User login
What’s next for COVID? Here’s what to know
As holiday celebrations wind down in the United States, COVID is on the rise.
Will there be another winter surge? If so, can we minimize it? How big a role might the boosters play in that? Are more mandates coming, along with a return to closed offices and businesses? Read on for a look at the latest info.
Cases, hospitalizations, deaths
As of Dec. 27, the latest statistics, the Centers for Disease Control and Prevention reports more than 487,000 weekly cases, compared to about 265,000 for the week ending Oct. 12. On average, 4,938 people were admitted to the hospital daily from Dec. 19 to 25, down about 6% from the 5,257 admitted daily the week before.
Deaths totaled 2,952 weekly as of Dec. 21, up from 2,699 on Dec. 14.
“What’s sobering overall is still seeing about 400 deaths a day in the U.S.,” said Peter Chin-Hong, MD, professor of medicine and infectious disease specialist at the University of California, San Francisco. “It’s still very high.”
As of Dec. 17, the variants predominating are BQ.1, BQ.1.1, and XBB. Experts said they are paying close attention to XBB, which is increasing quickly in the Northeast.
Predicting a winter surge
Experts tracking the pandemic agree there will be a surge.
“We are in the midst of it now,” said Eric Topol, MD, founder and director of the Scripps Research Translational Institute, La Jolla, Calif., and editor-in-chief of Medscape (MDedge’s sister site). “It’s not nearly like what we’ve had in Omicron or other waves; it’s not as severe. But it’s being particularly felt by seniors.”
One bit of good news: “Outside of that group it doesn’t look like – so far – it is going to be as bad a wave [as in the past],” Dr. Topol said.
Predicting the extent of the post-holiday surge “is the billion-dollar question right now,” said Katelyn Jetelina, PhD, a San Diego epidemiologist and author of the newsletter Your Local Epidemiologist.
“Much of these waves are not being driven by subvariants of concern but rather behavior,” she said.
People are opening up their social networks to gather for celebrations and family time. That’s unique to this winter, she said.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
Others point out that the surge doesn’t involve just COVID.
“We are expecting a Christmas surge and we are concerned it might be a triple surge,” said William Schaffner, MD, professor of infectious diseases at Vanderbilt University, Nashville, Tenn., referring to the rising cases of flu and RSV (respiratory syncytial virus).
Dr. Jetelina shares that concern, worrying that those illnesses may be what overwhelms hospital capacity.
Another wild card is the situation in China. With the easing of China’s “zero COVID” policies, cases there are rising dramatically. Some models are predicting up to 1 million COVID deaths could occur in China in 2023. (The United States is now requiring travelers from China to show a negative COVID test before entering. Italy and Japan have taken similar measures.)
“The suffering that is going to occur in China is not good news at all,” Dr. Topol said. “We are going to be seeing that for many weeks if not months ahead.”
Theoretically, uncontained spread such as what is expected there could generate a whole new family of variants, he said. But “the main hit is going to be in China,” he predicted. “But it’s hard to project with accuracy.”
“China is 20% of the global population, so we can’t ignore it,” Dr. Jetelina said. “The question is, what’s the probability of a subvariant of concern coming from China? I think the probability is pretty low, but the possibility is there.”
What happens with cases in China may “throw a wrench” in the transition from pandemic to endemic, Dr. Chin-Hong said. But even if the rising cases in China do result in a new variant, “there’s so much T cell and B cell immunity [here], your average person is still not going to get seriously ill, even if the variant looks really scary.”
Minimizing the damage
Experts echo the same advice on stemming the surge, especially for adults who are 65 or older: Get the bivalent booster, and get it now.
“The same with the influenza vaccine,” Dr. Schaffner said.
Both the booster vaccine and the flu vaccine have been underused this year, he said. “It’s part of the general vaccine fatigue.”
The low uptake of the booster vaccine is concerning, Dr. Topol said, especially among adults aged 65 and older, the age group most vulnerable to severe disease. Just 35.7% of U.S. adults 65 and older have gotten the booster, according to the CDC. Dr. Topol calls that a tragedy.
Younger people have not taken to the booster, either. Overall, only 14.1% of people aged 5 and up have gotten an updated booster dose, according to the CDC.
Recent studies find value in the boosters. One study looked only at adults age 65 or older, finding that the bivalent booster reduced the risk of hospitalization by 84% compared to someone not vaccinated, and 73% compared to someone who had received only the monovalent vaccine. Another study of adults found those who had gotten the bivalent were less likely to need COVID-related emergency room care or urgent care.
In a Dec. 21 report in the New England Journal of Medicine, researchers took plasma samples from people who had gotten either one or two monovalent boosters or the bivalent to determine how well they worked against the circulating Omicron subvariants BA.1, BA.5, BA.2.75.2, BQ.1.1, and XBB. The bivalent worked better than the monovalent against all the Omicron subvariants, but especially against BA.2.75.2, BQ.1.1, and XBB.
Rapid testing can help minimize transmission. On Dec. 15, the Biden administration announced its Winter Preparedness Plan, urging Americans to test before and after travel as well as indoor visiting with vulnerable individuals, providing another round of free at-home tests, continuing to make community testing available and continuing to provide vaccines.
Besides the general precautions, Dr. Schaffner suggested: “Look at yourself. Who are you? If you are older than 65, or have underlying illness or are immunocompromised, or are pregnant, please put your mask back on. And think about social distancing. It might be time to worship at home and stream a movie,” instead of going to the theaters, he said.
Back to mandates?
On Dec. 9, the New York City Commissioner of Health and Mental Hygiene urged a return to masking indoors, saying people “should” mask up, including in schools, stores, offices, and when in crowded outdoor settings.
On the same date, the County of Los Angeles Public Health urged a return to masking for everyone aged 2 and older when indoors, including at schools, in transit, or in work sites when around others.
While the CDC order requiring masks on public transportation is no longer in effect, the agency continues to recommend that those using public transportation do so.
But some are taking that further. In Philadelphia, for example, School Superintendent Tony B. Watlington Sr., EdD, announced before the winter break that indoor masking would be required for all students and staff for the first 2 weeks of school return, through Jan. 13, citing guidance from the Philadelphia Department of Public Health.
Universal masking in schools does reduce COVID transmission, as a study published in late November suggests. After Massachusetts dropped the statewide universal masking policy in public schools in February 2022, researchers compared the incidence of COVID in 70 school districts there that dropped the mandate with two school districts that kept it. In the 15 weeks after the policy was rescinded, the lifting of the mandate was linked with an additional 44.9 cases of COVID per 1,000 students and staff. That corresponded to an estimated 11,901 cases and to nearly 30% of the cases in all districts during that time.
That said, experts see mandates as the exception rather than the rule, at least for now, citing public backlash against mandates to mask or follow other restrictions.
“Mandating, we know, it shuts people off,” Dr. Topol said. “It’s unenforceable. If you have a very strong recommendation, that’s probably as good as you’re going to be able to do right now.”
There may be communities where mandates go over better than others, Dr. Schaffner said, such as communities where people have confidence in their public health authorities.
Glimmers of hope
Despite uncertainties, experts offered some not-so-dismal perspectives as well.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
A version of this article first appeared on WebMD.com.
As holiday celebrations wind down in the United States, COVID is on the rise.
Will there be another winter surge? If so, can we minimize it? How big a role might the boosters play in that? Are more mandates coming, along with a return to closed offices and businesses? Read on for a look at the latest info.
Cases, hospitalizations, deaths
As of Dec. 27, the latest statistics, the Centers for Disease Control and Prevention reports more than 487,000 weekly cases, compared to about 265,000 for the week ending Oct. 12. On average, 4,938 people were admitted to the hospital daily from Dec. 19 to 25, down about 6% from the 5,257 admitted daily the week before.
Deaths totaled 2,952 weekly as of Dec. 21, up from 2,699 on Dec. 14.
“What’s sobering overall is still seeing about 400 deaths a day in the U.S.,” said Peter Chin-Hong, MD, professor of medicine and infectious disease specialist at the University of California, San Francisco. “It’s still very high.”
As of Dec. 17, the variants predominating are BQ.1, BQ.1.1, and XBB. Experts said they are paying close attention to XBB, which is increasing quickly in the Northeast.
Predicting a winter surge
Experts tracking the pandemic agree there will be a surge.
“We are in the midst of it now,” said Eric Topol, MD, founder and director of the Scripps Research Translational Institute, La Jolla, Calif., and editor-in-chief of Medscape (MDedge’s sister site). “It’s not nearly like what we’ve had in Omicron or other waves; it’s not as severe. But it’s being particularly felt by seniors.”
One bit of good news: “Outside of that group it doesn’t look like – so far – it is going to be as bad a wave [as in the past],” Dr. Topol said.
Predicting the extent of the post-holiday surge “is the billion-dollar question right now,” said Katelyn Jetelina, PhD, a San Diego epidemiologist and author of the newsletter Your Local Epidemiologist.
“Much of these waves are not being driven by subvariants of concern but rather behavior,” she said.
People are opening up their social networks to gather for celebrations and family time. That’s unique to this winter, she said.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
Others point out that the surge doesn’t involve just COVID.
“We are expecting a Christmas surge and we are concerned it might be a triple surge,” said William Schaffner, MD, professor of infectious diseases at Vanderbilt University, Nashville, Tenn., referring to the rising cases of flu and RSV (respiratory syncytial virus).
Dr. Jetelina shares that concern, worrying that those illnesses may be what overwhelms hospital capacity.
Another wild card is the situation in China. With the easing of China’s “zero COVID” policies, cases there are rising dramatically. Some models are predicting up to 1 million COVID deaths could occur in China in 2023. (The United States is now requiring travelers from China to show a negative COVID test before entering. Italy and Japan have taken similar measures.)
“The suffering that is going to occur in China is not good news at all,” Dr. Topol said. “We are going to be seeing that for many weeks if not months ahead.”
Theoretically, uncontained spread such as what is expected there could generate a whole new family of variants, he said. But “the main hit is going to be in China,” he predicted. “But it’s hard to project with accuracy.”
“China is 20% of the global population, so we can’t ignore it,” Dr. Jetelina said. “The question is, what’s the probability of a subvariant of concern coming from China? I think the probability is pretty low, but the possibility is there.”
What happens with cases in China may “throw a wrench” in the transition from pandemic to endemic, Dr. Chin-Hong said. But even if the rising cases in China do result in a new variant, “there’s so much T cell and B cell immunity [here], your average person is still not going to get seriously ill, even if the variant looks really scary.”
Minimizing the damage
Experts echo the same advice on stemming the surge, especially for adults who are 65 or older: Get the bivalent booster, and get it now.
“The same with the influenza vaccine,” Dr. Schaffner said.
Both the booster vaccine and the flu vaccine have been underused this year, he said. “It’s part of the general vaccine fatigue.”
The low uptake of the booster vaccine is concerning, Dr. Topol said, especially among adults aged 65 and older, the age group most vulnerable to severe disease. Just 35.7% of U.S. adults 65 and older have gotten the booster, according to the CDC. Dr. Topol calls that a tragedy.
Younger people have not taken to the booster, either. Overall, only 14.1% of people aged 5 and up have gotten an updated booster dose, according to the CDC.
Recent studies find value in the boosters. One study looked only at adults age 65 or older, finding that the bivalent booster reduced the risk of hospitalization by 84% compared to someone not vaccinated, and 73% compared to someone who had received only the monovalent vaccine. Another study of adults found those who had gotten the bivalent were less likely to need COVID-related emergency room care or urgent care.
In a Dec. 21 report in the New England Journal of Medicine, researchers took plasma samples from people who had gotten either one or two monovalent boosters or the bivalent to determine how well they worked against the circulating Omicron subvariants BA.1, BA.5, BA.2.75.2, BQ.1.1, and XBB. The bivalent worked better than the monovalent against all the Omicron subvariants, but especially against BA.2.75.2, BQ.1.1, and XBB.
Rapid testing can help minimize transmission. On Dec. 15, the Biden administration announced its Winter Preparedness Plan, urging Americans to test before and after travel as well as indoor visiting with vulnerable individuals, providing another round of free at-home tests, continuing to make community testing available and continuing to provide vaccines.
Besides the general precautions, Dr. Schaffner suggested: “Look at yourself. Who are you? If you are older than 65, or have underlying illness or are immunocompromised, or are pregnant, please put your mask back on. And think about social distancing. It might be time to worship at home and stream a movie,” instead of going to the theaters, he said.
Back to mandates?
On Dec. 9, the New York City Commissioner of Health and Mental Hygiene urged a return to masking indoors, saying people “should” mask up, including in schools, stores, offices, and when in crowded outdoor settings.
On the same date, the County of Los Angeles Public Health urged a return to masking for everyone aged 2 and older when indoors, including at schools, in transit, or in work sites when around others.
While the CDC order requiring masks on public transportation is no longer in effect, the agency continues to recommend that those using public transportation do so.
But some are taking that further. In Philadelphia, for example, School Superintendent Tony B. Watlington Sr., EdD, announced before the winter break that indoor masking would be required for all students and staff for the first 2 weeks of school return, through Jan. 13, citing guidance from the Philadelphia Department of Public Health.
Universal masking in schools does reduce COVID transmission, as a study published in late November suggests. After Massachusetts dropped the statewide universal masking policy in public schools in February 2022, researchers compared the incidence of COVID in 70 school districts there that dropped the mandate with two school districts that kept it. In the 15 weeks after the policy was rescinded, the lifting of the mandate was linked with an additional 44.9 cases of COVID per 1,000 students and staff. That corresponded to an estimated 11,901 cases and to nearly 30% of the cases in all districts during that time.
That said, experts see mandates as the exception rather than the rule, at least for now, citing public backlash against mandates to mask or follow other restrictions.
“Mandating, we know, it shuts people off,” Dr. Topol said. “It’s unenforceable. If you have a very strong recommendation, that’s probably as good as you’re going to be able to do right now.”
There may be communities where mandates go over better than others, Dr. Schaffner said, such as communities where people have confidence in their public health authorities.
Glimmers of hope
Despite uncertainties, experts offered some not-so-dismal perspectives as well.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
A version of this article first appeared on WebMD.com.
As holiday celebrations wind down in the United States, COVID is on the rise.
Will there be another winter surge? If so, can we minimize it? How big a role might the boosters play in that? Are more mandates coming, along with a return to closed offices and businesses? Read on for a look at the latest info.
Cases, hospitalizations, deaths
As of Dec. 27, the latest statistics, the Centers for Disease Control and Prevention reports more than 487,000 weekly cases, compared to about 265,000 for the week ending Oct. 12. On average, 4,938 people were admitted to the hospital daily from Dec. 19 to 25, down about 6% from the 5,257 admitted daily the week before.
Deaths totaled 2,952 weekly as of Dec. 21, up from 2,699 on Dec. 14.
“What’s sobering overall is still seeing about 400 deaths a day in the U.S.,” said Peter Chin-Hong, MD, professor of medicine and infectious disease specialist at the University of California, San Francisco. “It’s still very high.”
As of Dec. 17, the variants predominating are BQ.1, BQ.1.1, and XBB. Experts said they are paying close attention to XBB, which is increasing quickly in the Northeast.
Predicting a winter surge
Experts tracking the pandemic agree there will be a surge.
“We are in the midst of it now,” said Eric Topol, MD, founder and director of the Scripps Research Translational Institute, La Jolla, Calif., and editor-in-chief of Medscape (MDedge’s sister site). “It’s not nearly like what we’ve had in Omicron or other waves; it’s not as severe. But it’s being particularly felt by seniors.”
One bit of good news: “Outside of that group it doesn’t look like – so far – it is going to be as bad a wave [as in the past],” Dr. Topol said.
Predicting the extent of the post-holiday surge “is the billion-dollar question right now,” said Katelyn Jetelina, PhD, a San Diego epidemiologist and author of the newsletter Your Local Epidemiologist.
“Much of these waves are not being driven by subvariants of concern but rather behavior,” she said.
People are opening up their social networks to gather for celebrations and family time. That’s unique to this winter, she said.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
Others point out that the surge doesn’t involve just COVID.
“We are expecting a Christmas surge and we are concerned it might be a triple surge,” said William Schaffner, MD, professor of infectious diseases at Vanderbilt University, Nashville, Tenn., referring to the rising cases of flu and RSV (respiratory syncytial virus).
Dr. Jetelina shares that concern, worrying that those illnesses may be what overwhelms hospital capacity.
Another wild card is the situation in China. With the easing of China’s “zero COVID” policies, cases there are rising dramatically. Some models are predicting up to 1 million COVID deaths could occur in China in 2023. (The United States is now requiring travelers from China to show a negative COVID test before entering. Italy and Japan have taken similar measures.)
“The suffering that is going to occur in China is not good news at all,” Dr. Topol said. “We are going to be seeing that for many weeks if not months ahead.”
Theoretically, uncontained spread such as what is expected there could generate a whole new family of variants, he said. But “the main hit is going to be in China,” he predicted. “But it’s hard to project with accuracy.”
“China is 20% of the global population, so we can’t ignore it,” Dr. Jetelina said. “The question is, what’s the probability of a subvariant of concern coming from China? I think the probability is pretty low, but the possibility is there.”
What happens with cases in China may “throw a wrench” in the transition from pandemic to endemic, Dr. Chin-Hong said. But even if the rising cases in China do result in a new variant, “there’s so much T cell and B cell immunity [here], your average person is still not going to get seriously ill, even if the variant looks really scary.”
Minimizing the damage
Experts echo the same advice on stemming the surge, especially for adults who are 65 or older: Get the bivalent booster, and get it now.
“The same with the influenza vaccine,” Dr. Schaffner said.
Both the booster vaccine and the flu vaccine have been underused this year, he said. “It’s part of the general vaccine fatigue.”
The low uptake of the booster vaccine is concerning, Dr. Topol said, especially among adults aged 65 and older, the age group most vulnerable to severe disease. Just 35.7% of U.S. adults 65 and older have gotten the booster, according to the CDC. Dr. Topol calls that a tragedy.
Younger people have not taken to the booster, either. Overall, only 14.1% of people aged 5 and up have gotten an updated booster dose, according to the CDC.
Recent studies find value in the boosters. One study looked only at adults age 65 or older, finding that the bivalent booster reduced the risk of hospitalization by 84% compared to someone not vaccinated, and 73% compared to someone who had received only the monovalent vaccine. Another study of adults found those who had gotten the bivalent were less likely to need COVID-related emergency room care or urgent care.
In a Dec. 21 report in the New England Journal of Medicine, researchers took plasma samples from people who had gotten either one or two monovalent boosters or the bivalent to determine how well they worked against the circulating Omicron subvariants BA.1, BA.5, BA.2.75.2, BQ.1.1, and XBB. The bivalent worked better than the monovalent against all the Omicron subvariants, but especially against BA.2.75.2, BQ.1.1, and XBB.
Rapid testing can help minimize transmission. On Dec. 15, the Biden administration announced its Winter Preparedness Plan, urging Americans to test before and after travel as well as indoor visiting with vulnerable individuals, providing another round of free at-home tests, continuing to make community testing available and continuing to provide vaccines.
Besides the general precautions, Dr. Schaffner suggested: “Look at yourself. Who are you? If you are older than 65, or have underlying illness or are immunocompromised, or are pregnant, please put your mask back on. And think about social distancing. It might be time to worship at home and stream a movie,” instead of going to the theaters, he said.
Back to mandates?
On Dec. 9, the New York City Commissioner of Health and Mental Hygiene urged a return to masking indoors, saying people “should” mask up, including in schools, stores, offices, and when in crowded outdoor settings.
On the same date, the County of Los Angeles Public Health urged a return to masking for everyone aged 2 and older when indoors, including at schools, in transit, or in work sites when around others.
While the CDC order requiring masks on public transportation is no longer in effect, the agency continues to recommend that those using public transportation do so.
But some are taking that further. In Philadelphia, for example, School Superintendent Tony B. Watlington Sr., EdD, announced before the winter break that indoor masking would be required for all students and staff for the first 2 weeks of school return, through Jan. 13, citing guidance from the Philadelphia Department of Public Health.
Universal masking in schools does reduce COVID transmission, as a study published in late November suggests. After Massachusetts dropped the statewide universal masking policy in public schools in February 2022, researchers compared the incidence of COVID in 70 school districts there that dropped the mandate with two school districts that kept it. In the 15 weeks after the policy was rescinded, the lifting of the mandate was linked with an additional 44.9 cases of COVID per 1,000 students and staff. That corresponded to an estimated 11,901 cases and to nearly 30% of the cases in all districts during that time.
That said, experts see mandates as the exception rather than the rule, at least for now, citing public backlash against mandates to mask or follow other restrictions.
“Mandating, we know, it shuts people off,” Dr. Topol said. “It’s unenforceable. If you have a very strong recommendation, that’s probably as good as you’re going to be able to do right now.”
There may be communities where mandates go over better than others, Dr. Schaffner said, such as communities where people have confidence in their public health authorities.
Glimmers of hope
Despite uncertainties, experts offered some not-so-dismal perspectives as well.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
A version of this article first appeared on WebMD.com.
IBD patients have limited protection against Omicron with third vaccine dose
For people with inflammatory bowel disease (IBD) taking immunosuppressive medication, a third dose of a COVID-19 mRNA vaccine significantly increases neutralizing antibodies against the original SARS-CoV-2 strain, but the picture is more complicated for protection against the Omicron variant, according to a research letter published in Gastroenterology.
“As further mutations in the viral genome accumulate over time, with the attendant risk of immune evasion, it remains important to continue to reappraise vaccination strategy, including the implementation of personalized approaches for some patients, such as those treated with anti-TNF drugs and JAK inhibitors,” wrote Zhigang Liu, PhD, a research associate in the department of metabolism, digestion, and reproduction at Imperial College London, and his colleagues. “Preferential use of bivalent vaccines may be especially valuable in IBD patients taking anti-TNF agents or JAK inhibitors,” they wrote. Their study did not assess neutralizing antibodies resulting from use of the bivalent vaccine, however.
The researchers tracked 268 participants, including 49 healthy participants serving as controls, from May 2021 through March 2022. The other participants had IBD and included 51 patients taking thiopurines, 36 patients taking infliximab, 39 taking both infliximab and thiopurines, 39 taking ustekinumab, 38 taking vedolizumab, and 16 taking tofacitinib. The IBD patients were all enrolled in the SARS-CoV-2 Vaccination Immunogenicity in Immunosuppressed Inflammatory Bowel Disease Patients (VIP) cohort.
None of the participants had evidence of a SARS-CoV-2 infection at baseline. All had received two doses of an mRNA COVID-19 vaccine (all received Pfizer, except two controls who received Moderna) or two doses of the AstraZeneca vaccine as their primary vaccination. All received an mRNA vaccine for their third dose. Among the IBD patients, 137 received the AstraZeneca in their primary two-dose series, and 82 received Pfizer.
First the researchers assessed the participants’ humoral response to the vaccine against the original SARS-CoV-2 strain and against the Omicron BA.1 variant. Neutralizing antibody titers rose significantly against both strains after the third vaccine dose for all participants.
“However, 50% neutralization titer (NT50) values were significantly lower against Omicron than against the ancestral strain in all study groups, irrespective of the immunosuppressive treatment regimen,” the authors reported. NT50 values are a measure that reflect a vaccine-induced humoral immunity against SARS-CoV-2 after vaccination.
Compared to the healthy controls, individuals receiving infliximab, tofacitinib, or infliximab/thiopurine combination therapy showed significantly lower responses after the second and third vaccine doses. Thirteen patients did not generate NT50 against Omicron after the second vaccine dose, and 7 of them were on infliximab monotherapy. They represented nearly 20% of all infliximab monotherapy participants.
Next the researchers assessed the risk of a breakthrough infection according to neutralizing titer thresholds. Individuals with an NT50 less than 500 had 1.6 times greater odds of a breakthrough infection than those with an NT50 above 500, they noted. After two vaccine doses, 46% of participants with IBD had an NT50 above 500 for the ancestral strain, which rose to 85% of those with IBD after a third dose.
In the healthy control group, 35% had an NT50 under 500 after two doses, and 14% of them had a breakthrough infection, all of which were mild and none of which required hospitalization. The NT50 in healthy controls, however, was not significantly associated with risk of breakthrough infection.
“In this study, neutralizing titers elicited against the omicron variant were generally poor for all individuals and were substantially lower in recipients of infliximab, infliximab/thiopurine combination, or tofacitinib therapy,” the authors concluded. “This raises concerns about whether currently available vaccines will be sufficient to protect against continually evolving SARS-CoV-2 variants, especially in patients established on certain immunosuppressive drugs.”
The small population sizes for each subgroup based on medication was one of the study’s limitations. Another was the fact that it was underpowered to conclusively determine whether an increased risk of breakthrough infection exists in IBD patients who have lower titers of neutralizing antibodies. A limitation for generalization to U.S. patients is that just 64% of the IBD patients received the AstraZeneca vaccine, which is not offered in the United States, for their first two doses before receiving the third mRNA (Pfizer) dose.
The study was funded by Pfizer in an independent research grant and by the NIHR Biomedical Research Centres in Imperial College London and Imperial College Healthcare NHS Trust and Cambridge, and the NIHR Clinical Research Facility Cambridge.
Dr. Liu and one other author had no disclosures. The other 18 authors have a range of disclosures related to various pharmaceutical companies, including Pfizer.
Understanding how inflammatory bowel disease (IBD) impacts COVID-19 infection risk and how IBD medications influence this risk remains an ever-evolving discussion, particularly with the emergence of new SARS-CoV-2 variants and booster vaccines. In this study, Liu et al. further shape this conversation: They show that a third mRNA COVID-19 vaccine dose increases neutralizing antibody levels against the Omicron variant in IBD patients compared to the level following a second vaccine dose, but that infliximab and tofacitinib significantly attenuate this response. They additionally suggest that IBD patients achieve lower neutralizing antibody levels after a third COVID-19 vaccine and may have a higher breakthrough infection risk compared to healthy controls without IBD.
Whether to change booster vaccination recommendations specifically for IBD patients on tofacitinib or infliximab, however, remains an unanswered question. The small sample of patients on tofacitinib precludes definitive conclusions regarding tofacitinib’s impact on vaccine response. Moreover, this humoral antibody-based study tells only half the story: We need analyses of the cell-mediated booster vaccine response to truly understand vaccine efficacy during immunosuppressant use. Lastly, future studies including the bivalent booster will provide the most up-to-date information on protecting our IBD patients from the Omicron variant.
Dr. Erica J. Brenner MD, MSCR is an Assistant Professor, Department of Pediatrics, Division of Pediatric Gastroenterology, University of North Carolina School of Medicine; and a cofounder of the Surveillance Epidemiology of Coronavirus Under Research Exclusion for Inflammatory Bowel Disease (SECURE-IBD) Registry. She has no relevant financial conflicts of interest.
Understanding how inflammatory bowel disease (IBD) impacts COVID-19 infection risk and how IBD medications influence this risk remains an ever-evolving discussion, particularly with the emergence of new SARS-CoV-2 variants and booster vaccines. In this study, Liu et al. further shape this conversation: They show that a third mRNA COVID-19 vaccine dose increases neutralizing antibody levels against the Omicron variant in IBD patients compared to the level following a second vaccine dose, but that infliximab and tofacitinib significantly attenuate this response. They additionally suggest that IBD patients achieve lower neutralizing antibody levels after a third COVID-19 vaccine and may have a higher breakthrough infection risk compared to healthy controls without IBD.
Whether to change booster vaccination recommendations specifically for IBD patients on tofacitinib or infliximab, however, remains an unanswered question. The small sample of patients on tofacitinib precludes definitive conclusions regarding tofacitinib’s impact on vaccine response. Moreover, this humoral antibody-based study tells only half the story: We need analyses of the cell-mediated booster vaccine response to truly understand vaccine efficacy during immunosuppressant use. Lastly, future studies including the bivalent booster will provide the most up-to-date information on protecting our IBD patients from the Omicron variant.
Dr. Erica J. Brenner MD, MSCR is an Assistant Professor, Department of Pediatrics, Division of Pediatric Gastroenterology, University of North Carolina School of Medicine; and a cofounder of the Surveillance Epidemiology of Coronavirus Under Research Exclusion for Inflammatory Bowel Disease (SECURE-IBD) Registry. She has no relevant financial conflicts of interest.
Understanding how inflammatory bowel disease (IBD) impacts COVID-19 infection risk and how IBD medications influence this risk remains an ever-evolving discussion, particularly with the emergence of new SARS-CoV-2 variants and booster vaccines. In this study, Liu et al. further shape this conversation: They show that a third mRNA COVID-19 vaccine dose increases neutralizing antibody levels against the Omicron variant in IBD patients compared to the level following a second vaccine dose, but that infliximab and tofacitinib significantly attenuate this response. They additionally suggest that IBD patients achieve lower neutralizing antibody levels after a third COVID-19 vaccine and may have a higher breakthrough infection risk compared to healthy controls without IBD.
Whether to change booster vaccination recommendations specifically for IBD patients on tofacitinib or infliximab, however, remains an unanswered question. The small sample of patients on tofacitinib precludes definitive conclusions regarding tofacitinib’s impact on vaccine response. Moreover, this humoral antibody-based study tells only half the story: We need analyses of the cell-mediated booster vaccine response to truly understand vaccine efficacy during immunosuppressant use. Lastly, future studies including the bivalent booster will provide the most up-to-date information on protecting our IBD patients from the Omicron variant.
Dr. Erica J. Brenner MD, MSCR is an Assistant Professor, Department of Pediatrics, Division of Pediatric Gastroenterology, University of North Carolina School of Medicine; and a cofounder of the Surveillance Epidemiology of Coronavirus Under Research Exclusion for Inflammatory Bowel Disease (SECURE-IBD) Registry. She has no relevant financial conflicts of interest.
For people with inflammatory bowel disease (IBD) taking immunosuppressive medication, a third dose of a COVID-19 mRNA vaccine significantly increases neutralizing antibodies against the original SARS-CoV-2 strain, but the picture is more complicated for protection against the Omicron variant, according to a research letter published in Gastroenterology.
“As further mutations in the viral genome accumulate over time, with the attendant risk of immune evasion, it remains important to continue to reappraise vaccination strategy, including the implementation of personalized approaches for some patients, such as those treated with anti-TNF drugs and JAK inhibitors,” wrote Zhigang Liu, PhD, a research associate in the department of metabolism, digestion, and reproduction at Imperial College London, and his colleagues. “Preferential use of bivalent vaccines may be especially valuable in IBD patients taking anti-TNF agents or JAK inhibitors,” they wrote. Their study did not assess neutralizing antibodies resulting from use of the bivalent vaccine, however.
The researchers tracked 268 participants, including 49 healthy participants serving as controls, from May 2021 through March 2022. The other participants had IBD and included 51 patients taking thiopurines, 36 patients taking infliximab, 39 taking both infliximab and thiopurines, 39 taking ustekinumab, 38 taking vedolizumab, and 16 taking tofacitinib. The IBD patients were all enrolled in the SARS-CoV-2 Vaccination Immunogenicity in Immunosuppressed Inflammatory Bowel Disease Patients (VIP) cohort.
None of the participants had evidence of a SARS-CoV-2 infection at baseline. All had received two doses of an mRNA COVID-19 vaccine (all received Pfizer, except two controls who received Moderna) or two doses of the AstraZeneca vaccine as their primary vaccination. All received an mRNA vaccine for their third dose. Among the IBD patients, 137 received the AstraZeneca in their primary two-dose series, and 82 received Pfizer.
First the researchers assessed the participants’ humoral response to the vaccine against the original SARS-CoV-2 strain and against the Omicron BA.1 variant. Neutralizing antibody titers rose significantly against both strains after the third vaccine dose for all participants.
“However, 50% neutralization titer (NT50) values were significantly lower against Omicron than against the ancestral strain in all study groups, irrespective of the immunosuppressive treatment regimen,” the authors reported. NT50 values are a measure that reflect a vaccine-induced humoral immunity against SARS-CoV-2 after vaccination.
Compared to the healthy controls, individuals receiving infliximab, tofacitinib, or infliximab/thiopurine combination therapy showed significantly lower responses after the second and third vaccine doses. Thirteen patients did not generate NT50 against Omicron after the second vaccine dose, and 7 of them were on infliximab monotherapy. They represented nearly 20% of all infliximab monotherapy participants.
Next the researchers assessed the risk of a breakthrough infection according to neutralizing titer thresholds. Individuals with an NT50 less than 500 had 1.6 times greater odds of a breakthrough infection than those with an NT50 above 500, they noted. After two vaccine doses, 46% of participants with IBD had an NT50 above 500 for the ancestral strain, which rose to 85% of those with IBD after a third dose.
In the healthy control group, 35% had an NT50 under 500 after two doses, and 14% of them had a breakthrough infection, all of which were mild and none of which required hospitalization. The NT50 in healthy controls, however, was not significantly associated with risk of breakthrough infection.
“In this study, neutralizing titers elicited against the omicron variant were generally poor for all individuals and were substantially lower in recipients of infliximab, infliximab/thiopurine combination, or tofacitinib therapy,” the authors concluded. “This raises concerns about whether currently available vaccines will be sufficient to protect against continually evolving SARS-CoV-2 variants, especially in patients established on certain immunosuppressive drugs.”
The small population sizes for each subgroup based on medication was one of the study’s limitations. Another was the fact that it was underpowered to conclusively determine whether an increased risk of breakthrough infection exists in IBD patients who have lower titers of neutralizing antibodies. A limitation for generalization to U.S. patients is that just 64% of the IBD patients received the AstraZeneca vaccine, which is not offered in the United States, for their first two doses before receiving the third mRNA (Pfizer) dose.
The study was funded by Pfizer in an independent research grant and by the NIHR Biomedical Research Centres in Imperial College London and Imperial College Healthcare NHS Trust and Cambridge, and the NIHR Clinical Research Facility Cambridge.
Dr. Liu and one other author had no disclosures. The other 18 authors have a range of disclosures related to various pharmaceutical companies, including Pfizer.
For people with inflammatory bowel disease (IBD) taking immunosuppressive medication, a third dose of a COVID-19 mRNA vaccine significantly increases neutralizing antibodies against the original SARS-CoV-2 strain, but the picture is more complicated for protection against the Omicron variant, according to a research letter published in Gastroenterology.
“As further mutations in the viral genome accumulate over time, with the attendant risk of immune evasion, it remains important to continue to reappraise vaccination strategy, including the implementation of personalized approaches for some patients, such as those treated with anti-TNF drugs and JAK inhibitors,” wrote Zhigang Liu, PhD, a research associate in the department of metabolism, digestion, and reproduction at Imperial College London, and his colleagues. “Preferential use of bivalent vaccines may be especially valuable in IBD patients taking anti-TNF agents or JAK inhibitors,” they wrote. Their study did not assess neutralizing antibodies resulting from use of the bivalent vaccine, however.
The researchers tracked 268 participants, including 49 healthy participants serving as controls, from May 2021 through March 2022. The other participants had IBD and included 51 patients taking thiopurines, 36 patients taking infliximab, 39 taking both infliximab and thiopurines, 39 taking ustekinumab, 38 taking vedolizumab, and 16 taking tofacitinib. The IBD patients were all enrolled in the SARS-CoV-2 Vaccination Immunogenicity in Immunosuppressed Inflammatory Bowel Disease Patients (VIP) cohort.
None of the participants had evidence of a SARS-CoV-2 infection at baseline. All had received two doses of an mRNA COVID-19 vaccine (all received Pfizer, except two controls who received Moderna) or two doses of the AstraZeneca vaccine as their primary vaccination. All received an mRNA vaccine for their third dose. Among the IBD patients, 137 received the AstraZeneca in their primary two-dose series, and 82 received Pfizer.
First the researchers assessed the participants’ humoral response to the vaccine against the original SARS-CoV-2 strain and against the Omicron BA.1 variant. Neutralizing antibody titers rose significantly against both strains after the third vaccine dose for all participants.
“However, 50% neutralization titer (NT50) values were significantly lower against Omicron than against the ancestral strain in all study groups, irrespective of the immunosuppressive treatment regimen,” the authors reported. NT50 values are a measure that reflect a vaccine-induced humoral immunity against SARS-CoV-2 after vaccination.
Compared to the healthy controls, individuals receiving infliximab, tofacitinib, or infliximab/thiopurine combination therapy showed significantly lower responses after the second and third vaccine doses. Thirteen patients did not generate NT50 against Omicron after the second vaccine dose, and 7 of them were on infliximab monotherapy. They represented nearly 20% of all infliximab monotherapy participants.
Next the researchers assessed the risk of a breakthrough infection according to neutralizing titer thresholds. Individuals with an NT50 less than 500 had 1.6 times greater odds of a breakthrough infection than those with an NT50 above 500, they noted. After two vaccine doses, 46% of participants with IBD had an NT50 above 500 for the ancestral strain, which rose to 85% of those with IBD after a third dose.
In the healthy control group, 35% had an NT50 under 500 after two doses, and 14% of them had a breakthrough infection, all of which were mild and none of which required hospitalization. The NT50 in healthy controls, however, was not significantly associated with risk of breakthrough infection.
“In this study, neutralizing titers elicited against the omicron variant were generally poor for all individuals and were substantially lower in recipients of infliximab, infliximab/thiopurine combination, or tofacitinib therapy,” the authors concluded. “This raises concerns about whether currently available vaccines will be sufficient to protect against continually evolving SARS-CoV-2 variants, especially in patients established on certain immunosuppressive drugs.”
The small population sizes for each subgroup based on medication was one of the study’s limitations. Another was the fact that it was underpowered to conclusively determine whether an increased risk of breakthrough infection exists in IBD patients who have lower titers of neutralizing antibodies. A limitation for generalization to U.S. patients is that just 64% of the IBD patients received the AstraZeneca vaccine, which is not offered in the United States, for their first two doses before receiving the third mRNA (Pfizer) dose.
The study was funded by Pfizer in an independent research grant and by the NIHR Biomedical Research Centres in Imperial College London and Imperial College Healthcare NHS Trust and Cambridge, and the NIHR Clinical Research Facility Cambridge.
Dr. Liu and one other author had no disclosures. The other 18 authors have a range of disclosures related to various pharmaceutical companies, including Pfizer.
FROM GASTROENTEROLOGY
Children and COVID: New cases fell as the old year ended
The end of 2022 saw a drop in new COVID-19 cases in children, even as rates of emergency department visits continued upward trends that began in late October.
New cases for the week of Dec. 23-29 fell for the first time since late November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP/CHA analysis of publicly available state data differs somewhat from figures reported by the Centers for Disease Control and Prevention, which has new cases for the latest available week, Dec.18-24, at just over 27,000 after 3 straight weeks of declines from a count of almost 63,000 for the week ending Nov. 26. The CDC, however, updates previously reported data on a regular basis, so that 27,000 is likely to increase in the coming weeks.
The CDC line on the graph also shows a peak for the week of Oct. 30 to Nov. 5 when new cases reached almost 50,000, compared with almost 30,000 reported for the week of Oct. 28 to Nov. 3 by the AAP and CHA in their report of state-level data. The AAP and CHA put the total number of child COVID cases since the start of the pandemic at 15.2 million as of Dec. 29, while the CDC reports 16.2 million cases as of Dec. 28.
There have been 1,975 deaths from COVID-19 in children aged 0-17 years, according to the CDC, which amounts to just over 0.2% of all COVID deaths for which age group data were available.
CDC data on emergency department visits involving diagnosed COVID-19 have been rising since late October. In children aged 0-11 years, for example, COVID was involved in 1.0% of ED visits (7-day average) as late as Nov. 4, but by Dec. 27 that rate was 2.6%. Children aged 12-15 years went from 0.6% on Oct. 28 to 1.5% on Dec. 27, while 16- to 17-year-olds had ED visit rates of 0.6% on Oct. 19 and 1.7% on Dec. 27, the CDC said on its COVID Data Tracker.
New hospital admissions with diagnosed COVID, which had been following the same upward trend as ED visits since late October, halted that rise in children aged 0-17 years and have gone no higher than 0.29 per 100,000 population since Dec. 9, the CDC data show.
The end of 2022 saw a drop in new COVID-19 cases in children, even as rates of emergency department visits continued upward trends that began in late October.
New cases for the week of Dec. 23-29 fell for the first time since late November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP/CHA analysis of publicly available state data differs somewhat from figures reported by the Centers for Disease Control and Prevention, which has new cases for the latest available week, Dec.18-24, at just over 27,000 after 3 straight weeks of declines from a count of almost 63,000 for the week ending Nov. 26. The CDC, however, updates previously reported data on a regular basis, so that 27,000 is likely to increase in the coming weeks.
The CDC line on the graph also shows a peak for the week of Oct. 30 to Nov. 5 when new cases reached almost 50,000, compared with almost 30,000 reported for the week of Oct. 28 to Nov. 3 by the AAP and CHA in their report of state-level data. The AAP and CHA put the total number of child COVID cases since the start of the pandemic at 15.2 million as of Dec. 29, while the CDC reports 16.2 million cases as of Dec. 28.
There have been 1,975 deaths from COVID-19 in children aged 0-17 years, according to the CDC, which amounts to just over 0.2% of all COVID deaths for which age group data were available.
CDC data on emergency department visits involving diagnosed COVID-19 have been rising since late October. In children aged 0-11 years, for example, COVID was involved in 1.0% of ED visits (7-day average) as late as Nov. 4, but by Dec. 27 that rate was 2.6%. Children aged 12-15 years went from 0.6% on Oct. 28 to 1.5% on Dec. 27, while 16- to 17-year-olds had ED visit rates of 0.6% on Oct. 19 and 1.7% on Dec. 27, the CDC said on its COVID Data Tracker.
New hospital admissions with diagnosed COVID, which had been following the same upward trend as ED visits since late October, halted that rise in children aged 0-17 years and have gone no higher than 0.29 per 100,000 population since Dec. 9, the CDC data show.
The end of 2022 saw a drop in new COVID-19 cases in children, even as rates of emergency department visits continued upward trends that began in late October.
New cases for the week of Dec. 23-29 fell for the first time since late November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP/CHA analysis of publicly available state data differs somewhat from figures reported by the Centers for Disease Control and Prevention, which has new cases for the latest available week, Dec.18-24, at just over 27,000 after 3 straight weeks of declines from a count of almost 63,000 for the week ending Nov. 26. The CDC, however, updates previously reported data on a regular basis, so that 27,000 is likely to increase in the coming weeks.
The CDC line on the graph also shows a peak for the week of Oct. 30 to Nov. 5 when new cases reached almost 50,000, compared with almost 30,000 reported for the week of Oct. 28 to Nov. 3 by the AAP and CHA in their report of state-level data. The AAP and CHA put the total number of child COVID cases since the start of the pandemic at 15.2 million as of Dec. 29, while the CDC reports 16.2 million cases as of Dec. 28.
There have been 1,975 deaths from COVID-19 in children aged 0-17 years, according to the CDC, which amounts to just over 0.2% of all COVID deaths for which age group data were available.
CDC data on emergency department visits involving diagnosed COVID-19 have been rising since late October. In children aged 0-11 years, for example, COVID was involved in 1.0% of ED visits (7-day average) as late as Nov. 4, but by Dec. 27 that rate was 2.6%. Children aged 12-15 years went from 0.6% on Oct. 28 to 1.5% on Dec. 27, while 16- to 17-year-olds had ED visit rates of 0.6% on Oct. 19 and 1.7% on Dec. 27, the CDC said on its COVID Data Tracker.
New hospital admissions with diagnosed COVID, which had been following the same upward trend as ED visits since late October, halted that rise in children aged 0-17 years and have gone no higher than 0.29 per 100,000 population since Dec. 9, the CDC data show.
SARS-CoV-2 seroprevalence grew rapidly in pandemic’s early waves
By August 2022, two-and-a-half years into the COVID-19 pandemic, most children as well as most adults under age 60 years had evidence of SARS-CoV-2 vaccination and/or infection, a Canadian seroprevalence study of almost 14,000 people over the first seven waves of the pandemic reports.
However, fewer than 50% people older than age 60, the age group most vulnerable to severe outcomes, showed evidence of immunity from infection or vaccination. The authors noted that older adults – who have the lowest infection rates but highest risk of severe outcomes – continue to warrant prioritized vaccination, writing online in the Canadian Medical Association Journal.
Previous evidence suggests that a combination of both infection and vaccination exposure may induce more robust and durable hybrid immunity than either exposure alone, according to lead author Danuta M. Skowronski, MD, MHSc, an epidemiologist at the British Columbia Centre for Disease Control in Vancouver.
“Our main objective was to chronicle the changing proportion of the population considered immunologically naive and therefore susceptible to SARS-CoV-2,” Dr. Skowronski said in an interview. “It’s relevant for risk assessment to know what proportion have acquired some priming for more efficient immune memory response to the virus because that reduces the likelihood of severe outcomes.” Standardized seroprevalence studies are essential to inform COVID-19 response, particularly in resource-limited regions.
The study
Conducted in British Columbia’s Greater Vancouver and Fraser Valley, the analysis found that in the first year of the pandemic, when extraordinary measures were in place to curtail transmission, virtually everyone remained immunologically naive. Thereafter, however, age-based vaccine rollouts dramatically changed the immuno-epidemiological landscape so that by September 2021, more than 80% of the study population had antibody evidence of immunological priming, while more than 85% remained uninfected.
By August 2022, after the Omicron-variant waves, overall vaccine- and infection-induced seroprevalence exceeded 95%, with 60% having been actually infected, including at least three-quarters of children. Fewer than 50% of older adults, however, showed immunological evidence of exposure.
The study results were based on anonymized residual sera from children and adults in an outpatient laboratory network. At least three immunoassays per serosurvey were used to detect antibodies to SARS-CoV-2 spike (from vaccine) and to nucleocapsid antibodies (from infection).
The researchers assessed any seroprevalence – vaccine-, infection-induced, or both – as defined by positivity on any two assays. Infection-induced seroprevalence was also defined by dual-assay positivity but required both antinucleocapsid and antispike detection. Their estimates of infection-induced seroprevalence indicated considerable under-ascertainment of infections by standard surveillance case reports.
Results
During the first year of the pandemic, fewer than 1% manifested seroprevalence during the first three snapshots and fewer than 5% by January 2021. With vaccine rollout, however, seroprevalence increased dramatically during the first half of 2021 to 56% by May/June 2021 and to 83% by September/October 2021.
In addition, infection-induced seroprevalence was low at less than 15% in September/October 2021 until the arrival of the Omicron waves, after which it rose to 42% by March 2022 and 61% by July/August 2022. Combined seroprevalence for vaccination or infection was more than 95% by the summer, with most children but less than half of adults older than 60 years showing evidence of having been infected.
“We found the highest infection rates among children, closely followed by young adults, which may reflect their greater interconnectedness, including between siblings and parents in the household, as well as with peers in schools and the community,” the authors wrote, adding that the low cumulative infection rates among older adults may reflect their higher vaccination rates and greater social isolation.
U.S. data show similar age-related infection rates, but data among children from other Canadian provinces are limited, the authors said.
Commenting on the survey but not involved in it, infectious diseases expert Marc Germain, MD, PhD, a vice president at Héma-Québec in Quebec City, believes the pattern observed in British Columbia is fairly representative of what happened across Canada and the United States, including the sweeping effect of the Omicron variant and the differential impact according to age.
“But regional differences might very well exist – for example, due to differential vaccine uptake – and are also probably related in part to the different testing platforms being used,” Dr. Germain told this news organization.
Caroline Quach-Tanh, MD, PhD, a pediatrician and epidemiologist/infectologist at the University of Montreal, pointed out that Quebec seroprevalence surveys using residual blood samples from children and adults visiting emergency departments for any reason showed higher rates of prior infection than did the BC surveys. “But Dr. Skowronski’s findings are likely applicable to settings where some nonpharmacological interventions were put in place, but without strict confinement – and thus are likely applicable to most settings in the U.S. and Canada.”
Dr. Quach-Tanh added that there is always a risk of bias with the use of residual blood samples, “but the fact that the study method was stable should have captured a similar population from time to time. It would be unlikely to result in a major overestimation in the proportion of individuals positive for SARS-CoV-2 antibodies.”
A recent global meta-analysis found that while global seroprevalence has risen considerably, albeit variably by region, more than a third of the world’s population is still seronegative to the SARS-CoV-2 virus.
Dr. Skowronski reported institutional grants from the Canadian Institutes of Health Research and the British Columbia Centre for Disease Control Foundation for Public Health for other SARSCoV-2 work. Coauthor Romina C. Reyes, MD, chairs the BC Diagnostic Accreditation Program committee. Coauthor Mel Krajden, MD, reported institutional grants from Roche, Hologic, and Siemens. Dr. Germain and Dr. Quach-Tanh disclosed no competing interests relevant to their comments.
By August 2022, two-and-a-half years into the COVID-19 pandemic, most children as well as most adults under age 60 years had evidence of SARS-CoV-2 vaccination and/or infection, a Canadian seroprevalence study of almost 14,000 people over the first seven waves of the pandemic reports.
However, fewer than 50% people older than age 60, the age group most vulnerable to severe outcomes, showed evidence of immunity from infection or vaccination. The authors noted that older adults – who have the lowest infection rates but highest risk of severe outcomes – continue to warrant prioritized vaccination, writing online in the Canadian Medical Association Journal.
Previous evidence suggests that a combination of both infection and vaccination exposure may induce more robust and durable hybrid immunity than either exposure alone, according to lead author Danuta M. Skowronski, MD, MHSc, an epidemiologist at the British Columbia Centre for Disease Control in Vancouver.
“Our main objective was to chronicle the changing proportion of the population considered immunologically naive and therefore susceptible to SARS-CoV-2,” Dr. Skowronski said in an interview. “It’s relevant for risk assessment to know what proportion have acquired some priming for more efficient immune memory response to the virus because that reduces the likelihood of severe outcomes.” Standardized seroprevalence studies are essential to inform COVID-19 response, particularly in resource-limited regions.
The study
Conducted in British Columbia’s Greater Vancouver and Fraser Valley, the analysis found that in the first year of the pandemic, when extraordinary measures were in place to curtail transmission, virtually everyone remained immunologically naive. Thereafter, however, age-based vaccine rollouts dramatically changed the immuno-epidemiological landscape so that by September 2021, more than 80% of the study population had antibody evidence of immunological priming, while more than 85% remained uninfected.
By August 2022, after the Omicron-variant waves, overall vaccine- and infection-induced seroprevalence exceeded 95%, with 60% having been actually infected, including at least three-quarters of children. Fewer than 50% of older adults, however, showed immunological evidence of exposure.
The study results were based on anonymized residual sera from children and adults in an outpatient laboratory network. At least three immunoassays per serosurvey were used to detect antibodies to SARS-CoV-2 spike (from vaccine) and to nucleocapsid antibodies (from infection).
The researchers assessed any seroprevalence – vaccine-, infection-induced, or both – as defined by positivity on any two assays. Infection-induced seroprevalence was also defined by dual-assay positivity but required both antinucleocapsid and antispike detection. Their estimates of infection-induced seroprevalence indicated considerable under-ascertainment of infections by standard surveillance case reports.
Results
During the first year of the pandemic, fewer than 1% manifested seroprevalence during the first three snapshots and fewer than 5% by January 2021. With vaccine rollout, however, seroprevalence increased dramatically during the first half of 2021 to 56% by May/June 2021 and to 83% by September/October 2021.
In addition, infection-induced seroprevalence was low at less than 15% in September/October 2021 until the arrival of the Omicron waves, after which it rose to 42% by March 2022 and 61% by July/August 2022. Combined seroprevalence for vaccination or infection was more than 95% by the summer, with most children but less than half of adults older than 60 years showing evidence of having been infected.
“We found the highest infection rates among children, closely followed by young adults, which may reflect their greater interconnectedness, including between siblings and parents in the household, as well as with peers in schools and the community,” the authors wrote, adding that the low cumulative infection rates among older adults may reflect their higher vaccination rates and greater social isolation.
U.S. data show similar age-related infection rates, but data among children from other Canadian provinces are limited, the authors said.
Commenting on the survey but not involved in it, infectious diseases expert Marc Germain, MD, PhD, a vice president at Héma-Québec in Quebec City, believes the pattern observed in British Columbia is fairly representative of what happened across Canada and the United States, including the sweeping effect of the Omicron variant and the differential impact according to age.
“But regional differences might very well exist – for example, due to differential vaccine uptake – and are also probably related in part to the different testing platforms being used,” Dr. Germain told this news organization.
Caroline Quach-Tanh, MD, PhD, a pediatrician and epidemiologist/infectologist at the University of Montreal, pointed out that Quebec seroprevalence surveys using residual blood samples from children and adults visiting emergency departments for any reason showed higher rates of prior infection than did the BC surveys. “But Dr. Skowronski’s findings are likely applicable to settings where some nonpharmacological interventions were put in place, but without strict confinement – and thus are likely applicable to most settings in the U.S. and Canada.”
Dr. Quach-Tanh added that there is always a risk of bias with the use of residual blood samples, “but the fact that the study method was stable should have captured a similar population from time to time. It would be unlikely to result in a major overestimation in the proportion of individuals positive for SARS-CoV-2 antibodies.”
A recent global meta-analysis found that while global seroprevalence has risen considerably, albeit variably by region, more than a third of the world’s population is still seronegative to the SARS-CoV-2 virus.
Dr. Skowronski reported institutional grants from the Canadian Institutes of Health Research and the British Columbia Centre for Disease Control Foundation for Public Health for other SARSCoV-2 work. Coauthor Romina C. Reyes, MD, chairs the BC Diagnostic Accreditation Program committee. Coauthor Mel Krajden, MD, reported institutional grants from Roche, Hologic, and Siemens. Dr. Germain and Dr. Quach-Tanh disclosed no competing interests relevant to their comments.
By August 2022, two-and-a-half years into the COVID-19 pandemic, most children as well as most adults under age 60 years had evidence of SARS-CoV-2 vaccination and/or infection, a Canadian seroprevalence study of almost 14,000 people over the first seven waves of the pandemic reports.
However, fewer than 50% people older than age 60, the age group most vulnerable to severe outcomes, showed evidence of immunity from infection or vaccination. The authors noted that older adults – who have the lowest infection rates but highest risk of severe outcomes – continue to warrant prioritized vaccination, writing online in the Canadian Medical Association Journal.
Previous evidence suggests that a combination of both infection and vaccination exposure may induce more robust and durable hybrid immunity than either exposure alone, according to lead author Danuta M. Skowronski, MD, MHSc, an epidemiologist at the British Columbia Centre for Disease Control in Vancouver.
“Our main objective was to chronicle the changing proportion of the population considered immunologically naive and therefore susceptible to SARS-CoV-2,” Dr. Skowronski said in an interview. “It’s relevant for risk assessment to know what proportion have acquired some priming for more efficient immune memory response to the virus because that reduces the likelihood of severe outcomes.” Standardized seroprevalence studies are essential to inform COVID-19 response, particularly in resource-limited regions.
The study
Conducted in British Columbia’s Greater Vancouver and Fraser Valley, the analysis found that in the first year of the pandemic, when extraordinary measures were in place to curtail transmission, virtually everyone remained immunologically naive. Thereafter, however, age-based vaccine rollouts dramatically changed the immuno-epidemiological landscape so that by September 2021, more than 80% of the study population had antibody evidence of immunological priming, while more than 85% remained uninfected.
By August 2022, after the Omicron-variant waves, overall vaccine- and infection-induced seroprevalence exceeded 95%, with 60% having been actually infected, including at least three-quarters of children. Fewer than 50% of older adults, however, showed immunological evidence of exposure.
The study results were based on anonymized residual sera from children and adults in an outpatient laboratory network. At least three immunoassays per serosurvey were used to detect antibodies to SARS-CoV-2 spike (from vaccine) and to nucleocapsid antibodies (from infection).
The researchers assessed any seroprevalence – vaccine-, infection-induced, or both – as defined by positivity on any two assays. Infection-induced seroprevalence was also defined by dual-assay positivity but required both antinucleocapsid and antispike detection. Their estimates of infection-induced seroprevalence indicated considerable under-ascertainment of infections by standard surveillance case reports.
Results
During the first year of the pandemic, fewer than 1% manifested seroprevalence during the first three snapshots and fewer than 5% by January 2021. With vaccine rollout, however, seroprevalence increased dramatically during the first half of 2021 to 56% by May/June 2021 and to 83% by September/October 2021.
In addition, infection-induced seroprevalence was low at less than 15% in September/October 2021 until the arrival of the Omicron waves, after which it rose to 42% by March 2022 and 61% by July/August 2022. Combined seroprevalence for vaccination or infection was more than 95% by the summer, with most children but less than half of adults older than 60 years showing evidence of having been infected.
“We found the highest infection rates among children, closely followed by young adults, which may reflect their greater interconnectedness, including between siblings and parents in the household, as well as with peers in schools and the community,” the authors wrote, adding that the low cumulative infection rates among older adults may reflect their higher vaccination rates and greater social isolation.
U.S. data show similar age-related infection rates, but data among children from other Canadian provinces are limited, the authors said.
Commenting on the survey but not involved in it, infectious diseases expert Marc Germain, MD, PhD, a vice president at Héma-Québec in Quebec City, believes the pattern observed in British Columbia is fairly representative of what happened across Canada and the United States, including the sweeping effect of the Omicron variant and the differential impact according to age.
“But regional differences might very well exist – for example, due to differential vaccine uptake – and are also probably related in part to the different testing platforms being used,” Dr. Germain told this news organization.
Caroline Quach-Tanh, MD, PhD, a pediatrician and epidemiologist/infectologist at the University of Montreal, pointed out that Quebec seroprevalence surveys using residual blood samples from children and adults visiting emergency departments for any reason showed higher rates of prior infection than did the BC surveys. “But Dr. Skowronski’s findings are likely applicable to settings where some nonpharmacological interventions were put in place, but without strict confinement – and thus are likely applicable to most settings in the U.S. and Canada.”
Dr. Quach-Tanh added that there is always a risk of bias with the use of residual blood samples, “but the fact that the study method was stable should have captured a similar population from time to time. It would be unlikely to result in a major overestimation in the proportion of individuals positive for SARS-CoV-2 antibodies.”
A recent global meta-analysis found that while global seroprevalence has risen considerably, albeit variably by region, more than a third of the world’s population is still seronegative to the SARS-CoV-2 virus.
Dr. Skowronski reported institutional grants from the Canadian Institutes of Health Research and the British Columbia Centre for Disease Control Foundation for Public Health for other SARSCoV-2 work. Coauthor Romina C. Reyes, MD, chairs the BC Diagnostic Accreditation Program committee. Coauthor Mel Krajden, MD, reported institutional grants from Roche, Hologic, and Siemens. Dr. Germain and Dr. Quach-Tanh disclosed no competing interests relevant to their comments.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
Study of beliefs about what causes cancer sparks debate
The study, entitled, “Everything Causes Cancer? Beliefs and Attitudes Towards Cancer Prevention Among Anti-Vaxxers, Flat Earthers, and Reptilian Conspiracists: Online Cross Sectional Survey,” was published in the Christmas 2022 issue of The British Medical Journal (BMJ).
The authors explain that they set out to evaluate “the patterns of beliefs about cancer among people who believed in conspiracies, rejected the COVID-19 vaccine, or preferred alternative medicine.”
They sought such people on social media and online chat platforms and asked them questions about real and mythical causes of cancer.
Almost half of survey participants agreed with the statement, “It seems like everything causes cancer.”
Overall, among all participants, awareness of the actual causes of cancer was greater than awareness of the mythical causes of cancer, the authors report. However, awareness of the actual causes of cancer was lower among the unvaccinated and members of conspiracy groups than among their counterparts.
The authors are concerned that their findings suggest “a direct connection between digital misinformation and consequent potential erroneous health decisions, which may represent a further preventable fraction of cancer.”
Backlash and criticism
The study “highlights the difficulty society encounters in distinguishing the actual causes of cancer from mythical causes,” The BMJ commented on Twitter.
However, both the study and the journal received some backlash.
This is a “horrible article seeking to smear people with concerns about COVID vaccines,” commented Clare Craig, a British consultant pathologist who specializes in cancer diagnostics.
The study and its methodology were also harshly criticized on Twitter by Normal Fenton, professor of risk information management at the Queen Mary University of London.
The senior author of the study, Laura Costas, a medical epidemiologist with the Catalan Institute of Oncology, Barcelona, told this news organization that the naysayers on social media, many of whom focused their comments on the COVID-19 vaccine, prove the purpose of the study – that misinformation spreads widely on the internet.
“Most comments focused on spreading COVID-19 myths, which were not the direct subject of the study, and questioned the motivations of BMJ authors and the scientific community, assuming they had a common malevolent hidden agenda,” Ms. Costas said.
“They stated the need of having critical thinking, a trait in common with the scientific method, but dogmatically dismissed any information that comes from official sources,” she added.
Ms. Costas commented that “society encounters difficulty in differentiating actual from mythical causes of cancer owing to mass information. We therefore planned this study with a certain satire, which is in line with the essence of The BMJ Christmas issue.”
The BMJ has a long history of publishing a lighthearted Christmas edition full of original, satirical, and nontraditional studies. Previous years have seen studies that explored potential harms from holly and ivy, survival time of chocolates on hospital wards, and the question, “Were James Bond’s drinks shaken because of alcohol induced tremor?”
Study details
Ms. Costas and colleagues sought participants for their survey from online forums that included 4chan and Reddit, which are known for their controversial content posted by anonymous users. Data were also collected from ForoCoches and HispaChan, well-known Spanish online forums. These online sites were intentionally chosen because researchers thought “conspiracy beliefs would be more prevalent,” according to Ms. Costas.
Across the multiple forums, there were 1,494 participants. Of these, 209 participants were unvaccinated against COVID-19, 112 preferred alternatives rather than conventional medicine, and 62 reported that they believed the earth was flat or believed that humanoids take reptilian forms to manipulate human societies.
The team then sought to assess beliefs about actual and mythical (nonestablished) causes of cancer by presenting the participants with the closed risk factor questions on two validated scales – the Cancer Awareness Measure (CAM) and CAM–Mythical Causes Scale (CAM-MYCS).
Responses to both were recorded on a five-point scale; answers ranged from “strongly disagree” to “strongly agree.”
The CAM assesses cancer risk perceptions of 11 established risk factors for cancer: smoking actively or passively, consuming alcohol, low levels of physical activity, consuming red or processed meat, getting sunburnt as a child, family history of cancer, human papillomavirus infection, being overweight, age greater than or equal to 70 years, and low vegetable and fruit consumption.
The CAM-MYCS measure includes 12 questions on risk perceptions of mythical causes of cancer – nonestablished causes that are commonly believed to cause cancer but for which there is no supporting scientific evidence, the authors explain. These items include drinking from plastic bottles; eating food containing artificial sweeteners or additives and genetically modified food; using microwave ovens, aerosol containers, mobile phones, and cleaning products; living near power lines; feeling stressed; experiencing physical trauma; and being exposed to electromagnetic frequencies/non-ionizing radiation, such as wi-fi networks, radio, and television.
The most endorsed mythical causes of cancer were eating food containing additives (63.9%) or sweeteners (50.7%), feeling stressed (59.7%), and eating genetically modified foods (38.4%).
A version of this article first appeared on Medscape.com.
The study, entitled, “Everything Causes Cancer? Beliefs and Attitudes Towards Cancer Prevention Among Anti-Vaxxers, Flat Earthers, and Reptilian Conspiracists: Online Cross Sectional Survey,” was published in the Christmas 2022 issue of The British Medical Journal (BMJ).
The authors explain that they set out to evaluate “the patterns of beliefs about cancer among people who believed in conspiracies, rejected the COVID-19 vaccine, or preferred alternative medicine.”
They sought such people on social media and online chat platforms and asked them questions about real and mythical causes of cancer.
Almost half of survey participants agreed with the statement, “It seems like everything causes cancer.”
Overall, among all participants, awareness of the actual causes of cancer was greater than awareness of the mythical causes of cancer, the authors report. However, awareness of the actual causes of cancer was lower among the unvaccinated and members of conspiracy groups than among their counterparts.
The authors are concerned that their findings suggest “a direct connection between digital misinformation and consequent potential erroneous health decisions, which may represent a further preventable fraction of cancer.”
Backlash and criticism
The study “highlights the difficulty society encounters in distinguishing the actual causes of cancer from mythical causes,” The BMJ commented on Twitter.
However, both the study and the journal received some backlash.
This is a “horrible article seeking to smear people with concerns about COVID vaccines,” commented Clare Craig, a British consultant pathologist who specializes in cancer diagnostics.
The study and its methodology were also harshly criticized on Twitter by Normal Fenton, professor of risk information management at the Queen Mary University of London.
The senior author of the study, Laura Costas, a medical epidemiologist with the Catalan Institute of Oncology, Barcelona, told this news organization that the naysayers on social media, many of whom focused their comments on the COVID-19 vaccine, prove the purpose of the study – that misinformation spreads widely on the internet.
“Most comments focused on spreading COVID-19 myths, which were not the direct subject of the study, and questioned the motivations of BMJ authors and the scientific community, assuming they had a common malevolent hidden agenda,” Ms. Costas said.
“They stated the need of having critical thinking, a trait in common with the scientific method, but dogmatically dismissed any information that comes from official sources,” she added.
Ms. Costas commented that “society encounters difficulty in differentiating actual from mythical causes of cancer owing to mass information. We therefore planned this study with a certain satire, which is in line with the essence of The BMJ Christmas issue.”
The BMJ has a long history of publishing a lighthearted Christmas edition full of original, satirical, and nontraditional studies. Previous years have seen studies that explored potential harms from holly and ivy, survival time of chocolates on hospital wards, and the question, “Were James Bond’s drinks shaken because of alcohol induced tremor?”
Study details
Ms. Costas and colleagues sought participants for their survey from online forums that included 4chan and Reddit, which are known for their controversial content posted by anonymous users. Data were also collected from ForoCoches and HispaChan, well-known Spanish online forums. These online sites were intentionally chosen because researchers thought “conspiracy beliefs would be more prevalent,” according to Ms. Costas.
Across the multiple forums, there were 1,494 participants. Of these, 209 participants were unvaccinated against COVID-19, 112 preferred alternatives rather than conventional medicine, and 62 reported that they believed the earth was flat or believed that humanoids take reptilian forms to manipulate human societies.
The team then sought to assess beliefs about actual and mythical (nonestablished) causes of cancer by presenting the participants with the closed risk factor questions on two validated scales – the Cancer Awareness Measure (CAM) and CAM–Mythical Causes Scale (CAM-MYCS).
Responses to both were recorded on a five-point scale; answers ranged from “strongly disagree” to “strongly agree.”
The CAM assesses cancer risk perceptions of 11 established risk factors for cancer: smoking actively or passively, consuming alcohol, low levels of physical activity, consuming red or processed meat, getting sunburnt as a child, family history of cancer, human papillomavirus infection, being overweight, age greater than or equal to 70 years, and low vegetable and fruit consumption.
The CAM-MYCS measure includes 12 questions on risk perceptions of mythical causes of cancer – nonestablished causes that are commonly believed to cause cancer but for which there is no supporting scientific evidence, the authors explain. These items include drinking from plastic bottles; eating food containing artificial sweeteners or additives and genetically modified food; using microwave ovens, aerosol containers, mobile phones, and cleaning products; living near power lines; feeling stressed; experiencing physical trauma; and being exposed to electromagnetic frequencies/non-ionizing radiation, such as wi-fi networks, radio, and television.
The most endorsed mythical causes of cancer were eating food containing additives (63.9%) or sweeteners (50.7%), feeling stressed (59.7%), and eating genetically modified foods (38.4%).
A version of this article first appeared on Medscape.com.
The study, entitled, “Everything Causes Cancer? Beliefs and Attitudes Towards Cancer Prevention Among Anti-Vaxxers, Flat Earthers, and Reptilian Conspiracists: Online Cross Sectional Survey,” was published in the Christmas 2022 issue of The British Medical Journal (BMJ).
The authors explain that they set out to evaluate “the patterns of beliefs about cancer among people who believed in conspiracies, rejected the COVID-19 vaccine, or preferred alternative medicine.”
They sought such people on social media and online chat platforms and asked them questions about real and mythical causes of cancer.
Almost half of survey participants agreed with the statement, “It seems like everything causes cancer.”
Overall, among all participants, awareness of the actual causes of cancer was greater than awareness of the mythical causes of cancer, the authors report. However, awareness of the actual causes of cancer was lower among the unvaccinated and members of conspiracy groups than among their counterparts.
The authors are concerned that their findings suggest “a direct connection between digital misinformation and consequent potential erroneous health decisions, which may represent a further preventable fraction of cancer.”
Backlash and criticism
The study “highlights the difficulty society encounters in distinguishing the actual causes of cancer from mythical causes,” The BMJ commented on Twitter.
However, both the study and the journal received some backlash.
This is a “horrible article seeking to smear people with concerns about COVID vaccines,” commented Clare Craig, a British consultant pathologist who specializes in cancer diagnostics.
The study and its methodology were also harshly criticized on Twitter by Normal Fenton, professor of risk information management at the Queen Mary University of London.
The senior author of the study, Laura Costas, a medical epidemiologist with the Catalan Institute of Oncology, Barcelona, told this news organization that the naysayers on social media, many of whom focused their comments on the COVID-19 vaccine, prove the purpose of the study – that misinformation spreads widely on the internet.
“Most comments focused on spreading COVID-19 myths, which were not the direct subject of the study, and questioned the motivations of BMJ authors and the scientific community, assuming they had a common malevolent hidden agenda,” Ms. Costas said.
“They stated the need of having critical thinking, a trait in common with the scientific method, but dogmatically dismissed any information that comes from official sources,” she added.
Ms. Costas commented that “society encounters difficulty in differentiating actual from mythical causes of cancer owing to mass information. We therefore planned this study with a certain satire, which is in line with the essence of The BMJ Christmas issue.”
The BMJ has a long history of publishing a lighthearted Christmas edition full of original, satirical, and nontraditional studies. Previous years have seen studies that explored potential harms from holly and ivy, survival time of chocolates on hospital wards, and the question, “Were James Bond’s drinks shaken because of alcohol induced tremor?”
Study details
Ms. Costas and colleagues sought participants for their survey from online forums that included 4chan and Reddit, which are known for their controversial content posted by anonymous users. Data were also collected from ForoCoches and HispaChan, well-known Spanish online forums. These online sites were intentionally chosen because researchers thought “conspiracy beliefs would be more prevalent,” according to Ms. Costas.
Across the multiple forums, there were 1,494 participants. Of these, 209 participants were unvaccinated against COVID-19, 112 preferred alternatives rather than conventional medicine, and 62 reported that they believed the earth was flat or believed that humanoids take reptilian forms to manipulate human societies.
The team then sought to assess beliefs about actual and mythical (nonestablished) causes of cancer by presenting the participants with the closed risk factor questions on two validated scales – the Cancer Awareness Measure (CAM) and CAM–Mythical Causes Scale (CAM-MYCS).
Responses to both were recorded on a five-point scale; answers ranged from “strongly disagree” to “strongly agree.”
The CAM assesses cancer risk perceptions of 11 established risk factors for cancer: smoking actively or passively, consuming alcohol, low levels of physical activity, consuming red or processed meat, getting sunburnt as a child, family history of cancer, human papillomavirus infection, being overweight, age greater than or equal to 70 years, and low vegetable and fruit consumption.
The CAM-MYCS measure includes 12 questions on risk perceptions of mythical causes of cancer – nonestablished causes that are commonly believed to cause cancer but for which there is no supporting scientific evidence, the authors explain. These items include drinking from plastic bottles; eating food containing artificial sweeteners or additives and genetically modified food; using microwave ovens, aerosol containers, mobile phones, and cleaning products; living near power lines; feeling stressed; experiencing physical trauma; and being exposed to electromagnetic frequencies/non-ionizing radiation, such as wi-fi networks, radio, and television.
The most endorsed mythical causes of cancer were eating food containing additives (63.9%) or sweeteners (50.7%), feeling stressed (59.7%), and eating genetically modified foods (38.4%).
A version of this article first appeared on Medscape.com.
COVID update: ASH experts discuss thrombosis, immunity
NEW ORLEANS –
In a presidential symposium at the annual meeting of the American Society of Hematology, La Jolla Institute of Immunology scientist Shane Crotty, PhD, explained that COVID-19 has a “superpower” that allows it to be “extraordinarily stealthy.”
The virus, he said, can sneak past the body’s innate immune system, which normally responds to viral invaders within minutes to hours. “This is why you have people with high viral loads who are presymptomatic. Their innate immune system hasn’t even recognized that these people are infected.”
The adaptive immune system kicks in later. As Dr. Crotty noted, adaptive immunity is composed of three branches: B cells (the source of antibodies), CD4 “helper” T cells, and CD8 “killer” T cells. In the first year of COVID-19, his team tracked 188 subjects post infection in what he said was the largest study of its kind ever for any viral infection.
“In 8 months, 95% of people who had been infected still had measurable immune memory. In fact, most of them had multiple different compartments of immune memory still detectable, and it was likely that these individuals would still have that memory years into the future. Based on that, we made the prediction that most people who have had COVID-19 would likely be protected from reinfection – at least by severe infections – for 3 years into the future. That prediction has widely held up even in the presence of variants which weren’t around at the time.”
How do vaccines fit into the immunity picture? Dr. Crotty’s lab has tracked subjects who received 4 vaccines – Moderna, Pfizer/BioNTech, Janssen/Johnson & Johnson, and Novavax. Researchers found that the mRNA vaccines, Moderna and Pfizer/BioNTech, “are fantastic at eliciting neutralizing antibodies quickly, but then they drop off rapidly at two doses and actually continue to drop for 10 months.”
Still, he said, “when we take a look at 6 months, actually the vaccines are doing pretty incredibly well. If we compare them to an average infected individual, the mRNA vaccines all have higher neutralizing antibody titers.”
What’s happening? According to Dr. Crotty, B cells are “making guesses about what other variants might look like.” But he said research suggests that an important component of this process – germinal centers – aren’t made in some vaccinated people who are immunocompromised. (Germinal centers have been described as “microbial boot camps” for B cells.)
The good news, Dr. Crotty noted, is that a greater understanding of how COVID-19 penetrates various layers of adaptive immune defenses will lead to better ways to protect the immunocompromised. “If you think about immunity in this layered defense way, there are various ways that it could be enhanced for individuals in different categories,” he said.
Hematologist Beverley J. Hunt, MD, OBE, of St. Thomas’ Hospital/King’s Healthcare Partners in London, spoke at the ASH presidential symposium about blood clots and COVID-19. As she noted, concern arose about vaccine-related blood clots. A British team “managed quickly to come up with a diagnostic criteria,” she said. “We looked at nearly 300 patients and essentially came up with a scoring system.”
The diagnostic criteria was based on an analysis of definite or probable cases of vaccine-induced immune thrombocytopenia and thrombosis (VITT) – all related to the AstraZeneca vaccine. The criteria appeared in a 2021 study in the New England Journal of Medicine.
The report’s data didn’t allow it to compare the efficacy of anticoagulants. However, Dr. Hunt noted that clinicians turned to plasma exchange in patients with low platelet counts and extensive thrombosis. The report stated “survival after plasma exchange was 90%, considerably better than would be predicted given the baseline characteristics.”
“Now we’re following up,” Dr. Hunt said. One question to answer: Is long-term anticoagulation helpful? “We have many patients,” she said, “who are taking an anti-platelet factor out of habit.”
Dr. Crotty and Dr. Hunt report no disclosures. This reporter is a paid participant in a COVID vaccine study run by Dr. Crotty’s lab.
NEW ORLEANS –
In a presidential symposium at the annual meeting of the American Society of Hematology, La Jolla Institute of Immunology scientist Shane Crotty, PhD, explained that COVID-19 has a “superpower” that allows it to be “extraordinarily stealthy.”
The virus, he said, can sneak past the body’s innate immune system, which normally responds to viral invaders within minutes to hours. “This is why you have people with high viral loads who are presymptomatic. Their innate immune system hasn’t even recognized that these people are infected.”
The adaptive immune system kicks in later. As Dr. Crotty noted, adaptive immunity is composed of three branches: B cells (the source of antibodies), CD4 “helper” T cells, and CD8 “killer” T cells. In the first year of COVID-19, his team tracked 188 subjects post infection in what he said was the largest study of its kind ever for any viral infection.
“In 8 months, 95% of people who had been infected still had measurable immune memory. In fact, most of them had multiple different compartments of immune memory still detectable, and it was likely that these individuals would still have that memory years into the future. Based on that, we made the prediction that most people who have had COVID-19 would likely be protected from reinfection – at least by severe infections – for 3 years into the future. That prediction has widely held up even in the presence of variants which weren’t around at the time.”
How do vaccines fit into the immunity picture? Dr. Crotty’s lab has tracked subjects who received 4 vaccines – Moderna, Pfizer/BioNTech, Janssen/Johnson & Johnson, and Novavax. Researchers found that the mRNA vaccines, Moderna and Pfizer/BioNTech, “are fantastic at eliciting neutralizing antibodies quickly, but then they drop off rapidly at two doses and actually continue to drop for 10 months.”
Still, he said, “when we take a look at 6 months, actually the vaccines are doing pretty incredibly well. If we compare them to an average infected individual, the mRNA vaccines all have higher neutralizing antibody titers.”
What’s happening? According to Dr. Crotty, B cells are “making guesses about what other variants might look like.” But he said research suggests that an important component of this process – germinal centers – aren’t made in some vaccinated people who are immunocompromised. (Germinal centers have been described as “microbial boot camps” for B cells.)
The good news, Dr. Crotty noted, is that a greater understanding of how COVID-19 penetrates various layers of adaptive immune defenses will lead to better ways to protect the immunocompromised. “If you think about immunity in this layered defense way, there are various ways that it could be enhanced for individuals in different categories,” he said.
Hematologist Beverley J. Hunt, MD, OBE, of St. Thomas’ Hospital/King’s Healthcare Partners in London, spoke at the ASH presidential symposium about blood clots and COVID-19. As she noted, concern arose about vaccine-related blood clots. A British team “managed quickly to come up with a diagnostic criteria,” she said. “We looked at nearly 300 patients and essentially came up with a scoring system.”
The diagnostic criteria was based on an analysis of definite or probable cases of vaccine-induced immune thrombocytopenia and thrombosis (VITT) – all related to the AstraZeneca vaccine. The criteria appeared in a 2021 study in the New England Journal of Medicine.
The report’s data didn’t allow it to compare the efficacy of anticoagulants. However, Dr. Hunt noted that clinicians turned to plasma exchange in patients with low platelet counts and extensive thrombosis. The report stated “survival after plasma exchange was 90%, considerably better than would be predicted given the baseline characteristics.”
“Now we’re following up,” Dr. Hunt said. One question to answer: Is long-term anticoagulation helpful? “We have many patients,” she said, “who are taking an anti-platelet factor out of habit.”
Dr. Crotty and Dr. Hunt report no disclosures. This reporter is a paid participant in a COVID vaccine study run by Dr. Crotty’s lab.
NEW ORLEANS –
In a presidential symposium at the annual meeting of the American Society of Hematology, La Jolla Institute of Immunology scientist Shane Crotty, PhD, explained that COVID-19 has a “superpower” that allows it to be “extraordinarily stealthy.”
The virus, he said, can sneak past the body’s innate immune system, which normally responds to viral invaders within minutes to hours. “This is why you have people with high viral loads who are presymptomatic. Their innate immune system hasn’t even recognized that these people are infected.”
The adaptive immune system kicks in later. As Dr. Crotty noted, adaptive immunity is composed of three branches: B cells (the source of antibodies), CD4 “helper” T cells, and CD8 “killer” T cells. In the first year of COVID-19, his team tracked 188 subjects post infection in what he said was the largest study of its kind ever for any viral infection.
“In 8 months, 95% of people who had been infected still had measurable immune memory. In fact, most of them had multiple different compartments of immune memory still detectable, and it was likely that these individuals would still have that memory years into the future. Based on that, we made the prediction that most people who have had COVID-19 would likely be protected from reinfection – at least by severe infections – for 3 years into the future. That prediction has widely held up even in the presence of variants which weren’t around at the time.”
How do vaccines fit into the immunity picture? Dr. Crotty’s lab has tracked subjects who received 4 vaccines – Moderna, Pfizer/BioNTech, Janssen/Johnson & Johnson, and Novavax. Researchers found that the mRNA vaccines, Moderna and Pfizer/BioNTech, “are fantastic at eliciting neutralizing antibodies quickly, but then they drop off rapidly at two doses and actually continue to drop for 10 months.”
Still, he said, “when we take a look at 6 months, actually the vaccines are doing pretty incredibly well. If we compare them to an average infected individual, the mRNA vaccines all have higher neutralizing antibody titers.”
What’s happening? According to Dr. Crotty, B cells are “making guesses about what other variants might look like.” But he said research suggests that an important component of this process – germinal centers – aren’t made in some vaccinated people who are immunocompromised. (Germinal centers have been described as “microbial boot camps” for B cells.)
The good news, Dr. Crotty noted, is that a greater understanding of how COVID-19 penetrates various layers of adaptive immune defenses will lead to better ways to protect the immunocompromised. “If you think about immunity in this layered defense way, there are various ways that it could be enhanced for individuals in different categories,” he said.
Hematologist Beverley J. Hunt, MD, OBE, of St. Thomas’ Hospital/King’s Healthcare Partners in London, spoke at the ASH presidential symposium about blood clots and COVID-19. As she noted, concern arose about vaccine-related blood clots. A British team “managed quickly to come up with a diagnostic criteria,” she said. “We looked at nearly 300 patients and essentially came up with a scoring system.”
The diagnostic criteria was based on an analysis of definite or probable cases of vaccine-induced immune thrombocytopenia and thrombosis (VITT) – all related to the AstraZeneca vaccine. The criteria appeared in a 2021 study in the New England Journal of Medicine.
The report’s data didn’t allow it to compare the efficacy of anticoagulants. However, Dr. Hunt noted that clinicians turned to plasma exchange in patients with low platelet counts and extensive thrombosis. The report stated “survival after plasma exchange was 90%, considerably better than would be predicted given the baseline characteristics.”
“Now we’re following up,” Dr. Hunt said. One question to answer: Is long-term anticoagulation helpful? “We have many patients,” she said, “who are taking an anti-platelet factor out of habit.”
Dr. Crotty and Dr. Hunt report no disclosures. This reporter is a paid participant in a COVID vaccine study run by Dr. Crotty’s lab.
AT ASH 2022
Endocarditis tied to drug use on the rise, spiked during COVID
A new study provides more evidence that endocarditis associated with drug use is a significant and growing health concern, and further demonstrates that this risk has been exacerbated by the COVID-19 pandemic.
The rate of infective endocarditis among individuals in the United States with opioid or cocaine use disorder increased in the 11-year period 2011 to 2022, with the steepest increase logged during the COVID-19 pandemic (2021-2022), according to the study.
A diagnosis of COVID-19 more than doubled the risk for a new diagnosis of endocarditis in patients with either cocaine (hazard ratio, 2.24) or opioid use disorder (HR, 2.23).
“Our data suggests that, in addition to the major social disruption from the pandemic, including disrupted access to health care, COVID-19 infection itself is a significant risk factor for new diagnosis of endocarditis in drug using populations,” authors Nora Volkow, MD, director of the National Institute on Drug Abuse, and colleagues wrote.
“Drug-using populations, particularly those who use cocaine or opioids, have some of the highest risk for endocarditis, and here we show that having a COVID-19 diagnoses further increases this risk,” they added.
The study was published online in Molecular Psychiatry.
The researchers analyzed electronic health record data collected from January 2011 to August 2022 for more than 109 million people across the United States, including more than 736,000 with an opioid use disorder and more than 379,000 with a cocaine use disorder.
In 2011, there were 4 cases of endocarditis per day for every 1 million people with opioid use disorder. By 2022, the rate had increased to 30 cases per day per 1 million people with opioid use disorder.
For people with cocaine use disorder, cases of endocarditis increased from 5 per 1 million in 2011 to 23 per 1 million in 2022.
Among individuals with cocaine or opioid use disorder, the risk of being hospitalized within 180 days following a diagnosis of endocarditis was higher in those with than without COVID-19 (67.5% vs. 58.7%; HR, 1.21).
The risk of dying within 180 days following new diagnosis of endocarditis was also higher in those with than without COVID-19 (9.2% vs. 8%; HR, 1.16).
The study also showed that Black and Hispanic individuals had a lower risk for COVID-19-associated endocarditis than non-Hispanic White individuals, which is consistent with a higher prevalence of injection drug use in non-Hispanic White populations, compared with Black or Hispanic populations, the researchers pointed out.
Dr. Volkow and colleagues said their findings highlight the need to screen drug users for endocarditis and link them to infectious disease and addiction treatment if they contract COVID-19.
“People with substance use disorder already face major impediments to proper health care due to lack of access and stigma,” Dr. Volkow said in a news release.
“Proven techniques like syringe service programs, which help people avoid infection from reused or shared injection equipment, can help prevent this often fatal and costly condition,” Dr. Volkow added.
The authors said it will also be important to determine exactly how SARS-CoV-2 viral infection exacerbates the risk for endocarditis in drug users.
Support for the study was provided by the National Institute on Aging, National Institute on Alcohol Abuse and Alcoholism, the Clinical and Translational Science Collaborative of Cleveland, and the National Cancer Institute Case Comprehensive Cancer Center. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study provides more evidence that endocarditis associated with drug use is a significant and growing health concern, and further demonstrates that this risk has been exacerbated by the COVID-19 pandemic.
The rate of infective endocarditis among individuals in the United States with opioid or cocaine use disorder increased in the 11-year period 2011 to 2022, with the steepest increase logged during the COVID-19 pandemic (2021-2022), according to the study.
A diagnosis of COVID-19 more than doubled the risk for a new diagnosis of endocarditis in patients with either cocaine (hazard ratio, 2.24) or opioid use disorder (HR, 2.23).
“Our data suggests that, in addition to the major social disruption from the pandemic, including disrupted access to health care, COVID-19 infection itself is a significant risk factor for new diagnosis of endocarditis in drug using populations,” authors Nora Volkow, MD, director of the National Institute on Drug Abuse, and colleagues wrote.
“Drug-using populations, particularly those who use cocaine or opioids, have some of the highest risk for endocarditis, and here we show that having a COVID-19 diagnoses further increases this risk,” they added.
The study was published online in Molecular Psychiatry.
The researchers analyzed electronic health record data collected from January 2011 to August 2022 for more than 109 million people across the United States, including more than 736,000 with an opioid use disorder and more than 379,000 with a cocaine use disorder.
In 2011, there were 4 cases of endocarditis per day for every 1 million people with opioid use disorder. By 2022, the rate had increased to 30 cases per day per 1 million people with opioid use disorder.
For people with cocaine use disorder, cases of endocarditis increased from 5 per 1 million in 2011 to 23 per 1 million in 2022.
Among individuals with cocaine or opioid use disorder, the risk of being hospitalized within 180 days following a diagnosis of endocarditis was higher in those with than without COVID-19 (67.5% vs. 58.7%; HR, 1.21).
The risk of dying within 180 days following new diagnosis of endocarditis was also higher in those with than without COVID-19 (9.2% vs. 8%; HR, 1.16).
The study also showed that Black and Hispanic individuals had a lower risk for COVID-19-associated endocarditis than non-Hispanic White individuals, which is consistent with a higher prevalence of injection drug use in non-Hispanic White populations, compared with Black or Hispanic populations, the researchers pointed out.
Dr. Volkow and colleagues said their findings highlight the need to screen drug users for endocarditis and link them to infectious disease and addiction treatment if they contract COVID-19.
“People with substance use disorder already face major impediments to proper health care due to lack of access and stigma,” Dr. Volkow said in a news release.
“Proven techniques like syringe service programs, which help people avoid infection from reused or shared injection equipment, can help prevent this often fatal and costly condition,” Dr. Volkow added.
The authors said it will also be important to determine exactly how SARS-CoV-2 viral infection exacerbates the risk for endocarditis in drug users.
Support for the study was provided by the National Institute on Aging, National Institute on Alcohol Abuse and Alcoholism, the Clinical and Translational Science Collaborative of Cleveland, and the National Cancer Institute Case Comprehensive Cancer Center. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study provides more evidence that endocarditis associated with drug use is a significant and growing health concern, and further demonstrates that this risk has been exacerbated by the COVID-19 pandemic.
The rate of infective endocarditis among individuals in the United States with opioid or cocaine use disorder increased in the 11-year period 2011 to 2022, with the steepest increase logged during the COVID-19 pandemic (2021-2022), according to the study.
A diagnosis of COVID-19 more than doubled the risk for a new diagnosis of endocarditis in patients with either cocaine (hazard ratio, 2.24) or opioid use disorder (HR, 2.23).
“Our data suggests that, in addition to the major social disruption from the pandemic, including disrupted access to health care, COVID-19 infection itself is a significant risk factor for new diagnosis of endocarditis in drug using populations,” authors Nora Volkow, MD, director of the National Institute on Drug Abuse, and colleagues wrote.
“Drug-using populations, particularly those who use cocaine or opioids, have some of the highest risk for endocarditis, and here we show that having a COVID-19 diagnoses further increases this risk,” they added.
The study was published online in Molecular Psychiatry.
The researchers analyzed electronic health record data collected from January 2011 to August 2022 for more than 109 million people across the United States, including more than 736,000 with an opioid use disorder and more than 379,000 with a cocaine use disorder.
In 2011, there were 4 cases of endocarditis per day for every 1 million people with opioid use disorder. By 2022, the rate had increased to 30 cases per day per 1 million people with opioid use disorder.
For people with cocaine use disorder, cases of endocarditis increased from 5 per 1 million in 2011 to 23 per 1 million in 2022.
Among individuals with cocaine or opioid use disorder, the risk of being hospitalized within 180 days following a diagnosis of endocarditis was higher in those with than without COVID-19 (67.5% vs. 58.7%; HR, 1.21).
The risk of dying within 180 days following new diagnosis of endocarditis was also higher in those with than without COVID-19 (9.2% vs. 8%; HR, 1.16).
The study also showed that Black and Hispanic individuals had a lower risk for COVID-19-associated endocarditis than non-Hispanic White individuals, which is consistent with a higher prevalence of injection drug use in non-Hispanic White populations, compared with Black or Hispanic populations, the researchers pointed out.
Dr. Volkow and colleagues said their findings highlight the need to screen drug users for endocarditis and link them to infectious disease and addiction treatment if they contract COVID-19.
“People with substance use disorder already face major impediments to proper health care due to lack of access and stigma,” Dr. Volkow said in a news release.
“Proven techniques like syringe service programs, which help people avoid infection from reused or shared injection equipment, can help prevent this often fatal and costly condition,” Dr. Volkow added.
The authors said it will also be important to determine exactly how SARS-CoV-2 viral infection exacerbates the risk for endocarditis in drug users.
Support for the study was provided by the National Institute on Aging, National Institute on Alcohol Abuse and Alcoholism, the Clinical and Translational Science Collaborative of Cleveland, and the National Cancer Institute Case Comprehensive Cancer Center. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM MOLECULAR PSYCHIATRY
How to have a safer and more joyful holiday season
This holiday season, I am looking forward to spending some time with family, as I have in the past. As I have chatted with others, many friends are looking forward to events that are potentially larger and potentially returning to prepandemic type gatherings.
Gathering is important and can bring joy, sense of community, and love to the lives of many. Unfortunately, the risks associated with gathering are not over. as our country faces many cases of respiratory syncytial virus (RSV), COVID-19, and influenza at the same time.
During the first week of December, cases of influenza were rising across the country1 and were rising faster than in previous years. Although getting the vaccine is an important method of influenza prevention and is recommended for everyone over the age of 6 months with rare exception, many have not gotten their vaccine this year.
Influenza
Thus far, “nearly 50% of reported flu-associated hospitalizations in women of childbearing age have been in women who are pregnant.” We are seeing this at a time with lower-than-average uptake of influenza vaccine leaving both the pregnant persons and their babies unprotected. In addition to utilizing vaccines as prevention, isolating when ill, cleaning surfaces, and practicing good hand hygiene can all decrease transmission.
RSV
In addition to rises of influenza, there are currently high rates of RSV in various parts of the country. Prior to 2020, RSV typically started in the fall and peaked in the winter months. However, since the pandemic, the typical seasonal pattern has not returned, and it is unclear when it will. Although RSV hits the very young, the old, and the immunocompromised the most, RSV can infect anyone. Unfortunately, we do not currently have a vaccine for everyone against this virus. Prevention of transmission includes, as with flu, isolating when ill, cleaning surfaces, and washing hands.2
COVID-19
Of course, the effects of the COVID-19 pandemic are also still here as well. During the first week of December, the CDC reported rising cases of COVID across the country. Within the past few months, there have been several developments, though, for protection. There are now bivalent vaccines available as either third doses or booster doses approved for all persons over 6 months of age. As of the first week of December, only 13.5% of those aged 5 and over had received an updated booster.
There is currently wider access to rapid testing, including at-home testing, which can allow individuals to identify if COVID positive. Additionally, there is access to medication to decrease the likelihood of severe disease – though this does not take the place of vaccinations.
If anyone does test positive for COVID, they should follow the most recent quarantine guidelines including wearing a well-fitted mask when they do begin returning to activities.3
With rising cases of all three of these viruses, some may be asking how we can safely gather. There are several things to consider and do to enjoy our events. The first thing everyone can do is to receive updated vaccinations for both influenza and COVID-19 if eligible. Although it may take some time to be effective, vaccination is still one of our most effective methods of disease prevention and is important this winter season. Vaccinations can also help decrease the risk of severe disease.
Although many have stopped masking, as cases rise, it is time to consider masking particularly when community levels of any of these viruses are high. Masks help with preventing and spreading more than just COVID-19. Using them can be especially important for those going places such as stores and to large public gatherings and when riding on buses, planes, or trains.
In summary
Preventing exposure by masking can help keep individuals healthy prior to celebrating the holidays with others. With access to rapid testing, it makes sense to consider testing prior to gathering with friends and family. Most importantly, although we all are looking forward to spending time with our loved ones, it is important to stay home if not feeling well. Following these recommendations will allow us to have a safer and more joyful holiday season.
Dr. Wheat is a family physician at Erie Family Health Center and program director of Northwestern University’s McGaw Family Medicine residency program, both in Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at [email protected].
References
1. Centers for Disease Control and Prevention. Influenza (flu). [Online] Dec. 1, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/flu/index.htm.
2. Respiratory syncytial virus. Respiratory syncytial virus infection (RSV). [Online] Oct. 28, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/rsv/index.html.
3. COVID-19. [Online] Dec. 7, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/coronavirus/2019-ncov/index.html.
This holiday season, I am looking forward to spending some time with family, as I have in the past. As I have chatted with others, many friends are looking forward to events that are potentially larger and potentially returning to prepandemic type gatherings.
Gathering is important and can bring joy, sense of community, and love to the lives of many. Unfortunately, the risks associated with gathering are not over. as our country faces many cases of respiratory syncytial virus (RSV), COVID-19, and influenza at the same time.
During the first week of December, cases of influenza were rising across the country1 and were rising faster than in previous years. Although getting the vaccine is an important method of influenza prevention and is recommended for everyone over the age of 6 months with rare exception, many have not gotten their vaccine this year.
Influenza
Thus far, “nearly 50% of reported flu-associated hospitalizations in women of childbearing age have been in women who are pregnant.” We are seeing this at a time with lower-than-average uptake of influenza vaccine leaving both the pregnant persons and their babies unprotected. In addition to utilizing vaccines as prevention, isolating when ill, cleaning surfaces, and practicing good hand hygiene can all decrease transmission.
RSV
In addition to rises of influenza, there are currently high rates of RSV in various parts of the country. Prior to 2020, RSV typically started in the fall and peaked in the winter months. However, since the pandemic, the typical seasonal pattern has not returned, and it is unclear when it will. Although RSV hits the very young, the old, and the immunocompromised the most, RSV can infect anyone. Unfortunately, we do not currently have a vaccine for everyone against this virus. Prevention of transmission includes, as with flu, isolating when ill, cleaning surfaces, and washing hands.2
COVID-19
Of course, the effects of the COVID-19 pandemic are also still here as well. During the first week of December, the CDC reported rising cases of COVID across the country. Within the past few months, there have been several developments, though, for protection. There are now bivalent vaccines available as either third doses or booster doses approved for all persons over 6 months of age. As of the first week of December, only 13.5% of those aged 5 and over had received an updated booster.
There is currently wider access to rapid testing, including at-home testing, which can allow individuals to identify if COVID positive. Additionally, there is access to medication to decrease the likelihood of severe disease – though this does not take the place of vaccinations.
If anyone does test positive for COVID, they should follow the most recent quarantine guidelines including wearing a well-fitted mask when they do begin returning to activities.3
With rising cases of all three of these viruses, some may be asking how we can safely gather. There are several things to consider and do to enjoy our events. The first thing everyone can do is to receive updated vaccinations for both influenza and COVID-19 if eligible. Although it may take some time to be effective, vaccination is still one of our most effective methods of disease prevention and is important this winter season. Vaccinations can also help decrease the risk of severe disease.
Although many have stopped masking, as cases rise, it is time to consider masking particularly when community levels of any of these viruses are high. Masks help with preventing and spreading more than just COVID-19. Using them can be especially important for those going places such as stores and to large public gatherings and when riding on buses, planes, or trains.
In summary
Preventing exposure by masking can help keep individuals healthy prior to celebrating the holidays with others. With access to rapid testing, it makes sense to consider testing prior to gathering with friends and family. Most importantly, although we all are looking forward to spending time with our loved ones, it is important to stay home if not feeling well. Following these recommendations will allow us to have a safer and more joyful holiday season.
Dr. Wheat is a family physician at Erie Family Health Center and program director of Northwestern University’s McGaw Family Medicine residency program, both in Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at [email protected].
References
1. Centers for Disease Control and Prevention. Influenza (flu). [Online] Dec. 1, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/flu/index.htm.
2. Respiratory syncytial virus. Respiratory syncytial virus infection (RSV). [Online] Oct. 28, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/rsv/index.html.
3. COVID-19. [Online] Dec. 7, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/coronavirus/2019-ncov/index.html.
This holiday season, I am looking forward to spending some time with family, as I have in the past. As I have chatted with others, many friends are looking forward to events that are potentially larger and potentially returning to prepandemic type gatherings.
Gathering is important and can bring joy, sense of community, and love to the lives of many. Unfortunately, the risks associated with gathering are not over. as our country faces many cases of respiratory syncytial virus (RSV), COVID-19, and influenza at the same time.
During the first week of December, cases of influenza were rising across the country1 and were rising faster than in previous years. Although getting the vaccine is an important method of influenza prevention and is recommended for everyone over the age of 6 months with rare exception, many have not gotten their vaccine this year.
Influenza
Thus far, “nearly 50% of reported flu-associated hospitalizations in women of childbearing age have been in women who are pregnant.” We are seeing this at a time with lower-than-average uptake of influenza vaccine leaving both the pregnant persons and their babies unprotected. In addition to utilizing vaccines as prevention, isolating when ill, cleaning surfaces, and practicing good hand hygiene can all decrease transmission.
RSV
In addition to rises of influenza, there are currently high rates of RSV in various parts of the country. Prior to 2020, RSV typically started in the fall and peaked in the winter months. However, since the pandemic, the typical seasonal pattern has not returned, and it is unclear when it will. Although RSV hits the very young, the old, and the immunocompromised the most, RSV can infect anyone. Unfortunately, we do not currently have a vaccine for everyone against this virus. Prevention of transmission includes, as with flu, isolating when ill, cleaning surfaces, and washing hands.2
COVID-19
Of course, the effects of the COVID-19 pandemic are also still here as well. During the first week of December, the CDC reported rising cases of COVID across the country. Within the past few months, there have been several developments, though, for protection. There are now bivalent vaccines available as either third doses or booster doses approved for all persons over 6 months of age. As of the first week of December, only 13.5% of those aged 5 and over had received an updated booster.
There is currently wider access to rapid testing, including at-home testing, which can allow individuals to identify if COVID positive. Additionally, there is access to medication to decrease the likelihood of severe disease – though this does not take the place of vaccinations.
If anyone does test positive for COVID, they should follow the most recent quarantine guidelines including wearing a well-fitted mask when they do begin returning to activities.3
With rising cases of all three of these viruses, some may be asking how we can safely gather. There are several things to consider and do to enjoy our events. The first thing everyone can do is to receive updated vaccinations for both influenza and COVID-19 if eligible. Although it may take some time to be effective, vaccination is still one of our most effective methods of disease prevention and is important this winter season. Vaccinations can also help decrease the risk of severe disease.
Although many have stopped masking, as cases rise, it is time to consider masking particularly when community levels of any of these viruses are high. Masks help with preventing and spreading more than just COVID-19. Using them can be especially important for those going places such as stores and to large public gatherings and when riding on buses, planes, or trains.
In summary
Preventing exposure by masking can help keep individuals healthy prior to celebrating the holidays with others. With access to rapid testing, it makes sense to consider testing prior to gathering with friends and family. Most importantly, although we all are looking forward to spending time with our loved ones, it is important to stay home if not feeling well. Following these recommendations will allow us to have a safer and more joyful holiday season.
Dr. Wheat is a family physician at Erie Family Health Center and program director of Northwestern University’s McGaw Family Medicine residency program, both in Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at [email protected].
References
1. Centers for Disease Control and Prevention. Influenza (flu). [Online] Dec. 1, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/flu/index.htm.
2. Respiratory syncytial virus. Respiratory syncytial virus infection (RSV). [Online] Oct. 28, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/rsv/index.html.
3. COVID-19. [Online] Dec. 7, 2022. [Cited: 2022 Dec 10.] https://www.cdc.gov/coronavirus/2019-ncov/index.html.
Cardiac injury caused by COVID-19 less common than thought
The study examined cardiac MRI scans in 31 patients before and after having COVID-19 infection and found no new evidence of myocardial injury in the post-COVID scans relative to the pre-COVID scans.
“To the best of our knowledge this is the first cardiac MRI study to assess myocardial injury pre- and post-COVID-19,” the authors stated.
They say that while this study cannot rule out the possibility of rare events of COVID-19–induced myocardial injury, “the complete absence of de novo late gadolinium enhancement lesions after COVID-19 in this cohort indicates that outside special circumstances, COVID-19–induced myocardial injury may be much less common than suggested by previous studies.”
The study was published online in JACC: Cardiovascular Imaging.
Coauthor Till F. Althoff, MD, Cardiovascular Institute, Clínic–University Hospital Barcelona, said in an interview that previous reports have found a high rate of cardiac lesions in patients undergoing imaging after having had COVID-19 infection.
“In some reports, this has been as high as 80% of patients even though they have not had severe COVID disease. These reports have been interpreted as showing the majority of patients have some COVID-induced cardiac damage, which is an alarming message,” he commented.
However, he pointed out that the patients in these reports did not undergo a cardiac MRI scan before they had COVID-19 so it wasn’t known whether these cardiac lesions were present before infection or not.
To try and gain more accurate information, the current study examined cardiac MRI scans in the same patients before and after they had COVID-19.
The researchers, from an arrhythmia unit, made use of the fact that all their patients have cardiac MRI data, so they used their large registry of patients in whom cardiac MRI had been performed, and cross referenced this to a health care database to identify those patients who had confirmed COVID-19 after they obtaining a cardiac scan at the arrhythmia unit. They then conducted another cardiac MRI scan in the 31 patients identified a median of 5 months after their COVID-19 infection.
“These 31 patients had a cardiac MRI scan pre-COVID and post COVID using exactly the same scanner with identical sequences, so the scans were absolutely comparable,” Dr. Althoff noted.
Of these 31 patients, 7 had been hospitalized at the time of acute presentation with COVID-19, of whom 2 required intensive care. Most patients (29) had been symptomatic, but none reported cardiac symptoms.
Results showed that, on the post–COVID-19 scan, late gadolinium enhancement lesions indicative of residual myocardial injury were encountered in 15 of the 31 patients (48%), which the researchers said is in line with previous reports.
However, intraindividual comparison with the pre–COVID-19 cardiac MRI scans showed all these lesions were preexisting with identical localization, pattern, and transmural distribution, and thus not COVID-19 related.
Quantitative analyses, performed independently, detected no increase in the size of individual lesions nor in the global left ventricular late gadolinium enhancement extent.
Comparison of pre- and post COVID-19 imaging sequences did not show any differences in ventricular functional or structural parameters.
“While this study only has 31 patients, the fact that we are conducting intra-individual comparisons, which rules out bias, means that we don’t need a large number of patients for reliable results,” Dr. Althoff said.
“These types of lesions are normal to see. We know that individuals without cardiac disease have these types of lesions, and they are not necessarily an indication of any specific pathology. I was kind of surprised by the interpretation of previous data, which is why we did the current study,” he added.
Dr. Althoff acknowledged that some cardiac injury may have been seen if much larger numbers of patients had been included. “But I think we can say from this data that COVID-induced cardiac damage is much less of an issue than we may have previously thought,” he added.
He also noted that most of the patients in this study had mild COVID-19, so the results cannot be extrapolated to severe COVID-19 infection.
However, Dr. Althoff pointed out that all the patients already had atrial fibrillation, so would have been at higher risk of cardiac injury from COVID-19.
“These patients had preexisting cardiac risk factors, and thus they would have been more susceptible to both a more severe course of COVID and an increased risk of myocardial damage due to COVID. The fact that we don’t find any myocardial injury due to COVID in this group is even more reassuring. The general population will be at even lower risk,” he commented.
“I think we can say that, in COVID patients who do not have any cardiac symptoms, our study suggests that the incidence of cardiac injury is very low,” Dr. Althoff said.
“Even in patients with severe COVID and myocardial involvement reflected by increased troponin levels, I wouldn’t be sure that they have any residual cardiac injury. While it has been reported that cardiac lesions have been found in such patients, pre-COVID MRI scans were not available so we don’t know if they were there before,” he added.
“We do not know the true incidence of cardiac injury after COVID, but I think we can say from this data that it is definitely not anywhere near the 40%-50% or even greater that some of the previous reports have suggested,” he stated.
Dr. Althoff suggested that, based on these data, some of the recommendations based on previous reports such the need for follow-up cardiac scans and caution about partaking in sports again after COVID-19 infection, are probably not necessary.
“Our data suggest that these concerns are unfounded, and we need to step back a bit and stop alarming patients about the risk of cardiac damage after COVID,” he said. “Yes, if patients have cardiac symptoms during or after COVID infection they should get checked out, but I do not think we need to do a cardiac risk assessment in patients without cardiac symptoms in COVID.”
This work is supported in part by grants from Instituto de Salud Carlos III, the Spanish government, Madrid, and Fundació la Marató de TV3 in Catalonia. Dr. Althoff has received research grants for investigator-initiated trials from Biosense Webster.
A version of this article first appeared on Medscape.com.
The study examined cardiac MRI scans in 31 patients before and after having COVID-19 infection and found no new evidence of myocardial injury in the post-COVID scans relative to the pre-COVID scans.
“To the best of our knowledge this is the first cardiac MRI study to assess myocardial injury pre- and post-COVID-19,” the authors stated.
They say that while this study cannot rule out the possibility of rare events of COVID-19–induced myocardial injury, “the complete absence of de novo late gadolinium enhancement lesions after COVID-19 in this cohort indicates that outside special circumstances, COVID-19–induced myocardial injury may be much less common than suggested by previous studies.”
The study was published online in JACC: Cardiovascular Imaging.
Coauthor Till F. Althoff, MD, Cardiovascular Institute, Clínic–University Hospital Barcelona, said in an interview that previous reports have found a high rate of cardiac lesions in patients undergoing imaging after having had COVID-19 infection.
“In some reports, this has been as high as 80% of patients even though they have not had severe COVID disease. These reports have been interpreted as showing the majority of patients have some COVID-induced cardiac damage, which is an alarming message,” he commented.
However, he pointed out that the patients in these reports did not undergo a cardiac MRI scan before they had COVID-19 so it wasn’t known whether these cardiac lesions were present before infection or not.
To try and gain more accurate information, the current study examined cardiac MRI scans in the same patients before and after they had COVID-19.
The researchers, from an arrhythmia unit, made use of the fact that all their patients have cardiac MRI data, so they used their large registry of patients in whom cardiac MRI had been performed, and cross referenced this to a health care database to identify those patients who had confirmed COVID-19 after they obtaining a cardiac scan at the arrhythmia unit. They then conducted another cardiac MRI scan in the 31 patients identified a median of 5 months after their COVID-19 infection.
“These 31 patients had a cardiac MRI scan pre-COVID and post COVID using exactly the same scanner with identical sequences, so the scans were absolutely comparable,” Dr. Althoff noted.
Of these 31 patients, 7 had been hospitalized at the time of acute presentation with COVID-19, of whom 2 required intensive care. Most patients (29) had been symptomatic, but none reported cardiac symptoms.
Results showed that, on the post–COVID-19 scan, late gadolinium enhancement lesions indicative of residual myocardial injury were encountered in 15 of the 31 patients (48%), which the researchers said is in line with previous reports.
However, intraindividual comparison with the pre–COVID-19 cardiac MRI scans showed all these lesions were preexisting with identical localization, pattern, and transmural distribution, and thus not COVID-19 related.
Quantitative analyses, performed independently, detected no increase in the size of individual lesions nor in the global left ventricular late gadolinium enhancement extent.
Comparison of pre- and post COVID-19 imaging sequences did not show any differences in ventricular functional or structural parameters.
“While this study only has 31 patients, the fact that we are conducting intra-individual comparisons, which rules out bias, means that we don’t need a large number of patients for reliable results,” Dr. Althoff said.
“These types of lesions are normal to see. We know that individuals without cardiac disease have these types of lesions, and they are not necessarily an indication of any specific pathology. I was kind of surprised by the interpretation of previous data, which is why we did the current study,” he added.
Dr. Althoff acknowledged that some cardiac injury may have been seen if much larger numbers of patients had been included. “But I think we can say from this data that COVID-induced cardiac damage is much less of an issue than we may have previously thought,” he added.
He also noted that most of the patients in this study had mild COVID-19, so the results cannot be extrapolated to severe COVID-19 infection.
However, Dr. Althoff pointed out that all the patients already had atrial fibrillation, so would have been at higher risk of cardiac injury from COVID-19.
“These patients had preexisting cardiac risk factors, and thus they would have been more susceptible to both a more severe course of COVID and an increased risk of myocardial damage due to COVID. The fact that we don’t find any myocardial injury due to COVID in this group is even more reassuring. The general population will be at even lower risk,” he commented.
“I think we can say that, in COVID patients who do not have any cardiac symptoms, our study suggests that the incidence of cardiac injury is very low,” Dr. Althoff said.
“Even in patients with severe COVID and myocardial involvement reflected by increased troponin levels, I wouldn’t be sure that they have any residual cardiac injury. While it has been reported that cardiac lesions have been found in such patients, pre-COVID MRI scans were not available so we don’t know if they were there before,” he added.
“We do not know the true incidence of cardiac injury after COVID, but I think we can say from this data that it is definitely not anywhere near the 40%-50% or even greater that some of the previous reports have suggested,” he stated.
Dr. Althoff suggested that, based on these data, some of the recommendations based on previous reports such the need for follow-up cardiac scans and caution about partaking in sports again after COVID-19 infection, are probably not necessary.
“Our data suggest that these concerns are unfounded, and we need to step back a bit and stop alarming patients about the risk of cardiac damage after COVID,” he said. “Yes, if patients have cardiac symptoms during or after COVID infection they should get checked out, but I do not think we need to do a cardiac risk assessment in patients without cardiac symptoms in COVID.”
This work is supported in part by grants from Instituto de Salud Carlos III, the Spanish government, Madrid, and Fundació la Marató de TV3 in Catalonia. Dr. Althoff has received research grants for investigator-initiated trials from Biosense Webster.
A version of this article first appeared on Medscape.com.
The study examined cardiac MRI scans in 31 patients before and after having COVID-19 infection and found no new evidence of myocardial injury in the post-COVID scans relative to the pre-COVID scans.
“To the best of our knowledge this is the first cardiac MRI study to assess myocardial injury pre- and post-COVID-19,” the authors stated.
They say that while this study cannot rule out the possibility of rare events of COVID-19–induced myocardial injury, “the complete absence of de novo late gadolinium enhancement lesions after COVID-19 in this cohort indicates that outside special circumstances, COVID-19–induced myocardial injury may be much less common than suggested by previous studies.”
The study was published online in JACC: Cardiovascular Imaging.
Coauthor Till F. Althoff, MD, Cardiovascular Institute, Clínic–University Hospital Barcelona, said in an interview that previous reports have found a high rate of cardiac lesions in patients undergoing imaging after having had COVID-19 infection.
“In some reports, this has been as high as 80% of patients even though they have not had severe COVID disease. These reports have been interpreted as showing the majority of patients have some COVID-induced cardiac damage, which is an alarming message,” he commented.
However, he pointed out that the patients in these reports did not undergo a cardiac MRI scan before they had COVID-19 so it wasn’t known whether these cardiac lesions were present before infection or not.
To try and gain more accurate information, the current study examined cardiac MRI scans in the same patients before and after they had COVID-19.
The researchers, from an arrhythmia unit, made use of the fact that all their patients have cardiac MRI data, so they used their large registry of patients in whom cardiac MRI had been performed, and cross referenced this to a health care database to identify those patients who had confirmed COVID-19 after they obtaining a cardiac scan at the arrhythmia unit. They then conducted another cardiac MRI scan in the 31 patients identified a median of 5 months after their COVID-19 infection.
“These 31 patients had a cardiac MRI scan pre-COVID and post COVID using exactly the same scanner with identical sequences, so the scans were absolutely comparable,” Dr. Althoff noted.
Of these 31 patients, 7 had been hospitalized at the time of acute presentation with COVID-19, of whom 2 required intensive care. Most patients (29) had been symptomatic, but none reported cardiac symptoms.
Results showed that, on the post–COVID-19 scan, late gadolinium enhancement lesions indicative of residual myocardial injury were encountered in 15 of the 31 patients (48%), which the researchers said is in line with previous reports.
However, intraindividual comparison with the pre–COVID-19 cardiac MRI scans showed all these lesions were preexisting with identical localization, pattern, and transmural distribution, and thus not COVID-19 related.
Quantitative analyses, performed independently, detected no increase in the size of individual lesions nor in the global left ventricular late gadolinium enhancement extent.
Comparison of pre- and post COVID-19 imaging sequences did not show any differences in ventricular functional or structural parameters.
“While this study only has 31 patients, the fact that we are conducting intra-individual comparisons, which rules out bias, means that we don’t need a large number of patients for reliable results,” Dr. Althoff said.
“These types of lesions are normal to see. We know that individuals without cardiac disease have these types of lesions, and they are not necessarily an indication of any specific pathology. I was kind of surprised by the interpretation of previous data, which is why we did the current study,” he added.
Dr. Althoff acknowledged that some cardiac injury may have been seen if much larger numbers of patients had been included. “But I think we can say from this data that COVID-induced cardiac damage is much less of an issue than we may have previously thought,” he added.
He also noted that most of the patients in this study had mild COVID-19, so the results cannot be extrapolated to severe COVID-19 infection.
However, Dr. Althoff pointed out that all the patients already had atrial fibrillation, so would have been at higher risk of cardiac injury from COVID-19.
“These patients had preexisting cardiac risk factors, and thus they would have been more susceptible to both a more severe course of COVID and an increased risk of myocardial damage due to COVID. The fact that we don’t find any myocardial injury due to COVID in this group is even more reassuring. The general population will be at even lower risk,” he commented.
“I think we can say that, in COVID patients who do not have any cardiac symptoms, our study suggests that the incidence of cardiac injury is very low,” Dr. Althoff said.
“Even in patients with severe COVID and myocardial involvement reflected by increased troponin levels, I wouldn’t be sure that they have any residual cardiac injury. While it has been reported that cardiac lesions have been found in such patients, pre-COVID MRI scans were not available so we don’t know if they were there before,” he added.
“We do not know the true incidence of cardiac injury after COVID, but I think we can say from this data that it is definitely not anywhere near the 40%-50% or even greater that some of the previous reports have suggested,” he stated.
Dr. Althoff suggested that, based on these data, some of the recommendations based on previous reports such the need for follow-up cardiac scans and caution about partaking in sports again after COVID-19 infection, are probably not necessary.
“Our data suggest that these concerns are unfounded, and we need to step back a bit and stop alarming patients about the risk of cardiac damage after COVID,” he said. “Yes, if patients have cardiac symptoms during or after COVID infection they should get checked out, but I do not think we need to do a cardiac risk assessment in patients without cardiac symptoms in COVID.”
This work is supported in part by grants from Instituto de Salud Carlos III, the Spanish government, Madrid, and Fundació la Marató de TV3 in Catalonia. Dr. Althoff has received research grants for investigator-initiated trials from Biosense Webster.
A version of this article first appeared on Medscape.com.
FROM JACC: CARDIOVASCULAR IMAGING
Children and COVID: New-case counts offer dueling narratives
New COVID-19 cases in children jumped by 66% during the first 2 weeks of December after an 8-week steady period lasting through October and November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
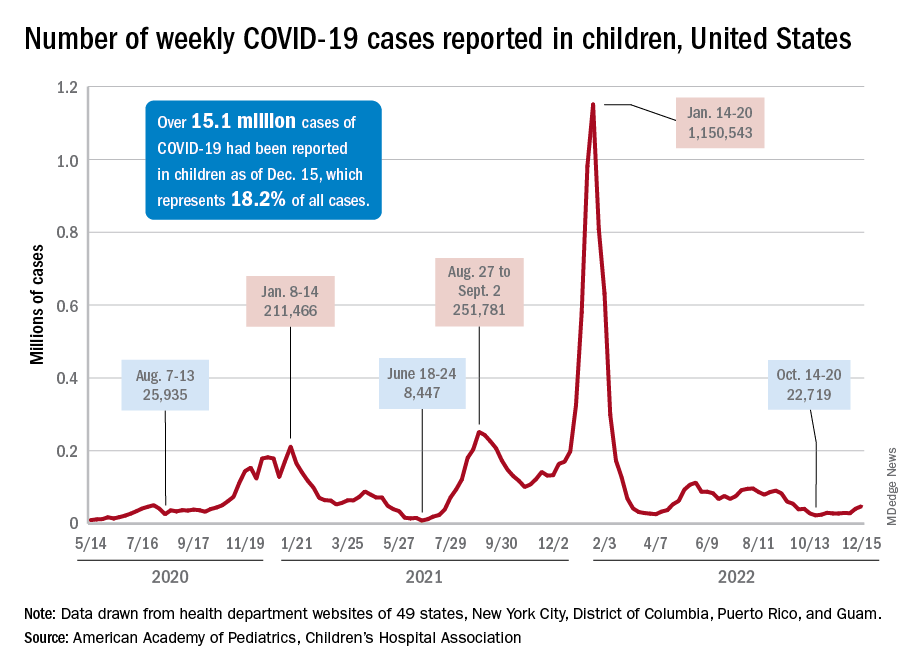
and totaling less than 29,000 for the week of Nov. 25 to Dec. 1. That increase of almost 19,000 cases is the largest over a 2-week period since late July, the AAP and CHA said in their weekly COVID report based on data collected from state and territorial health department websites.
[This publication has been following the AAP/CHA report since the summer of 2020 and continues to share the data for the sake of consistency, but it must be noted that a number of states are no longer updating their public COVID dashboards. As a result, there is now a considerable discrepancy between the AAP/CHA weekly figures and those reported by the Centers for Disease Control and Prevention, which has no such limitations on state data.]
The situation involving new cases over the last 2 weeks is quite different from the CDC’s perspective. The agency does not publish a weekly count, instead offering cumulative cases, which stood at almost 16.1 million as of Dec. 14. Calculating a 2-week total puts the new-case count for Dec. 1-14 at 113,572 among children aged 0-17 years. That is higher than the AAP/CHA count (88,629) for roughly the same period, but it is actually lower than the CDC’s figure (161,832) for the last 2 weeks of November.
The CDC data, in other words, suggest that new cases have gone down in the last 2 weeks, while the AAP and CHA, with their somewhat limited perspective, announced that new cases have gone up.
One COVID-related measure from the CDC that is not contradicted by other sources is hospitalization rates, which had climbed from 0.16 new admissions in children aged 0-17 years with confirmed COVID per 100,000 population on Oct. 22 to 0.29 per 100,000 on Dec. 9. Visits to the emergency department with diagnosed COVID, meanwhile, have been fairly steady so far through December in children, according to the CDC.
New COVID-19 cases in children jumped by 66% during the first 2 weeks of December after an 8-week steady period lasting through October and November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
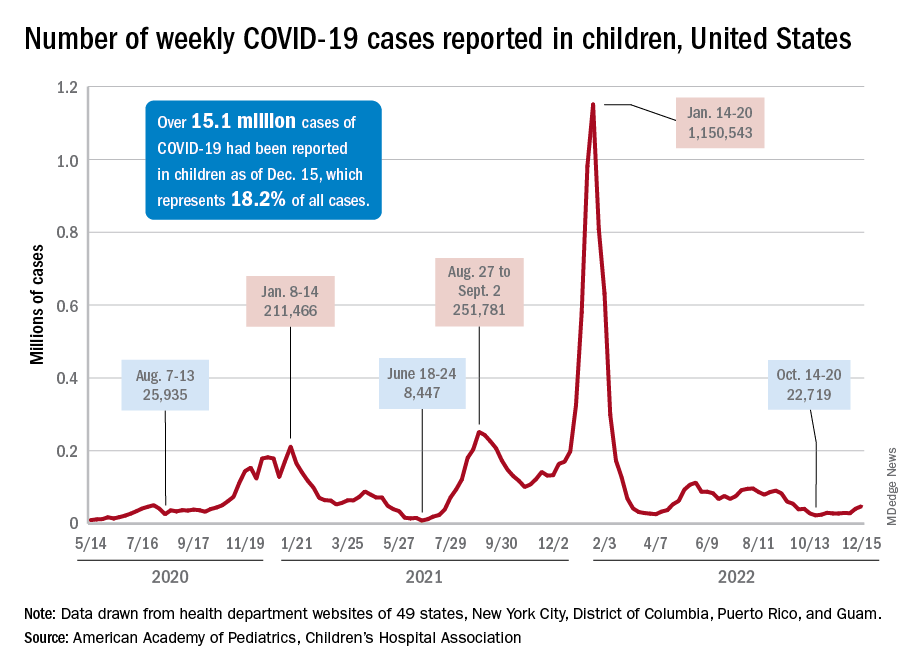
and totaling less than 29,000 for the week of Nov. 25 to Dec. 1. That increase of almost 19,000 cases is the largest over a 2-week period since late July, the AAP and CHA said in their weekly COVID report based on data collected from state and territorial health department websites.
[This publication has been following the AAP/CHA report since the summer of 2020 and continues to share the data for the sake of consistency, but it must be noted that a number of states are no longer updating their public COVID dashboards. As a result, there is now a considerable discrepancy between the AAP/CHA weekly figures and those reported by the Centers for Disease Control and Prevention, which has no such limitations on state data.]
The situation involving new cases over the last 2 weeks is quite different from the CDC’s perspective. The agency does not publish a weekly count, instead offering cumulative cases, which stood at almost 16.1 million as of Dec. 14. Calculating a 2-week total puts the new-case count for Dec. 1-14 at 113,572 among children aged 0-17 years. That is higher than the AAP/CHA count (88,629) for roughly the same period, but it is actually lower than the CDC’s figure (161,832) for the last 2 weeks of November.
The CDC data, in other words, suggest that new cases have gone down in the last 2 weeks, while the AAP and CHA, with their somewhat limited perspective, announced that new cases have gone up.
One COVID-related measure from the CDC that is not contradicted by other sources is hospitalization rates, which had climbed from 0.16 new admissions in children aged 0-17 years with confirmed COVID per 100,000 population on Oct. 22 to 0.29 per 100,000 on Dec. 9. Visits to the emergency department with diagnosed COVID, meanwhile, have been fairly steady so far through December in children, according to the CDC.
New COVID-19 cases in children jumped by 66% during the first 2 weeks of December after an 8-week steady period lasting through October and November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
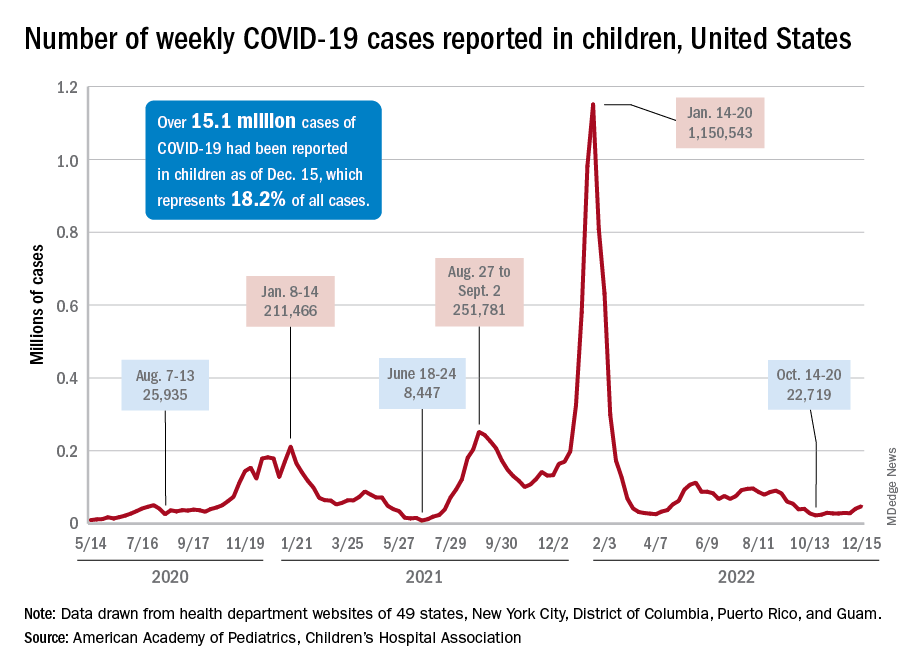
and totaling less than 29,000 for the week of Nov. 25 to Dec. 1. That increase of almost 19,000 cases is the largest over a 2-week period since late July, the AAP and CHA said in their weekly COVID report based on data collected from state and territorial health department websites.
[This publication has been following the AAP/CHA report since the summer of 2020 and continues to share the data for the sake of consistency, but it must be noted that a number of states are no longer updating their public COVID dashboards. As a result, there is now a considerable discrepancy between the AAP/CHA weekly figures and those reported by the Centers for Disease Control and Prevention, which has no such limitations on state data.]
The situation involving new cases over the last 2 weeks is quite different from the CDC’s perspective. The agency does not publish a weekly count, instead offering cumulative cases, which stood at almost 16.1 million as of Dec. 14. Calculating a 2-week total puts the new-case count for Dec. 1-14 at 113,572 among children aged 0-17 years. That is higher than the AAP/CHA count (88,629) for roughly the same period, but it is actually lower than the CDC’s figure (161,832) for the last 2 weeks of November.
The CDC data, in other words, suggest that new cases have gone down in the last 2 weeks, while the AAP and CHA, with their somewhat limited perspective, announced that new cases have gone up.
One COVID-related measure from the CDC that is not contradicted by other sources is hospitalization rates, which had climbed from 0.16 new admissions in children aged 0-17 years with confirmed COVID per 100,000 population on Oct. 22 to 0.29 per 100,000 on Dec. 9. Visits to the emergency department with diagnosed COVID, meanwhile, have been fairly steady so far through December in children, according to the CDC.








