User login
Ketamine promising for rare condition linked to autism
Also known as Helsmoortel–Van Der Aa syndrome, ADNP syndrome is caused by mutations in the ADNP gene. Studies in animal models suggest that low-dose ketamine increases expression of ADNP and is neuroprotective.
Intrigued by the preclinical evidence, Alexander Kolevzon, MD, clinical director of the Seaver Autism Center at Mount Sinai, New York, and colleagues treated 10 children with ADNP syndrome with a single low dose of ketamine (0.5mg/kg) infused intravenously over 40 minutes. The children ranged in ages 6-12 years.
Using parent-report instruments to assess treatment effects, ketamine was associated with “nominally significant” improvement in a variety of domains, including social behavior, attention-deficit and hyperactivity, restricted and repetitive behaviors, and sensory sensitivities.
Parent reports of improvement in these domains aligned with clinician-rated assessments based on the Clinical Global Impressions–Improvement scale.
The results also highlight the potential utility of electrophysiological measurement of auditory steady-state response and eye-tracking to track change with ketamine treatment, the researchers say.
The study was published online in Human Genetics and Genomic (HGG) Advances.
Hypothesis-generating
Ketamine was generally well tolerated. There were no clinically significant abnormalities in laboratory or cardiac monitoring, and there were no serious adverse events (AEs).
Treatment emergent AEs were all mild to moderate and no child required any interventions.
The most common AEs were elation/silliness in five children (50%), all of whom had a history of similar symptoms. Drowsiness and fatigue occurred in four children (40%) and two of them had a history of drowsiness. Aggression was likewise relatively common, reported in four children (40%), all of whom had aggression at baseline.
Decreased appetite emerged as a new AE in three children (30%), increased anxiety occurred in three children (30%), and irritability, nausea/vomiting, and restlessness each occurred in two children (20%).
The researchers caution that the findings are intended to be “hypothesis generating.”
“We are encouraged by these findings, which provide preliminary support for ketamine to help reduce negative effects of this devastating syndrome,” Dr. Kolevzon said in a news release from Mount Sinai.
Ketamine might help ease symptoms of ADNP syndrome “by increasing expression of the ADNP gene or by promoting synaptic plasticity through glutamatergic pathways,” Dr. Kolevzon told this news organization.
The next step, he said, is to get “a larger, placebo-controlled study approved for funding using repeated dosing over a longer duration of time. We are working with the FDA to get the design approved for an investigational new drug application.”
Support for the study was provided by the ADNP Kids Foundation and the Foundation for Mood Disorders. Support for mediKanren was provided by the National Center for Advancing Translational Sciences, and National Institutes of Health through the Biomedical Data Translator Program. Dr. Kolevzon is on the scientific advisory board of Ovid Therapeutics, Ritrova Therapeutics, and Jaguar Therapeutics and consults to Acadia, Alkermes, GW Pharmaceuticals, Neuren Pharmaceuticals, Clinilabs Drug Development Corporation, and Scioto Biosciences.
A version of this article first appeared on Medscape.com.
Also known as Helsmoortel–Van Der Aa syndrome, ADNP syndrome is caused by mutations in the ADNP gene. Studies in animal models suggest that low-dose ketamine increases expression of ADNP and is neuroprotective.
Intrigued by the preclinical evidence, Alexander Kolevzon, MD, clinical director of the Seaver Autism Center at Mount Sinai, New York, and colleagues treated 10 children with ADNP syndrome with a single low dose of ketamine (0.5mg/kg) infused intravenously over 40 minutes. The children ranged in ages 6-12 years.
Using parent-report instruments to assess treatment effects, ketamine was associated with “nominally significant” improvement in a variety of domains, including social behavior, attention-deficit and hyperactivity, restricted and repetitive behaviors, and sensory sensitivities.
Parent reports of improvement in these domains aligned with clinician-rated assessments based on the Clinical Global Impressions–Improvement scale.
The results also highlight the potential utility of electrophysiological measurement of auditory steady-state response and eye-tracking to track change with ketamine treatment, the researchers say.
The study was published online in Human Genetics and Genomic (HGG) Advances.
Hypothesis-generating
Ketamine was generally well tolerated. There were no clinically significant abnormalities in laboratory or cardiac monitoring, and there were no serious adverse events (AEs).
Treatment emergent AEs were all mild to moderate and no child required any interventions.
The most common AEs were elation/silliness in five children (50%), all of whom had a history of similar symptoms. Drowsiness and fatigue occurred in four children (40%) and two of them had a history of drowsiness. Aggression was likewise relatively common, reported in four children (40%), all of whom had aggression at baseline.
Decreased appetite emerged as a new AE in three children (30%), increased anxiety occurred in three children (30%), and irritability, nausea/vomiting, and restlessness each occurred in two children (20%).
The researchers caution that the findings are intended to be “hypothesis generating.”
“We are encouraged by these findings, which provide preliminary support for ketamine to help reduce negative effects of this devastating syndrome,” Dr. Kolevzon said in a news release from Mount Sinai.
Ketamine might help ease symptoms of ADNP syndrome “by increasing expression of the ADNP gene or by promoting synaptic plasticity through glutamatergic pathways,” Dr. Kolevzon told this news organization.
The next step, he said, is to get “a larger, placebo-controlled study approved for funding using repeated dosing over a longer duration of time. We are working with the FDA to get the design approved for an investigational new drug application.”
Support for the study was provided by the ADNP Kids Foundation and the Foundation for Mood Disorders. Support for mediKanren was provided by the National Center for Advancing Translational Sciences, and National Institutes of Health through the Biomedical Data Translator Program. Dr. Kolevzon is on the scientific advisory board of Ovid Therapeutics, Ritrova Therapeutics, and Jaguar Therapeutics and consults to Acadia, Alkermes, GW Pharmaceuticals, Neuren Pharmaceuticals, Clinilabs Drug Development Corporation, and Scioto Biosciences.
A version of this article first appeared on Medscape.com.
Also known as Helsmoortel–Van Der Aa syndrome, ADNP syndrome is caused by mutations in the ADNP gene. Studies in animal models suggest that low-dose ketamine increases expression of ADNP and is neuroprotective.
Intrigued by the preclinical evidence, Alexander Kolevzon, MD, clinical director of the Seaver Autism Center at Mount Sinai, New York, and colleagues treated 10 children with ADNP syndrome with a single low dose of ketamine (0.5mg/kg) infused intravenously over 40 minutes. The children ranged in ages 6-12 years.
Using parent-report instruments to assess treatment effects, ketamine was associated with “nominally significant” improvement in a variety of domains, including social behavior, attention-deficit and hyperactivity, restricted and repetitive behaviors, and sensory sensitivities.
Parent reports of improvement in these domains aligned with clinician-rated assessments based on the Clinical Global Impressions–Improvement scale.
The results also highlight the potential utility of electrophysiological measurement of auditory steady-state response and eye-tracking to track change with ketamine treatment, the researchers say.
The study was published online in Human Genetics and Genomic (HGG) Advances.
Hypothesis-generating
Ketamine was generally well tolerated. There were no clinically significant abnormalities in laboratory or cardiac monitoring, and there were no serious adverse events (AEs).
Treatment emergent AEs were all mild to moderate and no child required any interventions.
The most common AEs were elation/silliness in five children (50%), all of whom had a history of similar symptoms. Drowsiness and fatigue occurred in four children (40%) and two of them had a history of drowsiness. Aggression was likewise relatively common, reported in four children (40%), all of whom had aggression at baseline.
Decreased appetite emerged as a new AE in three children (30%), increased anxiety occurred in three children (30%), and irritability, nausea/vomiting, and restlessness each occurred in two children (20%).
The researchers caution that the findings are intended to be “hypothesis generating.”
“We are encouraged by these findings, which provide preliminary support for ketamine to help reduce negative effects of this devastating syndrome,” Dr. Kolevzon said in a news release from Mount Sinai.
Ketamine might help ease symptoms of ADNP syndrome “by increasing expression of the ADNP gene or by promoting synaptic plasticity through glutamatergic pathways,” Dr. Kolevzon told this news organization.
The next step, he said, is to get “a larger, placebo-controlled study approved for funding using repeated dosing over a longer duration of time. We are working with the FDA to get the design approved for an investigational new drug application.”
Support for the study was provided by the ADNP Kids Foundation and the Foundation for Mood Disorders. Support for mediKanren was provided by the National Center for Advancing Translational Sciences, and National Institutes of Health through the Biomedical Data Translator Program. Dr. Kolevzon is on the scientific advisory board of Ovid Therapeutics, Ritrova Therapeutics, and Jaguar Therapeutics and consults to Acadia, Alkermes, GW Pharmaceuticals, Neuren Pharmaceuticals, Clinilabs Drug Development Corporation, and Scioto Biosciences.
A version of this article first appeared on Medscape.com.
From Human Genetics and Genomic Advances
Children and COVID: New cases took a downturn in September
After 2 weeks of increases in the number of new COVID-19 cases in children – a trend that just happened to coincide with the start of a new school year – there were fewer cases reported during the first full week of September, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, the AAP and CHA said in their weekly COVID-19 report, noting also that seven states and the District of Columbia no longer update their online dashboards while others publish new data less often than every week.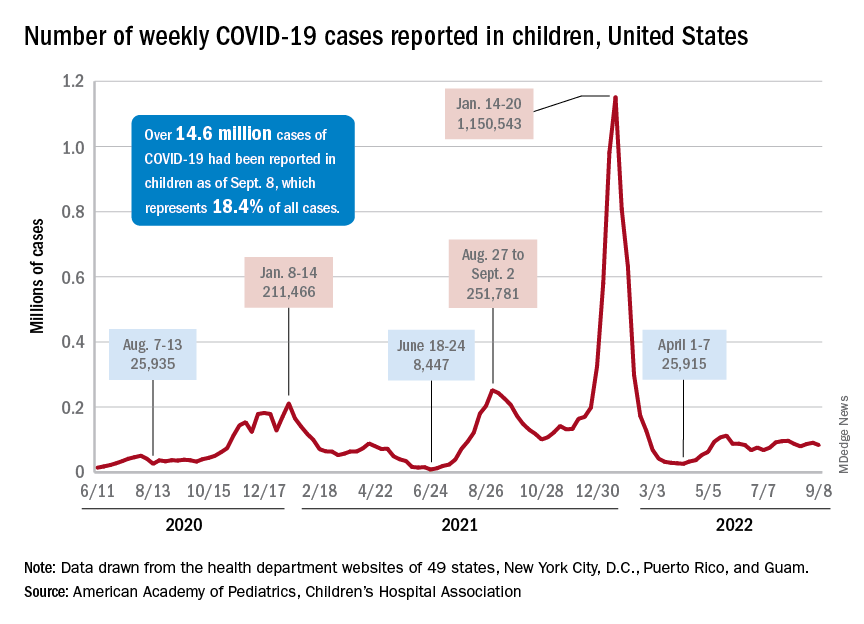
The drop in new cases was accompanied by declines in emergency department visits and hospital admissions, both of which had shown some signs of resurgence in mid- to late August. The brief rise in ED visits seemed to be age-related, occurring in those aged 12 years and older but not in younger children, whose ED visit rate fell steadily through August. Through the first week of September, however, 7-day averages were down for both those aged 12-15 and for 16- to 17-year-olds, the Centers for Disease Control and Prevention reported.
The rate of new hospital admissions of children with confirmed COVID-19, available only for ages 0-17 years, has declined every day since Aug. 28, when it reached 0.44 per 100,000 population after a week of climbing, the CDC said on its COVID Data Tracker.
Cumulatively, about 156,000 children were hospitalized with COVID from Aug. 1, 2020 to Sept. 10, 2022, according to the CDC, which puts the total number of pediatric cases at just over 15 million and deaths at 1,778. Those last two figures represent 17.4% and about 0.4% of all U.S. cases and deaths. The AAP and CHA estimate that about 14.6 million child cases have been reported so far, which is 18.4% of cases in all ages.
Vaccinations are slowly adding up
On the prevention side of the health care system’s response to COVID, the CDC’s cumulative numbers looked like this as of Sept. 6:
- 1.1 million children under age 5 (about 5.8% of the age group) had received at least one dose of vaccine, and 280,000 (1.4%) were fully vaccinated.
- Almost 11 million (38.2%) children aged 5-11 had gotten one dose, and 8.9 million (31.1%) were fully vaccinated.
- 17.9 million (70.8%) children aged 12-17 had received at least one dose, and 15.3 million (60.5%) were fully vaccinated.
Over the 14 days ending Sept. 7, children aged 2-4 years made up the largest group (21.4%) of Americans getting their first vaccine doses, while those aged 5-11 years were the third largest age group at 16.7% of all vaccinees (25- to 49-year-olds were second). The situation was reversed for vaccine completion over the last 2 weeks: Those aged 5-11 were first at 24.7%, and the 2- to 4-year-olds were third at 16.7% (those aged 25-49 were second again), according to the COVID Data Tracker.
After 2 weeks of increases in the number of new COVID-19 cases in children – a trend that just happened to coincide with the start of a new school year – there were fewer cases reported during the first full week of September, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, the AAP and CHA said in their weekly COVID-19 report, noting also that seven states and the District of Columbia no longer update their online dashboards while others publish new data less often than every week.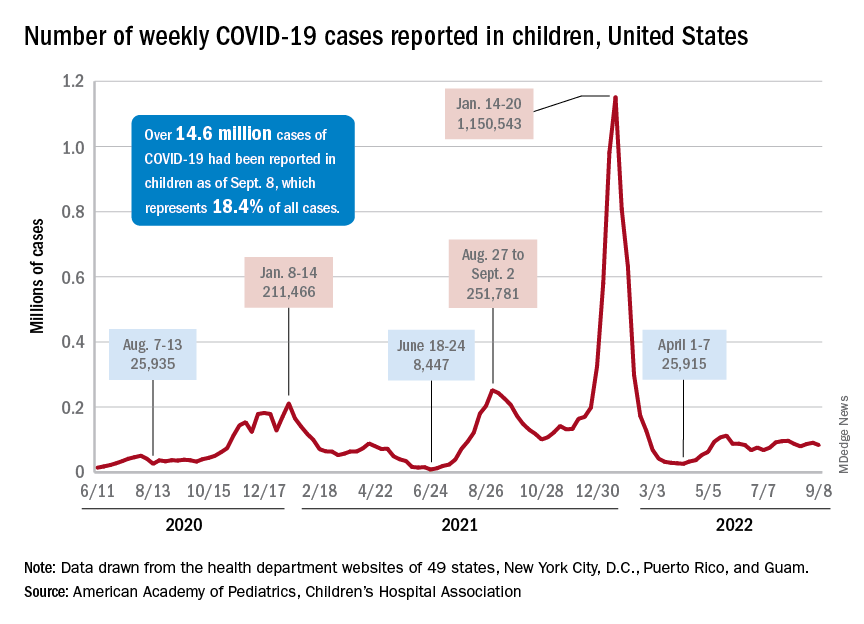
The drop in new cases was accompanied by declines in emergency department visits and hospital admissions, both of which had shown some signs of resurgence in mid- to late August. The brief rise in ED visits seemed to be age-related, occurring in those aged 12 years and older but not in younger children, whose ED visit rate fell steadily through August. Through the first week of September, however, 7-day averages were down for both those aged 12-15 and for 16- to 17-year-olds, the Centers for Disease Control and Prevention reported.
The rate of new hospital admissions of children with confirmed COVID-19, available only for ages 0-17 years, has declined every day since Aug. 28, when it reached 0.44 per 100,000 population after a week of climbing, the CDC said on its COVID Data Tracker.
Cumulatively, about 156,000 children were hospitalized with COVID from Aug. 1, 2020 to Sept. 10, 2022, according to the CDC, which puts the total number of pediatric cases at just over 15 million and deaths at 1,778. Those last two figures represent 17.4% and about 0.4% of all U.S. cases and deaths. The AAP and CHA estimate that about 14.6 million child cases have been reported so far, which is 18.4% of cases in all ages.
Vaccinations are slowly adding up
On the prevention side of the health care system’s response to COVID, the CDC’s cumulative numbers looked like this as of Sept. 6:
- 1.1 million children under age 5 (about 5.8% of the age group) had received at least one dose of vaccine, and 280,000 (1.4%) were fully vaccinated.
- Almost 11 million (38.2%) children aged 5-11 had gotten one dose, and 8.9 million (31.1%) were fully vaccinated.
- 17.9 million (70.8%) children aged 12-17 had received at least one dose, and 15.3 million (60.5%) were fully vaccinated.
Over the 14 days ending Sept. 7, children aged 2-4 years made up the largest group (21.4%) of Americans getting their first vaccine doses, while those aged 5-11 years were the third largest age group at 16.7% of all vaccinees (25- to 49-year-olds were second). The situation was reversed for vaccine completion over the last 2 weeks: Those aged 5-11 were first at 24.7%, and the 2- to 4-year-olds were third at 16.7% (those aged 25-49 were second again), according to the COVID Data Tracker.
After 2 weeks of increases in the number of new COVID-19 cases in children – a trend that just happened to coincide with the start of a new school year – there were fewer cases reported during the first full week of September, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, the AAP and CHA said in their weekly COVID-19 report, noting also that seven states and the District of Columbia no longer update their online dashboards while others publish new data less often than every week.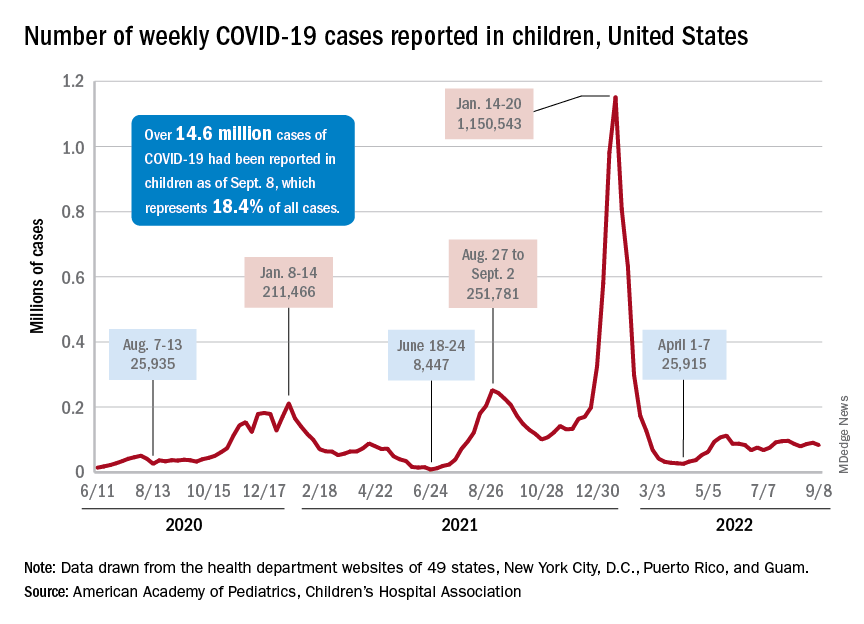
The drop in new cases was accompanied by declines in emergency department visits and hospital admissions, both of which had shown some signs of resurgence in mid- to late August. The brief rise in ED visits seemed to be age-related, occurring in those aged 12 years and older but not in younger children, whose ED visit rate fell steadily through August. Through the first week of September, however, 7-day averages were down for both those aged 12-15 and for 16- to 17-year-olds, the Centers for Disease Control and Prevention reported.
The rate of new hospital admissions of children with confirmed COVID-19, available only for ages 0-17 years, has declined every day since Aug. 28, when it reached 0.44 per 100,000 population after a week of climbing, the CDC said on its COVID Data Tracker.
Cumulatively, about 156,000 children were hospitalized with COVID from Aug. 1, 2020 to Sept. 10, 2022, according to the CDC, which puts the total number of pediatric cases at just over 15 million and deaths at 1,778. Those last two figures represent 17.4% and about 0.4% of all U.S. cases and deaths. The AAP and CHA estimate that about 14.6 million child cases have been reported so far, which is 18.4% of cases in all ages.
Vaccinations are slowly adding up
On the prevention side of the health care system’s response to COVID, the CDC’s cumulative numbers looked like this as of Sept. 6:
- 1.1 million children under age 5 (about 5.8% of the age group) had received at least one dose of vaccine, and 280,000 (1.4%) were fully vaccinated.
- Almost 11 million (38.2%) children aged 5-11 had gotten one dose, and 8.9 million (31.1%) were fully vaccinated.
- 17.9 million (70.8%) children aged 12-17 had received at least one dose, and 15.3 million (60.5%) were fully vaccinated.
Over the 14 days ending Sept. 7, children aged 2-4 years made up the largest group (21.4%) of Americans getting their first vaccine doses, while those aged 5-11 years were the third largest age group at 16.7% of all vaccinees (25- to 49-year-olds were second). The situation was reversed for vaccine completion over the last 2 weeks: Those aged 5-11 were first at 24.7%, and the 2- to 4-year-olds were third at 16.7% (those aged 25-49 were second again), according to the COVID Data Tracker.
CDC warns of enterovirus strain linked to polio-like condition
, according to a Health Network Alert advisory by the Centers for Disease Control and Prevention.
In August, health care providers and hospitals notified the CDC of an increase in severe respiratory illness in children who also tested positive for rhinovirus (RV) or enterovirus (EV). Additional testing revealed that some children were positive for EV-D68, which primarily causes acute respiratory illness. However, the virus has been associated with acute flaccid myelitis (AFM), a rare neurologic condition involving muscle weakness.
Also, in July and August 2022, surveillance networks reported an increase in EV-D68 activity compared with the same months in 2019, 2020, and 2021, the agency said in the alert. As of Aug. 30, the CDC has not received any reports of AFM beginning this year; however, spikes in EV-D68 typically come before cases of AFM, they said.
“Something we are always on the lookout for in the late summer and fall is AFM cases,” said Rick Malley, MD, of the division of infectious disease at Boston Children’s Hospital, in an interview with this news organization. “Unfortunately, we kind of expect them during enterovirus season,” he said. That season is thought to peak in the late summer and early fall.
Since the CDC began tracking AFM in August 2014, there have been 692 confirmed cases in the United States. AFM cases spiked in 2014, 2016, and 2018, mostly in young children. In 2021, there were 28 confirmed cases across 15 states. The CDC did not specify the age of those cases, but in 2018 – when EV-D68 most recently circulated at high levels – the median age of children who visited the emergency department or were hospitalized for EV-D68–associated respiratory illness was 3 years.
“[AFM] can be very severe and it can be very scary for the parents of children who have it,” Dr. Malley said, “but given the prevalence of enteroviruses in the community, you have to conclude it’s a relatively rare event in susceptible individuals. Why some get it and others don’t is unfortunately unclear at this moment.”
The CDC recommends that providers consider EV-D68 as a possible cause for acute, severe respiratory illness in children. If the cause of a respiratory illness in a severely ill patient is not clear, health professionals should test for RVs and EVs, if this is not already part of a typical diagnostic workflow, the agency said. Currently, there are no vaccines or specific treatments for RV or EV, and the CDC recommends supportive clinical management.
The advisory also urged providers to “strongly consider AFM in patients with acute flaccid limb weakness, especially after respiratory illness or fever, and between the months of August and November 2022.”
For any patient presenting with possible AFM, clinicians should collect samples from multiple sources, including cerebrospinal fluid, serum, stool, and a nasopharyngeal or oropharyngeal swab. Samples should be taken “as early as possible and preferably on the day of onset of limb weakness,” the alert said. There is currently no specific medicine for AFM, the agency said, though recommended interventions may vary for each patient.
A version of this article first appeared on Medscape.com.
, according to a Health Network Alert advisory by the Centers for Disease Control and Prevention.
In August, health care providers and hospitals notified the CDC of an increase in severe respiratory illness in children who also tested positive for rhinovirus (RV) or enterovirus (EV). Additional testing revealed that some children were positive for EV-D68, which primarily causes acute respiratory illness. However, the virus has been associated with acute flaccid myelitis (AFM), a rare neurologic condition involving muscle weakness.
Also, in July and August 2022, surveillance networks reported an increase in EV-D68 activity compared with the same months in 2019, 2020, and 2021, the agency said in the alert. As of Aug. 30, the CDC has not received any reports of AFM beginning this year; however, spikes in EV-D68 typically come before cases of AFM, they said.
“Something we are always on the lookout for in the late summer and fall is AFM cases,” said Rick Malley, MD, of the division of infectious disease at Boston Children’s Hospital, in an interview with this news organization. “Unfortunately, we kind of expect them during enterovirus season,” he said. That season is thought to peak in the late summer and early fall.
Since the CDC began tracking AFM in August 2014, there have been 692 confirmed cases in the United States. AFM cases spiked in 2014, 2016, and 2018, mostly in young children. In 2021, there were 28 confirmed cases across 15 states. The CDC did not specify the age of those cases, but in 2018 – when EV-D68 most recently circulated at high levels – the median age of children who visited the emergency department or were hospitalized for EV-D68–associated respiratory illness was 3 years.
“[AFM] can be very severe and it can be very scary for the parents of children who have it,” Dr. Malley said, “but given the prevalence of enteroviruses in the community, you have to conclude it’s a relatively rare event in susceptible individuals. Why some get it and others don’t is unfortunately unclear at this moment.”
The CDC recommends that providers consider EV-D68 as a possible cause for acute, severe respiratory illness in children. If the cause of a respiratory illness in a severely ill patient is not clear, health professionals should test for RVs and EVs, if this is not already part of a typical diagnostic workflow, the agency said. Currently, there are no vaccines or specific treatments for RV or EV, and the CDC recommends supportive clinical management.
The advisory also urged providers to “strongly consider AFM in patients with acute flaccid limb weakness, especially after respiratory illness or fever, and between the months of August and November 2022.”
For any patient presenting with possible AFM, clinicians should collect samples from multiple sources, including cerebrospinal fluid, serum, stool, and a nasopharyngeal or oropharyngeal swab. Samples should be taken “as early as possible and preferably on the day of onset of limb weakness,” the alert said. There is currently no specific medicine for AFM, the agency said, though recommended interventions may vary for each patient.
A version of this article first appeared on Medscape.com.
, according to a Health Network Alert advisory by the Centers for Disease Control and Prevention.
In August, health care providers and hospitals notified the CDC of an increase in severe respiratory illness in children who also tested positive for rhinovirus (RV) or enterovirus (EV). Additional testing revealed that some children were positive for EV-D68, which primarily causes acute respiratory illness. However, the virus has been associated with acute flaccid myelitis (AFM), a rare neurologic condition involving muscle weakness.
Also, in July and August 2022, surveillance networks reported an increase in EV-D68 activity compared with the same months in 2019, 2020, and 2021, the agency said in the alert. As of Aug. 30, the CDC has not received any reports of AFM beginning this year; however, spikes in EV-D68 typically come before cases of AFM, they said.
“Something we are always on the lookout for in the late summer and fall is AFM cases,” said Rick Malley, MD, of the division of infectious disease at Boston Children’s Hospital, in an interview with this news organization. “Unfortunately, we kind of expect them during enterovirus season,” he said. That season is thought to peak in the late summer and early fall.
Since the CDC began tracking AFM in August 2014, there have been 692 confirmed cases in the United States. AFM cases spiked in 2014, 2016, and 2018, mostly in young children. In 2021, there were 28 confirmed cases across 15 states. The CDC did not specify the age of those cases, but in 2018 – when EV-D68 most recently circulated at high levels – the median age of children who visited the emergency department or were hospitalized for EV-D68–associated respiratory illness was 3 years.
“[AFM] can be very severe and it can be very scary for the parents of children who have it,” Dr. Malley said, “but given the prevalence of enteroviruses in the community, you have to conclude it’s a relatively rare event in susceptible individuals. Why some get it and others don’t is unfortunately unclear at this moment.”
The CDC recommends that providers consider EV-D68 as a possible cause for acute, severe respiratory illness in children. If the cause of a respiratory illness in a severely ill patient is not clear, health professionals should test for RVs and EVs, if this is not already part of a typical diagnostic workflow, the agency said. Currently, there are no vaccines or specific treatments for RV or EV, and the CDC recommends supportive clinical management.
The advisory also urged providers to “strongly consider AFM in patients with acute flaccid limb weakness, especially after respiratory illness or fever, and between the months of August and November 2022.”
For any patient presenting with possible AFM, clinicians should collect samples from multiple sources, including cerebrospinal fluid, serum, stool, and a nasopharyngeal or oropharyngeal swab. Samples should be taken “as early as possible and preferably on the day of onset of limb weakness,” the alert said. There is currently no specific medicine for AFM, the agency said, though recommended interventions may vary for each patient.
A version of this article first appeared on Medscape.com.
Weight gain during pregnancy may play role in child ADHD risk
Obesity in women of reproductive age has emerged as one of the main risk factors associated with neonatal complications and long-term neuropsychiatric consequences in offspring, including attention-deficit/hyperactivity disorder.
Research has also linked pregestational diabetes and gestational diabetes mellitus (GDM) to an increased risk for ADHD in offspring. Now, an observational study of 1,036 singleton births at one hospital between 1998 and 2008 suggests that in the presence of GDM, maternal obesity combined with excessive weight gain during pregnancy may be jointly associated with increased risk of offspring ADHD. The median follow-up was 17.7 years.
Maternal obesity was independently associated with ADHD (adjusted hazard ratio, 1.66; 95% confidence interval: 1.07-2.60), but excessive weight gain during pregnancy and maternal overweight were not, reported Verónica Perea, MD, PhD, of the Hospital Universitari Mútua de Terrassa, Barcelona, and colleagues in the Journal of Clinical Endocrinology & Metabolism.
However, in women with pregestation obesity who gained more weight than recommended by the National Academy of Medicine (NAM), the risk of offspring ADHD was higher, compared with women of normal weight whose pregnancy weight stayed within NAM guidelines (adjusted hazard ratio, 2.13; 95% confidence interval: 1.14-4.01).
“The results of this study suggest that the negative repercussions of excessive weight gain on children within the setting of a high-risk population with GDM and obesity were not only observed during the prenatal period but also years later with a development of ADHD,” the researchers wrote.
The study also showed that when maternal weight gain did not exceed NAM guidelines, maternal obesity was no longer independently associated with ADHD in offspring (aHR, 1.36; 95% CI: 0.78-2.36). This finding conflicts with earlier studies focusing primarily on the role of pregestational maternal weight, the researchers said. A 2018 nationwide Finnish cohort study in newborns showed an increased long-term risk of ADHD in those born to women with GDM, compared with the nondiabetic population. This long-term risk of ADHD increased in the presence of pregestational obesity (HR, 1.64).
Similarly, evidence from systematic reviews and meta-analyses has demonstrated that antenatal lifestyle interventions to prevent excessive weight gain during pregnancy were associated with a reduction in adverse pregnancy outcomes. However, evidence on offspring mental health was lacking, especially in high-risk pregnancies with gestational diabetes, the study authors said.
Although causal inferences can’t be drawn from the current observational study, “it seems that the higher risk [of ADHD] observed would be explained by the role of gestational weight gain during the antenatal period,” Dr. Perea said in an interview. Importantly, the study highlights a window of opportunity for promoting healthy weight gain during pregnancy, Dr. Perea said. ”This should be a priority in the current management of gestation.”
Fatima Cody Stanford, MD, MPH, an associate professor of medicine and pediatrics at Harvard Medical School, Boston, agreed. “I think one of the key issues is that there’s very little attention paid to how weight gain is regulated during pregnancy,” she said in an interview. On many other points, however, Dr. Stanford, who is a specialist in obesity medicine at Massachusetts General Hospital Weight Center, did not agree.
The association between ADHD and obesity has already been well established by a 2019 meta-analysis and systematic review of studies over the last 10 years, she emphasized. “These studies were able to show a much stronger association between maternal obesity and ADHD in offspring because they were powered to detect differences.”
The current study does not say “anything new or novel,” Dr. Stanford added. “Maternal obesity and the association with an increased risk of ADHD in offspring is the main issue. I don’t think there was any appreciable increase when weight gain during pregnancy was factored in. It’s mild at best.”
Eran Bornstein, MD, vice-chair of obstetrics and gynecology at Lenox Hill Hospital, New York, expressed a similar point of view. Although the study findings “add to the current literature,” they should be interpreted “cautiously,” Dr. Bornstein said in an interview.
The size of the effect on ADHD risk attributable to maternal weight gain during pregnancy “was not clear,” he said. “Cohort studies of this sort are excellent for finding associations which help us generate the hypothesis, but this doesn’t demonstrate a cause and effect or a magnitude for this effect.”
Physicians should follow cumulative data suggesting that maternal obesity is associated with a number of pregnancy complications and neonatal outcomes in women with and without diabetes, Dr. Bornstein suggested. “Optimizing maternal weight prior to pregnancy and adhering to recommendations regarding weight gain has the potential to improve some of these outcomes.”
Treating obesity prior to conception mitigates GDM risk, agreed Dr. Stanford. “The issue,” she explained, “is that all of the drugs approved for the treatment of obesity are contraindicated in pregnancy and lifestyle modification fails in 96% of cases, even when there is no pregnancy.” Drugs such as metformin are being used off-label to treat obesity and to safely manage gestational weight gain, she said. “Those of us who practice obesity medicine know that metformin can be safely used throughout pregnancy with no harm to the fetus.”
This study was partially funded by Fundació Docència i Recerca MútuaTerrassa. Dr. Perea and study coauthors reporting have no conflicts of interest. Dr. Stanford disclosed relationships with Novo Nordisk, Eli Lilly, Boehringer Ingelheim, Gelesis, Pfizer, Currax, and Rhythm. Dr. Bornstein reported having no conflicts of interest.
This story was updated on 11/7/2022.
Obesity in women of reproductive age has emerged as one of the main risk factors associated with neonatal complications and long-term neuropsychiatric consequences in offspring, including attention-deficit/hyperactivity disorder.
Research has also linked pregestational diabetes and gestational diabetes mellitus (GDM) to an increased risk for ADHD in offspring. Now, an observational study of 1,036 singleton births at one hospital between 1998 and 2008 suggests that in the presence of GDM, maternal obesity combined with excessive weight gain during pregnancy may be jointly associated with increased risk of offspring ADHD. The median follow-up was 17.7 years.
Maternal obesity was independently associated with ADHD (adjusted hazard ratio, 1.66; 95% confidence interval: 1.07-2.60), but excessive weight gain during pregnancy and maternal overweight were not, reported Verónica Perea, MD, PhD, of the Hospital Universitari Mútua de Terrassa, Barcelona, and colleagues in the Journal of Clinical Endocrinology & Metabolism.
However, in women with pregestation obesity who gained more weight than recommended by the National Academy of Medicine (NAM), the risk of offspring ADHD was higher, compared with women of normal weight whose pregnancy weight stayed within NAM guidelines (adjusted hazard ratio, 2.13; 95% confidence interval: 1.14-4.01).
“The results of this study suggest that the negative repercussions of excessive weight gain on children within the setting of a high-risk population with GDM and obesity were not only observed during the prenatal period but also years later with a development of ADHD,” the researchers wrote.
The study also showed that when maternal weight gain did not exceed NAM guidelines, maternal obesity was no longer independently associated with ADHD in offspring (aHR, 1.36; 95% CI: 0.78-2.36). This finding conflicts with earlier studies focusing primarily on the role of pregestational maternal weight, the researchers said. A 2018 nationwide Finnish cohort study in newborns showed an increased long-term risk of ADHD in those born to women with GDM, compared with the nondiabetic population. This long-term risk of ADHD increased in the presence of pregestational obesity (HR, 1.64).
Similarly, evidence from systematic reviews and meta-analyses has demonstrated that antenatal lifestyle interventions to prevent excessive weight gain during pregnancy were associated with a reduction in adverse pregnancy outcomes. However, evidence on offspring mental health was lacking, especially in high-risk pregnancies with gestational diabetes, the study authors said.
Although causal inferences can’t be drawn from the current observational study, “it seems that the higher risk [of ADHD] observed would be explained by the role of gestational weight gain during the antenatal period,” Dr. Perea said in an interview. Importantly, the study highlights a window of opportunity for promoting healthy weight gain during pregnancy, Dr. Perea said. ”This should be a priority in the current management of gestation.”
Fatima Cody Stanford, MD, MPH, an associate professor of medicine and pediatrics at Harvard Medical School, Boston, agreed. “I think one of the key issues is that there’s very little attention paid to how weight gain is regulated during pregnancy,” she said in an interview. On many other points, however, Dr. Stanford, who is a specialist in obesity medicine at Massachusetts General Hospital Weight Center, did not agree.
The association between ADHD and obesity has already been well established by a 2019 meta-analysis and systematic review of studies over the last 10 years, she emphasized. “These studies were able to show a much stronger association between maternal obesity and ADHD in offspring because they were powered to detect differences.”
The current study does not say “anything new or novel,” Dr. Stanford added. “Maternal obesity and the association with an increased risk of ADHD in offspring is the main issue. I don’t think there was any appreciable increase when weight gain during pregnancy was factored in. It’s mild at best.”
Eran Bornstein, MD, vice-chair of obstetrics and gynecology at Lenox Hill Hospital, New York, expressed a similar point of view. Although the study findings “add to the current literature,” they should be interpreted “cautiously,” Dr. Bornstein said in an interview.
The size of the effect on ADHD risk attributable to maternal weight gain during pregnancy “was not clear,” he said. “Cohort studies of this sort are excellent for finding associations which help us generate the hypothesis, but this doesn’t demonstrate a cause and effect or a magnitude for this effect.”
Physicians should follow cumulative data suggesting that maternal obesity is associated with a number of pregnancy complications and neonatal outcomes in women with and without diabetes, Dr. Bornstein suggested. “Optimizing maternal weight prior to pregnancy and adhering to recommendations regarding weight gain has the potential to improve some of these outcomes.”
Treating obesity prior to conception mitigates GDM risk, agreed Dr. Stanford. “The issue,” she explained, “is that all of the drugs approved for the treatment of obesity are contraindicated in pregnancy and lifestyle modification fails in 96% of cases, even when there is no pregnancy.” Drugs such as metformin are being used off-label to treat obesity and to safely manage gestational weight gain, she said. “Those of us who practice obesity medicine know that metformin can be safely used throughout pregnancy with no harm to the fetus.”
This study was partially funded by Fundació Docència i Recerca MútuaTerrassa. Dr. Perea and study coauthors reporting have no conflicts of interest. Dr. Stanford disclosed relationships with Novo Nordisk, Eli Lilly, Boehringer Ingelheim, Gelesis, Pfizer, Currax, and Rhythm. Dr. Bornstein reported having no conflicts of interest.
This story was updated on 11/7/2022.
Obesity in women of reproductive age has emerged as one of the main risk factors associated with neonatal complications and long-term neuropsychiatric consequences in offspring, including attention-deficit/hyperactivity disorder.
Research has also linked pregestational diabetes and gestational diabetes mellitus (GDM) to an increased risk for ADHD in offspring. Now, an observational study of 1,036 singleton births at one hospital between 1998 and 2008 suggests that in the presence of GDM, maternal obesity combined with excessive weight gain during pregnancy may be jointly associated with increased risk of offspring ADHD. The median follow-up was 17.7 years.
Maternal obesity was independently associated with ADHD (adjusted hazard ratio, 1.66; 95% confidence interval: 1.07-2.60), but excessive weight gain during pregnancy and maternal overweight were not, reported Verónica Perea, MD, PhD, of the Hospital Universitari Mútua de Terrassa, Barcelona, and colleagues in the Journal of Clinical Endocrinology & Metabolism.
However, in women with pregestation obesity who gained more weight than recommended by the National Academy of Medicine (NAM), the risk of offspring ADHD was higher, compared with women of normal weight whose pregnancy weight stayed within NAM guidelines (adjusted hazard ratio, 2.13; 95% confidence interval: 1.14-4.01).
“The results of this study suggest that the negative repercussions of excessive weight gain on children within the setting of a high-risk population with GDM and obesity were not only observed during the prenatal period but also years later with a development of ADHD,” the researchers wrote.
The study also showed that when maternal weight gain did not exceed NAM guidelines, maternal obesity was no longer independently associated with ADHD in offspring (aHR, 1.36; 95% CI: 0.78-2.36). This finding conflicts with earlier studies focusing primarily on the role of pregestational maternal weight, the researchers said. A 2018 nationwide Finnish cohort study in newborns showed an increased long-term risk of ADHD in those born to women with GDM, compared with the nondiabetic population. This long-term risk of ADHD increased in the presence of pregestational obesity (HR, 1.64).
Similarly, evidence from systematic reviews and meta-analyses has demonstrated that antenatal lifestyle interventions to prevent excessive weight gain during pregnancy were associated with a reduction in adverse pregnancy outcomes. However, evidence on offspring mental health was lacking, especially in high-risk pregnancies with gestational diabetes, the study authors said.
Although causal inferences can’t be drawn from the current observational study, “it seems that the higher risk [of ADHD] observed would be explained by the role of gestational weight gain during the antenatal period,” Dr. Perea said in an interview. Importantly, the study highlights a window of opportunity for promoting healthy weight gain during pregnancy, Dr. Perea said. ”This should be a priority in the current management of gestation.”
Fatima Cody Stanford, MD, MPH, an associate professor of medicine and pediatrics at Harvard Medical School, Boston, agreed. “I think one of the key issues is that there’s very little attention paid to how weight gain is regulated during pregnancy,” she said in an interview. On many other points, however, Dr. Stanford, who is a specialist in obesity medicine at Massachusetts General Hospital Weight Center, did not agree.
The association between ADHD and obesity has already been well established by a 2019 meta-analysis and systematic review of studies over the last 10 years, she emphasized. “These studies were able to show a much stronger association between maternal obesity and ADHD in offspring because they were powered to detect differences.”
The current study does not say “anything new or novel,” Dr. Stanford added. “Maternal obesity and the association with an increased risk of ADHD in offspring is the main issue. I don’t think there was any appreciable increase when weight gain during pregnancy was factored in. It’s mild at best.”
Eran Bornstein, MD, vice-chair of obstetrics and gynecology at Lenox Hill Hospital, New York, expressed a similar point of view. Although the study findings “add to the current literature,” they should be interpreted “cautiously,” Dr. Bornstein said in an interview.
The size of the effect on ADHD risk attributable to maternal weight gain during pregnancy “was not clear,” he said. “Cohort studies of this sort are excellent for finding associations which help us generate the hypothesis, but this doesn’t demonstrate a cause and effect or a magnitude for this effect.”
Physicians should follow cumulative data suggesting that maternal obesity is associated with a number of pregnancy complications and neonatal outcomes in women with and without diabetes, Dr. Bornstein suggested. “Optimizing maternal weight prior to pregnancy and adhering to recommendations regarding weight gain has the potential to improve some of these outcomes.”
Treating obesity prior to conception mitigates GDM risk, agreed Dr. Stanford. “The issue,” she explained, “is that all of the drugs approved for the treatment of obesity are contraindicated in pregnancy and lifestyle modification fails in 96% of cases, even when there is no pregnancy.” Drugs such as metformin are being used off-label to treat obesity and to safely manage gestational weight gain, she said. “Those of us who practice obesity medicine know that metformin can be safely used throughout pregnancy with no harm to the fetus.”
This study was partially funded by Fundació Docència i Recerca MútuaTerrassa. Dr. Perea and study coauthors reporting have no conflicts of interest. Dr. Stanford disclosed relationships with Novo Nordisk, Eli Lilly, Boehringer Ingelheim, Gelesis, Pfizer, Currax, and Rhythm. Dr. Bornstein reported having no conflicts of interest.
This story was updated on 11/7/2022.
The Journal of Clinical Endocrinology & Metabolism
N.Y. governor declares state disaster emergency to boost polio vaccination
New York Governor Kathy Hochul declared a state disaster emergency on Sept. 9 after the polio virus has been detected in another county. The order allows EMS workers, midwives, and pharmacists to administer the vaccine and permits physicians and nurse practitioners to issue standing orders for polio vaccines.
“On polio, we simply cannot roll the dice,” New York State Health Commissioner Dr. Mary T. Bassett said in a news release. “If you or your child are unvaccinated or not up to date with vaccinations, the risk of paralytic disease is real. I urge New Yorkers to not accept any risk at all.”
In July, an unvaccinated adult man in Rockland County, which is north of New York City, was diagnosed with polio virus. It was the first confirmed case of the virus in the United States since 2013.
New York state health officials have not announced any additional polio cases. Since as early as April, polio has also been detected in wastewater samples in New York City and in Rockland, Orange, and Sullivan counties. In August, the virus was detected in wastewater from Nassau County on Long Island.
New York’s statewide polio vaccination rate is 79%, and the New York State Department of Health is aiming for a rate over 90%, the announcement said. In some counties, vaccination rates are far below the state average, including Rockland County (60%), Orange County (59%), and Sullivan County (62%). Nassau County’s polio vaccination rate is similar to the state average.
“Polio immunization is safe and effective – protecting nearly all people against disease who receive the recommended doses,” Dr. Basset said; “Do not wait to vaccinate.”
A version of this article first appeared on Medscape.com.
New York Governor Kathy Hochul declared a state disaster emergency on Sept. 9 after the polio virus has been detected in another county. The order allows EMS workers, midwives, and pharmacists to administer the vaccine and permits physicians and nurse practitioners to issue standing orders for polio vaccines.
“On polio, we simply cannot roll the dice,” New York State Health Commissioner Dr. Mary T. Bassett said in a news release. “If you or your child are unvaccinated or not up to date with vaccinations, the risk of paralytic disease is real. I urge New Yorkers to not accept any risk at all.”
In July, an unvaccinated adult man in Rockland County, which is north of New York City, was diagnosed with polio virus. It was the first confirmed case of the virus in the United States since 2013.
New York state health officials have not announced any additional polio cases. Since as early as April, polio has also been detected in wastewater samples in New York City and in Rockland, Orange, and Sullivan counties. In August, the virus was detected in wastewater from Nassau County on Long Island.
New York’s statewide polio vaccination rate is 79%, and the New York State Department of Health is aiming for a rate over 90%, the announcement said. In some counties, vaccination rates are far below the state average, including Rockland County (60%), Orange County (59%), and Sullivan County (62%). Nassau County’s polio vaccination rate is similar to the state average.
“Polio immunization is safe and effective – protecting nearly all people against disease who receive the recommended doses,” Dr. Basset said; “Do not wait to vaccinate.”
A version of this article first appeared on Medscape.com.
New York Governor Kathy Hochul declared a state disaster emergency on Sept. 9 after the polio virus has been detected in another county. The order allows EMS workers, midwives, and pharmacists to administer the vaccine and permits physicians and nurse practitioners to issue standing orders for polio vaccines.
“On polio, we simply cannot roll the dice,” New York State Health Commissioner Dr. Mary T. Bassett said in a news release. “If you or your child are unvaccinated or not up to date with vaccinations, the risk of paralytic disease is real. I urge New Yorkers to not accept any risk at all.”
In July, an unvaccinated adult man in Rockland County, which is north of New York City, was diagnosed with polio virus. It was the first confirmed case of the virus in the United States since 2013.
New York state health officials have not announced any additional polio cases. Since as early as April, polio has also been detected in wastewater samples in New York City and in Rockland, Orange, and Sullivan counties. In August, the virus was detected in wastewater from Nassau County on Long Island.
New York’s statewide polio vaccination rate is 79%, and the New York State Department of Health is aiming for a rate over 90%, the announcement said. In some counties, vaccination rates are far below the state average, including Rockland County (60%), Orange County (59%), and Sullivan County (62%). Nassau County’s polio vaccination rate is similar to the state average.
“Polio immunization is safe and effective – protecting nearly all people against disease who receive the recommended doses,” Dr. Basset said; “Do not wait to vaccinate.”
A version of this article first appeared on Medscape.com.
Parent training pays off for children with autism
“Referrals for parent training should now be considered the expected standard for medical practice,” said a member of the research team, Timothy B. Smith, PhD, a professor of psychology at Brigham Young University, Provo, Utah.
Programs that show parents how to teach functional skills and address maladaptive behaviors, also known as parent-mediated or parent-implemented interventions, offer an alternative to one-on-one professional services, which are in short supply, according to the paper, which was published in the Journal of Autism and Developmental Disorders.
Methods and results
The meta-analysis included 54 papers based on randomized clinical trials involving 2,895 children, which compared the effects of various parent interventions with professional treatment, treatment as usual, or being on a wait-list to receive an intervention.
Overall the research team reported “moderately strong” average benefits from the parent-mediated interventions (Hedges’ g, 0.553), indicating a medium effect size. Parent interventions had the greatest effect on outcomes involving positive behavior and social skills (0.603), followed by language and communication (0.545), maladaptive behavior (0.519), and life skills (0.239).
Similar benefits were observed regardless of a child’s age or sex or which parent or parents implemented an intervention. The effects also appeared to be consistent regardless of intervention characteristics, such as the number of training sessions parents received, although the researchers noted that many studies did not provide data on such details.
Paul Carbone, MD, a professor of pediatrics at the University of Utah, Salt Lake City, who was not involved in the review, said it demonstrates that such parental engagement is “vitally important” and pediatricians “should not hesitate to refer interested families.”
Dr. Carbone, who is the medical director of an assessment program for children with suspected developmental disabilities, said many training programs for parents have adopted telehealth, adding to their convenience. To make appropriate referrals, primary care clinicians should become acquainted with local programs and learn which outcomes they target, he said.
Dr. Smith noted that primary care physicians are “better trained now than ever” to identify autism spectrum disorder and therefore are among the first to identify those conditions and help parents understand “that their actions at home absolutely make a difference in the child’s development.”
Overcoming limitations, future research needs
The research team attempted to overcome limitations with previous reviews by using comprehensive search terms and other methods to identify relevant studies, including some that had not been published. They included only studies that reflect common practice of training multiple parents simultaneously, they wrote.
Dr. Smith noted that long-term outcomes data and further study to compare effects on children with mild, moderate, and severe autism are needed.
Although logic would suggest greater benefits for children with severe disease, there are no data to demonstrate that, he said.
The authors of the study and Dr. Carbone reported no relevant competing interests.
“Referrals for parent training should now be considered the expected standard for medical practice,” said a member of the research team, Timothy B. Smith, PhD, a professor of psychology at Brigham Young University, Provo, Utah.
Programs that show parents how to teach functional skills and address maladaptive behaviors, also known as parent-mediated or parent-implemented interventions, offer an alternative to one-on-one professional services, which are in short supply, according to the paper, which was published in the Journal of Autism and Developmental Disorders.
Methods and results
The meta-analysis included 54 papers based on randomized clinical trials involving 2,895 children, which compared the effects of various parent interventions with professional treatment, treatment as usual, or being on a wait-list to receive an intervention.
Overall the research team reported “moderately strong” average benefits from the parent-mediated interventions (Hedges’ g, 0.553), indicating a medium effect size. Parent interventions had the greatest effect on outcomes involving positive behavior and social skills (0.603), followed by language and communication (0.545), maladaptive behavior (0.519), and life skills (0.239).
Similar benefits were observed regardless of a child’s age or sex or which parent or parents implemented an intervention. The effects also appeared to be consistent regardless of intervention characteristics, such as the number of training sessions parents received, although the researchers noted that many studies did not provide data on such details.
Paul Carbone, MD, a professor of pediatrics at the University of Utah, Salt Lake City, who was not involved in the review, said it demonstrates that such parental engagement is “vitally important” and pediatricians “should not hesitate to refer interested families.”
Dr. Carbone, who is the medical director of an assessment program for children with suspected developmental disabilities, said many training programs for parents have adopted telehealth, adding to their convenience. To make appropriate referrals, primary care clinicians should become acquainted with local programs and learn which outcomes they target, he said.
Dr. Smith noted that primary care physicians are “better trained now than ever” to identify autism spectrum disorder and therefore are among the first to identify those conditions and help parents understand “that their actions at home absolutely make a difference in the child’s development.”
Overcoming limitations, future research needs
The research team attempted to overcome limitations with previous reviews by using comprehensive search terms and other methods to identify relevant studies, including some that had not been published. They included only studies that reflect common practice of training multiple parents simultaneously, they wrote.
Dr. Smith noted that long-term outcomes data and further study to compare effects on children with mild, moderate, and severe autism are needed.
Although logic would suggest greater benefits for children with severe disease, there are no data to demonstrate that, he said.
The authors of the study and Dr. Carbone reported no relevant competing interests.
“Referrals for parent training should now be considered the expected standard for medical practice,” said a member of the research team, Timothy B. Smith, PhD, a professor of psychology at Brigham Young University, Provo, Utah.
Programs that show parents how to teach functional skills and address maladaptive behaviors, also known as parent-mediated or parent-implemented interventions, offer an alternative to one-on-one professional services, which are in short supply, according to the paper, which was published in the Journal of Autism and Developmental Disorders.
Methods and results
The meta-analysis included 54 papers based on randomized clinical trials involving 2,895 children, which compared the effects of various parent interventions with professional treatment, treatment as usual, or being on a wait-list to receive an intervention.
Overall the research team reported “moderately strong” average benefits from the parent-mediated interventions (Hedges’ g, 0.553), indicating a medium effect size. Parent interventions had the greatest effect on outcomes involving positive behavior and social skills (0.603), followed by language and communication (0.545), maladaptive behavior (0.519), and life skills (0.239).
Similar benefits were observed regardless of a child’s age or sex or which parent or parents implemented an intervention. The effects also appeared to be consistent regardless of intervention characteristics, such as the number of training sessions parents received, although the researchers noted that many studies did not provide data on such details.
Paul Carbone, MD, a professor of pediatrics at the University of Utah, Salt Lake City, who was not involved in the review, said it demonstrates that such parental engagement is “vitally important” and pediatricians “should not hesitate to refer interested families.”
Dr. Carbone, who is the medical director of an assessment program for children with suspected developmental disabilities, said many training programs for parents have adopted telehealth, adding to their convenience. To make appropriate referrals, primary care clinicians should become acquainted with local programs and learn which outcomes they target, he said.
Dr. Smith noted that primary care physicians are “better trained now than ever” to identify autism spectrum disorder and therefore are among the first to identify those conditions and help parents understand “that their actions at home absolutely make a difference in the child’s development.”
Overcoming limitations, future research needs
The research team attempted to overcome limitations with previous reviews by using comprehensive search terms and other methods to identify relevant studies, including some that had not been published. They included only studies that reflect common practice of training multiple parents simultaneously, they wrote.
Dr. Smith noted that long-term outcomes data and further study to compare effects on children with mild, moderate, and severe autism are needed.
Although logic would suggest greater benefits for children with severe disease, there are no data to demonstrate that, he said.
The authors of the study and Dr. Carbone reported no relevant competing interests.
FROM JOURNAL OF AUTISM AND DEVELOPMENTAL DISORDERS
Candy, desserts: A ‘gateway’ to unhealthy eating among teens
Certain ultraprocessed foods – especially candy, prepackaged pastries, and frozen desserts – could be “gateway foods” for adolescents, leading them to increase their intake of other unhealthy foods, a new study suggests.
“For teens, gateway ultraprocessed foods (candy, store pastries, frozen desserts) should be prioritized for preventive dietary interventions as they increase intake across all other UPFs,” lead researcher Maria Balhara said in an interview.
“The good news,” said Ms. Balhara, is that even small changes, such as reducing how often gateway foods are consumed, may reduce overall intake of unhealthy foods and have a “big impact” on overall health.
Ms. Balhara has a unique perspective on adolescent eating habits: She’s 16 years old, from Florida, and conducted the study while dual-enrolled at Broward College and Cooper City High School.
Her study was released Sept. 7 ahead of presentation at the American Heart Association Hypertension Scientific Sessions 2022 in San Diego.
Blame the pandemic?
Over the past 30 years, there’s been a steady increase in consumption of UPFs worldwide, coupled with mounting evidence that diets rich in UPFs raise the risk for several chronic diseases, including weight gain, hypertension, and increased risk for heart disease and premature death.
For her research, Ms. Balhara asked 315 teenagers (42% male) from 12 high schools in South Florida how often they consumed UPFs over two time periods – before COVID in 2019 and after COVID restrictions were eased in 2022 – using a survey that she developed called the Processed Intake Evaluation (PIE).
More than 2 in 5 teens (43%) increased their consumption of UPFs between 2019 and 2022.
During this time, increased consumption of frozen desserts was associated with an 11% increase in consumption of all other UPFs, whereas increased consumption of prepackaged pastries and candy was associated with a 12% and 31%, respectively, increase in consumption of all other UPFs, Ms. Balhara found.
Encouragingly, 57% of teens decreased their consumption of UPFs between 2019 and 2022.
During this time, decreased consumption of processed meats was associated with an 8% decrease in consumption of all other UPFs, whereas decreased consumption of white bread and biscuits was associated with a 9% and 10%, respectively, decrease in consumption of all other UPFs.
The results provide initial evidence for a new “gateway food model,” Ms. Balhara told this news organization, in which certain UPFs, when increased, drive overall consumption of all UPFs among teens.
Limitations of the study include the self-reported dietary data and the fact that the PIE survey has not been validated.
Not all UPFs are bad
“I commend Ms. Balhara for her project, which highlights the importance of establishing good dietary patterns early in life,” Donna K. Arnett, PhD, past president of the AHA, said in a news release.
“The relationship between poor dietary quality and cardiovascular risk factors is well-established. While this is a small, preliminary study, it’s an important topic to continue to investigate and help us understand ways we can influence dietary behaviors to promote optimal cardiovascular health for all ages,” said Dr. Arnett, executive vice president for academic affairs and provost at the University of South Carolina, Columbia.
Offering perspective on the study, Taylor C. Wallace, PhD, with the department of nutrition and food studies, George Mason University, Fairfax, Va., made the point that “food processing and ultraprocessed foods aren’t the problem. The problem is the types of ultraprocessed foods on the market that people consume.”
“Remember, non-fat, vitamin D fortified yogurt is also ‘ultra-processed,’ and it’s very healthy,” he told this news organization.
Dr. Wallace said that it’s no surprise that teens increased their intake of UPFs during the pandemic.
“Of course, people increased processed food intake during the pandemic. Processed foods are shelf stable at a time when grocery stores were running out of things and supply chains weren’t able to keep up. Also, many were depressed and use food to indulge,” he noted.
The study had no funding. Ms. Balhara has no relevant disclosures. Dr. Wallace is principal and CEO of Think Healthy Group; chief food and nutrition scientist with Produce for Better Health Foundation; editor, Journal of Dietary Supplements; deputy editor, Journal of the American College of Nutrition; nutrition section editor, Annals of Medicine; and an advisory board member with Forbes Health.
A version of this article first appeared on Medscape.com.
Certain ultraprocessed foods – especially candy, prepackaged pastries, and frozen desserts – could be “gateway foods” for adolescents, leading them to increase their intake of other unhealthy foods, a new study suggests.
“For teens, gateway ultraprocessed foods (candy, store pastries, frozen desserts) should be prioritized for preventive dietary interventions as they increase intake across all other UPFs,” lead researcher Maria Balhara said in an interview.
“The good news,” said Ms. Balhara, is that even small changes, such as reducing how often gateway foods are consumed, may reduce overall intake of unhealthy foods and have a “big impact” on overall health.
Ms. Balhara has a unique perspective on adolescent eating habits: She’s 16 years old, from Florida, and conducted the study while dual-enrolled at Broward College and Cooper City High School.
Her study was released Sept. 7 ahead of presentation at the American Heart Association Hypertension Scientific Sessions 2022 in San Diego.
Blame the pandemic?
Over the past 30 years, there’s been a steady increase in consumption of UPFs worldwide, coupled with mounting evidence that diets rich in UPFs raise the risk for several chronic diseases, including weight gain, hypertension, and increased risk for heart disease and premature death.
For her research, Ms. Balhara asked 315 teenagers (42% male) from 12 high schools in South Florida how often they consumed UPFs over two time periods – before COVID in 2019 and after COVID restrictions were eased in 2022 – using a survey that she developed called the Processed Intake Evaluation (PIE).
More than 2 in 5 teens (43%) increased their consumption of UPFs between 2019 and 2022.
During this time, increased consumption of frozen desserts was associated with an 11% increase in consumption of all other UPFs, whereas increased consumption of prepackaged pastries and candy was associated with a 12% and 31%, respectively, increase in consumption of all other UPFs, Ms. Balhara found.
Encouragingly, 57% of teens decreased their consumption of UPFs between 2019 and 2022.
During this time, decreased consumption of processed meats was associated with an 8% decrease in consumption of all other UPFs, whereas decreased consumption of white bread and biscuits was associated with a 9% and 10%, respectively, decrease in consumption of all other UPFs.
The results provide initial evidence for a new “gateway food model,” Ms. Balhara told this news organization, in which certain UPFs, when increased, drive overall consumption of all UPFs among teens.
Limitations of the study include the self-reported dietary data and the fact that the PIE survey has not been validated.
Not all UPFs are bad
“I commend Ms. Balhara for her project, which highlights the importance of establishing good dietary patterns early in life,” Donna K. Arnett, PhD, past president of the AHA, said in a news release.
“The relationship between poor dietary quality and cardiovascular risk factors is well-established. While this is a small, preliminary study, it’s an important topic to continue to investigate and help us understand ways we can influence dietary behaviors to promote optimal cardiovascular health for all ages,” said Dr. Arnett, executive vice president for academic affairs and provost at the University of South Carolina, Columbia.
Offering perspective on the study, Taylor C. Wallace, PhD, with the department of nutrition and food studies, George Mason University, Fairfax, Va., made the point that “food processing and ultraprocessed foods aren’t the problem. The problem is the types of ultraprocessed foods on the market that people consume.”
“Remember, non-fat, vitamin D fortified yogurt is also ‘ultra-processed,’ and it’s very healthy,” he told this news organization.
Dr. Wallace said that it’s no surprise that teens increased their intake of UPFs during the pandemic.
“Of course, people increased processed food intake during the pandemic. Processed foods are shelf stable at a time when grocery stores were running out of things and supply chains weren’t able to keep up. Also, many were depressed and use food to indulge,” he noted.
The study had no funding. Ms. Balhara has no relevant disclosures. Dr. Wallace is principal and CEO of Think Healthy Group; chief food and nutrition scientist with Produce for Better Health Foundation; editor, Journal of Dietary Supplements; deputy editor, Journal of the American College of Nutrition; nutrition section editor, Annals of Medicine; and an advisory board member with Forbes Health.
A version of this article first appeared on Medscape.com.
Certain ultraprocessed foods – especially candy, prepackaged pastries, and frozen desserts – could be “gateway foods” for adolescents, leading them to increase their intake of other unhealthy foods, a new study suggests.
“For teens, gateway ultraprocessed foods (candy, store pastries, frozen desserts) should be prioritized for preventive dietary interventions as they increase intake across all other UPFs,” lead researcher Maria Balhara said in an interview.
“The good news,” said Ms. Balhara, is that even small changes, such as reducing how often gateway foods are consumed, may reduce overall intake of unhealthy foods and have a “big impact” on overall health.
Ms. Balhara has a unique perspective on adolescent eating habits: She’s 16 years old, from Florida, and conducted the study while dual-enrolled at Broward College and Cooper City High School.
Her study was released Sept. 7 ahead of presentation at the American Heart Association Hypertension Scientific Sessions 2022 in San Diego.
Blame the pandemic?
Over the past 30 years, there’s been a steady increase in consumption of UPFs worldwide, coupled with mounting evidence that diets rich in UPFs raise the risk for several chronic diseases, including weight gain, hypertension, and increased risk for heart disease and premature death.
For her research, Ms. Balhara asked 315 teenagers (42% male) from 12 high schools in South Florida how often they consumed UPFs over two time periods – before COVID in 2019 and after COVID restrictions were eased in 2022 – using a survey that she developed called the Processed Intake Evaluation (PIE).
More than 2 in 5 teens (43%) increased their consumption of UPFs between 2019 and 2022.
During this time, increased consumption of frozen desserts was associated with an 11% increase in consumption of all other UPFs, whereas increased consumption of prepackaged pastries and candy was associated with a 12% and 31%, respectively, increase in consumption of all other UPFs, Ms. Balhara found.
Encouragingly, 57% of teens decreased their consumption of UPFs between 2019 and 2022.
During this time, decreased consumption of processed meats was associated with an 8% decrease in consumption of all other UPFs, whereas decreased consumption of white bread and biscuits was associated with a 9% and 10%, respectively, decrease in consumption of all other UPFs.
The results provide initial evidence for a new “gateway food model,” Ms. Balhara told this news organization, in which certain UPFs, when increased, drive overall consumption of all UPFs among teens.
Limitations of the study include the self-reported dietary data and the fact that the PIE survey has not been validated.
Not all UPFs are bad
“I commend Ms. Balhara for her project, which highlights the importance of establishing good dietary patterns early in life,” Donna K. Arnett, PhD, past president of the AHA, said in a news release.
“The relationship between poor dietary quality and cardiovascular risk factors is well-established. While this is a small, preliminary study, it’s an important topic to continue to investigate and help us understand ways we can influence dietary behaviors to promote optimal cardiovascular health for all ages,” said Dr. Arnett, executive vice president for academic affairs and provost at the University of South Carolina, Columbia.
Offering perspective on the study, Taylor C. Wallace, PhD, with the department of nutrition and food studies, George Mason University, Fairfax, Va., made the point that “food processing and ultraprocessed foods aren’t the problem. The problem is the types of ultraprocessed foods on the market that people consume.”
“Remember, non-fat, vitamin D fortified yogurt is also ‘ultra-processed,’ and it’s very healthy,” he told this news organization.
Dr. Wallace said that it’s no surprise that teens increased their intake of UPFs during the pandemic.
“Of course, people increased processed food intake during the pandemic. Processed foods are shelf stable at a time when grocery stores were running out of things and supply chains weren’t able to keep up. Also, many were depressed and use food to indulge,” he noted.
The study had no funding. Ms. Balhara has no relevant disclosures. Dr. Wallace is principal and CEO of Think Healthy Group; chief food and nutrition scientist with Produce for Better Health Foundation; editor, Journal of Dietary Supplements; deputy editor, Journal of the American College of Nutrition; nutrition section editor, Annals of Medicine; and an advisory board member with Forbes Health.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION 2022
Fish in pregnancy not dangerous after all, says new study
A new study has called into question the decades-long official guidance advising pregnant women to limit consumption of certain fish because of their potentially high mercury content. That advice was based particularly on one 1997 study suggesting a correlation between fetal exposure to methylmercury and cognitive dysfunction at age 7.
The U.K’s National Health Service currently advises not only pregnant women but also all those who are potentially fertile (those “who are planning a pregnancy or may have a child one day”) to limit oily fish consumption to no more than two portions per week. During pregnancy and while trying to get pregnant, women are advised to avoid shark, swordfish, and marlin altogether.
Suspicions arose from study involving consumption of pilot whale
However, researchers from the University of Bristol (England) now suggest that assumptions generated by the original 1997 study – of a cohort of women in the Faroe Islands – were unwarranted. “It was clearly stated that the methylmercury levels were associated with consumption of pilot whale (a sea mammal, not a fish),” they said.
The pilot whale is a species known to concentrate cadmium and mercury, and indeed in 1989 Faroe Islanders themselves had been advised to limit consumption of both whale meat and blubber, and to abstain completely from liver and kidneys.
Yet, as the authors pointed out, following the 1997 study, “the subsequent assumptions were that seafood in general was responsible for increased mercury levels in the mother.”
New study shows ‘no evidence of harm’
Their new research, published in NeuroToxicology, has now shown that “there is no evidence of harm from these fish,” they said. They recommend that advice for pregnant women should now be revised.
The study drew together analyses on over 4,131 pregnant mothers from the Avon Longitudinal Study of Parents and Children (ALSPAC), also known as the ‘Children of the 90s’ study, with similar detailed studies conducted in the Seychelles. The two populations differ considerably in their frequency of fish consumption: fish is a major component of the diet in the Seychelles, but eaten less frequently in the Avon study area, centered on Bristol.
The team looked for studies using the data from these two contrasting cohorts where mercury levels had been measured during pregnancy and the children followed up at frequent intervals during their childhood. Longitudinal studies in the Seychelles “have not demonstrated harmful cognitive effects in children with increasing maternal mercury levels”, they reported.
The same proved true in the United Kingdom, a more-developed country where fish is eaten less frequently, they found. They summarized the results from various papers that used ALSPAC data and found no adverse associations between total mercury levels measured in maternal whole blood and umbilical cord tissue with children’s cognitive development, in terms of either IQ or scholastic abilities.
In addition, extensive dietary questionnaires during pregnancy had allowed estimates of total fish intake to be calculated, as well as variations in the amount of each type of seafood consumed. “Although seafood is a source of dietary mercury, it appeared to explain a relatively small proportion (9%) of the variation in total blood mercury in our U.K. study population,” they said – actually less than the variance attributable to socio-demographic characteristics of the mother (10.4%).
Positive benefits of eating fish irrespective of type
What mattered was not which types of fish were eaten but whether the woman ate fish or not, which emerged as the most important factor. The mother’s prenatal mercury level was positively associated with her child’s IQ if she had eaten fish in pregnancy, but not if she had not.
“Significantly beneficial associations with prenatal mercury levels were shown for total and performance IQ, mathematical/scientific reasoning, and birth weight, in fish-consuming versus non–fish-consuming mothers,” the authors said. “These beneficial findings are similar to those observed in the Seychelles, where fish consumption is high and prenatal mercury levels are 10 times higher than U.S. levels.”
Caroline Taylor, PhD, senior research fellow and coauthor of the study, said: “We found that the mother’s mercury level during pregnancy is likely to have no adverse effect on the development of the child provided that the mother eats fish. If she did not eat fish, then there was some evidence that her mercury level could have a harmful effect on the child.”
The team said that this was because the essential nutrients in the fish could be protective against the mercury content of the fish. “This could be because of the benefits from the mix of essential nutrients that fish provides, including long-chain fatty acids, iodine, vitamin D and selenium,” said Dr. Taylor.
Women stopped eating any fish ‘to be on the safe side’
The authors called for a change in official guidance. “Health advice to pregnant women concerning consumption of mercury-containing foods has resulted in anxiety, with subsequent avoidance of fish consumption during pregnancy.” Seafood contains many nutrients crucial for children’s growth and development, but “there is the possibility that some women will stop eating any fish ‘to be on the safe side.’ ”
The authors said: “Although advice to pregnant women was generally that fish was good, the accompanying caveat was to avoid fish with high levels of mercury. Psychologically, the latter was the message that women remembered, and the general reaction has been for women to reduce their intake of all seafood.”
Coauthor Jean Golding, emeritus professor of pediatric and perinatal epidemiology at the University of Bristol, said: “It is important that advisories from health professionals revise their advice warning against eating certain species of fish. There is no evidence of harm from these fish, but there is evidence from different countries that such advice can cause confusion in pregnant women. The guidance for pregnancy should highlight ‘Eat at least two portions of fish a week, one of which should be oily’ – and omit all warnings that certain fish should not be eaten.”
The study was funded via core support for ALSPAC by the UK Medical Research Council and the UK Wellcome Trust.
A version of this article first appeared on Medscape UK.
A new study has called into question the decades-long official guidance advising pregnant women to limit consumption of certain fish because of their potentially high mercury content. That advice was based particularly on one 1997 study suggesting a correlation between fetal exposure to methylmercury and cognitive dysfunction at age 7.
The U.K’s National Health Service currently advises not only pregnant women but also all those who are potentially fertile (those “who are planning a pregnancy or may have a child one day”) to limit oily fish consumption to no more than two portions per week. During pregnancy and while trying to get pregnant, women are advised to avoid shark, swordfish, and marlin altogether.
Suspicions arose from study involving consumption of pilot whale
However, researchers from the University of Bristol (England) now suggest that assumptions generated by the original 1997 study – of a cohort of women in the Faroe Islands – were unwarranted. “It was clearly stated that the methylmercury levels were associated with consumption of pilot whale (a sea mammal, not a fish),” they said.
The pilot whale is a species known to concentrate cadmium and mercury, and indeed in 1989 Faroe Islanders themselves had been advised to limit consumption of both whale meat and blubber, and to abstain completely from liver and kidneys.
Yet, as the authors pointed out, following the 1997 study, “the subsequent assumptions were that seafood in general was responsible for increased mercury levels in the mother.”
New study shows ‘no evidence of harm’
Their new research, published in NeuroToxicology, has now shown that “there is no evidence of harm from these fish,” they said. They recommend that advice for pregnant women should now be revised.
The study drew together analyses on over 4,131 pregnant mothers from the Avon Longitudinal Study of Parents and Children (ALSPAC), also known as the ‘Children of the 90s’ study, with similar detailed studies conducted in the Seychelles. The two populations differ considerably in their frequency of fish consumption: fish is a major component of the diet in the Seychelles, but eaten less frequently in the Avon study area, centered on Bristol.
The team looked for studies using the data from these two contrasting cohorts where mercury levels had been measured during pregnancy and the children followed up at frequent intervals during their childhood. Longitudinal studies in the Seychelles “have not demonstrated harmful cognitive effects in children with increasing maternal mercury levels”, they reported.
The same proved true in the United Kingdom, a more-developed country where fish is eaten less frequently, they found. They summarized the results from various papers that used ALSPAC data and found no adverse associations between total mercury levels measured in maternal whole blood and umbilical cord tissue with children’s cognitive development, in terms of either IQ or scholastic abilities.
In addition, extensive dietary questionnaires during pregnancy had allowed estimates of total fish intake to be calculated, as well as variations in the amount of each type of seafood consumed. “Although seafood is a source of dietary mercury, it appeared to explain a relatively small proportion (9%) of the variation in total blood mercury in our U.K. study population,” they said – actually less than the variance attributable to socio-demographic characteristics of the mother (10.4%).
Positive benefits of eating fish irrespective of type
What mattered was not which types of fish were eaten but whether the woman ate fish or not, which emerged as the most important factor. The mother’s prenatal mercury level was positively associated with her child’s IQ if she had eaten fish in pregnancy, but not if she had not.
“Significantly beneficial associations with prenatal mercury levels were shown for total and performance IQ, mathematical/scientific reasoning, and birth weight, in fish-consuming versus non–fish-consuming mothers,” the authors said. “These beneficial findings are similar to those observed in the Seychelles, where fish consumption is high and prenatal mercury levels are 10 times higher than U.S. levels.”
Caroline Taylor, PhD, senior research fellow and coauthor of the study, said: “We found that the mother’s mercury level during pregnancy is likely to have no adverse effect on the development of the child provided that the mother eats fish. If she did not eat fish, then there was some evidence that her mercury level could have a harmful effect on the child.”
The team said that this was because the essential nutrients in the fish could be protective against the mercury content of the fish. “This could be because of the benefits from the mix of essential nutrients that fish provides, including long-chain fatty acids, iodine, vitamin D and selenium,” said Dr. Taylor.
Women stopped eating any fish ‘to be on the safe side’
The authors called for a change in official guidance. “Health advice to pregnant women concerning consumption of mercury-containing foods has resulted in anxiety, with subsequent avoidance of fish consumption during pregnancy.” Seafood contains many nutrients crucial for children’s growth and development, but “there is the possibility that some women will stop eating any fish ‘to be on the safe side.’ ”
The authors said: “Although advice to pregnant women was generally that fish was good, the accompanying caveat was to avoid fish with high levels of mercury. Psychologically, the latter was the message that women remembered, and the general reaction has been for women to reduce their intake of all seafood.”
Coauthor Jean Golding, emeritus professor of pediatric and perinatal epidemiology at the University of Bristol, said: “It is important that advisories from health professionals revise their advice warning against eating certain species of fish. There is no evidence of harm from these fish, but there is evidence from different countries that such advice can cause confusion in pregnant women. The guidance for pregnancy should highlight ‘Eat at least two portions of fish a week, one of which should be oily’ – and omit all warnings that certain fish should not be eaten.”
The study was funded via core support for ALSPAC by the UK Medical Research Council and the UK Wellcome Trust.
A version of this article first appeared on Medscape UK.
A new study has called into question the decades-long official guidance advising pregnant women to limit consumption of certain fish because of their potentially high mercury content. That advice was based particularly on one 1997 study suggesting a correlation between fetal exposure to methylmercury and cognitive dysfunction at age 7.
The U.K’s National Health Service currently advises not only pregnant women but also all those who are potentially fertile (those “who are planning a pregnancy or may have a child one day”) to limit oily fish consumption to no more than two portions per week. During pregnancy and while trying to get pregnant, women are advised to avoid shark, swordfish, and marlin altogether.
Suspicions arose from study involving consumption of pilot whale
However, researchers from the University of Bristol (England) now suggest that assumptions generated by the original 1997 study – of a cohort of women in the Faroe Islands – were unwarranted. “It was clearly stated that the methylmercury levels were associated with consumption of pilot whale (a sea mammal, not a fish),” they said.
The pilot whale is a species known to concentrate cadmium and mercury, and indeed in 1989 Faroe Islanders themselves had been advised to limit consumption of both whale meat and blubber, and to abstain completely from liver and kidneys.
Yet, as the authors pointed out, following the 1997 study, “the subsequent assumptions were that seafood in general was responsible for increased mercury levels in the mother.”
New study shows ‘no evidence of harm’
Their new research, published in NeuroToxicology, has now shown that “there is no evidence of harm from these fish,” they said. They recommend that advice for pregnant women should now be revised.
The study drew together analyses on over 4,131 pregnant mothers from the Avon Longitudinal Study of Parents and Children (ALSPAC), also known as the ‘Children of the 90s’ study, with similar detailed studies conducted in the Seychelles. The two populations differ considerably in their frequency of fish consumption: fish is a major component of the diet in the Seychelles, but eaten less frequently in the Avon study area, centered on Bristol.
The team looked for studies using the data from these two contrasting cohorts where mercury levels had been measured during pregnancy and the children followed up at frequent intervals during their childhood. Longitudinal studies in the Seychelles “have not demonstrated harmful cognitive effects in children with increasing maternal mercury levels”, they reported.
The same proved true in the United Kingdom, a more-developed country where fish is eaten less frequently, they found. They summarized the results from various papers that used ALSPAC data and found no adverse associations between total mercury levels measured in maternal whole blood and umbilical cord tissue with children’s cognitive development, in terms of either IQ or scholastic abilities.
In addition, extensive dietary questionnaires during pregnancy had allowed estimates of total fish intake to be calculated, as well as variations in the amount of each type of seafood consumed. “Although seafood is a source of dietary mercury, it appeared to explain a relatively small proportion (9%) of the variation in total blood mercury in our U.K. study population,” they said – actually less than the variance attributable to socio-demographic characteristics of the mother (10.4%).
Positive benefits of eating fish irrespective of type
What mattered was not which types of fish were eaten but whether the woman ate fish or not, which emerged as the most important factor. The mother’s prenatal mercury level was positively associated with her child’s IQ if she had eaten fish in pregnancy, but not if she had not.
“Significantly beneficial associations with prenatal mercury levels were shown for total and performance IQ, mathematical/scientific reasoning, and birth weight, in fish-consuming versus non–fish-consuming mothers,” the authors said. “These beneficial findings are similar to those observed in the Seychelles, where fish consumption is high and prenatal mercury levels are 10 times higher than U.S. levels.”
Caroline Taylor, PhD, senior research fellow and coauthor of the study, said: “We found that the mother’s mercury level during pregnancy is likely to have no adverse effect on the development of the child provided that the mother eats fish. If she did not eat fish, then there was some evidence that her mercury level could have a harmful effect on the child.”
The team said that this was because the essential nutrients in the fish could be protective against the mercury content of the fish. “This could be because of the benefits from the mix of essential nutrients that fish provides, including long-chain fatty acids, iodine, vitamin D and selenium,” said Dr. Taylor.
Women stopped eating any fish ‘to be on the safe side’
The authors called for a change in official guidance. “Health advice to pregnant women concerning consumption of mercury-containing foods has resulted in anxiety, with subsequent avoidance of fish consumption during pregnancy.” Seafood contains many nutrients crucial for children’s growth and development, but “there is the possibility that some women will stop eating any fish ‘to be on the safe side.’ ”
The authors said: “Although advice to pregnant women was generally that fish was good, the accompanying caveat was to avoid fish with high levels of mercury. Psychologically, the latter was the message that women remembered, and the general reaction has been for women to reduce their intake of all seafood.”
Coauthor Jean Golding, emeritus professor of pediatric and perinatal epidemiology at the University of Bristol, said: “It is important that advisories from health professionals revise their advice warning against eating certain species of fish. There is no evidence of harm from these fish, but there is evidence from different countries that such advice can cause confusion in pregnant women. The guidance for pregnancy should highlight ‘Eat at least two portions of fish a week, one of which should be oily’ – and omit all warnings that certain fish should not be eaten.”
The study was funded via core support for ALSPAC by the UK Medical Research Council and the UK Wellcome Trust.
A version of this article first appeared on Medscape UK.
FROM NEUROTOXICOLOGY
AI and reality – diagnosing otitis media is a real challenge
Let’s pretend for a moment that you receive a call from one of your college roommates who thanks to his family connections has become a venture capitalist in California. His group is considering investing in a start-up that is developing a handheld instrument that it claims will use artificial intelligence to diagnose ear infections far more accurately than the human eye. He wonders if you would like to help him evaluate the company’s proposal and offers you a small percentage of the profits for your efforts should they choose to invest.
Your former roommate has done enough research on his own to understand that otitis media makes up a large chunk of a pediatrician’s workload and that making an accurate diagnosis can often be difficult in a struggling child. He describes his own experience watching a frustrated pediatrician attempting to remove wax from his child’s ear and eventually prescribing antibiotics “to be safe.”
You agree and review the prospectus, which includes a paper from a peer-reviewed journal. What you discover is that the investigators used more than 600 high-resolution images of tympanic membranes taken “during operative myringotomy and tympanostomy tube placement” and the findings at tympanocentesis to train a neural network.
Once trained, the model they developed could differentiate with 95% accuracy between an image of a tympanic membrane that covered a normal middle ear from one that merely contained fluid and from one that contained infected fluid. When these same images were shown to 39 clinicians, more than half of which were pediatricians and included both faculty-level staff and trainees, the average diagnostic accuracy was 65%.
The prospectus includes prediction that this technology could easily be developed into a handheld instrument similar to a traditional otoscope, which could then be linked to the operator’s smartphone, giving the clinician an instant treat or no-treat answer.
Now, remember you have nothing to lose except maybe a friendship. How would you advise your old college roommate?
My advice to your college buddy would be one of caution! Yes, there is a potential big upside because there is a real need for a device that could provide a diagnostic accuracy that this AI model promises. While I suspect that AI will always be more accurate in diagnosis using static images, I bet that most people, clinicians and nonclinicians, could improve their accuracy by linking photos with diagnoses with an hour of practice.
However, evaluating a high-resolution photograph taken through an operative scope inserted into the cerumenless ear canal of a sedated, afrebrile child is several orders of magnitude less difficult than the real-world environment in which the diagnosis of otitis media is usually made.
If the venture capitalists were still interested in getting into the otitis media marketplace, you might suggest they look into companies that have already developed image capture otoscopes. At this point I could only find one on the Internet that was portable and it certainly isn’t small-child friendly. Once we have a tool that can capture images in real-world situations, the next step is to train AI systems to interpret them using the approach these researchers have developed. I bet it can be done. It will be only a matter of time ... and money.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Let’s pretend for a moment that you receive a call from one of your college roommates who thanks to his family connections has become a venture capitalist in California. His group is considering investing in a start-up that is developing a handheld instrument that it claims will use artificial intelligence to diagnose ear infections far more accurately than the human eye. He wonders if you would like to help him evaluate the company’s proposal and offers you a small percentage of the profits for your efforts should they choose to invest.
Your former roommate has done enough research on his own to understand that otitis media makes up a large chunk of a pediatrician’s workload and that making an accurate diagnosis can often be difficult in a struggling child. He describes his own experience watching a frustrated pediatrician attempting to remove wax from his child’s ear and eventually prescribing antibiotics “to be safe.”
You agree and review the prospectus, which includes a paper from a peer-reviewed journal. What you discover is that the investigators used more than 600 high-resolution images of tympanic membranes taken “during operative myringotomy and tympanostomy tube placement” and the findings at tympanocentesis to train a neural network.
Once trained, the model they developed could differentiate with 95% accuracy between an image of a tympanic membrane that covered a normal middle ear from one that merely contained fluid and from one that contained infected fluid. When these same images were shown to 39 clinicians, more than half of which were pediatricians and included both faculty-level staff and trainees, the average diagnostic accuracy was 65%.
The prospectus includes prediction that this technology could easily be developed into a handheld instrument similar to a traditional otoscope, which could then be linked to the operator’s smartphone, giving the clinician an instant treat or no-treat answer.
Now, remember you have nothing to lose except maybe a friendship. How would you advise your old college roommate?
My advice to your college buddy would be one of caution! Yes, there is a potential big upside because there is a real need for a device that could provide a diagnostic accuracy that this AI model promises. While I suspect that AI will always be more accurate in diagnosis using static images, I bet that most people, clinicians and nonclinicians, could improve their accuracy by linking photos with diagnoses with an hour of practice.
However, evaluating a high-resolution photograph taken through an operative scope inserted into the cerumenless ear canal of a sedated, afrebrile child is several orders of magnitude less difficult than the real-world environment in which the diagnosis of otitis media is usually made.
If the venture capitalists were still interested in getting into the otitis media marketplace, you might suggest they look into companies that have already developed image capture otoscopes. At this point I could only find one on the Internet that was portable and it certainly isn’t small-child friendly. Once we have a tool that can capture images in real-world situations, the next step is to train AI systems to interpret them using the approach these researchers have developed. I bet it can be done. It will be only a matter of time ... and money.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Let’s pretend for a moment that you receive a call from one of your college roommates who thanks to his family connections has become a venture capitalist in California. His group is considering investing in a start-up that is developing a handheld instrument that it claims will use artificial intelligence to diagnose ear infections far more accurately than the human eye. He wonders if you would like to help him evaluate the company’s proposal and offers you a small percentage of the profits for your efforts should they choose to invest.
Your former roommate has done enough research on his own to understand that otitis media makes up a large chunk of a pediatrician’s workload and that making an accurate diagnosis can often be difficult in a struggling child. He describes his own experience watching a frustrated pediatrician attempting to remove wax from his child’s ear and eventually prescribing antibiotics “to be safe.”
You agree and review the prospectus, which includes a paper from a peer-reviewed journal. What you discover is that the investigators used more than 600 high-resolution images of tympanic membranes taken “during operative myringotomy and tympanostomy tube placement” and the findings at tympanocentesis to train a neural network.
Once trained, the model they developed could differentiate with 95% accuracy between an image of a tympanic membrane that covered a normal middle ear from one that merely contained fluid and from one that contained infected fluid. When these same images were shown to 39 clinicians, more than half of which were pediatricians and included both faculty-level staff and trainees, the average diagnostic accuracy was 65%.
The prospectus includes prediction that this technology could easily be developed into a handheld instrument similar to a traditional otoscope, which could then be linked to the operator’s smartphone, giving the clinician an instant treat or no-treat answer.
Now, remember you have nothing to lose except maybe a friendship. How would you advise your old college roommate?
My advice to your college buddy would be one of caution! Yes, there is a potential big upside because there is a real need for a device that could provide a diagnostic accuracy that this AI model promises. While I suspect that AI will always be more accurate in diagnosis using static images, I bet that most people, clinicians and nonclinicians, could improve their accuracy by linking photos with diagnoses with an hour of practice.
However, evaluating a high-resolution photograph taken through an operative scope inserted into the cerumenless ear canal of a sedated, afrebrile child is several orders of magnitude less difficult than the real-world environment in which the diagnosis of otitis media is usually made.
If the venture capitalists were still interested in getting into the otitis media marketplace, you might suggest they look into companies that have already developed image capture otoscopes. At this point I could only find one on the Internet that was portable and it certainly isn’t small-child friendly. Once we have a tool that can capture images in real-world situations, the next step is to train AI systems to interpret them using the approach these researchers have developed. I bet it can be done. It will be only a matter of time ... and money.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Where a child eats breakfast is important
We’ve been told for decades that a child who doesn’t start the day with a good breakfast is entering school at a serious disadvantage. The brain needs a good supply of energy to learn optimally. So the standard wisdom goes. Subsidized school breakfast programs have been built around this chestnut. But, is there solid evidence to support the notion that simply adding a morning meal to a child’s schedule will improve his or her school performance? It sounds like common sense, but is it just one of those old grandmother’s nuggets that doesn’t stand up under close scrutiny?
A recent study from Spain suggests that the relationship between breakfast and school performance is not merely related to the nutritional needs of a growing brain. Using data from nearly 4,000 Spanish children aged 4-14 collected in a 2017 national health survey, the investigators found “skipping breakfast and eating breakfast out of the home were linked to greater odds of psychosocial behavioral problems than eating breakfast at home.” And, we already know that, in general, children who misbehave in school don’t thrive academically.
There were also associations between the absence or presence of certain food groups in the morning meal with behavioral problems. But the data lacked the granularity to draw any firm conclusions – although the authors felt that what they consider a healthy Spanish diet may have had a positive influence on behavior.
The findings in this study may simply be another example of the many positive influences that have been associated with family meals and have little to do with what is actually consumed. The association may not have much to do with the family gathering together at a single Norman Rockwell sitting, a reality that I suspect seldom occurs. The apparent positive influence of breakfast may be that it reflects a family’s priorities: that food is important, that sleep is important, and that school is important – so important that scheduling the morning should focus on sending the child off well prepared. The child who is allowed to stay up to an unhealthy hour is likely to be difficult to arouse in the morning for breakfast and getting off to school.
It may be that the child’s behavior problems are so disruptive and taxing for the family that even with their best efforts, the parents can’t find the time and energy to provide a breakfast in the home.
On the other hand, the study doesn’t tell us how many children aren’t offered breakfast at home because their families simply can’t afford it. Obviously, the answer depends on the socioeconomic mix of a given community. In some localities this may represent a sizable percentage of the population.
So where does this leave us? Unfortunately, as I read through the discussion at the end of this paper I felt that the authors were leaning too much toward further research based on the potential associations between behavior and specific food groups their data suggested.
For me, the take-home message from this paper is that our existing efforts to improve academic success with food offered in school should also include strategies that promote eating breakfast at home. For example, the backpack take-home food distribution programs that seem to have been effective could include breakfast-targeted items packaged in a way that encourage families to provide breakfast at home.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
We’ve been told for decades that a child who doesn’t start the day with a good breakfast is entering school at a serious disadvantage. The brain needs a good supply of energy to learn optimally. So the standard wisdom goes. Subsidized school breakfast programs have been built around this chestnut. But, is there solid evidence to support the notion that simply adding a morning meal to a child’s schedule will improve his or her school performance? It sounds like common sense, but is it just one of those old grandmother’s nuggets that doesn’t stand up under close scrutiny?
A recent study from Spain suggests that the relationship between breakfast and school performance is not merely related to the nutritional needs of a growing brain. Using data from nearly 4,000 Spanish children aged 4-14 collected in a 2017 national health survey, the investigators found “skipping breakfast and eating breakfast out of the home were linked to greater odds of psychosocial behavioral problems than eating breakfast at home.” And, we already know that, in general, children who misbehave in school don’t thrive academically.
There were also associations between the absence or presence of certain food groups in the morning meal with behavioral problems. But the data lacked the granularity to draw any firm conclusions – although the authors felt that what they consider a healthy Spanish diet may have had a positive influence on behavior.
The findings in this study may simply be another example of the many positive influences that have been associated with family meals and have little to do with what is actually consumed. The association may not have much to do with the family gathering together at a single Norman Rockwell sitting, a reality that I suspect seldom occurs. The apparent positive influence of breakfast may be that it reflects a family’s priorities: that food is important, that sleep is important, and that school is important – so important that scheduling the morning should focus on sending the child off well prepared. The child who is allowed to stay up to an unhealthy hour is likely to be difficult to arouse in the morning for breakfast and getting off to school.
It may be that the child’s behavior problems are so disruptive and taxing for the family that even with their best efforts, the parents can’t find the time and energy to provide a breakfast in the home.
On the other hand, the study doesn’t tell us how many children aren’t offered breakfast at home because their families simply can’t afford it. Obviously, the answer depends on the socioeconomic mix of a given community. In some localities this may represent a sizable percentage of the population.
So where does this leave us? Unfortunately, as I read through the discussion at the end of this paper I felt that the authors were leaning too much toward further research based on the potential associations between behavior and specific food groups their data suggested.
For me, the take-home message from this paper is that our existing efforts to improve academic success with food offered in school should also include strategies that promote eating breakfast at home. For example, the backpack take-home food distribution programs that seem to have been effective could include breakfast-targeted items packaged in a way that encourage families to provide breakfast at home.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
We’ve been told for decades that a child who doesn’t start the day with a good breakfast is entering school at a serious disadvantage. The brain needs a good supply of energy to learn optimally. So the standard wisdom goes. Subsidized school breakfast programs have been built around this chestnut. But, is there solid evidence to support the notion that simply adding a morning meal to a child’s schedule will improve his or her school performance? It sounds like common sense, but is it just one of those old grandmother’s nuggets that doesn’t stand up under close scrutiny?
A recent study from Spain suggests that the relationship between breakfast and school performance is not merely related to the nutritional needs of a growing brain. Using data from nearly 4,000 Spanish children aged 4-14 collected in a 2017 national health survey, the investigators found “skipping breakfast and eating breakfast out of the home were linked to greater odds of psychosocial behavioral problems than eating breakfast at home.” And, we already know that, in general, children who misbehave in school don’t thrive academically.
There were also associations between the absence or presence of certain food groups in the morning meal with behavioral problems. But the data lacked the granularity to draw any firm conclusions – although the authors felt that what they consider a healthy Spanish diet may have had a positive influence on behavior.
The findings in this study may simply be another example of the many positive influences that have been associated with family meals and have little to do with what is actually consumed. The association may not have much to do with the family gathering together at a single Norman Rockwell sitting, a reality that I suspect seldom occurs. The apparent positive influence of breakfast may be that it reflects a family’s priorities: that food is important, that sleep is important, and that school is important – so important that scheduling the morning should focus on sending the child off well prepared. The child who is allowed to stay up to an unhealthy hour is likely to be difficult to arouse in the morning for breakfast and getting off to school.
It may be that the child’s behavior problems are so disruptive and taxing for the family that even with their best efforts, the parents can’t find the time and energy to provide a breakfast in the home.
On the other hand, the study doesn’t tell us how many children aren’t offered breakfast at home because their families simply can’t afford it. Obviously, the answer depends on the socioeconomic mix of a given community. In some localities this may represent a sizable percentage of the population.
So where does this leave us? Unfortunately, as I read through the discussion at the end of this paper I felt that the authors were leaning too much toward further research based on the potential associations between behavior and specific food groups their data suggested.
For me, the take-home message from this paper is that our existing efforts to improve academic success with food offered in school should also include strategies that promote eating breakfast at home. For example, the backpack take-home food distribution programs that seem to have been effective could include breakfast-targeted items packaged in a way that encourage families to provide breakfast at home.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].




