User login
VIDEO: Less follow-up proposed for low-risk thyroid cancer
BOSTON – , Bryan R. Haugen, MD, suggested in a keynote lecture during the World Congress on Thyroid Cancer.
Traditionally, thyroid cancer specialists have monitored these patients for persistent or recurrent disease as often as every 6 or 12 months. “But what we’ve realized with recent assessments of response to treatment is that some patients do well without a recurrence over many years; so, the concept of doing less monitoring and less imaging, especially in patients with an excellent response [to their initial treatment], is being studied,” Dr. Haugen said in a video interview following his talk.
He estimated that perhaps two-thirds or as many as three-quarters of patients with differentiated thyroid cancer fall into the category of having low- or intermediate-risk disease with an excellent or good response to treatment, and hence they are potential candidates for eventually transitioning to less frequent follow-up.
During his talk, Dr. Haugen suggested that after several years with no sign of disease recurrence, lower-risk patients with an excellent treatment response may be able to stop undergoing regular monitoring, and those with a good treatment response may be able to safely have their monitoring intervals extended.
According to the most recent (2015) guidelines for differentiated thyroid cancer management from the American Thyroid Association, lower-risk patients with an excellent treatment response should have their serum thyroglobulin measured every 12-24 months and undergo an ultrasound examination every 3-5 years, while patients with a good response are targeted for serum thyroglobulin measurement annually with an ultrasound every 1-3 years (Thyroid. 2016 Jan;26[1]:1-133). Dr. Haugen chaired the expert panel that wrote these guidelines.
In another provocative suggestion, Dr. Haugen proposed that once well-responsive, lower-risk patients have remained disease free for several years, their less frequent follow-up monitoring could be continued by a primary care physician or another less specialized clinician.
At some time in the future, “a patient’s primary care physician could follow a simple tumor marker, thyroglobulin, maybe once every 5 years,” said Dr. Haugen, professor of medicine and head of the division of endocrinology, metabolism, and diabetes at the University of Colorado in Aurora. “At the University of Colorado, we use advanced-practice providers to do long-term follow-up” for lower-risk, treatment-responsive patients, he said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
BOSTON – , Bryan R. Haugen, MD, suggested in a keynote lecture during the World Congress on Thyroid Cancer.
Traditionally, thyroid cancer specialists have monitored these patients for persistent or recurrent disease as often as every 6 or 12 months. “But what we’ve realized with recent assessments of response to treatment is that some patients do well without a recurrence over many years; so, the concept of doing less monitoring and less imaging, especially in patients with an excellent response [to their initial treatment], is being studied,” Dr. Haugen said in a video interview following his talk.
He estimated that perhaps two-thirds or as many as three-quarters of patients with differentiated thyroid cancer fall into the category of having low- or intermediate-risk disease with an excellent or good response to treatment, and hence they are potential candidates for eventually transitioning to less frequent follow-up.
During his talk, Dr. Haugen suggested that after several years with no sign of disease recurrence, lower-risk patients with an excellent treatment response may be able to stop undergoing regular monitoring, and those with a good treatment response may be able to safely have their monitoring intervals extended.
According to the most recent (2015) guidelines for differentiated thyroid cancer management from the American Thyroid Association, lower-risk patients with an excellent treatment response should have their serum thyroglobulin measured every 12-24 months and undergo an ultrasound examination every 3-5 years, while patients with a good response are targeted for serum thyroglobulin measurement annually with an ultrasound every 1-3 years (Thyroid. 2016 Jan;26[1]:1-133). Dr. Haugen chaired the expert panel that wrote these guidelines.
In another provocative suggestion, Dr. Haugen proposed that once well-responsive, lower-risk patients have remained disease free for several years, their less frequent follow-up monitoring could be continued by a primary care physician or another less specialized clinician.
At some time in the future, “a patient’s primary care physician could follow a simple tumor marker, thyroglobulin, maybe once every 5 years,” said Dr. Haugen, professor of medicine and head of the division of endocrinology, metabolism, and diabetes at the University of Colorado in Aurora. “At the University of Colorado, we use advanced-practice providers to do long-term follow-up” for lower-risk, treatment-responsive patients, he said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
BOSTON – , Bryan R. Haugen, MD, suggested in a keynote lecture during the World Congress on Thyroid Cancer.
Traditionally, thyroid cancer specialists have monitored these patients for persistent or recurrent disease as often as every 6 or 12 months. “But what we’ve realized with recent assessments of response to treatment is that some patients do well without a recurrence over many years; so, the concept of doing less monitoring and less imaging, especially in patients with an excellent response [to their initial treatment], is being studied,” Dr. Haugen said in a video interview following his talk.
He estimated that perhaps two-thirds or as many as three-quarters of patients with differentiated thyroid cancer fall into the category of having low- or intermediate-risk disease with an excellent or good response to treatment, and hence they are potential candidates for eventually transitioning to less frequent follow-up.
During his talk, Dr. Haugen suggested that after several years with no sign of disease recurrence, lower-risk patients with an excellent treatment response may be able to stop undergoing regular monitoring, and those with a good treatment response may be able to safely have their monitoring intervals extended.
According to the most recent (2015) guidelines for differentiated thyroid cancer management from the American Thyroid Association, lower-risk patients with an excellent treatment response should have their serum thyroglobulin measured every 12-24 months and undergo an ultrasound examination every 3-5 years, while patients with a good response are targeted for serum thyroglobulin measurement annually with an ultrasound every 1-3 years (Thyroid. 2016 Jan;26[1]:1-133). Dr. Haugen chaired the expert panel that wrote these guidelines.
In another provocative suggestion, Dr. Haugen proposed that once well-responsive, lower-risk patients have remained disease free for several years, their less frequent follow-up monitoring could be continued by a primary care physician or another less specialized clinician.
At some time in the future, “a patient’s primary care physician could follow a simple tumor marker, thyroglobulin, maybe once every 5 years,” said Dr. Haugen, professor of medicine and head of the division of endocrinology, metabolism, and diabetes at the University of Colorado in Aurora. “At the University of Colorado, we use advanced-practice providers to do long-term follow-up” for lower-risk, treatment-responsive patients, he said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT WCTC 2017
USPSTF: No thyroid cancer screening for asymptomatic adults
The U.S. Preventive Services Task Force recommends against screening asymptomatic adults for thyroid cancer, because the harms of such screening outweigh the benefits, according to a recommendation statement published May 9 in JAMA.
The USPSTF makes recommendations about the effectiveness of specific health care services for patients who don’t have related signs or symptoms. In this case, the recommendation statement addresses screening of adults who have no signs or symptoms of thyroid cancer by using neck palpation or ultrasonography, said Kirsten Bibbins-Domingo, MD, PhD, chair of the organization and lead author of the recommendation statement, and her associates (JAMA. 2017 May 9;317[18]:1882-7).
This document is an update of the previous USPSTF recommendation statement issued in 1996 and was undertaken because there have been several major advances related to the disease since that time.
However, despite a comprehensive review of the current literature, the group found no direct evidence supporting a change to their original advice against such screening.
They emphasized that this applies only to asymptomatic adults, not to those who have hoarseness, throat pain, difficulty swallowing, lumps in the neck, swelling, or asymmetry of the neck; nor to those who have a history of exposure to ionizing radiation, a family history of thyroid cancer, or a genetic susceptibility to the disease.
The results of the literature review were summarized in an evidence report by Jennifer S. Lin, MD, of Kaiser Permanente Center for Health Research, Portland, Ore., and her associates. They examined 67 studies involving nearly 584,000 patients, including 10 studies that addressed screening test performance, 3 that addressed the possible harms of screening, 2 that addressed treatment benefits, and 52 that addressed treatment harms.
No good-quality studies assessed the net benefit of thyroid cancer screening, nor whether “early” treatment of screen-detected cancers improved patient outcomes. However, the preponderance of evidence suggested that most thyroid cancers detected by screening are indolent.
So, treatment is likely unnecessary but exposes patients to “nontrivial” harms, including an increased risk of second primary malignancy, permanent adverse effects on the salivary glands, laryngeal nerve injury, hypoparathyroidism, and the need for lifelong thyroid replacement therapy and monitoring for cancer recurrence, Dr. Lin and her associates said in their evidence report (JAMA. 2017 May 9;317[18]:1888-1903).
The task force noted that no professional medical society currently recommends population-based screening for thyroid cancer. The American Cancer Society, American Thyroid Association, American Association of Clinical Endocrinologists, and American College of Endocrinology all have no specific recommendations for screening asymptomatic patients, while the American Academy of Family Physicians recommends against such screening, said Dr. Bibbins-Domingo, who is also a professor of medicine at the University of California, San Francisco, and her associates.
Further information regarding the recommendation statement and the evidence report is available at www.uspreventiveservicestaskforce.org.
The USPSTF is an independent voluntary group supported by the Agency for Healthcare Research and Quality. The authors’ conflict of interest disclosures are available at www.uspreventiveservicestaskforce.org.
The rationale for recommending against screening asymptomatic people for thyroid cancer is compelling, and the evidence clearly points to the harms outweighing the benefits.
But that doesn’t mean that the conversation about screening should stop. What the field needs is not a better means to detect thyroid nodules, but a noninvasive measure to distinguish nodules whose cells will leave the thyroid capsule and cause morbidity from nodules whose cells will not. That will spare patients with indolent cancers from unnecessary treatment, while steering the minority of patients with more aggressive cancers to early treatment.
Anne R. Cappola, MD, is in the division of endocrinology, diabetes, and metabolism at the University of Pennsylvania, Philadelphia, and is an associate editor of JAMA. She reported having no relevant financial disclosures. Dr. Cappola made these remarks in an editorial accompanying the recommendation statement and the evidence report (JAMA. 2017 May 9;317[18]:1840-1).
The rationale for recommending against screening asymptomatic people for thyroid cancer is compelling, and the evidence clearly points to the harms outweighing the benefits.
But that doesn’t mean that the conversation about screening should stop. What the field needs is not a better means to detect thyroid nodules, but a noninvasive measure to distinguish nodules whose cells will leave the thyroid capsule and cause morbidity from nodules whose cells will not. That will spare patients with indolent cancers from unnecessary treatment, while steering the minority of patients with more aggressive cancers to early treatment.
Anne R. Cappola, MD, is in the division of endocrinology, diabetes, and metabolism at the University of Pennsylvania, Philadelphia, and is an associate editor of JAMA. She reported having no relevant financial disclosures. Dr. Cappola made these remarks in an editorial accompanying the recommendation statement and the evidence report (JAMA. 2017 May 9;317[18]:1840-1).
The rationale for recommending against screening asymptomatic people for thyroid cancer is compelling, and the evidence clearly points to the harms outweighing the benefits.
But that doesn’t mean that the conversation about screening should stop. What the field needs is not a better means to detect thyroid nodules, but a noninvasive measure to distinguish nodules whose cells will leave the thyroid capsule and cause morbidity from nodules whose cells will not. That will spare patients with indolent cancers from unnecessary treatment, while steering the minority of patients with more aggressive cancers to early treatment.
Anne R. Cappola, MD, is in the division of endocrinology, diabetes, and metabolism at the University of Pennsylvania, Philadelphia, and is an associate editor of JAMA. She reported having no relevant financial disclosures. Dr. Cappola made these remarks in an editorial accompanying the recommendation statement and the evidence report (JAMA. 2017 May 9;317[18]:1840-1).
The U.S. Preventive Services Task Force recommends against screening asymptomatic adults for thyroid cancer, because the harms of such screening outweigh the benefits, according to a recommendation statement published May 9 in JAMA.
The USPSTF makes recommendations about the effectiveness of specific health care services for patients who don’t have related signs or symptoms. In this case, the recommendation statement addresses screening of adults who have no signs or symptoms of thyroid cancer by using neck palpation or ultrasonography, said Kirsten Bibbins-Domingo, MD, PhD, chair of the organization and lead author of the recommendation statement, and her associates (JAMA. 2017 May 9;317[18]:1882-7).
This document is an update of the previous USPSTF recommendation statement issued in 1996 and was undertaken because there have been several major advances related to the disease since that time.
However, despite a comprehensive review of the current literature, the group found no direct evidence supporting a change to their original advice against such screening.
They emphasized that this applies only to asymptomatic adults, not to those who have hoarseness, throat pain, difficulty swallowing, lumps in the neck, swelling, or asymmetry of the neck; nor to those who have a history of exposure to ionizing radiation, a family history of thyroid cancer, or a genetic susceptibility to the disease.
The results of the literature review were summarized in an evidence report by Jennifer S. Lin, MD, of Kaiser Permanente Center for Health Research, Portland, Ore., and her associates. They examined 67 studies involving nearly 584,000 patients, including 10 studies that addressed screening test performance, 3 that addressed the possible harms of screening, 2 that addressed treatment benefits, and 52 that addressed treatment harms.
No good-quality studies assessed the net benefit of thyroid cancer screening, nor whether “early” treatment of screen-detected cancers improved patient outcomes. However, the preponderance of evidence suggested that most thyroid cancers detected by screening are indolent.
So, treatment is likely unnecessary but exposes patients to “nontrivial” harms, including an increased risk of second primary malignancy, permanent adverse effects on the salivary glands, laryngeal nerve injury, hypoparathyroidism, and the need for lifelong thyroid replacement therapy and monitoring for cancer recurrence, Dr. Lin and her associates said in their evidence report (JAMA. 2017 May 9;317[18]:1888-1903).
The task force noted that no professional medical society currently recommends population-based screening for thyroid cancer. The American Cancer Society, American Thyroid Association, American Association of Clinical Endocrinologists, and American College of Endocrinology all have no specific recommendations for screening asymptomatic patients, while the American Academy of Family Physicians recommends against such screening, said Dr. Bibbins-Domingo, who is also a professor of medicine at the University of California, San Francisco, and her associates.
Further information regarding the recommendation statement and the evidence report is available at www.uspreventiveservicestaskforce.org.
The USPSTF is an independent voluntary group supported by the Agency for Healthcare Research and Quality. The authors’ conflict of interest disclosures are available at www.uspreventiveservicestaskforce.org.
The U.S. Preventive Services Task Force recommends against screening asymptomatic adults for thyroid cancer, because the harms of such screening outweigh the benefits, according to a recommendation statement published May 9 in JAMA.
The USPSTF makes recommendations about the effectiveness of specific health care services for patients who don’t have related signs or symptoms. In this case, the recommendation statement addresses screening of adults who have no signs or symptoms of thyroid cancer by using neck palpation or ultrasonography, said Kirsten Bibbins-Domingo, MD, PhD, chair of the organization and lead author of the recommendation statement, and her associates (JAMA. 2017 May 9;317[18]:1882-7).
This document is an update of the previous USPSTF recommendation statement issued in 1996 and was undertaken because there have been several major advances related to the disease since that time.
However, despite a comprehensive review of the current literature, the group found no direct evidence supporting a change to their original advice against such screening.
They emphasized that this applies only to asymptomatic adults, not to those who have hoarseness, throat pain, difficulty swallowing, lumps in the neck, swelling, or asymmetry of the neck; nor to those who have a history of exposure to ionizing radiation, a family history of thyroid cancer, or a genetic susceptibility to the disease.
The results of the literature review were summarized in an evidence report by Jennifer S. Lin, MD, of Kaiser Permanente Center for Health Research, Portland, Ore., and her associates. They examined 67 studies involving nearly 584,000 patients, including 10 studies that addressed screening test performance, 3 that addressed the possible harms of screening, 2 that addressed treatment benefits, and 52 that addressed treatment harms.
No good-quality studies assessed the net benefit of thyroid cancer screening, nor whether “early” treatment of screen-detected cancers improved patient outcomes. However, the preponderance of evidence suggested that most thyroid cancers detected by screening are indolent.
So, treatment is likely unnecessary but exposes patients to “nontrivial” harms, including an increased risk of second primary malignancy, permanent adverse effects on the salivary glands, laryngeal nerve injury, hypoparathyroidism, and the need for lifelong thyroid replacement therapy and monitoring for cancer recurrence, Dr. Lin and her associates said in their evidence report (JAMA. 2017 May 9;317[18]:1888-1903).
The task force noted that no professional medical society currently recommends population-based screening for thyroid cancer. The American Cancer Society, American Thyroid Association, American Association of Clinical Endocrinologists, and American College of Endocrinology all have no specific recommendations for screening asymptomatic patients, while the American Academy of Family Physicians recommends against such screening, said Dr. Bibbins-Domingo, who is also a professor of medicine at the University of California, San Francisco, and her associates.
Further information regarding the recommendation statement and the evidence report is available at www.uspreventiveservicestaskforce.org.
The USPSTF is an independent voluntary group supported by the Agency for Healthcare Research and Quality. The authors’ conflict of interest disclosures are available at www.uspreventiveservicestaskforce.org.
FROM JAMA
Key clinical point: The USPSTF recommends against screening asymptomatic adults for thyroid cancer because the harms outweigh the benefits.
Major finding: None of the 67 studies reviewed in the evidence report directly assessed the net benefit of thyroid cancer screening, nor whether “early” treatment of screen-detected cancers improved patient outcomes.
Data source: A recommendation statement based on a review of 67 studies published during 1996-2016 involving 583,914 patients.
Disclosures: The USPSTF is an independent voluntary group supported by the Agency for Healthcare Research and Quality. The authors’ conflict of interest disclosures are available at www.uspreventiveservicestaskforce.org.
Metformin linked with better survival in RCC patients with diabetes
Metformin use was associated with better survival for patients with renal cell carcinoma and diabetes in a meta-analysis, investigators report.
Yang Li, MD, and associates at Chongqing (China) Medical University, performed a pooled analysis of data from 254,329 patients with both localized and metastatic renal cell carcinoma, and found the risk of mortality was reduced in patients exposed to metformin (hazard ratio, 0.41; P less than .001).
However, there was significant heterogeneity among the eight eligible studies included in the meta-analysis, Dr. Li and associates reported (Int Urol Nephrol. 2017 Mar 7. doi: 10.1007/s11255-017-1548-4).
In a subgroup analysis, the association held in patients with localized disease, but was not significant in those with metastatic disease.
The current meta-analysis suggests that the use of metformin could improve the survival of kidney cancer patients, particularly those with localized disease; however, further studies are needed, the investigators conclude.
The authors declared that they had no conflicts of interest.
Metformin use was associated with better survival for patients with renal cell carcinoma and diabetes in a meta-analysis, investigators report.
Yang Li, MD, and associates at Chongqing (China) Medical University, performed a pooled analysis of data from 254,329 patients with both localized and metastatic renal cell carcinoma, and found the risk of mortality was reduced in patients exposed to metformin (hazard ratio, 0.41; P less than .001).
However, there was significant heterogeneity among the eight eligible studies included in the meta-analysis, Dr. Li and associates reported (Int Urol Nephrol. 2017 Mar 7. doi: 10.1007/s11255-017-1548-4).
In a subgroup analysis, the association held in patients with localized disease, but was not significant in those with metastatic disease.
The current meta-analysis suggests that the use of metformin could improve the survival of kidney cancer patients, particularly those with localized disease; however, further studies are needed, the investigators conclude.
The authors declared that they had no conflicts of interest.
Metformin use was associated with better survival for patients with renal cell carcinoma and diabetes in a meta-analysis, investigators report.
Yang Li, MD, and associates at Chongqing (China) Medical University, performed a pooled analysis of data from 254,329 patients with both localized and metastatic renal cell carcinoma, and found the risk of mortality was reduced in patients exposed to metformin (hazard ratio, 0.41; P less than .001).
However, there was significant heterogeneity among the eight eligible studies included in the meta-analysis, Dr. Li and associates reported (Int Urol Nephrol. 2017 Mar 7. doi: 10.1007/s11255-017-1548-4).
In a subgroup analysis, the association held in patients with localized disease, but was not significant in those with metastatic disease.
The current meta-analysis suggests that the use of metformin could improve the survival of kidney cancer patients, particularly those with localized disease; however, further studies are needed, the investigators conclude.
The authors declared that they had no conflicts of interest.
Key clinical point:
Major finding: In a pooled analysis of data from eight studies, the risk of mortality was reduced in patients exposed to metformin (hazard ratio, 0.41; P less than .001).
Data source: A meta-analysis of eight studies including 254,329 patients with renal cell carcinoma.
Disclosures: The authors declared that they had no conflicts of interest.
Temozolomide may help half of patients with aggressive pituitary tumors
ORLANDO – Temozolomide, an alkylating agent approved for glioblastoma, improved long-term survival in about half of patients who took it for aggressive pituitary tumors, a retrospective study has determined.
The study, conducted by members of the French Society of Endocrinology, comprised 43 patients. Of the 51% who responded to the treatment, the median overall survival time was 44 months, compared to just 16 months for patients who didn’t respond, Gérald Raverot, MD, said at the annual meeting of the Endocrine Society.
“Despite the very good response we saw in some patients, we also saw a high risk of recurrence, with a median of about 30 months,” for relapse, he noted. “And a second course of temozolomide always failed.”
When used for aggressive pituitary tumors, temozolomide is usually given in a conventional scheme of up to 12 cycles. It’s typically reserved for tumors that have responded poorly to other treatment regimens, Dr. Raverot said.
The drug has not been widely studied in patients with aggressive pituitary tumors, although there have been a number of case reports suggesting that can be beneficial. Data on about 90 patients have been published. The largest series to date appeared in 2015 and comprised 24 patients. It found about a 50% response rate to the drug. Two patients had a complete regression and seven patients had a partial regression of tumor mass. Tumor mass shrunk to less than 30% in three patients, less than 50% in three, and less than 75% in one.
Because of both the promise temozolomide shows in these very tough cases, and the paucity of descriptive and clinical data, Dr. Raverot and his colleagues conducted a multi-center study that spanned 21 facilities in France and comprised 43 patients who were treated from 2006-2016. The intent was to evaluate efficacy at the end of treatment, or at last follow-up in the case of those who were still being treated. Tumor response was defined as a decrease of more than 30% in the largest tumor diameter; hormonal response was more than a 50% decrease in baseline hormone levels. The endpoint was overall survival and relapse-free survival.
Of the 43 patients, 29 were men. The group’s mean age at diagnosis was 43 years, and the mean age at temozolomide treatment, 53 years. Fourteen of the tumors were carcinomas and 12 were silent or initially silent.
About half of the tumors (23) were adrenocorticotropic hormone-producing. Other tumor types were prolactin-secreting (13) and growth hormone-secreting (3); an additional three tumors secreted both prolactin and growth hormone.
Most patients (36) underwent a typical temozolomide protocol. This consisted of at least one 5-day cycle of 150 mg/m2/day every 28 days, followed by 250 mg/m2/day thereafter. The median number of cycles was 6.5, but this ranged from 1-24 cycles.
Six patients were treated according to the Stupp protocol for temozolomide in glioblastoma. This consists of daily temozolomide 75 mg/m2 with concomitant radiotherapy for 6 weeks, followed by a standard temozolomide protocol. Four patients underwent 6 cycles; one patient 12 cycles, and one patient, 17 cycles.
An additional four patients had concomitant radiotherapy within 4 months of their temozolomide treatment.
The overall response rate was 51% (22 patients). Dr. Raverot attempted to identify clinical characteristics predictive of response. There was no association with gender, age at diagnosis or age at temozolomide treatment, tumor type, whether or not the tumor was a carcinoma, or what type of hormone it secreted. Nor was there a response associated with hypermethylation of the O6-methylguanine-DNA-methyltransferase (MGMT) gene.
Dr. Raverot found only one positive association with response. Tumors that were silent or initially silent (12) were much less likely to respond than secreting tumors. Of the 21 nonresponsive tumors, 10 were silent (45%). Of the 22 responsive tumors, only 2 were silent (9%).
Dr. Raverot also analyzed response by protocol and found intriguing results. Of the 10 patients who had concomitant radiotherapy, seven responded and three did not. Patients who underwent the Stupp protocol also tended to do better, he said. “Of the six who had this, five responded, so this is interesting.”
However, he cautioned, both of these positive associations are based on such small numbers that it’s impossible to draw firm conclusions.
Dr. Raverot had survival data on 38 patients with a median follow-up of 16 months after the end of treatment. Of these, 20 were responders and 18 were non-responders. Death had occurred in 13 of the nonresponders and five responders.
Of the 20 responders, 10 were still controlled at the time of last follow-up, and 10 had relapsed at a median of 5 months after treatment cessation. Five of these patients had a second course of temozolomide, but none of them responded to it, Dr. Raverot said. Three of these patients have died and two are still living.
“We looked at other salvage treatments for them, but none of these therapies could control the disease. Unfortunately, we just don’t have good treatment options for these patients. And even among those with good treatment response, there is a risk of early recurrence, with a median time of 30 months to relapse. The second course of temozolomide always fails. So we have now some questions about who we should maintain on treatment. We don’t have this answered yet, and we need to.”
Dr. Raverot had no financial disclosures.
[email protected]
On Twitter @Alz_gal
ORLANDO – Temozolomide, an alkylating agent approved for glioblastoma, improved long-term survival in about half of patients who took it for aggressive pituitary tumors, a retrospective study has determined.
The study, conducted by members of the French Society of Endocrinology, comprised 43 patients. Of the 51% who responded to the treatment, the median overall survival time was 44 months, compared to just 16 months for patients who didn’t respond, Gérald Raverot, MD, said at the annual meeting of the Endocrine Society.
“Despite the very good response we saw in some patients, we also saw a high risk of recurrence, with a median of about 30 months,” for relapse, he noted. “And a second course of temozolomide always failed.”
When used for aggressive pituitary tumors, temozolomide is usually given in a conventional scheme of up to 12 cycles. It’s typically reserved for tumors that have responded poorly to other treatment regimens, Dr. Raverot said.
The drug has not been widely studied in patients with aggressive pituitary tumors, although there have been a number of case reports suggesting that can be beneficial. Data on about 90 patients have been published. The largest series to date appeared in 2015 and comprised 24 patients. It found about a 50% response rate to the drug. Two patients had a complete regression and seven patients had a partial regression of tumor mass. Tumor mass shrunk to less than 30% in three patients, less than 50% in three, and less than 75% in one.
Because of both the promise temozolomide shows in these very tough cases, and the paucity of descriptive and clinical data, Dr. Raverot and his colleagues conducted a multi-center study that spanned 21 facilities in France and comprised 43 patients who were treated from 2006-2016. The intent was to evaluate efficacy at the end of treatment, or at last follow-up in the case of those who were still being treated. Tumor response was defined as a decrease of more than 30% in the largest tumor diameter; hormonal response was more than a 50% decrease in baseline hormone levels. The endpoint was overall survival and relapse-free survival.
Of the 43 patients, 29 were men. The group’s mean age at diagnosis was 43 years, and the mean age at temozolomide treatment, 53 years. Fourteen of the tumors were carcinomas and 12 were silent or initially silent.
About half of the tumors (23) were adrenocorticotropic hormone-producing. Other tumor types were prolactin-secreting (13) and growth hormone-secreting (3); an additional three tumors secreted both prolactin and growth hormone.
Most patients (36) underwent a typical temozolomide protocol. This consisted of at least one 5-day cycle of 150 mg/m2/day every 28 days, followed by 250 mg/m2/day thereafter. The median number of cycles was 6.5, but this ranged from 1-24 cycles.
Six patients were treated according to the Stupp protocol for temozolomide in glioblastoma. This consists of daily temozolomide 75 mg/m2 with concomitant radiotherapy for 6 weeks, followed by a standard temozolomide protocol. Four patients underwent 6 cycles; one patient 12 cycles, and one patient, 17 cycles.
An additional four patients had concomitant radiotherapy within 4 months of their temozolomide treatment.
The overall response rate was 51% (22 patients). Dr. Raverot attempted to identify clinical characteristics predictive of response. There was no association with gender, age at diagnosis or age at temozolomide treatment, tumor type, whether or not the tumor was a carcinoma, or what type of hormone it secreted. Nor was there a response associated with hypermethylation of the O6-methylguanine-DNA-methyltransferase (MGMT) gene.
Dr. Raverot found only one positive association with response. Tumors that were silent or initially silent (12) were much less likely to respond than secreting tumors. Of the 21 nonresponsive tumors, 10 were silent (45%). Of the 22 responsive tumors, only 2 were silent (9%).
Dr. Raverot also analyzed response by protocol and found intriguing results. Of the 10 patients who had concomitant radiotherapy, seven responded and three did not. Patients who underwent the Stupp protocol also tended to do better, he said. “Of the six who had this, five responded, so this is interesting.”
However, he cautioned, both of these positive associations are based on such small numbers that it’s impossible to draw firm conclusions.
Dr. Raverot had survival data on 38 patients with a median follow-up of 16 months after the end of treatment. Of these, 20 were responders and 18 were non-responders. Death had occurred in 13 of the nonresponders and five responders.
Of the 20 responders, 10 were still controlled at the time of last follow-up, and 10 had relapsed at a median of 5 months after treatment cessation. Five of these patients had a second course of temozolomide, but none of them responded to it, Dr. Raverot said. Three of these patients have died and two are still living.
“We looked at other salvage treatments for them, but none of these therapies could control the disease. Unfortunately, we just don’t have good treatment options for these patients. And even among those with good treatment response, there is a risk of early recurrence, with a median time of 30 months to relapse. The second course of temozolomide always fails. So we have now some questions about who we should maintain on treatment. We don’t have this answered yet, and we need to.”
Dr. Raverot had no financial disclosures.
[email protected]
On Twitter @Alz_gal
ORLANDO – Temozolomide, an alkylating agent approved for glioblastoma, improved long-term survival in about half of patients who took it for aggressive pituitary tumors, a retrospective study has determined.
The study, conducted by members of the French Society of Endocrinology, comprised 43 patients. Of the 51% who responded to the treatment, the median overall survival time was 44 months, compared to just 16 months for patients who didn’t respond, Gérald Raverot, MD, said at the annual meeting of the Endocrine Society.
“Despite the very good response we saw in some patients, we also saw a high risk of recurrence, with a median of about 30 months,” for relapse, he noted. “And a second course of temozolomide always failed.”
When used for aggressive pituitary tumors, temozolomide is usually given in a conventional scheme of up to 12 cycles. It’s typically reserved for tumors that have responded poorly to other treatment regimens, Dr. Raverot said.
The drug has not been widely studied in patients with aggressive pituitary tumors, although there have been a number of case reports suggesting that can be beneficial. Data on about 90 patients have been published. The largest series to date appeared in 2015 and comprised 24 patients. It found about a 50% response rate to the drug. Two patients had a complete regression and seven patients had a partial regression of tumor mass. Tumor mass shrunk to less than 30% in three patients, less than 50% in three, and less than 75% in one.
Because of both the promise temozolomide shows in these very tough cases, and the paucity of descriptive and clinical data, Dr. Raverot and his colleagues conducted a multi-center study that spanned 21 facilities in France and comprised 43 patients who were treated from 2006-2016. The intent was to evaluate efficacy at the end of treatment, or at last follow-up in the case of those who were still being treated. Tumor response was defined as a decrease of more than 30% in the largest tumor diameter; hormonal response was more than a 50% decrease in baseline hormone levels. The endpoint was overall survival and relapse-free survival.
Of the 43 patients, 29 were men. The group’s mean age at diagnosis was 43 years, and the mean age at temozolomide treatment, 53 years. Fourteen of the tumors were carcinomas and 12 were silent or initially silent.
About half of the tumors (23) were adrenocorticotropic hormone-producing. Other tumor types were prolactin-secreting (13) and growth hormone-secreting (3); an additional three tumors secreted both prolactin and growth hormone.
Most patients (36) underwent a typical temozolomide protocol. This consisted of at least one 5-day cycle of 150 mg/m2/day every 28 days, followed by 250 mg/m2/day thereafter. The median number of cycles was 6.5, but this ranged from 1-24 cycles.
Six patients were treated according to the Stupp protocol for temozolomide in glioblastoma. This consists of daily temozolomide 75 mg/m2 with concomitant radiotherapy for 6 weeks, followed by a standard temozolomide protocol. Four patients underwent 6 cycles; one patient 12 cycles, and one patient, 17 cycles.
An additional four patients had concomitant radiotherapy within 4 months of their temozolomide treatment.
The overall response rate was 51% (22 patients). Dr. Raverot attempted to identify clinical characteristics predictive of response. There was no association with gender, age at diagnosis or age at temozolomide treatment, tumor type, whether or not the tumor was a carcinoma, or what type of hormone it secreted. Nor was there a response associated with hypermethylation of the O6-methylguanine-DNA-methyltransferase (MGMT) gene.
Dr. Raverot found only one positive association with response. Tumors that were silent or initially silent (12) were much less likely to respond than secreting tumors. Of the 21 nonresponsive tumors, 10 were silent (45%). Of the 22 responsive tumors, only 2 were silent (9%).
Dr. Raverot also analyzed response by protocol and found intriguing results. Of the 10 patients who had concomitant radiotherapy, seven responded and three did not. Patients who underwent the Stupp protocol also tended to do better, he said. “Of the six who had this, five responded, so this is interesting.”
However, he cautioned, both of these positive associations are based on such small numbers that it’s impossible to draw firm conclusions.
Dr. Raverot had survival data on 38 patients with a median follow-up of 16 months after the end of treatment. Of these, 20 were responders and 18 were non-responders. Death had occurred in 13 of the nonresponders and five responders.
Of the 20 responders, 10 were still controlled at the time of last follow-up, and 10 had relapsed at a median of 5 months after treatment cessation. Five of these patients had a second course of temozolomide, but none of them responded to it, Dr. Raverot said. Three of these patients have died and two are still living.
“We looked at other salvage treatments for them, but none of these therapies could control the disease. Unfortunately, we just don’t have good treatment options for these patients. And even among those with good treatment response, there is a risk of early recurrence, with a median time of 30 months to relapse. The second course of temozolomide always fails. So we have now some questions about who we should maintain on treatment. We don’t have this answered yet, and we need to.”
Dr. Raverot had no financial disclosures.
[email protected]
On Twitter @Alz_gal
AT ENDO 2017
Key clinical point:
Major finding: Of the 51% who responded to the treatment, the median overall survival time was 44 months, compared to just 16 months for patients who didn’t respond.
Data source: The retrospective study comprised 43 patients treated in France.
Disclosures: Dr. Raverot had no financial disclosures.
Thyroid cancer incidence: It’s not all good news
ORLANDO – The incidence of thyroid cancer in the United States between 2000-2013 has dropped in whites while increasing in blacks and Hispanics, Anupam Kotwal, MBBS, said during a press briefing at the annual meeting of the Endocrine Society.
Other recently reported data have shown a steady gradual incidence in thyroid cancer between 1974-2013 (JAMA. 2017 Mar 31. doi:10.1001/jama.2017.2719).
From 2000 to 2013, the incidence of thyroid cancer as a whole increased from 7.4 to 14.5 cases per 100,000 population with an annual percent increase of 6.7% from 2000-2009 (P less than .05) and 2.4% from 2010 to 2013 (P less than .05). In Hispanics and African-Americans, thyroid cancer incidence has continuously increased, with an annual percent increase of 4.7% (P less than .05) and 5.1% (P less than .05) respectively, whereas for non-Hispanic whites, the annual percent increase decelerated from 7.1% (P less than .05) before 2009 to 2.2% after 2009.
Looking at changes to incidence by age, non-Hispanic white women over the age of 75 are the only ones to see a decrease, from 6.5 cases per 100,000 in 2010 to 2.4 cases per 100,000 population in 2014. The investigations reported the same acceleration of incidence among everyone under the age of 20 years.
These findings are consistent with recent reports demonstrating that thyroid cancer is the 2nd most common cancer among Hispanic females, female adolescents and young adults.
Dr. Kotwal reported that he had no relevant conflicts of interest.
ORLANDO – The incidence of thyroid cancer in the United States between 2000-2013 has dropped in whites while increasing in blacks and Hispanics, Anupam Kotwal, MBBS, said during a press briefing at the annual meeting of the Endocrine Society.
Other recently reported data have shown a steady gradual incidence in thyroid cancer between 1974-2013 (JAMA. 2017 Mar 31. doi:10.1001/jama.2017.2719).
From 2000 to 2013, the incidence of thyroid cancer as a whole increased from 7.4 to 14.5 cases per 100,000 population with an annual percent increase of 6.7% from 2000-2009 (P less than .05) and 2.4% from 2010 to 2013 (P less than .05). In Hispanics and African-Americans, thyroid cancer incidence has continuously increased, with an annual percent increase of 4.7% (P less than .05) and 5.1% (P less than .05) respectively, whereas for non-Hispanic whites, the annual percent increase decelerated from 7.1% (P less than .05) before 2009 to 2.2% after 2009.
Looking at changes to incidence by age, non-Hispanic white women over the age of 75 are the only ones to see a decrease, from 6.5 cases per 100,000 in 2010 to 2.4 cases per 100,000 population in 2014. The investigations reported the same acceleration of incidence among everyone under the age of 20 years.
These findings are consistent with recent reports demonstrating that thyroid cancer is the 2nd most common cancer among Hispanic females, female adolescents and young adults.
Dr. Kotwal reported that he had no relevant conflicts of interest.
ORLANDO – The incidence of thyroid cancer in the United States between 2000-2013 has dropped in whites while increasing in blacks and Hispanics, Anupam Kotwal, MBBS, said during a press briefing at the annual meeting of the Endocrine Society.
Other recently reported data have shown a steady gradual incidence in thyroid cancer between 1974-2013 (JAMA. 2017 Mar 31. doi:10.1001/jama.2017.2719).
From 2000 to 2013, the incidence of thyroid cancer as a whole increased from 7.4 to 14.5 cases per 100,000 population with an annual percent increase of 6.7% from 2000-2009 (P less than .05) and 2.4% from 2010 to 2013 (P less than .05). In Hispanics and African-Americans, thyroid cancer incidence has continuously increased, with an annual percent increase of 4.7% (P less than .05) and 5.1% (P less than .05) respectively, whereas for non-Hispanic whites, the annual percent increase decelerated from 7.1% (P less than .05) before 2009 to 2.2% after 2009.
Looking at changes to incidence by age, non-Hispanic white women over the age of 75 are the only ones to see a decrease, from 6.5 cases per 100,000 in 2010 to 2.4 cases per 100,000 population in 2014. The investigations reported the same acceleration of incidence among everyone under the age of 20 years.
These findings are consistent with recent reports demonstrating that thyroid cancer is the 2nd most common cancer among Hispanic females, female adolescents and young adults.
Dr. Kotwal reported that he had no relevant conflicts of interest.
AT ENDO 2017
Key clinical point:
Major finding: The incidence of thyroid cancer has dropped from 7 cases per 100,000 in 2000 to 2.2 cases per 100,000 in 2013 among whites. Among blacks it has increased from 5 cases to 7 cases per 100,000 over that time frame and in Hispanics from 7 cases to 12 cases per 100,000.
Data source: Data from the National Cancer Institute’s Surveillance, Epidemiology, and End Results data base.
Disclosures: The study received no external funding. Dr. Kotwal reported he had no relevant financial conflicts of interest.
Peptide vaccine shows early promise in ovarian, endometrial cancers
NATIONAL HARBOR, MD. – The folate-binding protein vaccine E39+GM-CSF was well tolerated and exhibited a statistically significant, dose-dependent effect on recurrence and disease-free survival among patients with remitted primary ovarian or endometrial cancer, according to the results of a small prospective controlled phase I/IIa trial.
After a median follow-up of 12 months, cancer recurred in 41% of all vaccine recipients and 55% of controls (P = .41), G. Larry Maxwell, MD, reported at the annual meeting of the Society of Gynecologic Oncology. However, cancer recurred in only 13% of patients who received the highest (1,000 mcg) dose of peptide in the vaccine (P = .01 compared with the control group). A closer look showed that this survival benefit was limited to patients with primary disease, indicating that this vaccine has potential as an adjuvant to standard therapy for primary endometrial or ovarian cancer, he added.
Mortality from these cancers continues to rise in the United States despite conventional treatment with chemotherapy and radiation, noted Dr. Maxwell, who is chairman of the department of obstetrics and gynecology of Inova Fairfax Hospital in Annandale, Va.
“Targeted therapies have been evaluated, but durable response remains limited. Novel agents are needed,” he emphasized. He and his coinvestigators have focused on folate-binding protein, which is overexpressed by 20- to 80-fold in endometrial and ovarian tumors, compared with healthy tissue. To develop the vaccine, they combined E39, an immunogenic peptide of folate receptor 1 that amplifies the lymphocytic tumor response, with the immune adjuvant, granulocyte macrophage-colony stimulating factor (GM-CSF).
The trial included 51 patients, of whom 40 had primary ovarian or endometrial cancer and 11 had recurrent cancer. The 29 patients who were HLA-A2 positive were allocated to the vaccine group, receiving six intradermal inoculations of either 100-mcg, 500-mcg, or 1,000-mcg E39 plus 250-mcg GM-CSF, spaced by 21-28 days. Fifteen of these patients received 1,000-mcg E39, while 14 received 500- or 100-mcg doses. The treatment group also received two booster vaccines spaced 6 months apart. The 22 HLA-A2–negative patients were followed as controls. The intervention and control groups resembled each other clinically and demographically, Dr. Maxwell said.
Estimated rates of 2-year disease-free survival were 77% for patients in the 1,000 mcg–dose group, 44% for controls (P = .05), and 23% for patients who received less than 1,000 mcg vaccine (P = .005). Adverse events mainly included grade 1 or grade 2 myalgias, headaches, or reactions at the vaccination site. Mild adverse events were significantly more common at the 1,000-mcg E39 dose than at lower doses (P = .04). There was one grade 3 toxicity, and no grade 4 or 5 adverse events.
Delayed-type hypersensitivity reactions were more pronounced after vaccination, compared with baseline (5.7 ± 1.5 mm versus 10.3 ± 3.0 mm; P = .06), particularly in the 1,000-mcg group (3.8 ± 2.0 mm vs. 9.5 ± 3.5 mm, P = .03), Dr. Maxwell reported. Among patients whose cancer did not recur, delayed-type hypersensitivity was markedly higher after vaccination than at baseline (P = .06). “Our functional immunologic data show that vaccination is associated with delayed type hypersensitivity, but more important, it is associated with clinical outcome,” Dr. Maxwell said.
Low levels of folate-binding protein expression correlated with better disease-free survival, he also reported. “Possibly, this is because high levels of expression are associated with disease aggressiveness, which may outpace the immune response,” he said.
A phase Ib trial of the E39 folate-binding protein peptide vaccine is underway. Dr. Maxwell did not cite external funding sources and reported having no conflicts of interest.
NATIONAL HARBOR, MD. – The folate-binding protein vaccine E39+GM-CSF was well tolerated and exhibited a statistically significant, dose-dependent effect on recurrence and disease-free survival among patients with remitted primary ovarian or endometrial cancer, according to the results of a small prospective controlled phase I/IIa trial.
After a median follow-up of 12 months, cancer recurred in 41% of all vaccine recipients and 55% of controls (P = .41), G. Larry Maxwell, MD, reported at the annual meeting of the Society of Gynecologic Oncology. However, cancer recurred in only 13% of patients who received the highest (1,000 mcg) dose of peptide in the vaccine (P = .01 compared with the control group). A closer look showed that this survival benefit was limited to patients with primary disease, indicating that this vaccine has potential as an adjuvant to standard therapy for primary endometrial or ovarian cancer, he added.
Mortality from these cancers continues to rise in the United States despite conventional treatment with chemotherapy and radiation, noted Dr. Maxwell, who is chairman of the department of obstetrics and gynecology of Inova Fairfax Hospital in Annandale, Va.
“Targeted therapies have been evaluated, but durable response remains limited. Novel agents are needed,” he emphasized. He and his coinvestigators have focused on folate-binding protein, which is overexpressed by 20- to 80-fold in endometrial and ovarian tumors, compared with healthy tissue. To develop the vaccine, they combined E39, an immunogenic peptide of folate receptor 1 that amplifies the lymphocytic tumor response, with the immune adjuvant, granulocyte macrophage-colony stimulating factor (GM-CSF).
The trial included 51 patients, of whom 40 had primary ovarian or endometrial cancer and 11 had recurrent cancer. The 29 patients who were HLA-A2 positive were allocated to the vaccine group, receiving six intradermal inoculations of either 100-mcg, 500-mcg, or 1,000-mcg E39 plus 250-mcg GM-CSF, spaced by 21-28 days. Fifteen of these patients received 1,000-mcg E39, while 14 received 500- or 100-mcg doses. The treatment group also received two booster vaccines spaced 6 months apart. The 22 HLA-A2–negative patients were followed as controls. The intervention and control groups resembled each other clinically and demographically, Dr. Maxwell said.
Estimated rates of 2-year disease-free survival were 77% for patients in the 1,000 mcg–dose group, 44% for controls (P = .05), and 23% for patients who received less than 1,000 mcg vaccine (P = .005). Adverse events mainly included grade 1 or grade 2 myalgias, headaches, or reactions at the vaccination site. Mild adverse events were significantly more common at the 1,000-mcg E39 dose than at lower doses (P = .04). There was one grade 3 toxicity, and no grade 4 or 5 adverse events.
Delayed-type hypersensitivity reactions were more pronounced after vaccination, compared with baseline (5.7 ± 1.5 mm versus 10.3 ± 3.0 mm; P = .06), particularly in the 1,000-mcg group (3.8 ± 2.0 mm vs. 9.5 ± 3.5 mm, P = .03), Dr. Maxwell reported. Among patients whose cancer did not recur, delayed-type hypersensitivity was markedly higher after vaccination than at baseline (P = .06). “Our functional immunologic data show that vaccination is associated with delayed type hypersensitivity, but more important, it is associated with clinical outcome,” Dr. Maxwell said.
Low levels of folate-binding protein expression correlated with better disease-free survival, he also reported. “Possibly, this is because high levels of expression are associated with disease aggressiveness, which may outpace the immune response,” he said.
A phase Ib trial of the E39 folate-binding protein peptide vaccine is underway. Dr. Maxwell did not cite external funding sources and reported having no conflicts of interest.
NATIONAL HARBOR, MD. – The folate-binding protein vaccine E39+GM-CSF was well tolerated and exhibited a statistically significant, dose-dependent effect on recurrence and disease-free survival among patients with remitted primary ovarian or endometrial cancer, according to the results of a small prospective controlled phase I/IIa trial.
After a median follow-up of 12 months, cancer recurred in 41% of all vaccine recipients and 55% of controls (P = .41), G. Larry Maxwell, MD, reported at the annual meeting of the Society of Gynecologic Oncology. However, cancer recurred in only 13% of patients who received the highest (1,000 mcg) dose of peptide in the vaccine (P = .01 compared with the control group). A closer look showed that this survival benefit was limited to patients with primary disease, indicating that this vaccine has potential as an adjuvant to standard therapy for primary endometrial or ovarian cancer, he added.
Mortality from these cancers continues to rise in the United States despite conventional treatment with chemotherapy and radiation, noted Dr. Maxwell, who is chairman of the department of obstetrics and gynecology of Inova Fairfax Hospital in Annandale, Va.
“Targeted therapies have been evaluated, but durable response remains limited. Novel agents are needed,” he emphasized. He and his coinvestigators have focused on folate-binding protein, which is overexpressed by 20- to 80-fold in endometrial and ovarian tumors, compared with healthy tissue. To develop the vaccine, they combined E39, an immunogenic peptide of folate receptor 1 that amplifies the lymphocytic tumor response, with the immune adjuvant, granulocyte macrophage-colony stimulating factor (GM-CSF).
The trial included 51 patients, of whom 40 had primary ovarian or endometrial cancer and 11 had recurrent cancer. The 29 patients who were HLA-A2 positive were allocated to the vaccine group, receiving six intradermal inoculations of either 100-mcg, 500-mcg, or 1,000-mcg E39 plus 250-mcg GM-CSF, spaced by 21-28 days. Fifteen of these patients received 1,000-mcg E39, while 14 received 500- or 100-mcg doses. The treatment group also received two booster vaccines spaced 6 months apart. The 22 HLA-A2–negative patients were followed as controls. The intervention and control groups resembled each other clinically and demographically, Dr. Maxwell said.
Estimated rates of 2-year disease-free survival were 77% for patients in the 1,000 mcg–dose group, 44% for controls (P = .05), and 23% for patients who received less than 1,000 mcg vaccine (P = .005). Adverse events mainly included grade 1 or grade 2 myalgias, headaches, or reactions at the vaccination site. Mild adverse events were significantly more common at the 1,000-mcg E39 dose than at lower doses (P = .04). There was one grade 3 toxicity, and no grade 4 or 5 adverse events.
Delayed-type hypersensitivity reactions were more pronounced after vaccination, compared with baseline (5.7 ± 1.5 mm versus 10.3 ± 3.0 mm; P = .06), particularly in the 1,000-mcg group (3.8 ± 2.0 mm vs. 9.5 ± 3.5 mm, P = .03), Dr. Maxwell reported. Among patients whose cancer did not recur, delayed-type hypersensitivity was markedly higher after vaccination than at baseline (P = .06). “Our functional immunologic data show that vaccination is associated with delayed type hypersensitivity, but more important, it is associated with clinical outcome,” Dr. Maxwell said.
Low levels of folate-binding protein expression correlated with better disease-free survival, he also reported. “Possibly, this is because high levels of expression are associated with disease aggressiveness, which may outpace the immune response,” he said.
A phase Ib trial of the E39 folate-binding protein peptide vaccine is underway. Dr. Maxwell did not cite external funding sources and reported having no conflicts of interest.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: The folate-binding protein vaccine E39+GM-CSF was well tolerated and exhibited a statistically significant, dose-dependent effect on recurrence and disease-free survival among patients with remitted primary ovarian or endometrial cancer.
Major finding: Most adverse events were of grade 1 or grade 2 severity and were local, not systemic. After a median follow-up of 12 months, cancer recurred in 13% of patients who received the highest (1,000 mcg) dose of peptide in the vaccine, versus 55% controls (P = .01 compared with the control group).
Data source: A prospective controlled phase I/IIa trial of 51 patients with primary or recurrent ovarian or endometrial cancer.
Disclosures: Dr. Maxwell did not cite external funding sources and reported having no conflicts of interest.
Standardize opioid prescribing after endocrine neck surgery, researchers say
Twenty oral morphine equivalents is the best option for pain relief medication with which to discharge outpatients after thyroidectomy or parathyroidectomy surgery, according to researchers. The report was published online in Annals of Surgical Oncology.
Irene Lou, MD, of the department of surgery at the University of Wisconsin–Madison, and her coauthors conducted a prospective observational cohort study collecting data on pain scores and the oral morphine equivalents used by 313 adult patients undergoing thyroidectomy or parathyroidectomy at two large endocrine surgery centers.
While patients were prescribed a median of 30 oral morphine equivalents at discharge – with a range from 0 to 120 – the median number of equivalents taken was 3 (with a range of 0-60).
Overall, 68.4% of patients took at least one oral morphine equivalent. The majority of patients (83%) took 10 or fewer oral morphine equivalents, and only 7% of patients took more than 20 oral morphine equivalents (Ann Surg Oncol. 2017 Feb 3. doi: 10.1245/s10434-017-5781-y).
Among the patients who took more than 10 oral morphine equivalents, 85% said it was for incisional pain, 4% said it was for sore throat, and 11% said it was for some other pain.
While the overall mean pain score after surgery was 2, the study found that mean pain scores in the patients who took more than 10 oral morphine equivalents were significantly higher than in patients who took 10 or fewer. Among patients who used narcotic pain relief, 1% said they did so because they were instructed to despite having reported no pain.
Other factors predicting higher oral morphine equivalent use were age – patients tended to be younger than 45 years – total thyroidectomy, or a history of previous narcotic use.
“Based on our results, we have changed our practices to discharge all patients undergoing parathyroid or thyroid surgery and to request an oral narcotic prescription with no more than 20 equivalents, which translates to 20 tablets of hydrocodone/acetaminophen 5/325” the authors wrote.
Noting that the abuse and misuse of prescription opioids is the leading cause of overdose deaths in the United States, they argued that standardized prescribing practices are a way to not only reduce waste but also to improve patient safety.
“We also discovered that even between our two institutions, there was no standard prescribing pattern, with a wide range of prescriptions and number of equivalents dispensed.”
The authors also examined alternative and adjunctive methods of pain relief, pointing to previous studies suggesting benefits from preoperative gabapentin, postoperative music therapy, postoperative ice packs, and nonopioid analgesics.
They noted that because their study covered the breadth of endocrine neck operations, it did include patients who had minimally invasive surgery through to those who underwent total thyroidectomy with neck dissections. They also pointed out that the data pain scores and oral morphine equivalent use was based on patient recollection.
“Notwithstanding these limitations, our study is the first to examine outpatient narcotic pain medication use after thyroid and parathyroid surgery,” they said. “A standardized practice of prescribing stands to increase patient safety and minimize the risks of dependence and overdose.”
Two authors were supported by National Institutes of Health grants. No other conflicts of interest were declared.
Twenty oral morphine equivalents is the best option for pain relief medication with which to discharge outpatients after thyroidectomy or parathyroidectomy surgery, according to researchers. The report was published online in Annals of Surgical Oncology.
Irene Lou, MD, of the department of surgery at the University of Wisconsin–Madison, and her coauthors conducted a prospective observational cohort study collecting data on pain scores and the oral morphine equivalents used by 313 adult patients undergoing thyroidectomy or parathyroidectomy at two large endocrine surgery centers.
While patients were prescribed a median of 30 oral morphine equivalents at discharge – with a range from 0 to 120 – the median number of equivalents taken was 3 (with a range of 0-60).
Overall, 68.4% of patients took at least one oral morphine equivalent. The majority of patients (83%) took 10 or fewer oral morphine equivalents, and only 7% of patients took more than 20 oral morphine equivalents (Ann Surg Oncol. 2017 Feb 3. doi: 10.1245/s10434-017-5781-y).
Among the patients who took more than 10 oral morphine equivalents, 85% said it was for incisional pain, 4% said it was for sore throat, and 11% said it was for some other pain.
While the overall mean pain score after surgery was 2, the study found that mean pain scores in the patients who took more than 10 oral morphine equivalents were significantly higher than in patients who took 10 or fewer. Among patients who used narcotic pain relief, 1% said they did so because they were instructed to despite having reported no pain.
Other factors predicting higher oral morphine equivalent use were age – patients tended to be younger than 45 years – total thyroidectomy, or a history of previous narcotic use.
“Based on our results, we have changed our practices to discharge all patients undergoing parathyroid or thyroid surgery and to request an oral narcotic prescription with no more than 20 equivalents, which translates to 20 tablets of hydrocodone/acetaminophen 5/325” the authors wrote.
Noting that the abuse and misuse of prescription opioids is the leading cause of overdose deaths in the United States, they argued that standardized prescribing practices are a way to not only reduce waste but also to improve patient safety.
“We also discovered that even between our two institutions, there was no standard prescribing pattern, with a wide range of prescriptions and number of equivalents dispensed.”
The authors also examined alternative and adjunctive methods of pain relief, pointing to previous studies suggesting benefits from preoperative gabapentin, postoperative music therapy, postoperative ice packs, and nonopioid analgesics.
They noted that because their study covered the breadth of endocrine neck operations, it did include patients who had minimally invasive surgery through to those who underwent total thyroidectomy with neck dissections. They also pointed out that the data pain scores and oral morphine equivalent use was based on patient recollection.
“Notwithstanding these limitations, our study is the first to examine outpatient narcotic pain medication use after thyroid and parathyroid surgery,” they said. “A standardized practice of prescribing stands to increase patient safety and minimize the risks of dependence and overdose.”
Two authors were supported by National Institutes of Health grants. No other conflicts of interest were declared.
Twenty oral morphine equivalents is the best option for pain relief medication with which to discharge outpatients after thyroidectomy or parathyroidectomy surgery, according to researchers. The report was published online in Annals of Surgical Oncology.
Irene Lou, MD, of the department of surgery at the University of Wisconsin–Madison, and her coauthors conducted a prospective observational cohort study collecting data on pain scores and the oral morphine equivalents used by 313 adult patients undergoing thyroidectomy or parathyroidectomy at two large endocrine surgery centers.
While patients were prescribed a median of 30 oral morphine equivalents at discharge – with a range from 0 to 120 – the median number of equivalents taken was 3 (with a range of 0-60).
Overall, 68.4% of patients took at least one oral morphine equivalent. The majority of patients (83%) took 10 or fewer oral morphine equivalents, and only 7% of patients took more than 20 oral morphine equivalents (Ann Surg Oncol. 2017 Feb 3. doi: 10.1245/s10434-017-5781-y).
Among the patients who took more than 10 oral morphine equivalents, 85% said it was for incisional pain, 4% said it was for sore throat, and 11% said it was for some other pain.
While the overall mean pain score after surgery was 2, the study found that mean pain scores in the patients who took more than 10 oral morphine equivalents were significantly higher than in patients who took 10 or fewer. Among patients who used narcotic pain relief, 1% said they did so because they were instructed to despite having reported no pain.
Other factors predicting higher oral morphine equivalent use were age – patients tended to be younger than 45 years – total thyroidectomy, or a history of previous narcotic use.
“Based on our results, we have changed our practices to discharge all patients undergoing parathyroid or thyroid surgery and to request an oral narcotic prescription with no more than 20 equivalents, which translates to 20 tablets of hydrocodone/acetaminophen 5/325” the authors wrote.
Noting that the abuse and misuse of prescription opioids is the leading cause of overdose deaths in the United States, they argued that standardized prescribing practices are a way to not only reduce waste but also to improve patient safety.
“We also discovered that even between our two institutions, there was no standard prescribing pattern, with a wide range of prescriptions and number of equivalents dispensed.”
The authors also examined alternative and adjunctive methods of pain relief, pointing to previous studies suggesting benefits from preoperative gabapentin, postoperative music therapy, postoperative ice packs, and nonopioid analgesics.
They noted that because their study covered the breadth of endocrine neck operations, it did include patients who had minimally invasive surgery through to those who underwent total thyroidectomy with neck dissections. They also pointed out that the data pain scores and oral morphine equivalent use was based on patient recollection.
“Notwithstanding these limitations, our study is the first to examine outpatient narcotic pain medication use after thyroid and parathyroid surgery,” they said. “A standardized practice of prescribing stands to increase patient safety and minimize the risks of dependence and overdose.”
Two authors were supported by National Institutes of Health grants. No other conflicts of interest were declared.
FROM ANNALS OF SURGICAL ONCOLOGY
Key clinical point: Twenty oral morphine equivalents is the ideal amount of pain relief medication with which to discharge outpatients after thyroidectomy or parathyroidectomy surgery.
Major finding: Only 7% of patients who undergo thyroidectomy or parathyroidectomy use more than 20 oral morphine equivalents for postoperative pain relief.
Data source: Observational cohort study of 313 adult patients undergoing thyroidectomy or parathyroidectomy.
Disclosures: Two authors were supported by National Institutes of Health grants. No other conflicts of interest were declared.
Cabozantinib shows promise for carcinoid tumors, pNET
SAN FRANCISCO – Treatment with cabozantinib was associated with objective tumor responses and encouraging progression-free survival in patients with advanced carcinoid and pancreatic neuroendocrine tumors in a two-cohort phase II trial.
Of 41 patients in the carcinoid tumor cohort, 6 achieved RECIST-defined partial response (objective response rate, 15%), and 26 had stable disease. Median progression-free survival was 31.4 months.
Of 20 patients in the pancreatic neuroendocrine tumors (pNET) cohort, 3 achieved a partial response (objective response rate, 15%), and 15 had stable disease. Median progression-free survival was 21.8 months, Jennifer A. Chan, MD, reported at the symposium, sponsored by ASCO, ASTRO, the American Gastroenterological Association, and the Society of Surgical Oncology.
Although dose reduction was common – occurring in 81% of 53 patients who completed at least one treatment cycle – treatment was tolerable, said Dr. Chan of Dana-Farber Cancer Institute, Boston.
Study patients had progressive, well-differentiated grade 1-2 carcinoid tumors or pNET, and were treated with 60 mg of oral cabozantinib daily. There were no limits on prior therapy, and patients were restaged every 2 months for the first 6 months, then every 3 months thereafter.
The 41 patients with carcinoid tumors had a median age of 63 years and ECOG performance status of 0 or 1. Only 20 patients were enrolled in the pNET group, because accrual was halted, in part because of funding considerations. Patients in that group had a median age of 55 years, and also had ECOG performance status of 0 or 1, Dr. Chan said.
Carcinoid tumor patients completed a median of 8 28-day treatment cycles (range, 0-44), and pNET patients completed a median of 10 cycles (range, 0-25).
The most common reasons for discontinuation were progression or death in 51% of patients, withdrawal of consent or investigator decision in 28%, and adverse events in 21%, she noted.
The most common grade 3/4 toxicities included hypertension in 13% of patients, hypophosphatemia in 11%, and diarrhea in 10%.
Unexpected grade 3/4 events included heart failure and autoimmune hemolytic anemia, which each occurred in 1 patient.
This phase II study was initiated in light of promising preclinical work, Dr. Chan said.
“There has been much progress in recent years in the treatment of advanced neuroendocrine tumors,” she said. “The VEGF pathway inhibitors have been demonstrated to show activity, and the tyrosine kinase inhibitor sunitinib is approved for patients with progressive pancreatic neuroendocrine tumors.”
Recent studies also suggest that inhibition of MET may be an effective treatment strategy. MET activation has been shown to be associated with tumor growth, expression of MET has been observed in a significant proportion of neuroendocrine tumors, and increased expression of MET has been associated with decreased overall survival in pancreatic neuroendocrine tumors, she noted.
“Cabozantinib is a tyrosine kinase inhibitor that targets multiple receptors, including the VEGF receptors MET, ASL, and RET,” Dr. Chan explained. “It improves progression-free survival in advanced renal cell carcinoma in the first-line setting, compared with sunitinib, and also in the second-line setting, compared with everolimus in patients previously treated with anti-angiogenic therapy.” Cabozantinib is also approved for use in patients with progressive, metastatic medullary thyroid carcinoma, she added.
In preclinical models of neuroendocrine tumors, cabozantinib inhibited cell viability, and in a mouse model it decreased metastasis and invasion of pNET.
The current findings provide further evidence of cabozantinib’s safety and efficacy, Dr. Chan said. The progression-free survival in this phase II study is of particularly interest in the context of historical results, she added.
“Recognizing the limitations of interpreting progression-free survival data in an uncontrolled phase II trial, as well as comparing data to previous clinical trials, the progression-free survival results that we observed do appear encouraging,” she said. “It will be important to confirm the activity of cabozantinib in a randomized phase III setting.”
Dr. Chan reported having stock or other ownership interests in Merck; having a consulting or advisory role with Bayer, Ipsen, Novartis, Pfizer, and Pozen; and receiving research funding from Novartis and Sanofi.
SAN FRANCISCO – Treatment with cabozantinib was associated with objective tumor responses and encouraging progression-free survival in patients with advanced carcinoid and pancreatic neuroendocrine tumors in a two-cohort phase II trial.
Of 41 patients in the carcinoid tumor cohort, 6 achieved RECIST-defined partial response (objective response rate, 15%), and 26 had stable disease. Median progression-free survival was 31.4 months.
Of 20 patients in the pancreatic neuroendocrine tumors (pNET) cohort, 3 achieved a partial response (objective response rate, 15%), and 15 had stable disease. Median progression-free survival was 21.8 months, Jennifer A. Chan, MD, reported at the symposium, sponsored by ASCO, ASTRO, the American Gastroenterological Association, and the Society of Surgical Oncology.
Although dose reduction was common – occurring in 81% of 53 patients who completed at least one treatment cycle – treatment was tolerable, said Dr. Chan of Dana-Farber Cancer Institute, Boston.
Study patients had progressive, well-differentiated grade 1-2 carcinoid tumors or pNET, and were treated with 60 mg of oral cabozantinib daily. There were no limits on prior therapy, and patients were restaged every 2 months for the first 6 months, then every 3 months thereafter.
The 41 patients with carcinoid tumors had a median age of 63 years and ECOG performance status of 0 or 1. Only 20 patients were enrolled in the pNET group, because accrual was halted, in part because of funding considerations. Patients in that group had a median age of 55 years, and also had ECOG performance status of 0 or 1, Dr. Chan said.
Carcinoid tumor patients completed a median of 8 28-day treatment cycles (range, 0-44), and pNET patients completed a median of 10 cycles (range, 0-25).
The most common reasons for discontinuation were progression or death in 51% of patients, withdrawal of consent or investigator decision in 28%, and adverse events in 21%, she noted.
The most common grade 3/4 toxicities included hypertension in 13% of patients, hypophosphatemia in 11%, and diarrhea in 10%.
Unexpected grade 3/4 events included heart failure and autoimmune hemolytic anemia, which each occurred in 1 patient.
This phase II study was initiated in light of promising preclinical work, Dr. Chan said.
“There has been much progress in recent years in the treatment of advanced neuroendocrine tumors,” she said. “The VEGF pathway inhibitors have been demonstrated to show activity, and the tyrosine kinase inhibitor sunitinib is approved for patients with progressive pancreatic neuroendocrine tumors.”
Recent studies also suggest that inhibition of MET may be an effective treatment strategy. MET activation has been shown to be associated with tumor growth, expression of MET has been observed in a significant proportion of neuroendocrine tumors, and increased expression of MET has been associated with decreased overall survival in pancreatic neuroendocrine tumors, she noted.
“Cabozantinib is a tyrosine kinase inhibitor that targets multiple receptors, including the VEGF receptors MET, ASL, and RET,” Dr. Chan explained. “It improves progression-free survival in advanced renal cell carcinoma in the first-line setting, compared with sunitinib, and also in the second-line setting, compared with everolimus in patients previously treated with anti-angiogenic therapy.” Cabozantinib is also approved for use in patients with progressive, metastatic medullary thyroid carcinoma, she added.
In preclinical models of neuroendocrine tumors, cabozantinib inhibited cell viability, and in a mouse model it decreased metastasis and invasion of pNET.
The current findings provide further evidence of cabozantinib’s safety and efficacy, Dr. Chan said. The progression-free survival in this phase II study is of particularly interest in the context of historical results, she added.
“Recognizing the limitations of interpreting progression-free survival data in an uncontrolled phase II trial, as well as comparing data to previous clinical trials, the progression-free survival results that we observed do appear encouraging,” she said. “It will be important to confirm the activity of cabozantinib in a randomized phase III setting.”
Dr. Chan reported having stock or other ownership interests in Merck; having a consulting or advisory role with Bayer, Ipsen, Novartis, Pfizer, and Pozen; and receiving research funding from Novartis and Sanofi.
SAN FRANCISCO – Treatment with cabozantinib was associated with objective tumor responses and encouraging progression-free survival in patients with advanced carcinoid and pancreatic neuroendocrine tumors in a two-cohort phase II trial.
Of 41 patients in the carcinoid tumor cohort, 6 achieved RECIST-defined partial response (objective response rate, 15%), and 26 had stable disease. Median progression-free survival was 31.4 months.
Of 20 patients in the pancreatic neuroendocrine tumors (pNET) cohort, 3 achieved a partial response (objective response rate, 15%), and 15 had stable disease. Median progression-free survival was 21.8 months, Jennifer A. Chan, MD, reported at the symposium, sponsored by ASCO, ASTRO, the American Gastroenterological Association, and the Society of Surgical Oncology.
Although dose reduction was common – occurring in 81% of 53 patients who completed at least one treatment cycle – treatment was tolerable, said Dr. Chan of Dana-Farber Cancer Institute, Boston.
Study patients had progressive, well-differentiated grade 1-2 carcinoid tumors or pNET, and were treated with 60 mg of oral cabozantinib daily. There were no limits on prior therapy, and patients were restaged every 2 months for the first 6 months, then every 3 months thereafter.
The 41 patients with carcinoid tumors had a median age of 63 years and ECOG performance status of 0 or 1. Only 20 patients were enrolled in the pNET group, because accrual was halted, in part because of funding considerations. Patients in that group had a median age of 55 years, and also had ECOG performance status of 0 or 1, Dr. Chan said.
Carcinoid tumor patients completed a median of 8 28-day treatment cycles (range, 0-44), and pNET patients completed a median of 10 cycles (range, 0-25).
The most common reasons for discontinuation were progression or death in 51% of patients, withdrawal of consent or investigator decision in 28%, and adverse events in 21%, she noted.
The most common grade 3/4 toxicities included hypertension in 13% of patients, hypophosphatemia in 11%, and diarrhea in 10%.
Unexpected grade 3/4 events included heart failure and autoimmune hemolytic anemia, which each occurred in 1 patient.
This phase II study was initiated in light of promising preclinical work, Dr. Chan said.
“There has been much progress in recent years in the treatment of advanced neuroendocrine tumors,” she said. “The VEGF pathway inhibitors have been demonstrated to show activity, and the tyrosine kinase inhibitor sunitinib is approved for patients with progressive pancreatic neuroendocrine tumors.”
Recent studies also suggest that inhibition of MET may be an effective treatment strategy. MET activation has been shown to be associated with tumor growth, expression of MET has been observed in a significant proportion of neuroendocrine tumors, and increased expression of MET has been associated with decreased overall survival in pancreatic neuroendocrine tumors, she noted.
“Cabozantinib is a tyrosine kinase inhibitor that targets multiple receptors, including the VEGF receptors MET, ASL, and RET,” Dr. Chan explained. “It improves progression-free survival in advanced renal cell carcinoma in the first-line setting, compared with sunitinib, and also in the second-line setting, compared with everolimus in patients previously treated with anti-angiogenic therapy.” Cabozantinib is also approved for use in patients with progressive, metastatic medullary thyroid carcinoma, she added.
In preclinical models of neuroendocrine tumors, cabozantinib inhibited cell viability, and in a mouse model it decreased metastasis and invasion of pNET.
The current findings provide further evidence of cabozantinib’s safety and efficacy, Dr. Chan said. The progression-free survival in this phase II study is of particularly interest in the context of historical results, she added.
“Recognizing the limitations of interpreting progression-free survival data in an uncontrolled phase II trial, as well as comparing data to previous clinical trials, the progression-free survival results that we observed do appear encouraging,” she said. “It will be important to confirm the activity of cabozantinib in a randomized phase III setting.”
Dr. Chan reported having stock or other ownership interests in Merck; having a consulting or advisory role with Bayer, Ipsen, Novartis, Pfizer, and Pozen; and receiving research funding from Novartis and Sanofi.
Key clinical point:
Major finding: The objective response rate was 15% in both groups; median progression-free survival was 31.4 and 21.8 months in the carcinoid and pNET groups, respectively.
Data source: A phase II trial involving 61 patients.
Disclosures: Dr. Chan reported having stock or other ownership interests in Merck; having a consulting or advisory role with Bayer, Ipsen, Novartis, Pfizer, and Pozen; and receiving research funding from Novartis and Sanofi.
Increase brings flu activity back to seasonal high
for the week ending Jan. 21, compared with three states the week before, according to the Centers for Disease Control and Prevention.
Alabama, Kansas, New Jersey, Oklahoma, and South Carolina were at level 10 on the CDC’s 1-10 scale of ILI activity, with Oklahoma reaching that level for the third consecutive week. Georgia (level 9) and Louisiana, Minnesota, Missouri, and Tennessee (level 8) were also in the “high” range, the CDC reported.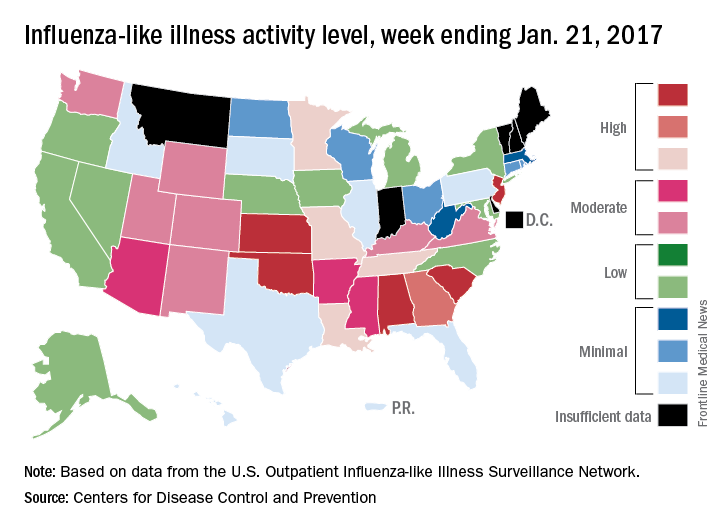
Three flu-related pediatric deaths were reported for the week, although two occurred during the week ending Jan. 14. The two earlier deaths were associated with an influenza A (H3) virus, and the more recent death was associated with an influenza B virus. For the 2016-2017 season so far, there have been a total of eight pediatric deaths, the CDC said.
for the week ending Jan. 21, compared with three states the week before, according to the Centers for Disease Control and Prevention.
Alabama, Kansas, New Jersey, Oklahoma, and South Carolina were at level 10 on the CDC’s 1-10 scale of ILI activity, with Oklahoma reaching that level for the third consecutive week. Georgia (level 9) and Louisiana, Minnesota, Missouri, and Tennessee (level 8) were also in the “high” range, the CDC reported.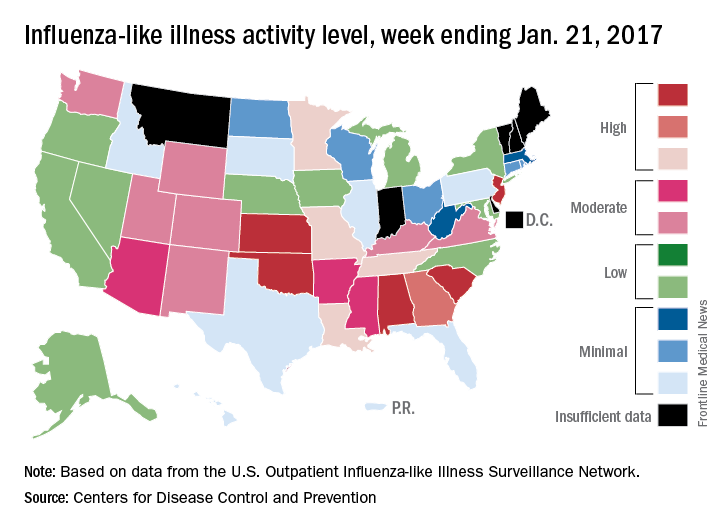
Three flu-related pediatric deaths were reported for the week, although two occurred during the week ending Jan. 14. The two earlier deaths were associated with an influenza A (H3) virus, and the more recent death was associated with an influenza B virus. For the 2016-2017 season so far, there have been a total of eight pediatric deaths, the CDC said.
for the week ending Jan. 21, compared with three states the week before, according to the Centers for Disease Control and Prevention.
Alabama, Kansas, New Jersey, Oklahoma, and South Carolina were at level 10 on the CDC’s 1-10 scale of ILI activity, with Oklahoma reaching that level for the third consecutive week. Georgia (level 9) and Louisiana, Minnesota, Missouri, and Tennessee (level 8) were also in the “high” range, the CDC reported.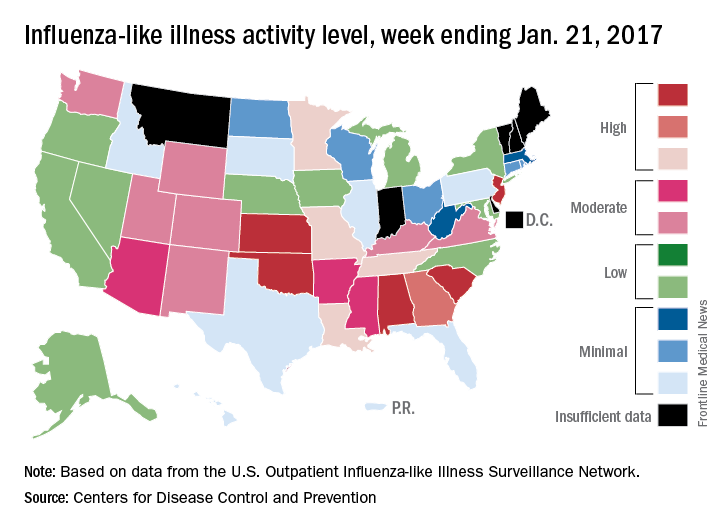
Three flu-related pediatric deaths were reported for the week, although two occurred during the week ending Jan. 14. The two earlier deaths were associated with an influenza A (H3) virus, and the more recent death was associated with an influenza B virus. For the 2016-2017 season so far, there have been a total of eight pediatric deaths, the CDC said.
VIDEO: Open, robotic, laparoscopic approaches equally effective in pancreatectomy
WASHINGTON – Minimally invasive surgery – whether robotic or laparoscopic – is just as effective as open surgery in pancreatectomy.
Both minimally invasive approaches had perioperative and oncologic outcomes that were similar to open approaches, as well as to each other, Katelin Mirkin, MD, reported at the annual clinical congress of the American College of Surgeons. And while minimally invasive surgery (MIS) techniques were associated with a slightly faster move to neoadjuvant chemotherapy, survival outcomes in all three surgical approaches were similar.
Dr. Mirkin, a surgery resident at Penn State Milton S. Hershey Medical Center, Hershey, Pa., plumbed the National Cancer Database for patients with stage I-III pancreatic cancer who were treated by surgical resection from 2010 to 2012. Her cohort comprised 9,047 patients; of these, 7,924 were treated with open surgery, 992 with laparoscopic surgery, and 131 with robotic surgery. She examined a number of factors including lymph node harvest and surgical margins, length of stay and time to adjuvant chemotherapy, and survival.
Patients who had MIS were older (67 vs. 66 years) and more often treated at an academic center, but otherwise there were no significant baseline differences.
Dr. Mirkin first compared the open surgeries with MIS. There were no significant associations with surgical approach and cancer stage. However, distal resections were significantly more likely to be dealt with by MIS, and Whipple procedures by open approaches. There were also more open than MIS total resections.
MIS was more likely to conclude with negative surgical margins (79% vs. 75%), and open surgery more likely to end with positive margins (22% vs. 19%).
Perioperative outcomes favored MIS approaches for all types of surgery, with a mean overall stay of 9.5 days vs. 11.3 days for open surgery. The mean length of stay for a distal resection was 7 days for MIS vs. 8 for open. For a Whipple procedure, the mean stay was 10.7 vs. 11.9 days. For a total resection, it was 10 vs. 11.8 days.
MIS was also associated with a significantly shorter time to the initiation of adjuvant chemotherapy overall (56 vs. 59 days). For a Whipple, time to chemotherapy was 58 vs. 60 days, respectively. For a distal resection, it was 52 vs. 56 days, and for a total resection, 52 vs. 58 days.
Neither approach offered a survival benefit over the other, Dr. Mirkin noted. For stage I cancers, less than 50% of MIS patients and less than 25% of open patients were alive by 50 months. For those with stage II tumors, less than 25% of each group was alive by 40 months. For stage III tumors, the 40-month survival rates were about 10% for MIS patients and 15% for open patients.
Dr. Mirkin then examined perioperative, oncologic, and survival outcomes among those who underwent laparoscopic and robotic surgeries. There were no demographic differences between these groups.
Oncologic outcomes were almost identical with regard to the number of positive regional nodes harvested (six), and surgical margins. Nodes were negative in 82% of robotic cases vs. 78% of laparoscopic cases and positive in 17.6% of robotic cases and 19.4% of laparoscopic cases.
Length of stay was significantly shorter for a laparoscopic approach overall (10 vs. 9.4 days) and particularly in distal resection (7 vs. 10 days). However, there were no differences in length of stay in any other surgery type. Nor was there any difference in the time to neoadjuvant chemotherapy.
Survival outcomes were similar as well. For stage I cancers, 40-month survival was about 40% in the laparoscopic group and 25% in the robotic group. For stage II cancers, 40-month survival was about 15% and 25%, respectively. For stage III tumors, 20-month survival in the robotic group was near 0 and 25% in the laparoscopic group. By 40 months almost all patients were deceased.
A multivariate survival analysis controlled for age, sex, race, comorbidities, facility type and location, surgery type, surgical margins, pathologic stage, and systemic therapy. It found only one significant association: Patients with 12 or more lymph nodes harvested were 19% more likely to die than those with fewer than 12 nodes harvested.
Time to chemotherapy (longer or shorter than 57 days) did not significantly impact survival, Dr. Mirkin said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @alz_gal
WASHINGTON – Minimally invasive surgery – whether robotic or laparoscopic – is just as effective as open surgery in pancreatectomy.
Both minimally invasive approaches had perioperative and oncologic outcomes that were similar to open approaches, as well as to each other, Katelin Mirkin, MD, reported at the annual clinical congress of the American College of Surgeons. And while minimally invasive surgery (MIS) techniques were associated with a slightly faster move to neoadjuvant chemotherapy, survival outcomes in all three surgical approaches were similar.
Dr. Mirkin, a surgery resident at Penn State Milton S. Hershey Medical Center, Hershey, Pa., plumbed the National Cancer Database for patients with stage I-III pancreatic cancer who were treated by surgical resection from 2010 to 2012. Her cohort comprised 9,047 patients; of these, 7,924 were treated with open surgery, 992 with laparoscopic surgery, and 131 with robotic surgery. She examined a number of factors including lymph node harvest and surgical margins, length of stay and time to adjuvant chemotherapy, and survival.
Patients who had MIS were older (67 vs. 66 years) and more often treated at an academic center, but otherwise there were no significant baseline differences.
Dr. Mirkin first compared the open surgeries with MIS. There were no significant associations with surgical approach and cancer stage. However, distal resections were significantly more likely to be dealt with by MIS, and Whipple procedures by open approaches. There were also more open than MIS total resections.
MIS was more likely to conclude with negative surgical margins (79% vs. 75%), and open surgery more likely to end with positive margins (22% vs. 19%).
Perioperative outcomes favored MIS approaches for all types of surgery, with a mean overall stay of 9.5 days vs. 11.3 days for open surgery. The mean length of stay for a distal resection was 7 days for MIS vs. 8 for open. For a Whipple procedure, the mean stay was 10.7 vs. 11.9 days. For a total resection, it was 10 vs. 11.8 days.
MIS was also associated with a significantly shorter time to the initiation of adjuvant chemotherapy overall (56 vs. 59 days). For a Whipple, time to chemotherapy was 58 vs. 60 days, respectively. For a distal resection, it was 52 vs. 56 days, and for a total resection, 52 vs. 58 days.
Neither approach offered a survival benefit over the other, Dr. Mirkin noted. For stage I cancers, less than 50% of MIS patients and less than 25% of open patients were alive by 50 months. For those with stage II tumors, less than 25% of each group was alive by 40 months. For stage III tumors, the 40-month survival rates were about 10% for MIS patients and 15% for open patients.
Dr. Mirkin then examined perioperative, oncologic, and survival outcomes among those who underwent laparoscopic and robotic surgeries. There were no demographic differences between these groups.
Oncologic outcomes were almost identical with regard to the number of positive regional nodes harvested (six), and surgical margins. Nodes were negative in 82% of robotic cases vs. 78% of laparoscopic cases and positive in 17.6% of robotic cases and 19.4% of laparoscopic cases.
Length of stay was significantly shorter for a laparoscopic approach overall (10 vs. 9.4 days) and particularly in distal resection (7 vs. 10 days). However, there were no differences in length of stay in any other surgery type. Nor was there any difference in the time to neoadjuvant chemotherapy.
Survival outcomes were similar as well. For stage I cancers, 40-month survival was about 40% in the laparoscopic group and 25% in the robotic group. For stage II cancers, 40-month survival was about 15% and 25%, respectively. For stage III tumors, 20-month survival in the robotic group was near 0 and 25% in the laparoscopic group. By 40 months almost all patients were deceased.
A multivariate survival analysis controlled for age, sex, race, comorbidities, facility type and location, surgery type, surgical margins, pathologic stage, and systemic therapy. It found only one significant association: Patients with 12 or more lymph nodes harvested were 19% more likely to die than those with fewer than 12 nodes harvested.
Time to chemotherapy (longer or shorter than 57 days) did not significantly impact survival, Dr. Mirkin said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @alz_gal
WASHINGTON – Minimally invasive surgery – whether robotic or laparoscopic – is just as effective as open surgery in pancreatectomy.
Both minimally invasive approaches had perioperative and oncologic outcomes that were similar to open approaches, as well as to each other, Katelin Mirkin, MD, reported at the annual clinical congress of the American College of Surgeons. And while minimally invasive surgery (MIS) techniques were associated with a slightly faster move to neoadjuvant chemotherapy, survival outcomes in all three surgical approaches were similar.
Dr. Mirkin, a surgery resident at Penn State Milton S. Hershey Medical Center, Hershey, Pa., plumbed the National Cancer Database for patients with stage I-III pancreatic cancer who were treated by surgical resection from 2010 to 2012. Her cohort comprised 9,047 patients; of these, 7,924 were treated with open surgery, 992 with laparoscopic surgery, and 131 with robotic surgery. She examined a number of factors including lymph node harvest and surgical margins, length of stay and time to adjuvant chemotherapy, and survival.
Patients who had MIS were older (67 vs. 66 years) and more often treated at an academic center, but otherwise there were no significant baseline differences.
Dr. Mirkin first compared the open surgeries with MIS. There were no significant associations with surgical approach and cancer stage. However, distal resections were significantly more likely to be dealt with by MIS, and Whipple procedures by open approaches. There were also more open than MIS total resections.
MIS was more likely to conclude with negative surgical margins (79% vs. 75%), and open surgery more likely to end with positive margins (22% vs. 19%).
Perioperative outcomes favored MIS approaches for all types of surgery, with a mean overall stay of 9.5 days vs. 11.3 days for open surgery. The mean length of stay for a distal resection was 7 days for MIS vs. 8 for open. For a Whipple procedure, the mean stay was 10.7 vs. 11.9 days. For a total resection, it was 10 vs. 11.8 days.
MIS was also associated with a significantly shorter time to the initiation of adjuvant chemotherapy overall (56 vs. 59 days). For a Whipple, time to chemotherapy was 58 vs. 60 days, respectively. For a distal resection, it was 52 vs. 56 days, and for a total resection, 52 vs. 58 days.
Neither approach offered a survival benefit over the other, Dr. Mirkin noted. For stage I cancers, less than 50% of MIS patients and less than 25% of open patients were alive by 50 months. For those with stage II tumors, less than 25% of each group was alive by 40 months. For stage III tumors, the 40-month survival rates were about 10% for MIS patients and 15% for open patients.
Dr. Mirkin then examined perioperative, oncologic, and survival outcomes among those who underwent laparoscopic and robotic surgeries. There were no demographic differences between these groups.
Oncologic outcomes were almost identical with regard to the number of positive regional nodes harvested (six), and surgical margins. Nodes were negative in 82% of robotic cases vs. 78% of laparoscopic cases and positive in 17.6% of robotic cases and 19.4% of laparoscopic cases.
Length of stay was significantly shorter for a laparoscopic approach overall (10 vs. 9.4 days) and particularly in distal resection (7 vs. 10 days). However, there were no differences in length of stay in any other surgery type. Nor was there any difference in the time to neoadjuvant chemotherapy.
Survival outcomes were similar as well. For stage I cancers, 40-month survival was about 40% in the laparoscopic group and 25% in the robotic group. For stage II cancers, 40-month survival was about 15% and 25%, respectively. For stage III tumors, 20-month survival in the robotic group was near 0 and 25% in the laparoscopic group. By 40 months almost all patients were deceased.
A multivariate survival analysis controlled for age, sex, race, comorbidities, facility type and location, surgery type, surgical margins, pathologic stage, and systemic therapy. It found only one significant association: Patients with 12 or more lymph nodes harvested were 19% more likely to die than those with fewer than 12 nodes harvested.
Time to chemotherapy (longer or shorter than 57 days) did not significantly impact survival, Dr. Mirkin said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @alz_gal
AT THE ACS CLINICAL CONGRESS
Key clinical point:
Major finding: For stage I cancers, less than 50% of minimally invasive surgery patients and less than 25% of open surgery patients were alive by 50 months. For those with stage II tumors, less than 25% of each group was alive by 40 months.
Data source: The database review comprised 9,047 cases.
Disclosures: Dr. Mirkin had no financial disclosures.