User login
Ophthalmologist who developed medical botox dies at 89
his family confirmed to National Public Radio.
Four decades ago, Alan Brown Scott, MD, a native of Berkeley, Calif., turned the drug, once a deadly poison, into a revolutionary treatment for obscure eye diseases. It later became a well-known blockbuster treatment for reducing the appearance of wrinkles and treating hyperhidrosis (excessive sweating). Other approved medical uses include treatment of overactive bladder and urinary incontinence.
According to the American Society of Plastic Surgeons, its popularity for cosmetic use was boosted further during the pandemic and it was the No. 1 minimally invasive cosmetic procedure performed in 2020. Among the 13.3 million procedures, 4.4 million involved Botox.
According to Bloomberg Businessweek, Ed Schantz, who was working in the military’s biological weapons program, was the one to first send the toxin to Dr. Scott, who wanted to explore its properties for medical use.
The same Bloomberg article also noted that the original botulinum toxin itself “is so powerful that a tiny amount can suffocate a person by paralyzing the muscles used for breathing.”
Dr. Scott was looking for a way to help his patients avoid extensive surgeries.
“Specifically, he was aiming to treat people with strabismus, or cross-eyes, and blepharospasm, which is an uncontrollable closure of eyes. Today, it’s also used as a treatment to help with migraines, hair loss, and drooling,” NPR reported.
The New York Times once described Botox as “medicine’s answer to duct tape.”
Dr. Scott was the executive director of the Smith-Kettlewell Eye Research Institute in San Francisco when he did his pioneering research with botulinum toxin in the 1970s and 1980s, according to a 2002 article in SFGate.
In 1991, Dr. Scott sold the drug to Allergan, when it was called Oculinum. The next year, the name was officially changed to Botox.
In 2002, Dr. Scott told SFGate, when asked about the more popular use for the drug, “I think that’s a charming, slightly frivolous use,” adding, “but it’s not along the lines of what I was into, applications for serious disorders.”
According to Scientific American in 2016, Dr. Scott, then age 83, kept working on the noncosmetic benefits of botulism-toxin injections for eye-related disorders at the Strabismus Research Foundation,
He told Scientific American he was proud that his efforts “are directly helpful to people.”
“There are interesting and difficult problems still to be solved, and I’m a practicing physician and I see them every day,” he said.
Dr. Scott’s daughter, Ann Scott, told NPR: “He definitely loved his work and he was also a really great father.” She said her dad involved his children in his research and work.
She added, “He was a really calm, more of a quiet reserved person,” and said he was committed to teaching his students, many of them international students.
“That was what he really loved,” she said.
Dr. Scott, who died Dec. 16, was in intensive care for the last 10 days from an unspecified illness, his daughter told NPR.
A version of this article first appeared on Medscape.com.
his family confirmed to National Public Radio.
Four decades ago, Alan Brown Scott, MD, a native of Berkeley, Calif., turned the drug, once a deadly poison, into a revolutionary treatment for obscure eye diseases. It later became a well-known blockbuster treatment for reducing the appearance of wrinkles and treating hyperhidrosis (excessive sweating). Other approved medical uses include treatment of overactive bladder and urinary incontinence.
According to the American Society of Plastic Surgeons, its popularity for cosmetic use was boosted further during the pandemic and it was the No. 1 minimally invasive cosmetic procedure performed in 2020. Among the 13.3 million procedures, 4.4 million involved Botox.
According to Bloomberg Businessweek, Ed Schantz, who was working in the military’s biological weapons program, was the one to first send the toxin to Dr. Scott, who wanted to explore its properties for medical use.
The same Bloomberg article also noted that the original botulinum toxin itself “is so powerful that a tiny amount can suffocate a person by paralyzing the muscles used for breathing.”
Dr. Scott was looking for a way to help his patients avoid extensive surgeries.
“Specifically, he was aiming to treat people with strabismus, or cross-eyes, and blepharospasm, which is an uncontrollable closure of eyes. Today, it’s also used as a treatment to help with migraines, hair loss, and drooling,” NPR reported.
The New York Times once described Botox as “medicine’s answer to duct tape.”
Dr. Scott was the executive director of the Smith-Kettlewell Eye Research Institute in San Francisco when he did his pioneering research with botulinum toxin in the 1970s and 1980s, according to a 2002 article in SFGate.
In 1991, Dr. Scott sold the drug to Allergan, when it was called Oculinum. The next year, the name was officially changed to Botox.
In 2002, Dr. Scott told SFGate, when asked about the more popular use for the drug, “I think that’s a charming, slightly frivolous use,” adding, “but it’s not along the lines of what I was into, applications for serious disorders.”
According to Scientific American in 2016, Dr. Scott, then age 83, kept working on the noncosmetic benefits of botulism-toxin injections for eye-related disorders at the Strabismus Research Foundation,
He told Scientific American he was proud that his efforts “are directly helpful to people.”
“There are interesting and difficult problems still to be solved, and I’m a practicing physician and I see them every day,” he said.
Dr. Scott’s daughter, Ann Scott, told NPR: “He definitely loved his work and he was also a really great father.” She said her dad involved his children in his research and work.
She added, “He was a really calm, more of a quiet reserved person,” and said he was committed to teaching his students, many of them international students.
“That was what he really loved,” she said.
Dr. Scott, who died Dec. 16, was in intensive care for the last 10 days from an unspecified illness, his daughter told NPR.
A version of this article first appeared on Medscape.com.
his family confirmed to National Public Radio.
Four decades ago, Alan Brown Scott, MD, a native of Berkeley, Calif., turned the drug, once a deadly poison, into a revolutionary treatment for obscure eye diseases. It later became a well-known blockbuster treatment for reducing the appearance of wrinkles and treating hyperhidrosis (excessive sweating). Other approved medical uses include treatment of overactive bladder and urinary incontinence.
According to the American Society of Plastic Surgeons, its popularity for cosmetic use was boosted further during the pandemic and it was the No. 1 minimally invasive cosmetic procedure performed in 2020. Among the 13.3 million procedures, 4.4 million involved Botox.
According to Bloomberg Businessweek, Ed Schantz, who was working in the military’s biological weapons program, was the one to first send the toxin to Dr. Scott, who wanted to explore its properties for medical use.
The same Bloomberg article also noted that the original botulinum toxin itself “is so powerful that a tiny amount can suffocate a person by paralyzing the muscles used for breathing.”
Dr. Scott was looking for a way to help his patients avoid extensive surgeries.
“Specifically, he was aiming to treat people with strabismus, or cross-eyes, and blepharospasm, which is an uncontrollable closure of eyes. Today, it’s also used as a treatment to help with migraines, hair loss, and drooling,” NPR reported.
The New York Times once described Botox as “medicine’s answer to duct tape.”
Dr. Scott was the executive director of the Smith-Kettlewell Eye Research Institute in San Francisco when he did his pioneering research with botulinum toxin in the 1970s and 1980s, according to a 2002 article in SFGate.
In 1991, Dr. Scott sold the drug to Allergan, when it was called Oculinum. The next year, the name was officially changed to Botox.
In 2002, Dr. Scott told SFGate, when asked about the more popular use for the drug, “I think that’s a charming, slightly frivolous use,” adding, “but it’s not along the lines of what I was into, applications for serious disorders.”
According to Scientific American in 2016, Dr. Scott, then age 83, kept working on the noncosmetic benefits of botulism-toxin injections for eye-related disorders at the Strabismus Research Foundation,
He told Scientific American he was proud that his efforts “are directly helpful to people.”
“There are interesting and difficult problems still to be solved, and I’m a practicing physician and I see them every day,” he said.
Dr. Scott’s daughter, Ann Scott, told NPR: “He definitely loved his work and he was also a really great father.” She said her dad involved his children in his research and work.
She added, “He was a really calm, more of a quiet reserved person,” and said he was committed to teaching his students, many of them international students.
“That was what he really loved,” she said.
Dr. Scott, who died Dec. 16, was in intensive care for the last 10 days from an unspecified illness, his daughter told NPR.
A version of this article first appeared on Medscape.com.
Dermatologists driving use of vascular lasers in the Medicare population
In addition, as a proportion of Medicare charges submitted that were reimbursed, the highest reimbursements were for dermatologists and those in the Western geographic region.
Those are among the key findings from an analysis that aimed to characterize trends in use and reimbursement patterns of vascular lasers in the Medicare-insured population.
“There are several modalities for vascular laser treatment, including the pulse dye laser, the frequency doubled KTP laser, and others,” presenting author Partik Singh, MD, MBA, said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “Laser treatment of vascular lesions may sometimes be covered by insurance, depending on the indication, but little is known about how and which clinicians are taking advantage of this covered treatment.”
Dr. Singh, a 2nd-year dermatology resident at the University of Rochester Medical Center, and coauthor Mara Weinstein Velez, MD, extracted data from the 2012-2018 Medicare Public Use File, which includes 100% fee-for-service, non–Medicare Advantage claims based on CPT codes, yet no information on patient data, clinical context, or indications. Outcomes of interest were total vascular laser claims per year, annual vascular laser claims per clinician, annual clinicians using vascular lasers, accepted reimbursements defined by the allowed charge or the submitted charge to Medicare, and clinical specialties and geographic location.
The researchers found that more than half of clinicians who used vascular lasers during the study period were dermatologists (55%), followed by general surgeons (6%), family practice/internal medicine physicians (5% each) and various others. Use of vascular lasers among all clinicians increased 10.5% annually during the study period, from 3,786 to 6,883, and was most pronounced among dermatologists, whose use increased 18.4% annually, from 1,878 to 5,182. “Nondermatologists did not have a big change in their overall utilization rate, but they did have a steady utilization of vascular lasers, roughly at almost 2,000 claims per year,” Dr. Singh said.
The researchers also observed that the use of vascular lasers on a per-clinician basis increased 7.4% annually among all clinicians during the study period, from 77.3 to 118.7. This was mostly driven by dermatologists, whose per-clinician use increased 10.4% annually, from 81.7 to 148.7. Use by nondermatologists remained about stable, with just a 0.1% increase annually, from 73.4 to 74. In addition, the number of clinicians who billed for vascular laser procedures increased 2.9% annually between 2012 and 2018, from 49 to 58. This growth was driven mostly by dermatologists, who increased their billing for vascular laser procedures by 7.2% annually, from 23 to 35 clinicians.
In other findings, dermatologists were reimbursed at 68.3% of submitted charges, compared with 59.3% of charges submitted by other clinicians (P = .0001), and reimbursement rates were greatest in the Western geographic region of the United States vs. the Northeast, Midwest, and Southern regions (73.1% vs. 50.2%, 65.4%, and 55.3%, respectively; P < .0001).
“Use of vascular lasers is increasing primarily among dermatologists, though there is steady use of these procedures by nondermatologists,” Dr. Singh concluded. “Medicare charges were more often fully reimbursed when billed by dermatologists and those in the Western U.S., perhaps suggesting a better familiarity with appropriate indications and better administrative resources for coverage of vascular laser procedures.”
After the meeting, Dr. Singh acknowledged certain limitations of the analysis, including the fact that it “was limited only to Medicare Part B fee-for-service claims, not including Medicare Advantage,” he told this news organization. “Our conclusions do not necessarily hold true for Medicaid or commercial insurers, for instance. Moreover, this dataset doesn’t provide patient-specific information, such as the indication for the procedure. Further studies are needed to characterize utilization of various lasers in not only Medicare beneficiaries, but also those with Medicaid, private insurance, and patients paying out-of-pocket. Additionally, study is also needed to explain why these differences in reimbursement hold true.”
The researchers reported having no relevant financial disclosures.
In addition, as a proportion of Medicare charges submitted that were reimbursed, the highest reimbursements were for dermatologists and those in the Western geographic region.
Those are among the key findings from an analysis that aimed to characterize trends in use and reimbursement patterns of vascular lasers in the Medicare-insured population.
“There are several modalities for vascular laser treatment, including the pulse dye laser, the frequency doubled KTP laser, and others,” presenting author Partik Singh, MD, MBA, said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “Laser treatment of vascular lesions may sometimes be covered by insurance, depending on the indication, but little is known about how and which clinicians are taking advantage of this covered treatment.”
Dr. Singh, a 2nd-year dermatology resident at the University of Rochester Medical Center, and coauthor Mara Weinstein Velez, MD, extracted data from the 2012-2018 Medicare Public Use File, which includes 100% fee-for-service, non–Medicare Advantage claims based on CPT codes, yet no information on patient data, clinical context, or indications. Outcomes of interest were total vascular laser claims per year, annual vascular laser claims per clinician, annual clinicians using vascular lasers, accepted reimbursements defined by the allowed charge or the submitted charge to Medicare, and clinical specialties and geographic location.
The researchers found that more than half of clinicians who used vascular lasers during the study period were dermatologists (55%), followed by general surgeons (6%), family practice/internal medicine physicians (5% each) and various others. Use of vascular lasers among all clinicians increased 10.5% annually during the study period, from 3,786 to 6,883, and was most pronounced among dermatologists, whose use increased 18.4% annually, from 1,878 to 5,182. “Nondermatologists did not have a big change in their overall utilization rate, but they did have a steady utilization of vascular lasers, roughly at almost 2,000 claims per year,” Dr. Singh said.
The researchers also observed that the use of vascular lasers on a per-clinician basis increased 7.4% annually among all clinicians during the study period, from 77.3 to 118.7. This was mostly driven by dermatologists, whose per-clinician use increased 10.4% annually, from 81.7 to 148.7. Use by nondermatologists remained about stable, with just a 0.1% increase annually, from 73.4 to 74. In addition, the number of clinicians who billed for vascular laser procedures increased 2.9% annually between 2012 and 2018, from 49 to 58. This growth was driven mostly by dermatologists, who increased their billing for vascular laser procedures by 7.2% annually, from 23 to 35 clinicians.
In other findings, dermatologists were reimbursed at 68.3% of submitted charges, compared with 59.3% of charges submitted by other clinicians (P = .0001), and reimbursement rates were greatest in the Western geographic region of the United States vs. the Northeast, Midwest, and Southern regions (73.1% vs. 50.2%, 65.4%, and 55.3%, respectively; P < .0001).
“Use of vascular lasers is increasing primarily among dermatologists, though there is steady use of these procedures by nondermatologists,” Dr. Singh concluded. “Medicare charges were more often fully reimbursed when billed by dermatologists and those in the Western U.S., perhaps suggesting a better familiarity with appropriate indications and better administrative resources for coverage of vascular laser procedures.”
After the meeting, Dr. Singh acknowledged certain limitations of the analysis, including the fact that it “was limited only to Medicare Part B fee-for-service claims, not including Medicare Advantage,” he told this news organization. “Our conclusions do not necessarily hold true for Medicaid or commercial insurers, for instance. Moreover, this dataset doesn’t provide patient-specific information, such as the indication for the procedure. Further studies are needed to characterize utilization of various lasers in not only Medicare beneficiaries, but also those with Medicaid, private insurance, and patients paying out-of-pocket. Additionally, study is also needed to explain why these differences in reimbursement hold true.”
The researchers reported having no relevant financial disclosures.
In addition, as a proportion of Medicare charges submitted that were reimbursed, the highest reimbursements were for dermatologists and those in the Western geographic region.
Those are among the key findings from an analysis that aimed to characterize trends in use and reimbursement patterns of vascular lasers in the Medicare-insured population.
“There are several modalities for vascular laser treatment, including the pulse dye laser, the frequency doubled KTP laser, and others,” presenting author Partik Singh, MD, MBA, said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “Laser treatment of vascular lesions may sometimes be covered by insurance, depending on the indication, but little is known about how and which clinicians are taking advantage of this covered treatment.”
Dr. Singh, a 2nd-year dermatology resident at the University of Rochester Medical Center, and coauthor Mara Weinstein Velez, MD, extracted data from the 2012-2018 Medicare Public Use File, which includes 100% fee-for-service, non–Medicare Advantage claims based on CPT codes, yet no information on patient data, clinical context, or indications. Outcomes of interest were total vascular laser claims per year, annual vascular laser claims per clinician, annual clinicians using vascular lasers, accepted reimbursements defined by the allowed charge or the submitted charge to Medicare, and clinical specialties and geographic location.
The researchers found that more than half of clinicians who used vascular lasers during the study period were dermatologists (55%), followed by general surgeons (6%), family practice/internal medicine physicians (5% each) and various others. Use of vascular lasers among all clinicians increased 10.5% annually during the study period, from 3,786 to 6,883, and was most pronounced among dermatologists, whose use increased 18.4% annually, from 1,878 to 5,182. “Nondermatologists did not have a big change in their overall utilization rate, but they did have a steady utilization of vascular lasers, roughly at almost 2,000 claims per year,” Dr. Singh said.
The researchers also observed that the use of vascular lasers on a per-clinician basis increased 7.4% annually among all clinicians during the study period, from 77.3 to 118.7. This was mostly driven by dermatologists, whose per-clinician use increased 10.4% annually, from 81.7 to 148.7. Use by nondermatologists remained about stable, with just a 0.1% increase annually, from 73.4 to 74. In addition, the number of clinicians who billed for vascular laser procedures increased 2.9% annually between 2012 and 2018, from 49 to 58. This growth was driven mostly by dermatologists, who increased their billing for vascular laser procedures by 7.2% annually, from 23 to 35 clinicians.
In other findings, dermatologists were reimbursed at 68.3% of submitted charges, compared with 59.3% of charges submitted by other clinicians (P = .0001), and reimbursement rates were greatest in the Western geographic region of the United States vs. the Northeast, Midwest, and Southern regions (73.1% vs. 50.2%, 65.4%, and 55.3%, respectively; P < .0001).
“Use of vascular lasers is increasing primarily among dermatologists, though there is steady use of these procedures by nondermatologists,” Dr. Singh concluded. “Medicare charges were more often fully reimbursed when billed by dermatologists and those in the Western U.S., perhaps suggesting a better familiarity with appropriate indications and better administrative resources for coverage of vascular laser procedures.”
After the meeting, Dr. Singh acknowledged certain limitations of the analysis, including the fact that it “was limited only to Medicare Part B fee-for-service claims, not including Medicare Advantage,” he told this news organization. “Our conclusions do not necessarily hold true for Medicaid or commercial insurers, for instance. Moreover, this dataset doesn’t provide patient-specific information, such as the indication for the procedure. Further studies are needed to characterize utilization of various lasers in not only Medicare beneficiaries, but also those with Medicaid, private insurance, and patients paying out-of-pocket. Additionally, study is also needed to explain why these differences in reimbursement hold true.”
The researchers reported having no relevant financial disclosures.
FROM ASDS 2021
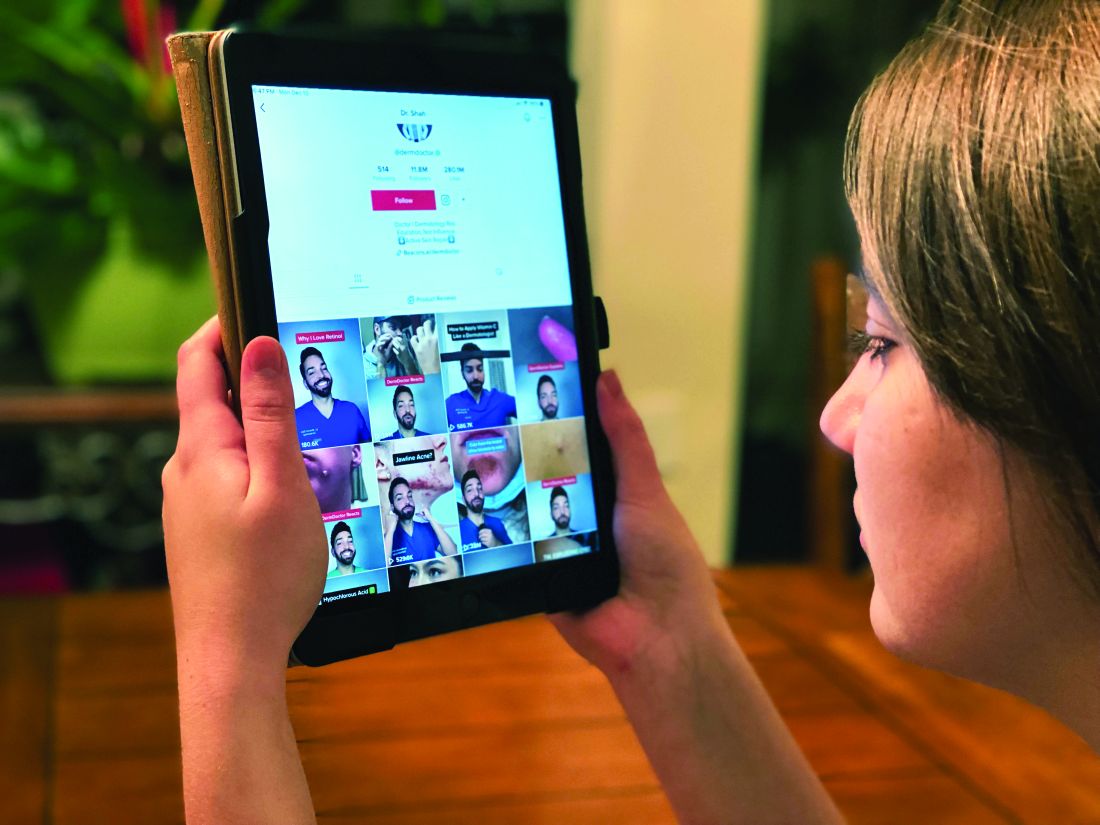
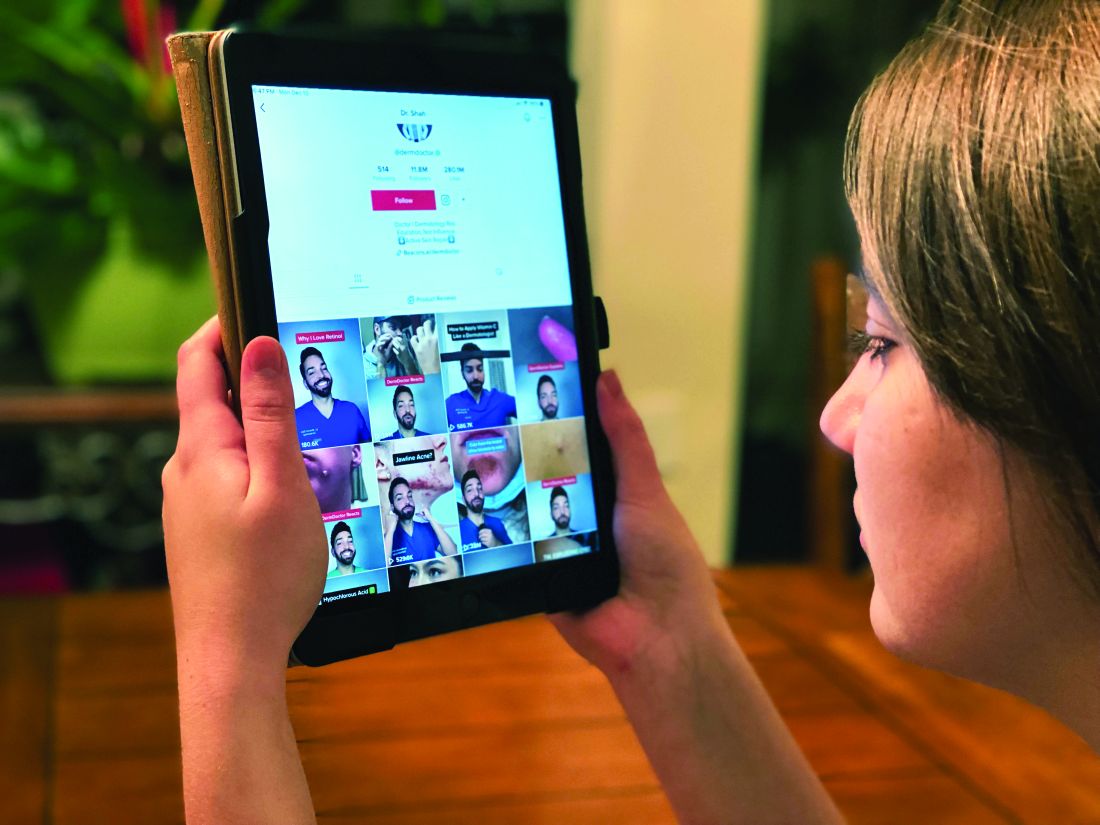
Dermatologists take to TikTok to share their own ‘hacks’
A young woman is having her lip swabbed with an unknown substance, smiling, on the TikTok video. Seconds later, another young woman, wearing gloves, pushes a hyaluron pen against the first woman’s lips, who, in the next cut, is smiling, happy. “My first syringe down and already 1,000x more confident,” the caption reads.
That video is one of thousands showing hyaluron pen use on TikTok. The pens are sold online and are unapproved – which led to a Food and Drug Administration warning in October 2021 that use could cause bleeding, infection, blood vessel occlusion that could result in blindness or stroke, allergic reactions, and other injuries.
The warning has not stopped many TikTokkers, who also use the medium to promote all sorts of skin and aesthetic products and procedures, a large number unproven, unapproved, or ill advised. which, more often than not, comes from “skinfluencers,” aestheticians, and other laypeople, not board-certified dermatologists.
The suggested “hacks” can be harmless or ineffective, but they also can be misleading, fraudulent, or even dangerous.
Skinfluencers take the lead
TikTok has a reported 1 billion monthly users. Two-thirds are aged 10-29 years, according to data reported in February 2021 in the Journal of the American Academy of Dermatology by David X. Zheng, BA, and colleagues at Case Western Reserve University, Cleveland, and the department of dermatology, Johns Hopkins University, Baltimore.
Visitors consume information in video bits that run from 15 seconds to up to 3 minutes and can follow their favorite TikTokkers, browse for people or hashtags with a search function, or click on content recommended by the platform, which uses algorithms based on the user’s viewing habits to determine what might be of interest.
Some of the biggest “skinfluencers” have millions of followers: Hyram Yarbro, (@skincarebyhyram) for instance, has 6.6 million followers and his own line of skin care products at Sephora. Mr. Yarbro is seen as a no-nonsense debunker of skin care myths, as is British influencer James Welsh, who has 124,000 followers.
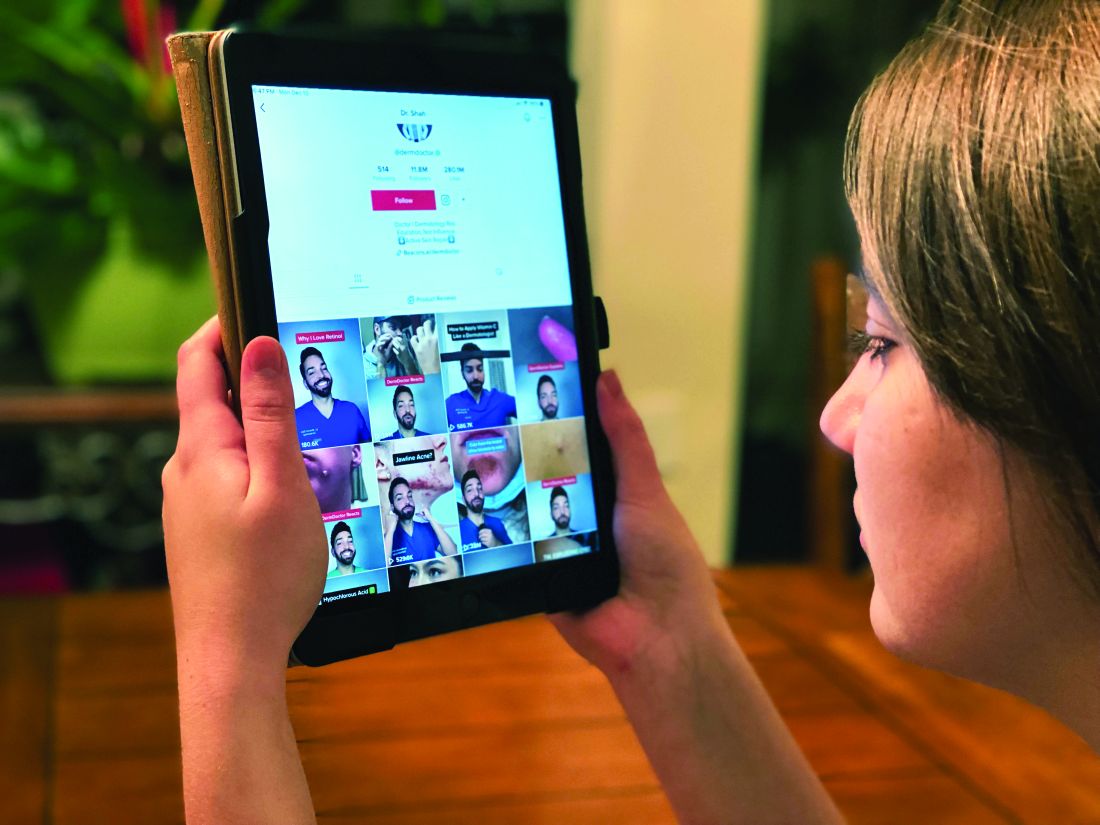
“The reason why people trust your average influencer person who’s not a doctor is because they’re relatable,” said Muneeb Shah, MD, a dermatology resident at Atlantic Dermatology in Wilmington, N.C. – known to his 11.4 million TikTok followers as @dermdoctor.
To Sandra Lee, MD, the popularity of nonprofessionals is easy to explain. “You have to think about the fact that a lot of people can’t see dermatologists – they don’t have the money, they don’t have the time to travel there, they don’t have health insurance, or they’re scared of doctors, so they’re willing to try to find an answer, and one of the easiest ways, one of the more entertaining ways to get information, is on social media.”
Dr. Lee is in private practice in Upland, Calif., but is better known as “Dr. Pimple Popper,” through her television show of the same name and her social media accounts, including on TikTok, where she has 14.4 million followers after having started in 2020.
“We’re all looking for that no-down-time, no-expense, no-lines, no-wrinkles, stay-young-forever magic bullet,” said Dr. Lee.
Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, agreed that people are looking for a quick fix. They don’t want to wait 12 weeks for an acne medication or 16 weeks for a biologic to work. “They want something simple, easy, do-it-yourself,” and “natural,” he said.
Laypeople are still the dominant producers – and have the most views – of dermatology content.
Morgan Nguyen, BA, at Northwestern University, Chicago, and colleagues looked at hashtags for the top 10 dermatologic diagnoses and procedures and analyzed the content of the first 40 TikTok videos in each category. About half the videos were produced by an individual, and 39% by a health care provider, according to the study, published in the International Journal of Women’s Dermatology. About 40% of the videos were educational, focusing on skin care, procedures, and disease treatment.
Viewership was highest for videos by laypeople, followed by those produced by business or industry accounts. Those produced by health care providers received only 18% of the views.
The most popular videos were about dermatologic diagnoses, with 2.5 billion views, followed by dermatologic procedures, with 708 million views.
Ms. Nguyen noted in the study that the most liked and most viewed posts were related to #skincare but that board-certified dermatologists produced only 2.5% of the #skincare videos.
Dermatologists take to TikTok
Some dermatologists have started their own TikTok accounts, seeking both to counteract misinformation and provide education.
Dr. Shah has become one of the top influencers on the platform. In a year-end wrap, TikTok put Dr. Shah at No. 7 on its top creators list for 2021.
The dermatology resident said that TikTok is a good tool for reaching patients who might not otherwise interact with dermatologists. He recounted the story of an individual who came into his office with the idea that they had hidradenitis suppurativa.
The person had self-diagnosed after seeing one of Dr. Shah’s TikTok videos on the condition. It was a pleasant surprise, said Dr. Shah. People with hidradenitis suppurativa often avoid treatment, and it’s underdiagnosed and improperly treated, despite an American Academy of Dermatology awareness campaign.
“Dermatologists on social media are almost like the communications department for dermatology,” Dr. Shah commented.
A key to making TikTok work to advance dermatologists’ goals is knowing what makes it unique.
Dr. Lee said she prefers it to Instagram, because TikTok’s algorithms and its younger-skewing audience help her reach a more specific audience.
The algorithm “creates a positive feedback loop in which popular content creators or viral trends are prioritized on the users’ homepages, in turn providing the creators of these videos with an even larger audience,” Mr. Zheng, of University Hospitals Cleveland Medical Center, and coauthors noted in their letter in the Journal of the American Academy of Dermatology.
TikTok also celebrates the everyday – someone doesn’t have to be a celebrity to make something go viral, said Dr. Lee. She believes that TikTok users are more accepting of average people with real problems – which helps when someone is TikTokking about a skin condition.
Doris Day, MD, who goes by @drdorisday on TikTok, agreed with Dr. Lee. “There are so many creative ways you can convey information with it that’s different than what you have on Instagram,” said Dr. Day, who is in private practice in New York. And, she added, “it does really lend itself to getting points out super-fast.”
Dermatologists on TikTok also said they like the “duets” and the “stitch” features, which allow users to add on to an existing video, essentially chiming in or responding to what might have already been posted, in a side-by-side format.
Dr. Shah said he often duets videos that have questionable content. “It allows me to directly respond to people. A lot of times, if something is going really viral and it’s not accurate, you’ll have a response from me or one of the other doctors” within hours or days.
Dr. Shah’s duets are labeled with “DermDoctor Reacts” or “DermDoctor Explains.” In one duet, with more than 2.8 million views, the upper half of the video is someone squeezing a blackhead, while Dr. Shah, in the bottom half, in green scrubs, opines over some hip-hop music: “This is just a blackhead. But once it gets to this point, they do need to be extracted because topical treatments won’t help.”
Dr. Lee – whose TikTok and other accounts capitalize on teens’ obsession with popping pimples – has a duet in which she advised that although popping will leave scars, there are more ideal times to pop, if they must. The duet has at least 21 million views.
Sometimes a TikTok video effectively takes on a trend without being a duet. Nurse practitioner Uy Dam (@uy.np) has a video that demonstrates the dangers of hyaluron pens. He uses both a pen and a needle to inject fluid into a block of jello. The pen delivers a scattershot load of differing depths, while the needle is exact. It’s visual and easy to understand and has at least 1.3 million views.
Still, TikTok, like other forms of social media, is full of misinformation and false accounts, including people who claim to be doctors. “It’s hard for the regular person, myself included, sometimes to be able to root through that and find out whether something is real or not,” said Dr. Lee.
Dr. Friedman said he’s concerned about the lack of accountability. A doctor could lose his or her license for promoting unproven cures, especially if they are harmful. But for influencers, “there’s no accountability for posting information that can actually hurt people.”
TikTok trends gone bad
And some people are being hurt by emulating what they see on TikTok.
Dr. Friedman had a patient with extreme irritant contact dermatitis, “almost like chemical burns to her underarms,” he said. He determined that she saw a video “hack” that recommended using baking soda to stop hyperhidrosis. The patient used so much that it burned her skin.
In 2020, do-it-yourself freckles – with henna or sewing needles impregnated with ink – went viral. Tilly Whitfeld, a 21-year-old reality TV star on Australia’s Big Brother show, told the New York Times that she tried it at home after seeing a TikTok video. She ordered brown tattoo ink online and later found out that it was contaminated with lead, according to the Times. Ms. Whitfeld developed an infection and temporary vision loss and has permanent scarring.
She has since put out a cautionary TikTok video that’s been viewed some 300,000 times.
TikTokkers have also flocked to the idea of using sunscreen to “contour” the face. Selected areas are left without sunscreen to burn or tan. In a duet, a plastic surgeon shakes his head as a young woman explains that “it works.”
Scalp-popping – in which the hair is yanked so hard that it pulls the galea off the skull – has been mostly shut down by TikTok. A search of “scalp popping” brings up the message: “Learn how to recognize harmful challenges and hoaxes.” At-home mole and skin tag removal, pimple-popping, and supposed acne cures such as drinking chlorophyll are all avidly documented and shared on TikTok.
Dr. Shah had a back-and-forth video dialog with someone who had stubbed a toe and then drilled a hole into the nail to drain the hematoma. In a reaction video, Dr. Shah said it was likely to turn into an infection. When it did, the man revealed the infection in a video where he tagged Dr. Shah and later posted a video at the podiatrist’s office having his nail removed, again tagging Dr. Shah.
“I think that pretty much no procedure for skin is good to do at home,” said Dr. Shah, who repeatedly admonishes against mole removal by a nonphysician. He tells followers that “it’s extremely dangerous – not only is it going to cause scarring, but you are potentially discarding a cancerous lesion.”
Unfortunately, most will not follow the advice, said Dr. Shah. That’s especially true of pimple-popping. Aiming for the least harm, he suggests in some TikTok videos that poppers keep the area clean, wear gloves, and consult a physician to get an antibiotic prescription. “You might as well at least guide them in the right direction,” he added.
Dr. Lee believes that lack of access to physicians, insurance, or money may play into how TikTok trends evolve. “Probably those people who injected their lips with this air gun thing, maybe they didn’t have the money necessarily to get filler,” she said.
Also, she noted, while TikTok may try to police its content, creators are incentivized to be outrageous. “The more inflammatory your post is, the more engagement you get.”
Dr. Shah thinks TikTok is self-correcting. “If you’re not being ethical or contradicting yourself, putting out information that’s not accurate, people are going to catch on very quickly,” he said. “The only value, the only currency you have on social media is the trust that you build with people that follow you.”
What it takes to be a TikTokker
For dermatologists, conveying their credentials and experience is one way to build that currency. Dr. Lee advised fellow doctors on TikTok to “showcase your training and how many years it took to become a dermatologist.”
Plunging into TikTok is not for everyone, though. It’s time consuming, said Dr. Lee, who now devotes most of her nonclinical time to TikTok. She creates her own content, leaving others to manage her Instagram account.
Many of those in the medical field who have dived into TikTok are residents, like Dr. Shah. “They are attuned to it and understand it more,” said Dr. Lee. “It’s harder for a lot of us who are older, who really weren’t involved that much in social media at all. It’s very hard to jump in.” There’s a learning curve, and it takes hours to create a single video. “You have to enjoy it and it has to be a part of your life,” she said.
Dr. Shah started experimenting with TikTok at the beginning of the pandemic in 2020 and has never turned back. Fast-talking, curious, and with an infectious sense of fun, he shares tidbits about his personal life – putting his wife in some of his videos – and always seems upbeat.
He said that, as his following grew, users began to see him as an authority figure and started “tagging” him more often, seeking his opinion on other videos. Although still a resident, he believes he has specialized knowledge to share. “Even if you’re not the world’s leading expert in a particular topic, you’re still adding value for the person who doesn’t know much.”
Dr. Shah also occasionally does promotional TikToks, identified as sponsored content. He said he only works with companies that he believes have legitimate products. “You do have to monetize at some point,” he said, noting that many dermatologists, himself included, are trading clinic time for TikTok. “There’s no universe where they can do this for free.”
Product endorsements are likely more rewarding for influencers and other users like Dr. Shah than the remuneration from TikTok, the company. The platform pays user accounts $20 per 1 million views, Dr. Shah said. “Financially, it’s not a big winner for a practicing dermatologist, but the educational outreach is worthwhile.”
To be successful also means understanding what drives viewership.
Using “trending” sounds has “been shown to increase the likelihood of a video amassing millions of views” and may increase engagement with dermatologists’ TikTok videos, wrote Bina Kassamali, BA, and colleagues at the Brigham and Women’s Hospital in Boston and the Ponce Health Science University School of Medicine in Ponce, Puerto Rico, in a letter published in the Journal of the American Academy of Dermatology in July 2021.
Certain content is more likely to engage viewers. In their analysis of top trending dermatologic hashtags, acne-related content was viewed 6.7 billion times, followed by alopecia, with 1.1 billion views. Psoriasis content had 84 million views, putting it eighth on the list of topics.
Dermatologists are still cracking TikTok. They are accumulating more followers on TikTok than on Instagram but have greater engagement on Instagram reels, wrote Mindy D. Szeto, MS, and colleagues at the University of Colorado at Denver, Aurora, and Rocky Vista University in Parker, Colo., in the Journal of the American Academy of Dermatology in April 2021.
Dr. Lee and Dr. Shah had the highest engagement rate on TikTok, according to Ms. Szeto. The engagement rate is calculated as (likes + comments per post)/(total followers) x 100.
“TikTok may currently be the leading avenue for audience education by dermatologist influencers,” they wrote, urging dermatologists to use the platform to answer the call as more of the public “continues to turn to social media for medical advice.”
Dr. Day said she will keep trying to build her TikTok audience. She has just 239 followers, compared with her 44,500 on Instagram. “The more I do TikTok, the more I do any of these mediums, the better I get at it,” she said. “We just have to put a little time and effort into it and try to get more followers and just keep sharing the information.”
Dr. Friedman sees it as a positive that some dermatologists have taken to TikTok to dispel myths and put “good information out there in small bites.” But to be more effective, they need more followers.
“The truth is that 14-year-old is probably going to listen more to a Hyram than a dermatologist,” he said. “Maybe we need to work with these other individuals who know how to take these messages and convert them to a language that can be digested by a 14-year-old, by a 12-year-old, by a 23-year-old. We need to come to the table together and not fight.”
A version of this article first appeared on Medscape.com.
A young woman is having her lip swabbed with an unknown substance, smiling, on the TikTok video. Seconds later, another young woman, wearing gloves, pushes a hyaluron pen against the first woman’s lips, who, in the next cut, is smiling, happy. “My first syringe down and already 1,000x more confident,” the caption reads.
That video is one of thousands showing hyaluron pen use on TikTok. The pens are sold online and are unapproved – which led to a Food and Drug Administration warning in October 2021 that use could cause bleeding, infection, blood vessel occlusion that could result in blindness or stroke, allergic reactions, and other injuries.
The warning has not stopped many TikTokkers, who also use the medium to promote all sorts of skin and aesthetic products and procedures, a large number unproven, unapproved, or ill advised. which, more often than not, comes from “skinfluencers,” aestheticians, and other laypeople, not board-certified dermatologists.
The suggested “hacks” can be harmless or ineffective, but they also can be misleading, fraudulent, or even dangerous.
Skinfluencers take the lead
TikTok has a reported 1 billion monthly users. Two-thirds are aged 10-29 years, according to data reported in February 2021 in the Journal of the American Academy of Dermatology by David X. Zheng, BA, and colleagues at Case Western Reserve University, Cleveland, and the department of dermatology, Johns Hopkins University, Baltimore.
Visitors consume information in video bits that run from 15 seconds to up to 3 minutes and can follow their favorite TikTokkers, browse for people or hashtags with a search function, or click on content recommended by the platform, which uses algorithms based on the user’s viewing habits to determine what might be of interest.
Some of the biggest “skinfluencers” have millions of followers: Hyram Yarbro, (@skincarebyhyram) for instance, has 6.6 million followers and his own line of skin care products at Sephora. Mr. Yarbro is seen as a no-nonsense debunker of skin care myths, as is British influencer James Welsh, who has 124,000 followers.
“The reason why people trust your average influencer person who’s not a doctor is because they’re relatable,” said Muneeb Shah, MD, a dermatology resident at Atlantic Dermatology in Wilmington, N.C. – known to his 11.4 million TikTok followers as @dermdoctor.
To Sandra Lee, MD, the popularity of nonprofessionals is easy to explain. “You have to think about the fact that a lot of people can’t see dermatologists – they don’t have the money, they don’t have the time to travel there, they don’t have health insurance, or they’re scared of doctors, so they’re willing to try to find an answer, and one of the easiest ways, one of the more entertaining ways to get information, is on social media.”
Dr. Lee is in private practice in Upland, Calif., but is better known as “Dr. Pimple Popper,” through her television show of the same name and her social media accounts, including on TikTok, where she has 14.4 million followers after having started in 2020.
“We’re all looking for that no-down-time, no-expense, no-lines, no-wrinkles, stay-young-forever magic bullet,” said Dr. Lee.
Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, agreed that people are looking for a quick fix. They don’t want to wait 12 weeks for an acne medication or 16 weeks for a biologic to work. “They want something simple, easy, do-it-yourself,” and “natural,” he said.
Laypeople are still the dominant producers – and have the most views – of dermatology content.
Morgan Nguyen, BA, at Northwestern University, Chicago, and colleagues looked at hashtags for the top 10 dermatologic diagnoses and procedures and analyzed the content of the first 40 TikTok videos in each category. About half the videos were produced by an individual, and 39% by a health care provider, according to the study, published in the International Journal of Women’s Dermatology. About 40% of the videos were educational, focusing on skin care, procedures, and disease treatment.
Viewership was highest for videos by laypeople, followed by those produced by business or industry accounts. Those produced by health care providers received only 18% of the views.
The most popular videos were about dermatologic diagnoses, with 2.5 billion views, followed by dermatologic procedures, with 708 million views.
Ms. Nguyen noted in the study that the most liked and most viewed posts were related to #skincare but that board-certified dermatologists produced only 2.5% of the #skincare videos.
Dermatologists take to TikTok
Some dermatologists have started their own TikTok accounts, seeking both to counteract misinformation and provide education.
Dr. Shah has become one of the top influencers on the platform. In a year-end wrap, TikTok put Dr. Shah at No. 7 on its top creators list for 2021.
The dermatology resident said that TikTok is a good tool for reaching patients who might not otherwise interact with dermatologists. He recounted the story of an individual who came into his office with the idea that they had hidradenitis suppurativa.
The person had self-diagnosed after seeing one of Dr. Shah’s TikTok videos on the condition. It was a pleasant surprise, said Dr. Shah. People with hidradenitis suppurativa often avoid treatment, and it’s underdiagnosed and improperly treated, despite an American Academy of Dermatology awareness campaign.
“Dermatologists on social media are almost like the communications department for dermatology,” Dr. Shah commented.
A key to making TikTok work to advance dermatologists’ goals is knowing what makes it unique.
Dr. Lee said she prefers it to Instagram, because TikTok’s algorithms and its younger-skewing audience help her reach a more specific audience.
The algorithm “creates a positive feedback loop in which popular content creators or viral trends are prioritized on the users’ homepages, in turn providing the creators of these videos with an even larger audience,” Mr. Zheng, of University Hospitals Cleveland Medical Center, and coauthors noted in their letter in the Journal of the American Academy of Dermatology.
TikTok also celebrates the everyday – someone doesn’t have to be a celebrity to make something go viral, said Dr. Lee. She believes that TikTok users are more accepting of average people with real problems – which helps when someone is TikTokking about a skin condition.
Doris Day, MD, who goes by @drdorisday on TikTok, agreed with Dr. Lee. “There are so many creative ways you can convey information with it that’s different than what you have on Instagram,” said Dr. Day, who is in private practice in New York. And, she added, “it does really lend itself to getting points out super-fast.”
Dermatologists on TikTok also said they like the “duets” and the “stitch” features, which allow users to add on to an existing video, essentially chiming in or responding to what might have already been posted, in a side-by-side format.
Dr. Shah said he often duets videos that have questionable content. “It allows me to directly respond to people. A lot of times, if something is going really viral and it’s not accurate, you’ll have a response from me or one of the other doctors” within hours or days.
Dr. Shah’s duets are labeled with “DermDoctor Reacts” or “DermDoctor Explains.” In one duet, with more than 2.8 million views, the upper half of the video is someone squeezing a blackhead, while Dr. Shah, in the bottom half, in green scrubs, opines over some hip-hop music: “This is just a blackhead. But once it gets to this point, they do need to be extracted because topical treatments won’t help.”
Dr. Lee – whose TikTok and other accounts capitalize on teens’ obsession with popping pimples – has a duet in which she advised that although popping will leave scars, there are more ideal times to pop, if they must. The duet has at least 21 million views.
Sometimes a TikTok video effectively takes on a trend without being a duet. Nurse practitioner Uy Dam (@uy.np) has a video that demonstrates the dangers of hyaluron pens. He uses both a pen and a needle to inject fluid into a block of jello. The pen delivers a scattershot load of differing depths, while the needle is exact. It’s visual and easy to understand and has at least 1.3 million views.
Still, TikTok, like other forms of social media, is full of misinformation and false accounts, including people who claim to be doctors. “It’s hard for the regular person, myself included, sometimes to be able to root through that and find out whether something is real or not,” said Dr. Lee.
Dr. Friedman said he’s concerned about the lack of accountability. A doctor could lose his or her license for promoting unproven cures, especially if they are harmful. But for influencers, “there’s no accountability for posting information that can actually hurt people.”
TikTok trends gone bad
And some people are being hurt by emulating what they see on TikTok.
Dr. Friedman had a patient with extreme irritant contact dermatitis, “almost like chemical burns to her underarms,” he said. He determined that she saw a video “hack” that recommended using baking soda to stop hyperhidrosis. The patient used so much that it burned her skin.
In 2020, do-it-yourself freckles – with henna or sewing needles impregnated with ink – went viral. Tilly Whitfeld, a 21-year-old reality TV star on Australia’s Big Brother show, told the New York Times that she tried it at home after seeing a TikTok video. She ordered brown tattoo ink online and later found out that it was contaminated with lead, according to the Times. Ms. Whitfeld developed an infection and temporary vision loss and has permanent scarring.
She has since put out a cautionary TikTok video that’s been viewed some 300,000 times.
TikTokkers have also flocked to the idea of using sunscreen to “contour” the face. Selected areas are left without sunscreen to burn or tan. In a duet, a plastic surgeon shakes his head as a young woman explains that “it works.”
Scalp-popping – in which the hair is yanked so hard that it pulls the galea off the skull – has been mostly shut down by TikTok. A search of “scalp popping” brings up the message: “Learn how to recognize harmful challenges and hoaxes.” At-home mole and skin tag removal, pimple-popping, and supposed acne cures such as drinking chlorophyll are all avidly documented and shared on TikTok.
Dr. Shah had a back-and-forth video dialog with someone who had stubbed a toe and then drilled a hole into the nail to drain the hematoma. In a reaction video, Dr. Shah said it was likely to turn into an infection. When it did, the man revealed the infection in a video where he tagged Dr. Shah and later posted a video at the podiatrist’s office having his nail removed, again tagging Dr. Shah.
“I think that pretty much no procedure for skin is good to do at home,” said Dr. Shah, who repeatedly admonishes against mole removal by a nonphysician. He tells followers that “it’s extremely dangerous – not only is it going to cause scarring, but you are potentially discarding a cancerous lesion.”
Unfortunately, most will not follow the advice, said Dr. Shah. That’s especially true of pimple-popping. Aiming for the least harm, he suggests in some TikTok videos that poppers keep the area clean, wear gloves, and consult a physician to get an antibiotic prescription. “You might as well at least guide them in the right direction,” he added.
Dr. Lee believes that lack of access to physicians, insurance, or money may play into how TikTok trends evolve. “Probably those people who injected their lips with this air gun thing, maybe they didn’t have the money necessarily to get filler,” she said.
Also, she noted, while TikTok may try to police its content, creators are incentivized to be outrageous. “The more inflammatory your post is, the more engagement you get.”
Dr. Shah thinks TikTok is self-correcting. “If you’re not being ethical or contradicting yourself, putting out information that’s not accurate, people are going to catch on very quickly,” he said. “The only value, the only currency you have on social media is the trust that you build with people that follow you.”
What it takes to be a TikTokker
For dermatologists, conveying their credentials and experience is one way to build that currency. Dr. Lee advised fellow doctors on TikTok to “showcase your training and how many years it took to become a dermatologist.”
Plunging into TikTok is not for everyone, though. It’s time consuming, said Dr. Lee, who now devotes most of her nonclinical time to TikTok. She creates her own content, leaving others to manage her Instagram account.
Many of those in the medical field who have dived into TikTok are residents, like Dr. Shah. “They are attuned to it and understand it more,” said Dr. Lee. “It’s harder for a lot of us who are older, who really weren’t involved that much in social media at all. It’s very hard to jump in.” There’s a learning curve, and it takes hours to create a single video. “You have to enjoy it and it has to be a part of your life,” she said.
Dr. Shah started experimenting with TikTok at the beginning of the pandemic in 2020 and has never turned back. Fast-talking, curious, and with an infectious sense of fun, he shares tidbits about his personal life – putting his wife in some of his videos – and always seems upbeat.
He said that, as his following grew, users began to see him as an authority figure and started “tagging” him more often, seeking his opinion on other videos. Although still a resident, he believes he has specialized knowledge to share. “Even if you’re not the world’s leading expert in a particular topic, you’re still adding value for the person who doesn’t know much.”
Dr. Shah also occasionally does promotional TikToks, identified as sponsored content. He said he only works with companies that he believes have legitimate products. “You do have to monetize at some point,” he said, noting that many dermatologists, himself included, are trading clinic time for TikTok. “There’s no universe where they can do this for free.”
Product endorsements are likely more rewarding for influencers and other users like Dr. Shah than the remuneration from TikTok, the company. The platform pays user accounts $20 per 1 million views, Dr. Shah said. “Financially, it’s not a big winner for a practicing dermatologist, but the educational outreach is worthwhile.”
To be successful also means understanding what drives viewership.
Using “trending” sounds has “been shown to increase the likelihood of a video amassing millions of views” and may increase engagement with dermatologists’ TikTok videos, wrote Bina Kassamali, BA, and colleagues at the Brigham and Women’s Hospital in Boston and the Ponce Health Science University School of Medicine in Ponce, Puerto Rico, in a letter published in the Journal of the American Academy of Dermatology in July 2021.
Certain content is more likely to engage viewers. In their analysis of top trending dermatologic hashtags, acne-related content was viewed 6.7 billion times, followed by alopecia, with 1.1 billion views. Psoriasis content had 84 million views, putting it eighth on the list of topics.
Dermatologists are still cracking TikTok. They are accumulating more followers on TikTok than on Instagram but have greater engagement on Instagram reels, wrote Mindy D. Szeto, MS, and colleagues at the University of Colorado at Denver, Aurora, and Rocky Vista University in Parker, Colo., in the Journal of the American Academy of Dermatology in April 2021.
Dr. Lee and Dr. Shah had the highest engagement rate on TikTok, according to Ms. Szeto. The engagement rate is calculated as (likes + comments per post)/(total followers) x 100.
“TikTok may currently be the leading avenue for audience education by dermatologist influencers,” they wrote, urging dermatologists to use the platform to answer the call as more of the public “continues to turn to social media for medical advice.”
Dr. Day said she will keep trying to build her TikTok audience. She has just 239 followers, compared with her 44,500 on Instagram. “The more I do TikTok, the more I do any of these mediums, the better I get at it,” she said. “We just have to put a little time and effort into it and try to get more followers and just keep sharing the information.”
Dr. Friedman sees it as a positive that some dermatologists have taken to TikTok to dispel myths and put “good information out there in small bites.” But to be more effective, they need more followers.
“The truth is that 14-year-old is probably going to listen more to a Hyram than a dermatologist,” he said. “Maybe we need to work with these other individuals who know how to take these messages and convert them to a language that can be digested by a 14-year-old, by a 12-year-old, by a 23-year-old. We need to come to the table together and not fight.”
A version of this article first appeared on Medscape.com.
A young woman is having her lip swabbed with an unknown substance, smiling, on the TikTok video. Seconds later, another young woman, wearing gloves, pushes a hyaluron pen against the first woman’s lips, who, in the next cut, is smiling, happy. “My first syringe down and already 1,000x more confident,” the caption reads.
That video is one of thousands showing hyaluron pen use on TikTok. The pens are sold online and are unapproved – which led to a Food and Drug Administration warning in October 2021 that use could cause bleeding, infection, blood vessel occlusion that could result in blindness or stroke, allergic reactions, and other injuries.
The warning has not stopped many TikTokkers, who also use the medium to promote all sorts of skin and aesthetic products and procedures, a large number unproven, unapproved, or ill advised. which, more often than not, comes from “skinfluencers,” aestheticians, and other laypeople, not board-certified dermatologists.
The suggested “hacks” can be harmless or ineffective, but they also can be misleading, fraudulent, or even dangerous.
Skinfluencers take the lead
TikTok has a reported 1 billion monthly users. Two-thirds are aged 10-29 years, according to data reported in February 2021 in the Journal of the American Academy of Dermatology by David X. Zheng, BA, and colleagues at Case Western Reserve University, Cleveland, and the department of dermatology, Johns Hopkins University, Baltimore.
Visitors consume information in video bits that run from 15 seconds to up to 3 minutes and can follow their favorite TikTokkers, browse for people or hashtags with a search function, or click on content recommended by the platform, which uses algorithms based on the user’s viewing habits to determine what might be of interest.
Some of the biggest “skinfluencers” have millions of followers: Hyram Yarbro, (@skincarebyhyram) for instance, has 6.6 million followers and his own line of skin care products at Sephora. Mr. Yarbro is seen as a no-nonsense debunker of skin care myths, as is British influencer James Welsh, who has 124,000 followers.
“The reason why people trust your average influencer person who’s not a doctor is because they’re relatable,” said Muneeb Shah, MD, a dermatology resident at Atlantic Dermatology in Wilmington, N.C. – known to his 11.4 million TikTok followers as @dermdoctor.
To Sandra Lee, MD, the popularity of nonprofessionals is easy to explain. “You have to think about the fact that a lot of people can’t see dermatologists – they don’t have the money, they don’t have the time to travel there, they don’t have health insurance, or they’re scared of doctors, so they’re willing to try to find an answer, and one of the easiest ways, one of the more entertaining ways to get information, is on social media.”
Dr. Lee is in private practice in Upland, Calif., but is better known as “Dr. Pimple Popper,” through her television show of the same name and her social media accounts, including on TikTok, where she has 14.4 million followers after having started in 2020.
“We’re all looking for that no-down-time, no-expense, no-lines, no-wrinkles, stay-young-forever magic bullet,” said Dr. Lee.
Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, agreed that people are looking for a quick fix. They don’t want to wait 12 weeks for an acne medication or 16 weeks for a biologic to work. “They want something simple, easy, do-it-yourself,” and “natural,” he said.
Laypeople are still the dominant producers – and have the most views – of dermatology content.
Morgan Nguyen, BA, at Northwestern University, Chicago, and colleagues looked at hashtags for the top 10 dermatologic diagnoses and procedures and analyzed the content of the first 40 TikTok videos in each category. About half the videos were produced by an individual, and 39% by a health care provider, according to the study, published in the International Journal of Women’s Dermatology. About 40% of the videos were educational, focusing on skin care, procedures, and disease treatment.
Viewership was highest for videos by laypeople, followed by those produced by business or industry accounts. Those produced by health care providers received only 18% of the views.
The most popular videos were about dermatologic diagnoses, with 2.5 billion views, followed by dermatologic procedures, with 708 million views.
Ms. Nguyen noted in the study that the most liked and most viewed posts were related to #skincare but that board-certified dermatologists produced only 2.5% of the #skincare videos.
Dermatologists take to TikTok
Some dermatologists have started their own TikTok accounts, seeking both to counteract misinformation and provide education.
Dr. Shah has become one of the top influencers on the platform. In a year-end wrap, TikTok put Dr. Shah at No. 7 on its top creators list for 2021.
The dermatology resident said that TikTok is a good tool for reaching patients who might not otherwise interact with dermatologists. He recounted the story of an individual who came into his office with the idea that they had hidradenitis suppurativa.
The person had self-diagnosed after seeing one of Dr. Shah’s TikTok videos on the condition. It was a pleasant surprise, said Dr. Shah. People with hidradenitis suppurativa often avoid treatment, and it’s underdiagnosed and improperly treated, despite an American Academy of Dermatology awareness campaign.
“Dermatologists on social media are almost like the communications department for dermatology,” Dr. Shah commented.
A key to making TikTok work to advance dermatologists’ goals is knowing what makes it unique.
Dr. Lee said she prefers it to Instagram, because TikTok’s algorithms and its younger-skewing audience help her reach a more specific audience.
The algorithm “creates a positive feedback loop in which popular content creators or viral trends are prioritized on the users’ homepages, in turn providing the creators of these videos with an even larger audience,” Mr. Zheng, of University Hospitals Cleveland Medical Center, and coauthors noted in their letter in the Journal of the American Academy of Dermatology.
TikTok also celebrates the everyday – someone doesn’t have to be a celebrity to make something go viral, said Dr. Lee. She believes that TikTok users are more accepting of average people with real problems – which helps when someone is TikTokking about a skin condition.
Doris Day, MD, who goes by @drdorisday on TikTok, agreed with Dr. Lee. “There are so many creative ways you can convey information with it that’s different than what you have on Instagram,” said Dr. Day, who is in private practice in New York. And, she added, “it does really lend itself to getting points out super-fast.”
Dermatologists on TikTok also said they like the “duets” and the “stitch” features, which allow users to add on to an existing video, essentially chiming in or responding to what might have already been posted, in a side-by-side format.
Dr. Shah said he often duets videos that have questionable content. “It allows me to directly respond to people. A lot of times, if something is going really viral and it’s not accurate, you’ll have a response from me or one of the other doctors” within hours or days.
Dr. Shah’s duets are labeled with “DermDoctor Reacts” or “DermDoctor Explains.” In one duet, with more than 2.8 million views, the upper half of the video is someone squeezing a blackhead, while Dr. Shah, in the bottom half, in green scrubs, opines over some hip-hop music: “This is just a blackhead. But once it gets to this point, they do need to be extracted because topical treatments won’t help.”
Dr. Lee – whose TikTok and other accounts capitalize on teens’ obsession with popping pimples – has a duet in which she advised that although popping will leave scars, there are more ideal times to pop, if they must. The duet has at least 21 million views.
Sometimes a TikTok video effectively takes on a trend without being a duet. Nurse practitioner Uy Dam (@uy.np) has a video that demonstrates the dangers of hyaluron pens. He uses both a pen and a needle to inject fluid into a block of jello. The pen delivers a scattershot load of differing depths, while the needle is exact. It’s visual and easy to understand and has at least 1.3 million views.
Still, TikTok, like other forms of social media, is full of misinformation and false accounts, including people who claim to be doctors. “It’s hard for the regular person, myself included, sometimes to be able to root through that and find out whether something is real or not,” said Dr. Lee.
Dr. Friedman said he’s concerned about the lack of accountability. A doctor could lose his or her license for promoting unproven cures, especially if they are harmful. But for influencers, “there’s no accountability for posting information that can actually hurt people.”
TikTok trends gone bad
And some people are being hurt by emulating what they see on TikTok.
Dr. Friedman had a patient with extreme irritant contact dermatitis, “almost like chemical burns to her underarms,” he said. He determined that she saw a video “hack” that recommended using baking soda to stop hyperhidrosis. The patient used so much that it burned her skin.
In 2020, do-it-yourself freckles – with henna or sewing needles impregnated with ink – went viral. Tilly Whitfeld, a 21-year-old reality TV star on Australia’s Big Brother show, told the New York Times that she tried it at home after seeing a TikTok video. She ordered brown tattoo ink online and later found out that it was contaminated with lead, according to the Times. Ms. Whitfeld developed an infection and temporary vision loss and has permanent scarring.
She has since put out a cautionary TikTok video that’s been viewed some 300,000 times.
TikTokkers have also flocked to the idea of using sunscreen to “contour” the face. Selected areas are left without sunscreen to burn or tan. In a duet, a plastic surgeon shakes his head as a young woman explains that “it works.”
Scalp-popping – in which the hair is yanked so hard that it pulls the galea off the skull – has been mostly shut down by TikTok. A search of “scalp popping” brings up the message: “Learn how to recognize harmful challenges and hoaxes.” At-home mole and skin tag removal, pimple-popping, and supposed acne cures such as drinking chlorophyll are all avidly documented and shared on TikTok.
Dr. Shah had a back-and-forth video dialog with someone who had stubbed a toe and then drilled a hole into the nail to drain the hematoma. In a reaction video, Dr. Shah said it was likely to turn into an infection. When it did, the man revealed the infection in a video where he tagged Dr. Shah and later posted a video at the podiatrist’s office having his nail removed, again tagging Dr. Shah.
“I think that pretty much no procedure for skin is good to do at home,” said Dr. Shah, who repeatedly admonishes against mole removal by a nonphysician. He tells followers that “it’s extremely dangerous – not only is it going to cause scarring, but you are potentially discarding a cancerous lesion.”
Unfortunately, most will not follow the advice, said Dr. Shah. That’s especially true of pimple-popping. Aiming for the least harm, he suggests in some TikTok videos that poppers keep the area clean, wear gloves, and consult a physician to get an antibiotic prescription. “You might as well at least guide them in the right direction,” he added.
Dr. Lee believes that lack of access to physicians, insurance, or money may play into how TikTok trends evolve. “Probably those people who injected their lips with this air gun thing, maybe they didn’t have the money necessarily to get filler,” she said.
Also, she noted, while TikTok may try to police its content, creators are incentivized to be outrageous. “The more inflammatory your post is, the more engagement you get.”
Dr. Shah thinks TikTok is self-correcting. “If you’re not being ethical or contradicting yourself, putting out information that’s not accurate, people are going to catch on very quickly,” he said. “The only value, the only currency you have on social media is the trust that you build with people that follow you.”
What it takes to be a TikTokker
For dermatologists, conveying their credentials and experience is one way to build that currency. Dr. Lee advised fellow doctors on TikTok to “showcase your training and how many years it took to become a dermatologist.”
Plunging into TikTok is not for everyone, though. It’s time consuming, said Dr. Lee, who now devotes most of her nonclinical time to TikTok. She creates her own content, leaving others to manage her Instagram account.
Many of those in the medical field who have dived into TikTok are residents, like Dr. Shah. “They are attuned to it and understand it more,” said Dr. Lee. “It’s harder for a lot of us who are older, who really weren’t involved that much in social media at all. It’s very hard to jump in.” There’s a learning curve, and it takes hours to create a single video. “You have to enjoy it and it has to be a part of your life,” she said.
Dr. Shah started experimenting with TikTok at the beginning of the pandemic in 2020 and has never turned back. Fast-talking, curious, and with an infectious sense of fun, he shares tidbits about his personal life – putting his wife in some of his videos – and always seems upbeat.
He said that, as his following grew, users began to see him as an authority figure and started “tagging” him more often, seeking his opinion on other videos. Although still a resident, he believes he has specialized knowledge to share. “Even if you’re not the world’s leading expert in a particular topic, you’re still adding value for the person who doesn’t know much.”
Dr. Shah also occasionally does promotional TikToks, identified as sponsored content. He said he only works with companies that he believes have legitimate products. “You do have to monetize at some point,” he said, noting that many dermatologists, himself included, are trading clinic time for TikTok. “There’s no universe where they can do this for free.”
Product endorsements are likely more rewarding for influencers and other users like Dr. Shah than the remuneration from TikTok, the company. The platform pays user accounts $20 per 1 million views, Dr. Shah said. “Financially, it’s not a big winner for a practicing dermatologist, but the educational outreach is worthwhile.”
To be successful also means understanding what drives viewership.
Using “trending” sounds has “been shown to increase the likelihood of a video amassing millions of views” and may increase engagement with dermatologists’ TikTok videos, wrote Bina Kassamali, BA, and colleagues at the Brigham and Women’s Hospital in Boston and the Ponce Health Science University School of Medicine in Ponce, Puerto Rico, in a letter published in the Journal of the American Academy of Dermatology in July 2021.
Certain content is more likely to engage viewers. In their analysis of top trending dermatologic hashtags, acne-related content was viewed 6.7 billion times, followed by alopecia, with 1.1 billion views. Psoriasis content had 84 million views, putting it eighth on the list of topics.
Dermatologists are still cracking TikTok. They are accumulating more followers on TikTok than on Instagram but have greater engagement on Instagram reels, wrote Mindy D. Szeto, MS, and colleagues at the University of Colorado at Denver, Aurora, and Rocky Vista University in Parker, Colo., in the Journal of the American Academy of Dermatology in April 2021.
Dr. Lee and Dr. Shah had the highest engagement rate on TikTok, according to Ms. Szeto. The engagement rate is calculated as (likes + comments per post)/(total followers) x 100.
“TikTok may currently be the leading avenue for audience education by dermatologist influencers,” they wrote, urging dermatologists to use the platform to answer the call as more of the public “continues to turn to social media for medical advice.”
Dr. Day said she will keep trying to build her TikTok audience. She has just 239 followers, compared with her 44,500 on Instagram. “The more I do TikTok, the more I do any of these mediums, the better I get at it,” she said. “We just have to put a little time and effort into it and try to get more followers and just keep sharing the information.”
Dr. Friedman sees it as a positive that some dermatologists have taken to TikTok to dispel myths and put “good information out there in small bites.” But to be more effective, they need more followers.
“The truth is that 14-year-old is probably going to listen more to a Hyram than a dermatologist,” he said. “Maybe we need to work with these other individuals who know how to take these messages and convert them to a language that can be digested by a 14-year-old, by a 12-year-old, by a 23-year-old. We need to come to the table together and not fight.”
A version of this article first appeared on Medscape.com.
Acid series: Azelaic acid
However, it has many positive qualities, including being gentle enough to use daily and is safe to use in pregnancy. It is antibacterial, comedolytic, keratolytic, and has antioxidant activity. Unfortunately, in the last decade the formulations of azelaic acid have not been changed considerably. The 20% cream, 15% gel, and 15% foam vehicles are often too irritating and drying to be used in the population it is intended for: those with rosacea, or with inflamed or sensitive skin.
Azelaic acid is a dicarboxylic acid produced by Pityrosporum ovale. It inhibits the synthesis of cellular proteins and is bactericidal against Propionibacterium acnes and Staphylococcus epidermidis. Azelaic acid is both keratolytic and comedolytic by decreasing keratohyalin granules and reducing filaggrin in the epidermis. It not only scavenges free oxygen radicals, thereby reducing inflammation, but is also a tyrosinase inhibitor – making it a safe, non–hydroquinone-based alternative to skin lightening.
Azelaic acid has little toxicity, it is ingested regularly as it is found in wheat, barley, and rye. Topical side effects are usually mild and can subside with increased use. The most common side effects include erythema, local stinging, pruritus, scaling, and a burning sensation. It is considered safe in pregnancy and a great alternative to medications for acne in pregnant or nursing patients.
The largest constraint with azelaic acid preparations on the market – and most likely the reason it has not been more widely used for acne, rosacea, antiaging, and hyperpigmentation – is the formulation. The foam and gel preparations are irritating and difficult to use on dry or sensitive skin. The 20% cream preparations are slightly better tolerated; however, in vitro skin-penetration studies have shown that cutaneous penetration of azelaic acid is greater after application of a 15% gel (aqueous-based vehicle) and 15% foam (hydrophilic oil-in-water emulsion) as compared with the 20% cream formulations.
In my clinical experience, azelaic acid can only be used in rosacea patients with oily or nonsensitive skin. The majority of my rosacea patients cannot tolerate the burning sensation, albeit transient and mild. Acne patients who do not have dry skin and pregnant patients with mild acne are a great population for integrating azelaic acid into an acne regimen. I also use azelaic acid as an alternative for mild melasma and lentigines in patients who are tapering off hydroquinone or cannot use hydroquinone. In the future, we need better, creamier, nonirritating formulations to be developed and more studies of higher concentrations of this acid for both prescription/patient at-home use, as well as more elegant in-office localized peel systems using azelaic acid.
Dr. Talakoub and Dr. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Fitton A and Goa KL. Drugs. 1991 May;41(5):780-98.
Del Rosso JQ. J Clin Aesthet Dermatol. 2017 Mar;10(3):37-40.
Breathnach AC et al. Clin Dermatol. Apr-Jun 1989;7(2):106-19.
However, it has many positive qualities, including being gentle enough to use daily and is safe to use in pregnancy. It is antibacterial, comedolytic, keratolytic, and has antioxidant activity. Unfortunately, in the last decade the formulations of azelaic acid have not been changed considerably. The 20% cream, 15% gel, and 15% foam vehicles are often too irritating and drying to be used in the population it is intended for: those with rosacea, or with inflamed or sensitive skin.
Azelaic acid is a dicarboxylic acid produced by Pityrosporum ovale. It inhibits the synthesis of cellular proteins and is bactericidal against Propionibacterium acnes and Staphylococcus epidermidis. Azelaic acid is both keratolytic and comedolytic by decreasing keratohyalin granules and reducing filaggrin in the epidermis. It not only scavenges free oxygen radicals, thereby reducing inflammation, but is also a tyrosinase inhibitor – making it a safe, non–hydroquinone-based alternative to skin lightening.
Azelaic acid has little toxicity, it is ingested regularly as it is found in wheat, barley, and rye. Topical side effects are usually mild and can subside with increased use. The most common side effects include erythema, local stinging, pruritus, scaling, and a burning sensation. It is considered safe in pregnancy and a great alternative to medications for acne in pregnant or nursing patients.
The largest constraint with azelaic acid preparations on the market – and most likely the reason it has not been more widely used for acne, rosacea, antiaging, and hyperpigmentation – is the formulation. The foam and gel preparations are irritating and difficult to use on dry or sensitive skin. The 20% cream preparations are slightly better tolerated; however, in vitro skin-penetration studies have shown that cutaneous penetration of azelaic acid is greater after application of a 15% gel (aqueous-based vehicle) and 15% foam (hydrophilic oil-in-water emulsion) as compared with the 20% cream formulations.
In my clinical experience, azelaic acid can only be used in rosacea patients with oily or nonsensitive skin. The majority of my rosacea patients cannot tolerate the burning sensation, albeit transient and mild. Acne patients who do not have dry skin and pregnant patients with mild acne are a great population for integrating azelaic acid into an acne regimen. I also use azelaic acid as an alternative for mild melasma and lentigines in patients who are tapering off hydroquinone or cannot use hydroquinone. In the future, we need better, creamier, nonirritating formulations to be developed and more studies of higher concentrations of this acid for both prescription/patient at-home use, as well as more elegant in-office localized peel systems using azelaic acid.
Dr. Talakoub and Dr. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Fitton A and Goa KL. Drugs. 1991 May;41(5):780-98.
Del Rosso JQ. J Clin Aesthet Dermatol. 2017 Mar;10(3):37-40.
Breathnach AC et al. Clin Dermatol. Apr-Jun 1989;7(2):106-19.
However, it has many positive qualities, including being gentle enough to use daily and is safe to use in pregnancy. It is antibacterial, comedolytic, keratolytic, and has antioxidant activity. Unfortunately, in the last decade the formulations of azelaic acid have not been changed considerably. The 20% cream, 15% gel, and 15% foam vehicles are often too irritating and drying to be used in the population it is intended for: those with rosacea, or with inflamed or sensitive skin.
Azelaic acid is a dicarboxylic acid produced by Pityrosporum ovale. It inhibits the synthesis of cellular proteins and is bactericidal against Propionibacterium acnes and Staphylococcus epidermidis. Azelaic acid is both keratolytic and comedolytic by decreasing keratohyalin granules and reducing filaggrin in the epidermis. It not only scavenges free oxygen radicals, thereby reducing inflammation, but is also a tyrosinase inhibitor – making it a safe, non–hydroquinone-based alternative to skin lightening.
Azelaic acid has little toxicity, it is ingested regularly as it is found in wheat, barley, and rye. Topical side effects are usually mild and can subside with increased use. The most common side effects include erythema, local stinging, pruritus, scaling, and a burning sensation. It is considered safe in pregnancy and a great alternative to medications for acne in pregnant or nursing patients.
The largest constraint with azelaic acid preparations on the market – and most likely the reason it has not been more widely used for acne, rosacea, antiaging, and hyperpigmentation – is the formulation. The foam and gel preparations are irritating and difficult to use on dry or sensitive skin. The 20% cream preparations are slightly better tolerated; however, in vitro skin-penetration studies have shown that cutaneous penetration of azelaic acid is greater after application of a 15% gel (aqueous-based vehicle) and 15% foam (hydrophilic oil-in-water emulsion) as compared with the 20% cream formulations.
In my clinical experience, azelaic acid can only be used in rosacea patients with oily or nonsensitive skin. The majority of my rosacea patients cannot tolerate the burning sensation, albeit transient and mild. Acne patients who do not have dry skin and pregnant patients with mild acne are a great population for integrating azelaic acid into an acne regimen. I also use azelaic acid as an alternative for mild melasma and lentigines in patients who are tapering off hydroquinone or cannot use hydroquinone. In the future, we need better, creamier, nonirritating formulations to be developed and more studies of higher concentrations of this acid for both prescription/patient at-home use, as well as more elegant in-office localized peel systems using azelaic acid.
Dr. Talakoub and Dr. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Fitton A and Goa KL. Drugs. 1991 May;41(5):780-98.
Del Rosso JQ. J Clin Aesthet Dermatol. 2017 Mar;10(3):37-40.
Breathnach AC et al. Clin Dermatol. Apr-Jun 1989;7(2):106-19.
Moisturizers and skin barrier repair
There are dozens of skin care products that claim to repair the barrier that do not have the science or ingredient content to back them up.
Does a skin barrier repair moisturizer really repair?
First, let’s briefly review what the skin barrier is. The stratum corneum (SC), the most superficial layer of the epidermis, averages approximately 15-cell layers in thickness.1,2 The keratinocytes reside there in a pattern resembling a brick wall. The “mortar” is composed of the lipid contents extruded from the lamellar granules. This protective barrier functions to prevent transepidermal water loss (TEWL) and entry of allergens, irritants, and pathogens into deeper layers of the skin. This column will focus briefly on the structure and function of the skin barrier and the barrier repair technologies that use synthetic lipids such as myristoyl-palmitoyl and myristyl/palmityl-oxo-stearamide/arachamide MEA.
Structure of the skin barrier
SC keratinocytes are surrounded by lamella made from lipid bilayers. The lipids have hydrophilic heads and hydrophobic tails; the bilayer arises when the hydrophobic tails face the center and the hydrophilic heads face out of the bilayer. This formation yields a disc-shaped hydrophobic lamellar center. There are actually several of these lamellar layers between keratinocytes.
The naturally occurring primary lipids of the bilayer lamellae are made up of an equal ratio of ceramides, cholesterol, and free fatty acid. Arranged in a 1:1:1 ratio, they fit together like pieces of a puzzle to achieve skin barrier homeostasis. The shape and size of these puzzle pieces is critical. An incorrect shape results in a hole in the skin barrier resulting in dehydration, inflammation, and sensitivity.
Ceramides
Ceramides are a complex family of lipids (sphingolipids – a sphingoid base and a fatty acid) involved in cell, as well as barrier, homeostasis and water-holding capacity. In fact, they are known to play a crucial role in cell proliferation, differentiation, and apoptosis.3 There are at least 16 types of naturally occurring ceramides. For years, they have been included in barrier repair moisturizers. They are difficult to work with in moisturizers for several reasons:
- Ceramides are abundant in brain tissue and the ceramides used in moisturizers in the past were derived from bovine brain tissue. Prior to the emergence of bovine spongiform encephalopathy (mad cow disease), many ceramides in skin-care products were animal derived, which made them expensive and undesirable.
- Ceramides in skin care that are made from plant sources are referred to as phyto-derived ceramides. Although they share a similar structure with ceramides that occur in human skin, there are differences in chain length, hydroxylation pattern, and the degree of unsaturation that lead to structural diversity.4 The shape of ceramides is critical for a strong skin barrier because the lipids in the skin barrier must fit together like puzzle pieces to form a water-tight barrier. Natural sources of ceramides include rice, wheat, potato, konjac, and maize. Standardization of ceramide shape and structure makes using phyto-derived ceramides in skin care products challenging.
- Ceramides, because of their waxy consistency, require heat during the mixing process of skin care product manufacturing. This heat can make other ingredients inactive in the skin care formulation. (Ceramides are typically added early in the formulation process, and the heat-sensitive ones are added later.)
- Many forms of ceramides are unstable in the product manufacturing and bottling processes.
- Skin penetration of ceramides depends on the shape and size of ceramides.
Synthetic ceramides have been developed to make ceramides safe, affordable, and more easily formulated into moisturizers. These formulations synthesized in the lab are sometimes called pseudoceramides because they are structurally different compounds that mimic the activity of ceramides. They are developed to be less expensive to manufacture, safer than those derived from animals, and easier to formulate, and they can be made into the specific shape of the ceramide puzzle piece.
Ceramides in skin care
The naturally occurring intercellular lipids of the SC are composed of approximately equal proportions of ceramides, cholesterol, and fatty acids (referred to in this article as the “three barrier lipids” for simplicity).5-9 Alterations in any of these three barrier lipids or their regulatory enzymes result in impairments in the function of the epidermal barrier. Therefore, any synthetic ceramide must mimic the shape of natural ceramides, or the three barrier lipids in the moisturizer must mimic the shape of the entire bilayer lamella. Unfortunately, most barrier repair moisturizers do not meet these criteria and are not true barrier repair moisturizers.
How do you know if a moisturizer repairs the skin barrier?
Clinical tests such as measuring transepidermal water loss (TEWL) with a Tewameter are usually done to support the barrier repair claim. However, occlusive ingredients like oils can lower TEWL without affecting the barrier. In fact, we believe that sebum on the skin can make an impaired barrier and result in normal TEWL even when the barrier is impaired. So, just because a product improved TEWL does not necessarily mean that it repairs the barrier.
One way to test the ability of a moisturizer to repair the barrier is to look at a structural analysis of the moisturizer to see if it forms the requisite bilayer lamellar shape. An easy way to do this testing is to look for the cross pattern under a cross polarized microscope. The cross pattern is known as optical anisotropy. 8
The best barrier repair creams
Optimal barrier repair creams either feature a 1:1:1 ratio of epidermal lipids or form a cross structure when viewed with a cross-polarized microscope.8 There are several categories of barrier repair moisturizers that meet these criteria.
Barrier repair creams with a 1:1:1 ratio of lipids:
Peter Elias, MD, holds the patent on barrier repair moisturizer technology that has a 1:1:1 ratio. His well-established technology is used in a prescription barrier repair cream called EpiCeram® which is approved by the Food and Drug Administration to treat eczema. There are no other moisturizers that I know of that contain this 1:1:1 lipid ratio.
There is a barrier repair cream on the market that contains a 2:4:2 ratio of lipids based on a study that showed that this ratio is effective in older skin with an impaired barrier. It is unknown if this moisturizer forms a cross pattern.
Barrier repair creams that demonstrate a cross pattern:
Multilamellar emulsion (MLE) technology: This barrier repair technology, invented in South Korea, contains the synthetic pseudoceramide called myristyl/palmityl-oxo-stearamide/arachamide MEA (C34H67NO3/C36H71NO3/C38H75NO3), or the pseudoceramide myristoyl-palmitoyl-oxostearamide-arachamide MEA.
In a 2019 pilot study by Ye and colleagues, the investigators treated 33 older volunteers twice daily for 30 days with approximately 3 mL of an emollient containing MLE technology. In addition, 30 untreated older subjects and 11 young volunteers served as controls. The investigators found that the topically applied barrier repair emollient significantly improved barrier function, as well as stratum corneum hydration. Circulating levels of the important, age-related plasma cytokines interleukin-1 beta and IL-6 were found to have normalized, while tumor necrosis factor–alpha decreased markedly. The investigators suggested that repair of the skin barrier might diminish circulating proinflammatory cytokine levels (such as amyloid A) in aged humans, potentially mitigating the development of chronic inflammatory conditions.10
MLE technology has also been shown to improve childhood atopic dermatitis and prevent steroid atrophy.11,12 The consistent use of MLE technology in moisturizers has been shown to alleviate inflammatory factors in the blood and is believed to lessen systemic inflammation.10
Physiologic (PSL) lipid repair technology: This technology was invented by one of the South Korean researchers who helped develop MLE technology. It contains pseudoceramides, fatty acids, and cholesterol. The figure of the cross pattern above, as seen under the cross polarized microscope, is an image taken of this PSL lipid repair technology.
Conclusion
Do not believe that a moisturizer repairs the barrier just because it says so on the label. Three of the most popular body moisturizes used to treat eczema do not actually have the proper formula to repair the barrier. Unfortunately, there are dozens of skin care products that claim to repair the barrier that do not have the science or ingredient content to back them up. To restore the skin barrier to a healthy condition, it is imperative that the barrier repair moisturizers that you are recommending for patients have the correct 1:1:1 ratio of epidermal lipids or contain bilayer lamella that mimic the natural multilamellar layers and display the cross pattern under a cross-polarized microscope.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions, a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Christophers E and Kligman AM. J Invest Dermatol. 1964;42:407-9.
2. Blair C. Br J Dermatol. 1968;80(7):430-6.
3. Morita O et al. Food Chem Toxicol. 2009 Apr;47(4):681-6.
4. Tessema E N et al. Skin pharmacology and physiology. 2017;30(3):115-38.
5. Coderch L et al. Am J Clin Dermatol. 2003;4(2):107-29.
6. Man MQ et al. Arch Dermatol. 1993;129(6):728-38.
7. Man MQ M et al. J Invest Dermatol. 1996 May;106(5):1096-101.
8. Park BD et al. J Invest Dermatol. 2003;121(4):794-801.
9. Proksch E and Jensen J. Skin as an organ of protection, in “Fitzpatrick’s Dermatology in General Medicine,” 7th ed. New York: McGraw-Hill, 2008, pp. 383-95.
10. Ye L et al. J Eur Acad Dermatol Venereol. 2019;33(11):2197-201.
11. Lee EJ et al. Ann Dermatol. 2003;15(4):133-8.
12. Ahn SK et al. J Dermatol. 2006;33(2):80-90.
There are dozens of skin care products that claim to repair the barrier that do not have the science or ingredient content to back them up.
Does a skin barrier repair moisturizer really repair?
First, let’s briefly review what the skin barrier is. The stratum corneum (SC), the most superficial layer of the epidermis, averages approximately 15-cell layers in thickness.1,2 The keratinocytes reside there in a pattern resembling a brick wall. The “mortar” is composed of the lipid contents extruded from the lamellar granules. This protective barrier functions to prevent transepidermal water loss (TEWL) and entry of allergens, irritants, and pathogens into deeper layers of the skin. This column will focus briefly on the structure and function of the skin barrier and the barrier repair technologies that use synthetic lipids such as myristoyl-palmitoyl and myristyl/palmityl-oxo-stearamide/arachamide MEA.
Structure of the skin barrier
SC keratinocytes are surrounded by lamella made from lipid bilayers. The lipids have hydrophilic heads and hydrophobic tails; the bilayer arises when the hydrophobic tails face the center and the hydrophilic heads face out of the bilayer. This formation yields a disc-shaped hydrophobic lamellar center. There are actually several of these lamellar layers between keratinocytes.
The naturally occurring primary lipids of the bilayer lamellae are made up of an equal ratio of ceramides, cholesterol, and free fatty acid. Arranged in a 1:1:1 ratio, they fit together like pieces of a puzzle to achieve skin barrier homeostasis. The shape and size of these puzzle pieces is critical. An incorrect shape results in a hole in the skin barrier resulting in dehydration, inflammation, and sensitivity.
Ceramides
Ceramides are a complex family of lipids (sphingolipids – a sphingoid base and a fatty acid) involved in cell, as well as barrier, homeostasis and water-holding capacity. In fact, they are known to play a crucial role in cell proliferation, differentiation, and apoptosis.3 There are at least 16 types of naturally occurring ceramides. For years, they have been included in barrier repair moisturizers. They are difficult to work with in moisturizers for several reasons:
- Ceramides are abundant in brain tissue and the ceramides used in moisturizers in the past were derived from bovine brain tissue. Prior to the emergence of bovine spongiform encephalopathy (mad cow disease), many ceramides in skin-care products were animal derived, which made them expensive and undesirable.
- Ceramides in skin care that are made from plant sources are referred to as phyto-derived ceramides. Although they share a similar structure with ceramides that occur in human skin, there are differences in chain length, hydroxylation pattern, and the degree of unsaturation that lead to structural diversity.4 The shape of ceramides is critical for a strong skin barrier because the lipids in the skin barrier must fit together like puzzle pieces to form a water-tight barrier. Natural sources of ceramides include rice, wheat, potato, konjac, and maize. Standardization of ceramide shape and structure makes using phyto-derived ceramides in skin care products challenging.
- Ceramides, because of their waxy consistency, require heat during the mixing process of skin care product manufacturing. This heat can make other ingredients inactive in the skin care formulation. (Ceramides are typically added early in the formulation process, and the heat-sensitive ones are added later.)
- Many forms of ceramides are unstable in the product manufacturing and bottling processes.
- Skin penetration of ceramides depends on the shape and size of ceramides.
Synthetic ceramides have been developed to make ceramides safe, affordable, and more easily formulated into moisturizers. These formulations synthesized in the lab are sometimes called pseudoceramides because they are structurally different compounds that mimic the activity of ceramides. They are developed to be less expensive to manufacture, safer than those derived from animals, and easier to formulate, and they can be made into the specific shape of the ceramide puzzle piece.
Ceramides in skin care
The naturally occurring intercellular lipids of the SC are composed of approximately equal proportions of ceramides, cholesterol, and fatty acids (referred to in this article as the “three barrier lipids” for simplicity).5-9 Alterations in any of these three barrier lipids or their regulatory enzymes result in impairments in the function of the epidermal barrier. Therefore, any synthetic ceramide must mimic the shape of natural ceramides, or the three barrier lipids in the moisturizer must mimic the shape of the entire bilayer lamella. Unfortunately, most barrier repair moisturizers do not meet these criteria and are not true barrier repair moisturizers.
How do you know if a moisturizer repairs the skin barrier?
Clinical tests such as measuring transepidermal water loss (TEWL) with a Tewameter are usually done to support the barrier repair claim. However, occlusive ingredients like oils can lower TEWL without affecting the barrier. In fact, we believe that sebum on the skin can make an impaired barrier and result in normal TEWL even when the barrier is impaired. So, just because a product improved TEWL does not necessarily mean that it repairs the barrier.
One way to test the ability of a moisturizer to repair the barrier is to look at a structural analysis of the moisturizer to see if it forms the requisite bilayer lamellar shape. An easy way to do this testing is to look for the cross pattern under a cross polarized microscope. The cross pattern is known as optical anisotropy. 8
The best barrier repair creams
Optimal barrier repair creams either feature a 1:1:1 ratio of epidermal lipids or form a cross structure when viewed with a cross-polarized microscope.8 There are several categories of barrier repair moisturizers that meet these criteria.
Barrier repair creams with a 1:1:1 ratio of lipids:
Peter Elias, MD, holds the patent on barrier repair moisturizer technology that has a 1:1:1 ratio. His well-established technology is used in a prescription barrier repair cream called EpiCeram® which is approved by the Food and Drug Administration to treat eczema. There are no other moisturizers that I know of that contain this 1:1:1 lipid ratio.
There is a barrier repair cream on the market that contains a 2:4:2 ratio of lipids based on a study that showed that this ratio is effective in older skin with an impaired barrier. It is unknown if this moisturizer forms a cross pattern.
Barrier repair creams that demonstrate a cross pattern:
Multilamellar emulsion (MLE) technology: This barrier repair technology, invented in South Korea, contains the synthetic pseudoceramide called myristyl/palmityl-oxo-stearamide/arachamide MEA (C34H67NO3/C36H71NO3/C38H75NO3), or the pseudoceramide myristoyl-palmitoyl-oxostearamide-arachamide MEA.
In a 2019 pilot study by Ye and colleagues, the investigators treated 33 older volunteers twice daily for 30 days with approximately 3 mL of an emollient containing MLE technology. In addition, 30 untreated older subjects and 11 young volunteers served as controls. The investigators found that the topically applied barrier repair emollient significantly improved barrier function, as well as stratum corneum hydration. Circulating levels of the important, age-related plasma cytokines interleukin-1 beta and IL-6 were found to have normalized, while tumor necrosis factor–alpha decreased markedly. The investigators suggested that repair of the skin barrier might diminish circulating proinflammatory cytokine levels (such as amyloid A) in aged humans, potentially mitigating the development of chronic inflammatory conditions.10
MLE technology has also been shown to improve childhood atopic dermatitis and prevent steroid atrophy.11,12 The consistent use of MLE technology in moisturizers has been shown to alleviate inflammatory factors in the blood and is believed to lessen systemic inflammation.10
Physiologic (PSL) lipid repair technology: This technology was invented by one of the South Korean researchers who helped develop MLE technology. It contains pseudoceramides, fatty acids, and cholesterol. The figure of the cross pattern above, as seen under the cross polarized microscope, is an image taken of this PSL lipid repair technology.
Conclusion
Do not believe that a moisturizer repairs the barrier just because it says so on the label. Three of the most popular body moisturizes used to treat eczema do not actually have the proper formula to repair the barrier. Unfortunately, there are dozens of skin care products that claim to repair the barrier that do not have the science or ingredient content to back them up. To restore the skin barrier to a healthy condition, it is imperative that the barrier repair moisturizers that you are recommending for patients have the correct 1:1:1 ratio of epidermal lipids or contain bilayer lamella that mimic the natural multilamellar layers and display the cross pattern under a cross-polarized microscope.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions, a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Christophers E and Kligman AM. J Invest Dermatol. 1964;42:407-9.
2. Blair C. Br J Dermatol. 1968;80(7):430-6.
3. Morita O et al. Food Chem Toxicol. 2009 Apr;47(4):681-6.
4. Tessema E N et al. Skin pharmacology and physiology. 2017;30(3):115-38.
5. Coderch L et al. Am J Clin Dermatol. 2003;4(2):107-29.
6. Man MQ et al. Arch Dermatol. 1993;129(6):728-38.
7. Man MQ M et al. J Invest Dermatol. 1996 May;106(5):1096-101.
8. Park BD et al. J Invest Dermatol. 2003;121(4):794-801.
9. Proksch E and Jensen J. Skin as an organ of protection, in “Fitzpatrick’s Dermatology in General Medicine,” 7th ed. New York: McGraw-Hill, 2008, pp. 383-95.
10. Ye L et al. J Eur Acad Dermatol Venereol. 2019;33(11):2197-201.
11. Lee EJ et al. Ann Dermatol. 2003;15(4):133-8.
12. Ahn SK et al. J Dermatol. 2006;33(2):80-90.
There are dozens of skin care products that claim to repair the barrier that do not have the science or ingredient content to back them up.
Does a skin barrier repair moisturizer really repair?
First, let’s briefly review what the skin barrier is. The stratum corneum (SC), the most superficial layer of the epidermis, averages approximately 15-cell layers in thickness.1,2 The keratinocytes reside there in a pattern resembling a brick wall. The “mortar” is composed of the lipid contents extruded from the lamellar granules. This protective barrier functions to prevent transepidermal water loss (TEWL) and entry of allergens, irritants, and pathogens into deeper layers of the skin. This column will focus briefly on the structure and function of the skin barrier and the barrier repair technologies that use synthetic lipids such as myristoyl-palmitoyl and myristyl/palmityl-oxo-stearamide/arachamide MEA.
Structure of the skin barrier
SC keratinocytes are surrounded by lamella made from lipid bilayers. The lipids have hydrophilic heads and hydrophobic tails; the bilayer arises when the hydrophobic tails face the center and the hydrophilic heads face out of the bilayer. This formation yields a disc-shaped hydrophobic lamellar center. There are actually several of these lamellar layers between keratinocytes.
The naturally occurring primary lipids of the bilayer lamellae are made up of an equal ratio of ceramides, cholesterol, and free fatty acid. Arranged in a 1:1:1 ratio, they fit together like pieces of a puzzle to achieve skin barrier homeostasis. The shape and size of these puzzle pieces is critical. An incorrect shape results in a hole in the skin barrier resulting in dehydration, inflammation, and sensitivity.
Ceramides
Ceramides are a complex family of lipids (sphingolipids – a sphingoid base and a fatty acid) involved in cell, as well as barrier, homeostasis and water-holding capacity. In fact, they are known to play a crucial role in cell proliferation, differentiation, and apoptosis.3 There are at least 16 types of naturally occurring ceramides. For years, they have been included in barrier repair moisturizers. They are difficult to work with in moisturizers for several reasons:
- Ceramides are abundant in brain tissue and the ceramides used in moisturizers in the past were derived from bovine brain tissue. Prior to the emergence of bovine spongiform encephalopathy (mad cow disease), many ceramides in skin-care products were animal derived, which made them expensive and undesirable.
- Ceramides in skin care that are made from plant sources are referred to as phyto-derived ceramides. Although they share a similar structure with ceramides that occur in human skin, there are differences in chain length, hydroxylation pattern, and the degree of unsaturation that lead to structural diversity.4 The shape of ceramides is critical for a strong skin barrier because the lipids in the skin barrier must fit together like puzzle pieces to form a water-tight barrier. Natural sources of ceramides include rice, wheat, potato, konjac, and maize. Standardization of ceramide shape and structure makes using phyto-derived ceramides in skin care products challenging.
- Ceramides, because of their waxy consistency, require heat during the mixing process of skin care product manufacturing. This heat can make other ingredients inactive in the skin care formulation. (Ceramides are typically added early in the formulation process, and the heat-sensitive ones are added later.)
- Many forms of ceramides are unstable in the product manufacturing and bottling processes.
- Skin penetration of ceramides depends on the shape and size of ceramides.
Synthetic ceramides have been developed to make ceramides safe, affordable, and more easily formulated into moisturizers. These formulations synthesized in the lab are sometimes called pseudoceramides because they are structurally different compounds that mimic the activity of ceramides. They are developed to be less expensive to manufacture, safer than those derived from animals, and easier to formulate, and they can be made into the specific shape of the ceramide puzzle piece.
Ceramides in skin care
The naturally occurring intercellular lipids of the SC are composed of approximately equal proportions of ceramides, cholesterol, and fatty acids (referred to in this article as the “three barrier lipids” for simplicity).5-9 Alterations in any of these three barrier lipids or their regulatory enzymes result in impairments in the function of the epidermal barrier. Therefore, any synthetic ceramide must mimic the shape of natural ceramides, or the three barrier lipids in the moisturizer must mimic the shape of the entire bilayer lamella. Unfortunately, most barrier repair moisturizers do not meet these criteria and are not true barrier repair moisturizers.
How do you know if a moisturizer repairs the skin barrier?
Clinical tests such as measuring transepidermal water loss (TEWL) with a Tewameter are usually done to support the barrier repair claim. However, occlusive ingredients like oils can lower TEWL without affecting the barrier. In fact, we believe that sebum on the skin can make an impaired barrier and result in normal TEWL even when the barrier is impaired. So, just because a product improved TEWL does not necessarily mean that it repairs the barrier.
One way to test the ability of a moisturizer to repair the barrier is to look at a structural analysis of the moisturizer to see if it forms the requisite bilayer lamellar shape. An easy way to do this testing is to look for the cross pattern under a cross polarized microscope. The cross pattern is known as optical anisotropy. 8
The best barrier repair creams
Optimal barrier repair creams either feature a 1:1:1 ratio of epidermal lipids or form a cross structure when viewed with a cross-polarized microscope.8 There are several categories of barrier repair moisturizers that meet these criteria.
Barrier repair creams with a 1:1:1 ratio of lipids:
Peter Elias, MD, holds the patent on barrier repair moisturizer technology that has a 1:1:1 ratio. His well-established technology is used in a prescription barrier repair cream called EpiCeram® which is approved by the Food and Drug Administration to treat eczema. There are no other moisturizers that I know of that contain this 1:1:1 lipid ratio.
There is a barrier repair cream on the market that contains a 2:4:2 ratio of lipids based on a study that showed that this ratio is effective in older skin with an impaired barrier. It is unknown if this moisturizer forms a cross pattern.
Barrier repair creams that demonstrate a cross pattern:
Multilamellar emulsion (MLE) technology: This barrier repair technology, invented in South Korea, contains the synthetic pseudoceramide called myristyl/palmityl-oxo-stearamide/arachamide MEA (C34H67NO3/C36H71NO3/C38H75NO3), or the pseudoceramide myristoyl-palmitoyl-oxostearamide-arachamide MEA.
In a 2019 pilot study by Ye and colleagues, the investigators treated 33 older volunteers twice daily for 30 days with approximately 3 mL of an emollient containing MLE technology. In addition, 30 untreated older subjects and 11 young volunteers served as controls. The investigators found that the topically applied barrier repair emollient significantly improved barrier function, as well as stratum corneum hydration. Circulating levels of the important, age-related plasma cytokines interleukin-1 beta and IL-6 were found to have normalized, while tumor necrosis factor–alpha decreased markedly. The investigators suggested that repair of the skin barrier might diminish circulating proinflammatory cytokine levels (such as amyloid A) in aged humans, potentially mitigating the development of chronic inflammatory conditions.10
MLE technology has also been shown to improve childhood atopic dermatitis and prevent steroid atrophy.11,12 The consistent use of MLE technology in moisturizers has been shown to alleviate inflammatory factors in the blood and is believed to lessen systemic inflammation.10
Physiologic (PSL) lipid repair technology: This technology was invented by one of the South Korean researchers who helped develop MLE technology. It contains pseudoceramides, fatty acids, and cholesterol. The figure of the cross pattern above, as seen under the cross polarized microscope, is an image taken of this PSL lipid repair technology.
Conclusion
Do not believe that a moisturizer repairs the barrier just because it says so on the label. Three of the most popular body moisturizes used to treat eczema do not actually have the proper formula to repair the barrier. Unfortunately, there are dozens of skin care products that claim to repair the barrier that do not have the science or ingredient content to back them up. To restore the skin barrier to a healthy condition, it is imperative that the barrier repair moisturizers that you are recommending for patients have the correct 1:1:1 ratio of epidermal lipids or contain bilayer lamella that mimic the natural multilamellar layers and display the cross pattern under a cross-polarized microscope.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions, a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Christophers E and Kligman AM. J Invest Dermatol. 1964;42:407-9.
2. Blair C. Br J Dermatol. 1968;80(7):430-6.
3. Morita O et al. Food Chem Toxicol. 2009 Apr;47(4):681-6.
4. Tessema E N et al. Skin pharmacology and physiology. 2017;30(3):115-38.
5. Coderch L et al. Am J Clin Dermatol. 2003;4(2):107-29.
6. Man MQ et al. Arch Dermatol. 1993;129(6):728-38.
7. Man MQ M et al. J Invest Dermatol. 1996 May;106(5):1096-101.
8. Park BD et al. J Invest Dermatol. 2003;121(4):794-801.
9. Proksch E and Jensen J. Skin as an organ of protection, in “Fitzpatrick’s Dermatology in General Medicine,” 7th ed. New York: McGraw-Hill, 2008, pp. 383-95.
10. Ye L et al. J Eur Acad Dermatol Venereol. 2019;33(11):2197-201.
11. Lee EJ et al. Ann Dermatol. 2003;15(4):133-8.
12. Ahn SK et al. J Dermatol. 2006;33(2):80-90.
Filler complications involving vascular necrosis, vision changes on the rise
analysis showed.
“The ASDS estimates that 1.6 million soft tissue filler procedures were performed in 2019, a 78% increase from 2012,” presenting author Michelle Xiong, a 4th-year student at Brown University, Providence, R.I., said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “The popularity of dermal fillers continues to increase. With that, there is increasing concern of possible associated adverse events. Most concerning are those related to vascular occlusion.”
Under the supervision of senior author Kachiu C. Lee, MD, MPH, of Main Line Center for Laser Surgery in Ardmore, Pa., Ms. Xiong and colleagues analyzed the Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database of medical device–related adverse event reports, to better understand and characterize dermal filler-related complications. They limited the analysis to adverse events involving injectable fillers from January 2014 to December 2020 and determined the number of complications by type per year and reviewed reports to identify injection site locations. Next, they used the binomial test to compare the proportion of complication categories from 2014 through 2016 and from 2017 through 2020.
In all, 5,994 reports were identified during the 7-year study period. To evaluate trends over time, the researchers estimated the rate of complications per 100 reports each year. While the absolute number of reports increased over time, the rate of adverse events per 100 reports decreased, suggesting an overall improvement in safety.
When the researchers focused on complications involving vascular occlusion, they found that vascular necrosis accounted for 3.5% of all complications, compared with vision changes (1.5% of all complications), and stroke (0.3% of all complications). When comparing the years 2014-2016 with 2017-2020, there was a significant increase in adverse events involving vascular necrosis (0.9%; P = .018) and vision changes (0.94%; P = .001), but no significant difference in the number of reports of stroke (-0.1%; P = .409). “This highlights that serious complications like necrosis and vision changes have increased over time,” Ms. Xiong said.
Overall, the three most common injection sites involving necrosis and vision changes were the cheek, the nose, and the nasolabial fold. The cheek was the most common site associated with stroke. “These findings are similar to those of previous studies, further emphasizing that the nose, nasolabial fold, and cheek are possibly challenging injection sites,” she said.
“In general, as the face is a highly vascular area with many anastomoses, it’s especially important to be aware of facial anatomy when injecting. In addition to awareness of anatomy, injection techniques can influence vascular complications. Unfortunately, the event narratives in the MAUDE database did not go into detail about the procedural technique.”
Ms. Xiong said that as the popularity of dermal fillers continues to grow, “it’s important for providers to understand the possible adverse events, both to better counsel patients and to improve safety management. The proportion of serious complications such as vascular necrosis and vision changes have increased from 2014 to 2020. This highlights an increased need for training to better understand facial anatomy and to emphasize practice techniques to minimize risk.”
Dr. Lee acknowledged certain limitations of the study, including that “submission of adverse events to the MAUDE database are not verified or standardized,” she told this news organization.
“With the ever-increasing popularity of fillers, it is not surprising that the absolute number of complications is rising, but it is also reassuring to see that the overall ratio of complications per hundred reports is down,” said Lawrence J. Green, MD, clinical professor of dermatology at George Washington University, Washington, who was asked to comment on the study. “I would be curious to know what proportion of filler complications are due to non–core practitioners compared to dermatologists and plastic surgeons.”
The researchers reported having no financial disclosures.
Dr. Green disclosed that he is a speaker, consultant, or investigator for numerous pharmaceutical companies.
analysis showed.
“The ASDS estimates that 1.6 million soft tissue filler procedures were performed in 2019, a 78% increase from 2012,” presenting author Michelle Xiong, a 4th-year student at Brown University, Providence, R.I., said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “The popularity of dermal fillers continues to increase. With that, there is increasing concern of possible associated adverse events. Most concerning are those related to vascular occlusion.”
Under the supervision of senior author Kachiu C. Lee, MD, MPH, of Main Line Center for Laser Surgery in Ardmore, Pa., Ms. Xiong and colleagues analyzed the Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database of medical device–related adverse event reports, to better understand and characterize dermal filler-related complications. They limited the analysis to adverse events involving injectable fillers from January 2014 to December 2020 and determined the number of complications by type per year and reviewed reports to identify injection site locations. Next, they used the binomial test to compare the proportion of complication categories from 2014 through 2016 and from 2017 through 2020.
In all, 5,994 reports were identified during the 7-year study period. To evaluate trends over time, the researchers estimated the rate of complications per 100 reports each year. While the absolute number of reports increased over time, the rate of adverse events per 100 reports decreased, suggesting an overall improvement in safety.
When the researchers focused on complications involving vascular occlusion, they found that vascular necrosis accounted for 3.5% of all complications, compared with vision changes (1.5% of all complications), and stroke (0.3% of all complications). When comparing the years 2014-2016 with 2017-2020, there was a significant increase in adverse events involving vascular necrosis (0.9%; P = .018) and vision changes (0.94%; P = .001), but no significant difference in the number of reports of stroke (-0.1%; P = .409). “This highlights that serious complications like necrosis and vision changes have increased over time,” Ms. Xiong said.
Overall, the three most common injection sites involving necrosis and vision changes were the cheek, the nose, and the nasolabial fold. The cheek was the most common site associated with stroke. “These findings are similar to those of previous studies, further emphasizing that the nose, nasolabial fold, and cheek are possibly challenging injection sites,” she said.
“In general, as the face is a highly vascular area with many anastomoses, it’s especially important to be aware of facial anatomy when injecting. In addition to awareness of anatomy, injection techniques can influence vascular complications. Unfortunately, the event narratives in the MAUDE database did not go into detail about the procedural technique.”
Ms. Xiong said that as the popularity of dermal fillers continues to grow, “it’s important for providers to understand the possible adverse events, both to better counsel patients and to improve safety management. The proportion of serious complications such as vascular necrosis and vision changes have increased from 2014 to 2020. This highlights an increased need for training to better understand facial anatomy and to emphasize practice techniques to minimize risk.”
Dr. Lee acknowledged certain limitations of the study, including that “submission of adverse events to the MAUDE database are not verified or standardized,” she told this news organization.
“With the ever-increasing popularity of fillers, it is not surprising that the absolute number of complications is rising, but it is also reassuring to see that the overall ratio of complications per hundred reports is down,” said Lawrence J. Green, MD, clinical professor of dermatology at George Washington University, Washington, who was asked to comment on the study. “I would be curious to know what proportion of filler complications are due to non–core practitioners compared to dermatologists and plastic surgeons.”
The researchers reported having no financial disclosures.
Dr. Green disclosed that he is a speaker, consultant, or investigator for numerous pharmaceutical companies.
analysis showed.
“The ASDS estimates that 1.6 million soft tissue filler procedures were performed in 2019, a 78% increase from 2012,” presenting author Michelle Xiong, a 4th-year student at Brown University, Providence, R.I., said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “The popularity of dermal fillers continues to increase. With that, there is increasing concern of possible associated adverse events. Most concerning are those related to vascular occlusion.”
Under the supervision of senior author Kachiu C. Lee, MD, MPH, of Main Line Center for Laser Surgery in Ardmore, Pa., Ms. Xiong and colleagues analyzed the Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database of medical device–related adverse event reports, to better understand and characterize dermal filler-related complications. They limited the analysis to adverse events involving injectable fillers from January 2014 to December 2020 and determined the number of complications by type per year and reviewed reports to identify injection site locations. Next, they used the binomial test to compare the proportion of complication categories from 2014 through 2016 and from 2017 through 2020.
In all, 5,994 reports were identified during the 7-year study period. To evaluate trends over time, the researchers estimated the rate of complications per 100 reports each year. While the absolute number of reports increased over time, the rate of adverse events per 100 reports decreased, suggesting an overall improvement in safety.
When the researchers focused on complications involving vascular occlusion, they found that vascular necrosis accounted for 3.5% of all complications, compared with vision changes (1.5% of all complications), and stroke (0.3% of all complications). When comparing the years 2014-2016 with 2017-2020, there was a significant increase in adverse events involving vascular necrosis (0.9%; P = .018) and vision changes (0.94%; P = .001), but no significant difference in the number of reports of stroke (-0.1%; P = .409). “This highlights that serious complications like necrosis and vision changes have increased over time,” Ms. Xiong said.
Overall, the three most common injection sites involving necrosis and vision changes were the cheek, the nose, and the nasolabial fold. The cheek was the most common site associated with stroke. “These findings are similar to those of previous studies, further emphasizing that the nose, nasolabial fold, and cheek are possibly challenging injection sites,” she said.
“In general, as the face is a highly vascular area with many anastomoses, it’s especially important to be aware of facial anatomy when injecting. In addition to awareness of anatomy, injection techniques can influence vascular complications. Unfortunately, the event narratives in the MAUDE database did not go into detail about the procedural technique.”
Ms. Xiong said that as the popularity of dermal fillers continues to grow, “it’s important for providers to understand the possible adverse events, both to better counsel patients and to improve safety management. The proportion of serious complications such as vascular necrosis and vision changes have increased from 2014 to 2020. This highlights an increased need for training to better understand facial anatomy and to emphasize practice techniques to minimize risk.”
Dr. Lee acknowledged certain limitations of the study, including that “submission of adverse events to the MAUDE database are not verified or standardized,” she told this news organization.
“With the ever-increasing popularity of fillers, it is not surprising that the absolute number of complications is rising, but it is also reassuring to see that the overall ratio of complications per hundred reports is down,” said Lawrence J. Green, MD, clinical professor of dermatology at George Washington University, Washington, who was asked to comment on the study. “I would be curious to know what proportion of filler complications are due to non–core practitioners compared to dermatologists and plastic surgeons.”
The researchers reported having no financial disclosures.
Dr. Green disclosed that he is a speaker, consultant, or investigator for numerous pharmaceutical companies.
FROM ASDS 2021
Review finds microneedling an effective add-on to topical melasma therapies
, results from a combined systematic review and meta-analysis suggest.
“Microneedling has a similar efficacy to other drug delivery methods, such as CO2 laser or intradermal microinjections, for the treatment of melasma,” presenting author Marcus G. Tan, MD, said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “When used in combination with topical depigmenting therapies, microneedling also demonstrated superior efficacy and a more favorable safety profile compared to oral tranexamic acid.”
For the study, Dr. Tan, a 5-year dermatology resident at the University of Ottawa, and colleagues searched MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials using the keywords “melasma” and “microneedling.” They limited their analysis to prospective, comparative studies incorporating the use of microneedling in the treatment of melasma and excluded those involving radiofrequency. The primary outcome was improvement in melasma severity, evaluated through the Melasma Area and Severity Index (MASI). The secondary outcomes were improvement in patient satisfaction, quality of life, and any reported adverse events.
Twelve studies involving 459 patients from seven countries were included in the final analysis. Of these, seven were randomized controlled studies and five were nonrandomized split-face studies. Topical treatments used in the studies included tranexamic acid (TXA), vitamin C, platelet-rich plasma, and hydroquinone-based depigmenting serums such as rucinol, sophora-alpha, and N-acetyl glucosamine. Of the 12 studies, 4 used mechanical microneedling and 8 used electric repeating microneedling. The most common needle length used was 1.5 mm, with a range from 0.1 to 1.5 mm, depending on the anatomic site treated. Topical anesthesia was applied 30-60 minutes prior to treatment. Treatment intervals were 2-4 weeks apart.
Their analysis found that microneedling alone resulted in a 23%-29% improvement in MASI. “Across all studies, adding topical therapies resulted in greater improvements in melasma severity, with a moderate effect at 8 weeks and a large effect at 12-16 weeks,” Dr. Tan said. “This also translated to higher patient satisfaction scores and improved patient-reported quality of life.”
A split-face study in the analysis, which compared topical TXA with microneedling to topical TXA with fractional CO2 laser, found that both approaches had similar efficacy and rates of adverse events. Another split-face study that evaluated recalcitrant melasma found that adding vitamin C with microneedling to a nonablative Q-switched Nd:YAG laser resulted in a further 38.3% greater improvement in MASI and a 12.5% lower recurrence rate at 6 months.
In two other studies, researchers compared microneedling to intradermal microinjections to deliver platelet-rich plasma or topical TXA. Both modalities were found to have similar efficacy. “However, microneedling was found to be better tolerated and had higher patient satisfaction as a result,” Dr. Tan said.
A separate analysis found that Tri-Luma (fluocinolone acetonide, hydroquinone, and tretinoin) cream with microneedling outperformed Tri-Luma plus oral TXA in terms of efficacy, patient satisfaction, and tolerability. “Interestingly, adding oral TXA to Tri-Luma with microneedling did not lead to further improvements,” Dr. Tan said.
The researchers found that microneedling was well tolerated in all 12 studies. Overall, no scarring or serious adverse events were reported. Mild-transient dyspigmentation occurred in 5%-12% of cases and herpes simplex virus reactivation was seen in a minority of patients.
Dr. Tan commented on three proposed mechanisms of action, which support the efficacy of microneedling for the treatment of melasma. “First, microneedling assists in the transcutaneous delivery of topical agents through the micropores,” he said. “Second, microneedling also assists in the transcutaneous elimination of melanin and other skin debris through the micropores. Third, the microinjuries stimulate the wound healing response, resulting in neocollagenesis, neoelastogenesis, and epidermal thickening.”
In an interview, Dr. Tan acknowledged certain limitations of the study, including the pooling of randomized and nonrandomized studies in the final meta-analysis, the heterogeneity in the treatment protocols and devices used, as well as the inclusion of studies with a moderate risk of bias. “Nonetheless, these limitations do not affect the conclusion that microneedling is a useful and safe adjuvant to topical therapies for melasma,” he said.
Catherine M. DiGiorgio, MD, who was asked to comment on the study, noted that melasma is a notoriously difficult condition to treat. “Many energy-based device treatments as well as other therapies have been proposed for treatment over the years. However, none have shown reliable, reproducible, and most importantly long-lasting results,” said Dr. DiGiorgio, a laser and cosmetic dermatologist at The Boston Center for Facial Rejuvenation. “Caution should be employed regarding the true efficacy of treatments for other than, at best, temporary results.”
The review included numerous studies without a clear definition of the strengths or methodologies of the studies, she added, noting that randomized controlled split-face studies with long-term follow up are the best way to assess the efficacy of treatments. “Further, regarding drug delivery, microneedling is the least effective method of delivery of drugs to the skin and laser-assisted drug delivery using ablative fractional lasers is the most effective. As with all melasma treatments, healthy skepticism is never a bad approach.”
Dr. Tan reported having no financial disclosures. Dr. DiGiorgio disclosed that she conducts research for Quthero Inc., and holds stock in the company.
, results from a combined systematic review and meta-analysis suggest.
“Microneedling has a similar efficacy to other drug delivery methods, such as CO2 laser or intradermal microinjections, for the treatment of melasma,” presenting author Marcus G. Tan, MD, said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “When used in combination with topical depigmenting therapies, microneedling also demonstrated superior efficacy and a more favorable safety profile compared to oral tranexamic acid.”
For the study, Dr. Tan, a 5-year dermatology resident at the University of Ottawa, and colleagues searched MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials using the keywords “melasma” and “microneedling.” They limited their analysis to prospective, comparative studies incorporating the use of microneedling in the treatment of melasma and excluded those involving radiofrequency. The primary outcome was improvement in melasma severity, evaluated through the Melasma Area and Severity Index (MASI). The secondary outcomes were improvement in patient satisfaction, quality of life, and any reported adverse events.
Twelve studies involving 459 patients from seven countries were included in the final analysis. Of these, seven were randomized controlled studies and five were nonrandomized split-face studies. Topical treatments used in the studies included tranexamic acid (TXA), vitamin C, platelet-rich plasma, and hydroquinone-based depigmenting serums such as rucinol, sophora-alpha, and N-acetyl glucosamine. Of the 12 studies, 4 used mechanical microneedling and 8 used electric repeating microneedling. The most common needle length used was 1.5 mm, with a range from 0.1 to 1.5 mm, depending on the anatomic site treated. Topical anesthesia was applied 30-60 minutes prior to treatment. Treatment intervals were 2-4 weeks apart.
Their analysis found that microneedling alone resulted in a 23%-29% improvement in MASI. “Across all studies, adding topical therapies resulted in greater improvements in melasma severity, with a moderate effect at 8 weeks and a large effect at 12-16 weeks,” Dr. Tan said. “This also translated to higher patient satisfaction scores and improved patient-reported quality of life.”
A split-face study in the analysis, which compared topical TXA with microneedling to topical TXA with fractional CO2 laser, found that both approaches had similar efficacy and rates of adverse events. Another split-face study that evaluated recalcitrant melasma found that adding vitamin C with microneedling to a nonablative Q-switched Nd:YAG laser resulted in a further 38.3% greater improvement in MASI and a 12.5% lower recurrence rate at 6 months.
In two other studies, researchers compared microneedling to intradermal microinjections to deliver platelet-rich plasma or topical TXA. Both modalities were found to have similar efficacy. “However, microneedling was found to be better tolerated and had higher patient satisfaction as a result,” Dr. Tan said.
A separate analysis found that Tri-Luma (fluocinolone acetonide, hydroquinone, and tretinoin) cream with microneedling outperformed Tri-Luma plus oral TXA in terms of efficacy, patient satisfaction, and tolerability. “Interestingly, adding oral TXA to Tri-Luma with microneedling did not lead to further improvements,” Dr. Tan said.
The researchers found that microneedling was well tolerated in all 12 studies. Overall, no scarring or serious adverse events were reported. Mild-transient dyspigmentation occurred in 5%-12% of cases and herpes simplex virus reactivation was seen in a minority of patients.
Dr. Tan commented on three proposed mechanisms of action, which support the efficacy of microneedling for the treatment of melasma. “First, microneedling assists in the transcutaneous delivery of topical agents through the micropores,” he said. “Second, microneedling also assists in the transcutaneous elimination of melanin and other skin debris through the micropores. Third, the microinjuries stimulate the wound healing response, resulting in neocollagenesis, neoelastogenesis, and epidermal thickening.”
In an interview, Dr. Tan acknowledged certain limitations of the study, including the pooling of randomized and nonrandomized studies in the final meta-analysis, the heterogeneity in the treatment protocols and devices used, as well as the inclusion of studies with a moderate risk of bias. “Nonetheless, these limitations do not affect the conclusion that microneedling is a useful and safe adjuvant to topical therapies for melasma,” he said.
Catherine M. DiGiorgio, MD, who was asked to comment on the study, noted that melasma is a notoriously difficult condition to treat. “Many energy-based device treatments as well as other therapies have been proposed for treatment over the years. However, none have shown reliable, reproducible, and most importantly long-lasting results,” said Dr. DiGiorgio, a laser and cosmetic dermatologist at The Boston Center for Facial Rejuvenation. “Caution should be employed regarding the true efficacy of treatments for other than, at best, temporary results.”
The review included numerous studies without a clear definition of the strengths or methodologies of the studies, she added, noting that randomized controlled split-face studies with long-term follow up are the best way to assess the efficacy of treatments. “Further, regarding drug delivery, microneedling is the least effective method of delivery of drugs to the skin and laser-assisted drug delivery using ablative fractional lasers is the most effective. As with all melasma treatments, healthy skepticism is never a bad approach.”
Dr. Tan reported having no financial disclosures. Dr. DiGiorgio disclosed that she conducts research for Quthero Inc., and holds stock in the company.
, results from a combined systematic review and meta-analysis suggest.
“Microneedling has a similar efficacy to other drug delivery methods, such as CO2 laser or intradermal microinjections, for the treatment of melasma,” presenting author Marcus G. Tan, MD, said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “When used in combination with topical depigmenting therapies, microneedling also demonstrated superior efficacy and a more favorable safety profile compared to oral tranexamic acid.”
For the study, Dr. Tan, a 5-year dermatology resident at the University of Ottawa, and colleagues searched MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials using the keywords “melasma” and “microneedling.” They limited their analysis to prospective, comparative studies incorporating the use of microneedling in the treatment of melasma and excluded those involving radiofrequency. The primary outcome was improvement in melasma severity, evaluated through the Melasma Area and Severity Index (MASI). The secondary outcomes were improvement in patient satisfaction, quality of life, and any reported adverse events.
Twelve studies involving 459 patients from seven countries were included in the final analysis. Of these, seven were randomized controlled studies and five were nonrandomized split-face studies. Topical treatments used in the studies included tranexamic acid (TXA), vitamin C, platelet-rich plasma, and hydroquinone-based depigmenting serums such as rucinol, sophora-alpha, and N-acetyl glucosamine. Of the 12 studies, 4 used mechanical microneedling and 8 used electric repeating microneedling. The most common needle length used was 1.5 mm, with a range from 0.1 to 1.5 mm, depending on the anatomic site treated. Topical anesthesia was applied 30-60 minutes prior to treatment. Treatment intervals were 2-4 weeks apart.
Their analysis found that microneedling alone resulted in a 23%-29% improvement in MASI. “Across all studies, adding topical therapies resulted in greater improvements in melasma severity, with a moderate effect at 8 weeks and a large effect at 12-16 weeks,” Dr. Tan said. “This also translated to higher patient satisfaction scores and improved patient-reported quality of life.”
A split-face study in the analysis, which compared topical TXA with microneedling to topical TXA with fractional CO2 laser, found that both approaches had similar efficacy and rates of adverse events. Another split-face study that evaluated recalcitrant melasma found that adding vitamin C with microneedling to a nonablative Q-switched Nd:YAG laser resulted in a further 38.3% greater improvement in MASI and a 12.5% lower recurrence rate at 6 months.
In two other studies, researchers compared microneedling to intradermal microinjections to deliver platelet-rich plasma or topical TXA. Both modalities were found to have similar efficacy. “However, microneedling was found to be better tolerated and had higher patient satisfaction as a result,” Dr. Tan said.
A separate analysis found that Tri-Luma (fluocinolone acetonide, hydroquinone, and tretinoin) cream with microneedling outperformed Tri-Luma plus oral TXA in terms of efficacy, patient satisfaction, and tolerability. “Interestingly, adding oral TXA to Tri-Luma with microneedling did not lead to further improvements,” Dr. Tan said.
The researchers found that microneedling was well tolerated in all 12 studies. Overall, no scarring or serious adverse events were reported. Mild-transient dyspigmentation occurred in 5%-12% of cases and herpes simplex virus reactivation was seen in a minority of patients.
Dr. Tan commented on three proposed mechanisms of action, which support the efficacy of microneedling for the treatment of melasma. “First, microneedling assists in the transcutaneous delivery of topical agents through the micropores,” he said. “Second, microneedling also assists in the transcutaneous elimination of melanin and other skin debris through the micropores. Third, the microinjuries stimulate the wound healing response, resulting in neocollagenesis, neoelastogenesis, and epidermal thickening.”
In an interview, Dr. Tan acknowledged certain limitations of the study, including the pooling of randomized and nonrandomized studies in the final meta-analysis, the heterogeneity in the treatment protocols and devices used, as well as the inclusion of studies with a moderate risk of bias. “Nonetheless, these limitations do not affect the conclusion that microneedling is a useful and safe adjuvant to topical therapies for melasma,” he said.
Catherine M. DiGiorgio, MD, who was asked to comment on the study, noted that melasma is a notoriously difficult condition to treat. “Many energy-based device treatments as well as other therapies have been proposed for treatment over the years. However, none have shown reliable, reproducible, and most importantly long-lasting results,” said Dr. DiGiorgio, a laser and cosmetic dermatologist at The Boston Center for Facial Rejuvenation. “Caution should be employed regarding the true efficacy of treatments for other than, at best, temporary results.”
The review included numerous studies without a clear definition of the strengths or methodologies of the studies, she added, noting that randomized controlled split-face studies with long-term follow up are the best way to assess the efficacy of treatments. “Further, regarding drug delivery, microneedling is the least effective method of delivery of drugs to the skin and laser-assisted drug delivery using ablative fractional lasers is the most effective. As with all melasma treatments, healthy skepticism is never a bad approach.”
Dr. Tan reported having no financial disclosures. Dr. DiGiorgio disclosed that she conducts research for Quthero Inc., and holds stock in the company.
FROM ASDS 2021
International panel backs energy-based devices as first-line treatment of acne scars
International consensus .
Peter R. Shumaker, MD, a dermatologist and dermatologic surgeon at the VA San Diego Healthcare System and one of the authors of the paper, noted that a panel of 24 international experts in dermatology and plastic surgery assembled to develop the recommendations for integrating EBDs into the management of acne scarring.
“The advent of fractional laser technology in the mid-2000s ushered in an exciting new period of exploration and advances in scar treatment with EBDs,” Dr. Shumaker said in an interview. “Despite intense interest and a wealth of available literature, international treatment guidelines and patient access to these potentially life-changing treatments are currently lagging behind our capabilities.”
One of the key recommendations of the paper is that EBDs should have an expanded role in the treatment of acne scars, according to Dr. Shumaker, associate clinical professor of dermatology at the University of California, San Diego. “Panel members were unanimous in their view that EBDs, particularly ablative and nonablative fractional lasers, vascular lasers, and fractional radiofrequency devices, have an important role in the management of acne scars and should be considered a first-line treatment for a variety of scar types,” he said.
The process leading to the recommendations included developing clinical questions, based on input from the panelists and a literature review, and using a two-step modified Delphi method, “an iterative process used to achieve consensus for a defined clinical problem where there is little or conflicting published evidence and where expert opinion is decisive,” the authors wrote. This involved email questionnaires highlighting different topics, including the role of EBDs in mitigating and treating acne scars in patients with active acne, the use of different EBDs for treating different types of acne scars, and considerations in treating skin of color.
The panel noted considerations in the treatment of acne scars in skin of color. “Regardless of the platform, patients with darker skin types may require treatment modifications including: a reduction in fluence/pulse energy; decreased microcolumn density; greater intervals between treatments; longer pulse durations; epidermal cooling with fastidious technique to ensure appropriate cooling, additional cooling in between passes to decrease bulk heating; and pretreatment and posttreatment topical regimens (e.g., retinoids, bleaching creams, etc.) and strict sun precautions,” wrote the authors.
Panelists agreed that there is an absence of large, well-controlled, multicenter comparative trials of various laser and energy treatments for acne scars. “Such trials would be helpful in establishing the relative utility and persistence of benefit of various laser treatments and also in comparing their effectiveness versus that of nonenergy treatments,” the authors noted.
Asked to comment on the paper, Andrei Metelitsa, MD, a dermatologist in Calgary, Alta., and clinical associate professor at the University of Calgary, said the consensus recommendations on EBDs in acne scarring are “providing an international expert perspective, potentially changing a long-perceived paradigm of treatments.”
Dr. Metelitsa pointed out that the authors are taking a solid position with respect to reducing the delay to initiation of laser treatment following isotretinoin therapy. “The authors take a strong stance against the old dogma of postponing laser resurfacing for at least 6 months post isotretinoin,” he said. “According to the authors, there is sufficient evidence to support the idea of safely starting laser therapies, including fractional ablative and nonablative, within 1 month post isotretinoin, much sooner than previously suggested.”
He added that the authors point to the fact most experts utilize vascular lasers, such as pulsed-dye, to treat active acne in combination with medical therapy, thus reducing duration and severity of inflammation and potentially reducing further scar formation. “According to this published consensus, such laser therapies can even be used while the patient is actively treated with isotretinoin,” he said.
Dr. Metelitsa noted that the consensus recommendations outline how the choice of device should be guided by the clinical subtype of acne scars.
Dr. Shumaker, Dr. Metelitsa, and the authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
International consensus .
Peter R. Shumaker, MD, a dermatologist and dermatologic surgeon at the VA San Diego Healthcare System and one of the authors of the paper, noted that a panel of 24 international experts in dermatology and plastic surgery assembled to develop the recommendations for integrating EBDs into the management of acne scarring.
“The advent of fractional laser technology in the mid-2000s ushered in an exciting new period of exploration and advances in scar treatment with EBDs,” Dr. Shumaker said in an interview. “Despite intense interest and a wealth of available literature, international treatment guidelines and patient access to these potentially life-changing treatments are currently lagging behind our capabilities.”
One of the key recommendations of the paper is that EBDs should have an expanded role in the treatment of acne scars, according to Dr. Shumaker, associate clinical professor of dermatology at the University of California, San Diego. “Panel members were unanimous in their view that EBDs, particularly ablative and nonablative fractional lasers, vascular lasers, and fractional radiofrequency devices, have an important role in the management of acne scars and should be considered a first-line treatment for a variety of scar types,” he said.
The process leading to the recommendations included developing clinical questions, based on input from the panelists and a literature review, and using a two-step modified Delphi method, “an iterative process used to achieve consensus for a defined clinical problem where there is little or conflicting published evidence and where expert opinion is decisive,” the authors wrote. This involved email questionnaires highlighting different topics, including the role of EBDs in mitigating and treating acne scars in patients with active acne, the use of different EBDs for treating different types of acne scars, and considerations in treating skin of color.
The panel noted considerations in the treatment of acne scars in skin of color. “Regardless of the platform, patients with darker skin types may require treatment modifications including: a reduction in fluence/pulse energy; decreased microcolumn density; greater intervals between treatments; longer pulse durations; epidermal cooling with fastidious technique to ensure appropriate cooling, additional cooling in between passes to decrease bulk heating; and pretreatment and posttreatment topical regimens (e.g., retinoids, bleaching creams, etc.) and strict sun precautions,” wrote the authors.
Panelists agreed that there is an absence of large, well-controlled, multicenter comparative trials of various laser and energy treatments for acne scars. “Such trials would be helpful in establishing the relative utility and persistence of benefit of various laser treatments and also in comparing their effectiveness versus that of nonenergy treatments,” the authors noted.
Asked to comment on the paper, Andrei Metelitsa, MD, a dermatologist in Calgary, Alta., and clinical associate professor at the University of Calgary, said the consensus recommendations on EBDs in acne scarring are “providing an international expert perspective, potentially changing a long-perceived paradigm of treatments.”
Dr. Metelitsa pointed out that the authors are taking a solid position with respect to reducing the delay to initiation of laser treatment following isotretinoin therapy. “The authors take a strong stance against the old dogma of postponing laser resurfacing for at least 6 months post isotretinoin,” he said. “According to the authors, there is sufficient evidence to support the idea of safely starting laser therapies, including fractional ablative and nonablative, within 1 month post isotretinoin, much sooner than previously suggested.”
He added that the authors point to the fact most experts utilize vascular lasers, such as pulsed-dye, to treat active acne in combination with medical therapy, thus reducing duration and severity of inflammation and potentially reducing further scar formation. “According to this published consensus, such laser therapies can even be used while the patient is actively treated with isotretinoin,” he said.
Dr. Metelitsa noted that the consensus recommendations outline how the choice of device should be guided by the clinical subtype of acne scars.
Dr. Shumaker, Dr. Metelitsa, and the authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
International consensus .
Peter R. Shumaker, MD, a dermatologist and dermatologic surgeon at the VA San Diego Healthcare System and one of the authors of the paper, noted that a panel of 24 international experts in dermatology and plastic surgery assembled to develop the recommendations for integrating EBDs into the management of acne scarring.
“The advent of fractional laser technology in the mid-2000s ushered in an exciting new period of exploration and advances in scar treatment with EBDs,” Dr. Shumaker said in an interview. “Despite intense interest and a wealth of available literature, international treatment guidelines and patient access to these potentially life-changing treatments are currently lagging behind our capabilities.”
One of the key recommendations of the paper is that EBDs should have an expanded role in the treatment of acne scars, according to Dr. Shumaker, associate clinical professor of dermatology at the University of California, San Diego. “Panel members were unanimous in their view that EBDs, particularly ablative and nonablative fractional lasers, vascular lasers, and fractional radiofrequency devices, have an important role in the management of acne scars and should be considered a first-line treatment for a variety of scar types,” he said.
The process leading to the recommendations included developing clinical questions, based on input from the panelists and a literature review, and using a two-step modified Delphi method, “an iterative process used to achieve consensus for a defined clinical problem where there is little or conflicting published evidence and where expert opinion is decisive,” the authors wrote. This involved email questionnaires highlighting different topics, including the role of EBDs in mitigating and treating acne scars in patients with active acne, the use of different EBDs for treating different types of acne scars, and considerations in treating skin of color.
The panel noted considerations in the treatment of acne scars in skin of color. “Regardless of the platform, patients with darker skin types may require treatment modifications including: a reduction in fluence/pulse energy; decreased microcolumn density; greater intervals between treatments; longer pulse durations; epidermal cooling with fastidious technique to ensure appropriate cooling, additional cooling in between passes to decrease bulk heating; and pretreatment and posttreatment topical regimens (e.g., retinoids, bleaching creams, etc.) and strict sun precautions,” wrote the authors.
Panelists agreed that there is an absence of large, well-controlled, multicenter comparative trials of various laser and energy treatments for acne scars. “Such trials would be helpful in establishing the relative utility and persistence of benefit of various laser treatments and also in comparing their effectiveness versus that of nonenergy treatments,” the authors noted.
Asked to comment on the paper, Andrei Metelitsa, MD, a dermatologist in Calgary, Alta., and clinical associate professor at the University of Calgary, said the consensus recommendations on EBDs in acne scarring are “providing an international expert perspective, potentially changing a long-perceived paradigm of treatments.”
Dr. Metelitsa pointed out that the authors are taking a solid position with respect to reducing the delay to initiation of laser treatment following isotretinoin therapy. “The authors take a strong stance against the old dogma of postponing laser resurfacing for at least 6 months post isotretinoin,” he said. “According to the authors, there is sufficient evidence to support the idea of safely starting laser therapies, including fractional ablative and nonablative, within 1 month post isotretinoin, much sooner than previously suggested.”
He added that the authors point to the fact most experts utilize vascular lasers, such as pulsed-dye, to treat active acne in combination with medical therapy, thus reducing duration and severity of inflammation and potentially reducing further scar formation. “According to this published consensus, such laser therapies can even be used while the patient is actively treated with isotretinoin,” he said.
Dr. Metelitsa noted that the consensus recommendations outline how the choice of device should be guided by the clinical subtype of acne scars.
Dr. Shumaker, Dr. Metelitsa, and the authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Characterizing Counterfeit Dermatologic Devices Sold on Popular E-commerce Websites
To the Editor:
Approved medical devices on the market are substantial capital investments for practitioners. E-commerce websites, such as Alibaba.com (https://www.alibaba.com/) and DHgate.com (https://www.dhgate.com/), sell sham medical devices at a fraction of the cost of authentic products, with sellers often echoing the same treatment claims as legitimate devices that have been cleared by the US Food and Drug Administration (FDA).
In dermatology, devices claiming to perform cryolipolysis, laser skin resurfacing, radiofrequency skin tightening, and more exist on e-commerce websites. These counterfeit medical devices might differ from legitimate devices in ways that affect patient safety and treatment efficacy.1,2 The degree of difference between counterfeit and legitimate devices remains unknown, and potential harm from so-called knockoff devices needs to be critically examined by providers.
In this exploratory study, we characterize counterfeit listings of devices commonly used in dermatology. Using the trademark name of devices as the key terms, we searched Alibaba.com and DHgate.com for listings of counterfeit products. We recorded the total number of listings; the listing name, catalog number, and unit price; and claims of FDA certification. Characteristics of counterfeit listings were summarized using standard descriptive statistics in Microsoft Excel. Continuous variables were summarized with means and ranges.
Six medical devices that had been cleared by the FDA between 2002 and 2012 for use in dermatology were explored, including systems for picosecond and fractionated lasers, monopolar and bipolar radiofrequency skin tightening, cryolipolysis, and nonablative radiofrequency skin resurfacing. Our search of these 6 representative dermatologic devices revealed 47,055 counterfeit product listings on Alibaba.com and DHgate.com. Upon searching these popular e-commerce websites using the device name as the search term, the number of listings varied considerably between the 2 e-commerce websites for the same device and from device to device on the same e-commerce website. On Alibaba.com, the greatest number of listings resulted for picosecond laser (23,622 listings), fractionated laser (15,269), and radiofrequency skin tightening devices (3555); cryolipolysis and nonablative radiofrequency resurfacing devices had notably fewer listings (35 and 38, respectively). On DHGate.com, a similar trend was noted with the most numerous listings for picosecond and fractionated laser systems (2429 and 1345, respectively).
Among the first 10 listings of products on Alibaba.com and DHgate.com for these 6 devices, 10.7% (11 of 103) had advertised claims of FDA clearance on the listing page. Of 103 counterfeit products, China was the country of origin for 100; South Korea for 2; and Thailand for 1. Unit pricing was heterogeneous between the 2 e-commerce websites for the counterfeit listings; pricing for duplicate fractionated laser systems was particularly dissimilar, with an average price on Alibab.com of US $8105.80 and an average price on DHgate.com of US $3409.14. Even on the same e-commerce website, the range of unit pricing differed greatly for dermatologic devices. For example, among the first 10 listings on Alibaba.com for a fractionated laser system, the price ranged from US $2300 to US $32,000.
Counterfeit medical devices are on the rise in dermatology.1,3 Although devices such as radiofrequency and laser systems had thousands of knockoff listings on 2 e-commerce websites, other devices, such as cryolipolysis and body contouring systems, had fewer listings, suggesting heterogeneity in the prevalence of different counterfeit dermatologic devices on the market.
The varied pricing of the top 10 listings for each product and spurious claims of FDA clearance for some listings highlight the lack of regulatory authority over consistent product information on e-commerce websites. Furthermore, differences between characteristics of counterfeit device listings can impede efforts to trace suppliers and increase the opacity of counterfeit purchasing.
Three criteria have been proposed for a device to be considered counterfeit3:
• The device has no proven safety or efficacy among consumers. For example, the substantial threat of copycat devices in dermatology has been demonstrated by reports of burns caused by fake cryolipolysis devices.2
• The device violates patent rights or copy trademarks. Due to the regional nature of intellectual property rights, country-specific filings of patents and trademarks are required if protections are sought internationally. In this study, counterfeit devices originated in China, South Korea, and Thailand, where patent and trademark protections for the original devices do not extend.
• The device is falsely claimed to have been cleared by the FDA or other clinical regulatory authorities. Legitimate medical devices are subject to rounds of safety and compatibility testing using standards set by regulatory bodies, such as the FDA’s Center for Devices and Radiological Health, the International Organization of Standardization, and the International Electrotechnical Commission. Compliance with these safety standards is lost, however, among unregulated internet sales of medical devices. Our search revealed that 10.7% of the top 10 counterfeit device listings for each product explicitly mentioned FDA clearance in the product description. Among the thousands of listings on e-commerce sites, even a fraction that make spurious FDA-clearance claims can mislead consumers.
The issue of counterfeit medical devices has not gone unrecognized globally. In 2013, the World Health Organization created the Global Surveillance and Monitoring System to unify international efforts for reporting substandard, unlicensed, or falsified medical products.4 Although universal monitoring systems can improve detection of counterfeit products, we highlight the alarming continuing ease of purchasing counterfeit dermatologic devices through e-commerce websites. Due to the widespread nature of counterfeiting across all domains of medicine, the onus of curbing counterfeit dermatologic devices might be on dermatology providers to recognize and report such occurrences.
This exploration of counterfeit dermatologic devices revealed a lack of consistency throughout product listings on 2 popular e-commerce websites, Alibaba.com and DHgate.com. Given the alarming availability of these devices on the internet, practitioners should approach the purchase of any device with concern about counterfeiting. Future avenues of study might explore the prevalence of counterfeit devices used in dermatology practices and offer insight on regulation and consumer safety efforts.
- Wang JV, Zachary CB, Saedi N. Counterfeit esthetic devices and patient safety in dermatology. J Cosmet Dermatol. 2018;17:396-397. doi:10.1111/jocd.12526
- Biesman BS, Patel N. Physician alert: beware of counterfeit medical devices. Lasers Surg Med. 2014;46:528‐530. doi:10.1002/lsm.22275
- Stevens WG, Spring MA, Macias LH. Counterfeit medical devices: the money you save up front will cost you big in the end. Aesthet Surg J. 2014;34:786‐788. doi:10.1177/1090820X14529960
- Pisani E. WHO Global Surveillance and Monitoring System for Substandard and Falsified Medical Products. World Health Organization; 2017. Accessed November 21, 2021. https://www.who.int/medicines/regulation/ssffc/publications/GSMSreport_EN.pdf?ua=1
To the Editor:
Approved medical devices on the market are substantial capital investments for practitioners. E-commerce websites, such as Alibaba.com (https://www.alibaba.com/) and DHgate.com (https://www.dhgate.com/), sell sham medical devices at a fraction of the cost of authentic products, with sellers often echoing the same treatment claims as legitimate devices that have been cleared by the US Food and Drug Administration (FDA).
In dermatology, devices claiming to perform cryolipolysis, laser skin resurfacing, radiofrequency skin tightening, and more exist on e-commerce websites. These counterfeit medical devices might differ from legitimate devices in ways that affect patient safety and treatment efficacy.1,2 The degree of difference between counterfeit and legitimate devices remains unknown, and potential harm from so-called knockoff devices needs to be critically examined by providers.
In this exploratory study, we characterize counterfeit listings of devices commonly used in dermatology. Using the trademark name of devices as the key terms, we searched Alibaba.com and DHgate.com for listings of counterfeit products. We recorded the total number of listings; the listing name, catalog number, and unit price; and claims of FDA certification. Characteristics of counterfeit listings were summarized using standard descriptive statistics in Microsoft Excel. Continuous variables were summarized with means and ranges.
Six medical devices that had been cleared by the FDA between 2002 and 2012 for use in dermatology were explored, including systems for picosecond and fractionated lasers, monopolar and bipolar radiofrequency skin tightening, cryolipolysis, and nonablative radiofrequency skin resurfacing. Our search of these 6 representative dermatologic devices revealed 47,055 counterfeit product listings on Alibaba.com and DHgate.com. Upon searching these popular e-commerce websites using the device name as the search term, the number of listings varied considerably between the 2 e-commerce websites for the same device and from device to device on the same e-commerce website. On Alibaba.com, the greatest number of listings resulted for picosecond laser (23,622 listings), fractionated laser (15,269), and radiofrequency skin tightening devices (3555); cryolipolysis and nonablative radiofrequency resurfacing devices had notably fewer listings (35 and 38, respectively). On DHGate.com, a similar trend was noted with the most numerous listings for picosecond and fractionated laser systems (2429 and 1345, respectively).
Among the first 10 listings of products on Alibaba.com and DHgate.com for these 6 devices, 10.7% (11 of 103) had advertised claims of FDA clearance on the listing page. Of 103 counterfeit products, China was the country of origin for 100; South Korea for 2; and Thailand for 1. Unit pricing was heterogeneous between the 2 e-commerce websites for the counterfeit listings; pricing for duplicate fractionated laser systems was particularly dissimilar, with an average price on Alibab.com of US $8105.80 and an average price on DHgate.com of US $3409.14. Even on the same e-commerce website, the range of unit pricing differed greatly for dermatologic devices. For example, among the first 10 listings on Alibaba.com for a fractionated laser system, the price ranged from US $2300 to US $32,000.
Counterfeit medical devices are on the rise in dermatology.1,3 Although devices such as radiofrequency and laser systems had thousands of knockoff listings on 2 e-commerce websites, other devices, such as cryolipolysis and body contouring systems, had fewer listings, suggesting heterogeneity in the prevalence of different counterfeit dermatologic devices on the market.
The varied pricing of the top 10 listings for each product and spurious claims of FDA clearance for some listings highlight the lack of regulatory authority over consistent product information on e-commerce websites. Furthermore, differences between characteristics of counterfeit device listings can impede efforts to trace suppliers and increase the opacity of counterfeit purchasing.
Three criteria have been proposed for a device to be considered counterfeit3:
• The device has no proven safety or efficacy among consumers. For example, the substantial threat of copycat devices in dermatology has been demonstrated by reports of burns caused by fake cryolipolysis devices.2
• The device violates patent rights or copy trademarks. Due to the regional nature of intellectual property rights, country-specific filings of patents and trademarks are required if protections are sought internationally. In this study, counterfeit devices originated in China, South Korea, and Thailand, where patent and trademark protections for the original devices do not extend.
• The device is falsely claimed to have been cleared by the FDA or other clinical regulatory authorities. Legitimate medical devices are subject to rounds of safety and compatibility testing using standards set by regulatory bodies, such as the FDA’s Center for Devices and Radiological Health, the International Organization of Standardization, and the International Electrotechnical Commission. Compliance with these safety standards is lost, however, among unregulated internet sales of medical devices. Our search revealed that 10.7% of the top 10 counterfeit device listings for each product explicitly mentioned FDA clearance in the product description. Among the thousands of listings on e-commerce sites, even a fraction that make spurious FDA-clearance claims can mislead consumers.
The issue of counterfeit medical devices has not gone unrecognized globally. In 2013, the World Health Organization created the Global Surveillance and Monitoring System to unify international efforts for reporting substandard, unlicensed, or falsified medical products.4 Although universal monitoring systems can improve detection of counterfeit products, we highlight the alarming continuing ease of purchasing counterfeit dermatologic devices through e-commerce websites. Due to the widespread nature of counterfeiting across all domains of medicine, the onus of curbing counterfeit dermatologic devices might be on dermatology providers to recognize and report such occurrences.
This exploration of counterfeit dermatologic devices revealed a lack of consistency throughout product listings on 2 popular e-commerce websites, Alibaba.com and DHgate.com. Given the alarming availability of these devices on the internet, practitioners should approach the purchase of any device with concern about counterfeiting. Future avenues of study might explore the prevalence of counterfeit devices used in dermatology practices and offer insight on regulation and consumer safety efforts.
To the Editor:
Approved medical devices on the market are substantial capital investments for practitioners. E-commerce websites, such as Alibaba.com (https://www.alibaba.com/) and DHgate.com (https://www.dhgate.com/), sell sham medical devices at a fraction of the cost of authentic products, with sellers often echoing the same treatment claims as legitimate devices that have been cleared by the US Food and Drug Administration (FDA).
In dermatology, devices claiming to perform cryolipolysis, laser skin resurfacing, radiofrequency skin tightening, and more exist on e-commerce websites. These counterfeit medical devices might differ from legitimate devices in ways that affect patient safety and treatment efficacy.1,2 The degree of difference between counterfeit and legitimate devices remains unknown, and potential harm from so-called knockoff devices needs to be critically examined by providers.
In this exploratory study, we characterize counterfeit listings of devices commonly used in dermatology. Using the trademark name of devices as the key terms, we searched Alibaba.com and DHgate.com for listings of counterfeit products. We recorded the total number of listings; the listing name, catalog number, and unit price; and claims of FDA certification. Characteristics of counterfeit listings were summarized using standard descriptive statistics in Microsoft Excel. Continuous variables were summarized with means and ranges.
Six medical devices that had been cleared by the FDA between 2002 and 2012 for use in dermatology were explored, including systems for picosecond and fractionated lasers, monopolar and bipolar radiofrequency skin tightening, cryolipolysis, and nonablative radiofrequency skin resurfacing. Our search of these 6 representative dermatologic devices revealed 47,055 counterfeit product listings on Alibaba.com and DHgate.com. Upon searching these popular e-commerce websites using the device name as the search term, the number of listings varied considerably between the 2 e-commerce websites for the same device and from device to device on the same e-commerce website. On Alibaba.com, the greatest number of listings resulted for picosecond laser (23,622 listings), fractionated laser (15,269), and radiofrequency skin tightening devices (3555); cryolipolysis and nonablative radiofrequency resurfacing devices had notably fewer listings (35 and 38, respectively). On DHGate.com, a similar trend was noted with the most numerous listings for picosecond and fractionated laser systems (2429 and 1345, respectively).
Among the first 10 listings of products on Alibaba.com and DHgate.com for these 6 devices, 10.7% (11 of 103) had advertised claims of FDA clearance on the listing page. Of 103 counterfeit products, China was the country of origin for 100; South Korea for 2; and Thailand for 1. Unit pricing was heterogeneous between the 2 e-commerce websites for the counterfeit listings; pricing for duplicate fractionated laser systems was particularly dissimilar, with an average price on Alibab.com of US $8105.80 and an average price on DHgate.com of US $3409.14. Even on the same e-commerce website, the range of unit pricing differed greatly for dermatologic devices. For example, among the first 10 listings on Alibaba.com for a fractionated laser system, the price ranged from US $2300 to US $32,000.
Counterfeit medical devices are on the rise in dermatology.1,3 Although devices such as radiofrequency and laser systems had thousands of knockoff listings on 2 e-commerce websites, other devices, such as cryolipolysis and body contouring systems, had fewer listings, suggesting heterogeneity in the prevalence of different counterfeit dermatologic devices on the market.
The varied pricing of the top 10 listings for each product and spurious claims of FDA clearance for some listings highlight the lack of regulatory authority over consistent product information on e-commerce websites. Furthermore, differences between characteristics of counterfeit device listings can impede efforts to trace suppliers and increase the opacity of counterfeit purchasing.
Three criteria have been proposed for a device to be considered counterfeit3:
• The device has no proven safety or efficacy among consumers. For example, the substantial threat of copycat devices in dermatology has been demonstrated by reports of burns caused by fake cryolipolysis devices.2
• The device violates patent rights or copy trademarks. Due to the regional nature of intellectual property rights, country-specific filings of patents and trademarks are required if protections are sought internationally. In this study, counterfeit devices originated in China, South Korea, and Thailand, where patent and trademark protections for the original devices do not extend.
• The device is falsely claimed to have been cleared by the FDA or other clinical regulatory authorities. Legitimate medical devices are subject to rounds of safety and compatibility testing using standards set by regulatory bodies, such as the FDA’s Center for Devices and Radiological Health, the International Organization of Standardization, and the International Electrotechnical Commission. Compliance with these safety standards is lost, however, among unregulated internet sales of medical devices. Our search revealed that 10.7% of the top 10 counterfeit device listings for each product explicitly mentioned FDA clearance in the product description. Among the thousands of listings on e-commerce sites, even a fraction that make spurious FDA-clearance claims can mislead consumers.
The issue of counterfeit medical devices has not gone unrecognized globally. In 2013, the World Health Organization created the Global Surveillance and Monitoring System to unify international efforts for reporting substandard, unlicensed, or falsified medical products.4 Although universal monitoring systems can improve detection of counterfeit products, we highlight the alarming continuing ease of purchasing counterfeit dermatologic devices through e-commerce websites. Due to the widespread nature of counterfeiting across all domains of medicine, the onus of curbing counterfeit dermatologic devices might be on dermatology providers to recognize and report such occurrences.
This exploration of counterfeit dermatologic devices revealed a lack of consistency throughout product listings on 2 popular e-commerce websites, Alibaba.com and DHgate.com. Given the alarming availability of these devices on the internet, practitioners should approach the purchase of any device with concern about counterfeiting. Future avenues of study might explore the prevalence of counterfeit devices used in dermatology practices and offer insight on regulation and consumer safety efforts.
- Wang JV, Zachary CB, Saedi N. Counterfeit esthetic devices and patient safety in dermatology. J Cosmet Dermatol. 2018;17:396-397. doi:10.1111/jocd.12526
- Biesman BS, Patel N. Physician alert: beware of counterfeit medical devices. Lasers Surg Med. 2014;46:528‐530. doi:10.1002/lsm.22275
- Stevens WG, Spring MA, Macias LH. Counterfeit medical devices: the money you save up front will cost you big in the end. Aesthet Surg J. 2014;34:786‐788. doi:10.1177/1090820X14529960
- Pisani E. WHO Global Surveillance and Monitoring System for Substandard and Falsified Medical Products. World Health Organization; 2017. Accessed November 21, 2021. https://www.who.int/medicines/regulation/ssffc/publications/GSMSreport_EN.pdf?ua=1
- Wang JV, Zachary CB, Saedi N. Counterfeit esthetic devices and patient safety in dermatology. J Cosmet Dermatol. 2018;17:396-397. doi:10.1111/jocd.12526
- Biesman BS, Patel N. Physician alert: beware of counterfeit medical devices. Lasers Surg Med. 2014;46:528‐530. doi:10.1002/lsm.22275
- Stevens WG, Spring MA, Macias LH. Counterfeit medical devices: the money you save up front will cost you big in the end. Aesthet Surg J. 2014;34:786‐788. doi:10.1177/1090820X14529960
- Pisani E. WHO Global Surveillance and Monitoring System for Substandard and Falsified Medical Products. World Health Organization; 2017. Accessed November 21, 2021. https://www.who.int/medicines/regulation/ssffc/publications/GSMSreport_EN.pdf?ua=1
Practice Points
- Among thousands of counterfeit dermatologic listings, there is great heterogeneity in the number of listings per different subtypes of dermatologic devices, device descriptions, and unit pricing, along with false claims of US Food and Drug Administration clearance.
- Given the prevalence of counterfeit medical devices readily available for purchase online, dermatology practitioners should be wary of the authenticity of any medical device purchased for clinical use.
Sea buckthorn: What is it and what is it good for?
To avoid jumping on the bandwagon of another ingredient trend, we sought to examine the scientific background and properties of sea buckthorn oil and it’s utility for the skin.
Sea buckthorn (Hippophae rhamnoides) – also known as a Siberian pineapple tree, and as sandthorn, sallowthorn, or seaberry – is a thorny, dioecious shrub (or tree) in the oleaster family. It can grow up to 23 feet high and is found in coastal sea cliff areas and on mountain slopes of Western Europe, and in dry sandy areas of Asia Minor and Central Asia, Siberia, China, and Tibet. Common sea buckthorn flowers in late April and early May, producing a large number of small, green and brown flowers, turning into edible, usually yellow or orange round berries. The berries have a bitter, sour taste and have a mild aroma, resembling that of a pineapple. The fruit contains a small stone that covers an oily seed.
The berries are a source of antioxidant vitamins, flavonoids, and organic acids, and when pressed, produce a juice that separates into three layers: a thick cream (upper layer), a combination of saturated and unsaturated fatty acids (middle layer), and juice that is a source of fat (lower layer). The berries contain mainly vitamin C, but also vitamin A (alpha- and beta-carotene) and a mixture of other carotenoids, as well as varying concentrations of tocopherols (vitamin E), folic acid, and vitamin B complex–group vitamins.
In addition to flavonoids, the berries contain catechins and procyanidins, cyclitols, phospholipids, tannins, sugars (galactose, fructose, xylose), organic acids (maleic acid, oxalic acid, malic acid, tartaric acid), phenolic acids (such as ferulic acid), and fatty oil. The amount of vitamin C content varies with the variety of the plant and where it is found. The oil of sea buckthorn may be extracted from two parts of the plant, with mechanical cold pressing of seeds (up to 12.5% weight as oil content) and fruit pulp (8%-12% oil content).
Among vegetable oils, sea buckthorn fruit oil has the highest content of palmitoleic acid (omega-7).
Fruit and seed oils contain tocotrienols and plant sterols. Pulp sea buckthorn oil has a high carotenoid content, as opposed to seed oil, and in Mongolia, Russia, and China, is used as a topical therapy for skin burns.
Other significant fatty acids found in sea buckthorn oil are saturated fatty acids (palmitic acid and stearic acid) and polyunsaturated fatty acids, which include alpha-linolenic acid (omega-3), gamma-linolenic acid (omega-6), linolic acid (omega-6), oleic acid (omega-9), and eicosanoic acid (omega-9). Gamma-linoleic acid in particular is reduced in dry skin conditions, such as aging and atopic dermatitis. The human body can produce some gamma-linolenic acid, oleic acid, and palmitoleic acid, but not linolic acid and alpha-linolenic acid. The addition of these substances to diet or skin care has been found to be beneficial in improving dryness and the skin barrier.
In addition, linolic acid, a natural component of human sebum, has been noted to be decreased in the sebum of people with acne-prone skin. Preliminary evidence indicates that dietary supplements containing fatty acids such as docosahexaenoic acid, sea buckthorn oil, and hemp seed oil may decrease the severity of atopic dermatitis.
Besides use in topical skin care and cosmetic preparations, sea buckthorn has also been used successfully in the treatment of chronic gastric ulcer disease, inflammation of the vagina and cervix, and cervical erosion. The bark and leaves of sea buckthorn used to be applied to treat diarrhea and dermatologic conditions, while berry oil has been applied topically or taken orally to soften the skin.
In traditional Indian, Chinese, and Tibetan medicines, sea buckthorn berries are used for medicinal purposes, as their ingredients were thought to have a beneficial effect on the function of the alimentary, respiratory, and circulatory systems. Current studies and uses are now confirming their utility experienced over hundreds of years.
Harvesting sea buckthorn fruit is difficult because of dense thorn arrangement among the berries. Therefore, sometimes the only way to obtain fruit is to remove the entire branch of the shrub, which reduces future crops. For this reason berries can only be harvested once every 2 years.
Sea buckthorn has interesting properties and could be of benefit in topical skin care, as long as it is not overharvested or harvested in a way that has a detrimental impact on the environment.
Dr. Wesley and Lily Talakoub, MD, are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
References
United States Department of Agriculture. PLANTS Profile for Hippophae rhamnoides (seaberry). 2007.
Zielińska A and Nowak I. Lipids Health Dis. 2017 May 19;16(1):95.
Reynolds KA et al. Int J Dermatol. 2019 Dec;58(12):1371-6.
To avoid jumping on the bandwagon of another ingredient trend, we sought to examine the scientific background and properties of sea buckthorn oil and it’s utility for the skin.
Sea buckthorn (Hippophae rhamnoides) – also known as a Siberian pineapple tree, and as sandthorn, sallowthorn, or seaberry – is a thorny, dioecious shrub (or tree) in the oleaster family. It can grow up to 23 feet high and is found in coastal sea cliff areas and on mountain slopes of Western Europe, and in dry sandy areas of Asia Minor and Central Asia, Siberia, China, and Tibet. Common sea buckthorn flowers in late April and early May, producing a large number of small, green and brown flowers, turning into edible, usually yellow or orange round berries. The berries have a bitter, sour taste and have a mild aroma, resembling that of a pineapple. The fruit contains a small stone that covers an oily seed.
The berries are a source of antioxidant vitamins, flavonoids, and organic acids, and when pressed, produce a juice that separates into three layers: a thick cream (upper layer), a combination of saturated and unsaturated fatty acids (middle layer), and juice that is a source of fat (lower layer). The berries contain mainly vitamin C, but also vitamin A (alpha- and beta-carotene) and a mixture of other carotenoids, as well as varying concentrations of tocopherols (vitamin E), folic acid, and vitamin B complex–group vitamins.
In addition to flavonoids, the berries contain catechins and procyanidins, cyclitols, phospholipids, tannins, sugars (galactose, fructose, xylose), organic acids (maleic acid, oxalic acid, malic acid, tartaric acid), phenolic acids (such as ferulic acid), and fatty oil. The amount of vitamin C content varies with the variety of the plant and where it is found. The oil of sea buckthorn may be extracted from two parts of the plant, with mechanical cold pressing of seeds (up to 12.5% weight as oil content) and fruit pulp (8%-12% oil content).
Among vegetable oils, sea buckthorn fruit oil has the highest content of palmitoleic acid (omega-7).
Fruit and seed oils contain tocotrienols and plant sterols. Pulp sea buckthorn oil has a high carotenoid content, as opposed to seed oil, and in Mongolia, Russia, and China, is used as a topical therapy for skin burns.
Other significant fatty acids found in sea buckthorn oil are saturated fatty acids (palmitic acid and stearic acid) and polyunsaturated fatty acids, which include alpha-linolenic acid (omega-3), gamma-linolenic acid (omega-6), linolic acid (omega-6), oleic acid (omega-9), and eicosanoic acid (omega-9). Gamma-linoleic acid in particular is reduced in dry skin conditions, such as aging and atopic dermatitis. The human body can produce some gamma-linolenic acid, oleic acid, and palmitoleic acid, but not linolic acid and alpha-linolenic acid. The addition of these substances to diet or skin care has been found to be beneficial in improving dryness and the skin barrier.
In addition, linolic acid, a natural component of human sebum, has been noted to be decreased in the sebum of people with acne-prone skin. Preliminary evidence indicates that dietary supplements containing fatty acids such as docosahexaenoic acid, sea buckthorn oil, and hemp seed oil may decrease the severity of atopic dermatitis.
Besides use in topical skin care and cosmetic preparations, sea buckthorn has also been used successfully in the treatment of chronic gastric ulcer disease, inflammation of the vagina and cervix, and cervical erosion. The bark and leaves of sea buckthorn used to be applied to treat diarrhea and dermatologic conditions, while berry oil has been applied topically or taken orally to soften the skin.
In traditional Indian, Chinese, and Tibetan medicines, sea buckthorn berries are used for medicinal purposes, as their ingredients were thought to have a beneficial effect on the function of the alimentary, respiratory, and circulatory systems. Current studies and uses are now confirming their utility experienced over hundreds of years.
Harvesting sea buckthorn fruit is difficult because of dense thorn arrangement among the berries. Therefore, sometimes the only way to obtain fruit is to remove the entire branch of the shrub, which reduces future crops. For this reason berries can only be harvested once every 2 years.
Sea buckthorn has interesting properties and could be of benefit in topical skin care, as long as it is not overharvested or harvested in a way that has a detrimental impact on the environment.
Dr. Wesley and Lily Talakoub, MD, are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
References
United States Department of Agriculture. PLANTS Profile for Hippophae rhamnoides (seaberry). 2007.
Zielińska A and Nowak I. Lipids Health Dis. 2017 May 19;16(1):95.
Reynolds KA et al. Int J Dermatol. 2019 Dec;58(12):1371-6.
To avoid jumping on the bandwagon of another ingredient trend, we sought to examine the scientific background and properties of sea buckthorn oil and it’s utility for the skin.
Sea buckthorn (Hippophae rhamnoides) – also known as a Siberian pineapple tree, and as sandthorn, sallowthorn, or seaberry – is a thorny, dioecious shrub (or tree) in the oleaster family. It can grow up to 23 feet high and is found in coastal sea cliff areas and on mountain slopes of Western Europe, and in dry sandy areas of Asia Minor and Central Asia, Siberia, China, and Tibet. Common sea buckthorn flowers in late April and early May, producing a large number of small, green and brown flowers, turning into edible, usually yellow or orange round berries. The berries have a bitter, sour taste and have a mild aroma, resembling that of a pineapple. The fruit contains a small stone that covers an oily seed.
The berries are a source of antioxidant vitamins, flavonoids, and organic acids, and when pressed, produce a juice that separates into three layers: a thick cream (upper layer), a combination of saturated and unsaturated fatty acids (middle layer), and juice that is a source of fat (lower layer). The berries contain mainly vitamin C, but also vitamin A (alpha- and beta-carotene) and a mixture of other carotenoids, as well as varying concentrations of tocopherols (vitamin E), folic acid, and vitamin B complex–group vitamins.
In addition to flavonoids, the berries contain catechins and procyanidins, cyclitols, phospholipids, tannins, sugars (galactose, fructose, xylose), organic acids (maleic acid, oxalic acid, malic acid, tartaric acid), phenolic acids (such as ferulic acid), and fatty oil. The amount of vitamin C content varies with the variety of the plant and where it is found. The oil of sea buckthorn may be extracted from two parts of the plant, with mechanical cold pressing of seeds (up to 12.5% weight as oil content) and fruit pulp (8%-12% oil content).
Among vegetable oils, sea buckthorn fruit oil has the highest content of palmitoleic acid (omega-7).
Fruit and seed oils contain tocotrienols and plant sterols. Pulp sea buckthorn oil has a high carotenoid content, as opposed to seed oil, and in Mongolia, Russia, and China, is used as a topical therapy for skin burns.
Other significant fatty acids found in sea buckthorn oil are saturated fatty acids (palmitic acid and stearic acid) and polyunsaturated fatty acids, which include alpha-linolenic acid (omega-3), gamma-linolenic acid (omega-6), linolic acid (omega-6), oleic acid (omega-9), and eicosanoic acid (omega-9). Gamma-linoleic acid in particular is reduced in dry skin conditions, such as aging and atopic dermatitis. The human body can produce some gamma-linolenic acid, oleic acid, and palmitoleic acid, but not linolic acid and alpha-linolenic acid. The addition of these substances to diet or skin care has been found to be beneficial in improving dryness and the skin barrier.
In addition, linolic acid, a natural component of human sebum, has been noted to be decreased in the sebum of people with acne-prone skin. Preliminary evidence indicates that dietary supplements containing fatty acids such as docosahexaenoic acid, sea buckthorn oil, and hemp seed oil may decrease the severity of atopic dermatitis.
Besides use in topical skin care and cosmetic preparations, sea buckthorn has also been used successfully in the treatment of chronic gastric ulcer disease, inflammation of the vagina and cervix, and cervical erosion. The bark and leaves of sea buckthorn used to be applied to treat diarrhea and dermatologic conditions, while berry oil has been applied topically or taken orally to soften the skin.
In traditional Indian, Chinese, and Tibetan medicines, sea buckthorn berries are used for medicinal purposes, as their ingredients were thought to have a beneficial effect on the function of the alimentary, respiratory, and circulatory systems. Current studies and uses are now confirming their utility experienced over hundreds of years.
Harvesting sea buckthorn fruit is difficult because of dense thorn arrangement among the berries. Therefore, sometimes the only way to obtain fruit is to remove the entire branch of the shrub, which reduces future crops. For this reason berries can only be harvested once every 2 years.
Sea buckthorn has interesting properties and could be of benefit in topical skin care, as long as it is not overharvested or harvested in a way that has a detrimental impact on the environment.
Dr. Wesley and Lily Talakoub, MD, are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
References
United States Department of Agriculture. PLANTS Profile for Hippophae rhamnoides (seaberry). 2007.
Zielińska A and Nowak I. Lipids Health Dis. 2017 May 19;16(1):95.
Reynolds KA et al. Int J Dermatol. 2019 Dec;58(12):1371-6.