User login
ID experts dole out practical advice to help with mask confusion
The Centers for Disease Control and Prevention’s latest guidance on what fully vaccinated people can do safely – including not socially distancing and not wearing a mask indoors or outdoors unless other regulations require it – has been widely misinterpreted and caused confusion, two infectious disease experts said at a briefing on May 20 hosted by the Infectious Diseases Society of America (IDSA).
The CDC did not ‘’lift” the mask mandate, but rather supplied guidance for those who are fully vaccinated. However, many questions and gray areas remain, and the experts addressed those. ‘’The CDC guidance is really directed at people who are fully vaccinated and who we know are likely to have a really solid response to the vaccine,” said Jeanne Marrazzo, MD, MPH, director of infectious diseases at the University of Alabama at Birmingham and an IDSA board member.
That message was largely lost, said Dr. Marrazzo and Jeffrey Duchin, MD, health officer of public health for Seattle and King County, Washington, and also an IDSA board member. Dr. Duchin said many people mistakenly regarded the new guidance as a message that the pandemic is over.
Among their practical tips on how to interpret the guidance:
To mask or not?
To make the decision, people need to think about not only the numbers of vaccinated versus unvaccinated individuals in their community but the local rates of disease, the experts said. And they need to know that the CDC guidance doesn’t apply if regulations by federal or state authorities or businesses and workplace are in conflict.
Deciding on mask use sometimes depends on where you are going. What about going into grocery stores or large bin stores without a mask? “If you are fully vaccinated and have no other conditions that compromise your immune system, and the rates of COVID are relatively low where you live, and the vaccination rates are high, I would be 100% fine” without a mask, Dr. Marrazzo said. But it’s important to think of all these factors in calculating your risk.
“I’m still wearing a mask when I go anywhere in public,” she said, citing vaccination rates that have not yet reached 50% in her area.
If that rate reached 80%, the typical percentage talked about for herd immunity, and new cases were low, Dr. Marrazzo said she might shed the mask.
The CDC also continues to recommend masks on mass transit for all.
One population that also must be considered, and who must evaluate their risk, even if vaccinated, are the immunocompromised, Dr. Marrazzo said. While people think of the immunocompromised as those with HIV or organ transplants, the numbers are actually much larger.
“A study a couple of years ago indicated up to 3% of Americans may actually have been told by their physician they have some of level of being immunocompromised,” she said. Among the examples are those who are on dialysis, on chemotherapy, or those taking any of the medications that modify the immune system.
“Millions of people fit this bill, and we have [very] little data on whether the vaccine works in them. We think it does,” Dr. Marrazzo said.
Still, she said, it’s a reason for these people to be cautious. For some other vaccines, the dose is modified for those who are immunocompromised. What’s not known yet is whether additional doses of the COVID vaccines might boost protection for those who are immunocompromised.
Many people, even after vaccination, may choose to keep wearing a mask especially in indoor, crowded settings, Dr. Duchin said. “We need to expect, accept, and respect continued mask wearing by anyone at any time.”
In most outdoor settings, he said, “I think masks are probably not necessary, vaccinated or not, regardless of age.” One exception: close face-to-face contact, such as in certain sports.
How to protect toddlers and infants
With masks not practical or recommended for infants and toddlers under 2 years old, Dr. Marrazzo said adults should remember that ‘’those very little kids don’t do poorly at all [even if infected], although there is not a ton of data.”
Adults should still treat young children as vulnerable, especially newborns. Adults not yet vaccinated should wear a mask when around them, she said.
J & J vaccine recipients
With less ‘’real world” data on the Johnson & Johnson vaccine, should those who got it think of themselves in a different risk group than those who got Moderna or Pfizer and adjust their behavior accordingly?
“The J&J vaccine, based on everything we know, does provide a great deal of protection,” Dr. Marrazzo said. ‘’We don’t know as much about prevention of transmission in the asymptomatic cases in the J&J.”
Most of that data, she said, is from the mRNA vaccines Pfizer and Moderna. “I think it’s an important area to study and learn about.” But all three vaccines, overall, provide a high level of protection, she said.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention’s latest guidance on what fully vaccinated people can do safely – including not socially distancing and not wearing a mask indoors or outdoors unless other regulations require it – has been widely misinterpreted and caused confusion, two infectious disease experts said at a briefing on May 20 hosted by the Infectious Diseases Society of America (IDSA).
The CDC did not ‘’lift” the mask mandate, but rather supplied guidance for those who are fully vaccinated. However, many questions and gray areas remain, and the experts addressed those. ‘’The CDC guidance is really directed at people who are fully vaccinated and who we know are likely to have a really solid response to the vaccine,” said Jeanne Marrazzo, MD, MPH, director of infectious diseases at the University of Alabama at Birmingham and an IDSA board member.
That message was largely lost, said Dr. Marrazzo and Jeffrey Duchin, MD, health officer of public health for Seattle and King County, Washington, and also an IDSA board member. Dr. Duchin said many people mistakenly regarded the new guidance as a message that the pandemic is over.
Among their practical tips on how to interpret the guidance:
To mask or not?
To make the decision, people need to think about not only the numbers of vaccinated versus unvaccinated individuals in their community but the local rates of disease, the experts said. And they need to know that the CDC guidance doesn’t apply if regulations by federal or state authorities or businesses and workplace are in conflict.
Deciding on mask use sometimes depends on where you are going. What about going into grocery stores or large bin stores without a mask? “If you are fully vaccinated and have no other conditions that compromise your immune system, and the rates of COVID are relatively low where you live, and the vaccination rates are high, I would be 100% fine” without a mask, Dr. Marrazzo said. But it’s important to think of all these factors in calculating your risk.
“I’m still wearing a mask when I go anywhere in public,” she said, citing vaccination rates that have not yet reached 50% in her area.
If that rate reached 80%, the typical percentage talked about for herd immunity, and new cases were low, Dr. Marrazzo said she might shed the mask.
The CDC also continues to recommend masks on mass transit for all.
One population that also must be considered, and who must evaluate their risk, even if vaccinated, are the immunocompromised, Dr. Marrazzo said. While people think of the immunocompromised as those with HIV or organ transplants, the numbers are actually much larger.
“A study a couple of years ago indicated up to 3% of Americans may actually have been told by their physician they have some of level of being immunocompromised,” she said. Among the examples are those who are on dialysis, on chemotherapy, or those taking any of the medications that modify the immune system.
“Millions of people fit this bill, and we have [very] little data on whether the vaccine works in them. We think it does,” Dr. Marrazzo said.
Still, she said, it’s a reason for these people to be cautious. For some other vaccines, the dose is modified for those who are immunocompromised. What’s not known yet is whether additional doses of the COVID vaccines might boost protection for those who are immunocompromised.
Many people, even after vaccination, may choose to keep wearing a mask especially in indoor, crowded settings, Dr. Duchin said. “We need to expect, accept, and respect continued mask wearing by anyone at any time.”
In most outdoor settings, he said, “I think masks are probably not necessary, vaccinated or not, regardless of age.” One exception: close face-to-face contact, such as in certain sports.
How to protect toddlers and infants
With masks not practical or recommended for infants and toddlers under 2 years old, Dr. Marrazzo said adults should remember that ‘’those very little kids don’t do poorly at all [even if infected], although there is not a ton of data.”
Adults should still treat young children as vulnerable, especially newborns. Adults not yet vaccinated should wear a mask when around them, she said.
J & J vaccine recipients
With less ‘’real world” data on the Johnson & Johnson vaccine, should those who got it think of themselves in a different risk group than those who got Moderna or Pfizer and adjust their behavior accordingly?
“The J&J vaccine, based on everything we know, does provide a great deal of protection,” Dr. Marrazzo said. ‘’We don’t know as much about prevention of transmission in the asymptomatic cases in the J&J.”
Most of that data, she said, is from the mRNA vaccines Pfizer and Moderna. “I think it’s an important area to study and learn about.” But all three vaccines, overall, provide a high level of protection, she said.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention’s latest guidance on what fully vaccinated people can do safely – including not socially distancing and not wearing a mask indoors or outdoors unless other regulations require it – has been widely misinterpreted and caused confusion, two infectious disease experts said at a briefing on May 20 hosted by the Infectious Diseases Society of America (IDSA).
The CDC did not ‘’lift” the mask mandate, but rather supplied guidance for those who are fully vaccinated. However, many questions and gray areas remain, and the experts addressed those. ‘’The CDC guidance is really directed at people who are fully vaccinated and who we know are likely to have a really solid response to the vaccine,” said Jeanne Marrazzo, MD, MPH, director of infectious diseases at the University of Alabama at Birmingham and an IDSA board member.
That message was largely lost, said Dr. Marrazzo and Jeffrey Duchin, MD, health officer of public health for Seattle and King County, Washington, and also an IDSA board member. Dr. Duchin said many people mistakenly regarded the new guidance as a message that the pandemic is over.
Among their practical tips on how to interpret the guidance:
To mask or not?
To make the decision, people need to think about not only the numbers of vaccinated versus unvaccinated individuals in their community but the local rates of disease, the experts said. And they need to know that the CDC guidance doesn’t apply if regulations by federal or state authorities or businesses and workplace are in conflict.
Deciding on mask use sometimes depends on where you are going. What about going into grocery stores or large bin stores without a mask? “If you are fully vaccinated and have no other conditions that compromise your immune system, and the rates of COVID are relatively low where you live, and the vaccination rates are high, I would be 100% fine” without a mask, Dr. Marrazzo said. But it’s important to think of all these factors in calculating your risk.
“I’m still wearing a mask when I go anywhere in public,” she said, citing vaccination rates that have not yet reached 50% in her area.
If that rate reached 80%, the typical percentage talked about for herd immunity, and new cases were low, Dr. Marrazzo said she might shed the mask.
The CDC also continues to recommend masks on mass transit for all.
One population that also must be considered, and who must evaluate their risk, even if vaccinated, are the immunocompromised, Dr. Marrazzo said. While people think of the immunocompromised as those with HIV or organ transplants, the numbers are actually much larger.
“A study a couple of years ago indicated up to 3% of Americans may actually have been told by their physician they have some of level of being immunocompromised,” she said. Among the examples are those who are on dialysis, on chemotherapy, or those taking any of the medications that modify the immune system.
“Millions of people fit this bill, and we have [very] little data on whether the vaccine works in them. We think it does,” Dr. Marrazzo said.
Still, she said, it’s a reason for these people to be cautious. For some other vaccines, the dose is modified for those who are immunocompromised. What’s not known yet is whether additional doses of the COVID vaccines might boost protection for those who are immunocompromised.
Many people, even after vaccination, may choose to keep wearing a mask especially in indoor, crowded settings, Dr. Duchin said. “We need to expect, accept, and respect continued mask wearing by anyone at any time.”
In most outdoor settings, he said, “I think masks are probably not necessary, vaccinated or not, regardless of age.” One exception: close face-to-face contact, such as in certain sports.
How to protect toddlers and infants
With masks not practical or recommended for infants and toddlers under 2 years old, Dr. Marrazzo said adults should remember that ‘’those very little kids don’t do poorly at all [even if infected], although there is not a ton of data.”
Adults should still treat young children as vulnerable, especially newborns. Adults not yet vaccinated should wear a mask when around them, she said.
J & J vaccine recipients
With less ‘’real world” data on the Johnson & Johnson vaccine, should those who got it think of themselves in a different risk group than those who got Moderna or Pfizer and adjust their behavior accordingly?
“The J&J vaccine, based on everything we know, does provide a great deal of protection,” Dr. Marrazzo said. ‘’We don’t know as much about prevention of transmission in the asymptomatic cases in the J&J.”
Most of that data, she said, is from the mRNA vaccines Pfizer and Moderna. “I think it’s an important area to study and learn about.” But all three vaccines, overall, provide a high level of protection, she said.
A version of this article first appeared on Medscape.com.
Care of post–acute COVID-19 patients requires multidisciplinary collaboration
In the wake of the COVID-19 pandemic, a population of patients has arisen with a range of symptoms and complications after surviving the acute phase of illness, according to Mezgebe Berhe, MD, of Baylor University Medical Center, Dallas.
Different terms have been used to describe this condition, including post COVID, long COVID, chronic COVID, and long-haulers, Dr. Berhe said in a presentation at SHM Converge, the annual conference of the Society of Hospital Medicine. However, the current medical consensus for a definition is post–acute COVID-19 syndrome.
Acute COVID-19 generally lasts for about 4 weeks after the onset of symptoms, and post–acute COVID-19 is generally defined as “persistent symptoms and/or delayed or long-term complications beyond 4 weeks from the onset of symptoms,” he said. The postacute period may be broken into a subacute phase with symptoms and abnormalities present from 4-12 weeks beyond the acute phase, and then a chronic or post–acute COVID-19 syndrome, with symptoms and abnormalities present beyond 12 weeks after the onset of acute COVID-19.
Patients in the subacute or post–COVID-19 phase of illness are polymerase chain reaction negative and may have multiorgan symptomatology, said Dr. Berhe. Physical symptoms include fatigue, decline in quality of life, joint pain, and muscle weakness; reported mental symptoms include anxiety and depression; sleep disturbance; PTSD; cognitive disturbance (described by patients as “brain fog”); and headaches.
Pulmonary symptoms in post–acute COVID-19 patients include dyspnea, cough, and persistent oxygen requirements; patients also have reported palpitations and chest pain. Thromboembolism, chronic kidney disease, and hair loss also have been reported in COVID-19 patients in the postacute period.
What studies show
Early reports on postacute consequences of COVID-19 have been reported in published studies from the United States, Europe, and China, and the current treatment recommendations are based on findings from these studies, Dr. Berhe said.
In an observational cohort study from 38 hospitals in Michigan, researchers assessed 60-day outcomes for 1,250 COVID-19 patients who were discharged alive from the hospital. The researchers used medical record abstraction and telephone surveys to assess long-term symptoms. Overall, 6.7% of the patients died and 15.1% required hospital readmission. A total of 488 patients completed the telephone survey. Of these, 32.6% reported persistent symptoms, 18.9% reported new or worsening symptoms, 22.9% reported dyspnea while walking up stairs, 15.4% reported a cough, and 13.1% reported a persistent loss of taste or smell.
Data from multiple countries in Europe have shown similar prevalence of post–acute COVID-19 syndrome, but Dr. Berhe highlighted an Italian study in which 87% of 143 patients discharged from hospitals after acute COVID-19 reported at least one symptom at 60 day. “A decline in quality of life, as measured by the EuroQol visual analog scale, was reported by 44.1% of patients” in the Italian study, Dr. Berhe noted.
In a prospective cohort study conducted in Wuhan, China, researchers conducted a comprehensive in-person evaluation of symptoms in 1,733 COVID-19 patients at 6 months from symptom onset, and found that 76% reported at least one symptom, said Dr. Berhe. “Similar to other studies, muscle weakness and fatigue were the most common symptoms, followed by sleep problems and anxiety/depression.
Dr. Berhe also cited a literature review published in Clinical Infectious Diseases that addressed COVID-19 in children; in one study of postacute COVID-19, approximately 12% of children had 5 weeks’ prevalence of persistent symptoms, compared with 22% of adults. This finding should remind clinicians that “Children can have devastating persistent symptoms following acute COVID-19 disease,” Dr. Berhe said.
In the post–acute COVID clinic
“Multidisciplinary collaboration is essential to provide integrated outpatient care to survivors of acute COVID-19,” Dr. Berhe said. Such collaboration includes pulmonary and cardiovascular symptom assessment through virtual or in-person follow-up at 4-6 weeks and at 12 weeks after hospital discharge. For those with dyspnea and persistent oxygen requirements at 12 weeks, consider the 6-minute walk test, pulmonary function test, chest x-ray, pulmonary embolism work-up, echocardiogram, and high-resolution CT of the chest as indicated.
With regard to neuropsychiatry, patients should be screened for anxiety, depression, PTSD, sleep disturbance, and cognitive impairment, said Dr. Berhe.
For hematology, “consider extended thromboprophylaxis for high-risk survivors based on shared decision-making,” he said. The incidence of thrombotic events post COVID is less than 5% so you have to be very selective and they should be in the highest-risk category.
COVID-19 patients with acute kidney infections should have a follow-up with a nephrologist soon after hospital discharge, he added.
From a primary care standpoint, early rehabilitation and patient education are important for managing symptoms; also consider recommending patient enrollment in research studies, Dr. Berhe said.
Dr. Berhe has been involved in multiple clinical trials of treating acute COVID-19 patients, but had no financial conflicts to disclose.
In the wake of the COVID-19 pandemic, a population of patients has arisen with a range of symptoms and complications after surviving the acute phase of illness, according to Mezgebe Berhe, MD, of Baylor University Medical Center, Dallas.
Different terms have been used to describe this condition, including post COVID, long COVID, chronic COVID, and long-haulers, Dr. Berhe said in a presentation at SHM Converge, the annual conference of the Society of Hospital Medicine. However, the current medical consensus for a definition is post–acute COVID-19 syndrome.
Acute COVID-19 generally lasts for about 4 weeks after the onset of symptoms, and post–acute COVID-19 is generally defined as “persistent symptoms and/or delayed or long-term complications beyond 4 weeks from the onset of symptoms,” he said. The postacute period may be broken into a subacute phase with symptoms and abnormalities present from 4-12 weeks beyond the acute phase, and then a chronic or post–acute COVID-19 syndrome, with symptoms and abnormalities present beyond 12 weeks after the onset of acute COVID-19.
Patients in the subacute or post–COVID-19 phase of illness are polymerase chain reaction negative and may have multiorgan symptomatology, said Dr. Berhe. Physical symptoms include fatigue, decline in quality of life, joint pain, and muscle weakness; reported mental symptoms include anxiety and depression; sleep disturbance; PTSD; cognitive disturbance (described by patients as “brain fog”); and headaches.
Pulmonary symptoms in post–acute COVID-19 patients include dyspnea, cough, and persistent oxygen requirements; patients also have reported palpitations and chest pain. Thromboembolism, chronic kidney disease, and hair loss also have been reported in COVID-19 patients in the postacute period.
What studies show
Early reports on postacute consequences of COVID-19 have been reported in published studies from the United States, Europe, and China, and the current treatment recommendations are based on findings from these studies, Dr. Berhe said.
In an observational cohort study from 38 hospitals in Michigan, researchers assessed 60-day outcomes for 1,250 COVID-19 patients who were discharged alive from the hospital. The researchers used medical record abstraction and telephone surveys to assess long-term symptoms. Overall, 6.7% of the patients died and 15.1% required hospital readmission. A total of 488 patients completed the telephone survey. Of these, 32.6% reported persistent symptoms, 18.9% reported new or worsening symptoms, 22.9% reported dyspnea while walking up stairs, 15.4% reported a cough, and 13.1% reported a persistent loss of taste or smell.
Data from multiple countries in Europe have shown similar prevalence of post–acute COVID-19 syndrome, but Dr. Berhe highlighted an Italian study in which 87% of 143 patients discharged from hospitals after acute COVID-19 reported at least one symptom at 60 day. “A decline in quality of life, as measured by the EuroQol visual analog scale, was reported by 44.1% of patients” in the Italian study, Dr. Berhe noted.
In a prospective cohort study conducted in Wuhan, China, researchers conducted a comprehensive in-person evaluation of symptoms in 1,733 COVID-19 patients at 6 months from symptom onset, and found that 76% reported at least one symptom, said Dr. Berhe. “Similar to other studies, muscle weakness and fatigue were the most common symptoms, followed by sleep problems and anxiety/depression.
Dr. Berhe also cited a literature review published in Clinical Infectious Diseases that addressed COVID-19 in children; in one study of postacute COVID-19, approximately 12% of children had 5 weeks’ prevalence of persistent symptoms, compared with 22% of adults. This finding should remind clinicians that “Children can have devastating persistent symptoms following acute COVID-19 disease,” Dr. Berhe said.
In the post–acute COVID clinic
“Multidisciplinary collaboration is essential to provide integrated outpatient care to survivors of acute COVID-19,” Dr. Berhe said. Such collaboration includes pulmonary and cardiovascular symptom assessment through virtual or in-person follow-up at 4-6 weeks and at 12 weeks after hospital discharge. For those with dyspnea and persistent oxygen requirements at 12 weeks, consider the 6-minute walk test, pulmonary function test, chest x-ray, pulmonary embolism work-up, echocardiogram, and high-resolution CT of the chest as indicated.
With regard to neuropsychiatry, patients should be screened for anxiety, depression, PTSD, sleep disturbance, and cognitive impairment, said Dr. Berhe.
For hematology, “consider extended thromboprophylaxis for high-risk survivors based on shared decision-making,” he said. The incidence of thrombotic events post COVID is less than 5% so you have to be very selective and they should be in the highest-risk category.
COVID-19 patients with acute kidney infections should have a follow-up with a nephrologist soon after hospital discharge, he added.
From a primary care standpoint, early rehabilitation and patient education are important for managing symptoms; also consider recommending patient enrollment in research studies, Dr. Berhe said.
Dr. Berhe has been involved in multiple clinical trials of treating acute COVID-19 patients, but had no financial conflicts to disclose.
In the wake of the COVID-19 pandemic, a population of patients has arisen with a range of symptoms and complications after surviving the acute phase of illness, according to Mezgebe Berhe, MD, of Baylor University Medical Center, Dallas.
Different terms have been used to describe this condition, including post COVID, long COVID, chronic COVID, and long-haulers, Dr. Berhe said in a presentation at SHM Converge, the annual conference of the Society of Hospital Medicine. However, the current medical consensus for a definition is post–acute COVID-19 syndrome.
Acute COVID-19 generally lasts for about 4 weeks after the onset of symptoms, and post–acute COVID-19 is generally defined as “persistent symptoms and/or delayed or long-term complications beyond 4 weeks from the onset of symptoms,” he said. The postacute period may be broken into a subacute phase with symptoms and abnormalities present from 4-12 weeks beyond the acute phase, and then a chronic or post–acute COVID-19 syndrome, with symptoms and abnormalities present beyond 12 weeks after the onset of acute COVID-19.
Patients in the subacute or post–COVID-19 phase of illness are polymerase chain reaction negative and may have multiorgan symptomatology, said Dr. Berhe. Physical symptoms include fatigue, decline in quality of life, joint pain, and muscle weakness; reported mental symptoms include anxiety and depression; sleep disturbance; PTSD; cognitive disturbance (described by patients as “brain fog”); and headaches.
Pulmonary symptoms in post–acute COVID-19 patients include dyspnea, cough, and persistent oxygen requirements; patients also have reported palpitations and chest pain. Thromboembolism, chronic kidney disease, and hair loss also have been reported in COVID-19 patients in the postacute period.
What studies show
Early reports on postacute consequences of COVID-19 have been reported in published studies from the United States, Europe, and China, and the current treatment recommendations are based on findings from these studies, Dr. Berhe said.
In an observational cohort study from 38 hospitals in Michigan, researchers assessed 60-day outcomes for 1,250 COVID-19 patients who were discharged alive from the hospital. The researchers used medical record abstraction and telephone surveys to assess long-term symptoms. Overall, 6.7% of the patients died and 15.1% required hospital readmission. A total of 488 patients completed the telephone survey. Of these, 32.6% reported persistent symptoms, 18.9% reported new or worsening symptoms, 22.9% reported dyspnea while walking up stairs, 15.4% reported a cough, and 13.1% reported a persistent loss of taste or smell.
Data from multiple countries in Europe have shown similar prevalence of post–acute COVID-19 syndrome, but Dr. Berhe highlighted an Italian study in which 87% of 143 patients discharged from hospitals after acute COVID-19 reported at least one symptom at 60 day. “A decline in quality of life, as measured by the EuroQol visual analog scale, was reported by 44.1% of patients” in the Italian study, Dr. Berhe noted.
In a prospective cohort study conducted in Wuhan, China, researchers conducted a comprehensive in-person evaluation of symptoms in 1,733 COVID-19 patients at 6 months from symptom onset, and found that 76% reported at least one symptom, said Dr. Berhe. “Similar to other studies, muscle weakness and fatigue were the most common symptoms, followed by sleep problems and anxiety/depression.
Dr. Berhe also cited a literature review published in Clinical Infectious Diseases that addressed COVID-19 in children; in one study of postacute COVID-19, approximately 12% of children had 5 weeks’ prevalence of persistent symptoms, compared with 22% of adults. This finding should remind clinicians that “Children can have devastating persistent symptoms following acute COVID-19 disease,” Dr. Berhe said.
In the post–acute COVID clinic
“Multidisciplinary collaboration is essential to provide integrated outpatient care to survivors of acute COVID-19,” Dr. Berhe said. Such collaboration includes pulmonary and cardiovascular symptom assessment through virtual or in-person follow-up at 4-6 weeks and at 12 weeks after hospital discharge. For those with dyspnea and persistent oxygen requirements at 12 weeks, consider the 6-minute walk test, pulmonary function test, chest x-ray, pulmonary embolism work-up, echocardiogram, and high-resolution CT of the chest as indicated.
With regard to neuropsychiatry, patients should be screened for anxiety, depression, PTSD, sleep disturbance, and cognitive impairment, said Dr. Berhe.
For hematology, “consider extended thromboprophylaxis for high-risk survivors based on shared decision-making,” he said. The incidence of thrombotic events post COVID is less than 5% so you have to be very selective and they should be in the highest-risk category.
COVID-19 patients with acute kidney infections should have a follow-up with a nephrologist soon after hospital discharge, he added.
From a primary care standpoint, early rehabilitation and patient education are important for managing symptoms; also consider recommending patient enrollment in research studies, Dr. Berhe said.
Dr. Berhe has been involved in multiple clinical trials of treating acute COVID-19 patients, but had no financial conflicts to disclose.
FROM SHM CONVERGE 2021
HHS to inject billions into mental health, substance use disorders
The U.S. Department of Health and Human Services will inject billions of dollars into programs designed to address mental health and substance use disorders, including $3 billion released to states as of May 18, said federal officials.
The American Rescue Plan, a COVID-relief package signed into law in March, contained the money, which will be divided equally between the Community Mental Health Services Block Grant Program and the Substance Abuse Prevention and Treatment Block Grant Program, said Tom Coderre, Acting Assistant Secretary for Mental Health and Substance Use, in a call with reporters.
The award amounts will vary by state.
The mental health program helps states and territories provide services for children with serious emotional issues and adults with serious mental illness.
The substance use program provides money to plan, implement, and evaluate prevention, intervention, treatment, and recovery services.
, which fueled an increase in anxiety, depression, and overdose, said Assistant Secretary for Health Rachel Levine, MD, on the call.
“We know multiple stressors during the pandemic – isolation, sickness, grief, job loss, food instability, and loss of routines – have devastated many Americans and presented the unprecedented behavioral health challenges across the nation,” said Dr. Levine.
The HHS also announced that it is re-establishing a Behavioral Health Coordinating Council (BHCC). Dr. Levine and Mr. Coderre will serve as cochairs of the Council, which will coordinate action-oriented approaches to addressing the HHS’s behavioral health efforts.
However, in 2014, the U.S. Government Accountability Office criticized the BHCC for only focusing on the HHS, and noted the lack of coordination across the federal government’s various efforts to address mental health.
‘A huge step forward’
The American Psychiatric Association welcomed the new money and the return of the council.
“In the wake of the pandemic an unprecedented, and as of yet untold, number of Americans are faced with mental health and substance use disorders, particularly in communities impacted by structural racism,” said APA President Vivian Pender, MD, in a statement. “With the creation of this Council and this investment in mental health, the administration is taking a huge step forward.”
APA CEO and Medical Director Saul Levin, MD, MPA, added: “This Council has great potential to ease the challenges we face as we begin to recover from the pandemic’s impact on our society, and [the] APA looks forward to assisting in their efforts.”
HHS Secretary Xavier Becerra noted in a statement that the COVID-19 pandemic “has made clear the need to invest resources in our nation’s mental health and address the inequities that still exist around behavioral health care.” He added, “This national problem calls for department-wide coordination to address the issue.”
Dr. Levine said the Council “will assure the right prioritization and guidelines are in place to provide pathways to prevention, intervention, treatment, and recovery services.”
A version of this article first appeared on Medscape.com.
The U.S. Department of Health and Human Services will inject billions of dollars into programs designed to address mental health and substance use disorders, including $3 billion released to states as of May 18, said federal officials.
The American Rescue Plan, a COVID-relief package signed into law in March, contained the money, which will be divided equally between the Community Mental Health Services Block Grant Program and the Substance Abuse Prevention and Treatment Block Grant Program, said Tom Coderre, Acting Assistant Secretary for Mental Health and Substance Use, in a call with reporters.
The award amounts will vary by state.
The mental health program helps states and territories provide services for children with serious emotional issues and adults with serious mental illness.
The substance use program provides money to plan, implement, and evaluate prevention, intervention, treatment, and recovery services.
, which fueled an increase in anxiety, depression, and overdose, said Assistant Secretary for Health Rachel Levine, MD, on the call.
“We know multiple stressors during the pandemic – isolation, sickness, grief, job loss, food instability, and loss of routines – have devastated many Americans and presented the unprecedented behavioral health challenges across the nation,” said Dr. Levine.
The HHS also announced that it is re-establishing a Behavioral Health Coordinating Council (BHCC). Dr. Levine and Mr. Coderre will serve as cochairs of the Council, which will coordinate action-oriented approaches to addressing the HHS’s behavioral health efforts.
However, in 2014, the U.S. Government Accountability Office criticized the BHCC for only focusing on the HHS, and noted the lack of coordination across the federal government’s various efforts to address mental health.
‘A huge step forward’
The American Psychiatric Association welcomed the new money and the return of the council.
“In the wake of the pandemic an unprecedented, and as of yet untold, number of Americans are faced with mental health and substance use disorders, particularly in communities impacted by structural racism,” said APA President Vivian Pender, MD, in a statement. “With the creation of this Council and this investment in mental health, the administration is taking a huge step forward.”
APA CEO and Medical Director Saul Levin, MD, MPA, added: “This Council has great potential to ease the challenges we face as we begin to recover from the pandemic’s impact on our society, and [the] APA looks forward to assisting in their efforts.”
HHS Secretary Xavier Becerra noted in a statement that the COVID-19 pandemic “has made clear the need to invest resources in our nation’s mental health and address the inequities that still exist around behavioral health care.” He added, “This national problem calls for department-wide coordination to address the issue.”
Dr. Levine said the Council “will assure the right prioritization and guidelines are in place to provide pathways to prevention, intervention, treatment, and recovery services.”
A version of this article first appeared on Medscape.com.
The U.S. Department of Health and Human Services will inject billions of dollars into programs designed to address mental health and substance use disorders, including $3 billion released to states as of May 18, said federal officials.
The American Rescue Plan, a COVID-relief package signed into law in March, contained the money, which will be divided equally between the Community Mental Health Services Block Grant Program and the Substance Abuse Prevention and Treatment Block Grant Program, said Tom Coderre, Acting Assistant Secretary for Mental Health and Substance Use, in a call with reporters.
The award amounts will vary by state.
The mental health program helps states and territories provide services for children with serious emotional issues and adults with serious mental illness.
The substance use program provides money to plan, implement, and evaluate prevention, intervention, treatment, and recovery services.
, which fueled an increase in anxiety, depression, and overdose, said Assistant Secretary for Health Rachel Levine, MD, on the call.
“We know multiple stressors during the pandemic – isolation, sickness, grief, job loss, food instability, and loss of routines – have devastated many Americans and presented the unprecedented behavioral health challenges across the nation,” said Dr. Levine.
The HHS also announced that it is re-establishing a Behavioral Health Coordinating Council (BHCC). Dr. Levine and Mr. Coderre will serve as cochairs of the Council, which will coordinate action-oriented approaches to addressing the HHS’s behavioral health efforts.
However, in 2014, the U.S. Government Accountability Office criticized the BHCC for only focusing on the HHS, and noted the lack of coordination across the federal government’s various efforts to address mental health.
‘A huge step forward’
The American Psychiatric Association welcomed the new money and the return of the council.
“In the wake of the pandemic an unprecedented, and as of yet untold, number of Americans are faced with mental health and substance use disorders, particularly in communities impacted by structural racism,” said APA President Vivian Pender, MD, in a statement. “With the creation of this Council and this investment in mental health, the administration is taking a huge step forward.”
APA CEO and Medical Director Saul Levin, MD, MPA, added: “This Council has great potential to ease the challenges we face as we begin to recover from the pandemic’s impact on our society, and [the] APA looks forward to assisting in their efforts.”
HHS Secretary Xavier Becerra noted in a statement that the COVID-19 pandemic “has made clear the need to invest resources in our nation’s mental health and address the inequities that still exist around behavioral health care.” He added, “This national problem calls for department-wide coordination to address the issue.”
Dr. Levine said the Council “will assure the right prioritization and guidelines are in place to provide pathways to prevention, intervention, treatment, and recovery services.”
A version of this article first appeared on Medscape.com.
Family physicians’ compensation levels stable in pandemic
to $236,000, up from $234,000 last year, even as many practices saw a decrease in hours and patient visits during the pandemic.
Only pediatricians earned less ($221,000) according to the Medscape Family Physician Compensation Report 2021. Plastic surgeons topped this year’s list, at $526,000, followed by orthopedists, at $511,000, and cardiologists, at $459,000.
Family physicians ranked in the middle of specialties in terms of the percentages of physicians who thought they were fairly compensated: 57% of family physicians said they were fairly paid, and 79% of oncologists said they were. Only 44% of infectious disease physicians said they were fairly compensated.
Survey answers indicate, though, that pay isn’t driving family physicians’ satisfaction.
Only 10% of family physicians in the survey said that “making good money at a job I like” was the most rewarding aspect of the job. The top two answers by far were “gratitude/relationships with patients” (chosen by 34%) and “knowing I’m making the world a better place” (27%). Respondents could choose more than one answer.
Despite the small uptick in earnings overall in the specialty, more than one-third of family physicians (36%) reported a decline in compensation in this year’s survey, which included 18,000 responses from physicians in 29 specialties.
Male family physicians continue to be paid much more than their female colleagues, this year 29% more, widening the gap from 26% last year. Overall, men in primary care earned 27% more than their female colleagues, and male specialists earned 33% more.
As for decline in patients seen in some specialties, family physicians are holding their own.
Whereas pediatricians have seen a drop of 18% in patient visits, family physicians saw a decline of just 5%, from an average of 81 to 77 patients per week.
Most expect return to normal pay within 3 years
Most family physicians (83%) who incurred financial losses this year said they expect that income will return to normal within 3 years. More than one-third of that group (38%) said they expect compensation to get back to normal in the next year.
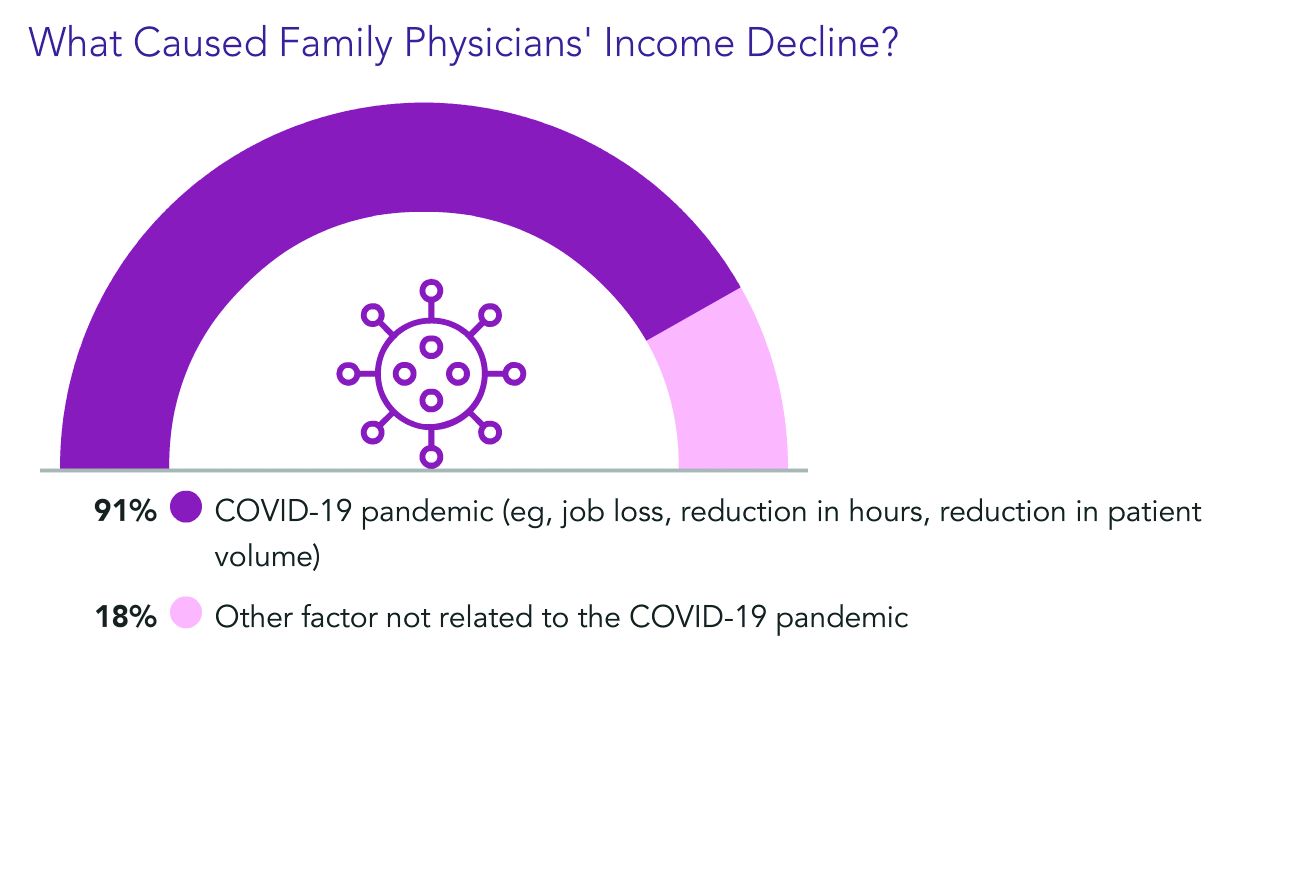
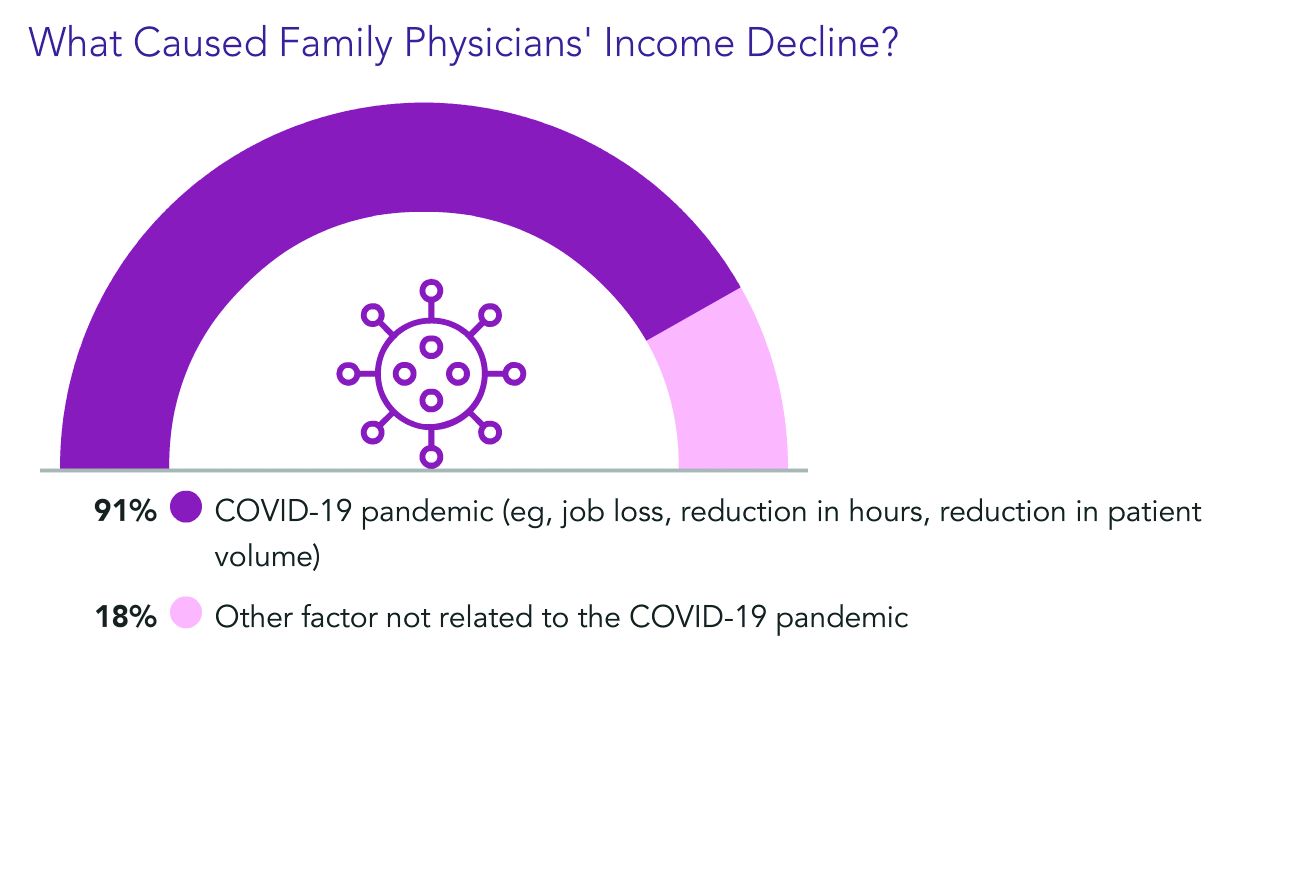
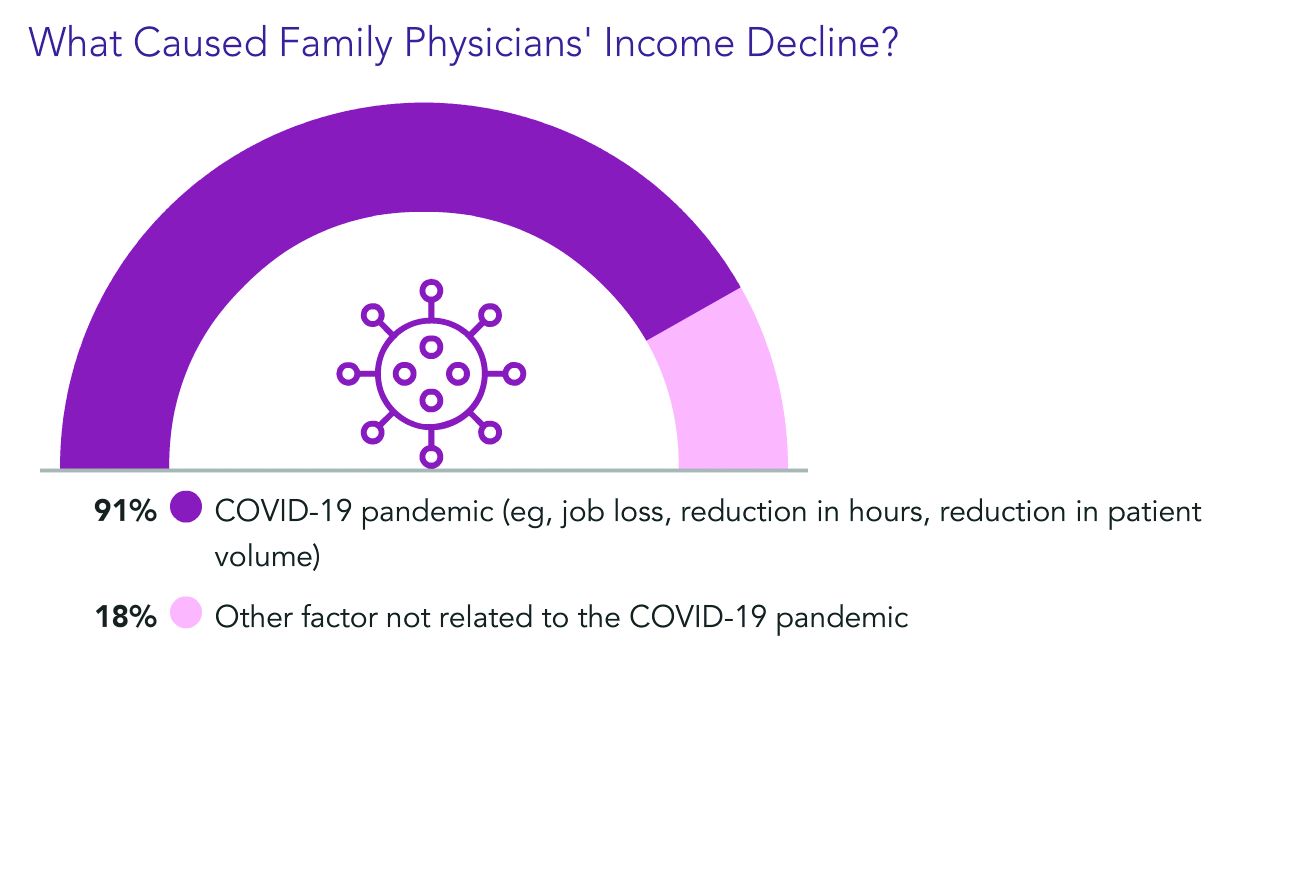
Almost all of the family physicians who lost income (91%) pointed the finger at COVID-19. Respondents could choose more than one answer, and 18% said other factors were also to blame.
Family physicians averaged $27,000 in incentive bonuses, higher than those in internal medicine, pediatrics, and psychiatry. Orthopedists had by far the highest bonuses, at $116,000.
For family physicians who received a bonus this year, the amount equaled about 12% of their salary, up from 10% last year. Bonuses are usually based on productivity but can also be tied to patient satisfaction, clinical processes, and other factors.
The number of family physicians who achieved more than three-quarters of their potential annual bonus rose to 61% this year, up from 55%.
17 hours a week on administrative tasks
The survey also ranked specialties by the amount of time physicians spent on paperwork and administrative tasks, including participation in professional organizations and clinical reading.
Family physicians fell squarely in the middle, with 17 hours per week spent on such tasks. Infectious disease physicians spent the most time, at 24.2 hours a week, and anesthesiologists spent the least, at 10.1.
Work hours declined for many physicians during the pandemic, and some were furloughed.
But, like most physicians, family physicians are once more working normal hours. They average 49 hours per week, which is slightly more than before the pandemic.
Specialists whose weekly hours are above normal are infectious disease physicians, intensivists, and public health and preventive medicine physicians; all are working 6 to 7 hours a week more than usual, according to the survey responses.
Responses also turned up some uncertainty on the future makeup of patient panels.
Most family physicians (69%) said they would continue to take new and current Medicare/Medicaid patients.
However, close to one-third of family physicians said they would stop treating at least some patients they already have and will not take new ones or haven’t decided yet.
A version of this article first appeared on Medscape.com.
to $236,000, up from $234,000 last year, even as many practices saw a decrease in hours and patient visits during the pandemic.
Only pediatricians earned less ($221,000) according to the Medscape Family Physician Compensation Report 2021. Plastic surgeons topped this year’s list, at $526,000, followed by orthopedists, at $511,000, and cardiologists, at $459,000.
Family physicians ranked in the middle of specialties in terms of the percentages of physicians who thought they were fairly compensated: 57% of family physicians said they were fairly paid, and 79% of oncologists said they were. Only 44% of infectious disease physicians said they were fairly compensated.
Survey answers indicate, though, that pay isn’t driving family physicians’ satisfaction.
Only 10% of family physicians in the survey said that “making good money at a job I like” was the most rewarding aspect of the job. The top two answers by far were “gratitude/relationships with patients” (chosen by 34%) and “knowing I’m making the world a better place” (27%). Respondents could choose more than one answer.
Despite the small uptick in earnings overall in the specialty, more than one-third of family physicians (36%) reported a decline in compensation in this year’s survey, which included 18,000 responses from physicians in 29 specialties.
Male family physicians continue to be paid much more than their female colleagues, this year 29% more, widening the gap from 26% last year. Overall, men in primary care earned 27% more than their female colleagues, and male specialists earned 33% more.
As for decline in patients seen in some specialties, family physicians are holding their own.
Whereas pediatricians have seen a drop of 18% in patient visits, family physicians saw a decline of just 5%, from an average of 81 to 77 patients per week.
Most expect return to normal pay within 3 years
Most family physicians (83%) who incurred financial losses this year said they expect that income will return to normal within 3 years. More than one-third of that group (38%) said they expect compensation to get back to normal in the next year.
Almost all of the family physicians who lost income (91%) pointed the finger at COVID-19. Respondents could choose more than one answer, and 18% said other factors were also to blame.
Family physicians averaged $27,000 in incentive bonuses, higher than those in internal medicine, pediatrics, and psychiatry. Orthopedists had by far the highest bonuses, at $116,000.
For family physicians who received a bonus this year, the amount equaled about 12% of their salary, up from 10% last year. Bonuses are usually based on productivity but can also be tied to patient satisfaction, clinical processes, and other factors.
The number of family physicians who achieved more than three-quarters of their potential annual bonus rose to 61% this year, up from 55%.
17 hours a week on administrative tasks
The survey also ranked specialties by the amount of time physicians spent on paperwork and administrative tasks, including participation in professional organizations and clinical reading.
Family physicians fell squarely in the middle, with 17 hours per week spent on such tasks. Infectious disease physicians spent the most time, at 24.2 hours a week, and anesthesiologists spent the least, at 10.1.
Work hours declined for many physicians during the pandemic, and some were furloughed.
But, like most physicians, family physicians are once more working normal hours. They average 49 hours per week, which is slightly more than before the pandemic.
Specialists whose weekly hours are above normal are infectious disease physicians, intensivists, and public health and preventive medicine physicians; all are working 6 to 7 hours a week more than usual, according to the survey responses.
Responses also turned up some uncertainty on the future makeup of patient panels.
Most family physicians (69%) said they would continue to take new and current Medicare/Medicaid patients.
However, close to one-third of family physicians said they would stop treating at least some patients they already have and will not take new ones or haven’t decided yet.
A version of this article first appeared on Medscape.com.
to $236,000, up from $234,000 last year, even as many practices saw a decrease in hours and patient visits during the pandemic.
Only pediatricians earned less ($221,000) according to the Medscape Family Physician Compensation Report 2021. Plastic surgeons topped this year’s list, at $526,000, followed by orthopedists, at $511,000, and cardiologists, at $459,000.
Family physicians ranked in the middle of specialties in terms of the percentages of physicians who thought they were fairly compensated: 57% of family physicians said they were fairly paid, and 79% of oncologists said they were. Only 44% of infectious disease physicians said they were fairly compensated.
Survey answers indicate, though, that pay isn’t driving family physicians’ satisfaction.
Only 10% of family physicians in the survey said that “making good money at a job I like” was the most rewarding aspect of the job. The top two answers by far were “gratitude/relationships with patients” (chosen by 34%) and “knowing I’m making the world a better place” (27%). Respondents could choose more than one answer.
Despite the small uptick in earnings overall in the specialty, more than one-third of family physicians (36%) reported a decline in compensation in this year’s survey, which included 18,000 responses from physicians in 29 specialties.
Male family physicians continue to be paid much more than their female colleagues, this year 29% more, widening the gap from 26% last year. Overall, men in primary care earned 27% more than their female colleagues, and male specialists earned 33% more.
As for decline in patients seen in some specialties, family physicians are holding their own.
Whereas pediatricians have seen a drop of 18% in patient visits, family physicians saw a decline of just 5%, from an average of 81 to 77 patients per week.
Most expect return to normal pay within 3 years
Most family physicians (83%) who incurred financial losses this year said they expect that income will return to normal within 3 years. More than one-third of that group (38%) said they expect compensation to get back to normal in the next year.
Almost all of the family physicians who lost income (91%) pointed the finger at COVID-19. Respondents could choose more than one answer, and 18% said other factors were also to blame.
Family physicians averaged $27,000 in incentive bonuses, higher than those in internal medicine, pediatrics, and psychiatry. Orthopedists had by far the highest bonuses, at $116,000.
For family physicians who received a bonus this year, the amount equaled about 12% of their salary, up from 10% last year. Bonuses are usually based on productivity but can also be tied to patient satisfaction, clinical processes, and other factors.
The number of family physicians who achieved more than three-quarters of their potential annual bonus rose to 61% this year, up from 55%.
17 hours a week on administrative tasks
The survey also ranked specialties by the amount of time physicians spent on paperwork and administrative tasks, including participation in professional organizations and clinical reading.
Family physicians fell squarely in the middle, with 17 hours per week spent on such tasks. Infectious disease physicians spent the most time, at 24.2 hours a week, and anesthesiologists spent the least, at 10.1.
Work hours declined for many physicians during the pandemic, and some were furloughed.
But, like most physicians, family physicians are once more working normal hours. They average 49 hours per week, which is slightly more than before the pandemic.
Specialists whose weekly hours are above normal are infectious disease physicians, intensivists, and public health and preventive medicine physicians; all are working 6 to 7 hours a week more than usual, according to the survey responses.
Responses also turned up some uncertainty on the future makeup of patient panels.
Most family physicians (69%) said they would continue to take new and current Medicare/Medicaid patients.
However, close to one-third of family physicians said they would stop treating at least some patients they already have and will not take new ones or haven’t decided yet.
A version of this article first appeared on Medscape.com.
Hospital outcomes for children with MIS-C unaffected by initial presentation site
Length of hospital stay and the need for intensive care for pediatric COVID-19 patients with multisystem inflammatory syndrome in children was not significantly different for those who presented first as outpatients or emergency patients, based on data from 34 children.
Multisystem inflammatory syndrome in children (MIS-C) can be challenging to diagnose, as the key characteristics of fever, elevated inflammatory markers, and involvement of at least two organ systems often overlap with other illnesses, said Erin B. Treemarcki, DO, of the University of Utah, Salt Lake City, and colleagues.
“Primary care and urgent care providers are often the first point of health care for children with symptoms of MIS-C,” the researchers wrote. In a study (Poster 142) presented at the annual meeting of the Pediatric Academic Societies, held virtually, the researchers conducted a retrospective review of 34 patients younger than 21 years who were hospitalized with MIS-C at a single center between April 2020 and December 2020. The average age of the patients was 7.9 years, 68% were male, 82% were White, and 53% first presented to an outpatient clinic.
Sixteen patients presented to an emergency department and 18 presented to an ambulatory setting. The length of hospitalization ranged from 3 to 16 days with a median of 6 days, and the PICU stay ranged from 1 to 10 days with a median of 2 days.
Overall, the length of hospital stay and rate of PICU admission were not significantly different between the emergency presentation and outpatient presentation groups. Twenty-four patients entered the PICU, 13 at admission and 11 as transfers. However, the median number of days of symptoms prior to admission was significantly higher for outpatient cases (6 days vs. 4 days, P = .03).
One patient was readmitted to the hospital within 30 days for aseptic meningitis, and none of the patients died.
Initial symptoms were not significantly different for outpatient vs. emergency department patients. The most common initial manifestations of MIS-C included fever (100%), gastrointestinal symptoms (85%), and mucocutaneous symptoms (88%). Mucocutaneous symptoms included rash, oral mucosal changes, conjunctivitis, and hand/foot edema. In addition, 65% of the patients met at least 3 criteria for Kawasaki disease, the researchers noted.
The most common elevated labs at presentation regardless of setting were D-dimer (100%), C-reactive protein (97%), ferritin (97%), procalcitonin (97%), and serum IL-6 (94%).
The study findings were limited by the small sample size and focus on data from a single center. However, the results emphasize the varied presentations of MIS-C and the importance that both primary care and urgent care providers know the signs, as they are often the first point of health care for children with MIS-C, the researchers noted.
Keep looking for factors that put children at risk
“MIS-C is probably the most serious complication of COVID in children, so we as pediatricians on the front line need to know what it looks like,” Karalyn Kinsella, MD, a pediatrician in Cheshire, Conn., said in an interview.
Dr. Kinsella said she was surprised by the study finding that children’s length of hospital stay was not affected by presentation setting.
“I would have thought the kids presenting in an outpatient setting would take longer to diagnose, and therefore have a longer hospital stay,” she noted. Instead, the take-home message is that whether the MIS-C diagnosis occurs in the outpatient or emergency setting, the length of stay is the same, and that the most common symptoms are fever, gastrointestinal, mucocutaneous, and cardiac symptoms regardless of initial presentation setting, she said.
More research is needed, and future studies should examine “any potential underlying factors making these particular kids susceptible to MIS-C,” Dr. Kinsella added.
The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts, but serves on the Pediatric News Editorial Advisory Board.
Length of hospital stay and the need for intensive care for pediatric COVID-19 patients with multisystem inflammatory syndrome in children was not significantly different for those who presented first as outpatients or emergency patients, based on data from 34 children.
Multisystem inflammatory syndrome in children (MIS-C) can be challenging to diagnose, as the key characteristics of fever, elevated inflammatory markers, and involvement of at least two organ systems often overlap with other illnesses, said Erin B. Treemarcki, DO, of the University of Utah, Salt Lake City, and colleagues.
“Primary care and urgent care providers are often the first point of health care for children with symptoms of MIS-C,” the researchers wrote. In a study (Poster 142) presented at the annual meeting of the Pediatric Academic Societies, held virtually, the researchers conducted a retrospective review of 34 patients younger than 21 years who were hospitalized with MIS-C at a single center between April 2020 and December 2020. The average age of the patients was 7.9 years, 68% were male, 82% were White, and 53% first presented to an outpatient clinic.
Sixteen patients presented to an emergency department and 18 presented to an ambulatory setting. The length of hospitalization ranged from 3 to 16 days with a median of 6 days, and the PICU stay ranged from 1 to 10 days with a median of 2 days.
Overall, the length of hospital stay and rate of PICU admission were not significantly different between the emergency presentation and outpatient presentation groups. Twenty-four patients entered the PICU, 13 at admission and 11 as transfers. However, the median number of days of symptoms prior to admission was significantly higher for outpatient cases (6 days vs. 4 days, P = .03).
One patient was readmitted to the hospital within 30 days for aseptic meningitis, and none of the patients died.
Initial symptoms were not significantly different for outpatient vs. emergency department patients. The most common initial manifestations of MIS-C included fever (100%), gastrointestinal symptoms (85%), and mucocutaneous symptoms (88%). Mucocutaneous symptoms included rash, oral mucosal changes, conjunctivitis, and hand/foot edema. In addition, 65% of the patients met at least 3 criteria for Kawasaki disease, the researchers noted.
The most common elevated labs at presentation regardless of setting were D-dimer (100%), C-reactive protein (97%), ferritin (97%), procalcitonin (97%), and serum IL-6 (94%).
The study findings were limited by the small sample size and focus on data from a single center. However, the results emphasize the varied presentations of MIS-C and the importance that both primary care and urgent care providers know the signs, as they are often the first point of health care for children with MIS-C, the researchers noted.
Keep looking for factors that put children at risk
“MIS-C is probably the most serious complication of COVID in children, so we as pediatricians on the front line need to know what it looks like,” Karalyn Kinsella, MD, a pediatrician in Cheshire, Conn., said in an interview.
Dr. Kinsella said she was surprised by the study finding that children’s length of hospital stay was not affected by presentation setting.
“I would have thought the kids presenting in an outpatient setting would take longer to diagnose, and therefore have a longer hospital stay,” she noted. Instead, the take-home message is that whether the MIS-C diagnosis occurs in the outpatient or emergency setting, the length of stay is the same, and that the most common symptoms are fever, gastrointestinal, mucocutaneous, and cardiac symptoms regardless of initial presentation setting, she said.
More research is needed, and future studies should examine “any potential underlying factors making these particular kids susceptible to MIS-C,” Dr. Kinsella added.
The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts, but serves on the Pediatric News Editorial Advisory Board.
Length of hospital stay and the need for intensive care for pediatric COVID-19 patients with multisystem inflammatory syndrome in children was not significantly different for those who presented first as outpatients or emergency patients, based on data from 34 children.
Multisystem inflammatory syndrome in children (MIS-C) can be challenging to diagnose, as the key characteristics of fever, elevated inflammatory markers, and involvement of at least two organ systems often overlap with other illnesses, said Erin B. Treemarcki, DO, of the University of Utah, Salt Lake City, and colleagues.
“Primary care and urgent care providers are often the first point of health care for children with symptoms of MIS-C,” the researchers wrote. In a study (Poster 142) presented at the annual meeting of the Pediatric Academic Societies, held virtually, the researchers conducted a retrospective review of 34 patients younger than 21 years who were hospitalized with MIS-C at a single center between April 2020 and December 2020. The average age of the patients was 7.9 years, 68% were male, 82% were White, and 53% first presented to an outpatient clinic.
Sixteen patients presented to an emergency department and 18 presented to an ambulatory setting. The length of hospitalization ranged from 3 to 16 days with a median of 6 days, and the PICU stay ranged from 1 to 10 days with a median of 2 days.
Overall, the length of hospital stay and rate of PICU admission were not significantly different between the emergency presentation and outpatient presentation groups. Twenty-four patients entered the PICU, 13 at admission and 11 as transfers. However, the median number of days of symptoms prior to admission was significantly higher for outpatient cases (6 days vs. 4 days, P = .03).
One patient was readmitted to the hospital within 30 days for aseptic meningitis, and none of the patients died.
Initial symptoms were not significantly different for outpatient vs. emergency department patients. The most common initial manifestations of MIS-C included fever (100%), gastrointestinal symptoms (85%), and mucocutaneous symptoms (88%). Mucocutaneous symptoms included rash, oral mucosal changes, conjunctivitis, and hand/foot edema. In addition, 65% of the patients met at least 3 criteria for Kawasaki disease, the researchers noted.
The most common elevated labs at presentation regardless of setting were D-dimer (100%), C-reactive protein (97%), ferritin (97%), procalcitonin (97%), and serum IL-6 (94%).
The study findings were limited by the small sample size and focus on data from a single center. However, the results emphasize the varied presentations of MIS-C and the importance that both primary care and urgent care providers know the signs, as they are often the first point of health care for children with MIS-C, the researchers noted.
Keep looking for factors that put children at risk
“MIS-C is probably the most serious complication of COVID in children, so we as pediatricians on the front line need to know what it looks like,” Karalyn Kinsella, MD, a pediatrician in Cheshire, Conn., said in an interview.
Dr. Kinsella said she was surprised by the study finding that children’s length of hospital stay was not affected by presentation setting.
“I would have thought the kids presenting in an outpatient setting would take longer to diagnose, and therefore have a longer hospital stay,” she noted. Instead, the take-home message is that whether the MIS-C diagnosis occurs in the outpatient or emergency setting, the length of stay is the same, and that the most common symptoms are fever, gastrointestinal, mucocutaneous, and cardiac symptoms regardless of initial presentation setting, she said.
More research is needed, and future studies should examine “any potential underlying factors making these particular kids susceptible to MIS-C,” Dr. Kinsella added.
The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts, but serves on the Pediatric News Editorial Advisory Board.
FROM PAS 2021
A new take on breathing and a performance-enhancing placebo
No ifs, ands, or butt ventilators
Breathing, on most days, is a pretty simple task. You inhale, the oxygen goes in, fills your lungs, becomes carbon dioxide, and is exhaled. But as certain recent events have made very clear, some diseases make this task difficult, which is where ventilators come in. The issue is, some patients can’t really use ventilators.
Enter a new study from Japan, which tested the ability of mice and pigs to absorb oxygen through the rectum. Yes, breathing through the butt. It’s not actually such a far-fetched idea; several aquatic animals such as sea cucumbers and catfish absorb oxygen through their intestines, and as any drunken frat boy can tell you after a good butt chug, other chemicals can absolutely be absorbed by human intestines.
After an initial successful experiment where a group of mice had their intestines scrubbed, had pure oxygen inserted enterally, and were exposed to a hypoxic environment, the researchers decided to step up their game and avoid the exhaustive act of digestive scrubbing by enlisting the aid of something out of science fiction: perfluorocarbon. If you haven’t seen “The Abyss,” this liquid can absorb massive amounts of oxygen, so you can actually breathe it in the same way you do with air.
In part two of the experiment, a group of hypoxic mice and pigs had perfluorocarbon inserted into their anuses, while another group got saline solution. The saline group did not fare well, but the animals that got perfluorocarbon had their hypoxic symptoms relieved within minutes.
The effectiveness of this procedure in humans clearly has yet to be tested, and while it may not be useful in all, or even most, situations, it is always beneficial to have more ways to combat a problem. Just don’t tell the frat boys: They’ll be hooking oxygen tanks up to their butts and chanting: “Breathe! Breathe! Breathe!”
Better, stronger, faster … pinker
Many people, most of whom aren’t even athletes, commit huge amounts of time, effort, and expense to improve their athletic performance. But what if there’s an easier way?
Research conducted at the University of Westminster (England) showed that participants could, with one fairly simple intervention, get on a treadmill and run 212 meters further in 30 minutes, increasing their speed by an average of 4.4%. Not only that, but “feelings of pleasure were also enhanced, meaning participants found running more enjoyable,” according to a statement from the university.
Is this amazing intervention a new wonder drug? No. Is it a super special nutritional supplement? Negatory. An energy drink that “gives you wiiings”? Nope. The latest designer steroid? Nyet.
Like we said, it’s simple, and it’s pink. Literally, the color pink. We will explain.
Each of the 10 study subjects completed two 30-minute trials on the treadmill. For one, they were given a clear, artificially sweetened drink while they were running. For the other, they received the exact same drink colored pink with food dye. Pink did better. So to recap the last month in our column, faster looks pink, and skinny smells like lemons.
Once again, science demonstrates that you can’t go wrong by fooling a brain. Next week, LOTME tries to find out if purple makes you funnier.
Hey … I’m singing here!
Noise pollution has been linked to plenty of negative outcomes, but the latest target is the poor baby zebra finch.
Researchers at the Max Planck Institute of Ornithology in Germany say traffic noise disrupts the timing of vocal development and impairs learning in the flying finches. The noise was also shown to suppress their immune systems, because of lingering stress.
The good news is that the birds with noise-induced stress sang as much as their peers in a control group, so the delay in development “was not due to a lack of vocal practice,” according to researchers. However, one long-term effect could be that zebra finch birdsongs could change over time due to noise-induced copying errors. Imagine a really long game of birdsong telephone – the song at the beginning is unlikely to be the song years from now.
While not mentioned in the study, one could also imagine that due to all that exposure to traffic, young zebra finches could be developing a salty dialect and impatience with fellow finches taking up too much space on the same tree branch. Hopefully, they don’t give others “the bird.”
Slimy soap
Remember at the beginning of the pandemic when it was almost impossible to find sufficient hand-washing supplies? Just when you thought you’d tried everything, there is soap made from snail slime.
Snail slime, surprisingly, has many beneficial properties for humans. The slime has antiaging and skin healing properties and is actually used in some Korean beauty supplies. The snails even use the slime to help fix their shells if they become damaged.
Happily, no snails are harmed in the slime extraction and making of the soap. Snail farmer Damien Desrochers says, “I only touch it with my finger, you see it’s not violent, it’s simple.”
As you can probably imagine, a lot of slime is needed to have a steady supply of this soap, so Mr. Desrochers has systems in place to get enough slime. Approximately 40 snails are needed to make 15 bars of soap, and he hopes to produce about 3,000 bars in the first year.
Nothing really surprises us anymore in the beauty world: People put eggs in their hair and bee venom on their skin, so what’s wrong with a little snail slime?
No ifs, ands, or butt ventilators
Breathing, on most days, is a pretty simple task. You inhale, the oxygen goes in, fills your lungs, becomes carbon dioxide, and is exhaled. But as certain recent events have made very clear, some diseases make this task difficult, which is where ventilators come in. The issue is, some patients can’t really use ventilators.
Enter a new study from Japan, which tested the ability of mice and pigs to absorb oxygen through the rectum. Yes, breathing through the butt. It’s not actually such a far-fetched idea; several aquatic animals such as sea cucumbers and catfish absorb oxygen through their intestines, and as any drunken frat boy can tell you after a good butt chug, other chemicals can absolutely be absorbed by human intestines.
After an initial successful experiment where a group of mice had their intestines scrubbed, had pure oxygen inserted enterally, and were exposed to a hypoxic environment, the researchers decided to step up their game and avoid the exhaustive act of digestive scrubbing by enlisting the aid of something out of science fiction: perfluorocarbon. If you haven’t seen “The Abyss,” this liquid can absorb massive amounts of oxygen, so you can actually breathe it in the same way you do with air.
In part two of the experiment, a group of hypoxic mice and pigs had perfluorocarbon inserted into their anuses, while another group got saline solution. The saline group did not fare well, but the animals that got perfluorocarbon had their hypoxic symptoms relieved within minutes.
The effectiveness of this procedure in humans clearly has yet to be tested, and while it may not be useful in all, or even most, situations, it is always beneficial to have more ways to combat a problem. Just don’t tell the frat boys: They’ll be hooking oxygen tanks up to their butts and chanting: “Breathe! Breathe! Breathe!”
Better, stronger, faster … pinker
Many people, most of whom aren’t even athletes, commit huge amounts of time, effort, and expense to improve their athletic performance. But what if there’s an easier way?
Research conducted at the University of Westminster (England) showed that participants could, with one fairly simple intervention, get on a treadmill and run 212 meters further in 30 minutes, increasing their speed by an average of 4.4%. Not only that, but “feelings of pleasure were also enhanced, meaning participants found running more enjoyable,” according to a statement from the university.
Is this amazing intervention a new wonder drug? No. Is it a super special nutritional supplement? Negatory. An energy drink that “gives you wiiings”? Nope. The latest designer steroid? Nyet.
Like we said, it’s simple, and it’s pink. Literally, the color pink. We will explain.
Each of the 10 study subjects completed two 30-minute trials on the treadmill. For one, they were given a clear, artificially sweetened drink while they were running. For the other, they received the exact same drink colored pink with food dye. Pink did better. So to recap the last month in our column, faster looks pink, and skinny smells like lemons.
Once again, science demonstrates that you can’t go wrong by fooling a brain. Next week, LOTME tries to find out if purple makes you funnier.
Hey … I’m singing here!
Noise pollution has been linked to plenty of negative outcomes, but the latest target is the poor baby zebra finch.
Researchers at the Max Planck Institute of Ornithology in Germany say traffic noise disrupts the timing of vocal development and impairs learning in the flying finches. The noise was also shown to suppress their immune systems, because of lingering stress.
The good news is that the birds with noise-induced stress sang as much as their peers in a control group, so the delay in development “was not due to a lack of vocal practice,” according to researchers. However, one long-term effect could be that zebra finch birdsongs could change over time due to noise-induced copying errors. Imagine a really long game of birdsong telephone – the song at the beginning is unlikely to be the song years from now.
While not mentioned in the study, one could also imagine that due to all that exposure to traffic, young zebra finches could be developing a salty dialect and impatience with fellow finches taking up too much space on the same tree branch. Hopefully, they don’t give others “the bird.”
Slimy soap
Remember at the beginning of the pandemic when it was almost impossible to find sufficient hand-washing supplies? Just when you thought you’d tried everything, there is soap made from snail slime.
Snail slime, surprisingly, has many beneficial properties for humans. The slime has antiaging and skin healing properties and is actually used in some Korean beauty supplies. The snails even use the slime to help fix their shells if they become damaged.
Happily, no snails are harmed in the slime extraction and making of the soap. Snail farmer Damien Desrochers says, “I only touch it with my finger, you see it’s not violent, it’s simple.”
As you can probably imagine, a lot of slime is needed to have a steady supply of this soap, so Mr. Desrochers has systems in place to get enough slime. Approximately 40 snails are needed to make 15 bars of soap, and he hopes to produce about 3,000 bars in the first year.
Nothing really surprises us anymore in the beauty world: People put eggs in their hair and bee venom on their skin, so what’s wrong with a little snail slime?
No ifs, ands, or butt ventilators
Breathing, on most days, is a pretty simple task. You inhale, the oxygen goes in, fills your lungs, becomes carbon dioxide, and is exhaled. But as certain recent events have made very clear, some diseases make this task difficult, which is where ventilators come in. The issue is, some patients can’t really use ventilators.
Enter a new study from Japan, which tested the ability of mice and pigs to absorb oxygen through the rectum. Yes, breathing through the butt. It’s not actually such a far-fetched idea; several aquatic animals such as sea cucumbers and catfish absorb oxygen through their intestines, and as any drunken frat boy can tell you after a good butt chug, other chemicals can absolutely be absorbed by human intestines.
After an initial successful experiment where a group of mice had their intestines scrubbed, had pure oxygen inserted enterally, and were exposed to a hypoxic environment, the researchers decided to step up their game and avoid the exhaustive act of digestive scrubbing by enlisting the aid of something out of science fiction: perfluorocarbon. If you haven’t seen “The Abyss,” this liquid can absorb massive amounts of oxygen, so you can actually breathe it in the same way you do with air.
In part two of the experiment, a group of hypoxic mice and pigs had perfluorocarbon inserted into their anuses, while another group got saline solution. The saline group did not fare well, but the animals that got perfluorocarbon had their hypoxic symptoms relieved within minutes.
The effectiveness of this procedure in humans clearly has yet to be tested, and while it may not be useful in all, or even most, situations, it is always beneficial to have more ways to combat a problem. Just don’t tell the frat boys: They’ll be hooking oxygen tanks up to their butts and chanting: “Breathe! Breathe! Breathe!”
Better, stronger, faster … pinker
Many people, most of whom aren’t even athletes, commit huge amounts of time, effort, and expense to improve their athletic performance. But what if there’s an easier way?
Research conducted at the University of Westminster (England) showed that participants could, with one fairly simple intervention, get on a treadmill and run 212 meters further in 30 minutes, increasing their speed by an average of 4.4%. Not only that, but “feelings of pleasure were also enhanced, meaning participants found running more enjoyable,” according to a statement from the university.
Is this amazing intervention a new wonder drug? No. Is it a super special nutritional supplement? Negatory. An energy drink that “gives you wiiings”? Nope. The latest designer steroid? Nyet.
Like we said, it’s simple, and it’s pink. Literally, the color pink. We will explain.
Each of the 10 study subjects completed two 30-minute trials on the treadmill. For one, they were given a clear, artificially sweetened drink while they were running. For the other, they received the exact same drink colored pink with food dye. Pink did better. So to recap the last month in our column, faster looks pink, and skinny smells like lemons.
Once again, science demonstrates that you can’t go wrong by fooling a brain. Next week, LOTME tries to find out if purple makes you funnier.
Hey … I’m singing here!
Noise pollution has been linked to plenty of negative outcomes, but the latest target is the poor baby zebra finch.
Researchers at the Max Planck Institute of Ornithology in Germany say traffic noise disrupts the timing of vocal development and impairs learning in the flying finches. The noise was also shown to suppress their immune systems, because of lingering stress.
The good news is that the birds with noise-induced stress sang as much as their peers in a control group, so the delay in development “was not due to a lack of vocal practice,” according to researchers. However, one long-term effect could be that zebra finch birdsongs could change over time due to noise-induced copying errors. Imagine a really long game of birdsong telephone – the song at the beginning is unlikely to be the song years from now.
While not mentioned in the study, one could also imagine that due to all that exposure to traffic, young zebra finches could be developing a salty dialect and impatience with fellow finches taking up too much space on the same tree branch. Hopefully, they don’t give others “the bird.”
Slimy soap
Remember at the beginning of the pandemic when it was almost impossible to find sufficient hand-washing supplies? Just when you thought you’d tried everything, there is soap made from snail slime.
Snail slime, surprisingly, has many beneficial properties for humans. The slime has antiaging and skin healing properties and is actually used in some Korean beauty supplies. The snails even use the slime to help fix their shells if they become damaged.
Happily, no snails are harmed in the slime extraction and making of the soap. Snail farmer Damien Desrochers says, “I only touch it with my finger, you see it’s not violent, it’s simple.”
As you can probably imagine, a lot of slime is needed to have a steady supply of this soap, so Mr. Desrochers has systems in place to get enough slime. Approximately 40 snails are needed to make 15 bars of soap, and he hopes to produce about 3,000 bars in the first year.
Nothing really surprises us anymore in the beauty world: People put eggs in their hair and bee venom on their skin, so what’s wrong with a little snail slime?
Coping with postpandemic school hesitancy
As the protective effect of the vaccines becomes increasingly apparent, a large number of school systems are beginning to return to prepandemic in-school learning. But anecdotal reports from around the country are making it clear that some children or their families are hesitant to return to the old norm of face to face learning (Goldstein D. “Schools Are Open, but Many Families Remain Hesitant to Return.” New York Times. 2021 May 9). The possible explanations for this hesitancy include a broad list that goes well beyond the obvious concern about the child contracting COVID-19.
I hear from my grandchildren that remote learning has for the most part been unpleasant and lacked the rigor of their in-class experiences. But, they admit that they have found that, in some situations, they prefer the environment at home because it is less distracting. They also acknowledge that, while they miss seeing their friends, at times the isolation has allowed them to be more efficient. Of course, their observations must be viewed in light of their personalities and the support provided by their parents. For these motivated teenagers, the bottom line is that they would prefer to be in school.
However, for the children who have always been a bit ambivalent about school either because they were anxious in social situations or because they found the academics too challenging, one can easily understand why they might prefer to remain in a less-intimidating home environment. For them, missing their friends may have little draw because they may not have had any friends. And, the negative feedback and bullying they have received at school is too overwhelming. A teenager for whom the pandemic has offered the out-of-school free time to explore her independence, feel more like an adult, and enjoy the benefits of having a job may be hesitant to return to the restrictions imposed by what she sees as the childishness of in-school learning.
Compounding the problem is the risk avoidance posture of some school systems and the hesitancy of some teachers to return to an environment that they continue to view as unsafe despite the evidence of the effectiveness of the vaccines and the minimal threat of in-school spread. It is going to be interesting to see how school administrators and politicians deal with this level of institutional hesitancy. Some schools may take what might be considered a hard-line approach and eliminate remote learning completely.
Regardless of how swiftly and thoughtfully schools return to in-class learning, a large number of children will eventually be faced with the stark reality of returning to a place in which they had felt painfully uncomfortable in the past. Pediatricians must be prepared to see this current wave of school hesitancy morph into a full-fledged tsunami of school refusals.
Successful management of a family whose child finds school too challenging emotionally has always required a combination of careful attention to the possible medical causes of the child’s complaints, consultation with a mental health practitioner, and thoughtful coordination with educators sensitive to the child’s school-generated distress.
It has never been easy to reassure the family of a child with frequent headaches or belly pain that his symptoms have no physical basis and then gently point out that the stress of school attendance may be a contributing factor. Some families who buy into the association may be fortunate enough to be able to offer their child home schooling as a solution to school refusal. But this strategy often requires that one parent remain home and has the temperament and the skills to teach.
Now that we have all seen that remote learning has the potential to work in a crisis, will some parents begin to demand it for their children with school refusal? Who will pay for it? I think you and I would prefer to see a solution that targeted therapeutic interventions aimed at getting the child back in school. But you and I also know those strategies don’t always work.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
As the protective effect of the vaccines becomes increasingly apparent, a large number of school systems are beginning to return to prepandemic in-school learning. But anecdotal reports from around the country are making it clear that some children or their families are hesitant to return to the old norm of face to face learning (Goldstein D. “Schools Are Open, but Many Families Remain Hesitant to Return.” New York Times. 2021 May 9). The possible explanations for this hesitancy include a broad list that goes well beyond the obvious concern about the child contracting COVID-19.
I hear from my grandchildren that remote learning has for the most part been unpleasant and lacked the rigor of their in-class experiences. But, they admit that they have found that, in some situations, they prefer the environment at home because it is less distracting. They also acknowledge that, while they miss seeing their friends, at times the isolation has allowed them to be more efficient. Of course, their observations must be viewed in light of their personalities and the support provided by their parents. For these motivated teenagers, the bottom line is that they would prefer to be in school.
However, for the children who have always been a bit ambivalent about school either because they were anxious in social situations or because they found the academics too challenging, one can easily understand why they might prefer to remain in a less-intimidating home environment. For them, missing their friends may have little draw because they may not have had any friends. And, the negative feedback and bullying they have received at school is too overwhelming. A teenager for whom the pandemic has offered the out-of-school free time to explore her independence, feel more like an adult, and enjoy the benefits of having a job may be hesitant to return to the restrictions imposed by what she sees as the childishness of in-school learning.
Compounding the problem is the risk avoidance posture of some school systems and the hesitancy of some teachers to return to an environment that they continue to view as unsafe despite the evidence of the effectiveness of the vaccines and the minimal threat of in-school spread. It is going to be interesting to see how school administrators and politicians deal with this level of institutional hesitancy. Some schools may take what might be considered a hard-line approach and eliminate remote learning completely.
Regardless of how swiftly and thoughtfully schools return to in-class learning, a large number of children will eventually be faced with the stark reality of returning to a place in which they had felt painfully uncomfortable in the past. Pediatricians must be prepared to see this current wave of school hesitancy morph into a full-fledged tsunami of school refusals.
Successful management of a family whose child finds school too challenging emotionally has always required a combination of careful attention to the possible medical causes of the child’s complaints, consultation with a mental health practitioner, and thoughtful coordination with educators sensitive to the child’s school-generated distress.
It has never been easy to reassure the family of a child with frequent headaches or belly pain that his symptoms have no physical basis and then gently point out that the stress of school attendance may be a contributing factor. Some families who buy into the association may be fortunate enough to be able to offer their child home schooling as a solution to school refusal. But this strategy often requires that one parent remain home and has the temperament and the skills to teach.
Now that we have all seen that remote learning has the potential to work in a crisis, will some parents begin to demand it for their children with school refusal? Who will pay for it? I think you and I would prefer to see a solution that targeted therapeutic interventions aimed at getting the child back in school. But you and I also know those strategies don’t always work.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
As the protective effect of the vaccines becomes increasingly apparent, a large number of school systems are beginning to return to prepandemic in-school learning. But anecdotal reports from around the country are making it clear that some children or their families are hesitant to return to the old norm of face to face learning (Goldstein D. “Schools Are Open, but Many Families Remain Hesitant to Return.” New York Times. 2021 May 9). The possible explanations for this hesitancy include a broad list that goes well beyond the obvious concern about the child contracting COVID-19.
I hear from my grandchildren that remote learning has for the most part been unpleasant and lacked the rigor of their in-class experiences. But, they admit that they have found that, in some situations, they prefer the environment at home because it is less distracting. They also acknowledge that, while they miss seeing their friends, at times the isolation has allowed them to be more efficient. Of course, their observations must be viewed in light of their personalities and the support provided by their parents. For these motivated teenagers, the bottom line is that they would prefer to be in school.
However, for the children who have always been a bit ambivalent about school either because they were anxious in social situations or because they found the academics too challenging, one can easily understand why they might prefer to remain in a less-intimidating home environment. For them, missing their friends may have little draw because they may not have had any friends. And, the negative feedback and bullying they have received at school is too overwhelming. A teenager for whom the pandemic has offered the out-of-school free time to explore her independence, feel more like an adult, and enjoy the benefits of having a job may be hesitant to return to the restrictions imposed by what she sees as the childishness of in-school learning.
Compounding the problem is the risk avoidance posture of some school systems and the hesitancy of some teachers to return to an environment that they continue to view as unsafe despite the evidence of the effectiveness of the vaccines and the minimal threat of in-school spread. It is going to be interesting to see how school administrators and politicians deal with this level of institutional hesitancy. Some schools may take what might be considered a hard-line approach and eliminate remote learning completely.
Regardless of how swiftly and thoughtfully schools return to in-class learning, a large number of children will eventually be faced with the stark reality of returning to a place in which they had felt painfully uncomfortable in the past. Pediatricians must be prepared to see this current wave of school hesitancy morph into a full-fledged tsunami of school refusals.
Successful management of a family whose child finds school too challenging emotionally has always required a combination of careful attention to the possible medical causes of the child’s complaints, consultation with a mental health practitioner, and thoughtful coordination with educators sensitive to the child’s school-generated distress.
It has never been easy to reassure the family of a child with frequent headaches or belly pain that his symptoms have no physical basis and then gently point out that the stress of school attendance may be a contributing factor. Some families who buy into the association may be fortunate enough to be able to offer their child home schooling as a solution to school refusal. But this strategy often requires that one parent remain home and has the temperament and the skills to teach.
Now that we have all seen that remote learning has the potential to work in a crisis, will some parents begin to demand it for their children with school refusal? Who will pay for it? I think you and I would prefer to see a solution that targeted therapeutic interventions aimed at getting the child back in school. But you and I also know those strategies don’t always work.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Mother-to-infant COVID-19 transmission is unlikely
Mothers with a history of COVID-19 exposure during pregnancy are not likely to transmit the infection to their newborns, based on data from more than 2,000 women.
“Uncertainty at the onset of the COVID-19 pandemic led to varying postnatal care recommendations for newborns exposed to SARS-CoV-2 in utero,” said Margaret H. Kyle, of Columbia University, New York, and colleagues.
The Columbia University Irving Medical Center, an early epicenter of the pandemic, allowed rooming-in and encouraged direct breastfeeding between infected mothers and their newborns while adopting extensive safety measures, the researchers said.
In a study presented at the virtual meeting of the Pediatric Academic Societies (Poster 141), the researchers conducted a retrospective chart review of all newborns born at the medical center from March 22, 2020, through August 7, 2020. The study was part of Columbia University’s ongoing COVID-19 Mother Baby Outcomes (COMBO) initiative to “describe the health and well-being of mother-infant dyads with and without prenatal SARS-CoV-2 infections,” according to the researchers.
During the study period, the researchers identified newborns of 327 women who tested positive for COVID-19 at any point during pregnancy and compared them to newborns of 2,125 unexposed women. Demographics were similar between the groups.
Overall, the total test positivity was 0.7% for exposed newborns; 1.0% tested positive on an initial test, and 0% were positive on retest. During the newborn hospital stay and a 2-week follow-up, 0% of all newborns showed clinical evidence of infection.
No significant differences were noted between exposed and unexposed newborns in clinical outcomes including gestational age, mode of delivery, 5-minute Apgar score, heart rate, respiratory rate, or temperature. Although more infants of COVID-19–exposed mothers compared with unexposed mothers had an emergency department visit within the first 14 days of life (6% vs. 3%, P = .002), none of the infants was diagnosed with COVID-19 during these visits. Cough, fever, congestion, or bilirubin were more frequent reasons for emergency department visits in the exposed infants compared with unexposed infants, but these differences were not significant.
The study findings were limited by several factors, including the retrospective design and the limited follow-up period to only the first 2 weeks of life, the researchers noted. In addition, perinatal transmission rates were available only for the 202 newborns who were followed up in the hospital system, they said. However, the results suggest that the risk of mother-to-newborn vertical transmission of COVID-19 remains low, even when mothers are breastfeeding and infants are rooming in, they concluded.
Study supports safety of rooming in
The study is important because of the value of mother and infant bonding, Karalyn Kinsella, MD, a pediatrician in Cheshire, Conn., said in an interview. “We know maternal and infant bonding and breastfeeding are extremely important in the first few days of life,” she said. “Initially, COVID-positive moms were separated from their babies during this important time.” Dr. Kinsella said she was not surprised by the study findings, as they reflect other research that newborns have not been getting infected with COVID-19 from their mothers.
Consequently, the take-home message is that newborns can room in with their mothers in the hospital setting, and they are at low risk for COVID-19 regardless of the mother’s exposure history, said Dr. Kinsella. Looking ahead, future areas of research could include examining SARS-CoV-2 antibodies in newborns, she noted.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose, but serves on the Pediatric News Editorial Advisory Board.
Mothers with a history of COVID-19 exposure during pregnancy are not likely to transmit the infection to their newborns, based on data from more than 2,000 women.
“Uncertainty at the onset of the COVID-19 pandemic led to varying postnatal care recommendations for newborns exposed to SARS-CoV-2 in utero,” said Margaret H. Kyle, of Columbia University, New York, and colleagues.
The Columbia University Irving Medical Center, an early epicenter of the pandemic, allowed rooming-in and encouraged direct breastfeeding between infected mothers and their newborns while adopting extensive safety measures, the researchers said.
In a study presented at the virtual meeting of the Pediatric Academic Societies (Poster 141), the researchers conducted a retrospective chart review of all newborns born at the medical center from March 22, 2020, through August 7, 2020. The study was part of Columbia University’s ongoing COVID-19 Mother Baby Outcomes (COMBO) initiative to “describe the health and well-being of mother-infant dyads with and without prenatal SARS-CoV-2 infections,” according to the researchers.
During the study period, the researchers identified newborns of 327 women who tested positive for COVID-19 at any point during pregnancy and compared them to newborns of 2,125 unexposed women. Demographics were similar between the groups.
Overall, the total test positivity was 0.7% for exposed newborns; 1.0% tested positive on an initial test, and 0% were positive on retest. During the newborn hospital stay and a 2-week follow-up, 0% of all newborns showed clinical evidence of infection.
No significant differences were noted between exposed and unexposed newborns in clinical outcomes including gestational age, mode of delivery, 5-minute Apgar score, heart rate, respiratory rate, or temperature. Although more infants of COVID-19–exposed mothers compared with unexposed mothers had an emergency department visit within the first 14 days of life (6% vs. 3%, P = .002), none of the infants was diagnosed with COVID-19 during these visits. Cough, fever, congestion, or bilirubin were more frequent reasons for emergency department visits in the exposed infants compared with unexposed infants, but these differences were not significant.
The study findings were limited by several factors, including the retrospective design and the limited follow-up period to only the first 2 weeks of life, the researchers noted. In addition, perinatal transmission rates were available only for the 202 newborns who were followed up in the hospital system, they said. However, the results suggest that the risk of mother-to-newborn vertical transmission of COVID-19 remains low, even when mothers are breastfeeding and infants are rooming in, they concluded.
Study supports safety of rooming in
The study is important because of the value of mother and infant bonding, Karalyn Kinsella, MD, a pediatrician in Cheshire, Conn., said in an interview. “We know maternal and infant bonding and breastfeeding are extremely important in the first few days of life,” she said. “Initially, COVID-positive moms were separated from their babies during this important time.” Dr. Kinsella said she was not surprised by the study findings, as they reflect other research that newborns have not been getting infected with COVID-19 from their mothers.
Consequently, the take-home message is that newborns can room in with their mothers in the hospital setting, and they are at low risk for COVID-19 regardless of the mother’s exposure history, said Dr. Kinsella. Looking ahead, future areas of research could include examining SARS-CoV-2 antibodies in newborns, she noted.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose, but serves on the Pediatric News Editorial Advisory Board.
Mothers with a history of COVID-19 exposure during pregnancy are not likely to transmit the infection to their newborns, based on data from more than 2,000 women.
“Uncertainty at the onset of the COVID-19 pandemic led to varying postnatal care recommendations for newborns exposed to SARS-CoV-2 in utero,” said Margaret H. Kyle, of Columbia University, New York, and colleagues.
The Columbia University Irving Medical Center, an early epicenter of the pandemic, allowed rooming-in and encouraged direct breastfeeding between infected mothers and their newborns while adopting extensive safety measures, the researchers said.
In a study presented at the virtual meeting of the Pediatric Academic Societies (Poster 141), the researchers conducted a retrospective chart review of all newborns born at the medical center from March 22, 2020, through August 7, 2020. The study was part of Columbia University’s ongoing COVID-19 Mother Baby Outcomes (COMBO) initiative to “describe the health and well-being of mother-infant dyads with and without prenatal SARS-CoV-2 infections,” according to the researchers.
During the study period, the researchers identified newborns of 327 women who tested positive for COVID-19 at any point during pregnancy and compared them to newborns of 2,125 unexposed women. Demographics were similar between the groups.
Overall, the total test positivity was 0.7% for exposed newborns; 1.0% tested positive on an initial test, and 0% were positive on retest. During the newborn hospital stay and a 2-week follow-up, 0% of all newborns showed clinical evidence of infection.
No significant differences were noted between exposed and unexposed newborns in clinical outcomes including gestational age, mode of delivery, 5-minute Apgar score, heart rate, respiratory rate, or temperature. Although more infants of COVID-19–exposed mothers compared with unexposed mothers had an emergency department visit within the first 14 days of life (6% vs. 3%, P = .002), none of the infants was diagnosed with COVID-19 during these visits. Cough, fever, congestion, or bilirubin were more frequent reasons for emergency department visits in the exposed infants compared with unexposed infants, but these differences were not significant.
The study findings were limited by several factors, including the retrospective design and the limited follow-up period to only the first 2 weeks of life, the researchers noted. In addition, perinatal transmission rates were available only for the 202 newborns who were followed up in the hospital system, they said. However, the results suggest that the risk of mother-to-newborn vertical transmission of COVID-19 remains low, even when mothers are breastfeeding and infants are rooming in, they concluded.
Study supports safety of rooming in
The study is important because of the value of mother and infant bonding, Karalyn Kinsella, MD, a pediatrician in Cheshire, Conn., said in an interview. “We know maternal and infant bonding and breastfeeding are extremely important in the first few days of life,” she said. “Initially, COVID-positive moms were separated from their babies during this important time.” Dr. Kinsella said she was not surprised by the study findings, as they reflect other research that newborns have not been getting infected with COVID-19 from their mothers.
Consequently, the take-home message is that newborns can room in with their mothers in the hospital setting, and they are at low risk for COVID-19 regardless of the mother’s exposure history, said Dr. Kinsella. Looking ahead, future areas of research could include examining SARS-CoV-2 antibodies in newborns, she noted.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose, but serves on the Pediatric News Editorial Advisory Board.
FROM PAS 2021
Acts of kindness, empathy bolster mental health
Sigmund Freud said, “Out of your vulnerabilities will come greatest strength.” What exactly did Dr. Freud mean by this?
Many aspects of mental health treatment include cognitive restructuring, behavioral changes, emotion processing, and setting boundaries. These are all critical aspects of treatment, but what about kindness and compassion?
We often forget that kindness requires us to be vulnerable and take a risk at times. Being kind to others is not always easy, and it is not always an automatic reaction. Vulnerability often involves risk, but the outcomes often outweigh fear.
Dr. Freud was highlighting that being kind, open, and honest will often result in strong character and resilience. In turn, it will help others. Psychology and psychiatry have proved time and time again that empathy, compassion, and kindness have numerous benefits for mental and physical health for both the giver and the receiver.
From a biological perspective, we know that acts of kindness signal the brain to release serotonin and dopamine, known as “feel good transmitters,” and endorphins, which in turn lessen pain, depression, and anxiety. According to Waguih W. Ishak, MD, a psychiatrist affiliated with Cedars-Sinai in Los Angeles,1 in addition to boosting oxytocin and dopamine, being kind can increase serotonin, a neurotransmitter that helps regulate mood. Kindness and compassion have been shown to release oxytocin, known as the “love hormone,” which increases self-esteem, trust, connection, and optimism. Oxytocin also reduces blood pressure and has been dubbed the “cardioprotective” hormone. According to Kelli Harding, MD, MPH, a psychiatrist affiliated with Columbia University in New York,2 kindness can extend the lifespan. Research from Emory University in Atlanta has shown that, when an individual is kind to another, the brain’s reward centers light up – resulting in a “helper’s high.” Thus, kindness is self-reinforcing.3
Kindness leads to a greater sense of connection to others and a lessening in feelings of isolation. Small acts of kindness build up compassion in oneself. Research indicates that kindness doesn’t just positively affect the giver and receiver but can also benefit onlookers. An article in Psychology Today,4 suggests that those who witness acts of kindness are also more likely to “pay it forward,” resulting in a domino effect. Along these same lines, altruistic people, specifically those who engage in charitable donations, expressed higher levels of overall happiness according to a 2010 Harvard Business School survey.5
“You can’t pour from an empty cup” is a trendy quote making its way around social media. Before we can be kind and compassionate to others, we must first be kind and compassionate to ourselves. In today’s world, productivity and pressure-filled environments consume us daily. We often find ourselves skipping meals, forgetting to connect with loved ones, missing breaks, and even neglecting our sleep. It is virtually impossible to care for others when we are depleted ourselves. Sometimes not prioritizing ourselves can result in collateral damage. We may become short-tempered, irritable, moody, and overwhelmed. At this point kindness, compassion, and empathy toward others are likely to be absent. Once we replenish ourselves, by taking time off, indulging in a nice meal, exercising, we are more likely to respond as opposed to react, ask others about themselves, and engage in overall positive interactions throughout our day. Kindness is best fostered by being kind to ourselves to sustain our own well-being and by being kind to others in order to maintain the cycle. For clinicians who have been pushed to respond to various aspects of the COVID-19 pandemic, self-care has never been more important.
COVID-19 has been difficult for everyone, particularly the elderly and vulnerable populations. However, kindness has proved to be an overwhelming response as many businesses and individuals have taken to volunteering time and resources for those in need. Even big corporations have chipped in. For example, Lyft and Uber – in a partnership with the White House – are now offering free rides to vaccine sites, and several local businesses have donated personal protective equipment to hospitals and assisted living facilities.
Kindness and empathy are ever present in the field of mental health, medicine, and substance use treatment. The very act of caring for another involves kindness. In medicine, empathy has been defined as “an emotional experience between an observer and a subject in which the observer, based on visual and auditory cues, identifies and transiently experiences the subject’s emotional state.”6
As mental health professionals, we receive empathy training early on in our schooling – increasingly so over the last decade. Research has indicated that trusting relationships between clinicians and patients result in optimal care. Evidence-based communication styles are being widely implemented. This entails using nonjudgmental language, open-ended questions, and active listening skills, for example. In addition, the mental health professionals have our conscious and unconscious judgments. If empathy training is provided, we can learn to acknowledge our biases and mitigate them. Lastly, empathy training has been proven to assist with destigmatization, increase in treatment seeking, and overall better outcomes.
Substance use treatment, which often focuses on cognition and behavior changing, boundaries, and family dynamics, also requires support and kindness. Although it is not an empirically based “treatment,” Alcoholics Anonymous (AA) has used kindness for decades.
Step 12 of AA’s 12-step program, which was developed by two people with alcohol use disorder in 1935 in Akron, Ohio, is as follows: “Having had a spiritual awakening as the result of these steps, we tried to carry this message to alcoholics, and to practice these principles in all our affairs.”
Once AA members are on solid ground with their sobriety, they are urged to help others in their recovery. This process provides many benefits. When individuals are concerned about someone else, they are less focused on themselves. This helps the individuals in recovery to decrease their rumination and “get out of themselves.” It also allows for the AA member to be kind and helpful to an individual who is suffering, thereby expressing kindness, compassion, and empathy. This act of “paying it forward” produces a domino effect that has withstood the test of time as evidenced by the ever-growing fellowship of Alcoholics Anonymous.
Several small acts of kindness can help us as clinicians and our patients:
1. Practice self-care.
2. Take a half day off from your practice.
3. Give staff a half day off.
4. Call a family member or friend and ask them how they are doing. Then engage in active listening and refrain from giving advice.
5. Donate to a homeless shelter or volunteer your time at a charity.
6. Give a stranger a compliment.
7. Surprise someone with a small gift.
8. Send a loved one a letter instead of a text.
9. Pick up litter.
10. Acknowledge family and friends who gave you extra support during the pandemic.
11. Take baked goods to your office.
12. Help a neighbor with groceries.
13. Leave a generous tip.
14. Play soft music in your office.
In conclusion, kindness, empathy, and compassion are vital concepts that are not just fluffy theories. They have vast mental, physical, and social benefits for us and our patients.
References
1. Cedars-Sinai staff. The Science of Kindness. 2019 Feb 13. Cedars-Sinai blog.
2. Harding K. The Rabbit Effect: Live Longer, Happier, and Healthier with the Groundbreaking Science of Kindness. Atria Books, 2019.
3. Ritvo E. BeKindr. Momosa Publishing, 2017.
4. Svoboda E. “Pay it Forward.” Psychology Today. Last reviewed 2016 Jun 9.
5. Aknin LB et al. “Prosocial spending and well-being: Cross-Cultural Evidence for a Psychological Universal.” Harvard Business School. Working Paper 11-038. 2010.
6. Hirsch EM. AMA J Ethics. Virtual Mentor. 2007;9(6):423-7.
Dr. Haji is a licensed clinical psychologist specializing in psychodiagnostic assessment, forensic assessment, dual diagnosis, serious and persistent mental illness, depression, anxiety, personality disorders, and substance abuse treatment. She practices in Miami and has no conflicts of interest.
Sigmund Freud said, “Out of your vulnerabilities will come greatest strength.” What exactly did Dr. Freud mean by this?
Many aspects of mental health treatment include cognitive restructuring, behavioral changes, emotion processing, and setting boundaries. These are all critical aspects of treatment, but what about kindness and compassion?
We often forget that kindness requires us to be vulnerable and take a risk at times. Being kind to others is not always easy, and it is not always an automatic reaction. Vulnerability often involves risk, but the outcomes often outweigh fear.
Dr. Freud was highlighting that being kind, open, and honest will often result in strong character and resilience. In turn, it will help others. Psychology and psychiatry have proved time and time again that empathy, compassion, and kindness have numerous benefits for mental and physical health for both the giver and the receiver.
From a biological perspective, we know that acts of kindness signal the brain to release serotonin and dopamine, known as “feel good transmitters,” and endorphins, which in turn lessen pain, depression, and anxiety. According to Waguih W. Ishak, MD, a psychiatrist affiliated with Cedars-Sinai in Los Angeles,1 in addition to boosting oxytocin and dopamine, being kind can increase serotonin, a neurotransmitter that helps regulate mood. Kindness and compassion have been shown to release oxytocin, known as the “love hormone,” which increases self-esteem, trust, connection, and optimism. Oxytocin also reduces blood pressure and has been dubbed the “cardioprotective” hormone. According to Kelli Harding, MD, MPH, a psychiatrist affiliated with Columbia University in New York,2 kindness can extend the lifespan. Research from Emory University in Atlanta has shown that, when an individual is kind to another, the brain’s reward centers light up – resulting in a “helper’s high.” Thus, kindness is self-reinforcing.3
Kindness leads to a greater sense of connection to others and a lessening in feelings of isolation. Small acts of kindness build up compassion in oneself. Research indicates that kindness doesn’t just positively affect the giver and receiver but can also benefit onlookers. An article in Psychology Today,4 suggests that those who witness acts of kindness are also more likely to “pay it forward,” resulting in a domino effect. Along these same lines, altruistic people, specifically those who engage in charitable donations, expressed higher levels of overall happiness according to a 2010 Harvard Business School survey.5
“You can’t pour from an empty cup” is a trendy quote making its way around social media. Before we can be kind and compassionate to others, we must first be kind and compassionate to ourselves. In today’s world, productivity and pressure-filled environments consume us daily. We often find ourselves skipping meals, forgetting to connect with loved ones, missing breaks, and even neglecting our sleep. It is virtually impossible to care for others when we are depleted ourselves. Sometimes not prioritizing ourselves can result in collateral damage. We may become short-tempered, irritable, moody, and overwhelmed. At this point kindness, compassion, and empathy toward others are likely to be absent. Once we replenish ourselves, by taking time off, indulging in a nice meal, exercising, we are more likely to respond as opposed to react, ask others about themselves, and engage in overall positive interactions throughout our day. Kindness is best fostered by being kind to ourselves to sustain our own well-being and by being kind to others in order to maintain the cycle. For clinicians who have been pushed to respond to various aspects of the COVID-19 pandemic, self-care has never been more important.
COVID-19 has been difficult for everyone, particularly the elderly and vulnerable populations. However, kindness has proved to be an overwhelming response as many businesses and individuals have taken to volunteering time and resources for those in need. Even big corporations have chipped in. For example, Lyft and Uber – in a partnership with the White House – are now offering free rides to vaccine sites, and several local businesses have donated personal protective equipment to hospitals and assisted living facilities.
Kindness and empathy are ever present in the field of mental health, medicine, and substance use treatment. The very act of caring for another involves kindness. In medicine, empathy has been defined as “an emotional experience between an observer and a subject in which the observer, based on visual and auditory cues, identifies and transiently experiences the subject’s emotional state.”6
As mental health professionals, we receive empathy training early on in our schooling – increasingly so over the last decade. Research has indicated that trusting relationships between clinicians and patients result in optimal care. Evidence-based communication styles are being widely implemented. This entails using nonjudgmental language, open-ended questions, and active listening skills, for example. In addition, the mental health professionals have our conscious and unconscious judgments. If empathy training is provided, we can learn to acknowledge our biases and mitigate them. Lastly, empathy training has been proven to assist with destigmatization, increase in treatment seeking, and overall better outcomes.
Substance use treatment, which often focuses on cognition and behavior changing, boundaries, and family dynamics, also requires support and kindness. Although it is not an empirically based “treatment,” Alcoholics Anonymous (AA) has used kindness for decades.
Step 12 of AA’s 12-step program, which was developed by two people with alcohol use disorder in 1935 in Akron, Ohio, is as follows: “Having had a spiritual awakening as the result of these steps, we tried to carry this message to alcoholics, and to practice these principles in all our affairs.”
Once AA members are on solid ground with their sobriety, they are urged to help others in their recovery. This process provides many benefits. When individuals are concerned about someone else, they are less focused on themselves. This helps the individuals in recovery to decrease their rumination and “get out of themselves.” It also allows for the AA member to be kind and helpful to an individual who is suffering, thereby expressing kindness, compassion, and empathy. This act of “paying it forward” produces a domino effect that has withstood the test of time as evidenced by the ever-growing fellowship of Alcoholics Anonymous.
Several small acts of kindness can help us as clinicians and our patients:
1. Practice self-care.
2. Take a half day off from your practice.
3. Give staff a half day off.
4. Call a family member or friend and ask them how they are doing. Then engage in active listening and refrain from giving advice.
5. Donate to a homeless shelter or volunteer your time at a charity.
6. Give a stranger a compliment.
7. Surprise someone with a small gift.
8. Send a loved one a letter instead of a text.
9. Pick up litter.
10. Acknowledge family and friends who gave you extra support during the pandemic.
11. Take baked goods to your office.
12. Help a neighbor with groceries.
13. Leave a generous tip.
14. Play soft music in your office.
In conclusion, kindness, empathy, and compassion are vital concepts that are not just fluffy theories. They have vast mental, physical, and social benefits for us and our patients.
References
1. Cedars-Sinai staff. The Science of Kindness. 2019 Feb 13. Cedars-Sinai blog.
2. Harding K. The Rabbit Effect: Live Longer, Happier, and Healthier with the Groundbreaking Science of Kindness. Atria Books, 2019.
3. Ritvo E. BeKindr. Momosa Publishing, 2017.
4. Svoboda E. “Pay it Forward.” Psychology Today. Last reviewed 2016 Jun 9.
5. Aknin LB et al. “Prosocial spending and well-being: Cross-Cultural Evidence for a Psychological Universal.” Harvard Business School. Working Paper 11-038. 2010.
6. Hirsch EM. AMA J Ethics. Virtual Mentor. 2007;9(6):423-7.
Dr. Haji is a licensed clinical psychologist specializing in psychodiagnostic assessment, forensic assessment, dual diagnosis, serious and persistent mental illness, depression, anxiety, personality disorders, and substance abuse treatment. She practices in Miami and has no conflicts of interest.
Sigmund Freud said, “Out of your vulnerabilities will come greatest strength.” What exactly did Dr. Freud mean by this?
Many aspects of mental health treatment include cognitive restructuring, behavioral changes, emotion processing, and setting boundaries. These are all critical aspects of treatment, but what about kindness and compassion?
We often forget that kindness requires us to be vulnerable and take a risk at times. Being kind to others is not always easy, and it is not always an automatic reaction. Vulnerability often involves risk, but the outcomes often outweigh fear.
Dr. Freud was highlighting that being kind, open, and honest will often result in strong character and resilience. In turn, it will help others. Psychology and psychiatry have proved time and time again that empathy, compassion, and kindness have numerous benefits for mental and physical health for both the giver and the receiver.
From a biological perspective, we know that acts of kindness signal the brain to release serotonin and dopamine, known as “feel good transmitters,” and endorphins, which in turn lessen pain, depression, and anxiety. According to Waguih W. Ishak, MD, a psychiatrist affiliated with Cedars-Sinai in Los Angeles,1 in addition to boosting oxytocin and dopamine, being kind can increase serotonin, a neurotransmitter that helps regulate mood. Kindness and compassion have been shown to release oxytocin, known as the “love hormone,” which increases self-esteem, trust, connection, and optimism. Oxytocin also reduces blood pressure and has been dubbed the “cardioprotective” hormone. According to Kelli Harding, MD, MPH, a psychiatrist affiliated with Columbia University in New York,2 kindness can extend the lifespan. Research from Emory University in Atlanta has shown that, when an individual is kind to another, the brain’s reward centers light up – resulting in a “helper’s high.” Thus, kindness is self-reinforcing.3
Kindness leads to a greater sense of connection to others and a lessening in feelings of isolation. Small acts of kindness build up compassion in oneself. Research indicates that kindness doesn’t just positively affect the giver and receiver but can also benefit onlookers. An article in Psychology Today,4 suggests that those who witness acts of kindness are also more likely to “pay it forward,” resulting in a domino effect. Along these same lines, altruistic people, specifically those who engage in charitable donations, expressed higher levels of overall happiness according to a 2010 Harvard Business School survey.5
“You can’t pour from an empty cup” is a trendy quote making its way around social media. Before we can be kind and compassionate to others, we must first be kind and compassionate to ourselves. In today’s world, productivity and pressure-filled environments consume us daily. We often find ourselves skipping meals, forgetting to connect with loved ones, missing breaks, and even neglecting our sleep. It is virtually impossible to care for others when we are depleted ourselves. Sometimes not prioritizing ourselves can result in collateral damage. We may become short-tempered, irritable, moody, and overwhelmed. At this point kindness, compassion, and empathy toward others are likely to be absent. Once we replenish ourselves, by taking time off, indulging in a nice meal, exercising, we are more likely to respond as opposed to react, ask others about themselves, and engage in overall positive interactions throughout our day. Kindness is best fostered by being kind to ourselves to sustain our own well-being and by being kind to others in order to maintain the cycle. For clinicians who have been pushed to respond to various aspects of the COVID-19 pandemic, self-care has never been more important.
COVID-19 has been difficult for everyone, particularly the elderly and vulnerable populations. However, kindness has proved to be an overwhelming response as many businesses and individuals have taken to volunteering time and resources for those in need. Even big corporations have chipped in. For example, Lyft and Uber – in a partnership with the White House – are now offering free rides to vaccine sites, and several local businesses have donated personal protective equipment to hospitals and assisted living facilities.
Kindness and empathy are ever present in the field of mental health, medicine, and substance use treatment. The very act of caring for another involves kindness. In medicine, empathy has been defined as “an emotional experience between an observer and a subject in which the observer, based on visual and auditory cues, identifies and transiently experiences the subject’s emotional state.”6
As mental health professionals, we receive empathy training early on in our schooling – increasingly so over the last decade. Research has indicated that trusting relationships between clinicians and patients result in optimal care. Evidence-based communication styles are being widely implemented. This entails using nonjudgmental language, open-ended questions, and active listening skills, for example. In addition, the mental health professionals have our conscious and unconscious judgments. If empathy training is provided, we can learn to acknowledge our biases and mitigate them. Lastly, empathy training has been proven to assist with destigmatization, increase in treatment seeking, and overall better outcomes.
Substance use treatment, which often focuses on cognition and behavior changing, boundaries, and family dynamics, also requires support and kindness. Although it is not an empirically based “treatment,” Alcoholics Anonymous (AA) has used kindness for decades.
Step 12 of AA’s 12-step program, which was developed by two people with alcohol use disorder in 1935 in Akron, Ohio, is as follows: “Having had a spiritual awakening as the result of these steps, we tried to carry this message to alcoholics, and to practice these principles in all our affairs.”
Once AA members are on solid ground with their sobriety, they are urged to help others in their recovery. This process provides many benefits. When individuals are concerned about someone else, they are less focused on themselves. This helps the individuals in recovery to decrease their rumination and “get out of themselves.” It also allows for the AA member to be kind and helpful to an individual who is suffering, thereby expressing kindness, compassion, and empathy. This act of “paying it forward” produces a domino effect that has withstood the test of time as evidenced by the ever-growing fellowship of Alcoholics Anonymous.
Several small acts of kindness can help us as clinicians and our patients:
1. Practice self-care.
2. Take a half day off from your practice.
3. Give staff a half day off.
4. Call a family member or friend and ask them how they are doing. Then engage in active listening and refrain from giving advice.
5. Donate to a homeless shelter or volunteer your time at a charity.
6. Give a stranger a compliment.
7. Surprise someone with a small gift.
8. Send a loved one a letter instead of a text.
9. Pick up litter.
10. Acknowledge family and friends who gave you extra support during the pandemic.
11. Take baked goods to your office.
12. Help a neighbor with groceries.
13. Leave a generous tip.
14. Play soft music in your office.
In conclusion, kindness, empathy, and compassion are vital concepts that are not just fluffy theories. They have vast mental, physical, and social benefits for us and our patients.
References
1. Cedars-Sinai staff. The Science of Kindness. 2019 Feb 13. Cedars-Sinai blog.
2. Harding K. The Rabbit Effect: Live Longer, Happier, and Healthier with the Groundbreaking Science of Kindness. Atria Books, 2019.
3. Ritvo E. BeKindr. Momosa Publishing, 2017.
4. Svoboda E. “Pay it Forward.” Psychology Today. Last reviewed 2016 Jun 9.
5. Aknin LB et al. “Prosocial spending and well-being: Cross-Cultural Evidence for a Psychological Universal.” Harvard Business School. Working Paper 11-038. 2010.
6. Hirsch EM. AMA J Ethics. Virtual Mentor. 2007;9(6):423-7.
Dr. Haji is a licensed clinical psychologist specializing in psychodiagnostic assessment, forensic assessment, dual diagnosis, serious and persistent mental illness, depression, anxiety, personality disorders, and substance abuse treatment. She practices in Miami and has no conflicts of interest.
Pressure on primary care expected to intensify with long-COVID
, experts say.
“It could be as many as 5% to 10% who are still having symptoms at 12 weeks. Those numbers are higher if you’re talking about patients who had been hospitalized with COVID-19,” Russ Phillips, MD, director of the Center for Primary Care at Harvard Medical School, Boston, said in an interview.
A recent study from the Centers for Disease Control and Prevention and Kaiser Permanente Georgia found that among 3,171 nonhospitalized adult patients with COVID-19, 69% had one or more outpatient visits 28 to 180 days after the diagnosis. Two-thirds had a visit for a new primary diagnosis, and about one-third had a new specialist visit. Symptom diagnoses included cough, shortness of breath, chest or throat pain, and fatigue.
These visits have come while cases of acute COVID continue to occur, and there has been an increase in patients returning to primary care after avoiding it while the pandemic surged. For these patients, delay in seeking care has often led a worsening of chronic conditions.
Dr. Phillips pointed to a shortcoming in primary care that will need to be addressed with regard to long-COVID: “We don’t have good systems to follow patients and their symptoms over time.”
Long-COVID will require that kind of care, but current payment systems don’t support proactively reaching out to patients to track them over time, he noted.
“We do a good job of identifying these issues for patients who come in, but it’s the patients who don’t that we worry about the most,” he said.
Dr. Phillips provided examples of the kind of management plans needed to improve outcomes for patients with long-COVID. In anticoagulation clinics, patients who receive blood thinners are monitored closely, and in mental health care, patients with depression are linked with social workers and are monitored regularly.
“Around COVID, those management plans are in their infancy,” he said.
John Brooks, MD, chief medical officer for the CDC’s COVID-19 response, testified in a congressional hearing at the end of April that interim guidance concerning protocols for long-COVID in primary care are forthcoming. He also noted that the CDC is working closely with the Centers for Medicare & Medicaid Services to develop medical coding for long-COVID.
In the meantime, Dr. Phillips said, one strategy is to have patients self-monitor their condition and relay results to primary care physicians electronically.
As an example, Dr. Phillips described a patient with long-COVID who was receiving supplemental oxygen and who wanted to resume her exercise regimen.
She checked her own oxygen saturation levels before and during exercise and reported the levels every few days through their patient portal.
“Very slowly we were able to cut down on her oxygen and increase her exercise capacity until she no longer needed oxygen and could go back to her usual activities of daily living,” he said.
Nurse practitioners, social workers, and other nonphysician care team members may be increasingly relied upon to provide care for long-COVID patients as well, he said.
Additionally, telehealth, which is currently reimbursed the same way as in-person visits are, enables easier access for checking in with patients, he said.
Empathy and listening needed
Sabrina Assoumou, MD, MPH, assistant professor of medicine at Boston University, told this news organization that it will be crucial to address health care disparities as long-COVID cases mount.
COVID disproportionately affects communities of color, and it stands to reason that this will be the case for long-COVID as well, she said. Diversifying the workforce will be vital, inasmuch as diagnosis may depend on how well a physician listens to patients as they describe their symptoms, continued Dr. Assoumou, whose primary care practice centers on HIV patients.
The symptoms of long-COVID are vague, she explained, and include brain fog, fatigue, and shortness of breath, and it takes longer to diagnose than many conditions.
Dr. Assoumou said some people were never tested for COVID and never received a diagnosis, yet they are now experiencing the extended effects.
“Long-COVID will force us to go back to the basics – like really listening to our patients,” she said. “We’re definitely going to need to be more empathetic.”
No large influx yet
Charles Vega, MD, health sciences clinical professor of family medicine at the University of California, Irvine, said he is skeptical that the primary care system will be overwhelmed with long-COVID cases.
Dr. Vega is a family physician working in the largest safety net clinic in Orange County, California. About 90% of his patients are LatinX, a population disproportionately burdened by COVID, yet he hasn’t seen a surge in long-COVID cases.
He said that may be because patients know there isn’t a treatment for long-COVID. They are well connected through online forums such as Body Politic COVID-19 Support Group and may not feel they need to see a doctor.
“It wasn’t scientists finding [long-COVID], it was patients who developed this disease model themselves,” he said. “That’s where most of the data sharing is.”
Yet, for long-COVID patients who do need care, primary care is the best home for them, Dr. Vega said.
He said the most common symptoms he sees are fatigue and poor activity tolerance. “They get winded going to the bathroom,” he said.
The most difficult symptom is dyspnea, he said. Patients describe being breathless, but it’s not bad enough to qualify for supplemental oxygen.
“Being breathless is a pretty desperate thing and hurts quality of life,” he said.
Most patients describe general malaise.
Care for long-COVID will require medical care and mental health care, Dr. Vega notes. Primary care is already set up to screen and to coordinate care with the appropriate provider.
“I think there’s a role for specialists, but primary care has to be involved,” he said.
Dr. Phillips, Dr. Assoumou, and Dr. Vega report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
, experts say.
“It could be as many as 5% to 10% who are still having symptoms at 12 weeks. Those numbers are higher if you’re talking about patients who had been hospitalized with COVID-19,” Russ Phillips, MD, director of the Center for Primary Care at Harvard Medical School, Boston, said in an interview.
A recent study from the Centers for Disease Control and Prevention and Kaiser Permanente Georgia found that among 3,171 nonhospitalized adult patients with COVID-19, 69% had one or more outpatient visits 28 to 180 days after the diagnosis. Two-thirds had a visit for a new primary diagnosis, and about one-third had a new specialist visit. Symptom diagnoses included cough, shortness of breath, chest or throat pain, and fatigue.
These visits have come while cases of acute COVID continue to occur, and there has been an increase in patients returning to primary care after avoiding it while the pandemic surged. For these patients, delay in seeking care has often led a worsening of chronic conditions.
Dr. Phillips pointed to a shortcoming in primary care that will need to be addressed with regard to long-COVID: “We don’t have good systems to follow patients and their symptoms over time.”
Long-COVID will require that kind of care, but current payment systems don’t support proactively reaching out to patients to track them over time, he noted.
“We do a good job of identifying these issues for patients who come in, but it’s the patients who don’t that we worry about the most,” he said.
Dr. Phillips provided examples of the kind of management plans needed to improve outcomes for patients with long-COVID. In anticoagulation clinics, patients who receive blood thinners are monitored closely, and in mental health care, patients with depression are linked with social workers and are monitored regularly.
“Around COVID, those management plans are in their infancy,” he said.
John Brooks, MD, chief medical officer for the CDC’s COVID-19 response, testified in a congressional hearing at the end of April that interim guidance concerning protocols for long-COVID in primary care are forthcoming. He also noted that the CDC is working closely with the Centers for Medicare & Medicaid Services to develop medical coding for long-COVID.
In the meantime, Dr. Phillips said, one strategy is to have patients self-monitor their condition and relay results to primary care physicians electronically.
As an example, Dr. Phillips described a patient with long-COVID who was receiving supplemental oxygen and who wanted to resume her exercise regimen.
She checked her own oxygen saturation levels before and during exercise and reported the levels every few days through their patient portal.
“Very slowly we were able to cut down on her oxygen and increase her exercise capacity until she no longer needed oxygen and could go back to her usual activities of daily living,” he said.
Nurse practitioners, social workers, and other nonphysician care team members may be increasingly relied upon to provide care for long-COVID patients as well, he said.
Additionally, telehealth, which is currently reimbursed the same way as in-person visits are, enables easier access for checking in with patients, he said.
Empathy and listening needed
Sabrina Assoumou, MD, MPH, assistant professor of medicine at Boston University, told this news organization that it will be crucial to address health care disparities as long-COVID cases mount.
COVID disproportionately affects communities of color, and it stands to reason that this will be the case for long-COVID as well, she said. Diversifying the workforce will be vital, inasmuch as diagnosis may depend on how well a physician listens to patients as they describe their symptoms, continued Dr. Assoumou, whose primary care practice centers on HIV patients.
The symptoms of long-COVID are vague, she explained, and include brain fog, fatigue, and shortness of breath, and it takes longer to diagnose than many conditions.
Dr. Assoumou said some people were never tested for COVID and never received a diagnosis, yet they are now experiencing the extended effects.
“Long-COVID will force us to go back to the basics – like really listening to our patients,” she said. “We’re definitely going to need to be more empathetic.”
No large influx yet
Charles Vega, MD, health sciences clinical professor of family medicine at the University of California, Irvine, said he is skeptical that the primary care system will be overwhelmed with long-COVID cases.
Dr. Vega is a family physician working in the largest safety net clinic in Orange County, California. About 90% of his patients are LatinX, a population disproportionately burdened by COVID, yet he hasn’t seen a surge in long-COVID cases.
He said that may be because patients know there isn’t a treatment for long-COVID. They are well connected through online forums such as Body Politic COVID-19 Support Group and may not feel they need to see a doctor.
“It wasn’t scientists finding [long-COVID], it was patients who developed this disease model themselves,” he said. “That’s where most of the data sharing is.”
Yet, for long-COVID patients who do need care, primary care is the best home for them, Dr. Vega said.
He said the most common symptoms he sees are fatigue and poor activity tolerance. “They get winded going to the bathroom,” he said.
The most difficult symptom is dyspnea, he said. Patients describe being breathless, but it’s not bad enough to qualify for supplemental oxygen.
“Being breathless is a pretty desperate thing and hurts quality of life,” he said.
Most patients describe general malaise.
Care for long-COVID will require medical care and mental health care, Dr. Vega notes. Primary care is already set up to screen and to coordinate care with the appropriate provider.
“I think there’s a role for specialists, but primary care has to be involved,” he said.
Dr. Phillips, Dr. Assoumou, and Dr. Vega report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
, experts say.
“It could be as many as 5% to 10% who are still having symptoms at 12 weeks. Those numbers are higher if you’re talking about patients who had been hospitalized with COVID-19,” Russ Phillips, MD, director of the Center for Primary Care at Harvard Medical School, Boston, said in an interview.
A recent study from the Centers for Disease Control and Prevention and Kaiser Permanente Georgia found that among 3,171 nonhospitalized adult patients with COVID-19, 69% had one or more outpatient visits 28 to 180 days after the diagnosis. Two-thirds had a visit for a new primary diagnosis, and about one-third had a new specialist visit. Symptom diagnoses included cough, shortness of breath, chest or throat pain, and fatigue.
These visits have come while cases of acute COVID continue to occur, and there has been an increase in patients returning to primary care after avoiding it while the pandemic surged. For these patients, delay in seeking care has often led a worsening of chronic conditions.
Dr. Phillips pointed to a shortcoming in primary care that will need to be addressed with regard to long-COVID: “We don’t have good systems to follow patients and their symptoms over time.”
Long-COVID will require that kind of care, but current payment systems don’t support proactively reaching out to patients to track them over time, he noted.
“We do a good job of identifying these issues for patients who come in, but it’s the patients who don’t that we worry about the most,” he said.
Dr. Phillips provided examples of the kind of management plans needed to improve outcomes for patients with long-COVID. In anticoagulation clinics, patients who receive blood thinners are monitored closely, and in mental health care, patients with depression are linked with social workers and are monitored regularly.
“Around COVID, those management plans are in their infancy,” he said.
John Brooks, MD, chief medical officer for the CDC’s COVID-19 response, testified in a congressional hearing at the end of April that interim guidance concerning protocols for long-COVID in primary care are forthcoming. He also noted that the CDC is working closely with the Centers for Medicare & Medicaid Services to develop medical coding for long-COVID.
In the meantime, Dr. Phillips said, one strategy is to have patients self-monitor their condition and relay results to primary care physicians electronically.
As an example, Dr. Phillips described a patient with long-COVID who was receiving supplemental oxygen and who wanted to resume her exercise regimen.
She checked her own oxygen saturation levels before and during exercise and reported the levels every few days through their patient portal.
“Very slowly we were able to cut down on her oxygen and increase her exercise capacity until she no longer needed oxygen and could go back to her usual activities of daily living,” he said.
Nurse practitioners, social workers, and other nonphysician care team members may be increasingly relied upon to provide care for long-COVID patients as well, he said.
Additionally, telehealth, which is currently reimbursed the same way as in-person visits are, enables easier access for checking in with patients, he said.
Empathy and listening needed
Sabrina Assoumou, MD, MPH, assistant professor of medicine at Boston University, told this news organization that it will be crucial to address health care disparities as long-COVID cases mount.
COVID disproportionately affects communities of color, and it stands to reason that this will be the case for long-COVID as well, she said. Diversifying the workforce will be vital, inasmuch as diagnosis may depend on how well a physician listens to patients as they describe their symptoms, continued Dr. Assoumou, whose primary care practice centers on HIV patients.
The symptoms of long-COVID are vague, she explained, and include brain fog, fatigue, and shortness of breath, and it takes longer to diagnose than many conditions.
Dr. Assoumou said some people were never tested for COVID and never received a diagnosis, yet they are now experiencing the extended effects.
“Long-COVID will force us to go back to the basics – like really listening to our patients,” she said. “We’re definitely going to need to be more empathetic.”
No large influx yet
Charles Vega, MD, health sciences clinical professor of family medicine at the University of California, Irvine, said he is skeptical that the primary care system will be overwhelmed with long-COVID cases.
Dr. Vega is a family physician working in the largest safety net clinic in Orange County, California. About 90% of his patients are LatinX, a population disproportionately burdened by COVID, yet he hasn’t seen a surge in long-COVID cases.
He said that may be because patients know there isn’t a treatment for long-COVID. They are well connected through online forums such as Body Politic COVID-19 Support Group and may not feel they need to see a doctor.
“It wasn’t scientists finding [long-COVID], it was patients who developed this disease model themselves,” he said. “That’s where most of the data sharing is.”
Yet, for long-COVID patients who do need care, primary care is the best home for them, Dr. Vega said.
He said the most common symptoms he sees are fatigue and poor activity tolerance. “They get winded going to the bathroom,” he said.
The most difficult symptom is dyspnea, he said. Patients describe being breathless, but it’s not bad enough to qualify for supplemental oxygen.
“Being breathless is a pretty desperate thing and hurts quality of life,” he said.
Most patients describe general malaise.
Care for long-COVID will require medical care and mental health care, Dr. Vega notes. Primary care is already set up to screen and to coordinate care with the appropriate provider.
“I think there’s a role for specialists, but primary care has to be involved,” he said.
Dr. Phillips, Dr. Assoumou, and Dr. Vega report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.