User login
Doctors hesitated to embrace biosimilar infliximab in first 2 years
Physicians have been slow to embrace biosimilar versions of infliximab, but are more likely to prescribe it to new patients, based on data from a review of nearly 50,000 infliximab claims through Medicare in the first 2 years that biosimilars were available in the United States.
“Although biosimilar versions are as safe and effective as the biologic, patients and physicians may be more reluctant to switch from a working biologic regimen in a chronic setting than an acute one,” wrote Alice J. Chen, PhD, of the University of Southern California, Los Angeles, and colleagues.
In a research letter published in JAMA Internal Medicine, the investigators examined prescribing patterns of physicians switching between the originator infliximab (Remicade) and two of its biosimilars (Inflectra and Renflexis).
They reviewed infliximab use and reimbursement in the 100% Medicare Part B quarterly claims database from Jan. 1, 2017, to Dec. 31, 2018. The study population included Medicare patients classified as new if they had no infliximab claims in the prior 6 months; those with claims were considered returning patients.
In a comparison of claims reflecting 49,771 patients and 4,289 physicians in 2018, a total of 1,418 new patients (17.4%) and 4,495 (10.8%) returning patients used a biosimilar. “Of returning patients, half used the biosimilar version exclusively, whereas the other half switched between biologic and biosimilar versions,” the researchers noted.
Of the 4,289 physicians who prescribed infliximab, 3,124 prescribed no biosimilars, 1,015 prescribed both biologics and biosimilars, and 150 prescribed biosimilars only. Of the physicians who prescribed both, approximately 61% switched some patients from the biologic to the biosimilar; “the remainder kept individual patients on only 1 version of the drug but treated patients with both versions,” the researchers wrote.
The adoption of biosimilars may be slower for chronic vs. acute conditions, the researchers noted. “Prescribers may hesitate to switch clinically stable chronic patients from biologic regimens if they are unfamiliar with the biosimilar or face financial disincentives from prescribing it.”
The study findings were limited by several factors including the use of only 2 years of data and a focus only on Medicare Part B. Switching medications may have been influenced by factors such as lower copays for patients and rebates or discounts for physicians; however, “further research is needed to better understand biosimilar pricing dynamics and the barriers to adopting biosimilars for chronic conditions,” they concluded.
The study was supported by the Leonard D. Schaeffer Center for Health Policy & Economics at the University of Southern California, Los Angeles, and the National Institute on Aging. Lead author Dr. Chen also disclosed receiving personal fees from Amgen outside of the current study.
SOURCE: Chen AJ et al. JAMA Intern Med. 2020 July 20. doi: 10.1001/jamainternmed.2020.3188.
Physicians have been slow to embrace biosimilar versions of infliximab, but are more likely to prescribe it to new patients, based on data from a review of nearly 50,000 infliximab claims through Medicare in the first 2 years that biosimilars were available in the United States.
“Although biosimilar versions are as safe and effective as the biologic, patients and physicians may be more reluctant to switch from a working biologic regimen in a chronic setting than an acute one,” wrote Alice J. Chen, PhD, of the University of Southern California, Los Angeles, and colleagues.
In a research letter published in JAMA Internal Medicine, the investigators examined prescribing patterns of physicians switching between the originator infliximab (Remicade) and two of its biosimilars (Inflectra and Renflexis).
They reviewed infliximab use and reimbursement in the 100% Medicare Part B quarterly claims database from Jan. 1, 2017, to Dec. 31, 2018. The study population included Medicare patients classified as new if they had no infliximab claims in the prior 6 months; those with claims were considered returning patients.
In a comparison of claims reflecting 49,771 patients and 4,289 physicians in 2018, a total of 1,418 new patients (17.4%) and 4,495 (10.8%) returning patients used a biosimilar. “Of returning patients, half used the biosimilar version exclusively, whereas the other half switched between biologic and biosimilar versions,” the researchers noted.
Of the 4,289 physicians who prescribed infliximab, 3,124 prescribed no biosimilars, 1,015 prescribed both biologics and biosimilars, and 150 prescribed biosimilars only. Of the physicians who prescribed both, approximately 61% switched some patients from the biologic to the biosimilar; “the remainder kept individual patients on only 1 version of the drug but treated patients with both versions,” the researchers wrote.
The adoption of biosimilars may be slower for chronic vs. acute conditions, the researchers noted. “Prescribers may hesitate to switch clinically stable chronic patients from biologic regimens if they are unfamiliar with the biosimilar or face financial disincentives from prescribing it.”
The study findings were limited by several factors including the use of only 2 years of data and a focus only on Medicare Part B. Switching medications may have been influenced by factors such as lower copays for patients and rebates or discounts for physicians; however, “further research is needed to better understand biosimilar pricing dynamics and the barriers to adopting biosimilars for chronic conditions,” they concluded.
The study was supported by the Leonard D. Schaeffer Center for Health Policy & Economics at the University of Southern California, Los Angeles, and the National Institute on Aging. Lead author Dr. Chen also disclosed receiving personal fees from Amgen outside of the current study.
SOURCE: Chen AJ et al. JAMA Intern Med. 2020 July 20. doi: 10.1001/jamainternmed.2020.3188.
Physicians have been slow to embrace biosimilar versions of infliximab, but are more likely to prescribe it to new patients, based on data from a review of nearly 50,000 infliximab claims through Medicare in the first 2 years that biosimilars were available in the United States.
“Although biosimilar versions are as safe and effective as the biologic, patients and physicians may be more reluctant to switch from a working biologic regimen in a chronic setting than an acute one,” wrote Alice J. Chen, PhD, of the University of Southern California, Los Angeles, and colleagues.
In a research letter published in JAMA Internal Medicine, the investigators examined prescribing patterns of physicians switching between the originator infliximab (Remicade) and two of its biosimilars (Inflectra and Renflexis).
They reviewed infliximab use and reimbursement in the 100% Medicare Part B quarterly claims database from Jan. 1, 2017, to Dec. 31, 2018. The study population included Medicare patients classified as new if they had no infliximab claims in the prior 6 months; those with claims were considered returning patients.
In a comparison of claims reflecting 49,771 patients and 4,289 physicians in 2018, a total of 1,418 new patients (17.4%) and 4,495 (10.8%) returning patients used a biosimilar. “Of returning patients, half used the biosimilar version exclusively, whereas the other half switched between biologic and biosimilar versions,” the researchers noted.
Of the 4,289 physicians who prescribed infliximab, 3,124 prescribed no biosimilars, 1,015 prescribed both biologics and biosimilars, and 150 prescribed biosimilars only. Of the physicians who prescribed both, approximately 61% switched some patients from the biologic to the biosimilar; “the remainder kept individual patients on only 1 version of the drug but treated patients with both versions,” the researchers wrote.
The adoption of biosimilars may be slower for chronic vs. acute conditions, the researchers noted. “Prescribers may hesitate to switch clinically stable chronic patients from biologic regimens if they are unfamiliar with the biosimilar or face financial disincentives from prescribing it.”
The study findings were limited by several factors including the use of only 2 years of data and a focus only on Medicare Part B. Switching medications may have been influenced by factors such as lower copays for patients and rebates or discounts for physicians; however, “further research is needed to better understand biosimilar pricing dynamics and the barriers to adopting biosimilars for chronic conditions,” they concluded.
The study was supported by the Leonard D. Schaeffer Center for Health Policy & Economics at the University of Southern California, Los Angeles, and the National Institute on Aging. Lead author Dr. Chen also disclosed receiving personal fees from Amgen outside of the current study.
SOURCE: Chen AJ et al. JAMA Intern Med. 2020 July 20. doi: 10.1001/jamainternmed.2020.3188.
FROM JAMA INTERNAL MEDICINE
Key clinical point: A total of 17% of patients new to infliximab received a biosimilar in 2018, compared with 11% of returning patients.
Major finding: Biosimilar infliximab accounted for 10% of the market share 2 years after the product was introduced.
Study details: The data come from a review of infliximab claims across 49,771 patients and 4,289 physicians who prescribed infliximab in 2018.
Disclosures: The study was supported by the Leonard D. Schaeffer Center for Health Policy & Economics at the University of Southern California, Los Angeles, and the National Institute on Aging. Lead author Dr. Chen also disclosed receiving personal fees from Amgen outside of the current study.
Source: Chen AJ et al. JAMA Intern Med. 2020 July 20. doi: 10.1001/jamainternmed.2020.3188.
Clinicians address psoriatic disease risk in the era of COVID-19
COVID-19 has posed serious questions for patients with psoriatic disease and the clinicians who treat them. Both have serious concerns over whether psoriasis or the medications used to treat it pose additional risk for contracting COVID-19 or experiencing worse outcomes with illness.
At the virtual annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis, experts gathered to discuss these concerns and what is known about the special risk factors for psoriatic disease patients.
Studies from a few registries have been done already among patients with autoimmune disease, and the results so far suggest that patients may be able to breathe a little easier. “I don’t see any data that suggests that use of immunosuppressives or having autoimmune disease increases your risk of acquiring it. I think most of the risk is driven by risk of exposure,” said Kevin Winthrop, MD, MPH, a professor of public health, infectious diseases, ophthalmology at Oregon Health & Science University, Portland, during a presentation.
That assertion was reinforced by data presented by Rebecca Haberman, MD, a rheumatologist at New York University Langone Health. Her group created the Web-Based Assessment of Autoimmune, Immune-Mediated, and Rheumatic Patients during the COVID-19 Pandemic (WARCOV) cohort study to address the question of whether patients with immune-mediated inflammatory disease (IMID), including inflammatory arthritis, psoriasis, or inflammatory bowel disease, should discontinue or modify their immunotherapy regimens in the face of potential exposure to COVID-19.
To date, the study has data on 1,122 patients; 604 with inflammatory arthritis, 128 of whom have tested positive for COVID-19. The team established a cohort using the first 86 IMID patients confirmed to have contracted COVID-19. The hospitalization rate was 16% overall, and use of corticosteroids was associated with increased hospitalization risk. A follow-up analysis looking at the first 103 inflammatory arthritis patients who contracted COVID-19 showed a hospitalization rate of 26% and a mortality of 4%. That hospitalization rate is similar to the general hospitalization rate estimated by the New York Department of Health, Dr. Haberman said in her presentation.
Risk factors associated with hospitalization included being older and having asthma or COPD, which is similar to the general population. Use of oral glucocorticoids was linked to a big increase in risk for hospitalization, even with doses less than 10 mg prednisone daily (odds ratio, 14.31; 95% confidence interval, 3.55-57.70). There were no links between use of any cytokine therapy and risk, but use of TNF inhibitors was associated with a reduced risk (OR, 0.35; 95% CI, 0.13-0.97), while use of JAK inhibitors was associated with greater risk (OR, 6.30; 95% CI, 1.68-23.69). The latter result is tentative because of a small sample size, and it was driven largely by the experiences of patients with psoriatic arthritis.
Another study, run by the COVID-19 Global Rheumatology Alliance, looked at 600 patients with rheumatic disease from 40 countries, and “found no smoking gun,” said Leonard Calabrese, DO, who leads the Cleveland Clinic’s section of clinical immunology, during his presentation. “People can develop this when they’re on hydroxychloroquine. They seem to do not remarkably bad or remarkably good. There is no adverse signal for biologics, but being on prednisone [at a dose of] more than 10 mg is not great,” said Dr. Calabrese, who also noted that other publications have supported these conclusions.
So given these findings, how should clinicians address patient concerns? In the absence of probable exposure, “we say it’s better to have a well-controlled IMID on therapy than a poorly-controlled IMID on submaximal therapy. We say stick to therapy and try to wean the prednisone down as low as possible,” Dr. Calabrese said.
More controversially, what should patients do if they have had a significant exposure, such as a close proximity, prolonged exposure encounter with an individual with documented COVID-19, or at high-risk of disease? Dr. Calabrese noted that the American College of Rheumatology (ACR) guidelines recommend that low-level immunomodulation can be continued, “with an asterisk if it’s hydroxychloroquine, and it is in most of our minds now that we know that it is not effective, and the toxicity in the COVID setting is still being worked out,” he said.
With respect to other immunosuppressants, the ACR recommends stopping them temporarily, although IL-6 inhibitors may be continued in select circumstances. Resumption of the therapeutics can resume after a negative COVID test or completion of a 2-week observation period.
When patients contract COVID-19, antimalarial medications can be continued because they have been studied. “But medium-level immunomodulators, in particular methotrexate, I have grave concerns about because it can inhibit the adaptive immune response and antibody formation,” he said. COVID-19 is a serious infection, and all serious biologics have a package insert saying to stop them in a serious infection. Again, IL-6 inhibitors may be considered an exception in the right circumstances. When to resume these medications remains unknown. “I think that’s a work in progress. Test-based versus clinic-based strategies are a matter of controversy,” Dr. Calabrese said.
Ultimately, the question of what to do with immunosuppressive therapies in this population will continue to be a challenge. “The only good answer is to follow the rules of social distancing and to wear a mask,” said Kristina Callis Duffin, MD, a cochair of the department of dermatology and associate professor of dermatology at the University of Utah, Salt Lake City.
COVID-19 has posed serious questions for patients with psoriatic disease and the clinicians who treat them. Both have serious concerns over whether psoriasis or the medications used to treat it pose additional risk for contracting COVID-19 or experiencing worse outcomes with illness.
At the virtual annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis, experts gathered to discuss these concerns and what is known about the special risk factors for psoriatic disease patients.
Studies from a few registries have been done already among patients with autoimmune disease, and the results so far suggest that patients may be able to breathe a little easier. “I don’t see any data that suggests that use of immunosuppressives or having autoimmune disease increases your risk of acquiring it. I think most of the risk is driven by risk of exposure,” said Kevin Winthrop, MD, MPH, a professor of public health, infectious diseases, ophthalmology at Oregon Health & Science University, Portland, during a presentation.
That assertion was reinforced by data presented by Rebecca Haberman, MD, a rheumatologist at New York University Langone Health. Her group created the Web-Based Assessment of Autoimmune, Immune-Mediated, and Rheumatic Patients during the COVID-19 Pandemic (WARCOV) cohort study to address the question of whether patients with immune-mediated inflammatory disease (IMID), including inflammatory arthritis, psoriasis, or inflammatory bowel disease, should discontinue or modify their immunotherapy regimens in the face of potential exposure to COVID-19.
To date, the study has data on 1,122 patients; 604 with inflammatory arthritis, 128 of whom have tested positive for COVID-19. The team established a cohort using the first 86 IMID patients confirmed to have contracted COVID-19. The hospitalization rate was 16% overall, and use of corticosteroids was associated with increased hospitalization risk. A follow-up analysis looking at the first 103 inflammatory arthritis patients who contracted COVID-19 showed a hospitalization rate of 26% and a mortality of 4%. That hospitalization rate is similar to the general hospitalization rate estimated by the New York Department of Health, Dr. Haberman said in her presentation.
Risk factors associated with hospitalization included being older and having asthma or COPD, which is similar to the general population. Use of oral glucocorticoids was linked to a big increase in risk for hospitalization, even with doses less than 10 mg prednisone daily (odds ratio, 14.31; 95% confidence interval, 3.55-57.70). There were no links between use of any cytokine therapy and risk, but use of TNF inhibitors was associated with a reduced risk (OR, 0.35; 95% CI, 0.13-0.97), while use of JAK inhibitors was associated with greater risk (OR, 6.30; 95% CI, 1.68-23.69). The latter result is tentative because of a small sample size, and it was driven largely by the experiences of patients with psoriatic arthritis.
Another study, run by the COVID-19 Global Rheumatology Alliance, looked at 600 patients with rheumatic disease from 40 countries, and “found no smoking gun,” said Leonard Calabrese, DO, who leads the Cleveland Clinic’s section of clinical immunology, during his presentation. “People can develop this when they’re on hydroxychloroquine. They seem to do not remarkably bad or remarkably good. There is no adverse signal for biologics, but being on prednisone [at a dose of] more than 10 mg is not great,” said Dr. Calabrese, who also noted that other publications have supported these conclusions.
So given these findings, how should clinicians address patient concerns? In the absence of probable exposure, “we say it’s better to have a well-controlled IMID on therapy than a poorly-controlled IMID on submaximal therapy. We say stick to therapy and try to wean the prednisone down as low as possible,” Dr. Calabrese said.
More controversially, what should patients do if they have had a significant exposure, such as a close proximity, prolonged exposure encounter with an individual with documented COVID-19, or at high-risk of disease? Dr. Calabrese noted that the American College of Rheumatology (ACR) guidelines recommend that low-level immunomodulation can be continued, “with an asterisk if it’s hydroxychloroquine, and it is in most of our minds now that we know that it is not effective, and the toxicity in the COVID setting is still being worked out,” he said.
With respect to other immunosuppressants, the ACR recommends stopping them temporarily, although IL-6 inhibitors may be continued in select circumstances. Resumption of the therapeutics can resume after a negative COVID test or completion of a 2-week observation period.
When patients contract COVID-19, antimalarial medications can be continued because they have been studied. “But medium-level immunomodulators, in particular methotrexate, I have grave concerns about because it can inhibit the adaptive immune response and antibody formation,” he said. COVID-19 is a serious infection, and all serious biologics have a package insert saying to stop them in a serious infection. Again, IL-6 inhibitors may be considered an exception in the right circumstances. When to resume these medications remains unknown. “I think that’s a work in progress. Test-based versus clinic-based strategies are a matter of controversy,” Dr. Calabrese said.
Ultimately, the question of what to do with immunosuppressive therapies in this population will continue to be a challenge. “The only good answer is to follow the rules of social distancing and to wear a mask,” said Kristina Callis Duffin, MD, a cochair of the department of dermatology and associate professor of dermatology at the University of Utah, Salt Lake City.
COVID-19 has posed serious questions for patients with psoriatic disease and the clinicians who treat them. Both have serious concerns over whether psoriasis or the medications used to treat it pose additional risk for contracting COVID-19 or experiencing worse outcomes with illness.
At the virtual annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis, experts gathered to discuss these concerns and what is known about the special risk factors for psoriatic disease patients.
Studies from a few registries have been done already among patients with autoimmune disease, and the results so far suggest that patients may be able to breathe a little easier. “I don’t see any data that suggests that use of immunosuppressives or having autoimmune disease increases your risk of acquiring it. I think most of the risk is driven by risk of exposure,” said Kevin Winthrop, MD, MPH, a professor of public health, infectious diseases, ophthalmology at Oregon Health & Science University, Portland, during a presentation.
That assertion was reinforced by data presented by Rebecca Haberman, MD, a rheumatologist at New York University Langone Health. Her group created the Web-Based Assessment of Autoimmune, Immune-Mediated, and Rheumatic Patients during the COVID-19 Pandemic (WARCOV) cohort study to address the question of whether patients with immune-mediated inflammatory disease (IMID), including inflammatory arthritis, psoriasis, or inflammatory bowel disease, should discontinue or modify their immunotherapy regimens in the face of potential exposure to COVID-19.
To date, the study has data on 1,122 patients; 604 with inflammatory arthritis, 128 of whom have tested positive for COVID-19. The team established a cohort using the first 86 IMID patients confirmed to have contracted COVID-19. The hospitalization rate was 16% overall, and use of corticosteroids was associated with increased hospitalization risk. A follow-up analysis looking at the first 103 inflammatory arthritis patients who contracted COVID-19 showed a hospitalization rate of 26% and a mortality of 4%. That hospitalization rate is similar to the general hospitalization rate estimated by the New York Department of Health, Dr. Haberman said in her presentation.
Risk factors associated with hospitalization included being older and having asthma or COPD, which is similar to the general population. Use of oral glucocorticoids was linked to a big increase in risk for hospitalization, even with doses less than 10 mg prednisone daily (odds ratio, 14.31; 95% confidence interval, 3.55-57.70). There were no links between use of any cytokine therapy and risk, but use of TNF inhibitors was associated with a reduced risk (OR, 0.35; 95% CI, 0.13-0.97), while use of JAK inhibitors was associated with greater risk (OR, 6.30; 95% CI, 1.68-23.69). The latter result is tentative because of a small sample size, and it was driven largely by the experiences of patients with psoriatic arthritis.
Another study, run by the COVID-19 Global Rheumatology Alliance, looked at 600 patients with rheumatic disease from 40 countries, and “found no smoking gun,” said Leonard Calabrese, DO, who leads the Cleveland Clinic’s section of clinical immunology, during his presentation. “People can develop this when they’re on hydroxychloroquine. They seem to do not remarkably bad or remarkably good. There is no adverse signal for biologics, but being on prednisone [at a dose of] more than 10 mg is not great,” said Dr. Calabrese, who also noted that other publications have supported these conclusions.
So given these findings, how should clinicians address patient concerns? In the absence of probable exposure, “we say it’s better to have a well-controlled IMID on therapy than a poorly-controlled IMID on submaximal therapy. We say stick to therapy and try to wean the prednisone down as low as possible,” Dr. Calabrese said.
More controversially, what should patients do if they have had a significant exposure, such as a close proximity, prolonged exposure encounter with an individual with documented COVID-19, or at high-risk of disease? Dr. Calabrese noted that the American College of Rheumatology (ACR) guidelines recommend that low-level immunomodulation can be continued, “with an asterisk if it’s hydroxychloroquine, and it is in most of our minds now that we know that it is not effective, and the toxicity in the COVID setting is still being worked out,” he said.
With respect to other immunosuppressants, the ACR recommends stopping them temporarily, although IL-6 inhibitors may be continued in select circumstances. Resumption of the therapeutics can resume after a negative COVID test or completion of a 2-week observation period.
When patients contract COVID-19, antimalarial medications can be continued because they have been studied. “But medium-level immunomodulators, in particular methotrexate, I have grave concerns about because it can inhibit the adaptive immune response and antibody formation,” he said. COVID-19 is a serious infection, and all serious biologics have a package insert saying to stop them in a serious infection. Again, IL-6 inhibitors may be considered an exception in the right circumstances. When to resume these medications remains unknown. “I think that’s a work in progress. Test-based versus clinic-based strategies are a matter of controversy,” Dr. Calabrese said.
Ultimately, the question of what to do with immunosuppressive therapies in this population will continue to be a challenge. “The only good answer is to follow the rules of social distancing and to wear a mask,” said Kristina Callis Duffin, MD, a cochair of the department of dermatology and associate professor of dermatology at the University of Utah, Salt Lake City.
FROM THE GRAPPA 2020 VIRTUAL ANNUAL MEETING
Ready for PRIME time? Newly ID’d cells predict RA flares
A newly identified circulating cell type may be a reliable marker for impending RA flares. The discovery and description of the cells, which bear a “striking” similarity to synovial fibroblasts, provide important clues to the origins of RA and progressive joint inflammation, investigators say.
By studying longitudinally collected blood samples from four patients with RA over 4 years, Dana E. Orange, MD and colleagues at Rockefeller University, New York, identified a pattern of B-cell activation and expansion of circulating cells that are negative for CD45 and CD31 expression, and positive for PDPN, dubbed preinflammatory mesenchymal or “PRIME” cells.
Expansion of PRIME cells in circulation increased dramatically in the weeks leading up to a flare and decreased during a flare, suggesting the possibility of a serum assay for predicting flares and allowing for early intervention to ameliorate or prevent disabling consequences, the investigators wrote in a study published in the New England Journal of Medicine.
“Our hope is that this will be a diagnostic in the future, but we need to study it in more patients to see how it will perform,” Dr. Orange said in an interview, adding that the cells, if shown to be pathogenic, could also be targets for new therapeutic strategies.
RNA sequencing
Dr. Orange and colleagues discovered the PRIME cells through a novel clinical and technical protocol involving home collection of blood by patients and longitudinal RNA sequencing to study gene expression profiles during times of both disease quiescence and flares, and noticed a distinct pattern of PRIME cell expansion, depletion, and gene expression.
“Looking at their gene expression profiles, they overlapped with fibroblasts that reside in inflamed rheumatoid arthritis synovium, and in an animal model those types of fibroblasts were important for allowing entry of inflammatory infiltrates around the joint,” she said.
PRIME cells may be a precursor of synovial fibroblasts, which have been implicated by some researchers in the spread of RA between joints, Dr. Orange added.
Patients do homework
The investigators began by enrolling four patients, followed for 1-4 years, who met 2010 American College of Rheumatology–European League Against Rheumatism criteria and who were seropositive for anti–cyclic citrullinated peptide antibodies.
They assessed disease activity from patient homes weekly or during escalation of flares up to four times daily, with the Routine Assessment of Patient Index Data 3 (RAPID3) questionnaire, as well as monthly clinic visits. At clinic visits during flares, disease activity was assessed using both the RAPID3 and 28-joint Disease Activity Score.
The patients performed fingerstick blood collection and mailed the samples overnight each week to Rockefeller University, where RNA was extracted and sequenced. The investigators identified gene transcripts that were differentially expressed in blood prior to flares, and compared them with data profiles derived from synovial single-cell RNA sequencing.
To validate the findings, the researchers used flow cytometry and sorted blood-cell RNA sequencing of samples from an additional 19 patients with RA.
They found that a total of 2,613 genes were differentially expressed during a flare, compared with baseline, and that expression of 1,437 of these genes was increased during a flare, with the remaining 1,176 decreased during flares.
Before the storm
Focusing on two flare-antecedent clusters of genes, they identified one cluster of transcripts that increased 2 weeks before a flare, enriched with genes coding for developmental pathways for naive B cells (that is, not yet exposed to antigens) and leukocytes.
The second cluster included gene transcripts that increased during the week before a flare, then decreased over the duration of the flare. Genes in this cluster were enriched for pathways that were unexpected in typical blood specimens, including genes involved in cartilage morphogenesis, endochondral bone growth, and extracellular matrix organization. The gene activity suggested the presence of a mesenchymal cell, they wrote.
The RNA expression profiles of these newly identified PRIME cells were very similar to those of synovial fibroblasts, and the investigators speculated that PRIME cells may be synovial fibroblast precursors.
They proposed a model of RA exacerbation in which PRIME cells become activated by B cells in the weeks immediately preceding a flare, and then migrate out of blood into the synovium.
The investigators are currently investigating “how reproducible this signature is in different flares in patients on different types of background therapy, and then we’re very interested in looking at the upstream triggers of the B cell and the PRIME cell,” Dr. Orange said.
“One of the reasons this is very exciting is that there are these signatures that can be found when patients are clearly asymptomatic but about to flare, and if we can intervene at that time, then the patients won’t have to live through a flare, they won’t have to have that experience,” she said.
Pros and cons
In an editorial accompanying the study, Ellen M. Gravallese, MD, from Brigham and Women’s Hospital in Boston and William H. Robinson, MD, PhD, from Stanford (Calif.) University and the Veterans Affairs Palo Alto (Calif.) Health Care System wrote that the study demonstrates an important method for identifying genetic contributions to many different types of disease.
“Orange and colleagues show that intensively collected longitudinal data from a small sample of patients can be used to identify dysregulated transcriptional signatures that are not recognized by classical cross-sectional studies. This study illustrates the exciting potential of longitudinal genomics to identify key antecedents of disease flares in an approach that may be applicable to the investigation of pathogenic and protective immune responses in a wide range of human diseases,” they wrote.
Rheumatology researcher Christopher D. Buckley, MBBS, DPhil, from the University of Birmingham (England), who was not involved in the study, said that the use of blood samples is both a strength and a weakness of the study.
“Blood is much easier to get than synovial tissue, but synovial tissue is important. If I’m trying to look at the blood and trying to make an inference about what’s going on in the synovium, if I don’t look at the synovium I don’t know what the link between the blood and synovium is,” he said in an interview.
On the plus side, “the big advantage about looking at blood is that you do multiple time points, which is really cool,” he said.
Dr. Buckley is a coauthor of a recent paper in Nature Medicine – published after the study by Dr. Orange and colleagues was accepted by the New England Journal of Medicine – showing that a population of macrophages in synovium was highly predictive of remission in patients with RA, and that therapeutic modulation of these macrophages has the potential as a treatment strategy for RA.
“We are very keen to understand the cellular basis of disease. We’re very good at understanding genes, but genes have to work in cells, and cells make organs, so the cells are critical,” he said.
The paper adds fuel to a controversy that has been raging among rheumatology researchers for more than a decade: the “flying fibroblast” hypothesis, which suggests that fibroblasts can migrate from one joint to another, hence spreading the disease in a manner akin to cancer metastases.
“It’s been quite controversial whether these cells like fibroblasts can exist in the blood, or whether they’re found in sufficient number in the blood,” Dr. Buckley said. “The fact that they have identified these PRIME cells is fascinating, because that’s going to cause us to go back and reinvestigate the whole flying fibroblast story.”
His colleague John Isaacs, MBBS, PhD, from Newcastle (England) University, is principal investigator for the BIO-FLARE study, in which participants with RA stop taking their disease-modifying antirheumatic drugs under close supervision of researchers. The investigators then study the patients looking for flare signals as well as the biology of flares themselves.
“As it happens, our protocols would not pick up this particular cell, because we have not been focusing on the stroma, at least not in peripheral blood. We’ve all been looking at synovium as part of BIO-FLARE,” he said in an interview. “We will be looking for this cell now that we have seen this research, and certainly we would want to replicate.”
He agreed with Dr. Buckley’s observation that the PRIME cell data may revive the flying fibroblast hypothesis. “This is a great paper in a top clinical journal. What isn’t there is mechanism. That’s the thing we’re all going to want to understand now: Where do the cells come from, how do they actually trigger flares, and how do they go down as flare starts?”
Both Dr. Buckley and Dr. Isaacs agreed that the study findings point to important new avenues of research, but also noted that the study was small, involving a total of only 23 patients, and that replication of the findings and elucidation of the mechanism of PRIME cell generation and disposition will be required.
The study was supported by grants from the National Institutes of Health, Simons Foundation, Robertson Foundation, Rheumatology Research Foundation, Bernard and Irene Schwartz Foundation, the Iris and Junming Le Foundation, and Rockefeller University. Dr. Orange disclosed a provisional patent for the discovery of the PRIME cells. Dr. Buckley and Dr. Isaacs reported no relevant conflicts of interest.
SOURCE: Orange DE et al. N Engl J Med. 2020 Jul 15. doi: 10.1056/NEJMoa2004114.
A newly identified circulating cell type may be a reliable marker for impending RA flares. The discovery and description of the cells, which bear a “striking” similarity to synovial fibroblasts, provide important clues to the origins of RA and progressive joint inflammation, investigators say.
By studying longitudinally collected blood samples from four patients with RA over 4 years, Dana E. Orange, MD and colleagues at Rockefeller University, New York, identified a pattern of B-cell activation and expansion of circulating cells that are negative for CD45 and CD31 expression, and positive for PDPN, dubbed preinflammatory mesenchymal or “PRIME” cells.
Expansion of PRIME cells in circulation increased dramatically in the weeks leading up to a flare and decreased during a flare, suggesting the possibility of a serum assay for predicting flares and allowing for early intervention to ameliorate or prevent disabling consequences, the investigators wrote in a study published in the New England Journal of Medicine.
“Our hope is that this will be a diagnostic in the future, but we need to study it in more patients to see how it will perform,” Dr. Orange said in an interview, adding that the cells, if shown to be pathogenic, could also be targets for new therapeutic strategies.
RNA sequencing
Dr. Orange and colleagues discovered the PRIME cells through a novel clinical and technical protocol involving home collection of blood by patients and longitudinal RNA sequencing to study gene expression profiles during times of both disease quiescence and flares, and noticed a distinct pattern of PRIME cell expansion, depletion, and gene expression.
“Looking at their gene expression profiles, they overlapped with fibroblasts that reside in inflamed rheumatoid arthritis synovium, and in an animal model those types of fibroblasts were important for allowing entry of inflammatory infiltrates around the joint,” she said.
PRIME cells may be a precursor of synovial fibroblasts, which have been implicated by some researchers in the spread of RA between joints, Dr. Orange added.
Patients do homework
The investigators began by enrolling four patients, followed for 1-4 years, who met 2010 American College of Rheumatology–European League Against Rheumatism criteria and who were seropositive for anti–cyclic citrullinated peptide antibodies.
They assessed disease activity from patient homes weekly or during escalation of flares up to four times daily, with the Routine Assessment of Patient Index Data 3 (RAPID3) questionnaire, as well as monthly clinic visits. At clinic visits during flares, disease activity was assessed using both the RAPID3 and 28-joint Disease Activity Score.
The patients performed fingerstick blood collection and mailed the samples overnight each week to Rockefeller University, where RNA was extracted and sequenced. The investigators identified gene transcripts that were differentially expressed in blood prior to flares, and compared them with data profiles derived from synovial single-cell RNA sequencing.
To validate the findings, the researchers used flow cytometry and sorted blood-cell RNA sequencing of samples from an additional 19 patients with RA.
They found that a total of 2,613 genes were differentially expressed during a flare, compared with baseline, and that expression of 1,437 of these genes was increased during a flare, with the remaining 1,176 decreased during flares.
Before the storm
Focusing on two flare-antecedent clusters of genes, they identified one cluster of transcripts that increased 2 weeks before a flare, enriched with genes coding for developmental pathways for naive B cells (that is, not yet exposed to antigens) and leukocytes.
The second cluster included gene transcripts that increased during the week before a flare, then decreased over the duration of the flare. Genes in this cluster were enriched for pathways that were unexpected in typical blood specimens, including genes involved in cartilage morphogenesis, endochondral bone growth, and extracellular matrix organization. The gene activity suggested the presence of a mesenchymal cell, they wrote.
The RNA expression profiles of these newly identified PRIME cells were very similar to those of synovial fibroblasts, and the investigators speculated that PRIME cells may be synovial fibroblast precursors.
They proposed a model of RA exacerbation in which PRIME cells become activated by B cells in the weeks immediately preceding a flare, and then migrate out of blood into the synovium.
The investigators are currently investigating “how reproducible this signature is in different flares in patients on different types of background therapy, and then we’re very interested in looking at the upstream triggers of the B cell and the PRIME cell,” Dr. Orange said.
“One of the reasons this is very exciting is that there are these signatures that can be found when patients are clearly asymptomatic but about to flare, and if we can intervene at that time, then the patients won’t have to live through a flare, they won’t have to have that experience,” she said.
Pros and cons
In an editorial accompanying the study, Ellen M. Gravallese, MD, from Brigham and Women’s Hospital in Boston and William H. Robinson, MD, PhD, from Stanford (Calif.) University and the Veterans Affairs Palo Alto (Calif.) Health Care System wrote that the study demonstrates an important method for identifying genetic contributions to many different types of disease.
“Orange and colleagues show that intensively collected longitudinal data from a small sample of patients can be used to identify dysregulated transcriptional signatures that are not recognized by classical cross-sectional studies. This study illustrates the exciting potential of longitudinal genomics to identify key antecedents of disease flares in an approach that may be applicable to the investigation of pathogenic and protective immune responses in a wide range of human diseases,” they wrote.
Rheumatology researcher Christopher D. Buckley, MBBS, DPhil, from the University of Birmingham (England), who was not involved in the study, said that the use of blood samples is both a strength and a weakness of the study.
“Blood is much easier to get than synovial tissue, but synovial tissue is important. If I’m trying to look at the blood and trying to make an inference about what’s going on in the synovium, if I don’t look at the synovium I don’t know what the link between the blood and synovium is,” he said in an interview.
On the plus side, “the big advantage about looking at blood is that you do multiple time points, which is really cool,” he said.
Dr. Buckley is a coauthor of a recent paper in Nature Medicine – published after the study by Dr. Orange and colleagues was accepted by the New England Journal of Medicine – showing that a population of macrophages in synovium was highly predictive of remission in patients with RA, and that therapeutic modulation of these macrophages has the potential as a treatment strategy for RA.
“We are very keen to understand the cellular basis of disease. We’re very good at understanding genes, but genes have to work in cells, and cells make organs, so the cells are critical,” he said.
The paper adds fuel to a controversy that has been raging among rheumatology researchers for more than a decade: the “flying fibroblast” hypothesis, which suggests that fibroblasts can migrate from one joint to another, hence spreading the disease in a manner akin to cancer metastases.
“It’s been quite controversial whether these cells like fibroblasts can exist in the blood, or whether they’re found in sufficient number in the blood,” Dr. Buckley said. “The fact that they have identified these PRIME cells is fascinating, because that’s going to cause us to go back and reinvestigate the whole flying fibroblast story.”
His colleague John Isaacs, MBBS, PhD, from Newcastle (England) University, is principal investigator for the BIO-FLARE study, in which participants with RA stop taking their disease-modifying antirheumatic drugs under close supervision of researchers. The investigators then study the patients looking for flare signals as well as the biology of flares themselves.
“As it happens, our protocols would not pick up this particular cell, because we have not been focusing on the stroma, at least not in peripheral blood. We’ve all been looking at synovium as part of BIO-FLARE,” he said in an interview. “We will be looking for this cell now that we have seen this research, and certainly we would want to replicate.”
He agreed with Dr. Buckley’s observation that the PRIME cell data may revive the flying fibroblast hypothesis. “This is a great paper in a top clinical journal. What isn’t there is mechanism. That’s the thing we’re all going to want to understand now: Where do the cells come from, how do they actually trigger flares, and how do they go down as flare starts?”
Both Dr. Buckley and Dr. Isaacs agreed that the study findings point to important new avenues of research, but also noted that the study was small, involving a total of only 23 patients, and that replication of the findings and elucidation of the mechanism of PRIME cell generation and disposition will be required.
The study was supported by grants from the National Institutes of Health, Simons Foundation, Robertson Foundation, Rheumatology Research Foundation, Bernard and Irene Schwartz Foundation, the Iris and Junming Le Foundation, and Rockefeller University. Dr. Orange disclosed a provisional patent for the discovery of the PRIME cells. Dr. Buckley and Dr. Isaacs reported no relevant conflicts of interest.
SOURCE: Orange DE et al. N Engl J Med. 2020 Jul 15. doi: 10.1056/NEJMoa2004114.
A newly identified circulating cell type may be a reliable marker for impending RA flares. The discovery and description of the cells, which bear a “striking” similarity to synovial fibroblasts, provide important clues to the origins of RA and progressive joint inflammation, investigators say.
By studying longitudinally collected blood samples from four patients with RA over 4 years, Dana E. Orange, MD and colleagues at Rockefeller University, New York, identified a pattern of B-cell activation and expansion of circulating cells that are negative for CD45 and CD31 expression, and positive for PDPN, dubbed preinflammatory mesenchymal or “PRIME” cells.
Expansion of PRIME cells in circulation increased dramatically in the weeks leading up to a flare and decreased during a flare, suggesting the possibility of a serum assay for predicting flares and allowing for early intervention to ameliorate or prevent disabling consequences, the investigators wrote in a study published in the New England Journal of Medicine.
“Our hope is that this will be a diagnostic in the future, but we need to study it in more patients to see how it will perform,” Dr. Orange said in an interview, adding that the cells, if shown to be pathogenic, could also be targets for new therapeutic strategies.
RNA sequencing
Dr. Orange and colleagues discovered the PRIME cells through a novel clinical and technical protocol involving home collection of blood by patients and longitudinal RNA sequencing to study gene expression profiles during times of both disease quiescence and flares, and noticed a distinct pattern of PRIME cell expansion, depletion, and gene expression.
“Looking at their gene expression profiles, they overlapped with fibroblasts that reside in inflamed rheumatoid arthritis synovium, and in an animal model those types of fibroblasts were important for allowing entry of inflammatory infiltrates around the joint,” she said.
PRIME cells may be a precursor of synovial fibroblasts, which have been implicated by some researchers in the spread of RA between joints, Dr. Orange added.
Patients do homework
The investigators began by enrolling four patients, followed for 1-4 years, who met 2010 American College of Rheumatology–European League Against Rheumatism criteria and who were seropositive for anti–cyclic citrullinated peptide antibodies.
They assessed disease activity from patient homes weekly or during escalation of flares up to four times daily, with the Routine Assessment of Patient Index Data 3 (RAPID3) questionnaire, as well as monthly clinic visits. At clinic visits during flares, disease activity was assessed using both the RAPID3 and 28-joint Disease Activity Score.
The patients performed fingerstick blood collection and mailed the samples overnight each week to Rockefeller University, where RNA was extracted and sequenced. The investigators identified gene transcripts that were differentially expressed in blood prior to flares, and compared them with data profiles derived from synovial single-cell RNA sequencing.
To validate the findings, the researchers used flow cytometry and sorted blood-cell RNA sequencing of samples from an additional 19 patients with RA.
They found that a total of 2,613 genes were differentially expressed during a flare, compared with baseline, and that expression of 1,437 of these genes was increased during a flare, with the remaining 1,176 decreased during flares.
Before the storm
Focusing on two flare-antecedent clusters of genes, they identified one cluster of transcripts that increased 2 weeks before a flare, enriched with genes coding for developmental pathways for naive B cells (that is, not yet exposed to antigens) and leukocytes.
The second cluster included gene transcripts that increased during the week before a flare, then decreased over the duration of the flare. Genes in this cluster were enriched for pathways that were unexpected in typical blood specimens, including genes involved in cartilage morphogenesis, endochondral bone growth, and extracellular matrix organization. The gene activity suggested the presence of a mesenchymal cell, they wrote.
The RNA expression profiles of these newly identified PRIME cells were very similar to those of synovial fibroblasts, and the investigators speculated that PRIME cells may be synovial fibroblast precursors.
They proposed a model of RA exacerbation in which PRIME cells become activated by B cells in the weeks immediately preceding a flare, and then migrate out of blood into the synovium.
The investigators are currently investigating “how reproducible this signature is in different flares in patients on different types of background therapy, and then we’re very interested in looking at the upstream triggers of the B cell and the PRIME cell,” Dr. Orange said.
“One of the reasons this is very exciting is that there are these signatures that can be found when patients are clearly asymptomatic but about to flare, and if we can intervene at that time, then the patients won’t have to live through a flare, they won’t have to have that experience,” she said.
Pros and cons
In an editorial accompanying the study, Ellen M. Gravallese, MD, from Brigham and Women’s Hospital in Boston and William H. Robinson, MD, PhD, from Stanford (Calif.) University and the Veterans Affairs Palo Alto (Calif.) Health Care System wrote that the study demonstrates an important method for identifying genetic contributions to many different types of disease.
“Orange and colleagues show that intensively collected longitudinal data from a small sample of patients can be used to identify dysregulated transcriptional signatures that are not recognized by classical cross-sectional studies. This study illustrates the exciting potential of longitudinal genomics to identify key antecedents of disease flares in an approach that may be applicable to the investigation of pathogenic and protective immune responses in a wide range of human diseases,” they wrote.
Rheumatology researcher Christopher D. Buckley, MBBS, DPhil, from the University of Birmingham (England), who was not involved in the study, said that the use of blood samples is both a strength and a weakness of the study.
“Blood is much easier to get than synovial tissue, but synovial tissue is important. If I’m trying to look at the blood and trying to make an inference about what’s going on in the synovium, if I don’t look at the synovium I don’t know what the link between the blood and synovium is,” he said in an interview.
On the plus side, “the big advantage about looking at blood is that you do multiple time points, which is really cool,” he said.
Dr. Buckley is a coauthor of a recent paper in Nature Medicine – published after the study by Dr. Orange and colleagues was accepted by the New England Journal of Medicine – showing that a population of macrophages in synovium was highly predictive of remission in patients with RA, and that therapeutic modulation of these macrophages has the potential as a treatment strategy for RA.
“We are very keen to understand the cellular basis of disease. We’re very good at understanding genes, but genes have to work in cells, and cells make organs, so the cells are critical,” he said.
The paper adds fuel to a controversy that has been raging among rheumatology researchers for more than a decade: the “flying fibroblast” hypothesis, which suggests that fibroblasts can migrate from one joint to another, hence spreading the disease in a manner akin to cancer metastases.
“It’s been quite controversial whether these cells like fibroblasts can exist in the blood, or whether they’re found in sufficient number in the blood,” Dr. Buckley said. “The fact that they have identified these PRIME cells is fascinating, because that’s going to cause us to go back and reinvestigate the whole flying fibroblast story.”
His colleague John Isaacs, MBBS, PhD, from Newcastle (England) University, is principal investigator for the BIO-FLARE study, in which participants with RA stop taking their disease-modifying antirheumatic drugs under close supervision of researchers. The investigators then study the patients looking for flare signals as well as the biology of flares themselves.
“As it happens, our protocols would not pick up this particular cell, because we have not been focusing on the stroma, at least not in peripheral blood. We’ve all been looking at synovium as part of BIO-FLARE,” he said in an interview. “We will be looking for this cell now that we have seen this research, and certainly we would want to replicate.”
He agreed with Dr. Buckley’s observation that the PRIME cell data may revive the flying fibroblast hypothesis. “This is a great paper in a top clinical journal. What isn’t there is mechanism. That’s the thing we’re all going to want to understand now: Where do the cells come from, how do they actually trigger flares, and how do they go down as flare starts?”
Both Dr. Buckley and Dr. Isaacs agreed that the study findings point to important new avenues of research, but also noted that the study was small, involving a total of only 23 patients, and that replication of the findings and elucidation of the mechanism of PRIME cell generation and disposition will be required.
The study was supported by grants from the National Institutes of Health, Simons Foundation, Robertson Foundation, Rheumatology Research Foundation, Bernard and Irene Schwartz Foundation, the Iris and Junming Le Foundation, and Rockefeller University. Dr. Orange disclosed a provisional patent for the discovery of the PRIME cells. Dr. Buckley and Dr. Isaacs reported no relevant conflicts of interest.
SOURCE: Orange DE et al. N Engl J Med. 2020 Jul 15. doi: 10.1056/NEJMoa2004114.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: A newly identified cell type may be predictive of RA flares.
Major finding: Preinflammatory mesenchymal cells were expanded in the week preceding a flare and decreased during the flare.
Study details: A longitudinal observational study of 23 patients with RA.
Disclosures: The study was supported by grants from the National Institutes of Health, Simons Foundation, Robertson Foundation, Rheumatology Research Foundation, Bernard and Irene Schwartz Foundation, the Iris and Junming Le Foundation, and Rockefeller University. Dr. Orange disclosed a provisional patent for the discovery of the preinflammatory mesenchymal cells.
Source: Orange DE et al. N Engl J Med. 2020 Jul 15. doi: 10.1056/NEJMoa2004114.
Move over supplements, here come medical foods
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.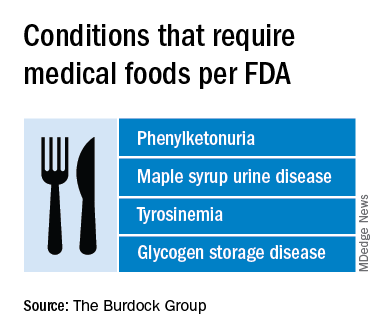
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.
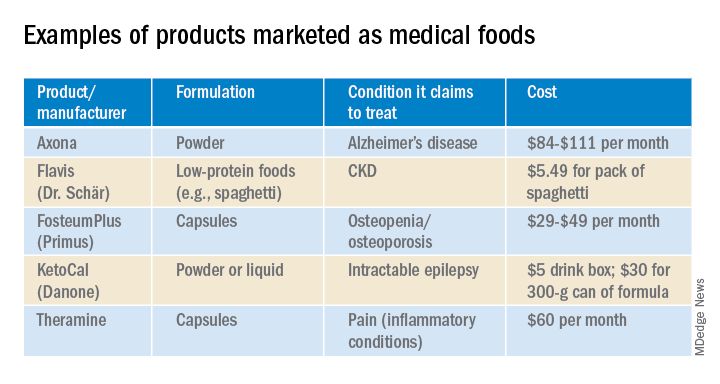
In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.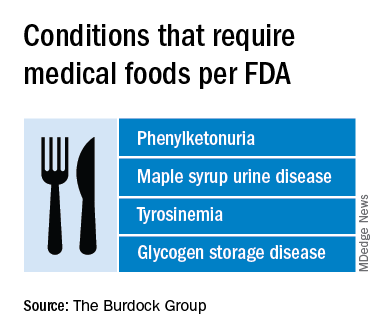
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.
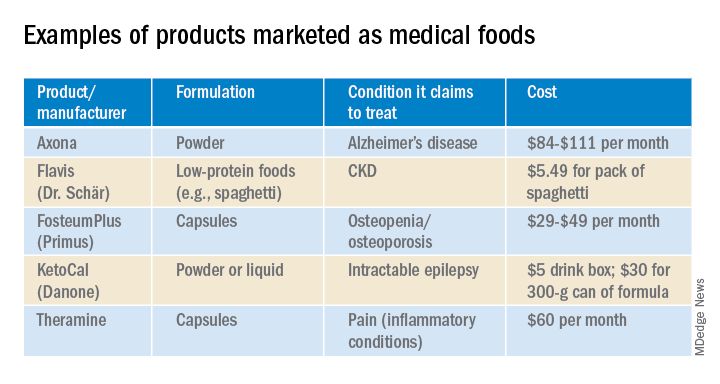
In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.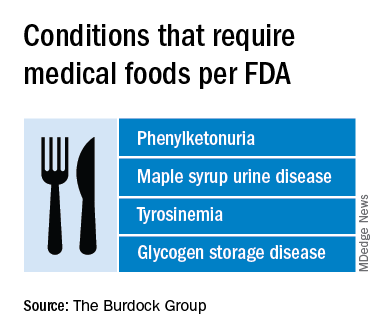
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.
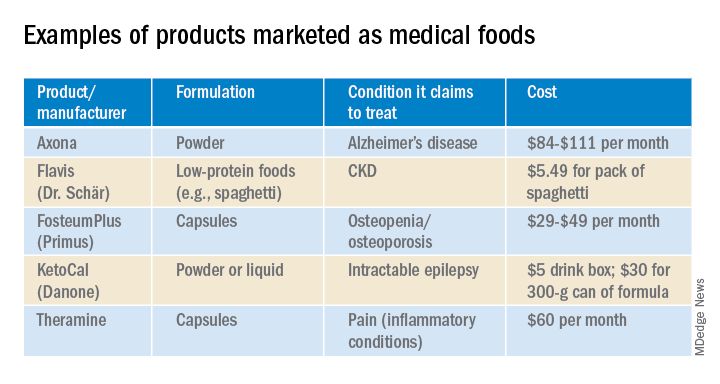
In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
FDA approves Tremfya (guselkumab) for psoriatic arthritis
, according to a July 14 announcement from its manufacturer, Janssen.
The FDA’s approval marks the second indication for guselkumab, which was first approved for adults with plaque psoriasis in 2017.
The agency based its approval on two pivotal phase 3 clinical trials, DISCOVER-1 and DISCOVER-2, which tested the biologic in 1,120 adults with active PsA who were naive to biologics (both trials) or had an inadequate response or intolerance to one or two tumor necrosis factor inhibitors (in about 30% of patients in DISCOVER-1). Part of this pretrial standard treatment could include at least 4 months of Otezla (apremilast), at least 3 months of nonbiologic disease-modifying antirheumatic drugs (DMARDs), or at least 4 weeks of NSAIDs. In both trials, about 58% of patients took methotrexate.
Participants who took guselkumab achieved 20% improvement in American College of Rheumatology response criteria at week 24 at rates of 52% in DISCOVER-1 and 64% in DISCOVER-2, whereas placebo-treated patients had rates of 22% and 33%, respectively.
Guselkumab improved patients’ other symptoms, including skin manifestations of psoriasis, physical functioning, enthesitis, dactylitis, and fatigue, according to the Janssen release.
Guselkumab, a fully human monoclonal antibody that selectively binds to the p19 subunit of IL-23, is administered as a 100-mg subcutaneous injection every 8 weeks, following two starter doses at weeks 0 and 4, and can be used alone or in combination with a conventional DMARD.
In guselkumab clinical trials of patients with PsA, a minority had bronchitis or a decreased neutrophil count, but the safety profile was otherwise generally consistent with what has been seen in patients with plaque psoriasis, according to the company release. Other common side effects described in 1% or more of patients have included upper respiratory infections, headache, injection-site reactions, arthralgia, diarrhea, gastroenteritis, tinea infections, and herpes simplex infections.
, according to a July 14 announcement from its manufacturer, Janssen.
The FDA’s approval marks the second indication for guselkumab, which was first approved for adults with plaque psoriasis in 2017.
The agency based its approval on two pivotal phase 3 clinical trials, DISCOVER-1 and DISCOVER-2, which tested the biologic in 1,120 adults with active PsA who were naive to biologics (both trials) or had an inadequate response or intolerance to one or two tumor necrosis factor inhibitors (in about 30% of patients in DISCOVER-1). Part of this pretrial standard treatment could include at least 4 months of Otezla (apremilast), at least 3 months of nonbiologic disease-modifying antirheumatic drugs (DMARDs), or at least 4 weeks of NSAIDs. In both trials, about 58% of patients took methotrexate.
Participants who took guselkumab achieved 20% improvement in American College of Rheumatology response criteria at week 24 at rates of 52% in DISCOVER-1 and 64% in DISCOVER-2, whereas placebo-treated patients had rates of 22% and 33%, respectively.
Guselkumab improved patients’ other symptoms, including skin manifestations of psoriasis, physical functioning, enthesitis, dactylitis, and fatigue, according to the Janssen release.
Guselkumab, a fully human monoclonal antibody that selectively binds to the p19 subunit of IL-23, is administered as a 100-mg subcutaneous injection every 8 weeks, following two starter doses at weeks 0 and 4, and can be used alone or in combination with a conventional DMARD.
In guselkumab clinical trials of patients with PsA, a minority had bronchitis or a decreased neutrophil count, but the safety profile was otherwise generally consistent with what has been seen in patients with plaque psoriasis, according to the company release. Other common side effects described in 1% or more of patients have included upper respiratory infections, headache, injection-site reactions, arthralgia, diarrhea, gastroenteritis, tinea infections, and herpes simplex infections.
, according to a July 14 announcement from its manufacturer, Janssen.
The FDA’s approval marks the second indication for guselkumab, which was first approved for adults with plaque psoriasis in 2017.
The agency based its approval on two pivotal phase 3 clinical trials, DISCOVER-1 and DISCOVER-2, which tested the biologic in 1,120 adults with active PsA who were naive to biologics (both trials) or had an inadequate response or intolerance to one or two tumor necrosis factor inhibitors (in about 30% of patients in DISCOVER-1). Part of this pretrial standard treatment could include at least 4 months of Otezla (apremilast), at least 3 months of nonbiologic disease-modifying antirheumatic drugs (DMARDs), or at least 4 weeks of NSAIDs. In both trials, about 58% of patients took methotrexate.
Participants who took guselkumab achieved 20% improvement in American College of Rheumatology response criteria at week 24 at rates of 52% in DISCOVER-1 and 64% in DISCOVER-2, whereas placebo-treated patients had rates of 22% and 33%, respectively.
Guselkumab improved patients’ other symptoms, including skin manifestations of psoriasis, physical functioning, enthesitis, dactylitis, and fatigue, according to the Janssen release.
Guselkumab, a fully human monoclonal antibody that selectively binds to the p19 subunit of IL-23, is administered as a 100-mg subcutaneous injection every 8 weeks, following two starter doses at weeks 0 and 4, and can be used alone or in combination with a conventional DMARD.
In guselkumab clinical trials of patients with PsA, a minority had bronchitis or a decreased neutrophil count, but the safety profile was otherwise generally consistent with what has been seen in patients with plaque psoriasis, according to the company release. Other common side effects described in 1% or more of patients have included upper respiratory infections, headache, injection-site reactions, arthralgia, diarrhea, gastroenteritis, tinea infections, and herpes simplex infections.
PASDAS beats DAS28 in measuring psoriatic arthritis treat-to-target success
Measuring success with a treat-to-target strategy in psoriatic arthritis patients proved to be more comprehensive with the Psoriatic Arthritis Disease Activity Score (PASDAS) than it was with the Disease Activity Score in 28 joints (DAS28), according to findings from a prospective cohort study.
Fewer patients had a low disease activity score according to DAS28, and a higher percentage of patients deemed adequately treated according to DAS28 were found to have residual disease activity, compared with the number of patients so categorized according to PASDAS, researcher Michelle Mulder reported in her presentation of the study at the virtual annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA).
“PASDAS implementation in a tightly monitored PsA [psoriatic arthritis] cohort suggests relevant residual disease burden, even though DAS28 was measured at every visit previously,” said Ms. Mulder, an MD/PhD student at Sint Maartenskliniek in Nijmegen, The Netherlands.
The presentation was convincing to Philip Helliwell, MD, PhD, who is a professor of clinical rheumatology at Leeds (England) University, and was also one of the developers of PASDAS. “We know it can be used in clinical practice with a certain amount of organization and clinical staff to help you,” he said during another presentation at GRAPPA.
Treat to target is a widely accepted therapeutic strategy. It’s particularly common in rheumatoid arthritis, but increasing evidence suggests that it improves patient outcomes in psoriatic arthritis. DAS28 is frequently used in treat-to-target approaches in rheumatoid arthritis, and often gets applied to psoriatic arthritis since rheumatologists are already comfortable with it, according to Ms. Mulder. “However, DAS28 has shown some limitations when used in psoriatic arthritis. For example, its joint count is limited to only 28 joints, and it does not take all PsA domains into account,” she said.
DAS28 was previously used at Sint Maartenskliniek in combination with psoriatic arthritis–specific assessment recommendations, but the institution opted in 2019 to switch to PASDAS, which was developed by GRAPPA and the European League Against Rheumatism. “To better adhere to international PsA guidelines, we chose to implement PASDAS in our cohort with the assumption that it might improve patient care,” Ms. Mulder said.
With DAS28, clinicians measured the C-reactive protein (CRP) and Patient Global Visual Analog Scale (VAS) domains and were advised to examine 28 joints for tender and swollen joint count domains. Under the PASDAS guidance, clinicians examined 68 joints for tenderness, 66 joints for swelling, CRP, Patient Global VAS, Physician Global VAS, Leeds Enthesitis Index, dactylitis, and the 12-item Short Form Physical Composite Scale. They also examined the skin, nails, and axial disease.
To examine the effects of the switch from DAS28 to PASDAS, the researchers compared outcomes in 855 patients before and after the change during March to December 2019. The mean age of patients was 55 years, and 46% were female. The mean disease duration was 10 years, and the mean PASDAS score was 3.1. A total of 96% of participants were negative for anti-cyclic citrullinated peptide. Overall, 30% had arthritis, 9% had axial disease, 3% had dactylitis, 21% had enthesitis, 51% had skin disease, and 42% had nail disease.
About three-quarters (77.4%) of patients reached the threshold of low disease activity (LDA) according to the DAS28 measure, while 53.1% did so using the PASDAS. High disease activity occurred in 7.8% of patients according to DAS28, compared with 2.7% as measured by PASDAS. Patients who reached only the DAS28 LDA target but not the PASDAS target, compared with patients who reached the LDA target in both measures, had significantly worse counts for swelling in 66 joints (0.7 vs. 0.2; P < .001) and tenderness in 68 joints (2.1 vs. 0.7; P < .001), as well as worse scores for enthesitis (0.5 vs. 0.1; P < .001), dactylitis (4% vs. 1%; P = .005), patient global VAS (44.0 vs. 14.4; P < .001), Health Assessment Questionnaire (0.8 vs. 0.4; P < .001) and Patient Acceptable Symptom State (unacceptable score in 17% vs. 3%; P < .001).
Ms. Mulder acknowledged that PASDAS imposes a significant burden on clinicians, and noted that Sint Maartenskliniek created patient infrastructure to handle the load. “It’s very important that you set up your clinic in a specific way. When the patient comes in, we draw blood immediately and we ask them to fill in the questionnaires, and then they go to a specialized nurse who measures all the different components of the PASDAS. It took a lot of time to train the specialized nurses and to implement the PASDAS score in our electronic health records. After we did those things, it was quite easy because we have this whole setup. It takes time and it is difficult, but it is definitely possible to do it,” Ms. Mulder said during a live Q&A following her prerecorded presentation.
The study received no funding. Ms. Mulder had no relevant financial disclosures. Dr. Helliwell has financial ties to AbbVie, Amgen, Celgen, Galapagos, Janssen, Novartis, Pfizer, and UCB.
SOURCE: Mulder M et al. GRAPPA 2020 Virtual Annual Meeting.
Measuring success with a treat-to-target strategy in psoriatic arthritis patients proved to be more comprehensive with the Psoriatic Arthritis Disease Activity Score (PASDAS) than it was with the Disease Activity Score in 28 joints (DAS28), according to findings from a prospective cohort study.
Fewer patients had a low disease activity score according to DAS28, and a higher percentage of patients deemed adequately treated according to DAS28 were found to have residual disease activity, compared with the number of patients so categorized according to PASDAS, researcher Michelle Mulder reported in her presentation of the study at the virtual annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA).
“PASDAS implementation in a tightly monitored PsA [psoriatic arthritis] cohort suggests relevant residual disease burden, even though DAS28 was measured at every visit previously,” said Ms. Mulder, an MD/PhD student at Sint Maartenskliniek in Nijmegen, The Netherlands.
The presentation was convincing to Philip Helliwell, MD, PhD, who is a professor of clinical rheumatology at Leeds (England) University, and was also one of the developers of PASDAS. “We know it can be used in clinical practice with a certain amount of organization and clinical staff to help you,” he said during another presentation at GRAPPA.
Treat to target is a widely accepted therapeutic strategy. It’s particularly common in rheumatoid arthritis, but increasing evidence suggests that it improves patient outcomes in psoriatic arthritis. DAS28 is frequently used in treat-to-target approaches in rheumatoid arthritis, and often gets applied to psoriatic arthritis since rheumatologists are already comfortable with it, according to Ms. Mulder. “However, DAS28 has shown some limitations when used in psoriatic arthritis. For example, its joint count is limited to only 28 joints, and it does not take all PsA domains into account,” she said.
DAS28 was previously used at Sint Maartenskliniek in combination with psoriatic arthritis–specific assessment recommendations, but the institution opted in 2019 to switch to PASDAS, which was developed by GRAPPA and the European League Against Rheumatism. “To better adhere to international PsA guidelines, we chose to implement PASDAS in our cohort with the assumption that it might improve patient care,” Ms. Mulder said.
With DAS28, clinicians measured the C-reactive protein (CRP) and Patient Global Visual Analog Scale (VAS) domains and were advised to examine 28 joints for tender and swollen joint count domains. Under the PASDAS guidance, clinicians examined 68 joints for tenderness, 66 joints for swelling, CRP, Patient Global VAS, Physician Global VAS, Leeds Enthesitis Index, dactylitis, and the 12-item Short Form Physical Composite Scale. They also examined the skin, nails, and axial disease.
To examine the effects of the switch from DAS28 to PASDAS, the researchers compared outcomes in 855 patients before and after the change during March to December 2019. The mean age of patients was 55 years, and 46% were female. The mean disease duration was 10 years, and the mean PASDAS score was 3.1. A total of 96% of participants were negative for anti-cyclic citrullinated peptide. Overall, 30% had arthritis, 9% had axial disease, 3% had dactylitis, 21% had enthesitis, 51% had skin disease, and 42% had nail disease.
About three-quarters (77.4%) of patients reached the threshold of low disease activity (LDA) according to the DAS28 measure, while 53.1% did so using the PASDAS. High disease activity occurred in 7.8% of patients according to DAS28, compared with 2.7% as measured by PASDAS. Patients who reached only the DAS28 LDA target but not the PASDAS target, compared with patients who reached the LDA target in both measures, had significantly worse counts for swelling in 66 joints (0.7 vs. 0.2; P < .001) and tenderness in 68 joints (2.1 vs. 0.7; P < .001), as well as worse scores for enthesitis (0.5 vs. 0.1; P < .001), dactylitis (4% vs. 1%; P = .005), patient global VAS (44.0 vs. 14.4; P < .001), Health Assessment Questionnaire (0.8 vs. 0.4; P < .001) and Patient Acceptable Symptom State (unacceptable score in 17% vs. 3%; P < .001).
Ms. Mulder acknowledged that PASDAS imposes a significant burden on clinicians, and noted that Sint Maartenskliniek created patient infrastructure to handle the load. “It’s very important that you set up your clinic in a specific way. When the patient comes in, we draw blood immediately and we ask them to fill in the questionnaires, and then they go to a specialized nurse who measures all the different components of the PASDAS. It took a lot of time to train the specialized nurses and to implement the PASDAS score in our electronic health records. After we did those things, it was quite easy because we have this whole setup. It takes time and it is difficult, but it is definitely possible to do it,” Ms. Mulder said during a live Q&A following her prerecorded presentation.
The study received no funding. Ms. Mulder had no relevant financial disclosures. Dr. Helliwell has financial ties to AbbVie, Amgen, Celgen, Galapagos, Janssen, Novartis, Pfizer, and UCB.
SOURCE: Mulder M et al. GRAPPA 2020 Virtual Annual Meeting.
Measuring success with a treat-to-target strategy in psoriatic arthritis patients proved to be more comprehensive with the Psoriatic Arthritis Disease Activity Score (PASDAS) than it was with the Disease Activity Score in 28 joints (DAS28), according to findings from a prospective cohort study.
Fewer patients had a low disease activity score according to DAS28, and a higher percentage of patients deemed adequately treated according to DAS28 were found to have residual disease activity, compared with the number of patients so categorized according to PASDAS, researcher Michelle Mulder reported in her presentation of the study at the virtual annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA).
“PASDAS implementation in a tightly monitored PsA [psoriatic arthritis] cohort suggests relevant residual disease burden, even though DAS28 was measured at every visit previously,” said Ms. Mulder, an MD/PhD student at Sint Maartenskliniek in Nijmegen, The Netherlands.
The presentation was convincing to Philip Helliwell, MD, PhD, who is a professor of clinical rheumatology at Leeds (England) University, and was also one of the developers of PASDAS. “We know it can be used in clinical practice with a certain amount of organization and clinical staff to help you,” he said during another presentation at GRAPPA.
Treat to target is a widely accepted therapeutic strategy. It’s particularly common in rheumatoid arthritis, but increasing evidence suggests that it improves patient outcomes in psoriatic arthritis. DAS28 is frequently used in treat-to-target approaches in rheumatoid arthritis, and often gets applied to psoriatic arthritis since rheumatologists are already comfortable with it, according to Ms. Mulder. “However, DAS28 has shown some limitations when used in psoriatic arthritis. For example, its joint count is limited to only 28 joints, and it does not take all PsA domains into account,” she said.
DAS28 was previously used at Sint Maartenskliniek in combination with psoriatic arthritis–specific assessment recommendations, but the institution opted in 2019 to switch to PASDAS, which was developed by GRAPPA and the European League Against Rheumatism. “To better adhere to international PsA guidelines, we chose to implement PASDAS in our cohort with the assumption that it might improve patient care,” Ms. Mulder said.
With DAS28, clinicians measured the C-reactive protein (CRP) and Patient Global Visual Analog Scale (VAS) domains and were advised to examine 28 joints for tender and swollen joint count domains. Under the PASDAS guidance, clinicians examined 68 joints for tenderness, 66 joints for swelling, CRP, Patient Global VAS, Physician Global VAS, Leeds Enthesitis Index, dactylitis, and the 12-item Short Form Physical Composite Scale. They also examined the skin, nails, and axial disease.
To examine the effects of the switch from DAS28 to PASDAS, the researchers compared outcomes in 855 patients before and after the change during March to December 2019. The mean age of patients was 55 years, and 46% were female. The mean disease duration was 10 years, and the mean PASDAS score was 3.1. A total of 96% of participants were negative for anti-cyclic citrullinated peptide. Overall, 30% had arthritis, 9% had axial disease, 3% had dactylitis, 21% had enthesitis, 51% had skin disease, and 42% had nail disease.
About three-quarters (77.4%) of patients reached the threshold of low disease activity (LDA) according to the DAS28 measure, while 53.1% did so using the PASDAS. High disease activity occurred in 7.8% of patients according to DAS28, compared with 2.7% as measured by PASDAS. Patients who reached only the DAS28 LDA target but not the PASDAS target, compared with patients who reached the LDA target in both measures, had significantly worse counts for swelling in 66 joints (0.7 vs. 0.2; P < .001) and tenderness in 68 joints (2.1 vs. 0.7; P < .001), as well as worse scores for enthesitis (0.5 vs. 0.1; P < .001), dactylitis (4% vs. 1%; P = .005), patient global VAS (44.0 vs. 14.4; P < .001), Health Assessment Questionnaire (0.8 vs. 0.4; P < .001) and Patient Acceptable Symptom State (unacceptable score in 17% vs. 3%; P < .001).
Ms. Mulder acknowledged that PASDAS imposes a significant burden on clinicians, and noted that Sint Maartenskliniek created patient infrastructure to handle the load. “It’s very important that you set up your clinic in a specific way. When the patient comes in, we draw blood immediately and we ask them to fill in the questionnaires, and then they go to a specialized nurse who measures all the different components of the PASDAS. It took a lot of time to train the specialized nurses and to implement the PASDAS score in our electronic health records. After we did those things, it was quite easy because we have this whole setup. It takes time and it is difficult, but it is definitely possible to do it,” Ms. Mulder said during a live Q&A following her prerecorded presentation.
The study received no funding. Ms. Mulder had no relevant financial disclosures. Dr. Helliwell has financial ties to AbbVie, Amgen, Celgen, Galapagos, Janssen, Novartis, Pfizer, and UCB.
SOURCE: Mulder M et al. GRAPPA 2020 Virtual Annual Meeting.
FROM GRAPPA 2020 VIRTUAL ANNUAL MEETING
Cardiac CT scans can be used for osteoporosis screening
A new study has determined a benefit of cardiac CT scans beyond assessing heart health: Evaluating fracture rate and potential osteoporosis through the bone mineral density (BMD) of thoracic vertebrae.
“Our results represent a step toward appraisal and recognition of the clinical utility of opportunistic BMD screening from cardiac CT,” wrote Josephine Therkildsen, MD, of Hospital Unit West in Herning, Denmark, and coauthors. The study was published July 14 in Radiology.
To determine if further analysis of cardiac CT could help determine BMD and its association with fracture rate, the investigators launched a prospective observational study of 1,487 Danish patients with potential coronary artery disease who underwent cardiac CT scans between September 2014 and March 2016. Their mean age was 57 years (standard deviation, 9; range, 40-80). Nearly all of the patients were white, and 52.5% (n = 781) were women.
All participants underwent a noncontrast-enhanced cardiac CT, from which volumetric BMD of three thoracic vertebrae was measured via commercially available semiautomatic software. Their mean BMD was 119 mg/cm3 (SD, 34) with no significant difference noted between male and female patients. Of the 1,487 participants, 695 were defined as having normal BMD (> 120 mg/cm3), 613 as having low BMD (80-120 mg/cm3), and 179 as having very low BMD (< 80 mg/cm3). Median follow-up was 3.1 years (interquartile range, 2.7-3.4).
Incident fracture occurred in 80 patients (5.4%), of whom 48 were women and 32 were men. Patients who suffered fractures were significantly older than patients with no fractures (mean 59 years vs. 57 years; P = .03). Of the 80 patients with fractures, 31 were osteoporosis related.
In an unadjusted analysis, participants with very low BMD had a greater rate of any fracture (hazard ratio [HR], 2.6; 95% confidence interval, 1.4-4.7; P = .002) and of osteoporosis-related fracture (HR, 8.1; 95% CI, 2.4-27.0; P = .001). After adjustment for age and sex, their rates remained significantly greater for any fracture (HR, 2.1; 95% CI, 1.1-4.2; P = .03) and for osteoporosis-related fracture (HR, 4.0; 95% CI, 1.1-15.0; P = .04).
“Opportunistic” use of scans benefits both physicians and patients
“The concept of using a CT scan that was done for a different purpose allows you to be opportunistic,” Ethel S. Siris, MD, the Madeline C. Stabile Professor of Clinical Medicine in the department of medicine at Columbia University and director of the Toni Stabile Osteoporosis Center of the Columbia University Medical Center, New York–Presbyterian Hospital, New York, said in an interview. “If you’re dealing with older patients, and if you have the software for your radiologist to use to reanalyze the CT scan and say something about the bone, it’s certainly a way of estimating who may be at risk of future fractures.
“From a practical point of view, it’s hard to imagine that it would ever replace conventional bone mineral density testing via DXA [dual-energy x-ray absorptiometry],” she added. “That said, osteoporosis is woefully underdiagnosed because people don’t get DXA tested. This study showed that, if you have access to the scan of the thoracic or even the lumbar spine and if you have the necessary software, you can make legitimate statements about the numbers being low or very low. What that would lead to, I would hope, is some internists to say, ‘This could be a predictor of fracture risk. We should put you on treatment.’ And then follow up with a conventional DXA test.
“Is that going to happen? I don’t know. But the bottom line of the study is: Anything that may enhance the physician’s drive to evaluate a patient for fracture risk is good.”
Whatever the reason for the scan, CT can help diagnose osteoporosis
This study reinforces that CT exams – of the chest, in particular – can serve a valuable dual purpose as osteoporosis screenings, Miriam A. Bredella, MD, professor of radiology at Harvard Medical School and vice chair of the department of radiology at Massachusetts General Hospital, Boston, wrote in an accompanying editorial.
“In the United States, more than 80 million CT examinations are performed each year, many of which could be used to screen for osteoporosis without additional costs or radiation exposure,” she wrote. And thanks to the findings of the study by Therkildsen et al., which relied on both established and new BMD thresholds, the link between thoracic spine BMD and fracture risk is clearer than ever.
“I hope this study will ignite interest in using chest CT examinations performed for other purposes, such as lung cancer screening, for opportunistic osteoporosis screening and prediction of fractures in vulnerable populations,” she added.
The authors acknowledged their study’s limitations, including a small number of fracture events overall and the inability to evaluate associations between BMD and fracture rate at specific locations. In addition, their cohort was largely made up of white participants with a certain coronary artery disease risk profile; because of ethnical differences in BMD measurements, their results “cannot be extrapolated to other ethnical groups.”
Several of the study’s authors reported potential conflicts of interest, including receiving grants and money for consultancies and board memberships from various councils, associations, and pharmaceutical companies. Dr. Bredella reported no conflicts of interest. Dr. Siris has no relevant disclosures.
SOURCE: Therkildsen J et al. Radiology. 2020 Jul 14. doi: 10.1148/radiol.2020192706.
A new study has determined a benefit of cardiac CT scans beyond assessing heart health: Evaluating fracture rate and potential osteoporosis through the bone mineral density (BMD) of thoracic vertebrae.
“Our results represent a step toward appraisal and recognition of the clinical utility of opportunistic BMD screening from cardiac CT,” wrote Josephine Therkildsen, MD, of Hospital Unit West in Herning, Denmark, and coauthors. The study was published July 14 in Radiology.
To determine if further analysis of cardiac CT could help determine BMD and its association with fracture rate, the investigators launched a prospective observational study of 1,487 Danish patients with potential coronary artery disease who underwent cardiac CT scans between September 2014 and March 2016. Their mean age was 57 years (standard deviation, 9; range, 40-80). Nearly all of the patients were white, and 52.5% (n = 781) were women.
All participants underwent a noncontrast-enhanced cardiac CT, from which volumetric BMD of three thoracic vertebrae was measured via commercially available semiautomatic software. Their mean BMD was 119 mg/cm3 (SD, 34) with no significant difference noted between male and female patients. Of the 1,487 participants, 695 were defined as having normal BMD (> 120 mg/cm3), 613 as having low BMD (80-120 mg/cm3), and 179 as having very low BMD (< 80 mg/cm3). Median follow-up was 3.1 years (interquartile range, 2.7-3.4).
Incident fracture occurred in 80 patients (5.4%), of whom 48 were women and 32 were men. Patients who suffered fractures were significantly older than patients with no fractures (mean 59 years vs. 57 years; P = .03). Of the 80 patients with fractures, 31 were osteoporosis related.
In an unadjusted analysis, participants with very low BMD had a greater rate of any fracture (hazard ratio [HR], 2.6; 95% confidence interval, 1.4-4.7; P = .002) and of osteoporosis-related fracture (HR, 8.1; 95% CI, 2.4-27.0; P = .001). After adjustment for age and sex, their rates remained significantly greater for any fracture (HR, 2.1; 95% CI, 1.1-4.2; P = .03) and for osteoporosis-related fracture (HR, 4.0; 95% CI, 1.1-15.0; P = .04).
“Opportunistic” use of scans benefits both physicians and patients
“The concept of using a CT scan that was done for a different purpose allows you to be opportunistic,” Ethel S. Siris, MD, the Madeline C. Stabile Professor of Clinical Medicine in the department of medicine at Columbia University and director of the Toni Stabile Osteoporosis Center of the Columbia University Medical Center, New York–Presbyterian Hospital, New York, said in an interview. “If you’re dealing with older patients, and if you have the software for your radiologist to use to reanalyze the CT scan and say something about the bone, it’s certainly a way of estimating who may be at risk of future fractures.
“From a practical point of view, it’s hard to imagine that it would ever replace conventional bone mineral density testing via DXA [dual-energy x-ray absorptiometry],” she added. “That said, osteoporosis is woefully underdiagnosed because people don’t get DXA tested. This study showed that, if you have access to the scan of the thoracic or even the lumbar spine and if you have the necessary software, you can make legitimate statements about the numbers being low or very low. What that would lead to, I would hope, is some internists to say, ‘This could be a predictor of fracture risk. We should put you on treatment.’ And then follow up with a conventional DXA test.
“Is that going to happen? I don’t know. But the bottom line of the study is: Anything that may enhance the physician’s drive to evaluate a patient for fracture risk is good.”
Whatever the reason for the scan, CT can help diagnose osteoporosis
This study reinforces that CT exams – of the chest, in particular – can serve a valuable dual purpose as osteoporosis screenings, Miriam A. Bredella, MD, professor of radiology at Harvard Medical School and vice chair of the department of radiology at Massachusetts General Hospital, Boston, wrote in an accompanying editorial.
“In the United States, more than 80 million CT examinations are performed each year, many of which could be used to screen for osteoporosis without additional costs or radiation exposure,” she wrote. And thanks to the findings of the study by Therkildsen et al., which relied on both established and new BMD thresholds, the link between thoracic spine BMD and fracture risk is clearer than ever.
“I hope this study will ignite interest in using chest CT examinations performed for other purposes, such as lung cancer screening, for opportunistic osteoporosis screening and prediction of fractures in vulnerable populations,” she added.
The authors acknowledged their study’s limitations, including a small number of fracture events overall and the inability to evaluate associations between BMD and fracture rate at specific locations. In addition, their cohort was largely made up of white participants with a certain coronary artery disease risk profile; because of ethnical differences in BMD measurements, their results “cannot be extrapolated to other ethnical groups.”
Several of the study’s authors reported potential conflicts of interest, including receiving grants and money for consultancies and board memberships from various councils, associations, and pharmaceutical companies. Dr. Bredella reported no conflicts of interest. Dr. Siris has no relevant disclosures.
SOURCE: Therkildsen J et al. Radiology. 2020 Jul 14. doi: 10.1148/radiol.2020192706.
A new study has determined a benefit of cardiac CT scans beyond assessing heart health: Evaluating fracture rate and potential osteoporosis through the bone mineral density (BMD) of thoracic vertebrae.
“Our results represent a step toward appraisal and recognition of the clinical utility of opportunistic BMD screening from cardiac CT,” wrote Josephine Therkildsen, MD, of Hospital Unit West in Herning, Denmark, and coauthors. The study was published July 14 in Radiology.
To determine if further analysis of cardiac CT could help determine BMD and its association with fracture rate, the investigators launched a prospective observational study of 1,487 Danish patients with potential coronary artery disease who underwent cardiac CT scans between September 2014 and March 2016. Their mean age was 57 years (standard deviation, 9; range, 40-80). Nearly all of the patients were white, and 52.5% (n = 781) were women.
All participants underwent a noncontrast-enhanced cardiac CT, from which volumetric BMD of three thoracic vertebrae was measured via commercially available semiautomatic software. Their mean BMD was 119 mg/cm3 (SD, 34) with no significant difference noted between male and female patients. Of the 1,487 participants, 695 were defined as having normal BMD (> 120 mg/cm3), 613 as having low BMD (80-120 mg/cm3), and 179 as having very low BMD (< 80 mg/cm3). Median follow-up was 3.1 years (interquartile range, 2.7-3.4).
Incident fracture occurred in 80 patients (5.4%), of whom 48 were women and 32 were men. Patients who suffered fractures were significantly older than patients with no fractures (mean 59 years vs. 57 years; P = .03). Of the 80 patients with fractures, 31 were osteoporosis related.
In an unadjusted analysis, participants with very low BMD had a greater rate of any fracture (hazard ratio [HR], 2.6; 95% confidence interval, 1.4-4.7; P = .002) and of osteoporosis-related fracture (HR, 8.1; 95% CI, 2.4-27.0; P = .001). After adjustment for age and sex, their rates remained significantly greater for any fracture (HR, 2.1; 95% CI, 1.1-4.2; P = .03) and for osteoporosis-related fracture (HR, 4.0; 95% CI, 1.1-15.0; P = .04).
“Opportunistic” use of scans benefits both physicians and patients
“The concept of using a CT scan that was done for a different purpose allows you to be opportunistic,” Ethel S. Siris, MD, the Madeline C. Stabile Professor of Clinical Medicine in the department of medicine at Columbia University and director of the Toni Stabile Osteoporosis Center of the Columbia University Medical Center, New York–Presbyterian Hospital, New York, said in an interview. “If you’re dealing with older patients, and if you have the software for your radiologist to use to reanalyze the CT scan and say something about the bone, it’s certainly a way of estimating who may be at risk of future fractures.
“From a practical point of view, it’s hard to imagine that it would ever replace conventional bone mineral density testing via DXA [dual-energy x-ray absorptiometry],” she added. “That said, osteoporosis is woefully underdiagnosed because people don’t get DXA tested. This study showed that, if you have access to the scan of the thoracic or even the lumbar spine and if you have the necessary software, you can make legitimate statements about the numbers being low or very low. What that would lead to, I would hope, is some internists to say, ‘This could be a predictor of fracture risk. We should put you on treatment.’ And then follow up with a conventional DXA test.
“Is that going to happen? I don’t know. But the bottom line of the study is: Anything that may enhance the physician’s drive to evaluate a patient for fracture risk is good.”
Whatever the reason for the scan, CT can help diagnose osteoporosis
This study reinforces that CT exams – of the chest, in particular – can serve a valuable dual purpose as osteoporosis screenings, Miriam A. Bredella, MD, professor of radiology at Harvard Medical School and vice chair of the department of radiology at Massachusetts General Hospital, Boston, wrote in an accompanying editorial.
“In the United States, more than 80 million CT examinations are performed each year, many of which could be used to screen for osteoporosis without additional costs or radiation exposure,” she wrote. And thanks to the findings of the study by Therkildsen et al., which relied on both established and new BMD thresholds, the link between thoracic spine BMD and fracture risk is clearer than ever.
“I hope this study will ignite interest in using chest CT examinations performed for other purposes, such as lung cancer screening, for opportunistic osteoporosis screening and prediction of fractures in vulnerable populations,” she added.
The authors acknowledged their study’s limitations, including a small number of fracture events overall and the inability to evaluate associations between BMD and fracture rate at specific locations. In addition, their cohort was largely made up of white participants with a certain coronary artery disease risk profile; because of ethnical differences in BMD measurements, their results “cannot be extrapolated to other ethnical groups.”
Several of the study’s authors reported potential conflicts of interest, including receiving grants and money for consultancies and board memberships from various councils, associations, and pharmaceutical companies. Dr. Bredella reported no conflicts of interest. Dr. Siris has no relevant disclosures.
SOURCE: Therkildsen J et al. Radiology. 2020 Jul 14. doi: 10.1148/radiol.2020192706.
FROM RADIOLOGY
Steroids linked to increased hypertension in RA
Although the adverse effects of systemic glucocorticoids (GCs) are well known, their association with hypertension in rheumatoid arthritis (RA) has been unclear. Now, a large population-based study shows that the drugs are linked to a 17% overall increased risk for incident hypertension among patients with RA.
Further, when the researchers stratified participants by dose category, they found that doses higher than 7.5 mg were significantly associated with hypertension. Cumulative dosage was not tied to any clear pattern of risk.
The authors, led by Ruth E. Costello, a researcher at the Centre for Epidemiology Versus Arthritis in the Centre for Musculoskeletal Research at the University of Manchester (England) concluded that patients who are taking these drugs for the treatment of RA should be monitored for high blood pressure, which is an important but modifiable cardiovascular risk factor, and treated appropriately.
The results of Ms. Costello and colleagues’ study were published June 27 in Rheumatology.
“While fractures associated with these steroid drugs are well studied, hypertension is a side effect that seems to have been less well studied, and yet it is an important cardiovascular risk factor that can be managed,” Ms. Costello said in an interview.
To better understand the possible association, Ms. Costello and colleagues identified 17,760 patients who were newly diagnosed with RA between 1992 and 2019 and were included in the Clinical Practice Research Datalink, which represents about 7% of the U.K. population. None of the patients had hypertension at initial RA diagnosis. Slightly more than two-thirds were women (68.1%), and the mean age was 56.3 years.
Of those patients, 7,421 (41.8%) were prescribed GCs during postdiagnosis follow-up. Most patients (73%) were followed for at least 2 years.
Patients who used GCs were slightly older than never-users (mean age, 57.7 vs. 55.3 years), were predominantly women, had a history of smoking, and had more comorbidities.
The overall incidence rate (IR) of hypertension was 64.1 per 1,000 person-years (95% confidence interval, 62.5-65.7). There were 6,243 cases of incident hypertension over 97,547 person-years of follow-up.
Among those exposed to GCs, 1,321 patients developed hypertension, for an IR of 87.6 per 1,000 person-years. Among unexposed participants, the IR for hypertension was 59.7 per 1,000 person-years. In Cox proportional hazards modeling, GC use was associated with a 17% increased risk for hypertension (hazard ratio, 1.17; 95% CI, 1.10-1.24).
The researchers noted that 40% of GC users with hypertension were not prescribed an antihypertensive agent at any point during the study. “Whilst some may have been offered lifestyle advice, left untreated this has important implications in terms of addressing modifiable risk factors in an RA population already at increased risk of CV disease,” they wrote.
They noted that cardiovascular disease is a major driver of the elevated mortality risk seen among adults with RA compared with the general population and that recent treatment recommendations address management of cardiovascular risks in these patients.
“There are several routes by which GCs may promote cardiovascular disease, including hypertension, metabolic changes, diabetes, and weight gain. We don’t currently know the extent to which each of these individual mechanisms may be increasing cardiovascular disease,” said Ms. Costello.
“Glucocorticoids increase fluid retention and promote obesity and hypertension,” said Rajat S. Bhatt, MD, a rheumatologist at Prime Rheumatology and Memorial Hermann Katy Hospital in Richmond, Texas, who sees hypertension in GC users in his clinical practice. “So patients need to be monitored for these risk factors,” he said in an interview.
Although hypertension may be a significant factor in the increase in cardiovascular disease in the RA population, Dr. Bhatt said the major driver is likely the intrinsic inflammatory state caused by the disease itself. As to why the GC-hypertension connection has flown under the radar in RA, he added, “That specific link has been difficult to tease out since RA patients are often on multiple medications.”
In regard to the role of dosage, Dr. Bhatt said that hypertension risk increases with higher GC doses, as the U.K. study indicates, and usually subsides when patients stop using GCs.
“Whether the observed dose association is causal or influenced by the underlying disease severity, our results suggest we should be vigilant in patients on all doses of GC, especially higher doses,” Ms. Costello added.
In regard to using drugs that are less cardiotoxic than GCs, Dr. Bhatt said that there are clinical scenarios in which GC therapy is the best choice, so just switching to nonsteroidal drugs is no panacea. “All RA drugs have adverse side effects, and anyway, the goal of rheumatology treatment is always to get patients off corticosteroids as soon as possible,” he said.
Ms. Costello and colleagues noted that their results are consonant with earlier research, including a single-center, cross-sectional study in which less than 6 months’ use of prednisolone at a median dose of 7.5 mg was associated with hypertension. In a German registry study, among patients who received doses of less than 7.5 mg for less than 6 months, there were higher rates of self-reported elevations in blood pressure.
The findings are at odds, however, with a recent matched-cohort study, which also used data from the Clinical Practice Research Datalink. That study found no association between GC use and hypertension.
GCs have come under increasing scrutiny in regard to several diseases. A study published July 7 found that even short-term courses of a few days’ duration entail risks for serious adverse events.
Ms. Costello’s group says that an estimate of GC-related incident hypertension in RA should allow more informed treatment decisions and that their findings highlight the ongoing need to monitor for and address this risk.
The study was supported by the Centre for Epidemiology Versus Arthritis and by the National Institute for Health Research Manchester Biomedical Research Centre. Coauthor William G. Dixon, PhD, has received consultancy fees from Google and Bayer unrelated to this study. Dr. Bhatt has disclosed no relevant financial relationships.
SOURCE: Costello RE et al. Rheumatology. 2020 June 27. doi: 10.1093/rheumatology/keaa209.
A version of this article originally appeared on Medscape.com.
Although the adverse effects of systemic glucocorticoids (GCs) are well known, their association with hypertension in rheumatoid arthritis (RA) has been unclear. Now, a large population-based study shows that the drugs are linked to a 17% overall increased risk for incident hypertension among patients with RA.
Further, when the researchers stratified participants by dose category, they found that doses higher than 7.5 mg were significantly associated with hypertension. Cumulative dosage was not tied to any clear pattern of risk.
The authors, led by Ruth E. Costello, a researcher at the Centre for Epidemiology Versus Arthritis in the Centre for Musculoskeletal Research at the University of Manchester (England) concluded that patients who are taking these drugs for the treatment of RA should be monitored for high blood pressure, which is an important but modifiable cardiovascular risk factor, and treated appropriately.
The results of Ms. Costello and colleagues’ study were published June 27 in Rheumatology.
“While fractures associated with these steroid drugs are well studied, hypertension is a side effect that seems to have been less well studied, and yet it is an important cardiovascular risk factor that can be managed,” Ms. Costello said in an interview.
To better understand the possible association, Ms. Costello and colleagues identified 17,760 patients who were newly diagnosed with RA between 1992 and 2019 and were included in the Clinical Practice Research Datalink, which represents about 7% of the U.K. population. None of the patients had hypertension at initial RA diagnosis. Slightly more than two-thirds were women (68.1%), and the mean age was 56.3 years.
Of those patients, 7,421 (41.8%) were prescribed GCs during postdiagnosis follow-up. Most patients (73%) were followed for at least 2 years.
Patients who used GCs were slightly older than never-users (mean age, 57.7 vs. 55.3 years), were predominantly women, had a history of smoking, and had more comorbidities.
The overall incidence rate (IR) of hypertension was 64.1 per 1,000 person-years (95% confidence interval, 62.5-65.7). There were 6,243 cases of incident hypertension over 97,547 person-years of follow-up.
Among those exposed to GCs, 1,321 patients developed hypertension, for an IR of 87.6 per 1,000 person-years. Among unexposed participants, the IR for hypertension was 59.7 per 1,000 person-years. In Cox proportional hazards modeling, GC use was associated with a 17% increased risk for hypertension (hazard ratio, 1.17; 95% CI, 1.10-1.24).
The researchers noted that 40% of GC users with hypertension were not prescribed an antihypertensive agent at any point during the study. “Whilst some may have been offered lifestyle advice, left untreated this has important implications in terms of addressing modifiable risk factors in an RA population already at increased risk of CV disease,” they wrote.
They noted that cardiovascular disease is a major driver of the elevated mortality risk seen among adults with RA compared with the general population and that recent treatment recommendations address management of cardiovascular risks in these patients.
“There are several routes by which GCs may promote cardiovascular disease, including hypertension, metabolic changes, diabetes, and weight gain. We don’t currently know the extent to which each of these individual mechanisms may be increasing cardiovascular disease,” said Ms. Costello.
“Glucocorticoids increase fluid retention and promote obesity and hypertension,” said Rajat S. Bhatt, MD, a rheumatologist at Prime Rheumatology and Memorial Hermann Katy Hospital in Richmond, Texas, who sees hypertension in GC users in his clinical practice. “So patients need to be monitored for these risk factors,” he said in an interview.
Although hypertension may be a significant factor in the increase in cardiovascular disease in the RA population, Dr. Bhatt said the major driver is likely the intrinsic inflammatory state caused by the disease itself. As to why the GC-hypertension connection has flown under the radar in RA, he added, “That specific link has been difficult to tease out since RA patients are often on multiple medications.”
In regard to the role of dosage, Dr. Bhatt said that hypertension risk increases with higher GC doses, as the U.K. study indicates, and usually subsides when patients stop using GCs.
“Whether the observed dose association is causal or influenced by the underlying disease severity, our results suggest we should be vigilant in patients on all doses of GC, especially higher doses,” Ms. Costello added.
In regard to using drugs that are less cardiotoxic than GCs, Dr. Bhatt said that there are clinical scenarios in which GC therapy is the best choice, so just switching to nonsteroidal drugs is no panacea. “All RA drugs have adverse side effects, and anyway, the goal of rheumatology treatment is always to get patients off corticosteroids as soon as possible,” he said.
Ms. Costello and colleagues noted that their results are consonant with earlier research, including a single-center, cross-sectional study in which less than 6 months’ use of prednisolone at a median dose of 7.5 mg was associated with hypertension. In a German registry study, among patients who received doses of less than 7.5 mg for less than 6 months, there were higher rates of self-reported elevations in blood pressure.
The findings are at odds, however, with a recent matched-cohort study, which also used data from the Clinical Practice Research Datalink. That study found no association between GC use and hypertension.
GCs have come under increasing scrutiny in regard to several diseases. A study published July 7 found that even short-term courses of a few days’ duration entail risks for serious adverse events.
Ms. Costello’s group says that an estimate of GC-related incident hypertension in RA should allow more informed treatment decisions and that their findings highlight the ongoing need to monitor for and address this risk.
The study was supported by the Centre for Epidemiology Versus Arthritis and by the National Institute for Health Research Manchester Biomedical Research Centre. Coauthor William G. Dixon, PhD, has received consultancy fees from Google and Bayer unrelated to this study. Dr. Bhatt has disclosed no relevant financial relationships.
SOURCE: Costello RE et al. Rheumatology. 2020 June 27. doi: 10.1093/rheumatology/keaa209.
A version of this article originally appeared on Medscape.com.
Although the adverse effects of systemic glucocorticoids (GCs) are well known, their association with hypertension in rheumatoid arthritis (RA) has been unclear. Now, a large population-based study shows that the drugs are linked to a 17% overall increased risk for incident hypertension among patients with RA.
Further, when the researchers stratified participants by dose category, they found that doses higher than 7.5 mg were significantly associated with hypertension. Cumulative dosage was not tied to any clear pattern of risk.
The authors, led by Ruth E. Costello, a researcher at the Centre for Epidemiology Versus Arthritis in the Centre for Musculoskeletal Research at the University of Manchester (England) concluded that patients who are taking these drugs for the treatment of RA should be monitored for high blood pressure, which is an important but modifiable cardiovascular risk factor, and treated appropriately.
The results of Ms. Costello and colleagues’ study were published June 27 in Rheumatology.
“While fractures associated with these steroid drugs are well studied, hypertension is a side effect that seems to have been less well studied, and yet it is an important cardiovascular risk factor that can be managed,” Ms. Costello said in an interview.
To better understand the possible association, Ms. Costello and colleagues identified 17,760 patients who were newly diagnosed with RA between 1992 and 2019 and were included in the Clinical Practice Research Datalink, which represents about 7% of the U.K. population. None of the patients had hypertension at initial RA diagnosis. Slightly more than two-thirds were women (68.1%), and the mean age was 56.3 years.
Of those patients, 7,421 (41.8%) were prescribed GCs during postdiagnosis follow-up. Most patients (73%) were followed for at least 2 years.
Patients who used GCs were slightly older than never-users (mean age, 57.7 vs. 55.3 years), were predominantly women, had a history of smoking, and had more comorbidities.
The overall incidence rate (IR) of hypertension was 64.1 per 1,000 person-years (95% confidence interval, 62.5-65.7). There were 6,243 cases of incident hypertension over 97,547 person-years of follow-up.
Among those exposed to GCs, 1,321 patients developed hypertension, for an IR of 87.6 per 1,000 person-years. Among unexposed participants, the IR for hypertension was 59.7 per 1,000 person-years. In Cox proportional hazards modeling, GC use was associated with a 17% increased risk for hypertension (hazard ratio, 1.17; 95% CI, 1.10-1.24).
The researchers noted that 40% of GC users with hypertension were not prescribed an antihypertensive agent at any point during the study. “Whilst some may have been offered lifestyle advice, left untreated this has important implications in terms of addressing modifiable risk factors in an RA population already at increased risk of CV disease,” they wrote.
They noted that cardiovascular disease is a major driver of the elevated mortality risk seen among adults with RA compared with the general population and that recent treatment recommendations address management of cardiovascular risks in these patients.
“There are several routes by which GCs may promote cardiovascular disease, including hypertension, metabolic changes, diabetes, and weight gain. We don’t currently know the extent to which each of these individual mechanisms may be increasing cardiovascular disease,” said Ms. Costello.
“Glucocorticoids increase fluid retention and promote obesity and hypertension,” said Rajat S. Bhatt, MD, a rheumatologist at Prime Rheumatology and Memorial Hermann Katy Hospital in Richmond, Texas, who sees hypertension in GC users in his clinical practice. “So patients need to be monitored for these risk factors,” he said in an interview.
Although hypertension may be a significant factor in the increase in cardiovascular disease in the RA population, Dr. Bhatt said the major driver is likely the intrinsic inflammatory state caused by the disease itself. As to why the GC-hypertension connection has flown under the radar in RA, he added, “That specific link has been difficult to tease out since RA patients are often on multiple medications.”
In regard to the role of dosage, Dr. Bhatt said that hypertension risk increases with higher GC doses, as the U.K. study indicates, and usually subsides when patients stop using GCs.
“Whether the observed dose association is causal or influenced by the underlying disease severity, our results suggest we should be vigilant in patients on all doses of GC, especially higher doses,” Ms. Costello added.
In regard to using drugs that are less cardiotoxic than GCs, Dr. Bhatt said that there are clinical scenarios in which GC therapy is the best choice, so just switching to nonsteroidal drugs is no panacea. “All RA drugs have adverse side effects, and anyway, the goal of rheumatology treatment is always to get patients off corticosteroids as soon as possible,” he said.
Ms. Costello and colleagues noted that their results are consonant with earlier research, including a single-center, cross-sectional study in which less than 6 months’ use of prednisolone at a median dose of 7.5 mg was associated with hypertension. In a German registry study, among patients who received doses of less than 7.5 mg for less than 6 months, there were higher rates of self-reported elevations in blood pressure.
The findings are at odds, however, with a recent matched-cohort study, which also used data from the Clinical Practice Research Datalink. That study found no association between GC use and hypertension.
GCs have come under increasing scrutiny in regard to several diseases. A study published July 7 found that even short-term courses of a few days’ duration entail risks for serious adverse events.
Ms. Costello’s group says that an estimate of GC-related incident hypertension in RA should allow more informed treatment decisions and that their findings highlight the ongoing need to monitor for and address this risk.
The study was supported by the Centre for Epidemiology Versus Arthritis and by the National Institute for Health Research Manchester Biomedical Research Centre. Coauthor William G. Dixon, PhD, has received consultancy fees from Google and Bayer unrelated to this study. Dr. Bhatt has disclosed no relevant financial relationships.
SOURCE: Costello RE et al. Rheumatology. 2020 June 27. doi: 10.1093/rheumatology/keaa209.
A version of this article originally appeared on Medscape.com.
FROM RHEUMATOLOGY
Even a few days of steroids may be risky, new study suggests
Extended use of corticosteroids for chronic inflammatory conditions puts patients at risk for serious adverse events (AEs), including cardiovascular disease, osteoporosis, cataracts, and diabetes. Now, a growing body of evidence suggests that even short bursts of these drugs are associated with serious risks.
Most recently, a population-based study of more than 2.6 million people found that taking corticosteroids for 14 days or less was associated with a substantially greater risk for gastrointestinal (GI) bleeding, sepsis, and heart failure, particularly within the first 30 days after therapy.
In the study, Tsung-Chieh Yao, MD, PhD, a professor in the division of allergy, asthma, and rheumatology in the department of pediatrics at Chang Gung Memorial Hospital in Taoyuan, Taiwan, and colleagues used a self-controlled case series to analyze data from Taiwan’s National Health Insurance Research Database of medical claims. They compared patients’ conditions in the period from 5 to 90 days before treatment to conditions from the periods from 5 to 30 days and from 31 to 90 days after therapy.
With a median duration of 3 days of treatment, the incidence rate ratios (IRRs) were 1.80 (95% confidence interval, 1.75-1.84) for GI bleeding, 1.99 (95% CI, 1.70-2.32) for sepsis, and 2.37 (95% CI, 2.13-2.63) for heart failure.
Given the findings, physicians should weigh the benefits against the risks of rare but potentially serious consequences of these anti-inflammatory drugs, according to the authors.
“After initiating patients on oral steroid bursts, physicians should be on the lookout for these severe adverse events, particularly within the first month after initiation of steroid therapy,” Dr. Yao said in an interview.
The findings were published online July 6 in Annals of Internal Medicine.
Of the 15,859,129 adult Asians in the Taiwanese database, the study included 2,623,327 adults aged 20-64 years who received single steroid bursts (14 days or less) between Jan. 1, 2013, and Dec. 31, 2015.
Almost 60% of the indications were for skin disorders, such as eczema and urticaria, and for respiratory tract infections, such as sinusitis and acute pharyngitis. Among specialties, dermatology, otolaryngology, family practice, internal medicine, and pediatrics accounted for 88% of prescriptions.
“Our findings are important for physicians and guideline developers because short-term use of oral corticosteroids is common and the real-world safety of this approach remains unclear,” the authors wrote. They acknowledged that the database did not provide information on such potential confounders as disease severity and lifestyle factors, nor did it include children and vulnerable individuals, which may limit the generalizability of the results.
The findings echo those of a 2017 cohort study conducted by researchers at the University of Michigan in Ann Arbor. That study, by Akbar K. Waljee, MD, assistant professor of gastroenterology, University of Michigan, Ann Arbor, and colleagues, included data on more than 1.5 million privately insured U.S. adults. The researchers included somewhat longer steroid bursts of up to 30 days’ duration and found that use of the drugs was associated with a greater than fivefold increased risk for sepsis, a more than threefold increased risk for venous thromboembolism, and a nearly twofold increased risk for fracture within 30 days of starting treatment.
Furthermore, the elevated risk persisted at prednisone-equivalent doses of less than 20 mg/d (IRR, 4.02 for sepsis, 3.61 for venous thromboembolism, and 1.83 for fracture; all P < .001).
The U.S. study also found that during the 3-year period from 2012 to 2014, more than 20% of patients were prescribed short-term oral corticosteroids.
“Both studies indicate that these short-term regimens are more common in the real world than was previously thought and are not risk free,” Dr. Yao said.
Recognition that corticosteroids are associated with adverse events has been building for decades, according to the authors of an editorial that accompanies the new study.
“However, we commonly use short corticosteroid ‘bursts’ for minor ailments despite a lack of evidence for meaningful benefit. We are now learning that bursts as short as 3 days may increase risk for serious AEs, even in young and healthy people,” wrote editorialists Beth I. Wallace, MD, of the Center for Clinical Management Research at the VA Ann Arbor Healthcare System and the Institute for Healthcare Policy and Innovation at Michigan Medicine, Ann Arbor, and Dr. Waljee, who led the 2017 study.
Dr. Wallace and Dr. Waljee drew parallels between corticosteroid bursts and other short-term regimens, such as of antibiotics and opiates, in which prescriber preference and sometimes patient pressure play a role. “All of these treatments have well-defined indications but can cause net harm when used. We can thus conceive of a corticosteroid stewardship model of targeted interventions that aims to reduce inappropriate prescribing,” they wrote.
In an interview, Dr. Wallace, a rheumatologist who prescribes oral steroids fairly frequently, noted that the Taiwan study is the first to investigate steroid bursts. “Up till now, these very short courses have flown under the radar. Clinicians very commonly prescribe short courses to help relieve symptoms of self-limited conditions like bronchitis, and we assume that because the exposure duration is short, the risks are low, especially for patients who are otherwise healthy.”
She warned that the data in the current study indicate that these short bursts – even at the lower end of the 1- to 2-week courses American physicians prescribe most often – carry small but real increases in risk for serious AEs. “And these increases were seen in young, healthy people, not just in people with preexisting conditions,” she said. “So, we might need to start thinking harder about how we are prescribing even these very short courses of steroids and try to use steroids only when their meaningful benefits really outweigh the risk.”
She noted that a patient with a chronic inflammatory condition such as rheumatoid arthritis may benefit substantially from short-term steroids to treat a disease flare. In that specific case, the benefits of short-term steroids may outweigh the risks, Dr. Wallace said.
But not everyone thinks a new strategy is needed. For Whitney A. High, MD, associate professor of dermatology and pathology at the University of Colorado at Denver, Aurora, the overprescribing of short-term corticosteroids is not a problem, and dermatologists are already exercising caution.
“I only prescribe these drugs short term to, at a guess, about 1 in 40 patients and only when a patient is miserable and quality of life is being seriously affected,” he said in an interview. “And that’s something that can’t be measured in a database study like the one from Taiwan but only in a risk-benefit analysis,” he said.
Furthermore, dermatologists have other drugs and technologies in their armamentarium, including topical steroids with occlusion or with wet wraps, phototherapy, phosphodiesterase inhibitors, calcipotriene, methotrexate and other immunosuppressive agents, and biologics. “In fact, many of these agents are specifically referred to as steroid-sparing,” Dr. High said.
Nor does he experience much pressure from patients to prescribe these drugs. “While occasionally I may encounter a patient who places pressure on me for oral steroids, it’s probably not nearly as frequently as providers in other fields are pressured to prescribe antibiotics or narcotics,” he said.
According to the Taiwanese researchers, the next step is to conduct more studies, including clinical trials, to determine optimal use of corticosteroids by monitoring adverse events. In the meantime, for practitioners such as Dr. Wallace and Dr. High, there is ample evidence from several recent studies of the harms of short-term corticosteroids, whereas the benefits for patients with self-limiting conditions remain uncertain. “This and other studies like it quite appropriately remind providers to avoid oral steroids when they’re not necessary and to seek alternatives where possible,” Dr. High said.
The study was supported by the National Health Research Institutes of Taiwan, the Ministry of Science and Technology of Taiwan, the Chang Gung Medical Foundation, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (NIH). Dr. Yao has disclosed no relevant financial relationships. Dr. Wu has received grants from GlaxoSmithKline outside the submitted work. The editorialists and Dr. High have disclosed no relevant financial relationships. Dr. Wallace received an NIH grant during the writing of the editorial.
A version of this article originally appeared on Medscape.com.
Extended use of corticosteroids for chronic inflammatory conditions puts patients at risk for serious adverse events (AEs), including cardiovascular disease, osteoporosis, cataracts, and diabetes. Now, a growing body of evidence suggests that even short bursts of these drugs are associated with serious risks.
Most recently, a population-based study of more than 2.6 million people found that taking corticosteroids for 14 days or less was associated with a substantially greater risk for gastrointestinal (GI) bleeding, sepsis, and heart failure, particularly within the first 30 days after therapy.
In the study, Tsung-Chieh Yao, MD, PhD, a professor in the division of allergy, asthma, and rheumatology in the department of pediatrics at Chang Gung Memorial Hospital in Taoyuan, Taiwan, and colleagues used a self-controlled case series to analyze data from Taiwan’s National Health Insurance Research Database of medical claims. They compared patients’ conditions in the period from 5 to 90 days before treatment to conditions from the periods from 5 to 30 days and from 31 to 90 days after therapy.
With a median duration of 3 days of treatment, the incidence rate ratios (IRRs) were 1.80 (95% confidence interval, 1.75-1.84) for GI bleeding, 1.99 (95% CI, 1.70-2.32) for sepsis, and 2.37 (95% CI, 2.13-2.63) for heart failure.
Given the findings, physicians should weigh the benefits against the risks of rare but potentially serious consequences of these anti-inflammatory drugs, according to the authors.
“After initiating patients on oral steroid bursts, physicians should be on the lookout for these severe adverse events, particularly within the first month after initiation of steroid therapy,” Dr. Yao said in an interview.
The findings were published online July 6 in Annals of Internal Medicine.
Of the 15,859,129 adult Asians in the Taiwanese database, the study included 2,623,327 adults aged 20-64 years who received single steroid bursts (14 days or less) between Jan. 1, 2013, and Dec. 31, 2015.
Almost 60% of the indications were for skin disorders, such as eczema and urticaria, and for respiratory tract infections, such as sinusitis and acute pharyngitis. Among specialties, dermatology, otolaryngology, family practice, internal medicine, and pediatrics accounted for 88% of prescriptions.
“Our findings are important for physicians and guideline developers because short-term use of oral corticosteroids is common and the real-world safety of this approach remains unclear,” the authors wrote. They acknowledged that the database did not provide information on such potential confounders as disease severity and lifestyle factors, nor did it include children and vulnerable individuals, which may limit the generalizability of the results.
The findings echo those of a 2017 cohort study conducted by researchers at the University of Michigan in Ann Arbor. That study, by Akbar K. Waljee, MD, assistant professor of gastroenterology, University of Michigan, Ann Arbor, and colleagues, included data on more than 1.5 million privately insured U.S. adults. The researchers included somewhat longer steroid bursts of up to 30 days’ duration and found that use of the drugs was associated with a greater than fivefold increased risk for sepsis, a more than threefold increased risk for venous thromboembolism, and a nearly twofold increased risk for fracture within 30 days of starting treatment.
Furthermore, the elevated risk persisted at prednisone-equivalent doses of less than 20 mg/d (IRR, 4.02 for sepsis, 3.61 for venous thromboembolism, and 1.83 for fracture; all P < .001).
The U.S. study also found that during the 3-year period from 2012 to 2014, more than 20% of patients were prescribed short-term oral corticosteroids.
“Both studies indicate that these short-term regimens are more common in the real world than was previously thought and are not risk free,” Dr. Yao said.
Recognition that corticosteroids are associated with adverse events has been building for decades, according to the authors of an editorial that accompanies the new study.
“However, we commonly use short corticosteroid ‘bursts’ for minor ailments despite a lack of evidence for meaningful benefit. We are now learning that bursts as short as 3 days may increase risk for serious AEs, even in young and healthy people,” wrote editorialists Beth I. Wallace, MD, of the Center for Clinical Management Research at the VA Ann Arbor Healthcare System and the Institute for Healthcare Policy and Innovation at Michigan Medicine, Ann Arbor, and Dr. Waljee, who led the 2017 study.
Dr. Wallace and Dr. Waljee drew parallels between corticosteroid bursts and other short-term regimens, such as of antibiotics and opiates, in which prescriber preference and sometimes patient pressure play a role. “All of these treatments have well-defined indications but can cause net harm when used. We can thus conceive of a corticosteroid stewardship model of targeted interventions that aims to reduce inappropriate prescribing,” they wrote.
In an interview, Dr. Wallace, a rheumatologist who prescribes oral steroids fairly frequently, noted that the Taiwan study is the first to investigate steroid bursts. “Up till now, these very short courses have flown under the radar. Clinicians very commonly prescribe short courses to help relieve symptoms of self-limited conditions like bronchitis, and we assume that because the exposure duration is short, the risks are low, especially for patients who are otherwise healthy.”
She warned that the data in the current study indicate that these short bursts – even at the lower end of the 1- to 2-week courses American physicians prescribe most often – carry small but real increases in risk for serious AEs. “And these increases were seen in young, healthy people, not just in people with preexisting conditions,” she said. “So, we might need to start thinking harder about how we are prescribing even these very short courses of steroids and try to use steroids only when their meaningful benefits really outweigh the risk.”
She noted that a patient with a chronic inflammatory condition such as rheumatoid arthritis may benefit substantially from short-term steroids to treat a disease flare. In that specific case, the benefits of short-term steroids may outweigh the risks, Dr. Wallace said.
But not everyone thinks a new strategy is needed. For Whitney A. High, MD, associate professor of dermatology and pathology at the University of Colorado at Denver, Aurora, the overprescribing of short-term corticosteroids is not a problem, and dermatologists are already exercising caution.
“I only prescribe these drugs short term to, at a guess, about 1 in 40 patients and only when a patient is miserable and quality of life is being seriously affected,” he said in an interview. “And that’s something that can’t be measured in a database study like the one from Taiwan but only in a risk-benefit analysis,” he said.
Furthermore, dermatologists have other drugs and technologies in their armamentarium, including topical steroids with occlusion or with wet wraps, phototherapy, phosphodiesterase inhibitors, calcipotriene, methotrexate and other immunosuppressive agents, and biologics. “In fact, many of these agents are specifically referred to as steroid-sparing,” Dr. High said.
Nor does he experience much pressure from patients to prescribe these drugs. “While occasionally I may encounter a patient who places pressure on me for oral steroids, it’s probably not nearly as frequently as providers in other fields are pressured to prescribe antibiotics or narcotics,” he said.
According to the Taiwanese researchers, the next step is to conduct more studies, including clinical trials, to determine optimal use of corticosteroids by monitoring adverse events. In the meantime, for practitioners such as Dr. Wallace and Dr. High, there is ample evidence from several recent studies of the harms of short-term corticosteroids, whereas the benefits for patients with self-limiting conditions remain uncertain. “This and other studies like it quite appropriately remind providers to avoid oral steroids when they’re not necessary and to seek alternatives where possible,” Dr. High said.
The study was supported by the National Health Research Institutes of Taiwan, the Ministry of Science and Technology of Taiwan, the Chang Gung Medical Foundation, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (NIH). Dr. Yao has disclosed no relevant financial relationships. Dr. Wu has received grants from GlaxoSmithKline outside the submitted work. The editorialists and Dr. High have disclosed no relevant financial relationships. Dr. Wallace received an NIH grant during the writing of the editorial.
A version of this article originally appeared on Medscape.com.
Extended use of corticosteroids for chronic inflammatory conditions puts patients at risk for serious adverse events (AEs), including cardiovascular disease, osteoporosis, cataracts, and diabetes. Now, a growing body of evidence suggests that even short bursts of these drugs are associated with serious risks.
Most recently, a population-based study of more than 2.6 million people found that taking corticosteroids for 14 days or less was associated with a substantially greater risk for gastrointestinal (GI) bleeding, sepsis, and heart failure, particularly within the first 30 days after therapy.
In the study, Tsung-Chieh Yao, MD, PhD, a professor in the division of allergy, asthma, and rheumatology in the department of pediatrics at Chang Gung Memorial Hospital in Taoyuan, Taiwan, and colleagues used a self-controlled case series to analyze data from Taiwan’s National Health Insurance Research Database of medical claims. They compared patients’ conditions in the period from 5 to 90 days before treatment to conditions from the periods from 5 to 30 days and from 31 to 90 days after therapy.
With a median duration of 3 days of treatment, the incidence rate ratios (IRRs) were 1.80 (95% confidence interval, 1.75-1.84) for GI bleeding, 1.99 (95% CI, 1.70-2.32) for sepsis, and 2.37 (95% CI, 2.13-2.63) for heart failure.
Given the findings, physicians should weigh the benefits against the risks of rare but potentially serious consequences of these anti-inflammatory drugs, according to the authors.
“After initiating patients on oral steroid bursts, physicians should be on the lookout for these severe adverse events, particularly within the first month after initiation of steroid therapy,” Dr. Yao said in an interview.
The findings were published online July 6 in Annals of Internal Medicine.
Of the 15,859,129 adult Asians in the Taiwanese database, the study included 2,623,327 adults aged 20-64 years who received single steroid bursts (14 days or less) between Jan. 1, 2013, and Dec. 31, 2015.
Almost 60% of the indications were for skin disorders, such as eczema and urticaria, and for respiratory tract infections, such as sinusitis and acute pharyngitis. Among specialties, dermatology, otolaryngology, family practice, internal medicine, and pediatrics accounted for 88% of prescriptions.
“Our findings are important for physicians and guideline developers because short-term use of oral corticosteroids is common and the real-world safety of this approach remains unclear,” the authors wrote. They acknowledged that the database did not provide information on such potential confounders as disease severity and lifestyle factors, nor did it include children and vulnerable individuals, which may limit the generalizability of the results.
The findings echo those of a 2017 cohort study conducted by researchers at the University of Michigan in Ann Arbor. That study, by Akbar K. Waljee, MD, assistant professor of gastroenterology, University of Michigan, Ann Arbor, and colleagues, included data on more than 1.5 million privately insured U.S. adults. The researchers included somewhat longer steroid bursts of up to 30 days’ duration and found that use of the drugs was associated with a greater than fivefold increased risk for sepsis, a more than threefold increased risk for venous thromboembolism, and a nearly twofold increased risk for fracture within 30 days of starting treatment.
Furthermore, the elevated risk persisted at prednisone-equivalent doses of less than 20 mg/d (IRR, 4.02 for sepsis, 3.61 for venous thromboembolism, and 1.83 for fracture; all P < .001).
The U.S. study also found that during the 3-year period from 2012 to 2014, more than 20% of patients were prescribed short-term oral corticosteroids.
“Both studies indicate that these short-term regimens are more common in the real world than was previously thought and are not risk free,” Dr. Yao said.
Recognition that corticosteroids are associated with adverse events has been building for decades, according to the authors of an editorial that accompanies the new study.
“However, we commonly use short corticosteroid ‘bursts’ for minor ailments despite a lack of evidence for meaningful benefit. We are now learning that bursts as short as 3 days may increase risk for serious AEs, even in young and healthy people,” wrote editorialists Beth I. Wallace, MD, of the Center for Clinical Management Research at the VA Ann Arbor Healthcare System and the Institute for Healthcare Policy and Innovation at Michigan Medicine, Ann Arbor, and Dr. Waljee, who led the 2017 study.
Dr. Wallace and Dr. Waljee drew parallels between corticosteroid bursts and other short-term regimens, such as of antibiotics and opiates, in which prescriber preference and sometimes patient pressure play a role. “All of these treatments have well-defined indications but can cause net harm when used. We can thus conceive of a corticosteroid stewardship model of targeted interventions that aims to reduce inappropriate prescribing,” they wrote.
In an interview, Dr. Wallace, a rheumatologist who prescribes oral steroids fairly frequently, noted that the Taiwan study is the first to investigate steroid bursts. “Up till now, these very short courses have flown under the radar. Clinicians very commonly prescribe short courses to help relieve symptoms of self-limited conditions like bronchitis, and we assume that because the exposure duration is short, the risks are low, especially for patients who are otherwise healthy.”
She warned that the data in the current study indicate that these short bursts – even at the lower end of the 1- to 2-week courses American physicians prescribe most often – carry small but real increases in risk for serious AEs. “And these increases were seen in young, healthy people, not just in people with preexisting conditions,” she said. “So, we might need to start thinking harder about how we are prescribing even these very short courses of steroids and try to use steroids only when their meaningful benefits really outweigh the risk.”
She noted that a patient with a chronic inflammatory condition such as rheumatoid arthritis may benefit substantially from short-term steroids to treat a disease flare. In that specific case, the benefits of short-term steroids may outweigh the risks, Dr. Wallace said.
But not everyone thinks a new strategy is needed. For Whitney A. High, MD, associate professor of dermatology and pathology at the University of Colorado at Denver, Aurora, the overprescribing of short-term corticosteroids is not a problem, and dermatologists are already exercising caution.
“I only prescribe these drugs short term to, at a guess, about 1 in 40 patients and only when a patient is miserable and quality of life is being seriously affected,” he said in an interview. “And that’s something that can’t be measured in a database study like the one from Taiwan but only in a risk-benefit analysis,” he said.
Furthermore, dermatologists have other drugs and technologies in their armamentarium, including topical steroids with occlusion or with wet wraps, phototherapy, phosphodiesterase inhibitors, calcipotriene, methotrexate and other immunosuppressive agents, and biologics. “In fact, many of these agents are specifically referred to as steroid-sparing,” Dr. High said.
Nor does he experience much pressure from patients to prescribe these drugs. “While occasionally I may encounter a patient who places pressure on me for oral steroids, it’s probably not nearly as frequently as providers in other fields are pressured to prescribe antibiotics or narcotics,” he said.
According to the Taiwanese researchers, the next step is to conduct more studies, including clinical trials, to determine optimal use of corticosteroids by monitoring adverse events. In the meantime, for practitioners such as Dr. Wallace and Dr. High, there is ample evidence from several recent studies of the harms of short-term corticosteroids, whereas the benefits for patients with self-limiting conditions remain uncertain. “This and other studies like it quite appropriately remind providers to avoid oral steroids when they’re not necessary and to seek alternatives where possible,” Dr. High said.
The study was supported by the National Health Research Institutes of Taiwan, the Ministry of Science and Technology of Taiwan, the Chang Gung Medical Foundation, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (NIH). Dr. Yao has disclosed no relevant financial relationships. Dr. Wu has received grants from GlaxoSmithKline outside the submitted work. The editorialists and Dr. High have disclosed no relevant financial relationships. Dr. Wallace received an NIH grant during the writing of the editorial.
A version of this article originally appeared on Medscape.com.
Pulmonary function tests can’t substitute for high-resolution CT in early systemic sclerosis ILD screening
Clinicians shouldn’t rely on pulmonary function tests (PFTs) alone to screen for interstitial lung disease (ILD). The tests performed poorly in a retrospective study of 212 patients with systemic sclerosis, reinforcing the findings of previous studies.
Any screening algorithm should include high-resolution CT (HRCT), which is good at prognosticating disease, the investigators wrote in Arthritis & Rheumatology. “I think all newly diagnosed systemic sclerosis patients should have a full set of PFTs (spirometry, lung volumes, and diffusion capacity) and an HRCT at baseline to evaluate for ILD,” the study’s lead author, Elana J. Bernstein, MD, said in an interview.
ILD is a leading cause of death in systemic sclerosis (SSc) patients, affecting 40%-60% of those with the disease. HRCT is currently the preferred option for detection of ILD. PFTs are commonly used to screen for ILD but haven’t performed well in previous studies. “Someone can have abnormalities on HRCT that are consistent with ILD but still have PFTs that are in the ‘normal’ range,” explained Dr. Bernstein of Columbia University, New York. One cross-sectional study of 102 SSc patients found that the test’s sensitivity for the detection of ILD on HRCT was just 37.5% when forced vital capacity (FVC) <80% predicted.
Investigators sought to assess performance characteristics of PFTs in patients with early diffuse cutaneous SSc, a cohort at high risk of developing ILD. The study enlisted patients from the Prospective Registry of Early Systemic Sclerosis (PRESS), a multicenter, prospective cohort study of adults with early diffuse cutaneous SSc. Overall, 212 patients at 11 U.S. academic medical centers participated in the study from April 2012 to January 2019.
All patients had spirometry (PFT) and HRCT chest scans. PFTs were conducted per American Thoracic Society/European Respiratory Society guidelines. The investigators calculated test characteristics for single PFT and combinations of PFT parameters for the detection of ILD on HRCT. The HRCTs were ordered at the discretion of treating physicians, and scrutinized for ILD features such as reticular changes, honeycombing, traction bronchiectasis, and ground-glass opacities. The investigators defined the lower limit of normal for FVC, total lung capacity, and diffusion capacity for carbon monoxide (DLCO) as 80% predicted.
Overall, Dr. Bernstein and her colleagues found that PFTs lacked sufficient sensitivity and negative predictive value for the detection of ILD on HRCT in these patients.
An FVC <80% predicted performed at only 63% sensitivity and an false negative rate of 37%. Total lung capacity or DLCO <80% predicted had a sensitivity of 46% and 80%, respectively. The combination of FVC or DLCO <80% predicted raised sensitivity to 85%. However, the addition of total lung capacity to this combination did not improve results.
Overall, PFTs had a positive predictive value of 64%-74% and an negative predictive value of 61%-70%. “This means that PFT alone will not accurately predict the presence of ILD in about 35%, and not be correctly negative in about 35%,” observed Daniel E. Furst, MD, professor of medicine (emeritus) at the University of California, Los Angeles, and professor of rheumatology at the University of California, Los Angeles.
While the combination of FVC <80% predicted or DLCO <80% predicted performed better than the other parameters, the sensitivity “is inadequate for an ILD screening test as it results in an false negative rate of 15%, thereby falsely reassuring 15% of patients that they do not have ILD when in fact they do,” the investigators observed.
“This study reinforces the notion that PFTs alone are ineffective screening tools for ILD in the presence of systemic sclerosis, particularly for patients with early systemic sclerosis,” said Elizabeth Volkmann, MD, MS, assistant professor and codirector of the CTD-ILD program in the division of rheumatology at the University of California, Los Angeles.
The study’s scope was relatively small, yet the results provide further evidence to show that HRCT should be performed in all SSc patients to screen for the presence of ILD, Dr. Volkmann said in an interview.
Other research has demonstrated the value of baseline HRCT as a prognosticator of ILD outcomes. The method provides useful information about the degree of fibrosis and degree of damage in early-stage disease, said Dr. Furst, also an adjunct professor at the University of Washington, Seattle, and a research professor at the University of Florence (Italy). “If there’s honeycombing, that’s a bad prognosis. If it’s ground glass or reticular changes, the prognosis is better.
“Once there’s a lot of damage, it’s much harder to interpret disease with HRCT,” he added.
HRCT and PFT work well together to assess what’s happening in patients, Dr. Furst explained. HRCT provides an idea of anatomic changes, whereas PFT outlines aspects of functional change to diagnose early ILD in early diffuse SSc. The study results should not apply to patients with later disease who have more developed ILD, he noted.
The investigators acknowledged that they weren’t able to categorize and analyze patients according to disease extent because they didn’t quantify the extent of ILD. Another limitation was that the HRCTs and PFTs were ordered at the discretion of individual physicians, which means that not all participants received the tests.
“Although the tests were done in 90% of the population, there is still a probability of a significant selection bias,” Dr. Furst said.
Dr. Bernstein and several other coauthors in the study received grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases to support their work. Dr. Furst disclosed receiving grant/research support from and/or consulting for AbbVie, Actelion, Amgen, Bristol-Myers Squibb, Corbus, the National Institutes of Health, Novartis, Pfizer, and Roche/Genentech. Dr. Volkmann disclosed consulting for and/or receiving grant support from Boehringer Ingelheim, Corbus, and Forbius.
SOURCE: Bernstein EJ et al. Arthritis Rheumatol. 2020 Jun 25. doi: 10.1002/art.41415.
Clinicians shouldn’t rely on pulmonary function tests (PFTs) alone to screen for interstitial lung disease (ILD). The tests performed poorly in a retrospective study of 212 patients with systemic sclerosis, reinforcing the findings of previous studies.
Any screening algorithm should include high-resolution CT (HRCT), which is good at prognosticating disease, the investigators wrote in Arthritis & Rheumatology. “I think all newly diagnosed systemic sclerosis patients should have a full set of PFTs (spirometry, lung volumes, and diffusion capacity) and an HRCT at baseline to evaluate for ILD,” the study’s lead author, Elana J. Bernstein, MD, said in an interview.
ILD is a leading cause of death in systemic sclerosis (SSc) patients, affecting 40%-60% of those with the disease. HRCT is currently the preferred option for detection of ILD. PFTs are commonly used to screen for ILD but haven’t performed well in previous studies. “Someone can have abnormalities on HRCT that are consistent with ILD but still have PFTs that are in the ‘normal’ range,” explained Dr. Bernstein of Columbia University, New York. One cross-sectional study of 102 SSc patients found that the test’s sensitivity for the detection of ILD on HRCT was just 37.5% when forced vital capacity (FVC) <80% predicted.
Investigators sought to assess performance characteristics of PFTs in patients with early diffuse cutaneous SSc, a cohort at high risk of developing ILD. The study enlisted patients from the Prospective Registry of Early Systemic Sclerosis (PRESS), a multicenter, prospective cohort study of adults with early diffuse cutaneous SSc. Overall, 212 patients at 11 U.S. academic medical centers participated in the study from April 2012 to January 2019.
All patients had spirometry (PFT) and HRCT chest scans. PFTs were conducted per American Thoracic Society/European Respiratory Society guidelines. The investigators calculated test characteristics for single PFT and combinations of PFT parameters for the detection of ILD on HRCT. The HRCTs were ordered at the discretion of treating physicians, and scrutinized for ILD features such as reticular changes, honeycombing, traction bronchiectasis, and ground-glass opacities. The investigators defined the lower limit of normal for FVC, total lung capacity, and diffusion capacity for carbon monoxide (DLCO) as 80% predicted.
Overall, Dr. Bernstein and her colleagues found that PFTs lacked sufficient sensitivity and negative predictive value for the detection of ILD on HRCT in these patients.
An FVC <80% predicted performed at only 63% sensitivity and an false negative rate of 37%. Total lung capacity or DLCO <80% predicted had a sensitivity of 46% and 80%, respectively. The combination of FVC or DLCO <80% predicted raised sensitivity to 85%. However, the addition of total lung capacity to this combination did not improve results.
Overall, PFTs had a positive predictive value of 64%-74% and an negative predictive value of 61%-70%. “This means that PFT alone will not accurately predict the presence of ILD in about 35%, and not be correctly negative in about 35%,” observed Daniel E. Furst, MD, professor of medicine (emeritus) at the University of California, Los Angeles, and professor of rheumatology at the University of California, Los Angeles.
While the combination of FVC <80% predicted or DLCO <80% predicted performed better than the other parameters, the sensitivity “is inadequate for an ILD screening test as it results in an false negative rate of 15%, thereby falsely reassuring 15% of patients that they do not have ILD when in fact they do,” the investigators observed.
“This study reinforces the notion that PFTs alone are ineffective screening tools for ILD in the presence of systemic sclerosis, particularly for patients with early systemic sclerosis,” said Elizabeth Volkmann, MD, MS, assistant professor and codirector of the CTD-ILD program in the division of rheumatology at the University of California, Los Angeles.
The study’s scope was relatively small, yet the results provide further evidence to show that HRCT should be performed in all SSc patients to screen for the presence of ILD, Dr. Volkmann said in an interview.
Other research has demonstrated the value of baseline HRCT as a prognosticator of ILD outcomes. The method provides useful information about the degree of fibrosis and degree of damage in early-stage disease, said Dr. Furst, also an adjunct professor at the University of Washington, Seattle, and a research professor at the University of Florence (Italy). “If there’s honeycombing, that’s a bad prognosis. If it’s ground glass or reticular changes, the prognosis is better.
“Once there’s a lot of damage, it’s much harder to interpret disease with HRCT,” he added.
HRCT and PFT work well together to assess what’s happening in patients, Dr. Furst explained. HRCT provides an idea of anatomic changes, whereas PFT outlines aspects of functional change to diagnose early ILD in early diffuse SSc. The study results should not apply to patients with later disease who have more developed ILD, he noted.
The investigators acknowledged that they weren’t able to categorize and analyze patients according to disease extent because they didn’t quantify the extent of ILD. Another limitation was that the HRCTs and PFTs were ordered at the discretion of individual physicians, which means that not all participants received the tests.
“Although the tests were done in 90% of the population, there is still a probability of a significant selection bias,” Dr. Furst said.
Dr. Bernstein and several other coauthors in the study received grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases to support their work. Dr. Furst disclosed receiving grant/research support from and/or consulting for AbbVie, Actelion, Amgen, Bristol-Myers Squibb, Corbus, the National Institutes of Health, Novartis, Pfizer, and Roche/Genentech. Dr. Volkmann disclosed consulting for and/or receiving grant support from Boehringer Ingelheim, Corbus, and Forbius.
SOURCE: Bernstein EJ et al. Arthritis Rheumatol. 2020 Jun 25. doi: 10.1002/art.41415.
Clinicians shouldn’t rely on pulmonary function tests (PFTs) alone to screen for interstitial lung disease (ILD). The tests performed poorly in a retrospective study of 212 patients with systemic sclerosis, reinforcing the findings of previous studies.
Any screening algorithm should include high-resolution CT (HRCT), which is good at prognosticating disease, the investigators wrote in Arthritis & Rheumatology. “I think all newly diagnosed systemic sclerosis patients should have a full set of PFTs (spirometry, lung volumes, and diffusion capacity) and an HRCT at baseline to evaluate for ILD,” the study’s lead author, Elana J. Bernstein, MD, said in an interview.
ILD is a leading cause of death in systemic sclerosis (SSc) patients, affecting 40%-60% of those with the disease. HRCT is currently the preferred option for detection of ILD. PFTs are commonly used to screen for ILD but haven’t performed well in previous studies. “Someone can have abnormalities on HRCT that are consistent with ILD but still have PFTs that are in the ‘normal’ range,” explained Dr. Bernstein of Columbia University, New York. One cross-sectional study of 102 SSc patients found that the test’s sensitivity for the detection of ILD on HRCT was just 37.5% when forced vital capacity (FVC) <80% predicted.
Investigators sought to assess performance characteristics of PFTs in patients with early diffuse cutaneous SSc, a cohort at high risk of developing ILD. The study enlisted patients from the Prospective Registry of Early Systemic Sclerosis (PRESS), a multicenter, prospective cohort study of adults with early diffuse cutaneous SSc. Overall, 212 patients at 11 U.S. academic medical centers participated in the study from April 2012 to January 2019.
All patients had spirometry (PFT) and HRCT chest scans. PFTs were conducted per American Thoracic Society/European Respiratory Society guidelines. The investigators calculated test characteristics for single PFT and combinations of PFT parameters for the detection of ILD on HRCT. The HRCTs were ordered at the discretion of treating physicians, and scrutinized for ILD features such as reticular changes, honeycombing, traction bronchiectasis, and ground-glass opacities. The investigators defined the lower limit of normal for FVC, total lung capacity, and diffusion capacity for carbon monoxide (DLCO) as 80% predicted.
Overall, Dr. Bernstein and her colleagues found that PFTs lacked sufficient sensitivity and negative predictive value for the detection of ILD on HRCT in these patients.
An FVC <80% predicted performed at only 63% sensitivity and an false negative rate of 37%. Total lung capacity or DLCO <80% predicted had a sensitivity of 46% and 80%, respectively. The combination of FVC or DLCO <80% predicted raised sensitivity to 85%. However, the addition of total lung capacity to this combination did not improve results.
Overall, PFTs had a positive predictive value of 64%-74% and an negative predictive value of 61%-70%. “This means that PFT alone will not accurately predict the presence of ILD in about 35%, and not be correctly negative in about 35%,” observed Daniel E. Furst, MD, professor of medicine (emeritus) at the University of California, Los Angeles, and professor of rheumatology at the University of California, Los Angeles.
While the combination of FVC <80% predicted or DLCO <80% predicted performed better than the other parameters, the sensitivity “is inadequate for an ILD screening test as it results in an false negative rate of 15%, thereby falsely reassuring 15% of patients that they do not have ILD when in fact they do,” the investigators observed.
“This study reinforces the notion that PFTs alone are ineffective screening tools for ILD in the presence of systemic sclerosis, particularly for patients with early systemic sclerosis,” said Elizabeth Volkmann, MD, MS, assistant professor and codirector of the CTD-ILD program in the division of rheumatology at the University of California, Los Angeles.
The study’s scope was relatively small, yet the results provide further evidence to show that HRCT should be performed in all SSc patients to screen for the presence of ILD, Dr. Volkmann said in an interview.
Other research has demonstrated the value of baseline HRCT as a prognosticator of ILD outcomes. The method provides useful information about the degree of fibrosis and degree of damage in early-stage disease, said Dr. Furst, also an adjunct professor at the University of Washington, Seattle, and a research professor at the University of Florence (Italy). “If there’s honeycombing, that’s a bad prognosis. If it’s ground glass or reticular changes, the prognosis is better.
“Once there’s a lot of damage, it’s much harder to interpret disease with HRCT,” he added.
HRCT and PFT work well together to assess what’s happening in patients, Dr. Furst explained. HRCT provides an idea of anatomic changes, whereas PFT outlines aspects of functional change to diagnose early ILD in early diffuse SSc. The study results should not apply to patients with later disease who have more developed ILD, he noted.
The investigators acknowledged that they weren’t able to categorize and analyze patients according to disease extent because they didn’t quantify the extent of ILD. Another limitation was that the HRCTs and PFTs were ordered at the discretion of individual physicians, which means that not all participants received the tests.
“Although the tests were done in 90% of the population, there is still a probability of a significant selection bias,” Dr. Furst said.
Dr. Bernstein and several other coauthors in the study received grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases to support their work. Dr. Furst disclosed receiving grant/research support from and/or consulting for AbbVie, Actelion, Amgen, Bristol-Myers Squibb, Corbus, the National Institutes of Health, Novartis, Pfizer, and Roche/Genentech. Dr. Volkmann disclosed consulting for and/or receiving grant support from Boehringer Ingelheim, Corbus, and Forbius.
SOURCE: Bernstein EJ et al. Arthritis Rheumatol. 2020 Jun 25. doi: 10.1002/art.41415.
FROM ARTHRITIS & RHEUMATOLOGY















