User login
More on How to Decrease Dermatology Interview Costs
To the Editor:
Ongoing concern about the high costs of dermatology residency interviews has led to several cost-saving proposals, as presented by Hussain1 in the Cutis article, “Reducing the Cost of Dermatology Residency Applications: An Applicant’s Perspective.” Additional strategies to reduce applicant costs include eliminating travel costs through video or telephone interviews, interviewing students who are visiting during their away rotation, and developing and implementing a mechanism to exempt students from participating in the Electronic Residency Application Service (
First, because applicants would be limited to 1 application to participate in the early decision program, they must realistically consider the strength of their application and weigh their chances for acceptance to that program. Programs could facilitate the process by becoming more transparent about the type of applicants that have previously matched in their program.2 If an early-decision applicant successfully matches, that applicant would be prohibited from applying to additional dermatology residency programs through
Second, early-decision actions by programs—probably by August 1, a time when most third-year medical students have completed their academic year—would be determined before ERAS releases applications to residency programs. This timeline would remove successful applicants in the early decision program from going to additional interviews and incurring the associated travel costs.
Third, early decision could be potentially beneficial to applicants who are tied to a specific geographic region for training and to programs with specific program needs, such as expertise in specific areas of dermatology research or areas of clinical need (eg, adding a dermatopathologist, plastic surgeon, internist, or a pediatrician to the residency program who now wants dermatology training) or other program needs.
Fourth, application costs could potentially be lower for early-decision applicants than through the present application process if participating institutions waived application fees. Applicants would still be responsible for submitting requested academic transcripts, letters of recommendation, and travel expenses if an on-site interview is requested by the program.
Finally, highly desirable applicants who are offered a position through early decision would result in more opportunities for other applicants to interview for the remaining available residency positions through ERAS/NRMP.
Downsides to early decision for dermatology residency include the inability of applicants to compare programs to one another through their personal experiences, such as prior rotations or interviews, and for programs to compare applicants though the interview process and away rotations. In addition, US Medical Licensing Examination Step 2 scores and Alpha Omega Alpha honor medical society status and other academic honors may not be available to programs to consider at the time of early decision. Cooperation would be needed with ERAS and NRMP to create an early decision program for dermatology residency.
One other potential consequence of the early match could involve instances of strained relationships between research fellows and their sponsoring institution or dermatology program. Research fellows often match at their research institution, and failing to early match could potentially sour the relationship between the applicant and the program, thus leading to a less productive year. However, many programs participating in an early match will probably have additional residency positions remaining in the traditional match that would be still available to the fellows.
The concept of an early-binding residency match process has the potential to save both time and money for programs and applicants. Although an early-match process would have many positive effects, there also would be inherent downsides that accompany such a system. Nonetheless, an early-match process in dermatology has the prospect of efficiently pairing applicants and programs that feel strongly about each other while simplifying the match process and reducing costs for all parties involved.
References
1. Hussain AN.
2. Weisert E, Phan M. Thoughts on reducing the cost for dermatology residency applications. DIG@UTMB blog. http://digutmb.blogspot.com/2019/12/thoughts-on-reducing-cost-for.html. Published December 23, 2019. Accessed April 17, 2020.
3. Early decision program. Association of American Medical Colleges website. https://students-residents.aamc.org/applying-medical-school/article/early-decision-program/. Accessed April 8, 2020.
Author’s Response
The early decision option for dermatology residency applications would be a welcomed addition to the process but may be complicated by 2 recent events: the coronavirus disease 2019 (COVID-19) pandemic and the change of US Medical Licensing Examination (USMLE) Step 1 score reporting to a pass/fail system.
The COVID-19 pandemic has caused remarkable economic distress and likely affects medical students more acutely given their high levels of debt. As Ryan and Wagner observed, one advantage of the early-decision option would be financial relief for certain students. If applicants successfully match during the early-decision phase, they will not need to apply to any additional dermatology programs and also can target their preliminary-year applications to the geographic region where they have already matched.
In addition, the COVID-19 pandemic may further reduce early applicants’ ability to visit programs in person. Various medical schools have curtailed away rotations, and programs may opt for virtual interviews in accordance with social distancing guidelines.1 Thus, early applicants will have even fewer opportunities to compare programs before they must make a binding decision about their residency placement. Although away rotations and interview travel are some of the largest drivers of application cost,2 reducing costs in this way might shortchange both students and programs.
Arguably, the change in USMLE Step 1 score reporting beginning in 2022 may impact residency selection for a longer period of time than the COVID-19 pandemic. Program directors cited USMLE Step 1 scores as one of the main factors determining which applicants may be invited to interview.3 The lack of numerical USMLE Step 1 scores may encourage programs to place more weight on other metrics such as USMLE Step 2 CK scores or Alpha Omega Alpha membership.4 However, as Ryan and Wagner point out, such metrics may not be available in time for early-decision applicants.
As such, future program directors will have precious little information to screen early-decision applicants and may need to conduct holistic application review. This would require increased time and manpower compared to screening based on traditional metrics but may lead to a better “fit” for an applicant with a residency.
In general, implementation of any early decision program would benefit dermatology applicants as a group by removing elite candidates from the applicant pool. According to National Resident Matching Program data, just 3% of dermatology applicants account for more than 12% of overall interviews.5 In other words, a small group of the strongest applicants receives a lion’s share of interviews, crowding out many other candidates. Removing these top-tier applicants likely would provide remaining applicants with a higher return on investment per application, and students may choose to save money by applying to fewer programs.
Adopting early-decision options within the dermatology match may be complicated given the COVID-19 pandemic and USMLE score changes but may spur positive changes in the process while also reducing the financial burden on applicants.
Aamir N. Hussain, MD, MAPP
From Northwell Health, Manhasset, New York.
The author reports no conflict of interest.
Correspondence: Aamir N. Hussain, MD, MAPP ([email protected]).
References
1. Coronavirus (COVID-19) and the VSLO program. Association of American Medical Colleges website. https://students-residents.aamc.org/attending-medical-school/article/coronavirus-covid-19-and-vslo-program/. Accessed April 17, 2020.
2. Mansouri B, Walker GD, Mitchell J, et al. The cost of applying to dermatology residency: 2014 data estimates. J Am Acad Dermatol. 2016;74:754-756.
3. National Resident Matching Program, Data Release and Research Committee. Results of the 2018 NRMP Program Director Survey. Washington, DC: National Resident Matching Program; 2018. https://www.nrmp.org/wp-content/uploads/2018/07/NRMP-2018-Program-Director-Survey-for-WWW.pdf. Published June 2018. Accessed April 17, 2020.
4. Crane MA, Chang HA, Azamfirei R. Medical education takes a step in the right direction: where does that leave students? [published online March 6, 2020]. JAMA. doi:10.1001/jama.2020.2950.
5. Lee AH, Young P, Liao R, et al. I dream of Gini: quantifying inequality in otolaryngology residency interviews. Laryngoscope. 2019;129:627-633.
To the Editor:
Ongoing concern about the high costs of dermatology residency interviews has led to several cost-saving proposals, as presented by Hussain1 in the Cutis article, “Reducing the Cost of Dermatology Residency Applications: An Applicant’s Perspective.” Additional strategies to reduce applicant costs include eliminating travel costs through video or telephone interviews, interviewing students who are visiting during their away rotation, and developing and implementing a mechanism to exempt students from participating in the Electronic Residency Application Service (
First, because applicants would be limited to 1 application to participate in the early decision program, they must realistically consider the strength of their application and weigh their chances for acceptance to that program. Programs could facilitate the process by becoming more transparent about the type of applicants that have previously matched in their program.2 If an early-decision applicant successfully matches, that applicant would be prohibited from applying to additional dermatology residency programs through
Second, early-decision actions by programs—probably by August 1, a time when most third-year medical students have completed their academic year—would be determined before ERAS releases applications to residency programs. This timeline would remove successful applicants in the early decision program from going to additional interviews and incurring the associated travel costs.
Third, early decision could be potentially beneficial to applicants who are tied to a specific geographic region for training and to programs with specific program needs, such as expertise in specific areas of dermatology research or areas of clinical need (eg, adding a dermatopathologist, plastic surgeon, internist, or a pediatrician to the residency program who now wants dermatology training) or other program needs.
Fourth, application costs could potentially be lower for early-decision applicants than through the present application process if participating institutions waived application fees. Applicants would still be responsible for submitting requested academic transcripts, letters of recommendation, and travel expenses if an on-site interview is requested by the program.
Finally, highly desirable applicants who are offered a position through early decision would result in more opportunities for other applicants to interview for the remaining available residency positions through ERAS/NRMP.
Downsides to early decision for dermatology residency include the inability of applicants to compare programs to one another through their personal experiences, such as prior rotations or interviews, and for programs to compare applicants though the interview process and away rotations. In addition, US Medical Licensing Examination Step 2 scores and Alpha Omega Alpha honor medical society status and other academic honors may not be available to programs to consider at the time of early decision. Cooperation would be needed with ERAS and NRMP to create an early decision program for dermatology residency.
One other potential consequence of the early match could involve instances of strained relationships between research fellows and their sponsoring institution or dermatology program. Research fellows often match at their research institution, and failing to early match could potentially sour the relationship between the applicant and the program, thus leading to a less productive year. However, many programs participating in an early match will probably have additional residency positions remaining in the traditional match that would be still available to the fellows.
The concept of an early-binding residency match process has the potential to save both time and money for programs and applicants. Although an early-match process would have many positive effects, there also would be inherent downsides that accompany such a system. Nonetheless, an early-match process in dermatology has the prospect of efficiently pairing applicants and programs that feel strongly about each other while simplifying the match process and reducing costs for all parties involved.
References
1. Hussain AN.
2. Weisert E, Phan M. Thoughts on reducing the cost for dermatology residency applications. DIG@UTMB blog. http://digutmb.blogspot.com/2019/12/thoughts-on-reducing-cost-for.html. Published December 23, 2019. Accessed April 17, 2020.
3. Early decision program. Association of American Medical Colleges website. https://students-residents.aamc.org/applying-medical-school/article/early-decision-program/. Accessed April 8, 2020.
Author’s Response
The early decision option for dermatology residency applications would be a welcomed addition to the process but may be complicated by 2 recent events: the coronavirus disease 2019 (COVID-19) pandemic and the change of US Medical Licensing Examination (USMLE) Step 1 score reporting to a pass/fail system.
The COVID-19 pandemic has caused remarkable economic distress and likely affects medical students more acutely given their high levels of debt. As Ryan and Wagner observed, one advantage of the early-decision option would be financial relief for certain students. If applicants successfully match during the early-decision phase, they will not need to apply to any additional dermatology programs and also can target their preliminary-year applications to the geographic region where they have already matched.
In addition, the COVID-19 pandemic may further reduce early applicants’ ability to visit programs in person. Various medical schools have curtailed away rotations, and programs may opt for virtual interviews in accordance with social distancing guidelines.1 Thus, early applicants will have even fewer opportunities to compare programs before they must make a binding decision about their residency placement. Although away rotations and interview travel are some of the largest drivers of application cost,2 reducing costs in this way might shortchange both students and programs.
Arguably, the change in USMLE Step 1 score reporting beginning in 2022 may impact residency selection for a longer period of time than the COVID-19 pandemic. Program directors cited USMLE Step 1 scores as one of the main factors determining which applicants may be invited to interview.3 The lack of numerical USMLE Step 1 scores may encourage programs to place more weight on other metrics such as USMLE Step 2 CK scores or Alpha Omega Alpha membership.4 However, as Ryan and Wagner point out, such metrics may not be available in time for early-decision applicants.
As such, future program directors will have precious little information to screen early-decision applicants and may need to conduct holistic application review. This would require increased time and manpower compared to screening based on traditional metrics but may lead to a better “fit” for an applicant with a residency.
In general, implementation of any early decision program would benefit dermatology applicants as a group by removing elite candidates from the applicant pool. According to National Resident Matching Program data, just 3% of dermatology applicants account for more than 12% of overall interviews.5 In other words, a small group of the strongest applicants receives a lion’s share of interviews, crowding out many other candidates. Removing these top-tier applicants likely would provide remaining applicants with a higher return on investment per application, and students may choose to save money by applying to fewer programs.
Adopting early-decision options within the dermatology match may be complicated given the COVID-19 pandemic and USMLE score changes but may spur positive changes in the process while also reducing the financial burden on applicants.
Aamir N. Hussain, MD, MAPP
From Northwell Health, Manhasset, New York.
The author reports no conflict of interest.
Correspondence: Aamir N. Hussain, MD, MAPP ([email protected]).
References
1. Coronavirus (COVID-19) and the VSLO program. Association of American Medical Colleges website. https://students-residents.aamc.org/attending-medical-school/article/coronavirus-covid-19-and-vslo-program/. Accessed April 17, 2020.
2. Mansouri B, Walker GD, Mitchell J, et al. The cost of applying to dermatology residency: 2014 data estimates. J Am Acad Dermatol. 2016;74:754-756.
3. National Resident Matching Program, Data Release and Research Committee. Results of the 2018 NRMP Program Director Survey. Washington, DC: National Resident Matching Program; 2018. https://www.nrmp.org/wp-content/uploads/2018/07/NRMP-2018-Program-Director-Survey-for-WWW.pdf. Published June 2018. Accessed April 17, 2020.
4. Crane MA, Chang HA, Azamfirei R. Medical education takes a step in the right direction: where does that leave students? [published online March 6, 2020]. JAMA. doi:10.1001/jama.2020.2950.
5. Lee AH, Young P, Liao R, et al. I dream of Gini: quantifying inequality in otolaryngology residency interviews. Laryngoscope. 2019;129:627-633.
To the Editor:
Ongoing concern about the high costs of dermatology residency interviews has led to several cost-saving proposals, as presented by Hussain1 in the Cutis article, “Reducing the Cost of Dermatology Residency Applications: An Applicant’s Perspective.” Additional strategies to reduce applicant costs include eliminating travel costs through video or telephone interviews, interviewing students who are visiting during their away rotation, and developing and implementing a mechanism to exempt students from participating in the Electronic Residency Application Service (
First, because applicants would be limited to 1 application to participate in the early decision program, they must realistically consider the strength of their application and weigh their chances for acceptance to that program. Programs could facilitate the process by becoming more transparent about the type of applicants that have previously matched in their program.2 If an early-decision applicant successfully matches, that applicant would be prohibited from applying to additional dermatology residency programs through
Second, early-decision actions by programs—probably by August 1, a time when most third-year medical students have completed their academic year—would be determined before ERAS releases applications to residency programs. This timeline would remove successful applicants in the early decision program from going to additional interviews and incurring the associated travel costs.
Third, early decision could be potentially beneficial to applicants who are tied to a specific geographic region for training and to programs with specific program needs, such as expertise in specific areas of dermatology research or areas of clinical need (eg, adding a dermatopathologist, plastic surgeon, internist, or a pediatrician to the residency program who now wants dermatology training) or other program needs.
Fourth, application costs could potentially be lower for early-decision applicants than through the present application process if participating institutions waived application fees. Applicants would still be responsible for submitting requested academic transcripts, letters of recommendation, and travel expenses if an on-site interview is requested by the program.
Finally, highly desirable applicants who are offered a position through early decision would result in more opportunities for other applicants to interview for the remaining available residency positions through ERAS/NRMP.
Downsides to early decision for dermatology residency include the inability of applicants to compare programs to one another through their personal experiences, such as prior rotations or interviews, and for programs to compare applicants though the interview process and away rotations. In addition, US Medical Licensing Examination Step 2 scores and Alpha Omega Alpha honor medical society status and other academic honors may not be available to programs to consider at the time of early decision. Cooperation would be needed with ERAS and NRMP to create an early decision program for dermatology residency.
One other potential consequence of the early match could involve instances of strained relationships between research fellows and their sponsoring institution or dermatology program. Research fellows often match at their research institution, and failing to early match could potentially sour the relationship between the applicant and the program, thus leading to a less productive year. However, many programs participating in an early match will probably have additional residency positions remaining in the traditional match that would be still available to the fellows.
The concept of an early-binding residency match process has the potential to save both time and money for programs and applicants. Although an early-match process would have many positive effects, there also would be inherent downsides that accompany such a system. Nonetheless, an early-match process in dermatology has the prospect of efficiently pairing applicants and programs that feel strongly about each other while simplifying the match process and reducing costs for all parties involved.
References
1. Hussain AN.
2. Weisert E, Phan M. Thoughts on reducing the cost for dermatology residency applications. DIG@UTMB blog. http://digutmb.blogspot.com/2019/12/thoughts-on-reducing-cost-for.html. Published December 23, 2019. Accessed April 17, 2020.
3. Early decision program. Association of American Medical Colleges website. https://students-residents.aamc.org/applying-medical-school/article/early-decision-program/. Accessed April 8, 2020.
Author’s Response
The early decision option for dermatology residency applications would be a welcomed addition to the process but may be complicated by 2 recent events: the coronavirus disease 2019 (COVID-19) pandemic and the change of US Medical Licensing Examination (USMLE) Step 1 score reporting to a pass/fail system.
The COVID-19 pandemic has caused remarkable economic distress and likely affects medical students more acutely given their high levels of debt. As Ryan and Wagner observed, one advantage of the early-decision option would be financial relief for certain students. If applicants successfully match during the early-decision phase, they will not need to apply to any additional dermatology programs and also can target their preliminary-year applications to the geographic region where they have already matched.
In addition, the COVID-19 pandemic may further reduce early applicants’ ability to visit programs in person. Various medical schools have curtailed away rotations, and programs may opt for virtual interviews in accordance with social distancing guidelines.1 Thus, early applicants will have even fewer opportunities to compare programs before they must make a binding decision about their residency placement. Although away rotations and interview travel are some of the largest drivers of application cost,2 reducing costs in this way might shortchange both students and programs.
Arguably, the change in USMLE Step 1 score reporting beginning in 2022 may impact residency selection for a longer period of time than the COVID-19 pandemic. Program directors cited USMLE Step 1 scores as one of the main factors determining which applicants may be invited to interview.3 The lack of numerical USMLE Step 1 scores may encourage programs to place more weight on other metrics such as USMLE Step 2 CK scores or Alpha Omega Alpha membership.4 However, as Ryan and Wagner point out, such metrics may not be available in time for early-decision applicants.
As such, future program directors will have precious little information to screen early-decision applicants and may need to conduct holistic application review. This would require increased time and manpower compared to screening based on traditional metrics but may lead to a better “fit” for an applicant with a residency.
In general, implementation of any early decision program would benefit dermatology applicants as a group by removing elite candidates from the applicant pool. According to National Resident Matching Program data, just 3% of dermatology applicants account for more than 12% of overall interviews.5 In other words, a small group of the strongest applicants receives a lion’s share of interviews, crowding out many other candidates. Removing these top-tier applicants likely would provide remaining applicants with a higher return on investment per application, and students may choose to save money by applying to fewer programs.
Adopting early-decision options within the dermatology match may be complicated given the COVID-19 pandemic and USMLE score changes but may spur positive changes in the process while also reducing the financial burden on applicants.
Aamir N. Hussain, MD, MAPP
From Northwell Health, Manhasset, New York.
The author reports no conflict of interest.
Correspondence: Aamir N. Hussain, MD, MAPP ([email protected]).
References
1. Coronavirus (COVID-19) and the VSLO program. Association of American Medical Colleges website. https://students-residents.aamc.org/attending-medical-school/article/coronavirus-covid-19-and-vslo-program/. Accessed April 17, 2020.
2. Mansouri B, Walker GD, Mitchell J, et al. The cost of applying to dermatology residency: 2014 data estimates. J Am Acad Dermatol. 2016;74:754-756.
3. National Resident Matching Program, Data Release and Research Committee. Results of the 2018 NRMP Program Director Survey. Washington, DC: National Resident Matching Program; 2018. https://www.nrmp.org/wp-content/uploads/2018/07/NRMP-2018-Program-Director-Survey-for-WWW.pdf. Published June 2018. Accessed April 17, 2020.
4. Crane MA, Chang HA, Azamfirei R. Medical education takes a step in the right direction: where does that leave students? [published online March 6, 2020]. JAMA. doi:10.1001/jama.2020.2950.
5. Lee AH, Young P, Liao R, et al. I dream of Gini: quantifying inequality in otolaryngology residency interviews. Laryngoscope. 2019;129:627-633.
The American maternal mortality crisis: The role of racism and bias
April 11-17 marked the third annual national Black Maternal Health Week, an event launched in 2017 by the Atlanta-based Black Mamas Matter Alliance (BMMA), in part to “deepen the national conversation about black maternal health.”
Around the same time, emerging data showing higher mortality rates among black patients versus patients of other races with COVID-19 opened similar dialogue fraught with questions about what might explain the disturbing health disparities.
“It’s kind of surprising to me that people are shocked by these [COVID-19] disparities,” Rebekah Gee, MD, an ob.gyn. who is director of the Louisiana State University Health System in New Orleans and a driving force behind initiatives addressing racial disparities in maternal health, said in an interview. If this is it, great – and certainly every moment is a moment for learning – but these COVID-19 disparities should not be surprising to people who have been looking at data.”
Veronica Gillispie, MD, an ob.gyn. and medical director of the Louisiana Perinatal Quality Collaborative and Pregnancy-Associated Mortality Review, was similarly baffled that the news was treated as a revelation.
That news includes outcomes data from New York showing that in March there were 92.3 and 74.3 deaths per 100,000 black and Hispanic COVID-19 patients, respectively, compared with 45.2 per 100,000 white patients.
“Now there’s a task force and all these initiatives to look at why this is happening, and I think those of us who work in maternal mortality are all saying, ‘We know why it’s happening,’ ” she said. “It’s the same thing we’ve been telling people why it’s been happening in maternal mortality.
“It’s implicit bias and structural racism.”
Facing hard numbers, harder conversations
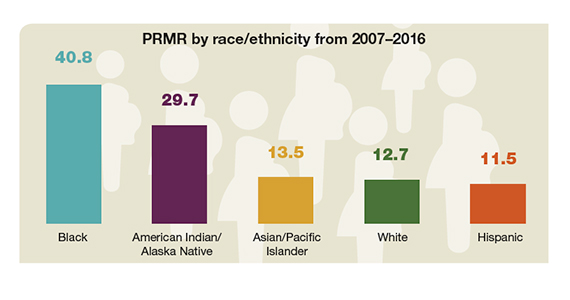
The U.S. maternal mortality rate in 2018 was 17 per 100,000 live births – the highest of any similarly wealthy industrialized nation, the Centers for Disease Control and Prevention’s National Center for Health Statistics (NCHS) reported in January. That’s a striking statistic in its own right. Perhaps more striking is the breakdown by race.
Hispanic women had the lowest maternal mortality rate at 12 per 100,000 live births, followed by non-Hispanic white women at 15.
The rate for non-Hispanic black women was 37 per 100,000 live births.
Numerous factors contribute to these disparities. Among those listed by the American College of Obstetricians and Gynecologists’ chief executive officer Maureen G. Phipps, MD, in a press statement on the NCHS data, are care access issues, lack of standardization of care, bias, and racism. All of these must be addressed if the disparities in maternal and other areas of care are to be eliminated, according to Dr. Phipps.
“The NCHS data confirmed what we have known from other data sources: The rate of maternal deaths for non-Hispanic black women is substantially higher than the rates for non-Hispanic white women,” she wrote. “Continued efforts to improve the standardization of data and review processes related to U.S. maternal mortality are a necessary step to achieving the goal of eliminating disparities and preventable maternal mortality.”
However, such efforts frequently encounter roadblocks constructed by the reluctance among “many academics, policy makers, scientists, elected officials, journalists, and others responsible for defining and responding to the public discourse” to identify racism as a root cause of health disparities, according to Zinzi D. Bailey, ScD, former director of research and evaluation for the New York City Department of Health and Mental Hygiene, and colleagues.
In the third of a three-part conceptual report in The Lancet, entitled America: Equity and Equality in Health, Dr. Bailey and colleagues argued that advancing health equity requires a focus on structural racism – which they defined as “the totality of ways in which societies foster racial discrimination via mutually reinforcing inequitable systems (e.g., in housing, education, employment, earning, benefits, credit, media, healthcare, and criminal justice, etc.) that in turn reinforce discriminatory beliefs, values, and distribution of resources.”
In their series, the authors peeled back layer upon layer of sociological and political contributors to structural racism throughout history, revealing how each laid a foundation for health inequity over time. They particularly home in on health care quality and access.
“Interpersonal racism, bias, and discrimination in healthcare settings can directly affect health through poor health care,” they wrote, noting that “almost 15 years ago, the Institute of Medicine report entitled Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, documented systematic and pervasive bias in the treatment of people of color resulting in substandard care.”
That report concluded that “bias, stereotyping, prejudice, and clinical uncertainty on the part of healthcare providers” likely play a role in the continuation of health disparities. More recent data – including the NCHS maternal mortality data – show an ongoing crisis.
A study of 210 experienced primary care providers and 190 community members in the Denver area, for example, found substantial evidence of implicit bias against both Latino and African American patients. The authors defined implicit bias as “unintentional and even unconscious” negative evaluation of one group and its members relative to another that is expressed implicitly, such as through negative nonverbal behavior.
“Activated by situational cues (e.g., a person’s skin color), implicit bias can quickly and unknowingly exert its influence on perception, memory, and behavior,” they wrote.
In their study, Implicit Association Test and self-report measures of bias showed similar rates of implicit bias among the providers and community members, with only a slight weakening of ethnic/racial bias among providers after adjustment for background characteristics, which suggests “a wider societal problem,” they said.
A specific example of how implicit bias can manifest was described in a 2016 report addressing the well-documented under-treatment of pain among black versus white patients. Kelly M. Hoffman, PhD, and colleagues demonstrated that a substantial number of individuals with at least some medical training endorse false beliefs regarding biological differences between black and white patients. For example, 25% of 28 white residents surveyed agreed black individuals have thicker skin, and 4% believed black individuals have faster blood coagulation and less sensitivity in their nerve endings.
Those who more strongly endorsed such erroneous beliefs were more likely to underestimate and undertreat pain among black patients, the authors found.
Another study, which underscored the insidiousness of structural racism, was reported in Science. The authors identified significant racial bias in an algorithm widely used by health systems, insurers, and practitioners to allocate health care resources for patients with complex health needs. The algorithm, which affects millions of patients, uses predictions of future health care costs rather than future illness to determine who should receive extra medical care.
The problem is that unequal care access for black patients skews lower the foundational cost data used for making those predictions. Correcting the algorithm would increase the percentage of black patients receiving additional medical help from 17.7% to 46.5%, the authors concluded.
This evidence of persistent racism and bias in medicine, however, doesn’t mean progress is lacking.
ACOG has partnered with numerous other organizations to promote awareness and change, including through legislation. A recent win was the enactment of the Preventing Maternal Deaths Act of 2018, a bipartisan bill designed to promote and support maternal mortality review committees in every state. A major focus of BMMA’s Black Maternal Health Week was the Black Maternal Health Momnibus Act of 2020, a nine-bill package introduced in March to comprehensively address the crisis.
But efforts like these, whether they aim to elucidate the contributors to health disparities or to directly target structural and overt racism and root out implicit bias in medical care, are nothing new. As Dr. Bailey and colleagues noted, a challenge is getting the message across because efforts to avoid tough conversations around these topics are nothing new, either.
Dr. Gee attested to that during a maternal mortality panel discussion at the 2019 ACOG meeting where she spoke about the resistance she encountered in 2016 when she was appointed secretary of the Louisiana Health Department and worked to make racism and bias a foundational part of the discussion on improving maternal and fetal outcomes.
She established the first Office of Health Equity in the state – and the first in the nation to not only require measurement outcomes by race but also explicitly address racial bias at the outset. The goal wasn’t just to talk about it but to “plan for addressing equity in every single aspect of what we do with ... our case equity action teams.”
“At our first maternal mortality quality meetings we insisted on focusing on equity at the very outset, and we had people that left when we started talking about racism,” she said, noting that others said it was “too political” to discuss during an election year or that equity was something to address later.
“We said no. We insisted on it, and I think that was very important because all ships don’t rise with the tide, not with health disparities,” she said, recounting an earlier experience when she led the Louisiana Birth Outcomes Initiative: “I asked to have a brown-bag focused on racism at the department so we could talk about the impact of implicit bias on decision making, and I was told that I was a Yankee who didn’t understand the South and that racism didn’t really exist here, and what did I know about it – and I couldn’t have the brown-bag.”
That was in 2011.
Fast-forward to April 24, 2020. As Dr. Gee shared her perspective on addressing racism and bias in medicine, she was preparing for a call regarding the racial disparities in COVID-19 outcomes – the first health equity action sanctioned by Louisiana Governor John Bel Edwards (D).
“I think we really set the stage for these discussions,” she said.
Addressing equity to enact change
The efforts in Louisiana also set the stage for better maternal outcomes. At the 2019 ACOG meeting where she spoke as part of the President’s Panel, Dr. Gee said Louisiana had the highest maternal mortality rates in the nation. The NCHC data released in January, however, suggest that may no longer be the case.
Inconsistencies in how the latest and prior data were reported, including in how maternal mortality was defined, make direct comparison impossible. But in the latest report, Louisiana ranked seventh among states with available data.
“Ninety percent of the deliveries in the state happen at hospitals that we worked with,” Dr. Gee said, highlighting the reach of the efforts to improve outcomes there.
She also described a recent case involving an anemic patient whose bleeding risk was identified early thanks to the programs put in place. That enabled early preparation in the event of complications.
The patient experienced a massive hemorrhage, but the preparation, including having units of blood on hand in case of such an emergency, saved her life.
“So we clearly have not just data, but individual stories of people whose lives have been saved by this work,” she said.
More tangible data on maternal morbidity further show that the efforts in the state are making a difference, Dr. Gillispie said, citing preliminary outcomes data from the Pregnancy-Associated Mortality Review launched in 2018.
“We started with an initial goal of reducing severe maternal morbidity related to hypertension and hemorrhage by 20%, as well as reducing the black/white disparity gap by Mother’s Day 2020,” she said.
Final analyses have been delayed because of COVID-19, but early assessments showed a reduction in the disparity gap, she said, again highlighting the importance of focusing on equity.
“Definitely from the standpoint of the Quality Collaborative side ... we’ve been working with our facilities to make them aware of what implicit bias is, helping them to also do the Harvard Implicit Bias Test so they can figure out what their own biases are, start working to acknowledge them and address them, and start working to fight against letting that bias change how they treat individuals,” Dr. Gillispie said.
The work started through these initiatives will continue because there is much left to be done, she said.
Indeed, the surprised reactions in recent weeks to the reports of disparities in COVID-19 outcomes further underscore that reality, and the maternal mortality statistics – with use of the voices of those directly affected by structural and overt racism and bias in maternal care as a megaphone – speak for themselves.
Hearing implicit bias from patients’ perspective
Just ask Timoria McQueen Saba, a black woman who nearly died from a postpartum hemorrhage in 2010. At ACOG 2019, she spoke about how she had to switch ob.gyns. three times during her first pregnancy because she felt she had not received quality care – one doctor neglected to tell her she had placenta previa. She also experienced excessive wait times at prenatal appointments and had been on the receiving end of microaggressions and degrading questions such as “Are you still married?” and “Is your husband your baby’s father?” – and these are all things her white friends who recommended those physicians never experienced, she said.
“The health care system has just sometimes beaten people down so much, just like the world has – people of color, especially – to where you’re dismissed, your concerns are invalidated,” she said. “Some doctors don’t even think black people feel pain [or that] our pain is less.”
Mrs. Saba also spoke about how her health care “improved a billion percent” when her white husband accompanied her to appointments.
Just ask Charles S. Johnson IV, whose wife Kira Dixon Johnson died in 2016 during surgery for postpartum bleeding complications – after he and other family members spent 10 hours pleading for help for her.
Speaking at the ACOG panel discussion with Mrs. Saba, Mr. Johnson described “a clear disconnect” between the medical staff at the hospital and the way they viewed and valued Kira. He shared his frustration in wanting to advocate for his wife, but knowing that, as an African American male, he risked being seen as a threat and removed from the hospital if he didn’t stay calm, if he “tapped into those natural instincts as a man and a husband who wants to just protect his family.”
He fought back emotions, struggling to get the words out, saying that’s what haunts him and keeps him up at night – wondering if he should have “fought harder, grabbed the doctor by the collar, raised his voice, slammed on the counter.
“Maybe they would have done something,” he said.
Such experiences cross all socioeconomic boundaries. Ask U.S. Track and Field Olympic gold medalist Allyson Felix, who testified at a U.S. House Ways and Means Committee hearing on May 16, 2019 after developing severe preeclampsia that threatened her life and that of her baby. Ask tennis champion Serena Williams, who demanded assessment for pulmonary embolism following the birth of her child; she knew the signs, but her health care providers initially dismissed her concerns.
Their experiences aren’t just anecdotal. Data consistently show how racism and bias affect patient treatment and outcomes. Dr. Gee, for example, shared findings from a retrospective assessment of 47 confirmed pregnancy-related deaths in Louisiana between 2011 and 2016 that looked specifically at whether the deaths could potentially have been prevented if blood was given sooner, cardiomyopathy was recognized sooner, hypertension was treated on time, or other changes were made to care.
The answer was “Yes” in 9% of cases involving white patients – and in 59% of cases involving black patients (odds ratio, 14.6).
The study, reported in February in Obstetrics & Gynecology, showed that 27 of the deaths (58%) occurred at level III or IV birth facilities and that those deaths were not less likely than those at level I or II facilities to be categorized as preventable (OR, 2.0).
Findings from the Giving Voice to Mothers study, published in Reproductive Health in 2019, showed how mistreatment during childbirth might contribute to such outcomes.
In an online cross-sectional survey of more than 2,100 U.S. women, one in six reported at least one type of mistreatment, such as loss of autonomy, being yelled at or threatened, being ignored or having requests for help ignored, Saraswathi Vedam, SciD, of the Birth Place Lab at the University of British Columbia, Vancouver, and colleagues reported.
Race was among the factors associated with likelihood of mistreatment, and the rates of mistreatment for women of color were consistently higher – even when looking at interactions between race and other characteristics, such as socioeconomic status (SES). For example, 27.2% of women of color with low SES, compared with 18.7% of white women with low SES, reported mistreatment. Having a partner who was black, regardless of maternal race, was also associated with an increased rate of mistreatment, the authors found.
“I often get the question, ‘Do you think Kira would be alive if she was white,’ ” Mr. Johnson said. “The first way I respond to that question is [by saying that] the simple fact that you have to ask me is a problem.
“When this first happened, I was in so much pain that I couldn’t process the fact that something so egregious and outrageous happened to my wife because of the color of her skin, but as I began to process and really think about it and unpack this scenario, I have to be really frank ... do I think that she would have sat there for 10 hours while we begged and pleaded? Absolutely not.”
He stressed that his words aren’t “an indictment of the profession.”
“This is not an indictment saying that all people are racist or prejudiced,” he said. “But here’s the reality: If you are in this profession, if you are responsible for the well-being of patients and their families, and you are not able to see them in the same way that you see your mother, your wife, your sister, you have two options – you need to find something else to do or you need to take steps to get better.”
Fixing systems, finding solutions
Dr. Gee acknowledged the work that physicians need to do to help improve outcomes.
“The average time we give a patient to talk is 11 seconds before we interrupt them,” she said, as one example. “We have to recognize that.”
But efforts to improve outcomes shouldn’t just focus on changing physician behavior, she said.
“We really need to focus, as has the U.K. – very effectively – on using midwives, doulas, other health care professionals as complements to physicians to make sure that we have women-centered birth experiences.
“So, instead of just blaming the doctors, I think we need to change the system,” Dr. Gee emphasized.
The disruptions in health systems caused by COVID-19 present a unique opportunity to do that, she said. There is now an opportunity to build them back.
“We have a chance to build the systems back, and when we do so, we ought to build them back correcting for implicit bias and some of the systemic issues that lead to poor outcomes for people of color in our country,” she said.
Solutions proposed by Dr. Gee and others include more diversity in the workforce, more inclusion of patient advocates in maternal care, development of culturally appropriate literacy and numeracy communications, measurement by race (and action on the outcomes), standardization of care, and development of new ways to improve care access.
We will focus more specifically on these solutions in Part 2 of this article in our maternal mortality series. Previous articles in the series are available at mdedge.com/obgyn/maternal-mortality.
April 11-17 marked the third annual national Black Maternal Health Week, an event launched in 2017 by the Atlanta-based Black Mamas Matter Alliance (BMMA), in part to “deepen the national conversation about black maternal health.”
Around the same time, emerging data showing higher mortality rates among black patients versus patients of other races with COVID-19 opened similar dialogue fraught with questions about what might explain the disturbing health disparities.
“It’s kind of surprising to me that people are shocked by these [COVID-19] disparities,” Rebekah Gee, MD, an ob.gyn. who is director of the Louisiana State University Health System in New Orleans and a driving force behind initiatives addressing racial disparities in maternal health, said in an interview. If this is it, great – and certainly every moment is a moment for learning – but these COVID-19 disparities should not be surprising to people who have been looking at data.”
Veronica Gillispie, MD, an ob.gyn. and medical director of the Louisiana Perinatal Quality Collaborative and Pregnancy-Associated Mortality Review, was similarly baffled that the news was treated as a revelation.
That news includes outcomes data from New York showing that in March there were 92.3 and 74.3 deaths per 100,000 black and Hispanic COVID-19 patients, respectively, compared with 45.2 per 100,000 white patients.
“Now there’s a task force and all these initiatives to look at why this is happening, and I think those of us who work in maternal mortality are all saying, ‘We know why it’s happening,’ ” she said. “It’s the same thing we’ve been telling people why it’s been happening in maternal mortality.
“It’s implicit bias and structural racism.”
Facing hard numbers, harder conversations
The U.S. maternal mortality rate in 2018 was 17 per 100,000 live births – the highest of any similarly wealthy industrialized nation, the Centers for Disease Control and Prevention’s National Center for Health Statistics (NCHS) reported in January. That’s a striking statistic in its own right. Perhaps more striking is the breakdown by race.
Hispanic women had the lowest maternal mortality rate at 12 per 100,000 live births, followed by non-Hispanic white women at 15.
The rate for non-Hispanic black women was 37 per 100,000 live births.
Numerous factors contribute to these disparities. Among those listed by the American College of Obstetricians and Gynecologists’ chief executive officer Maureen G. Phipps, MD, in a press statement on the NCHS data, are care access issues, lack of standardization of care, bias, and racism. All of these must be addressed if the disparities in maternal and other areas of care are to be eliminated, according to Dr. Phipps.
“The NCHS data confirmed what we have known from other data sources: The rate of maternal deaths for non-Hispanic black women is substantially higher than the rates for non-Hispanic white women,” she wrote. “Continued efforts to improve the standardization of data and review processes related to U.S. maternal mortality are a necessary step to achieving the goal of eliminating disparities and preventable maternal mortality.”
However, such efforts frequently encounter roadblocks constructed by the reluctance among “many academics, policy makers, scientists, elected officials, journalists, and others responsible for defining and responding to the public discourse” to identify racism as a root cause of health disparities, according to Zinzi D. Bailey, ScD, former director of research and evaluation for the New York City Department of Health and Mental Hygiene, and colleagues.
In the third of a three-part conceptual report in The Lancet, entitled America: Equity and Equality in Health, Dr. Bailey and colleagues argued that advancing health equity requires a focus on structural racism – which they defined as “the totality of ways in which societies foster racial discrimination via mutually reinforcing inequitable systems (e.g., in housing, education, employment, earning, benefits, credit, media, healthcare, and criminal justice, etc.) that in turn reinforce discriminatory beliefs, values, and distribution of resources.”
In their series, the authors peeled back layer upon layer of sociological and political contributors to structural racism throughout history, revealing how each laid a foundation for health inequity over time. They particularly home in on health care quality and access.
“Interpersonal racism, bias, and discrimination in healthcare settings can directly affect health through poor health care,” they wrote, noting that “almost 15 years ago, the Institute of Medicine report entitled Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, documented systematic and pervasive bias in the treatment of people of color resulting in substandard care.”
That report concluded that “bias, stereotyping, prejudice, and clinical uncertainty on the part of healthcare providers” likely play a role in the continuation of health disparities. More recent data – including the NCHS maternal mortality data – show an ongoing crisis.
A study of 210 experienced primary care providers and 190 community members in the Denver area, for example, found substantial evidence of implicit bias against both Latino and African American patients. The authors defined implicit bias as “unintentional and even unconscious” negative evaluation of one group and its members relative to another that is expressed implicitly, such as through negative nonverbal behavior.
“Activated by situational cues (e.g., a person’s skin color), implicit bias can quickly and unknowingly exert its influence on perception, memory, and behavior,” they wrote.
In their study, Implicit Association Test and self-report measures of bias showed similar rates of implicit bias among the providers and community members, with only a slight weakening of ethnic/racial bias among providers after adjustment for background characteristics, which suggests “a wider societal problem,” they said.
A specific example of how implicit bias can manifest was described in a 2016 report addressing the well-documented under-treatment of pain among black versus white patients. Kelly M. Hoffman, PhD, and colleagues demonstrated that a substantial number of individuals with at least some medical training endorse false beliefs regarding biological differences between black and white patients. For example, 25% of 28 white residents surveyed agreed black individuals have thicker skin, and 4% believed black individuals have faster blood coagulation and less sensitivity in their nerve endings.
Those who more strongly endorsed such erroneous beliefs were more likely to underestimate and undertreat pain among black patients, the authors found.
Another study, which underscored the insidiousness of structural racism, was reported in Science. The authors identified significant racial bias in an algorithm widely used by health systems, insurers, and practitioners to allocate health care resources for patients with complex health needs. The algorithm, which affects millions of patients, uses predictions of future health care costs rather than future illness to determine who should receive extra medical care.
The problem is that unequal care access for black patients skews lower the foundational cost data used for making those predictions. Correcting the algorithm would increase the percentage of black patients receiving additional medical help from 17.7% to 46.5%, the authors concluded.
This evidence of persistent racism and bias in medicine, however, doesn’t mean progress is lacking.
ACOG has partnered with numerous other organizations to promote awareness and change, including through legislation. A recent win was the enactment of the Preventing Maternal Deaths Act of 2018, a bipartisan bill designed to promote and support maternal mortality review committees in every state. A major focus of BMMA’s Black Maternal Health Week was the Black Maternal Health Momnibus Act of 2020, a nine-bill package introduced in March to comprehensively address the crisis.
But efforts like these, whether they aim to elucidate the contributors to health disparities or to directly target structural and overt racism and root out implicit bias in medical care, are nothing new. As Dr. Bailey and colleagues noted, a challenge is getting the message across because efforts to avoid tough conversations around these topics are nothing new, either.
Dr. Gee attested to that during a maternal mortality panel discussion at the 2019 ACOG meeting where she spoke about the resistance she encountered in 2016 when she was appointed secretary of the Louisiana Health Department and worked to make racism and bias a foundational part of the discussion on improving maternal and fetal outcomes.
She established the first Office of Health Equity in the state – and the first in the nation to not only require measurement outcomes by race but also explicitly address racial bias at the outset. The goal wasn’t just to talk about it but to “plan for addressing equity in every single aspect of what we do with ... our case equity action teams.”
“At our first maternal mortality quality meetings we insisted on focusing on equity at the very outset, and we had people that left when we started talking about racism,” she said, noting that others said it was “too political” to discuss during an election year or that equity was something to address later.
“We said no. We insisted on it, and I think that was very important because all ships don’t rise with the tide, not with health disparities,” she said, recounting an earlier experience when she led the Louisiana Birth Outcomes Initiative: “I asked to have a brown-bag focused on racism at the department so we could talk about the impact of implicit bias on decision making, and I was told that I was a Yankee who didn’t understand the South and that racism didn’t really exist here, and what did I know about it – and I couldn’t have the brown-bag.”
That was in 2011.
Fast-forward to April 24, 2020. As Dr. Gee shared her perspective on addressing racism and bias in medicine, she was preparing for a call regarding the racial disparities in COVID-19 outcomes – the first health equity action sanctioned by Louisiana Governor John Bel Edwards (D).
“I think we really set the stage for these discussions,” she said.
Addressing equity to enact change
The efforts in Louisiana also set the stage for better maternal outcomes. At the 2019 ACOG meeting where she spoke as part of the President’s Panel, Dr. Gee said Louisiana had the highest maternal mortality rates in the nation. The NCHC data released in January, however, suggest that may no longer be the case.
Inconsistencies in how the latest and prior data were reported, including in how maternal mortality was defined, make direct comparison impossible. But in the latest report, Louisiana ranked seventh among states with available data.
“Ninety percent of the deliveries in the state happen at hospitals that we worked with,” Dr. Gee said, highlighting the reach of the efforts to improve outcomes there.
She also described a recent case involving an anemic patient whose bleeding risk was identified early thanks to the programs put in place. That enabled early preparation in the event of complications.
The patient experienced a massive hemorrhage, but the preparation, including having units of blood on hand in case of such an emergency, saved her life.
“So we clearly have not just data, but individual stories of people whose lives have been saved by this work,” she said.
More tangible data on maternal morbidity further show that the efforts in the state are making a difference, Dr. Gillispie said, citing preliminary outcomes data from the Pregnancy-Associated Mortality Review launched in 2018.
“We started with an initial goal of reducing severe maternal morbidity related to hypertension and hemorrhage by 20%, as well as reducing the black/white disparity gap by Mother’s Day 2020,” she said.
Final analyses have been delayed because of COVID-19, but early assessments showed a reduction in the disparity gap, she said, again highlighting the importance of focusing on equity.
“Definitely from the standpoint of the Quality Collaborative side ... we’ve been working with our facilities to make them aware of what implicit bias is, helping them to also do the Harvard Implicit Bias Test so they can figure out what their own biases are, start working to acknowledge them and address them, and start working to fight against letting that bias change how they treat individuals,” Dr. Gillispie said.
The work started through these initiatives will continue because there is much left to be done, she said.
Indeed, the surprised reactions in recent weeks to the reports of disparities in COVID-19 outcomes further underscore that reality, and the maternal mortality statistics – with use of the voices of those directly affected by structural and overt racism and bias in maternal care as a megaphone – speak for themselves.
Hearing implicit bias from patients’ perspective
Just ask Timoria McQueen Saba, a black woman who nearly died from a postpartum hemorrhage in 2010. At ACOG 2019, she spoke about how she had to switch ob.gyns. three times during her first pregnancy because she felt she had not received quality care – one doctor neglected to tell her she had placenta previa. She also experienced excessive wait times at prenatal appointments and had been on the receiving end of microaggressions and degrading questions such as “Are you still married?” and “Is your husband your baby’s father?” – and these are all things her white friends who recommended those physicians never experienced, she said.
“The health care system has just sometimes beaten people down so much, just like the world has – people of color, especially – to where you’re dismissed, your concerns are invalidated,” she said. “Some doctors don’t even think black people feel pain [or that] our pain is less.”
Mrs. Saba also spoke about how her health care “improved a billion percent” when her white husband accompanied her to appointments.
Just ask Charles S. Johnson IV, whose wife Kira Dixon Johnson died in 2016 during surgery for postpartum bleeding complications – after he and other family members spent 10 hours pleading for help for her.
Speaking at the ACOG panel discussion with Mrs. Saba, Mr. Johnson described “a clear disconnect” between the medical staff at the hospital and the way they viewed and valued Kira. He shared his frustration in wanting to advocate for his wife, but knowing that, as an African American male, he risked being seen as a threat and removed from the hospital if he didn’t stay calm, if he “tapped into those natural instincts as a man and a husband who wants to just protect his family.”
He fought back emotions, struggling to get the words out, saying that’s what haunts him and keeps him up at night – wondering if he should have “fought harder, grabbed the doctor by the collar, raised his voice, slammed on the counter.
“Maybe they would have done something,” he said.
Such experiences cross all socioeconomic boundaries. Ask U.S. Track and Field Olympic gold medalist Allyson Felix, who testified at a U.S. House Ways and Means Committee hearing on May 16, 2019 after developing severe preeclampsia that threatened her life and that of her baby. Ask tennis champion Serena Williams, who demanded assessment for pulmonary embolism following the birth of her child; she knew the signs, but her health care providers initially dismissed her concerns.
Their experiences aren’t just anecdotal. Data consistently show how racism and bias affect patient treatment and outcomes. Dr. Gee, for example, shared findings from a retrospective assessment of 47 confirmed pregnancy-related deaths in Louisiana between 2011 and 2016 that looked specifically at whether the deaths could potentially have been prevented if blood was given sooner, cardiomyopathy was recognized sooner, hypertension was treated on time, or other changes were made to care.
The answer was “Yes” in 9% of cases involving white patients – and in 59% of cases involving black patients (odds ratio, 14.6).
The study, reported in February in Obstetrics & Gynecology, showed that 27 of the deaths (58%) occurred at level III or IV birth facilities and that those deaths were not less likely than those at level I or II facilities to be categorized as preventable (OR, 2.0).
Findings from the Giving Voice to Mothers study, published in Reproductive Health in 2019, showed how mistreatment during childbirth might contribute to such outcomes.
In an online cross-sectional survey of more than 2,100 U.S. women, one in six reported at least one type of mistreatment, such as loss of autonomy, being yelled at or threatened, being ignored or having requests for help ignored, Saraswathi Vedam, SciD, of the Birth Place Lab at the University of British Columbia, Vancouver, and colleagues reported.
Race was among the factors associated with likelihood of mistreatment, and the rates of mistreatment for women of color were consistently higher – even when looking at interactions between race and other characteristics, such as socioeconomic status (SES). For example, 27.2% of women of color with low SES, compared with 18.7% of white women with low SES, reported mistreatment. Having a partner who was black, regardless of maternal race, was also associated with an increased rate of mistreatment, the authors found.
“I often get the question, ‘Do you think Kira would be alive if she was white,’ ” Mr. Johnson said. “The first way I respond to that question is [by saying that] the simple fact that you have to ask me is a problem.
“When this first happened, I was in so much pain that I couldn’t process the fact that something so egregious and outrageous happened to my wife because of the color of her skin, but as I began to process and really think about it and unpack this scenario, I have to be really frank ... do I think that she would have sat there for 10 hours while we begged and pleaded? Absolutely not.”
He stressed that his words aren’t “an indictment of the profession.”
“This is not an indictment saying that all people are racist or prejudiced,” he said. “But here’s the reality: If you are in this profession, if you are responsible for the well-being of patients and their families, and you are not able to see them in the same way that you see your mother, your wife, your sister, you have two options – you need to find something else to do or you need to take steps to get better.”
Fixing systems, finding solutions
Dr. Gee acknowledged the work that physicians need to do to help improve outcomes.
“The average time we give a patient to talk is 11 seconds before we interrupt them,” she said, as one example. “We have to recognize that.”
But efforts to improve outcomes shouldn’t just focus on changing physician behavior, she said.
“We really need to focus, as has the U.K. – very effectively – on using midwives, doulas, other health care professionals as complements to physicians to make sure that we have women-centered birth experiences.
“So, instead of just blaming the doctors, I think we need to change the system,” Dr. Gee emphasized.
The disruptions in health systems caused by COVID-19 present a unique opportunity to do that, she said. There is now an opportunity to build them back.
“We have a chance to build the systems back, and when we do so, we ought to build them back correcting for implicit bias and some of the systemic issues that lead to poor outcomes for people of color in our country,” she said.
Solutions proposed by Dr. Gee and others include more diversity in the workforce, more inclusion of patient advocates in maternal care, development of culturally appropriate literacy and numeracy communications, measurement by race (and action on the outcomes), standardization of care, and development of new ways to improve care access.
We will focus more specifically on these solutions in Part 2 of this article in our maternal mortality series. Previous articles in the series are available at mdedge.com/obgyn/maternal-mortality.
April 11-17 marked the third annual national Black Maternal Health Week, an event launched in 2017 by the Atlanta-based Black Mamas Matter Alliance (BMMA), in part to “deepen the national conversation about black maternal health.”
Around the same time, emerging data showing higher mortality rates among black patients versus patients of other races with COVID-19 opened similar dialogue fraught with questions about what might explain the disturbing health disparities.
“It’s kind of surprising to me that people are shocked by these [COVID-19] disparities,” Rebekah Gee, MD, an ob.gyn. who is director of the Louisiana State University Health System in New Orleans and a driving force behind initiatives addressing racial disparities in maternal health, said in an interview. If this is it, great – and certainly every moment is a moment for learning – but these COVID-19 disparities should not be surprising to people who have been looking at data.”
Veronica Gillispie, MD, an ob.gyn. and medical director of the Louisiana Perinatal Quality Collaborative and Pregnancy-Associated Mortality Review, was similarly baffled that the news was treated as a revelation.
That news includes outcomes data from New York showing that in March there were 92.3 and 74.3 deaths per 100,000 black and Hispanic COVID-19 patients, respectively, compared with 45.2 per 100,000 white patients.
“Now there’s a task force and all these initiatives to look at why this is happening, and I think those of us who work in maternal mortality are all saying, ‘We know why it’s happening,’ ” she said. “It’s the same thing we’ve been telling people why it’s been happening in maternal mortality.
“It’s implicit bias and structural racism.”
Facing hard numbers, harder conversations
The U.S. maternal mortality rate in 2018 was 17 per 100,000 live births – the highest of any similarly wealthy industrialized nation, the Centers for Disease Control and Prevention’s National Center for Health Statistics (NCHS) reported in January. That’s a striking statistic in its own right. Perhaps more striking is the breakdown by race.
Hispanic women had the lowest maternal mortality rate at 12 per 100,000 live births, followed by non-Hispanic white women at 15.
The rate for non-Hispanic black women was 37 per 100,000 live births.
Numerous factors contribute to these disparities. Among those listed by the American College of Obstetricians and Gynecologists’ chief executive officer Maureen G. Phipps, MD, in a press statement on the NCHS data, are care access issues, lack of standardization of care, bias, and racism. All of these must be addressed if the disparities in maternal and other areas of care are to be eliminated, according to Dr. Phipps.
“The NCHS data confirmed what we have known from other data sources: The rate of maternal deaths for non-Hispanic black women is substantially higher than the rates for non-Hispanic white women,” she wrote. “Continued efforts to improve the standardization of data and review processes related to U.S. maternal mortality are a necessary step to achieving the goal of eliminating disparities and preventable maternal mortality.”
However, such efforts frequently encounter roadblocks constructed by the reluctance among “many academics, policy makers, scientists, elected officials, journalists, and others responsible for defining and responding to the public discourse” to identify racism as a root cause of health disparities, according to Zinzi D. Bailey, ScD, former director of research and evaluation for the New York City Department of Health and Mental Hygiene, and colleagues.
In the third of a three-part conceptual report in The Lancet, entitled America: Equity and Equality in Health, Dr. Bailey and colleagues argued that advancing health equity requires a focus on structural racism – which they defined as “the totality of ways in which societies foster racial discrimination via mutually reinforcing inequitable systems (e.g., in housing, education, employment, earning, benefits, credit, media, healthcare, and criminal justice, etc.) that in turn reinforce discriminatory beliefs, values, and distribution of resources.”
In their series, the authors peeled back layer upon layer of sociological and political contributors to structural racism throughout history, revealing how each laid a foundation for health inequity over time. They particularly home in on health care quality and access.
“Interpersonal racism, bias, and discrimination in healthcare settings can directly affect health through poor health care,” they wrote, noting that “almost 15 years ago, the Institute of Medicine report entitled Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, documented systematic and pervasive bias in the treatment of people of color resulting in substandard care.”
That report concluded that “bias, stereotyping, prejudice, and clinical uncertainty on the part of healthcare providers” likely play a role in the continuation of health disparities. More recent data – including the NCHS maternal mortality data – show an ongoing crisis.
A study of 210 experienced primary care providers and 190 community members in the Denver area, for example, found substantial evidence of implicit bias against both Latino and African American patients. The authors defined implicit bias as “unintentional and even unconscious” negative evaluation of one group and its members relative to another that is expressed implicitly, such as through negative nonverbal behavior.
“Activated by situational cues (e.g., a person’s skin color), implicit bias can quickly and unknowingly exert its influence on perception, memory, and behavior,” they wrote.
In their study, Implicit Association Test and self-report measures of bias showed similar rates of implicit bias among the providers and community members, with only a slight weakening of ethnic/racial bias among providers after adjustment for background characteristics, which suggests “a wider societal problem,” they said.
A specific example of how implicit bias can manifest was described in a 2016 report addressing the well-documented under-treatment of pain among black versus white patients. Kelly M. Hoffman, PhD, and colleagues demonstrated that a substantial number of individuals with at least some medical training endorse false beliefs regarding biological differences between black and white patients. For example, 25% of 28 white residents surveyed agreed black individuals have thicker skin, and 4% believed black individuals have faster blood coagulation and less sensitivity in their nerve endings.
Those who more strongly endorsed such erroneous beliefs were more likely to underestimate and undertreat pain among black patients, the authors found.
Another study, which underscored the insidiousness of structural racism, was reported in Science. The authors identified significant racial bias in an algorithm widely used by health systems, insurers, and practitioners to allocate health care resources for patients with complex health needs. The algorithm, which affects millions of patients, uses predictions of future health care costs rather than future illness to determine who should receive extra medical care.
The problem is that unequal care access for black patients skews lower the foundational cost data used for making those predictions. Correcting the algorithm would increase the percentage of black patients receiving additional medical help from 17.7% to 46.5%, the authors concluded.
This evidence of persistent racism and bias in medicine, however, doesn’t mean progress is lacking.
ACOG has partnered with numerous other organizations to promote awareness and change, including through legislation. A recent win was the enactment of the Preventing Maternal Deaths Act of 2018, a bipartisan bill designed to promote and support maternal mortality review committees in every state. A major focus of BMMA’s Black Maternal Health Week was the Black Maternal Health Momnibus Act of 2020, a nine-bill package introduced in March to comprehensively address the crisis.
But efforts like these, whether they aim to elucidate the contributors to health disparities or to directly target structural and overt racism and root out implicit bias in medical care, are nothing new. As Dr. Bailey and colleagues noted, a challenge is getting the message across because efforts to avoid tough conversations around these topics are nothing new, either.
Dr. Gee attested to that during a maternal mortality panel discussion at the 2019 ACOG meeting where she spoke about the resistance she encountered in 2016 when she was appointed secretary of the Louisiana Health Department and worked to make racism and bias a foundational part of the discussion on improving maternal and fetal outcomes.
She established the first Office of Health Equity in the state – and the first in the nation to not only require measurement outcomes by race but also explicitly address racial bias at the outset. The goal wasn’t just to talk about it but to “plan for addressing equity in every single aspect of what we do with ... our case equity action teams.”
“At our first maternal mortality quality meetings we insisted on focusing on equity at the very outset, and we had people that left when we started talking about racism,” she said, noting that others said it was “too political” to discuss during an election year or that equity was something to address later.
“We said no. We insisted on it, and I think that was very important because all ships don’t rise with the tide, not with health disparities,” she said, recounting an earlier experience when she led the Louisiana Birth Outcomes Initiative: “I asked to have a brown-bag focused on racism at the department so we could talk about the impact of implicit bias on decision making, and I was told that I was a Yankee who didn’t understand the South and that racism didn’t really exist here, and what did I know about it – and I couldn’t have the brown-bag.”
That was in 2011.
Fast-forward to April 24, 2020. As Dr. Gee shared her perspective on addressing racism and bias in medicine, she was preparing for a call regarding the racial disparities in COVID-19 outcomes – the first health equity action sanctioned by Louisiana Governor John Bel Edwards (D).
“I think we really set the stage for these discussions,” she said.
Addressing equity to enact change
The efforts in Louisiana also set the stage for better maternal outcomes. At the 2019 ACOG meeting where she spoke as part of the President’s Panel, Dr. Gee said Louisiana had the highest maternal mortality rates in the nation. The NCHC data released in January, however, suggest that may no longer be the case.
Inconsistencies in how the latest and prior data were reported, including in how maternal mortality was defined, make direct comparison impossible. But in the latest report, Louisiana ranked seventh among states with available data.
“Ninety percent of the deliveries in the state happen at hospitals that we worked with,” Dr. Gee said, highlighting the reach of the efforts to improve outcomes there.
She also described a recent case involving an anemic patient whose bleeding risk was identified early thanks to the programs put in place. That enabled early preparation in the event of complications.
The patient experienced a massive hemorrhage, but the preparation, including having units of blood on hand in case of such an emergency, saved her life.
“So we clearly have not just data, but individual stories of people whose lives have been saved by this work,” she said.
More tangible data on maternal morbidity further show that the efforts in the state are making a difference, Dr. Gillispie said, citing preliminary outcomes data from the Pregnancy-Associated Mortality Review launched in 2018.
“We started with an initial goal of reducing severe maternal morbidity related to hypertension and hemorrhage by 20%, as well as reducing the black/white disparity gap by Mother’s Day 2020,” she said.
Final analyses have been delayed because of COVID-19, but early assessments showed a reduction in the disparity gap, she said, again highlighting the importance of focusing on equity.
“Definitely from the standpoint of the Quality Collaborative side ... we’ve been working with our facilities to make them aware of what implicit bias is, helping them to also do the Harvard Implicit Bias Test so they can figure out what their own biases are, start working to acknowledge them and address them, and start working to fight against letting that bias change how they treat individuals,” Dr. Gillispie said.
The work started through these initiatives will continue because there is much left to be done, she said.
Indeed, the surprised reactions in recent weeks to the reports of disparities in COVID-19 outcomes further underscore that reality, and the maternal mortality statistics – with use of the voices of those directly affected by structural and overt racism and bias in maternal care as a megaphone – speak for themselves.
Hearing implicit bias from patients’ perspective
Just ask Timoria McQueen Saba, a black woman who nearly died from a postpartum hemorrhage in 2010. At ACOG 2019, she spoke about how she had to switch ob.gyns. three times during her first pregnancy because she felt she had not received quality care – one doctor neglected to tell her she had placenta previa. She also experienced excessive wait times at prenatal appointments and had been on the receiving end of microaggressions and degrading questions such as “Are you still married?” and “Is your husband your baby’s father?” – and these are all things her white friends who recommended those physicians never experienced, she said.
“The health care system has just sometimes beaten people down so much, just like the world has – people of color, especially – to where you’re dismissed, your concerns are invalidated,” she said. “Some doctors don’t even think black people feel pain [or that] our pain is less.”
Mrs. Saba also spoke about how her health care “improved a billion percent” when her white husband accompanied her to appointments.
Just ask Charles S. Johnson IV, whose wife Kira Dixon Johnson died in 2016 during surgery for postpartum bleeding complications – after he and other family members spent 10 hours pleading for help for her.
Speaking at the ACOG panel discussion with Mrs. Saba, Mr. Johnson described “a clear disconnect” between the medical staff at the hospital and the way they viewed and valued Kira. He shared his frustration in wanting to advocate for his wife, but knowing that, as an African American male, he risked being seen as a threat and removed from the hospital if he didn’t stay calm, if he “tapped into those natural instincts as a man and a husband who wants to just protect his family.”
He fought back emotions, struggling to get the words out, saying that’s what haunts him and keeps him up at night – wondering if he should have “fought harder, grabbed the doctor by the collar, raised his voice, slammed on the counter.
“Maybe they would have done something,” he said.
Such experiences cross all socioeconomic boundaries. Ask U.S. Track and Field Olympic gold medalist Allyson Felix, who testified at a U.S. House Ways and Means Committee hearing on May 16, 2019 after developing severe preeclampsia that threatened her life and that of her baby. Ask tennis champion Serena Williams, who demanded assessment for pulmonary embolism following the birth of her child; she knew the signs, but her health care providers initially dismissed her concerns.
Their experiences aren’t just anecdotal. Data consistently show how racism and bias affect patient treatment and outcomes. Dr. Gee, for example, shared findings from a retrospective assessment of 47 confirmed pregnancy-related deaths in Louisiana between 2011 and 2016 that looked specifically at whether the deaths could potentially have been prevented if blood was given sooner, cardiomyopathy was recognized sooner, hypertension was treated on time, or other changes were made to care.
The answer was “Yes” in 9% of cases involving white patients – and in 59% of cases involving black patients (odds ratio, 14.6).
The study, reported in February in Obstetrics & Gynecology, showed that 27 of the deaths (58%) occurred at level III or IV birth facilities and that those deaths were not less likely than those at level I or II facilities to be categorized as preventable (OR, 2.0).
Findings from the Giving Voice to Mothers study, published in Reproductive Health in 2019, showed how mistreatment during childbirth might contribute to such outcomes.
In an online cross-sectional survey of more than 2,100 U.S. women, one in six reported at least one type of mistreatment, such as loss of autonomy, being yelled at or threatened, being ignored or having requests for help ignored, Saraswathi Vedam, SciD, of the Birth Place Lab at the University of British Columbia, Vancouver, and colleagues reported.
Race was among the factors associated with likelihood of mistreatment, and the rates of mistreatment for women of color were consistently higher – even when looking at interactions between race and other characteristics, such as socioeconomic status (SES). For example, 27.2% of women of color with low SES, compared with 18.7% of white women with low SES, reported mistreatment. Having a partner who was black, regardless of maternal race, was also associated with an increased rate of mistreatment, the authors found.
“I often get the question, ‘Do you think Kira would be alive if she was white,’ ” Mr. Johnson said. “The first way I respond to that question is [by saying that] the simple fact that you have to ask me is a problem.
“When this first happened, I was in so much pain that I couldn’t process the fact that something so egregious and outrageous happened to my wife because of the color of her skin, but as I began to process and really think about it and unpack this scenario, I have to be really frank ... do I think that she would have sat there for 10 hours while we begged and pleaded? Absolutely not.”
He stressed that his words aren’t “an indictment of the profession.”
“This is not an indictment saying that all people are racist or prejudiced,” he said. “But here’s the reality: If you are in this profession, if you are responsible for the well-being of patients and their families, and you are not able to see them in the same way that you see your mother, your wife, your sister, you have two options – you need to find something else to do or you need to take steps to get better.”
Fixing systems, finding solutions
Dr. Gee acknowledged the work that physicians need to do to help improve outcomes.
“The average time we give a patient to talk is 11 seconds before we interrupt them,” she said, as one example. “We have to recognize that.”
But efforts to improve outcomes shouldn’t just focus on changing physician behavior, she said.
“We really need to focus, as has the U.K. – very effectively – on using midwives, doulas, other health care professionals as complements to physicians to make sure that we have women-centered birth experiences.
“So, instead of just blaming the doctors, I think we need to change the system,” Dr. Gee emphasized.
The disruptions in health systems caused by COVID-19 present a unique opportunity to do that, she said. There is now an opportunity to build them back.
“We have a chance to build the systems back, and when we do so, we ought to build them back correcting for implicit bias and some of the systemic issues that lead to poor outcomes for people of color in our country,” she said.
Solutions proposed by Dr. Gee and others include more diversity in the workforce, more inclusion of patient advocates in maternal care, development of culturally appropriate literacy and numeracy communications, measurement by race (and action on the outcomes), standardization of care, and development of new ways to improve care access.
We will focus more specifically on these solutions in Part 2 of this article in our maternal mortality series. Previous articles in the series are available at mdedge.com/obgyn/maternal-mortality.
Hair Care Products Used by Women of African Descent: Review of Ingredients
In the African American and African communities, information regarding the care and treatment of hair and skin often is obtained from relatives as well as Internet videos and bloggers.1 Moreover, fewer than half of African American women surveyed believe that their physician understands African American hair.2 In addition to proficiency in the diagnosis and treatment of hair and scalp disorders in this population, dermatologists must be aware of common hair and scalp beliefs, misconceptions, care, and product use to ensure culturally competent interactions and treatment.
When a patient of African descent refers to their hair as “natural,” he/she is referring to its texture compared with hair that is chemically treated with straighteners (ie, “relaxed” or “permed” hair). Natural hair refers to hair that has not been altered with chemical treatments that permanently break and re-form disulfide bonds of the hair.1 In 2003, it was estimated that 80% of African American women treated their hair with a chemical relaxer.3 However, this preference has changed over the last decade, with a larger percentage of African American women choosing to wear a natural hairstyle.4
Regardless of preferred hairstyle, a multitude of products can be used to obtain and maintain the particular style. According to US Food and Drug Administration regulations, a product’s ingredients must appear on an information panel in descending order of predominance. Additionally, products must be accurately labeled without misleading information. However, one study found that hair care products commonly used by African American women contain mixtures of endocrine-disrupting chemicals, and 84% of detected chemicals are not listed on the label.5
Properties of Hair Care Products
Women of African descent use hair grooming products for cleansing and moisturizing the hair and scalp, detangling, and styling. Products to achieve these goals comprise shampoos, leave-in and rinse-out conditioners, creams, pomades, oils, and gels. In August 2018 we performed a Google search of the most popular hair care products used for natural hair and chemically relaxed African American hair. Key terms used in our search included popular natural hair products, best natural hair products, top natural hair products, products for permed hair, shampoos for permed hair, conditioner for permed hair, popular detanglers for African American hair, popular products for natural hair, detanglers used for permed hair, gels for relaxed hair, moisturizers for relaxed hair, gels for natural hair, and popular moisturizers for African American hair. We reviewed all websites generated by the search and compared the most popular brands, compiled a list of products, and reviewed them for availability in 2 beauty supply stores in Philadelphia, Pennsylvania; 1 Walmart in Hershey, Pennsylvania; and 1 Walmart in Willow Grove, Pennsylvania. Of the 80 products identified, we selected 57 products to be reviewed for ingredients based on which ones were most commonly seen in search results. Table 1 highlights several randomly chosen popular hair care products used by African American women to familiarize dermatologists with specific products and manufacturers.
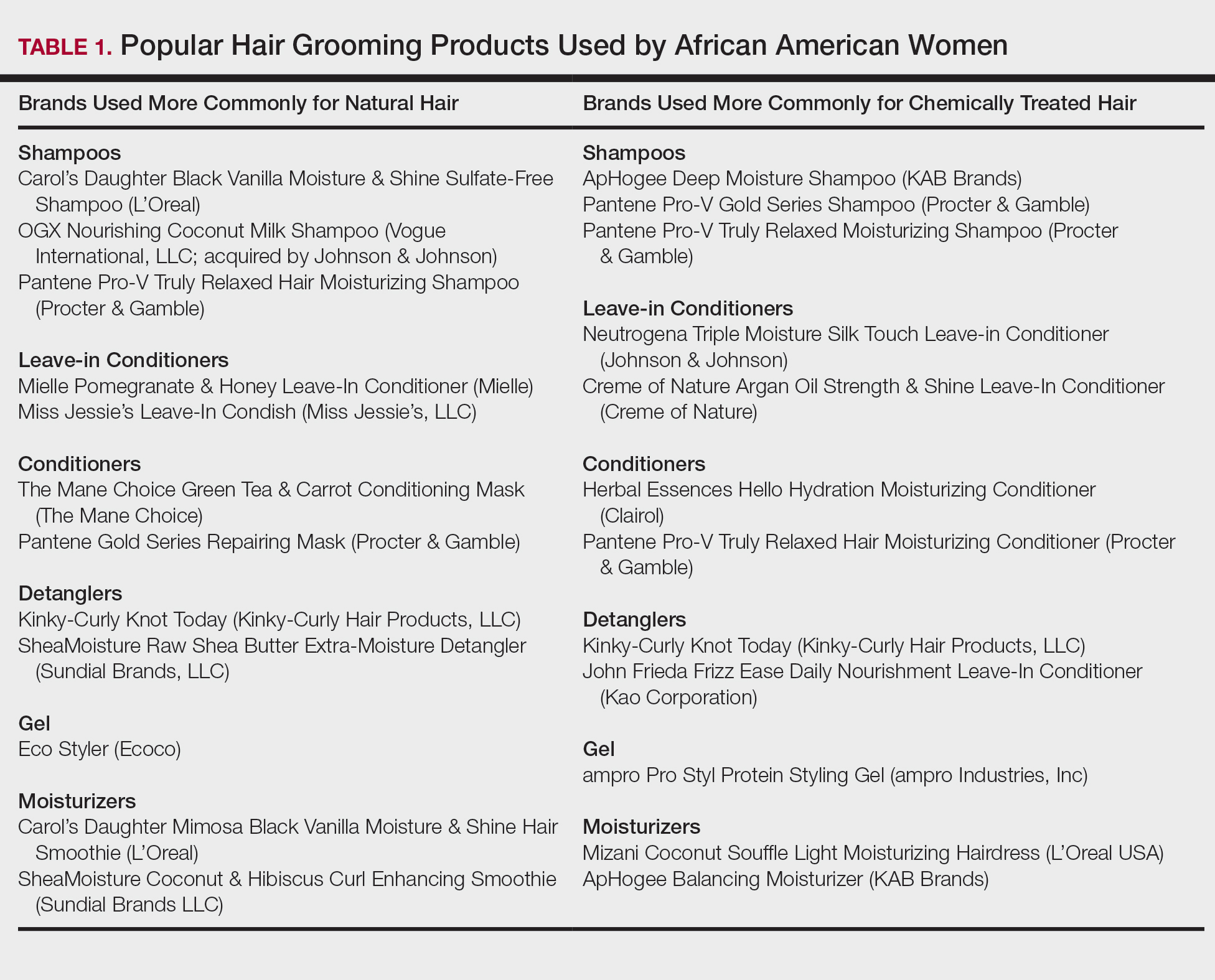
Tightly coiled hair, common among women of African descent, is considered fragile because of decreased water content and tensile strength.6 Fragility is exacerbated by manipulation during styling, excessive heat, and harsh shampoos that strip the hair of moisture, as well as chemical treatments that lead to protein deficiency.4,6,7 Because tightly coiled hair is naturally dry and fragile, women of African descent have a particular preference for products that reduce hair dryness and breakage, which has led to the popularity of sulfate-free shampoos that minimize loss of moisture in hair; moisturizers, oils, and conditioners also are used to enhance moisture retention in hair. Conditioners also provide protein substances that can help strengthen hair.4
Consumers’ concerns about the inclusion of potentially harmful ingredients have resulted in reformulation of many products. Our review of products demonstrated that natural hair consumers used fewer products containing silicones, parabens, and sulfates, compared to consumers with chemically relaxed hair. Another tool used by manufacturers to address these concerns is the inclusion of an additional label to distinguish the product as sulfate free, silicone free, paraben free, petroleum free, or a combination of these terms. Although many patients believe that there are “good” and “bad” products, they should be made aware that there are pros and cons of ingredients frequently found in hair-grooming products. Popular ingredients in hair care products include sulfates, cationic surfactants and cationic polymers, silicone, oils, and parabens.
Sulfates
Sulfates are anion detergents in shampoo that remove sebum from the scalp and hair. The number of sulfates in a shampoo positively correlates to cleansing strength.1 However, sulfates can cause excessive sebum removal and lead to hair that is hard, rough, dull, and prone to tangle and breakage.6 Sulfates also dissolve oil on the hair, causing additional dryness and breakage.7
There are a variety of sulfate compounds with different sebum-removal capabilities. Lauryl sulfates are commonly used in shampoos for oily hair. Tightly coiled hair that has been overly cleansed with these ingredients can become exceedingly dry and unmanageable, which explains why products with lauryl sulfates are avoided. Table 1 includes only 1 product containing lauryl sulfate (Pantene Pro-V Gold Series Shampoo). Patients using a lauryl sulfate–containing shampoo can select a product that also contains a conditioning agent in the formulation.6 Alternatively, sulfate-free shampoos that contain surfactants with less detergency can be used.8 There are no published studies of the cleansing ability of sulfate-free shampoos or their effects on hair shaft fragility.9
At the opposite end of the spectrum is sodium laureth sulfate, commonly used as a primary detergent in shampoos designed for normal to dry hair.10 Sodium laureth sulfate, which provides excellent cleansing and leaves the hair better moisturized and manageable compared to lauryl sulfates,10 is a common ingredient in the products in Table 1 (ApHogee Deep Moisture Shampoo, Pantene Pro-V Gold Series Shampoo, and Pantene Pro-V Truly Relaxed Moisturizing Shampoo).
An ingredient that might be confused for a sulfate is behentrimonium methosulfate, a cationic quaternary ammonium salt that is not used to cleanse the hair, unlike sodium lauryl sulfate and sodium laureth sulfate, but serves as an antistatic conditioning agent to keep hair moisturized and frizz free.11 Behentrimonium methosulfate is found in conditioners and detanglers in Table 1 (The Mane Choice Green Tea & Carrot Conditioning Mask, Kinky-Curly Knot Today, Miss Jessie’s Leave-In Condish, SheaMoisture Raw Shea Butter Extra-Moisture Detangler, Mielle Pomegranate & Honey Leave-In Conditioner). Patients should be informed that behentrimonium methosulfate is not water soluble, which suggests that it can lead to buildup of residue.
Cationic Surfactants and Cationic Polymers
Cationic surfactants and cationic polymers are found in many hair products and improve manageability by softening and detangling hair.6,10 Hair consists of negatively charged keratin proteins7 that electrostatically attract the positively charged polar group of cationic surfactants and cationic polymers. These surfactants and polymers then adhere to and normalize hair surface charges, resulting in improved texture and reduced friction between strands.6 For African American patients with natural hair, cationic surfactants and polymers help to maintain curl patterns and assist in detangling.6 Polyquaternium is a cationic polymer that is found in several products in Table 1 (Carol’s Daughter Black Vanilla Moisture & Shine Sulfate-Free Shampoo, OGX Nourishing Coconut Milk Shampoo, ApHogee Deep Moisture Shampoo, Pantene Pro-V Gold Series Shampoo, Neutrogena Triple Moisture Silk Touch Leave-In Conditioner, Creme of Nature Argan Oil Strength & Shine Leave-in Conditioner, and John Frieda Frizz Ease Daily Nourishment Leave-In Conditioner).
The surfactants triethanolamine and tetrasodium ethylenediaminetetraacetic acid (EDTA) are ingredients in some styling gels and have been reported as potential carcinogens.12 However, there are inadequate human or animal data to support the carcinogenicity of either ingredient at this time. Of note, tetrasodium EDTA has been reported to increase the penetration of other chemicals through the skin, which might lead to toxicity.12
Silicone
Silicone agents can be found in a variety of hair care products, including shampoos, detanglers, hair conditioners, leave-in conditioners, and moisturizers. Of the 22 products listed in Table 1, silicones are found in 14 products. Common silicones include dimethicone, amodimethicone, cyclopentasiloxane, and dimethiconol. Silicones form hydrophobic films that create smoothness and shine.6,8 Silicone-containing products help reduce frizz and provide protection against breakage and heat damage in chemically relaxed hair.6,7 For patients with natural hair, silicones aid in hair detangling.
Frequent use of silicone products can result in residue buildup due to the insolubility of silicone in water. Preventatively, some products include water-soluble silicones with the same benefits, such as silicones with the prefixes PPG- or PEG-, laurylmethicone copolyol, and dimethicone copolyol.7 Dimethicone copolyol was found in 1 of our reviewed products (OGX Nourishing Coconut Milk Shampoo); 10 products in Table 1 contain ingredients with the prefixes PPG- or PEG-. Several products in our review contain both water-soluble and water-insoluble silicones (eg, Creme of Nature Argan Oil Strength & Shine Leave-In Conditioner).
Oils
Oils in hair care products prevent hair breakage by coating the hair shaft and sealing in moisture. There are various types of oils in hair care products. Essential oils are volatile liquid-aroma substances derived most commonly from plants through dry or steam distillation or by other mechanical processes.13 Essential oils are used to seal and moisturize the hair and often are used to produce fragrance in hair products.6 Examples of essential oils that are ingredients in cosmetics include tea tree oil (TTO), peppermint oil, rosemary oil, and thyme oil. Vegetable oils can be used to dilute essential oils because essential oils can irritate skin.14
Tea tree oil is an essential oil obtained through steam distillation of the leaves of the coastal tree Melaleuca alternifolia. The molecule terpinen-4-ol is a major component of TTO thought to exhibit antiseptic and anti-inflammatory properties.15 Pazyar et al16 reviewed several studies that propose the use of TTO to treat acne vulgaris, seborrheic dermatitis, and chronic gingivitis. Although this herbal oil seemingly has many possible dermatologic applications, dermatologists should be aware that reports have linked TTO to allergic contact dermatitis due to 1,8-cineole, another constituent of TTO.17 Tea tree oil is an ingredient in several of the hair care products that we reviewed. With growing patient interest in the benefits of TTO, further research is necessary to establish guidelines on its use for seborrheic dermatitis.
Castor oil is a vegetable oil pressed from the seeds of the castor oil plant. Its primary fatty acid group—ricinoleic acid—along with certain salts and esters function primarily as skin-conditioning agents, emulsion stabilizers, and surfactants in cosmetic products.18 Jamaican black castor oil is a popular moisturizing oil in the African American natural hair community. It differs in color from standard castor oil because of the manner in which the oil is processed. Anecdotally, it is sometimes advertised as a hair growth serum; some patients admit to applying Jamaican black castor oil on the scalp as self-treatment of alopecia. The basis for such claims might stem from research showing that ricinoleic acid exhibits anti-inflammatory and analgesic properties in some mice and guinea pig models with repeated topical application.17 Scientific evidence does not, however, support claims that castor oil or Jamaican black castor oil can treat alopecia.
Mineral oils have a lubricant base and are refined from petroleum crude oils. The composition of crude oil varies; to remove impurities, it must undergo treatment with different degrees of refinement. When products are highly treated, the result is a substantially decreased level of impurities.19 Although they are beneficial in coating the hair shaft and preventing hair damage, consumers tend to avoid products containing mineral oil because of its carcinogenic potential if untreated or mildly treated.20
Although cosmetics with mineral oils are highly treated, a study showed that mineral oil is the largest contaminant in the human body, with cosmetics being a possible source.21 Studies also have revealed that mineral oils do not prevent hair breakage compared to other oils, such as essential oils and coconut oil.22,23 Many consumers therefore choose to avoid mineral oil because alternative oils exist that are beneficial in preventing hair damage but do not present carcinogenic risk. An example of a mineral oil–free product in Table 1 is Mizani Coconut Souffle Light Moisturizing Hairdress. Only 8 of the 57 products we reviewed did not contain oil, including the following 5 included in Table 1: Carol’s Daughter Black Vanilla Moisture & Shine Sulfate-Free Shampoo, Miss Jessie’s Leave-In Condish, Kinky-Curly Knot Today (although this product did have behentrimonium made from rapeseed oil), Herbal Essences Hello Hydration Moisturizing Conditioner, and ampro Pro Styl Protein Styling Gel.
Parabens
Parabens are preservatives used to prevent growth of pathogens in and prevent decomposition of cosmetic products. Parabens have attracted a lot of criticism because of their possible link to breast cancer.24 In vitro and in vivo studies of parabens have demonstrated weak estrogenic activity that increased proportionally with increased length and branching of alkyl side chains. In vivo animal studies demonstrated weak estrogenic activity—100,000-fold less potent than 17β-estradiol.25 Ongoing research examines the relationship between the estrogenic properties of parabens, endocrine disruption, and cancer in human breast epithelial cells.5,24 The Cosmetic Ingredient Review and the US Food and Drug Administration uphold that parabens are safe to use in cosmetics.26 Several products that include parabens are listed in Table 1 (ApHogee Deep Moisture Shampoo, Neutrogena Triple Moisture Silk Touch Leave-In Conditioner, John Frieda Frizz Ease Daily Nourishment Leave-In Conditioner, and ampro Pro Styl Protein Styling Gel).
Our Recommendations
Table 2 (although not exhaustive) includes the authors’ recommendations of hair care products for individuals of African descent. Dermatologists should discuss the pros and cons of the use of products with ingredients that have controversial health effects, namely parabens, triethanolamine, tetrasodium EDTA, and mineral oils. Our recommendations do not include products that contain the prior ingredients. For many women of African descent, their hair type and therefore product use changes with the season, health of their hair, and normal changes to hair throughout their lifetime. There is no magic product for all: Each patient has specific individual styling preferences and a distinctive hair type. Decisions about which products to use can be guided with the assistance of a dermatologist but will ultimately be left up to the patient.
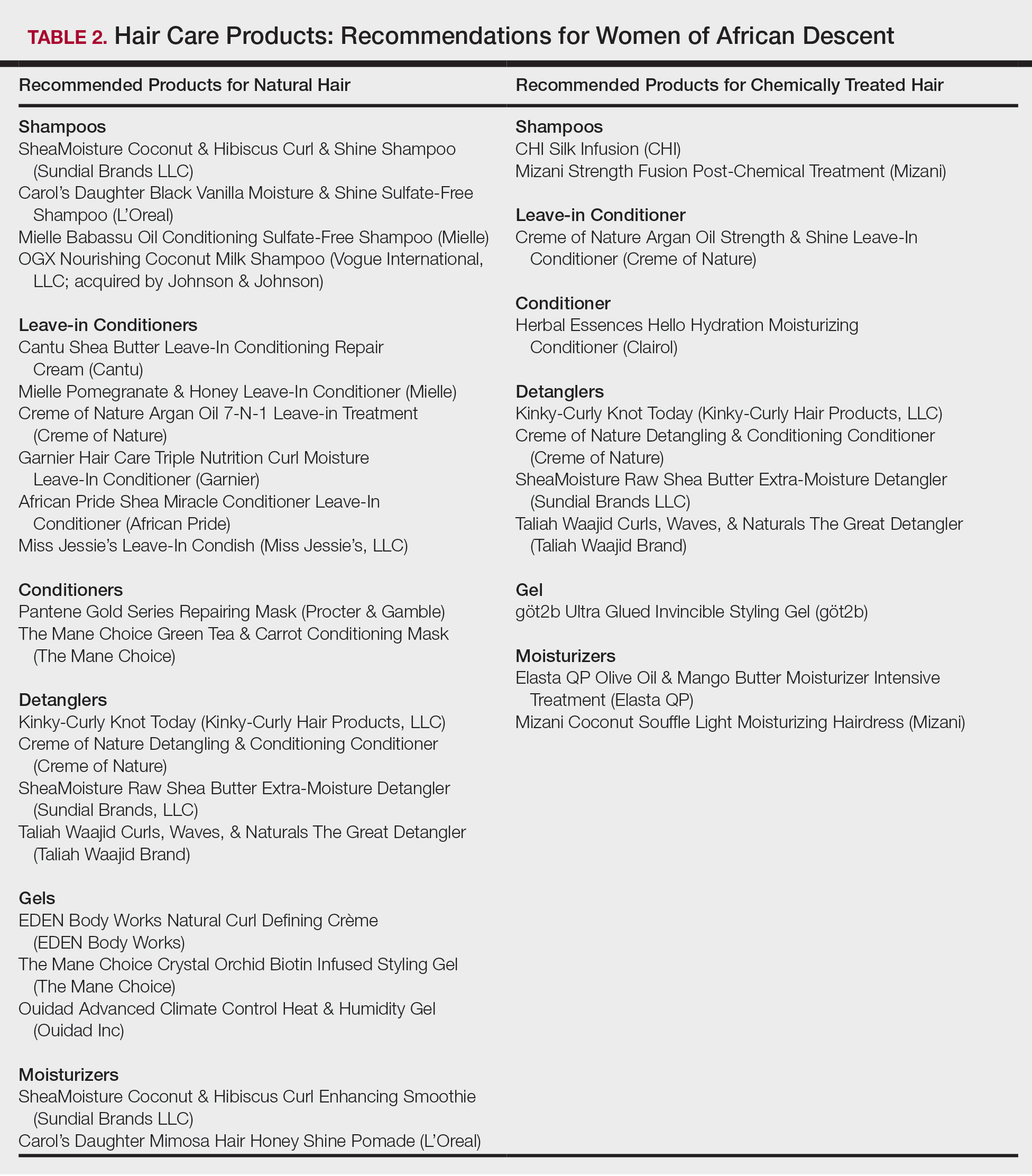
Conclusion
Given the array of hair and scalp care products, it is helpful for dermatologists to become familiar with several of the most popular ingredients and commonly used products. It might be helpful to ask patients which products they use and which ones have been effective for their unique hair concerns. Thus, you become armed with a catalogue of product recommendations for your patients.
- Taylor S, Kelly AP, Lim HW, et al. Taylor and Kelly’s Dermatology for Skin of Color. 2nd ed. New York, NY: McGraw-Hill; 2009.
- Gathers RC, Mahan MG. African American women, hair care, and health barriers. J Clin Aesthet Dermatol. 2014;7:26-29.
- Quinn CR, Quinn TM, Kelly AP. Hair care practices in African American women. Cutis. 2003;72:280-282, 285-289.
- Griffin M, Lenzy Y. Contemporary African-American hair care practices. Pract Dermatol. http://practicaldermatology.com/2015/05/contemporary-african-american-hair-care-practices/. May 2015. Accessed March 19, 2020.
- Helm JS, Nishioka M, Brody JG, et al. Measurement of endocrine disrupting and asthma-associated chemicals in hair products used by black women. Environ Res. 2018;165:448-458.
- Crawford K, Hernandez C. A review of hair care products for black individuals. Cutis. 2014;93:289-293.
- Bosley RE, Daveluy S. A primer to natural hair care practices in black patients. Cutis. 2015;95:78-80, 106.
- Cline A, Uwakwe L, McMichael A. No sulfates, no parabens, and the “no-poo” method: a new patient perspective on common shampoo ingredients. Cutis. 2018;101:22-26.
- Gavazzoni Dias MFR. Hair cosmetics: an overview. Int J Trichology. 2015;7:2-15.
- Draelos ZD. Essentials of hair care often neglected: hair cleansing.Int J Trichology. 2010;2:24-29.
- Becker L, Bergfeld W, Belsito D, et al. Safety assessment of trimoniums as used in cosmetics. Int J Toxicol. 2012;31(6 suppl):296S-341S.
- National Center for Biotechnology Information. PubChem Database. Edetate sodium, CID=6144. https://pubchem.ncbi.nlm.nih.gov/compound/EDTA_
tetrasodium#section=FDA-Requirements. Accessed March 19, 2020. - Lanigan RS, Yamarik TA. Final report on the safety assessment of EDTA, calcium disodium EDTA, diammonium EDTA, dipotassium EDTA, disodium EDTA, TEA-EDTA, tetrasodium EDTA, tripotassium EDTA, trisodium EDTA, HEDTA, and trisodium HEDTA. Int J Toxicol. 2002;21(suppl 2):95-142.
- Vasireddy L, Bingle LEH, Davies MS. Antimicrobial activity of essential oils against multidrug-resistant clinical isolates of the Burkholderia cepacia complex. PLoS One. 2018;13:e0201835.
- Mondello F, De Bernardis F, Girolamo A, et al. In vivo activity of terpinen-4-ol, the main bioactive component of Melaleuca alternifolia Cheel (tea tree) oil against azole-susceptible and -resistant human pathogenic Candida species. BMC Infect Dis. 2006;6:158.
- Pazyar N, Yaghoobi R, Bagherani N, et al. A review of applications of tea tree oil in dermatology. Int J Dermatol. 2013;52:784-790.
- Selvaag E, Eriksen B, Thune P. Contact allergy due to tea tree oil and cross-sensitization to colophony. Contact Dermatitis. 1994;31:124-125.
- Vieira C, Fetzer S, Sauer SK, et al. Pro- and anti-inflammatory actions of ricinoleic acid: similarities and differences with capsaicin. Naunyn Schmiedebergs Arch Pharmacol. 2001;364:87-95.
- International Agency for Research on Cancer, IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Polynuclear Aromatic Hydrocarbons, Part 2, Carbon Blacks, Mineral Oils (Lubricant Base Oils and Derived Products) and Sorne Nitroarenes. Vol 33. Lyon, France: International Agency for Research on Cancer; April 1984. https://monographs.iarc.fr/wp-content/uploads/2018/06/mono33.pdf. Accessed March 19, 2020.
- Vieira C, Evangelista S, Cirillo R, et al. Effect of ricinoleic acid in acute and subchronic experimental models of inflammation. Mediators Inflamm. 2000;9:223-228.
- Concin N, Hofstetter G, Plattner B, et al. Evidence for cosmetics as a source of mineral oil contamination in women. J Womens Health (Larchmt). 2011;20:1713-1719.
- Biedermann M, Barp L, Kornauth C, et al. Mineral oil in human tissues, part II: characterization of the accumulated hydrocarbons by comprehensive two-dimensional gas chromatography. Sci Total Environ. 2015;506-507:644-655.
- Ruetsch SB, Kamath YK, Rele AS, et al. Secondary ion mass spectrometric investigation of penetration of coconut and mineral oils into human hair fibers: relevance to hair damage. J Cosmet Sci. 2001;52:169-184.
- Darbre PD, Aljarrah A, Miller WR, et al. Concentrations of parabens in human breast tumours. J Appl Toxicol. 2004;24:5-13.
- Routledge EJ, Parker J, Odum J, et al. Some alkyl hydroxy benzoate preservatives (parabens) are estrogenic. Toxicol Appl Pharmacol. 1998;153:12-19.
- Centers for Disease Control and Prevention. Parabens factsheet. https://www.cdc.gov/biomonitoring/Parabens_FactSheet.html. Updated April 7, 2017. Accessed March 19, 2020.
In the African American and African communities, information regarding the care and treatment of hair and skin often is obtained from relatives as well as Internet videos and bloggers.1 Moreover, fewer than half of African American women surveyed believe that their physician understands African American hair.2 In addition to proficiency in the diagnosis and treatment of hair and scalp disorders in this population, dermatologists must be aware of common hair and scalp beliefs, misconceptions, care, and product use to ensure culturally competent interactions and treatment.
When a patient of African descent refers to their hair as “natural,” he/she is referring to its texture compared with hair that is chemically treated with straighteners (ie, “relaxed” or “permed” hair). Natural hair refers to hair that has not been altered with chemical treatments that permanently break and re-form disulfide bonds of the hair.1 In 2003, it was estimated that 80% of African American women treated their hair with a chemical relaxer.3 However, this preference has changed over the last decade, with a larger percentage of African American women choosing to wear a natural hairstyle.4
Regardless of preferred hairstyle, a multitude of products can be used to obtain and maintain the particular style. According to US Food and Drug Administration regulations, a product’s ingredients must appear on an information panel in descending order of predominance. Additionally, products must be accurately labeled without misleading information. However, one study found that hair care products commonly used by African American women contain mixtures of endocrine-disrupting chemicals, and 84% of detected chemicals are not listed on the label.5
Properties of Hair Care Products
Women of African descent use hair grooming products for cleansing and moisturizing the hair and scalp, detangling, and styling. Products to achieve these goals comprise shampoos, leave-in and rinse-out conditioners, creams, pomades, oils, and gels. In August 2018 we performed a Google search of the most popular hair care products used for natural hair and chemically relaxed African American hair. Key terms used in our search included popular natural hair products, best natural hair products, top natural hair products, products for permed hair, shampoos for permed hair, conditioner for permed hair, popular detanglers for African American hair, popular products for natural hair, detanglers used for permed hair, gels for relaxed hair, moisturizers for relaxed hair, gels for natural hair, and popular moisturizers for African American hair. We reviewed all websites generated by the search and compared the most popular brands, compiled a list of products, and reviewed them for availability in 2 beauty supply stores in Philadelphia, Pennsylvania; 1 Walmart in Hershey, Pennsylvania; and 1 Walmart in Willow Grove, Pennsylvania. Of the 80 products identified, we selected 57 products to be reviewed for ingredients based on which ones were most commonly seen in search results. Table 1 highlights several randomly chosen popular hair care products used by African American women to familiarize dermatologists with specific products and manufacturers.
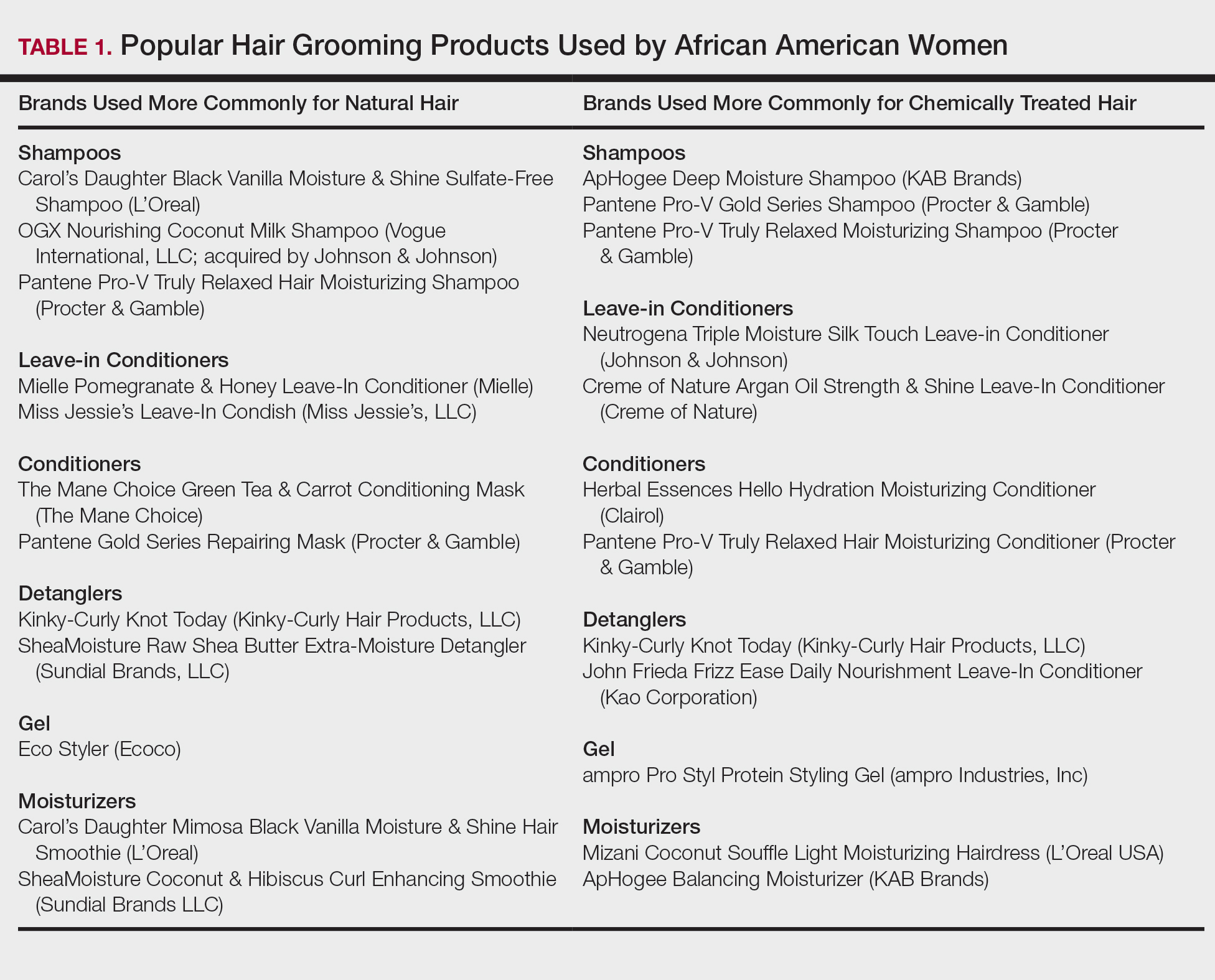
Tightly coiled hair, common among women of African descent, is considered fragile because of decreased water content and tensile strength.6 Fragility is exacerbated by manipulation during styling, excessive heat, and harsh shampoos that strip the hair of moisture, as well as chemical treatments that lead to protein deficiency.4,6,7 Because tightly coiled hair is naturally dry and fragile, women of African descent have a particular preference for products that reduce hair dryness and breakage, which has led to the popularity of sulfate-free shampoos that minimize loss of moisture in hair; moisturizers, oils, and conditioners also are used to enhance moisture retention in hair. Conditioners also provide protein substances that can help strengthen hair.4
Consumers’ concerns about the inclusion of potentially harmful ingredients have resulted in reformulation of many products. Our review of products demonstrated that natural hair consumers used fewer products containing silicones, parabens, and sulfates, compared to consumers with chemically relaxed hair. Another tool used by manufacturers to address these concerns is the inclusion of an additional label to distinguish the product as sulfate free, silicone free, paraben free, petroleum free, or a combination of these terms. Although many patients believe that there are “good” and “bad” products, they should be made aware that there are pros and cons of ingredients frequently found in hair-grooming products. Popular ingredients in hair care products include sulfates, cationic surfactants and cationic polymers, silicone, oils, and parabens.
Sulfates
Sulfates are anion detergents in shampoo that remove sebum from the scalp and hair. The number of sulfates in a shampoo positively correlates to cleansing strength.1 However, sulfates can cause excessive sebum removal and lead to hair that is hard, rough, dull, and prone to tangle and breakage.6 Sulfates also dissolve oil on the hair, causing additional dryness and breakage.7
There are a variety of sulfate compounds with different sebum-removal capabilities. Lauryl sulfates are commonly used in shampoos for oily hair. Tightly coiled hair that has been overly cleansed with these ingredients can become exceedingly dry and unmanageable, which explains why products with lauryl sulfates are avoided. Table 1 includes only 1 product containing lauryl sulfate (Pantene Pro-V Gold Series Shampoo). Patients using a lauryl sulfate–containing shampoo can select a product that also contains a conditioning agent in the formulation.6 Alternatively, sulfate-free shampoos that contain surfactants with less detergency can be used.8 There are no published studies of the cleansing ability of sulfate-free shampoos or their effects on hair shaft fragility.9
At the opposite end of the spectrum is sodium laureth sulfate, commonly used as a primary detergent in shampoos designed for normal to dry hair.10 Sodium laureth sulfate, which provides excellent cleansing and leaves the hair better moisturized and manageable compared to lauryl sulfates,10 is a common ingredient in the products in Table 1 (ApHogee Deep Moisture Shampoo, Pantene Pro-V Gold Series Shampoo, and Pantene Pro-V Truly Relaxed Moisturizing Shampoo).
An ingredient that might be confused for a sulfate is behentrimonium methosulfate, a cationic quaternary ammonium salt that is not used to cleanse the hair, unlike sodium lauryl sulfate and sodium laureth sulfate, but serves as an antistatic conditioning agent to keep hair moisturized and frizz free.11 Behentrimonium methosulfate is found in conditioners and detanglers in Table 1 (The Mane Choice Green Tea & Carrot Conditioning Mask, Kinky-Curly Knot Today, Miss Jessie’s Leave-In Condish, SheaMoisture Raw Shea Butter Extra-Moisture Detangler, Mielle Pomegranate & Honey Leave-In Conditioner). Patients should be informed that behentrimonium methosulfate is not water soluble, which suggests that it can lead to buildup of residue.
Cationic Surfactants and Cationic Polymers
Cationic surfactants and cationic polymers are found in many hair products and improve manageability by softening and detangling hair.6,10 Hair consists of negatively charged keratin proteins7 that electrostatically attract the positively charged polar group of cationic surfactants and cationic polymers. These surfactants and polymers then adhere to and normalize hair surface charges, resulting in improved texture and reduced friction between strands.6 For African American patients with natural hair, cationic surfactants and polymers help to maintain curl patterns and assist in detangling.6 Polyquaternium is a cationic polymer that is found in several products in Table 1 (Carol’s Daughter Black Vanilla Moisture & Shine Sulfate-Free Shampoo, OGX Nourishing Coconut Milk Shampoo, ApHogee Deep Moisture Shampoo, Pantene Pro-V Gold Series Shampoo, Neutrogena Triple Moisture Silk Touch Leave-In Conditioner, Creme of Nature Argan Oil Strength & Shine Leave-in Conditioner, and John Frieda Frizz Ease Daily Nourishment Leave-In Conditioner).
The surfactants triethanolamine and tetrasodium ethylenediaminetetraacetic acid (EDTA) are ingredients in some styling gels and have been reported as potential carcinogens.12 However, there are inadequate human or animal data to support the carcinogenicity of either ingredient at this time. Of note, tetrasodium EDTA has been reported to increase the penetration of other chemicals through the skin, which might lead to toxicity.12
Silicone
Silicone agents can be found in a variety of hair care products, including shampoos, detanglers, hair conditioners, leave-in conditioners, and moisturizers. Of the 22 products listed in Table 1, silicones are found in 14 products. Common silicones include dimethicone, amodimethicone, cyclopentasiloxane, and dimethiconol. Silicones form hydrophobic films that create smoothness and shine.6,8 Silicone-containing products help reduce frizz and provide protection against breakage and heat damage in chemically relaxed hair.6,7 For patients with natural hair, silicones aid in hair detangling.
Frequent use of silicone products can result in residue buildup due to the insolubility of silicone in water. Preventatively, some products include water-soluble silicones with the same benefits, such as silicones with the prefixes PPG- or PEG-, laurylmethicone copolyol, and dimethicone copolyol.7 Dimethicone copolyol was found in 1 of our reviewed products (OGX Nourishing Coconut Milk Shampoo); 10 products in Table 1 contain ingredients with the prefixes PPG- or PEG-. Several products in our review contain both water-soluble and water-insoluble silicones (eg, Creme of Nature Argan Oil Strength & Shine Leave-In Conditioner).
Oils
Oils in hair care products prevent hair breakage by coating the hair shaft and sealing in moisture. There are various types of oils in hair care products. Essential oils are volatile liquid-aroma substances derived most commonly from plants through dry or steam distillation or by other mechanical processes.13 Essential oils are used to seal and moisturize the hair and often are used to produce fragrance in hair products.6 Examples of essential oils that are ingredients in cosmetics include tea tree oil (TTO), peppermint oil, rosemary oil, and thyme oil. Vegetable oils can be used to dilute essential oils because essential oils can irritate skin.14
Tea tree oil is an essential oil obtained through steam distillation of the leaves of the coastal tree Melaleuca alternifolia. The molecule terpinen-4-ol is a major component of TTO thought to exhibit antiseptic and anti-inflammatory properties.15 Pazyar et al16 reviewed several studies that propose the use of TTO to treat acne vulgaris, seborrheic dermatitis, and chronic gingivitis. Although this herbal oil seemingly has many possible dermatologic applications, dermatologists should be aware that reports have linked TTO to allergic contact dermatitis due to 1,8-cineole, another constituent of TTO.17 Tea tree oil is an ingredient in several of the hair care products that we reviewed. With growing patient interest in the benefits of TTO, further research is necessary to establish guidelines on its use for seborrheic dermatitis.
Castor oil is a vegetable oil pressed from the seeds of the castor oil plant. Its primary fatty acid group—ricinoleic acid—along with certain salts and esters function primarily as skin-conditioning agents, emulsion stabilizers, and surfactants in cosmetic products.18 Jamaican black castor oil is a popular moisturizing oil in the African American natural hair community. It differs in color from standard castor oil because of the manner in which the oil is processed. Anecdotally, it is sometimes advertised as a hair growth serum; some patients admit to applying Jamaican black castor oil on the scalp as self-treatment of alopecia. The basis for such claims might stem from research showing that ricinoleic acid exhibits anti-inflammatory and analgesic properties in some mice and guinea pig models with repeated topical application.17 Scientific evidence does not, however, support claims that castor oil or Jamaican black castor oil can treat alopecia.
Mineral oils have a lubricant base and are refined from petroleum crude oils. The composition of crude oil varies; to remove impurities, it must undergo treatment with different degrees of refinement. When products are highly treated, the result is a substantially decreased level of impurities.19 Although they are beneficial in coating the hair shaft and preventing hair damage, consumers tend to avoid products containing mineral oil because of its carcinogenic potential if untreated or mildly treated.20
Although cosmetics with mineral oils are highly treated, a study showed that mineral oil is the largest contaminant in the human body, with cosmetics being a possible source.21 Studies also have revealed that mineral oils do not prevent hair breakage compared to other oils, such as essential oils and coconut oil.22,23 Many consumers therefore choose to avoid mineral oil because alternative oils exist that are beneficial in preventing hair damage but do not present carcinogenic risk. An example of a mineral oil–free product in Table 1 is Mizani Coconut Souffle Light Moisturizing Hairdress. Only 8 of the 57 products we reviewed did not contain oil, including the following 5 included in Table 1: Carol’s Daughter Black Vanilla Moisture & Shine Sulfate-Free Shampoo, Miss Jessie’s Leave-In Condish, Kinky-Curly Knot Today (although this product did have behentrimonium made from rapeseed oil), Herbal Essences Hello Hydration Moisturizing Conditioner, and ampro Pro Styl Protein Styling Gel.
Parabens
Parabens are preservatives used to prevent growth of pathogens in and prevent decomposition of cosmetic products. Parabens have attracted a lot of criticism because of their possible link to breast cancer.24 In vitro and in vivo studies of parabens have demonstrated weak estrogenic activity that increased proportionally with increased length and branching of alkyl side chains. In vivo animal studies demonstrated weak estrogenic activity—100,000-fold less potent than 17β-estradiol.25 Ongoing research examines the relationship between the estrogenic properties of parabens, endocrine disruption, and cancer in human breast epithelial cells.5,24 The Cosmetic Ingredient Review and the US Food and Drug Administration uphold that parabens are safe to use in cosmetics.26 Several products that include parabens are listed in Table 1 (ApHogee Deep Moisture Shampoo, Neutrogena Triple Moisture Silk Touch Leave-In Conditioner, John Frieda Frizz Ease Daily Nourishment Leave-In Conditioner, and ampro Pro Styl Protein Styling Gel).
Our Recommendations
Table 2 (although not exhaustive) includes the authors’ recommendations of hair care products for individuals of African descent. Dermatologists should discuss the pros and cons of the use of products with ingredients that have controversial health effects, namely parabens, triethanolamine, tetrasodium EDTA, and mineral oils. Our recommendations do not include products that contain the prior ingredients. For many women of African descent, their hair type and therefore product use changes with the season, health of their hair, and normal changes to hair throughout their lifetime. There is no magic product for all: Each patient has specific individual styling preferences and a distinctive hair type. Decisions about which products to use can be guided with the assistance of a dermatologist but will ultimately be left up to the patient.
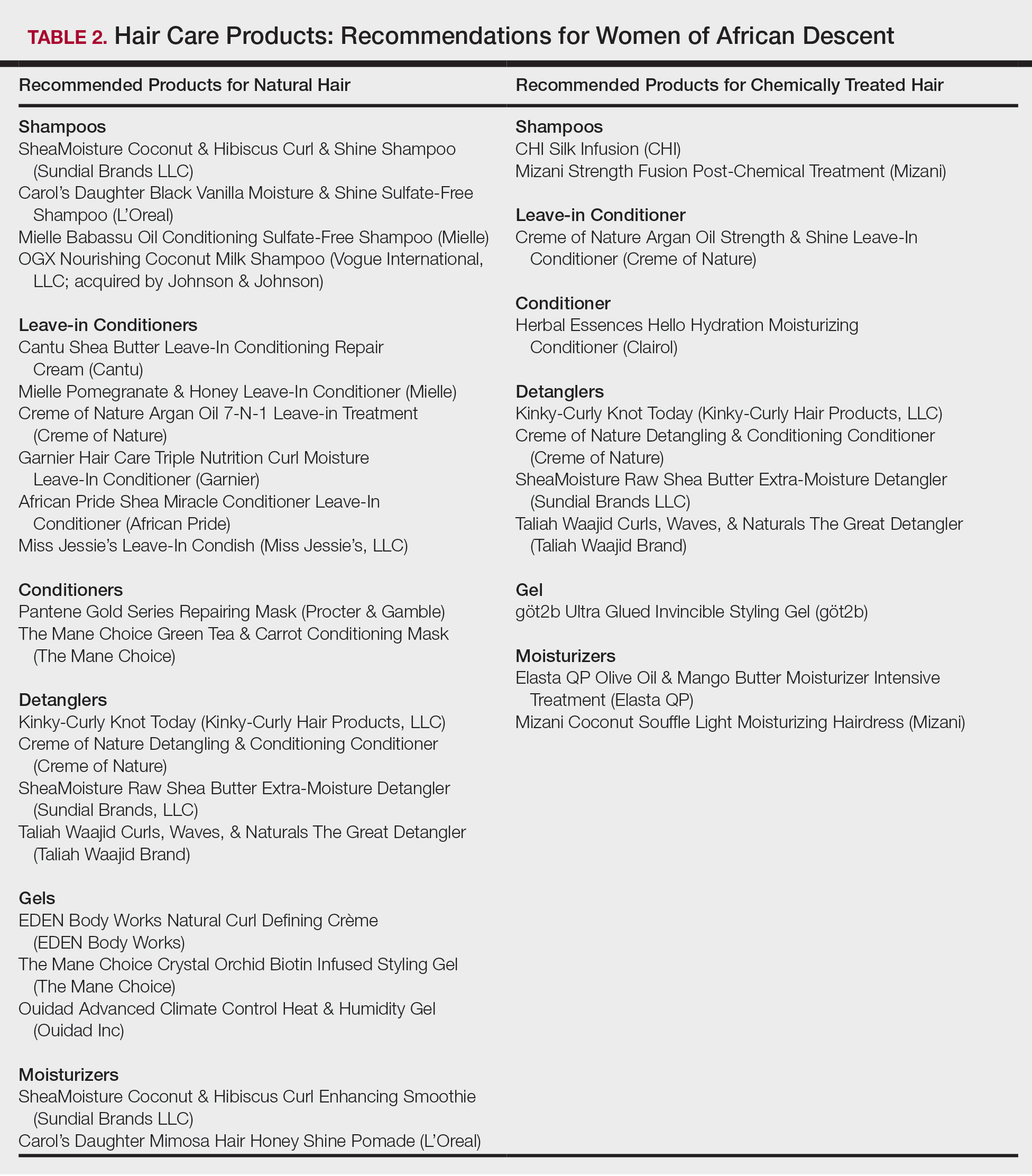
Conclusion
Given the array of hair and scalp care products, it is helpful for dermatologists to become familiar with several of the most popular ingredients and commonly used products. It might be helpful to ask patients which products they use and which ones have been effective for their unique hair concerns. Thus, you become armed with a catalogue of product recommendations for your patients.
In the African American and African communities, information regarding the care and treatment of hair and skin often is obtained from relatives as well as Internet videos and bloggers.1 Moreover, fewer than half of African American women surveyed believe that their physician understands African American hair.2 In addition to proficiency in the diagnosis and treatment of hair and scalp disorders in this population, dermatologists must be aware of common hair and scalp beliefs, misconceptions, care, and product use to ensure culturally competent interactions and treatment.
When a patient of African descent refers to their hair as “natural,” he/she is referring to its texture compared with hair that is chemically treated with straighteners (ie, “relaxed” or “permed” hair). Natural hair refers to hair that has not been altered with chemical treatments that permanently break and re-form disulfide bonds of the hair.1 In 2003, it was estimated that 80% of African American women treated their hair with a chemical relaxer.3 However, this preference has changed over the last decade, with a larger percentage of African American women choosing to wear a natural hairstyle.4
Regardless of preferred hairstyle, a multitude of products can be used to obtain and maintain the particular style. According to US Food and Drug Administration regulations, a product’s ingredients must appear on an information panel in descending order of predominance. Additionally, products must be accurately labeled without misleading information. However, one study found that hair care products commonly used by African American women contain mixtures of endocrine-disrupting chemicals, and 84% of detected chemicals are not listed on the label.5
Properties of Hair Care Products
Women of African descent use hair grooming products for cleansing and moisturizing the hair and scalp, detangling, and styling. Products to achieve these goals comprise shampoos, leave-in and rinse-out conditioners, creams, pomades, oils, and gels. In August 2018 we performed a Google search of the most popular hair care products used for natural hair and chemically relaxed African American hair. Key terms used in our search included popular natural hair products, best natural hair products, top natural hair products, products for permed hair, shampoos for permed hair, conditioner for permed hair, popular detanglers for African American hair, popular products for natural hair, detanglers used for permed hair, gels for relaxed hair, moisturizers for relaxed hair, gels for natural hair, and popular moisturizers for African American hair. We reviewed all websites generated by the search and compared the most popular brands, compiled a list of products, and reviewed them for availability in 2 beauty supply stores in Philadelphia, Pennsylvania; 1 Walmart in Hershey, Pennsylvania; and 1 Walmart in Willow Grove, Pennsylvania. Of the 80 products identified, we selected 57 products to be reviewed for ingredients based on which ones were most commonly seen in search results. Table 1 highlights several randomly chosen popular hair care products used by African American women to familiarize dermatologists with specific products and manufacturers.
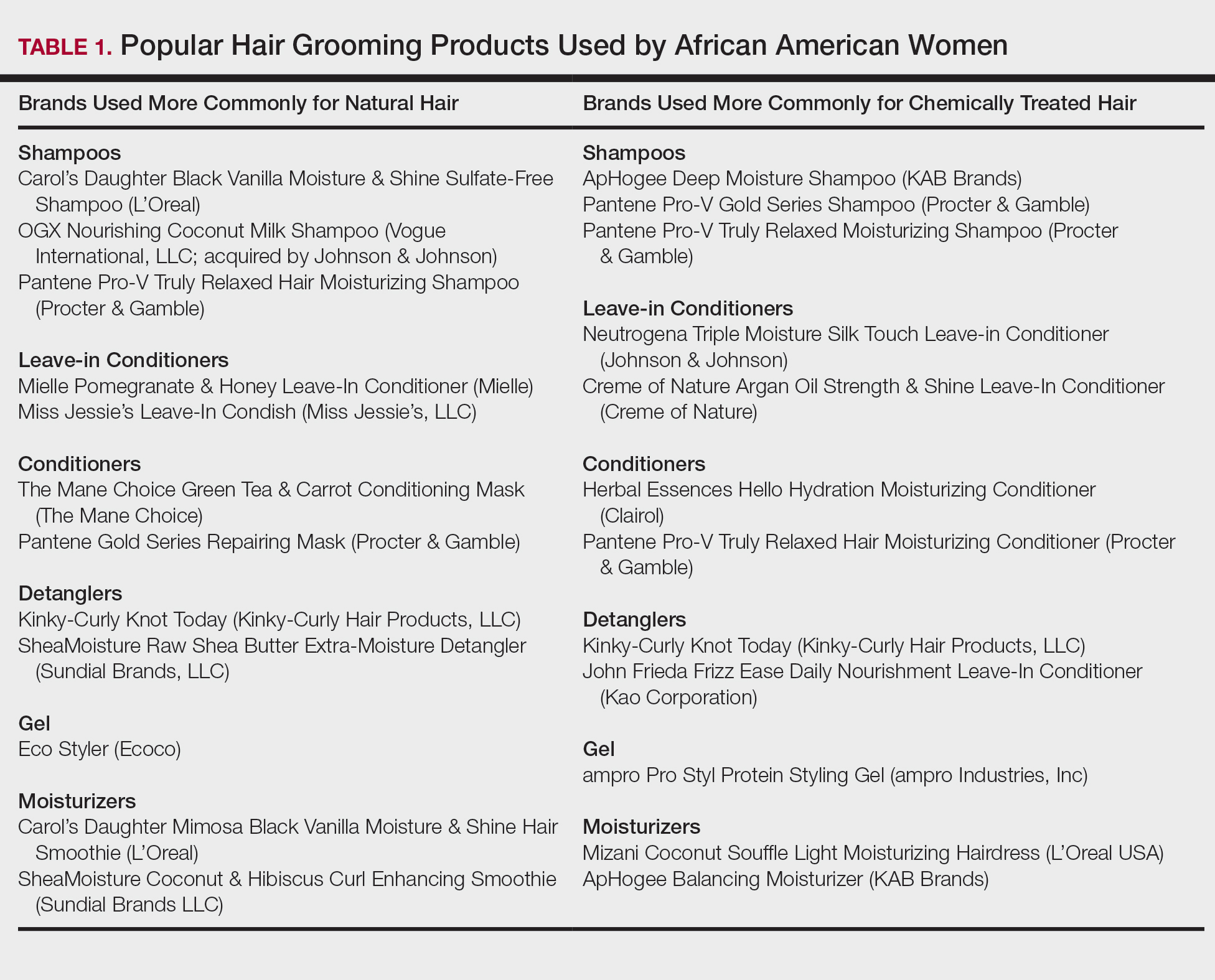
Tightly coiled hair, common among women of African descent, is considered fragile because of decreased water content and tensile strength.6 Fragility is exacerbated by manipulation during styling, excessive heat, and harsh shampoos that strip the hair of moisture, as well as chemical treatments that lead to protein deficiency.4,6,7 Because tightly coiled hair is naturally dry and fragile, women of African descent have a particular preference for products that reduce hair dryness and breakage, which has led to the popularity of sulfate-free shampoos that minimize loss of moisture in hair; moisturizers, oils, and conditioners also are used to enhance moisture retention in hair. Conditioners also provide protein substances that can help strengthen hair.4
Consumers’ concerns about the inclusion of potentially harmful ingredients have resulted in reformulation of many products. Our review of products demonstrated that natural hair consumers used fewer products containing silicones, parabens, and sulfates, compared to consumers with chemically relaxed hair. Another tool used by manufacturers to address these concerns is the inclusion of an additional label to distinguish the product as sulfate free, silicone free, paraben free, petroleum free, or a combination of these terms. Although many patients believe that there are “good” and “bad” products, they should be made aware that there are pros and cons of ingredients frequently found in hair-grooming products. Popular ingredients in hair care products include sulfates, cationic surfactants and cationic polymers, silicone, oils, and parabens.
Sulfates
Sulfates are anion detergents in shampoo that remove sebum from the scalp and hair. The number of sulfates in a shampoo positively correlates to cleansing strength.1 However, sulfates can cause excessive sebum removal and lead to hair that is hard, rough, dull, and prone to tangle and breakage.6 Sulfates also dissolve oil on the hair, causing additional dryness and breakage.7
There are a variety of sulfate compounds with different sebum-removal capabilities. Lauryl sulfates are commonly used in shampoos for oily hair. Tightly coiled hair that has been overly cleansed with these ingredients can become exceedingly dry and unmanageable, which explains why products with lauryl sulfates are avoided. Table 1 includes only 1 product containing lauryl sulfate (Pantene Pro-V Gold Series Shampoo). Patients using a lauryl sulfate–containing shampoo can select a product that also contains a conditioning agent in the formulation.6 Alternatively, sulfate-free shampoos that contain surfactants with less detergency can be used.8 There are no published studies of the cleansing ability of sulfate-free shampoos or their effects on hair shaft fragility.9
At the opposite end of the spectrum is sodium laureth sulfate, commonly used as a primary detergent in shampoos designed for normal to dry hair.10 Sodium laureth sulfate, which provides excellent cleansing and leaves the hair better moisturized and manageable compared to lauryl sulfates,10 is a common ingredient in the products in Table 1 (ApHogee Deep Moisture Shampoo, Pantene Pro-V Gold Series Shampoo, and Pantene Pro-V Truly Relaxed Moisturizing Shampoo).
An ingredient that might be confused for a sulfate is behentrimonium methosulfate, a cationic quaternary ammonium salt that is not used to cleanse the hair, unlike sodium lauryl sulfate and sodium laureth sulfate, but serves as an antistatic conditioning agent to keep hair moisturized and frizz free.11 Behentrimonium methosulfate is found in conditioners and detanglers in Table 1 (The Mane Choice Green Tea & Carrot Conditioning Mask, Kinky-Curly Knot Today, Miss Jessie’s Leave-In Condish, SheaMoisture Raw Shea Butter Extra-Moisture Detangler, Mielle Pomegranate & Honey Leave-In Conditioner). Patients should be informed that behentrimonium methosulfate is not water soluble, which suggests that it can lead to buildup of residue.
Cationic Surfactants and Cationic Polymers
Cationic surfactants and cationic polymers are found in many hair products and improve manageability by softening and detangling hair.6,10 Hair consists of negatively charged keratin proteins7 that electrostatically attract the positively charged polar group of cationic surfactants and cationic polymers. These surfactants and polymers then adhere to and normalize hair surface charges, resulting in improved texture and reduced friction between strands.6 For African American patients with natural hair, cationic surfactants and polymers help to maintain curl patterns and assist in detangling.6 Polyquaternium is a cationic polymer that is found in several products in Table 1 (Carol’s Daughter Black Vanilla Moisture & Shine Sulfate-Free Shampoo, OGX Nourishing Coconut Milk Shampoo, ApHogee Deep Moisture Shampoo, Pantene Pro-V Gold Series Shampoo, Neutrogena Triple Moisture Silk Touch Leave-In Conditioner, Creme of Nature Argan Oil Strength & Shine Leave-in Conditioner, and John Frieda Frizz Ease Daily Nourishment Leave-In Conditioner).
The surfactants triethanolamine and tetrasodium ethylenediaminetetraacetic acid (EDTA) are ingredients in some styling gels and have been reported as potential carcinogens.12 However, there are inadequate human or animal data to support the carcinogenicity of either ingredient at this time. Of note, tetrasodium EDTA has been reported to increase the penetration of other chemicals through the skin, which might lead to toxicity.12
Silicone
Silicone agents can be found in a variety of hair care products, including shampoos, detanglers, hair conditioners, leave-in conditioners, and moisturizers. Of the 22 products listed in Table 1, silicones are found in 14 products. Common silicones include dimethicone, amodimethicone, cyclopentasiloxane, and dimethiconol. Silicones form hydrophobic films that create smoothness and shine.6,8 Silicone-containing products help reduce frizz and provide protection against breakage and heat damage in chemically relaxed hair.6,7 For patients with natural hair, silicones aid in hair detangling.
Frequent use of silicone products can result in residue buildup due to the insolubility of silicone in water. Preventatively, some products include water-soluble silicones with the same benefits, such as silicones with the prefixes PPG- or PEG-, laurylmethicone copolyol, and dimethicone copolyol.7 Dimethicone copolyol was found in 1 of our reviewed products (OGX Nourishing Coconut Milk Shampoo); 10 products in Table 1 contain ingredients with the prefixes PPG- or PEG-. Several products in our review contain both water-soluble and water-insoluble silicones (eg, Creme of Nature Argan Oil Strength & Shine Leave-In Conditioner).
Oils
Oils in hair care products prevent hair breakage by coating the hair shaft and sealing in moisture. There are various types of oils in hair care products. Essential oils are volatile liquid-aroma substances derived most commonly from plants through dry or steam distillation or by other mechanical processes.13 Essential oils are used to seal and moisturize the hair and often are used to produce fragrance in hair products.6 Examples of essential oils that are ingredients in cosmetics include tea tree oil (TTO), peppermint oil, rosemary oil, and thyme oil. Vegetable oils can be used to dilute essential oils because essential oils can irritate skin.14
Tea tree oil is an essential oil obtained through steam distillation of the leaves of the coastal tree Melaleuca alternifolia. The molecule terpinen-4-ol is a major component of TTO thought to exhibit antiseptic and anti-inflammatory properties.15 Pazyar et al16 reviewed several studies that propose the use of TTO to treat acne vulgaris, seborrheic dermatitis, and chronic gingivitis. Although this herbal oil seemingly has many possible dermatologic applications, dermatologists should be aware that reports have linked TTO to allergic contact dermatitis due to 1,8-cineole, another constituent of TTO.17 Tea tree oil is an ingredient in several of the hair care products that we reviewed. With growing patient interest in the benefits of TTO, further research is necessary to establish guidelines on its use for seborrheic dermatitis.
Castor oil is a vegetable oil pressed from the seeds of the castor oil plant. Its primary fatty acid group—ricinoleic acid—along with certain salts and esters function primarily as skin-conditioning agents, emulsion stabilizers, and surfactants in cosmetic products.18 Jamaican black castor oil is a popular moisturizing oil in the African American natural hair community. It differs in color from standard castor oil because of the manner in which the oil is processed. Anecdotally, it is sometimes advertised as a hair growth serum; some patients admit to applying Jamaican black castor oil on the scalp as self-treatment of alopecia. The basis for such claims might stem from research showing that ricinoleic acid exhibits anti-inflammatory and analgesic properties in some mice and guinea pig models with repeated topical application.17 Scientific evidence does not, however, support claims that castor oil or Jamaican black castor oil can treat alopecia.
Mineral oils have a lubricant base and are refined from petroleum crude oils. The composition of crude oil varies; to remove impurities, it must undergo treatment with different degrees of refinement. When products are highly treated, the result is a substantially decreased level of impurities.19 Although they are beneficial in coating the hair shaft and preventing hair damage, consumers tend to avoid products containing mineral oil because of its carcinogenic potential if untreated or mildly treated.20
Although cosmetics with mineral oils are highly treated, a study showed that mineral oil is the largest contaminant in the human body, with cosmetics being a possible source.21 Studies also have revealed that mineral oils do not prevent hair breakage compared to other oils, such as essential oils and coconut oil.22,23 Many consumers therefore choose to avoid mineral oil because alternative oils exist that are beneficial in preventing hair damage but do not present carcinogenic risk. An example of a mineral oil–free product in Table 1 is Mizani Coconut Souffle Light Moisturizing Hairdress. Only 8 of the 57 products we reviewed did not contain oil, including the following 5 included in Table 1: Carol’s Daughter Black Vanilla Moisture & Shine Sulfate-Free Shampoo, Miss Jessie’s Leave-In Condish, Kinky-Curly Knot Today (although this product did have behentrimonium made from rapeseed oil), Herbal Essences Hello Hydration Moisturizing Conditioner, and ampro Pro Styl Protein Styling Gel.
Parabens
Parabens are preservatives used to prevent growth of pathogens in and prevent decomposition of cosmetic products. Parabens have attracted a lot of criticism because of their possible link to breast cancer.24 In vitro and in vivo studies of parabens have demonstrated weak estrogenic activity that increased proportionally with increased length and branching of alkyl side chains. In vivo animal studies demonstrated weak estrogenic activity—100,000-fold less potent than 17β-estradiol.25 Ongoing research examines the relationship between the estrogenic properties of parabens, endocrine disruption, and cancer in human breast epithelial cells.5,24 The Cosmetic Ingredient Review and the US Food and Drug Administration uphold that parabens are safe to use in cosmetics.26 Several products that include parabens are listed in Table 1 (ApHogee Deep Moisture Shampoo, Neutrogena Triple Moisture Silk Touch Leave-In Conditioner, John Frieda Frizz Ease Daily Nourishment Leave-In Conditioner, and ampro Pro Styl Protein Styling Gel).
Our Recommendations
Table 2 (although not exhaustive) includes the authors’ recommendations of hair care products for individuals of African descent. Dermatologists should discuss the pros and cons of the use of products with ingredients that have controversial health effects, namely parabens, triethanolamine, tetrasodium EDTA, and mineral oils. Our recommendations do not include products that contain the prior ingredients. For many women of African descent, their hair type and therefore product use changes with the season, health of their hair, and normal changes to hair throughout their lifetime. There is no magic product for all: Each patient has specific individual styling preferences and a distinctive hair type. Decisions about which products to use can be guided with the assistance of a dermatologist but will ultimately be left up to the patient.
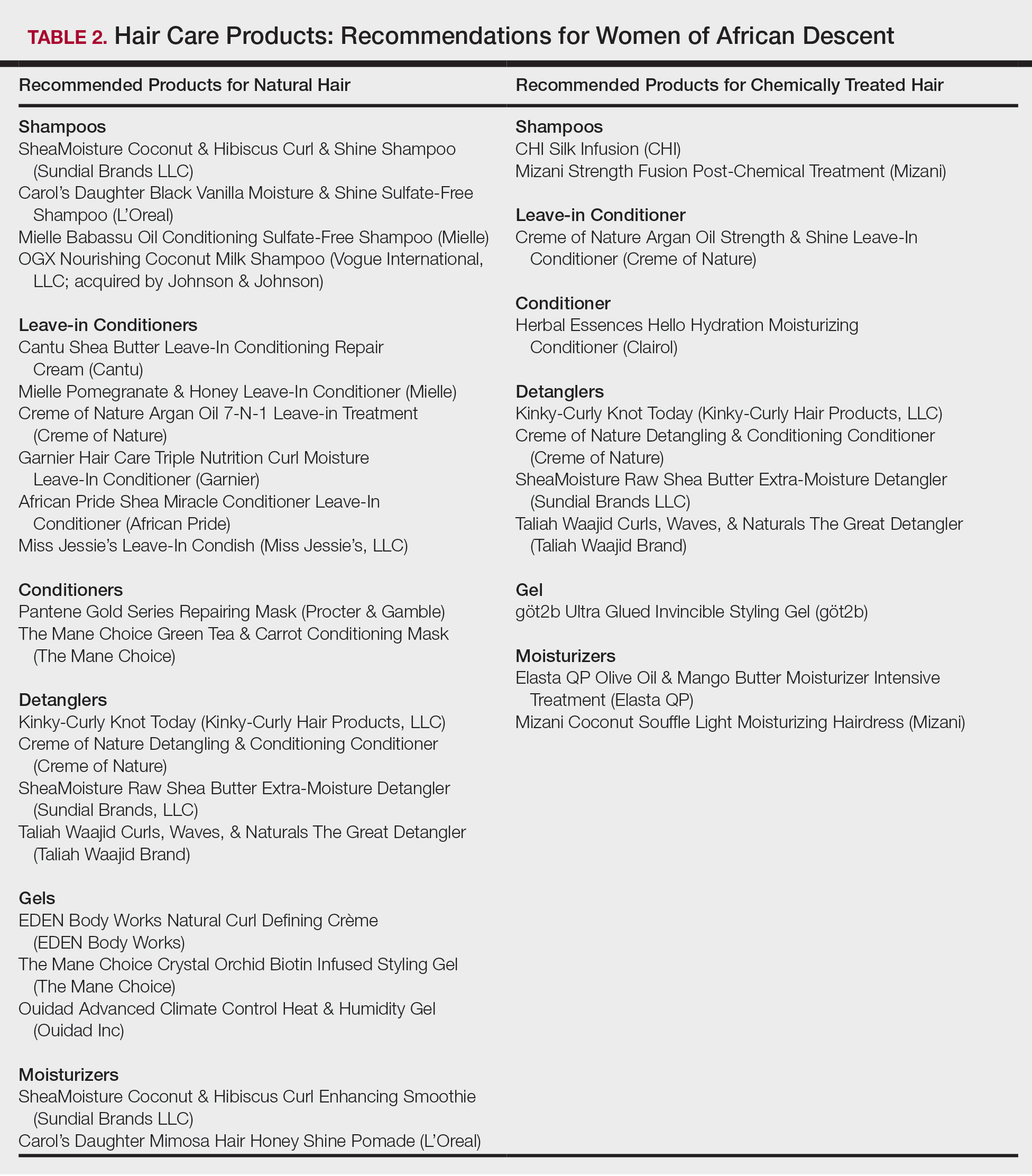
Conclusion
Given the array of hair and scalp care products, it is helpful for dermatologists to become familiar with several of the most popular ingredients and commonly used products. It might be helpful to ask patients which products they use and which ones have been effective for their unique hair concerns. Thus, you become armed with a catalogue of product recommendations for your patients.
- Taylor S, Kelly AP, Lim HW, et al. Taylor and Kelly’s Dermatology for Skin of Color. 2nd ed. New York, NY: McGraw-Hill; 2009.
- Gathers RC, Mahan MG. African American women, hair care, and health barriers. J Clin Aesthet Dermatol. 2014;7:26-29.
- Quinn CR, Quinn TM, Kelly AP. Hair care practices in African American women. Cutis. 2003;72:280-282, 285-289.
- Griffin M, Lenzy Y. Contemporary African-American hair care practices. Pract Dermatol. http://practicaldermatology.com/2015/05/contemporary-african-american-hair-care-practices/. May 2015. Accessed March 19, 2020.
- Helm JS, Nishioka M, Brody JG, et al. Measurement of endocrine disrupting and asthma-associated chemicals in hair products used by black women. Environ Res. 2018;165:448-458.
- Crawford K, Hernandez C. A review of hair care products for black individuals. Cutis. 2014;93:289-293.
- Bosley RE, Daveluy S. A primer to natural hair care practices in black patients. Cutis. 2015;95:78-80, 106.
- Cline A, Uwakwe L, McMichael A. No sulfates, no parabens, and the “no-poo” method: a new patient perspective on common shampoo ingredients. Cutis. 2018;101:22-26.
- Gavazzoni Dias MFR. Hair cosmetics: an overview. Int J Trichology. 2015;7:2-15.
- Draelos ZD. Essentials of hair care often neglected: hair cleansing.Int J Trichology. 2010;2:24-29.
- Becker L, Bergfeld W, Belsito D, et al. Safety assessment of trimoniums as used in cosmetics. Int J Toxicol. 2012;31(6 suppl):296S-341S.
- National Center for Biotechnology Information. PubChem Database. Edetate sodium, CID=6144. https://pubchem.ncbi.nlm.nih.gov/compound/EDTA_
tetrasodium#section=FDA-Requirements. Accessed March 19, 2020. - Lanigan RS, Yamarik TA. Final report on the safety assessment of EDTA, calcium disodium EDTA, diammonium EDTA, dipotassium EDTA, disodium EDTA, TEA-EDTA, tetrasodium EDTA, tripotassium EDTA, trisodium EDTA, HEDTA, and trisodium HEDTA. Int J Toxicol. 2002;21(suppl 2):95-142.
- Vasireddy L, Bingle LEH, Davies MS. Antimicrobial activity of essential oils against multidrug-resistant clinical isolates of the Burkholderia cepacia complex. PLoS One. 2018;13:e0201835.
- Mondello F, De Bernardis F, Girolamo A, et al. In vivo activity of terpinen-4-ol, the main bioactive component of Melaleuca alternifolia Cheel (tea tree) oil against azole-susceptible and -resistant human pathogenic Candida species. BMC Infect Dis. 2006;6:158.
- Pazyar N, Yaghoobi R, Bagherani N, et al. A review of applications of tea tree oil in dermatology. Int J Dermatol. 2013;52:784-790.
- Selvaag E, Eriksen B, Thune P. Contact allergy due to tea tree oil and cross-sensitization to colophony. Contact Dermatitis. 1994;31:124-125.
- Vieira C, Fetzer S, Sauer SK, et al. Pro- and anti-inflammatory actions of ricinoleic acid: similarities and differences with capsaicin. Naunyn Schmiedebergs Arch Pharmacol. 2001;364:87-95.
- International Agency for Research on Cancer, IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Polynuclear Aromatic Hydrocarbons, Part 2, Carbon Blacks, Mineral Oils (Lubricant Base Oils and Derived Products) and Sorne Nitroarenes. Vol 33. Lyon, France: International Agency for Research on Cancer; April 1984. https://monographs.iarc.fr/wp-content/uploads/2018/06/mono33.pdf. Accessed March 19, 2020.
- Vieira C, Evangelista S, Cirillo R, et al. Effect of ricinoleic acid in acute and subchronic experimental models of inflammation. Mediators Inflamm. 2000;9:223-228.
- Concin N, Hofstetter G, Plattner B, et al. Evidence for cosmetics as a source of mineral oil contamination in women. J Womens Health (Larchmt). 2011;20:1713-1719.
- Biedermann M, Barp L, Kornauth C, et al. Mineral oil in human tissues, part II: characterization of the accumulated hydrocarbons by comprehensive two-dimensional gas chromatography. Sci Total Environ. 2015;506-507:644-655.
- Ruetsch SB, Kamath YK, Rele AS, et al. Secondary ion mass spectrometric investigation of penetration of coconut and mineral oils into human hair fibers: relevance to hair damage. J Cosmet Sci. 2001;52:169-184.
- Darbre PD, Aljarrah A, Miller WR, et al. Concentrations of parabens in human breast tumours. J Appl Toxicol. 2004;24:5-13.
- Routledge EJ, Parker J, Odum J, et al. Some alkyl hydroxy benzoate preservatives (parabens) are estrogenic. Toxicol Appl Pharmacol. 1998;153:12-19.
- Centers for Disease Control and Prevention. Parabens factsheet. https://www.cdc.gov/biomonitoring/Parabens_FactSheet.html. Updated April 7, 2017. Accessed March 19, 2020.
- Taylor S, Kelly AP, Lim HW, et al. Taylor and Kelly’s Dermatology for Skin of Color. 2nd ed. New York, NY: McGraw-Hill; 2009.
- Gathers RC, Mahan MG. African American women, hair care, and health barriers. J Clin Aesthet Dermatol. 2014;7:26-29.
- Quinn CR, Quinn TM, Kelly AP. Hair care practices in African American women. Cutis. 2003;72:280-282, 285-289.
- Griffin M, Lenzy Y. Contemporary African-American hair care practices. Pract Dermatol. http://practicaldermatology.com/2015/05/contemporary-african-american-hair-care-practices/. May 2015. Accessed March 19, 2020.
- Helm JS, Nishioka M, Brody JG, et al. Measurement of endocrine disrupting and asthma-associated chemicals in hair products used by black women. Environ Res. 2018;165:448-458.
- Crawford K, Hernandez C. A review of hair care products for black individuals. Cutis. 2014;93:289-293.
- Bosley RE, Daveluy S. A primer to natural hair care practices in black patients. Cutis. 2015;95:78-80, 106.
- Cline A, Uwakwe L, McMichael A. No sulfates, no parabens, and the “no-poo” method: a new patient perspective on common shampoo ingredients. Cutis. 2018;101:22-26.
- Gavazzoni Dias MFR. Hair cosmetics: an overview. Int J Trichology. 2015;7:2-15.
- Draelos ZD. Essentials of hair care often neglected: hair cleansing.Int J Trichology. 2010;2:24-29.
- Becker L, Bergfeld W, Belsito D, et al. Safety assessment of trimoniums as used in cosmetics. Int J Toxicol. 2012;31(6 suppl):296S-341S.
- National Center for Biotechnology Information. PubChem Database. Edetate sodium, CID=6144. https://pubchem.ncbi.nlm.nih.gov/compound/EDTA_
tetrasodium#section=FDA-Requirements. Accessed March 19, 2020. - Lanigan RS, Yamarik TA. Final report on the safety assessment of EDTA, calcium disodium EDTA, diammonium EDTA, dipotassium EDTA, disodium EDTA, TEA-EDTA, tetrasodium EDTA, tripotassium EDTA, trisodium EDTA, HEDTA, and trisodium HEDTA. Int J Toxicol. 2002;21(suppl 2):95-142.
- Vasireddy L, Bingle LEH, Davies MS. Antimicrobial activity of essential oils against multidrug-resistant clinical isolates of the Burkholderia cepacia complex. PLoS One. 2018;13:e0201835.
- Mondello F, De Bernardis F, Girolamo A, et al. In vivo activity of terpinen-4-ol, the main bioactive component of Melaleuca alternifolia Cheel (tea tree) oil against azole-susceptible and -resistant human pathogenic Candida species. BMC Infect Dis. 2006;6:158.
- Pazyar N, Yaghoobi R, Bagherani N, et al. A review of applications of tea tree oil in dermatology. Int J Dermatol. 2013;52:784-790.
- Selvaag E, Eriksen B, Thune P. Contact allergy due to tea tree oil and cross-sensitization to colophony. Contact Dermatitis. 1994;31:124-125.
- Vieira C, Fetzer S, Sauer SK, et al. Pro- and anti-inflammatory actions of ricinoleic acid: similarities and differences with capsaicin. Naunyn Schmiedebergs Arch Pharmacol. 2001;364:87-95.
- International Agency for Research on Cancer, IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Polynuclear Aromatic Hydrocarbons, Part 2, Carbon Blacks, Mineral Oils (Lubricant Base Oils and Derived Products) and Sorne Nitroarenes. Vol 33. Lyon, France: International Agency for Research on Cancer; April 1984. https://monographs.iarc.fr/wp-content/uploads/2018/06/mono33.pdf. Accessed March 19, 2020.
- Vieira C, Evangelista S, Cirillo R, et al. Effect of ricinoleic acid in acute and subchronic experimental models of inflammation. Mediators Inflamm. 2000;9:223-228.
- Concin N, Hofstetter G, Plattner B, et al. Evidence for cosmetics as a source of mineral oil contamination in women. J Womens Health (Larchmt). 2011;20:1713-1719.
- Biedermann M, Barp L, Kornauth C, et al. Mineral oil in human tissues, part II: characterization of the accumulated hydrocarbons by comprehensive two-dimensional gas chromatography. Sci Total Environ. 2015;506-507:644-655.
- Ruetsch SB, Kamath YK, Rele AS, et al. Secondary ion mass spectrometric investigation of penetration of coconut and mineral oils into human hair fibers: relevance to hair damage. J Cosmet Sci. 2001;52:169-184.
- Darbre PD, Aljarrah A, Miller WR, et al. Concentrations of parabens in human breast tumours. J Appl Toxicol. 2004;24:5-13.
- Routledge EJ, Parker J, Odum J, et al. Some alkyl hydroxy benzoate preservatives (parabens) are estrogenic. Toxicol Appl Pharmacol. 1998;153:12-19.
- Centers for Disease Control and Prevention. Parabens factsheet. https://www.cdc.gov/biomonitoring/Parabens_FactSheet.html. Updated April 7, 2017. Accessed March 19, 2020.
Practice Points
- Dermatologists must be aware of common hair and scalp beliefs, misconceptions, care, and product use to ensure culturally competent patient interactions and treatment.
- Common ingredients in popular hair care products used by African Americans include sulfates, cationic surfactants and polymers, silicone, oils, and parabens.
Breach of migrant youths’ confidentiality is unethical, unacceptable
We are in the healing profession. We practice a trade. We are doctors, therapists, counselors. We work with children, adults, and couples. We document the physical form of our patient after examination, setting the stage for interventions that heal and alleviate suffering. With those who we do not touch physically, we hold out our psychological arms to embrace them in a therapeutic relationship.
We are privileged to appreciate their deeper selves through voice, unsaid words, and body language. A trust evolves (or might not); deeper exploration where our intuition and technical skill discover what troubles the soul. Healing begins as a delicate dance: As trust is earned, our patients risk vulnerability by revealing their weakest selves.
As healers, we often find ourselves adrift with our own insecurities, our own histories that make us human; our styles may differ but training and the tenets and guidelines set by our professional societies keep us in safe waters. These guidelines are informed by the science of health care research and vetted through centuries of observation and experience of process. “Do no harm” is perhaps one of the major rules of engaging with patients. The scaffolding that our code of ethics provides healing professions trumps external pressures to deviate. If you violate these codes, the consequences are borne by the patient and the potential loss of your license.
Some of you may have read about Kevin Euceda, an adolescent who reportedly was waiting for his immigration interview and ordered to undergo mandatory therapy as part of the immigration protocol. Kevin revealed to his therapist the history of violence he experienced as a child growing up in Honduras. His subsequent initiation into a gang was the only option he had to escape a violent death. Those of us who work with youth from gang cultures know fully that allegiance to a gang is a means to find an identity and brotherhood with the payment by a lifestyle of violence. A therapist faced with this information does not judge but helps the person deal with PTSD, nightmares, and guilt that become part of an identity just as the memories of mines blowing up in the face of combat affect veterans.
But the therapist, who reportedly holds a master’s in rehabilitation counseling and was “a year away from passing her licensing exam,” according to an article published in the Washington Post, followed policy of the Office of Refugee Resettlement. The therapist betrayed Kevin by reporting the information he shared with her confidentially to Immigration and Customs Enforcement. The reason the therapist gave for the breach was that she was compelled do so because Kevin reported participating in gang activity in Honduras. Subsequently, Kevin was sent to a high-security detention center – and is now facing deportation.
Betraying a patient, profession
Therapy begins as a contract between patient and therapist. The contract stipulates that all that transpires in the process of therapy (usually a 50-minute block of time, usually weekly) is information held by the therapist and patient – and is not to be shared with anyone, including parents, guardians, legal entities, and health care agencies. This allows the gradual sharing of events, emotions, behaviors, and reactions akin to peeling an onion. Memories, reactions, and feelings assist the therapist as they start their quest of discovery of the conflict and how to resolve it. Trust is the central tenet of this journey. The patient thinks: “You will hear me; you will see me you will understand me and help me understand myself.” The doctor responds: “Even I don’t yet know fully what ails you; we will discover that together. … I will not fail your trust.”
So how does this interface with external pressures? The constitution of a free country provides some inviolable protections that prevent derailment of the codes of ethics based on science. The fine line between what are considered sacrosanct ethics of a field – be it health care, climatology, or architecture – and what could be sacrificed in the name of prevailing forces (political or otherwise) has to be under constant scrutiny by the members of the guild. In health care, when patients cannot trust the science, its implementation, or is let down by the clinician, they are unlikely to benefit from treatment. A foundation of distrust paves the way for future therapeutic relationships that are stained with distrust and noncompliance.
The ethics guidelines of the American Academy of Psychiatry and the Law specify that psychiatrists in forensic roles “should be clear about limitations on confidentiality in the treatment relationship and ensure that these limitations are communicated to the patient.” Again, the therapist in this case is not a psychiatrist, but I would argue that the same rules would apply.
It is reassuring to know that several key groups, including the American Psychiatric Association, American Academy of Child and Adolescent Psychiatry, and the American Psychological Association, have all condemned the therapist’s actions. Psychiatrists and other mental health professionals must do no harm. We must not stand idly by and allow the kind of professional breach that happened to Kevin continue. Patients who confide in mental health professionals with the promise of confidentiality must be able to do so without fear. Only with confidentiality can the therapeutic relationship thrive.
Dr. Sood is professor of psychiatry and pediatrics, and senior professor of child mental health policy, at Virginia Commonwealth University, Richmond.
We are in the healing profession. We practice a trade. We are doctors, therapists, counselors. We work with children, adults, and couples. We document the physical form of our patient after examination, setting the stage for interventions that heal and alleviate suffering. With those who we do not touch physically, we hold out our psychological arms to embrace them in a therapeutic relationship.
We are privileged to appreciate their deeper selves through voice, unsaid words, and body language. A trust evolves (or might not); deeper exploration where our intuition and technical skill discover what troubles the soul. Healing begins as a delicate dance: As trust is earned, our patients risk vulnerability by revealing their weakest selves.
As healers, we often find ourselves adrift with our own insecurities, our own histories that make us human; our styles may differ but training and the tenets and guidelines set by our professional societies keep us in safe waters. These guidelines are informed by the science of health care research and vetted through centuries of observation and experience of process. “Do no harm” is perhaps one of the major rules of engaging with patients. The scaffolding that our code of ethics provides healing professions trumps external pressures to deviate. If you violate these codes, the consequences are borne by the patient and the potential loss of your license.
Some of you may have read about Kevin Euceda, an adolescent who reportedly was waiting for his immigration interview and ordered to undergo mandatory therapy as part of the immigration protocol. Kevin revealed to his therapist the history of violence he experienced as a child growing up in Honduras. His subsequent initiation into a gang was the only option he had to escape a violent death. Those of us who work with youth from gang cultures know fully that allegiance to a gang is a means to find an identity and brotherhood with the payment by a lifestyle of violence. A therapist faced with this information does not judge but helps the person deal with PTSD, nightmares, and guilt that become part of an identity just as the memories of mines blowing up in the face of combat affect veterans.
But the therapist, who reportedly holds a master’s in rehabilitation counseling and was “a year away from passing her licensing exam,” according to an article published in the Washington Post, followed policy of the Office of Refugee Resettlement. The therapist betrayed Kevin by reporting the information he shared with her confidentially to Immigration and Customs Enforcement. The reason the therapist gave for the breach was that she was compelled do so because Kevin reported participating in gang activity in Honduras. Subsequently, Kevin was sent to a high-security detention center – and is now facing deportation.
Betraying a patient, profession
Therapy begins as a contract between patient and therapist. The contract stipulates that all that transpires in the process of therapy (usually a 50-minute block of time, usually weekly) is information held by the therapist and patient – and is not to be shared with anyone, including parents, guardians, legal entities, and health care agencies. This allows the gradual sharing of events, emotions, behaviors, and reactions akin to peeling an onion. Memories, reactions, and feelings assist the therapist as they start their quest of discovery of the conflict and how to resolve it. Trust is the central tenet of this journey. The patient thinks: “You will hear me; you will see me you will understand me and help me understand myself.” The doctor responds: “Even I don’t yet know fully what ails you; we will discover that together. … I will not fail your trust.”
So how does this interface with external pressures? The constitution of a free country provides some inviolable protections that prevent derailment of the codes of ethics based on science. The fine line between what are considered sacrosanct ethics of a field – be it health care, climatology, or architecture – and what could be sacrificed in the name of prevailing forces (political or otherwise) has to be under constant scrutiny by the members of the guild. In health care, when patients cannot trust the science, its implementation, or is let down by the clinician, they are unlikely to benefit from treatment. A foundation of distrust paves the way for future therapeutic relationships that are stained with distrust and noncompliance.
The ethics guidelines of the American Academy of Psychiatry and the Law specify that psychiatrists in forensic roles “should be clear about limitations on confidentiality in the treatment relationship and ensure that these limitations are communicated to the patient.” Again, the therapist in this case is not a psychiatrist, but I would argue that the same rules would apply.
It is reassuring to know that several key groups, including the American Psychiatric Association, American Academy of Child and Adolescent Psychiatry, and the American Psychological Association, have all condemned the therapist’s actions. Psychiatrists and other mental health professionals must do no harm. We must not stand idly by and allow the kind of professional breach that happened to Kevin continue. Patients who confide in mental health professionals with the promise of confidentiality must be able to do so without fear. Only with confidentiality can the therapeutic relationship thrive.
Dr. Sood is professor of psychiatry and pediatrics, and senior professor of child mental health policy, at Virginia Commonwealth University, Richmond.
We are in the healing profession. We practice a trade. We are doctors, therapists, counselors. We work with children, adults, and couples. We document the physical form of our patient after examination, setting the stage for interventions that heal and alleviate suffering. With those who we do not touch physically, we hold out our psychological arms to embrace them in a therapeutic relationship.
We are privileged to appreciate their deeper selves through voice, unsaid words, and body language. A trust evolves (or might not); deeper exploration where our intuition and technical skill discover what troubles the soul. Healing begins as a delicate dance: As trust is earned, our patients risk vulnerability by revealing their weakest selves.
As healers, we often find ourselves adrift with our own insecurities, our own histories that make us human; our styles may differ but training and the tenets and guidelines set by our professional societies keep us in safe waters. These guidelines are informed by the science of health care research and vetted through centuries of observation and experience of process. “Do no harm” is perhaps one of the major rules of engaging with patients. The scaffolding that our code of ethics provides healing professions trumps external pressures to deviate. If you violate these codes, the consequences are borne by the patient and the potential loss of your license.
Some of you may have read about Kevin Euceda, an adolescent who reportedly was waiting for his immigration interview and ordered to undergo mandatory therapy as part of the immigration protocol. Kevin revealed to his therapist the history of violence he experienced as a child growing up in Honduras. His subsequent initiation into a gang was the only option he had to escape a violent death. Those of us who work with youth from gang cultures know fully that allegiance to a gang is a means to find an identity and brotherhood with the payment by a lifestyle of violence. A therapist faced with this information does not judge but helps the person deal with PTSD, nightmares, and guilt that become part of an identity just as the memories of mines blowing up in the face of combat affect veterans.
But the therapist, who reportedly holds a master’s in rehabilitation counseling and was “a year away from passing her licensing exam,” according to an article published in the Washington Post, followed policy of the Office of Refugee Resettlement. The therapist betrayed Kevin by reporting the information he shared with her confidentially to Immigration and Customs Enforcement. The reason the therapist gave for the breach was that she was compelled do so because Kevin reported participating in gang activity in Honduras. Subsequently, Kevin was sent to a high-security detention center – and is now facing deportation.
Betraying a patient, profession
Therapy begins as a contract between patient and therapist. The contract stipulates that all that transpires in the process of therapy (usually a 50-minute block of time, usually weekly) is information held by the therapist and patient – and is not to be shared with anyone, including parents, guardians, legal entities, and health care agencies. This allows the gradual sharing of events, emotions, behaviors, and reactions akin to peeling an onion. Memories, reactions, and feelings assist the therapist as they start their quest of discovery of the conflict and how to resolve it. Trust is the central tenet of this journey. The patient thinks: “You will hear me; you will see me you will understand me and help me understand myself.” The doctor responds: “Even I don’t yet know fully what ails you; we will discover that together. … I will not fail your trust.”
So how does this interface with external pressures? The constitution of a free country provides some inviolable protections that prevent derailment of the codes of ethics based on science. The fine line between what are considered sacrosanct ethics of a field – be it health care, climatology, or architecture – and what could be sacrificed in the name of prevailing forces (political or otherwise) has to be under constant scrutiny by the members of the guild. In health care, when patients cannot trust the science, its implementation, or is let down by the clinician, they are unlikely to benefit from treatment. A foundation of distrust paves the way for future therapeutic relationships that are stained with distrust and noncompliance.
The ethics guidelines of the American Academy of Psychiatry and the Law specify that psychiatrists in forensic roles “should be clear about limitations on confidentiality in the treatment relationship and ensure that these limitations are communicated to the patient.” Again, the therapist in this case is not a psychiatrist, but I would argue that the same rules would apply.
It is reassuring to know that several key groups, including the American Psychiatric Association, American Academy of Child and Adolescent Psychiatry, and the American Psychological Association, have all condemned the therapist’s actions. Psychiatrists and other mental health professionals must do no harm. We must not stand idly by and allow the kind of professional breach that happened to Kevin continue. Patients who confide in mental health professionals with the promise of confidentiality must be able to do so without fear. Only with confidentiality can the therapeutic relationship thrive.
Dr. Sood is professor of psychiatry and pediatrics, and senior professor of child mental health policy, at Virginia Commonwealth University, Richmond.
Meeting the mental health needs of American Muslim patients
Nearly 3.5 million adherents to the religion of Islam (Muslims) live in the United States, and this number is projected to more than double to 8.1 million by 2050.1 As of 2017, an estimated 58% of American Muslims were immigrants, but nearly 25% were born in the United States to parents who also were US-born, including many African American Muslims.1 American Muslims face a rise of Islamophobia, hate crimes, and discrimination at school, work, and the communities in which they live.2 This population may experience feelings of anger as well as rejection and abandonment by the country they call home. They may also wrestle with conforming to American social norms while maintaining their Muslim identity.
When providing psychiatric care to American Muslim patients, clinicians need to understand these patients’ specific stressors. American Muslim patients may experience a variety of mental health conditions, including posttraumatic stress disorder, major depressive disorder, generalized anxiety disorder, panic attacks, adjustment disorder, and somatization.2 Unfortunately, American Muslims may be less likely to seek psychiatric help because the stigma of mental illness remains a barrier to care in this community.3 In addition, entrenched cultural beliefs about mental illness may discourage many from seeking treatment. Because of a paucity of data on the psychiatric care of American Muslim patients, there is a great need to understand how to treat this vulnerable, often marginalized population.
Suggestions for improving care
Based on my clinical experience, I recommend the following practices for clinicians to consider when caring for American Muslim patients:
- Ensure that your assessment accounts for religious and cultural factors to help understand your patient’s perception of his/her illness.4 Consider using the DSM-IV Outline for Culture Formulation,5 DSM-5 Cultural Formulation Interview,6 or the American Academy of Child and Adolescent Psychiatry Practice Parameter for Cultural Competence in Child and Adolescent Psychiatric Practice.7
- Be sensitive to your patient’s family hierarchy and history. Often, extended family members will accompany an American Muslim patient for input and support during a clinical visit.
- Provide appropriate psychoeducation, because some patients may shun medication, especially those who think that medication should be reserved for severe illness that requires long-term inpatient stays.
- Listen for somatic symptoms that may mask distress.8
- Be mindful of your patient’s preferences regarding gender roles. For example, a female patient may prefer to receive care from a female clinician.
- Align therapy with your patient’s religious and cultural beliefs. Some research shows that for Muslim patients, modified short-term psychodynamic therapy fares better than classic long-term psychoanalysis.9 Therapy should focus on family dynamics, conflicts, and relationships.9
- Consider employing cognitive-behavioral therapy, solution-focused therapy, modeling, and behavioral techniques such as behavioral modification, systemic desensitization, and flooding because these may be effective for Muslim patients.9,10
- Suggest guided imagery and relaxation techniques because some Muslim patients may find that these could be a natural extension of prayer and meditation.9
- Work with local Imams (Muslim spiritual leaders) to recognize mental illness, overcome stigma in the community, dispel misinformation, and refer patients.11
- If the patient has a “traditional healer,” such as a Sheikh or Imam, understand the extent of this individual’s involvement. Some healers may tell patients that mental illness is a problem of faith or being possessed by a spirit (ie, “jinn” or Satan-like spirits).
- Use an interpreter if English is not the patient’s primary language.
- Respect the patient’s religious practices. When possible, offer alternative treatments to medication formulations that include pork (most gelatins). Also, patients may want to adjust their medication schedule during Ramadan, when many Muslims fast from dawn to dusk.
Future goals: Increasing access, reducing stigma
More research on the mental health needs of American Muslim patients is needed, especially as discrimination and hate crimes against this population continue to rise. Clinicians should tailor their assessments and recommended treatments to these patients’ preferences, and address how religious and cultural connectedness may impact their patient’s mental health. Increasing access to services and reducing stigma associated with mental health care are critical for improving outcomes among Muslim patients.
1. Pew Research Center. Demographic portrait of Muslim Americans. https://www.pewforum.org/2017/07/26/demographic-portrait-of-muslim-americans. Published November 9, 2017. Accessed January 15 , 2019.
2. Moffic HS, Peteet J, Hankir AZ, eds. Islamophobia and psychiatry: recognition, prevention, and treatment. Cham, Switzerland: Springer; 2019:171-181,335-345.
3. Ciftci A, Jones N, Corrigan PW. Mental health stigma in the Muslim community. Journal of Muslim Mental Health. 2013;7(1). doi: 10.3998/jmmh.10381607.0007.102.
4. Ahmed SR, Amer MM, Killawi A. The ecosystems perspective in social work: Implications for culturally competent practice with American Muslims. J Relig Spiritual Soc Work. 2017;36(1-2):48-72.
5. Outline for Cultural Formulation. In: Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994:845-846.
6. Lewis-Fernández R, Aggarwal NK, Hinton L, et al, eds. DSM-5 handbook on the Cultural Formulation Interview. Washington, DC: American Psychiatric Association Publishing; 2016.
7. Pumariega AJ, Rothe E, Mian A, et al; American Academy of Child and Adolescent Psychiatry (AACAP) Committee on Quality Issues (CQI). Practice Parameter for Cultural Competence in Child and Adolescent Psychiatric Practice. J Am Acad Child Adolesc Psychiatry. 2013;52(10):1101-1115.
8. Basit A, Hamid M. Mental health issues of American Muslims. J IMA. 2010;42(3):106-110.
9. Amer MM, Jalal B. Individual psychotherapy/counseling. In: Ahmed S, Amer MM, eds. Counseling Muslims: handbook of mental health issues and interventions. New York, NY: Routledge; 2013:87-117.
10. Chaudhry S, Li C. Is solution-focused brief therapy culturally appropriate for Muslim American counselees? J Contemp Psychotherapy. 2011;41(2):109-113.
11. Ali OM. The Imam and the mental health of Muslims: learning from research with other clergy. Journal of Muslim Mental Health. 2016;10(1). doi: 10.3998/jmmh.10381607.0010.106.
Nearly 3.5 million adherents to the religion of Islam (Muslims) live in the United States, and this number is projected to more than double to 8.1 million by 2050.1 As of 2017, an estimated 58% of American Muslims were immigrants, but nearly 25% were born in the United States to parents who also were US-born, including many African American Muslims.1 American Muslims face a rise of Islamophobia, hate crimes, and discrimination at school, work, and the communities in which they live.2 This population may experience feelings of anger as well as rejection and abandonment by the country they call home. They may also wrestle with conforming to American social norms while maintaining their Muslim identity.
When providing psychiatric care to American Muslim patients, clinicians need to understand these patients’ specific stressors. American Muslim patients may experience a variety of mental health conditions, including posttraumatic stress disorder, major depressive disorder, generalized anxiety disorder, panic attacks, adjustment disorder, and somatization.2 Unfortunately, American Muslims may be less likely to seek psychiatric help because the stigma of mental illness remains a barrier to care in this community.3 In addition, entrenched cultural beliefs about mental illness may discourage many from seeking treatment. Because of a paucity of data on the psychiatric care of American Muslim patients, there is a great need to understand how to treat this vulnerable, often marginalized population.
Suggestions for improving care
Based on my clinical experience, I recommend the following practices for clinicians to consider when caring for American Muslim patients:
- Ensure that your assessment accounts for religious and cultural factors to help understand your patient’s perception of his/her illness.4 Consider using the DSM-IV Outline for Culture Formulation,5 DSM-5 Cultural Formulation Interview,6 or the American Academy of Child and Adolescent Psychiatry Practice Parameter for Cultural Competence in Child and Adolescent Psychiatric Practice.7
- Be sensitive to your patient’s family hierarchy and history. Often, extended family members will accompany an American Muslim patient for input and support during a clinical visit.
- Provide appropriate psychoeducation, because some patients may shun medication, especially those who think that medication should be reserved for severe illness that requires long-term inpatient stays.
- Listen for somatic symptoms that may mask distress.8
- Be mindful of your patient’s preferences regarding gender roles. For example, a female patient may prefer to receive care from a female clinician.
- Align therapy with your patient’s religious and cultural beliefs. Some research shows that for Muslim patients, modified short-term psychodynamic therapy fares better than classic long-term psychoanalysis.9 Therapy should focus on family dynamics, conflicts, and relationships.9
- Consider employing cognitive-behavioral therapy, solution-focused therapy, modeling, and behavioral techniques such as behavioral modification, systemic desensitization, and flooding because these may be effective for Muslim patients.9,10
- Suggest guided imagery and relaxation techniques because some Muslim patients may find that these could be a natural extension of prayer and meditation.9
- Work with local Imams (Muslim spiritual leaders) to recognize mental illness, overcome stigma in the community, dispel misinformation, and refer patients.11
- If the patient has a “traditional healer,” such as a Sheikh or Imam, understand the extent of this individual’s involvement. Some healers may tell patients that mental illness is a problem of faith or being possessed by a spirit (ie, “jinn” or Satan-like spirits).
- Use an interpreter if English is not the patient’s primary language.
- Respect the patient’s religious practices. When possible, offer alternative treatments to medication formulations that include pork (most gelatins). Also, patients may want to adjust their medication schedule during Ramadan, when many Muslims fast from dawn to dusk.
Future goals: Increasing access, reducing stigma
More research on the mental health needs of American Muslim patients is needed, especially as discrimination and hate crimes against this population continue to rise. Clinicians should tailor their assessments and recommended treatments to these patients’ preferences, and address how religious and cultural connectedness may impact their patient’s mental health. Increasing access to services and reducing stigma associated with mental health care are critical for improving outcomes among Muslim patients.
Nearly 3.5 million adherents to the religion of Islam (Muslims) live in the United States, and this number is projected to more than double to 8.1 million by 2050.1 As of 2017, an estimated 58% of American Muslims were immigrants, but nearly 25% were born in the United States to parents who also were US-born, including many African American Muslims.1 American Muslims face a rise of Islamophobia, hate crimes, and discrimination at school, work, and the communities in which they live.2 This population may experience feelings of anger as well as rejection and abandonment by the country they call home. They may also wrestle with conforming to American social norms while maintaining their Muslim identity.
When providing psychiatric care to American Muslim patients, clinicians need to understand these patients’ specific stressors. American Muslim patients may experience a variety of mental health conditions, including posttraumatic stress disorder, major depressive disorder, generalized anxiety disorder, panic attacks, adjustment disorder, and somatization.2 Unfortunately, American Muslims may be less likely to seek psychiatric help because the stigma of mental illness remains a barrier to care in this community.3 In addition, entrenched cultural beliefs about mental illness may discourage many from seeking treatment. Because of a paucity of data on the psychiatric care of American Muslim patients, there is a great need to understand how to treat this vulnerable, often marginalized population.
Suggestions for improving care
Based on my clinical experience, I recommend the following practices for clinicians to consider when caring for American Muslim patients:
- Ensure that your assessment accounts for religious and cultural factors to help understand your patient’s perception of his/her illness.4 Consider using the DSM-IV Outline for Culture Formulation,5 DSM-5 Cultural Formulation Interview,6 or the American Academy of Child and Adolescent Psychiatry Practice Parameter for Cultural Competence in Child and Adolescent Psychiatric Practice.7
- Be sensitive to your patient’s family hierarchy and history. Often, extended family members will accompany an American Muslim patient for input and support during a clinical visit.
- Provide appropriate psychoeducation, because some patients may shun medication, especially those who think that medication should be reserved for severe illness that requires long-term inpatient stays.
- Listen for somatic symptoms that may mask distress.8
- Be mindful of your patient’s preferences regarding gender roles. For example, a female patient may prefer to receive care from a female clinician.
- Align therapy with your patient’s religious and cultural beliefs. Some research shows that for Muslim patients, modified short-term psychodynamic therapy fares better than classic long-term psychoanalysis.9 Therapy should focus on family dynamics, conflicts, and relationships.9
- Consider employing cognitive-behavioral therapy, solution-focused therapy, modeling, and behavioral techniques such as behavioral modification, systemic desensitization, and flooding because these may be effective for Muslim patients.9,10
- Suggest guided imagery and relaxation techniques because some Muslim patients may find that these could be a natural extension of prayer and meditation.9
- Work with local Imams (Muslim spiritual leaders) to recognize mental illness, overcome stigma in the community, dispel misinformation, and refer patients.11
- If the patient has a “traditional healer,” such as a Sheikh or Imam, understand the extent of this individual’s involvement. Some healers may tell patients that mental illness is a problem of faith or being possessed by a spirit (ie, “jinn” or Satan-like spirits).
- Use an interpreter if English is not the patient’s primary language.
- Respect the patient’s religious practices. When possible, offer alternative treatments to medication formulations that include pork (most gelatins). Also, patients may want to adjust their medication schedule during Ramadan, when many Muslims fast from dawn to dusk.
Future goals: Increasing access, reducing stigma
More research on the mental health needs of American Muslim patients is needed, especially as discrimination and hate crimes against this population continue to rise. Clinicians should tailor their assessments and recommended treatments to these patients’ preferences, and address how religious and cultural connectedness may impact their patient’s mental health. Increasing access to services and reducing stigma associated with mental health care are critical for improving outcomes among Muslim patients.
1. Pew Research Center. Demographic portrait of Muslim Americans. https://www.pewforum.org/2017/07/26/demographic-portrait-of-muslim-americans. Published November 9, 2017. Accessed January 15 , 2019.
2. Moffic HS, Peteet J, Hankir AZ, eds. Islamophobia and psychiatry: recognition, prevention, and treatment. Cham, Switzerland: Springer; 2019:171-181,335-345.
3. Ciftci A, Jones N, Corrigan PW. Mental health stigma in the Muslim community. Journal of Muslim Mental Health. 2013;7(1). doi: 10.3998/jmmh.10381607.0007.102.
4. Ahmed SR, Amer MM, Killawi A. The ecosystems perspective in social work: Implications for culturally competent practice with American Muslims. J Relig Spiritual Soc Work. 2017;36(1-2):48-72.
5. Outline for Cultural Formulation. In: Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994:845-846.
6. Lewis-Fernández R, Aggarwal NK, Hinton L, et al, eds. DSM-5 handbook on the Cultural Formulation Interview. Washington, DC: American Psychiatric Association Publishing; 2016.
7. Pumariega AJ, Rothe E, Mian A, et al; American Academy of Child and Adolescent Psychiatry (AACAP) Committee on Quality Issues (CQI). Practice Parameter for Cultural Competence in Child and Adolescent Psychiatric Practice. J Am Acad Child Adolesc Psychiatry. 2013;52(10):1101-1115.
8. Basit A, Hamid M. Mental health issues of American Muslims. J IMA. 2010;42(3):106-110.
9. Amer MM, Jalal B. Individual psychotherapy/counseling. In: Ahmed S, Amer MM, eds. Counseling Muslims: handbook of mental health issues and interventions. New York, NY: Routledge; 2013:87-117.
10. Chaudhry S, Li C. Is solution-focused brief therapy culturally appropriate for Muslim American counselees? J Contemp Psychotherapy. 2011;41(2):109-113.
11. Ali OM. The Imam and the mental health of Muslims: learning from research with other clergy. Journal of Muslim Mental Health. 2016;10(1). doi: 10.3998/jmmh.10381607.0010.106.
1. Pew Research Center. Demographic portrait of Muslim Americans. https://www.pewforum.org/2017/07/26/demographic-portrait-of-muslim-americans. Published November 9, 2017. Accessed January 15 , 2019.
2. Moffic HS, Peteet J, Hankir AZ, eds. Islamophobia and psychiatry: recognition, prevention, and treatment. Cham, Switzerland: Springer; 2019:171-181,335-345.
3. Ciftci A, Jones N, Corrigan PW. Mental health stigma in the Muslim community. Journal of Muslim Mental Health. 2013;7(1). doi: 10.3998/jmmh.10381607.0007.102.
4. Ahmed SR, Amer MM, Killawi A. The ecosystems perspective in social work: Implications for culturally competent practice with American Muslims. J Relig Spiritual Soc Work. 2017;36(1-2):48-72.
5. Outline for Cultural Formulation. In: Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994:845-846.
6. Lewis-Fernández R, Aggarwal NK, Hinton L, et al, eds. DSM-5 handbook on the Cultural Formulation Interview. Washington, DC: American Psychiatric Association Publishing; 2016.
7. Pumariega AJ, Rothe E, Mian A, et al; American Academy of Child and Adolescent Psychiatry (AACAP) Committee on Quality Issues (CQI). Practice Parameter for Cultural Competence in Child and Adolescent Psychiatric Practice. J Am Acad Child Adolesc Psychiatry. 2013;52(10):1101-1115.
8. Basit A, Hamid M. Mental health issues of American Muslims. J IMA. 2010;42(3):106-110.
9. Amer MM, Jalal B. Individual psychotherapy/counseling. In: Ahmed S, Amer MM, eds. Counseling Muslims: handbook of mental health issues and interventions. New York, NY: Routledge; 2013:87-117.
10. Chaudhry S, Li C. Is solution-focused brief therapy culturally appropriate for Muslim American counselees? J Contemp Psychotherapy. 2011;41(2):109-113.
11. Ali OM. The Imam and the mental health of Muslims: learning from research with other clergy. Journal of Muslim Mental Health. 2016;10(1). doi: 10.3998/jmmh.10381607.0010.106.
Primary care can embrace gender-affirming policies, approaches
In a new “blueprint” for practices planning to implement a transgender care program, Anna M. Morenz, MD, and her coauthors emphasized that more than technical skills are needed to build an effective and welcoming transgender health practice.
All patient-facing staff – from schedulers and receptionists to nurses and billers – should “receive a foundational level of training in cultural sensitivity and effective communication with transgender and gender-diverse persons,” they wrote. In addition, they emphasized, “the workplace culture must ensure that chatter behind closed doors does not differ from patient-facing language.”
One thing that’s become clear over time, noted the authors of the blueprint, is that transgender care is no longer limited to the endocrinologist’s office. “After years of referring transgender and gender-diverse patients to specialty clinics and endocrinologists, transgender health experts have come to agree that gender-affirming hormone therapy can be safely delivered as part of routine care by a trained primary care clinician,” wrote Dr. Morenz, an internal medicine resident at the University of Washington, Seattle, and her coauthors.
Nor do most adults receiving gender-affirming care require mental health services, unless the patient or the primary care clinician sees a need or utility for psychological care. The blueprint was published in the Annals of Family Medicine.
The first step to setting up transgender services within a primary care practice is to conduct a needs assessment, suggested Dr. Morenz and her colleagues. Whether in-person focus groups or online surveys or questionnaires are best might depend on the community climate, they wrote. When stigma is high, the opportunity for anonymity might provide more robust results. Other considerations include whether there’s a concentration of transgender people with particularly high need or risk in the community – for example, transgender women of color, who might be at higher risk of HIV/AIDS than the general population. Depending on the needs of a particular community, initial transgender care efforts may have a focus on such a population.
A practice also should conduct a realistic appraisal of its own strengths and areas of weakness: Is signage inclusive? Do intake forms afford flexibility in gender and pronoun preference? Are front office staff comfortable greeting members of the lesbian-gay-bisexual-transgender-queer-intersex-asexual (LGBTQIA) community? What about restroom signage – is there a gender-inclusive option?
Competent provision of trauma-informed care goes hand in hand with assessment and preparation for providing transgender care, noted the blueprint authors, because “transgender and gender-diverse people experience high levels of trauma and stress related to minority status.”
Performing outreach within an organization and community also can unearth existing services, so that a primary care transgender practice dovetails with and complements those ongoing efforts, avoiding unnecessarily duplicative services. “All transgender health programs can benefit from developing broad relationships with external agencies, community-based organizatons, and individual practitioners who provide a range of services and can function as a network for knowledge-sharing and referrals,” noted Dr. Morenz and her coauthors.
“Starting a new program, especially one focused on a stigmatized population, can generate staff concerns and resistance,” acknowledged Dr. Morenz and her colleagues. Efforts at getting organizational buy-in can emphasize that providing transgender care helps meet ethical obligations within medicine. Emphasizing that making such care available is really at the vanguard of best practices might help overcome some resistance, they said.
, with at least one champion having a leadership role within the organization, wrote Dr. Morenz and her colleagues.
A variety of care models can work when a practice is initiating transgender care, depending on community needs, internal resources, and the commitment level of various stakeholders. An evening clinic staffed by a small number of clinicians can be a good way to test the waters in some cases. Other facilities might wish to identify clinicians who are competent to offer hormone therapy, while still other clinics might be able to incorporate transgender care more globally within their practice. Regardless of which service model a practice opts for, however, it’s crucial to have staff members who are savvy navigators of insurance reimbursement for gender-affirming care.
And when transgender care is nested within a practice, those patients must not feel like second-class citizens of the clinic, or that they’re receiving care that’s somehow different or substandard. For example, wrote Dr. Morenz and her coauthors, a facility must consider what will happen when a transgender patient presents for urgent health needs and the primary care clinician is not available.
The nuts and bolts of providing safe and effective gender-affirming hormone therapy, said the blueprint authors, can be mastered with training and practice. “Despite common concerns that transgender health care is complicated, it is in fact as straightforward as managing common chronic diseases.”
The first step, they said, is providing risk-benefit education and counseling to patients, and reviewing fertility preservation considerations and options. Then, either estradiol or testosterone is initiated; Further suppression of endogenous hormones also might be indicated in feminization therapy in particular. The authors provided several continuing education resources for clinicians and other health care team members, and noted that a “train the trainer” model can prove effective, with a core team training others once they’ve become comfortable with the ins and outs of hormone prescribing and monitoring.
Having a staff that looks like the patient panel can go a long way toward promoting authentic inclusivity, but Dr. Morenz and her colleagues cautioned against hiring practices that amount to tokenism, or expecting transgender or gender-diverse staff to be ambassadors or spokespeople for others.
Taken together, the start-up costs for providing transgender care can be “minimal,” wrote the blueprint authors, because many free and low-cost educational resources are available. Some of the only real outlays may come from altering restroom signage and tweaking the electronic health record to accommodate gender diversity.
A practice that goes forward with transgender care, they conclude, “will provide a unique opportunity to holistically improve wellness and quality of life for transgender and gender-diverse people,” joining the “growing and passionate network of clinical practice teams who are committed to health care, innovation, and equity for transgender and gender-diverse communities.”
Dr. Morenz reported no outside sources of funding and reported that she has no relevant conflicts of interest.
SOURCE: Morenz AM et al. Ann Fam Med. 2020 Jan;18(1):73-9.
In a new “blueprint” for practices planning to implement a transgender care program, Anna M. Morenz, MD, and her coauthors emphasized that more than technical skills are needed to build an effective and welcoming transgender health practice.
All patient-facing staff – from schedulers and receptionists to nurses and billers – should “receive a foundational level of training in cultural sensitivity and effective communication with transgender and gender-diverse persons,” they wrote. In addition, they emphasized, “the workplace culture must ensure that chatter behind closed doors does not differ from patient-facing language.”
One thing that’s become clear over time, noted the authors of the blueprint, is that transgender care is no longer limited to the endocrinologist’s office. “After years of referring transgender and gender-diverse patients to specialty clinics and endocrinologists, transgender health experts have come to agree that gender-affirming hormone therapy can be safely delivered as part of routine care by a trained primary care clinician,” wrote Dr. Morenz, an internal medicine resident at the University of Washington, Seattle, and her coauthors.
Nor do most adults receiving gender-affirming care require mental health services, unless the patient or the primary care clinician sees a need or utility for psychological care. The blueprint was published in the Annals of Family Medicine.
The first step to setting up transgender services within a primary care practice is to conduct a needs assessment, suggested Dr. Morenz and her colleagues. Whether in-person focus groups or online surveys or questionnaires are best might depend on the community climate, they wrote. When stigma is high, the opportunity for anonymity might provide more robust results. Other considerations include whether there’s a concentration of transgender people with particularly high need or risk in the community – for example, transgender women of color, who might be at higher risk of HIV/AIDS than the general population. Depending on the needs of a particular community, initial transgender care efforts may have a focus on such a population.
A practice also should conduct a realistic appraisal of its own strengths and areas of weakness: Is signage inclusive? Do intake forms afford flexibility in gender and pronoun preference? Are front office staff comfortable greeting members of the lesbian-gay-bisexual-transgender-queer-intersex-asexual (LGBTQIA) community? What about restroom signage – is there a gender-inclusive option?
Competent provision of trauma-informed care goes hand in hand with assessment and preparation for providing transgender care, noted the blueprint authors, because “transgender and gender-diverse people experience high levels of trauma and stress related to minority status.”
Performing outreach within an organization and community also can unearth existing services, so that a primary care transgender practice dovetails with and complements those ongoing efforts, avoiding unnecessarily duplicative services. “All transgender health programs can benefit from developing broad relationships with external agencies, community-based organizatons, and individual practitioners who provide a range of services and can function as a network for knowledge-sharing and referrals,” noted Dr. Morenz and her coauthors.
“Starting a new program, especially one focused on a stigmatized population, can generate staff concerns and resistance,” acknowledged Dr. Morenz and her colleagues. Efforts at getting organizational buy-in can emphasize that providing transgender care helps meet ethical obligations within medicine. Emphasizing that making such care available is really at the vanguard of best practices might help overcome some resistance, they said.
, with at least one champion having a leadership role within the organization, wrote Dr. Morenz and her colleagues.
A variety of care models can work when a practice is initiating transgender care, depending on community needs, internal resources, and the commitment level of various stakeholders. An evening clinic staffed by a small number of clinicians can be a good way to test the waters in some cases. Other facilities might wish to identify clinicians who are competent to offer hormone therapy, while still other clinics might be able to incorporate transgender care more globally within their practice. Regardless of which service model a practice opts for, however, it’s crucial to have staff members who are savvy navigators of insurance reimbursement for gender-affirming care.
And when transgender care is nested within a practice, those patients must not feel like second-class citizens of the clinic, or that they’re receiving care that’s somehow different or substandard. For example, wrote Dr. Morenz and her coauthors, a facility must consider what will happen when a transgender patient presents for urgent health needs and the primary care clinician is not available.
The nuts and bolts of providing safe and effective gender-affirming hormone therapy, said the blueprint authors, can be mastered with training and practice. “Despite common concerns that transgender health care is complicated, it is in fact as straightforward as managing common chronic diseases.”
The first step, they said, is providing risk-benefit education and counseling to patients, and reviewing fertility preservation considerations and options. Then, either estradiol or testosterone is initiated; Further suppression of endogenous hormones also might be indicated in feminization therapy in particular. The authors provided several continuing education resources for clinicians and other health care team members, and noted that a “train the trainer” model can prove effective, with a core team training others once they’ve become comfortable with the ins and outs of hormone prescribing and monitoring.
Having a staff that looks like the patient panel can go a long way toward promoting authentic inclusivity, but Dr. Morenz and her colleagues cautioned against hiring practices that amount to tokenism, or expecting transgender or gender-diverse staff to be ambassadors or spokespeople for others.
Taken together, the start-up costs for providing transgender care can be “minimal,” wrote the blueprint authors, because many free and low-cost educational resources are available. Some of the only real outlays may come from altering restroom signage and tweaking the electronic health record to accommodate gender diversity.
A practice that goes forward with transgender care, they conclude, “will provide a unique opportunity to holistically improve wellness and quality of life for transgender and gender-diverse people,” joining the “growing and passionate network of clinical practice teams who are committed to health care, innovation, and equity for transgender and gender-diverse communities.”
Dr. Morenz reported no outside sources of funding and reported that she has no relevant conflicts of interest.
SOURCE: Morenz AM et al. Ann Fam Med. 2020 Jan;18(1):73-9.
In a new “blueprint” for practices planning to implement a transgender care program, Anna M. Morenz, MD, and her coauthors emphasized that more than technical skills are needed to build an effective and welcoming transgender health practice.
All patient-facing staff – from schedulers and receptionists to nurses and billers – should “receive a foundational level of training in cultural sensitivity and effective communication with transgender and gender-diverse persons,” they wrote. In addition, they emphasized, “the workplace culture must ensure that chatter behind closed doors does not differ from patient-facing language.”
One thing that’s become clear over time, noted the authors of the blueprint, is that transgender care is no longer limited to the endocrinologist’s office. “After years of referring transgender and gender-diverse patients to specialty clinics and endocrinologists, transgender health experts have come to agree that gender-affirming hormone therapy can be safely delivered as part of routine care by a trained primary care clinician,” wrote Dr. Morenz, an internal medicine resident at the University of Washington, Seattle, and her coauthors.
Nor do most adults receiving gender-affirming care require mental health services, unless the patient or the primary care clinician sees a need or utility for psychological care. The blueprint was published in the Annals of Family Medicine.
The first step to setting up transgender services within a primary care practice is to conduct a needs assessment, suggested Dr. Morenz and her colleagues. Whether in-person focus groups or online surveys or questionnaires are best might depend on the community climate, they wrote. When stigma is high, the opportunity for anonymity might provide more robust results. Other considerations include whether there’s a concentration of transgender people with particularly high need or risk in the community – for example, transgender women of color, who might be at higher risk of HIV/AIDS than the general population. Depending on the needs of a particular community, initial transgender care efforts may have a focus on such a population.
A practice also should conduct a realistic appraisal of its own strengths and areas of weakness: Is signage inclusive? Do intake forms afford flexibility in gender and pronoun preference? Are front office staff comfortable greeting members of the lesbian-gay-bisexual-transgender-queer-intersex-asexual (LGBTQIA) community? What about restroom signage – is there a gender-inclusive option?
Competent provision of trauma-informed care goes hand in hand with assessment and preparation for providing transgender care, noted the blueprint authors, because “transgender and gender-diverse people experience high levels of trauma and stress related to minority status.”
Performing outreach within an organization and community also can unearth existing services, so that a primary care transgender practice dovetails with and complements those ongoing efforts, avoiding unnecessarily duplicative services. “All transgender health programs can benefit from developing broad relationships with external agencies, community-based organizatons, and individual practitioners who provide a range of services and can function as a network for knowledge-sharing and referrals,” noted Dr. Morenz and her coauthors.
“Starting a new program, especially one focused on a stigmatized population, can generate staff concerns and resistance,” acknowledged Dr. Morenz and her colleagues. Efforts at getting organizational buy-in can emphasize that providing transgender care helps meet ethical obligations within medicine. Emphasizing that making such care available is really at the vanguard of best practices might help overcome some resistance, they said.
, with at least one champion having a leadership role within the organization, wrote Dr. Morenz and her colleagues.
A variety of care models can work when a practice is initiating transgender care, depending on community needs, internal resources, and the commitment level of various stakeholders. An evening clinic staffed by a small number of clinicians can be a good way to test the waters in some cases. Other facilities might wish to identify clinicians who are competent to offer hormone therapy, while still other clinics might be able to incorporate transgender care more globally within their practice. Regardless of which service model a practice opts for, however, it’s crucial to have staff members who are savvy navigators of insurance reimbursement for gender-affirming care.
And when transgender care is nested within a practice, those patients must not feel like second-class citizens of the clinic, or that they’re receiving care that’s somehow different or substandard. For example, wrote Dr. Morenz and her coauthors, a facility must consider what will happen when a transgender patient presents for urgent health needs and the primary care clinician is not available.
The nuts and bolts of providing safe and effective gender-affirming hormone therapy, said the blueprint authors, can be mastered with training and practice. “Despite common concerns that transgender health care is complicated, it is in fact as straightforward as managing common chronic diseases.”
The first step, they said, is providing risk-benefit education and counseling to patients, and reviewing fertility preservation considerations and options. Then, either estradiol or testosterone is initiated; Further suppression of endogenous hormones also might be indicated in feminization therapy in particular. The authors provided several continuing education resources for clinicians and other health care team members, and noted that a “train the trainer” model can prove effective, with a core team training others once they’ve become comfortable with the ins and outs of hormone prescribing and monitoring.
Having a staff that looks like the patient panel can go a long way toward promoting authentic inclusivity, but Dr. Morenz and her colleagues cautioned against hiring practices that amount to tokenism, or expecting transgender or gender-diverse staff to be ambassadors or spokespeople for others.
Taken together, the start-up costs for providing transgender care can be “minimal,” wrote the blueprint authors, because many free and low-cost educational resources are available. Some of the only real outlays may come from altering restroom signage and tweaking the electronic health record to accommodate gender diversity.
A practice that goes forward with transgender care, they conclude, “will provide a unique opportunity to holistically improve wellness and quality of life for transgender and gender-diverse people,” joining the “growing and passionate network of clinical practice teams who are committed to health care, innovation, and equity for transgender and gender-diverse communities.”
Dr. Morenz reported no outside sources of funding and reported that she has no relevant conflicts of interest.
SOURCE: Morenz AM et al. Ann Fam Med. 2020 Jan;18(1):73-9.
FROM THE ANNALS OF FAMILY MEDICINE
Social determinants of health and the hospitalist
Are access to housing and food as important as therapeutics?
While physicians acknowledge that the social determinants of health can impact outcomes from medical care, some may feel that trying to address factors such as homelessness, food insecurity, or lack of ready access to transportation or pharmacy services is just not part of the doctor’s job. A majority of 621 physicians surveyed in the summer of 2017 by Salt Lake City–based health care intelligence firm Leavitt Partners say they are neither capable of nor responsible for addressing such issues.1
But that view may become unsustainable as the U.S. health care system continues to advance toward value- and population-based models of health care and as evidence mounts that social factors are important contributors to costly outcomes, such as avoidable hospital readmissions or emergency room visits. A recent report from the Robert Wood Johnson Foundation estimates that at least 40% of health outcomes are the result of social and economic factors, while only 20% can be attributed to medical care.2
“This is a hot topic – getting a lot of attention these days,” said hospitalist and care transitions expert Ramon Jacobs-Shaw, MD, MPA, regional medical officer for CareMore Health, a California-based physician-led health delivery organization and subsidiary of Anthem. “If you go around the country, some doctors still see social factors as the realm of the social worker. But large health care organizations are coming to recognize that social determinants are huge contributors to the health of their members and to the outcomes of their care.”
Hospitalists could be the natural providers to delve into the specific psychosocial aspects of their patients’ lives, or try to figure out how those factors contribute to health care needs, Dr. Jacobs-Shaw said. They typically confront such issues while the patient is in the hospital bed, but what are the steps that led to the hospitalization in the first place? What will happen after the patient is discharged?
“For example, if patients lack transportation, how can they get to their follow-up medical appointment in the primary care office in order to manage their diabetes? If you can’t follow up with them, their diabetes could get out of control, with complications as a result, such as an infected wound,” he said. Another big issue is access to affordable medications. “CareMore has pharmacists embedded on our care teams. They try to figure out the best medicine for the patient but at the lowest cost. They meet individually with patients and do medication counseling, particularly for those with polypharmacy issues.”
Making health care more equitable
Dr. Jacobs-Shaw has long held a personal interest in issues of inclusiveness, diversity, and how to make health care more equitable for historically underserved groups. Asking how to have a bigger impact on these issues is what brought him, after 13 years as a hospitalist on the East Coast, to CareMore, a company that has made addressing social needs central to its care model. “In California, where I am based, we are a wrap-around for patients who are covered by Medicare Advantage plans. We are whatever the patient needs us to be.”
He oversees a group of hospitalists, dubbed extensivists, who provide advanced patient care and chronic disease management. In the extensivist model, physicians and advanced practice nurses provide comprehensive and coordinated care to patients with complex medical issues, taking their scope of practice beyond the hospital into homes, post-acute care facilities, and other settings, with a focus on keeping patients healthier and reducing readmission.3
“Our patients get access to extra services and resources, some of which are available at our care centers – which are one-stop outpatient facilities. We also focus on a lot of things physicians didn’t historically think were within their wheelhouse. Hospitalists deal with these kinds of issues every day, but may not label them as social determinants of health,” Dr. Jacobs-Shaw said. He emphasized that hospitalists should realize that they are not powerless to address these issues, working in partnership with other groups in and out of the hospital. They should also know that health care payers increasingly are dedicating resources to these issues.
“We just started trying to address homelessness through a pilot in Orange County, working with nonprofit organizations and philanthropy to offer a transitional site of care for our patients who are being discharged from the hospital and have housing insecurity issues, to get them transitioned into more secure housing,” Dr. Jacobs-Shaw said. CareMore also has a transportation collaborative that offers no-cost, nonemergency transportation to medical appointments. “That’s meeting them where they are at, based on an assessment of their needs and resources.”
What are social determinants?
The social determinants of health – social, environmental, and other nonmedical factors that contribute to overall health status and medical need – have been defined by the World Health Organization as: “conditions in which people are born, grow, live, work, and age.” That is a broad complex of overlapping social and systems issues, but it provides a context for a broader understanding of the patient’s health and response to medical interventions.
Socioeconomic status is a huge determinant. Level of education may be more important than income if the person lacks the health literacy to navigate the system and access needed care. Housing instability may include poor sanitation, substandard dwellings, or unsafe neighborhoods – all of which can affect a person’s well-being. Environmental health may include compromised air quality – which can impact pulmonary health. Other issues include access to employment and child care, utility needs, and interpersonal violence.
A 2014 paper in Annals of Internal Medicine found that residence within a disadvantaged neighborhood was a factor in hospital readmission rates as often as was chronic pulmonary disease.4 A recent report on social determinants of health by the National Institute for Health Care Management notes that patients with food insecurity are 2.4 times more likely to go to the emergency room, while those with transportation needs are 2.6 times more likely.5
What can health care leaders do to better equip their clinicians and teams to help patients deal with this array of complex needs? Intermountain Healthcare, based in Salt Lake City, spearheaded in 2018 the development of the Alliance for the Determinants of Health, starting in the communities of Ogden and St. George, Utah. The Alliance seeks to promote health, improve access to care, and decrease health care costs through a charitable contribution of $12 million over 3 years to seed collaborative demonstration projects.
Lisa Nichols, assistant vice president for community health at Intermountain, said that, while hospitalists were not directly involved in planning the Alliance, hospitalists and ED physicians have become essential to the patient-screening process for health and social needs.
“We met with hospitalists, emergency departments, and hospital administrators, because we wanted their feedback on how to raise awareness of the social needs of patients,” she said. “They have good ideas. They see the patients who come in from the homeless shelters.”
Other hospitals are subsidizing apartments for homeless patients being discharged from the hospital. CommonSpirit Health, the new national Catholic health care organization formed by the 2019 merger of Dignity Health and Catholic Health Initiatives, has explored how to help create and sustain affordable housing in the communities it serves. Investments like this have inspired others, such as Kaiser Permanente, to get involved in supporting housing initiatives.6
Comprehensive community care
David Meltzer, MD, PhD, a hospitalist and professor of medicine at the University of Chicago, said most hospitalists these days believe social determinants of health are part of their job responsibilities.
“That’s not to say we all do it well. We may fail at addressing some of the barriers our patients face. But I don’t know anyone who still says it’s not their job,” he said.
Since 2012, Dr. Meltzer has led a pilot called Comprehensive Care Physicians (CCP), in which the same physician cares for patients with chronic health problems in the clinic and in the hospital, working with a team of nurse practitioners, social workers, care coordinators, and other specialists. A total of 2,000 patients with chronic health problems were enrolled in the study from 2012 to 2016, half assigned to standard care and half assigned to five CCP doctors. The result: The CCP model has shown large improvements in outcomes – particularly among the more vulnerable, less activated patients, is preferred by patients, and has significantly reduced health care utilization.
The next step for the research team is another randomized controlled trial called Comprehensive Care, Community, and Culture, designed to address unmet social needs. Study group patients will also be screened for unmet social needs and have access to a community health worker and to the initiative’s Artful Living Program, which includes community and cultural activities like yoga and dance classes, cooking classes, art classes, and music concerts. To address the complex dimensions and determinants of health, Dr. Meltzer explained, efforts to improve health must extend to sectors far beyond traditional health care.
“I think trying to understand your patients’ social and nonmedical needs starts with getting to know them, and asking about their needs,” he said. “The better you know them, the better you are able to make medical decisions that will promote positive outcomes.”
Sound Physicians, a national hospitalist company based in Tacoma, Wash., and working in 350 hospitals in 41 states, recently published a blog post on its website about the importance of social determinants of health.7 Sound Physicians participates in value-based care through bundled Medicare/Medicaid contracts based on episodes of care for hospitalized patients with certain diagnoses or DRGs, explained John Dickey, MD, the company’s chief medical officer for population health.
“We’ve been heavily involved in trying to improve cost and outcomes of care since 2015. Social determinants absolutely play into trying to lower costs of care and reduce rates of readmissions, which are often multifactorial in cause,” he said. Hospitalists are uniquely equipped to impact post-acute outcomes, Dr. Dickey said, working in partnership with a position Sound Physicians calls the clinical performance nurse.
“We can also partner with primary care providers, provide education for our hospitalist staff, and work with in-home care supports for patients such as these, who otherwise might end up in a skilled nursing facility – even though they’d rather be at home,” he said.
Innovations at Northwell Health
Northwell Health, a multihospital comprehensive health system serving the New York City metro area and Long Island, has shown innovative leadership in addressing social factors. The 23-hospital system initiated in early 2019 a 15-item Self-Reported Social Determinants Screening Tool, which is now used with hospitalized patients to connect them with the support they need to fully recover and avoid readmissions.
Northwell is also providing professional education on social determinants for different constituencies across its system, said Johanna Martinez, MD, MS, a hospitalist and GME Director of Diversity and Health Equity at the Zucker School of Medicine at Hofstra/Northwell. A day-long training retreat was offered to GME faculty, and learning platforms have been developed for physicians, social workers, nurses, and others.
“One of the questions that comes up is that if you find social needs, what do you do about them?” Dr. Martinez explained. That’s more a difficult challenge, she said, so at Northwell, orthopedic surgeons are now asking patients questions like: “What’s going to happen when you go home? What are your social supports? Can you get to the physical therapist’s office?”
Another example of Northwell’s innovations is its Food as Health Program, initially piloted at Long Island Jewish Hospital in Valley Stream, N.Y. Hospitalized patients are asked two questions using a validated screening tool called the Hunger Vital Sign to identify their food insecurities.8 Those who answer yes are referred to a dietitian, and if they have a nutrition-related diagnosis, they enter the multidisciplinary wraparound program.
A key element is the food and health center, located on the hospital campus, where they can get food to take home and referrals to other services, with culturally tailored, disease-specific food education incorporated into the discharge plan. One of the partnering organizations is Island Harvest Food Bank, which helps about 1 in every 10 residents of Long Island with their food insecurity issues.
“When I talk to clinicians, most of us went into medicine to save lives and cure people. Yet the research shows that no matter who we are, we can’t do the best work that our patients need unless we consider their social determinants,” Dr. Martinez said. Ultimately, she noted, there is a need to change the culture of health care. “We have to create system change, reimbursement change, policy change.”
Omolara Uwemedimo, MD, MPH, associate professor of pediatrics and occupational medicine at Northwell and a former nocturnist, said the treatment of illness and health improvement don’t begin in the hospital, they begin in the community. Identifying where people are struggling and what communities they come from requires a broader view of the provider’s role. “Are patients who are readmitted to the hospital generally coming from certain demographics or from certain zip codes?” she asked. “Start there. How can we better connect with those communities?”
Education is key
In 2020 and beyond, hospitalists will hear more about the social determinants of health, Dr. Jacobs-Shaw concluded. “Without addressing those social determinants, we aren’t going to be able to meaningfully impact outcomes or be effective stewards of health care costs – addressing the psychosocial factors and root causes of patients coming in and out of the hospital.”
He added that self-education is key for hospitalists and the teams they work with – to be more aware of the link between health outcomes and social determinants. Guidelines and other resources on social determinants of health are available from the American College of Physicians and the American Association of Family Physicians. ACP issued a position paper on addressing social determinants of health to improve patient care,while AAFP has a research page on its website dedicated to social determinants of health, highlighting a number of initiatives and resources for physicians and others.9
The American Hospital Association has produced fact sheets on ICD-10CM code categories for social determinants of health, including 11 ICD-10 “Z” codes, numbered Z55-Z65, which can be used for coding interventions to address social determinants of health. Other experts are looking at how to adapt the electronic health record to capture sociodemographic and behavioral factors, and then trigger referrals to resources in the hospital and the broader community, and how to mobilize artificial intelligence and machine learning to better identify social needs.
“Our doctors really want to be able to take care of the whole patient, while being stewards of health care resources. But sometimes we feel powerless and wonder how we can have a bigger impact on people, on populations” Dr. Jacobs-Shaw said. “Remember it only takes one voice within an organization to start to elevate this topic.”
References
1. Rappleye E. Physicians say social determinants of health are not their responsibility. Becker’s Hospital Review. 2018 May 15.
2. Robert Wood Johnson Foundation, University of Wisconsin Population Health Institute. County Health Rankings, 2014.
3. Freeman, GA. The extensivist model. Health Leaders Magazine, 2016 Sep 15.
4. Kind AJ et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: A retrospective cohort study. Ann Intern Med. 2014 Dec 2;161(11):765-74.
5. National Institute for Health Care Management. Addressing social determinants of health can improve community health & reduce costs.
6. Vial PB. Boundless collaboration: A philosophy for sustainable and stabilizing housing investment strategies. Health Progress: Journal of the Catholic Health Association of the United States. September-October 2019.
7. Social determinants of health: New solutions for growing complexities. Op-Med, a blog by Sound Physicians. 2019 Aug 1.
8. The hunger vital sign: A new standard of care for preventive health.
9. Daniel H et al. Addressing social determinants to improve patient care and promote health equity: An American College of Physicians position paper. Ann Intern Med. 2018;168:557-578.
Are access to housing and food as important as therapeutics?
Are access to housing and food as important as therapeutics?
While physicians acknowledge that the social determinants of health can impact outcomes from medical care, some may feel that trying to address factors such as homelessness, food insecurity, or lack of ready access to transportation or pharmacy services is just not part of the doctor’s job. A majority of 621 physicians surveyed in the summer of 2017 by Salt Lake City–based health care intelligence firm Leavitt Partners say they are neither capable of nor responsible for addressing such issues.1
But that view may become unsustainable as the U.S. health care system continues to advance toward value- and population-based models of health care and as evidence mounts that social factors are important contributors to costly outcomes, such as avoidable hospital readmissions or emergency room visits. A recent report from the Robert Wood Johnson Foundation estimates that at least 40% of health outcomes are the result of social and economic factors, while only 20% can be attributed to medical care.2
“This is a hot topic – getting a lot of attention these days,” said hospitalist and care transitions expert Ramon Jacobs-Shaw, MD, MPA, regional medical officer for CareMore Health, a California-based physician-led health delivery organization and subsidiary of Anthem. “If you go around the country, some doctors still see social factors as the realm of the social worker. But large health care organizations are coming to recognize that social determinants are huge contributors to the health of their members and to the outcomes of their care.”
Hospitalists could be the natural providers to delve into the specific psychosocial aspects of their patients’ lives, or try to figure out how those factors contribute to health care needs, Dr. Jacobs-Shaw said. They typically confront such issues while the patient is in the hospital bed, but what are the steps that led to the hospitalization in the first place? What will happen after the patient is discharged?
“For example, if patients lack transportation, how can they get to their follow-up medical appointment in the primary care office in order to manage their diabetes? If you can’t follow up with them, their diabetes could get out of control, with complications as a result, such as an infected wound,” he said. Another big issue is access to affordable medications. “CareMore has pharmacists embedded on our care teams. They try to figure out the best medicine for the patient but at the lowest cost. They meet individually with patients and do medication counseling, particularly for those with polypharmacy issues.”
Making health care more equitable
Dr. Jacobs-Shaw has long held a personal interest in issues of inclusiveness, diversity, and how to make health care more equitable for historically underserved groups. Asking how to have a bigger impact on these issues is what brought him, after 13 years as a hospitalist on the East Coast, to CareMore, a company that has made addressing social needs central to its care model. “In California, where I am based, we are a wrap-around for patients who are covered by Medicare Advantage plans. We are whatever the patient needs us to be.”
He oversees a group of hospitalists, dubbed extensivists, who provide advanced patient care and chronic disease management. In the extensivist model, physicians and advanced practice nurses provide comprehensive and coordinated care to patients with complex medical issues, taking their scope of practice beyond the hospital into homes, post-acute care facilities, and other settings, with a focus on keeping patients healthier and reducing readmission.3
“Our patients get access to extra services and resources, some of which are available at our care centers – which are one-stop outpatient facilities. We also focus on a lot of things physicians didn’t historically think were within their wheelhouse. Hospitalists deal with these kinds of issues every day, but may not label them as social determinants of health,” Dr. Jacobs-Shaw said. He emphasized that hospitalists should realize that they are not powerless to address these issues, working in partnership with other groups in and out of the hospital. They should also know that health care payers increasingly are dedicating resources to these issues.
“We just started trying to address homelessness through a pilot in Orange County, working with nonprofit organizations and philanthropy to offer a transitional site of care for our patients who are being discharged from the hospital and have housing insecurity issues, to get them transitioned into more secure housing,” Dr. Jacobs-Shaw said. CareMore also has a transportation collaborative that offers no-cost, nonemergency transportation to medical appointments. “That’s meeting them where they are at, based on an assessment of their needs and resources.”
What are social determinants?
The social determinants of health – social, environmental, and other nonmedical factors that contribute to overall health status and medical need – have been defined by the World Health Organization as: “conditions in which people are born, grow, live, work, and age.” That is a broad complex of overlapping social and systems issues, but it provides a context for a broader understanding of the patient’s health and response to medical interventions.
Socioeconomic status is a huge determinant. Level of education may be more important than income if the person lacks the health literacy to navigate the system and access needed care. Housing instability may include poor sanitation, substandard dwellings, or unsafe neighborhoods – all of which can affect a person’s well-being. Environmental health may include compromised air quality – which can impact pulmonary health. Other issues include access to employment and child care, utility needs, and interpersonal violence.
A 2014 paper in Annals of Internal Medicine found that residence within a disadvantaged neighborhood was a factor in hospital readmission rates as often as was chronic pulmonary disease.4 A recent report on social determinants of health by the National Institute for Health Care Management notes that patients with food insecurity are 2.4 times more likely to go to the emergency room, while those with transportation needs are 2.6 times more likely.5
What can health care leaders do to better equip their clinicians and teams to help patients deal with this array of complex needs? Intermountain Healthcare, based in Salt Lake City, spearheaded in 2018 the development of the Alliance for the Determinants of Health, starting in the communities of Ogden and St. George, Utah. The Alliance seeks to promote health, improve access to care, and decrease health care costs through a charitable contribution of $12 million over 3 years to seed collaborative demonstration projects.
Lisa Nichols, assistant vice president for community health at Intermountain, said that, while hospitalists were not directly involved in planning the Alliance, hospitalists and ED physicians have become essential to the patient-screening process for health and social needs.
“We met with hospitalists, emergency departments, and hospital administrators, because we wanted their feedback on how to raise awareness of the social needs of patients,” she said. “They have good ideas. They see the patients who come in from the homeless shelters.”
Other hospitals are subsidizing apartments for homeless patients being discharged from the hospital. CommonSpirit Health, the new national Catholic health care organization formed by the 2019 merger of Dignity Health and Catholic Health Initiatives, has explored how to help create and sustain affordable housing in the communities it serves. Investments like this have inspired others, such as Kaiser Permanente, to get involved in supporting housing initiatives.6
Comprehensive community care
David Meltzer, MD, PhD, a hospitalist and professor of medicine at the University of Chicago, said most hospitalists these days believe social determinants of health are part of their job responsibilities.
“That’s not to say we all do it well. We may fail at addressing some of the barriers our patients face. But I don’t know anyone who still says it’s not their job,” he said.
Since 2012, Dr. Meltzer has led a pilot called Comprehensive Care Physicians (CCP), in which the same physician cares for patients with chronic health problems in the clinic and in the hospital, working with a team of nurse practitioners, social workers, care coordinators, and other specialists. A total of 2,000 patients with chronic health problems were enrolled in the study from 2012 to 2016, half assigned to standard care and half assigned to five CCP doctors. The result: The CCP model has shown large improvements in outcomes – particularly among the more vulnerable, less activated patients, is preferred by patients, and has significantly reduced health care utilization.
The next step for the research team is another randomized controlled trial called Comprehensive Care, Community, and Culture, designed to address unmet social needs. Study group patients will also be screened for unmet social needs and have access to a community health worker and to the initiative’s Artful Living Program, which includes community and cultural activities like yoga and dance classes, cooking classes, art classes, and music concerts. To address the complex dimensions and determinants of health, Dr. Meltzer explained, efforts to improve health must extend to sectors far beyond traditional health care.
“I think trying to understand your patients’ social and nonmedical needs starts with getting to know them, and asking about their needs,” he said. “The better you know them, the better you are able to make medical decisions that will promote positive outcomes.”
Sound Physicians, a national hospitalist company based in Tacoma, Wash., and working in 350 hospitals in 41 states, recently published a blog post on its website about the importance of social determinants of health.7 Sound Physicians participates in value-based care through bundled Medicare/Medicaid contracts based on episodes of care for hospitalized patients with certain diagnoses or DRGs, explained John Dickey, MD, the company’s chief medical officer for population health.
“We’ve been heavily involved in trying to improve cost and outcomes of care since 2015. Social determinants absolutely play into trying to lower costs of care and reduce rates of readmissions, which are often multifactorial in cause,” he said. Hospitalists are uniquely equipped to impact post-acute outcomes, Dr. Dickey said, working in partnership with a position Sound Physicians calls the clinical performance nurse.
“We can also partner with primary care providers, provide education for our hospitalist staff, and work with in-home care supports for patients such as these, who otherwise might end up in a skilled nursing facility – even though they’d rather be at home,” he said.
Innovations at Northwell Health
Northwell Health, a multihospital comprehensive health system serving the New York City metro area and Long Island, has shown innovative leadership in addressing social factors. The 23-hospital system initiated in early 2019 a 15-item Self-Reported Social Determinants Screening Tool, which is now used with hospitalized patients to connect them with the support they need to fully recover and avoid readmissions.
Northwell is also providing professional education on social determinants for different constituencies across its system, said Johanna Martinez, MD, MS, a hospitalist and GME Director of Diversity and Health Equity at the Zucker School of Medicine at Hofstra/Northwell. A day-long training retreat was offered to GME faculty, and learning platforms have been developed for physicians, social workers, nurses, and others.
“One of the questions that comes up is that if you find social needs, what do you do about them?” Dr. Martinez explained. That’s more a difficult challenge, she said, so at Northwell, orthopedic surgeons are now asking patients questions like: “What’s going to happen when you go home? What are your social supports? Can you get to the physical therapist’s office?”
Another example of Northwell’s innovations is its Food as Health Program, initially piloted at Long Island Jewish Hospital in Valley Stream, N.Y. Hospitalized patients are asked two questions using a validated screening tool called the Hunger Vital Sign to identify their food insecurities.8 Those who answer yes are referred to a dietitian, and if they have a nutrition-related diagnosis, they enter the multidisciplinary wraparound program.
A key element is the food and health center, located on the hospital campus, where they can get food to take home and referrals to other services, with culturally tailored, disease-specific food education incorporated into the discharge plan. One of the partnering organizations is Island Harvest Food Bank, which helps about 1 in every 10 residents of Long Island with their food insecurity issues.
“When I talk to clinicians, most of us went into medicine to save lives and cure people. Yet the research shows that no matter who we are, we can’t do the best work that our patients need unless we consider their social determinants,” Dr. Martinez said. Ultimately, she noted, there is a need to change the culture of health care. “We have to create system change, reimbursement change, policy change.”
Omolara Uwemedimo, MD, MPH, associate professor of pediatrics and occupational medicine at Northwell and a former nocturnist, said the treatment of illness and health improvement don’t begin in the hospital, they begin in the community. Identifying where people are struggling and what communities they come from requires a broader view of the provider’s role. “Are patients who are readmitted to the hospital generally coming from certain demographics or from certain zip codes?” she asked. “Start there. How can we better connect with those communities?”
Education is key
In 2020 and beyond, hospitalists will hear more about the social determinants of health, Dr. Jacobs-Shaw concluded. “Without addressing those social determinants, we aren’t going to be able to meaningfully impact outcomes or be effective stewards of health care costs – addressing the psychosocial factors and root causes of patients coming in and out of the hospital.”
He added that self-education is key for hospitalists and the teams they work with – to be more aware of the link between health outcomes and social determinants. Guidelines and other resources on social determinants of health are available from the American College of Physicians and the American Association of Family Physicians. ACP issued a position paper on addressing social determinants of health to improve patient care,while AAFP has a research page on its website dedicated to social determinants of health, highlighting a number of initiatives and resources for physicians and others.9
The American Hospital Association has produced fact sheets on ICD-10CM code categories for social determinants of health, including 11 ICD-10 “Z” codes, numbered Z55-Z65, which can be used for coding interventions to address social determinants of health. Other experts are looking at how to adapt the electronic health record to capture sociodemographic and behavioral factors, and then trigger referrals to resources in the hospital and the broader community, and how to mobilize artificial intelligence and machine learning to better identify social needs.
“Our doctors really want to be able to take care of the whole patient, while being stewards of health care resources. But sometimes we feel powerless and wonder how we can have a bigger impact on people, on populations” Dr. Jacobs-Shaw said. “Remember it only takes one voice within an organization to start to elevate this topic.”
References
1. Rappleye E. Physicians say social determinants of health are not their responsibility. Becker’s Hospital Review. 2018 May 15.
2. Robert Wood Johnson Foundation, University of Wisconsin Population Health Institute. County Health Rankings, 2014.
3. Freeman, GA. The extensivist model. Health Leaders Magazine, 2016 Sep 15.
4. Kind AJ et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: A retrospective cohort study. Ann Intern Med. 2014 Dec 2;161(11):765-74.
5. National Institute for Health Care Management. Addressing social determinants of health can improve community health & reduce costs.
6. Vial PB. Boundless collaboration: A philosophy for sustainable and stabilizing housing investment strategies. Health Progress: Journal of the Catholic Health Association of the United States. September-October 2019.
7. Social determinants of health: New solutions for growing complexities. Op-Med, a blog by Sound Physicians. 2019 Aug 1.
8. The hunger vital sign: A new standard of care for preventive health.
9. Daniel H et al. Addressing social determinants to improve patient care and promote health equity: An American College of Physicians position paper. Ann Intern Med. 2018;168:557-578.
While physicians acknowledge that the social determinants of health can impact outcomes from medical care, some may feel that trying to address factors such as homelessness, food insecurity, or lack of ready access to transportation or pharmacy services is just not part of the doctor’s job. A majority of 621 physicians surveyed in the summer of 2017 by Salt Lake City–based health care intelligence firm Leavitt Partners say they are neither capable of nor responsible for addressing such issues.1
But that view may become unsustainable as the U.S. health care system continues to advance toward value- and population-based models of health care and as evidence mounts that social factors are important contributors to costly outcomes, such as avoidable hospital readmissions or emergency room visits. A recent report from the Robert Wood Johnson Foundation estimates that at least 40% of health outcomes are the result of social and economic factors, while only 20% can be attributed to medical care.2
“This is a hot topic – getting a lot of attention these days,” said hospitalist and care transitions expert Ramon Jacobs-Shaw, MD, MPA, regional medical officer for CareMore Health, a California-based physician-led health delivery organization and subsidiary of Anthem. “If you go around the country, some doctors still see social factors as the realm of the social worker. But large health care organizations are coming to recognize that social determinants are huge contributors to the health of their members and to the outcomes of their care.”
Hospitalists could be the natural providers to delve into the specific psychosocial aspects of their patients’ lives, or try to figure out how those factors contribute to health care needs, Dr. Jacobs-Shaw said. They typically confront such issues while the patient is in the hospital bed, but what are the steps that led to the hospitalization in the first place? What will happen after the patient is discharged?
“For example, if patients lack transportation, how can they get to their follow-up medical appointment in the primary care office in order to manage their diabetes? If you can’t follow up with them, their diabetes could get out of control, with complications as a result, such as an infected wound,” he said. Another big issue is access to affordable medications. “CareMore has pharmacists embedded on our care teams. They try to figure out the best medicine for the patient but at the lowest cost. They meet individually with patients and do medication counseling, particularly for those with polypharmacy issues.”
Making health care more equitable
Dr. Jacobs-Shaw has long held a personal interest in issues of inclusiveness, diversity, and how to make health care more equitable for historically underserved groups. Asking how to have a bigger impact on these issues is what brought him, after 13 years as a hospitalist on the East Coast, to CareMore, a company that has made addressing social needs central to its care model. “In California, where I am based, we are a wrap-around for patients who are covered by Medicare Advantage plans. We are whatever the patient needs us to be.”
He oversees a group of hospitalists, dubbed extensivists, who provide advanced patient care and chronic disease management. In the extensivist model, physicians and advanced practice nurses provide comprehensive and coordinated care to patients with complex medical issues, taking their scope of practice beyond the hospital into homes, post-acute care facilities, and other settings, with a focus on keeping patients healthier and reducing readmission.3
“Our patients get access to extra services and resources, some of which are available at our care centers – which are one-stop outpatient facilities. We also focus on a lot of things physicians didn’t historically think were within their wheelhouse. Hospitalists deal with these kinds of issues every day, but may not label them as social determinants of health,” Dr. Jacobs-Shaw said. He emphasized that hospitalists should realize that they are not powerless to address these issues, working in partnership with other groups in and out of the hospital. They should also know that health care payers increasingly are dedicating resources to these issues.
“We just started trying to address homelessness through a pilot in Orange County, working with nonprofit organizations and philanthropy to offer a transitional site of care for our patients who are being discharged from the hospital and have housing insecurity issues, to get them transitioned into more secure housing,” Dr. Jacobs-Shaw said. CareMore also has a transportation collaborative that offers no-cost, nonemergency transportation to medical appointments. “That’s meeting them where they are at, based on an assessment of their needs and resources.”
What are social determinants?
The social determinants of health – social, environmental, and other nonmedical factors that contribute to overall health status and medical need – have been defined by the World Health Organization as: “conditions in which people are born, grow, live, work, and age.” That is a broad complex of overlapping social and systems issues, but it provides a context for a broader understanding of the patient’s health and response to medical interventions.
Socioeconomic status is a huge determinant. Level of education may be more important than income if the person lacks the health literacy to navigate the system and access needed care. Housing instability may include poor sanitation, substandard dwellings, or unsafe neighborhoods – all of which can affect a person’s well-being. Environmental health may include compromised air quality – which can impact pulmonary health. Other issues include access to employment and child care, utility needs, and interpersonal violence.
A 2014 paper in Annals of Internal Medicine found that residence within a disadvantaged neighborhood was a factor in hospital readmission rates as often as was chronic pulmonary disease.4 A recent report on social determinants of health by the National Institute for Health Care Management notes that patients with food insecurity are 2.4 times more likely to go to the emergency room, while those with transportation needs are 2.6 times more likely.5
What can health care leaders do to better equip their clinicians and teams to help patients deal with this array of complex needs? Intermountain Healthcare, based in Salt Lake City, spearheaded in 2018 the development of the Alliance for the Determinants of Health, starting in the communities of Ogden and St. George, Utah. The Alliance seeks to promote health, improve access to care, and decrease health care costs through a charitable contribution of $12 million over 3 years to seed collaborative demonstration projects.
Lisa Nichols, assistant vice president for community health at Intermountain, said that, while hospitalists were not directly involved in planning the Alliance, hospitalists and ED physicians have become essential to the patient-screening process for health and social needs.
“We met with hospitalists, emergency departments, and hospital administrators, because we wanted their feedback on how to raise awareness of the social needs of patients,” she said. “They have good ideas. They see the patients who come in from the homeless shelters.”
Other hospitals are subsidizing apartments for homeless patients being discharged from the hospital. CommonSpirit Health, the new national Catholic health care organization formed by the 2019 merger of Dignity Health and Catholic Health Initiatives, has explored how to help create and sustain affordable housing in the communities it serves. Investments like this have inspired others, such as Kaiser Permanente, to get involved in supporting housing initiatives.6
Comprehensive community care
David Meltzer, MD, PhD, a hospitalist and professor of medicine at the University of Chicago, said most hospitalists these days believe social determinants of health are part of their job responsibilities.
“That’s not to say we all do it well. We may fail at addressing some of the barriers our patients face. But I don’t know anyone who still says it’s not their job,” he said.
Since 2012, Dr. Meltzer has led a pilot called Comprehensive Care Physicians (CCP), in which the same physician cares for patients with chronic health problems in the clinic and in the hospital, working with a team of nurse practitioners, social workers, care coordinators, and other specialists. A total of 2,000 patients with chronic health problems were enrolled in the study from 2012 to 2016, half assigned to standard care and half assigned to five CCP doctors. The result: The CCP model has shown large improvements in outcomes – particularly among the more vulnerable, less activated patients, is preferred by patients, and has significantly reduced health care utilization.
The next step for the research team is another randomized controlled trial called Comprehensive Care, Community, and Culture, designed to address unmet social needs. Study group patients will also be screened for unmet social needs and have access to a community health worker and to the initiative’s Artful Living Program, which includes community and cultural activities like yoga and dance classes, cooking classes, art classes, and music concerts. To address the complex dimensions and determinants of health, Dr. Meltzer explained, efforts to improve health must extend to sectors far beyond traditional health care.
“I think trying to understand your patients’ social and nonmedical needs starts with getting to know them, and asking about their needs,” he said. “The better you know them, the better you are able to make medical decisions that will promote positive outcomes.”
Sound Physicians, a national hospitalist company based in Tacoma, Wash., and working in 350 hospitals in 41 states, recently published a blog post on its website about the importance of social determinants of health.7 Sound Physicians participates in value-based care through bundled Medicare/Medicaid contracts based on episodes of care for hospitalized patients with certain diagnoses or DRGs, explained John Dickey, MD, the company’s chief medical officer for population health.
“We’ve been heavily involved in trying to improve cost and outcomes of care since 2015. Social determinants absolutely play into trying to lower costs of care and reduce rates of readmissions, which are often multifactorial in cause,” he said. Hospitalists are uniquely equipped to impact post-acute outcomes, Dr. Dickey said, working in partnership with a position Sound Physicians calls the clinical performance nurse.
“We can also partner with primary care providers, provide education for our hospitalist staff, and work with in-home care supports for patients such as these, who otherwise might end up in a skilled nursing facility – even though they’d rather be at home,” he said.
Innovations at Northwell Health
Northwell Health, a multihospital comprehensive health system serving the New York City metro area and Long Island, has shown innovative leadership in addressing social factors. The 23-hospital system initiated in early 2019 a 15-item Self-Reported Social Determinants Screening Tool, which is now used with hospitalized patients to connect them with the support they need to fully recover and avoid readmissions.
Northwell is also providing professional education on social determinants for different constituencies across its system, said Johanna Martinez, MD, MS, a hospitalist and GME Director of Diversity and Health Equity at the Zucker School of Medicine at Hofstra/Northwell. A day-long training retreat was offered to GME faculty, and learning platforms have been developed for physicians, social workers, nurses, and others.
“One of the questions that comes up is that if you find social needs, what do you do about them?” Dr. Martinez explained. That’s more a difficult challenge, she said, so at Northwell, orthopedic surgeons are now asking patients questions like: “What’s going to happen when you go home? What are your social supports? Can you get to the physical therapist’s office?”
Another example of Northwell’s innovations is its Food as Health Program, initially piloted at Long Island Jewish Hospital in Valley Stream, N.Y. Hospitalized patients are asked two questions using a validated screening tool called the Hunger Vital Sign to identify their food insecurities.8 Those who answer yes are referred to a dietitian, and if they have a nutrition-related diagnosis, they enter the multidisciplinary wraparound program.
A key element is the food and health center, located on the hospital campus, where they can get food to take home and referrals to other services, with culturally tailored, disease-specific food education incorporated into the discharge plan. One of the partnering organizations is Island Harvest Food Bank, which helps about 1 in every 10 residents of Long Island with their food insecurity issues.
“When I talk to clinicians, most of us went into medicine to save lives and cure people. Yet the research shows that no matter who we are, we can’t do the best work that our patients need unless we consider their social determinants,” Dr. Martinez said. Ultimately, she noted, there is a need to change the culture of health care. “We have to create system change, reimbursement change, policy change.”
Omolara Uwemedimo, MD, MPH, associate professor of pediatrics and occupational medicine at Northwell and a former nocturnist, said the treatment of illness and health improvement don’t begin in the hospital, they begin in the community. Identifying where people are struggling and what communities they come from requires a broader view of the provider’s role. “Are patients who are readmitted to the hospital generally coming from certain demographics or from certain zip codes?” she asked. “Start there. How can we better connect with those communities?”
Education is key
In 2020 and beyond, hospitalists will hear more about the social determinants of health, Dr. Jacobs-Shaw concluded. “Without addressing those social determinants, we aren’t going to be able to meaningfully impact outcomes or be effective stewards of health care costs – addressing the psychosocial factors and root causes of patients coming in and out of the hospital.”
He added that self-education is key for hospitalists and the teams they work with – to be more aware of the link between health outcomes and social determinants. Guidelines and other resources on social determinants of health are available from the American College of Physicians and the American Association of Family Physicians. ACP issued a position paper on addressing social determinants of health to improve patient care,while AAFP has a research page on its website dedicated to social determinants of health, highlighting a number of initiatives and resources for physicians and others.9
The American Hospital Association has produced fact sheets on ICD-10CM code categories for social determinants of health, including 11 ICD-10 “Z” codes, numbered Z55-Z65, which can be used for coding interventions to address social determinants of health. Other experts are looking at how to adapt the electronic health record to capture sociodemographic and behavioral factors, and then trigger referrals to resources in the hospital and the broader community, and how to mobilize artificial intelligence and machine learning to better identify social needs.
“Our doctors really want to be able to take care of the whole patient, while being stewards of health care resources. But sometimes we feel powerless and wonder how we can have a bigger impact on people, on populations” Dr. Jacobs-Shaw said. “Remember it only takes one voice within an organization to start to elevate this topic.”
References
1. Rappleye E. Physicians say social determinants of health are not their responsibility. Becker’s Hospital Review. 2018 May 15.
2. Robert Wood Johnson Foundation, University of Wisconsin Population Health Institute. County Health Rankings, 2014.
3. Freeman, GA. The extensivist model. Health Leaders Magazine, 2016 Sep 15.
4. Kind AJ et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: A retrospective cohort study. Ann Intern Med. 2014 Dec 2;161(11):765-74.
5. National Institute for Health Care Management. Addressing social determinants of health can improve community health & reduce costs.
6. Vial PB. Boundless collaboration: A philosophy for sustainable and stabilizing housing investment strategies. Health Progress: Journal of the Catholic Health Association of the United States. September-October 2019.
7. Social determinants of health: New solutions for growing complexities. Op-Med, a blog by Sound Physicians. 2019 Aug 1.
8. The hunger vital sign: A new standard of care for preventive health.
9. Daniel H et al. Addressing social determinants to improve patient care and promote health equity: An American College of Physicians position paper. Ann Intern Med. 2018;168:557-578.
Racial Limitations of Fitzpatrick Skin Type
Fitzpatrick skin type (FST) is the most commonly used classification system in dermatologic practice. It was developed by Thomas B. Fitzpatrick, MD, PhD, in 1975 to assess the propensity of the skin to burn during phototherapy.1 Fitzpatrick skin type also can be used to assess the clinical benefits and efficacy of cosmetic procedures, including laser hair removal, chemical peel and dermabrasion, tattoo removal, spray tanning, and laser resurfacing for acne scarring.2 The original FST classifications included skin types I through IV; skin types V and VI were later added to include individuals of Asian, Indian, and African origin.1 As a result, FST often is used by providers as a means of describing constitutive skin color and ethnicity.3
How did FST transition from describing the propensity of the skin to burn from UV light exposure to categorizing skin color, thereby becoming a proxy for race? It most likely occurred because there has not been another widely adopted classification system for describing skin color that can be applied to all skin types. Even when the FST classification scale is used as intended, there are inconsistencies with its accuracy; for example, self-reported FSTs have correlated poorly with sunburn risk as well as physician-reported FSTs.4,5 Although physician-reported FSTs have been demonstrated to correlate with race, race does not consistently correlate with objective measures of pigmentation or self-reported FSTs.5 For example, Japanese women often self-identify as FST type II, but Asian skin generally is considered to be nonwhite.1 Fitzpatrick himself acknowledged that race and ethnicity are cultural and political terms with no scientific basis.6 Fitzpatrick skin type also has been demonstrated to correlate poorly with constitutive skin color and minimal erythema dose values.7
We conducted an anonymous survey of dermatologists and dermatology trainees to evaluate how providers use FST in their clinical practice as well as how it is used to describe race and ethnicity.
Methods
The survey was distributed electronically to dermatologists and dermatology trainees from March 13 to March 28, 2019, using the Association of Professors of Dermatology listserv, as well as in person at the annual Skin of Color Society meeting in Washington, DC, on February 28, 2019. The 8-item survey included questions about physician demographics (ie, primary practice setting, board certification, and geographic location); whether the respondent identified as an individual with skin of color; and how the respondent utilized FST in clinical notes (ie, describing race/ethnicity, skin cancer risk, and constitutive [baseline] skin color; determining initial phototherapy dosage and suitability for laser treatments, and likelihood of skin burning). A t test was used to determine whether dermatologists who identified as having skin of color utilized FST differently.
Results
A total of 141 surveys were returned, and 140 respondents were included in the final analysis. Given the methods used to distribute the survey, a response rate could not be calculated. The respondents included more board-certified dermatologists (70%) than dermatology trainees (30%). Ninety-three percent of respondents indicated an academic institution as their primary practice location. Notably, 26% of respondents self-identified as having skin of color.
Forty-one percent of all respondents agreed that FST should be included in their clinical documentation. In response to the question “In what scenarios would you refer to FST in a clinical note?” 31% said they used FST to describe patients’ race or ethnicity, 47% used it to describe patients’ constitutive skin color, and 22% utilized it in both scenarios. Respondents who did not identify as having skin of color were more likely to use FST to describe constitutive skin color, though this finding was not statistically significant (P=.063). Anecdotally, providers also included FST in clinical notes on postinflammatory hyperpigmentation, melasma, and treatment with cryotherapy.
Comment
The US Census Bureau has estimated that half of the US population will be of non-European descent by 2050.8 As racial and ethnic distinctions continue to be blurred, attempts to include all nonwhite skin types under the umbrella term skin of color becomes increasingly problematic. The true number of skin colors is unknown but likely is infinite, as Brazilian artist Angélica Dass has demonstrated with her photographic project “Humanae” (Figure). Given this shift in demographics and the limitations of the FST, alternative methods of describing skin color must be developed.

© Angélica Dass | Humanae Work in Progress (Courtesy of the artist).
The results of our survey suggest that approximately one-third to half of academic dermatologists/dermatology trainees use FST to describe race/ethnicity and/or constitutive skin color. This misuse of FST may occur more frequently among physicians who do not identify as having skin of color. Additionally, misuse of FST in academic settings may be problematic and confusing for medical students who may learn to use this common dermatologic tool outside of its original intent.
We acknowledge that the conundrum of how to classify individuals with nonwhite skin or skin of color is not simply answered. Several alternative skin classification models have been proposed to improve the sensitivity and specificity of identifying patients with skin of color (Table). Refining FST classification is one approach. Employing terms such as skin irritation, tenderness, itching, or skin becoming darker from sun exposure rather than painful burn or tanning may result in better identification.1,4 A study conducted in India modified the FST questionnaire to acknowledge cultural behaviors.15 Because lighter skin is culturally valued in this population, patient experience with purposeful sun exposure was limited; thus, the questionnaire was modified to remove questions on the use of tanning booths and/or creams as well as sun exposure and instead included more objective questions regarding dark brown eye color, black and dark brown hair color, and dark brown skin color.15 Other studies have suggested that patient-reported photosensitivity assessed via a questionnaire is a valid measure for assessing FST but is associated with an overestimation of skin color, known as “the dark shift.”20

Sharma et al15 utilized reflectance spectrophotometry as an objective measure of melanin and skin erythema. The melanin index consistently showed a positive correlation with FSTs as opposed to the erythema index, which correlated poorly.15 Although reflectance spectrometry accurately identifies skin color in patients with nonwhite skin,21,22 it is an impractical and cost-prohibitive tool for daily practice. A more practical tool for the clinical setting would be a visual color scale with skin hues spanning FST types I to VI, including bands of increasingly darker gradations that would be particularly useful in assessing skin of color. Once such tool is the Taylor Hyperpigmentation Scale.17 Although currently not widely available, this tool could be further refined with additional skin hues.
Conclusion
Other investigators have criticized the various limitations of FST, including physician vs patient assessment, interview vs questionnaire, and phrasing of questions on skin type.23 Our findings suggest that medical providers should be cognizant of conflating race and ethnicity with FST. Two authors of this report (O.R.W. and J.E.D.) are medical students with skin of color and frequently have observed the addition of FST to the medical records of patients who were not receiving phototherapy as a proxy for race. We believe that more culturally appropriate and clinically relevant methods for describing skin of color need to be developed and, in the interim, the original intent of FST should be emphasized and incorporated in medical school and resident education.
Acknowledgment
The authors thank Adewole Adamson, MD (Austin, Texas), for discussion and feedback.
- Goldsmith LA, Katz SI, Gilchrest BA, et al, eds. Fitzpatrick’s Dermatology in General Medicine. 8th ed. New York, NY: The McGraw-Hill Companies; 2012.
- Sachdeva S. Fitzpatrick skin typing: applications in dermatology. Indian J Dermatol Venereol Leprol. 2009;75:93-96.
- Everett JS, Budescu M, Sommers MS. Making sense of skin color in clinical care. Clin Nurs Res. 2012;21:495-516.
- Eilers S, Bach DQ, Gaber R, et al. Accuracy of self-report in assessingFitzpatrick skin phototypes I through VI. JAMA Dermatol. 2013;149:1289-1294.
- He SY, McCulloch CE, Boscardin WJ, et al. Self-reported pigmentary phenotypes and race are significant but incomplete predictors of Fitzpatrick skin phototype in an ethnically diverse population. J Am Acad Dermatol. 2014;71:731-737.
- Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869-871.
- Leenutaphong V. Relationship between skin color and cutaneous response to ultraviolet radiation in Thai. Photodermatol Photoimmunol Photomed. 1996;11:198-203.
- Colby SL, Ortman JM. Projections of the Size and Composition of the US Population: 2014 to 2060. Washington, DC: US Census Bureau; 2015.
- Baumann L. Understanding and treating various skin types: the Baumann Skin Type Indicator. Dermatol Clin. 2008;26:359-373.
- Fanous N. A new patient classification for laser resurfacing and peels: predicting responses, risks, and results. Aesthetic Plast Surg. 2002;26:99-104.
- Glogau RG. Chemical peeling and aging skin. J Geriatric Dermatol. 1994;2:30-35.
- Goldman M. Universal classification of skin type. In: Shiffman M, Mirrafati S, Lam S, et al, eds. Simplified Facial Rejuvenation. Berlin, Heidelberg, Germany: Springer; 2008:47-50.
- Kawada A. UVB-induced erythema, delayed tanning, and UVA-induced immediate tanning in Japanese skin. Photodermatol. 1986;3:327-333.
- Lancer HA. Lancer Ethnicity Scale (LES). Lasers Surg Med. 1998;22:9.
- Sharma VK, Gupta V, Jangid BL, et al. Modification of the Fitzpatrick system of skin phototype classification for the Indian population, and its correlation with narrowband diffuse reflectance spectrophotometry. Clin Exp Dermatol. 2018;43:274-280.
- Roberts WE. The Roberts Skin Type Classification System. J Drugs Dermatol. 2008;7:452-456.
- Taylor SC, Arsonnaud S, Czernielewski J. The Taylor hyperpigmentation scale: a new visual assessment tool for the evaluation of skin color and pigmentation. Cutis. 2005;76:270-274.
- Treesirichod A, Chansakulporn S, Wattanapan P. Correlation between skin color evaluation by skin color scale chart and narrowband reflectance spectrophotometer. Indian J Dermatol. 2014;59:339-342.
- Willis I, Earles RM. A new classification system relevant to people of African descent. J Cosmet Dermatol. 2005;18:209-216.
- Reeder AI, Hammond VA, Gray AR. Questionnaire items to assess skin color and erythemal sensitivity: reliability, validity, and “the dark shift.” Cancer Epidemiol Biomarkers Prev. 2010;19:1167-1173.
- Dwyer T, Muller HK, Blizzard L, et al. The use of spectrophotometry to estimate melanin density in Caucasians. Cancer Epidemiol Biomarkers Prev. 1998;7:203-206.
- Pershing LK, Tirumala VP, Nelson JL, et al. Reflectance spectrophotometer: the dermatologists’ sphygmomanometer for skin phototyping? J Invest Dermatol. 2008;128:1633-1640.
- Trakatelli M, Bylaite-Bucinskiene M, Correia O, et al. Clinical assessment of skin phototypes: watch your words! Eur J Dermatol. 2017;27:615-619.
Fitzpatrick skin type (FST) is the most commonly used classification system in dermatologic practice. It was developed by Thomas B. Fitzpatrick, MD, PhD, in 1975 to assess the propensity of the skin to burn during phototherapy.1 Fitzpatrick skin type also can be used to assess the clinical benefits and efficacy of cosmetic procedures, including laser hair removal, chemical peel and dermabrasion, tattoo removal, spray tanning, and laser resurfacing for acne scarring.2 The original FST classifications included skin types I through IV; skin types V and VI were later added to include individuals of Asian, Indian, and African origin.1 As a result, FST often is used by providers as a means of describing constitutive skin color and ethnicity.3
How did FST transition from describing the propensity of the skin to burn from UV light exposure to categorizing skin color, thereby becoming a proxy for race? It most likely occurred because there has not been another widely adopted classification system for describing skin color that can be applied to all skin types. Even when the FST classification scale is used as intended, there are inconsistencies with its accuracy; for example, self-reported FSTs have correlated poorly with sunburn risk as well as physician-reported FSTs.4,5 Although physician-reported FSTs have been demonstrated to correlate with race, race does not consistently correlate with objective measures of pigmentation or self-reported FSTs.5 For example, Japanese women often self-identify as FST type II, but Asian skin generally is considered to be nonwhite.1 Fitzpatrick himself acknowledged that race and ethnicity are cultural and political terms with no scientific basis.6 Fitzpatrick skin type also has been demonstrated to correlate poorly with constitutive skin color and minimal erythema dose values.7
We conducted an anonymous survey of dermatologists and dermatology trainees to evaluate how providers use FST in their clinical practice as well as how it is used to describe race and ethnicity.
Methods
The survey was distributed electronically to dermatologists and dermatology trainees from March 13 to March 28, 2019, using the Association of Professors of Dermatology listserv, as well as in person at the annual Skin of Color Society meeting in Washington, DC, on February 28, 2019. The 8-item survey included questions about physician demographics (ie, primary practice setting, board certification, and geographic location); whether the respondent identified as an individual with skin of color; and how the respondent utilized FST in clinical notes (ie, describing race/ethnicity, skin cancer risk, and constitutive [baseline] skin color; determining initial phototherapy dosage and suitability for laser treatments, and likelihood of skin burning). A t test was used to determine whether dermatologists who identified as having skin of color utilized FST differently.
Results
A total of 141 surveys were returned, and 140 respondents were included in the final analysis. Given the methods used to distribute the survey, a response rate could not be calculated. The respondents included more board-certified dermatologists (70%) than dermatology trainees (30%). Ninety-three percent of respondents indicated an academic institution as their primary practice location. Notably, 26% of respondents self-identified as having skin of color.
Forty-one percent of all respondents agreed that FST should be included in their clinical documentation. In response to the question “In what scenarios would you refer to FST in a clinical note?” 31% said they used FST to describe patients’ race or ethnicity, 47% used it to describe patients’ constitutive skin color, and 22% utilized it in both scenarios. Respondents who did not identify as having skin of color were more likely to use FST to describe constitutive skin color, though this finding was not statistically significant (P=.063). Anecdotally, providers also included FST in clinical notes on postinflammatory hyperpigmentation, melasma, and treatment with cryotherapy.
Comment
The US Census Bureau has estimated that half of the US population will be of non-European descent by 2050.8 As racial and ethnic distinctions continue to be blurred, attempts to include all nonwhite skin types under the umbrella term skin of color becomes increasingly problematic. The true number of skin colors is unknown but likely is infinite, as Brazilian artist Angélica Dass has demonstrated with her photographic project “Humanae” (Figure). Given this shift in demographics and the limitations of the FST, alternative methods of describing skin color must be developed.

© Angélica Dass | Humanae Work in Progress (Courtesy of the artist).
The results of our survey suggest that approximately one-third to half of academic dermatologists/dermatology trainees use FST to describe race/ethnicity and/or constitutive skin color. This misuse of FST may occur more frequently among physicians who do not identify as having skin of color. Additionally, misuse of FST in academic settings may be problematic and confusing for medical students who may learn to use this common dermatologic tool outside of its original intent.
We acknowledge that the conundrum of how to classify individuals with nonwhite skin or skin of color is not simply answered. Several alternative skin classification models have been proposed to improve the sensitivity and specificity of identifying patients with skin of color (Table). Refining FST classification is one approach. Employing terms such as skin irritation, tenderness, itching, or skin becoming darker from sun exposure rather than painful burn or tanning may result in better identification.1,4 A study conducted in India modified the FST questionnaire to acknowledge cultural behaviors.15 Because lighter skin is culturally valued in this population, patient experience with purposeful sun exposure was limited; thus, the questionnaire was modified to remove questions on the use of tanning booths and/or creams as well as sun exposure and instead included more objective questions regarding dark brown eye color, black and dark brown hair color, and dark brown skin color.15 Other studies have suggested that patient-reported photosensitivity assessed via a questionnaire is a valid measure for assessing FST but is associated with an overestimation of skin color, known as “the dark shift.”20

Sharma et al15 utilized reflectance spectrophotometry as an objective measure of melanin and skin erythema. The melanin index consistently showed a positive correlation with FSTs as opposed to the erythema index, which correlated poorly.15 Although reflectance spectrometry accurately identifies skin color in patients with nonwhite skin,21,22 it is an impractical and cost-prohibitive tool for daily practice. A more practical tool for the clinical setting would be a visual color scale with skin hues spanning FST types I to VI, including bands of increasingly darker gradations that would be particularly useful in assessing skin of color. Once such tool is the Taylor Hyperpigmentation Scale.17 Although currently not widely available, this tool could be further refined with additional skin hues.
Conclusion
Other investigators have criticized the various limitations of FST, including physician vs patient assessment, interview vs questionnaire, and phrasing of questions on skin type.23 Our findings suggest that medical providers should be cognizant of conflating race and ethnicity with FST. Two authors of this report (O.R.W. and J.E.D.) are medical students with skin of color and frequently have observed the addition of FST to the medical records of patients who were not receiving phototherapy as a proxy for race. We believe that more culturally appropriate and clinically relevant methods for describing skin of color need to be developed and, in the interim, the original intent of FST should be emphasized and incorporated in medical school and resident education.
Acknowledgment
The authors thank Adewole Adamson, MD (Austin, Texas), for discussion and feedback.
Fitzpatrick skin type (FST) is the most commonly used classification system in dermatologic practice. It was developed by Thomas B. Fitzpatrick, MD, PhD, in 1975 to assess the propensity of the skin to burn during phototherapy.1 Fitzpatrick skin type also can be used to assess the clinical benefits and efficacy of cosmetic procedures, including laser hair removal, chemical peel and dermabrasion, tattoo removal, spray tanning, and laser resurfacing for acne scarring.2 The original FST classifications included skin types I through IV; skin types V and VI were later added to include individuals of Asian, Indian, and African origin.1 As a result, FST often is used by providers as a means of describing constitutive skin color and ethnicity.3
How did FST transition from describing the propensity of the skin to burn from UV light exposure to categorizing skin color, thereby becoming a proxy for race? It most likely occurred because there has not been another widely adopted classification system for describing skin color that can be applied to all skin types. Even when the FST classification scale is used as intended, there are inconsistencies with its accuracy; for example, self-reported FSTs have correlated poorly with sunburn risk as well as physician-reported FSTs.4,5 Although physician-reported FSTs have been demonstrated to correlate with race, race does not consistently correlate with objective measures of pigmentation or self-reported FSTs.5 For example, Japanese women often self-identify as FST type II, but Asian skin generally is considered to be nonwhite.1 Fitzpatrick himself acknowledged that race and ethnicity are cultural and political terms with no scientific basis.6 Fitzpatrick skin type also has been demonstrated to correlate poorly with constitutive skin color and minimal erythema dose values.7
We conducted an anonymous survey of dermatologists and dermatology trainees to evaluate how providers use FST in their clinical practice as well as how it is used to describe race and ethnicity.
Methods
The survey was distributed electronically to dermatologists and dermatology trainees from March 13 to March 28, 2019, using the Association of Professors of Dermatology listserv, as well as in person at the annual Skin of Color Society meeting in Washington, DC, on February 28, 2019. The 8-item survey included questions about physician demographics (ie, primary practice setting, board certification, and geographic location); whether the respondent identified as an individual with skin of color; and how the respondent utilized FST in clinical notes (ie, describing race/ethnicity, skin cancer risk, and constitutive [baseline] skin color; determining initial phototherapy dosage and suitability for laser treatments, and likelihood of skin burning). A t test was used to determine whether dermatologists who identified as having skin of color utilized FST differently.
Results
A total of 141 surveys were returned, and 140 respondents were included in the final analysis. Given the methods used to distribute the survey, a response rate could not be calculated. The respondents included more board-certified dermatologists (70%) than dermatology trainees (30%). Ninety-three percent of respondents indicated an academic institution as their primary practice location. Notably, 26% of respondents self-identified as having skin of color.
Forty-one percent of all respondents agreed that FST should be included in their clinical documentation. In response to the question “In what scenarios would you refer to FST in a clinical note?” 31% said they used FST to describe patients’ race or ethnicity, 47% used it to describe patients’ constitutive skin color, and 22% utilized it in both scenarios. Respondents who did not identify as having skin of color were more likely to use FST to describe constitutive skin color, though this finding was not statistically significant (P=.063). Anecdotally, providers also included FST in clinical notes on postinflammatory hyperpigmentation, melasma, and treatment with cryotherapy.
Comment
The US Census Bureau has estimated that half of the US population will be of non-European descent by 2050.8 As racial and ethnic distinctions continue to be blurred, attempts to include all nonwhite skin types under the umbrella term skin of color becomes increasingly problematic. The true number of skin colors is unknown but likely is infinite, as Brazilian artist Angélica Dass has demonstrated with her photographic project “Humanae” (Figure). Given this shift in demographics and the limitations of the FST, alternative methods of describing skin color must be developed.

© Angélica Dass | Humanae Work in Progress (Courtesy of the artist).
The results of our survey suggest that approximately one-third to half of academic dermatologists/dermatology trainees use FST to describe race/ethnicity and/or constitutive skin color. This misuse of FST may occur more frequently among physicians who do not identify as having skin of color. Additionally, misuse of FST in academic settings may be problematic and confusing for medical students who may learn to use this common dermatologic tool outside of its original intent.
We acknowledge that the conundrum of how to classify individuals with nonwhite skin or skin of color is not simply answered. Several alternative skin classification models have been proposed to improve the sensitivity and specificity of identifying patients with skin of color (Table). Refining FST classification is one approach. Employing terms such as skin irritation, tenderness, itching, or skin becoming darker from sun exposure rather than painful burn or tanning may result in better identification.1,4 A study conducted in India modified the FST questionnaire to acknowledge cultural behaviors.15 Because lighter skin is culturally valued in this population, patient experience with purposeful sun exposure was limited; thus, the questionnaire was modified to remove questions on the use of tanning booths and/or creams as well as sun exposure and instead included more objective questions regarding dark brown eye color, black and dark brown hair color, and dark brown skin color.15 Other studies have suggested that patient-reported photosensitivity assessed via a questionnaire is a valid measure for assessing FST but is associated with an overestimation of skin color, known as “the dark shift.”20

Sharma et al15 utilized reflectance spectrophotometry as an objective measure of melanin and skin erythema. The melanin index consistently showed a positive correlation with FSTs as opposed to the erythema index, which correlated poorly.15 Although reflectance spectrometry accurately identifies skin color in patients with nonwhite skin,21,22 it is an impractical and cost-prohibitive tool for daily practice. A more practical tool for the clinical setting would be a visual color scale with skin hues spanning FST types I to VI, including bands of increasingly darker gradations that would be particularly useful in assessing skin of color. Once such tool is the Taylor Hyperpigmentation Scale.17 Although currently not widely available, this tool could be further refined with additional skin hues.
Conclusion
Other investigators have criticized the various limitations of FST, including physician vs patient assessment, interview vs questionnaire, and phrasing of questions on skin type.23 Our findings suggest that medical providers should be cognizant of conflating race and ethnicity with FST. Two authors of this report (O.R.W. and J.E.D.) are medical students with skin of color and frequently have observed the addition of FST to the medical records of patients who were not receiving phototherapy as a proxy for race. We believe that more culturally appropriate and clinically relevant methods for describing skin of color need to be developed and, in the interim, the original intent of FST should be emphasized and incorporated in medical school and resident education.
Acknowledgment
The authors thank Adewole Adamson, MD (Austin, Texas), for discussion and feedback.
- Goldsmith LA, Katz SI, Gilchrest BA, et al, eds. Fitzpatrick’s Dermatology in General Medicine. 8th ed. New York, NY: The McGraw-Hill Companies; 2012.
- Sachdeva S. Fitzpatrick skin typing: applications in dermatology. Indian J Dermatol Venereol Leprol. 2009;75:93-96.
- Everett JS, Budescu M, Sommers MS. Making sense of skin color in clinical care. Clin Nurs Res. 2012;21:495-516.
- Eilers S, Bach DQ, Gaber R, et al. Accuracy of self-report in assessingFitzpatrick skin phototypes I through VI. JAMA Dermatol. 2013;149:1289-1294.
- He SY, McCulloch CE, Boscardin WJ, et al. Self-reported pigmentary phenotypes and race are significant but incomplete predictors of Fitzpatrick skin phototype in an ethnically diverse population. J Am Acad Dermatol. 2014;71:731-737.
- Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869-871.
- Leenutaphong V. Relationship between skin color and cutaneous response to ultraviolet radiation in Thai. Photodermatol Photoimmunol Photomed. 1996;11:198-203.
- Colby SL, Ortman JM. Projections of the Size and Composition of the US Population: 2014 to 2060. Washington, DC: US Census Bureau; 2015.
- Baumann L. Understanding and treating various skin types: the Baumann Skin Type Indicator. Dermatol Clin. 2008;26:359-373.
- Fanous N. A new patient classification for laser resurfacing and peels: predicting responses, risks, and results. Aesthetic Plast Surg. 2002;26:99-104.
- Glogau RG. Chemical peeling and aging skin. J Geriatric Dermatol. 1994;2:30-35.
- Goldman M. Universal classification of skin type. In: Shiffman M, Mirrafati S, Lam S, et al, eds. Simplified Facial Rejuvenation. Berlin, Heidelberg, Germany: Springer; 2008:47-50.
- Kawada A. UVB-induced erythema, delayed tanning, and UVA-induced immediate tanning in Japanese skin. Photodermatol. 1986;3:327-333.
- Lancer HA. Lancer Ethnicity Scale (LES). Lasers Surg Med. 1998;22:9.
- Sharma VK, Gupta V, Jangid BL, et al. Modification of the Fitzpatrick system of skin phototype classification for the Indian population, and its correlation with narrowband diffuse reflectance spectrophotometry. Clin Exp Dermatol. 2018;43:274-280.
- Roberts WE. The Roberts Skin Type Classification System. J Drugs Dermatol. 2008;7:452-456.
- Taylor SC, Arsonnaud S, Czernielewski J. The Taylor hyperpigmentation scale: a new visual assessment tool for the evaluation of skin color and pigmentation. Cutis. 2005;76:270-274.
- Treesirichod A, Chansakulporn S, Wattanapan P. Correlation between skin color evaluation by skin color scale chart and narrowband reflectance spectrophotometer. Indian J Dermatol. 2014;59:339-342.
- Willis I, Earles RM. A new classification system relevant to people of African descent. J Cosmet Dermatol. 2005;18:209-216.
- Reeder AI, Hammond VA, Gray AR. Questionnaire items to assess skin color and erythemal sensitivity: reliability, validity, and “the dark shift.” Cancer Epidemiol Biomarkers Prev. 2010;19:1167-1173.
- Dwyer T, Muller HK, Blizzard L, et al. The use of spectrophotometry to estimate melanin density in Caucasians. Cancer Epidemiol Biomarkers Prev. 1998;7:203-206.
- Pershing LK, Tirumala VP, Nelson JL, et al. Reflectance spectrophotometer: the dermatologists’ sphygmomanometer for skin phototyping? J Invest Dermatol. 2008;128:1633-1640.
- Trakatelli M, Bylaite-Bucinskiene M, Correia O, et al. Clinical assessment of skin phototypes: watch your words! Eur J Dermatol. 2017;27:615-619.
- Goldsmith LA, Katz SI, Gilchrest BA, et al, eds. Fitzpatrick’s Dermatology in General Medicine. 8th ed. New York, NY: The McGraw-Hill Companies; 2012.
- Sachdeva S. Fitzpatrick skin typing: applications in dermatology. Indian J Dermatol Venereol Leprol. 2009;75:93-96.
- Everett JS, Budescu M, Sommers MS. Making sense of skin color in clinical care. Clin Nurs Res. 2012;21:495-516.
- Eilers S, Bach DQ, Gaber R, et al. Accuracy of self-report in assessingFitzpatrick skin phototypes I through VI. JAMA Dermatol. 2013;149:1289-1294.
- He SY, McCulloch CE, Boscardin WJ, et al. Self-reported pigmentary phenotypes and race are significant but incomplete predictors of Fitzpatrick skin phototype in an ethnically diverse population. J Am Acad Dermatol. 2014;71:731-737.
- Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869-871.
- Leenutaphong V. Relationship between skin color and cutaneous response to ultraviolet radiation in Thai. Photodermatol Photoimmunol Photomed. 1996;11:198-203.
- Colby SL, Ortman JM. Projections of the Size and Composition of the US Population: 2014 to 2060. Washington, DC: US Census Bureau; 2015.
- Baumann L. Understanding and treating various skin types: the Baumann Skin Type Indicator. Dermatol Clin. 2008;26:359-373.
- Fanous N. A new patient classification for laser resurfacing and peels: predicting responses, risks, and results. Aesthetic Plast Surg. 2002;26:99-104.
- Glogau RG. Chemical peeling and aging skin. J Geriatric Dermatol. 1994;2:30-35.
- Goldman M. Universal classification of skin type. In: Shiffman M, Mirrafati S, Lam S, et al, eds. Simplified Facial Rejuvenation. Berlin, Heidelberg, Germany: Springer; 2008:47-50.
- Kawada A. UVB-induced erythema, delayed tanning, and UVA-induced immediate tanning in Japanese skin. Photodermatol. 1986;3:327-333.
- Lancer HA. Lancer Ethnicity Scale (LES). Lasers Surg Med. 1998;22:9.
- Sharma VK, Gupta V, Jangid BL, et al. Modification of the Fitzpatrick system of skin phototype classification for the Indian population, and its correlation with narrowband diffuse reflectance spectrophotometry. Clin Exp Dermatol. 2018;43:274-280.
- Roberts WE. The Roberts Skin Type Classification System. J Drugs Dermatol. 2008;7:452-456.
- Taylor SC, Arsonnaud S, Czernielewski J. The Taylor hyperpigmentation scale: a new visual assessment tool for the evaluation of skin color and pigmentation. Cutis. 2005;76:270-274.
- Treesirichod A, Chansakulporn S, Wattanapan P. Correlation between skin color evaluation by skin color scale chart and narrowband reflectance spectrophotometer. Indian J Dermatol. 2014;59:339-342.
- Willis I, Earles RM. A new classification system relevant to people of African descent. J Cosmet Dermatol. 2005;18:209-216.
- Reeder AI, Hammond VA, Gray AR. Questionnaire items to assess skin color and erythemal sensitivity: reliability, validity, and “the dark shift.” Cancer Epidemiol Biomarkers Prev. 2010;19:1167-1173.
- Dwyer T, Muller HK, Blizzard L, et al. The use of spectrophotometry to estimate melanin density in Caucasians. Cancer Epidemiol Biomarkers Prev. 1998;7:203-206.
- Pershing LK, Tirumala VP, Nelson JL, et al. Reflectance spectrophotometer: the dermatologists’ sphygmomanometer for skin phototyping? J Invest Dermatol. 2008;128:1633-1640.
- Trakatelli M, Bylaite-Bucinskiene M, Correia O, et al. Clinical assessment of skin phototypes: watch your words! Eur J Dermatol. 2017;27:615-619.
Practice Points
- Medical providers should be cognizant of conflating race and ethnicity with Fitzpatrick skin type (FST).
- Misuse of FST may occur more frequently among physicians who do not identify as having skin of color.
- Although alternative skin type classification systems have been proposed, more clinically relevant methods for describing skin of color need to be developed.
Racial disparities in pregnancy-related death
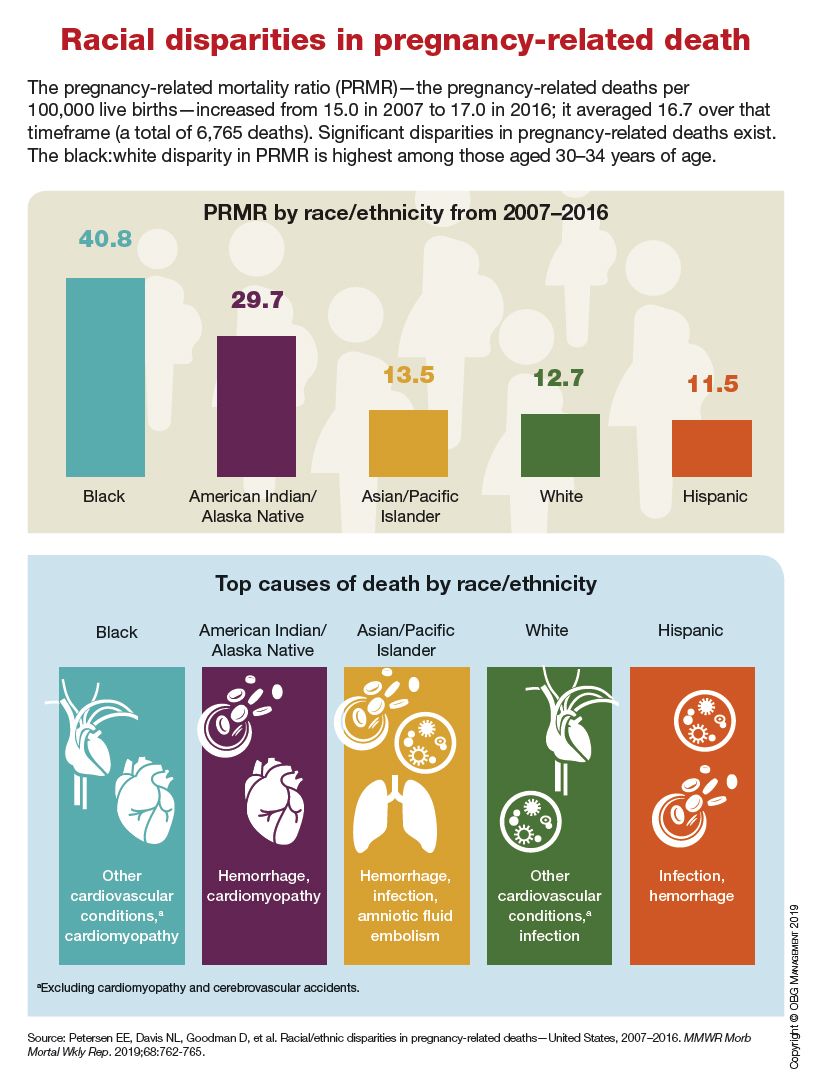
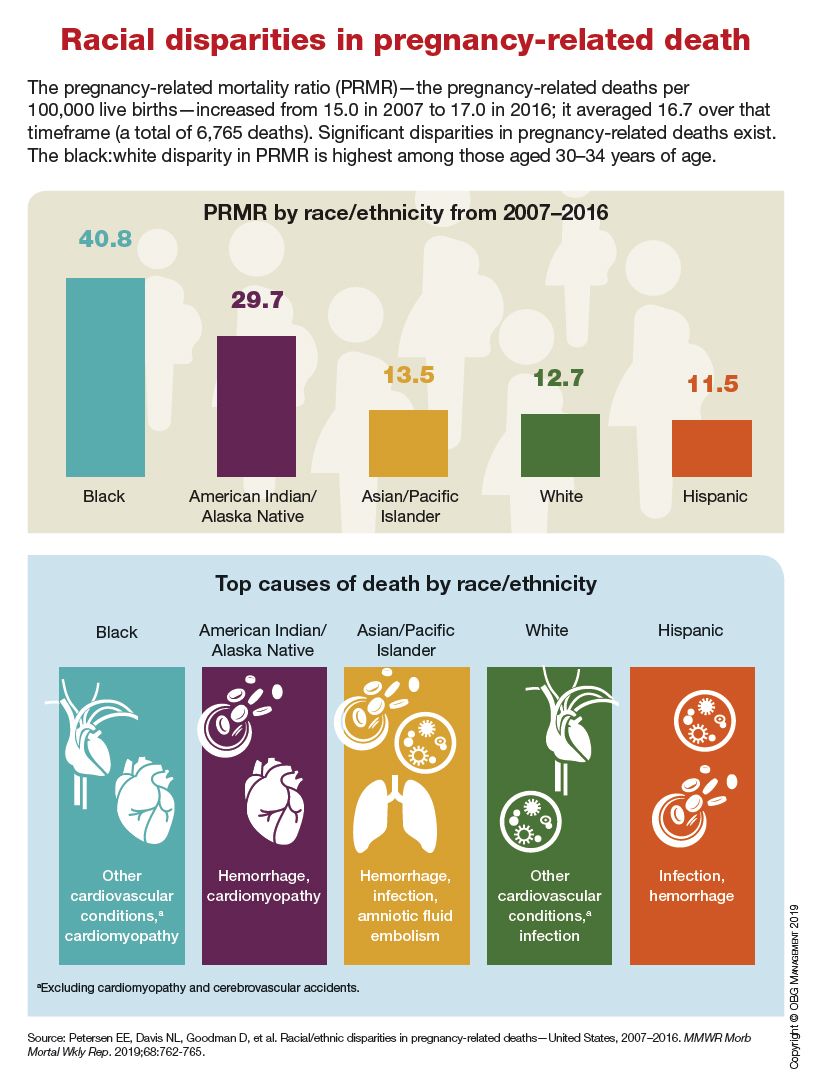
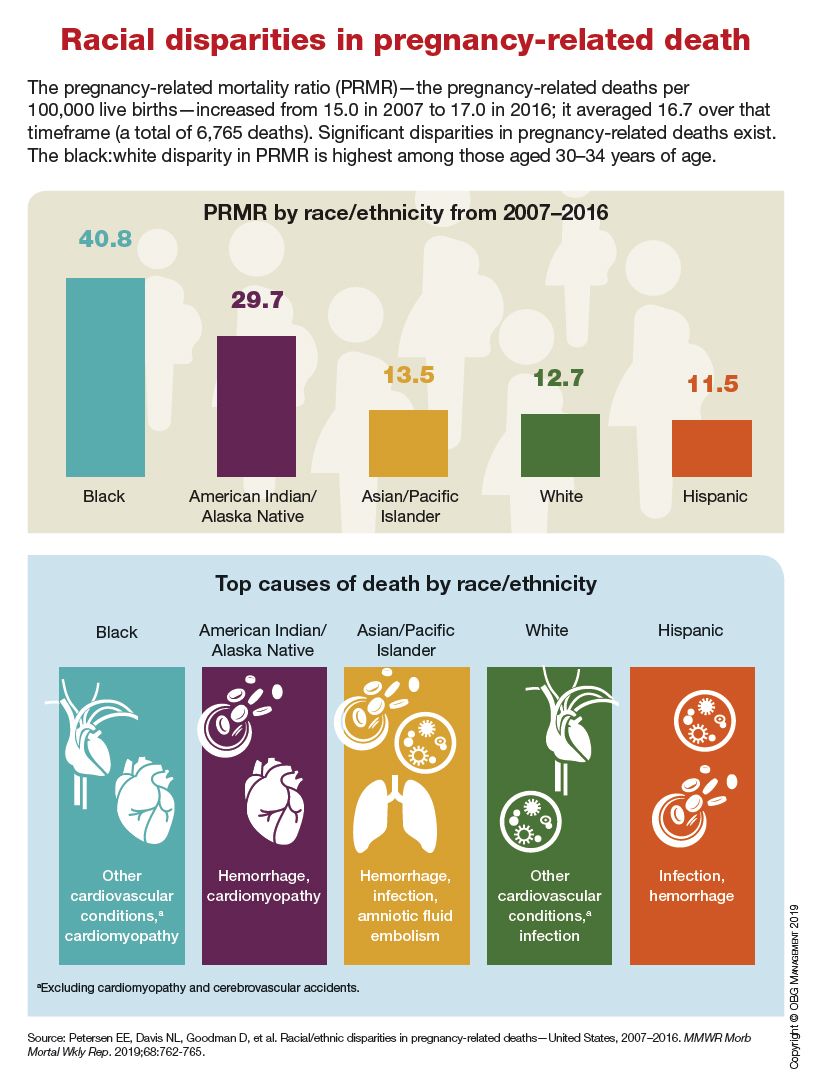
A reflection on Ghana’s mental health system
In recent years, the delivery of mental health services in Ghana has expanded substantially, especially since the passing of the Mental Health Act in 2012. In this article, I reflect on my experience as a visiting psychiatry resident in August 2018 at 2 Ghanaian hospitals located in Accra and Navrongo. Evident strengths of the mental health system were family support for patients and the scope of psychiatrists, while the most prominent weakness was the inadequate funding. As treatment of mental illness expands, more funding, psychiatrists, and mental health workers will be critical for the continued success of Ghana’s mental health system.
Psychiatric treatment in Ghana
Ghana has a population of approximately 28 million people, yet the country has an estimated 18 to 25 psychiatrists, up from 11 psychiatrists in 2011.1-3 Compared with the United States, which has 10.54 psychiatrists per 100,000 people (approximately 1 psychiatrist per 9,500 people), Ghana has .058 psychiatrists per 100,000 people (approximately 1 psychiatrist per 1.7 million people).4 In Ghana, most psychiatric care is delivered by mental health nurses, community mental health officers (CMHOs), and clinical psychiatric officers; supervision by psychiatrists is limited.3 Due to low public awareness, a scarcity of clinicians, and limited access to diagnostic services and medications, individuals with psychiatric illness in Ghana are often stigmatized, undertreated, and mistreated. To address this, in March 2012, Ghana passed Mental Health Act 846, which established a mental health commission and outlined protections for individuals with mental health needs.5 Since then, the number of people seeking treatment and the number of clinicians have expanded, but there are still significant challenges, such as a lack of funding for medications and facilities, and limited clinicians.6
During my last year of psychiatry residency at Mount Sinai Hospital in New York, I spent several weeks in Ghana at 2 institutions, observing and supervising the provision of psychiatric services. This was my first experience with the country’s health care system; therefore, my objectives were to:
- assess the current state of psychiatric services through observation and interviews with clinical staff
- provide instruction to clinicians in areas of need.
Two-thirds of my time was spent at the Accra Psychiatric Hospital, 1 of only 3 psychiatric hospitals in Ghana, all of which are located in the southern region of the country. The remainder of my time was spent at the Navrongo War Memorial Hospital in Ghana’s Northern Region.
The Accra Psychiatric Hospital is a sprawling complex near the center of the capital city. Every morning I walked through a large outdoor waiting area to the examination room, which was filled with at least 30 patients by 9
Navrongo War Memorial Hospital. There are no practicing psychiatrists in the northern region of the country; therefore, all mental health care is delivered by mental health nurses and CMHOs. CMHOs have 1 year of training plus a minimum of 2 years of service. They focus on identifying psychiatric cases in the community and coordinating treatment. Nurses have prescribing rights. A psychiatrist should be scheduled to visit the various districts in the region every 6 months to provide supervision, but this is not always feasible.
When I visited, I was the only psychiatrist who had been to this hospital in more than 1 year. During my time there, I reviewed the treatment protocols and gave lectures on the management of psychiatric emergencies and motivational interviewing, because addiction to alcohol and tramadol are 2 of the most pressing mental health problems in the country.7 I also saw patients with nurses, and supervised them on their assessment and treatment.
Continue to: In Ghana...
In Ghana, psychiatric services are often delivered using the community mental health model, in which many patients are visited in their homes. One morning, we went to a prayer camp to see if there were any individuals who would benefit from psychiatric services. There were no cases that day, but during the visit I sat under a tree where a few years before it was not uncommon to find a person who was psychotic or agitated chained to the tree. Several years of outreach by the local nurses has resulted in the camp leaders better recognizing mental illness early and contacting the nurses, as opposed to locking a person in chains for an extended period.
On one occasion, we answered a crisis call where a person experiencing a psychotic episode had locked himself in his house. The team talked with the individual through a locked screen door for 30 minutes, after which he eventually came out of the home to speak with us. A few days later, the patient accepted fluphenazine decanoate injection at his home. Two weeks later, he came to the outpatient clinic to continue treatment. Four months later, the patient was still in treatment and had started an apprenticeship for repairing cars.
As I was walking out of the hospital on my last day, I was called back to see a woman with a seizure who had been brought to the hospital. Unfortunately, there was no more diazepam in stock with which to treat her. This event highlighted the lack of resources available in this setting.
3 Take-home messages
My experience at both hospitals led me to reflect on 3 important factors impacting the mental health system in Ghana:
Family support. For at least 80% of appointments, patients were accompanied by family members or friends. The family hierarchy is still dominant in the Ghanaian culture, and clinicians often need the buy-in of the family, especially when financial support is required. More often than not, families enhanced patients’ treatment, but in some instances, they were a barrier.
Continue to: The types of cases
The types of cases. Most of the patients coming to both hospitals had diagnoses of bipolar disorder, schizophrenia, substance use disorder, or epilepsy. My impression was that patients or family members sought treatment for disorders that were conspicuous. I saw <5 cases of depression or anxiety. I wonder if this was because:
- patients with these disorders were referred to psychologists
- patients sought out faith-based treatment
- there was a lower incidence of these disorders, or these disorders were detected less frequently.
Inadequate funding. Despite the clinicians’ astute observations and diagnoses, they faced challenges, including a lack of access to medications because pharmacies were out of stock, or the patient or hospital could not afford the medication. At times, these challenges resulted in patients admitted to the hospital not receiving medications. When Mental Health Act 846 was implemented, it was widely purported that mental health care would be available to everyone, but the funding mechanism was not firmly established.8,9 Currently, laboratory workup, mental health treatment, and medications are not covered by health insurance, and government funding for mental health is insufficient. Therefore, in most areas, the entire cost burden of psychiatric care falls on patients and their families, or on hospitals.
Making progress despite barriers
In her inaugural address, former American Psychiatric Association President Altha J. Stewart, MD, named expanding the organization’s work in global mental health as one of her 3 primary goals.10 There are several means by which American psychiatrists can support the work of psychiatrists in Ghana and elsewhere. One way is by helping the mental health commission and other entities within the country petition the government and health insurance companies to expand coverage for mental health services. Teleconferencing, in which psychiatrists in Ghana or other parts of the world provide supervision to mid-level clinicians, has been piloted in other countries such as Liberia and could be implemented to address the critical shortages of psychiatrists in certain regions.11
In the past 7 years, Ghana has made significant strides in destigmatizing mental illness, and as a result more individuals are seeking treatment and more clinicians at all levels are being trained. Despite significant barriers, physicians, nurses, and other mental health workers deliver empathic and evidence-based treatment in a manner that defies the mental health system’s current limitations.
1. Ofori-Atta A, Attafuah J, Jack H, et al. Joining psychiatric care and faith healing in a prayer camp in Ghana: randomised trial. Br J Psychiatry. 2018;212(1):34-41.
2. Ghana has only 18 psychiatrists; experts beg government for more funds. GhanaWeb. https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Ghana-has-only-18-psychiatrists-experts-beg-government-for-more-funds-591732. Published October 17, 2017. Accessed July 24, 2019.
3. Agyapong VIO, Farren C, McAuliffe E. Improving Ghana’s mental healthcare through task-shifting-psychiatrists and health policy directors perceptions about government’s commitment and the role of community mental health workers. Global Health. 2016;12:57.
4. World Health Organization. Global Health Observatory data repository. http://apps.who.int/gho/data/node.main.MHHR?lang=en. Published April 25, 2019. Accessed July 24, 2019.
5. Walker GH, Osei A. Mental health law in Ghana. BJPsych Int. 2017;14(2):38-39.
6. Doku VC, Wusu-Takyi A, Awakame J. Implementing the Mental Health Act in Ghana: any challenges ahead? Ghana Med J. 2012;46(4):241-250.
7. Kissiedu E. High dose Tramadol floods market. Business Day. http://businessdayghana.com/high-dose-tramadol-floods-market/. Published September 25, 2017. Accessed July 24, 2019.
8. Badu E, O’Brien AP, Mitchell R. An integrative review of potential enablers and barriers to accessing mental health services in Ghana. Health Res Policy Syst. 2018;16(1):110.
9. Ghana mental health care delivery risks collapse for lack of funds. News Ghana. https://www.newsghana.com.gh/ghana-mental-health-care-delivery-risks-collapse-for-lack-of-funds/. Published May 29, 2018. Accessed July 24, 2019.
10. Stewart AJ. Response to the Presidential Address. Am J Psychiatry. 2018;175(8):726-727.
11. Katz, CL, Washington FB, Sacco M, et al. A resident-based telepsychiatry supervision pilot program in Liberia. Psychiatr Serv. 2018;70(3):243-246.
In recent years, the delivery of mental health services in Ghana has expanded substantially, especially since the passing of the Mental Health Act in 2012. In this article, I reflect on my experience as a visiting psychiatry resident in August 2018 at 2 Ghanaian hospitals located in Accra and Navrongo. Evident strengths of the mental health system were family support for patients and the scope of psychiatrists, while the most prominent weakness was the inadequate funding. As treatment of mental illness expands, more funding, psychiatrists, and mental health workers will be critical for the continued success of Ghana’s mental health system.
Psychiatric treatment in Ghana
Ghana has a population of approximately 28 million people, yet the country has an estimated 18 to 25 psychiatrists, up from 11 psychiatrists in 2011.1-3 Compared with the United States, which has 10.54 psychiatrists per 100,000 people (approximately 1 psychiatrist per 9,500 people), Ghana has .058 psychiatrists per 100,000 people (approximately 1 psychiatrist per 1.7 million people).4 In Ghana, most psychiatric care is delivered by mental health nurses, community mental health officers (CMHOs), and clinical psychiatric officers; supervision by psychiatrists is limited.3 Due to low public awareness, a scarcity of clinicians, and limited access to diagnostic services and medications, individuals with psychiatric illness in Ghana are often stigmatized, undertreated, and mistreated. To address this, in March 2012, Ghana passed Mental Health Act 846, which established a mental health commission and outlined protections for individuals with mental health needs.5 Since then, the number of people seeking treatment and the number of clinicians have expanded, but there are still significant challenges, such as a lack of funding for medications and facilities, and limited clinicians.6
During my last year of psychiatry residency at Mount Sinai Hospital in New York, I spent several weeks in Ghana at 2 institutions, observing and supervising the provision of psychiatric services. This was my first experience with the country’s health care system; therefore, my objectives were to:
- assess the current state of psychiatric services through observation and interviews with clinical staff
- provide instruction to clinicians in areas of need.
Two-thirds of my time was spent at the Accra Psychiatric Hospital, 1 of only 3 psychiatric hospitals in Ghana, all of which are located in the southern region of the country. The remainder of my time was spent at the Navrongo War Memorial Hospital in Ghana’s Northern Region.
The Accra Psychiatric Hospital is a sprawling complex near the center of the capital city. Every morning I walked through a large outdoor waiting area to the examination room, which was filled with at least 30 patients by 9
Navrongo War Memorial Hospital. There are no practicing psychiatrists in the northern region of the country; therefore, all mental health care is delivered by mental health nurses and CMHOs. CMHOs have 1 year of training plus a minimum of 2 years of service. They focus on identifying psychiatric cases in the community and coordinating treatment. Nurses have prescribing rights. A psychiatrist should be scheduled to visit the various districts in the region every 6 months to provide supervision, but this is not always feasible.
When I visited, I was the only psychiatrist who had been to this hospital in more than 1 year. During my time there, I reviewed the treatment protocols and gave lectures on the management of psychiatric emergencies and motivational interviewing, because addiction to alcohol and tramadol are 2 of the most pressing mental health problems in the country.7 I also saw patients with nurses, and supervised them on their assessment and treatment.
Continue to: In Ghana...
In Ghana, psychiatric services are often delivered using the community mental health model, in which many patients are visited in their homes. One morning, we went to a prayer camp to see if there were any individuals who would benefit from psychiatric services. There were no cases that day, but during the visit I sat under a tree where a few years before it was not uncommon to find a person who was psychotic or agitated chained to the tree. Several years of outreach by the local nurses has resulted in the camp leaders better recognizing mental illness early and contacting the nurses, as opposed to locking a person in chains for an extended period.
On one occasion, we answered a crisis call where a person experiencing a psychotic episode had locked himself in his house. The team talked with the individual through a locked screen door for 30 minutes, after which he eventually came out of the home to speak with us. A few days later, the patient accepted fluphenazine decanoate injection at his home. Two weeks later, he came to the outpatient clinic to continue treatment. Four months later, the patient was still in treatment and had started an apprenticeship for repairing cars.
As I was walking out of the hospital on my last day, I was called back to see a woman with a seizure who had been brought to the hospital. Unfortunately, there was no more diazepam in stock with which to treat her. This event highlighted the lack of resources available in this setting.
3 Take-home messages
My experience at both hospitals led me to reflect on 3 important factors impacting the mental health system in Ghana:
Family support. For at least 80% of appointments, patients were accompanied by family members or friends. The family hierarchy is still dominant in the Ghanaian culture, and clinicians often need the buy-in of the family, especially when financial support is required. More often than not, families enhanced patients’ treatment, but in some instances, they were a barrier.
Continue to: The types of cases
The types of cases. Most of the patients coming to both hospitals had diagnoses of bipolar disorder, schizophrenia, substance use disorder, or epilepsy. My impression was that patients or family members sought treatment for disorders that were conspicuous. I saw <5 cases of depression or anxiety. I wonder if this was because:
- patients with these disorders were referred to psychologists
- patients sought out faith-based treatment
- there was a lower incidence of these disorders, or these disorders were detected less frequently.
Inadequate funding. Despite the clinicians’ astute observations and diagnoses, they faced challenges, including a lack of access to medications because pharmacies were out of stock, or the patient or hospital could not afford the medication. At times, these challenges resulted in patients admitted to the hospital not receiving medications. When Mental Health Act 846 was implemented, it was widely purported that mental health care would be available to everyone, but the funding mechanism was not firmly established.8,9 Currently, laboratory workup, mental health treatment, and medications are not covered by health insurance, and government funding for mental health is insufficient. Therefore, in most areas, the entire cost burden of psychiatric care falls on patients and their families, or on hospitals.
Making progress despite barriers
In her inaugural address, former American Psychiatric Association President Altha J. Stewart, MD, named expanding the organization’s work in global mental health as one of her 3 primary goals.10 There are several means by which American psychiatrists can support the work of psychiatrists in Ghana and elsewhere. One way is by helping the mental health commission and other entities within the country petition the government and health insurance companies to expand coverage for mental health services. Teleconferencing, in which psychiatrists in Ghana or other parts of the world provide supervision to mid-level clinicians, has been piloted in other countries such as Liberia and could be implemented to address the critical shortages of psychiatrists in certain regions.11
In the past 7 years, Ghana has made significant strides in destigmatizing mental illness, and as a result more individuals are seeking treatment and more clinicians at all levels are being trained. Despite significant barriers, physicians, nurses, and other mental health workers deliver empathic and evidence-based treatment in a manner that defies the mental health system’s current limitations.
In recent years, the delivery of mental health services in Ghana has expanded substantially, especially since the passing of the Mental Health Act in 2012. In this article, I reflect on my experience as a visiting psychiatry resident in August 2018 at 2 Ghanaian hospitals located in Accra and Navrongo. Evident strengths of the mental health system were family support for patients and the scope of psychiatrists, while the most prominent weakness was the inadequate funding. As treatment of mental illness expands, more funding, psychiatrists, and mental health workers will be critical for the continued success of Ghana’s mental health system.
Psychiatric treatment in Ghana
Ghana has a population of approximately 28 million people, yet the country has an estimated 18 to 25 psychiatrists, up from 11 psychiatrists in 2011.1-3 Compared with the United States, which has 10.54 psychiatrists per 100,000 people (approximately 1 psychiatrist per 9,500 people), Ghana has .058 psychiatrists per 100,000 people (approximately 1 psychiatrist per 1.7 million people).4 In Ghana, most psychiatric care is delivered by mental health nurses, community mental health officers (CMHOs), and clinical psychiatric officers; supervision by psychiatrists is limited.3 Due to low public awareness, a scarcity of clinicians, and limited access to diagnostic services and medications, individuals with psychiatric illness in Ghana are often stigmatized, undertreated, and mistreated. To address this, in March 2012, Ghana passed Mental Health Act 846, which established a mental health commission and outlined protections for individuals with mental health needs.5 Since then, the number of people seeking treatment and the number of clinicians have expanded, but there are still significant challenges, such as a lack of funding for medications and facilities, and limited clinicians.6
During my last year of psychiatry residency at Mount Sinai Hospital in New York, I spent several weeks in Ghana at 2 institutions, observing and supervising the provision of psychiatric services. This was my first experience with the country’s health care system; therefore, my objectives were to:
- assess the current state of psychiatric services through observation and interviews with clinical staff
- provide instruction to clinicians in areas of need.
Two-thirds of my time was spent at the Accra Psychiatric Hospital, 1 of only 3 psychiatric hospitals in Ghana, all of which are located in the southern region of the country. The remainder of my time was spent at the Navrongo War Memorial Hospital in Ghana’s Northern Region.
The Accra Psychiatric Hospital is a sprawling complex near the center of the capital city. Every morning I walked through a large outdoor waiting area to the examination room, which was filled with at least 30 patients by 9
Navrongo War Memorial Hospital. There are no practicing psychiatrists in the northern region of the country; therefore, all mental health care is delivered by mental health nurses and CMHOs. CMHOs have 1 year of training plus a minimum of 2 years of service. They focus on identifying psychiatric cases in the community and coordinating treatment. Nurses have prescribing rights. A psychiatrist should be scheduled to visit the various districts in the region every 6 months to provide supervision, but this is not always feasible.
When I visited, I was the only psychiatrist who had been to this hospital in more than 1 year. During my time there, I reviewed the treatment protocols and gave lectures on the management of psychiatric emergencies and motivational interviewing, because addiction to alcohol and tramadol are 2 of the most pressing mental health problems in the country.7 I also saw patients with nurses, and supervised them on their assessment and treatment.
Continue to: In Ghana...
In Ghana, psychiatric services are often delivered using the community mental health model, in which many patients are visited in their homes. One morning, we went to a prayer camp to see if there were any individuals who would benefit from psychiatric services. There were no cases that day, but during the visit I sat under a tree where a few years before it was not uncommon to find a person who was psychotic or agitated chained to the tree. Several years of outreach by the local nurses has resulted in the camp leaders better recognizing mental illness early and contacting the nurses, as opposed to locking a person in chains for an extended period.
On one occasion, we answered a crisis call where a person experiencing a psychotic episode had locked himself in his house. The team talked with the individual through a locked screen door for 30 minutes, after which he eventually came out of the home to speak with us. A few days later, the patient accepted fluphenazine decanoate injection at his home. Two weeks later, he came to the outpatient clinic to continue treatment. Four months later, the patient was still in treatment and had started an apprenticeship for repairing cars.
As I was walking out of the hospital on my last day, I was called back to see a woman with a seizure who had been brought to the hospital. Unfortunately, there was no more diazepam in stock with which to treat her. This event highlighted the lack of resources available in this setting.
3 Take-home messages
My experience at both hospitals led me to reflect on 3 important factors impacting the mental health system in Ghana:
Family support. For at least 80% of appointments, patients were accompanied by family members or friends. The family hierarchy is still dominant in the Ghanaian culture, and clinicians often need the buy-in of the family, especially when financial support is required. More often than not, families enhanced patients’ treatment, but in some instances, they were a barrier.
Continue to: The types of cases
The types of cases. Most of the patients coming to both hospitals had diagnoses of bipolar disorder, schizophrenia, substance use disorder, or epilepsy. My impression was that patients or family members sought treatment for disorders that were conspicuous. I saw <5 cases of depression or anxiety. I wonder if this was because:
- patients with these disorders were referred to psychologists
- patients sought out faith-based treatment
- there was a lower incidence of these disorders, or these disorders were detected less frequently.
Inadequate funding. Despite the clinicians’ astute observations and diagnoses, they faced challenges, including a lack of access to medications because pharmacies were out of stock, or the patient or hospital could not afford the medication. At times, these challenges resulted in patients admitted to the hospital not receiving medications. When Mental Health Act 846 was implemented, it was widely purported that mental health care would be available to everyone, but the funding mechanism was not firmly established.8,9 Currently, laboratory workup, mental health treatment, and medications are not covered by health insurance, and government funding for mental health is insufficient. Therefore, in most areas, the entire cost burden of psychiatric care falls on patients and their families, or on hospitals.
Making progress despite barriers
In her inaugural address, former American Psychiatric Association President Altha J. Stewart, MD, named expanding the organization’s work in global mental health as one of her 3 primary goals.10 There are several means by which American psychiatrists can support the work of psychiatrists in Ghana and elsewhere. One way is by helping the mental health commission and other entities within the country petition the government and health insurance companies to expand coverage for mental health services. Teleconferencing, in which psychiatrists in Ghana or other parts of the world provide supervision to mid-level clinicians, has been piloted in other countries such as Liberia and could be implemented to address the critical shortages of psychiatrists in certain regions.11
In the past 7 years, Ghana has made significant strides in destigmatizing mental illness, and as a result more individuals are seeking treatment and more clinicians at all levels are being trained. Despite significant barriers, physicians, nurses, and other mental health workers deliver empathic and evidence-based treatment in a manner that defies the mental health system’s current limitations.
1. Ofori-Atta A, Attafuah J, Jack H, et al. Joining psychiatric care and faith healing in a prayer camp in Ghana: randomised trial. Br J Psychiatry. 2018;212(1):34-41.
2. Ghana has only 18 psychiatrists; experts beg government for more funds. GhanaWeb. https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Ghana-has-only-18-psychiatrists-experts-beg-government-for-more-funds-591732. Published October 17, 2017. Accessed July 24, 2019.
3. Agyapong VIO, Farren C, McAuliffe E. Improving Ghana’s mental healthcare through task-shifting-psychiatrists and health policy directors perceptions about government’s commitment and the role of community mental health workers. Global Health. 2016;12:57.
4. World Health Organization. Global Health Observatory data repository. http://apps.who.int/gho/data/node.main.MHHR?lang=en. Published April 25, 2019. Accessed July 24, 2019.
5. Walker GH, Osei A. Mental health law in Ghana. BJPsych Int. 2017;14(2):38-39.
6. Doku VC, Wusu-Takyi A, Awakame J. Implementing the Mental Health Act in Ghana: any challenges ahead? Ghana Med J. 2012;46(4):241-250.
7. Kissiedu E. High dose Tramadol floods market. Business Day. http://businessdayghana.com/high-dose-tramadol-floods-market/. Published September 25, 2017. Accessed July 24, 2019.
8. Badu E, O’Brien AP, Mitchell R. An integrative review of potential enablers and barriers to accessing mental health services in Ghana. Health Res Policy Syst. 2018;16(1):110.
9. Ghana mental health care delivery risks collapse for lack of funds. News Ghana. https://www.newsghana.com.gh/ghana-mental-health-care-delivery-risks-collapse-for-lack-of-funds/. Published May 29, 2018. Accessed July 24, 2019.
10. Stewart AJ. Response to the Presidential Address. Am J Psychiatry. 2018;175(8):726-727.
11. Katz, CL, Washington FB, Sacco M, et al. A resident-based telepsychiatry supervision pilot program in Liberia. Psychiatr Serv. 2018;70(3):243-246.
1. Ofori-Atta A, Attafuah J, Jack H, et al. Joining psychiatric care and faith healing in a prayer camp in Ghana: randomised trial. Br J Psychiatry. 2018;212(1):34-41.
2. Ghana has only 18 psychiatrists; experts beg government for more funds. GhanaWeb. https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Ghana-has-only-18-psychiatrists-experts-beg-government-for-more-funds-591732. Published October 17, 2017. Accessed July 24, 2019.
3. Agyapong VIO, Farren C, McAuliffe E. Improving Ghana’s mental healthcare through task-shifting-psychiatrists and health policy directors perceptions about government’s commitment and the role of community mental health workers. Global Health. 2016;12:57.
4. World Health Organization. Global Health Observatory data repository. http://apps.who.int/gho/data/node.main.MHHR?lang=en. Published April 25, 2019. Accessed July 24, 2019.
5. Walker GH, Osei A. Mental health law in Ghana. BJPsych Int. 2017;14(2):38-39.
6. Doku VC, Wusu-Takyi A, Awakame J. Implementing the Mental Health Act in Ghana: any challenges ahead? Ghana Med J. 2012;46(4):241-250.
7. Kissiedu E. High dose Tramadol floods market. Business Day. http://businessdayghana.com/high-dose-tramadol-floods-market/. Published September 25, 2017. Accessed July 24, 2019.
8. Badu E, O’Brien AP, Mitchell R. An integrative review of potential enablers and barriers to accessing mental health services in Ghana. Health Res Policy Syst. 2018;16(1):110.
9. Ghana mental health care delivery risks collapse for lack of funds. News Ghana. https://www.newsghana.com.gh/ghana-mental-health-care-delivery-risks-collapse-for-lack-of-funds/. Published May 29, 2018. Accessed July 24, 2019.
10. Stewart AJ. Response to the Presidential Address. Am J Psychiatry. 2018;175(8):726-727.
11. Katz, CL, Washington FB, Sacco M, et al. A resident-based telepsychiatry supervision pilot program in Liberia. Psychiatr Serv. 2018;70(3):243-246.