User login
Family Physician: Abortion care is health and primary care
I am aware of how intersecting social, economic, familial, and environmental factors influence what is best for patient’s lives, and I consider having this awareness to be part of being a family medicine physician.
People being able to make choices about their reproductive health and their reproductive futures without unnecessary and harmful barriers is a part of a person’s overall health that family medicine physicians should recognize and prioritize. Helping people achieve their reproductive health care goals includes helping patients access abortion care if that is the care that they decide that they need.
According to the Guttmacher Institute, 2021 was “the worst year for abortion rights in almost half a century” as 108 abortion restrictions were enacted throughout the country. The most damaging restriction was introduced in Texas in the fall of 2021 called SB8, which has virtually stopped all abortion care in person for any person with a pregnancy greater than 6 weeks’ gestation. Now, in 2022 we are seeing several other states, including Idaho and Oklahoma, set to pass similar laws that will essentially halt most abortion care in the clinical setting in those states.
Abortion access had already been a problem in much of the country prior to 2021 because of burdensome and not medically necessary restrictions. Based on current political trends we are getting to a place where it is not hard to imagine that up to half of the states in this country will not allow their communities to access abortion care in the clinical setting at all in the very near future. This is not reproductive freedom, and I am outraged that people are being forced to travel hundreds of miles for their abortion care, forced to continue pregnancies that they don’t want, or forced to find other ways to obtain medication abortion pills.
While obtaining medication abortion pills online and managing the abortion process at home is safe and recognized as safe by the World Health Organization, no one should be forced to utilize a certain type of care based on their state of residence, in my opinion.
Providing evidence-based medicine to patients is ‘my duty’
Abortion care is health care and is primary care. One in four women will have an abortion by the age of 45, and we know that transgender, nonbinary, and gender-expansive people also have abortions. That means on any given day as family medicine physicians we are likely taking care of more than one person who has had an abortion, will have an abortion, and/or is considering an abortion. Therefore, all family medicine physicians need to be prepared to counsel patients about all of their pregnancy options, answer questions about pregnancy and abortion, and help people get the compassionate care that they deserve.
Our patients turn to us as trusted sources of information. When they reach out to us, I consider providing evidence-based medicine to patients – that includes factual information about abortion care if and when our patients need it – to be my duty as a family medicine physician.
Resources on abortion care for family medicine physicians
For family medicine physicians who did not have adequate exposure to abortion care during residency, there are many evidence-based resources to review in order to become more knowledgeable in abortion care.
In many areas of medicine, we have to continue to learn and seek out references, and abortion care is no different. One could argue that understanding abortion care and providing patients with factual information about their options and abortion care is even more important because of stigma surrounding abortion care and the rampant lies about abortion care that are easily accessible and that even other medical professionals and politicians spread. There are even fake clinics, often called “crisis pregnancy centers”, that intimidate, lie about abortion, and coerce patients to make decisions that are against their desires. Thus, being that trusted source of factual information about abortion care is even more important in the face of so many lies.
There are several organizations that are dedicated to education surrounding abortion care, in particular within the primary care setting. The Reproductive Health Access Project (RHAP), Reproductive Health Education in Family Medicine (RHEDI), and Training in Early Abortion for Comprehensive Healthcare (TEACH) all provide free resources on abortion care, how to incorporate abortion care into primary care, and how to teach medical students and residents about abortion care.
In addition, the National Network of Abortion Funds connects people to community-led organizations that provide assistance related to direct financial and logistical support for obtaining abortion care. I believe it is critical that we familiarize ourselves with our local abortion funds and share what we learn about these resources with our patients.
As abortion access continues to be further stripped away from many people that we take care of, I think standing up for what is right and what is our duty as physicians becomes more important. That duty is to provide our patients with evidence-based medicine and compassionate care so that our communities can obtain reproductive health outcomes and freedom that are best for their lives.
Dr. Lockley is a family physician currently living in Harlem, N.Y., and a member of the editorial advisory board of Family Practice News. She currently works for Public Health Solutions’ Sexual and Reproductive Health Centers in Brooklyn, providing primary care and reproductive health care services there, and as an abortion provider throughout the New York region. She completed both medical school and residency in Philadelphia and then did a fellowship in reproductive health care and advocacy through the Family Health Center of Harlem and the Reproductive Health Access Project. She can be reached at [email protected].
I am aware of how intersecting social, economic, familial, and environmental factors influence what is best for patient’s lives, and I consider having this awareness to be part of being a family medicine physician.
People being able to make choices about their reproductive health and their reproductive futures without unnecessary and harmful barriers is a part of a person’s overall health that family medicine physicians should recognize and prioritize. Helping people achieve their reproductive health care goals includes helping patients access abortion care if that is the care that they decide that they need.
According to the Guttmacher Institute, 2021 was “the worst year for abortion rights in almost half a century” as 108 abortion restrictions were enacted throughout the country. The most damaging restriction was introduced in Texas in the fall of 2021 called SB8, which has virtually stopped all abortion care in person for any person with a pregnancy greater than 6 weeks’ gestation. Now, in 2022 we are seeing several other states, including Idaho and Oklahoma, set to pass similar laws that will essentially halt most abortion care in the clinical setting in those states.
Abortion access had already been a problem in much of the country prior to 2021 because of burdensome and not medically necessary restrictions. Based on current political trends we are getting to a place where it is not hard to imagine that up to half of the states in this country will not allow their communities to access abortion care in the clinical setting at all in the very near future. This is not reproductive freedom, and I am outraged that people are being forced to travel hundreds of miles for their abortion care, forced to continue pregnancies that they don’t want, or forced to find other ways to obtain medication abortion pills.
While obtaining medication abortion pills online and managing the abortion process at home is safe and recognized as safe by the World Health Organization, no one should be forced to utilize a certain type of care based on their state of residence, in my opinion.
Providing evidence-based medicine to patients is ‘my duty’
Abortion care is health care and is primary care. One in four women will have an abortion by the age of 45, and we know that transgender, nonbinary, and gender-expansive people also have abortions. That means on any given day as family medicine physicians we are likely taking care of more than one person who has had an abortion, will have an abortion, and/or is considering an abortion. Therefore, all family medicine physicians need to be prepared to counsel patients about all of their pregnancy options, answer questions about pregnancy and abortion, and help people get the compassionate care that they deserve.
Our patients turn to us as trusted sources of information. When they reach out to us, I consider providing evidence-based medicine to patients – that includes factual information about abortion care if and when our patients need it – to be my duty as a family medicine physician.
Resources on abortion care for family medicine physicians
For family medicine physicians who did not have adequate exposure to abortion care during residency, there are many evidence-based resources to review in order to become more knowledgeable in abortion care.
In many areas of medicine, we have to continue to learn and seek out references, and abortion care is no different. One could argue that understanding abortion care and providing patients with factual information about their options and abortion care is even more important because of stigma surrounding abortion care and the rampant lies about abortion care that are easily accessible and that even other medical professionals and politicians spread. There are even fake clinics, often called “crisis pregnancy centers”, that intimidate, lie about abortion, and coerce patients to make decisions that are against their desires. Thus, being that trusted source of factual information about abortion care is even more important in the face of so many lies.
There are several organizations that are dedicated to education surrounding abortion care, in particular within the primary care setting. The Reproductive Health Access Project (RHAP), Reproductive Health Education in Family Medicine (RHEDI), and Training in Early Abortion for Comprehensive Healthcare (TEACH) all provide free resources on abortion care, how to incorporate abortion care into primary care, and how to teach medical students and residents about abortion care.
In addition, the National Network of Abortion Funds connects people to community-led organizations that provide assistance related to direct financial and logistical support for obtaining abortion care. I believe it is critical that we familiarize ourselves with our local abortion funds and share what we learn about these resources with our patients.
As abortion access continues to be further stripped away from many people that we take care of, I think standing up for what is right and what is our duty as physicians becomes more important. That duty is to provide our patients with evidence-based medicine and compassionate care so that our communities can obtain reproductive health outcomes and freedom that are best for their lives.
Dr. Lockley is a family physician currently living in Harlem, N.Y., and a member of the editorial advisory board of Family Practice News. She currently works for Public Health Solutions’ Sexual and Reproductive Health Centers in Brooklyn, providing primary care and reproductive health care services there, and as an abortion provider throughout the New York region. She completed both medical school and residency in Philadelphia and then did a fellowship in reproductive health care and advocacy through the Family Health Center of Harlem and the Reproductive Health Access Project. She can be reached at [email protected].
I am aware of how intersecting social, economic, familial, and environmental factors influence what is best for patient’s lives, and I consider having this awareness to be part of being a family medicine physician.
People being able to make choices about their reproductive health and their reproductive futures without unnecessary and harmful barriers is a part of a person’s overall health that family medicine physicians should recognize and prioritize. Helping people achieve their reproductive health care goals includes helping patients access abortion care if that is the care that they decide that they need.
According to the Guttmacher Institute, 2021 was “the worst year for abortion rights in almost half a century” as 108 abortion restrictions were enacted throughout the country. The most damaging restriction was introduced in Texas in the fall of 2021 called SB8, which has virtually stopped all abortion care in person for any person with a pregnancy greater than 6 weeks’ gestation. Now, in 2022 we are seeing several other states, including Idaho and Oklahoma, set to pass similar laws that will essentially halt most abortion care in the clinical setting in those states.
Abortion access had already been a problem in much of the country prior to 2021 because of burdensome and not medically necessary restrictions. Based on current political trends we are getting to a place where it is not hard to imagine that up to half of the states in this country will not allow their communities to access abortion care in the clinical setting at all in the very near future. This is not reproductive freedom, and I am outraged that people are being forced to travel hundreds of miles for their abortion care, forced to continue pregnancies that they don’t want, or forced to find other ways to obtain medication abortion pills.
While obtaining medication abortion pills online and managing the abortion process at home is safe and recognized as safe by the World Health Organization, no one should be forced to utilize a certain type of care based on their state of residence, in my opinion.
Providing evidence-based medicine to patients is ‘my duty’
Abortion care is health care and is primary care. One in four women will have an abortion by the age of 45, and we know that transgender, nonbinary, and gender-expansive people also have abortions. That means on any given day as family medicine physicians we are likely taking care of more than one person who has had an abortion, will have an abortion, and/or is considering an abortion. Therefore, all family medicine physicians need to be prepared to counsel patients about all of their pregnancy options, answer questions about pregnancy and abortion, and help people get the compassionate care that they deserve.
Our patients turn to us as trusted sources of information. When they reach out to us, I consider providing evidence-based medicine to patients – that includes factual information about abortion care if and when our patients need it – to be my duty as a family medicine physician.
Resources on abortion care for family medicine physicians
For family medicine physicians who did not have adequate exposure to abortion care during residency, there are many evidence-based resources to review in order to become more knowledgeable in abortion care.
In many areas of medicine, we have to continue to learn and seek out references, and abortion care is no different. One could argue that understanding abortion care and providing patients with factual information about their options and abortion care is even more important because of stigma surrounding abortion care and the rampant lies about abortion care that are easily accessible and that even other medical professionals and politicians spread. There are even fake clinics, often called “crisis pregnancy centers”, that intimidate, lie about abortion, and coerce patients to make decisions that are against their desires. Thus, being that trusted source of factual information about abortion care is even more important in the face of so many lies.
There are several organizations that are dedicated to education surrounding abortion care, in particular within the primary care setting. The Reproductive Health Access Project (RHAP), Reproductive Health Education in Family Medicine (RHEDI), and Training in Early Abortion for Comprehensive Healthcare (TEACH) all provide free resources on abortion care, how to incorporate abortion care into primary care, and how to teach medical students and residents about abortion care.
In addition, the National Network of Abortion Funds connects people to community-led organizations that provide assistance related to direct financial and logistical support for obtaining abortion care. I believe it is critical that we familiarize ourselves with our local abortion funds and share what we learn about these resources with our patients.
As abortion access continues to be further stripped away from many people that we take care of, I think standing up for what is right and what is our duty as physicians becomes more important. That duty is to provide our patients with evidence-based medicine and compassionate care so that our communities can obtain reproductive health outcomes and freedom that are best for their lives.
Dr. Lockley is a family physician currently living in Harlem, N.Y., and a member of the editorial advisory board of Family Practice News. She currently works for Public Health Solutions’ Sexual and Reproductive Health Centers in Brooklyn, providing primary care and reproductive health care services there, and as an abortion provider throughout the New York region. She completed both medical school and residency in Philadelphia and then did a fellowship in reproductive health care and advocacy through the Family Health Center of Harlem and the Reproductive Health Access Project. She can be reached at [email protected].
ACC looks to build inclusive, bully-free cardiology workplaces
The American College of Cardiology has issued a new health policy statement directed at eliminating the bias, discrimination, bullying, and harassment that hamstrings the delivery of quality cardiovascular care.
“We pay a lot of attention, of course, to our patients and patient care issues but our ability to care optimally for patients is limited if the workforce is handicapped in any way,” said Pamela S. Douglas, MD, of Duke University, Durham, N.C., who cochaired the writing committee.
The document is the second in the ACC’s diversity inclusion initiative, following the 2019 report on equal compensation and opportunity in cardiology, but the foundation for the work actually started 5 years ago, she told this news organization.
“Unfortunately, COVID and other world events have created a climate in the United States where people don’t treat each other terribly well,” Dr. Douglas said. “It’s divisive and confrontational often, when it should be collaborative. So this document, at this time, was serendipitous but wonderful timing.”
The 2022 ACC Health Policy Statement on Building Respect, Civility, and Inclusion in the Cardiovascular Workforce was published online March 17 in the Journal of the American College of Cardiology.
The 63-page document provides 12 principles for building a better workplace, starting with the belief that civil behavior and respect are inherent in its core values of teamwork, collaboration, and professionalism.
The ACC calls on all organizations and individuals involved in providing cardiovascular care, education, or research to recognize the “ubiquity” of uncivil behavior and the continuum of bias, discrimination, bullying, and harassment (BDBH) that characterize it.
Some of the recommendations they offer to eliminate these behaviors include:
- Creating institutional policies and resources to ensure hiring decisions, evaluations, and departmental/program/center reviews are objective.
- Including assessments of personal behaviors related to respect and civility in performance reviews.
- Establishing confidential, fair, and transparent mechanisms for reporting and investigating individuals and/or departments suspected of BDBH.
- Adopting longitudinal metrics and accurate data collection to track progress and inform future policy and interventions.
- Encouraging independent evaluation of institutional culture and efforts to reduce BDBH.
- Celebrating those who promote and achieve excellence in reducing BDBH.
Patients behaving badly
What’s new, especially since the COVID-19 pandemic, is the number of patients who themselves engage in disrespectful and uncivil behavior, observed Dr. Douglas.
“As physicians, it was the patient’s always right. So you work to do backflips to accommodate the patient,” she said. “But when the patient says: I don’t want to be treated by anybody that comes from outside the United States, that’s not our society anymore. And that has to be addressed and dealt with.”
The policy statement features a suite of online tools and resources including 15 case examples and 30 sample policies from institutions that have been anonymized and some provide an action framework for addressing this type of patient behavior, Dr. Douglas said. An individual, for example, can ask the patient why they made the remark, explaining that the provider is qualified and someone they’d like to have care for their own family. If it was a trainee on the receiving end, it’s fair for them to go back to their supervisor, mentor, or training director.
“They should back you up and explain to the patient that it’s not who we are at this hospital and that they’re happy to provide care, but they are part of the hospital and need to obey the rules and environment in this hospital,” she said.
Writing committee cochair Michael J. Mack, MD, of Baylor Scott & White Health, Plano, Tex., told tthis news organization that “one of the concepts that I hadn’t heard before that resonated with me was the term ‘upstander’ – that you can’t just be a bystander and watch this happen and do nothing. If you’re witness to this in the workplace, if it’s gender bias or racial bias, you need to get involved and reach out to that individual and see what you can do to help and be a reporter of it.”
But it’s all too costly
Financial constraints are often cited as a reason not to focus on bias, discrimination, bullying, and harassment in the workplace or to shelve initiatives, but it’s a false argument, say Dr. Mack and Dr. Douglas.
“One of the case examples is a cardiology practice that is suffering a decline in finances, and the board makes the recommendation that the efforts at diversity and civil workplaces need to be the first to go,” Dr. Mack explained. “And the point that’s being made in this is you can’t afford not to do it because it ends up being more costly to the business in the long run.”
Part of that cost is associated with losing valuable employees that were contributing but left because there wasn’t a culture of respectfulness and positivity in their workplace. While that’s always been a risk, it’s become a particularly compelling issue because of the workforce shortages present 3 years on in the pandemic, he said.
“There’s a new reexamination to be sure that we have a positive work environment that people want to come to work at every day,” he said. “I run our Research Institute, and normally we have a 5% vacancy rate, and our unfilled-position rate is 25% right now.”
Health care is delivered as a team today, but if a member feels disrespected, or worse – harassed, bullied, or discriminated against – they’re not going to contribute at the top of their game, Dr. Douglas said.
“It’s very well documented that bad behavior exists and that it has negative consequences for patient care for institutions, who are at great risk legally and regulatory wise,” she said. “And the document makes that clear that that risk is increasing.”
Dr. Douglas pointed out that the Joint Commission now requires good behavior in institutions that it accredits and that the Accreditation Council for Graduate Medical Education requires education around professionalism and evidence that their trainees are treated as professionals.
Funding agencies like the National Institutes of Health have also jumped into this space, recently establishing a hotline to report harassment, discrimination, and bullying perpetrated by an NIH-funded investigator, and giving institutions 30 days to investigate.
“In the last 2 years they have defunded, taken away the grants of 75 investigators, compared to zero in the 5 years before that,” Dr. Douglas said. “So I think, even though the bad behavior may be escalating, the consequences are escalating too.”
The new “2022 ACC Health Policy Statement on Building Respect, Civility, and Inclusion in the Cardiovascular Workplace” will be discussed in a session at the ACC 2022 Scientific Sessions on April 2 at 4:15 p.m. ET.
A version of this article first appeared on Medscape.com.
The American College of Cardiology has issued a new health policy statement directed at eliminating the bias, discrimination, bullying, and harassment that hamstrings the delivery of quality cardiovascular care.
“We pay a lot of attention, of course, to our patients and patient care issues but our ability to care optimally for patients is limited if the workforce is handicapped in any way,” said Pamela S. Douglas, MD, of Duke University, Durham, N.C., who cochaired the writing committee.
The document is the second in the ACC’s diversity inclusion initiative, following the 2019 report on equal compensation and opportunity in cardiology, but the foundation for the work actually started 5 years ago, she told this news organization.
“Unfortunately, COVID and other world events have created a climate in the United States where people don’t treat each other terribly well,” Dr. Douglas said. “It’s divisive and confrontational often, when it should be collaborative. So this document, at this time, was serendipitous but wonderful timing.”
The 2022 ACC Health Policy Statement on Building Respect, Civility, and Inclusion in the Cardiovascular Workforce was published online March 17 in the Journal of the American College of Cardiology.
The 63-page document provides 12 principles for building a better workplace, starting with the belief that civil behavior and respect are inherent in its core values of teamwork, collaboration, and professionalism.
The ACC calls on all organizations and individuals involved in providing cardiovascular care, education, or research to recognize the “ubiquity” of uncivil behavior and the continuum of bias, discrimination, bullying, and harassment (BDBH) that characterize it.
Some of the recommendations they offer to eliminate these behaviors include:
- Creating institutional policies and resources to ensure hiring decisions, evaluations, and departmental/program/center reviews are objective.
- Including assessments of personal behaviors related to respect and civility in performance reviews.
- Establishing confidential, fair, and transparent mechanisms for reporting and investigating individuals and/or departments suspected of BDBH.
- Adopting longitudinal metrics and accurate data collection to track progress and inform future policy and interventions.
- Encouraging independent evaluation of institutional culture and efforts to reduce BDBH.
- Celebrating those who promote and achieve excellence in reducing BDBH.
Patients behaving badly
What’s new, especially since the COVID-19 pandemic, is the number of patients who themselves engage in disrespectful and uncivil behavior, observed Dr. Douglas.
“As physicians, it was the patient’s always right. So you work to do backflips to accommodate the patient,” she said. “But when the patient says: I don’t want to be treated by anybody that comes from outside the United States, that’s not our society anymore. And that has to be addressed and dealt with.”
The policy statement features a suite of online tools and resources including 15 case examples and 30 sample policies from institutions that have been anonymized and some provide an action framework for addressing this type of patient behavior, Dr. Douglas said. An individual, for example, can ask the patient why they made the remark, explaining that the provider is qualified and someone they’d like to have care for their own family. If it was a trainee on the receiving end, it’s fair for them to go back to their supervisor, mentor, or training director.
“They should back you up and explain to the patient that it’s not who we are at this hospital and that they’re happy to provide care, but they are part of the hospital and need to obey the rules and environment in this hospital,” she said.
Writing committee cochair Michael J. Mack, MD, of Baylor Scott & White Health, Plano, Tex., told tthis news organization that “one of the concepts that I hadn’t heard before that resonated with me was the term ‘upstander’ – that you can’t just be a bystander and watch this happen and do nothing. If you’re witness to this in the workplace, if it’s gender bias or racial bias, you need to get involved and reach out to that individual and see what you can do to help and be a reporter of it.”
But it’s all too costly
Financial constraints are often cited as a reason not to focus on bias, discrimination, bullying, and harassment in the workplace or to shelve initiatives, but it’s a false argument, say Dr. Mack and Dr. Douglas.
“One of the case examples is a cardiology practice that is suffering a decline in finances, and the board makes the recommendation that the efforts at diversity and civil workplaces need to be the first to go,” Dr. Mack explained. “And the point that’s being made in this is you can’t afford not to do it because it ends up being more costly to the business in the long run.”
Part of that cost is associated with losing valuable employees that were contributing but left because there wasn’t a culture of respectfulness and positivity in their workplace. While that’s always been a risk, it’s become a particularly compelling issue because of the workforce shortages present 3 years on in the pandemic, he said.
“There’s a new reexamination to be sure that we have a positive work environment that people want to come to work at every day,” he said. “I run our Research Institute, and normally we have a 5% vacancy rate, and our unfilled-position rate is 25% right now.”
Health care is delivered as a team today, but if a member feels disrespected, or worse – harassed, bullied, or discriminated against – they’re not going to contribute at the top of their game, Dr. Douglas said.
“It’s very well documented that bad behavior exists and that it has negative consequences for patient care for institutions, who are at great risk legally and regulatory wise,” she said. “And the document makes that clear that that risk is increasing.”
Dr. Douglas pointed out that the Joint Commission now requires good behavior in institutions that it accredits and that the Accreditation Council for Graduate Medical Education requires education around professionalism and evidence that their trainees are treated as professionals.
Funding agencies like the National Institutes of Health have also jumped into this space, recently establishing a hotline to report harassment, discrimination, and bullying perpetrated by an NIH-funded investigator, and giving institutions 30 days to investigate.
“In the last 2 years they have defunded, taken away the grants of 75 investigators, compared to zero in the 5 years before that,” Dr. Douglas said. “So I think, even though the bad behavior may be escalating, the consequences are escalating too.”
The new “2022 ACC Health Policy Statement on Building Respect, Civility, and Inclusion in the Cardiovascular Workplace” will be discussed in a session at the ACC 2022 Scientific Sessions on April 2 at 4:15 p.m. ET.
A version of this article first appeared on Medscape.com.
The American College of Cardiology has issued a new health policy statement directed at eliminating the bias, discrimination, bullying, and harassment that hamstrings the delivery of quality cardiovascular care.
“We pay a lot of attention, of course, to our patients and patient care issues but our ability to care optimally for patients is limited if the workforce is handicapped in any way,” said Pamela S. Douglas, MD, of Duke University, Durham, N.C., who cochaired the writing committee.
The document is the second in the ACC’s diversity inclusion initiative, following the 2019 report on equal compensation and opportunity in cardiology, but the foundation for the work actually started 5 years ago, she told this news organization.
“Unfortunately, COVID and other world events have created a climate in the United States where people don’t treat each other terribly well,” Dr. Douglas said. “It’s divisive and confrontational often, when it should be collaborative. So this document, at this time, was serendipitous but wonderful timing.”
The 2022 ACC Health Policy Statement on Building Respect, Civility, and Inclusion in the Cardiovascular Workforce was published online March 17 in the Journal of the American College of Cardiology.
The 63-page document provides 12 principles for building a better workplace, starting with the belief that civil behavior and respect are inherent in its core values of teamwork, collaboration, and professionalism.
The ACC calls on all organizations and individuals involved in providing cardiovascular care, education, or research to recognize the “ubiquity” of uncivil behavior and the continuum of bias, discrimination, bullying, and harassment (BDBH) that characterize it.
Some of the recommendations they offer to eliminate these behaviors include:
- Creating institutional policies and resources to ensure hiring decisions, evaluations, and departmental/program/center reviews are objective.
- Including assessments of personal behaviors related to respect and civility in performance reviews.
- Establishing confidential, fair, and transparent mechanisms for reporting and investigating individuals and/or departments suspected of BDBH.
- Adopting longitudinal metrics and accurate data collection to track progress and inform future policy and interventions.
- Encouraging independent evaluation of institutional culture and efforts to reduce BDBH.
- Celebrating those who promote and achieve excellence in reducing BDBH.
Patients behaving badly
What’s new, especially since the COVID-19 pandemic, is the number of patients who themselves engage in disrespectful and uncivil behavior, observed Dr. Douglas.
“As physicians, it was the patient’s always right. So you work to do backflips to accommodate the patient,” she said. “But when the patient says: I don’t want to be treated by anybody that comes from outside the United States, that’s not our society anymore. And that has to be addressed and dealt with.”
The policy statement features a suite of online tools and resources including 15 case examples and 30 sample policies from institutions that have been anonymized and some provide an action framework for addressing this type of patient behavior, Dr. Douglas said. An individual, for example, can ask the patient why they made the remark, explaining that the provider is qualified and someone they’d like to have care for their own family. If it was a trainee on the receiving end, it’s fair for them to go back to their supervisor, mentor, or training director.
“They should back you up and explain to the patient that it’s not who we are at this hospital and that they’re happy to provide care, but they are part of the hospital and need to obey the rules and environment in this hospital,” she said.
Writing committee cochair Michael J. Mack, MD, of Baylor Scott & White Health, Plano, Tex., told tthis news organization that “one of the concepts that I hadn’t heard before that resonated with me was the term ‘upstander’ – that you can’t just be a bystander and watch this happen and do nothing. If you’re witness to this in the workplace, if it’s gender bias or racial bias, you need to get involved and reach out to that individual and see what you can do to help and be a reporter of it.”
But it’s all too costly
Financial constraints are often cited as a reason not to focus on bias, discrimination, bullying, and harassment in the workplace or to shelve initiatives, but it’s a false argument, say Dr. Mack and Dr. Douglas.
“One of the case examples is a cardiology practice that is suffering a decline in finances, and the board makes the recommendation that the efforts at diversity and civil workplaces need to be the first to go,” Dr. Mack explained. “And the point that’s being made in this is you can’t afford not to do it because it ends up being more costly to the business in the long run.”
Part of that cost is associated with losing valuable employees that were contributing but left because there wasn’t a culture of respectfulness and positivity in their workplace. While that’s always been a risk, it’s become a particularly compelling issue because of the workforce shortages present 3 years on in the pandemic, he said.
“There’s a new reexamination to be sure that we have a positive work environment that people want to come to work at every day,” he said. “I run our Research Institute, and normally we have a 5% vacancy rate, and our unfilled-position rate is 25% right now.”
Health care is delivered as a team today, but if a member feels disrespected, or worse – harassed, bullied, or discriminated against – they’re not going to contribute at the top of their game, Dr. Douglas said.
“It’s very well documented that bad behavior exists and that it has negative consequences for patient care for institutions, who are at great risk legally and regulatory wise,” she said. “And the document makes that clear that that risk is increasing.”
Dr. Douglas pointed out that the Joint Commission now requires good behavior in institutions that it accredits and that the Accreditation Council for Graduate Medical Education requires education around professionalism and evidence that their trainees are treated as professionals.
Funding agencies like the National Institutes of Health have also jumped into this space, recently establishing a hotline to report harassment, discrimination, and bullying perpetrated by an NIH-funded investigator, and giving institutions 30 days to investigate.
“In the last 2 years they have defunded, taken away the grants of 75 investigators, compared to zero in the 5 years before that,” Dr. Douglas said. “So I think, even though the bad behavior may be escalating, the consequences are escalating too.”
The new “2022 ACC Health Policy Statement on Building Respect, Civility, and Inclusion in the Cardiovascular Workplace” will be discussed in a session at the ACC 2022 Scientific Sessions on April 2 at 4:15 p.m. ET.
A version of this article first appeared on Medscape.com.
FROM JACC
Racial disparities seen in pediatric postoperative mortality rates
Among Black and White children, higher socioeconomic status (SES) was associated with lower pediatric postoperative mortality, according to a cohort study published in JAMA Network Open. However, this association was not equitable when comparing Black and White children.
The results showed that postoperative mortality rates were significantly higher in Black children in the highest income category, compared with White children in the same category.
“[We] assessed whether increasing family SES is associated with lower pediatric postoperative mortality and, if so, whether this association is equitable among Black and White children,” Brittany L. Willer, MD, of Nationwide Children’s Hospital in Columbus, Ohio, and colleagues wrote.
The researchers retrospectively analyzed data from 51 pediatric tertiary care hospitals apart of the Children’s Hospital Association Pediatric Health Information System. The cohort included children younger than 18 years who underwent inpatient surgical procedures between January 2004 and December 2020.
The exposures of interest were race and parental income quartile; the primary endpoint was risk-adjusted in-hospital mortality rates by race and parental income quartile.
Results
The study cohort included 1,378,111 participants, including 248,464 (18.0%) Black and 1,129,647 (82.0%) White children, respectively.
The overall mortality rate was 1.2%, and rates decreased as income quartile increased (1.4% in quartile 1 [lowest income]; 1.3% in quartile 2; 1.0% in quartile 3; and 0.9% in quartile 4 [highest income]; P < .001).
Among participants in the three lowest income quartiles, Black children had 33% greater odds of postoperative death versus White children (adjusted odds ratio, 1.33; 95% confidence interval, 1.27-1.39; P < .001). This difference persisted in children in the highest income quartile (aOR, 1.39; 95% CI, 1.25-1.54; P < .001).
In addition, postoperative mortality rates in Black children in the highest income quartile (1.30%; 95% CI, 1.19%-1.42%) were similar to those of White children in the lowest income quartile (1.20%; 95% CI, 1.16%-1.25%).
“These findings suggest that increasing family SES did not provide equitable advantage to Black, compared with White children, and interventions that target socioeconomic inequities alone may not fully address persistent racial disparities in pediatric postoperative mortality,” wrote Dr. Willer and colleagues. “A multifaceted approach that includes dismantling of socioeconomic barriers, equitable availability of comprehensive pediatric surgical care, and personalized care for children of all races is needed.”
The researchers acknowledged that a potential limitation of the study was the use of zip code–level median household income as a proxy for family SES.
A perspective
In an interview, Timothy Joos, MD, a Seattle internist and pediatrician in private practice, said “there is a fair dose of racism and classism inside all of us – recognizing and coming to terms with it are steps toward improving equity issues.
“As providers, we have to remind ourselves to give our most prompt and thorough care to the patients with the most acute and severe illnesses,” Dr. Joos said. “As organizations, we have to pursue feedback from all our clients, but with special outreach to those that are used to not having their voices heard.”
No funding sources were reported. The authors reported no relevant disclosures. Dr. Joos is a member of the Pediatric News editorial advisory board but had no other disclosures.
Among Black and White children, higher socioeconomic status (SES) was associated with lower pediatric postoperative mortality, according to a cohort study published in JAMA Network Open. However, this association was not equitable when comparing Black and White children.
The results showed that postoperative mortality rates were significantly higher in Black children in the highest income category, compared with White children in the same category.
“[We] assessed whether increasing family SES is associated with lower pediatric postoperative mortality and, if so, whether this association is equitable among Black and White children,” Brittany L. Willer, MD, of Nationwide Children’s Hospital in Columbus, Ohio, and colleagues wrote.
The researchers retrospectively analyzed data from 51 pediatric tertiary care hospitals apart of the Children’s Hospital Association Pediatric Health Information System. The cohort included children younger than 18 years who underwent inpatient surgical procedures between January 2004 and December 2020.
The exposures of interest were race and parental income quartile; the primary endpoint was risk-adjusted in-hospital mortality rates by race and parental income quartile.
Results
The study cohort included 1,378,111 participants, including 248,464 (18.0%) Black and 1,129,647 (82.0%) White children, respectively.
The overall mortality rate was 1.2%, and rates decreased as income quartile increased (1.4% in quartile 1 [lowest income]; 1.3% in quartile 2; 1.0% in quartile 3; and 0.9% in quartile 4 [highest income]; P < .001).
Among participants in the three lowest income quartiles, Black children had 33% greater odds of postoperative death versus White children (adjusted odds ratio, 1.33; 95% confidence interval, 1.27-1.39; P < .001). This difference persisted in children in the highest income quartile (aOR, 1.39; 95% CI, 1.25-1.54; P < .001).
In addition, postoperative mortality rates in Black children in the highest income quartile (1.30%; 95% CI, 1.19%-1.42%) were similar to those of White children in the lowest income quartile (1.20%; 95% CI, 1.16%-1.25%).
“These findings suggest that increasing family SES did not provide equitable advantage to Black, compared with White children, and interventions that target socioeconomic inequities alone may not fully address persistent racial disparities in pediatric postoperative mortality,” wrote Dr. Willer and colleagues. “A multifaceted approach that includes dismantling of socioeconomic barriers, equitable availability of comprehensive pediatric surgical care, and personalized care for children of all races is needed.”
The researchers acknowledged that a potential limitation of the study was the use of zip code–level median household income as a proxy for family SES.
A perspective
In an interview, Timothy Joos, MD, a Seattle internist and pediatrician in private practice, said “there is a fair dose of racism and classism inside all of us – recognizing and coming to terms with it are steps toward improving equity issues.
“As providers, we have to remind ourselves to give our most prompt and thorough care to the patients with the most acute and severe illnesses,” Dr. Joos said. “As organizations, we have to pursue feedback from all our clients, but with special outreach to those that are used to not having their voices heard.”
No funding sources were reported. The authors reported no relevant disclosures. Dr. Joos is a member of the Pediatric News editorial advisory board but had no other disclosures.
Among Black and White children, higher socioeconomic status (SES) was associated with lower pediatric postoperative mortality, according to a cohort study published in JAMA Network Open. However, this association was not equitable when comparing Black and White children.
The results showed that postoperative mortality rates were significantly higher in Black children in the highest income category, compared with White children in the same category.
“[We] assessed whether increasing family SES is associated with lower pediatric postoperative mortality and, if so, whether this association is equitable among Black and White children,” Brittany L. Willer, MD, of Nationwide Children’s Hospital in Columbus, Ohio, and colleagues wrote.
The researchers retrospectively analyzed data from 51 pediatric tertiary care hospitals apart of the Children’s Hospital Association Pediatric Health Information System. The cohort included children younger than 18 years who underwent inpatient surgical procedures between January 2004 and December 2020.
The exposures of interest were race and parental income quartile; the primary endpoint was risk-adjusted in-hospital mortality rates by race and parental income quartile.
Results
The study cohort included 1,378,111 participants, including 248,464 (18.0%) Black and 1,129,647 (82.0%) White children, respectively.
The overall mortality rate was 1.2%, and rates decreased as income quartile increased (1.4% in quartile 1 [lowest income]; 1.3% in quartile 2; 1.0% in quartile 3; and 0.9% in quartile 4 [highest income]; P < .001).
Among participants in the three lowest income quartiles, Black children had 33% greater odds of postoperative death versus White children (adjusted odds ratio, 1.33; 95% confidence interval, 1.27-1.39; P < .001). This difference persisted in children in the highest income quartile (aOR, 1.39; 95% CI, 1.25-1.54; P < .001).
In addition, postoperative mortality rates in Black children in the highest income quartile (1.30%; 95% CI, 1.19%-1.42%) were similar to those of White children in the lowest income quartile (1.20%; 95% CI, 1.16%-1.25%).
“These findings suggest that increasing family SES did not provide equitable advantage to Black, compared with White children, and interventions that target socioeconomic inequities alone may not fully address persistent racial disparities in pediatric postoperative mortality,” wrote Dr. Willer and colleagues. “A multifaceted approach that includes dismantling of socioeconomic barriers, equitable availability of comprehensive pediatric surgical care, and personalized care for children of all races is needed.”
The researchers acknowledged that a potential limitation of the study was the use of zip code–level median household income as a proxy for family SES.
A perspective
In an interview, Timothy Joos, MD, a Seattle internist and pediatrician in private practice, said “there is a fair dose of racism and classism inside all of us – recognizing and coming to terms with it are steps toward improving equity issues.
“As providers, we have to remind ourselves to give our most prompt and thorough care to the patients with the most acute and severe illnesses,” Dr. Joos said. “As organizations, we have to pursue feedback from all our clients, but with special outreach to those that are used to not having their voices heard.”
No funding sources were reported. The authors reported no relevant disclosures. Dr. Joos is a member of the Pediatric News editorial advisory board but had no other disclosures.
FROM JAMA NETWORK OPEN
U.S. primary care seen lagging in key markers
In delivery of primary care, including access and coordination, the U.S. trails well behind 10 other wealthy countries, according to a new report from the Commonwealth Fund.
The document, released March 15, concludes that the shortcomings in the U.S. system – from a lack of a relationship with a primary care physician to unequal access to after-hours care – “disproportionately affect Black and Latinx communities and rural areas, exacerbating disparities that have widened during the COVID-19 pandemic.”
“This report really shows that the U.S. is falling behind. We know that a strong primary care system yields better health outcomes. We have a lot to learn from other high-income countries,” coauthor Munira Z. Gunja, MPH, a senior researcher for the Commonwealth Fund’s International Program in Health Policy and Practice Innovations, told this news organization. “At baseline, we really need to make sure that everyone has health insurance in this country so they can actually use primary care services, and we need to increase the supply of those services.”
The report draws from the Commonwealth Fund’s 2019 and 2020 International Health Policy Surveys and the 2020 International Profiles of Health Care Systems. Among the main points:
- U.S. adults are the least likely to have a regular physician or place of care or a long-standing relationship with a primary care provider: 43% of American adults have a long-term relationship with a primary care doctor, compared with highs of 71% in Germany and the Netherlands.
- Access to home visits or after-hours care – excluding emergency department visits – is lowest in the United States (45%). In the Netherlands, Norway, New Zealand, and Germany, the rate is 90% to 96%.
- Half of primary care providers in the United States report adequate coordination with specialists and hospitals – around the average for the 11 countries studied.
‘Dismal mess’
Experts reacted to the report with a mix of concern and frustration – but not surprise.
“The results in this report are not surprising, and we have known them all for a number of years now,” Timothy Hoff, PhD, a health policy expert at Northeastern University, Boston, said. “Primary care doctors remain the backbone of our primary care system. But there are too few of them in the United States, and there likely will remain too few of them in the future. This opens the door to other and more diverse forms of innovation that will be required to help complement the work they do.”
Dr. Hoff, author of Searching for the Family Doctor: Primary Care on the Brink, added that comparing the United States to smaller countries like Norway or the United Kingdom is “somewhat problematic.”
“Our system has to take care of several hundred million people, trapped in a fragmented and market-based delivery system focused on specialty care, each of whom may have a different insurance plan,” he said. “Doing some of the things very small countries with government-funded insurance and a history of strong primary care delivery do in taking care of far fewer citizens is not realistic.”
Jeffrey Borkan, MD, PhD, chair and professor in the department of family medicine at the Alpert Medical School of Brown University, Providence, R.I., said the most shocking finding in the report is that despite spending far more on health care than any other country, “we cannot manage to provide one of the least expensive and most efficacious services: a relationship with a primary care doctor.”
Arthur Caplan, PhD, director of the Division of Medical Ethics at New York University Langone Medical Center, called primary care in this country “a dismal mess. It has been for many years. This is especially so in mental health. Access in many counties is nonexistent, and many primary care physicians are opting into boutique care.”
R. Shawn Martin, CEO of the 133,000-member American Academy of Family Physicians, said, “None of this surprises me. I think these are trendlines; we have been following this for many, many years here at the Academy.”
Mr. Martin added that he was disappointed that the recent, large investments in sharing and digitizing information have not closed the gaps that hinder the efficient and widespread delivery of primary care.
The findings in the report weren’t all bad. More primary care providers in the United States (30%) screen their patients for social needs such as housing, food security, and transportation – the highest among all 11 nations studied.
Also, Commonwealth Fund said the proportion of patients who said they received information on meeting their social needs and screening for domestic violence or social isolation was low everywhere. However, the percentage in the United States, Canada, and Norway was the highest, at 9%. Sweden had the lowest rate for such screenings, at 1%.
The researchers noted that social determinants of health account for as much as 55% of health outcomes. “In some countries, like the United States, the higher rates of receiving such information may be a response to the higher rates of material hardship, along with a weaker safety net,” the report states.
Ms. Gunja and her colleagues suggested several options for changes in policies, including narrowing the wage gap between primary care providers and higher-paid specialists; subsidizing medical school tuition to give students incentives to enter primary care; investing in telehealth to make primary care more accessible; and rewarding and holding providers accountable for continuity of care.
“The U.S. had the largest wage gap and highest tuition fees among the countries we studied,” Ms. Gunja told this news organization..
Researchers noted that U.S. patients could benefit from the introduction of incentives such as those paid in New Zealand to primary health organizations, which receive additional funding per capita to promote health and coordinate care.
But Dr. Caplan was skeptical that those measures would do much to correct the problems.
“We have no will to fix this ongoing, scandalous situation,” he said. “Specialist care still pays inordinately large salaries. Nurses and physician extenders are underused. Academic prestige does little to reward primary care. Plus, patients are not pressing for better access. Sorry, but I see no solutions pending in the current climate. Obamacare barely survived.”
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In delivery of primary care, including access and coordination, the U.S. trails well behind 10 other wealthy countries, according to a new report from the Commonwealth Fund.
The document, released March 15, concludes that the shortcomings in the U.S. system – from a lack of a relationship with a primary care physician to unequal access to after-hours care – “disproportionately affect Black and Latinx communities and rural areas, exacerbating disparities that have widened during the COVID-19 pandemic.”
“This report really shows that the U.S. is falling behind. We know that a strong primary care system yields better health outcomes. We have a lot to learn from other high-income countries,” coauthor Munira Z. Gunja, MPH, a senior researcher for the Commonwealth Fund’s International Program in Health Policy and Practice Innovations, told this news organization. “At baseline, we really need to make sure that everyone has health insurance in this country so they can actually use primary care services, and we need to increase the supply of those services.”
The report draws from the Commonwealth Fund’s 2019 and 2020 International Health Policy Surveys and the 2020 International Profiles of Health Care Systems. Among the main points:
- U.S. adults are the least likely to have a regular physician or place of care or a long-standing relationship with a primary care provider: 43% of American adults have a long-term relationship with a primary care doctor, compared with highs of 71% in Germany and the Netherlands.
- Access to home visits or after-hours care – excluding emergency department visits – is lowest in the United States (45%). In the Netherlands, Norway, New Zealand, and Germany, the rate is 90% to 96%.
- Half of primary care providers in the United States report adequate coordination with specialists and hospitals – around the average for the 11 countries studied.
‘Dismal mess’
Experts reacted to the report with a mix of concern and frustration – but not surprise.
“The results in this report are not surprising, and we have known them all for a number of years now,” Timothy Hoff, PhD, a health policy expert at Northeastern University, Boston, said. “Primary care doctors remain the backbone of our primary care system. But there are too few of them in the United States, and there likely will remain too few of them in the future. This opens the door to other and more diverse forms of innovation that will be required to help complement the work they do.”
Dr. Hoff, author of Searching for the Family Doctor: Primary Care on the Brink, added that comparing the United States to smaller countries like Norway or the United Kingdom is “somewhat problematic.”
“Our system has to take care of several hundred million people, trapped in a fragmented and market-based delivery system focused on specialty care, each of whom may have a different insurance plan,” he said. “Doing some of the things very small countries with government-funded insurance and a history of strong primary care delivery do in taking care of far fewer citizens is not realistic.”
Jeffrey Borkan, MD, PhD, chair and professor in the department of family medicine at the Alpert Medical School of Brown University, Providence, R.I., said the most shocking finding in the report is that despite spending far more on health care than any other country, “we cannot manage to provide one of the least expensive and most efficacious services: a relationship with a primary care doctor.”
Arthur Caplan, PhD, director of the Division of Medical Ethics at New York University Langone Medical Center, called primary care in this country “a dismal mess. It has been for many years. This is especially so in mental health. Access in many counties is nonexistent, and many primary care physicians are opting into boutique care.”
R. Shawn Martin, CEO of the 133,000-member American Academy of Family Physicians, said, “None of this surprises me. I think these are trendlines; we have been following this for many, many years here at the Academy.”
Mr. Martin added that he was disappointed that the recent, large investments in sharing and digitizing information have not closed the gaps that hinder the efficient and widespread delivery of primary care.
The findings in the report weren’t all bad. More primary care providers in the United States (30%) screen their patients for social needs such as housing, food security, and transportation – the highest among all 11 nations studied.
Also, Commonwealth Fund said the proportion of patients who said they received information on meeting their social needs and screening for domestic violence or social isolation was low everywhere. However, the percentage in the United States, Canada, and Norway was the highest, at 9%. Sweden had the lowest rate for such screenings, at 1%.
The researchers noted that social determinants of health account for as much as 55% of health outcomes. “In some countries, like the United States, the higher rates of receiving such information may be a response to the higher rates of material hardship, along with a weaker safety net,” the report states.
Ms. Gunja and her colleagues suggested several options for changes in policies, including narrowing the wage gap between primary care providers and higher-paid specialists; subsidizing medical school tuition to give students incentives to enter primary care; investing in telehealth to make primary care more accessible; and rewarding and holding providers accountable for continuity of care.
“The U.S. had the largest wage gap and highest tuition fees among the countries we studied,” Ms. Gunja told this news organization..
Researchers noted that U.S. patients could benefit from the introduction of incentives such as those paid in New Zealand to primary health organizations, which receive additional funding per capita to promote health and coordinate care.
But Dr. Caplan was skeptical that those measures would do much to correct the problems.
“We have no will to fix this ongoing, scandalous situation,” he said. “Specialist care still pays inordinately large salaries. Nurses and physician extenders are underused. Academic prestige does little to reward primary care. Plus, patients are not pressing for better access. Sorry, but I see no solutions pending in the current climate. Obamacare barely survived.”
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In delivery of primary care, including access and coordination, the U.S. trails well behind 10 other wealthy countries, according to a new report from the Commonwealth Fund.
The document, released March 15, concludes that the shortcomings in the U.S. system – from a lack of a relationship with a primary care physician to unequal access to after-hours care – “disproportionately affect Black and Latinx communities and rural areas, exacerbating disparities that have widened during the COVID-19 pandemic.”
“This report really shows that the U.S. is falling behind. We know that a strong primary care system yields better health outcomes. We have a lot to learn from other high-income countries,” coauthor Munira Z. Gunja, MPH, a senior researcher for the Commonwealth Fund’s International Program in Health Policy and Practice Innovations, told this news organization. “At baseline, we really need to make sure that everyone has health insurance in this country so they can actually use primary care services, and we need to increase the supply of those services.”
The report draws from the Commonwealth Fund’s 2019 and 2020 International Health Policy Surveys and the 2020 International Profiles of Health Care Systems. Among the main points:
- U.S. adults are the least likely to have a regular physician or place of care or a long-standing relationship with a primary care provider: 43% of American adults have a long-term relationship with a primary care doctor, compared with highs of 71% in Germany and the Netherlands.
- Access to home visits or after-hours care – excluding emergency department visits – is lowest in the United States (45%). In the Netherlands, Norway, New Zealand, and Germany, the rate is 90% to 96%.
- Half of primary care providers in the United States report adequate coordination with specialists and hospitals – around the average for the 11 countries studied.
‘Dismal mess’
Experts reacted to the report with a mix of concern and frustration – but not surprise.
“The results in this report are not surprising, and we have known them all for a number of years now,” Timothy Hoff, PhD, a health policy expert at Northeastern University, Boston, said. “Primary care doctors remain the backbone of our primary care system. But there are too few of them in the United States, and there likely will remain too few of them in the future. This opens the door to other and more diverse forms of innovation that will be required to help complement the work they do.”
Dr. Hoff, author of Searching for the Family Doctor: Primary Care on the Brink, added that comparing the United States to smaller countries like Norway or the United Kingdom is “somewhat problematic.”
“Our system has to take care of several hundred million people, trapped in a fragmented and market-based delivery system focused on specialty care, each of whom may have a different insurance plan,” he said. “Doing some of the things very small countries with government-funded insurance and a history of strong primary care delivery do in taking care of far fewer citizens is not realistic.”
Jeffrey Borkan, MD, PhD, chair and professor in the department of family medicine at the Alpert Medical School of Brown University, Providence, R.I., said the most shocking finding in the report is that despite spending far more on health care than any other country, “we cannot manage to provide one of the least expensive and most efficacious services: a relationship with a primary care doctor.”
Arthur Caplan, PhD, director of the Division of Medical Ethics at New York University Langone Medical Center, called primary care in this country “a dismal mess. It has been for many years. This is especially so in mental health. Access in many counties is nonexistent, and many primary care physicians are opting into boutique care.”
R. Shawn Martin, CEO of the 133,000-member American Academy of Family Physicians, said, “None of this surprises me. I think these are trendlines; we have been following this for many, many years here at the Academy.”
Mr. Martin added that he was disappointed that the recent, large investments in sharing and digitizing information have not closed the gaps that hinder the efficient and widespread delivery of primary care.
The findings in the report weren’t all bad. More primary care providers in the United States (30%) screen their patients for social needs such as housing, food security, and transportation – the highest among all 11 nations studied.
Also, Commonwealth Fund said the proportion of patients who said they received information on meeting their social needs and screening for domestic violence or social isolation was low everywhere. However, the percentage in the United States, Canada, and Norway was the highest, at 9%. Sweden had the lowest rate for such screenings, at 1%.
The researchers noted that social determinants of health account for as much as 55% of health outcomes. “In some countries, like the United States, the higher rates of receiving such information may be a response to the higher rates of material hardship, along with a weaker safety net,” the report states.
Ms. Gunja and her colleagues suggested several options for changes in policies, including narrowing the wage gap between primary care providers and higher-paid specialists; subsidizing medical school tuition to give students incentives to enter primary care; investing in telehealth to make primary care more accessible; and rewarding and holding providers accountable for continuity of care.
“The U.S. had the largest wage gap and highest tuition fees among the countries we studied,” Ms. Gunja told this news organization..
Researchers noted that U.S. patients could benefit from the introduction of incentives such as those paid in New Zealand to primary health organizations, which receive additional funding per capita to promote health and coordinate care.
But Dr. Caplan was skeptical that those measures would do much to correct the problems.
“We have no will to fix this ongoing, scandalous situation,” he said. “Specialist care still pays inordinately large salaries. Nurses and physician extenders are underused. Academic prestige does little to reward primary care. Plus, patients are not pressing for better access. Sorry, but I see no solutions pending in the current climate. Obamacare barely survived.”
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiologists say rights to maternity leave violated
A survey of 323 women cardiologists who were working while they were pregnant showed that nearly 75% experienced discriminatory maternity-leave practices, some of which were likely violations of the Family and Medical Leave Act (FMLA).
More than 40% saw their salaries decreased during their year of pregnancy, 38% were required to perform extra service or call before taking maternity leave, exposing them to occupational hazards such as radiation, and 40% experienced a pregnancy complication, significantly higher than the general population and other medical specialties.
Additionally, of those who performed extra service or call, 18% were placed on bedrest before delivery, compared with 7.4% who did not perform extra service or call.
More than half of respondents reported that pregnancy negatively impacted their careers, and 42.4% said they experienced pressure to return to work and a delay in promotions, both illegal practices under the FMLA.
The survey is published in the Journal of the American College of Cardiology.
“Childbearing is difficult for women in cardiology with more than double the rate of gestational complications of the U.S. population, frequent income loss out of proportion to reduced productivity, and for nearly half, has an adverse impact on their career,” lead author Martha Gulati, MD, University of Arizona, Phoenix, said in a statement.
“While many professions struggle to create environments supportive of pregnancy and child-rearing, the prevalence of illegal behavior in cardiology is quite high and presents substantial legal risk for employers,” Dr. Gulati added.
C. Noel Bairey Merz, MD, professor of cardiology at Cedars-Sinai Smidt Heart Institute, Los Angeles, and a coauthor of the survey, told this news organization that it’s not surprising that such a situation exists, even “in this day and age.”
“I’m not surprised as a woman in cardiology myself. I was told by my training director that if I took off more than my allowed sick leave when I had my first and second children, I would have to repeat the year of training, so not surprised at all. I hear this from colleagues all the time,” Dr. Bairey Merz said.
The exchange left her feeling fearful for her career.
“Who wants to repeat a year? It pushes you back from a career standpoint, financially, everything. It also made me angry. I had a colleague who busted his leg in a motorcycle accident. He was unable to do any procedures for 16 weeks, and he didn’t have to repeat the year,” she pointed out.
The challenge that pregnancy represents is frequently cited by women as a deterrent for applying for a cardiology fellowship, Laxmi S. Mehta, MD, Ohio State University, Columbus, and colleagues wrote in an accompanying editorial.
The findings from the survey “reveal restrictive maternity leave data in a profession that has historically and currently continues to have a diversity problem,” they wrote.
“Maternity and pregnancy issues are a thing in cardiology,” Dr. Mehta said in an interview. “It’s one of the reasons why women get deterred from going into the field. It makes it challenging to choose cardiology if you perceive that the culture is negative, that it’s hard to be pregnant, or to bear children, or to take care of them post partum. It is problematic and it should not be occurring now.”
Leadership that condones such restrictive policies or even promotes them through ignorance and inaction needs to be held accountable, she added.
“We need to move forward from this negativity and make it more warm and welcoming to have families, whether you are a trainee or a practicing cardiologist, male or female. We need transparent and consistent parental leave policies and things like lactation support when a woman returns to work. That is a big issue,” Dr. Mehta said.
Having cardiovascular leaders champion the cause of adequate maternity and paternity leave are crucial to creating a newer, inclusive environment in cardiology.
As an example, Dr. Mehta recounted her own experience when she was in training 17 years ago.
“When I interviewed for a cardiology fellowship, one of the female program directors asked me if I was planning to have children, because if I did, the other fellows wouldn’t like it if they had to cover for me,” she said. “I ended up doing my fellowship where the chief of cardiology encouraged me to have children. He said: ‘Have your children during training, we will support you.’ And he did. I still had to do all of the call make-up and that stuff, but I worked in a supportive environment, and it made all the difference.”
“It’s about allyship,” she added. “You will have some people who are supportive and some who are not, but when you have the chief supporting you, you have a strong ally.”
The researchers suggest that one strategy is to temporarily replace cardiologists on maternity leave with locums, or “deepen the bench of coverage for clinical work, as is done for other absences. Given the expanding coverage of parental and family medical leaves, and awareness of these issues nationally, the need for this is likely to become less of an exception and more the rule.”
For example, nine states and Washington, D.C. now provide paid parental leave, they wrote, “and there is pending legislation in others.”
Dr. Bairey Merz and Dr. Mehta reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A survey of 323 women cardiologists who were working while they were pregnant showed that nearly 75% experienced discriminatory maternity-leave practices, some of which were likely violations of the Family and Medical Leave Act (FMLA).
More than 40% saw their salaries decreased during their year of pregnancy, 38% were required to perform extra service or call before taking maternity leave, exposing them to occupational hazards such as radiation, and 40% experienced a pregnancy complication, significantly higher than the general population and other medical specialties.
Additionally, of those who performed extra service or call, 18% were placed on bedrest before delivery, compared with 7.4% who did not perform extra service or call.
More than half of respondents reported that pregnancy negatively impacted their careers, and 42.4% said they experienced pressure to return to work and a delay in promotions, both illegal practices under the FMLA.
The survey is published in the Journal of the American College of Cardiology.
“Childbearing is difficult for women in cardiology with more than double the rate of gestational complications of the U.S. population, frequent income loss out of proportion to reduced productivity, and for nearly half, has an adverse impact on their career,” lead author Martha Gulati, MD, University of Arizona, Phoenix, said in a statement.
“While many professions struggle to create environments supportive of pregnancy and child-rearing, the prevalence of illegal behavior in cardiology is quite high and presents substantial legal risk for employers,” Dr. Gulati added.
C. Noel Bairey Merz, MD, professor of cardiology at Cedars-Sinai Smidt Heart Institute, Los Angeles, and a coauthor of the survey, told this news organization that it’s not surprising that such a situation exists, even “in this day and age.”
“I’m not surprised as a woman in cardiology myself. I was told by my training director that if I took off more than my allowed sick leave when I had my first and second children, I would have to repeat the year of training, so not surprised at all. I hear this from colleagues all the time,” Dr. Bairey Merz said.
The exchange left her feeling fearful for her career.
“Who wants to repeat a year? It pushes you back from a career standpoint, financially, everything. It also made me angry. I had a colleague who busted his leg in a motorcycle accident. He was unable to do any procedures for 16 weeks, and he didn’t have to repeat the year,” she pointed out.
The challenge that pregnancy represents is frequently cited by women as a deterrent for applying for a cardiology fellowship, Laxmi S. Mehta, MD, Ohio State University, Columbus, and colleagues wrote in an accompanying editorial.
The findings from the survey “reveal restrictive maternity leave data in a profession that has historically and currently continues to have a diversity problem,” they wrote.
“Maternity and pregnancy issues are a thing in cardiology,” Dr. Mehta said in an interview. “It’s one of the reasons why women get deterred from going into the field. It makes it challenging to choose cardiology if you perceive that the culture is negative, that it’s hard to be pregnant, or to bear children, or to take care of them post partum. It is problematic and it should not be occurring now.”
Leadership that condones such restrictive policies or even promotes them through ignorance and inaction needs to be held accountable, she added.
“We need to move forward from this negativity and make it more warm and welcoming to have families, whether you are a trainee or a practicing cardiologist, male or female. We need transparent and consistent parental leave policies and things like lactation support when a woman returns to work. That is a big issue,” Dr. Mehta said.
Having cardiovascular leaders champion the cause of adequate maternity and paternity leave are crucial to creating a newer, inclusive environment in cardiology.
As an example, Dr. Mehta recounted her own experience when she was in training 17 years ago.
“When I interviewed for a cardiology fellowship, one of the female program directors asked me if I was planning to have children, because if I did, the other fellows wouldn’t like it if they had to cover for me,” she said. “I ended up doing my fellowship where the chief of cardiology encouraged me to have children. He said: ‘Have your children during training, we will support you.’ And he did. I still had to do all of the call make-up and that stuff, but I worked in a supportive environment, and it made all the difference.”
“It’s about allyship,” she added. “You will have some people who are supportive and some who are not, but when you have the chief supporting you, you have a strong ally.”
The researchers suggest that one strategy is to temporarily replace cardiologists on maternity leave with locums, or “deepen the bench of coverage for clinical work, as is done for other absences. Given the expanding coverage of parental and family medical leaves, and awareness of these issues nationally, the need for this is likely to become less of an exception and more the rule.”
For example, nine states and Washington, D.C. now provide paid parental leave, they wrote, “and there is pending legislation in others.”
Dr. Bairey Merz and Dr. Mehta reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A survey of 323 women cardiologists who were working while they were pregnant showed that nearly 75% experienced discriminatory maternity-leave practices, some of which were likely violations of the Family and Medical Leave Act (FMLA).
More than 40% saw their salaries decreased during their year of pregnancy, 38% were required to perform extra service or call before taking maternity leave, exposing them to occupational hazards such as radiation, and 40% experienced a pregnancy complication, significantly higher than the general population and other medical specialties.
Additionally, of those who performed extra service or call, 18% were placed on bedrest before delivery, compared with 7.4% who did not perform extra service or call.
More than half of respondents reported that pregnancy negatively impacted their careers, and 42.4% said they experienced pressure to return to work and a delay in promotions, both illegal practices under the FMLA.
The survey is published in the Journal of the American College of Cardiology.
“Childbearing is difficult for women in cardiology with more than double the rate of gestational complications of the U.S. population, frequent income loss out of proportion to reduced productivity, and for nearly half, has an adverse impact on their career,” lead author Martha Gulati, MD, University of Arizona, Phoenix, said in a statement.
“While many professions struggle to create environments supportive of pregnancy and child-rearing, the prevalence of illegal behavior in cardiology is quite high and presents substantial legal risk for employers,” Dr. Gulati added.
C. Noel Bairey Merz, MD, professor of cardiology at Cedars-Sinai Smidt Heart Institute, Los Angeles, and a coauthor of the survey, told this news organization that it’s not surprising that such a situation exists, even “in this day and age.”
“I’m not surprised as a woman in cardiology myself. I was told by my training director that if I took off more than my allowed sick leave when I had my first and second children, I would have to repeat the year of training, so not surprised at all. I hear this from colleagues all the time,” Dr. Bairey Merz said.
The exchange left her feeling fearful for her career.
“Who wants to repeat a year? It pushes you back from a career standpoint, financially, everything. It also made me angry. I had a colleague who busted his leg in a motorcycle accident. He was unable to do any procedures for 16 weeks, and he didn’t have to repeat the year,” she pointed out.
The challenge that pregnancy represents is frequently cited by women as a deterrent for applying for a cardiology fellowship, Laxmi S. Mehta, MD, Ohio State University, Columbus, and colleagues wrote in an accompanying editorial.
The findings from the survey “reveal restrictive maternity leave data in a profession that has historically and currently continues to have a diversity problem,” they wrote.
“Maternity and pregnancy issues are a thing in cardiology,” Dr. Mehta said in an interview. “It’s one of the reasons why women get deterred from going into the field. It makes it challenging to choose cardiology if you perceive that the culture is negative, that it’s hard to be pregnant, or to bear children, or to take care of them post partum. It is problematic and it should not be occurring now.”
Leadership that condones such restrictive policies or even promotes them through ignorance and inaction needs to be held accountable, she added.
“We need to move forward from this negativity and make it more warm and welcoming to have families, whether you are a trainee or a practicing cardiologist, male or female. We need transparent and consistent parental leave policies and things like lactation support when a woman returns to work. That is a big issue,” Dr. Mehta said.
Having cardiovascular leaders champion the cause of adequate maternity and paternity leave are crucial to creating a newer, inclusive environment in cardiology.
As an example, Dr. Mehta recounted her own experience when she was in training 17 years ago.
“When I interviewed for a cardiology fellowship, one of the female program directors asked me if I was planning to have children, because if I did, the other fellows wouldn’t like it if they had to cover for me,” she said. “I ended up doing my fellowship where the chief of cardiology encouraged me to have children. He said: ‘Have your children during training, we will support you.’ And he did. I still had to do all of the call make-up and that stuff, but I worked in a supportive environment, and it made all the difference.”
“It’s about allyship,” she added. “You will have some people who are supportive and some who are not, but when you have the chief supporting you, you have a strong ally.”
The researchers suggest that one strategy is to temporarily replace cardiologists on maternity leave with locums, or “deepen the bench of coverage for clinical work, as is done for other absences. Given the expanding coverage of parental and family medical leaves, and awareness of these issues nationally, the need for this is likely to become less of an exception and more the rule.”
For example, nine states and Washington, D.C. now provide paid parental leave, they wrote, “and there is pending legislation in others.”
Dr. Bairey Merz and Dr. Mehta reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Food insecurity linked to metabolic syndrome in Hispanic/Latino youth
Severe food insecurity was associated with metabolic syndrome and unfavorable cardiometabolic markers in Hispanic/Latino youth, researchers report.
The findings, published March 16 in Pediatrics, highlight the need to investigate interventions that address food insecurity among Hispanic/Latino youth, a segment of the U.S. population at high risk of cardiometabolic complications.
“Among Hispanic/Latino youth, no study, to our knowledge has evaluated food insecurity’s role in metabolic syndrome and metabolic syndrome–relevant cardiometabolic markers in this population,” lead author Luis E. Maldonado, PhD, of the University of North Carolina at Chapel Hill, and colleagues explained.
The researchers conducted a cross-sectional study to evaluate the associations between lower household and child food security and metabolic syndrome, as well as clinically measured cardiometabolic markers, including fasting plasma glucose, waist circumference, triglycerides, systolic and diastolic blood pressure, and high-density lipoprotein cholesterol (HDL-C).
Household food security (high, marginal, low, very low) and child food security (high, marginal, low/very low) measures were evaluated separately, and were adjusted for participant age, sex, site, parental education, and poverty-income ratio.
Data were obtained from the Hispanic Community Children’s Health Study/Study of Latino Youth, a study of offspring of adults enrolled in the Hispanic Community Health Survey/Study of Latinos.
Results
The study cohort included 1,325 Hispanic/Latino youth aged 8-16 years. For both household food security and child food security, youth in the lowest food security category had significantly lower HDL-C compared with youth with high food security (household food security, –3.17; 95% confidence interval, –5.65 to –0.70; child food security, –1.81; 95% CI, –3.54 to –0.09).
In addition, low/very low compared with high child food security was associated with higher triglycerides (beta, 8.68; 95% CI, 1.75-15.61), higher fasting plasma glucose (beta, 1.37; 95% CI, 0.08-2.65), and metabolic syndrome composite variable expected log counts (beta, 2.12; 95% CI, 0.02-0.45).
Furthermore, the researchers found statistically significant interactions between each of the two food security measures and receipt of any food assistance in the previous year in models of triglycerides (P for interactions: household food security, .03 and child food security, .005) and HDL-C (P for interactions: household food security, .01 and child food security, .04).
After evaluating the effect of parental place of birth, they found a statistically significant association for triglycerides only (P for interactions: household food security, .05 and child food security, .008).
“Our study is among the first to document adverse associations between household and child food security measures with a metabolic syndrome score variable and several metabolic syndrome–relevant cardiometabolic markers among US Hispanic/Latino youth,” the researchers wrote.
The researchers acknowledged that the cross-sectional nature of the study was a key limitation; thus, causality could not be inferred.
“In the future, we plan to conduct more qualitative work to better understand how Hispanic/Latino families respond to food insecurity, which may identify the factors that shape their response,” study author Sandra S. Albrecht, PhD, of Columbia University, New York, NY, said in an interview.
Recommendations for pediatricians
Food insecurity researcher Yankun Wang, PhD candidate at Indiana University, Bloomington, commented: “I would recommend pediatricians pay more attention to children from low-income households since they are more likely to have mental and physical health issues due to food insecurity.
“It can be very helpful if pediatricians could help families obtain SNAP benefits, enroll youth in the school breakfast and lunch programs, and promote nutrition education in schools,” Mr. Wang added.
This study was supported by grant funding from the National Heart, Lung, and Blood Institute. The authors reported no relevant disclosures.
Severe food insecurity was associated with metabolic syndrome and unfavorable cardiometabolic markers in Hispanic/Latino youth, researchers report.
The findings, published March 16 in Pediatrics, highlight the need to investigate interventions that address food insecurity among Hispanic/Latino youth, a segment of the U.S. population at high risk of cardiometabolic complications.
“Among Hispanic/Latino youth, no study, to our knowledge has evaluated food insecurity’s role in metabolic syndrome and metabolic syndrome–relevant cardiometabolic markers in this population,” lead author Luis E. Maldonado, PhD, of the University of North Carolina at Chapel Hill, and colleagues explained.
The researchers conducted a cross-sectional study to evaluate the associations between lower household and child food security and metabolic syndrome, as well as clinically measured cardiometabolic markers, including fasting plasma glucose, waist circumference, triglycerides, systolic and diastolic blood pressure, and high-density lipoprotein cholesterol (HDL-C).
Household food security (high, marginal, low, very low) and child food security (high, marginal, low/very low) measures were evaluated separately, and were adjusted for participant age, sex, site, parental education, and poverty-income ratio.
Data were obtained from the Hispanic Community Children’s Health Study/Study of Latino Youth, a study of offspring of adults enrolled in the Hispanic Community Health Survey/Study of Latinos.
Results
The study cohort included 1,325 Hispanic/Latino youth aged 8-16 years. For both household food security and child food security, youth in the lowest food security category had significantly lower HDL-C compared with youth with high food security (household food security, –3.17; 95% confidence interval, –5.65 to –0.70; child food security, –1.81; 95% CI, –3.54 to –0.09).
In addition, low/very low compared with high child food security was associated with higher triglycerides (beta, 8.68; 95% CI, 1.75-15.61), higher fasting plasma glucose (beta, 1.37; 95% CI, 0.08-2.65), and metabolic syndrome composite variable expected log counts (beta, 2.12; 95% CI, 0.02-0.45).
Furthermore, the researchers found statistically significant interactions between each of the two food security measures and receipt of any food assistance in the previous year in models of triglycerides (P for interactions: household food security, .03 and child food security, .005) and HDL-C (P for interactions: household food security, .01 and child food security, .04).
After evaluating the effect of parental place of birth, they found a statistically significant association for triglycerides only (P for interactions: household food security, .05 and child food security, .008).
“Our study is among the first to document adverse associations between household and child food security measures with a metabolic syndrome score variable and several metabolic syndrome–relevant cardiometabolic markers among US Hispanic/Latino youth,” the researchers wrote.
The researchers acknowledged that the cross-sectional nature of the study was a key limitation; thus, causality could not be inferred.
“In the future, we plan to conduct more qualitative work to better understand how Hispanic/Latino families respond to food insecurity, which may identify the factors that shape their response,” study author Sandra S. Albrecht, PhD, of Columbia University, New York, NY, said in an interview.
Recommendations for pediatricians
Food insecurity researcher Yankun Wang, PhD candidate at Indiana University, Bloomington, commented: “I would recommend pediatricians pay more attention to children from low-income households since they are more likely to have mental and physical health issues due to food insecurity.
“It can be very helpful if pediatricians could help families obtain SNAP benefits, enroll youth in the school breakfast and lunch programs, and promote nutrition education in schools,” Mr. Wang added.
This study was supported by grant funding from the National Heart, Lung, and Blood Institute. The authors reported no relevant disclosures.
Severe food insecurity was associated with metabolic syndrome and unfavorable cardiometabolic markers in Hispanic/Latino youth, researchers report.
The findings, published March 16 in Pediatrics, highlight the need to investigate interventions that address food insecurity among Hispanic/Latino youth, a segment of the U.S. population at high risk of cardiometabolic complications.
“Among Hispanic/Latino youth, no study, to our knowledge has evaluated food insecurity’s role in metabolic syndrome and metabolic syndrome–relevant cardiometabolic markers in this population,” lead author Luis E. Maldonado, PhD, of the University of North Carolina at Chapel Hill, and colleagues explained.
The researchers conducted a cross-sectional study to evaluate the associations between lower household and child food security and metabolic syndrome, as well as clinically measured cardiometabolic markers, including fasting plasma glucose, waist circumference, triglycerides, systolic and diastolic blood pressure, and high-density lipoprotein cholesterol (HDL-C).
Household food security (high, marginal, low, very low) and child food security (high, marginal, low/very low) measures were evaluated separately, and were adjusted for participant age, sex, site, parental education, and poverty-income ratio.
Data were obtained from the Hispanic Community Children’s Health Study/Study of Latino Youth, a study of offspring of adults enrolled in the Hispanic Community Health Survey/Study of Latinos.
Results
The study cohort included 1,325 Hispanic/Latino youth aged 8-16 years. For both household food security and child food security, youth in the lowest food security category had significantly lower HDL-C compared with youth with high food security (household food security, –3.17; 95% confidence interval, –5.65 to –0.70; child food security, –1.81; 95% CI, –3.54 to –0.09).
In addition, low/very low compared with high child food security was associated with higher triglycerides (beta, 8.68; 95% CI, 1.75-15.61), higher fasting plasma glucose (beta, 1.37; 95% CI, 0.08-2.65), and metabolic syndrome composite variable expected log counts (beta, 2.12; 95% CI, 0.02-0.45).
Furthermore, the researchers found statistically significant interactions between each of the two food security measures and receipt of any food assistance in the previous year in models of triglycerides (P for interactions: household food security, .03 and child food security, .005) and HDL-C (P for interactions: household food security, .01 and child food security, .04).
After evaluating the effect of parental place of birth, they found a statistically significant association for triglycerides only (P for interactions: household food security, .05 and child food security, .008).
“Our study is among the first to document adverse associations between household and child food security measures with a metabolic syndrome score variable and several metabolic syndrome–relevant cardiometabolic markers among US Hispanic/Latino youth,” the researchers wrote.
The researchers acknowledged that the cross-sectional nature of the study was a key limitation; thus, causality could not be inferred.
“In the future, we plan to conduct more qualitative work to better understand how Hispanic/Latino families respond to food insecurity, which may identify the factors that shape their response,” study author Sandra S. Albrecht, PhD, of Columbia University, New York, NY, said in an interview.
Recommendations for pediatricians
Food insecurity researcher Yankun Wang, PhD candidate at Indiana University, Bloomington, commented: “I would recommend pediatricians pay more attention to children from low-income households since they are more likely to have mental and physical health issues due to food insecurity.
“It can be very helpful if pediatricians could help families obtain SNAP benefits, enroll youth in the school breakfast and lunch programs, and promote nutrition education in schools,” Mr. Wang added.
This study was supported by grant funding from the National Heart, Lung, and Blood Institute. The authors reported no relevant disclosures.
FROM PEDIATRICS
Morphology of Mycosis Fungoides and Sézary Syndrome in Skin of Color
Mycosis fungoides (MF) and Sézary syndrome (SS) are non-Hodgkin T-cell lymphomas that make up the majority of cutaneous T-cell lymphomas. These conditions commonly affect Black patients, with an incidence rate of 12.6 cases of cutaneous T-cell lymphomas per million individuals vs 9.8 per million individuals in non–skin of color (SoC) patients.1 However, educational resources tend to focus on the clinical manifestations of MF/SS in lighter skin types, describing MF as erythematous patches, plaques, or tumors presenting in non–sun-exposed areas of the skin and SS as generalized erythroderma.2 Skin of color, comprised of Fitzpatrick skin types (FSTs) IV to VI,3 is poorly represented across dermatology textbooks,4,5 medical student resources,6 and peer-reviewed publications,7 raising awareness for the need to address this disparity.
Skin of color patients with MF/SS display variable morphologies, including features such as hyperpigmentation and hypopigmentation,8 the latter being exceedingly rare in non-SoC patients.9 Familiarity with these differences among providers is essential to allow for equitable diagnosis and treatment across all skin types, especially in light of data predicting that by 2044 more than 50% of the US population will be people of color.10 Patients with SoC are of many ethnic and racial backgrounds, including Black, Hispanic, American Indian, Pacific Islander, and Asian.11
Along with morphologic differences, there also are several racial disparities in the prognosis and survival of patients with MF/SS. Black patients diagnosed with MF present with greater body surface area affected, and Black women with MF have reduced survival rates compared to their White counterparts.12 Given these racial disparities in survival and representation in educational resources, we aimed to quantify the frequency of various morphologic characteristics of MF/SS in patients with SoC vs non-SoC patients to facilitate better recognition of early MF/SS in SoC patients by medical providers.
Methods
We performed a retrospective chart review following approval from the institutional review board at Northwestern University (Chicago, Illinois). We identified all patients with FSTs IV to VI and biopsy-proven MF/SS who had been clinically photographed in our clinic from January 1998 to December 2019. Only photographs that were high quality enough to review morphologic features were included in our review. Fitzpatrick skin type was determined based on electronic medical record documentation. If photographs were available from multiple visits for the same patient, only those showing posttreatment nonactive lesions were included. Additionally, 36 patients with FSTs I to III (non-SoC) and biopsy-proven MF/SS were included in our review as a comparison with the SoC cohort. The primary outcomes for this study included the presence of scale, erythema, hyperpigmentation, hypopigmentation, violaceous color, lichenification, silver hue, dyschromia, alopecia, poikiloderma, atrophy, and ulceration in active lesions. Dyschromia was defined by the presence of both hypopigmentation and hyperpigmentation. Poikiloderma was defined by hypopigmentation and hyperpigmentation, telangiectasia, and atrophy. Secondary outcomes included evaluation of those same characteristics in posttreatment nonactive lesions. All photographs were independently assessed by 3 authors (M.L.E., C.J.W., J.M.M.), and discrepancies were resolved by further review of the photograph in question and discussion.
Statistical Analysis—Summary statistics were applied to describe demographic and clinical characteristics. The χ2 test was used for categorical variables. Results achieving P<.05 were considered statistically significant.
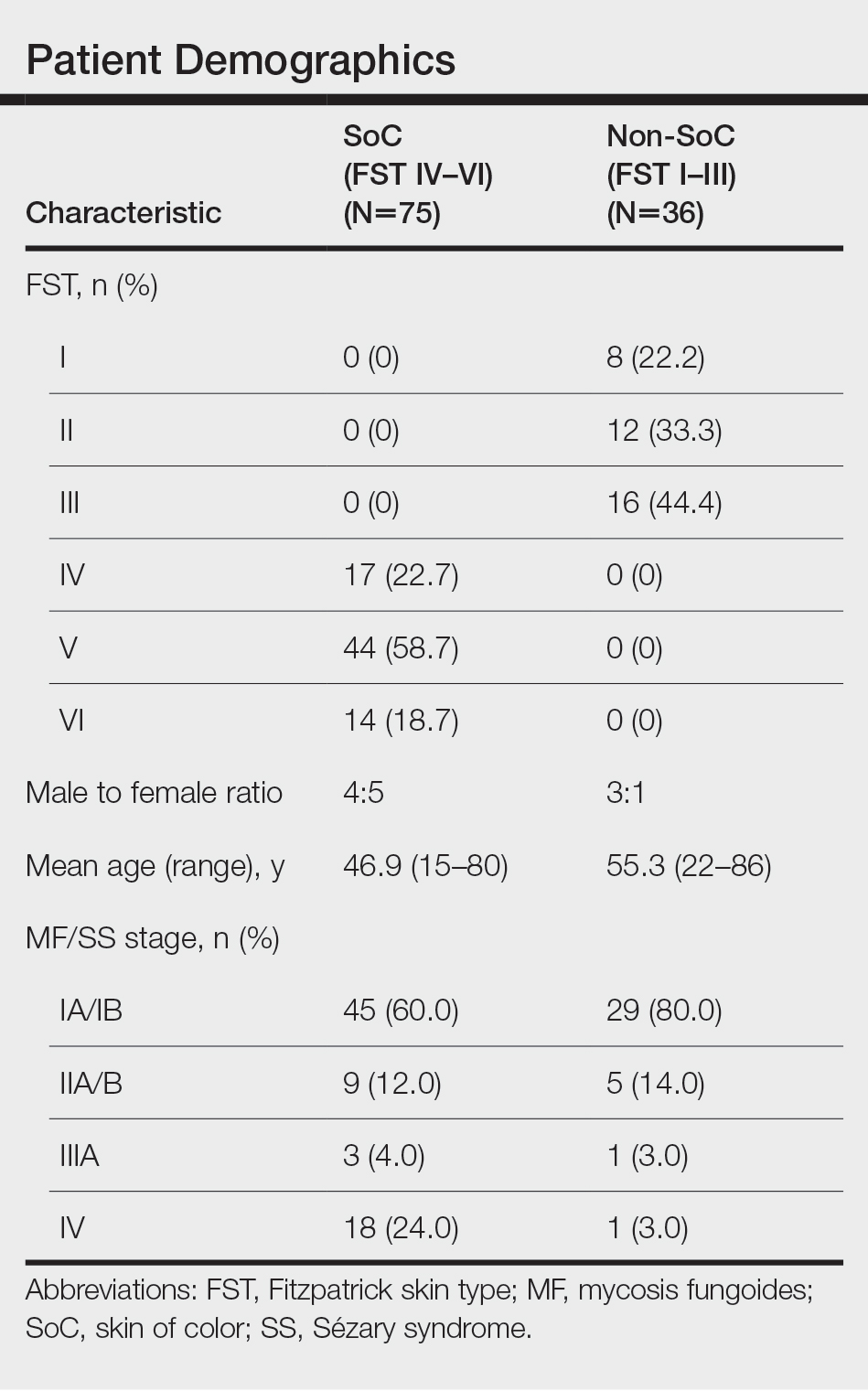
Results
We reviewed photographs of 111 patients across all skin types (8, FST I; 12, FST II; 16, FST III; 17, FST IV; 44, FST V; 14, FST VI). The cohort was 47% female, and the mean age was 49.7 years (range, 15–86 years). The majority of the cohort had early-stage MF (stage IA or IB). There were more cases of SS in the SoC cohort than the non-SoC cohort (Table). Only 5 photographs had discrepancies and required discussion among the reviewers to achieve consensus.
![Frequency of morphologic features found in skin of color (SoC [Fitzpatrick skin types IV–VI]) vs non-SoC (Fitzpatrick skin types I–III) patients with mycosis fungoides/Sézary syndrome Frequency of morphologic features found in skin of color (SoC [Fitzpatrick skin types IV–VI]) vs non-SoC (Fitzpatrick skin types I–III) patients with mycosis fungoides/Sézary syndrome](https://cdn.mdedge.com/files/s3fs-public/Espinosa_1.JPG)
Regarding morphologic characteristics in active lesions (Figure 1), scale was present in almost all patients (99% in SoC, 94% in non-SoC). Erythema was present in nearly all non-SoC patients (94%) but only in 69% of SoC patients (P=.003). Poikiloderma also was found to be present at higher frequencies in non-SoC patients compared with SoC patients (19% and 4%, respectively [P=.008]). However, hyperpigmentation (80% vs 39%), lichenification (43% vs 17%), and silver hue (25% vs 3%) were more common in SoC patients than non-SoC patients (P<.05). There were no significant differences in the remaining features, including hypopigmentation (39% vs 25%), dyschromia (24% vs 19%), violaceous color (44% vs 25%), atrophy (11% vs 22%), alopecia (23% vs 31%), and ulceration (16% vs 8%) between SoC and non-SoC patients (P>.05). Photographs of MF in patients with SoC can be seen in Figure 2.
![Representative photographs of mycosis fungoides (MF) in skin of color (Fitzpatrick skin types [FSTs] IV–VI) Representative photographs of mycosis fungoides (MF) in skin of color (Fitzpatrick skin types [FSTs] IV–VI)](https://cdn.mdedge.com/files/s3fs-public/CT109003003_e_Fig2_ABCDE.JPG)
Posttreatment (nonactive) photographs were available for 26 patients (6 non-SoC, 20 SoC). We found that across all FST groups, hyperpigmentation was more common than hypopigmentation in areas of previously active disease. Statistical analysis was not completed given that few non-SoC photographs were available for comparison.
Comment
This qualitative review demonstrates the heterogeneity of MF/SS in SoC patients and that these conditions do not present in this population with the classic erythematous patches and plaques found in non-SoC patients. We found that hyperpigmentation, lichenification, and silver hue were present at higher rates in patients with FSTs IV to VI compared to those with FSTs I to III, which had higher rates of erythema and poikiloderma. Familiarity with these morphologic features along with increased exposure to clinical photographs of MF/SS in SoC patients will aid in the visual recognition required for this diagnosis, since erythema is harder to identify in darker skin types. Recognizing the unique findings of MF in patients with SoC as well as in patients with lighter skin types will enable earlier diagnosis and treatment of MF/SS across all skin types. If MF is diagnosed and treated early, life expectancy is similar to that of patients without MF.13 However, the 5-year survival rate for advanced-stage MF/SS is 52% across all skin types, and studies have found that Black patients with advanced-stage disease have worse outcomes despite accounting for demographic factors and tumor stage.14,15 Given the worse outcomes in SoC patients with advanced-stage MF/SS, earlier diagnosis could help address this disparity.8,13,14 Similar morphologic features could be used in diagnosing other inflammatory conditions; studies have shown that the lack of recognition of erythema in Black children has led to delayed diagnosis of atopic dermatitis and subsequent inadequate treatment.16,17
The morphologic presentation of MF/SS in SoC patients also can influence an optimal treatment plan for this population. Hypopigmented MF responds better to phototherapy than hyperpigmented MF, as phototherapy has been shown to have decreased efficacy with increasing FST.18 Therefore, for patients with FSTs IV to VI, topical agents such as nitrogen mustard or bexarotene may be more suitable treatment options, as the efficacy of these treatments is independent of skin color.8 However, nitrogen mustard commonly leads to postinflammatory hyperpigmentation, and topical bexarotene may lead to erythema or irritation; therefore, providers must counsel patients on these possible side effects. For refractory disease, adjunct systemic treatments such as oral bexarotene, subcutaneous interferon, methotrexate, or radiation therapy may be considered.8
In addition to aiding in the prompt diagnosis and treatment of MF/SS in SoC patients, our findings may be used to better assess the extent of disease and distinguish between active MF/SS lesions vs xerosis cutis or residual dyschromia from previously treated lesions. It is important to note that these morphologic features must be taken into account with a complete history and work-up. The differential diagnosis of MF/SS includes conditions such as atopic dermatitis, psoriasis, tinea corporis, and drug reactions, which may have similar morphology in SoC.19
Limitations of our study include the single-center design and the use of photographs instead of in-person examination; however, our cutaneous lymphoma clinic serves a diverse patient population, and our 3 reviewers rated the photographs independently. Discussion amongst the reviewers to address discrepancies was only required for 5 photographs, indicating the high inter-reviewer reliability. Additionally, the original purpose of FST was to assess for the propensity of the skin to burn when undergoing phototherapy, not to serve as a marker for skin color. We recommend trainees and clinicians be mindful about the purpose of FST and to use inclusive language (eg, using the terms skin irritation, skin tenderness, or skin becoming darker from the sun instead of tanning) when determining FST in darker-skinned individuals.20 Future directions include examining if certain treatments are associated with prolonged dyschromia.
Conclusion
In our single-institution retrospective study, we found differences in the morphologic presentation of MF/SS in SoC patients vs non-SoC patients. While erythema is a common feature in non-SoC patients, clinical features of hyperpigmentation, lichenification, and silver hue should be carefully evaluated in the diagnosis of MF/SS in SoC patients. Knowledge of the heterogenous presentation of MF/SS in patients with SoC allows for expedited diagnosis and treatment, leading to better clinical outcomes. Valuable resources, including Taylor and Kelly’s Dermatology for Skin of Color, the Skin of Color Society, and VisualDx educate providers on how dermatologic conditions present in darker skin types. However, there is still work to be done to enhance diversity in educational resources in order to provide equitable care to patients of all skin types.
- Korgavkar K, Xiong M, Weinstock M. Changing incidence trends of cutaneous T-cell lymphoma. JAMA Dermatol. 2013;149:1295-1299. doi:10.1001/jamadermatol.2013.5526
- Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part I. diagnosis: clinical and histopathologic features and new molecular and biologic markers. J Am Acad Dermatol. 2014;70:205.E1-E16; quiz 221-222. doi:10.1016/j.jaad.2013.07.049
- Tull RZ, Kerby E, Subash JJ, et al. Ethnic skin centers in the United States: where are we in 2020?. J Am Acad Dermatol. 2020;83:1757-1759. doi:10.1016/j.jaad.2020.03.054
- Adelekun A, Onyekaba G, Lipoff JB. Skin color in dermatology textbooks: an updated evaluation and analysis. J Am Acad Dermatol. 2021;84:194-196. doi:10.1016/j.jaad.2020.04.084
- Ebede T, Papier A. Disparities in dermatology educational resources. J Am Acad Dermatol. 2006;55:687-690. doi:10.1016/j.jaad.2005.10.068
- Jones VA, Clark KA, Shobajo MT, et al. Skin of color representation in medical education: an analysis of popular preparatory materials used for United States medical licensing examinations. J Am Acad Dermatol. 2021;85:773-775. doi:10.1016/j.jaad.2020.07.112
- Montgomery SN, Elbuluk N. A quantitative analysis of research publications focused on the top chief complaints in skin of color patients. J Am Acad Dermatol. 2021;85:241-242. doi:10.1016/j.jaad.2020.08.031
- Hinds GA, Heald P. Cutaneous T-cell lymphoma in skin of color. J Am Acad Dermatol. 2009;60:359-375; quiz 376-378. doi:10.1016/j.jaad.2008.10.031
- Ardigó M, Borroni G, Muscardin L, et al. Hypopigmented mycosis fungoides in Caucasian patients: a clinicopathologic study of 7 cases. J Am Acad Dermatol. 2003;49:264-270. doi:10.1067/s0190-9622(03)00907-1
- Colby SL, Ortman JM. Projections of the size and composition of the U.S. population: 2014 to 2060. United States Census Bureau website. Updated October 8, 2021. Accessed February 28, 2022. https://www.census.gov/library/publications/2015/demo/p25-1143.html
- Taylor SC, Kyei A. Defining skin of color. In: Kelly AP, Taylor SC, Lim HW, et al, eds. Taylor and Kelly’s Dermatology for Skin of Color. 2nd ed. McGraw-Hill Education; 2016.
- Huang AH, Kwatra SG, Khanna R, et al. Racial disparities in the clinical presentation and prognosis of patients with mycosis fungoides. J Natl Med Assoc. 2019;111:633-639. doi:10.1016/j.jnma.2019.08.006
- Kim YH, Jensen RA, Watanabe GL, et al. Clinical stage IA (limited patch and plaque) mycosis fungoides. a long-term outcome analysis. Arch Dermatol. 1996;132:1309-1313.
- Scarisbrick JJ, Prince HM, Vermeer MH, et al. Cutaneous lymphoma international consortium study of outcome in advanced stages of mycosis fungoides and Sézary syndrome: effect of specific prognostic markers on survival and development of a prognostic model. J Clin Oncol. 2015;33:3766-3773. doi:10.1200/JCO.2015.61.7142
- Nath SK, Yu JB, Wilson LD. Poorer prognosis of African-American patients with mycosis fungoides: an analysis of the SEER dataset, 1988 to 2008. Clin Lymphoma Myeloma Leuk. 2014;14:419-423. doi:10.1016/j.clml.2013.12.018
- Ben-Gashir MA, Hay RJ. Reliance on erythema scores may mask severe atopic dermatitis in black children compared with their white counterparts. Br J Dermatol. 2002;147:920-925. doi:10.1046/j.1365-2133.2002.04965.x
- Poladian K, De Souza B, McMichael AJ. Atopic dermatitis in adolescents with skin of color. Cutis. 2019;104:164-168.
- Yones SS, Palmer RA, Garibaldinos TT, et al. Randomized double-blind trial of the treatment of chronic plaque psoriasis: efficacy of psoralen-UV-A therapy vs narrowband UV-B therapy. Arch Dermatol. 2006;142:836-842. doi:10.1001/archderm.142.7.836
- Currimbhoy S, Pandya AG. Cutaneous T-cell lymphoma. In: Kelly AP, Taylor SC, Lim HW, et al, eds. Taylor and Kelly’s Dermatology for Skin of Color. 2nd ed. McGraw-Hill Education; 2016.
- Ware OR, Dawson JE, Shinohara MM, et al. Racial limitations of Fitzpatrick skin type. Cutis. 2020;105:77-80.
Mycosis fungoides (MF) and Sézary syndrome (SS) are non-Hodgkin T-cell lymphomas that make up the majority of cutaneous T-cell lymphomas. These conditions commonly affect Black patients, with an incidence rate of 12.6 cases of cutaneous T-cell lymphomas per million individuals vs 9.8 per million individuals in non–skin of color (SoC) patients.1 However, educational resources tend to focus on the clinical manifestations of MF/SS in lighter skin types, describing MF as erythematous patches, plaques, or tumors presenting in non–sun-exposed areas of the skin and SS as generalized erythroderma.2 Skin of color, comprised of Fitzpatrick skin types (FSTs) IV to VI,3 is poorly represented across dermatology textbooks,4,5 medical student resources,6 and peer-reviewed publications,7 raising awareness for the need to address this disparity.
Skin of color patients with MF/SS display variable morphologies, including features such as hyperpigmentation and hypopigmentation,8 the latter being exceedingly rare in non-SoC patients.9 Familiarity with these differences among providers is essential to allow for equitable diagnosis and treatment across all skin types, especially in light of data predicting that by 2044 more than 50% of the US population will be people of color.10 Patients with SoC are of many ethnic and racial backgrounds, including Black, Hispanic, American Indian, Pacific Islander, and Asian.11
Along with morphologic differences, there also are several racial disparities in the prognosis and survival of patients with MF/SS. Black patients diagnosed with MF present with greater body surface area affected, and Black women with MF have reduced survival rates compared to their White counterparts.12 Given these racial disparities in survival and representation in educational resources, we aimed to quantify the frequency of various morphologic characteristics of MF/SS in patients with SoC vs non-SoC patients to facilitate better recognition of early MF/SS in SoC patients by medical providers.
Methods
We performed a retrospective chart review following approval from the institutional review board at Northwestern University (Chicago, Illinois). We identified all patients with FSTs IV to VI and biopsy-proven MF/SS who had been clinically photographed in our clinic from January 1998 to December 2019. Only photographs that were high quality enough to review morphologic features were included in our review. Fitzpatrick skin type was determined based on electronic medical record documentation. If photographs were available from multiple visits for the same patient, only those showing posttreatment nonactive lesions were included. Additionally, 36 patients with FSTs I to III (non-SoC) and biopsy-proven MF/SS were included in our review as a comparison with the SoC cohort. The primary outcomes for this study included the presence of scale, erythema, hyperpigmentation, hypopigmentation, violaceous color, lichenification, silver hue, dyschromia, alopecia, poikiloderma, atrophy, and ulceration in active lesions. Dyschromia was defined by the presence of both hypopigmentation and hyperpigmentation. Poikiloderma was defined by hypopigmentation and hyperpigmentation, telangiectasia, and atrophy. Secondary outcomes included evaluation of those same characteristics in posttreatment nonactive lesions. All photographs were independently assessed by 3 authors (M.L.E., C.J.W., J.M.M.), and discrepancies were resolved by further review of the photograph in question and discussion.
Statistical Analysis—Summary statistics were applied to describe demographic and clinical characteristics. The χ2 test was used for categorical variables. Results achieving P<.05 were considered statistically significant.
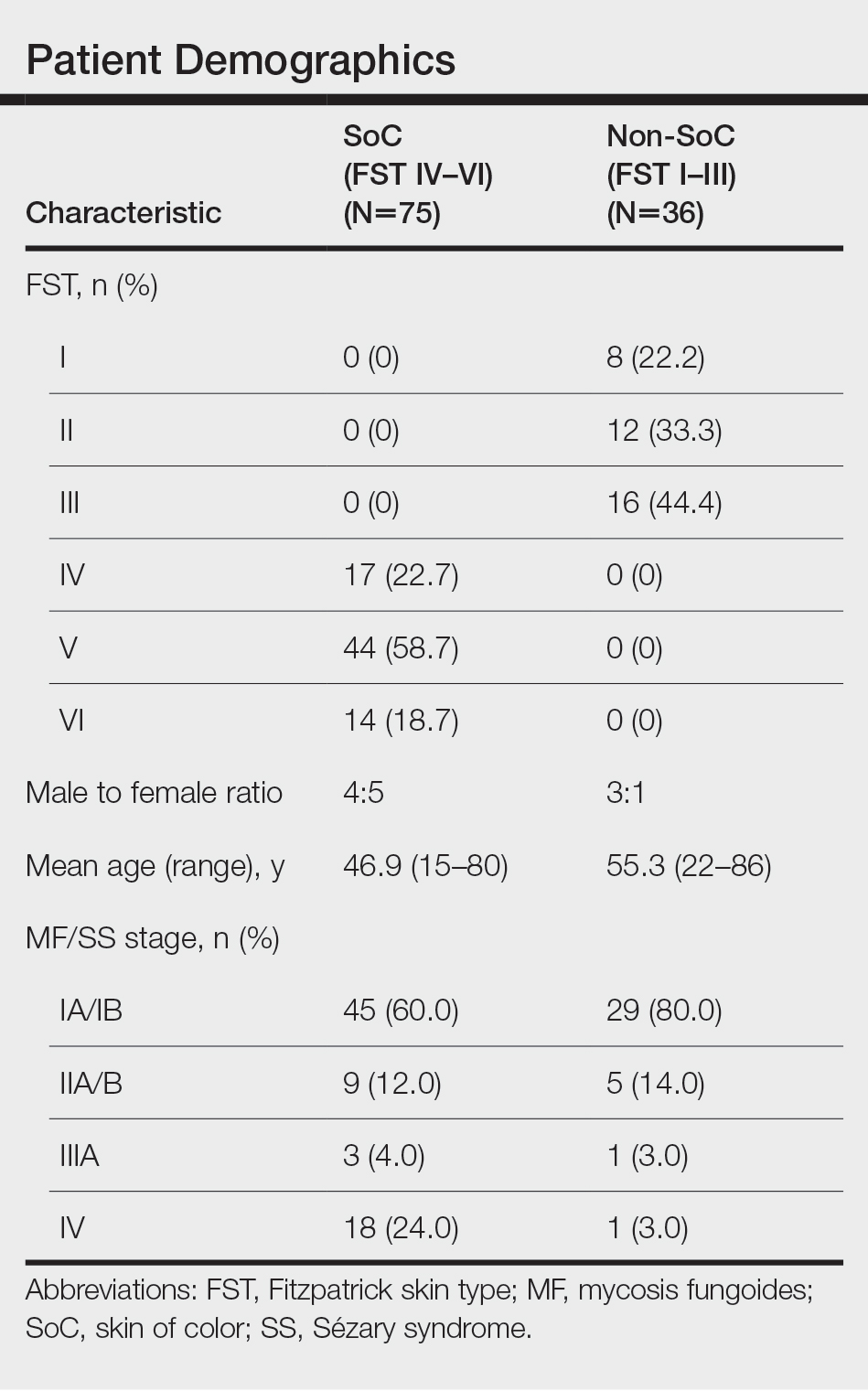
Results
We reviewed photographs of 111 patients across all skin types (8, FST I; 12, FST II; 16, FST III; 17, FST IV; 44, FST V; 14, FST VI). The cohort was 47% female, and the mean age was 49.7 years (range, 15–86 years). The majority of the cohort had early-stage MF (stage IA or IB). There were more cases of SS in the SoC cohort than the non-SoC cohort (Table). Only 5 photographs had discrepancies and required discussion among the reviewers to achieve consensus.
![Frequency of morphologic features found in skin of color (SoC [Fitzpatrick skin types IV–VI]) vs non-SoC (Fitzpatrick skin types I–III) patients with mycosis fungoides/Sézary syndrome Frequency of morphologic features found in skin of color (SoC [Fitzpatrick skin types IV–VI]) vs non-SoC (Fitzpatrick skin types I–III) patients with mycosis fungoides/Sézary syndrome](https://cdn.mdedge.com/files/s3fs-public/Espinosa_1.JPG)
Regarding morphologic characteristics in active lesions (Figure 1), scale was present in almost all patients (99% in SoC, 94% in non-SoC). Erythema was present in nearly all non-SoC patients (94%) but only in 69% of SoC patients (P=.003). Poikiloderma also was found to be present at higher frequencies in non-SoC patients compared with SoC patients (19% and 4%, respectively [P=.008]). However, hyperpigmentation (80% vs 39%), lichenification (43% vs 17%), and silver hue (25% vs 3%) were more common in SoC patients than non-SoC patients (P<.05). There were no significant differences in the remaining features, including hypopigmentation (39% vs 25%), dyschromia (24% vs 19%), violaceous color (44% vs 25%), atrophy (11% vs 22%), alopecia (23% vs 31%), and ulceration (16% vs 8%) between SoC and non-SoC patients (P>.05). Photographs of MF in patients with SoC can be seen in Figure 2.
![Representative photographs of mycosis fungoides (MF) in skin of color (Fitzpatrick skin types [FSTs] IV–VI) Representative photographs of mycosis fungoides (MF) in skin of color (Fitzpatrick skin types [FSTs] IV–VI)](https://cdn.mdedge.com/files/s3fs-public/CT109003003_e_Fig2_ABCDE.JPG)
Posttreatment (nonactive) photographs were available for 26 patients (6 non-SoC, 20 SoC). We found that across all FST groups, hyperpigmentation was more common than hypopigmentation in areas of previously active disease. Statistical analysis was not completed given that few non-SoC photographs were available for comparison.
Comment
This qualitative review demonstrates the heterogeneity of MF/SS in SoC patients and that these conditions do not present in this population with the classic erythematous patches and plaques found in non-SoC patients. We found that hyperpigmentation, lichenification, and silver hue were present at higher rates in patients with FSTs IV to VI compared to those with FSTs I to III, which had higher rates of erythema and poikiloderma. Familiarity with these morphologic features along with increased exposure to clinical photographs of MF/SS in SoC patients will aid in the visual recognition required for this diagnosis, since erythema is harder to identify in darker skin types. Recognizing the unique findings of MF in patients with SoC as well as in patients with lighter skin types will enable earlier diagnosis and treatment of MF/SS across all skin types. If MF is diagnosed and treated early, life expectancy is similar to that of patients without MF.13 However, the 5-year survival rate for advanced-stage MF/SS is 52% across all skin types, and studies have found that Black patients with advanced-stage disease have worse outcomes despite accounting for demographic factors and tumor stage.14,15 Given the worse outcomes in SoC patients with advanced-stage MF/SS, earlier diagnosis could help address this disparity.8,13,14 Similar morphologic features could be used in diagnosing other inflammatory conditions; studies have shown that the lack of recognition of erythema in Black children has led to delayed diagnosis of atopic dermatitis and subsequent inadequate treatment.16,17
The morphologic presentation of MF/SS in SoC patients also can influence an optimal treatment plan for this population. Hypopigmented MF responds better to phototherapy than hyperpigmented MF, as phototherapy has been shown to have decreased efficacy with increasing FST.18 Therefore, for patients with FSTs IV to VI, topical agents such as nitrogen mustard or bexarotene may be more suitable treatment options, as the efficacy of these treatments is independent of skin color.8 However, nitrogen mustard commonly leads to postinflammatory hyperpigmentation, and topical bexarotene may lead to erythema or irritation; therefore, providers must counsel patients on these possible side effects. For refractory disease, adjunct systemic treatments such as oral bexarotene, subcutaneous interferon, methotrexate, or radiation therapy may be considered.8
In addition to aiding in the prompt diagnosis and treatment of MF/SS in SoC patients, our findings may be used to better assess the extent of disease and distinguish between active MF/SS lesions vs xerosis cutis or residual dyschromia from previously treated lesions. It is important to note that these morphologic features must be taken into account with a complete history and work-up. The differential diagnosis of MF/SS includes conditions such as atopic dermatitis, psoriasis, tinea corporis, and drug reactions, which may have similar morphology in SoC.19
Limitations of our study include the single-center design and the use of photographs instead of in-person examination; however, our cutaneous lymphoma clinic serves a diverse patient population, and our 3 reviewers rated the photographs independently. Discussion amongst the reviewers to address discrepancies was only required for 5 photographs, indicating the high inter-reviewer reliability. Additionally, the original purpose of FST was to assess for the propensity of the skin to burn when undergoing phototherapy, not to serve as a marker for skin color. We recommend trainees and clinicians be mindful about the purpose of FST and to use inclusive language (eg, using the terms skin irritation, skin tenderness, or skin becoming darker from the sun instead of tanning) when determining FST in darker-skinned individuals.20 Future directions include examining if certain treatments are associated with prolonged dyschromia.
Conclusion
In our single-institution retrospective study, we found differences in the morphologic presentation of MF/SS in SoC patients vs non-SoC patients. While erythema is a common feature in non-SoC patients, clinical features of hyperpigmentation, lichenification, and silver hue should be carefully evaluated in the diagnosis of MF/SS in SoC patients. Knowledge of the heterogenous presentation of MF/SS in patients with SoC allows for expedited diagnosis and treatment, leading to better clinical outcomes. Valuable resources, including Taylor and Kelly’s Dermatology for Skin of Color, the Skin of Color Society, and VisualDx educate providers on how dermatologic conditions present in darker skin types. However, there is still work to be done to enhance diversity in educational resources in order to provide equitable care to patients of all skin types.
Mycosis fungoides (MF) and Sézary syndrome (SS) are non-Hodgkin T-cell lymphomas that make up the majority of cutaneous T-cell lymphomas. These conditions commonly affect Black patients, with an incidence rate of 12.6 cases of cutaneous T-cell lymphomas per million individuals vs 9.8 per million individuals in non–skin of color (SoC) patients.1 However, educational resources tend to focus on the clinical manifestations of MF/SS in lighter skin types, describing MF as erythematous patches, plaques, or tumors presenting in non–sun-exposed areas of the skin and SS as generalized erythroderma.2 Skin of color, comprised of Fitzpatrick skin types (FSTs) IV to VI,3 is poorly represented across dermatology textbooks,4,5 medical student resources,6 and peer-reviewed publications,7 raising awareness for the need to address this disparity.
Skin of color patients with MF/SS display variable morphologies, including features such as hyperpigmentation and hypopigmentation,8 the latter being exceedingly rare in non-SoC patients.9 Familiarity with these differences among providers is essential to allow for equitable diagnosis and treatment across all skin types, especially in light of data predicting that by 2044 more than 50% of the US population will be people of color.10 Patients with SoC are of many ethnic and racial backgrounds, including Black, Hispanic, American Indian, Pacific Islander, and Asian.11
Along with morphologic differences, there also are several racial disparities in the prognosis and survival of patients with MF/SS. Black patients diagnosed with MF present with greater body surface area affected, and Black women with MF have reduced survival rates compared to their White counterparts.12 Given these racial disparities in survival and representation in educational resources, we aimed to quantify the frequency of various morphologic characteristics of MF/SS in patients with SoC vs non-SoC patients to facilitate better recognition of early MF/SS in SoC patients by medical providers.
Methods
We performed a retrospective chart review following approval from the institutional review board at Northwestern University (Chicago, Illinois). We identified all patients with FSTs IV to VI and biopsy-proven MF/SS who had been clinically photographed in our clinic from January 1998 to December 2019. Only photographs that were high quality enough to review morphologic features were included in our review. Fitzpatrick skin type was determined based on electronic medical record documentation. If photographs were available from multiple visits for the same patient, only those showing posttreatment nonactive lesions were included. Additionally, 36 patients with FSTs I to III (non-SoC) and biopsy-proven MF/SS were included in our review as a comparison with the SoC cohort. The primary outcomes for this study included the presence of scale, erythema, hyperpigmentation, hypopigmentation, violaceous color, lichenification, silver hue, dyschromia, alopecia, poikiloderma, atrophy, and ulceration in active lesions. Dyschromia was defined by the presence of both hypopigmentation and hyperpigmentation. Poikiloderma was defined by hypopigmentation and hyperpigmentation, telangiectasia, and atrophy. Secondary outcomes included evaluation of those same characteristics in posttreatment nonactive lesions. All photographs were independently assessed by 3 authors (M.L.E., C.J.W., J.M.M.), and discrepancies were resolved by further review of the photograph in question and discussion.
Statistical Analysis—Summary statistics were applied to describe demographic and clinical characteristics. The χ2 test was used for categorical variables. Results achieving P<.05 were considered statistically significant.
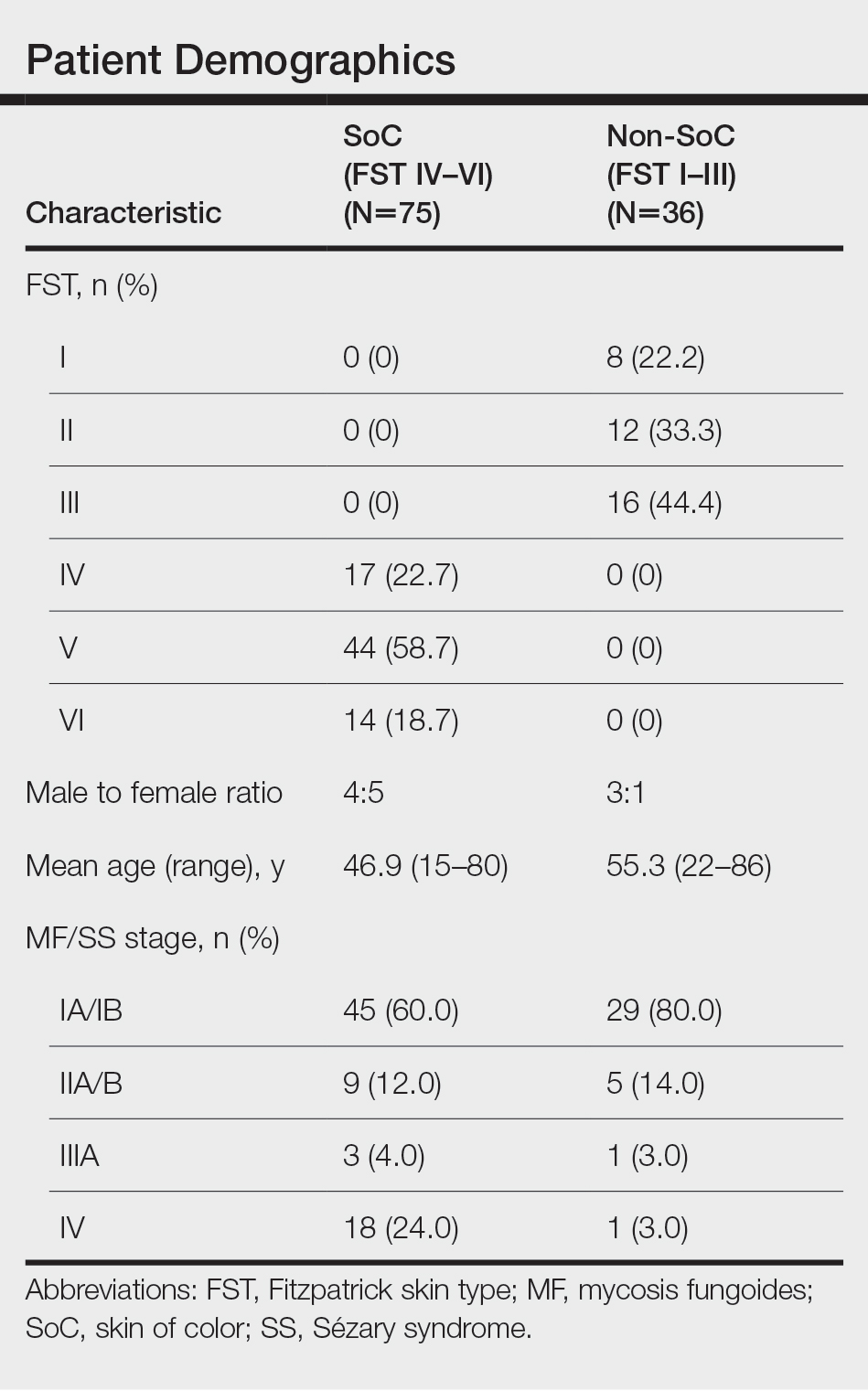
Results
We reviewed photographs of 111 patients across all skin types (8, FST I; 12, FST II; 16, FST III; 17, FST IV; 44, FST V; 14, FST VI). The cohort was 47% female, and the mean age was 49.7 years (range, 15–86 years). The majority of the cohort had early-stage MF (stage IA or IB). There were more cases of SS in the SoC cohort than the non-SoC cohort (Table). Only 5 photographs had discrepancies and required discussion among the reviewers to achieve consensus.
![Frequency of morphologic features found in skin of color (SoC [Fitzpatrick skin types IV–VI]) vs non-SoC (Fitzpatrick skin types I–III) patients with mycosis fungoides/Sézary syndrome Frequency of morphologic features found in skin of color (SoC [Fitzpatrick skin types IV–VI]) vs non-SoC (Fitzpatrick skin types I–III) patients with mycosis fungoides/Sézary syndrome](https://cdn.mdedge.com/files/s3fs-public/Espinosa_1.JPG)
Regarding morphologic characteristics in active lesions (Figure 1), scale was present in almost all patients (99% in SoC, 94% in non-SoC). Erythema was present in nearly all non-SoC patients (94%) but only in 69% of SoC patients (P=.003). Poikiloderma also was found to be present at higher frequencies in non-SoC patients compared with SoC patients (19% and 4%, respectively [P=.008]). However, hyperpigmentation (80% vs 39%), lichenification (43% vs 17%), and silver hue (25% vs 3%) were more common in SoC patients than non-SoC patients (P<.05). There were no significant differences in the remaining features, including hypopigmentation (39% vs 25%), dyschromia (24% vs 19%), violaceous color (44% vs 25%), atrophy (11% vs 22%), alopecia (23% vs 31%), and ulceration (16% vs 8%) between SoC and non-SoC patients (P>.05). Photographs of MF in patients with SoC can be seen in Figure 2.
![Representative photographs of mycosis fungoides (MF) in skin of color (Fitzpatrick skin types [FSTs] IV–VI) Representative photographs of mycosis fungoides (MF) in skin of color (Fitzpatrick skin types [FSTs] IV–VI)](https://cdn.mdedge.com/files/s3fs-public/CT109003003_e_Fig2_ABCDE.JPG)
Posttreatment (nonactive) photographs were available for 26 patients (6 non-SoC, 20 SoC). We found that across all FST groups, hyperpigmentation was more common than hypopigmentation in areas of previously active disease. Statistical analysis was not completed given that few non-SoC photographs were available for comparison.
Comment
This qualitative review demonstrates the heterogeneity of MF/SS in SoC patients and that these conditions do not present in this population with the classic erythematous patches and plaques found in non-SoC patients. We found that hyperpigmentation, lichenification, and silver hue were present at higher rates in patients with FSTs IV to VI compared to those with FSTs I to III, which had higher rates of erythema and poikiloderma. Familiarity with these morphologic features along with increased exposure to clinical photographs of MF/SS in SoC patients will aid in the visual recognition required for this diagnosis, since erythema is harder to identify in darker skin types. Recognizing the unique findings of MF in patients with SoC as well as in patients with lighter skin types will enable earlier diagnosis and treatment of MF/SS across all skin types. If MF is diagnosed and treated early, life expectancy is similar to that of patients without MF.13 However, the 5-year survival rate for advanced-stage MF/SS is 52% across all skin types, and studies have found that Black patients with advanced-stage disease have worse outcomes despite accounting for demographic factors and tumor stage.14,15 Given the worse outcomes in SoC patients with advanced-stage MF/SS, earlier diagnosis could help address this disparity.8,13,14 Similar morphologic features could be used in diagnosing other inflammatory conditions; studies have shown that the lack of recognition of erythema in Black children has led to delayed diagnosis of atopic dermatitis and subsequent inadequate treatment.16,17
The morphologic presentation of MF/SS in SoC patients also can influence an optimal treatment plan for this population. Hypopigmented MF responds better to phototherapy than hyperpigmented MF, as phototherapy has been shown to have decreased efficacy with increasing FST.18 Therefore, for patients with FSTs IV to VI, topical agents such as nitrogen mustard or bexarotene may be more suitable treatment options, as the efficacy of these treatments is independent of skin color.8 However, nitrogen mustard commonly leads to postinflammatory hyperpigmentation, and topical bexarotene may lead to erythema or irritation; therefore, providers must counsel patients on these possible side effects. For refractory disease, adjunct systemic treatments such as oral bexarotene, subcutaneous interferon, methotrexate, or radiation therapy may be considered.8
In addition to aiding in the prompt diagnosis and treatment of MF/SS in SoC patients, our findings may be used to better assess the extent of disease and distinguish between active MF/SS lesions vs xerosis cutis or residual dyschromia from previously treated lesions. It is important to note that these morphologic features must be taken into account with a complete history and work-up. The differential diagnosis of MF/SS includes conditions such as atopic dermatitis, psoriasis, tinea corporis, and drug reactions, which may have similar morphology in SoC.19
Limitations of our study include the single-center design and the use of photographs instead of in-person examination; however, our cutaneous lymphoma clinic serves a diverse patient population, and our 3 reviewers rated the photographs independently. Discussion amongst the reviewers to address discrepancies was only required for 5 photographs, indicating the high inter-reviewer reliability. Additionally, the original purpose of FST was to assess for the propensity of the skin to burn when undergoing phototherapy, not to serve as a marker for skin color. We recommend trainees and clinicians be mindful about the purpose of FST and to use inclusive language (eg, using the terms skin irritation, skin tenderness, or skin becoming darker from the sun instead of tanning) when determining FST in darker-skinned individuals.20 Future directions include examining if certain treatments are associated with prolonged dyschromia.
Conclusion
In our single-institution retrospective study, we found differences in the morphologic presentation of MF/SS in SoC patients vs non-SoC patients. While erythema is a common feature in non-SoC patients, clinical features of hyperpigmentation, lichenification, and silver hue should be carefully evaluated in the diagnosis of MF/SS in SoC patients. Knowledge of the heterogenous presentation of MF/SS in patients with SoC allows for expedited diagnosis and treatment, leading to better clinical outcomes. Valuable resources, including Taylor and Kelly’s Dermatology for Skin of Color, the Skin of Color Society, and VisualDx educate providers on how dermatologic conditions present in darker skin types. However, there is still work to be done to enhance diversity in educational resources in order to provide equitable care to patients of all skin types.
- Korgavkar K, Xiong M, Weinstock M. Changing incidence trends of cutaneous T-cell lymphoma. JAMA Dermatol. 2013;149:1295-1299. doi:10.1001/jamadermatol.2013.5526
- Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part I. diagnosis: clinical and histopathologic features and new molecular and biologic markers. J Am Acad Dermatol. 2014;70:205.E1-E16; quiz 221-222. doi:10.1016/j.jaad.2013.07.049
- Tull RZ, Kerby E, Subash JJ, et al. Ethnic skin centers in the United States: where are we in 2020?. J Am Acad Dermatol. 2020;83:1757-1759. doi:10.1016/j.jaad.2020.03.054
- Adelekun A, Onyekaba G, Lipoff JB. Skin color in dermatology textbooks: an updated evaluation and analysis. J Am Acad Dermatol. 2021;84:194-196. doi:10.1016/j.jaad.2020.04.084
- Ebede T, Papier A. Disparities in dermatology educational resources. J Am Acad Dermatol. 2006;55:687-690. doi:10.1016/j.jaad.2005.10.068
- Jones VA, Clark KA, Shobajo MT, et al. Skin of color representation in medical education: an analysis of popular preparatory materials used for United States medical licensing examinations. J Am Acad Dermatol. 2021;85:773-775. doi:10.1016/j.jaad.2020.07.112
- Montgomery SN, Elbuluk N. A quantitative analysis of research publications focused on the top chief complaints in skin of color patients. J Am Acad Dermatol. 2021;85:241-242. doi:10.1016/j.jaad.2020.08.031
- Hinds GA, Heald P. Cutaneous T-cell lymphoma in skin of color. J Am Acad Dermatol. 2009;60:359-375; quiz 376-378. doi:10.1016/j.jaad.2008.10.031
- Ardigó M, Borroni G, Muscardin L, et al. Hypopigmented mycosis fungoides in Caucasian patients: a clinicopathologic study of 7 cases. J Am Acad Dermatol. 2003;49:264-270. doi:10.1067/s0190-9622(03)00907-1
- Colby SL, Ortman JM. Projections of the size and composition of the U.S. population: 2014 to 2060. United States Census Bureau website. Updated October 8, 2021. Accessed February 28, 2022. https://www.census.gov/library/publications/2015/demo/p25-1143.html
- Taylor SC, Kyei A. Defining skin of color. In: Kelly AP, Taylor SC, Lim HW, et al, eds. Taylor and Kelly’s Dermatology for Skin of Color. 2nd ed. McGraw-Hill Education; 2016.
- Huang AH, Kwatra SG, Khanna R, et al. Racial disparities in the clinical presentation and prognosis of patients with mycosis fungoides. J Natl Med Assoc. 2019;111:633-639. doi:10.1016/j.jnma.2019.08.006
- Kim YH, Jensen RA, Watanabe GL, et al. Clinical stage IA (limited patch and plaque) mycosis fungoides. a long-term outcome analysis. Arch Dermatol. 1996;132:1309-1313.
- Scarisbrick JJ, Prince HM, Vermeer MH, et al. Cutaneous lymphoma international consortium study of outcome in advanced stages of mycosis fungoides and Sézary syndrome: effect of specific prognostic markers on survival and development of a prognostic model. J Clin Oncol. 2015;33:3766-3773. doi:10.1200/JCO.2015.61.7142
- Nath SK, Yu JB, Wilson LD. Poorer prognosis of African-American patients with mycosis fungoides: an analysis of the SEER dataset, 1988 to 2008. Clin Lymphoma Myeloma Leuk. 2014;14:419-423. doi:10.1016/j.clml.2013.12.018
- Ben-Gashir MA, Hay RJ. Reliance on erythema scores may mask severe atopic dermatitis in black children compared with their white counterparts. Br J Dermatol. 2002;147:920-925. doi:10.1046/j.1365-2133.2002.04965.x
- Poladian K, De Souza B, McMichael AJ. Atopic dermatitis in adolescents with skin of color. Cutis. 2019;104:164-168.
- Yones SS, Palmer RA, Garibaldinos TT, et al. Randomized double-blind trial of the treatment of chronic plaque psoriasis: efficacy of psoralen-UV-A therapy vs narrowband UV-B therapy. Arch Dermatol. 2006;142:836-842. doi:10.1001/archderm.142.7.836
- Currimbhoy S, Pandya AG. Cutaneous T-cell lymphoma. In: Kelly AP, Taylor SC, Lim HW, et al, eds. Taylor and Kelly’s Dermatology for Skin of Color. 2nd ed. McGraw-Hill Education; 2016.
- Ware OR, Dawson JE, Shinohara MM, et al. Racial limitations of Fitzpatrick skin type. Cutis. 2020;105:77-80.
- Korgavkar K, Xiong M, Weinstock M. Changing incidence trends of cutaneous T-cell lymphoma. JAMA Dermatol. 2013;149:1295-1299. doi:10.1001/jamadermatol.2013.5526
- Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part I. diagnosis: clinical and histopathologic features and new molecular and biologic markers. J Am Acad Dermatol. 2014;70:205.E1-E16; quiz 221-222. doi:10.1016/j.jaad.2013.07.049
- Tull RZ, Kerby E, Subash JJ, et al. Ethnic skin centers in the United States: where are we in 2020?. J Am Acad Dermatol. 2020;83:1757-1759. doi:10.1016/j.jaad.2020.03.054
- Adelekun A, Onyekaba G, Lipoff JB. Skin color in dermatology textbooks: an updated evaluation and analysis. J Am Acad Dermatol. 2021;84:194-196. doi:10.1016/j.jaad.2020.04.084
- Ebede T, Papier A. Disparities in dermatology educational resources. J Am Acad Dermatol. 2006;55:687-690. doi:10.1016/j.jaad.2005.10.068
- Jones VA, Clark KA, Shobajo MT, et al. Skin of color representation in medical education: an analysis of popular preparatory materials used for United States medical licensing examinations. J Am Acad Dermatol. 2021;85:773-775. doi:10.1016/j.jaad.2020.07.112
- Montgomery SN, Elbuluk N. A quantitative analysis of research publications focused on the top chief complaints in skin of color patients. J Am Acad Dermatol. 2021;85:241-242. doi:10.1016/j.jaad.2020.08.031
- Hinds GA, Heald P. Cutaneous T-cell lymphoma in skin of color. J Am Acad Dermatol. 2009;60:359-375; quiz 376-378. doi:10.1016/j.jaad.2008.10.031
- Ardigó M, Borroni G, Muscardin L, et al. Hypopigmented mycosis fungoides in Caucasian patients: a clinicopathologic study of 7 cases. J Am Acad Dermatol. 2003;49:264-270. doi:10.1067/s0190-9622(03)00907-1
- Colby SL, Ortman JM. Projections of the size and composition of the U.S. population: 2014 to 2060. United States Census Bureau website. Updated October 8, 2021. Accessed February 28, 2022. https://www.census.gov/library/publications/2015/demo/p25-1143.html
- Taylor SC, Kyei A. Defining skin of color. In: Kelly AP, Taylor SC, Lim HW, et al, eds. Taylor and Kelly’s Dermatology for Skin of Color. 2nd ed. McGraw-Hill Education; 2016.
- Huang AH, Kwatra SG, Khanna R, et al. Racial disparities in the clinical presentation and prognosis of patients with mycosis fungoides. J Natl Med Assoc. 2019;111:633-639. doi:10.1016/j.jnma.2019.08.006
- Kim YH, Jensen RA, Watanabe GL, et al. Clinical stage IA (limited patch and plaque) mycosis fungoides. a long-term outcome analysis. Arch Dermatol. 1996;132:1309-1313.
- Scarisbrick JJ, Prince HM, Vermeer MH, et al. Cutaneous lymphoma international consortium study of outcome in advanced stages of mycosis fungoides and Sézary syndrome: effect of specific prognostic markers on survival and development of a prognostic model. J Clin Oncol. 2015;33:3766-3773. doi:10.1200/JCO.2015.61.7142
- Nath SK, Yu JB, Wilson LD. Poorer prognosis of African-American patients with mycosis fungoides: an analysis of the SEER dataset, 1988 to 2008. Clin Lymphoma Myeloma Leuk. 2014;14:419-423. doi:10.1016/j.clml.2013.12.018
- Ben-Gashir MA, Hay RJ. Reliance on erythema scores may mask severe atopic dermatitis in black children compared with their white counterparts. Br J Dermatol. 2002;147:920-925. doi:10.1046/j.1365-2133.2002.04965.x
- Poladian K, De Souza B, McMichael AJ. Atopic dermatitis in adolescents with skin of color. Cutis. 2019;104:164-168.
- Yones SS, Palmer RA, Garibaldinos TT, et al. Randomized double-blind trial of the treatment of chronic plaque psoriasis: efficacy of psoralen-UV-A therapy vs narrowband UV-B therapy. Arch Dermatol. 2006;142:836-842. doi:10.1001/archderm.142.7.836
- Currimbhoy S, Pandya AG. Cutaneous T-cell lymphoma. In: Kelly AP, Taylor SC, Lim HW, et al, eds. Taylor and Kelly’s Dermatology for Skin of Color. 2nd ed. McGraw-Hill Education; 2016.
- Ware OR, Dawson JE, Shinohara MM, et al. Racial limitations of Fitzpatrick skin type. Cutis. 2020;105:77-80.
Practice Points
- Dermatologists should be familiar with the variable morphology of mycosis fungoides (MF)/Sézary syndrome (SS) exhibited by patients of all skin types to ensure prompt diagnosis and treatment.
- Patients with skin of color (SoC)(Fitzpatrick skin types IV–VI) with MF/SS are more likely than non-SoC patients (Fitzpatrick skin types I–III) to present with hyperpigmentation, a silver hue, and lichenification, whereas non-SoC patients commonly present with erythema and poikiloderma.
Women still missing from CV clinical trial leadership
Although women were well represented on panels, and chaired or cochaired sessions, thanks to the ACC’s ongoing efforts to promote gender diversity and inclusion, they rarely got to give the big talks.
“Unfortunately, women continue to be underrepresented among CV clinical trial leadership, leading to a lack of subject diversity,” Mary Norine Walsh, MD, medical director of heart failure and cardiac transplantation at Ascension St. Vincent Heart Center, Indianapolis, Ind., wrote in a review published online Feb. 28 in the Journal of the American College of Cardiology.
An analysis of cardiovascular trials published during the past 4 years showed that women comprised only 10.1% of clinical trial leadership committees, and more than half of the trials had no women at all as part of the trial leadership team. About 10% of the trials had a woman as first or senior author.
In an interview, Dr. Walsh said she was prompted to write her review because she found the absence of women presenters at ACC 21 so striking.
“ACC 21 was held virtually because of COVID. This gave me the opportunity to easily view all of the research sessions. I attended all of the late-breaking clinical trials and featured clinical research sessions live while they were being presented, and it slowly dawned on me as I was watching that the vast majority of the presenters were men,” she said.
“The ACC does what it can to ensure a good gender mix of panelists and session chairs, but what it cannot control is who presents the data. The fact that 93% of these talks were given by men was astonishing to me,” Dr. Walsh said.
Of the three trials presented by women, one was on sex-specific outcomes in high-risk patients receiving ticagrelor with or without aspirin after percutaneous coronary intervention (a subanalysis of the TWILIGHT study); one was on the impact of COVID-19 on the global cardiovascular workforce (the ACC 2020 Well Being Study); and one was on the prevention of cardiac dysfunction during adjuvanttherapy with candesartan and metoprolol (the PRADA study).
Most of the presenters were regulars at the ACC podium. As Dr. Walsh observed: “This was assuredly not the inaugural turn at the international podium for these male trial presenters.”
So why are women so noticeably absent among the leaders of cardiovascular clinical trials research?
The root cause for this underrepresentation begins with the low number of women who lead clinical trials in cardiovascular medicine and surgery, and the fact that there are fewer female cardiologists than male cardiologists to begin with.
Then there is the lack of mentorship, which, Dr. Walsh said, “really does occur along gendered lines, with men mentoring men.”
In addition, industry-funded trials tend to feed a nondiverse investigator pipeline and other research collaborations often encompass established networks, Dr. Walsh noted.
“When industry is embarking on a new trial of a drug or device, it tends to lean back on who they have had led before. It really gets down to who you know, so getting new people in is fairly difficult,” she said.
Several initiatives to increase diversity in CV clinical trial leadership are ongoing by the ACC and other organizations.
For example, Women as One gives “escalator awards” to boost or escalate the training of highly qualified female cardiologists through targeted funding, mentorship, and networking.
The ACC’s “Clinical Trial Research: Upping Your Game” program aims to develop and train the next generation of a diverse and inclusive clinical trials workforce, focusing not only on women but on other traditionally underrepresented groups.
“We’re now in our third cohort of investigators who are early in their careers. We’re arming them with the skills to become successful in becoming investigators and then going up the chain to trial leadership. We are focusing our efforts on those who are underrepresented in cardiology – women, native Americans, Latinx, and Black investigators. We are hoping to increase diversity through that way, but more still needs to be done,” she said.
Trial sponsors, whether federally funded or industry sponsored, need to insist on diversity of the trial steering committee, and principal investigators need to consider diversity.
“A rethinking of who is eligible to present important trial results is needed,” Dr. Walsh said.
“The informal, or formal, pecking order of CV trial leadership needs to be reworked. All members of the steering committee should be possible presenters, and women should not be asked to report late-breaking results of trials that are reporting sex-specific results or data that are pertinent only to a female population.”
A version of this article first appeared on Medscape.com.
Although women were well represented on panels, and chaired or cochaired sessions, thanks to the ACC’s ongoing efforts to promote gender diversity and inclusion, they rarely got to give the big talks.
“Unfortunately, women continue to be underrepresented among CV clinical trial leadership, leading to a lack of subject diversity,” Mary Norine Walsh, MD, medical director of heart failure and cardiac transplantation at Ascension St. Vincent Heart Center, Indianapolis, Ind., wrote in a review published online Feb. 28 in the Journal of the American College of Cardiology.
An analysis of cardiovascular trials published during the past 4 years showed that women comprised only 10.1% of clinical trial leadership committees, and more than half of the trials had no women at all as part of the trial leadership team. About 10% of the trials had a woman as first or senior author.
In an interview, Dr. Walsh said she was prompted to write her review because she found the absence of women presenters at ACC 21 so striking.
“ACC 21 was held virtually because of COVID. This gave me the opportunity to easily view all of the research sessions. I attended all of the late-breaking clinical trials and featured clinical research sessions live while they were being presented, and it slowly dawned on me as I was watching that the vast majority of the presenters were men,” she said.
“The ACC does what it can to ensure a good gender mix of panelists and session chairs, but what it cannot control is who presents the data. The fact that 93% of these talks were given by men was astonishing to me,” Dr. Walsh said.
Of the three trials presented by women, one was on sex-specific outcomes in high-risk patients receiving ticagrelor with or without aspirin after percutaneous coronary intervention (a subanalysis of the TWILIGHT study); one was on the impact of COVID-19 on the global cardiovascular workforce (the ACC 2020 Well Being Study); and one was on the prevention of cardiac dysfunction during adjuvanttherapy with candesartan and metoprolol (the PRADA study).
Most of the presenters were regulars at the ACC podium. As Dr. Walsh observed: “This was assuredly not the inaugural turn at the international podium for these male trial presenters.”
So why are women so noticeably absent among the leaders of cardiovascular clinical trials research?
The root cause for this underrepresentation begins with the low number of women who lead clinical trials in cardiovascular medicine and surgery, and the fact that there are fewer female cardiologists than male cardiologists to begin with.
Then there is the lack of mentorship, which, Dr. Walsh said, “really does occur along gendered lines, with men mentoring men.”
In addition, industry-funded trials tend to feed a nondiverse investigator pipeline and other research collaborations often encompass established networks, Dr. Walsh noted.
“When industry is embarking on a new trial of a drug or device, it tends to lean back on who they have had led before. It really gets down to who you know, so getting new people in is fairly difficult,” she said.
Several initiatives to increase diversity in CV clinical trial leadership are ongoing by the ACC and other organizations.
For example, Women as One gives “escalator awards” to boost or escalate the training of highly qualified female cardiologists through targeted funding, mentorship, and networking.
The ACC’s “Clinical Trial Research: Upping Your Game” program aims to develop and train the next generation of a diverse and inclusive clinical trials workforce, focusing not only on women but on other traditionally underrepresented groups.
“We’re now in our third cohort of investigators who are early in their careers. We’re arming them with the skills to become successful in becoming investigators and then going up the chain to trial leadership. We are focusing our efforts on those who are underrepresented in cardiology – women, native Americans, Latinx, and Black investigators. We are hoping to increase diversity through that way, but more still needs to be done,” she said.
Trial sponsors, whether federally funded or industry sponsored, need to insist on diversity of the trial steering committee, and principal investigators need to consider diversity.
“A rethinking of who is eligible to present important trial results is needed,” Dr. Walsh said.
“The informal, or formal, pecking order of CV trial leadership needs to be reworked. All members of the steering committee should be possible presenters, and women should not be asked to report late-breaking results of trials that are reporting sex-specific results or data that are pertinent only to a female population.”
A version of this article first appeared on Medscape.com.
Although women were well represented on panels, and chaired or cochaired sessions, thanks to the ACC’s ongoing efforts to promote gender diversity and inclusion, they rarely got to give the big talks.
“Unfortunately, women continue to be underrepresented among CV clinical trial leadership, leading to a lack of subject diversity,” Mary Norine Walsh, MD, medical director of heart failure and cardiac transplantation at Ascension St. Vincent Heart Center, Indianapolis, Ind., wrote in a review published online Feb. 28 in the Journal of the American College of Cardiology.
An analysis of cardiovascular trials published during the past 4 years showed that women comprised only 10.1% of clinical trial leadership committees, and more than half of the trials had no women at all as part of the trial leadership team. About 10% of the trials had a woman as first or senior author.
In an interview, Dr. Walsh said she was prompted to write her review because she found the absence of women presenters at ACC 21 so striking.
“ACC 21 was held virtually because of COVID. This gave me the opportunity to easily view all of the research sessions. I attended all of the late-breaking clinical trials and featured clinical research sessions live while they were being presented, and it slowly dawned on me as I was watching that the vast majority of the presenters were men,” she said.
“The ACC does what it can to ensure a good gender mix of panelists and session chairs, but what it cannot control is who presents the data. The fact that 93% of these talks were given by men was astonishing to me,” Dr. Walsh said.
Of the three trials presented by women, one was on sex-specific outcomes in high-risk patients receiving ticagrelor with or without aspirin after percutaneous coronary intervention (a subanalysis of the TWILIGHT study); one was on the impact of COVID-19 on the global cardiovascular workforce (the ACC 2020 Well Being Study); and one was on the prevention of cardiac dysfunction during adjuvanttherapy with candesartan and metoprolol (the PRADA study).
Most of the presenters were regulars at the ACC podium. As Dr. Walsh observed: “This was assuredly not the inaugural turn at the international podium for these male trial presenters.”
So why are women so noticeably absent among the leaders of cardiovascular clinical trials research?
The root cause for this underrepresentation begins with the low number of women who lead clinical trials in cardiovascular medicine and surgery, and the fact that there are fewer female cardiologists than male cardiologists to begin with.
Then there is the lack of mentorship, which, Dr. Walsh said, “really does occur along gendered lines, with men mentoring men.”
In addition, industry-funded trials tend to feed a nondiverse investigator pipeline and other research collaborations often encompass established networks, Dr. Walsh noted.
“When industry is embarking on a new trial of a drug or device, it tends to lean back on who they have had led before. It really gets down to who you know, so getting new people in is fairly difficult,” she said.
Several initiatives to increase diversity in CV clinical trial leadership are ongoing by the ACC and other organizations.
For example, Women as One gives “escalator awards” to boost or escalate the training of highly qualified female cardiologists through targeted funding, mentorship, and networking.
The ACC’s “Clinical Trial Research: Upping Your Game” program aims to develop and train the next generation of a diverse and inclusive clinical trials workforce, focusing not only on women but on other traditionally underrepresented groups.
“We’re now in our third cohort of investigators who are early in their careers. We’re arming them with the skills to become successful in becoming investigators and then going up the chain to trial leadership. We are focusing our efforts on those who are underrepresented in cardiology – women, native Americans, Latinx, and Black investigators. We are hoping to increase diversity through that way, but more still needs to be done,” she said.
Trial sponsors, whether federally funded or industry sponsored, need to insist on diversity of the trial steering committee, and principal investigators need to consider diversity.
“A rethinking of who is eligible to present important trial results is needed,” Dr. Walsh said.
“The informal, or formal, pecking order of CV trial leadership needs to be reworked. All members of the steering committee should be possible presenters, and women should not be asked to report late-breaking results of trials that are reporting sex-specific results or data that are pertinent only to a female population.”
A version of this article first appeared on Medscape.com.
Discoid lupus
THE COMPARISON
A Multicolored (pink, brown, and white) indurated plaques in a butterfly distribution on the face of a 30-year-old woman with a darker skin tone.
B Pink, elevated, indurated plaques with hypopigmentation in a butterfly distribution on the face of a 19-year-old woman with a lighter skin tone.
Cutaneous lupus erythematosus may occur with or without systemic lupus erythematosus. Discoid lupus erythematosus (DLE), a form of chronic cutaneous lupus, is most commonly found on the scalp, face, and ears.1

Epidemiology
DLE is most common in adult women (age range, 20–40 years).2 It occurs more frequently in women of African descent.3,4
Key clinical features in people with darker skin tones
Clinical features of DLE lesions include erythema, induration, follicular plugging, dyspigmentation, and scarring alopecia.1 In patients of African descent, lesions may be annular and hypopigmented to depigmented centrally with a border of hyperpigmentation. Active lesions may be painful and/or pruritic.2
DLE lesions occur in photodistributed areas, although not exclusively. Photoprotective clothing and sunscreen are an important part of the treatment plan.1 Although sunscreen is recommended for patients with DLE, those with darker skin tones may find some sunscreens cosmetically unappealing due to a mismatch with their normal skin color.5 Tinted sunscreens may be beneficial additions.
Worth noting
Approximately 5% to 25% of patients with cutaneous lupus go on to develop systemic lupus erythematosus.6
Health disparity highlight
Discoid lesions may cause cutaneous scars that are quite disfiguring and may negatively impact quality of life. Some patients may have a few scattered lesions, whereas others have extensive disease covering most of the scalp. DLE lesions of the scalp have classic clinical features including hair loss, erythema, hypopigmentation, and hyperpigmentation. The clinician’s comfort with performing a scalp examination with cultural humility is an important acquired skill and is especially important when the examination is performed on patients with more tightly coiled hair.7 For example, physicians may adopt the “compliment, discuss, and suggest” method when counseling patients.8
1. Bolognia JL, Jorizzo JJ, Schaffer JV, et al. Dermatology. 3rd ed. Elsevier; 2012.
2. Otberg N, Wu W-Y, McElwee KJ, et al. Diagnosis and management of primary cicatricial alopecia: part I. Skinmed. 2008;7:19-26. doi:10.1111/j.1540-9740.2007.07163.x
3. Callen JP. Chronic cutaneous lupus erythematosus. clinical, laboratory, therapeutic, and prognostic examination of 62 patients. Arch Dermatol. 1982;118:412-416. doi:10.1001/archderm.118.6.412
4. McCarty DJ, Manzi S, Medsger TA Jr, et al. Incidence of systemic lupus erythematosus. race and gender differences. Arthritis Rheum. 1995;38:1260-1270. doi:10.1002/art.1780380914
5. Morquette AJ, Waples ER, Heath CR. The importance of cosmetically elegant sunscreen in skin of color populations. J Cosmet Dermatol. In press.
6. Zhou W, Wu H, Zhao M, et al. New insights into the progression from cutaneous lupus to systemic lupus erythematosus. Expert Rev Clin Immunol. 2020;16:829-837. doi:10.1080/17446 66X.2020.1805316
7. Grayson C, Heath C. An approach to examining tightly coiled hair among patients with hair loss in race-discordant patient-physician interactions. JAMA Dermatol. 2021;157:505-506. doi:10.1001/jamadermatol.2021.0338
8. Grayson C, Heath CR. Counseling about traction alopecia: a “compliment, discuss, and suggest” method. Cutis. 2021;108:20-22.
THE COMPARISON
A Multicolored (pink, brown, and white) indurated plaques in a butterfly distribution on the face of a 30-year-old woman with a darker skin tone.
B Pink, elevated, indurated plaques with hypopigmentation in a butterfly distribution on the face of a 19-year-old woman with a lighter skin tone.
Cutaneous lupus erythematosus may occur with or without systemic lupus erythematosus. Discoid lupus erythematosus (DLE), a form of chronic cutaneous lupus, is most commonly found on the scalp, face, and ears.1

Epidemiology
DLE is most common in adult women (age range, 20–40 years).2 It occurs more frequently in women of African descent.3,4
Key clinical features in people with darker skin tones
Clinical features of DLE lesions include erythema, induration, follicular plugging, dyspigmentation, and scarring alopecia.1 In patients of African descent, lesions may be annular and hypopigmented to depigmented centrally with a border of hyperpigmentation. Active lesions may be painful and/or pruritic.2
DLE lesions occur in photodistributed areas, although not exclusively. Photoprotective clothing and sunscreen are an important part of the treatment plan.1 Although sunscreen is recommended for patients with DLE, those with darker skin tones may find some sunscreens cosmetically unappealing due to a mismatch with their normal skin color.5 Tinted sunscreens may be beneficial additions.
Worth noting
Approximately 5% to 25% of patients with cutaneous lupus go on to develop systemic lupus erythematosus.6
Health disparity highlight
Discoid lesions may cause cutaneous scars that are quite disfiguring and may negatively impact quality of life. Some patients may have a few scattered lesions, whereas others have extensive disease covering most of the scalp. DLE lesions of the scalp have classic clinical features including hair loss, erythema, hypopigmentation, and hyperpigmentation. The clinician’s comfort with performing a scalp examination with cultural humility is an important acquired skill and is especially important when the examination is performed on patients with more tightly coiled hair.7 For example, physicians may adopt the “compliment, discuss, and suggest” method when counseling patients.8
THE COMPARISON
A Multicolored (pink, brown, and white) indurated plaques in a butterfly distribution on the face of a 30-year-old woman with a darker skin tone.
B Pink, elevated, indurated plaques with hypopigmentation in a butterfly distribution on the face of a 19-year-old woman with a lighter skin tone.
Cutaneous lupus erythematosus may occur with or without systemic lupus erythematosus. Discoid lupus erythematosus (DLE), a form of chronic cutaneous lupus, is most commonly found on the scalp, face, and ears.1

Epidemiology
DLE is most common in adult women (age range, 20–40 years).2 It occurs more frequently in women of African descent.3,4
Key clinical features in people with darker skin tones
Clinical features of DLE lesions include erythema, induration, follicular plugging, dyspigmentation, and scarring alopecia.1 In patients of African descent, lesions may be annular and hypopigmented to depigmented centrally with a border of hyperpigmentation. Active lesions may be painful and/or pruritic.2
DLE lesions occur in photodistributed areas, although not exclusively. Photoprotective clothing and sunscreen are an important part of the treatment plan.1 Although sunscreen is recommended for patients with DLE, those with darker skin tones may find some sunscreens cosmetically unappealing due to a mismatch with their normal skin color.5 Tinted sunscreens may be beneficial additions.
Worth noting
Approximately 5% to 25% of patients with cutaneous lupus go on to develop systemic lupus erythematosus.6
Health disparity highlight
Discoid lesions may cause cutaneous scars that are quite disfiguring and may negatively impact quality of life. Some patients may have a few scattered lesions, whereas others have extensive disease covering most of the scalp. DLE lesions of the scalp have classic clinical features including hair loss, erythema, hypopigmentation, and hyperpigmentation. The clinician’s comfort with performing a scalp examination with cultural humility is an important acquired skill and is especially important when the examination is performed on patients with more tightly coiled hair.7 For example, physicians may adopt the “compliment, discuss, and suggest” method when counseling patients.8
1. Bolognia JL, Jorizzo JJ, Schaffer JV, et al. Dermatology. 3rd ed. Elsevier; 2012.
2. Otberg N, Wu W-Y, McElwee KJ, et al. Diagnosis and management of primary cicatricial alopecia: part I. Skinmed. 2008;7:19-26. doi:10.1111/j.1540-9740.2007.07163.x
3. Callen JP. Chronic cutaneous lupus erythematosus. clinical, laboratory, therapeutic, and prognostic examination of 62 patients. Arch Dermatol. 1982;118:412-416. doi:10.1001/archderm.118.6.412
4. McCarty DJ, Manzi S, Medsger TA Jr, et al. Incidence of systemic lupus erythematosus. race and gender differences. Arthritis Rheum. 1995;38:1260-1270. doi:10.1002/art.1780380914
5. Morquette AJ, Waples ER, Heath CR. The importance of cosmetically elegant sunscreen in skin of color populations. J Cosmet Dermatol. In press.
6. Zhou W, Wu H, Zhao M, et al. New insights into the progression from cutaneous lupus to systemic lupus erythematosus. Expert Rev Clin Immunol. 2020;16:829-837. doi:10.1080/17446 66X.2020.1805316
7. Grayson C, Heath C. An approach to examining tightly coiled hair among patients with hair loss in race-discordant patient-physician interactions. JAMA Dermatol. 2021;157:505-506. doi:10.1001/jamadermatol.2021.0338
8. Grayson C, Heath CR. Counseling about traction alopecia: a “compliment, discuss, and suggest” method. Cutis. 2021;108:20-22.
1. Bolognia JL, Jorizzo JJ, Schaffer JV, et al. Dermatology. 3rd ed. Elsevier; 2012.
2. Otberg N, Wu W-Y, McElwee KJ, et al. Diagnosis and management of primary cicatricial alopecia: part I. Skinmed. 2008;7:19-26. doi:10.1111/j.1540-9740.2007.07163.x
3. Callen JP. Chronic cutaneous lupus erythematosus. clinical, laboratory, therapeutic, and prognostic examination of 62 patients. Arch Dermatol. 1982;118:412-416. doi:10.1001/archderm.118.6.412
4. McCarty DJ, Manzi S, Medsger TA Jr, et al. Incidence of systemic lupus erythematosus. race and gender differences. Arthritis Rheum. 1995;38:1260-1270. doi:10.1002/art.1780380914
5. Morquette AJ, Waples ER, Heath CR. The importance of cosmetically elegant sunscreen in skin of color populations. J Cosmet Dermatol. In press.
6. Zhou W, Wu H, Zhao M, et al. New insights into the progression from cutaneous lupus to systemic lupus erythematosus. Expert Rev Clin Immunol. 2020;16:829-837. doi:10.1080/17446 66X.2020.1805316
7. Grayson C, Heath C. An approach to examining tightly coiled hair among patients with hair loss in race-discordant patient-physician interactions. JAMA Dermatol. 2021;157:505-506. doi:10.1001/jamadermatol.2021.0338
8. Grayson C, Heath CR. Counseling about traction alopecia: a “compliment, discuss, and suggest” method. Cutis. 2021;108:20-22.
All in the family
Six female doctors from two families share their journeys through medicine.
When Annie Uhing, MD, is stressed about work, she can call her mom. She and her mom are close, yes, but her mom is also a physician and understands the ups and downs of medical education and the unique challenges of being a woman in medicine.
“My mom and I were talking about this the other day – I don’t think we know any other mother-daughter pairs of doctors,” said Dr. Uhing.
In the United States, the number of female physicians has risen steadily since the mid- and late-20th century. As of 2019, women made up more than half of medical school classes across the country and 36.3% of the physician workforce.
Still, most female physicians are concentrated in a handful of specialties (such as pediatrics and obstetrics and gynecology) while the percentages of women in other areas remains extremely low (urology and orthopedic surgery). Many female physicians share anecdotal stories about not being taken seriously, like when a patient mistook them for a nurse, or preferred the advice of a male colleague to their own.
To celebrate International Women’s Day, this news organization talked to two families of female doctors about their experiences in medicine and how they inspire and support one another inside and outside the hospital.
Deborah, Charlene, and Annie
When Deborah Gaebler-Spira, MD, started medical school at the University of Illinois in 1975, women made up just 15% of her class. “For me, the idea that as a woman you could have a vocation that could be quite meaningful and self-directed – that was very important,” said Dr. Gaebler-Spira, now a pediatric rehabilitation physician at the Shirley Ryan Ability Lab and professor at Northwestern University in Chicago.
She blocked out a lot of discouragement along the way. In undergrad, the dean of the college warned Dr. Gaebler-Spira she’d never make it as a doctor. In medical school interviews, administrators could be hostile. “There was this feeling that you were taking a place of someone who really deserved it,” she said. When selecting a residency, Dr. Gaebler-Spira decided against a career in obstetrics because of the overt misogyny in the field at the time.
Instead, she went into pediatrics and physical medicine and rehabilitation, eventually working to become an expert in cerebral palsy. Along the way, Dr. Gaebler-Spira made lifelong friends with other female physicians and found strong female mentors, including Billie Adams, MD, and Helen Emery, MD.
When her sister, Charlene Gaebler-Uhing, MD, also decided to go into medicine, Dr. Gaebler-Spira said she “thought it was a sign of sanity as she was always much more competitive than I was! And if I could do it, no question she was able!”
Dr. Gaebler-Uhing, now an adolescent medicine specialist at Children’s Wisconsin in Milwaukee, followed her older sister’s footsteps to medical school in 1983, after first considering a career in social work.
While there were now more women going into medicine – her medical school class was about 25% women – problems persisted. During clinical rotations in residency, Dr. Gaebler-Uhing was often the only woman on a team and made the conscious decision to go professionally by her nickname, Charlie. “If a woman’s name was on the consult, her opinion and insights did not get the same value or respect as a male physician’s,” she said. “The only way they knew I was a woman was if they really knew me.”
The Gaebler sisters leaned on each other professionally and personally throughout their careers. When both sisters practiced in Chicago, they referred patients to one another. And Dr. Gaebler-Uhing said her older sister was a great role model for how to balance the dual roles of physician and parent, as few of the older female doctors who trained her were married or had a child.
Now Dr. Gaebler-Uhing’s daughter, Annie Uhing, MD, is entering medicine herself. She is currently pediatric resident at the University of Wisconsin American Family Hospital. She plans to do a chief year and then a pediatric endocrinology fellowship.
Growing up, Dr. Uhing wasn’t always sure she wanted to work as much as her parents, who are both doctors. But her mom provided a great example few of her friends had at home: “If you want to work, you should work and do what you want to do and it’s not wrong to want to have a really high-powered job as a woman,” said Dr. Uhing.
Kathryn, Susan, and Rita
The three sisters Kathryn Hudson, MD, Susan Schmidt, MD, and Rita Butler, MD, were inspired to go into medicine by their mother, Rita Watson, MD, who was one of the first female interventional cardiologists in the United States.
“I think we had a front row seat to what being a doctor was like,” said Dr. Hudson, a hematologist and oncologist and director of survivorship at Texas Oncology in Austin. Both parents were MDs – their dad was a pharmaceutical researcher at Merck – and they would excitedly discuss patient cases and drug development at the dinner table, said Dr. Butler, an interventional cardiology fellow at the Lankenau Heart Institute in Wynnewood, Pa.
All three sisters have vivid memories of ‘Take Your Daughter to Work Day’ at their mom’s hospital. “I remember going to Take Your Daughter to Work Day with her and watching her in action and thinking, oh my gosh, my mom is so cool and I want to be like her,” said Dr. Schmidt, a pediatric critical care specialist at St. Christopher’s Hospital for Children in Philadelphia. “I’ve always felt special that my mom was doing something really cool and really saving lives,” said Dr. Schmidt.
Their fourth sibling, John, isn’t a physician and “I honestly wonder if it’s because he never went to Take Your Daughter to Work Day!” said Dr. Butler.
Having a mother who had both a high-powered medical career and a family helped the three women know they could do the same. “It is a difficult journey, don’t get me wrong, but I never questioned that I could do it because my mom did it first,” said Dr. Hudson.
As adults, the sisters confide in one another as they navigate modern motherhood and careers, switching between discussing medical cases and parenting advice.
As hard as their mom worked while they were growing up, she didn’t have the pressure of living up to the “super mom” ideal we have now, said Dr. Butler. “Everyone wants women to work like they don’t have kids and everyone wants women to parent like they don’t have a job,” she said. Having two sisters who can provide reassurance and advice in that area goes a long way, she said.
“I think sharing that experience of navigating motherhood, a medical career, and marriage, and adult life with sisters who are going through all the same things is really special and I feel really fortunate for that,” said Dr. Schmidt.
*This story was updated on 3/8/2022.
Six female doctors from two families share their journeys through medicine.
Six female doctors from two families share their journeys through medicine.
When Annie Uhing, MD, is stressed about work, she can call her mom. She and her mom are close, yes, but her mom is also a physician and understands the ups and downs of medical education and the unique challenges of being a woman in medicine.
“My mom and I were talking about this the other day – I don’t think we know any other mother-daughter pairs of doctors,” said Dr. Uhing.
In the United States, the number of female physicians has risen steadily since the mid- and late-20th century. As of 2019, women made up more than half of medical school classes across the country and 36.3% of the physician workforce.
Still, most female physicians are concentrated in a handful of specialties (such as pediatrics and obstetrics and gynecology) while the percentages of women in other areas remains extremely low (urology and orthopedic surgery). Many female physicians share anecdotal stories about not being taken seriously, like when a patient mistook them for a nurse, or preferred the advice of a male colleague to their own.
To celebrate International Women’s Day, this news organization talked to two families of female doctors about their experiences in medicine and how they inspire and support one another inside and outside the hospital.
Deborah, Charlene, and Annie
When Deborah Gaebler-Spira, MD, started medical school at the University of Illinois in 1975, women made up just 15% of her class. “For me, the idea that as a woman you could have a vocation that could be quite meaningful and self-directed – that was very important,” said Dr. Gaebler-Spira, now a pediatric rehabilitation physician at the Shirley Ryan Ability Lab and professor at Northwestern University in Chicago.
She blocked out a lot of discouragement along the way. In undergrad, the dean of the college warned Dr. Gaebler-Spira she’d never make it as a doctor. In medical school interviews, administrators could be hostile. “There was this feeling that you were taking a place of someone who really deserved it,” she said. When selecting a residency, Dr. Gaebler-Spira decided against a career in obstetrics because of the overt misogyny in the field at the time.
Instead, she went into pediatrics and physical medicine and rehabilitation, eventually working to become an expert in cerebral palsy. Along the way, Dr. Gaebler-Spira made lifelong friends with other female physicians and found strong female mentors, including Billie Adams, MD, and Helen Emery, MD.
When her sister, Charlene Gaebler-Uhing, MD, also decided to go into medicine, Dr. Gaebler-Spira said she “thought it was a sign of sanity as she was always much more competitive than I was! And if I could do it, no question she was able!”
Dr. Gaebler-Uhing, now an adolescent medicine specialist at Children’s Wisconsin in Milwaukee, followed her older sister’s footsteps to medical school in 1983, after first considering a career in social work.
While there were now more women going into medicine – her medical school class was about 25% women – problems persisted. During clinical rotations in residency, Dr. Gaebler-Uhing was often the only woman on a team and made the conscious decision to go professionally by her nickname, Charlie. “If a woman’s name was on the consult, her opinion and insights did not get the same value or respect as a male physician’s,” she said. “The only way they knew I was a woman was if they really knew me.”
The Gaebler sisters leaned on each other professionally and personally throughout their careers. When both sisters practiced in Chicago, they referred patients to one another. And Dr. Gaebler-Uhing said her older sister was a great role model for how to balance the dual roles of physician and parent, as few of the older female doctors who trained her were married or had a child.
Now Dr. Gaebler-Uhing’s daughter, Annie Uhing, MD, is entering medicine herself. She is currently pediatric resident at the University of Wisconsin American Family Hospital. She plans to do a chief year and then a pediatric endocrinology fellowship.
Growing up, Dr. Uhing wasn’t always sure she wanted to work as much as her parents, who are both doctors. But her mom provided a great example few of her friends had at home: “If you want to work, you should work and do what you want to do and it’s not wrong to want to have a really high-powered job as a woman,” said Dr. Uhing.
Kathryn, Susan, and Rita
The three sisters Kathryn Hudson, MD, Susan Schmidt, MD, and Rita Butler, MD, were inspired to go into medicine by their mother, Rita Watson, MD, who was one of the first female interventional cardiologists in the United States.
“I think we had a front row seat to what being a doctor was like,” said Dr. Hudson, a hematologist and oncologist and director of survivorship at Texas Oncology in Austin. Both parents were MDs – their dad was a pharmaceutical researcher at Merck – and they would excitedly discuss patient cases and drug development at the dinner table, said Dr. Butler, an interventional cardiology fellow at the Lankenau Heart Institute in Wynnewood, Pa.
All three sisters have vivid memories of ‘Take Your Daughter to Work Day’ at their mom’s hospital. “I remember going to Take Your Daughter to Work Day with her and watching her in action and thinking, oh my gosh, my mom is so cool and I want to be like her,” said Dr. Schmidt, a pediatric critical care specialist at St. Christopher’s Hospital for Children in Philadelphia. “I’ve always felt special that my mom was doing something really cool and really saving lives,” said Dr. Schmidt.
Their fourth sibling, John, isn’t a physician and “I honestly wonder if it’s because he never went to Take Your Daughter to Work Day!” said Dr. Butler.
Having a mother who had both a high-powered medical career and a family helped the three women know they could do the same. “It is a difficult journey, don’t get me wrong, but I never questioned that I could do it because my mom did it first,” said Dr. Hudson.
As adults, the sisters confide in one another as they navigate modern motherhood and careers, switching between discussing medical cases and parenting advice.
As hard as their mom worked while they were growing up, she didn’t have the pressure of living up to the “super mom” ideal we have now, said Dr. Butler. “Everyone wants women to work like they don’t have kids and everyone wants women to parent like they don’t have a job,” she said. Having two sisters who can provide reassurance and advice in that area goes a long way, she said.
“I think sharing that experience of navigating motherhood, a medical career, and marriage, and adult life with sisters who are going through all the same things is really special and I feel really fortunate for that,” said Dr. Schmidt.
*This story was updated on 3/8/2022.
When Annie Uhing, MD, is stressed about work, she can call her mom. She and her mom are close, yes, but her mom is also a physician and understands the ups and downs of medical education and the unique challenges of being a woman in medicine.
“My mom and I were talking about this the other day – I don’t think we know any other mother-daughter pairs of doctors,” said Dr. Uhing.
In the United States, the number of female physicians has risen steadily since the mid- and late-20th century. As of 2019, women made up more than half of medical school classes across the country and 36.3% of the physician workforce.
Still, most female physicians are concentrated in a handful of specialties (such as pediatrics and obstetrics and gynecology) while the percentages of women in other areas remains extremely low (urology and orthopedic surgery). Many female physicians share anecdotal stories about not being taken seriously, like when a patient mistook them for a nurse, or preferred the advice of a male colleague to their own.
To celebrate International Women’s Day, this news organization talked to two families of female doctors about their experiences in medicine and how they inspire and support one another inside and outside the hospital.
Deborah, Charlene, and Annie
When Deborah Gaebler-Spira, MD, started medical school at the University of Illinois in 1975, women made up just 15% of her class. “For me, the idea that as a woman you could have a vocation that could be quite meaningful and self-directed – that was very important,” said Dr. Gaebler-Spira, now a pediatric rehabilitation physician at the Shirley Ryan Ability Lab and professor at Northwestern University in Chicago.
She blocked out a lot of discouragement along the way. In undergrad, the dean of the college warned Dr. Gaebler-Spira she’d never make it as a doctor. In medical school interviews, administrators could be hostile. “There was this feeling that you were taking a place of someone who really deserved it,” she said. When selecting a residency, Dr. Gaebler-Spira decided against a career in obstetrics because of the overt misogyny in the field at the time.
Instead, she went into pediatrics and physical medicine and rehabilitation, eventually working to become an expert in cerebral palsy. Along the way, Dr. Gaebler-Spira made lifelong friends with other female physicians and found strong female mentors, including Billie Adams, MD, and Helen Emery, MD.
When her sister, Charlene Gaebler-Uhing, MD, also decided to go into medicine, Dr. Gaebler-Spira said she “thought it was a sign of sanity as she was always much more competitive than I was! And if I could do it, no question she was able!”
Dr. Gaebler-Uhing, now an adolescent medicine specialist at Children’s Wisconsin in Milwaukee, followed her older sister’s footsteps to medical school in 1983, after first considering a career in social work.
While there were now more women going into medicine – her medical school class was about 25% women – problems persisted. During clinical rotations in residency, Dr. Gaebler-Uhing was often the only woman on a team and made the conscious decision to go professionally by her nickname, Charlie. “If a woman’s name was on the consult, her opinion and insights did not get the same value or respect as a male physician’s,” she said. “The only way they knew I was a woman was if they really knew me.”
The Gaebler sisters leaned on each other professionally and personally throughout their careers. When both sisters practiced in Chicago, they referred patients to one another. And Dr. Gaebler-Uhing said her older sister was a great role model for how to balance the dual roles of physician and parent, as few of the older female doctors who trained her were married or had a child.
Now Dr. Gaebler-Uhing’s daughter, Annie Uhing, MD, is entering medicine herself. She is currently pediatric resident at the University of Wisconsin American Family Hospital. She plans to do a chief year and then a pediatric endocrinology fellowship.
Growing up, Dr. Uhing wasn’t always sure she wanted to work as much as her parents, who are both doctors. But her mom provided a great example few of her friends had at home: “If you want to work, you should work and do what you want to do and it’s not wrong to want to have a really high-powered job as a woman,” said Dr. Uhing.
Kathryn, Susan, and Rita
The three sisters Kathryn Hudson, MD, Susan Schmidt, MD, and Rita Butler, MD, were inspired to go into medicine by their mother, Rita Watson, MD, who was one of the first female interventional cardiologists in the United States.
“I think we had a front row seat to what being a doctor was like,” said Dr. Hudson, a hematologist and oncologist and director of survivorship at Texas Oncology in Austin. Both parents were MDs – their dad was a pharmaceutical researcher at Merck – and they would excitedly discuss patient cases and drug development at the dinner table, said Dr. Butler, an interventional cardiology fellow at the Lankenau Heart Institute in Wynnewood, Pa.
All three sisters have vivid memories of ‘Take Your Daughter to Work Day’ at their mom’s hospital. “I remember going to Take Your Daughter to Work Day with her and watching her in action and thinking, oh my gosh, my mom is so cool and I want to be like her,” said Dr. Schmidt, a pediatric critical care specialist at St. Christopher’s Hospital for Children in Philadelphia. “I’ve always felt special that my mom was doing something really cool and really saving lives,” said Dr. Schmidt.
Their fourth sibling, John, isn’t a physician and “I honestly wonder if it’s because he never went to Take Your Daughter to Work Day!” said Dr. Butler.
Having a mother who had both a high-powered medical career and a family helped the three women know they could do the same. “It is a difficult journey, don’t get me wrong, but I never questioned that I could do it because my mom did it first,” said Dr. Hudson.
As adults, the sisters confide in one another as they navigate modern motherhood and careers, switching between discussing medical cases and parenting advice.
As hard as their mom worked while they were growing up, she didn’t have the pressure of living up to the “super mom” ideal we have now, said Dr. Butler. “Everyone wants women to work like they don’t have kids and everyone wants women to parent like they don’t have a job,” she said. Having two sisters who can provide reassurance and advice in that area goes a long way, she said.
“I think sharing that experience of navigating motherhood, a medical career, and marriage, and adult life with sisters who are going through all the same things is really special and I feel really fortunate for that,” said Dr. Schmidt.
*This story was updated on 3/8/2022.