User login
Striae gravidarum: More than a ‘nuisance,’ say researchers
In the study of healthy pregnant women, “we found that SG can be associated with a host of negative reactions reflecting increased psychological and emotional distress,” reported Kaveri Karhade, MD, from the Berman Skin Institute, Los Altos, Calif., and coauthors from the University of Michigan, Ann Arbor. Dr. Karhade was with the department of dermatology at the University of Michigan at the time the study was conducted.
“We suggest that health care providers should avoid thinking of SG as merely a cosmetic ‘nuisance,’ ” they wrote in an article published in the International Journal of Women’s Dermatology. “Instead, it would be reasonable for providers to approach SG like other dermatologic concerns, and to consider asking patients whether SG cause emotional distress and whether prevention or treatment strategies should be attempted, even if not completely effective and potentially costly.”
The investigators did not evaluate treatments, but Frank Wang, MD, senior author of the study and professor of clinical dermatology at the University of Michigan Medicine, said in an interview that, “while they aren’t completely effective, some treatments can still help.” In addition, “recommending something also shows that you are listening to patients’ concerns – taking their concerns and skin lesions seriously,” he said.
Patient survey
The authors conducted a cross-sectional survey of 116 healthy pregnant women with SG. Participants were asked about the emotional and psychological effects of the lesions and how SG affects quality of life. The survey was modeled on questions from the Dermatology Life Quality Index, which asks about the impact of skin disease on embarrassment/self-consciousness, clothing choice, leisure activities, and interpersonal problems. “Content of questions was also devised from direct discussion with pregnant women attending clinic appointments or participating in other research studies on SG at our institution, and discussion with expert colleagues in obstetrics and dermatology,” the authors explained.
The survey consisted of 35 questions concerning demographics, pregnancy characteristics, personal and family history of SG, specific physical concerns about SG, impact of SG on attitude toward pregnancy, willingness to prevent SG or seek treatment, severity of SG (self-evaluated), the impact of SG on specific life-quality facets, and the location of lesions.
About two-thirds of respondents were aged 25-36 years and were White; the remainder self-identified as Asian, Black, Native American, or “other.” Most women reported “average” weight gain during the current pregnancy. Almost half of participants (45%) reporting a history of SG from prior pregnancies, and 65% reported a family history of SG.
The abdomen was identified most frequently as the location of SG (75%), followed by the breasts (43%), hips (43%), thighs (36%), buttocks (19%), and other areas (6%).
For most women (75%), permanency of the lesions was their top concern. About half (51%) reported that they had attempted to prevent SG, mostly with topical creams or oils. Three-quarters (75%) expressed interest in seeking treatment for SG, but this percentage dropped significantly to 33% (P =.008) if that treatment would not be covered by insurance.
Regarding the psychological impact of SG, embarrassment/self-consciousness correlated most strongly with lesion severity, followed by general quality of life, impact on choice of attire, impact on self-image/self-esteem, feelings of anxiety/depression related to SG, alteration of social/leisure activities related to SG (all P < .0001), and creation of interpersonal problems related to SG (P = .02).
The investigators also found that an increase in the effect of SG on self-image/self-esteem was “moderately associated” with younger age (P < .001) and that increased embarrassment related to SG was “moderately associated” with weight gain during pregnancy (P < .001).
“For years, stretch marks have been a topic to avoid and something many women try to hide,” Timothy Johnson, MD, professor of obstetrics and gynecology at the University of Michigan and coauthor of the study, said in a press release from the university. “Pregnant women talk about stretch marks with me every single week at clinic, and it’s time we break the stigma and start talking about them openly with all patients. ... By doing this study, we have an opportunity to normalize stretch marks in the context of all other dermatological conditions.”
Asked to comment on the findings, Tina Alster, MD, director of the Washington Institute of Dermatologic Laser Surgery and clinical professor of dermatology at Georgetown University, Washington, said her 3 decades of clinical experience support the authors’ findings. “Most patients who have striae are very self-conscious about them and report that their presence has negatively impacted their quality of life and self-confidence,” she said in an interview. “Of course, patients who come to my office are interested in having them treated, so my patient subset is skewed.”
She said treatment strategies that she discusses with patients include topical retinol/retinoids, which she said provide “low clinical response”; microneedling, which provides “marked” clinical response; and nonablative laser treatment, which provides “good” clinical response.
Considering particular patient characteristics, including budget, Dr. Alster said, “For those on a limited budget, I would propose daily use of a topical retinol, despite the low clinical effect. Many retinol-containing products are available over the counter. Prescription-strength retinoic acid tends to be pricey, often costing as much as in-office treatments.” Medical microneedling (not the cosmetic “roller” microneedling performed by aestheticians), she added, “gives the best results for the money and produces clinical results that mirror those achieved with lasers.”
Dr. Wang agreed that even recommending less expensive and less efficacious options such as over-the-counter creams can help alleviate patients’ concerns. “It shows that you are being holistic – not just caring for medical issues around pregnancy, but that you also take the emotional/psychological concerns of pregnant individuals and new parents seriously and that you recognize the impact of skin problems on quality of life. In the end, recommending something – in other words, providing some options, like creams or other therapies, for instance – is still, in my opinion, better than not recommending anything.”
Dr. Wang is involved with a study that is currently enrolling patients and that is evaluating the formation of early SG, which includes performing skin biopsies as soon as lesions appear.
The study had no funding. The study authors and Dr. Alster disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In the study of healthy pregnant women, “we found that SG can be associated with a host of negative reactions reflecting increased psychological and emotional distress,” reported Kaveri Karhade, MD, from the Berman Skin Institute, Los Altos, Calif., and coauthors from the University of Michigan, Ann Arbor. Dr. Karhade was with the department of dermatology at the University of Michigan at the time the study was conducted.
“We suggest that health care providers should avoid thinking of SG as merely a cosmetic ‘nuisance,’ ” they wrote in an article published in the International Journal of Women’s Dermatology. “Instead, it would be reasonable for providers to approach SG like other dermatologic concerns, and to consider asking patients whether SG cause emotional distress and whether prevention or treatment strategies should be attempted, even if not completely effective and potentially costly.”
The investigators did not evaluate treatments, but Frank Wang, MD, senior author of the study and professor of clinical dermatology at the University of Michigan Medicine, said in an interview that, “while they aren’t completely effective, some treatments can still help.” In addition, “recommending something also shows that you are listening to patients’ concerns – taking their concerns and skin lesions seriously,” he said.
Patient survey
The authors conducted a cross-sectional survey of 116 healthy pregnant women with SG. Participants were asked about the emotional and psychological effects of the lesions and how SG affects quality of life. The survey was modeled on questions from the Dermatology Life Quality Index, which asks about the impact of skin disease on embarrassment/self-consciousness, clothing choice, leisure activities, and interpersonal problems. “Content of questions was also devised from direct discussion with pregnant women attending clinic appointments or participating in other research studies on SG at our institution, and discussion with expert colleagues in obstetrics and dermatology,” the authors explained.
The survey consisted of 35 questions concerning demographics, pregnancy characteristics, personal and family history of SG, specific physical concerns about SG, impact of SG on attitude toward pregnancy, willingness to prevent SG or seek treatment, severity of SG (self-evaluated), the impact of SG on specific life-quality facets, and the location of lesions.
About two-thirds of respondents were aged 25-36 years and were White; the remainder self-identified as Asian, Black, Native American, or “other.” Most women reported “average” weight gain during the current pregnancy. Almost half of participants (45%) reporting a history of SG from prior pregnancies, and 65% reported a family history of SG.
The abdomen was identified most frequently as the location of SG (75%), followed by the breasts (43%), hips (43%), thighs (36%), buttocks (19%), and other areas (6%).
For most women (75%), permanency of the lesions was their top concern. About half (51%) reported that they had attempted to prevent SG, mostly with topical creams or oils. Three-quarters (75%) expressed interest in seeking treatment for SG, but this percentage dropped significantly to 33% (P =.008) if that treatment would not be covered by insurance.
Regarding the psychological impact of SG, embarrassment/self-consciousness correlated most strongly with lesion severity, followed by general quality of life, impact on choice of attire, impact on self-image/self-esteem, feelings of anxiety/depression related to SG, alteration of social/leisure activities related to SG (all P < .0001), and creation of interpersonal problems related to SG (P = .02).
The investigators also found that an increase in the effect of SG on self-image/self-esteem was “moderately associated” with younger age (P < .001) and that increased embarrassment related to SG was “moderately associated” with weight gain during pregnancy (P < .001).
“For years, stretch marks have been a topic to avoid and something many women try to hide,” Timothy Johnson, MD, professor of obstetrics and gynecology at the University of Michigan and coauthor of the study, said in a press release from the university. “Pregnant women talk about stretch marks with me every single week at clinic, and it’s time we break the stigma and start talking about them openly with all patients. ... By doing this study, we have an opportunity to normalize stretch marks in the context of all other dermatological conditions.”
Asked to comment on the findings, Tina Alster, MD, director of the Washington Institute of Dermatologic Laser Surgery and clinical professor of dermatology at Georgetown University, Washington, said her 3 decades of clinical experience support the authors’ findings. “Most patients who have striae are very self-conscious about them and report that their presence has negatively impacted their quality of life and self-confidence,” she said in an interview. “Of course, patients who come to my office are interested in having them treated, so my patient subset is skewed.”
She said treatment strategies that she discusses with patients include topical retinol/retinoids, which she said provide “low clinical response”; microneedling, which provides “marked” clinical response; and nonablative laser treatment, which provides “good” clinical response.
Considering particular patient characteristics, including budget, Dr. Alster said, “For those on a limited budget, I would propose daily use of a topical retinol, despite the low clinical effect. Many retinol-containing products are available over the counter. Prescription-strength retinoic acid tends to be pricey, often costing as much as in-office treatments.” Medical microneedling (not the cosmetic “roller” microneedling performed by aestheticians), she added, “gives the best results for the money and produces clinical results that mirror those achieved with lasers.”
Dr. Wang agreed that even recommending less expensive and less efficacious options such as over-the-counter creams can help alleviate patients’ concerns. “It shows that you are being holistic – not just caring for medical issues around pregnancy, but that you also take the emotional/psychological concerns of pregnant individuals and new parents seriously and that you recognize the impact of skin problems on quality of life. In the end, recommending something – in other words, providing some options, like creams or other therapies, for instance – is still, in my opinion, better than not recommending anything.”
Dr. Wang is involved with a study that is currently enrolling patients and that is evaluating the formation of early SG, which includes performing skin biopsies as soon as lesions appear.
The study had no funding. The study authors and Dr. Alster disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In the study of healthy pregnant women, “we found that SG can be associated with a host of negative reactions reflecting increased psychological and emotional distress,” reported Kaveri Karhade, MD, from the Berman Skin Institute, Los Altos, Calif., and coauthors from the University of Michigan, Ann Arbor. Dr. Karhade was with the department of dermatology at the University of Michigan at the time the study was conducted.
“We suggest that health care providers should avoid thinking of SG as merely a cosmetic ‘nuisance,’ ” they wrote in an article published in the International Journal of Women’s Dermatology. “Instead, it would be reasonable for providers to approach SG like other dermatologic concerns, and to consider asking patients whether SG cause emotional distress and whether prevention or treatment strategies should be attempted, even if not completely effective and potentially costly.”
The investigators did not evaluate treatments, but Frank Wang, MD, senior author of the study and professor of clinical dermatology at the University of Michigan Medicine, said in an interview that, “while they aren’t completely effective, some treatments can still help.” In addition, “recommending something also shows that you are listening to patients’ concerns – taking their concerns and skin lesions seriously,” he said.
Patient survey
The authors conducted a cross-sectional survey of 116 healthy pregnant women with SG. Participants were asked about the emotional and psychological effects of the lesions and how SG affects quality of life. The survey was modeled on questions from the Dermatology Life Quality Index, which asks about the impact of skin disease on embarrassment/self-consciousness, clothing choice, leisure activities, and interpersonal problems. “Content of questions was also devised from direct discussion with pregnant women attending clinic appointments or participating in other research studies on SG at our institution, and discussion with expert colleagues in obstetrics and dermatology,” the authors explained.
The survey consisted of 35 questions concerning demographics, pregnancy characteristics, personal and family history of SG, specific physical concerns about SG, impact of SG on attitude toward pregnancy, willingness to prevent SG or seek treatment, severity of SG (self-evaluated), the impact of SG on specific life-quality facets, and the location of lesions.
About two-thirds of respondents were aged 25-36 years and were White; the remainder self-identified as Asian, Black, Native American, or “other.” Most women reported “average” weight gain during the current pregnancy. Almost half of participants (45%) reporting a history of SG from prior pregnancies, and 65% reported a family history of SG.
The abdomen was identified most frequently as the location of SG (75%), followed by the breasts (43%), hips (43%), thighs (36%), buttocks (19%), and other areas (6%).
For most women (75%), permanency of the lesions was their top concern. About half (51%) reported that they had attempted to prevent SG, mostly with topical creams or oils. Three-quarters (75%) expressed interest in seeking treatment for SG, but this percentage dropped significantly to 33% (P =.008) if that treatment would not be covered by insurance.
Regarding the psychological impact of SG, embarrassment/self-consciousness correlated most strongly with lesion severity, followed by general quality of life, impact on choice of attire, impact on self-image/self-esteem, feelings of anxiety/depression related to SG, alteration of social/leisure activities related to SG (all P < .0001), and creation of interpersonal problems related to SG (P = .02).
The investigators also found that an increase in the effect of SG on self-image/self-esteem was “moderately associated” with younger age (P < .001) and that increased embarrassment related to SG was “moderately associated” with weight gain during pregnancy (P < .001).
“For years, stretch marks have been a topic to avoid and something many women try to hide,” Timothy Johnson, MD, professor of obstetrics and gynecology at the University of Michigan and coauthor of the study, said in a press release from the university. “Pregnant women talk about stretch marks with me every single week at clinic, and it’s time we break the stigma and start talking about them openly with all patients. ... By doing this study, we have an opportunity to normalize stretch marks in the context of all other dermatological conditions.”
Asked to comment on the findings, Tina Alster, MD, director of the Washington Institute of Dermatologic Laser Surgery and clinical professor of dermatology at Georgetown University, Washington, said her 3 decades of clinical experience support the authors’ findings. “Most patients who have striae are very self-conscious about them and report that their presence has negatively impacted their quality of life and self-confidence,” she said in an interview. “Of course, patients who come to my office are interested in having them treated, so my patient subset is skewed.”
She said treatment strategies that she discusses with patients include topical retinol/retinoids, which she said provide “low clinical response”; microneedling, which provides “marked” clinical response; and nonablative laser treatment, which provides “good” clinical response.
Considering particular patient characteristics, including budget, Dr. Alster said, “For those on a limited budget, I would propose daily use of a topical retinol, despite the low clinical effect. Many retinol-containing products are available over the counter. Prescription-strength retinoic acid tends to be pricey, often costing as much as in-office treatments.” Medical microneedling (not the cosmetic “roller” microneedling performed by aestheticians), she added, “gives the best results for the money and produces clinical results that mirror those achieved with lasers.”
Dr. Wang agreed that even recommending less expensive and less efficacious options such as over-the-counter creams can help alleviate patients’ concerns. “It shows that you are being holistic – not just caring for medical issues around pregnancy, but that you also take the emotional/psychological concerns of pregnant individuals and new parents seriously and that you recognize the impact of skin problems on quality of life. In the end, recommending something – in other words, providing some options, like creams or other therapies, for instance – is still, in my opinion, better than not recommending anything.”
Dr. Wang is involved with a study that is currently enrolling patients and that is evaluating the formation of early SG, which includes performing skin biopsies as soon as lesions appear.
The study had no funding. The study authors and Dr. Alster disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Does the use of frankincense make sense in dermatology?
The Boswellia serrata exudate or gum (known in India as “guggulu”) that forms an aromatic resin traditionally used as incense – and known as frankincense (especially when retrieved from Boswellia species found in Eritrea and Somalia but also from the Indian variety) – has been considered for thousands of years to possess therapeutic properties. It is used in Ayurvedic medicine, as well as in traditional medicine in China and the Middle East, particularly for its anti-inflammatory effects to treat chronic conditions.1-8 In fact, such essential oils have been used since 2800 BC to treat various inflammatory conditions, including skin sores and wounds, as well as in perfumes and incense.2,9 In the West, use of frankincense dates back to thousands of years as well, more often found in the form of incense for religious and cultural ceremonies.7 Over the past 2 decades, .3 This column focuses on some of the emerging data on this ancient botanical agent.
Chemical constituents
Terpenoids and essential oils are the primary components of frankincense and are known to impart anti-inflammatory and anticancer activity. The same is true for myrrh, which has been combined with frankincense in traditional Chinese medicine as a single medication for millennia, with the two acting synergistically and considered still to be a potent combination in conferring various biological benefits.7
In 2010, in a systematic review of the anti-inflammatory and anticancer activities of Boswellia species and their chemical ingredients, Efferth and Oesch found that frankincense blocks the production of leukotrienes, cyclooxygenase (COX) 1 and 2, as well as 5-lipoxygenase; and oxidative stress. It also contributes to regulation of immune cells from the innate and acquired immune systems and exerts anticancer activity by influencing signaling transduction responsible for cell cycle arrest, as well as inhibition of proliferation, angiogenesis, invasion, and metastasis. The investigators also reported on clinical trial results that have found efficacy of frankincense and its constituents in ameliorating symptoms of psoriasis and erythematous eczema, among other disorders.3
Anti-inflammatory activity
Li et al. completed a study in 2016 to identify the active ingredients responsible for the anti-inflammatory and analgesic effects of frankincense. They found that alpha-pinene, linalool, and 1-octanol were key contributors. These constituents were noted for suppressing COX-2 overexpression in mice, as well as nociceptive stimulus-induced inflammatory infiltrates.10
Noting the increasing popularity of frankincense essential oil in skin care, despite a paucity of data, in 2017, Han et al. evaluated the biological activities of the essential oil in pre-inflamed human dermal fibroblasts using 17 key protein biomarkers. Frankincense essential oil displayed significant antiproliferative activity and suppressed collagen III, interferon gamma-induced protein 10, and intracellular adhesion molecule 1. The investigators referred to the overall encouraging potential of frankincense essential oil to exert influence over inflammation and tissue remodeling in human skin and called for additional research into its mechanisms of action and active constituents.11
Anticancer activity
The main active ingredient in frankincense, boswellic acid, has been shown to promote apoptosis, suppress matrix metalloproteinase secretion, and hinder migration in metastatic melanoma cell lines in mice.6,12
In 2019, Hakkim et al. demonstrated that frankincense essential oil yielded substantial antimelanoma activity in vitro and in vivo and ameliorated hepatotoxicity caused by acetaminophen.13
There is one case report in the literature on the use of frankincense as a treatment for skin cancer. A 56-year-old man received frankincense oil multiple times a day for 4 months to treat a nodular basal cell carcinoma on one arm (which resolved) and an infiltrative BCC on the chest (some focal residual tumor remained).6,14 Topical frankincense or boswellic acid has been given a grade D recommendation for treating skin cancer, however, because of only one level-of-evidence-5 study.6
Antimicrobial activity
In 2012, de Rapper et al. collected samples of three essential oils of frankincense (Boswellia rivae, Boswellia neglecta, and Boswellia papyrifera) and two essential oil samples of myrrh and sweet myrrh from different regions of Ethiopia to study their anti-infective properties alone and in combination. The investigators observed synergistic and additive effects, particularly between B. papyrifera and Commiphora myrrha. While noting the long history of the combined use of frankincense and myrrh essential oils since 1500 BC, the investigators highlighted their study as the first antimicrobial work to verify the effectiveness of this combination, validating the use of this combination to thwart particular pathogens.15
Just 2 years ago, Ljaljević Grbić et al. evaluated the in vitro antimicrobial potential of the liquid and vapor phases of B. carteri and C. myrrha (frankincense and myrrh, respectively) essential oils, finding that frankincense demonstrated marked capacity to act as a natural antimicrobial agent.9
Transdermal delivery
In 2017, Zhu et al. showed that frankincense and myrrh essential oils promoted the permeability of the Chinese herb Chuanxiong and may facilitate drug elimination from the epidermis via dermal capillaries by dint of improved cutaneous blood flow, thereby augmenting transdermal drug delivery.16 The same team also showed that frankincense and myrrh essential oils, by fostering permeation by enhancing drug delivery across the stratum corneum, can also alter the structure of the stratum corneum.17
Conclusion
The use of frankincense in traditional medicine has a long and impressive track record. Recent research provides reason for optimism, and further investigating the possible incorporation of this botanical agent into modern dermatologic therapies appears warranted. Clearly, however, much more research is needed.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Kimmatkar N et al. Phytomedicine. 2003 Jan;10(1):3-7.
2. Ammon HP. Wien Med Wochenschr. 2002;152(15-16):373-8.
3. Efferth T & Oesch F. Semin Cancer Biol. 2020 Feb 4;S1044-579X(20)30034-1.
4. Banno N et al. J Ethnopharmacol. 2006 Sep 19;107(2):249-53.
5. Poeckel D & Werz O. Curr Med Chem. 2006;13(28):3359-69.
6. Li JY, Kampp JT. Dermatol Surg. 2019 Jan;45(1):58-67.
7. Cao B et al. Molecules. 2019 Aug 24;24(17): 3076.
8. Mertens M et al. Flavour Fragr J. 2009;24:279-300.
9. Ljaljević Grbić M et al. J Ethnopharmacol. 2018 Jun 12;219:1-14.
10. Li XJ et al. J Ethnopharmacol. 2016 Feb 17;179:22-6.
11. Han X et al. Biochim Open. 2017 Feb 3;4:31-5.
12. Zhao W et al. Cancer Detect Prev. 2003;27:67-75.
13. Hakkim FL et al. Oncotarget. 2019 May 28;10(37):3472-90.
14. Fung K et al. OA Altern Med 2013;1:14.
15. de Rapper S et al. Lett Appl Microbiol. 2012 Apr;54(4):352-8.
16. Zhu XF et al. Zhongguo Zhong Yao Za Zhi. 2017 Feb;42(4):680-5.
17. Guan YM et al. Zhongguo Zhong Yao Za Zhi. 2017 Sep;42(17):3350-5.
The Boswellia serrata exudate or gum (known in India as “guggulu”) that forms an aromatic resin traditionally used as incense – and known as frankincense (especially when retrieved from Boswellia species found in Eritrea and Somalia but also from the Indian variety) – has been considered for thousands of years to possess therapeutic properties. It is used in Ayurvedic medicine, as well as in traditional medicine in China and the Middle East, particularly for its anti-inflammatory effects to treat chronic conditions.1-8 In fact, such essential oils have been used since 2800 BC to treat various inflammatory conditions, including skin sores and wounds, as well as in perfumes and incense.2,9 In the West, use of frankincense dates back to thousands of years as well, more often found in the form of incense for religious and cultural ceremonies.7 Over the past 2 decades, .3 This column focuses on some of the emerging data on this ancient botanical agent.
Chemical constituents
Terpenoids and essential oils are the primary components of frankincense and are known to impart anti-inflammatory and anticancer activity. The same is true for myrrh, which has been combined with frankincense in traditional Chinese medicine as a single medication for millennia, with the two acting synergistically and considered still to be a potent combination in conferring various biological benefits.7
In 2010, in a systematic review of the anti-inflammatory and anticancer activities of Boswellia species and their chemical ingredients, Efferth and Oesch found that frankincense blocks the production of leukotrienes, cyclooxygenase (COX) 1 and 2, as well as 5-lipoxygenase; and oxidative stress. It also contributes to regulation of immune cells from the innate and acquired immune systems and exerts anticancer activity by influencing signaling transduction responsible for cell cycle arrest, as well as inhibition of proliferation, angiogenesis, invasion, and metastasis. The investigators also reported on clinical trial results that have found efficacy of frankincense and its constituents in ameliorating symptoms of psoriasis and erythematous eczema, among other disorders.3
Anti-inflammatory activity
Li et al. completed a study in 2016 to identify the active ingredients responsible for the anti-inflammatory and analgesic effects of frankincense. They found that alpha-pinene, linalool, and 1-octanol were key contributors. These constituents were noted for suppressing COX-2 overexpression in mice, as well as nociceptive stimulus-induced inflammatory infiltrates.10
Noting the increasing popularity of frankincense essential oil in skin care, despite a paucity of data, in 2017, Han et al. evaluated the biological activities of the essential oil in pre-inflamed human dermal fibroblasts using 17 key protein biomarkers. Frankincense essential oil displayed significant antiproliferative activity and suppressed collagen III, interferon gamma-induced protein 10, and intracellular adhesion molecule 1. The investigators referred to the overall encouraging potential of frankincense essential oil to exert influence over inflammation and tissue remodeling in human skin and called for additional research into its mechanisms of action and active constituents.11
Anticancer activity
The main active ingredient in frankincense, boswellic acid, has been shown to promote apoptosis, suppress matrix metalloproteinase secretion, and hinder migration in metastatic melanoma cell lines in mice.6,12
In 2019, Hakkim et al. demonstrated that frankincense essential oil yielded substantial antimelanoma activity in vitro and in vivo and ameliorated hepatotoxicity caused by acetaminophen.13
There is one case report in the literature on the use of frankincense as a treatment for skin cancer. A 56-year-old man received frankincense oil multiple times a day for 4 months to treat a nodular basal cell carcinoma on one arm (which resolved) and an infiltrative BCC on the chest (some focal residual tumor remained).6,14 Topical frankincense or boswellic acid has been given a grade D recommendation for treating skin cancer, however, because of only one level-of-evidence-5 study.6
Antimicrobial activity
In 2012, de Rapper et al. collected samples of three essential oils of frankincense (Boswellia rivae, Boswellia neglecta, and Boswellia papyrifera) and two essential oil samples of myrrh and sweet myrrh from different regions of Ethiopia to study their anti-infective properties alone and in combination. The investigators observed synergistic and additive effects, particularly between B. papyrifera and Commiphora myrrha. While noting the long history of the combined use of frankincense and myrrh essential oils since 1500 BC, the investigators highlighted their study as the first antimicrobial work to verify the effectiveness of this combination, validating the use of this combination to thwart particular pathogens.15
Just 2 years ago, Ljaljević Grbić et al. evaluated the in vitro antimicrobial potential of the liquid and vapor phases of B. carteri and C. myrrha (frankincense and myrrh, respectively) essential oils, finding that frankincense demonstrated marked capacity to act as a natural antimicrobial agent.9
Transdermal delivery
In 2017, Zhu et al. showed that frankincense and myrrh essential oils promoted the permeability of the Chinese herb Chuanxiong and may facilitate drug elimination from the epidermis via dermal capillaries by dint of improved cutaneous blood flow, thereby augmenting transdermal drug delivery.16 The same team also showed that frankincense and myrrh essential oils, by fostering permeation by enhancing drug delivery across the stratum corneum, can also alter the structure of the stratum corneum.17
Conclusion
The use of frankincense in traditional medicine has a long and impressive track record. Recent research provides reason for optimism, and further investigating the possible incorporation of this botanical agent into modern dermatologic therapies appears warranted. Clearly, however, much more research is needed.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Kimmatkar N et al. Phytomedicine. 2003 Jan;10(1):3-7.
2. Ammon HP. Wien Med Wochenschr. 2002;152(15-16):373-8.
3. Efferth T & Oesch F. Semin Cancer Biol. 2020 Feb 4;S1044-579X(20)30034-1.
4. Banno N et al. J Ethnopharmacol. 2006 Sep 19;107(2):249-53.
5. Poeckel D & Werz O. Curr Med Chem. 2006;13(28):3359-69.
6. Li JY, Kampp JT. Dermatol Surg. 2019 Jan;45(1):58-67.
7. Cao B et al. Molecules. 2019 Aug 24;24(17): 3076.
8. Mertens M et al. Flavour Fragr J. 2009;24:279-300.
9. Ljaljević Grbić M et al. J Ethnopharmacol. 2018 Jun 12;219:1-14.
10. Li XJ et al. J Ethnopharmacol. 2016 Feb 17;179:22-6.
11. Han X et al. Biochim Open. 2017 Feb 3;4:31-5.
12. Zhao W et al. Cancer Detect Prev. 2003;27:67-75.
13. Hakkim FL et al. Oncotarget. 2019 May 28;10(37):3472-90.
14. Fung K et al. OA Altern Med 2013;1:14.
15. de Rapper S et al. Lett Appl Microbiol. 2012 Apr;54(4):352-8.
16. Zhu XF et al. Zhongguo Zhong Yao Za Zhi. 2017 Feb;42(4):680-5.
17. Guan YM et al. Zhongguo Zhong Yao Za Zhi. 2017 Sep;42(17):3350-5.
The Boswellia serrata exudate or gum (known in India as “guggulu”) that forms an aromatic resin traditionally used as incense – and known as frankincense (especially when retrieved from Boswellia species found in Eritrea and Somalia but also from the Indian variety) – has been considered for thousands of years to possess therapeutic properties. It is used in Ayurvedic medicine, as well as in traditional medicine in China and the Middle East, particularly for its anti-inflammatory effects to treat chronic conditions.1-8 In fact, such essential oils have been used since 2800 BC to treat various inflammatory conditions, including skin sores and wounds, as well as in perfumes and incense.2,9 In the West, use of frankincense dates back to thousands of years as well, more often found in the form of incense for religious and cultural ceremonies.7 Over the past 2 decades, .3 This column focuses on some of the emerging data on this ancient botanical agent.
Chemical constituents
Terpenoids and essential oils are the primary components of frankincense and are known to impart anti-inflammatory and anticancer activity. The same is true for myrrh, which has been combined with frankincense in traditional Chinese medicine as a single medication for millennia, with the two acting synergistically and considered still to be a potent combination in conferring various biological benefits.7
In 2010, in a systematic review of the anti-inflammatory and anticancer activities of Boswellia species and their chemical ingredients, Efferth and Oesch found that frankincense blocks the production of leukotrienes, cyclooxygenase (COX) 1 and 2, as well as 5-lipoxygenase; and oxidative stress. It also contributes to regulation of immune cells from the innate and acquired immune systems and exerts anticancer activity by influencing signaling transduction responsible for cell cycle arrest, as well as inhibition of proliferation, angiogenesis, invasion, and metastasis. The investigators also reported on clinical trial results that have found efficacy of frankincense and its constituents in ameliorating symptoms of psoriasis and erythematous eczema, among other disorders.3
Anti-inflammatory activity
Li et al. completed a study in 2016 to identify the active ingredients responsible for the anti-inflammatory and analgesic effects of frankincense. They found that alpha-pinene, linalool, and 1-octanol were key contributors. These constituents were noted for suppressing COX-2 overexpression in mice, as well as nociceptive stimulus-induced inflammatory infiltrates.10
Noting the increasing popularity of frankincense essential oil in skin care, despite a paucity of data, in 2017, Han et al. evaluated the biological activities of the essential oil in pre-inflamed human dermal fibroblasts using 17 key protein biomarkers. Frankincense essential oil displayed significant antiproliferative activity and suppressed collagen III, interferon gamma-induced protein 10, and intracellular adhesion molecule 1. The investigators referred to the overall encouraging potential of frankincense essential oil to exert influence over inflammation and tissue remodeling in human skin and called for additional research into its mechanisms of action and active constituents.11
Anticancer activity
The main active ingredient in frankincense, boswellic acid, has been shown to promote apoptosis, suppress matrix metalloproteinase secretion, and hinder migration in metastatic melanoma cell lines in mice.6,12
In 2019, Hakkim et al. demonstrated that frankincense essential oil yielded substantial antimelanoma activity in vitro and in vivo and ameliorated hepatotoxicity caused by acetaminophen.13
There is one case report in the literature on the use of frankincense as a treatment for skin cancer. A 56-year-old man received frankincense oil multiple times a day for 4 months to treat a nodular basal cell carcinoma on one arm (which resolved) and an infiltrative BCC on the chest (some focal residual tumor remained).6,14 Topical frankincense or boswellic acid has been given a grade D recommendation for treating skin cancer, however, because of only one level-of-evidence-5 study.6
Antimicrobial activity
In 2012, de Rapper et al. collected samples of three essential oils of frankincense (Boswellia rivae, Boswellia neglecta, and Boswellia papyrifera) and two essential oil samples of myrrh and sweet myrrh from different regions of Ethiopia to study their anti-infective properties alone and in combination. The investigators observed synergistic and additive effects, particularly between B. papyrifera and Commiphora myrrha. While noting the long history of the combined use of frankincense and myrrh essential oils since 1500 BC, the investigators highlighted their study as the first antimicrobial work to verify the effectiveness of this combination, validating the use of this combination to thwart particular pathogens.15
Just 2 years ago, Ljaljević Grbić et al. evaluated the in vitro antimicrobial potential of the liquid and vapor phases of B. carteri and C. myrrha (frankincense and myrrh, respectively) essential oils, finding that frankincense demonstrated marked capacity to act as a natural antimicrobial agent.9
Transdermal delivery
In 2017, Zhu et al. showed that frankincense and myrrh essential oils promoted the permeability of the Chinese herb Chuanxiong and may facilitate drug elimination from the epidermis via dermal capillaries by dint of improved cutaneous blood flow, thereby augmenting transdermal drug delivery.16 The same team also showed that frankincense and myrrh essential oils, by fostering permeation by enhancing drug delivery across the stratum corneum, can also alter the structure of the stratum corneum.17
Conclusion
The use of frankincense in traditional medicine has a long and impressive track record. Recent research provides reason for optimism, and further investigating the possible incorporation of this botanical agent into modern dermatologic therapies appears warranted. Clearly, however, much more research is needed.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Kimmatkar N et al. Phytomedicine. 2003 Jan;10(1):3-7.
2. Ammon HP. Wien Med Wochenschr. 2002;152(15-16):373-8.
3. Efferth T & Oesch F. Semin Cancer Biol. 2020 Feb 4;S1044-579X(20)30034-1.
4. Banno N et al. J Ethnopharmacol. 2006 Sep 19;107(2):249-53.
5. Poeckel D & Werz O. Curr Med Chem. 2006;13(28):3359-69.
6. Li JY, Kampp JT. Dermatol Surg. 2019 Jan;45(1):58-67.
7. Cao B et al. Molecules. 2019 Aug 24;24(17): 3076.
8. Mertens M et al. Flavour Fragr J. 2009;24:279-300.
9. Ljaljević Grbić M et al. J Ethnopharmacol. 2018 Jun 12;219:1-14.
10. Li XJ et al. J Ethnopharmacol. 2016 Feb 17;179:22-6.
11. Han X et al. Biochim Open. 2017 Feb 3;4:31-5.
12. Zhao W et al. Cancer Detect Prev. 2003;27:67-75.
13. Hakkim FL et al. Oncotarget. 2019 May 28;10(37):3472-90.
14. Fung K et al. OA Altern Med 2013;1:14.
15. de Rapper S et al. Lett Appl Microbiol. 2012 Apr;54(4):352-8.
16. Zhu XF et al. Zhongguo Zhong Yao Za Zhi. 2017 Feb;42(4):680-5.
17. Guan YM et al. Zhongguo Zhong Yao Za Zhi. 2017 Sep;42(17):3350-5.
What are the legal risks of practicing laser cutaneous surgery?
The physician-patient relationship is a key factor in preventing litigation following cutaneous laser surgery, according to Mathew M. Avram, MD, JD.
“Numerous studies indicate that good communication and rapport are the most important means to avoid a lawsuit,” Dr. Avram, director of laser, cosmetics, and dermatologic surgery at Massachusetts General Hospital, Boston, said during a virtual course on laser and aesthetic skin therapy. “It is helpful to say that the outcome was not optimal or what you were anticipating. Communicate your plan [for the complication] clearly and honestly to your patient. The patient may not understand the severity of the complication. If they don’t, they will either leave it alone or they will go elsewhere and may receive poor care.” He added that in New England, “we have some stoic patients who may say ‘I don’t want to bother the doctor’ or ‘It’s my fault for having the procedure done.’ ”
Establishing effective communication with patients from the outset is good practice, he continued, because 75% of physicians in low-risk specialties will face a malpractice claim by age 65. Nearly a decade ago Dr. Avram, H. Ray Jalian, MD, and Chris Jalian, JD, published results from a national legal database analysis identifying common errors and risk factors for litigation in cutaneous surgery. Their search yielded 1,807 documents with 174 unique legal claims involving injury from a cutaneous laser treatment, from 1985 to 2012. The most common litigated procedures were laser hair removal, rejuvenation (mostly related to intense pulsed-light treatments), and laser treatment of leg veins, while the most common injuries sustained were burns, scars, and pigmentary changes. The most common causes of legal action were lack of informed consent and fraud.
Among the 120 cases with public decisions, cases favored the plaintiff 51% of the time. “That’s unusual,” said Dr. Avram, president of American Society for Dermatologic Surgery. “Usually, physicians do better, but I think the fact that they’re cosmetic cases probably shades things a little bit.” The median monetary award was $350,000 and ranged from $5,000 to $2,145,000. The two largest judgments were for improper use of topical anesthesia that led to deaths of patients in laser hair removal cases.
In a separate analysis, the same authors searched an online national database to identify the incidence of medical professional liability claims resulting from cutaneous laser surgery performed by nonphysician operators (NPOs) from 1999 to 2012. Among the 175 cases identified, 43% involved an NPO. “In fact, the cases involving NPOs exploded over a 4-year period; they grew from 36% in 2008 of cases to 78% in 2011,” Dr. Avram said. “This was even more true for laser hair removal.”
The practice setting turned out to be a factor. Only 23% of NPO litigation involving laser procedures arose in medical office settings, while 77% of cases involving NPOs were performed outside of traditional medical settings such as in salons and medical spas – mostly for laser hair removal. “We updated this information by examining the setting for nonphysician operator litigation between 2012 and 2017 and found that 66% of cases involving NPOs were performed outside of a traditional medical setting, while 34% of NPO litigation arose in medical office settings,” Dr. Avram said during the meeting, which was named What’s the Truth? and sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “That’s close to a 2 to 1 ratio.”
In an analysis of medical professional liability claims involving Mohs surgery from 1989 to 2011, 26 of the 42 cases identified involved a primary defendant who was not a Mohs surgeon. In the 26 cases, the most common reasons for lawsuits were failure or delay of diagnosis of a skin cancer, cosmetic outcome issues, lack of informed consent, and delay or failure to refer to a Mohs surgeon. Of the cases that involved Mohs surgeons, the most common causes were lack of proper informed consent and cosmetic outcome issues, but “these cases were overwhelmingly decided in favor of the surgeons,” said Dr. Avram, one of the study authors.
On a related note, Dr. Avram underscored the importance of biopsy-site photography, “because patients and physicians misidentify biopsy sites too commonly,” he said. In a single-center study of 34 biopsy sites of cutaneous head and neck malignancies, patients misidentified the biopsy site 4-7 weeks out in 29% of the cases. Blinded dermatologists and the patient misidentified the biopsy site in 12% of the cases. “Good biopsy site photography should be mandatory in your practice,” he advised.
Clinicians can avoid cutaneous laser surgery complications only by not treating patients. “Complications and side effects are inevitable; you need to know your limits,” he said. “Even in skilled hands, if you treat enough patients, you will encounter challenging side effects. Do not perform a procedure that might produce a side effect that you cannot recognize and treat.”
The best way to avoid complications is to trust your eyes – not the laser – since the same device made by the same manufacturer may produce highly different outputs at the same setting (see J Am Acad Dermatol. 2016;74[5]:807-19).
“Moreover, lasers can produce much different energies after they have been serviced,” Dr. Avram said. “Do not memorize settings. Do not blindly replicate recommended settings from a colleague or a device manufacturer,” he advised. “Some devices are not externally calibrated. Therefore, the settings on one device may not translate the same way to yours. Often, device manufacturers underplay the settings. Safe and unsafe laser endpoints and close observation are the best means to avoiding clinical complications. That means you follow clinical endpoints, not fluences. The key clinical finding is the endpoint, not the energy setting.”
Temporary and expected side effects include erythema, edema, and purpura. “With these it’s just handholding and unlikely to lead to any legal consequences,” he continued. “With temporary hyperpigmentation that can occur with laser hair removal, time is one your side, because typically this will resolve before any litigation progresses. Permanent side effects from lasers and light sources and injectables are a different issue, things like permanent hypopigmentation, depigmentation, and scarring. These are most likely to produce liability.”
In Dr. Avram’s opinion, complications are best handled with widespread communication. “There is a temptation to avoid a patient with a poor outcome or side effect,” he said. “This is bad medicine and rightfully angers your patient and increases the risk of a lawsuit. [Resist] the temptation to avoid showing a poor outcome to a colleague. Many complications can be significantly improved or cleared with timely and appropriate interventions. You should always document your efforts.”
Dr. Avram disclosed that he has received consulting fees from Allergan and Galderma. He is a member of the scientific advisory board for Allergan and Soliton, is an investigator for Endo, and holds stock options in La Jolla NanoMedical Inc.
The physician-patient relationship is a key factor in preventing litigation following cutaneous laser surgery, according to Mathew M. Avram, MD, JD.
“Numerous studies indicate that good communication and rapport are the most important means to avoid a lawsuit,” Dr. Avram, director of laser, cosmetics, and dermatologic surgery at Massachusetts General Hospital, Boston, said during a virtual course on laser and aesthetic skin therapy. “It is helpful to say that the outcome was not optimal or what you were anticipating. Communicate your plan [for the complication] clearly and honestly to your patient. The patient may not understand the severity of the complication. If they don’t, they will either leave it alone or they will go elsewhere and may receive poor care.” He added that in New England, “we have some stoic patients who may say ‘I don’t want to bother the doctor’ or ‘It’s my fault for having the procedure done.’ ”
Establishing effective communication with patients from the outset is good practice, he continued, because 75% of physicians in low-risk specialties will face a malpractice claim by age 65. Nearly a decade ago Dr. Avram, H. Ray Jalian, MD, and Chris Jalian, JD, published results from a national legal database analysis identifying common errors and risk factors for litigation in cutaneous surgery. Their search yielded 1,807 documents with 174 unique legal claims involving injury from a cutaneous laser treatment, from 1985 to 2012. The most common litigated procedures were laser hair removal, rejuvenation (mostly related to intense pulsed-light treatments), and laser treatment of leg veins, while the most common injuries sustained were burns, scars, and pigmentary changes. The most common causes of legal action were lack of informed consent and fraud.
Among the 120 cases with public decisions, cases favored the plaintiff 51% of the time. “That’s unusual,” said Dr. Avram, president of American Society for Dermatologic Surgery. “Usually, physicians do better, but I think the fact that they’re cosmetic cases probably shades things a little bit.” The median monetary award was $350,000 and ranged from $5,000 to $2,145,000. The two largest judgments were for improper use of topical anesthesia that led to deaths of patients in laser hair removal cases.
In a separate analysis, the same authors searched an online national database to identify the incidence of medical professional liability claims resulting from cutaneous laser surgery performed by nonphysician operators (NPOs) from 1999 to 2012. Among the 175 cases identified, 43% involved an NPO. “In fact, the cases involving NPOs exploded over a 4-year period; they grew from 36% in 2008 of cases to 78% in 2011,” Dr. Avram said. “This was even more true for laser hair removal.”
The practice setting turned out to be a factor. Only 23% of NPO litigation involving laser procedures arose in medical office settings, while 77% of cases involving NPOs were performed outside of traditional medical settings such as in salons and medical spas – mostly for laser hair removal. “We updated this information by examining the setting for nonphysician operator litigation between 2012 and 2017 and found that 66% of cases involving NPOs were performed outside of a traditional medical setting, while 34% of NPO litigation arose in medical office settings,” Dr. Avram said during the meeting, which was named What’s the Truth? and sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “That’s close to a 2 to 1 ratio.”
In an analysis of medical professional liability claims involving Mohs surgery from 1989 to 2011, 26 of the 42 cases identified involved a primary defendant who was not a Mohs surgeon. In the 26 cases, the most common reasons for lawsuits were failure or delay of diagnosis of a skin cancer, cosmetic outcome issues, lack of informed consent, and delay or failure to refer to a Mohs surgeon. Of the cases that involved Mohs surgeons, the most common causes were lack of proper informed consent and cosmetic outcome issues, but “these cases were overwhelmingly decided in favor of the surgeons,” said Dr. Avram, one of the study authors.
On a related note, Dr. Avram underscored the importance of biopsy-site photography, “because patients and physicians misidentify biopsy sites too commonly,” he said. In a single-center study of 34 biopsy sites of cutaneous head and neck malignancies, patients misidentified the biopsy site 4-7 weeks out in 29% of the cases. Blinded dermatologists and the patient misidentified the biopsy site in 12% of the cases. “Good biopsy site photography should be mandatory in your practice,” he advised.
Clinicians can avoid cutaneous laser surgery complications only by not treating patients. “Complications and side effects are inevitable; you need to know your limits,” he said. “Even in skilled hands, if you treat enough patients, you will encounter challenging side effects. Do not perform a procedure that might produce a side effect that you cannot recognize and treat.”
The best way to avoid complications is to trust your eyes – not the laser – since the same device made by the same manufacturer may produce highly different outputs at the same setting (see J Am Acad Dermatol. 2016;74[5]:807-19).
“Moreover, lasers can produce much different energies after they have been serviced,” Dr. Avram said. “Do not memorize settings. Do not blindly replicate recommended settings from a colleague or a device manufacturer,” he advised. “Some devices are not externally calibrated. Therefore, the settings on one device may not translate the same way to yours. Often, device manufacturers underplay the settings. Safe and unsafe laser endpoints and close observation are the best means to avoiding clinical complications. That means you follow clinical endpoints, not fluences. The key clinical finding is the endpoint, not the energy setting.”
Temporary and expected side effects include erythema, edema, and purpura. “With these it’s just handholding and unlikely to lead to any legal consequences,” he continued. “With temporary hyperpigmentation that can occur with laser hair removal, time is one your side, because typically this will resolve before any litigation progresses. Permanent side effects from lasers and light sources and injectables are a different issue, things like permanent hypopigmentation, depigmentation, and scarring. These are most likely to produce liability.”
In Dr. Avram’s opinion, complications are best handled with widespread communication. “There is a temptation to avoid a patient with a poor outcome or side effect,” he said. “This is bad medicine and rightfully angers your patient and increases the risk of a lawsuit. [Resist] the temptation to avoid showing a poor outcome to a colleague. Many complications can be significantly improved or cleared with timely and appropriate interventions. You should always document your efforts.”
Dr. Avram disclosed that he has received consulting fees from Allergan and Galderma. He is a member of the scientific advisory board for Allergan and Soliton, is an investigator for Endo, and holds stock options in La Jolla NanoMedical Inc.
The physician-patient relationship is a key factor in preventing litigation following cutaneous laser surgery, according to Mathew M. Avram, MD, JD.
“Numerous studies indicate that good communication and rapport are the most important means to avoid a lawsuit,” Dr. Avram, director of laser, cosmetics, and dermatologic surgery at Massachusetts General Hospital, Boston, said during a virtual course on laser and aesthetic skin therapy. “It is helpful to say that the outcome was not optimal or what you were anticipating. Communicate your plan [for the complication] clearly and honestly to your patient. The patient may not understand the severity of the complication. If they don’t, they will either leave it alone or they will go elsewhere and may receive poor care.” He added that in New England, “we have some stoic patients who may say ‘I don’t want to bother the doctor’ or ‘It’s my fault for having the procedure done.’ ”
Establishing effective communication with patients from the outset is good practice, he continued, because 75% of physicians in low-risk specialties will face a malpractice claim by age 65. Nearly a decade ago Dr. Avram, H. Ray Jalian, MD, and Chris Jalian, JD, published results from a national legal database analysis identifying common errors and risk factors for litigation in cutaneous surgery. Their search yielded 1,807 documents with 174 unique legal claims involving injury from a cutaneous laser treatment, from 1985 to 2012. The most common litigated procedures were laser hair removal, rejuvenation (mostly related to intense pulsed-light treatments), and laser treatment of leg veins, while the most common injuries sustained were burns, scars, and pigmentary changes. The most common causes of legal action were lack of informed consent and fraud.
Among the 120 cases with public decisions, cases favored the plaintiff 51% of the time. “That’s unusual,” said Dr. Avram, president of American Society for Dermatologic Surgery. “Usually, physicians do better, but I think the fact that they’re cosmetic cases probably shades things a little bit.” The median monetary award was $350,000 and ranged from $5,000 to $2,145,000. The two largest judgments were for improper use of topical anesthesia that led to deaths of patients in laser hair removal cases.
In a separate analysis, the same authors searched an online national database to identify the incidence of medical professional liability claims resulting from cutaneous laser surgery performed by nonphysician operators (NPOs) from 1999 to 2012. Among the 175 cases identified, 43% involved an NPO. “In fact, the cases involving NPOs exploded over a 4-year period; they grew from 36% in 2008 of cases to 78% in 2011,” Dr. Avram said. “This was even more true for laser hair removal.”
The practice setting turned out to be a factor. Only 23% of NPO litigation involving laser procedures arose in medical office settings, while 77% of cases involving NPOs were performed outside of traditional medical settings such as in salons and medical spas – mostly for laser hair removal. “We updated this information by examining the setting for nonphysician operator litigation between 2012 and 2017 and found that 66% of cases involving NPOs were performed outside of a traditional medical setting, while 34% of NPO litigation arose in medical office settings,” Dr. Avram said during the meeting, which was named What’s the Truth? and sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “That’s close to a 2 to 1 ratio.”
In an analysis of medical professional liability claims involving Mohs surgery from 1989 to 2011, 26 of the 42 cases identified involved a primary defendant who was not a Mohs surgeon. In the 26 cases, the most common reasons for lawsuits were failure or delay of diagnosis of a skin cancer, cosmetic outcome issues, lack of informed consent, and delay or failure to refer to a Mohs surgeon. Of the cases that involved Mohs surgeons, the most common causes were lack of proper informed consent and cosmetic outcome issues, but “these cases were overwhelmingly decided in favor of the surgeons,” said Dr. Avram, one of the study authors.
On a related note, Dr. Avram underscored the importance of biopsy-site photography, “because patients and physicians misidentify biopsy sites too commonly,” he said. In a single-center study of 34 biopsy sites of cutaneous head and neck malignancies, patients misidentified the biopsy site 4-7 weeks out in 29% of the cases. Blinded dermatologists and the patient misidentified the biopsy site in 12% of the cases. “Good biopsy site photography should be mandatory in your practice,” he advised.
Clinicians can avoid cutaneous laser surgery complications only by not treating patients. “Complications and side effects are inevitable; you need to know your limits,” he said. “Even in skilled hands, if you treat enough patients, you will encounter challenging side effects. Do not perform a procedure that might produce a side effect that you cannot recognize and treat.”
The best way to avoid complications is to trust your eyes – not the laser – since the same device made by the same manufacturer may produce highly different outputs at the same setting (see J Am Acad Dermatol. 2016;74[5]:807-19).
“Moreover, lasers can produce much different energies after they have been serviced,” Dr. Avram said. “Do not memorize settings. Do not blindly replicate recommended settings from a colleague or a device manufacturer,” he advised. “Some devices are not externally calibrated. Therefore, the settings on one device may not translate the same way to yours. Often, device manufacturers underplay the settings. Safe and unsafe laser endpoints and close observation are the best means to avoiding clinical complications. That means you follow clinical endpoints, not fluences. The key clinical finding is the endpoint, not the energy setting.”
Temporary and expected side effects include erythema, edema, and purpura. “With these it’s just handholding and unlikely to lead to any legal consequences,” he continued. “With temporary hyperpigmentation that can occur with laser hair removal, time is one your side, because typically this will resolve before any litigation progresses. Permanent side effects from lasers and light sources and injectables are a different issue, things like permanent hypopigmentation, depigmentation, and scarring. These are most likely to produce liability.”
In Dr. Avram’s opinion, complications are best handled with widespread communication. “There is a temptation to avoid a patient with a poor outcome or side effect,” he said. “This is bad medicine and rightfully angers your patient and increases the risk of a lawsuit. [Resist] the temptation to avoid showing a poor outcome to a colleague. Many complications can be significantly improved or cleared with timely and appropriate interventions. You should always document your efforts.”
Dr. Avram disclosed that he has received consulting fees from Allergan and Galderma. He is a member of the scientific advisory board for Allergan and Soliton, is an investigator for Endo, and holds stock options in La Jolla NanoMedical Inc.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Expert shares eye protection tips for cutaneous laser surgery
Suzanne L. Kilmer, MD, will never forget the day when the center of her vision became blurry after performing cutaneous laser surgery.
The laser light reflected off the patient’s protective eye shield and caused a photo-induced foveal injury to Dr. Kilmer’s eye even though she was wearing protective goggles. “It was like the central part of my vision was browned out,” Dr. Kilmer, director of the Laser and Skin Surgery Center of Northern California, Sacramento, recalled during a virtual course on laser and aesthetic skin therapy. “My injury completely resolved, but you may not get so lucky. You can really get into trouble with longer pulse widths and higher-energy lasers.”
The injury occurred, she said, because the goggles she wore were sufficient for 1,064-nm wavelengths, but she was treating the patient with a 532 nm–wavelength laser. “I did not have the protection I needed,” she said. “You have to make sure to check the glasses yourself before you treat so that what happened to me doesn’t happen to you.”
Dr. Kilmer, who is also a clinical professor of dermatology at the University of California, Davis, said that during cutaneous laser surgery, “we want to pay attention all the time to minimize our risk.” She also recommended to make sure “all personnel in the room have had good safety training and have baseline eye exams. The door needs to be closed. The windows need to be covered, and you need a warning sign on the door that contains the specific wavelength, pulse width, and energy being used.”
The most important element of the sign, she added, pertains to the wavelength, because that determines the most appropriate goggles or eyewear to use “to ensure that you have an optical density high enough to protect your eyes.”
She advised using only eyewear designed for the specific laser wavelength being used, and to check the optical density prior to firing the laser. “You want the optical density to be greater than 4-6; you want as much protection as possible,” Dr. Kilmer said. “If you’re using a 1,064-nm laser and a 532-nm laser, you want glasses that protect you from both of those wavelengths. Multi- and dual-wavelength glasses are now available. The newer eyewear also allows you to see much better so there’s less risk with you taking it off the goggles [during the procedure].”
Dr. Kilmer recommends keeping a set of goggles outside of the procedure room door that matches every set of goggles being used in the room. “In one room, you may have several different lasers,” she said. “So you want some way to ‘attach’ the goggles to that particular laser, whether it’s a tray or some type of a coding system – some way to keep those together.”
For eye shield protection, the David-Baker lid clamp and the Jaeger plate are appropriate for ablative laser resurfacing, but most dermatologists use individual steel eye shields that are placed externally or internally. “Make sure you have different-sized eye shields on hand,” she advised during the meeting, which was named What’s the Truth? and sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine.
“Depending on what you’re performing, you will need anywhere from neonate size to larger adult size. Some adults may require child-size shields,” she said, noting that there are external eye shields that can be cleaned after each use. “But we tend to use LASER-Aid disposable eye shields, which have metal in the middle and stick over the eyelid. You only use these when you’re working outside of the orbital rim. If you’re treating within the orbital rim, you have to use an internal eye shield.”
She reported having no relevant financial disclosures related to her presentation.
Suzanne L. Kilmer, MD, will never forget the day when the center of her vision became blurry after performing cutaneous laser surgery.
The laser light reflected off the patient’s protective eye shield and caused a photo-induced foveal injury to Dr. Kilmer’s eye even though she was wearing protective goggles. “It was like the central part of my vision was browned out,” Dr. Kilmer, director of the Laser and Skin Surgery Center of Northern California, Sacramento, recalled during a virtual course on laser and aesthetic skin therapy. “My injury completely resolved, but you may not get so lucky. You can really get into trouble with longer pulse widths and higher-energy lasers.”
The injury occurred, she said, because the goggles she wore were sufficient for 1,064-nm wavelengths, but she was treating the patient with a 532 nm–wavelength laser. “I did not have the protection I needed,” she said. “You have to make sure to check the glasses yourself before you treat so that what happened to me doesn’t happen to you.”
Dr. Kilmer, who is also a clinical professor of dermatology at the University of California, Davis, said that during cutaneous laser surgery, “we want to pay attention all the time to minimize our risk.” She also recommended to make sure “all personnel in the room have had good safety training and have baseline eye exams. The door needs to be closed. The windows need to be covered, and you need a warning sign on the door that contains the specific wavelength, pulse width, and energy being used.”
The most important element of the sign, she added, pertains to the wavelength, because that determines the most appropriate goggles or eyewear to use “to ensure that you have an optical density high enough to protect your eyes.”
She advised using only eyewear designed for the specific laser wavelength being used, and to check the optical density prior to firing the laser. “You want the optical density to be greater than 4-6; you want as much protection as possible,” Dr. Kilmer said. “If you’re using a 1,064-nm laser and a 532-nm laser, you want glasses that protect you from both of those wavelengths. Multi- and dual-wavelength glasses are now available. The newer eyewear also allows you to see much better so there’s less risk with you taking it off the goggles [during the procedure].”
Dr. Kilmer recommends keeping a set of goggles outside of the procedure room door that matches every set of goggles being used in the room. “In one room, you may have several different lasers,” she said. “So you want some way to ‘attach’ the goggles to that particular laser, whether it’s a tray or some type of a coding system – some way to keep those together.”
For eye shield protection, the David-Baker lid clamp and the Jaeger plate are appropriate for ablative laser resurfacing, but most dermatologists use individual steel eye shields that are placed externally or internally. “Make sure you have different-sized eye shields on hand,” she advised during the meeting, which was named What’s the Truth? and sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine.
“Depending on what you’re performing, you will need anywhere from neonate size to larger adult size. Some adults may require child-size shields,” she said, noting that there are external eye shields that can be cleaned after each use. “But we tend to use LASER-Aid disposable eye shields, which have metal in the middle and stick over the eyelid. You only use these when you’re working outside of the orbital rim. If you’re treating within the orbital rim, you have to use an internal eye shield.”
She reported having no relevant financial disclosures related to her presentation.
Suzanne L. Kilmer, MD, will never forget the day when the center of her vision became blurry after performing cutaneous laser surgery.
The laser light reflected off the patient’s protective eye shield and caused a photo-induced foveal injury to Dr. Kilmer’s eye even though she was wearing protective goggles. “It was like the central part of my vision was browned out,” Dr. Kilmer, director of the Laser and Skin Surgery Center of Northern California, Sacramento, recalled during a virtual course on laser and aesthetic skin therapy. “My injury completely resolved, but you may not get so lucky. You can really get into trouble with longer pulse widths and higher-energy lasers.”
The injury occurred, she said, because the goggles she wore were sufficient for 1,064-nm wavelengths, but she was treating the patient with a 532 nm–wavelength laser. “I did not have the protection I needed,” she said. “You have to make sure to check the glasses yourself before you treat so that what happened to me doesn’t happen to you.”
Dr. Kilmer, who is also a clinical professor of dermatology at the University of California, Davis, said that during cutaneous laser surgery, “we want to pay attention all the time to minimize our risk.” She also recommended to make sure “all personnel in the room have had good safety training and have baseline eye exams. The door needs to be closed. The windows need to be covered, and you need a warning sign on the door that contains the specific wavelength, pulse width, and energy being used.”
The most important element of the sign, she added, pertains to the wavelength, because that determines the most appropriate goggles or eyewear to use “to ensure that you have an optical density high enough to protect your eyes.”
She advised using only eyewear designed for the specific laser wavelength being used, and to check the optical density prior to firing the laser. “You want the optical density to be greater than 4-6; you want as much protection as possible,” Dr. Kilmer said. “If you’re using a 1,064-nm laser and a 532-nm laser, you want glasses that protect you from both of those wavelengths. Multi- and dual-wavelength glasses are now available. The newer eyewear also allows you to see much better so there’s less risk with you taking it off the goggles [during the procedure].”
Dr. Kilmer recommends keeping a set of goggles outside of the procedure room door that matches every set of goggles being used in the room. “In one room, you may have several different lasers,” she said. “So you want some way to ‘attach’ the goggles to that particular laser, whether it’s a tray or some type of a coding system – some way to keep those together.”
For eye shield protection, the David-Baker lid clamp and the Jaeger plate are appropriate for ablative laser resurfacing, but most dermatologists use individual steel eye shields that are placed externally or internally. “Make sure you have different-sized eye shields on hand,” she advised during the meeting, which was named What’s the Truth? and sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine.
“Depending on what you’re performing, you will need anywhere from neonate size to larger adult size. Some adults may require child-size shields,” she said, noting that there are external eye shields that can be cleaned after each use. “But we tend to use LASER-Aid disposable eye shields, which have metal in the middle and stick over the eyelid. You only use these when you’re working outside of the orbital rim. If you’re treating within the orbital rim, you have to use an internal eye shield.”
She reported having no relevant financial disclosures related to her presentation.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
FDA issues stronger safety requirements for breast implants
The Food and Drug Administration on Oct. 27 announced stronger safety requirements for breast implants, restricting sales of implants only to providers and health facilities that review potential risks of the devices with patients before surgery, via a “Patient Decision Checklist.” The agency also placed a boxed warning – the strongest warning that the FDA requires – on all legally marketed breast implants.
“Protecting patients’ health when they are treated with a medical device is our most important priority,” Binita Ashar, MD, director of the Office of Surgical and Infection Control Devices in the FDA’s Center for Devices and Radiological Health, said in a press release. “In recent years, the FDA has sought more ways to increase patients’ access to clear and understandable information about the benefits and risks of breast implants. By strengthening the safety requirements for manufacturers, the FDA is working to close information gaps for anyone who may be considering breast implant surgery.”
This announcement comes 10 years after the FDA issued a comprehensive safety update on silicone gel–filled implants, which reported a possible association between these devices and anaplastic large cell lymphoma (ALCL). The studies reviewed in the 2011 document also noted that a “significant percentage of women who receive silicone gel–filled breast implants experience complications and adverse outcomes,” the most common being repeat operation, implant removal, rupture, or capsular contracture (scar tissue tightening around the implant).
Breast augmentation has been one of the top five cosmetic procedures in the United States since 2006, according to the American Society for Plastic Surgery, with more than 400,000 people getting breast implants in 2019. Nearly 300,000 were for cosmetic reasons, and more than 100,000 were for breast reconstruction after mastectomies.
In 2019, the FDA proposed adding a boxed warning for breast implants, stating that the devices do not last an entire lifetime; that over time the risk for complications increases; and that breast implants have been associated with ALCL, and also may be associated with systemic symptoms such as fatigue, joint pain, and brain fog. The Oct. 27 FDA action now requires that manufacturers update breast implant packaging to include that information in a boxed warning, as well as the following:
- A patient-decision checklist
- Updated silicone gel–filled breast implant rupture screening recommendations
- A device description including materials used in the device
- Patient device ID cards
The updated label changes must be present on manufacturers’ websites in 30 days, the FDA said.
The new requirements have received largely positive reactions from both physicians and patient organizations. In an emailed statement to this news organization, Lynn Jeffers, MD, MBA, the immediate past president of the American Society of Plastic Surgeons, said that “ASPS has always supported patients being fully informed about their choices and the risks, benefits, and alternatives of the options available. “We look forward to our continued collaboration with the FDA on the safety of implants and other devices.”
Maria Gmitro, president and cofounder of the Breast Implant Safety Alliance, an all-volunteer nonprofit based in Charleston, S.C., said that some of the language in the patient checklist could be stronger, especially when referring to breast implant–associated ALCL.
To inform patients of risks more clearly, “it’s the words like ‘associated with’ that we feel need to be stronger” she said in an interview. She also noted that women who already have breast implants may not be aware of these potential complications, which these new FDA requirements do not address.
But overall, the nonprofit was “thrilled” with the announcement, Ms. Gmitro said. “Placing restrictions on breast implants is a really big step, and we applaud the FDA’s efforts. This is information that every patient considering breast implants should know, and we’ve been advocating for better informed consent.”
A version of this article first appeared on Medscape.com.
The Food and Drug Administration on Oct. 27 announced stronger safety requirements for breast implants, restricting sales of implants only to providers and health facilities that review potential risks of the devices with patients before surgery, via a “Patient Decision Checklist.” The agency also placed a boxed warning – the strongest warning that the FDA requires – on all legally marketed breast implants.
“Protecting patients’ health when they are treated with a medical device is our most important priority,” Binita Ashar, MD, director of the Office of Surgical and Infection Control Devices in the FDA’s Center for Devices and Radiological Health, said in a press release. “In recent years, the FDA has sought more ways to increase patients’ access to clear and understandable information about the benefits and risks of breast implants. By strengthening the safety requirements for manufacturers, the FDA is working to close information gaps for anyone who may be considering breast implant surgery.”
This announcement comes 10 years after the FDA issued a comprehensive safety update on silicone gel–filled implants, which reported a possible association between these devices and anaplastic large cell lymphoma (ALCL). The studies reviewed in the 2011 document also noted that a “significant percentage of women who receive silicone gel–filled breast implants experience complications and adverse outcomes,” the most common being repeat operation, implant removal, rupture, or capsular contracture (scar tissue tightening around the implant).
Breast augmentation has been one of the top five cosmetic procedures in the United States since 2006, according to the American Society for Plastic Surgery, with more than 400,000 people getting breast implants in 2019. Nearly 300,000 were for cosmetic reasons, and more than 100,000 were for breast reconstruction after mastectomies.
In 2019, the FDA proposed adding a boxed warning for breast implants, stating that the devices do not last an entire lifetime; that over time the risk for complications increases; and that breast implants have been associated with ALCL, and also may be associated with systemic symptoms such as fatigue, joint pain, and brain fog. The Oct. 27 FDA action now requires that manufacturers update breast implant packaging to include that information in a boxed warning, as well as the following:
- A patient-decision checklist
- Updated silicone gel–filled breast implant rupture screening recommendations
- A device description including materials used in the device
- Patient device ID cards
The updated label changes must be present on manufacturers’ websites in 30 days, the FDA said.
The new requirements have received largely positive reactions from both physicians and patient organizations. In an emailed statement to this news organization, Lynn Jeffers, MD, MBA, the immediate past president of the American Society of Plastic Surgeons, said that “ASPS has always supported patients being fully informed about their choices and the risks, benefits, and alternatives of the options available. “We look forward to our continued collaboration with the FDA on the safety of implants and other devices.”
Maria Gmitro, president and cofounder of the Breast Implant Safety Alliance, an all-volunteer nonprofit based in Charleston, S.C., said that some of the language in the patient checklist could be stronger, especially when referring to breast implant–associated ALCL.
To inform patients of risks more clearly, “it’s the words like ‘associated with’ that we feel need to be stronger” she said in an interview. She also noted that women who already have breast implants may not be aware of these potential complications, which these new FDA requirements do not address.
But overall, the nonprofit was “thrilled” with the announcement, Ms. Gmitro said. “Placing restrictions on breast implants is a really big step, and we applaud the FDA’s efforts. This is information that every patient considering breast implants should know, and we’ve been advocating for better informed consent.”
A version of this article first appeared on Medscape.com.
The Food and Drug Administration on Oct. 27 announced stronger safety requirements for breast implants, restricting sales of implants only to providers and health facilities that review potential risks of the devices with patients before surgery, via a “Patient Decision Checklist.” The agency also placed a boxed warning – the strongest warning that the FDA requires – on all legally marketed breast implants.
“Protecting patients’ health when they are treated with a medical device is our most important priority,” Binita Ashar, MD, director of the Office of Surgical and Infection Control Devices in the FDA’s Center for Devices and Radiological Health, said in a press release. “In recent years, the FDA has sought more ways to increase patients’ access to clear and understandable information about the benefits and risks of breast implants. By strengthening the safety requirements for manufacturers, the FDA is working to close information gaps for anyone who may be considering breast implant surgery.”
This announcement comes 10 years after the FDA issued a comprehensive safety update on silicone gel–filled implants, which reported a possible association between these devices and anaplastic large cell lymphoma (ALCL). The studies reviewed in the 2011 document also noted that a “significant percentage of women who receive silicone gel–filled breast implants experience complications and adverse outcomes,” the most common being repeat operation, implant removal, rupture, or capsular contracture (scar tissue tightening around the implant).
Breast augmentation has been one of the top five cosmetic procedures in the United States since 2006, according to the American Society for Plastic Surgery, with more than 400,000 people getting breast implants in 2019. Nearly 300,000 were for cosmetic reasons, and more than 100,000 were for breast reconstruction after mastectomies.
In 2019, the FDA proposed adding a boxed warning for breast implants, stating that the devices do not last an entire lifetime; that over time the risk for complications increases; and that breast implants have been associated with ALCL, and also may be associated with systemic symptoms such as fatigue, joint pain, and brain fog. The Oct. 27 FDA action now requires that manufacturers update breast implant packaging to include that information in a boxed warning, as well as the following:
- A patient-decision checklist
- Updated silicone gel–filled breast implant rupture screening recommendations
- A device description including materials used in the device
- Patient device ID cards
The updated label changes must be present on manufacturers’ websites in 30 days, the FDA said.
The new requirements have received largely positive reactions from both physicians and patient organizations. In an emailed statement to this news organization, Lynn Jeffers, MD, MBA, the immediate past president of the American Society of Plastic Surgeons, said that “ASPS has always supported patients being fully informed about their choices and the risks, benefits, and alternatives of the options available. “We look forward to our continued collaboration with the FDA on the safety of implants and other devices.”
Maria Gmitro, president and cofounder of the Breast Implant Safety Alliance, an all-volunteer nonprofit based in Charleston, S.C., said that some of the language in the patient checklist could be stronger, especially when referring to breast implant–associated ALCL.
To inform patients of risks more clearly, “it’s the words like ‘associated with’ that we feel need to be stronger” she said in an interview. She also noted that women who already have breast implants may not be aware of these potential complications, which these new FDA requirements do not address.
But overall, the nonprofit was “thrilled” with the announcement, Ms. Gmitro said. “Placing restrictions on breast implants is a really big step, and we applaud the FDA’s efforts. This is information that every patient considering breast implants should know, and we’ve been advocating for better informed consent.”
A version of this article first appeared on Medscape.com.
Selective cooling technology being used to remove age spots
, according to Arisa E. Ortiz, MD.
“What’s unique about this device is that I can see results without any downtime,” Dr. Ortiz, director of laser and cosmetic dermatology at the University of California, San Diego, said during a virtual course on laser and aesthetic skin therapy. “Most other devices are not like that. It was well tolerated; there was minimal pain. There was no postinflammatory hyperpigmentation; it really is customizable to the patients’ needs.”
First cleared by the Food and Drug Administration in 2016 to remove benign lesions of the skin, Glacial Rx received an expanded indication in 2020 to temporarily reduce pain, swelling, and inflammation. The device, which was developed by R2 Technologies, relies on cryomodulation, a concept developed at Massachusetts General Hospital and the Wellman Center for Photomedicine, Boston, to improve skin appearance and freeze melanin at the source. “Cryomodulation pauses melanin production, but the melanocyte function is preserved, the epidermal barrier is not disrupted, and there is no persistent inflammatory response, which is key, because it decreases the risk of postinflammatory hyperpigmentation, especially in darker skin types,” Dr. Ortiz said.
Here’s how it works: The handpiece of the device is placed on top of the skin and cooling is delivered to targeted solar lentigos and other benign lesions. Ice nucleation takes place within the dendrites. As cell turnover takes place, melanin-free cells migrate upward and appear as new skin. “Clinically, this appears as clearance of the lesion,” Dr. Ortiz said.
She discussed her clinical experience treating 15 patients with a beta version of the device. Since that time, Glacial Rx was redesigned to include a smaller-tipped handpiece, easier and faster prep time, and a proprietary water-based gel to facilitate ice crystal propagation, which is applied to the targeted lesions just prior to treatment.
For the trial at UCSD, the researchers performed 29 treatment sessions on 15 patients with Fitzpatrick skin types I-IV, to gain clinical experience and evaluate the effectiveness of the device. They found that the treatment was well tolerated, with minimal discomfort. The amount of heat extracted ranged from 107 to 166 kJ/cm2. No long-term dyschromia was observed, and some patients had lesion clearance after just one treatment.
“The settings are able to be titrated to where you have zero downtime, but you still get a lightening effect,” Dr. Ortiz said during the meeting, named “Laser & Aesthetic Skin Therapy: What’s the Truth?” sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “With other devices such as intense pulsed light, if you don’t see darkening than it probably didn’t work. With this device, you can titrate the length of the cooling and the temperature of the cooling.”
Posttreatment side effects commonly observed in the study were mild erythema, swelling, itching, and darkening. “There was minimal erythema in the higher settings, and some reports of itching and transient darkening in some of the higher settings,” she said.
Future indications for Glacial Rx may include psoriasis, acne, and rosacea. “We did try to use this for melasma,” she said. “It was effective, but I wouldn’t say it’s a cure for melasma. Melasma is very stubborn and requires a combination treatment, but it’s something we can use in our armamentarium.”
Dr. Ortiz reported having received consulting fees from R2 Technologies. She has been a paid consultant for and has received equipment from many device companies.
, according to Arisa E. Ortiz, MD.
“What’s unique about this device is that I can see results without any downtime,” Dr. Ortiz, director of laser and cosmetic dermatology at the University of California, San Diego, said during a virtual course on laser and aesthetic skin therapy. “Most other devices are not like that. It was well tolerated; there was minimal pain. There was no postinflammatory hyperpigmentation; it really is customizable to the patients’ needs.”
First cleared by the Food and Drug Administration in 2016 to remove benign lesions of the skin, Glacial Rx received an expanded indication in 2020 to temporarily reduce pain, swelling, and inflammation. The device, which was developed by R2 Technologies, relies on cryomodulation, a concept developed at Massachusetts General Hospital and the Wellman Center for Photomedicine, Boston, to improve skin appearance and freeze melanin at the source. “Cryomodulation pauses melanin production, but the melanocyte function is preserved, the epidermal barrier is not disrupted, and there is no persistent inflammatory response, which is key, because it decreases the risk of postinflammatory hyperpigmentation, especially in darker skin types,” Dr. Ortiz said.
Here’s how it works: The handpiece of the device is placed on top of the skin and cooling is delivered to targeted solar lentigos and other benign lesions. Ice nucleation takes place within the dendrites. As cell turnover takes place, melanin-free cells migrate upward and appear as new skin. “Clinically, this appears as clearance of the lesion,” Dr. Ortiz said.
She discussed her clinical experience treating 15 patients with a beta version of the device. Since that time, Glacial Rx was redesigned to include a smaller-tipped handpiece, easier and faster prep time, and a proprietary water-based gel to facilitate ice crystal propagation, which is applied to the targeted lesions just prior to treatment.
For the trial at UCSD, the researchers performed 29 treatment sessions on 15 patients with Fitzpatrick skin types I-IV, to gain clinical experience and evaluate the effectiveness of the device. They found that the treatment was well tolerated, with minimal discomfort. The amount of heat extracted ranged from 107 to 166 kJ/cm2. No long-term dyschromia was observed, and some patients had lesion clearance after just one treatment.
“The settings are able to be titrated to where you have zero downtime, but you still get a lightening effect,” Dr. Ortiz said during the meeting, named “Laser & Aesthetic Skin Therapy: What’s the Truth?” sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “With other devices such as intense pulsed light, if you don’t see darkening than it probably didn’t work. With this device, you can titrate the length of the cooling and the temperature of the cooling.”
Posttreatment side effects commonly observed in the study were mild erythema, swelling, itching, and darkening. “There was minimal erythema in the higher settings, and some reports of itching and transient darkening in some of the higher settings,” she said.
Future indications for Glacial Rx may include psoriasis, acne, and rosacea. “We did try to use this for melasma,” she said. “It was effective, but I wouldn’t say it’s a cure for melasma. Melasma is very stubborn and requires a combination treatment, but it’s something we can use in our armamentarium.”
Dr. Ortiz reported having received consulting fees from R2 Technologies. She has been a paid consultant for and has received equipment from many device companies.
, according to Arisa E. Ortiz, MD.
“What’s unique about this device is that I can see results without any downtime,” Dr. Ortiz, director of laser and cosmetic dermatology at the University of California, San Diego, said during a virtual course on laser and aesthetic skin therapy. “Most other devices are not like that. It was well tolerated; there was minimal pain. There was no postinflammatory hyperpigmentation; it really is customizable to the patients’ needs.”
First cleared by the Food and Drug Administration in 2016 to remove benign lesions of the skin, Glacial Rx received an expanded indication in 2020 to temporarily reduce pain, swelling, and inflammation. The device, which was developed by R2 Technologies, relies on cryomodulation, a concept developed at Massachusetts General Hospital and the Wellman Center for Photomedicine, Boston, to improve skin appearance and freeze melanin at the source. “Cryomodulation pauses melanin production, but the melanocyte function is preserved, the epidermal barrier is not disrupted, and there is no persistent inflammatory response, which is key, because it decreases the risk of postinflammatory hyperpigmentation, especially in darker skin types,” Dr. Ortiz said.
Here’s how it works: The handpiece of the device is placed on top of the skin and cooling is delivered to targeted solar lentigos and other benign lesions. Ice nucleation takes place within the dendrites. As cell turnover takes place, melanin-free cells migrate upward and appear as new skin. “Clinically, this appears as clearance of the lesion,” Dr. Ortiz said.
She discussed her clinical experience treating 15 patients with a beta version of the device. Since that time, Glacial Rx was redesigned to include a smaller-tipped handpiece, easier and faster prep time, and a proprietary water-based gel to facilitate ice crystal propagation, which is applied to the targeted lesions just prior to treatment.
For the trial at UCSD, the researchers performed 29 treatment sessions on 15 patients with Fitzpatrick skin types I-IV, to gain clinical experience and evaluate the effectiveness of the device. They found that the treatment was well tolerated, with minimal discomfort. The amount of heat extracted ranged from 107 to 166 kJ/cm2. No long-term dyschromia was observed, and some patients had lesion clearance after just one treatment.
“The settings are able to be titrated to where you have zero downtime, but you still get a lightening effect,” Dr. Ortiz said during the meeting, named “Laser & Aesthetic Skin Therapy: What’s the Truth?” sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “With other devices such as intense pulsed light, if you don’t see darkening than it probably didn’t work. With this device, you can titrate the length of the cooling and the temperature of the cooling.”
Posttreatment side effects commonly observed in the study were mild erythema, swelling, itching, and darkening. “There was minimal erythema in the higher settings, and some reports of itching and transient darkening in some of the higher settings,” she said.
Future indications for Glacial Rx may include psoriasis, acne, and rosacea. “We did try to use this for melasma,” she said. “It was effective, but I wouldn’t say it’s a cure for melasma. Melasma is very stubborn and requires a combination treatment, but it’s something we can use in our armamentarium.”
Dr. Ortiz reported having received consulting fees from R2 Technologies. She has been a paid consultant for and has received equipment from many device companies.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Disinclined to offer laser hair removal? An expert makes the case to think otherwise
Omar A. Ibrahimi, MD, PhD, hears some dermatology colleagues say they don’t bother to offer laser hair removal in their practices because they figure that the procedure is under the purview of medical spas, but he sees it differently.
“I offer laser hair removal in my practice as a way to protect my patients from being picked off by medical spas,” Dr. Ibrahimi, a dermatologist and medical director of the Connecticut Skin Institute, said during a virtual course on laser and aesthetic skin therapy. “These patients are going to want to get laser hair removal. If they’re not going to have the opportunity to get it at your practice, they’re going to seek it elsewhere. When they go elsewhere, they’re going to be picked off for other procedures as well.”
First developed in 1995 by R. Rox Anderson, MD, and colleagues at The Wellman Center for Photomedicine, laser hair removal has become the gold standard for permanent hair destruction, and ranks as the most common energy-based procedure performed in the world, Dr. Ibrahimi said. “Results are very long lasting and durable beyond 2 years after treatment,” he said. “These patients tend to be highly satisfied and have permanence with these treatments.”
Treatment goal, patient selection
While the target chromophore for the procedure is melanin, the goal is to destroy the stem cells located in the hair bulge and the hair bulb. “This is technically called the extended theory of selective photothermolysis, but it’s the same concept except that our target chromophore and our desired target for destruction are slightly spatially separated,” he said.
Proper patient selection is key, so a focused medical history and physical exam are essential prior to the procedure. If unwanted hair is located on the face, jawline, or chest of a female, consider and ask about potential endocrine-related dysfunctions such as polycystic ovary syndrome (PCOS). “Getting those addressed can often help the hypertrichosis as well,” he said. “Another condition is explosive hypertrichosis where hair growth starts very suddenly. It’s uncommon but it’s something to think about.”
Pregnancy is not an absolute contraindication for laser hair removal, Dr. Ibrahimi continued, but he elects not to perform the procedure on pregnant patients. He also asks patients about any history of photosensitivity, active infection at the intended treatment site, keloids, or hypertrophic scarring. Past methods of hair removal also matter. “What we’re targeting is the pigment in the hair shafts,” he said. “So, if your patient is waxing or plucking or epilating or removing the hair in some manner, they’re actually removing the target chromophore.”
Patients with darker Fitzpatrick skin types can be treated safely but tanned individuals face a risk of complications because of active melanocytes. “As we approach summer in New England, we slow down the amount of hair removal we do because it’s a riskier procedure,” he said. “I recommend that my patients not get any significant amount of sun exposure a month before or after treatment.”
The color and quality of hair also drive treatment success. Black and brown terminal hairs absorb the millisecond laser energy, but white, gray, red, and light blond hairs lack adequate melanin to make them suitable target chromophores.
Excessive and unwanted body hair ranges in severity and can usually be classified as either hypertrichosis or hirsutism.
The desired clinical endpoint is perifollicular edema and erythema. Treatment parameters that can be varied with Food and Drug Administration–cleared devices include wavelength, fluence, pulse duration, spot size, and skin cooling. The most popular devices are the Alexandrite 755 nm laser; the diode 800 nm laser; and the 1064 nm Nd:YAG laser, which is safe for all skin types. “Often you have to use higher relative fluences to treat patients with the 1064 nm Nd:YAG because on the absorption spectrum, the 1064-nm wavelength has a relatively lower absorption for melanin compared to the alexandrite. However, you can still get effective, long-term hair reduction with the Nd:YAG laser,” he said (Arch Dermatol. 2008 Oct;144[10]:1323-7).
More recently, Dr. Ibrahimi and colleagues found that a 1060-nm diode laser system with multiple handpieces for permanent hair reduction was safe for all skin types, in an open label prospective study.
Higher fluences have been correlated with greater rates of permanent hair removal, but they also are more likely to cause undesired side effects. Dr. Ibrahimi advises clinicians new to laser hair removal to conduct a few different test spots and look for the desired clinical endpoint of perifollicular erythema and edema. “The highest fluence that gives you that endpoint without any adverse reactions is going to the best fluence for treatment,” he said at the meeting, which was named “Laser & Aesthetic Skin Therapy: What’s the Truth” and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “Do a few test spots, bring them back a week later and see which ones were tolerated well without any side effects and which weren’t. That gives you a good starting point for your treatment.”
Cooling down the epidermal melanin not only keeps the procedure safe, it’s a salve for pain. “There are a variety of methods of passive and active cooling,” said Dr. Ibrahimi, a member of the American Society for Dermatologic Surgery board of directors. “You can use something as simple as cold gel, but the active methods are better because once the method of passive application of cold gel warms up, you lose that cooling effect. You can use forced chilled air. Many commercial devices come with a cold tip which cools down the epidermal melanin. Others use dynamic cooling, which emit cryogen spray from a separate part of the handpiece. It hits right where the laser pulse is going to go, is absorbed by the skin, and it cools down the epidermal melanin.”
Treatment complications
Complications that can occur from treatment include pigmentary changes such as hyperpigmentation and hypopigmentation. “In lighter skinned individuals, sometimes excess fluence can lead to an erythematous appearance,” he said. “In darker-skinned individuals, this often manifests as hyperpigmentation and can be very long-lasting.” Dr. Ibrahimi ranks improper technique as a complication, “because ideally you want to lay your pulses down with 10%-15% overlap during treatment,” he explained. “If you don’t overlap, you’re going to have zones that don’t get any of the laser photons. If you do, then your patient is not going to be happy with you.”
Paradoxical hypertrichosis occurs in 1%-5% of patients, typically in women from Mediterranean, Middle Eastern, or South Asian ethnic backgrounds. This tends to develop on the lateral or jawline part of the face. “Often it occurs in the setting where they come in and want these vellus hairs treated,” he said. “Somehow the laser, instead of destroying the hair shaft, triggers it and stimulates it and can’t differentiate a vellus hair from a terminal hair. This is important to discuss during your informed consent, especially when you’re treating on the lateral jawline or the sideburn area. If this happens, you can treat through it.”
Transgender patients and future directions
Dr. Ibrahimi pointed out that increasing numbers of transgender patients are visiting dermatologists seeking laser hair removal. About 16 million Americans are estimated to have a gender identity that differs from the one assigned to them at birth, yet they face several barriers to care, “ranging from ignorance on our end to maybe our own biases being transposed onto these patients,” he said. “We really need to do a better job for them. We really have an obligation to provide good care for all of our patients.”
Transgender women typically seek hair removal on the face and neck as well as in the genital area to remove hairs in preparation for vaginoplasty. Transgender men typically seek hair reduction on the forearm or on the thigh, because those are graft sites in preparation for phalloplasty. As a resource for transgender care, he recommends the UCSF Transgender Care website.
As for future directions in the field, Dr. Ibrahimi predicted that hair removal devices for home use will continue to improve and become more widespread. “This raises a host of considerations, from the risk of eye damage to the risk for paradoxical hypertrichosis, and what happens when pigmented lesions get treated with these low-powered machines compared to the ones we have in our office,” he said. “I also think we’re going to see office-based devices with larger spot sizes, smarter devices that are capable of taking over more of the functions we do. I’m most excited about the potential for treating nonpigmented white hair or poorly pigmented blond or reddish hair in the future.”
Dr. Ibrahimi disclosed that he has received research funding and speaker honoraria from Lutronic, Lumenis, Cutera, and Syneron-Candela. He also holds stock in AVAVA Inc.
Omar A. Ibrahimi, MD, PhD, hears some dermatology colleagues say they don’t bother to offer laser hair removal in their practices because they figure that the procedure is under the purview of medical spas, but he sees it differently.
“I offer laser hair removal in my practice as a way to protect my patients from being picked off by medical spas,” Dr. Ibrahimi, a dermatologist and medical director of the Connecticut Skin Institute, said during a virtual course on laser and aesthetic skin therapy. “These patients are going to want to get laser hair removal. If they’re not going to have the opportunity to get it at your practice, they’re going to seek it elsewhere. When they go elsewhere, they’re going to be picked off for other procedures as well.”
First developed in 1995 by R. Rox Anderson, MD, and colleagues at The Wellman Center for Photomedicine, laser hair removal has become the gold standard for permanent hair destruction, and ranks as the most common energy-based procedure performed in the world, Dr. Ibrahimi said. “Results are very long lasting and durable beyond 2 years after treatment,” he said. “These patients tend to be highly satisfied and have permanence with these treatments.”
Treatment goal, patient selection
While the target chromophore for the procedure is melanin, the goal is to destroy the stem cells located in the hair bulge and the hair bulb. “This is technically called the extended theory of selective photothermolysis, but it’s the same concept except that our target chromophore and our desired target for destruction are slightly spatially separated,” he said.
Proper patient selection is key, so a focused medical history and physical exam are essential prior to the procedure. If unwanted hair is located on the face, jawline, or chest of a female, consider and ask about potential endocrine-related dysfunctions such as polycystic ovary syndrome (PCOS). “Getting those addressed can often help the hypertrichosis as well,” he said. “Another condition is explosive hypertrichosis where hair growth starts very suddenly. It’s uncommon but it’s something to think about.”
Pregnancy is not an absolute contraindication for laser hair removal, Dr. Ibrahimi continued, but he elects not to perform the procedure on pregnant patients. He also asks patients about any history of photosensitivity, active infection at the intended treatment site, keloids, or hypertrophic scarring. Past methods of hair removal also matter. “What we’re targeting is the pigment in the hair shafts,” he said. “So, if your patient is waxing or plucking or epilating or removing the hair in some manner, they’re actually removing the target chromophore.”
Patients with darker Fitzpatrick skin types can be treated safely but tanned individuals face a risk of complications because of active melanocytes. “As we approach summer in New England, we slow down the amount of hair removal we do because it’s a riskier procedure,” he said. “I recommend that my patients not get any significant amount of sun exposure a month before or after treatment.”
The color and quality of hair also drive treatment success. Black and brown terminal hairs absorb the millisecond laser energy, but white, gray, red, and light blond hairs lack adequate melanin to make them suitable target chromophores.
Excessive and unwanted body hair ranges in severity and can usually be classified as either hypertrichosis or hirsutism.
The desired clinical endpoint is perifollicular edema and erythema. Treatment parameters that can be varied with Food and Drug Administration–cleared devices include wavelength, fluence, pulse duration, spot size, and skin cooling. The most popular devices are the Alexandrite 755 nm laser; the diode 800 nm laser; and the 1064 nm Nd:YAG laser, which is safe for all skin types. “Often you have to use higher relative fluences to treat patients with the 1064 nm Nd:YAG because on the absorption spectrum, the 1064-nm wavelength has a relatively lower absorption for melanin compared to the alexandrite. However, you can still get effective, long-term hair reduction with the Nd:YAG laser,” he said (Arch Dermatol. 2008 Oct;144[10]:1323-7).
More recently, Dr. Ibrahimi and colleagues found that a 1060-nm diode laser system with multiple handpieces for permanent hair reduction was safe for all skin types, in an open label prospective study.
Higher fluences have been correlated with greater rates of permanent hair removal, but they also are more likely to cause undesired side effects. Dr. Ibrahimi advises clinicians new to laser hair removal to conduct a few different test spots and look for the desired clinical endpoint of perifollicular erythema and edema. “The highest fluence that gives you that endpoint without any adverse reactions is going to the best fluence for treatment,” he said at the meeting, which was named “Laser & Aesthetic Skin Therapy: What’s the Truth” and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “Do a few test spots, bring them back a week later and see which ones were tolerated well without any side effects and which weren’t. That gives you a good starting point for your treatment.”
Cooling down the epidermal melanin not only keeps the procedure safe, it’s a salve for pain. “There are a variety of methods of passive and active cooling,” said Dr. Ibrahimi, a member of the American Society for Dermatologic Surgery board of directors. “You can use something as simple as cold gel, but the active methods are better because once the method of passive application of cold gel warms up, you lose that cooling effect. You can use forced chilled air. Many commercial devices come with a cold tip which cools down the epidermal melanin. Others use dynamic cooling, which emit cryogen spray from a separate part of the handpiece. It hits right where the laser pulse is going to go, is absorbed by the skin, and it cools down the epidermal melanin.”
Treatment complications
Complications that can occur from treatment include pigmentary changes such as hyperpigmentation and hypopigmentation. “In lighter skinned individuals, sometimes excess fluence can lead to an erythematous appearance,” he said. “In darker-skinned individuals, this often manifests as hyperpigmentation and can be very long-lasting.” Dr. Ibrahimi ranks improper technique as a complication, “because ideally you want to lay your pulses down with 10%-15% overlap during treatment,” he explained. “If you don’t overlap, you’re going to have zones that don’t get any of the laser photons. If you do, then your patient is not going to be happy with you.”
Paradoxical hypertrichosis occurs in 1%-5% of patients, typically in women from Mediterranean, Middle Eastern, or South Asian ethnic backgrounds. This tends to develop on the lateral or jawline part of the face. “Often it occurs in the setting where they come in and want these vellus hairs treated,” he said. “Somehow the laser, instead of destroying the hair shaft, triggers it and stimulates it and can’t differentiate a vellus hair from a terminal hair. This is important to discuss during your informed consent, especially when you’re treating on the lateral jawline or the sideburn area. If this happens, you can treat through it.”
Transgender patients and future directions
Dr. Ibrahimi pointed out that increasing numbers of transgender patients are visiting dermatologists seeking laser hair removal. About 16 million Americans are estimated to have a gender identity that differs from the one assigned to them at birth, yet they face several barriers to care, “ranging from ignorance on our end to maybe our own biases being transposed onto these patients,” he said. “We really need to do a better job for them. We really have an obligation to provide good care for all of our patients.”
Transgender women typically seek hair removal on the face and neck as well as in the genital area to remove hairs in preparation for vaginoplasty. Transgender men typically seek hair reduction on the forearm or on the thigh, because those are graft sites in preparation for phalloplasty. As a resource for transgender care, he recommends the UCSF Transgender Care website.
As for future directions in the field, Dr. Ibrahimi predicted that hair removal devices for home use will continue to improve and become more widespread. “This raises a host of considerations, from the risk of eye damage to the risk for paradoxical hypertrichosis, and what happens when pigmented lesions get treated with these low-powered machines compared to the ones we have in our office,” he said. “I also think we’re going to see office-based devices with larger spot sizes, smarter devices that are capable of taking over more of the functions we do. I’m most excited about the potential for treating nonpigmented white hair or poorly pigmented blond or reddish hair in the future.”
Dr. Ibrahimi disclosed that he has received research funding and speaker honoraria from Lutronic, Lumenis, Cutera, and Syneron-Candela. He also holds stock in AVAVA Inc.
Omar A. Ibrahimi, MD, PhD, hears some dermatology colleagues say they don’t bother to offer laser hair removal in their practices because they figure that the procedure is under the purview of medical spas, but he sees it differently.
“I offer laser hair removal in my practice as a way to protect my patients from being picked off by medical spas,” Dr. Ibrahimi, a dermatologist and medical director of the Connecticut Skin Institute, said during a virtual course on laser and aesthetic skin therapy. “These patients are going to want to get laser hair removal. If they’re not going to have the opportunity to get it at your practice, they’re going to seek it elsewhere. When they go elsewhere, they’re going to be picked off for other procedures as well.”
First developed in 1995 by R. Rox Anderson, MD, and colleagues at The Wellman Center for Photomedicine, laser hair removal has become the gold standard for permanent hair destruction, and ranks as the most common energy-based procedure performed in the world, Dr. Ibrahimi said. “Results are very long lasting and durable beyond 2 years after treatment,” he said. “These patients tend to be highly satisfied and have permanence with these treatments.”
Treatment goal, patient selection
While the target chromophore for the procedure is melanin, the goal is to destroy the stem cells located in the hair bulge and the hair bulb. “This is technically called the extended theory of selective photothermolysis, but it’s the same concept except that our target chromophore and our desired target for destruction are slightly spatially separated,” he said.
Proper patient selection is key, so a focused medical history and physical exam are essential prior to the procedure. If unwanted hair is located on the face, jawline, or chest of a female, consider and ask about potential endocrine-related dysfunctions such as polycystic ovary syndrome (PCOS). “Getting those addressed can often help the hypertrichosis as well,” he said. “Another condition is explosive hypertrichosis where hair growth starts very suddenly. It’s uncommon but it’s something to think about.”
Pregnancy is not an absolute contraindication for laser hair removal, Dr. Ibrahimi continued, but he elects not to perform the procedure on pregnant patients. He also asks patients about any history of photosensitivity, active infection at the intended treatment site, keloids, or hypertrophic scarring. Past methods of hair removal also matter. “What we’re targeting is the pigment in the hair shafts,” he said. “So, if your patient is waxing or plucking or epilating or removing the hair in some manner, they’re actually removing the target chromophore.”
Patients with darker Fitzpatrick skin types can be treated safely but tanned individuals face a risk of complications because of active melanocytes. “As we approach summer in New England, we slow down the amount of hair removal we do because it’s a riskier procedure,” he said. “I recommend that my patients not get any significant amount of sun exposure a month before or after treatment.”
The color and quality of hair also drive treatment success. Black and brown terminal hairs absorb the millisecond laser energy, but white, gray, red, and light blond hairs lack adequate melanin to make them suitable target chromophores.
Excessive and unwanted body hair ranges in severity and can usually be classified as either hypertrichosis or hirsutism.
The desired clinical endpoint is perifollicular edema and erythema. Treatment parameters that can be varied with Food and Drug Administration–cleared devices include wavelength, fluence, pulse duration, spot size, and skin cooling. The most popular devices are the Alexandrite 755 nm laser; the diode 800 nm laser; and the 1064 nm Nd:YAG laser, which is safe for all skin types. “Often you have to use higher relative fluences to treat patients with the 1064 nm Nd:YAG because on the absorption spectrum, the 1064-nm wavelength has a relatively lower absorption for melanin compared to the alexandrite. However, you can still get effective, long-term hair reduction with the Nd:YAG laser,” he said (Arch Dermatol. 2008 Oct;144[10]:1323-7).
More recently, Dr. Ibrahimi and colleagues found that a 1060-nm diode laser system with multiple handpieces for permanent hair reduction was safe for all skin types, in an open label prospective study.
Higher fluences have been correlated with greater rates of permanent hair removal, but they also are more likely to cause undesired side effects. Dr. Ibrahimi advises clinicians new to laser hair removal to conduct a few different test spots and look for the desired clinical endpoint of perifollicular erythema and edema. “The highest fluence that gives you that endpoint without any adverse reactions is going to the best fluence for treatment,” he said at the meeting, which was named “Laser & Aesthetic Skin Therapy: What’s the Truth” and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “Do a few test spots, bring them back a week later and see which ones were tolerated well without any side effects and which weren’t. That gives you a good starting point for your treatment.”
Cooling down the epidermal melanin not only keeps the procedure safe, it’s a salve for pain. “There are a variety of methods of passive and active cooling,” said Dr. Ibrahimi, a member of the American Society for Dermatologic Surgery board of directors. “You can use something as simple as cold gel, but the active methods are better because once the method of passive application of cold gel warms up, you lose that cooling effect. You can use forced chilled air. Many commercial devices come with a cold tip which cools down the epidermal melanin. Others use dynamic cooling, which emit cryogen spray from a separate part of the handpiece. It hits right where the laser pulse is going to go, is absorbed by the skin, and it cools down the epidermal melanin.”
Treatment complications
Complications that can occur from treatment include pigmentary changes such as hyperpigmentation and hypopigmentation. “In lighter skinned individuals, sometimes excess fluence can lead to an erythematous appearance,” he said. “In darker-skinned individuals, this often manifests as hyperpigmentation and can be very long-lasting.” Dr. Ibrahimi ranks improper technique as a complication, “because ideally you want to lay your pulses down with 10%-15% overlap during treatment,” he explained. “If you don’t overlap, you’re going to have zones that don’t get any of the laser photons. If you do, then your patient is not going to be happy with you.”
Paradoxical hypertrichosis occurs in 1%-5% of patients, typically in women from Mediterranean, Middle Eastern, or South Asian ethnic backgrounds. This tends to develop on the lateral or jawline part of the face. “Often it occurs in the setting where they come in and want these vellus hairs treated,” he said. “Somehow the laser, instead of destroying the hair shaft, triggers it and stimulates it and can’t differentiate a vellus hair from a terminal hair. This is important to discuss during your informed consent, especially when you’re treating on the lateral jawline or the sideburn area. If this happens, you can treat through it.”
Transgender patients and future directions
Dr. Ibrahimi pointed out that increasing numbers of transgender patients are visiting dermatologists seeking laser hair removal. About 16 million Americans are estimated to have a gender identity that differs from the one assigned to them at birth, yet they face several barriers to care, “ranging from ignorance on our end to maybe our own biases being transposed onto these patients,” he said. “We really need to do a better job for them. We really have an obligation to provide good care for all of our patients.”
Transgender women typically seek hair removal on the face and neck as well as in the genital area to remove hairs in preparation for vaginoplasty. Transgender men typically seek hair reduction on the forearm or on the thigh, because those are graft sites in preparation for phalloplasty. As a resource for transgender care, he recommends the UCSF Transgender Care website.
As for future directions in the field, Dr. Ibrahimi predicted that hair removal devices for home use will continue to improve and become more widespread. “This raises a host of considerations, from the risk of eye damage to the risk for paradoxical hypertrichosis, and what happens when pigmented lesions get treated with these low-powered machines compared to the ones we have in our office,” he said. “I also think we’re going to see office-based devices with larger spot sizes, smarter devices that are capable of taking over more of the functions we do. I’m most excited about the potential for treating nonpigmented white hair or poorly pigmented blond or reddish hair in the future.”
Dr. Ibrahimi disclosed that he has received research funding and speaker honoraria from Lutronic, Lumenis, Cutera, and Syneron-Candela. He also holds stock in AVAVA Inc.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Major increase seen in cosmeceutical alternatives to topical hydroquinone
along with new strategies to improve their efficacy, according to a report at the Skin of Color Update 2021.
“Ten or 15 years ago, I was showing a slide with five [alternatives to hydroquinone]. Now there are dozens,” reported Heather Woolery-Lloyd, MD, director of the skin of color division in the department of dermatology at the University of Miami.
The growth in alternatives to hydroquinone is timely. After threats to do so for more than a decade, the Food and Drug Administration finally banned hydroquinone from OTC products in 2020. The ban was folded into the Coronavirus Aid, Relief, and Economic Security (CARES) Act passed in March of 2020 and then implemented the following September.
Until the ban of hydroquinone, OTC products with this compound were widely sought by many individuals with darker skin tones to self-treat melasma and other forms of hyperpigmentation, according to Dr. Woolery-Lloyd. Hydroquinone is still available in prescription products, but she is often asked for OTC alternatives, and she says the list is long and getting longer.
Niacinamide
Detailing the products she has been recommending most frequently as substitutes, Dr. Woolery-Lloyd reported that several are supported by high quality studies. One example is niacinamide.
Of the several controlled studies she cited, one double-blind randomized trial found niacinamide to be equivalent to hydroquinone for melasma on the basis of colorimetric measures. The study compared 4% niacinamide cream applied on one side of the face with 4% hydroquinone cream applied on the other side in 27 patients with melasma. Although the proportion of responses rated good or excellent on a subjective basis was lower with niacinamide (44% vs. 55%), the difference was not statistically significant and niacinamide cream was clearly active, producing objective improvements in mast cell infiltrate and solar elastosis in melasma skin as well. Both were well tolerated.
In other studies, niacinamide has been shown to be effective in the treatment of melasma when combined with other active agents such as tranexamic acid, said Dr. Woolery-Lloyd, who added that OTC products containing niacinamide are now “among my favorites” when directing patients to cosmeceuticals for hyperpigmentation.
Topical vitamin C
Topical vitamin C or ascorbic acid is another. Like niacinamide, topical vitamin C has also been compared with hydroquinone in a double-blind, randomized trial. Although the niacinamide trial and this study were performed 10 or more years ago, these data have new relevance with the ban of OTC hydroquinone.
In the study, 5% ascorbic acid cream on one side of the face was compared with 4% hydroquinone cream, applied on the other side, in 16 women with melasma. Again, there were no statistical differences in colorimetric measures, but good to excellent results were reported for 93% of the sides of the face treated with hydroquinone versus 62.5% of the sides treated with vitamin C (P < .05). “Hydroquinone performed better, but the vitamin C was active and very well tolerated,” Dr. Woolery-Lloyd said.
However, the ascorbic acid cream was better tolerated, with a far lower rate of adverse events (6.2% vs. 68.7%), an advantage that makes it easy to recommend to patients, said Dr. Woolery-Lloyd, who now uses it frequently in her own practice.
Liquiritin, a licorice extract, is another lightening agent increasingly included in OTC products that she also recommends. In two older studies in medical journals published in Pakistan, both the 2% and 4% strengths of liquiritin cream outperformed hydroquinone on the basis of a Melasma Area and Severity Index (MASI) rating. The liquiritin cream was well tolerated in both studies.
Azelaic acid, tranexamic acid
OTC products containing azelaic acid are also effective for hyperpigmentation based on published trials in which they were compared with hydroquinone for treating melasma. In one study of 29 women with melasma cited by Dr. Woolery-Lloyd, 20% azelaic acid cream was more effective than hydroquinone 4% cream after 2 months of treatment on the basis of the mean MASI score (6.2 vs. 3.8).
The list also includes cysteamine, silymarin, and tranexamic acid.
In the case of tranexamic acid, Dr. Woolery-Lloyd cited a relatively recent study of 60 patients with melasma, comparing two strategies for applying tranexamic acid to treatment with hydroquinone over 12 weeks. Compared with 2% hydroquinone (applied nightly) or 1.8% liposomal tranexamic acid (applied twice a day), 5% tranexamic acid solution with microneedling (weekly) had a slightly greater rate of success defined as more than a 50% improvement in hyperpigmentation in an Asian population (30%, 27.8%, and 33.3%, respectively).
“Microneedling is a newer technology that appears to be effective at improving absorption,” said Dr. Woolery-Lloyd. She predicts that microneedling will be used with increasing frequency in combination with topical cosmeceuticals.
She also predicted that these topical agents will be increasingly employed in combinations as the field of cosmeceuticals becomes increasingly more sophisticated. “When it comes to skin quality, cosmeceuticals remain our first-line therapy, especially in skin of color,” she said.
The rapid growth and utility of OTC cosmeceuticals is an area that dermatologists need to be following, according to Darius Mehregan, MD, chair of the department of dermatology, Wayne State University, Detroit, who was senior author of an article published last year that reviewed the ingredients of popular OTC cosmeceuticals.
“Our patients have a great interest in cosmeceuticals and are looking to us for guidance. I think we have a responsibility to help them identify products supported by evidence and to warn them about potential side effects,” Dr. Mehregan, who was not at the meeting, said in an interview.
He agreed that the removal of hydroquinone from OTC products will create a specific need in the area of cosmeceuticals.
“Hydroquinone has for a long time been one of the most effective agents in OTC products for melasma, so patients are going to be looking for alternatives. Identifying which drugs have shown efficacy in controlled studies will be very helpful,” he said.
Dr. Woolery-Lloyd reports financial relationships with Ortho Dermatologics, L’Oréal, Galderma, Allergan, and Somabella Laboratories. Dr. Mehregan reports no potential conflicts of interest.
along with new strategies to improve their efficacy, according to a report at the Skin of Color Update 2021.
“Ten or 15 years ago, I was showing a slide with five [alternatives to hydroquinone]. Now there are dozens,” reported Heather Woolery-Lloyd, MD, director of the skin of color division in the department of dermatology at the University of Miami.
The growth in alternatives to hydroquinone is timely. After threats to do so for more than a decade, the Food and Drug Administration finally banned hydroquinone from OTC products in 2020. The ban was folded into the Coronavirus Aid, Relief, and Economic Security (CARES) Act passed in March of 2020 and then implemented the following September.
Until the ban of hydroquinone, OTC products with this compound were widely sought by many individuals with darker skin tones to self-treat melasma and other forms of hyperpigmentation, according to Dr. Woolery-Lloyd. Hydroquinone is still available in prescription products, but she is often asked for OTC alternatives, and she says the list is long and getting longer.
Niacinamide
Detailing the products she has been recommending most frequently as substitutes, Dr. Woolery-Lloyd reported that several are supported by high quality studies. One example is niacinamide.
Of the several controlled studies she cited, one double-blind randomized trial found niacinamide to be equivalent to hydroquinone for melasma on the basis of colorimetric measures. The study compared 4% niacinamide cream applied on one side of the face with 4% hydroquinone cream applied on the other side in 27 patients with melasma. Although the proportion of responses rated good or excellent on a subjective basis was lower with niacinamide (44% vs. 55%), the difference was not statistically significant and niacinamide cream was clearly active, producing objective improvements in mast cell infiltrate and solar elastosis in melasma skin as well. Both were well tolerated.
In other studies, niacinamide has been shown to be effective in the treatment of melasma when combined with other active agents such as tranexamic acid, said Dr. Woolery-Lloyd, who added that OTC products containing niacinamide are now “among my favorites” when directing patients to cosmeceuticals for hyperpigmentation.
Topical vitamin C
Topical vitamin C or ascorbic acid is another. Like niacinamide, topical vitamin C has also been compared with hydroquinone in a double-blind, randomized trial. Although the niacinamide trial and this study were performed 10 or more years ago, these data have new relevance with the ban of OTC hydroquinone.
In the study, 5% ascorbic acid cream on one side of the face was compared with 4% hydroquinone cream, applied on the other side, in 16 women with melasma. Again, there were no statistical differences in colorimetric measures, but good to excellent results were reported for 93% of the sides of the face treated with hydroquinone versus 62.5% of the sides treated with vitamin C (P < .05). “Hydroquinone performed better, but the vitamin C was active and very well tolerated,” Dr. Woolery-Lloyd said.
However, the ascorbic acid cream was better tolerated, with a far lower rate of adverse events (6.2% vs. 68.7%), an advantage that makes it easy to recommend to patients, said Dr. Woolery-Lloyd, who now uses it frequently in her own practice.
Liquiritin, a licorice extract, is another lightening agent increasingly included in OTC products that she also recommends. In two older studies in medical journals published in Pakistan, both the 2% and 4% strengths of liquiritin cream outperformed hydroquinone on the basis of a Melasma Area and Severity Index (MASI) rating. The liquiritin cream was well tolerated in both studies.
Azelaic acid, tranexamic acid
OTC products containing azelaic acid are also effective for hyperpigmentation based on published trials in which they were compared with hydroquinone for treating melasma. In one study of 29 women with melasma cited by Dr. Woolery-Lloyd, 20% azelaic acid cream was more effective than hydroquinone 4% cream after 2 months of treatment on the basis of the mean MASI score (6.2 vs. 3.8).
The list also includes cysteamine, silymarin, and tranexamic acid.
In the case of tranexamic acid, Dr. Woolery-Lloyd cited a relatively recent study of 60 patients with melasma, comparing two strategies for applying tranexamic acid to treatment with hydroquinone over 12 weeks. Compared with 2% hydroquinone (applied nightly) or 1.8% liposomal tranexamic acid (applied twice a day), 5% tranexamic acid solution with microneedling (weekly) had a slightly greater rate of success defined as more than a 50% improvement in hyperpigmentation in an Asian population (30%, 27.8%, and 33.3%, respectively).
“Microneedling is a newer technology that appears to be effective at improving absorption,” said Dr. Woolery-Lloyd. She predicts that microneedling will be used with increasing frequency in combination with topical cosmeceuticals.
She also predicted that these topical agents will be increasingly employed in combinations as the field of cosmeceuticals becomes increasingly more sophisticated. “When it comes to skin quality, cosmeceuticals remain our first-line therapy, especially in skin of color,” she said.
The rapid growth and utility of OTC cosmeceuticals is an area that dermatologists need to be following, according to Darius Mehregan, MD, chair of the department of dermatology, Wayne State University, Detroit, who was senior author of an article published last year that reviewed the ingredients of popular OTC cosmeceuticals.
“Our patients have a great interest in cosmeceuticals and are looking to us for guidance. I think we have a responsibility to help them identify products supported by evidence and to warn them about potential side effects,” Dr. Mehregan, who was not at the meeting, said in an interview.
He agreed that the removal of hydroquinone from OTC products will create a specific need in the area of cosmeceuticals.
“Hydroquinone has for a long time been one of the most effective agents in OTC products for melasma, so patients are going to be looking for alternatives. Identifying which drugs have shown efficacy in controlled studies will be very helpful,” he said.
Dr. Woolery-Lloyd reports financial relationships with Ortho Dermatologics, L’Oréal, Galderma, Allergan, and Somabella Laboratories. Dr. Mehregan reports no potential conflicts of interest.
along with new strategies to improve their efficacy, according to a report at the Skin of Color Update 2021.
“Ten or 15 years ago, I was showing a slide with five [alternatives to hydroquinone]. Now there are dozens,” reported Heather Woolery-Lloyd, MD, director of the skin of color division in the department of dermatology at the University of Miami.
The growth in alternatives to hydroquinone is timely. After threats to do so for more than a decade, the Food and Drug Administration finally banned hydroquinone from OTC products in 2020. The ban was folded into the Coronavirus Aid, Relief, and Economic Security (CARES) Act passed in March of 2020 and then implemented the following September.
Until the ban of hydroquinone, OTC products with this compound were widely sought by many individuals with darker skin tones to self-treat melasma and other forms of hyperpigmentation, according to Dr. Woolery-Lloyd. Hydroquinone is still available in prescription products, but she is often asked for OTC alternatives, and she says the list is long and getting longer.
Niacinamide
Detailing the products she has been recommending most frequently as substitutes, Dr. Woolery-Lloyd reported that several are supported by high quality studies. One example is niacinamide.
Of the several controlled studies she cited, one double-blind randomized trial found niacinamide to be equivalent to hydroquinone for melasma on the basis of colorimetric measures. The study compared 4% niacinamide cream applied on one side of the face with 4% hydroquinone cream applied on the other side in 27 patients with melasma. Although the proportion of responses rated good or excellent on a subjective basis was lower with niacinamide (44% vs. 55%), the difference was not statistically significant and niacinamide cream was clearly active, producing objective improvements in mast cell infiltrate and solar elastosis in melasma skin as well. Both were well tolerated.
In other studies, niacinamide has been shown to be effective in the treatment of melasma when combined with other active agents such as tranexamic acid, said Dr. Woolery-Lloyd, who added that OTC products containing niacinamide are now “among my favorites” when directing patients to cosmeceuticals for hyperpigmentation.
Topical vitamin C
Topical vitamin C or ascorbic acid is another. Like niacinamide, topical vitamin C has also been compared with hydroquinone in a double-blind, randomized trial. Although the niacinamide trial and this study were performed 10 or more years ago, these data have new relevance with the ban of OTC hydroquinone.
In the study, 5% ascorbic acid cream on one side of the face was compared with 4% hydroquinone cream, applied on the other side, in 16 women with melasma. Again, there were no statistical differences in colorimetric measures, but good to excellent results were reported for 93% of the sides of the face treated with hydroquinone versus 62.5% of the sides treated with vitamin C (P < .05). “Hydroquinone performed better, but the vitamin C was active and very well tolerated,” Dr. Woolery-Lloyd said.
However, the ascorbic acid cream was better tolerated, with a far lower rate of adverse events (6.2% vs. 68.7%), an advantage that makes it easy to recommend to patients, said Dr. Woolery-Lloyd, who now uses it frequently in her own practice.
Liquiritin, a licorice extract, is another lightening agent increasingly included in OTC products that she also recommends. In two older studies in medical journals published in Pakistan, both the 2% and 4% strengths of liquiritin cream outperformed hydroquinone on the basis of a Melasma Area and Severity Index (MASI) rating. The liquiritin cream was well tolerated in both studies.
Azelaic acid, tranexamic acid
OTC products containing azelaic acid are also effective for hyperpigmentation based on published trials in which they were compared with hydroquinone for treating melasma. In one study of 29 women with melasma cited by Dr. Woolery-Lloyd, 20% azelaic acid cream was more effective than hydroquinone 4% cream after 2 months of treatment on the basis of the mean MASI score (6.2 vs. 3.8).
The list also includes cysteamine, silymarin, and tranexamic acid.
In the case of tranexamic acid, Dr. Woolery-Lloyd cited a relatively recent study of 60 patients with melasma, comparing two strategies for applying tranexamic acid to treatment with hydroquinone over 12 weeks. Compared with 2% hydroquinone (applied nightly) or 1.8% liposomal tranexamic acid (applied twice a day), 5% tranexamic acid solution with microneedling (weekly) had a slightly greater rate of success defined as more than a 50% improvement in hyperpigmentation in an Asian population (30%, 27.8%, and 33.3%, respectively).
“Microneedling is a newer technology that appears to be effective at improving absorption,” said Dr. Woolery-Lloyd. She predicts that microneedling will be used with increasing frequency in combination with topical cosmeceuticals.
She also predicted that these topical agents will be increasingly employed in combinations as the field of cosmeceuticals becomes increasingly more sophisticated. “When it comes to skin quality, cosmeceuticals remain our first-line therapy, especially in skin of color,” she said.
The rapid growth and utility of OTC cosmeceuticals is an area that dermatologists need to be following, according to Darius Mehregan, MD, chair of the department of dermatology, Wayne State University, Detroit, who was senior author of an article published last year that reviewed the ingredients of popular OTC cosmeceuticals.
“Our patients have a great interest in cosmeceuticals and are looking to us for guidance. I think we have a responsibility to help them identify products supported by evidence and to warn them about potential side effects,” Dr. Mehregan, who was not at the meeting, said in an interview.
He agreed that the removal of hydroquinone from OTC products will create a specific need in the area of cosmeceuticals.
“Hydroquinone has for a long time been one of the most effective agents in OTC products for melasma, so patients are going to be looking for alternatives. Identifying which drugs have shown efficacy in controlled studies will be very helpful,” he said.
Dr. Woolery-Lloyd reports financial relationships with Ortho Dermatologics, L’Oréal, Galderma, Allergan, and Somabella Laboratories. Dr. Mehregan reports no potential conflicts of interest.
FROM SOC 2021
Transgender use of dermatologic procedures has strong gender tilt
, according to the results of a recent survey.
Transfeminine persons – those assigned male at birth – were much more likely to report a previous dermatologic procedure, compared with transmasculine respondents, by a margin of 64.9%-7.5%, Laura Ragmanauskaite, MD, and associates reported.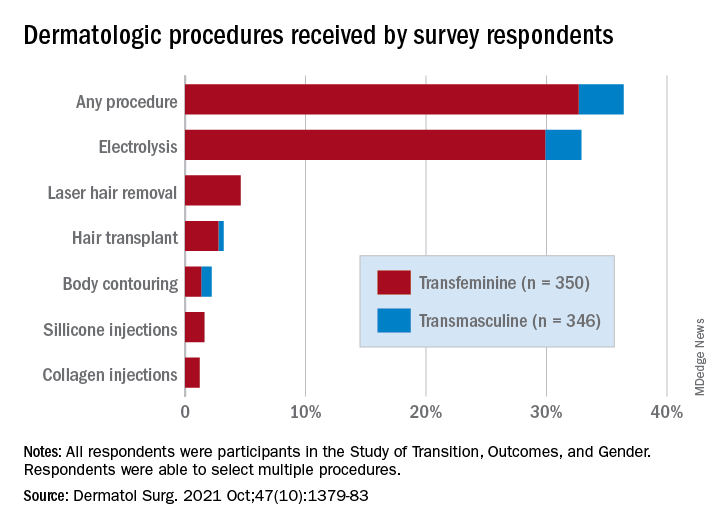
“Hair removal was the most frequently reported procedure type, with electrolysis being more common than laser hair removal,” they said, noting that “previous research on hair removal treatments among gender minority persons did not detect differences in the use of electrolysis and laser hair removal.”
Just under one-third of all respondents (32.9%) said that they had undergone electrolysis and 4.6% reported previous laser hair removal. For electrolysis, that works out to 59.4% of transfeminine and 6.1% of transmasculine respondents, while 9.1% of all transfeminine and no transmasculine persons had received laser hair removal, Dr. Ragmanauskaite of the department of dermatology, Emory University, Atlanta, and her coauthors said.
Those who had undergone gender-affirming surgery were significantly more likely to report electrolysis (78.6%) than were persons who had received no gender-affirming surgery or hormone therapy alone (47.4%), a statistically significant difference (P < .01). All of the other, less common procedures included in the online survey – 696 responses were received from 350 transfeminine and 346 transmasculine persons participating in the Study of Transition, Outcomes, and Gender – were reported more often by the transfeminine respondents. The procedure with the closest gender distribution was body contouring, reported by nine transfeminine and six transmasculine persons, the researchers said.
Use of dermal fillers was even less common (2.8% among all respondents, all transfeminine persons), with just 11 reporting having received silicone and 8 reporting having received collagen, although the survey did not ask about how the injections were obtained. In a previous study, the prevalence of illicit filler injection in transgender women was 16.9%, they pointed out.
These types of noninvasive, gender-affirming procedures “may contribute to higher levels of self-confidence and [reduce] gender dysphoria. Future studies should examine motivations, barriers, and optimal timing” for such procedures in transgender persons, Dr. Ragmanauskaite and associates wrote.
The authors reported that they had no relevant disclosures.
, according to the results of a recent survey.
Transfeminine persons – those assigned male at birth – were much more likely to report a previous dermatologic procedure, compared with transmasculine respondents, by a margin of 64.9%-7.5%, Laura Ragmanauskaite, MD, and associates reported.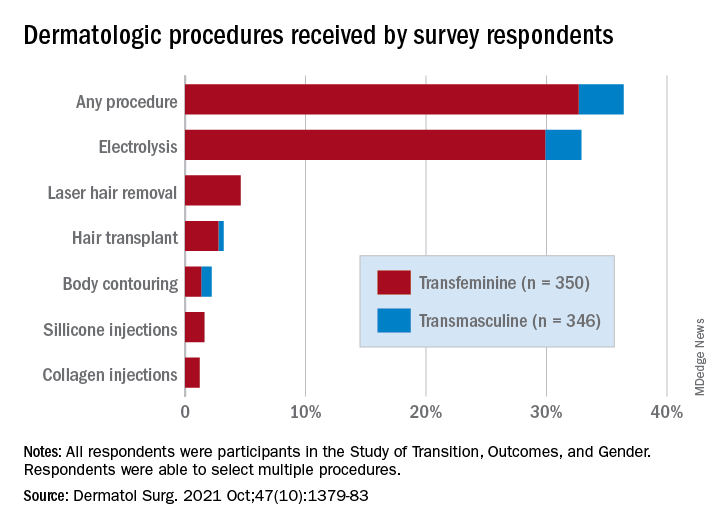
“Hair removal was the most frequently reported procedure type, with electrolysis being more common than laser hair removal,” they said, noting that “previous research on hair removal treatments among gender minority persons did not detect differences in the use of electrolysis and laser hair removal.”
Just under one-third of all respondents (32.9%) said that they had undergone electrolysis and 4.6% reported previous laser hair removal. For electrolysis, that works out to 59.4% of transfeminine and 6.1% of transmasculine respondents, while 9.1% of all transfeminine and no transmasculine persons had received laser hair removal, Dr. Ragmanauskaite of the department of dermatology, Emory University, Atlanta, and her coauthors said.
Those who had undergone gender-affirming surgery were significantly more likely to report electrolysis (78.6%) than were persons who had received no gender-affirming surgery or hormone therapy alone (47.4%), a statistically significant difference (P < .01). All of the other, less common procedures included in the online survey – 696 responses were received from 350 transfeminine and 346 transmasculine persons participating in the Study of Transition, Outcomes, and Gender – were reported more often by the transfeminine respondents. The procedure with the closest gender distribution was body contouring, reported by nine transfeminine and six transmasculine persons, the researchers said.
Use of dermal fillers was even less common (2.8% among all respondents, all transfeminine persons), with just 11 reporting having received silicone and 8 reporting having received collagen, although the survey did not ask about how the injections were obtained. In a previous study, the prevalence of illicit filler injection in transgender women was 16.9%, they pointed out.
These types of noninvasive, gender-affirming procedures “may contribute to higher levels of self-confidence and [reduce] gender dysphoria. Future studies should examine motivations, barriers, and optimal timing” for such procedures in transgender persons, Dr. Ragmanauskaite and associates wrote.
The authors reported that they had no relevant disclosures.
, according to the results of a recent survey.
Transfeminine persons – those assigned male at birth – were much more likely to report a previous dermatologic procedure, compared with transmasculine respondents, by a margin of 64.9%-7.5%, Laura Ragmanauskaite, MD, and associates reported.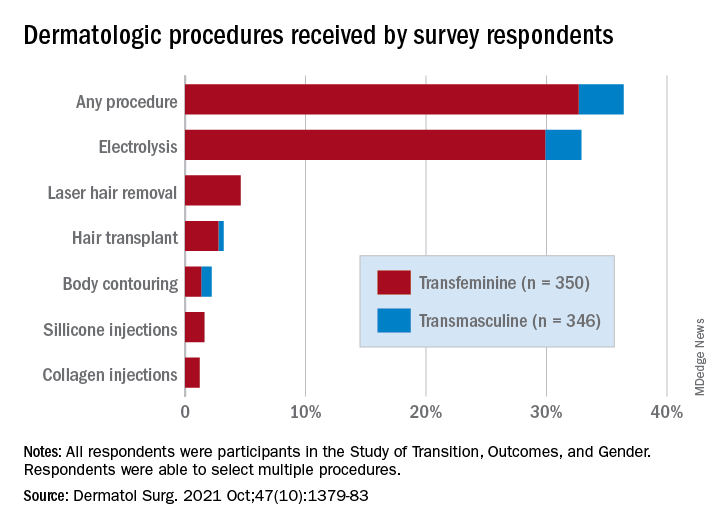
“Hair removal was the most frequently reported procedure type, with electrolysis being more common than laser hair removal,” they said, noting that “previous research on hair removal treatments among gender minority persons did not detect differences in the use of electrolysis and laser hair removal.”
Just under one-third of all respondents (32.9%) said that they had undergone electrolysis and 4.6% reported previous laser hair removal. For electrolysis, that works out to 59.4% of transfeminine and 6.1% of transmasculine respondents, while 9.1% of all transfeminine and no transmasculine persons had received laser hair removal, Dr. Ragmanauskaite of the department of dermatology, Emory University, Atlanta, and her coauthors said.
Those who had undergone gender-affirming surgery were significantly more likely to report electrolysis (78.6%) than were persons who had received no gender-affirming surgery or hormone therapy alone (47.4%), a statistically significant difference (P < .01). All of the other, less common procedures included in the online survey – 696 responses were received from 350 transfeminine and 346 transmasculine persons participating in the Study of Transition, Outcomes, and Gender – were reported more often by the transfeminine respondents. The procedure with the closest gender distribution was body contouring, reported by nine transfeminine and six transmasculine persons, the researchers said.
Use of dermal fillers was even less common (2.8% among all respondents, all transfeminine persons), with just 11 reporting having received silicone and 8 reporting having received collagen, although the survey did not ask about how the injections were obtained. In a previous study, the prevalence of illicit filler injection in transgender women was 16.9%, they pointed out.
These types of noninvasive, gender-affirming procedures “may contribute to higher levels of self-confidence and [reduce] gender dysphoria. Future studies should examine motivations, barriers, and optimal timing” for such procedures in transgender persons, Dr. Ragmanauskaite and associates wrote.
The authors reported that they had no relevant disclosures.
FROM DERMATOLOGIC SURGERY
Study finds plume generated during laser tattoo removal generally viewed as safe
Results of a new .
While tattoo removal plume has not been previously studied, an analysis from 2016 found that laser hair removal plume contains toxic compounds, including carcinogens and environmental toxins, underscoring the importance of using smoke evacuators, good ventilation, and respiratory protection. “Ultrafine particles can become lodged in human alveoli in the lungs,” the study’s senior author, Mathew M. Avram, MD, JD, said during a virtual course on laser and aesthetic skin therapy. “This travels over distances, so it is potentially affecting people in your waiting room and others in areas within the clinic.”
For the study of laser tattoo removal plume, Yakir S. Levin, MD, PhD, a dermatologist at the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston; Dr. Avram, director of laser, cosmetics, and dermatologic surgery at MGH; and coinvestigators from NIOSH, conducted air sampling to determine the gaseous, particulate, and microbiological content of laser tattoo removal plume. They performed the study in ex vivo pig skin and in humans undergoing routine laser tattoo removal, and measured ultrafine particulate concentrations, metals, volatile organic compounds, and airborne bacteria.
For the swine portion of the study, they found that levels of metals including aluminum, copper, manganese, phosphorus, potassium, titanium, and zirconium were all below occupational exposure limits. All organic compounds including acetone and benzene were also below occupational exposure limits. “This is different than what we found in the study of laser plume generated during hair removal,” Dr. Avram said. “In laser hair removal, these were all elevated to a concerning extent.”
For the human part of the study, particle concentrations for ultrafine particulates were higher in the dermatologist’s breathing zone and near the tattoo removal site than in the rest of the treatment room or outside of the room. Concentrations were 30 times lower for human skin than for pig skin. “We’re not sure why, but there were higher levels of ultrafine particulates right around the area we treated,” Dr. Avram said. “Still, they were all below exposure limits that would be concerning in terms of NIOSH. So, although they were elevated, they were still considered safe. That was the case for organic compounds as well.”
He pointed out that the study, which was supported by a grant from the American Society for Dermatologic Surgery (ASDS), did not include an analysis of viral particles generated during later tattoo removal “so there is a question about that,” and it is something worth studying, he said.
Dr. Avram, the current president of ASDS, noted that 17% of the estimated 40 million-plus Americans with tattoos have “tattoo regret,” and many turn to dermatologic surgeons for removal, which requires multiple treatments, and is painful and expensive.
Picosecond lasers
“One thing that’s changed in the past several years is the development of picosecond lasers, which produce extraordinarily high energy for an extraordinarily short period of time,” he said at the meeting, named “Laser & Aesthetic Skin Therapy: What’s the Truth?” and sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. The desired endpoint is dermal whitening with cavitation and rupture. “You don’t want to see splatter with the epidermis flying off,” he said.
Several devices are commercially available with wavelengths of 532, 680, 755, 785, and 1064 nm, and pulse durations ranging from 300 to 750 picoseconds. Nd:Yag lasers target red and black ink, while alexandrite and ruby wavelengths target green and blue ink.
“After the treatment, we use simple Vaseline on top of the tattoo and a nonadherent Telfa dressing with paper tape over it,” Dr. Avram said. For patients with skin of color, he said, “occasionally I will add a steroid. Inflammation and redness can lead to hyperpigmentation. The steroid decreases some of that inflammation and therefore decreases the risk of hyperpigmentation.”
In his clinical experience, picosecond lasers are more effective at tattoo removal than Q-switched nanosecond lasers overall. With a picosecond laser, “you get some nonselective targeting of other pigments such as yellow to improve, even though you really don’t have the correct wavelength. I also think they are more effective for faded tattoos than the Q-switched nanosecond lasers, but they are significantly more expensive, so you need to think about that, and to what extent you are doing tattoo removal. In any event, it’s a multi-treatment process. You do it for multiple weeks between treatments and it takes time and patience. During the consultation, it is crucial to let patients know that.”
In 2012, R. Rox Anderson, MD, director of the Wellman Center for Photomedicine, and colleagues first described the R20 method for tattoo removal, which consists of four consecutive treatment passes with a Q-switched alexandrite laser separated by 20 minutes. “On the first treatment pass, there was an immediate whitening reaction “with little or no whitening on subsequent passes,” said Dr. Avram, who was not involved with the study. “Three months later, treatment with the R20 method was much more effective than conventional single-pass laser treatment. Light microscopy showed greater dispersion of the ink with the R20 method.” A follow-up study conducted at the Wellman Center did not completely support these findings, but a subsequent study led by Suzanne L. Kilmer, MD, was more supportive.
This concept has led to new treatment paradigms for tattoo removal, including the Food and Drug Administration–cleared perfluorodecalin patch, a transparent PFD-infused silicone patch that helps reduce scatter and improves efficacy. “It also allows for performing of repeat laser treatments at the same visit without waiting 20 minutes as you would with the R20 method,” Dr. Avram said. In a pilot study, 11 of the 17 patients showed more rapid clearance with the PFD patch than the control side versus one pass without the PFD patch. “It’s important to note that they used only one wavelength, and some of the tattoos weren’t appropriate for that wavelength, so 11 out of 17 is actually better than it might seem,” he said.
Ablative fractional resurfacing can play a role with tattoo removal, but Dr. Avram typically limits this option to recalcitrant tattoos. “Remember: You’re creating a zone of ablation with a cuff of coagulation, so you’re going to remove some of the tattoo just by creating those areas of clearance and vaporization,” he said. “You can do that in combination with the Q-switched or picosecond laser, which has better efficacy. The best way to do this is to start with the pigment laser – the picosecond or nanosecond laser – and then do the ablative fractional resurfacing afterward. You should never use IPL or laser hair removal lasers to remove tattoos, though. I see that occasionally. You’re going to burn your patients.”
Another approach is to use an Nd:Yag picosecond laser followed by microneedling. “What we’re trying to do here is get an egress of the tattoo pigments,” he explained. “We’re trying to mobilize the ink, get it out of the skin, and get it out of the macrophages to get improvement.”
In 2019, Soliton’s Rapid Acoustic Pulse (RAP) device was cleared by the FDA for tattoo removal. The device is indicated as an accessory to the 1064-nm Q-switched laser for black ink tattoo removal on the arms, legs, and torso in Fitzpatrick skin type I-III individuals. “It’s an application for 1 minute and that allows for additional laser passes,” Dr. Avram said. “You do the laser treatment, you do the acoustic shock wave device, and you do this as multiple passes. This is getting back to the R20 method, the idea that you are going to treat repeatedly. The rapid acoustic pulses result in dispersion and destruction of dermal vacuoles, which enables multiple laser passes in a single treatment session. If you can see the ink, you can ablate the ink.”
Dr. Avram disclosed that he has received consulting fees from Allergan, Merz, and Galderma. He is a member of the scientific advisory board for Allergan and Soliton, is an investigator for Endo, and holds stock options in La Jolla NanoMedical Inc.
Results of a new .
While tattoo removal plume has not been previously studied, an analysis from 2016 found that laser hair removal plume contains toxic compounds, including carcinogens and environmental toxins, underscoring the importance of using smoke evacuators, good ventilation, and respiratory protection. “Ultrafine particles can become lodged in human alveoli in the lungs,” the study’s senior author, Mathew M. Avram, MD, JD, said during a virtual course on laser and aesthetic skin therapy. “This travels over distances, so it is potentially affecting people in your waiting room and others in areas within the clinic.”
For the study of laser tattoo removal plume, Yakir S. Levin, MD, PhD, a dermatologist at the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston; Dr. Avram, director of laser, cosmetics, and dermatologic surgery at MGH; and coinvestigators from NIOSH, conducted air sampling to determine the gaseous, particulate, and microbiological content of laser tattoo removal plume. They performed the study in ex vivo pig skin and in humans undergoing routine laser tattoo removal, and measured ultrafine particulate concentrations, metals, volatile organic compounds, and airborne bacteria.
For the swine portion of the study, they found that levels of metals including aluminum, copper, manganese, phosphorus, potassium, titanium, and zirconium were all below occupational exposure limits. All organic compounds including acetone and benzene were also below occupational exposure limits. “This is different than what we found in the study of laser plume generated during hair removal,” Dr. Avram said. “In laser hair removal, these were all elevated to a concerning extent.”
For the human part of the study, particle concentrations for ultrafine particulates were higher in the dermatologist’s breathing zone and near the tattoo removal site than in the rest of the treatment room or outside of the room. Concentrations were 30 times lower for human skin than for pig skin. “We’re not sure why, but there were higher levels of ultrafine particulates right around the area we treated,” Dr. Avram said. “Still, they were all below exposure limits that would be concerning in terms of NIOSH. So, although they were elevated, they were still considered safe. That was the case for organic compounds as well.”
He pointed out that the study, which was supported by a grant from the American Society for Dermatologic Surgery (ASDS), did not include an analysis of viral particles generated during later tattoo removal “so there is a question about that,” and it is something worth studying, he said.
Dr. Avram, the current president of ASDS, noted that 17% of the estimated 40 million-plus Americans with tattoos have “tattoo regret,” and many turn to dermatologic surgeons for removal, which requires multiple treatments, and is painful and expensive.
Picosecond lasers
“One thing that’s changed in the past several years is the development of picosecond lasers, which produce extraordinarily high energy for an extraordinarily short period of time,” he said at the meeting, named “Laser & Aesthetic Skin Therapy: What’s the Truth?” and sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. The desired endpoint is dermal whitening with cavitation and rupture. “You don’t want to see splatter with the epidermis flying off,” he said.
Several devices are commercially available with wavelengths of 532, 680, 755, 785, and 1064 nm, and pulse durations ranging from 300 to 750 picoseconds. Nd:Yag lasers target red and black ink, while alexandrite and ruby wavelengths target green and blue ink.
“After the treatment, we use simple Vaseline on top of the tattoo and a nonadherent Telfa dressing with paper tape over it,” Dr. Avram said. For patients with skin of color, he said, “occasionally I will add a steroid. Inflammation and redness can lead to hyperpigmentation. The steroid decreases some of that inflammation and therefore decreases the risk of hyperpigmentation.”
In his clinical experience, picosecond lasers are more effective at tattoo removal than Q-switched nanosecond lasers overall. With a picosecond laser, “you get some nonselective targeting of other pigments such as yellow to improve, even though you really don’t have the correct wavelength. I also think they are more effective for faded tattoos than the Q-switched nanosecond lasers, but they are significantly more expensive, so you need to think about that, and to what extent you are doing tattoo removal. In any event, it’s a multi-treatment process. You do it for multiple weeks between treatments and it takes time and patience. During the consultation, it is crucial to let patients know that.”
In 2012, R. Rox Anderson, MD, director of the Wellman Center for Photomedicine, and colleagues first described the R20 method for tattoo removal, which consists of four consecutive treatment passes with a Q-switched alexandrite laser separated by 20 minutes. “On the first treatment pass, there was an immediate whitening reaction “with little or no whitening on subsequent passes,” said Dr. Avram, who was not involved with the study. “Three months later, treatment with the R20 method was much more effective than conventional single-pass laser treatment. Light microscopy showed greater dispersion of the ink with the R20 method.” A follow-up study conducted at the Wellman Center did not completely support these findings, but a subsequent study led by Suzanne L. Kilmer, MD, was more supportive.
This concept has led to new treatment paradigms for tattoo removal, including the Food and Drug Administration–cleared perfluorodecalin patch, a transparent PFD-infused silicone patch that helps reduce scatter and improves efficacy. “It also allows for performing of repeat laser treatments at the same visit without waiting 20 minutes as you would with the R20 method,” Dr. Avram said. In a pilot study, 11 of the 17 patients showed more rapid clearance with the PFD patch than the control side versus one pass without the PFD patch. “It’s important to note that they used only one wavelength, and some of the tattoos weren’t appropriate for that wavelength, so 11 out of 17 is actually better than it might seem,” he said.
Ablative fractional resurfacing can play a role with tattoo removal, but Dr. Avram typically limits this option to recalcitrant tattoos. “Remember: You’re creating a zone of ablation with a cuff of coagulation, so you’re going to remove some of the tattoo just by creating those areas of clearance and vaporization,” he said. “You can do that in combination with the Q-switched or picosecond laser, which has better efficacy. The best way to do this is to start with the pigment laser – the picosecond or nanosecond laser – and then do the ablative fractional resurfacing afterward. You should never use IPL or laser hair removal lasers to remove tattoos, though. I see that occasionally. You’re going to burn your patients.”
Another approach is to use an Nd:Yag picosecond laser followed by microneedling. “What we’re trying to do here is get an egress of the tattoo pigments,” he explained. “We’re trying to mobilize the ink, get it out of the skin, and get it out of the macrophages to get improvement.”
In 2019, Soliton’s Rapid Acoustic Pulse (RAP) device was cleared by the FDA for tattoo removal. The device is indicated as an accessory to the 1064-nm Q-switched laser for black ink tattoo removal on the arms, legs, and torso in Fitzpatrick skin type I-III individuals. “It’s an application for 1 minute and that allows for additional laser passes,” Dr. Avram said. “You do the laser treatment, you do the acoustic shock wave device, and you do this as multiple passes. This is getting back to the R20 method, the idea that you are going to treat repeatedly. The rapid acoustic pulses result in dispersion and destruction of dermal vacuoles, which enables multiple laser passes in a single treatment session. If you can see the ink, you can ablate the ink.”
Dr. Avram disclosed that he has received consulting fees from Allergan, Merz, and Galderma. He is a member of the scientific advisory board for Allergan and Soliton, is an investigator for Endo, and holds stock options in La Jolla NanoMedical Inc.
Results of a new .
While tattoo removal plume has not been previously studied, an analysis from 2016 found that laser hair removal plume contains toxic compounds, including carcinogens and environmental toxins, underscoring the importance of using smoke evacuators, good ventilation, and respiratory protection. “Ultrafine particles can become lodged in human alveoli in the lungs,” the study’s senior author, Mathew M. Avram, MD, JD, said during a virtual course on laser and aesthetic skin therapy. “This travels over distances, so it is potentially affecting people in your waiting room and others in areas within the clinic.”
For the study of laser tattoo removal plume, Yakir S. Levin, MD, PhD, a dermatologist at the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston; Dr. Avram, director of laser, cosmetics, and dermatologic surgery at MGH; and coinvestigators from NIOSH, conducted air sampling to determine the gaseous, particulate, and microbiological content of laser tattoo removal plume. They performed the study in ex vivo pig skin and in humans undergoing routine laser tattoo removal, and measured ultrafine particulate concentrations, metals, volatile organic compounds, and airborne bacteria.
For the swine portion of the study, they found that levels of metals including aluminum, copper, manganese, phosphorus, potassium, titanium, and zirconium were all below occupational exposure limits. All organic compounds including acetone and benzene were also below occupational exposure limits. “This is different than what we found in the study of laser plume generated during hair removal,” Dr. Avram said. “In laser hair removal, these were all elevated to a concerning extent.”
For the human part of the study, particle concentrations for ultrafine particulates were higher in the dermatologist’s breathing zone and near the tattoo removal site than in the rest of the treatment room or outside of the room. Concentrations were 30 times lower for human skin than for pig skin. “We’re not sure why, but there were higher levels of ultrafine particulates right around the area we treated,” Dr. Avram said. “Still, they were all below exposure limits that would be concerning in terms of NIOSH. So, although they were elevated, they were still considered safe. That was the case for organic compounds as well.”
He pointed out that the study, which was supported by a grant from the American Society for Dermatologic Surgery (ASDS), did not include an analysis of viral particles generated during later tattoo removal “so there is a question about that,” and it is something worth studying, he said.
Dr. Avram, the current president of ASDS, noted that 17% of the estimated 40 million-plus Americans with tattoos have “tattoo regret,” and many turn to dermatologic surgeons for removal, which requires multiple treatments, and is painful and expensive.
Picosecond lasers
“One thing that’s changed in the past several years is the development of picosecond lasers, which produce extraordinarily high energy for an extraordinarily short period of time,” he said at the meeting, named “Laser & Aesthetic Skin Therapy: What’s the Truth?” and sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. The desired endpoint is dermal whitening with cavitation and rupture. “You don’t want to see splatter with the epidermis flying off,” he said.
Several devices are commercially available with wavelengths of 532, 680, 755, 785, and 1064 nm, and pulse durations ranging from 300 to 750 picoseconds. Nd:Yag lasers target red and black ink, while alexandrite and ruby wavelengths target green and blue ink.
“After the treatment, we use simple Vaseline on top of the tattoo and a nonadherent Telfa dressing with paper tape over it,” Dr. Avram said. For patients with skin of color, he said, “occasionally I will add a steroid. Inflammation and redness can lead to hyperpigmentation. The steroid decreases some of that inflammation and therefore decreases the risk of hyperpigmentation.”
In his clinical experience, picosecond lasers are more effective at tattoo removal than Q-switched nanosecond lasers overall. With a picosecond laser, “you get some nonselective targeting of other pigments such as yellow to improve, even though you really don’t have the correct wavelength. I also think they are more effective for faded tattoos than the Q-switched nanosecond lasers, but they are significantly more expensive, so you need to think about that, and to what extent you are doing tattoo removal. In any event, it’s a multi-treatment process. You do it for multiple weeks between treatments and it takes time and patience. During the consultation, it is crucial to let patients know that.”
In 2012, R. Rox Anderson, MD, director of the Wellman Center for Photomedicine, and colleagues first described the R20 method for tattoo removal, which consists of four consecutive treatment passes with a Q-switched alexandrite laser separated by 20 minutes. “On the first treatment pass, there was an immediate whitening reaction “with little or no whitening on subsequent passes,” said Dr. Avram, who was not involved with the study. “Three months later, treatment with the R20 method was much more effective than conventional single-pass laser treatment. Light microscopy showed greater dispersion of the ink with the R20 method.” A follow-up study conducted at the Wellman Center did not completely support these findings, but a subsequent study led by Suzanne L. Kilmer, MD, was more supportive.
This concept has led to new treatment paradigms for tattoo removal, including the Food and Drug Administration–cleared perfluorodecalin patch, a transparent PFD-infused silicone patch that helps reduce scatter and improves efficacy. “It also allows for performing of repeat laser treatments at the same visit without waiting 20 minutes as you would with the R20 method,” Dr. Avram said. In a pilot study, 11 of the 17 patients showed more rapid clearance with the PFD patch than the control side versus one pass without the PFD patch. “It’s important to note that they used only one wavelength, and some of the tattoos weren’t appropriate for that wavelength, so 11 out of 17 is actually better than it might seem,” he said.
Ablative fractional resurfacing can play a role with tattoo removal, but Dr. Avram typically limits this option to recalcitrant tattoos. “Remember: You’re creating a zone of ablation with a cuff of coagulation, so you’re going to remove some of the tattoo just by creating those areas of clearance and vaporization,” he said. “You can do that in combination with the Q-switched or picosecond laser, which has better efficacy. The best way to do this is to start with the pigment laser – the picosecond or nanosecond laser – and then do the ablative fractional resurfacing afterward. You should never use IPL or laser hair removal lasers to remove tattoos, though. I see that occasionally. You’re going to burn your patients.”
Another approach is to use an Nd:Yag picosecond laser followed by microneedling. “What we’re trying to do here is get an egress of the tattoo pigments,” he explained. “We’re trying to mobilize the ink, get it out of the skin, and get it out of the macrophages to get improvement.”
In 2019, Soliton’s Rapid Acoustic Pulse (RAP) device was cleared by the FDA for tattoo removal. The device is indicated as an accessory to the 1064-nm Q-switched laser for black ink tattoo removal on the arms, legs, and torso in Fitzpatrick skin type I-III individuals. “It’s an application for 1 minute and that allows for additional laser passes,” Dr. Avram said. “You do the laser treatment, you do the acoustic shock wave device, and you do this as multiple passes. This is getting back to the R20 method, the idea that you are going to treat repeatedly. The rapid acoustic pulses result in dispersion and destruction of dermal vacuoles, which enables multiple laser passes in a single treatment session. If you can see the ink, you can ablate the ink.”
Dr. Avram disclosed that he has received consulting fees from Allergan, Merz, and Galderma. He is a member of the scientific advisory board for Allergan and Soliton, is an investigator for Endo, and holds stock options in La Jolla NanoMedical Inc.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE














