User login
Small study: MRIs okay with pacemakers and defibrillators
VANCOUVER, B.C. – When done safely, MRI imaging has an important role to play in patients with pacemakers and implanted cardioverter defibrillators, according to a study of 32 patients who underwent the procedure without complications at Allegheny General Hospital in Pittsburgh.
"It looks like this is safe in the right situation," based on the results and ongoing research elsewhere. "There are occasions – more often than you might think – when" MRI imaging of such patients has "potentially life-saving consequences. I would suggest it is probably no longer taboo," said lead investigator Dr. Robert Biederman, director of cardiovascular MRI at Allegheny and an associate professor of medicine at Drexel University in Philadelphia.
Among the 32 patients in the study, 23 underwent neurologic MRI imaging, and 9 underwent cardiac MRI imaging.
The neurologic MRI imaging picked up a case of Creutzfeldt–Jakob disease in one with unexplained altered mental status, and a syrinx in another who had unexplained arm weakness, a finding that made a "huge difference neurosurgically." Overall, neurologic imaging made or altered diagnoses in 15 patients, and confirmed them in eight, Dr. Biederman said at the 18th World Congress on Heart Disease.
Cardiac MRI imaging picked up cardiac sarcoidosis in one, and constrictive pericarditis in another. In six cases, it simply confirmed provisional diagnoses. Even so, "there is value in confirming for surgeons, patients, and family members that they are doing the right thing," he said.
Often, in the absence of a solid diagnosis, the "patients were going to die." Imaging was only done, however, after conversations that sometimes ran more than an hour with patients and family members about the risks of MRIs with pacemakers (PM) and automated implantable cardioverter-defibrillators (AICD), including tissue cauterization, fibrosis, lethal tachycardia, and device misfire. "This was absolutely done with the patient’s full knowledge of risk," he said.
Although MRIs have caused at least 12 deaths in patients with PMs and AICDs over the last 3 decades, ongoing research with newer devices is beginning to suggest it’s safe if proper device and MRI adjustments are made; well over 1,000 patients have undergone MRIs in recent years with no complications. Even so, "assuming it is safe, no one’s asked if it makes a difference. This is the first time to my knowledge that anyone has stepped beyond the question of safety to see if results from MRIs" in these patients "warrant the risk," Dr. Biederman said (e.g., Am. Heart J. 2013;165:266-72).
Four of the patients had combination PM/AICDs, 18 had dual-chamber PMs, three dependent PMs, five AICDs, and two just single pacer leads. Only one patient had a Revo MRI SureScan Pacing System, the only pacer FDA- approved for MRI use. Scans ran an average of a half hour, plus or minus 15 minutes; a few patients were scanned twice.
The MRIs were performed in a dedicated cardiovascular MRI suite with continuous ECG, blood pressure, heart rate, and oxygen saturation monitoring. "We turned all the defibrillator technology off, and tried to turn the pacemaker off. If we couldn’t, we turned it to an asynchronous mode." Sequences were done at a specific absorption rate (SAR) of less than 2 W/kg, because "there is less radiofrequency energy being sent at a slower rate, so [it’s] less likely" to heat the device. "We try to keep the specific absorption rate as low as possible," Dr. Biederman said.
Devices were reset and tested after the procedure to ensure that impedance, thresholds, amplitudes, and shock impedances were the same as before the scans.
Dr. Biederman said he has no disclosures.
VANCOUVER, B.C. – When done safely, MRI imaging has an important role to play in patients with pacemakers and implanted cardioverter defibrillators, according to a study of 32 patients who underwent the procedure without complications at Allegheny General Hospital in Pittsburgh.
"It looks like this is safe in the right situation," based on the results and ongoing research elsewhere. "There are occasions – more often than you might think – when" MRI imaging of such patients has "potentially life-saving consequences. I would suggest it is probably no longer taboo," said lead investigator Dr. Robert Biederman, director of cardiovascular MRI at Allegheny and an associate professor of medicine at Drexel University in Philadelphia.
Among the 32 patients in the study, 23 underwent neurologic MRI imaging, and 9 underwent cardiac MRI imaging.
The neurologic MRI imaging picked up a case of Creutzfeldt–Jakob disease in one with unexplained altered mental status, and a syrinx in another who had unexplained arm weakness, a finding that made a "huge difference neurosurgically." Overall, neurologic imaging made or altered diagnoses in 15 patients, and confirmed them in eight, Dr. Biederman said at the 18th World Congress on Heart Disease.
Cardiac MRI imaging picked up cardiac sarcoidosis in one, and constrictive pericarditis in another. In six cases, it simply confirmed provisional diagnoses. Even so, "there is value in confirming for surgeons, patients, and family members that they are doing the right thing," he said.
Often, in the absence of a solid diagnosis, the "patients were going to die." Imaging was only done, however, after conversations that sometimes ran more than an hour with patients and family members about the risks of MRIs with pacemakers (PM) and automated implantable cardioverter-defibrillators (AICD), including tissue cauterization, fibrosis, lethal tachycardia, and device misfire. "This was absolutely done with the patient’s full knowledge of risk," he said.
Although MRIs have caused at least 12 deaths in patients with PMs and AICDs over the last 3 decades, ongoing research with newer devices is beginning to suggest it’s safe if proper device and MRI adjustments are made; well over 1,000 patients have undergone MRIs in recent years with no complications. Even so, "assuming it is safe, no one’s asked if it makes a difference. This is the first time to my knowledge that anyone has stepped beyond the question of safety to see if results from MRIs" in these patients "warrant the risk," Dr. Biederman said (e.g., Am. Heart J. 2013;165:266-72).
Four of the patients had combination PM/AICDs, 18 had dual-chamber PMs, three dependent PMs, five AICDs, and two just single pacer leads. Only one patient had a Revo MRI SureScan Pacing System, the only pacer FDA- approved for MRI use. Scans ran an average of a half hour, plus or minus 15 minutes; a few patients were scanned twice.
The MRIs were performed in a dedicated cardiovascular MRI suite with continuous ECG, blood pressure, heart rate, and oxygen saturation monitoring. "We turned all the defibrillator technology off, and tried to turn the pacemaker off. If we couldn’t, we turned it to an asynchronous mode." Sequences were done at a specific absorption rate (SAR) of less than 2 W/kg, because "there is less radiofrequency energy being sent at a slower rate, so [it’s] less likely" to heat the device. "We try to keep the specific absorption rate as low as possible," Dr. Biederman said.
Devices were reset and tested after the procedure to ensure that impedance, thresholds, amplitudes, and shock impedances were the same as before the scans.
Dr. Biederman said he has no disclosures.
VANCOUVER, B.C. – When done safely, MRI imaging has an important role to play in patients with pacemakers and implanted cardioverter defibrillators, according to a study of 32 patients who underwent the procedure without complications at Allegheny General Hospital in Pittsburgh.
"It looks like this is safe in the right situation," based on the results and ongoing research elsewhere. "There are occasions – more often than you might think – when" MRI imaging of such patients has "potentially life-saving consequences. I would suggest it is probably no longer taboo," said lead investigator Dr. Robert Biederman, director of cardiovascular MRI at Allegheny and an associate professor of medicine at Drexel University in Philadelphia.
Among the 32 patients in the study, 23 underwent neurologic MRI imaging, and 9 underwent cardiac MRI imaging.
The neurologic MRI imaging picked up a case of Creutzfeldt–Jakob disease in one with unexplained altered mental status, and a syrinx in another who had unexplained arm weakness, a finding that made a "huge difference neurosurgically." Overall, neurologic imaging made or altered diagnoses in 15 patients, and confirmed them in eight, Dr. Biederman said at the 18th World Congress on Heart Disease.
Cardiac MRI imaging picked up cardiac sarcoidosis in one, and constrictive pericarditis in another. In six cases, it simply confirmed provisional diagnoses. Even so, "there is value in confirming for surgeons, patients, and family members that they are doing the right thing," he said.
Often, in the absence of a solid diagnosis, the "patients were going to die." Imaging was only done, however, after conversations that sometimes ran more than an hour with patients and family members about the risks of MRIs with pacemakers (PM) and automated implantable cardioverter-defibrillators (AICD), including tissue cauterization, fibrosis, lethal tachycardia, and device misfire. "This was absolutely done with the patient’s full knowledge of risk," he said.
Although MRIs have caused at least 12 deaths in patients with PMs and AICDs over the last 3 decades, ongoing research with newer devices is beginning to suggest it’s safe if proper device and MRI adjustments are made; well over 1,000 patients have undergone MRIs in recent years with no complications. Even so, "assuming it is safe, no one’s asked if it makes a difference. This is the first time to my knowledge that anyone has stepped beyond the question of safety to see if results from MRIs" in these patients "warrant the risk," Dr. Biederman said (e.g., Am. Heart J. 2013;165:266-72).
Four of the patients had combination PM/AICDs, 18 had dual-chamber PMs, three dependent PMs, five AICDs, and two just single pacer leads. Only one patient had a Revo MRI SureScan Pacing System, the only pacer FDA- approved for MRI use. Scans ran an average of a half hour, plus or minus 15 minutes; a few patients were scanned twice.
The MRIs were performed in a dedicated cardiovascular MRI suite with continuous ECG, blood pressure, heart rate, and oxygen saturation monitoring. "We turned all the defibrillator technology off, and tried to turn the pacemaker off. If we couldn’t, we turned it to an asynchronous mode." Sequences were done at a specific absorption rate (SAR) of less than 2 W/kg, because "there is less radiofrequency energy being sent at a slower rate, so [it’s] less likely" to heat the device. "We try to keep the specific absorption rate as low as possible," Dr. Biederman said.
Devices were reset and tested after the procedure to ensure that impedance, thresholds, amplitudes, and shock impedances were the same as before the scans.
Dr. Biederman said he has no disclosures.
AT THE 18TH WORLD CONGRESS ON HEART DISEASE
Major finding: MRIs made or altered neurologic diagnoses in 15 of 23 patients with pacemakers or implanted defibrillators. They confirmed diagnoses in the rest. There were no imaging complications.
Data Source: Prospective study of 32 patients with the devices who underwent MRIs
Disclosures: The lead investigator has no disclosures.
Neck–Shoulder Crossover: How Often Do Neck and Shoulder Pathology Masquerade as Each Other?
Traumatic Obterator Hip Traumatic Obterator Hip Dislocation in a 9-Year-Old Boy Dislocation in a 9-Year-Old Boy
Avoiding Unplanned Resections of Wrist Sarcomas: An Algorithm for Evaluating Dorsal Wrist Masses
Severe Left Shoulder Pain After a Fall
Diffuse Abdominal Pain and Pleural Effusion
Fever, dyspnea, and a new heart murmur
A 35-year-old man presented to the emergency department because of night sweats, fever, chills, and shortness of breath. He also had an acute onset of blue discoloration of his right fourth finger. His symptoms (except for the finger discoloration) had begun about 6 months previously and had rapidly progressed despite several courses of different antibiotics of different types, given both intravenously in the hospital and orally at home. He had lost 20 lb during this time. Previously, he had been healthy.
About 1 month after his symptoms began, he had consulted his primary care physician, who detected a new grade 4/6 systolic and diastolic murmur. Transthoracic echocardiography about 2 months after that demonstrated mild aortic and mitral insufficiency but no echocardiographic features supporting infective endocarditis. Of note, the patient had no risk factors for endocarditis such as illicit drug use or poor dental health.
In the emergency department, his temperature was 99.4°F (37.4°C), pulse 109 beats per minute, and blood pressure 126/60 mm Hg. He had a grade 3/6 harsh holosystolic murmur best heard at the right upper sternal border, a grade 3/4 holodiastolic murmur audible across the precordium, and a grade 3/4 holosystolic blowing murmur best heard at the cardiac apex. Other findings included signs of aortic insufficiency—the Duroziez sign (a diastolic murmur heard over the femoral artery when compressed), Watson’s water-hammer pulse (indicating a wide pulse pressure), and the Müller sign (pulsation of the uvula)—and small Janeway lesions on the inner aspect of his right arm and palm.
Electrocardiography showed normal sinus rhythm, PR interval 128 ms, QRS complex 100 ms, QT interval 360 ms, and corrected QT interval 473 ms.
Blood cultures grew Streptococcus sanguinis. Both transthoracic and transesophageal echocardiography were done promptly and revealed multiple mobile echodensities attached to a trileaflet aortic valve, consistent with vegetations and valve leaflet destruction; severe (4+) aortic regurgitation with flow reversal in the abdominal aorta; mild mitral regurgitation; and a mitral valve aneurysm with mild mitral regurgitation (Figure 1).
INFECTIVE ENDOCARDITIS: WORTH CONSIDERING
S sanguinis is a member of the group of viridans streptococci. As a normal inhabitant of the healthy human mouth, it is found in dental plaque. It may enter the bloodstream during dental cleaning and may colonize the heart valves, particularly the mitral and aortic valves, where it is the most common cause of subacute bacterial endocarditis.
Infective endocarditis is often diagnosed clinically with the Duke criteria (www.med-calc.com/endocarditis.html).1 However, the variability of the clinical presentation and the nonspecific nature of the initial workup often create a diagnostic challenge for the evaluating physician.1,2
In cases of recurrent persistent fever and a new heart murmur, infective endocarditis must always be considered. Blood cultures should be ordered early and repeatedly. If blood cultures are positive, transesophageal echocardiography should be done without delay if transthoracic echocardiography was unremarkable. Prompt diagnosis and surgical intervention prevent complications.
MITRAL VALVE ANEURYSM IN AORTIC VALVE ENDOCARDITIS
Aortic valve endocarditis often also involves the mitral valve; mitral valve endocarditis is seen in 17% of patients undergoing surgery for aortic valve endocarditis.3 Proposed mechanisms for this association include jet lesions from aortic regurgitation, vegetation prolapse with direct contact between the aortic valve and anterior mitral leaflet (“kissing lesions”), and direct local spread of infection.4–7
One of every five patients with mitral valve involvement in aortic valve endocarditis has a mitral valve aneurysm.3 This is a serious finding, as it can lead to septic embolization. Also, the weakened lining of the mitral valve aneurysm can rupture, resulting in severe mitral regurgitation, acute pulmonary edema, and precipitous cardiopulmonary decompensation.5
Transesophageal echocardiography is more sensitive than transthoracic echocardiography for detecting mitral valve aneurysm.8 On two-dimensional echocardiography, the lesion appears as a narrow-necked, saccular echolucency with systolic protrusion into the left atrium. Color Doppler imaging often shows turbulent, high-velocity flow.
Differential diagnosis of mitral valve aneurysm
Differential diagnostic considerations include a valvular blood cyst, a congenital cardiac diverticulum, and mitral valve prolapse.
Valvular blood cysts are extremely rare in adults.9 These benign, congenital tumors are most often found on the atrioventricular valves in infants, in whom the reported incidence is between 25% and 100%. In almost all cases, these cysts are believed to regress spontaneously with time.
In almost all reported cases, the cyst involved the valvular apparatus or papillary muscle of the tricuspid, pulmonary, or mitral valve.10 Cysts consist of a benign diverticulum lined with flattened, cobblestone-shaped endothelium and are filled with blood. They can cause heart murmurs in otherwise asymptomatic patients.
On echocardiography, a blood cyst appears as an oval mass (often at the interatrial septum), often with normal cardiac function. In the rare case in which a blood cyst is found incidentally during echocardiography, the hemodynamic impact, if any, should be determined by Doppler techniques.
When benign, a valvular blood cyst can be safely monitored with echocardiographic follow-up.11 Treatment involves surgical resection of the mass in symptomatic patients in whom cardiac function is impaired by the presence of the cyst.
Congenital cardiac diverticuli are extremely rare, most often seen in children, and associated with a midline thoracoabdominal defect. Echocardiography can differentiate a ventricular diverticulum from an aneurysm or a pseudoaneurysm.
A ventricular diverticulum has a fibrous, narrow neck connecting with the ventricle, and a small circular echo-free space that communicates with the ventricle via this narrow neck.2 Doppler imaging shows systolic flow from the diverticulum to the ventricle, and systolic contractility may also be seen during cardiac catheterization. Congenital diverticulum is typically confused with ventricular aneurysm and, to a lesser degree, with mitral valve aneurysm.
Mitral valve prolapse is characterized by interchordal ballooning or hooding of the mitral valve leaflets that occurs when one or both floppy, enlarged leaflets prolapse into the left atrium during systole.
BACK TO OUR PATIENT
The patient underwent open heart surgery, with successful repair of the aortic root, replacement of the aortic valve, and repair of the mitral valve. An abscess was found within the aneurysmal cavity.
- Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med 1994; 96:200–209.
- Prendergast BD. Diagnostic criteria and problems in infective endocarditis. Heart 2004; 90:611–613.
- Gonzalez-Lavin L, Lise M, Ross D. The importance of the ‘jet lesion’ in bacterial endocarditis involving the left heart. Surgical considerations. J Thorac Cardiovasc Surg 1970; 59:185–192.
- Silbiger JJ. Review: mitral valve aneurysms in infective endocarditis: mechanisms, clinical recognition, and treatment. J Heart Valve Dis 2009; 18:476–480.
- Reid CL, Chandraratna AN, Harrison E, et al. Mitral valve aneurysm: clinical features, echocardiographic-pathologic correlations. J Am Coll Cardiol 1983; 2:460–464.
- Rodbard S. Blood velocity and endocarditis. Circulation 1963; 27:18–28.
- Piper C, Hetzer R, Körfer R, Bergemann R, Horstkotte D. The importance of secondary mitral valve involvement in primary aortic valve endocarditis; the mitral kissing vegetation. Eur Heart J 2002; 23:79–86.
- Cziner DG, Rosenzweig BP, Katz ES, Keller AM, Daniel WG, Kronzon I. Transesophageal versus transthoracic echocardiography for diagnosing mitral valve perforation. Am J Cardiol 1992; 69:1495–1497.
- Roberts PF, Serra AJ, McNicholas KW, Shapira N, Lemole GM. Atrial blood cyst: a rare finding. Ann Thorac Surg 1996; 62:880–882.
- Grimaldi A, Capritti E, Pappalardo F, et al. Images in cardiovascular medicine: blood cyst of the mitral valve. J Cardiovasc Med 2012; 3:46.
- Boyd WC, Rosengart TK, Hartman GS. Isolated left ventricular diverticulum in an adult. J Cardiothorac Vasc Anesth 1999; 13:468–470.
A 35-year-old man presented to the emergency department because of night sweats, fever, chills, and shortness of breath. He also had an acute onset of blue discoloration of his right fourth finger. His symptoms (except for the finger discoloration) had begun about 6 months previously and had rapidly progressed despite several courses of different antibiotics of different types, given both intravenously in the hospital and orally at home. He had lost 20 lb during this time. Previously, he had been healthy.
About 1 month after his symptoms began, he had consulted his primary care physician, who detected a new grade 4/6 systolic and diastolic murmur. Transthoracic echocardiography about 2 months after that demonstrated mild aortic and mitral insufficiency but no echocardiographic features supporting infective endocarditis. Of note, the patient had no risk factors for endocarditis such as illicit drug use or poor dental health.
In the emergency department, his temperature was 99.4°F (37.4°C), pulse 109 beats per minute, and blood pressure 126/60 mm Hg. He had a grade 3/6 harsh holosystolic murmur best heard at the right upper sternal border, a grade 3/4 holodiastolic murmur audible across the precordium, and a grade 3/4 holosystolic blowing murmur best heard at the cardiac apex. Other findings included signs of aortic insufficiency—the Duroziez sign (a diastolic murmur heard over the femoral artery when compressed), Watson’s water-hammer pulse (indicating a wide pulse pressure), and the Müller sign (pulsation of the uvula)—and small Janeway lesions on the inner aspect of his right arm and palm.
Electrocardiography showed normal sinus rhythm, PR interval 128 ms, QRS complex 100 ms, QT interval 360 ms, and corrected QT interval 473 ms.
Blood cultures grew Streptococcus sanguinis. Both transthoracic and transesophageal echocardiography were done promptly and revealed multiple mobile echodensities attached to a trileaflet aortic valve, consistent with vegetations and valve leaflet destruction; severe (4+) aortic regurgitation with flow reversal in the abdominal aorta; mild mitral regurgitation; and a mitral valve aneurysm with mild mitral regurgitation (Figure 1).
INFECTIVE ENDOCARDITIS: WORTH CONSIDERING
S sanguinis is a member of the group of viridans streptococci. As a normal inhabitant of the healthy human mouth, it is found in dental plaque. It may enter the bloodstream during dental cleaning and may colonize the heart valves, particularly the mitral and aortic valves, where it is the most common cause of subacute bacterial endocarditis.
Infective endocarditis is often diagnosed clinically with the Duke criteria (www.med-calc.com/endocarditis.html).1 However, the variability of the clinical presentation and the nonspecific nature of the initial workup often create a diagnostic challenge for the evaluating physician.1,2
In cases of recurrent persistent fever and a new heart murmur, infective endocarditis must always be considered. Blood cultures should be ordered early and repeatedly. If blood cultures are positive, transesophageal echocardiography should be done without delay if transthoracic echocardiography was unremarkable. Prompt diagnosis and surgical intervention prevent complications.
MITRAL VALVE ANEURYSM IN AORTIC VALVE ENDOCARDITIS
Aortic valve endocarditis often also involves the mitral valve; mitral valve endocarditis is seen in 17% of patients undergoing surgery for aortic valve endocarditis.3 Proposed mechanisms for this association include jet lesions from aortic regurgitation, vegetation prolapse with direct contact between the aortic valve and anterior mitral leaflet (“kissing lesions”), and direct local spread of infection.4–7
One of every five patients with mitral valve involvement in aortic valve endocarditis has a mitral valve aneurysm.3 This is a serious finding, as it can lead to septic embolization. Also, the weakened lining of the mitral valve aneurysm can rupture, resulting in severe mitral regurgitation, acute pulmonary edema, and precipitous cardiopulmonary decompensation.5
Transesophageal echocardiography is more sensitive than transthoracic echocardiography for detecting mitral valve aneurysm.8 On two-dimensional echocardiography, the lesion appears as a narrow-necked, saccular echolucency with systolic protrusion into the left atrium. Color Doppler imaging often shows turbulent, high-velocity flow.
Differential diagnosis of mitral valve aneurysm
Differential diagnostic considerations include a valvular blood cyst, a congenital cardiac diverticulum, and mitral valve prolapse.
Valvular blood cysts are extremely rare in adults.9 These benign, congenital tumors are most often found on the atrioventricular valves in infants, in whom the reported incidence is between 25% and 100%. In almost all cases, these cysts are believed to regress spontaneously with time.
In almost all reported cases, the cyst involved the valvular apparatus or papillary muscle of the tricuspid, pulmonary, or mitral valve.10 Cysts consist of a benign diverticulum lined with flattened, cobblestone-shaped endothelium and are filled with blood. They can cause heart murmurs in otherwise asymptomatic patients.
On echocardiography, a blood cyst appears as an oval mass (often at the interatrial septum), often with normal cardiac function. In the rare case in which a blood cyst is found incidentally during echocardiography, the hemodynamic impact, if any, should be determined by Doppler techniques.
When benign, a valvular blood cyst can be safely monitored with echocardiographic follow-up.11 Treatment involves surgical resection of the mass in symptomatic patients in whom cardiac function is impaired by the presence of the cyst.
Congenital cardiac diverticuli are extremely rare, most often seen in children, and associated with a midline thoracoabdominal defect. Echocardiography can differentiate a ventricular diverticulum from an aneurysm or a pseudoaneurysm.
A ventricular diverticulum has a fibrous, narrow neck connecting with the ventricle, and a small circular echo-free space that communicates with the ventricle via this narrow neck.2 Doppler imaging shows systolic flow from the diverticulum to the ventricle, and systolic contractility may also be seen during cardiac catheterization. Congenital diverticulum is typically confused with ventricular aneurysm and, to a lesser degree, with mitral valve aneurysm.
Mitral valve prolapse is characterized by interchordal ballooning or hooding of the mitral valve leaflets that occurs when one or both floppy, enlarged leaflets prolapse into the left atrium during systole.
BACK TO OUR PATIENT
The patient underwent open heart surgery, with successful repair of the aortic root, replacement of the aortic valve, and repair of the mitral valve. An abscess was found within the aneurysmal cavity.
A 35-year-old man presented to the emergency department because of night sweats, fever, chills, and shortness of breath. He also had an acute onset of blue discoloration of his right fourth finger. His symptoms (except for the finger discoloration) had begun about 6 months previously and had rapidly progressed despite several courses of different antibiotics of different types, given both intravenously in the hospital and orally at home. He had lost 20 lb during this time. Previously, he had been healthy.
About 1 month after his symptoms began, he had consulted his primary care physician, who detected a new grade 4/6 systolic and diastolic murmur. Transthoracic echocardiography about 2 months after that demonstrated mild aortic and mitral insufficiency but no echocardiographic features supporting infective endocarditis. Of note, the patient had no risk factors for endocarditis such as illicit drug use or poor dental health.
In the emergency department, his temperature was 99.4°F (37.4°C), pulse 109 beats per minute, and blood pressure 126/60 mm Hg. He had a grade 3/6 harsh holosystolic murmur best heard at the right upper sternal border, a grade 3/4 holodiastolic murmur audible across the precordium, and a grade 3/4 holosystolic blowing murmur best heard at the cardiac apex. Other findings included signs of aortic insufficiency—the Duroziez sign (a diastolic murmur heard over the femoral artery when compressed), Watson’s water-hammer pulse (indicating a wide pulse pressure), and the Müller sign (pulsation of the uvula)—and small Janeway lesions on the inner aspect of his right arm and palm.
Electrocardiography showed normal sinus rhythm, PR interval 128 ms, QRS complex 100 ms, QT interval 360 ms, and corrected QT interval 473 ms.
Blood cultures grew Streptococcus sanguinis. Both transthoracic and transesophageal echocardiography were done promptly and revealed multiple mobile echodensities attached to a trileaflet aortic valve, consistent with vegetations and valve leaflet destruction; severe (4+) aortic regurgitation with flow reversal in the abdominal aorta; mild mitral regurgitation; and a mitral valve aneurysm with mild mitral regurgitation (Figure 1).
INFECTIVE ENDOCARDITIS: WORTH CONSIDERING
S sanguinis is a member of the group of viridans streptococci. As a normal inhabitant of the healthy human mouth, it is found in dental plaque. It may enter the bloodstream during dental cleaning and may colonize the heart valves, particularly the mitral and aortic valves, where it is the most common cause of subacute bacterial endocarditis.
Infective endocarditis is often diagnosed clinically with the Duke criteria (www.med-calc.com/endocarditis.html).1 However, the variability of the clinical presentation and the nonspecific nature of the initial workup often create a diagnostic challenge for the evaluating physician.1,2
In cases of recurrent persistent fever and a new heart murmur, infective endocarditis must always be considered. Blood cultures should be ordered early and repeatedly. If blood cultures are positive, transesophageal echocardiography should be done without delay if transthoracic echocardiography was unremarkable. Prompt diagnosis and surgical intervention prevent complications.
MITRAL VALVE ANEURYSM IN AORTIC VALVE ENDOCARDITIS
Aortic valve endocarditis often also involves the mitral valve; mitral valve endocarditis is seen in 17% of patients undergoing surgery for aortic valve endocarditis.3 Proposed mechanisms for this association include jet lesions from aortic regurgitation, vegetation prolapse with direct contact between the aortic valve and anterior mitral leaflet (“kissing lesions”), and direct local spread of infection.4–7
One of every five patients with mitral valve involvement in aortic valve endocarditis has a mitral valve aneurysm.3 This is a serious finding, as it can lead to septic embolization. Also, the weakened lining of the mitral valve aneurysm can rupture, resulting in severe mitral regurgitation, acute pulmonary edema, and precipitous cardiopulmonary decompensation.5
Transesophageal echocardiography is more sensitive than transthoracic echocardiography for detecting mitral valve aneurysm.8 On two-dimensional echocardiography, the lesion appears as a narrow-necked, saccular echolucency with systolic protrusion into the left atrium. Color Doppler imaging often shows turbulent, high-velocity flow.
Differential diagnosis of mitral valve aneurysm
Differential diagnostic considerations include a valvular blood cyst, a congenital cardiac diverticulum, and mitral valve prolapse.
Valvular blood cysts are extremely rare in adults.9 These benign, congenital tumors are most often found on the atrioventricular valves in infants, in whom the reported incidence is between 25% and 100%. In almost all cases, these cysts are believed to regress spontaneously with time.
In almost all reported cases, the cyst involved the valvular apparatus or papillary muscle of the tricuspid, pulmonary, or mitral valve.10 Cysts consist of a benign diverticulum lined with flattened, cobblestone-shaped endothelium and are filled with blood. They can cause heart murmurs in otherwise asymptomatic patients.
On echocardiography, a blood cyst appears as an oval mass (often at the interatrial septum), often with normal cardiac function. In the rare case in which a blood cyst is found incidentally during echocardiography, the hemodynamic impact, if any, should be determined by Doppler techniques.
When benign, a valvular blood cyst can be safely monitored with echocardiographic follow-up.11 Treatment involves surgical resection of the mass in symptomatic patients in whom cardiac function is impaired by the presence of the cyst.
Congenital cardiac diverticuli are extremely rare, most often seen in children, and associated with a midline thoracoabdominal defect. Echocardiography can differentiate a ventricular diverticulum from an aneurysm or a pseudoaneurysm.
A ventricular diverticulum has a fibrous, narrow neck connecting with the ventricle, and a small circular echo-free space that communicates with the ventricle via this narrow neck.2 Doppler imaging shows systolic flow from the diverticulum to the ventricle, and systolic contractility may also be seen during cardiac catheterization. Congenital diverticulum is typically confused with ventricular aneurysm and, to a lesser degree, with mitral valve aneurysm.
Mitral valve prolapse is characterized by interchordal ballooning or hooding of the mitral valve leaflets that occurs when one or both floppy, enlarged leaflets prolapse into the left atrium during systole.
BACK TO OUR PATIENT
The patient underwent open heart surgery, with successful repair of the aortic root, replacement of the aortic valve, and repair of the mitral valve. An abscess was found within the aneurysmal cavity.
- Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med 1994; 96:200–209.
- Prendergast BD. Diagnostic criteria and problems in infective endocarditis. Heart 2004; 90:611–613.
- Gonzalez-Lavin L, Lise M, Ross D. The importance of the ‘jet lesion’ in bacterial endocarditis involving the left heart. Surgical considerations. J Thorac Cardiovasc Surg 1970; 59:185–192.
- Silbiger JJ. Review: mitral valve aneurysms in infective endocarditis: mechanisms, clinical recognition, and treatment. J Heart Valve Dis 2009; 18:476–480.
- Reid CL, Chandraratna AN, Harrison E, et al. Mitral valve aneurysm: clinical features, echocardiographic-pathologic correlations. J Am Coll Cardiol 1983; 2:460–464.
- Rodbard S. Blood velocity and endocarditis. Circulation 1963; 27:18–28.
- Piper C, Hetzer R, Körfer R, Bergemann R, Horstkotte D. The importance of secondary mitral valve involvement in primary aortic valve endocarditis; the mitral kissing vegetation. Eur Heart J 2002; 23:79–86.
- Cziner DG, Rosenzweig BP, Katz ES, Keller AM, Daniel WG, Kronzon I. Transesophageal versus transthoracic echocardiography for diagnosing mitral valve perforation. Am J Cardiol 1992; 69:1495–1497.
- Roberts PF, Serra AJ, McNicholas KW, Shapira N, Lemole GM. Atrial blood cyst: a rare finding. Ann Thorac Surg 1996; 62:880–882.
- Grimaldi A, Capritti E, Pappalardo F, et al. Images in cardiovascular medicine: blood cyst of the mitral valve. J Cardiovasc Med 2012; 3:46.
- Boyd WC, Rosengart TK, Hartman GS. Isolated left ventricular diverticulum in an adult. J Cardiothorac Vasc Anesth 1999; 13:468–470.
- Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med 1994; 96:200–209.
- Prendergast BD. Diagnostic criteria and problems in infective endocarditis. Heart 2004; 90:611–613.
- Gonzalez-Lavin L, Lise M, Ross D. The importance of the ‘jet lesion’ in bacterial endocarditis involving the left heart. Surgical considerations. J Thorac Cardiovasc Surg 1970; 59:185–192.
- Silbiger JJ. Review: mitral valve aneurysms in infective endocarditis: mechanisms, clinical recognition, and treatment. J Heart Valve Dis 2009; 18:476–480.
- Reid CL, Chandraratna AN, Harrison E, et al. Mitral valve aneurysm: clinical features, echocardiographic-pathologic correlations. J Am Coll Cardiol 1983; 2:460–464.
- Rodbard S. Blood velocity and endocarditis. Circulation 1963; 27:18–28.
- Piper C, Hetzer R, Körfer R, Bergemann R, Horstkotte D. The importance of secondary mitral valve involvement in primary aortic valve endocarditis; the mitral kissing vegetation. Eur Heart J 2002; 23:79–86.
- Cziner DG, Rosenzweig BP, Katz ES, Keller AM, Daniel WG, Kronzon I. Transesophageal versus transthoracic echocardiography for diagnosing mitral valve perforation. Am J Cardiol 1992; 69:1495–1497.
- Roberts PF, Serra AJ, McNicholas KW, Shapira N, Lemole GM. Atrial blood cyst: a rare finding. Ann Thorac Surg 1996; 62:880–882.
- Grimaldi A, Capritti E, Pappalardo F, et al. Images in cardiovascular medicine: blood cyst of the mitral valve. J Cardiovasc Med 2012; 3:46.
- Boyd WC, Rosengart TK, Hartman GS. Isolated left ventricular diverticulum in an adult. J Cardiothorac Vasc Anesth 1999; 13:468–470.
Transient ischemic attack: Omen and opportunity
A transient ischemic attack (TIA), like an episode of unstable angina, is an ominous portent of future morbidity and death even though, by definition, the event leaves no residual neurologic deficit.
But there is a positive side. When a patient presents with a TIA, the physician has the rare opportunity to reduce the risk of a disabling outcome—in this case, stroke. Therefore, patients deserve a rapid and thorough evaluation and appropriate stroke-preventive treatment.
MANY ‘TIAs’ ARE ACTUALLY STROKES
TIA has traditionally been described as a sudden focal neurologic deficit that lasts less than 24 hours, is presumed to be of vascular origin, and is confined to an area of the brain, spinal cord, or eye perfused by a specific artery. This symptom-based definition was based on the arbitrary and inaccurate assumption that brief symptoms would not be associated with damage to brain parenchyma.
The definition has since been updated and made more rational based on new concepts of brain ischemia informed by imaging, especially diffusion-weighted magnetic resonance imaging (MRI).1 One-third of episodes characterized as a TIA according to the classic definition would be considered an infarction on the basis of diffusion-weighted MRI.2 The new tissue-based definition characterizes TIA as a brief episode of neurologic dysfunction caused by focal ischemia of the brain, spinal cord, or retina, with clinical symptoms lasting less than 24 hours and without evidence of acute infarction.3
AN OPPORTUNITY TO INTERVENE
Most TIAs resolve in less than 30 minutes. The US National Institute of Neurological Disorders and Stroke trial of tissue plasminogen activator found that if symptoms of cerebral ischemia had not resolved by 1 hour or had not rapidly improved within 3 hours, complete resolution was rare (only 2% at 24 hours).4 Hence, physicians evaluating and treating patients with TIAs should treat these episodes with the urgency they deserve.
Moreover, half of the strokes that follow TIAs occur within 48 hours.5 A rapid and thorough evaluation and the initiation of secondary preventive treatments have been shown to reduce the early occurrence of stroke by up to 80%.6 Hence, the correct diagnosis of TIA gives the clinician the best opportunity to prevent stroke and its personal, social, and sometimes fatal consequences.
STROKES OUTNUMBER TIAs, BUT TIAs ARE UNDERREPORTED
According to 2012 statistics, nearly 795,000 strokes occur in the United States each year, 610,000 of which are first attacks and 185,000 are recurrences. Every 40 seconds, someone in the United States has a stroke.7
In comparison, the incidence of TIA in the United States is estimated at 200,000 to 500,000 per year, though the true number is difficult to know because of underreporting.8,9 About half of patients who experience a TIA fail to report it to their health care provider—a lost opportunity for intervention and stroke prevention.10,11
A meta-analysis showed that the risk of stroke after TIA was 9.9% at 2 days, 13.4% at 30 days, and 17.3% at 90 days.12
Interestingly, the risk of stroke after TIA exceeds the risk of recurrent stroke after a first stroke. This was shown in a study that found that patients who had made a substantial recovery within 24 hours (ie, patients with a TIA) were more likely to suffer neurologic deterioration in the next 3 months than were those who did not have significant early improvement.13
RISK FACTORS FOR TIA ARE THE SAME AS FOR STROKE
The risk of cerebrovascular disease increases with age and is higher in men14 and in blacks and Hispanics.15
The risk factors and clinical presentation do not differ between TIA and stroke, so the evaluation and treatment should not differ either. These two events represent a continuum of the same disease entity.
Some risk factors for TIA are modifiable, others are not.
Nonmodifiable risk factors
Nonmodifiable risk factors for TIA include older age, male sex, African American race, low birth weight, Hispanic ethnicity, and family history. If the patient has nonmodifiable risk factors, we should try all the harder to correct the modifiable ones.
Older age. The risk of ischemic stroke and intracranial hemorrhage doubles with each decade after age 55 in both sexes.16
Sex. Men have a significantly higher incidence of TIA than women,11 whereas the opposite is true for stroke: women have a higher lifetime risk of stroke than men.17
African Americans have an incidence of stroke (all types) 38% higher than that of whites,18 and an incidence of TIA (inpatient and out-of-hospital) 40% higher than the overall age- and sex-adjusted rate in the white population.11
Low birth weight. The odds of stroke are more than twice as high in people who weighed less than 2,500 g at birth compared with those who weighed 4,000 g or more, probably because of a correlation between low birth weight and hypertension.19
A family history of stroke increases the risk of stroke by nearly 30%, the association being stronger with large-vessel and smallvessel stroke than with cardioembolic stroke.20
Modifiable risk factors
Modifiable risk factors include cigarette smoking, hypertension, diabetes, lipid abnormalities, atrial fibrillation, carotid stenosis, and dietary and hormonal factors. Detecting these factors, which often coexist, is the first step in trying to modify them and reduce the patient’s risk.
Cigarette smoking approximately doubles the risk of ischemic stroke.21–23
Hypertension has a relationship with stroke risk that is strong, continuous, graded, consistent, and significant.24
Diabetes increases stroke risk nearly six times.25
Lipid abnormalities. Most studies have found an association between lipid levels (total cholesterol and low-density lipoprotein cholesterol) and the risk of death from ischemic stroke,26–28 and an inverse relationship between high-density lipoprotein cholesterol levels and stroke risk.29
Atrial fibrillation increases the risk of ischemic stroke up to fivefold, even in the absence of cardiac valvular disease. The mechanism is embolism of stasis-induced thrombi that form in the left atrial appendage.30
Carotid stenosis. Asymptomatic carotid atherosclerotic stenotic lesions in the extracranial internal carotid artery or carotid bulb are associated with a higher risk of stroke.24,31
Lifestyle factors. Diets that lower blood pressure have been found to decrease stroke risk.24 Exercise in men and women reduces the risk of stroke or death by 25% to 30% compared with inactive people.32 Weight reduction has been found to lower blood pressure and reduce stroke risk.24
Other potentially modifiable risk factors include migraine with aura, metabolic syndrome, excess alcohol consumption (and, paradoxically, complete abstinence from alcohol), drug abuse, sleep-disordered breathing, hyperhomocysteinemia, high lipoprotein (a) levels, hypercoagulability, infection with organisms such as Chlamydia pneumoniae, cytomegalovirus, and Helicobacter pylori, and acute infections such as respiratory and urinary infections.26
Conditions in certain demographic groups
Patients in certain demographic groups present with rarer conditions associated with stroke and TIA.
Sickle cell disease. Eleven percent of patients with sickle cell disease have clinical strokes, and a substantial number have “silent” infarcts identified on neuroimaging.33,34
Postmenopausal hormone replacement therapy with any product containing conjugated equine estrogen carries a risk of cerebrovascular events,35 and the higher the dose, the higher the risk.36 Also, oral contraceptives may be harmful in women who have additional risk factors such as cigarette smoking, prior thromboembolic events, or migraine with aura.37,38
THREE CAUSES OF STROKE AND TIA
Stroke and TIA should not be considered diagnoses in themselves, but rather the end point of many other diseases. The diagnosis lies in identifying the mechanism of the cerebrovascular event. The three main mechanisms are thrombosis, embolism, and decreased perfusion.
Thrombosis is caused by obstruction of blood flow within one or more blood vessels, the most common cause being atherosclerosis. Large-artery atherosclerosis, such as in the carotid bifurcation or extracranial internal carotid, causes TIAs that occur over a period of weeks or months with a variety of presentations in that vascular territory, from years of gradual accumulation of atherosclerotic plaque.39
In patients with small-artery or penetrating artery disease, hypertension is the primary risk factor and the pathology, specific to small arterioles, is lipohyalinosis rather than atherosclerosis. These patients may present with a stuttering clinical course, and episodes are more stereotypical.
Less common obstructive vascular pathologies include fibromuscular dysplasia, arteritides, and dissection.
Embolism can occur from a proximal source such as the heart or from proximal vessels such as the aorta, carotid, or vertebral arteries. The embolic particle may form on heart valves or lesions within the heart (eg, clot, tumor), or in the venous circulation and paradoxically cross over to the arterial side through an intracardiac or transpulmonary shunt. Embolism may also be due to a hypercoagulable state.40 Embolic stroke is suspected when multiple vascular territories within the brain are clinically or radiographically affected.
Decreased systemic perfusion caused by severe heart failure or systemic hypotension can cause ischemia to the brain diffusely and bilaterally, limiting the ability of the blood-stream to wash out microemboli, especially in the border zones (also known as “watershed areas”), thus leading to ischemia or infarction.41 Decreased perfusion can also be local, due to a fixed vessel stenosis.
Using another classification system, a study in Rochester, MN, found the following incident rates of stroke subtypes, adjusted for age and sex, per 100,000 population42:
- Large-vessel cervical or intracranial atherosclerosis with more than 50% stenosis—27
- Cardioembolism—40
- Lacunar, small-vessel disease—25
- Uncertain cause—52
- Other identifiable cause—4.
THREE CLINICAL FEATURES SUGGEST TIA
TIAs can be hard to distinguish from nonischemic neurologic events in the acute setting such as an emergency room. Up to 60% of patients suspected of having a TIA actually have a nonischemic cause of their symptoms.43
Three clinical features suggest a TIA during the emergency room evaluation:
- Rapid onset of symptoms—“like lightning” or “in seconds,” in contrast to migraine and seizures, which develop over minutes
- No history of similar episodes in the past
- Absence of nonspecific symptoms—eg, stomach upset or tightness in the chest.
CLINICAL DIAGNOSIS
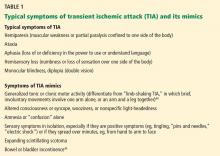
Because most TIA symptoms and signs have already resolved by the time of evaluation, the diagnosis depends on a careful history with special attention to the pace of onset and resolution, the duration and nature of the symptoms, circumstances at the time of symptom onset, previous similar episodes, associated features, vascular risk factors, and family history (Table 1).44,45
A detailed neurologic examination is imperative and should include fundoscopy. A cardiovascular assessment should include cardiac rhythm, bruits in the neck, orbits, and groin, peripheral pulses, and electrocardiography.
Do neurologists do a better job at diagnosing TIA and stroke?
Primary care physicians, internists, and emergency department physicians are often the ones to carry out the clinical assessment of possible TIA.
Determining if transient neurologic symptoms are caused by ischemia can be a challenge. When in doubt, referral to a neurologist with subspecialty training in cerebrovascular disease should be considered.
But do neurologists really do a better job? A recent study sought to compare the accuracy of diagnosis of TIA made by general practitioners, emergency physicians, and neurologists. The nonneurologists considered “confusion” and “unexplained fall” suggestive of TIA and “lower facial palsy” and “monocular blindness” less suggestive of TIA—whereas the opposite is true. This shows that nonneurologists often label minor strokes and several nonvascular transient neurologic disturbances as TIAs, and up to half of patients could be mislabeled as a result.46
Differences in diagnosing cerebrovascular events between emergency room physicians and attending neurologists have been tested,47 with an accuracy of diagnosis as low as 38% by emergency department physicians in one study.48 However, other studies did not show such a trend.49,50
A study at a university-based teaching hospital found the sensitivity of emergency room physician diagnosis to be 98.6% with a positive predictive value of 94.8%,49 showing that at a large teaching hospital with a comprehensive stroke intervention program, emergency physicians could identify patients with stroke, particularly hemorrhagic stroke, very accurately.
Improving the diagnosis of stroke and TIA
Routine use of imaging and involvement of a neurologist increase the sensitivity and accuracy of diagnosis. Education and written guidelines for acute stroke treatment both in the emergency department and in out-of-hospital settings seem to dramatically improve the rates of diagnostic accuracy and appropriate treatment.50
Emergency medical service personnel use two screening tools in the field to identify TIA and stroke symptoms:
- The Cincinnati Prehospital Stroke Scale, a three-item scale based on three signs: facial droop, arm drift, and slurring of speech51
- The Los Angeles Prehospital Stroke Screen, which uses screening questions and asymmetry in the face, hand grip strength, and arm drift.52
Knowing that the patient is having a minor stroke or TIA is important. Urgent treatment of these conditions decreases the risk of stroke in the next 90 days, which was 10.5% in one study.5 Urgent assessment and early intervention could reduce this risk of subsequent stroke down to 2%.6
ASSESSING RISK OF STROKE AFTER TIA
There is a practical need for prediction of stroke during the first few days after the event. The ABCD and ABCD2 scores were developed to stratify the short-term risk of stroke in patients with recent TIA.
The ABCD score
The ABCD score53 was derived to allow primary care physicians and other physicians to identify which patients with a suspected diagnosis of TIA should be referred for emergency assessment, to allow secondary-care physicians to determine which patients with probable or definite TIA need emergency investigation and treatment, to allow public education about the need for medical attention after a TIA, and to identify people at high risk.
The ABCD2 score
The ABCD2 score predicts the short-term risk of stroke following a TIA.54 Points are assigned as follows:
- Age > 60 years: 1 point
- Blood pressure (systolic) > 140 mm Hg or diastolic blood pressure > 90 mm Hg: 1 point
- Clinical factors: unilateral weakness with or without speech impairment: 2 points (1 point for speech impairment without weakness)
- Duration of symptoms > 60 minutes: 2 points (1 point for 10–59 minutes)
- Diabetes: 1 point.
Thus, the possible total ranges from 0 to 7 points. Higher scores indicate a greater risk of stroke at 2, 7, 30, and 90 days:
- Total score 0, 1, 2, or 3: 2-day stroke risk 1.0% (low risk)
- Total score 4 or 5: 2-day stroke risk 4.1% (moderate risk)
- Total score 6 or 7: 2-day stroke risk 8.1% (high risk).
WHO SHOULD BE HOSPITALIZED?
It has been suggested that the ABCD2 score can help in triaging patients to hospital admission or outpatient care, though no randomized trial has actually evaluated the utility of the ABCD2 score in this way.3
A study of consecutive TIA patients admitted over 12 months55 found that patients with an ABCD2 score of 3 or less had the same chance of requiring hospitalization (based on positive diffusion-weighted MRI studies, risk factor identification, and treatment initiation) as those with a score of 4 to 7. Hence, admitting TIA patients on the basis of the ABCD2 score alone requires further study. However, such decisions, though informed by clinical data, depend heavily on societal input (eg, from insurance companies, national health protocols) and may be outside the purview of clinical investigation.
The benefits of hospitalization include the ability to rapidly carry out tests such as cardiac monitoring for atrial fibrillation; to detect atherosclerosis, aortic arch atheroma, and paradoxical emboli; and to quickly start secondary prevention treatments and education about the importance of adhering to them. Early endarterectomy in the case of carotid stenosis can be offered. Additionally, if stroke symptoms recur, thrombolytic drug therapy can be started quickly.
Nguyen-Huynh et al56 analyzed the cost utility of 24-hour hospitalization for patients diagnosed with a recent TIA who were candidates for tissue plasminogen activator if a stroke occurred. They found hospitalization to be borderline cost-effective on the whole, with definite cost-effectiveness found in patients with higher stroke risk.
If patients come to medical attention several days after the TIA, then assessing risk with the ABCD2 score may no longer be reliable.57
INVESTIGATIONS
Parenchymal neuroimaging
Computed tomography (CT) without contrast is the most widely used neuroimaging test in the acute setting, since it is widely available, fast, and relatively low-cost. It will not show any abnormality in TIA or early ischemic stroke. However, it is helpful as a screening tool to rule out intracranial lesions such as hemorrhage or tumor. It may also show evidence of established infarction, which would indicate that the ischemia probably had been present for at least 6 to 12 hours.
MRI is clearly superior to noncontrast CT for detecting small areas of ischemia in patients with TIA, and it should be used unless the patient has a contraindication to it. Roughly one-third of TIA patients have lesions detectable on diffusion-weighted imaging, which helps to confirm that the episode was caused by cerebral ischemia, but nearly half of the diffusion MRI changes may be fully reversible.58 Evidence of prior stroke, leukoaraiosis, or white matter disease on fluid-attenuated inversion recovery and T2 sequences and microhemorrhages (on gradient echo sequences) help to determine a mechanistic diagnosis.
Subcategorizing TIA patients on the basis of the findings on diffusion-weighted MRI and the ABCD2 score is prognostically helpful.59 It can help to determine which patients need hospitalization and aggressive treatment, and in the case of identified diffusion-weighted MRI-positive stroke, it helps to localize and elucidate the mechanism of stroke. Hence, MRI is the preferred neuroimaging study for evaluating patients with TIA.3
Vascular imaging
Establishing the status of both intracranial and extracranial vessels is important for understanding the etiology, estimating the risk of future ischemic events, and formulating a treatment plan—eg, carotid endarterectomy in cases of significant stenosis (70% to 99%), which reduces the risk of ipsilateral stroke.60 Imaging studies include CT angiography, magnetic resonance angiography, extracranial and transcranial ultrasonography, and conventional catheter-based angiography.
CT angiography has higher spatial resolution, but vessels may be obscured by calcification associated with atherosclerotic plaque. It has the advantage of wide availability, low cost, short scanning time, and excellent patient tolerability.
Magnetic resonance angiography with gadolinium enhancement offers good quality imaging from the great vessels in the chest to the medium-sized vessels distal to the circle of Willis.
The contrast agents used in MRI and CT can have negative consequences in patients with renal disease. MRI contrast has been associated with nephrogenic fibrosing dermopathy, 61 and CT contrast can cause contrast-induced nephropathy.62
Carotid ultrasonography and transcranial Doppler ultrasonography are noninvasive and are not associated with significant adverse events. They can be used safely in patients with renal dysfunction, and they provide physiologic information that cannot be obtained with MRI and CT, which are static imaging techniques. Detecting microemboli on transcranial Doppler is an independent predictor of recurrent ischemic events.63,64
Catheter-based angiography is occasionally needed in confusing or more complicated cases, but it is invasive and occasionally is associated with iatrogenic stroke and other vascular complications.
Cardiac and aortic imaging
Echocardiography is used to detect lesions that can be sources of embolism such as regional wall-motion abnormalities, cardiac thrombus or mass, endocarditis, aortic arch atheroma, and patent foramen ovale. In patients with cryptogenic TIA or stroke, those with patent foramen ovale alone were found to have a lower risk of recurrent stroke than those who had both atrial septal aneurysm and patent foramen ovale.65
Transesophageal echocardiography is more sensitive than transthoracic echocardiography for detecting cardioembolic lesions, especially patent foramen ovale.66 In patients with cerebral ischemia and normal transthoracic findings, cardiac sources of embolism may be detected in about 40% of patients with transesophageal echocardiography.67
Cardiac rhythm monitoring
Electrocardiography and prolonged telemetry are recommended in patients with cryptogenic TIA to detect cardiac ischemia and paroxysmal atrial fibrillation. In one study, Holter monitoring detected atrial fibrillation in 6% of patients hospitalized with ischemic stroke or TIA.68 In another study, atrial fibrillation was detected after a median of 21 days of outpatient cardiac monitoring in 23% of patients.69
The optimal duration of outpatient telemetry has not yet been established, but studies have found significant increases in detection of paroxysms of atrial fibrillation with monitoring for 7 or longer.70
Laboratory tests in the acute setting
These include lipid profile, hemoglobin A1c, and cardiac enzymes. The advantages of hospitalization are early detection of these modifiable risk factors and early initiation of treatment.
Tests for rarer disorders
Tests for rarer disorders are sometimes indicated in unusual cases, such as ischemic symptoms occurring in young patients without other common risk factors. This includes testing for prothrombotic states, toxicology, blood cultures, inflammatory markers, hemoglobin electrophoresis, and lumbar puncture. The benefit of routine testing for thrombophilic disorders in cerebrovascular disease remains uncertain, with no clear association demonstrated with arterial stroke, but testing is more relevant in the case of venous (and paradoxical) thromboembolism.71
TREAT THE UNDERLYING DISORDER
Treatment depends on the mechanism that is thought to be responsible for the ischemic event. Vascular risk factors are important to identify and modify for all stroke subtypes.
Illustrating the importance of treating TIA and minor stroke, one study72 found that for antiplatelet therapy (aspirin, dipyridamole, or aspirin plus dipyridamole), the number needed to treat for 2 years was around 18.
Anticoagulation for cardioembolism
Atrial fibrillation, especially following a cerebrovascular ischemic event, should be treated with long-term anticoagulation with warfarin (Coumadin), dabigatran (Pradaxa), rivaroxaban (Xarelto), or apixaban (Eliquis).73 If the patient cannot tolerate anticoagulation, aspirin is recommended, and if he or she cannot tolerate aspirin, clopidogrel (Plavix) is recommended.
Antiplatelet therapy for large-vessel atherosclerosis and small-vessel disease
In the acute phase, aspirin 81 mg to 325 mg orally can be given. If the patient is allergic to aspirin, a loading dose of clopidogrel 300 mg and then 75 mg daily may be given.
A pilot study of loading with aspirin 325 mg or clopidogrel 375 mg in acute ischemic stroke and TIA patients showed that these treatments were safe when given within 36 hours and decreased the risk of neurologic deterioration.74 The patient should continue on aspirin 81 mg or clopidogrel 75 mg, as suggested by the Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER) trial.75 In the long term, an antiplatelet drug such as aspirin or clopidogrel or the combination of aspirin and extended-release dipyridamole is reasonable.76
Cilostazol (Pletal) is not inferior and is possibly superior to aspirin in preventing noncardioembolic ischemic stroke. It is used off-label for secondary prevention of stroke of noncardioembolic origin.77
Statins
In the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial, high-dose atorvastatin (Lipitor)—80 mg daily—was found to reduce the risk of subsequent stroke and other cardiovascular events in patients with recent stroke irrespective of low-density lipoprotein cholesterol (LDL-C) level, but there was a small increase in the risk of hemorrhagic stroke.78
In patients with hyperlipidemia, current recommendations suggest a target LDL-C level lower than 100 mg/dL in patients with atherosclerotic stroke or TIA, and lower than 70 mg/dL in those with concomitant diabetes.79
Antihypertensive therapy
In the acute period, ie, the first 24 hours after symptoms, guidelines have advocated allowing high blood pressure to remain high (“permissive hypertension”) unless the systolic pressure is greater than 200 mm Hg or the diastolic pressure is greater than 120 mm Hg or the patient is receiving thrombolytic therapy.80 However, this has recently been challenged by findings in randomized trials.81 Permissive hypertension and avoidance of dehydration with intravenous normal saline may improve cerebral perfusion, which is especially important in patients with high-grade intracranial or extracranial stenosis. Within the parameters outlined above, we recommend against aggressively treating high blood pressure in the acute phase.
In the long term, antihypertensive therapy reduces the risk of recurrent stroke or TIA.82 The goal is to keep blood pressure lower than 140/90 mm Hg, or lower than 130/80 mm Hg in patients with diabetes. A study of patients with ischemic noncardioembolic stroke showed a higher risk of recurrent stroke if the systolic blood pressure was lower than 120 or higher than 140 mm Hg.83
Some classes of antihypertensive medication may be more beneficial than others. There is some evidence that angiotensin-converting enzyme (ACE) inhibitors alone or in combination with a diuretic or an angiotensin receptor blocker are superior to other regimens, possibly because of neuroprotective mechanisms.84 A recent meta-analysis found angiotensin receptor blockers to be more effective than either ACE inhibitors or beta-blockers in stroke prevention; however, calcium channel blockers were superior to renin-angiotensin system blockers (ACE inhibitors and angiotensin receptor blockers).85
Lifestyle modifications
Smoking cessation and cardiovascular exercise for more than 10 minutes more than 3 times per week is strongly recommended.
For patients with diabetes, the goal is to keep the fasting blood glucose level lower than 126 mg/dL.
Moderate alcohol intake has been shown to decrease stroke risk compared with excessive intake or none at all.86
Carotid endarterectomy
Carotid endarterectomy has been recommended within 2 weeks of cerebral or retinal TIA in those cases attributable to high-grade internal carotid artery stenosis in patients who have low surgical risk.87 This risk can be estimated on the basis of patient factors, surgeon factors, and hospital volume. The specific recommendations are as follows:
- 70% to 99% carotid stenosis: carotid endarterectomy recommended
- 50% to 69% carotid stenosis: carotid endarterectomy recommended in select patients with a perioperative complication rate < 6%
- < 50% carotid stenosis: carotid endarterectomy not routinely recommended.
Carotid artery angioplasty and stenting with distal embolic protection device
Data from the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST) and European stenting trials indicate that in patients over age 70, carotid endarterectomy appears to be superior to carotid artery stenting, whereas in younger patients the periprocedural risks of stroke and death are similar. Hence, carotid artery stenting performed by an interventionist with a low complication rate is a reasonable alternative to carotid endarterectomy.88,89
- Albers GW, Caplan LR, Easton JD, et al; TIA Working Group. Transient ischemic attack—proposal for a new definition. N Engl J Med 2002; 347:1713–1716.
- Ovbiagele B, Kidwell CS, Saver JL. Epidemiological impact in the United States of a tissue-based definition of transient ischemic attack. Stroke 2003; 34:919–924.
- Easton JD, Saver JL, Albers GW, et al; American Heart Association. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke 2009; 40:2276–2293.
- Marler JR, Tilley BC, Lu M, et al. Early stroke treatment associated with better outcome: the NINDS rt-PA stroke study. Neurology 2000; 55:1649–1655.
- Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA 2000; 284:2901–2906.
- Rothwell PM, Giles MF, Chandratheva A, et al; Early use of Existing Preventive Strategies for Stroke (EXPRESS) study. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007; 370:1432–1442.
- Roger VL, Go AS, Lloyd-Jones DM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 2012; 125:e2–e220.
- Johnston SC. Clinical practice. Transient ischemic attack. N Engl J Med 2002; 347:1687–1692.
- Johnston SC, Fayad PB, Gorelick PB, et al. Prevalence and knowledge of transient ischemic attack among US adults. Neurology 2003; 60:1429–1434.
- Eliasziw M, Kennedy J, Hill MD, Buchan AM, Barnett HJ; North American Symptomatic Carotid Endarterectomy Trial Group. Early risk of stroke after a transient ischemic attack in patients with internal carotid artery disease. CMAJ 2004; 170:1105–1109.
- Kleindorfer D, Panagos P, Pancioli A, et al. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke 2005; 36:720–723.
- Wu CM, McLaughlin K, Lorenzetti DL, Hill MD, Manns BJ, Ghali WA. Early risk of stroke after transient ischemic attack: a systematic review and meta-analysis. Arch Intern Med 2007; 167:2417–2422.
- Johnston SC, Leira EC, Hansen MD, Adams HP. Early recovery after cerebral ischemia risk of subsequent neurological deterioration. Ann Neurol 2003; 54:439–444.
- Bots ML, van der Wilk EC, Koudstaal PJ, Hofman A, Grobbee DE. Transient neurological attacks in the general population. Prevalence, risk factors, and clinical relevance. Stroke 1997; 28:768–773.
- White H, Boden-Albala B, Wang C, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation 2005; 111:1327–1331.
- Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Stroke incidence, prevalence, and survival: secular trends in Rochester, Minnesota, through 1989. Stroke 1996; 27:373–380.
- Seshadri S, Beiser A, Kelly-Hayes M, et al. The lifetime risk of stroke: estimates from the Framingham Study. Stroke 2006; 37:345–350.
- Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke 1999; 30:736–743.
- Lackland DT, Egan BM, Ferguson PL. Low birth weight as a risk factor for hypertension. J Clin Hypertens (Greenwich) 2003; 5:133–136.
- Flossmann E, Schulz UG, Rothwell PM. Systematic review of methods and results of studies of the genetic epidemiology of ischemic stroke. Stroke 2004; 35:212–227.
- Rodriguez BL, D’Agostino R, Abbott RD, et al. Risk of hospitalized stroke in men enrolled in the Honolulu Heart Program and the Framingham Study: a comparison of incidence and risk factor effects. Stroke 2002; 33:230–236.
- Manolio TA, Kronmal RA, Burke GL, O’Leary DH, Price TR. Short-term predictors of incident stroke in older adults. The Cardiovascular Health Study. Stroke 1996; 27:1479–1486.
- Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke 1991; 22:312–318.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572.
- Allen TW. Guide to clinical preventive services. Report of the US Preventive Services Task Force. J Am Osteopath Assoc 1991; 91:281–289.
- Goldstein LB, Bushnell CD, Adams RJ, et al; American Heart Association Stroke Council. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42:517–584.
- Iso H, Jacobs DR, Wentworth D, Neaton JD, Cohen JD. Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the multiple risk factor intervention trial. N Engl J Med 1989; 320:904–910.
- Zhang X, Patel A, Horibe H, et al; Asia Pacific Cohort Studies Collaboration. Cholesterol, coronary heart disease, and stroke in the Asia Pacific region. Int J Epidemiol 2003; 32:563–572.
- Sanossian N, Saver JL, Navab M, Ovbiagele B. High-density lipoprotein cholesterol: an emerging target for stroke treatment. Stroke 2007; 38:1104–1109.
- Kannel WB, Benjamin EJ. Status of the epidemiology of atrial fibrillation. Med Clin North Am 2008; 92:17–40.
- Inzitari D, Eliasziw M, Gates P, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 2000; 342:1693–1700.
- Physical Activity Guidelines Advisory Committee report, 2008. To the Secretary of Health and Human Services. Part A: executive summary. Nutr Rev 2009; 67:114–120.
- Armstrong FD, Thompson RJ, Wang W, et al. Cognitive functioning and brain magnetic resonance imaging in children with sickle cell disease. Neuropsychology Committee of the Cooperative Study of Sickle Cell Disease. Pediatrics 1996; 97:864–870.
- Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood 1998; 91:288–294.
- Mosca L, Banka CL, Benjamin EJ, et al; Expert Panel/Writing Group; American Heart Association; American Academy of Family Physicians; American College of Obstetricians and Gynecologists; American College of Cardiology Foundation; Society of Thoracic Surgeons; American Medical Women's Association; Centers for Disease Control and Prevention; Office of Research on Women's Health; Association of Black Cardiologists; American College of Physicians; World Heart Federation; National Heart, Lung, and Blood Institute; American College of Nurse Practitioners. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation 2007; 115:1481–1501.
- Lidegaard Ø, Løkkegaard E, Jensen A, Skovlund CW, Keiding N. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med 2012; 366:2257–2266.
- Chan WS, Ray J, Wai EK, et al. Risk of stroke in women exposed to low-dose oral contraceptives: a critical evaluation of the evidence. Arch Intern Med 2004; 164:741–747.
- Bousser MG, Conard J, Kittner S, et al. Recommendations on the risk of ischaemic stroke associated with use of combined oral contraceptives and hormone replacement therapy in women with migraine. The International Headache Society Task Force on Combined Oral Contraceptives & Hormone Replacement Therapy. Cephalalgia 2000; 20:155–156.
- Mohr JP, Caplan LR, Melski JW, et al. The Harvard Cooperative Stroke Registry: a prospective registry. Neurology 1978; 28:754–762.
- Caplan LR. Brain embolism, revisited. Neurology 1993; 43:1281–1287.
- Caplan LR, Hennerici M. Impaired clearance of emboli (washout) is an important link between hypoperfusion, embolism, and ischemic stroke. Arch Neurol 1998; 55:1475–1482.
- Petty GW, Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke 1999; 30:2513–2516.
- Prabhakaran S, Silver AJ, Warrior L, McClenathan B, Lee VH. Misdiagnosis of transient ischemic attacks in the emergency room. Cerebrovasc Dis 2008; 26:630–635.
- Baquis GD, Pessin MS, Scott RM. Limb shaking—a carotid TIA. Stroke 1985; 16:444–448.
- Luengo-Fernandez R, Gray AM, Rothwell PM. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): a prospective population-based sequential comparison. Lancet Neurol 2009; 8:235–243.
- Ferro JM, Falcão I, Rodrigues G, et al. Diagnosis of transient ischemic attack by the nonneurologist. A validation study. Stroke 1996; 27:2225–2229.
- Norris JW, Hachinski VC. Misdiagnosis of stroke. Lancet 1982; 1:328–331.
- Ferro JM, Pinto AN, Falcão I, et al. Diagnosis of stroke by the nonneurologist. A validation study. Stroke 1998; 29:1106–1109.
- Kothari RU, Brott T, Broderick JP, Hamilton CA. Emergency physicians. Accuracy in the diagnosis of stroke. Stroke 1995; 26:2238–2241.
- Artto V, Putaala J, Strbian D, et al; Helsinki Stroke Thrombolysis Registry Group. Stroke mimics and intravenous thrombolysis. Ann Emerg Med 2012; 59:27–32.
- Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med 1999; 33:373–378.
- Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke 2000; 31:71–76.
- Rothwell PM, Giles MF, Flossmann E, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet 2005; 366:29–36.
- Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet 2007; 369:283–292.
- Lou M, Safdar A, Edlow JA, et al. Can ABCD score predict the need for in-hospital intervention in patients with transient ischemic attacks? Int J Emerg Med 2010; 3:75–80.
- Nguyen-Huynh MN, Johnston SC. Is hospitalization after TIA cost-effective on the basis of treatment with tPA? Neurology 2005; 65:1799–1801.
- Calvet D, Lamy C, Touzé E, Oppenheim C, Meder JF, Mas JL. Management and outcome of patients with transient ischemic attack admitted to a stroke unit. Cerebrovasc Dis 2007; 24:80–85.
- Kidwell CS, Alger JR, Di Salle F, et al. Diffusion MRI in patients with transient ischemic attacks. Stroke 1999; 30:1174–1180.
- Giles MF, Albers GW, Amarenco P, et al. Early stroke risk and ABCD2 score performance in tissue- vs time-defined TIA: a multicenter study. Neurology 2011; 77:1222–1228.
- Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 1998; 351:1379–1387.
- Thomsen HS. Nephrogenic systemic fibrosis: history and epidemiology. Radiol Clin North Am 2009; 47:827–831.
- Barrett BJ, Parfrey PS. Clinical practice. Preventing nephropathy induced by contrast medium. N Engl J Med 2006; 354:379–386.
- Valton L, Larrue V, le Traon AP, Massabuau P, Géraud G. Microembolic signals and risk of early recurrence in patients with stroke or transient ischemic attack. Stroke 1998; 29:2125–2128.
- Gao S, Wong KS, Hansberg T, Lam WW, Droste DW, Ringelstein EB. Microembolic signal predicts recurrent cerebral ischemic events in acute stroke patients with middle cerebral artery stenosis. Stroke 2004; 35:2832–2836.
- Mas JL, Zuber M. Recurrent cerebrovascular events in patients with patent foramen ovale, atrial septal aneurysm, or both and cryptogenic stroke or transient ischemic attack. French Study Group on Patent Foramen Ovale and Atrial Septal Aneurysm. Am Heart J 1995; 130:1083–1088.
- Di Tullio M, Sacco RL, Venketasubramanian N, Sherman D, Mohr JP, Homma S. Comparison of diagnostic techniques for the detection of a patent foramen ovale in stroke patients. Stroke 1993; 24:1020–1024.
- de Bruijn SF, Agema WR, Lammers GJ, et al. Transesophageal echocardiography is superior to transthoracic echocardiography in management of patients of any age with transient ischemic attack or stroke. Stroke 2006; 37:2531–2534.
- Lazzaro MA, Krishnan K, Prabhakaran S. Detection of atrial fibrillation with concurrent Holter monitoring and continuous cardiac telemetry following ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 2012; 21:89–93.
- Tayal AH, Tian M, Kelly KM, et al. Atrial fibrillation detected by mobile cardiac outpatient telemetry in cryptogenic TIA or stroke. Neurology 2008; 71:1696–1701.
- Seet RC, Friedman PA, Rabinstein AA. Prolonged rhythm monitoring for the detection of occult paroxysmal atrial fibrillation in ischemic stroke of unknown cause. Circulation 2011; 124:477–486.
- Morris JG, Singh S, Fisher M. Testing for inherited thrombophilias in arterial stroke: can it cause more harm than good? Stroke 2010; 41:2985–2990.
- Diener HC, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci 1996; 143:1–13.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009; 361:1139–1151.
- Meyer DM, Albright KC, Allison TA, Grotta JC. LOAD: a pilot study of the safety of loading of aspirin and clopidogrel in acute ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 2008; 17:26–29.
- Kennedy J, Hill MD, Ryckborst KJ, Eliasziw M, Demchuk AM, Buchan AM; FASTER Investigators. Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER): a randomised controlled pilot trial. Lancet Neurol 2007; 6:961–969.
- Sacco RL, Diener HC, Yusuf S, et al; PRoFESS Study Group. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med 2008; 359:1238–1251.
- Shinohara Y, Katayama Y, Uchiyama S, et al; CSPS 2 group. Cilostazol for prevention of secondary stroke (CSPS 2): an aspirin-controlled, double-blind, randomised non-inferiority trial. Lancet Neurol 2010; 9:959–968.
- Amarenco P, Bogousslavsky J, Callahan A, et al; Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 2006; 355:549–559.
- Furie KL, Kasner SE, Adams RJ, et al; American Heart Association Stroke Council, Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42:227–276.
- Koenig MA, Geocadin RG, de Grouchy M, et al. Safety of induced hypertension therapy in patients with acute ischemic stroke. Neurocrit Care 2006; 4:3–7.
- Elijovich F, Laffer CL. Acute stroke: lower blood pressure looks better and better. Hypertension 2010; 56:808–810.
- Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke: an overview of published reviews. Stroke 2004; 35:1024.
- Ovbiagele B, Diener HC, Yusuf S, et al; PROFESS Investigators. Level of systolic blood pressure within the normal range and risk of recurrent stroke. JAMA 2011; 306:2137–2144.
- Chrysant SG. The pathophysiologic role of the brain renin-angiotensin system in stroke protection: clinical implications. J Clin Hypertens (Greenwich) 2007; 9:454–459.
- Verdecchia P, Gentile G, Angeli F, Reboldi G. Beyond blood pressure: evidence for cardiovascular, cerebrovascular, and renal protective effects of renin-angiotensin system blockers. Ther Adv Cardiovasc Dis 2012; 6:81–91.
- Elkind MS, Sciacca R, Boden-Albala B, Rundek T, Paik MC, Sacco RL. Moderate alcohol consumption reduces risk of ischemic stroke: the Northern Manhattan Study. Stroke 2006; 37:13–19.
- Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJ; Carotid Endarterectomy Trialists Collaboration. Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet 2004; 363:915–924.
- Brott TG, Hobson RW, Howard G, et al; CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 2010; 363:11–23.
- Carotid Stenting Trialists’ Collaboration; Bonati LH, Dobson J, Algra A, et al. Short-term outcome after stenting versus endarterectomy for symptomatic carotid stenosis: a preplanned meta-analysis of individual patient data. Lancet 2010; 376:1062–1073.
A transient ischemic attack (TIA), like an episode of unstable angina, is an ominous portent of future morbidity and death even though, by definition, the event leaves no residual neurologic deficit.
But there is a positive side. When a patient presents with a TIA, the physician has the rare opportunity to reduce the risk of a disabling outcome—in this case, stroke. Therefore, patients deserve a rapid and thorough evaluation and appropriate stroke-preventive treatment.
MANY ‘TIAs’ ARE ACTUALLY STROKES
TIA has traditionally been described as a sudden focal neurologic deficit that lasts less than 24 hours, is presumed to be of vascular origin, and is confined to an area of the brain, spinal cord, or eye perfused by a specific artery. This symptom-based definition was based on the arbitrary and inaccurate assumption that brief symptoms would not be associated with damage to brain parenchyma.
The definition has since been updated and made more rational based on new concepts of brain ischemia informed by imaging, especially diffusion-weighted magnetic resonance imaging (MRI).1 One-third of episodes characterized as a TIA according to the classic definition would be considered an infarction on the basis of diffusion-weighted MRI.2 The new tissue-based definition characterizes TIA as a brief episode of neurologic dysfunction caused by focal ischemia of the brain, spinal cord, or retina, with clinical symptoms lasting less than 24 hours and without evidence of acute infarction.3
AN OPPORTUNITY TO INTERVENE
Most TIAs resolve in less than 30 minutes. The US National Institute of Neurological Disorders and Stroke trial of tissue plasminogen activator found that if symptoms of cerebral ischemia had not resolved by 1 hour or had not rapidly improved within 3 hours, complete resolution was rare (only 2% at 24 hours).4 Hence, physicians evaluating and treating patients with TIAs should treat these episodes with the urgency they deserve.
Moreover, half of the strokes that follow TIAs occur within 48 hours.5 A rapid and thorough evaluation and the initiation of secondary preventive treatments have been shown to reduce the early occurrence of stroke by up to 80%.6 Hence, the correct diagnosis of TIA gives the clinician the best opportunity to prevent stroke and its personal, social, and sometimes fatal consequences.
STROKES OUTNUMBER TIAs, BUT TIAs ARE UNDERREPORTED
According to 2012 statistics, nearly 795,000 strokes occur in the United States each year, 610,000 of which are first attacks and 185,000 are recurrences. Every 40 seconds, someone in the United States has a stroke.7
In comparison, the incidence of TIA in the United States is estimated at 200,000 to 500,000 per year, though the true number is difficult to know because of underreporting.8,9 About half of patients who experience a TIA fail to report it to their health care provider—a lost opportunity for intervention and stroke prevention.10,11
A meta-analysis showed that the risk of stroke after TIA was 9.9% at 2 days, 13.4% at 30 days, and 17.3% at 90 days.12
Interestingly, the risk of stroke after TIA exceeds the risk of recurrent stroke after a first stroke. This was shown in a study that found that patients who had made a substantial recovery within 24 hours (ie, patients with a TIA) were more likely to suffer neurologic deterioration in the next 3 months than were those who did not have significant early improvement.13
RISK FACTORS FOR TIA ARE THE SAME AS FOR STROKE
The risk of cerebrovascular disease increases with age and is higher in men14 and in blacks and Hispanics.15
The risk factors and clinical presentation do not differ between TIA and stroke, so the evaluation and treatment should not differ either. These two events represent a continuum of the same disease entity.
Some risk factors for TIA are modifiable, others are not.
Nonmodifiable risk factors
Nonmodifiable risk factors for TIA include older age, male sex, African American race, low birth weight, Hispanic ethnicity, and family history. If the patient has nonmodifiable risk factors, we should try all the harder to correct the modifiable ones.
Older age. The risk of ischemic stroke and intracranial hemorrhage doubles with each decade after age 55 in both sexes.16
Sex. Men have a significantly higher incidence of TIA than women,11 whereas the opposite is true for stroke: women have a higher lifetime risk of stroke than men.17
African Americans have an incidence of stroke (all types) 38% higher than that of whites,18 and an incidence of TIA (inpatient and out-of-hospital) 40% higher than the overall age- and sex-adjusted rate in the white population.11
Low birth weight. The odds of stroke are more than twice as high in people who weighed less than 2,500 g at birth compared with those who weighed 4,000 g or more, probably because of a correlation between low birth weight and hypertension.19
A family history of stroke increases the risk of stroke by nearly 30%, the association being stronger with large-vessel and smallvessel stroke than with cardioembolic stroke.20
Modifiable risk factors
Modifiable risk factors include cigarette smoking, hypertension, diabetes, lipid abnormalities, atrial fibrillation, carotid stenosis, and dietary and hormonal factors. Detecting these factors, which often coexist, is the first step in trying to modify them and reduce the patient’s risk.
Cigarette smoking approximately doubles the risk of ischemic stroke.21–23
Hypertension has a relationship with stroke risk that is strong, continuous, graded, consistent, and significant.24
Diabetes increases stroke risk nearly six times.25
Lipid abnormalities. Most studies have found an association between lipid levels (total cholesterol and low-density lipoprotein cholesterol) and the risk of death from ischemic stroke,26–28 and an inverse relationship between high-density lipoprotein cholesterol levels and stroke risk.29
Atrial fibrillation increases the risk of ischemic stroke up to fivefold, even in the absence of cardiac valvular disease. The mechanism is embolism of stasis-induced thrombi that form in the left atrial appendage.30
Carotid stenosis. Asymptomatic carotid atherosclerotic stenotic lesions in the extracranial internal carotid artery or carotid bulb are associated with a higher risk of stroke.24,31
Lifestyle factors. Diets that lower blood pressure have been found to decrease stroke risk.24 Exercise in men and women reduces the risk of stroke or death by 25% to 30% compared with inactive people.32 Weight reduction has been found to lower blood pressure and reduce stroke risk.24
Other potentially modifiable risk factors include migraine with aura, metabolic syndrome, excess alcohol consumption (and, paradoxically, complete abstinence from alcohol), drug abuse, sleep-disordered breathing, hyperhomocysteinemia, high lipoprotein (a) levels, hypercoagulability, infection with organisms such as Chlamydia pneumoniae, cytomegalovirus, and Helicobacter pylori, and acute infections such as respiratory and urinary infections.26
Conditions in certain demographic groups
Patients in certain demographic groups present with rarer conditions associated with stroke and TIA.
Sickle cell disease. Eleven percent of patients with sickle cell disease have clinical strokes, and a substantial number have “silent” infarcts identified on neuroimaging.33,34
Postmenopausal hormone replacement therapy with any product containing conjugated equine estrogen carries a risk of cerebrovascular events,35 and the higher the dose, the higher the risk.36 Also, oral contraceptives may be harmful in women who have additional risk factors such as cigarette smoking, prior thromboembolic events, or migraine with aura.37,38
THREE CAUSES OF STROKE AND TIA
Stroke and TIA should not be considered diagnoses in themselves, but rather the end point of many other diseases. The diagnosis lies in identifying the mechanism of the cerebrovascular event. The three main mechanisms are thrombosis, embolism, and decreased perfusion.
Thrombosis is caused by obstruction of blood flow within one or more blood vessels, the most common cause being atherosclerosis. Large-artery atherosclerosis, such as in the carotid bifurcation or extracranial internal carotid, causes TIAs that occur over a period of weeks or months with a variety of presentations in that vascular territory, from years of gradual accumulation of atherosclerotic plaque.39
In patients with small-artery or penetrating artery disease, hypertension is the primary risk factor and the pathology, specific to small arterioles, is lipohyalinosis rather than atherosclerosis. These patients may present with a stuttering clinical course, and episodes are more stereotypical.
Less common obstructive vascular pathologies include fibromuscular dysplasia, arteritides, and dissection.
Embolism can occur from a proximal source such as the heart or from proximal vessels such as the aorta, carotid, or vertebral arteries. The embolic particle may form on heart valves or lesions within the heart (eg, clot, tumor), or in the venous circulation and paradoxically cross over to the arterial side through an intracardiac or transpulmonary shunt. Embolism may also be due to a hypercoagulable state.40 Embolic stroke is suspected when multiple vascular territories within the brain are clinically or radiographically affected.
Decreased systemic perfusion caused by severe heart failure or systemic hypotension can cause ischemia to the brain diffusely and bilaterally, limiting the ability of the blood-stream to wash out microemboli, especially in the border zones (also known as “watershed areas”), thus leading to ischemia or infarction.41 Decreased perfusion can also be local, due to a fixed vessel stenosis.
Using another classification system, a study in Rochester, MN, found the following incident rates of stroke subtypes, adjusted for age and sex, per 100,000 population42:
- Large-vessel cervical or intracranial atherosclerosis with more than 50% stenosis—27
- Cardioembolism—40
- Lacunar, small-vessel disease—25
- Uncertain cause—52
- Other identifiable cause—4.
THREE CLINICAL FEATURES SUGGEST TIA
TIAs can be hard to distinguish from nonischemic neurologic events in the acute setting such as an emergency room. Up to 60% of patients suspected of having a TIA actually have a nonischemic cause of their symptoms.43
Three clinical features suggest a TIA during the emergency room evaluation:
- Rapid onset of symptoms—“like lightning” or “in seconds,” in contrast to migraine and seizures, which develop over minutes
- No history of similar episodes in the past
- Absence of nonspecific symptoms—eg, stomach upset or tightness in the chest.
CLINICAL DIAGNOSIS
Because most TIA symptoms and signs have already resolved by the time of evaluation, the diagnosis depends on a careful history with special attention to the pace of onset and resolution, the duration and nature of the symptoms, circumstances at the time of symptom onset, previous similar episodes, associated features, vascular risk factors, and family history (Table 1).44,45
A detailed neurologic examination is imperative and should include fundoscopy. A cardiovascular assessment should include cardiac rhythm, bruits in the neck, orbits, and groin, peripheral pulses, and electrocardiography.
Do neurologists do a better job at diagnosing TIA and stroke?
Primary care physicians, internists, and emergency department physicians are often the ones to carry out the clinical assessment of possible TIA.
Determining if transient neurologic symptoms are caused by ischemia can be a challenge. When in doubt, referral to a neurologist with subspecialty training in cerebrovascular disease should be considered.
But do neurologists really do a better job? A recent study sought to compare the accuracy of diagnosis of TIA made by general practitioners, emergency physicians, and neurologists. The nonneurologists considered “confusion” and “unexplained fall” suggestive of TIA and “lower facial palsy” and “monocular blindness” less suggestive of TIA—whereas the opposite is true. This shows that nonneurologists often label minor strokes and several nonvascular transient neurologic disturbances as TIAs, and up to half of patients could be mislabeled as a result.46
Differences in diagnosing cerebrovascular events between emergency room physicians and attending neurologists have been tested,47 with an accuracy of diagnosis as low as 38% by emergency department physicians in one study.48 However, other studies did not show such a trend.49,50
A study at a university-based teaching hospital found the sensitivity of emergency room physician diagnosis to be 98.6% with a positive predictive value of 94.8%,49 showing that at a large teaching hospital with a comprehensive stroke intervention program, emergency physicians could identify patients with stroke, particularly hemorrhagic stroke, very accurately.
Improving the diagnosis of stroke and TIA
Routine use of imaging and involvement of a neurologist increase the sensitivity and accuracy of diagnosis. Education and written guidelines for acute stroke treatment both in the emergency department and in out-of-hospital settings seem to dramatically improve the rates of diagnostic accuracy and appropriate treatment.50
Emergency medical service personnel use two screening tools in the field to identify TIA and stroke symptoms:
- The Cincinnati Prehospital Stroke Scale, a three-item scale based on three signs: facial droop, arm drift, and slurring of speech51
- The Los Angeles Prehospital Stroke Screen, which uses screening questions and asymmetry in the face, hand grip strength, and arm drift.52
Knowing that the patient is having a minor stroke or TIA is important. Urgent treatment of these conditions decreases the risk of stroke in the next 90 days, which was 10.5% in one study.5 Urgent assessment and early intervention could reduce this risk of subsequent stroke down to 2%.6
ASSESSING RISK OF STROKE AFTER TIA
There is a practical need for prediction of stroke during the first few days after the event. The ABCD and ABCD2 scores were developed to stratify the short-term risk of stroke in patients with recent TIA.
The ABCD score
The ABCD score53 was derived to allow primary care physicians and other physicians to identify which patients with a suspected diagnosis of TIA should be referred for emergency assessment, to allow secondary-care physicians to determine which patients with probable or definite TIA need emergency investigation and treatment, to allow public education about the need for medical attention after a TIA, and to identify people at high risk.
The ABCD2 score
The ABCD2 score predicts the short-term risk of stroke following a TIA.54 Points are assigned as follows:
- Age > 60 years: 1 point
- Blood pressure (systolic) > 140 mm Hg or diastolic blood pressure > 90 mm Hg: 1 point
- Clinical factors: unilateral weakness with or without speech impairment: 2 points (1 point for speech impairment without weakness)
- Duration of symptoms > 60 minutes: 2 points (1 point for 10–59 minutes)
- Diabetes: 1 point.
Thus, the possible total ranges from 0 to 7 points. Higher scores indicate a greater risk of stroke at 2, 7, 30, and 90 days:
- Total score 0, 1, 2, or 3: 2-day stroke risk 1.0% (low risk)
- Total score 4 or 5: 2-day stroke risk 4.1% (moderate risk)
- Total score 6 or 7: 2-day stroke risk 8.1% (high risk).
WHO SHOULD BE HOSPITALIZED?
It has been suggested that the ABCD2 score can help in triaging patients to hospital admission or outpatient care, though no randomized trial has actually evaluated the utility of the ABCD2 score in this way.3
A study of consecutive TIA patients admitted over 12 months55 found that patients with an ABCD2 score of 3 or less had the same chance of requiring hospitalization (based on positive diffusion-weighted MRI studies, risk factor identification, and treatment initiation) as those with a score of 4 to 7. Hence, admitting TIA patients on the basis of the ABCD2 score alone requires further study. However, such decisions, though informed by clinical data, depend heavily on societal input (eg, from insurance companies, national health protocols) and may be outside the purview of clinical investigation.
The benefits of hospitalization include the ability to rapidly carry out tests such as cardiac monitoring for atrial fibrillation; to detect atherosclerosis, aortic arch atheroma, and paradoxical emboli; and to quickly start secondary prevention treatments and education about the importance of adhering to them. Early endarterectomy in the case of carotid stenosis can be offered. Additionally, if stroke symptoms recur, thrombolytic drug therapy can be started quickly.
Nguyen-Huynh et al56 analyzed the cost utility of 24-hour hospitalization for patients diagnosed with a recent TIA who were candidates for tissue plasminogen activator if a stroke occurred. They found hospitalization to be borderline cost-effective on the whole, with definite cost-effectiveness found in patients with higher stroke risk.
If patients come to medical attention several days after the TIA, then assessing risk with the ABCD2 score may no longer be reliable.57
INVESTIGATIONS
Parenchymal neuroimaging
Computed tomography (CT) without contrast is the most widely used neuroimaging test in the acute setting, since it is widely available, fast, and relatively low-cost. It will not show any abnormality in TIA or early ischemic stroke. However, it is helpful as a screening tool to rule out intracranial lesions such as hemorrhage or tumor. It may also show evidence of established infarction, which would indicate that the ischemia probably had been present for at least 6 to 12 hours.
MRI is clearly superior to noncontrast CT for detecting small areas of ischemia in patients with TIA, and it should be used unless the patient has a contraindication to it. Roughly one-third of TIA patients have lesions detectable on diffusion-weighted imaging, which helps to confirm that the episode was caused by cerebral ischemia, but nearly half of the diffusion MRI changes may be fully reversible.58 Evidence of prior stroke, leukoaraiosis, or white matter disease on fluid-attenuated inversion recovery and T2 sequences and microhemorrhages (on gradient echo sequences) help to determine a mechanistic diagnosis.
Subcategorizing TIA patients on the basis of the findings on diffusion-weighted MRI and the ABCD2 score is prognostically helpful.59 It can help to determine which patients need hospitalization and aggressive treatment, and in the case of identified diffusion-weighted MRI-positive stroke, it helps to localize and elucidate the mechanism of stroke. Hence, MRI is the preferred neuroimaging study for evaluating patients with TIA.3
Vascular imaging
Establishing the status of both intracranial and extracranial vessels is important for understanding the etiology, estimating the risk of future ischemic events, and formulating a treatment plan—eg, carotid endarterectomy in cases of significant stenosis (70% to 99%), which reduces the risk of ipsilateral stroke.60 Imaging studies include CT angiography, magnetic resonance angiography, extracranial and transcranial ultrasonography, and conventional catheter-based angiography.
CT angiography has higher spatial resolution, but vessels may be obscured by calcification associated with atherosclerotic plaque. It has the advantage of wide availability, low cost, short scanning time, and excellent patient tolerability.
Magnetic resonance angiography with gadolinium enhancement offers good quality imaging from the great vessels in the chest to the medium-sized vessels distal to the circle of Willis.
The contrast agents used in MRI and CT can have negative consequences in patients with renal disease. MRI contrast has been associated with nephrogenic fibrosing dermopathy, 61 and CT contrast can cause contrast-induced nephropathy.62
Carotid ultrasonography and transcranial Doppler ultrasonography are noninvasive and are not associated with significant adverse events. They can be used safely in patients with renal dysfunction, and they provide physiologic information that cannot be obtained with MRI and CT, which are static imaging techniques. Detecting microemboli on transcranial Doppler is an independent predictor of recurrent ischemic events.63,64
Catheter-based angiography is occasionally needed in confusing or more complicated cases, but it is invasive and occasionally is associated with iatrogenic stroke and other vascular complications.
Cardiac and aortic imaging
Echocardiography is used to detect lesions that can be sources of embolism such as regional wall-motion abnormalities, cardiac thrombus or mass, endocarditis, aortic arch atheroma, and patent foramen ovale. In patients with cryptogenic TIA or stroke, those with patent foramen ovale alone were found to have a lower risk of recurrent stroke than those who had both atrial septal aneurysm and patent foramen ovale.65
Transesophageal echocardiography is more sensitive than transthoracic echocardiography for detecting cardioembolic lesions, especially patent foramen ovale.66 In patients with cerebral ischemia and normal transthoracic findings, cardiac sources of embolism may be detected in about 40% of patients with transesophageal echocardiography.67
Cardiac rhythm monitoring
Electrocardiography and prolonged telemetry are recommended in patients with cryptogenic TIA to detect cardiac ischemia and paroxysmal atrial fibrillation. In one study, Holter monitoring detected atrial fibrillation in 6% of patients hospitalized with ischemic stroke or TIA.68 In another study, atrial fibrillation was detected after a median of 21 days of outpatient cardiac monitoring in 23% of patients.69
The optimal duration of outpatient telemetry has not yet been established, but studies have found significant increases in detection of paroxysms of atrial fibrillation with monitoring for 7 or longer.70
Laboratory tests in the acute setting
These include lipid profile, hemoglobin A1c, and cardiac enzymes. The advantages of hospitalization are early detection of these modifiable risk factors and early initiation of treatment.
Tests for rarer disorders
Tests for rarer disorders are sometimes indicated in unusual cases, such as ischemic symptoms occurring in young patients without other common risk factors. This includes testing for prothrombotic states, toxicology, blood cultures, inflammatory markers, hemoglobin electrophoresis, and lumbar puncture. The benefit of routine testing for thrombophilic disorders in cerebrovascular disease remains uncertain, with no clear association demonstrated with arterial stroke, but testing is more relevant in the case of venous (and paradoxical) thromboembolism.71
TREAT THE UNDERLYING DISORDER
Treatment depends on the mechanism that is thought to be responsible for the ischemic event. Vascular risk factors are important to identify and modify for all stroke subtypes.
Illustrating the importance of treating TIA and minor stroke, one study72 found that for antiplatelet therapy (aspirin, dipyridamole, or aspirin plus dipyridamole), the number needed to treat for 2 years was around 18.
Anticoagulation for cardioembolism
Atrial fibrillation, especially following a cerebrovascular ischemic event, should be treated with long-term anticoagulation with warfarin (Coumadin), dabigatran (Pradaxa), rivaroxaban (Xarelto), or apixaban (Eliquis).73 If the patient cannot tolerate anticoagulation, aspirin is recommended, and if he or she cannot tolerate aspirin, clopidogrel (Plavix) is recommended.
Antiplatelet therapy for large-vessel atherosclerosis and small-vessel disease
In the acute phase, aspirin 81 mg to 325 mg orally can be given. If the patient is allergic to aspirin, a loading dose of clopidogrel 300 mg and then 75 mg daily may be given.
A pilot study of loading with aspirin 325 mg or clopidogrel 375 mg in acute ischemic stroke and TIA patients showed that these treatments were safe when given within 36 hours and decreased the risk of neurologic deterioration.74 The patient should continue on aspirin 81 mg or clopidogrel 75 mg, as suggested by the Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER) trial.75 In the long term, an antiplatelet drug such as aspirin or clopidogrel or the combination of aspirin and extended-release dipyridamole is reasonable.76
Cilostazol (Pletal) is not inferior and is possibly superior to aspirin in preventing noncardioembolic ischemic stroke. It is used off-label for secondary prevention of stroke of noncardioembolic origin.77
Statins
In the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial, high-dose atorvastatin (Lipitor)—80 mg daily—was found to reduce the risk of subsequent stroke and other cardiovascular events in patients with recent stroke irrespective of low-density lipoprotein cholesterol (LDL-C) level, but there was a small increase in the risk of hemorrhagic stroke.78
In patients with hyperlipidemia, current recommendations suggest a target LDL-C level lower than 100 mg/dL in patients with atherosclerotic stroke or TIA, and lower than 70 mg/dL in those with concomitant diabetes.79
Antihypertensive therapy
In the acute period, ie, the first 24 hours after symptoms, guidelines have advocated allowing high blood pressure to remain high (“permissive hypertension”) unless the systolic pressure is greater than 200 mm Hg or the diastolic pressure is greater than 120 mm Hg or the patient is receiving thrombolytic therapy.80 However, this has recently been challenged by findings in randomized trials.81 Permissive hypertension and avoidance of dehydration with intravenous normal saline may improve cerebral perfusion, which is especially important in patients with high-grade intracranial or extracranial stenosis. Within the parameters outlined above, we recommend against aggressively treating high blood pressure in the acute phase.
In the long term, antihypertensive therapy reduces the risk of recurrent stroke or TIA.82 The goal is to keep blood pressure lower than 140/90 mm Hg, or lower than 130/80 mm Hg in patients with diabetes. A study of patients with ischemic noncardioembolic stroke showed a higher risk of recurrent stroke if the systolic blood pressure was lower than 120 or higher than 140 mm Hg.83
Some classes of antihypertensive medication may be more beneficial than others. There is some evidence that angiotensin-converting enzyme (ACE) inhibitors alone or in combination with a diuretic or an angiotensin receptor blocker are superior to other regimens, possibly because of neuroprotective mechanisms.84 A recent meta-analysis found angiotensin receptor blockers to be more effective than either ACE inhibitors or beta-blockers in stroke prevention; however, calcium channel blockers were superior to renin-angiotensin system blockers (ACE inhibitors and angiotensin receptor blockers).85
Lifestyle modifications
Smoking cessation and cardiovascular exercise for more than 10 minutes more than 3 times per week is strongly recommended.
For patients with diabetes, the goal is to keep the fasting blood glucose level lower than 126 mg/dL.
Moderate alcohol intake has been shown to decrease stroke risk compared with excessive intake or none at all.86
Carotid endarterectomy
Carotid endarterectomy has been recommended within 2 weeks of cerebral or retinal TIA in those cases attributable to high-grade internal carotid artery stenosis in patients who have low surgical risk.87 This risk can be estimated on the basis of patient factors, surgeon factors, and hospital volume. The specific recommendations are as follows:
- 70% to 99% carotid stenosis: carotid endarterectomy recommended
- 50% to 69% carotid stenosis: carotid endarterectomy recommended in select patients with a perioperative complication rate < 6%
- < 50% carotid stenosis: carotid endarterectomy not routinely recommended.
Carotid artery angioplasty and stenting with distal embolic protection device
Data from the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST) and European stenting trials indicate that in patients over age 70, carotid endarterectomy appears to be superior to carotid artery stenting, whereas in younger patients the periprocedural risks of stroke and death are similar. Hence, carotid artery stenting performed by an interventionist with a low complication rate is a reasonable alternative to carotid endarterectomy.88,89
A transient ischemic attack (TIA), like an episode of unstable angina, is an ominous portent of future morbidity and death even though, by definition, the event leaves no residual neurologic deficit.
But there is a positive side. When a patient presents with a TIA, the physician has the rare opportunity to reduce the risk of a disabling outcome—in this case, stroke. Therefore, patients deserve a rapid and thorough evaluation and appropriate stroke-preventive treatment.
MANY ‘TIAs’ ARE ACTUALLY STROKES
TIA has traditionally been described as a sudden focal neurologic deficit that lasts less than 24 hours, is presumed to be of vascular origin, and is confined to an area of the brain, spinal cord, or eye perfused by a specific artery. This symptom-based definition was based on the arbitrary and inaccurate assumption that brief symptoms would not be associated with damage to brain parenchyma.
The definition has since been updated and made more rational based on new concepts of brain ischemia informed by imaging, especially diffusion-weighted magnetic resonance imaging (MRI).1 One-third of episodes characterized as a TIA according to the classic definition would be considered an infarction on the basis of diffusion-weighted MRI.2 The new tissue-based definition characterizes TIA as a brief episode of neurologic dysfunction caused by focal ischemia of the brain, spinal cord, or retina, with clinical symptoms lasting less than 24 hours and without evidence of acute infarction.3
AN OPPORTUNITY TO INTERVENE
Most TIAs resolve in less than 30 minutes. The US National Institute of Neurological Disorders and Stroke trial of tissue plasminogen activator found that if symptoms of cerebral ischemia had not resolved by 1 hour or had not rapidly improved within 3 hours, complete resolution was rare (only 2% at 24 hours).4 Hence, physicians evaluating and treating patients with TIAs should treat these episodes with the urgency they deserve.
Moreover, half of the strokes that follow TIAs occur within 48 hours.5 A rapid and thorough evaluation and the initiation of secondary preventive treatments have been shown to reduce the early occurrence of stroke by up to 80%.6 Hence, the correct diagnosis of TIA gives the clinician the best opportunity to prevent stroke and its personal, social, and sometimes fatal consequences.
STROKES OUTNUMBER TIAs, BUT TIAs ARE UNDERREPORTED
According to 2012 statistics, nearly 795,000 strokes occur in the United States each year, 610,000 of which are first attacks and 185,000 are recurrences. Every 40 seconds, someone in the United States has a stroke.7
In comparison, the incidence of TIA in the United States is estimated at 200,000 to 500,000 per year, though the true number is difficult to know because of underreporting.8,9 About half of patients who experience a TIA fail to report it to their health care provider—a lost opportunity for intervention and stroke prevention.10,11
A meta-analysis showed that the risk of stroke after TIA was 9.9% at 2 days, 13.4% at 30 days, and 17.3% at 90 days.12
Interestingly, the risk of stroke after TIA exceeds the risk of recurrent stroke after a first stroke. This was shown in a study that found that patients who had made a substantial recovery within 24 hours (ie, patients with a TIA) were more likely to suffer neurologic deterioration in the next 3 months than were those who did not have significant early improvement.13
RISK FACTORS FOR TIA ARE THE SAME AS FOR STROKE
The risk of cerebrovascular disease increases with age and is higher in men14 and in blacks and Hispanics.15
The risk factors and clinical presentation do not differ between TIA and stroke, so the evaluation and treatment should not differ either. These two events represent a continuum of the same disease entity.
Some risk factors for TIA are modifiable, others are not.
Nonmodifiable risk factors
Nonmodifiable risk factors for TIA include older age, male sex, African American race, low birth weight, Hispanic ethnicity, and family history. If the patient has nonmodifiable risk factors, we should try all the harder to correct the modifiable ones.
Older age. The risk of ischemic stroke and intracranial hemorrhage doubles with each decade after age 55 in both sexes.16
Sex. Men have a significantly higher incidence of TIA than women,11 whereas the opposite is true for stroke: women have a higher lifetime risk of stroke than men.17
African Americans have an incidence of stroke (all types) 38% higher than that of whites,18 and an incidence of TIA (inpatient and out-of-hospital) 40% higher than the overall age- and sex-adjusted rate in the white population.11
Low birth weight. The odds of stroke are more than twice as high in people who weighed less than 2,500 g at birth compared with those who weighed 4,000 g or more, probably because of a correlation between low birth weight and hypertension.19
A family history of stroke increases the risk of stroke by nearly 30%, the association being stronger with large-vessel and smallvessel stroke than with cardioembolic stroke.20
Modifiable risk factors
Modifiable risk factors include cigarette smoking, hypertension, diabetes, lipid abnormalities, atrial fibrillation, carotid stenosis, and dietary and hormonal factors. Detecting these factors, which often coexist, is the first step in trying to modify them and reduce the patient’s risk.
Cigarette smoking approximately doubles the risk of ischemic stroke.21–23
Hypertension has a relationship with stroke risk that is strong, continuous, graded, consistent, and significant.24
Diabetes increases stroke risk nearly six times.25
Lipid abnormalities. Most studies have found an association between lipid levels (total cholesterol and low-density lipoprotein cholesterol) and the risk of death from ischemic stroke,26–28 and an inverse relationship between high-density lipoprotein cholesterol levels and stroke risk.29
Atrial fibrillation increases the risk of ischemic stroke up to fivefold, even in the absence of cardiac valvular disease. The mechanism is embolism of stasis-induced thrombi that form in the left atrial appendage.30
Carotid stenosis. Asymptomatic carotid atherosclerotic stenotic lesions in the extracranial internal carotid artery or carotid bulb are associated with a higher risk of stroke.24,31
Lifestyle factors. Diets that lower blood pressure have been found to decrease stroke risk.24 Exercise in men and women reduces the risk of stroke or death by 25% to 30% compared with inactive people.32 Weight reduction has been found to lower blood pressure and reduce stroke risk.24
Other potentially modifiable risk factors include migraine with aura, metabolic syndrome, excess alcohol consumption (and, paradoxically, complete abstinence from alcohol), drug abuse, sleep-disordered breathing, hyperhomocysteinemia, high lipoprotein (a) levels, hypercoagulability, infection with organisms such as Chlamydia pneumoniae, cytomegalovirus, and Helicobacter pylori, and acute infections such as respiratory and urinary infections.26
Conditions in certain demographic groups
Patients in certain demographic groups present with rarer conditions associated with stroke and TIA.
Sickle cell disease. Eleven percent of patients with sickle cell disease have clinical strokes, and a substantial number have “silent” infarcts identified on neuroimaging.33,34
Postmenopausal hormone replacement therapy with any product containing conjugated equine estrogen carries a risk of cerebrovascular events,35 and the higher the dose, the higher the risk.36 Also, oral contraceptives may be harmful in women who have additional risk factors such as cigarette smoking, prior thromboembolic events, or migraine with aura.37,38
THREE CAUSES OF STROKE AND TIA
Stroke and TIA should not be considered diagnoses in themselves, but rather the end point of many other diseases. The diagnosis lies in identifying the mechanism of the cerebrovascular event. The three main mechanisms are thrombosis, embolism, and decreased perfusion.
Thrombosis is caused by obstruction of blood flow within one or more blood vessels, the most common cause being atherosclerosis. Large-artery atherosclerosis, such as in the carotid bifurcation or extracranial internal carotid, causes TIAs that occur over a period of weeks or months with a variety of presentations in that vascular territory, from years of gradual accumulation of atherosclerotic plaque.39
In patients with small-artery or penetrating artery disease, hypertension is the primary risk factor and the pathology, specific to small arterioles, is lipohyalinosis rather than atherosclerosis. These patients may present with a stuttering clinical course, and episodes are more stereotypical.
Less common obstructive vascular pathologies include fibromuscular dysplasia, arteritides, and dissection.
Embolism can occur from a proximal source such as the heart or from proximal vessels such as the aorta, carotid, or vertebral arteries. The embolic particle may form on heart valves or lesions within the heart (eg, clot, tumor), or in the venous circulation and paradoxically cross over to the arterial side through an intracardiac or transpulmonary shunt. Embolism may also be due to a hypercoagulable state.40 Embolic stroke is suspected when multiple vascular territories within the brain are clinically or radiographically affected.
Decreased systemic perfusion caused by severe heart failure or systemic hypotension can cause ischemia to the brain diffusely and bilaterally, limiting the ability of the blood-stream to wash out microemboli, especially in the border zones (also known as “watershed areas”), thus leading to ischemia or infarction.41 Decreased perfusion can also be local, due to a fixed vessel stenosis.
Using another classification system, a study in Rochester, MN, found the following incident rates of stroke subtypes, adjusted for age and sex, per 100,000 population42:
- Large-vessel cervical or intracranial atherosclerosis with more than 50% stenosis—27
- Cardioembolism—40
- Lacunar, small-vessel disease—25
- Uncertain cause—52
- Other identifiable cause—4.
THREE CLINICAL FEATURES SUGGEST TIA
TIAs can be hard to distinguish from nonischemic neurologic events in the acute setting such as an emergency room. Up to 60% of patients suspected of having a TIA actually have a nonischemic cause of their symptoms.43
Three clinical features suggest a TIA during the emergency room evaluation:
- Rapid onset of symptoms—“like lightning” or “in seconds,” in contrast to migraine and seizures, which develop over minutes
- No history of similar episodes in the past
- Absence of nonspecific symptoms—eg, stomach upset or tightness in the chest.
CLINICAL DIAGNOSIS
Because most TIA symptoms and signs have already resolved by the time of evaluation, the diagnosis depends on a careful history with special attention to the pace of onset and resolution, the duration and nature of the symptoms, circumstances at the time of symptom onset, previous similar episodes, associated features, vascular risk factors, and family history (Table 1).44,45
A detailed neurologic examination is imperative and should include fundoscopy. A cardiovascular assessment should include cardiac rhythm, bruits in the neck, orbits, and groin, peripheral pulses, and electrocardiography.
Do neurologists do a better job at diagnosing TIA and stroke?
Primary care physicians, internists, and emergency department physicians are often the ones to carry out the clinical assessment of possible TIA.
Determining if transient neurologic symptoms are caused by ischemia can be a challenge. When in doubt, referral to a neurologist with subspecialty training in cerebrovascular disease should be considered.
But do neurologists really do a better job? A recent study sought to compare the accuracy of diagnosis of TIA made by general practitioners, emergency physicians, and neurologists. The nonneurologists considered “confusion” and “unexplained fall” suggestive of TIA and “lower facial palsy” and “monocular blindness” less suggestive of TIA—whereas the opposite is true. This shows that nonneurologists often label minor strokes and several nonvascular transient neurologic disturbances as TIAs, and up to half of patients could be mislabeled as a result.46
Differences in diagnosing cerebrovascular events between emergency room physicians and attending neurologists have been tested,47 with an accuracy of diagnosis as low as 38% by emergency department physicians in one study.48 However, other studies did not show such a trend.49,50
A study at a university-based teaching hospital found the sensitivity of emergency room physician diagnosis to be 98.6% with a positive predictive value of 94.8%,49 showing that at a large teaching hospital with a comprehensive stroke intervention program, emergency physicians could identify patients with stroke, particularly hemorrhagic stroke, very accurately.
Improving the diagnosis of stroke and TIA
Routine use of imaging and involvement of a neurologist increase the sensitivity and accuracy of diagnosis. Education and written guidelines for acute stroke treatment both in the emergency department and in out-of-hospital settings seem to dramatically improve the rates of diagnostic accuracy and appropriate treatment.50
Emergency medical service personnel use two screening tools in the field to identify TIA and stroke symptoms:
- The Cincinnati Prehospital Stroke Scale, a three-item scale based on three signs: facial droop, arm drift, and slurring of speech51
- The Los Angeles Prehospital Stroke Screen, which uses screening questions and asymmetry in the face, hand grip strength, and arm drift.52
Knowing that the patient is having a minor stroke or TIA is important. Urgent treatment of these conditions decreases the risk of stroke in the next 90 days, which was 10.5% in one study.5 Urgent assessment and early intervention could reduce this risk of subsequent stroke down to 2%.6
ASSESSING RISK OF STROKE AFTER TIA
There is a practical need for prediction of stroke during the first few days after the event. The ABCD and ABCD2 scores were developed to stratify the short-term risk of stroke in patients with recent TIA.
The ABCD score
The ABCD score53 was derived to allow primary care physicians and other physicians to identify which patients with a suspected diagnosis of TIA should be referred for emergency assessment, to allow secondary-care physicians to determine which patients with probable or definite TIA need emergency investigation and treatment, to allow public education about the need for medical attention after a TIA, and to identify people at high risk.
The ABCD2 score
The ABCD2 score predicts the short-term risk of stroke following a TIA.54 Points are assigned as follows:
- Age > 60 years: 1 point
- Blood pressure (systolic) > 140 mm Hg or diastolic blood pressure > 90 mm Hg: 1 point
- Clinical factors: unilateral weakness with or without speech impairment: 2 points (1 point for speech impairment without weakness)
- Duration of symptoms > 60 minutes: 2 points (1 point for 10–59 minutes)
- Diabetes: 1 point.
Thus, the possible total ranges from 0 to 7 points. Higher scores indicate a greater risk of stroke at 2, 7, 30, and 90 days:
- Total score 0, 1, 2, or 3: 2-day stroke risk 1.0% (low risk)
- Total score 4 or 5: 2-day stroke risk 4.1% (moderate risk)
- Total score 6 or 7: 2-day stroke risk 8.1% (high risk).
WHO SHOULD BE HOSPITALIZED?
It has been suggested that the ABCD2 score can help in triaging patients to hospital admission or outpatient care, though no randomized trial has actually evaluated the utility of the ABCD2 score in this way.3
A study of consecutive TIA patients admitted over 12 months55 found that patients with an ABCD2 score of 3 or less had the same chance of requiring hospitalization (based on positive diffusion-weighted MRI studies, risk factor identification, and treatment initiation) as those with a score of 4 to 7. Hence, admitting TIA patients on the basis of the ABCD2 score alone requires further study. However, such decisions, though informed by clinical data, depend heavily on societal input (eg, from insurance companies, national health protocols) and may be outside the purview of clinical investigation.
The benefits of hospitalization include the ability to rapidly carry out tests such as cardiac monitoring for atrial fibrillation; to detect atherosclerosis, aortic arch atheroma, and paradoxical emboli; and to quickly start secondary prevention treatments and education about the importance of adhering to them. Early endarterectomy in the case of carotid stenosis can be offered. Additionally, if stroke symptoms recur, thrombolytic drug therapy can be started quickly.
Nguyen-Huynh et al56 analyzed the cost utility of 24-hour hospitalization for patients diagnosed with a recent TIA who were candidates for tissue plasminogen activator if a stroke occurred. They found hospitalization to be borderline cost-effective on the whole, with definite cost-effectiveness found in patients with higher stroke risk.
If patients come to medical attention several days after the TIA, then assessing risk with the ABCD2 score may no longer be reliable.57
INVESTIGATIONS
Parenchymal neuroimaging
Computed tomography (CT) without contrast is the most widely used neuroimaging test in the acute setting, since it is widely available, fast, and relatively low-cost. It will not show any abnormality in TIA or early ischemic stroke. However, it is helpful as a screening tool to rule out intracranial lesions such as hemorrhage or tumor. It may also show evidence of established infarction, which would indicate that the ischemia probably had been present for at least 6 to 12 hours.
MRI is clearly superior to noncontrast CT for detecting small areas of ischemia in patients with TIA, and it should be used unless the patient has a contraindication to it. Roughly one-third of TIA patients have lesions detectable on diffusion-weighted imaging, which helps to confirm that the episode was caused by cerebral ischemia, but nearly half of the diffusion MRI changes may be fully reversible.58 Evidence of prior stroke, leukoaraiosis, or white matter disease on fluid-attenuated inversion recovery and T2 sequences and microhemorrhages (on gradient echo sequences) help to determine a mechanistic diagnosis.
Subcategorizing TIA patients on the basis of the findings on diffusion-weighted MRI and the ABCD2 score is prognostically helpful.59 It can help to determine which patients need hospitalization and aggressive treatment, and in the case of identified diffusion-weighted MRI-positive stroke, it helps to localize and elucidate the mechanism of stroke. Hence, MRI is the preferred neuroimaging study for evaluating patients with TIA.3
Vascular imaging
Establishing the status of both intracranial and extracranial vessels is important for understanding the etiology, estimating the risk of future ischemic events, and formulating a treatment plan—eg, carotid endarterectomy in cases of significant stenosis (70% to 99%), which reduces the risk of ipsilateral stroke.60 Imaging studies include CT angiography, magnetic resonance angiography, extracranial and transcranial ultrasonography, and conventional catheter-based angiography.
CT angiography has higher spatial resolution, but vessels may be obscured by calcification associated with atherosclerotic plaque. It has the advantage of wide availability, low cost, short scanning time, and excellent patient tolerability.
Magnetic resonance angiography with gadolinium enhancement offers good quality imaging from the great vessels in the chest to the medium-sized vessels distal to the circle of Willis.
The contrast agents used in MRI and CT can have negative consequences in patients with renal disease. MRI contrast has been associated with nephrogenic fibrosing dermopathy, 61 and CT contrast can cause contrast-induced nephropathy.62
Carotid ultrasonography and transcranial Doppler ultrasonography are noninvasive and are not associated with significant adverse events. They can be used safely in patients with renal dysfunction, and they provide physiologic information that cannot be obtained with MRI and CT, which are static imaging techniques. Detecting microemboli on transcranial Doppler is an independent predictor of recurrent ischemic events.63,64
Catheter-based angiography is occasionally needed in confusing or more complicated cases, but it is invasive and occasionally is associated with iatrogenic stroke and other vascular complications.
Cardiac and aortic imaging
Echocardiography is used to detect lesions that can be sources of embolism such as regional wall-motion abnormalities, cardiac thrombus or mass, endocarditis, aortic arch atheroma, and patent foramen ovale. In patients with cryptogenic TIA or stroke, those with patent foramen ovale alone were found to have a lower risk of recurrent stroke than those who had both atrial septal aneurysm and patent foramen ovale.65
Transesophageal echocardiography is more sensitive than transthoracic echocardiography for detecting cardioembolic lesions, especially patent foramen ovale.66 In patients with cerebral ischemia and normal transthoracic findings, cardiac sources of embolism may be detected in about 40% of patients with transesophageal echocardiography.67
Cardiac rhythm monitoring
Electrocardiography and prolonged telemetry are recommended in patients with cryptogenic TIA to detect cardiac ischemia and paroxysmal atrial fibrillation. In one study, Holter monitoring detected atrial fibrillation in 6% of patients hospitalized with ischemic stroke or TIA.68 In another study, atrial fibrillation was detected after a median of 21 days of outpatient cardiac monitoring in 23% of patients.69
The optimal duration of outpatient telemetry has not yet been established, but studies have found significant increases in detection of paroxysms of atrial fibrillation with monitoring for 7 or longer.70
Laboratory tests in the acute setting
These include lipid profile, hemoglobin A1c, and cardiac enzymes. The advantages of hospitalization are early detection of these modifiable risk factors and early initiation of treatment.
Tests for rarer disorders
Tests for rarer disorders are sometimes indicated in unusual cases, such as ischemic symptoms occurring in young patients without other common risk factors. This includes testing for prothrombotic states, toxicology, blood cultures, inflammatory markers, hemoglobin electrophoresis, and lumbar puncture. The benefit of routine testing for thrombophilic disorders in cerebrovascular disease remains uncertain, with no clear association demonstrated with arterial stroke, but testing is more relevant in the case of venous (and paradoxical) thromboembolism.71
TREAT THE UNDERLYING DISORDER
Treatment depends on the mechanism that is thought to be responsible for the ischemic event. Vascular risk factors are important to identify and modify for all stroke subtypes.
Illustrating the importance of treating TIA and minor stroke, one study72 found that for antiplatelet therapy (aspirin, dipyridamole, or aspirin plus dipyridamole), the number needed to treat for 2 years was around 18.
Anticoagulation for cardioembolism
Atrial fibrillation, especially following a cerebrovascular ischemic event, should be treated with long-term anticoagulation with warfarin (Coumadin), dabigatran (Pradaxa), rivaroxaban (Xarelto), or apixaban (Eliquis).73 If the patient cannot tolerate anticoagulation, aspirin is recommended, and if he or she cannot tolerate aspirin, clopidogrel (Plavix) is recommended.
Antiplatelet therapy for large-vessel atherosclerosis and small-vessel disease
In the acute phase, aspirin 81 mg to 325 mg orally can be given. If the patient is allergic to aspirin, a loading dose of clopidogrel 300 mg and then 75 mg daily may be given.
A pilot study of loading with aspirin 325 mg or clopidogrel 375 mg in acute ischemic stroke and TIA patients showed that these treatments were safe when given within 36 hours and decreased the risk of neurologic deterioration.74 The patient should continue on aspirin 81 mg or clopidogrel 75 mg, as suggested by the Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER) trial.75 In the long term, an antiplatelet drug such as aspirin or clopidogrel or the combination of aspirin and extended-release dipyridamole is reasonable.76
Cilostazol (Pletal) is not inferior and is possibly superior to aspirin in preventing noncardioembolic ischemic stroke. It is used off-label for secondary prevention of stroke of noncardioembolic origin.77
Statins
In the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial, high-dose atorvastatin (Lipitor)—80 mg daily—was found to reduce the risk of subsequent stroke and other cardiovascular events in patients with recent stroke irrespective of low-density lipoprotein cholesterol (LDL-C) level, but there was a small increase in the risk of hemorrhagic stroke.78
In patients with hyperlipidemia, current recommendations suggest a target LDL-C level lower than 100 mg/dL in patients with atherosclerotic stroke or TIA, and lower than 70 mg/dL in those with concomitant diabetes.79
Antihypertensive therapy
In the acute period, ie, the first 24 hours after symptoms, guidelines have advocated allowing high blood pressure to remain high (“permissive hypertension”) unless the systolic pressure is greater than 200 mm Hg or the diastolic pressure is greater than 120 mm Hg or the patient is receiving thrombolytic therapy.80 However, this has recently been challenged by findings in randomized trials.81 Permissive hypertension and avoidance of dehydration with intravenous normal saline may improve cerebral perfusion, which is especially important in patients with high-grade intracranial or extracranial stenosis. Within the parameters outlined above, we recommend against aggressively treating high blood pressure in the acute phase.
In the long term, antihypertensive therapy reduces the risk of recurrent stroke or TIA.82 The goal is to keep blood pressure lower than 140/90 mm Hg, or lower than 130/80 mm Hg in patients with diabetes. A study of patients with ischemic noncardioembolic stroke showed a higher risk of recurrent stroke if the systolic blood pressure was lower than 120 or higher than 140 mm Hg.83
Some classes of antihypertensive medication may be more beneficial than others. There is some evidence that angiotensin-converting enzyme (ACE) inhibitors alone or in combination with a diuretic or an angiotensin receptor blocker are superior to other regimens, possibly because of neuroprotective mechanisms.84 A recent meta-analysis found angiotensin receptor blockers to be more effective than either ACE inhibitors or beta-blockers in stroke prevention; however, calcium channel blockers were superior to renin-angiotensin system blockers (ACE inhibitors and angiotensin receptor blockers).85
Lifestyle modifications
Smoking cessation and cardiovascular exercise for more than 10 minutes more than 3 times per week is strongly recommended.
For patients with diabetes, the goal is to keep the fasting blood glucose level lower than 126 mg/dL.
Moderate alcohol intake has been shown to decrease stroke risk compared with excessive intake or none at all.86
Carotid endarterectomy
Carotid endarterectomy has been recommended within 2 weeks of cerebral or retinal TIA in those cases attributable to high-grade internal carotid artery stenosis in patients who have low surgical risk.87 This risk can be estimated on the basis of patient factors, surgeon factors, and hospital volume. The specific recommendations are as follows:
- 70% to 99% carotid stenosis: carotid endarterectomy recommended
- 50% to 69% carotid stenosis: carotid endarterectomy recommended in select patients with a perioperative complication rate < 6%
- < 50% carotid stenosis: carotid endarterectomy not routinely recommended.
Carotid artery angioplasty and stenting with distal embolic protection device
Data from the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST) and European stenting trials indicate that in patients over age 70, carotid endarterectomy appears to be superior to carotid artery stenting, whereas in younger patients the periprocedural risks of stroke and death are similar. Hence, carotid artery stenting performed by an interventionist with a low complication rate is a reasonable alternative to carotid endarterectomy.88,89
- Albers GW, Caplan LR, Easton JD, et al; TIA Working Group. Transient ischemic attack—proposal for a new definition. N Engl J Med 2002; 347:1713–1716.
- Ovbiagele B, Kidwell CS, Saver JL. Epidemiological impact in the United States of a tissue-based definition of transient ischemic attack. Stroke 2003; 34:919–924.
- Easton JD, Saver JL, Albers GW, et al; American Heart Association. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke 2009; 40:2276–2293.
- Marler JR, Tilley BC, Lu M, et al. Early stroke treatment associated with better outcome: the NINDS rt-PA stroke study. Neurology 2000; 55:1649–1655.
- Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA 2000; 284:2901–2906.
- Rothwell PM, Giles MF, Chandratheva A, et al; Early use of Existing Preventive Strategies for Stroke (EXPRESS) study. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007; 370:1432–1442.
- Roger VL, Go AS, Lloyd-Jones DM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 2012; 125:e2–e220.
- Johnston SC. Clinical practice. Transient ischemic attack. N Engl J Med 2002; 347:1687–1692.
- Johnston SC, Fayad PB, Gorelick PB, et al. Prevalence and knowledge of transient ischemic attack among US adults. Neurology 2003; 60:1429–1434.
- Eliasziw M, Kennedy J, Hill MD, Buchan AM, Barnett HJ; North American Symptomatic Carotid Endarterectomy Trial Group. Early risk of stroke after a transient ischemic attack in patients with internal carotid artery disease. CMAJ 2004; 170:1105–1109.
- Kleindorfer D, Panagos P, Pancioli A, et al. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke 2005; 36:720–723.
- Wu CM, McLaughlin K, Lorenzetti DL, Hill MD, Manns BJ, Ghali WA. Early risk of stroke after transient ischemic attack: a systematic review and meta-analysis. Arch Intern Med 2007; 167:2417–2422.
- Johnston SC, Leira EC, Hansen MD, Adams HP. Early recovery after cerebral ischemia risk of subsequent neurological deterioration. Ann Neurol 2003; 54:439–444.
- Bots ML, van der Wilk EC, Koudstaal PJ, Hofman A, Grobbee DE. Transient neurological attacks in the general population. Prevalence, risk factors, and clinical relevance. Stroke 1997; 28:768–773.
- White H, Boden-Albala B, Wang C, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation 2005; 111:1327–1331.
- Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Stroke incidence, prevalence, and survival: secular trends in Rochester, Minnesota, through 1989. Stroke 1996; 27:373–380.
- Seshadri S, Beiser A, Kelly-Hayes M, et al. The lifetime risk of stroke: estimates from the Framingham Study. Stroke 2006; 37:345–350.
- Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke 1999; 30:736–743.
- Lackland DT, Egan BM, Ferguson PL. Low birth weight as a risk factor for hypertension. J Clin Hypertens (Greenwich) 2003; 5:133–136.
- Flossmann E, Schulz UG, Rothwell PM. Systematic review of methods and results of studies of the genetic epidemiology of ischemic stroke. Stroke 2004; 35:212–227.
- Rodriguez BL, D’Agostino R, Abbott RD, et al. Risk of hospitalized stroke in men enrolled in the Honolulu Heart Program and the Framingham Study: a comparison of incidence and risk factor effects. Stroke 2002; 33:230–236.
- Manolio TA, Kronmal RA, Burke GL, O’Leary DH, Price TR. Short-term predictors of incident stroke in older adults. The Cardiovascular Health Study. Stroke 1996; 27:1479–1486.
- Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke 1991; 22:312–318.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572.
- Allen TW. Guide to clinical preventive services. Report of the US Preventive Services Task Force. J Am Osteopath Assoc 1991; 91:281–289.
- Goldstein LB, Bushnell CD, Adams RJ, et al; American Heart Association Stroke Council. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42:517–584.
- Iso H, Jacobs DR, Wentworth D, Neaton JD, Cohen JD. Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the multiple risk factor intervention trial. N Engl J Med 1989; 320:904–910.
- Zhang X, Patel A, Horibe H, et al; Asia Pacific Cohort Studies Collaboration. Cholesterol, coronary heart disease, and stroke in the Asia Pacific region. Int J Epidemiol 2003; 32:563–572.
- Sanossian N, Saver JL, Navab M, Ovbiagele B. High-density lipoprotein cholesterol: an emerging target for stroke treatment. Stroke 2007; 38:1104–1109.
- Kannel WB, Benjamin EJ. Status of the epidemiology of atrial fibrillation. Med Clin North Am 2008; 92:17–40.
- Inzitari D, Eliasziw M, Gates P, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 2000; 342:1693–1700.
- Physical Activity Guidelines Advisory Committee report, 2008. To the Secretary of Health and Human Services. Part A: executive summary. Nutr Rev 2009; 67:114–120.
- Armstrong FD, Thompson RJ, Wang W, et al. Cognitive functioning and brain magnetic resonance imaging in children with sickle cell disease. Neuropsychology Committee of the Cooperative Study of Sickle Cell Disease. Pediatrics 1996; 97:864–870.
- Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood 1998; 91:288–294.
- Mosca L, Banka CL, Benjamin EJ, et al; Expert Panel/Writing Group; American Heart Association; American Academy of Family Physicians; American College of Obstetricians and Gynecologists; American College of Cardiology Foundation; Society of Thoracic Surgeons; American Medical Women's Association; Centers for Disease Control and Prevention; Office of Research on Women's Health; Association of Black Cardiologists; American College of Physicians; World Heart Federation; National Heart, Lung, and Blood Institute; American College of Nurse Practitioners. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation 2007; 115:1481–1501.
- Lidegaard Ø, Løkkegaard E, Jensen A, Skovlund CW, Keiding N. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med 2012; 366:2257–2266.
- Chan WS, Ray J, Wai EK, et al. Risk of stroke in women exposed to low-dose oral contraceptives: a critical evaluation of the evidence. Arch Intern Med 2004; 164:741–747.
- Bousser MG, Conard J, Kittner S, et al. Recommendations on the risk of ischaemic stroke associated with use of combined oral contraceptives and hormone replacement therapy in women with migraine. The International Headache Society Task Force on Combined Oral Contraceptives & Hormone Replacement Therapy. Cephalalgia 2000; 20:155–156.
- Mohr JP, Caplan LR, Melski JW, et al. The Harvard Cooperative Stroke Registry: a prospective registry. Neurology 1978; 28:754–762.
- Caplan LR. Brain embolism, revisited. Neurology 1993; 43:1281–1287.
- Caplan LR, Hennerici M. Impaired clearance of emboli (washout) is an important link between hypoperfusion, embolism, and ischemic stroke. Arch Neurol 1998; 55:1475–1482.
- Petty GW, Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke 1999; 30:2513–2516.
- Prabhakaran S, Silver AJ, Warrior L, McClenathan B, Lee VH. Misdiagnosis of transient ischemic attacks in the emergency room. Cerebrovasc Dis 2008; 26:630–635.
- Baquis GD, Pessin MS, Scott RM. Limb shaking—a carotid TIA. Stroke 1985; 16:444–448.
- Luengo-Fernandez R, Gray AM, Rothwell PM. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): a prospective population-based sequential comparison. Lancet Neurol 2009; 8:235–243.
- Ferro JM, Falcão I, Rodrigues G, et al. Diagnosis of transient ischemic attack by the nonneurologist. A validation study. Stroke 1996; 27:2225–2229.
- Norris JW, Hachinski VC. Misdiagnosis of stroke. Lancet 1982; 1:328–331.
- Ferro JM, Pinto AN, Falcão I, et al. Diagnosis of stroke by the nonneurologist. A validation study. Stroke 1998; 29:1106–1109.
- Kothari RU, Brott T, Broderick JP, Hamilton CA. Emergency physicians. Accuracy in the diagnosis of stroke. Stroke 1995; 26:2238–2241.
- Artto V, Putaala J, Strbian D, et al; Helsinki Stroke Thrombolysis Registry Group. Stroke mimics and intravenous thrombolysis. Ann Emerg Med 2012; 59:27–32.
- Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med 1999; 33:373–378.
- Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke 2000; 31:71–76.
- Rothwell PM, Giles MF, Flossmann E, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet 2005; 366:29–36.
- Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet 2007; 369:283–292.
- Lou M, Safdar A, Edlow JA, et al. Can ABCD score predict the need for in-hospital intervention in patients with transient ischemic attacks? Int J Emerg Med 2010; 3:75–80.
- Nguyen-Huynh MN, Johnston SC. Is hospitalization after TIA cost-effective on the basis of treatment with tPA? Neurology 2005; 65:1799–1801.
- Calvet D, Lamy C, Touzé E, Oppenheim C, Meder JF, Mas JL. Management and outcome of patients with transient ischemic attack admitted to a stroke unit. Cerebrovasc Dis 2007; 24:80–85.
- Kidwell CS, Alger JR, Di Salle F, et al. Diffusion MRI in patients with transient ischemic attacks. Stroke 1999; 30:1174–1180.
- Giles MF, Albers GW, Amarenco P, et al. Early stroke risk and ABCD2 score performance in tissue- vs time-defined TIA: a multicenter study. Neurology 2011; 77:1222–1228.
- Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 1998; 351:1379–1387.
- Thomsen HS. Nephrogenic systemic fibrosis: history and epidemiology. Radiol Clin North Am 2009; 47:827–831.
- Barrett BJ, Parfrey PS. Clinical practice. Preventing nephropathy induced by contrast medium. N Engl J Med 2006; 354:379–386.
- Valton L, Larrue V, le Traon AP, Massabuau P, Géraud G. Microembolic signals and risk of early recurrence in patients with stroke or transient ischemic attack. Stroke 1998; 29:2125–2128.
- Gao S, Wong KS, Hansberg T, Lam WW, Droste DW, Ringelstein EB. Microembolic signal predicts recurrent cerebral ischemic events in acute stroke patients with middle cerebral artery stenosis. Stroke 2004; 35:2832–2836.
- Mas JL, Zuber M. Recurrent cerebrovascular events in patients with patent foramen ovale, atrial septal aneurysm, or both and cryptogenic stroke or transient ischemic attack. French Study Group on Patent Foramen Ovale and Atrial Septal Aneurysm. Am Heart J 1995; 130:1083–1088.
- Di Tullio M, Sacco RL, Venketasubramanian N, Sherman D, Mohr JP, Homma S. Comparison of diagnostic techniques for the detection of a patent foramen ovale in stroke patients. Stroke 1993; 24:1020–1024.
- de Bruijn SF, Agema WR, Lammers GJ, et al. Transesophageal echocardiography is superior to transthoracic echocardiography in management of patients of any age with transient ischemic attack or stroke. Stroke 2006; 37:2531–2534.
- Lazzaro MA, Krishnan K, Prabhakaran S. Detection of atrial fibrillation with concurrent Holter monitoring and continuous cardiac telemetry following ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 2012; 21:89–93.
- Tayal AH, Tian M, Kelly KM, et al. Atrial fibrillation detected by mobile cardiac outpatient telemetry in cryptogenic TIA or stroke. Neurology 2008; 71:1696–1701.
- Seet RC, Friedman PA, Rabinstein AA. Prolonged rhythm monitoring for the detection of occult paroxysmal atrial fibrillation in ischemic stroke of unknown cause. Circulation 2011; 124:477–486.
- Morris JG, Singh S, Fisher M. Testing for inherited thrombophilias in arterial stroke: can it cause more harm than good? Stroke 2010; 41:2985–2990.
- Diener HC, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci 1996; 143:1–13.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009; 361:1139–1151.
- Meyer DM, Albright KC, Allison TA, Grotta JC. LOAD: a pilot study of the safety of loading of aspirin and clopidogrel in acute ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 2008; 17:26–29.
- Kennedy J, Hill MD, Ryckborst KJ, Eliasziw M, Demchuk AM, Buchan AM; FASTER Investigators. Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER): a randomised controlled pilot trial. Lancet Neurol 2007; 6:961–969.
- Sacco RL, Diener HC, Yusuf S, et al; PRoFESS Study Group. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med 2008; 359:1238–1251.
- Shinohara Y, Katayama Y, Uchiyama S, et al; CSPS 2 group. Cilostazol for prevention of secondary stroke (CSPS 2): an aspirin-controlled, double-blind, randomised non-inferiority trial. Lancet Neurol 2010; 9:959–968.
- Amarenco P, Bogousslavsky J, Callahan A, et al; Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 2006; 355:549–559.
- Furie KL, Kasner SE, Adams RJ, et al; American Heart Association Stroke Council, Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42:227–276.
- Koenig MA, Geocadin RG, de Grouchy M, et al. Safety of induced hypertension therapy in patients with acute ischemic stroke. Neurocrit Care 2006; 4:3–7.
- Elijovich F, Laffer CL. Acute stroke: lower blood pressure looks better and better. Hypertension 2010; 56:808–810.
- Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke: an overview of published reviews. Stroke 2004; 35:1024.
- Ovbiagele B, Diener HC, Yusuf S, et al; PROFESS Investigators. Level of systolic blood pressure within the normal range and risk of recurrent stroke. JAMA 2011; 306:2137–2144.
- Chrysant SG. The pathophysiologic role of the brain renin-angiotensin system in stroke protection: clinical implications. J Clin Hypertens (Greenwich) 2007; 9:454–459.
- Verdecchia P, Gentile G, Angeli F, Reboldi G. Beyond blood pressure: evidence for cardiovascular, cerebrovascular, and renal protective effects of renin-angiotensin system blockers. Ther Adv Cardiovasc Dis 2012; 6:81–91.
- Elkind MS, Sciacca R, Boden-Albala B, Rundek T, Paik MC, Sacco RL. Moderate alcohol consumption reduces risk of ischemic stroke: the Northern Manhattan Study. Stroke 2006; 37:13–19.
- Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJ; Carotid Endarterectomy Trialists Collaboration. Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet 2004; 363:915–924.
- Brott TG, Hobson RW, Howard G, et al; CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 2010; 363:11–23.
- Carotid Stenting Trialists’ Collaboration; Bonati LH, Dobson J, Algra A, et al. Short-term outcome after stenting versus endarterectomy for symptomatic carotid stenosis: a preplanned meta-analysis of individual patient data. Lancet 2010; 376:1062–1073.
- Albers GW, Caplan LR, Easton JD, et al; TIA Working Group. Transient ischemic attack—proposal for a new definition. N Engl J Med 2002; 347:1713–1716.
- Ovbiagele B, Kidwell CS, Saver JL. Epidemiological impact in the United States of a tissue-based definition of transient ischemic attack. Stroke 2003; 34:919–924.
- Easton JD, Saver JL, Albers GW, et al; American Heart Association. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke 2009; 40:2276–2293.
- Marler JR, Tilley BC, Lu M, et al. Early stroke treatment associated with better outcome: the NINDS rt-PA stroke study. Neurology 2000; 55:1649–1655.
- Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA 2000; 284:2901–2906.
- Rothwell PM, Giles MF, Chandratheva A, et al; Early use of Existing Preventive Strategies for Stroke (EXPRESS) study. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007; 370:1432–1442.
- Roger VL, Go AS, Lloyd-Jones DM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 2012; 125:e2–e220.
- Johnston SC. Clinical practice. Transient ischemic attack. N Engl J Med 2002; 347:1687–1692.
- Johnston SC, Fayad PB, Gorelick PB, et al. Prevalence and knowledge of transient ischemic attack among US adults. Neurology 2003; 60:1429–1434.
- Eliasziw M, Kennedy J, Hill MD, Buchan AM, Barnett HJ; North American Symptomatic Carotid Endarterectomy Trial Group. Early risk of stroke after a transient ischemic attack in patients with internal carotid artery disease. CMAJ 2004; 170:1105–1109.
- Kleindorfer D, Panagos P, Pancioli A, et al. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke 2005; 36:720–723.
- Wu CM, McLaughlin K, Lorenzetti DL, Hill MD, Manns BJ, Ghali WA. Early risk of stroke after transient ischemic attack: a systematic review and meta-analysis. Arch Intern Med 2007; 167:2417–2422.
- Johnston SC, Leira EC, Hansen MD, Adams HP. Early recovery after cerebral ischemia risk of subsequent neurological deterioration. Ann Neurol 2003; 54:439–444.
- Bots ML, van der Wilk EC, Koudstaal PJ, Hofman A, Grobbee DE. Transient neurological attacks in the general population. Prevalence, risk factors, and clinical relevance. Stroke 1997; 28:768–773.
- White H, Boden-Albala B, Wang C, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation 2005; 111:1327–1331.
- Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Stroke incidence, prevalence, and survival: secular trends in Rochester, Minnesota, through 1989. Stroke 1996; 27:373–380.
- Seshadri S, Beiser A, Kelly-Hayes M, et al. The lifetime risk of stroke: estimates from the Framingham Study. Stroke 2006; 37:345–350.
- Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke 1999; 30:736–743.
- Lackland DT, Egan BM, Ferguson PL. Low birth weight as a risk factor for hypertension. J Clin Hypertens (Greenwich) 2003; 5:133–136.
- Flossmann E, Schulz UG, Rothwell PM. Systematic review of methods and results of studies of the genetic epidemiology of ischemic stroke. Stroke 2004; 35:212–227.
- Rodriguez BL, D’Agostino R, Abbott RD, et al. Risk of hospitalized stroke in men enrolled in the Honolulu Heart Program and the Framingham Study: a comparison of incidence and risk factor effects. Stroke 2002; 33:230–236.
- Manolio TA, Kronmal RA, Burke GL, O’Leary DH, Price TR. Short-term predictors of incident stroke in older adults. The Cardiovascular Health Study. Stroke 1996; 27:1479–1486.
- Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke 1991; 22:312–318.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572.
- Allen TW. Guide to clinical preventive services. Report of the US Preventive Services Task Force. J Am Osteopath Assoc 1991; 91:281–289.
- Goldstein LB, Bushnell CD, Adams RJ, et al; American Heart Association Stroke Council. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42:517–584.
- Iso H, Jacobs DR, Wentworth D, Neaton JD, Cohen JD. Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the multiple risk factor intervention trial. N Engl J Med 1989; 320:904–910.
- Zhang X, Patel A, Horibe H, et al; Asia Pacific Cohort Studies Collaboration. Cholesterol, coronary heart disease, and stroke in the Asia Pacific region. Int J Epidemiol 2003; 32:563–572.
- Sanossian N, Saver JL, Navab M, Ovbiagele B. High-density lipoprotein cholesterol: an emerging target for stroke treatment. Stroke 2007; 38:1104–1109.
- Kannel WB, Benjamin EJ. Status of the epidemiology of atrial fibrillation. Med Clin North Am 2008; 92:17–40.
- Inzitari D, Eliasziw M, Gates P, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 2000; 342:1693–1700.
- Physical Activity Guidelines Advisory Committee report, 2008. To the Secretary of Health and Human Services. Part A: executive summary. Nutr Rev 2009; 67:114–120.
- Armstrong FD, Thompson RJ, Wang W, et al. Cognitive functioning and brain magnetic resonance imaging in children with sickle cell disease. Neuropsychology Committee of the Cooperative Study of Sickle Cell Disease. Pediatrics 1996; 97:864–870.
- Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood 1998; 91:288–294.
- Mosca L, Banka CL, Benjamin EJ, et al; Expert Panel/Writing Group; American Heart Association; American Academy of Family Physicians; American College of Obstetricians and Gynecologists; American College of Cardiology Foundation; Society of Thoracic Surgeons; American Medical Women's Association; Centers for Disease Control and Prevention; Office of Research on Women's Health; Association of Black Cardiologists; American College of Physicians; World Heart Federation; National Heart, Lung, and Blood Institute; American College of Nurse Practitioners. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation 2007; 115:1481–1501.
- Lidegaard Ø, Løkkegaard E, Jensen A, Skovlund CW, Keiding N. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med 2012; 366:2257–2266.
- Chan WS, Ray J, Wai EK, et al. Risk of stroke in women exposed to low-dose oral contraceptives: a critical evaluation of the evidence. Arch Intern Med 2004; 164:741–747.
- Bousser MG, Conard J, Kittner S, et al. Recommendations on the risk of ischaemic stroke associated with use of combined oral contraceptives and hormone replacement therapy in women with migraine. The International Headache Society Task Force on Combined Oral Contraceptives & Hormone Replacement Therapy. Cephalalgia 2000; 20:155–156.
- Mohr JP, Caplan LR, Melski JW, et al. The Harvard Cooperative Stroke Registry: a prospective registry. Neurology 1978; 28:754–762.
- Caplan LR. Brain embolism, revisited. Neurology 1993; 43:1281–1287.
- Caplan LR, Hennerici M. Impaired clearance of emboli (washout) is an important link between hypoperfusion, embolism, and ischemic stroke. Arch Neurol 1998; 55:1475–1482.
- Petty GW, Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke 1999; 30:2513–2516.
- Prabhakaran S, Silver AJ, Warrior L, McClenathan B, Lee VH. Misdiagnosis of transient ischemic attacks in the emergency room. Cerebrovasc Dis 2008; 26:630–635.
- Baquis GD, Pessin MS, Scott RM. Limb shaking—a carotid TIA. Stroke 1985; 16:444–448.
- Luengo-Fernandez R, Gray AM, Rothwell PM. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): a prospective population-based sequential comparison. Lancet Neurol 2009; 8:235–243.
- Ferro JM, Falcão I, Rodrigues G, et al. Diagnosis of transient ischemic attack by the nonneurologist. A validation study. Stroke 1996; 27:2225–2229.
- Norris JW, Hachinski VC. Misdiagnosis of stroke. Lancet 1982; 1:328–331.
- Ferro JM, Pinto AN, Falcão I, et al. Diagnosis of stroke by the nonneurologist. A validation study. Stroke 1998; 29:1106–1109.
- Kothari RU, Brott T, Broderick JP, Hamilton CA. Emergency physicians. Accuracy in the diagnosis of stroke. Stroke 1995; 26:2238–2241.
- Artto V, Putaala J, Strbian D, et al; Helsinki Stroke Thrombolysis Registry Group. Stroke mimics and intravenous thrombolysis. Ann Emerg Med 2012; 59:27–32.
- Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med 1999; 33:373–378.
- Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke 2000; 31:71–76.
- Rothwell PM, Giles MF, Flossmann E, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet 2005; 366:29–36.
- Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet 2007; 369:283–292.
- Lou M, Safdar A, Edlow JA, et al. Can ABCD score predict the need for in-hospital intervention in patients with transient ischemic attacks? Int J Emerg Med 2010; 3:75–80.
- Nguyen-Huynh MN, Johnston SC. Is hospitalization after TIA cost-effective on the basis of treatment with tPA? Neurology 2005; 65:1799–1801.
- Calvet D, Lamy C, Touzé E, Oppenheim C, Meder JF, Mas JL. Management and outcome of patients with transient ischemic attack admitted to a stroke unit. Cerebrovasc Dis 2007; 24:80–85.
- Kidwell CS, Alger JR, Di Salle F, et al. Diffusion MRI in patients with transient ischemic attacks. Stroke 1999; 30:1174–1180.
- Giles MF, Albers GW, Amarenco P, et al. Early stroke risk and ABCD2 score performance in tissue- vs time-defined TIA: a multicenter study. Neurology 2011; 77:1222–1228.
- Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 1998; 351:1379–1387.
- Thomsen HS. Nephrogenic systemic fibrosis: history and epidemiology. Radiol Clin North Am 2009; 47:827–831.
- Barrett BJ, Parfrey PS. Clinical practice. Preventing nephropathy induced by contrast medium. N Engl J Med 2006; 354:379–386.
- Valton L, Larrue V, le Traon AP, Massabuau P, Géraud G. Microembolic signals and risk of early recurrence in patients with stroke or transient ischemic attack. Stroke 1998; 29:2125–2128.
- Gao S, Wong KS, Hansberg T, Lam WW, Droste DW, Ringelstein EB. Microembolic signal predicts recurrent cerebral ischemic events in acute stroke patients with middle cerebral artery stenosis. Stroke 2004; 35:2832–2836.
- Mas JL, Zuber M. Recurrent cerebrovascular events in patients with patent foramen ovale, atrial septal aneurysm, or both and cryptogenic stroke or transient ischemic attack. French Study Group on Patent Foramen Ovale and Atrial Septal Aneurysm. Am Heart J 1995; 130:1083–1088.
- Di Tullio M, Sacco RL, Venketasubramanian N, Sherman D, Mohr JP, Homma S. Comparison of diagnostic techniques for the detection of a patent foramen ovale in stroke patients. Stroke 1993; 24:1020–1024.
- de Bruijn SF, Agema WR, Lammers GJ, et al. Transesophageal echocardiography is superior to transthoracic echocardiography in management of patients of any age with transient ischemic attack or stroke. Stroke 2006; 37:2531–2534.
- Lazzaro MA, Krishnan K, Prabhakaran S. Detection of atrial fibrillation with concurrent Holter monitoring and continuous cardiac telemetry following ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 2012; 21:89–93.
- Tayal AH, Tian M, Kelly KM, et al. Atrial fibrillation detected by mobile cardiac outpatient telemetry in cryptogenic TIA or stroke. Neurology 2008; 71:1696–1701.
- Seet RC, Friedman PA, Rabinstein AA. Prolonged rhythm monitoring for the detection of occult paroxysmal atrial fibrillation in ischemic stroke of unknown cause. Circulation 2011; 124:477–486.
- Morris JG, Singh S, Fisher M. Testing for inherited thrombophilias in arterial stroke: can it cause more harm than good? Stroke 2010; 41:2985–2990.
- Diener HC, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci 1996; 143:1–13.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009; 361:1139–1151.
- Meyer DM, Albright KC, Allison TA, Grotta JC. LOAD: a pilot study of the safety of loading of aspirin and clopidogrel in acute ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis 2008; 17:26–29.
- Kennedy J, Hill MD, Ryckborst KJ, Eliasziw M, Demchuk AM, Buchan AM; FASTER Investigators. Fast Assessment of Stroke and Transient Ischaemic Attack to Prevent Early Recurrence (FASTER): a randomised controlled pilot trial. Lancet Neurol 2007; 6:961–969.
- Sacco RL, Diener HC, Yusuf S, et al; PRoFESS Study Group. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med 2008; 359:1238–1251.
- Shinohara Y, Katayama Y, Uchiyama S, et al; CSPS 2 group. Cilostazol for prevention of secondary stroke (CSPS 2): an aspirin-controlled, double-blind, randomised non-inferiority trial. Lancet Neurol 2010; 9:959–968.
- Amarenco P, Bogousslavsky J, Callahan A, et al; Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 2006; 355:549–559.
- Furie KL, Kasner SE, Adams RJ, et al; American Heart Association Stroke Council, Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42:227–276.
- Koenig MA, Geocadin RG, de Grouchy M, et al. Safety of induced hypertension therapy in patients with acute ischemic stroke. Neurocrit Care 2006; 4:3–7.
- Elijovich F, Laffer CL. Acute stroke: lower blood pressure looks better and better. Hypertension 2010; 56:808–810.
- Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke: an overview of published reviews. Stroke 2004; 35:1024.
- Ovbiagele B, Diener HC, Yusuf S, et al; PROFESS Investigators. Level of systolic blood pressure within the normal range and risk of recurrent stroke. JAMA 2011; 306:2137–2144.
- Chrysant SG. The pathophysiologic role of the brain renin-angiotensin system in stroke protection: clinical implications. J Clin Hypertens (Greenwich) 2007; 9:454–459.
- Verdecchia P, Gentile G, Angeli F, Reboldi G. Beyond blood pressure: evidence for cardiovascular, cerebrovascular, and renal protective effects of renin-angiotensin system blockers. Ther Adv Cardiovasc Dis 2012; 6:81–91.
- Elkind MS, Sciacca R, Boden-Albala B, Rundek T, Paik MC, Sacco RL. Moderate alcohol consumption reduces risk of ischemic stroke: the Northern Manhattan Study. Stroke 2006; 37:13–19.
- Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJ; Carotid Endarterectomy Trialists Collaboration. Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet 2004; 363:915–924.
- Brott TG, Hobson RW, Howard G, et al; CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 2010; 363:11–23.
- Carotid Stenting Trialists’ Collaboration; Bonati LH, Dobson J, Algra A, et al. Short-term outcome after stenting versus endarterectomy for symptomatic carotid stenosis: a preplanned meta-analysis of individual patient data. Lancet 2010; 376:1062–1073.
KEY POINTS
- Modifiable risk factors for stroke and TIA include cigarette smoking, hypertension, diabetes, lipid abnormalities, atrial fibrillation, carotid stenosis, and dietary and hormonal factors.
- The three major mechanisms of stroke and TIA are thrombosis, embolism, and decreased systemic perfusion.
- Typical symptoms of TIA include hemiparesis, hemisensory loss, aphasia, vision loss, ataxia, and diplopia. Three clinical features that suggest TIA are rapid onset of symptoms, no history of similar episodes in the past, and the absence of nonspecific symptoms.
- In suspected TIA, magnetic resonance imaging is clearly superior to noncontrast computed tomography (CT) for detecting small areas of ischemia; this test should be used unless contraindicated.
- Imaging studies of the blood vessels include CT angiography, magnetic resonance angiography, conventional angiography, and extracranial and transcranial ultrasonography.
LV fibrosis predicts mortality in atrial fib patients
Left ventricular late gadolinium enhancement – a marker of myocardial fibrosis – occurs commonly and may predict mortality in patients with atrial fibrillation, a prospective observational study has shown.
Of 664 consecutive patients with atrial fibrillation and no known prior myocardial infarction who were referred for radiofrequency ablation of the pulmonary veins between September 2006 and June 2011, 88 (13%) had unanticipated left ventricular late gadolinium enhancement (LV LGE) identified via cardiac magnetic resonance imaging, and 68 died over a median follow-up of 42 months. The mortality rate was 8.1% among those with LV LGE, compared with 2.3% among those without LV LGE, Dr. Thomas G. Neilan of Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, and his colleagues reported online Aug. 28 in the Journal of the American College of Cardiology.
After adjustment for key variables, including sex, diabetes, and heart failure, the presence of LV LGE was significantly linked with mortality. Age and the extent of LGE were the strongest independent predictors of mortality (hazard ratios, 1.05 and 1.15, respectively), the investigators said (J. Am. Coll. Cardiol. 2013 Aug. 28 [doi.org/10.1016/j.jacc.2013.07.067 ]).
The presence of LV LGE provided strong prognostic information, they said, noting that each 1% increase in LGE was associated with a 15% increased risk of death.
The findings were similar when an additional 56 patients with a history of myocardial infarction were included in the analysis, they noted.
Patients in the study had an average age of 56 years. Most (73%) were men.
The pattern of LV LGE was ischemic in 59% and nonischemic in 41%; among those with no history of myocardial infarction, the pattern was ischemic in 50% and nonischemic in 50%.
The findings provide needed information about the presence, pattern, and prognostic significance of left ventricular myocardial fibrosis in patients with atrial fibrillation.
The presence of LV LGE provides "strong and complementary" prognostic information in patients with several conditions, such as congenital heart disease, myocardial infarction, and myocarditis to name a few, but limited data are available regarding the presence and prognostic significance of LV LGE in patients with atrial fibrillation, the investigators said.
The current findings highlight the frequency of LV LGE in this population and its strong association with mortality, and support "the robust and additive prognostic information" provided by cardiac magnetic resonance imaging in patients being referred for pulmonary vein isolation, they concluded, adding that the findings also may support further study in this high-risk cohort.
These findings by Dr. Neilan and his colleagues suggest that the presence of late gadolinium enhancement on cardiac magnetic resonance has important consequences, but the causal link between atrial fibrillation and left ventricular fibrosis is difficult to ascertain, Dr. Zhiyu Ling and Dr. Harikrishna Tandri wrote in an editorial.
The findings, which are the result of "an attempt to connect the dots between AF and all cause mortality," also suggest that cardiac magnetic resonance may be the preferred imaging modality for certain higher-risk patients undergoing catheter ablation for AF, they said (J. Am. Coll. Cardiol. 2013 Aug. 28 [doi.org/10.1016/j.jacc.2013.08.692]).
"The finding of LGE in the LV might identify patients with occult coronary disease or a cardiomyopathy, or trigger aggressive risk factor management of modifiable risks such as sleep apnea and hypertension. Whether this strategy will better risk stratify patients at risk of mortality and thus change the observed outcomes needs to be tested in prospective studies designed specifically to answer this question," they wrote.
Additional study is also warranted to investigate the prevalence of LV LGE and its association with cardiovascular mortality in patients with persistent AF and severe comorbidities and to "establish whether LGE is a major independent predictive factor of cardiovascular mortality in patients with AF," they said.
Dr. Ling and Dr. Tandri are with Johns Hopkins Hospital, Baltimore. They reported having no relevant financial disclosures.
These findings by Dr. Neilan and his colleagues suggest that the presence of late gadolinium enhancement on cardiac magnetic resonance has important consequences, but the causal link between atrial fibrillation and left ventricular fibrosis is difficult to ascertain, Dr. Zhiyu Ling and Dr. Harikrishna Tandri wrote in an editorial.
The findings, which are the result of "an attempt to connect the dots between AF and all cause mortality," also suggest that cardiac magnetic resonance may be the preferred imaging modality for certain higher-risk patients undergoing catheter ablation for AF, they said (J. Am. Coll. Cardiol. 2013 Aug. 28 [doi.org/10.1016/j.jacc.2013.08.692]).
"The finding of LGE in the LV might identify patients with occult coronary disease or a cardiomyopathy, or trigger aggressive risk factor management of modifiable risks such as sleep apnea and hypertension. Whether this strategy will better risk stratify patients at risk of mortality and thus change the observed outcomes needs to be tested in prospective studies designed specifically to answer this question," they wrote.
Additional study is also warranted to investigate the prevalence of LV LGE and its association with cardiovascular mortality in patients with persistent AF and severe comorbidities and to "establish whether LGE is a major independent predictive factor of cardiovascular mortality in patients with AF," they said.
Dr. Ling and Dr. Tandri are with Johns Hopkins Hospital, Baltimore. They reported having no relevant financial disclosures.
These findings by Dr. Neilan and his colleagues suggest that the presence of late gadolinium enhancement on cardiac magnetic resonance has important consequences, but the causal link between atrial fibrillation and left ventricular fibrosis is difficult to ascertain, Dr. Zhiyu Ling and Dr. Harikrishna Tandri wrote in an editorial.
The findings, which are the result of "an attempt to connect the dots between AF and all cause mortality," also suggest that cardiac magnetic resonance may be the preferred imaging modality for certain higher-risk patients undergoing catheter ablation for AF, they said (J. Am. Coll. Cardiol. 2013 Aug. 28 [doi.org/10.1016/j.jacc.2013.08.692]).
"The finding of LGE in the LV might identify patients with occult coronary disease or a cardiomyopathy, or trigger aggressive risk factor management of modifiable risks such as sleep apnea and hypertension. Whether this strategy will better risk stratify patients at risk of mortality and thus change the observed outcomes needs to be tested in prospective studies designed specifically to answer this question," they wrote.
Additional study is also warranted to investigate the prevalence of LV LGE and its association with cardiovascular mortality in patients with persistent AF and severe comorbidities and to "establish whether LGE is a major independent predictive factor of cardiovascular mortality in patients with AF," they said.
Dr. Ling and Dr. Tandri are with Johns Hopkins Hospital, Baltimore. They reported having no relevant financial disclosures.
Left ventricular late gadolinium enhancement – a marker of myocardial fibrosis – occurs commonly and may predict mortality in patients with atrial fibrillation, a prospective observational study has shown.
Of 664 consecutive patients with atrial fibrillation and no known prior myocardial infarction who were referred for radiofrequency ablation of the pulmonary veins between September 2006 and June 2011, 88 (13%) had unanticipated left ventricular late gadolinium enhancement (LV LGE) identified via cardiac magnetic resonance imaging, and 68 died over a median follow-up of 42 months. The mortality rate was 8.1% among those with LV LGE, compared with 2.3% among those without LV LGE, Dr. Thomas G. Neilan of Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, and his colleagues reported online Aug. 28 in the Journal of the American College of Cardiology.
After adjustment for key variables, including sex, diabetes, and heart failure, the presence of LV LGE was significantly linked with mortality. Age and the extent of LGE were the strongest independent predictors of mortality (hazard ratios, 1.05 and 1.15, respectively), the investigators said (J. Am. Coll. Cardiol. 2013 Aug. 28 [doi.org/10.1016/j.jacc.2013.07.067 ]).
The presence of LV LGE provided strong prognostic information, they said, noting that each 1% increase in LGE was associated with a 15% increased risk of death.
The findings were similar when an additional 56 patients with a history of myocardial infarction were included in the analysis, they noted.
Patients in the study had an average age of 56 years. Most (73%) were men.
The pattern of LV LGE was ischemic in 59% and nonischemic in 41%; among those with no history of myocardial infarction, the pattern was ischemic in 50% and nonischemic in 50%.
The findings provide needed information about the presence, pattern, and prognostic significance of left ventricular myocardial fibrosis in patients with atrial fibrillation.
The presence of LV LGE provides "strong and complementary" prognostic information in patients with several conditions, such as congenital heart disease, myocardial infarction, and myocarditis to name a few, but limited data are available regarding the presence and prognostic significance of LV LGE in patients with atrial fibrillation, the investigators said.
The current findings highlight the frequency of LV LGE in this population and its strong association with mortality, and support "the robust and additive prognostic information" provided by cardiac magnetic resonance imaging in patients being referred for pulmonary vein isolation, they concluded, adding that the findings also may support further study in this high-risk cohort.
Left ventricular late gadolinium enhancement – a marker of myocardial fibrosis – occurs commonly and may predict mortality in patients with atrial fibrillation, a prospective observational study has shown.
Of 664 consecutive patients with atrial fibrillation and no known prior myocardial infarction who were referred for radiofrequency ablation of the pulmonary veins between September 2006 and June 2011, 88 (13%) had unanticipated left ventricular late gadolinium enhancement (LV LGE) identified via cardiac magnetic resonance imaging, and 68 died over a median follow-up of 42 months. The mortality rate was 8.1% among those with LV LGE, compared with 2.3% among those without LV LGE, Dr. Thomas G. Neilan of Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, and his colleagues reported online Aug. 28 in the Journal of the American College of Cardiology.
After adjustment for key variables, including sex, diabetes, and heart failure, the presence of LV LGE was significantly linked with mortality. Age and the extent of LGE were the strongest independent predictors of mortality (hazard ratios, 1.05 and 1.15, respectively), the investigators said (J. Am. Coll. Cardiol. 2013 Aug. 28 [doi.org/10.1016/j.jacc.2013.07.067 ]).
The presence of LV LGE provided strong prognostic information, they said, noting that each 1% increase in LGE was associated with a 15% increased risk of death.
The findings were similar when an additional 56 patients with a history of myocardial infarction were included in the analysis, they noted.
Patients in the study had an average age of 56 years. Most (73%) were men.
The pattern of LV LGE was ischemic in 59% and nonischemic in 41%; among those with no history of myocardial infarction, the pattern was ischemic in 50% and nonischemic in 50%.
The findings provide needed information about the presence, pattern, and prognostic significance of left ventricular myocardial fibrosis in patients with atrial fibrillation.
The presence of LV LGE provides "strong and complementary" prognostic information in patients with several conditions, such as congenital heart disease, myocardial infarction, and myocarditis to name a few, but limited data are available regarding the presence and prognostic significance of LV LGE in patients with atrial fibrillation, the investigators said.
The current findings highlight the frequency of LV LGE in this population and its strong association with mortality, and support "the robust and additive prognostic information" provided by cardiac magnetic resonance imaging in patients being referred for pulmonary vein isolation, they concluded, adding that the findings also may support further study in this high-risk cohort.
FROM jOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Major finding: Mortality was 8.1% in the patients with LV VGE identified via cardiac magnetic resonance imaging, vs. 2.3% in those without LV LGE.
Data source: A prospective cohort study in 720 AF patients.
Disclosures: This study was supported by a Fellow to Faculty grant from the American Heart Association, and by project grants from the National Institutes of Health to study coauthors M. Jerosch-Herold, Ph.D., and Dr. Raymond Y. Kwong. The remaining authors reported having no relevant financial disclosures.
Vitamin C protects kidneys against angiography contrast
Ascorbic acid may protect against contrast-induced-acute kidney injury in patients undergoing coronary angiography, a meta-analysis of nine randomized controlled trials has shown.
The overall incidence of contrast-induced acute kidney injury (CI-AKI) among 740 patients who received ascorbic acid and who were included in the final analysis was 9.6%, compared with 16.8% in 796 patients who received placebo or an alternative pharmacologic treatment, Dr. Umar Sadat of Cambridge (England) University Hospitals NHS Foundation Trust, and colleagues reported.
"In the pooled analysis using random effects model, patients receiving ascorbic acid had 33% less risk of CI-AKI compared to the control group (risk ratio, 0.672)," a statistically significant difference, the investigators wrote.
The findings were published online Aug. 28 in the Journal of the American College of Cardiology.
The investigators systematically reviewed Medline, Embase, and Cochrane central databases for studies published from inception to May 2013 on the incidence of CI-AKI in patients undergoing coronary angiography. Studies that were included in the meta-analysis had at least one arm that involved treatment with ascorbic acid alone or in combination with saline hydration. Ultimately, nine studies involving a total of 1,536 patients with baseline renal impairment were included (J. Am. Coll. Cardiol. 2013 Aug. 28).
The findings, which provide "robust evidence that ascorbic acid reduces the risk of CI-AKI, albeit by a small magnitude," suggest that ascorbic acid has nephroprotective qualities and could form a part of effective prophylactic pharmacologic regimens to protect patients undergoing coronary angiography against CI-AKI.
It makes sense that ascorbic acid – a form of vitamin C – could provide nephroprotection, because strong evidence suggests it acts as a potent antioxidant by scavenging physiologically relevant reactive oxygen species (ROS), they explained, noting that ROS-induced oxidative stress and renal vasoconstriction have been implicated in the etiology of CI-AKI.
The findings are important, because the incidence of CI-AKI is rising in tandem with the increasing number of contrast media–enhanced radiologic procedures and with a rise in the octogenarian population with comorbidities such as hypertension, diabetes, and renovascular disease that predispose patients to renal impairment, the investigators said.
However, further investigation regarding the optimal dosage and route of administration of ascorbic acid in order to assess its full potential as a nephroprotective agent is warranted, they concluded.
The findings of this meta-analysis represent an advancement in the field, and frame ascorbic acid as a potential therapy to be evaluated in large-scale clinical trials, according to Dr. Peter A. McCullough and Dr. Krittapoom Akrawinthawong.
This is important given the lack of "bona fide preventive approaches" to protect against CK-AKI until less-toxic iodinated contrast becomes available, they wrote in an editorial (J. Am. Coll. Cardiol. 2013 Aug. 28).
However, several questions about the potential benefits of ascorbic acid in this setting remain unanswered, they noted.
The key question remains: "If we prevent or lessen CI-AKI as determined by serum creatinine, will we reduce the rates of clinical outcomes including end-stage renal disease, mortality, and more secondary events including the development of heart failure, recurrent acute coronary syndromes, or stroke?"
This question can be answered only by large-scale trials with effective therapies and adequate follow-up, they said.
Dr. McCullough is with Providence Hospitals and Medical Centers, Southfield and Novi, Mich. Dr. Akrawinthawong is with St. John Hospital and Medical Center, Detroit. They said they had no relevant financial disclosures.
The findings of this meta-analysis represent an advancement in the field, and frame ascorbic acid as a potential therapy to be evaluated in large-scale clinical trials, according to Dr. Peter A. McCullough and Dr. Krittapoom Akrawinthawong.
This is important given the lack of "bona fide preventive approaches" to protect against CK-AKI until less-toxic iodinated contrast becomes available, they wrote in an editorial (J. Am. Coll. Cardiol. 2013 Aug. 28).
However, several questions about the potential benefits of ascorbic acid in this setting remain unanswered, they noted.
The key question remains: "If we prevent or lessen CI-AKI as determined by serum creatinine, will we reduce the rates of clinical outcomes including end-stage renal disease, mortality, and more secondary events including the development of heart failure, recurrent acute coronary syndromes, or stroke?"
This question can be answered only by large-scale trials with effective therapies and adequate follow-up, they said.
Dr. McCullough is with Providence Hospitals and Medical Centers, Southfield and Novi, Mich. Dr. Akrawinthawong is with St. John Hospital and Medical Center, Detroit. They said they had no relevant financial disclosures.
The findings of this meta-analysis represent an advancement in the field, and frame ascorbic acid as a potential therapy to be evaluated in large-scale clinical trials, according to Dr. Peter A. McCullough and Dr. Krittapoom Akrawinthawong.
This is important given the lack of "bona fide preventive approaches" to protect against CK-AKI until less-toxic iodinated contrast becomes available, they wrote in an editorial (J. Am. Coll. Cardiol. 2013 Aug. 28).
However, several questions about the potential benefits of ascorbic acid in this setting remain unanswered, they noted.
The key question remains: "If we prevent or lessen CI-AKI as determined by serum creatinine, will we reduce the rates of clinical outcomes including end-stage renal disease, mortality, and more secondary events including the development of heart failure, recurrent acute coronary syndromes, or stroke?"
This question can be answered only by large-scale trials with effective therapies and adequate follow-up, they said.
Dr. McCullough is with Providence Hospitals and Medical Centers, Southfield and Novi, Mich. Dr. Akrawinthawong is with St. John Hospital and Medical Center, Detroit. They said they had no relevant financial disclosures.
Ascorbic acid may protect against contrast-induced-acute kidney injury in patients undergoing coronary angiography, a meta-analysis of nine randomized controlled trials has shown.
The overall incidence of contrast-induced acute kidney injury (CI-AKI) among 740 patients who received ascorbic acid and who were included in the final analysis was 9.6%, compared with 16.8% in 796 patients who received placebo or an alternative pharmacologic treatment, Dr. Umar Sadat of Cambridge (England) University Hospitals NHS Foundation Trust, and colleagues reported.
"In the pooled analysis using random effects model, patients receiving ascorbic acid had 33% less risk of CI-AKI compared to the control group (risk ratio, 0.672)," a statistically significant difference, the investigators wrote.
The findings were published online Aug. 28 in the Journal of the American College of Cardiology.
The investigators systematically reviewed Medline, Embase, and Cochrane central databases for studies published from inception to May 2013 on the incidence of CI-AKI in patients undergoing coronary angiography. Studies that were included in the meta-analysis had at least one arm that involved treatment with ascorbic acid alone or in combination with saline hydration. Ultimately, nine studies involving a total of 1,536 patients with baseline renal impairment were included (J. Am. Coll. Cardiol. 2013 Aug. 28).
The findings, which provide "robust evidence that ascorbic acid reduces the risk of CI-AKI, albeit by a small magnitude," suggest that ascorbic acid has nephroprotective qualities and could form a part of effective prophylactic pharmacologic regimens to protect patients undergoing coronary angiography against CI-AKI.
It makes sense that ascorbic acid – a form of vitamin C – could provide nephroprotection, because strong evidence suggests it acts as a potent antioxidant by scavenging physiologically relevant reactive oxygen species (ROS), they explained, noting that ROS-induced oxidative stress and renal vasoconstriction have been implicated in the etiology of CI-AKI.
The findings are important, because the incidence of CI-AKI is rising in tandem with the increasing number of contrast media–enhanced radiologic procedures and with a rise in the octogenarian population with comorbidities such as hypertension, diabetes, and renovascular disease that predispose patients to renal impairment, the investigators said.
However, further investigation regarding the optimal dosage and route of administration of ascorbic acid in order to assess its full potential as a nephroprotective agent is warranted, they concluded.
Ascorbic acid may protect against contrast-induced-acute kidney injury in patients undergoing coronary angiography, a meta-analysis of nine randomized controlled trials has shown.
The overall incidence of contrast-induced acute kidney injury (CI-AKI) among 740 patients who received ascorbic acid and who were included in the final analysis was 9.6%, compared with 16.8% in 796 patients who received placebo or an alternative pharmacologic treatment, Dr. Umar Sadat of Cambridge (England) University Hospitals NHS Foundation Trust, and colleagues reported.
"In the pooled analysis using random effects model, patients receiving ascorbic acid had 33% less risk of CI-AKI compared to the control group (risk ratio, 0.672)," a statistically significant difference, the investigators wrote.
The findings were published online Aug. 28 in the Journal of the American College of Cardiology.
The investigators systematically reviewed Medline, Embase, and Cochrane central databases for studies published from inception to May 2013 on the incidence of CI-AKI in patients undergoing coronary angiography. Studies that were included in the meta-analysis had at least one arm that involved treatment with ascorbic acid alone or in combination with saline hydration. Ultimately, nine studies involving a total of 1,536 patients with baseline renal impairment were included (J. Am. Coll. Cardiol. 2013 Aug. 28).
The findings, which provide "robust evidence that ascorbic acid reduces the risk of CI-AKI, albeit by a small magnitude," suggest that ascorbic acid has nephroprotective qualities and could form a part of effective prophylactic pharmacologic regimens to protect patients undergoing coronary angiography against CI-AKI.
It makes sense that ascorbic acid – a form of vitamin C – could provide nephroprotection, because strong evidence suggests it acts as a potent antioxidant by scavenging physiologically relevant reactive oxygen species (ROS), they explained, noting that ROS-induced oxidative stress and renal vasoconstriction have been implicated in the etiology of CI-AKI.
The findings are important, because the incidence of CI-AKI is rising in tandem with the increasing number of contrast media–enhanced radiologic procedures and with a rise in the octogenarian population with comorbidities such as hypertension, diabetes, and renovascular disease that predispose patients to renal impairment, the investigators said.
However, further investigation regarding the optimal dosage and route of administration of ascorbic acid in order to assess its full potential as a nephroprotective agent is warranted, they concluded.
FROM JACC
Major finding: Ascorbic acid treatment was associated with a 33% reduction in CI-AKI risk.
Data source: A meta-analysis of nine randomized controlled trials involving 1,536 patients.
Disclosures: The investigators reported having no relevant financial disclosures.