User login
Patient With Severe Headache After IV Immunoglobulin
A 35-year-old woman with a history of hypothyroidism and idiopathic small fiber autonomic and sensory neuropathy presented to the emergency department (ED) 48 hours after IV immunoglobulin (IG) infusion with a severe headache, nausea, neck stiffness, photophobia, and episodes of intense positional eye pressure. The patient reported previous episodes of headaches post-IVIG infusion but not nearly as severe. On ED arrival, the patient was afebrile with vital signs within normal limits. Initial laboratory results were notable for levels within reference range parameters: 5.9 × 109/L white blood cell (WBC) count, 13.3 g/dL hemoglobin, 38.7% hematocrit, and 279 × 109/L platelet count; there were no abnormal urinalysis findings, and she was negative for human chorionic gonadotropin.
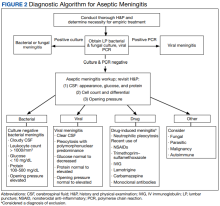
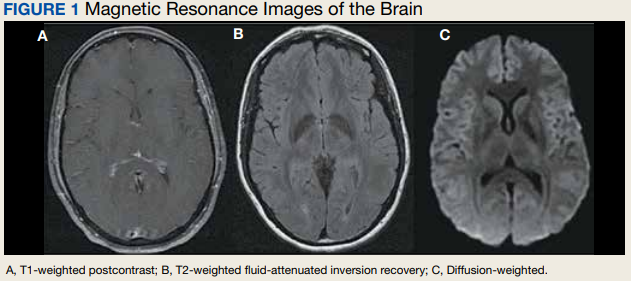
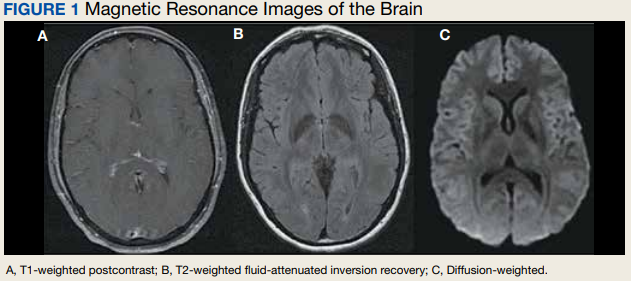
Due to the patient’s symptoms concerning for an acute intracranial process, a brain computed tomography (CT) without contrast was ordered. The CT demonstrated no intracranial abnormalities, but the patient’s symptoms continued to worsen. The patient was started on IV fluids and 1 g IV acetaminophen and underwent a lumbar puncture (LP). Her opening pressure was elevated at 29 cm H2O (reference range, 6-20 cm), and the fluid was notably clear. During the LP, 25 mL of cerebrospinal fluid (CSF) was collected for laboratory analysis to include a polymerase chain reaction (PCR) panel and cultures, and a closing pressure of 12 cm H2O was recorded at the end of the procedure with the patient reporting some relief of pressure. The patient was admitted to the medicine ward for further workup and observations.The patient’s meningitis/encephalitis PCR panel detected no pathogens in the CSF, but her WBC count was 84 × 109/L (reference range, 4-11) with 30 segmented neutrophils (reference range, 0-6) and red blood cell count of 24 (reference range, 0-1); her normal glucose at 60 mg/dL (reference range, 40-70) and protein of 33 mg/dL (reference range, 15-45) were within normal parameters. Brain magnetic resonance images with and without contrast was inconsistent with any acute intracranial pathology to include subarachnoid hemorrhage or central nervous system neoplasm (Figure 1). Bacterial and fungal cultures were negative.
- What is your diagnosis?
- How would you treat this patient?
Discussion
Aseptic meningitis presents with a typical clinical picture of meningitis to include headache, stiffened neck, and photophobia. In the event of negative CSF bacterial and fungal cultures and negative viral PCR, a diagnosis of aseptic meningitis is considered.1 Though the differential for aseptic meningitis is broad, in the immunocompetent patient, the most common etiology of aseptic meningitis in the United States is by far viral, and specifically, enterovirus (50.9%). It is less commonly caused by herpes simplex virus (8.3%), varicella zoster virus, and finally, the mosquito-borne St. Louis encephalitis and West Nile viruses typically acquired in the summer or early fall months. Other infectious agents that can present with aseptic meningitis are spirochetes (Lyme disease and syphilis), tuberculous meningitis, fungal infections (cryptococcal meningitis), and other bacterial infections that have a negative culture.
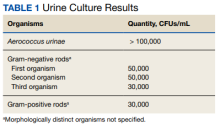
The patient’s history, physical examination, vital signs, imaging, and lumbar puncture findings were most concerning for drug-induced aseptic meningitis (DIAM) secondary to her recent IVIG infusion. An algorithm can be used to work through the diagnostic approach (Figure 2).3,4
Immediate and delayed adverse reactions to IVIG are known risks for IVIG therapy. About 1% to 15% of patients who receive IVIG will experience mild immediate reactions to the infusion.6 These immediate reactions include fever (78.6%), acrocyanosis (71.4%), rash (64.3%), headache (57.1%), shortness of breath (42.8%), hypotension (35.7%), and chest pain (21.4%).
IVIG is an increasingly used biologic pharmacologic agent used for a variety of medical conditions. This can be attributed to its multifaceted properties and ability to fight infection when given as replacement therapy and provide immunomodulation in conjunction with its more well-known anti-inflammatory properties.8 The number of conditions that can potentially benefit from IVIG is so vast that the American Academy of Allergy, Asthma and Immunology had to divide the indication for IVIG therapy into definitely beneficial, probably beneficial, may provide benefit, and unlikely to provide benefit categories.8
Conclusions
We encourage heightened clinical suspicion of DIAM in patients who have recently undergone IVIG infusion and present with meningeal signs (stiff neck, headache, photophobia, and ear/eye pressure) without any evidence of infection on physical examination or laboratory results. With such, we hope to improve clinician suspicion, detection, as well as patient education and outcomes in cases of DIAM.
1. Kareva L, Mironska K, Stavric K, Hasani A. Adverse reactions to intravenous immunoglobulins—our experience. Open Access Maced J Med Sci. 2018;6(12):2359-2362. doi:10.3889/oamjms.2018.513
2. Mount HR, Boyle SD. Aseptic and bacterial meningitis: evaluation, treatment, and prevention. Am Fam Physician. 2017;96(5):314-322.
3. Seehusen DA, Reeves MM, Fomin DA. Cerebrospinal fluid analysis. Am Fam Physician. 2003;68(6):1103-1108.
4. Connolly KJ, Hammer SM. The acute aseptic meningitis syndrome. Infect Dis Clin North Am. 1990;4(4):599-622.
5. Jolles S, Sewell WA, Leighton C. Drug-induced aseptic meningitis: diagnosis and management. Drug Saf. 2000;22(3):215-226. doi:10.2165/00002018-200022030-00005
6. Yelehe-Okouma M, Czmil-Garon J, Pape E, Petitpain N, Gillet P. Drug-induced aseptic meningitis: a mini-review. Fundam Clin Pharmacol. 2018;32(3):252-260. doi:10.1111/fcp.12349
7. Kepa L, Oczko-Grzesik B, Stolarz W, Sobala-Szczygiel B. Drug-induced aseptic meningitis in suspected central nervous system infections. J Clin Neurosci. 2005;12(5):562-564. doi:10.1016/j.jocn.2004.08.024
8. Perez EE, Orange JS, Bonilla F, et al. Update on the use of immunoglobulin in human disease: a review of evidence. J Allergy Clin Immunol. 2017;139(3S):S1-S46. doi:10.1016/j.jaci.2016.09.023
9. Kaarthigeyan K, Burli VV. Aseptic meningitis following intravenous immunoglobulin therapy of common variable immunodeficiency. J Pediatr Neurosci. 2011;6(2):160-161. doi:10.4103/1817-1745.92858
A 35-year-old woman with a history of hypothyroidism and idiopathic small fiber autonomic and sensory neuropathy presented to the emergency department (ED) 48 hours after IV immunoglobulin (IG) infusion with a severe headache, nausea, neck stiffness, photophobia, and episodes of intense positional eye pressure. The patient reported previous episodes of headaches post-IVIG infusion but not nearly as severe. On ED arrival, the patient was afebrile with vital signs within normal limits. Initial laboratory results were notable for levels within reference range parameters: 5.9 × 109/L white blood cell (WBC) count, 13.3 g/dL hemoglobin, 38.7% hematocrit, and 279 × 109/L platelet count; there were no abnormal urinalysis findings, and she was negative for human chorionic gonadotropin.
Due to the patient’s symptoms concerning for an acute intracranial process, a brain computed tomography (CT) without contrast was ordered. The CT demonstrated no intracranial abnormalities, but the patient’s symptoms continued to worsen. The patient was started on IV fluids and 1 g IV acetaminophen and underwent a lumbar puncture (LP). Her opening pressure was elevated at 29 cm H2O (reference range, 6-20 cm), and the fluid was notably clear. During the LP, 25 mL of cerebrospinal fluid (CSF) was collected for laboratory analysis to include a polymerase chain reaction (PCR) panel and cultures, and a closing pressure of 12 cm H2O was recorded at the end of the procedure with the patient reporting some relief of pressure. The patient was admitted to the medicine ward for further workup and observations.The patient’s meningitis/encephalitis PCR panel detected no pathogens in the CSF, but her WBC count was 84 × 109/L (reference range, 4-11) with 30 segmented neutrophils (reference range, 0-6) and red blood cell count of 24 (reference range, 0-1); her normal glucose at 60 mg/dL (reference range, 40-70) and protein of 33 mg/dL (reference range, 15-45) were within normal parameters. Brain magnetic resonance images with and without contrast was inconsistent with any acute intracranial pathology to include subarachnoid hemorrhage or central nervous system neoplasm (Figure 1). Bacterial and fungal cultures were negative.
- What is your diagnosis?
- How would you treat this patient?
Discussion
Aseptic meningitis presents with a typical clinical picture of meningitis to include headache, stiffened neck, and photophobia. In the event of negative CSF bacterial and fungal cultures and negative viral PCR, a diagnosis of aseptic meningitis is considered.1 Though the differential for aseptic meningitis is broad, in the immunocompetent patient, the most common etiology of aseptic meningitis in the United States is by far viral, and specifically, enterovirus (50.9%). It is less commonly caused by herpes simplex virus (8.3%), varicella zoster virus, and finally, the mosquito-borne St. Louis encephalitis and West Nile viruses typically acquired in the summer or early fall months. Other infectious agents that can present with aseptic meningitis are spirochetes (Lyme disease and syphilis), tuberculous meningitis, fungal infections (cryptococcal meningitis), and other bacterial infections that have a negative culture.
The patient’s history, physical examination, vital signs, imaging, and lumbar puncture findings were most concerning for drug-induced aseptic meningitis (DIAM) secondary to her recent IVIG infusion. An algorithm can be used to work through the diagnostic approach (Figure 2).3,4
Immediate and delayed adverse reactions to IVIG are known risks for IVIG therapy. About 1% to 15% of patients who receive IVIG will experience mild immediate reactions to the infusion.6 These immediate reactions include fever (78.6%), acrocyanosis (71.4%), rash (64.3%), headache (57.1%), shortness of breath (42.8%), hypotension (35.7%), and chest pain (21.4%).
IVIG is an increasingly used biologic pharmacologic agent used for a variety of medical conditions. This can be attributed to its multifaceted properties and ability to fight infection when given as replacement therapy and provide immunomodulation in conjunction with its more well-known anti-inflammatory properties.8 The number of conditions that can potentially benefit from IVIG is so vast that the American Academy of Allergy, Asthma and Immunology had to divide the indication for IVIG therapy into definitely beneficial, probably beneficial, may provide benefit, and unlikely to provide benefit categories.8
Conclusions
We encourage heightened clinical suspicion of DIAM in patients who have recently undergone IVIG infusion and present with meningeal signs (stiff neck, headache, photophobia, and ear/eye pressure) without any evidence of infection on physical examination or laboratory results. With such, we hope to improve clinician suspicion, detection, as well as patient education and outcomes in cases of DIAM.
A 35-year-old woman with a history of hypothyroidism and idiopathic small fiber autonomic and sensory neuropathy presented to the emergency department (ED) 48 hours after IV immunoglobulin (IG) infusion with a severe headache, nausea, neck stiffness, photophobia, and episodes of intense positional eye pressure. The patient reported previous episodes of headaches post-IVIG infusion but not nearly as severe. On ED arrival, the patient was afebrile with vital signs within normal limits. Initial laboratory results were notable for levels within reference range parameters: 5.9 × 109/L white blood cell (WBC) count, 13.3 g/dL hemoglobin, 38.7% hematocrit, and 279 × 109/L platelet count; there were no abnormal urinalysis findings, and she was negative for human chorionic gonadotropin.
Due to the patient’s symptoms concerning for an acute intracranial process, a brain computed tomography (CT) without contrast was ordered. The CT demonstrated no intracranial abnormalities, but the patient’s symptoms continued to worsen. The patient was started on IV fluids and 1 g IV acetaminophen and underwent a lumbar puncture (LP). Her opening pressure was elevated at 29 cm H2O (reference range, 6-20 cm), and the fluid was notably clear. During the LP, 25 mL of cerebrospinal fluid (CSF) was collected for laboratory analysis to include a polymerase chain reaction (PCR) panel and cultures, and a closing pressure of 12 cm H2O was recorded at the end of the procedure with the patient reporting some relief of pressure. The patient was admitted to the medicine ward for further workup and observations.The patient’s meningitis/encephalitis PCR panel detected no pathogens in the CSF, but her WBC count was 84 × 109/L (reference range, 4-11) with 30 segmented neutrophils (reference range, 0-6) and red blood cell count of 24 (reference range, 0-1); her normal glucose at 60 mg/dL (reference range, 40-70) and protein of 33 mg/dL (reference range, 15-45) were within normal parameters. Brain magnetic resonance images with and without contrast was inconsistent with any acute intracranial pathology to include subarachnoid hemorrhage or central nervous system neoplasm (Figure 1). Bacterial and fungal cultures were negative.
- What is your diagnosis?
- How would you treat this patient?
Discussion
Aseptic meningitis presents with a typical clinical picture of meningitis to include headache, stiffened neck, and photophobia. In the event of negative CSF bacterial and fungal cultures and negative viral PCR, a diagnosis of aseptic meningitis is considered.1 Though the differential for aseptic meningitis is broad, in the immunocompetent patient, the most common etiology of aseptic meningitis in the United States is by far viral, and specifically, enterovirus (50.9%). It is less commonly caused by herpes simplex virus (8.3%), varicella zoster virus, and finally, the mosquito-borne St. Louis encephalitis and West Nile viruses typically acquired in the summer or early fall months. Other infectious agents that can present with aseptic meningitis are spirochetes (Lyme disease and syphilis), tuberculous meningitis, fungal infections (cryptococcal meningitis), and other bacterial infections that have a negative culture.
The patient’s history, physical examination, vital signs, imaging, and lumbar puncture findings were most concerning for drug-induced aseptic meningitis (DIAM) secondary to her recent IVIG infusion. An algorithm can be used to work through the diagnostic approach (Figure 2).3,4
Immediate and delayed adverse reactions to IVIG are known risks for IVIG therapy. About 1% to 15% of patients who receive IVIG will experience mild immediate reactions to the infusion.6 These immediate reactions include fever (78.6%), acrocyanosis (71.4%), rash (64.3%), headache (57.1%), shortness of breath (42.8%), hypotension (35.7%), and chest pain (21.4%).
IVIG is an increasingly used biologic pharmacologic agent used for a variety of medical conditions. This can be attributed to its multifaceted properties and ability to fight infection when given as replacement therapy and provide immunomodulation in conjunction with its more well-known anti-inflammatory properties.8 The number of conditions that can potentially benefit from IVIG is so vast that the American Academy of Allergy, Asthma and Immunology had to divide the indication for IVIG therapy into definitely beneficial, probably beneficial, may provide benefit, and unlikely to provide benefit categories.8
Conclusions
We encourage heightened clinical suspicion of DIAM in patients who have recently undergone IVIG infusion and present with meningeal signs (stiff neck, headache, photophobia, and ear/eye pressure) without any evidence of infection on physical examination or laboratory results. With such, we hope to improve clinician suspicion, detection, as well as patient education and outcomes in cases of DIAM.
1. Kareva L, Mironska K, Stavric K, Hasani A. Adverse reactions to intravenous immunoglobulins—our experience. Open Access Maced J Med Sci. 2018;6(12):2359-2362. doi:10.3889/oamjms.2018.513
2. Mount HR, Boyle SD. Aseptic and bacterial meningitis: evaluation, treatment, and prevention. Am Fam Physician. 2017;96(5):314-322.
3. Seehusen DA, Reeves MM, Fomin DA. Cerebrospinal fluid analysis. Am Fam Physician. 2003;68(6):1103-1108.
4. Connolly KJ, Hammer SM. The acute aseptic meningitis syndrome. Infect Dis Clin North Am. 1990;4(4):599-622.
5. Jolles S, Sewell WA, Leighton C. Drug-induced aseptic meningitis: diagnosis and management. Drug Saf. 2000;22(3):215-226. doi:10.2165/00002018-200022030-00005
6. Yelehe-Okouma M, Czmil-Garon J, Pape E, Petitpain N, Gillet P. Drug-induced aseptic meningitis: a mini-review. Fundam Clin Pharmacol. 2018;32(3):252-260. doi:10.1111/fcp.12349
7. Kepa L, Oczko-Grzesik B, Stolarz W, Sobala-Szczygiel B. Drug-induced aseptic meningitis in suspected central nervous system infections. J Clin Neurosci. 2005;12(5):562-564. doi:10.1016/j.jocn.2004.08.024
8. Perez EE, Orange JS, Bonilla F, et al. Update on the use of immunoglobulin in human disease: a review of evidence. J Allergy Clin Immunol. 2017;139(3S):S1-S46. doi:10.1016/j.jaci.2016.09.023
9. Kaarthigeyan K, Burli VV. Aseptic meningitis following intravenous immunoglobulin therapy of common variable immunodeficiency. J Pediatr Neurosci. 2011;6(2):160-161. doi:10.4103/1817-1745.92858
1. Kareva L, Mironska K, Stavric K, Hasani A. Adverse reactions to intravenous immunoglobulins—our experience. Open Access Maced J Med Sci. 2018;6(12):2359-2362. doi:10.3889/oamjms.2018.513
2. Mount HR, Boyle SD. Aseptic and bacterial meningitis: evaluation, treatment, and prevention. Am Fam Physician. 2017;96(5):314-322.
3. Seehusen DA, Reeves MM, Fomin DA. Cerebrospinal fluid analysis. Am Fam Physician. 2003;68(6):1103-1108.
4. Connolly KJ, Hammer SM. The acute aseptic meningitis syndrome. Infect Dis Clin North Am. 1990;4(4):599-622.
5. Jolles S, Sewell WA, Leighton C. Drug-induced aseptic meningitis: diagnosis and management. Drug Saf. 2000;22(3):215-226. doi:10.2165/00002018-200022030-00005
6. Yelehe-Okouma M, Czmil-Garon J, Pape E, Petitpain N, Gillet P. Drug-induced aseptic meningitis: a mini-review. Fundam Clin Pharmacol. 2018;32(3):252-260. doi:10.1111/fcp.12349
7. Kepa L, Oczko-Grzesik B, Stolarz W, Sobala-Szczygiel B. Drug-induced aseptic meningitis in suspected central nervous system infections. J Clin Neurosci. 2005;12(5):562-564. doi:10.1016/j.jocn.2004.08.024
8. Perez EE, Orange JS, Bonilla F, et al. Update on the use of immunoglobulin in human disease: a review of evidence. J Allergy Clin Immunol. 2017;139(3S):S1-S46. doi:10.1016/j.jaci.2016.09.023
9. Kaarthigeyan K, Burli VV. Aseptic meningitis following intravenous immunoglobulin therapy of common variable immunodeficiency. J Pediatr Neurosci. 2011;6(2):160-161. doi:10.4103/1817-1745.92858
Oral Therapy for Aerococcus urinae Bacteremia and Thoracic Spondylodiscitis of Presumed Urinary Origin
Aerococcus urinae (A urinae), a gram-positive coccus readily mistaken for a Staphylococcus species, was first identified in 1992.1-3 It now reportedly accounts for 0.2% to 0.8% of clinical urine isolates.4-6 A urinae bacteriuria is typically asymptomatic and mainly occurs in women.7-9 Symptomatic A urinae urinary tract infection (UTI) occurs predominantly in older men with underlying urologic abnormalities.4-10
Serious A urinae infections are rare. The first 2 reported cases involved men with A urinae endocarditis, one of whom died.11,12 To date, only 8 cases of spondylodiscitis due to A urinae have been reported.13-20 Optimal treatment for invasive A urinae infection is undefined; however, the reported cases were treated successfully with diverse antibiotic regimen combinations; all including a β-lactam and beginning with at least 2 weeks of IV antibiotics.13-20 We describe a man with A urinae bacteremia and spondylodiscitis, presumably arising from a urinary source in the setting of bladder outlet obstruction, who was treated successfully.
Case Presentation
A 74-year-old man with morbid obesity, type 2 diabetes mellitus, stage 2 chronic kidney disease, and tobacco use presented to the emergency department after 2 weeks of progressive, nonradiating, midthoracic back pain, lower extremity weakness, gait imbalance, fatigue, anorexia, rigors, and subjective fevers. On presentation, he was afebrile and hemodynamically stable. A physical examination revealed point tenderness of the midthoracic vertebrae, nontender costovertebral angles, diffusely decreased strength, nonsustained clonus in both lower extremities, inguinal intertrigo, and a buried penis with purulent meatal discharge.
Laboratory results indicated a white blood cell (WBC) count of 13.5 K/μL (reference range, 4.0-11.0), absolute neutrophil count of 11.48 K/μL (reference range, 2.0-7.7), C-reactive protein (CRP) level of 225.3 mg/L (reference range, ≤ 5.0), erythrocyte sedimentation rate of 85 mm/h (reference range, 5-15), serum blood urea nitrogen of 76 mg/dL (reference range, 8-26), and serum creatinine (SCr) of 1.9 mg/dL (reference range, 1.1-1.4). A urinalysis showed positive leukocyte esterase, WBC clumps, and little bacteria. Abdominal/pelvic computed tomography showed spondylodiscitis-like changes at T7-T8, bilateral perinephric fat stranding, bladder distension, and bladder wall thickening.
The patient was presumed to have discitis secondary to a UTI, with possible pyelonephritis, and was given empiric vancomycin and ceftriaxone. Spinal magnetic resonance imaging with contrast supported spondylodiscitis at T7-T8, extending to T8-T9. Preliminary results from the admission blood and urine cultures showed gram-positive cocci in clusters, which were presumed initially to be Staphylococcus aureus (S aureus).
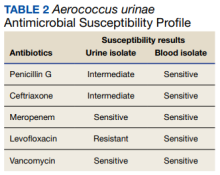
The final urine culture report listed multiple organisms, predominantly A urinae (Table 1);
On hospital day 6, the patient’s back pain had resolved, micturition was normal, appetite had normalized, and SCr was minimally above baseline (1.4 mg/dL). He insisted on completing antibiotic treatment at home and had no other medical indication for continued hospitalization. Thus, antibiotic therapy was changed to an all-oral regimen of amoxicillin 1 g 3 times daily for 10 days and levofloxacin 750 mg daily for 6 weeks, and the patient was discharged to home.
The patient returned 5 days postdischarge due to anuria. Investigation showed severe acute kidney injury (SCr, 6.8 mg/dL) and bladder outlet obstruction due to phimosis and urethral meatal stenosis. Urinalysis was unremarkable. His CRP had declined from 225 mg/L (initial admission) to 154 mg/L. A urinae culture and 2 sets of blood cultures were finalized as no growth. He was diagnosed with postrenal acute kidney injury and underwent meatal dilation and Foley catheterization but declined surgical correction. When seen in the clinic 2 months postantimicrobial therapy, the patient had normal micturition, no symptoms or signs of infection, and steadily down-trending inflammatory markers.
Discussion
A urinae, historically considered a rare pathogen, has been identified with increasing frequency in urine cultures due to improved microbiologic diagnostic techniques. However, there are only 8 reported cases of A urinae spondylodiscitis. Urinary pathology is an accepted risk factor for A urinae infections; consequently, we suspect that our patient’s urinary outflow obstruction and poor genitourinary hygiene were related to his invasive A urinae infection.10,21,22 We surmise that he had a chronic urinary outflow obstruction contributing to his infection, as evidenced by imaging findings, while the phimosis and urethral meatal stenosis were most likely infectious sequelae considering his anuria and acute kidney injury 5 days postdischarge. Indeed, the correlation between A urinae and urinary tract pathology may justify an evaluation for urinary pathology in any man with A urinae infection, regardless of the presence of symptoms.
By contrast, the implications of A urinae bacteriuria remain unclear. From a public health perspective, A urinae bacteriuria is rare, but the infectious mechanism remains undetermined with a case report suggesting the possibility of sexual transmission.4-6,23 In our case, the patient was not sexually active and had no clear origin of infection. Considering the potential severity of infection, more studies are needed to determine the infectious mechanism of A urinae.
In terms of infectious morbidity, the results seem to vary by sex. In a retrospective study of about 30,000 clinical urine samples, 62 (58 from women, 4 from men) yielded A urinae. The 62 corresponding patients lacked systemic infectious complications, leading the authors to conclude that A urinae is a relatively avirulent organism.24 Although possibly true in women, we are wary of drawing conclusions, especially regarding men, from a study that included only 62 urine samples were A urinae–positive, with only 4 from men. More evidence is needed to define the prognostic implications of A urinae bacteriuria in men.
As illustrated by the present case and previous reports, severe A urinae infections can occur, and the contributory factors deserve consideration. In our patient, the actual mechanism for bacteremia remains unclear. The initial concern for acute pyelonephritis was prompted by a computed tomography finding of bilateral perinephric fat stranding. This finding was questioned because it is common in older patients without infection, hence, is highly nonspecific. A correlation with urinary outflow obstruction may be an important clue in cases like this one.25,26
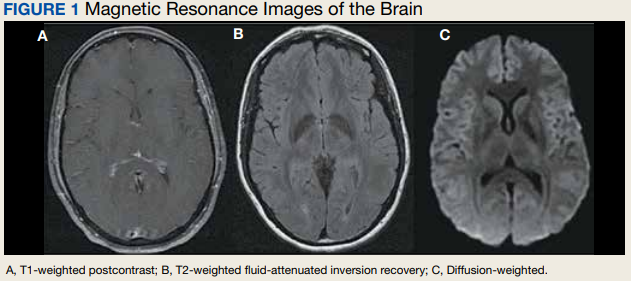
Furthermore, whether the urinary tract truly was the source of the patient’s bacteremia is clouded by the differing antimicrobial susceptibility patterns of the A urinae blood and urine isolates. The simplest explanation for this discordance may be that all the isolates shared a common initial origin but adapted to different environments in the host (perhaps over time) or laboratory, producing phenotypic variation. Alternatively, the infection could have been polyclonal from the onset, with sampling error leading to the differing detected susceptibility patterns, or the blood and urine isolates may have represented independent acquisition events, involving distinct A urinae strains. Unfortunately (from an academic perspective), given patient preferences and recommendations from the infectious disease consultant, no bone biopsy was done for histology and culture to confirm infection and to allow comparative strain identification if A urinae was isolated.
Optimal treatment for A urinae spondylodiscitis has yet to be established. β-lactams have shown good clinical efficacy despite being bacteriostatic in vitro.27 Early in vitro studies showed synergistic bactericidal synergistic activity with penicillin plus aminoglycoside combination therapies.27-30 Cases of endocarditis have been successfully treated mainly with the combination of a β-lactam plus aminoglycoside combination therapy.30,31 Previous cases of spondylodiscitis have been treated successfully with diverse antimicrobial agents, including clindamycin, β-lactams, cephalosporins, fluoroquinolones, and aminoglycosides.14
Our patient improved rapidly while receiving empiric therapy with vancomycin and ceftriaxone and tolerated a rapid transition to oral amoxicillin and levofloxacin. This is the shortest IV treatment course for A urinae spondylodiscitis reported to date. We suspect that such rapid IV-to-oral transitions will suffice in most stable patients with A urinae spondylodiscitis or other invasive A urinae infections in line with the results of the OVIVA and POET trials.32,33
Conclusions
We believe A urinae UTI in the absence of obvious predisposing factors should prompt evaluation for urinary outflow obstruction. Despite improved laboratory diagnostic techniques, spondylodiscitis related to A urinae remains a rare entity and thus definitive treatment recommendations are difficult to make. However, we suspect that in many cases it is reasonable to extrapolate from the results of the POET and OVIVA trials and rapidly transition therapy of A urinae spondylodiscitis from IV to oral antibiotics. We suspect a review of the US Department of Veterans Affairs population might uncover a higher incidence of A urinae infection than previously estimated due to the population demographics and the epidemiology of A urinae.
1. Christensen JJ, Korner B, Kjaergaard H. Aerococcus-like organism—an unnoticed urinary tract pathogen. APMIS. 1989;97(6):539-546. doi:10.1111/j.1699-0463.1989.tb00828.x
2. Aguirre M, Collins MD. Phylogenetic analysis of some Aerococcus-like organisms from urinary tract infections: description of Aerococcus urinae sp. nov. J Gen Microbiol. 1992;138(2):401-405. doi:10.1099/00221287-138-2-401
3. Williams RE, Hirch A, Cowan ST. Aerococcus, a new bacterial genus. J Gen Microbiol. 1953;8(3):475-480. doi:10.1099/00221287-8-3-475
4. Kline KA, Lewis AL. Gram-positive uropathogens, polymicrobial urinary tract infection, and the emerging microbiota of the urinary tract. Microbiol Spectr. 2016;4(2). doi:10.1128/microbiolspec.UTI-0012-2012
5. Schuur PM, Kasteren ME, Sabbe L, Vos MC, Janssens MM, Buiting AG. Urinary tract infections with Aerococcus urinae in the south of The Netherlands. Eur J Clin Microbiol Infect Dis. 1997;16(12):871-875. doi:10.1007/BF01700552
6. Grude N, Tveten Y. Aerococcus urinae og urinveisinfeksjon [Aerococcus urinae and urinary tract infection]. Tidsskr Nor Laegeforen. 2002;122(2):174-175.
7. Narayanasamy S, King K, Dennison A, Spelman DW, Aung AK. Clinical characteristics and laboratory identification of Aerococcus infections: an Australian tertiary centre perspective. Int J Microbiol. 2017;2017. doi:10.1155/2017/5684614
8. Hilt EE, McKinley K, Pearce MM, et al. Urine is not sterile: use of enhanced urine culture techniques to detect resident bacterial flora in the adult female bladder. J Clin Microbiol. 2014;52(3):871-876. doi:10.1128/JCM.02876-13
9. Pearce MM, Hilt EE, Rosenfeld AB, et al. The female urinary microbiome: a comparison of women with and without urgency urinary incontinence. mBio. 2014;5(4):e01283-14. doi:10.1128/mBio.01283-14
10. Sahu KK, Lal A, Mishra AK, Abraham GM. Aerococcus-related infections and their significance: a 9-year retrospective study. J Microsc Ultrastruct. 2021;9(1):18-25. doi:10.4103/JMAU.JMAU_61_19
11. Skov RL, Klarlund M, Thorsen S. Fatal endocarditis due to Aerococcus urinae. Diagn Microbiol Infect Dis. 1995;21(4):219-221. doi:10.1016/0732-8893(95)00037-b
12. Kristensen B, Nielsen G. Endocarditis caused by Aerococcus urinae, a newly recognized pathogen. Eur J Clin Microbiol Infect Dis. 1995;14(1):49-51. doi:10.1007/BF02112619
13. Astudillo L, Sailler L, Porte L, Lefevre JC, Massip P, Arlet-Suau E. Spondylodiscitis due to Aerococcus urinae: a first report. Scand J Infect Dis. 2003;35(11-12):890-891. doi:10.1080/00365540310016664
14. Lyagoubi A, Souffi C, Baroiller V, Vallee E. Spondylodiscitis: an increasingly described localization. EJIFCC. 2020;31(2):169-173.
15. Jerome M, Slim J, Sison R, Marton R. A case of Aerococcus urinae vertebral osteomyelitis. J Glob Infect Dis. 2015;7(2):85-86. doi:10.4103/0974-777X.157246
16. Tekin A, Tekin G, Turunç T, Demiroğlu Z, Kizilkiliç O. Infective endocarditis and spondylodiscitis in a patient due to Aerococcus urinae: first report. Int J Cardiol. 2007;115(3):402-403. doi:10.1016/j.ijcard.2006.01.046
17. Rougier E, Braud A, Argemi X, et al. Spondylodiscitis due to Aerococcus urinae and literature review. Infection. 2018;46(3):419-421. doi:10.1007/s15010-017-1106-0
18. Degroote E, Yildiz H, Lecouvet F, Verroken A, Belkhir L. Aerococcus urinae: an underestimated cause of spine infection? Case report and review of the literature. Acta Clin Belg. 2018;73(6):444-447. doi:10.1080/17843286.2018.1443003
19. Torres-Martos E, Pérez-Cortés S, Sánchez-Calvo JM, López-Prieto MD. Spondylodiscitis due to Aerococcus urinae infection in an elderly immunocompetent patient. Enferm Infecc Microbiol Clin. 2017;35(10):682-684. doi:10.1016/j.eimc.2017.02.005
20. Senneby E, Petersson AC, Rasmussen M. Clinical and microbiological features of bacteraemia with Aerococcus urinae. Clin Microbiol Infect. 2012;18(6):546-550. doi:10.1111/j.1469-0691.2011.03609.x
21. Sunnerhagen T, Nilson B, Olaison L, Rasmussen M. Clinical and microbiological features of infective endocarditis caused by aerococci. Infection. 2016;44(2):167-173. doi:10.1007/s15010-015-0812-8
22. de Jong MF, Soetekouw R, ten Kate RW, Veenendaal D. Aerococcus urinae: severe and fatal bloodstream infections and endocarditis. J Clin Microbiol. 2010;48(9):3445-3447. doi:10.1128/JCM.00835-10
23. Babaeer AA, Nader C, Iacoviello V, Tomera K. Necrotizing urethritis due to Aerococcus urinae. Case Rep Urol. 2015;2015:136147. doi:10.1155/2015/136147
24. Sierra-Hoffman M, Watkins K, Jinadatha C, Fader R, Carpenter JL. Clinical significance of Aerococcus urinae: a retrospective review. Diagn Microbiol Infect Dis. 2005;53(4):289-292. doi:10.1016/j.diagmicrobio.2005.06.021
25. Fukami H, Takeuchi Y, Kagaya S, et al. Perirenal fat stranding is not a powerful diagnostic tool for acute pyelonephritis. Int J Gen Med. 2017;10:137-144. doi:10.2147/IJGM.S133685
26. Han NY, Sung DJ, Kim MJ, Park BJ, Sim KC, Cho SB. Perirenal fat stranding on CT: is there an association with bladder outlet obstruction? Br J Radiol. 2016;89(1063):20160195. doi:10.1259/bjr.20160195
27. Hirzel C, Hirzberger L, Furrer H, Endimiani A. Bactericidal activity of penicillin, ceftriaxone, gentamicin and daptomycin alone and in combination against Aerococcus urinae. Int J Antimicrob Agents. 2016;48(3):271-276. doi:10.1016/j.ijantimicag.2016.05.007
28. Zbinden R, Santanam P, Hunziker L, Leuzinger B, von Graevenitz A. Endocarditis due to Aerococcus urinae: diagnostic tests, fatty acid composition and killing kinetics. Infection. 1999;27(2):122-124. doi:10.1007/BF02560511
29. Skov R, Christensen JJ, Korner B, Frimodt-Møller N, Espersen F. In vitro antimicrobial susceptibility of Aerococcus urinae to 14 antibiotics, and time-kill curves for penicillin, gentamicin and vancomycin. J Antimicrob Chemother. 2001;48(5):653-658. doi:10.1093/jac/48.5.653
30. Ebnöther C, Altwegg M, Gottschalk J, Seebach JD, Kronenberg A. Aerococcus urinae endocarditis: case report and review of the literature. Infection. 2002;30(5):310-313. doi:10.1007/s15010-002-3106-x
31. Tai DBG, Go JR, Fida M, Saleh OA. Management and treatment of Aerococcus bacteremia and endocarditis. Int J Infect Dis. 2021;102:584-589. doi:10.1016/j.ijid.2020.10.096
32. Li H-K, Rombach I, Zambellas R, et al; OVIVA Trial Collaborators. Oral versus intravenous antibiotics for bone and joint infection. N Engl J Med. 2019;380(5):425-436. doi:10.1056/NEJMoa1710926
33. Iversen K, Ihlemann N, Gill SU, et al. Partial oral versus intravenous antibiotic treatment of endocarditis. N Engl J Med. 2019;380(5):415-424. doi:10.1056/NEJMoa1808312
Aerococcus urinae (A urinae), a gram-positive coccus readily mistaken for a Staphylococcus species, was first identified in 1992.1-3 It now reportedly accounts for 0.2% to 0.8% of clinical urine isolates.4-6 A urinae bacteriuria is typically asymptomatic and mainly occurs in women.7-9 Symptomatic A urinae urinary tract infection (UTI) occurs predominantly in older men with underlying urologic abnormalities.4-10
Serious A urinae infections are rare. The first 2 reported cases involved men with A urinae endocarditis, one of whom died.11,12 To date, only 8 cases of spondylodiscitis due to A urinae have been reported.13-20 Optimal treatment for invasive A urinae infection is undefined; however, the reported cases were treated successfully with diverse antibiotic regimen combinations; all including a β-lactam and beginning with at least 2 weeks of IV antibiotics.13-20 We describe a man with A urinae bacteremia and spondylodiscitis, presumably arising from a urinary source in the setting of bladder outlet obstruction, who was treated successfully.
Case Presentation
A 74-year-old man with morbid obesity, type 2 diabetes mellitus, stage 2 chronic kidney disease, and tobacco use presented to the emergency department after 2 weeks of progressive, nonradiating, midthoracic back pain, lower extremity weakness, gait imbalance, fatigue, anorexia, rigors, and subjective fevers. On presentation, he was afebrile and hemodynamically stable. A physical examination revealed point tenderness of the midthoracic vertebrae, nontender costovertebral angles, diffusely decreased strength, nonsustained clonus in both lower extremities, inguinal intertrigo, and a buried penis with purulent meatal discharge.
Laboratory results indicated a white blood cell (WBC) count of 13.5 K/μL (reference range, 4.0-11.0), absolute neutrophil count of 11.48 K/μL (reference range, 2.0-7.7), C-reactive protein (CRP) level of 225.3 mg/L (reference range, ≤ 5.0), erythrocyte sedimentation rate of 85 mm/h (reference range, 5-15), serum blood urea nitrogen of 76 mg/dL (reference range, 8-26), and serum creatinine (SCr) of 1.9 mg/dL (reference range, 1.1-1.4). A urinalysis showed positive leukocyte esterase, WBC clumps, and little bacteria. Abdominal/pelvic computed tomography showed spondylodiscitis-like changes at T7-T8, bilateral perinephric fat stranding, bladder distension, and bladder wall thickening.
The patient was presumed to have discitis secondary to a UTI, with possible pyelonephritis, and was given empiric vancomycin and ceftriaxone. Spinal magnetic resonance imaging with contrast supported spondylodiscitis at T7-T8, extending to T8-T9. Preliminary results from the admission blood and urine cultures showed gram-positive cocci in clusters, which were presumed initially to be Staphylococcus aureus (S aureus).
The final urine culture report listed multiple organisms, predominantly A urinae (Table 1);
On hospital day 6, the patient’s back pain had resolved, micturition was normal, appetite had normalized, and SCr was minimally above baseline (1.4 mg/dL). He insisted on completing antibiotic treatment at home and had no other medical indication for continued hospitalization. Thus, antibiotic therapy was changed to an all-oral regimen of amoxicillin 1 g 3 times daily for 10 days and levofloxacin 750 mg daily for 6 weeks, and the patient was discharged to home.
The patient returned 5 days postdischarge due to anuria. Investigation showed severe acute kidney injury (SCr, 6.8 mg/dL) and bladder outlet obstruction due to phimosis and urethral meatal stenosis. Urinalysis was unremarkable. His CRP had declined from 225 mg/L (initial admission) to 154 mg/L. A urinae culture and 2 sets of blood cultures were finalized as no growth. He was diagnosed with postrenal acute kidney injury and underwent meatal dilation and Foley catheterization but declined surgical correction. When seen in the clinic 2 months postantimicrobial therapy, the patient had normal micturition, no symptoms or signs of infection, and steadily down-trending inflammatory markers.
Discussion
A urinae, historically considered a rare pathogen, has been identified with increasing frequency in urine cultures due to improved microbiologic diagnostic techniques. However, there are only 8 reported cases of A urinae spondylodiscitis. Urinary pathology is an accepted risk factor for A urinae infections; consequently, we suspect that our patient’s urinary outflow obstruction and poor genitourinary hygiene were related to his invasive A urinae infection.10,21,22 We surmise that he had a chronic urinary outflow obstruction contributing to his infection, as evidenced by imaging findings, while the phimosis and urethral meatal stenosis were most likely infectious sequelae considering his anuria and acute kidney injury 5 days postdischarge. Indeed, the correlation between A urinae and urinary tract pathology may justify an evaluation for urinary pathology in any man with A urinae infection, regardless of the presence of symptoms.
By contrast, the implications of A urinae bacteriuria remain unclear. From a public health perspective, A urinae bacteriuria is rare, but the infectious mechanism remains undetermined with a case report suggesting the possibility of sexual transmission.4-6,23 In our case, the patient was not sexually active and had no clear origin of infection. Considering the potential severity of infection, more studies are needed to determine the infectious mechanism of A urinae.
In terms of infectious morbidity, the results seem to vary by sex. In a retrospective study of about 30,000 clinical urine samples, 62 (58 from women, 4 from men) yielded A urinae. The 62 corresponding patients lacked systemic infectious complications, leading the authors to conclude that A urinae is a relatively avirulent organism.24 Although possibly true in women, we are wary of drawing conclusions, especially regarding men, from a study that included only 62 urine samples were A urinae–positive, with only 4 from men. More evidence is needed to define the prognostic implications of A urinae bacteriuria in men.
As illustrated by the present case and previous reports, severe A urinae infections can occur, and the contributory factors deserve consideration. In our patient, the actual mechanism for bacteremia remains unclear. The initial concern for acute pyelonephritis was prompted by a computed tomography finding of bilateral perinephric fat stranding. This finding was questioned because it is common in older patients without infection, hence, is highly nonspecific. A correlation with urinary outflow obstruction may be an important clue in cases like this one.25,26
Furthermore, whether the urinary tract truly was the source of the patient’s bacteremia is clouded by the differing antimicrobial susceptibility patterns of the A urinae blood and urine isolates. The simplest explanation for this discordance may be that all the isolates shared a common initial origin but adapted to different environments in the host (perhaps over time) or laboratory, producing phenotypic variation. Alternatively, the infection could have been polyclonal from the onset, with sampling error leading to the differing detected susceptibility patterns, or the blood and urine isolates may have represented independent acquisition events, involving distinct A urinae strains. Unfortunately (from an academic perspective), given patient preferences and recommendations from the infectious disease consultant, no bone biopsy was done for histology and culture to confirm infection and to allow comparative strain identification if A urinae was isolated.
Optimal treatment for A urinae spondylodiscitis has yet to be established. β-lactams have shown good clinical efficacy despite being bacteriostatic in vitro.27 Early in vitro studies showed synergistic bactericidal synergistic activity with penicillin plus aminoglycoside combination therapies.27-30 Cases of endocarditis have been successfully treated mainly with the combination of a β-lactam plus aminoglycoside combination therapy.30,31 Previous cases of spondylodiscitis have been treated successfully with diverse antimicrobial agents, including clindamycin, β-lactams, cephalosporins, fluoroquinolones, and aminoglycosides.14
Our patient improved rapidly while receiving empiric therapy with vancomycin and ceftriaxone and tolerated a rapid transition to oral amoxicillin and levofloxacin. This is the shortest IV treatment course for A urinae spondylodiscitis reported to date. We suspect that such rapid IV-to-oral transitions will suffice in most stable patients with A urinae spondylodiscitis or other invasive A urinae infections in line with the results of the OVIVA and POET trials.32,33
Conclusions
We believe A urinae UTI in the absence of obvious predisposing factors should prompt evaluation for urinary outflow obstruction. Despite improved laboratory diagnostic techniques, spondylodiscitis related to A urinae remains a rare entity and thus definitive treatment recommendations are difficult to make. However, we suspect that in many cases it is reasonable to extrapolate from the results of the POET and OVIVA trials and rapidly transition therapy of A urinae spondylodiscitis from IV to oral antibiotics. We suspect a review of the US Department of Veterans Affairs population might uncover a higher incidence of A urinae infection than previously estimated due to the population demographics and the epidemiology of A urinae.
Aerococcus urinae (A urinae), a gram-positive coccus readily mistaken for a Staphylococcus species, was first identified in 1992.1-3 It now reportedly accounts for 0.2% to 0.8% of clinical urine isolates.4-6 A urinae bacteriuria is typically asymptomatic and mainly occurs in women.7-9 Symptomatic A urinae urinary tract infection (UTI) occurs predominantly in older men with underlying urologic abnormalities.4-10
Serious A urinae infections are rare. The first 2 reported cases involved men with A urinae endocarditis, one of whom died.11,12 To date, only 8 cases of spondylodiscitis due to A urinae have been reported.13-20 Optimal treatment for invasive A urinae infection is undefined; however, the reported cases were treated successfully with diverse antibiotic regimen combinations; all including a β-lactam and beginning with at least 2 weeks of IV antibiotics.13-20 We describe a man with A urinae bacteremia and spondylodiscitis, presumably arising from a urinary source in the setting of bladder outlet obstruction, who was treated successfully.
Case Presentation
A 74-year-old man with morbid obesity, type 2 diabetes mellitus, stage 2 chronic kidney disease, and tobacco use presented to the emergency department after 2 weeks of progressive, nonradiating, midthoracic back pain, lower extremity weakness, gait imbalance, fatigue, anorexia, rigors, and subjective fevers. On presentation, he was afebrile and hemodynamically stable. A physical examination revealed point tenderness of the midthoracic vertebrae, nontender costovertebral angles, diffusely decreased strength, nonsustained clonus in both lower extremities, inguinal intertrigo, and a buried penis with purulent meatal discharge.
Laboratory results indicated a white blood cell (WBC) count of 13.5 K/μL (reference range, 4.0-11.0), absolute neutrophil count of 11.48 K/μL (reference range, 2.0-7.7), C-reactive protein (CRP) level of 225.3 mg/L (reference range, ≤ 5.0), erythrocyte sedimentation rate of 85 mm/h (reference range, 5-15), serum blood urea nitrogen of 76 mg/dL (reference range, 8-26), and serum creatinine (SCr) of 1.9 mg/dL (reference range, 1.1-1.4). A urinalysis showed positive leukocyte esterase, WBC clumps, and little bacteria. Abdominal/pelvic computed tomography showed spondylodiscitis-like changes at T7-T8, bilateral perinephric fat stranding, bladder distension, and bladder wall thickening.
The patient was presumed to have discitis secondary to a UTI, with possible pyelonephritis, and was given empiric vancomycin and ceftriaxone. Spinal magnetic resonance imaging with contrast supported spondylodiscitis at T7-T8, extending to T8-T9. Preliminary results from the admission blood and urine cultures showed gram-positive cocci in clusters, which were presumed initially to be Staphylococcus aureus (S aureus).
The final urine culture report listed multiple organisms, predominantly A urinae (Table 1);
On hospital day 6, the patient’s back pain had resolved, micturition was normal, appetite had normalized, and SCr was minimally above baseline (1.4 mg/dL). He insisted on completing antibiotic treatment at home and had no other medical indication for continued hospitalization. Thus, antibiotic therapy was changed to an all-oral regimen of amoxicillin 1 g 3 times daily for 10 days and levofloxacin 750 mg daily for 6 weeks, and the patient was discharged to home.
The patient returned 5 days postdischarge due to anuria. Investigation showed severe acute kidney injury (SCr, 6.8 mg/dL) and bladder outlet obstruction due to phimosis and urethral meatal stenosis. Urinalysis was unremarkable. His CRP had declined from 225 mg/L (initial admission) to 154 mg/L. A urinae culture and 2 sets of blood cultures were finalized as no growth. He was diagnosed with postrenal acute kidney injury and underwent meatal dilation and Foley catheterization but declined surgical correction. When seen in the clinic 2 months postantimicrobial therapy, the patient had normal micturition, no symptoms or signs of infection, and steadily down-trending inflammatory markers.
Discussion
A urinae, historically considered a rare pathogen, has been identified with increasing frequency in urine cultures due to improved microbiologic diagnostic techniques. However, there are only 8 reported cases of A urinae spondylodiscitis. Urinary pathology is an accepted risk factor for A urinae infections; consequently, we suspect that our patient’s urinary outflow obstruction and poor genitourinary hygiene were related to his invasive A urinae infection.10,21,22 We surmise that he had a chronic urinary outflow obstruction contributing to his infection, as evidenced by imaging findings, while the phimosis and urethral meatal stenosis were most likely infectious sequelae considering his anuria and acute kidney injury 5 days postdischarge. Indeed, the correlation between A urinae and urinary tract pathology may justify an evaluation for urinary pathology in any man with A urinae infection, regardless of the presence of symptoms.
By contrast, the implications of A urinae bacteriuria remain unclear. From a public health perspective, A urinae bacteriuria is rare, but the infectious mechanism remains undetermined with a case report suggesting the possibility of sexual transmission.4-6,23 In our case, the patient was not sexually active and had no clear origin of infection. Considering the potential severity of infection, more studies are needed to determine the infectious mechanism of A urinae.
In terms of infectious morbidity, the results seem to vary by sex. In a retrospective study of about 30,000 clinical urine samples, 62 (58 from women, 4 from men) yielded A urinae. The 62 corresponding patients lacked systemic infectious complications, leading the authors to conclude that A urinae is a relatively avirulent organism.24 Although possibly true in women, we are wary of drawing conclusions, especially regarding men, from a study that included only 62 urine samples were A urinae–positive, with only 4 from men. More evidence is needed to define the prognostic implications of A urinae bacteriuria in men.
As illustrated by the present case and previous reports, severe A urinae infections can occur, and the contributory factors deserve consideration. In our patient, the actual mechanism for bacteremia remains unclear. The initial concern for acute pyelonephritis was prompted by a computed tomography finding of bilateral perinephric fat stranding. This finding was questioned because it is common in older patients without infection, hence, is highly nonspecific. A correlation with urinary outflow obstruction may be an important clue in cases like this one.25,26
Furthermore, whether the urinary tract truly was the source of the patient’s bacteremia is clouded by the differing antimicrobial susceptibility patterns of the A urinae blood and urine isolates. The simplest explanation for this discordance may be that all the isolates shared a common initial origin but adapted to different environments in the host (perhaps over time) or laboratory, producing phenotypic variation. Alternatively, the infection could have been polyclonal from the onset, with sampling error leading to the differing detected susceptibility patterns, or the blood and urine isolates may have represented independent acquisition events, involving distinct A urinae strains. Unfortunately (from an academic perspective), given patient preferences and recommendations from the infectious disease consultant, no bone biopsy was done for histology and culture to confirm infection and to allow comparative strain identification if A urinae was isolated.
Optimal treatment for A urinae spondylodiscitis has yet to be established. β-lactams have shown good clinical efficacy despite being bacteriostatic in vitro.27 Early in vitro studies showed synergistic bactericidal synergistic activity with penicillin plus aminoglycoside combination therapies.27-30 Cases of endocarditis have been successfully treated mainly with the combination of a β-lactam plus aminoglycoside combination therapy.30,31 Previous cases of spondylodiscitis have been treated successfully with diverse antimicrobial agents, including clindamycin, β-lactams, cephalosporins, fluoroquinolones, and aminoglycosides.14
Our patient improved rapidly while receiving empiric therapy with vancomycin and ceftriaxone and tolerated a rapid transition to oral amoxicillin and levofloxacin. This is the shortest IV treatment course for A urinae spondylodiscitis reported to date. We suspect that such rapid IV-to-oral transitions will suffice in most stable patients with A urinae spondylodiscitis or other invasive A urinae infections in line with the results of the OVIVA and POET trials.32,33
Conclusions
We believe A urinae UTI in the absence of obvious predisposing factors should prompt evaluation for urinary outflow obstruction. Despite improved laboratory diagnostic techniques, spondylodiscitis related to A urinae remains a rare entity and thus definitive treatment recommendations are difficult to make. However, we suspect that in many cases it is reasonable to extrapolate from the results of the POET and OVIVA trials and rapidly transition therapy of A urinae spondylodiscitis from IV to oral antibiotics. We suspect a review of the US Department of Veterans Affairs population might uncover a higher incidence of A urinae infection than previously estimated due to the population demographics and the epidemiology of A urinae.
1. Christensen JJ, Korner B, Kjaergaard H. Aerococcus-like organism—an unnoticed urinary tract pathogen. APMIS. 1989;97(6):539-546. doi:10.1111/j.1699-0463.1989.tb00828.x
2. Aguirre M, Collins MD. Phylogenetic analysis of some Aerococcus-like organisms from urinary tract infections: description of Aerococcus urinae sp. nov. J Gen Microbiol. 1992;138(2):401-405. doi:10.1099/00221287-138-2-401
3. Williams RE, Hirch A, Cowan ST. Aerococcus, a new bacterial genus. J Gen Microbiol. 1953;8(3):475-480. doi:10.1099/00221287-8-3-475
4. Kline KA, Lewis AL. Gram-positive uropathogens, polymicrobial urinary tract infection, and the emerging microbiota of the urinary tract. Microbiol Spectr. 2016;4(2). doi:10.1128/microbiolspec.UTI-0012-2012
5. Schuur PM, Kasteren ME, Sabbe L, Vos MC, Janssens MM, Buiting AG. Urinary tract infections with Aerococcus urinae in the south of The Netherlands. Eur J Clin Microbiol Infect Dis. 1997;16(12):871-875. doi:10.1007/BF01700552
6. Grude N, Tveten Y. Aerococcus urinae og urinveisinfeksjon [Aerococcus urinae and urinary tract infection]. Tidsskr Nor Laegeforen. 2002;122(2):174-175.
7. Narayanasamy S, King K, Dennison A, Spelman DW, Aung AK. Clinical characteristics and laboratory identification of Aerococcus infections: an Australian tertiary centre perspective. Int J Microbiol. 2017;2017. doi:10.1155/2017/5684614
8. Hilt EE, McKinley K, Pearce MM, et al. Urine is not sterile: use of enhanced urine culture techniques to detect resident bacterial flora in the adult female bladder. J Clin Microbiol. 2014;52(3):871-876. doi:10.1128/JCM.02876-13
9. Pearce MM, Hilt EE, Rosenfeld AB, et al. The female urinary microbiome: a comparison of women with and without urgency urinary incontinence. mBio. 2014;5(4):e01283-14. doi:10.1128/mBio.01283-14
10. Sahu KK, Lal A, Mishra AK, Abraham GM. Aerococcus-related infections and their significance: a 9-year retrospective study. J Microsc Ultrastruct. 2021;9(1):18-25. doi:10.4103/JMAU.JMAU_61_19
11. Skov RL, Klarlund M, Thorsen S. Fatal endocarditis due to Aerococcus urinae. Diagn Microbiol Infect Dis. 1995;21(4):219-221. doi:10.1016/0732-8893(95)00037-b
12. Kristensen B, Nielsen G. Endocarditis caused by Aerococcus urinae, a newly recognized pathogen. Eur J Clin Microbiol Infect Dis. 1995;14(1):49-51. doi:10.1007/BF02112619
13. Astudillo L, Sailler L, Porte L, Lefevre JC, Massip P, Arlet-Suau E. Spondylodiscitis due to Aerococcus urinae: a first report. Scand J Infect Dis. 2003;35(11-12):890-891. doi:10.1080/00365540310016664
14. Lyagoubi A, Souffi C, Baroiller V, Vallee E. Spondylodiscitis: an increasingly described localization. EJIFCC. 2020;31(2):169-173.
15. Jerome M, Slim J, Sison R, Marton R. A case of Aerococcus urinae vertebral osteomyelitis. J Glob Infect Dis. 2015;7(2):85-86. doi:10.4103/0974-777X.157246
16. Tekin A, Tekin G, Turunç T, Demiroğlu Z, Kizilkiliç O. Infective endocarditis and spondylodiscitis in a patient due to Aerococcus urinae: first report. Int J Cardiol. 2007;115(3):402-403. doi:10.1016/j.ijcard.2006.01.046
17. Rougier E, Braud A, Argemi X, et al. Spondylodiscitis due to Aerococcus urinae and literature review. Infection. 2018;46(3):419-421. doi:10.1007/s15010-017-1106-0
18. Degroote E, Yildiz H, Lecouvet F, Verroken A, Belkhir L. Aerococcus urinae: an underestimated cause of spine infection? Case report and review of the literature. Acta Clin Belg. 2018;73(6):444-447. doi:10.1080/17843286.2018.1443003
19. Torres-Martos E, Pérez-Cortés S, Sánchez-Calvo JM, López-Prieto MD. Spondylodiscitis due to Aerococcus urinae infection in an elderly immunocompetent patient. Enferm Infecc Microbiol Clin. 2017;35(10):682-684. doi:10.1016/j.eimc.2017.02.005
20. Senneby E, Petersson AC, Rasmussen M. Clinical and microbiological features of bacteraemia with Aerococcus urinae. Clin Microbiol Infect. 2012;18(6):546-550. doi:10.1111/j.1469-0691.2011.03609.x
21. Sunnerhagen T, Nilson B, Olaison L, Rasmussen M. Clinical and microbiological features of infective endocarditis caused by aerococci. Infection. 2016;44(2):167-173. doi:10.1007/s15010-015-0812-8
22. de Jong MF, Soetekouw R, ten Kate RW, Veenendaal D. Aerococcus urinae: severe and fatal bloodstream infections and endocarditis. J Clin Microbiol. 2010;48(9):3445-3447. doi:10.1128/JCM.00835-10
23. Babaeer AA, Nader C, Iacoviello V, Tomera K. Necrotizing urethritis due to Aerococcus urinae. Case Rep Urol. 2015;2015:136147. doi:10.1155/2015/136147
24. Sierra-Hoffman M, Watkins K, Jinadatha C, Fader R, Carpenter JL. Clinical significance of Aerococcus urinae: a retrospective review. Diagn Microbiol Infect Dis. 2005;53(4):289-292. doi:10.1016/j.diagmicrobio.2005.06.021
25. Fukami H, Takeuchi Y, Kagaya S, et al. Perirenal fat stranding is not a powerful diagnostic tool for acute pyelonephritis. Int J Gen Med. 2017;10:137-144. doi:10.2147/IJGM.S133685
26. Han NY, Sung DJ, Kim MJ, Park BJ, Sim KC, Cho SB. Perirenal fat stranding on CT: is there an association with bladder outlet obstruction? Br J Radiol. 2016;89(1063):20160195. doi:10.1259/bjr.20160195
27. Hirzel C, Hirzberger L, Furrer H, Endimiani A. Bactericidal activity of penicillin, ceftriaxone, gentamicin and daptomycin alone and in combination against Aerococcus urinae. Int J Antimicrob Agents. 2016;48(3):271-276. doi:10.1016/j.ijantimicag.2016.05.007
28. Zbinden R, Santanam P, Hunziker L, Leuzinger B, von Graevenitz A. Endocarditis due to Aerococcus urinae: diagnostic tests, fatty acid composition and killing kinetics. Infection. 1999;27(2):122-124. doi:10.1007/BF02560511
29. Skov R, Christensen JJ, Korner B, Frimodt-Møller N, Espersen F. In vitro antimicrobial susceptibility of Aerococcus urinae to 14 antibiotics, and time-kill curves for penicillin, gentamicin and vancomycin. J Antimicrob Chemother. 2001;48(5):653-658. doi:10.1093/jac/48.5.653
30. Ebnöther C, Altwegg M, Gottschalk J, Seebach JD, Kronenberg A. Aerococcus urinae endocarditis: case report and review of the literature. Infection. 2002;30(5):310-313. doi:10.1007/s15010-002-3106-x
31. Tai DBG, Go JR, Fida M, Saleh OA. Management and treatment of Aerococcus bacteremia and endocarditis. Int J Infect Dis. 2021;102:584-589. doi:10.1016/j.ijid.2020.10.096
32. Li H-K, Rombach I, Zambellas R, et al; OVIVA Trial Collaborators. Oral versus intravenous antibiotics for bone and joint infection. N Engl J Med. 2019;380(5):425-436. doi:10.1056/NEJMoa1710926
33. Iversen K, Ihlemann N, Gill SU, et al. Partial oral versus intravenous antibiotic treatment of endocarditis. N Engl J Med. 2019;380(5):415-424. doi:10.1056/NEJMoa1808312
1. Christensen JJ, Korner B, Kjaergaard H. Aerococcus-like organism—an unnoticed urinary tract pathogen. APMIS. 1989;97(6):539-546. doi:10.1111/j.1699-0463.1989.tb00828.x
2. Aguirre M, Collins MD. Phylogenetic analysis of some Aerococcus-like organisms from urinary tract infections: description of Aerococcus urinae sp. nov. J Gen Microbiol. 1992;138(2):401-405. doi:10.1099/00221287-138-2-401
3. Williams RE, Hirch A, Cowan ST. Aerococcus, a new bacterial genus. J Gen Microbiol. 1953;8(3):475-480. doi:10.1099/00221287-8-3-475
4. Kline KA, Lewis AL. Gram-positive uropathogens, polymicrobial urinary tract infection, and the emerging microbiota of the urinary tract. Microbiol Spectr. 2016;4(2). doi:10.1128/microbiolspec.UTI-0012-2012
5. Schuur PM, Kasteren ME, Sabbe L, Vos MC, Janssens MM, Buiting AG. Urinary tract infections with Aerococcus urinae in the south of The Netherlands. Eur J Clin Microbiol Infect Dis. 1997;16(12):871-875. doi:10.1007/BF01700552
6. Grude N, Tveten Y. Aerococcus urinae og urinveisinfeksjon [Aerococcus urinae and urinary tract infection]. Tidsskr Nor Laegeforen. 2002;122(2):174-175.
7. Narayanasamy S, King K, Dennison A, Spelman DW, Aung AK. Clinical characteristics and laboratory identification of Aerococcus infections: an Australian tertiary centre perspective. Int J Microbiol. 2017;2017. doi:10.1155/2017/5684614
8. Hilt EE, McKinley K, Pearce MM, et al. Urine is not sterile: use of enhanced urine culture techniques to detect resident bacterial flora in the adult female bladder. J Clin Microbiol. 2014;52(3):871-876. doi:10.1128/JCM.02876-13
9. Pearce MM, Hilt EE, Rosenfeld AB, et al. The female urinary microbiome: a comparison of women with and without urgency urinary incontinence. mBio. 2014;5(4):e01283-14. doi:10.1128/mBio.01283-14
10. Sahu KK, Lal A, Mishra AK, Abraham GM. Aerococcus-related infections and their significance: a 9-year retrospective study. J Microsc Ultrastruct. 2021;9(1):18-25. doi:10.4103/JMAU.JMAU_61_19
11. Skov RL, Klarlund M, Thorsen S. Fatal endocarditis due to Aerococcus urinae. Diagn Microbiol Infect Dis. 1995;21(4):219-221. doi:10.1016/0732-8893(95)00037-b
12. Kristensen B, Nielsen G. Endocarditis caused by Aerococcus urinae, a newly recognized pathogen. Eur J Clin Microbiol Infect Dis. 1995;14(1):49-51. doi:10.1007/BF02112619
13. Astudillo L, Sailler L, Porte L, Lefevre JC, Massip P, Arlet-Suau E. Spondylodiscitis due to Aerococcus urinae: a first report. Scand J Infect Dis. 2003;35(11-12):890-891. doi:10.1080/00365540310016664
14. Lyagoubi A, Souffi C, Baroiller V, Vallee E. Spondylodiscitis: an increasingly described localization. EJIFCC. 2020;31(2):169-173.
15. Jerome M, Slim J, Sison R, Marton R. A case of Aerococcus urinae vertebral osteomyelitis. J Glob Infect Dis. 2015;7(2):85-86. doi:10.4103/0974-777X.157246
16. Tekin A, Tekin G, Turunç T, Demiroğlu Z, Kizilkiliç O. Infective endocarditis and spondylodiscitis in a patient due to Aerococcus urinae: first report. Int J Cardiol. 2007;115(3):402-403. doi:10.1016/j.ijcard.2006.01.046
17. Rougier E, Braud A, Argemi X, et al. Spondylodiscitis due to Aerococcus urinae and literature review. Infection. 2018;46(3):419-421. doi:10.1007/s15010-017-1106-0
18. Degroote E, Yildiz H, Lecouvet F, Verroken A, Belkhir L. Aerococcus urinae: an underestimated cause of spine infection? Case report and review of the literature. Acta Clin Belg. 2018;73(6):444-447. doi:10.1080/17843286.2018.1443003
19. Torres-Martos E, Pérez-Cortés S, Sánchez-Calvo JM, López-Prieto MD. Spondylodiscitis due to Aerococcus urinae infection in an elderly immunocompetent patient. Enferm Infecc Microbiol Clin. 2017;35(10):682-684. doi:10.1016/j.eimc.2017.02.005
20. Senneby E, Petersson AC, Rasmussen M. Clinical and microbiological features of bacteraemia with Aerococcus urinae. Clin Microbiol Infect. 2012;18(6):546-550. doi:10.1111/j.1469-0691.2011.03609.x
21. Sunnerhagen T, Nilson B, Olaison L, Rasmussen M. Clinical and microbiological features of infective endocarditis caused by aerococci. Infection. 2016;44(2):167-173. doi:10.1007/s15010-015-0812-8
22. de Jong MF, Soetekouw R, ten Kate RW, Veenendaal D. Aerococcus urinae: severe and fatal bloodstream infections and endocarditis. J Clin Microbiol. 2010;48(9):3445-3447. doi:10.1128/JCM.00835-10
23. Babaeer AA, Nader C, Iacoviello V, Tomera K. Necrotizing urethritis due to Aerococcus urinae. Case Rep Urol. 2015;2015:136147. doi:10.1155/2015/136147
24. Sierra-Hoffman M, Watkins K, Jinadatha C, Fader R, Carpenter JL. Clinical significance of Aerococcus urinae: a retrospective review. Diagn Microbiol Infect Dis. 2005;53(4):289-292. doi:10.1016/j.diagmicrobio.2005.06.021
25. Fukami H, Takeuchi Y, Kagaya S, et al. Perirenal fat stranding is not a powerful diagnostic tool for acute pyelonephritis. Int J Gen Med. 2017;10:137-144. doi:10.2147/IJGM.S133685
26. Han NY, Sung DJ, Kim MJ, Park BJ, Sim KC, Cho SB. Perirenal fat stranding on CT: is there an association with bladder outlet obstruction? Br J Radiol. 2016;89(1063):20160195. doi:10.1259/bjr.20160195
27. Hirzel C, Hirzberger L, Furrer H, Endimiani A. Bactericidal activity of penicillin, ceftriaxone, gentamicin and daptomycin alone and in combination against Aerococcus urinae. Int J Antimicrob Agents. 2016;48(3):271-276. doi:10.1016/j.ijantimicag.2016.05.007
28. Zbinden R, Santanam P, Hunziker L, Leuzinger B, von Graevenitz A. Endocarditis due to Aerococcus urinae: diagnostic tests, fatty acid composition and killing kinetics. Infection. 1999;27(2):122-124. doi:10.1007/BF02560511
29. Skov R, Christensen JJ, Korner B, Frimodt-Møller N, Espersen F. In vitro antimicrobial susceptibility of Aerococcus urinae to 14 antibiotics, and time-kill curves for penicillin, gentamicin and vancomycin. J Antimicrob Chemother. 2001;48(5):653-658. doi:10.1093/jac/48.5.653
30. Ebnöther C, Altwegg M, Gottschalk J, Seebach JD, Kronenberg A. Aerococcus urinae endocarditis: case report and review of the literature. Infection. 2002;30(5):310-313. doi:10.1007/s15010-002-3106-x
31. Tai DBG, Go JR, Fida M, Saleh OA. Management and treatment of Aerococcus bacteremia and endocarditis. Int J Infect Dis. 2021;102:584-589. doi:10.1016/j.ijid.2020.10.096
32. Li H-K, Rombach I, Zambellas R, et al; OVIVA Trial Collaborators. Oral versus intravenous antibiotics for bone and joint infection. N Engl J Med. 2019;380(5):425-436. doi:10.1056/NEJMoa1710926
33. Iversen K, Ihlemann N, Gill SU, et al. Partial oral versus intravenous antibiotic treatment of endocarditis. N Engl J Med. 2019;380(5):415-424. doi:10.1056/NEJMoa1808312
HIV vaccine trial makes pivotal leap toward making ‘super antibodies’
The announcement comes from the journal Science, which published phase 1 results of a small clinical trial for a vaccine technology that aims to cause the body to create a rare kind of cell.
“At the most general level, the trial results show that one can design vaccines that induce antibodies with prespecified genetic features, and this may herald a new era of precision vaccines,” William Schief, PhD, a researcher at the Scripps Research Institute and study coauthor, told the American Association for the Advancement of Science.
The study was the first to test the approach in humans and was effective in 97% – or 35 of 36 – participants. The vaccine technology is called “germline targeting.” Trial results show that “one can design a vaccine that elicits made-to-order antibodies in humans,” Dr. Schief said in a news release.
In addition to possibly being a breakthrough for the treatment of HIV, the vaccine technology could also impact the development of treatments for flu, hepatitis C, and coronaviruses, study authors wrote.
There is no cure for HIV, but there are treatments to manage how the disease progresses. HIV attacks the body’s immune system, destroys white blood cells, and increases susceptibility to other infections, AAAS summarized. More than 1 million people in the United States and 38 million people worldwide have HIV.
Previous HIV vaccine attempts were not able to cause the production of specialized cells known as “broadly neutralizing antibodies,” CNN reported.
“Call them super antibodies, if you want,” University of Minnesota HIV researcher Timothy Schacker, MD, who was not involved in the research, told CNN. “The hope is that if you can induce this kind of immunity in people, you can protect them from some of these viruses that we’ve had a very hard time designing vaccines for that are effective. So this is an important step forward.”
Study authors said this is just the first step in the multiphase vaccine design, which so far is a theory. Further study is needed to see if the next steps also work in humans, and then if all the steps can be linked together and can be effective against HIV.
A version of this article first appeared on WebMD.com.
The announcement comes from the journal Science, which published phase 1 results of a small clinical trial for a vaccine technology that aims to cause the body to create a rare kind of cell.
“At the most general level, the trial results show that one can design vaccines that induce antibodies with prespecified genetic features, and this may herald a new era of precision vaccines,” William Schief, PhD, a researcher at the Scripps Research Institute and study coauthor, told the American Association for the Advancement of Science.
The study was the first to test the approach in humans and was effective in 97% – or 35 of 36 – participants. The vaccine technology is called “germline targeting.” Trial results show that “one can design a vaccine that elicits made-to-order antibodies in humans,” Dr. Schief said in a news release.
In addition to possibly being a breakthrough for the treatment of HIV, the vaccine technology could also impact the development of treatments for flu, hepatitis C, and coronaviruses, study authors wrote.
There is no cure for HIV, but there are treatments to manage how the disease progresses. HIV attacks the body’s immune system, destroys white blood cells, and increases susceptibility to other infections, AAAS summarized. More than 1 million people in the United States and 38 million people worldwide have HIV.
Previous HIV vaccine attempts were not able to cause the production of specialized cells known as “broadly neutralizing antibodies,” CNN reported.
“Call them super antibodies, if you want,” University of Minnesota HIV researcher Timothy Schacker, MD, who was not involved in the research, told CNN. “The hope is that if you can induce this kind of immunity in people, you can protect them from some of these viruses that we’ve had a very hard time designing vaccines for that are effective. So this is an important step forward.”
Study authors said this is just the first step in the multiphase vaccine design, which so far is a theory. Further study is needed to see if the next steps also work in humans, and then if all the steps can be linked together and can be effective against HIV.
A version of this article first appeared on WebMD.com.
The announcement comes from the journal Science, which published phase 1 results of a small clinical trial for a vaccine technology that aims to cause the body to create a rare kind of cell.
“At the most general level, the trial results show that one can design vaccines that induce antibodies with prespecified genetic features, and this may herald a new era of precision vaccines,” William Schief, PhD, a researcher at the Scripps Research Institute and study coauthor, told the American Association for the Advancement of Science.
The study was the first to test the approach in humans and was effective in 97% – or 35 of 36 – participants. The vaccine technology is called “germline targeting.” Trial results show that “one can design a vaccine that elicits made-to-order antibodies in humans,” Dr. Schief said in a news release.
In addition to possibly being a breakthrough for the treatment of HIV, the vaccine technology could also impact the development of treatments for flu, hepatitis C, and coronaviruses, study authors wrote.
There is no cure for HIV, but there are treatments to manage how the disease progresses. HIV attacks the body’s immune system, destroys white blood cells, and increases susceptibility to other infections, AAAS summarized. More than 1 million people in the United States and 38 million people worldwide have HIV.
Previous HIV vaccine attempts were not able to cause the production of specialized cells known as “broadly neutralizing antibodies,” CNN reported.
“Call them super antibodies, if you want,” University of Minnesota HIV researcher Timothy Schacker, MD, who was not involved in the research, told CNN. “The hope is that if you can induce this kind of immunity in people, you can protect them from some of these viruses that we’ve had a very hard time designing vaccines for that are effective. So this is an important step forward.”
Study authors said this is just the first step in the multiphase vaccine design, which so far is a theory. Further study is needed to see if the next steps also work in humans, and then if all the steps can be linked together and can be effective against HIV.
A version of this article first appeared on WebMD.com.
FROM SCIENCE
CAB-LA’s full potential for HIV prevention hits snags
, say authors of a new review article.
CAB-LA “represents the most important breakthrough in HIV prevention in recent years,” write Geoffroy Liegeon, MD, and Jade Ghosn, MD, PhD, with Université Paris Cité, in this month’s HIV Medicine.
It has been found to be safe, and more effective in phase 3 trials than oral PrEP, and is well-accepted in men who have sex with men, and transgender and cisgender women.
Reductions in stigma
Surveys show patients at high risk for HIV – especially those who see PrEP as burdensome – are highly interested in long-acting injectable drugs. Reduced stigma with the injections also appears to steer the choice toward a long-acting agent and may attract more people to HIV prevention programs.
The first two injections are given 4 weeks apart, followed by an injection every 8 weeks.
Models designed to increase uptake, adherence, and persistence when on and after discontinuing CAB-LA will be important for wider rollout, as will better patient education and demonstrated efficacy and safety in populations not included in clinical trials, Dr. Liegeon and Dr. Ghosn note.
Still, they point out that its broader integration into clinical routine is held back by factors including breakthrough infections despite timely injections, complexity of follow-up, logistical considerations, and its cost-effectiveness compared with oral PrEP.
A hefty price tag
“[T]he cost effectiveness compared with TDF-FTC [tenofovir/emtricitabine] generics may not support its use at the current price in many settings,” the authors write.
For low- and middle-income countries, the TDF/FTC price is about $55, according to the World Health Organization’s Global Price Reporting, while the current price of CAB-LA in the United States is about $22,000, according to Dr. Ghosn. He said in an interview that because the cost of generics can reach $400-$500 per year in the United States, depending on the pharmaceutical companies, the price for CAB-LA is almost 60 times higher than TDF/FTC in the Untied States.
The biggest hope for the price reduction, at least in lower-income countries, he said, is a new licensing agreement.
ViiV Healthcare signed a new voluntary licensing agreement with the Medicines Patent Pool in July to help access in low-income, lower-middle-income, and sub-Saharan African countries, he explained.
The authors summarize: “[E]stablishing the effectiveness of CAB-LA does not guarantee its uptake into clinical routine.”
Because of the combined issues, the WHO recommended CAB-LA as an additional prevention choice for PrEP in its recent guidelines, pending further studies.
Barriers frustrate providers
Lauren Fontana, DO, assistant professor at the University of Minnesota, Minneapolis, and infectious disease physician at M Health Fairview, said in an interview that “as a health care provider, cost and insurance barriers can be frustrating, especially when CAB-LA is identified as the best option for a patient.”
Lack of nonphysician-led initiatives, such as nurse- or pharmacy-led services for CAB-LA, may limit availability to marginalized and at-risk populations, she said.
“If a clinic can acquire CAB-LA, clinic protocols need to be developed and considerations of missed visits and doses must be thought about when implementing a program,” Dr. Fontana said.
Clinics need resources to engage with patients to promote retention in the program with case management and pharmacy support, she added.
“Simplification processes need to be developed to make CAB-LA an option for more clinics and patients,” she continued. “We are still learning about the incidence of breakthrough HIV infections, patterns of HIV seroconversion, and how to optimize testing so that HIV infections are detected early.”
Dr. Liegeon, Dr. Ghosn, and Dr. Fontana report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, say authors of a new review article.
CAB-LA “represents the most important breakthrough in HIV prevention in recent years,” write Geoffroy Liegeon, MD, and Jade Ghosn, MD, PhD, with Université Paris Cité, in this month’s HIV Medicine.
It has been found to be safe, and more effective in phase 3 trials than oral PrEP, and is well-accepted in men who have sex with men, and transgender and cisgender women.
Reductions in stigma
Surveys show patients at high risk for HIV – especially those who see PrEP as burdensome – are highly interested in long-acting injectable drugs. Reduced stigma with the injections also appears to steer the choice toward a long-acting agent and may attract more people to HIV prevention programs.
The first two injections are given 4 weeks apart, followed by an injection every 8 weeks.
Models designed to increase uptake, adherence, and persistence when on and after discontinuing CAB-LA will be important for wider rollout, as will better patient education and demonstrated efficacy and safety in populations not included in clinical trials, Dr. Liegeon and Dr. Ghosn note.
Still, they point out that its broader integration into clinical routine is held back by factors including breakthrough infections despite timely injections, complexity of follow-up, logistical considerations, and its cost-effectiveness compared with oral PrEP.
A hefty price tag
“[T]he cost effectiveness compared with TDF-FTC [tenofovir/emtricitabine] generics may not support its use at the current price in many settings,” the authors write.
For low- and middle-income countries, the TDF/FTC price is about $55, according to the World Health Organization’s Global Price Reporting, while the current price of CAB-LA in the United States is about $22,000, according to Dr. Ghosn. He said in an interview that because the cost of generics can reach $400-$500 per year in the United States, depending on the pharmaceutical companies, the price for CAB-LA is almost 60 times higher than TDF/FTC in the Untied States.
The biggest hope for the price reduction, at least in lower-income countries, he said, is a new licensing agreement.
ViiV Healthcare signed a new voluntary licensing agreement with the Medicines Patent Pool in July to help access in low-income, lower-middle-income, and sub-Saharan African countries, he explained.
The authors summarize: “[E]stablishing the effectiveness of CAB-LA does not guarantee its uptake into clinical routine.”
Because of the combined issues, the WHO recommended CAB-LA as an additional prevention choice for PrEP in its recent guidelines, pending further studies.
Barriers frustrate providers
Lauren Fontana, DO, assistant professor at the University of Minnesota, Minneapolis, and infectious disease physician at M Health Fairview, said in an interview that “as a health care provider, cost and insurance barriers can be frustrating, especially when CAB-LA is identified as the best option for a patient.”
Lack of nonphysician-led initiatives, such as nurse- or pharmacy-led services for CAB-LA, may limit availability to marginalized and at-risk populations, she said.
“If a clinic can acquire CAB-LA, clinic protocols need to be developed and considerations of missed visits and doses must be thought about when implementing a program,” Dr. Fontana said.
Clinics need resources to engage with patients to promote retention in the program with case management and pharmacy support, she added.
“Simplification processes need to be developed to make CAB-LA an option for more clinics and patients,” she continued. “We are still learning about the incidence of breakthrough HIV infections, patterns of HIV seroconversion, and how to optimize testing so that HIV infections are detected early.”
Dr. Liegeon, Dr. Ghosn, and Dr. Fontana report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, say authors of a new review article.
CAB-LA “represents the most important breakthrough in HIV prevention in recent years,” write Geoffroy Liegeon, MD, and Jade Ghosn, MD, PhD, with Université Paris Cité, in this month’s HIV Medicine.
It has been found to be safe, and more effective in phase 3 trials than oral PrEP, and is well-accepted in men who have sex with men, and transgender and cisgender women.
Reductions in stigma
Surveys show patients at high risk for HIV – especially those who see PrEP as burdensome – are highly interested in long-acting injectable drugs. Reduced stigma with the injections also appears to steer the choice toward a long-acting agent and may attract more people to HIV prevention programs.
The first two injections are given 4 weeks apart, followed by an injection every 8 weeks.
Models designed to increase uptake, adherence, and persistence when on and after discontinuing CAB-LA will be important for wider rollout, as will better patient education and demonstrated efficacy and safety in populations not included in clinical trials, Dr. Liegeon and Dr. Ghosn note.
Still, they point out that its broader integration into clinical routine is held back by factors including breakthrough infections despite timely injections, complexity of follow-up, logistical considerations, and its cost-effectiveness compared with oral PrEP.
A hefty price tag
“[T]he cost effectiveness compared with TDF-FTC [tenofovir/emtricitabine] generics may not support its use at the current price in many settings,” the authors write.
For low- and middle-income countries, the TDF/FTC price is about $55, according to the World Health Organization’s Global Price Reporting, while the current price of CAB-LA in the United States is about $22,000, according to Dr. Ghosn. He said in an interview that because the cost of generics can reach $400-$500 per year in the United States, depending on the pharmaceutical companies, the price for CAB-LA is almost 60 times higher than TDF/FTC in the Untied States.
The biggest hope for the price reduction, at least in lower-income countries, he said, is a new licensing agreement.
ViiV Healthcare signed a new voluntary licensing agreement with the Medicines Patent Pool in July to help access in low-income, lower-middle-income, and sub-Saharan African countries, he explained.
The authors summarize: “[E]stablishing the effectiveness of CAB-LA does not guarantee its uptake into clinical routine.”
Because of the combined issues, the WHO recommended CAB-LA as an additional prevention choice for PrEP in its recent guidelines, pending further studies.
Barriers frustrate providers
Lauren Fontana, DO, assistant professor at the University of Minnesota, Minneapolis, and infectious disease physician at M Health Fairview, said in an interview that “as a health care provider, cost and insurance barriers can be frustrating, especially when CAB-LA is identified as the best option for a patient.”
Lack of nonphysician-led initiatives, such as nurse- or pharmacy-led services for CAB-LA, may limit availability to marginalized and at-risk populations, she said.
“If a clinic can acquire CAB-LA, clinic protocols need to be developed and considerations of missed visits and doses must be thought about when implementing a program,” Dr. Fontana said.
Clinics need resources to engage with patients to promote retention in the program with case management and pharmacy support, she added.
“Simplification processes need to be developed to make CAB-LA an option for more clinics and patients,” she continued. “We are still learning about the incidence of breakthrough HIV infections, patterns of HIV seroconversion, and how to optimize testing so that HIV infections are detected early.”
Dr. Liegeon, Dr. Ghosn, and Dr. Fontana report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HIV MEDICINE
Pregnancy outcomes on long-acting antiretroviral
In a cautiously optimistic report,
Among 10 live births, there was one birth defect (congenital ptosis, or droopy eyelid), which was not attributed to the trial drugs. There were no instances of perinatal HIV transmission at delivery or during the 1-year follow-up.
“Long-acting cabotegravir-rilpivirine is the first and only complete injectable regimen potentially available for pregnant women,” first author Parul Patel, PharmD, global medical affairs director for cabotegravir at ViiV Healthcare, said in an interview. The regimen was approved by the U.S. Food and Drug Administration in January 2021 for injections every 4 weeks and in February 2022 for injections every 8 weeks.
“Importantly, it can be dosed monthly or every 2 months,” Patel said. “This could be advantageous for women who are experiencing constant change during pregnancy. This could be a consideration for women who might have problems tolerating oral pills during pregnancy or might have problems with emesis.”
The study was published in HIV Medicine.
“We are really pursuing the development of the long-acting version of cabotegravir in combination with rilpivirine,” Dr. Patel said. “It’s an industry standard during initial development that you start very conservatively and not allow a woman who is pregnant to continue dosing of a drug while still evaluating its overall safety profile. We really want to understand the use of this agent in nonpregnant adults before exposing pregnant women to active treatment.”
Pregnancies in trials excluding pregnant women
In the paper, Dr. Patel and her coauthors noted the limited data on pregnant women exposed to CAB + RPV. They analyzed pregnancies in four phase 2b/3/3b clinical trials sponsored by ViiV Healthcare and a compassionate use program. All clinical trial participants first received oral CAB + RPV daily for 4 weeks to assess individual tolerance before the experimental long-acting injection of CAB + RPV every 4 weeks or every 8 weeks.
Women participants were required to use highly effective contraception during the trials and for at least 52 weeks after the last injection. Urine pregnancy tests were given at baseline, before each injection, and when pregnancy was suspected. If a pregnancy was detected, CAB + RPV (oral or long-acting injections) was discontinued and the woman switched to an alternative oral antiretroviral, unless she and her physician decided to continue with injections in the compassionate use program.
Pregnancy outcomes
Among 25 reported pregnancies in 22 women during the trial, there were 10 live births. Nine of the mothers who delivered their babies at term had switched to an alternative antiretroviral regimen and maintained virologic suppression throughout pregnancy and post partum, or the last available viral load assessment.
The 10th participant remained on long-acting CAB + RPV during her pregnancy and had a live birth with congenital ptosis that was resolving without treatment at the 4-month ophthalmology consult, the authors wrote. The mother experienced persistent low-level viremia before and throughout her pregnancy.
Two of the pregnancies occurred after the last monthly injection, during the washout period. Other studies have reported that each long-acting drug, CAB and RPV, can be detected more than 1 year after the last injection. In the new report, plasma CAB and RPV washout concentrations during pregnancy were within the range of those in nonpregnant women, the authors wrote.
Among the 14 participants with non–live birth outcomes, 13 switched to an alternative antiretroviral regimen during pregnancy and maintained virologic suppression through pregnancy and post partum, or until their last viral assessment. The remaining participant received long-acting CAB + RPV and continued this treatment for the duration of their pregnancy.
“It’s a very limited data set, so we’re not in a position to be able to make definitive conclusions around long-acting cabotegravir-rilpivirine in pregnancy,” Dr. Patel acknowledged. “But the data that we presented among the 25 women who were exposed to cabotegravir-rilpivirine looks reassuring.”
Planned studies during pregnancy
Vani Vannappagari, MBBS, MPH, PhD, global head of epidemiology and real-world evidence at ViiV Healthcare and study coauthor, said in an interview that the initial results are spurring promising new research.
“We are working with an external IMPAACT [International Maternal Pediatric Adolescent AIDS Clinical Trials Network] group on a clinical trial ... to try to determine the appropriate dose of long-acting cabotegravir-rilpivirine during pregnancy,” Dr. Vannappagari said. “The clinical trial will give us the immediate safety, dose information, and viral suppression rates for both the mother and the infant. But long-term safety, especially birth defects and any adverse pregnancy and neonatal outcomes, will come from our antiretroviral pregnancy registry and other noninterventional studies.
“In the very small cohort studied, [in] pregnancies that were continued after exposure to long-acting cabotegravir and rilpivirine in the first trimester, there were no significant adverse fetal outcomes identified,” he said. “That’s reassuring, as is the fact that at the time these patients were switched in early pregnancy, their viral loads were all undetectable at the time that their pregnancies were diagnosed.”
Neil Silverman, MD, professor of clinical obstetrics and gynecology and director of the Infections in Pregnancy Program at the University of California, Los Angeles, Medical Center, who was not associated with the study, provided a comment to this news organization.
“The larger question still remains why pregnant women were so actively excluded from the original study design when this trial was evaluating a newer long-acting preparation of two anti-HIV medications that otherwise would be perfectly fine to use during pregnancy?”
Dr. Silverman continued, “In this case, it’s particularly frustrating since the present study was simply evaluating established medications currently being used to manage HIV infection, but in a newer longer-acting mode of administration by an injection every 2 months. If a patient had already been successfully managed on an oral antiviral regimen containing an integrase inhibitor and a non-nucleoside reverse transcriptase inhibitor, like the two drugs studied here, it would not be considered reasonable to switch that regimen simply because she was found to be pregnant.”
Dr. Patel and Dr. Vannappagari are employees of ViiV Healthcare and stockholders of GlaxoSmithKline.
This analysis was funded by ViiV Healthcare, and all studies were cofunded by ViiV Healthcare and Janssen Research & Development. Dr. Silverman reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a cautiously optimistic report,
Among 10 live births, there was one birth defect (congenital ptosis, or droopy eyelid), which was not attributed to the trial drugs. There were no instances of perinatal HIV transmission at delivery or during the 1-year follow-up.
“Long-acting cabotegravir-rilpivirine is the first and only complete injectable regimen potentially available for pregnant women,” first author Parul Patel, PharmD, global medical affairs director for cabotegravir at ViiV Healthcare, said in an interview. The regimen was approved by the U.S. Food and Drug Administration in January 2021 for injections every 4 weeks and in February 2022 for injections every 8 weeks.
“Importantly, it can be dosed monthly or every 2 months,” Patel said. “This could be advantageous for women who are experiencing constant change during pregnancy. This could be a consideration for women who might have problems tolerating oral pills during pregnancy or might have problems with emesis.”
The study was published in HIV Medicine.
“We are really pursuing the development of the long-acting version of cabotegravir in combination with rilpivirine,” Dr. Patel said. “It’s an industry standard during initial development that you start very conservatively and not allow a woman who is pregnant to continue dosing of a drug while still evaluating its overall safety profile. We really want to understand the use of this agent in nonpregnant adults before exposing pregnant women to active treatment.”
Pregnancies in trials excluding pregnant women
In the paper, Dr. Patel and her coauthors noted the limited data on pregnant women exposed to CAB + RPV. They analyzed pregnancies in four phase 2b/3/3b clinical trials sponsored by ViiV Healthcare and a compassionate use program. All clinical trial participants first received oral CAB + RPV daily for 4 weeks to assess individual tolerance before the experimental long-acting injection of CAB + RPV every 4 weeks or every 8 weeks.
Women participants were required to use highly effective contraception during the trials and for at least 52 weeks after the last injection. Urine pregnancy tests were given at baseline, before each injection, and when pregnancy was suspected. If a pregnancy was detected, CAB + RPV (oral or long-acting injections) was discontinued and the woman switched to an alternative oral antiretroviral, unless she and her physician decided to continue with injections in the compassionate use program.
Pregnancy outcomes
Among 25 reported pregnancies in 22 women during the trial, there were 10 live births. Nine of the mothers who delivered their babies at term had switched to an alternative antiretroviral regimen and maintained virologic suppression throughout pregnancy and post partum, or the last available viral load assessment.
The 10th participant remained on long-acting CAB + RPV during her pregnancy and had a live birth with congenital ptosis that was resolving without treatment at the 4-month ophthalmology consult, the authors wrote. The mother experienced persistent low-level viremia before and throughout her pregnancy.
Two of the pregnancies occurred after the last monthly injection, during the washout period. Other studies have reported that each long-acting drug, CAB and RPV, can be detected more than 1 year after the last injection. In the new report, plasma CAB and RPV washout concentrations during pregnancy were within the range of those in nonpregnant women, the authors wrote.
Among the 14 participants with non–live birth outcomes, 13 switched to an alternative antiretroviral regimen during pregnancy and maintained virologic suppression through pregnancy and post partum, or until their last viral assessment. The remaining participant received long-acting CAB + RPV and continued this treatment for the duration of their pregnancy.
“It’s a very limited data set, so we’re not in a position to be able to make definitive conclusions around long-acting cabotegravir-rilpivirine in pregnancy,” Dr. Patel acknowledged. “But the data that we presented among the 25 women who were exposed to cabotegravir-rilpivirine looks reassuring.”
Planned studies during pregnancy
Vani Vannappagari, MBBS, MPH, PhD, global head of epidemiology and real-world evidence at ViiV Healthcare and study coauthor, said in an interview that the initial results are spurring promising new research.
“We are working with an external IMPAACT [International Maternal Pediatric Adolescent AIDS Clinical Trials Network] group on a clinical trial ... to try to determine the appropriate dose of long-acting cabotegravir-rilpivirine during pregnancy,” Dr. Vannappagari said. “The clinical trial will give us the immediate safety, dose information, and viral suppression rates for both the mother and the infant. But long-term safety, especially birth defects and any adverse pregnancy and neonatal outcomes, will come from our antiretroviral pregnancy registry and other noninterventional studies.
“In the very small cohort studied, [in] pregnancies that were continued after exposure to long-acting cabotegravir and rilpivirine in the first trimester, there were no significant adverse fetal outcomes identified,” he said. “That’s reassuring, as is the fact that at the time these patients were switched in early pregnancy, their viral loads were all undetectable at the time that their pregnancies were diagnosed.”
Neil Silverman, MD, professor of clinical obstetrics and gynecology and director of the Infections in Pregnancy Program at the University of California, Los Angeles, Medical Center, who was not associated with the study, provided a comment to this news organization.
“The larger question still remains why pregnant women were so actively excluded from the original study design when this trial was evaluating a newer long-acting preparation of two anti-HIV medications that otherwise would be perfectly fine to use during pregnancy?”
Dr. Silverman continued, “In this case, it’s particularly frustrating since the present study was simply evaluating established medications currently being used to manage HIV infection, but in a newer longer-acting mode of administration by an injection every 2 months. If a patient had already been successfully managed on an oral antiviral regimen containing an integrase inhibitor and a non-nucleoside reverse transcriptase inhibitor, like the two drugs studied here, it would not be considered reasonable to switch that regimen simply because she was found to be pregnant.”
Dr. Patel and Dr. Vannappagari are employees of ViiV Healthcare and stockholders of GlaxoSmithKline.
This analysis was funded by ViiV Healthcare, and all studies were cofunded by ViiV Healthcare and Janssen Research & Development. Dr. Silverman reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a cautiously optimistic report,
Among 10 live births, there was one birth defect (congenital ptosis, or droopy eyelid), which was not attributed to the trial drugs. There were no instances of perinatal HIV transmission at delivery or during the 1-year follow-up.
“Long-acting cabotegravir-rilpivirine is the first and only complete injectable regimen potentially available for pregnant women,” first author Parul Patel, PharmD, global medical affairs director for cabotegravir at ViiV Healthcare, said in an interview. The regimen was approved by the U.S. Food and Drug Administration in January 2021 for injections every 4 weeks and in February 2022 for injections every 8 weeks.
“Importantly, it can be dosed monthly or every 2 months,” Patel said. “This could be advantageous for women who are experiencing constant change during pregnancy. This could be a consideration for women who might have problems tolerating oral pills during pregnancy or might have problems with emesis.”
The study was published in HIV Medicine.
“We are really pursuing the development of the long-acting version of cabotegravir in combination with rilpivirine,” Dr. Patel said. “It’s an industry standard during initial development that you start very conservatively and not allow a woman who is pregnant to continue dosing of a drug while still evaluating its overall safety profile. We really want to understand the use of this agent in nonpregnant adults before exposing pregnant women to active treatment.”
Pregnancies in trials excluding pregnant women
In the paper, Dr. Patel and her coauthors noted the limited data on pregnant women exposed to CAB + RPV. They analyzed pregnancies in four phase 2b/3/3b clinical trials sponsored by ViiV Healthcare and a compassionate use program. All clinical trial participants first received oral CAB + RPV daily for 4 weeks to assess individual tolerance before the experimental long-acting injection of CAB + RPV every 4 weeks or every 8 weeks.
Women participants were required to use highly effective contraception during the trials and for at least 52 weeks after the last injection. Urine pregnancy tests were given at baseline, before each injection, and when pregnancy was suspected. If a pregnancy was detected, CAB + RPV (oral or long-acting injections) was discontinued and the woman switched to an alternative oral antiretroviral, unless she and her physician decided to continue with injections in the compassionate use program.
Pregnancy outcomes
Among 25 reported pregnancies in 22 women during the trial, there were 10 live births. Nine of the mothers who delivered their babies at term had switched to an alternative antiretroviral regimen and maintained virologic suppression throughout pregnancy and post partum, or the last available viral load assessment.
The 10th participant remained on long-acting CAB + RPV during her pregnancy and had a live birth with congenital ptosis that was resolving without treatment at the 4-month ophthalmology consult, the authors wrote. The mother experienced persistent low-level viremia before and throughout her pregnancy.
Two of the pregnancies occurred after the last monthly injection, during the washout period. Other studies have reported that each long-acting drug, CAB and RPV, can be detected more than 1 year after the last injection. In the new report, plasma CAB and RPV washout concentrations during pregnancy were within the range of those in nonpregnant women, the authors wrote.
Among the 14 participants with non–live birth outcomes, 13 switched to an alternative antiretroviral regimen during pregnancy and maintained virologic suppression through pregnancy and post partum, or until their last viral assessment. The remaining participant received long-acting CAB + RPV and continued this treatment for the duration of their pregnancy.
“It’s a very limited data set, so we’re not in a position to be able to make definitive conclusions around long-acting cabotegravir-rilpivirine in pregnancy,” Dr. Patel acknowledged. “But the data that we presented among the 25 women who were exposed to cabotegravir-rilpivirine looks reassuring.”
Planned studies during pregnancy
Vani Vannappagari, MBBS, MPH, PhD, global head of epidemiology and real-world evidence at ViiV Healthcare and study coauthor, said in an interview that the initial results are spurring promising new research.
“We are working with an external IMPAACT [International Maternal Pediatric Adolescent AIDS Clinical Trials Network] group on a clinical trial ... to try to determine the appropriate dose of long-acting cabotegravir-rilpivirine during pregnancy,” Dr. Vannappagari said. “The clinical trial will give us the immediate safety, dose information, and viral suppression rates for both the mother and the infant. But long-term safety, especially birth defects and any adverse pregnancy and neonatal outcomes, will come from our antiretroviral pregnancy registry and other noninterventional studies.
“In the very small cohort studied, [in] pregnancies that were continued after exposure to long-acting cabotegravir and rilpivirine in the first trimester, there were no significant adverse fetal outcomes identified,” he said. “That’s reassuring, as is the fact that at the time these patients were switched in early pregnancy, their viral loads were all undetectable at the time that their pregnancies were diagnosed.”
Neil Silverman, MD, professor of clinical obstetrics and gynecology and director of the Infections in Pregnancy Program at the University of California, Los Angeles, Medical Center, who was not associated with the study, provided a comment to this news organization.
“The larger question still remains why pregnant women were so actively excluded from the original study design when this trial was evaluating a newer long-acting preparation of two anti-HIV medications that otherwise would be perfectly fine to use during pregnancy?”
Dr. Silverman continued, “In this case, it’s particularly frustrating since the present study was simply evaluating established medications currently being used to manage HIV infection, but in a newer longer-acting mode of administration by an injection every 2 months. If a patient had already been successfully managed on an oral antiviral regimen containing an integrase inhibitor and a non-nucleoside reverse transcriptase inhibitor, like the two drugs studied here, it would not be considered reasonable to switch that regimen simply because she was found to be pregnant.”
Dr. Patel and Dr. Vannappagari are employees of ViiV Healthcare and stockholders of GlaxoSmithKline.
This analysis was funded by ViiV Healthcare, and all studies were cofunded by ViiV Healthcare and Janssen Research & Development. Dr. Silverman reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HIV MEDICINE
U.S. sees most flu hospitalizations in a decade
But the number of deaths and outpatient visits for flu or flu-like illnesses was down slightly from the week before, the CDC said in its weekly FluView report.
There were almost 26,000 new hospital admissions involving laboratory-confirmed influenza over those 7 days, up by over 31% from the previous week, based on data from 5,000 hospitals in the HHS Protect system, which tracks and shares COVID-19 data.
The cumulative hospitalization rate for the 2022-2023 season is 26.0 per 100,000 people, the highest seen at this time of year since 2010-2011, the CDC said, based on data from its Influenza Hospitalization Surveillance Network, which includes hospitals in select counties in 13 states.
At this point in the 2019-2020 season, just before the COVID-19 pandemic began, the cumulative rate was 3.1 per 100,000 people, the CDC’s data show.
On the positive side, the proportion of outpatient visits for influenza-like illness dropped slightly to 7.2%, from 7.5% the week before. But these cases from the CDC’s Outpatient Influenza-like Illness Surveillance Network are not laboratory confirmed, so the data could include people with the flu, COVID-19, or respiratory syncytial virus.
The number of confirmed flu deaths for the week of Nov. 27 to Dec. 3 also fell slightly from the last full week of November, 246 vs. 255, but the number of pediatric deaths rose from 2 to 7, and total deaths in children are already up to 21 for 2022-2023. That’s compared to 44 that were reported during all of the 2021-2022 season, the CDC said.
“So far this season, there have been at least 13 million illnesses, 120,000 hospitalizations, and 7,300 deaths from flu,” the agency estimated.
A version of this article first appeared on Medscape.com.
But the number of deaths and outpatient visits for flu or flu-like illnesses was down slightly from the week before, the CDC said in its weekly FluView report.
There were almost 26,000 new hospital admissions involving laboratory-confirmed influenza over those 7 days, up by over 31% from the previous week, based on data from 5,000 hospitals in the HHS Protect system, which tracks and shares COVID-19 data.
The cumulative hospitalization rate for the 2022-2023 season is 26.0 per 100,000 people, the highest seen at this time of year since 2010-2011, the CDC said, based on data from its Influenza Hospitalization Surveillance Network, which includes hospitals in select counties in 13 states.
At this point in the 2019-2020 season, just before the COVID-19 pandemic began, the cumulative rate was 3.1 per 100,000 people, the CDC’s data show.
On the positive side, the proportion of outpatient visits for influenza-like illness dropped slightly to 7.2%, from 7.5% the week before. But these cases from the CDC’s Outpatient Influenza-like Illness Surveillance Network are not laboratory confirmed, so the data could include people with the flu, COVID-19, or respiratory syncytial virus.
The number of confirmed flu deaths for the week of Nov. 27 to Dec. 3 also fell slightly from the last full week of November, 246 vs. 255, but the number of pediatric deaths rose from 2 to 7, and total deaths in children are already up to 21 for 2022-2023. That’s compared to 44 that were reported during all of the 2021-2022 season, the CDC said.
“So far this season, there have been at least 13 million illnesses, 120,000 hospitalizations, and 7,300 deaths from flu,” the agency estimated.
A version of this article first appeared on Medscape.com.
But the number of deaths and outpatient visits for flu or flu-like illnesses was down slightly from the week before, the CDC said in its weekly FluView report.
There were almost 26,000 new hospital admissions involving laboratory-confirmed influenza over those 7 days, up by over 31% from the previous week, based on data from 5,000 hospitals in the HHS Protect system, which tracks and shares COVID-19 data.
The cumulative hospitalization rate for the 2022-2023 season is 26.0 per 100,000 people, the highest seen at this time of year since 2010-2011, the CDC said, based on data from its Influenza Hospitalization Surveillance Network, which includes hospitals in select counties in 13 states.
At this point in the 2019-2020 season, just before the COVID-19 pandemic began, the cumulative rate was 3.1 per 100,000 people, the CDC’s data show.
On the positive side, the proportion of outpatient visits for influenza-like illness dropped slightly to 7.2%, from 7.5% the week before. But these cases from the CDC’s Outpatient Influenza-like Illness Surveillance Network are not laboratory confirmed, so the data could include people with the flu, COVID-19, or respiratory syncytial virus.
The number of confirmed flu deaths for the week of Nov. 27 to Dec. 3 also fell slightly from the last full week of November, 246 vs. 255, but the number of pediatric deaths rose from 2 to 7, and total deaths in children are already up to 21 for 2022-2023. That’s compared to 44 that were reported during all of the 2021-2022 season, the CDC said.
“So far this season, there have been at least 13 million illnesses, 120,000 hospitalizations, and 7,300 deaths from flu,” the agency estimated.
A version of this article first appeared on Medscape.com.
As COVID treatments dwindle, are new ones waiting in the wings?
It was the last monoclonal antibody treatment standing. But less than 10 months after the U.S. Food and Drug Administration gave bebtelovimab its emergency use authorization (EUA) to fight COVID-19, it earlier this month de-authorized it, just as it had for other monoclonal antibody treatments, and for the same reason:
Bebtelovimab couldn’t neutralize the Omicron subvariants BQ.1 and BQ.1.1, the cause of nearly 60% of COVID cases nationally as of November 30.
Next on the chopping block, some predict, will be Evusheld, the combination of tixagevimab and cilgavimab given as a preventive monoclonal antibody to people who are immunocompromised and at high risk of contracting COVID and to those who can’t take the vaccine. In October, the FDA warned that Evusheld was not neutralizing circulating COVID variants.
As the options for treating and preventing COVID decline, will companies rally quickly to develop new ones, or cut their losses in developing treatments that may work for only a few months, given the speed of viral mutations?
But although monoclonal antibody treatments are off the table, at least for now, antiviral drugs – including Paxlovid – are still very much available, and some say underused.
Others suggest it’s time to resurrect interest in convalescent plasma, a treatment used early in the pandemic before drugs or vaccines were here and still authorized for use in those who are immunosuppressed or receiving immunosuppressive treatment.
And on the prevention front, staying up to date with booster vaccines, masking, and taking other precautions should be stressed more, others say, regardless of the number of treatment options, and especially now, as cases rise and people gather for the winter holidays.
‘A major setback’
The bebtelovimab de-authorization was “a major setback,” but an understandable one, said Arturo Casadevall, MD, PhD, professor and chair of molecular microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health in Baltimore. “Monoclonal antibodies are great drugs. We are in an unfortunate situation in that they are vulnerable to changes in the virus” and can’t offer long-lasting protection.
Supplies of bebtelovimab will be retained, according to the FDA, in case variants susceptible to it return.
“What happened to bebtelovimab is no surprise,” agreed Amesh Adalja, MD, senior scholar at Johns Hopkins Center for Health Security. “This is what is going to happen when you are targeting a virus that mutates a lot.”
Monoclonal antibodies work by binding to the spike protein on the virus surface to prevent it from entering cells.
However, Dr. Adalja doesn’t view the disappearance of monoclonal antibody treatments as a major setback. Monoclonal antibodies were not the primary way COVID was treated, he said.
While he does believe it’s important that more monoclonal antibody treatments be developed, “I think it’s important to remember we still have Paxlovid while everyone is lamenting the loss of bebtelovimab.’’
Antivirals: What’s here, what’s coming
Compared with monoclonal antibodies, “Paxlovid remains a much easier drug to give,” Dr. Adalja told this news organization, because it is taken orally, not intravenously.
And it’s effective. In a recent study, researchers found that adults diagnosed with COVID given Paxlovid within 5 days of diagnosis had a 51% lower hospitalization rate within the next 30 days than those not given it. Another study shows it could also reduce a person’s risk of developing long COVID by 26%.
Paxlovid is underused, Dr. Adalja said, partly because the rebound potential got more press than the effectiveness. When a celebrity got rebound from Paxlovid, he said, that would make the news, overshadowing the research on its effectiveness.
Besides Paxlovid, the antivirals remdesivir (Veklury), given intravenously for 3 days, and molnupiravir (Lagevrio), taken orally, are also still available. Antivirals work by targeting specific parts of the virus to prevent it from multiplying.
In the lab, remdesivir, molnupiravir, and another antiviral, nirmatrelvir, all appear to be effective against both BQ.1.1 (a BA.5 subvariant) and XBB (a BA.2 subvariant), both rapidly rising in the United States, according to a report last week in the New England Journal of Medicine.
The researchers also tested several monoclonal antibodies and found they did not neutralize either of the subvariants BQ.1.1 and XBB.
A new oral antiviral, Xocova (ensitrelvir fumaric acid), from Japanese manufacturer Shionogi, received emergency approval in Japan on November 22. It’s taken once a day for 5 days. The goal is to expand access to it globally, according to the company.
Pardes Biosciences launched a phase 2 trial in September for its oral antiviral drug (PBI-0451), under study as a treatment and preventive for COVID. It expects data by the first quarter of 2023.
Pfizer, which makes Paxlovid, has partnered with Clear Creek Bio to develop another oral antiviral COVID drug.
Other approaches
A receptor protein known as ACE2 (angiotensin-converting enzyme 2) is the main “doorway” that SARS-CoV-2 uses to enter and infect cells.
Dana-Farber Cancer Institute scientists are developing a “decoy” drug that works by mimicking the ACE2 receptor on the surface of cells; when the virus tries to bind to it, the spike protein is destroyed. Human trials have not yet started.
Other researchers are investigating whether an already-approved drug used to treat a liver disease, Actigall (UDCA/ursodeoxycholic acid), could protect against COVID infection by reducing ACE2.
So far, the researchers have found in early research that people taking UDCA for liver conditions were less likely than those not taking the drug to have severe COVID. They also found that UDCA reduced SARS-CoV-2 infection in human lungs maintained outside the body.
Monoclonal antibody treatments?
After the FDA decision to withdraw the bebtelovimab EUA, which Eli Lilly said it agreed with, the company issued a statement, promising it wasn’t giving up on monoclonal antibody treatments.
“Lilly will continue to search and evaluate monoclonal antibodies to identify potential candidates for clinical development against new variants,” it read in part.
AstraZeneca, which makes Evusheld, is also continuing to work on monoclonal antibody development. According to a spokesperson, “We are also developing a new long-acting antibody combination – AZD5156 – which has been shown in the lab to neutralize emerging new variants and all known variants to date. We are working to accelerate the development of AZD5156 to make it available at the end of 2023.”
The AstraZeneca spokesperson said he could share no more information about what the combination would include.
A convalescent plasma comeback?
Although Paxlovid can help, there are many contraindications to it, such as drug-drug interactions, Dr. Casadevall told this news organization. And now that the monoclonal antibody treatments have been paused, convalescent plasma “is the only antibody-based therapy that is reliably available. Convalescent plasma includes thousands of different antibodies.”
With his colleagues, Dr. Casadevall evaluated plasma samples from 740 patients. Some had received booster vaccines and been infected with Omicron, others had received boosters and not been infected, and still others had not been vaccinated and became infected.
In a report (not yet peer-reviewed), they found the plasma from those who had been infected or boosted within the past 6 months neutralized the new Omicron variants BQ.1.1, XBB.1, and BF.7.
A push for boosters, masks
To get through the coming months, taking precautions like masking and distancing and staying up to date on booster vaccinations, especially for older adults, can make a difference, other experts say.
In a Twitter thread in early December, Peter Hotez, MD, PhD, professor of pediatrics and molecular virology and microbiology at Baylor College of Medicine, Houston, urged people to take COVID seriously as holiday parties and gatherings occur.
“The single most impactful thing you can do is get your bivalent booster,” he tweeted, as well as give your kids the booster, citing preliminary research that the bivalent mRNA booster broadens immunity against the Omicron subvariants.
For seniors, he said, ‘‘if you get breakthrough COVID, [it’s] really important to get Paxlovid.” Masks will help not only for COVID but also influenza, respiratory syncytial virus (RSV), and other conditions.
Mitigation measures have largely been abandoned, according to Eric Topol, MD, director of the Scripps Research Translational Institute, La Jolla, Calif., and editor-in-chief of Medscape. In an op-ed in the Los Angeles Times, and on his Twitter feed, he reminds people about masking and urges people to get the bivalent booster.
According to the Centers for Disease Control and Prevention, as of Dec. 8, only 13.5% of people aged 5 and older have gotten an updated booster, despite research that shows an increase in antibodies to BQ.1.1. Recent research has found that the bivalent booster increases antibodies to BQ.1.1 by up to 10-fold, Dr. Topol said.
Dr. Adalja is on advisory boards for Shionogi, GSK, and Pardes. Dr. Casadevall reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It was the last monoclonal antibody treatment standing. But less than 10 months after the U.S. Food and Drug Administration gave bebtelovimab its emergency use authorization (EUA) to fight COVID-19, it earlier this month de-authorized it, just as it had for other monoclonal antibody treatments, and for the same reason:
Bebtelovimab couldn’t neutralize the Omicron subvariants BQ.1 and BQ.1.1, the cause of nearly 60% of COVID cases nationally as of November 30.
Next on the chopping block, some predict, will be Evusheld, the combination of tixagevimab and cilgavimab given as a preventive monoclonal antibody to people who are immunocompromised and at high risk of contracting COVID and to those who can’t take the vaccine. In October, the FDA warned that Evusheld was not neutralizing circulating COVID variants.
As the options for treating and preventing COVID decline, will companies rally quickly to develop new ones, or cut their losses in developing treatments that may work for only a few months, given the speed of viral mutations?
But although monoclonal antibody treatments are off the table, at least for now, antiviral drugs – including Paxlovid – are still very much available, and some say underused.
Others suggest it’s time to resurrect interest in convalescent plasma, a treatment used early in the pandemic before drugs or vaccines were here and still authorized for use in those who are immunosuppressed or receiving immunosuppressive treatment.
And on the prevention front, staying up to date with booster vaccines, masking, and taking other precautions should be stressed more, others say, regardless of the number of treatment options, and especially now, as cases rise and people gather for the winter holidays.
‘A major setback’
The bebtelovimab de-authorization was “a major setback,” but an understandable one, said Arturo Casadevall, MD, PhD, professor and chair of molecular microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health in Baltimore. “Monoclonal antibodies are great drugs. We are in an unfortunate situation in that they are vulnerable to changes in the virus” and can’t offer long-lasting protection.
Supplies of bebtelovimab will be retained, according to the FDA, in case variants susceptible to it return.
“What happened to bebtelovimab is no surprise,” agreed Amesh Adalja, MD, senior scholar at Johns Hopkins Center for Health Security. “This is what is going to happen when you are targeting a virus that mutates a lot.”
Monoclonal antibodies work by binding to the spike protein on the virus surface to prevent it from entering cells.
However, Dr. Adalja doesn’t view the disappearance of monoclonal antibody treatments as a major setback. Monoclonal antibodies were not the primary way COVID was treated, he said.
While he does believe it’s important that more monoclonal antibody treatments be developed, “I think it’s important to remember we still have Paxlovid while everyone is lamenting the loss of bebtelovimab.’’
Antivirals: What’s here, what’s coming
Compared with monoclonal antibodies, “Paxlovid remains a much easier drug to give,” Dr. Adalja told this news organization, because it is taken orally, not intravenously.
And it’s effective. In a recent study, researchers found that adults diagnosed with COVID given Paxlovid within 5 days of diagnosis had a 51% lower hospitalization rate within the next 30 days than those not given it. Another study shows it could also reduce a person’s risk of developing long COVID by 26%.
Paxlovid is underused, Dr. Adalja said, partly because the rebound potential got more press than the effectiveness. When a celebrity got rebound from Paxlovid, he said, that would make the news, overshadowing the research on its effectiveness.
Besides Paxlovid, the antivirals remdesivir (Veklury), given intravenously for 3 days, and molnupiravir (Lagevrio), taken orally, are also still available. Antivirals work by targeting specific parts of the virus to prevent it from multiplying.
In the lab, remdesivir, molnupiravir, and another antiviral, nirmatrelvir, all appear to be effective against both BQ.1.1 (a BA.5 subvariant) and XBB (a BA.2 subvariant), both rapidly rising in the United States, according to a report last week in the New England Journal of Medicine.
The researchers also tested several monoclonal antibodies and found they did not neutralize either of the subvariants BQ.1.1 and XBB.
A new oral antiviral, Xocova (ensitrelvir fumaric acid), from Japanese manufacturer Shionogi, received emergency approval in Japan on November 22. It’s taken once a day for 5 days. The goal is to expand access to it globally, according to the company.
Pardes Biosciences launched a phase 2 trial in September for its oral antiviral drug (PBI-0451), under study as a treatment and preventive for COVID. It expects data by the first quarter of 2023.
Pfizer, which makes Paxlovid, has partnered with Clear Creek Bio to develop another oral antiviral COVID drug.
Other approaches
A receptor protein known as ACE2 (angiotensin-converting enzyme 2) is the main “doorway” that SARS-CoV-2 uses to enter and infect cells.
Dana-Farber Cancer Institute scientists are developing a “decoy” drug that works by mimicking the ACE2 receptor on the surface of cells; when the virus tries to bind to it, the spike protein is destroyed. Human trials have not yet started.
Other researchers are investigating whether an already-approved drug used to treat a liver disease, Actigall (UDCA/ursodeoxycholic acid), could protect against COVID infection by reducing ACE2.
So far, the researchers have found in early research that people taking UDCA for liver conditions were less likely than those not taking the drug to have severe COVID. They also found that UDCA reduced SARS-CoV-2 infection in human lungs maintained outside the body.
Monoclonal antibody treatments?
After the FDA decision to withdraw the bebtelovimab EUA, which Eli Lilly said it agreed with, the company issued a statement, promising it wasn’t giving up on monoclonal antibody treatments.
“Lilly will continue to search and evaluate monoclonal antibodies to identify potential candidates for clinical development against new variants,” it read in part.
AstraZeneca, which makes Evusheld, is also continuing to work on monoclonal antibody development. According to a spokesperson, “We are also developing a new long-acting antibody combination – AZD5156 – which has been shown in the lab to neutralize emerging new variants and all known variants to date. We are working to accelerate the development of AZD5156 to make it available at the end of 2023.”
The AstraZeneca spokesperson said he could share no more information about what the combination would include.
A convalescent plasma comeback?
Although Paxlovid can help, there are many contraindications to it, such as drug-drug interactions, Dr. Casadevall told this news organization. And now that the monoclonal antibody treatments have been paused, convalescent plasma “is the only antibody-based therapy that is reliably available. Convalescent plasma includes thousands of different antibodies.”
With his colleagues, Dr. Casadevall evaluated plasma samples from 740 patients. Some had received booster vaccines and been infected with Omicron, others had received boosters and not been infected, and still others had not been vaccinated and became infected.
In a report (not yet peer-reviewed), they found the plasma from those who had been infected or boosted within the past 6 months neutralized the new Omicron variants BQ.1.1, XBB.1, and BF.7.
A push for boosters, masks
To get through the coming months, taking precautions like masking and distancing and staying up to date on booster vaccinations, especially for older adults, can make a difference, other experts say.
In a Twitter thread in early December, Peter Hotez, MD, PhD, professor of pediatrics and molecular virology and microbiology at Baylor College of Medicine, Houston, urged people to take COVID seriously as holiday parties and gatherings occur.
“The single most impactful thing you can do is get your bivalent booster,” he tweeted, as well as give your kids the booster, citing preliminary research that the bivalent mRNA booster broadens immunity against the Omicron subvariants.
For seniors, he said, ‘‘if you get breakthrough COVID, [it’s] really important to get Paxlovid.” Masks will help not only for COVID but also influenza, respiratory syncytial virus (RSV), and other conditions.
Mitigation measures have largely been abandoned, according to Eric Topol, MD, director of the Scripps Research Translational Institute, La Jolla, Calif., and editor-in-chief of Medscape. In an op-ed in the Los Angeles Times, and on his Twitter feed, he reminds people about masking and urges people to get the bivalent booster.
According to the Centers for Disease Control and Prevention, as of Dec. 8, only 13.5% of people aged 5 and older have gotten an updated booster, despite research that shows an increase in antibodies to BQ.1.1. Recent research has found that the bivalent booster increases antibodies to BQ.1.1 by up to 10-fold, Dr. Topol said.
Dr. Adalja is on advisory boards for Shionogi, GSK, and Pardes. Dr. Casadevall reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It was the last monoclonal antibody treatment standing. But less than 10 months after the U.S. Food and Drug Administration gave bebtelovimab its emergency use authorization (EUA) to fight COVID-19, it earlier this month de-authorized it, just as it had for other monoclonal antibody treatments, and for the same reason:
Bebtelovimab couldn’t neutralize the Omicron subvariants BQ.1 and BQ.1.1, the cause of nearly 60% of COVID cases nationally as of November 30.
Next on the chopping block, some predict, will be Evusheld, the combination of tixagevimab and cilgavimab given as a preventive monoclonal antibody to people who are immunocompromised and at high risk of contracting COVID and to those who can’t take the vaccine. In October, the FDA warned that Evusheld was not neutralizing circulating COVID variants.
As the options for treating and preventing COVID decline, will companies rally quickly to develop new ones, or cut their losses in developing treatments that may work for only a few months, given the speed of viral mutations?
But although monoclonal antibody treatments are off the table, at least for now, antiviral drugs – including Paxlovid – are still very much available, and some say underused.
Others suggest it’s time to resurrect interest in convalescent plasma, a treatment used early in the pandemic before drugs or vaccines were here and still authorized for use in those who are immunosuppressed or receiving immunosuppressive treatment.
And on the prevention front, staying up to date with booster vaccines, masking, and taking other precautions should be stressed more, others say, regardless of the number of treatment options, and especially now, as cases rise and people gather for the winter holidays.
‘A major setback’
The bebtelovimab de-authorization was “a major setback,” but an understandable one, said Arturo Casadevall, MD, PhD, professor and chair of molecular microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health in Baltimore. “Monoclonal antibodies are great drugs. We are in an unfortunate situation in that they are vulnerable to changes in the virus” and can’t offer long-lasting protection.
Supplies of bebtelovimab will be retained, according to the FDA, in case variants susceptible to it return.
“What happened to bebtelovimab is no surprise,” agreed Amesh Adalja, MD, senior scholar at Johns Hopkins Center for Health Security. “This is what is going to happen when you are targeting a virus that mutates a lot.”
Monoclonal antibodies work by binding to the spike protein on the virus surface to prevent it from entering cells.
However, Dr. Adalja doesn’t view the disappearance of monoclonal antibody treatments as a major setback. Monoclonal antibodies were not the primary way COVID was treated, he said.
While he does believe it’s important that more monoclonal antibody treatments be developed, “I think it’s important to remember we still have Paxlovid while everyone is lamenting the loss of bebtelovimab.’’
Antivirals: What’s here, what’s coming
Compared with monoclonal antibodies, “Paxlovid remains a much easier drug to give,” Dr. Adalja told this news organization, because it is taken orally, not intravenously.
And it’s effective. In a recent study, researchers found that adults diagnosed with COVID given Paxlovid within 5 days of diagnosis had a 51% lower hospitalization rate within the next 30 days than those not given it. Another study shows it could also reduce a person’s risk of developing long COVID by 26%.
Paxlovid is underused, Dr. Adalja said, partly because the rebound potential got more press than the effectiveness. When a celebrity got rebound from Paxlovid, he said, that would make the news, overshadowing the research on its effectiveness.
Besides Paxlovid, the antivirals remdesivir (Veklury), given intravenously for 3 days, and molnupiravir (Lagevrio), taken orally, are also still available. Antivirals work by targeting specific parts of the virus to prevent it from multiplying.
In the lab, remdesivir, molnupiravir, and another antiviral, nirmatrelvir, all appear to be effective against both BQ.1.1 (a BA.5 subvariant) and XBB (a BA.2 subvariant), both rapidly rising in the United States, according to a report last week in the New England Journal of Medicine.
The researchers also tested several monoclonal antibodies and found they did not neutralize either of the subvariants BQ.1.1 and XBB.
A new oral antiviral, Xocova (ensitrelvir fumaric acid), from Japanese manufacturer Shionogi, received emergency approval in Japan on November 22. It’s taken once a day for 5 days. The goal is to expand access to it globally, according to the company.
Pardes Biosciences launched a phase 2 trial in September for its oral antiviral drug (PBI-0451), under study as a treatment and preventive for COVID. It expects data by the first quarter of 2023.
Pfizer, which makes Paxlovid, has partnered with Clear Creek Bio to develop another oral antiviral COVID drug.
Other approaches
A receptor protein known as ACE2 (angiotensin-converting enzyme 2) is the main “doorway” that SARS-CoV-2 uses to enter and infect cells.
Dana-Farber Cancer Institute scientists are developing a “decoy” drug that works by mimicking the ACE2 receptor on the surface of cells; when the virus tries to bind to it, the spike protein is destroyed. Human trials have not yet started.
Other researchers are investigating whether an already-approved drug used to treat a liver disease, Actigall (UDCA/ursodeoxycholic acid), could protect against COVID infection by reducing ACE2.
So far, the researchers have found in early research that people taking UDCA for liver conditions were less likely than those not taking the drug to have severe COVID. They also found that UDCA reduced SARS-CoV-2 infection in human lungs maintained outside the body.
Monoclonal antibody treatments?
After the FDA decision to withdraw the bebtelovimab EUA, which Eli Lilly said it agreed with, the company issued a statement, promising it wasn’t giving up on monoclonal antibody treatments.
“Lilly will continue to search and evaluate monoclonal antibodies to identify potential candidates for clinical development against new variants,” it read in part.
AstraZeneca, which makes Evusheld, is also continuing to work on monoclonal antibody development. According to a spokesperson, “We are also developing a new long-acting antibody combination – AZD5156 – which has been shown in the lab to neutralize emerging new variants and all known variants to date. We are working to accelerate the development of AZD5156 to make it available at the end of 2023.”
The AstraZeneca spokesperson said he could share no more information about what the combination would include.
A convalescent plasma comeback?
Although Paxlovid can help, there are many contraindications to it, such as drug-drug interactions, Dr. Casadevall told this news organization. And now that the monoclonal antibody treatments have been paused, convalescent plasma “is the only antibody-based therapy that is reliably available. Convalescent plasma includes thousands of different antibodies.”
With his colleagues, Dr. Casadevall evaluated plasma samples from 740 patients. Some had received booster vaccines and been infected with Omicron, others had received boosters and not been infected, and still others had not been vaccinated and became infected.
In a report (not yet peer-reviewed), they found the plasma from those who had been infected or boosted within the past 6 months neutralized the new Omicron variants BQ.1.1, XBB.1, and BF.7.
A push for boosters, masks
To get through the coming months, taking precautions like masking and distancing and staying up to date on booster vaccinations, especially for older adults, can make a difference, other experts say.
In a Twitter thread in early December, Peter Hotez, MD, PhD, professor of pediatrics and molecular virology and microbiology at Baylor College of Medicine, Houston, urged people to take COVID seriously as holiday parties and gatherings occur.
“The single most impactful thing you can do is get your bivalent booster,” he tweeted, as well as give your kids the booster, citing preliminary research that the bivalent mRNA booster broadens immunity against the Omicron subvariants.
For seniors, he said, ‘‘if you get breakthrough COVID, [it’s] really important to get Paxlovid.” Masks will help not only for COVID but also influenza, respiratory syncytial virus (RSV), and other conditions.
Mitigation measures have largely been abandoned, according to Eric Topol, MD, director of the Scripps Research Translational Institute, La Jolla, Calif., and editor-in-chief of Medscape. In an op-ed in the Los Angeles Times, and on his Twitter feed, he reminds people about masking and urges people to get the bivalent booster.
According to the Centers for Disease Control and Prevention, as of Dec. 8, only 13.5% of people aged 5 and older have gotten an updated booster, despite research that shows an increase in antibodies to BQ.1.1. Recent research has found that the bivalent booster increases antibodies to BQ.1.1 by up to 10-fold, Dr. Topol said.
Dr. Adalja is on advisory boards for Shionogi, GSK, and Pardes. Dr. Casadevall reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Direct-acting antivirals tied to better outcomes in chronic Hep C
Eiichi Ogawa, MD, PhD, with the department of general internal medicine, Kyushu University Hospital in Fukuoka, Japan, led the retrospective study of 245,596 adults with CHC. In the new research, which was published in JAMA Internal Medicine, the authors analyzed data from the Optum Clinformatics Data Mart (CDM) database, 2010-2021.
It was important to do the study because of limited and conflicting information – mostly from case reports – on safety of the DAAs when they were approved for CHC in 2014, said coauthor Mindie H. Nguyen, MD, in an interview.
‘DAA treatment is safe’
“The main message is that DAA treatment is safe,” said Dr. Nguyen, of the division of gastroenterology and hepatology at Stanford (Calif.) University Medical Center in Palo Alto. In the early days of treatment, physicians were treating the sickest patients with the DAAs, which may have introduced patient selection bias and caused lasting misperceptions about poor safety, she noted.
“I really hope to dispel this myth,” she said, adding that this study also shows improved liver and nonliver outcomes.
Of the total cohort in this study, 40,654 patients had one or more prescriptions for a DAA (without interferon) and 204,942 patients had not been treated.
All-cause mortality reduced by 57%
DAA treatment, vs. no treatment, was linked with a large and significant reduction (57%) in all-cause mortality. That finding was particularly notable, because it was seen regardless of age, sex, race and ethnicity, comorbidities, alcohol use, and presence of hepatocellular carcinoma or cirrhosis.
The authors noted that patients without cirrhosis are a population previously considered to receive less benefit from an HCV cure than patients with cirrhosis.
DAAs were associated with lower risk of hepatocellular carcinoma and decompensation as well as risk of nonliver outcomes, including diabetes, cardiovascular disease (CVD), and chronic kidney disease (CKD).
Lower risk of poor nonliver outcomes
The researchers found that when they compared DAA-treated patients with untreated patients, the incidences per 1,000 person-years of having diabetes were 30.2 vs. 37.2 (P less than .001), and of having kidney disease was 31.1 vs. 34.1 (P less than .001), respectively.
“This retrospective cohort study provides valuable information to physicians,” Noel Deep, MD, chief medical officer at Aspirus Langlade Hospital in Antigo, Wis., said, in an interview.
The study’s size helps confirm DAAs’ safety and benefit, and previously unknown added benefits, in treating CHC, he continued.
Large study confirms, introduces DAA benefits
Dr. Deep, who was not part of the study, noted that DAAs now show much promise in efficacy and tolerability in most people with chronic hepatitis C, including those with concomitant conditions such as CKD.
“Previous studies did not have such large-scale nationwide data. [The findings of the new study] greatly enhance our knowledge of DAA treatment for chronic hepatitis C patients across the spectrum from noncirrhotic to compensated cirrhotic to decompensated cirrhotic,” Dr. Deep said. “The added benefit of improved outcomes for diabetes, CVD, CKD, and nonliver cancers truly surprised me.”
Dr. Deep pointed out some limitations of the study, including that, as the authors acknowledge, only privately insured patients were included so results may not be generalizable to the underinsured/uninsured “who might have other risk factors, poorer health, and fewer resources.”
He added: “The data also may not be reflective of the outcomes in Asians who were, in my opinion, also underrepresented in this study.”
The authors cited the insurance claims database they used as a strength of the study, due to it containing information on 61 million people from across all regions of the United States.
Dr. Ogawa reports grants from Gilead Sciences outside the submitted work. Coauthor Dr. Nguyen reports institutional grants and advisory board fees from Gilead Sciences outside the submitted work. Another coauthor reports speaking/consulting fees from Gilead and Merck Sharp & Dohme outside the submitted work. No other disclosures were reported.
The Stanford Center for Population Health Sciences (PHS) supported this study by providing access to the PHS Data Core.
Dr. Deep reports no relevant financial relationships. He serves on the editorial advisory board of Internal Medicine News.
Eiichi Ogawa, MD, PhD, with the department of general internal medicine, Kyushu University Hospital in Fukuoka, Japan, led the retrospective study of 245,596 adults with CHC. In the new research, which was published in JAMA Internal Medicine, the authors analyzed data from the Optum Clinformatics Data Mart (CDM) database, 2010-2021.
It was important to do the study because of limited and conflicting information – mostly from case reports – on safety of the DAAs when they were approved for CHC in 2014, said coauthor Mindie H. Nguyen, MD, in an interview.
‘DAA treatment is safe’
“The main message is that DAA treatment is safe,” said Dr. Nguyen, of the division of gastroenterology and hepatology at Stanford (Calif.) University Medical Center in Palo Alto. In the early days of treatment, physicians were treating the sickest patients with the DAAs, which may have introduced patient selection bias and caused lasting misperceptions about poor safety, she noted.
“I really hope to dispel this myth,” she said, adding that this study also shows improved liver and nonliver outcomes.
Of the total cohort in this study, 40,654 patients had one or more prescriptions for a DAA (without interferon) and 204,942 patients had not been treated.
All-cause mortality reduced by 57%
DAA treatment, vs. no treatment, was linked with a large and significant reduction (57%) in all-cause mortality. That finding was particularly notable, because it was seen regardless of age, sex, race and ethnicity, comorbidities, alcohol use, and presence of hepatocellular carcinoma or cirrhosis.
The authors noted that patients without cirrhosis are a population previously considered to receive less benefit from an HCV cure than patients with cirrhosis.
DAAs were associated with lower risk of hepatocellular carcinoma and decompensation as well as risk of nonliver outcomes, including diabetes, cardiovascular disease (CVD), and chronic kidney disease (CKD).
Lower risk of poor nonliver outcomes
The researchers found that when they compared DAA-treated patients with untreated patients, the incidences per 1,000 person-years of having diabetes were 30.2 vs. 37.2 (P less than .001), and of having kidney disease was 31.1 vs. 34.1 (P less than .001), respectively.
“This retrospective cohort study provides valuable information to physicians,” Noel Deep, MD, chief medical officer at Aspirus Langlade Hospital in Antigo, Wis., said, in an interview.
The study’s size helps confirm DAAs’ safety and benefit, and previously unknown added benefits, in treating CHC, he continued.
Large study confirms, introduces DAA benefits
Dr. Deep, who was not part of the study, noted that DAAs now show much promise in efficacy and tolerability in most people with chronic hepatitis C, including those with concomitant conditions such as CKD.
“Previous studies did not have such large-scale nationwide data. [The findings of the new study] greatly enhance our knowledge of DAA treatment for chronic hepatitis C patients across the spectrum from noncirrhotic to compensated cirrhotic to decompensated cirrhotic,” Dr. Deep said. “The added benefit of improved outcomes for diabetes, CVD, CKD, and nonliver cancers truly surprised me.”
Dr. Deep pointed out some limitations of the study, including that, as the authors acknowledge, only privately insured patients were included so results may not be generalizable to the underinsured/uninsured “who might have other risk factors, poorer health, and fewer resources.”
He added: “The data also may not be reflective of the outcomes in Asians who were, in my opinion, also underrepresented in this study.”
The authors cited the insurance claims database they used as a strength of the study, due to it containing information on 61 million people from across all regions of the United States.
Dr. Ogawa reports grants from Gilead Sciences outside the submitted work. Coauthor Dr. Nguyen reports institutional grants and advisory board fees from Gilead Sciences outside the submitted work. Another coauthor reports speaking/consulting fees from Gilead and Merck Sharp & Dohme outside the submitted work. No other disclosures were reported.
The Stanford Center for Population Health Sciences (PHS) supported this study by providing access to the PHS Data Core.
Dr. Deep reports no relevant financial relationships. He serves on the editorial advisory board of Internal Medicine News.
Eiichi Ogawa, MD, PhD, with the department of general internal medicine, Kyushu University Hospital in Fukuoka, Japan, led the retrospective study of 245,596 adults with CHC. In the new research, which was published in JAMA Internal Medicine, the authors analyzed data from the Optum Clinformatics Data Mart (CDM) database, 2010-2021.
It was important to do the study because of limited and conflicting information – mostly from case reports – on safety of the DAAs when they were approved for CHC in 2014, said coauthor Mindie H. Nguyen, MD, in an interview.
‘DAA treatment is safe’
“The main message is that DAA treatment is safe,” said Dr. Nguyen, of the division of gastroenterology and hepatology at Stanford (Calif.) University Medical Center in Palo Alto. In the early days of treatment, physicians were treating the sickest patients with the DAAs, which may have introduced patient selection bias and caused lasting misperceptions about poor safety, she noted.
“I really hope to dispel this myth,” she said, adding that this study also shows improved liver and nonliver outcomes.
Of the total cohort in this study, 40,654 patients had one or more prescriptions for a DAA (without interferon) and 204,942 patients had not been treated.
All-cause mortality reduced by 57%
DAA treatment, vs. no treatment, was linked with a large and significant reduction (57%) in all-cause mortality. That finding was particularly notable, because it was seen regardless of age, sex, race and ethnicity, comorbidities, alcohol use, and presence of hepatocellular carcinoma or cirrhosis.
The authors noted that patients without cirrhosis are a population previously considered to receive less benefit from an HCV cure than patients with cirrhosis.
DAAs were associated with lower risk of hepatocellular carcinoma and decompensation as well as risk of nonliver outcomes, including diabetes, cardiovascular disease (CVD), and chronic kidney disease (CKD).
Lower risk of poor nonliver outcomes
The researchers found that when they compared DAA-treated patients with untreated patients, the incidences per 1,000 person-years of having diabetes were 30.2 vs. 37.2 (P less than .001), and of having kidney disease was 31.1 vs. 34.1 (P less than .001), respectively.
“This retrospective cohort study provides valuable information to physicians,” Noel Deep, MD, chief medical officer at Aspirus Langlade Hospital in Antigo, Wis., said, in an interview.
The study’s size helps confirm DAAs’ safety and benefit, and previously unknown added benefits, in treating CHC, he continued.
Large study confirms, introduces DAA benefits
Dr. Deep, who was not part of the study, noted that DAAs now show much promise in efficacy and tolerability in most people with chronic hepatitis C, including those with concomitant conditions such as CKD.
“Previous studies did not have such large-scale nationwide data. [The findings of the new study] greatly enhance our knowledge of DAA treatment for chronic hepatitis C patients across the spectrum from noncirrhotic to compensated cirrhotic to decompensated cirrhotic,” Dr. Deep said. “The added benefit of improved outcomes for diabetes, CVD, CKD, and nonliver cancers truly surprised me.”
Dr. Deep pointed out some limitations of the study, including that, as the authors acknowledge, only privately insured patients were included so results may not be generalizable to the underinsured/uninsured “who might have other risk factors, poorer health, and fewer resources.”
He added: “The data also may not be reflective of the outcomes in Asians who were, in my opinion, also underrepresented in this study.”
The authors cited the insurance claims database they used as a strength of the study, due to it containing information on 61 million people from across all regions of the United States.
Dr. Ogawa reports grants from Gilead Sciences outside the submitted work. Coauthor Dr. Nguyen reports institutional grants and advisory board fees from Gilead Sciences outside the submitted work. Another coauthor reports speaking/consulting fees from Gilead and Merck Sharp & Dohme outside the submitted work. No other disclosures were reported.
The Stanford Center for Population Health Sciences (PHS) supported this study by providing access to the PHS Data Core.
Dr. Deep reports no relevant financial relationships. He serves on the editorial advisory board of Internal Medicine News.
FROM JAMA INTERNAL MEDICINE
A bold national plan to eliminate HCV by 2050
WASHINGTON – “We don’t get to use the ‘eliminate’ word all that often with a disease that’s taking thousands or tens of thousands – or worldwide, hundreds of thousands – of lives every year, but we have that opportunity with hepatitis C.”
So said Francis S. Collins, MD, PhD, special projects advisor to the Executive Office of the President of the United States, and former director of the National Institutes of Health, speaking at a special session outlining ambitious goals for a national plan to eliminate hepatitis C virus (HCV) infections by the year 2050.
The session was held at the annual meeting of the American Association for the Study of Liver Diseases.
A public health crisis
Dr. Collins labeled HCV a public health crisis, citing statistics from the Centers for Disease Control and Prevention that show that the rate of reported acute HCV infection cases increased 400% between 2010 and 2020, with the highest rates among young adults aged 20-39 years.
In addition, an estimated 2.4 million people in the United States are living with chronic HCV infections, but as many as 40% of these people are unaware of their infection, despite broad recommendations for the screening of all adults aged 18 years and older, he said.
“Our goal is to try to do something to change this,” Dr. Collins said. He noted that for the past 8 years we have had highly effective oral agents that don’t just treat the disease but cure it – 95%-97% of the time, with only 8-12 weeks of oral therapy and relatively few side effects.
“A wonderful story, one of the most exciting stories that’s come out of biomedical research in the last couple of decades,” he said.
Yet Dr. Collins also acknowledged that the task of developing a national plan is daunting, despite that pharmaceutical triumph.
National pharmacy claims data show that the number of persons treated for HCV with direct-acting antiviral agents (DAAs) in the United States declined from a high of 164,247 in 2015 to 83,740 in 2020.
Furthermore, CDC data from 2019 and 2020 show that, of persons with a diagnosis of HCV infection, only 23% of those on Medicaid, 28% of those on Medicare, and 35% of those with private insurance were treated for their infections.
“We have a huge gap here between the ability to know you have the disease and to get treatment, and we don’t see the numbers here for the uninsured, or people in prisons, but they’re probably much worse,” he said.
Obstacles abound, as do ways to overcome them
Current barriers to treatment include the aforementioned lack of awareness of infection, a “clunky” two-step diagnosis requiring an antibody test followed by an RNA or core antigen test necessitating three visits often separated by several weeks, and the high cost of treatment (around $90,000 per patient).
In addition, insurers commonly require proof that patients remain sober for extended periods, insist that treatment monitoring be performed by specialists only, and often approve treatment only for those patients who have documented evidence of liver damage.
“Does that make sense to you?” Dr. Collins asked. “You’ve got a cure for a liver disease, and you have to wait and show that the liver’s been damaged before you receive it? That just doesn’t fit,” he said.
Dr. Collins also pointed out that we’re dealing with hard-to-reach populations (underserved, uninsured, justice-involved), and people who are in tough times. “Anything that you put in the way as a barrier is going to make this worse in terms of its ability to be implemented,” he said.
To demonstrate how a coordinated HCV-elimination program could work, Dr. Collins pointed to a Medicaid cohort study in Louisiana conducted from July 2019 through December 2021, in which 8,867 patients started on therapy, 7,763 (88%) completed therapy, and 5,882 (66%) returned for testing. Of those tested, 5,285 (90%) had sustained virologic responses.
Another model of a hepatitis C elimination program was provided by the Veterans Health Administration. They received funding for an effort for all veterans, and in the space of 7 years were able to reach out even to some of their difficult-to-reach populations and achieve high diagnosis and treatment rates in a way that could be a model for what we would want to do across the nation, Dr. Collins noted.
Doing the math
Also at the session, Jagpreet Chhatwal, PhD, director of the Massachusetts General Hospital Institute for Technology Assessment and associate professor of radiology at Harvard Medical School, Boston, described outcomes projected by a mathematical simulation model of the HCV epidemic that he and his colleagues developed.
The HEP-SIM (Hepatitis C Disease Burden Simulation) model evaluates HCV prevalence trends, the number needed to screen and treat to eliminate HCV, HCV-associated clinical outcomes, the cost of an elimination program, and the cost savings that could be realized from preventing long-term complications.
The model seeks to determine whether the upfront costs of a national HCV elimination program could be offset by savings down the road. Specifically, it assumes that within the next 5 years 1.31 million individuals would be diagnosed with HCV and projects that within that time frame 1.52 million would need to be treated to meet HCV elimination goals.
The model shows that, compared with the status quo, a concerted campaign of screening and treatment would prevent more than 10,000 HCV-related deaths by 2030, and 91,000 deaths by 2050.
A coordinated screening program is also projected to prevent 17,000 cases of hepatocellular carcinoma by 2030 and 108,000 cases by 2050, as well as avert 29,000 cases of decompensated cirrhosis by 2030 and 93,000 such cases by 2050.
The cost savings associated with an HCV elimination plan would also be substantial, Dr. Chhatwal said.
According to the model, over the next decade the cumulative costs associated with HCV would decline by $14.2 billion, compared with the status quo. Nearly 80% of those savings ($11.2 billion) would be in Medicare and Medicaid.
The total projected savings from 2024 through 2050 – in disease management, testing, treatment, and pragmatic costs – are estimated at $59.3 billion, Dr. Chhatwal said.
“This is unprecedented,” he said.
Getting it done
Rachael L. Fleurence, PhD, MSc, a health economist currently serving as a senior advisor in the Executive Office of the President, summarized efforts to build a national HCV elimination program with input from federal health care agencies, state health leaders, patients, advocacy groups, drug manufacturers, and insurers.
She noted that a large component and focus of the program will be working on diagnostic test development but also accelerating bringing tests into the United States that are currently unavailable here. “These include point-of-care RNA diagnostic tests, as well as core antigen laboratory tests,” she said.
The program will be designed to offer broad access to curative anti-HCV drugs through a national subscription model that would make DAAs available to Medicaid recipients, justice-involved populations, the uninsured, and American Indians and Alaskan Natives who receive care through the Indian Health Service.
“On the Medicare and commercial insurance fronts, we’re still exploring different approaches, including potentially a co-pay assistance for Medicare beneficiaries, as well as working with commercial insurers to reduce barriers to access,” she said.
The program would also involve screening strategies extending to more settings, especially for high-risk populations, expanding the number of providers allowed to screen and treat HCV infections through telehealth, ensuring incentives for providers, and increasing the number of community health workers and case workers to improve linkage to care.
The next steps for the program would include funding to support the NIH’s RADx diagnostics program to accelerate access to testing, planning for the subscription model for DAA purchase, and launching pilot programs with the CDC, the Health Resources and Services Administration, the Substance Abuse and Mental Health Services Administration, and the Indian Health Service.
A call to action
Dr. Collins ended this portion of the program with an exhortation to AASLD members to do their part.
“We need your help,” Dr. Collins said. “This is a bold initiative, but it’s an opportunity. It’s even a responsibility. If we can actually succeed at this kind of outreach and save lives, and at the same time save money, how can we not do that?”
Dr. Collins, Dr. Chhatwal, and Dr. Fleurence each reported having no financial conflicts.
A version of this article first appeared on Medscape.com.
WASHINGTON – “We don’t get to use the ‘eliminate’ word all that often with a disease that’s taking thousands or tens of thousands – or worldwide, hundreds of thousands – of lives every year, but we have that opportunity with hepatitis C.”
So said Francis S. Collins, MD, PhD, special projects advisor to the Executive Office of the President of the United States, and former director of the National Institutes of Health, speaking at a special session outlining ambitious goals for a national plan to eliminate hepatitis C virus (HCV) infections by the year 2050.
The session was held at the annual meeting of the American Association for the Study of Liver Diseases.
A public health crisis
Dr. Collins labeled HCV a public health crisis, citing statistics from the Centers for Disease Control and Prevention that show that the rate of reported acute HCV infection cases increased 400% between 2010 and 2020, with the highest rates among young adults aged 20-39 years.
In addition, an estimated 2.4 million people in the United States are living with chronic HCV infections, but as many as 40% of these people are unaware of their infection, despite broad recommendations for the screening of all adults aged 18 years and older, he said.
“Our goal is to try to do something to change this,” Dr. Collins said. He noted that for the past 8 years we have had highly effective oral agents that don’t just treat the disease but cure it – 95%-97% of the time, with only 8-12 weeks of oral therapy and relatively few side effects.
“A wonderful story, one of the most exciting stories that’s come out of biomedical research in the last couple of decades,” he said.
Yet Dr. Collins also acknowledged that the task of developing a national plan is daunting, despite that pharmaceutical triumph.
National pharmacy claims data show that the number of persons treated for HCV with direct-acting antiviral agents (DAAs) in the United States declined from a high of 164,247 in 2015 to 83,740 in 2020.
Furthermore, CDC data from 2019 and 2020 show that, of persons with a diagnosis of HCV infection, only 23% of those on Medicaid, 28% of those on Medicare, and 35% of those with private insurance were treated for their infections.
“We have a huge gap here between the ability to know you have the disease and to get treatment, and we don’t see the numbers here for the uninsured, or people in prisons, but they’re probably much worse,” he said.
Obstacles abound, as do ways to overcome them
Current barriers to treatment include the aforementioned lack of awareness of infection, a “clunky” two-step diagnosis requiring an antibody test followed by an RNA or core antigen test necessitating three visits often separated by several weeks, and the high cost of treatment (around $90,000 per patient).
In addition, insurers commonly require proof that patients remain sober for extended periods, insist that treatment monitoring be performed by specialists only, and often approve treatment only for those patients who have documented evidence of liver damage.
“Does that make sense to you?” Dr. Collins asked. “You’ve got a cure for a liver disease, and you have to wait and show that the liver’s been damaged before you receive it? That just doesn’t fit,” he said.
Dr. Collins also pointed out that we’re dealing with hard-to-reach populations (underserved, uninsured, justice-involved), and people who are in tough times. “Anything that you put in the way as a barrier is going to make this worse in terms of its ability to be implemented,” he said.
To demonstrate how a coordinated HCV-elimination program could work, Dr. Collins pointed to a Medicaid cohort study in Louisiana conducted from July 2019 through December 2021, in which 8,867 patients started on therapy, 7,763 (88%) completed therapy, and 5,882 (66%) returned for testing. Of those tested, 5,285 (90%) had sustained virologic responses.
Another model of a hepatitis C elimination program was provided by the Veterans Health Administration. They received funding for an effort for all veterans, and in the space of 7 years were able to reach out even to some of their difficult-to-reach populations and achieve high diagnosis and treatment rates in a way that could be a model for what we would want to do across the nation, Dr. Collins noted.
Doing the math
Also at the session, Jagpreet Chhatwal, PhD, director of the Massachusetts General Hospital Institute for Technology Assessment and associate professor of radiology at Harvard Medical School, Boston, described outcomes projected by a mathematical simulation model of the HCV epidemic that he and his colleagues developed.
The HEP-SIM (Hepatitis C Disease Burden Simulation) model evaluates HCV prevalence trends, the number needed to screen and treat to eliminate HCV, HCV-associated clinical outcomes, the cost of an elimination program, and the cost savings that could be realized from preventing long-term complications.
The model seeks to determine whether the upfront costs of a national HCV elimination program could be offset by savings down the road. Specifically, it assumes that within the next 5 years 1.31 million individuals would be diagnosed with HCV and projects that within that time frame 1.52 million would need to be treated to meet HCV elimination goals.
The model shows that, compared with the status quo, a concerted campaign of screening and treatment would prevent more than 10,000 HCV-related deaths by 2030, and 91,000 deaths by 2050.
A coordinated screening program is also projected to prevent 17,000 cases of hepatocellular carcinoma by 2030 and 108,000 cases by 2050, as well as avert 29,000 cases of decompensated cirrhosis by 2030 and 93,000 such cases by 2050.
The cost savings associated with an HCV elimination plan would also be substantial, Dr. Chhatwal said.
According to the model, over the next decade the cumulative costs associated with HCV would decline by $14.2 billion, compared with the status quo. Nearly 80% of those savings ($11.2 billion) would be in Medicare and Medicaid.
The total projected savings from 2024 through 2050 – in disease management, testing, treatment, and pragmatic costs – are estimated at $59.3 billion, Dr. Chhatwal said.
“This is unprecedented,” he said.
Getting it done
Rachael L. Fleurence, PhD, MSc, a health economist currently serving as a senior advisor in the Executive Office of the President, summarized efforts to build a national HCV elimination program with input from federal health care agencies, state health leaders, patients, advocacy groups, drug manufacturers, and insurers.
She noted that a large component and focus of the program will be working on diagnostic test development but also accelerating bringing tests into the United States that are currently unavailable here. “These include point-of-care RNA diagnostic tests, as well as core antigen laboratory tests,” she said.
The program will be designed to offer broad access to curative anti-HCV drugs through a national subscription model that would make DAAs available to Medicaid recipients, justice-involved populations, the uninsured, and American Indians and Alaskan Natives who receive care through the Indian Health Service.
“On the Medicare and commercial insurance fronts, we’re still exploring different approaches, including potentially a co-pay assistance for Medicare beneficiaries, as well as working with commercial insurers to reduce barriers to access,” she said.
The program would also involve screening strategies extending to more settings, especially for high-risk populations, expanding the number of providers allowed to screen and treat HCV infections through telehealth, ensuring incentives for providers, and increasing the number of community health workers and case workers to improve linkage to care.
The next steps for the program would include funding to support the NIH’s RADx diagnostics program to accelerate access to testing, planning for the subscription model for DAA purchase, and launching pilot programs with the CDC, the Health Resources and Services Administration, the Substance Abuse and Mental Health Services Administration, and the Indian Health Service.
A call to action
Dr. Collins ended this portion of the program with an exhortation to AASLD members to do their part.
“We need your help,” Dr. Collins said. “This is a bold initiative, but it’s an opportunity. It’s even a responsibility. If we can actually succeed at this kind of outreach and save lives, and at the same time save money, how can we not do that?”
Dr. Collins, Dr. Chhatwal, and Dr. Fleurence each reported having no financial conflicts.
A version of this article first appeared on Medscape.com.
WASHINGTON – “We don’t get to use the ‘eliminate’ word all that often with a disease that’s taking thousands or tens of thousands – or worldwide, hundreds of thousands – of lives every year, but we have that opportunity with hepatitis C.”
So said Francis S. Collins, MD, PhD, special projects advisor to the Executive Office of the President of the United States, and former director of the National Institutes of Health, speaking at a special session outlining ambitious goals for a national plan to eliminate hepatitis C virus (HCV) infections by the year 2050.
The session was held at the annual meeting of the American Association for the Study of Liver Diseases.
A public health crisis
Dr. Collins labeled HCV a public health crisis, citing statistics from the Centers for Disease Control and Prevention that show that the rate of reported acute HCV infection cases increased 400% between 2010 and 2020, with the highest rates among young adults aged 20-39 years.
In addition, an estimated 2.4 million people in the United States are living with chronic HCV infections, but as many as 40% of these people are unaware of their infection, despite broad recommendations for the screening of all adults aged 18 years and older, he said.
“Our goal is to try to do something to change this,” Dr. Collins said. He noted that for the past 8 years we have had highly effective oral agents that don’t just treat the disease but cure it – 95%-97% of the time, with only 8-12 weeks of oral therapy and relatively few side effects.
“A wonderful story, one of the most exciting stories that’s come out of biomedical research in the last couple of decades,” he said.
Yet Dr. Collins also acknowledged that the task of developing a national plan is daunting, despite that pharmaceutical triumph.
National pharmacy claims data show that the number of persons treated for HCV with direct-acting antiviral agents (DAAs) in the United States declined from a high of 164,247 in 2015 to 83,740 in 2020.
Furthermore, CDC data from 2019 and 2020 show that, of persons with a diagnosis of HCV infection, only 23% of those on Medicaid, 28% of those on Medicare, and 35% of those with private insurance were treated for their infections.
“We have a huge gap here between the ability to know you have the disease and to get treatment, and we don’t see the numbers here for the uninsured, or people in prisons, but they’re probably much worse,” he said.
Obstacles abound, as do ways to overcome them
Current barriers to treatment include the aforementioned lack of awareness of infection, a “clunky” two-step diagnosis requiring an antibody test followed by an RNA or core antigen test necessitating three visits often separated by several weeks, and the high cost of treatment (around $90,000 per patient).
In addition, insurers commonly require proof that patients remain sober for extended periods, insist that treatment monitoring be performed by specialists only, and often approve treatment only for those patients who have documented evidence of liver damage.
“Does that make sense to you?” Dr. Collins asked. “You’ve got a cure for a liver disease, and you have to wait and show that the liver’s been damaged before you receive it? That just doesn’t fit,” he said.
Dr. Collins also pointed out that we’re dealing with hard-to-reach populations (underserved, uninsured, justice-involved), and people who are in tough times. “Anything that you put in the way as a barrier is going to make this worse in terms of its ability to be implemented,” he said.
To demonstrate how a coordinated HCV-elimination program could work, Dr. Collins pointed to a Medicaid cohort study in Louisiana conducted from July 2019 through December 2021, in which 8,867 patients started on therapy, 7,763 (88%) completed therapy, and 5,882 (66%) returned for testing. Of those tested, 5,285 (90%) had sustained virologic responses.
Another model of a hepatitis C elimination program was provided by the Veterans Health Administration. They received funding for an effort for all veterans, and in the space of 7 years were able to reach out even to some of their difficult-to-reach populations and achieve high diagnosis and treatment rates in a way that could be a model for what we would want to do across the nation, Dr. Collins noted.
Doing the math
Also at the session, Jagpreet Chhatwal, PhD, director of the Massachusetts General Hospital Institute for Technology Assessment and associate professor of radiology at Harvard Medical School, Boston, described outcomes projected by a mathematical simulation model of the HCV epidemic that he and his colleagues developed.
The HEP-SIM (Hepatitis C Disease Burden Simulation) model evaluates HCV prevalence trends, the number needed to screen and treat to eliminate HCV, HCV-associated clinical outcomes, the cost of an elimination program, and the cost savings that could be realized from preventing long-term complications.
The model seeks to determine whether the upfront costs of a national HCV elimination program could be offset by savings down the road. Specifically, it assumes that within the next 5 years 1.31 million individuals would be diagnosed with HCV and projects that within that time frame 1.52 million would need to be treated to meet HCV elimination goals.
The model shows that, compared with the status quo, a concerted campaign of screening and treatment would prevent more than 10,000 HCV-related deaths by 2030, and 91,000 deaths by 2050.
A coordinated screening program is also projected to prevent 17,000 cases of hepatocellular carcinoma by 2030 and 108,000 cases by 2050, as well as avert 29,000 cases of decompensated cirrhosis by 2030 and 93,000 such cases by 2050.
The cost savings associated with an HCV elimination plan would also be substantial, Dr. Chhatwal said.
According to the model, over the next decade the cumulative costs associated with HCV would decline by $14.2 billion, compared with the status quo. Nearly 80% of those savings ($11.2 billion) would be in Medicare and Medicaid.
The total projected savings from 2024 through 2050 – in disease management, testing, treatment, and pragmatic costs – are estimated at $59.3 billion, Dr. Chhatwal said.
“This is unprecedented,” he said.
Getting it done
Rachael L. Fleurence, PhD, MSc, a health economist currently serving as a senior advisor in the Executive Office of the President, summarized efforts to build a national HCV elimination program with input from federal health care agencies, state health leaders, patients, advocacy groups, drug manufacturers, and insurers.
She noted that a large component and focus of the program will be working on diagnostic test development but also accelerating bringing tests into the United States that are currently unavailable here. “These include point-of-care RNA diagnostic tests, as well as core antigen laboratory tests,” she said.
The program will be designed to offer broad access to curative anti-HCV drugs through a national subscription model that would make DAAs available to Medicaid recipients, justice-involved populations, the uninsured, and American Indians and Alaskan Natives who receive care through the Indian Health Service.
“On the Medicare and commercial insurance fronts, we’re still exploring different approaches, including potentially a co-pay assistance for Medicare beneficiaries, as well as working with commercial insurers to reduce barriers to access,” she said.
The program would also involve screening strategies extending to more settings, especially for high-risk populations, expanding the number of providers allowed to screen and treat HCV infections through telehealth, ensuring incentives for providers, and increasing the number of community health workers and case workers to improve linkage to care.
The next steps for the program would include funding to support the NIH’s RADx diagnostics program to accelerate access to testing, planning for the subscription model for DAA purchase, and launching pilot programs with the CDC, the Health Resources and Services Administration, the Substance Abuse and Mental Health Services Administration, and the Indian Health Service.
A call to action
Dr. Collins ended this portion of the program with an exhortation to AASLD members to do their part.
“We need your help,” Dr. Collins said. “This is a bold initiative, but it’s an opportunity. It’s even a responsibility. If we can actually succeed at this kind of outreach and save lives, and at the same time save money, how can we not do that?”
Dr. Collins, Dr. Chhatwal, and Dr. Fleurence each reported having no financial conflicts.
A version of this article first appeared on Medscape.com.
AT THE LIVER MEETING
Hospital financial decisions play a role in the critical shortage of pediatric beds for RSV patients
The dire shortage of pediatric hospital beds plaguing the nation in the fall of 2022 is a byproduct of financial decisions made by hospitals over the past decade, as they shuttered children’s wards, which often operate in the red, and expanded the number of beds available for more profitable endeavors like joint replacements and cancer care.
To cope with the flood of young patients sickened by a sweeping convergence of nasty bugs – especially respiratory syncytial virus, influenza, and coronavirus – medical centers nationwide have deployed triage tents, delayed elective surgeries, and transferred critically ill children out of state.
A major factor in the bed shortage is a years-long trend among hospitals of eliminating pediatric units, which tend to be less profitable than adult units, said Mark Wietecha, MS, MBA, CEO of the Children’s Hospital Association. Hospitals optimize revenue by striving to keep their beds 100% full – and filled with patients whose conditions command generous insurance reimbursements.
“It really has to do with dollars,” said Scott Krugman, MD, MS, vice chair of pediatrics at the Herman and Walter Samuelson Children’s Hospital at Sinai in Baltimore. “Hospitals rely on high-volume, high-reimbursement procedures from good payers to make money. There’s no incentive for hospitals to provide money-losing services.”
The number of pediatric inpatient units in hospitals fell 19% from 2008 to 2018, according to a study published in 2021 in the journal Pediatrics. Just this year, hospitals have closed pediatric units in Boston and Springfield, Mass.; Richmond, Va.; and Tulsa, Okla.
The current surge in dangerous respiratory illnesses among children is yet another example of how COVID-19 has upended the health care system. The lockdowns and isolation that marked the first years of the pandemic left kids largely unexposed – and still vulnerable – to viruses other than COVID for two winters, and doctors are now essentially treating multiple years’ worth of respiratory ailments.
The pandemic also accelerated changes in the health care industry that have left many communities with fewer hospital beds available for children who are acutely ill, along with fewer doctors and nurses to care for them.
When intensive care units were flooded with older COVID patients in 2020, some hospitals began using children’s beds to treat adults. Many of those pediatric beds haven’t been restored, said Daniel Rauch, MD, chair of the American Academy of Pediatrics’ committee on hospital care.
In addition, the relentless pace of the pandemic has spurred more than 230,000 health care providers – including doctors, nurses, and physician assistants – to quit. Before the pandemic, about 10% of nurses left their jobs every year; the rate has risen to about 20%, Dr. Wietecha said. He estimates that pediatric hospitals are unable to maintain as many as 10% of their beds because of staffing shortages.
“There is just not enough space for all the kids who need beds,” said Megan Ranney, MD, MPH, who works in several emergency departments in Providence, R.I., including Hasbro Children’s Hospital. The number of children seeking emergency care in recent weeks was 25% higher than the hospital’s previous record.
“We have doctors who are cleaning beds so we can get children into them faster,” said Dr. Ranney, a deputy dean at Brown University’s School of Public Health.
There’s not great money in treating kids. About 40% of U.S. children are covered by Medicaid, a joint federal-state program for low-income patients and people with disabilities. Base Medicaid rates are typically more than 20% below those paid by Medicare, the government insurance program for older adults, and are even lower when compared with private insurance. While specialty care for a range of common adult procedures, from knee and hip replacements to heart surgeries and cancer treatments, generates major profits for medical centers, hospitals complain they typically lose money on inpatient pediatric care.
When Tufts Children’s Hospital closed 41 pediatric beds this summer, hospital officials assured residents that young patients could receive care at nearby Boston Children’s Hospital. Now, Boston Children’s is delaying some elective surgeries to make room for kids who are acutely ill.
Dr. Rauch noted that children’s hospitals, which specialize in treating rare and serious conditions such as pediatric cancer, cystic fibrosis, and heart defects, simply aren’t designed to handle this season’s crush of kids acutely ill with respiratory bugs.
Even before the autumn’s viral trifecta, pediatric units were straining to absorb rising numbers of young people in acute mental distress. Stories abound of children in mental crises being marooned for weeks in emergency departments while awaiting transfer to a pediatric psychiatric unit. On a good day, Dr. Ranney said, 20% of pediatric emergency room beds at Hasbro Children’s Hospital are occupied by children experiencing mental health issues.
In hopes of adding pediatric capacity, the American Academy of Pediatrics joined the Children’s Hospital Association last month in calling on the White House to declare a national emergency due to child respiratory infections and provide additional resources to help cover the costs of care. The Biden administration has said that the flexibility hospital systems and providers have been given during the pandemic to sidestep certain staffing requirements also applies to RSV and flu.
Doernbecher Children’s Hospital at Oregon Health & Science University has shifted to “crisis standards of care,” enabling intensive care nurses to treat more patients than they’re usually assigned. Hospitals in Atlanta, Pittsburgh, and Aurora, Colorado, meanwhile, have resorted to treating young patients in overflow tents in parking lots.
Alex Kon, MD, a pediatric critical care physician at Community Medical Center in Missoula, Mont., said providers there have made plans to care for older kids in the adult intensive care unit, and to divert ambulances to other facilities when necessary. With only three pediatric ICUs in the state, that means young patients may be flown as far as Seattle or Spokane, Wash., or Idaho.
Hollis Lillard took her 1-year-old son, Calder, to an Army hospital in Northern Virginia last month after he experienced several days of fever, coughing, and labored breathing. They spent 7 anguished hours in the emergency room before the hospital found an open bed and transferred them by ambulance to Walter Reed National Military Medical Center in Maryland.
With proper therapy and instructions for home care, Calder’s virus was readily treatable: He recovered after he was given oxygen and treated with steroids, which fight inflammation, and albuterol, which counteracts bronchospasms. He was discharged the next day.
Although hospitalizations for RSV are falling, rates remain well above the norm for this time of year. And hospitals may not get much relief.
People can be infected with RSV more than once a year, and Dr. Krugman worries about a resurgence in the months to come. Because of the coronavirus, which competes with other viruses, “the usual seasonal pattern of viruses has gone out the window,” he said.
Like RSV, influenza arrived early this season. Both viruses usually peak around January. Three strains of flu are circulating and have caused an estimated 8.7 million illnesses, 78,000 hospitalizations, and 4,500 deaths, according to the Centers for Disease Control and Prevention.
Dr. Krugman doubts the health care industry will learn any quick lessons from the current crisis. “Unless there is a radical change in how we pay for pediatric hospital care,” Dr. Krugman said, “the bed shortage is only going to get worse.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The dire shortage of pediatric hospital beds plaguing the nation in the fall of 2022 is a byproduct of financial decisions made by hospitals over the past decade, as they shuttered children’s wards, which often operate in the red, and expanded the number of beds available for more profitable endeavors like joint replacements and cancer care.
To cope with the flood of young patients sickened by a sweeping convergence of nasty bugs – especially respiratory syncytial virus, influenza, and coronavirus – medical centers nationwide have deployed triage tents, delayed elective surgeries, and transferred critically ill children out of state.
A major factor in the bed shortage is a years-long trend among hospitals of eliminating pediatric units, which tend to be less profitable than adult units, said Mark Wietecha, MS, MBA, CEO of the Children’s Hospital Association. Hospitals optimize revenue by striving to keep their beds 100% full – and filled with patients whose conditions command generous insurance reimbursements.
“It really has to do with dollars,” said Scott Krugman, MD, MS, vice chair of pediatrics at the Herman and Walter Samuelson Children’s Hospital at Sinai in Baltimore. “Hospitals rely on high-volume, high-reimbursement procedures from good payers to make money. There’s no incentive for hospitals to provide money-losing services.”
The number of pediatric inpatient units in hospitals fell 19% from 2008 to 2018, according to a study published in 2021 in the journal Pediatrics. Just this year, hospitals have closed pediatric units in Boston and Springfield, Mass.; Richmond, Va.; and Tulsa, Okla.
The current surge in dangerous respiratory illnesses among children is yet another example of how COVID-19 has upended the health care system. The lockdowns and isolation that marked the first years of the pandemic left kids largely unexposed – and still vulnerable – to viruses other than COVID for two winters, and doctors are now essentially treating multiple years’ worth of respiratory ailments.
The pandemic also accelerated changes in the health care industry that have left many communities with fewer hospital beds available for children who are acutely ill, along with fewer doctors and nurses to care for them.
When intensive care units were flooded with older COVID patients in 2020, some hospitals began using children’s beds to treat adults. Many of those pediatric beds haven’t been restored, said Daniel Rauch, MD, chair of the American Academy of Pediatrics’ committee on hospital care.
In addition, the relentless pace of the pandemic has spurred more than 230,000 health care providers – including doctors, nurses, and physician assistants – to quit. Before the pandemic, about 10% of nurses left their jobs every year; the rate has risen to about 20%, Dr. Wietecha said. He estimates that pediatric hospitals are unable to maintain as many as 10% of their beds because of staffing shortages.
“There is just not enough space for all the kids who need beds,” said Megan Ranney, MD, MPH, who works in several emergency departments in Providence, R.I., including Hasbro Children’s Hospital. The number of children seeking emergency care in recent weeks was 25% higher than the hospital’s previous record.
“We have doctors who are cleaning beds so we can get children into them faster,” said Dr. Ranney, a deputy dean at Brown University’s School of Public Health.
There’s not great money in treating kids. About 40% of U.S. children are covered by Medicaid, a joint federal-state program for low-income patients and people with disabilities. Base Medicaid rates are typically more than 20% below those paid by Medicare, the government insurance program for older adults, and are even lower when compared with private insurance. While specialty care for a range of common adult procedures, from knee and hip replacements to heart surgeries and cancer treatments, generates major profits for medical centers, hospitals complain they typically lose money on inpatient pediatric care.
When Tufts Children’s Hospital closed 41 pediatric beds this summer, hospital officials assured residents that young patients could receive care at nearby Boston Children’s Hospital. Now, Boston Children’s is delaying some elective surgeries to make room for kids who are acutely ill.
Dr. Rauch noted that children’s hospitals, which specialize in treating rare and serious conditions such as pediatric cancer, cystic fibrosis, and heart defects, simply aren’t designed to handle this season’s crush of kids acutely ill with respiratory bugs.
Even before the autumn’s viral trifecta, pediatric units were straining to absorb rising numbers of young people in acute mental distress. Stories abound of children in mental crises being marooned for weeks in emergency departments while awaiting transfer to a pediatric psychiatric unit. On a good day, Dr. Ranney said, 20% of pediatric emergency room beds at Hasbro Children’s Hospital are occupied by children experiencing mental health issues.
In hopes of adding pediatric capacity, the American Academy of Pediatrics joined the Children’s Hospital Association last month in calling on the White House to declare a national emergency due to child respiratory infections and provide additional resources to help cover the costs of care. The Biden administration has said that the flexibility hospital systems and providers have been given during the pandemic to sidestep certain staffing requirements also applies to RSV and flu.
Doernbecher Children’s Hospital at Oregon Health & Science University has shifted to “crisis standards of care,” enabling intensive care nurses to treat more patients than they’re usually assigned. Hospitals in Atlanta, Pittsburgh, and Aurora, Colorado, meanwhile, have resorted to treating young patients in overflow tents in parking lots.
Alex Kon, MD, a pediatric critical care physician at Community Medical Center in Missoula, Mont., said providers there have made plans to care for older kids in the adult intensive care unit, and to divert ambulances to other facilities when necessary. With only three pediatric ICUs in the state, that means young patients may be flown as far as Seattle or Spokane, Wash., or Idaho.
Hollis Lillard took her 1-year-old son, Calder, to an Army hospital in Northern Virginia last month after he experienced several days of fever, coughing, and labored breathing. They spent 7 anguished hours in the emergency room before the hospital found an open bed and transferred them by ambulance to Walter Reed National Military Medical Center in Maryland.
With proper therapy and instructions for home care, Calder’s virus was readily treatable: He recovered after he was given oxygen and treated with steroids, which fight inflammation, and albuterol, which counteracts bronchospasms. He was discharged the next day.
Although hospitalizations for RSV are falling, rates remain well above the norm for this time of year. And hospitals may not get much relief.
People can be infected with RSV more than once a year, and Dr. Krugman worries about a resurgence in the months to come. Because of the coronavirus, which competes with other viruses, “the usual seasonal pattern of viruses has gone out the window,” he said.
Like RSV, influenza arrived early this season. Both viruses usually peak around January. Three strains of flu are circulating and have caused an estimated 8.7 million illnesses, 78,000 hospitalizations, and 4,500 deaths, according to the Centers for Disease Control and Prevention.
Dr. Krugman doubts the health care industry will learn any quick lessons from the current crisis. “Unless there is a radical change in how we pay for pediatric hospital care,” Dr. Krugman said, “the bed shortage is only going to get worse.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The dire shortage of pediatric hospital beds plaguing the nation in the fall of 2022 is a byproduct of financial decisions made by hospitals over the past decade, as they shuttered children’s wards, which often operate in the red, and expanded the number of beds available for more profitable endeavors like joint replacements and cancer care.
To cope with the flood of young patients sickened by a sweeping convergence of nasty bugs – especially respiratory syncytial virus, influenza, and coronavirus – medical centers nationwide have deployed triage tents, delayed elective surgeries, and transferred critically ill children out of state.
A major factor in the bed shortage is a years-long trend among hospitals of eliminating pediatric units, which tend to be less profitable than adult units, said Mark Wietecha, MS, MBA, CEO of the Children’s Hospital Association. Hospitals optimize revenue by striving to keep their beds 100% full – and filled with patients whose conditions command generous insurance reimbursements.
“It really has to do with dollars,” said Scott Krugman, MD, MS, vice chair of pediatrics at the Herman and Walter Samuelson Children’s Hospital at Sinai in Baltimore. “Hospitals rely on high-volume, high-reimbursement procedures from good payers to make money. There’s no incentive for hospitals to provide money-losing services.”
The number of pediatric inpatient units in hospitals fell 19% from 2008 to 2018, according to a study published in 2021 in the journal Pediatrics. Just this year, hospitals have closed pediatric units in Boston and Springfield, Mass.; Richmond, Va.; and Tulsa, Okla.
The current surge in dangerous respiratory illnesses among children is yet another example of how COVID-19 has upended the health care system. The lockdowns and isolation that marked the first years of the pandemic left kids largely unexposed – and still vulnerable – to viruses other than COVID for two winters, and doctors are now essentially treating multiple years’ worth of respiratory ailments.
The pandemic also accelerated changes in the health care industry that have left many communities with fewer hospital beds available for children who are acutely ill, along with fewer doctors and nurses to care for them.
When intensive care units were flooded with older COVID patients in 2020, some hospitals began using children’s beds to treat adults. Many of those pediatric beds haven’t been restored, said Daniel Rauch, MD, chair of the American Academy of Pediatrics’ committee on hospital care.
In addition, the relentless pace of the pandemic has spurred more than 230,000 health care providers – including doctors, nurses, and physician assistants – to quit. Before the pandemic, about 10% of nurses left their jobs every year; the rate has risen to about 20%, Dr. Wietecha said. He estimates that pediatric hospitals are unable to maintain as many as 10% of their beds because of staffing shortages.
“There is just not enough space for all the kids who need beds,” said Megan Ranney, MD, MPH, who works in several emergency departments in Providence, R.I., including Hasbro Children’s Hospital. The number of children seeking emergency care in recent weeks was 25% higher than the hospital’s previous record.
“We have doctors who are cleaning beds so we can get children into them faster,” said Dr. Ranney, a deputy dean at Brown University’s School of Public Health.
There’s not great money in treating kids. About 40% of U.S. children are covered by Medicaid, a joint federal-state program for low-income patients and people with disabilities. Base Medicaid rates are typically more than 20% below those paid by Medicare, the government insurance program for older adults, and are even lower when compared with private insurance. While specialty care for a range of common adult procedures, from knee and hip replacements to heart surgeries and cancer treatments, generates major profits for medical centers, hospitals complain they typically lose money on inpatient pediatric care.
When Tufts Children’s Hospital closed 41 pediatric beds this summer, hospital officials assured residents that young patients could receive care at nearby Boston Children’s Hospital. Now, Boston Children’s is delaying some elective surgeries to make room for kids who are acutely ill.
Dr. Rauch noted that children’s hospitals, which specialize in treating rare and serious conditions such as pediatric cancer, cystic fibrosis, and heart defects, simply aren’t designed to handle this season’s crush of kids acutely ill with respiratory bugs.
Even before the autumn’s viral trifecta, pediatric units were straining to absorb rising numbers of young people in acute mental distress. Stories abound of children in mental crises being marooned for weeks in emergency departments while awaiting transfer to a pediatric psychiatric unit. On a good day, Dr. Ranney said, 20% of pediatric emergency room beds at Hasbro Children’s Hospital are occupied by children experiencing mental health issues.
In hopes of adding pediatric capacity, the American Academy of Pediatrics joined the Children’s Hospital Association last month in calling on the White House to declare a national emergency due to child respiratory infections and provide additional resources to help cover the costs of care. The Biden administration has said that the flexibility hospital systems and providers have been given during the pandemic to sidestep certain staffing requirements also applies to RSV and flu.
Doernbecher Children’s Hospital at Oregon Health & Science University has shifted to “crisis standards of care,” enabling intensive care nurses to treat more patients than they’re usually assigned. Hospitals in Atlanta, Pittsburgh, and Aurora, Colorado, meanwhile, have resorted to treating young patients in overflow tents in parking lots.
Alex Kon, MD, a pediatric critical care physician at Community Medical Center in Missoula, Mont., said providers there have made plans to care for older kids in the adult intensive care unit, and to divert ambulances to other facilities when necessary. With only three pediatric ICUs in the state, that means young patients may be flown as far as Seattle or Spokane, Wash., or Idaho.
Hollis Lillard took her 1-year-old son, Calder, to an Army hospital in Northern Virginia last month after he experienced several days of fever, coughing, and labored breathing. They spent 7 anguished hours in the emergency room before the hospital found an open bed and transferred them by ambulance to Walter Reed National Military Medical Center in Maryland.
With proper therapy and instructions for home care, Calder’s virus was readily treatable: He recovered after he was given oxygen and treated with steroids, which fight inflammation, and albuterol, which counteracts bronchospasms. He was discharged the next day.
Although hospitalizations for RSV are falling, rates remain well above the norm for this time of year. And hospitals may not get much relief.
People can be infected with RSV more than once a year, and Dr. Krugman worries about a resurgence in the months to come. Because of the coronavirus, which competes with other viruses, “the usual seasonal pattern of viruses has gone out the window,” he said.
Like RSV, influenza arrived early this season. Both viruses usually peak around January. Three strains of flu are circulating and have caused an estimated 8.7 million illnesses, 78,000 hospitalizations, and 4,500 deaths, according to the Centers for Disease Control and Prevention.
Dr. Krugman doubts the health care industry will learn any quick lessons from the current crisis. “Unless there is a radical change in how we pay for pediatric hospital care,” Dr. Krugman said, “the bed shortage is only going to get worse.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.