User login
Higher ‘chemical restraint’ rates in Black psych patients in the ED
Black patients presenting with psychiatric disorders to hospital emergency departments across the United States have significantly higher rates of chemical restraint than their White counterparts, new research shows.
The investigators also found White patients were more likely to receive chemical sedation at hospitals with a higher proportion of Black patients – a finding that suggests hospital demographics influence practice patterns and that structural racism may be a root cause.
“There is a large disparity in the rates at which patients who presented to EDs nationally in the United States are restrained by race. You are 63% more likely, for the same set of chief complaints, to be chemically sedated if you are Black versus if you’re White,” senior investigator Ari Friedman, MD, PhD, an assistant professor of emergency medicine, and medical ethics and health policy, University of Pennsylvania, Philadelphia, told this news organization.
“The major mediator of that difference is the institution you are at – hospitals that primarily serve Black patients are more likely to chemically sedate their patients for these chief complaints – including White patients. So, it’s mediated by the practice pattern and environment,” Dr. Friedman added.
The study was published in the May issue of Annals of Epidemiology.
First large-scale study
Chemical sedation, also known as chemical restraint, is used to calm and help protect patients from harming themselves or others. Previous research on racial differences in the care of ED psychiatric patients with agitation suggests that there may be treatment disparities.
“Previous research from single institutions [has] shown that Black patients are more likely than White patients to be physically restrained, and this has been shown to be true among adult patients and pediatric patients,” lead author Utsha Khatri, MD, assistant professor of emergency medicine at the Icahn School of Medicine, New York, told this news organization.
Specifically, two single-institution studies within the last year revealed similar disparities, with higher rates of physical restraint for Black and Hispanic psychiatric patients in the ED. Another recent study showed an association with race, ethnicity, and pharmacological restraint use among pediatric patients presenting to the ED for mental health concerns.
“There has been work in psychiatry on disparities in this context, although there is less work in emergency departments,” said Dr. Friedman. “We looked across all U.S. EDs as opposed to within a single health system. The major trade-offs for us were that we weren’t able to observe restraint orders, which don’t find their way into national datasets, so we had to make some inferences based on the type of medications given.”
For the study the investigators analyzed data from 2008-2018 through the National Hospital Ambulatory Medical Survey (NHAMCS) database. They examined the association of race and the administration of chemical sedation, with either an antipsychotic or ketamine, in ED visits for psychiatric disorders. These were any visit where the reason for the visit was “symptoms referable to psychological and mental disorders.”
Of the 76.2 million total ED visits evaluated, the researchers found that Black patients presenting with a psychiatric disorder were significantly more likely to receive chemical sedation with antipsychotics or ketamine than White patients presenting with the same conditions (5.3% vs. 3.0%; P < .01). This difference remained significant when accounting for admission or transfer to psychiatric facilities.
Combatting the forces of racism
When researchers accounted for the percent of hospital population that was Black, they found that patient race no longer affected the likelihood of chemical restraint.
“We found the key source of this racial disparity in use of chemical sedation is accounted for by the fact that hospitals that treat a higher proportion of Black patients tend to use more sedation,” said Dr. Khatri.
“Our findings suggest that patients who present to hospitals that serve a patient population that is 60% Black would have [a] roughly 1.8 times likelihood of getting chemically sedated, compared with a hospital that serves a population that is 10% Black,” she added.
“When a hospital has fewer resources, they often don’t have the staff or time to de-escalate a patient in distress and can have to resort to chemical sedation more quickly than a hospital with ample staff and resources,” said Dr. Friedman in a release.
Dr. Khatri added that the study highlights the need to combat the forces of racism by focusing not just on provider bias but by addressing the “underlying structural issues that lead to Black patients getting worse care based on where they live.”
“Hospitals have unequal distribution of resources and quality, largely patterned on the racial makeup of their patients. Dedicated training and funding for de-escalation techniques as well as sufficient staffing and availability of outpatient mental health care may help keep both patients and staff safe by reducing the use of physical restraint and chemical sedation in appropriate circumstances,” said Dr. Khatri.
Dr. Friedman noted that there will always be a need for restraint use to facilitate rapid medical evaluation and stabilization of patients, but “we want to make it as humane, thoughtful, and rare as possible, and to have a large armamentarium of alternative strategies that can be equitably applied across emergency departments.”
Need for widespread, systemic change
Commenting on the findings, Regina James, MD, the American Psychiatric Association’s chief of Diversity and Health Equity and deputy medical director, said the large-scale study confirms the widespread existence of racial and ethnic disparities in patients with psychiatric disorders.
“This study and previous studies, not only in psychiatry but in other areas of medicine, all bring to light that there continues to be evidence of racial and ethnic disparities in health care, and this is consistent across a range of illnesses and health care services,” said Dr. James.
“It’s important that as we think about the solution, we also think about the etiology of the problem and the layers that have contributed to it – understanding, embracing, and recognizing that these differences didn’t just come up de novo. It’s policies, practices, and behaviors that got us to this point, and it’s going to be policies, practices, and behaviors that are going to move us away from this point,” noted Dr. James.
She added that future research should focus on further understanding which factors exacerbate agitation among patients and what resources directed at the hospital level, including de-escalation training, nursing staff, and waiting room crowding, may be effective at reducing the use of chemical sedation when clinically appropriate.
The authors and Dr. James report no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
Black patients presenting with psychiatric disorders to hospital emergency departments across the United States have significantly higher rates of chemical restraint than their White counterparts, new research shows.
The investigators also found White patients were more likely to receive chemical sedation at hospitals with a higher proportion of Black patients – a finding that suggests hospital demographics influence practice patterns and that structural racism may be a root cause.
“There is a large disparity in the rates at which patients who presented to EDs nationally in the United States are restrained by race. You are 63% more likely, for the same set of chief complaints, to be chemically sedated if you are Black versus if you’re White,” senior investigator Ari Friedman, MD, PhD, an assistant professor of emergency medicine, and medical ethics and health policy, University of Pennsylvania, Philadelphia, told this news organization.
“The major mediator of that difference is the institution you are at – hospitals that primarily serve Black patients are more likely to chemically sedate their patients for these chief complaints – including White patients. So, it’s mediated by the practice pattern and environment,” Dr. Friedman added.
The study was published in the May issue of Annals of Epidemiology.
First large-scale study
Chemical sedation, also known as chemical restraint, is used to calm and help protect patients from harming themselves or others. Previous research on racial differences in the care of ED psychiatric patients with agitation suggests that there may be treatment disparities.
“Previous research from single institutions [has] shown that Black patients are more likely than White patients to be physically restrained, and this has been shown to be true among adult patients and pediatric patients,” lead author Utsha Khatri, MD, assistant professor of emergency medicine at the Icahn School of Medicine, New York, told this news organization.
Specifically, two single-institution studies within the last year revealed similar disparities, with higher rates of physical restraint for Black and Hispanic psychiatric patients in the ED. Another recent study showed an association with race, ethnicity, and pharmacological restraint use among pediatric patients presenting to the ED for mental health concerns.
“There has been work in psychiatry on disparities in this context, although there is less work in emergency departments,” said Dr. Friedman. “We looked across all U.S. EDs as opposed to within a single health system. The major trade-offs for us were that we weren’t able to observe restraint orders, which don’t find their way into national datasets, so we had to make some inferences based on the type of medications given.”
For the study the investigators analyzed data from 2008-2018 through the National Hospital Ambulatory Medical Survey (NHAMCS) database. They examined the association of race and the administration of chemical sedation, with either an antipsychotic or ketamine, in ED visits for psychiatric disorders. These were any visit where the reason for the visit was “symptoms referable to psychological and mental disorders.”
Of the 76.2 million total ED visits evaluated, the researchers found that Black patients presenting with a psychiatric disorder were significantly more likely to receive chemical sedation with antipsychotics or ketamine than White patients presenting with the same conditions (5.3% vs. 3.0%; P < .01). This difference remained significant when accounting for admission or transfer to psychiatric facilities.
Combatting the forces of racism
When researchers accounted for the percent of hospital population that was Black, they found that patient race no longer affected the likelihood of chemical restraint.
“We found the key source of this racial disparity in use of chemical sedation is accounted for by the fact that hospitals that treat a higher proportion of Black patients tend to use more sedation,” said Dr. Khatri.
“Our findings suggest that patients who present to hospitals that serve a patient population that is 60% Black would have [a] roughly 1.8 times likelihood of getting chemically sedated, compared with a hospital that serves a population that is 10% Black,” she added.
“When a hospital has fewer resources, they often don’t have the staff or time to de-escalate a patient in distress and can have to resort to chemical sedation more quickly than a hospital with ample staff and resources,” said Dr. Friedman in a release.
Dr. Khatri added that the study highlights the need to combat the forces of racism by focusing not just on provider bias but by addressing the “underlying structural issues that lead to Black patients getting worse care based on where they live.”
“Hospitals have unequal distribution of resources and quality, largely patterned on the racial makeup of their patients. Dedicated training and funding for de-escalation techniques as well as sufficient staffing and availability of outpatient mental health care may help keep both patients and staff safe by reducing the use of physical restraint and chemical sedation in appropriate circumstances,” said Dr. Khatri.
Dr. Friedman noted that there will always be a need for restraint use to facilitate rapid medical evaluation and stabilization of patients, but “we want to make it as humane, thoughtful, and rare as possible, and to have a large armamentarium of alternative strategies that can be equitably applied across emergency departments.”
Need for widespread, systemic change
Commenting on the findings, Regina James, MD, the American Psychiatric Association’s chief of Diversity and Health Equity and deputy medical director, said the large-scale study confirms the widespread existence of racial and ethnic disparities in patients with psychiatric disorders.
“This study and previous studies, not only in psychiatry but in other areas of medicine, all bring to light that there continues to be evidence of racial and ethnic disparities in health care, and this is consistent across a range of illnesses and health care services,” said Dr. James.
“It’s important that as we think about the solution, we also think about the etiology of the problem and the layers that have contributed to it – understanding, embracing, and recognizing that these differences didn’t just come up de novo. It’s policies, practices, and behaviors that got us to this point, and it’s going to be policies, practices, and behaviors that are going to move us away from this point,” noted Dr. James.
She added that future research should focus on further understanding which factors exacerbate agitation among patients and what resources directed at the hospital level, including de-escalation training, nursing staff, and waiting room crowding, may be effective at reducing the use of chemical sedation when clinically appropriate.
The authors and Dr. James report no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
Black patients presenting with psychiatric disorders to hospital emergency departments across the United States have significantly higher rates of chemical restraint than their White counterparts, new research shows.
The investigators also found White patients were more likely to receive chemical sedation at hospitals with a higher proportion of Black patients – a finding that suggests hospital demographics influence practice patterns and that structural racism may be a root cause.
“There is a large disparity in the rates at which patients who presented to EDs nationally in the United States are restrained by race. You are 63% more likely, for the same set of chief complaints, to be chemically sedated if you are Black versus if you’re White,” senior investigator Ari Friedman, MD, PhD, an assistant professor of emergency medicine, and medical ethics and health policy, University of Pennsylvania, Philadelphia, told this news organization.
“The major mediator of that difference is the institution you are at – hospitals that primarily serve Black patients are more likely to chemically sedate their patients for these chief complaints – including White patients. So, it’s mediated by the practice pattern and environment,” Dr. Friedman added.
The study was published in the May issue of Annals of Epidemiology.
First large-scale study
Chemical sedation, also known as chemical restraint, is used to calm and help protect patients from harming themselves or others. Previous research on racial differences in the care of ED psychiatric patients with agitation suggests that there may be treatment disparities.
“Previous research from single institutions [has] shown that Black patients are more likely than White patients to be physically restrained, and this has been shown to be true among adult patients and pediatric patients,” lead author Utsha Khatri, MD, assistant professor of emergency medicine at the Icahn School of Medicine, New York, told this news organization.
Specifically, two single-institution studies within the last year revealed similar disparities, with higher rates of physical restraint for Black and Hispanic psychiatric patients in the ED. Another recent study showed an association with race, ethnicity, and pharmacological restraint use among pediatric patients presenting to the ED for mental health concerns.
“There has been work in psychiatry on disparities in this context, although there is less work in emergency departments,” said Dr. Friedman. “We looked across all U.S. EDs as opposed to within a single health system. The major trade-offs for us were that we weren’t able to observe restraint orders, which don’t find their way into national datasets, so we had to make some inferences based on the type of medications given.”
For the study the investigators analyzed data from 2008-2018 through the National Hospital Ambulatory Medical Survey (NHAMCS) database. They examined the association of race and the administration of chemical sedation, with either an antipsychotic or ketamine, in ED visits for psychiatric disorders. These were any visit where the reason for the visit was “symptoms referable to psychological and mental disorders.”
Of the 76.2 million total ED visits evaluated, the researchers found that Black patients presenting with a psychiatric disorder were significantly more likely to receive chemical sedation with antipsychotics or ketamine than White patients presenting with the same conditions (5.3% vs. 3.0%; P < .01). This difference remained significant when accounting for admission or transfer to psychiatric facilities.
Combatting the forces of racism
When researchers accounted for the percent of hospital population that was Black, they found that patient race no longer affected the likelihood of chemical restraint.
“We found the key source of this racial disparity in use of chemical sedation is accounted for by the fact that hospitals that treat a higher proportion of Black patients tend to use more sedation,” said Dr. Khatri.
“Our findings suggest that patients who present to hospitals that serve a patient population that is 60% Black would have [a] roughly 1.8 times likelihood of getting chemically sedated, compared with a hospital that serves a population that is 10% Black,” she added.
“When a hospital has fewer resources, they often don’t have the staff or time to de-escalate a patient in distress and can have to resort to chemical sedation more quickly than a hospital with ample staff and resources,” said Dr. Friedman in a release.
Dr. Khatri added that the study highlights the need to combat the forces of racism by focusing not just on provider bias but by addressing the “underlying structural issues that lead to Black patients getting worse care based on where they live.”
“Hospitals have unequal distribution of resources and quality, largely patterned on the racial makeup of their patients. Dedicated training and funding for de-escalation techniques as well as sufficient staffing and availability of outpatient mental health care may help keep both patients and staff safe by reducing the use of physical restraint and chemical sedation in appropriate circumstances,” said Dr. Khatri.
Dr. Friedman noted that there will always be a need for restraint use to facilitate rapid medical evaluation and stabilization of patients, but “we want to make it as humane, thoughtful, and rare as possible, and to have a large armamentarium of alternative strategies that can be equitably applied across emergency departments.”
Need for widespread, systemic change
Commenting on the findings, Regina James, MD, the American Psychiatric Association’s chief of Diversity and Health Equity and deputy medical director, said the large-scale study confirms the widespread existence of racial and ethnic disparities in patients with psychiatric disorders.
“This study and previous studies, not only in psychiatry but in other areas of medicine, all bring to light that there continues to be evidence of racial and ethnic disparities in health care, and this is consistent across a range of illnesses and health care services,” said Dr. James.
“It’s important that as we think about the solution, we also think about the etiology of the problem and the layers that have contributed to it – understanding, embracing, and recognizing that these differences didn’t just come up de novo. It’s policies, practices, and behaviors that got us to this point, and it’s going to be policies, practices, and behaviors that are going to move us away from this point,” noted Dr. James.
She added that future research should focus on further understanding which factors exacerbate agitation among patients and what resources directed at the hospital level, including de-escalation training, nursing staff, and waiting room crowding, may be effective at reducing the use of chemical sedation when clinically appropriate.
The authors and Dr. James report no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
Antibiotic prescriptions to Black and Hispanic/Latinx patients in the U.S. are often inappropriate
LISBON – Two-thirds of antibiotic prescriptions written for Black patients and more than half of antibiotic prescriptions for Hispanic/Latinx patients are inappropriate, according to data from a study of antibiotic prescribing habits in U.S. doctors’ offices, hospital clinics, and emergency departments.
Eric Young, PharmD, PhD, from the University of Texas at Austin, and UT Health, San Antonio, presented his work as a poster at the 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) 2022.
“We were really surprised mainly by the racial findings, because Black patients have the highest overall and the highest inappropriate prescribing of antibiotics,” he told this news organization. “There was also a difference seen for age [across all ethnicities].”
Pediatric patients were found to have high overall prescribing but, notably, the lowest inappropriate prescribing among all the patient groups, reported Dr. Young. “This is interesting because oftentimes we think the more antibiotics are prescribed, then surely the greater the inappropriate prescribing would be too, but pediatricians actually have one of the lowest rates of inappropriate antibiotic prescribing. They do a great job.”
The study included more than 7 billion patient visits, 11.3% of which involved an antibiotic prescription.
The rate of antibiotic prescribing was 122 per 1,000 visits in Black patients and 139 per 1,000 visits in Hispanic patients, while in White patients, the rate was 109 per 1,000 visits. The rate was 114 per 1,000 visits in patients younger than 18 years and 170 per 1,000 visits in females.
Dr. Young found that almost 64% of antibiotic prescriptions written for Black patients and 58% for Hispanic patients were inappropriate. For White patients, the rate of inappropriate antibiotic prescribing was 56%. Similarly, 74% of prescriptions dispensed to patients aged 65 years and older and 58% to males were deemed inappropriate.
Kajal Bhakta, PharmD, BCACP, ambulatory care clinical pharmacist, University Health System, UT Health Science Center San Antonio, who was not involved in the study, pointed out that antibiotics are frequently prescribed without confirmation of an infection, owing to the fact that the verification process may delay care, especially in the outpatient setting.
Dr. Bhakta said that overprescribing in the elderly population and in certain ethnic groups was “likely due to socioeconomic and cultural factors. These prescribing methods may lead to unnecessary drug side effects and/or antimicrobial resistance.”
Regarding the patient-doctor consultation process, she pointed out that “older patients may have trouble describing their symptoms, and when those symptoms remain unresolved, providers may be more inclined to prescribe antibiotics to help.”
Sometimes overprescribing can occur because of the logistics involved in getting to the doctor’s office in the outpatient setting. “Sometimes patients struggle with transportation, as two separate trips to the doctor and pharmacy may not be feasible. Additionally, these same patients may have limited access to health care and therefore may use an urgent care facility for their acute infection–like symptoms,” Dr. Bhakta explained.
Dr. Young, who is of Asian descent, first became interested in disparities in health care when he noticed that ethnic minority groups showed greater hesitancy toward COVID-19 vaccination. “I noticed that there weren’t many Asians involved in previous trials and realized at this point that disparities were rampant.”
Dr. Young had been involved in investigating the overall use and the inappropriate use of antibiotics across the whole U.S. population when his interest in health disparities prompted him to study these patterns in specific demographic groups.
“Most previous data are derived from inpatient studies where the physician is giving the antibiotics,” said Dr. Young, who looked specifically at outpatient prescribing.
Dr. Young used prescribing data from the Centers for Disease Control and Prevention’s National Ambulatory Medical Care Survey, which covers more than 5.7 billion adult (aged 18 and older) and 1.3 billion child visits to outpatient practices between 2009 and 2016 across all 50 U.S. states and Washington, D.C.
He gathered patient data on ICD-9-CM and ICD-10 diagnostic codes for infections and for diagnoses that “appeared like infections.” All of the patients who were included had received at least one oral antibiotic. Antibiotic prescribing was defined as visits that included an antibiotic per 1,000 total patient visits.
On the basis of previous research, Dr. Young and his colleagues then determined whether each antibiotic prescription was appropriate, possibly appropriate, or inappropriate. Patient demographics included age (younger than 18 years, 18-64 years, and older than 64 years), sex (male or female), race, and ethnicity (White, Black, more than one race, Hispanic/Latinx, and other). These data were used to evaluate overall and inappropriate use.
“The health care community needs to be really careful with the judicious use of antibiotics,” Dr. Young said. “We have good guidelines on antimicrobial stewardship both in the inpatient and outpatient settings, but sometimes we overlook the disparities and cultural implications held by some patients.”
Typical examples of socioeconomic and cultural factors at play included patients not being able to afford the antibiotics, having limited access to care, or not returning for a follow-up visit for whatever reason.
“Patients of Black and Hispanic descent often don’t have the same degree of established care that many White patients have,” Dr. Young noted.
In the future, Dr. Young wants to conduct research into whether patients are actually taking their prescribed antibiotics, as well as their outcomes. For example, he would like to investigate whether rates of antibiotic resistance or Clostridioides difficile infection are higher among Black patients.
Dr. Young and Dr. Bhakta have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LISBON – Two-thirds of antibiotic prescriptions written for Black patients and more than half of antibiotic prescriptions for Hispanic/Latinx patients are inappropriate, according to data from a study of antibiotic prescribing habits in U.S. doctors’ offices, hospital clinics, and emergency departments.
Eric Young, PharmD, PhD, from the University of Texas at Austin, and UT Health, San Antonio, presented his work as a poster at the 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) 2022.
“We were really surprised mainly by the racial findings, because Black patients have the highest overall and the highest inappropriate prescribing of antibiotics,” he told this news organization. “There was also a difference seen for age [across all ethnicities].”
Pediatric patients were found to have high overall prescribing but, notably, the lowest inappropriate prescribing among all the patient groups, reported Dr. Young. “This is interesting because oftentimes we think the more antibiotics are prescribed, then surely the greater the inappropriate prescribing would be too, but pediatricians actually have one of the lowest rates of inappropriate antibiotic prescribing. They do a great job.”
The study included more than 7 billion patient visits, 11.3% of which involved an antibiotic prescription.
The rate of antibiotic prescribing was 122 per 1,000 visits in Black patients and 139 per 1,000 visits in Hispanic patients, while in White patients, the rate was 109 per 1,000 visits. The rate was 114 per 1,000 visits in patients younger than 18 years and 170 per 1,000 visits in females.
Dr. Young found that almost 64% of antibiotic prescriptions written for Black patients and 58% for Hispanic patients were inappropriate. For White patients, the rate of inappropriate antibiotic prescribing was 56%. Similarly, 74% of prescriptions dispensed to patients aged 65 years and older and 58% to males were deemed inappropriate.
Kajal Bhakta, PharmD, BCACP, ambulatory care clinical pharmacist, University Health System, UT Health Science Center San Antonio, who was not involved in the study, pointed out that antibiotics are frequently prescribed without confirmation of an infection, owing to the fact that the verification process may delay care, especially in the outpatient setting.
Dr. Bhakta said that overprescribing in the elderly population and in certain ethnic groups was “likely due to socioeconomic and cultural factors. These prescribing methods may lead to unnecessary drug side effects and/or antimicrobial resistance.”
Regarding the patient-doctor consultation process, she pointed out that “older patients may have trouble describing their symptoms, and when those symptoms remain unresolved, providers may be more inclined to prescribe antibiotics to help.”
Sometimes overprescribing can occur because of the logistics involved in getting to the doctor’s office in the outpatient setting. “Sometimes patients struggle with transportation, as two separate trips to the doctor and pharmacy may not be feasible. Additionally, these same patients may have limited access to health care and therefore may use an urgent care facility for their acute infection–like symptoms,” Dr. Bhakta explained.
Dr. Young, who is of Asian descent, first became interested in disparities in health care when he noticed that ethnic minority groups showed greater hesitancy toward COVID-19 vaccination. “I noticed that there weren’t many Asians involved in previous trials and realized at this point that disparities were rampant.”
Dr. Young had been involved in investigating the overall use and the inappropriate use of antibiotics across the whole U.S. population when his interest in health disparities prompted him to study these patterns in specific demographic groups.
“Most previous data are derived from inpatient studies where the physician is giving the antibiotics,” said Dr. Young, who looked specifically at outpatient prescribing.
Dr. Young used prescribing data from the Centers for Disease Control and Prevention’s National Ambulatory Medical Care Survey, which covers more than 5.7 billion adult (aged 18 and older) and 1.3 billion child visits to outpatient practices between 2009 and 2016 across all 50 U.S. states and Washington, D.C.
He gathered patient data on ICD-9-CM and ICD-10 diagnostic codes for infections and for diagnoses that “appeared like infections.” All of the patients who were included had received at least one oral antibiotic. Antibiotic prescribing was defined as visits that included an antibiotic per 1,000 total patient visits.
On the basis of previous research, Dr. Young and his colleagues then determined whether each antibiotic prescription was appropriate, possibly appropriate, or inappropriate. Patient demographics included age (younger than 18 years, 18-64 years, and older than 64 years), sex (male or female), race, and ethnicity (White, Black, more than one race, Hispanic/Latinx, and other). These data were used to evaluate overall and inappropriate use.
“The health care community needs to be really careful with the judicious use of antibiotics,” Dr. Young said. “We have good guidelines on antimicrobial stewardship both in the inpatient and outpatient settings, but sometimes we overlook the disparities and cultural implications held by some patients.”
Typical examples of socioeconomic and cultural factors at play included patients not being able to afford the antibiotics, having limited access to care, or not returning for a follow-up visit for whatever reason.
“Patients of Black and Hispanic descent often don’t have the same degree of established care that many White patients have,” Dr. Young noted.
In the future, Dr. Young wants to conduct research into whether patients are actually taking their prescribed antibiotics, as well as their outcomes. For example, he would like to investigate whether rates of antibiotic resistance or Clostridioides difficile infection are higher among Black patients.
Dr. Young and Dr. Bhakta have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LISBON – Two-thirds of antibiotic prescriptions written for Black patients and more than half of antibiotic prescriptions for Hispanic/Latinx patients are inappropriate, according to data from a study of antibiotic prescribing habits in U.S. doctors’ offices, hospital clinics, and emergency departments.
Eric Young, PharmD, PhD, from the University of Texas at Austin, and UT Health, San Antonio, presented his work as a poster at the 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) 2022.
“We were really surprised mainly by the racial findings, because Black patients have the highest overall and the highest inappropriate prescribing of antibiotics,” he told this news organization. “There was also a difference seen for age [across all ethnicities].”
Pediatric patients were found to have high overall prescribing but, notably, the lowest inappropriate prescribing among all the patient groups, reported Dr. Young. “This is interesting because oftentimes we think the more antibiotics are prescribed, then surely the greater the inappropriate prescribing would be too, but pediatricians actually have one of the lowest rates of inappropriate antibiotic prescribing. They do a great job.”
The study included more than 7 billion patient visits, 11.3% of which involved an antibiotic prescription.
The rate of antibiotic prescribing was 122 per 1,000 visits in Black patients and 139 per 1,000 visits in Hispanic patients, while in White patients, the rate was 109 per 1,000 visits. The rate was 114 per 1,000 visits in patients younger than 18 years and 170 per 1,000 visits in females.
Dr. Young found that almost 64% of antibiotic prescriptions written for Black patients and 58% for Hispanic patients were inappropriate. For White patients, the rate of inappropriate antibiotic prescribing was 56%. Similarly, 74% of prescriptions dispensed to patients aged 65 years and older and 58% to males were deemed inappropriate.
Kajal Bhakta, PharmD, BCACP, ambulatory care clinical pharmacist, University Health System, UT Health Science Center San Antonio, who was not involved in the study, pointed out that antibiotics are frequently prescribed without confirmation of an infection, owing to the fact that the verification process may delay care, especially in the outpatient setting.
Dr. Bhakta said that overprescribing in the elderly population and in certain ethnic groups was “likely due to socioeconomic and cultural factors. These prescribing methods may lead to unnecessary drug side effects and/or antimicrobial resistance.”
Regarding the patient-doctor consultation process, she pointed out that “older patients may have trouble describing their symptoms, and when those symptoms remain unresolved, providers may be more inclined to prescribe antibiotics to help.”
Sometimes overprescribing can occur because of the logistics involved in getting to the doctor’s office in the outpatient setting. “Sometimes patients struggle with transportation, as two separate trips to the doctor and pharmacy may not be feasible. Additionally, these same patients may have limited access to health care and therefore may use an urgent care facility for their acute infection–like symptoms,” Dr. Bhakta explained.
Dr. Young, who is of Asian descent, first became interested in disparities in health care when he noticed that ethnic minority groups showed greater hesitancy toward COVID-19 vaccination. “I noticed that there weren’t many Asians involved in previous trials and realized at this point that disparities were rampant.”
Dr. Young had been involved in investigating the overall use and the inappropriate use of antibiotics across the whole U.S. population when his interest in health disparities prompted him to study these patterns in specific demographic groups.
“Most previous data are derived from inpatient studies where the physician is giving the antibiotics,” said Dr. Young, who looked specifically at outpatient prescribing.
Dr. Young used prescribing data from the Centers for Disease Control and Prevention’s National Ambulatory Medical Care Survey, which covers more than 5.7 billion adult (aged 18 and older) and 1.3 billion child visits to outpatient practices between 2009 and 2016 across all 50 U.S. states and Washington, D.C.
He gathered patient data on ICD-9-CM and ICD-10 diagnostic codes for infections and for diagnoses that “appeared like infections.” All of the patients who were included had received at least one oral antibiotic. Antibiotic prescribing was defined as visits that included an antibiotic per 1,000 total patient visits.
On the basis of previous research, Dr. Young and his colleagues then determined whether each antibiotic prescription was appropriate, possibly appropriate, or inappropriate. Patient demographics included age (younger than 18 years, 18-64 years, and older than 64 years), sex (male or female), race, and ethnicity (White, Black, more than one race, Hispanic/Latinx, and other). These data were used to evaluate overall and inappropriate use.
“The health care community needs to be really careful with the judicious use of antibiotics,” Dr. Young said. “We have good guidelines on antimicrobial stewardship both in the inpatient and outpatient settings, but sometimes we overlook the disparities and cultural implications held by some patients.”
Typical examples of socioeconomic and cultural factors at play included patients not being able to afford the antibiotics, having limited access to care, or not returning for a follow-up visit for whatever reason.
“Patients of Black and Hispanic descent often don’t have the same degree of established care that many White patients have,” Dr. Young noted.
In the future, Dr. Young wants to conduct research into whether patients are actually taking their prescribed antibiotics, as well as their outcomes. For example, he would like to investigate whether rates of antibiotic resistance or Clostridioides difficile infection are higher among Black patients.
Dr. Young and Dr. Bhakta have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ECCMID 2022
How to address social determinants of health, according to expert panel
This patient is on prednisone for her RA because she can’t afford better drugs, and she has been occasionally skipping her insulin, Dr. Candler said during her presentation, at the annual meeting of the American College of Physicians
Plus, her first language is Turkish, and she’s missed many doctor appointments because she lives too far from the center-city clinics, said Dr. Candler, who is the care team medical director at Iora Primary Care in Houston.
How are this woman’s needs supposed to be met in a fee-for-service system that allows medical staff 15 to 30 minutes to help solve her problems?
Potential regulatory fixes
A panel of experts talked about potential policies and regulatory fixes that take into account the impact of “social determinants of health.” Some of these are gaining traction, but there is still a huge gap between how medicine in practiced in the United States and the health needs of people in the community, the panelists said.
The ACO REACH (Realizing Equity, Access and Community Health) model is a recent step forward, said Josh Liao, MD, MSc, associate chair for health systems at the University of Washington, Seattle. The accountable care organization model pays doctors more for caring for Medicare patients in underserved communities.
“To me, it represents that at least we’re moving in the direction where we’re acknowledging directly that social environment matters,” he said.
The American College of Physicians’ Medical Practice and Quality Committee helped improve payment for telehealth, an important step for equity to the underserved, said William Fox, MD, at Fox and Brantley Internal Medicine in Charlottesville, Va., and chair of the committee for ACP’s Virginia chapter. But many policies require much more work, he said.
One aim is getting to universal health coverage – 31 million people in the United States still don’t have health insurance, a number that is greatly improved since the Affordable Care Act but has plateaued recently.
Another is to invest more in primary care – which accounts for about 5% of spending even though 35% of patient visits are to primary care.
Dr. Fox said the U.S. system also needs to evolve beyond fee-for-service, invest in information technology to bridge the gap between the access for the rich and poor, continue to expand telehealth, and reform payment programs to recognize social factors.
“The current finance system and the quality payment program are focused on downstream impacts of poor health,” Dr. Fox said.
Primary care needs to shed the expectation that it must show that it reduces costs in order to be valued, he continued. Care sometimes is necessary but doesn’t reduce cost. Also, cost reduction is often seen in the long run, but studied only in the short term, and therefore the evidence for cost reduction can be elusive.
What can internists do to help?
Dr. Candler said internal medicine physicians can do their part by collecting data on patients and staff and measuring outcomes to identify disparities. Additionally, they could run their practices with community and cultural needs in mind, she said.
“Some of that might mean hiring differently. Think about it – if you’re in a position to start building new practices, go where they need you,” Dr. Candler explained. “It might mean a little bit more of a commute for you. But your patients are already doing that with their untreated cataracts, so who’s safer on the roads?”
George Abraham, MD, MPH – president of ACP and professor of medicine at the University of Massachusetts , Boston, who did not present in the session – suggested physicians should be looking at their own practice style, location, and the way their practice runs, and see where there are opportunities to be more in touch.
“I’m sure we all have practices where we have a diverse patient population,” he said. What doctors can do is to specifically focus on their minority population and ask: ‘What do they experience that others don’t experience as my patient coming into my office?’ he said.
Dr. Abraham, who received his medical degree in India and is ACP’s first president who is an international medical graduate, pointed to ACP’s emphasis on diversifying the internal medicine workforce to reflect the communities.
Recent measures have included the creation of an ACP international medical graduate task force and establishing an antiharassment policy and reporting process.
“The conversation has started a lot more,” he said.
Dr. Candler reports financial relationships with Abbott, AbbVie, Johnson & Johnson, Merck, Medtronic, Pfizer, and other companies. She is also a member of the editorial advisory board of Internal Medicine News. Dr. Fox reports financial relationships with Obagi Cosmeceuticals. Dr. Liao reports financial relationships with Eli Lilly, Gilead, Johnson & Johnson, Novavax, and other companies. Dr. Abraham reports no relevant financial relationships.
This patient is on prednisone for her RA because she can’t afford better drugs, and she has been occasionally skipping her insulin, Dr. Candler said during her presentation, at the annual meeting of the American College of Physicians
Plus, her first language is Turkish, and she’s missed many doctor appointments because she lives too far from the center-city clinics, said Dr. Candler, who is the care team medical director at Iora Primary Care in Houston.
How are this woman’s needs supposed to be met in a fee-for-service system that allows medical staff 15 to 30 minutes to help solve her problems?
Potential regulatory fixes
A panel of experts talked about potential policies and regulatory fixes that take into account the impact of “social determinants of health.” Some of these are gaining traction, but there is still a huge gap between how medicine in practiced in the United States and the health needs of people in the community, the panelists said.
The ACO REACH (Realizing Equity, Access and Community Health) model is a recent step forward, said Josh Liao, MD, MSc, associate chair for health systems at the University of Washington, Seattle. The accountable care organization model pays doctors more for caring for Medicare patients in underserved communities.
“To me, it represents that at least we’re moving in the direction where we’re acknowledging directly that social environment matters,” he said.
The American College of Physicians’ Medical Practice and Quality Committee helped improve payment for telehealth, an important step for equity to the underserved, said William Fox, MD, at Fox and Brantley Internal Medicine in Charlottesville, Va., and chair of the committee for ACP’s Virginia chapter. But many policies require much more work, he said.
One aim is getting to universal health coverage – 31 million people in the United States still don’t have health insurance, a number that is greatly improved since the Affordable Care Act but has plateaued recently.
Another is to invest more in primary care – which accounts for about 5% of spending even though 35% of patient visits are to primary care.
Dr. Fox said the U.S. system also needs to evolve beyond fee-for-service, invest in information technology to bridge the gap between the access for the rich and poor, continue to expand telehealth, and reform payment programs to recognize social factors.
“The current finance system and the quality payment program are focused on downstream impacts of poor health,” Dr. Fox said.
Primary care needs to shed the expectation that it must show that it reduces costs in order to be valued, he continued. Care sometimes is necessary but doesn’t reduce cost. Also, cost reduction is often seen in the long run, but studied only in the short term, and therefore the evidence for cost reduction can be elusive.
What can internists do to help?
Dr. Candler said internal medicine physicians can do their part by collecting data on patients and staff and measuring outcomes to identify disparities. Additionally, they could run their practices with community and cultural needs in mind, she said.
“Some of that might mean hiring differently. Think about it – if you’re in a position to start building new practices, go where they need you,” Dr. Candler explained. “It might mean a little bit more of a commute for you. But your patients are already doing that with their untreated cataracts, so who’s safer on the roads?”
George Abraham, MD, MPH – president of ACP and professor of medicine at the University of Massachusetts , Boston, who did not present in the session – suggested physicians should be looking at their own practice style, location, and the way their practice runs, and see where there are opportunities to be more in touch.
“I’m sure we all have practices where we have a diverse patient population,” he said. What doctors can do is to specifically focus on their minority population and ask: ‘What do they experience that others don’t experience as my patient coming into my office?’ he said.
Dr. Abraham, who received his medical degree in India and is ACP’s first president who is an international medical graduate, pointed to ACP’s emphasis on diversifying the internal medicine workforce to reflect the communities.
Recent measures have included the creation of an ACP international medical graduate task force and establishing an antiharassment policy and reporting process.
“The conversation has started a lot more,” he said.
Dr. Candler reports financial relationships with Abbott, AbbVie, Johnson & Johnson, Merck, Medtronic, Pfizer, and other companies. She is also a member of the editorial advisory board of Internal Medicine News. Dr. Fox reports financial relationships with Obagi Cosmeceuticals. Dr. Liao reports financial relationships with Eli Lilly, Gilead, Johnson & Johnson, Novavax, and other companies. Dr. Abraham reports no relevant financial relationships.
This patient is on prednisone for her RA because she can’t afford better drugs, and she has been occasionally skipping her insulin, Dr. Candler said during her presentation, at the annual meeting of the American College of Physicians
Plus, her first language is Turkish, and she’s missed many doctor appointments because she lives too far from the center-city clinics, said Dr. Candler, who is the care team medical director at Iora Primary Care in Houston.
How are this woman’s needs supposed to be met in a fee-for-service system that allows medical staff 15 to 30 minutes to help solve her problems?
Potential regulatory fixes
A panel of experts talked about potential policies and regulatory fixes that take into account the impact of “social determinants of health.” Some of these are gaining traction, but there is still a huge gap between how medicine in practiced in the United States and the health needs of people in the community, the panelists said.
The ACO REACH (Realizing Equity, Access and Community Health) model is a recent step forward, said Josh Liao, MD, MSc, associate chair for health systems at the University of Washington, Seattle. The accountable care organization model pays doctors more for caring for Medicare patients in underserved communities.
“To me, it represents that at least we’re moving in the direction where we’re acknowledging directly that social environment matters,” he said.
The American College of Physicians’ Medical Practice and Quality Committee helped improve payment for telehealth, an important step for equity to the underserved, said William Fox, MD, at Fox and Brantley Internal Medicine in Charlottesville, Va., and chair of the committee for ACP’s Virginia chapter. But many policies require much more work, he said.
One aim is getting to universal health coverage – 31 million people in the United States still don’t have health insurance, a number that is greatly improved since the Affordable Care Act but has plateaued recently.
Another is to invest more in primary care – which accounts for about 5% of spending even though 35% of patient visits are to primary care.
Dr. Fox said the U.S. system also needs to evolve beyond fee-for-service, invest in information technology to bridge the gap between the access for the rich and poor, continue to expand telehealth, and reform payment programs to recognize social factors.
“The current finance system and the quality payment program are focused on downstream impacts of poor health,” Dr. Fox said.
Primary care needs to shed the expectation that it must show that it reduces costs in order to be valued, he continued. Care sometimes is necessary but doesn’t reduce cost. Also, cost reduction is often seen in the long run, but studied only in the short term, and therefore the evidence for cost reduction can be elusive.
What can internists do to help?
Dr. Candler said internal medicine physicians can do their part by collecting data on patients and staff and measuring outcomes to identify disparities. Additionally, they could run their practices with community and cultural needs in mind, she said.
“Some of that might mean hiring differently. Think about it – if you’re in a position to start building new practices, go where they need you,” Dr. Candler explained. “It might mean a little bit more of a commute for you. But your patients are already doing that with their untreated cataracts, so who’s safer on the roads?”
George Abraham, MD, MPH – president of ACP and professor of medicine at the University of Massachusetts , Boston, who did not present in the session – suggested physicians should be looking at their own practice style, location, and the way their practice runs, and see where there are opportunities to be more in touch.
“I’m sure we all have practices where we have a diverse patient population,” he said. What doctors can do is to specifically focus on their minority population and ask: ‘What do they experience that others don’t experience as my patient coming into my office?’ he said.
Dr. Abraham, who received his medical degree in India and is ACP’s first president who is an international medical graduate, pointed to ACP’s emphasis on diversifying the internal medicine workforce to reflect the communities.
Recent measures have included the creation of an ACP international medical graduate task force and establishing an antiharassment policy and reporting process.
“The conversation has started a lot more,” he said.
Dr. Candler reports financial relationships with Abbott, AbbVie, Johnson & Johnson, Merck, Medtronic, Pfizer, and other companies. She is also a member of the editorial advisory board of Internal Medicine News. Dr. Fox reports financial relationships with Obagi Cosmeceuticals. Dr. Liao reports financial relationships with Eli Lilly, Gilead, Johnson & Johnson, Novavax, and other companies. Dr. Abraham reports no relevant financial relationships.
AT INTERNAL MEDICINE 2022
Internet intervention improved insomnia in Black women
Data from previous studies suggest that women are up to 40% more likely to experience insomnia disorder compared with men, Eric S. Zhou, PhD, of Harvard Medical School, Boston, and colleagues wrote. The risk is even higher among Black women, but research on tailored treatments for this particular population has been limited.
In their study, published in JAMA Psychiatry, the researchers recruited women with elevated insomnia symptoms who were enrolled in the Black Women’s Health Study, an ongoing national, longitudinal research cohort in the United States. Participants were recruited between October 2019 and June 2020.The participants were randomized to an Internet-delivered behavior intervention (108 women), a stakeholder-informed Internet intervention tailored to Black women (110 women), or non-Internet patient education about sleep (115 women).
The Internet intervention, known as Sleep Healthy Using the Internet (SHUTi), was a 6-session program lasting 45-60 minutes per session and delivered over 6-9 weeks. The program included core elements of cognitive behavioral therapy and took into account information provided by patients about their baseline sleep function, treatment adherence, and sleep progress.
The tailored version of SHUTi for Black women (SHUTi-BWHS) was similar, but included Black actors for video vignettes and the inclusion of content about the cultural and social contexts in which insomnia often occurs for Black women, such while managing neighborhood noise and or living in crowded environments.
A third group received standard patient education material about sleep through a noninteractive website, and served as the control group.
The primary outcome of insomnia severity was measured using the Insomnia Severity Index (ISI), a 0- to 28-point scale. Scores for the ISI are based on responses to seven questions, including some that ask participants to rate the severity of their insomnia symptoms.
Clinically significant improvement in insomnia was defined as a reduction in score of more than 7 points. Patients were assessed at baseline, at 9 weeks, and again at approximately 6 months.
Significantly greater reductions in insomnia severity seen in intervention groups vs. control group
Overall, women randomized to SHUTi or SHUTi-BWHS) reported a significantly greater reduction in insomnia symptoms from baseline to 6 months, compared with the control group (P < .001), with ISI score decreases of 10.0, 9.3, and 3.6, respectively. No statistically significant differences in ISI score changes appeared between the between the SHUTi-BWHS and SHUTi groups.
Also, significantly more women in the SHUTi-BWHS group than in the SHUTi group completed the intervention (78.2% vs. 64.8%).
Treatment response was similar between the SHUTI-BWHS and SHUTi groups; 47.3% and 46.3%, respectively, had a decrease in ISI score of more than 7 points. In addition, 37% of women in the SHUTi-BWHS and 38% of women in the SHUTi groups reached ISI scores of less than 8 points, defined as full resolution of insomnia, by the last follow-up visit.
Both the SHUTi and SHUTi-BWHS interventions had dramatic effects on insomnia, but the increased number of women who completed the intervention in the SHUTi-BWHS group supports the value of tailored intervention, the researchers noted. “Similar to prior SHUTi trials, there was a direct association between the participant’s level of intervention engagement and their improvement in sleep.”
The average age of the participants was 60 years, 62% were single, and 44% had a graduate degree or higher. Approximately 5% were being actively treated for sleep apnea.
The study findings were limited by several factors including the relatively high socioeconomic status of the study participants, lack of data on medical mistrust, and inability to detect smaller differences between SHUTi and SHUTi-BWHS, the researchers noted.
Choose Internet-based CBT first for insomnia
“This was an excellent paper that sought to see the relative efficacy of standard version of Internet-delivered CBT-I [cognitive-behavioral therapy for insomnia] versus a culturally tailored version for Black women,” said Neil Skolnik, MD, professor of family and community medicine at Thomas Jefferson University, Philadelphia, in an interview. “The trial confirmed that, compared with sleep education, which was used as the control, Internet-delivered CBT-I is effective in the treatment of insomnia.”
“These results demonstrate two important things,” said Dr. Skolnik. “The most important is that Internet-delivered CBT-I works, and since it is both safe and effective, should be the first-line therapy for patients who want treatment for insomnia.”
Secondly, “the fact that more people completed culturally tailored versions suggests that, when culturally tailored versions are available, their use is preferable, as it might facilitate a higher proportion of patients being successful in their insomnia treatment,” he added.
The study was supported by the Patient-Centered Outcomes Research Institute. The Black Women’s Health Study is supported by the National Cancer Institute. Dr. Zhou disclosed support from both PCORI and the NCI during the study. Dr. Skolnik, who was not involved in the study, disclosed serving on the advisory board for Idorsia Pharmaceuticals. He is also a member of the editorial advisory board of Family Practice News.
Data from previous studies suggest that women are up to 40% more likely to experience insomnia disorder compared with men, Eric S. Zhou, PhD, of Harvard Medical School, Boston, and colleagues wrote. The risk is even higher among Black women, but research on tailored treatments for this particular population has been limited.
In their study, published in JAMA Psychiatry, the researchers recruited women with elevated insomnia symptoms who were enrolled in the Black Women’s Health Study, an ongoing national, longitudinal research cohort in the United States. Participants were recruited between October 2019 and June 2020.The participants were randomized to an Internet-delivered behavior intervention (108 women), a stakeholder-informed Internet intervention tailored to Black women (110 women), or non-Internet patient education about sleep (115 women).
The Internet intervention, known as Sleep Healthy Using the Internet (SHUTi), was a 6-session program lasting 45-60 minutes per session and delivered over 6-9 weeks. The program included core elements of cognitive behavioral therapy and took into account information provided by patients about their baseline sleep function, treatment adherence, and sleep progress.
The tailored version of SHUTi for Black women (SHUTi-BWHS) was similar, but included Black actors for video vignettes and the inclusion of content about the cultural and social contexts in which insomnia often occurs for Black women, such while managing neighborhood noise and or living in crowded environments.
A third group received standard patient education material about sleep through a noninteractive website, and served as the control group.
The primary outcome of insomnia severity was measured using the Insomnia Severity Index (ISI), a 0- to 28-point scale. Scores for the ISI are based on responses to seven questions, including some that ask participants to rate the severity of their insomnia symptoms.
Clinically significant improvement in insomnia was defined as a reduction in score of more than 7 points. Patients were assessed at baseline, at 9 weeks, and again at approximately 6 months.
Significantly greater reductions in insomnia severity seen in intervention groups vs. control group
Overall, women randomized to SHUTi or SHUTi-BWHS) reported a significantly greater reduction in insomnia symptoms from baseline to 6 months, compared with the control group (P < .001), with ISI score decreases of 10.0, 9.3, and 3.6, respectively. No statistically significant differences in ISI score changes appeared between the between the SHUTi-BWHS and SHUTi groups.
Also, significantly more women in the SHUTi-BWHS group than in the SHUTi group completed the intervention (78.2% vs. 64.8%).
Treatment response was similar between the SHUTI-BWHS and SHUTi groups; 47.3% and 46.3%, respectively, had a decrease in ISI score of more than 7 points. In addition, 37% of women in the SHUTi-BWHS and 38% of women in the SHUTi groups reached ISI scores of less than 8 points, defined as full resolution of insomnia, by the last follow-up visit.
Both the SHUTi and SHUTi-BWHS interventions had dramatic effects on insomnia, but the increased number of women who completed the intervention in the SHUTi-BWHS group supports the value of tailored intervention, the researchers noted. “Similar to prior SHUTi trials, there was a direct association between the participant’s level of intervention engagement and their improvement in sleep.”
The average age of the participants was 60 years, 62% were single, and 44% had a graduate degree or higher. Approximately 5% were being actively treated for sleep apnea.
The study findings were limited by several factors including the relatively high socioeconomic status of the study participants, lack of data on medical mistrust, and inability to detect smaller differences between SHUTi and SHUTi-BWHS, the researchers noted.
Choose Internet-based CBT first for insomnia
“This was an excellent paper that sought to see the relative efficacy of standard version of Internet-delivered CBT-I [cognitive-behavioral therapy for insomnia] versus a culturally tailored version for Black women,” said Neil Skolnik, MD, professor of family and community medicine at Thomas Jefferson University, Philadelphia, in an interview. “The trial confirmed that, compared with sleep education, which was used as the control, Internet-delivered CBT-I is effective in the treatment of insomnia.”
“These results demonstrate two important things,” said Dr. Skolnik. “The most important is that Internet-delivered CBT-I works, and since it is both safe and effective, should be the first-line therapy for patients who want treatment for insomnia.”
Secondly, “the fact that more people completed culturally tailored versions suggests that, when culturally tailored versions are available, their use is preferable, as it might facilitate a higher proportion of patients being successful in their insomnia treatment,” he added.
The study was supported by the Patient-Centered Outcomes Research Institute. The Black Women’s Health Study is supported by the National Cancer Institute. Dr. Zhou disclosed support from both PCORI and the NCI during the study. Dr. Skolnik, who was not involved in the study, disclosed serving on the advisory board for Idorsia Pharmaceuticals. He is also a member of the editorial advisory board of Family Practice News.
Data from previous studies suggest that women are up to 40% more likely to experience insomnia disorder compared with men, Eric S. Zhou, PhD, of Harvard Medical School, Boston, and colleagues wrote. The risk is even higher among Black women, but research on tailored treatments for this particular population has been limited.
In their study, published in JAMA Psychiatry, the researchers recruited women with elevated insomnia symptoms who were enrolled in the Black Women’s Health Study, an ongoing national, longitudinal research cohort in the United States. Participants were recruited between October 2019 and June 2020.The participants were randomized to an Internet-delivered behavior intervention (108 women), a stakeholder-informed Internet intervention tailored to Black women (110 women), or non-Internet patient education about sleep (115 women).
The Internet intervention, known as Sleep Healthy Using the Internet (SHUTi), was a 6-session program lasting 45-60 minutes per session and delivered over 6-9 weeks. The program included core elements of cognitive behavioral therapy and took into account information provided by patients about their baseline sleep function, treatment adherence, and sleep progress.
The tailored version of SHUTi for Black women (SHUTi-BWHS) was similar, but included Black actors for video vignettes and the inclusion of content about the cultural and social contexts in which insomnia often occurs for Black women, such while managing neighborhood noise and or living in crowded environments.
A third group received standard patient education material about sleep through a noninteractive website, and served as the control group.
The primary outcome of insomnia severity was measured using the Insomnia Severity Index (ISI), a 0- to 28-point scale. Scores for the ISI are based on responses to seven questions, including some that ask participants to rate the severity of their insomnia symptoms.
Clinically significant improvement in insomnia was defined as a reduction in score of more than 7 points. Patients were assessed at baseline, at 9 weeks, and again at approximately 6 months.
Significantly greater reductions in insomnia severity seen in intervention groups vs. control group
Overall, women randomized to SHUTi or SHUTi-BWHS) reported a significantly greater reduction in insomnia symptoms from baseline to 6 months, compared with the control group (P < .001), with ISI score decreases of 10.0, 9.3, and 3.6, respectively. No statistically significant differences in ISI score changes appeared between the between the SHUTi-BWHS and SHUTi groups.
Also, significantly more women in the SHUTi-BWHS group than in the SHUTi group completed the intervention (78.2% vs. 64.8%).
Treatment response was similar between the SHUTI-BWHS and SHUTi groups; 47.3% and 46.3%, respectively, had a decrease in ISI score of more than 7 points. In addition, 37% of women in the SHUTi-BWHS and 38% of women in the SHUTi groups reached ISI scores of less than 8 points, defined as full resolution of insomnia, by the last follow-up visit.
Both the SHUTi and SHUTi-BWHS interventions had dramatic effects on insomnia, but the increased number of women who completed the intervention in the SHUTi-BWHS group supports the value of tailored intervention, the researchers noted. “Similar to prior SHUTi trials, there was a direct association between the participant’s level of intervention engagement and their improvement in sleep.”
The average age of the participants was 60 years, 62% were single, and 44% had a graduate degree or higher. Approximately 5% were being actively treated for sleep apnea.
The study findings were limited by several factors including the relatively high socioeconomic status of the study participants, lack of data on medical mistrust, and inability to detect smaller differences between SHUTi and SHUTi-BWHS, the researchers noted.
Choose Internet-based CBT first for insomnia
“This was an excellent paper that sought to see the relative efficacy of standard version of Internet-delivered CBT-I [cognitive-behavioral therapy for insomnia] versus a culturally tailored version for Black women,” said Neil Skolnik, MD, professor of family and community medicine at Thomas Jefferson University, Philadelphia, in an interview. “The trial confirmed that, compared with sleep education, which was used as the control, Internet-delivered CBT-I is effective in the treatment of insomnia.”
“These results demonstrate two important things,” said Dr. Skolnik. “The most important is that Internet-delivered CBT-I works, and since it is both safe and effective, should be the first-line therapy for patients who want treatment for insomnia.”
Secondly, “the fact that more people completed culturally tailored versions suggests that, when culturally tailored versions are available, their use is preferable, as it might facilitate a higher proportion of patients being successful in their insomnia treatment,” he added.
The study was supported by the Patient-Centered Outcomes Research Institute. The Black Women’s Health Study is supported by the National Cancer Institute. Dr. Zhou disclosed support from both PCORI and the NCI during the study. Dr. Skolnik, who was not involved in the study, disclosed serving on the advisory board for Idorsia Pharmaceuticals. He is also a member of the editorial advisory board of Family Practice News.
FROM JAMA PSYCHIATRY
Black, senior patients more likely to get unneeded antibiotics
Black and senior patients are more likely to be overprescribed antibiotics, according to a new study of 7 billion trips to health care centers – findings that doctors say warrant a further look into unequal prescription practices.
Researchers at the University of Texas Health Science Center found that 64% of antibiotic prescriptions to Black patients and 74% of antibiotic prescriptions to patients aged 65 years and older were deemed inappropriate. White patients, meanwhile, received prescriptions that were deemed inappropriate 56% of the time.
Most of those prescriptions were written for conditions like nonbacterial skin problems, viral respiratory tract infections, and bronchitis – none of which can be treated with antibiotics.
The study – which used data from visits to U.S. doctors’ offices, hospitals, and EDs – will be presented at the 2022 European Congress of Clinical Microbiology & Infectious Diseases in Lisbon.
Researchers also found that 58% of antibiotic prescriptions to patients with a Hispanic or Latin American background were also not appropriate for use.
“Our results suggest that Black and [Hispanic/Latino] patients may be not be properly treated and are receiving antibiotic prescriptions even when not indicated,” researcher Eric Young, PharmD, said in a news release.
Doctors typically will prescribe an antibiotic if they fear a patient’s symptoms may lead to an infection, Dr. Young said. This is particularly true if the doctor believes a patient is unlikely to return for a follow-up, which, he says, “more frequently happens in minority populations.”
The Centers for Disease Control and Prevention estimates that at least 30% of outpatient antibiotic prescriptions are not needed, and up to 50% of antibiotics prescribed are either unnecessary or the wrong type and/or dosage.
Overprescribing of antibiotics has long plagued the medical field. In 2015, the administration of then-President Barack Obama released a National Action Plan for Combating Antibiotic-Resistant Bacteria, with a goal to cut unneeded outpatient antibiotic use by at least half by 2020.
When antibiotics are overused, bacteria that infect us evolve to become stronger and defeat the drugs meant to save us.
Though the findings still need more study, at first glance they provide a concerning but unsurprising look at health inequities, said Rachel Villanueva, MD, president of the National Medical Association, the leading organization representing doctors and patients of African descent.
“We do know that these kind of inequities have existed for a long time in our society,” said Dr. Villanueva, a clinical assistant professor at the New York University. “They’re not new and have been well documented for many, many years. But this deserves further research and further evaluation.”
“This is just the first step – we need to do some more evaluation on how different communities are treated in the health care system. Why is this occurring?”
For patients 65 and older, it may be less about bias and more about having a hard time diagnosing certain conditions within that population, said Preeti Malani, MD, a professor of infectious diseases at the University of Michigan, Ann Arbor, and director of the National Poll on Healthy Aging.
For example, she said, some older patients may have a harder time describing their symptoms. In some cases, doctors may give these patients a prescription to fill in case the issue does not clear up, because it could be harder for them to get back into the office.
“Sometimes it’s hard to know exactly what’s going on,” Dr. Malani said. “Something I’ve done in my own practice in the past is say, ‘I’m giving you a prescription, but I don’t want you to fill it yet.’”
Dr. Malani said inappropriately prescribing antibiotics can be especially dangerous for people 65 and older because of drug interactions and complications like Achilles tendon rupture and a Clostridioides difficile infection, which can arise after antibiotic use.
“We need more information on what drives this in older adults,” she said.
A version of this article first appeared on Medscape.com.
Black and senior patients are more likely to be overprescribed antibiotics, according to a new study of 7 billion trips to health care centers – findings that doctors say warrant a further look into unequal prescription practices.
Researchers at the University of Texas Health Science Center found that 64% of antibiotic prescriptions to Black patients and 74% of antibiotic prescriptions to patients aged 65 years and older were deemed inappropriate. White patients, meanwhile, received prescriptions that were deemed inappropriate 56% of the time.
Most of those prescriptions were written for conditions like nonbacterial skin problems, viral respiratory tract infections, and bronchitis – none of which can be treated with antibiotics.
The study – which used data from visits to U.S. doctors’ offices, hospitals, and EDs – will be presented at the 2022 European Congress of Clinical Microbiology & Infectious Diseases in Lisbon.
Researchers also found that 58% of antibiotic prescriptions to patients with a Hispanic or Latin American background were also not appropriate for use.
“Our results suggest that Black and [Hispanic/Latino] patients may be not be properly treated and are receiving antibiotic prescriptions even when not indicated,” researcher Eric Young, PharmD, said in a news release.
Doctors typically will prescribe an antibiotic if they fear a patient’s symptoms may lead to an infection, Dr. Young said. This is particularly true if the doctor believes a patient is unlikely to return for a follow-up, which, he says, “more frequently happens in minority populations.”
The Centers for Disease Control and Prevention estimates that at least 30% of outpatient antibiotic prescriptions are not needed, and up to 50% of antibiotics prescribed are either unnecessary or the wrong type and/or dosage.
Overprescribing of antibiotics has long plagued the medical field. In 2015, the administration of then-President Barack Obama released a National Action Plan for Combating Antibiotic-Resistant Bacteria, with a goal to cut unneeded outpatient antibiotic use by at least half by 2020.
When antibiotics are overused, bacteria that infect us evolve to become stronger and defeat the drugs meant to save us.
Though the findings still need more study, at first glance they provide a concerning but unsurprising look at health inequities, said Rachel Villanueva, MD, president of the National Medical Association, the leading organization representing doctors and patients of African descent.
“We do know that these kind of inequities have existed for a long time in our society,” said Dr. Villanueva, a clinical assistant professor at the New York University. “They’re not new and have been well documented for many, many years. But this deserves further research and further evaluation.”
“This is just the first step – we need to do some more evaluation on how different communities are treated in the health care system. Why is this occurring?”
For patients 65 and older, it may be less about bias and more about having a hard time diagnosing certain conditions within that population, said Preeti Malani, MD, a professor of infectious diseases at the University of Michigan, Ann Arbor, and director of the National Poll on Healthy Aging.
For example, she said, some older patients may have a harder time describing their symptoms. In some cases, doctors may give these patients a prescription to fill in case the issue does not clear up, because it could be harder for them to get back into the office.
“Sometimes it’s hard to know exactly what’s going on,” Dr. Malani said. “Something I’ve done in my own practice in the past is say, ‘I’m giving you a prescription, but I don’t want you to fill it yet.’”
Dr. Malani said inappropriately prescribing antibiotics can be especially dangerous for people 65 and older because of drug interactions and complications like Achilles tendon rupture and a Clostridioides difficile infection, which can arise after antibiotic use.
“We need more information on what drives this in older adults,” she said.
A version of this article first appeared on Medscape.com.
Black and senior patients are more likely to be overprescribed antibiotics, according to a new study of 7 billion trips to health care centers – findings that doctors say warrant a further look into unequal prescription practices.
Researchers at the University of Texas Health Science Center found that 64% of antibiotic prescriptions to Black patients and 74% of antibiotic prescriptions to patients aged 65 years and older were deemed inappropriate. White patients, meanwhile, received prescriptions that were deemed inappropriate 56% of the time.
Most of those prescriptions were written for conditions like nonbacterial skin problems, viral respiratory tract infections, and bronchitis – none of which can be treated with antibiotics.
The study – which used data from visits to U.S. doctors’ offices, hospitals, and EDs – will be presented at the 2022 European Congress of Clinical Microbiology & Infectious Diseases in Lisbon.
Researchers also found that 58% of antibiotic prescriptions to patients with a Hispanic or Latin American background were also not appropriate for use.
“Our results suggest that Black and [Hispanic/Latino] patients may be not be properly treated and are receiving antibiotic prescriptions even when not indicated,” researcher Eric Young, PharmD, said in a news release.
Doctors typically will prescribe an antibiotic if they fear a patient’s symptoms may lead to an infection, Dr. Young said. This is particularly true if the doctor believes a patient is unlikely to return for a follow-up, which, he says, “more frequently happens in minority populations.”
The Centers for Disease Control and Prevention estimates that at least 30% of outpatient antibiotic prescriptions are not needed, and up to 50% of antibiotics prescribed are either unnecessary or the wrong type and/or dosage.
Overprescribing of antibiotics has long plagued the medical field. In 2015, the administration of then-President Barack Obama released a National Action Plan for Combating Antibiotic-Resistant Bacteria, with a goal to cut unneeded outpatient antibiotic use by at least half by 2020.
When antibiotics are overused, bacteria that infect us evolve to become stronger and defeat the drugs meant to save us.
Though the findings still need more study, at first glance they provide a concerning but unsurprising look at health inequities, said Rachel Villanueva, MD, president of the National Medical Association, the leading organization representing doctors and patients of African descent.
“We do know that these kind of inequities have existed for a long time in our society,” said Dr. Villanueva, a clinical assistant professor at the New York University. “They’re not new and have been well documented for many, many years. But this deserves further research and further evaluation.”
“This is just the first step – we need to do some more evaluation on how different communities are treated in the health care system. Why is this occurring?”
For patients 65 and older, it may be less about bias and more about having a hard time diagnosing certain conditions within that population, said Preeti Malani, MD, a professor of infectious diseases at the University of Michigan, Ann Arbor, and director of the National Poll on Healthy Aging.
For example, she said, some older patients may have a harder time describing their symptoms. In some cases, doctors may give these patients a prescription to fill in case the issue does not clear up, because it could be harder for them to get back into the office.
“Sometimes it’s hard to know exactly what’s going on,” Dr. Malani said. “Something I’ve done in my own practice in the past is say, ‘I’m giving you a prescription, but I don’t want you to fill it yet.’”
Dr. Malani said inappropriately prescribing antibiotics can be especially dangerous for people 65 and older because of drug interactions and complications like Achilles tendon rupture and a Clostridioides difficile infection, which can arise after antibiotic use.
“We need more information on what drives this in older adults,” she said.
A version of this article first appeared on Medscape.com.
Fetuses suffer the effects of poverty in the womb
Poverty is known to be associated with poor health outcomes throughout life. Now, new research has shown that, from as early as the second trimester of pregnancy, fetuses are already feeling the effects of poverty.
“There is a well-recognized health inequality where quality and duration of life are lower among the most poor. This divide is present both within and between countries,” said Steve Turner, who led the study.
Given the association of poverty and low birth weight, the authors of the new multi-national study, published in the Journal of Epidemiology and Community Health, hypothesized that “individuals from highest household income compared to those with lowest household income will have increased fetal size in the second and third trimester and birth.”
For their study, researchers from the University of Aberdeen gathered details of ante-natal and birth size – second and third trimester fetal ultrasound measurements of estimated fetal weight, biparietal diameter, and femur length, as well as birth measurements of weight, occipitofrontal circumference, and crown heel length – from eight cohorts that included 21,714 individuals from nations including Scotland, England, Saudi Arabia, the U.S., Netherlands, Spain, Norway, Sweden, and France.
They then related these to household income, taking into account other factors, including mother’s age, height, number of other children, and smoking, analyzing the data using cross-sectional two-stage individual patient data analyses and a longitudinal one-stage individual patient data analysis.
Household income closely related to birth size
The authors found that higher household income was associated with larger fetal head size and weight but not length, from the second half of pregnancy, compared with lowest household income. They said that their results argue for “a relationship where household income is closely related to birth size.”
The results showed that, across the countries studied, babies were smaller at birth if they came from a lower income household, and this discrepancy in size was already apparent at 20 weeks gestation.
“This is the first time that size differences have been found at such an early stage of development,” the authors said, “and also the first time it has been compared across continents.”
Professor Turner pointed out that “what this study shows is that the inequality, as seen by reduced size in fetal life, is present long before birth, and this poverty gap widens between twenty weeks gestation and birth.”
He added: “Basically, regardless of whether you live in Saudi, the U.S., or Europe, and accounting for things that might affect fetal growth, if your parents are poor, you will be smaller before birth and at birth compared to if your parents were not poor.”
Increase engagement with pregnant mothers living in poverty
He emphasized how this was problematic, as small size before and after birth puts an individual at “increased risk for many serious illnesses in later life.”
The authors hope that this study will encourage health care providers to recognize the health risks associated with lower income for mothers and their unborn children and to provide more support and guidance to mitigate the risks.
They said, “interventions aimed at softening the impact of poverty on pregnant mothers could reduce incidence of small for gestational age and the associated burden of excessive morbidity and mortality throughout the life course.”
Professor Turner described how the mechanisms that drive this inequity may be explained by pregnant mothers from poor households having difficulty in accessing or engaging with antenatal care.
“We would like to see health care providers around the world strive to increase engagement with pregnant mothers living in poverty,” he said. “This engagement will reward all of society by putting unborn children on a trajectory to longer and healthier lives.”
A version of this article first appeared on Medscape UK.
Poverty is known to be associated with poor health outcomes throughout life. Now, new research has shown that, from as early as the second trimester of pregnancy, fetuses are already feeling the effects of poverty.
“There is a well-recognized health inequality where quality and duration of life are lower among the most poor. This divide is present both within and between countries,” said Steve Turner, who led the study.
Given the association of poverty and low birth weight, the authors of the new multi-national study, published in the Journal of Epidemiology and Community Health, hypothesized that “individuals from highest household income compared to those with lowest household income will have increased fetal size in the second and third trimester and birth.”
For their study, researchers from the University of Aberdeen gathered details of ante-natal and birth size – second and third trimester fetal ultrasound measurements of estimated fetal weight, biparietal diameter, and femur length, as well as birth measurements of weight, occipitofrontal circumference, and crown heel length – from eight cohorts that included 21,714 individuals from nations including Scotland, England, Saudi Arabia, the U.S., Netherlands, Spain, Norway, Sweden, and France.
They then related these to household income, taking into account other factors, including mother’s age, height, number of other children, and smoking, analyzing the data using cross-sectional two-stage individual patient data analyses and a longitudinal one-stage individual patient data analysis.
Household income closely related to birth size
The authors found that higher household income was associated with larger fetal head size and weight but not length, from the second half of pregnancy, compared with lowest household income. They said that their results argue for “a relationship where household income is closely related to birth size.”
The results showed that, across the countries studied, babies were smaller at birth if they came from a lower income household, and this discrepancy in size was already apparent at 20 weeks gestation.
“This is the first time that size differences have been found at such an early stage of development,” the authors said, “and also the first time it has been compared across continents.”
Professor Turner pointed out that “what this study shows is that the inequality, as seen by reduced size in fetal life, is present long before birth, and this poverty gap widens between twenty weeks gestation and birth.”
He added: “Basically, regardless of whether you live in Saudi, the U.S., or Europe, and accounting for things that might affect fetal growth, if your parents are poor, you will be smaller before birth and at birth compared to if your parents were not poor.”
Increase engagement with pregnant mothers living in poverty
He emphasized how this was problematic, as small size before and after birth puts an individual at “increased risk for many serious illnesses in later life.”
The authors hope that this study will encourage health care providers to recognize the health risks associated with lower income for mothers and their unborn children and to provide more support and guidance to mitigate the risks.
They said, “interventions aimed at softening the impact of poverty on pregnant mothers could reduce incidence of small for gestational age and the associated burden of excessive morbidity and mortality throughout the life course.”
Professor Turner described how the mechanisms that drive this inequity may be explained by pregnant mothers from poor households having difficulty in accessing or engaging with antenatal care.
“We would like to see health care providers around the world strive to increase engagement with pregnant mothers living in poverty,” he said. “This engagement will reward all of society by putting unborn children on a trajectory to longer and healthier lives.”
A version of this article first appeared on Medscape UK.
Poverty is known to be associated with poor health outcomes throughout life. Now, new research has shown that, from as early as the second trimester of pregnancy, fetuses are already feeling the effects of poverty.
“There is a well-recognized health inequality where quality and duration of life are lower among the most poor. This divide is present both within and between countries,” said Steve Turner, who led the study.
Given the association of poverty and low birth weight, the authors of the new multi-national study, published in the Journal of Epidemiology and Community Health, hypothesized that “individuals from highest household income compared to those with lowest household income will have increased fetal size in the second and third trimester and birth.”
For their study, researchers from the University of Aberdeen gathered details of ante-natal and birth size – second and third trimester fetal ultrasound measurements of estimated fetal weight, biparietal diameter, and femur length, as well as birth measurements of weight, occipitofrontal circumference, and crown heel length – from eight cohorts that included 21,714 individuals from nations including Scotland, England, Saudi Arabia, the U.S., Netherlands, Spain, Norway, Sweden, and France.
They then related these to household income, taking into account other factors, including mother’s age, height, number of other children, and smoking, analyzing the data using cross-sectional two-stage individual patient data analyses and a longitudinal one-stage individual patient data analysis.
Household income closely related to birth size
The authors found that higher household income was associated with larger fetal head size and weight but not length, from the second half of pregnancy, compared with lowest household income. They said that their results argue for “a relationship where household income is closely related to birth size.”
The results showed that, across the countries studied, babies were smaller at birth if they came from a lower income household, and this discrepancy in size was already apparent at 20 weeks gestation.
“This is the first time that size differences have been found at such an early stage of development,” the authors said, “and also the first time it has been compared across continents.”
Professor Turner pointed out that “what this study shows is that the inequality, as seen by reduced size in fetal life, is present long before birth, and this poverty gap widens between twenty weeks gestation and birth.”
He added: “Basically, regardless of whether you live in Saudi, the U.S., or Europe, and accounting for things that might affect fetal growth, if your parents are poor, you will be smaller before birth and at birth compared to if your parents were not poor.”
Increase engagement with pregnant mothers living in poverty
He emphasized how this was problematic, as small size before and after birth puts an individual at “increased risk for many serious illnesses in later life.”
The authors hope that this study will encourage health care providers to recognize the health risks associated with lower income for mothers and their unborn children and to provide more support and guidance to mitigate the risks.
They said, “interventions aimed at softening the impact of poverty on pregnant mothers could reduce incidence of small for gestational age and the associated burden of excessive morbidity and mortality throughout the life course.”
Professor Turner described how the mechanisms that drive this inequity may be explained by pregnant mothers from poor households having difficulty in accessing or engaging with antenatal care.
“We would like to see health care providers around the world strive to increase engagement with pregnant mothers living in poverty,” he said. “This engagement will reward all of society by putting unborn children on a trajectory to longer and healthier lives.”
A version of this article first appeared on Medscape UK.
FROM THE JOURNAL OF EPIDEMIOLOGY AND COMMUNITY HEALTH
Women in rheumatology: A look back, a look forward
Jean Liew, MD, recalls the long list of women mentors who have guided her career in rheumatology.
It started during her residency, when Jennifer Barton, MD, at Oregon Health & Science University, Portland, exposed her to new ways of conducting clinical research on patient outcomes.
In fellowship, she met Lianne Gensler, MD, a leader in axial spondyloarthritis, at the annual meeting of the American College of Rheumatology. Through Dr. Gensler’s mentorship and sponsorship, she was introduced to Maureen Dubreuil, MD, at Boston University, whose research focuses on pharmacoepidemiologic approaches using large databases.
Dr. Liew currently practices rheumatology under the leadership of Tuhina Neogi, MD, a world-renowned expert in osteoarthritis and gout. “She’s my research mentor,” Dr. Liew, an assistant professor of medicine at Boston University, said in an interview.
Her academic timeline reflects the powerful network and influence of women rheumatologists, who represent half of the adult rheumatology workforce in the United States. “In the research arena, many experts are women and they serve as role models and mentors to many,” Dr. Liew said.
But there’s more work to do, she and others acknowledged.
Rheumatology faces ongoing workforce shortages while struggling with a gender gap that’s closing but not as quickly as many women rheumatologists would like to see.
The gap persists, despite overall gains in the field of medicine, Vaneet Sandhu, MD, a rheumatologist with Loma Linda (Calif.) University, said in an interview. Women have exceeded men as enrollees in medical colleges, reported the Association of American Medical Colleges. And yet, “our colleagues reported last year that, in academic rheumatology, women are less likely to be full or associate professors than men,” she said.
The odds of being a fellowship program director or division director is similar in both males and females. “So, we’ve had some gains, but there’s always room for more,” Dr. Sandhu said.
Too few physicians
The next 10 years forecasts a dearth in American physicians.
AAMC projects a shortage of 124,000 doctors in the United States by 2034. Following on a similar trajectory, the ACR in 2015 anticipated a 25% drop in the supply of rheumatology clinical providers by 2030, with demand exceeding supply by more than 4,100 clinical employees.
The ACR’s workforce study projected that more women would come into rheumatology, noted Marcy Bolster, MD, director of the rheumatology fellowship training program at Massachusetts General Hospital, Boston. Women make up at least 50% of the workforce and 66% of fellows If these numbers hold, “we’ll definitely see an increase in the percent of women in the workforce” moving forward, Dr. Bolster said in an interview.
Women have helped the shortage to a great extent, said Nilanjana Bose, MD, a rheumatologist at Lonestar Rheumatology, Houston.
The work-life balance that rheumatology offers, combined with its focus on the cognitive part of internal medicine, explains why the field has attracted so many women. Rheumatology provides flexible work options. Women “get to teach or do rounds in the hospital or have a private practice where you’re mostly outpatient with some hospital work,” Dr. Bose said in an interview.
With anticipated shortages looming over the next decade, the profession needs to be cognizant of the different demands women face in their careers and how it can accommodate the workforce to meet the needs of its providers and maintain access for patients, Dr. Bolster said.
There are many innovative ways to match the demand for access. One thought is to create shared positions. Instead of employing four full-time physicians and one person part time, have two people who are working part time, Dr. Bolster suggested. “It is also important to not only expand our workforce with advanced practice providers, but to ensure their retention in the rheumatology workforce, to improve access to care for those with rheumatic diseases.”
Increasing the number of residency positions is another step toward addressing the shortage, Dr. Sandhu offered.
Women rheumatologists should make their voices heard by contacting members of Congress to support legislation that advocates for workforce shortage solutions, “in addition to generally supporting women’s rights and growth in the workplace,” she said.
The gender divide continues
Rosalind Ramsey-Goldman, MD, DrPH, remembers being the only woman in a group of five during her fellowship in the mid-1980s. Few women role models existed within the ACR, especially those in academic careers. “Now, most fellowships have more than 50% women, reflecting the number of women going to medical school,” said Dr. Ramsey-Goldman, Gallagher Research Professor in Rheumatology at Northwestern University and Northwestern Medicine, Chicago.
As more women enter the profession, women rheumatologists in academic rheumatology have started to outpace men in recent years. Some research suggests they’ve made headway in gaining leadership spots at institutions.
One recent paper, a cross-sectional national study of more than 6,100 rheumatologists, found that women had similar odds of attaining fellowship program or division director positions as men. As directors of training programs, women in rheumatology “instill this collaborative and growth mindset that encourages learners to self-reflect and work as a team,” Dr. Sandhu said.
Women bring a different perspective to training, and how curriculum works, Dr. Bose said. Studies have shown that women tend to be more empathic. They ask more questions. “That’s not to say men aren’t good. Women just have an inborn ability for connecting,” and this perspective helps to enrich the educational experience for trainees.
Women who lead training programs are also attuned to realities that female trainees confront, such as dealing with the challenges of achieving the best possible education while also raising a family, noted Graciela S. Alarcón, MD, MPH, who holds emeritus positions at the University of Alabama at Birmingham and the Universidad Peruana Cayetano Heredia in Lima, Peru.
“These program directors cultivate the ability to relate to women trainees in a very personal manner, supporting them in their efforts to achieve a balance between their training demands and their family/personal responsibilities,” she said.
Other research suggests the gender gap hasn’t gone away. Women continue to have lower odds of holding a higher-level professorship, receiving a federal grant, or speaking at academic conferences. They are also less likely to serve as first authors on rheumatology guidelines or recommendations.
Some studies suggest that women see fewer patients and earn less than their male counterparts. At peak difference, men can earn up to $100,000+ more than women. “My own impression is that it takes more efforts for women to reach the same level of recognition than men, and although overt discrimination is rare nowadays, subtle discrimination still occurs,” according to Dr. Alarcón.
Over a lifetime, female physicians can expect to earn less than their male counterparts, with clear implications for different retirement income levels, she said.
Fixing a leaky academic pipeline
The reality is the academic pipeline, and especially the physician-scientist pipeline, “continues to be leaky,” Dr. Liew said. “We know that caregivers to young children have larger barriers to surmount in academics and in research, and that there is a gender disparity present.” The toll of academic medicine on early career women who are parents is especially pronounced. While the pandemic has intensified this problem, it was around pre-COVID, she added.
Women who start in academia as academic clinicians or clinician researchers aren’t always able to meet their goals for promotion within the appropriate time frame. This is because of inequities in the system and lack of support related to maternity leave, childcare, and other issues. As a result, they leave academia and go into private practice or industry, Dr. Liew said.
The ACR in its 2015 survey projected that more women would be seeking part-time positions.
The good news is many academic institutions are taking a more equitable view about different career paths, offering equal parental leave to both men and women, Dr. Bolster noted. “It is essential that workforce planning encompasses the changing responsibilities within families and account for more parental leave by both men and women.” If certain projections come true, with 50% of the profession retiring between 2015 and 2030, combined with more men and women working part time, “it is requisite that workforce strategies plan for this.”
When Dr. Ramsey-Goldman was a trainee and junior faculty, there were no formal maternity leave policies.
Now, this benefit is available, she said. In another critical change, the ACR has made childcare services and a lactation room available for young mothers during its annual meeting. “Virtual meetings afford further ways to interact with colleagues,” she added.
Whether women choose to stay in academia or go into clinical practice is a very personal decision. “But it is also fair that, in some programs, training directors and faculty members can encourage trainees toward academia and its fascinating research possibilities,” Dr. Alarcón offered.
Making gains in research
Women are increasingly driving groundbreaking rheumatology research at all levels, Dr. Sandhu said. “And women empower women. Not infrequently, our female leaders, veterans in rheumatology research, seek younger female rheumatologists to help them grow in their niches. This has been one of the most beautiful things of the sisterhood in rheumatology that I have been blessed to be part of.”
In pediatric rheumatology, young female researchers are leading global research efforts. Some standouts include Kate Webb, MD, a pediatric rheumatologist in Cape Town, South Africa, and scientist who has worked on multisystem inflammatory syndrome during the pandemic. Sheila Angeles-Han, MD, who works on uveitis in juvenile idiopathic arthritis, had a role in recent ACR guidelines. Laura Lewandowski, MD, has also contributed to global rheumatology efforts, especially in low- and middle-income countries, Dr. Liew said.
The 2021 ACR annual meeting highlighted the research efforts of women rheumatologists from around the world. A global rheumatology summit at the meeting featured many women voices, including Dzifa Dey, MD, from Ghana, who received the ACR Distinguished International Rheumatology Professional Award. Ashira Blazer, MD, and Irene Blanco, MD, have spearheaded the ACR’s diversity, equity, and inclusion initiatives.
Women researchers have many opportunities to study rheumatologic diseases that disproportionately affect women, Dr. Alarcón said.
Lupus, for example, affects women in a much higher proportion than men (90% vs. 10%). This may be an attractive target for the best and brightest among future women researchers, Dr. Alarcón suggested. “It is a fact that publications related to lupus in leading internal medicine and rheumatology journals often include women either as first or senior authors. In that context, it can be said that several advances in the study of lupus worldwide can be attributed to women.”
This applies to disparities in social determinants of health that account for extremely complex outcomes in lupus among women of color, compared with White women, in addition to the costs associated with the disease and its impact on morbidity, mortality, and quality of life.
Women rheumatologists have advanced the work in reproductive management of rheumatic diseases, including a recent ACR-endorsed publication that provides formal guidance on managing reproductive health in women with rheumatic disease, Dr. Sandhu said. “One thing is clear: Without women, the work on reproductive diseases in rheumatology to date would not likely be where it is.”
Dr. Ramsey-Goldman added that “this critical work will not only set the stage for clinical care of both women and men regarding their reproductive health but will also inform education strategies for trainees and future research activities, and help direct policy regarding access to care, medication development, and costs of treatment.”
Obtaining grant funding to support salaries and researcher endeavors remains a challenge, Dr. Liew said. “It takes working evenings, weekends, and holidays to meet those goals within a set time frame. So you can see why a female faculty member with children might be disadvantaged, compared to a male counterpart without children.”
Competition for grant funding remains fierce as budgets become tighter, she added.
“We will lose a lot more brilliant and compassionate rheumatologists (clinicians, physician-scientists, and scientists alike) if we do not think of ways to make things more equitable or do not acknowledge the privileges that support some to continued career successes and leave others behind,” Dr. Liew said.
Women who choose a research field should seek out mentor and financial support that will allow them enough protected time to balance out research with other clinical activities, such as teaching and patient care, Dr. Alarcón said.
Training directors, mentors, and faculty should prioritize the needs of current and future women researchers, she said. “The guidance provided to young female trainees toward a successful research career is a formidable challenge that may provide, in turn, enormous satisfaction. There are established avenues to seek funding as new investigators.”
Progress in diversity
Rheumatology as a field is attracting more candidates and all races and genders, Dr. Bose said. “I think in the coming years we will see more and more women from minorities being incorporated into the rheumatology workforce.”
Others would like to see further improvements in diversity and attracting women from historically excluded backgrounds. Patients will benefit from rheumatologists who are able to connect with them through shared languages, cultures, and other life experiences, Dr. Liew said. “It is imperative that we work on recruitment, mentorship, and retention in this regard.”
While the representation of women of color is still inadequate, there has been some progress, Dr. Sandhu said. The number of female Hispanic, Latinx, and Black or African American graduates from medical school has seen a steady rise since 2017. And, AAMC has established task forces such as the Women of Color Initiative to identify strategies for furthering the careers of women of color in academic medicine.
“There’s still a lot of room to grow. I am, however, proud to say we will finally have a woman of color as the president of ACR in 2023,” said Dr. Sandhu, referring to Deborah Dyett Desir, MD.
Dr. Desir discussed the importance of diversifying the ACR in a recent interview.
All rheumatologists know that there is a place for them in the ACR, she stressed. “The demographics of our membership should reflect that of our population.”
As growth in diverse representation occurs, so will recruitment, retention, and a greater awareness and distribution of knowledge and means to address implicit biases and microaggressions, Dr. Sandhu said. “We will see a greater quality of health care, where patients may feel more connected to someone they can identify with.”
Looking ahead
Dr. Alarcón expects women to continue to play a major role in rheumatology, not just in research, education, and patient care but in leadership of academic societies and professional organizations.
“Women in rheumatology have come a long way – a piece of history that I have been fortunate to witness from my beginnings in the early 1970s. We have, I think, paved the way for the next generations of leaders in our beloved specialty field.”
Dr. Bolster is a member of the ACR board of directors and board liaison of the ACR Workforce Solutions Committee. Dr. Ramsey-Goldman has been a GlaxoSmithKline consultant for lupus studies, a consultant and site investigator with Exagen Diagnostics for lupus biomarker studies, and a site investigator for Xencor and Horizon Pharma lupus trials. Dr. Sandhu serves on the ACR’s Committee on Rheumatology Training and Workforce Issues.
Related article
Pioneer days of rheumatology: One veteran looks back
Patricia Woo, CBE, FMedSci, FRCP, has seen it all.
As a member of the British Rheumatology Society and fellow of the Royal College of Physicians, she presented the case for and obtained official training approval for pediatric rheumatology in the 1990s. She also set the wheels in motion to form the Paediatric Rheumatology International Trials Organisation and the Paediatric Rheumatology European Society.
Now 74, Dr. Woo remembers the discrimination she faced in the 1970s. “I was told I couldn’t become an investigator or consultant if I were to marry or have children.” Around the same time, she found out a male clinician researcher didn’t want to work with her, not because of her qualifications, but because she was a woman.
That wouldn’t happen now with all the antidiscrimination laws in place, noted Dr. Woo, an emeritus professor of pediatric rheumatology and previous head of the Centre for Paediatric and Adolescent Rheumatology at UCL, London. Looking at the advances made by women in rheumatology, “there’s a major difference between 3 decades ago and today. If anyone discriminates today, they are called out.”
As the founding president of the Paediatric Rheumatology European Society, Dr. Woo is one of many early trailblazers who weathered many changes and made gains in the profession.
It’s important to recognize the work of Barbara Ansell, MD, the founder of pediatric rheumatology in the Canadian Red Cross Memorial Hospital, said Dr. Woo. Back in the 1960s, this wasn’t even a subspecialty. “Sick kids in general were taken either to pediatricians who didn’t know much about undescribed rheumatological conditions, and rheumatologists who didn’t know or have facilities for pediatric care.”
Dr. Ansell started this work, and Dr. Woo took over when she retired. With her colleagues, she set up a syllabus for pediatric rheumatology to formalize training for all junior doctors. This established a model of multidisciplinary clinical care and research. “Over the years, more women doctors have been attracted to pediatric rheumatology and have done well,” she said.
The rise of female leaders in rheumatology over the past few decades has been exponential, she continued. Women have become presidents of rheumatologic societies. Some established themselves as leaders in specific disciplines.
Carol Black, MD, from the United Kingdom is renowned for her international collaborative work in scleroderma research and clinical care. Patience White, MD in Washington, D.C., started research on the process of transitioning from childhood to adolescent to adult clinical care, a discipline that now has a strong international presence, Dr. Woo said.
The European Alliance of Associations for Rheumatology, which created a task force on gender equity in academic rheumatology, is evolving, she continued. The Academy of Medical Sciences in the United Kingdom also has active gender equality and mentoring programs, including a program to boost the careers of all researchers.
It’s also much easier now for women to become lead authors on papers since many are heads of lab or clinical services, Dr. Woo continued. “I don’t think there’s much discrimination if you’re a good clinician, and/or a good scientist. If women do their work well, they get the appropriate acknowledgment.”
Jean Liew, MD, recalls the long list of women mentors who have guided her career in rheumatology.
It started during her residency, when Jennifer Barton, MD, at Oregon Health & Science University, Portland, exposed her to new ways of conducting clinical research on patient outcomes.
In fellowship, she met Lianne Gensler, MD, a leader in axial spondyloarthritis, at the annual meeting of the American College of Rheumatology. Through Dr. Gensler’s mentorship and sponsorship, she was introduced to Maureen Dubreuil, MD, at Boston University, whose research focuses on pharmacoepidemiologic approaches using large databases.
Dr. Liew currently practices rheumatology under the leadership of Tuhina Neogi, MD, a world-renowned expert in osteoarthritis and gout. “She’s my research mentor,” Dr. Liew, an assistant professor of medicine at Boston University, said in an interview.
Her academic timeline reflects the powerful network and influence of women rheumatologists, who represent half of the adult rheumatology workforce in the United States. “In the research arena, many experts are women and they serve as role models and mentors to many,” Dr. Liew said.
But there’s more work to do, she and others acknowledged.
Rheumatology faces ongoing workforce shortages while struggling with a gender gap that’s closing but not as quickly as many women rheumatologists would like to see.
The gap persists, despite overall gains in the field of medicine, Vaneet Sandhu, MD, a rheumatologist with Loma Linda (Calif.) University, said in an interview. Women have exceeded men as enrollees in medical colleges, reported the Association of American Medical Colleges. And yet, “our colleagues reported last year that, in academic rheumatology, women are less likely to be full or associate professors than men,” she said.
The odds of being a fellowship program director or division director is similar in both males and females. “So, we’ve had some gains, but there’s always room for more,” Dr. Sandhu said.
Too few physicians
The next 10 years forecasts a dearth in American physicians.
AAMC projects a shortage of 124,000 doctors in the United States by 2034. Following on a similar trajectory, the ACR in 2015 anticipated a 25% drop in the supply of rheumatology clinical providers by 2030, with demand exceeding supply by more than 4,100 clinical employees.
The ACR’s workforce study projected that more women would come into rheumatology, noted Marcy Bolster, MD, director of the rheumatology fellowship training program at Massachusetts General Hospital, Boston. Women make up at least 50% of the workforce and 66% of fellows If these numbers hold, “we’ll definitely see an increase in the percent of women in the workforce” moving forward, Dr. Bolster said in an interview.
Women have helped the shortage to a great extent, said Nilanjana Bose, MD, a rheumatologist at Lonestar Rheumatology, Houston.
The work-life balance that rheumatology offers, combined with its focus on the cognitive part of internal medicine, explains why the field has attracted so many women. Rheumatology provides flexible work options. Women “get to teach or do rounds in the hospital or have a private practice where you’re mostly outpatient with some hospital work,” Dr. Bose said in an interview.
With anticipated shortages looming over the next decade, the profession needs to be cognizant of the different demands women face in their careers and how it can accommodate the workforce to meet the needs of its providers and maintain access for patients, Dr. Bolster said.
There are many innovative ways to match the demand for access. One thought is to create shared positions. Instead of employing four full-time physicians and one person part time, have two people who are working part time, Dr. Bolster suggested. “It is also important to not only expand our workforce with advanced practice providers, but to ensure their retention in the rheumatology workforce, to improve access to care for those with rheumatic diseases.”
Increasing the number of residency positions is another step toward addressing the shortage, Dr. Sandhu offered.
Women rheumatologists should make their voices heard by contacting members of Congress to support legislation that advocates for workforce shortage solutions, “in addition to generally supporting women’s rights and growth in the workplace,” she said.
The gender divide continues
Rosalind Ramsey-Goldman, MD, DrPH, remembers being the only woman in a group of five during her fellowship in the mid-1980s. Few women role models existed within the ACR, especially those in academic careers. “Now, most fellowships have more than 50% women, reflecting the number of women going to medical school,” said Dr. Ramsey-Goldman, Gallagher Research Professor in Rheumatology at Northwestern University and Northwestern Medicine, Chicago.
As more women enter the profession, women rheumatologists in academic rheumatology have started to outpace men in recent years. Some research suggests they’ve made headway in gaining leadership spots at institutions.
One recent paper, a cross-sectional national study of more than 6,100 rheumatologists, found that women had similar odds of attaining fellowship program or division director positions as men. As directors of training programs, women in rheumatology “instill this collaborative and growth mindset that encourages learners to self-reflect and work as a team,” Dr. Sandhu said.
Women bring a different perspective to training, and how curriculum works, Dr. Bose said. Studies have shown that women tend to be more empathic. They ask more questions. “That’s not to say men aren’t good. Women just have an inborn ability for connecting,” and this perspective helps to enrich the educational experience for trainees.
Women who lead training programs are also attuned to realities that female trainees confront, such as dealing with the challenges of achieving the best possible education while also raising a family, noted Graciela S. Alarcón, MD, MPH, who holds emeritus positions at the University of Alabama at Birmingham and the Universidad Peruana Cayetano Heredia in Lima, Peru.
“These program directors cultivate the ability to relate to women trainees in a very personal manner, supporting them in their efforts to achieve a balance between their training demands and their family/personal responsibilities,” she said.
Other research suggests the gender gap hasn’t gone away. Women continue to have lower odds of holding a higher-level professorship, receiving a federal grant, or speaking at academic conferences. They are also less likely to serve as first authors on rheumatology guidelines or recommendations.
Some studies suggest that women see fewer patients and earn less than their male counterparts. At peak difference, men can earn up to $100,000+ more than women. “My own impression is that it takes more efforts for women to reach the same level of recognition than men, and although overt discrimination is rare nowadays, subtle discrimination still occurs,” according to Dr. Alarcón.
Over a lifetime, female physicians can expect to earn less than their male counterparts, with clear implications for different retirement income levels, she said.
Fixing a leaky academic pipeline
The reality is the academic pipeline, and especially the physician-scientist pipeline, “continues to be leaky,” Dr. Liew said. “We know that caregivers to young children have larger barriers to surmount in academics and in research, and that there is a gender disparity present.” The toll of academic medicine on early career women who are parents is especially pronounced. While the pandemic has intensified this problem, it was around pre-COVID, she added.
Women who start in academia as academic clinicians or clinician researchers aren’t always able to meet their goals for promotion within the appropriate time frame. This is because of inequities in the system and lack of support related to maternity leave, childcare, and other issues. As a result, they leave academia and go into private practice or industry, Dr. Liew said.
The ACR in its 2015 survey projected that more women would be seeking part-time positions.
The good news is many academic institutions are taking a more equitable view about different career paths, offering equal parental leave to both men and women, Dr. Bolster noted. “It is essential that workforce planning encompasses the changing responsibilities within families and account for more parental leave by both men and women.” If certain projections come true, with 50% of the profession retiring between 2015 and 2030, combined with more men and women working part time, “it is requisite that workforce strategies plan for this.”
When Dr. Ramsey-Goldman was a trainee and junior faculty, there were no formal maternity leave policies.
Now, this benefit is available, she said. In another critical change, the ACR has made childcare services and a lactation room available for young mothers during its annual meeting. “Virtual meetings afford further ways to interact with colleagues,” she added.
Whether women choose to stay in academia or go into clinical practice is a very personal decision. “But it is also fair that, in some programs, training directors and faculty members can encourage trainees toward academia and its fascinating research possibilities,” Dr. Alarcón offered.
Making gains in research
Women are increasingly driving groundbreaking rheumatology research at all levels, Dr. Sandhu said. “And women empower women. Not infrequently, our female leaders, veterans in rheumatology research, seek younger female rheumatologists to help them grow in their niches. This has been one of the most beautiful things of the sisterhood in rheumatology that I have been blessed to be part of.”
In pediatric rheumatology, young female researchers are leading global research efforts. Some standouts include Kate Webb, MD, a pediatric rheumatologist in Cape Town, South Africa, and scientist who has worked on multisystem inflammatory syndrome during the pandemic. Sheila Angeles-Han, MD, who works on uveitis in juvenile idiopathic arthritis, had a role in recent ACR guidelines. Laura Lewandowski, MD, has also contributed to global rheumatology efforts, especially in low- and middle-income countries, Dr. Liew said.
The 2021 ACR annual meeting highlighted the research efforts of women rheumatologists from around the world. A global rheumatology summit at the meeting featured many women voices, including Dzifa Dey, MD, from Ghana, who received the ACR Distinguished International Rheumatology Professional Award. Ashira Blazer, MD, and Irene Blanco, MD, have spearheaded the ACR’s diversity, equity, and inclusion initiatives.
Women researchers have many opportunities to study rheumatologic diseases that disproportionately affect women, Dr. Alarcón said.
Lupus, for example, affects women in a much higher proportion than men (90% vs. 10%). This may be an attractive target for the best and brightest among future women researchers, Dr. Alarcón suggested. “It is a fact that publications related to lupus in leading internal medicine and rheumatology journals often include women either as first or senior authors. In that context, it can be said that several advances in the study of lupus worldwide can be attributed to women.”
This applies to disparities in social determinants of health that account for extremely complex outcomes in lupus among women of color, compared with White women, in addition to the costs associated with the disease and its impact on morbidity, mortality, and quality of life.
Women rheumatologists have advanced the work in reproductive management of rheumatic diseases, including a recent ACR-endorsed publication that provides formal guidance on managing reproductive health in women with rheumatic disease, Dr. Sandhu said. “One thing is clear: Without women, the work on reproductive diseases in rheumatology to date would not likely be where it is.”
Dr. Ramsey-Goldman added that “this critical work will not only set the stage for clinical care of both women and men regarding their reproductive health but will also inform education strategies for trainees and future research activities, and help direct policy regarding access to care, medication development, and costs of treatment.”
Obtaining grant funding to support salaries and researcher endeavors remains a challenge, Dr. Liew said. “It takes working evenings, weekends, and holidays to meet those goals within a set time frame. So you can see why a female faculty member with children might be disadvantaged, compared to a male counterpart without children.”
Competition for grant funding remains fierce as budgets become tighter, she added.
“We will lose a lot more brilliant and compassionate rheumatologists (clinicians, physician-scientists, and scientists alike) if we do not think of ways to make things more equitable or do not acknowledge the privileges that support some to continued career successes and leave others behind,” Dr. Liew said.
Women who choose a research field should seek out mentor and financial support that will allow them enough protected time to balance out research with other clinical activities, such as teaching and patient care, Dr. Alarcón said.
Training directors, mentors, and faculty should prioritize the needs of current and future women researchers, she said. “The guidance provided to young female trainees toward a successful research career is a formidable challenge that may provide, in turn, enormous satisfaction. There are established avenues to seek funding as new investigators.”
Progress in diversity
Rheumatology as a field is attracting more candidates and all races and genders, Dr. Bose said. “I think in the coming years we will see more and more women from minorities being incorporated into the rheumatology workforce.”
Others would like to see further improvements in diversity and attracting women from historically excluded backgrounds. Patients will benefit from rheumatologists who are able to connect with them through shared languages, cultures, and other life experiences, Dr. Liew said. “It is imperative that we work on recruitment, mentorship, and retention in this regard.”
While the representation of women of color is still inadequate, there has been some progress, Dr. Sandhu said. The number of female Hispanic, Latinx, and Black or African American graduates from medical school has seen a steady rise since 2017. And, AAMC has established task forces such as the Women of Color Initiative to identify strategies for furthering the careers of women of color in academic medicine.
“There’s still a lot of room to grow. I am, however, proud to say we will finally have a woman of color as the president of ACR in 2023,” said Dr. Sandhu, referring to Deborah Dyett Desir, MD.
Dr. Desir discussed the importance of diversifying the ACR in a recent interview.
All rheumatologists know that there is a place for them in the ACR, she stressed. “The demographics of our membership should reflect that of our population.”
As growth in diverse representation occurs, so will recruitment, retention, and a greater awareness and distribution of knowledge and means to address implicit biases and microaggressions, Dr. Sandhu said. “We will see a greater quality of health care, where patients may feel more connected to someone they can identify with.”
Looking ahead
Dr. Alarcón expects women to continue to play a major role in rheumatology, not just in research, education, and patient care but in leadership of academic societies and professional organizations.
“Women in rheumatology have come a long way – a piece of history that I have been fortunate to witness from my beginnings in the early 1970s. We have, I think, paved the way for the next generations of leaders in our beloved specialty field.”
Dr. Bolster is a member of the ACR board of directors and board liaison of the ACR Workforce Solutions Committee. Dr. Ramsey-Goldman has been a GlaxoSmithKline consultant for lupus studies, a consultant and site investigator with Exagen Diagnostics for lupus biomarker studies, and a site investigator for Xencor and Horizon Pharma lupus trials. Dr. Sandhu serves on the ACR’s Committee on Rheumatology Training and Workforce Issues.
Related article
Pioneer days of rheumatology: One veteran looks back
Patricia Woo, CBE, FMedSci, FRCP, has seen it all.
As a member of the British Rheumatology Society and fellow of the Royal College of Physicians, she presented the case for and obtained official training approval for pediatric rheumatology in the 1990s. She also set the wheels in motion to form the Paediatric Rheumatology International Trials Organisation and the Paediatric Rheumatology European Society.
Now 74, Dr. Woo remembers the discrimination she faced in the 1970s. “I was told I couldn’t become an investigator or consultant if I were to marry or have children.” Around the same time, she found out a male clinician researcher didn’t want to work with her, not because of her qualifications, but because she was a woman.
That wouldn’t happen now with all the antidiscrimination laws in place, noted Dr. Woo, an emeritus professor of pediatric rheumatology and previous head of the Centre for Paediatric and Adolescent Rheumatology at UCL, London. Looking at the advances made by women in rheumatology, “there’s a major difference between 3 decades ago and today. If anyone discriminates today, they are called out.”
As the founding president of the Paediatric Rheumatology European Society, Dr. Woo is one of many early trailblazers who weathered many changes and made gains in the profession.
It’s important to recognize the work of Barbara Ansell, MD, the founder of pediatric rheumatology in the Canadian Red Cross Memorial Hospital, said Dr. Woo. Back in the 1960s, this wasn’t even a subspecialty. “Sick kids in general were taken either to pediatricians who didn’t know much about undescribed rheumatological conditions, and rheumatologists who didn’t know or have facilities for pediatric care.”
Dr. Ansell started this work, and Dr. Woo took over when she retired. With her colleagues, she set up a syllabus for pediatric rheumatology to formalize training for all junior doctors. This established a model of multidisciplinary clinical care and research. “Over the years, more women doctors have been attracted to pediatric rheumatology and have done well,” she said.
The rise of female leaders in rheumatology over the past few decades has been exponential, she continued. Women have become presidents of rheumatologic societies. Some established themselves as leaders in specific disciplines.
Carol Black, MD, from the United Kingdom is renowned for her international collaborative work in scleroderma research and clinical care. Patience White, MD in Washington, D.C., started research on the process of transitioning from childhood to adolescent to adult clinical care, a discipline that now has a strong international presence, Dr. Woo said.
The European Alliance of Associations for Rheumatology, which created a task force on gender equity in academic rheumatology, is evolving, she continued. The Academy of Medical Sciences in the United Kingdom also has active gender equality and mentoring programs, including a program to boost the careers of all researchers.
It’s also much easier now for women to become lead authors on papers since many are heads of lab or clinical services, Dr. Woo continued. “I don’t think there’s much discrimination if you’re a good clinician, and/or a good scientist. If women do their work well, they get the appropriate acknowledgment.”
Jean Liew, MD, recalls the long list of women mentors who have guided her career in rheumatology.
It started during her residency, when Jennifer Barton, MD, at Oregon Health & Science University, Portland, exposed her to new ways of conducting clinical research on patient outcomes.
In fellowship, she met Lianne Gensler, MD, a leader in axial spondyloarthritis, at the annual meeting of the American College of Rheumatology. Through Dr. Gensler’s mentorship and sponsorship, she was introduced to Maureen Dubreuil, MD, at Boston University, whose research focuses on pharmacoepidemiologic approaches using large databases.
Dr. Liew currently practices rheumatology under the leadership of Tuhina Neogi, MD, a world-renowned expert in osteoarthritis and gout. “She’s my research mentor,” Dr. Liew, an assistant professor of medicine at Boston University, said in an interview.
Her academic timeline reflects the powerful network and influence of women rheumatologists, who represent half of the adult rheumatology workforce in the United States. “In the research arena, many experts are women and they serve as role models and mentors to many,” Dr. Liew said.
But there’s more work to do, she and others acknowledged.
Rheumatology faces ongoing workforce shortages while struggling with a gender gap that’s closing but not as quickly as many women rheumatologists would like to see.
The gap persists, despite overall gains in the field of medicine, Vaneet Sandhu, MD, a rheumatologist with Loma Linda (Calif.) University, said in an interview. Women have exceeded men as enrollees in medical colleges, reported the Association of American Medical Colleges. And yet, “our colleagues reported last year that, in academic rheumatology, women are less likely to be full or associate professors than men,” she said.
The odds of being a fellowship program director or division director is similar in both males and females. “So, we’ve had some gains, but there’s always room for more,” Dr. Sandhu said.
Too few physicians
The next 10 years forecasts a dearth in American physicians.
AAMC projects a shortage of 124,000 doctors in the United States by 2034. Following on a similar trajectory, the ACR in 2015 anticipated a 25% drop in the supply of rheumatology clinical providers by 2030, with demand exceeding supply by more than 4,100 clinical employees.
The ACR’s workforce study projected that more women would come into rheumatology, noted Marcy Bolster, MD, director of the rheumatology fellowship training program at Massachusetts General Hospital, Boston. Women make up at least 50% of the workforce and 66% of fellows If these numbers hold, “we’ll definitely see an increase in the percent of women in the workforce” moving forward, Dr. Bolster said in an interview.
Women have helped the shortage to a great extent, said Nilanjana Bose, MD, a rheumatologist at Lonestar Rheumatology, Houston.
The work-life balance that rheumatology offers, combined with its focus on the cognitive part of internal medicine, explains why the field has attracted so many women. Rheumatology provides flexible work options. Women “get to teach or do rounds in the hospital or have a private practice where you’re mostly outpatient with some hospital work,” Dr. Bose said in an interview.
With anticipated shortages looming over the next decade, the profession needs to be cognizant of the different demands women face in their careers and how it can accommodate the workforce to meet the needs of its providers and maintain access for patients, Dr. Bolster said.
There are many innovative ways to match the demand for access. One thought is to create shared positions. Instead of employing four full-time physicians and one person part time, have two people who are working part time, Dr. Bolster suggested. “It is also important to not only expand our workforce with advanced practice providers, but to ensure their retention in the rheumatology workforce, to improve access to care for those with rheumatic diseases.”
Increasing the number of residency positions is another step toward addressing the shortage, Dr. Sandhu offered.
Women rheumatologists should make their voices heard by contacting members of Congress to support legislation that advocates for workforce shortage solutions, “in addition to generally supporting women’s rights and growth in the workplace,” she said.
The gender divide continues
Rosalind Ramsey-Goldman, MD, DrPH, remembers being the only woman in a group of five during her fellowship in the mid-1980s. Few women role models existed within the ACR, especially those in academic careers. “Now, most fellowships have more than 50% women, reflecting the number of women going to medical school,” said Dr. Ramsey-Goldman, Gallagher Research Professor in Rheumatology at Northwestern University and Northwestern Medicine, Chicago.
As more women enter the profession, women rheumatologists in academic rheumatology have started to outpace men in recent years. Some research suggests they’ve made headway in gaining leadership spots at institutions.
One recent paper, a cross-sectional national study of more than 6,100 rheumatologists, found that women had similar odds of attaining fellowship program or division director positions as men. As directors of training programs, women in rheumatology “instill this collaborative and growth mindset that encourages learners to self-reflect and work as a team,” Dr. Sandhu said.
Women bring a different perspective to training, and how curriculum works, Dr. Bose said. Studies have shown that women tend to be more empathic. They ask more questions. “That’s not to say men aren’t good. Women just have an inborn ability for connecting,” and this perspective helps to enrich the educational experience for trainees.
Women who lead training programs are also attuned to realities that female trainees confront, such as dealing with the challenges of achieving the best possible education while also raising a family, noted Graciela S. Alarcón, MD, MPH, who holds emeritus positions at the University of Alabama at Birmingham and the Universidad Peruana Cayetano Heredia in Lima, Peru.
“These program directors cultivate the ability to relate to women trainees in a very personal manner, supporting them in their efforts to achieve a balance between their training demands and their family/personal responsibilities,” she said.
Other research suggests the gender gap hasn’t gone away. Women continue to have lower odds of holding a higher-level professorship, receiving a federal grant, or speaking at academic conferences. They are also less likely to serve as first authors on rheumatology guidelines or recommendations.
Some studies suggest that women see fewer patients and earn less than their male counterparts. At peak difference, men can earn up to $100,000+ more than women. “My own impression is that it takes more efforts for women to reach the same level of recognition than men, and although overt discrimination is rare nowadays, subtle discrimination still occurs,” according to Dr. Alarcón.
Over a lifetime, female physicians can expect to earn less than their male counterparts, with clear implications for different retirement income levels, she said.
Fixing a leaky academic pipeline
The reality is the academic pipeline, and especially the physician-scientist pipeline, “continues to be leaky,” Dr. Liew said. “We know that caregivers to young children have larger barriers to surmount in academics and in research, and that there is a gender disparity present.” The toll of academic medicine on early career women who are parents is especially pronounced. While the pandemic has intensified this problem, it was around pre-COVID, she added.
Women who start in academia as academic clinicians or clinician researchers aren’t always able to meet their goals for promotion within the appropriate time frame. This is because of inequities in the system and lack of support related to maternity leave, childcare, and other issues. As a result, they leave academia and go into private practice or industry, Dr. Liew said.
The ACR in its 2015 survey projected that more women would be seeking part-time positions.
The good news is many academic institutions are taking a more equitable view about different career paths, offering equal parental leave to both men and women, Dr. Bolster noted. “It is essential that workforce planning encompasses the changing responsibilities within families and account for more parental leave by both men and women.” If certain projections come true, with 50% of the profession retiring between 2015 and 2030, combined with more men and women working part time, “it is requisite that workforce strategies plan for this.”
When Dr. Ramsey-Goldman was a trainee and junior faculty, there were no formal maternity leave policies.
Now, this benefit is available, she said. In another critical change, the ACR has made childcare services and a lactation room available for young mothers during its annual meeting. “Virtual meetings afford further ways to interact with colleagues,” she added.
Whether women choose to stay in academia or go into clinical practice is a very personal decision. “But it is also fair that, in some programs, training directors and faculty members can encourage trainees toward academia and its fascinating research possibilities,” Dr. Alarcón offered.
Making gains in research
Women are increasingly driving groundbreaking rheumatology research at all levels, Dr. Sandhu said. “And women empower women. Not infrequently, our female leaders, veterans in rheumatology research, seek younger female rheumatologists to help them grow in their niches. This has been one of the most beautiful things of the sisterhood in rheumatology that I have been blessed to be part of.”
In pediatric rheumatology, young female researchers are leading global research efforts. Some standouts include Kate Webb, MD, a pediatric rheumatologist in Cape Town, South Africa, and scientist who has worked on multisystem inflammatory syndrome during the pandemic. Sheila Angeles-Han, MD, who works on uveitis in juvenile idiopathic arthritis, had a role in recent ACR guidelines. Laura Lewandowski, MD, has also contributed to global rheumatology efforts, especially in low- and middle-income countries, Dr. Liew said.
The 2021 ACR annual meeting highlighted the research efforts of women rheumatologists from around the world. A global rheumatology summit at the meeting featured many women voices, including Dzifa Dey, MD, from Ghana, who received the ACR Distinguished International Rheumatology Professional Award. Ashira Blazer, MD, and Irene Blanco, MD, have spearheaded the ACR’s diversity, equity, and inclusion initiatives.
Women researchers have many opportunities to study rheumatologic diseases that disproportionately affect women, Dr. Alarcón said.
Lupus, for example, affects women in a much higher proportion than men (90% vs. 10%). This may be an attractive target for the best and brightest among future women researchers, Dr. Alarcón suggested. “It is a fact that publications related to lupus in leading internal medicine and rheumatology journals often include women either as first or senior authors. In that context, it can be said that several advances in the study of lupus worldwide can be attributed to women.”
This applies to disparities in social determinants of health that account for extremely complex outcomes in lupus among women of color, compared with White women, in addition to the costs associated with the disease and its impact on morbidity, mortality, and quality of life.
Women rheumatologists have advanced the work in reproductive management of rheumatic diseases, including a recent ACR-endorsed publication that provides formal guidance on managing reproductive health in women with rheumatic disease, Dr. Sandhu said. “One thing is clear: Without women, the work on reproductive diseases in rheumatology to date would not likely be where it is.”
Dr. Ramsey-Goldman added that “this critical work will not only set the stage for clinical care of both women and men regarding their reproductive health but will also inform education strategies for trainees and future research activities, and help direct policy regarding access to care, medication development, and costs of treatment.”
Obtaining grant funding to support salaries and researcher endeavors remains a challenge, Dr. Liew said. “It takes working evenings, weekends, and holidays to meet those goals within a set time frame. So you can see why a female faculty member with children might be disadvantaged, compared to a male counterpart without children.”
Competition for grant funding remains fierce as budgets become tighter, she added.
“We will lose a lot more brilliant and compassionate rheumatologists (clinicians, physician-scientists, and scientists alike) if we do not think of ways to make things more equitable or do not acknowledge the privileges that support some to continued career successes and leave others behind,” Dr. Liew said.
Women who choose a research field should seek out mentor and financial support that will allow them enough protected time to balance out research with other clinical activities, such as teaching and patient care, Dr. Alarcón said.
Training directors, mentors, and faculty should prioritize the needs of current and future women researchers, she said. “The guidance provided to young female trainees toward a successful research career is a formidable challenge that may provide, in turn, enormous satisfaction. There are established avenues to seek funding as new investigators.”
Progress in diversity
Rheumatology as a field is attracting more candidates and all races and genders, Dr. Bose said. “I think in the coming years we will see more and more women from minorities being incorporated into the rheumatology workforce.”
Others would like to see further improvements in diversity and attracting women from historically excluded backgrounds. Patients will benefit from rheumatologists who are able to connect with them through shared languages, cultures, and other life experiences, Dr. Liew said. “It is imperative that we work on recruitment, mentorship, and retention in this regard.”
While the representation of women of color is still inadequate, there has been some progress, Dr. Sandhu said. The number of female Hispanic, Latinx, and Black or African American graduates from medical school has seen a steady rise since 2017. And, AAMC has established task forces such as the Women of Color Initiative to identify strategies for furthering the careers of women of color in academic medicine.
“There’s still a lot of room to grow. I am, however, proud to say we will finally have a woman of color as the president of ACR in 2023,” said Dr. Sandhu, referring to Deborah Dyett Desir, MD.
Dr. Desir discussed the importance of diversifying the ACR in a recent interview.
All rheumatologists know that there is a place for them in the ACR, she stressed. “The demographics of our membership should reflect that of our population.”
As growth in diverse representation occurs, so will recruitment, retention, and a greater awareness and distribution of knowledge and means to address implicit biases and microaggressions, Dr. Sandhu said. “We will see a greater quality of health care, where patients may feel more connected to someone they can identify with.”
Looking ahead
Dr. Alarcón expects women to continue to play a major role in rheumatology, not just in research, education, and patient care but in leadership of academic societies and professional organizations.
“Women in rheumatology have come a long way – a piece of history that I have been fortunate to witness from my beginnings in the early 1970s. We have, I think, paved the way for the next generations of leaders in our beloved specialty field.”
Dr. Bolster is a member of the ACR board of directors and board liaison of the ACR Workforce Solutions Committee. Dr. Ramsey-Goldman has been a GlaxoSmithKline consultant for lupus studies, a consultant and site investigator with Exagen Diagnostics for lupus biomarker studies, and a site investigator for Xencor and Horizon Pharma lupus trials. Dr. Sandhu serves on the ACR’s Committee on Rheumatology Training and Workforce Issues.
Related article
Pioneer days of rheumatology: One veteran looks back
Patricia Woo, CBE, FMedSci, FRCP, has seen it all.
As a member of the British Rheumatology Society and fellow of the Royal College of Physicians, she presented the case for and obtained official training approval for pediatric rheumatology in the 1990s. She also set the wheels in motion to form the Paediatric Rheumatology International Trials Organisation and the Paediatric Rheumatology European Society.
Now 74, Dr. Woo remembers the discrimination she faced in the 1970s. “I was told I couldn’t become an investigator or consultant if I were to marry or have children.” Around the same time, she found out a male clinician researcher didn’t want to work with her, not because of her qualifications, but because she was a woman.
That wouldn’t happen now with all the antidiscrimination laws in place, noted Dr. Woo, an emeritus professor of pediatric rheumatology and previous head of the Centre for Paediatric and Adolescent Rheumatology at UCL, London. Looking at the advances made by women in rheumatology, “there’s a major difference between 3 decades ago and today. If anyone discriminates today, they are called out.”
As the founding president of the Paediatric Rheumatology European Society, Dr. Woo is one of many early trailblazers who weathered many changes and made gains in the profession.
It’s important to recognize the work of Barbara Ansell, MD, the founder of pediatric rheumatology in the Canadian Red Cross Memorial Hospital, said Dr. Woo. Back in the 1960s, this wasn’t even a subspecialty. “Sick kids in general were taken either to pediatricians who didn’t know much about undescribed rheumatological conditions, and rheumatologists who didn’t know or have facilities for pediatric care.”
Dr. Ansell started this work, and Dr. Woo took over when she retired. With her colleagues, she set up a syllabus for pediatric rheumatology to formalize training for all junior doctors. This established a model of multidisciplinary clinical care and research. “Over the years, more women doctors have been attracted to pediatric rheumatology and have done well,” she said.
The rise of female leaders in rheumatology over the past few decades has been exponential, she continued. Women have become presidents of rheumatologic societies. Some established themselves as leaders in specific disciplines.
Carol Black, MD, from the United Kingdom is renowned for her international collaborative work in scleroderma research and clinical care. Patience White, MD in Washington, D.C., started research on the process of transitioning from childhood to adolescent to adult clinical care, a discipline that now has a strong international presence, Dr. Woo said.
The European Alliance of Associations for Rheumatology, which created a task force on gender equity in academic rheumatology, is evolving, she continued. The Academy of Medical Sciences in the United Kingdom also has active gender equality and mentoring programs, including a program to boost the careers of all researchers.
It’s also much easier now for women to become lead authors on papers since many are heads of lab or clinical services, Dr. Woo continued. “I don’t think there’s much discrimination if you’re a good clinician, and/or a good scientist. If women do their work well, they get the appropriate acknowledgment.”
More medical schools build training in transgender care
Klay Noto wants to be the kind of doctor he never had when he began to question his gender identity.
A second-year student at Tulane University in New Orleans, he wants to listen compassionately to patients’ concerns and recognize the hurt when they question who they are. He will be the kind of doctor who knows that a breast exam can be traumatizing if someone has been breast binding or that instructing a patient to take everything off and put on a gown can be triggering for someone with gender dysphoria.
Being in the room for hard conversations is part of why he pursued med school. “There aren’t many LGBT people in medicine and as I started to understand all the dynamics that go into it, I started to see that I could do it and I could be that different kind of doctor,” he told this news organization.
Mr. Noto, who transitioned after college, wants to see more transgender people like himself teaching gender medicine, and for all medical students to be trained in what it means to be transgender and how to give compassionate and comprehensive care to all patients.
Gains have been made in providing curriculum in transgender care that trains medical students in such concepts as how to approach gender identity with sensitivity and how to manage hormone therapy and surgery for transitioning patients who request that, according to those interviewed for this story.
But they agree there’s a long way to go to having widespread medical school integration of the health care needs of about 1.4 million transgender people in the United States.
According to the Association of American Medical Colleges (AAMC) Curriculum Inventory data collected from 131 U.S. medical schools, more than 65% offered some form of transgender-related education in 2018, and more than 80% of those provided such curriculum in required courses.
Lack of transgender, nonbinary faculty
Jason Klein, MD, is a pediatric endocrinologist and medical director of the Transgender Youth Health Program at New York (N.Y.) University.
He said in an interview that the number of programs nationally that have gender medicine as a structured part of their curriculum has increased over the last 5-10 years, but that education is not standardized from program to program.
The program at NYU includes lecture-style learning, case presentations, real-world conversations with people in the community, group discussions, and patient care, Dr. Klein said. There are formal lectures as part of adolescent medicine where students learn the differences between gender and sexual identity, and education on medical treatment of transgender and nonbinary adolescents, starting with puberty blockers and moving into affirming hormones.
Doctors also learn to know their limits and decide when to refer patients to a specialist.
“The focus is really about empathic and supportive care,” said Dr. Klein, assistant professor in the department of pediatrics at Hassenfeld Children’s Hospital at NYU Langone Health. “It’s about communication and understanding and the language we use and how to deliver affirming care in a health care setting in general.”
Imagine the potential stressors, he said, of a transgender person entering a typical health care setting. The electronic health record may only have room for the legal name of a person and not the name a person may currently be using. The intake form typically asks patients to check either male or female. The bathrooms give the same two choices.
“Every physician should know how to speak with, treat, emote with, and empathize with care for the trans and nonbinary individual,” Dr. Klein said.
Dr. Klein noted there is a glaring shortage of trans and nonbinary physicians to lead efforts to expand education on integrating the medical, psychological, and psychosocial care that patients will receive.
Currently, gender medicine is not included on board exams for adolescent medicine or endocrinology, he said.
“Adding formal training in gender medicine to board exams would really help solidify the importance of this arena of medicine,” he noted.
First AAMC standards
In 2014, the AAMC released the first standards to guide curricula across medical school and residency to support training doctors to be competent in caring for transgender patients.
The standards include recommending that all doctors be able to communicate with patients related to their gender identity and understand how to deliver high-quality care to transgender and gender-diverse patients within their specialty, Kristen L. Eckstrand, MD, a coauthor of the guidelines, told this news organization.
“Many medical schools have developed their own curricula to meet these standards,” said Dr. Eckstrand, medical director for LGBTQIA+ Health at the University of Pittsburgh Medical Center.
Norma Poll-Hunter, PhD, AAMC’s senior director for workforce diversity, noted that the organization recently released its diversity, equity, and inclusion competencies that guide the medical education of students, residents, and faculty.
Dr. Poll-Hunter told this news organization that AAMC partners with the Building the Next Generation of Academic Physicians LGBT Health Workforce Conference “to support safe spaces for scholarly efforts and mentorship to advance this area of work.”
Team approach at Rutgers
Among the medical schools that incorporate comprehensive transgender care into the curriculum is Rutgers University’s Robert Wood Johnson Medical School in New Brunswick, N.J.
Gloria Bachmann, MD, is professor of obstetrics and gynecology at the school and medical director of its partner, the PROUD Gender Center of New Jersey. PROUD stands for “Promoting Respect, Outreach, Understanding, and Dignity,” and the center provides comprehensive care for transgender and nonbinary patients in one location.
Dr. Bachmann said Rutgers takes a team approach with both instructors and learners teaching medical students about transgender care. The teachers are not only professors in traditional classroom lectures, but patient navigators and nurses at the PROUD center, established as part of the medical school in 2020. Students learn from the navigators, for instance, how to help patients through the spectrum of inpatient and outpatient care.
“All of our learners do get to care for individuals who identify as transgender,” said Dr. Bachmann.
Among the improvements in educating students on transgender care over the years, she said, is the emphasis on social determinants of health. In the transgender population, initial questions may include whether the person is able to access care through insurance as laws vary widely on what care and procedures are covered.
As another example, Dr. Bachmann cites: “If they are seen on an emergency basis and are sent home with medication and follow-up, can they afford it?”
Another consideration is whether there is a home to which they can return.
“Many individuals who are transgender may not have a home. Their family may not be accepting of them. Therefore, it’s the social determinants of health as well as their transgender identity that have to be put into the equation of best care,” she said.
Giving back to the trans community
Mr. Noto doesn’t know whether he will specialize in gender medicine, but he is committed to serving the transgender community in whatever physician path he chooses.
He said he realizes he is fortunate to have strong family support and good insurance and that he can afford fees, such as the copay to see transgender care specialists. Many in the community do not have those resources and are likely to get care “only if they have to.”
At Tulane, training in transgender care starts during orientation week and continues on different levels, with different options, throughout medical school and residency, he added.
Mr. Noto said he would like to see more mandatory learning such as a “queer-centered exam, where you have to give an organ inventory and you have to ask patients if it’s OK to talk about X, Y, and Z.” He’d also like more opportunities for clinical interaction with transgender patients, such as queer-centered rotations.
When physicians aren’t well trained in transgender care, you have patients educating the doctors, which, Mr. Noto said, should not be acceptable.
“People come to you on their worst day. And to not be informed about them in my mind is negligent. In what other population can you choose not to learn about someone just because you don’t want to?” he said.
A version of this article first appeared on Medscape.com.
Klay Noto wants to be the kind of doctor he never had when he began to question his gender identity.
A second-year student at Tulane University in New Orleans, he wants to listen compassionately to patients’ concerns and recognize the hurt when they question who they are. He will be the kind of doctor who knows that a breast exam can be traumatizing if someone has been breast binding or that instructing a patient to take everything off and put on a gown can be triggering for someone with gender dysphoria.
Being in the room for hard conversations is part of why he pursued med school. “There aren’t many LGBT people in medicine and as I started to understand all the dynamics that go into it, I started to see that I could do it and I could be that different kind of doctor,” he told this news organization.
Mr. Noto, who transitioned after college, wants to see more transgender people like himself teaching gender medicine, and for all medical students to be trained in what it means to be transgender and how to give compassionate and comprehensive care to all patients.
Gains have been made in providing curriculum in transgender care that trains medical students in such concepts as how to approach gender identity with sensitivity and how to manage hormone therapy and surgery for transitioning patients who request that, according to those interviewed for this story.
But they agree there’s a long way to go to having widespread medical school integration of the health care needs of about 1.4 million transgender people in the United States.
According to the Association of American Medical Colleges (AAMC) Curriculum Inventory data collected from 131 U.S. medical schools, more than 65% offered some form of transgender-related education in 2018, and more than 80% of those provided such curriculum in required courses.
Lack of transgender, nonbinary faculty
Jason Klein, MD, is a pediatric endocrinologist and medical director of the Transgender Youth Health Program at New York (N.Y.) University.
He said in an interview that the number of programs nationally that have gender medicine as a structured part of their curriculum has increased over the last 5-10 years, but that education is not standardized from program to program.
The program at NYU includes lecture-style learning, case presentations, real-world conversations with people in the community, group discussions, and patient care, Dr. Klein said. There are formal lectures as part of adolescent medicine where students learn the differences between gender and sexual identity, and education on medical treatment of transgender and nonbinary adolescents, starting with puberty blockers and moving into affirming hormones.
Doctors also learn to know their limits and decide when to refer patients to a specialist.
“The focus is really about empathic and supportive care,” said Dr. Klein, assistant professor in the department of pediatrics at Hassenfeld Children’s Hospital at NYU Langone Health. “It’s about communication and understanding and the language we use and how to deliver affirming care in a health care setting in general.”
Imagine the potential stressors, he said, of a transgender person entering a typical health care setting. The electronic health record may only have room for the legal name of a person and not the name a person may currently be using. The intake form typically asks patients to check either male or female. The bathrooms give the same two choices.
“Every physician should know how to speak with, treat, emote with, and empathize with care for the trans and nonbinary individual,” Dr. Klein said.
Dr. Klein noted there is a glaring shortage of trans and nonbinary physicians to lead efforts to expand education on integrating the medical, psychological, and psychosocial care that patients will receive.
Currently, gender medicine is not included on board exams for adolescent medicine or endocrinology, he said.
“Adding formal training in gender medicine to board exams would really help solidify the importance of this arena of medicine,” he noted.
First AAMC standards
In 2014, the AAMC released the first standards to guide curricula across medical school and residency to support training doctors to be competent in caring for transgender patients.
The standards include recommending that all doctors be able to communicate with patients related to their gender identity and understand how to deliver high-quality care to transgender and gender-diverse patients within their specialty, Kristen L. Eckstrand, MD, a coauthor of the guidelines, told this news organization.
“Many medical schools have developed their own curricula to meet these standards,” said Dr. Eckstrand, medical director for LGBTQIA+ Health at the University of Pittsburgh Medical Center.
Norma Poll-Hunter, PhD, AAMC’s senior director for workforce diversity, noted that the organization recently released its diversity, equity, and inclusion competencies that guide the medical education of students, residents, and faculty.
Dr. Poll-Hunter told this news organization that AAMC partners with the Building the Next Generation of Academic Physicians LGBT Health Workforce Conference “to support safe spaces for scholarly efforts and mentorship to advance this area of work.”
Team approach at Rutgers
Among the medical schools that incorporate comprehensive transgender care into the curriculum is Rutgers University’s Robert Wood Johnson Medical School in New Brunswick, N.J.
Gloria Bachmann, MD, is professor of obstetrics and gynecology at the school and medical director of its partner, the PROUD Gender Center of New Jersey. PROUD stands for “Promoting Respect, Outreach, Understanding, and Dignity,” and the center provides comprehensive care for transgender and nonbinary patients in one location.
Dr. Bachmann said Rutgers takes a team approach with both instructors and learners teaching medical students about transgender care. The teachers are not only professors in traditional classroom lectures, but patient navigators and nurses at the PROUD center, established as part of the medical school in 2020. Students learn from the navigators, for instance, how to help patients through the spectrum of inpatient and outpatient care.
“All of our learners do get to care for individuals who identify as transgender,” said Dr. Bachmann.
Among the improvements in educating students on transgender care over the years, she said, is the emphasis on social determinants of health. In the transgender population, initial questions may include whether the person is able to access care through insurance as laws vary widely on what care and procedures are covered.
As another example, Dr. Bachmann cites: “If they are seen on an emergency basis and are sent home with medication and follow-up, can they afford it?”
Another consideration is whether there is a home to which they can return.
“Many individuals who are transgender may not have a home. Their family may not be accepting of them. Therefore, it’s the social determinants of health as well as their transgender identity that have to be put into the equation of best care,” she said.
Giving back to the trans community
Mr. Noto doesn’t know whether he will specialize in gender medicine, but he is committed to serving the transgender community in whatever physician path he chooses.
He said he realizes he is fortunate to have strong family support and good insurance and that he can afford fees, such as the copay to see transgender care specialists. Many in the community do not have those resources and are likely to get care “only if they have to.”
At Tulane, training in transgender care starts during orientation week and continues on different levels, with different options, throughout medical school and residency, he added.
Mr. Noto said he would like to see more mandatory learning such as a “queer-centered exam, where you have to give an organ inventory and you have to ask patients if it’s OK to talk about X, Y, and Z.” He’d also like more opportunities for clinical interaction with transgender patients, such as queer-centered rotations.
When physicians aren’t well trained in transgender care, you have patients educating the doctors, which, Mr. Noto said, should not be acceptable.
“People come to you on their worst day. And to not be informed about them in my mind is negligent. In what other population can you choose not to learn about someone just because you don’t want to?” he said.
A version of this article first appeared on Medscape.com.
Klay Noto wants to be the kind of doctor he never had when he began to question his gender identity.
A second-year student at Tulane University in New Orleans, he wants to listen compassionately to patients’ concerns and recognize the hurt when they question who they are. He will be the kind of doctor who knows that a breast exam can be traumatizing if someone has been breast binding or that instructing a patient to take everything off and put on a gown can be triggering for someone with gender dysphoria.
Being in the room for hard conversations is part of why he pursued med school. “There aren’t many LGBT people in medicine and as I started to understand all the dynamics that go into it, I started to see that I could do it and I could be that different kind of doctor,” he told this news organization.
Mr. Noto, who transitioned after college, wants to see more transgender people like himself teaching gender medicine, and for all medical students to be trained in what it means to be transgender and how to give compassionate and comprehensive care to all patients.
Gains have been made in providing curriculum in transgender care that trains medical students in such concepts as how to approach gender identity with sensitivity and how to manage hormone therapy and surgery for transitioning patients who request that, according to those interviewed for this story.
But they agree there’s a long way to go to having widespread medical school integration of the health care needs of about 1.4 million transgender people in the United States.
According to the Association of American Medical Colleges (AAMC) Curriculum Inventory data collected from 131 U.S. medical schools, more than 65% offered some form of transgender-related education in 2018, and more than 80% of those provided such curriculum in required courses.
Lack of transgender, nonbinary faculty
Jason Klein, MD, is a pediatric endocrinologist and medical director of the Transgender Youth Health Program at New York (N.Y.) University.
He said in an interview that the number of programs nationally that have gender medicine as a structured part of their curriculum has increased over the last 5-10 years, but that education is not standardized from program to program.
The program at NYU includes lecture-style learning, case presentations, real-world conversations with people in the community, group discussions, and patient care, Dr. Klein said. There are formal lectures as part of adolescent medicine where students learn the differences between gender and sexual identity, and education on medical treatment of transgender and nonbinary adolescents, starting with puberty blockers and moving into affirming hormones.
Doctors also learn to know their limits and decide when to refer patients to a specialist.
“The focus is really about empathic and supportive care,” said Dr. Klein, assistant professor in the department of pediatrics at Hassenfeld Children’s Hospital at NYU Langone Health. “It’s about communication and understanding and the language we use and how to deliver affirming care in a health care setting in general.”
Imagine the potential stressors, he said, of a transgender person entering a typical health care setting. The electronic health record may only have room for the legal name of a person and not the name a person may currently be using. The intake form typically asks patients to check either male or female. The bathrooms give the same two choices.
“Every physician should know how to speak with, treat, emote with, and empathize with care for the trans and nonbinary individual,” Dr. Klein said.
Dr. Klein noted there is a glaring shortage of trans and nonbinary physicians to lead efforts to expand education on integrating the medical, psychological, and psychosocial care that patients will receive.
Currently, gender medicine is not included on board exams for adolescent medicine or endocrinology, he said.
“Adding formal training in gender medicine to board exams would really help solidify the importance of this arena of medicine,” he noted.
First AAMC standards
In 2014, the AAMC released the first standards to guide curricula across medical school and residency to support training doctors to be competent in caring for transgender patients.
The standards include recommending that all doctors be able to communicate with patients related to their gender identity and understand how to deliver high-quality care to transgender and gender-diverse patients within their specialty, Kristen L. Eckstrand, MD, a coauthor of the guidelines, told this news organization.
“Many medical schools have developed their own curricula to meet these standards,” said Dr. Eckstrand, medical director for LGBTQIA+ Health at the University of Pittsburgh Medical Center.
Norma Poll-Hunter, PhD, AAMC’s senior director for workforce diversity, noted that the organization recently released its diversity, equity, and inclusion competencies that guide the medical education of students, residents, and faculty.
Dr. Poll-Hunter told this news organization that AAMC partners with the Building the Next Generation of Academic Physicians LGBT Health Workforce Conference “to support safe spaces for scholarly efforts and mentorship to advance this area of work.”
Team approach at Rutgers
Among the medical schools that incorporate comprehensive transgender care into the curriculum is Rutgers University’s Robert Wood Johnson Medical School in New Brunswick, N.J.
Gloria Bachmann, MD, is professor of obstetrics and gynecology at the school and medical director of its partner, the PROUD Gender Center of New Jersey. PROUD stands for “Promoting Respect, Outreach, Understanding, and Dignity,” and the center provides comprehensive care for transgender and nonbinary patients in one location.
Dr. Bachmann said Rutgers takes a team approach with both instructors and learners teaching medical students about transgender care. The teachers are not only professors in traditional classroom lectures, but patient navigators and nurses at the PROUD center, established as part of the medical school in 2020. Students learn from the navigators, for instance, how to help patients through the spectrum of inpatient and outpatient care.
“All of our learners do get to care for individuals who identify as transgender,” said Dr. Bachmann.
Among the improvements in educating students on transgender care over the years, she said, is the emphasis on social determinants of health. In the transgender population, initial questions may include whether the person is able to access care through insurance as laws vary widely on what care and procedures are covered.
As another example, Dr. Bachmann cites: “If they are seen on an emergency basis and are sent home with medication and follow-up, can they afford it?”
Another consideration is whether there is a home to which they can return.
“Many individuals who are transgender may not have a home. Their family may not be accepting of them. Therefore, it’s the social determinants of health as well as their transgender identity that have to be put into the equation of best care,” she said.
Giving back to the trans community
Mr. Noto doesn’t know whether he will specialize in gender medicine, but he is committed to serving the transgender community in whatever physician path he chooses.
He said he realizes he is fortunate to have strong family support and good insurance and that he can afford fees, such as the copay to see transgender care specialists. Many in the community do not have those resources and are likely to get care “only if they have to.”
At Tulane, training in transgender care starts during orientation week and continues on different levels, with different options, throughout medical school and residency, he added.
Mr. Noto said he would like to see more mandatory learning such as a “queer-centered exam, where you have to give an organ inventory and you have to ask patients if it’s OK to talk about X, Y, and Z.” He’d also like more opportunities for clinical interaction with transgender patients, such as queer-centered rotations.
When physicians aren’t well trained in transgender care, you have patients educating the doctors, which, Mr. Noto said, should not be acceptable.
“People come to you on their worst day. And to not be informed about them in my mind is negligent. In what other population can you choose not to learn about someone just because you don’t want to?” he said.
A version of this article first appeared on Medscape.com.
Central centrifugal cicatricial alopecia
THE PRESENTATION
A Early central centrifugal cicatricial alopecia with a small central patch of hair loss in a 45-year-old Black woman.
B Late central centrifugal cicatricial alopecia with a large central patch of hair loss in a 43-year-old Black woman.
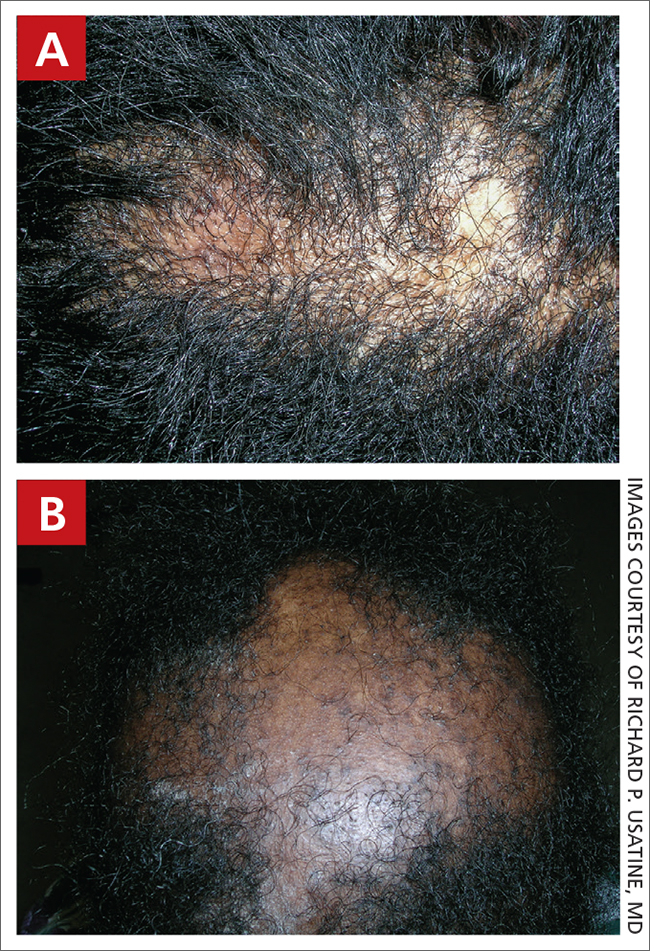
Scarring alopecia is a collection of hair loss disorders including chronic cutaneous lupus erythematosus (discoid lupus), lichen planopilaris, dissecting cellulitis, acne keloidalis, and central centrifugal cicatricial alopecia.1 CCCA (formerly hot comb alopecia or follicular degeneration syndrome) is a progressive, scarring, inflammatory alopecia and represents the most common form of scarring alopecia in women of African descent. It results in permanent destruction of hair follicles.
Epidemiology
CCCA predominantly affects women of African descent but also may affect men. The prevalence of CCCA in those of African descent has varied in the literature. Khumalo2 reported a prevalence of 1.2% for women younger than 50 years and 6.7% in women older than 50 years. CCCA has been reported in other ethnic groups, such as those of Asian descent.3
Historically, hair care practices that are more common in those of African descent, such as high-tension hairstyles as well as heat and chemical hair relaxers, were implicated in the development of CCCA. However, the causes of CCCA are most likely multifactorial, including family history, genetic mutations, and hair care practices.4-7 PADI3 mutations likely predispose some women to CCCA. Mutations in PADI3, which encodes peptidyl arginine deiminase 3 (an enzyme that modifies proteins crucial for the formation of hair shafts), were found in some patients with CCCA.8 Moreover, other genetic defects also likely play a role.7
Key clinical features
Early recognition is key for patients with CCCA.
- CCCA begins in the central scalp (crown area, vertex) and spreads centrifugally.
- Scalp symptoms such as tenderness, pain, a tingling or crawling sensation, and itching may occur.9 Some patients may not have any symptoms at all, and hair loss may progress painlessly.
- Central hair breakage—forme fruste CCCA—may be a presenting sign of CCCA.9
- Loss of follicular ostia and mottled hypopigmented and hyperpigmented macules are common findings.6
- CCCA can be diagnosed clinically and by histopathology.
Worth noting
Patients may experience hair loss and scalp symptoms for years before seeking medical evaluation. In some cultures, hair breakage or itching on the top of the scalp may be viewed as a normal occurrence in life.
It is important to set patient expectations that CCCA is a scarring alopecia, and the initial goal often is to maintain the patient's existing hair. However, hair and areas responding to treatment should still be treated. Without any intervention, the resulting scarring from CCCA may permanently scar follicles on the entire scalp.
Continue to: Due to the inflammatory...
Due to the inflammatory nature of CCCA, potent topical corticosteroids (eg, clobetasol propionate), intralesional corticosteroids (eg, triamcinolone acetonide), and oral antiinflammatory agents (eg, doxycycline) are utilized in the treatment of CCCA. Minoxidil is another treatment option. Adjuvant therapies such as topical metformin also have been tried.10 Importantly, treatment of CCCA may halt further permanent destruction of hair follicles, but scalp symptoms may reappear periodically and require re-treatment with anti-inflammatory agents.
Health care highlight
Thorough scalp examination and awareness of clinical features of CCCA may prompt earlier diagnosis and prevent future severe permanent alopecia. Clinicians should encourage patients with suggestive signs or symptoms of CCCA to seek care from a dermatologist.
1. Sperling LC. Scarring alopecia and the dermatopathologist. J Cutan Pathol. 2001;28:333-342. doi:10.1034/ j.1600-0560.2001.280701.x
2. Khumalo NP. Prevalence of central centrifugal cicatricial alopecia. Arch Dermatol. 2011;147:1453-1454. doi:10.1001/ archderm.147.12.1453
3. Su HJ, Cheng AY, Liu CH, et al. Primary scarring alopecia: a retrospective study of 89 patients in Taiwan [published online January 16, 2018]. J Dermatol. 2018;45:450-455. doi:10.1111/ 1346-8138.14217
4. Sperling LC, Cowper SE. The histopathology of primary cicatricial alopecia. Semin Cutan Med Surg. 2006;25:41-50
5. Dlova NC, Forder M. Central centrifugal cicatricial alopecia: possible familial aetiology in two African families from South Africa. Int J Dermatol. 2012;51(supp 1):17-20, 20-23.
6. Ogunleye TA, Quinn CR, McMichael A. Alopecia. In: Taylor SC, Kelly AP, Lim HW, et al, eds. Dermatology for Skin of Color. McGraw Hill; 2016:253-264.
7. Uitto J. Genetic susceptibility to alopecia [published online February 13, 2019]. N Engl J Med. 2019;380:873-876. doi:10.1056/ NEJMe1900042
8. Malki L, Sarig O, Romano MT, et al. Variant PADI3 in central centrifugal cicatricial alopecia. N Engl J Med. 2019;380:833-841.
9. Callender VD, Wright DR, Davis EC, et al. Hair breakage as a presenting sign of early or occult central centrifugal cicatricial alopecia: clinicopathologic findings in 9 patients. Arch Dermatol. 2012;148:1047-1052.
10. Araoye EF, Thomas JAL, Aguh CU. Hair regrowth in 2 patients with recalcitrant central centrifugal cicatricial alopecia after use of topical metformin. JAAD Case Rep. 2020;6:106-108. doi:10.1016/ j.jdcr.2019.12.008.
THE PRESENTATION
A Early central centrifugal cicatricial alopecia with a small central patch of hair loss in a 45-year-old Black woman.
B Late central centrifugal cicatricial alopecia with a large central patch of hair loss in a 43-year-old Black woman.
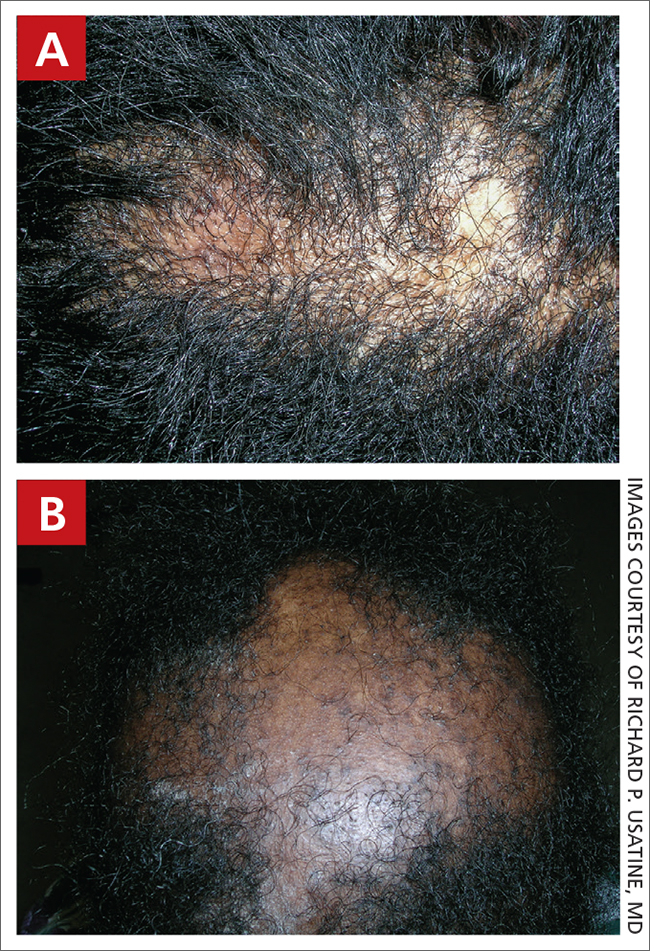
Scarring alopecia is a collection of hair loss disorders including chronic cutaneous lupus erythematosus (discoid lupus), lichen planopilaris, dissecting cellulitis, acne keloidalis, and central centrifugal cicatricial alopecia.1 CCCA (formerly hot comb alopecia or follicular degeneration syndrome) is a progressive, scarring, inflammatory alopecia and represents the most common form of scarring alopecia in women of African descent. It results in permanent destruction of hair follicles.
Epidemiology
CCCA predominantly affects women of African descent but also may affect men. The prevalence of CCCA in those of African descent has varied in the literature. Khumalo2 reported a prevalence of 1.2% for women younger than 50 years and 6.7% in women older than 50 years. CCCA has been reported in other ethnic groups, such as those of Asian descent.3
Historically, hair care practices that are more common in those of African descent, such as high-tension hairstyles as well as heat and chemical hair relaxers, were implicated in the development of CCCA. However, the causes of CCCA are most likely multifactorial, including family history, genetic mutations, and hair care practices.4-7 PADI3 mutations likely predispose some women to CCCA. Mutations in PADI3, which encodes peptidyl arginine deiminase 3 (an enzyme that modifies proteins crucial for the formation of hair shafts), were found in some patients with CCCA.8 Moreover, other genetic defects also likely play a role.7
Key clinical features
Early recognition is key for patients with CCCA.
- CCCA begins in the central scalp (crown area, vertex) and spreads centrifugally.
- Scalp symptoms such as tenderness, pain, a tingling or crawling sensation, and itching may occur.9 Some patients may not have any symptoms at all, and hair loss may progress painlessly.
- Central hair breakage—forme fruste CCCA—may be a presenting sign of CCCA.9
- Loss of follicular ostia and mottled hypopigmented and hyperpigmented macules are common findings.6
- CCCA can be diagnosed clinically and by histopathology.
Worth noting
Patients may experience hair loss and scalp symptoms for years before seeking medical evaluation. In some cultures, hair breakage or itching on the top of the scalp may be viewed as a normal occurrence in life.
It is important to set patient expectations that CCCA is a scarring alopecia, and the initial goal often is to maintain the patient's existing hair. However, hair and areas responding to treatment should still be treated. Without any intervention, the resulting scarring from CCCA may permanently scar follicles on the entire scalp.
Continue to: Due to the inflammatory...
Due to the inflammatory nature of CCCA, potent topical corticosteroids (eg, clobetasol propionate), intralesional corticosteroids (eg, triamcinolone acetonide), and oral antiinflammatory agents (eg, doxycycline) are utilized in the treatment of CCCA. Minoxidil is another treatment option. Adjuvant therapies such as topical metformin also have been tried.10 Importantly, treatment of CCCA may halt further permanent destruction of hair follicles, but scalp symptoms may reappear periodically and require re-treatment with anti-inflammatory agents.
Health care highlight
Thorough scalp examination and awareness of clinical features of CCCA may prompt earlier diagnosis and prevent future severe permanent alopecia. Clinicians should encourage patients with suggestive signs or symptoms of CCCA to seek care from a dermatologist.
THE PRESENTATION
A Early central centrifugal cicatricial alopecia with a small central patch of hair loss in a 45-year-old Black woman.
B Late central centrifugal cicatricial alopecia with a large central patch of hair loss in a 43-year-old Black woman.
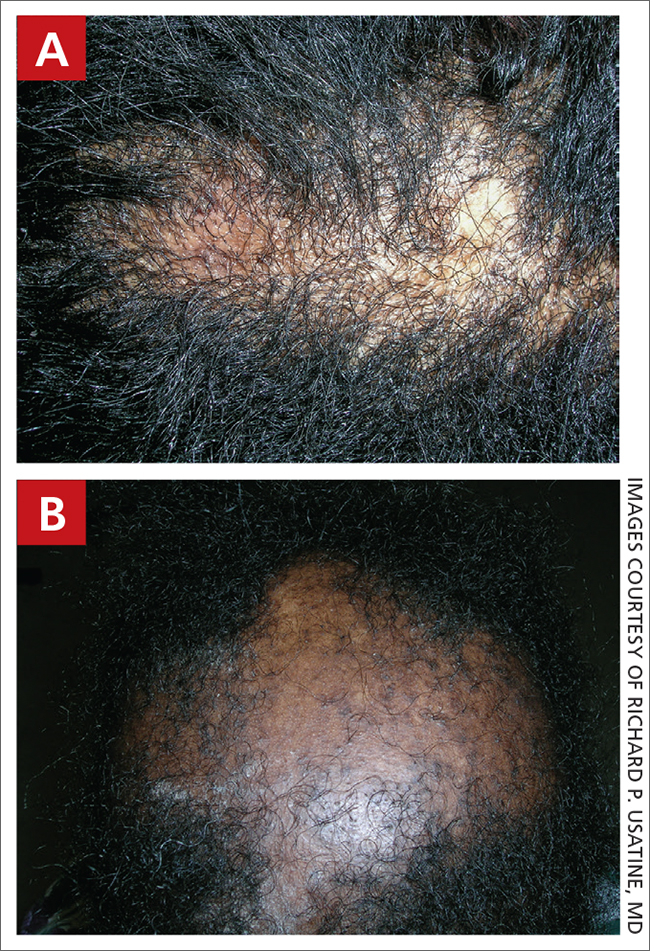
Scarring alopecia is a collection of hair loss disorders including chronic cutaneous lupus erythematosus (discoid lupus), lichen planopilaris, dissecting cellulitis, acne keloidalis, and central centrifugal cicatricial alopecia.1 CCCA (formerly hot comb alopecia or follicular degeneration syndrome) is a progressive, scarring, inflammatory alopecia and represents the most common form of scarring alopecia in women of African descent. It results in permanent destruction of hair follicles.
Epidemiology
CCCA predominantly affects women of African descent but also may affect men. The prevalence of CCCA in those of African descent has varied in the literature. Khumalo2 reported a prevalence of 1.2% for women younger than 50 years and 6.7% in women older than 50 years. CCCA has been reported in other ethnic groups, such as those of Asian descent.3
Historically, hair care practices that are more common in those of African descent, such as high-tension hairstyles as well as heat and chemical hair relaxers, were implicated in the development of CCCA. However, the causes of CCCA are most likely multifactorial, including family history, genetic mutations, and hair care practices.4-7 PADI3 mutations likely predispose some women to CCCA. Mutations in PADI3, which encodes peptidyl arginine deiminase 3 (an enzyme that modifies proteins crucial for the formation of hair shafts), were found in some patients with CCCA.8 Moreover, other genetic defects also likely play a role.7
Key clinical features
Early recognition is key for patients with CCCA.
- CCCA begins in the central scalp (crown area, vertex) and spreads centrifugally.
- Scalp symptoms such as tenderness, pain, a tingling or crawling sensation, and itching may occur.9 Some patients may not have any symptoms at all, and hair loss may progress painlessly.
- Central hair breakage—forme fruste CCCA—may be a presenting sign of CCCA.9
- Loss of follicular ostia and mottled hypopigmented and hyperpigmented macules are common findings.6
- CCCA can be diagnosed clinically and by histopathology.
Worth noting
Patients may experience hair loss and scalp symptoms for years before seeking medical evaluation. In some cultures, hair breakage or itching on the top of the scalp may be viewed as a normal occurrence in life.
It is important to set patient expectations that CCCA is a scarring alopecia, and the initial goal often is to maintain the patient's existing hair. However, hair and areas responding to treatment should still be treated. Without any intervention, the resulting scarring from CCCA may permanently scar follicles on the entire scalp.
Continue to: Due to the inflammatory...
Due to the inflammatory nature of CCCA, potent topical corticosteroids (eg, clobetasol propionate), intralesional corticosteroids (eg, triamcinolone acetonide), and oral antiinflammatory agents (eg, doxycycline) are utilized in the treatment of CCCA. Minoxidil is another treatment option. Adjuvant therapies such as topical metformin also have been tried.10 Importantly, treatment of CCCA may halt further permanent destruction of hair follicles, but scalp symptoms may reappear periodically and require re-treatment with anti-inflammatory agents.
Health care highlight
Thorough scalp examination and awareness of clinical features of CCCA may prompt earlier diagnosis and prevent future severe permanent alopecia. Clinicians should encourage patients with suggestive signs or symptoms of CCCA to seek care from a dermatologist.
1. Sperling LC. Scarring alopecia and the dermatopathologist. J Cutan Pathol. 2001;28:333-342. doi:10.1034/ j.1600-0560.2001.280701.x
2. Khumalo NP. Prevalence of central centrifugal cicatricial alopecia. Arch Dermatol. 2011;147:1453-1454. doi:10.1001/ archderm.147.12.1453
3. Su HJ, Cheng AY, Liu CH, et al. Primary scarring alopecia: a retrospective study of 89 patients in Taiwan [published online January 16, 2018]. J Dermatol. 2018;45:450-455. doi:10.1111/ 1346-8138.14217
4. Sperling LC, Cowper SE. The histopathology of primary cicatricial alopecia. Semin Cutan Med Surg. 2006;25:41-50
5. Dlova NC, Forder M. Central centrifugal cicatricial alopecia: possible familial aetiology in two African families from South Africa. Int J Dermatol. 2012;51(supp 1):17-20, 20-23.
6. Ogunleye TA, Quinn CR, McMichael A. Alopecia. In: Taylor SC, Kelly AP, Lim HW, et al, eds. Dermatology for Skin of Color. McGraw Hill; 2016:253-264.
7. Uitto J. Genetic susceptibility to alopecia [published online February 13, 2019]. N Engl J Med. 2019;380:873-876. doi:10.1056/ NEJMe1900042
8. Malki L, Sarig O, Romano MT, et al. Variant PADI3 in central centrifugal cicatricial alopecia. N Engl J Med. 2019;380:833-841.
9. Callender VD, Wright DR, Davis EC, et al. Hair breakage as a presenting sign of early or occult central centrifugal cicatricial alopecia: clinicopathologic findings in 9 patients. Arch Dermatol. 2012;148:1047-1052.
10. Araoye EF, Thomas JAL, Aguh CU. Hair regrowth in 2 patients with recalcitrant central centrifugal cicatricial alopecia after use of topical metformin. JAAD Case Rep. 2020;6:106-108. doi:10.1016/ j.jdcr.2019.12.008.
1. Sperling LC. Scarring alopecia and the dermatopathologist. J Cutan Pathol. 2001;28:333-342. doi:10.1034/ j.1600-0560.2001.280701.x
2. Khumalo NP. Prevalence of central centrifugal cicatricial alopecia. Arch Dermatol. 2011;147:1453-1454. doi:10.1001/ archderm.147.12.1453
3. Su HJ, Cheng AY, Liu CH, et al. Primary scarring alopecia: a retrospective study of 89 patients in Taiwan [published online January 16, 2018]. J Dermatol. 2018;45:450-455. doi:10.1111/ 1346-8138.14217
4. Sperling LC, Cowper SE. The histopathology of primary cicatricial alopecia. Semin Cutan Med Surg. 2006;25:41-50
5. Dlova NC, Forder M. Central centrifugal cicatricial alopecia: possible familial aetiology in two African families from South Africa. Int J Dermatol. 2012;51(supp 1):17-20, 20-23.
6. Ogunleye TA, Quinn CR, McMichael A. Alopecia. In: Taylor SC, Kelly AP, Lim HW, et al, eds. Dermatology for Skin of Color. McGraw Hill; 2016:253-264.
7. Uitto J. Genetic susceptibility to alopecia [published online February 13, 2019]. N Engl J Med. 2019;380:873-876. doi:10.1056/ NEJMe1900042
8. Malki L, Sarig O, Romano MT, et al. Variant PADI3 in central centrifugal cicatricial alopecia. N Engl J Med. 2019;380:833-841.
9. Callender VD, Wright DR, Davis EC, et al. Hair breakage as a presenting sign of early or occult central centrifugal cicatricial alopecia: clinicopathologic findings in 9 patients. Arch Dermatol. 2012;148:1047-1052.
10. Araoye EF, Thomas JAL, Aguh CU. Hair regrowth in 2 patients with recalcitrant central centrifugal cicatricial alopecia after use of topical metformin. JAAD Case Rep. 2020;6:106-108. doi:10.1016/ j.jdcr.2019.12.008.
Sex differences in COPD slow to be recognized, treated
When Sigmund Freud claimed that “anatomy is destiny” he was referring to anatomical sex as a determinant of personality traits. Expert consensus statements have previously offered some recommendations for managing these syndromes, but clinical data are scarce, so the present review “is intended to establish a starting point for future research,”
That notion has been widely discredited, but Freud appears to be inadvertently right in one respect: When it comes to chronic obstructive pulmonary disease (COPD), anatomy really is destiny, and sex may be as well, pulmonary researchers say.
There is a growing body of evidence to indicate that COPD affects men and women differently, and that men and women patients with COPD require different clinical management. Yet women are often underdiagnosed or misdiagnosed, partly because of poorly understood sex differences, but also because of cultural biases.
But plunging any farther into the weeds, it’s important to define terms. Although various investigators have used the terms “sex” and “gender” interchangeably, sex is the preferred term when referring to biological attributes of individual patients, while gender refers to personal identity.
These distinctions are important, contended Amik Sodhi, MBBS, MPH, from the division of allergy, pulmonology, and critical care medicine at the University of Wisconsin–Madison.
“Sex is essentially a biologic construct, so it’s got to do with the sex chromosomes, the genetics of that person, and it refers to the anatomic variations that can change susceptibility to different diseases,” she said in an interview.
An example of sex differences or “sexual dimorphism” can be found in a recent meta-analysis of sex-based genetic associations by Megan Hardin, MD, MPH from Brigham & Women’s Hospital in Boston and colleagues.
They reported that CELSR1, a gene involved in fetal lung development, was expressed more among women than among men and that a single nucleotide polymorphism in the gene was associated with COPD among women smokers, but not among men smokers.
The finding points to a potential risk locus for COPD in women, and could help shed light on sexual dimorphism in COPD, Dr. Hardin and colleagues said.
In contrast to sex, “gender is more of a psychosocial construct which can impact how diseases manifest themselves, how they are potentially managed, and what outcomes might occur for that particular disease,” Dr. Sodhi said.
She and her colleagues recently published a review of sex and gender in common lung disorders and sleep in the journal CHEST, where they wrote that the “influence of sex and gender is portrayed in epidemiological data, disease pathogenesis and pathophysiology, clinical manifestations, response to treatment, access to care, and health outcomes. Hence, sex and gender should be considered in all types of research, clinical practice and educational curricula.”
For example, as previously reported at the 2021 annual meeting of the American Thoracic Society, sex-specific differences in the severity of symptoms and prevalence of comorbidities in patients with COPD may point to different criteria for diagnosing cardiac comorbidities in women and men.
Those conclusions came from a retrospective analysis of data on 795 women and 1,251 men with GOLD (Global Initiative for Chronic Obstructive Lung Disease) class 1-3 disease.
The investigators looked at the patients’ clinical history, comorbidities, lung function, COPD Assessment Test scores, and modified Medical Research Council (mMRC) dyspnea score, and found significant differences between men and women for most functional parameters and comorbidities, and for CAT items of cough, phlegm, and energy.
In logistic regression analysis, predictors for cardiac disease in men were energy, mMRC score, smoking status, body mass index, age, and spirometric lung function, but in women only age was significantly predictive for cardiac disease.
An example of gender effects on COPD differences in men and women is the increase in cigarette advertising aimed at women in the 1960s and the advent of women-targeted brands such as Virginia Slims, which in turn lead to increased smoking rates among women. In addition, in the developing world, where the sex/gender gap in COPD is narrowing, women tend to have greater exposure to wood smoke and cooking fuels in unventilated or poorly ventilated spaces, compared with men.
Increasing incidence among women
According to the Centers for Disease Control and Prevention, chronic lower respiratory diseases, primarily COPD, were the fourth-leading cause of death in women in the United States in 2018, following only heart disease, cancer, and accidents/injuries.
And as a CDC analysis of data from the 2013 Behavioral Risk Factor Surveillance System showed, women were more likely to report being told by a physician that they had COPD than did men (6.6%, compared with 5.4%).
Dr. Sodhi and colleagues noted that, at all time points examined from 2005 to 2014, women had a higher proportion than men of COPD hospitalizations and in-hospital deaths. They also noted that female sex is associated with a threefold risk for severe early-onset COPD, and that women with COPD have lower diffusion capacity of lungs for carbon monoxide, despite having higher predicted forced expiratory volume in 1 second, compared with men.
“Historically, COPD wasn’t a disease that was so prevalent in women. It’s been in the past 20 years that the trends have changed,” said Patricia Silveyra, MSc, PhD, ATSF, associate professor of environmental and occupational health at Indiana University, Bloomington.
The increasing prevalence of COPD among women cannot be explained by smoking alone, she said in an interview.
“It used to be thought that it was because more women smoked, but actually a lot of women who don’t smoke can develop COPD, so it appears to be probably something environmental, but because it used to be a disease of older men, in the clinic there was also a bias to diagnose men with COPD, and women with asthma, so a lot of women went underdiagnosed,” Dr. Silveyra said.
In their review, Dr. Sodhi and colleagues noted that women with COPD “may be underdiagnosed as a result of having different symptoms from those classically recognized. Reasons for underdiagnosis or a delay in diagnosis may also be due to lack of a formal evaluation with spirometry, women seeking care later in the course of disease, physician bias, or associated fatigue or depression misdirecting diagnostic strategies. Underdiagnosis may be associated with psychological distress and worse health-related quality of life.”
Although the evidence is mixed, women tend to present more frequently with the chronic bronchitis phenotype of COPD, compared with the emphysema phenotype, and women tend to have greater degrees of pulmonary function impairment when exposed to tobacco smoke, even after controlling for differences in height and weight.
“For the same amount of exposure to tobacco smoke, females are likely to develop more severe airflow limitation at an earlier age than males, and have more exacerbation,” Dr. Sodhi and colleagues wrote.
Both Dr. Silveyra and Dr. Sodhi said that reason why men and women differ in their physiological reactions to smoke are still unknown.
Sex differences in drug responses
There is only limited evidence to indicate that women and men respond differently to various therapeutic agents, but what is clear is that more research into this area is needed, Dr. Sodhi and Dr. Silveyra said.
For example, among the few studies that have documented sex differences, one showed no sex differences in the efficacy of salmeterol/fluticasone combination therapy for reducing exacerbations or improving quality of life, whereas another showed that women were more likely than men to experience COPD symptoms or exacerbations after stopping inhaled corticosteroids, Dr. Sodhi and colleagues noted.
Both Dr. Sodhi and Dr. Silveyra emphasized the need for clinical trials that study the effects of sex on treatment outcomes in COPD, which could lead to better, more personalized therapeutic regimens that take sex and gender into account.
Dr. Sodhi and colleagues offered the following advice to clinicians: “Interaction with female patients should take into account that their symptoms may not conform to traditionally accepted presentations. Challenges exist for female patients at all levels of health care interaction and as clinicians we need to acknowledge the bias and willfully work toward recognition and elimination of unconscious and conscious bias. Empowering our patients to have frank discussions with their health care team when they perceive bias is another step to help promote equity.”
The review by Dr. Sodhi and colleagues was supported by grants from the National Institutes of Health. Dr. Sodhi and Dr. Silveyra reported having no conflicts of interest to disclose.
When Sigmund Freud claimed that “anatomy is destiny” he was referring to anatomical sex as a determinant of personality traits. Expert consensus statements have previously offered some recommendations for managing these syndromes, but clinical data are scarce, so the present review “is intended to establish a starting point for future research,”
That notion has been widely discredited, but Freud appears to be inadvertently right in one respect: When it comes to chronic obstructive pulmonary disease (COPD), anatomy really is destiny, and sex may be as well, pulmonary researchers say.
There is a growing body of evidence to indicate that COPD affects men and women differently, and that men and women patients with COPD require different clinical management. Yet women are often underdiagnosed or misdiagnosed, partly because of poorly understood sex differences, but also because of cultural biases.
But plunging any farther into the weeds, it’s important to define terms. Although various investigators have used the terms “sex” and “gender” interchangeably, sex is the preferred term when referring to biological attributes of individual patients, while gender refers to personal identity.
These distinctions are important, contended Amik Sodhi, MBBS, MPH, from the division of allergy, pulmonology, and critical care medicine at the University of Wisconsin–Madison.
“Sex is essentially a biologic construct, so it’s got to do with the sex chromosomes, the genetics of that person, and it refers to the anatomic variations that can change susceptibility to different diseases,” she said in an interview.
An example of sex differences or “sexual dimorphism” can be found in a recent meta-analysis of sex-based genetic associations by Megan Hardin, MD, MPH from Brigham & Women’s Hospital in Boston and colleagues.
They reported that CELSR1, a gene involved in fetal lung development, was expressed more among women than among men and that a single nucleotide polymorphism in the gene was associated with COPD among women smokers, but not among men smokers.
The finding points to a potential risk locus for COPD in women, and could help shed light on sexual dimorphism in COPD, Dr. Hardin and colleagues said.
In contrast to sex, “gender is more of a psychosocial construct which can impact how diseases manifest themselves, how they are potentially managed, and what outcomes might occur for that particular disease,” Dr. Sodhi said.
She and her colleagues recently published a review of sex and gender in common lung disorders and sleep in the journal CHEST, where they wrote that the “influence of sex and gender is portrayed in epidemiological data, disease pathogenesis and pathophysiology, clinical manifestations, response to treatment, access to care, and health outcomes. Hence, sex and gender should be considered in all types of research, clinical practice and educational curricula.”
For example, as previously reported at the 2021 annual meeting of the American Thoracic Society, sex-specific differences in the severity of symptoms and prevalence of comorbidities in patients with COPD may point to different criteria for diagnosing cardiac comorbidities in women and men.
Those conclusions came from a retrospective analysis of data on 795 women and 1,251 men with GOLD (Global Initiative for Chronic Obstructive Lung Disease) class 1-3 disease.
The investigators looked at the patients’ clinical history, comorbidities, lung function, COPD Assessment Test scores, and modified Medical Research Council (mMRC) dyspnea score, and found significant differences between men and women for most functional parameters and comorbidities, and for CAT items of cough, phlegm, and energy.
In logistic regression analysis, predictors for cardiac disease in men were energy, mMRC score, smoking status, body mass index, age, and spirometric lung function, but in women only age was significantly predictive for cardiac disease.
An example of gender effects on COPD differences in men and women is the increase in cigarette advertising aimed at women in the 1960s and the advent of women-targeted brands such as Virginia Slims, which in turn lead to increased smoking rates among women. In addition, in the developing world, where the sex/gender gap in COPD is narrowing, women tend to have greater exposure to wood smoke and cooking fuels in unventilated or poorly ventilated spaces, compared with men.
Increasing incidence among women
According to the Centers for Disease Control and Prevention, chronic lower respiratory diseases, primarily COPD, were the fourth-leading cause of death in women in the United States in 2018, following only heart disease, cancer, and accidents/injuries.
And as a CDC analysis of data from the 2013 Behavioral Risk Factor Surveillance System showed, women were more likely to report being told by a physician that they had COPD than did men (6.6%, compared with 5.4%).
Dr. Sodhi and colleagues noted that, at all time points examined from 2005 to 2014, women had a higher proportion than men of COPD hospitalizations and in-hospital deaths. They also noted that female sex is associated with a threefold risk for severe early-onset COPD, and that women with COPD have lower diffusion capacity of lungs for carbon monoxide, despite having higher predicted forced expiratory volume in 1 second, compared with men.
“Historically, COPD wasn’t a disease that was so prevalent in women. It’s been in the past 20 years that the trends have changed,” said Patricia Silveyra, MSc, PhD, ATSF, associate professor of environmental and occupational health at Indiana University, Bloomington.
The increasing prevalence of COPD among women cannot be explained by smoking alone, she said in an interview.
“It used to be thought that it was because more women smoked, but actually a lot of women who don’t smoke can develop COPD, so it appears to be probably something environmental, but because it used to be a disease of older men, in the clinic there was also a bias to diagnose men with COPD, and women with asthma, so a lot of women went underdiagnosed,” Dr. Silveyra said.
In their review, Dr. Sodhi and colleagues noted that women with COPD “may be underdiagnosed as a result of having different symptoms from those classically recognized. Reasons for underdiagnosis or a delay in diagnosis may also be due to lack of a formal evaluation with spirometry, women seeking care later in the course of disease, physician bias, or associated fatigue or depression misdirecting diagnostic strategies. Underdiagnosis may be associated with psychological distress and worse health-related quality of life.”
Although the evidence is mixed, women tend to present more frequently with the chronic bronchitis phenotype of COPD, compared with the emphysema phenotype, and women tend to have greater degrees of pulmonary function impairment when exposed to tobacco smoke, even after controlling for differences in height and weight.
“For the same amount of exposure to tobacco smoke, females are likely to develop more severe airflow limitation at an earlier age than males, and have more exacerbation,” Dr. Sodhi and colleagues wrote.
Both Dr. Silveyra and Dr. Sodhi said that reason why men and women differ in their physiological reactions to smoke are still unknown.
Sex differences in drug responses
There is only limited evidence to indicate that women and men respond differently to various therapeutic agents, but what is clear is that more research into this area is needed, Dr. Sodhi and Dr. Silveyra said.
For example, among the few studies that have documented sex differences, one showed no sex differences in the efficacy of salmeterol/fluticasone combination therapy for reducing exacerbations or improving quality of life, whereas another showed that women were more likely than men to experience COPD symptoms or exacerbations after stopping inhaled corticosteroids, Dr. Sodhi and colleagues noted.
Both Dr. Sodhi and Dr. Silveyra emphasized the need for clinical trials that study the effects of sex on treatment outcomes in COPD, which could lead to better, more personalized therapeutic regimens that take sex and gender into account.
Dr. Sodhi and colleagues offered the following advice to clinicians: “Interaction with female patients should take into account that their symptoms may not conform to traditionally accepted presentations. Challenges exist for female patients at all levels of health care interaction and as clinicians we need to acknowledge the bias and willfully work toward recognition and elimination of unconscious and conscious bias. Empowering our patients to have frank discussions with their health care team when they perceive bias is another step to help promote equity.”
The review by Dr. Sodhi and colleagues was supported by grants from the National Institutes of Health. Dr. Sodhi and Dr. Silveyra reported having no conflicts of interest to disclose.
When Sigmund Freud claimed that “anatomy is destiny” he was referring to anatomical sex as a determinant of personality traits. Expert consensus statements have previously offered some recommendations for managing these syndromes, but clinical data are scarce, so the present review “is intended to establish a starting point for future research,”
That notion has been widely discredited, but Freud appears to be inadvertently right in one respect: When it comes to chronic obstructive pulmonary disease (COPD), anatomy really is destiny, and sex may be as well, pulmonary researchers say.
There is a growing body of evidence to indicate that COPD affects men and women differently, and that men and women patients with COPD require different clinical management. Yet women are often underdiagnosed or misdiagnosed, partly because of poorly understood sex differences, but also because of cultural biases.
But plunging any farther into the weeds, it’s important to define terms. Although various investigators have used the terms “sex” and “gender” interchangeably, sex is the preferred term when referring to biological attributes of individual patients, while gender refers to personal identity.
These distinctions are important, contended Amik Sodhi, MBBS, MPH, from the division of allergy, pulmonology, and critical care medicine at the University of Wisconsin–Madison.
“Sex is essentially a biologic construct, so it’s got to do with the sex chromosomes, the genetics of that person, and it refers to the anatomic variations that can change susceptibility to different diseases,” she said in an interview.
An example of sex differences or “sexual dimorphism” can be found in a recent meta-analysis of sex-based genetic associations by Megan Hardin, MD, MPH from Brigham & Women’s Hospital in Boston and colleagues.
They reported that CELSR1, a gene involved in fetal lung development, was expressed more among women than among men and that a single nucleotide polymorphism in the gene was associated with COPD among women smokers, but not among men smokers.
The finding points to a potential risk locus for COPD in women, and could help shed light on sexual dimorphism in COPD, Dr. Hardin and colleagues said.
In contrast to sex, “gender is more of a psychosocial construct which can impact how diseases manifest themselves, how they are potentially managed, and what outcomes might occur for that particular disease,” Dr. Sodhi said.
She and her colleagues recently published a review of sex and gender in common lung disorders and sleep in the journal CHEST, where they wrote that the “influence of sex and gender is portrayed in epidemiological data, disease pathogenesis and pathophysiology, clinical manifestations, response to treatment, access to care, and health outcomes. Hence, sex and gender should be considered in all types of research, clinical practice and educational curricula.”
For example, as previously reported at the 2021 annual meeting of the American Thoracic Society, sex-specific differences in the severity of symptoms and prevalence of comorbidities in patients with COPD may point to different criteria for diagnosing cardiac comorbidities in women and men.
Those conclusions came from a retrospective analysis of data on 795 women and 1,251 men with GOLD (Global Initiative for Chronic Obstructive Lung Disease) class 1-3 disease.
The investigators looked at the patients’ clinical history, comorbidities, lung function, COPD Assessment Test scores, and modified Medical Research Council (mMRC) dyspnea score, and found significant differences between men and women for most functional parameters and comorbidities, and for CAT items of cough, phlegm, and energy.
In logistic regression analysis, predictors for cardiac disease in men were energy, mMRC score, smoking status, body mass index, age, and spirometric lung function, but in women only age was significantly predictive for cardiac disease.
An example of gender effects on COPD differences in men and women is the increase in cigarette advertising aimed at women in the 1960s and the advent of women-targeted brands such as Virginia Slims, which in turn lead to increased smoking rates among women. In addition, in the developing world, where the sex/gender gap in COPD is narrowing, women tend to have greater exposure to wood smoke and cooking fuels in unventilated or poorly ventilated spaces, compared with men.
Increasing incidence among women
According to the Centers for Disease Control and Prevention, chronic lower respiratory diseases, primarily COPD, were the fourth-leading cause of death in women in the United States in 2018, following only heart disease, cancer, and accidents/injuries.
And as a CDC analysis of data from the 2013 Behavioral Risk Factor Surveillance System showed, women were more likely to report being told by a physician that they had COPD than did men (6.6%, compared with 5.4%).
Dr. Sodhi and colleagues noted that, at all time points examined from 2005 to 2014, women had a higher proportion than men of COPD hospitalizations and in-hospital deaths. They also noted that female sex is associated with a threefold risk for severe early-onset COPD, and that women with COPD have lower diffusion capacity of lungs for carbon monoxide, despite having higher predicted forced expiratory volume in 1 second, compared with men.
“Historically, COPD wasn’t a disease that was so prevalent in women. It’s been in the past 20 years that the trends have changed,” said Patricia Silveyra, MSc, PhD, ATSF, associate professor of environmental and occupational health at Indiana University, Bloomington.
The increasing prevalence of COPD among women cannot be explained by smoking alone, she said in an interview.
“It used to be thought that it was because more women smoked, but actually a lot of women who don’t smoke can develop COPD, so it appears to be probably something environmental, but because it used to be a disease of older men, in the clinic there was also a bias to diagnose men with COPD, and women with asthma, so a lot of women went underdiagnosed,” Dr. Silveyra said.
In their review, Dr. Sodhi and colleagues noted that women with COPD “may be underdiagnosed as a result of having different symptoms from those classically recognized. Reasons for underdiagnosis or a delay in diagnosis may also be due to lack of a formal evaluation with spirometry, women seeking care later in the course of disease, physician bias, or associated fatigue or depression misdirecting diagnostic strategies. Underdiagnosis may be associated with psychological distress and worse health-related quality of life.”
Although the evidence is mixed, women tend to present more frequently with the chronic bronchitis phenotype of COPD, compared with the emphysema phenotype, and women tend to have greater degrees of pulmonary function impairment when exposed to tobacco smoke, even after controlling for differences in height and weight.
“For the same amount of exposure to tobacco smoke, females are likely to develop more severe airflow limitation at an earlier age than males, and have more exacerbation,” Dr. Sodhi and colleagues wrote.
Both Dr. Silveyra and Dr. Sodhi said that reason why men and women differ in their physiological reactions to smoke are still unknown.
Sex differences in drug responses
There is only limited evidence to indicate that women and men respond differently to various therapeutic agents, but what is clear is that more research into this area is needed, Dr. Sodhi and Dr. Silveyra said.
For example, among the few studies that have documented sex differences, one showed no sex differences in the efficacy of salmeterol/fluticasone combination therapy for reducing exacerbations or improving quality of life, whereas another showed that women were more likely than men to experience COPD symptoms or exacerbations after stopping inhaled corticosteroids, Dr. Sodhi and colleagues noted.
Both Dr. Sodhi and Dr. Silveyra emphasized the need for clinical trials that study the effects of sex on treatment outcomes in COPD, which could lead to better, more personalized therapeutic regimens that take sex and gender into account.
Dr. Sodhi and colleagues offered the following advice to clinicians: “Interaction with female patients should take into account that their symptoms may not conform to traditionally accepted presentations. Challenges exist for female patients at all levels of health care interaction and as clinicians we need to acknowledge the bias and willfully work toward recognition and elimination of unconscious and conscious bias. Empowering our patients to have frank discussions with their health care team when they perceive bias is another step to help promote equity.”
The review by Dr. Sodhi and colleagues was supported by grants from the National Institutes of Health. Dr. Sodhi and Dr. Silveyra reported having no conflicts of interest to disclose.