User login
I’m a physician battling long COVID. I can assure you it’s real
One in 5. It almost seems unimaginable that this is the real number of people who are struggling with long COVID, especially considering how many people in the United States have had COVID-19 at this point (more than 96 million).
Even more unimaginable at this time is that it’s happening to me. I’ve experienced not only the disabling effects of long COVID, but I’ve also seen, firsthand, the frustration of navigating diagnosis and treatment. It’s given me a taste of what millions of other patients are going through.
Vaxxed, masked, and (too) relaxed
I caught COVID-19 (probably Omicron BA.5) that presented as sniffles, making me think it was probably just allergies. However, my resting heart rate was up on my Garmin watch, so of course I got tested and was positive.
With my symptoms virtually nonexistent, it seemed, at the time, merely an inconvenience, because I was forced to isolate away from family and friends, who all stayed negative.
But 2 weeks later, I began to have urticaria – hives – after physical exertion. Did that mean my mast cells were angry? There’s some evidence these immune cells become overactivated in some patients with COVID. Next, I began to experience lightheadedness and the rapid heartbeat of tachycardia. The tachycardia was especially bad any time I physically exerted myself, including on a walk. Imagine me – a lover of all bargain shopping – cutting short a trip to the outlet mall on a particularly bad day when my heart rate was 140 after taking just a few steps. This was orthostatic intolerance.
Then came the severe worsening of my migraines – which are often vestibular, making me nauseated and dizzy on top of the throbbing.
I was of course familiar with these symptoms, as professor and chair of the department of rehabilitation medicine at the Joe R. and Teresa Lozano Long School of Medicine at University of Texas Health Science Center, San Antonio. I developed a post-COVID recovery clinic to help patients.
So I knew about postexertional malaise (PEM) and postexertional symptom exacerbation (PESE), but I was now experiencing these distressing symptoms firsthand.
Clinicians really need to look for this cardinal sign of long COVID as well as evidence of myalgic encephalomyelitis or chronic fatigue syndrome (ME/CFS). ME/CFS is marked by exacerbation of fatigue or symptoms after an activity that could previously be done without these aftereffects. In my case, as an All-American Masters miler with several marathons under my belt, running 5 miles is a walk in the park. But now, I pay for those 5 miles for the rest of the day on the couch or with palpitations, dizziness, and fatigue the following day. Busy clinic day full of procedures? I would have to be sitting by the end of it. Bed by 9 PM was not always early enough.
Becoming a statistic
Here I am, one of the leading experts in the country on caring for people with long COVID, featured in the national news and having testified in front of Congress, and now I am part of that lived experience. Me – a healthy athlete, with no comorbidities, a normal BMI, vaccinated and boosted, and after an almost asymptomatic bout of COVID-19, a victim to long COVID.
You just never know how your body is going to react. Neuroinflammation occurred in studies with mice with mild respiratory COVID and could be happening to me. I did not want a chronic immune-mediated vasculopathy.
So, I did what any other hyperaware physician-researcher would do. I enrolled in the RECOVER trial – a study my own institution is taking part in and one that I recommend to my own patients.
I also decided that I need to access care and not just ignore my symptoms or try to treat them myself.
That’s when things got difficult. There was a wait of at least a month to see my primary care provider – but I was able to use my privileged position as a physician to get in sooner.
My provider said that she had limited knowledge of long COVID, and she hesitated to order some of the tests and treatments that I recommended because they were not yet considered standard of care. I can understand the hesitation. It is engrained in medical education to follow evidence based on the highest-quality research studies. We are slowly learning more about long COVID, but acknowledging the learning curve offers little to patients who need help now.
This has made me realize that we cannot wait on an evidence-based approach – which can take decades to develop – while people are suffering. And it’s important that everyone on the front line learn about some of the manifestations and disease management of long COVID.
I left this first physician visit feeling more defeated than anything and decided to try to push through. That, I quickly realized, was not the right thing to do.
So again, after a couple of significant crashes and days of severe migraines, I phoned a friend: Ratna Bhavaraju-Sanka, MD, the amazing neurologist who treats patients with long COVID alongside me. She squeezed me in on a non-clinic day. Again, I had the privilege to see a specialist most people wait half a year to see. I was diagnosed with both autonomic dysfunction and intractable migraine.
She ordered some intravenous fluids and IV magnesium that would probably help both. But then another obstacle arose. My institution’s infusion center is focused on patients with cancer, and I was unable to schedule treatments there.
Luckily, I knew about the concierge mobile IV hydration therapy companies that come to your house – mostly offering a hangover treatment service. And I am thankful that I had the health literacy and financial ability to pay for some fluids at home.
On another particularly bad day, I phoned other friends – higher-ups at the hospital – who expedited a slot at the hospital infusion center and approval for the IV magnesium.
Thanks to my access, knowledge, and other privileges, I got fairly quick if imperfect care, enrolled in a research trial, and received medications. I knew to pace myself. The vast majority of others with long COVID lack these advantages.
The patient with long COVID
Things I have learned that others can learn, too:
- Acknowledge and recognize that long COVID is a disease that is affecting 1 in 5 Americans who catch COVID. Many look completely “normal on the outside.” Please listen to your patients.
- Autonomic dysfunction is a common manifestation of long COVID. A 10-minute stand test goes a long way in diagnosing this condition, from the American Academy of Physical Medicine and Rehabilitation. It is not just anxiety.
- “That’s only in research” is dismissive and harmful. Think outside the box. Follow guidelines. Consider encouraging patients to sign up for trials.
- Screen for PEM/PESE and teach your patients to pace themselves, because pushing through it or doing graded exercises will be harmful.
- We need to train more physicians to treat postacute sequelae of SARS-CoV-2 infection () and other postinfectious conditions, such as ME/CFS.
If long COVID is hard for physicians to understand and deal with, imagine how difficult it is for patients with no expertise in this area.
It is exponentially harder for those with fewer resources, time, and health literacy. My lived experience with long COVID has shown me that being a patient is never easy. You put your body and fate into the hands of trusted professionals and expect validation and assistance, not gaslighting or gatekeeping.
Along with millions of others, I am tired of waiting.
Dr. Gutierrez is Professor and Distinguished Chair, department of rehabilitation medicine, University of Texas Health Science Center at San Antonio. She reported receiving honoraria for lecturing on long COVID and receiving a research grant from Co-PI for the NIH RECOVER trial.
A version of this article first appeared on Medscape.com.
One in 5. It almost seems unimaginable that this is the real number of people who are struggling with long COVID, especially considering how many people in the United States have had COVID-19 at this point (more than 96 million).
Even more unimaginable at this time is that it’s happening to me. I’ve experienced not only the disabling effects of long COVID, but I’ve also seen, firsthand, the frustration of navigating diagnosis and treatment. It’s given me a taste of what millions of other patients are going through.
Vaxxed, masked, and (too) relaxed
I caught COVID-19 (probably Omicron BA.5) that presented as sniffles, making me think it was probably just allergies. However, my resting heart rate was up on my Garmin watch, so of course I got tested and was positive.
With my symptoms virtually nonexistent, it seemed, at the time, merely an inconvenience, because I was forced to isolate away from family and friends, who all stayed negative.
But 2 weeks later, I began to have urticaria – hives – after physical exertion. Did that mean my mast cells were angry? There’s some evidence these immune cells become overactivated in some patients with COVID. Next, I began to experience lightheadedness and the rapid heartbeat of tachycardia. The tachycardia was especially bad any time I physically exerted myself, including on a walk. Imagine me – a lover of all bargain shopping – cutting short a trip to the outlet mall on a particularly bad day when my heart rate was 140 after taking just a few steps. This was orthostatic intolerance.
Then came the severe worsening of my migraines – which are often vestibular, making me nauseated and dizzy on top of the throbbing.
I was of course familiar with these symptoms, as professor and chair of the department of rehabilitation medicine at the Joe R. and Teresa Lozano Long School of Medicine at University of Texas Health Science Center, San Antonio. I developed a post-COVID recovery clinic to help patients.
So I knew about postexertional malaise (PEM) and postexertional symptom exacerbation (PESE), but I was now experiencing these distressing symptoms firsthand.
Clinicians really need to look for this cardinal sign of long COVID as well as evidence of myalgic encephalomyelitis or chronic fatigue syndrome (ME/CFS). ME/CFS is marked by exacerbation of fatigue or symptoms after an activity that could previously be done without these aftereffects. In my case, as an All-American Masters miler with several marathons under my belt, running 5 miles is a walk in the park. But now, I pay for those 5 miles for the rest of the day on the couch or with palpitations, dizziness, and fatigue the following day. Busy clinic day full of procedures? I would have to be sitting by the end of it. Bed by 9 PM was not always early enough.
Becoming a statistic
Here I am, one of the leading experts in the country on caring for people with long COVID, featured in the national news and having testified in front of Congress, and now I am part of that lived experience. Me – a healthy athlete, with no comorbidities, a normal BMI, vaccinated and boosted, and after an almost asymptomatic bout of COVID-19, a victim to long COVID.
You just never know how your body is going to react. Neuroinflammation occurred in studies with mice with mild respiratory COVID and could be happening to me. I did not want a chronic immune-mediated vasculopathy.
So, I did what any other hyperaware physician-researcher would do. I enrolled in the RECOVER trial – a study my own institution is taking part in and one that I recommend to my own patients.
I also decided that I need to access care and not just ignore my symptoms or try to treat them myself.
That’s when things got difficult. There was a wait of at least a month to see my primary care provider – but I was able to use my privileged position as a physician to get in sooner.
My provider said that she had limited knowledge of long COVID, and she hesitated to order some of the tests and treatments that I recommended because they were not yet considered standard of care. I can understand the hesitation. It is engrained in medical education to follow evidence based on the highest-quality research studies. We are slowly learning more about long COVID, but acknowledging the learning curve offers little to patients who need help now.
This has made me realize that we cannot wait on an evidence-based approach – which can take decades to develop – while people are suffering. And it’s important that everyone on the front line learn about some of the manifestations and disease management of long COVID.
I left this first physician visit feeling more defeated than anything and decided to try to push through. That, I quickly realized, was not the right thing to do.
So again, after a couple of significant crashes and days of severe migraines, I phoned a friend: Ratna Bhavaraju-Sanka, MD, the amazing neurologist who treats patients with long COVID alongside me. She squeezed me in on a non-clinic day. Again, I had the privilege to see a specialist most people wait half a year to see. I was diagnosed with both autonomic dysfunction and intractable migraine.
She ordered some intravenous fluids and IV magnesium that would probably help both. But then another obstacle arose. My institution’s infusion center is focused on patients with cancer, and I was unable to schedule treatments there.
Luckily, I knew about the concierge mobile IV hydration therapy companies that come to your house – mostly offering a hangover treatment service. And I am thankful that I had the health literacy and financial ability to pay for some fluids at home.
On another particularly bad day, I phoned other friends – higher-ups at the hospital – who expedited a slot at the hospital infusion center and approval for the IV magnesium.
Thanks to my access, knowledge, and other privileges, I got fairly quick if imperfect care, enrolled in a research trial, and received medications. I knew to pace myself. The vast majority of others with long COVID lack these advantages.
The patient with long COVID
Things I have learned that others can learn, too:
- Acknowledge and recognize that long COVID is a disease that is affecting 1 in 5 Americans who catch COVID. Many look completely “normal on the outside.” Please listen to your patients.
- Autonomic dysfunction is a common manifestation of long COVID. A 10-minute stand test goes a long way in diagnosing this condition, from the American Academy of Physical Medicine and Rehabilitation. It is not just anxiety.
- “That’s only in research” is dismissive and harmful. Think outside the box. Follow guidelines. Consider encouraging patients to sign up for trials.
- Screen for PEM/PESE and teach your patients to pace themselves, because pushing through it or doing graded exercises will be harmful.
- We need to train more physicians to treat postacute sequelae of SARS-CoV-2 infection () and other postinfectious conditions, such as ME/CFS.
If long COVID is hard for physicians to understand and deal with, imagine how difficult it is for patients with no expertise in this area.
It is exponentially harder for those with fewer resources, time, and health literacy. My lived experience with long COVID has shown me that being a patient is never easy. You put your body and fate into the hands of trusted professionals and expect validation and assistance, not gaslighting or gatekeeping.
Along with millions of others, I am tired of waiting.
Dr. Gutierrez is Professor and Distinguished Chair, department of rehabilitation medicine, University of Texas Health Science Center at San Antonio. She reported receiving honoraria for lecturing on long COVID and receiving a research grant from Co-PI for the NIH RECOVER trial.
A version of this article first appeared on Medscape.com.
One in 5. It almost seems unimaginable that this is the real number of people who are struggling with long COVID, especially considering how many people in the United States have had COVID-19 at this point (more than 96 million).
Even more unimaginable at this time is that it’s happening to me. I’ve experienced not only the disabling effects of long COVID, but I’ve also seen, firsthand, the frustration of navigating diagnosis and treatment. It’s given me a taste of what millions of other patients are going through.
Vaxxed, masked, and (too) relaxed
I caught COVID-19 (probably Omicron BA.5) that presented as sniffles, making me think it was probably just allergies. However, my resting heart rate was up on my Garmin watch, so of course I got tested and was positive.
With my symptoms virtually nonexistent, it seemed, at the time, merely an inconvenience, because I was forced to isolate away from family and friends, who all stayed negative.
But 2 weeks later, I began to have urticaria – hives – after physical exertion. Did that mean my mast cells were angry? There’s some evidence these immune cells become overactivated in some patients with COVID. Next, I began to experience lightheadedness and the rapid heartbeat of tachycardia. The tachycardia was especially bad any time I physically exerted myself, including on a walk. Imagine me – a lover of all bargain shopping – cutting short a trip to the outlet mall on a particularly bad day when my heart rate was 140 after taking just a few steps. This was orthostatic intolerance.
Then came the severe worsening of my migraines – which are often vestibular, making me nauseated and dizzy on top of the throbbing.
I was of course familiar with these symptoms, as professor and chair of the department of rehabilitation medicine at the Joe R. and Teresa Lozano Long School of Medicine at University of Texas Health Science Center, San Antonio. I developed a post-COVID recovery clinic to help patients.
So I knew about postexertional malaise (PEM) and postexertional symptom exacerbation (PESE), but I was now experiencing these distressing symptoms firsthand.
Clinicians really need to look for this cardinal sign of long COVID as well as evidence of myalgic encephalomyelitis or chronic fatigue syndrome (ME/CFS). ME/CFS is marked by exacerbation of fatigue or symptoms after an activity that could previously be done without these aftereffects. In my case, as an All-American Masters miler with several marathons under my belt, running 5 miles is a walk in the park. But now, I pay for those 5 miles for the rest of the day on the couch or with palpitations, dizziness, and fatigue the following day. Busy clinic day full of procedures? I would have to be sitting by the end of it. Bed by 9 PM was not always early enough.
Becoming a statistic
Here I am, one of the leading experts in the country on caring for people with long COVID, featured in the national news and having testified in front of Congress, and now I am part of that lived experience. Me – a healthy athlete, with no comorbidities, a normal BMI, vaccinated and boosted, and after an almost asymptomatic bout of COVID-19, a victim to long COVID.
You just never know how your body is going to react. Neuroinflammation occurred in studies with mice with mild respiratory COVID and could be happening to me. I did not want a chronic immune-mediated vasculopathy.
So, I did what any other hyperaware physician-researcher would do. I enrolled in the RECOVER trial – a study my own institution is taking part in and one that I recommend to my own patients.
I also decided that I need to access care and not just ignore my symptoms or try to treat them myself.
That’s when things got difficult. There was a wait of at least a month to see my primary care provider – but I was able to use my privileged position as a physician to get in sooner.
My provider said that she had limited knowledge of long COVID, and she hesitated to order some of the tests and treatments that I recommended because they were not yet considered standard of care. I can understand the hesitation. It is engrained in medical education to follow evidence based on the highest-quality research studies. We are slowly learning more about long COVID, but acknowledging the learning curve offers little to patients who need help now.
This has made me realize that we cannot wait on an evidence-based approach – which can take decades to develop – while people are suffering. And it’s important that everyone on the front line learn about some of the manifestations and disease management of long COVID.
I left this first physician visit feeling more defeated than anything and decided to try to push through. That, I quickly realized, was not the right thing to do.
So again, after a couple of significant crashes and days of severe migraines, I phoned a friend: Ratna Bhavaraju-Sanka, MD, the amazing neurologist who treats patients with long COVID alongside me. She squeezed me in on a non-clinic day. Again, I had the privilege to see a specialist most people wait half a year to see. I was diagnosed with both autonomic dysfunction and intractable migraine.
She ordered some intravenous fluids and IV magnesium that would probably help both. But then another obstacle arose. My institution’s infusion center is focused on patients with cancer, and I was unable to schedule treatments there.
Luckily, I knew about the concierge mobile IV hydration therapy companies that come to your house – mostly offering a hangover treatment service. And I am thankful that I had the health literacy and financial ability to pay for some fluids at home.
On another particularly bad day, I phoned other friends – higher-ups at the hospital – who expedited a slot at the hospital infusion center and approval for the IV magnesium.
Thanks to my access, knowledge, and other privileges, I got fairly quick if imperfect care, enrolled in a research trial, and received medications. I knew to pace myself. The vast majority of others with long COVID lack these advantages.
The patient with long COVID
Things I have learned that others can learn, too:
- Acknowledge and recognize that long COVID is a disease that is affecting 1 in 5 Americans who catch COVID. Many look completely “normal on the outside.” Please listen to your patients.
- Autonomic dysfunction is a common manifestation of long COVID. A 10-minute stand test goes a long way in diagnosing this condition, from the American Academy of Physical Medicine and Rehabilitation. It is not just anxiety.
- “That’s only in research” is dismissive and harmful. Think outside the box. Follow guidelines. Consider encouraging patients to sign up for trials.
- Screen for PEM/PESE and teach your patients to pace themselves, because pushing through it or doing graded exercises will be harmful.
- We need to train more physicians to treat postacute sequelae of SARS-CoV-2 infection () and other postinfectious conditions, such as ME/CFS.
If long COVID is hard for physicians to understand and deal with, imagine how difficult it is for patients with no expertise in this area.
It is exponentially harder for those with fewer resources, time, and health literacy. My lived experience with long COVID has shown me that being a patient is never easy. You put your body and fate into the hands of trusted professionals and expect validation and assistance, not gaslighting or gatekeeping.
Along with millions of others, I am tired of waiting.
Dr. Gutierrez is Professor and Distinguished Chair, department of rehabilitation medicine, University of Texas Health Science Center at San Antonio. She reported receiving honoraria for lecturing on long COVID and receiving a research grant from Co-PI for the NIH RECOVER trial.
A version of this article first appeared on Medscape.com.
Has the pandemic affected babies’ brain development?
There’s some good overall news in a large analysis that looked at whether a mother’s COVID-19 infection or birth during the pandemic could affect a baby’s brain development.
Researchers studied 21,419 infants who had neurodevelopmental screening during the pandemic (from January 2020 to January 2021) and compared them with babies born before the pandemic (2015-2019).
They found in an analysis of eight studies that, generally, brain development in infants ages 6-12 months old was not changed by COVID-19.
Communication skill scores lower than prepandemic
However, one area did see a significant difference when they looked at answers to the Ages and Stages Questionnaire, 3rd edition (ASQ-3): Scores were lower in communication skills.
Compared with the prepandemic babies, the pandemic group of babies was more likely to have communication impairment (odds were 1.7 times higher).
Additionally, mothers’ SARS-CoV-2 infection was not associated with significant differences in any neurodevelopment sector in offspring, with one exception: Odds were 3.5 times higher for fine motor impairment in the pandemic baby group.
The babies in this study were either exposed in the womb to the SARS-CoV-2 infection or screened during the pandemic regardless of whether they were exposed to the virus.
The study, led by Kamran Hessami, MD, with the Maternal Fetal Care Center at Boston Children’s Hospital and Harvard Medical School in Boston, was published in JAMA Network Open.
Potential reasons for lower communication skills
The study points to some factors of the pandemic that may be tied to impaired communication skills.
“Higher levels of COVID-19–related stress were reported for both mothers and fathers of infants aged 0-6 months and were associated with insensitive parenting practices, including decreased emotional responsiveness in only mothers, which could lessen the reciprocal exchanges that support language development in early childhood,” they write. “Additionally, opportunities to promote language and social development through new experiences outside the home, including visits with extended family and friends or attendance at a child care center, were lessened for many during the pandemic.”
Viviana M. Fajardo Martinez, MD, with neonatal/perinatal medicine at University of California, Los Angeles, Health, told this publication her team is also studying child development before and after the pandemic over a 3-year period, and delayed communication skills is something she is seeing in clinic there.
She says some parents have been concerned, saying their babies aren’t talking enough or are behind in vocabulary.
Babies can catch up after 12 months
One thing she tells parents is that babies who are a bit delayed at 12 months can catch up.
Up to 18 months, they can catch up, she said, adding that they can be reevaluated then for improvement. If, at that point, the baby is not catching up, “that’s when we refer for early intervention,” she said.
Dr. Martinez also tells parents concerned about their infant’s communication skills that it’s important to talk, read, and sing to their child. She said amid pandemic stress, corners may have been cut in asking children to use language skills.
For instance, if a child points to an apple, a stressed parent may just give the child the apple instead of asking the child to request it by name and repeat the word several times.
She also said a limitation of this study is the use of the ASQ-3 questionnaire, which is filled out by parents. Answers are subjective, she notes, and sometimes differ between one child’s two parents. The questionnaire was commonly used during the pandemic because a more objective, professional evaluation has been more difficult.
However, a measure like the Bayley Scales of Infant and Toddler Development Screening Test adds objectivity and will likely give a better picture as research progresses, Dr. Martinez said.
Some information missing
Andréane Lavallée, PhD, and Dani Dumitriu, MD, PhD, both with the department of pediatrics at Columbia University, New York, write in an invited commentary that the overall positive message of the study “should not make researchers complacent” and results should be viewed with caution.
They point out that the precise effects of this novel virus are still unclear and the age group and variables studied may not tell the whole story.
“It should be noted that this systematic review did not consider timing of exposure during pregnancy, maternal infection severity, or exposure to various SARS-CoV-2 variants – all factors that could eventually be proven to contribute to subtle adverse neurodevelopmental outcomes,” they write.
Additionally, past pandemics “such as the 1918 Spanish flu, 1964 rubella, and 2009 H1N1” have taught researchers to watch for increases in diagnoses such as autism spectrum disorder (ASD) and schizophrenia in subsequent years.
“ASD is generally diagnosed at age 3-5 years (and often not until early teens), while schizophrenia is generally diagnosed in mid-to-late 20s,” the editorialists point out. The authors agree and emphasize the need for long-term studies.
Authors report no relevant financial relationships. Editorialist Dr. Dumitriu reports grants from National Institute of Mental Health, the U.S. Centers for Disease Control and Prevention, and the W. K. Kellogg Foundation; and has received gift funds from Einhorn Collaborative during the conduct of the study to the Nurture Science Program, for which Dr Dumitriu serves as director. Dr. Dumitriu received personal fees from Medela outside the submitted work; and is the corresponding author for one of the studies (Shuffrey et al., 2022) included in the systematic review conducted by Dr. Hessami et al. Dr. Lavallée reports grants from the Canadian Institutes of Health Research. Dr. Martinez reports no relevant financial relationships.
There’s some good overall news in a large analysis that looked at whether a mother’s COVID-19 infection or birth during the pandemic could affect a baby’s brain development.
Researchers studied 21,419 infants who had neurodevelopmental screening during the pandemic (from January 2020 to January 2021) and compared them with babies born before the pandemic (2015-2019).
They found in an analysis of eight studies that, generally, brain development in infants ages 6-12 months old was not changed by COVID-19.
Communication skill scores lower than prepandemic
However, one area did see a significant difference when they looked at answers to the Ages and Stages Questionnaire, 3rd edition (ASQ-3): Scores were lower in communication skills.
Compared with the prepandemic babies, the pandemic group of babies was more likely to have communication impairment (odds were 1.7 times higher).
Additionally, mothers’ SARS-CoV-2 infection was not associated with significant differences in any neurodevelopment sector in offspring, with one exception: Odds were 3.5 times higher for fine motor impairment in the pandemic baby group.
The babies in this study were either exposed in the womb to the SARS-CoV-2 infection or screened during the pandemic regardless of whether they were exposed to the virus.
The study, led by Kamran Hessami, MD, with the Maternal Fetal Care Center at Boston Children’s Hospital and Harvard Medical School in Boston, was published in JAMA Network Open.
Potential reasons for lower communication skills
The study points to some factors of the pandemic that may be tied to impaired communication skills.
“Higher levels of COVID-19–related stress were reported for both mothers and fathers of infants aged 0-6 months and were associated with insensitive parenting practices, including decreased emotional responsiveness in only mothers, which could lessen the reciprocal exchanges that support language development in early childhood,” they write. “Additionally, opportunities to promote language and social development through new experiences outside the home, including visits with extended family and friends or attendance at a child care center, were lessened for many during the pandemic.”
Viviana M. Fajardo Martinez, MD, with neonatal/perinatal medicine at University of California, Los Angeles, Health, told this publication her team is also studying child development before and after the pandemic over a 3-year period, and delayed communication skills is something she is seeing in clinic there.
She says some parents have been concerned, saying their babies aren’t talking enough or are behind in vocabulary.
Babies can catch up after 12 months
One thing she tells parents is that babies who are a bit delayed at 12 months can catch up.
Up to 18 months, they can catch up, she said, adding that they can be reevaluated then for improvement. If, at that point, the baby is not catching up, “that’s when we refer for early intervention,” she said.
Dr. Martinez also tells parents concerned about their infant’s communication skills that it’s important to talk, read, and sing to their child. She said amid pandemic stress, corners may have been cut in asking children to use language skills.
For instance, if a child points to an apple, a stressed parent may just give the child the apple instead of asking the child to request it by name and repeat the word several times.
She also said a limitation of this study is the use of the ASQ-3 questionnaire, which is filled out by parents. Answers are subjective, she notes, and sometimes differ between one child’s two parents. The questionnaire was commonly used during the pandemic because a more objective, professional evaluation has been more difficult.
However, a measure like the Bayley Scales of Infant and Toddler Development Screening Test adds objectivity and will likely give a better picture as research progresses, Dr. Martinez said.
Some information missing
Andréane Lavallée, PhD, and Dani Dumitriu, MD, PhD, both with the department of pediatrics at Columbia University, New York, write in an invited commentary that the overall positive message of the study “should not make researchers complacent” and results should be viewed with caution.
They point out that the precise effects of this novel virus are still unclear and the age group and variables studied may not tell the whole story.
“It should be noted that this systematic review did not consider timing of exposure during pregnancy, maternal infection severity, or exposure to various SARS-CoV-2 variants – all factors that could eventually be proven to contribute to subtle adverse neurodevelopmental outcomes,” they write.
Additionally, past pandemics “such as the 1918 Spanish flu, 1964 rubella, and 2009 H1N1” have taught researchers to watch for increases in diagnoses such as autism spectrum disorder (ASD) and schizophrenia in subsequent years.
“ASD is generally diagnosed at age 3-5 years (and often not until early teens), while schizophrenia is generally diagnosed in mid-to-late 20s,” the editorialists point out. The authors agree and emphasize the need for long-term studies.
Authors report no relevant financial relationships. Editorialist Dr. Dumitriu reports grants from National Institute of Mental Health, the U.S. Centers for Disease Control and Prevention, and the W. K. Kellogg Foundation; and has received gift funds from Einhorn Collaborative during the conduct of the study to the Nurture Science Program, for which Dr Dumitriu serves as director. Dr. Dumitriu received personal fees from Medela outside the submitted work; and is the corresponding author for one of the studies (Shuffrey et al., 2022) included in the systematic review conducted by Dr. Hessami et al. Dr. Lavallée reports grants from the Canadian Institutes of Health Research. Dr. Martinez reports no relevant financial relationships.
There’s some good overall news in a large analysis that looked at whether a mother’s COVID-19 infection or birth during the pandemic could affect a baby’s brain development.
Researchers studied 21,419 infants who had neurodevelopmental screening during the pandemic (from January 2020 to January 2021) and compared them with babies born before the pandemic (2015-2019).
They found in an analysis of eight studies that, generally, brain development in infants ages 6-12 months old was not changed by COVID-19.
Communication skill scores lower than prepandemic
However, one area did see a significant difference when they looked at answers to the Ages and Stages Questionnaire, 3rd edition (ASQ-3): Scores were lower in communication skills.
Compared with the prepandemic babies, the pandemic group of babies was more likely to have communication impairment (odds were 1.7 times higher).
Additionally, mothers’ SARS-CoV-2 infection was not associated with significant differences in any neurodevelopment sector in offspring, with one exception: Odds were 3.5 times higher for fine motor impairment in the pandemic baby group.
The babies in this study were either exposed in the womb to the SARS-CoV-2 infection or screened during the pandemic regardless of whether they were exposed to the virus.
The study, led by Kamran Hessami, MD, with the Maternal Fetal Care Center at Boston Children’s Hospital and Harvard Medical School in Boston, was published in JAMA Network Open.
Potential reasons for lower communication skills
The study points to some factors of the pandemic that may be tied to impaired communication skills.
“Higher levels of COVID-19–related stress were reported for both mothers and fathers of infants aged 0-6 months and were associated with insensitive parenting practices, including decreased emotional responsiveness in only mothers, which could lessen the reciprocal exchanges that support language development in early childhood,” they write. “Additionally, opportunities to promote language and social development through new experiences outside the home, including visits with extended family and friends or attendance at a child care center, were lessened for many during the pandemic.”
Viviana M. Fajardo Martinez, MD, with neonatal/perinatal medicine at University of California, Los Angeles, Health, told this publication her team is also studying child development before and after the pandemic over a 3-year period, and delayed communication skills is something she is seeing in clinic there.
She says some parents have been concerned, saying their babies aren’t talking enough or are behind in vocabulary.
Babies can catch up after 12 months
One thing she tells parents is that babies who are a bit delayed at 12 months can catch up.
Up to 18 months, they can catch up, she said, adding that they can be reevaluated then for improvement. If, at that point, the baby is not catching up, “that’s when we refer for early intervention,” she said.
Dr. Martinez also tells parents concerned about their infant’s communication skills that it’s important to talk, read, and sing to their child. She said amid pandemic stress, corners may have been cut in asking children to use language skills.
For instance, if a child points to an apple, a stressed parent may just give the child the apple instead of asking the child to request it by name and repeat the word several times.
She also said a limitation of this study is the use of the ASQ-3 questionnaire, which is filled out by parents. Answers are subjective, she notes, and sometimes differ between one child’s two parents. The questionnaire was commonly used during the pandemic because a more objective, professional evaluation has been more difficult.
However, a measure like the Bayley Scales of Infant and Toddler Development Screening Test adds objectivity and will likely give a better picture as research progresses, Dr. Martinez said.
Some information missing
Andréane Lavallée, PhD, and Dani Dumitriu, MD, PhD, both with the department of pediatrics at Columbia University, New York, write in an invited commentary that the overall positive message of the study “should not make researchers complacent” and results should be viewed with caution.
They point out that the precise effects of this novel virus are still unclear and the age group and variables studied may not tell the whole story.
“It should be noted that this systematic review did not consider timing of exposure during pregnancy, maternal infection severity, or exposure to various SARS-CoV-2 variants – all factors that could eventually be proven to contribute to subtle adverse neurodevelopmental outcomes,” they write.
Additionally, past pandemics “such as the 1918 Spanish flu, 1964 rubella, and 2009 H1N1” have taught researchers to watch for increases in diagnoses such as autism spectrum disorder (ASD) and schizophrenia in subsequent years.
“ASD is generally diagnosed at age 3-5 years (and often not until early teens), while schizophrenia is generally diagnosed in mid-to-late 20s,” the editorialists point out. The authors agree and emphasize the need for long-term studies.
Authors report no relevant financial relationships. Editorialist Dr. Dumitriu reports grants from National Institute of Mental Health, the U.S. Centers for Disease Control and Prevention, and the W. K. Kellogg Foundation; and has received gift funds from Einhorn Collaborative during the conduct of the study to the Nurture Science Program, for which Dr Dumitriu serves as director. Dr. Dumitriu received personal fees from Medela outside the submitted work; and is the corresponding author for one of the studies (Shuffrey et al., 2022) included in the systematic review conducted by Dr. Hessami et al. Dr. Lavallée reports grants from the Canadian Institutes of Health Research. Dr. Martinez reports no relevant financial relationships.
FROM JAMA NETWORK OPEN
Finerenone: ‘Striking’ cut in pneumonia, COVID-19 risks
The nonsteroidal mineralocorticoid receptor antagonist finerenone (Kerendia) unexpectedly showed that it might protect against incident infective pneumonia and COVID-19. The finding was based on secondary analyses run on more than 13,000 people enrolled in the two pivotal trials for finerenone.
Finerenone was approved by the Food and Drug Administration in 2021 for slowing progressive renal dysfunction and preventing cardiovascular events in adults with type 2 diabetes and chronic kidney disease (CKD).
‘Striking reduction in the risk of pneumonia’
The “striking reduction in risk of pneumonia” in a new analysis suggests that “the propagation of pulmonary infection into lobar or bronchial consolidation may be reduced by finerenone,” write Bertram Pitt, MD, and coauthors in a report published on October 26 in JAMA Network Open.
They also suggest that if further studies confirm that finerenone treatment reduces complications from pneumonia and COVID-19, it would have “significant medical implications,” especially because of the limited treatment options now available for complications from COVID-19.
The new analyses used the FIDELITY dataset, a prespecified merging of results from the FIDELIO-DKD and FIGARO-DKD trials, which together enrolled 13,026 people with type 2 diabetes and CKD, as determined on the basis of the patients’ having a urine albumin-to-creatinine ratio of at least 30 mg/g.
The primary outcomes of these trials showed that treatment with finerenone led to significant slowing of the progression of CKD and a significant reduction in the incidence of cardiovascular events, compared with placebo during median follow-up of 3 years.
The new, secondary analyses focused on the 6.0% of participants in whom there was evidence of pneumonia and the 1.6% in whom there was evidence of having COVID-19. Pneumonia was the most common serious adverse event in the two trials, a finding consistent with the documented risk for pneumonia faced by people with CKD.
Finerenone linked with a 29% relative reduction in pneumonia
When analyzed by treatment, the incidence of pneumonia was 4.7% among those who received finerenone and 6.7% among those who received placebo. This translated into a significant relative risk reduction of 29% associated with finerenone treatment.
Analysis of COVID-19 adverse events showed a 1.3% incidence among those who received finerenone and a 1.8% incidence among those in the placebo group, which translated into a significant 27% relative risk reduction linked with finerenone treatment.
In contrast, the data showed no reduced incidence of several other respiratory infections among the finerenone recipients, including nasopharyngitis, bronchitis, and influenza. The data also showed no signal that pneumonia or COVID-19 was more severe among the people who did not receive finerenone, nor did finerenone treatment appear to affect pneumonia recovery.
Analysis based on adverse events reports
These secondary analyses are far from definitive. The authors relied on pneumonia and COVID-19 being reported as adverse events. Each investigator diagnosed pneumonia at their discretion, and the trials did not specify diagnostic criteria. The authors also acknowledge that testing for COVID-19 was “not widespread” and that one of the two pivotal trials largely ran prior to the onset of the COVID-19 pandemic so that only 6 participants developed COVID-19 symptoms out of more than 5,700 enrolled.
The authors hypothesize that several actions of finerenone might potentially help mediate an effect on pneumonia and COVID-19: improvements in pulmonary inflammation and fibrosis, upregulation of expression of angiotensin converting enzyme 2, and amelioration of right heart pressure and pulmonary congestion. Also, antagonizing the mineralocorticoid receptor on monocytes and macrophages may block macrophage infiltration and accumulation of active macrophages, which can mediate the pulmonary tissue damage caused by COVID-19.
The FIDELIO-DKD and FIGARO-DKD trials and the FIDELITY combined database were sponsored by Bayer, the company that markets finerenone (Kerendia). Dr. Pitt has received personal fees from Bayer and personal fees and stock options from numerous other companies. Several coauthors reported having a financial relationship with Bayer, as well as with other companies.
A version of this article first appeared on Medscape.com.
The nonsteroidal mineralocorticoid receptor antagonist finerenone (Kerendia) unexpectedly showed that it might protect against incident infective pneumonia and COVID-19. The finding was based on secondary analyses run on more than 13,000 people enrolled in the two pivotal trials for finerenone.
Finerenone was approved by the Food and Drug Administration in 2021 for slowing progressive renal dysfunction and preventing cardiovascular events in adults with type 2 diabetes and chronic kidney disease (CKD).
‘Striking reduction in the risk of pneumonia’
The “striking reduction in risk of pneumonia” in a new analysis suggests that “the propagation of pulmonary infection into lobar or bronchial consolidation may be reduced by finerenone,” write Bertram Pitt, MD, and coauthors in a report published on October 26 in JAMA Network Open.
They also suggest that if further studies confirm that finerenone treatment reduces complications from pneumonia and COVID-19, it would have “significant medical implications,” especially because of the limited treatment options now available for complications from COVID-19.
The new analyses used the FIDELITY dataset, a prespecified merging of results from the FIDELIO-DKD and FIGARO-DKD trials, which together enrolled 13,026 people with type 2 diabetes and CKD, as determined on the basis of the patients’ having a urine albumin-to-creatinine ratio of at least 30 mg/g.
The primary outcomes of these trials showed that treatment with finerenone led to significant slowing of the progression of CKD and a significant reduction in the incidence of cardiovascular events, compared with placebo during median follow-up of 3 years.
The new, secondary analyses focused on the 6.0% of participants in whom there was evidence of pneumonia and the 1.6% in whom there was evidence of having COVID-19. Pneumonia was the most common serious adverse event in the two trials, a finding consistent with the documented risk for pneumonia faced by people with CKD.
Finerenone linked with a 29% relative reduction in pneumonia
When analyzed by treatment, the incidence of pneumonia was 4.7% among those who received finerenone and 6.7% among those who received placebo. This translated into a significant relative risk reduction of 29% associated with finerenone treatment.
Analysis of COVID-19 adverse events showed a 1.3% incidence among those who received finerenone and a 1.8% incidence among those in the placebo group, which translated into a significant 27% relative risk reduction linked with finerenone treatment.
In contrast, the data showed no reduced incidence of several other respiratory infections among the finerenone recipients, including nasopharyngitis, bronchitis, and influenza. The data also showed no signal that pneumonia or COVID-19 was more severe among the people who did not receive finerenone, nor did finerenone treatment appear to affect pneumonia recovery.
Analysis based on adverse events reports
These secondary analyses are far from definitive. The authors relied on pneumonia and COVID-19 being reported as adverse events. Each investigator diagnosed pneumonia at their discretion, and the trials did not specify diagnostic criteria. The authors also acknowledge that testing for COVID-19 was “not widespread” and that one of the two pivotal trials largely ran prior to the onset of the COVID-19 pandemic so that only 6 participants developed COVID-19 symptoms out of more than 5,700 enrolled.
The authors hypothesize that several actions of finerenone might potentially help mediate an effect on pneumonia and COVID-19: improvements in pulmonary inflammation and fibrosis, upregulation of expression of angiotensin converting enzyme 2, and amelioration of right heart pressure and pulmonary congestion. Also, antagonizing the mineralocorticoid receptor on monocytes and macrophages may block macrophage infiltration and accumulation of active macrophages, which can mediate the pulmonary tissue damage caused by COVID-19.
The FIDELIO-DKD and FIGARO-DKD trials and the FIDELITY combined database were sponsored by Bayer, the company that markets finerenone (Kerendia). Dr. Pitt has received personal fees from Bayer and personal fees and stock options from numerous other companies. Several coauthors reported having a financial relationship with Bayer, as well as with other companies.
A version of this article first appeared on Medscape.com.
The nonsteroidal mineralocorticoid receptor antagonist finerenone (Kerendia) unexpectedly showed that it might protect against incident infective pneumonia and COVID-19. The finding was based on secondary analyses run on more than 13,000 people enrolled in the two pivotal trials for finerenone.
Finerenone was approved by the Food and Drug Administration in 2021 for slowing progressive renal dysfunction and preventing cardiovascular events in adults with type 2 diabetes and chronic kidney disease (CKD).
‘Striking reduction in the risk of pneumonia’
The “striking reduction in risk of pneumonia” in a new analysis suggests that “the propagation of pulmonary infection into lobar or bronchial consolidation may be reduced by finerenone,” write Bertram Pitt, MD, and coauthors in a report published on October 26 in JAMA Network Open.
They also suggest that if further studies confirm that finerenone treatment reduces complications from pneumonia and COVID-19, it would have “significant medical implications,” especially because of the limited treatment options now available for complications from COVID-19.
The new analyses used the FIDELITY dataset, a prespecified merging of results from the FIDELIO-DKD and FIGARO-DKD trials, which together enrolled 13,026 people with type 2 diabetes and CKD, as determined on the basis of the patients’ having a urine albumin-to-creatinine ratio of at least 30 mg/g.
The primary outcomes of these trials showed that treatment with finerenone led to significant slowing of the progression of CKD and a significant reduction in the incidence of cardiovascular events, compared with placebo during median follow-up of 3 years.
The new, secondary analyses focused on the 6.0% of participants in whom there was evidence of pneumonia and the 1.6% in whom there was evidence of having COVID-19. Pneumonia was the most common serious adverse event in the two trials, a finding consistent with the documented risk for pneumonia faced by people with CKD.
Finerenone linked with a 29% relative reduction in pneumonia
When analyzed by treatment, the incidence of pneumonia was 4.7% among those who received finerenone and 6.7% among those who received placebo. This translated into a significant relative risk reduction of 29% associated with finerenone treatment.
Analysis of COVID-19 adverse events showed a 1.3% incidence among those who received finerenone and a 1.8% incidence among those in the placebo group, which translated into a significant 27% relative risk reduction linked with finerenone treatment.
In contrast, the data showed no reduced incidence of several other respiratory infections among the finerenone recipients, including nasopharyngitis, bronchitis, and influenza. The data also showed no signal that pneumonia or COVID-19 was more severe among the people who did not receive finerenone, nor did finerenone treatment appear to affect pneumonia recovery.
Analysis based on adverse events reports
These secondary analyses are far from definitive. The authors relied on pneumonia and COVID-19 being reported as adverse events. Each investigator diagnosed pneumonia at their discretion, and the trials did not specify diagnostic criteria. The authors also acknowledge that testing for COVID-19 was “not widespread” and that one of the two pivotal trials largely ran prior to the onset of the COVID-19 pandemic so that only 6 participants developed COVID-19 symptoms out of more than 5,700 enrolled.
The authors hypothesize that several actions of finerenone might potentially help mediate an effect on pneumonia and COVID-19: improvements in pulmonary inflammation and fibrosis, upregulation of expression of angiotensin converting enzyme 2, and amelioration of right heart pressure and pulmonary congestion. Also, antagonizing the mineralocorticoid receptor on monocytes and macrophages may block macrophage infiltration and accumulation of active macrophages, which can mediate the pulmonary tissue damage caused by COVID-19.
The FIDELIO-DKD and FIGARO-DKD trials and the FIDELITY combined database were sponsored by Bayer, the company that markets finerenone (Kerendia). Dr. Pitt has received personal fees from Bayer and personal fees and stock options from numerous other companies. Several coauthors reported having a financial relationship with Bayer, as well as with other companies.
A version of this article first appeared on Medscape.com.
Is it flu, RSV, or COVID? Experts fear the ‘tripledemic’
Just when we thought this holiday season, finally, would be the back-to-normal one, some infectious disease experts are warning that a so-called “tripledemic” – influenza, COVID-19, and RSV – may be in the forecast.
The warning isn’t without basis.
The flu season has gotten an early start. As of Oct. 21, early increases in seasonal flu activity have been reported in most of the country, the Centers for Disease Control and Prevention said, with the southeast and south-central areas having the highest activity levels.
Children’s hospitals and EDs are seeing a surge in children with RSV.
COVID-19 cases are trending down, according to the CDC, but epidemiologists – scientists who study disease outbreaks – always have their eyes on emerging variants.
said Justin Lessler, PhD, a professor of epidemiology at the University of North Carolina at Chapel Hill. Dr. Lessler is on the coordinating team for the COVID-19 Scenario Modeling Hub, which aims to predict the course COVID-19, and the Flu Scenario Modeling Hub, which does the same for influenza.
For COVID-19, some models are predicting some spikes before Christmas, he said, and others see a new wave in 2023. For the flu, the model is predicting an earlier-than-usual start, as the CDC has reported.
While flu activity is relatively low, the CDC said, the season is off to an early start. For the week ending Oct. 21, 1,674 patients were hospitalized for flu, higher than in the summer months but fewer than the 2,675 hospitalizations for the week of May 15, 2022.
As of Oct. 20, COVID-19 cases have declined 12% over the last 2 weeks, nationwide. But hospitalizations are up 10% in much of the Northeast, The New York Times reports, and the improvement in cases and deaths has been slowing down.
As of Oct. 15, 15% of RSV tests reported nationwide were positive, compared with about 11% at that time in 2021, the CDC said. The surveillance collects information from 75 counties in 12 states.
Experts point out that the viruses – all three are respiratory viruses – are simply playing catchup.
“They spread the same way and along with lots of other viruses, and you tend to see an increase in them during the cold months,” said Timothy Brewer, MD, professor of medicine and epidemiology at UCLA.
The increase in all three viruses “is almost predictable at this point in the pandemic,” said Dean Blumberg, MD, a professor and chief of pediatric infectious diseases at the University of California Davis Health. “All the respiratory viruses are out of whack.”
Last year, RSV cases were up, too, and began to appear very early, he said, in the summer instead of in the cooler months. Flu also appeared early in 2021, as it has in 2022.
That contrasts with the flu season of 2020-2021, when COVID precautions were nearly universal, and cases were down. At UC Davis, “we didn’t have one pediatric admission due to influenza in the 2020-2021 [flu] season,” Dr. Blumberg said.
The number of pediatric flu deaths usually range from 37 to 199 per year, according to CDC records. But in the 2020-2021 season, the CDC recorded one pediatric flu death in the U.S.
Both children and adults have had less contact with others the past two seasons, Dr. Blumberg said, “and they don’t get the immunity they got with those infections [previously]. That’s why we are seeing out-of-season, early season [viruses].”
Eventually, he said, the cases of flu and RSV will return to previous levels. “It could be as soon as next year,” Dr. Blumberg said. And COVID-19, hopefully, will become like influenza, he said.
“RSV has always come around in the fall and winter,” said Elizabeth Murray, DO, a pediatric emergency medicine doctor at the University of Rochester (N.Y.) Medical Center and a spokesperson for the American Academy of Pediatrics. In 2022, children are back in school and for the most part not masking. “It’s a perfect storm for all the germs to spread now. They’ve just been waiting for their opportunity to come back.”
Self-care vs. not
RSV can pose a risk for anyone, but most at risk are children under age 5, especially infants under age 1, and adults over age 65. There is no vaccine for it. Symptoms include a runny nose, decreased appetite, coughing, sneezing, fever, and wheezing. But in young infants, there may only be decreased activity, crankiness, and breathing issues, the CDC said.
Keep an eye on the breathing if RSV is suspected, Dr. Murray tells parents. If your child can’t breathe easily, is unable to lie down comfortably, can’t speak clearly, or is sucking in the chest muscles to breathe, get medical help. Most kids with RSV can stay home and recover, she said, but often will need to be checked by a medical professional.
She advises against getting an oximeter to measure oxygen levels for home use. “They are often not accurate,” she said. If in doubt about how serious your child’s symptoms are, “don’t wait it out,” and don’t hesitate to call 911.
Symptoms of flu, COVID, and RSV can overlap. But each can involve breathing problems, which can be an emergency.
“It’s important to seek medical attention for any concerning symptoms, but especially severe shortness of breath or difficulty breathing, as these could signal the need for supplemental oxygen or other emergency interventions,” said Mandy De Vries, a respiratory therapist and director of education at the American Association for Respiratory Care. Inhalation treatment or mechanical ventilation may be needed for severe respiratory issues.
Precautions
To avoid the tripledemic – or any single infection – Timothy Brewer, MD, a professor of medicine and epidemiology at the University of California, Los Angeles, suggests some familiar measures: “Stay home if you’re feeling sick. Make sure you are up to date on your vaccinations. Wear a mask indoors.”
A version of this article first appeared on Medscape.com.
Just when we thought this holiday season, finally, would be the back-to-normal one, some infectious disease experts are warning that a so-called “tripledemic” – influenza, COVID-19, and RSV – may be in the forecast.
The warning isn’t without basis.
The flu season has gotten an early start. As of Oct. 21, early increases in seasonal flu activity have been reported in most of the country, the Centers for Disease Control and Prevention said, with the southeast and south-central areas having the highest activity levels.
Children’s hospitals and EDs are seeing a surge in children with RSV.
COVID-19 cases are trending down, according to the CDC, but epidemiologists – scientists who study disease outbreaks – always have their eyes on emerging variants.
said Justin Lessler, PhD, a professor of epidemiology at the University of North Carolina at Chapel Hill. Dr. Lessler is on the coordinating team for the COVID-19 Scenario Modeling Hub, which aims to predict the course COVID-19, and the Flu Scenario Modeling Hub, which does the same for influenza.
For COVID-19, some models are predicting some spikes before Christmas, he said, and others see a new wave in 2023. For the flu, the model is predicting an earlier-than-usual start, as the CDC has reported.
While flu activity is relatively low, the CDC said, the season is off to an early start. For the week ending Oct. 21, 1,674 patients were hospitalized for flu, higher than in the summer months but fewer than the 2,675 hospitalizations for the week of May 15, 2022.
As of Oct. 20, COVID-19 cases have declined 12% over the last 2 weeks, nationwide. But hospitalizations are up 10% in much of the Northeast, The New York Times reports, and the improvement in cases and deaths has been slowing down.
As of Oct. 15, 15% of RSV tests reported nationwide were positive, compared with about 11% at that time in 2021, the CDC said. The surveillance collects information from 75 counties in 12 states.
Experts point out that the viruses – all three are respiratory viruses – are simply playing catchup.
“They spread the same way and along with lots of other viruses, and you tend to see an increase in them during the cold months,” said Timothy Brewer, MD, professor of medicine and epidemiology at UCLA.
The increase in all three viruses “is almost predictable at this point in the pandemic,” said Dean Blumberg, MD, a professor and chief of pediatric infectious diseases at the University of California Davis Health. “All the respiratory viruses are out of whack.”
Last year, RSV cases were up, too, and began to appear very early, he said, in the summer instead of in the cooler months. Flu also appeared early in 2021, as it has in 2022.
That contrasts with the flu season of 2020-2021, when COVID precautions were nearly universal, and cases were down. At UC Davis, “we didn’t have one pediatric admission due to influenza in the 2020-2021 [flu] season,” Dr. Blumberg said.
The number of pediatric flu deaths usually range from 37 to 199 per year, according to CDC records. But in the 2020-2021 season, the CDC recorded one pediatric flu death in the U.S.
Both children and adults have had less contact with others the past two seasons, Dr. Blumberg said, “and they don’t get the immunity they got with those infections [previously]. That’s why we are seeing out-of-season, early season [viruses].”
Eventually, he said, the cases of flu and RSV will return to previous levels. “It could be as soon as next year,” Dr. Blumberg said. And COVID-19, hopefully, will become like influenza, he said.
“RSV has always come around in the fall and winter,” said Elizabeth Murray, DO, a pediatric emergency medicine doctor at the University of Rochester (N.Y.) Medical Center and a spokesperson for the American Academy of Pediatrics. In 2022, children are back in school and for the most part not masking. “It’s a perfect storm for all the germs to spread now. They’ve just been waiting for their opportunity to come back.”
Self-care vs. not
RSV can pose a risk for anyone, but most at risk are children under age 5, especially infants under age 1, and adults over age 65. There is no vaccine for it. Symptoms include a runny nose, decreased appetite, coughing, sneezing, fever, and wheezing. But in young infants, there may only be decreased activity, crankiness, and breathing issues, the CDC said.
Keep an eye on the breathing if RSV is suspected, Dr. Murray tells parents. If your child can’t breathe easily, is unable to lie down comfortably, can’t speak clearly, or is sucking in the chest muscles to breathe, get medical help. Most kids with RSV can stay home and recover, she said, but often will need to be checked by a medical professional.
She advises against getting an oximeter to measure oxygen levels for home use. “They are often not accurate,” she said. If in doubt about how serious your child’s symptoms are, “don’t wait it out,” and don’t hesitate to call 911.
Symptoms of flu, COVID, and RSV can overlap. But each can involve breathing problems, which can be an emergency.
“It’s important to seek medical attention for any concerning symptoms, but especially severe shortness of breath or difficulty breathing, as these could signal the need for supplemental oxygen or other emergency interventions,” said Mandy De Vries, a respiratory therapist and director of education at the American Association for Respiratory Care. Inhalation treatment or mechanical ventilation may be needed for severe respiratory issues.
Precautions
To avoid the tripledemic – or any single infection – Timothy Brewer, MD, a professor of medicine and epidemiology at the University of California, Los Angeles, suggests some familiar measures: “Stay home if you’re feeling sick. Make sure you are up to date on your vaccinations. Wear a mask indoors.”
A version of this article first appeared on Medscape.com.
Just when we thought this holiday season, finally, would be the back-to-normal one, some infectious disease experts are warning that a so-called “tripledemic” – influenza, COVID-19, and RSV – may be in the forecast.
The warning isn’t without basis.
The flu season has gotten an early start. As of Oct. 21, early increases in seasonal flu activity have been reported in most of the country, the Centers for Disease Control and Prevention said, with the southeast and south-central areas having the highest activity levels.
Children’s hospitals and EDs are seeing a surge in children with RSV.
COVID-19 cases are trending down, according to the CDC, but epidemiologists – scientists who study disease outbreaks – always have their eyes on emerging variants.
said Justin Lessler, PhD, a professor of epidemiology at the University of North Carolina at Chapel Hill. Dr. Lessler is on the coordinating team for the COVID-19 Scenario Modeling Hub, which aims to predict the course COVID-19, and the Flu Scenario Modeling Hub, which does the same for influenza.
For COVID-19, some models are predicting some spikes before Christmas, he said, and others see a new wave in 2023. For the flu, the model is predicting an earlier-than-usual start, as the CDC has reported.
While flu activity is relatively low, the CDC said, the season is off to an early start. For the week ending Oct. 21, 1,674 patients were hospitalized for flu, higher than in the summer months but fewer than the 2,675 hospitalizations for the week of May 15, 2022.
As of Oct. 20, COVID-19 cases have declined 12% over the last 2 weeks, nationwide. But hospitalizations are up 10% in much of the Northeast, The New York Times reports, and the improvement in cases and deaths has been slowing down.
As of Oct. 15, 15% of RSV tests reported nationwide were positive, compared with about 11% at that time in 2021, the CDC said. The surveillance collects information from 75 counties in 12 states.
Experts point out that the viruses – all three are respiratory viruses – are simply playing catchup.
“They spread the same way and along with lots of other viruses, and you tend to see an increase in them during the cold months,” said Timothy Brewer, MD, professor of medicine and epidemiology at UCLA.
The increase in all three viruses “is almost predictable at this point in the pandemic,” said Dean Blumberg, MD, a professor and chief of pediatric infectious diseases at the University of California Davis Health. “All the respiratory viruses are out of whack.”
Last year, RSV cases were up, too, and began to appear very early, he said, in the summer instead of in the cooler months. Flu also appeared early in 2021, as it has in 2022.
That contrasts with the flu season of 2020-2021, when COVID precautions were nearly universal, and cases were down. At UC Davis, “we didn’t have one pediatric admission due to influenza in the 2020-2021 [flu] season,” Dr. Blumberg said.
The number of pediatric flu deaths usually range from 37 to 199 per year, according to CDC records. But in the 2020-2021 season, the CDC recorded one pediatric flu death in the U.S.
Both children and adults have had less contact with others the past two seasons, Dr. Blumberg said, “and they don’t get the immunity they got with those infections [previously]. That’s why we are seeing out-of-season, early season [viruses].”
Eventually, he said, the cases of flu and RSV will return to previous levels. “It could be as soon as next year,” Dr. Blumberg said. And COVID-19, hopefully, will become like influenza, he said.
“RSV has always come around in the fall and winter,” said Elizabeth Murray, DO, a pediatric emergency medicine doctor at the University of Rochester (N.Y.) Medical Center and a spokesperson for the American Academy of Pediatrics. In 2022, children are back in school and for the most part not masking. “It’s a perfect storm for all the germs to spread now. They’ve just been waiting for their opportunity to come back.”
Self-care vs. not
RSV can pose a risk for anyone, but most at risk are children under age 5, especially infants under age 1, and adults over age 65. There is no vaccine for it. Symptoms include a runny nose, decreased appetite, coughing, sneezing, fever, and wheezing. But in young infants, there may only be decreased activity, crankiness, and breathing issues, the CDC said.
Keep an eye on the breathing if RSV is suspected, Dr. Murray tells parents. If your child can’t breathe easily, is unable to lie down comfortably, can’t speak clearly, or is sucking in the chest muscles to breathe, get medical help. Most kids with RSV can stay home and recover, she said, but often will need to be checked by a medical professional.
She advises against getting an oximeter to measure oxygen levels for home use. “They are often not accurate,” she said. If in doubt about how serious your child’s symptoms are, “don’t wait it out,” and don’t hesitate to call 911.
Symptoms of flu, COVID, and RSV can overlap. But each can involve breathing problems, which can be an emergency.
“It’s important to seek medical attention for any concerning symptoms, but especially severe shortness of breath or difficulty breathing, as these could signal the need for supplemental oxygen or other emergency interventions,” said Mandy De Vries, a respiratory therapist and director of education at the American Association for Respiratory Care. Inhalation treatment or mechanical ventilation may be needed for severe respiratory issues.
Precautions
To avoid the tripledemic – or any single infection – Timothy Brewer, MD, a professor of medicine and epidemiology at the University of California, Los Angeles, suggests some familiar measures: “Stay home if you’re feeling sick. Make sure you are up to date on your vaccinations. Wear a mask indoors.”
A version of this article first appeared on Medscape.com.
Ivermectin for COVID-19: Final nail in the coffin
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
It began in a petri dish.
Ivermectin, a widely available, cheap, and well-tolerated drug on the WHO’s list of essential medicines for its critical role in treating river blindness, was shown to dramatically reduce the proliferation of SARS-CoV-2 virus in cell culture.
You know the rest of the story. Despite the fact that the median inhibitory concentration in cell culture is about 100-fold higher than what one can achieve with oral dosing in humans, anecdotal reports of miraculous cures proliferated.
Cohort studies suggested that people who got ivermectin did very well in terms of COVID outcomes.
A narrative started to develop online – one that is still quite present today – that authorities were suppressing the good news about ivermectin in order to line their own pockets and those of the execs at Big Pharma. The official Twitter account of the Food and Drug Administration clapped back, reminding the populace that we are not horses or cows.
And every time a study came out that seemed like the nail in the coffin for the so-called horse paste, it rose again, vampire-like, feasting on the blood of social media outrage.
The truth is that, while excitement for ivermectin mounted online, it crashed quite quickly in scientific circles. Most randomized trials showed no effect of the drug. A couple of larger trials which seemed to show dramatic effects were subsequently shown to be fraudulent.
Then the TOGETHER trial was published. The 1,400-patient study from Brazil, which treated outpatients with COVID-19, found no significant difference in hospitalization or ER visits – the primary outcome – between those randomized to ivermectin vs. placebo or another therapy.
But still, Brazil. Different population than the United States. Different health systems. And very different rates of Strongyloides infections (this is a parasite that may be incidentally treated by ivermectin, leading to improvement independent of the drug’s effect on COVID). We all wanted a U.S. trial.
And now we have it. ACTIV-6 was published Oct. 21 in JAMA, a study randomizing outpatients with COVID-19 from 93 sites around the United States to ivermectin or placebo.
A total of 1,591 individuals – median age 47, 60% female – with confirmed symptomatic COVID-19 were randomized from June 2021 to February 2022. About half had been vaccinated.
The primary outcome was straightforward: time to clinical recovery. The time to recovery, defined as having three symptom-free days, was 12 days in the ivermectin group and 13 days in the placebo group – that’s within the margin of error.
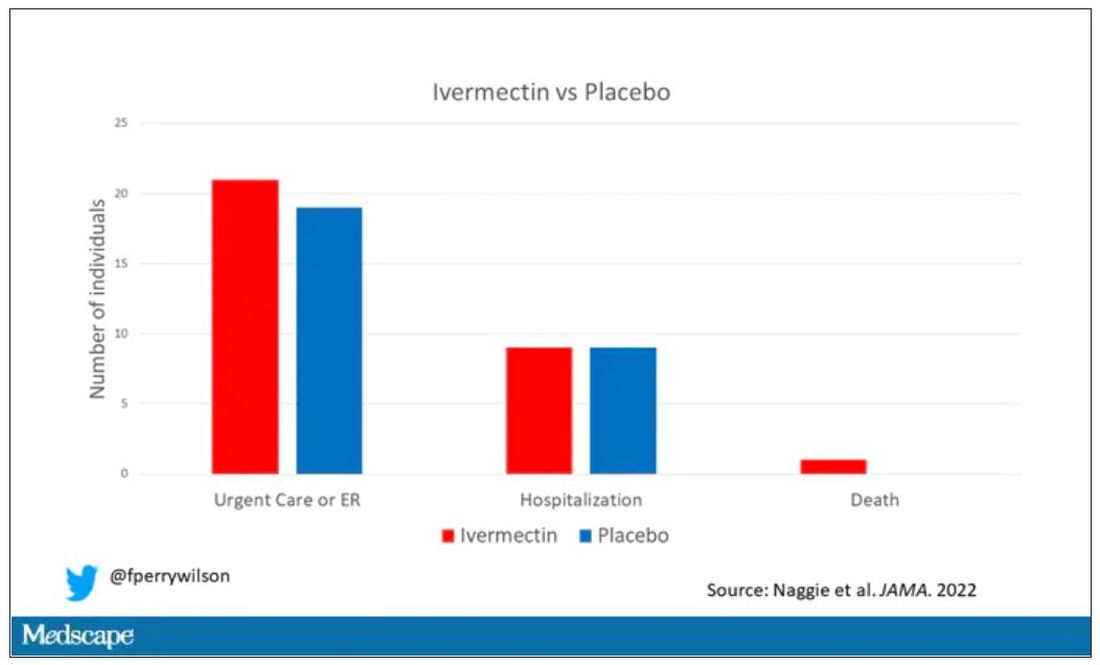
But overall, everyone in the trial did fairly well. Serious outcomes, like death, hospitalization, urgent care, or ER visits, occurred in 32 people in the ivermectin group and 28 in the placebo group. Death itself was rare – just one occurred in the trial, in someone receiving ivermectin.OK, are we done with this drug yet? Is this nice U.S. randomized trial enough to convince people that results from a petri dish don’t always transfer to humans, regardless of the presence or absence of an evil pharmaceutical cabal?
No, of course not. At this point, I can predict the responses. The dose wasn’t high enough. It wasn’t given early enough. The patients weren’t sick enough, or they were too sick. This is motivated reasoning, plain and simple. It’s not to say that there isn’t a chance that this drug has some off-target effects on COVID that we haven’t adequately measured, but studies like ACTIV-6 effectively rule out the idea that it’s a miracle cure. And you know what? That’s OK. Miracle cures are vanishingly rare. Most things that work in medicine work OK; they make us a little better, and we learn why they do that and improve on them, and try again and again. It’s not flashy; it doesn’t have that allure of secret knowledge. But it’s what separates science from magic.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator; his science communication work can be found in the Huffington Post, on NPR, and on Medscape.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
It began in a petri dish.
Ivermectin, a widely available, cheap, and well-tolerated drug on the WHO’s list of essential medicines for its critical role in treating river blindness, was shown to dramatically reduce the proliferation of SARS-CoV-2 virus in cell culture.
You know the rest of the story. Despite the fact that the median inhibitory concentration in cell culture is about 100-fold higher than what one can achieve with oral dosing in humans, anecdotal reports of miraculous cures proliferated.
Cohort studies suggested that people who got ivermectin did very well in terms of COVID outcomes.
A narrative started to develop online – one that is still quite present today – that authorities were suppressing the good news about ivermectin in order to line their own pockets and those of the execs at Big Pharma. The official Twitter account of the Food and Drug Administration clapped back, reminding the populace that we are not horses or cows.
And every time a study came out that seemed like the nail in the coffin for the so-called horse paste, it rose again, vampire-like, feasting on the blood of social media outrage.
The truth is that, while excitement for ivermectin mounted online, it crashed quite quickly in scientific circles. Most randomized trials showed no effect of the drug. A couple of larger trials which seemed to show dramatic effects were subsequently shown to be fraudulent.
Then the TOGETHER trial was published. The 1,400-patient study from Brazil, which treated outpatients with COVID-19, found no significant difference in hospitalization or ER visits – the primary outcome – between those randomized to ivermectin vs. placebo or another therapy.
But still, Brazil. Different population than the United States. Different health systems. And very different rates of Strongyloides infections (this is a parasite that may be incidentally treated by ivermectin, leading to improvement independent of the drug’s effect on COVID). We all wanted a U.S. trial.
And now we have it. ACTIV-6 was published Oct. 21 in JAMA, a study randomizing outpatients with COVID-19 from 93 sites around the United States to ivermectin or placebo.
A total of 1,591 individuals – median age 47, 60% female – with confirmed symptomatic COVID-19 were randomized from June 2021 to February 2022. About half had been vaccinated.
The primary outcome was straightforward: time to clinical recovery. The time to recovery, defined as having three symptom-free days, was 12 days in the ivermectin group and 13 days in the placebo group – that’s within the margin of error.
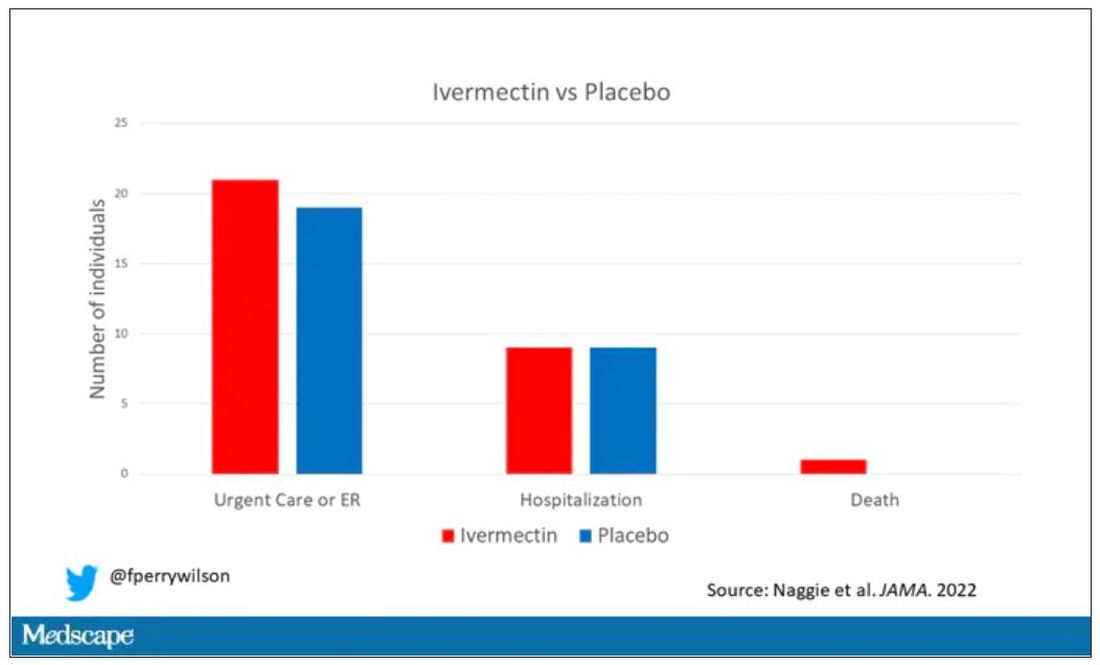
But overall, everyone in the trial did fairly well. Serious outcomes, like death, hospitalization, urgent care, or ER visits, occurred in 32 people in the ivermectin group and 28 in the placebo group. Death itself was rare – just one occurred in the trial, in someone receiving ivermectin.OK, are we done with this drug yet? Is this nice U.S. randomized trial enough to convince people that results from a petri dish don’t always transfer to humans, regardless of the presence or absence of an evil pharmaceutical cabal?
No, of course not. At this point, I can predict the responses. The dose wasn’t high enough. It wasn’t given early enough. The patients weren’t sick enough, or they were too sick. This is motivated reasoning, plain and simple. It’s not to say that there isn’t a chance that this drug has some off-target effects on COVID that we haven’t adequately measured, but studies like ACTIV-6 effectively rule out the idea that it’s a miracle cure. And you know what? That’s OK. Miracle cures are vanishingly rare. Most things that work in medicine work OK; they make us a little better, and we learn why they do that and improve on them, and try again and again. It’s not flashy; it doesn’t have that allure of secret knowledge. But it’s what separates science from magic.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator; his science communication work can be found in the Huffington Post, on NPR, and on Medscape.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
It began in a petri dish.
Ivermectin, a widely available, cheap, and well-tolerated drug on the WHO’s list of essential medicines for its critical role in treating river blindness, was shown to dramatically reduce the proliferation of SARS-CoV-2 virus in cell culture.
You know the rest of the story. Despite the fact that the median inhibitory concentration in cell culture is about 100-fold higher than what one can achieve with oral dosing in humans, anecdotal reports of miraculous cures proliferated.
Cohort studies suggested that people who got ivermectin did very well in terms of COVID outcomes.
A narrative started to develop online – one that is still quite present today – that authorities were suppressing the good news about ivermectin in order to line their own pockets and those of the execs at Big Pharma. The official Twitter account of the Food and Drug Administration clapped back, reminding the populace that we are not horses or cows.
And every time a study came out that seemed like the nail in the coffin for the so-called horse paste, it rose again, vampire-like, feasting on the blood of social media outrage.
The truth is that, while excitement for ivermectin mounted online, it crashed quite quickly in scientific circles. Most randomized trials showed no effect of the drug. A couple of larger trials which seemed to show dramatic effects were subsequently shown to be fraudulent.
Then the TOGETHER trial was published. The 1,400-patient study from Brazil, which treated outpatients with COVID-19, found no significant difference in hospitalization or ER visits – the primary outcome – between those randomized to ivermectin vs. placebo or another therapy.
But still, Brazil. Different population than the United States. Different health systems. And very different rates of Strongyloides infections (this is a parasite that may be incidentally treated by ivermectin, leading to improvement independent of the drug’s effect on COVID). We all wanted a U.S. trial.
And now we have it. ACTIV-6 was published Oct. 21 in JAMA, a study randomizing outpatients with COVID-19 from 93 sites around the United States to ivermectin or placebo.
A total of 1,591 individuals – median age 47, 60% female – with confirmed symptomatic COVID-19 were randomized from June 2021 to February 2022. About half had been vaccinated.
The primary outcome was straightforward: time to clinical recovery. The time to recovery, defined as having three symptom-free days, was 12 days in the ivermectin group and 13 days in the placebo group – that’s within the margin of error.
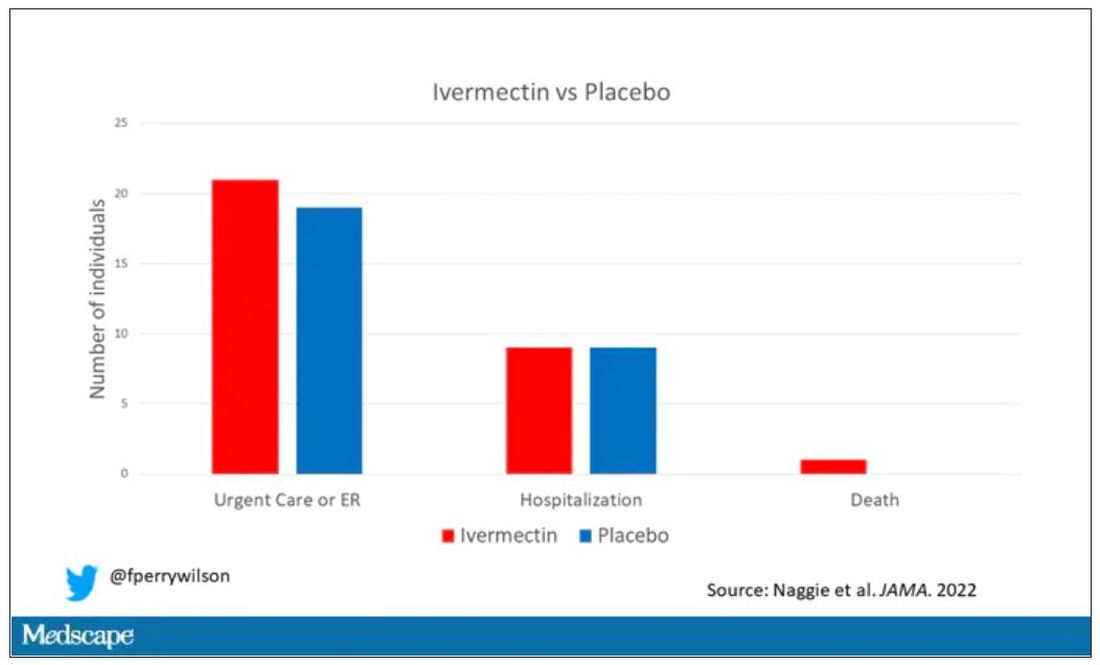
But overall, everyone in the trial did fairly well. Serious outcomes, like death, hospitalization, urgent care, or ER visits, occurred in 32 people in the ivermectin group and 28 in the placebo group. Death itself was rare – just one occurred in the trial, in someone receiving ivermectin.OK, are we done with this drug yet? Is this nice U.S. randomized trial enough to convince people that results from a petri dish don’t always transfer to humans, regardless of the presence or absence of an evil pharmaceutical cabal?
No, of course not. At this point, I can predict the responses. The dose wasn’t high enough. It wasn’t given early enough. The patients weren’t sick enough, or they were too sick. This is motivated reasoning, plain and simple. It’s not to say that there isn’t a chance that this drug has some off-target effects on COVID that we haven’t adequately measured, but studies like ACTIV-6 effectively rule out the idea that it’s a miracle cure. And you know what? That’s OK. Miracle cures are vanishingly rare. Most things that work in medicine work OK; they make us a little better, and we learn why they do that and improve on them, and try again and again. It’s not flashy; it doesn’t have that allure of secret knowledge. But it’s what separates science from magic.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator; his science communication work can be found in the Huffington Post, on NPR, and on Medscape.
A version of this article first appeared on Medscape.com.
Side effects from COVID vaccine show its effectiveness
It means your body had a greater antibody response than people who had just a little pain or rash at the injection site, or no reaction at all.
That’s according to new research published in the journal JAMA Network Open .
“These findings support reframing postvaccination symptoms as signals of vaccine effectiveness and reinforce guidelines for vaccine boosters in older adults,” researchers from Columbia University in New York, the University of Vermont, and Boston University wrote.
The vaccines provided strong protection regardless of the level of reaction, researchers said. Almost all the study’s 928 adult participants had a positive antibody response after receiving two doses of vaccine.
“I don’t want a patient to tell me that, ‘Golly, I didn’t get any reaction, my arm wasn’t sore, I didn’t have fever. The vaccine didn’t work.’ I don’t want that conclusion to be out there,” William Schaffner, MD, a professor in the division of infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn., told CNN.
“This is more to reassure people who have had a reaction that that’s their immune system responding, actually in a rather good way, to the vaccine, even though it has caused them some discomfort,” said Dr. Schaffner, who was not involved in the study.
A version of this article first appeared on WebMD.com.
It means your body had a greater antibody response than people who had just a little pain or rash at the injection site, or no reaction at all.
That’s according to new research published in the journal JAMA Network Open .
“These findings support reframing postvaccination symptoms as signals of vaccine effectiveness and reinforce guidelines for vaccine boosters in older adults,” researchers from Columbia University in New York, the University of Vermont, and Boston University wrote.
The vaccines provided strong protection regardless of the level of reaction, researchers said. Almost all the study’s 928 adult participants had a positive antibody response after receiving two doses of vaccine.
“I don’t want a patient to tell me that, ‘Golly, I didn’t get any reaction, my arm wasn’t sore, I didn’t have fever. The vaccine didn’t work.’ I don’t want that conclusion to be out there,” William Schaffner, MD, a professor in the division of infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn., told CNN.
“This is more to reassure people who have had a reaction that that’s their immune system responding, actually in a rather good way, to the vaccine, even though it has caused them some discomfort,” said Dr. Schaffner, who was not involved in the study.
A version of this article first appeared on WebMD.com.
It means your body had a greater antibody response than people who had just a little pain or rash at the injection site, or no reaction at all.
That’s according to new research published in the journal JAMA Network Open .
“These findings support reframing postvaccination symptoms as signals of vaccine effectiveness and reinforce guidelines for vaccine boosters in older adults,” researchers from Columbia University in New York, the University of Vermont, and Boston University wrote.
The vaccines provided strong protection regardless of the level of reaction, researchers said. Almost all the study’s 928 adult participants had a positive antibody response after receiving two doses of vaccine.
“I don’t want a patient to tell me that, ‘Golly, I didn’t get any reaction, my arm wasn’t sore, I didn’t have fever. The vaccine didn’t work.’ I don’t want that conclusion to be out there,” William Schaffner, MD, a professor in the division of infectious diseases at Vanderbilt University Medical Center, Nashville, Tenn., told CNN.
“This is more to reassure people who have had a reaction that that’s their immune system responding, actually in a rather good way, to the vaccine, even though it has caused them some discomfort,” said Dr. Schaffner, who was not involved in the study.
A version of this article first appeared on WebMD.com.
FROM JAMA NETWORK OPEN
Children and COVID: Weekly cases fall to lowest level in over a year
With the third autumn of the COVID era now upon us, the discussion has turned again to a possible influenza/COVID twindemic, as well as the new-for-2022 influenza/COVID/respiratory syncytial virus tripledemic. It appears, however, that COVID may have missed the memo.
For the sixth time in the last 7 weeks, the number of new COVID cases in children fell, with just under 23,000 reported during the week of Oct. 14-20, according to the American Academy of Pediatrics and the Children’s Hospital Association. That is the lowest weekly count so far this year, and the lowest since early July of 2021, just as the Delta surge was starting. New pediatric cases had dipped to 8,500, the lowest for any week during the pandemic, a couple of weeks before that, the AAP/CHA data show.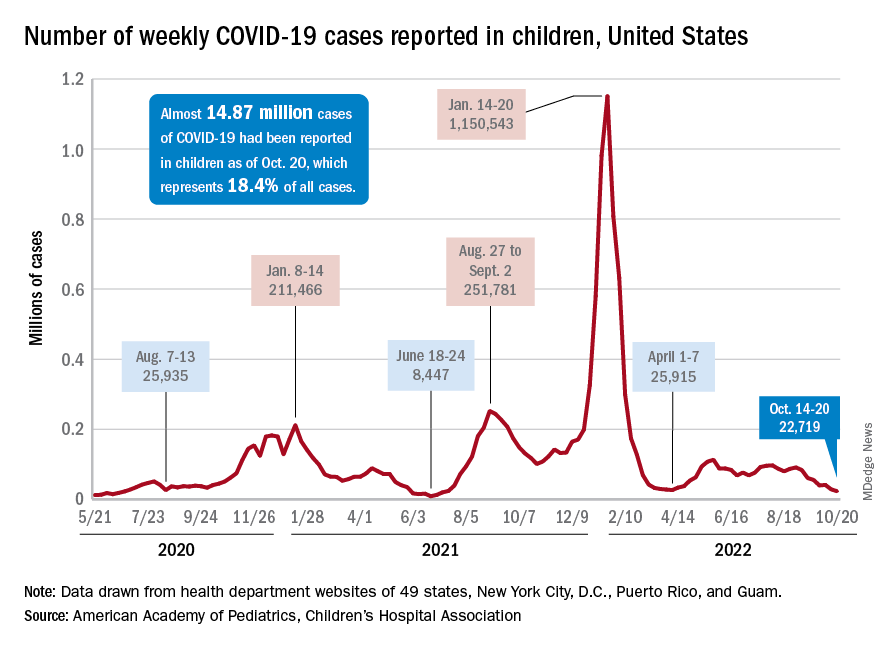
Weekly cases have fallen by almost 75% since over 90,000 were reported for the week of Aug. 26 to Sept. 1, even as children have returned to school and vaccine uptake remains slow in the youngest age groups. Rates of emergency department visits with diagnosed COVID also have continued to drop, as have new admissions, and both are nearing their 2021 lows, according to the Centers for Disease Control and Prevention.
New vaccinations in children under age 5 years were up slightly for the most recent week (Oct. 13-19), but total uptake for that age group is only 7.1% for an initial dose and 2.9% for full vaccination. Among children aged 5-11 years, 38.7% have received at least one dose and 31.6% have completed the primary series, with corresponding figures of 71.2% and 60.9% for those aged 12-17, the CDC said on its COVID Data Tracker.
Despite the low overall numbers, though, the youngest children are, in one respect, punching above their weight when it comes to vaccinations. In the 2 weeks from Oct. 6 to Oct. 19, children under 5 years of age, who represent 5.9% of the U.S. population, received 9.2% of the initial vaccine doses administered. Children aged 5-11 years, who represent 8.7% of the total population, got just 4.2% of all first doses over those same 2 weeks, while 12- to 17-year-olds, who make up 7.6% of the population, got 3.4% of the vaccine doses, the CDC reported.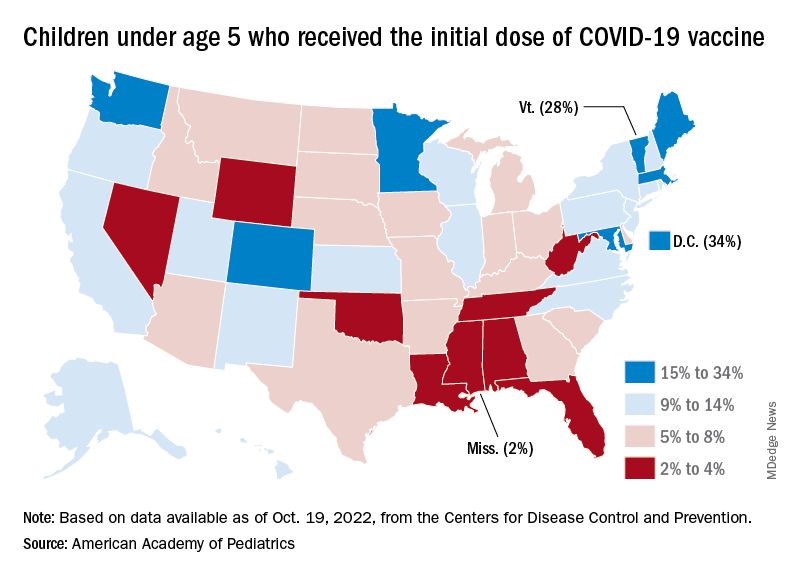
On the vaccine-approval front, the Food and Drug Administration recently announced that the new bivalent COVID-19 vaccines are now included in the emergency use authorizations for children who have completed primary or booster vaccination. The Moderna vaccine is authorized as a single-dose booster for children as young as 6 years and the Pfizer-BioNTech vaccine can be given as a single booster dose in children as young as 5 years, the FDA said.
“These bivalent COVID-19 vaccines include an mRNA component of the original strain to provide an immune response that is broadly protective against COVID-19 and an mRNA component in common between the omicron variant BA.4 and BA.5 lineages,” the FDA said.
With the third autumn of the COVID era now upon us, the discussion has turned again to a possible influenza/COVID twindemic, as well as the new-for-2022 influenza/COVID/respiratory syncytial virus tripledemic. It appears, however, that COVID may have missed the memo.
For the sixth time in the last 7 weeks, the number of new COVID cases in children fell, with just under 23,000 reported during the week of Oct. 14-20, according to the American Academy of Pediatrics and the Children’s Hospital Association. That is the lowest weekly count so far this year, and the lowest since early July of 2021, just as the Delta surge was starting. New pediatric cases had dipped to 8,500, the lowest for any week during the pandemic, a couple of weeks before that, the AAP/CHA data show.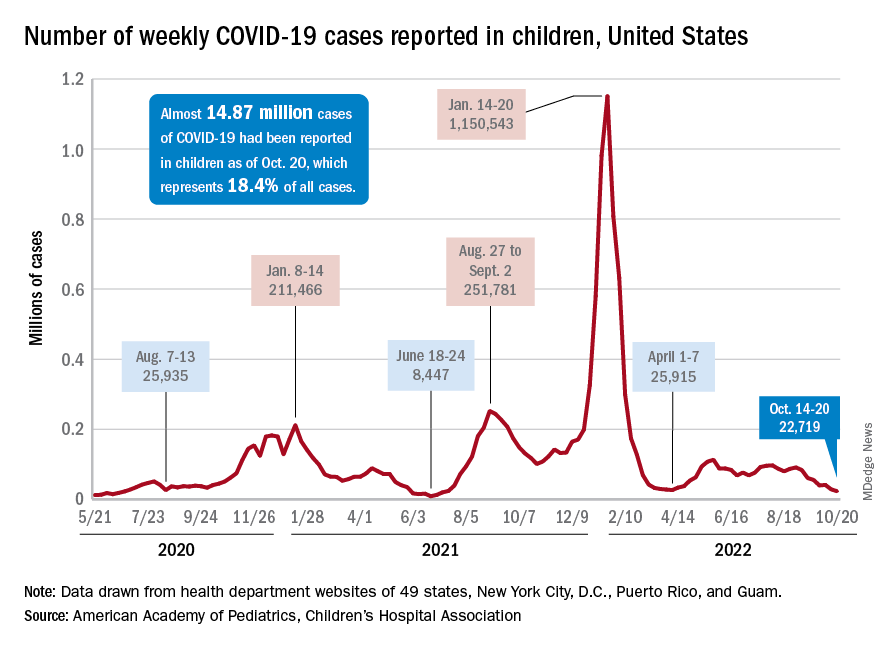
Weekly cases have fallen by almost 75% since over 90,000 were reported for the week of Aug. 26 to Sept. 1, even as children have returned to school and vaccine uptake remains slow in the youngest age groups. Rates of emergency department visits with diagnosed COVID also have continued to drop, as have new admissions, and both are nearing their 2021 lows, according to the Centers for Disease Control and Prevention.
New vaccinations in children under age 5 years were up slightly for the most recent week (Oct. 13-19), but total uptake for that age group is only 7.1% for an initial dose and 2.9% for full vaccination. Among children aged 5-11 years, 38.7% have received at least one dose and 31.6% have completed the primary series, with corresponding figures of 71.2% and 60.9% for those aged 12-17, the CDC said on its COVID Data Tracker.
Despite the low overall numbers, though, the youngest children are, in one respect, punching above their weight when it comes to vaccinations. In the 2 weeks from Oct. 6 to Oct. 19, children under 5 years of age, who represent 5.9% of the U.S. population, received 9.2% of the initial vaccine doses administered. Children aged 5-11 years, who represent 8.7% of the total population, got just 4.2% of all first doses over those same 2 weeks, while 12- to 17-year-olds, who make up 7.6% of the population, got 3.4% of the vaccine doses, the CDC reported.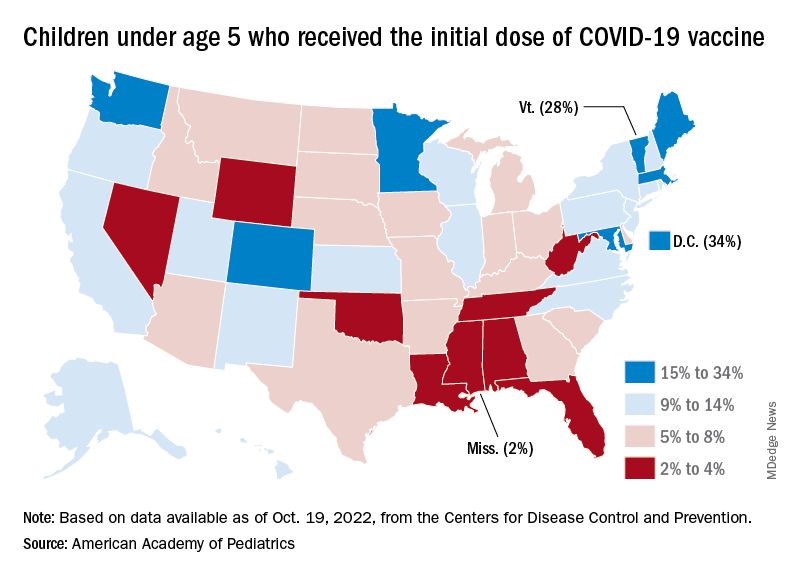
On the vaccine-approval front, the Food and Drug Administration recently announced that the new bivalent COVID-19 vaccines are now included in the emergency use authorizations for children who have completed primary or booster vaccination. The Moderna vaccine is authorized as a single-dose booster for children as young as 6 years and the Pfizer-BioNTech vaccine can be given as a single booster dose in children as young as 5 years, the FDA said.
“These bivalent COVID-19 vaccines include an mRNA component of the original strain to provide an immune response that is broadly protective against COVID-19 and an mRNA component in common between the omicron variant BA.4 and BA.5 lineages,” the FDA said.
With the third autumn of the COVID era now upon us, the discussion has turned again to a possible influenza/COVID twindemic, as well as the new-for-2022 influenza/COVID/respiratory syncytial virus tripledemic. It appears, however, that COVID may have missed the memo.
For the sixth time in the last 7 weeks, the number of new COVID cases in children fell, with just under 23,000 reported during the week of Oct. 14-20, according to the American Academy of Pediatrics and the Children’s Hospital Association. That is the lowest weekly count so far this year, and the lowest since early July of 2021, just as the Delta surge was starting. New pediatric cases had dipped to 8,500, the lowest for any week during the pandemic, a couple of weeks before that, the AAP/CHA data show.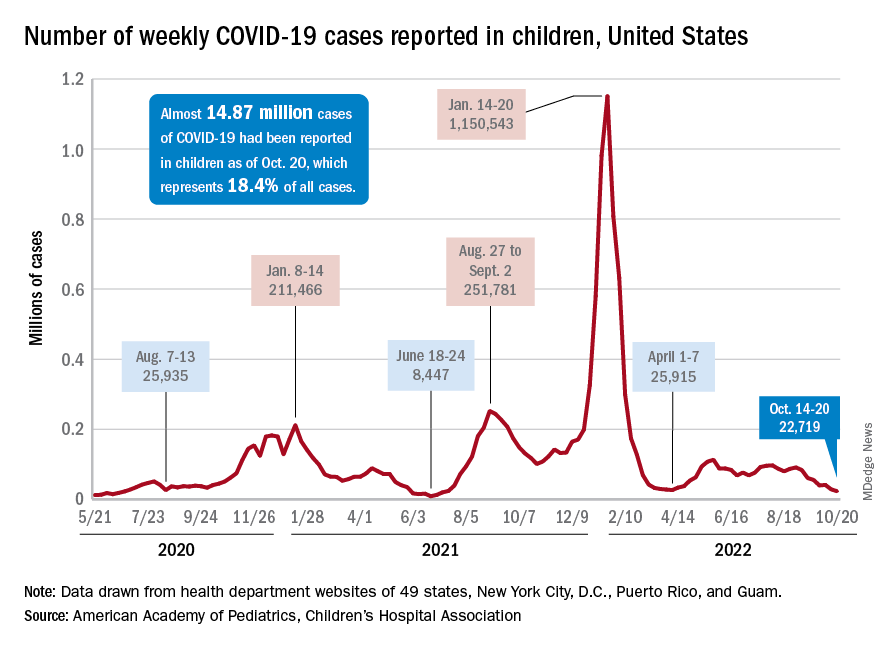
Weekly cases have fallen by almost 75% since over 90,000 were reported for the week of Aug. 26 to Sept. 1, even as children have returned to school and vaccine uptake remains slow in the youngest age groups. Rates of emergency department visits with diagnosed COVID also have continued to drop, as have new admissions, and both are nearing their 2021 lows, according to the Centers for Disease Control and Prevention.
New vaccinations in children under age 5 years were up slightly for the most recent week (Oct. 13-19), but total uptake for that age group is only 7.1% for an initial dose and 2.9% for full vaccination. Among children aged 5-11 years, 38.7% have received at least one dose and 31.6% have completed the primary series, with corresponding figures of 71.2% and 60.9% for those aged 12-17, the CDC said on its COVID Data Tracker.
Despite the low overall numbers, though, the youngest children are, in one respect, punching above their weight when it comes to vaccinations. In the 2 weeks from Oct. 6 to Oct. 19, children under 5 years of age, who represent 5.9% of the U.S. population, received 9.2% of the initial vaccine doses administered. Children aged 5-11 years, who represent 8.7% of the total population, got just 4.2% of all first doses over those same 2 weeks, while 12- to 17-year-olds, who make up 7.6% of the population, got 3.4% of the vaccine doses, the CDC reported.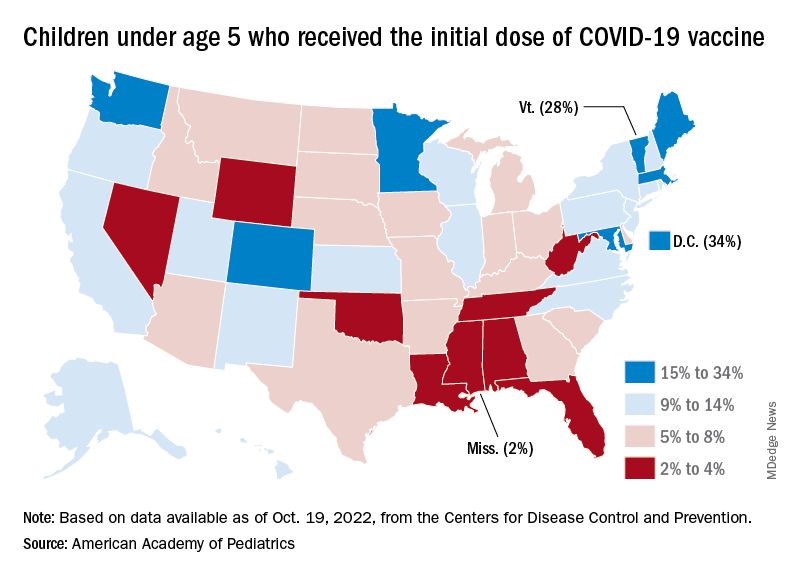
On the vaccine-approval front, the Food and Drug Administration recently announced that the new bivalent COVID-19 vaccines are now included in the emergency use authorizations for children who have completed primary or booster vaccination. The Moderna vaccine is authorized as a single-dose booster for children as young as 6 years and the Pfizer-BioNTech vaccine can be given as a single booster dose in children as young as 5 years, the FDA said.
“These bivalent COVID-19 vaccines include an mRNA component of the original strain to provide an immune response that is broadly protective against COVID-19 and an mRNA component in common between the omicron variant BA.4 and BA.5 lineages,” the FDA said.
Healthy diet, less news helped prevent anxiety, depression during COVID
VIENNA –
Results from a longitudinal Spanish survey study of more than 1,000 adults showed that being outside, relaxing, participating in physical activities, and drinking plenty of water were also beneficial. However, social contact with friends and relatives, following a routine, and pursuing hobbies had no significant impact.
“This was a little surprising,” lead author Joaquim Radua, MD, PhD, August Pi i Sunyer Biomedical Research Institute (IDIBAPS), Barcelona, said in a release.
“Like many people, we had assumed that personal contact would play a bigger part in avoiding anxiety and depression during stressful times,” he added.
However, Dr. Radua said that because the study was conducted during the COVID-19 pandemic, “people who socialized may also have been anxious about getting infected.”
Consequently, “it may be that this specific behavior cannot be extrapolated to other times, when there is no pandemic,” he said.
The findings were presented at the 35th European College of Neuropsychopharmacology (ECNP) Congress.
Correlational versus longitudinal studies
Dr. Radua emphasized that individuals “should socialize,” of course.
“We think it’s important that people continue to follow what works for them and that if you enjoy seeing friends or following a hobby, you continue to do so,” he said.
“Our work was centered on COVID, but we now need to see if these factors apply to other stressful circumstances. These simple behaviors may prevent anxiety and depression, and prevention is better than cure,” he added.
The researchers note that, in “times of uncertainty” such as the COVID-19 pandemic, many individuals experience increases in both anxiety and depressive symptoms.
Although a range of behaviors are recommended to help people cope, the investigators add that some of the recommendations are based on correlational studies.
Indeed, the researchers previously identified a correlation between following a healthy/balanced diet, among other measures, and lower anxiety and depressive symptoms during the pandemic.
However, it is unclear from cross-sectional studies whether the behavior alters the symptoms, in which case the behavior could be considered “helpful,” or conversely whether the symptoms alter an individual’s behavior, in which case the behaviors “may be useless,” the investigators note.
The investigative team therefore set out to provide more robust evidence for making recommendations and conducted a prospective longitudinal study.
They recruited 1,049 adults online via social networks, matching them to the regional, age and sex, and urbanicity distribution of the overall Spanish population.
Every 2 weeks for 12 months, the researchers administered the General Anxiety Disorder (GAD)-7, the Patient Health Questionnaire (PHQ)-9, and a two-item ecological momentary assessment to minimize recall bias, among other measures. They also asked about 10 self-report coping behaviors.
Significant coping behaviors
The study was completed by 942 individuals, indicating a retention of 90%.
Among both completers and non-completers there was an over-representation of individuals aged 18-34 years and women, compared with the general population, and fewer participants aged at least 65 years.
Pre-recruitment, the mean baseline GAD-7 score among completers was 7.4, falling to around 5.5 at the time of the first questionnaire. Scores on the PHQ-9 were 7.6 and 5.6, respectively.
Performing population-weighted autoregressive moving average models to analyze the relationship between the current frequency of the coping behaviors and future changes in anxiety and depressive symptoms, the investigators found that the greatest effect was from following a healthy, balanced diet, with an impact size of 0.95.
This was followed by avoiding too much stressful news (impact size, 0.91), staying outdoors or looking outside (0.40), doing relaxing activities (0.33), participating in physical exercise (0.32), and drinking water to hydrate (0.25).
Overall, these coping behaviors were associated with a significant reduction in anxiety and depressive symptoms (all, P < .001).
On the other hand, there was no impact on future symptoms from socializing with friends and relatives, whether or not they lived in the same household. There was also no effect from following a routine, pursuing hobbies, or performing home tasks.
The researchers note that similar results were obtained when excluding participants with hazardous alcohol consumption, defined as a score on the Alcohol Use Disorders Identification Test of 8 or higher.
However, they point out that despite its prospective design and large cohort, the study was not interventional. Therefore, they “cannot rule out the possibility that decreasing the frequency of a behavior is an early sign of some mechanism that later leads to increased anxiety and depression symptoms.”
Nevertheless, they believe that possibility “seems unlikely.”
Reflective of a unique time?
Commenting on the findings, Catherine Harmer, PhD, director of the Psychopharmacology and Emotional Research Lab, department of psychiatry, University of Oxford (England), said in the release this was an “interesting study” that “provides some important insights as to which behaviors may protect our mental health during times of significant stress.”
She said the finding that social contact was not beneficial was “surprising” but may reflect the fact that, during the pandemic, it was “stressful even to have those social contacts, even if we managed to meet a friend outside.”
The results of the study may therefore be “reflective of the unique experience” of the COVID-19 pandemic, said Dr. Harmer, who was not involved with the research.
“I wouldn’t think that reading too much news would generally be something that has a negative impact on depression and anxiety, but I think it was very much at the time,” she said.
With the pandemic overwhelming one country after another, “the more you read about it, the more frightening it was,” she added, noting that it is “easy to forget how frightened we were at the beginning.”
Dr. Harmer noted that “it would be interesting” if the study was repeated and the same factors came out – or if they were unique to that time.
This would be “useful to know, as these times may come again. And the more information we have to cope with a pandemic, the better,” she concluded.
The research was supported by the AXA Research Fund via an AXA Award granted to Dr. Radua from the call for projects “mitigating risk in the wake of the COVID-19 pandemic.” The investigators and Dr. Harmer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
VIENNA –
Results from a longitudinal Spanish survey study of more than 1,000 adults showed that being outside, relaxing, participating in physical activities, and drinking plenty of water were also beneficial. However, social contact with friends and relatives, following a routine, and pursuing hobbies had no significant impact.
“This was a little surprising,” lead author Joaquim Radua, MD, PhD, August Pi i Sunyer Biomedical Research Institute (IDIBAPS), Barcelona, said in a release.
“Like many people, we had assumed that personal contact would play a bigger part in avoiding anxiety and depression during stressful times,” he added.
However, Dr. Radua said that because the study was conducted during the COVID-19 pandemic, “people who socialized may also have been anxious about getting infected.”
Consequently, “it may be that this specific behavior cannot be extrapolated to other times, when there is no pandemic,” he said.
The findings were presented at the 35th European College of Neuropsychopharmacology (ECNP) Congress.
Correlational versus longitudinal studies
Dr. Radua emphasized that individuals “should socialize,” of course.
“We think it’s important that people continue to follow what works for them and that if you enjoy seeing friends or following a hobby, you continue to do so,” he said.
“Our work was centered on COVID, but we now need to see if these factors apply to other stressful circumstances. These simple behaviors may prevent anxiety and depression, and prevention is better than cure,” he added.
The researchers note that, in “times of uncertainty” such as the COVID-19 pandemic, many individuals experience increases in both anxiety and depressive symptoms.
Although a range of behaviors are recommended to help people cope, the investigators add that some of the recommendations are based on correlational studies.
Indeed, the researchers previously identified a correlation between following a healthy/balanced diet, among other measures, and lower anxiety and depressive symptoms during the pandemic.
However, it is unclear from cross-sectional studies whether the behavior alters the symptoms, in which case the behavior could be considered “helpful,” or conversely whether the symptoms alter an individual’s behavior, in which case the behaviors “may be useless,” the investigators note.
The investigative team therefore set out to provide more robust evidence for making recommendations and conducted a prospective longitudinal study.
They recruited 1,049 adults online via social networks, matching them to the regional, age and sex, and urbanicity distribution of the overall Spanish population.
Every 2 weeks for 12 months, the researchers administered the General Anxiety Disorder (GAD)-7, the Patient Health Questionnaire (PHQ)-9, and a two-item ecological momentary assessment to minimize recall bias, among other measures. They also asked about 10 self-report coping behaviors.
Significant coping behaviors
The study was completed by 942 individuals, indicating a retention of 90%.
Among both completers and non-completers there was an over-representation of individuals aged 18-34 years and women, compared with the general population, and fewer participants aged at least 65 years.
Pre-recruitment, the mean baseline GAD-7 score among completers was 7.4, falling to around 5.5 at the time of the first questionnaire. Scores on the PHQ-9 were 7.6 and 5.6, respectively.
Performing population-weighted autoregressive moving average models to analyze the relationship between the current frequency of the coping behaviors and future changes in anxiety and depressive symptoms, the investigators found that the greatest effect was from following a healthy, balanced diet, with an impact size of 0.95.
This was followed by avoiding too much stressful news (impact size, 0.91), staying outdoors or looking outside (0.40), doing relaxing activities (0.33), participating in physical exercise (0.32), and drinking water to hydrate (0.25).
Overall, these coping behaviors were associated with a significant reduction in anxiety and depressive symptoms (all, P < .001).
On the other hand, there was no impact on future symptoms from socializing with friends and relatives, whether or not they lived in the same household. There was also no effect from following a routine, pursuing hobbies, or performing home tasks.
The researchers note that similar results were obtained when excluding participants with hazardous alcohol consumption, defined as a score on the Alcohol Use Disorders Identification Test of 8 or higher.
However, they point out that despite its prospective design and large cohort, the study was not interventional. Therefore, they “cannot rule out the possibility that decreasing the frequency of a behavior is an early sign of some mechanism that later leads to increased anxiety and depression symptoms.”
Nevertheless, they believe that possibility “seems unlikely.”
Reflective of a unique time?
Commenting on the findings, Catherine Harmer, PhD, director of the Psychopharmacology and Emotional Research Lab, department of psychiatry, University of Oxford (England), said in the release this was an “interesting study” that “provides some important insights as to which behaviors may protect our mental health during times of significant stress.”
She said the finding that social contact was not beneficial was “surprising” but may reflect the fact that, during the pandemic, it was “stressful even to have those social contacts, even if we managed to meet a friend outside.”
The results of the study may therefore be “reflective of the unique experience” of the COVID-19 pandemic, said Dr. Harmer, who was not involved with the research.
“I wouldn’t think that reading too much news would generally be something that has a negative impact on depression and anxiety, but I think it was very much at the time,” she said.
With the pandemic overwhelming one country after another, “the more you read about it, the more frightening it was,” she added, noting that it is “easy to forget how frightened we were at the beginning.”
Dr. Harmer noted that “it would be interesting” if the study was repeated and the same factors came out – or if they were unique to that time.
This would be “useful to know, as these times may come again. And the more information we have to cope with a pandemic, the better,” she concluded.
The research was supported by the AXA Research Fund via an AXA Award granted to Dr. Radua from the call for projects “mitigating risk in the wake of the COVID-19 pandemic.” The investigators and Dr. Harmer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
VIENNA –
Results from a longitudinal Spanish survey study of more than 1,000 adults showed that being outside, relaxing, participating in physical activities, and drinking plenty of water were also beneficial. However, social contact with friends and relatives, following a routine, and pursuing hobbies had no significant impact.
“This was a little surprising,” lead author Joaquim Radua, MD, PhD, August Pi i Sunyer Biomedical Research Institute (IDIBAPS), Barcelona, said in a release.
“Like many people, we had assumed that personal contact would play a bigger part in avoiding anxiety and depression during stressful times,” he added.
However, Dr. Radua said that because the study was conducted during the COVID-19 pandemic, “people who socialized may also have been anxious about getting infected.”
Consequently, “it may be that this specific behavior cannot be extrapolated to other times, when there is no pandemic,” he said.
The findings were presented at the 35th European College of Neuropsychopharmacology (ECNP) Congress.
Correlational versus longitudinal studies
Dr. Radua emphasized that individuals “should socialize,” of course.
“We think it’s important that people continue to follow what works for them and that if you enjoy seeing friends or following a hobby, you continue to do so,” he said.
“Our work was centered on COVID, but we now need to see if these factors apply to other stressful circumstances. These simple behaviors may prevent anxiety and depression, and prevention is better than cure,” he added.
The researchers note that, in “times of uncertainty” such as the COVID-19 pandemic, many individuals experience increases in both anxiety and depressive symptoms.
Although a range of behaviors are recommended to help people cope, the investigators add that some of the recommendations are based on correlational studies.
Indeed, the researchers previously identified a correlation between following a healthy/balanced diet, among other measures, and lower anxiety and depressive symptoms during the pandemic.
However, it is unclear from cross-sectional studies whether the behavior alters the symptoms, in which case the behavior could be considered “helpful,” or conversely whether the symptoms alter an individual’s behavior, in which case the behaviors “may be useless,” the investigators note.
The investigative team therefore set out to provide more robust evidence for making recommendations and conducted a prospective longitudinal study.
They recruited 1,049 adults online via social networks, matching them to the regional, age and sex, and urbanicity distribution of the overall Spanish population.
Every 2 weeks for 12 months, the researchers administered the General Anxiety Disorder (GAD)-7, the Patient Health Questionnaire (PHQ)-9, and a two-item ecological momentary assessment to minimize recall bias, among other measures. They also asked about 10 self-report coping behaviors.
Significant coping behaviors
The study was completed by 942 individuals, indicating a retention of 90%.
Among both completers and non-completers there was an over-representation of individuals aged 18-34 years and women, compared with the general population, and fewer participants aged at least 65 years.
Pre-recruitment, the mean baseline GAD-7 score among completers was 7.4, falling to around 5.5 at the time of the first questionnaire. Scores on the PHQ-9 were 7.6 and 5.6, respectively.
Performing population-weighted autoregressive moving average models to analyze the relationship between the current frequency of the coping behaviors and future changes in anxiety and depressive symptoms, the investigators found that the greatest effect was from following a healthy, balanced diet, with an impact size of 0.95.
This was followed by avoiding too much stressful news (impact size, 0.91), staying outdoors or looking outside (0.40), doing relaxing activities (0.33), participating in physical exercise (0.32), and drinking water to hydrate (0.25).
Overall, these coping behaviors were associated with a significant reduction in anxiety and depressive symptoms (all, P < .001).
On the other hand, there was no impact on future symptoms from socializing with friends and relatives, whether or not they lived in the same household. There was also no effect from following a routine, pursuing hobbies, or performing home tasks.
The researchers note that similar results were obtained when excluding participants with hazardous alcohol consumption, defined as a score on the Alcohol Use Disorders Identification Test of 8 or higher.
However, they point out that despite its prospective design and large cohort, the study was not interventional. Therefore, they “cannot rule out the possibility that decreasing the frequency of a behavior is an early sign of some mechanism that later leads to increased anxiety and depression symptoms.”
Nevertheless, they believe that possibility “seems unlikely.”
Reflective of a unique time?
Commenting on the findings, Catherine Harmer, PhD, director of the Psychopharmacology and Emotional Research Lab, department of psychiatry, University of Oxford (England), said in the release this was an “interesting study” that “provides some important insights as to which behaviors may protect our mental health during times of significant stress.”
She said the finding that social contact was not beneficial was “surprising” but may reflect the fact that, during the pandemic, it was “stressful even to have those social contacts, even if we managed to meet a friend outside.”
The results of the study may therefore be “reflective of the unique experience” of the COVID-19 pandemic, said Dr. Harmer, who was not involved with the research.
“I wouldn’t think that reading too much news would generally be something that has a negative impact on depression and anxiety, but I think it was very much at the time,” she said.
With the pandemic overwhelming one country after another, “the more you read about it, the more frightening it was,” she added, noting that it is “easy to forget how frightened we were at the beginning.”
Dr. Harmer noted that “it would be interesting” if the study was repeated and the same factors came out – or if they were unique to that time.
This would be “useful to know, as these times may come again. And the more information we have to cope with a pandemic, the better,” she concluded.
The research was supported by the AXA Research Fund via an AXA Award granted to Dr. Radua from the call for projects “mitigating risk in the wake of the COVID-19 pandemic.” The investigators and Dr. Harmer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ECNP 2022
Myocarditis after COVID vax rare and mild in teens
New data from Israel provide further evidence that myocarditis is a rare adverse event of vaccination with the Pfizer/BioNTech mRNA COVID-19 vaccine in adolescents – one that predominantly occurs in males and typically after the second dose.
The new data also indicate a “mild and benign” clinical course of myocarditis after vaccination, with “favorable” long-term prognosis based on cardiac imaging findings.
Guy Witberg, MD, MPH, Rabin Medical Center, Petah Tikva, Israel, and colleagues report their latest observations in correspondence in The New England Journal of Medicine, online.
The group previously reported in December 2021 that the incidence of myocarditis in Israel after receipt of the Pfizer/BioNTech BNT162b2 mRNA COVID-19 vaccine was highest among males between the ages of 16 and 29 (10.7 cases per 100,000).
The vaccine has since been approved for adolescents aged 12-15. Initial evidence for this age group, reported by Dr. Witberg and colleagues in March 2022, suggests a similar low incidence and mild course of myocarditis, although follow-up was limited to 30 days.
In their latest report, with follow-up out to 6 months, Dr. Witberg and colleagues identified nine probable or definite cases of myocarditis among 182,605 Israeli adolescents aged 12-15 who received the Pfizer/BioNTech mRNA vaccine – an incidence of 4.8 cases per 100,000.
Eight cases occurred after the second vaccine dose. All nine cases were mild.
Cardiac and inflammatory markers were elevated in all adolescent patients and electrocardiographic results were abnormal in two-thirds.
Eight patients had a normal ejection fraction, and four had a pericardial effusion. The patients spent 2-4 days hospitalized, and the in-hospital course was uneventful.
Echocardiographic findings were available a median of 10 days after discharge for eight patients. All echocardiograms showed a normal ejection fraction and resolution of pericardial effusion.
Five patients underwent cardiac MRI, including three scans performed at a median of 104 days after discharge. The scans showed “minimal evidence” of myocardial scarring or fibrosis, with evidence of late gadolinium enhancement ranging from 0% to 2%.
At a median of 206 days following discharge, all of the patients were alive, and none had been readmitted to the hospital, Dr. Witberg and colleagues report.
This research had no specific funding. Five authors have received research grants from Pfizer.
A version of this article first appeared on Medscape.com.
New data from Israel provide further evidence that myocarditis is a rare adverse event of vaccination with the Pfizer/BioNTech mRNA COVID-19 vaccine in adolescents – one that predominantly occurs in males and typically after the second dose.
The new data also indicate a “mild and benign” clinical course of myocarditis after vaccination, with “favorable” long-term prognosis based on cardiac imaging findings.
Guy Witberg, MD, MPH, Rabin Medical Center, Petah Tikva, Israel, and colleagues report their latest observations in correspondence in The New England Journal of Medicine, online.
The group previously reported in December 2021 that the incidence of myocarditis in Israel after receipt of the Pfizer/BioNTech BNT162b2 mRNA COVID-19 vaccine was highest among males between the ages of 16 and 29 (10.7 cases per 100,000).
The vaccine has since been approved for adolescents aged 12-15. Initial evidence for this age group, reported by Dr. Witberg and colleagues in March 2022, suggests a similar low incidence and mild course of myocarditis, although follow-up was limited to 30 days.
In their latest report, with follow-up out to 6 months, Dr. Witberg and colleagues identified nine probable or definite cases of myocarditis among 182,605 Israeli adolescents aged 12-15 who received the Pfizer/BioNTech mRNA vaccine – an incidence of 4.8 cases per 100,000.
Eight cases occurred after the second vaccine dose. All nine cases were mild.
Cardiac and inflammatory markers were elevated in all adolescent patients and electrocardiographic results were abnormal in two-thirds.
Eight patients had a normal ejection fraction, and four had a pericardial effusion. The patients spent 2-4 days hospitalized, and the in-hospital course was uneventful.
Echocardiographic findings were available a median of 10 days after discharge for eight patients. All echocardiograms showed a normal ejection fraction and resolution of pericardial effusion.
Five patients underwent cardiac MRI, including three scans performed at a median of 104 days after discharge. The scans showed “minimal evidence” of myocardial scarring or fibrosis, with evidence of late gadolinium enhancement ranging from 0% to 2%.
At a median of 206 days following discharge, all of the patients were alive, and none had been readmitted to the hospital, Dr. Witberg and colleagues report.
This research had no specific funding. Five authors have received research grants from Pfizer.
A version of this article first appeared on Medscape.com.
New data from Israel provide further evidence that myocarditis is a rare adverse event of vaccination with the Pfizer/BioNTech mRNA COVID-19 vaccine in adolescents – one that predominantly occurs in males and typically after the second dose.
The new data also indicate a “mild and benign” clinical course of myocarditis after vaccination, with “favorable” long-term prognosis based on cardiac imaging findings.
Guy Witberg, MD, MPH, Rabin Medical Center, Petah Tikva, Israel, and colleagues report their latest observations in correspondence in The New England Journal of Medicine, online.
The group previously reported in December 2021 that the incidence of myocarditis in Israel after receipt of the Pfizer/BioNTech BNT162b2 mRNA COVID-19 vaccine was highest among males between the ages of 16 and 29 (10.7 cases per 100,000).
The vaccine has since been approved for adolescents aged 12-15. Initial evidence for this age group, reported by Dr. Witberg and colleagues in March 2022, suggests a similar low incidence and mild course of myocarditis, although follow-up was limited to 30 days.
In their latest report, with follow-up out to 6 months, Dr. Witberg and colleagues identified nine probable or definite cases of myocarditis among 182,605 Israeli adolescents aged 12-15 who received the Pfizer/BioNTech mRNA vaccine – an incidence of 4.8 cases per 100,000.
Eight cases occurred after the second vaccine dose. All nine cases were mild.
Cardiac and inflammatory markers were elevated in all adolescent patients and electrocardiographic results were abnormal in two-thirds.
Eight patients had a normal ejection fraction, and four had a pericardial effusion. The patients spent 2-4 days hospitalized, and the in-hospital course was uneventful.
Echocardiographic findings were available a median of 10 days after discharge for eight patients. All echocardiograms showed a normal ejection fraction and resolution of pericardial effusion.
Five patients underwent cardiac MRI, including three scans performed at a median of 104 days after discharge. The scans showed “minimal evidence” of myocardial scarring or fibrosis, with evidence of late gadolinium enhancement ranging from 0% to 2%.
At a median of 206 days following discharge, all of the patients were alive, and none had been readmitted to the hospital, Dr. Witberg and colleagues report.
This research had no specific funding. Five authors have received research grants from Pfizer.
A version of this article first appeared on Medscape.com.
Worse COVID outcomes seen with gout, particularly in women
People with gout, especially women, appear to be at higher risk for poor COVID-19 outcomes, including hospitalization and death, regardless of COVID-19 vaccination status, researchers suggest.
“We found that the risks of SARS-CoV-2 infection, 30-day hospitalization, and 30-day death among individuals with gout were higher than the general population irrespective of the vaccination status,” lead study author Dongxing Xie, MD, PhD, Xiangya Hospital, Central South University, Changsha, China, and his colleagues write in their large population study. “This finding informs individuals with gout, especially women, that additional measures, even after vaccination, should be considered in order to mitigate the risk of SARS-CoV-2 infection and its severe sequelae.”
People with gout, the most common inflammatory arthritis, often have other conditions that are linked to higher risk for SARS-CoV-2 infection and poor outcomes as well, including obesity, cardiovascular disease, and chronic kidney disease, the authors write. And elevated serum urate may contribute to inflammation and possible COVID-19 complications. But unlike in the case of diseases such as lupus and rheumatoid arthritis, little is known about SARS-CoV-2 infection risk among patients with gout.
As reported in Arthritis & Rheumatology, Dr. Xie and his research team used the Health Improvement Network ([THIN], now called IQVIA Medical Research Database) repository of medical conditions, demographics, and other details of around 17 million people in the United Kingdom to estimate the risk for SARS-CoV-2 infection, hospitalization, and death in people with gout. They compared those outcomes with outcomes of people without gout and compared outcomes of vaccinated vs. nonvaccinated participants.
From December 2020 through October 2021, the researchers investigated the risk for SARS-CoV-2 breakthrough infection in vaccinated people between age 18 and 90 years who had gout and were hospitalized within 30 days after the infection diagnosis or who died within 30 days after the diagnosis. They compared these outcomes with the outcomes of people in the general population without gout after COVID-19 vaccination. They also compared the risk for SARS-CoV-2 infection and its severe outcomes between individuals with gout and the general population among unvaccinated people.
They weighted these comparisons on the basis of age, sex, body mass index, socioeconomic deprivation index score, region, and number of previous COVID-19 tests in one model. A more fully adjusted model also weighted the comparisons for lifestyle factors, comorbidities, medications, and healthcare utilization.
The vaccinated cohort consisted of 54,576 people with gout and 1,336,377 without gout from the general population. The unvaccinated cohort included 61,111 individuals with gout and 1,697,168 individuals without gout from the general population.
Women more likely to be hospitalized and die
The risk for breakthrough infection in the vaccinated cohort was significantly higher among people with gout than among those without gout in the general population, particularly for men, who had hazard ratios (HRs) ranging from 1.22 with a fully adjusted exposure score to 1.30 with a partially adjusted score, but this was not seen in women. The overall incidence of breakthrough infection per 1,000 person-months for these groups was 4.68 with gout vs. 3.76 without gout.
The researchers showed a similar pattern of a higher rate of hospitalizations for people with gout vs. without (0.42/1,000 person-months vs. 0.28); in this case, women had higher risks than did men, with HRs for women ranging from 1.55 with a fully adjusted exposure score to 1.91 with a partially adjusted score, compared with 1.22 and 1.43 for men, respectively.
People with gout had significantly higher mortality than did those without (0.06/1,000 person-months vs. 0.04), but the risk for death was only higher for women, with HRs calculated to be 2.23 in fully adjusted exposure scores and 3.01 in partially adjusted scores.
These same comparisons in the unvaccinated cohort all went in the same direction as did those in the vaccinated cohort but showed higher rates for infection (8.69/1,000 person-months vs. 6.89), hospitalization (2.57/1,000 person-months vs. 1.71), and death (0.65/1,000 person-months vs. 0.53). Similar sex-specific links between gout and risks for SARS-CoV-2 infection, hospitalization, and death were seen in the unvaccinated cohort.
Patients with gout and COVID-19 need close monitoring
Four experts who were not involved in the study encourage greater attention to the needs of patients with gout.
Pamela B. Davis, MD, PhD, research professor at Case Western Reserve University, Cleveland, told this news organization, “This study brings to attention yet another potentially vulnerable group for physicians to monitor closely if they are infected with SARS-CoV-2.
“It is not clear why women with gout are more vulnerable, but fewer women than men were in the cohort with gout, and the confidence intervals for the results in women were, in general, larger,” she said.
“The authors suggest that women with gout tend to be older and have more comorbidities than men with gout,” Dr. Davis added. “The excess risk diminishes when the model is fully adjusted for comorbidities, such as obesity, hypertension, or heart disease, suggesting that already-known antecedents of infection severity account for a great deal of the excess risk.”
Kevin D. Deane, MD, PhD, associate professor of medicine and chair in rheumatology research at the University of Colorado at Denver, Aurora, advises physicians to keep in mind other conditions linked with increased risk for severe COVID-19, including advanced age; heart, lung, or kidney problems; and autoimmune diseases.
“I would be very cautious about the finding that there was not a difference in outcomes in individuals with gout based on vaccination status,” he cautioned, urging clinicians to “still strongly recommend vaccines according to guidelines.”
Sarah E. Waldman, MD, associate clinical professor of infectious diseases at UC Davis Health in Sacramento, Calif., called the study interesting but not surprising.
“The reason for increased risk for COVID-19 infection among those with gout may have to do with their underlying inflammatory state. Additional research needs to be done on this topic.
“Retrospective population-based cohort studies can be difficult to interpret due to biases,” she added. Associations identified in this type of study do not determine causation.
“As the researchers noted, those with gout tend to have additional comorbidities as well as advanced age,” she said. “They may also seek medical care more often and be tested for SARS-CoV-2 more frequently.”
Dr. Waldman advises clinicians to counsel patients with gout about their potential increased infection risk and ways they can protect themselves, including COVID-19 vaccinations.
“The strong association between gout and COVID-19 infection could involve coexisting conditions such as diabetes, hypertension, cardiovascular disease, and chronic kidney disease,” Dr. Aung added.
Earlier studies show links between gout and severe COVID-19 outcomes
Lead author Kanon Jatuworapruk, MD, PhD, of Thammasat University in Pathumthani, Thailand, and his colleagues investigated characteristics and outcomes of people with gout who were hospitalized for COVID-19 between March 2020 and October 2021, using data from the COVID-19 Global Rheumatology Alliance registry.
“This cohort of people with gout and COVID-19 who were hospitalized had high frequencies of ventilatory support and death,” the authors write in ACR Open Rheumatology . “This suggests that patients with gout who were hospitalized for COVID-19 may be at risk of poor outcomes, perhaps related to known risk factors for poor outcomes, such as age and presence of comorbidity.”
In their study, the average age of the 163 patients was 63 years, and 85% were men. Most lived in the Western Pacific Region and North America, and 46% had two or more comorbidities, most commonly hypertension, cardiovascular disease, diabetes, chronic kidney disease, and obesity. The researchers found that:
- Sixty-eight percent of the cohort required supplemental oxygen or ventilatory support during hospitalization.
- Sixteen percent of deaths were related to COVID-19, with 73% of deaths occurring in people with two or more comorbidities.
Ruth K. Topless, assistant research fellow in the department of biochemistry at the University of Otago in Dunedin, New Zealand, is the lead author on a study she and her colleagues are conducting using the UK Biobank databases of 459,837 participants in the United Kingdom, including 15,871 people with gout, through April 6, 2021, to investigate whether gout is a risk factor for diagnosis of COVID-19 and COVID-19–related death.
“Gout is a risk factor for COVID-19-related death in the UK Biobank cohort, with an increased risk in women with gout, which was driven by risk factors independent of the metabolic comorbidities of gout,” the researchers conclude in The Lancet Rheumatology.
In their study, gout was linked with COVID-19 diagnosis (odds ratio, 1.20; 95% confidence interval, 1.11-1.29) but not with risk for COVID-19–related death in the group of patients with COVID-19 (OR, 1.20; 95% CI, 0.96-1.51). In the entire cohort, gout was linked with COVID-19–related death (OR, 1.29; 95% CI, 1.06-1.56); women with gout were at increased risk for COVID-19–related death (OR, 1.98; 95% CI, 1.34-2.94), but men with gout were not (OR, 1.16; 95% CI, 0.93-1.45). The risk for COVID-19 diagnosis was significant in the nonvaccinated group (OR, 1.21; 95% CI, 1.11-1.30) but not in the vaccinated group (OR, 1.09; 95% CI, 0.65-1.85).
Editorial authors join in recommending further related research
In a commentary in The Lancet Rheumatology about the UK Biobank and other related research, Christoffer B. Nissen, MD, of University Hospital of Southern Denmark in Sonderborg, and his co-authors call the Topless and colleagues study “an elegantly conducted analysis of data from the UK Biobank supporting the hypothesis that gout needs attention in patients with COVID-19.”
Further studies are needed to investigate to what degree a diagnosis of gout is a risk factor for COVID-19 and whether treatment modifies the risk of a severe disease course,” they write. “However, in the interim, the results of this study could be considered when risk stratifying patients with gout in view of vaccination recommendations and early treatment interventions.”
Each of the three studies received grant funding. Several of the authors of the studies report financial involvements with pharmaceutical companies. All outside experts commented by email and report no relevant financial involvements.
A version of this article first appeared on Medscape.com.
People with gout, especially women, appear to be at higher risk for poor COVID-19 outcomes, including hospitalization and death, regardless of COVID-19 vaccination status, researchers suggest.
“We found that the risks of SARS-CoV-2 infection, 30-day hospitalization, and 30-day death among individuals with gout were higher than the general population irrespective of the vaccination status,” lead study author Dongxing Xie, MD, PhD, Xiangya Hospital, Central South University, Changsha, China, and his colleagues write in their large population study. “This finding informs individuals with gout, especially women, that additional measures, even after vaccination, should be considered in order to mitigate the risk of SARS-CoV-2 infection and its severe sequelae.”
People with gout, the most common inflammatory arthritis, often have other conditions that are linked to higher risk for SARS-CoV-2 infection and poor outcomes as well, including obesity, cardiovascular disease, and chronic kidney disease, the authors write. And elevated serum urate may contribute to inflammation and possible COVID-19 complications. But unlike in the case of diseases such as lupus and rheumatoid arthritis, little is known about SARS-CoV-2 infection risk among patients with gout.
As reported in Arthritis & Rheumatology, Dr. Xie and his research team used the Health Improvement Network ([THIN], now called IQVIA Medical Research Database) repository of medical conditions, demographics, and other details of around 17 million people in the United Kingdom to estimate the risk for SARS-CoV-2 infection, hospitalization, and death in people with gout. They compared those outcomes with outcomes of people without gout and compared outcomes of vaccinated vs. nonvaccinated participants.
From December 2020 through October 2021, the researchers investigated the risk for SARS-CoV-2 breakthrough infection in vaccinated people between age 18 and 90 years who had gout and were hospitalized within 30 days after the infection diagnosis or who died within 30 days after the diagnosis. They compared these outcomes with the outcomes of people in the general population without gout after COVID-19 vaccination. They also compared the risk for SARS-CoV-2 infection and its severe outcomes between individuals with gout and the general population among unvaccinated people.
They weighted these comparisons on the basis of age, sex, body mass index, socioeconomic deprivation index score, region, and number of previous COVID-19 tests in one model. A more fully adjusted model also weighted the comparisons for lifestyle factors, comorbidities, medications, and healthcare utilization.
The vaccinated cohort consisted of 54,576 people with gout and 1,336,377 without gout from the general population. The unvaccinated cohort included 61,111 individuals with gout and 1,697,168 individuals without gout from the general population.
Women more likely to be hospitalized and die
The risk for breakthrough infection in the vaccinated cohort was significantly higher among people with gout than among those without gout in the general population, particularly for men, who had hazard ratios (HRs) ranging from 1.22 with a fully adjusted exposure score to 1.30 with a partially adjusted score, but this was not seen in women. The overall incidence of breakthrough infection per 1,000 person-months for these groups was 4.68 with gout vs. 3.76 without gout.
The researchers showed a similar pattern of a higher rate of hospitalizations for people with gout vs. without (0.42/1,000 person-months vs. 0.28); in this case, women had higher risks than did men, with HRs for women ranging from 1.55 with a fully adjusted exposure score to 1.91 with a partially adjusted score, compared with 1.22 and 1.43 for men, respectively.
People with gout had significantly higher mortality than did those without (0.06/1,000 person-months vs. 0.04), but the risk for death was only higher for women, with HRs calculated to be 2.23 in fully adjusted exposure scores and 3.01 in partially adjusted scores.
These same comparisons in the unvaccinated cohort all went in the same direction as did those in the vaccinated cohort but showed higher rates for infection (8.69/1,000 person-months vs. 6.89), hospitalization (2.57/1,000 person-months vs. 1.71), and death (0.65/1,000 person-months vs. 0.53). Similar sex-specific links between gout and risks for SARS-CoV-2 infection, hospitalization, and death were seen in the unvaccinated cohort.
Patients with gout and COVID-19 need close monitoring
Four experts who were not involved in the study encourage greater attention to the needs of patients with gout.
Pamela B. Davis, MD, PhD, research professor at Case Western Reserve University, Cleveland, told this news organization, “This study brings to attention yet another potentially vulnerable group for physicians to monitor closely if they are infected with SARS-CoV-2.
“It is not clear why women with gout are more vulnerable, but fewer women than men were in the cohort with gout, and the confidence intervals for the results in women were, in general, larger,” she said.
“The authors suggest that women with gout tend to be older and have more comorbidities than men with gout,” Dr. Davis added. “The excess risk diminishes when the model is fully adjusted for comorbidities, such as obesity, hypertension, or heart disease, suggesting that already-known antecedents of infection severity account for a great deal of the excess risk.”
Kevin D. Deane, MD, PhD, associate professor of medicine and chair in rheumatology research at the University of Colorado at Denver, Aurora, advises physicians to keep in mind other conditions linked with increased risk for severe COVID-19, including advanced age; heart, lung, or kidney problems; and autoimmune diseases.
“I would be very cautious about the finding that there was not a difference in outcomes in individuals with gout based on vaccination status,” he cautioned, urging clinicians to “still strongly recommend vaccines according to guidelines.”
Sarah E. Waldman, MD, associate clinical professor of infectious diseases at UC Davis Health in Sacramento, Calif., called the study interesting but not surprising.
“The reason for increased risk for COVID-19 infection among those with gout may have to do with their underlying inflammatory state. Additional research needs to be done on this topic.
“Retrospective population-based cohort studies can be difficult to interpret due to biases,” she added. Associations identified in this type of study do not determine causation.
“As the researchers noted, those with gout tend to have additional comorbidities as well as advanced age,” she said. “They may also seek medical care more often and be tested for SARS-CoV-2 more frequently.”
Dr. Waldman advises clinicians to counsel patients with gout about their potential increased infection risk and ways they can protect themselves, including COVID-19 vaccinations.
“The strong association between gout and COVID-19 infection could involve coexisting conditions such as diabetes, hypertension, cardiovascular disease, and chronic kidney disease,” Dr. Aung added.
Earlier studies show links between gout and severe COVID-19 outcomes
Lead author Kanon Jatuworapruk, MD, PhD, of Thammasat University in Pathumthani, Thailand, and his colleagues investigated characteristics and outcomes of people with gout who were hospitalized for COVID-19 between March 2020 and October 2021, using data from the COVID-19 Global Rheumatology Alliance registry.
“This cohort of people with gout and COVID-19 who were hospitalized had high frequencies of ventilatory support and death,” the authors write in ACR Open Rheumatology . “This suggests that patients with gout who were hospitalized for COVID-19 may be at risk of poor outcomes, perhaps related to known risk factors for poor outcomes, such as age and presence of comorbidity.”
In their study, the average age of the 163 patients was 63 years, and 85% were men. Most lived in the Western Pacific Region and North America, and 46% had two or more comorbidities, most commonly hypertension, cardiovascular disease, diabetes, chronic kidney disease, and obesity. The researchers found that:
- Sixty-eight percent of the cohort required supplemental oxygen or ventilatory support during hospitalization.
- Sixteen percent of deaths were related to COVID-19, with 73% of deaths occurring in people with two or more comorbidities.
Ruth K. Topless, assistant research fellow in the department of biochemistry at the University of Otago in Dunedin, New Zealand, is the lead author on a study she and her colleagues are conducting using the UK Biobank databases of 459,837 participants in the United Kingdom, including 15,871 people with gout, through April 6, 2021, to investigate whether gout is a risk factor for diagnosis of COVID-19 and COVID-19–related death.
“Gout is a risk factor for COVID-19-related death in the UK Biobank cohort, with an increased risk in women with gout, which was driven by risk factors independent of the metabolic comorbidities of gout,” the researchers conclude in The Lancet Rheumatology.
In their study, gout was linked with COVID-19 diagnosis (odds ratio, 1.20; 95% confidence interval, 1.11-1.29) but not with risk for COVID-19–related death in the group of patients with COVID-19 (OR, 1.20; 95% CI, 0.96-1.51). In the entire cohort, gout was linked with COVID-19–related death (OR, 1.29; 95% CI, 1.06-1.56); women with gout were at increased risk for COVID-19–related death (OR, 1.98; 95% CI, 1.34-2.94), but men with gout were not (OR, 1.16; 95% CI, 0.93-1.45). The risk for COVID-19 diagnosis was significant in the nonvaccinated group (OR, 1.21; 95% CI, 1.11-1.30) but not in the vaccinated group (OR, 1.09; 95% CI, 0.65-1.85).
Editorial authors join in recommending further related research
In a commentary in The Lancet Rheumatology about the UK Biobank and other related research, Christoffer B. Nissen, MD, of University Hospital of Southern Denmark in Sonderborg, and his co-authors call the Topless and colleagues study “an elegantly conducted analysis of data from the UK Biobank supporting the hypothesis that gout needs attention in patients with COVID-19.”
Further studies are needed to investigate to what degree a diagnosis of gout is a risk factor for COVID-19 and whether treatment modifies the risk of a severe disease course,” they write. “However, in the interim, the results of this study could be considered when risk stratifying patients with gout in view of vaccination recommendations and early treatment interventions.”
Each of the three studies received grant funding. Several of the authors of the studies report financial involvements with pharmaceutical companies. All outside experts commented by email and report no relevant financial involvements.
A version of this article first appeared on Medscape.com.
People with gout, especially women, appear to be at higher risk for poor COVID-19 outcomes, including hospitalization and death, regardless of COVID-19 vaccination status, researchers suggest.
“We found that the risks of SARS-CoV-2 infection, 30-day hospitalization, and 30-day death among individuals with gout were higher than the general population irrespective of the vaccination status,” lead study author Dongxing Xie, MD, PhD, Xiangya Hospital, Central South University, Changsha, China, and his colleagues write in their large population study. “This finding informs individuals with gout, especially women, that additional measures, even after vaccination, should be considered in order to mitigate the risk of SARS-CoV-2 infection and its severe sequelae.”
People with gout, the most common inflammatory arthritis, often have other conditions that are linked to higher risk for SARS-CoV-2 infection and poor outcomes as well, including obesity, cardiovascular disease, and chronic kidney disease, the authors write. And elevated serum urate may contribute to inflammation and possible COVID-19 complications. But unlike in the case of diseases such as lupus and rheumatoid arthritis, little is known about SARS-CoV-2 infection risk among patients with gout.
As reported in Arthritis & Rheumatology, Dr. Xie and his research team used the Health Improvement Network ([THIN], now called IQVIA Medical Research Database) repository of medical conditions, demographics, and other details of around 17 million people in the United Kingdom to estimate the risk for SARS-CoV-2 infection, hospitalization, and death in people with gout. They compared those outcomes with outcomes of people without gout and compared outcomes of vaccinated vs. nonvaccinated participants.
From December 2020 through October 2021, the researchers investigated the risk for SARS-CoV-2 breakthrough infection in vaccinated people between age 18 and 90 years who had gout and were hospitalized within 30 days after the infection diagnosis or who died within 30 days after the diagnosis. They compared these outcomes with the outcomes of people in the general population without gout after COVID-19 vaccination. They also compared the risk for SARS-CoV-2 infection and its severe outcomes between individuals with gout and the general population among unvaccinated people.
They weighted these comparisons on the basis of age, sex, body mass index, socioeconomic deprivation index score, region, and number of previous COVID-19 tests in one model. A more fully adjusted model also weighted the comparisons for lifestyle factors, comorbidities, medications, and healthcare utilization.
The vaccinated cohort consisted of 54,576 people with gout and 1,336,377 without gout from the general population. The unvaccinated cohort included 61,111 individuals with gout and 1,697,168 individuals without gout from the general population.
Women more likely to be hospitalized and die
The risk for breakthrough infection in the vaccinated cohort was significantly higher among people with gout than among those without gout in the general population, particularly for men, who had hazard ratios (HRs) ranging from 1.22 with a fully adjusted exposure score to 1.30 with a partially adjusted score, but this was not seen in women. The overall incidence of breakthrough infection per 1,000 person-months for these groups was 4.68 with gout vs. 3.76 without gout.
The researchers showed a similar pattern of a higher rate of hospitalizations for people with gout vs. without (0.42/1,000 person-months vs. 0.28); in this case, women had higher risks than did men, with HRs for women ranging from 1.55 with a fully adjusted exposure score to 1.91 with a partially adjusted score, compared with 1.22 and 1.43 for men, respectively.
People with gout had significantly higher mortality than did those without (0.06/1,000 person-months vs. 0.04), but the risk for death was only higher for women, with HRs calculated to be 2.23 in fully adjusted exposure scores and 3.01 in partially adjusted scores.
These same comparisons in the unvaccinated cohort all went in the same direction as did those in the vaccinated cohort but showed higher rates for infection (8.69/1,000 person-months vs. 6.89), hospitalization (2.57/1,000 person-months vs. 1.71), and death (0.65/1,000 person-months vs. 0.53). Similar sex-specific links between gout and risks for SARS-CoV-2 infection, hospitalization, and death were seen in the unvaccinated cohort.
Patients with gout and COVID-19 need close monitoring
Four experts who were not involved in the study encourage greater attention to the needs of patients with gout.
Pamela B. Davis, MD, PhD, research professor at Case Western Reserve University, Cleveland, told this news organization, “This study brings to attention yet another potentially vulnerable group for physicians to monitor closely if they are infected with SARS-CoV-2.
“It is not clear why women with gout are more vulnerable, but fewer women than men were in the cohort with gout, and the confidence intervals for the results in women were, in general, larger,” she said.
“The authors suggest that women with gout tend to be older and have more comorbidities than men with gout,” Dr. Davis added. “The excess risk diminishes when the model is fully adjusted for comorbidities, such as obesity, hypertension, or heart disease, suggesting that already-known antecedents of infection severity account for a great deal of the excess risk.”
Kevin D. Deane, MD, PhD, associate professor of medicine and chair in rheumatology research at the University of Colorado at Denver, Aurora, advises physicians to keep in mind other conditions linked with increased risk for severe COVID-19, including advanced age; heart, lung, or kidney problems; and autoimmune diseases.
“I would be very cautious about the finding that there was not a difference in outcomes in individuals with gout based on vaccination status,” he cautioned, urging clinicians to “still strongly recommend vaccines according to guidelines.”
Sarah E. Waldman, MD, associate clinical professor of infectious diseases at UC Davis Health in Sacramento, Calif., called the study interesting but not surprising.
“The reason for increased risk for COVID-19 infection among those with gout may have to do with their underlying inflammatory state. Additional research needs to be done on this topic.
“Retrospective population-based cohort studies can be difficult to interpret due to biases,” she added. Associations identified in this type of study do not determine causation.
“As the researchers noted, those with gout tend to have additional comorbidities as well as advanced age,” she said. “They may also seek medical care more often and be tested for SARS-CoV-2 more frequently.”
Dr. Waldman advises clinicians to counsel patients with gout about their potential increased infection risk and ways they can protect themselves, including COVID-19 vaccinations.
“The strong association between gout and COVID-19 infection could involve coexisting conditions such as diabetes, hypertension, cardiovascular disease, and chronic kidney disease,” Dr. Aung added.
Earlier studies show links between gout and severe COVID-19 outcomes
Lead author Kanon Jatuworapruk, MD, PhD, of Thammasat University in Pathumthani, Thailand, and his colleagues investigated characteristics and outcomes of people with gout who were hospitalized for COVID-19 between March 2020 and October 2021, using data from the COVID-19 Global Rheumatology Alliance registry.
“This cohort of people with gout and COVID-19 who were hospitalized had high frequencies of ventilatory support and death,” the authors write in ACR Open Rheumatology . “This suggests that patients with gout who were hospitalized for COVID-19 may be at risk of poor outcomes, perhaps related to known risk factors for poor outcomes, such as age and presence of comorbidity.”
In their study, the average age of the 163 patients was 63 years, and 85% were men. Most lived in the Western Pacific Region and North America, and 46% had two or more comorbidities, most commonly hypertension, cardiovascular disease, diabetes, chronic kidney disease, and obesity. The researchers found that:
- Sixty-eight percent of the cohort required supplemental oxygen or ventilatory support during hospitalization.
- Sixteen percent of deaths were related to COVID-19, with 73% of deaths occurring in people with two or more comorbidities.
Ruth K. Topless, assistant research fellow in the department of biochemistry at the University of Otago in Dunedin, New Zealand, is the lead author on a study she and her colleagues are conducting using the UK Biobank databases of 459,837 participants in the United Kingdom, including 15,871 people with gout, through April 6, 2021, to investigate whether gout is a risk factor for diagnosis of COVID-19 and COVID-19–related death.
“Gout is a risk factor for COVID-19-related death in the UK Biobank cohort, with an increased risk in women with gout, which was driven by risk factors independent of the metabolic comorbidities of gout,” the researchers conclude in The Lancet Rheumatology.
In their study, gout was linked with COVID-19 diagnosis (odds ratio, 1.20; 95% confidence interval, 1.11-1.29) but not with risk for COVID-19–related death in the group of patients with COVID-19 (OR, 1.20; 95% CI, 0.96-1.51). In the entire cohort, gout was linked with COVID-19–related death (OR, 1.29; 95% CI, 1.06-1.56); women with gout were at increased risk for COVID-19–related death (OR, 1.98; 95% CI, 1.34-2.94), but men with gout were not (OR, 1.16; 95% CI, 0.93-1.45). The risk for COVID-19 diagnosis was significant in the nonvaccinated group (OR, 1.21; 95% CI, 1.11-1.30) but not in the vaccinated group (OR, 1.09; 95% CI, 0.65-1.85).
Editorial authors join in recommending further related research
In a commentary in The Lancet Rheumatology about the UK Biobank and other related research, Christoffer B. Nissen, MD, of University Hospital of Southern Denmark in Sonderborg, and his co-authors call the Topless and colleagues study “an elegantly conducted analysis of data from the UK Biobank supporting the hypothesis that gout needs attention in patients with COVID-19.”
Further studies are needed to investigate to what degree a diagnosis of gout is a risk factor for COVID-19 and whether treatment modifies the risk of a severe disease course,” they write. “However, in the interim, the results of this study could be considered when risk stratifying patients with gout in view of vaccination recommendations and early treatment interventions.”
Each of the three studies received grant funding. Several of the authors of the studies report financial involvements with pharmaceutical companies. All outside experts commented by email and report no relevant financial involvements.
A version of this article first appeared on Medscape.com.