19).
On multivariate analysis and after adjusting for diabetes, smoking, age, and other potential confounders, the antibiotic group was 54% less likely than the no-prep group to develop an SSI (odds ratio 0.46), 26% less likely to be readmitted (OR 0.74), and more likely to leave the hospital earlier, at about 4 days instead of 5 (OR 0.90). SSIs and readmissions were only slightly less likely in the mechanical prep–only group, compared with the no-prep group, and there was no difference in length of stay.
There were fewer anastomotic leaks, fewer cases of sepsis, less significant bleeding, and other benefits for oral antibiotics with mechanical preparation. In addition, there was a protective effect against 30-day mortality in open procedures.
“Even in the minimally invasive group,” about two-thirds of patients, “oral antibiotic prep … was protective for surgical site infections,” Dr. Morris said at the annual clinical congress of the American College of Surgeons.
Still, bowel prep remains “a very controversial topic.” Nationwide some surgeons prep, some don’t. “People have very strong beliefs that may or may not be rooted in the data,” she said.
There are concerns about fluid and electrolyte disturbances, Clostridium difficile overgrowth, and other potential problems. Plus, mechanical preparation hasn’t worked any better than placebo in recent studies, but many of those studies didn’t include oral antibiotics. Effective bowel prep includes both, Dr. Morris said.
It’s possible that confounders might have been at work in the Alabama study. Perhaps surgeons shied away from bowel prep in older, sicker patients, but the rate of acute renal injury was the same in all three study groups at about 0.9%, suggesting similar background comorbidities.
“I don’t think confounding issues” explain the findings. Previously, “we’ve shown the benefit of oral antibiotic bowel prep in a [Veterans Affairs] cohort, and now we’ve shown it in this national cohort,” Dr. Morris said (Dis. Colon. Rectum 2012;55:1160-6).
After a marked reduction in surgical site infections in the VA study, “we changed our practices. We now do mechanical and oral antibiotic preps and have seen a 50% reduction in our SSI rate. We don’t feel like we are doing anything else differently,” she said.
Dr. Morris has no disclosures.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Effective bowel prep must include oral antibiotics as well as laxatives.
Major finding: Prepping colorectal surgery patients with both oral antibiotics and laxatives halves the risk of surgery site infections (OR 0.46, 95% CI 0.36-0.59, P < .001),
Data source: Review of 8,415 cases in the National Surgery Quality Improvement Program
Disclosures: Dr. Morris has no relevant financial disclosures.
Low-stage colon cancers need to be followed post surgery for recurrence
SAN FRANCISCO – Patients with stage I colorectal cancer should be followed as closely as patients with higher-stage primary tumors after resection, according to a prospective 6-year surveillance study of 1,202 British patients.
The reason is that the incidence of recurrences that can be treated surgically with curative intent is the same in stage I patients as it is in patients with stage II and III primaries, about 6% (J. Am. Coll. Surg. 2014:219;e46-47).
Following resection with clear margins, the patients were randomized about 300 per group to either serial CT surveillance, serial carcinoembryonic antigen (CEA) monitoring, both, or minimum surveillance, and followed for a median of 4.4 years. About a quarter of the subjects had Dukes’ A primaries and a quarter Dukes’ C primaries, and about half had Dukes’ B primaries. The A, B, C designations are similar to the stage I, II, and III designations more common in the United States.
On both sides of the Atlantic, guidelines focus on active surveillance for higher-stage primaries, but are ambivalent about monitoring stage I tumors because they are less likely to recur and the benefit of follow-up has been uncertain.
That needs to change because treatable recurrences are what matters, and they are as likely in low-stage disease as in high-stage disease, lead investigator Dr. Sian Pugh, a colorectal surgeon at the University of Southampton (England), said at the annual clinical congress of the American College of Surgeons.
“Picking up recurrences that are not treatable doesn’t help anyone; it just gives you bad news earlier,” she said. The benefit of follow-up is “finding treatable disease, and that’s independent of the stage of the primary tumor. We recommend equivalent follow-up for all patients with resected Dukes’ A-C colorectal cancer. The guidelines [should] be reconsidered,” she asserted.
Her team also thinks that the most cost-effective way to monitor patients is probably with CEA monitoring every 3 months for the first 2 years, CEA monitoring every 6 months thereafter until year 5, and a single CT at 12-18 months to catch recurrences that don’t express CEA. That strategy was three times more likely than minimal surveillance to find treatable recurrences, about the same as serial CTs and serial CTs with regular CEA monitoring.
“We don’t think patients need to be followed up quite as intensively as the guidelines suggest,” – for instance, CT scans every 6 months – “but we are waiting for more health economic analysis,” Dr. Pugh said.
Although treatable recurrences were equally likely in all the groups, they were more common in patients with lower-stage primary cancers. Among recurrences in patients with Dukes’ A primary tumors, 50% (13/26) were treated surgically with curative intent, compared with 40% (32/81) in patients with Dukes’ B primaries and 24% (20/82) in those with Dukes’ C.
Pulmonary recurrence was most frequent with rectal primary tumors, and multisite recurrence was most common from right-colonic cancers. Median survival following recurrence was 2.28 years and was influenced by stage and site of primary. Following recurrence, survival was highest in those with lower-stage and rectal primaries, and lowest in patients with higher-stage primaries and recurrence from the right colon.
Dr. Pugh had no disclosures. The work was funded by the U.K. National Health Service.
There’s a lot of heterogeneity in the United States with regard to how frequently people get surveillance imaging and CEA for colon cancer recurrence. The study is helpful because it presents data that inform the decision.
These data suggest that CEA on a regular basis and a CT scan at 1 year are enough. This may be a more rational, cost-effective way to screen people and still achieve what we’re trying to achieve: picking up treatable recurrences.
Dr. Timothy Pawlik is chief of the division of surgical oncology and a professor of surgery at Johns Hopkins University, Baltimore.
There’s a lot of heterogeneity in the United States with regard to how frequently people get surveillance imaging and CEA for colon cancer recurrence. The study is helpful because it presents data that inform the decision.
These data suggest that CEA on a regular basis and a CT scan at 1 year are enough. This may be a more rational, cost-effective way to screen people and still achieve what we’re trying to achieve: picking up treatable recurrences.
Dr. Timothy Pawlik is chief of the division of surgical oncology and a professor of surgery at Johns Hopkins University, Baltimore.
There’s a lot of heterogeneity in the United States with regard to how frequently people get surveillance imaging and CEA for colon cancer recurrence. The study is helpful because it presents data that inform the decision.
These data suggest that CEA on a regular basis and a CT scan at 1 year are enough. This may be a more rational, cost-effective way to screen people and still achieve what we’re trying to achieve: picking up treatable recurrences.
Dr. Timothy Pawlik is chief of the division of surgical oncology and a professor of surgery at Johns Hopkins University, Baltimore.
SAN FRANCISCO – Patients with stage I colorectal cancer should be followed as closely as patients with higher-stage primary tumors after resection, according to a prospective 6-year surveillance study of 1,202 British patients.
The reason is that the incidence of recurrences that can be treated surgically with curative intent is the same in stage I patients as it is in patients with stage II and III primaries, about 6% (J. Am. Coll. Surg. 2014:219;e46-47).
Following resection with clear margins, the patients were randomized about 300 per group to either serial CT surveillance, serial carcinoembryonic antigen (CEA) monitoring, both, or minimum surveillance, and followed for a median of 4.4 years. About a quarter of the subjects had Dukes’ A primaries and a quarter Dukes’ C primaries, and about half had Dukes’ B primaries. The A, B, C designations are similar to the stage I, II, and III designations more common in the United States.
On both sides of the Atlantic, guidelines focus on active surveillance for higher-stage primaries, but are ambivalent about monitoring stage I tumors because they are less likely to recur and the benefit of follow-up has been uncertain.
That needs to change because treatable recurrences are what matters, and they are as likely in low-stage disease as in high-stage disease, lead investigator Dr. Sian Pugh, a colorectal surgeon at the University of Southampton (England), said at the annual clinical congress of the American College of Surgeons.
“Picking up recurrences that are not treatable doesn’t help anyone; it just gives you bad news earlier,” she said. The benefit of follow-up is “finding treatable disease, and that’s independent of the stage of the primary tumor. We recommend equivalent follow-up for all patients with resected Dukes’ A-C colorectal cancer. The guidelines [should] be reconsidered,” she asserted.
Her team also thinks that the most cost-effective way to monitor patients is probably with CEA monitoring every 3 months for the first 2 years, CEA monitoring every 6 months thereafter until year 5, and a single CT at 12-18 months to catch recurrences that don’t express CEA. That strategy was three times more likely than minimal surveillance to find treatable recurrences, about the same as serial CTs and serial CTs with regular CEA monitoring.
“We don’t think patients need to be followed up quite as intensively as the guidelines suggest,” – for instance, CT scans every 6 months – “but we are waiting for more health economic analysis,” Dr. Pugh said.
Although treatable recurrences were equally likely in all the groups, they were more common in patients with lower-stage primary cancers. Among recurrences in patients with Dukes’ A primary tumors, 50% (13/26) were treated surgically with curative intent, compared with 40% (32/81) in patients with Dukes’ B primaries and 24% (20/82) in those with Dukes’ C.
Pulmonary recurrence was most frequent with rectal primary tumors, and multisite recurrence was most common from right-colonic cancers. Median survival following recurrence was 2.28 years and was influenced by stage and site of primary. Following recurrence, survival was highest in those with lower-stage and rectal primaries, and lowest in patients with higher-stage primaries and recurrence from the right colon.
Dr. Pugh had no disclosures. The work was funded by the U.K. National Health Service.
SAN FRANCISCO – Patients with stage I colorectal cancer should be followed as closely as patients with higher-stage primary tumors after resection, according to a prospective 6-year surveillance study of 1,202 British patients.
The reason is that the incidence of recurrences that can be treated surgically with curative intent is the same in stage I patients as it is in patients with stage II and III primaries, about 6% (J. Am. Coll. Surg. 2014:219;e46-47).
Following resection with clear margins, the patients were randomized about 300 per group to either serial CT surveillance, serial carcinoembryonic antigen (CEA) monitoring, both, or minimum surveillance, and followed for a median of 4.4 years. About a quarter of the subjects had Dukes’ A primaries and a quarter Dukes’ C primaries, and about half had Dukes’ B primaries. The A, B, C designations are similar to the stage I, II, and III designations more common in the United States.
On both sides of the Atlantic, guidelines focus on active surveillance for higher-stage primaries, but are ambivalent about monitoring stage I tumors because they are less likely to recur and the benefit of follow-up has been uncertain.
That needs to change because treatable recurrences are what matters, and they are as likely in low-stage disease as in high-stage disease, lead investigator Dr. Sian Pugh, a colorectal surgeon at the University of Southampton (England), said at the annual clinical congress of the American College of Surgeons.
“Picking up recurrences that are not treatable doesn’t help anyone; it just gives you bad news earlier,” she said. The benefit of follow-up is “finding treatable disease, and that’s independent of the stage of the primary tumor. We recommend equivalent follow-up for all patients with resected Dukes’ A-C colorectal cancer. The guidelines [should] be reconsidered,” she asserted.
Her team also thinks that the most cost-effective way to monitor patients is probably with CEA monitoring every 3 months for the first 2 years, CEA monitoring every 6 months thereafter until year 5, and a single CT at 12-18 months to catch recurrences that don’t express CEA. That strategy was three times more likely than minimal surveillance to find treatable recurrences, about the same as serial CTs and serial CTs with regular CEA monitoring.
“We don’t think patients need to be followed up quite as intensively as the guidelines suggest,” – for instance, CT scans every 6 months – “but we are waiting for more health economic analysis,” Dr. Pugh said.
Although treatable recurrences were equally likely in all the groups, they were more common in patients with lower-stage primary cancers. Among recurrences in patients with Dukes’ A primary tumors, 50% (13/26) were treated surgically with curative intent, compared with 40% (32/81) in patients with Dukes’ B primaries and 24% (20/82) in those with Dukes’ C.
Pulmonary recurrence was most frequent with rectal primary tumors, and multisite recurrence was most common from right-colonic cancers. Median survival following recurrence was 2.28 years and was influenced by stage and site of primary. Following recurrence, survival was highest in those with lower-stage and rectal primaries, and lowest in patients with higher-stage primaries and recurrence from the right colon.
Dr. Pugh had no disclosures. The work was funded by the U.K. National Health Service.
Key clinical point: The incidence of treatable recurrence is the same regardless of the stage of the primary colon tumor.
Major finding: Six percent of recurrent stage I, II, and III colon cancers can be treated surgically with curative intent.
Data source: Randomized surveillance study of 1,202 British colon cancer patients after removal of their primary tumors.
Disclosures: Dr. Pugh had no disclosures. The work was funded by the U.K. National Health Service.
Presurgical BMI doesn’t predict diabetes remission
A patient’s body mass index before bariatric surgery is unrelated to remission of his or her diabetes afterward, according to a report published online in Annals of Surgery.
In a meta-analysis of 94 observational and interventional clinical studies, the efficacy of the surgery as a metabolic procedure had nothing to do with baseline body mass index (BMI) and instead depended on the degree of diabetic compromise at baseline. “We believe therefore that the use of baseline BMIs to gauge the metabolic effect of surgery is misleading and should be avoided,” said Simona Panunzi, Ph.D., of the Italian National Council of Research-Institute of Systems Analysis and Computer Sciences, Biomathematics Laboratory, Rome, and her associates.
At present, baseline BMI is considered the only valid selection criterion for bariatric surgery in diabetic adults, even though numerous studies have reported that neither BMI nor body weight are good predictors of diabetes remission. In contrast, many other studies have reported that body fat distribution, and visceral obesity in particular, directly affects glycemic control, insulin resistance, and the metabolic syndrome, the investigators commented (Ann. Surg. 2014 Oct. 30 [E-pub ahead of print]).
To assess which factors best predict diabetes remission after bariatric surgery, Dr. Panunzi and her associates performed a systematic review and meta-analysis of the literature. They screened 1,437 articles and focused on 94: 35 studies included patients with a baseline BMI of less than 35 kg/m2, 56 studies included patients with a baseline BMI of 35 kg/m2 or more, and 3 studies included patients with any baseline BMI. There were a total of 94,579 patients, of whom 4,944 had type 2 diabetes.
The mean age of the study participants was approximately 46 years. Bariatric procedures included sleeve gastrectomy, Roux-en-Y gastric bypass, biliopancreatic diversion, laparoscopic gastric banding, and duodenal-jejunal bypass. Across all the studies, the percent reduction in mean BMI after surgery was 17% for patients with a baseline BMI of less than 35 kg/m2 (group 1) and 35% for those with a baseline BMI of 35 kg/m2 or more (group 2).
Diabetes remitted in 72% of the patients in group 1 and 71% of those in group 2, a nonsignificant difference. The only factor found to predict remission, defined as the normalization of HbA1c, was the severity of diabetes as measured by fasting levels of glucose, insulin, and HbA1c at baseline, the investigators said.
“The appropriateness of the BMI criterion proposed by the National Institutes of Health for determining the eligibility of patients with diabetes for bariatric surgery has already been challenged by other authors. However, until now there was no direct evidence of its lack of relevance. It seems clear from the results of [our] study that baseline BMI does not carry prognostic information for diabetes resolution after bariatric surgery,” they added.
This meta-analysis was limited in that few of the reviewed studies reported diabetes duration, a well-known predictor of remission. And the definition of diabetes remission varied widely among the studies, from simple withdrawal of diabetes medications to various specific plasma glucose or HbA1c levels, the investigators noted.
A patient’s body mass index before bariatric surgery is unrelated to remission of his or her diabetes afterward, according to a report published online in Annals of Surgery.
In a meta-analysis of 94 observational and interventional clinical studies, the efficacy of the surgery as a metabolic procedure had nothing to do with baseline body mass index (BMI) and instead depended on the degree of diabetic compromise at baseline. “We believe therefore that the use of baseline BMIs to gauge the metabolic effect of surgery is misleading and should be avoided,” said Simona Panunzi, Ph.D., of the Italian National Council of Research-Institute of Systems Analysis and Computer Sciences, Biomathematics Laboratory, Rome, and her associates.
At present, baseline BMI is considered the only valid selection criterion for bariatric surgery in diabetic adults, even though numerous studies have reported that neither BMI nor body weight are good predictors of diabetes remission. In contrast, many other studies have reported that body fat distribution, and visceral obesity in particular, directly affects glycemic control, insulin resistance, and the metabolic syndrome, the investigators commented (Ann. Surg. 2014 Oct. 30 [E-pub ahead of print]).
To assess which factors best predict diabetes remission after bariatric surgery, Dr. Panunzi and her associates performed a systematic review and meta-analysis of the literature. They screened 1,437 articles and focused on 94: 35 studies included patients with a baseline BMI of less than 35 kg/m2, 56 studies included patients with a baseline BMI of 35 kg/m2 or more, and 3 studies included patients with any baseline BMI. There were a total of 94,579 patients, of whom 4,944 had type 2 diabetes.
The mean age of the study participants was approximately 46 years. Bariatric procedures included sleeve gastrectomy, Roux-en-Y gastric bypass, biliopancreatic diversion, laparoscopic gastric banding, and duodenal-jejunal bypass. Across all the studies, the percent reduction in mean BMI after surgery was 17% for patients with a baseline BMI of less than 35 kg/m2 (group 1) and 35% for those with a baseline BMI of 35 kg/m2 or more (group 2).
Diabetes remitted in 72% of the patients in group 1 and 71% of those in group 2, a nonsignificant difference. The only factor found to predict remission, defined as the normalization of HbA1c, was the severity of diabetes as measured by fasting levels of glucose, insulin, and HbA1c at baseline, the investigators said.
“The appropriateness of the BMI criterion proposed by the National Institutes of Health for determining the eligibility of patients with diabetes for bariatric surgery has already been challenged by other authors. However, until now there was no direct evidence of its lack of relevance. It seems clear from the results of [our] study that baseline BMI does not carry prognostic information for diabetes resolution after bariatric surgery,” they added.
This meta-analysis was limited in that few of the reviewed studies reported diabetes duration, a well-known predictor of remission. And the definition of diabetes remission varied widely among the studies, from simple withdrawal of diabetes medications to various specific plasma glucose or HbA1c levels, the investigators noted.
A patient’s body mass index before bariatric surgery is unrelated to remission of his or her diabetes afterward, according to a report published online in Annals of Surgery.
In a meta-analysis of 94 observational and interventional clinical studies, the efficacy of the surgery as a metabolic procedure had nothing to do with baseline body mass index (BMI) and instead depended on the degree of diabetic compromise at baseline. “We believe therefore that the use of baseline BMIs to gauge the metabolic effect of surgery is misleading and should be avoided,” said Simona Panunzi, Ph.D., of the Italian National Council of Research-Institute of Systems Analysis and Computer Sciences, Biomathematics Laboratory, Rome, and her associates.
At present, baseline BMI is considered the only valid selection criterion for bariatric surgery in diabetic adults, even though numerous studies have reported that neither BMI nor body weight are good predictors of diabetes remission. In contrast, many other studies have reported that body fat distribution, and visceral obesity in particular, directly affects glycemic control, insulin resistance, and the metabolic syndrome, the investigators commented (Ann. Surg. 2014 Oct. 30 [E-pub ahead of print]).
To assess which factors best predict diabetes remission after bariatric surgery, Dr. Panunzi and her associates performed a systematic review and meta-analysis of the literature. They screened 1,437 articles and focused on 94: 35 studies included patients with a baseline BMI of less than 35 kg/m2, 56 studies included patients with a baseline BMI of 35 kg/m2 or more, and 3 studies included patients with any baseline BMI. There were a total of 94,579 patients, of whom 4,944 had type 2 diabetes.
The mean age of the study participants was approximately 46 years. Bariatric procedures included sleeve gastrectomy, Roux-en-Y gastric bypass, biliopancreatic diversion, laparoscopic gastric banding, and duodenal-jejunal bypass. Across all the studies, the percent reduction in mean BMI after surgery was 17% for patients with a baseline BMI of less than 35 kg/m2 (group 1) and 35% for those with a baseline BMI of 35 kg/m2 or more (group 2).
Diabetes remitted in 72% of the patients in group 1 and 71% of those in group 2, a nonsignificant difference. The only factor found to predict remission, defined as the normalization of HbA1c, was the severity of diabetes as measured by fasting levels of glucose, insulin, and HbA1c at baseline, the investigators said.
“The appropriateness of the BMI criterion proposed by the National Institutes of Health for determining the eligibility of patients with diabetes for bariatric surgery has already been challenged by other authors. However, until now there was no direct evidence of its lack of relevance. It seems clear from the results of [our] study that baseline BMI does not carry prognostic information for diabetes resolution after bariatric surgery,” they added.
This meta-analysis was limited in that few of the reviewed studies reported diabetes duration, a well-known predictor of remission. And the definition of diabetes remission varied widely among the studies, from simple withdrawal of diabetes medications to various specific plasma glucose or HbA1c levels, the investigators noted.
FROM ANNALS OF SURGERY
Key clinical point: BMI before bariatric surgery is unrelated to diabetes remission afterward.
Major finding: Diabetes remitted in 72% of the patients with a baseline BMI under 35 kg/m2 and 71% of those with a baseline BMI of 35 kg/m2 or more.
Data source: A meta-analysis of 94 clinical studies reporting bariatric surgery results for 94,579 overweight/obese patients, including 4,944 who had diabetes.
Disclosures: This study received no financial support from external sponsors. Dr. Panunzi and her associates reported having no financial disclosures.
Running history doesn’t contribute to knee OA risk
BOSTON– A history of current or past running did not contribute to a higher odds of developing knee osteoarthritis and may even have a slight protective effect, researchers found in a cross-sectional study of participants in the Osteoarthritis Initiative.
“Although this study does not address the question of whether or not running is harmful in people who do have preexisting knee OA [osteoarthritis], among people who do not have knee OA, [the study indicates that] there is no reason to restrict participation in habitual running at any time in life from the perspective that it does not appear to be harmful to the knee joint,” lead author Dr. Grace Hsiao-Wei Lo said at a press briefing at the annual meeting of the American College of Rheumatology.
Physical activities guidelines from the Centers for Disease Control and Prevention recommend that adults get at least 75 minutes per week of physical activity at a vigorous intensity, which includes running or jogging, noted Dr. Lo of the section of immunology, allergy, and rheumatology at Baylor College of Medicine, Houston.
The study, which is among the first to examine the potential relationship between running and OA in a population-based study of nonelite or high-level runners, included 2,683 participants (44% male) with a mean age of 64 years and mean body-mass index (BMI) of 28 kg/m2. The investigators found that 29% self-identified as runners as some point in their life up to their inclusion into study, with running history occurring in 49% of those aged older than 50 years, 31% in those aged 35-49 years, 15% in those aged 19-34 years, and 9% in those aged 12-18 years. Patients were identified as runners if they listed it as one of their top three activities during those periods. Runners were slightly younger than the overall population with a mean age of 62 years and were more often male (62%). Nonrunners had a mean age of 65 years and were less often male (36%). BMI did not differ between the two.
Knee pain was significantly less prevalent in runners than in nonrunners (35% vs. 42%, respectively), and runners were 13% less likely to have knee pain (odds ratio, 0.87). The relationship did not change after controlling for age, sex, and BMI.
Radiographic knee OA with a Kellgren-Lawrence grade of 2 or more also was significantly less common among runners than among nonrunners (54% vs. 60%), but the relationship was not significant after controlling for the same variables.
Symptomatic radiographic OA – defined as having at least one knee with both radiographic knee OA and frequent knee pain – occurred in 23% of runners and 30% of nonrunners. The significantly lower likelihood for runners to develop symptomatic knee OA than non-runners (OR, 0.83) was slightly attenuated after controlling for age, sex, and BMI, but remained statistically significant.
“When we did look at each individual age range, the results were very similar. Some of the results were no longer statistically significant, but the results were generally in the same direction,” Dr. Lo noted.
Previous studies that have examined the relationship between running and the development of knee OA have been limited in their generalizability to the general population because of the inclusion of elite runners and those with a high level of running as well as small sample size, Dr. Lo said. Self-selection as runners is an important limitation of this cross-sectional, observational study because “there’s always the possibility that people stopped running because they developed knee symptoms,” she said.
Dr. Lo said that her work on the study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. None of the other authors had disclosures.
BOSTON– A history of current or past running did not contribute to a higher odds of developing knee osteoarthritis and may even have a slight protective effect, researchers found in a cross-sectional study of participants in the Osteoarthritis Initiative.
“Although this study does not address the question of whether or not running is harmful in people who do have preexisting knee OA [osteoarthritis], among people who do not have knee OA, [the study indicates that] there is no reason to restrict participation in habitual running at any time in life from the perspective that it does not appear to be harmful to the knee joint,” lead author Dr. Grace Hsiao-Wei Lo said at a press briefing at the annual meeting of the American College of Rheumatology.
Physical activities guidelines from the Centers for Disease Control and Prevention recommend that adults get at least 75 minutes per week of physical activity at a vigorous intensity, which includes running or jogging, noted Dr. Lo of the section of immunology, allergy, and rheumatology at Baylor College of Medicine, Houston.
The study, which is among the first to examine the potential relationship between running and OA in a population-based study of nonelite or high-level runners, included 2,683 participants (44% male) with a mean age of 64 years and mean body-mass index (BMI) of 28 kg/m2. The investigators found that 29% self-identified as runners as some point in their life up to their inclusion into study, with running history occurring in 49% of those aged older than 50 years, 31% in those aged 35-49 years, 15% in those aged 19-34 years, and 9% in those aged 12-18 years. Patients were identified as runners if they listed it as one of their top three activities during those periods. Runners were slightly younger than the overall population with a mean age of 62 years and were more often male (62%). Nonrunners had a mean age of 65 years and were less often male (36%). BMI did not differ between the two.
Knee pain was significantly less prevalent in runners than in nonrunners (35% vs. 42%, respectively), and runners were 13% less likely to have knee pain (odds ratio, 0.87). The relationship did not change after controlling for age, sex, and BMI.
Radiographic knee OA with a Kellgren-Lawrence grade of 2 or more also was significantly less common among runners than among nonrunners (54% vs. 60%), but the relationship was not significant after controlling for the same variables.
Symptomatic radiographic OA – defined as having at least one knee with both radiographic knee OA and frequent knee pain – occurred in 23% of runners and 30% of nonrunners. The significantly lower likelihood for runners to develop symptomatic knee OA than non-runners (OR, 0.83) was slightly attenuated after controlling for age, sex, and BMI, but remained statistically significant.
“When we did look at each individual age range, the results were very similar. Some of the results were no longer statistically significant, but the results were generally in the same direction,” Dr. Lo noted.
Previous studies that have examined the relationship between running and the development of knee OA have been limited in their generalizability to the general population because of the inclusion of elite runners and those with a high level of running as well as small sample size, Dr. Lo said. Self-selection as runners is an important limitation of this cross-sectional, observational study because “there’s always the possibility that people stopped running because they developed knee symptoms,” she said.
Dr. Lo said that her work on the study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. None of the other authors had disclosures.
BOSTON– A history of current or past running did not contribute to a higher odds of developing knee osteoarthritis and may even have a slight protective effect, researchers found in a cross-sectional study of participants in the Osteoarthritis Initiative.
“Although this study does not address the question of whether or not running is harmful in people who do have preexisting knee OA [osteoarthritis], among people who do not have knee OA, [the study indicates that] there is no reason to restrict participation in habitual running at any time in life from the perspective that it does not appear to be harmful to the knee joint,” lead author Dr. Grace Hsiao-Wei Lo said at a press briefing at the annual meeting of the American College of Rheumatology.
Physical activities guidelines from the Centers for Disease Control and Prevention recommend that adults get at least 75 minutes per week of physical activity at a vigorous intensity, which includes running or jogging, noted Dr. Lo of the section of immunology, allergy, and rheumatology at Baylor College of Medicine, Houston.
The study, which is among the first to examine the potential relationship between running and OA in a population-based study of nonelite or high-level runners, included 2,683 participants (44% male) with a mean age of 64 years and mean body-mass index (BMI) of 28 kg/m2. The investigators found that 29% self-identified as runners as some point in their life up to their inclusion into study, with running history occurring in 49% of those aged older than 50 years, 31% in those aged 35-49 years, 15% in those aged 19-34 years, and 9% in those aged 12-18 years. Patients were identified as runners if they listed it as one of their top three activities during those periods. Runners were slightly younger than the overall population with a mean age of 62 years and were more often male (62%). Nonrunners had a mean age of 65 years and were less often male (36%). BMI did not differ between the two.
Knee pain was significantly less prevalent in runners than in nonrunners (35% vs. 42%, respectively), and runners were 13% less likely to have knee pain (odds ratio, 0.87). The relationship did not change after controlling for age, sex, and BMI.
Radiographic knee OA with a Kellgren-Lawrence grade of 2 or more also was significantly less common among runners than among nonrunners (54% vs. 60%), but the relationship was not significant after controlling for the same variables.
Symptomatic radiographic OA – defined as having at least one knee with both radiographic knee OA and frequent knee pain – occurred in 23% of runners and 30% of nonrunners. The significantly lower likelihood for runners to develop symptomatic knee OA than non-runners (OR, 0.83) was slightly attenuated after controlling for age, sex, and BMI, but remained statistically significant.
“When we did look at each individual age range, the results were very similar. Some of the results were no longer statistically significant, but the results were generally in the same direction,” Dr. Lo noted.
Previous studies that have examined the relationship between running and the development of knee OA have been limited in their generalizability to the general population because of the inclusion of elite runners and those with a high level of running as well as small sample size, Dr. Lo said. Self-selection as runners is an important limitation of this cross-sectional, observational study because “there’s always the possibility that people stopped running because they developed knee symptoms,” she said.
Dr. Lo said that her work on the study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. None of the other authors had disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point: There’s no need to restrict habitual running in people who don’t already have knee OA.
Major finding: Symptomatic radiographic OA occurred in 23% of runners and 30% of nonrunners
Data source: A cross-sectional study of 2,683 community-dwelling participants in the Osteoarthritis Initiative.
Disclosures: Dr. Lo said that her work on the study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. None of the other authors had disclosures.
Biomarkers may predict course after blunt trauma
Differences in circulating biomarkers distinguished blunt trauma patients who improved over time from those who instead developed serial persistent infections and multiple organ failures in a single-center retrospective cohort study published online in Annals of Surgery.
The distinctly different patterns in biomarkers were already becoming apparent in blood samples taken at admission to the ICU, and they evolved over the first week of hospitalization. The patterns in patients who went on to develop infections and organ failures most likely reflect an excessive inflammatory response to injury, which caused further immune dysregulation and impairment of host physiological function that rendered patients susceptible to severe infection.
“We propose that a combination of traditional parameters of inflammation, such as white blood cell differential, combined with a novel subset of circulating biomarkers measured upon presentation and over the initial 24 hours, could be used to stratify ICU patients for either more or less intensive care and monitoring,” wrote the investigators. This would optimize both resource utilization and patient outcomes, wrote the investigators, led by Dr. Rami A. Namas of the department of surgery and Center for Inflammation and Regenerative Modeling, McGowan Institute for Regenerative Medicine, University of Pittsburgh (Ann. Surg. 2014 Nov. 3).
They analyzed blood test results from 472 adults who survived severe blunt trauma and were admitted to the emergency department of a trauma center during an 8-year period. A total of 127 (27%) went on to develop persistent nosocomial infections – including 79 cases of pneumonia, 39 of urinary tract infections, 15 of bloodstream infections, 5 of wound infections, 2 of empyema, and 1 of Clostridium difficile infection – and organ failure. The study participants had undergone blood sampling via central venous or arterial catheters at least three times during the first 24 hours in the ICU, as well as at frequent intervals for at least a week. Samples were tested for the levels of 26 inflammatory biomarkers.
The investigators then performed a case-control analysis differentiating the blood test results between a subgroup of 44 patients who never developed nosocomial infections from 44 who had. They excluded patients who received blood transfusions or underwent emergency surgery within the first 24 hours, “to avoid the confounding impact of these interventions on the overall inflammatory response.” They also selected only patients whose trauma was caused by a motor vehicle accident, to avoid confounding factors related to the mechanism of injury. The two study groups were rigorously matched for patient age, patient sex, and Injury Severity Score.
Overall, injury severity was comparable between the two study groups. The severity of brain injury in particular, as reflected in Glasgow Coma Scores, was not significantly worse for patients who developed persistent infections. Both groups also showed a virtually identical pattern of elevation in the chemokines MIG/CXCL9, IL-8/CXCL8, and eotaxins, beginning at admission and continuing throughout the first week of ICU care. This suggests that these mediators are a component of a normal immune response to injury.
However, patients who developed persistent infections had “larger and more highly connected networks of systemic inflammation biomarkers” than did the other patients, suggesting that “mounting an adequately robust inflammatory response is essential for effective restoration of homeostasis after injury, [but] an overly exuberant and sustained immune response may be detrimental,” the investigators said.
At admission, the patients who later developed persistent infections had much higher levels than did the patients who recovered of the biomarkers IL-6, MCP-1/CCL2, HMGB1, and IL-1RA. “The early peak suggests that these mediators are produced in response to preexisting factors or variables associated with injury mechanism/pattern or prehospital management that are not revealed in our analysis. It is unclear, for example, if this pattern reflects the higher incidence of thoracic trauma in the [persistent infection] group,” Dr. Namas and his associates wrote.
After 12 hours, this pattern of biomarkers gave way to an increase in cytokines either produced by lymphoid cells or involved in the regulation of lymphocyte responses. This relatively early engagement of the lymphocyte response correlated with the development of multiple organ dysfunction beginning on day 2, which progressed over time in the infection group but rapidly resolved in the group that had an uncomplicated recovery. “We speculate that the gradual elevations of cytokines such as IL-1beta and TNF-alpha ... could reflect the response to microbes in the early phases of infection, though further studies are needed to test this hypothesis,” the researchers said. Compared with the patients who recovered, those who developed persistent infections also showed significant elevations in total leukocyte counts and polymorphonuclear neutrophils percentage, beginning at admission and continuing throughout the first week. They showed sustained lymphopenia from admission through 2 weeks of ICU care. This suggests that lymphocyte depletion “plays a detrimental role in the evolution of nosocomial sepsis-induced multiple organ failure after traumatic injury,” they noted.
Differences in circulating biomarkers distinguished blunt trauma patients who improved over time from those who instead developed serial persistent infections and multiple organ failures in a single-center retrospective cohort study published online in Annals of Surgery.
The distinctly different patterns in biomarkers were already becoming apparent in blood samples taken at admission to the ICU, and they evolved over the first week of hospitalization. The patterns in patients who went on to develop infections and organ failures most likely reflect an excessive inflammatory response to injury, which caused further immune dysregulation and impairment of host physiological function that rendered patients susceptible to severe infection.
“We propose that a combination of traditional parameters of inflammation, such as white blood cell differential, combined with a novel subset of circulating biomarkers measured upon presentation and over the initial 24 hours, could be used to stratify ICU patients for either more or less intensive care and monitoring,” wrote the investigators. This would optimize both resource utilization and patient outcomes, wrote the investigators, led by Dr. Rami A. Namas of the department of surgery and Center for Inflammation and Regenerative Modeling, McGowan Institute for Regenerative Medicine, University of Pittsburgh (Ann. Surg. 2014 Nov. 3).
They analyzed blood test results from 472 adults who survived severe blunt trauma and were admitted to the emergency department of a trauma center during an 8-year period. A total of 127 (27%) went on to develop persistent nosocomial infections – including 79 cases of pneumonia, 39 of urinary tract infections, 15 of bloodstream infections, 5 of wound infections, 2 of empyema, and 1 of Clostridium difficile infection – and organ failure. The study participants had undergone blood sampling via central venous or arterial catheters at least three times during the first 24 hours in the ICU, as well as at frequent intervals for at least a week. Samples were tested for the levels of 26 inflammatory biomarkers.
The investigators then performed a case-control analysis differentiating the blood test results between a subgroup of 44 patients who never developed nosocomial infections from 44 who had. They excluded patients who received blood transfusions or underwent emergency surgery within the first 24 hours, “to avoid the confounding impact of these interventions on the overall inflammatory response.” They also selected only patients whose trauma was caused by a motor vehicle accident, to avoid confounding factors related to the mechanism of injury. The two study groups were rigorously matched for patient age, patient sex, and Injury Severity Score.
Overall, injury severity was comparable between the two study groups. The severity of brain injury in particular, as reflected in Glasgow Coma Scores, was not significantly worse for patients who developed persistent infections. Both groups also showed a virtually identical pattern of elevation in the chemokines MIG/CXCL9, IL-8/CXCL8, and eotaxins, beginning at admission and continuing throughout the first week of ICU care. This suggests that these mediators are a component of a normal immune response to injury.
However, patients who developed persistent infections had “larger and more highly connected networks of systemic inflammation biomarkers” than did the other patients, suggesting that “mounting an adequately robust inflammatory response is essential for effective restoration of homeostasis after injury, [but] an overly exuberant and sustained immune response may be detrimental,” the investigators said.
At admission, the patients who later developed persistent infections had much higher levels than did the patients who recovered of the biomarkers IL-6, MCP-1/CCL2, HMGB1, and IL-1RA. “The early peak suggests that these mediators are produced in response to preexisting factors or variables associated with injury mechanism/pattern or prehospital management that are not revealed in our analysis. It is unclear, for example, if this pattern reflects the higher incidence of thoracic trauma in the [persistent infection] group,” Dr. Namas and his associates wrote.
After 12 hours, this pattern of biomarkers gave way to an increase in cytokines either produced by lymphoid cells or involved in the regulation of lymphocyte responses. This relatively early engagement of the lymphocyte response correlated with the development of multiple organ dysfunction beginning on day 2, which progressed over time in the infection group but rapidly resolved in the group that had an uncomplicated recovery. “We speculate that the gradual elevations of cytokines such as IL-1beta and TNF-alpha ... could reflect the response to microbes in the early phases of infection, though further studies are needed to test this hypothesis,” the researchers said. Compared with the patients who recovered, those who developed persistent infections also showed significant elevations in total leukocyte counts and polymorphonuclear neutrophils percentage, beginning at admission and continuing throughout the first week. They showed sustained lymphopenia from admission through 2 weeks of ICU care. This suggests that lymphocyte depletion “plays a detrimental role in the evolution of nosocomial sepsis-induced multiple organ failure after traumatic injury,” they noted.
Differences in circulating biomarkers distinguished blunt trauma patients who improved over time from those who instead developed serial persistent infections and multiple organ failures in a single-center retrospective cohort study published online in Annals of Surgery.
The distinctly different patterns in biomarkers were already becoming apparent in blood samples taken at admission to the ICU, and they evolved over the first week of hospitalization. The patterns in patients who went on to develop infections and organ failures most likely reflect an excessive inflammatory response to injury, which caused further immune dysregulation and impairment of host physiological function that rendered patients susceptible to severe infection.
“We propose that a combination of traditional parameters of inflammation, such as white blood cell differential, combined with a novel subset of circulating biomarkers measured upon presentation and over the initial 24 hours, could be used to stratify ICU patients for either more or less intensive care and monitoring,” wrote the investigators. This would optimize both resource utilization and patient outcomes, wrote the investigators, led by Dr. Rami A. Namas of the department of surgery and Center for Inflammation and Regenerative Modeling, McGowan Institute for Regenerative Medicine, University of Pittsburgh (Ann. Surg. 2014 Nov. 3).
They analyzed blood test results from 472 adults who survived severe blunt trauma and were admitted to the emergency department of a trauma center during an 8-year period. A total of 127 (27%) went on to develop persistent nosocomial infections – including 79 cases of pneumonia, 39 of urinary tract infections, 15 of bloodstream infections, 5 of wound infections, 2 of empyema, and 1 of Clostridium difficile infection – and organ failure. The study participants had undergone blood sampling via central venous or arterial catheters at least three times during the first 24 hours in the ICU, as well as at frequent intervals for at least a week. Samples were tested for the levels of 26 inflammatory biomarkers.
The investigators then performed a case-control analysis differentiating the blood test results between a subgroup of 44 patients who never developed nosocomial infections from 44 who had. They excluded patients who received blood transfusions or underwent emergency surgery within the first 24 hours, “to avoid the confounding impact of these interventions on the overall inflammatory response.” They also selected only patients whose trauma was caused by a motor vehicle accident, to avoid confounding factors related to the mechanism of injury. The two study groups were rigorously matched for patient age, patient sex, and Injury Severity Score.
Overall, injury severity was comparable between the two study groups. The severity of brain injury in particular, as reflected in Glasgow Coma Scores, was not significantly worse for patients who developed persistent infections. Both groups also showed a virtually identical pattern of elevation in the chemokines MIG/CXCL9, IL-8/CXCL8, and eotaxins, beginning at admission and continuing throughout the first week of ICU care. This suggests that these mediators are a component of a normal immune response to injury.
However, patients who developed persistent infections had “larger and more highly connected networks of systemic inflammation biomarkers” than did the other patients, suggesting that “mounting an adequately robust inflammatory response is essential for effective restoration of homeostasis after injury, [but] an overly exuberant and sustained immune response may be detrimental,” the investigators said.
At admission, the patients who later developed persistent infections had much higher levels than did the patients who recovered of the biomarkers IL-6, MCP-1/CCL2, HMGB1, and IL-1RA. “The early peak suggests that these mediators are produced in response to preexisting factors or variables associated with injury mechanism/pattern or prehospital management that are not revealed in our analysis. It is unclear, for example, if this pattern reflects the higher incidence of thoracic trauma in the [persistent infection] group,” Dr. Namas and his associates wrote.
After 12 hours, this pattern of biomarkers gave way to an increase in cytokines either produced by lymphoid cells or involved in the regulation of lymphocyte responses. This relatively early engagement of the lymphocyte response correlated with the development of multiple organ dysfunction beginning on day 2, which progressed over time in the infection group but rapidly resolved in the group that had an uncomplicated recovery. “We speculate that the gradual elevations of cytokines such as IL-1beta and TNF-alpha ... could reflect the response to microbes in the early phases of infection, though further studies are needed to test this hypothesis,” the researchers said. Compared with the patients who recovered, those who developed persistent infections also showed significant elevations in total leukocyte counts and polymorphonuclear neutrophils percentage, beginning at admission and continuing throughout the first week. They showed sustained lymphopenia from admission through 2 weeks of ICU care. This suggests that lymphocyte depletion “plays a detrimental role in the evolution of nosocomial sepsis-induced multiple organ failure after traumatic injury,” they noted.
Key clinical point: Blood biomarkers appear to predict which blunt trauma patients will have an abnormal inflammatory response to their injuries, predisposing them to serial infections and multiple organ failures.
Major finding: Patients who had complicated ICU courses had higher levels of IL-6, MCP-1/CCL2, HMGB1, and IL-1RA at admission; increased lymphoid cytokines at 12 hours that correlated with multiple organ dysfunction; and elevated total leukocyte counts, elevated PMN percentage, and sustained lymphopenia throughout their ICU stay.
Data source: A retrospective single-center cohort study involving 472 blunt trauma patients treated over an 8-year period, of whom 127 developed nosocomial infections and multiple organ failure.
Disclosures: This study was supported by the National Institutes of Health. Dr. Namas and his associates reported having no financial disclosures.