User login
Checkpoint inhibitors’ ‘big picture’ safety shown with preexisting autoimmune diseases
Patients with advanced melanoma and preexisting autoimmune diseases (AIDs) who were treated with immune checkpoint inhibitors (ICIs) responded well and did not suffer more grade 3 or higher immune-related adverse events than patients without an AID, a new study finds, although some concerns were raised regarding patients with inflammatory bowel disease (IBD).
“To our knowledge, this is the first study to bridge this knowledge gap by presenting ‘real-world’ data on the safety and efficacy of ICI on a national scale,” wrote Monique K. van der Kooij, MD, of Leiden (the Netherlands) University Medical Center and coauthors. The study was published online in Annals of Internal Medicine.
To investigate ICI use and response among this specific subset of melanoma patients, the researchers launched a nationwide cohort study set in the Netherlands. Data were gathered via the Dutch Melanoma Treatment Registry (DMTR), in which 4,367 patients with advanced melanoma were enrolled between July 2013 and July 2018.
Within that cohort, 415 (9.5%) had preexisting AIDs. Nearly 55% had rheumatologic AIDs (n = 227) – which included RA, systemic lupus erythematosus, scleroderma, sarcoidosis, and vasculitis – with the next most frequent being endocrine AID (n = 143) and IBD (n = 55). Patients with AID were older than patients without (67 vs. 63 years) and were more likely to be female (53% vs. 41%).
The ICIs used in the study included anti-CTLA4 (ipilimumab), anti–programmed death 1 (PD-1) (nivolumab or pembrolizumab), or a combination of nivolumab and ipilimumab. Of the patients with AID, 55% (n = 228) were treated with ICI, compared with 58% of patients without AID. A total of 87 AID patients were treated with anti-CTLA4, 187 received anti-PD-1, and 34 received the combination. The combination was not readily available in the Netherlands until 2017, the authors stated, acknowledging that it may be wise to revisit its effects in the coming years.
Incidence of immune-related adverse events
The incidence of immune-related adverse events (irAEs) grade 3 and above for patients with and without AID who were given anti-CTLA4 was 30%. The incidence rate of irAEs was also similar for patients with (17%; 95% confidence interval, 12%-23%) and without (13%; 95% CI, 12%-15%) AID on anti-PD-1. Patients with AIDs who took anti-PD-1 therapy discontinued it more often because of toxicity than did the patients without AIDs.
The combination group had irAE incidence rates of 44% (95% CI, 27%-62%) for patients with AID, compared with 48% (95% CI, 43%-53%) for patients without AIDs. Overall, no patients with AIDs on ICIs died of toxicity, compared with three deaths among patients without AID on anti-CTLA4, five deaths among patients on anti-PD-1, and one patient on the combination.
Patients with IBD had a notably higher risk of anti-PD-1–induced colitis (19%; 95% CI, 7%-37%), compared with patients with other AIDs (3%; 95% CI, 0%-6%) and patients without AIDs (2%; 95% CI, 2%-3%). IBD patients were also more likely than all other groups on ICIs to stop treatment because of toxicity, leading the researchers to note that “close monitoring in patients with IBD is advised.”
Overall survival after diagnosis was similar in patients with AIDs (median, 13 months; 95% CI, 10-16 months) and without (median, 14 months; 95% CI, 13-15 months), as was the objective response rate to anti-CTLA4 treatment (10% vs. 16%), anti-PD-1 treatment (40% vs. 44%), and combination therapy (39% vs. 43%).
Study largely bypasses the effects of checkpoint inhibitors on RA patients
“For detail, you can’t look to this study,” Anne R. Bass, MD, of the division of rheumatology at the Hospital for Special Surgery in New York, said in an interview. “But for a big-picture look at ‘how safe are checkpoint inhibitors,’ I think it’s an important one.”
Dr. Bass noted that the investigators lumped certain elements together and bypassed others, including their focus on grade 3 or higher adverse events. That was a decision the authors themselves recognized as a potential limitation of their research.
“Understandably, they were worried about life-threatening adverse events, and that’s fine,” she said. But for patients with arthritis who flare, their events are usually grade 2 or even grade 1 and therefore not captured or analyzed in the study. “This does not really address the risk of flare in an RA patient.”
She also questioned their grouping of AIDs, with a bevy of rheumatic diseases categorized as one cluster and the “other” group being particularly broad in its inclusion of “all AIDs not listed” – though only eight patients were placed into that group.
That said, the researchers relied on an oncology database, not one aimed at AID or adverse events. “The numbers are so much bigger than any other study in this area that’s been done,” she said. “It’s both a strength and a weakness of this kind of database.”
Indeed, the authors considered their use of nationwide, population-based data from the DMTR a benefit, calling it “a strength of our approach.”
The DMTR was funded by a grant from the Netherlands Organization for Health Research and Development and sponsored by Bristol-Myers Squibb, Novartis, Roche Nederland, Merck Sharp & Dohme, and Pierre Fabre via the Dutch Institute for Clinical Auditing.
Patients with advanced melanoma and preexisting autoimmune diseases (AIDs) who were treated with immune checkpoint inhibitors (ICIs) responded well and did not suffer more grade 3 or higher immune-related adverse events than patients without an AID, a new study finds, although some concerns were raised regarding patients with inflammatory bowel disease (IBD).
“To our knowledge, this is the first study to bridge this knowledge gap by presenting ‘real-world’ data on the safety and efficacy of ICI on a national scale,” wrote Monique K. van der Kooij, MD, of Leiden (the Netherlands) University Medical Center and coauthors. The study was published online in Annals of Internal Medicine.
To investigate ICI use and response among this specific subset of melanoma patients, the researchers launched a nationwide cohort study set in the Netherlands. Data were gathered via the Dutch Melanoma Treatment Registry (DMTR), in which 4,367 patients with advanced melanoma were enrolled between July 2013 and July 2018.
Within that cohort, 415 (9.5%) had preexisting AIDs. Nearly 55% had rheumatologic AIDs (n = 227) – which included RA, systemic lupus erythematosus, scleroderma, sarcoidosis, and vasculitis – with the next most frequent being endocrine AID (n = 143) and IBD (n = 55). Patients with AID were older than patients without (67 vs. 63 years) and were more likely to be female (53% vs. 41%).
The ICIs used in the study included anti-CTLA4 (ipilimumab), anti–programmed death 1 (PD-1) (nivolumab or pembrolizumab), or a combination of nivolumab and ipilimumab. Of the patients with AID, 55% (n = 228) were treated with ICI, compared with 58% of patients without AID. A total of 87 AID patients were treated with anti-CTLA4, 187 received anti-PD-1, and 34 received the combination. The combination was not readily available in the Netherlands until 2017, the authors stated, acknowledging that it may be wise to revisit its effects in the coming years.
Incidence of immune-related adverse events
The incidence of immune-related adverse events (irAEs) grade 3 and above for patients with and without AID who were given anti-CTLA4 was 30%. The incidence rate of irAEs was also similar for patients with (17%; 95% confidence interval, 12%-23%) and without (13%; 95% CI, 12%-15%) AID on anti-PD-1. Patients with AIDs who took anti-PD-1 therapy discontinued it more often because of toxicity than did the patients without AIDs.
The combination group had irAE incidence rates of 44% (95% CI, 27%-62%) for patients with AID, compared with 48% (95% CI, 43%-53%) for patients without AIDs. Overall, no patients with AIDs on ICIs died of toxicity, compared with three deaths among patients without AID on anti-CTLA4, five deaths among patients on anti-PD-1, and one patient on the combination.
Patients with IBD had a notably higher risk of anti-PD-1–induced colitis (19%; 95% CI, 7%-37%), compared with patients with other AIDs (3%; 95% CI, 0%-6%) and patients without AIDs (2%; 95% CI, 2%-3%). IBD patients were also more likely than all other groups on ICIs to stop treatment because of toxicity, leading the researchers to note that “close monitoring in patients with IBD is advised.”
Overall survival after diagnosis was similar in patients with AIDs (median, 13 months; 95% CI, 10-16 months) and without (median, 14 months; 95% CI, 13-15 months), as was the objective response rate to anti-CTLA4 treatment (10% vs. 16%), anti-PD-1 treatment (40% vs. 44%), and combination therapy (39% vs. 43%).
Study largely bypasses the effects of checkpoint inhibitors on RA patients
“For detail, you can’t look to this study,” Anne R. Bass, MD, of the division of rheumatology at the Hospital for Special Surgery in New York, said in an interview. “But for a big-picture look at ‘how safe are checkpoint inhibitors,’ I think it’s an important one.”
Dr. Bass noted that the investigators lumped certain elements together and bypassed others, including their focus on grade 3 or higher adverse events. That was a decision the authors themselves recognized as a potential limitation of their research.
“Understandably, they were worried about life-threatening adverse events, and that’s fine,” she said. But for patients with arthritis who flare, their events are usually grade 2 or even grade 1 and therefore not captured or analyzed in the study. “This does not really address the risk of flare in an RA patient.”
She also questioned their grouping of AIDs, with a bevy of rheumatic diseases categorized as one cluster and the “other” group being particularly broad in its inclusion of “all AIDs not listed” – though only eight patients were placed into that group.
That said, the researchers relied on an oncology database, not one aimed at AID or adverse events. “The numbers are so much bigger than any other study in this area that’s been done,” she said. “It’s both a strength and a weakness of this kind of database.”
Indeed, the authors considered their use of nationwide, population-based data from the DMTR a benefit, calling it “a strength of our approach.”
The DMTR was funded by a grant from the Netherlands Organization for Health Research and Development and sponsored by Bristol-Myers Squibb, Novartis, Roche Nederland, Merck Sharp & Dohme, and Pierre Fabre via the Dutch Institute for Clinical Auditing.
Patients with advanced melanoma and preexisting autoimmune diseases (AIDs) who were treated with immune checkpoint inhibitors (ICIs) responded well and did not suffer more grade 3 or higher immune-related adverse events than patients without an AID, a new study finds, although some concerns were raised regarding patients with inflammatory bowel disease (IBD).
“To our knowledge, this is the first study to bridge this knowledge gap by presenting ‘real-world’ data on the safety and efficacy of ICI on a national scale,” wrote Monique K. van der Kooij, MD, of Leiden (the Netherlands) University Medical Center and coauthors. The study was published online in Annals of Internal Medicine.
To investigate ICI use and response among this specific subset of melanoma patients, the researchers launched a nationwide cohort study set in the Netherlands. Data were gathered via the Dutch Melanoma Treatment Registry (DMTR), in which 4,367 patients with advanced melanoma were enrolled between July 2013 and July 2018.
Within that cohort, 415 (9.5%) had preexisting AIDs. Nearly 55% had rheumatologic AIDs (n = 227) – which included RA, systemic lupus erythematosus, scleroderma, sarcoidosis, and vasculitis – with the next most frequent being endocrine AID (n = 143) and IBD (n = 55). Patients with AID were older than patients without (67 vs. 63 years) and were more likely to be female (53% vs. 41%).
The ICIs used in the study included anti-CTLA4 (ipilimumab), anti–programmed death 1 (PD-1) (nivolumab or pembrolizumab), or a combination of nivolumab and ipilimumab. Of the patients with AID, 55% (n = 228) were treated with ICI, compared with 58% of patients without AID. A total of 87 AID patients were treated with anti-CTLA4, 187 received anti-PD-1, and 34 received the combination. The combination was not readily available in the Netherlands until 2017, the authors stated, acknowledging that it may be wise to revisit its effects in the coming years.
Incidence of immune-related adverse events
The incidence of immune-related adverse events (irAEs) grade 3 and above for patients with and without AID who were given anti-CTLA4 was 30%. The incidence rate of irAEs was also similar for patients with (17%; 95% confidence interval, 12%-23%) and without (13%; 95% CI, 12%-15%) AID on anti-PD-1. Patients with AIDs who took anti-PD-1 therapy discontinued it more often because of toxicity than did the patients without AIDs.
The combination group had irAE incidence rates of 44% (95% CI, 27%-62%) for patients with AID, compared with 48% (95% CI, 43%-53%) for patients without AIDs. Overall, no patients with AIDs on ICIs died of toxicity, compared with three deaths among patients without AID on anti-CTLA4, five deaths among patients on anti-PD-1, and one patient on the combination.
Patients with IBD had a notably higher risk of anti-PD-1–induced colitis (19%; 95% CI, 7%-37%), compared with patients with other AIDs (3%; 95% CI, 0%-6%) and patients without AIDs (2%; 95% CI, 2%-3%). IBD patients were also more likely than all other groups on ICIs to stop treatment because of toxicity, leading the researchers to note that “close monitoring in patients with IBD is advised.”
Overall survival after diagnosis was similar in patients with AIDs (median, 13 months; 95% CI, 10-16 months) and without (median, 14 months; 95% CI, 13-15 months), as was the objective response rate to anti-CTLA4 treatment (10% vs. 16%), anti-PD-1 treatment (40% vs. 44%), and combination therapy (39% vs. 43%).
Study largely bypasses the effects of checkpoint inhibitors on RA patients
“For detail, you can’t look to this study,” Anne R. Bass, MD, of the division of rheumatology at the Hospital for Special Surgery in New York, said in an interview. “But for a big-picture look at ‘how safe are checkpoint inhibitors,’ I think it’s an important one.”
Dr. Bass noted that the investigators lumped certain elements together and bypassed others, including their focus on grade 3 or higher adverse events. That was a decision the authors themselves recognized as a potential limitation of their research.
“Understandably, they were worried about life-threatening adverse events, and that’s fine,” she said. But for patients with arthritis who flare, their events are usually grade 2 or even grade 1 and therefore not captured or analyzed in the study. “This does not really address the risk of flare in an RA patient.”
She also questioned their grouping of AIDs, with a bevy of rheumatic diseases categorized as one cluster and the “other” group being particularly broad in its inclusion of “all AIDs not listed” – though only eight patients were placed into that group.
That said, the researchers relied on an oncology database, not one aimed at AID or adverse events. “The numbers are so much bigger than any other study in this area that’s been done,” she said. “It’s both a strength and a weakness of this kind of database.”
Indeed, the authors considered their use of nationwide, population-based data from the DMTR a benefit, calling it “a strength of our approach.”
The DMTR was funded by a grant from the Netherlands Organization for Health Research and Development and sponsored by Bristol-Myers Squibb, Novartis, Roche Nederland, Merck Sharp & Dohme, and Pierre Fabre via the Dutch Institute for Clinical Auditing.
FROM ANNALS OF INTERNAL MEDICINE
Cumulative exposure to high-potency topical steroid doses drives osteoporosis fractures
In support of previously published case reports, in a dose-response relationship.
In a stepwise manner, the hazard ratios for major osteoporotic fracture (MOF) were found to start climbing incrementally for those with a cumulative topical steroid dose equivalent of more than 500 g of mometasone furoate when compared with exposure of 200-499 g, according to the team of investigators from the University of Copenhagen.
“Use of these drugs is very common, and we found an estimated population-attributable risk of as much as 4.3%,” the investigators reported in the study, published in JAMA Dermatology.
The retrospective cohort study drew data from the Danish National Patient Registry, which covers 99% of the country’s population. It was linked to the Danish National Prescription Registry, which captures data on pharmacy-dispensed medications. Data collected from the beginning of 2003 to the end of 2017 were evaluated.
Exposures to potent or very potent topical corticosteroids were converted into a single standard with potency equivalent to 1 mg/g of mometasone furoate. Four strata of exposure were compared to a reference exposure of 200-499 g. These were 500-999 g, 1,000-1,999 g, 2,000-9,999 g, and 10,000 g or greater.
For the first strata, the small increased risk for MOF did not reach significance (HR, 1.01; 95% confidence interval, 0.99-1.03), but each of the others did. These climbed from a 5% greater risk (HR 1.05 95% CI 1.02-1.08) for a cumulative exposure of 1,000 to 1,999 g, to a 10% greater risk (HR, 1.10; 95% CI, 1.07-1.13) for a cumulative exposure of 2,000-9,999 g, and finally to a 27% greater risk (HR, 1.27; 95% CI, 1.19-1.35) for a cumulative exposure of 10,000 g or higher.
The study included more than 700,000 individuals exposed to topical mometasone at a potency equivalent of 200 g or more over the study period. The reference group (200-499 g) was the largest (317,907 individuals). The first strata (500-999 g) included 186,359 patients; the second (1,000-1,999 g), 111,203 patients; the third (2,000-9,999 g), 94,334 patients; and the fifth (10,000 g or more), 13,448 patients.
“A 3% increase in the relative risk of osteoporosis and MOF was observed per doubling of the TCS dose,” according to the investigators.
Patients exposed to doses of high-potency topical steroids that put them at risk of MOF is limited but substantial, according to the senior author, Alexander Egeberg, MD, PhD, of the department of dermatology and allergy at Herlev and Gentofte Hospital, Copenhagen.
“It is true that the risk is modest for the average user of topical steroids,” Dr. Egeberg said in an interview. However, despite the fact that topical steroids are intended for short-term use, “2% of all our users had been exposed to the equivalent of 10,000 g of mometasone, which mean 100 tubes of 100 g.”
If the other two strata at significantly increased risk of MOF (greater than 1,000 g) are included, an additional 28% of all users are facing the potential for clinically significant osteoporosis, according to the Danish data.
The adverse effect of steroids on bone metabolism has been established previously, and several studies have linked systemic corticosteroid exposure, including inhaled corticosteroids, with increased risk of osteoporotic fracture. For example, one study showed that patients with chronic obstructive pulmonary disease on daily inhaled doses of the equivalent of fluticasone at or above 1,000 mcg for more than 4 years had about a 10% increased risk of MOF relative to those not exposed.
The data associate topical steroids with increased risk of osteoporotic fracture, but Dr. Egeberg said osteoporosis is not the only reason to use topical steroids prudently.
“It is important to keep in mind that osteoporosis and fractures are at the extreme end of the side-effect profile and that other side effects, such as striae formation, skin thinning, and dysregulated diabetes, can occur with much lower quantities of topical steroids,” Dr. Egeberg said
For avoiding this risk, “there are no specific cutoffs” recommended for topical steroids in current guidelines, but dermatologists should be aware that many of the indications for topical steroids, such as psoriasis and atopic dermatitis, involve skin with an impaired barrier function, exposing patients to an increased likelihood of absorption, according to Dr. Egeberg.
“A general rule of thumb that we use is that, if a patient with persistent disease activity requires a new prescription of the equivalent of 100 g mometasone every 1-2 months, it might be worth considering if there is a suitable alternative,” Dr. Egeberg said.
In an accompanying editorial, Rebecca D. Jackson, MD, of the division of endocrinology, diabetes, and metabolism in the department of internal medicine at Ohio State University, Columbus, agreed that no guidelines specific to avoiding the risks of topical corticosteroids are currently available, but she advised clinicians to be considering these risks nonetheless. In general, she suggested that topical steroids, like oral steroids, should be used at “the lowest dose for the shortest duration necessary to manage the underlying medical condition.”
The correlation between topical corticosteroids and increased risk of osteoporotic fracture, although not established previously in a large study, is not surprising, according to Victoria Werth, MD, chief of dermatology at the Philadelphia Veterans Affairs Hospital and professor of dermatology at the University of Pennsylvania, also in Philadelphia.
“Systemic absorption of potent topical steroids has previously been demonstrated with a rapid decrease in serum cortisol levels,” Dr. Werth said in an interview. She indicated that concern about the risk of osteoporosis imposed by use of potent steroids over large body surface areas is appropriate.
To minimize this risk, “it is reasonable to use the lowest dose of steroid possible and to try to substitute other medications when possible,” she said.
Dr. Egeberg reported financial relationships with Abbvie, Almirall, Bristol-Myers Squibb, Dermavant Sciences, Galderma, Janssen Pharmaceuticals, Eli Lilly, Novartis, Pfizer, Samsung, Bioepis, and UCB. Five authors had disclosures related to some of those pharmaceutical companies and/or others. Dr. Jackson had no disclosures.
In support of previously published case reports, in a dose-response relationship.
In a stepwise manner, the hazard ratios for major osteoporotic fracture (MOF) were found to start climbing incrementally for those with a cumulative topical steroid dose equivalent of more than 500 g of mometasone furoate when compared with exposure of 200-499 g, according to the team of investigators from the University of Copenhagen.
“Use of these drugs is very common, and we found an estimated population-attributable risk of as much as 4.3%,” the investigators reported in the study, published in JAMA Dermatology.
The retrospective cohort study drew data from the Danish National Patient Registry, which covers 99% of the country’s population. It was linked to the Danish National Prescription Registry, which captures data on pharmacy-dispensed medications. Data collected from the beginning of 2003 to the end of 2017 were evaluated.
Exposures to potent or very potent topical corticosteroids were converted into a single standard with potency equivalent to 1 mg/g of mometasone furoate. Four strata of exposure were compared to a reference exposure of 200-499 g. These were 500-999 g, 1,000-1,999 g, 2,000-9,999 g, and 10,000 g or greater.
For the first strata, the small increased risk for MOF did not reach significance (HR, 1.01; 95% confidence interval, 0.99-1.03), but each of the others did. These climbed from a 5% greater risk (HR 1.05 95% CI 1.02-1.08) for a cumulative exposure of 1,000 to 1,999 g, to a 10% greater risk (HR, 1.10; 95% CI, 1.07-1.13) for a cumulative exposure of 2,000-9,999 g, and finally to a 27% greater risk (HR, 1.27; 95% CI, 1.19-1.35) for a cumulative exposure of 10,000 g or higher.
The study included more than 700,000 individuals exposed to topical mometasone at a potency equivalent of 200 g or more over the study period. The reference group (200-499 g) was the largest (317,907 individuals). The first strata (500-999 g) included 186,359 patients; the second (1,000-1,999 g), 111,203 patients; the third (2,000-9,999 g), 94,334 patients; and the fifth (10,000 g or more), 13,448 patients.
“A 3% increase in the relative risk of osteoporosis and MOF was observed per doubling of the TCS dose,” according to the investigators.
Patients exposed to doses of high-potency topical steroids that put them at risk of MOF is limited but substantial, according to the senior author, Alexander Egeberg, MD, PhD, of the department of dermatology and allergy at Herlev and Gentofte Hospital, Copenhagen.
“It is true that the risk is modest for the average user of topical steroids,” Dr. Egeberg said in an interview. However, despite the fact that topical steroids are intended for short-term use, “2% of all our users had been exposed to the equivalent of 10,000 g of mometasone, which mean 100 tubes of 100 g.”
If the other two strata at significantly increased risk of MOF (greater than 1,000 g) are included, an additional 28% of all users are facing the potential for clinically significant osteoporosis, according to the Danish data.
The adverse effect of steroids on bone metabolism has been established previously, and several studies have linked systemic corticosteroid exposure, including inhaled corticosteroids, with increased risk of osteoporotic fracture. For example, one study showed that patients with chronic obstructive pulmonary disease on daily inhaled doses of the equivalent of fluticasone at or above 1,000 mcg for more than 4 years had about a 10% increased risk of MOF relative to those not exposed.
The data associate topical steroids with increased risk of osteoporotic fracture, but Dr. Egeberg said osteoporosis is not the only reason to use topical steroids prudently.
“It is important to keep in mind that osteoporosis and fractures are at the extreme end of the side-effect profile and that other side effects, such as striae formation, skin thinning, and dysregulated diabetes, can occur with much lower quantities of topical steroids,” Dr. Egeberg said
For avoiding this risk, “there are no specific cutoffs” recommended for topical steroids in current guidelines, but dermatologists should be aware that many of the indications for topical steroids, such as psoriasis and atopic dermatitis, involve skin with an impaired barrier function, exposing patients to an increased likelihood of absorption, according to Dr. Egeberg.
“A general rule of thumb that we use is that, if a patient with persistent disease activity requires a new prescription of the equivalent of 100 g mometasone every 1-2 months, it might be worth considering if there is a suitable alternative,” Dr. Egeberg said.
In an accompanying editorial, Rebecca D. Jackson, MD, of the division of endocrinology, diabetes, and metabolism in the department of internal medicine at Ohio State University, Columbus, agreed that no guidelines specific to avoiding the risks of topical corticosteroids are currently available, but she advised clinicians to be considering these risks nonetheless. In general, she suggested that topical steroids, like oral steroids, should be used at “the lowest dose for the shortest duration necessary to manage the underlying medical condition.”
The correlation between topical corticosteroids and increased risk of osteoporotic fracture, although not established previously in a large study, is not surprising, according to Victoria Werth, MD, chief of dermatology at the Philadelphia Veterans Affairs Hospital and professor of dermatology at the University of Pennsylvania, also in Philadelphia.
“Systemic absorption of potent topical steroids has previously been demonstrated with a rapid decrease in serum cortisol levels,” Dr. Werth said in an interview. She indicated that concern about the risk of osteoporosis imposed by use of potent steroids over large body surface areas is appropriate.
To minimize this risk, “it is reasonable to use the lowest dose of steroid possible and to try to substitute other medications when possible,” she said.
Dr. Egeberg reported financial relationships with Abbvie, Almirall, Bristol-Myers Squibb, Dermavant Sciences, Galderma, Janssen Pharmaceuticals, Eli Lilly, Novartis, Pfizer, Samsung, Bioepis, and UCB. Five authors had disclosures related to some of those pharmaceutical companies and/or others. Dr. Jackson had no disclosures.
In support of previously published case reports, in a dose-response relationship.
In a stepwise manner, the hazard ratios for major osteoporotic fracture (MOF) were found to start climbing incrementally for those with a cumulative topical steroid dose equivalent of more than 500 g of mometasone furoate when compared with exposure of 200-499 g, according to the team of investigators from the University of Copenhagen.
“Use of these drugs is very common, and we found an estimated population-attributable risk of as much as 4.3%,” the investigators reported in the study, published in JAMA Dermatology.
The retrospective cohort study drew data from the Danish National Patient Registry, which covers 99% of the country’s population. It was linked to the Danish National Prescription Registry, which captures data on pharmacy-dispensed medications. Data collected from the beginning of 2003 to the end of 2017 were evaluated.
Exposures to potent or very potent topical corticosteroids were converted into a single standard with potency equivalent to 1 mg/g of mometasone furoate. Four strata of exposure were compared to a reference exposure of 200-499 g. These were 500-999 g, 1,000-1,999 g, 2,000-9,999 g, and 10,000 g or greater.
For the first strata, the small increased risk for MOF did not reach significance (HR, 1.01; 95% confidence interval, 0.99-1.03), but each of the others did. These climbed from a 5% greater risk (HR 1.05 95% CI 1.02-1.08) for a cumulative exposure of 1,000 to 1,999 g, to a 10% greater risk (HR, 1.10; 95% CI, 1.07-1.13) for a cumulative exposure of 2,000-9,999 g, and finally to a 27% greater risk (HR, 1.27; 95% CI, 1.19-1.35) for a cumulative exposure of 10,000 g or higher.
The study included more than 700,000 individuals exposed to topical mometasone at a potency equivalent of 200 g or more over the study period. The reference group (200-499 g) was the largest (317,907 individuals). The first strata (500-999 g) included 186,359 patients; the second (1,000-1,999 g), 111,203 patients; the third (2,000-9,999 g), 94,334 patients; and the fifth (10,000 g or more), 13,448 patients.
“A 3% increase in the relative risk of osteoporosis and MOF was observed per doubling of the TCS dose,” according to the investigators.
Patients exposed to doses of high-potency topical steroids that put them at risk of MOF is limited but substantial, according to the senior author, Alexander Egeberg, MD, PhD, of the department of dermatology and allergy at Herlev and Gentofte Hospital, Copenhagen.
“It is true that the risk is modest for the average user of topical steroids,” Dr. Egeberg said in an interview. However, despite the fact that topical steroids are intended for short-term use, “2% of all our users had been exposed to the equivalent of 10,000 g of mometasone, which mean 100 tubes of 100 g.”
If the other two strata at significantly increased risk of MOF (greater than 1,000 g) are included, an additional 28% of all users are facing the potential for clinically significant osteoporosis, according to the Danish data.
The adverse effect of steroids on bone metabolism has been established previously, and several studies have linked systemic corticosteroid exposure, including inhaled corticosteroids, with increased risk of osteoporotic fracture. For example, one study showed that patients with chronic obstructive pulmonary disease on daily inhaled doses of the equivalent of fluticasone at or above 1,000 mcg for more than 4 years had about a 10% increased risk of MOF relative to those not exposed.
The data associate topical steroids with increased risk of osteoporotic fracture, but Dr. Egeberg said osteoporosis is not the only reason to use topical steroids prudently.
“It is important to keep in mind that osteoporosis and fractures are at the extreme end of the side-effect profile and that other side effects, such as striae formation, skin thinning, and dysregulated diabetes, can occur with much lower quantities of topical steroids,” Dr. Egeberg said
For avoiding this risk, “there are no specific cutoffs” recommended for topical steroids in current guidelines, but dermatologists should be aware that many of the indications for topical steroids, such as psoriasis and atopic dermatitis, involve skin with an impaired barrier function, exposing patients to an increased likelihood of absorption, according to Dr. Egeberg.
“A general rule of thumb that we use is that, if a patient with persistent disease activity requires a new prescription of the equivalent of 100 g mometasone every 1-2 months, it might be worth considering if there is a suitable alternative,” Dr. Egeberg said.
In an accompanying editorial, Rebecca D. Jackson, MD, of the division of endocrinology, diabetes, and metabolism in the department of internal medicine at Ohio State University, Columbus, agreed that no guidelines specific to avoiding the risks of topical corticosteroids are currently available, but she advised clinicians to be considering these risks nonetheless. In general, she suggested that topical steroids, like oral steroids, should be used at “the lowest dose for the shortest duration necessary to manage the underlying medical condition.”
The correlation between topical corticosteroids and increased risk of osteoporotic fracture, although not established previously in a large study, is not surprising, according to Victoria Werth, MD, chief of dermatology at the Philadelphia Veterans Affairs Hospital and professor of dermatology at the University of Pennsylvania, also in Philadelphia.
“Systemic absorption of potent topical steroids has previously been demonstrated with a rapid decrease in serum cortisol levels,” Dr. Werth said in an interview. She indicated that concern about the risk of osteoporosis imposed by use of potent steroids over large body surface areas is appropriate.
To minimize this risk, “it is reasonable to use the lowest dose of steroid possible and to try to substitute other medications when possible,” she said.
Dr. Egeberg reported financial relationships with Abbvie, Almirall, Bristol-Myers Squibb, Dermavant Sciences, Galderma, Janssen Pharmaceuticals, Eli Lilly, Novartis, Pfizer, Samsung, Bioepis, and UCB. Five authors had disclosures related to some of those pharmaceutical companies and/or others. Dr. Jackson had no disclosures.
FROM JAMA DERMATOLOGY
TNF inhibitors may slow spinal progression in axial spondyloarthritis
Patients with axial spondyloarthritis showed reduced spinal radiographic progression after treatment with tumor necrosis factor (TNF) inhibitors, based on data from 314 adults in a prospective cohort study.
Evidence of a link between inflammation and axial damage in patients with axial spondyloarthritis (axSpA) has been reported, and these patients are routinely treated with NSAIDs and TNF inhibitors (TNFi), wrote Alexandre Sepriano, MD, PhD, of Leiden (the Netherlands) University Medical Center, and colleagues.
“However, and despite significant efforts, it remains to be clarified whether there is also an effect of these drugs on axial damage accrual,” they noted.
In a study published in Arthritis & Rheumatology, the researchers recruited consecutive patients from rheumatology practices in Northern Alberta to enroll in the Follow Up Research Cohort in Ankylosing Spondylitis Treatment (ALBERTA FORCAST) observational cohort study. The average age of the patients was 41 years, 74% were men, 83% were HLA-B27 positive, and the average duration of symptoms was 18 years.
Progression was measured via spine radiographs every 2 years for up to 10 years; the radiographs were scored using the modified Stoke Ankylosing Spondylitis Spine Score (mSASSS). In addition, the researchers assessed the interaction between TNFi exposure and clinical disease activity using the Ankylosing Spondylitis Disease Activity Score (ASDAS) and the impact on mSASSS every 2 years. The analysis included 442 2-year intervals.
Overall, the researchers found a significant interaction between ASDAS and TNFi at the start of the interval, followed by gradient effect of ASDAS at the start of the interval on mSASSS 2 years later, which was more than twice as high in patients never treated with TNFi (beta = 0.41), compared with patients who were continuously treated with a TNFi (beta = 0.16).
“Similarly, patients treated with TNFi were 30% less likely to develop a new syndesmophyte 2 years later compared to those not treated,” the researchers said.
TNFi also directly slowed progression, as treated patients averaged 0.85 mSASSS units less 2 years later, compared with untreated patients.
Of note, “treatment with NSAIDs during follow-up was neither associated with the outcome nor did it modify or confound the association between TNFi and mSASSS,” the researchers said. In addition, “the direct effect of TNFi on mSASSS was still present after adjusting for a propensity score,” they wrote.
The study results were limited by several factors including the observational design, lack of data on long-term treatment effects, and inability to assess individual TNFi drugs separately, the researchers noted.
However, “the present study informs the rheumatology community by addressing the question as to whether or not TNFi inhibit radiographic progression in axSpA and if this effect is mediated solely by their effects on inflammation, as measured by the ASDAS, or whether additional mechanisms may be relevant,” they emphasized.
“A better understanding of these mechanisms might open avenues to further treatment strategies that might finally lead to effective disease modification in axial SpA,” they concluded.
The ALBERTA FORCAST study was supported by AbbVie. Several authors disclosed financial relationships with AbbVie and other manufacturers of TNFi.
Patients with axial spondyloarthritis showed reduced spinal radiographic progression after treatment with tumor necrosis factor (TNF) inhibitors, based on data from 314 adults in a prospective cohort study.
Evidence of a link between inflammation and axial damage in patients with axial spondyloarthritis (axSpA) has been reported, and these patients are routinely treated with NSAIDs and TNF inhibitors (TNFi), wrote Alexandre Sepriano, MD, PhD, of Leiden (the Netherlands) University Medical Center, and colleagues.
“However, and despite significant efforts, it remains to be clarified whether there is also an effect of these drugs on axial damage accrual,” they noted.
In a study published in Arthritis & Rheumatology, the researchers recruited consecutive patients from rheumatology practices in Northern Alberta to enroll in the Follow Up Research Cohort in Ankylosing Spondylitis Treatment (ALBERTA FORCAST) observational cohort study. The average age of the patients was 41 years, 74% were men, 83% were HLA-B27 positive, and the average duration of symptoms was 18 years.
Progression was measured via spine radiographs every 2 years for up to 10 years; the radiographs were scored using the modified Stoke Ankylosing Spondylitis Spine Score (mSASSS). In addition, the researchers assessed the interaction between TNFi exposure and clinical disease activity using the Ankylosing Spondylitis Disease Activity Score (ASDAS) and the impact on mSASSS every 2 years. The analysis included 442 2-year intervals.
Overall, the researchers found a significant interaction between ASDAS and TNFi at the start of the interval, followed by gradient effect of ASDAS at the start of the interval on mSASSS 2 years later, which was more than twice as high in patients never treated with TNFi (beta = 0.41), compared with patients who were continuously treated with a TNFi (beta = 0.16).
“Similarly, patients treated with TNFi were 30% less likely to develop a new syndesmophyte 2 years later compared to those not treated,” the researchers said.
TNFi also directly slowed progression, as treated patients averaged 0.85 mSASSS units less 2 years later, compared with untreated patients.
Of note, “treatment with NSAIDs during follow-up was neither associated with the outcome nor did it modify or confound the association between TNFi and mSASSS,” the researchers said. In addition, “the direct effect of TNFi on mSASSS was still present after adjusting for a propensity score,” they wrote.
The study results were limited by several factors including the observational design, lack of data on long-term treatment effects, and inability to assess individual TNFi drugs separately, the researchers noted.
However, “the present study informs the rheumatology community by addressing the question as to whether or not TNFi inhibit radiographic progression in axSpA and if this effect is mediated solely by their effects on inflammation, as measured by the ASDAS, or whether additional mechanisms may be relevant,” they emphasized.
“A better understanding of these mechanisms might open avenues to further treatment strategies that might finally lead to effective disease modification in axial SpA,” they concluded.
The ALBERTA FORCAST study was supported by AbbVie. Several authors disclosed financial relationships with AbbVie and other manufacturers of TNFi.
Patients with axial spondyloarthritis showed reduced spinal radiographic progression after treatment with tumor necrosis factor (TNF) inhibitors, based on data from 314 adults in a prospective cohort study.
Evidence of a link between inflammation and axial damage in patients with axial spondyloarthritis (axSpA) has been reported, and these patients are routinely treated with NSAIDs and TNF inhibitors (TNFi), wrote Alexandre Sepriano, MD, PhD, of Leiden (the Netherlands) University Medical Center, and colleagues.
“However, and despite significant efforts, it remains to be clarified whether there is also an effect of these drugs on axial damage accrual,” they noted.
In a study published in Arthritis & Rheumatology, the researchers recruited consecutive patients from rheumatology practices in Northern Alberta to enroll in the Follow Up Research Cohort in Ankylosing Spondylitis Treatment (ALBERTA FORCAST) observational cohort study. The average age of the patients was 41 years, 74% were men, 83% were HLA-B27 positive, and the average duration of symptoms was 18 years.
Progression was measured via spine radiographs every 2 years for up to 10 years; the radiographs were scored using the modified Stoke Ankylosing Spondylitis Spine Score (mSASSS). In addition, the researchers assessed the interaction between TNFi exposure and clinical disease activity using the Ankylosing Spondylitis Disease Activity Score (ASDAS) and the impact on mSASSS every 2 years. The analysis included 442 2-year intervals.
Overall, the researchers found a significant interaction between ASDAS and TNFi at the start of the interval, followed by gradient effect of ASDAS at the start of the interval on mSASSS 2 years later, which was more than twice as high in patients never treated with TNFi (beta = 0.41), compared with patients who were continuously treated with a TNFi (beta = 0.16).
“Similarly, patients treated with TNFi were 30% less likely to develop a new syndesmophyte 2 years later compared to those not treated,” the researchers said.
TNFi also directly slowed progression, as treated patients averaged 0.85 mSASSS units less 2 years later, compared with untreated patients.
Of note, “treatment with NSAIDs during follow-up was neither associated with the outcome nor did it modify or confound the association between TNFi and mSASSS,” the researchers said. In addition, “the direct effect of TNFi on mSASSS was still present after adjusting for a propensity score,” they wrote.
The study results were limited by several factors including the observational design, lack of data on long-term treatment effects, and inability to assess individual TNFi drugs separately, the researchers noted.
However, “the present study informs the rheumatology community by addressing the question as to whether or not TNFi inhibit radiographic progression in axSpA and if this effect is mediated solely by their effects on inflammation, as measured by the ASDAS, or whether additional mechanisms may be relevant,” they emphasized.
“A better understanding of these mechanisms might open avenues to further treatment strategies that might finally lead to effective disease modification in axial SpA,” they concluded.
The ALBERTA FORCAST study was supported by AbbVie. Several authors disclosed financial relationships with AbbVie and other manufacturers of TNFi.
FROM ARTHRITIS & RHEUMATOLOGY
Rheumatologic disease activity an important influencer of COVID-19 death risk
People with rheumatic and musculoskeletal diseases (RMDs) who contract the SARS-CoV-2 virus appear more likely to die from COVID-19 if their rheumatologic condition is not being well controlled at the time of their infection.
New data from the COVID-19 Global Rheumatology Alliance (GRA) physician registry reported in Annals of the Rheumatic Diseases have found that the odds of dying from COVID-19 were 87% higher in individuals recorded as having moderate to high disease activity versus those reported to be in remission or having low disease activity.
“I think this really highlights the importance of continuing to appropriately, and actively, treat our patients, and the importance of controlling their disease,” Pedro Machado, MD, PhD, said in an interview. Dr. Machado, an associate professor in rheumatology and muscle diseases at University College London and a consultant rheumatologist at several U.K. hospitals, has been involved in the GRA physician registry from the start, and sits on the GRA steering committee.
Alongside higher disease activity, several other important factors were found to be associated with increased odds of dying from COVID-19 – older age, male gender, and the presence of one or more comorbidities, such as hypertension combined with cardiovascular disease or chronic lung disease.
These demographic and disease-based factors have been linked to an increased risk for COVID-19–related hospitalization before, both in people with RMDs and in the general population, but the latest GRA physician registry data now take that a step further, and link them also to an increased risk for death, together with several other factors more specific to RMDs.
Logging COVID-19 rheumatologic cases
Since the start of the global pandemic, the potential effects that SARS-CoV-2 infection might have on people with RMDs in particular has concerned the rheumatology community. The main worries being that, either because of the underlying RMD itself or to its treatment, there may be immunoregulatory deficits or other risk factors that would make individuals more susceptible to not only infection but also to developing more severe COVID-19 than the general population.
These concerns led to the rapid formation of the GRA and the COVID-19 GRA physician registry in March 2020 to collect and analyze data on adults with rheumatic disease and confirmed or presumptive COVID-19. Entries into the registry are made by or under the direction of rheumatologists, and this is a voluntary process.
“This population cannot ever be entirely representative of the population of patients with rheumatic diseases,” Dr. Machado acknowledged. There will be selection and other biases that affect the reported data. That said, it’s the largest database of reported COVID-19 cases in adult rheumatology patients across the world, with more than 9,000 cases so far included from multiple registries, including those based in Europe and North and South America. Data from one of these – the French RMD cohort – have also recently been published in Annals of the Rheumatic Diseases, showing much the same findings but on a national level.
Hospitalization was the focus of a previous report because “you need large sample sizes” to look at endpoints that occur less frequently. When the first analysis was done, there were around 600 cases from 40 countries in the registry with sufficient data that could be used. Now, with a greater number of recorded cases, factors influencing the risk for death could be examined.
Death rate and risk factors found
Data on 3,729 COVID-19 cases in people with RMDs were included in the current analysis, all recorded in the first few months of the registry being open and up until July 1, 2020. In all, 390 (10.5%) of people died. While this is “clearly higher” than reported in the general population in most countries, the analysis was not designed to calculate a precise estimate.
“It should not be taken as an estimate of the overall death rate among patients with rheumatic diseases and COVID-19,” Dr. Machado and coauthors have been keen to point out.
“Age is always the biggest risk factor,” Dr. Machado explained. “There’s always a gradient: the older the patient, the worse the outcome.”
Indeed, there was a threefold increased risk for death among those aged 66-75 years versus those who were 65 years or younger (odds ratio, 3.00), and a sixfold increased risk for patients older than 75, compared with the younger age group (OR, 6.18).
Having both hypertension and cardiovascular disease was associated with an OR of 1.89, and coexisting chronic lung disease also significantly increased the chances of dying from COVID-19 (OR, 1.68).
Being of male sex was associated with a 46% increased risk for death from COVID-19 versus being of female sex.
The risk for COVID-19 death also rose with the use of corticosteroids. Compared with no steroid use, there was a 69% increased risk for with death at doses of 10 mg or more prednisolone equivalent per day.
“The finding about moderate to high doses of steroids being associated with a worse outcome is consistent with the first report; it was the same for hospitalization,” Dr. Machado observed.
The general consensus on steroid use in the COVID-19 setting is that they should be continued as needed, but at the lowest possible dose, as outlined in provisional recommendations set out by the recently renamed European Alliance of Associations for Rheumatology.
The GRA physician registry findings provide further support for this, suggesting that disease control should be optimized with disease-modifying antirheumatic drugs, ideally without increasing the dose of steroids.
Surprise over sulfasalazine risk
“Taking all medications into account – such as methotrexate, leflunomide, hydroxychloroquine, [tumor necrosis factor] blockers, interleukin-6 blockers, and [Janus kinase] inhibitors – it is quite reassuring because we did not see an association with worse outcome with those drugs overall,” Dr. Machado said.
However, treatment with rituximab (OR, 4.0), sulfasalazine (OR, 3.6), and immunosuppressive agents such as azathioprine, cyclophosphamide, cyclosporine, mycophenolate, or tacrolimus (OR, 2.2), were associated with higher odds of dying from COVID-19 when compared with treatment with methotrexate alone.
The findings for rituximab and immunosuppressant use were perhaps not unexpected, but the possible association between sulfasalazine and COVID-19 death was “a bit intriguing,” Dr. Machado observed. “Sulfasalazine is believed to have low immunosuppressive effect.”
This warrants further investigation, but there are likely a range of confounding factors at play. One could be that people considered to be at higher risk may have been more often prescribed sulfasalazine because it was thought to be less immunosuppressive. Another might be because people taking sulfasalazine were more likely to be smokers, and they were also not advised to protect themselves from exposure to the virus (shielding) during the first wave of the pandemic, at least not in the United Kingdom.
Rituximab caution and vaccination
“Rituximab is a concern,” Dr. Machado acknowledged. “It is a concern that rheumatologists are now aware of and they are addressing, but then it’s a concern for a very specific subgroup of patients.”
While rheumatologists are, and will continue to prescribe it, there will be even more careful consideration over when, in whom, and how to use it during, and possibly even after, the pandemic.
“COVID is here to stay, it will become endemic, and it’s going to be part of our lives like the flu virus is,” Dr. Machado predicted.
Then there is the issue on vaccinating people against COVID-19, should those on rituximab still receive it? The answer is a yes, but, as with other vaccinations it’s all about the timing of when the vaccination is given.
Societies such as the British Society for Rheumatology have already begun to include guidance on this, recommending one of the available COVID-19 vaccines is given at least a month before the next or first dose of rituximab is due. As rituximab is given every few months, with doses sometimes spaced as much as 9 months or even a year apart, this should not be too much of a problem, but it is “better to have the vaccine first,” Dr. Machado said.
Has COVID-19 care improved in RMDs?
In separate research published in The Lancet Rheumatology, April Jorge, MD, of Massachusetts General Hospital and Harvard Medical School, both in Boston, and associates found that the risks of severe COVID-19 outcomes have improved over time, although they still “remain substantial.”
Dr. Jorge and colleagues looked at temporal trends in COVID-19 outcomes in patients with RMDs over the course of the first 6 months of the pandemic in 2020, using data from a large, multicenter, electronic health record network (TriNetX).
They formed two patient cohorts – a late (diagnosed from April 20 to July 20) and an early (diagnosed from January 20 to April 20) cohort – to see if outcomes had improved and discovered lower relative risks among patients in the late cohort for hospitalization (0.67), admission to the ICU (0.56), mechanical ventilation (0.39), acute kidney injury (0.66), renal replacement (0.53), and death (0.39).
“These results are encouraging,” but it’s difficult to match these different populations of patients, Dr. Machado said. “There are always factors that you cannot match for” and were not included in the U.S. analysis.
While there are important caveats in how the analysis was performed and thus in interpreting these data, they do “suggest that one of the reasons why outcomes have improved is because we have become better at treating these patients,” Dr. Machado added.
“Our treatment has improved, and our capacity to treat the complications has improved. We understand better how the disease behaves – we know that they can have thromboembolic complications that we can manage, and we are now able to manage ventilation issues better.”
Moreover, Dr. Machado said that, not only were clinicians more aware of what they should or should not do, there were treatments that were being used routinely or in some cases based on recent clinical trial results. “I think we are indeed treating these patients better.”
The COVID-19 GRA physician registry is financially supported by the American College of Rheumatology and EULAR. Dr. Machado had no relevant conflicts of interest.
People with rheumatic and musculoskeletal diseases (RMDs) who contract the SARS-CoV-2 virus appear more likely to die from COVID-19 if their rheumatologic condition is not being well controlled at the time of their infection.
New data from the COVID-19 Global Rheumatology Alliance (GRA) physician registry reported in Annals of the Rheumatic Diseases have found that the odds of dying from COVID-19 were 87% higher in individuals recorded as having moderate to high disease activity versus those reported to be in remission or having low disease activity.
“I think this really highlights the importance of continuing to appropriately, and actively, treat our patients, and the importance of controlling their disease,” Pedro Machado, MD, PhD, said in an interview. Dr. Machado, an associate professor in rheumatology and muscle diseases at University College London and a consultant rheumatologist at several U.K. hospitals, has been involved in the GRA physician registry from the start, and sits on the GRA steering committee.
Alongside higher disease activity, several other important factors were found to be associated with increased odds of dying from COVID-19 – older age, male gender, and the presence of one or more comorbidities, such as hypertension combined with cardiovascular disease or chronic lung disease.
These demographic and disease-based factors have been linked to an increased risk for COVID-19–related hospitalization before, both in people with RMDs and in the general population, but the latest GRA physician registry data now take that a step further, and link them also to an increased risk for death, together with several other factors more specific to RMDs.
Logging COVID-19 rheumatologic cases
Since the start of the global pandemic, the potential effects that SARS-CoV-2 infection might have on people with RMDs in particular has concerned the rheumatology community. The main worries being that, either because of the underlying RMD itself or to its treatment, there may be immunoregulatory deficits or other risk factors that would make individuals more susceptible to not only infection but also to developing more severe COVID-19 than the general population.
These concerns led to the rapid formation of the GRA and the COVID-19 GRA physician registry in March 2020 to collect and analyze data on adults with rheumatic disease and confirmed or presumptive COVID-19. Entries into the registry are made by or under the direction of rheumatologists, and this is a voluntary process.
“This population cannot ever be entirely representative of the population of patients with rheumatic diseases,” Dr. Machado acknowledged. There will be selection and other biases that affect the reported data. That said, it’s the largest database of reported COVID-19 cases in adult rheumatology patients across the world, with more than 9,000 cases so far included from multiple registries, including those based in Europe and North and South America. Data from one of these – the French RMD cohort – have also recently been published in Annals of the Rheumatic Diseases, showing much the same findings but on a national level.
Hospitalization was the focus of a previous report because “you need large sample sizes” to look at endpoints that occur less frequently. When the first analysis was done, there were around 600 cases from 40 countries in the registry with sufficient data that could be used. Now, with a greater number of recorded cases, factors influencing the risk for death could be examined.
Death rate and risk factors found
Data on 3,729 COVID-19 cases in people with RMDs were included in the current analysis, all recorded in the first few months of the registry being open and up until July 1, 2020. In all, 390 (10.5%) of people died. While this is “clearly higher” than reported in the general population in most countries, the analysis was not designed to calculate a precise estimate.
“It should not be taken as an estimate of the overall death rate among patients with rheumatic diseases and COVID-19,” Dr. Machado and coauthors have been keen to point out.
“Age is always the biggest risk factor,” Dr. Machado explained. “There’s always a gradient: the older the patient, the worse the outcome.”
Indeed, there was a threefold increased risk for death among those aged 66-75 years versus those who were 65 years or younger (odds ratio, 3.00), and a sixfold increased risk for patients older than 75, compared with the younger age group (OR, 6.18).
Having both hypertension and cardiovascular disease was associated with an OR of 1.89, and coexisting chronic lung disease also significantly increased the chances of dying from COVID-19 (OR, 1.68).
Being of male sex was associated with a 46% increased risk for death from COVID-19 versus being of female sex.
The risk for COVID-19 death also rose with the use of corticosteroids. Compared with no steroid use, there was a 69% increased risk for with death at doses of 10 mg or more prednisolone equivalent per day.
“The finding about moderate to high doses of steroids being associated with a worse outcome is consistent with the first report; it was the same for hospitalization,” Dr. Machado observed.
The general consensus on steroid use in the COVID-19 setting is that they should be continued as needed, but at the lowest possible dose, as outlined in provisional recommendations set out by the recently renamed European Alliance of Associations for Rheumatology.
The GRA physician registry findings provide further support for this, suggesting that disease control should be optimized with disease-modifying antirheumatic drugs, ideally without increasing the dose of steroids.
Surprise over sulfasalazine risk
“Taking all medications into account – such as methotrexate, leflunomide, hydroxychloroquine, [tumor necrosis factor] blockers, interleukin-6 blockers, and [Janus kinase] inhibitors – it is quite reassuring because we did not see an association with worse outcome with those drugs overall,” Dr. Machado said.
However, treatment with rituximab (OR, 4.0), sulfasalazine (OR, 3.6), and immunosuppressive agents such as azathioprine, cyclophosphamide, cyclosporine, mycophenolate, or tacrolimus (OR, 2.2), were associated with higher odds of dying from COVID-19 when compared with treatment with methotrexate alone.
The findings for rituximab and immunosuppressant use were perhaps not unexpected, but the possible association between sulfasalazine and COVID-19 death was “a bit intriguing,” Dr. Machado observed. “Sulfasalazine is believed to have low immunosuppressive effect.”
This warrants further investigation, but there are likely a range of confounding factors at play. One could be that people considered to be at higher risk may have been more often prescribed sulfasalazine because it was thought to be less immunosuppressive. Another might be because people taking sulfasalazine were more likely to be smokers, and they were also not advised to protect themselves from exposure to the virus (shielding) during the first wave of the pandemic, at least not in the United Kingdom.
Rituximab caution and vaccination
“Rituximab is a concern,” Dr. Machado acknowledged. “It is a concern that rheumatologists are now aware of and they are addressing, but then it’s a concern for a very specific subgroup of patients.”
While rheumatologists are, and will continue to prescribe it, there will be even more careful consideration over when, in whom, and how to use it during, and possibly even after, the pandemic.
“COVID is here to stay, it will become endemic, and it’s going to be part of our lives like the flu virus is,” Dr. Machado predicted.
Then there is the issue on vaccinating people against COVID-19, should those on rituximab still receive it? The answer is a yes, but, as with other vaccinations it’s all about the timing of when the vaccination is given.
Societies such as the British Society for Rheumatology have already begun to include guidance on this, recommending one of the available COVID-19 vaccines is given at least a month before the next or first dose of rituximab is due. As rituximab is given every few months, with doses sometimes spaced as much as 9 months or even a year apart, this should not be too much of a problem, but it is “better to have the vaccine first,” Dr. Machado said.
Has COVID-19 care improved in RMDs?
In separate research published in The Lancet Rheumatology, April Jorge, MD, of Massachusetts General Hospital and Harvard Medical School, both in Boston, and associates found that the risks of severe COVID-19 outcomes have improved over time, although they still “remain substantial.”
Dr. Jorge and colleagues looked at temporal trends in COVID-19 outcomes in patients with RMDs over the course of the first 6 months of the pandemic in 2020, using data from a large, multicenter, electronic health record network (TriNetX).
They formed two patient cohorts – a late (diagnosed from April 20 to July 20) and an early (diagnosed from January 20 to April 20) cohort – to see if outcomes had improved and discovered lower relative risks among patients in the late cohort for hospitalization (0.67), admission to the ICU (0.56), mechanical ventilation (0.39), acute kidney injury (0.66), renal replacement (0.53), and death (0.39).
“These results are encouraging,” but it’s difficult to match these different populations of patients, Dr. Machado said. “There are always factors that you cannot match for” and were not included in the U.S. analysis.
While there are important caveats in how the analysis was performed and thus in interpreting these data, they do “suggest that one of the reasons why outcomes have improved is because we have become better at treating these patients,” Dr. Machado added.
“Our treatment has improved, and our capacity to treat the complications has improved. We understand better how the disease behaves – we know that they can have thromboembolic complications that we can manage, and we are now able to manage ventilation issues better.”
Moreover, Dr. Machado said that, not only were clinicians more aware of what they should or should not do, there were treatments that were being used routinely or in some cases based on recent clinical trial results. “I think we are indeed treating these patients better.”
The COVID-19 GRA physician registry is financially supported by the American College of Rheumatology and EULAR. Dr. Machado had no relevant conflicts of interest.
People with rheumatic and musculoskeletal diseases (RMDs) who contract the SARS-CoV-2 virus appear more likely to die from COVID-19 if their rheumatologic condition is not being well controlled at the time of their infection.
New data from the COVID-19 Global Rheumatology Alliance (GRA) physician registry reported in Annals of the Rheumatic Diseases have found that the odds of dying from COVID-19 were 87% higher in individuals recorded as having moderate to high disease activity versus those reported to be in remission or having low disease activity.
“I think this really highlights the importance of continuing to appropriately, and actively, treat our patients, and the importance of controlling their disease,” Pedro Machado, MD, PhD, said in an interview. Dr. Machado, an associate professor in rheumatology and muscle diseases at University College London and a consultant rheumatologist at several U.K. hospitals, has been involved in the GRA physician registry from the start, and sits on the GRA steering committee.
Alongside higher disease activity, several other important factors were found to be associated with increased odds of dying from COVID-19 – older age, male gender, and the presence of one or more comorbidities, such as hypertension combined with cardiovascular disease or chronic lung disease.
These demographic and disease-based factors have been linked to an increased risk for COVID-19–related hospitalization before, both in people with RMDs and in the general population, but the latest GRA physician registry data now take that a step further, and link them also to an increased risk for death, together with several other factors more specific to RMDs.
Logging COVID-19 rheumatologic cases
Since the start of the global pandemic, the potential effects that SARS-CoV-2 infection might have on people with RMDs in particular has concerned the rheumatology community. The main worries being that, either because of the underlying RMD itself or to its treatment, there may be immunoregulatory deficits or other risk factors that would make individuals more susceptible to not only infection but also to developing more severe COVID-19 than the general population.
These concerns led to the rapid formation of the GRA and the COVID-19 GRA physician registry in March 2020 to collect and analyze data on adults with rheumatic disease and confirmed or presumptive COVID-19. Entries into the registry are made by or under the direction of rheumatologists, and this is a voluntary process.
“This population cannot ever be entirely representative of the population of patients with rheumatic diseases,” Dr. Machado acknowledged. There will be selection and other biases that affect the reported data. That said, it’s the largest database of reported COVID-19 cases in adult rheumatology patients across the world, with more than 9,000 cases so far included from multiple registries, including those based in Europe and North and South America. Data from one of these – the French RMD cohort – have also recently been published in Annals of the Rheumatic Diseases, showing much the same findings but on a national level.
Hospitalization was the focus of a previous report because “you need large sample sizes” to look at endpoints that occur less frequently. When the first analysis was done, there were around 600 cases from 40 countries in the registry with sufficient data that could be used. Now, with a greater number of recorded cases, factors influencing the risk for death could be examined.
Death rate and risk factors found
Data on 3,729 COVID-19 cases in people with RMDs were included in the current analysis, all recorded in the first few months of the registry being open and up until July 1, 2020. In all, 390 (10.5%) of people died. While this is “clearly higher” than reported in the general population in most countries, the analysis was not designed to calculate a precise estimate.
“It should not be taken as an estimate of the overall death rate among patients with rheumatic diseases and COVID-19,” Dr. Machado and coauthors have been keen to point out.
“Age is always the biggest risk factor,” Dr. Machado explained. “There’s always a gradient: the older the patient, the worse the outcome.”
Indeed, there was a threefold increased risk for death among those aged 66-75 years versus those who were 65 years or younger (odds ratio, 3.00), and a sixfold increased risk for patients older than 75, compared with the younger age group (OR, 6.18).
Having both hypertension and cardiovascular disease was associated with an OR of 1.89, and coexisting chronic lung disease also significantly increased the chances of dying from COVID-19 (OR, 1.68).
Being of male sex was associated with a 46% increased risk for death from COVID-19 versus being of female sex.
The risk for COVID-19 death also rose with the use of corticosteroids. Compared with no steroid use, there was a 69% increased risk for with death at doses of 10 mg or more prednisolone equivalent per day.
“The finding about moderate to high doses of steroids being associated with a worse outcome is consistent with the first report; it was the same for hospitalization,” Dr. Machado observed.
The general consensus on steroid use in the COVID-19 setting is that they should be continued as needed, but at the lowest possible dose, as outlined in provisional recommendations set out by the recently renamed European Alliance of Associations for Rheumatology.
The GRA physician registry findings provide further support for this, suggesting that disease control should be optimized with disease-modifying antirheumatic drugs, ideally without increasing the dose of steroids.
Surprise over sulfasalazine risk
“Taking all medications into account – such as methotrexate, leflunomide, hydroxychloroquine, [tumor necrosis factor] blockers, interleukin-6 blockers, and [Janus kinase] inhibitors – it is quite reassuring because we did not see an association with worse outcome with those drugs overall,” Dr. Machado said.
However, treatment with rituximab (OR, 4.0), sulfasalazine (OR, 3.6), and immunosuppressive agents such as azathioprine, cyclophosphamide, cyclosporine, mycophenolate, or tacrolimus (OR, 2.2), were associated with higher odds of dying from COVID-19 when compared with treatment with methotrexate alone.
The findings for rituximab and immunosuppressant use were perhaps not unexpected, but the possible association between sulfasalazine and COVID-19 death was “a bit intriguing,” Dr. Machado observed. “Sulfasalazine is believed to have low immunosuppressive effect.”
This warrants further investigation, but there are likely a range of confounding factors at play. One could be that people considered to be at higher risk may have been more often prescribed sulfasalazine because it was thought to be less immunosuppressive. Another might be because people taking sulfasalazine were more likely to be smokers, and they were also not advised to protect themselves from exposure to the virus (shielding) during the first wave of the pandemic, at least not in the United Kingdom.
Rituximab caution and vaccination
“Rituximab is a concern,” Dr. Machado acknowledged. “It is a concern that rheumatologists are now aware of and they are addressing, but then it’s a concern for a very specific subgroup of patients.”
While rheumatologists are, and will continue to prescribe it, there will be even more careful consideration over when, in whom, and how to use it during, and possibly even after, the pandemic.
“COVID is here to stay, it will become endemic, and it’s going to be part of our lives like the flu virus is,” Dr. Machado predicted.
Then there is the issue on vaccinating people against COVID-19, should those on rituximab still receive it? The answer is a yes, but, as with other vaccinations it’s all about the timing of when the vaccination is given.
Societies such as the British Society for Rheumatology have already begun to include guidance on this, recommending one of the available COVID-19 vaccines is given at least a month before the next or first dose of rituximab is due. As rituximab is given every few months, with doses sometimes spaced as much as 9 months or even a year apart, this should not be too much of a problem, but it is “better to have the vaccine first,” Dr. Machado said.
Has COVID-19 care improved in RMDs?
In separate research published in The Lancet Rheumatology, April Jorge, MD, of Massachusetts General Hospital and Harvard Medical School, both in Boston, and associates found that the risks of severe COVID-19 outcomes have improved over time, although they still “remain substantial.”
Dr. Jorge and colleagues looked at temporal trends in COVID-19 outcomes in patients with RMDs over the course of the first 6 months of the pandemic in 2020, using data from a large, multicenter, electronic health record network (TriNetX).
They formed two patient cohorts – a late (diagnosed from April 20 to July 20) and an early (diagnosed from January 20 to April 20) cohort – to see if outcomes had improved and discovered lower relative risks among patients in the late cohort for hospitalization (0.67), admission to the ICU (0.56), mechanical ventilation (0.39), acute kidney injury (0.66), renal replacement (0.53), and death (0.39).
“These results are encouraging,” but it’s difficult to match these different populations of patients, Dr. Machado said. “There are always factors that you cannot match for” and were not included in the U.S. analysis.
While there are important caveats in how the analysis was performed and thus in interpreting these data, they do “suggest that one of the reasons why outcomes have improved is because we have become better at treating these patients,” Dr. Machado added.
“Our treatment has improved, and our capacity to treat the complications has improved. We understand better how the disease behaves – we know that they can have thromboembolic complications that we can manage, and we are now able to manage ventilation issues better.”
Moreover, Dr. Machado said that, not only were clinicians more aware of what they should or should not do, there were treatments that were being used routinely or in some cases based on recent clinical trial results. “I think we are indeed treating these patients better.”
The COVID-19 GRA physician registry is financially supported by the American College of Rheumatology and EULAR. Dr. Machado had no relevant conflicts of interest.
FROM ANNALS OF THE RHEUMATIC DISEASES
FDA alert confirms heart and cancer risks with tofacitinib (Xeljanz)
The Food and Drug Administration has alerted the public to an increased risk of serious heart-related problems and cancer risk associated with the Janus kinase inhibitor tofacitinib (Xeljanz, Xeljanz XR), based on early results from a safety clinical trial comparing tofacitinib and tumor necrosis factor inhibitors in patients with rheumatoid arthritis (RA).
The FDA is awaiting further results from the trial, but in a safety communication issued on Feb. 4, the agency advised patients not to discontinue tofacitinib without consulting their health care providers and advised health care professionals to weigh the risks and benefits when prescribing the drug and continue to follow the current prescribing information.
Tofacitinib was approved for treatment of RA in 2012 at a 5-mg dose. After this approval, the FDA required drug manufacturer Pfizer to conduct a safety clinical trial that included the 5-mg twice-daily dose and a 10-mg twice-daily dose that is currently approved only for ulcerative colitis. In addition to RA and ulcerative colitis, tofacitinib is approved for adults with active psoriatic arthritis and patients aged 2 years or older with active polyarticular course juvenile idiopathic arthritis.
Pfizer announced partial results of the study, known as the ORAL Surveillance trial, in a press release on Jan. 27. The randomized trial included 4,362 RA patients aged 50 years and older who received either 5-mg or 10-mg doses of tofacitinib or a TNF inhibitor (adalimumab or etanercept).
The full results have yet to be released, but based on data from approximately 10,000 person-years for the combined tofacitinib groups and approximately 5,000 person-years for the TNF inhibitor group, the rate of major cardiovascular adverse events was significantly higher in the combined tofacitinib group, compared with the TNF inhibitor group (0.98 vs. 0.73 per 100 person-years; hazard ratio, 1.33). In addition, the rate of adjudicated malignancies was significantly higher in the tofacitinib group, compared with the TNF inhibitor group (1.13 vs. 0.77 per 100 person-years; HR, 1.48).
In February 2019, the FDA issued a warning stating an increased risk of pulmonary embolism and death associated with the 10-mg twice-daily dose of tofacitinib, following interims results from the safety study.
In July 2019, the FDA added a boxed warning to tofacitinib advising of the increased risk for pulmonary embolism and death associated with the 10-mg twice-daily dose.
The FDA encouraged health care professionals and patients to report any side effects from tofacitinib or other medications through the FDA MedWatch program online or by phone at 1-800-332-1088.
Until nuances revealed, no change in practice
The preliminary study findings contain some nuances that are a bit complicated from a statistical standpoint, according to Daniel Furst, MD, professor emeritus of medicine at the University of California, Los Angeles; adjunct professor at the University of Washington, Seattle; and research professor at the University of Florence (Italy).
This is supposed to be a noninferiority study, so something might not be noninferior, “but that doesn’t mean it is inferior,” explained Dr. Furst, who is also a member of the MDedge Rheumatology Editorial Advisory Board.
Dr. Furst said he was surprised by the study findings, because “I didn’t expect there to be any differences, and in fact it is not clear how great the differences are” among the groups in the study, he said.
When the complete findings are released, in one of the instances, “the statistics may show a very small statistical difference that indicates we may have to be more careful in this particularly high-risk group,” Dr. Furst noted.
“When we understand the data more closely, we may find that there are some nuances we need to be careful about,” he said. However, “until those data are out, I would not make any changes in my practice.”
Whether the current study findings represent a class effect is “impossible to say,” since tofacitinib affects three enzymes, while other JAK inhibitors affect only one or two, he noted.
Dr. Furst disclosed receiving grant/research support from and/or consulting for AbbVie, Actelion, Amgen, Bristol-Myers Squibb, Corbus, the National Institutes of Health, Novartis, Pfizer, and Roche/Genentech.
Updated on 2/8/2021.
The Food and Drug Administration has alerted the public to an increased risk of serious heart-related problems and cancer risk associated with the Janus kinase inhibitor tofacitinib (Xeljanz, Xeljanz XR), based on early results from a safety clinical trial comparing tofacitinib and tumor necrosis factor inhibitors in patients with rheumatoid arthritis (RA).
The FDA is awaiting further results from the trial, but in a safety communication issued on Feb. 4, the agency advised patients not to discontinue tofacitinib without consulting their health care providers and advised health care professionals to weigh the risks and benefits when prescribing the drug and continue to follow the current prescribing information.
Tofacitinib was approved for treatment of RA in 2012 at a 5-mg dose. After this approval, the FDA required drug manufacturer Pfizer to conduct a safety clinical trial that included the 5-mg twice-daily dose and a 10-mg twice-daily dose that is currently approved only for ulcerative colitis. In addition to RA and ulcerative colitis, tofacitinib is approved for adults with active psoriatic arthritis and patients aged 2 years or older with active polyarticular course juvenile idiopathic arthritis.
Pfizer announced partial results of the study, known as the ORAL Surveillance trial, in a press release on Jan. 27. The randomized trial included 4,362 RA patients aged 50 years and older who received either 5-mg or 10-mg doses of tofacitinib or a TNF inhibitor (adalimumab or etanercept).
The full results have yet to be released, but based on data from approximately 10,000 person-years for the combined tofacitinib groups and approximately 5,000 person-years for the TNF inhibitor group, the rate of major cardiovascular adverse events was significantly higher in the combined tofacitinib group, compared with the TNF inhibitor group (0.98 vs. 0.73 per 100 person-years; hazard ratio, 1.33). In addition, the rate of adjudicated malignancies was significantly higher in the tofacitinib group, compared with the TNF inhibitor group (1.13 vs. 0.77 per 100 person-years; HR, 1.48).
In February 2019, the FDA issued a warning stating an increased risk of pulmonary embolism and death associated with the 10-mg twice-daily dose of tofacitinib, following interims results from the safety study.
In July 2019, the FDA added a boxed warning to tofacitinib advising of the increased risk for pulmonary embolism and death associated with the 10-mg twice-daily dose.
The FDA encouraged health care professionals and patients to report any side effects from tofacitinib or other medications through the FDA MedWatch program online or by phone at 1-800-332-1088.
Until nuances revealed, no change in practice
The preliminary study findings contain some nuances that are a bit complicated from a statistical standpoint, according to Daniel Furst, MD, professor emeritus of medicine at the University of California, Los Angeles; adjunct professor at the University of Washington, Seattle; and research professor at the University of Florence (Italy).
This is supposed to be a noninferiority study, so something might not be noninferior, “but that doesn’t mean it is inferior,” explained Dr. Furst, who is also a member of the MDedge Rheumatology Editorial Advisory Board.
Dr. Furst said he was surprised by the study findings, because “I didn’t expect there to be any differences, and in fact it is not clear how great the differences are” among the groups in the study, he said.
When the complete findings are released, in one of the instances, “the statistics may show a very small statistical difference that indicates we may have to be more careful in this particularly high-risk group,” Dr. Furst noted.
“When we understand the data more closely, we may find that there are some nuances we need to be careful about,” he said. However, “until those data are out, I would not make any changes in my practice.”
Whether the current study findings represent a class effect is “impossible to say,” since tofacitinib affects three enzymes, while other JAK inhibitors affect only one or two, he noted.
Dr. Furst disclosed receiving grant/research support from and/or consulting for AbbVie, Actelion, Amgen, Bristol-Myers Squibb, Corbus, the National Institutes of Health, Novartis, Pfizer, and Roche/Genentech.
Updated on 2/8/2021.
The Food and Drug Administration has alerted the public to an increased risk of serious heart-related problems and cancer risk associated with the Janus kinase inhibitor tofacitinib (Xeljanz, Xeljanz XR), based on early results from a safety clinical trial comparing tofacitinib and tumor necrosis factor inhibitors in patients with rheumatoid arthritis (RA).
The FDA is awaiting further results from the trial, but in a safety communication issued on Feb. 4, the agency advised patients not to discontinue tofacitinib without consulting their health care providers and advised health care professionals to weigh the risks and benefits when prescribing the drug and continue to follow the current prescribing information.
Tofacitinib was approved for treatment of RA in 2012 at a 5-mg dose. After this approval, the FDA required drug manufacturer Pfizer to conduct a safety clinical trial that included the 5-mg twice-daily dose and a 10-mg twice-daily dose that is currently approved only for ulcerative colitis. In addition to RA and ulcerative colitis, tofacitinib is approved for adults with active psoriatic arthritis and patients aged 2 years or older with active polyarticular course juvenile idiopathic arthritis.
Pfizer announced partial results of the study, known as the ORAL Surveillance trial, in a press release on Jan. 27. The randomized trial included 4,362 RA patients aged 50 years and older who received either 5-mg or 10-mg doses of tofacitinib or a TNF inhibitor (adalimumab or etanercept).
The full results have yet to be released, but based on data from approximately 10,000 person-years for the combined tofacitinib groups and approximately 5,000 person-years for the TNF inhibitor group, the rate of major cardiovascular adverse events was significantly higher in the combined tofacitinib group, compared with the TNF inhibitor group (0.98 vs. 0.73 per 100 person-years; hazard ratio, 1.33). In addition, the rate of adjudicated malignancies was significantly higher in the tofacitinib group, compared with the TNF inhibitor group (1.13 vs. 0.77 per 100 person-years; HR, 1.48).
In February 2019, the FDA issued a warning stating an increased risk of pulmonary embolism and death associated with the 10-mg twice-daily dose of tofacitinib, following interims results from the safety study.
In July 2019, the FDA added a boxed warning to tofacitinib advising of the increased risk for pulmonary embolism and death associated with the 10-mg twice-daily dose.
The FDA encouraged health care professionals and patients to report any side effects from tofacitinib or other medications through the FDA MedWatch program online or by phone at 1-800-332-1088.
Until nuances revealed, no change in practice
The preliminary study findings contain some nuances that are a bit complicated from a statistical standpoint, according to Daniel Furst, MD, professor emeritus of medicine at the University of California, Los Angeles; adjunct professor at the University of Washington, Seattle; and research professor at the University of Florence (Italy).
This is supposed to be a noninferiority study, so something might not be noninferior, “but that doesn’t mean it is inferior,” explained Dr. Furst, who is also a member of the MDedge Rheumatology Editorial Advisory Board.
Dr. Furst said he was surprised by the study findings, because “I didn’t expect there to be any differences, and in fact it is not clear how great the differences are” among the groups in the study, he said.
When the complete findings are released, in one of the instances, “the statistics may show a very small statistical difference that indicates we may have to be more careful in this particularly high-risk group,” Dr. Furst noted.
“When we understand the data more closely, we may find that there are some nuances we need to be careful about,” he said. However, “until those data are out, I would not make any changes in my practice.”
Whether the current study findings represent a class effect is “impossible to say,” since tofacitinib affects three enzymes, while other JAK inhibitors affect only one or two, he noted.
Dr. Furst disclosed receiving grant/research support from and/or consulting for AbbVie, Actelion, Amgen, Bristol-Myers Squibb, Corbus, the National Institutes of Health, Novartis, Pfizer, and Roche/Genentech.
Updated on 2/8/2021.
COVID-19: Another study links colchicine to better results
The gout drug colchicine appears to lower the severity of COVID-19, a small new Brazilian study finds, adding to evidence that the familiar medication holds promise as a treatment for hospitalized patients.
Patients who received colchicine in this randomized, double-blinded, placebo-controlled clinical trial presented better evolution in terms of the need for supplemental oxygen and the length of hospitalisation. ... Colchicine was safe and well tolerated,” the study authors wrote in RMD Open. However, deaths were rare in the trial, they added, and it is impossible to “evaluate the capacity of colchicine to avoid admission to ICU and reduce mortality.”
The oral anti-inflammatory colchicine, widely used as treatment in rheumatic disease, was first approved in the United States 60 years ago. Researchers began to explore its potential as a COVID-19 treatment in the early months of the pandemic.
On Jan. 25, an international team of researchers reported in a press release – but not yet a published paper – that the drug seemed to reduce hospitalizations, mechanical ventilation, and deaths in the ColCORONA trial. Earlier, a much-smaller, randomized, open-label, Greek trial linked the drug to reduced time to clinical deterioration and hospital stay.
The Brazilian authors of the new study, led by Maria Isabel Lopes of the University of São Paulo’s Ribeirão Preto Medical School, randomly assigned 75 hospitalized patients with moderate to severe COVID-19 to colchicine or placebo. A total of 72 subjects completed the April-August 2020 trial: 36 received colchicine (typically 0.5 mg three times for 5 days, then 0.5 mg twice daily for 5 days; doses were adjusted in low-weight patients and those with chronic kidney disease). The other 36 received the placebo.
(In the United States, 0.6-mg tablets of generic colchicine cost as little as $1.90 each with free coupons, according to goodrx.com.)
The median age in the groups was similar (55 years); and the placebo group had more women (61% vs. 47% in the colchicine group, P = .34). All 72 patients received the same COVID-19 treatment at the time of the trial: azithromycin, hydroxychloroquine, and unfractionated heparin. Most patients, about two-thirds in both groups, also received methylprednisolone because they needed higher amounts of supplemental oxygen.
Patients in the colchicine group needed supplemental oxygen for less time: Their median time of need was 4.0 days (interquartile range [IQR], 2.0-6.0) vs. 6.5 days (IQR, 4.0-9.0) for the placebo group (P < .001). The median time for hospitalization was also lower at 7.0 days (IQR, 5.0–9.0) for the colchicine group vs. 9.0 (IQR, 7.0–12.0) for the placebo group (log rank test, 10.6; P = .001).
The researchers also reported the percentage of patients who needed supplemental oxygen at day 2 as 67% with colchicine vs. 86% with placebo, and at day 7 as 9% vs. 42% (log rank test, 10.6; P = .001). Two patients in the placebo group died, both from ventilator-associated pneumonia.
As for side effects, new or worsened diarrhea was reported more often in the colchicine group (17% vs. 6% with placebo), but the difference was not statistically significant (P = .26), and diarrhea was controlled via medication.
The researchers reported that limitations include the exclusion criteria and their inability to link colchicine to rates of ICU admissions and death.
The drug appears to help patients with COVID-19, the study authors wrote, by “inhibiting inflammasome, reducing neutrophil migration and activation, or preventing endothelial damage.”
A “well-conceived and well-designed” study
In an interview, NYU Langone Health rheumatologist Michael H. Pillinger, MD – an investigator with the ColCORONA trial – praised the Brazilian study. It “appears well-conceived and well-designed, and was enrolled at a rate that was greater than the sample size that was estimated to be needed based on power analysis,” he said.
The Brazilian study is small, he noted. (In contrast, the ColCORONA trial had 4,488 outpatient participants.) “This study differs from ColCORONA in several ways – the most important being that it is a study of inpatients with moderate to severe COVID (really mostly moderate),” he added. “ColCORONA is looking at a target audience that is much larger – outpatients with mild to moderate COVID with risk factors for hospitalization. Both questions are really important and certainly not mutually exclusive, since our care remains inadequate in both venues. This study also adds value in that several other studies have been conducted in hospital patients with enrollment criteria relatively similar to this one, and all showed benefit, but those were open-label or retrospective, and this is blinded and placebo-controlled.”
Using colchicine in patients with COVID-19
Should physicians turn to colchicine in patients with COVID-19? “I would rather that it still be used in the context of research until formal recommendations can be made by bodies like the NIH and CDC,” Dr. Pillinger said. “But certainly, there may be times when physicians feel compelled to treat patients off label.”
He cautioned, however, that colchicine should never be used with some other drugs. Its interaction with the antibiotic clarithromycin can be fatal, he noted. And, he said, the drug must be monitored in general since it can cause rare, severe problems.
“Overall, colchicine probably works on the overabundant inflammatory response to COVID, and it may be that it can be combined with other drugs that affect viral replication or promote immunity – e.g. vaccines,” Dr. Pillinger said. “So far, it seems as if there is no safety problem with combining colchicine with other approaches, but this has not been studied in a rigorous manner.”
Moving forward, he said, the drug’s very low price outside of the United States “could provide resource-poor countries with a way to help keep patients out of precious hospital beds – or help them go home sooner once admitted.” For now, however, “we need a large-scale inpatient study, and one is currently going on in Great Britain. We also need validation of the outpatient ColCORONA study, and studies to look at whether colchicine can work in conjunction with other strategies.”
The study was funded by grants from the São Paulo Research Foundation, Brazilian National Council for Scientific and Technological Development, and CAPES Foundation. No disclosures are reported. Dr. Pillinger reports serving as an investigator for the ColCORONA trial and receiving a unrelated investigator-initiated grant from Hikma, a colchicine manufacturer.
The gout drug colchicine appears to lower the severity of COVID-19, a small new Brazilian study finds, adding to evidence that the familiar medication holds promise as a treatment for hospitalized patients.
Patients who received colchicine in this randomized, double-blinded, placebo-controlled clinical trial presented better evolution in terms of the need for supplemental oxygen and the length of hospitalisation. ... Colchicine was safe and well tolerated,” the study authors wrote in RMD Open. However, deaths were rare in the trial, they added, and it is impossible to “evaluate the capacity of colchicine to avoid admission to ICU and reduce mortality.”
The oral anti-inflammatory colchicine, widely used as treatment in rheumatic disease, was first approved in the United States 60 years ago. Researchers began to explore its potential as a COVID-19 treatment in the early months of the pandemic.
On Jan. 25, an international team of researchers reported in a press release – but not yet a published paper – that the drug seemed to reduce hospitalizations, mechanical ventilation, and deaths in the ColCORONA trial. Earlier, a much-smaller, randomized, open-label, Greek trial linked the drug to reduced time to clinical deterioration and hospital stay.
The Brazilian authors of the new study, led by Maria Isabel Lopes of the University of São Paulo’s Ribeirão Preto Medical School, randomly assigned 75 hospitalized patients with moderate to severe COVID-19 to colchicine or placebo. A total of 72 subjects completed the April-August 2020 trial: 36 received colchicine (typically 0.5 mg three times for 5 days, then 0.5 mg twice daily for 5 days; doses were adjusted in low-weight patients and those with chronic kidney disease). The other 36 received the placebo.
(In the United States, 0.6-mg tablets of generic colchicine cost as little as $1.90 each with free coupons, according to goodrx.com.)
The median age in the groups was similar (55 years); and the placebo group had more women (61% vs. 47% in the colchicine group, P = .34). All 72 patients received the same COVID-19 treatment at the time of the trial: azithromycin, hydroxychloroquine, and unfractionated heparin. Most patients, about two-thirds in both groups, also received methylprednisolone because they needed higher amounts of supplemental oxygen.
Patients in the colchicine group needed supplemental oxygen for less time: Their median time of need was 4.0 days (interquartile range [IQR], 2.0-6.0) vs. 6.5 days (IQR, 4.0-9.0) for the placebo group (P < .001). The median time for hospitalization was also lower at 7.0 days (IQR, 5.0–9.0) for the colchicine group vs. 9.0 (IQR, 7.0–12.0) for the placebo group (log rank test, 10.6; P = .001).
The researchers also reported the percentage of patients who needed supplemental oxygen at day 2 as 67% with colchicine vs. 86% with placebo, and at day 7 as 9% vs. 42% (log rank test, 10.6; P = .001). Two patients in the placebo group died, both from ventilator-associated pneumonia.
As for side effects, new or worsened diarrhea was reported more often in the colchicine group (17% vs. 6% with placebo), but the difference was not statistically significant (P = .26), and diarrhea was controlled via medication.
The researchers reported that limitations include the exclusion criteria and their inability to link colchicine to rates of ICU admissions and death.
The drug appears to help patients with COVID-19, the study authors wrote, by “inhibiting inflammasome, reducing neutrophil migration and activation, or preventing endothelial damage.”
A “well-conceived and well-designed” study
In an interview, NYU Langone Health rheumatologist Michael H. Pillinger, MD – an investigator with the ColCORONA trial – praised the Brazilian study. It “appears well-conceived and well-designed, and was enrolled at a rate that was greater than the sample size that was estimated to be needed based on power analysis,” he said.
The Brazilian study is small, he noted. (In contrast, the ColCORONA trial had 4,488 outpatient participants.) “This study differs from ColCORONA in several ways – the most important being that it is a study of inpatients with moderate to severe COVID (really mostly moderate),” he added. “ColCORONA is looking at a target audience that is much larger – outpatients with mild to moderate COVID with risk factors for hospitalization. Both questions are really important and certainly not mutually exclusive, since our care remains inadequate in both venues. This study also adds value in that several other studies have been conducted in hospital patients with enrollment criteria relatively similar to this one, and all showed benefit, but those were open-label or retrospective, and this is blinded and placebo-controlled.”
Using colchicine in patients with COVID-19
Should physicians turn to colchicine in patients with COVID-19? “I would rather that it still be used in the context of research until formal recommendations can be made by bodies like the NIH and CDC,” Dr. Pillinger said. “But certainly, there may be times when physicians feel compelled to treat patients off label.”
He cautioned, however, that colchicine should never be used with some other drugs. Its interaction with the antibiotic clarithromycin can be fatal, he noted. And, he said, the drug must be monitored in general since it can cause rare, severe problems.
“Overall, colchicine probably works on the overabundant inflammatory response to COVID, and it may be that it can be combined with other drugs that affect viral replication or promote immunity – e.g. vaccines,” Dr. Pillinger said. “So far, it seems as if there is no safety problem with combining colchicine with other approaches, but this has not been studied in a rigorous manner.”
Moving forward, he said, the drug’s very low price outside of the United States “could provide resource-poor countries with a way to help keep patients out of precious hospital beds – or help them go home sooner once admitted.” For now, however, “we need a large-scale inpatient study, and one is currently going on in Great Britain. We also need validation of the outpatient ColCORONA study, and studies to look at whether colchicine can work in conjunction with other strategies.”
The study was funded by grants from the São Paulo Research Foundation, Brazilian National Council for Scientific and Technological Development, and CAPES Foundation. No disclosures are reported. Dr. Pillinger reports serving as an investigator for the ColCORONA trial and receiving a unrelated investigator-initiated grant from Hikma, a colchicine manufacturer.
The gout drug colchicine appears to lower the severity of COVID-19, a small new Brazilian study finds, adding to evidence that the familiar medication holds promise as a treatment for hospitalized patients.
Patients who received colchicine in this randomized, double-blinded, placebo-controlled clinical trial presented better evolution in terms of the need for supplemental oxygen and the length of hospitalisation. ... Colchicine was safe and well tolerated,” the study authors wrote in RMD Open. However, deaths were rare in the trial, they added, and it is impossible to “evaluate the capacity of colchicine to avoid admission to ICU and reduce mortality.”
The oral anti-inflammatory colchicine, widely used as treatment in rheumatic disease, was first approved in the United States 60 years ago. Researchers began to explore its potential as a COVID-19 treatment in the early months of the pandemic.
On Jan. 25, an international team of researchers reported in a press release – but not yet a published paper – that the drug seemed to reduce hospitalizations, mechanical ventilation, and deaths in the ColCORONA trial. Earlier, a much-smaller, randomized, open-label, Greek trial linked the drug to reduced time to clinical deterioration and hospital stay.
The Brazilian authors of the new study, led by Maria Isabel Lopes of the University of São Paulo’s Ribeirão Preto Medical School, randomly assigned 75 hospitalized patients with moderate to severe COVID-19 to colchicine or placebo. A total of 72 subjects completed the April-August 2020 trial: 36 received colchicine (typically 0.5 mg three times for 5 days, then 0.5 mg twice daily for 5 days; doses were adjusted in low-weight patients and those with chronic kidney disease). The other 36 received the placebo.
(In the United States, 0.6-mg tablets of generic colchicine cost as little as $1.90 each with free coupons, according to goodrx.com.)
The median age in the groups was similar (55 years); and the placebo group had more women (61% vs. 47% in the colchicine group, P = .34). All 72 patients received the same COVID-19 treatment at the time of the trial: azithromycin, hydroxychloroquine, and unfractionated heparin. Most patients, about two-thirds in both groups, also received methylprednisolone because they needed higher amounts of supplemental oxygen.
Patients in the colchicine group needed supplemental oxygen for less time: Their median time of need was 4.0 days (interquartile range [IQR], 2.0-6.0) vs. 6.5 days (IQR, 4.0-9.0) for the placebo group (P < .001). The median time for hospitalization was also lower at 7.0 days (IQR, 5.0–9.0) for the colchicine group vs. 9.0 (IQR, 7.0–12.0) for the placebo group (log rank test, 10.6; P = .001).
The researchers also reported the percentage of patients who needed supplemental oxygen at day 2 as 67% with colchicine vs. 86% with placebo, and at day 7 as 9% vs. 42% (log rank test, 10.6; P = .001). Two patients in the placebo group died, both from ventilator-associated pneumonia.
As for side effects, new or worsened diarrhea was reported more often in the colchicine group (17% vs. 6% with placebo), but the difference was not statistically significant (P = .26), and diarrhea was controlled via medication.
The researchers reported that limitations include the exclusion criteria and their inability to link colchicine to rates of ICU admissions and death.
The drug appears to help patients with COVID-19, the study authors wrote, by “inhibiting inflammasome, reducing neutrophil migration and activation, or preventing endothelial damage.”
A “well-conceived and well-designed” study
In an interview, NYU Langone Health rheumatologist Michael H. Pillinger, MD – an investigator with the ColCORONA trial – praised the Brazilian study. It “appears well-conceived and well-designed, and was enrolled at a rate that was greater than the sample size that was estimated to be needed based on power analysis,” he said.
The Brazilian study is small, he noted. (In contrast, the ColCORONA trial had 4,488 outpatient participants.) “This study differs from ColCORONA in several ways – the most important being that it is a study of inpatients with moderate to severe COVID (really mostly moderate),” he added. “ColCORONA is looking at a target audience that is much larger – outpatients with mild to moderate COVID with risk factors for hospitalization. Both questions are really important and certainly not mutually exclusive, since our care remains inadequate in both venues. This study also adds value in that several other studies have been conducted in hospital patients with enrollment criteria relatively similar to this one, and all showed benefit, but those were open-label or retrospective, and this is blinded and placebo-controlled.”
Using colchicine in patients with COVID-19
Should physicians turn to colchicine in patients with COVID-19? “I would rather that it still be used in the context of research until formal recommendations can be made by bodies like the NIH and CDC,” Dr. Pillinger said. “But certainly, there may be times when physicians feel compelled to treat patients off label.”
He cautioned, however, that colchicine should never be used with some other drugs. Its interaction with the antibiotic clarithromycin can be fatal, he noted. And, he said, the drug must be monitored in general since it can cause rare, severe problems.
“Overall, colchicine probably works on the overabundant inflammatory response to COVID, and it may be that it can be combined with other drugs that affect viral replication or promote immunity – e.g. vaccines,” Dr. Pillinger said. “So far, it seems as if there is no safety problem with combining colchicine with other approaches, but this has not been studied in a rigorous manner.”
Moving forward, he said, the drug’s very low price outside of the United States “could provide resource-poor countries with a way to help keep patients out of precious hospital beds – or help them go home sooner once admitted.” For now, however, “we need a large-scale inpatient study, and one is currently going on in Great Britain. We also need validation of the outpatient ColCORONA study, and studies to look at whether colchicine can work in conjunction with other strategies.”
The study was funded by grants from the São Paulo Research Foundation, Brazilian National Council for Scientific and Technological Development, and CAPES Foundation. No disclosures are reported. Dr. Pillinger reports serving as an investigator for the ColCORONA trial and receiving a unrelated investigator-initiated grant from Hikma, a colchicine manufacturer.
FROM RMD OPEN
Dan Kastner wins Crafoord Prize in Polyarthritis
“for establishing the concept of autoinflammatory diseases.” The prize, named after the donor Holger Crafoord because of his bout with severe rheumatoid arthritis toward the end of his life, is for 6 million Swedish kronor (approximately USD $700,000).
Dr. Kastner, scientific director at the U.S. National Human Genome Research Institute’s division of intramural research, received the award for identifying the mechanisms responsible for familial Mediterranean fever, tumor necrosis factor receptor–associated periodic syndrome, and other diagnoses within the group of autoinflammatory diseases.
“Dan Kastner is often called the father of autoinflammatory diseases, a title that he thoroughly deserves. His discoveries have taught us a great deal about the immune system and its functions, contributing to effective treatments that reduce the symptoms of diseases from which patients previously suffered enormously, sometimes leading to premature death,” Olle Kämpe, chair of the prize committee, said in a press announcement.
While the Crafoord Prize normally is awarded on a 3-year rotating basis for achievements in mathematics and astronomy, geosciences, and biosciences, the prize in polyarthritis is “only awarded when there has been scientific progress that motivates a prize,” according to the press release.
“for establishing the concept of autoinflammatory diseases.” The prize, named after the donor Holger Crafoord because of his bout with severe rheumatoid arthritis toward the end of his life, is for 6 million Swedish kronor (approximately USD $700,000).
Dr. Kastner, scientific director at the U.S. National Human Genome Research Institute’s division of intramural research, received the award for identifying the mechanisms responsible for familial Mediterranean fever, tumor necrosis factor receptor–associated periodic syndrome, and other diagnoses within the group of autoinflammatory diseases.
“Dan Kastner is often called the father of autoinflammatory diseases, a title that he thoroughly deserves. His discoveries have taught us a great deal about the immune system and its functions, contributing to effective treatments that reduce the symptoms of diseases from which patients previously suffered enormously, sometimes leading to premature death,” Olle Kämpe, chair of the prize committee, said in a press announcement.
While the Crafoord Prize normally is awarded on a 3-year rotating basis for achievements in mathematics and astronomy, geosciences, and biosciences, the prize in polyarthritis is “only awarded when there has been scientific progress that motivates a prize,” according to the press release.
“for establishing the concept of autoinflammatory diseases.” The prize, named after the donor Holger Crafoord because of his bout with severe rheumatoid arthritis toward the end of his life, is for 6 million Swedish kronor (approximately USD $700,000).
Dr. Kastner, scientific director at the U.S. National Human Genome Research Institute’s division of intramural research, received the award for identifying the mechanisms responsible for familial Mediterranean fever, tumor necrosis factor receptor–associated periodic syndrome, and other diagnoses within the group of autoinflammatory diseases.
“Dan Kastner is often called the father of autoinflammatory diseases, a title that he thoroughly deserves. His discoveries have taught us a great deal about the immune system and its functions, contributing to effective treatments that reduce the symptoms of diseases from which patients previously suffered enormously, sometimes leading to premature death,” Olle Kämpe, chair of the prize committee, said in a press announcement.
While the Crafoord Prize normally is awarded on a 3-year rotating basis for achievements in mathematics and astronomy, geosciences, and biosciences, the prize in polyarthritis is “only awarded when there has been scientific progress that motivates a prize,” according to the press release.
Patients with early arthritis may need tailored treatments
Patients with early, undifferentiated arthritis may benefit from milder or stronger treatments, depending on the number of their risk factors for developing rheumatoid arthritis, researchers say.
If the finding is borne out by further research, clinicians could consider treating some of these patients with hydroxychloroquine, steroids, or nonsteroidal anti-inflammatory drugs (NSAIDs) rather than methotrexate, said Pascal de Jong, MD, PhD, a rheumatologist at Erasmus Medical Center in Rotterdam, the Netherlands.
“Maybe those patients with fewer risk factors should get less intensive treatment,” he said in an interview. The study by de Jong and colleagues was published online Jan. 23 in Rheumatology.
The European Alliance of Associations for Rheumatology recommends starting treatment with methotrexate for patients who are at risk for persistent arthritis, which it says is “factually synonymous” with rheumatoid arthritis.
But these recommendations are based on studies involving patients with established rheumatoid arthritis, Dr. de Jong said.
In an earlier study, he and his colleagues found that hydroxychloroquine can be just as effective as methotrexate for patients newly diagnosed with rheumatoid arthritis who don’t have autoantibodies. This led them to wonder whether their findings might apply to some subgroups of patients with early arthritis.
As an initial test of this idea, they identified 130 patients from the Rotterdam Early Arthritis Cohort (tREACH) trial who had at least one swollen joint but who did meet the diagnostic criteria for rheumatoid arthritis.
They sorted the patients into groups on the basis of the number of risk factors for persistent arthritis. The risk factors were autoantibody positivity (rheumatoid factor and/or anticitrullinated protein antibody), polyarthritis (more than four swollen joints), erosive disease, and elevations in levels of acute-phase reactants.
Thirty-one patients had none of these risk factors, 66 patients had one risk factor, and the remaining 33 patients had at least two risk factors.
After 2 years of follow-up, 74% of the patients who had had no risk factors had recovered from their arthritis and had not taken disease-modifying antirheumatic drugs (DMARDs) for at least 6 months (DMARD-free remission). Among the patients who had had one risk factor, 48% achieved DMARD-free remission. Among those who had had two risk factors, 45% achieved DMARD-free remission. The differences between the group that had had no risk factors and the other two groups were statistically significant (P < .05).
The researchers found that those patients who had been experiencing their symptoms for fewer than 6 months were more likely to achieve disease-free remission.
They also sorted patients into different groups on the basis of the treatments they received. One group of 30 comprised all patients who had been initially treated with methotrexate and included patients who had also received other drugs. One group of 40 received hydroxychloroquine initially, and one group of 60 comprised patients who had received no DMARDs initially and included those who had received NSAIDs or glucocorticoids.
There was no statistically significant difference in DMARD-free remission rates among the treatment groups. However, among those patients who were not treated initially with DMARDs, the chance of sustaining DMARD-free remission for more than a year was lower in comparison with the patients who received methotrexate initially (odds ratio, 4.28; 95% confidence interval, 1.34-13.72; P < .05).
Those patients who had fewer baseline risk factors were more likely to have their medication dosages tapered, and they were at lower risk for flares. Patients with more risk factors were more likely to require an intensificiation of treatment, such as with the use of biologicals.
Methotrexate is more likely to cause side effects such as nausea, fatigue, and hair loss than hydroxychloroquine, Dr. de Jong said. “If the medication is better tolerated, it also influences the compliance of the patient,” he said.
The study could help rheumatologists determine which patients need the most aggressive treatment, agreed Kevin Deane, MD, PhD, associate professor of medicine, division of rheumatology, the University of Colorado, Aurora.
“That’s a common clinical problem,” he said. “Somebody comes in with sort of mild arthritis, and you don’t quite know what it is yet.”
But he added that more research is needed to understand what treatment works best for those patients whose arthritis has not yet been differentiated. Primary care physicians who suspect inflammatory arthritis should refer their patients to rheumatologists and should test for rheumatoid factors and anticyclic citrullinated peptide, Dr. Deane said.
The authors and Dr. Deane have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with early, undifferentiated arthritis may benefit from milder or stronger treatments, depending on the number of their risk factors for developing rheumatoid arthritis, researchers say.
If the finding is borne out by further research, clinicians could consider treating some of these patients with hydroxychloroquine, steroids, or nonsteroidal anti-inflammatory drugs (NSAIDs) rather than methotrexate, said Pascal de Jong, MD, PhD, a rheumatologist at Erasmus Medical Center in Rotterdam, the Netherlands.
“Maybe those patients with fewer risk factors should get less intensive treatment,” he said in an interview. The study by de Jong and colleagues was published online Jan. 23 in Rheumatology.
The European Alliance of Associations for Rheumatology recommends starting treatment with methotrexate for patients who are at risk for persistent arthritis, which it says is “factually synonymous” with rheumatoid arthritis.
But these recommendations are based on studies involving patients with established rheumatoid arthritis, Dr. de Jong said.
In an earlier study, he and his colleagues found that hydroxychloroquine can be just as effective as methotrexate for patients newly diagnosed with rheumatoid arthritis who don’t have autoantibodies. This led them to wonder whether their findings might apply to some subgroups of patients with early arthritis.
As an initial test of this idea, they identified 130 patients from the Rotterdam Early Arthritis Cohort (tREACH) trial who had at least one swollen joint but who did meet the diagnostic criteria for rheumatoid arthritis.
They sorted the patients into groups on the basis of the number of risk factors for persistent arthritis. The risk factors were autoantibody positivity (rheumatoid factor and/or anticitrullinated protein antibody), polyarthritis (more than four swollen joints), erosive disease, and elevations in levels of acute-phase reactants.
Thirty-one patients had none of these risk factors, 66 patients had one risk factor, and the remaining 33 patients had at least two risk factors.
After 2 years of follow-up, 74% of the patients who had had no risk factors had recovered from their arthritis and had not taken disease-modifying antirheumatic drugs (DMARDs) for at least 6 months (DMARD-free remission). Among the patients who had had one risk factor, 48% achieved DMARD-free remission. Among those who had had two risk factors, 45% achieved DMARD-free remission. The differences between the group that had had no risk factors and the other two groups were statistically significant (P < .05).
The researchers found that those patients who had been experiencing their symptoms for fewer than 6 months were more likely to achieve disease-free remission.
They also sorted patients into different groups on the basis of the treatments they received. One group of 30 comprised all patients who had been initially treated with methotrexate and included patients who had also received other drugs. One group of 40 received hydroxychloroquine initially, and one group of 60 comprised patients who had received no DMARDs initially and included those who had received NSAIDs or glucocorticoids.
There was no statistically significant difference in DMARD-free remission rates among the treatment groups. However, among those patients who were not treated initially with DMARDs, the chance of sustaining DMARD-free remission for more than a year was lower in comparison with the patients who received methotrexate initially (odds ratio, 4.28; 95% confidence interval, 1.34-13.72; P < .05).
Those patients who had fewer baseline risk factors were more likely to have their medication dosages tapered, and they were at lower risk for flares. Patients with more risk factors were more likely to require an intensificiation of treatment, such as with the use of biologicals.
Methotrexate is more likely to cause side effects such as nausea, fatigue, and hair loss than hydroxychloroquine, Dr. de Jong said. “If the medication is better tolerated, it also influences the compliance of the patient,” he said.
The study could help rheumatologists determine which patients need the most aggressive treatment, agreed Kevin Deane, MD, PhD, associate professor of medicine, division of rheumatology, the University of Colorado, Aurora.
“That’s a common clinical problem,” he said. “Somebody comes in with sort of mild arthritis, and you don’t quite know what it is yet.”
But he added that more research is needed to understand what treatment works best for those patients whose arthritis has not yet been differentiated. Primary care physicians who suspect inflammatory arthritis should refer their patients to rheumatologists and should test for rheumatoid factors and anticyclic citrullinated peptide, Dr. Deane said.
The authors and Dr. Deane have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with early, undifferentiated arthritis may benefit from milder or stronger treatments, depending on the number of their risk factors for developing rheumatoid arthritis, researchers say.
If the finding is borne out by further research, clinicians could consider treating some of these patients with hydroxychloroquine, steroids, or nonsteroidal anti-inflammatory drugs (NSAIDs) rather than methotrexate, said Pascal de Jong, MD, PhD, a rheumatologist at Erasmus Medical Center in Rotterdam, the Netherlands.
“Maybe those patients with fewer risk factors should get less intensive treatment,” he said in an interview. The study by de Jong and colleagues was published online Jan. 23 in Rheumatology.
The European Alliance of Associations for Rheumatology recommends starting treatment with methotrexate for patients who are at risk for persistent arthritis, which it says is “factually synonymous” with rheumatoid arthritis.
But these recommendations are based on studies involving patients with established rheumatoid arthritis, Dr. de Jong said.
In an earlier study, he and his colleagues found that hydroxychloroquine can be just as effective as methotrexate for patients newly diagnosed with rheumatoid arthritis who don’t have autoantibodies. This led them to wonder whether their findings might apply to some subgroups of patients with early arthritis.
As an initial test of this idea, they identified 130 patients from the Rotterdam Early Arthritis Cohort (tREACH) trial who had at least one swollen joint but who did meet the diagnostic criteria for rheumatoid arthritis.
They sorted the patients into groups on the basis of the number of risk factors for persistent arthritis. The risk factors were autoantibody positivity (rheumatoid factor and/or anticitrullinated protein antibody), polyarthritis (more than four swollen joints), erosive disease, and elevations in levels of acute-phase reactants.
Thirty-one patients had none of these risk factors, 66 patients had one risk factor, and the remaining 33 patients had at least two risk factors.
After 2 years of follow-up, 74% of the patients who had had no risk factors had recovered from their arthritis and had not taken disease-modifying antirheumatic drugs (DMARDs) for at least 6 months (DMARD-free remission). Among the patients who had had one risk factor, 48% achieved DMARD-free remission. Among those who had had two risk factors, 45% achieved DMARD-free remission. The differences between the group that had had no risk factors and the other two groups were statistically significant (P < .05).
The researchers found that those patients who had been experiencing their symptoms for fewer than 6 months were more likely to achieve disease-free remission.
They also sorted patients into different groups on the basis of the treatments they received. One group of 30 comprised all patients who had been initially treated with methotrexate and included patients who had also received other drugs. One group of 40 received hydroxychloroquine initially, and one group of 60 comprised patients who had received no DMARDs initially and included those who had received NSAIDs or glucocorticoids.
There was no statistically significant difference in DMARD-free remission rates among the treatment groups. However, among those patients who were not treated initially with DMARDs, the chance of sustaining DMARD-free remission for more than a year was lower in comparison with the patients who received methotrexate initially (odds ratio, 4.28; 95% confidence interval, 1.34-13.72; P < .05).
Those patients who had fewer baseline risk factors were more likely to have their medication dosages tapered, and they were at lower risk for flares. Patients with more risk factors were more likely to require an intensificiation of treatment, such as with the use of biologicals.
Methotrexate is more likely to cause side effects such as nausea, fatigue, and hair loss than hydroxychloroquine, Dr. de Jong said. “If the medication is better tolerated, it also influences the compliance of the patient,” he said.
The study could help rheumatologists determine which patients need the most aggressive treatment, agreed Kevin Deane, MD, PhD, associate professor of medicine, division of rheumatology, the University of Colorado, Aurora.
“That’s a common clinical problem,” he said. “Somebody comes in with sort of mild arthritis, and you don’t quite know what it is yet.”
But he added that more research is needed to understand what treatment works best for those patients whose arthritis has not yet been differentiated. Primary care physicians who suspect inflammatory arthritis should refer their patients to rheumatologists and should test for rheumatoid factors and anticyclic citrullinated peptide, Dr. Deane said.
The authors and Dr. Deane have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Tofacitinib for RA misses the mark in safety study
Daily treatment with tofacitinib (Xeljanz) led to more malignancies and adverse cardiovascular events in older rheumatoid arthritis patients compared with treatment with a tumor necrosis factor (TNF) inhibitor, according to the partial results of a safety study announced last week by Pfizer.
The postmarketing study known as ORAL Surveillance began in 2014 to evaluate the safety of the Janus kinase (JAK) inhibitor tofacitinib compared to a TNF inhibitor in RA patients 50 years of age or older with at least one additional cardiovascular risk factor. Its 4,362 participants were randomized to either daily doses of 5 mg (n = 1,455) or 10 mg (n = 1,456) of tofacitinib or the TNFi (n = 1,451), which was adalimumab for patients in the United States, Canada, and Puerto Rico, and etanercept elsewhere. During analysis, adverse events were pooled for all patients on tofacitinib.
Overall, 135 patients developed major adverse cardiovascular events (MACE) and 164 developed malignancies – excluding nonmelanoma skin cancer. The incidence of adjudicated malignancies was significantly higher in the tofacitinib group, compared with the TNFi group (1.13 vs. 0.77 per 100 person-years; hazard ratio, 1.48; 95% confidence interval, 1.04-2.09). The rate of MACE was also higher in the combined tofacitinib group (0.98 vs. 0.73 per 100 person-years; HR, 1.33; 95% CI, 0.91-1.94). Both rates for tofacitinib did not meet the trial’s noninferiority criteria.
Among the patients on tofacitinib, the most reported MACE was myocardial infarction and the most reported malignancy was lung cancer. Study participants with noted risk factors – including older age and smoking – were more likely to experience adverse events.
In February 2019, patients in the 10-mg tofacitinib group were switched to the 5-mg because of a safety signal indicating increased risk of pulmonary embolism and death.
Tofacitinib was approved for RA in November 2012, though concerns about serious side effects had been noted during clinical trials and a boxed warning was ultimately added to the drug’s label. Tofacitinib is also approved for adults with active psoriatic arthritis, adults with moderately to severely active ulcerative colitis, and patients aged 2 years or older with active polyarticular course juvenile idiopathic arthritis. Other JAK inhibitors such as baricitinib and upadacitinib have been approved for RA in the interim as well, though the higher dose of baricitinib was rejected in committee because of safety concerns and both their boxes also warn against infections, thrombosis, and cancer.
A postmarketing safety study on baricitinib is expected to be completed in 2025.
The full results of the ORAL Surveillance study – which should address safety regarding pulmonary embolism and mortality, as well as efficacy data – have not yet been released. “Pfizer is working with the [FDA] and other regulatory agencies to review the full results and analyses as they become available,” the press release said.
Daily treatment with tofacitinib (Xeljanz) led to more malignancies and adverse cardiovascular events in older rheumatoid arthritis patients compared with treatment with a tumor necrosis factor (TNF) inhibitor, according to the partial results of a safety study announced last week by Pfizer.
The postmarketing study known as ORAL Surveillance began in 2014 to evaluate the safety of the Janus kinase (JAK) inhibitor tofacitinib compared to a TNF inhibitor in RA patients 50 years of age or older with at least one additional cardiovascular risk factor. Its 4,362 participants were randomized to either daily doses of 5 mg (n = 1,455) or 10 mg (n = 1,456) of tofacitinib or the TNFi (n = 1,451), which was adalimumab for patients in the United States, Canada, and Puerto Rico, and etanercept elsewhere. During analysis, adverse events were pooled for all patients on tofacitinib.
Overall, 135 patients developed major adverse cardiovascular events (MACE) and 164 developed malignancies – excluding nonmelanoma skin cancer. The incidence of adjudicated malignancies was significantly higher in the tofacitinib group, compared with the TNFi group (1.13 vs. 0.77 per 100 person-years; hazard ratio, 1.48; 95% confidence interval, 1.04-2.09). The rate of MACE was also higher in the combined tofacitinib group (0.98 vs. 0.73 per 100 person-years; HR, 1.33; 95% CI, 0.91-1.94). Both rates for tofacitinib did not meet the trial’s noninferiority criteria.
Among the patients on tofacitinib, the most reported MACE was myocardial infarction and the most reported malignancy was lung cancer. Study participants with noted risk factors – including older age and smoking – were more likely to experience adverse events.
In February 2019, patients in the 10-mg tofacitinib group were switched to the 5-mg because of a safety signal indicating increased risk of pulmonary embolism and death.
Tofacitinib was approved for RA in November 2012, though concerns about serious side effects had been noted during clinical trials and a boxed warning was ultimately added to the drug’s label. Tofacitinib is also approved for adults with active psoriatic arthritis, adults with moderately to severely active ulcerative colitis, and patients aged 2 years or older with active polyarticular course juvenile idiopathic arthritis. Other JAK inhibitors such as baricitinib and upadacitinib have been approved for RA in the interim as well, though the higher dose of baricitinib was rejected in committee because of safety concerns and both their boxes also warn against infections, thrombosis, and cancer.
A postmarketing safety study on baricitinib is expected to be completed in 2025.
The full results of the ORAL Surveillance study – which should address safety regarding pulmonary embolism and mortality, as well as efficacy data – have not yet been released. “Pfizer is working with the [FDA] and other regulatory agencies to review the full results and analyses as they become available,” the press release said.
Daily treatment with tofacitinib (Xeljanz) led to more malignancies and adverse cardiovascular events in older rheumatoid arthritis patients compared with treatment with a tumor necrosis factor (TNF) inhibitor, according to the partial results of a safety study announced last week by Pfizer.
The postmarketing study known as ORAL Surveillance began in 2014 to evaluate the safety of the Janus kinase (JAK) inhibitor tofacitinib compared to a TNF inhibitor in RA patients 50 years of age or older with at least one additional cardiovascular risk factor. Its 4,362 participants were randomized to either daily doses of 5 mg (n = 1,455) or 10 mg (n = 1,456) of tofacitinib or the TNFi (n = 1,451), which was adalimumab for patients in the United States, Canada, and Puerto Rico, and etanercept elsewhere. During analysis, adverse events were pooled for all patients on tofacitinib.
Overall, 135 patients developed major adverse cardiovascular events (MACE) and 164 developed malignancies – excluding nonmelanoma skin cancer. The incidence of adjudicated malignancies was significantly higher in the tofacitinib group, compared with the TNFi group (1.13 vs. 0.77 per 100 person-years; hazard ratio, 1.48; 95% confidence interval, 1.04-2.09). The rate of MACE was also higher in the combined tofacitinib group (0.98 vs. 0.73 per 100 person-years; HR, 1.33; 95% CI, 0.91-1.94). Both rates for tofacitinib did not meet the trial’s noninferiority criteria.
Among the patients on tofacitinib, the most reported MACE was myocardial infarction and the most reported malignancy was lung cancer. Study participants with noted risk factors – including older age and smoking – were more likely to experience adverse events.
In February 2019, patients in the 10-mg tofacitinib group were switched to the 5-mg because of a safety signal indicating increased risk of pulmonary embolism and death.
Tofacitinib was approved for RA in November 2012, though concerns about serious side effects had been noted during clinical trials and a boxed warning was ultimately added to the drug’s label. Tofacitinib is also approved for adults with active psoriatic arthritis, adults with moderately to severely active ulcerative colitis, and patients aged 2 years or older with active polyarticular course juvenile idiopathic arthritis. Other JAK inhibitors such as baricitinib and upadacitinib have been approved for RA in the interim as well, though the higher dose of baricitinib was rejected in committee because of safety concerns and both their boxes also warn against infections, thrombosis, and cancer.
A postmarketing safety study on baricitinib is expected to be completed in 2025.
The full results of the ORAL Surveillance study – which should address safety regarding pulmonary embolism and mortality, as well as efficacy data – have not yet been released. “Pfizer is working with the [FDA] and other regulatory agencies to review the full results and analyses as they become available,” the press release said.
Meta-analysis finds much less lupus than expected
The prevalence of systemic lupus erythematosus (SLE) appears to be much lower than previously believed and may pose “a potential risk to research funding for the disease,” according to results of a meta-analysis involving a network of population-based registries.
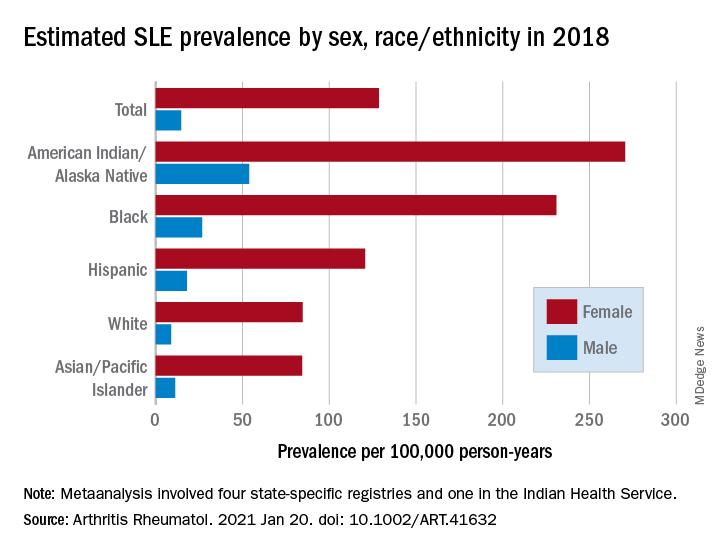
“When we started this study, a widely cited lupus statistic was that approximately 1.5 million Americans were affected. Our meta-analysis found the actual prevalence to be slightly more than 200,000: a number that approaches the [Food and Drug Administration’s] definition of a rare disease,” Emily Somers, PhD, ScM, senior author and associate professor of rheumatology and environmental health sciences at the University of Michigan, Ann Arbor, said in a written statement.
Their estimates, published online in Arthritis & Rheumatology, put the overall SLE prevalence in the United States at 72.8 per 100,000 person-years in 2018, with nearly nine times more females affected (128.7 cases per 100,000) than males (14.6 per 100,000). Race and ethnicity also play a role, as prevalence was highest among American Indian/Alaska Native and Black females, with Hispanic females lower but still higher than White and Asian/Pacific Islander females, Peter M. Izmirly, MD, MSc, of New York University, the lead author, and associates said.
SLE prevalence was distributed similarly in men, although there was a greater relative margin between American Indians/Alaska Natives (53.8 cases per 100,000 person-years) and Blacks (26.7 per 100,000), and Asians/Pacific Islanders were higher than Whites (11.2 vs. 8.9), the investigators reported.
The meta-analysis leveraged data from the Centers for Disease Control and Prevention’s national lupus registries, which include four state-specific SLE registries and a fifth in the Indian Health Service. All cases of SLE occurred in 2002-2009, and the data were age adjusted to the 2000 U.S. population and separately extrapolated to the 2018 U.S. Census population, they explained.
The analysis was funded by cooperative agreements between the New York City Department of Health and Mental Hygiene and New York University, and the CDC and National Institute of Health.
The prevalence of systemic lupus erythematosus (SLE) appears to be much lower than previously believed and may pose “a potential risk to research funding for the disease,” according to results of a meta-analysis involving a network of population-based registries.
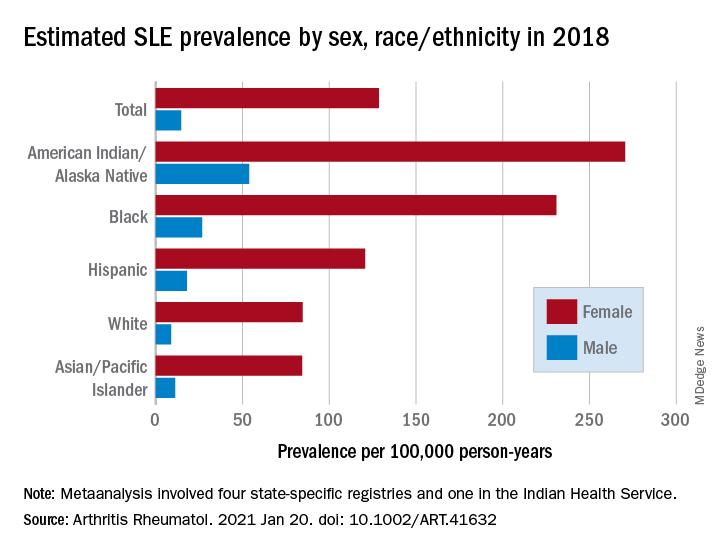
“When we started this study, a widely cited lupus statistic was that approximately 1.5 million Americans were affected. Our meta-analysis found the actual prevalence to be slightly more than 200,000: a number that approaches the [Food and Drug Administration’s] definition of a rare disease,” Emily Somers, PhD, ScM, senior author and associate professor of rheumatology and environmental health sciences at the University of Michigan, Ann Arbor, said in a written statement.
Their estimates, published online in Arthritis & Rheumatology, put the overall SLE prevalence in the United States at 72.8 per 100,000 person-years in 2018, with nearly nine times more females affected (128.7 cases per 100,000) than males (14.6 per 100,000). Race and ethnicity also play a role, as prevalence was highest among American Indian/Alaska Native and Black females, with Hispanic females lower but still higher than White and Asian/Pacific Islander females, Peter M. Izmirly, MD, MSc, of New York University, the lead author, and associates said.
SLE prevalence was distributed similarly in men, although there was a greater relative margin between American Indians/Alaska Natives (53.8 cases per 100,000 person-years) and Blacks (26.7 per 100,000), and Asians/Pacific Islanders were higher than Whites (11.2 vs. 8.9), the investigators reported.
The meta-analysis leveraged data from the Centers for Disease Control and Prevention’s national lupus registries, which include four state-specific SLE registries and a fifth in the Indian Health Service. All cases of SLE occurred in 2002-2009, and the data were age adjusted to the 2000 U.S. population and separately extrapolated to the 2018 U.S. Census population, they explained.
The analysis was funded by cooperative agreements between the New York City Department of Health and Mental Hygiene and New York University, and the CDC and National Institute of Health.
The prevalence of systemic lupus erythematosus (SLE) appears to be much lower than previously believed and may pose “a potential risk to research funding for the disease,” according to results of a meta-analysis involving a network of population-based registries.
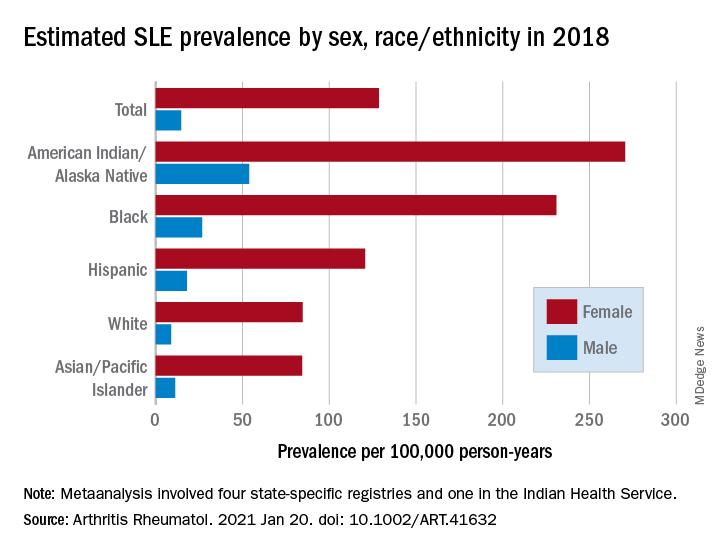
“When we started this study, a widely cited lupus statistic was that approximately 1.5 million Americans were affected. Our meta-analysis found the actual prevalence to be slightly more than 200,000: a number that approaches the [Food and Drug Administration’s] definition of a rare disease,” Emily Somers, PhD, ScM, senior author and associate professor of rheumatology and environmental health sciences at the University of Michigan, Ann Arbor, said in a written statement.
Their estimates, published online in Arthritis & Rheumatology, put the overall SLE prevalence in the United States at 72.8 per 100,000 person-years in 2018, with nearly nine times more females affected (128.7 cases per 100,000) than males (14.6 per 100,000). Race and ethnicity also play a role, as prevalence was highest among American Indian/Alaska Native and Black females, with Hispanic females lower but still higher than White and Asian/Pacific Islander females, Peter M. Izmirly, MD, MSc, of New York University, the lead author, and associates said.
SLE prevalence was distributed similarly in men, although there was a greater relative margin between American Indians/Alaska Natives (53.8 cases per 100,000 person-years) and Blacks (26.7 per 100,000), and Asians/Pacific Islanders were higher than Whites (11.2 vs. 8.9), the investigators reported.
The meta-analysis leveraged data from the Centers for Disease Control and Prevention’s national lupus registries, which include four state-specific SLE registries and a fifth in the Indian Health Service. All cases of SLE occurred in 2002-2009, and the data were age adjusted to the 2000 U.S. population and separately extrapolated to the 2018 U.S. Census population, they explained.
The analysis was funded by cooperative agreements between the New York City Department of Health and Mental Hygiene and New York University, and the CDC and National Institute of Health.
FROM ARTHRITIS & RHEUMATOLOGY











