User login
Dr. Eve Espey: Some good news in her 2019 contraceptive update
NASHVILLE, TENN. – There’s some good news on the contraception and reproductive health front, according to a recent update from Eve Espey, MD.
The unintended pregnancy rate in the United States, including among adolescents and young women, is declining, and the U.S. abortion rate is at its lowest level since Roe v. Wade, she said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
A 2016 article based on 2008-2011 data showed that after hovering around 50% for nearly 3 decades, the unintended pregnancy rate dropped “for the first time in a very long period of time,” said Dr. Espey, professor and chair of the department of obstetrics & gynecology, division of family planning at the University of New Mexico, Albuquerque (N Engl J Med. 2016; 374[9]:843-52).
“It doesn’t look that impressive – it basically went down to 45%, but considering the scope and the number of women who are affected by unplanned pregnancy, this is actually a huge public health achievement,” she said. “And I think ... in the next cycles of the [Center for Disease Control and Prevention’s] National Survey of Family Growth ... we’ll hopefully continue to see this and potentially more [decline].”
As for abortion rates, an increase occurred following Roe v. Wade, but rates are now down to pre-Roe levels.
“One of the things that we know about the abortion rate is that the most important determinant ... is access to contraceptives,” Dr. Espey said, noting that both the abortion and unintended pregnancy rate declines are attributable to better and more consistent use of contraceptives, increased abstinence as teens are waiting longer to have sex, and the “meteoric rise in long-acting reversible contraceptive (LARC) use.”
Importantly, while improvements in public health have traditionally only impacted upper-class white women, a reduction is finally occurring in disparities with women of color, but those disparities still remain,” she added. “Just like we’re focusing so much on this relative to maternal mortality, the same kinds of disparities occur in access to reproductive health.”
Dr. Espey also provided updates on other aspects of contraception.
IUDs and other LARC methods
The use of LARCs increased from 2% of contraceptive types used by reproductive-aged women in 2002 to 12% in 2012. The majority of that change was in IUD use, with a small increase in implant use, she said, noting that the latest data from the 2015-2017 cycle of the National Survey of Family Growth shows that the rate is now up to 16%.
“The rise has been nothing that I ever imagined that I would see, certainly in my professional career,” she said.
The huge impact of LARCs on the unintended pregnancy rate is attributable to consistent effectiveness over time, compared with an increasing failure rate over time with short-acting contraceptive methods, she said, explaining that while the failure rate with oral contraceptives is about 8%-9% over the first 3 years, it increases to 53% at 8 years.
It’s a matter of looking at both “typical use” effectiveness and continuation rates: LARCs have continuation rates of about 75%-85%; Depot-Provera, for example, has a 25%-30% continuation rate at 1 year, she noted.
Dr. Espey also attributed the gains to improved access via the Affordable Care Act’s contraceptive mandate, which has been shown in numerous studies to have improved access and consistency of contraceptive use, but which is “currently being chipped away,” and to the federal Title X program that covers family planning care for low income women, including undocumented women.
“These two programs have made a huge impact for us, and I hope that we as ob.gyns. will continue to support them,” she said.
Reproductive justice
Despite their effectiveness, it is important to remember that LARC methods are not right for everyone, Dr. Espey said.
“It’s not all about effectiveness. Women have many reasons for accessing contraception, and our job is not to reduce unintended pregnancy. ... The idea really is that we empower women. ... We should really give choices and trust women to make the best choices for them,” she explained.
Barriers to IUD removal also should be eliminated, she noted, explaining that a woman who wants her IUD removed a month after insertion should have that option.
She said she has “changed her language,” from asking why a woman wants an $800 IUD removed after a month to asking whether she would like to hear about ways to make it better or if she is “just ready to have it removed.”
For those not interested in a discussion about birth control, she suggested providing information about the bedsider.org site.
“This is a great resource for patients,” she said, noting that it is available in both English and Spanish.
U.S. Medical Eligibility Criteria and Selected Practice Recommendations on contraceptive use
The MEC contraceptive guidance, a regularly updated, evidence-based project of the CDC, provides “best practices” information on candidate selection, or the “who” of contraceptive selection (who is a candidate for a particular method), Dr. Espy said, noting that it’s a “handy resource” for in-office use.
The SPR is more of a “how-to” guide that provides specifics on contraceptive use, such as when a woman can rely on the pill for contraception after she starts taking it, or how a woman should be followed after IUD placement, she said.
A free CDC app provides access to both.
Emergency contraception
The best overall emergency contraceptive method is the copper IUD, but often it is less accessible than oral methods, of which ulipristal acetate (ella), is the best choice, Dr. Espy said.
“Ulipristal is kind of a best-kept secret. It’s a selective estrogen-receptor modulator – it actually works better and longer than Plan B (levonorgestrel). What’s great about Plan B is that you can get it over the counter, but ulipristal delays ovulation longer,” she explained.
Contraceptives and obesity
Oral contraceptive efficacy is “so much more about adherence,” than about weight, she said.
With respect to the contraceptive patch, limited evidence suggests that obesity may reduce effectiveness, but “it’s still way better than barrier methods,” and for the contraceptive ring, no evidence suggests that obesity affects efficacy, she said.
For emergency contraception, evidence suggests that ulipristal is more effective than Plan B in women with high body mass index.
OTC contraceptive access
Pharmacy and OTC access are a good idea, Dr. Espy said.
“ACOG now supports both, which is great, and there are now a number of states where women can access contraception through the pharmacy. There are a lot of barriers there as well, and really the answer is OTC access,” she said. “There is a pill right now that is seeking [Food and Drug Administration] approval; it will be a progestin-only pill – the first one to be available over the counter, so I think this is something that we’ll see in the next 5-10 years.”
Additional future directions
One technology in development is a longer-acting injectable, such as a 6- or 9-month Depot-type shot.
Biodegradable implants also are in development. “What a cool idea – it just disappears in your arm, no need to remove it,” Dr. Espey said, adding that nonsurgical permanent sterilization is another possible advance, which would be “a holy grail.”
As for male contraception?
“I’ve been saying for about 25 years that in 5 years we’ll have a male contraceptive, so I’m not going to say it anymore with any kind of time frame, but it’s possible,” she said.
Dr. Espey reported having no financial disclosures.
NASHVILLE, TENN. – There’s some good news on the contraception and reproductive health front, according to a recent update from Eve Espey, MD.
The unintended pregnancy rate in the United States, including among adolescents and young women, is declining, and the U.S. abortion rate is at its lowest level since Roe v. Wade, she said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
A 2016 article based on 2008-2011 data showed that after hovering around 50% for nearly 3 decades, the unintended pregnancy rate dropped “for the first time in a very long period of time,” said Dr. Espey, professor and chair of the department of obstetrics & gynecology, division of family planning at the University of New Mexico, Albuquerque (N Engl J Med. 2016; 374[9]:843-52).
“It doesn’t look that impressive – it basically went down to 45%, but considering the scope and the number of women who are affected by unplanned pregnancy, this is actually a huge public health achievement,” she said. “And I think ... in the next cycles of the [Center for Disease Control and Prevention’s] National Survey of Family Growth ... we’ll hopefully continue to see this and potentially more [decline].”
As for abortion rates, an increase occurred following Roe v. Wade, but rates are now down to pre-Roe levels.
“One of the things that we know about the abortion rate is that the most important determinant ... is access to contraceptives,” Dr. Espey said, noting that both the abortion and unintended pregnancy rate declines are attributable to better and more consistent use of contraceptives, increased abstinence as teens are waiting longer to have sex, and the “meteoric rise in long-acting reversible contraceptive (LARC) use.”
Importantly, while improvements in public health have traditionally only impacted upper-class white women, a reduction is finally occurring in disparities with women of color, but those disparities still remain,” she added. “Just like we’re focusing so much on this relative to maternal mortality, the same kinds of disparities occur in access to reproductive health.”
Dr. Espey also provided updates on other aspects of contraception.
IUDs and other LARC methods
The use of LARCs increased from 2% of contraceptive types used by reproductive-aged women in 2002 to 12% in 2012. The majority of that change was in IUD use, with a small increase in implant use, she said, noting that the latest data from the 2015-2017 cycle of the National Survey of Family Growth shows that the rate is now up to 16%.
“The rise has been nothing that I ever imagined that I would see, certainly in my professional career,” she said.
The huge impact of LARCs on the unintended pregnancy rate is attributable to consistent effectiveness over time, compared with an increasing failure rate over time with short-acting contraceptive methods, she said, explaining that while the failure rate with oral contraceptives is about 8%-9% over the first 3 years, it increases to 53% at 8 years.
It’s a matter of looking at both “typical use” effectiveness and continuation rates: LARCs have continuation rates of about 75%-85%; Depot-Provera, for example, has a 25%-30% continuation rate at 1 year, she noted.
Dr. Espey also attributed the gains to improved access via the Affordable Care Act’s contraceptive mandate, which has been shown in numerous studies to have improved access and consistency of contraceptive use, but which is “currently being chipped away,” and to the federal Title X program that covers family planning care for low income women, including undocumented women.
“These two programs have made a huge impact for us, and I hope that we as ob.gyns. will continue to support them,” she said.
Reproductive justice
Despite their effectiveness, it is important to remember that LARC methods are not right for everyone, Dr. Espey said.
“It’s not all about effectiveness. Women have many reasons for accessing contraception, and our job is not to reduce unintended pregnancy. ... The idea really is that we empower women. ... We should really give choices and trust women to make the best choices for them,” she explained.
Barriers to IUD removal also should be eliminated, she noted, explaining that a woman who wants her IUD removed a month after insertion should have that option.
She said she has “changed her language,” from asking why a woman wants an $800 IUD removed after a month to asking whether she would like to hear about ways to make it better or if she is “just ready to have it removed.”
For those not interested in a discussion about birth control, she suggested providing information about the bedsider.org site.
“This is a great resource for patients,” she said, noting that it is available in both English and Spanish.
U.S. Medical Eligibility Criteria and Selected Practice Recommendations on contraceptive use
The MEC contraceptive guidance, a regularly updated, evidence-based project of the CDC, provides “best practices” information on candidate selection, or the “who” of contraceptive selection (who is a candidate for a particular method), Dr. Espy said, noting that it’s a “handy resource” for in-office use.
The SPR is more of a “how-to” guide that provides specifics on contraceptive use, such as when a woman can rely on the pill for contraception after she starts taking it, or how a woman should be followed after IUD placement, she said.
A free CDC app provides access to both.
Emergency contraception
The best overall emergency contraceptive method is the copper IUD, but often it is less accessible than oral methods, of which ulipristal acetate (ella), is the best choice, Dr. Espy said.
“Ulipristal is kind of a best-kept secret. It’s a selective estrogen-receptor modulator – it actually works better and longer than Plan B (levonorgestrel). What’s great about Plan B is that you can get it over the counter, but ulipristal delays ovulation longer,” she explained.
Contraceptives and obesity
Oral contraceptive efficacy is “so much more about adherence,” than about weight, she said.
With respect to the contraceptive patch, limited evidence suggests that obesity may reduce effectiveness, but “it’s still way better than barrier methods,” and for the contraceptive ring, no evidence suggests that obesity affects efficacy, she said.
For emergency contraception, evidence suggests that ulipristal is more effective than Plan B in women with high body mass index.
OTC contraceptive access
Pharmacy and OTC access are a good idea, Dr. Espy said.
“ACOG now supports both, which is great, and there are now a number of states where women can access contraception through the pharmacy. There are a lot of barriers there as well, and really the answer is OTC access,” she said. “There is a pill right now that is seeking [Food and Drug Administration] approval; it will be a progestin-only pill – the first one to be available over the counter, so I think this is something that we’ll see in the next 5-10 years.”
Additional future directions
One technology in development is a longer-acting injectable, such as a 6- or 9-month Depot-type shot.
Biodegradable implants also are in development. “What a cool idea – it just disappears in your arm, no need to remove it,” Dr. Espey said, adding that nonsurgical permanent sterilization is another possible advance, which would be “a holy grail.”
As for male contraception?
“I’ve been saying for about 25 years that in 5 years we’ll have a male contraceptive, so I’m not going to say it anymore with any kind of time frame, but it’s possible,” she said.
Dr. Espey reported having no financial disclosures.
NASHVILLE, TENN. – There’s some good news on the contraception and reproductive health front, according to a recent update from Eve Espey, MD.
The unintended pregnancy rate in the United States, including among adolescents and young women, is declining, and the U.S. abortion rate is at its lowest level since Roe v. Wade, she said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
A 2016 article based on 2008-2011 data showed that after hovering around 50% for nearly 3 decades, the unintended pregnancy rate dropped “for the first time in a very long period of time,” said Dr. Espey, professor and chair of the department of obstetrics & gynecology, division of family planning at the University of New Mexico, Albuquerque (N Engl J Med. 2016; 374[9]:843-52).
“It doesn’t look that impressive – it basically went down to 45%, but considering the scope and the number of women who are affected by unplanned pregnancy, this is actually a huge public health achievement,” she said. “And I think ... in the next cycles of the [Center for Disease Control and Prevention’s] National Survey of Family Growth ... we’ll hopefully continue to see this and potentially more [decline].”
As for abortion rates, an increase occurred following Roe v. Wade, but rates are now down to pre-Roe levels.
“One of the things that we know about the abortion rate is that the most important determinant ... is access to contraceptives,” Dr. Espey said, noting that both the abortion and unintended pregnancy rate declines are attributable to better and more consistent use of contraceptives, increased abstinence as teens are waiting longer to have sex, and the “meteoric rise in long-acting reversible contraceptive (LARC) use.”
Importantly, while improvements in public health have traditionally only impacted upper-class white women, a reduction is finally occurring in disparities with women of color, but those disparities still remain,” she added. “Just like we’re focusing so much on this relative to maternal mortality, the same kinds of disparities occur in access to reproductive health.”
Dr. Espey also provided updates on other aspects of contraception.
IUDs and other LARC methods
The use of LARCs increased from 2% of contraceptive types used by reproductive-aged women in 2002 to 12% in 2012. The majority of that change was in IUD use, with a small increase in implant use, she said, noting that the latest data from the 2015-2017 cycle of the National Survey of Family Growth shows that the rate is now up to 16%.
“The rise has been nothing that I ever imagined that I would see, certainly in my professional career,” she said.
The huge impact of LARCs on the unintended pregnancy rate is attributable to consistent effectiveness over time, compared with an increasing failure rate over time with short-acting contraceptive methods, she said, explaining that while the failure rate with oral contraceptives is about 8%-9% over the first 3 years, it increases to 53% at 8 years.
It’s a matter of looking at both “typical use” effectiveness and continuation rates: LARCs have continuation rates of about 75%-85%; Depot-Provera, for example, has a 25%-30% continuation rate at 1 year, she noted.
Dr. Espey also attributed the gains to improved access via the Affordable Care Act’s contraceptive mandate, which has been shown in numerous studies to have improved access and consistency of contraceptive use, but which is “currently being chipped away,” and to the federal Title X program that covers family planning care for low income women, including undocumented women.
“These two programs have made a huge impact for us, and I hope that we as ob.gyns. will continue to support them,” she said.
Reproductive justice
Despite their effectiveness, it is important to remember that LARC methods are not right for everyone, Dr. Espey said.
“It’s not all about effectiveness. Women have many reasons for accessing contraception, and our job is not to reduce unintended pregnancy. ... The idea really is that we empower women. ... We should really give choices and trust women to make the best choices for them,” she explained.
Barriers to IUD removal also should be eliminated, she noted, explaining that a woman who wants her IUD removed a month after insertion should have that option.
She said she has “changed her language,” from asking why a woman wants an $800 IUD removed after a month to asking whether she would like to hear about ways to make it better or if she is “just ready to have it removed.”
For those not interested in a discussion about birth control, she suggested providing information about the bedsider.org site.
“This is a great resource for patients,” she said, noting that it is available in both English and Spanish.
U.S. Medical Eligibility Criteria and Selected Practice Recommendations on contraceptive use
The MEC contraceptive guidance, a regularly updated, evidence-based project of the CDC, provides “best practices” information on candidate selection, or the “who” of contraceptive selection (who is a candidate for a particular method), Dr. Espy said, noting that it’s a “handy resource” for in-office use.
The SPR is more of a “how-to” guide that provides specifics on contraceptive use, such as when a woman can rely on the pill for contraception after she starts taking it, or how a woman should be followed after IUD placement, she said.
A free CDC app provides access to both.
Emergency contraception
The best overall emergency contraceptive method is the copper IUD, but often it is less accessible than oral methods, of which ulipristal acetate (ella), is the best choice, Dr. Espy said.
“Ulipristal is kind of a best-kept secret. It’s a selective estrogen-receptor modulator – it actually works better and longer than Plan B (levonorgestrel). What’s great about Plan B is that you can get it over the counter, but ulipristal delays ovulation longer,” she explained.
Contraceptives and obesity
Oral contraceptive efficacy is “so much more about adherence,” than about weight, she said.
With respect to the contraceptive patch, limited evidence suggests that obesity may reduce effectiveness, but “it’s still way better than barrier methods,” and for the contraceptive ring, no evidence suggests that obesity affects efficacy, she said.
For emergency contraception, evidence suggests that ulipristal is more effective than Plan B in women with high body mass index.
OTC contraceptive access
Pharmacy and OTC access are a good idea, Dr. Espy said.
“ACOG now supports both, which is great, and there are now a number of states where women can access contraception through the pharmacy. There are a lot of barriers there as well, and really the answer is OTC access,” she said. “There is a pill right now that is seeking [Food and Drug Administration] approval; it will be a progestin-only pill – the first one to be available over the counter, so I think this is something that we’ll see in the next 5-10 years.”
Additional future directions
One technology in development is a longer-acting injectable, such as a 6- or 9-month Depot-type shot.
Biodegradable implants also are in development. “What a cool idea – it just disappears in your arm, no need to remove it,” Dr. Espey said, adding that nonsurgical permanent sterilization is another possible advance, which would be “a holy grail.”
As for male contraception?
“I’ve been saying for about 25 years that in 5 years we’ll have a male contraceptive, so I’m not going to say it anymore with any kind of time frame, but it’s possible,” she said.
Dr. Espey reported having no financial disclosures.
EXPERT ANALYSIS FROM ACOG 2019
Survey: Patient-provider communication regarding dyspareunia disappoints
NASHVILLE, TENN. – Many women with endometriosis experience dyspareunia, but they are largely unsatisfied when it comes to discussions with health care providers about their symptoms, the results of an online survey suggest.
Of 638 women with self-reported endometriosis who responded to the survey, 81% said they always or usually experience pain during intercourse, 51% described their pain as severe, and 49% said they experience pain lasting more than 24 hours, Roberta Renzelli-Cain, DO, reported during a poster session at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
“The results of our survey suggest that said Dr. Renzelli-Cain, director of the West Virginia National Center of Excellence in Women’s Health and an ob.gyn. at West Virginia University, Morgantown.
In fact, survey responses suggested that dyspareunia has a marked impact on quality of life; 69% of respondents said they find sexual intercourse unpleasant, 31% said they always or usually avoid intercourse, 44% strongly agreed that dyspareunia has affected their relationship with their spouse or partner, 63% said they worry that their spouse or partner will leave, and 63% said they feel depressed because of their dyspareunia, she and her colleagues found.
Most respondents (88%) discussed their symptoms with health care providers (HCPs), and 85% did so with their ob.gyn. Among the other HCPs who respondents spoke with about their dyspareunia were primary care physicians, nurse practitioners, emergency department doctors, fertility specialists, and pain specialists.
Among the reasons given for avoiding discussions with HCPs about painful intercourse were embarrassment (34% of respondents), thinking nothing would help (26%), the physician was a man (5%), and a feeling that the provider was not understanding (3%).
Overall, 18% of respondents said they received no advice from their HCPs regarding how to deal with their dyspareunia, and 39% found nothing that their HCPs suggested to be effective.
Advice given by HCPs included surgery, lubricant use, over-the-counter pain medication, and trying different sexual positions. The percentages of respondents receiving this advice, and the percentages who considered the advice effective, respectively, were 46%, 25% for surgery; 32%, 21% for lubricant use; 36%, 18% for OTC medication; and 21%, 14% for trying different sexual positions, the investigators said.
Importantly, 42% of respondent said they felt it would be easier to discuss dyspareunia if their HCP initiated the subject.
The findings are notable given that 6%-10% of women of childbearing age are affected by endometriosis, and about 30% of those women have related dyspareunia – a “challenging symptom associated with lower sexual functioning, as well as lower self-esteem, and body image,” the investigators wrote.
The 24-question English-language survey was conducted online among women aged 19 years or older who reported having endometriosis and dyspareunia. Participants were recruited via a social network for women with endometriosis (MyEndometriosisTeam.com) and invited by e-mail to participate.
Of the 32,865 invited participants, 361 U.S.-based women and 277 women from outside the United States completed the survey. Most (83%) were aged 19-29 years.
In this online survey, the majority of women reported suboptimal communication with HCPs when seeking help for dyspareunia, the investigators said, concluding that “these results were similar between the U.S.- and non-U.S.–based women, highlighting the need for better medical communication between patients and HCPs, and better advice for patients regarding dyspareunia.”
Dr. Renzelli-Cain reported having no relevant financial disclosures.
NASHVILLE, TENN. – Many women with endometriosis experience dyspareunia, but they are largely unsatisfied when it comes to discussions with health care providers about their symptoms, the results of an online survey suggest.
Of 638 women with self-reported endometriosis who responded to the survey, 81% said they always or usually experience pain during intercourse, 51% described their pain as severe, and 49% said they experience pain lasting more than 24 hours, Roberta Renzelli-Cain, DO, reported during a poster session at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
“The results of our survey suggest that said Dr. Renzelli-Cain, director of the West Virginia National Center of Excellence in Women’s Health and an ob.gyn. at West Virginia University, Morgantown.
In fact, survey responses suggested that dyspareunia has a marked impact on quality of life; 69% of respondents said they find sexual intercourse unpleasant, 31% said they always or usually avoid intercourse, 44% strongly agreed that dyspareunia has affected their relationship with their spouse or partner, 63% said they worry that their spouse or partner will leave, and 63% said they feel depressed because of their dyspareunia, she and her colleagues found.
Most respondents (88%) discussed their symptoms with health care providers (HCPs), and 85% did so with their ob.gyn. Among the other HCPs who respondents spoke with about their dyspareunia were primary care physicians, nurse practitioners, emergency department doctors, fertility specialists, and pain specialists.
Among the reasons given for avoiding discussions with HCPs about painful intercourse were embarrassment (34% of respondents), thinking nothing would help (26%), the physician was a man (5%), and a feeling that the provider was not understanding (3%).
Overall, 18% of respondents said they received no advice from their HCPs regarding how to deal with their dyspareunia, and 39% found nothing that their HCPs suggested to be effective.
Advice given by HCPs included surgery, lubricant use, over-the-counter pain medication, and trying different sexual positions. The percentages of respondents receiving this advice, and the percentages who considered the advice effective, respectively, were 46%, 25% for surgery; 32%, 21% for lubricant use; 36%, 18% for OTC medication; and 21%, 14% for trying different sexual positions, the investigators said.
Importantly, 42% of respondent said they felt it would be easier to discuss dyspareunia if their HCP initiated the subject.
The findings are notable given that 6%-10% of women of childbearing age are affected by endometriosis, and about 30% of those women have related dyspareunia – a “challenging symptom associated with lower sexual functioning, as well as lower self-esteem, and body image,” the investigators wrote.
The 24-question English-language survey was conducted online among women aged 19 years or older who reported having endometriosis and dyspareunia. Participants were recruited via a social network for women with endometriosis (MyEndometriosisTeam.com) and invited by e-mail to participate.
Of the 32,865 invited participants, 361 U.S.-based women and 277 women from outside the United States completed the survey. Most (83%) were aged 19-29 years.
In this online survey, the majority of women reported suboptimal communication with HCPs when seeking help for dyspareunia, the investigators said, concluding that “these results were similar between the U.S.- and non-U.S.–based women, highlighting the need for better medical communication between patients and HCPs, and better advice for patients regarding dyspareunia.”
Dr. Renzelli-Cain reported having no relevant financial disclosures.
NASHVILLE, TENN. – Many women with endometriosis experience dyspareunia, but they are largely unsatisfied when it comes to discussions with health care providers about their symptoms, the results of an online survey suggest.
Of 638 women with self-reported endometriosis who responded to the survey, 81% said they always or usually experience pain during intercourse, 51% described their pain as severe, and 49% said they experience pain lasting more than 24 hours, Roberta Renzelli-Cain, DO, reported during a poster session at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
“The results of our survey suggest that said Dr. Renzelli-Cain, director of the West Virginia National Center of Excellence in Women’s Health and an ob.gyn. at West Virginia University, Morgantown.
In fact, survey responses suggested that dyspareunia has a marked impact on quality of life; 69% of respondents said they find sexual intercourse unpleasant, 31% said they always or usually avoid intercourse, 44% strongly agreed that dyspareunia has affected their relationship with their spouse or partner, 63% said they worry that their spouse or partner will leave, and 63% said they feel depressed because of their dyspareunia, she and her colleagues found.
Most respondents (88%) discussed their symptoms with health care providers (HCPs), and 85% did so with their ob.gyn. Among the other HCPs who respondents spoke with about their dyspareunia were primary care physicians, nurse practitioners, emergency department doctors, fertility specialists, and pain specialists.
Among the reasons given for avoiding discussions with HCPs about painful intercourse were embarrassment (34% of respondents), thinking nothing would help (26%), the physician was a man (5%), and a feeling that the provider was not understanding (3%).
Overall, 18% of respondents said they received no advice from their HCPs regarding how to deal with their dyspareunia, and 39% found nothing that their HCPs suggested to be effective.
Advice given by HCPs included surgery, lubricant use, over-the-counter pain medication, and trying different sexual positions. The percentages of respondents receiving this advice, and the percentages who considered the advice effective, respectively, were 46%, 25% for surgery; 32%, 21% for lubricant use; 36%, 18% for OTC medication; and 21%, 14% for trying different sexual positions, the investigators said.
Importantly, 42% of respondent said they felt it would be easier to discuss dyspareunia if their HCP initiated the subject.
The findings are notable given that 6%-10% of women of childbearing age are affected by endometriosis, and about 30% of those women have related dyspareunia – a “challenging symptom associated with lower sexual functioning, as well as lower self-esteem, and body image,” the investigators wrote.
The 24-question English-language survey was conducted online among women aged 19 years or older who reported having endometriosis and dyspareunia. Participants were recruited via a social network for women with endometriosis (MyEndometriosisTeam.com) and invited by e-mail to participate.
Of the 32,865 invited participants, 361 U.S.-based women and 277 women from outside the United States completed the survey. Most (83%) were aged 19-29 years.
In this online survey, the majority of women reported suboptimal communication with HCPs when seeking help for dyspareunia, the investigators said, concluding that “these results were similar between the U.S.- and non-U.S.–based women, highlighting the need for better medical communication between patients and HCPs, and better advice for patients regarding dyspareunia.”
Dr. Renzelli-Cain reported having no relevant financial disclosures.
REPORTING FROM ACOG 2019
Substantial reductions in HPV infections, CIN2+ after vaccination
The introduction of the human papillomavirus according to a meta-analysis of data from more than 60 million individuals worldwide.
Mélanie Drolet, PhD, from the Centre de recherche du CHU de Québec–Université Laval, and coauthors of the HPV Vaccination Impact Study Group reported the results of a systematic review and meta-analysis of 65 studies showing pre- and postvaccination frequency of at least one HPV-related endpoint published in the Lancet. The studies were conducted in 14 high-income countries, 12 of which were vaccinating only women and girls, with the results at 5-8 years published in the Lancet.
At 5-8 years after a vaccination program was implemented, there was a significant 83% reduction in the prevalence of HPV 16 and 18, both of which are targeted by the vaccine, among girls aged 13-19 years; a 66% reduction among women aged 20-24 years; and a 37% reduction in women aged 25-29 years, even though most of these women were unvaccinated.
There also were significant decreases at 5-8 years in the prevalence of HPV subtypes 31, 33, and 45, which are not included in the vaccine but against which the vaccine appears to offer cross-protection. Among girls aged 13-19 years, there was a significant 54% reduction in the prevalence of these subtypes, among women aged 20-24 years there was a nonsignificant 28% decrease, but among women aged 25-29 years, there was no significant decrease.
The analysis also found significant declines in the prevalence of cervical intraepithelial neoplasias (CINs) of grade 2 or above. At 5-9 years after vaccination was introduced, CIN2+ decreased by 51% among girls aged 15-19 years who also were screened for cervical cancer, and by 31% among women aged 20-24 years.
However, over the same time period, the rates of CIN2+ increased by a significant 19% among mostly unvaccinated women aged 25-29 years and 23% among mostly unvaccinated women aged 30-39 years, despite both groups being screened for cervical abnormalities.
While most of the countries in the study vaccinated only girls and women, two studies did find nonsignificant decreases in the prevalence of HPV 16, 18, 31, 33, and 45 among boys aged 16-19 years, but not among men aged 20-24 years.
HPV vaccination also was associated with significant declines in the incidence of anogenital warts among both males and females. In the first 4 years alone, vaccination was associated with significant reductions in anogenital wart diagnoses among females aged 15-29 years, as well as nonsignificant but “substantial” reductions in unvaccinated boys aged 15-19 years.
After 5-8 years, anogenital wart diagnoses decreased by 67% among girls aged 15-19 years, significantly by 54% among women aged 20-24 years, and 31% among women aged 25-29 years – all significant changes. Among boys aged 15-19 years, anogenital wart diagnoses decreased by a significant 48%, and among men aged 20-24 years they decreased by a significant 32%.
The decreases in anogenital wart diagnoses were even greater in countries that implemented vaccination among multiple cohorts simultaneously and achieved high vaccination coverage, compared with countries that vaccinated only one cohort at a time or had low routine vaccination coverage.
“Our study is the first to show the real-world additional benefit of multicohort HPV vaccination and high routine vaccination coverage, and the fast and substantial herd effects of vaccination in countries which implement these measures,” wrote Dr. Drolet and coauthors. “The greater impact of multicohort vaccination was similar when restricting the analyses to countries with high routine vaccination coverage.”
They pointed to the World Health Organization’s recently revised position on HPV vaccination, which now recommends vaccination of multiple cohorts of girls aged 9-14 years, although they raised the question of what might be the optimal number of age cohorts. “Number needed to vaccinate and cost-effectiveness analyses in high-income countries suggest that vaccinating multiple cohorts of individuals up to 18 years of age is highly efficient and cost effective.”
This analysis by Drolet et al. “provides compelling evidence for HPV vaccine efficacy on all outcomes explored and for almost all age strata,” Dr. Silvia de Sanjose, of PATH in Seattle, and Dr. Sinead Delany-Moretlwe of the Wits Reproductive Health and HIV Institute at the University of Witwatersrand in Johannesburg, said in an accompanying editorial (Lancet. 2019 Jun 26. doi: 10.1016/ S0140-6736[19]30549-5). This study shows just how effective HPV vaccination can be across a range of outcomes and ages, and also demonstrates the herd immunity benefits, particularly when multiple cohorts are vaccinated and there is high vaccination coverage.
One key limitation of this analysis is the lack of data from low- and middle-income countries. The data by Drolet et al. “emphasise the importance of redoubling our efforts to tackle the fiscal, supply, and programmatic barriers that currently limit HPV vaccine programmes; with these efforts, HPV vaccination could become a hallmark investment of cancer prevention in the 21st century,” Dr. de Sanjose and Dr. Delany-Moretlwe concluded.
The study was funded by WHO, Canadian Institutes of Health Research, and Fonds de recherche du Québec–Santé. No conflicts of interest were declared.
Dr. de Sanjose declared previous institutional support from Merck.
SOURCE: Drolet M et al. Lancet 2019 Jun 26. doi: 10.1016/ S0140-6736(19)30298-3.
The introduction of the human papillomavirus according to a meta-analysis of data from more than 60 million individuals worldwide.
Mélanie Drolet, PhD, from the Centre de recherche du CHU de Québec–Université Laval, and coauthors of the HPV Vaccination Impact Study Group reported the results of a systematic review and meta-analysis of 65 studies showing pre- and postvaccination frequency of at least one HPV-related endpoint published in the Lancet. The studies were conducted in 14 high-income countries, 12 of which were vaccinating only women and girls, with the results at 5-8 years published in the Lancet.
At 5-8 years after a vaccination program was implemented, there was a significant 83% reduction in the prevalence of HPV 16 and 18, both of which are targeted by the vaccine, among girls aged 13-19 years; a 66% reduction among women aged 20-24 years; and a 37% reduction in women aged 25-29 years, even though most of these women were unvaccinated.
There also were significant decreases at 5-8 years in the prevalence of HPV subtypes 31, 33, and 45, which are not included in the vaccine but against which the vaccine appears to offer cross-protection. Among girls aged 13-19 years, there was a significant 54% reduction in the prevalence of these subtypes, among women aged 20-24 years there was a nonsignificant 28% decrease, but among women aged 25-29 years, there was no significant decrease.
The analysis also found significant declines in the prevalence of cervical intraepithelial neoplasias (CINs) of grade 2 or above. At 5-9 years after vaccination was introduced, CIN2+ decreased by 51% among girls aged 15-19 years who also were screened for cervical cancer, and by 31% among women aged 20-24 years.
However, over the same time period, the rates of CIN2+ increased by a significant 19% among mostly unvaccinated women aged 25-29 years and 23% among mostly unvaccinated women aged 30-39 years, despite both groups being screened for cervical abnormalities.
While most of the countries in the study vaccinated only girls and women, two studies did find nonsignificant decreases in the prevalence of HPV 16, 18, 31, 33, and 45 among boys aged 16-19 years, but not among men aged 20-24 years.
HPV vaccination also was associated with significant declines in the incidence of anogenital warts among both males and females. In the first 4 years alone, vaccination was associated with significant reductions in anogenital wart diagnoses among females aged 15-29 years, as well as nonsignificant but “substantial” reductions in unvaccinated boys aged 15-19 years.
After 5-8 years, anogenital wart diagnoses decreased by 67% among girls aged 15-19 years, significantly by 54% among women aged 20-24 years, and 31% among women aged 25-29 years – all significant changes. Among boys aged 15-19 years, anogenital wart diagnoses decreased by a significant 48%, and among men aged 20-24 years they decreased by a significant 32%.
The decreases in anogenital wart diagnoses were even greater in countries that implemented vaccination among multiple cohorts simultaneously and achieved high vaccination coverage, compared with countries that vaccinated only one cohort at a time or had low routine vaccination coverage.
“Our study is the first to show the real-world additional benefit of multicohort HPV vaccination and high routine vaccination coverage, and the fast and substantial herd effects of vaccination in countries which implement these measures,” wrote Dr. Drolet and coauthors. “The greater impact of multicohort vaccination was similar when restricting the analyses to countries with high routine vaccination coverage.”
They pointed to the World Health Organization’s recently revised position on HPV vaccination, which now recommends vaccination of multiple cohorts of girls aged 9-14 years, although they raised the question of what might be the optimal number of age cohorts. “Number needed to vaccinate and cost-effectiveness analyses in high-income countries suggest that vaccinating multiple cohorts of individuals up to 18 years of age is highly efficient and cost effective.”
This analysis by Drolet et al. “provides compelling evidence for HPV vaccine efficacy on all outcomes explored and for almost all age strata,” Dr. Silvia de Sanjose, of PATH in Seattle, and Dr. Sinead Delany-Moretlwe of the Wits Reproductive Health and HIV Institute at the University of Witwatersrand in Johannesburg, said in an accompanying editorial (Lancet. 2019 Jun 26. doi: 10.1016/ S0140-6736[19]30549-5). This study shows just how effective HPV vaccination can be across a range of outcomes and ages, and also demonstrates the herd immunity benefits, particularly when multiple cohorts are vaccinated and there is high vaccination coverage.
One key limitation of this analysis is the lack of data from low- and middle-income countries. The data by Drolet et al. “emphasise the importance of redoubling our efforts to tackle the fiscal, supply, and programmatic barriers that currently limit HPV vaccine programmes; with these efforts, HPV vaccination could become a hallmark investment of cancer prevention in the 21st century,” Dr. de Sanjose and Dr. Delany-Moretlwe concluded.
The study was funded by WHO, Canadian Institutes of Health Research, and Fonds de recherche du Québec–Santé. No conflicts of interest were declared.
Dr. de Sanjose declared previous institutional support from Merck.
SOURCE: Drolet M et al. Lancet 2019 Jun 26. doi: 10.1016/ S0140-6736(19)30298-3.
The introduction of the human papillomavirus according to a meta-analysis of data from more than 60 million individuals worldwide.
Mélanie Drolet, PhD, from the Centre de recherche du CHU de Québec–Université Laval, and coauthors of the HPV Vaccination Impact Study Group reported the results of a systematic review and meta-analysis of 65 studies showing pre- and postvaccination frequency of at least one HPV-related endpoint published in the Lancet. The studies were conducted in 14 high-income countries, 12 of which were vaccinating only women and girls, with the results at 5-8 years published in the Lancet.
At 5-8 years after a vaccination program was implemented, there was a significant 83% reduction in the prevalence of HPV 16 and 18, both of which are targeted by the vaccine, among girls aged 13-19 years; a 66% reduction among women aged 20-24 years; and a 37% reduction in women aged 25-29 years, even though most of these women were unvaccinated.
There also were significant decreases at 5-8 years in the prevalence of HPV subtypes 31, 33, and 45, which are not included in the vaccine but against which the vaccine appears to offer cross-protection. Among girls aged 13-19 years, there was a significant 54% reduction in the prevalence of these subtypes, among women aged 20-24 years there was a nonsignificant 28% decrease, but among women aged 25-29 years, there was no significant decrease.
The analysis also found significant declines in the prevalence of cervical intraepithelial neoplasias (CINs) of grade 2 or above. At 5-9 years after vaccination was introduced, CIN2+ decreased by 51% among girls aged 15-19 years who also were screened for cervical cancer, and by 31% among women aged 20-24 years.
However, over the same time period, the rates of CIN2+ increased by a significant 19% among mostly unvaccinated women aged 25-29 years and 23% among mostly unvaccinated women aged 30-39 years, despite both groups being screened for cervical abnormalities.
While most of the countries in the study vaccinated only girls and women, two studies did find nonsignificant decreases in the prevalence of HPV 16, 18, 31, 33, and 45 among boys aged 16-19 years, but not among men aged 20-24 years.
HPV vaccination also was associated with significant declines in the incidence of anogenital warts among both males and females. In the first 4 years alone, vaccination was associated with significant reductions in anogenital wart diagnoses among females aged 15-29 years, as well as nonsignificant but “substantial” reductions in unvaccinated boys aged 15-19 years.
After 5-8 years, anogenital wart diagnoses decreased by 67% among girls aged 15-19 years, significantly by 54% among women aged 20-24 years, and 31% among women aged 25-29 years – all significant changes. Among boys aged 15-19 years, anogenital wart diagnoses decreased by a significant 48%, and among men aged 20-24 years they decreased by a significant 32%.
The decreases in anogenital wart diagnoses were even greater in countries that implemented vaccination among multiple cohorts simultaneously and achieved high vaccination coverage, compared with countries that vaccinated only one cohort at a time or had low routine vaccination coverage.
“Our study is the first to show the real-world additional benefit of multicohort HPV vaccination and high routine vaccination coverage, and the fast and substantial herd effects of vaccination in countries which implement these measures,” wrote Dr. Drolet and coauthors. “The greater impact of multicohort vaccination was similar when restricting the analyses to countries with high routine vaccination coverage.”
They pointed to the World Health Organization’s recently revised position on HPV vaccination, which now recommends vaccination of multiple cohorts of girls aged 9-14 years, although they raised the question of what might be the optimal number of age cohorts. “Number needed to vaccinate and cost-effectiveness analyses in high-income countries suggest that vaccinating multiple cohorts of individuals up to 18 years of age is highly efficient and cost effective.”
This analysis by Drolet et al. “provides compelling evidence for HPV vaccine efficacy on all outcomes explored and for almost all age strata,” Dr. Silvia de Sanjose, of PATH in Seattle, and Dr. Sinead Delany-Moretlwe of the Wits Reproductive Health and HIV Institute at the University of Witwatersrand in Johannesburg, said in an accompanying editorial (Lancet. 2019 Jun 26. doi: 10.1016/ S0140-6736[19]30549-5). This study shows just how effective HPV vaccination can be across a range of outcomes and ages, and also demonstrates the herd immunity benefits, particularly when multiple cohorts are vaccinated and there is high vaccination coverage.
One key limitation of this analysis is the lack of data from low- and middle-income countries. The data by Drolet et al. “emphasise the importance of redoubling our efforts to tackle the fiscal, supply, and programmatic barriers that currently limit HPV vaccine programmes; with these efforts, HPV vaccination could become a hallmark investment of cancer prevention in the 21st century,” Dr. de Sanjose and Dr. Delany-Moretlwe concluded.
The study was funded by WHO, Canadian Institutes of Health Research, and Fonds de recherche du Québec–Santé. No conflicts of interest were declared.
Dr. de Sanjose declared previous institutional support from Merck.
SOURCE: Drolet M et al. Lancet 2019 Jun 26. doi: 10.1016/ S0140-6736(19)30298-3.
FROM THE LANCET
Key clinical point: Significant declines in HPV infections, CIN2+, and anogenital warts have occurred after the introduction of HPV vaccine programs, some because of herd effects.
Major finding: The HPV vaccination program is associated with a significant 83% reduction in the prevalence of HPV 16 and 18 among girls aged 13-19 years in 14 high-income countries.
Study details: Systematic review and meta-analysis of 65 studies involving more than 60 million individuals in 14 countries.
Disclosures: The study was funded by World Health Organization, Canadian Institutes of Health Research, and Fonds de recherche du Québec – Santé. No conflicts of interest were declared.
Source: Drolet M et al. Lancet 2019 Jun 26. doi: 10.1016/ S0140-6736(19)30298-3.
About one in four youths prescribed stimulants also use the drugs nonmedically
SAN ANTONIO – Of 196 U.S. youth who reported use of at least one prescribed stimulant in their lifetimes, 25% also said they used the drugs nonmedically, based on a survey of children and adolescents aged 10-17 years.
Another 5% of the youth surveyed reported exclusively nonmedical use of stimulants. The survey participants lived in six U.S. cities and their outlying areas.
“Parents of both users and nonusers should warn their children of the dangers of using others’ stimulants and giving their own stimulants to others,” concluded Linda B. Cottler, PhD, MPH of the University of Florida, and colleagues.
“Physicians and pharmacists should make users and their families aware of the need to take medications as prescribed and not to share medications with others,” they wrote in their research poster at the annual meeting of the College on Problems of Drug Dependence. “Continuous monitoring of these medications in the community should be a priority.”
Though prevalence research has shown increasing stimulant misuse among youth, little data exist for younger children, the researchers noted. They therefore conducted a survey of 1,777 youth aged 10-17 years from September to October 2018 in six cities in California, Texas, and Florida, the most populous U.S. states.
The participants included youth from urban, rural, and suburban areas of Los Angeles, Dallas, Houston, Tampa, Orlando, and Miami. Trained graduate students and professional raters approached the respondents in entertainment venues and obtained assent but did not require parental consent. The respondents received $30 for completing the survey.
A total of 11.1% of respondents reporting having used prescription stimulants in their lifetime, and 7.6% had done so in the past 30 days. Just under a third of those who used stimulants (30.1%) did so for nonmedical purposes, defined as taking the stimulant nonorally (except for the patch Daytrana), getting the stimulant from someone else, or taking more of the drug than prescribed.
A quarter of the respondents who used stimulants reported both medical use and nonmedical use. And 5.1% of these youths reported only using stimulants nonmedically.
Among those with any lifetime stimulant use, 13.8% reported nonoral administration, including 9.7% who snorted or sniffed the drugs, 4.1% who smoked them, and 1.0% who injected them. Just over half (51.8%) of those reporting nonoral use had also used prescription stimulants orally.
The likelihood of using stimulants nonmedically increased with age (P less than .0001). The researchers found no significant associations between nonmedical use and geography or race/ethnicity. Among 10- to 12-year-olds, 3.1% reported only medical use of stimulants, and 0.7% (2 of 286 respondents in this age group) reported any nonmedical use of stimulants.
Of those aged 13-15 years, 2.1% reported any nonmedical stimulant use.
Nonmedical stimulant use was reported by twice as many boys (67.8%) as girls (32.2%), though this finding may not be surprising as the majority of nonmedical users were also medical users and stimulants are prescribed more frequently to boys than to girls (P less than .0006).
The research was funded by Arbor Pharmaceuticals. The authors noted no conflicts of interest.
SAN ANTONIO – Of 196 U.S. youth who reported use of at least one prescribed stimulant in their lifetimes, 25% also said they used the drugs nonmedically, based on a survey of children and adolescents aged 10-17 years.
Another 5% of the youth surveyed reported exclusively nonmedical use of stimulants. The survey participants lived in six U.S. cities and their outlying areas.
“Parents of both users and nonusers should warn their children of the dangers of using others’ stimulants and giving their own stimulants to others,” concluded Linda B. Cottler, PhD, MPH of the University of Florida, and colleagues.
“Physicians and pharmacists should make users and their families aware of the need to take medications as prescribed and not to share medications with others,” they wrote in their research poster at the annual meeting of the College on Problems of Drug Dependence. “Continuous monitoring of these medications in the community should be a priority.”
Though prevalence research has shown increasing stimulant misuse among youth, little data exist for younger children, the researchers noted. They therefore conducted a survey of 1,777 youth aged 10-17 years from September to October 2018 in six cities in California, Texas, and Florida, the most populous U.S. states.
The participants included youth from urban, rural, and suburban areas of Los Angeles, Dallas, Houston, Tampa, Orlando, and Miami. Trained graduate students and professional raters approached the respondents in entertainment venues and obtained assent but did not require parental consent. The respondents received $30 for completing the survey.
A total of 11.1% of respondents reporting having used prescription stimulants in their lifetime, and 7.6% had done so in the past 30 days. Just under a third of those who used stimulants (30.1%) did so for nonmedical purposes, defined as taking the stimulant nonorally (except for the patch Daytrana), getting the stimulant from someone else, or taking more of the drug than prescribed.
A quarter of the respondents who used stimulants reported both medical use and nonmedical use. And 5.1% of these youths reported only using stimulants nonmedically.
Among those with any lifetime stimulant use, 13.8% reported nonoral administration, including 9.7% who snorted or sniffed the drugs, 4.1% who smoked them, and 1.0% who injected them. Just over half (51.8%) of those reporting nonoral use had also used prescription stimulants orally.
The likelihood of using stimulants nonmedically increased with age (P less than .0001). The researchers found no significant associations between nonmedical use and geography or race/ethnicity. Among 10- to 12-year-olds, 3.1% reported only medical use of stimulants, and 0.7% (2 of 286 respondents in this age group) reported any nonmedical use of stimulants.
Of those aged 13-15 years, 2.1% reported any nonmedical stimulant use.
Nonmedical stimulant use was reported by twice as many boys (67.8%) as girls (32.2%), though this finding may not be surprising as the majority of nonmedical users were also medical users and stimulants are prescribed more frequently to boys than to girls (P less than .0006).
The research was funded by Arbor Pharmaceuticals. The authors noted no conflicts of interest.
SAN ANTONIO – Of 196 U.S. youth who reported use of at least one prescribed stimulant in their lifetimes, 25% also said they used the drugs nonmedically, based on a survey of children and adolescents aged 10-17 years.
Another 5% of the youth surveyed reported exclusively nonmedical use of stimulants. The survey participants lived in six U.S. cities and their outlying areas.
“Parents of both users and nonusers should warn their children of the dangers of using others’ stimulants and giving their own stimulants to others,” concluded Linda B. Cottler, PhD, MPH of the University of Florida, and colleagues.
“Physicians and pharmacists should make users and their families aware of the need to take medications as prescribed and not to share medications with others,” they wrote in their research poster at the annual meeting of the College on Problems of Drug Dependence. “Continuous monitoring of these medications in the community should be a priority.”
Though prevalence research has shown increasing stimulant misuse among youth, little data exist for younger children, the researchers noted. They therefore conducted a survey of 1,777 youth aged 10-17 years from September to October 2018 in six cities in California, Texas, and Florida, the most populous U.S. states.
The participants included youth from urban, rural, and suburban areas of Los Angeles, Dallas, Houston, Tampa, Orlando, and Miami. Trained graduate students and professional raters approached the respondents in entertainment venues and obtained assent but did not require parental consent. The respondents received $30 for completing the survey.
A total of 11.1% of respondents reporting having used prescription stimulants in their lifetime, and 7.6% had done so in the past 30 days. Just under a third of those who used stimulants (30.1%) did so for nonmedical purposes, defined as taking the stimulant nonorally (except for the patch Daytrana), getting the stimulant from someone else, or taking more of the drug than prescribed.
A quarter of the respondents who used stimulants reported both medical use and nonmedical use. And 5.1% of these youths reported only using stimulants nonmedically.
Among those with any lifetime stimulant use, 13.8% reported nonoral administration, including 9.7% who snorted or sniffed the drugs, 4.1% who smoked them, and 1.0% who injected them. Just over half (51.8%) of those reporting nonoral use had also used prescription stimulants orally.
The likelihood of using stimulants nonmedically increased with age (P less than .0001). The researchers found no significant associations between nonmedical use and geography or race/ethnicity. Among 10- to 12-year-olds, 3.1% reported only medical use of stimulants, and 0.7% (2 of 286 respondents in this age group) reported any nonmedical use of stimulants.
Of those aged 13-15 years, 2.1% reported any nonmedical stimulant use.
Nonmedical stimulant use was reported by twice as many boys (67.8%) as girls (32.2%), though this finding may not be surprising as the majority of nonmedical users were also medical users and stimulants are prescribed more frequently to boys than to girls (P less than .0006).
The research was funded by Arbor Pharmaceuticals. The authors noted no conflicts of interest.
REPORTING FROM CPDD 2019
Cannabis vaping among teens tied to tobacco use
and that practice is associated with cigars, waterpipe and e-cigarette use, findings from a survey of nearly 3,000 adolescents have shown.
“Although the prevalence of e-cigarette use among youth has increased dramatically in the past decade, little epidemiologic data exist on the prevalence of using e-cigarette devices or other specialised devices to vaporise (‘vape’) cannabis in the form of hash oil, tetrahydrocannabinol (THC) wax or oil, or dried cannabis buds or leaves,” wrote Sarah D. Kowitt, PhD, of the University of North Carolina, Chapel Hill, and colleagues. “This is surprising given that (1) cannabis (also referred to as marijuana) and e-cigarettes are the most commonly used substances by adolescents in the USA, (2) evidence exists that adolescents dual use both tobacco e-cigarettes and cannabis, and (3) longitudinal research suggests that use of e-cigarettes is associated with progression to use of cannabis.”
In a study published in BMJ Open, the researchers used data from the 2017 North Carolina Youth Tobacco Survey, a school-based survey of students in grades 6-12. The study population included 2,835 adolescents in grades 9-12.
Overall, 9.6% of students reported ever vaping cannabis. In multivariate analysis, cannabis vaping was significantly more likely among adolescents who reported using e-cigarettes (adjusted odds ratio 3.18), cigars (aOR 3.76), or water pipes (aOR 2.32) in the past 30 days, compared with peers who didn’t use tobacco.
The researchers found no significant association between smokeless tobacco use or traditional cigarette use in the past 30 days and vaping cannabis.
In a bivariate analysis, vaping cannabis was significantly more common among males vs. females (11% vs. 8.2%) and among non-Hispanic white students (11.3%), Hispanic students (10.5%), and other non-Hispanic students (11.8%) compared with non-Hispanic black students (5.0%).
In addition, prevalence of cannabis vaping increased with grade level, from 4.7% of 9th graders to 15.5% of 12th graders.
The health impacts of vaping cannabis are not well researched, but the researchers note that among the potential safety issues are earlier initiation of tobacco or cannabis use, concomitant tobacco and cannabis use, increased frequency of use or misuse of tobacco or cannabis, or increased potency of cannabis.
The results of the study were limited by several factors including the use of data only from the state of North Carolina, the lack of data on frequency or current vaping cannabis behavior, lack of data on specific products, and lack of data on whether teens used specialized devices or e-cigarettes for cannabis vaping. However, the findings are consistent with studies on prevalence of cannabis vaping in other states such as Connecticut and California. “No studies to our knowledge have examined how adolescents who vape cannabis use other specific tobacco products (i.e., cigarettes, cigars, waterpipe, smokeless tobacco),” the researchers wrote.
The findings confirm that a large number of adolescents who use tobacco products have vaped cannabis as well, and this growing public health issue “is likely to affect and be affected by tobacco control and cannabis policies in states and at the federal level in the USA,” the researchers concluded.
“Increased research investigating how youth use e-cigarette devices for other purposes beyond vaping nicotine, like the current study, is needed,” they added.
The study was supported in part by the National Cancer Institute and the Food and Drug Administration’s Center for Tobacco Products. The researchers had no financial conflicts to disclose.
SOURCE: Kowitt SD et al. BMJ Open. 2019 Jun 13. doi: 10.1136/bmjopen-2018-028535.
and that practice is associated with cigars, waterpipe and e-cigarette use, findings from a survey of nearly 3,000 adolescents have shown.
“Although the prevalence of e-cigarette use among youth has increased dramatically in the past decade, little epidemiologic data exist on the prevalence of using e-cigarette devices or other specialised devices to vaporise (‘vape’) cannabis in the form of hash oil, tetrahydrocannabinol (THC) wax or oil, or dried cannabis buds or leaves,” wrote Sarah D. Kowitt, PhD, of the University of North Carolina, Chapel Hill, and colleagues. “This is surprising given that (1) cannabis (also referred to as marijuana) and e-cigarettes are the most commonly used substances by adolescents in the USA, (2) evidence exists that adolescents dual use both tobacco e-cigarettes and cannabis, and (3) longitudinal research suggests that use of e-cigarettes is associated with progression to use of cannabis.”
In a study published in BMJ Open, the researchers used data from the 2017 North Carolina Youth Tobacco Survey, a school-based survey of students in grades 6-12. The study population included 2,835 adolescents in grades 9-12.
Overall, 9.6% of students reported ever vaping cannabis. In multivariate analysis, cannabis vaping was significantly more likely among adolescents who reported using e-cigarettes (adjusted odds ratio 3.18), cigars (aOR 3.76), or water pipes (aOR 2.32) in the past 30 days, compared with peers who didn’t use tobacco.
The researchers found no significant association between smokeless tobacco use or traditional cigarette use in the past 30 days and vaping cannabis.
In a bivariate analysis, vaping cannabis was significantly more common among males vs. females (11% vs. 8.2%) and among non-Hispanic white students (11.3%), Hispanic students (10.5%), and other non-Hispanic students (11.8%) compared with non-Hispanic black students (5.0%).
In addition, prevalence of cannabis vaping increased with grade level, from 4.7% of 9th graders to 15.5% of 12th graders.
The health impacts of vaping cannabis are not well researched, but the researchers note that among the potential safety issues are earlier initiation of tobacco or cannabis use, concomitant tobacco and cannabis use, increased frequency of use or misuse of tobacco or cannabis, or increased potency of cannabis.
The results of the study were limited by several factors including the use of data only from the state of North Carolina, the lack of data on frequency or current vaping cannabis behavior, lack of data on specific products, and lack of data on whether teens used specialized devices or e-cigarettes for cannabis vaping. However, the findings are consistent with studies on prevalence of cannabis vaping in other states such as Connecticut and California. “No studies to our knowledge have examined how adolescents who vape cannabis use other specific tobacco products (i.e., cigarettes, cigars, waterpipe, smokeless tobacco),” the researchers wrote.
The findings confirm that a large number of adolescents who use tobacco products have vaped cannabis as well, and this growing public health issue “is likely to affect and be affected by tobacco control and cannabis policies in states and at the federal level in the USA,” the researchers concluded.
“Increased research investigating how youth use e-cigarette devices for other purposes beyond vaping nicotine, like the current study, is needed,” they added.
The study was supported in part by the National Cancer Institute and the Food and Drug Administration’s Center for Tobacco Products. The researchers had no financial conflicts to disclose.
SOURCE: Kowitt SD et al. BMJ Open. 2019 Jun 13. doi: 10.1136/bmjopen-2018-028535.
and that practice is associated with cigars, waterpipe and e-cigarette use, findings from a survey of nearly 3,000 adolescents have shown.
“Although the prevalence of e-cigarette use among youth has increased dramatically in the past decade, little epidemiologic data exist on the prevalence of using e-cigarette devices or other specialised devices to vaporise (‘vape’) cannabis in the form of hash oil, tetrahydrocannabinol (THC) wax or oil, or dried cannabis buds or leaves,” wrote Sarah D. Kowitt, PhD, of the University of North Carolina, Chapel Hill, and colleagues. “This is surprising given that (1) cannabis (also referred to as marijuana) and e-cigarettes are the most commonly used substances by adolescents in the USA, (2) evidence exists that adolescents dual use both tobacco e-cigarettes and cannabis, and (3) longitudinal research suggests that use of e-cigarettes is associated with progression to use of cannabis.”
In a study published in BMJ Open, the researchers used data from the 2017 North Carolina Youth Tobacco Survey, a school-based survey of students in grades 6-12. The study population included 2,835 adolescents in grades 9-12.
Overall, 9.6% of students reported ever vaping cannabis. In multivariate analysis, cannabis vaping was significantly more likely among adolescents who reported using e-cigarettes (adjusted odds ratio 3.18), cigars (aOR 3.76), or water pipes (aOR 2.32) in the past 30 days, compared with peers who didn’t use tobacco.
The researchers found no significant association between smokeless tobacco use or traditional cigarette use in the past 30 days and vaping cannabis.
In a bivariate analysis, vaping cannabis was significantly more common among males vs. females (11% vs. 8.2%) and among non-Hispanic white students (11.3%), Hispanic students (10.5%), and other non-Hispanic students (11.8%) compared with non-Hispanic black students (5.0%).
In addition, prevalence of cannabis vaping increased with grade level, from 4.7% of 9th graders to 15.5% of 12th graders.
The health impacts of vaping cannabis are not well researched, but the researchers note that among the potential safety issues are earlier initiation of tobacco or cannabis use, concomitant tobacco and cannabis use, increased frequency of use or misuse of tobacco or cannabis, or increased potency of cannabis.
The results of the study were limited by several factors including the use of data only from the state of North Carolina, the lack of data on frequency or current vaping cannabis behavior, lack of data on specific products, and lack of data on whether teens used specialized devices or e-cigarettes for cannabis vaping. However, the findings are consistent with studies on prevalence of cannabis vaping in other states such as Connecticut and California. “No studies to our knowledge have examined how adolescents who vape cannabis use other specific tobacco products (i.e., cigarettes, cigars, waterpipe, smokeless tobacco),” the researchers wrote.
The findings confirm that a large number of adolescents who use tobacco products have vaped cannabis as well, and this growing public health issue “is likely to affect and be affected by tobacco control and cannabis policies in states and at the federal level in the USA,” the researchers concluded.
“Increased research investigating how youth use e-cigarette devices for other purposes beyond vaping nicotine, like the current study, is needed,” they added.
The study was supported in part by the National Cancer Institute and the Food and Drug Administration’s Center for Tobacco Products. The researchers had no financial conflicts to disclose.
SOURCE: Kowitt SD et al. BMJ Open. 2019 Jun 13. doi: 10.1136/bmjopen-2018-028535.
FROM BMJ OPEN
Key clinical point: Use of tobacco products was significantly associated with cannabis vaping in teens.
Major finding: Approximately 10% of adolescents reported vaping cannabis.
Study details: The data come from a survey of 2,835 adolescents in North Carolina.
Disclosures: The study was supported in part by the National Cancer Institute and the FDA Center for Tobacco Products. The researchers had no financial conflicts to disclose.
Source: Kowitt SD et al. BMJ Open. 2019 Jun 13. doi: 10.1136/bmjopen-2018-028535.
Appeals court allows Title X restrictions to take effect
The panel ruled that the Trump administration’s funding restrictions were a reasonable interpretation of the federal Title X statute and that the administration is likely to prevail in its argument that lower courts erroneously halted the rules from taking effect. The ruling means the restrictions can take effect in every state except for Maryland, which passed a 2019 measure approving the use of state funds to replace federal Title X money if the new rule is enacted.
Alex Azar, secretary of the Department of Health & Human Services, said agency officials were pleased the 9th Circuit recognized there was no need to hold up the new family planning rules that simply enforce laws already on the books.
“We are also pleased that the [9th] Circuit agreed that the three preliminary injunctions against the new rules, including two nationwide injunctions, were inappropriate,” Mr. Azar said in the statement. “This decision is a major step toward the Trump administration being able to ensure that all Title X projects comply with the Title X statute and do not support abortion as a method of family planning.”
Leana Wen, MD, president for the Planned Parenthood Federation of America called the court ruling “devastating” for the millions of patients who rely on Title X health centers for cancer screenings, HIV tests, affordable birth control, and other critical primary and preventive care.
“We will be immediately seeking emergency relief from the [U.S.] Court of Appeals,” Dr. Wen said in a statement. “Planned Parenthood will not let the government censor our doctors and nurses from informing patients where and how they can access health care. We will continue to fight the Trump administration in the courts and alongside champions in Congress to protect everyone’s fundamental right to health care.”
The changes to the Title X program – originally scheduled to take effect May 3 – make health clinics ineligible for Title X funding if they offer, promote, or support abortion as a method of family planning. Title X grants generally go to health centers that provide reproductive health care – such as STD testing, cancer screenings, and contraception – to low-income families. Under the rule, the government would withdraw financial assistance to clinics if they allow counseling or referrals associated with abortion, regardless of whether the money is used for other health care services.
More than 20 states and several abortion rights organizations sued over the rules in four separate states. District judges in Oregon, Washington, and California temporarily blocked the rules from taking effect. The 9th Circuit ruling overturns these injunctions.
The American College of Physicians, the American Academy of Family Physicians, the American College of Obstetricians and Gynecologists, the American Academy of Pediatrics, and other groups have voiced their opposition to the Title X restrictions.
In a joint court brief, the medical societies wrote that the Trump administration’s limitations to the Title X program will create cultural, geographic, and financial barriers to care; erode the physician-patient relationship; and cause extreme, immediate, and irreparable harm to millions of patients.
The panel ruled that the Trump administration’s funding restrictions were a reasonable interpretation of the federal Title X statute and that the administration is likely to prevail in its argument that lower courts erroneously halted the rules from taking effect. The ruling means the restrictions can take effect in every state except for Maryland, which passed a 2019 measure approving the use of state funds to replace federal Title X money if the new rule is enacted.
Alex Azar, secretary of the Department of Health & Human Services, said agency officials were pleased the 9th Circuit recognized there was no need to hold up the new family planning rules that simply enforce laws already on the books.
“We are also pleased that the [9th] Circuit agreed that the three preliminary injunctions against the new rules, including two nationwide injunctions, were inappropriate,” Mr. Azar said in the statement. “This decision is a major step toward the Trump administration being able to ensure that all Title X projects comply with the Title X statute and do not support abortion as a method of family planning.”
Leana Wen, MD, president for the Planned Parenthood Federation of America called the court ruling “devastating” for the millions of patients who rely on Title X health centers for cancer screenings, HIV tests, affordable birth control, and other critical primary and preventive care.
“We will be immediately seeking emergency relief from the [U.S.] Court of Appeals,” Dr. Wen said in a statement. “Planned Parenthood will not let the government censor our doctors and nurses from informing patients where and how they can access health care. We will continue to fight the Trump administration in the courts and alongside champions in Congress to protect everyone’s fundamental right to health care.”
The changes to the Title X program – originally scheduled to take effect May 3 – make health clinics ineligible for Title X funding if they offer, promote, or support abortion as a method of family planning. Title X grants generally go to health centers that provide reproductive health care – such as STD testing, cancer screenings, and contraception – to low-income families. Under the rule, the government would withdraw financial assistance to clinics if they allow counseling or referrals associated with abortion, regardless of whether the money is used for other health care services.
More than 20 states and several abortion rights organizations sued over the rules in four separate states. District judges in Oregon, Washington, and California temporarily blocked the rules from taking effect. The 9th Circuit ruling overturns these injunctions.
The American College of Physicians, the American Academy of Family Physicians, the American College of Obstetricians and Gynecologists, the American Academy of Pediatrics, and other groups have voiced their opposition to the Title X restrictions.
In a joint court brief, the medical societies wrote that the Trump administration’s limitations to the Title X program will create cultural, geographic, and financial barriers to care; erode the physician-patient relationship; and cause extreme, immediate, and irreparable harm to millions of patients.
The panel ruled that the Trump administration’s funding restrictions were a reasonable interpretation of the federal Title X statute and that the administration is likely to prevail in its argument that lower courts erroneously halted the rules from taking effect. The ruling means the restrictions can take effect in every state except for Maryland, which passed a 2019 measure approving the use of state funds to replace federal Title X money if the new rule is enacted.
Alex Azar, secretary of the Department of Health & Human Services, said agency officials were pleased the 9th Circuit recognized there was no need to hold up the new family planning rules that simply enforce laws already on the books.
“We are also pleased that the [9th] Circuit agreed that the three preliminary injunctions against the new rules, including two nationwide injunctions, were inappropriate,” Mr. Azar said in the statement. “This decision is a major step toward the Trump administration being able to ensure that all Title X projects comply with the Title X statute and do not support abortion as a method of family planning.”
Leana Wen, MD, president for the Planned Parenthood Federation of America called the court ruling “devastating” for the millions of patients who rely on Title X health centers for cancer screenings, HIV tests, affordable birth control, and other critical primary and preventive care.
“We will be immediately seeking emergency relief from the [U.S.] Court of Appeals,” Dr. Wen said in a statement. “Planned Parenthood will not let the government censor our doctors and nurses from informing patients where and how they can access health care. We will continue to fight the Trump administration in the courts and alongside champions in Congress to protect everyone’s fundamental right to health care.”
The changes to the Title X program – originally scheduled to take effect May 3 – make health clinics ineligible for Title X funding if they offer, promote, or support abortion as a method of family planning. Title X grants generally go to health centers that provide reproductive health care – such as STD testing, cancer screenings, and contraception – to low-income families. Under the rule, the government would withdraw financial assistance to clinics if they allow counseling or referrals associated with abortion, regardless of whether the money is used for other health care services.
More than 20 states and several abortion rights organizations sued over the rules in four separate states. District judges in Oregon, Washington, and California temporarily blocked the rules from taking effect. The 9th Circuit ruling overturns these injunctions.
The American College of Physicians, the American Academy of Family Physicians, the American College of Obstetricians and Gynecologists, the American Academy of Pediatrics, and other groups have voiced their opposition to the Title X restrictions.
In a joint court brief, the medical societies wrote that the Trump administration’s limitations to the Title X program will create cultural, geographic, and financial barriers to care; erode the physician-patient relationship; and cause extreme, immediate, and irreparable harm to millions of patients.
Medical cannabis laws appear no longer tied to drop in opioid overdose mortality
Correlations do not hold when analysis is expanded to 2017
Contrary to previous research indicating that medical cannabis laws reduced opioid overdose mortality, the association between these two has reversed, with opioid overdose mortality increased in states with comprehensive medical cannabis laws, according to Chelsea L. Shover, PhD, and associates.
The original research by Marcus A. Bachhuber, MD, and associates showed that the introduction of state medical cannabis laws was associated with a 24.8% reduction in opioid overdose deaths per 100,000 population between 1999 and 2010. In contrast, the new research – which looked at a longer time period than the original research did – found that the association between state medical cannabis laws and opioid overdose mortality reversed direction, from –21% to +23%.
“We find it unlikely that medical cannabis – used by about 2.5% of the U.S. population – has exerted large conflicting effects on opioid overdose mortality,” wrote Dr. Shover, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University, and associates. “A more plausible interpretation is that this association is spurious.” Their study was published in the Proceedings of the National Academy of Sciences.
To conduct their analysis, Dr. Shover and associates extended the timeline reviewed by Dr. Bachhuber and associates to 2017. During 2010-2017, 32 states enacted medical cannabis laws, including 17 allowing only medical cannabis with low levels of tetrahydrocannabinol (THC), and 8 legalized recreational marijuana. In the expanded timeline during 1999-2017, states possessing a comprehensive medical marijuana law saw an increase in opioid overdose mortality of 28.2%. Meanwhile, states with recreational marijuana laws saw a decrease of 14.7% in opioid overdose mortality, and states with low-THC medical cannabis laws saw a decrease of 7.1%. However, the investigators noted that those values had wide confidence intervals, which indicates “compatibility with large range of true associations.”
Corporate actors with deep pockets have substantial ability to promote congenial results, and suffering people are desperate for effective solutions. Cannabinoids have demonstrated therapeutic benefits, but reducing population-level opioid overdose mortality does not appear to be among them,” Dr. Shover and associates noted.
Dr. Shover reported receiving support from National Institute on Drug Abuse and the Wu Tsai Neurosciences Institute. Another coauthor received support from the Veterans Health Administration, Wu Tsai Neurosciences Institute, and the Esther Ting Memorial Professorship at Stanford.
SOURCE: Shover CL et al. Proc Natl Acad Sci U S A. 2019 Jun 10. doi: 10.1073/pnas.1903434116.
Correlations do not hold when analysis is expanded to 2017
Correlations do not hold when analysis is expanded to 2017
Contrary to previous research indicating that medical cannabis laws reduced opioid overdose mortality, the association between these two has reversed, with opioid overdose mortality increased in states with comprehensive medical cannabis laws, according to Chelsea L. Shover, PhD, and associates.
The original research by Marcus A. Bachhuber, MD, and associates showed that the introduction of state medical cannabis laws was associated with a 24.8% reduction in opioid overdose deaths per 100,000 population between 1999 and 2010. In contrast, the new research – which looked at a longer time period than the original research did – found that the association between state medical cannabis laws and opioid overdose mortality reversed direction, from –21% to +23%.
“We find it unlikely that medical cannabis – used by about 2.5% of the U.S. population – has exerted large conflicting effects on opioid overdose mortality,” wrote Dr. Shover, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University, and associates. “A more plausible interpretation is that this association is spurious.” Their study was published in the Proceedings of the National Academy of Sciences.
To conduct their analysis, Dr. Shover and associates extended the timeline reviewed by Dr. Bachhuber and associates to 2017. During 2010-2017, 32 states enacted medical cannabis laws, including 17 allowing only medical cannabis with low levels of tetrahydrocannabinol (THC), and 8 legalized recreational marijuana. In the expanded timeline during 1999-2017, states possessing a comprehensive medical marijuana law saw an increase in opioid overdose mortality of 28.2%. Meanwhile, states with recreational marijuana laws saw a decrease of 14.7% in opioid overdose mortality, and states with low-THC medical cannabis laws saw a decrease of 7.1%. However, the investigators noted that those values had wide confidence intervals, which indicates “compatibility with large range of true associations.”
Corporate actors with deep pockets have substantial ability to promote congenial results, and suffering people are desperate for effective solutions. Cannabinoids have demonstrated therapeutic benefits, but reducing population-level opioid overdose mortality does not appear to be among them,” Dr. Shover and associates noted.
Dr. Shover reported receiving support from National Institute on Drug Abuse and the Wu Tsai Neurosciences Institute. Another coauthor received support from the Veterans Health Administration, Wu Tsai Neurosciences Institute, and the Esther Ting Memorial Professorship at Stanford.
SOURCE: Shover CL et al. Proc Natl Acad Sci U S A. 2019 Jun 10. doi: 10.1073/pnas.1903434116.
Contrary to previous research indicating that medical cannabis laws reduced opioid overdose mortality, the association between these two has reversed, with opioid overdose mortality increased in states with comprehensive medical cannabis laws, according to Chelsea L. Shover, PhD, and associates.
The original research by Marcus A. Bachhuber, MD, and associates showed that the introduction of state medical cannabis laws was associated with a 24.8% reduction in opioid overdose deaths per 100,000 population between 1999 and 2010. In contrast, the new research – which looked at a longer time period than the original research did – found that the association between state medical cannabis laws and opioid overdose mortality reversed direction, from –21% to +23%.
“We find it unlikely that medical cannabis – used by about 2.5% of the U.S. population – has exerted large conflicting effects on opioid overdose mortality,” wrote Dr. Shover, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University, and associates. “A more plausible interpretation is that this association is spurious.” Their study was published in the Proceedings of the National Academy of Sciences.
To conduct their analysis, Dr. Shover and associates extended the timeline reviewed by Dr. Bachhuber and associates to 2017. During 2010-2017, 32 states enacted medical cannabis laws, including 17 allowing only medical cannabis with low levels of tetrahydrocannabinol (THC), and 8 legalized recreational marijuana. In the expanded timeline during 1999-2017, states possessing a comprehensive medical marijuana law saw an increase in opioid overdose mortality of 28.2%. Meanwhile, states with recreational marijuana laws saw a decrease of 14.7% in opioid overdose mortality, and states with low-THC medical cannabis laws saw a decrease of 7.1%. However, the investigators noted that those values had wide confidence intervals, which indicates “compatibility with large range of true associations.”
Corporate actors with deep pockets have substantial ability to promote congenial results, and suffering people are desperate for effective solutions. Cannabinoids have demonstrated therapeutic benefits, but reducing population-level opioid overdose mortality does not appear to be among them,” Dr. Shover and associates noted.
Dr. Shover reported receiving support from National Institute on Drug Abuse and the Wu Tsai Neurosciences Institute. Another coauthor received support from the Veterans Health Administration, Wu Tsai Neurosciences Institute, and the Esther Ting Memorial Professorship at Stanford.
SOURCE: Shover CL et al. Proc Natl Acad Sci U S A. 2019 Jun 10. doi: 10.1073/pnas.1903434116.
FROM PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
Vaping among teens increased significantly from 2017 to 2018
according to data from national cross-sectional surveys.
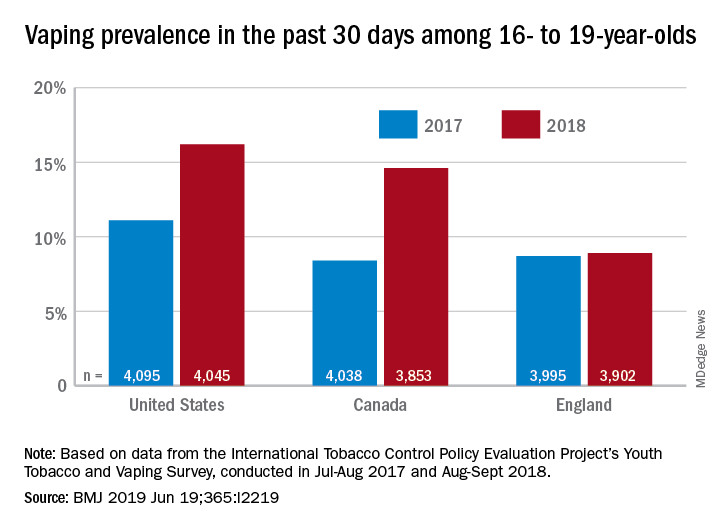
The prevalence of vaping in the past 30 days rose from 11% to 16% in the United States and from 8% to 14.6% in Canada, while use in England showed an nonsignificant increase of 8.7% to 8.9%, David Hammond, PhD, of the University of Waterloo (Canada) and associates said in the BMJ.
Embedded in those U.S. and Canadian increases is the recent evolution of the vaping market brought about by “the growth of JUUL e-cigarettes and similar products [that use] benzoic acid and nicotine salt technology to deliver higher concentrations of nicotine than conventional e-cigarettes,” they explained.
In England, the JUUL system is limited to less than half the nicotine concentration, at 20 mg/mL, compared with more than 50 mg/mL in the United States and Canada, and it was not available at all types of retail outlets at the time of the surveys. That situation changed in March 2019, when the company expanded to convenience stores, the investigators noted.
In the United States, JUUL was the second-most popular product among past–30-day vapers who had a usual brand in 2017, with 9% reporting use. In 2018, JUUL was the most popular brand and use was up to 28%. In Canada, the brand was not among the top five in 2017, but was third in 2018 at 10% in those who reported vaping in the past 30 days. The leading Canadian brand in 2018 was Smok, which released a nicotine-salt version in March of 2018, Dr. Hammond and associates reported.
“Before 2018, there was relatively little evidence of regular vaping among adolescents that might be indicative of nicotine addiction; however, the emergence of JUUL and nicotine salt–based products might signal a change,” they wrote.
The International Tobacco Control Policy Evaluation Project’s Youth Tobacco and Vaping Survey was conducted online in each country in two waves – July to August 2017 and August to September 2018 – with a sample size of approximately 12,000 for each.
The study was funded by the U.S. National Institutes of Health. Dr. Hammond is supported by a Canadian Institutes of Health Research–Public Health Agency of Canada applied public health research chair. The investigators said that they had no other financial disclosures to report, but several have served as paid witnesses in legal challenges against tobacco companies.
SOURCE: Hammond D et al. BMJ 2019 Jun 19. doi: 10.1136/bmj.l2219.
according to data from national cross-sectional surveys.
The prevalence of vaping in the past 30 days rose from 11% to 16% in the United States and from 8% to 14.6% in Canada, while use in England showed an nonsignificant increase of 8.7% to 8.9%, David Hammond, PhD, of the University of Waterloo (Canada) and associates said in the BMJ.
Embedded in those U.S. and Canadian increases is the recent evolution of the vaping market brought about by “the growth of JUUL e-cigarettes and similar products [that use] benzoic acid and nicotine salt technology to deliver higher concentrations of nicotine than conventional e-cigarettes,” they explained.
In England, the JUUL system is limited to less than half the nicotine concentration, at 20 mg/mL, compared with more than 50 mg/mL in the United States and Canada, and it was not available at all types of retail outlets at the time of the surveys. That situation changed in March 2019, when the company expanded to convenience stores, the investigators noted.
In the United States, JUUL was the second-most popular product among past–30-day vapers who had a usual brand in 2017, with 9% reporting use. In 2018, JUUL was the most popular brand and use was up to 28%. In Canada, the brand was not among the top five in 2017, but was third in 2018 at 10% in those who reported vaping in the past 30 days. The leading Canadian brand in 2018 was Smok, which released a nicotine-salt version in March of 2018, Dr. Hammond and associates reported.
“Before 2018, there was relatively little evidence of regular vaping among adolescents that might be indicative of nicotine addiction; however, the emergence of JUUL and nicotine salt–based products might signal a change,” they wrote.
The International Tobacco Control Policy Evaluation Project’s Youth Tobacco and Vaping Survey was conducted online in each country in two waves – July to August 2017 and August to September 2018 – with a sample size of approximately 12,000 for each.
The study was funded by the U.S. National Institutes of Health. Dr. Hammond is supported by a Canadian Institutes of Health Research–Public Health Agency of Canada applied public health research chair. The investigators said that they had no other financial disclosures to report, but several have served as paid witnesses in legal challenges against tobacco companies.
SOURCE: Hammond D et al. BMJ 2019 Jun 19. doi: 10.1136/bmj.l2219.
according to data from national cross-sectional surveys.
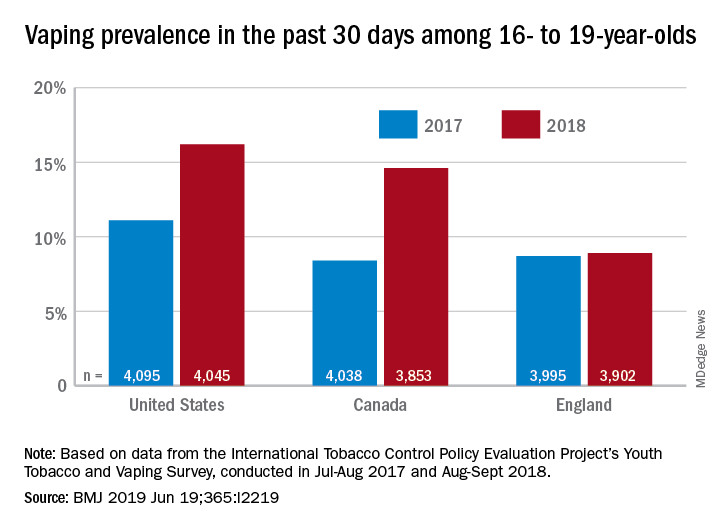
The prevalence of vaping in the past 30 days rose from 11% to 16% in the United States and from 8% to 14.6% in Canada, while use in England showed an nonsignificant increase of 8.7% to 8.9%, David Hammond, PhD, of the University of Waterloo (Canada) and associates said in the BMJ.
Embedded in those U.S. and Canadian increases is the recent evolution of the vaping market brought about by “the growth of JUUL e-cigarettes and similar products [that use] benzoic acid and nicotine salt technology to deliver higher concentrations of nicotine than conventional e-cigarettes,” they explained.
In England, the JUUL system is limited to less than half the nicotine concentration, at 20 mg/mL, compared with more than 50 mg/mL in the United States and Canada, and it was not available at all types of retail outlets at the time of the surveys. That situation changed in March 2019, when the company expanded to convenience stores, the investigators noted.
In the United States, JUUL was the second-most popular product among past–30-day vapers who had a usual brand in 2017, with 9% reporting use. In 2018, JUUL was the most popular brand and use was up to 28%. In Canada, the brand was not among the top five in 2017, but was third in 2018 at 10% in those who reported vaping in the past 30 days. The leading Canadian brand in 2018 was Smok, which released a nicotine-salt version in March of 2018, Dr. Hammond and associates reported.
“Before 2018, there was relatively little evidence of regular vaping among adolescents that might be indicative of nicotine addiction; however, the emergence of JUUL and nicotine salt–based products might signal a change,” they wrote.
The International Tobacco Control Policy Evaluation Project’s Youth Tobacco and Vaping Survey was conducted online in each country in two waves – July to August 2017 and August to September 2018 – with a sample size of approximately 12,000 for each.
The study was funded by the U.S. National Institutes of Health. Dr. Hammond is supported by a Canadian Institutes of Health Research–Public Health Agency of Canada applied public health research chair. The investigators said that they had no other financial disclosures to report, but several have served as paid witnesses in legal challenges against tobacco companies.
SOURCE: Hammond D et al. BMJ 2019 Jun 19. doi: 10.1136/bmj.l2219.
FROM THE BMJ
Key clinical point: Recent increases in vaping prevalence among teens “might be indicative of nicotine addiction.”
Major finding: Vaping prevalence increased from 11% to 16% in the United States and from 8% to 14.6% in Canada.
Study details: Two waves of a national, cross-sectional survey that included approximately 12,000 respondents each.
Disclosures: The study was funded by the U.S. National Institutes of Health. Dr. Hammond is supported by a Canadian Institutes of Health Research–Public Health Agency of Canada applied public health research chair. The investigators said that they had no other financial disclosures to report, but several have served as paid witnesses in legal challenges against tobacco companies.
Source: Hammond D et al. BMJ. 2019 Jun 19. doi: 10.1136/bmj.l2219.
Suicide rates rise in U.S. adolescents and young adults
Suicides in teens and young adults reached 6,241 in 2017, the highest since 2000, according to data from a review of the Centers for Disease Control and Prevention Underlying Cause of Death database.
The suicide rate overall was 12 per 100,000 in 2017 for 15-19 year olds.
Although suicide rates have increased across all age groups in the United States since 2000, “adolescents are of particular concern, with increases in social media use, anxiety, depression, and self-inflicted injuries,” wrote Oren Miron of Harvard Medical School, Boston, and colleagues.
In a research letter published in JAMA, the researchers analyzed trends in teen and young adult suicides from 2000 to 2017. The combined suicide rate for males and females aged 15-19 years in 2000 was 8 per 100,000 with no significant changes until 2007, followed by an annual percentage change (APC) of 3% from 2007 to 2014 and 10% from 2014 to 2017.
When the data were broken out by gender, Of note, these young men showed a decreasing trend in APC of –2% from 2000 to 2007 before increasing.
Among females aged 15-19 years, no increase was noted until 2010, then researchers identified an APC of 8% from 2010 to 2017.
For ages 20-24 years, the combined suicide rate for males and females was 13 per 100,000 in 2000, which rose to 17 per 100,000 in 2017. The APC in the older group was 1% from 2000 to 2013 and 6% from 2013 to 2017. Increasing trends were observed for both males and females over the study period.
The study was limited by the potential inaccuracy in cause of death listed on death certificates, such as mistaking a suicide for an accidental overdose, and the increased suicide rate could reflect more accurate reporting, the researchers noted.
Nonetheless, the results support the need for more studies of contributing factors to teen and young adult suicides to help develop prevention strategies and analysis of factors that may have contributed to declines in suicide rates in the past, they said.
Coauthor Dr. Yu was supported by the Harvard Data Science Fellowship. The researchers had no relevant financial disclosures.
SOURCE: Miron O et al. JAMA. 2019 Jun 28;321:2362-4.
Suicides in teens and young adults reached 6,241 in 2017, the highest since 2000, according to data from a review of the Centers for Disease Control and Prevention Underlying Cause of Death database.
The suicide rate overall was 12 per 100,000 in 2017 for 15-19 year olds.
Although suicide rates have increased across all age groups in the United States since 2000, “adolescents are of particular concern, with increases in social media use, anxiety, depression, and self-inflicted injuries,” wrote Oren Miron of Harvard Medical School, Boston, and colleagues.
In a research letter published in JAMA, the researchers analyzed trends in teen and young adult suicides from 2000 to 2017. The combined suicide rate for males and females aged 15-19 years in 2000 was 8 per 100,000 with no significant changes until 2007, followed by an annual percentage change (APC) of 3% from 2007 to 2014 and 10% from 2014 to 2017.
When the data were broken out by gender, Of note, these young men showed a decreasing trend in APC of –2% from 2000 to 2007 before increasing.
Among females aged 15-19 years, no increase was noted until 2010, then researchers identified an APC of 8% from 2010 to 2017.
For ages 20-24 years, the combined suicide rate for males and females was 13 per 100,000 in 2000, which rose to 17 per 100,000 in 2017. The APC in the older group was 1% from 2000 to 2013 and 6% from 2013 to 2017. Increasing trends were observed for both males and females over the study period.
The study was limited by the potential inaccuracy in cause of death listed on death certificates, such as mistaking a suicide for an accidental overdose, and the increased suicide rate could reflect more accurate reporting, the researchers noted.
Nonetheless, the results support the need for more studies of contributing factors to teen and young adult suicides to help develop prevention strategies and analysis of factors that may have contributed to declines in suicide rates in the past, they said.
Coauthor Dr. Yu was supported by the Harvard Data Science Fellowship. The researchers had no relevant financial disclosures.
SOURCE: Miron O et al. JAMA. 2019 Jun 28;321:2362-4.
Suicides in teens and young adults reached 6,241 in 2017, the highest since 2000, according to data from a review of the Centers for Disease Control and Prevention Underlying Cause of Death database.
The suicide rate overall was 12 per 100,000 in 2017 for 15-19 year olds.
Although suicide rates have increased across all age groups in the United States since 2000, “adolescents are of particular concern, with increases in social media use, anxiety, depression, and self-inflicted injuries,” wrote Oren Miron of Harvard Medical School, Boston, and colleagues.
In a research letter published in JAMA, the researchers analyzed trends in teen and young adult suicides from 2000 to 2017. The combined suicide rate for males and females aged 15-19 years in 2000 was 8 per 100,000 with no significant changes until 2007, followed by an annual percentage change (APC) of 3% from 2007 to 2014 and 10% from 2014 to 2017.
When the data were broken out by gender, Of note, these young men showed a decreasing trend in APC of –2% from 2000 to 2007 before increasing.
Among females aged 15-19 years, no increase was noted until 2010, then researchers identified an APC of 8% from 2010 to 2017.
For ages 20-24 years, the combined suicide rate for males and females was 13 per 100,000 in 2000, which rose to 17 per 100,000 in 2017. The APC in the older group was 1% from 2000 to 2013 and 6% from 2013 to 2017. Increasing trends were observed for both males and females over the study period.
The study was limited by the potential inaccuracy in cause of death listed on death certificates, such as mistaking a suicide for an accidental overdose, and the increased suicide rate could reflect more accurate reporting, the researchers noted.
Nonetheless, the results support the need for more studies of contributing factors to teen and young adult suicides to help develop prevention strategies and analysis of factors that may have contributed to declines in suicide rates in the past, they said.
Coauthor Dr. Yu was supported by the Harvard Data Science Fellowship. The researchers had no relevant financial disclosures.
SOURCE: Miron O et al. JAMA. 2019 Jun 28;321:2362-4.
FROM JAMA
Key clinical point: Suicide rates in U.S. adolescents and young adults have increased since 2000.
Major finding: The combined suicide rate for males and females aged 15-19 years underwent an annual percentage change of 3% from 2007 to 2014 and 10% from 2014 to 2017.
Study details: The data come from the CDC Underlying Cause of Death database.
Disclosures: Coauthor Dr. Yu was supported by the Harvard Data Science Fellowship. The researchers had no relevant financial disclosures.
Source: Miron O et al. JAMA. 2019 Jun 28;321:2362-4.
Ovarian reserve markers fall on isotretinoin, but rebound after stopping treatment
MILAN – according to data presented at the World Congress of Dermatology.
Although markers for ovarian reserve, including anti-Müllerian hormone (AMH) serum levels, ovarian volume, and antral follicle count, were significantly lower during a period of isotretinoin use than at baseline, these values were were not significantly different from pretreatment levels by 1 month after stopping isotretinoin.
For patients taking isotretinoin at a dose of 0.5 mg/kg/day, AMH levels fell from a baseline level of 5.29 ng/mL to 4.16 ng/mL during treatment, but rebounded to 4.77 ng/mL 1 month after stopping treatment (P less than .001 for difference between baseline and on-drug values), Tuğba Özkök Akbulut, MD, said during a late-breaking abstracts session.
For women taking isotretinoin 1 mg/kg/day, AMH levels went from 5.14 ng/mL at baseline to 4.24 ng/mL on treatment, to 4.65 ng/mL 1 month after treatment (P less than .001 for difference between baseline and on-drug values), reported Dr. Akbulut a dermatologist at the Haseki Training Research Hospital, Istanbul.
Women on the higher dose of isotretinoin had a similar pattern of decline while on treatment and rebound after ceasing isotretinoin for ovarian volume and antral follicle count (P less than .001 for all values). These differences were not statistically significant for women taking 0.5 mg/kg/day of isotretinoin, except for right ovarian volume (P = 0.013).
Although values were numerically lower for many markers of ovarian reserve after ceasing treatment, compared with baseline figures, these differences were not statistically significantly different. Markers of ovarian reserve did not change significantly for a control group of women without acne.
Dr. Akbulut and her colleagues conducted this prospective case-control study of 42 women of reproductive age who sought dermatologist care for severe acne unresponsive to conservative therapy; 26 women who did not have acne constituted the control group. Smokers, patients with thyroid disease, and those with known polycystic ovary syndrome were excluded from participation.
The women with acne received oral isotretinoin dosed either at 0.5 or 1.0 mg/kg/day, with treatment lasting 5-9 months. For each patient, treatment was stopped when the cumulative dose reached 120 mg/kg.
After an initial visit at which blood was collected from all participants to measure serum AMH levels, those receiving isotretinoin were seen every 4 weeks to check serum lipid and liver enzyme levels.
At the 3-month mark during the study period and 1 month after the end of completing isotretinoin treatment, or at the end of the study period for the control group, blood samples also were drawn for AMH levels.
To measure hormone levels, also blood was drawn between days 2 and 5 of the follicular phase of the menstrual cycle. Participants received ultrasounds to measure antral follicle count and ovarian volume between days 2 and 5 of the menstrual cycle at the initial visit, at the 3-month visit, and at the final visit. Results were interpreted by a trained gynecologist.
Patients, who were mostly in their early 20s, had a mean body mass index of about 22 kg/m2. Hormone levels, ovarian volume, and antral follicle count did not differ among study arms at baseline.
“There are contradictory reports in the literature regarding the effect of retinoic acid on ovarian reserve,” noted Dr. Akbulut. Some preclinical studies found that retinoic acid increased fertility and ovarian reserve in rodents; however, some human studies had shown lower serum AMH concentrations in patients using isotretinoin.
This new demonstration of the reversibility of isotretinoin’s negative effect on ovarian reserve helps clarify a confused picture in the medical literature, said Dr. Akbulut. “The results of our study demonstrated that systemic isotretinoin had a reversible effect on ovarian reserve.”
Dr. Akbulut reported no outside sources of funding and that she had no relevant financial disclosures.
MILAN – according to data presented at the World Congress of Dermatology.
Although markers for ovarian reserve, including anti-Müllerian hormone (AMH) serum levels, ovarian volume, and antral follicle count, were significantly lower during a period of isotretinoin use than at baseline, these values were were not significantly different from pretreatment levels by 1 month after stopping isotretinoin.
For patients taking isotretinoin at a dose of 0.5 mg/kg/day, AMH levels fell from a baseline level of 5.29 ng/mL to 4.16 ng/mL during treatment, but rebounded to 4.77 ng/mL 1 month after stopping treatment (P less than .001 for difference between baseline and on-drug values), Tuğba Özkök Akbulut, MD, said during a late-breaking abstracts session.
For women taking isotretinoin 1 mg/kg/day, AMH levels went from 5.14 ng/mL at baseline to 4.24 ng/mL on treatment, to 4.65 ng/mL 1 month after treatment (P less than .001 for difference between baseline and on-drug values), reported Dr. Akbulut a dermatologist at the Haseki Training Research Hospital, Istanbul.
Women on the higher dose of isotretinoin had a similar pattern of decline while on treatment and rebound after ceasing isotretinoin for ovarian volume and antral follicle count (P less than .001 for all values). These differences were not statistically significant for women taking 0.5 mg/kg/day of isotretinoin, except for right ovarian volume (P = 0.013).
Although values were numerically lower for many markers of ovarian reserve after ceasing treatment, compared with baseline figures, these differences were not statistically significantly different. Markers of ovarian reserve did not change significantly for a control group of women without acne.
Dr. Akbulut and her colleagues conducted this prospective case-control study of 42 women of reproductive age who sought dermatologist care for severe acne unresponsive to conservative therapy; 26 women who did not have acne constituted the control group. Smokers, patients with thyroid disease, and those with known polycystic ovary syndrome were excluded from participation.
The women with acne received oral isotretinoin dosed either at 0.5 or 1.0 mg/kg/day, with treatment lasting 5-9 months. For each patient, treatment was stopped when the cumulative dose reached 120 mg/kg.
After an initial visit at which blood was collected from all participants to measure serum AMH levels, those receiving isotretinoin were seen every 4 weeks to check serum lipid and liver enzyme levels.
At the 3-month mark during the study period and 1 month after the end of completing isotretinoin treatment, or at the end of the study period for the control group, blood samples also were drawn for AMH levels.
To measure hormone levels, also blood was drawn between days 2 and 5 of the follicular phase of the menstrual cycle. Participants received ultrasounds to measure antral follicle count and ovarian volume between days 2 and 5 of the menstrual cycle at the initial visit, at the 3-month visit, and at the final visit. Results were interpreted by a trained gynecologist.
Patients, who were mostly in their early 20s, had a mean body mass index of about 22 kg/m2. Hormone levels, ovarian volume, and antral follicle count did not differ among study arms at baseline.
“There are contradictory reports in the literature regarding the effect of retinoic acid on ovarian reserve,” noted Dr. Akbulut. Some preclinical studies found that retinoic acid increased fertility and ovarian reserve in rodents; however, some human studies had shown lower serum AMH concentrations in patients using isotretinoin.
This new demonstration of the reversibility of isotretinoin’s negative effect on ovarian reserve helps clarify a confused picture in the medical literature, said Dr. Akbulut. “The results of our study demonstrated that systemic isotretinoin had a reversible effect on ovarian reserve.”
Dr. Akbulut reported no outside sources of funding and that she had no relevant financial disclosures.
MILAN – according to data presented at the World Congress of Dermatology.
Although markers for ovarian reserve, including anti-Müllerian hormone (AMH) serum levels, ovarian volume, and antral follicle count, were significantly lower during a period of isotretinoin use than at baseline, these values were were not significantly different from pretreatment levels by 1 month after stopping isotretinoin.
For patients taking isotretinoin at a dose of 0.5 mg/kg/day, AMH levels fell from a baseline level of 5.29 ng/mL to 4.16 ng/mL during treatment, but rebounded to 4.77 ng/mL 1 month after stopping treatment (P less than .001 for difference between baseline and on-drug values), Tuğba Özkök Akbulut, MD, said during a late-breaking abstracts session.
For women taking isotretinoin 1 mg/kg/day, AMH levels went from 5.14 ng/mL at baseline to 4.24 ng/mL on treatment, to 4.65 ng/mL 1 month after treatment (P less than .001 for difference between baseline and on-drug values), reported Dr. Akbulut a dermatologist at the Haseki Training Research Hospital, Istanbul.
Women on the higher dose of isotretinoin had a similar pattern of decline while on treatment and rebound after ceasing isotretinoin for ovarian volume and antral follicle count (P less than .001 for all values). These differences were not statistically significant for women taking 0.5 mg/kg/day of isotretinoin, except for right ovarian volume (P = 0.013).
Although values were numerically lower for many markers of ovarian reserve after ceasing treatment, compared with baseline figures, these differences were not statistically significantly different. Markers of ovarian reserve did not change significantly for a control group of women without acne.
Dr. Akbulut and her colleagues conducted this prospective case-control study of 42 women of reproductive age who sought dermatologist care for severe acne unresponsive to conservative therapy; 26 women who did not have acne constituted the control group. Smokers, patients with thyroid disease, and those with known polycystic ovary syndrome were excluded from participation.
The women with acne received oral isotretinoin dosed either at 0.5 or 1.0 mg/kg/day, with treatment lasting 5-9 months. For each patient, treatment was stopped when the cumulative dose reached 120 mg/kg.
After an initial visit at which blood was collected from all participants to measure serum AMH levels, those receiving isotretinoin were seen every 4 weeks to check serum lipid and liver enzyme levels.
At the 3-month mark during the study period and 1 month after the end of completing isotretinoin treatment, or at the end of the study period for the control group, blood samples also were drawn for AMH levels.
To measure hormone levels, also blood was drawn between days 2 and 5 of the follicular phase of the menstrual cycle. Participants received ultrasounds to measure antral follicle count and ovarian volume between days 2 and 5 of the menstrual cycle at the initial visit, at the 3-month visit, and at the final visit. Results were interpreted by a trained gynecologist.
Patients, who were mostly in their early 20s, had a mean body mass index of about 22 kg/m2. Hormone levels, ovarian volume, and antral follicle count did not differ among study arms at baseline.
“There are contradictory reports in the literature regarding the effect of retinoic acid on ovarian reserve,” noted Dr. Akbulut. Some preclinical studies found that retinoic acid increased fertility and ovarian reserve in rodents; however, some human studies had shown lower serum AMH concentrations in patients using isotretinoin.
This new demonstration of the reversibility of isotretinoin’s negative effect on ovarian reserve helps clarify a confused picture in the medical literature, said Dr. Akbulut. “The results of our study demonstrated that systemic isotretinoin had a reversible effect on ovarian reserve.”
Dr. Akbulut reported no outside sources of funding and that she had no relevant financial disclosures.
REPORTING FROM WCD2019