User login
Long COVID symptoms reported by 6% of pediatric patients
The prevalence of long COVID in children has been unclear, and is complicated by the lack of a consistent definition, said Anna Funk, PhD, an epidemiologist at the University of Calgary (Alba.), during her online presentation of the findings at the 31st European Congress of Clinical Microbiology & Infectious Diseases.
In the several small studies conducted to date, rates range from 0% to 67% 2-4 months after infection, Dr. Funk reported.
To examine prevalence, she and her colleagues, as part of the Pediatric Emergency Research Network (PERN) global research consortium, assessed more than 10,500 children who were screened for SARS-CoV-2 when they presented to the ED at 1 of 41 study sites in 10 countries – Australia, Canada, Indonesia, the United States, plus three countries in Latin America and three in Western Europe – from March 2020 to June 15, 2021.
PERN researchers are following up with the more than 3,100 children who tested positive 14, 30, and 90 days after testing, tracking respiratory, neurologic, and psychobehavioral sequelae.
Dr. Funk presented data on the 1,884 children who tested positive for SARS-CoV-2 before Jan. 20, 2021, and who had completed 90-day follow-up; 447 of those children were hospitalized and 1,437 were not.
Symptoms were reported more often by children admitted to the hospital than not admitted (9.8% vs. 4.6%). Common persistent symptoms were respiratory in 2% of cases, systemic (such as fatigue and fever) in 2%, neurologic (such as headache, seizures, and continued loss of taste or smell) in 1%, and psychological (such as new-onset depression and anxiety) in 1%.
“This study provides the first good epidemiological data on persistent symptoms among SARS-CoV-2–infected children, regardless of severity,” said Kevin Messacar, MD, a pediatric infectious disease clinician and researcher at Children’s Hospital Colorado in Aurora, who was not involved in the study.
And the findings show that, although severe COVID and chronic symptoms are less common in children than in adults, they are “not nonexistent and need to be taken seriously,” he said in an interview.
After adjustment for country of enrollment, children aged 10-17 years were more likely to experience persistent symptoms than children younger than 1 year (odds ratio, 2.4; P = .002).
Hospitalized children were more than twice as likely to experience persistent symptoms as nonhospitalized children (OR, 2.5; P < .001). And children who presented to the ED with at least seven symptoms were four times more likely to have long-term symptoms than those who presented with fewer symptoms (OR, 4.02; P = .01).
‘Some reassurance’
“Given that COVID is new and is known to have acute cardiac and neurologic effects, particularly in children with [multisystem inflammatory syndrome], there were initially concerns about persistent cardiovascular and neurologic effects in any infected child,” Dr. Messacar explained. “These data provide some reassurance that this is uncommon among children with mild or moderate infections who are not hospitalized.”
But “the risk is not zero,” he added. “Getting children vaccinated when it is available to them and taking precautions to prevent unvaccinated children getting COVID is the best way to reduce the risk of severe disease or persistent symptoms.”
The study was limited by its lack of data on variants, reliance on self-reported symptoms, and a population drawn solely from EDs, Dr. Funk acknowledged.
No external funding source was noted. Dr. Messacar and Dr. Funk disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The prevalence of long COVID in children has been unclear, and is complicated by the lack of a consistent definition, said Anna Funk, PhD, an epidemiologist at the University of Calgary (Alba.), during her online presentation of the findings at the 31st European Congress of Clinical Microbiology & Infectious Diseases.
In the several small studies conducted to date, rates range from 0% to 67% 2-4 months after infection, Dr. Funk reported.
To examine prevalence, she and her colleagues, as part of the Pediatric Emergency Research Network (PERN) global research consortium, assessed more than 10,500 children who were screened for SARS-CoV-2 when they presented to the ED at 1 of 41 study sites in 10 countries – Australia, Canada, Indonesia, the United States, plus three countries in Latin America and three in Western Europe – from March 2020 to June 15, 2021.
PERN researchers are following up with the more than 3,100 children who tested positive 14, 30, and 90 days after testing, tracking respiratory, neurologic, and psychobehavioral sequelae.
Dr. Funk presented data on the 1,884 children who tested positive for SARS-CoV-2 before Jan. 20, 2021, and who had completed 90-day follow-up; 447 of those children were hospitalized and 1,437 were not.
Symptoms were reported more often by children admitted to the hospital than not admitted (9.8% vs. 4.6%). Common persistent symptoms were respiratory in 2% of cases, systemic (such as fatigue and fever) in 2%, neurologic (such as headache, seizures, and continued loss of taste or smell) in 1%, and psychological (such as new-onset depression and anxiety) in 1%.
“This study provides the first good epidemiological data on persistent symptoms among SARS-CoV-2–infected children, regardless of severity,” said Kevin Messacar, MD, a pediatric infectious disease clinician and researcher at Children’s Hospital Colorado in Aurora, who was not involved in the study.
And the findings show that, although severe COVID and chronic symptoms are less common in children than in adults, they are “not nonexistent and need to be taken seriously,” he said in an interview.
After adjustment for country of enrollment, children aged 10-17 years were more likely to experience persistent symptoms than children younger than 1 year (odds ratio, 2.4; P = .002).
Hospitalized children were more than twice as likely to experience persistent symptoms as nonhospitalized children (OR, 2.5; P < .001). And children who presented to the ED with at least seven symptoms were four times more likely to have long-term symptoms than those who presented with fewer symptoms (OR, 4.02; P = .01).
‘Some reassurance’
“Given that COVID is new and is known to have acute cardiac and neurologic effects, particularly in children with [multisystem inflammatory syndrome], there were initially concerns about persistent cardiovascular and neurologic effects in any infected child,” Dr. Messacar explained. “These data provide some reassurance that this is uncommon among children with mild or moderate infections who are not hospitalized.”
But “the risk is not zero,” he added. “Getting children vaccinated when it is available to them and taking precautions to prevent unvaccinated children getting COVID is the best way to reduce the risk of severe disease or persistent symptoms.”
The study was limited by its lack of data on variants, reliance on self-reported symptoms, and a population drawn solely from EDs, Dr. Funk acknowledged.
No external funding source was noted. Dr. Messacar and Dr. Funk disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The prevalence of long COVID in children has been unclear, and is complicated by the lack of a consistent definition, said Anna Funk, PhD, an epidemiologist at the University of Calgary (Alba.), during her online presentation of the findings at the 31st European Congress of Clinical Microbiology & Infectious Diseases.
In the several small studies conducted to date, rates range from 0% to 67% 2-4 months after infection, Dr. Funk reported.
To examine prevalence, she and her colleagues, as part of the Pediatric Emergency Research Network (PERN) global research consortium, assessed more than 10,500 children who were screened for SARS-CoV-2 when they presented to the ED at 1 of 41 study sites in 10 countries – Australia, Canada, Indonesia, the United States, plus three countries in Latin America and three in Western Europe – from March 2020 to June 15, 2021.
PERN researchers are following up with the more than 3,100 children who tested positive 14, 30, and 90 days after testing, tracking respiratory, neurologic, and psychobehavioral sequelae.
Dr. Funk presented data on the 1,884 children who tested positive for SARS-CoV-2 before Jan. 20, 2021, and who had completed 90-day follow-up; 447 of those children were hospitalized and 1,437 were not.
Symptoms were reported more often by children admitted to the hospital than not admitted (9.8% vs. 4.6%). Common persistent symptoms were respiratory in 2% of cases, systemic (such as fatigue and fever) in 2%, neurologic (such as headache, seizures, and continued loss of taste or smell) in 1%, and psychological (such as new-onset depression and anxiety) in 1%.
“This study provides the first good epidemiological data on persistent symptoms among SARS-CoV-2–infected children, regardless of severity,” said Kevin Messacar, MD, a pediatric infectious disease clinician and researcher at Children’s Hospital Colorado in Aurora, who was not involved in the study.
And the findings show that, although severe COVID and chronic symptoms are less common in children than in adults, they are “not nonexistent and need to be taken seriously,” he said in an interview.
After adjustment for country of enrollment, children aged 10-17 years were more likely to experience persistent symptoms than children younger than 1 year (odds ratio, 2.4; P = .002).
Hospitalized children were more than twice as likely to experience persistent symptoms as nonhospitalized children (OR, 2.5; P < .001). And children who presented to the ED with at least seven symptoms were four times more likely to have long-term symptoms than those who presented with fewer symptoms (OR, 4.02; P = .01).
‘Some reassurance’
“Given that COVID is new and is known to have acute cardiac and neurologic effects, particularly in children with [multisystem inflammatory syndrome], there were initially concerns about persistent cardiovascular and neurologic effects in any infected child,” Dr. Messacar explained. “These data provide some reassurance that this is uncommon among children with mild or moderate infections who are not hospitalized.”
But “the risk is not zero,” he added. “Getting children vaccinated when it is available to them and taking precautions to prevent unvaccinated children getting COVID is the best way to reduce the risk of severe disease or persistent symptoms.”
The study was limited by its lack of data on variants, reliance on self-reported symptoms, and a population drawn solely from EDs, Dr. Funk acknowledged.
No external funding source was noted. Dr. Messacar and Dr. Funk disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rising rates of T1D in children: Is COVID to blame?
In early 2020, the COVID-19 pandemic changed everything about life as we know it, with widespread shutdowns across the globe. The U.S. health care system quickly adapted, pivoting to telehealth visits when able and proactively managing outpatient conditions to prevent overwhelming hospital resources and utilization. Meanwhile, at my practice, the typical rate of about one new-onset pediatric type 1 diabetes (T1D) case per week increased to about two per week.
However, the new diabetes cases continued to accumulate, and I saw more patients being diagnosed who did not have a known family history of autoimmunity. I began to ask friends at other centers whether they were noticing the same trend.
One colleague documented a 36% increase in her large center compared with the previous year. Another noted a 40% rise at his children’s hospital. We observed that there was often a respiratory illness reported several weeks before presenting with T1D. Sometimes the child was known to be COVID-positive. Sometimes the child had not been tested. Sometimes we suspected that COVID had been a preceding illness and then found negative SARS-CoV-2 antibodies – but we were not certain whether the result was meaningful given the time lapsed since infection.
Soon, reports emerged of large increases in severe diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state at initial presentation, a trend reported in other countries.
Is COVID-19 a trigger for T1D?
There is known precedent for increased risk for T1D after viral infections in patients who are already genetically susceptible. Mechanisms of immune-mediated islet cell failure would make sense following SARS-CoV-2 infection; direct islet toxicity was noted with SARS-CoV-1 and has been suspected with SARS-CoV-2 but not proven. Some have suggested that hypercoagulability with COVID-19 may lead to ischemic damage to the pancreas.
With multiple potential pathways for islet damage, increases in insulin-dependent diabetes would logically follow. Still, whether this is the case remains unclear. There is not yet definitive evidence that there is uptake of SARS-CoV-2 via receptors in the pancreatic beta cells.
Our current understanding of T1D pathogenesis is that susceptible individuals develop autoimmunity in response to an environmental trigger, with beta-cell failure developing over months to years. Perhaps vulnerable patients with genetic risk for pancreatic autoimmunity were stressed by SARS-CoV-2 infection and were diagnosed earlier than they might have been, showing some lead-time bias. Adult patients with COVID-19 demonstrated hyperglycemia that has been reversible in some cases, like the stress hyperglycemia seen with other infections and surgery in response to proinflammatory states.
The true question seems to be whether there is a unique type of diabetes related to direct viral toxicity. Do newly diagnosed patients have measurable traditional antibodies, like anti-glutamic acid decarboxylase or anti-islet cell antibodies? Is there proof of preceding SARS-CoV-2 infection? In the new cases that I thought were unusual at first glance, I found typical pancreatic autoimmunity and negative SARS-CoV-2 antibodies. The small cohorts reported thus far have had similar findings.
A stronger case can be made for the risk of developing diabetes (types 1 and 2) with rapid weight gain. Another marked pattern that pediatric endocrinologists have observed has been increased weight gain in children with closed schools, decreased activity, and more social isolation. I have seen weight change as great as 100 lb in a teen over the past year; 30- to 50-lb weight increases over the course of the pandemic have been common. Considering the “accelerator hypothesis” of faster onset of type 2 diabetes with rapid weight gain, implications for hastening of T1D with weight gain have also been considered. The full impact of these dramatic weight changes will take time to understand.
The true story may not emerge for years
Anecdotes and theoretical concerns may give us pause, but they are far from scientific truth. Efforts are underway to explore this perceived trend with international registries, including the CoviDIAB Registry as well as T1D Exchange. The true story may not emerge until years have passed to see the cumulative fallout of COVID-19. Regardless, these troubling observations should be considered as pandemic safeguards continue to loosen.
While pediatric mortality from COVID-19 has been relatively low (though sadly not zero), some have placed too little focus on possible morbidity. Long-term effects like long COVID and neuropsychiatric sequelae are becoming evident in all populations, including children. If a lifelong illness like diabetes can be directly linked to COVID-19, protecting children from infection with measures like masks becomes all the more crucial until vaccines are more readily available. Despite our rapid progress with understanding COVID-19 disease, there is still much left to learn.
A version of this article first appeared on Medscape.com.
In early 2020, the COVID-19 pandemic changed everything about life as we know it, with widespread shutdowns across the globe. The U.S. health care system quickly adapted, pivoting to telehealth visits when able and proactively managing outpatient conditions to prevent overwhelming hospital resources and utilization. Meanwhile, at my practice, the typical rate of about one new-onset pediatric type 1 diabetes (T1D) case per week increased to about two per week.
However, the new diabetes cases continued to accumulate, and I saw more patients being diagnosed who did not have a known family history of autoimmunity. I began to ask friends at other centers whether they were noticing the same trend.
One colleague documented a 36% increase in her large center compared with the previous year. Another noted a 40% rise at his children’s hospital. We observed that there was often a respiratory illness reported several weeks before presenting with T1D. Sometimes the child was known to be COVID-positive. Sometimes the child had not been tested. Sometimes we suspected that COVID had been a preceding illness and then found negative SARS-CoV-2 antibodies – but we were not certain whether the result was meaningful given the time lapsed since infection.
Soon, reports emerged of large increases in severe diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state at initial presentation, a trend reported in other countries.
Is COVID-19 a trigger for T1D?
There is known precedent for increased risk for T1D after viral infections in patients who are already genetically susceptible. Mechanisms of immune-mediated islet cell failure would make sense following SARS-CoV-2 infection; direct islet toxicity was noted with SARS-CoV-1 and has been suspected with SARS-CoV-2 but not proven. Some have suggested that hypercoagulability with COVID-19 may lead to ischemic damage to the pancreas.
With multiple potential pathways for islet damage, increases in insulin-dependent diabetes would logically follow. Still, whether this is the case remains unclear. There is not yet definitive evidence that there is uptake of SARS-CoV-2 via receptors in the pancreatic beta cells.
Our current understanding of T1D pathogenesis is that susceptible individuals develop autoimmunity in response to an environmental trigger, with beta-cell failure developing over months to years. Perhaps vulnerable patients with genetic risk for pancreatic autoimmunity were stressed by SARS-CoV-2 infection and were diagnosed earlier than they might have been, showing some lead-time bias. Adult patients with COVID-19 demonstrated hyperglycemia that has been reversible in some cases, like the stress hyperglycemia seen with other infections and surgery in response to proinflammatory states.
The true question seems to be whether there is a unique type of diabetes related to direct viral toxicity. Do newly diagnosed patients have measurable traditional antibodies, like anti-glutamic acid decarboxylase or anti-islet cell antibodies? Is there proof of preceding SARS-CoV-2 infection? In the new cases that I thought were unusual at first glance, I found typical pancreatic autoimmunity and negative SARS-CoV-2 antibodies. The small cohorts reported thus far have had similar findings.
A stronger case can be made for the risk of developing diabetes (types 1 and 2) with rapid weight gain. Another marked pattern that pediatric endocrinologists have observed has been increased weight gain in children with closed schools, decreased activity, and more social isolation. I have seen weight change as great as 100 lb in a teen over the past year; 30- to 50-lb weight increases over the course of the pandemic have been common. Considering the “accelerator hypothesis” of faster onset of type 2 diabetes with rapid weight gain, implications for hastening of T1D with weight gain have also been considered. The full impact of these dramatic weight changes will take time to understand.
The true story may not emerge for years
Anecdotes and theoretical concerns may give us pause, but they are far from scientific truth. Efforts are underway to explore this perceived trend with international registries, including the CoviDIAB Registry as well as T1D Exchange. The true story may not emerge until years have passed to see the cumulative fallout of COVID-19. Regardless, these troubling observations should be considered as pandemic safeguards continue to loosen.
While pediatric mortality from COVID-19 has been relatively low (though sadly not zero), some have placed too little focus on possible morbidity. Long-term effects like long COVID and neuropsychiatric sequelae are becoming evident in all populations, including children. If a lifelong illness like diabetes can be directly linked to COVID-19, protecting children from infection with measures like masks becomes all the more crucial until vaccines are more readily available. Despite our rapid progress with understanding COVID-19 disease, there is still much left to learn.
A version of this article first appeared on Medscape.com.
In early 2020, the COVID-19 pandemic changed everything about life as we know it, with widespread shutdowns across the globe. The U.S. health care system quickly adapted, pivoting to telehealth visits when able and proactively managing outpatient conditions to prevent overwhelming hospital resources and utilization. Meanwhile, at my practice, the typical rate of about one new-onset pediatric type 1 diabetes (T1D) case per week increased to about two per week.
However, the new diabetes cases continued to accumulate, and I saw more patients being diagnosed who did not have a known family history of autoimmunity. I began to ask friends at other centers whether they were noticing the same trend.
One colleague documented a 36% increase in her large center compared with the previous year. Another noted a 40% rise at his children’s hospital. We observed that there was often a respiratory illness reported several weeks before presenting with T1D. Sometimes the child was known to be COVID-positive. Sometimes the child had not been tested. Sometimes we suspected that COVID had been a preceding illness and then found negative SARS-CoV-2 antibodies – but we were not certain whether the result was meaningful given the time lapsed since infection.
Soon, reports emerged of large increases in severe diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state at initial presentation, a trend reported in other countries.
Is COVID-19 a trigger for T1D?
There is known precedent for increased risk for T1D after viral infections in patients who are already genetically susceptible. Mechanisms of immune-mediated islet cell failure would make sense following SARS-CoV-2 infection; direct islet toxicity was noted with SARS-CoV-1 and has been suspected with SARS-CoV-2 but not proven. Some have suggested that hypercoagulability with COVID-19 may lead to ischemic damage to the pancreas.
With multiple potential pathways for islet damage, increases in insulin-dependent diabetes would logically follow. Still, whether this is the case remains unclear. There is not yet definitive evidence that there is uptake of SARS-CoV-2 via receptors in the pancreatic beta cells.
Our current understanding of T1D pathogenesis is that susceptible individuals develop autoimmunity in response to an environmental trigger, with beta-cell failure developing over months to years. Perhaps vulnerable patients with genetic risk for pancreatic autoimmunity were stressed by SARS-CoV-2 infection and were diagnosed earlier than they might have been, showing some lead-time bias. Adult patients with COVID-19 demonstrated hyperglycemia that has been reversible in some cases, like the stress hyperglycemia seen with other infections and surgery in response to proinflammatory states.
The true question seems to be whether there is a unique type of diabetes related to direct viral toxicity. Do newly diagnosed patients have measurable traditional antibodies, like anti-glutamic acid decarboxylase or anti-islet cell antibodies? Is there proof of preceding SARS-CoV-2 infection? In the new cases that I thought were unusual at first glance, I found typical pancreatic autoimmunity and negative SARS-CoV-2 antibodies. The small cohorts reported thus far have had similar findings.
A stronger case can be made for the risk of developing diabetes (types 1 and 2) with rapid weight gain. Another marked pattern that pediatric endocrinologists have observed has been increased weight gain in children with closed schools, decreased activity, and more social isolation. I have seen weight change as great as 100 lb in a teen over the past year; 30- to 50-lb weight increases over the course of the pandemic have been common. Considering the “accelerator hypothesis” of faster onset of type 2 diabetes with rapid weight gain, implications for hastening of T1D with weight gain have also been considered. The full impact of these dramatic weight changes will take time to understand.
The true story may not emerge for years
Anecdotes and theoretical concerns may give us pause, but they are far from scientific truth. Efforts are underway to explore this perceived trend with international registries, including the CoviDIAB Registry as well as T1D Exchange. The true story may not emerge until years have passed to see the cumulative fallout of COVID-19. Regardless, these troubling observations should be considered as pandemic safeguards continue to loosen.
While pediatric mortality from COVID-19 has been relatively low (though sadly not zero), some have placed too little focus on possible morbidity. Long-term effects like long COVID and neuropsychiatric sequelae are becoming evident in all populations, including children. If a lifelong illness like diabetes can be directly linked to COVID-19, protecting children from infection with measures like masks becomes all the more crucial until vaccines are more readily available. Despite our rapid progress with understanding COVID-19 disease, there is still much left to learn.
A version of this article first appeared on Medscape.com.
Children and COVID: New vaccinations drop as the case count rises
With only a quarter of all children aged 12-15 years fully vaccinated against COVID-19, first vaccinations continued to drop and new cases for all children rose for the second consecutive week.
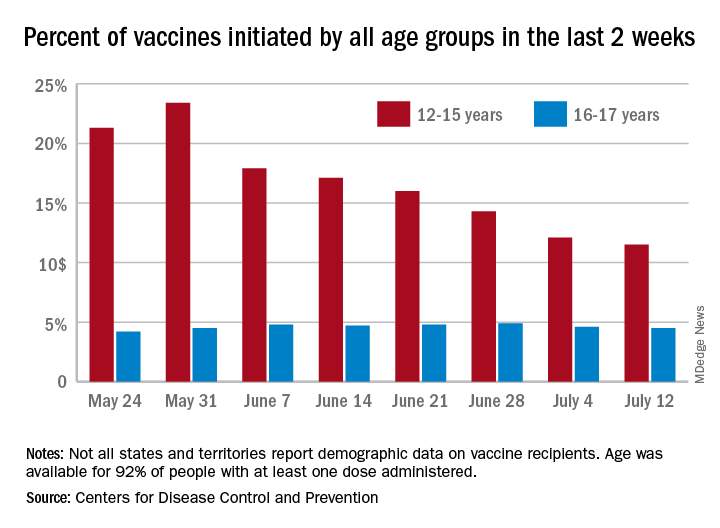
Just under 25% of children aged 12-15 had completed the vaccine regimen as of July 12, and just over one-third (33.5%) had received at least one dose. Meanwhile, that age group represented 11.5% of people who initiated vaccination during the 2 weeks ending July 12, down from 12.1% a week earlier, the Centers for Disease Control and Prevention said. The total number of new vaccinations for the week ending July 12 was just over 201,000, compared with 307,000 for the previous week.
New cases of COVID-19, however, were on the rise in children. The 19,000 new cases reported for the week ending July 8 were up from 12,000 a week earlier and 8,000 the week before that, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
That report also shows that children made up 22.3% of all new cases during the week of July 2-8, compared with 16.8% the previous week, and that there were nine deaths in children that same week, the most since March. COVID-related deaths among children total 344 in the 46 jurisdictions (43 states, New York City, Puerto Rico, and Guam) that are reporting such data by age. “It is not possible to standardize more detailed age ranges for children based on what is publicly available from the states,” the two groups noted.
Such data are available from the CDC’s COVID Data Tracker, however, and they show that children aged 16-17 years, who became eligible for COVID vaccination before the younger age group, are further ahead in the process. Among the older children, almost 46% had gotten at least one dose and 37% were fully vaccinated by July 12.
With only a quarter of all children aged 12-15 years fully vaccinated against COVID-19, first vaccinations continued to drop and new cases for all children rose for the second consecutive week.
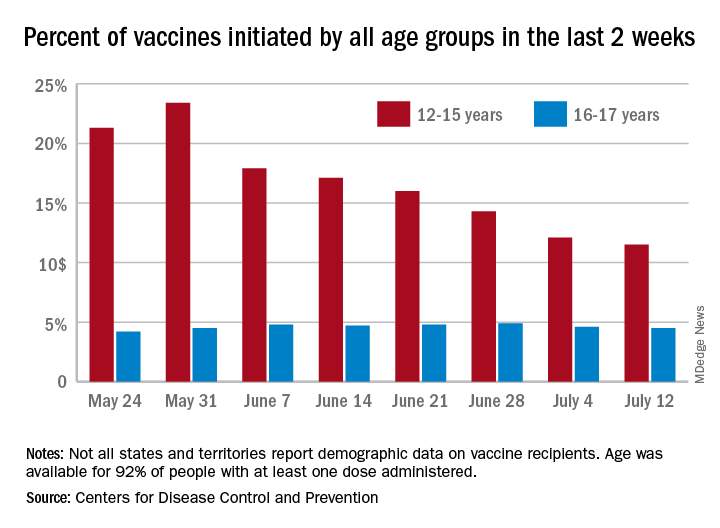
Just under 25% of children aged 12-15 had completed the vaccine regimen as of July 12, and just over one-third (33.5%) had received at least one dose. Meanwhile, that age group represented 11.5% of people who initiated vaccination during the 2 weeks ending July 12, down from 12.1% a week earlier, the Centers for Disease Control and Prevention said. The total number of new vaccinations for the week ending July 12 was just over 201,000, compared with 307,000 for the previous week.
New cases of COVID-19, however, were on the rise in children. The 19,000 new cases reported for the week ending July 8 were up from 12,000 a week earlier and 8,000 the week before that, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
That report also shows that children made up 22.3% of all new cases during the week of July 2-8, compared with 16.8% the previous week, and that there were nine deaths in children that same week, the most since March. COVID-related deaths among children total 344 in the 46 jurisdictions (43 states, New York City, Puerto Rico, and Guam) that are reporting such data by age. “It is not possible to standardize more detailed age ranges for children based on what is publicly available from the states,” the two groups noted.
Such data are available from the CDC’s COVID Data Tracker, however, and they show that children aged 16-17 years, who became eligible for COVID vaccination before the younger age group, are further ahead in the process. Among the older children, almost 46% had gotten at least one dose and 37% were fully vaccinated by July 12.
With only a quarter of all children aged 12-15 years fully vaccinated against COVID-19, first vaccinations continued to drop and new cases for all children rose for the second consecutive week.
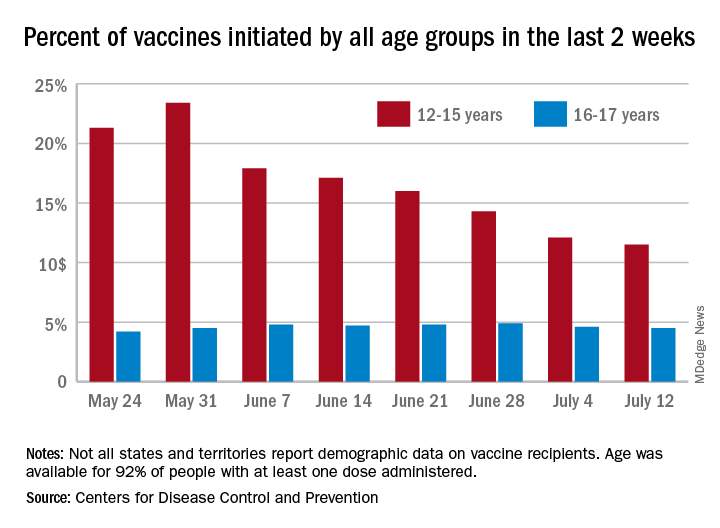
Just under 25% of children aged 12-15 had completed the vaccine regimen as of July 12, and just over one-third (33.5%) had received at least one dose. Meanwhile, that age group represented 11.5% of people who initiated vaccination during the 2 weeks ending July 12, down from 12.1% a week earlier, the Centers for Disease Control and Prevention said. The total number of new vaccinations for the week ending July 12 was just over 201,000, compared with 307,000 for the previous week.
New cases of COVID-19, however, were on the rise in children. The 19,000 new cases reported for the week ending July 8 were up from 12,000 a week earlier and 8,000 the week before that, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
That report also shows that children made up 22.3% of all new cases during the week of July 2-8, compared with 16.8% the previous week, and that there were nine deaths in children that same week, the most since March. COVID-related deaths among children total 344 in the 46 jurisdictions (43 states, New York City, Puerto Rico, and Guam) that are reporting such data by age. “It is not possible to standardize more detailed age ranges for children based on what is publicly available from the states,” the two groups noted.
Such data are available from the CDC’s COVID Data Tracker, however, and they show that children aged 16-17 years, who became eligible for COVID vaccination before the younger age group, are further ahead in the process. Among the older children, almost 46% had gotten at least one dose and 37% were fully vaccinated by July 12.
Patients on methotrexate show T-cell response to Pfizer vaccine
People taking methotrexate had low antibody responses after the first dose of the Pfizer-BioNTech mRNA COVID-19 vaccine, but did show evidence of T-cell–mediated immune responses, findings from a small study show.
The common immunosuppressant has previously been linked to poor antibody responses to mRNA COVID-19 vaccines, but this appears to be the first study to look at T-cell responses in people taking methotrexate.
The study findings were presented online July 11 at the 31st European Congress of Clinical Microbiology & Infectious Diseases and published in The Lancet Rheumatology.
“These findings indicate that seroconversion alone might not adequately reflect vaccine immunogenicity in individuals with immune-mediated inflammatory diseases receiving therapeutic immunosuppression, and caution against routine use of seroconversion data in isolation in clinical practice,” Satveer K. Mahil, MBBChir, PhD, from St. John’s Institute of Dermatology, Guy’s and St. Thomas’ NHS Foundation Trust, London, and colleagues wrote.
“When taking into account functional humoral immunity and T-cell responses, our data suggest that targeted biologics do not impair vaccine responses and provide some reassurance to this vulnerable population,” they wrote. “Notably, although methotrexate attenuated humoral immunity, cellular responses were preserved.”
Dr. Mahil and colleagues assessed 84 consecutive patients from a psoriasis specialist clinic that serves London and southeast England. Median age of the cohort was 43 years, and 85% were White. All had a confirmed psoriasis diagnosis, received the first dose of the Pfizer-BioNTech COVID-19 vaccine, and were taking either methotrexate (17 patients) or a targeted biologic (27 were taking a tumor necrosis factor inhibitor, 15 an interleukin-17 inhibitor, and 25 an IL-23 inhibitor). In addition, 17 healthy patients not receiving immunosuppression therapy who received the Pfizer-BioNTech vaccine served as the control group.
Four weeks after the study participants received their first dose of the vaccine, 78% of the immunosuppressed patients underwent seroconversion – producing measurable antibodies – as did 100% of the control group. Patients taking methotrexate had the lowest seroconversion rate at 47%, compared with 79% with TNF inhibitors, 83% with IL-23 inhibitors, and 100% with IL-17 inhibitors.
Participants taking methotrexate also had lower neutralizing activity against SARS-CoV-2 than control subjects and those taking a targeted biologic, who had similar levels of neutralizing activity.
All participants had low neutralizing titers against the alpha (B.1.1.7) variant.
The researchers also assessed cellular immunity, “defined as the presence of T cells secreting interferon-gamma, IL-2, or IL-21 in response to stimulation with two peptide pools spanning the entire length of the SARS-CoV-2 spike glycoprotein.”
A T-cell response was seen in 84% of participants taking immunosuppressants, including 93% of those in the methotrexate group and 69% of control subjects.
‘Some protection is better than none’
These findings regarding antibodies match what has been seen in other research, said Ignacio Sanz, MD, director of the Lowance Center for Human Immunology at Emory University, Atlanta.
It would be helpful to see antibody responses after the second doses, he added. Those data will be reported later, according to Dr. Mahil and colleagues.
“The authors make the valid point that T-cell immunity should also be measured. The information is meaningful and supports the idea that there could be protection still provided,” Dr. Sanz said in an interview, adding that it would have been helpful to see CD8 T-cell response as well.
“My message to patients, still, is that some protection is better than none, and that, indeed, protection may be afforded in different ways, including T-cell immunity, which, to the extent tested, seems to be induced,” he said. But discussion of B cells independent of their role in producing antibodies is missing.
“When it comes to B-cell responses, antibodies are the easier and more direct measurement. However, it is perfectly possible that the vaccine may fail to induce high antibody titers and still generate good B-cell immunity,” in the same way virus-specific memory B cells do, he explained. “They would not directly produce antibodies, yet they would be available for a good and quick response in the case of subsequent encounter with the virus and, incidentally, in the case of a booster dose. It is possible that the generation of antibody-producing plasma cells might be uncoupled from the generation of memory B cells.”
Temporarily stopping methotrexate
It is well known that methotrexate impairs humoral responses to influenza and pneumococcal vaccines, write Caoilfhionn M. Connolly, MD, and Julie J. Paik, MD, both from the Johns Hopkins University, Baltimore, in an accompanying comment.
Research has also shown that temporarily stopping methotrexate therapy for 2 weeks enhances response to the flu vaccine in patients with rheumatoid arthritis, which prompted the American College of Rheumatology to recommended temporary interruption of methotrexate for 1 week after each dose of the COVID-19 vaccine, the pair notes.
“Although it is encouraging that cellular responses appear to be preserved even in patients with poor humoral responses, these findings are not consistent across study groups,” Dr. Connolly and Dr. Paik explained. “During this period of clinical uncertainty, patients might remain vulnerable, especially after the first dose, and should engage in risk mitigation strategies.”
Mild adverse events after vaccination were reported by 75% of the immunosuppressed patients – most commonly injection-site pain, headache, and fatigue – and by 94% of control subjects. No participants reported moderate or severe adverse effects.
However, 11% of immunosuppressed patients reported a worsening of psoriasis symptoms after vaccination.
This research was funded by the U.K. National Institute for Health Research. Dr. Mahil has received departmental income from AbbVie, Celgene, Eli Lilly, Janssen-Cilag, Novartis, Sano, and UCB unrelated to this study. Seven other authors have relationships with a wide range of pharmaceutical and other companies. Dr. Sanz, Dr. Connolly, and Dr. Paik disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People taking methotrexate had low antibody responses after the first dose of the Pfizer-BioNTech mRNA COVID-19 vaccine, but did show evidence of T-cell–mediated immune responses, findings from a small study show.
The common immunosuppressant has previously been linked to poor antibody responses to mRNA COVID-19 vaccines, but this appears to be the first study to look at T-cell responses in people taking methotrexate.
The study findings were presented online July 11 at the 31st European Congress of Clinical Microbiology & Infectious Diseases and published in The Lancet Rheumatology.
“These findings indicate that seroconversion alone might not adequately reflect vaccine immunogenicity in individuals with immune-mediated inflammatory diseases receiving therapeutic immunosuppression, and caution against routine use of seroconversion data in isolation in clinical practice,” Satveer K. Mahil, MBBChir, PhD, from St. John’s Institute of Dermatology, Guy’s and St. Thomas’ NHS Foundation Trust, London, and colleagues wrote.
“When taking into account functional humoral immunity and T-cell responses, our data suggest that targeted biologics do not impair vaccine responses and provide some reassurance to this vulnerable population,” they wrote. “Notably, although methotrexate attenuated humoral immunity, cellular responses were preserved.”
Dr. Mahil and colleagues assessed 84 consecutive patients from a psoriasis specialist clinic that serves London and southeast England. Median age of the cohort was 43 years, and 85% were White. All had a confirmed psoriasis diagnosis, received the first dose of the Pfizer-BioNTech COVID-19 vaccine, and were taking either methotrexate (17 patients) or a targeted biologic (27 were taking a tumor necrosis factor inhibitor, 15 an interleukin-17 inhibitor, and 25 an IL-23 inhibitor). In addition, 17 healthy patients not receiving immunosuppression therapy who received the Pfizer-BioNTech vaccine served as the control group.
Four weeks after the study participants received their first dose of the vaccine, 78% of the immunosuppressed patients underwent seroconversion – producing measurable antibodies – as did 100% of the control group. Patients taking methotrexate had the lowest seroconversion rate at 47%, compared with 79% with TNF inhibitors, 83% with IL-23 inhibitors, and 100% with IL-17 inhibitors.
Participants taking methotrexate also had lower neutralizing activity against SARS-CoV-2 than control subjects and those taking a targeted biologic, who had similar levels of neutralizing activity.
All participants had low neutralizing titers against the alpha (B.1.1.7) variant.
The researchers also assessed cellular immunity, “defined as the presence of T cells secreting interferon-gamma, IL-2, or IL-21 in response to stimulation with two peptide pools spanning the entire length of the SARS-CoV-2 spike glycoprotein.”
A T-cell response was seen in 84% of participants taking immunosuppressants, including 93% of those in the methotrexate group and 69% of control subjects.
‘Some protection is better than none’
These findings regarding antibodies match what has been seen in other research, said Ignacio Sanz, MD, director of the Lowance Center for Human Immunology at Emory University, Atlanta.
It would be helpful to see antibody responses after the second doses, he added. Those data will be reported later, according to Dr. Mahil and colleagues.
“The authors make the valid point that T-cell immunity should also be measured. The information is meaningful and supports the idea that there could be protection still provided,” Dr. Sanz said in an interview, adding that it would have been helpful to see CD8 T-cell response as well.
“My message to patients, still, is that some protection is better than none, and that, indeed, protection may be afforded in different ways, including T-cell immunity, which, to the extent tested, seems to be induced,” he said. But discussion of B cells independent of their role in producing antibodies is missing.
“When it comes to B-cell responses, antibodies are the easier and more direct measurement. However, it is perfectly possible that the vaccine may fail to induce high antibody titers and still generate good B-cell immunity,” in the same way virus-specific memory B cells do, he explained. “They would not directly produce antibodies, yet they would be available for a good and quick response in the case of subsequent encounter with the virus and, incidentally, in the case of a booster dose. It is possible that the generation of antibody-producing plasma cells might be uncoupled from the generation of memory B cells.”
Temporarily stopping methotrexate
It is well known that methotrexate impairs humoral responses to influenza and pneumococcal vaccines, write Caoilfhionn M. Connolly, MD, and Julie J. Paik, MD, both from the Johns Hopkins University, Baltimore, in an accompanying comment.
Research has also shown that temporarily stopping methotrexate therapy for 2 weeks enhances response to the flu vaccine in patients with rheumatoid arthritis, which prompted the American College of Rheumatology to recommended temporary interruption of methotrexate for 1 week after each dose of the COVID-19 vaccine, the pair notes.
“Although it is encouraging that cellular responses appear to be preserved even in patients with poor humoral responses, these findings are not consistent across study groups,” Dr. Connolly and Dr. Paik explained. “During this period of clinical uncertainty, patients might remain vulnerable, especially after the first dose, and should engage in risk mitigation strategies.”
Mild adverse events after vaccination were reported by 75% of the immunosuppressed patients – most commonly injection-site pain, headache, and fatigue – and by 94% of control subjects. No participants reported moderate or severe adverse effects.
However, 11% of immunosuppressed patients reported a worsening of psoriasis symptoms after vaccination.
This research was funded by the U.K. National Institute for Health Research. Dr. Mahil has received departmental income from AbbVie, Celgene, Eli Lilly, Janssen-Cilag, Novartis, Sano, and UCB unrelated to this study. Seven other authors have relationships with a wide range of pharmaceutical and other companies. Dr. Sanz, Dr. Connolly, and Dr. Paik disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People taking methotrexate had low antibody responses after the first dose of the Pfizer-BioNTech mRNA COVID-19 vaccine, but did show evidence of T-cell–mediated immune responses, findings from a small study show.
The common immunosuppressant has previously been linked to poor antibody responses to mRNA COVID-19 vaccines, but this appears to be the first study to look at T-cell responses in people taking methotrexate.
The study findings were presented online July 11 at the 31st European Congress of Clinical Microbiology & Infectious Diseases and published in The Lancet Rheumatology.
“These findings indicate that seroconversion alone might not adequately reflect vaccine immunogenicity in individuals with immune-mediated inflammatory diseases receiving therapeutic immunosuppression, and caution against routine use of seroconversion data in isolation in clinical practice,” Satveer K. Mahil, MBBChir, PhD, from St. John’s Institute of Dermatology, Guy’s and St. Thomas’ NHS Foundation Trust, London, and colleagues wrote.
“When taking into account functional humoral immunity and T-cell responses, our data suggest that targeted biologics do not impair vaccine responses and provide some reassurance to this vulnerable population,” they wrote. “Notably, although methotrexate attenuated humoral immunity, cellular responses were preserved.”
Dr. Mahil and colleagues assessed 84 consecutive patients from a psoriasis specialist clinic that serves London and southeast England. Median age of the cohort was 43 years, and 85% were White. All had a confirmed psoriasis diagnosis, received the first dose of the Pfizer-BioNTech COVID-19 vaccine, and were taking either methotrexate (17 patients) or a targeted biologic (27 were taking a tumor necrosis factor inhibitor, 15 an interleukin-17 inhibitor, and 25 an IL-23 inhibitor). In addition, 17 healthy patients not receiving immunosuppression therapy who received the Pfizer-BioNTech vaccine served as the control group.
Four weeks after the study participants received their first dose of the vaccine, 78% of the immunosuppressed patients underwent seroconversion – producing measurable antibodies – as did 100% of the control group. Patients taking methotrexate had the lowest seroconversion rate at 47%, compared with 79% with TNF inhibitors, 83% with IL-23 inhibitors, and 100% with IL-17 inhibitors.
Participants taking methotrexate also had lower neutralizing activity against SARS-CoV-2 than control subjects and those taking a targeted biologic, who had similar levels of neutralizing activity.
All participants had low neutralizing titers against the alpha (B.1.1.7) variant.
The researchers also assessed cellular immunity, “defined as the presence of T cells secreting interferon-gamma, IL-2, or IL-21 in response to stimulation with two peptide pools spanning the entire length of the SARS-CoV-2 spike glycoprotein.”
A T-cell response was seen in 84% of participants taking immunosuppressants, including 93% of those in the methotrexate group and 69% of control subjects.
‘Some protection is better than none’
These findings regarding antibodies match what has been seen in other research, said Ignacio Sanz, MD, director of the Lowance Center for Human Immunology at Emory University, Atlanta.
It would be helpful to see antibody responses after the second doses, he added. Those data will be reported later, according to Dr. Mahil and colleagues.
“The authors make the valid point that T-cell immunity should also be measured. The information is meaningful and supports the idea that there could be protection still provided,” Dr. Sanz said in an interview, adding that it would have been helpful to see CD8 T-cell response as well.
“My message to patients, still, is that some protection is better than none, and that, indeed, protection may be afforded in different ways, including T-cell immunity, which, to the extent tested, seems to be induced,” he said. But discussion of B cells independent of their role in producing antibodies is missing.
“When it comes to B-cell responses, antibodies are the easier and more direct measurement. However, it is perfectly possible that the vaccine may fail to induce high antibody titers and still generate good B-cell immunity,” in the same way virus-specific memory B cells do, he explained. “They would not directly produce antibodies, yet they would be available for a good and quick response in the case of subsequent encounter with the virus and, incidentally, in the case of a booster dose. It is possible that the generation of antibody-producing plasma cells might be uncoupled from the generation of memory B cells.”
Temporarily stopping methotrexate
It is well known that methotrexate impairs humoral responses to influenza and pneumococcal vaccines, write Caoilfhionn M. Connolly, MD, and Julie J. Paik, MD, both from the Johns Hopkins University, Baltimore, in an accompanying comment.
Research has also shown that temporarily stopping methotrexate therapy for 2 weeks enhances response to the flu vaccine in patients with rheumatoid arthritis, which prompted the American College of Rheumatology to recommended temporary interruption of methotrexate for 1 week after each dose of the COVID-19 vaccine, the pair notes.
“Although it is encouraging that cellular responses appear to be preserved even in patients with poor humoral responses, these findings are not consistent across study groups,” Dr. Connolly and Dr. Paik explained. “During this period of clinical uncertainty, patients might remain vulnerable, especially after the first dose, and should engage in risk mitigation strategies.”
Mild adverse events after vaccination were reported by 75% of the immunosuppressed patients – most commonly injection-site pain, headache, and fatigue – and by 94% of control subjects. No participants reported moderate or severe adverse effects.
However, 11% of immunosuppressed patients reported a worsening of psoriasis symptoms after vaccination.
This research was funded by the U.K. National Institute for Health Research. Dr. Mahil has received departmental income from AbbVie, Celgene, Eli Lilly, Janssen-Cilag, Novartis, Sano, and UCB unrelated to this study. Seven other authors have relationships with a wide range of pharmaceutical and other companies. Dr. Sanz, Dr. Connolly, and Dr. Paik disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA to warn J&J that vaccine can increase Guillain-Barré risk: Media
as early as July 13, according to multiple media reports.
Although the FDA is projected to add the new warning to the labeling for the vaccine, the agency still calculates the benefit of vaccination with the J&J product continues to outweigh the risk. Benefits include protection against the Delta variant and serious COVID-19 outcomes.
More than 100 cases of Guillain-Barré reported to the Vaccine Adverse Event Reporting System, a federal program for reporting vaccine issues, spurred the FDA to act.
Men and people older than 50 appear to be at highest risk, according to reports of a July 12 Centers for Disease Control and Prevention statement. The CDC also revealed that most cases occur about 2 weeks following immunization.
Guillain-Barré syndrome often causes muscle weakness and sometimes temporary paralysis. Most people who develop the rare syndrome recover.
Such was not the case for a 57-year-old man, the New York Times reported July 12. He had a history of both a heart attack and stroke in the previous 4 years and died in April after vaccination with the J&J vaccine and developing Guillain-Barré.
The new warning comes in the wake of a number of setbacks for the company’s COVID-19 vaccine. On April 13, the FDA and CDC both recommended a 10-day pause on administration of the J&J vaccine after reports of rare blood clot events emerged. In mid-June, the FDA requested that Johnson and Johnson discard millions of vaccine doses produced at a manufacturing facility in Baltimore.
The mRNA vaccines from Pfizer/BioNTech and Moderna are not affected by the new FDA warning.
The Biden administration is expected to make a formal announcement of the new warning for the Johnson and Johnson vaccine as early as July 13, the Times reports.
A version of this article first appeared on Medscape.com.
as early as July 13, according to multiple media reports.
Although the FDA is projected to add the new warning to the labeling for the vaccine, the agency still calculates the benefit of vaccination with the J&J product continues to outweigh the risk. Benefits include protection against the Delta variant and serious COVID-19 outcomes.
More than 100 cases of Guillain-Barré reported to the Vaccine Adverse Event Reporting System, a federal program for reporting vaccine issues, spurred the FDA to act.
Men and people older than 50 appear to be at highest risk, according to reports of a July 12 Centers for Disease Control and Prevention statement. The CDC also revealed that most cases occur about 2 weeks following immunization.
Guillain-Barré syndrome often causes muscle weakness and sometimes temporary paralysis. Most people who develop the rare syndrome recover.
Such was not the case for a 57-year-old man, the New York Times reported July 12. He had a history of both a heart attack and stroke in the previous 4 years and died in April after vaccination with the J&J vaccine and developing Guillain-Barré.
The new warning comes in the wake of a number of setbacks for the company’s COVID-19 vaccine. On April 13, the FDA and CDC both recommended a 10-day pause on administration of the J&J vaccine after reports of rare blood clot events emerged. In mid-June, the FDA requested that Johnson and Johnson discard millions of vaccine doses produced at a manufacturing facility in Baltimore.
The mRNA vaccines from Pfizer/BioNTech and Moderna are not affected by the new FDA warning.
The Biden administration is expected to make a formal announcement of the new warning for the Johnson and Johnson vaccine as early as July 13, the Times reports.
A version of this article first appeared on Medscape.com.
as early as July 13, according to multiple media reports.
Although the FDA is projected to add the new warning to the labeling for the vaccine, the agency still calculates the benefit of vaccination with the J&J product continues to outweigh the risk. Benefits include protection against the Delta variant and serious COVID-19 outcomes.
More than 100 cases of Guillain-Barré reported to the Vaccine Adverse Event Reporting System, a federal program for reporting vaccine issues, spurred the FDA to act.
Men and people older than 50 appear to be at highest risk, according to reports of a July 12 Centers for Disease Control and Prevention statement. The CDC also revealed that most cases occur about 2 weeks following immunization.
Guillain-Barré syndrome often causes muscle weakness and sometimes temporary paralysis. Most people who develop the rare syndrome recover.
Such was not the case for a 57-year-old man, the New York Times reported July 12. He had a history of both a heart attack and stroke in the previous 4 years and died in April after vaccination with the J&J vaccine and developing Guillain-Barré.
The new warning comes in the wake of a number of setbacks for the company’s COVID-19 vaccine. On April 13, the FDA and CDC both recommended a 10-day pause on administration of the J&J vaccine after reports of rare blood clot events emerged. In mid-June, the FDA requested that Johnson and Johnson discard millions of vaccine doses produced at a manufacturing facility in Baltimore.
The mRNA vaccines from Pfizer/BioNTech and Moderna are not affected by the new FDA warning.
The Biden administration is expected to make a formal announcement of the new warning for the Johnson and Johnson vaccine as early as July 13, the Times reports.
A version of this article first appeared on Medscape.com.
‘Long haul’ COVID recovery worse than cancer rehab for some: CDC
People experiencing ongoing or “long-haul” symptoms after COVID-19 illness were more likely to report pain, challenges with physical activities, and “substantially worse health,” compared with people needing rehabilitation because of cancer, lead author Jessica Rogers-Brown, PhD, and colleagues report.
The study was published online July 9 in Morbidity and Mortality Weekly Report (MMWR).
The CDC investigators compared the self-reported physical and mental health symptoms, physical endurance, and use of health services of 1,295 outpatients recovering from COVID-19 and a control group of another 2,395 outpatients rehabilitating from a previous or current cancer diagnosis who had not experienced COVID-19.
Researchers used electronic health record data from January 2020 to March 2021 in the Select Medical network of outpatient clinics. The study included patients from 36 states and the District of Columbia.
Compared with people referred for cancer rehabilitation, those with COVID-19 symptoms lasting beyond 4 weeks were 2.3 times more likely to report pain, 1.8 times more likely to report worse physical health, and 1.6 times more likely to report difficulty with physical activities, an adjusted odds ratio analysis reveals.
The COVID-19 rehabilitation group also performed significantly worse on a 6-minute walk test, suggesting less physical endurance than people recovering from cancer (P < .001). They also used more rehabilitation services overall than the control group.
The researchers suggest services tailored to the unique physical and mental health rehabilitation needs of the post–COVID-19 patient population could be warranted.
The study does not suggest all people recovering with COVID-19 will fare worse than people recovering from cancer, the authors caution. They note that “these results should not be interpreted to mean that post–COVID-19 patients overall had poorer physical and mental health than patients with cancer.”
“Instead, results indicate that post–COVID-19 patients specifically referred to a large physical rehabilitation network had poorer health measures than those referred for cancer, which indicates that some patients recovering from COVID-19 had substantial rehabilitation needs.”
A version of this article first appeared on Medscape.com.
People experiencing ongoing or “long-haul” symptoms after COVID-19 illness were more likely to report pain, challenges with physical activities, and “substantially worse health,” compared with people needing rehabilitation because of cancer, lead author Jessica Rogers-Brown, PhD, and colleagues report.
The study was published online July 9 in Morbidity and Mortality Weekly Report (MMWR).
The CDC investigators compared the self-reported physical and mental health symptoms, physical endurance, and use of health services of 1,295 outpatients recovering from COVID-19 and a control group of another 2,395 outpatients rehabilitating from a previous or current cancer diagnosis who had not experienced COVID-19.
Researchers used electronic health record data from January 2020 to March 2021 in the Select Medical network of outpatient clinics. The study included patients from 36 states and the District of Columbia.
Compared with people referred for cancer rehabilitation, those with COVID-19 symptoms lasting beyond 4 weeks were 2.3 times more likely to report pain, 1.8 times more likely to report worse physical health, and 1.6 times more likely to report difficulty with physical activities, an adjusted odds ratio analysis reveals.
The COVID-19 rehabilitation group also performed significantly worse on a 6-minute walk test, suggesting less physical endurance than people recovering from cancer (P < .001). They also used more rehabilitation services overall than the control group.
The researchers suggest services tailored to the unique physical and mental health rehabilitation needs of the post–COVID-19 patient population could be warranted.
The study does not suggest all people recovering with COVID-19 will fare worse than people recovering from cancer, the authors caution. They note that “these results should not be interpreted to mean that post–COVID-19 patients overall had poorer physical and mental health than patients with cancer.”
“Instead, results indicate that post–COVID-19 patients specifically referred to a large physical rehabilitation network had poorer health measures than those referred for cancer, which indicates that some patients recovering from COVID-19 had substantial rehabilitation needs.”
A version of this article first appeared on Medscape.com.
People experiencing ongoing or “long-haul” symptoms after COVID-19 illness were more likely to report pain, challenges with physical activities, and “substantially worse health,” compared with people needing rehabilitation because of cancer, lead author Jessica Rogers-Brown, PhD, and colleagues report.
The study was published online July 9 in Morbidity and Mortality Weekly Report (MMWR).
The CDC investigators compared the self-reported physical and mental health symptoms, physical endurance, and use of health services of 1,295 outpatients recovering from COVID-19 and a control group of another 2,395 outpatients rehabilitating from a previous or current cancer diagnosis who had not experienced COVID-19.
Researchers used electronic health record data from January 2020 to March 2021 in the Select Medical network of outpatient clinics. The study included patients from 36 states and the District of Columbia.
Compared with people referred for cancer rehabilitation, those with COVID-19 symptoms lasting beyond 4 weeks were 2.3 times more likely to report pain, 1.8 times more likely to report worse physical health, and 1.6 times more likely to report difficulty with physical activities, an adjusted odds ratio analysis reveals.
The COVID-19 rehabilitation group also performed significantly worse on a 6-minute walk test, suggesting less physical endurance than people recovering from cancer (P < .001). They also used more rehabilitation services overall than the control group.
The researchers suggest services tailored to the unique physical and mental health rehabilitation needs of the post–COVID-19 patient population could be warranted.
The study does not suggest all people recovering with COVID-19 will fare worse than people recovering from cancer, the authors caution. They note that “these results should not be interpreted to mean that post–COVID-19 patients overall had poorer physical and mental health than patients with cancer.”
“Instead, results indicate that post–COVID-19 patients specifically referred to a large physical rehabilitation network had poorer health measures than those referred for cancer, which indicates that some patients recovering from COVID-19 had substantial rehabilitation needs.”
A version of this article first appeared on Medscape.com.
Malpractice claims from the COVID-19 pandemic: More questions than answers
Editor’s note: This article has been provided by The Doctors Company, the exclusively endorsed medical malpractice carrier for the Society of Hospital Medicine.
The pandemic has raised pressing questions around preventive measures, vaccines, and safe treatment, but it has also obscured one key lingering uncertainty for medical professionals: Where are all the medical malpractice claims?
A variety of factors create a cloud of uncertainty around when, if ever, we will see the claims we expected from care provided just before the pandemic, much less claims deriving from care during the pandemic of both COVID-19 and non–COVID-19 patients.
Malpractice claims take time to surface
We won’t know until 2022 or later whether there will be an increase in claims related to the pandemic. When a medical error occurs, it’s not like an automobile accident. Everybody nearby knows when there’s been an automobile accident because they hear screeching tires, a loud crash, and then sirens. But when a medical error occurs, generally speaking, neither the doctor nor the patient immediately knows that something is amiss. It can take months or years for people to realize that something untoward has occurred.
Claims from medical errors that occurred before the pandemic bring additional uncertainties. In 2020, we saw fewer than expected overall claims filed from events occurring 18-24 months before the pandemic. In total, 20% fewer claims were filed than in 2019. This may have had to do with courts shutting down, people being reluctant to meet with attorneys to discuss a claim, and/or lawyers working from home. We may see these claims filed later than expected, or maybe we won’t see them at all.
But without a doubt, pandemic-related claims will be filed. The pandemic’s impact on physicians increases the risk of claims. Burnout is a major cause of medical errors, and a recent study found that out of 60 countries, U.S. health care providers showed the highest rates of burnout. We’re concerned about the stress affecting physicians’ performance – not just the physical stress of the demands put on them while treating COVID-19 patients, but all of the worry. For instance, a lot of doctors at the start of this pandemic stayed at hotels because they didn’t want to bring the virus home to their families – if they got exposed. Those sorts of stressors from life disruptions, on top of the stress of treating COVID-19 patients and the stress of treating non–COVID-19 patients within overtaxed health care systems, contribute to the possibilities for error.
Immunity protections are not fail-safe
And while health care providers have medical liability protections during the pandemic, these protections may not prevent claims. Health care provider pandemic-related liability laws vary from state to state, and they will be tested in the courts as to whether they’re constitutional. For example, there is pending legislation in New York state that would repeal the provider protections created there at the start of the pandemic. Further, some expert witnesses will couch their statements in terms of what it takes to get around one of these statutes. Therefore, physicians do have reason for concern, even in states with strong liability protections.
The following case example, which is one of about 40 COVID-19–related claims made against our members so far, is a poster child for why these protections are necessary: A quadriplegic patient with COVID-19 had reached the point of organ failure before he reached the ED. There was really nothing medical science could do for him at that point, in terms of a chance at recovery. Therefore, the patient’s physician and conservator placed him in assisted living for palliative care. This was a sad but reasonable decision during a pandemic, with hospital beds needed for patients with a shot at surviving. Following that patient’s death, the physician is being sued.
Defending claims regarding treatment vs. regarding infection control
We are very confident in our ability to protect our members against claims where they are being sued over the treatment of the disease. Claims arising out of treatment are not concerning to us because there is no cure for COVID-19 – one can only treat the symptoms as the virus runs its course.
On the other hand, suits harder to defend would be those that revolve around transmitting the disease because providers didn’t follow guidelines from the Centers for Disease Control and Prevention or there wasn’t enough personal protective equipment. That’s why we stress the importance of following CDC guidelines, and why we’ve taken proactive steps to communicate with the entire medical community throughout the pandemic as part of our commitment to serve those who provide care.
Mr. White is chief operating officer at The Doctors Company. The guidelines suggested here are not rules, do not constitute legal advice, and do not ensure a successful outcome. The ultimate decision regarding the appropriateness of any treatment must be made by each health care provider considering the circumstances of the individual situation and in accordance with the laws of the jurisdiction in which the care is rendered.
Editor’s note: This article has been provided by The Doctors Company, the exclusively endorsed medical malpractice carrier for the Society of Hospital Medicine.
The pandemic has raised pressing questions around preventive measures, vaccines, and safe treatment, but it has also obscured one key lingering uncertainty for medical professionals: Where are all the medical malpractice claims?
A variety of factors create a cloud of uncertainty around when, if ever, we will see the claims we expected from care provided just before the pandemic, much less claims deriving from care during the pandemic of both COVID-19 and non–COVID-19 patients.
Malpractice claims take time to surface
We won’t know until 2022 or later whether there will be an increase in claims related to the pandemic. When a medical error occurs, it’s not like an automobile accident. Everybody nearby knows when there’s been an automobile accident because they hear screeching tires, a loud crash, and then sirens. But when a medical error occurs, generally speaking, neither the doctor nor the patient immediately knows that something is amiss. It can take months or years for people to realize that something untoward has occurred.
Claims from medical errors that occurred before the pandemic bring additional uncertainties. In 2020, we saw fewer than expected overall claims filed from events occurring 18-24 months before the pandemic. In total, 20% fewer claims were filed than in 2019. This may have had to do with courts shutting down, people being reluctant to meet with attorneys to discuss a claim, and/or lawyers working from home. We may see these claims filed later than expected, or maybe we won’t see them at all.
But without a doubt, pandemic-related claims will be filed. The pandemic’s impact on physicians increases the risk of claims. Burnout is a major cause of medical errors, and a recent study found that out of 60 countries, U.S. health care providers showed the highest rates of burnout. We’re concerned about the stress affecting physicians’ performance – not just the physical stress of the demands put on them while treating COVID-19 patients, but all of the worry. For instance, a lot of doctors at the start of this pandemic stayed at hotels because they didn’t want to bring the virus home to their families – if they got exposed. Those sorts of stressors from life disruptions, on top of the stress of treating COVID-19 patients and the stress of treating non–COVID-19 patients within overtaxed health care systems, contribute to the possibilities for error.
Immunity protections are not fail-safe
And while health care providers have medical liability protections during the pandemic, these protections may not prevent claims. Health care provider pandemic-related liability laws vary from state to state, and they will be tested in the courts as to whether they’re constitutional. For example, there is pending legislation in New York state that would repeal the provider protections created there at the start of the pandemic. Further, some expert witnesses will couch their statements in terms of what it takes to get around one of these statutes. Therefore, physicians do have reason for concern, even in states with strong liability protections.
The following case example, which is one of about 40 COVID-19–related claims made against our members so far, is a poster child for why these protections are necessary: A quadriplegic patient with COVID-19 had reached the point of organ failure before he reached the ED. There was really nothing medical science could do for him at that point, in terms of a chance at recovery. Therefore, the patient’s physician and conservator placed him in assisted living for palliative care. This was a sad but reasonable decision during a pandemic, with hospital beds needed for patients with a shot at surviving. Following that patient’s death, the physician is being sued.
Defending claims regarding treatment vs. regarding infection control
We are very confident in our ability to protect our members against claims where they are being sued over the treatment of the disease. Claims arising out of treatment are not concerning to us because there is no cure for COVID-19 – one can only treat the symptoms as the virus runs its course.
On the other hand, suits harder to defend would be those that revolve around transmitting the disease because providers didn’t follow guidelines from the Centers for Disease Control and Prevention or there wasn’t enough personal protective equipment. That’s why we stress the importance of following CDC guidelines, and why we’ve taken proactive steps to communicate with the entire medical community throughout the pandemic as part of our commitment to serve those who provide care.
Mr. White is chief operating officer at The Doctors Company. The guidelines suggested here are not rules, do not constitute legal advice, and do not ensure a successful outcome. The ultimate decision regarding the appropriateness of any treatment must be made by each health care provider considering the circumstances of the individual situation and in accordance with the laws of the jurisdiction in which the care is rendered.
Editor’s note: This article has been provided by The Doctors Company, the exclusively endorsed medical malpractice carrier for the Society of Hospital Medicine.
The pandemic has raised pressing questions around preventive measures, vaccines, and safe treatment, but it has also obscured one key lingering uncertainty for medical professionals: Where are all the medical malpractice claims?
A variety of factors create a cloud of uncertainty around when, if ever, we will see the claims we expected from care provided just before the pandemic, much less claims deriving from care during the pandemic of both COVID-19 and non–COVID-19 patients.
Malpractice claims take time to surface
We won’t know until 2022 or later whether there will be an increase in claims related to the pandemic. When a medical error occurs, it’s not like an automobile accident. Everybody nearby knows when there’s been an automobile accident because they hear screeching tires, a loud crash, and then sirens. But when a medical error occurs, generally speaking, neither the doctor nor the patient immediately knows that something is amiss. It can take months or years for people to realize that something untoward has occurred.
Claims from medical errors that occurred before the pandemic bring additional uncertainties. In 2020, we saw fewer than expected overall claims filed from events occurring 18-24 months before the pandemic. In total, 20% fewer claims were filed than in 2019. This may have had to do with courts shutting down, people being reluctant to meet with attorneys to discuss a claim, and/or lawyers working from home. We may see these claims filed later than expected, or maybe we won’t see them at all.
But without a doubt, pandemic-related claims will be filed. The pandemic’s impact on physicians increases the risk of claims. Burnout is a major cause of medical errors, and a recent study found that out of 60 countries, U.S. health care providers showed the highest rates of burnout. We’re concerned about the stress affecting physicians’ performance – not just the physical stress of the demands put on them while treating COVID-19 patients, but all of the worry. For instance, a lot of doctors at the start of this pandemic stayed at hotels because they didn’t want to bring the virus home to their families – if they got exposed. Those sorts of stressors from life disruptions, on top of the stress of treating COVID-19 patients and the stress of treating non–COVID-19 patients within overtaxed health care systems, contribute to the possibilities for error.
Immunity protections are not fail-safe
And while health care providers have medical liability protections during the pandemic, these protections may not prevent claims. Health care provider pandemic-related liability laws vary from state to state, and they will be tested in the courts as to whether they’re constitutional. For example, there is pending legislation in New York state that would repeal the provider protections created there at the start of the pandemic. Further, some expert witnesses will couch their statements in terms of what it takes to get around one of these statutes. Therefore, physicians do have reason for concern, even in states with strong liability protections.
The following case example, which is one of about 40 COVID-19–related claims made against our members so far, is a poster child for why these protections are necessary: A quadriplegic patient with COVID-19 had reached the point of organ failure before he reached the ED. There was really nothing medical science could do for him at that point, in terms of a chance at recovery. Therefore, the patient’s physician and conservator placed him in assisted living for palliative care. This was a sad but reasonable decision during a pandemic, with hospital beds needed for patients with a shot at surviving. Following that patient’s death, the physician is being sued.
Defending claims regarding treatment vs. regarding infection control
We are very confident in our ability to protect our members against claims where they are being sued over the treatment of the disease. Claims arising out of treatment are not concerning to us because there is no cure for COVID-19 – one can only treat the symptoms as the virus runs its course.
On the other hand, suits harder to defend would be those that revolve around transmitting the disease because providers didn’t follow guidelines from the Centers for Disease Control and Prevention or there wasn’t enough personal protective equipment. That’s why we stress the importance of following CDC guidelines, and why we’ve taken proactive steps to communicate with the entire medical community throughout the pandemic as part of our commitment to serve those who provide care.
Mr. White is chief operating officer at The Doctors Company. The guidelines suggested here are not rules, do not constitute legal advice, and do not ensure a successful outcome. The ultimate decision regarding the appropriateness of any treatment must be made by each health care provider considering the circumstances of the individual situation and in accordance with the laws of the jurisdiction in which the care is rendered.
Are oncologists liable for pandemic-related treatment delays?
Albuquerque oncologist Barbara McAneny, MD, has a patient in his 30s who experienced rectal bleeding for 6 months in 2020 but didn’t see a physician because he was afraid of catching COVID-19. He hoped it was just hemorrhoids.
When he finally came in to see her recently, Dr. McAneny diagnosed a large colon cancer. She fears the delay could prove fatal. “We’ll do our best to cure him, but I don’t know if he’ll be treatable,” she said. “Six months absolutely can make a difference.”
She and other oncologists around the country are seeing many patients in the past few months with advanced breast, colon, lung, and other cancers who were not diagnosed and treated during the COVID-19 pandemic because the patients didn’t want to come in, or because medical facilities weren’t taking nonemergency or non-COVID patients.
Given that failure to diagnose cancer is among the most common medical malpractice allegations, should oncologists be worried that they are at legal risk?
Pandemic provides ‘safe harbor’
In a March survey done by medical malpractice insurer The Doctors Company, one-third of physicians said they were very concerned or somewhat concerned that malpractice claims related to care during the pandemic will rise.
But in most of these cases, physicians and hospitals have little to worry about in terms of medical malpractice liability, according to veteran plaintiff and defense attorneys and the head of a large medical liability insurer.
“You had people with diseases like cancer not getting care because health care systems were overwhelmed,” said Sean Domnick, JD, a malpractice plaintiff attorney in Boca Raton, Fla. “Will those lead to successful malpractice lawsuits? Most likely not.”
“The risks will be low because it’s hard to pin it on the doctor if the patient didn’t want to come in or facilities weren’t scheduling appointments because of the public health emergency,” said Richard Roberts, MD, JD, a professor of family medicine at the University of Wisconsin–Madison who is also a malpractice defense attorney.
In addition, liability protections enacted in more than 30 states because of the COVID-19 pandemic will help shield clinicians from lawsuits. Those laws generally require allegations of gross negligence or reckless conduct far beyond ordinary negligence, which are hard to prove. But the immunity provisions remain largely untested in the courts, and it’s unclear how they will affect cases involving care for conditions other than COVID-19.
Another helpful factor is the widespread public appreciation of the valiant work by health care professionals throughout the pandemic, though that halo effect could fade over the next several years as malpractice claims from the pandemic period are filed and tried.
“In many circumstances, the pandemic will prove to be a safe harbor for providers,” said Steven Wigrizer, JD, a malpractice plaintiff attorney in Philadelphia. “Jurors will be reluctant to impose liability on providers who were doing their best in a global pandemic the world hadn’t seen in 100 years.”
Risky situations
These predictions from liability experts should reassure physicians who are anxious over reports that many cancer diagnoses were missed as a result of the COVID-19 pandemic.
Still, there are situations where physicians and hospitals could be vulnerable to malpractice claims despite the pandemic conditions. The highest-risk cases are those where patients recognized a potential cancer symptom like a breast lump or rectal bleeding, and tried to visit a doctor’s office or hospital, but were told they couldn’t be seen.
“Those kinds of cases lend themselves to delayed diagnosis claims,” said Richard Anderson, MD, an oncologist who is chairman and CEO of The Doctors Company. “My guess is we will see claims,” though he expects a reduced number arising from 2020 care scenarios, compared with previous years.
So far, his company has seen 20% fewer claims in 2020, which he said isn’t surprising given that the volume of physician and hospital visits plummeted.
Another risky situation is where physicians – particularly primary care physicians but also specialists like gynecologists and urologists – did not inform patients about concerning test results and order a follow-up test or visit. That is dangerous even if the physician did try to schedule a visit but the patient canceled the appointment.
“The jury will ask, ‘What did you do to get the patient back?’ ” said Sean Byrne, JD, a malpractice defense attorney in Richmond, Va. “The provider will say: ‘I’m sure we called.’ But it’s a difficult defense to say the patient didn’t return the call. I need written proof.”
Mr. Domnick said failures to follow up on suspicious test results could produce viable malpractice claims, pandemic or not. “The question becomes to what extent doctors will try to hide behind COVID to explain otherwise run-of-the-mill negligence,” he said. “We’ll have to see how that plays out.”
There are also worries about missed cancer diagnoses during telemedicine visits. “On telemedicine, I can’t feel a lymph node, I can’t palpate a breast mass, and I can’t see if someone’s liver is enlarged,” Dr. McAneny fretted. “I think you’ll get suits because you’ll miss stuff.”
One other area of exposure cited by the experts: Radiologists and pathologists could be sued for missing tumors in reading imaging tests. “The COVID-19 demand on resources has been immense,” Mr. Byrne said. “If that production pressure resulted in any quality loss in testing services, we could see claims.”
Patient protocols provide protection
There’s no question that cancer screenings dropped sharply during the pandemic. In June 2020, the National Cancer Institute estimated there was a 75% decrease in mammograms and colonoscopies during the first few months of the pandemic. It projected that delays in screenings, diagnoses, and treatment likely would result in 10,000 more breast and colorectal cancer deaths than otherwise expected over the next decade.
Delays of even 1 month in treatment for seven common forms of cancer can increase mortality risk by 6%-13%, according to a BMJ study.
While many medical facilities stopped doing preventive screening tests during the height of the pandemic last year, health care professionals still found ways to bring in patients with diagnosed cancers or who were at heightened cancer risk for tests and treatment.
Most facilities convened multidisciplinary tumor boards to decide which patients could wait for treatment, which patients could be maintained on drug therapy, and which ones needed immediate surgery, said Carla Fisher, MD, director of breast surgery at Indiana University, Indianapolis. For breast cancer, they used guidelines from her professional group, the American Society of Breast Surgeons.
Following such protocols for prioritizing patients for treatment during the pandemic should help protect against liability, experts said.
Even if it can be shown that a clinician’s negligence led to delayed diagnosis or treatment of a patient’s cancer, plaintiff attorneys will be wary about filing such claims. That is because it is difficult in most cases to prove that the delay significantly worsened the course of the patient’s disease or the odds of survival. Showing harm may be more possible with certain cancers known to be particularly aggressive.
“The plaintiff attorney will have to get an expert to say that the 3-month delay in getting the patient a mammogram caused her great harm,” said Dr. Roberts. “But it’s hard to calculate that scientifically, and it’s really hard to lay that all on the doctor or health system, because they were supposed to lock down during the pandemic.”
Playing catch-up
With patients now feeling more comfortable about coming in for physician visits, Mr. Byrne urges clinicians to make a special effort to mitigate potential liability arising from the past year. Physicians should carefully review patients’ charts and make sure to catch them up on preventive screenings. Some health systems, like Kaiser Permanente, have been doing proactive patient outreach for cancer screening throughout the pandemic.
“Providers may need to be extra diligent, and consider expanding the exam into a wellness visit and remind patients about cancer surveillance,” he said.
Overall, however, the expert consensus is that physicians should focus on providing the best quality care going forward, and not worry excessively about the care they wish they could have delivered over the past year during the extraordinary pandemic conditions.
“Liability risks will be decreased, because state laws have changed and doctors will be cut some slack, not just by judges and juries but by patients themselves,” Dr. Roberts said. “As you are running down the hall to take care of the next person, don’t be looking over your shoulder or you’ll run into the wall.”
A version of this article first appeared on Medscape.com.
Albuquerque oncologist Barbara McAneny, MD, has a patient in his 30s who experienced rectal bleeding for 6 months in 2020 but didn’t see a physician because he was afraid of catching COVID-19. He hoped it was just hemorrhoids.
When he finally came in to see her recently, Dr. McAneny diagnosed a large colon cancer. She fears the delay could prove fatal. “We’ll do our best to cure him, but I don’t know if he’ll be treatable,” she said. “Six months absolutely can make a difference.”
She and other oncologists around the country are seeing many patients in the past few months with advanced breast, colon, lung, and other cancers who were not diagnosed and treated during the COVID-19 pandemic because the patients didn’t want to come in, or because medical facilities weren’t taking nonemergency or non-COVID patients.
Given that failure to diagnose cancer is among the most common medical malpractice allegations, should oncologists be worried that they are at legal risk?
Pandemic provides ‘safe harbor’
In a March survey done by medical malpractice insurer The Doctors Company, one-third of physicians said they were very concerned or somewhat concerned that malpractice claims related to care during the pandemic will rise.
But in most of these cases, physicians and hospitals have little to worry about in terms of medical malpractice liability, according to veteran plaintiff and defense attorneys and the head of a large medical liability insurer.
“You had people with diseases like cancer not getting care because health care systems were overwhelmed,” said Sean Domnick, JD, a malpractice plaintiff attorney in Boca Raton, Fla. “Will those lead to successful malpractice lawsuits? Most likely not.”
“The risks will be low because it’s hard to pin it on the doctor if the patient didn’t want to come in or facilities weren’t scheduling appointments because of the public health emergency,” said Richard Roberts, MD, JD, a professor of family medicine at the University of Wisconsin–Madison who is also a malpractice defense attorney.
In addition, liability protections enacted in more than 30 states because of the COVID-19 pandemic will help shield clinicians from lawsuits. Those laws generally require allegations of gross negligence or reckless conduct far beyond ordinary negligence, which are hard to prove. But the immunity provisions remain largely untested in the courts, and it’s unclear how they will affect cases involving care for conditions other than COVID-19.
Another helpful factor is the widespread public appreciation of the valiant work by health care professionals throughout the pandemic, though that halo effect could fade over the next several years as malpractice claims from the pandemic period are filed and tried.
“In many circumstances, the pandemic will prove to be a safe harbor for providers,” said Steven Wigrizer, JD, a malpractice plaintiff attorney in Philadelphia. “Jurors will be reluctant to impose liability on providers who were doing their best in a global pandemic the world hadn’t seen in 100 years.”
Risky situations
These predictions from liability experts should reassure physicians who are anxious over reports that many cancer diagnoses were missed as a result of the COVID-19 pandemic.
Still, there are situations where physicians and hospitals could be vulnerable to malpractice claims despite the pandemic conditions. The highest-risk cases are those where patients recognized a potential cancer symptom like a breast lump or rectal bleeding, and tried to visit a doctor’s office or hospital, but were told they couldn’t be seen.
“Those kinds of cases lend themselves to delayed diagnosis claims,” said Richard Anderson, MD, an oncologist who is chairman and CEO of The Doctors Company. “My guess is we will see claims,” though he expects a reduced number arising from 2020 care scenarios, compared with previous years.
So far, his company has seen 20% fewer claims in 2020, which he said isn’t surprising given that the volume of physician and hospital visits plummeted.
Another risky situation is where physicians – particularly primary care physicians but also specialists like gynecologists and urologists – did not inform patients about concerning test results and order a follow-up test or visit. That is dangerous even if the physician did try to schedule a visit but the patient canceled the appointment.
“The jury will ask, ‘What did you do to get the patient back?’ ” said Sean Byrne, JD, a malpractice defense attorney in Richmond, Va. “The provider will say: ‘I’m sure we called.’ But it’s a difficult defense to say the patient didn’t return the call. I need written proof.”
Mr. Domnick said failures to follow up on suspicious test results could produce viable malpractice claims, pandemic or not. “The question becomes to what extent doctors will try to hide behind COVID to explain otherwise run-of-the-mill negligence,” he said. “We’ll have to see how that plays out.”
There are also worries about missed cancer diagnoses during telemedicine visits. “On telemedicine, I can’t feel a lymph node, I can’t palpate a breast mass, and I can’t see if someone’s liver is enlarged,” Dr. McAneny fretted. “I think you’ll get suits because you’ll miss stuff.”
One other area of exposure cited by the experts: Radiologists and pathologists could be sued for missing tumors in reading imaging tests. “The COVID-19 demand on resources has been immense,” Mr. Byrne said. “If that production pressure resulted in any quality loss in testing services, we could see claims.”
Patient protocols provide protection
There’s no question that cancer screenings dropped sharply during the pandemic. In June 2020, the National Cancer Institute estimated there was a 75% decrease in mammograms and colonoscopies during the first few months of the pandemic. It projected that delays in screenings, diagnoses, and treatment likely would result in 10,000 more breast and colorectal cancer deaths than otherwise expected over the next decade.
Delays of even 1 month in treatment for seven common forms of cancer can increase mortality risk by 6%-13%, according to a BMJ study.
While many medical facilities stopped doing preventive screening tests during the height of the pandemic last year, health care professionals still found ways to bring in patients with diagnosed cancers or who were at heightened cancer risk for tests and treatment.
Most facilities convened multidisciplinary tumor boards to decide which patients could wait for treatment, which patients could be maintained on drug therapy, and which ones needed immediate surgery, said Carla Fisher, MD, director of breast surgery at Indiana University, Indianapolis. For breast cancer, they used guidelines from her professional group, the American Society of Breast Surgeons.
Following such protocols for prioritizing patients for treatment during the pandemic should help protect against liability, experts said.
Even if it can be shown that a clinician’s negligence led to delayed diagnosis or treatment of a patient’s cancer, plaintiff attorneys will be wary about filing such claims. That is because it is difficult in most cases to prove that the delay significantly worsened the course of the patient’s disease or the odds of survival. Showing harm may be more possible with certain cancers known to be particularly aggressive.
“The plaintiff attorney will have to get an expert to say that the 3-month delay in getting the patient a mammogram caused her great harm,” said Dr. Roberts. “But it’s hard to calculate that scientifically, and it’s really hard to lay that all on the doctor or health system, because they were supposed to lock down during the pandemic.”
Playing catch-up
With patients now feeling more comfortable about coming in for physician visits, Mr. Byrne urges clinicians to make a special effort to mitigate potential liability arising from the past year. Physicians should carefully review patients’ charts and make sure to catch them up on preventive screenings. Some health systems, like Kaiser Permanente, have been doing proactive patient outreach for cancer screening throughout the pandemic.
“Providers may need to be extra diligent, and consider expanding the exam into a wellness visit and remind patients about cancer surveillance,” he said.
Overall, however, the expert consensus is that physicians should focus on providing the best quality care going forward, and not worry excessively about the care they wish they could have delivered over the past year during the extraordinary pandemic conditions.
“Liability risks will be decreased, because state laws have changed and doctors will be cut some slack, not just by judges and juries but by patients themselves,” Dr. Roberts said. “As you are running down the hall to take care of the next person, don’t be looking over your shoulder or you’ll run into the wall.”
A version of this article first appeared on Medscape.com.
Albuquerque oncologist Barbara McAneny, MD, has a patient in his 30s who experienced rectal bleeding for 6 months in 2020 but didn’t see a physician because he was afraid of catching COVID-19. He hoped it was just hemorrhoids.
When he finally came in to see her recently, Dr. McAneny diagnosed a large colon cancer. She fears the delay could prove fatal. “We’ll do our best to cure him, but I don’t know if he’ll be treatable,” she said. “Six months absolutely can make a difference.”
She and other oncologists around the country are seeing many patients in the past few months with advanced breast, colon, lung, and other cancers who were not diagnosed and treated during the COVID-19 pandemic because the patients didn’t want to come in, or because medical facilities weren’t taking nonemergency or non-COVID patients.
Given that failure to diagnose cancer is among the most common medical malpractice allegations, should oncologists be worried that they are at legal risk?
Pandemic provides ‘safe harbor’
In a March survey done by medical malpractice insurer The Doctors Company, one-third of physicians said they were very concerned or somewhat concerned that malpractice claims related to care during the pandemic will rise.
But in most of these cases, physicians and hospitals have little to worry about in terms of medical malpractice liability, according to veteran plaintiff and defense attorneys and the head of a large medical liability insurer.
“You had people with diseases like cancer not getting care because health care systems were overwhelmed,” said Sean Domnick, JD, a malpractice plaintiff attorney in Boca Raton, Fla. “Will those lead to successful malpractice lawsuits? Most likely not.”
“The risks will be low because it’s hard to pin it on the doctor if the patient didn’t want to come in or facilities weren’t scheduling appointments because of the public health emergency,” said Richard Roberts, MD, JD, a professor of family medicine at the University of Wisconsin–Madison who is also a malpractice defense attorney.
In addition, liability protections enacted in more than 30 states because of the COVID-19 pandemic will help shield clinicians from lawsuits. Those laws generally require allegations of gross negligence or reckless conduct far beyond ordinary negligence, which are hard to prove. But the immunity provisions remain largely untested in the courts, and it’s unclear how they will affect cases involving care for conditions other than COVID-19.
Another helpful factor is the widespread public appreciation of the valiant work by health care professionals throughout the pandemic, though that halo effect could fade over the next several years as malpractice claims from the pandemic period are filed and tried.
“In many circumstances, the pandemic will prove to be a safe harbor for providers,” said Steven Wigrizer, JD, a malpractice plaintiff attorney in Philadelphia. “Jurors will be reluctant to impose liability on providers who were doing their best in a global pandemic the world hadn’t seen in 100 years.”
Risky situations
These predictions from liability experts should reassure physicians who are anxious over reports that many cancer diagnoses were missed as a result of the COVID-19 pandemic.
Still, there are situations where physicians and hospitals could be vulnerable to malpractice claims despite the pandemic conditions. The highest-risk cases are those where patients recognized a potential cancer symptom like a breast lump or rectal bleeding, and tried to visit a doctor’s office or hospital, but were told they couldn’t be seen.
“Those kinds of cases lend themselves to delayed diagnosis claims,” said Richard Anderson, MD, an oncologist who is chairman and CEO of The Doctors Company. “My guess is we will see claims,” though he expects a reduced number arising from 2020 care scenarios, compared with previous years.
So far, his company has seen 20% fewer claims in 2020, which he said isn’t surprising given that the volume of physician and hospital visits plummeted.
Another risky situation is where physicians – particularly primary care physicians but also specialists like gynecologists and urologists – did not inform patients about concerning test results and order a follow-up test or visit. That is dangerous even if the physician did try to schedule a visit but the patient canceled the appointment.
“The jury will ask, ‘What did you do to get the patient back?’ ” said Sean Byrne, JD, a malpractice defense attorney in Richmond, Va. “The provider will say: ‘I’m sure we called.’ But it’s a difficult defense to say the patient didn’t return the call. I need written proof.”
Mr. Domnick said failures to follow up on suspicious test results could produce viable malpractice claims, pandemic or not. “The question becomes to what extent doctors will try to hide behind COVID to explain otherwise run-of-the-mill negligence,” he said. “We’ll have to see how that plays out.”
There are also worries about missed cancer diagnoses during telemedicine visits. “On telemedicine, I can’t feel a lymph node, I can’t palpate a breast mass, and I can’t see if someone’s liver is enlarged,” Dr. McAneny fretted. “I think you’ll get suits because you’ll miss stuff.”
One other area of exposure cited by the experts: Radiologists and pathologists could be sued for missing tumors in reading imaging tests. “The COVID-19 demand on resources has been immense,” Mr. Byrne said. “If that production pressure resulted in any quality loss in testing services, we could see claims.”
Patient protocols provide protection
There’s no question that cancer screenings dropped sharply during the pandemic. In June 2020, the National Cancer Institute estimated there was a 75% decrease in mammograms and colonoscopies during the first few months of the pandemic. It projected that delays in screenings, diagnoses, and treatment likely would result in 10,000 more breast and colorectal cancer deaths than otherwise expected over the next decade.
Delays of even 1 month in treatment for seven common forms of cancer can increase mortality risk by 6%-13%, according to a BMJ study.
While many medical facilities stopped doing preventive screening tests during the height of the pandemic last year, health care professionals still found ways to bring in patients with diagnosed cancers or who were at heightened cancer risk for tests and treatment.
Most facilities convened multidisciplinary tumor boards to decide which patients could wait for treatment, which patients could be maintained on drug therapy, and which ones needed immediate surgery, said Carla Fisher, MD, director of breast surgery at Indiana University, Indianapolis. For breast cancer, they used guidelines from her professional group, the American Society of Breast Surgeons.
Following such protocols for prioritizing patients for treatment during the pandemic should help protect against liability, experts said.
Even if it can be shown that a clinician’s negligence led to delayed diagnosis or treatment of a patient’s cancer, plaintiff attorneys will be wary about filing such claims. That is because it is difficult in most cases to prove that the delay significantly worsened the course of the patient’s disease or the odds of survival. Showing harm may be more possible with certain cancers known to be particularly aggressive.
“The plaintiff attorney will have to get an expert to say that the 3-month delay in getting the patient a mammogram caused her great harm,” said Dr. Roberts. “But it’s hard to calculate that scientifically, and it’s really hard to lay that all on the doctor or health system, because they were supposed to lock down during the pandemic.”
Playing catch-up
With patients now feeling more comfortable about coming in for physician visits, Mr. Byrne urges clinicians to make a special effort to mitigate potential liability arising from the past year. Physicians should carefully review patients’ charts and make sure to catch them up on preventive screenings. Some health systems, like Kaiser Permanente, have been doing proactive patient outreach for cancer screening throughout the pandemic.
“Providers may need to be extra diligent, and consider expanding the exam into a wellness visit and remind patients about cancer surveillance,” he said.
Overall, however, the expert consensus is that physicians should focus on providing the best quality care going forward, and not worry excessively about the care they wish they could have delivered over the past year during the extraordinary pandemic conditions.
“Liability risks will be decreased, because state laws have changed and doctors will be cut some slack, not just by judges and juries but by patients themselves,” Dr. Roberts said. “As you are running down the hall to take care of the next person, don’t be looking over your shoulder or you’ll run into the wall.”
A version of this article first appeared on Medscape.com.
Fitbit stats show lingering physiologic hit after COVID-19
People infected with SARS-CoV-2 can experience lingering physiologic effects after they recover, according to early data from an ongoing study that is harnessing the power of Fitbits and other wearable trackers to gauge long-term effects of COVID-19.
“To our knowledge, this is the first study to examine longer duration wearable sensor data. We found a prolonged physiological impact of COVID-19 infection, lasting approximately 2-3 months, on average, but with substantial intra-individual variability,” report Jennifer Radin, PhD, MPH, and colleagues with the Scripps Research Translational Institute, San Diego.
The study was published online July 7 in JAMA Network Open.
The DETECT study is enrolling adults from all over the United States and is collecting their health data from different wearable devices to better understand changes associated with viral illness, including COVID-19.
The current analysis focuses on a subset of 875 device wearers who reported symptoms of an acute respiratory illness and underwent testing for SARS-CoV-2. A total of 234 individuals tested positive for SARS-CoV-2; 641 were presumed to have other viral infections (COVID-19-negative symptomatic individuals).
The investigators found that among people with COVID-19, it took longer to return to baseline status with respect to resting heart rate (RHR), sleep, and activity compared with those who had symptoms of viral illness but who did not have COVID-19.
“This difference was most marked for RHR, with COVID-19-positive individuals initially experiencing a transient bradycardia followed by a prolonged relative tachycardia that did not return to baseline, on average, until 79 days after symptom onset,” Dr. Radin and colleagues reported.
Step count and sleep quantity returned to baseline values sooner than RHR, at 32 days and 24 days, respectively.
Among people with COVID-19, during recovery, trajectories differed with respect to return of RHR to normal in comparison with persons who did not have COVID-19.
The RHR of 32 COVID-19–positive participants (13.7%) remained 5 beats/min greater than their baseline RHR for more than 133 days, on average. During the acute phase of COVID-19, these individuals were more apt to report cough, body ache, and shortness of breath compared with other groups.
Limitation
The researchers say a limitation of this analysis is that symptom data were collected only during the acute phase of infection, which limits the ability to compare long-term physiologic and behavioral changes with long-term symptoms.
“In the future, with larger sample sizes and more comprehensive participant-reported outcomes, it will be possible to better understand factors associated with inter-individualized variability in COVID-19 recovery,” they concluded.
Earlier data from the DETECT study showed that pairing wearable tracker data with self-reported symptoms can improve COVID-19 prediction.
As previously reported by this news organization, DETECT investigators found that associating participant-reported symptoms with personal sensor data, such as deviation from normal sleep duration and RHR, resulted in an area under the curve of 0.80 for differentiating between symptomatic individuals who were positive and those who were negative for COVID-19.
Funding for the current study was provided by a grant from the National Center for Advancing Translational Sciences at the National Institutes of Health. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People infected with SARS-CoV-2 can experience lingering physiologic effects after they recover, according to early data from an ongoing study that is harnessing the power of Fitbits and other wearable trackers to gauge long-term effects of COVID-19.
“To our knowledge, this is the first study to examine longer duration wearable sensor data. We found a prolonged physiological impact of COVID-19 infection, lasting approximately 2-3 months, on average, but with substantial intra-individual variability,” report Jennifer Radin, PhD, MPH, and colleagues with the Scripps Research Translational Institute, San Diego.
The study was published online July 7 in JAMA Network Open.
The DETECT study is enrolling adults from all over the United States and is collecting their health data from different wearable devices to better understand changes associated with viral illness, including COVID-19.
The current analysis focuses on a subset of 875 device wearers who reported symptoms of an acute respiratory illness and underwent testing for SARS-CoV-2. A total of 234 individuals tested positive for SARS-CoV-2; 641 were presumed to have other viral infections (COVID-19-negative symptomatic individuals).
The investigators found that among people with COVID-19, it took longer to return to baseline status with respect to resting heart rate (RHR), sleep, and activity compared with those who had symptoms of viral illness but who did not have COVID-19.
“This difference was most marked for RHR, with COVID-19-positive individuals initially experiencing a transient bradycardia followed by a prolonged relative tachycardia that did not return to baseline, on average, until 79 days after symptom onset,” Dr. Radin and colleagues reported.
Step count and sleep quantity returned to baseline values sooner than RHR, at 32 days and 24 days, respectively.
Among people with COVID-19, during recovery, trajectories differed with respect to return of RHR to normal in comparison with persons who did not have COVID-19.
The RHR of 32 COVID-19–positive participants (13.7%) remained 5 beats/min greater than their baseline RHR for more than 133 days, on average. During the acute phase of COVID-19, these individuals were more apt to report cough, body ache, and shortness of breath compared with other groups.
Limitation
The researchers say a limitation of this analysis is that symptom data were collected only during the acute phase of infection, which limits the ability to compare long-term physiologic and behavioral changes with long-term symptoms.
“In the future, with larger sample sizes and more comprehensive participant-reported outcomes, it will be possible to better understand factors associated with inter-individualized variability in COVID-19 recovery,” they concluded.
Earlier data from the DETECT study showed that pairing wearable tracker data with self-reported symptoms can improve COVID-19 prediction.
As previously reported by this news organization, DETECT investigators found that associating participant-reported symptoms with personal sensor data, such as deviation from normal sleep duration and RHR, resulted in an area under the curve of 0.80 for differentiating between symptomatic individuals who were positive and those who were negative for COVID-19.
Funding for the current study was provided by a grant from the National Center for Advancing Translational Sciences at the National Institutes of Health. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People infected with SARS-CoV-2 can experience lingering physiologic effects after they recover, according to early data from an ongoing study that is harnessing the power of Fitbits and other wearable trackers to gauge long-term effects of COVID-19.
“To our knowledge, this is the first study to examine longer duration wearable sensor data. We found a prolonged physiological impact of COVID-19 infection, lasting approximately 2-3 months, on average, but with substantial intra-individual variability,” report Jennifer Radin, PhD, MPH, and colleagues with the Scripps Research Translational Institute, San Diego.
The study was published online July 7 in JAMA Network Open.
The DETECT study is enrolling adults from all over the United States and is collecting their health data from different wearable devices to better understand changes associated with viral illness, including COVID-19.
The current analysis focuses on a subset of 875 device wearers who reported symptoms of an acute respiratory illness and underwent testing for SARS-CoV-2. A total of 234 individuals tested positive for SARS-CoV-2; 641 were presumed to have other viral infections (COVID-19-negative symptomatic individuals).
The investigators found that among people with COVID-19, it took longer to return to baseline status with respect to resting heart rate (RHR), sleep, and activity compared with those who had symptoms of viral illness but who did not have COVID-19.
“This difference was most marked for RHR, with COVID-19-positive individuals initially experiencing a transient bradycardia followed by a prolonged relative tachycardia that did not return to baseline, on average, until 79 days after symptom onset,” Dr. Radin and colleagues reported.
Step count and sleep quantity returned to baseline values sooner than RHR, at 32 days and 24 days, respectively.
Among people with COVID-19, during recovery, trajectories differed with respect to return of RHR to normal in comparison with persons who did not have COVID-19.
The RHR of 32 COVID-19–positive participants (13.7%) remained 5 beats/min greater than their baseline RHR for more than 133 days, on average. During the acute phase of COVID-19, these individuals were more apt to report cough, body ache, and shortness of breath compared with other groups.
Limitation
The researchers say a limitation of this analysis is that symptom data were collected only during the acute phase of infection, which limits the ability to compare long-term physiologic and behavioral changes with long-term symptoms.
“In the future, with larger sample sizes and more comprehensive participant-reported outcomes, it will be possible to better understand factors associated with inter-individualized variability in COVID-19 recovery,” they concluded.
Earlier data from the DETECT study showed that pairing wearable tracker data with self-reported symptoms can improve COVID-19 prediction.
As previously reported by this news organization, DETECT investigators found that associating participant-reported symptoms with personal sensor data, such as deviation from normal sleep duration and RHR, resulted in an area under the curve of 0.80 for differentiating between symptomatic individuals who were positive and those who were negative for COVID-19.
Funding for the current study was provided by a grant from the National Center for Advancing Translational Sciences at the National Institutes of Health. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Isotretinoin Meets COVID-19: Revisiting a Fragmented Paradigm
We cannot solve our problems with the same thinking we used when we created them.
Albert Einstein
Amidst the myriad of disruptions and corollary solutions budding from the ongoing global COVID-19 pandemic, management of acne with isotretinoin underwent a makeover. Firstly, as with any pharmaceutical prescribed in the last 1 to 2 years, patients asked the compelling question, “Will this prescription put me at higher risk for COVID-19?”, resulting in a complex set of answers from both clinical and basic science perspectives. Further, the practical use of telemedicine for clinical visits and pregnancy test reporting altered the shape of isotretinoin physician-patient communication and follow-up. Finally, the combination of these circumstances spurred us to revisit common quandaries in prescribing this drug: Can we trust what patients tell us when they are taking isotretinoin? Do we need to monitor laboratory values and follow patients on isotretinoin as closely and as frequently as we have in the past? Does the Risk Evaluation and Mitigation Strategy (REMS) program of iPLEDGE hold true utility?
Impact of COVID-19 on Isotretinoin Use
Isotretinoin may have varying influence on the ease of host entry and virulence of COVID-19. Because the majority of patients experience some degree of mucous membrane desiccation on isotretinoin, it originally was postulated that disruption of the nasal mucosa, thereby uncovering the basal epithelial layer where angiotensin-converting enzyme 2 (ACE2) receptors are expressed, could increase the risk for viral invasion, as ACE2 is the host receptor for COVID-19 entry.1,2 On the other hand, a study of 672 medications and their effect on regulation of ACE2 levels stratified isotretinoin in the highest category of ACE2 downregulators, therefore theoretically preventing cellular entry and replication of the virus.3 In conferring with many of my colleagues and reviewing available literature, I found that these data did not summarily deter providers from initiating or continuing isotretinoin during the pandemic, and research is ongoing to particularly earmark isotretinoin as a possible COVID-19 therapy option.4,5 Despite this, and despite the lower risk for COVID-19 in the customary isotretinoin adolescent and young adult age range, an Italian study reported that 14.7% of patients (5/34) prematurely interrupted isotretinoin therapy during lockdown because of fear of COVID-19 infection.6 Data also suggest that college towns (akin to where I practice, rife with isotretinoin-eligible patients) reflected higher COVID-19 infection and death rates, likely due to dense cohabitation and intermittent migration of students and staff to and from campuses and within their communities.7 Approximately 30% of my patients on isotretinoin in the last 18 months reported having COVID-19 at some point during the pandemic, though no data exist to guide us on whether isotretinoin should be discontinued in this scenario; my patients typically continued the drug unless their primary health care team discouraged it, and in those cases, all of them resumed it after COVID-19 symptomatology resolved.
Last spring, the US Department of Health and Human Services and the US Food and Drug Administration announced that health care professionals who prescribe and/or dispense drugs subject to REMS with laboratory testing or imaging requirements should consider whether there are compelling reasons not to complete the required testing/imaging during the current public health emergency and use their best medical judgment in weighing the benefits and risks of continuing treatment in the absence of these tests. It also was stressed that prescribers should effectively communicate with their patients regarding these benefits, risks, and altered protocols.8 Further, the iPLEDGE program concurred that telemedicine was an acceptable visit type for both initiating and maintaining isotretinoin, and home pregnancy tests were valid for females of childbearing potential if an accurate testing date and results were communicated by patients to the prescriber in the required reporting windows.9 This allowed dermatologists to foster what was one of our most important roles as outpatient clinicians during the pandemic: to maintain normalcy, continuity, and support for as many patients as possible.
Isotretinoin and Telemedicine
During the pandemic, continuation of isotretinoin therapy proved easier than initiating it, given that patients could access and maintain a clear connection to the online visit platform, display understanding of the REMS mandates (along with a guardian present for a minor), perform a home pregnancy test and report the result followed by the quiz (for females), and collect the prescription in the allotted window. For new patients, the absence of a detailed in-person examination and rapport with the patient (and guardians when applicable) as well as misalignment of the date of iPLEDGE registration with the timing of the pregnancy test results and prescribing window were more onerous using digital or mailed versions of consent forms and photodocumentation of urine pregnancy test results. This tangle of requirements perpetuated missed prescribing windows, increased patient portal and phone messages, resulted in more time on the phone with the iPLEDGE help desk, and intensified angst for clinical staff.
These telemedicine visits also required validation of the patient’s geographic location to verify the billability of the visit and whether the patient was in a secure location to have a US Health Insurance Portability and Accountability Act–compliant conversation as well as the abstract notion that the timing and result of the pregnancy tests for females reflected a true nonpregnant state.10,11 Verification of the pregnancy tests in these situations was approached by either the patient reporting the outcome verbally or displaying the pregnancy test kit result in a video or photograph form for the medical record, all of which leave room for error, doubt, and lower sensitivity than laboratory-based collection. That being said, the increased implementation of telemedicine visits during the pandemic sustained patient access, decreased cost with less laboratory testing and reduced time away from work or school, and resulted in high patient satisfaction with their care.12 Additionally, it allowed providers to continue to more comfortably inch away from frequent in-person serologic cholesterol and hepatic testing during therapy based on mounting data that it is not indicated.13
Accordingly, the complicated concepts of trust, practicality, and sustainability for the safe and effective management of isotretinoin patients re-emerged. For example, prior to COVID-19, we trusted patients who said they were regularly taking their oral contraceptives or were truly practicing abstinence as a form of contraception. During the pandemic, we then added a layer of trust with home pregnancy test reporting. If the patient or guardian signed the isotretinoin consent form and understood the risks of the medication, ideally the physician-patient relationship fostered the optimal goals of honest conversation, adherence to the drug, safety, and clear skin. However, there is yet another trust assay: iPLEDGE, in turn, trusts that we are reporting patient data accurately, provoking us to reiterate questions we asked ourselves before the pandemic. Is the extra provider and staff clerical work and validation necessary, compounded by prior data that iPLEDGE’s capacity to limit pregnancy-related morbidity with isotretinoin has been called into question in the last decade?14 Do males need to be followed every month? Is laboratory monitoring still necessary for all isotretinoin candidates? Will post–COVID-19 data show that during various versions of the lockdown, an increased number of isotretinoin patients developed unmonitored morbidity, including transaminitis, hypertriglyceridemia, and an increase in pregnancies? How long will telemedicine visits for isotretinoin be reimbursable beyond the pandemic? Are there other models to enhance and improve isotretinoin teledermatology and compliance?15
Final Thoughts
Dermatologists’ experience managing high volumes of isotretinoin patients paired with the creativity to maintain meaningful (and truthful) patient connections and decrease administrative burden lie front and center in 2021. Because the COVID-19 pandemic remains ambient with a dearth of data to guide us, I pose the questions above as points for commiseration and catapults for future study, discussion, collaboration, and innovation. Perhaps the neo–COVID-19 world provided us with the spark we needed to metaphorically clean up the dusty isotretinoin tenets that have frayed our time and patience so we can maintain excellent care for this worthy population.
- Hamming I, Timens W, Bulthuis MLC, et al. Tissue disruption of ACE2 protein, the functional receptor for SARS coronavirus. a first step in understanding SARS pathogenesis. J Pathol. 2004;203:631-637.
- British Association of Dermatologists. COVID-19—isotretinoin guidance. Published March 26, 2020. Accessed June 21, 2021. https://www.bad.org.uk/shared/get-file.ashx?itemtype=document&id=6661
- Sinha S, Cheng K, Schäffer AA, et al. In vitro and in vivo identification of clinically approved drugs that modify ACE2 expression. Mol Syst Biol. 2020;16:E9628.
- Öǧüt ND, Kutlu Ö, Erbaǧcı E. Oral isotretinoin treatment in patients with acne vulgaris during the COVID-19 pandemic: a retrospective cohort study in a tertiary care hospital [published online April 22, 2021]. J Cosmet Dermatol. doi:10.1111/jocd.14168
- Isotretinoin in treatment of COVID-19. National Library of Medicine website. ClinicalTrials.gov identifier: NCT04361422. Updated September 23, 2020. Accessed June 21, 2021. https://clinicaltrials.gov/ct2/show/NCT04361422
- Donnarumma M, Nocerino M, Lauro W, et al. Isotretinoin in acne treatment during the coronavirus disease 2019 (COVID-19): a retrospective analysis of adherence to therapy and side effects [published online December 22, 2020]. Dermatol Ther. 2021;34:E14677.
- Ivory D, Gebeloff R, Mervosh S. Young people have less COVID-19 risk, but in college towns, deaths rose fast. The New York Times. December 12, 2020. Accessed June 21, 2021. https://www.nytimes.com/2020/12/12/us/covid-colleges-nursing-homes.html
- US Food and Drug Administration. Coronavirus (COVID-19) update: FDA provides update on patient access to certain REMS drugs during COVID-19 public health emergency. Published March 22, 2020. Accessed June 21, 2021. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-provides-update-patient-access-certain-rems-drugs-during-covid-19
- Haelle T. iPledge allows at-home pregnancy tests during pandemic. Dermatology News. Published April 3, 2020. Accessed June 28, 2021. https://www.mdedge.com/dermatology/article/220186/acne/ipledge-allows-home-pregnancy-tests-during-pandemic
- Bressler MY, Siegel DM, Markowitz O. Virtual dermatology: a COVID-19 update. Cutis. 2020;105:163-164; E2.
- Telemedicine key issues and policy. Federation of State Medical Boards website. Accessed June 28, 2021. https://www.fsmb.org/advocacy/telemedicine
- Ruggiero A, Megna M, Annunziata MC, et al. Teledermatology for acne during COVID-19: high patients’ satisfaction in spite of the emergency. J Eur Acad Dermatol Venereol. 2020;34:E662-E663.
- Barbieri JS, Shin DB, Wang S, et al. The clinical utility of laboratory monitoring during isotretinoin therapy for acne and changes to monitoring practices over time. J Am Acad Dermatol. 2020;82:72-79.
- Tkachenko E, Singer S, Sharma P, et al. US Food and Drug Administration reports of pregnancy and pregnancy-related adverse events associated with isotretinoin. JAMA Dermatol. 2019;155:1175-1179.
- Das S, et al. Asynchronous telemedicine for isotretinoin management: a direct care pilot [published online January 21, 2021]. J Am Acad Dermatol. doi:10.1016/j.jaad.2021.01.039
We cannot solve our problems with the same thinking we used when we created them.
Albert Einstein
Amidst the myriad of disruptions and corollary solutions budding from the ongoing global COVID-19 pandemic, management of acne with isotretinoin underwent a makeover. Firstly, as with any pharmaceutical prescribed in the last 1 to 2 years, patients asked the compelling question, “Will this prescription put me at higher risk for COVID-19?”, resulting in a complex set of answers from both clinical and basic science perspectives. Further, the practical use of telemedicine for clinical visits and pregnancy test reporting altered the shape of isotretinoin physician-patient communication and follow-up. Finally, the combination of these circumstances spurred us to revisit common quandaries in prescribing this drug: Can we trust what patients tell us when they are taking isotretinoin? Do we need to monitor laboratory values and follow patients on isotretinoin as closely and as frequently as we have in the past? Does the Risk Evaluation and Mitigation Strategy (REMS) program of iPLEDGE hold true utility?
Impact of COVID-19 on Isotretinoin Use
Isotretinoin may have varying influence on the ease of host entry and virulence of COVID-19. Because the majority of patients experience some degree of mucous membrane desiccation on isotretinoin, it originally was postulated that disruption of the nasal mucosa, thereby uncovering the basal epithelial layer where angiotensin-converting enzyme 2 (ACE2) receptors are expressed, could increase the risk for viral invasion, as ACE2 is the host receptor for COVID-19 entry.1,2 On the other hand, a study of 672 medications and their effect on regulation of ACE2 levels stratified isotretinoin in the highest category of ACE2 downregulators, therefore theoretically preventing cellular entry and replication of the virus.3 In conferring with many of my colleagues and reviewing available literature, I found that these data did not summarily deter providers from initiating or continuing isotretinoin during the pandemic, and research is ongoing to particularly earmark isotretinoin as a possible COVID-19 therapy option.4,5 Despite this, and despite the lower risk for COVID-19 in the customary isotretinoin adolescent and young adult age range, an Italian study reported that 14.7% of patients (5/34) prematurely interrupted isotretinoin therapy during lockdown because of fear of COVID-19 infection.6 Data also suggest that college towns (akin to where I practice, rife with isotretinoin-eligible patients) reflected higher COVID-19 infection and death rates, likely due to dense cohabitation and intermittent migration of students and staff to and from campuses and within their communities.7 Approximately 30% of my patients on isotretinoin in the last 18 months reported having COVID-19 at some point during the pandemic, though no data exist to guide us on whether isotretinoin should be discontinued in this scenario; my patients typically continued the drug unless their primary health care team discouraged it, and in those cases, all of them resumed it after COVID-19 symptomatology resolved.
Last spring, the US Department of Health and Human Services and the US Food and Drug Administration announced that health care professionals who prescribe and/or dispense drugs subject to REMS with laboratory testing or imaging requirements should consider whether there are compelling reasons not to complete the required testing/imaging during the current public health emergency and use their best medical judgment in weighing the benefits and risks of continuing treatment in the absence of these tests. It also was stressed that prescribers should effectively communicate with their patients regarding these benefits, risks, and altered protocols.8 Further, the iPLEDGE program concurred that telemedicine was an acceptable visit type for both initiating and maintaining isotretinoin, and home pregnancy tests were valid for females of childbearing potential if an accurate testing date and results were communicated by patients to the prescriber in the required reporting windows.9 This allowed dermatologists to foster what was one of our most important roles as outpatient clinicians during the pandemic: to maintain normalcy, continuity, and support for as many patients as possible.
Isotretinoin and Telemedicine
During the pandemic, continuation of isotretinoin therapy proved easier than initiating it, given that patients could access and maintain a clear connection to the online visit platform, display understanding of the REMS mandates (along with a guardian present for a minor), perform a home pregnancy test and report the result followed by the quiz (for females), and collect the prescription in the allotted window. For new patients, the absence of a detailed in-person examination and rapport with the patient (and guardians when applicable) as well as misalignment of the date of iPLEDGE registration with the timing of the pregnancy test results and prescribing window were more onerous using digital or mailed versions of consent forms and photodocumentation of urine pregnancy test results. This tangle of requirements perpetuated missed prescribing windows, increased patient portal and phone messages, resulted in more time on the phone with the iPLEDGE help desk, and intensified angst for clinical staff.
These telemedicine visits also required validation of the patient’s geographic location to verify the billability of the visit and whether the patient was in a secure location to have a US Health Insurance Portability and Accountability Act–compliant conversation as well as the abstract notion that the timing and result of the pregnancy tests for females reflected a true nonpregnant state.10,11 Verification of the pregnancy tests in these situations was approached by either the patient reporting the outcome verbally or displaying the pregnancy test kit result in a video or photograph form for the medical record, all of which leave room for error, doubt, and lower sensitivity than laboratory-based collection. That being said, the increased implementation of telemedicine visits during the pandemic sustained patient access, decreased cost with less laboratory testing and reduced time away from work or school, and resulted in high patient satisfaction with their care.12 Additionally, it allowed providers to continue to more comfortably inch away from frequent in-person serologic cholesterol and hepatic testing during therapy based on mounting data that it is not indicated.13
Accordingly, the complicated concepts of trust, practicality, and sustainability for the safe and effective management of isotretinoin patients re-emerged. For example, prior to COVID-19, we trusted patients who said they were regularly taking their oral contraceptives or were truly practicing abstinence as a form of contraception. During the pandemic, we then added a layer of trust with home pregnancy test reporting. If the patient or guardian signed the isotretinoin consent form and understood the risks of the medication, ideally the physician-patient relationship fostered the optimal goals of honest conversation, adherence to the drug, safety, and clear skin. However, there is yet another trust assay: iPLEDGE, in turn, trusts that we are reporting patient data accurately, provoking us to reiterate questions we asked ourselves before the pandemic. Is the extra provider and staff clerical work and validation necessary, compounded by prior data that iPLEDGE’s capacity to limit pregnancy-related morbidity with isotretinoin has been called into question in the last decade?14 Do males need to be followed every month? Is laboratory monitoring still necessary for all isotretinoin candidates? Will post–COVID-19 data show that during various versions of the lockdown, an increased number of isotretinoin patients developed unmonitored morbidity, including transaminitis, hypertriglyceridemia, and an increase in pregnancies? How long will telemedicine visits for isotretinoin be reimbursable beyond the pandemic? Are there other models to enhance and improve isotretinoin teledermatology and compliance?15
Final Thoughts
Dermatologists’ experience managing high volumes of isotretinoin patients paired with the creativity to maintain meaningful (and truthful) patient connections and decrease administrative burden lie front and center in 2021. Because the COVID-19 pandemic remains ambient with a dearth of data to guide us, I pose the questions above as points for commiseration and catapults for future study, discussion, collaboration, and innovation. Perhaps the neo–COVID-19 world provided us with the spark we needed to metaphorically clean up the dusty isotretinoin tenets that have frayed our time and patience so we can maintain excellent care for this worthy population.
We cannot solve our problems with the same thinking we used when we created them.
Albert Einstein
Amidst the myriad of disruptions and corollary solutions budding from the ongoing global COVID-19 pandemic, management of acne with isotretinoin underwent a makeover. Firstly, as with any pharmaceutical prescribed in the last 1 to 2 years, patients asked the compelling question, “Will this prescription put me at higher risk for COVID-19?”, resulting in a complex set of answers from both clinical and basic science perspectives. Further, the practical use of telemedicine for clinical visits and pregnancy test reporting altered the shape of isotretinoin physician-patient communication and follow-up. Finally, the combination of these circumstances spurred us to revisit common quandaries in prescribing this drug: Can we trust what patients tell us when they are taking isotretinoin? Do we need to monitor laboratory values and follow patients on isotretinoin as closely and as frequently as we have in the past? Does the Risk Evaluation and Mitigation Strategy (REMS) program of iPLEDGE hold true utility?
Impact of COVID-19 on Isotretinoin Use
Isotretinoin may have varying influence on the ease of host entry and virulence of COVID-19. Because the majority of patients experience some degree of mucous membrane desiccation on isotretinoin, it originally was postulated that disruption of the nasal mucosa, thereby uncovering the basal epithelial layer where angiotensin-converting enzyme 2 (ACE2) receptors are expressed, could increase the risk for viral invasion, as ACE2 is the host receptor for COVID-19 entry.1,2 On the other hand, a study of 672 medications and their effect on regulation of ACE2 levels stratified isotretinoin in the highest category of ACE2 downregulators, therefore theoretically preventing cellular entry and replication of the virus.3 In conferring with many of my colleagues and reviewing available literature, I found that these data did not summarily deter providers from initiating or continuing isotretinoin during the pandemic, and research is ongoing to particularly earmark isotretinoin as a possible COVID-19 therapy option.4,5 Despite this, and despite the lower risk for COVID-19 in the customary isotretinoin adolescent and young adult age range, an Italian study reported that 14.7% of patients (5/34) prematurely interrupted isotretinoin therapy during lockdown because of fear of COVID-19 infection.6 Data also suggest that college towns (akin to where I practice, rife with isotretinoin-eligible patients) reflected higher COVID-19 infection and death rates, likely due to dense cohabitation and intermittent migration of students and staff to and from campuses and within their communities.7 Approximately 30% of my patients on isotretinoin in the last 18 months reported having COVID-19 at some point during the pandemic, though no data exist to guide us on whether isotretinoin should be discontinued in this scenario; my patients typically continued the drug unless their primary health care team discouraged it, and in those cases, all of them resumed it after COVID-19 symptomatology resolved.
Last spring, the US Department of Health and Human Services and the US Food and Drug Administration announced that health care professionals who prescribe and/or dispense drugs subject to REMS with laboratory testing or imaging requirements should consider whether there are compelling reasons not to complete the required testing/imaging during the current public health emergency and use their best medical judgment in weighing the benefits and risks of continuing treatment in the absence of these tests. It also was stressed that prescribers should effectively communicate with their patients regarding these benefits, risks, and altered protocols.8 Further, the iPLEDGE program concurred that telemedicine was an acceptable visit type for both initiating and maintaining isotretinoin, and home pregnancy tests were valid for females of childbearing potential if an accurate testing date and results were communicated by patients to the prescriber in the required reporting windows.9 This allowed dermatologists to foster what was one of our most important roles as outpatient clinicians during the pandemic: to maintain normalcy, continuity, and support for as many patients as possible.
Isotretinoin and Telemedicine
During the pandemic, continuation of isotretinoin therapy proved easier than initiating it, given that patients could access and maintain a clear connection to the online visit platform, display understanding of the REMS mandates (along with a guardian present for a minor), perform a home pregnancy test and report the result followed by the quiz (for females), and collect the prescription in the allotted window. For new patients, the absence of a detailed in-person examination and rapport with the patient (and guardians when applicable) as well as misalignment of the date of iPLEDGE registration with the timing of the pregnancy test results and prescribing window were more onerous using digital or mailed versions of consent forms and photodocumentation of urine pregnancy test results. This tangle of requirements perpetuated missed prescribing windows, increased patient portal and phone messages, resulted in more time on the phone with the iPLEDGE help desk, and intensified angst for clinical staff.
These telemedicine visits also required validation of the patient’s geographic location to verify the billability of the visit and whether the patient was in a secure location to have a US Health Insurance Portability and Accountability Act–compliant conversation as well as the abstract notion that the timing and result of the pregnancy tests for females reflected a true nonpregnant state.10,11 Verification of the pregnancy tests in these situations was approached by either the patient reporting the outcome verbally or displaying the pregnancy test kit result in a video or photograph form for the medical record, all of which leave room for error, doubt, and lower sensitivity than laboratory-based collection. That being said, the increased implementation of telemedicine visits during the pandemic sustained patient access, decreased cost with less laboratory testing and reduced time away from work or school, and resulted in high patient satisfaction with their care.12 Additionally, it allowed providers to continue to more comfortably inch away from frequent in-person serologic cholesterol and hepatic testing during therapy based on mounting data that it is not indicated.13
Accordingly, the complicated concepts of trust, practicality, and sustainability for the safe and effective management of isotretinoin patients re-emerged. For example, prior to COVID-19, we trusted patients who said they were regularly taking their oral contraceptives or were truly practicing abstinence as a form of contraception. During the pandemic, we then added a layer of trust with home pregnancy test reporting. If the patient or guardian signed the isotretinoin consent form and understood the risks of the medication, ideally the physician-patient relationship fostered the optimal goals of honest conversation, adherence to the drug, safety, and clear skin. However, there is yet another trust assay: iPLEDGE, in turn, trusts that we are reporting patient data accurately, provoking us to reiterate questions we asked ourselves before the pandemic. Is the extra provider and staff clerical work and validation necessary, compounded by prior data that iPLEDGE’s capacity to limit pregnancy-related morbidity with isotretinoin has been called into question in the last decade?14 Do males need to be followed every month? Is laboratory monitoring still necessary for all isotretinoin candidates? Will post–COVID-19 data show that during various versions of the lockdown, an increased number of isotretinoin patients developed unmonitored morbidity, including transaminitis, hypertriglyceridemia, and an increase in pregnancies? How long will telemedicine visits for isotretinoin be reimbursable beyond the pandemic? Are there other models to enhance and improve isotretinoin teledermatology and compliance?15
Final Thoughts
Dermatologists’ experience managing high volumes of isotretinoin patients paired with the creativity to maintain meaningful (and truthful) patient connections and decrease administrative burden lie front and center in 2021. Because the COVID-19 pandemic remains ambient with a dearth of data to guide us, I pose the questions above as points for commiseration and catapults for future study, discussion, collaboration, and innovation. Perhaps the neo–COVID-19 world provided us with the spark we needed to metaphorically clean up the dusty isotretinoin tenets that have frayed our time and patience so we can maintain excellent care for this worthy population.
- Hamming I, Timens W, Bulthuis MLC, et al. Tissue disruption of ACE2 protein, the functional receptor for SARS coronavirus. a first step in understanding SARS pathogenesis. J Pathol. 2004;203:631-637.
- British Association of Dermatologists. COVID-19—isotretinoin guidance. Published March 26, 2020. Accessed June 21, 2021. https://www.bad.org.uk/shared/get-file.ashx?itemtype=document&id=6661
- Sinha S, Cheng K, Schäffer AA, et al. In vitro and in vivo identification of clinically approved drugs that modify ACE2 expression. Mol Syst Biol. 2020;16:E9628.
- Öǧüt ND, Kutlu Ö, Erbaǧcı E. Oral isotretinoin treatment in patients with acne vulgaris during the COVID-19 pandemic: a retrospective cohort study in a tertiary care hospital [published online April 22, 2021]. J Cosmet Dermatol. doi:10.1111/jocd.14168
- Isotretinoin in treatment of COVID-19. National Library of Medicine website. ClinicalTrials.gov identifier: NCT04361422. Updated September 23, 2020. Accessed June 21, 2021. https://clinicaltrials.gov/ct2/show/NCT04361422
- Donnarumma M, Nocerino M, Lauro W, et al. Isotretinoin in acne treatment during the coronavirus disease 2019 (COVID-19): a retrospective analysis of adherence to therapy and side effects [published online December 22, 2020]. Dermatol Ther. 2021;34:E14677.
- Ivory D, Gebeloff R, Mervosh S. Young people have less COVID-19 risk, but in college towns, deaths rose fast. The New York Times. December 12, 2020. Accessed June 21, 2021. https://www.nytimes.com/2020/12/12/us/covid-colleges-nursing-homes.html
- US Food and Drug Administration. Coronavirus (COVID-19) update: FDA provides update on patient access to certain REMS drugs during COVID-19 public health emergency. Published March 22, 2020. Accessed June 21, 2021. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-provides-update-patient-access-certain-rems-drugs-during-covid-19
- Haelle T. iPledge allows at-home pregnancy tests during pandemic. Dermatology News. Published April 3, 2020. Accessed June 28, 2021. https://www.mdedge.com/dermatology/article/220186/acne/ipledge-allows-home-pregnancy-tests-during-pandemic
- Bressler MY, Siegel DM, Markowitz O. Virtual dermatology: a COVID-19 update. Cutis. 2020;105:163-164; E2.
- Telemedicine key issues and policy. Federation of State Medical Boards website. Accessed June 28, 2021. https://www.fsmb.org/advocacy/telemedicine
- Ruggiero A, Megna M, Annunziata MC, et al. Teledermatology for acne during COVID-19: high patients’ satisfaction in spite of the emergency. J Eur Acad Dermatol Venereol. 2020;34:E662-E663.
- Barbieri JS, Shin DB, Wang S, et al. The clinical utility of laboratory monitoring during isotretinoin therapy for acne and changes to monitoring practices over time. J Am Acad Dermatol. 2020;82:72-79.
- Tkachenko E, Singer S, Sharma P, et al. US Food and Drug Administration reports of pregnancy and pregnancy-related adverse events associated with isotretinoin. JAMA Dermatol. 2019;155:1175-1179.
- Das S, et al. Asynchronous telemedicine for isotretinoin management: a direct care pilot [published online January 21, 2021]. J Am Acad Dermatol. doi:10.1016/j.jaad.2021.01.039
- Hamming I, Timens W, Bulthuis MLC, et al. Tissue disruption of ACE2 protein, the functional receptor for SARS coronavirus. a first step in understanding SARS pathogenesis. J Pathol. 2004;203:631-637.
- British Association of Dermatologists. COVID-19—isotretinoin guidance. Published March 26, 2020. Accessed June 21, 2021. https://www.bad.org.uk/shared/get-file.ashx?itemtype=document&id=6661
- Sinha S, Cheng K, Schäffer AA, et al. In vitro and in vivo identification of clinically approved drugs that modify ACE2 expression. Mol Syst Biol. 2020;16:E9628.
- Öǧüt ND, Kutlu Ö, Erbaǧcı E. Oral isotretinoin treatment in patients with acne vulgaris during the COVID-19 pandemic: a retrospective cohort study in a tertiary care hospital [published online April 22, 2021]. J Cosmet Dermatol. doi:10.1111/jocd.14168
- Isotretinoin in treatment of COVID-19. National Library of Medicine website. ClinicalTrials.gov identifier: NCT04361422. Updated September 23, 2020. Accessed June 21, 2021. https://clinicaltrials.gov/ct2/show/NCT04361422
- Donnarumma M, Nocerino M, Lauro W, et al. Isotretinoin in acne treatment during the coronavirus disease 2019 (COVID-19): a retrospective analysis of adherence to therapy and side effects [published online December 22, 2020]. Dermatol Ther. 2021;34:E14677.
- Ivory D, Gebeloff R, Mervosh S. Young people have less COVID-19 risk, but in college towns, deaths rose fast. The New York Times. December 12, 2020. Accessed June 21, 2021. https://www.nytimes.com/2020/12/12/us/covid-colleges-nursing-homes.html
- US Food and Drug Administration. Coronavirus (COVID-19) update: FDA provides update on patient access to certain REMS drugs during COVID-19 public health emergency. Published March 22, 2020. Accessed June 21, 2021. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-provides-update-patient-access-certain-rems-drugs-during-covid-19
- Haelle T. iPledge allows at-home pregnancy tests during pandemic. Dermatology News. Published April 3, 2020. Accessed June 28, 2021. https://www.mdedge.com/dermatology/article/220186/acne/ipledge-allows-home-pregnancy-tests-during-pandemic
- Bressler MY, Siegel DM, Markowitz O. Virtual dermatology: a COVID-19 update. Cutis. 2020;105:163-164; E2.
- Telemedicine key issues and policy. Federation of State Medical Boards website. Accessed June 28, 2021. https://www.fsmb.org/advocacy/telemedicine
- Ruggiero A, Megna M, Annunziata MC, et al. Teledermatology for acne during COVID-19: high patients’ satisfaction in spite of the emergency. J Eur Acad Dermatol Venereol. 2020;34:E662-E663.
- Barbieri JS, Shin DB, Wang S, et al. The clinical utility of laboratory monitoring during isotretinoin therapy for acne and changes to monitoring practices over time. J Am Acad Dermatol. 2020;82:72-79.
- Tkachenko E, Singer S, Sharma P, et al. US Food and Drug Administration reports of pregnancy and pregnancy-related adverse events associated with isotretinoin. JAMA Dermatol. 2019;155:1175-1179.
- Das S, et al. Asynchronous telemedicine for isotretinoin management: a direct care pilot [published online January 21, 2021]. J Am Acad Dermatol. doi:10.1016/j.jaad.2021.01.039

