User login
Automated RA image scoring could be coming
A novel program that aims to automate the Sharp-van der Heijde scoring of radiographs of patients with rheumatoid arthritis has shown good reliability in identifying regions of interest and matching human reader scoring for joint-space narrowing, according to a report given at the annual European Congress of Rheumatology, held online this year because of COVID-19.
First author and presenter Thomas Deimel, MD, and colleagues at the Medical University of Vienna said their program, called autoscoRA, may be a solution to the problem of readers having to make subjective calls on the severity of damage seen on radiographs.
Although the work continues to be validated, Dr. Deimel, a resident at the university, is confident in the system as is. “I think for joint space narrowing, we’re there at the point where this could be used and could be as good as a human reader in terms of reliability,” he said in an interview. To find out, the group plans to compare the variability between autoscoRA and a gold-standard human reader against the variability seen between human readers. If the two measures of variability are similar, it would provide a strong endorsement.
The effort is far from the first to develop an automatic scoring system for RA images, but no fully automated system has emerged as reliable, according to Dr. Deimel. He thinks one main issue for others has been lack of access to a sufficient data set to train systems. It can be difficult to find enough training images because many types of joint damage are comparatively uncommon. The problem is made even worse because images can be hard to interpret: The shapes that the system must decipher can be misleading, especially in positions of tendon insertion or ligament attachment that can resemble damage. Differing angles of view between various training images can also complicate matters.
The autoscoRA program is based on modifications of a form of convolutional neural network called the VGG16 architecture. The team used 2,207 images from 270 patients to train autoscoRA, 1,150 images from 133 patients for validation, and 1,834 images from 237 patients to test it.
The group had access to a high-quality data set of almost 6,000 hand radiographs from their institution, the result of foresight of principal investigator Daniel Aletaha, MD, and his predecessor Josef Smolen, MD. They “thought ahead and started collecting data and had all of it scored,” Dr. Deimel said. The work wasn’t all completed ahead of time, though. Dr. Deimel had to pull images from the hospital’s system sort through them manually.
The group also benefited from close proximity to computer scientists, including coauthor Georg Langs from the Medical University of Vienna’s computational imaging research lab. “We were lucky that we have a computer science department that is very much involved in medical imaging,” Dr. Deimel said.
The trained system successfully identified regions of interest in 96% of joints. It calculated the same score as the human reader in 80.5% of metacarpophalangeal joints and 72.3% of proximal interphalangeal joints. It deviated by more than 1 point from the gold-standard score in just 1.8% of metacarpophalangeal joints and 1.7% of proximal interphalangeal joints.
The researchers aim next to extend the program to bone erosions and also to images of the wrists and feet. They also hope to use scores from the program in clinical trials to measure a treatment’s effect, in registries of routine patient visits where thousands of such images along with clinical data could form the basis of informative observational studies, and in clinical practice, though likely with human oversight.
The study received no outside financial support. Dr. Deimel had no relevant financial disclosures. Mr. Langs reported being cofounder and shareholder of contextflow and receiving grants from Novartis, Siemens Healthineers, and NVIDIA. Dr. Aletaha reported financial relationships with many companies marketing drugs for rheumatoid arthritis.
SOURCE: Deimel T et al. Ann Rheum Dis. 2020 Jun;79(suppl 1):39-40.
A novel program that aims to automate the Sharp-van der Heijde scoring of radiographs of patients with rheumatoid arthritis has shown good reliability in identifying regions of interest and matching human reader scoring for joint-space narrowing, according to a report given at the annual European Congress of Rheumatology, held online this year because of COVID-19.
First author and presenter Thomas Deimel, MD, and colleagues at the Medical University of Vienna said their program, called autoscoRA, may be a solution to the problem of readers having to make subjective calls on the severity of damage seen on radiographs.
Although the work continues to be validated, Dr. Deimel, a resident at the university, is confident in the system as is. “I think for joint space narrowing, we’re there at the point where this could be used and could be as good as a human reader in terms of reliability,” he said in an interview. To find out, the group plans to compare the variability between autoscoRA and a gold-standard human reader against the variability seen between human readers. If the two measures of variability are similar, it would provide a strong endorsement.
The effort is far from the first to develop an automatic scoring system for RA images, but no fully automated system has emerged as reliable, according to Dr. Deimel. He thinks one main issue for others has been lack of access to a sufficient data set to train systems. It can be difficult to find enough training images because many types of joint damage are comparatively uncommon. The problem is made even worse because images can be hard to interpret: The shapes that the system must decipher can be misleading, especially in positions of tendon insertion or ligament attachment that can resemble damage. Differing angles of view between various training images can also complicate matters.
The autoscoRA program is based on modifications of a form of convolutional neural network called the VGG16 architecture. The team used 2,207 images from 270 patients to train autoscoRA, 1,150 images from 133 patients for validation, and 1,834 images from 237 patients to test it.
The group had access to a high-quality data set of almost 6,000 hand radiographs from their institution, the result of foresight of principal investigator Daniel Aletaha, MD, and his predecessor Josef Smolen, MD. They “thought ahead and started collecting data and had all of it scored,” Dr. Deimel said. The work wasn’t all completed ahead of time, though. Dr. Deimel had to pull images from the hospital’s system sort through them manually.
The group also benefited from close proximity to computer scientists, including coauthor Georg Langs from the Medical University of Vienna’s computational imaging research lab. “We were lucky that we have a computer science department that is very much involved in medical imaging,” Dr. Deimel said.
The trained system successfully identified regions of interest in 96% of joints. It calculated the same score as the human reader in 80.5% of metacarpophalangeal joints and 72.3% of proximal interphalangeal joints. It deviated by more than 1 point from the gold-standard score in just 1.8% of metacarpophalangeal joints and 1.7% of proximal interphalangeal joints.
The researchers aim next to extend the program to bone erosions and also to images of the wrists and feet. They also hope to use scores from the program in clinical trials to measure a treatment’s effect, in registries of routine patient visits where thousands of such images along with clinical data could form the basis of informative observational studies, and in clinical practice, though likely with human oversight.
The study received no outside financial support. Dr. Deimel had no relevant financial disclosures. Mr. Langs reported being cofounder and shareholder of contextflow and receiving grants from Novartis, Siemens Healthineers, and NVIDIA. Dr. Aletaha reported financial relationships with many companies marketing drugs for rheumatoid arthritis.
SOURCE: Deimel T et al. Ann Rheum Dis. 2020 Jun;79(suppl 1):39-40.
A novel program that aims to automate the Sharp-van der Heijde scoring of radiographs of patients with rheumatoid arthritis has shown good reliability in identifying regions of interest and matching human reader scoring for joint-space narrowing, according to a report given at the annual European Congress of Rheumatology, held online this year because of COVID-19.
First author and presenter Thomas Deimel, MD, and colleagues at the Medical University of Vienna said their program, called autoscoRA, may be a solution to the problem of readers having to make subjective calls on the severity of damage seen on radiographs.
Although the work continues to be validated, Dr. Deimel, a resident at the university, is confident in the system as is. “I think for joint space narrowing, we’re there at the point where this could be used and could be as good as a human reader in terms of reliability,” he said in an interview. To find out, the group plans to compare the variability between autoscoRA and a gold-standard human reader against the variability seen between human readers. If the two measures of variability are similar, it would provide a strong endorsement.
The effort is far from the first to develop an automatic scoring system for RA images, but no fully automated system has emerged as reliable, according to Dr. Deimel. He thinks one main issue for others has been lack of access to a sufficient data set to train systems. It can be difficult to find enough training images because many types of joint damage are comparatively uncommon. The problem is made even worse because images can be hard to interpret: The shapes that the system must decipher can be misleading, especially in positions of tendon insertion or ligament attachment that can resemble damage. Differing angles of view between various training images can also complicate matters.
The autoscoRA program is based on modifications of a form of convolutional neural network called the VGG16 architecture. The team used 2,207 images from 270 patients to train autoscoRA, 1,150 images from 133 patients for validation, and 1,834 images from 237 patients to test it.
The group had access to a high-quality data set of almost 6,000 hand radiographs from their institution, the result of foresight of principal investigator Daniel Aletaha, MD, and his predecessor Josef Smolen, MD. They “thought ahead and started collecting data and had all of it scored,” Dr. Deimel said. The work wasn’t all completed ahead of time, though. Dr. Deimel had to pull images from the hospital’s system sort through them manually.
The group also benefited from close proximity to computer scientists, including coauthor Georg Langs from the Medical University of Vienna’s computational imaging research lab. “We were lucky that we have a computer science department that is very much involved in medical imaging,” Dr. Deimel said.
The trained system successfully identified regions of interest in 96% of joints. It calculated the same score as the human reader in 80.5% of metacarpophalangeal joints and 72.3% of proximal interphalangeal joints. It deviated by more than 1 point from the gold-standard score in just 1.8% of metacarpophalangeal joints and 1.7% of proximal interphalangeal joints.
The researchers aim next to extend the program to bone erosions and also to images of the wrists and feet. They also hope to use scores from the program in clinical trials to measure a treatment’s effect, in registries of routine patient visits where thousands of such images along with clinical data could form the basis of informative observational studies, and in clinical practice, though likely with human oversight.
The study received no outside financial support. Dr. Deimel had no relevant financial disclosures. Mr. Langs reported being cofounder and shareholder of contextflow and receiving grants from Novartis, Siemens Healthineers, and NVIDIA. Dr. Aletaha reported financial relationships with many companies marketing drugs for rheumatoid arthritis.
SOURCE: Deimel T et al. Ann Rheum Dis. 2020 Jun;79(suppl 1):39-40.
FROM THE EULAR 2020 E-CONGRESS
Daily Recap: Transgender patients turn to DIY treatments; ACIP plans priority vaccine groups
Here are the stories our MDedge editors across specialties think you need to know about today:
Ignored by doctors, transgender patients turn to DIY treatments
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
Treating gender dysphoria should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.” Read more.
ACIP plans priority groups in advance of COVID-19 vaccine
Early plans for prioritizing vaccination when a COVID-19 vaccine becomes available include placing critical health care workers in the first tier, according to Sarah Mbaeyi, MD, MPH, of the CDC’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said. Read more.
‘Nietzsche was wrong’: Past stressors do not create psychological resilience.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop PTSD and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” said Stephen L. Buka, PhD. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.” Read more.
High-impact training can build bone in older women
Older adults, particularly postmenopausal women, are often advised to pursue low-impact, low-intensity exercise as a way to preserve joint health, but that approach might actually contribute to a decline in bone mineral density, researchers report.
Concerns about falls and fracture risk have led many clinicians to advise against higher-impact activities, like jumping, but that is exactly the type of activity that improves bone density and physical function, said Belinda Beck, PhD, professor at the Griffith University School of Allied Health Sciences in Southport, Australia. But new findings show that high-intensity resistance and impact training was a safe and effective way to improve bone mass.
“Once women hit 60, they’re somehow regarded as frail, but that becomes a self-fulfilling prophecy when we take this kinder, gentler approach to exercise,” said Vanessa Yingling, PhD. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Ignored by doctors, transgender patients turn to DIY treatments
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
Treating gender dysphoria should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.” Read more.
ACIP plans priority groups in advance of COVID-19 vaccine
Early plans for prioritizing vaccination when a COVID-19 vaccine becomes available include placing critical health care workers in the first tier, according to Sarah Mbaeyi, MD, MPH, of the CDC’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said. Read more.
‘Nietzsche was wrong’: Past stressors do not create psychological resilience.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop PTSD and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” said Stephen L. Buka, PhD. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.” Read more.
High-impact training can build bone in older women
Older adults, particularly postmenopausal women, are often advised to pursue low-impact, low-intensity exercise as a way to preserve joint health, but that approach might actually contribute to a decline in bone mineral density, researchers report.
Concerns about falls and fracture risk have led many clinicians to advise against higher-impact activities, like jumping, but that is exactly the type of activity that improves bone density and physical function, said Belinda Beck, PhD, professor at the Griffith University School of Allied Health Sciences in Southport, Australia. But new findings show that high-intensity resistance and impact training was a safe and effective way to improve bone mass.
“Once women hit 60, they’re somehow regarded as frail, but that becomes a self-fulfilling prophecy when we take this kinder, gentler approach to exercise,” said Vanessa Yingling, PhD. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Ignored by doctors, transgender patients turn to DIY treatments
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
Treating gender dysphoria should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.” Read more.
ACIP plans priority groups in advance of COVID-19 vaccine
Early plans for prioritizing vaccination when a COVID-19 vaccine becomes available include placing critical health care workers in the first tier, according to Sarah Mbaeyi, MD, MPH, of the CDC’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said. Read more.
‘Nietzsche was wrong’: Past stressors do not create psychological resilience.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop PTSD and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” said Stephen L. Buka, PhD. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.” Read more.
High-impact training can build bone in older women
Older adults, particularly postmenopausal women, are often advised to pursue low-impact, low-intensity exercise as a way to preserve joint health, but that approach might actually contribute to a decline in bone mineral density, researchers report.
Concerns about falls and fracture risk have led many clinicians to advise against higher-impact activities, like jumping, but that is exactly the type of activity that improves bone density and physical function, said Belinda Beck, PhD, professor at the Griffith University School of Allied Health Sciences in Southport, Australia. But new findings show that high-intensity resistance and impact training was a safe and effective way to improve bone mass.
“Once women hit 60, they’re somehow regarded as frail, but that becomes a self-fulfilling prophecy when we take this kinder, gentler approach to exercise,” said Vanessa Yingling, PhD. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
High-impact training can build bone in older women
Older adults, particularly postmenopausal women, are often advised to pursue low-impact, low-intensity exercise as a way to preserve joint health, but that approach might actually contribute to a decline in bone mineral density, researchers report.
Concerns about falls and fracture risk have led many clinicians to advise against higher-impact activities, like jumping, but that is exactly the type of activity that improves bone density and physical function, said Belinda Beck, PhD, professor at the Griffith University School of Allied Health Sciences in Southport, Australia.
“There has always been a quandary in terms of pursuing research on this,” she said in an interview. “We know from animal studies that bone only responds to high-intensity activity, but we worry about advising that for people with low bone mass, so instead we give them medications.”
“But not everyone likes to go on meds, they’re not 100% effective, and they’re not free of side effects,” said Beck, who is also the owner and director of The Bone Clinic in Brisbane, Australia.
In 2014, to assess whether high-intensity resistance and impact training (HiRIT) was a safe and effective way to improve bone mass, Beck and her colleagues conducted the LIFTMOR study of 101 postmenopausal women. The researchers showed that bone mineral density in the lumbar spine and femoral neck regions and functional performance measures were significantly better in the 49 participants randomized to HiRIT for 8 months than in the 52 randomized to low-intensity training.
Three years after the completion of LIFTMOR, the researchers looked at bone mineral density in 23 women from the HiRIT group in their retrospective observational study, the results of which were presented at the virtual American College of Sports Medicine 2020 Annual Meeting.
Ongoing gains were significantly better for the seven participants who continued with HiRIT (at least 25% compliance) than for the 16 who did not when looking at both bone mineral density of the lumbar spine (8.63% vs. 2.18%; P = .042) and femoral neck (3.67% vs. 2.85%; P = 0.14).
However, the women who discontinued HiRIT after 8 months maintained the gains in bone mineral density that they had achieved 3 years earlier.
Functional outcomes in the women who continued HiRIT were better than those in the women who did not, but the differences were not significant.
“The takeaway here is that this type of exercise appears to be a highly effective therapy to reduce risk of osteoporotic fracture, since it improves bone mass,” Beck said.
Jump more, lose less bone density
Given the widespread reluctance to suggest HiRIT-type activity to those with low bone mass, this research is significant, said Vanessa Yingling, PhD, from the Department of Kinesiology at California State University, East Bay.
“Once women hit 60, they’re somehow regarded as frail, but that becomes a self-fulfilling prophecy when we take this kinder, gentler approach to exercise,” Yingling said in an interview. “Building bone density in older adults is important, but maintaining current bone density is just as crucial. Without high-impact activity, we are likely to see decelerating density at a faster rate.”
The other key to the recent research is the functional testing, Yingling added. In addition to bone density measures, high-intensity activity can improve mobility and muscle strength, as the study noted.
This type of activity can be done in shorter bursts, making these workouts more efficient, she explained. For example, a Tabata high-intensity interval training session usually takes about 10 minutes, warm-up and cool-down included.
“A HiRIT workout even once or twice a week would likely improve function, strength, and bone density maintenance,” Beck said. “The result of that would be better fall prevention and potentially less medication usage for BMD issues.”
Both men and women can benefit from a HiRIT workout, Beck and Yingling said. Initially, supervision by a knowledgeable trainer or physical therapist is ideal, they added.
This article first appeared on Medscape.com.
Older adults, particularly postmenopausal women, are often advised to pursue low-impact, low-intensity exercise as a way to preserve joint health, but that approach might actually contribute to a decline in bone mineral density, researchers report.
Concerns about falls and fracture risk have led many clinicians to advise against higher-impact activities, like jumping, but that is exactly the type of activity that improves bone density and physical function, said Belinda Beck, PhD, professor at the Griffith University School of Allied Health Sciences in Southport, Australia.
“There has always been a quandary in terms of pursuing research on this,” she said in an interview. “We know from animal studies that bone only responds to high-intensity activity, but we worry about advising that for people with low bone mass, so instead we give them medications.”
“But not everyone likes to go on meds, they’re not 100% effective, and they’re not free of side effects,” said Beck, who is also the owner and director of The Bone Clinic in Brisbane, Australia.
In 2014, to assess whether high-intensity resistance and impact training (HiRIT) was a safe and effective way to improve bone mass, Beck and her colleagues conducted the LIFTMOR study of 101 postmenopausal women. The researchers showed that bone mineral density in the lumbar spine and femoral neck regions and functional performance measures were significantly better in the 49 participants randomized to HiRIT for 8 months than in the 52 randomized to low-intensity training.
Three years after the completion of LIFTMOR, the researchers looked at bone mineral density in 23 women from the HiRIT group in their retrospective observational study, the results of which were presented at the virtual American College of Sports Medicine 2020 Annual Meeting.
Ongoing gains were significantly better for the seven participants who continued with HiRIT (at least 25% compliance) than for the 16 who did not when looking at both bone mineral density of the lumbar spine (8.63% vs. 2.18%; P = .042) and femoral neck (3.67% vs. 2.85%; P = 0.14).
However, the women who discontinued HiRIT after 8 months maintained the gains in bone mineral density that they had achieved 3 years earlier.
Functional outcomes in the women who continued HiRIT were better than those in the women who did not, but the differences were not significant.
“The takeaway here is that this type of exercise appears to be a highly effective therapy to reduce risk of osteoporotic fracture, since it improves bone mass,” Beck said.
Jump more, lose less bone density
Given the widespread reluctance to suggest HiRIT-type activity to those with low bone mass, this research is significant, said Vanessa Yingling, PhD, from the Department of Kinesiology at California State University, East Bay.
“Once women hit 60, they’re somehow regarded as frail, but that becomes a self-fulfilling prophecy when we take this kinder, gentler approach to exercise,” Yingling said in an interview. “Building bone density in older adults is important, but maintaining current bone density is just as crucial. Without high-impact activity, we are likely to see decelerating density at a faster rate.”
The other key to the recent research is the functional testing, Yingling added. In addition to bone density measures, high-intensity activity can improve mobility and muscle strength, as the study noted.
This type of activity can be done in shorter bursts, making these workouts more efficient, she explained. For example, a Tabata high-intensity interval training session usually takes about 10 minutes, warm-up and cool-down included.
“A HiRIT workout even once or twice a week would likely improve function, strength, and bone density maintenance,” Beck said. “The result of that would be better fall prevention and potentially less medication usage for BMD issues.”
Both men and women can benefit from a HiRIT workout, Beck and Yingling said. Initially, supervision by a knowledgeable trainer or physical therapist is ideal, they added.
This article first appeared on Medscape.com.
Older adults, particularly postmenopausal women, are often advised to pursue low-impact, low-intensity exercise as a way to preserve joint health, but that approach might actually contribute to a decline in bone mineral density, researchers report.
Concerns about falls and fracture risk have led many clinicians to advise against higher-impact activities, like jumping, but that is exactly the type of activity that improves bone density and physical function, said Belinda Beck, PhD, professor at the Griffith University School of Allied Health Sciences in Southport, Australia.
“There has always been a quandary in terms of pursuing research on this,” she said in an interview. “We know from animal studies that bone only responds to high-intensity activity, but we worry about advising that for people with low bone mass, so instead we give them medications.”
“But not everyone likes to go on meds, they’re not 100% effective, and they’re not free of side effects,” said Beck, who is also the owner and director of The Bone Clinic in Brisbane, Australia.
In 2014, to assess whether high-intensity resistance and impact training (HiRIT) was a safe and effective way to improve bone mass, Beck and her colleagues conducted the LIFTMOR study of 101 postmenopausal women. The researchers showed that bone mineral density in the lumbar spine and femoral neck regions and functional performance measures were significantly better in the 49 participants randomized to HiRIT for 8 months than in the 52 randomized to low-intensity training.
Three years after the completion of LIFTMOR, the researchers looked at bone mineral density in 23 women from the HiRIT group in their retrospective observational study, the results of which were presented at the virtual American College of Sports Medicine 2020 Annual Meeting.
Ongoing gains were significantly better for the seven participants who continued with HiRIT (at least 25% compliance) than for the 16 who did not when looking at both bone mineral density of the lumbar spine (8.63% vs. 2.18%; P = .042) and femoral neck (3.67% vs. 2.85%; P = 0.14).
However, the women who discontinued HiRIT after 8 months maintained the gains in bone mineral density that they had achieved 3 years earlier.
Functional outcomes in the women who continued HiRIT were better than those in the women who did not, but the differences were not significant.
“The takeaway here is that this type of exercise appears to be a highly effective therapy to reduce risk of osteoporotic fracture, since it improves bone mass,” Beck said.
Jump more, lose less bone density
Given the widespread reluctance to suggest HiRIT-type activity to those with low bone mass, this research is significant, said Vanessa Yingling, PhD, from the Department of Kinesiology at California State University, East Bay.
“Once women hit 60, they’re somehow regarded as frail, but that becomes a self-fulfilling prophecy when we take this kinder, gentler approach to exercise,” Yingling said in an interview. “Building bone density in older adults is important, but maintaining current bone density is just as crucial. Without high-impact activity, we are likely to see decelerating density at a faster rate.”
The other key to the recent research is the functional testing, Yingling added. In addition to bone density measures, high-intensity activity can improve mobility and muscle strength, as the study noted.
This type of activity can be done in shorter bursts, making these workouts more efficient, she explained. For example, a Tabata high-intensity interval training session usually takes about 10 minutes, warm-up and cool-down included.
“A HiRIT workout even once or twice a week would likely improve function, strength, and bone density maintenance,” Beck said. “The result of that would be better fall prevention and potentially less medication usage for BMD issues.”
Both men and women can benefit from a HiRIT workout, Beck and Yingling said. Initially, supervision by a knowledgeable trainer or physical therapist is ideal, they added.
This article first appeared on Medscape.com.
First validated classification criteria for discoid lupus erythematosus unveiled
The first validated classification criteria for discoid lupus erythematosus has a sensitivity that ranges between 73.9% and 84.1% and a specificity that ranges between 75.9% and 92.9%.
“Discoid lupus erythematosus [DLE] is the most common type of chronic cutaneous lupus,” lead study author Scott A. Elman, MD, said during the virtual annual meeting of the American Academy of Dermatology. “It’s one of the most potentially disfiguring forms of cutaneous lupus erythematosus [CLE], which can lead to scarring, hair loss, and dyspigmentation if not treated early or promptly. It has a significant impact on patient quality of life and there are currently no classification criteria for DLE, which has led to problematic heterogeneity in observational and interventional research efforts. As there is increasing interest in drug development programs for CLE and DLE, there is a need to develop classification criteria.”
Dr. Elman, of the Harvard combined medicine-dermatology training program at Brigham and Women’s Hospital, Boston, pointed out that classification criteria are the standard definitions that are primarily intended to enroll uniform cohorts for research. “These emphasize high specificity, whereas diagnostic criteria reflect a more broad and variable set of features of a given disease, and therefore require a higher sensitivity,” he explained. “While classification criteria are not synonymous with diagnostic criteria, they typically mirror the list of criteria that are used for diagnosis.”
In 2017, Dr. Elman and colleagues generated an item list of 12 potential classification criteria using an international Delphi consensus process: 5 criteria represented disease morphology, 2 represented discoid lupus location, and 5 represented histopathology (J Am Acad Dermatol. 2017 Aug 1;77[2]:261-7). The purpose of the current study, which was presented as a late-breaking abstract, was to validate the proposed classification criteria in a multicenter, international trial. “The point is to be able to differentiate between discoid lupus and its disease mimickers, which could be confused in enrollment in clinical trials,” he said.
At nine participating sites, patients were identified at clinical visits as having either DLE or a DLE mimicker. After each visit, dermatologists determined if morphological features were present. One dermatopathologist at each site reviewed pathology, if available, to see if the histopathologic features were present. Diagnosis by clinical features and dermatopathology were tabulated and presented as counts and percentages. Clinical features among those with and without DLE were calculated and compared with chi-square or Fisher’s exact tests. The researchers used best subsets logistic regression analysis to identify candidate models.
A total of 215 patients were enrolled: 94 that were consistent with DLE and 121 that were consistent with a DLE mimicker. Most cases (83%) were from North America, 11% were from Asia, and 6% were from Europe. Only 86 cases (40%) had biopsies for dermatopathology review.
The following clinical features were found to be more commonly associated with DLE, compared with DLE mimickers: atrophic scarring (83% vs. 24%; P < .001), dyspigmentation (84% vs. 55%; P < .001), follicular hyperkeratosis/plugging (43% vs. 11%; P < .001), scarring alopecia (61% vs. 21%; P < .001), location in the conchal bowl (49% vs. 10%; P < .001), preference for the head and neck (87% vs. 49%; P < .001), and erythematous to violaceous in color (93% vs. 85%, a nonsignificant difference; P = .09).
When histopathological items were assessed, the following features were found to be more commonly associated with DLE, compared with DLE mimickers: interface/vacuolar dermatitis (83% vs. 53%; P = .004), perivascular and/or periappendageal lymphohistiocytic infiltrate (95% vs. 84%, a nonsignificant difference; P = .18), follicular keratin plugs (57% vs. 20%; P < .001), mucin deposition (73% vs. 39%; P = .002), and basement membrane thickening (57% vs. 14%; P < .001).
“There was good agreement between the diagnoses made by dermatologists and dermatopathologists, with a Cohen’s kappa statistic of 0.83,” Dr. Elman added. “Similarly, in many of the cases, the dermatopathologists and the dermatologists felt confident in their diagnosis.”
For the final model, the researchers excluded patients who had any missing data as well as those who had a diagnosis that was uncertain. This left 200 cases in the final model. Clinical variables associated with DLE were: atrophic scarring (odds ratio, 8.70; P < .001), location in the conchal bowl (OR, 6.80; P < .001), preference for head and neck (OR, 9.41; P < .001), dyspigmentation (OR, 3.23; P = .020), follicular hyperkeratosis/plugging (OR, 2.94; P = .054), and erythematous to violaceous in color (OR, 3.44; P = .056). The area under the curve for the model was 0.91.
According to Dr. Elman, the final model is a points-based model with 3 points assigned to atrophic scarring, 2 points assigned to location in the conchal bowl, 2 points assigned to preference for head and neck, 1 point assigned to dyspigmentation, 1 point assigned to follicular hyperkeratosis/plugging, and 1 point assigned to erythematous to violaceous in color. A score of 5 or greater yields a classification as DLE with 84.1% sensitivity and 75.9% specificity, while a score of 7 or greater yields a 73.9% sensitivity and 92.9% specificity.
Dr. Elman acknowledged certain limitations of the study, including the fact that information related to histopathology was not included in the final model. “This was a result of having only 40% of cases with relevant dermatopathology,” he said. “This limited our ability to meaningfully incorporate these items into a classification criteria set. However, with the data we’ve collected, efforts are under way to make a DLE-specific histopathology classification criteria.”
Another limitation is that the researchers relied on expert diagnosis as the preferred option. “Similarly, many of the cases came from large referral centers, and no demographic data were obtained, so this limits the generalizability of our study,” he said.
Dr. Elman reported having no financial disclosures.
The first validated classification criteria for discoid lupus erythematosus has a sensitivity that ranges between 73.9% and 84.1% and a specificity that ranges between 75.9% and 92.9%.
“Discoid lupus erythematosus [DLE] is the most common type of chronic cutaneous lupus,” lead study author Scott A. Elman, MD, said during the virtual annual meeting of the American Academy of Dermatology. “It’s one of the most potentially disfiguring forms of cutaneous lupus erythematosus [CLE], which can lead to scarring, hair loss, and dyspigmentation if not treated early or promptly. It has a significant impact on patient quality of life and there are currently no classification criteria for DLE, which has led to problematic heterogeneity in observational and interventional research efforts. As there is increasing interest in drug development programs for CLE and DLE, there is a need to develop classification criteria.”
Dr. Elman, of the Harvard combined medicine-dermatology training program at Brigham and Women’s Hospital, Boston, pointed out that classification criteria are the standard definitions that are primarily intended to enroll uniform cohorts for research. “These emphasize high specificity, whereas diagnostic criteria reflect a more broad and variable set of features of a given disease, and therefore require a higher sensitivity,” he explained. “While classification criteria are not synonymous with diagnostic criteria, they typically mirror the list of criteria that are used for diagnosis.”
In 2017, Dr. Elman and colleagues generated an item list of 12 potential classification criteria using an international Delphi consensus process: 5 criteria represented disease morphology, 2 represented discoid lupus location, and 5 represented histopathology (J Am Acad Dermatol. 2017 Aug 1;77[2]:261-7). The purpose of the current study, which was presented as a late-breaking abstract, was to validate the proposed classification criteria in a multicenter, international trial. “The point is to be able to differentiate between discoid lupus and its disease mimickers, which could be confused in enrollment in clinical trials,” he said.
At nine participating sites, patients were identified at clinical visits as having either DLE or a DLE mimicker. After each visit, dermatologists determined if morphological features were present. One dermatopathologist at each site reviewed pathology, if available, to see if the histopathologic features were present. Diagnosis by clinical features and dermatopathology were tabulated and presented as counts and percentages. Clinical features among those with and without DLE were calculated and compared with chi-square or Fisher’s exact tests. The researchers used best subsets logistic regression analysis to identify candidate models.
A total of 215 patients were enrolled: 94 that were consistent with DLE and 121 that were consistent with a DLE mimicker. Most cases (83%) were from North America, 11% were from Asia, and 6% were from Europe. Only 86 cases (40%) had biopsies for dermatopathology review.
The following clinical features were found to be more commonly associated with DLE, compared with DLE mimickers: atrophic scarring (83% vs. 24%; P < .001), dyspigmentation (84% vs. 55%; P < .001), follicular hyperkeratosis/plugging (43% vs. 11%; P < .001), scarring alopecia (61% vs. 21%; P < .001), location in the conchal bowl (49% vs. 10%; P < .001), preference for the head and neck (87% vs. 49%; P < .001), and erythematous to violaceous in color (93% vs. 85%, a nonsignificant difference; P = .09).
When histopathological items were assessed, the following features were found to be more commonly associated with DLE, compared with DLE mimickers: interface/vacuolar dermatitis (83% vs. 53%; P = .004), perivascular and/or periappendageal lymphohistiocytic infiltrate (95% vs. 84%, a nonsignificant difference; P = .18), follicular keratin plugs (57% vs. 20%; P < .001), mucin deposition (73% vs. 39%; P = .002), and basement membrane thickening (57% vs. 14%; P < .001).
“There was good agreement between the diagnoses made by dermatologists and dermatopathologists, with a Cohen’s kappa statistic of 0.83,” Dr. Elman added. “Similarly, in many of the cases, the dermatopathologists and the dermatologists felt confident in their diagnosis.”
For the final model, the researchers excluded patients who had any missing data as well as those who had a diagnosis that was uncertain. This left 200 cases in the final model. Clinical variables associated with DLE were: atrophic scarring (odds ratio, 8.70; P < .001), location in the conchal bowl (OR, 6.80; P < .001), preference for head and neck (OR, 9.41; P < .001), dyspigmentation (OR, 3.23; P = .020), follicular hyperkeratosis/plugging (OR, 2.94; P = .054), and erythematous to violaceous in color (OR, 3.44; P = .056). The area under the curve for the model was 0.91.
According to Dr. Elman, the final model is a points-based model with 3 points assigned to atrophic scarring, 2 points assigned to location in the conchal bowl, 2 points assigned to preference for head and neck, 1 point assigned to dyspigmentation, 1 point assigned to follicular hyperkeratosis/plugging, and 1 point assigned to erythematous to violaceous in color. A score of 5 or greater yields a classification as DLE with 84.1% sensitivity and 75.9% specificity, while a score of 7 or greater yields a 73.9% sensitivity and 92.9% specificity.
Dr. Elman acknowledged certain limitations of the study, including the fact that information related to histopathology was not included in the final model. “This was a result of having only 40% of cases with relevant dermatopathology,” he said. “This limited our ability to meaningfully incorporate these items into a classification criteria set. However, with the data we’ve collected, efforts are under way to make a DLE-specific histopathology classification criteria.”
Another limitation is that the researchers relied on expert diagnosis as the preferred option. “Similarly, many of the cases came from large referral centers, and no demographic data were obtained, so this limits the generalizability of our study,” he said.
Dr. Elman reported having no financial disclosures.
The first validated classification criteria for discoid lupus erythematosus has a sensitivity that ranges between 73.9% and 84.1% and a specificity that ranges between 75.9% and 92.9%.
“Discoid lupus erythematosus [DLE] is the most common type of chronic cutaneous lupus,” lead study author Scott A. Elman, MD, said during the virtual annual meeting of the American Academy of Dermatology. “It’s one of the most potentially disfiguring forms of cutaneous lupus erythematosus [CLE], which can lead to scarring, hair loss, and dyspigmentation if not treated early or promptly. It has a significant impact on patient quality of life and there are currently no classification criteria for DLE, which has led to problematic heterogeneity in observational and interventional research efforts. As there is increasing interest in drug development programs for CLE and DLE, there is a need to develop classification criteria.”
Dr. Elman, of the Harvard combined medicine-dermatology training program at Brigham and Women’s Hospital, Boston, pointed out that classification criteria are the standard definitions that are primarily intended to enroll uniform cohorts for research. “These emphasize high specificity, whereas diagnostic criteria reflect a more broad and variable set of features of a given disease, and therefore require a higher sensitivity,” he explained. “While classification criteria are not synonymous with diagnostic criteria, they typically mirror the list of criteria that are used for diagnosis.”
In 2017, Dr. Elman and colleagues generated an item list of 12 potential classification criteria using an international Delphi consensus process: 5 criteria represented disease morphology, 2 represented discoid lupus location, and 5 represented histopathology (J Am Acad Dermatol. 2017 Aug 1;77[2]:261-7). The purpose of the current study, which was presented as a late-breaking abstract, was to validate the proposed classification criteria in a multicenter, international trial. “The point is to be able to differentiate between discoid lupus and its disease mimickers, which could be confused in enrollment in clinical trials,” he said.
At nine participating sites, patients were identified at clinical visits as having either DLE or a DLE mimicker. After each visit, dermatologists determined if morphological features were present. One dermatopathologist at each site reviewed pathology, if available, to see if the histopathologic features were present. Diagnosis by clinical features and dermatopathology were tabulated and presented as counts and percentages. Clinical features among those with and without DLE were calculated and compared with chi-square or Fisher’s exact tests. The researchers used best subsets logistic regression analysis to identify candidate models.
A total of 215 patients were enrolled: 94 that were consistent with DLE and 121 that were consistent with a DLE mimicker. Most cases (83%) were from North America, 11% were from Asia, and 6% were from Europe. Only 86 cases (40%) had biopsies for dermatopathology review.
The following clinical features were found to be more commonly associated with DLE, compared with DLE mimickers: atrophic scarring (83% vs. 24%; P < .001), dyspigmentation (84% vs. 55%; P < .001), follicular hyperkeratosis/plugging (43% vs. 11%; P < .001), scarring alopecia (61% vs. 21%; P < .001), location in the conchal bowl (49% vs. 10%; P < .001), preference for the head and neck (87% vs. 49%; P < .001), and erythematous to violaceous in color (93% vs. 85%, a nonsignificant difference; P = .09).
When histopathological items were assessed, the following features were found to be more commonly associated with DLE, compared with DLE mimickers: interface/vacuolar dermatitis (83% vs. 53%; P = .004), perivascular and/or periappendageal lymphohistiocytic infiltrate (95% vs. 84%, a nonsignificant difference; P = .18), follicular keratin plugs (57% vs. 20%; P < .001), mucin deposition (73% vs. 39%; P = .002), and basement membrane thickening (57% vs. 14%; P < .001).
“There was good agreement between the diagnoses made by dermatologists and dermatopathologists, with a Cohen’s kappa statistic of 0.83,” Dr. Elman added. “Similarly, in many of the cases, the dermatopathologists and the dermatologists felt confident in their diagnosis.”
For the final model, the researchers excluded patients who had any missing data as well as those who had a diagnosis that was uncertain. This left 200 cases in the final model. Clinical variables associated with DLE were: atrophic scarring (odds ratio, 8.70; P < .001), location in the conchal bowl (OR, 6.80; P < .001), preference for head and neck (OR, 9.41; P < .001), dyspigmentation (OR, 3.23; P = .020), follicular hyperkeratosis/plugging (OR, 2.94; P = .054), and erythematous to violaceous in color (OR, 3.44; P = .056). The area under the curve for the model was 0.91.
According to Dr. Elman, the final model is a points-based model with 3 points assigned to atrophic scarring, 2 points assigned to location in the conchal bowl, 2 points assigned to preference for head and neck, 1 point assigned to dyspigmentation, 1 point assigned to follicular hyperkeratosis/plugging, and 1 point assigned to erythematous to violaceous in color. A score of 5 or greater yields a classification as DLE with 84.1% sensitivity and 75.9% specificity, while a score of 7 or greater yields a 73.9% sensitivity and 92.9% specificity.
Dr. Elman acknowledged certain limitations of the study, including the fact that information related to histopathology was not included in the final model. “This was a result of having only 40% of cases with relevant dermatopathology,” he said. “This limited our ability to meaningfully incorporate these items into a classification criteria set. However, with the data we’ve collected, efforts are under way to make a DLE-specific histopathology classification criteria.”
Another limitation is that the researchers relied on expert diagnosis as the preferred option. “Similarly, many of the cases came from large referral centers, and no demographic data were obtained, so this limits the generalizability of our study,” he said.
Dr. Elman reported having no financial disclosures.
FROM AAD 20
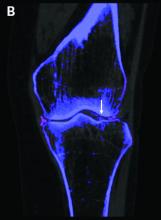
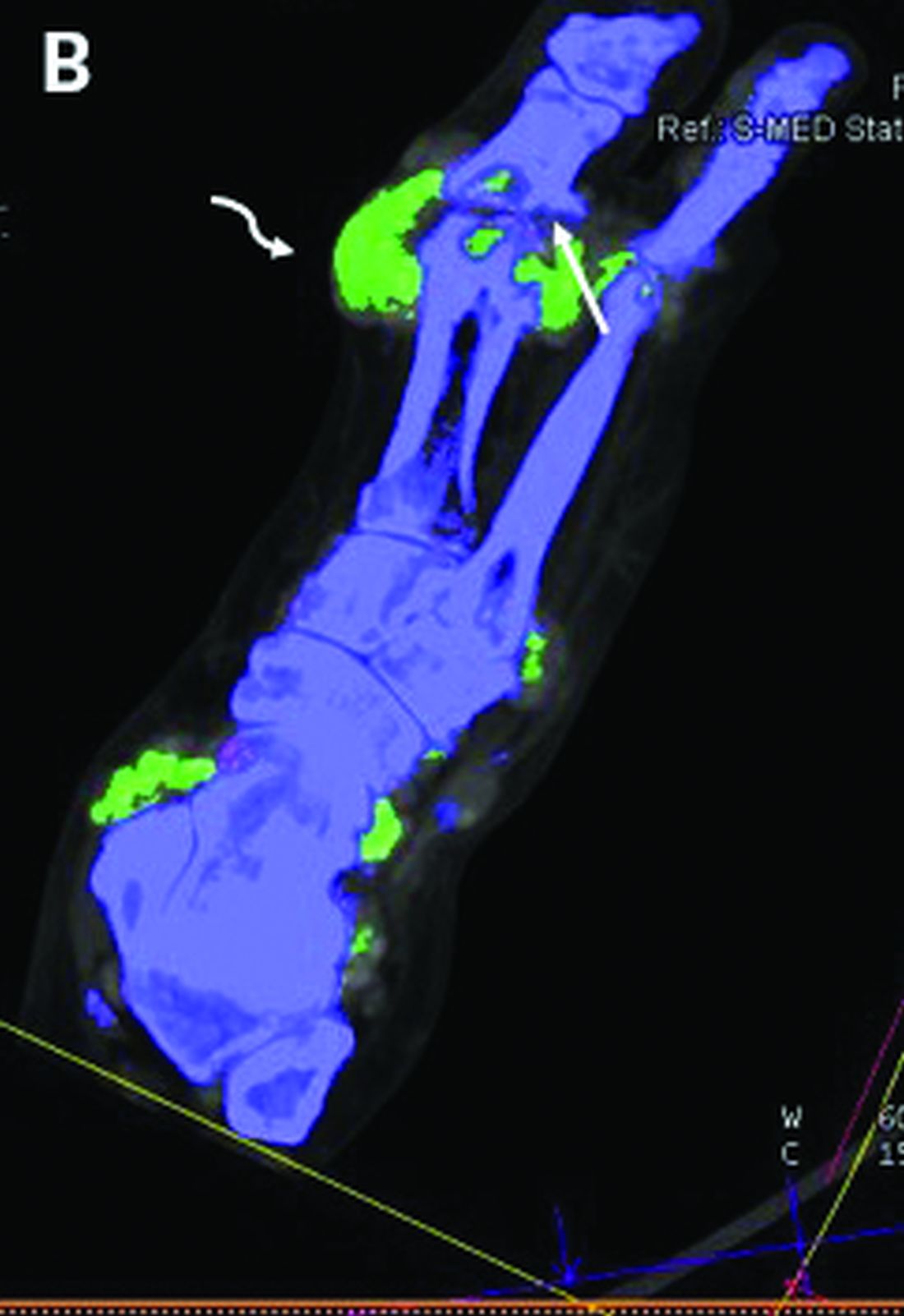
DECT has mixed performance in differentiating gout vs. CPPD
Dual-energy computed tomography (DECT) appears to have limited utility for differentiating between gout and calcium pyrophosphate deposition disease (CPPD), according to a German prospective cohort study. Findings were reported at the annual European Congress of Rheumatology, held online this year because of COVID-19.
“Differentiation of gout and pseudogout, or CPPD, is sometimes difficult,” said presenting investigator Valentin S. Schäfer, MD, associate professor of internal medicine and head of the department of rheumatology and clinical immunology at University Hospital Bonn (Germany).
“Arthrocentesis and subsequent polarization microscopy remains the gold standard,” he noted. “Novel diagnostic approaches, such as DECT, have recently been validated for gout, but limited data [are] available on the use of DECT in patients with CPPD.”
The investigators studied 30 patients: 22 with suspected gout and 8 with suspected CPPD. All underwent arthrocentesis with subsequent polarization microscopy for definitive diagnosis, plus clinical examination, ultrasound examination, conventional radiography, DECT, and assessment of 12 laboratory parameters.
For diagnosis of gout, DECT had a sensitivity and specificity of 59.1% and 100%, respectively, Dr. Schäfer reported, noting that this sensitivity falls considerably short of the 90% previously reported for gout.
Corresponding sensitivity and specificity were 90.9% and 75% for ultrasound, 58.8% and 100% for conventional radiography, and 81.8% and 87.5% for the rheumatologists’ suspected clinical diagnosis.
For diagnosis of CPPD, DECT had sensitivity of 37.5% and specificity of 81.8%. Corresponding values were 87.5% and 91% for ultrasound, 0% and 94.1% for conventional radiography, and 75.0% and 100% for suspected clinical diagnosis.
None of the 12 laboratory parameters studied – uric acid, C-reactive protein, organic phosphate, and leukocytes, among others – significantly differentiated between conditions.
“Both ultrasound and suspected clinical diagnosis had higher sensitivities than DECT for gout and CPPD,” Dr. Schäfer concluded. “Further studies with larger patient cohorts and perhaps modified scan protocols are needed in order to determine the diagnostic utility of DECT in CPPD.”
Findings in context
“Noninvasive, accurate methods for distinguishing between gout and CPPD will improve clinical care,” Sara K. Tedeschi, MD, MPH, predicted in an interview.
“Arthrocentesis is painful in an acutely inflamed joint, can be difficult to perform on small joints, and is underutilized in clinical practice,” she elaborated. And ultrasound is operator dependent and does not quantify crystal volume in and around the joint.
The question addressed by the study is therefore clinically relevant, according to Dr. Tedeschi, a rheumatologist at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School, Boston.
However, among the patients with CPPD, the study did not report specific phenotypes (acute inflammatory arthritis, chronic inflammatory arthritis, and osteoarthritis with calcium pyrophosphate deposits), she noted. “It is difficult to draw conclusions about the sensitivity or specificity of DECT for CPPD without this information, especially among just 8 CPPD patients.”
In addition, among the patients with gout, the proportion having new-onset disease with flare duration less than 6 weeks and the proportion with tophi were unknown, both of which affected DECT sensitivity in the previous study that reported 90% sensitivity. “Based on the 95% confidence interval in the present study, it is possible that with a larger sample size, DECT sensitivity for gout would have been higher,” she pointed out. “We also do not know the DECT software settings, which impact DECT interpretation as positive or negative for the crystal of interest.”
Finally, “it would be relevant to know what joints were aspirated and imaged in each group,” Dr. Tedeschi said. “For example, if the first metatarsophalangeal (MTP) joint was aspirated and imaged for half of the gout patients but for none of the CPPD patients, that may affect the study interpretation.”
The study did not receive any specific funding. Dr. Schäfer disclosed a variety of financial relationships with multiple pharmaceutical companies. Dr. Tedeschi disclosed receiving grant support from the National Institutes of Health to study imaging modalities for CPPD, and being first author on a study comparing the sensitivity of DECT, ultrasound, and x-ray for acute CPP crystal arthritis.
SOURCE: Kravchenko D et al. Ann Rheum Dis. 2020 Jun;79[suppl 1]:196.
Dual-energy computed tomography (DECT) appears to have limited utility for differentiating between gout and calcium pyrophosphate deposition disease (CPPD), according to a German prospective cohort study. Findings were reported at the annual European Congress of Rheumatology, held online this year because of COVID-19.
“Differentiation of gout and pseudogout, or CPPD, is sometimes difficult,” said presenting investigator Valentin S. Schäfer, MD, associate professor of internal medicine and head of the department of rheumatology and clinical immunology at University Hospital Bonn (Germany).
“Arthrocentesis and subsequent polarization microscopy remains the gold standard,” he noted. “Novel diagnostic approaches, such as DECT, have recently been validated for gout, but limited data [are] available on the use of DECT in patients with CPPD.”
The investigators studied 30 patients: 22 with suspected gout and 8 with suspected CPPD. All underwent arthrocentesis with subsequent polarization microscopy for definitive diagnosis, plus clinical examination, ultrasound examination, conventional radiography, DECT, and assessment of 12 laboratory parameters.
For diagnosis of gout, DECT had a sensitivity and specificity of 59.1% and 100%, respectively, Dr. Schäfer reported, noting that this sensitivity falls considerably short of the 90% previously reported for gout.
Corresponding sensitivity and specificity were 90.9% and 75% for ultrasound, 58.8% and 100% for conventional radiography, and 81.8% and 87.5% for the rheumatologists’ suspected clinical diagnosis.
For diagnosis of CPPD, DECT had sensitivity of 37.5% and specificity of 81.8%. Corresponding values were 87.5% and 91% for ultrasound, 0% and 94.1% for conventional radiography, and 75.0% and 100% for suspected clinical diagnosis.
None of the 12 laboratory parameters studied – uric acid, C-reactive protein, organic phosphate, and leukocytes, among others – significantly differentiated between conditions.
“Both ultrasound and suspected clinical diagnosis had higher sensitivities than DECT for gout and CPPD,” Dr. Schäfer concluded. “Further studies with larger patient cohorts and perhaps modified scan protocols are needed in order to determine the diagnostic utility of DECT in CPPD.”
Findings in context
“Noninvasive, accurate methods for distinguishing between gout and CPPD will improve clinical care,” Sara K. Tedeschi, MD, MPH, predicted in an interview.
“Arthrocentesis is painful in an acutely inflamed joint, can be difficult to perform on small joints, and is underutilized in clinical practice,” she elaborated. And ultrasound is operator dependent and does not quantify crystal volume in and around the joint.
The question addressed by the study is therefore clinically relevant, according to Dr. Tedeschi, a rheumatologist at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School, Boston.
However, among the patients with CPPD, the study did not report specific phenotypes (acute inflammatory arthritis, chronic inflammatory arthritis, and osteoarthritis with calcium pyrophosphate deposits), she noted. “It is difficult to draw conclusions about the sensitivity or specificity of DECT for CPPD without this information, especially among just 8 CPPD patients.”
In addition, among the patients with gout, the proportion having new-onset disease with flare duration less than 6 weeks and the proportion with tophi were unknown, both of which affected DECT sensitivity in the previous study that reported 90% sensitivity. “Based on the 95% confidence interval in the present study, it is possible that with a larger sample size, DECT sensitivity for gout would have been higher,” she pointed out. “We also do not know the DECT software settings, which impact DECT interpretation as positive or negative for the crystal of interest.”
Finally, “it would be relevant to know what joints were aspirated and imaged in each group,” Dr. Tedeschi said. “For example, if the first metatarsophalangeal (MTP) joint was aspirated and imaged for half of the gout patients but for none of the CPPD patients, that may affect the study interpretation.”
The study did not receive any specific funding. Dr. Schäfer disclosed a variety of financial relationships with multiple pharmaceutical companies. Dr. Tedeschi disclosed receiving grant support from the National Institutes of Health to study imaging modalities for CPPD, and being first author on a study comparing the sensitivity of DECT, ultrasound, and x-ray for acute CPP crystal arthritis.
SOURCE: Kravchenko D et al. Ann Rheum Dis. 2020 Jun;79[suppl 1]:196.
Dual-energy computed tomography (DECT) appears to have limited utility for differentiating between gout and calcium pyrophosphate deposition disease (CPPD), according to a German prospective cohort study. Findings were reported at the annual European Congress of Rheumatology, held online this year because of COVID-19.
“Differentiation of gout and pseudogout, or CPPD, is sometimes difficult,” said presenting investigator Valentin S. Schäfer, MD, associate professor of internal medicine and head of the department of rheumatology and clinical immunology at University Hospital Bonn (Germany).
“Arthrocentesis and subsequent polarization microscopy remains the gold standard,” he noted. “Novel diagnostic approaches, such as DECT, have recently been validated for gout, but limited data [are] available on the use of DECT in patients with CPPD.”
The investigators studied 30 patients: 22 with suspected gout and 8 with suspected CPPD. All underwent arthrocentesis with subsequent polarization microscopy for definitive diagnosis, plus clinical examination, ultrasound examination, conventional radiography, DECT, and assessment of 12 laboratory parameters.
For diagnosis of gout, DECT had a sensitivity and specificity of 59.1% and 100%, respectively, Dr. Schäfer reported, noting that this sensitivity falls considerably short of the 90% previously reported for gout.
Corresponding sensitivity and specificity were 90.9% and 75% for ultrasound, 58.8% and 100% for conventional radiography, and 81.8% and 87.5% for the rheumatologists’ suspected clinical diagnosis.
For diagnosis of CPPD, DECT had sensitivity of 37.5% and specificity of 81.8%. Corresponding values were 87.5% and 91% for ultrasound, 0% and 94.1% for conventional radiography, and 75.0% and 100% for suspected clinical diagnosis.
None of the 12 laboratory parameters studied – uric acid, C-reactive protein, organic phosphate, and leukocytes, among others – significantly differentiated between conditions.
“Both ultrasound and suspected clinical diagnosis had higher sensitivities than DECT for gout and CPPD,” Dr. Schäfer concluded. “Further studies with larger patient cohorts and perhaps modified scan protocols are needed in order to determine the diagnostic utility of DECT in CPPD.”
Findings in context
“Noninvasive, accurate methods for distinguishing between gout and CPPD will improve clinical care,” Sara K. Tedeschi, MD, MPH, predicted in an interview.
“Arthrocentesis is painful in an acutely inflamed joint, can be difficult to perform on small joints, and is underutilized in clinical practice,” she elaborated. And ultrasound is operator dependent and does not quantify crystal volume in and around the joint.
The question addressed by the study is therefore clinically relevant, according to Dr. Tedeschi, a rheumatologist at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School, Boston.
However, among the patients with CPPD, the study did not report specific phenotypes (acute inflammatory arthritis, chronic inflammatory arthritis, and osteoarthritis with calcium pyrophosphate deposits), she noted. “It is difficult to draw conclusions about the sensitivity or specificity of DECT for CPPD without this information, especially among just 8 CPPD patients.”
In addition, among the patients with gout, the proportion having new-onset disease with flare duration less than 6 weeks and the proportion with tophi were unknown, both of which affected DECT sensitivity in the previous study that reported 90% sensitivity. “Based on the 95% confidence interval in the present study, it is possible that with a larger sample size, DECT sensitivity for gout would have been higher,” she pointed out. “We also do not know the DECT software settings, which impact DECT interpretation as positive or negative for the crystal of interest.”
Finally, “it would be relevant to know what joints were aspirated and imaged in each group,” Dr. Tedeschi said. “For example, if the first metatarsophalangeal (MTP) joint was aspirated and imaged for half of the gout patients but for none of the CPPD patients, that may affect the study interpretation.”
The study did not receive any specific funding. Dr. Schäfer disclosed a variety of financial relationships with multiple pharmaceutical companies. Dr. Tedeschi disclosed receiving grant support from the National Institutes of Health to study imaging modalities for CPPD, and being first author on a study comparing the sensitivity of DECT, ultrasound, and x-ray for acute CPP crystal arthritis.
SOURCE: Kravchenko D et al. Ann Rheum Dis. 2020 Jun;79[suppl 1]:196.
FROM THE EULAR 2020 E-CONGRESS
In scleroderma, GERD questionnaires are essential tools
Every rheumatologist ought to be comfortable in using a validated gastrointestinal symptom scale for evaluation of gastroesophageal reflux disease in patients with scleroderma, Tracy M. Frech, MD, declared at the virtual edition of the American College of Rheumatology’s 2020 State-of-the-Art Clinical Symposium.
About 90% of scleroderma patients will develop GI tract involvement during the course of their connective tissue disease. And while any portion of the GI tract from esophagus to anus can be involved, the most common GI manifestation is gastroesophageal reflux disease (GERD), affecting up to 90% of scleroderma patients, observed Dr. Frech, a rheumatologist and director of the systemic sclerosis clinic at the University of Utah and the George E. Wahlen Department of Veterans Affairs Medical Center, both in Salt Lake City.
“It is essential to ask scleroderma patients questions in order to understand their gastrointestinal tract symptoms. The questionnaires are really critical for us to grade the severity and then properly order tests,” she explained. “The goal is symptom identification, ideally with minimal time burden and at no cost, to guide decisions that move our patients’ care forward.”
Three of the most useful validated instruments for assessment of GERD symptoms in scleroderma patients in routine clinical practice are the GerdQ, the University of California, Los Angeles, Scleroderma Clinical Trial Consortium GI Tract Questionnaire (UCLA GIT) 2.0 reflux scale, and the Patient-Reported Outcomes Measurement Information System (PROMIS) reflux scale.
The GerdQ is a six-item, self-administered questionnaire in which patients specify how many days in the past week they have experienced heartburn, regurgitation, nausea, sleep interference, upper abdominal pain, and need for medication. A free online tool is available for calculating the likelihood of having GERD based upon GerdQ score. A score of 8 or more points out of a possible 18 has the highest sensitivity and specificity for diagnosis of GERD.
The UCLA GIT 2.0 – the most commonly used instrument for GI symptom assessment in scleroderma patients – includes 34 items. It takes 6-8 minutes to complete the whole thing, but patients being assessed for GERD only need answer the eight GERD-specific questions. Six of these eight questions are the same as in the GerdQ. One of the two extra questions asks about difficulty in swallowing solid food, which if answered affirmatively warrants early referral to a gastroenterologist. The other question inquires about any food triggers for the reflux, providing an opportunity for a rheumatologist to educate the patient about the importance of avoiding acidic foods, such as tomatoes, and other food and drink generally considered healthy but which actually exacerbate GERD.
The National Institutes of Health PROMIS scale, the newest of the three instruments, is a 60-item questionnaire; however, only 20 questions relate to reflux and dysphagia and are thus germane to a focused GERD assessment in scleroderma.
When a clinical diagnosis of GERD is made in a scleroderma patient based upon symptoms elicited by questionnaire, guidelines recommend a trial of empiric proton pump inhibitor therapy and behavioral interventions, such as raising the head of the bed, in order to confirm the diagnosis. If the patient reports feeling better after these basic interventions, the diagnosis is confirmed. If not, it’s time to make a referral to a gastroenterologist for specialized care, Dr. Frech said.
Dr. Frech was a coinvestigator in an international, prospective, longitudinal study of patient-reported outcomes measures in 116 patients with scleroderma and GERD. All study participants had to complete the UCLA GIT 2.0, the PROMIS reflux scale, and a third patient-reported GERD measure both before and after the therapeutic intervention. The UCLA GIT 2.0 and PROMIS instruments demonstrated similarly robust sensitivity for identifying changes in GERD symptoms after therapeutic intervention.
“It doesn’t really matter what questionnaire we’re using,” according to the rheumatologist. “But I will point out that there is significant overlap in symptoms among GERD, gastroparesis, functional dyspepsia, and eosinophilic esophagitis, all of which cause symptoms of heartburn and regurgitation. So we don’t want to ask these questions just once, we want to make an intervention and then reask the questions to ensure that we’re continuously moving forward with the gastrointestinal tract management plan.”
Dr. Frech reported having no financial conflicts regarding her presentation.
Every rheumatologist ought to be comfortable in using a validated gastrointestinal symptom scale for evaluation of gastroesophageal reflux disease in patients with scleroderma, Tracy M. Frech, MD, declared at the virtual edition of the American College of Rheumatology’s 2020 State-of-the-Art Clinical Symposium.
About 90% of scleroderma patients will develop GI tract involvement during the course of their connective tissue disease. And while any portion of the GI tract from esophagus to anus can be involved, the most common GI manifestation is gastroesophageal reflux disease (GERD), affecting up to 90% of scleroderma patients, observed Dr. Frech, a rheumatologist and director of the systemic sclerosis clinic at the University of Utah and the George E. Wahlen Department of Veterans Affairs Medical Center, both in Salt Lake City.
“It is essential to ask scleroderma patients questions in order to understand their gastrointestinal tract symptoms. The questionnaires are really critical for us to grade the severity and then properly order tests,” she explained. “The goal is symptom identification, ideally with minimal time burden and at no cost, to guide decisions that move our patients’ care forward.”
Three of the most useful validated instruments for assessment of GERD symptoms in scleroderma patients in routine clinical practice are the GerdQ, the University of California, Los Angeles, Scleroderma Clinical Trial Consortium GI Tract Questionnaire (UCLA GIT) 2.0 reflux scale, and the Patient-Reported Outcomes Measurement Information System (PROMIS) reflux scale.
The GerdQ is a six-item, self-administered questionnaire in which patients specify how many days in the past week they have experienced heartburn, regurgitation, nausea, sleep interference, upper abdominal pain, and need for medication. A free online tool is available for calculating the likelihood of having GERD based upon GerdQ score. A score of 8 or more points out of a possible 18 has the highest sensitivity and specificity for diagnosis of GERD.
The UCLA GIT 2.0 – the most commonly used instrument for GI symptom assessment in scleroderma patients – includes 34 items. It takes 6-8 minutes to complete the whole thing, but patients being assessed for GERD only need answer the eight GERD-specific questions. Six of these eight questions are the same as in the GerdQ. One of the two extra questions asks about difficulty in swallowing solid food, which if answered affirmatively warrants early referral to a gastroenterologist. The other question inquires about any food triggers for the reflux, providing an opportunity for a rheumatologist to educate the patient about the importance of avoiding acidic foods, such as tomatoes, and other food and drink generally considered healthy but which actually exacerbate GERD.
The National Institutes of Health PROMIS scale, the newest of the three instruments, is a 60-item questionnaire; however, only 20 questions relate to reflux and dysphagia and are thus germane to a focused GERD assessment in scleroderma.
When a clinical diagnosis of GERD is made in a scleroderma patient based upon symptoms elicited by questionnaire, guidelines recommend a trial of empiric proton pump inhibitor therapy and behavioral interventions, such as raising the head of the bed, in order to confirm the diagnosis. If the patient reports feeling better after these basic interventions, the diagnosis is confirmed. If not, it’s time to make a referral to a gastroenterologist for specialized care, Dr. Frech said.
Dr. Frech was a coinvestigator in an international, prospective, longitudinal study of patient-reported outcomes measures in 116 patients with scleroderma and GERD. All study participants had to complete the UCLA GIT 2.0, the PROMIS reflux scale, and a third patient-reported GERD measure both before and after the therapeutic intervention. The UCLA GIT 2.0 and PROMIS instruments demonstrated similarly robust sensitivity for identifying changes in GERD symptoms after therapeutic intervention.
“It doesn’t really matter what questionnaire we’re using,” according to the rheumatologist. “But I will point out that there is significant overlap in symptoms among GERD, gastroparesis, functional dyspepsia, and eosinophilic esophagitis, all of which cause symptoms of heartburn and regurgitation. So we don’t want to ask these questions just once, we want to make an intervention and then reask the questions to ensure that we’re continuously moving forward with the gastrointestinal tract management plan.”
Dr. Frech reported having no financial conflicts regarding her presentation.
Every rheumatologist ought to be comfortable in using a validated gastrointestinal symptom scale for evaluation of gastroesophageal reflux disease in patients with scleroderma, Tracy M. Frech, MD, declared at the virtual edition of the American College of Rheumatology’s 2020 State-of-the-Art Clinical Symposium.
About 90% of scleroderma patients will develop GI tract involvement during the course of their connective tissue disease. And while any portion of the GI tract from esophagus to anus can be involved, the most common GI manifestation is gastroesophageal reflux disease (GERD), affecting up to 90% of scleroderma patients, observed Dr. Frech, a rheumatologist and director of the systemic sclerosis clinic at the University of Utah and the George E. Wahlen Department of Veterans Affairs Medical Center, both in Salt Lake City.
“It is essential to ask scleroderma patients questions in order to understand their gastrointestinal tract symptoms. The questionnaires are really critical for us to grade the severity and then properly order tests,” she explained. “The goal is symptom identification, ideally with minimal time burden and at no cost, to guide decisions that move our patients’ care forward.”
Three of the most useful validated instruments for assessment of GERD symptoms in scleroderma patients in routine clinical practice are the GerdQ, the University of California, Los Angeles, Scleroderma Clinical Trial Consortium GI Tract Questionnaire (UCLA GIT) 2.0 reflux scale, and the Patient-Reported Outcomes Measurement Information System (PROMIS) reflux scale.
The GerdQ is a six-item, self-administered questionnaire in which patients specify how many days in the past week they have experienced heartburn, regurgitation, nausea, sleep interference, upper abdominal pain, and need for medication. A free online tool is available for calculating the likelihood of having GERD based upon GerdQ score. A score of 8 or more points out of a possible 18 has the highest sensitivity and specificity for diagnosis of GERD.
The UCLA GIT 2.0 – the most commonly used instrument for GI symptom assessment in scleroderma patients – includes 34 items. It takes 6-8 minutes to complete the whole thing, but patients being assessed for GERD only need answer the eight GERD-specific questions. Six of these eight questions are the same as in the GerdQ. One of the two extra questions asks about difficulty in swallowing solid food, which if answered affirmatively warrants early referral to a gastroenterologist. The other question inquires about any food triggers for the reflux, providing an opportunity for a rheumatologist to educate the patient about the importance of avoiding acidic foods, such as tomatoes, and other food and drink generally considered healthy but which actually exacerbate GERD.
The National Institutes of Health PROMIS scale, the newest of the three instruments, is a 60-item questionnaire; however, only 20 questions relate to reflux and dysphagia and are thus germane to a focused GERD assessment in scleroderma.
When a clinical diagnosis of GERD is made in a scleroderma patient based upon symptoms elicited by questionnaire, guidelines recommend a trial of empiric proton pump inhibitor therapy and behavioral interventions, such as raising the head of the bed, in order to confirm the diagnosis. If the patient reports feeling better after these basic interventions, the diagnosis is confirmed. If not, it’s time to make a referral to a gastroenterologist for specialized care, Dr. Frech said.
Dr. Frech was a coinvestigator in an international, prospective, longitudinal study of patient-reported outcomes measures in 116 patients with scleroderma and GERD. All study participants had to complete the UCLA GIT 2.0, the PROMIS reflux scale, and a third patient-reported GERD measure both before and after the therapeutic intervention. The UCLA GIT 2.0 and PROMIS instruments demonstrated similarly robust sensitivity for identifying changes in GERD symptoms after therapeutic intervention.
“It doesn’t really matter what questionnaire we’re using,” according to the rheumatologist. “But I will point out that there is significant overlap in symptoms among GERD, gastroparesis, functional dyspepsia, and eosinophilic esophagitis, all of which cause symptoms of heartburn and regurgitation. So we don’t want to ask these questions just once, we want to make an intervention and then reask the questions to ensure that we’re continuously moving forward with the gastrointestinal tract management plan.”
Dr. Frech reported having no financial conflicts regarding her presentation.
FROM SOTA 2020
ACR issues guidances for MIS-C and pediatric rheumatic disease during pandemic
Two new clinical guidance documents from the American College of Rheumatology provide evidence-based recommendations for managing pediatric rheumatic disease during the COVID-19 pandemic as well as diagnostic and treatment recommendations for multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19 infection.
Although several children’s hospitals have published their treatment protocols for MIS-C since the condition’s initial discovery, the ACR appears to be the first medical organization to review all the most current evidence to issue interim guidance with the expectations that it will change as more data become available.
“It is challenging having to make recommendations not having a lot of scientific evidence, but we still felt we had to use whatever’s out there to the best of our ability and use our experience to put together these recommendations,” Dawn M. Wahezi, MD, chief of pediatric rheumatology at Children’s Hospital at Montefiore and an associate professor of pediatrics at Albert Einstein College of Medicine, New York, said in an interview.
“We wanted to be mindful of the fact that there are things we know and things we don’t know, and we have to be careful about what we’re recommending,” said Dr. Wahezi, a member of the ACR working group that assembled the recommendations for pediatric rheumatic disease management during the pandemic. “We’re recommending the best we can at this moment, but if there are new studies that come out and suggest otherwise, we will definitely have to go back and amend the document.”
The foremost priority of the pediatric rheumatic disease guidance focuses on maintaining control of the disease and avoiding flares that may put children at greater risk of infection. Dr. Wahezi said the ACR has received many calls from patients and clinicians asking whether patients should continue their immunosuppressant medications. Fear of the coronavirus infection, medication shortages, difficulty getting to the pharmacy, uneasiness about going to the clinic or hospital for infusions, and other barriers may have led to gaps in medication.
“We didn’t want people to be too quick to hold patients’ medications just because they were scared of COVID,” Dr. Wahezi said. “If they did have medication stopped for one reason or another and their disease flared, having active disease, regardless of which disease it is, actually puts you at higher risk for infection. By controlling their disease, that would be the way to protect them the most.”
A key takeaway in the guidance on MIS-C, meanwhile, is an emphasis on its rarity lest physicians be too quick to diagnose it and miss another serious condition with overlapping symptoms, explained Lauren Henderson, MD, an attending rheumatologist at Boston Children’s Hospital and assistant professor of pediatrics at Harvard Medical School, Boston. Dr. Henderson participated in the ACR group that wrote the MIS-C guidance.
“The first thing we want to be thoughtful about clinically is to recognize that children in general with the acute infectious phase of SARS-CoV-2 have mild symptoms and generally do well,” Dr. Henderson said. “From what we can tell from all the data, MIS-C is rare. That really needs to be considered when clinicians on the ground are doing the diagnostic evaluation” because of concerns that clinicians “could rush to diagnose and treat patients with MIS-C and miss important diagnoses like malignancies and infections.”
Management of pediatric rheumatic disease during the pandemic
The COVID-19 clinical guidance for managing pediatric rheumatic disease grew from the work of the North American Pediatric Rheumatology Clinical Guidance Task Force, which included seven pediatric rheumatologists, two pediatric infectious disease physicians, one adult rheumatologist, and one pediatric nurse practitioner. The general guidance covers usual preventive measures for reducing risk for COVID-19 infection, the recommendation that children continue to receive recommended vaccines unless contraindicated by medication, and routine in-person visits for ophthalmologic surveillance of those with a history of uveitis or at high risk for chronic uveitis. The guidance also notes the risk of mental health concerns, such as depression and anxiety, related to quarantine and the pandemic.
The top recommendation is initiation or continuation of all medications necessary to control underlying disease, including NSAIDs, hydroxychloroquine, ACE inhibitors/angiotensin II receptor blockers, colchicine, conventional disease-modifying antirheumatic drugs (cDMARDs), biologic DMARDs, and targeted synthetic DMARDs. Even patients who may have had exposure to COVID-19 or who have an asymptomatic COVID-19 infection should continue to take these medications with the exception of ACEi/ARBs.
In those with pediatric rheumatic disease who have a symptomatic COVID-19 infection, “NSAIDs, HCQ, and colchicine may be continued, if necessary, to control underlying disease,” as can interleukin (IL)-1 and IL-6 inhibitors, but “cDMARDs, bDMARDs [except IL-1 and IL-6 inhibitors] and tsDMARDs should be temporarily delayed or withheld,” according to the guidance. Glucocorticoids can be continued at the lowest possible dose to control disease.
“There’s nothing in the literature that suggests people who have rheumatic disease, especially children, and people who are on these medications, really are at increased risk for COVID-19,” Dr. Wahezi said. “That’s why we didn’t want people to be overcautious in stopping medications when the main priority is to control their disease.”
She noted some experts’ speculations that these medications may actually benefit patients with rheumatic disease who develop a COVID-19 infection because the medications keep the immune response in check. “If you allow them to have this dysregulated immune response and have active disease, you’re potentially putting them at greater risk,” Dr. Wahezi said, although she stressed that inadequate evidence exists to support these speculations right now.
Lack of evidence has been the biggest challenge all around with developing this guidance, she said.
“Because this is such an unprecedented situation and because people are so desperate to find treatments both for the illness and to protect those at risk for it, there are lots of people trying to put evidence out there, but it may not be the best-quality evidence,” Dr. Wahezi said.
Insufficient evidence also drove the group’s determination that “SARS-CoV-2 antibody testing is not useful in informing on the history of infection or risk of reinfection,” as the guidance states. Too much variability in the assays exist, Dr. Wahezi said, and, further, it’s unclear what the clinical significance of a positive test would be.
“We didn’t want anyone to feel they had to make clinical decisions based on the results of that antibody testing,” she said. “Even if the test is accurate, we don’t know how to interpret it because it’s so new.”
The guidance also notes that patients with stable disease and previously stable lab markers on stable doses of their medication may be able to extend the interval for medication toxicity lab testing a few months if there is concern about exposure to COVID-19 to get the blood work.
“If you’re just starting a medicine or there’s someone who’s had abnormalities with the medicine in the past or you’re making medication adjustments, you wouldn’t do it in those scenarios, but if there’s someone who’s been on the drug for a long time and are nervous to get [blood] drawn, it’s probably okay to delay it,” Dr. Wahezi said. Lab work for disease activity measures, on the other hand, remain particularly important, especially since telemedicine visits may require clinicians to rely on lab results more than previously.
Management of MIS-C associated with COVID-19
The task force that developed guidance for the new inflammatory condition recently linked to SARS-CoV-2 infections in children included nine pediatric rheumatologists, two adult rheumatologists, two pediatric cardiologists, two pediatric infectious disease specialists, and one pediatric critical care physician.
The guidance includes a figure for the diagnostic pathway in evaluating children suspected of having MIS-C and extensive detail on diagnostic work-up, but the task force intentionally avoided providing a case definition for the condition. Existing case definitions from the Centers for Disease Control and Prevention, World Health Organization, and the United Kingdom’s Royal College of Paediatrics and Child Health differ from one another and are based on unclear evidence, Dr. Henderson noted. “We really don’t have enough data to know the sensitivity and specificity of each parameter, and until that’s available, we didn’t want to add to the confusion,” she said.
The guidance also stresses that MIS-C is a rare complication, so patients suspected of having the condition who do not have “life-threatening manifestations should undergo diagnostic evaluation for MIS-C as well as other possible infectious and noninfectious etiologies before immunomodulatory treatment is initiated,” the guidance states.
Unless a child is in shock or otherwise requires urgent care, physicians should take the time to complete the diagnostic work-up while monitoring the child, Dr. Henderson said. If the child does have MIS-C, the guidance currently recommends intravenous immunoglobulin (IVIG) and/or glucocorticoids to prevent coronary artery aneurysms, the same treatment other institutions have been recommending.
“We don’t have rigorous comparative studies looking at different types of treatments,” Dr. Henderson said, noting that the vast majority of children in the literature received IVIG and/or glucocorticoid treatment. “Often children really responded quite forcefully to those treatments, but we don’t have high-quality data yet to know that this treatment is better than supportive care or another medication.”
Dr. Henderson also stressed the importance of children receiving care at a facility with the necessary expertise to manage MIS-C and receiving long-term follow-up care from a multidisciplinary clinical team that includes a rheumatologist, an infectious disease doctor, a cardiologist, and possibly a hematologist.
“Making sure children are admitted to a hospital that has the resources and are followed by physicians with expertise or understanding of the intricacies of MIS-C is really important,” she said, particularly for children with cardiac involvement. “We don’t know if all the kids presenting with left ventricular dysfunction and shock are at risk for having myocardial fibrosis down the line,” she noted. “There is so much we do not understand and very little data to guide us on what to do, so these children really need to be under the care of a cardiologist and rheumatologist to make sure that their care is tailored to them.”
Although MIS-C shares overlapping symptoms with Kawasaki disease, it’s still unclear how similar or different the two conditions are, Dr. Henderson said.
“We can definitely say that when we look at MIS-C and compare it to historical groups of Kawasaki disease before the pandemic, there are definitely different features in the MIS-C group,” she said. Kawasaki disease generally only affects children under age 5, whereas MIS-C patients run the gamut from age 1-17. Racial demographics are also different, with a higher proportion of black children affected by MIS-C.
It’s possible that the pathophysiology of both conditions will turn out to be similar, particularly given the hypothesis that Kawasaki disease is triggered by infections in genetically predisposed people. However, the severity of symptoms and risk of aneurysms appear greater with MIS-C so far.
“The degree to which these patients are presenting with left ventricular dysfunction and shock is much higher than what we’ve seen previously,” Dr. Henderson said. “Children can have aneurysms even if they don’t meet all the Kawasaki disease features, which makes it feel that this is somehow clinically different from what we’ve seen before. It’s not just the kids who have the rash and the conjunctivitis and the extremity changes and oral changes who have the aneurysms.”
The reason for including both IVIG and glucocorticoids as possible first-line drugs to prevent aneurysms is that some evidence suggests children with MIS-C may have higher levels of IVIG resistance, she said.
Like Dr. Wahezi, Dr. Henderson emphasized the necessarily transient nature of these recommendations.
“These recommendations will almost certainly change based on evolving understanding of MIS-C and the data,” Dr. Henderson said, adding that this new, unique condition highlights the importance of including children in allocating funding for research and in clinical trials.
“Children are not always identical to adults, and it’s really important that we have high-quality data to inform our decisions about how to care for them,” she said.
Dr. Wahezi had no disclosures. Dr. Henderson has consulted for Sobi and Adaptive Technologies. The guidelines did not note other disclosures for members of the ACR groups.
SOURCES: COVID-19 Clinical Guidance for Pediatric Patients with Rheumatic Disease and Clinical Guidance for Pediatric Patients with Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with SARS-CoV-2 and Hyperinflammation in COVID-19
Two new clinical guidance documents from the American College of Rheumatology provide evidence-based recommendations for managing pediatric rheumatic disease during the COVID-19 pandemic as well as diagnostic and treatment recommendations for multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19 infection.
Although several children’s hospitals have published their treatment protocols for MIS-C since the condition’s initial discovery, the ACR appears to be the first medical organization to review all the most current evidence to issue interim guidance with the expectations that it will change as more data become available.
“It is challenging having to make recommendations not having a lot of scientific evidence, but we still felt we had to use whatever’s out there to the best of our ability and use our experience to put together these recommendations,” Dawn M. Wahezi, MD, chief of pediatric rheumatology at Children’s Hospital at Montefiore and an associate professor of pediatrics at Albert Einstein College of Medicine, New York, said in an interview.
“We wanted to be mindful of the fact that there are things we know and things we don’t know, and we have to be careful about what we’re recommending,” said Dr. Wahezi, a member of the ACR working group that assembled the recommendations for pediatric rheumatic disease management during the pandemic. “We’re recommending the best we can at this moment, but if there are new studies that come out and suggest otherwise, we will definitely have to go back and amend the document.”
The foremost priority of the pediatric rheumatic disease guidance focuses on maintaining control of the disease and avoiding flares that may put children at greater risk of infection. Dr. Wahezi said the ACR has received many calls from patients and clinicians asking whether patients should continue their immunosuppressant medications. Fear of the coronavirus infection, medication shortages, difficulty getting to the pharmacy, uneasiness about going to the clinic or hospital for infusions, and other barriers may have led to gaps in medication.
“We didn’t want people to be too quick to hold patients’ medications just because they were scared of COVID,” Dr. Wahezi said. “If they did have medication stopped for one reason or another and their disease flared, having active disease, regardless of which disease it is, actually puts you at higher risk for infection. By controlling their disease, that would be the way to protect them the most.”
A key takeaway in the guidance on MIS-C, meanwhile, is an emphasis on its rarity lest physicians be too quick to diagnose it and miss another serious condition with overlapping symptoms, explained Lauren Henderson, MD, an attending rheumatologist at Boston Children’s Hospital and assistant professor of pediatrics at Harvard Medical School, Boston. Dr. Henderson participated in the ACR group that wrote the MIS-C guidance.
“The first thing we want to be thoughtful about clinically is to recognize that children in general with the acute infectious phase of SARS-CoV-2 have mild symptoms and generally do well,” Dr. Henderson said. “From what we can tell from all the data, MIS-C is rare. That really needs to be considered when clinicians on the ground are doing the diagnostic evaluation” because of concerns that clinicians “could rush to diagnose and treat patients with MIS-C and miss important diagnoses like malignancies and infections.”
Management of pediatric rheumatic disease during the pandemic
The COVID-19 clinical guidance for managing pediatric rheumatic disease grew from the work of the North American Pediatric Rheumatology Clinical Guidance Task Force, which included seven pediatric rheumatologists, two pediatric infectious disease physicians, one adult rheumatologist, and one pediatric nurse practitioner. The general guidance covers usual preventive measures for reducing risk for COVID-19 infection, the recommendation that children continue to receive recommended vaccines unless contraindicated by medication, and routine in-person visits for ophthalmologic surveillance of those with a history of uveitis or at high risk for chronic uveitis. The guidance also notes the risk of mental health concerns, such as depression and anxiety, related to quarantine and the pandemic.
The top recommendation is initiation or continuation of all medications necessary to control underlying disease, including NSAIDs, hydroxychloroquine, ACE inhibitors/angiotensin II receptor blockers, colchicine, conventional disease-modifying antirheumatic drugs (cDMARDs), biologic DMARDs, and targeted synthetic DMARDs. Even patients who may have had exposure to COVID-19 or who have an asymptomatic COVID-19 infection should continue to take these medications with the exception of ACEi/ARBs.
In those with pediatric rheumatic disease who have a symptomatic COVID-19 infection, “NSAIDs, HCQ, and colchicine may be continued, if necessary, to control underlying disease,” as can interleukin (IL)-1 and IL-6 inhibitors, but “cDMARDs, bDMARDs [except IL-1 and IL-6 inhibitors] and tsDMARDs should be temporarily delayed or withheld,” according to the guidance. Glucocorticoids can be continued at the lowest possible dose to control disease.
“There’s nothing in the literature that suggests people who have rheumatic disease, especially children, and people who are on these medications, really are at increased risk for COVID-19,” Dr. Wahezi said. “That’s why we didn’t want people to be overcautious in stopping medications when the main priority is to control their disease.”
She noted some experts’ speculations that these medications may actually benefit patients with rheumatic disease who develop a COVID-19 infection because the medications keep the immune response in check. “If you allow them to have this dysregulated immune response and have active disease, you’re potentially putting them at greater risk,” Dr. Wahezi said, although she stressed that inadequate evidence exists to support these speculations right now.
Lack of evidence has been the biggest challenge all around with developing this guidance, she said.
“Because this is such an unprecedented situation and because people are so desperate to find treatments both for the illness and to protect those at risk for it, there are lots of people trying to put evidence out there, but it may not be the best-quality evidence,” Dr. Wahezi said.
Insufficient evidence also drove the group’s determination that “SARS-CoV-2 antibody testing is not useful in informing on the history of infection or risk of reinfection,” as the guidance states. Too much variability in the assays exist, Dr. Wahezi said, and, further, it’s unclear what the clinical significance of a positive test would be.
“We didn’t want anyone to feel they had to make clinical decisions based on the results of that antibody testing,” she said. “Even if the test is accurate, we don’t know how to interpret it because it’s so new.”
The guidance also notes that patients with stable disease and previously stable lab markers on stable doses of their medication may be able to extend the interval for medication toxicity lab testing a few months if there is concern about exposure to COVID-19 to get the blood work.
“If you’re just starting a medicine or there’s someone who’s had abnormalities with the medicine in the past or you’re making medication adjustments, you wouldn’t do it in those scenarios, but if there’s someone who’s been on the drug for a long time and are nervous to get [blood] drawn, it’s probably okay to delay it,” Dr. Wahezi said. Lab work for disease activity measures, on the other hand, remain particularly important, especially since telemedicine visits may require clinicians to rely on lab results more than previously.
Management of MIS-C associated with COVID-19
The task force that developed guidance for the new inflammatory condition recently linked to SARS-CoV-2 infections in children included nine pediatric rheumatologists, two adult rheumatologists, two pediatric cardiologists, two pediatric infectious disease specialists, and one pediatric critical care physician.
The guidance includes a figure for the diagnostic pathway in evaluating children suspected of having MIS-C and extensive detail on diagnostic work-up, but the task force intentionally avoided providing a case definition for the condition. Existing case definitions from the Centers for Disease Control and Prevention, World Health Organization, and the United Kingdom’s Royal College of Paediatrics and Child Health differ from one another and are based on unclear evidence, Dr. Henderson noted. “We really don’t have enough data to know the sensitivity and specificity of each parameter, and until that’s available, we didn’t want to add to the confusion,” she said.
The guidance also stresses that MIS-C is a rare complication, so patients suspected of having the condition who do not have “life-threatening manifestations should undergo diagnostic evaluation for MIS-C as well as other possible infectious and noninfectious etiologies before immunomodulatory treatment is initiated,” the guidance states.
Unless a child is in shock or otherwise requires urgent care, physicians should take the time to complete the diagnostic work-up while monitoring the child, Dr. Henderson said. If the child does have MIS-C, the guidance currently recommends intravenous immunoglobulin (IVIG) and/or glucocorticoids to prevent coronary artery aneurysms, the same treatment other institutions have been recommending.
“We don’t have rigorous comparative studies looking at different types of treatments,” Dr. Henderson said, noting that the vast majority of children in the literature received IVIG and/or glucocorticoid treatment. “Often children really responded quite forcefully to those treatments, but we don’t have high-quality data yet to know that this treatment is better than supportive care or another medication.”
Dr. Henderson also stressed the importance of children receiving care at a facility with the necessary expertise to manage MIS-C and receiving long-term follow-up care from a multidisciplinary clinical team that includes a rheumatologist, an infectious disease doctor, a cardiologist, and possibly a hematologist.
“Making sure children are admitted to a hospital that has the resources and are followed by physicians with expertise or understanding of the intricacies of MIS-C is really important,” she said, particularly for children with cardiac involvement. “We don’t know if all the kids presenting with left ventricular dysfunction and shock are at risk for having myocardial fibrosis down the line,” she noted. “There is so much we do not understand and very little data to guide us on what to do, so these children really need to be under the care of a cardiologist and rheumatologist to make sure that their care is tailored to them.”
Although MIS-C shares overlapping symptoms with Kawasaki disease, it’s still unclear how similar or different the two conditions are, Dr. Henderson said.
“We can definitely say that when we look at MIS-C and compare it to historical groups of Kawasaki disease before the pandemic, there are definitely different features in the MIS-C group,” she said. Kawasaki disease generally only affects children under age 5, whereas MIS-C patients run the gamut from age 1-17. Racial demographics are also different, with a higher proportion of black children affected by MIS-C.
It’s possible that the pathophysiology of both conditions will turn out to be similar, particularly given the hypothesis that Kawasaki disease is triggered by infections in genetically predisposed people. However, the severity of symptoms and risk of aneurysms appear greater with MIS-C so far.
“The degree to which these patients are presenting with left ventricular dysfunction and shock is much higher than what we’ve seen previously,” Dr. Henderson said. “Children can have aneurysms even if they don’t meet all the Kawasaki disease features, which makes it feel that this is somehow clinically different from what we’ve seen before. It’s not just the kids who have the rash and the conjunctivitis and the extremity changes and oral changes who have the aneurysms.”
The reason for including both IVIG and glucocorticoids as possible first-line drugs to prevent aneurysms is that some evidence suggests children with MIS-C may have higher levels of IVIG resistance, she said.
Like Dr. Wahezi, Dr. Henderson emphasized the necessarily transient nature of these recommendations.
“These recommendations will almost certainly change based on evolving understanding of MIS-C and the data,” Dr. Henderson said, adding that this new, unique condition highlights the importance of including children in allocating funding for research and in clinical trials.
“Children are not always identical to adults, and it’s really important that we have high-quality data to inform our decisions about how to care for them,” she said.
Dr. Wahezi had no disclosures. Dr. Henderson has consulted for Sobi and Adaptive Technologies. The guidelines did not note other disclosures for members of the ACR groups.
SOURCES: COVID-19 Clinical Guidance for Pediatric Patients with Rheumatic Disease and Clinical Guidance for Pediatric Patients with Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with SARS-CoV-2 and Hyperinflammation in COVID-19
Two new clinical guidance documents from the American College of Rheumatology provide evidence-based recommendations for managing pediatric rheumatic disease during the COVID-19 pandemic as well as diagnostic and treatment recommendations for multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19 infection.
Although several children’s hospitals have published their treatment protocols for MIS-C since the condition’s initial discovery, the ACR appears to be the first medical organization to review all the most current evidence to issue interim guidance with the expectations that it will change as more data become available.
“It is challenging having to make recommendations not having a lot of scientific evidence, but we still felt we had to use whatever’s out there to the best of our ability and use our experience to put together these recommendations,” Dawn M. Wahezi, MD, chief of pediatric rheumatology at Children’s Hospital at Montefiore and an associate professor of pediatrics at Albert Einstein College of Medicine, New York, said in an interview.
“We wanted to be mindful of the fact that there are things we know and things we don’t know, and we have to be careful about what we’re recommending,” said Dr. Wahezi, a member of the ACR working group that assembled the recommendations for pediatric rheumatic disease management during the pandemic. “We’re recommending the best we can at this moment, but if there are new studies that come out and suggest otherwise, we will definitely have to go back and amend the document.”
The foremost priority of the pediatric rheumatic disease guidance focuses on maintaining control of the disease and avoiding flares that may put children at greater risk of infection. Dr. Wahezi said the ACR has received many calls from patients and clinicians asking whether patients should continue their immunosuppressant medications. Fear of the coronavirus infection, medication shortages, difficulty getting to the pharmacy, uneasiness about going to the clinic or hospital for infusions, and other barriers may have led to gaps in medication.
“We didn’t want people to be too quick to hold patients’ medications just because they were scared of COVID,” Dr. Wahezi said. “If they did have medication stopped for one reason or another and their disease flared, having active disease, regardless of which disease it is, actually puts you at higher risk for infection. By controlling their disease, that would be the way to protect them the most.”
A key takeaway in the guidance on MIS-C, meanwhile, is an emphasis on its rarity lest physicians be too quick to diagnose it and miss another serious condition with overlapping symptoms, explained Lauren Henderson, MD, an attending rheumatologist at Boston Children’s Hospital and assistant professor of pediatrics at Harvard Medical School, Boston. Dr. Henderson participated in the ACR group that wrote the MIS-C guidance.
“The first thing we want to be thoughtful about clinically is to recognize that children in general with the acute infectious phase of SARS-CoV-2 have mild symptoms and generally do well,” Dr. Henderson said. “From what we can tell from all the data, MIS-C is rare. That really needs to be considered when clinicians on the ground are doing the diagnostic evaluation” because of concerns that clinicians “could rush to diagnose and treat patients with MIS-C and miss important diagnoses like malignancies and infections.”
Management of pediatric rheumatic disease during the pandemic
The COVID-19 clinical guidance for managing pediatric rheumatic disease grew from the work of the North American Pediatric Rheumatology Clinical Guidance Task Force, which included seven pediatric rheumatologists, two pediatric infectious disease physicians, one adult rheumatologist, and one pediatric nurse practitioner. The general guidance covers usual preventive measures for reducing risk for COVID-19 infection, the recommendation that children continue to receive recommended vaccines unless contraindicated by medication, and routine in-person visits for ophthalmologic surveillance of those with a history of uveitis or at high risk for chronic uveitis. The guidance also notes the risk of mental health concerns, such as depression and anxiety, related to quarantine and the pandemic.
The top recommendation is initiation or continuation of all medications necessary to control underlying disease, including NSAIDs, hydroxychloroquine, ACE inhibitors/angiotensin II receptor blockers, colchicine, conventional disease-modifying antirheumatic drugs (cDMARDs), biologic DMARDs, and targeted synthetic DMARDs. Even patients who may have had exposure to COVID-19 or who have an asymptomatic COVID-19 infection should continue to take these medications with the exception of ACEi/ARBs.
In those with pediatric rheumatic disease who have a symptomatic COVID-19 infection, “NSAIDs, HCQ, and colchicine may be continued, if necessary, to control underlying disease,” as can interleukin (IL)-1 and IL-6 inhibitors, but “cDMARDs, bDMARDs [except IL-1 and IL-6 inhibitors] and tsDMARDs should be temporarily delayed or withheld,” according to the guidance. Glucocorticoids can be continued at the lowest possible dose to control disease.
“There’s nothing in the literature that suggests people who have rheumatic disease, especially children, and people who are on these medications, really are at increased risk for COVID-19,” Dr. Wahezi said. “That’s why we didn’t want people to be overcautious in stopping medications when the main priority is to control their disease.”
She noted some experts’ speculations that these medications may actually benefit patients with rheumatic disease who develop a COVID-19 infection because the medications keep the immune response in check. “If you allow them to have this dysregulated immune response and have active disease, you’re potentially putting them at greater risk,” Dr. Wahezi said, although she stressed that inadequate evidence exists to support these speculations right now.
Lack of evidence has been the biggest challenge all around with developing this guidance, she said.
“Because this is such an unprecedented situation and because people are so desperate to find treatments both for the illness and to protect those at risk for it, there are lots of people trying to put evidence out there, but it may not be the best-quality evidence,” Dr. Wahezi said.
Insufficient evidence also drove the group’s determination that “SARS-CoV-2 antibody testing is not useful in informing on the history of infection or risk of reinfection,” as the guidance states. Too much variability in the assays exist, Dr. Wahezi said, and, further, it’s unclear what the clinical significance of a positive test would be.
“We didn’t want anyone to feel they had to make clinical decisions based on the results of that antibody testing,” she said. “Even if the test is accurate, we don’t know how to interpret it because it’s so new.”
The guidance also notes that patients with stable disease and previously stable lab markers on stable doses of their medication may be able to extend the interval for medication toxicity lab testing a few months if there is concern about exposure to COVID-19 to get the blood work.
“If you’re just starting a medicine or there’s someone who’s had abnormalities with the medicine in the past or you’re making medication adjustments, you wouldn’t do it in those scenarios, but if there’s someone who’s been on the drug for a long time and are nervous to get [blood] drawn, it’s probably okay to delay it,” Dr. Wahezi said. Lab work for disease activity measures, on the other hand, remain particularly important, especially since telemedicine visits may require clinicians to rely on lab results more than previously.
Management of MIS-C associated with COVID-19
The task force that developed guidance for the new inflammatory condition recently linked to SARS-CoV-2 infections in children included nine pediatric rheumatologists, two adult rheumatologists, two pediatric cardiologists, two pediatric infectious disease specialists, and one pediatric critical care physician.
The guidance includes a figure for the diagnostic pathway in evaluating children suspected of having MIS-C and extensive detail on diagnostic work-up, but the task force intentionally avoided providing a case definition for the condition. Existing case definitions from the Centers for Disease Control and Prevention, World Health Organization, and the United Kingdom’s Royal College of Paediatrics and Child Health differ from one another and are based on unclear evidence, Dr. Henderson noted. “We really don’t have enough data to know the sensitivity and specificity of each parameter, and until that’s available, we didn’t want to add to the confusion,” she said.
The guidance also stresses that MIS-C is a rare complication, so patients suspected of having the condition who do not have “life-threatening manifestations should undergo diagnostic evaluation for MIS-C as well as other possible infectious and noninfectious etiologies before immunomodulatory treatment is initiated,” the guidance states.
Unless a child is in shock or otherwise requires urgent care, physicians should take the time to complete the diagnostic work-up while monitoring the child, Dr. Henderson said. If the child does have MIS-C, the guidance currently recommends intravenous immunoglobulin (IVIG) and/or glucocorticoids to prevent coronary artery aneurysms, the same treatment other institutions have been recommending.
“We don’t have rigorous comparative studies looking at different types of treatments,” Dr. Henderson said, noting that the vast majority of children in the literature received IVIG and/or glucocorticoid treatment. “Often children really responded quite forcefully to those treatments, but we don’t have high-quality data yet to know that this treatment is better than supportive care or another medication.”
Dr. Henderson also stressed the importance of children receiving care at a facility with the necessary expertise to manage MIS-C and receiving long-term follow-up care from a multidisciplinary clinical team that includes a rheumatologist, an infectious disease doctor, a cardiologist, and possibly a hematologist.
“Making sure children are admitted to a hospital that has the resources and are followed by physicians with expertise or understanding of the intricacies of MIS-C is really important,” she said, particularly for children with cardiac involvement. “We don’t know if all the kids presenting with left ventricular dysfunction and shock are at risk for having myocardial fibrosis down the line,” she noted. “There is so much we do not understand and very little data to guide us on what to do, so these children really need to be under the care of a cardiologist and rheumatologist to make sure that their care is tailored to them.”
Although MIS-C shares overlapping symptoms with Kawasaki disease, it’s still unclear how similar or different the two conditions are, Dr. Henderson said.
“We can definitely say that when we look at MIS-C and compare it to historical groups of Kawasaki disease before the pandemic, there are definitely different features in the MIS-C group,” she said. Kawasaki disease generally only affects children under age 5, whereas MIS-C patients run the gamut from age 1-17. Racial demographics are also different, with a higher proportion of black children affected by MIS-C.
It’s possible that the pathophysiology of both conditions will turn out to be similar, particularly given the hypothesis that Kawasaki disease is triggered by infections in genetically predisposed people. However, the severity of symptoms and risk of aneurysms appear greater with MIS-C so far.
“The degree to which these patients are presenting with left ventricular dysfunction and shock is much higher than what we’ve seen previously,” Dr. Henderson said. “Children can have aneurysms even if they don’t meet all the Kawasaki disease features, which makes it feel that this is somehow clinically different from what we’ve seen before. It’s not just the kids who have the rash and the conjunctivitis and the extremity changes and oral changes who have the aneurysms.”
The reason for including both IVIG and glucocorticoids as possible first-line drugs to prevent aneurysms is that some evidence suggests children with MIS-C may have higher levels of IVIG resistance, she said.
Like Dr. Wahezi, Dr. Henderson emphasized the necessarily transient nature of these recommendations.
“These recommendations will almost certainly change based on evolving understanding of MIS-C and the data,” Dr. Henderson said, adding that this new, unique condition highlights the importance of including children in allocating funding for research and in clinical trials.
“Children are not always identical to adults, and it’s really important that we have high-quality data to inform our decisions about how to care for them,” she said.
Dr. Wahezi had no disclosures. Dr. Henderson has consulted for Sobi and Adaptive Technologies. The guidelines did not note other disclosures for members of the ACR groups.
SOURCES: COVID-19 Clinical Guidance for Pediatric Patients with Rheumatic Disease and Clinical Guidance for Pediatric Patients with Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with SARS-CoV-2 and Hyperinflammation in COVID-19
EULAR gives pointers on intra-articular injection best practices
New EULAR recommendations for the intra-articular (IA) treatment of arthropathies aim to facilitate uniformity and quality of care for this mainstay of rheumatologic practice, according to a report on the new guidance that was presented at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Until now there were no official recommendations on how best to use it in everyday practice. “This is the first time that there’s been a joint effort to develop evidence-based recommendations,” Jacqueline Usón, MD, PhD, associate professor medicine at Rey Juan Carlos University in Madrid, said in an interview. “Everything that we are saying is pretty logical, but it’s nice to see it put in recommendations based on evidence.”
IA therapy has been around for decades and is key for treating adults with a number of different conditions where synovitis, effusion, pain, or all three, are present, such as inflammatory arthritis and osteoarthritis, Dr. Usón observed during her presentation.
“Today, commonly used injectables are not only corticosteroids but also local anesthetics, hyaluronic acid, blood products, and maybe pharmaceuticals,” she said, adding that “there is a wide variation in the way intra-articular therapies are used and delivered to patients.” Health professionals also have very different views and habits depending on geographic locations and health care systems, she observed. Ironing out the variation was one of the main objectives of the recommendations.
As one of the two conveners of the EULAR task force behind the recommendations, Dr. Usón, herself a rheumatologist at University Hospital of Móstoles, pointed out that the task force brought together a range of specialties – rheumatologists, orthopedic surgeons, radiologists, nuclear medicine specialists, among others, as well as patients – to ensure that the best advice could be given.
The task force followed EULAR standard operating procedures for developing recommendations, with discussion groups, systematic literature reviews, and Delphi technique-based consensus all being employed. The literature search considered publications from 1946 up until 2019.
“We agreed on the need for more background information from health professionals and patients, so we developed two surveys: One for health professionals with 160 items, [for which] we obtained 186 responses from 26 countries; and the patient survey was made up of 44 items, translated into 10 different languages, and we obtained 200 responses,” she said.
The results of the systematic literature review and surveys were used to help form expert consensus, leading to 5 overarching principles and 11 recommendations that look at before, during, and after intra-articular therapy.
Five overarching principles
The first overarching principle recognizes the widespread use of IA therapies and that their use is specific to the disease that is being treated and “may not be interchangeable across indications,” Dr. Usón said. The second principle concerns improving patient-centered outcomes, which are “those that are relevant to the patient,” and include the benefits, harms, preferences, or implications for self-management.
“Contextual factors are important and contribute to the effect of IAT [intra-articular treatment],” she said, discussing the third principle. “These include effective communication, patient expectations, or settings [where the procedure takes place]. In addition, one should take into account that the route of delivery has in itself a placebo effect. We found that in different RCTs [randomized controlled trials], the pooled placebo effect of IA saline is moderate to large.”
The fourth principle looks at ensuring that patients and clinicians make an informed and shared decision, which is again highlighted by the first recommendation. The fifth, and last, overarching principle acknowledges that IA injections may be given by a range of health care professionals.
Advice for before, during, and after injection
Patients need to be “fully informed of the nature of the procedure, the injectable used, and potential effects – benefits and risks – [and] informed consent should be obtained and documented,” said Dr. Usón, outlining the first recommendation. “That seems common,” she said in the interview, “but when we did the survey, we realize that many patients didn’t [give consent], and the doctors didn’t even ask for it. This is why it’s a very general statement, and it’s our first recommendation. The agreement was 99%!”
The recommendations also look at the optimal settings for performing injections, such as providing a professional and private, well-lighted room, and having a resuscitation kit nearby in case patients faint. Accuracy is important, Dr. Usón said, and imaging, such as ultrasound, should be used where available to ensure accurate injection into the joint. This is an area where further research could be performed, she said, urging young rheumatologists and health professionals to consider this. “Intra-articular therapy is something that you learn and do, but you never really investigate in it,” she said.
One recommendation states that when intra-articular injections are being given to pregnant patients, the safety of injected compound must be considered, both for the mother and for the fetus. There is another recommendation on the need to perform IA injections under aseptic conditions, and another stating that patients should be offered local anesthetics, after explaining the pros and cons.
Special populations of patients are also considered, Dr. Usón said. For example, the guidance advises warning patients with diabetes of the risk of transient glycemia after IA glucocorticoids and the need to monitor their blood glucose levels carefully for a couple of days afterward.
As a rule, “IAT is not a contraindication to people with clotting or bleeding disorders, or taking antithrombotic medications,” she said, unless they are at a high risk of bleeding.
Importantly, the recommendations cover when IAT can be performed after joint replacement surgery (after at least 3 months), and the need to “avoid overuse of injected joints” while also avoiding complete immobilization for at least 24 hours afterward. The recommendations very generally cover re-injections, but not how long intervals between injections should be. When asked about interval duration after her presentation, Dr. Usón said that the usual advice is to give IA injections no more than 2-3 times a year, but it depends on the injectable.
“It wasn’t our intention to review the efficacy and the safety of the different injectables, nor to review the use of IAT in different types of joint diseases,” she said. “We do lack a lot of information, a lot of evidence in this, and I really would hope that new rheumatologists start looking into and start investigating in this topic,” she added.
Recommendations will increase awareness of good clinical practice
“IA injections are commonly administered in the rheumatology setting. This is because [IA injection] is often a useful treatment for acute flare of arthritis, particularly when it is limited to a few joints,” observed Ai Lyn Tan, MD, associate professor and honorary consultant rheumatologist at the Leeds (England) Institute of Rheumatic and Musculoskeletal Medicine.
IA injection “also relieves symptoms relatively quickly for patients; however, the response can be variable, and there are side effects associated with IA injections,” Dr. Tan added in an interview.
There is a lack of universally accepted recommendations, Dr. Tan observed, noting that while there might be some local guidelines on how to safely perform IA injections these were often not standardized and were subject to being continually updated to try to improve the experience for patients.
“It is therefore timely to learn about the new EULAR recommendations for IA injections. The advantage of this will be to increase awareness of good clinical practice for performing IA injections.”
Dr. Tan had no relevant conflicts of interest.
SOURCE: EULAR COVID-19 Recommendations. E-congress content available until Sept. 1, 2020.
New EULAR recommendations for the intra-articular (IA) treatment of arthropathies aim to facilitate uniformity and quality of care for this mainstay of rheumatologic practice, according to a report on the new guidance that was presented at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Until now there were no official recommendations on how best to use it in everyday practice. “This is the first time that there’s been a joint effort to develop evidence-based recommendations,” Jacqueline Usón, MD, PhD, associate professor medicine at Rey Juan Carlos University in Madrid, said in an interview. “Everything that we are saying is pretty logical, but it’s nice to see it put in recommendations based on evidence.”
IA therapy has been around for decades and is key for treating adults with a number of different conditions where synovitis, effusion, pain, or all three, are present, such as inflammatory arthritis and osteoarthritis, Dr. Usón observed during her presentation.
“Today, commonly used injectables are not only corticosteroids but also local anesthetics, hyaluronic acid, blood products, and maybe pharmaceuticals,” she said, adding that “there is a wide variation in the way intra-articular therapies are used and delivered to patients.” Health professionals also have very different views and habits depending on geographic locations and health care systems, she observed. Ironing out the variation was one of the main objectives of the recommendations.
As one of the two conveners of the EULAR task force behind the recommendations, Dr. Usón, herself a rheumatologist at University Hospital of Móstoles, pointed out that the task force brought together a range of specialties – rheumatologists, orthopedic surgeons, radiologists, nuclear medicine specialists, among others, as well as patients – to ensure that the best advice could be given.
The task force followed EULAR standard operating procedures for developing recommendations, with discussion groups, systematic literature reviews, and Delphi technique-based consensus all being employed. The literature search considered publications from 1946 up until 2019.
“We agreed on the need for more background information from health professionals and patients, so we developed two surveys: One for health professionals with 160 items, [for which] we obtained 186 responses from 26 countries; and the patient survey was made up of 44 items, translated into 10 different languages, and we obtained 200 responses,” she said.
The results of the systematic literature review and surveys were used to help form expert consensus, leading to 5 overarching principles and 11 recommendations that look at before, during, and after intra-articular therapy.
Five overarching principles
The first overarching principle recognizes the widespread use of IA therapies and that their use is specific to the disease that is being treated and “may not be interchangeable across indications,” Dr. Usón said. The second principle concerns improving patient-centered outcomes, which are “those that are relevant to the patient,” and include the benefits, harms, preferences, or implications for self-management.
“Contextual factors are important and contribute to the effect of IAT [intra-articular treatment],” she said, discussing the third principle. “These include effective communication, patient expectations, or settings [where the procedure takes place]. In addition, one should take into account that the route of delivery has in itself a placebo effect. We found that in different RCTs [randomized controlled trials], the pooled placebo effect of IA saline is moderate to large.”
The fourth principle looks at ensuring that patients and clinicians make an informed and shared decision, which is again highlighted by the first recommendation. The fifth, and last, overarching principle acknowledges that IA injections may be given by a range of health care professionals.
Advice for before, during, and after injection
Patients need to be “fully informed of the nature of the procedure, the injectable used, and potential effects – benefits and risks – [and] informed consent should be obtained and documented,” said Dr. Usón, outlining the first recommendation. “That seems common,” she said in the interview, “but when we did the survey, we realize that many patients didn’t [give consent], and the doctors didn’t even ask for it. This is why it’s a very general statement, and it’s our first recommendation. The agreement was 99%!”
The recommendations also look at the optimal settings for performing injections, such as providing a professional and private, well-lighted room, and having a resuscitation kit nearby in case patients faint. Accuracy is important, Dr. Usón said, and imaging, such as ultrasound, should be used where available to ensure accurate injection into the joint. This is an area where further research could be performed, she said, urging young rheumatologists and health professionals to consider this. “Intra-articular therapy is something that you learn and do, but you never really investigate in it,” she said.
One recommendation states that when intra-articular injections are being given to pregnant patients, the safety of injected compound must be considered, both for the mother and for the fetus. There is another recommendation on the need to perform IA injections under aseptic conditions, and another stating that patients should be offered local anesthetics, after explaining the pros and cons.
Special populations of patients are also considered, Dr. Usón said. For example, the guidance advises warning patients with diabetes of the risk of transient glycemia after IA glucocorticoids and the need to monitor their blood glucose levels carefully for a couple of days afterward.
As a rule, “IAT is not a contraindication to people with clotting or bleeding disorders, or taking antithrombotic medications,” she said, unless they are at a high risk of bleeding.
Importantly, the recommendations cover when IAT can be performed after joint replacement surgery (after at least 3 months), and the need to “avoid overuse of injected joints” while also avoiding complete immobilization for at least 24 hours afterward. The recommendations very generally cover re-injections, but not how long intervals between injections should be. When asked about interval duration after her presentation, Dr. Usón said that the usual advice is to give IA injections no more than 2-3 times a year, but it depends on the injectable.
“It wasn’t our intention to review the efficacy and the safety of the different injectables, nor to review the use of IAT in different types of joint diseases,” she said. “We do lack a lot of information, a lot of evidence in this, and I really would hope that new rheumatologists start looking into and start investigating in this topic,” she added.
Recommendations will increase awareness of good clinical practice
“IA injections are commonly administered in the rheumatology setting. This is because [IA injection] is often a useful treatment for acute flare of arthritis, particularly when it is limited to a few joints,” observed Ai Lyn Tan, MD, associate professor and honorary consultant rheumatologist at the Leeds (England) Institute of Rheumatic and Musculoskeletal Medicine.
IA injection “also relieves symptoms relatively quickly for patients; however, the response can be variable, and there are side effects associated with IA injections,” Dr. Tan added in an interview.
There is a lack of universally accepted recommendations, Dr. Tan observed, noting that while there might be some local guidelines on how to safely perform IA injections these were often not standardized and were subject to being continually updated to try to improve the experience for patients.
“It is therefore timely to learn about the new EULAR recommendations for IA injections. The advantage of this will be to increase awareness of good clinical practice for performing IA injections.”
Dr. Tan had no relevant conflicts of interest.
SOURCE: EULAR COVID-19 Recommendations. E-congress content available until Sept. 1, 2020.
New EULAR recommendations for the intra-articular (IA) treatment of arthropathies aim to facilitate uniformity and quality of care for this mainstay of rheumatologic practice, according to a report on the new guidance that was presented at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Until now there were no official recommendations on how best to use it in everyday practice. “This is the first time that there’s been a joint effort to develop evidence-based recommendations,” Jacqueline Usón, MD, PhD, associate professor medicine at Rey Juan Carlos University in Madrid, said in an interview. “Everything that we are saying is pretty logical, but it’s nice to see it put in recommendations based on evidence.”
IA therapy has been around for decades and is key for treating adults with a number of different conditions where synovitis, effusion, pain, or all three, are present, such as inflammatory arthritis and osteoarthritis, Dr. Usón observed during her presentation.
“Today, commonly used injectables are not only corticosteroids but also local anesthetics, hyaluronic acid, blood products, and maybe pharmaceuticals,” she said, adding that “there is a wide variation in the way intra-articular therapies are used and delivered to patients.” Health professionals also have very different views and habits depending on geographic locations and health care systems, she observed. Ironing out the variation was one of the main objectives of the recommendations.
As one of the two conveners of the EULAR task force behind the recommendations, Dr. Usón, herself a rheumatologist at University Hospital of Móstoles, pointed out that the task force brought together a range of specialties – rheumatologists, orthopedic surgeons, radiologists, nuclear medicine specialists, among others, as well as patients – to ensure that the best advice could be given.
The task force followed EULAR standard operating procedures for developing recommendations, with discussion groups, systematic literature reviews, and Delphi technique-based consensus all being employed. The literature search considered publications from 1946 up until 2019.
“We agreed on the need for more background information from health professionals and patients, so we developed two surveys: One for health professionals with 160 items, [for which] we obtained 186 responses from 26 countries; and the patient survey was made up of 44 items, translated into 10 different languages, and we obtained 200 responses,” she said.
The results of the systematic literature review and surveys were used to help form expert consensus, leading to 5 overarching principles and 11 recommendations that look at before, during, and after intra-articular therapy.
Five overarching principles
The first overarching principle recognizes the widespread use of IA therapies and that their use is specific to the disease that is being treated and “may not be interchangeable across indications,” Dr. Usón said. The second principle concerns improving patient-centered outcomes, which are “those that are relevant to the patient,” and include the benefits, harms, preferences, or implications for self-management.
“Contextual factors are important and contribute to the effect of IAT [intra-articular treatment],” she said, discussing the third principle. “These include effective communication, patient expectations, or settings [where the procedure takes place]. In addition, one should take into account that the route of delivery has in itself a placebo effect. We found that in different RCTs [randomized controlled trials], the pooled placebo effect of IA saline is moderate to large.”
The fourth principle looks at ensuring that patients and clinicians make an informed and shared decision, which is again highlighted by the first recommendation. The fifth, and last, overarching principle acknowledges that IA injections may be given by a range of health care professionals.
Advice for before, during, and after injection
Patients need to be “fully informed of the nature of the procedure, the injectable used, and potential effects – benefits and risks – [and] informed consent should be obtained and documented,” said Dr. Usón, outlining the first recommendation. “That seems common,” she said in the interview, “but when we did the survey, we realize that many patients didn’t [give consent], and the doctors didn’t even ask for it. This is why it’s a very general statement, and it’s our first recommendation. The agreement was 99%!”
The recommendations also look at the optimal settings for performing injections, such as providing a professional and private, well-lighted room, and having a resuscitation kit nearby in case patients faint. Accuracy is important, Dr. Usón said, and imaging, such as ultrasound, should be used where available to ensure accurate injection into the joint. This is an area where further research could be performed, she said, urging young rheumatologists and health professionals to consider this. “Intra-articular therapy is something that you learn and do, but you never really investigate in it,” she said.
One recommendation states that when intra-articular injections are being given to pregnant patients, the safety of injected compound must be considered, both for the mother and for the fetus. There is another recommendation on the need to perform IA injections under aseptic conditions, and another stating that patients should be offered local anesthetics, after explaining the pros and cons.
Special populations of patients are also considered, Dr. Usón said. For example, the guidance advises warning patients with diabetes of the risk of transient glycemia after IA glucocorticoids and the need to monitor their blood glucose levels carefully for a couple of days afterward.
As a rule, “IAT is not a contraindication to people with clotting or bleeding disorders, or taking antithrombotic medications,” she said, unless they are at a high risk of bleeding.
Importantly, the recommendations cover when IAT can be performed after joint replacement surgery (after at least 3 months), and the need to “avoid overuse of injected joints” while also avoiding complete immobilization for at least 24 hours afterward. The recommendations very generally cover re-injections, but not how long intervals between injections should be. When asked about interval duration after her presentation, Dr. Usón said that the usual advice is to give IA injections no more than 2-3 times a year, but it depends on the injectable.
“It wasn’t our intention to review the efficacy and the safety of the different injectables, nor to review the use of IAT in different types of joint diseases,” she said. “We do lack a lot of information, a lot of evidence in this, and I really would hope that new rheumatologists start looking into and start investigating in this topic,” she added.
Recommendations will increase awareness of good clinical practice
“IA injections are commonly administered in the rheumatology setting. This is because [IA injection] is often a useful treatment for acute flare of arthritis, particularly when it is limited to a few joints,” observed Ai Lyn Tan, MD, associate professor and honorary consultant rheumatologist at the Leeds (England) Institute of Rheumatic and Musculoskeletal Medicine.
IA injection “also relieves symptoms relatively quickly for patients; however, the response can be variable, and there are side effects associated with IA injections,” Dr. Tan added in an interview.
There is a lack of universally accepted recommendations, Dr. Tan observed, noting that while there might be some local guidelines on how to safely perform IA injections these were often not standardized and were subject to being continually updated to try to improve the experience for patients.
“It is therefore timely to learn about the new EULAR recommendations for IA injections. The advantage of this will be to increase awareness of good clinical practice for performing IA injections.”
Dr. Tan had no relevant conflicts of interest.
SOURCE: EULAR COVID-19 Recommendations. E-congress content available until Sept. 1, 2020.
FROM THE EULAR 2020 E-CONGRESS
Belimumab safely improved renal function in lupus nephritis patients
compared with control patients who only received standard therapy, in a randomized, multicenter trial with 446 evaluable patients, a finding that may help extend this treatment to a new group of lupus patients.
“The largest” treatment study of lupus nephritis reported to date showed that belimumab, approved by the Food and Drug Administration in 2011 for treating patients with systemic lupus erythematosus (SLE), administered at a standard dosage of 10 mg intravenously every 4 weeks, “significantly improved multiple lupus nephritis renal responses versus standard therapy alone while maintaining an acceptable safety profile,” Richard A. Furie, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
The study’s primary endpoint was a composite measure that Dr. Furie and associates called the Primary Endpoint Renal Response, which required patients to have achieved a urinary protein-to-creatinine ratio of 0.7 or less (compared with an enrollment level of 1.0 or greater), an estimated glomerular filtration rate (eGFR) of at least 60 mL/min/1.73 kg/m2 and no more than 20% below its preflare level, and continuation on the assigned treatment regimen. After 104 weeks on this treatment, which followed a 60-day induction phase that included treatment with a high-dose glucocorticoid, the percentages of patients who met the Primary Endpoint Renal Response criteria were 32% in the control arm who received standard treatment at the discretion of their treating clinicians plus placebo infusions and 43% in patients who received belimumab infusions in addition to their standard care. This calculated out to a 55% relative increase in this response with belimumab, a statistically significant result, reported Dr. Furie, professor of medicine at Hofstra University, Hempstead, N.Y., and chief of rheumatology at Northwell Health in Manhasset, N.Y.
Patients who received belimumab also had similar and statistically significant levels of improvement for several secondary endpoints, including one called Complete Renal Response, which required a protein-to-creatinine ratio of no greater than 0.5, an eGFR of at least 90 mL/min per 1.73 kg/m2 and no more than 10% below its preflare level, and maintaining the assigned treatment. The Complete Renal Response after 104 weeks was 20% among control patients and 30% among those maintained on belimumab, a 74% relative improvement that was statistically significant. The total percentage of patients with any renal-related event after 104 weeks was 28% among the control patients and 16% among those who received belimumab, a statistically significant difference.
“The fact that the primary and all key secondary endpoints were successfully attained is a major accomplishment in lupus nephritis as well as in any SLE study,” Dr. Furie said in an interview. The study’s 2-year design “provided insight into the durability of the response,” and the steady divergence of the endpoint events in the two study arms beginning after about 24 weeks into the randomized phase “provided data regarding the rapidity of onset of action.” Collectively, the endpoints “mimic our real-life treatment goals: reduce disease activity, prevent flares, preserve renal function, lower steroid treatment, and do it all safely,” he concluded.
Results confirm benefit to subset of patients
“Belimumab is a safe and effective treatment for a significant subset of patients with lupus. We already knew that. Now we have even more confirmation,” commented Joan T. Merrill, MD, a professor of medicine at the University of Oklahoma Health Sciences Center and a rheumatologist who specializes in SLE at the Oklahoma Medical Research Foundation, both in Oklahoma City. “There have already been at least four international trials demonstrating belimumab’s efficacy in general lupus. Some patients in these earlier trials had nephritis, so it should not be surprising to see similar results in a trial restricted to patients with active nephritis, given the drug’s mechanism of action. Belimumab has repeatedly shown early and sustained benefits above what background treatments achieve, and belimumab has also proven to be safe to add to standard-of-care treatments,” she said in an interview.
The BLISS-LN (Efficacy and Safety of Belimumab in Patients With Active Lupus Nephritis) study enrolled patients at any of 118 centers in 20 countries, including the United States. All patients enrolled in the trial were adults with biopsy-confirmed, clinically active lupus nephritis and a urinary protein-to-creatinine ratio of at least 1.0, and need for induction therapy. The 60-day induction run-in phase began with high-dose glucocorticoids plus either cyclophosphamide or mycophenolate mofetil (CellCept), followed by maintenance on low-dose glucocorticoids and either azathioprine or mycophenolate mofetil. Nearly three-quarters of patients received mycophenolate mofetil–based induction. Once treatment with either belimumab or placebo began in the study’s main phase, the glucocorticoid dosage had to drop with tapering to no more than 10 mg/day within 24 weeks or the patient was considered a treatment failure.
Thoughts on current and future use of belimumab
The current labeled indication for belimumab is for “treatment of patients aged 5 years and older with active, autoantibody-positive systemic lupus erythematosus who are receiving standard therapy,” an inclusive SLE population, but the label also adds this caveat: “Limitations of use: The efficacy of Benlysta has not been evaluated in patients with severe active lupus nephritis or severe active central nervous system lupus.” According to Dr. Furie’s report, GlaxoSmithKline, the company that markets belimumab, plans to seek a labeled indication for lupus nephritis for the drug during 2020.
“I doubt the drug is widely used as yet in clinical practice for lupus nephritis,” although it is being prescribed to selected SLE patients in current, routine practice, said Dr. Merrill, a coinvestigator on some belimumab studies. What also remains unknown is the efficacy of belimumab monotherapy. “We don’t know which subset of patients might benefit from belimumab alone,” she noted. Nor is it known whether belimumab treatment of patients with SLE but without lupus nephritis will forestall later development of lupus nephritis.
“With the introduction of the subcutaneous formulation a few years ago, there has been greater belimumab use” overall in patients with SLE, said Dr. Furie, and with a safety and efficacy record now established in five separate, reported studies in addition to the new BLISS-LN study: BLISS-52, BLISS-76, BLISS-SC, BLISS-NE ASIA, and PLUTO. “The pivotal studies [BLISS-52 and BLISS-76] were done in patients with SLE but without nephritis in need of aggressive induction therapy. About 15% of the trial cohorts had low-level renal involvement,” and post hoc analyses suggested that the benefit in those patients was similar to patients without renal involvement, which led to the BLISS-LN study. “In theory, no SLE patients with high-level nephritis should be on belimumab at this time,” based on its labeling, although some SLE patients with low-level renal disease may now receive the drug because they also have other affected organs, such as skin and joints, Dr. Furie said.
“These are encouraging results,” commented George K. Bertsias, MD, a rheumatologist and SLE specialist at the University of Crete in Heraklion, Greece. He particularly cited the “significant effect from add-on belimumab” on top of treatment with mycophenolate mofetil, an “established and effective treatment for lupus nephritis. The data provide additional evidence for the efficacy of belimumab in SLE, and also in lupus nephritis,” he said in an interview, and “having an official labeled indication for active nephritis will enhance use of the drug” in such patients. “Considering the favorable effects of the drug on SLE, especially preventing major flares, and on lupus nephritis it is possible that the drug will be particularly suitable for SLE patients who are at high risk for developing lupus nephritis, although such an effect remains to be determined.” Until now, belimumab has generally been prescribed to SLE patients who have disease manifestations in organs outside of the kidneys, he noted.
BLISS-LN was sponsored by GlaxoSmithKline. Dr. Furie is a consultant to and has received research funding from GlaxoSmithKline, and several of the study’s coauthors are employees of the company. Dr. Merrill has been a consultant to GlaxoSmithKline as well as to several other companies and has been a coinvestigator on belimumab studies. Dr. Bertsias has been a consultant to Novartis and has received research funding from GlaxoSmithKline.
SOURCE: Furie RA et al. Ann Rheum Dis. 2020 Jun;79[suppl 1]:103, Abstract OP0164.
compared with control patients who only received standard therapy, in a randomized, multicenter trial with 446 evaluable patients, a finding that may help extend this treatment to a new group of lupus patients.
“The largest” treatment study of lupus nephritis reported to date showed that belimumab, approved by the Food and Drug Administration in 2011 for treating patients with systemic lupus erythematosus (SLE), administered at a standard dosage of 10 mg intravenously every 4 weeks, “significantly improved multiple lupus nephritis renal responses versus standard therapy alone while maintaining an acceptable safety profile,” Richard A. Furie, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
The study’s primary endpoint was a composite measure that Dr. Furie and associates called the Primary Endpoint Renal Response, which required patients to have achieved a urinary protein-to-creatinine ratio of 0.7 or less (compared with an enrollment level of 1.0 or greater), an estimated glomerular filtration rate (eGFR) of at least 60 mL/min/1.73 kg/m2 and no more than 20% below its preflare level, and continuation on the assigned treatment regimen. After 104 weeks on this treatment, which followed a 60-day induction phase that included treatment with a high-dose glucocorticoid, the percentages of patients who met the Primary Endpoint Renal Response criteria were 32% in the control arm who received standard treatment at the discretion of their treating clinicians plus placebo infusions and 43% in patients who received belimumab infusions in addition to their standard care. This calculated out to a 55% relative increase in this response with belimumab, a statistically significant result, reported Dr. Furie, professor of medicine at Hofstra University, Hempstead, N.Y., and chief of rheumatology at Northwell Health in Manhasset, N.Y.
Patients who received belimumab also had similar and statistically significant levels of improvement for several secondary endpoints, including one called Complete Renal Response, which required a protein-to-creatinine ratio of no greater than 0.5, an eGFR of at least 90 mL/min per 1.73 kg/m2 and no more than 10% below its preflare level, and maintaining the assigned treatment. The Complete Renal Response after 104 weeks was 20% among control patients and 30% among those maintained on belimumab, a 74% relative improvement that was statistically significant. The total percentage of patients with any renal-related event after 104 weeks was 28% among the control patients and 16% among those who received belimumab, a statistically significant difference.
“The fact that the primary and all key secondary endpoints were successfully attained is a major accomplishment in lupus nephritis as well as in any SLE study,” Dr. Furie said in an interview. The study’s 2-year design “provided insight into the durability of the response,” and the steady divergence of the endpoint events in the two study arms beginning after about 24 weeks into the randomized phase “provided data regarding the rapidity of onset of action.” Collectively, the endpoints “mimic our real-life treatment goals: reduce disease activity, prevent flares, preserve renal function, lower steroid treatment, and do it all safely,” he concluded.
Results confirm benefit to subset of patients
“Belimumab is a safe and effective treatment for a significant subset of patients with lupus. We already knew that. Now we have even more confirmation,” commented Joan T. Merrill, MD, a professor of medicine at the University of Oklahoma Health Sciences Center and a rheumatologist who specializes in SLE at the Oklahoma Medical Research Foundation, both in Oklahoma City. “There have already been at least four international trials demonstrating belimumab’s efficacy in general lupus. Some patients in these earlier trials had nephritis, so it should not be surprising to see similar results in a trial restricted to patients with active nephritis, given the drug’s mechanism of action. Belimumab has repeatedly shown early and sustained benefits above what background treatments achieve, and belimumab has also proven to be safe to add to standard-of-care treatments,” she said in an interview.
The BLISS-LN (Efficacy and Safety of Belimumab in Patients With Active Lupus Nephritis) study enrolled patients at any of 118 centers in 20 countries, including the United States. All patients enrolled in the trial were adults with biopsy-confirmed, clinically active lupus nephritis and a urinary protein-to-creatinine ratio of at least 1.0, and need for induction therapy. The 60-day induction run-in phase began with high-dose glucocorticoids plus either cyclophosphamide or mycophenolate mofetil (CellCept), followed by maintenance on low-dose glucocorticoids and either azathioprine or mycophenolate mofetil. Nearly three-quarters of patients received mycophenolate mofetil–based induction. Once treatment with either belimumab or placebo began in the study’s main phase, the glucocorticoid dosage had to drop with tapering to no more than 10 mg/day within 24 weeks or the patient was considered a treatment failure.
Thoughts on current and future use of belimumab
The current labeled indication for belimumab is for “treatment of patients aged 5 years and older with active, autoantibody-positive systemic lupus erythematosus who are receiving standard therapy,” an inclusive SLE population, but the label also adds this caveat: “Limitations of use: The efficacy of Benlysta has not been evaluated in patients with severe active lupus nephritis or severe active central nervous system lupus.” According to Dr. Furie’s report, GlaxoSmithKline, the company that markets belimumab, plans to seek a labeled indication for lupus nephritis for the drug during 2020.
“I doubt the drug is widely used as yet in clinical practice for lupus nephritis,” although it is being prescribed to selected SLE patients in current, routine practice, said Dr. Merrill, a coinvestigator on some belimumab studies. What also remains unknown is the efficacy of belimumab monotherapy. “We don’t know which subset of patients might benefit from belimumab alone,” she noted. Nor is it known whether belimumab treatment of patients with SLE but without lupus nephritis will forestall later development of lupus nephritis.
“With the introduction of the subcutaneous formulation a few years ago, there has been greater belimumab use” overall in patients with SLE, said Dr. Furie, and with a safety and efficacy record now established in five separate, reported studies in addition to the new BLISS-LN study: BLISS-52, BLISS-76, BLISS-SC, BLISS-NE ASIA, and PLUTO. “The pivotal studies [BLISS-52 and BLISS-76] were done in patients with SLE but without nephritis in need of aggressive induction therapy. About 15% of the trial cohorts had low-level renal involvement,” and post hoc analyses suggested that the benefit in those patients was similar to patients without renal involvement, which led to the BLISS-LN study. “In theory, no SLE patients with high-level nephritis should be on belimumab at this time,” based on its labeling, although some SLE patients with low-level renal disease may now receive the drug because they also have other affected organs, such as skin and joints, Dr. Furie said.
“These are encouraging results,” commented George K. Bertsias, MD, a rheumatologist and SLE specialist at the University of Crete in Heraklion, Greece. He particularly cited the “significant effect from add-on belimumab” on top of treatment with mycophenolate mofetil, an “established and effective treatment for lupus nephritis. The data provide additional evidence for the efficacy of belimumab in SLE, and also in lupus nephritis,” he said in an interview, and “having an official labeled indication for active nephritis will enhance use of the drug” in such patients. “Considering the favorable effects of the drug on SLE, especially preventing major flares, and on lupus nephritis it is possible that the drug will be particularly suitable for SLE patients who are at high risk for developing lupus nephritis, although such an effect remains to be determined.” Until now, belimumab has generally been prescribed to SLE patients who have disease manifestations in organs outside of the kidneys, he noted.
BLISS-LN was sponsored by GlaxoSmithKline. Dr. Furie is a consultant to and has received research funding from GlaxoSmithKline, and several of the study’s coauthors are employees of the company. Dr. Merrill has been a consultant to GlaxoSmithKline as well as to several other companies and has been a coinvestigator on belimumab studies. Dr. Bertsias has been a consultant to Novartis and has received research funding from GlaxoSmithKline.
SOURCE: Furie RA et al. Ann Rheum Dis. 2020 Jun;79[suppl 1]:103, Abstract OP0164.
compared with control patients who only received standard therapy, in a randomized, multicenter trial with 446 evaluable patients, a finding that may help extend this treatment to a new group of lupus patients.
“The largest” treatment study of lupus nephritis reported to date showed that belimumab, approved by the Food and Drug Administration in 2011 for treating patients with systemic lupus erythematosus (SLE), administered at a standard dosage of 10 mg intravenously every 4 weeks, “significantly improved multiple lupus nephritis renal responses versus standard therapy alone while maintaining an acceptable safety profile,” Richard A. Furie, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
The study’s primary endpoint was a composite measure that Dr. Furie and associates called the Primary Endpoint Renal Response, which required patients to have achieved a urinary protein-to-creatinine ratio of 0.7 or less (compared with an enrollment level of 1.0 or greater), an estimated glomerular filtration rate (eGFR) of at least 60 mL/min/1.73 kg/m2 and no more than 20% below its preflare level, and continuation on the assigned treatment regimen. After 104 weeks on this treatment, which followed a 60-day induction phase that included treatment with a high-dose glucocorticoid, the percentages of patients who met the Primary Endpoint Renal Response criteria were 32% in the control arm who received standard treatment at the discretion of their treating clinicians plus placebo infusions and 43% in patients who received belimumab infusions in addition to their standard care. This calculated out to a 55% relative increase in this response with belimumab, a statistically significant result, reported Dr. Furie, professor of medicine at Hofstra University, Hempstead, N.Y., and chief of rheumatology at Northwell Health in Manhasset, N.Y.
Patients who received belimumab also had similar and statistically significant levels of improvement for several secondary endpoints, including one called Complete Renal Response, which required a protein-to-creatinine ratio of no greater than 0.5, an eGFR of at least 90 mL/min per 1.73 kg/m2 and no more than 10% below its preflare level, and maintaining the assigned treatment. The Complete Renal Response after 104 weeks was 20% among control patients and 30% among those maintained on belimumab, a 74% relative improvement that was statistically significant. The total percentage of patients with any renal-related event after 104 weeks was 28% among the control patients and 16% among those who received belimumab, a statistically significant difference.
“The fact that the primary and all key secondary endpoints were successfully attained is a major accomplishment in lupus nephritis as well as in any SLE study,” Dr. Furie said in an interview. The study’s 2-year design “provided insight into the durability of the response,” and the steady divergence of the endpoint events in the two study arms beginning after about 24 weeks into the randomized phase “provided data regarding the rapidity of onset of action.” Collectively, the endpoints “mimic our real-life treatment goals: reduce disease activity, prevent flares, preserve renal function, lower steroid treatment, and do it all safely,” he concluded.
Results confirm benefit to subset of patients
“Belimumab is a safe and effective treatment for a significant subset of patients with lupus. We already knew that. Now we have even more confirmation,” commented Joan T. Merrill, MD, a professor of medicine at the University of Oklahoma Health Sciences Center and a rheumatologist who specializes in SLE at the Oklahoma Medical Research Foundation, both in Oklahoma City. “There have already been at least four international trials demonstrating belimumab’s efficacy in general lupus. Some patients in these earlier trials had nephritis, so it should not be surprising to see similar results in a trial restricted to patients with active nephritis, given the drug’s mechanism of action. Belimumab has repeatedly shown early and sustained benefits above what background treatments achieve, and belimumab has also proven to be safe to add to standard-of-care treatments,” she said in an interview.
The BLISS-LN (Efficacy and Safety of Belimumab in Patients With Active Lupus Nephritis) study enrolled patients at any of 118 centers in 20 countries, including the United States. All patients enrolled in the trial were adults with biopsy-confirmed, clinically active lupus nephritis and a urinary protein-to-creatinine ratio of at least 1.0, and need for induction therapy. The 60-day induction run-in phase began with high-dose glucocorticoids plus either cyclophosphamide or mycophenolate mofetil (CellCept), followed by maintenance on low-dose glucocorticoids and either azathioprine or mycophenolate mofetil. Nearly three-quarters of patients received mycophenolate mofetil–based induction. Once treatment with either belimumab or placebo began in the study’s main phase, the glucocorticoid dosage had to drop with tapering to no more than 10 mg/day within 24 weeks or the patient was considered a treatment failure.
Thoughts on current and future use of belimumab
The current labeled indication for belimumab is for “treatment of patients aged 5 years and older with active, autoantibody-positive systemic lupus erythematosus who are receiving standard therapy,” an inclusive SLE population, but the label also adds this caveat: “Limitations of use: The efficacy of Benlysta has not been evaluated in patients with severe active lupus nephritis or severe active central nervous system lupus.” According to Dr. Furie’s report, GlaxoSmithKline, the company that markets belimumab, plans to seek a labeled indication for lupus nephritis for the drug during 2020.
“I doubt the drug is widely used as yet in clinical practice for lupus nephritis,” although it is being prescribed to selected SLE patients in current, routine practice, said Dr. Merrill, a coinvestigator on some belimumab studies. What also remains unknown is the efficacy of belimumab monotherapy. “We don’t know which subset of patients might benefit from belimumab alone,” she noted. Nor is it known whether belimumab treatment of patients with SLE but without lupus nephritis will forestall later development of lupus nephritis.
“With the introduction of the subcutaneous formulation a few years ago, there has been greater belimumab use” overall in patients with SLE, said Dr. Furie, and with a safety and efficacy record now established in five separate, reported studies in addition to the new BLISS-LN study: BLISS-52, BLISS-76, BLISS-SC, BLISS-NE ASIA, and PLUTO. “The pivotal studies [BLISS-52 and BLISS-76] were done in patients with SLE but without nephritis in need of aggressive induction therapy. About 15% of the trial cohorts had low-level renal involvement,” and post hoc analyses suggested that the benefit in those patients was similar to patients without renal involvement, which led to the BLISS-LN study. “In theory, no SLE patients with high-level nephritis should be on belimumab at this time,” based on its labeling, although some SLE patients with low-level renal disease may now receive the drug because they also have other affected organs, such as skin and joints, Dr. Furie said.
“These are encouraging results,” commented George K. Bertsias, MD, a rheumatologist and SLE specialist at the University of Crete in Heraklion, Greece. He particularly cited the “significant effect from add-on belimumab” on top of treatment with mycophenolate mofetil, an “established and effective treatment for lupus nephritis. The data provide additional evidence for the efficacy of belimumab in SLE, and also in lupus nephritis,” he said in an interview, and “having an official labeled indication for active nephritis will enhance use of the drug” in such patients. “Considering the favorable effects of the drug on SLE, especially preventing major flares, and on lupus nephritis it is possible that the drug will be particularly suitable for SLE patients who are at high risk for developing lupus nephritis, although such an effect remains to be determined.” Until now, belimumab has generally been prescribed to SLE patients who have disease manifestations in organs outside of the kidneys, he noted.
BLISS-LN was sponsored by GlaxoSmithKline. Dr. Furie is a consultant to and has received research funding from GlaxoSmithKline, and several of the study’s coauthors are employees of the company. Dr. Merrill has been a consultant to GlaxoSmithKline as well as to several other companies and has been a coinvestigator on belimumab studies. Dr. Bertsias has been a consultant to Novartis and has received research funding from GlaxoSmithKline.
SOURCE: Furie RA et al. Ann Rheum Dis. 2020 Jun;79[suppl 1]:103, Abstract OP0164.
FROM THE EULAR 2020 E-CONGRESS
New registry focuses on rheumatic immune-related AEs of cancer therapy
Its first findings were reported at the annual European Congress of Rheumatology, held online this year due to COVID-19.
“We have limited knowledge on the interrelationships between malignant and rheumatic diseases on both the clinical and molecular level, and we have a large unmet need for management guidelines in the case of the coincidence of both disease entities,” noted lead author Karolina Benesova, MD, of the department of hematology, oncology, and rheumatology at University Hospital Heidelberg (Germany).
The TRheuMa registry – Therapy-Induced Rheumatic Symptoms in Patients with Malignancy – is one of three registries in a multicenter observational project exploring various contexts between malignant and rheumatic diseases. Over its first 22 months, the registry recruited 69 patients having rheumatic symptoms as a result of immune checkpoint inhibitor therapy or other cancer therapies.
Registry findings
The largest shares of patients had non–small cell lung cancer (38%) or melanoma (33%), Dr. Benesova reported. The immune checkpoint inhibitors most commonly received were pembrolizumab (Keytruda), nivolumab (Opdivo), and ipilimumab (Yervoy).
The immune-related adverse events usually presented with symptoms of de novo spondyloarthritis or psoriatic arthritis (42%), late-onset RA (17%), or polymyalgia rheumatica (14%). But 16% of the patients were experiencing a flare of a preexisting rheumatic and musculoskeletal disease.
Laboratory findings differed somewhat from those of classical rheumatic and musculoskeletal diseases, according to Dr. Benesova. Specific findings were rare; in particular, most patients did not have detectable autoantibodies. However, 76% had an elevated C-reactive protein level and 39% had an elevated soluble CD25 level. In addition, nearly all patients (96%) undergoing joint ultrasound had pathologic findings.
“Based on our experiences from interdisciplinary care together with our local oncologists, we have developed a therapeutic algorithm for rheumatic immune-related adverse events,” she reported, noting that the algorithm is consistent with recently published recommendations in this area.
The large majority of patients were adequately treated with prednisone at a dose greater than 10 mg (40%) or at a dose of 10 mg or less with or without an NSAID (40%), while some received NSAID monotherapy (14%).
“We have a growing proportion of patients on conventional or biological [disease-modifying antirheumatic drugs],” Dr. Benesova noted. “These are mostly patients with preexisting rheumatic and musculoskeletal disease or highly suspected de novo classical rheumatic and musculoskeletal disease under checkpoint inhibitor therapy.”
Patients with melanoma having a rheumatic immune-related adverse event had a better response to their therapy than historical counterparts who did not have such events: 39% of the former had a complete response, relative to merely 4% of the latter.
Only a small proportion of patients overall (9%) had to discontinue immune checkpoint inhibitor therapy because of their adverse event, and some of them may be eligible for rechallenge if their cancer progresses, Dr. Benesova noted.
“There is still a lot to be done,” she stated, such as better elucidating the nature of these adverse events [whether transient side effects or a triggering of chronic rheumatic and musculoskeletal diseases], the need for a defensive treatment strategy, and the advisability of closer monitoring of high-risk patients given immune checkpoint inhibitors. “We are aiming at solving these questions in the next few years,” she concluded.
Findings in context
“Registries are important to gain prospective data on patient outcomes,” Sabina Sandigursky, MD, an instructor in the division of rheumatology at the Laura and Isaac Perlmutter Cancer Center at New York University, commented in an interview. “One must be careful, while interpreting these data, especially since they are not randomized, controlled trials.”
Patterns may differ at other centers, too, she pointed out. “The German registry reported a predominance of spondyloarthritis-like disease; however, our patients have a predominance of small-joint involvement. It is unclear what accounts for this difference.”
Individual institutions in North America are similarly collecting data on this patient population, with efforts underway to compile those data to provide a larger picture, according to Dr. Sandigursky.
“Many of the syndromes that we consider to be rheumatic immune-related adverse events have been well described by groups from the U.S., Canada, Australia, and European Union,” she concluded. “From this registry, we can observe how patients are being treated in real time since this information is largely consensus based.”
The study did not receive any specific funding. Dr. Benesova disclosed grant/research support from AbbVie, Novartis, Rheumaliga Baden-Wurttemberg, and the University of Heidelberg, and consultancies, speaker fees, and/or travel reimbursements from AbbVie, Bristol-Myers Squibb, Gilead, Janssen, Medac, Merck Sharp & Dohme, Mundipharma, Novartis, Pfizer, Roche, and UCB. Some of her coauthors also disclosed financial relationships with industry. Dr. Sandigursky disclosed having no relevant conflicts of interest.
SOURCE: Benesova K et al. Ann Rheum Dis 2020;79[suppl 1]:168-9, Abstract OP0270.
Its first findings were reported at the annual European Congress of Rheumatology, held online this year due to COVID-19.
“We have limited knowledge on the interrelationships between malignant and rheumatic diseases on both the clinical and molecular level, and we have a large unmet need for management guidelines in the case of the coincidence of both disease entities,” noted lead author Karolina Benesova, MD, of the department of hematology, oncology, and rheumatology at University Hospital Heidelberg (Germany).
The TRheuMa registry – Therapy-Induced Rheumatic Symptoms in Patients with Malignancy – is one of three registries in a multicenter observational project exploring various contexts between malignant and rheumatic diseases. Over its first 22 months, the registry recruited 69 patients having rheumatic symptoms as a result of immune checkpoint inhibitor therapy or other cancer therapies.
Registry findings
The largest shares of patients had non–small cell lung cancer (38%) or melanoma (33%), Dr. Benesova reported. The immune checkpoint inhibitors most commonly received were pembrolizumab (Keytruda), nivolumab (Opdivo), and ipilimumab (Yervoy).
The immune-related adverse events usually presented with symptoms of de novo spondyloarthritis or psoriatic arthritis (42%), late-onset RA (17%), or polymyalgia rheumatica (14%). But 16% of the patients were experiencing a flare of a preexisting rheumatic and musculoskeletal disease.
Laboratory findings differed somewhat from those of classical rheumatic and musculoskeletal diseases, according to Dr. Benesova. Specific findings were rare; in particular, most patients did not have detectable autoantibodies. However, 76% had an elevated C-reactive protein level and 39% had an elevated soluble CD25 level. In addition, nearly all patients (96%) undergoing joint ultrasound had pathologic findings.
“Based on our experiences from interdisciplinary care together with our local oncologists, we have developed a therapeutic algorithm for rheumatic immune-related adverse events,” she reported, noting that the algorithm is consistent with recently published recommendations in this area.
The large majority of patients were adequately treated with prednisone at a dose greater than 10 mg (40%) or at a dose of 10 mg or less with or without an NSAID (40%), while some received NSAID monotherapy (14%).
“We have a growing proportion of patients on conventional or biological [disease-modifying antirheumatic drugs],” Dr. Benesova noted. “These are mostly patients with preexisting rheumatic and musculoskeletal disease or highly suspected de novo classical rheumatic and musculoskeletal disease under checkpoint inhibitor therapy.”
Patients with melanoma having a rheumatic immune-related adverse event had a better response to their therapy than historical counterparts who did not have such events: 39% of the former had a complete response, relative to merely 4% of the latter.
Only a small proportion of patients overall (9%) had to discontinue immune checkpoint inhibitor therapy because of their adverse event, and some of them may be eligible for rechallenge if their cancer progresses, Dr. Benesova noted.
“There is still a lot to be done,” she stated, such as better elucidating the nature of these adverse events [whether transient side effects or a triggering of chronic rheumatic and musculoskeletal diseases], the need for a defensive treatment strategy, and the advisability of closer monitoring of high-risk patients given immune checkpoint inhibitors. “We are aiming at solving these questions in the next few years,” she concluded.
Findings in context
“Registries are important to gain prospective data on patient outcomes,” Sabina Sandigursky, MD, an instructor in the division of rheumatology at the Laura and Isaac Perlmutter Cancer Center at New York University, commented in an interview. “One must be careful, while interpreting these data, especially since they are not randomized, controlled trials.”
Patterns may differ at other centers, too, she pointed out. “The German registry reported a predominance of spondyloarthritis-like disease; however, our patients have a predominance of small-joint involvement. It is unclear what accounts for this difference.”
Individual institutions in North America are similarly collecting data on this patient population, with efforts underway to compile those data to provide a larger picture, according to Dr. Sandigursky.
“Many of the syndromes that we consider to be rheumatic immune-related adverse events have been well described by groups from the U.S., Canada, Australia, and European Union,” she concluded. “From this registry, we can observe how patients are being treated in real time since this information is largely consensus based.”
The study did not receive any specific funding. Dr. Benesova disclosed grant/research support from AbbVie, Novartis, Rheumaliga Baden-Wurttemberg, and the University of Heidelberg, and consultancies, speaker fees, and/or travel reimbursements from AbbVie, Bristol-Myers Squibb, Gilead, Janssen, Medac, Merck Sharp & Dohme, Mundipharma, Novartis, Pfizer, Roche, and UCB. Some of her coauthors also disclosed financial relationships with industry. Dr. Sandigursky disclosed having no relevant conflicts of interest.
SOURCE: Benesova K et al. Ann Rheum Dis 2020;79[suppl 1]:168-9, Abstract OP0270.
Its first findings were reported at the annual European Congress of Rheumatology, held online this year due to COVID-19.
“We have limited knowledge on the interrelationships between malignant and rheumatic diseases on both the clinical and molecular level, and we have a large unmet need for management guidelines in the case of the coincidence of both disease entities,” noted lead author Karolina Benesova, MD, of the department of hematology, oncology, and rheumatology at University Hospital Heidelberg (Germany).
The TRheuMa registry – Therapy-Induced Rheumatic Symptoms in Patients with Malignancy – is one of three registries in a multicenter observational project exploring various contexts between malignant and rheumatic diseases. Over its first 22 months, the registry recruited 69 patients having rheumatic symptoms as a result of immune checkpoint inhibitor therapy or other cancer therapies.
Registry findings
The largest shares of patients had non–small cell lung cancer (38%) or melanoma (33%), Dr. Benesova reported. The immune checkpoint inhibitors most commonly received were pembrolizumab (Keytruda), nivolumab (Opdivo), and ipilimumab (Yervoy).
The immune-related adverse events usually presented with symptoms of de novo spondyloarthritis or psoriatic arthritis (42%), late-onset RA (17%), or polymyalgia rheumatica (14%). But 16% of the patients were experiencing a flare of a preexisting rheumatic and musculoskeletal disease.
Laboratory findings differed somewhat from those of classical rheumatic and musculoskeletal diseases, according to Dr. Benesova. Specific findings were rare; in particular, most patients did not have detectable autoantibodies. However, 76% had an elevated C-reactive protein level and 39% had an elevated soluble CD25 level. In addition, nearly all patients (96%) undergoing joint ultrasound had pathologic findings.
“Based on our experiences from interdisciplinary care together with our local oncologists, we have developed a therapeutic algorithm for rheumatic immune-related adverse events,” she reported, noting that the algorithm is consistent with recently published recommendations in this area.
The large majority of patients were adequately treated with prednisone at a dose greater than 10 mg (40%) or at a dose of 10 mg or less with or without an NSAID (40%), while some received NSAID monotherapy (14%).
“We have a growing proportion of patients on conventional or biological [disease-modifying antirheumatic drugs],” Dr. Benesova noted. “These are mostly patients with preexisting rheumatic and musculoskeletal disease or highly suspected de novo classical rheumatic and musculoskeletal disease under checkpoint inhibitor therapy.”
Patients with melanoma having a rheumatic immune-related adverse event had a better response to their therapy than historical counterparts who did not have such events: 39% of the former had a complete response, relative to merely 4% of the latter.
Only a small proportion of patients overall (9%) had to discontinue immune checkpoint inhibitor therapy because of their adverse event, and some of them may be eligible for rechallenge if their cancer progresses, Dr. Benesova noted.
“There is still a lot to be done,” she stated, such as better elucidating the nature of these adverse events [whether transient side effects or a triggering of chronic rheumatic and musculoskeletal diseases], the need for a defensive treatment strategy, and the advisability of closer monitoring of high-risk patients given immune checkpoint inhibitors. “We are aiming at solving these questions in the next few years,” she concluded.
Findings in context
“Registries are important to gain prospective data on patient outcomes,” Sabina Sandigursky, MD, an instructor in the division of rheumatology at the Laura and Isaac Perlmutter Cancer Center at New York University, commented in an interview. “One must be careful, while interpreting these data, especially since they are not randomized, controlled trials.”
Patterns may differ at other centers, too, she pointed out. “The German registry reported a predominance of spondyloarthritis-like disease; however, our patients have a predominance of small-joint involvement. It is unclear what accounts for this difference.”
Individual institutions in North America are similarly collecting data on this patient population, with efforts underway to compile those data to provide a larger picture, according to Dr. Sandigursky.
“Many of the syndromes that we consider to be rheumatic immune-related adverse events have been well described by groups from the U.S., Canada, Australia, and European Union,” she concluded. “From this registry, we can observe how patients are being treated in real time since this information is largely consensus based.”
The study did not receive any specific funding. Dr. Benesova disclosed grant/research support from AbbVie, Novartis, Rheumaliga Baden-Wurttemberg, and the University of Heidelberg, and consultancies, speaker fees, and/or travel reimbursements from AbbVie, Bristol-Myers Squibb, Gilead, Janssen, Medac, Merck Sharp & Dohme, Mundipharma, Novartis, Pfizer, Roche, and UCB. Some of her coauthors also disclosed financial relationships with industry. Dr. Sandigursky disclosed having no relevant conflicts of interest.
SOURCE: Benesova K et al. Ann Rheum Dis 2020;79[suppl 1]:168-9, Abstract OP0270.
FROM THE EULAR 2020 E-CONGRESS