User login
Elevated inflammation common in children’s severe COVID-19 disease
according to data from 50 patients at a single tertiary care center.
“Risk factors for severe disease in pediatric populations have not been clearly identified and the high prevalence of SARS-CoV-2 in NYC offers an opportunity to describe severe pediatric disease in more detail,” wrote Philip Zachariah, MD, of New York–Presbyterian Hospital, New York, and colleagues.
In a retrospective case series published in JAMA Pediatrics, the researchers reviewed data from 50 patients: 41 classified as severe and 9 classified as nonsevere. Among the patients, 27 were male and 25 were Hispanic. The patient population had a median of 2 days from symptom onset to hospital admission. The most common symptoms were fever (80%) and respiratory symptoms (64%). Seventy-six percent of patients had a median length of stay of 3 days (range 1-30 days).
At hospital admission, children with severe disease had significantly higher levels of several inflammatory markers compared with those without severe disease, notably C-reactive protein (median 8.978 mg/dL vs. 0.64 mg/dL) and procalcitonin (median 0.31 ng/mL vs. 0.17 ng/mL, (P < .001 for both). High mean peak levels of C-reactive protein, procalcitonin, interleukin 6, ferritin, and D-dimer were seen among the nine children (16%) who required mechanical ventilation, Dr. Zachariah and associates said.
None of the 14 infants and 1 of the 8 immunocompromised children in the study had severe disease, the researchers wrote.
Bacterial coinfections detected while patients were hospitalized were bacteremia in 6%, suspected bacterial pneumonia in 18%, urinary tract infections in 10%, skin and soft tissue infections in 6%, and streptococcus pharyngitis in 2%, Dr. Zachariah and associates reported.
Overall, 61% of the children had comorbidities identified in previous COVID-19 studies, of which obesity was the most common (22%); other comorbidities included asthma, sickle cell disease, cardiac disease, and diabetes. Obesity also was significantly associated with the need for mechanical ventilation in children aged 2 years and older (67%). A total of 16 patients required respiratory support, 9 of these were placed on mechanical ventilation; 6 of these 9 children were obese.
Fifteen patients (30%) who met criteria for increased oxygen requirements and respiratory distress received hydroxychloroquine, but the small sample size did not allow for assessment of treatment efficacy, the researchers said.
“Expanding our knowledge of COVID-19 [disease] in children will potentially permit early recognition of SARS-CoV-2 infection, understanding of the natural history of disease, and potential complications, said Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. This review of 50 SARS-CoV-2 infected children (less than 21 years of age) “provides insight into the short period of symptoms prior to hospitalization, challenges the concept that infants less than 1 year are at greatest risk of severe disease (as from the experience in China), and suggests rapid recovery in many children, as median length of stay was 3 days.
“The review revealed two findings that were surprising to me. First, the median length of stay of 3 days. As nearly 20% of the children required mechanical ventilation, it suggests many of the children were discharged quickly after evaluation, suggesting that we need to identify markers of severity to predict those children likely to have progressive disease and require respiratory support,” Dr. Pelton noted.
“The second observation suggests high rates of bacterial infection (bacteremia, pneumonia, UTI, and skin and soft tissue infection). I do not think this has been widely reported in adults, and may represent a difference between child and adult disease. More studies such as this will be required to identify how common coinfection with bacteria is,” he said.
“The take-home message is that although most children with COVID-19 have a mild or even asymptomatic course, some become severely ill requiring ventilator support and potentially ECMO [extracorporeal membrane oxygenation]. Potential predictors of severity include high C-reactive protein, obesity, and older age [adolescence], said Dr. Pelton, who was not involved in the study.
What additional research is needed? Dr. Pelton said that better markers of severe disease are needed, as well as an understanding of why obesity is a risk factor for severe disease in both children and adults. Are these prediabetic patients? he asked.
The study findings were limited by the small sample size and high proportion of Hispanic patients, which may limit generalizability, and some symptoms and comorbidities may have been missed because of the retrospective nature of the study, the researchers noted. However, the results support the need for hospitals to remain vigilant to the variable presentations of COVID-19 infections in children.
“Therapeutic considerations need to [include] the risk of toxicity, control of antiviral replication, and early recognition and management of immune dysregulation,” they concluded.
The study received no outside funding. Dr. Zachariah had no financial conflicts to disclose. Two coauthors reported ties with various pharmaceutical companies and organizations. Dr. Pelton said he had no relevant financial disclosures.
SOURCE: Zachariah P et al. JAMA Pediatr. 2020 June 3. doi:10.1001/jamapediatrics.2020.2430.
according to data from 50 patients at a single tertiary care center.
“Risk factors for severe disease in pediatric populations have not been clearly identified and the high prevalence of SARS-CoV-2 in NYC offers an opportunity to describe severe pediatric disease in more detail,” wrote Philip Zachariah, MD, of New York–Presbyterian Hospital, New York, and colleagues.
In a retrospective case series published in JAMA Pediatrics, the researchers reviewed data from 50 patients: 41 classified as severe and 9 classified as nonsevere. Among the patients, 27 were male and 25 were Hispanic. The patient population had a median of 2 days from symptom onset to hospital admission. The most common symptoms were fever (80%) and respiratory symptoms (64%). Seventy-six percent of patients had a median length of stay of 3 days (range 1-30 days).
At hospital admission, children with severe disease had significantly higher levels of several inflammatory markers compared with those without severe disease, notably C-reactive protein (median 8.978 mg/dL vs. 0.64 mg/dL) and procalcitonin (median 0.31 ng/mL vs. 0.17 ng/mL, (P < .001 for both). High mean peak levels of C-reactive protein, procalcitonin, interleukin 6, ferritin, and D-dimer were seen among the nine children (16%) who required mechanical ventilation, Dr. Zachariah and associates said.
None of the 14 infants and 1 of the 8 immunocompromised children in the study had severe disease, the researchers wrote.
Bacterial coinfections detected while patients were hospitalized were bacteremia in 6%, suspected bacterial pneumonia in 18%, urinary tract infections in 10%, skin and soft tissue infections in 6%, and streptococcus pharyngitis in 2%, Dr. Zachariah and associates reported.
Overall, 61% of the children had comorbidities identified in previous COVID-19 studies, of which obesity was the most common (22%); other comorbidities included asthma, sickle cell disease, cardiac disease, and diabetes. Obesity also was significantly associated with the need for mechanical ventilation in children aged 2 years and older (67%). A total of 16 patients required respiratory support, 9 of these were placed on mechanical ventilation; 6 of these 9 children were obese.
Fifteen patients (30%) who met criteria for increased oxygen requirements and respiratory distress received hydroxychloroquine, but the small sample size did not allow for assessment of treatment efficacy, the researchers said.
“Expanding our knowledge of COVID-19 [disease] in children will potentially permit early recognition of SARS-CoV-2 infection, understanding of the natural history of disease, and potential complications, said Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. This review of 50 SARS-CoV-2 infected children (less than 21 years of age) “provides insight into the short period of symptoms prior to hospitalization, challenges the concept that infants less than 1 year are at greatest risk of severe disease (as from the experience in China), and suggests rapid recovery in many children, as median length of stay was 3 days.
“The review revealed two findings that were surprising to me. First, the median length of stay of 3 days. As nearly 20% of the children required mechanical ventilation, it suggests many of the children were discharged quickly after evaluation, suggesting that we need to identify markers of severity to predict those children likely to have progressive disease and require respiratory support,” Dr. Pelton noted.
“The second observation suggests high rates of bacterial infection (bacteremia, pneumonia, UTI, and skin and soft tissue infection). I do not think this has been widely reported in adults, and may represent a difference between child and adult disease. More studies such as this will be required to identify how common coinfection with bacteria is,” he said.
“The take-home message is that although most children with COVID-19 have a mild or even asymptomatic course, some become severely ill requiring ventilator support and potentially ECMO [extracorporeal membrane oxygenation]. Potential predictors of severity include high C-reactive protein, obesity, and older age [adolescence], said Dr. Pelton, who was not involved in the study.
What additional research is needed? Dr. Pelton said that better markers of severe disease are needed, as well as an understanding of why obesity is a risk factor for severe disease in both children and adults. Are these prediabetic patients? he asked.
The study findings were limited by the small sample size and high proportion of Hispanic patients, which may limit generalizability, and some symptoms and comorbidities may have been missed because of the retrospective nature of the study, the researchers noted. However, the results support the need for hospitals to remain vigilant to the variable presentations of COVID-19 infections in children.
“Therapeutic considerations need to [include] the risk of toxicity, control of antiviral replication, and early recognition and management of immune dysregulation,” they concluded.
The study received no outside funding. Dr. Zachariah had no financial conflicts to disclose. Two coauthors reported ties with various pharmaceutical companies and organizations. Dr. Pelton said he had no relevant financial disclosures.
SOURCE: Zachariah P et al. JAMA Pediatr. 2020 June 3. doi:10.1001/jamapediatrics.2020.2430.
according to data from 50 patients at a single tertiary care center.
“Risk factors for severe disease in pediatric populations have not been clearly identified and the high prevalence of SARS-CoV-2 in NYC offers an opportunity to describe severe pediatric disease in more detail,” wrote Philip Zachariah, MD, of New York–Presbyterian Hospital, New York, and colleagues.
In a retrospective case series published in JAMA Pediatrics, the researchers reviewed data from 50 patients: 41 classified as severe and 9 classified as nonsevere. Among the patients, 27 were male and 25 were Hispanic. The patient population had a median of 2 days from symptom onset to hospital admission. The most common symptoms were fever (80%) and respiratory symptoms (64%). Seventy-six percent of patients had a median length of stay of 3 days (range 1-30 days).
At hospital admission, children with severe disease had significantly higher levels of several inflammatory markers compared with those without severe disease, notably C-reactive protein (median 8.978 mg/dL vs. 0.64 mg/dL) and procalcitonin (median 0.31 ng/mL vs. 0.17 ng/mL, (P < .001 for both). High mean peak levels of C-reactive protein, procalcitonin, interleukin 6, ferritin, and D-dimer were seen among the nine children (16%) who required mechanical ventilation, Dr. Zachariah and associates said.
None of the 14 infants and 1 of the 8 immunocompromised children in the study had severe disease, the researchers wrote.
Bacterial coinfections detected while patients were hospitalized were bacteremia in 6%, suspected bacterial pneumonia in 18%, urinary tract infections in 10%, skin and soft tissue infections in 6%, and streptococcus pharyngitis in 2%, Dr. Zachariah and associates reported.
Overall, 61% of the children had comorbidities identified in previous COVID-19 studies, of which obesity was the most common (22%); other comorbidities included asthma, sickle cell disease, cardiac disease, and diabetes. Obesity also was significantly associated with the need for mechanical ventilation in children aged 2 years and older (67%). A total of 16 patients required respiratory support, 9 of these were placed on mechanical ventilation; 6 of these 9 children were obese.
Fifteen patients (30%) who met criteria for increased oxygen requirements and respiratory distress received hydroxychloroquine, but the small sample size did not allow for assessment of treatment efficacy, the researchers said.
“Expanding our knowledge of COVID-19 [disease] in children will potentially permit early recognition of SARS-CoV-2 infection, understanding of the natural history of disease, and potential complications, said Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. This review of 50 SARS-CoV-2 infected children (less than 21 years of age) “provides insight into the short period of symptoms prior to hospitalization, challenges the concept that infants less than 1 year are at greatest risk of severe disease (as from the experience in China), and suggests rapid recovery in many children, as median length of stay was 3 days.
“The review revealed two findings that were surprising to me. First, the median length of stay of 3 days. As nearly 20% of the children required mechanical ventilation, it suggests many of the children were discharged quickly after evaluation, suggesting that we need to identify markers of severity to predict those children likely to have progressive disease and require respiratory support,” Dr. Pelton noted.
“The second observation suggests high rates of bacterial infection (bacteremia, pneumonia, UTI, and skin and soft tissue infection). I do not think this has been widely reported in adults, and may represent a difference between child and adult disease. More studies such as this will be required to identify how common coinfection with bacteria is,” he said.
“The take-home message is that although most children with COVID-19 have a mild or even asymptomatic course, some become severely ill requiring ventilator support and potentially ECMO [extracorporeal membrane oxygenation]. Potential predictors of severity include high C-reactive protein, obesity, and older age [adolescence], said Dr. Pelton, who was not involved in the study.
What additional research is needed? Dr. Pelton said that better markers of severe disease are needed, as well as an understanding of why obesity is a risk factor for severe disease in both children and adults. Are these prediabetic patients? he asked.
The study findings were limited by the small sample size and high proportion of Hispanic patients, which may limit generalizability, and some symptoms and comorbidities may have been missed because of the retrospective nature of the study, the researchers noted. However, the results support the need for hospitals to remain vigilant to the variable presentations of COVID-19 infections in children.
“Therapeutic considerations need to [include] the risk of toxicity, control of antiviral replication, and early recognition and management of immune dysregulation,” they concluded.
The study received no outside funding. Dr. Zachariah had no financial conflicts to disclose. Two coauthors reported ties with various pharmaceutical companies and organizations. Dr. Pelton said he had no relevant financial disclosures.
SOURCE: Zachariah P et al. JAMA Pediatr. 2020 June 3. doi:10.1001/jamapediatrics.2020.2430.
FROM JAMA PEDIATRICS
Preliminary evidence indicates famotidine might improve COVID-19 symptoms
High-dose oral famotidine might improve cardinal symptoms of COVID-19 infection, according to the findings of a small outpatient case series and a subsequent retrospective study.
After developing COVID-19 symptoms, the 10 patients in the case series began self-medicating with 60-240 mg famotidine daily over a median of 11 days. “All patients reported marked improvements of disease-related symptoms after starting famotidine,” first author Tobias Janowitz, MD, PhD, of Cold Spring Harbor Laboratory, N.Y., and associates wrote in Gut.
Improvements began within 24-48 hours of starting on the histamine-2 receptor antagonist. By 14 days after treatment initiation, all patients reported near-normalization of both respiratory and systemic symptoms, the researchers reported.
The patients were 23-71 years old. Seven tested positive for COVID-19, two had antibodies to COVID-19, and one had a clinical diagnosis of COVID-19 without laboratory confirmation. Over a median of 11 days (range, 5-21 days), six patients self-administered 80 mg famotidine three times daily and four self-administered lower amounts – from 60 to 150 mg of famotidine daily, divided into two or three doses. Patients started on famotidine between 2 and 26 days after symptom onset.
Through phone interviews and questionnaires, the researchers ascertained changes in cough, dyspnea, fatigue, headache, anosmia, and general unwellness by using a modified four-point Eastern Cooperative Oncology Group (ECOG) performance status scale. Improvements were seen across all symptom categories, and respiratory symptoms improved faster than systemic symptoms. Apart from two cases of persistent anosmia, symptoms resolved completely within 14 days of starting famotidine.
Seven patients reported no side effects of famotidine; one reported grade 1 dizziness and infrequent perceptions of tachycardia; one reported grade 1 dizziness, dry skin, and insomnia; and one reported grade 1 gastrointestinal symptoms and temporary forgetfulness. “Other than forgetfulness, all of these side effects are listed in the prescription information for famotidine, and all side effects resolved on discontinuation of famotidine,” the investigators wrote.
While the findings are intriguing, Dr. Janowitz and associates cautioned against overinterpretation of them. Another expert agreed: “This is a preliminary study based on a hypothesized antiviral effect. It’s important to know that it doesn’t really prove it works,” said Amesh Adalja, MD, senior scholar at the Johns Hopkins University Center for Health Security, Baltimore, and a spokesperson for the Infectious Diseases Society of America, during an interview with MDedge.
These patients might have improved anyway, without self-administering famotidine, said Dr. Adalja, who was not involved in the study.
Furthermore, the mechanism by which famotidine might act on COVID-19 remains unclear. The drug “could have a viral target, for example, one of the viral proteases, or a host target, resulting, for example, in modulation of the immunological response to the virus,” Dr. Janowitz and associates wrote.
Dr. Adalja noted that many compounds show effects against COVID-19 that are not well understood. He called for randomized trials to evaluate the biological plausibility of famotidine use, and its potential efficacy.
“This is a cheap, over-the-counter drug, but no drug is without side effects,” he added. “We need to know whether it works.”
Based on the case series findings, researchers conducted another retrospective study of patients hospitalized with COVID-19 infection. Those who were incidentally taking famotidine before or at hospitalization had a significantly reduced risk of intubation or death, with a hazard ratio of 0.43 (Gastroenterology. 2020 May 22. doi: 10.1053/j.gastro.2020.05.053)
The National Institutes of Health provided partial support. The investigators reported having no conflicts of interest.
SOURCE: Janowitz T et al. Gut. 2020 Jun 4. doi: 10.1136/gutjnl-2020-321852.
High-dose oral famotidine might improve cardinal symptoms of COVID-19 infection, according to the findings of a small outpatient case series and a subsequent retrospective study.
After developing COVID-19 symptoms, the 10 patients in the case series began self-medicating with 60-240 mg famotidine daily over a median of 11 days. “All patients reported marked improvements of disease-related symptoms after starting famotidine,” first author Tobias Janowitz, MD, PhD, of Cold Spring Harbor Laboratory, N.Y., and associates wrote in Gut.
Improvements began within 24-48 hours of starting on the histamine-2 receptor antagonist. By 14 days after treatment initiation, all patients reported near-normalization of both respiratory and systemic symptoms, the researchers reported.
The patients were 23-71 years old. Seven tested positive for COVID-19, two had antibodies to COVID-19, and one had a clinical diagnosis of COVID-19 without laboratory confirmation. Over a median of 11 days (range, 5-21 days), six patients self-administered 80 mg famotidine three times daily and four self-administered lower amounts – from 60 to 150 mg of famotidine daily, divided into two or three doses. Patients started on famotidine between 2 and 26 days after symptom onset.
Through phone interviews and questionnaires, the researchers ascertained changes in cough, dyspnea, fatigue, headache, anosmia, and general unwellness by using a modified four-point Eastern Cooperative Oncology Group (ECOG) performance status scale. Improvements were seen across all symptom categories, and respiratory symptoms improved faster than systemic symptoms. Apart from two cases of persistent anosmia, symptoms resolved completely within 14 days of starting famotidine.
Seven patients reported no side effects of famotidine; one reported grade 1 dizziness and infrequent perceptions of tachycardia; one reported grade 1 dizziness, dry skin, and insomnia; and one reported grade 1 gastrointestinal symptoms and temporary forgetfulness. “Other than forgetfulness, all of these side effects are listed in the prescription information for famotidine, and all side effects resolved on discontinuation of famotidine,” the investigators wrote.
While the findings are intriguing, Dr. Janowitz and associates cautioned against overinterpretation of them. Another expert agreed: “This is a preliminary study based on a hypothesized antiviral effect. It’s important to know that it doesn’t really prove it works,” said Amesh Adalja, MD, senior scholar at the Johns Hopkins University Center for Health Security, Baltimore, and a spokesperson for the Infectious Diseases Society of America, during an interview with MDedge.
These patients might have improved anyway, without self-administering famotidine, said Dr. Adalja, who was not involved in the study.
Furthermore, the mechanism by which famotidine might act on COVID-19 remains unclear. The drug “could have a viral target, for example, one of the viral proteases, or a host target, resulting, for example, in modulation of the immunological response to the virus,” Dr. Janowitz and associates wrote.
Dr. Adalja noted that many compounds show effects against COVID-19 that are not well understood. He called for randomized trials to evaluate the biological plausibility of famotidine use, and its potential efficacy.
“This is a cheap, over-the-counter drug, but no drug is without side effects,” he added. “We need to know whether it works.”
Based on the case series findings, researchers conducted another retrospective study of patients hospitalized with COVID-19 infection. Those who were incidentally taking famotidine before or at hospitalization had a significantly reduced risk of intubation or death, with a hazard ratio of 0.43 (Gastroenterology. 2020 May 22. doi: 10.1053/j.gastro.2020.05.053)
The National Institutes of Health provided partial support. The investigators reported having no conflicts of interest.
SOURCE: Janowitz T et al. Gut. 2020 Jun 4. doi: 10.1136/gutjnl-2020-321852.
High-dose oral famotidine might improve cardinal symptoms of COVID-19 infection, according to the findings of a small outpatient case series and a subsequent retrospective study.
After developing COVID-19 symptoms, the 10 patients in the case series began self-medicating with 60-240 mg famotidine daily over a median of 11 days. “All patients reported marked improvements of disease-related symptoms after starting famotidine,” first author Tobias Janowitz, MD, PhD, of Cold Spring Harbor Laboratory, N.Y., and associates wrote in Gut.
Improvements began within 24-48 hours of starting on the histamine-2 receptor antagonist. By 14 days after treatment initiation, all patients reported near-normalization of both respiratory and systemic symptoms, the researchers reported.
The patients were 23-71 years old. Seven tested positive for COVID-19, two had antibodies to COVID-19, and one had a clinical diagnosis of COVID-19 without laboratory confirmation. Over a median of 11 days (range, 5-21 days), six patients self-administered 80 mg famotidine three times daily and four self-administered lower amounts – from 60 to 150 mg of famotidine daily, divided into two or three doses. Patients started on famotidine between 2 and 26 days after symptom onset.
Through phone interviews and questionnaires, the researchers ascertained changes in cough, dyspnea, fatigue, headache, anosmia, and general unwellness by using a modified four-point Eastern Cooperative Oncology Group (ECOG) performance status scale. Improvements were seen across all symptom categories, and respiratory symptoms improved faster than systemic symptoms. Apart from two cases of persistent anosmia, symptoms resolved completely within 14 days of starting famotidine.
Seven patients reported no side effects of famotidine; one reported grade 1 dizziness and infrequent perceptions of tachycardia; one reported grade 1 dizziness, dry skin, and insomnia; and one reported grade 1 gastrointestinal symptoms and temporary forgetfulness. “Other than forgetfulness, all of these side effects are listed in the prescription information for famotidine, and all side effects resolved on discontinuation of famotidine,” the investigators wrote.
While the findings are intriguing, Dr. Janowitz and associates cautioned against overinterpretation of them. Another expert agreed: “This is a preliminary study based on a hypothesized antiviral effect. It’s important to know that it doesn’t really prove it works,” said Amesh Adalja, MD, senior scholar at the Johns Hopkins University Center for Health Security, Baltimore, and a spokesperson for the Infectious Diseases Society of America, during an interview with MDedge.
These patients might have improved anyway, without self-administering famotidine, said Dr. Adalja, who was not involved in the study.
Furthermore, the mechanism by which famotidine might act on COVID-19 remains unclear. The drug “could have a viral target, for example, one of the viral proteases, or a host target, resulting, for example, in modulation of the immunological response to the virus,” Dr. Janowitz and associates wrote.
Dr. Adalja noted that many compounds show effects against COVID-19 that are not well understood. He called for randomized trials to evaluate the biological plausibility of famotidine use, and its potential efficacy.
“This is a cheap, over-the-counter drug, but no drug is without side effects,” he added. “We need to know whether it works.”
Based on the case series findings, researchers conducted another retrospective study of patients hospitalized with COVID-19 infection. Those who were incidentally taking famotidine before or at hospitalization had a significantly reduced risk of intubation or death, with a hazard ratio of 0.43 (Gastroenterology. 2020 May 22. doi: 10.1053/j.gastro.2020.05.053)
The National Institutes of Health provided partial support. The investigators reported having no conflicts of interest.
SOURCE: Janowitz T et al. Gut. 2020 Jun 4. doi: 10.1136/gutjnl-2020-321852.
FROM GUT
WHO: Asymptomatic COVID-19 spread deemed ‘rare’
An official with the World Health Organization (WHO) has stated that it appears to be “rare” that an asymptomatic individual can pass SARS-CoV-2 to someone else.
“From the data we have, it still seems to be rare that an asymptomatic person actually transmits onward to a secondary individual,” Maria Van Kerkhove, PhD, WHO’s COVID-19 technical lead and an infectious disease epidemiologist, said June 8 at a news briefing from the agency’s Geneva headquarters.
This announcement came on the heels of the publication of an analysis in the Annals of Internal Medicine, which suggested that as many as 40-45% of COVID-19 cases may be asymptomatic. In this paper, the authors, Daniel P. Oran, AM, and Eric J. Topol, MD, of the Scripps Research Translational Institute in La Jolla, Calif stated: “The likelihood that approximately 40%-45% of those infected with SARS-CoV-2 will remain asymptomatic suggests that the virus might have greater potential than previously estimated to spread silently and deeply through human populations.”
"The early data that we have assembled on the prevalence of asymptomatic SARS-CoV-2 infection suggest that this is a significant factor in the rapid progression of the COVID-19 pandemic," the authors concluded.
Dr. Van Kerkhove also made comments suggesting otherwise on Twitter, citing a new summary by WHO: “@WHO recently published a summary of transmission of #COVID19, incl. symptomatic, pre-symptomatic and asymptomatic transmission.”
She also tweeted the following lines from the WHO summary: “Comprehensive studies on transmission from asymptomatic individuals are difficult to conduct, but the available evidence from contact tracing reported by Member States suggests that asymptomatically-infected individuals are much less likely to transmit the virus than those who develop symptoms.”
In an additional post, Dr. Van Kerkhove added: “In these data, it is important to breakdown truly asymptomatic vs pre-symptomatic vs mildly symptomatic... also to note that the [percentage] reported or estimated to be ‘asymptomatic’ is not the same as the [percentage] that are asymptomatic that actually transmit.”
In the paper published in the Annals of Internal Medicine, Mr. Oran and Dr. Topol analyzed data of asymptomatic individuals from 16 cohorts between April 19 and May 26, 2020 – a wide-ranging group consisting of residents of cities, health care workers, individuals in homeless shelters, obstetric patients, residents of a nursing home, crew members of aircraft carriers, passengers on cruise ships, and inmates in correctional facilities. Each cohort had varying rates of asymptomatic or presymptomatic cases..
When residents of Iceland were tested, 43 of 100 individuals who tested positive for SARS-CoV-2 did not show symptoms. In Vo’, Italy, 30 of 73 people (41.1%) with positive SARS-CoV-2 test results did not have symptoms in a first round of testing, and 13 of 29 (44.8%) had no symptoms in a second round of testing. Over half of residents of San Francisco’s Mission District who received testing (39 of 74; 52.7%) did not have symptoms, while slightly less than half of Indiana residents tested showed no symptoms (35 of 78; 44.8%).
A majority of 41 individuals (65.9%) who were mostly health care workers at Rutgers University reported no symptoms of COVID-19 at the time of testing. Data from homeless shelters in Boston (129 of 147; 87.7%) and Los Angeles (27 of 43; 62.7%) also showed a high rate of individuals without symptoms. Among 33 obstetric patients in New York City who tested positive for SARS-CoV-2, 29 women (87.9%) were asymptomatic during a median 2-day length of stay. In a Washington state nursing facility, 12 of 23 individuals (52.1%) were positive for SARS-CoV-2 without showing symptoms in a first round of testing, with another 15 of 24 residents (62.5%) not showing symptoms in a second round of testing. Of these residents, 24 individuals (88.9%) later went on to show symptoms of COVID-19.
Most of the 783 Greek citizens who tested positive for SARS-CoV-2 after being evacuated from Spain, Turkey, and the United Kingdom showed no symptoms of COVID-19 (35 of 40; 87.5%). A group of 565 Japanese citizens evacuated from Wuhan, China, had a lower number of cases without initial symptoms – 13 people were positive for SARS-CoV-2, and 4 of 13 (30.8%) had no symptoms.
In closed cohorts, there appeared to also be a high rate of COVID-19 cases without initial symptoms. Of 3,277 inmates from correctional facilities in Arkansas, North Carolina, Ohio, and Virginia, 3,146 individuals (96%) had no symptoms at the time of testing. There was also a large percentage of passengers and crew of the Diamond Princess cruise ship (331 of 712; 46.5%) and an Argentine cruise ship (104 of 128; 81.3%) who were positive for SARS-CoV-2 without symptoms. On the aircraft carrier U.S.S. Theodore Roosevelt, 60% of 856 individuals, while on the French aircraft carrier Charles de Gaulle, nearly 50% of individuals were asymptomatic.
It is difficult to tell the difference between people who are presymptomatic and will later go on to develop symptoms of COVID-19 and those who will remain asymptomatic. “The simple solution to this conundrum is longitudinal testing – that is, repeated observations of the individual over time,” but only 5 of 16 cohorts studied had longitudinal data on individuals, Mr. Oran and Dr. Topol said.
Seth Trueger, MD, an emergency physician and assistant professor of emergency medicine at Northwestern University, Chicago, who was not involved in the study, said it was important to see this information all in one place, even if the data isn’t new.
“I think we’ve certainly kind of seen from the beginning there’s some level of asymptomatic and presymptomatic spread,” Dr. Trueger said. “In health care, we’ve been lucky to get those lessons early on and start to think of things like universal masking in hospitals, and unfortunate things like limiting visitors.”
A more nuanced understanding of how SARS-CoV-2 spreads has been difficult to capture, in part because of operating under a shortened time frame and handicapped testing capacity, he noted. “[Even] in the best of possible circumstances, trying to figure out epidemiology in people who don’t have symptoms is really tough,” Dr. Truegar said.
“Even the best studies are still relatively decent samples, and not totally representative,” he added.
Another limitation to capturing accurate data is method of testing. Real-time reverse transcriptase polymerase chain reaction using nasopharyngeal swabs can detect RNA fragments from SARS-CoV-2, which could potentially affect the results. “It’s really hard to know what is actually infected virus versus just fragments of RNA that make the test positive,” Dr. Trueger said.
If the rate of asymptomatic cases is higher than previously thought, it’s a “double-edged sword,” he noted. It may mean the infection fatality rate is lower than predicted, but “even at high levels of what we think community levels might be, we’re far from herd immunity.”
The study authors and Dr. Trueger reported no relevant conflicts of interest.
SOURCE: Oran DP, Topol EJ. Ann Intern Med. 2020 Jun 3. doi: 10.7326/M20-3012.
This article was updated 6/8/20.
An official with the World Health Organization (WHO) has stated that it appears to be “rare” that an asymptomatic individual can pass SARS-CoV-2 to someone else.
“From the data we have, it still seems to be rare that an asymptomatic person actually transmits onward to a secondary individual,” Maria Van Kerkhove, PhD, WHO’s COVID-19 technical lead and an infectious disease epidemiologist, said June 8 at a news briefing from the agency’s Geneva headquarters.
This announcement came on the heels of the publication of an analysis in the Annals of Internal Medicine, which suggested that as many as 40-45% of COVID-19 cases may be asymptomatic. In this paper, the authors, Daniel P. Oran, AM, and Eric J. Topol, MD, of the Scripps Research Translational Institute in La Jolla, Calif stated: “The likelihood that approximately 40%-45% of those infected with SARS-CoV-2 will remain asymptomatic suggests that the virus might have greater potential than previously estimated to spread silently and deeply through human populations.”
"The early data that we have assembled on the prevalence of asymptomatic SARS-CoV-2 infection suggest that this is a significant factor in the rapid progression of the COVID-19 pandemic," the authors concluded.
Dr. Van Kerkhove also made comments suggesting otherwise on Twitter, citing a new summary by WHO: “@WHO recently published a summary of transmission of #COVID19, incl. symptomatic, pre-symptomatic and asymptomatic transmission.”
She also tweeted the following lines from the WHO summary: “Comprehensive studies on transmission from asymptomatic individuals are difficult to conduct, but the available evidence from contact tracing reported by Member States suggests that asymptomatically-infected individuals are much less likely to transmit the virus than those who develop symptoms.”
In an additional post, Dr. Van Kerkhove added: “In these data, it is important to breakdown truly asymptomatic vs pre-symptomatic vs mildly symptomatic... also to note that the [percentage] reported or estimated to be ‘asymptomatic’ is not the same as the [percentage] that are asymptomatic that actually transmit.”
In the paper published in the Annals of Internal Medicine, Mr. Oran and Dr. Topol analyzed data of asymptomatic individuals from 16 cohorts between April 19 and May 26, 2020 – a wide-ranging group consisting of residents of cities, health care workers, individuals in homeless shelters, obstetric patients, residents of a nursing home, crew members of aircraft carriers, passengers on cruise ships, and inmates in correctional facilities. Each cohort had varying rates of asymptomatic or presymptomatic cases..
When residents of Iceland were tested, 43 of 100 individuals who tested positive for SARS-CoV-2 did not show symptoms. In Vo’, Italy, 30 of 73 people (41.1%) with positive SARS-CoV-2 test results did not have symptoms in a first round of testing, and 13 of 29 (44.8%) had no symptoms in a second round of testing. Over half of residents of San Francisco’s Mission District who received testing (39 of 74; 52.7%) did not have symptoms, while slightly less than half of Indiana residents tested showed no symptoms (35 of 78; 44.8%).
A majority of 41 individuals (65.9%) who were mostly health care workers at Rutgers University reported no symptoms of COVID-19 at the time of testing. Data from homeless shelters in Boston (129 of 147; 87.7%) and Los Angeles (27 of 43; 62.7%) also showed a high rate of individuals without symptoms. Among 33 obstetric patients in New York City who tested positive for SARS-CoV-2, 29 women (87.9%) were asymptomatic during a median 2-day length of stay. In a Washington state nursing facility, 12 of 23 individuals (52.1%) were positive for SARS-CoV-2 without showing symptoms in a first round of testing, with another 15 of 24 residents (62.5%) not showing symptoms in a second round of testing. Of these residents, 24 individuals (88.9%) later went on to show symptoms of COVID-19.
Most of the 783 Greek citizens who tested positive for SARS-CoV-2 after being evacuated from Spain, Turkey, and the United Kingdom showed no symptoms of COVID-19 (35 of 40; 87.5%). A group of 565 Japanese citizens evacuated from Wuhan, China, had a lower number of cases without initial symptoms – 13 people were positive for SARS-CoV-2, and 4 of 13 (30.8%) had no symptoms.
In closed cohorts, there appeared to also be a high rate of COVID-19 cases without initial symptoms. Of 3,277 inmates from correctional facilities in Arkansas, North Carolina, Ohio, and Virginia, 3,146 individuals (96%) had no symptoms at the time of testing. There was also a large percentage of passengers and crew of the Diamond Princess cruise ship (331 of 712; 46.5%) and an Argentine cruise ship (104 of 128; 81.3%) who were positive for SARS-CoV-2 without symptoms. On the aircraft carrier U.S.S. Theodore Roosevelt, 60% of 856 individuals, while on the French aircraft carrier Charles de Gaulle, nearly 50% of individuals were asymptomatic.
It is difficult to tell the difference between people who are presymptomatic and will later go on to develop symptoms of COVID-19 and those who will remain asymptomatic. “The simple solution to this conundrum is longitudinal testing – that is, repeated observations of the individual over time,” but only 5 of 16 cohorts studied had longitudinal data on individuals, Mr. Oran and Dr. Topol said.
Seth Trueger, MD, an emergency physician and assistant professor of emergency medicine at Northwestern University, Chicago, who was not involved in the study, said it was important to see this information all in one place, even if the data isn’t new.
“I think we’ve certainly kind of seen from the beginning there’s some level of asymptomatic and presymptomatic spread,” Dr. Trueger said. “In health care, we’ve been lucky to get those lessons early on and start to think of things like universal masking in hospitals, and unfortunate things like limiting visitors.”
A more nuanced understanding of how SARS-CoV-2 spreads has been difficult to capture, in part because of operating under a shortened time frame and handicapped testing capacity, he noted. “[Even] in the best of possible circumstances, trying to figure out epidemiology in people who don’t have symptoms is really tough,” Dr. Truegar said.
“Even the best studies are still relatively decent samples, and not totally representative,” he added.
Another limitation to capturing accurate data is method of testing. Real-time reverse transcriptase polymerase chain reaction using nasopharyngeal swabs can detect RNA fragments from SARS-CoV-2, which could potentially affect the results. “It’s really hard to know what is actually infected virus versus just fragments of RNA that make the test positive,” Dr. Trueger said.
If the rate of asymptomatic cases is higher than previously thought, it’s a “double-edged sword,” he noted. It may mean the infection fatality rate is lower than predicted, but “even at high levels of what we think community levels might be, we’re far from herd immunity.”
The study authors and Dr. Trueger reported no relevant conflicts of interest.
SOURCE: Oran DP, Topol EJ. Ann Intern Med. 2020 Jun 3. doi: 10.7326/M20-3012.
This article was updated 6/8/20.
An official with the World Health Organization (WHO) has stated that it appears to be “rare” that an asymptomatic individual can pass SARS-CoV-2 to someone else.
“From the data we have, it still seems to be rare that an asymptomatic person actually transmits onward to a secondary individual,” Maria Van Kerkhove, PhD, WHO’s COVID-19 technical lead and an infectious disease epidemiologist, said June 8 at a news briefing from the agency’s Geneva headquarters.
This announcement came on the heels of the publication of an analysis in the Annals of Internal Medicine, which suggested that as many as 40-45% of COVID-19 cases may be asymptomatic. In this paper, the authors, Daniel P. Oran, AM, and Eric J. Topol, MD, of the Scripps Research Translational Institute in La Jolla, Calif stated: “The likelihood that approximately 40%-45% of those infected with SARS-CoV-2 will remain asymptomatic suggests that the virus might have greater potential than previously estimated to spread silently and deeply through human populations.”
"The early data that we have assembled on the prevalence of asymptomatic SARS-CoV-2 infection suggest that this is a significant factor in the rapid progression of the COVID-19 pandemic," the authors concluded.
Dr. Van Kerkhove also made comments suggesting otherwise on Twitter, citing a new summary by WHO: “@WHO recently published a summary of transmission of #COVID19, incl. symptomatic, pre-symptomatic and asymptomatic transmission.”
She also tweeted the following lines from the WHO summary: “Comprehensive studies on transmission from asymptomatic individuals are difficult to conduct, but the available evidence from contact tracing reported by Member States suggests that asymptomatically-infected individuals are much less likely to transmit the virus than those who develop symptoms.”
In an additional post, Dr. Van Kerkhove added: “In these data, it is important to breakdown truly asymptomatic vs pre-symptomatic vs mildly symptomatic... also to note that the [percentage] reported or estimated to be ‘asymptomatic’ is not the same as the [percentage] that are asymptomatic that actually transmit.”
In the paper published in the Annals of Internal Medicine, Mr. Oran and Dr. Topol analyzed data of asymptomatic individuals from 16 cohorts between April 19 and May 26, 2020 – a wide-ranging group consisting of residents of cities, health care workers, individuals in homeless shelters, obstetric patients, residents of a nursing home, crew members of aircraft carriers, passengers on cruise ships, and inmates in correctional facilities. Each cohort had varying rates of asymptomatic or presymptomatic cases..
When residents of Iceland were tested, 43 of 100 individuals who tested positive for SARS-CoV-2 did not show symptoms. In Vo’, Italy, 30 of 73 people (41.1%) with positive SARS-CoV-2 test results did not have symptoms in a first round of testing, and 13 of 29 (44.8%) had no symptoms in a second round of testing. Over half of residents of San Francisco’s Mission District who received testing (39 of 74; 52.7%) did not have symptoms, while slightly less than half of Indiana residents tested showed no symptoms (35 of 78; 44.8%).
A majority of 41 individuals (65.9%) who were mostly health care workers at Rutgers University reported no symptoms of COVID-19 at the time of testing. Data from homeless shelters in Boston (129 of 147; 87.7%) and Los Angeles (27 of 43; 62.7%) also showed a high rate of individuals without symptoms. Among 33 obstetric patients in New York City who tested positive for SARS-CoV-2, 29 women (87.9%) were asymptomatic during a median 2-day length of stay. In a Washington state nursing facility, 12 of 23 individuals (52.1%) were positive for SARS-CoV-2 without showing symptoms in a first round of testing, with another 15 of 24 residents (62.5%) not showing symptoms in a second round of testing. Of these residents, 24 individuals (88.9%) later went on to show symptoms of COVID-19.
Most of the 783 Greek citizens who tested positive for SARS-CoV-2 after being evacuated from Spain, Turkey, and the United Kingdom showed no symptoms of COVID-19 (35 of 40; 87.5%). A group of 565 Japanese citizens evacuated from Wuhan, China, had a lower number of cases without initial symptoms – 13 people were positive for SARS-CoV-2, and 4 of 13 (30.8%) had no symptoms.
In closed cohorts, there appeared to also be a high rate of COVID-19 cases without initial symptoms. Of 3,277 inmates from correctional facilities in Arkansas, North Carolina, Ohio, and Virginia, 3,146 individuals (96%) had no symptoms at the time of testing. There was also a large percentage of passengers and crew of the Diamond Princess cruise ship (331 of 712; 46.5%) and an Argentine cruise ship (104 of 128; 81.3%) who were positive for SARS-CoV-2 without symptoms. On the aircraft carrier U.S.S. Theodore Roosevelt, 60% of 856 individuals, while on the French aircraft carrier Charles de Gaulle, nearly 50% of individuals were asymptomatic.
It is difficult to tell the difference between people who are presymptomatic and will later go on to develop symptoms of COVID-19 and those who will remain asymptomatic. “The simple solution to this conundrum is longitudinal testing – that is, repeated observations of the individual over time,” but only 5 of 16 cohorts studied had longitudinal data on individuals, Mr. Oran and Dr. Topol said.
Seth Trueger, MD, an emergency physician and assistant professor of emergency medicine at Northwestern University, Chicago, who was not involved in the study, said it was important to see this information all in one place, even if the data isn’t new.
“I think we’ve certainly kind of seen from the beginning there’s some level of asymptomatic and presymptomatic spread,” Dr. Trueger said. “In health care, we’ve been lucky to get those lessons early on and start to think of things like universal masking in hospitals, and unfortunate things like limiting visitors.”
A more nuanced understanding of how SARS-CoV-2 spreads has been difficult to capture, in part because of operating under a shortened time frame and handicapped testing capacity, he noted. “[Even] in the best of possible circumstances, trying to figure out epidemiology in people who don’t have symptoms is really tough,” Dr. Truegar said.
“Even the best studies are still relatively decent samples, and not totally representative,” he added.
Another limitation to capturing accurate data is method of testing. Real-time reverse transcriptase polymerase chain reaction using nasopharyngeal swabs can detect RNA fragments from SARS-CoV-2, which could potentially affect the results. “It’s really hard to know what is actually infected virus versus just fragments of RNA that make the test positive,” Dr. Trueger said.
If the rate of asymptomatic cases is higher than previously thought, it’s a “double-edged sword,” he noted. It may mean the infection fatality rate is lower than predicted, but “even at high levels of what we think community levels might be, we’re far from herd immunity.”
The study authors and Dr. Trueger reported no relevant conflicts of interest.
SOURCE: Oran DP, Topol EJ. Ann Intern Med. 2020 Jun 3. doi: 10.7326/M20-3012.
This article was updated 6/8/20.
FROM ANNALS OF INTERNAL MEDICINE
JAK inhibitors have top risk for herpes zoster among newer RA DMARDs
Patients with rheumatoid arthritis (RA) who are treated with Janus kinase (JAK) inhibitors had the highest risk of developing herpes zoster among newer disease-modifying antirheumatic drugs (DMARDs), according to data released from the German biologics registry.
These are believed to be the first European data on the risk of herpes zoster with JAK inhibitors and showed that the crude incidence rate of herpes zoster per 1,000 patient-years was 24.9 with JAK inhibitors, compared with just 5.8 for controls taking conventional synthetic (cs) DMARDs.
The risk of herpes zoster was also increased with other biologic (b) and targeted synthetic (ts) DMARDs that were assessed, with crude rates per 1,000 patient-years of 10.4 for monoclonal tumor necrosis factor inhibitors (TNFi), 10.5 for B-cell targeted therapies, 9.4 for T-cell costimulation modulators, 9.0 for soluble TNF receptors, and 8.5 for interleukin (IL)-6 inhibitors.
Overall, JAK inhibitor treatment was associated with a fivefold higher risk of herpes zoster (hazard ratio, 5.0; P < .0001), compared with the control csDMARD population after adjustment using an inverse probability weights (IPW) method.
“The general risk of herpes zoster is [twofold] higher in patients with rheumatoid arthritis when you compare it with the general population,” said Anja Strangfeld, MD of the German Research Center, Berlin, and one of the three RABBIT [Rheumatoide Arthritis: Biobachtung der Biologika-Therapie] principal investigators.
“If you think of all the treatments that RA patients get, then the risk is further increased with bDMARD and [JAK inhibitor] treatments,” she added in an interview. While the risk was highest with JAK inhibitors, “we also saw that monoclonal TNF antibodies as well as all the other biologic DMARD treatments have a higher risk of herpes zoster in RA patients, compared to csDMARD therapy,” Dr. Strangfeld said.
Adjusted IPW HR for the other RA treatments showed an increased herpes zoster risk for all but the soluble TNF receptor agents, at 1.6 for IL-6 inhibitors (P = .0045) and monoclonal TNFi antibodies (P = .0003), and 1.7 for B-cell targeted therapies (P = .00026) and T-cell costimulation modulators (P = .0048).
Dr. Strangfeld presented these data during the annual European Congress of Rheumatology, held online this year due to COVID-19. The analysis included 12,470 patients with RA enrolled in RABBIT from 2007 onward and who had been treated with monoclonal TNF inhibitor antibodies, cell-targeted therapies, and tsDMARDs such as JAK inhibitors. In all, at the data cutoff at the end of April 2019, 452 cases of herpes zoster were recorded in 433 patients, of which 52 cases were serious.
“The reactivation of the varicella zoster virus causing the herpes zoster is triggered by a decline of cellular immunity. This can be due to aging or immune suppression of any kind,” Dr. Strangfeld said in her presentation.
“The Cox regression [analysis] revealed that higher age and intake of glucocorticoids were associated with an increased risk of herpes zoster,” she reported, with a dose dependent increase with glucocorticoids. IPW HR for age per 10 years was 1.3 (P < .0001) and 1.9 (P = .0022) for higher doses of glucocorticoids (>10 vs. 0 mg/day).
Commenting on the study, rheumatologist and epidemiologist Loreto Carmona, MD, PhD, said: “This is a very interesting study. The results are confident and precise. The frequency of herpes zoster infection [based on crude incidence rate estimates] is very high. However, we must focus on the [multivariable with IPW] analysis after taking into account baseline risk.”
Dr. Carmona, who is the chair of the congress’s Abstract Selection Committee and is the scientific director of the Instituto de Salud Musculoesquelética in Madrid, added: “Having a disease with high levels of activity or a disease refractory to treatments [both of which were very likely used in creating the IPW] levels off the risk a bit. Also, because RA by itself, glucocorticoids, and age all increase the risk. Still, jakinibs [JAK inhibitors] stand out as the treatment related to higher risk of herpes zoster infection.”
Dr. Strangfeld and fellow RABBIT investigators have previously looked at the risk of herpes zoster in patients treated with anti–TNF-alpha agents (JAMA. 2009;301[7]:737-44). They found that monoclonal anti–TNF-alpha agents may be associated with increased risk of herpes zoster, which is now confirmed by the current analysis. The reason for looking at herpes zoster risk again is that since that first analysis, many more therapies have become available for RA during the past 10 years, notably the tsDMARDs.
Herpes zoster may not always be a serious event, Dr. Strangfeld said in the interview, “but it diminishes your quality of life; it can also be associated with pain and may be followed by postherpetic neuralgia, which is very painful.” With new herpes zoster vaccinations available, it is now possible to vaccinate patients more easily. “This is advisable for all kinds of treatments,” she said.
“What we found was quite in agreement with the data that we know from the U.S., from the observational studies, for example from the Corrona database,” Dr. Strangfeld stated. The key finding is that the risk of herpes zoster is increased to some level, almost regardless of which drug is chosen, she said. “This gives a clear message that systematic herpes zoster vaccination should be done in patients with RA,” she suggested.
The German biologics registry RABBIT is supported by a joint unconditional grant from AbbVie, Amgen, Bristol-Myers Squibb, Celltrion, Hexal, Lilly, Merck Sharp & Dohme, Mylan, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Strangfeld has received speaker fees from AbbVie, Bristol-Myers Squibb, Merck Sharp & Dohme, Pfizer, Roche, Sanofi-Aventis, and UCB. Dr. Carmona had no relevant conflicts of interest to disclose.
SOURCE: Strangfeld A et al. Ann Rheum Dis. 2020;79[suppl 1]:150. Abstract OP0238.
Patients with rheumatoid arthritis (RA) who are treated with Janus kinase (JAK) inhibitors had the highest risk of developing herpes zoster among newer disease-modifying antirheumatic drugs (DMARDs), according to data released from the German biologics registry.
These are believed to be the first European data on the risk of herpes zoster with JAK inhibitors and showed that the crude incidence rate of herpes zoster per 1,000 patient-years was 24.9 with JAK inhibitors, compared with just 5.8 for controls taking conventional synthetic (cs) DMARDs.
The risk of herpes zoster was also increased with other biologic (b) and targeted synthetic (ts) DMARDs that were assessed, with crude rates per 1,000 patient-years of 10.4 for monoclonal tumor necrosis factor inhibitors (TNFi), 10.5 for B-cell targeted therapies, 9.4 for T-cell costimulation modulators, 9.0 for soluble TNF receptors, and 8.5 for interleukin (IL)-6 inhibitors.
Overall, JAK inhibitor treatment was associated with a fivefold higher risk of herpes zoster (hazard ratio, 5.0; P < .0001), compared with the control csDMARD population after adjustment using an inverse probability weights (IPW) method.
“The general risk of herpes zoster is [twofold] higher in patients with rheumatoid arthritis when you compare it with the general population,” said Anja Strangfeld, MD of the German Research Center, Berlin, and one of the three RABBIT [Rheumatoide Arthritis: Biobachtung der Biologika-Therapie] principal investigators.
“If you think of all the treatments that RA patients get, then the risk is further increased with bDMARD and [JAK inhibitor] treatments,” she added in an interview. While the risk was highest with JAK inhibitors, “we also saw that monoclonal TNF antibodies as well as all the other biologic DMARD treatments have a higher risk of herpes zoster in RA patients, compared to csDMARD therapy,” Dr. Strangfeld said.
Adjusted IPW HR for the other RA treatments showed an increased herpes zoster risk for all but the soluble TNF receptor agents, at 1.6 for IL-6 inhibitors (P = .0045) and monoclonal TNFi antibodies (P = .0003), and 1.7 for B-cell targeted therapies (P = .00026) and T-cell costimulation modulators (P = .0048).
Dr. Strangfeld presented these data during the annual European Congress of Rheumatology, held online this year due to COVID-19. The analysis included 12,470 patients with RA enrolled in RABBIT from 2007 onward and who had been treated with monoclonal TNF inhibitor antibodies, cell-targeted therapies, and tsDMARDs such as JAK inhibitors. In all, at the data cutoff at the end of April 2019, 452 cases of herpes zoster were recorded in 433 patients, of which 52 cases were serious.
“The reactivation of the varicella zoster virus causing the herpes zoster is triggered by a decline of cellular immunity. This can be due to aging or immune suppression of any kind,” Dr. Strangfeld said in her presentation.
“The Cox regression [analysis] revealed that higher age and intake of glucocorticoids were associated with an increased risk of herpes zoster,” she reported, with a dose dependent increase with glucocorticoids. IPW HR for age per 10 years was 1.3 (P < .0001) and 1.9 (P = .0022) for higher doses of glucocorticoids (>10 vs. 0 mg/day).
Commenting on the study, rheumatologist and epidemiologist Loreto Carmona, MD, PhD, said: “This is a very interesting study. The results are confident and precise. The frequency of herpes zoster infection [based on crude incidence rate estimates] is very high. However, we must focus on the [multivariable with IPW] analysis after taking into account baseline risk.”
Dr. Carmona, who is the chair of the congress’s Abstract Selection Committee and is the scientific director of the Instituto de Salud Musculoesquelética in Madrid, added: “Having a disease with high levels of activity or a disease refractory to treatments [both of which were very likely used in creating the IPW] levels off the risk a bit. Also, because RA by itself, glucocorticoids, and age all increase the risk. Still, jakinibs [JAK inhibitors] stand out as the treatment related to higher risk of herpes zoster infection.”
Dr. Strangfeld and fellow RABBIT investigators have previously looked at the risk of herpes zoster in patients treated with anti–TNF-alpha agents (JAMA. 2009;301[7]:737-44). They found that monoclonal anti–TNF-alpha agents may be associated with increased risk of herpes zoster, which is now confirmed by the current analysis. The reason for looking at herpes zoster risk again is that since that first analysis, many more therapies have become available for RA during the past 10 years, notably the tsDMARDs.
Herpes zoster may not always be a serious event, Dr. Strangfeld said in the interview, “but it diminishes your quality of life; it can also be associated with pain and may be followed by postherpetic neuralgia, which is very painful.” With new herpes zoster vaccinations available, it is now possible to vaccinate patients more easily. “This is advisable for all kinds of treatments,” she said.
“What we found was quite in agreement with the data that we know from the U.S., from the observational studies, for example from the Corrona database,” Dr. Strangfeld stated. The key finding is that the risk of herpes zoster is increased to some level, almost regardless of which drug is chosen, she said. “This gives a clear message that systematic herpes zoster vaccination should be done in patients with RA,” she suggested.
The German biologics registry RABBIT is supported by a joint unconditional grant from AbbVie, Amgen, Bristol-Myers Squibb, Celltrion, Hexal, Lilly, Merck Sharp & Dohme, Mylan, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Strangfeld has received speaker fees from AbbVie, Bristol-Myers Squibb, Merck Sharp & Dohme, Pfizer, Roche, Sanofi-Aventis, and UCB. Dr. Carmona had no relevant conflicts of interest to disclose.
SOURCE: Strangfeld A et al. Ann Rheum Dis. 2020;79[suppl 1]:150. Abstract OP0238.
Patients with rheumatoid arthritis (RA) who are treated with Janus kinase (JAK) inhibitors had the highest risk of developing herpes zoster among newer disease-modifying antirheumatic drugs (DMARDs), according to data released from the German biologics registry.
These are believed to be the first European data on the risk of herpes zoster with JAK inhibitors and showed that the crude incidence rate of herpes zoster per 1,000 patient-years was 24.9 with JAK inhibitors, compared with just 5.8 for controls taking conventional synthetic (cs) DMARDs.
The risk of herpes zoster was also increased with other biologic (b) and targeted synthetic (ts) DMARDs that were assessed, with crude rates per 1,000 patient-years of 10.4 for monoclonal tumor necrosis factor inhibitors (TNFi), 10.5 for B-cell targeted therapies, 9.4 for T-cell costimulation modulators, 9.0 for soluble TNF receptors, and 8.5 for interleukin (IL)-6 inhibitors.
Overall, JAK inhibitor treatment was associated with a fivefold higher risk of herpes zoster (hazard ratio, 5.0; P < .0001), compared with the control csDMARD population after adjustment using an inverse probability weights (IPW) method.
“The general risk of herpes zoster is [twofold] higher in patients with rheumatoid arthritis when you compare it with the general population,” said Anja Strangfeld, MD of the German Research Center, Berlin, and one of the three RABBIT [Rheumatoide Arthritis: Biobachtung der Biologika-Therapie] principal investigators.
“If you think of all the treatments that RA patients get, then the risk is further increased with bDMARD and [JAK inhibitor] treatments,” she added in an interview. While the risk was highest with JAK inhibitors, “we also saw that monoclonal TNF antibodies as well as all the other biologic DMARD treatments have a higher risk of herpes zoster in RA patients, compared to csDMARD therapy,” Dr. Strangfeld said.
Adjusted IPW HR for the other RA treatments showed an increased herpes zoster risk for all but the soluble TNF receptor agents, at 1.6 for IL-6 inhibitors (P = .0045) and monoclonal TNFi antibodies (P = .0003), and 1.7 for B-cell targeted therapies (P = .00026) and T-cell costimulation modulators (P = .0048).
Dr. Strangfeld presented these data during the annual European Congress of Rheumatology, held online this year due to COVID-19. The analysis included 12,470 patients with RA enrolled in RABBIT from 2007 onward and who had been treated with monoclonal TNF inhibitor antibodies, cell-targeted therapies, and tsDMARDs such as JAK inhibitors. In all, at the data cutoff at the end of April 2019, 452 cases of herpes zoster were recorded in 433 patients, of which 52 cases were serious.
“The reactivation of the varicella zoster virus causing the herpes zoster is triggered by a decline of cellular immunity. This can be due to aging or immune suppression of any kind,” Dr. Strangfeld said in her presentation.
“The Cox regression [analysis] revealed that higher age and intake of glucocorticoids were associated with an increased risk of herpes zoster,” she reported, with a dose dependent increase with glucocorticoids. IPW HR for age per 10 years was 1.3 (P < .0001) and 1.9 (P = .0022) for higher doses of glucocorticoids (>10 vs. 0 mg/day).
Commenting on the study, rheumatologist and epidemiologist Loreto Carmona, MD, PhD, said: “This is a very interesting study. The results are confident and precise. The frequency of herpes zoster infection [based on crude incidence rate estimates] is very high. However, we must focus on the [multivariable with IPW] analysis after taking into account baseline risk.”
Dr. Carmona, who is the chair of the congress’s Abstract Selection Committee and is the scientific director of the Instituto de Salud Musculoesquelética in Madrid, added: “Having a disease with high levels of activity or a disease refractory to treatments [both of which were very likely used in creating the IPW] levels off the risk a bit. Also, because RA by itself, glucocorticoids, and age all increase the risk. Still, jakinibs [JAK inhibitors] stand out as the treatment related to higher risk of herpes zoster infection.”
Dr. Strangfeld and fellow RABBIT investigators have previously looked at the risk of herpes zoster in patients treated with anti–TNF-alpha agents (JAMA. 2009;301[7]:737-44). They found that monoclonal anti–TNF-alpha agents may be associated with increased risk of herpes zoster, which is now confirmed by the current analysis. The reason for looking at herpes zoster risk again is that since that first analysis, many more therapies have become available for RA during the past 10 years, notably the tsDMARDs.
Herpes zoster may not always be a serious event, Dr. Strangfeld said in the interview, “but it diminishes your quality of life; it can also be associated with pain and may be followed by postherpetic neuralgia, which is very painful.” With new herpes zoster vaccinations available, it is now possible to vaccinate patients more easily. “This is advisable for all kinds of treatments,” she said.
“What we found was quite in agreement with the data that we know from the U.S., from the observational studies, for example from the Corrona database,” Dr. Strangfeld stated. The key finding is that the risk of herpes zoster is increased to some level, almost regardless of which drug is chosen, she said. “This gives a clear message that systematic herpes zoster vaccination should be done in patients with RA,” she suggested.
The German biologics registry RABBIT is supported by a joint unconditional grant from AbbVie, Amgen, Bristol-Myers Squibb, Celltrion, Hexal, Lilly, Merck Sharp & Dohme, Mylan, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Strangfeld has received speaker fees from AbbVie, Bristol-Myers Squibb, Merck Sharp & Dohme, Pfizer, Roche, Sanofi-Aventis, and UCB. Dr. Carmona had no relevant conflicts of interest to disclose.
SOURCE: Strangfeld A et al. Ann Rheum Dis. 2020;79[suppl 1]:150. Abstract OP0238.
FROM EULAR 2020 E-CONGRESS
FDA approves new antibiotic for HABP/VABP treatment
in people aged 18 years and older.
Approval for Recarbrio was based on results of a randomized, controlled clinical trial of 535 hospitalized adults with hospital-acquired and ventilator-associated bacterial pneumonia who received either Recarbrio or piperacillin-tazobactam. After 28 days, 16% of patients who received Recarbrio and 21% of patients who received piperacillin-tazobactam had died.
The most common adverse events associated with Recarbrio are increased alanine aminotransferase/ aspartate aminotransferase, anemia, diarrhea, hypokalemia, and hyponatremia. Recarbrio was previously approved by the FDA to treat patients with complicated urinary tract infections and complicated intra-abdominal infections who have limited or no alternative treatment options, according to an FDA press release.
“As a public health agency, the FDA addresses the threat of antimicrobial-resistant infections by facilitating the development of safe and effective new treatments. These efforts provide more options to fight serious bacterial infections and get new, safe and effective therapies to patients as soon as possible,” said Sumathi Nambiar, MD, MPH, director of the division of anti-infectives within the office of infectious disease at the Center for Drug Evaluation and Research.
in people aged 18 years and older.
Approval for Recarbrio was based on results of a randomized, controlled clinical trial of 535 hospitalized adults with hospital-acquired and ventilator-associated bacterial pneumonia who received either Recarbrio or piperacillin-tazobactam. After 28 days, 16% of patients who received Recarbrio and 21% of patients who received piperacillin-tazobactam had died.
The most common adverse events associated with Recarbrio are increased alanine aminotransferase/ aspartate aminotransferase, anemia, diarrhea, hypokalemia, and hyponatremia. Recarbrio was previously approved by the FDA to treat patients with complicated urinary tract infections and complicated intra-abdominal infections who have limited or no alternative treatment options, according to an FDA press release.
“As a public health agency, the FDA addresses the threat of antimicrobial-resistant infections by facilitating the development of safe and effective new treatments. These efforts provide more options to fight serious bacterial infections and get new, safe and effective therapies to patients as soon as possible,” said Sumathi Nambiar, MD, MPH, director of the division of anti-infectives within the office of infectious disease at the Center for Drug Evaluation and Research.
in people aged 18 years and older.
Approval for Recarbrio was based on results of a randomized, controlled clinical trial of 535 hospitalized adults with hospital-acquired and ventilator-associated bacterial pneumonia who received either Recarbrio or piperacillin-tazobactam. After 28 days, 16% of patients who received Recarbrio and 21% of patients who received piperacillin-tazobactam had died.
The most common adverse events associated with Recarbrio are increased alanine aminotransferase/ aspartate aminotransferase, anemia, diarrhea, hypokalemia, and hyponatremia. Recarbrio was previously approved by the FDA to treat patients with complicated urinary tract infections and complicated intra-abdominal infections who have limited or no alternative treatment options, according to an FDA press release.
“As a public health agency, the FDA addresses the threat of antimicrobial-resistant infections by facilitating the development of safe and effective new treatments. These efforts provide more options to fight serious bacterial infections and get new, safe and effective therapies to patients as soon as possible,” said Sumathi Nambiar, MD, MPH, director of the division of anti-infectives within the office of infectious disease at the Center for Drug Evaluation and Research.
FLU/SAL inhalers for COPD carry greater pneumonia risk
For well over a decade the elevated risk of pneumonia from inhaled corticosteroids for moderate to very severe COPD has been well documented, although the pneumonia risks from different types of ICSs have not been well understood.
Researchers from Taiwan have taken a step in to investigate this question with a nationwide cohort study that reported inhalers with budesonide and beclomethasone may have a lower pneumonia risk than that of fluticasone propionate/salmeterol inhalers (CHEST. 2020;157:117-29).
The study is the first to include beclomethasone-containing inhalers in a comparison of ICS/long-acting beta2-agonist (LABA) fixed combinations to evaluate pneumonia risk, along with dose and drug properties, wrote Ting-Yu Chang, MS, of the Graduate Institute of Clinical Pharmacology at the College of Medicine, National Taiwan University in Taipei, and colleagues.
The study evaluated 42,393 people with COPD in the National Health Insurance Research Database who got at least two continuous prescriptions for three different types of inhalers:
- Budesonide/formoterol (BUD/FOR).
- Beclomethasone/formoterol (BEC/FOR).
- Fluticasone propionate/salmeterol (FLU/SAL).
The study included patients aged 40 years and older who used a metered-dose inhaler (MDI) or dry-powder inhaler (DPI) between January 2011 and June 2015.
Patient experience with adverse events (AEs) was a factor in risk stratification, Mr. Chang and colleagues noted. “For the comparison between the BEC/FOR MDI and FLU/SAL MDI, the lower risk associated with the BEC/FOR MDI was more prominent in patients without severe AE in the past year,” they wrote.
The study found that BUD/FOR DPI users had a 17% lower risk of severe pneumonia and a 12% lower risk of severe AEs than that of FLU/SAL DPI users. The risk difference in pneumonia remained significant after adjustment for the ICS-equivalent daily dose, but the spread for AEs didn’t.
BEC/FOR MDI users were 31% less likely to get severe pneumonia and 18% less likely to have severe AEs than were FLU/SAL MDI users, but that difference declined and became nonsignificant after adjustment for the ICS-equivalent daily dose.
The study also found that a high average daily dose (> 500 mcg/d) of FLU/SAL MDI carried a 66% greater risk of severe pneumonia, compared with that of low-dose users. Also, medium-dose BEC/FOR MDI users (FLU equivalent 299-499 mcg/d) had a 38% greater risk of severe pneumonia than low-dose (< 200 mcg/d) users.
The variable pneumonia risks may be linked to each ICS’s pharmacokinetics, specifically their distinct lipophilic properties, Mr. Chang and colleagues wrote. Fluticasone propionate is known to be more lipophilic than budesonide, and while beclomethasone is more lipophilic than both, as a prodrug it rapidly converts to lower lipophilicity upon contact with bronchial secretions. “In general, a lipophilic ICS has a longer retention time within the airway or lung tissue to exert local immunosuppression and reduce inflammation,” Mr. Chang and colleagues stated.
The Taiwan Ministry of Science and Technology provided partial support for the study. Mr. Chang and colleagues have no relationships to disclose.
SOURCE: Chang TY et al. CHEST. 2020;157:117-29.
For well over a decade the elevated risk of pneumonia from inhaled corticosteroids for moderate to very severe COPD has been well documented, although the pneumonia risks from different types of ICSs have not been well understood.
Researchers from Taiwan have taken a step in to investigate this question with a nationwide cohort study that reported inhalers with budesonide and beclomethasone may have a lower pneumonia risk than that of fluticasone propionate/salmeterol inhalers (CHEST. 2020;157:117-29).
The study is the first to include beclomethasone-containing inhalers in a comparison of ICS/long-acting beta2-agonist (LABA) fixed combinations to evaluate pneumonia risk, along with dose and drug properties, wrote Ting-Yu Chang, MS, of the Graduate Institute of Clinical Pharmacology at the College of Medicine, National Taiwan University in Taipei, and colleagues.
The study evaluated 42,393 people with COPD in the National Health Insurance Research Database who got at least two continuous prescriptions for three different types of inhalers:
- Budesonide/formoterol (BUD/FOR).
- Beclomethasone/formoterol (BEC/FOR).
- Fluticasone propionate/salmeterol (FLU/SAL).
The study included patients aged 40 years and older who used a metered-dose inhaler (MDI) or dry-powder inhaler (DPI) between January 2011 and June 2015.
Patient experience with adverse events (AEs) was a factor in risk stratification, Mr. Chang and colleagues noted. “For the comparison between the BEC/FOR MDI and FLU/SAL MDI, the lower risk associated with the BEC/FOR MDI was more prominent in patients without severe AE in the past year,” they wrote.
The study found that BUD/FOR DPI users had a 17% lower risk of severe pneumonia and a 12% lower risk of severe AEs than that of FLU/SAL DPI users. The risk difference in pneumonia remained significant after adjustment for the ICS-equivalent daily dose, but the spread for AEs didn’t.
BEC/FOR MDI users were 31% less likely to get severe pneumonia and 18% less likely to have severe AEs than were FLU/SAL MDI users, but that difference declined and became nonsignificant after adjustment for the ICS-equivalent daily dose.
The study also found that a high average daily dose (> 500 mcg/d) of FLU/SAL MDI carried a 66% greater risk of severe pneumonia, compared with that of low-dose users. Also, medium-dose BEC/FOR MDI users (FLU equivalent 299-499 mcg/d) had a 38% greater risk of severe pneumonia than low-dose (< 200 mcg/d) users.
The variable pneumonia risks may be linked to each ICS’s pharmacokinetics, specifically their distinct lipophilic properties, Mr. Chang and colleagues wrote. Fluticasone propionate is known to be more lipophilic than budesonide, and while beclomethasone is more lipophilic than both, as a prodrug it rapidly converts to lower lipophilicity upon contact with bronchial secretions. “In general, a lipophilic ICS has a longer retention time within the airway or lung tissue to exert local immunosuppression and reduce inflammation,” Mr. Chang and colleagues stated.
The Taiwan Ministry of Science and Technology provided partial support for the study. Mr. Chang and colleagues have no relationships to disclose.
SOURCE: Chang TY et al. CHEST. 2020;157:117-29.
For well over a decade the elevated risk of pneumonia from inhaled corticosteroids for moderate to very severe COPD has been well documented, although the pneumonia risks from different types of ICSs have not been well understood.
Researchers from Taiwan have taken a step in to investigate this question with a nationwide cohort study that reported inhalers with budesonide and beclomethasone may have a lower pneumonia risk than that of fluticasone propionate/salmeterol inhalers (CHEST. 2020;157:117-29).
The study is the first to include beclomethasone-containing inhalers in a comparison of ICS/long-acting beta2-agonist (LABA) fixed combinations to evaluate pneumonia risk, along with dose and drug properties, wrote Ting-Yu Chang, MS, of the Graduate Institute of Clinical Pharmacology at the College of Medicine, National Taiwan University in Taipei, and colleagues.
The study evaluated 42,393 people with COPD in the National Health Insurance Research Database who got at least two continuous prescriptions for three different types of inhalers:
- Budesonide/formoterol (BUD/FOR).
- Beclomethasone/formoterol (BEC/FOR).
- Fluticasone propionate/salmeterol (FLU/SAL).
The study included patients aged 40 years and older who used a metered-dose inhaler (MDI) or dry-powder inhaler (DPI) between January 2011 and June 2015.
Patient experience with adverse events (AEs) was a factor in risk stratification, Mr. Chang and colleagues noted. “For the comparison between the BEC/FOR MDI and FLU/SAL MDI, the lower risk associated with the BEC/FOR MDI was more prominent in patients without severe AE in the past year,” they wrote.
The study found that BUD/FOR DPI users had a 17% lower risk of severe pneumonia and a 12% lower risk of severe AEs than that of FLU/SAL DPI users. The risk difference in pneumonia remained significant after adjustment for the ICS-equivalent daily dose, but the spread for AEs didn’t.
BEC/FOR MDI users were 31% less likely to get severe pneumonia and 18% less likely to have severe AEs than were FLU/SAL MDI users, but that difference declined and became nonsignificant after adjustment for the ICS-equivalent daily dose.
The study also found that a high average daily dose (> 500 mcg/d) of FLU/SAL MDI carried a 66% greater risk of severe pneumonia, compared with that of low-dose users. Also, medium-dose BEC/FOR MDI users (FLU equivalent 299-499 mcg/d) had a 38% greater risk of severe pneumonia than low-dose (< 200 mcg/d) users.
The variable pneumonia risks may be linked to each ICS’s pharmacokinetics, specifically their distinct lipophilic properties, Mr. Chang and colleagues wrote. Fluticasone propionate is known to be more lipophilic than budesonide, and while beclomethasone is more lipophilic than both, as a prodrug it rapidly converts to lower lipophilicity upon contact with bronchial secretions. “In general, a lipophilic ICS has a longer retention time within the airway or lung tissue to exert local immunosuppression and reduce inflammation,” Mr. Chang and colleagues stated.
The Taiwan Ministry of Science and Technology provided partial support for the study. Mr. Chang and colleagues have no relationships to disclose.
SOURCE: Chang TY et al. CHEST. 2020;157:117-29.
FROM CHEST
Today’s top news highlights: COVID-19 could worsen gambling problems, food allergies less common than thought
Here are the stories our MDedge editors across specialties think you need to know about today:
Could COVID-19 worsen gambling problems?
Take isolation, add excess available time and anxiety about illness or finances and you get the potential to increase problem gambling behaviors during the COVID-19 pandemic. A call to action, recently published in the Journal of Addiction Medicine, says it’s essential to gather data and supply guidance on this issue. “People are likely to be experiencing stress at levels they haven’t experienced previously,” said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said. Read more.
Food allergies in children are less frequent than expected
Food allergies appear to be less common than previously reported among 6- to 10-year-olds in Europe, according to a recent study. Prevalance ranged from a low of 1.4% to a high of 3.8%, both of which are “considerably lower” than the 16% rate based on parental reports of symptoms such as rash, itching, or diarrhea, Linus Grabenhenrich, MD, MPH, and colleagues reported in Allergy. The most commonly reported allergies were to peanuts and hazelnuts, with a prevalence of just over 5% for both. Previous research on pediatric food allergy prevalence has largely consisted of single-center studies with heterogeneous designs, the researchers noted. Read more.
The grocery store hug
William G. Wilkoff, MD, grew up in a family that didn’t embrace hugging, but as a small-town pediatrician he warmed up to the concept so much that he would frequently hug a passing acquaintance at the grocery store. That’s something he misses in the current environment and that he doesn’t expect will return. “[N]early every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship,” Dr. Wilkoff wrote in a column on MDedge. “Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child. I’m sure you have your own list of people who send off that we-need-to-hug spark.” Read more.
Identifying structural lesions of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that show a high degree of specificity in identifying such lesions in the disease. “Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19. “The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort.” Read more.
Making the world’s skin crawl
Clinicians should be aware of the skin manifestations of COVID-19, especially when triaging patients. In a commentary published on MDedge, Kathleen M. Coerdt and Amor Khachemoune, MD, describe the dermatologic implications of COVID-19, including the clinical manifestations of the disease, risk reduction techniques for patients and providers, personal protective equipment-associated adverse reactions, and the financial impact on dermatologists. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Could COVID-19 worsen gambling problems?
Take isolation, add excess available time and anxiety about illness or finances and you get the potential to increase problem gambling behaviors during the COVID-19 pandemic. A call to action, recently published in the Journal of Addiction Medicine, says it’s essential to gather data and supply guidance on this issue. “People are likely to be experiencing stress at levels they haven’t experienced previously,” said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said. Read more.
Food allergies in children are less frequent than expected
Food allergies appear to be less common than previously reported among 6- to 10-year-olds in Europe, according to a recent study. Prevalance ranged from a low of 1.4% to a high of 3.8%, both of which are “considerably lower” than the 16% rate based on parental reports of symptoms such as rash, itching, or diarrhea, Linus Grabenhenrich, MD, MPH, and colleagues reported in Allergy. The most commonly reported allergies were to peanuts and hazelnuts, with a prevalence of just over 5% for both. Previous research on pediatric food allergy prevalence has largely consisted of single-center studies with heterogeneous designs, the researchers noted. Read more.
The grocery store hug
William G. Wilkoff, MD, grew up in a family that didn’t embrace hugging, but as a small-town pediatrician he warmed up to the concept so much that he would frequently hug a passing acquaintance at the grocery store. That’s something he misses in the current environment and that he doesn’t expect will return. “[N]early every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship,” Dr. Wilkoff wrote in a column on MDedge. “Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child. I’m sure you have your own list of people who send off that we-need-to-hug spark.” Read more.
Identifying structural lesions of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that show a high degree of specificity in identifying such lesions in the disease. “Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19. “The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort.” Read more.
Making the world’s skin crawl
Clinicians should be aware of the skin manifestations of COVID-19, especially when triaging patients. In a commentary published on MDedge, Kathleen M. Coerdt and Amor Khachemoune, MD, describe the dermatologic implications of COVID-19, including the clinical manifestations of the disease, risk reduction techniques for patients and providers, personal protective equipment-associated adverse reactions, and the financial impact on dermatologists. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Could COVID-19 worsen gambling problems?
Take isolation, add excess available time and anxiety about illness or finances and you get the potential to increase problem gambling behaviors during the COVID-19 pandemic. A call to action, recently published in the Journal of Addiction Medicine, says it’s essential to gather data and supply guidance on this issue. “People are likely to be experiencing stress at levels they haven’t experienced previously,” said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said. Read more.
Food allergies in children are less frequent than expected
Food allergies appear to be less common than previously reported among 6- to 10-year-olds in Europe, according to a recent study. Prevalance ranged from a low of 1.4% to a high of 3.8%, both of which are “considerably lower” than the 16% rate based on parental reports of symptoms such as rash, itching, or diarrhea, Linus Grabenhenrich, MD, MPH, and colleagues reported in Allergy. The most commonly reported allergies were to peanuts and hazelnuts, with a prevalence of just over 5% for both. Previous research on pediatric food allergy prevalence has largely consisted of single-center studies with heterogeneous designs, the researchers noted. Read more.
The grocery store hug
William G. Wilkoff, MD, grew up in a family that didn’t embrace hugging, but as a small-town pediatrician he warmed up to the concept so much that he would frequently hug a passing acquaintance at the grocery store. That’s something he misses in the current environment and that he doesn’t expect will return. “[N]early every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship,” Dr. Wilkoff wrote in a column on MDedge. “Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child. I’m sure you have your own list of people who send off that we-need-to-hug spark.” Read more.
Identifying structural lesions of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that show a high degree of specificity in identifying such lesions in the disease. “Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19. “The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort.” Read more.
Making the world’s skin crawl
Clinicians should be aware of the skin manifestations of COVID-19, especially when triaging patients. In a commentary published on MDedge, Kathleen M. Coerdt and Amor Khachemoune, MD, describe the dermatologic implications of COVID-19, including the clinical manifestations of the disease, risk reduction techniques for patients and providers, personal protective equipment-associated adverse reactions, and the financial impact on dermatologists. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Bullous Eruption Caused by an Exotic Hedgehog Purchased as a Household Pet
Case Report
A 37-year-old woman presented to the dermatology clinic with an itchy rash involving the right hand. The rash had been present for 10 days but had become increasingly pruritic and vesicular over the last 5 days. She denied new exposures or other household members with similar symptoms. The patient reported that she had purchased a 4-toed, white-bellied African pygmy hedgehog (Atelerix albiventris) approximately 4 months prior. Upon questioning, she stated that she handled the hedgehog a couple of times a week and always washed her hands with soap and water immediately after. The patient’s medical and personal history were otherwise unremarkable.
Review of systems, including fevers, chills, and night sweats, was negative. Clinical examination revealed erythema with overlying vesicles and pustules on the right radial palm, radial dorsal hand, and interdigital web space of the first and second digit (Figure 1). The eruption was actively discharging serous exudate. No other lesions were present.

Unspecified acute contact dermatitis was the preliminary diagnosis based on clinical presentation and history. Other entities considered before making the diagnosis included psoriasis, eczema, and an infectious cause. Specimens were taken for bacterial and fungal cultures as well as a specimen for herpes simplex virus by polymerase chain reaction. Due to the intense pruritus and vesicular nature of the rash, the patient was treatedwith a 2-week, 60-40-20 prednisone taper and clobetasol propionate ointment 0.05% twice daily.
At 1-week follow-up, the eruption had improved, but the patient was still experiencing mild pruritus. Physical examination of the affected areas showed erythematous, violaceous, annular patches with slight scale at the periphery; all bullous lesions had resolved (Figure 2). Bacterial culture and herpes simplex virus by polymerase chain reaction were negative.

Two weeks after initial consultation, the fungal culture returned positive and showed growth of Trichophyton mentagrophytes. The patient was contacted and returned for re-evaluation. Physical examination showed decreased erythema and no bullous lesions; however, there was increased fine scale throughout the affected area on the right palm and first and second interdigital spaces (Figure 3). She reported mild pruritus. A confirmatory potassium hydroxide (KOH) preparation was positive for fungal hyphae. The patient was subsequently diagnosed with bullous tinea secondary to domestic hedgehog exposure that was now presenting as tinea manuum incognita. After 2 weeks of appropriate systemic and topical antifungal therapy, the patient’s skin eruption markedly improved (Figure 4).

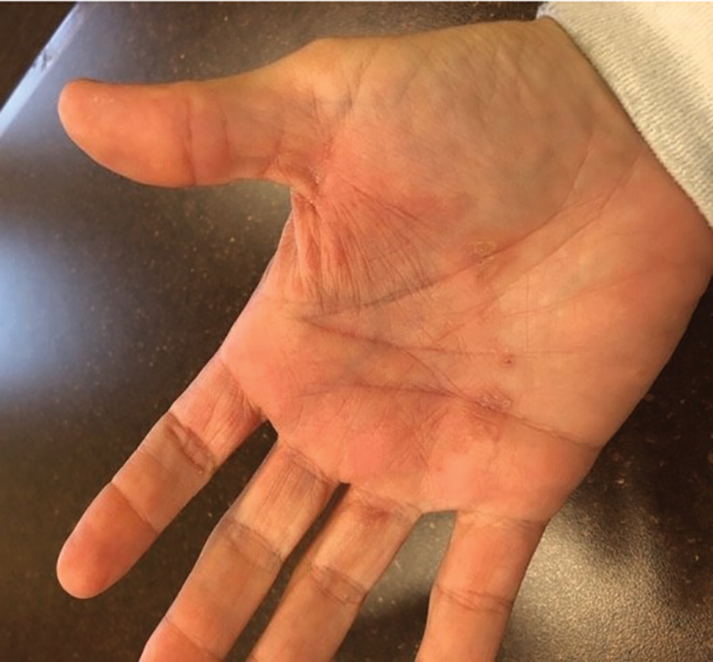
Comment
Tinea manuum is a dermatophytic epidermal infection of the hand. The most common causative organisms are Trichophyton rubrum, T mentagrophytes, and Epidermophyton floccosum. Infection can be acquired from contact with an infected person or animal, fomites, soil, or autoinoculation. Tinea manuum often is associated with tinea pedis. The hand that is used to excoriate the pruritic feet becomes infected, resulting in the classic two feet–one hand syndrome, which this patient did not have.1
Dermatophytes colonize keratin-containing tissues—skin, hair, and nails—utilizing the keratin for nutrients, and they do not invade living tissue in immunocompetent hosts. Dermatophytes cause clinical disease from an allergic host response to fungal antigens or their metabolic products.1 Tinea incognito results from the use of corticosteroids to treat a cutaneous fungal infection. The immunomodulatory effects of corticosteroids alter the appearance of the lesion. Hallmark signs and symptoms of a tinea infection, including scale, prominent border, erythema, and pruritus, can be reduced with corticosteroid use, giving the false impression that the lesion is resolving.2,3
The diagnosis of tinea manuum can be made clinically and often is supported with the findings of a KOH preparation. Scraping from an active scaling border generally provides the best results for obtaining fungal elements. For vesiculobullous lesions, the roof of a vesicle can provide an adequate specimen. Fungal culture and specific dermatophyte testing mediums can be used as confirmatory tests or allow for speciation, which help establish the diagnosis.1
Trichophyton mentagrophytes is a species complex—a group of closely related organisms that share morphologic appearance to the point that boundaries between them often are unclear. It can be identified by gross and microscopic morphology; however, variants of T mentagrophytes (eg, Trichophyton interdigitale, Trichophyton erinacei) require a confirmatory test or molecular analysis to be correctly identified.4-6 The laboratory used at our facility does not routinely attempt to identify the variant due to of lack of clinical significance.7,8
Anthropophilic fungi such as T rubrum, E floccosum, and T interdigitale generally do not cause a robust immunologic reaction. Infection usually is chronic in nature, though cases of pustular and vesicular tinea have been described.9,10Trichophyton erinacei and T mentagrophytes are zoophilic dermatophytes that cause an acute host response and are more likely to present with vesiculobullous lesions. Trichophyton erinacei is the most common fungal pathogen associated with A albiventris and has been isolated from its epidermal mites and quills,11,12 which likely facilitates interspecies transmission and compromises the cutaneous barrier of human hosts when the hedgehog is handled.
Atelerix albiventris is the most common domesticated hedgehog in the United States. These mild-mannered, nocturnal insectivores are unique, low-maintenance pets that have recently gained popularity. They are notable for their propensity to curl into a ball when frightened (Figure 5). The spines are not barbed and do not detach, as those of a porcupine do, but are still capable of piercing the skin. Atelerix albiventris is known to cause zoonotic dermatosis in humans and should be handled with gloves.13 Performing a KOH preparation early in the diagnostic workup can help initiate antifungal therapy, as results of fungal culture can take several weeks.

Conclusion
This case illustrates the importance of close follow-up of skin lesions that only partially respond to initial treatment and maintaining a high index of suspicion as exotic pets become popular.
- Elewski BE, Hughey LC, Hunt KM, et al. Fungal diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:1329-1363.
- Habif T. Superficial fungal infections. In: Habif T. Clinical Dermatology. 6th ed. Philadelphia, PA: Elsevier; 2016:487-533.
- Lange M, Jasiel‐Walikowska E, Nowicki R, et al. Tinea incognito due to Trichophyton mentagrophytes. Mycoses. 2010;53:455-457.
- Pchelin IM, Azarov DV, Churina MA, et al. Species boundaries in the Trichophyton mentagrophytes/T. interdigitale species complex. Med Mycol. 2019;57:781-789.
- Makimura K, Mochizuki T, Hasegawa A, et al. Phylogenetic classification of Trichophyton mentagrophytes complex strains based on DNA sequences of nuclear ribosomal internal transcribed spacer 1 regions. J Clin Microbiol. 1998;36:2629-2633.
- de Hoog GS, Dukik K, Monod M, et al. Toward a novel multilocus phylogenetic taxonomy for the dermatophytes. Mycopathologia. 2017;182:5-31.
- Rudramurthy SM, Shankarnarayan SA, Dogra S, et al. Mutation in the squalene epoxidase gene of Trichophyton interdigitale and Trichophyton rubrum associated with allylamine resistance. Antimicrob Agents Chemother. 2018;62:e02522-17.
- Singh A, Masih A, Khurana A, et al. High terbinafine resistance in Trichophyton interdigitale isolates in Delhi, India harbouring mutations in the squalene epoxidase gene. Mycoses. 2018;61:477-484.
- Kawakami Y, Oyama N, Sakai E, et al. Childhood tinea incognito caused by Trichophyton mentagrophytes var. interdigitale mimicking pustular psoriasis. Pediatr Dermatol. 2011;28:738-739.
- Neri I, Piraccini BM, Guareschi E, et al. Bullous tinea pedis in two children. Mycoses. 2004;47:475-478.
- Abarca ML, Castellá G, Martorell J, et al. Trichophyton erinacei in pet hedgehogs in Spain: occurrence and revision of its taxonomic status. Med Mycol. 2016;55:164-172.
- Morris P, English MP. Transmission and course of Trichophyton erinacei infections in British hedgehogs. Sabouraudia. 1973;11:42-47.
- Riley PY, Chomel BB. Hedgehog zoonoses. Emerg Infect Dis. 2005;11:1-5.
Case Report
A 37-year-old woman presented to the dermatology clinic with an itchy rash involving the right hand. The rash had been present for 10 days but had become increasingly pruritic and vesicular over the last 5 days. She denied new exposures or other household members with similar symptoms. The patient reported that she had purchased a 4-toed, white-bellied African pygmy hedgehog (Atelerix albiventris) approximately 4 months prior. Upon questioning, she stated that she handled the hedgehog a couple of times a week and always washed her hands with soap and water immediately after. The patient’s medical and personal history were otherwise unremarkable.
Review of systems, including fevers, chills, and night sweats, was negative. Clinical examination revealed erythema with overlying vesicles and pustules on the right radial palm, radial dorsal hand, and interdigital web space of the first and second digit (Figure 1). The eruption was actively discharging serous exudate. No other lesions were present.

Unspecified acute contact dermatitis was the preliminary diagnosis based on clinical presentation and history. Other entities considered before making the diagnosis included psoriasis, eczema, and an infectious cause. Specimens were taken for bacterial and fungal cultures as well as a specimen for herpes simplex virus by polymerase chain reaction. Due to the intense pruritus and vesicular nature of the rash, the patient was treatedwith a 2-week, 60-40-20 prednisone taper and clobetasol propionate ointment 0.05% twice daily.
At 1-week follow-up, the eruption had improved, but the patient was still experiencing mild pruritus. Physical examination of the affected areas showed erythematous, violaceous, annular patches with slight scale at the periphery; all bullous lesions had resolved (Figure 2). Bacterial culture and herpes simplex virus by polymerase chain reaction were negative.

Two weeks after initial consultation, the fungal culture returned positive and showed growth of Trichophyton mentagrophytes. The patient was contacted and returned for re-evaluation. Physical examination showed decreased erythema and no bullous lesions; however, there was increased fine scale throughout the affected area on the right palm and first and second interdigital spaces (Figure 3). She reported mild pruritus. A confirmatory potassium hydroxide (KOH) preparation was positive for fungal hyphae. The patient was subsequently diagnosed with bullous tinea secondary to domestic hedgehog exposure that was now presenting as tinea manuum incognita. After 2 weeks of appropriate systemic and topical antifungal therapy, the patient’s skin eruption markedly improved (Figure 4).

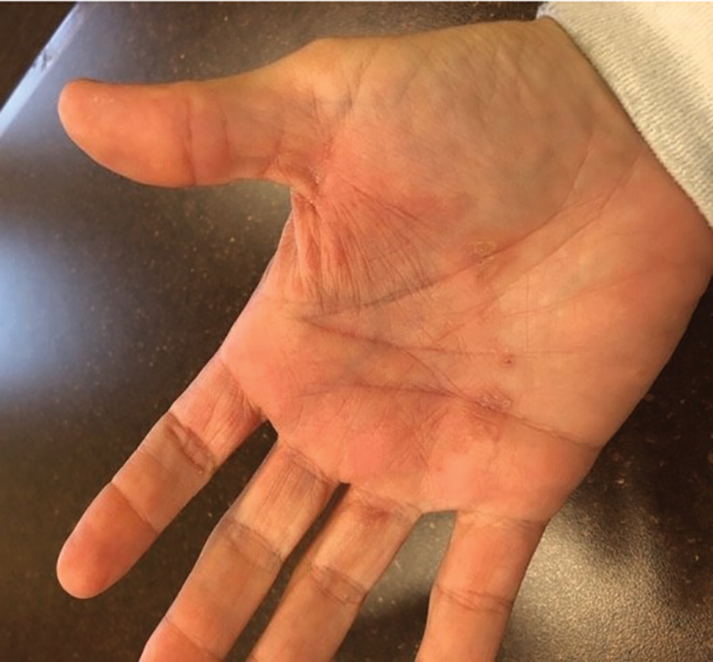
Comment
Tinea manuum is a dermatophytic epidermal infection of the hand. The most common causative organisms are Trichophyton rubrum, T mentagrophytes, and Epidermophyton floccosum. Infection can be acquired from contact with an infected person or animal, fomites, soil, or autoinoculation. Tinea manuum often is associated with tinea pedis. The hand that is used to excoriate the pruritic feet becomes infected, resulting in the classic two feet–one hand syndrome, which this patient did not have.1
Dermatophytes colonize keratin-containing tissues—skin, hair, and nails—utilizing the keratin for nutrients, and they do not invade living tissue in immunocompetent hosts. Dermatophytes cause clinical disease from an allergic host response to fungal antigens or their metabolic products.1 Tinea incognito results from the use of corticosteroids to treat a cutaneous fungal infection. The immunomodulatory effects of corticosteroids alter the appearance of the lesion. Hallmark signs and symptoms of a tinea infection, including scale, prominent border, erythema, and pruritus, can be reduced with corticosteroid use, giving the false impression that the lesion is resolving.2,3
The diagnosis of tinea manuum can be made clinically and often is supported with the findings of a KOH preparation. Scraping from an active scaling border generally provides the best results for obtaining fungal elements. For vesiculobullous lesions, the roof of a vesicle can provide an adequate specimen. Fungal culture and specific dermatophyte testing mediums can be used as confirmatory tests or allow for speciation, which help establish the diagnosis.1
Trichophyton mentagrophytes is a species complex—a group of closely related organisms that share morphologic appearance to the point that boundaries between them often are unclear. It can be identified by gross and microscopic morphology; however, variants of T mentagrophytes (eg, Trichophyton interdigitale, Trichophyton erinacei) require a confirmatory test or molecular analysis to be correctly identified.4-6 The laboratory used at our facility does not routinely attempt to identify the variant due to of lack of clinical significance.7,8
Anthropophilic fungi such as T rubrum, E floccosum, and T interdigitale generally do not cause a robust immunologic reaction. Infection usually is chronic in nature, though cases of pustular and vesicular tinea have been described.9,10Trichophyton erinacei and T mentagrophytes are zoophilic dermatophytes that cause an acute host response and are more likely to present with vesiculobullous lesions. Trichophyton erinacei is the most common fungal pathogen associated with A albiventris and has been isolated from its epidermal mites and quills,11,12 which likely facilitates interspecies transmission and compromises the cutaneous barrier of human hosts when the hedgehog is handled.
Atelerix albiventris is the most common domesticated hedgehog in the United States. These mild-mannered, nocturnal insectivores are unique, low-maintenance pets that have recently gained popularity. They are notable for their propensity to curl into a ball when frightened (Figure 5). The spines are not barbed and do not detach, as those of a porcupine do, but are still capable of piercing the skin. Atelerix albiventris is known to cause zoonotic dermatosis in humans and should be handled with gloves.13 Performing a KOH preparation early in the diagnostic workup can help initiate antifungal therapy, as results of fungal culture can take several weeks.

Conclusion
This case illustrates the importance of close follow-up of skin lesions that only partially respond to initial treatment and maintaining a high index of suspicion as exotic pets become popular.
Case Report
A 37-year-old woman presented to the dermatology clinic with an itchy rash involving the right hand. The rash had been present for 10 days but had become increasingly pruritic and vesicular over the last 5 days. She denied new exposures or other household members with similar symptoms. The patient reported that she had purchased a 4-toed, white-bellied African pygmy hedgehog (Atelerix albiventris) approximately 4 months prior. Upon questioning, she stated that she handled the hedgehog a couple of times a week and always washed her hands with soap and water immediately after. The patient’s medical and personal history were otherwise unremarkable.
Review of systems, including fevers, chills, and night sweats, was negative. Clinical examination revealed erythema with overlying vesicles and pustules on the right radial palm, radial dorsal hand, and interdigital web space of the first and second digit (Figure 1). The eruption was actively discharging serous exudate. No other lesions were present.

Unspecified acute contact dermatitis was the preliminary diagnosis based on clinical presentation and history. Other entities considered before making the diagnosis included psoriasis, eczema, and an infectious cause. Specimens were taken for bacterial and fungal cultures as well as a specimen for herpes simplex virus by polymerase chain reaction. Due to the intense pruritus and vesicular nature of the rash, the patient was treatedwith a 2-week, 60-40-20 prednisone taper and clobetasol propionate ointment 0.05% twice daily.
At 1-week follow-up, the eruption had improved, but the patient was still experiencing mild pruritus. Physical examination of the affected areas showed erythematous, violaceous, annular patches with slight scale at the periphery; all bullous lesions had resolved (Figure 2). Bacterial culture and herpes simplex virus by polymerase chain reaction were negative.

Two weeks after initial consultation, the fungal culture returned positive and showed growth of Trichophyton mentagrophytes. The patient was contacted and returned for re-evaluation. Physical examination showed decreased erythema and no bullous lesions; however, there was increased fine scale throughout the affected area on the right palm and first and second interdigital spaces (Figure 3). She reported mild pruritus. A confirmatory potassium hydroxide (KOH) preparation was positive for fungal hyphae. The patient was subsequently diagnosed with bullous tinea secondary to domestic hedgehog exposure that was now presenting as tinea manuum incognita. After 2 weeks of appropriate systemic and topical antifungal therapy, the patient’s skin eruption markedly improved (Figure 4).

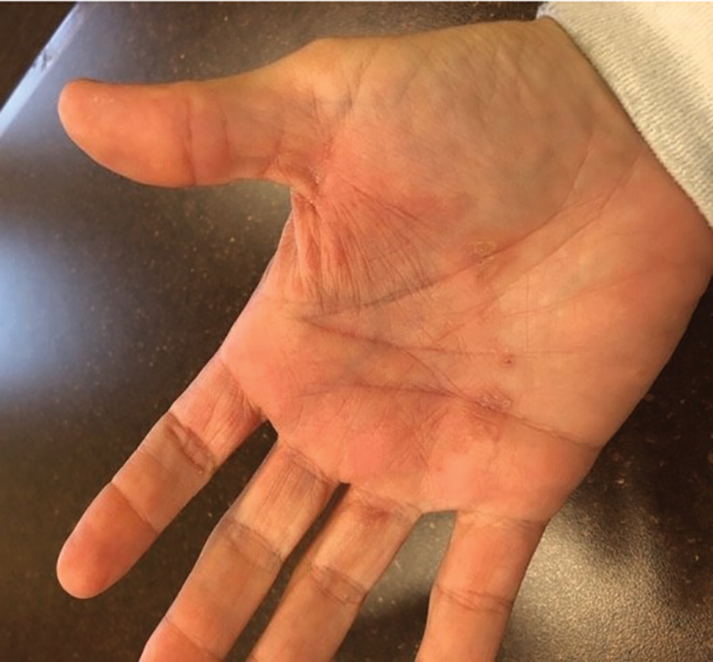
Comment
Tinea manuum is a dermatophytic epidermal infection of the hand. The most common causative organisms are Trichophyton rubrum, T mentagrophytes, and Epidermophyton floccosum. Infection can be acquired from contact with an infected person or animal, fomites, soil, or autoinoculation. Tinea manuum often is associated with tinea pedis. The hand that is used to excoriate the pruritic feet becomes infected, resulting in the classic two feet–one hand syndrome, which this patient did not have.1
Dermatophytes colonize keratin-containing tissues—skin, hair, and nails—utilizing the keratin for nutrients, and they do not invade living tissue in immunocompetent hosts. Dermatophytes cause clinical disease from an allergic host response to fungal antigens or their metabolic products.1 Tinea incognito results from the use of corticosteroids to treat a cutaneous fungal infection. The immunomodulatory effects of corticosteroids alter the appearance of the lesion. Hallmark signs and symptoms of a tinea infection, including scale, prominent border, erythema, and pruritus, can be reduced with corticosteroid use, giving the false impression that the lesion is resolving.2,3
The diagnosis of tinea manuum can be made clinically and often is supported with the findings of a KOH preparation. Scraping from an active scaling border generally provides the best results for obtaining fungal elements. For vesiculobullous lesions, the roof of a vesicle can provide an adequate specimen. Fungal culture and specific dermatophyte testing mediums can be used as confirmatory tests or allow for speciation, which help establish the diagnosis.1
Trichophyton mentagrophytes is a species complex—a group of closely related organisms that share morphologic appearance to the point that boundaries between them often are unclear. It can be identified by gross and microscopic morphology; however, variants of T mentagrophytes (eg, Trichophyton interdigitale, Trichophyton erinacei) require a confirmatory test or molecular analysis to be correctly identified.4-6 The laboratory used at our facility does not routinely attempt to identify the variant due to of lack of clinical significance.7,8
Anthropophilic fungi such as T rubrum, E floccosum, and T interdigitale generally do not cause a robust immunologic reaction. Infection usually is chronic in nature, though cases of pustular and vesicular tinea have been described.9,10Trichophyton erinacei and T mentagrophytes are zoophilic dermatophytes that cause an acute host response and are more likely to present with vesiculobullous lesions. Trichophyton erinacei is the most common fungal pathogen associated with A albiventris and has been isolated from its epidermal mites and quills,11,12 which likely facilitates interspecies transmission and compromises the cutaneous barrier of human hosts when the hedgehog is handled.
Atelerix albiventris is the most common domesticated hedgehog in the United States. These mild-mannered, nocturnal insectivores are unique, low-maintenance pets that have recently gained popularity. They are notable for their propensity to curl into a ball when frightened (Figure 5). The spines are not barbed and do not detach, as those of a porcupine do, but are still capable of piercing the skin. Atelerix albiventris is known to cause zoonotic dermatosis in humans and should be handled with gloves.13 Performing a KOH preparation early in the diagnostic workup can help initiate antifungal therapy, as results of fungal culture can take several weeks.

Conclusion
This case illustrates the importance of close follow-up of skin lesions that only partially respond to initial treatment and maintaining a high index of suspicion as exotic pets become popular.
- Elewski BE, Hughey LC, Hunt KM, et al. Fungal diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:1329-1363.
- Habif T. Superficial fungal infections. In: Habif T. Clinical Dermatology. 6th ed. Philadelphia, PA: Elsevier; 2016:487-533.
- Lange M, Jasiel‐Walikowska E, Nowicki R, et al. Tinea incognito due to Trichophyton mentagrophytes. Mycoses. 2010;53:455-457.
- Pchelin IM, Azarov DV, Churina MA, et al. Species boundaries in the Trichophyton mentagrophytes/T. interdigitale species complex. Med Mycol. 2019;57:781-789.
- Makimura K, Mochizuki T, Hasegawa A, et al. Phylogenetic classification of Trichophyton mentagrophytes complex strains based on DNA sequences of nuclear ribosomal internal transcribed spacer 1 regions. J Clin Microbiol. 1998;36:2629-2633.
- de Hoog GS, Dukik K, Monod M, et al. Toward a novel multilocus phylogenetic taxonomy for the dermatophytes. Mycopathologia. 2017;182:5-31.
- Rudramurthy SM, Shankarnarayan SA, Dogra S, et al. Mutation in the squalene epoxidase gene of Trichophyton interdigitale and Trichophyton rubrum associated with allylamine resistance. Antimicrob Agents Chemother. 2018;62:e02522-17.
- Singh A, Masih A, Khurana A, et al. High terbinafine resistance in Trichophyton interdigitale isolates in Delhi, India harbouring mutations in the squalene epoxidase gene. Mycoses. 2018;61:477-484.
- Kawakami Y, Oyama N, Sakai E, et al. Childhood tinea incognito caused by Trichophyton mentagrophytes var. interdigitale mimicking pustular psoriasis. Pediatr Dermatol. 2011;28:738-739.
- Neri I, Piraccini BM, Guareschi E, et al. Bullous tinea pedis in two children. Mycoses. 2004;47:475-478.
- Abarca ML, Castellá G, Martorell J, et al. Trichophyton erinacei in pet hedgehogs in Spain: occurrence and revision of its taxonomic status. Med Mycol. 2016;55:164-172.
- Morris P, English MP. Transmission and course of Trichophyton erinacei infections in British hedgehogs. Sabouraudia. 1973;11:42-47.
- Riley PY, Chomel BB. Hedgehog zoonoses. Emerg Infect Dis. 2005;11:1-5.
- Elewski BE, Hughey LC, Hunt KM, et al. Fungal diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:1329-1363.
- Habif T. Superficial fungal infections. In: Habif T. Clinical Dermatology. 6th ed. Philadelphia, PA: Elsevier; 2016:487-533.
- Lange M, Jasiel‐Walikowska E, Nowicki R, et al. Tinea incognito due to Trichophyton mentagrophytes. Mycoses. 2010;53:455-457.
- Pchelin IM, Azarov DV, Churina MA, et al. Species boundaries in the Trichophyton mentagrophytes/T. interdigitale species complex. Med Mycol. 2019;57:781-789.
- Makimura K, Mochizuki T, Hasegawa A, et al. Phylogenetic classification of Trichophyton mentagrophytes complex strains based on DNA sequences of nuclear ribosomal internal transcribed spacer 1 regions. J Clin Microbiol. 1998;36:2629-2633.
- de Hoog GS, Dukik K, Monod M, et al. Toward a novel multilocus phylogenetic taxonomy for the dermatophytes. Mycopathologia. 2017;182:5-31.
- Rudramurthy SM, Shankarnarayan SA, Dogra S, et al. Mutation in the squalene epoxidase gene of Trichophyton interdigitale and Trichophyton rubrum associated with allylamine resistance. Antimicrob Agents Chemother. 2018;62:e02522-17.
- Singh A, Masih A, Khurana A, et al. High terbinafine resistance in Trichophyton interdigitale isolates in Delhi, India harbouring mutations in the squalene epoxidase gene. Mycoses. 2018;61:477-484.
- Kawakami Y, Oyama N, Sakai E, et al. Childhood tinea incognito caused by Trichophyton mentagrophytes var. interdigitale mimicking pustular psoriasis. Pediatr Dermatol. 2011;28:738-739.
- Neri I, Piraccini BM, Guareschi E, et al. Bullous tinea pedis in two children. Mycoses. 2004;47:475-478.
- Abarca ML, Castellá G, Martorell J, et al. Trichophyton erinacei in pet hedgehogs in Spain: occurrence and revision of its taxonomic status. Med Mycol. 2016;55:164-172.
- Morris P, English MP. Transmission and course of Trichophyton erinacei infections in British hedgehogs. Sabouraudia. 1973;11:42-47.
- Riley PY, Chomel BB. Hedgehog zoonoses. Emerg Infect Dis. 2005;11:1-5.
Practice Points
- Bullous tinea may present with little or no scale, which can lead to confusion with acute contact dermatitis.
- The recent popularity of exotic pets may increase the incidence of fungal zoonotic dermatitis.
- Prompt recognition of tinea incognito is essential when treating lesions with corticosteroids.
- Skin lesions not responding appropriately to therapy warrant reassessment and further evaluation.
Evaluating complications of midline catheters
Background: Midline catheters have gained popularity in inpatient medical settings as a convenient alternative to PICC lines. This is primarily because of the ability to avoid central line–associated bloodstream infections (CLABSI) since these catheters terminate in the peripheral veins and cannot be reported as such. Additionally, they are potentially able to dwell longer than are traditional peripheral intravenous catheters. However, insufficient data exist to accurately describe the rate of complications in these catheters, as prior studies are based on single-center experiences.
Study design: Multicenter prospective cohort study.
Setting: Hospital medicine ward or medical ICU.
Synopsis: With use of a large database of adult patients from a quality initiative supported by Blue Cross Blue Shield of Michigan and Blue Care Network, this study identified 1,161 patients who had midline catheters placed and showed a 10.3% complication rate, of which 66.7% were minor (dislodgment, leaking, infiltration, or superficial thrombophlebitis) rather than major complications (occlusion, symptomatic upper-extremity deep venous thrombosis, or bloodstream infection). However, a similar rate of removal of the catheters was reported for major and minor complications (53.8% vs. 52.5%; P = .90). Across sites, there was substantial variation in utilization rates (0.97%-12.92%; P less than .001), dwell time and indication for use, and complication rates (3.4%-16.7%; P = .07).
The article does not provide guidance on when and how midline catheters should be used in order to minimize risk; nor does it include a comparison with traditional peripheral intravenous catheters or with PICC lines. Further studies are needed to guide indications and practices for catheter placement in order to minimize risk. Providers should continue to carefully consider the risks and benefits of midline catheter placement in individual cases.
Bottom line: Midline catheter placement more commonly leads to minor rather than major complications, though patterns of use and outcomes vary substantially across sites.
Citation: Chopra V et al. Variation in use and outcomes related to midline catheters: results from a multicentre pilot study. BMJ Qual Saf. 2019 Mar 18. doi: 10.1136/bmjqs-2018-008554.
Dr. Marcantonio is a Med-Peds hospitalist at Duke University Health System.
Background: Midline catheters have gained popularity in inpatient medical settings as a convenient alternative to PICC lines. This is primarily because of the ability to avoid central line–associated bloodstream infections (CLABSI) since these catheters terminate in the peripheral veins and cannot be reported as such. Additionally, they are potentially able to dwell longer than are traditional peripheral intravenous catheters. However, insufficient data exist to accurately describe the rate of complications in these catheters, as prior studies are based on single-center experiences.
Study design: Multicenter prospective cohort study.
Setting: Hospital medicine ward or medical ICU.
Synopsis: With use of a large database of adult patients from a quality initiative supported by Blue Cross Blue Shield of Michigan and Blue Care Network, this study identified 1,161 patients who had midline catheters placed and showed a 10.3% complication rate, of which 66.7% were minor (dislodgment, leaking, infiltration, or superficial thrombophlebitis) rather than major complications (occlusion, symptomatic upper-extremity deep venous thrombosis, or bloodstream infection). However, a similar rate of removal of the catheters was reported for major and minor complications (53.8% vs. 52.5%; P = .90). Across sites, there was substantial variation in utilization rates (0.97%-12.92%; P less than .001), dwell time and indication for use, and complication rates (3.4%-16.7%; P = .07).
The article does not provide guidance on when and how midline catheters should be used in order to minimize risk; nor does it include a comparison with traditional peripheral intravenous catheters or with PICC lines. Further studies are needed to guide indications and practices for catheter placement in order to minimize risk. Providers should continue to carefully consider the risks and benefits of midline catheter placement in individual cases.
Bottom line: Midline catheter placement more commonly leads to minor rather than major complications, though patterns of use and outcomes vary substantially across sites.
Citation: Chopra V et al. Variation in use and outcomes related to midline catheters: results from a multicentre pilot study. BMJ Qual Saf. 2019 Mar 18. doi: 10.1136/bmjqs-2018-008554.
Dr. Marcantonio is a Med-Peds hospitalist at Duke University Health System.
Background: Midline catheters have gained popularity in inpatient medical settings as a convenient alternative to PICC lines. This is primarily because of the ability to avoid central line–associated bloodstream infections (CLABSI) since these catheters terminate in the peripheral veins and cannot be reported as such. Additionally, they are potentially able to dwell longer than are traditional peripheral intravenous catheters. However, insufficient data exist to accurately describe the rate of complications in these catheters, as prior studies are based on single-center experiences.
Study design: Multicenter prospective cohort study.
Setting: Hospital medicine ward or medical ICU.
Synopsis: With use of a large database of adult patients from a quality initiative supported by Blue Cross Blue Shield of Michigan and Blue Care Network, this study identified 1,161 patients who had midline catheters placed and showed a 10.3% complication rate, of which 66.7% were minor (dislodgment, leaking, infiltration, or superficial thrombophlebitis) rather than major complications (occlusion, symptomatic upper-extremity deep venous thrombosis, or bloodstream infection). However, a similar rate of removal of the catheters was reported for major and minor complications (53.8% vs. 52.5%; P = .90). Across sites, there was substantial variation in utilization rates (0.97%-12.92%; P less than .001), dwell time and indication for use, and complication rates (3.4%-16.7%; P = .07).
The article does not provide guidance on when and how midline catheters should be used in order to minimize risk; nor does it include a comparison with traditional peripheral intravenous catheters or with PICC lines. Further studies are needed to guide indications and practices for catheter placement in order to minimize risk. Providers should continue to carefully consider the risks and benefits of midline catheter placement in individual cases.
Bottom line: Midline catheter placement more commonly leads to minor rather than major complications, though patterns of use and outcomes vary substantially across sites.
Citation: Chopra V et al. Variation in use and outcomes related to midline catheters: results from a multicentre pilot study. BMJ Qual Saf. 2019 Mar 18. doi: 10.1136/bmjqs-2018-008554.
Dr. Marcantonio is a Med-Peds hospitalist at Duke University Health System.
COVID-19: Problematic gambling could worsen
The confluence of isolation, excess available time, and anxiety about illness or finances as a result of the COVID-19 pandemic have the potential to increase problem gambling behaviors during this public health emergency, so it’s essential to gather data and supply guidance on this issue, according to a call to action published May 18 in the Journal of Addiction Medicine.
“When facing an unforeseen situation with confinement, fear of disease, and financial uncertainty for the future, problem gambling may be an important health hazard to monitor and prevent during and following the COVID-19 crisis, especially given current online gambling availability,” wrote Anders Håkansson, PhD, of Lund University in Sweden and coauthors.
Both stress and trauma have been linked to gambling problems, and both are occurring during the pandemic, said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn., in an interview.
“People are likely to be experiencing stress at levels they haven’t experienced previously,” Dr. Potenza said. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said.
David Hodgins, PhD, CPsych, a professor of psychology at the University of Calgary in Alberta, who was not involved with the commentary, noted that gambling relapse is triggered by “negative emotional states, interpersonal stress, and financial stress” – all three of which the pandemic contributes to.
Financial stress can especially “inflame erroneous gambling-related cognitions,” he said in an interview, including “beliefs such as the idea that gambling can solve financial problems, even when this is statistically almost impossible as debt increases, and that debt has been caused by gambling.”
Increased social isolation also is particularly problematic, pointed out Shane W. Kraus, PhD, from the University of Nevada, Las Vegas. Dr. Kraus also was not involved with the paper.
“If someone is already struggling with already negative emotions, negative feelings, thoughts, and depression, and you’re now isolating them quite a bit, that’s not going to be a recipe for success,” Dr. Kraus said in an interview.
Dr. Potenza said.
“We should be mindful of ways in which people develop addictions in these settings,” he said. “One of the aspects of the pandemic is that many people are at home for longer periods of time, and they use digital technologies more frequently.”
The use of digital technologies can include interaction on social media platforms and on meeting applications such as Zoom, but such use also offers opportunities for problematic gambling, gaming, and pornography use. The World Health Organization recognizes addiction disorders for gambling and for gaming, and online gaming platforms and pornography sites have reported substantial increases in their traffic during the pandemic, Dr. Potenza said.
The increase in frequency is unsurprising and not necessarily a concern by itself, Dr. Kraus said.
“It’s all about loss of control or difficulty engaging or disengaging,” Dr. Kraus said. “When you can’t stop doing something even if you like it or love it, when it interferes with your day-to-day activities and relationships, that’s when it’s a problem.”
Gambling online: Easy, available
The authors note that past research has identified increased gambling problems during economic crises in other countries.
“While currently speculative, financial hardships may promote gambling as individuals may be motivated to gamble to try to win money,” the authors suggested. “Although presently limited, existing data suggest that COVID-19–related financial concerns may increase gambling-related harms, and this possibility merits systematic research.”
But trends and characteristics of the gambling market, including direct effects from the pandemic, can potentially influence behaviors, too. Most casinos have closed during the pandemic, and most of the sports that people bet on have been canceled or postponed.
“Fewer people are gambling on sports, but they turn then to other areas,” Dr. Potenza said. “If they can’t bet on major league type sports, they might gamble on more local sporting events, or they may bet on other activities going on in society during the pandemic.”
But online gambling poses greater risk.
“Properties of online gambling may constitute a particular health hazard when many people are confined to their homes and have had rapid changes in working conditions, psychosocial stress, anxiety, and depression, as has been described in China,” the paper’s authors wrote. “Online gambling may be particularly concerning due to its availability and velocity” and association with higher debt levels.
In addition to online gaming’s ease and availability, past research has found patients report boredom and escapism as reasons they turned to it.
Again, boredom on its own is not necessarily a problem, but for those who already struggle with addictive behaviors, it can be a trigger, Dr. Kraus said.
“Boredom is very tough for them because it’s often associated with negative emotions,” such as dwelling on things not going well in their lives, he said. “In a pandemic, people are by themselves quite a bit, socially isolated, so for those who are struggling already with some depression or anxiety, it’s only going to be increased.”
Online gaming trends may vary with demographics, however. Dr. Kraus noted that his former clinic at the Veterans Administration has been seeing lower gambling in patients with addictive disorders, but those patients are also older and primarily frequented casinos.
“It’s going to depend on age and familiarity with technology,” he said, but even if older problem gamblers are not going to the Internet now, “let’s wait and see what happens in the next 2 or 3 months.”
The authors noted results from a small survey of patients in treatment for gambling addiction at the Bellvitge University Hospital in Barcelona, Spain, where two of the coauthors work. They conducted telephone surveys with 26 patients about the first 4 weeks of sheltering in place because of the coronavirus. All but four of the patients were male, and their average age was 45 years.
“Most presented worries about increased uncertainties, such as the negative impact on their work, risk of COVID-19 infection of themselves or their loved ones and their treatment,” the authors reported.
Although 19% were completely abstinent, an additional 12% (n = 3) reported worsened gambling. In addition, almost half (46%) reported anxiety symptoms and more than a quarter (27%) had depressive symptoms.
Appropriate care
A particularly complicating factor of the pandemic is how it has disrupted traditional ways of seeking health care, particularly with how much mental health and other medical care has shifted to telehealth and online delivery, Dr. Potenza pointed out.
“This is a change for many people, and it’s important for both caretakers and people in treatment to be mindful of this and to try to ensure that appropriate services are maintained for people during this time,” he said.
For example, 12-step programs traditionally meet in person, which is largely impossible during the pandemic. Some have moved meetings online, and other programs have turned to apps, such as the Addiction Policy Forum’s app Connections, an empirically validated digital therapy platform that lets patients and clinicians remain connected with remote check-ins.
The move to more telehealth may actually increase access, suggested Dr. Hodgins.
“There is no evidence that this is less effective, and in fact, its convenience might be an advantage in reaching more people,” he said. “More challenging is offering group therapies remotely, but this is also feasible.”
The treatment with the strongest evidence remains cognitive-behavioral therapy (CBT), Dr. Hodgins said.
“This therapy, in part, helps people become aware of their erroneous cognitions and to challenge them, but also helps people restructure their activities to change their habits,” he said. He also noted the rise of online therapy, whether supported by a therapist or entirely self-directed, such as Gambling Self-help.
“These programs typically provide cognitive behavior content but also content that comes from studying how people recover from gambling problems,” he said. “The challenge of completely self-directed approaches is follow-through. Like most online content, people tend to flit around more than they might in therapy.” Still, he added, research has shown good outcomes from these programs.
Dr. Potenza also noted that several organizations, including the International Society of Addiction Medicine and Children and Screens, have been hosting webinars related to COVID-19 coping and/or addiction that clinicians and patients might find helpful.
Identification of problematic behaviors
One challenge in watching for problematic gambling behaviors during the pandemic is the set of unusual living circumstances for most people right now. At almost no other time in history have people been primarily confined to their homes, many unable to go to work or working from home, with extra leisure time and nowhere to go.
“With the COVID-19 pandemic, a lot of daily life has changed,” Dr. Potenza said. “It’s unclear whether certain behaviors that have become habitual during the pandemic, such as gaming or online gambling, will then interfere with daily life when the pandemic subsides.”
“The problem is, a small proportion of people who are very vulnerable will develop a disorder and might maintain it,” Dr. Kraus said. Those who already struggle with mental health and may be out of work have greater potential for problematic behaviors.
Dr. Potenza collaborated with other psychiatrists in drafting consensus guidelines on maintaining healthy use of the Internet specifically during the pandemic (Compr Psychiatry. 2020 Jul. doi: 10.10161/comppsych.2020.152180).
“It’s important to think about where one draws the line between normative everyday behaviors – behaviors that are not interfering with life functioning – and those that do interfere with life functioning,” Dr. Potenza said. “If someone is having difficulty making work or family or school obligations, these are important signs that the behavior may be problematic.”
He offered suggestions for things people can do to promote their health during the pandemic, such as having regular routines that include getting physical exercise and social interaction, dining with family if isolating together, and making time for self-care. He also recommended setting limits on the use of digital devices and aiming for a healthy balance in keeping up with the news. The idea is to stay aware of what’s happening without getting burned out or traumatized by news coverage.
Guidance for clinicians
An urgent need for research and guidelines related to gambling and the pandemic exists, the authors argued.
In the meantime, aside from various validated screeners available, Dr. Kraus offered some practical advice for clinicians checking in with their patients: “Ask your patients what they have been doing to cope with this difficult time.”
Some might mention their faith, family, or friends, and others might not have an answer or mention drinking, gaming, or engaging in other activities. “We all do things to cope. Sometimes you use healthy coping and sometimes you use unhealthy coping,” Dr. Kraus said. “I would have a dialogue with my patients around, ‘How are you getting through? What’s helping you? What are some things you’ve tried that are tripping you up?’ ”
If gambling in particular is a possible concern, he encouraged clinicians to ask their patients whether they have tried to quit or what would happen if they stopped gambling.
“What we’d expect is the problem gamblers will have more irritability, crankiness, difficulty with quitting,” he said.
Dr. Hodgins agreed that checking in on how patients’ lives and activities have changed, and their emotion reactions to those changes, is prudent.
“The change in activities might be healthy or might include increased addictive behaviors, including increased use of substances, gaming, pornography, food, and gambling,” he said.
In addition, the paper authors list several examples of guidelines that might be considered in drafting guidance for clinicians, including the following:
- Limiting the extent of gambling
- Not gambling to regulate negative emotions
- Not gambling in order to try to solve financial problems or financial concerns
- Not gambling under the influence of alcohol or drugs
- Carefully monitoring gambling-related time and financial expenditures
- Maintaining and establishing daily routines involving activities other than gambling
- Minding gambling-related attitudes and behaviors in the presence of minors
- Not starting to gamble because of stressors
The research did not receive external funding. Dr. Håkansson has received research funding from the Swedish Sport Foundation, the Swedish alcohol monopoly Systembolaget, and the Swedish state-owned gambling operator AB Svenska Spel. He is working with the company Kontigo Care on devices for gambling addiction follow-up care. Dr. Potenza has received consulting or advisory compensation from several entities, including the Addiction Policy Forum, AXA Gaming, Idorsia, Opiant, and RiverMend Health. Dr. Potenza has received research funding from Mohegan Sun casino and the National Center for Responsible Gaming. No other authors or outside sources had industry-related disclosures.
SOURCE: Håkansson A et al. J Addict Med. 2020 May 18. doi: 10.1097/ADM.0000000000000690.
The confluence of isolation, excess available time, and anxiety about illness or finances as a result of the COVID-19 pandemic have the potential to increase problem gambling behaviors during this public health emergency, so it’s essential to gather data and supply guidance on this issue, according to a call to action published May 18 in the Journal of Addiction Medicine.
“When facing an unforeseen situation with confinement, fear of disease, and financial uncertainty for the future, problem gambling may be an important health hazard to monitor and prevent during and following the COVID-19 crisis, especially given current online gambling availability,” wrote Anders Håkansson, PhD, of Lund University in Sweden and coauthors.
Both stress and trauma have been linked to gambling problems, and both are occurring during the pandemic, said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn., in an interview.
“People are likely to be experiencing stress at levels they haven’t experienced previously,” Dr. Potenza said. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said.
David Hodgins, PhD, CPsych, a professor of psychology at the University of Calgary in Alberta, who was not involved with the commentary, noted that gambling relapse is triggered by “negative emotional states, interpersonal stress, and financial stress” – all three of which the pandemic contributes to.
Financial stress can especially “inflame erroneous gambling-related cognitions,” he said in an interview, including “beliefs such as the idea that gambling can solve financial problems, even when this is statistically almost impossible as debt increases, and that debt has been caused by gambling.”
Increased social isolation also is particularly problematic, pointed out Shane W. Kraus, PhD, from the University of Nevada, Las Vegas. Dr. Kraus also was not involved with the paper.
“If someone is already struggling with already negative emotions, negative feelings, thoughts, and depression, and you’re now isolating them quite a bit, that’s not going to be a recipe for success,” Dr. Kraus said in an interview.
Dr. Potenza said.
“We should be mindful of ways in which people develop addictions in these settings,” he said. “One of the aspects of the pandemic is that many people are at home for longer periods of time, and they use digital technologies more frequently.”
The use of digital technologies can include interaction on social media platforms and on meeting applications such as Zoom, but such use also offers opportunities for problematic gambling, gaming, and pornography use. The World Health Organization recognizes addiction disorders for gambling and for gaming, and online gaming platforms and pornography sites have reported substantial increases in their traffic during the pandemic, Dr. Potenza said.
The increase in frequency is unsurprising and not necessarily a concern by itself, Dr. Kraus said.
“It’s all about loss of control or difficulty engaging or disengaging,” Dr. Kraus said. “When you can’t stop doing something even if you like it or love it, when it interferes with your day-to-day activities and relationships, that’s when it’s a problem.”
Gambling online: Easy, available
The authors note that past research has identified increased gambling problems during economic crises in other countries.
“While currently speculative, financial hardships may promote gambling as individuals may be motivated to gamble to try to win money,” the authors suggested. “Although presently limited, existing data suggest that COVID-19–related financial concerns may increase gambling-related harms, and this possibility merits systematic research.”
But trends and characteristics of the gambling market, including direct effects from the pandemic, can potentially influence behaviors, too. Most casinos have closed during the pandemic, and most of the sports that people bet on have been canceled or postponed.
“Fewer people are gambling on sports, but they turn then to other areas,” Dr. Potenza said. “If they can’t bet on major league type sports, they might gamble on more local sporting events, or they may bet on other activities going on in society during the pandemic.”
But online gambling poses greater risk.
“Properties of online gambling may constitute a particular health hazard when many people are confined to their homes and have had rapid changes in working conditions, psychosocial stress, anxiety, and depression, as has been described in China,” the paper’s authors wrote. “Online gambling may be particularly concerning due to its availability and velocity” and association with higher debt levels.
In addition to online gaming’s ease and availability, past research has found patients report boredom and escapism as reasons they turned to it.
Again, boredom on its own is not necessarily a problem, but for those who already struggle with addictive behaviors, it can be a trigger, Dr. Kraus said.
“Boredom is very tough for them because it’s often associated with negative emotions,” such as dwelling on things not going well in their lives, he said. “In a pandemic, people are by themselves quite a bit, socially isolated, so for those who are struggling already with some depression or anxiety, it’s only going to be increased.”
Online gaming trends may vary with demographics, however. Dr. Kraus noted that his former clinic at the Veterans Administration has been seeing lower gambling in patients with addictive disorders, but those patients are also older and primarily frequented casinos.
“It’s going to depend on age and familiarity with technology,” he said, but even if older problem gamblers are not going to the Internet now, “let’s wait and see what happens in the next 2 or 3 months.”
The authors noted results from a small survey of patients in treatment for gambling addiction at the Bellvitge University Hospital in Barcelona, Spain, where two of the coauthors work. They conducted telephone surveys with 26 patients about the first 4 weeks of sheltering in place because of the coronavirus. All but four of the patients were male, and their average age was 45 years.
“Most presented worries about increased uncertainties, such as the negative impact on their work, risk of COVID-19 infection of themselves or their loved ones and their treatment,” the authors reported.
Although 19% were completely abstinent, an additional 12% (n = 3) reported worsened gambling. In addition, almost half (46%) reported anxiety symptoms and more than a quarter (27%) had depressive symptoms.
Appropriate care
A particularly complicating factor of the pandemic is how it has disrupted traditional ways of seeking health care, particularly with how much mental health and other medical care has shifted to telehealth and online delivery, Dr. Potenza pointed out.
“This is a change for many people, and it’s important for both caretakers and people in treatment to be mindful of this and to try to ensure that appropriate services are maintained for people during this time,” he said.
For example, 12-step programs traditionally meet in person, which is largely impossible during the pandemic. Some have moved meetings online, and other programs have turned to apps, such as the Addiction Policy Forum’s app Connections, an empirically validated digital therapy platform that lets patients and clinicians remain connected with remote check-ins.
The move to more telehealth may actually increase access, suggested Dr. Hodgins.
“There is no evidence that this is less effective, and in fact, its convenience might be an advantage in reaching more people,” he said. “More challenging is offering group therapies remotely, but this is also feasible.”
The treatment with the strongest evidence remains cognitive-behavioral therapy (CBT), Dr. Hodgins said.
“This therapy, in part, helps people become aware of their erroneous cognitions and to challenge them, but also helps people restructure their activities to change their habits,” he said. He also noted the rise of online therapy, whether supported by a therapist or entirely self-directed, such as Gambling Self-help.
“These programs typically provide cognitive behavior content but also content that comes from studying how people recover from gambling problems,” he said. “The challenge of completely self-directed approaches is follow-through. Like most online content, people tend to flit around more than they might in therapy.” Still, he added, research has shown good outcomes from these programs.
Dr. Potenza also noted that several organizations, including the International Society of Addiction Medicine and Children and Screens, have been hosting webinars related to COVID-19 coping and/or addiction that clinicians and patients might find helpful.
Identification of problematic behaviors
One challenge in watching for problematic gambling behaviors during the pandemic is the set of unusual living circumstances for most people right now. At almost no other time in history have people been primarily confined to their homes, many unable to go to work or working from home, with extra leisure time and nowhere to go.
“With the COVID-19 pandemic, a lot of daily life has changed,” Dr. Potenza said. “It’s unclear whether certain behaviors that have become habitual during the pandemic, such as gaming or online gambling, will then interfere with daily life when the pandemic subsides.”
“The problem is, a small proportion of people who are very vulnerable will develop a disorder and might maintain it,” Dr. Kraus said. Those who already struggle with mental health and may be out of work have greater potential for problematic behaviors.
Dr. Potenza collaborated with other psychiatrists in drafting consensus guidelines on maintaining healthy use of the Internet specifically during the pandemic (Compr Psychiatry. 2020 Jul. doi: 10.10161/comppsych.2020.152180).
“It’s important to think about where one draws the line between normative everyday behaviors – behaviors that are not interfering with life functioning – and those that do interfere with life functioning,” Dr. Potenza said. “If someone is having difficulty making work or family or school obligations, these are important signs that the behavior may be problematic.”
He offered suggestions for things people can do to promote their health during the pandemic, such as having regular routines that include getting physical exercise and social interaction, dining with family if isolating together, and making time for self-care. He also recommended setting limits on the use of digital devices and aiming for a healthy balance in keeping up with the news. The idea is to stay aware of what’s happening without getting burned out or traumatized by news coverage.
Guidance for clinicians
An urgent need for research and guidelines related to gambling and the pandemic exists, the authors argued.
In the meantime, aside from various validated screeners available, Dr. Kraus offered some practical advice for clinicians checking in with their patients: “Ask your patients what they have been doing to cope with this difficult time.”
Some might mention their faith, family, or friends, and others might not have an answer or mention drinking, gaming, or engaging in other activities. “We all do things to cope. Sometimes you use healthy coping and sometimes you use unhealthy coping,” Dr. Kraus said. “I would have a dialogue with my patients around, ‘How are you getting through? What’s helping you? What are some things you’ve tried that are tripping you up?’ ”
If gambling in particular is a possible concern, he encouraged clinicians to ask their patients whether they have tried to quit or what would happen if they stopped gambling.
“What we’d expect is the problem gamblers will have more irritability, crankiness, difficulty with quitting,” he said.
Dr. Hodgins agreed that checking in on how patients’ lives and activities have changed, and their emotion reactions to those changes, is prudent.
“The change in activities might be healthy or might include increased addictive behaviors, including increased use of substances, gaming, pornography, food, and gambling,” he said.
In addition, the paper authors list several examples of guidelines that might be considered in drafting guidance for clinicians, including the following:
- Limiting the extent of gambling
- Not gambling to regulate negative emotions
- Not gambling in order to try to solve financial problems or financial concerns
- Not gambling under the influence of alcohol or drugs
- Carefully monitoring gambling-related time and financial expenditures
- Maintaining and establishing daily routines involving activities other than gambling
- Minding gambling-related attitudes and behaviors in the presence of minors
- Not starting to gamble because of stressors
The research did not receive external funding. Dr. Håkansson has received research funding from the Swedish Sport Foundation, the Swedish alcohol monopoly Systembolaget, and the Swedish state-owned gambling operator AB Svenska Spel. He is working with the company Kontigo Care on devices for gambling addiction follow-up care. Dr. Potenza has received consulting or advisory compensation from several entities, including the Addiction Policy Forum, AXA Gaming, Idorsia, Opiant, and RiverMend Health. Dr. Potenza has received research funding from Mohegan Sun casino and the National Center for Responsible Gaming. No other authors or outside sources had industry-related disclosures.
SOURCE: Håkansson A et al. J Addict Med. 2020 May 18. doi: 10.1097/ADM.0000000000000690.
The confluence of isolation, excess available time, and anxiety about illness or finances as a result of the COVID-19 pandemic have the potential to increase problem gambling behaviors during this public health emergency, so it’s essential to gather data and supply guidance on this issue, according to a call to action published May 18 in the Journal of Addiction Medicine.
“When facing an unforeseen situation with confinement, fear of disease, and financial uncertainty for the future, problem gambling may be an important health hazard to monitor and prevent during and following the COVID-19 crisis, especially given current online gambling availability,” wrote Anders Håkansson, PhD, of Lund University in Sweden and coauthors.
Both stress and trauma have been linked to gambling problems, and both are occurring during the pandemic, said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn., in an interview.
“People are likely to be experiencing stress at levels they haven’t experienced previously,” Dr. Potenza said. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said.
David Hodgins, PhD, CPsych, a professor of psychology at the University of Calgary in Alberta, who was not involved with the commentary, noted that gambling relapse is triggered by “negative emotional states, interpersonal stress, and financial stress” – all three of which the pandemic contributes to.
Financial stress can especially “inflame erroneous gambling-related cognitions,” he said in an interview, including “beliefs such as the idea that gambling can solve financial problems, even when this is statistically almost impossible as debt increases, and that debt has been caused by gambling.”
Increased social isolation also is particularly problematic, pointed out Shane W. Kraus, PhD, from the University of Nevada, Las Vegas. Dr. Kraus also was not involved with the paper.
“If someone is already struggling with already negative emotions, negative feelings, thoughts, and depression, and you’re now isolating them quite a bit, that’s not going to be a recipe for success,” Dr. Kraus said in an interview.
Dr. Potenza said.
“We should be mindful of ways in which people develop addictions in these settings,” he said. “One of the aspects of the pandemic is that many people are at home for longer periods of time, and they use digital technologies more frequently.”
The use of digital technologies can include interaction on social media platforms and on meeting applications such as Zoom, but such use also offers opportunities for problematic gambling, gaming, and pornography use. The World Health Organization recognizes addiction disorders for gambling and for gaming, and online gaming platforms and pornography sites have reported substantial increases in their traffic during the pandemic, Dr. Potenza said.
The increase in frequency is unsurprising and not necessarily a concern by itself, Dr. Kraus said.
“It’s all about loss of control or difficulty engaging or disengaging,” Dr. Kraus said. “When you can’t stop doing something even if you like it or love it, when it interferes with your day-to-day activities and relationships, that’s when it’s a problem.”
Gambling online: Easy, available
The authors note that past research has identified increased gambling problems during economic crises in other countries.
“While currently speculative, financial hardships may promote gambling as individuals may be motivated to gamble to try to win money,” the authors suggested. “Although presently limited, existing data suggest that COVID-19–related financial concerns may increase gambling-related harms, and this possibility merits systematic research.”
But trends and characteristics of the gambling market, including direct effects from the pandemic, can potentially influence behaviors, too. Most casinos have closed during the pandemic, and most of the sports that people bet on have been canceled or postponed.
“Fewer people are gambling on sports, but they turn then to other areas,” Dr. Potenza said. “If they can’t bet on major league type sports, they might gamble on more local sporting events, or they may bet on other activities going on in society during the pandemic.”
But online gambling poses greater risk.
“Properties of online gambling may constitute a particular health hazard when many people are confined to their homes and have had rapid changes in working conditions, psychosocial stress, anxiety, and depression, as has been described in China,” the paper’s authors wrote. “Online gambling may be particularly concerning due to its availability and velocity” and association with higher debt levels.
In addition to online gaming’s ease and availability, past research has found patients report boredom and escapism as reasons they turned to it.
Again, boredom on its own is not necessarily a problem, but for those who already struggle with addictive behaviors, it can be a trigger, Dr. Kraus said.
“Boredom is very tough for them because it’s often associated with negative emotions,” such as dwelling on things not going well in their lives, he said. “In a pandemic, people are by themselves quite a bit, socially isolated, so for those who are struggling already with some depression or anxiety, it’s only going to be increased.”
Online gaming trends may vary with demographics, however. Dr. Kraus noted that his former clinic at the Veterans Administration has been seeing lower gambling in patients with addictive disorders, but those patients are also older and primarily frequented casinos.
“It’s going to depend on age and familiarity with technology,” he said, but even if older problem gamblers are not going to the Internet now, “let’s wait and see what happens in the next 2 or 3 months.”
The authors noted results from a small survey of patients in treatment for gambling addiction at the Bellvitge University Hospital in Barcelona, Spain, where two of the coauthors work. They conducted telephone surveys with 26 patients about the first 4 weeks of sheltering in place because of the coronavirus. All but four of the patients were male, and their average age was 45 years.
“Most presented worries about increased uncertainties, such as the negative impact on their work, risk of COVID-19 infection of themselves or their loved ones and their treatment,” the authors reported.
Although 19% were completely abstinent, an additional 12% (n = 3) reported worsened gambling. In addition, almost half (46%) reported anxiety symptoms and more than a quarter (27%) had depressive symptoms.
Appropriate care
A particularly complicating factor of the pandemic is how it has disrupted traditional ways of seeking health care, particularly with how much mental health and other medical care has shifted to telehealth and online delivery, Dr. Potenza pointed out.
“This is a change for many people, and it’s important for both caretakers and people in treatment to be mindful of this and to try to ensure that appropriate services are maintained for people during this time,” he said.
For example, 12-step programs traditionally meet in person, which is largely impossible during the pandemic. Some have moved meetings online, and other programs have turned to apps, such as the Addiction Policy Forum’s app Connections, an empirically validated digital therapy platform that lets patients and clinicians remain connected with remote check-ins.
The move to more telehealth may actually increase access, suggested Dr. Hodgins.
“There is no evidence that this is less effective, and in fact, its convenience might be an advantage in reaching more people,” he said. “More challenging is offering group therapies remotely, but this is also feasible.”
The treatment with the strongest evidence remains cognitive-behavioral therapy (CBT), Dr. Hodgins said.
“This therapy, in part, helps people become aware of their erroneous cognitions and to challenge them, but also helps people restructure their activities to change their habits,” he said. He also noted the rise of online therapy, whether supported by a therapist or entirely self-directed, such as Gambling Self-help.
“These programs typically provide cognitive behavior content but also content that comes from studying how people recover from gambling problems,” he said. “The challenge of completely self-directed approaches is follow-through. Like most online content, people tend to flit around more than they might in therapy.” Still, he added, research has shown good outcomes from these programs.
Dr. Potenza also noted that several organizations, including the International Society of Addiction Medicine and Children and Screens, have been hosting webinars related to COVID-19 coping and/or addiction that clinicians and patients might find helpful.
Identification of problematic behaviors
One challenge in watching for problematic gambling behaviors during the pandemic is the set of unusual living circumstances for most people right now. At almost no other time in history have people been primarily confined to their homes, many unable to go to work or working from home, with extra leisure time and nowhere to go.
“With the COVID-19 pandemic, a lot of daily life has changed,” Dr. Potenza said. “It’s unclear whether certain behaviors that have become habitual during the pandemic, such as gaming or online gambling, will then interfere with daily life when the pandemic subsides.”
“The problem is, a small proportion of people who are very vulnerable will develop a disorder and might maintain it,” Dr. Kraus said. Those who already struggle with mental health and may be out of work have greater potential for problematic behaviors.
Dr. Potenza collaborated with other psychiatrists in drafting consensus guidelines on maintaining healthy use of the Internet specifically during the pandemic (Compr Psychiatry. 2020 Jul. doi: 10.10161/comppsych.2020.152180).
“It’s important to think about where one draws the line between normative everyday behaviors – behaviors that are not interfering with life functioning – and those that do interfere with life functioning,” Dr. Potenza said. “If someone is having difficulty making work or family or school obligations, these are important signs that the behavior may be problematic.”
He offered suggestions for things people can do to promote their health during the pandemic, such as having regular routines that include getting physical exercise and social interaction, dining with family if isolating together, and making time for self-care. He also recommended setting limits on the use of digital devices and aiming for a healthy balance in keeping up with the news. The idea is to stay aware of what’s happening without getting burned out or traumatized by news coverage.
Guidance for clinicians
An urgent need for research and guidelines related to gambling and the pandemic exists, the authors argued.
In the meantime, aside from various validated screeners available, Dr. Kraus offered some practical advice for clinicians checking in with their patients: “Ask your patients what they have been doing to cope with this difficult time.”
Some might mention their faith, family, or friends, and others might not have an answer or mention drinking, gaming, or engaging in other activities. “We all do things to cope. Sometimes you use healthy coping and sometimes you use unhealthy coping,” Dr. Kraus said. “I would have a dialogue with my patients around, ‘How are you getting through? What’s helping you? What are some things you’ve tried that are tripping you up?’ ”
If gambling in particular is a possible concern, he encouraged clinicians to ask their patients whether they have tried to quit or what would happen if they stopped gambling.
“What we’d expect is the problem gamblers will have more irritability, crankiness, difficulty with quitting,” he said.
Dr. Hodgins agreed that checking in on how patients’ lives and activities have changed, and their emotion reactions to those changes, is prudent.
“The change in activities might be healthy or might include increased addictive behaviors, including increased use of substances, gaming, pornography, food, and gambling,” he said.
In addition, the paper authors list several examples of guidelines that might be considered in drafting guidance for clinicians, including the following:
- Limiting the extent of gambling
- Not gambling to regulate negative emotions
- Not gambling in order to try to solve financial problems or financial concerns
- Not gambling under the influence of alcohol or drugs
- Carefully monitoring gambling-related time and financial expenditures
- Maintaining and establishing daily routines involving activities other than gambling
- Minding gambling-related attitudes and behaviors in the presence of minors
- Not starting to gamble because of stressors
The research did not receive external funding. Dr. Håkansson has received research funding from the Swedish Sport Foundation, the Swedish alcohol monopoly Systembolaget, and the Swedish state-owned gambling operator AB Svenska Spel. He is working with the company Kontigo Care on devices for gambling addiction follow-up care. Dr. Potenza has received consulting or advisory compensation from several entities, including the Addiction Policy Forum, AXA Gaming, Idorsia, Opiant, and RiverMend Health. Dr. Potenza has received research funding from Mohegan Sun casino and the National Center for Responsible Gaming. No other authors or outside sources had industry-related disclosures.
SOURCE: Håkansson A et al. J Addict Med. 2020 May 18. doi: 10.1097/ADM.0000000000000690.
FROM THE JOURNAL OF ADDICTION MEDICINE