User login
Combination approach to melasma treatment yields best results
When establishing a treatment plan for patients with melasma, counseling them about realistic expectations is key.
“It’s important that they understand that this is a chronic condition, so it does require long-term maintenance therapy,” Arisa E. Ortiz, MD, said at the virtual annual Masters of Aesthetics Symposium. “We can improve melasma, but it’s difficult to cure melasma.”
While hydroquinone and other bleaching agents are typical treatment mainstays, chemical peels with glycolic acid, trichloroacetic acid, and salicylic acid can benefit some individuals. “For chemical peels, I really like glycolic acid peels because there is no downtime; it peels at the microscopic level,” said Dr. Ortiz, who is director of laser and cosmetic dermatology at the University of California, San Diego. “This is something they may need to repeat monthly, and having a week of peeling may be difficult to go through every month.”
Other common melasma treatments include lasers, intense pulsed light (IPL), and oral medications. “I personally am not impressed with microdermabrasion for melasma, so I don’t use that very much,” she said. “With laser treatment, you want to make sure you’re using low-energy lasers so that it doesn’t exacerbate or make them relapse or rebound.”
While hydroquinone is a mainstay of therapy, “you can’t use it chronically because of the risk of ochronosis (permanent darkening), so you do need to take drug holidays,” Dr. Ortiz said. “During those drug holidays, you want to make sure patients have a nonhydroquinone bleaching agent so that they don’t flare.” Options include lignin peroxidase, oligopeptide, Lytera, Melaplex, 4-n-butylresorcinol, Cysteamine cream, tranexamic acid, and oral antioxidants.
In a study sponsored by SkinMedica, investigators conducted a randomized, double-blind, half-face study in females with moderate to severe facial hyperpigmentation to assess the efficacy and tolerability of three new skin brightener formulations containing SMA-432, a prostaglandin E2 inhibitor, compared with topical 4% hydroquinone (J Drugs Dermatol 2012 Dec;11[12]:1478-82). They found that the nonhydroquinone skin formulations were better tolerated and were just as effective as 4% hydroquinone.
In a separate unpublished study of 22 females, investigators assessed the efficacy of the U.SK Advanced Defense Booster, which contains ferulic acid, maslinic acid, peptides, and olive leaf extract. They observed that 98% of patients saw improvement after 28 days of treatment.
When it comes to using lasers for melasma treatment, low-energy devices provide the best outcomes. “I prefer using something like the 1927-nm fractional diode lasers at 3.75% density, really low densities because there’s less risk for rebound,” Dr. Ortiz said. “They also enhance skin permeability for the use of topicals.”
In an observational study of 27 female patients with refractory melasma, Arielle Kauvar, MD, director of New York Laser & Skin Care, combined microdermabrasion with the Q-switched Nd:YAG (Lasers in Surgery and Medicine 2012; 44:117-24). “The settings she used were very low fluence, so there was no clinical endpoint or no whitening,” Dr. Ortiz said. Specifically, she used a laser at 1.6-2 J/cm2 with a 5- or 6-mm spot size immediately following microdermabrasion for 4 weeks. “She got a good improvement using a skin care regimen of sunscreen, hydroquinone, and tretinoin or vitamin C,” she said. “Remission lasted at least 6 months.”
In a study presented at the 2019 annual meeting of the America Society for Laser Medicine and Surgery, Dr. Ortiz and Tanya Greywal, MD, of the University of California, San Diego, used three passes of the 10764-nm Nd:YAG laser to treat 10 subjects with melasma skin types 2-5. The device has a 650-microsecond pulse duration, a 6-mm spot size, and an energy mode of 11-14 J/cm3. “There was no downtime with these patients, and they saw a mean improvement of 26%-50% as early as 3 weeks,” she said. “Patients did require multiple treatments to see adequate resolution, but no anesthesia or numbing cream was required. This is a good option for patients who need chronic maintenance treatment.”
Topicals also play a key role following the laser treatment of melasma. Dr. Ortiz characterized clobetasol as “kind of like the magic ointment.” She uses one application immediately post procedure “whenever I’m worried about a patient having postinflammatory hyperpigmentation or if I don’t want melasma patients to rebound. It can help reduce swelling and inflammation to decrease the risk of postinflammatory hyperpigmentation.”
Researchers have discovered that there is a vascular component to melasma. Paul M. Friedman, MD, of the Dermatology and Laser Surgery Center, Houston, and his colleagues used spectrocolorimetry to detect an underlying prominent vascular component in 11 patients with melasma (Lasers Surg Med 2017 Jan;49[1]:20-6). They determined that melasma lesions exhibiting subtle or subclinical telangiectatic erythema may be improved by combined vascular-targeted laser therapy together with fractional low-powered diode laser therapy. “A parallel improvement in telangiectatic erythema suggests a relationship between the underlying vasculature and hyperpigmentation,” said Dr. Ortiz, who was not affiliated with the study. “So, patients who have a vascular component to their melasma actually can get improved efficacy.”
Another strategy for melasma patients involves oral treatment with Polypodium leucotomos extract (PLE), a fern from the Polypodiaceae family with antioxidant properties that has been shown to be photoprotective against UVA and UVB radiation. “I like to think of it as an internal sunscreen,” Dr. Ortiz said. “It does not replace your external sunscreen, but it adds extra protection. It has been shown to significantly reduce the severity of sunburn and decrease the risk of UV radiation–induced skin cancer, as well as prevent skin aging.” The purported mechanism of action includes decreasing UV-mediated oxidative damage to DNA, enhancing the activity of endogenous antioxidant systems, increasing the minimal erythema dose, blocking UV radiation–induced cyclooxygenase-2 expression, reducing UV-induced immune suppression, and promoting p53 suppressor gene expression.
In a pilot placebo-controlled study of melasma patients on their normal regimen of hydroquinone and sunscreen, 40 Asian patients with melasma were randomized to receive either oral PLE supplementation or placebo for 12 weeks (J Clin Aesthet Dermatol 2018 Mar;11[3]:14-9). They found that PLE significantly improved and accelerated the outcome reached with hydroquinone and sunscreen from the first month of treatment, compared with placebo.
Dr. Ortiz next discussed the role of oral tranexamic acid, an antifibrinolytic, procoagulant agent that is approved by the Food and Drug Administration for the treatment of menorrhagia and for prevention of hemorrhage in patients with hemophilia undergoing tooth extractions. “It is a synthetic lysine derivative that inhibits plasminogen activation by blocking lysine-binding sites on the plasminogen molecule, and it’s a game changer for melasma treatment,” she said. “One of the side effects is that it inhibits melanogenesis and neovascularization. It’s been effective for melasma, but its use is limited by the risk for thromboembolism. It’s a slight increased risk, something patients should be aware of, but not something that should scare us away from prescribing it.”
In a study of 561 patients with melasma, 90% improved after a median treatment duration of 4 months, and only 7% had side effects (J Am Acad Dermatol 2016;75:385-92). The most common side effects were abdominal bloating and pain. One patient developed a DVT during treatment, but that person was found to have a protein S deficiency.
The daily dosing of tranexamic acid for menorrhagia is 3,900 mg daily, while the dose for melasma has ranged from 500 mg-1,500 mg per day, Dr. Ortiz said. It’s available as a 650-mg pill in the United States. “I prescribe 325 mg twice a day, but studies have shown that 650 mg once a day is just as effective,” she said.
Prior to prescribing tranexamic acid, Dr. Ortiz does not order labs, but she performs an extensive history of present illness. She does not prescribe it in patients with an increased risk of clotting, including people who smoke and those who take oral contraceptives or are on hormone supplementation. Use is also contraindicated in people with a current malignancy, those with a history of stroke or DVT, and those who have any clotting disorder.
She concluded her presentation by noting that she favors a combination approach to treating melasma patients that starts with a broad spectrum sunscreen and PLE. “For bleaching, I like to use 12% hydroquinone with 6% kojic acid in VersaBase,” she said. “Once I get them in better control, then I switch them to 4% hydroquinone for maintenance. I use glycolic peels, low-energy lasers, and tranexamic acid if the melasma is severe, and they have no contraindications. A combination approach really achieves the best results, and counseling is key.”
Dr. Ortiz disclosed having financial relationships with numerous pharmaceutical and device companies. She is also cochair of MOA.
When establishing a treatment plan for patients with melasma, counseling them about realistic expectations is key.
“It’s important that they understand that this is a chronic condition, so it does require long-term maintenance therapy,” Arisa E. Ortiz, MD, said at the virtual annual Masters of Aesthetics Symposium. “We can improve melasma, but it’s difficult to cure melasma.”
While hydroquinone and other bleaching agents are typical treatment mainstays, chemical peels with glycolic acid, trichloroacetic acid, and salicylic acid can benefit some individuals. “For chemical peels, I really like glycolic acid peels because there is no downtime; it peels at the microscopic level,” said Dr. Ortiz, who is director of laser and cosmetic dermatology at the University of California, San Diego. “This is something they may need to repeat monthly, and having a week of peeling may be difficult to go through every month.”
Other common melasma treatments include lasers, intense pulsed light (IPL), and oral medications. “I personally am not impressed with microdermabrasion for melasma, so I don’t use that very much,” she said. “With laser treatment, you want to make sure you’re using low-energy lasers so that it doesn’t exacerbate or make them relapse or rebound.”
While hydroquinone is a mainstay of therapy, “you can’t use it chronically because of the risk of ochronosis (permanent darkening), so you do need to take drug holidays,” Dr. Ortiz said. “During those drug holidays, you want to make sure patients have a nonhydroquinone bleaching agent so that they don’t flare.” Options include lignin peroxidase, oligopeptide, Lytera, Melaplex, 4-n-butylresorcinol, Cysteamine cream, tranexamic acid, and oral antioxidants.
In a study sponsored by SkinMedica, investigators conducted a randomized, double-blind, half-face study in females with moderate to severe facial hyperpigmentation to assess the efficacy and tolerability of three new skin brightener formulations containing SMA-432, a prostaglandin E2 inhibitor, compared with topical 4% hydroquinone (J Drugs Dermatol 2012 Dec;11[12]:1478-82). They found that the nonhydroquinone skin formulations were better tolerated and were just as effective as 4% hydroquinone.
In a separate unpublished study of 22 females, investigators assessed the efficacy of the U.SK Advanced Defense Booster, which contains ferulic acid, maslinic acid, peptides, and olive leaf extract. They observed that 98% of patients saw improvement after 28 days of treatment.
When it comes to using lasers for melasma treatment, low-energy devices provide the best outcomes. “I prefer using something like the 1927-nm fractional diode lasers at 3.75% density, really low densities because there’s less risk for rebound,” Dr. Ortiz said. “They also enhance skin permeability for the use of topicals.”
In an observational study of 27 female patients with refractory melasma, Arielle Kauvar, MD, director of New York Laser & Skin Care, combined microdermabrasion with the Q-switched Nd:YAG (Lasers in Surgery and Medicine 2012; 44:117-24). “The settings she used were very low fluence, so there was no clinical endpoint or no whitening,” Dr. Ortiz said. Specifically, she used a laser at 1.6-2 J/cm2 with a 5- or 6-mm spot size immediately following microdermabrasion for 4 weeks. “She got a good improvement using a skin care regimen of sunscreen, hydroquinone, and tretinoin or vitamin C,” she said. “Remission lasted at least 6 months.”
In a study presented at the 2019 annual meeting of the America Society for Laser Medicine and Surgery, Dr. Ortiz and Tanya Greywal, MD, of the University of California, San Diego, used three passes of the 10764-nm Nd:YAG laser to treat 10 subjects with melasma skin types 2-5. The device has a 650-microsecond pulse duration, a 6-mm spot size, and an energy mode of 11-14 J/cm3. “There was no downtime with these patients, and they saw a mean improvement of 26%-50% as early as 3 weeks,” she said. “Patients did require multiple treatments to see adequate resolution, but no anesthesia or numbing cream was required. This is a good option for patients who need chronic maintenance treatment.”
Topicals also play a key role following the laser treatment of melasma. Dr. Ortiz characterized clobetasol as “kind of like the magic ointment.” She uses one application immediately post procedure “whenever I’m worried about a patient having postinflammatory hyperpigmentation or if I don’t want melasma patients to rebound. It can help reduce swelling and inflammation to decrease the risk of postinflammatory hyperpigmentation.”
Researchers have discovered that there is a vascular component to melasma. Paul M. Friedman, MD, of the Dermatology and Laser Surgery Center, Houston, and his colleagues used spectrocolorimetry to detect an underlying prominent vascular component in 11 patients with melasma (Lasers Surg Med 2017 Jan;49[1]:20-6). They determined that melasma lesions exhibiting subtle or subclinical telangiectatic erythema may be improved by combined vascular-targeted laser therapy together with fractional low-powered diode laser therapy. “A parallel improvement in telangiectatic erythema suggests a relationship between the underlying vasculature and hyperpigmentation,” said Dr. Ortiz, who was not affiliated with the study. “So, patients who have a vascular component to their melasma actually can get improved efficacy.”
Another strategy for melasma patients involves oral treatment with Polypodium leucotomos extract (PLE), a fern from the Polypodiaceae family with antioxidant properties that has been shown to be photoprotective against UVA and UVB radiation. “I like to think of it as an internal sunscreen,” Dr. Ortiz said. “It does not replace your external sunscreen, but it adds extra protection. It has been shown to significantly reduce the severity of sunburn and decrease the risk of UV radiation–induced skin cancer, as well as prevent skin aging.” The purported mechanism of action includes decreasing UV-mediated oxidative damage to DNA, enhancing the activity of endogenous antioxidant systems, increasing the minimal erythema dose, blocking UV radiation–induced cyclooxygenase-2 expression, reducing UV-induced immune suppression, and promoting p53 suppressor gene expression.
In a pilot placebo-controlled study of melasma patients on their normal regimen of hydroquinone and sunscreen, 40 Asian patients with melasma were randomized to receive either oral PLE supplementation or placebo for 12 weeks (J Clin Aesthet Dermatol 2018 Mar;11[3]:14-9). They found that PLE significantly improved and accelerated the outcome reached with hydroquinone and sunscreen from the first month of treatment, compared with placebo.
Dr. Ortiz next discussed the role of oral tranexamic acid, an antifibrinolytic, procoagulant agent that is approved by the Food and Drug Administration for the treatment of menorrhagia and for prevention of hemorrhage in patients with hemophilia undergoing tooth extractions. “It is a synthetic lysine derivative that inhibits plasminogen activation by blocking lysine-binding sites on the plasminogen molecule, and it’s a game changer for melasma treatment,” she said. “One of the side effects is that it inhibits melanogenesis and neovascularization. It’s been effective for melasma, but its use is limited by the risk for thromboembolism. It’s a slight increased risk, something patients should be aware of, but not something that should scare us away from prescribing it.”
In a study of 561 patients with melasma, 90% improved after a median treatment duration of 4 months, and only 7% had side effects (J Am Acad Dermatol 2016;75:385-92). The most common side effects were abdominal bloating and pain. One patient developed a DVT during treatment, but that person was found to have a protein S deficiency.
The daily dosing of tranexamic acid for menorrhagia is 3,900 mg daily, while the dose for melasma has ranged from 500 mg-1,500 mg per day, Dr. Ortiz said. It’s available as a 650-mg pill in the United States. “I prescribe 325 mg twice a day, but studies have shown that 650 mg once a day is just as effective,” she said.
Prior to prescribing tranexamic acid, Dr. Ortiz does not order labs, but she performs an extensive history of present illness. She does not prescribe it in patients with an increased risk of clotting, including people who smoke and those who take oral contraceptives or are on hormone supplementation. Use is also contraindicated in people with a current malignancy, those with a history of stroke or DVT, and those who have any clotting disorder.
She concluded her presentation by noting that she favors a combination approach to treating melasma patients that starts with a broad spectrum sunscreen and PLE. “For bleaching, I like to use 12% hydroquinone with 6% kojic acid in VersaBase,” she said. “Once I get them in better control, then I switch them to 4% hydroquinone for maintenance. I use glycolic peels, low-energy lasers, and tranexamic acid if the melasma is severe, and they have no contraindications. A combination approach really achieves the best results, and counseling is key.”
Dr. Ortiz disclosed having financial relationships with numerous pharmaceutical and device companies. She is also cochair of MOA.
When establishing a treatment plan for patients with melasma, counseling them about realistic expectations is key.
“It’s important that they understand that this is a chronic condition, so it does require long-term maintenance therapy,” Arisa E. Ortiz, MD, said at the virtual annual Masters of Aesthetics Symposium. “We can improve melasma, but it’s difficult to cure melasma.”
While hydroquinone and other bleaching agents are typical treatment mainstays, chemical peels with glycolic acid, trichloroacetic acid, and salicylic acid can benefit some individuals. “For chemical peels, I really like glycolic acid peels because there is no downtime; it peels at the microscopic level,” said Dr. Ortiz, who is director of laser and cosmetic dermatology at the University of California, San Diego. “This is something they may need to repeat monthly, and having a week of peeling may be difficult to go through every month.”
Other common melasma treatments include lasers, intense pulsed light (IPL), and oral medications. “I personally am not impressed with microdermabrasion for melasma, so I don’t use that very much,” she said. “With laser treatment, you want to make sure you’re using low-energy lasers so that it doesn’t exacerbate or make them relapse or rebound.”
While hydroquinone is a mainstay of therapy, “you can’t use it chronically because of the risk of ochronosis (permanent darkening), so you do need to take drug holidays,” Dr. Ortiz said. “During those drug holidays, you want to make sure patients have a nonhydroquinone bleaching agent so that they don’t flare.” Options include lignin peroxidase, oligopeptide, Lytera, Melaplex, 4-n-butylresorcinol, Cysteamine cream, tranexamic acid, and oral antioxidants.
In a study sponsored by SkinMedica, investigators conducted a randomized, double-blind, half-face study in females with moderate to severe facial hyperpigmentation to assess the efficacy and tolerability of three new skin brightener formulations containing SMA-432, a prostaglandin E2 inhibitor, compared with topical 4% hydroquinone (J Drugs Dermatol 2012 Dec;11[12]:1478-82). They found that the nonhydroquinone skin formulations were better tolerated and were just as effective as 4% hydroquinone.
In a separate unpublished study of 22 females, investigators assessed the efficacy of the U.SK Advanced Defense Booster, which contains ferulic acid, maslinic acid, peptides, and olive leaf extract. They observed that 98% of patients saw improvement after 28 days of treatment.
When it comes to using lasers for melasma treatment, low-energy devices provide the best outcomes. “I prefer using something like the 1927-nm fractional diode lasers at 3.75% density, really low densities because there’s less risk for rebound,” Dr. Ortiz said. “They also enhance skin permeability for the use of topicals.”
In an observational study of 27 female patients with refractory melasma, Arielle Kauvar, MD, director of New York Laser & Skin Care, combined microdermabrasion with the Q-switched Nd:YAG (Lasers in Surgery and Medicine 2012; 44:117-24). “The settings she used were very low fluence, so there was no clinical endpoint or no whitening,” Dr. Ortiz said. Specifically, she used a laser at 1.6-2 J/cm2 with a 5- or 6-mm spot size immediately following microdermabrasion for 4 weeks. “She got a good improvement using a skin care regimen of sunscreen, hydroquinone, and tretinoin or vitamin C,” she said. “Remission lasted at least 6 months.”
In a study presented at the 2019 annual meeting of the America Society for Laser Medicine and Surgery, Dr. Ortiz and Tanya Greywal, MD, of the University of California, San Diego, used three passes of the 10764-nm Nd:YAG laser to treat 10 subjects with melasma skin types 2-5. The device has a 650-microsecond pulse duration, a 6-mm spot size, and an energy mode of 11-14 J/cm3. “There was no downtime with these patients, and they saw a mean improvement of 26%-50% as early as 3 weeks,” she said. “Patients did require multiple treatments to see adequate resolution, but no anesthesia or numbing cream was required. This is a good option for patients who need chronic maintenance treatment.”
Topicals also play a key role following the laser treatment of melasma. Dr. Ortiz characterized clobetasol as “kind of like the magic ointment.” She uses one application immediately post procedure “whenever I’m worried about a patient having postinflammatory hyperpigmentation or if I don’t want melasma patients to rebound. It can help reduce swelling and inflammation to decrease the risk of postinflammatory hyperpigmentation.”
Researchers have discovered that there is a vascular component to melasma. Paul M. Friedman, MD, of the Dermatology and Laser Surgery Center, Houston, and his colleagues used spectrocolorimetry to detect an underlying prominent vascular component in 11 patients with melasma (Lasers Surg Med 2017 Jan;49[1]:20-6). They determined that melasma lesions exhibiting subtle or subclinical telangiectatic erythema may be improved by combined vascular-targeted laser therapy together with fractional low-powered diode laser therapy. “A parallel improvement in telangiectatic erythema suggests a relationship between the underlying vasculature and hyperpigmentation,” said Dr. Ortiz, who was not affiliated with the study. “So, patients who have a vascular component to their melasma actually can get improved efficacy.”
Another strategy for melasma patients involves oral treatment with Polypodium leucotomos extract (PLE), a fern from the Polypodiaceae family with antioxidant properties that has been shown to be photoprotective against UVA and UVB radiation. “I like to think of it as an internal sunscreen,” Dr. Ortiz said. “It does not replace your external sunscreen, but it adds extra protection. It has been shown to significantly reduce the severity of sunburn and decrease the risk of UV radiation–induced skin cancer, as well as prevent skin aging.” The purported mechanism of action includes decreasing UV-mediated oxidative damage to DNA, enhancing the activity of endogenous antioxidant systems, increasing the minimal erythema dose, blocking UV radiation–induced cyclooxygenase-2 expression, reducing UV-induced immune suppression, and promoting p53 suppressor gene expression.
In a pilot placebo-controlled study of melasma patients on their normal regimen of hydroquinone and sunscreen, 40 Asian patients with melasma were randomized to receive either oral PLE supplementation or placebo for 12 weeks (J Clin Aesthet Dermatol 2018 Mar;11[3]:14-9). They found that PLE significantly improved and accelerated the outcome reached with hydroquinone and sunscreen from the first month of treatment, compared with placebo.
Dr. Ortiz next discussed the role of oral tranexamic acid, an antifibrinolytic, procoagulant agent that is approved by the Food and Drug Administration for the treatment of menorrhagia and for prevention of hemorrhage in patients with hemophilia undergoing tooth extractions. “It is a synthetic lysine derivative that inhibits plasminogen activation by blocking lysine-binding sites on the plasminogen molecule, and it’s a game changer for melasma treatment,” she said. “One of the side effects is that it inhibits melanogenesis and neovascularization. It’s been effective for melasma, but its use is limited by the risk for thromboembolism. It’s a slight increased risk, something patients should be aware of, but not something that should scare us away from prescribing it.”
In a study of 561 patients with melasma, 90% improved after a median treatment duration of 4 months, and only 7% had side effects (J Am Acad Dermatol 2016;75:385-92). The most common side effects were abdominal bloating and pain. One patient developed a DVT during treatment, but that person was found to have a protein S deficiency.
The daily dosing of tranexamic acid for menorrhagia is 3,900 mg daily, while the dose for melasma has ranged from 500 mg-1,500 mg per day, Dr. Ortiz said. It’s available as a 650-mg pill in the United States. “I prescribe 325 mg twice a day, but studies have shown that 650 mg once a day is just as effective,” she said.
Prior to prescribing tranexamic acid, Dr. Ortiz does not order labs, but she performs an extensive history of present illness. She does not prescribe it in patients with an increased risk of clotting, including people who smoke and those who take oral contraceptives or are on hormone supplementation. Use is also contraindicated in people with a current malignancy, those with a history of stroke or DVT, and those who have any clotting disorder.
She concluded her presentation by noting that she favors a combination approach to treating melasma patients that starts with a broad spectrum sunscreen and PLE. “For bleaching, I like to use 12% hydroquinone with 6% kojic acid in VersaBase,” she said. “Once I get them in better control, then I switch them to 4% hydroquinone for maintenance. I use glycolic peels, low-energy lasers, and tranexamic acid if the melasma is severe, and they have no contraindications. A combination approach really achieves the best results, and counseling is key.”
Dr. Ortiz disclosed having financial relationships with numerous pharmaceutical and device companies. She is also cochair of MOA.
EXPERT ANALYSIS FROM MOA 2020
Novel smart needle system designed to reduce risk of filler complications
In the very near future, clinicians injecting
That is the goal of an experienced team composed of leading clinicians, academics, and researchers developing S3 Inject, a first-in-class safety innovation that has entered human trials.
“When physicians inject the fillers, they hope experience and technique will enable them to avoid adverse events,” Irina Erenburg, PhD, said during the virtual annual Masters of Aesthetics Symposium. “If they inadvertently hit a blood vessel, the filler can actually occlude that vessel and cause either an infarct of the skin or, in certain serious cases, blindness. This is a challenging adverse event that every injector is focused on avoiding. While hyaluronidase is used as a rescue [medication] in certain cases, the risk is real,” she added.
Vision abnormalities, including blindness, and necrosis are among the adverse events associated with dermal fillers that have been reported to the Food and Drug Administration.
S3 Inject is a sensing needle that can differentiate tissues such as fat, blood vessels, and muscle. Its proprietary algorithms provide immediate feedback via a micro LED light embedded in the needle hub. Results from recent human trials demonstrate that, as the needle tip passes through different biological tissues and fluids, “it senses changes in specific electrical properties and with that information sends a very precise signal to the needle hub,” said Dr. Erenburg, CEO and President of Waltham, Mass.–based Blossom Innovations, a company focused on developing early stage medical devices in dermatology. “With that information, the physician can make real-time treatment decisions.”
Currently, in order to determine if the needle is in a blood vessel, physicians pull back on the syringe and look for a flash of blood. “In speaking with physicians, the pull back technique has limitations, in part, because filler in the syringe can limit easy pull back to check the presence of a blood vessel,” she said. “Our needles provide an immediate response for a safer injection.”
Blossom Innovations has developed a proprietary manufacturing process that will initially target 27 gauge needles, but over time it plans to introduce multiple sizes, as well as cannulas.
“The physicians in our industry are committed to patient safety and they’re looking for better outcomes with a solution that does not impact their technique,” said Dr. Erenburg, who founded Blossom Innovations along with R. Rox Anderson, MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston; Dieter Manstein, MD, PhD, also at Massachusetts General Hospital; and Henry H.L. Chan, MD, PhD, of the Hong Kong Dermatology and Laser Center. During market research for S3 Inject, which was conducted with 15 leading injectors, thought leaders, and trend makers, the country’s leading injectors expressed strong interest in “solutions that allow them to provide additional safety for their patients and provide personal reassurance to the physician,” she said. “They definitely would want to train all their physicians and injectors on its use.”
As clinical testing continues, the company is preparing to submit data to the FDA’s Premarket Notification program, known as the 510(k) process. “Our intent is to create a scale-up manufacturing over the course of the coming year in time for our clearance, with a planned launch at the end of 2021,” Dr. Erenburg said. “Based on our clinical research and physician discussions, we are confident that S3 Inject is a breakthrough safety technology which will drive a better outcome for patients.”
Dr. Erenburg is an employee of Blossom Innovations.
In the very near future, clinicians injecting
That is the goal of an experienced team composed of leading clinicians, academics, and researchers developing S3 Inject, a first-in-class safety innovation that has entered human trials.
“When physicians inject the fillers, they hope experience and technique will enable them to avoid adverse events,” Irina Erenburg, PhD, said during the virtual annual Masters of Aesthetics Symposium. “If they inadvertently hit a blood vessel, the filler can actually occlude that vessel and cause either an infarct of the skin or, in certain serious cases, blindness. This is a challenging adverse event that every injector is focused on avoiding. While hyaluronidase is used as a rescue [medication] in certain cases, the risk is real,” she added.
Vision abnormalities, including blindness, and necrosis are among the adverse events associated with dermal fillers that have been reported to the Food and Drug Administration.
S3 Inject is a sensing needle that can differentiate tissues such as fat, blood vessels, and muscle. Its proprietary algorithms provide immediate feedback via a micro LED light embedded in the needle hub. Results from recent human trials demonstrate that, as the needle tip passes through different biological tissues and fluids, “it senses changes in specific electrical properties and with that information sends a very precise signal to the needle hub,” said Dr. Erenburg, CEO and President of Waltham, Mass.–based Blossom Innovations, a company focused on developing early stage medical devices in dermatology. “With that information, the physician can make real-time treatment decisions.”
Currently, in order to determine if the needle is in a blood vessel, physicians pull back on the syringe and look for a flash of blood. “In speaking with physicians, the pull back technique has limitations, in part, because filler in the syringe can limit easy pull back to check the presence of a blood vessel,” she said. “Our needles provide an immediate response for a safer injection.”
Blossom Innovations has developed a proprietary manufacturing process that will initially target 27 gauge needles, but over time it plans to introduce multiple sizes, as well as cannulas.
“The physicians in our industry are committed to patient safety and they’re looking for better outcomes with a solution that does not impact their technique,” said Dr. Erenburg, who founded Blossom Innovations along with R. Rox Anderson, MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston; Dieter Manstein, MD, PhD, also at Massachusetts General Hospital; and Henry H.L. Chan, MD, PhD, of the Hong Kong Dermatology and Laser Center. During market research for S3 Inject, which was conducted with 15 leading injectors, thought leaders, and trend makers, the country’s leading injectors expressed strong interest in “solutions that allow them to provide additional safety for their patients and provide personal reassurance to the physician,” she said. “They definitely would want to train all their physicians and injectors on its use.”
As clinical testing continues, the company is preparing to submit data to the FDA’s Premarket Notification program, known as the 510(k) process. “Our intent is to create a scale-up manufacturing over the course of the coming year in time for our clearance, with a planned launch at the end of 2021,” Dr. Erenburg said. “Based on our clinical research and physician discussions, we are confident that S3 Inject is a breakthrough safety technology which will drive a better outcome for patients.”
Dr. Erenburg is an employee of Blossom Innovations.
In the very near future, clinicians injecting
That is the goal of an experienced team composed of leading clinicians, academics, and researchers developing S3 Inject, a first-in-class safety innovation that has entered human trials.
“When physicians inject the fillers, they hope experience and technique will enable them to avoid adverse events,” Irina Erenburg, PhD, said during the virtual annual Masters of Aesthetics Symposium. “If they inadvertently hit a blood vessel, the filler can actually occlude that vessel and cause either an infarct of the skin or, in certain serious cases, blindness. This is a challenging adverse event that every injector is focused on avoiding. While hyaluronidase is used as a rescue [medication] in certain cases, the risk is real,” she added.
Vision abnormalities, including blindness, and necrosis are among the adverse events associated with dermal fillers that have been reported to the Food and Drug Administration.
S3 Inject is a sensing needle that can differentiate tissues such as fat, blood vessels, and muscle. Its proprietary algorithms provide immediate feedback via a micro LED light embedded in the needle hub. Results from recent human trials demonstrate that, as the needle tip passes through different biological tissues and fluids, “it senses changes in specific electrical properties and with that information sends a very precise signal to the needle hub,” said Dr. Erenburg, CEO and President of Waltham, Mass.–based Blossom Innovations, a company focused on developing early stage medical devices in dermatology. “With that information, the physician can make real-time treatment decisions.”
Currently, in order to determine if the needle is in a blood vessel, physicians pull back on the syringe and look for a flash of blood. “In speaking with physicians, the pull back technique has limitations, in part, because filler in the syringe can limit easy pull back to check the presence of a blood vessel,” she said. “Our needles provide an immediate response for a safer injection.”
Blossom Innovations has developed a proprietary manufacturing process that will initially target 27 gauge needles, but over time it plans to introduce multiple sizes, as well as cannulas.
“The physicians in our industry are committed to patient safety and they’re looking for better outcomes with a solution that does not impact their technique,” said Dr. Erenburg, who founded Blossom Innovations along with R. Rox Anderson, MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston; Dieter Manstein, MD, PhD, also at Massachusetts General Hospital; and Henry H.L. Chan, MD, PhD, of the Hong Kong Dermatology and Laser Center. During market research for S3 Inject, which was conducted with 15 leading injectors, thought leaders, and trend makers, the country’s leading injectors expressed strong interest in “solutions that allow them to provide additional safety for their patients and provide personal reassurance to the physician,” she said. “They definitely would want to train all their physicians and injectors on its use.”
As clinical testing continues, the company is preparing to submit data to the FDA’s Premarket Notification program, known as the 510(k) process. “Our intent is to create a scale-up manufacturing over the course of the coming year in time for our clearance, with a planned launch at the end of 2021,” Dr. Erenburg said. “Based on our clinical research and physician discussions, we are confident that S3 Inject is a breakthrough safety technology which will drive a better outcome for patients.”
Dr. Erenburg is an employee of Blossom Innovations.
REPORTING FROM MOA 2020
The interesting history of dermatologist-developed skin care
Those of you who have visited my dermatology practice in Miami know that the art in my office is dedicated to the history of the skin care industry. I collect , and I have written this historical column in honor of the 50th anniversary of Dermatology News.
The first doctor to market his own cosmetic product, Erasmus Wilson, MD, faced scrutiny from his colleagues. Although he had contributed much to the field of dermatology, he was criticized by other dermatologists when he promoted a hair wash. The next doctor in my story, William Pusey, MD, was criticized for helping the company that manufactured Camay soap because he allowed his name to be used in Camay advertisements. The scrutiny that these two well-respected dermatologists endured from their colleagues deterred dermatologists from entering the skin care business for decades. The professional jealousy from dermatologic colleagues left the skin care field wide open for imposters, charlatans, and nondermatologists who had no concern for efficacy and patient outcomes to flourish. This is the story of a group of brilliant entrepreneurial dermatologists and one chiropractor who misrepresented himself as a dermatologist and how they influenced skin care as we know it.
Erasmus Wilson, MD1 (1809-1884): In 1840, Erasmus Wilson2 was a physician in London who chose to specialize in dermatology at a time when that specialization was frowned upon. He was a subeditor for The Lancet and wrote several books on dermatology including “Diseases of the Skin – A Practical and Theoretical Treatise,” “Portraits of the Diseases of the Skin,” and “Student’s Book on Diseases of the Skin.” He was the first professor of dermatology in the College of Surgeons and by 1869, was the leading English-speaking dermatologist in the world. He contributed much to dermatology, including his pioneering characterizations of Demodex mites, lichen planus, exfoliative dermatitis, neurotic excoriations, and roseola. Dr. Wilson was knighted in 1881 for his good works and notable generosity. (He was known for giving his poor patients money for food, endowing chairs in dermatology, and donating a famous obelisk in London).
In 1854, Dr. Wilson wrote a book for laypeople called “Healthy Skin: A Popular Treatise on the Skin and Hair, Their Preservation and Management,” in which he advocated cleanliness and bathing, which led to the popularity of Turkish baths and bathing resorts in Europe. Despite his undeniable contributions to dermatology, he was widely criticized by his colleagues for promoting a “Hair Wash” and a turtle oil soap. I cannot find any information about whether or not he developed the hair wash and turtle soap himself, but it seems that he earned income from sales of these two products, even though he was said to have donated it all to charities.
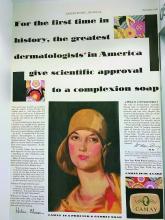
William A. Pusey MD (1865-1940): Dr. Pusey was the first chairman of dermatology at the University of Illinois College of Medicine, Chicago. He published several books, including “Care of the Skin and Hair,” “Syphilis as a Modern Problem,” “The Principles and Practices of Dermatology,” and “History of Dermatology” among others. He is best known for his work in developing the use of x-rays (roentgen rays) and phototherapy in dermatology, and in 1907, he was the first dermatologist to describe the use of solid carbon dioxide to treat skin lesions. He was president of the American Dermatological Association in 1910, president of the Chicago Medical Society in 1918, editor of the Archives of Dermatology in 1920, and president of the American Medical Association in 1924.
In the early 1920s, skin care companies were beginning to advertise their products using endorsements from celebrities and socialites, and were making misleading claims. Dr. Pusey wanted to work with these companies to help them perform evidence-based trials so they could make scientifically correct claims. Proctor & Gamble asked Dr. Pusey to advise them on how they could advertise honestly about their new soap, “Camay.” In Dr. Pusey’s words,3 “they (Proctor & Gamble) wanted to give the public authoritative advice about the use of soap and water. They suggested that I get a group of dermatologists of my selection to examine the soap and prepare instructions for bathing and the use of soap, and, if they found this soap was of high quality, to certify to that effect.” The research was performed as he suggested, and he allowed his name to be used in the Camay soap ads from 1926 to 1929. He said that he allowed them to use his name hoping to promote the need for evidence-based research, in contrast to the skin care products endorsed by socialites and celebrities that were flooding the market around that time.
Herbert Rattner, MD, at Northwestern University, Chicago, was his friend and one of the many dermatologists who criticized Dr. Pusey for allowing his name to be used in the Camay ads. Dr. Pusey’s reply to the criticism (according to Dr. Rattner) was that Proctor & Gamble was “proposing to do what the medical profession always is criticizing commercial concerns for not doing, namely, coming to physicians for information on medical matters. Could the profession hope to have any influence with business concerns if it was always eager to criticize bad commercial practices but never willing to support good ones?”3
While Dr. Pusey felt his reasons for adding his name to the Camay ads and research were justified, many of his friends stated that in hindsight, he regretted the action because of the negative response of his colleagues. It was years before dermatologists began providing input again into the skin care industry. During that time, radio, television and print ads were rampant with misleading claims – which led the way for a dermatologic imposter to make a fortune on skin care.
John Woodbury (1851-1909): John Woodbury, a chiropractor, never went to medical school, but that did not stop him from claiming he was a dermatologist and cosmetic surgeon. In 1889, he opened the John H. Woodbury Dermatological Institute in New York City, and over the next few years, opened Woodbury Dermatological Institutes in at least 5 states and employed 25 “physicians” who were not licensed to practice medicine. He came out with face soaps, tonics, and cold creams and spent a fortune on advertising these products and his institutes. In 1901, he sold his “Woodbury Soap” to the Andrew Jergens Company for $212,500 and 10% in royalties.
Multiple lawsuits occurred from 1898 to 1907 because he continued using the Woodbury name on his own products, despite having sold the “Woodbury” trademark to Jergens. He was sued for practicing medicine without a medical license and claiming to be a dermatologist when he was not. He lost most of these lawsuits, including one in 1907 in which the court ruled that corporations may not employ unlicensed professionals to practice medicine. In 1909, John Woodbury committed suicide. The Woodbury Soap company flourished in the 1930s and 1940s, as part of Jergens, until the brand was discontinued in 1970 when Jergens was acquired by American Brands.
The next dermatologists to come along did not make the same mistakes as those of their predecessors. They all made scientific discoveries through their basic science research in the laboratory, filed patents, formed skin care companies, perfected the formulations, and conducted research trials of the final product. Their marketing focused on science and efficacy and only rarely used their names and images in advertising, allowing them to maintain their reputations in the dermatology field.
Eugene Van Scott, MD (1922-present): Dermatologist Dr. Van Scott and dermatopharmacologist Ruey Yu, PhD, filed a method patent in the early 1970s on the effectiveness of alpha hydroxy acids to treat ichthyosis. They invented the abbreviation “AHA” and have continued their work on organic acids to this day. They now have more than 125 patents, which they have licensed to 60 companies in the cosmetics and pharmaceutical industries.
In 1988, 14 years after their initial publication, they founded the company they named Polystrata, which grew into today’s NeoStrata.4 Over the years, they had to defend their patents because many personal care companies used their technologies without licensing them. In 2007, they won a $41 million settlement in a patent infringement suit against Mary Kay filed in March 2005. They have both been very philanthropic in the dermatology world5 and are highly respected in the field. Among many other honors, Dr. Van Scott was named a Master Dermatologist by the American Academy of Dermatology in 1998 and received the Dermatology Foundation’s Distinguished Service Medallion in 2004.
Sheldon Pinnell, MD (1937-2013): After Dr. Pinnell completed his dermatology residency at Harvard Medical School, he spent 2 years studying collagen chemistry at the Max Planck Institute in Munich, Germany. In 1973, he returned to Duke University where he had earned his undergraduate degree before attending Yale University. He remained at Duke for the duration of his career and was professor and chief of dermatology there for many years. Early in his career, he focused on the role of vitamin C in collagen biosynthesis and discovered some of the mechanisms by which sun exposure causes photoaging. He described the use of the first (and most popular) topically applied L-ascorbic acid (vitamin C) to prevent and treat skin aging.
Dr. Pinnell’s many discoveries include showing that the addition of ascorbic acid to fibroblast cultures increases collagen production and that topically applied L-ascorbic acid penetrates into the skin best at a pH of 2-2.5. Dr. Pinnell changed the way the world uses topical antioxidants today; he was widely respected and was a member of the American Dermatological Association and an honorary member of the Society of Investigative Dermatology. He published more than 200 scientific articles and held 10 patents. He started the skin care company Skinceuticals, based on his antioxidant technologies. It was acquired by L’Oreal in 2005.
Richard Fitzpatrick, MD (1944-2014): The dermatologist affectionately known as “Fitz” is credited with being the first to use lasers for skin resurfacing. He went to medical school at Emory University and did his dermatology residency at the University of California, Los Angeles. He authored more than 130 publications and was one of the first doctors to specialize in cosmetic dermatology. He realized that fibroblast cell cultures used to produce the collagen filler CosmoPlast (no longer on the market) generated many growth factors that could rejuvenate the skin, and in 1999, he launched the skin care brand SkinMedica. In 2000, he received a patent for fibroblast-derived growth factors used topically for antiaging – a formula he called Tissue Nutrient Solution. In 2001, the popular product TNS Recovery Complex was launched based on the patented growth factor technology. It is still the most popular growth factor technology on the market.
What can we learn from these pioneers? I have had several interesting discussions about this topic with Leonard Hoenig, MD, section editor for Reflections on Dermatology: Past, Present, and Future, in Clinics in Dermatology. (Dr. Hoenig told me the interesting story that Listerine mouthwash was named in honor of Joseph Lister but accounts vary as to whether he gave permission to do so. This makes Dr. Lister the most famous physician to endorse a personal care product.) When Dr. Hoenig and I discussed the ethics of dermatologists creating a skin care line or retailing skin care in their medical practice, he stated my sentiments perfectly: “We should rely on professional, ethical, and legal guidelines to help us do what is right. Most importantly, we should have the best interests of our patients at heart when recommending any treatments.”
Dermatologists have unique knowledge, experience, and perspective on treating the skin with topical agents and have the true desire to improve skin health. If we do not discover, research, patent, and develop efficacious skin care products, someone else will do it – and I do not think they will do it as well as a dermatologist can.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Everett MA. Int J Dermatol. 1978 May;17(4):345-52.
2. Moxon RK. N Engl J Med. 1976 Apr 1;294(14):762-4.
3. Rattner H. Arch Derm Syphilol. 1937;35(1):25-66.
4. Neostrata: More than Hope, by Elaine Strauss, U.S. 1 Newspaper, Feb. 24, 1999.
5. Two legends in the field of dermatology provide $1 million gift to Temple University school of medicine’s department of dermatology, Temple University, June 5, 2015.
Those of you who have visited my dermatology practice in Miami know that the art in my office is dedicated to the history of the skin care industry. I collect , and I have written this historical column in honor of the 50th anniversary of Dermatology News.
The first doctor to market his own cosmetic product, Erasmus Wilson, MD, faced scrutiny from his colleagues. Although he had contributed much to the field of dermatology, he was criticized by other dermatologists when he promoted a hair wash. The next doctor in my story, William Pusey, MD, was criticized for helping the company that manufactured Camay soap because he allowed his name to be used in Camay advertisements. The scrutiny that these two well-respected dermatologists endured from their colleagues deterred dermatologists from entering the skin care business for decades. The professional jealousy from dermatologic colleagues left the skin care field wide open for imposters, charlatans, and nondermatologists who had no concern for efficacy and patient outcomes to flourish. This is the story of a group of brilliant entrepreneurial dermatologists and one chiropractor who misrepresented himself as a dermatologist and how they influenced skin care as we know it.
Erasmus Wilson, MD1 (1809-1884): In 1840, Erasmus Wilson2 was a physician in London who chose to specialize in dermatology at a time when that specialization was frowned upon. He was a subeditor for The Lancet and wrote several books on dermatology including “Diseases of the Skin – A Practical and Theoretical Treatise,” “Portraits of the Diseases of the Skin,” and “Student’s Book on Diseases of the Skin.” He was the first professor of dermatology in the College of Surgeons and by 1869, was the leading English-speaking dermatologist in the world. He contributed much to dermatology, including his pioneering characterizations of Demodex mites, lichen planus, exfoliative dermatitis, neurotic excoriations, and roseola. Dr. Wilson was knighted in 1881 for his good works and notable generosity. (He was known for giving his poor patients money for food, endowing chairs in dermatology, and donating a famous obelisk in London).
In 1854, Dr. Wilson wrote a book for laypeople called “Healthy Skin: A Popular Treatise on the Skin and Hair, Their Preservation and Management,” in which he advocated cleanliness and bathing, which led to the popularity of Turkish baths and bathing resorts in Europe. Despite his undeniable contributions to dermatology, he was widely criticized by his colleagues for promoting a “Hair Wash” and a turtle oil soap. I cannot find any information about whether or not he developed the hair wash and turtle soap himself, but it seems that he earned income from sales of these two products, even though he was said to have donated it all to charities.
William A. Pusey MD (1865-1940): Dr. Pusey was the first chairman of dermatology at the University of Illinois College of Medicine, Chicago. He published several books, including “Care of the Skin and Hair,” “Syphilis as a Modern Problem,” “The Principles and Practices of Dermatology,” and “History of Dermatology” among others. He is best known for his work in developing the use of x-rays (roentgen rays) and phototherapy in dermatology, and in 1907, he was the first dermatologist to describe the use of solid carbon dioxide to treat skin lesions. He was president of the American Dermatological Association in 1910, president of the Chicago Medical Society in 1918, editor of the Archives of Dermatology in 1920, and president of the American Medical Association in 1924.
In the early 1920s, skin care companies were beginning to advertise their products using endorsements from celebrities and socialites, and were making misleading claims. Dr. Pusey wanted to work with these companies to help them perform evidence-based trials so they could make scientifically correct claims. Proctor & Gamble asked Dr. Pusey to advise them on how they could advertise honestly about their new soap, “Camay.” In Dr. Pusey’s words,3 “they (Proctor & Gamble) wanted to give the public authoritative advice about the use of soap and water. They suggested that I get a group of dermatologists of my selection to examine the soap and prepare instructions for bathing and the use of soap, and, if they found this soap was of high quality, to certify to that effect.” The research was performed as he suggested, and he allowed his name to be used in the Camay soap ads from 1926 to 1929. He said that he allowed them to use his name hoping to promote the need for evidence-based research, in contrast to the skin care products endorsed by socialites and celebrities that were flooding the market around that time.
Herbert Rattner, MD, at Northwestern University, Chicago, was his friend and one of the many dermatologists who criticized Dr. Pusey for allowing his name to be used in the Camay ads. Dr. Pusey’s reply to the criticism (according to Dr. Rattner) was that Proctor & Gamble was “proposing to do what the medical profession always is criticizing commercial concerns for not doing, namely, coming to physicians for information on medical matters. Could the profession hope to have any influence with business concerns if it was always eager to criticize bad commercial practices but never willing to support good ones?”3
While Dr. Pusey felt his reasons for adding his name to the Camay ads and research were justified, many of his friends stated that in hindsight, he regretted the action because of the negative response of his colleagues. It was years before dermatologists began providing input again into the skin care industry. During that time, radio, television and print ads were rampant with misleading claims – which led the way for a dermatologic imposter to make a fortune on skin care.
John Woodbury (1851-1909): John Woodbury, a chiropractor, never went to medical school, but that did not stop him from claiming he was a dermatologist and cosmetic surgeon. In 1889, he opened the John H. Woodbury Dermatological Institute in New York City, and over the next few years, opened Woodbury Dermatological Institutes in at least 5 states and employed 25 “physicians” who were not licensed to practice medicine. He came out with face soaps, tonics, and cold creams and spent a fortune on advertising these products and his institutes. In 1901, he sold his “Woodbury Soap” to the Andrew Jergens Company for $212,500 and 10% in royalties.
Multiple lawsuits occurred from 1898 to 1907 because he continued using the Woodbury name on his own products, despite having sold the “Woodbury” trademark to Jergens. He was sued for practicing medicine without a medical license and claiming to be a dermatologist when he was not. He lost most of these lawsuits, including one in 1907 in which the court ruled that corporations may not employ unlicensed professionals to practice medicine. In 1909, John Woodbury committed suicide. The Woodbury Soap company flourished in the 1930s and 1940s, as part of Jergens, until the brand was discontinued in 1970 when Jergens was acquired by American Brands.
The next dermatologists to come along did not make the same mistakes as those of their predecessors. They all made scientific discoveries through their basic science research in the laboratory, filed patents, formed skin care companies, perfected the formulations, and conducted research trials of the final product. Their marketing focused on science and efficacy and only rarely used their names and images in advertising, allowing them to maintain their reputations in the dermatology field.
Eugene Van Scott, MD (1922-present): Dermatologist Dr. Van Scott and dermatopharmacologist Ruey Yu, PhD, filed a method patent in the early 1970s on the effectiveness of alpha hydroxy acids to treat ichthyosis. They invented the abbreviation “AHA” and have continued their work on organic acids to this day. They now have more than 125 patents, which they have licensed to 60 companies in the cosmetics and pharmaceutical industries.
In 1988, 14 years after their initial publication, they founded the company they named Polystrata, which grew into today’s NeoStrata.4 Over the years, they had to defend their patents because many personal care companies used their technologies without licensing them. In 2007, they won a $41 million settlement in a patent infringement suit against Mary Kay filed in March 2005. They have both been very philanthropic in the dermatology world5 and are highly respected in the field. Among many other honors, Dr. Van Scott was named a Master Dermatologist by the American Academy of Dermatology in 1998 and received the Dermatology Foundation’s Distinguished Service Medallion in 2004.
Sheldon Pinnell, MD (1937-2013): After Dr. Pinnell completed his dermatology residency at Harvard Medical School, he spent 2 years studying collagen chemistry at the Max Planck Institute in Munich, Germany. In 1973, he returned to Duke University where he had earned his undergraduate degree before attending Yale University. He remained at Duke for the duration of his career and was professor and chief of dermatology there for many years. Early in his career, he focused on the role of vitamin C in collagen biosynthesis and discovered some of the mechanisms by which sun exposure causes photoaging. He described the use of the first (and most popular) topically applied L-ascorbic acid (vitamin C) to prevent and treat skin aging.
Dr. Pinnell’s many discoveries include showing that the addition of ascorbic acid to fibroblast cultures increases collagen production and that topically applied L-ascorbic acid penetrates into the skin best at a pH of 2-2.5. Dr. Pinnell changed the way the world uses topical antioxidants today; he was widely respected and was a member of the American Dermatological Association and an honorary member of the Society of Investigative Dermatology. He published more than 200 scientific articles and held 10 patents. He started the skin care company Skinceuticals, based on his antioxidant technologies. It was acquired by L’Oreal in 2005.
Richard Fitzpatrick, MD (1944-2014): The dermatologist affectionately known as “Fitz” is credited with being the first to use lasers for skin resurfacing. He went to medical school at Emory University and did his dermatology residency at the University of California, Los Angeles. He authored more than 130 publications and was one of the first doctors to specialize in cosmetic dermatology. He realized that fibroblast cell cultures used to produce the collagen filler CosmoPlast (no longer on the market) generated many growth factors that could rejuvenate the skin, and in 1999, he launched the skin care brand SkinMedica. In 2000, he received a patent for fibroblast-derived growth factors used topically for antiaging – a formula he called Tissue Nutrient Solution. In 2001, the popular product TNS Recovery Complex was launched based on the patented growth factor technology. It is still the most popular growth factor technology on the market.
What can we learn from these pioneers? I have had several interesting discussions about this topic with Leonard Hoenig, MD, section editor for Reflections on Dermatology: Past, Present, and Future, in Clinics in Dermatology. (Dr. Hoenig told me the interesting story that Listerine mouthwash was named in honor of Joseph Lister but accounts vary as to whether he gave permission to do so. This makes Dr. Lister the most famous physician to endorse a personal care product.) When Dr. Hoenig and I discussed the ethics of dermatologists creating a skin care line or retailing skin care in their medical practice, he stated my sentiments perfectly: “We should rely on professional, ethical, and legal guidelines to help us do what is right. Most importantly, we should have the best interests of our patients at heart when recommending any treatments.”
Dermatologists have unique knowledge, experience, and perspective on treating the skin with topical agents and have the true desire to improve skin health. If we do not discover, research, patent, and develop efficacious skin care products, someone else will do it – and I do not think they will do it as well as a dermatologist can.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Everett MA. Int J Dermatol. 1978 May;17(4):345-52.
2. Moxon RK. N Engl J Med. 1976 Apr 1;294(14):762-4.
3. Rattner H. Arch Derm Syphilol. 1937;35(1):25-66.
4. Neostrata: More than Hope, by Elaine Strauss, U.S. 1 Newspaper, Feb. 24, 1999.
5. Two legends in the field of dermatology provide $1 million gift to Temple University school of medicine’s department of dermatology, Temple University, June 5, 2015.
Those of you who have visited my dermatology practice in Miami know that the art in my office is dedicated to the history of the skin care industry. I collect , and I have written this historical column in honor of the 50th anniversary of Dermatology News.
The first doctor to market his own cosmetic product, Erasmus Wilson, MD, faced scrutiny from his colleagues. Although he had contributed much to the field of dermatology, he was criticized by other dermatologists when he promoted a hair wash. The next doctor in my story, William Pusey, MD, was criticized for helping the company that manufactured Camay soap because he allowed his name to be used in Camay advertisements. The scrutiny that these two well-respected dermatologists endured from their colleagues deterred dermatologists from entering the skin care business for decades. The professional jealousy from dermatologic colleagues left the skin care field wide open for imposters, charlatans, and nondermatologists who had no concern for efficacy and patient outcomes to flourish. This is the story of a group of brilliant entrepreneurial dermatologists and one chiropractor who misrepresented himself as a dermatologist and how they influenced skin care as we know it.
Erasmus Wilson, MD1 (1809-1884): In 1840, Erasmus Wilson2 was a physician in London who chose to specialize in dermatology at a time when that specialization was frowned upon. He was a subeditor for The Lancet and wrote several books on dermatology including “Diseases of the Skin – A Practical and Theoretical Treatise,” “Portraits of the Diseases of the Skin,” and “Student’s Book on Diseases of the Skin.” He was the first professor of dermatology in the College of Surgeons and by 1869, was the leading English-speaking dermatologist in the world. He contributed much to dermatology, including his pioneering characterizations of Demodex mites, lichen planus, exfoliative dermatitis, neurotic excoriations, and roseola. Dr. Wilson was knighted in 1881 for his good works and notable generosity. (He was known for giving his poor patients money for food, endowing chairs in dermatology, and donating a famous obelisk in London).
In 1854, Dr. Wilson wrote a book for laypeople called “Healthy Skin: A Popular Treatise on the Skin and Hair, Their Preservation and Management,” in which he advocated cleanliness and bathing, which led to the popularity of Turkish baths and bathing resorts in Europe. Despite his undeniable contributions to dermatology, he was widely criticized by his colleagues for promoting a “Hair Wash” and a turtle oil soap. I cannot find any information about whether or not he developed the hair wash and turtle soap himself, but it seems that he earned income from sales of these two products, even though he was said to have donated it all to charities.
William A. Pusey MD (1865-1940): Dr. Pusey was the first chairman of dermatology at the University of Illinois College of Medicine, Chicago. He published several books, including “Care of the Skin and Hair,” “Syphilis as a Modern Problem,” “The Principles and Practices of Dermatology,” and “History of Dermatology” among others. He is best known for his work in developing the use of x-rays (roentgen rays) and phototherapy in dermatology, and in 1907, he was the first dermatologist to describe the use of solid carbon dioxide to treat skin lesions. He was president of the American Dermatological Association in 1910, president of the Chicago Medical Society in 1918, editor of the Archives of Dermatology in 1920, and president of the American Medical Association in 1924.
In the early 1920s, skin care companies were beginning to advertise their products using endorsements from celebrities and socialites, and were making misleading claims. Dr. Pusey wanted to work with these companies to help them perform evidence-based trials so they could make scientifically correct claims. Proctor & Gamble asked Dr. Pusey to advise them on how they could advertise honestly about their new soap, “Camay.” In Dr. Pusey’s words,3 “they (Proctor & Gamble) wanted to give the public authoritative advice about the use of soap and water. They suggested that I get a group of dermatologists of my selection to examine the soap and prepare instructions for bathing and the use of soap, and, if they found this soap was of high quality, to certify to that effect.” The research was performed as he suggested, and he allowed his name to be used in the Camay soap ads from 1926 to 1929. He said that he allowed them to use his name hoping to promote the need for evidence-based research, in contrast to the skin care products endorsed by socialites and celebrities that were flooding the market around that time.
Herbert Rattner, MD, at Northwestern University, Chicago, was his friend and one of the many dermatologists who criticized Dr. Pusey for allowing his name to be used in the Camay ads. Dr. Pusey’s reply to the criticism (according to Dr. Rattner) was that Proctor & Gamble was “proposing to do what the medical profession always is criticizing commercial concerns for not doing, namely, coming to physicians for information on medical matters. Could the profession hope to have any influence with business concerns if it was always eager to criticize bad commercial practices but never willing to support good ones?”3
While Dr. Pusey felt his reasons for adding his name to the Camay ads and research were justified, many of his friends stated that in hindsight, he regretted the action because of the negative response of his colleagues. It was years before dermatologists began providing input again into the skin care industry. During that time, radio, television and print ads were rampant with misleading claims – which led the way for a dermatologic imposter to make a fortune on skin care.
John Woodbury (1851-1909): John Woodbury, a chiropractor, never went to medical school, but that did not stop him from claiming he was a dermatologist and cosmetic surgeon. In 1889, he opened the John H. Woodbury Dermatological Institute in New York City, and over the next few years, opened Woodbury Dermatological Institutes in at least 5 states and employed 25 “physicians” who were not licensed to practice medicine. He came out with face soaps, tonics, and cold creams and spent a fortune on advertising these products and his institutes. In 1901, he sold his “Woodbury Soap” to the Andrew Jergens Company for $212,500 and 10% in royalties.
Multiple lawsuits occurred from 1898 to 1907 because he continued using the Woodbury name on his own products, despite having sold the “Woodbury” trademark to Jergens. He was sued for practicing medicine without a medical license and claiming to be a dermatologist when he was not. He lost most of these lawsuits, including one in 1907 in which the court ruled that corporations may not employ unlicensed professionals to practice medicine. In 1909, John Woodbury committed suicide. The Woodbury Soap company flourished in the 1930s and 1940s, as part of Jergens, until the brand was discontinued in 1970 when Jergens was acquired by American Brands.
The next dermatologists to come along did not make the same mistakes as those of their predecessors. They all made scientific discoveries through their basic science research in the laboratory, filed patents, formed skin care companies, perfected the formulations, and conducted research trials of the final product. Their marketing focused on science and efficacy and only rarely used their names and images in advertising, allowing them to maintain their reputations in the dermatology field.
Eugene Van Scott, MD (1922-present): Dermatologist Dr. Van Scott and dermatopharmacologist Ruey Yu, PhD, filed a method patent in the early 1970s on the effectiveness of alpha hydroxy acids to treat ichthyosis. They invented the abbreviation “AHA” and have continued their work on organic acids to this day. They now have more than 125 patents, which they have licensed to 60 companies in the cosmetics and pharmaceutical industries.
In 1988, 14 years after their initial publication, they founded the company they named Polystrata, which grew into today’s NeoStrata.4 Over the years, they had to defend their patents because many personal care companies used their technologies without licensing them. In 2007, they won a $41 million settlement in a patent infringement suit against Mary Kay filed in March 2005. They have both been very philanthropic in the dermatology world5 and are highly respected in the field. Among many other honors, Dr. Van Scott was named a Master Dermatologist by the American Academy of Dermatology in 1998 and received the Dermatology Foundation’s Distinguished Service Medallion in 2004.
Sheldon Pinnell, MD (1937-2013): After Dr. Pinnell completed his dermatology residency at Harvard Medical School, he spent 2 years studying collagen chemistry at the Max Planck Institute in Munich, Germany. In 1973, he returned to Duke University where he had earned his undergraduate degree before attending Yale University. He remained at Duke for the duration of his career and was professor and chief of dermatology there for many years. Early in his career, he focused on the role of vitamin C in collagen biosynthesis and discovered some of the mechanisms by which sun exposure causes photoaging. He described the use of the first (and most popular) topically applied L-ascorbic acid (vitamin C) to prevent and treat skin aging.
Dr. Pinnell’s many discoveries include showing that the addition of ascorbic acid to fibroblast cultures increases collagen production and that topically applied L-ascorbic acid penetrates into the skin best at a pH of 2-2.5. Dr. Pinnell changed the way the world uses topical antioxidants today; he was widely respected and was a member of the American Dermatological Association and an honorary member of the Society of Investigative Dermatology. He published more than 200 scientific articles and held 10 patents. He started the skin care company Skinceuticals, based on his antioxidant technologies. It was acquired by L’Oreal in 2005.
Richard Fitzpatrick, MD (1944-2014): The dermatologist affectionately known as “Fitz” is credited with being the first to use lasers for skin resurfacing. He went to medical school at Emory University and did his dermatology residency at the University of California, Los Angeles. He authored more than 130 publications and was one of the first doctors to specialize in cosmetic dermatology. He realized that fibroblast cell cultures used to produce the collagen filler CosmoPlast (no longer on the market) generated many growth factors that could rejuvenate the skin, and in 1999, he launched the skin care brand SkinMedica. In 2000, he received a patent for fibroblast-derived growth factors used topically for antiaging – a formula he called Tissue Nutrient Solution. In 2001, the popular product TNS Recovery Complex was launched based on the patented growth factor technology. It is still the most popular growth factor technology on the market.
What can we learn from these pioneers? I have had several interesting discussions about this topic with Leonard Hoenig, MD, section editor for Reflections on Dermatology: Past, Present, and Future, in Clinics in Dermatology. (Dr. Hoenig told me the interesting story that Listerine mouthwash was named in honor of Joseph Lister but accounts vary as to whether he gave permission to do so. This makes Dr. Lister the most famous physician to endorse a personal care product.) When Dr. Hoenig and I discussed the ethics of dermatologists creating a skin care line or retailing skin care in their medical practice, he stated my sentiments perfectly: “We should rely on professional, ethical, and legal guidelines to help us do what is right. Most importantly, we should have the best interests of our patients at heart when recommending any treatments.”
Dermatologists have unique knowledge, experience, and perspective on treating the skin with topical agents and have the true desire to improve skin health. If we do not discover, research, patent, and develop efficacious skin care products, someone else will do it – and I do not think they will do it as well as a dermatologist can.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Everett MA. Int J Dermatol. 1978 May;17(4):345-52.
2. Moxon RK. N Engl J Med. 1976 Apr 1;294(14):762-4.
3. Rattner H. Arch Derm Syphilol. 1937;35(1):25-66.
4. Neostrata: More than Hope, by Elaine Strauss, U.S. 1 Newspaper, Feb. 24, 1999.
5. Two legends in the field of dermatology provide $1 million gift to Temple University school of medicine’s department of dermatology, Temple University, June 5, 2015.
Biologic responses to metal implants: Dermatologic implications
Hypersensitivity to implantable devices, albeit rare, is a growing problem. according to a report on biological responses to metal implants released by the Food and Drug Administration in September 2019. Large controlled studies are lacking, and the FDA has initiated extensive postmarketing reviews of certain metal implants in response to safety concerns. Further research is needed on the composition of these implants, the diverse spectrum of metals used, the physical environment in which they are implanted, and the immune response associated with implants.
Local and systemic type IV hypersensitivity reactions can result from exposure to metal ions, which are thought to act as haptens and bind to proteins. The hapten-protein complex acts as the antigen for the T cell. Additionally, both acute and chronic inflammatory responses secondary to wound healing and foreign body reactions can occur. Neutrophils and macrophages elicit a tissue response, which can cause aseptic infection, loosening of joints, and tissue damage. Furthermore, corrosion of metal implants can lead to release of metal ions, which can have genotoxic and carcinogenic effects.
Clinical and subclinical effects of implantable devices depend on the device itself, the composition of the device, the tissue type, and an individual’s immune characteristics. Metal debris released from implants can activate innate and adaptive immune responses through a variety of different mechanisms, depending on the implant type and in what tissues the implant is placed. In the case of orthopedic implants, the most common implants, osteoclasts can sense metal and induce proinflammatory cytokines, which can result in corrosion and uptake of metal particles. Metal devices used in the central nervous system, such as intracerebral electrodes, can cause inflammatory responses leading to tissue encapsulation of electrodes. Corrosion of electrodes and release of metal ions can also impede ion channels in the CNS, blocking critical neuron-signaling pathways. Inflammatory reactions surrounding cardiac and vascular implants containing metal activate coagulation cascades, resulting in endothelial injury and activation of thrombi.
Despite the commonly used term “metal allergy” that delineates a type IV hypersensitivity reaction, reports in the literature supports the existence of both innate and adaptive immune responses to metal implanted in tissues. The recommended terminology is “adverse reactions to metal debris.” The clinical presentation may not be straightforward or easily attributed to the implant. Diagnostic tools are limited and may not detect a causal relationship.
Clinical symptoms can range from local rashes and pruritus to cardiac damage, depression, vertigo, and neurologic symptoms; autoimmune/autoinflammatory reactions including chronic fatigue and autoimmune-like systemic symptoms, such as joint pain, headaches, and hair loss, have also been reported in association with implants containing metal. In addition to pruritus, dermatologic manifestations can include erythema, edema, papules, vesicles, as well as systemic hypersensitivity reactions. Typically, cutaneous reactions usually present within 2 days to 24 months of implantation and may be considered surgical-site infections. Although these reactions can be treated with topical or oral corticosteroids, removal of the device is frequently needed for complete clearance.
In clinical practice, it has been frustrating that potential adverse reactions to metal implants are often overlooked because they are thought to be so rare. There are case series documenting metal implant hypersensitivity, but the actual prevalence of hypersensitivity or autoinflammatory reactions is not known. Testing methods are often inaccurate; therefore, identification of at-risk individuals and management of symptomatic patients with implants is important.
The 2016 American Contact Dermatitis Society guidelines do not recommend preimplantation patch testing unless there is a suspected metal allergy. However, patch testing cannot identify the extent of corrosion, autoinflammatory reactions, and foreign body reactions that can occur.
We must keep an open mind in patients who have implanted devices and have unusual or otherwise undefined symptoms. Often, the symptoms do not directly correspond to the site of implantation and the only way to discern whether the implant is the cause and to treat symptoms is removal of the implanted device.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Food and Drug Administration. Biological Responses to Metal Implants. 2019 Sep. https://www.fda.gov/media/131150/download.
Atwater AR, Reeder M. Cutis. 2020 Feb;105(2):68-70.
Schalock PC et al. Dermatitis. Sep-Oct 2016;27(5):241-7.
Hypersensitivity to implantable devices, albeit rare, is a growing problem. according to a report on biological responses to metal implants released by the Food and Drug Administration in September 2019. Large controlled studies are lacking, and the FDA has initiated extensive postmarketing reviews of certain metal implants in response to safety concerns. Further research is needed on the composition of these implants, the diverse spectrum of metals used, the physical environment in which they are implanted, and the immune response associated with implants.
Local and systemic type IV hypersensitivity reactions can result from exposure to metal ions, which are thought to act as haptens and bind to proteins. The hapten-protein complex acts as the antigen for the T cell. Additionally, both acute and chronic inflammatory responses secondary to wound healing and foreign body reactions can occur. Neutrophils and macrophages elicit a tissue response, which can cause aseptic infection, loosening of joints, and tissue damage. Furthermore, corrosion of metal implants can lead to release of metal ions, which can have genotoxic and carcinogenic effects.
Clinical and subclinical effects of implantable devices depend on the device itself, the composition of the device, the tissue type, and an individual’s immune characteristics. Metal debris released from implants can activate innate and adaptive immune responses through a variety of different mechanisms, depending on the implant type and in what tissues the implant is placed. In the case of orthopedic implants, the most common implants, osteoclasts can sense metal and induce proinflammatory cytokines, which can result in corrosion and uptake of metal particles. Metal devices used in the central nervous system, such as intracerebral electrodes, can cause inflammatory responses leading to tissue encapsulation of electrodes. Corrosion of electrodes and release of metal ions can also impede ion channels in the CNS, blocking critical neuron-signaling pathways. Inflammatory reactions surrounding cardiac and vascular implants containing metal activate coagulation cascades, resulting in endothelial injury and activation of thrombi.
Despite the commonly used term “metal allergy” that delineates a type IV hypersensitivity reaction, reports in the literature supports the existence of both innate and adaptive immune responses to metal implanted in tissues. The recommended terminology is “adverse reactions to metal debris.” The clinical presentation may not be straightforward or easily attributed to the implant. Diagnostic tools are limited and may not detect a causal relationship.
Clinical symptoms can range from local rashes and pruritus to cardiac damage, depression, vertigo, and neurologic symptoms; autoimmune/autoinflammatory reactions including chronic fatigue and autoimmune-like systemic symptoms, such as joint pain, headaches, and hair loss, have also been reported in association with implants containing metal. In addition to pruritus, dermatologic manifestations can include erythema, edema, papules, vesicles, as well as systemic hypersensitivity reactions. Typically, cutaneous reactions usually present within 2 days to 24 months of implantation and may be considered surgical-site infections. Although these reactions can be treated with topical or oral corticosteroids, removal of the device is frequently needed for complete clearance.
In clinical practice, it has been frustrating that potential adverse reactions to metal implants are often overlooked because they are thought to be so rare. There are case series documenting metal implant hypersensitivity, but the actual prevalence of hypersensitivity or autoinflammatory reactions is not known. Testing methods are often inaccurate; therefore, identification of at-risk individuals and management of symptomatic patients with implants is important.
The 2016 American Contact Dermatitis Society guidelines do not recommend preimplantation patch testing unless there is a suspected metal allergy. However, patch testing cannot identify the extent of corrosion, autoinflammatory reactions, and foreign body reactions that can occur.
We must keep an open mind in patients who have implanted devices and have unusual or otherwise undefined symptoms. Often, the symptoms do not directly correspond to the site of implantation and the only way to discern whether the implant is the cause and to treat symptoms is removal of the implanted device.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Food and Drug Administration. Biological Responses to Metal Implants. 2019 Sep. https://www.fda.gov/media/131150/download.
Atwater AR, Reeder M. Cutis. 2020 Feb;105(2):68-70.
Schalock PC et al. Dermatitis. Sep-Oct 2016;27(5):241-7.
Hypersensitivity to implantable devices, albeit rare, is a growing problem. according to a report on biological responses to metal implants released by the Food and Drug Administration in September 2019. Large controlled studies are lacking, and the FDA has initiated extensive postmarketing reviews of certain metal implants in response to safety concerns. Further research is needed on the composition of these implants, the diverse spectrum of metals used, the physical environment in which they are implanted, and the immune response associated with implants.
Local and systemic type IV hypersensitivity reactions can result from exposure to metal ions, which are thought to act as haptens and bind to proteins. The hapten-protein complex acts as the antigen for the T cell. Additionally, both acute and chronic inflammatory responses secondary to wound healing and foreign body reactions can occur. Neutrophils and macrophages elicit a tissue response, which can cause aseptic infection, loosening of joints, and tissue damage. Furthermore, corrosion of metal implants can lead to release of metal ions, which can have genotoxic and carcinogenic effects.
Clinical and subclinical effects of implantable devices depend on the device itself, the composition of the device, the tissue type, and an individual’s immune characteristics. Metal debris released from implants can activate innate and adaptive immune responses through a variety of different mechanisms, depending on the implant type and in what tissues the implant is placed. In the case of orthopedic implants, the most common implants, osteoclasts can sense metal and induce proinflammatory cytokines, which can result in corrosion and uptake of metal particles. Metal devices used in the central nervous system, such as intracerebral electrodes, can cause inflammatory responses leading to tissue encapsulation of electrodes. Corrosion of electrodes and release of metal ions can also impede ion channels in the CNS, blocking critical neuron-signaling pathways. Inflammatory reactions surrounding cardiac and vascular implants containing metal activate coagulation cascades, resulting in endothelial injury and activation of thrombi.
Despite the commonly used term “metal allergy” that delineates a type IV hypersensitivity reaction, reports in the literature supports the existence of both innate and adaptive immune responses to metal implanted in tissues. The recommended terminology is “adverse reactions to metal debris.” The clinical presentation may not be straightforward or easily attributed to the implant. Diagnostic tools are limited and may not detect a causal relationship.
Clinical symptoms can range from local rashes and pruritus to cardiac damage, depression, vertigo, and neurologic symptoms; autoimmune/autoinflammatory reactions including chronic fatigue and autoimmune-like systemic symptoms, such as joint pain, headaches, and hair loss, have also been reported in association with implants containing metal. In addition to pruritus, dermatologic manifestations can include erythema, edema, papules, vesicles, as well as systemic hypersensitivity reactions. Typically, cutaneous reactions usually present within 2 days to 24 months of implantation and may be considered surgical-site infections. Although these reactions can be treated with topical or oral corticosteroids, removal of the device is frequently needed for complete clearance.
In clinical practice, it has been frustrating that potential adverse reactions to metal implants are often overlooked because they are thought to be so rare. There are case series documenting metal implant hypersensitivity, but the actual prevalence of hypersensitivity or autoinflammatory reactions is not known. Testing methods are often inaccurate; therefore, identification of at-risk individuals and management of symptomatic patients with implants is important.
The 2016 American Contact Dermatitis Society guidelines do not recommend preimplantation patch testing unless there is a suspected metal allergy. However, patch testing cannot identify the extent of corrosion, autoinflammatory reactions, and foreign body reactions that can occur.
We must keep an open mind in patients who have implanted devices and have unusual or otherwise undefined symptoms. Often, the symptoms do not directly correspond to the site of implantation and the only way to discern whether the implant is the cause and to treat symptoms is removal of the implanted device.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Food and Drug Administration. Biological Responses to Metal Implants. 2019 Sep. https://www.fda.gov/media/131150/download.
Atwater AR, Reeder M. Cutis. 2020 Feb;105(2):68-70.
Schalock PC et al. Dermatitis. Sep-Oct 2016;27(5):241-7.
Novel botulinum toxin type A earns high marks for forehead lines
, Jeremy B. Green, MD, said at the virtual annual meeting of the American Academy of Dermatology.
When the study is completed, conclusions can be reached about the investigational product’s durability of benefit for treatment of dynamic forehead lines, which are notoriously challenging to treat. However, much is already known about the product’s durability for treatment of glabellar lines, as demonstrated in SAKURA 1 and SAKURA 2, two pivotal, phase 3, multicenter, randomized, double-blind, placebo-controlled trials totaling 609 patients.
In SAKURA 1 and 2, glabellar line severity didn’t return to baseline until a median of 28 and 26 weeks after injection. In contrast, as the study authors noted, the majority of patients whose glabellar lines are treated with the currently available botulinum toxin type A products are no longer responders by 3-4 months after treatment. Since surveys indicate most patients receive repeated injections every 5-6 months, that means they’re walking around with suboptimal results for the last 2-3 months before their next treatment session (Plast Reconstr Surg. 2020 Jan;145[1]:45-58).
This investigational neuromodulator, known as DaxibotulinumtoxinA for Injection, or DAXI, is composed of a highly purified 150-KDa botulinum toxin type A coupled with a proprietary stabilizing peptide. The product is formulated without human serum albumin and, once reconstituted, is stable at room temperature.
Dr. Green, a dermatologist in private practice in Coral Gables, Fla., reported on 61 participants in the phase 2 study, all with moderate or severe forehead lines and glabellar lines as assessed by both investigators and patients on structured scales. The patients’ glabellar lines were treated with 40 U of DAXI at baseline. Then 2 weeks later, their dynamic forehead lines were treated with either 12 U, 18 U, 24 U, or 30 U of DAXI. This sequential treatment recapitulates the approach widely used in clinical practice, he noted.
At baseline, two-thirds of patients had severe forehead lines at maximum eyebrow elevation as determined by Investigator Global Assessment – Forehead Wrinkle Severity and Patient Forehead Wrinkle Severity. The other third of participants had moderate forehead lines.
The primary endpoint was the presence of no or mild forehead lines by investigator assessment 4 weeks after treatment. This was achieved in 86% of patients who received 12 U of DAXI, 87% who recieved 18 U, 94% who received 24 U, and 100% of those who received 30 U.
“There appears to be a dose-dependent response, but this hasn’t yet been statistically analyzed,” Dr. Green said.
By patient assessment, there were no or only mild forehead lines at 4 weeks in 57% of those who received the lowest dose of DAXI, with rates of 80%, 100%, and 93% in those who received 18 U, 24 U, and 30 U.
At week 4, 57% of patients who got 12 U of DAXI pronounced themselves “satisfied” or “very satisfied” with DAXI therapy, as did 73%, 100%, and 93% of those who got the higher doses.
The treatment-related adverse events consisted of a smattering of cases of edema, erythema, or headache, similar to what’s described in the product labeling of all the neuromodulators.
Revance Therapeutics has applied to the Food and Drug Administration for marketing approval of DAXI for the treatment of glabellar lines. A regulatory decision is expected in late November. The company is also developing DAXI for the treatment of variety of neurologic and musculoskeletal conditions, including poststroke upper limb spasticity.
In an interview, Dr. Green said he was favorably impressed with DAXI’s durability for amelioration of forehead lines in the patients he personally treated in the ongoing phase 2 study, although there was no head-to-head comparison with other neuromodulators in the trial. He’s not aware of any planned phase 3 trial aimed at obtaining a forehead line indication.
“Of course, all four of the neuromodulators currently approved in the U.S. have glabellar line indications, but all are also used off-label in other locations, so I would imagine that DAXI will be used similarly if and when it is FDA-approved,” the dermatologist added.
He reported serving as a paid investigator for Revance.
, Jeremy B. Green, MD, said at the virtual annual meeting of the American Academy of Dermatology.
When the study is completed, conclusions can be reached about the investigational product’s durability of benefit for treatment of dynamic forehead lines, which are notoriously challenging to treat. However, much is already known about the product’s durability for treatment of glabellar lines, as demonstrated in SAKURA 1 and SAKURA 2, two pivotal, phase 3, multicenter, randomized, double-blind, placebo-controlled trials totaling 609 patients.
In SAKURA 1 and 2, glabellar line severity didn’t return to baseline until a median of 28 and 26 weeks after injection. In contrast, as the study authors noted, the majority of patients whose glabellar lines are treated with the currently available botulinum toxin type A products are no longer responders by 3-4 months after treatment. Since surveys indicate most patients receive repeated injections every 5-6 months, that means they’re walking around with suboptimal results for the last 2-3 months before their next treatment session (Plast Reconstr Surg. 2020 Jan;145[1]:45-58).
This investigational neuromodulator, known as DaxibotulinumtoxinA for Injection, or DAXI, is composed of a highly purified 150-KDa botulinum toxin type A coupled with a proprietary stabilizing peptide. The product is formulated without human serum albumin and, once reconstituted, is stable at room temperature.
Dr. Green, a dermatologist in private practice in Coral Gables, Fla., reported on 61 participants in the phase 2 study, all with moderate or severe forehead lines and glabellar lines as assessed by both investigators and patients on structured scales. The patients’ glabellar lines were treated with 40 U of DAXI at baseline. Then 2 weeks later, their dynamic forehead lines were treated with either 12 U, 18 U, 24 U, or 30 U of DAXI. This sequential treatment recapitulates the approach widely used in clinical practice, he noted.
At baseline, two-thirds of patients had severe forehead lines at maximum eyebrow elevation as determined by Investigator Global Assessment – Forehead Wrinkle Severity and Patient Forehead Wrinkle Severity. The other third of participants had moderate forehead lines.
The primary endpoint was the presence of no or mild forehead lines by investigator assessment 4 weeks after treatment. This was achieved in 86% of patients who received 12 U of DAXI, 87% who recieved 18 U, 94% who received 24 U, and 100% of those who received 30 U.
“There appears to be a dose-dependent response, but this hasn’t yet been statistically analyzed,” Dr. Green said.
By patient assessment, there were no or only mild forehead lines at 4 weeks in 57% of those who received the lowest dose of DAXI, with rates of 80%, 100%, and 93% in those who received 18 U, 24 U, and 30 U.
At week 4, 57% of patients who got 12 U of DAXI pronounced themselves “satisfied” or “very satisfied” with DAXI therapy, as did 73%, 100%, and 93% of those who got the higher doses.
The treatment-related adverse events consisted of a smattering of cases of edema, erythema, or headache, similar to what’s described in the product labeling of all the neuromodulators.
Revance Therapeutics has applied to the Food and Drug Administration for marketing approval of DAXI for the treatment of glabellar lines. A regulatory decision is expected in late November. The company is also developing DAXI for the treatment of variety of neurologic and musculoskeletal conditions, including poststroke upper limb spasticity.
In an interview, Dr. Green said he was favorably impressed with DAXI’s durability for amelioration of forehead lines in the patients he personally treated in the ongoing phase 2 study, although there was no head-to-head comparison with other neuromodulators in the trial. He’s not aware of any planned phase 3 trial aimed at obtaining a forehead line indication.
“Of course, all four of the neuromodulators currently approved in the U.S. have glabellar line indications, but all are also used off-label in other locations, so I would imagine that DAXI will be used similarly if and when it is FDA-approved,” the dermatologist added.
He reported serving as a paid investigator for Revance.
, Jeremy B. Green, MD, said at the virtual annual meeting of the American Academy of Dermatology.
When the study is completed, conclusions can be reached about the investigational product’s durability of benefit for treatment of dynamic forehead lines, which are notoriously challenging to treat. However, much is already known about the product’s durability for treatment of glabellar lines, as demonstrated in SAKURA 1 and SAKURA 2, two pivotal, phase 3, multicenter, randomized, double-blind, placebo-controlled trials totaling 609 patients.
In SAKURA 1 and 2, glabellar line severity didn’t return to baseline until a median of 28 and 26 weeks after injection. In contrast, as the study authors noted, the majority of patients whose glabellar lines are treated with the currently available botulinum toxin type A products are no longer responders by 3-4 months after treatment. Since surveys indicate most patients receive repeated injections every 5-6 months, that means they’re walking around with suboptimal results for the last 2-3 months before their next treatment session (Plast Reconstr Surg. 2020 Jan;145[1]:45-58).
This investigational neuromodulator, known as DaxibotulinumtoxinA for Injection, or DAXI, is composed of a highly purified 150-KDa botulinum toxin type A coupled with a proprietary stabilizing peptide. The product is formulated without human serum albumin and, once reconstituted, is stable at room temperature.
Dr. Green, a dermatologist in private practice in Coral Gables, Fla., reported on 61 participants in the phase 2 study, all with moderate or severe forehead lines and glabellar lines as assessed by both investigators and patients on structured scales. The patients’ glabellar lines were treated with 40 U of DAXI at baseline. Then 2 weeks later, their dynamic forehead lines were treated with either 12 U, 18 U, 24 U, or 30 U of DAXI. This sequential treatment recapitulates the approach widely used in clinical practice, he noted.
At baseline, two-thirds of patients had severe forehead lines at maximum eyebrow elevation as determined by Investigator Global Assessment – Forehead Wrinkle Severity and Patient Forehead Wrinkle Severity. The other third of participants had moderate forehead lines.
The primary endpoint was the presence of no or mild forehead lines by investigator assessment 4 weeks after treatment. This was achieved in 86% of patients who received 12 U of DAXI, 87% who recieved 18 U, 94% who received 24 U, and 100% of those who received 30 U.
“There appears to be a dose-dependent response, but this hasn’t yet been statistically analyzed,” Dr. Green said.
By patient assessment, there were no or only mild forehead lines at 4 weeks in 57% of those who received the lowest dose of DAXI, with rates of 80%, 100%, and 93% in those who received 18 U, 24 U, and 30 U.
At week 4, 57% of patients who got 12 U of DAXI pronounced themselves “satisfied” or “very satisfied” with DAXI therapy, as did 73%, 100%, and 93% of those who got the higher doses.
The treatment-related adverse events consisted of a smattering of cases of edema, erythema, or headache, similar to what’s described in the product labeling of all the neuromodulators.
Revance Therapeutics has applied to the Food and Drug Administration for marketing approval of DAXI for the treatment of glabellar lines. A regulatory decision is expected in late November. The company is also developing DAXI for the treatment of variety of neurologic and musculoskeletal conditions, including poststroke upper limb spasticity.
In an interview, Dr. Green said he was favorably impressed with DAXI’s durability for amelioration of forehead lines in the patients he personally treated in the ongoing phase 2 study, although there was no head-to-head comparison with other neuromodulators in the trial. He’s not aware of any planned phase 3 trial aimed at obtaining a forehead line indication.
“Of course, all four of the neuromodulators currently approved in the U.S. have glabellar line indications, but all are also used off-label in other locations, so I would imagine that DAXI will be used similarly if and when it is FDA-approved,” the dermatologist added.
He reported serving as a paid investigator for Revance.
FROM AAD 20
Are You Up-to-date on Dermal Fillers?
The popularity of injectable fillers for aesthetic use continues to rise, and cosmetic injectors must select from an increasing range of options to achieve optimal outcomes. In addition to formulating a treatment plan and having an intimate knowledge of the facial anatomy, filler selection is critical along with an appreciation of both approved and off-label indications for these products. Appropriate patient selection and treatment technique can minimize adverse events (AEs) and allow for the best outcomes.
The US Food and Drug Administration (FDA) approved the first injectable hyaluronic acid (HA) filler in 2003, the first addition since the approval of bovine collagen in 1981. To date, there are now 4 groups of approved fillers: (1) HA (Belotero Balance [Merz North America, Inc], Juvèderm products [Allergan], Restylane products [Galderma Laboratories, LP], Resilient HA products [Revance Therapeutics Inc and Teoxane SA]), (2) calcium hydroxylapatite (Radiesse [Merz North America, Inc]), (3) poly-L-lactic acid (Sculptra Aesthetic [Galderma Laboratories, LP]), and (4) polymethylmethacrylate (Bellafill [Suneva Medical, Inc]).1-3 Given the versatility of this wide portfolio of products, which often are used in combination with one another, we have advanced from the early goals of filling isolated lines or wrinkles on the face to the 3-dimensional restructuring of an entire treatment area. The increasing diversity of products, particularly the range of rheologic properties of HA fillers, allows the injector to strategically select the type of filler and depth of injection to achieve the desired treatment outcome. The duration of the treatment effects also is related to the properties of the filler.4,5
Advancements in injectable fillers also have led to new applications both on and off the face. Many pivotal clinical trials of fillers were performed in isolated anatomic areas, most commonly the nasolabial folds, leading to FDA approval of this indication. Other FDA-approved indications for fillers include lip augmentation (Juvèderm Ultra, Juvèderm Volbella, Restylane, Restylane Silk, Restylane Kysse), human immunodeficiency virus–associated lipoatrophy (Sculptra Aesthetic, Radiesse), volumization of the dorsal hands (Radiesse, Restylane Lyft), acne scarring (Bellafill), and age-related volume loss of the midface (Juvèderm Voluma, Restylane Lyft). Although it is considered off label, treatment of the temples, brows, tear troughs, jawline, horizontal neck lines, and etched-in radial cheek lines has been reported.6-9 It is legal to use fillers to treat these areas, but data have not yet been evaluated by the FDA to officially grant their approval, which likely will change with the conclusion of many ongoing industry-sponsored trials.
Adverse events from filler injections range from the anticipated transient tenderness, swelling, and bruising, which are likely to resolve in a matter of days, to the most severe complications—intravascular occlusion with permanent sequelae, namely tissue necrosis, blindness or visual compromise, and stroke. It is critical to obtain written informed consent prior to proceeding with dermal filler injections. Masterful knowledge of the facial anatomy, in particular the location and depth of key vascular structures, is critical in minimizing these severe AEs. Injection technique, including use of a microcannula, can reduce the risk, in addition to administration of small volumes of filler at a time, aspiration prior to injection, and use of a retrograde injection technique. There also are variations in the predicted courses of vascular structures, as demonstrated in a cadaveric study showing 4 variants of the course of the angular artery.10
Hyaluronic acid fillers are the most commonly used of the available products, and hyaluronidase, which can dissolve the filler, can be utilized to manage emergent and nonemergent AEs.11 Physical examination findings related to impending necrosis include blanching of the skin in the distribution of a key vessel with a mottled or reticulated purple discoloration. Hyaluronidase, on the order of hundreds of units, may be injected into the area of vascular compromise until reperfusion is achieved, in addition to administering aspirin and applying warm compresses to the area.11,12 The most severe AEs are blindness and/or stroke, associated with findings such as immediate vision loss, pain, nausea, vomiting, and neurologic compromise. Although the glabella, nose, nasolabial folds, and forehead are the most common anatomic areas associated with these AEs (in order of frequency), injections in all areas of the face have been associated with blindness.13,14 Retrobulbar and/or peribulbar injection of hyaluronidase for management of vision changes has been reported, but in most cases vision loss associated with dermal filler injections is not reversible.14,15
Nonemergent uses of enzyme reversal of filler placement include correcting undesirable aesthetic outcomes, such as asymmetry, misplaced filler, or even delayed granulomatous reactions. Hyaluronidase dosage should be determined by the amount and type of filler that was delivered to the patient. All HA fillers are not created equally, and evidence from dosing studies indicates that higher cross-linked and more cohesive fillers require higher doses of hyaluronidase.11 For example, Juvèderm Voluma, created as a mixture of low- and high-molecular-weight HA, has a higher cross-linking ratio. Approximately 30 U of hyaluronidase are suggested to dissolve 0.1 cc of Juvèderm Voluma as compared to 10 U of hyaluronidase for 0.1 cc of Juvèderm Ultra and 5 U for 0.1 cc of Restylane.11
Treatment with dermal fillers generally is safe and effective, and as new fillers come to the market, we must identify how they will help further our goal of improving patient outcomes. The effects of coronavirus disease 19 on aesthetic medicine are still unclear, yet this uncertainty should not deflect treating clinicians from overlooking the fundamentals of dermal fillers. In addition to considering the appropriate use of each filler based on its unique characteristics and indications, we must be sure that we are prepared with the tools to manage any and all possible complications.
- Jiang B, Ramirez M, Ranjit-Reeves R, et al. Noncollagen dermal fillers: a summary of the clinical trials used for their FDA approval. Dermatol Surg. 2019;45:1585-1596.
- Monheit G, Kaufman-Janette J, Joseph J, et al. Efficacy and safety of two resilient hyaluronic acid fillers in the treatment of moderate-to-severe nasolabial folds [published online March 24, 2020]. Dermatol Surg. doi:10.1097/DSS0000000000002391.
- Kaufman-Janette J, Taylor SC, Cox SE, et al. Efficacy and safety of a new resilient hyaluronic acid dermal filler, in the correction of moderate-to-severe nasolabial folds: a 64-week, prospective, multicenter, controlled, randomized, double-blind and within-subject study. J Cosmet Dermatol. 2019;18:1244-1253.
- Jones D, Murphy D. Volumizing hyaluronic acid filler for midface volume deficit: 2 year results from a pivotal single-blind randomized controlled study. Dermatol Surg. 2013;39:1602-1611.
- Hausauer AK, Jones DH. Long-term correction of iatrogenic lipoatrophy with volumizing hyaluronic acid filler. Dermatol Surg. 2018;44(suppl 1):S60-S62.
- Black J, Jones D. Cohesive polydensified matrix hyaluronic acid for the treatment of etched-in fine facial lines: a 6-month, open-label clinical trial. Dermatol Surg. 2018;44:1002-1011.
- Breithaupt A, Jones D, Braz A, et al. Anatomic basis for safe and effective volumization of the temple. Dermatol Surg. 2015;41:S278-S283.
- Dallara JM, Baspeyras M, Bui P, et al. Calcium hydroxylapatite for jawline rejuvenation: consensus recommendations. J Cosmet Dermatol. 2014;13:3-14.
- Minokadeh A, Black J, Jones D. Effacement of transverse neck lines with VYC-15L and a cohesive polydensified matrix hyaluronic acid. Dermatol Surg. 2019;45:941-948.
- Kim YS, Choi DY, Gil YC, et al. The anatomical origin and course of the angular artery regarding its clinical implications. Dermatol Surg. 2014;40:1070-1076.
- Jones DH. Update on emergency and nonemergency use of hyaluronidase in aesthetic dermatology. JAMA Dermatol. 2018;154:763-764.
- Cohen JL, Biesman BS, Dayan SH, et al. Treatment of hyaluronic acid filler-induced impending necrosis with hyaluronidase: consensus recommendations. Aesthet Surg J. 2015;35:844-849.
- Beleznay K, Carruthers J, Humphrey S, et al. Avoiding and treating blindness from fillers: a review of the world literature. Dermatol Surg. 2015;41:1097-1117.
- Beleznay K, Carruthers J, Humphrey S, et al. Update on avoiding and treating blindness from fillers: a recent review of the world literature. Aesthet Surg J. 2019;39:662-674.
- Chestnut C. Restoration of visual loss with retrobulblar hyaluronidase injection after hyaluronic acid filler. Dermatol Surg. 2018;44:435-437.
The popularity of injectable fillers for aesthetic use continues to rise, and cosmetic injectors must select from an increasing range of options to achieve optimal outcomes. In addition to formulating a treatment plan and having an intimate knowledge of the facial anatomy, filler selection is critical along with an appreciation of both approved and off-label indications for these products. Appropriate patient selection and treatment technique can minimize adverse events (AEs) and allow for the best outcomes.
The US Food and Drug Administration (FDA) approved the first injectable hyaluronic acid (HA) filler in 2003, the first addition since the approval of bovine collagen in 1981. To date, there are now 4 groups of approved fillers: (1) HA (Belotero Balance [Merz North America, Inc], Juvèderm products [Allergan], Restylane products [Galderma Laboratories, LP], Resilient HA products [Revance Therapeutics Inc and Teoxane SA]), (2) calcium hydroxylapatite (Radiesse [Merz North America, Inc]), (3) poly-L-lactic acid (Sculptra Aesthetic [Galderma Laboratories, LP]), and (4) polymethylmethacrylate (Bellafill [Suneva Medical, Inc]).1-3 Given the versatility of this wide portfolio of products, which often are used in combination with one another, we have advanced from the early goals of filling isolated lines or wrinkles on the face to the 3-dimensional restructuring of an entire treatment area. The increasing diversity of products, particularly the range of rheologic properties of HA fillers, allows the injector to strategically select the type of filler and depth of injection to achieve the desired treatment outcome. The duration of the treatment effects also is related to the properties of the filler.4,5
Advancements in injectable fillers also have led to new applications both on and off the face. Many pivotal clinical trials of fillers were performed in isolated anatomic areas, most commonly the nasolabial folds, leading to FDA approval of this indication. Other FDA-approved indications for fillers include lip augmentation (Juvèderm Ultra, Juvèderm Volbella, Restylane, Restylane Silk, Restylane Kysse), human immunodeficiency virus–associated lipoatrophy (Sculptra Aesthetic, Radiesse), volumization of the dorsal hands (Radiesse, Restylane Lyft), acne scarring (Bellafill), and age-related volume loss of the midface (Juvèderm Voluma, Restylane Lyft). Although it is considered off label, treatment of the temples, brows, tear troughs, jawline, horizontal neck lines, and etched-in radial cheek lines has been reported.6-9 It is legal to use fillers to treat these areas, but data have not yet been evaluated by the FDA to officially grant their approval, which likely will change with the conclusion of many ongoing industry-sponsored trials.
Adverse events from filler injections range from the anticipated transient tenderness, swelling, and bruising, which are likely to resolve in a matter of days, to the most severe complications—intravascular occlusion with permanent sequelae, namely tissue necrosis, blindness or visual compromise, and stroke. It is critical to obtain written informed consent prior to proceeding with dermal filler injections. Masterful knowledge of the facial anatomy, in particular the location and depth of key vascular structures, is critical in minimizing these severe AEs. Injection technique, including use of a microcannula, can reduce the risk, in addition to administration of small volumes of filler at a time, aspiration prior to injection, and use of a retrograde injection technique. There also are variations in the predicted courses of vascular structures, as demonstrated in a cadaveric study showing 4 variants of the course of the angular artery.10
Hyaluronic acid fillers are the most commonly used of the available products, and hyaluronidase, which can dissolve the filler, can be utilized to manage emergent and nonemergent AEs.11 Physical examination findings related to impending necrosis include blanching of the skin in the distribution of a key vessel with a mottled or reticulated purple discoloration. Hyaluronidase, on the order of hundreds of units, may be injected into the area of vascular compromise until reperfusion is achieved, in addition to administering aspirin and applying warm compresses to the area.11,12 The most severe AEs are blindness and/or stroke, associated with findings such as immediate vision loss, pain, nausea, vomiting, and neurologic compromise. Although the glabella, nose, nasolabial folds, and forehead are the most common anatomic areas associated with these AEs (in order of frequency), injections in all areas of the face have been associated with blindness.13,14 Retrobulbar and/or peribulbar injection of hyaluronidase for management of vision changes has been reported, but in most cases vision loss associated with dermal filler injections is not reversible.14,15
Nonemergent uses of enzyme reversal of filler placement include correcting undesirable aesthetic outcomes, such as asymmetry, misplaced filler, or even delayed granulomatous reactions. Hyaluronidase dosage should be determined by the amount and type of filler that was delivered to the patient. All HA fillers are not created equally, and evidence from dosing studies indicates that higher cross-linked and more cohesive fillers require higher doses of hyaluronidase.11 For example, Juvèderm Voluma, created as a mixture of low- and high-molecular-weight HA, has a higher cross-linking ratio. Approximately 30 U of hyaluronidase are suggested to dissolve 0.1 cc of Juvèderm Voluma as compared to 10 U of hyaluronidase for 0.1 cc of Juvèderm Ultra and 5 U for 0.1 cc of Restylane.11
Treatment with dermal fillers generally is safe and effective, and as new fillers come to the market, we must identify how they will help further our goal of improving patient outcomes. The effects of coronavirus disease 19 on aesthetic medicine are still unclear, yet this uncertainty should not deflect treating clinicians from overlooking the fundamentals of dermal fillers. In addition to considering the appropriate use of each filler based on its unique characteristics and indications, we must be sure that we are prepared with the tools to manage any and all possible complications.
The popularity of injectable fillers for aesthetic use continues to rise, and cosmetic injectors must select from an increasing range of options to achieve optimal outcomes. In addition to formulating a treatment plan and having an intimate knowledge of the facial anatomy, filler selection is critical along with an appreciation of both approved and off-label indications for these products. Appropriate patient selection and treatment technique can minimize adverse events (AEs) and allow for the best outcomes.
The US Food and Drug Administration (FDA) approved the first injectable hyaluronic acid (HA) filler in 2003, the first addition since the approval of bovine collagen in 1981. To date, there are now 4 groups of approved fillers: (1) HA (Belotero Balance [Merz North America, Inc], Juvèderm products [Allergan], Restylane products [Galderma Laboratories, LP], Resilient HA products [Revance Therapeutics Inc and Teoxane SA]), (2) calcium hydroxylapatite (Radiesse [Merz North America, Inc]), (3) poly-L-lactic acid (Sculptra Aesthetic [Galderma Laboratories, LP]), and (4) polymethylmethacrylate (Bellafill [Suneva Medical, Inc]).1-3 Given the versatility of this wide portfolio of products, which often are used in combination with one another, we have advanced from the early goals of filling isolated lines or wrinkles on the face to the 3-dimensional restructuring of an entire treatment area. The increasing diversity of products, particularly the range of rheologic properties of HA fillers, allows the injector to strategically select the type of filler and depth of injection to achieve the desired treatment outcome. The duration of the treatment effects also is related to the properties of the filler.4,5
Advancements in injectable fillers also have led to new applications both on and off the face. Many pivotal clinical trials of fillers were performed in isolated anatomic areas, most commonly the nasolabial folds, leading to FDA approval of this indication. Other FDA-approved indications for fillers include lip augmentation (Juvèderm Ultra, Juvèderm Volbella, Restylane, Restylane Silk, Restylane Kysse), human immunodeficiency virus–associated lipoatrophy (Sculptra Aesthetic, Radiesse), volumization of the dorsal hands (Radiesse, Restylane Lyft), acne scarring (Bellafill), and age-related volume loss of the midface (Juvèderm Voluma, Restylane Lyft). Although it is considered off label, treatment of the temples, brows, tear troughs, jawline, horizontal neck lines, and etched-in radial cheek lines has been reported.6-9 It is legal to use fillers to treat these areas, but data have not yet been evaluated by the FDA to officially grant their approval, which likely will change with the conclusion of many ongoing industry-sponsored trials.
Adverse events from filler injections range from the anticipated transient tenderness, swelling, and bruising, which are likely to resolve in a matter of days, to the most severe complications—intravascular occlusion with permanent sequelae, namely tissue necrosis, blindness or visual compromise, and stroke. It is critical to obtain written informed consent prior to proceeding with dermal filler injections. Masterful knowledge of the facial anatomy, in particular the location and depth of key vascular structures, is critical in minimizing these severe AEs. Injection technique, including use of a microcannula, can reduce the risk, in addition to administration of small volumes of filler at a time, aspiration prior to injection, and use of a retrograde injection technique. There also are variations in the predicted courses of vascular structures, as demonstrated in a cadaveric study showing 4 variants of the course of the angular artery.10
Hyaluronic acid fillers are the most commonly used of the available products, and hyaluronidase, which can dissolve the filler, can be utilized to manage emergent and nonemergent AEs.11 Physical examination findings related to impending necrosis include blanching of the skin in the distribution of a key vessel with a mottled or reticulated purple discoloration. Hyaluronidase, on the order of hundreds of units, may be injected into the area of vascular compromise until reperfusion is achieved, in addition to administering aspirin and applying warm compresses to the area.11,12 The most severe AEs are blindness and/or stroke, associated with findings such as immediate vision loss, pain, nausea, vomiting, and neurologic compromise. Although the glabella, nose, nasolabial folds, and forehead are the most common anatomic areas associated with these AEs (in order of frequency), injections in all areas of the face have been associated with blindness.13,14 Retrobulbar and/or peribulbar injection of hyaluronidase for management of vision changes has been reported, but in most cases vision loss associated with dermal filler injections is not reversible.14,15
Nonemergent uses of enzyme reversal of filler placement include correcting undesirable aesthetic outcomes, such as asymmetry, misplaced filler, or even delayed granulomatous reactions. Hyaluronidase dosage should be determined by the amount and type of filler that was delivered to the patient. All HA fillers are not created equally, and evidence from dosing studies indicates that higher cross-linked and more cohesive fillers require higher doses of hyaluronidase.11 For example, Juvèderm Voluma, created as a mixture of low- and high-molecular-weight HA, has a higher cross-linking ratio. Approximately 30 U of hyaluronidase are suggested to dissolve 0.1 cc of Juvèderm Voluma as compared to 10 U of hyaluronidase for 0.1 cc of Juvèderm Ultra and 5 U for 0.1 cc of Restylane.11
Treatment with dermal fillers generally is safe and effective, and as new fillers come to the market, we must identify how they will help further our goal of improving patient outcomes. The effects of coronavirus disease 19 on aesthetic medicine are still unclear, yet this uncertainty should not deflect treating clinicians from overlooking the fundamentals of dermal fillers. In addition to considering the appropriate use of each filler based on its unique characteristics and indications, we must be sure that we are prepared with the tools to manage any and all possible complications.
- Jiang B, Ramirez M, Ranjit-Reeves R, et al. Noncollagen dermal fillers: a summary of the clinical trials used for their FDA approval. Dermatol Surg. 2019;45:1585-1596.
- Monheit G, Kaufman-Janette J, Joseph J, et al. Efficacy and safety of two resilient hyaluronic acid fillers in the treatment of moderate-to-severe nasolabial folds [published online March 24, 2020]. Dermatol Surg. doi:10.1097/DSS0000000000002391.
- Kaufman-Janette J, Taylor SC, Cox SE, et al. Efficacy and safety of a new resilient hyaluronic acid dermal filler, in the correction of moderate-to-severe nasolabial folds: a 64-week, prospective, multicenter, controlled, randomized, double-blind and within-subject study. J Cosmet Dermatol. 2019;18:1244-1253.
- Jones D, Murphy D. Volumizing hyaluronic acid filler for midface volume deficit: 2 year results from a pivotal single-blind randomized controlled study. Dermatol Surg. 2013;39:1602-1611.
- Hausauer AK, Jones DH. Long-term correction of iatrogenic lipoatrophy with volumizing hyaluronic acid filler. Dermatol Surg. 2018;44(suppl 1):S60-S62.
- Black J, Jones D. Cohesive polydensified matrix hyaluronic acid for the treatment of etched-in fine facial lines: a 6-month, open-label clinical trial. Dermatol Surg. 2018;44:1002-1011.
- Breithaupt A, Jones D, Braz A, et al. Anatomic basis for safe and effective volumization of the temple. Dermatol Surg. 2015;41:S278-S283.
- Dallara JM, Baspeyras M, Bui P, et al. Calcium hydroxylapatite for jawline rejuvenation: consensus recommendations. J Cosmet Dermatol. 2014;13:3-14.
- Minokadeh A, Black J, Jones D. Effacement of transverse neck lines with VYC-15L and a cohesive polydensified matrix hyaluronic acid. Dermatol Surg. 2019;45:941-948.
- Kim YS, Choi DY, Gil YC, et al. The anatomical origin and course of the angular artery regarding its clinical implications. Dermatol Surg. 2014;40:1070-1076.
- Jones DH. Update on emergency and nonemergency use of hyaluronidase in aesthetic dermatology. JAMA Dermatol. 2018;154:763-764.
- Cohen JL, Biesman BS, Dayan SH, et al. Treatment of hyaluronic acid filler-induced impending necrosis with hyaluronidase: consensus recommendations. Aesthet Surg J. 2015;35:844-849.
- Beleznay K, Carruthers J, Humphrey S, et al. Avoiding and treating blindness from fillers: a review of the world literature. Dermatol Surg. 2015;41:1097-1117.
- Beleznay K, Carruthers J, Humphrey S, et al. Update on avoiding and treating blindness from fillers: a recent review of the world literature. Aesthet Surg J. 2019;39:662-674.
- Chestnut C. Restoration of visual loss with retrobulblar hyaluronidase injection after hyaluronic acid filler. Dermatol Surg. 2018;44:435-437.
- Jiang B, Ramirez M, Ranjit-Reeves R, et al. Noncollagen dermal fillers: a summary of the clinical trials used for their FDA approval. Dermatol Surg. 2019;45:1585-1596.
- Monheit G, Kaufman-Janette J, Joseph J, et al. Efficacy and safety of two resilient hyaluronic acid fillers in the treatment of moderate-to-severe nasolabial folds [published online March 24, 2020]. Dermatol Surg. doi:10.1097/DSS0000000000002391.
- Kaufman-Janette J, Taylor SC, Cox SE, et al. Efficacy and safety of a new resilient hyaluronic acid dermal filler, in the correction of moderate-to-severe nasolabial folds: a 64-week, prospective, multicenter, controlled, randomized, double-blind and within-subject study. J Cosmet Dermatol. 2019;18:1244-1253.
- Jones D, Murphy D. Volumizing hyaluronic acid filler for midface volume deficit: 2 year results from a pivotal single-blind randomized controlled study. Dermatol Surg. 2013;39:1602-1611.
- Hausauer AK, Jones DH. Long-term correction of iatrogenic lipoatrophy with volumizing hyaluronic acid filler. Dermatol Surg. 2018;44(suppl 1):S60-S62.
- Black J, Jones D. Cohesive polydensified matrix hyaluronic acid for the treatment of etched-in fine facial lines: a 6-month, open-label clinical trial. Dermatol Surg. 2018;44:1002-1011.
- Breithaupt A, Jones D, Braz A, et al. Anatomic basis for safe and effective volumization of the temple. Dermatol Surg. 2015;41:S278-S283.
- Dallara JM, Baspeyras M, Bui P, et al. Calcium hydroxylapatite for jawline rejuvenation: consensus recommendations. J Cosmet Dermatol. 2014;13:3-14.
- Minokadeh A, Black J, Jones D. Effacement of transverse neck lines with VYC-15L and a cohesive polydensified matrix hyaluronic acid. Dermatol Surg. 2019;45:941-948.
- Kim YS, Choi DY, Gil YC, et al. The anatomical origin and course of the angular artery regarding its clinical implications. Dermatol Surg. 2014;40:1070-1076.
- Jones DH. Update on emergency and nonemergency use of hyaluronidase in aesthetic dermatology. JAMA Dermatol. 2018;154:763-764.
- Cohen JL, Biesman BS, Dayan SH, et al. Treatment of hyaluronic acid filler-induced impending necrosis with hyaluronidase: consensus recommendations. Aesthet Surg J. 2015;35:844-849.
- Beleznay K, Carruthers J, Humphrey S, et al. Avoiding and treating blindness from fillers: a review of the world literature. Dermatol Surg. 2015;41:1097-1117.
- Beleznay K, Carruthers J, Humphrey S, et al. Update on avoiding and treating blindness from fillers: a recent review of the world literature. Aesthet Surg J. 2019;39:662-674.
- Chestnut C. Restoration of visual loss with retrobulblar hyaluronidase injection after hyaluronic acid filler. Dermatol Surg. 2018;44:435-437.
Botulinum toxin associated with antidepressant effects across indications, injection sites
, according to the study’s authors.
Their results show that the antidepressant effect of botulinum toxin “administered for various indications goes beyond the control of the intended disease states and does not depend on the location of the injection,” according to Tigran Makunts, PharmD, of the Skaggs School of Pharmacy and Pharmaceutical Sciences at the University of California, San Diego, and coauthors.
Previous high-quality studies have found botulinum toxin treatment has been associated with antidepressant effects when administered to the glabellar region of the face, they noted. The study was published in Scientific Reports.
The researchers evaluated adverse events reported to the Food and Drug Administration’s current adverse event reporting system (FAERS) between September 2012 and December 2019, and the FDA’s previous adverse event reporting system between January 2004 and August 2012. Overall, they analyzed 174,243 reports, which were divided into eight treatment-related groups based on the indication for botulinum toxin: Cosmetic use (20,684 patients), migraine (4,180 patients), spasms and spasticity not involving facial muscles (2,335 patients), neurological and urinary bladder disorders (915 patients), torticollis (1,360 patients), hyperhidrosis (601 patients), blepharospasm (487 patients), and sialorrhea (157 patients). Each group was matched to controls from the FAERS database, who had different treatments for the same indications. (Reports in which patients were on an antidepressant or where depression was listed as an indication were not included).
In nearly all treatment groups, reports of depression and depression-related adverse events were significantly lower among those who received botulinum toxin, compared with controls: For those who received botulinum toxin injections in facial muscles for cosmetic uses, the reporting odds ratio was 0.46 (95% confidence interval, 0.27-0.78). Significant effects were also see in the following groups: those who received injections into facial and head muscles for migraine (ROR, 0.60; 95% CI, 0.48-0.74), injections into the upper and lower limbs for spasms and spasticity (ROR, 0.28; 95% CI, 0.18-0.42), injections into neck muscles for torticollis and neck pain (ROR, 0.30; 95% CI, 0.20-0.44), injections into eyelid muscles for blepharospasm (ROR, 0.13; 95% CI, 0.05-0.39), and injections into the axilla and palm for hyperhidrosis (ROR, 0.12; 95% CI, 0.04-0.33).
There were no cases of depression or depression-related adverse event reports among those treated with botulinum toxin for sialorrhea with injections into the parotid and submandibular glands, and there were decreased reports of depression among those who received detrusor muscle injections for neurological and urinary bladder disorders, but the results in both groups were not statistically significant, according to the researchers.
In an interview, Ruben Abagyan, PhD, study coauthor and professor at Skaggs School of Pharmacy and Pharmaceutical Sciences, said the study’s finding go “beyond breaking a positive feedback loop between depression and the ‘frown’ wrinkles in the glabellar region of the forehead.” The data showing efficacy with botulinum toxin injected in other areas of the body can help clinicians “expand their search for the most effective injection location and dose beyond the facial injections to improve the depression-related therapeutic outcomes.”
Another takeaway from the study, he noted, is that botulinum toxin can have effects beyond the local effect seen near an injection site. Administering botulinum toxin for spasms and spasticity, excessive sweating, migraine, urinary bladder disorders, blepharospasm, or excessive salivation/drooling could result in reduced depression and improved systemic neurological effects.
“Severe depression remains a very difficult condition to treat. The existing drugs have dangerous side effects, the onset of the therapeutic action is delayed by at least a month, and the adherence to the medication is suboptimal. Therefore, finding new ways to treat depression is critical,” Dr. Abagyan said. “Botulinum toxin opens up a new physiological mechanism to be tried to reduce depression.”
Michelle Magid, MD, MBA, of the department of psychiatry at the University of Texas at Austin, said in an interview that, although the study was retrospective, “physicians can feel confident that botulinum toxin treatment will not cause depression; it may very well lead to improved mood in some of their patients.” Dr. Magid was not an author of this study, but has studied botulinum toxin as a possible treatment of depression.
“Previous studies have shown that botulinum toxin injected into the forehead region can improve symptoms of depression. The studies were small and confined to treating the glabellar region only,” she added. “This is a large retrospective study showing that botulinum toxin injected into other regions, such as the neck, underarms, bladder, hands, arms, and legs, can also have an antidepressant effect.”
Dr. Magid agreed that the use of botulinum toxin as an antidepressant should be investigated further, and could be a tool for patients who do not respond well to traditional antidepressant medications.
In their paper, the authors offered several plausible mechanisms for the antidepressant effects of botulinum toxin, including transneuronal transport to the parts of the central nervous system that regulate mood and emotion, systemic distribution, distributed muscle stress memory, and efficacy in the primary indication treatment. Although the mechanism of action is not well understood, Dr. Magid noted it could be the removal of somatic symptoms that contribute to an improvement in mood.
“It is possible that alleviating the psychological distress associated with neck spasms, excessive sweating [and so on] can be causing the antidepressive effects,” she said. “However, it is also possible that depression is actualized by a series of somatic symptoms – body aches, insomnia, sweating, for example. By removing somatic symptoms, one may also remove the correlating mood dysregulation.”
The study “certainly raises a lot of questions,” particularly about the “apparent multiple mechanisms of action of BoNT that we don’t understand yet,” Mark Rubin, MD, a cosmetic dermatologist who practices in Beverly Hills, Calif., said in an interview. “I believe it lends great deal of credence to the use of [botulinum toxin] for depression and certainly validates the need for more robust clinical trials for that indication,” he added.
“I think what we all as clinicians need to take away from this paper is that there is a great deal we don’t understand about the global pharmacologic effects of [botulinum toxin] and equally important, that there are apparently other pharmacologic pathways we need to explore in the treatment of depression, said Dr. Rubin, of the department of dermatology at the University of California, San Diego, who was not an investigator in the study.
One author reported being a consultant for Allergan. Dr. Makunts and the other author report no relevant conflicts of interest; Dr. Magid reported being a consultant for Allergan and a speaker for Ipsen. Dr. Rubin had no related disclosures.
SOURCE: Makunts T et al. Sci Rep. 2020 Jul 30;10(1):12851. doi: 10.1038/s41598-020-69773-7.
, according to the study’s authors.
Their results show that the antidepressant effect of botulinum toxin “administered for various indications goes beyond the control of the intended disease states and does not depend on the location of the injection,” according to Tigran Makunts, PharmD, of the Skaggs School of Pharmacy and Pharmaceutical Sciences at the University of California, San Diego, and coauthors.
Previous high-quality studies have found botulinum toxin treatment has been associated with antidepressant effects when administered to the glabellar region of the face, they noted. The study was published in Scientific Reports.
The researchers evaluated adverse events reported to the Food and Drug Administration’s current adverse event reporting system (FAERS) between September 2012 and December 2019, and the FDA’s previous adverse event reporting system between January 2004 and August 2012. Overall, they analyzed 174,243 reports, which were divided into eight treatment-related groups based on the indication for botulinum toxin: Cosmetic use (20,684 patients), migraine (4,180 patients), spasms and spasticity not involving facial muscles (2,335 patients), neurological and urinary bladder disorders (915 patients), torticollis (1,360 patients), hyperhidrosis (601 patients), blepharospasm (487 patients), and sialorrhea (157 patients). Each group was matched to controls from the FAERS database, who had different treatments for the same indications. (Reports in which patients were on an antidepressant or where depression was listed as an indication were not included).
In nearly all treatment groups, reports of depression and depression-related adverse events were significantly lower among those who received botulinum toxin, compared with controls: For those who received botulinum toxin injections in facial muscles for cosmetic uses, the reporting odds ratio was 0.46 (95% confidence interval, 0.27-0.78). Significant effects were also see in the following groups: those who received injections into facial and head muscles for migraine (ROR, 0.60; 95% CI, 0.48-0.74), injections into the upper and lower limbs for spasms and spasticity (ROR, 0.28; 95% CI, 0.18-0.42), injections into neck muscles for torticollis and neck pain (ROR, 0.30; 95% CI, 0.20-0.44), injections into eyelid muscles for blepharospasm (ROR, 0.13; 95% CI, 0.05-0.39), and injections into the axilla and palm for hyperhidrosis (ROR, 0.12; 95% CI, 0.04-0.33).
There were no cases of depression or depression-related adverse event reports among those treated with botulinum toxin for sialorrhea with injections into the parotid and submandibular glands, and there were decreased reports of depression among those who received detrusor muscle injections for neurological and urinary bladder disorders, but the results in both groups were not statistically significant, according to the researchers.
In an interview, Ruben Abagyan, PhD, study coauthor and professor at Skaggs School of Pharmacy and Pharmaceutical Sciences, said the study’s finding go “beyond breaking a positive feedback loop between depression and the ‘frown’ wrinkles in the glabellar region of the forehead.” The data showing efficacy with botulinum toxin injected in other areas of the body can help clinicians “expand their search for the most effective injection location and dose beyond the facial injections to improve the depression-related therapeutic outcomes.”
Another takeaway from the study, he noted, is that botulinum toxin can have effects beyond the local effect seen near an injection site. Administering botulinum toxin for spasms and spasticity, excessive sweating, migraine, urinary bladder disorders, blepharospasm, or excessive salivation/drooling could result in reduced depression and improved systemic neurological effects.
“Severe depression remains a very difficult condition to treat. The existing drugs have dangerous side effects, the onset of the therapeutic action is delayed by at least a month, and the adherence to the medication is suboptimal. Therefore, finding new ways to treat depression is critical,” Dr. Abagyan said. “Botulinum toxin opens up a new physiological mechanism to be tried to reduce depression.”
Michelle Magid, MD, MBA, of the department of psychiatry at the University of Texas at Austin, said in an interview that, although the study was retrospective, “physicians can feel confident that botulinum toxin treatment will not cause depression; it may very well lead to improved mood in some of their patients.” Dr. Magid was not an author of this study, but has studied botulinum toxin as a possible treatment of depression.
“Previous studies have shown that botulinum toxin injected into the forehead region can improve symptoms of depression. The studies were small and confined to treating the glabellar region only,” she added. “This is a large retrospective study showing that botulinum toxin injected into other regions, such as the neck, underarms, bladder, hands, arms, and legs, can also have an antidepressant effect.”
Dr. Magid agreed that the use of botulinum toxin as an antidepressant should be investigated further, and could be a tool for patients who do not respond well to traditional antidepressant medications.
In their paper, the authors offered several plausible mechanisms for the antidepressant effects of botulinum toxin, including transneuronal transport to the parts of the central nervous system that regulate mood and emotion, systemic distribution, distributed muscle stress memory, and efficacy in the primary indication treatment. Although the mechanism of action is not well understood, Dr. Magid noted it could be the removal of somatic symptoms that contribute to an improvement in mood.
“It is possible that alleviating the psychological distress associated with neck spasms, excessive sweating [and so on] can be causing the antidepressive effects,” she said. “However, it is also possible that depression is actualized by a series of somatic symptoms – body aches, insomnia, sweating, for example. By removing somatic symptoms, one may also remove the correlating mood dysregulation.”
The study “certainly raises a lot of questions,” particularly about the “apparent multiple mechanisms of action of BoNT that we don’t understand yet,” Mark Rubin, MD, a cosmetic dermatologist who practices in Beverly Hills, Calif., said in an interview. “I believe it lends great deal of credence to the use of [botulinum toxin] for depression and certainly validates the need for more robust clinical trials for that indication,” he added.
“I think what we all as clinicians need to take away from this paper is that there is a great deal we don’t understand about the global pharmacologic effects of [botulinum toxin] and equally important, that there are apparently other pharmacologic pathways we need to explore in the treatment of depression, said Dr. Rubin, of the department of dermatology at the University of California, San Diego, who was not an investigator in the study.
One author reported being a consultant for Allergan. Dr. Makunts and the other author report no relevant conflicts of interest; Dr. Magid reported being a consultant for Allergan and a speaker for Ipsen. Dr. Rubin had no related disclosures.
SOURCE: Makunts T et al. Sci Rep. 2020 Jul 30;10(1):12851. doi: 10.1038/s41598-020-69773-7.
, according to the study’s authors.
Their results show that the antidepressant effect of botulinum toxin “administered for various indications goes beyond the control of the intended disease states and does not depend on the location of the injection,” according to Tigran Makunts, PharmD, of the Skaggs School of Pharmacy and Pharmaceutical Sciences at the University of California, San Diego, and coauthors.
Previous high-quality studies have found botulinum toxin treatment has been associated with antidepressant effects when administered to the glabellar region of the face, they noted. The study was published in Scientific Reports.
The researchers evaluated adverse events reported to the Food and Drug Administration’s current adverse event reporting system (FAERS) between September 2012 and December 2019, and the FDA’s previous adverse event reporting system between January 2004 and August 2012. Overall, they analyzed 174,243 reports, which were divided into eight treatment-related groups based on the indication for botulinum toxin: Cosmetic use (20,684 patients), migraine (4,180 patients), spasms and spasticity not involving facial muscles (2,335 patients), neurological and urinary bladder disorders (915 patients), torticollis (1,360 patients), hyperhidrosis (601 patients), blepharospasm (487 patients), and sialorrhea (157 patients). Each group was matched to controls from the FAERS database, who had different treatments for the same indications. (Reports in which patients were on an antidepressant or where depression was listed as an indication were not included).
In nearly all treatment groups, reports of depression and depression-related adverse events were significantly lower among those who received botulinum toxin, compared with controls: For those who received botulinum toxin injections in facial muscles for cosmetic uses, the reporting odds ratio was 0.46 (95% confidence interval, 0.27-0.78). Significant effects were also see in the following groups: those who received injections into facial and head muscles for migraine (ROR, 0.60; 95% CI, 0.48-0.74), injections into the upper and lower limbs for spasms and spasticity (ROR, 0.28; 95% CI, 0.18-0.42), injections into neck muscles for torticollis and neck pain (ROR, 0.30; 95% CI, 0.20-0.44), injections into eyelid muscles for blepharospasm (ROR, 0.13; 95% CI, 0.05-0.39), and injections into the axilla and palm for hyperhidrosis (ROR, 0.12; 95% CI, 0.04-0.33).
There were no cases of depression or depression-related adverse event reports among those treated with botulinum toxin for sialorrhea with injections into the parotid and submandibular glands, and there were decreased reports of depression among those who received detrusor muscle injections for neurological and urinary bladder disorders, but the results in both groups were not statistically significant, according to the researchers.
In an interview, Ruben Abagyan, PhD, study coauthor and professor at Skaggs School of Pharmacy and Pharmaceutical Sciences, said the study’s finding go “beyond breaking a positive feedback loop between depression and the ‘frown’ wrinkles in the glabellar region of the forehead.” The data showing efficacy with botulinum toxin injected in other areas of the body can help clinicians “expand their search for the most effective injection location and dose beyond the facial injections to improve the depression-related therapeutic outcomes.”
Another takeaway from the study, he noted, is that botulinum toxin can have effects beyond the local effect seen near an injection site. Administering botulinum toxin for spasms and spasticity, excessive sweating, migraine, urinary bladder disorders, blepharospasm, or excessive salivation/drooling could result in reduced depression and improved systemic neurological effects.
“Severe depression remains a very difficult condition to treat. The existing drugs have dangerous side effects, the onset of the therapeutic action is delayed by at least a month, and the adherence to the medication is suboptimal. Therefore, finding new ways to treat depression is critical,” Dr. Abagyan said. “Botulinum toxin opens up a new physiological mechanism to be tried to reduce depression.”
Michelle Magid, MD, MBA, of the department of psychiatry at the University of Texas at Austin, said in an interview that, although the study was retrospective, “physicians can feel confident that botulinum toxin treatment will not cause depression; it may very well lead to improved mood in some of their patients.” Dr. Magid was not an author of this study, but has studied botulinum toxin as a possible treatment of depression.
“Previous studies have shown that botulinum toxin injected into the forehead region can improve symptoms of depression. The studies were small and confined to treating the glabellar region only,” she added. “This is a large retrospective study showing that botulinum toxin injected into other regions, such as the neck, underarms, bladder, hands, arms, and legs, can also have an antidepressant effect.”
Dr. Magid agreed that the use of botulinum toxin as an antidepressant should be investigated further, and could be a tool for patients who do not respond well to traditional antidepressant medications.
In their paper, the authors offered several plausible mechanisms for the antidepressant effects of botulinum toxin, including transneuronal transport to the parts of the central nervous system that regulate mood and emotion, systemic distribution, distributed muscle stress memory, and efficacy in the primary indication treatment. Although the mechanism of action is not well understood, Dr. Magid noted it could be the removal of somatic symptoms that contribute to an improvement in mood.
“It is possible that alleviating the psychological distress associated with neck spasms, excessive sweating [and so on] can be causing the antidepressive effects,” she said. “However, it is also possible that depression is actualized by a series of somatic symptoms – body aches, insomnia, sweating, for example. By removing somatic symptoms, one may also remove the correlating mood dysregulation.”
The study “certainly raises a lot of questions,” particularly about the “apparent multiple mechanisms of action of BoNT that we don’t understand yet,” Mark Rubin, MD, a cosmetic dermatologist who practices in Beverly Hills, Calif., said in an interview. “I believe it lends great deal of credence to the use of [botulinum toxin] for depression and certainly validates the need for more robust clinical trials for that indication,” he added.
“I think what we all as clinicians need to take away from this paper is that there is a great deal we don’t understand about the global pharmacologic effects of [botulinum toxin] and equally important, that there are apparently other pharmacologic pathways we need to explore in the treatment of depression, said Dr. Rubin, of the department of dermatology at the University of California, San Diego, who was not an investigator in the study.
One author reported being a consultant for Allergan. Dr. Makunts and the other author report no relevant conflicts of interest; Dr. Magid reported being a consultant for Allergan and a speaker for Ipsen. Dr. Rubin had no related disclosures.
SOURCE: Makunts T et al. Sci Rep. 2020 Jul 30;10(1):12851. doi: 10.1038/s41598-020-69773-7.
FROM SCIENTIFIC REPORTS
Colorism and dermatology
With the world currently really listening and engaged (hopefully) on making positive changes with regards to racism and systemic racial injustices, skin color has come to the forefront. Racism because of skin color has been an unfortunate part of our history and foundation of the United States with a capitalist society built and thriving on the profits of slavery, and a democracy founded on equality – unless you had black skin. These issues are at the forefront in the United States, but have also significantly impacted other parts of the world, including the Caribbean and South America having a significant African slave trade history and impacts, with Brazil currently facing the same systemic racial injustices and police brutality among black men, and King Leopold II of Belgium slaughtering an estimated 10-15 million Congolese people in the name of colonialism, slavery, and robbing resources (natural resources as well as servitude) in the Congo as late as the early 1900s.
These are just a few of the many historical examples of racial injustice, which remains ingrained in many parts of our society today. With this worldwide history, it has been advantageous for people to have lighter skin with regards to money, politics, jobs, education, the justice system, modeling/acting opportunities and contracts, home ownership, and opportunities for generational wealth for years to come. It has ingrained some unfortunate beliefs among some that having lighter skin is better, advantageous, and will make them more desirable or more beautiful.
and across the African continent. It is estimated that 77% of women in Nigeria and 55% of women in China use bleaching creams to achieve overall skin lightening. Unilever’s Fair & Lovely skin-whitening cream has long been a popular over-the-counter product in India, with an estimated market worth of 270 billion rupees ($4 billion USD). On June 25, 2020, Unilever vowed to rename and rebrand Fair & Lovely. With such an offensive name for a product that further promotes colorism, this is an effort in the right direction and has been a long time coming since its debut in 1975. Unilever’s Fair and Lovely Foundation for women’s causes still exists, and has not been renamed at the time of this writing.
Controversy remains on whether this product and other products such as these should exist for the purposes they are used for. Johnson & Johnson has decided that it will no longer produce and sell the Neutrogena Fine Fairness line, sold only in Asia and the Middle East, and the Clean & Clear Fairness line, sold in India. There are arguments to the contrary that halting production of skin-lightening products altogether may result in an influx of unsafe alternatives.
As dermatologists, we use skin-lightening products appropriately for the purposes of treating skin conditions such as postinflammatory hyperpigmentation, melasma, and photoaging. This is where the use of such products should largely end. While it is up to individuals about what they do with their skin and their bodies, we, as health care skin professionals, should be furthering the notion that all skin colors and types are beautiful. Moreover, we should not be encouraging the use of these products for overall skin whitening. Part of the issue is that these products are available often at high concentrations over the counter or in the illegal market, especially in parts of Asia and Africa where colorism is more common and skin whitening is more commonly practiced. The dangers are not only the risk of ochronosis with high concentrations or long term use of hydroquinone, but also what the Centre for Science and Environment found in a 2014 study, that 44% of the skin “fairness” creams in India contained mercury, which is illegal and a health concern.
In my practice, I have also had patients (several originally from Nigeria) who have admitted to long term use of skin-bleaching products for the purposes of all over face- and body-skin lightening who now suffer from very sensitive skin and experience bouts of eczematous dermatitis from time to time, despite having stopped using lightening cream. While there are adverse physical effects resulting from the use of these topicals for this purpose, the effects on the psyche are what concern me the most.
The beauty industry has also been an unfortunate part of furthering thoughts and attitudes concerning colorism over the years with lighter skin and Caucasian ideals being set as standards of beauty. One of many examples is a deodorant ad in the Middle East with the tagline “White is Purity” on a woman, which was pulled by Nivea in 2017 after it was slammed as racist. Another is the 2017 Dove ad for body wash that showed a smiling black woman peel off her brown shirt to reveal a white woman in a lighter-color shirt.
A shift has occurred in recent years with more ethnic images of beauty appearing in magazines and film. However, such opportunities are still less plentiful, pay discrepancies still occur, and sexual objectification of women of color as opposed to beautification is still rampant. As such, it is also up to us to do our part in studying and utilizing ethnic and racial differences in skin and beauty to maximize our efforts in promoting what is inherently beautiful as opposed to one standard of beauty. The education begins with the images we see, what we teach our children, loving ourselves, and as doctors, being knowledgeable about the right aesthetic choices for patients with different skin colors and types.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
With the world currently really listening and engaged (hopefully) on making positive changes with regards to racism and systemic racial injustices, skin color has come to the forefront. Racism because of skin color has been an unfortunate part of our history and foundation of the United States with a capitalist society built and thriving on the profits of slavery, and a democracy founded on equality – unless you had black skin. These issues are at the forefront in the United States, but have also significantly impacted other parts of the world, including the Caribbean and South America having a significant African slave trade history and impacts, with Brazil currently facing the same systemic racial injustices and police brutality among black men, and King Leopold II of Belgium slaughtering an estimated 10-15 million Congolese people in the name of colonialism, slavery, and robbing resources (natural resources as well as servitude) in the Congo as late as the early 1900s.
These are just a few of the many historical examples of racial injustice, which remains ingrained in many parts of our society today. With this worldwide history, it has been advantageous for people to have lighter skin with regards to money, politics, jobs, education, the justice system, modeling/acting opportunities and contracts, home ownership, and opportunities for generational wealth for years to come. It has ingrained some unfortunate beliefs among some that having lighter skin is better, advantageous, and will make them more desirable or more beautiful.
and across the African continent. It is estimated that 77% of women in Nigeria and 55% of women in China use bleaching creams to achieve overall skin lightening. Unilever’s Fair & Lovely skin-whitening cream has long been a popular over-the-counter product in India, with an estimated market worth of 270 billion rupees ($4 billion USD). On June 25, 2020, Unilever vowed to rename and rebrand Fair & Lovely. With such an offensive name for a product that further promotes colorism, this is an effort in the right direction and has been a long time coming since its debut in 1975. Unilever’s Fair and Lovely Foundation for women’s causes still exists, and has not been renamed at the time of this writing.
Controversy remains on whether this product and other products such as these should exist for the purposes they are used for. Johnson & Johnson has decided that it will no longer produce and sell the Neutrogena Fine Fairness line, sold only in Asia and the Middle East, and the Clean & Clear Fairness line, sold in India. There are arguments to the contrary that halting production of skin-lightening products altogether may result in an influx of unsafe alternatives.
As dermatologists, we use skin-lightening products appropriately for the purposes of treating skin conditions such as postinflammatory hyperpigmentation, melasma, and photoaging. This is where the use of such products should largely end. While it is up to individuals about what they do with their skin and their bodies, we, as health care skin professionals, should be furthering the notion that all skin colors and types are beautiful. Moreover, we should not be encouraging the use of these products for overall skin whitening. Part of the issue is that these products are available often at high concentrations over the counter or in the illegal market, especially in parts of Asia and Africa where colorism is more common and skin whitening is more commonly practiced. The dangers are not only the risk of ochronosis with high concentrations or long term use of hydroquinone, but also what the Centre for Science and Environment found in a 2014 study, that 44% of the skin “fairness” creams in India contained mercury, which is illegal and a health concern.
In my practice, I have also had patients (several originally from Nigeria) who have admitted to long term use of skin-bleaching products for the purposes of all over face- and body-skin lightening who now suffer from very sensitive skin and experience bouts of eczematous dermatitis from time to time, despite having stopped using lightening cream. While there are adverse physical effects resulting from the use of these topicals for this purpose, the effects on the psyche are what concern me the most.
The beauty industry has also been an unfortunate part of furthering thoughts and attitudes concerning colorism over the years with lighter skin and Caucasian ideals being set as standards of beauty. One of many examples is a deodorant ad in the Middle East with the tagline “White is Purity” on a woman, which was pulled by Nivea in 2017 after it was slammed as racist. Another is the 2017 Dove ad for body wash that showed a smiling black woman peel off her brown shirt to reveal a white woman in a lighter-color shirt.
A shift has occurred in recent years with more ethnic images of beauty appearing in magazines and film. However, such opportunities are still less plentiful, pay discrepancies still occur, and sexual objectification of women of color as opposed to beautification is still rampant. As such, it is also up to us to do our part in studying and utilizing ethnic and racial differences in skin and beauty to maximize our efforts in promoting what is inherently beautiful as opposed to one standard of beauty. The education begins with the images we see, what we teach our children, loving ourselves, and as doctors, being knowledgeable about the right aesthetic choices for patients with different skin colors and types.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
With the world currently really listening and engaged (hopefully) on making positive changes with regards to racism and systemic racial injustices, skin color has come to the forefront. Racism because of skin color has been an unfortunate part of our history and foundation of the United States with a capitalist society built and thriving on the profits of slavery, and a democracy founded on equality – unless you had black skin. These issues are at the forefront in the United States, but have also significantly impacted other parts of the world, including the Caribbean and South America having a significant African slave trade history and impacts, with Brazil currently facing the same systemic racial injustices and police brutality among black men, and King Leopold II of Belgium slaughtering an estimated 10-15 million Congolese people in the name of colonialism, slavery, and robbing resources (natural resources as well as servitude) in the Congo as late as the early 1900s.
These are just a few of the many historical examples of racial injustice, which remains ingrained in many parts of our society today. With this worldwide history, it has been advantageous for people to have lighter skin with regards to money, politics, jobs, education, the justice system, modeling/acting opportunities and contracts, home ownership, and opportunities for generational wealth for years to come. It has ingrained some unfortunate beliefs among some that having lighter skin is better, advantageous, and will make them more desirable or more beautiful.
and across the African continent. It is estimated that 77% of women in Nigeria and 55% of women in China use bleaching creams to achieve overall skin lightening. Unilever’s Fair & Lovely skin-whitening cream has long been a popular over-the-counter product in India, with an estimated market worth of 270 billion rupees ($4 billion USD). On June 25, 2020, Unilever vowed to rename and rebrand Fair & Lovely. With such an offensive name for a product that further promotes colorism, this is an effort in the right direction and has been a long time coming since its debut in 1975. Unilever’s Fair and Lovely Foundation for women’s causes still exists, and has not been renamed at the time of this writing.
Controversy remains on whether this product and other products such as these should exist for the purposes they are used for. Johnson & Johnson has decided that it will no longer produce and sell the Neutrogena Fine Fairness line, sold only in Asia and the Middle East, and the Clean & Clear Fairness line, sold in India. There are arguments to the contrary that halting production of skin-lightening products altogether may result in an influx of unsafe alternatives.
As dermatologists, we use skin-lightening products appropriately for the purposes of treating skin conditions such as postinflammatory hyperpigmentation, melasma, and photoaging. This is where the use of such products should largely end. While it is up to individuals about what they do with their skin and their bodies, we, as health care skin professionals, should be furthering the notion that all skin colors and types are beautiful. Moreover, we should not be encouraging the use of these products for overall skin whitening. Part of the issue is that these products are available often at high concentrations over the counter or in the illegal market, especially in parts of Asia and Africa where colorism is more common and skin whitening is more commonly practiced. The dangers are not only the risk of ochronosis with high concentrations or long term use of hydroquinone, but also what the Centre for Science and Environment found in a 2014 study, that 44% of the skin “fairness” creams in India contained mercury, which is illegal and a health concern.
In my practice, I have also had patients (several originally from Nigeria) who have admitted to long term use of skin-bleaching products for the purposes of all over face- and body-skin lightening who now suffer from very sensitive skin and experience bouts of eczematous dermatitis from time to time, despite having stopped using lightening cream. While there are adverse physical effects resulting from the use of these topicals for this purpose, the effects on the psyche are what concern me the most.
The beauty industry has also been an unfortunate part of furthering thoughts and attitudes concerning colorism over the years with lighter skin and Caucasian ideals being set as standards of beauty. One of many examples is a deodorant ad in the Middle East with the tagline “White is Purity” on a woman, which was pulled by Nivea in 2017 after it was slammed as racist. Another is the 2017 Dove ad for body wash that showed a smiling black woman peel off her brown shirt to reveal a white woman in a lighter-color shirt.
A shift has occurred in recent years with more ethnic images of beauty appearing in magazines and film. However, such opportunities are still less plentiful, pay discrepancies still occur, and sexual objectification of women of color as opposed to beautification is still rampant. As such, it is also up to us to do our part in studying and utilizing ethnic and racial differences in skin and beauty to maximize our efforts in promoting what is inherently beautiful as opposed to one standard of beauty. The education begins with the images we see, what we teach our children, loving ourselves, and as doctors, being knowledgeable about the right aesthetic choices for patients with different skin colors and types.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Is bufexamac worth the risk?
Bufexamac, a nonsteroidal anti-inflammatory drug agent used cutaneously and rectally, is well known globally as an initiator of allergic contact dermatitis. In fact, it has been removed from the European market (except Switzerland) for inducing allergic reactions, and is also banned in Japan, New Zealand, and the United States (where it was never approved).1 This column will primarily discuss recent findings in human trials and weigh in on the issue.
Antioxidant activity
. In 2003, Trommer and Neubert demonstrated that bufexamac displayed antioxidant activity in lipid models and HaCaT keratinocytes, as measured through mass spectrometry.2 In a 2005 in vitro study of the impact of 47 drugs, plant extracts and ingredients, and polysaccharides on lipid peroxidation engendered by UV irradiation, Trommer and Neubert found that bufexamac was among the drugs shown to exhibit antioxidant activity.3
Minor allergen? Worth using?
In a 2009 study on the prevalence and risk factors for allergic contact dermatitis to topical atopic dermatitis (AD) treatments, Mailhol et al. patch tested 641 children with AD using seven then-common ingredients (chlorhexidine, hexamidine, budesonide, tixocortol pivalate, bufexamac, sodium fusidate and with the current emollient used by the child). Bufexamac was identified as an allergen in only 2.5% of the 41 positive patch tests.4
To ban or not to ban
In 2012, the European Medicines Agency’s Committee for Medicinal Products for Human Use recommended that the marketing of formulations containing bufexamac be disallowed throughout the European Union because of a tendency toward inducing severe allergic contact dermatitis.5
Given its continuing use in Australia for the local treatment of several dermatoses, Pan and Nixon, in 2012, retrospectively reviewed patch-test data at the Skin and Cancer Foundation Inc. and found 19 cases of positive reactions to bufexamac (5% petrolatum) from 451 people patch tested. In 13 of 19 patients (68%), the reaction to bufexamac was considered to be associated with the identified dermatitis. The authors concluded that allergic contact dermatitis from bufexamac exposure is underreported in the English-language literature and cautioned that physicians should consider bufexamac allergy in patients who have a history of exposure.5
Bufexamac remained available over the counter in topical formulations in Australia as of early 2019. In response, Harris et al. presented several cases of patients who experienced severe skin eruptions after using such preparations in support of their advocacy to the Therapeutic Goods Administration in Australia to ban its use.6
In the middle of that year, Wong et al. reported on the hospitalization of a 41-year-old administrative worker who applied a first aid cream containing bufexamac (5%), lignocaine (1%), and chlorhexidine (0.1%) to a superficial right foot abrasion and who developed facial edema and widespread polymorphic eruptions 2 hours later. The authors suggested that this case reinforced the need to remove bufexamac from the markets where it remains because of the tendency to provoke severe allergic contact dermatoses and lack of efficacy.1
Conclusion
Bufexamac offers the somewhat rare opportunity for advocacy. That is to say, I think there is sufficient evidence to justify the removal of this potent allergen from the market in Australia, Switzerland, and other countries where it may be available.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. She had no relevant disclosures. Write to her at [email protected].
References
1. Wong GN et al. Contact Dermatitis. 2019 Jun;80(6):395-7.
2. Trommer H et al. J Pharm Pharmacol. 2003 Oct;55(10):1379-88.
3. Trommer H, Neubert RH. J Pharm Pharm Sci. 2005 Sep 15;8(3):494-506.
4. Mailhol C et al. Allergy. 2009 May;64(5):801-6.
5. Pan Y, Nixon R. Australas J Dermatol. 2012 Aug;53(3):207-10.
6. Harris AG et al. Australas J Dermatol. 2019 Feb;60(1):53-6.
Bufexamac, a nonsteroidal anti-inflammatory drug agent used cutaneously and rectally, is well known globally as an initiator of allergic contact dermatitis. In fact, it has been removed from the European market (except Switzerland) for inducing allergic reactions, and is also banned in Japan, New Zealand, and the United States (where it was never approved).1 This column will primarily discuss recent findings in human trials and weigh in on the issue.
Antioxidant activity
. In 2003, Trommer and Neubert demonstrated that bufexamac displayed antioxidant activity in lipid models and HaCaT keratinocytes, as measured through mass spectrometry.2 In a 2005 in vitro study of the impact of 47 drugs, plant extracts and ingredients, and polysaccharides on lipid peroxidation engendered by UV irradiation, Trommer and Neubert found that bufexamac was among the drugs shown to exhibit antioxidant activity.3
Minor allergen? Worth using?
In a 2009 study on the prevalence and risk factors for allergic contact dermatitis to topical atopic dermatitis (AD) treatments, Mailhol et al. patch tested 641 children with AD using seven then-common ingredients (chlorhexidine, hexamidine, budesonide, tixocortol pivalate, bufexamac, sodium fusidate and with the current emollient used by the child). Bufexamac was identified as an allergen in only 2.5% of the 41 positive patch tests.4
To ban or not to ban
In 2012, the European Medicines Agency’s Committee for Medicinal Products for Human Use recommended that the marketing of formulations containing bufexamac be disallowed throughout the European Union because of a tendency toward inducing severe allergic contact dermatitis.5
Given its continuing use in Australia for the local treatment of several dermatoses, Pan and Nixon, in 2012, retrospectively reviewed patch-test data at the Skin and Cancer Foundation Inc. and found 19 cases of positive reactions to bufexamac (5% petrolatum) from 451 people patch tested. In 13 of 19 patients (68%), the reaction to bufexamac was considered to be associated with the identified dermatitis. The authors concluded that allergic contact dermatitis from bufexamac exposure is underreported in the English-language literature and cautioned that physicians should consider bufexamac allergy in patients who have a history of exposure.5
Bufexamac remained available over the counter in topical formulations in Australia as of early 2019. In response, Harris et al. presented several cases of patients who experienced severe skin eruptions after using such preparations in support of their advocacy to the Therapeutic Goods Administration in Australia to ban its use.6
In the middle of that year, Wong et al. reported on the hospitalization of a 41-year-old administrative worker who applied a first aid cream containing bufexamac (5%), lignocaine (1%), and chlorhexidine (0.1%) to a superficial right foot abrasion and who developed facial edema and widespread polymorphic eruptions 2 hours later. The authors suggested that this case reinforced the need to remove bufexamac from the markets where it remains because of the tendency to provoke severe allergic contact dermatoses and lack of efficacy.1
Conclusion
Bufexamac offers the somewhat rare opportunity for advocacy. That is to say, I think there is sufficient evidence to justify the removal of this potent allergen from the market in Australia, Switzerland, and other countries where it may be available.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. She had no relevant disclosures. Write to her at [email protected].
References
1. Wong GN et al. Contact Dermatitis. 2019 Jun;80(6):395-7.
2. Trommer H et al. J Pharm Pharmacol. 2003 Oct;55(10):1379-88.
3. Trommer H, Neubert RH. J Pharm Pharm Sci. 2005 Sep 15;8(3):494-506.
4. Mailhol C et al. Allergy. 2009 May;64(5):801-6.
5. Pan Y, Nixon R. Australas J Dermatol. 2012 Aug;53(3):207-10.
6. Harris AG et al. Australas J Dermatol. 2019 Feb;60(1):53-6.
Bufexamac, a nonsteroidal anti-inflammatory drug agent used cutaneously and rectally, is well known globally as an initiator of allergic contact dermatitis. In fact, it has been removed from the European market (except Switzerland) for inducing allergic reactions, and is also banned in Japan, New Zealand, and the United States (where it was never approved).1 This column will primarily discuss recent findings in human trials and weigh in on the issue.
Antioxidant activity
. In 2003, Trommer and Neubert demonstrated that bufexamac displayed antioxidant activity in lipid models and HaCaT keratinocytes, as measured through mass spectrometry.2 In a 2005 in vitro study of the impact of 47 drugs, plant extracts and ingredients, and polysaccharides on lipid peroxidation engendered by UV irradiation, Trommer and Neubert found that bufexamac was among the drugs shown to exhibit antioxidant activity.3
Minor allergen? Worth using?
In a 2009 study on the prevalence and risk factors for allergic contact dermatitis to topical atopic dermatitis (AD) treatments, Mailhol et al. patch tested 641 children with AD using seven then-common ingredients (chlorhexidine, hexamidine, budesonide, tixocortol pivalate, bufexamac, sodium fusidate and with the current emollient used by the child). Bufexamac was identified as an allergen in only 2.5% of the 41 positive patch tests.4
To ban or not to ban
In 2012, the European Medicines Agency’s Committee for Medicinal Products for Human Use recommended that the marketing of formulations containing bufexamac be disallowed throughout the European Union because of a tendency toward inducing severe allergic contact dermatitis.5
Given its continuing use in Australia for the local treatment of several dermatoses, Pan and Nixon, in 2012, retrospectively reviewed patch-test data at the Skin and Cancer Foundation Inc. and found 19 cases of positive reactions to bufexamac (5% petrolatum) from 451 people patch tested. In 13 of 19 patients (68%), the reaction to bufexamac was considered to be associated with the identified dermatitis. The authors concluded that allergic contact dermatitis from bufexamac exposure is underreported in the English-language literature and cautioned that physicians should consider bufexamac allergy in patients who have a history of exposure.5
Bufexamac remained available over the counter in topical formulations in Australia as of early 2019. In response, Harris et al. presented several cases of patients who experienced severe skin eruptions after using such preparations in support of their advocacy to the Therapeutic Goods Administration in Australia to ban its use.6
In the middle of that year, Wong et al. reported on the hospitalization of a 41-year-old administrative worker who applied a first aid cream containing bufexamac (5%), lignocaine (1%), and chlorhexidine (0.1%) to a superficial right foot abrasion and who developed facial edema and widespread polymorphic eruptions 2 hours later. The authors suggested that this case reinforced the need to remove bufexamac from the markets where it remains because of the tendency to provoke severe allergic contact dermatoses and lack of efficacy.1
Conclusion
Bufexamac offers the somewhat rare opportunity for advocacy. That is to say, I think there is sufficient evidence to justify the removal of this potent allergen from the market in Australia, Switzerland, and other countries where it may be available.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. She had no relevant disclosures. Write to her at [email protected].
References
1. Wong GN et al. Contact Dermatitis. 2019 Jun;80(6):395-7.
2. Trommer H et al. J Pharm Pharmacol. 2003 Oct;55(10):1379-88.
3. Trommer H, Neubert RH. J Pharm Pharm Sci. 2005 Sep 15;8(3):494-506.
4. Mailhol C et al. Allergy. 2009 May;64(5):801-6.
5. Pan Y, Nixon R. Australas J Dermatol. 2012 Aug;53(3):207-10.
6. Harris AG et al. Australas J Dermatol. 2019 Feb;60(1):53-6.
FDA approves Qwo for treatment of cellulite
. The drug is the first injectable treatment for cellulite to receive regulatory approval.
In cellulite, fibrous septae are a primary contributing factor. The septae make up the fibrous connective tissue that connects the skin perpendicularly to the fascia below and tether the skin, drawing it downward and leading to a mattress-like appearance, commonly referred to as “dimpling.” When injected into the treatment area, Qwo is thought to release the fibrous septae enzymatically by specifically targeting types 1 and 3 collagen, which may result in smoothing of the skin and an improved appearance of cellulite.
The most common side effects of Qwo include injection site bruising, pain, areas of hardness, itching, redness, discoloration, swelling, and warmth in the treatment area.
Qwo is expected to be available throughout the United States at aesthetic health care practitioner’s offices starting in Spring 2021.
“Qwo could be a game-changer for many women with cellulite,” Anne Chapas, MD, a board-certified dermatologist at Union Square Laser Dermatology in New York, said in a press release. “I am thrilled there will now be an FDA-approved injectable treatment option proven to address a root cause of cellulite. What is exciting about Qwo is that it is a cutting-edge cellulite treatment, without the cutting,” Dr. Chapas, said.
. The drug is the first injectable treatment for cellulite to receive regulatory approval.
In cellulite, fibrous septae are a primary contributing factor. The septae make up the fibrous connective tissue that connects the skin perpendicularly to the fascia below and tether the skin, drawing it downward and leading to a mattress-like appearance, commonly referred to as “dimpling.” When injected into the treatment area, Qwo is thought to release the fibrous septae enzymatically by specifically targeting types 1 and 3 collagen, which may result in smoothing of the skin and an improved appearance of cellulite.
The most common side effects of Qwo include injection site bruising, pain, areas of hardness, itching, redness, discoloration, swelling, and warmth in the treatment area.
Qwo is expected to be available throughout the United States at aesthetic health care practitioner’s offices starting in Spring 2021.
“Qwo could be a game-changer for many women with cellulite,” Anne Chapas, MD, a board-certified dermatologist at Union Square Laser Dermatology in New York, said in a press release. “I am thrilled there will now be an FDA-approved injectable treatment option proven to address a root cause of cellulite. What is exciting about Qwo is that it is a cutting-edge cellulite treatment, without the cutting,” Dr. Chapas, said.
. The drug is the first injectable treatment for cellulite to receive regulatory approval.
In cellulite, fibrous septae are a primary contributing factor. The septae make up the fibrous connective tissue that connects the skin perpendicularly to the fascia below and tether the skin, drawing it downward and leading to a mattress-like appearance, commonly referred to as “dimpling.” When injected into the treatment area, Qwo is thought to release the fibrous septae enzymatically by specifically targeting types 1 and 3 collagen, which may result in smoothing of the skin and an improved appearance of cellulite.
The most common side effects of Qwo include injection site bruising, pain, areas of hardness, itching, redness, discoloration, swelling, and warmth in the treatment area.
Qwo is expected to be available throughout the United States at aesthetic health care practitioner’s offices starting in Spring 2021.
“Qwo could be a game-changer for many women with cellulite,” Anne Chapas, MD, a board-certified dermatologist at Union Square Laser Dermatology in New York, said in a press release. “I am thrilled there will now be an FDA-approved injectable treatment option proven to address a root cause of cellulite. What is exciting about Qwo is that it is a cutting-edge cellulite treatment, without the cutting,” Dr. Chapas, said.