User login
PROs in lung cancer and how to administer trastuzumab
In this edition of “How I will treat my next patient,” I take a look at two recent trials – one summarizes a presentation at the European Lung Cancer Congress on the value of durvalumab as adjuvant treatment in patients with locally-advanced non–small cell lung cancer and the other confirms the safety and efficacy of subcutaneously-administered trastuzumab as neoadjuvant treatment in HER2/-positive breast cancer patients.
PACIFIC trial
In the PACIFIC trial, 713 patients with unresectable, stage III non–small cell lung cancer (NSCLC) who received concurrent chemoradiation were randomized to receive adjuvant durvalumab or an identical placebo, for a year after radiation ended. The results were dramatic in favor of durvalumab (N Engl J Med. 2018;379:2342-50).
Durvalumab showed 24-month overall survival of 66.3% versus 55.6% with placebo (hazard ratio, 0.68, P = .0025) and progression-free survival of 17.2 months versus 5. 6 months (HR, 0.51). As expected, there were more grade 3-4 toxicities and treatment discontinuations with durvalumab than with placebo, but the toxicity seemed modest, given the substantial improvements in tumor-related outcomes.
At the recent European Lung Cancer Congress, Marina Garassino, MD, reported on Patient-Reported Outcomes (PRO) in PACIFIC. PROs were analyzed by PD-L1 level. A total of 63% of patients had PD-L1 tumor expression data for analysis. Overall, there were no major differences in PROs by PD-L1. Global quality of life did not differ by PD-L1 expression cohort.
These data support adjuvant durvalumab for stage III, chemoradiation-treated NSCLC patients, not only from efficacy and toxicity viewpoints, but also from the standpoint of the patient experience, independent of PD-L1 tumor expression.
What this means in practice
From every relevant perspective, regardless of histology and molecular features associated with their particular tumor, it is worthwhile for us to recommend – and for our patients to receive – durvalumab adjuvant therapy for up to 1 year after radiation ends, with close follow-up and adherence to the criteria for treatment modification or discontinuation as performed in the PACIFIC trial. These new data remove any lingering concerns about the value of this life-prolonging treatment.
Subcutaneous vs. IV trastuzumab
In this international phase 3 trial in early breast cancer patients, neoadjuvant chemotherapy was paired with either standard IV trastuzumab or subcutaneous trastuzumab at intervals of every 3 weeks. After the cytotoxic chemotherapy concluded, patients completed a 12-month course of trastuzumab with either the IV or subcutaneous administration, as previously randomized. The 6-year event-free survival and overall survival were 65% and 84%, respectively, for both the IV and subcutaneous treatment administration.
The authors concluded that these results are relevant to patients with low-risk HER2-positive breast cancer patients, for whom T-DM1 is not needed (JAMA Oncol. 2019 Apr 18. doi: 10.1001/jamaoncol.2019.0339).
What this means in practice
These long-term data from the HannaH trial show persuasively that patients should be offered the more convenient, hopefully cheaper, subcutaneous route of administration. Since relapses beyond year 6 are unlikely, these data are unlikely to change with further follow-up. At our hospital, we recently made the decision to add subcutaneous trastuzumab to our formulary.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers, and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I will treat my next patient,” I take a look at two recent trials – one summarizes a presentation at the European Lung Cancer Congress on the value of durvalumab as adjuvant treatment in patients with locally-advanced non–small cell lung cancer and the other confirms the safety and efficacy of subcutaneously-administered trastuzumab as neoadjuvant treatment in HER2/-positive breast cancer patients.
PACIFIC trial
In the PACIFIC trial, 713 patients with unresectable, stage III non–small cell lung cancer (NSCLC) who received concurrent chemoradiation were randomized to receive adjuvant durvalumab or an identical placebo, for a year after radiation ended. The results were dramatic in favor of durvalumab (N Engl J Med. 2018;379:2342-50).
Durvalumab showed 24-month overall survival of 66.3% versus 55.6% with placebo (hazard ratio, 0.68, P = .0025) and progression-free survival of 17.2 months versus 5. 6 months (HR, 0.51). As expected, there were more grade 3-4 toxicities and treatment discontinuations with durvalumab than with placebo, but the toxicity seemed modest, given the substantial improvements in tumor-related outcomes.
At the recent European Lung Cancer Congress, Marina Garassino, MD, reported on Patient-Reported Outcomes (PRO) in PACIFIC. PROs were analyzed by PD-L1 level. A total of 63% of patients had PD-L1 tumor expression data for analysis. Overall, there were no major differences in PROs by PD-L1. Global quality of life did not differ by PD-L1 expression cohort.
These data support adjuvant durvalumab for stage III, chemoradiation-treated NSCLC patients, not only from efficacy and toxicity viewpoints, but also from the standpoint of the patient experience, independent of PD-L1 tumor expression.
What this means in practice
From every relevant perspective, regardless of histology and molecular features associated with their particular tumor, it is worthwhile for us to recommend – and for our patients to receive – durvalumab adjuvant therapy for up to 1 year after radiation ends, with close follow-up and adherence to the criteria for treatment modification or discontinuation as performed in the PACIFIC trial. These new data remove any lingering concerns about the value of this life-prolonging treatment.
Subcutaneous vs. IV trastuzumab
In this international phase 3 trial in early breast cancer patients, neoadjuvant chemotherapy was paired with either standard IV trastuzumab or subcutaneous trastuzumab at intervals of every 3 weeks. After the cytotoxic chemotherapy concluded, patients completed a 12-month course of trastuzumab with either the IV or subcutaneous administration, as previously randomized. The 6-year event-free survival and overall survival were 65% and 84%, respectively, for both the IV and subcutaneous treatment administration.
The authors concluded that these results are relevant to patients with low-risk HER2-positive breast cancer patients, for whom T-DM1 is not needed (JAMA Oncol. 2019 Apr 18. doi: 10.1001/jamaoncol.2019.0339).
What this means in practice
These long-term data from the HannaH trial show persuasively that patients should be offered the more convenient, hopefully cheaper, subcutaneous route of administration. Since relapses beyond year 6 are unlikely, these data are unlikely to change with further follow-up. At our hospital, we recently made the decision to add subcutaneous trastuzumab to our formulary.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers, and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I will treat my next patient,” I take a look at two recent trials – one summarizes a presentation at the European Lung Cancer Congress on the value of durvalumab as adjuvant treatment in patients with locally-advanced non–small cell lung cancer and the other confirms the safety and efficacy of subcutaneously-administered trastuzumab as neoadjuvant treatment in HER2/-positive breast cancer patients.
PACIFIC trial
In the PACIFIC trial, 713 patients with unresectable, stage III non–small cell lung cancer (NSCLC) who received concurrent chemoradiation were randomized to receive adjuvant durvalumab or an identical placebo, for a year after radiation ended. The results were dramatic in favor of durvalumab (N Engl J Med. 2018;379:2342-50).
Durvalumab showed 24-month overall survival of 66.3% versus 55.6% with placebo (hazard ratio, 0.68, P = .0025) and progression-free survival of 17.2 months versus 5. 6 months (HR, 0.51). As expected, there were more grade 3-4 toxicities and treatment discontinuations with durvalumab than with placebo, but the toxicity seemed modest, given the substantial improvements in tumor-related outcomes.
At the recent European Lung Cancer Congress, Marina Garassino, MD, reported on Patient-Reported Outcomes (PRO) in PACIFIC. PROs were analyzed by PD-L1 level. A total of 63% of patients had PD-L1 tumor expression data for analysis. Overall, there were no major differences in PROs by PD-L1. Global quality of life did not differ by PD-L1 expression cohort.
These data support adjuvant durvalumab for stage III, chemoradiation-treated NSCLC patients, not only from efficacy and toxicity viewpoints, but also from the standpoint of the patient experience, independent of PD-L1 tumor expression.
What this means in practice
From every relevant perspective, regardless of histology and molecular features associated with their particular tumor, it is worthwhile for us to recommend – and for our patients to receive – durvalumab adjuvant therapy for up to 1 year after radiation ends, with close follow-up and adherence to the criteria for treatment modification or discontinuation as performed in the PACIFIC trial. These new data remove any lingering concerns about the value of this life-prolonging treatment.
Subcutaneous vs. IV trastuzumab
In this international phase 3 trial in early breast cancer patients, neoadjuvant chemotherapy was paired with either standard IV trastuzumab or subcutaneous trastuzumab at intervals of every 3 weeks. After the cytotoxic chemotherapy concluded, patients completed a 12-month course of trastuzumab with either the IV or subcutaneous administration, as previously randomized. The 6-year event-free survival and overall survival were 65% and 84%, respectively, for both the IV and subcutaneous treatment administration.
The authors concluded that these results are relevant to patients with low-risk HER2-positive breast cancer patients, for whom T-DM1 is not needed (JAMA Oncol. 2019 Apr 18. doi: 10.1001/jamaoncol.2019.0339).
What this means in practice
These long-term data from the HannaH trial show persuasively that patients should be offered the more convenient, hopefully cheaper, subcutaneous route of administration. Since relapses beyond year 6 are unlikely, these data are unlikely to change with further follow-up. At our hospital, we recently made the decision to add subcutaneous trastuzumab to our formulary.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers, and in expanding access to clinical trials to medically underserved populations.
A telemedicine compromise
It’s late on a Thursday afternoon. Even through the six walls that separate you from the waiting room you can feel the impatient throng of families as you struggle to see the tympanic membrane of a feverish and uncooperative 3-year-old. You already have scraped his auditory canal once with your curette. Your gut tells you that he must have an otitis but deeper in your soul there are other voices reminding you that to make the diagnosis you must visualize his ear drum. Your skill and the technology on hand has failed you.
It’s a Sunday morning, weekend hours, and you are seeing a 12-year-old with a sore throat and fever. Her physical exam suggests that she has strep pharyngitis but the team member in charge of restocking supplies has forgotten to reorder rapid strep kits and you used the last one yesterday afternoon.
Do you ignore your training and treat these sick children with antibiotics?
If you are someone who perceives the world in black and white, your response to these scenarios is simple because you NEVER prescribe antibiotics without seeing a tympanic membrane or confirming your suspicion with a rapid strep test. There are unrealistic solutions that could include requesting an immediate ear/nose/throat consult or sending the patient on an hour-long odyssey to the hospital lab. But for the rest of us who see in shades of gray, we may have to compromise our principles and temporarily become poor antibiotic stewards. The question is, how often do you compromise? Once a week, once a month, twice a year, or twice a day?
A study published in Pediatrics looks at the issue of antibiotic stewardship as it relates to telemedicine (“Antibiotic Prescribing During Pediatrics Direct-to-Consumer Telemedicine Visits,” Pediatrics. 2019 May. doi: 10.1542/peds.2018-2491).
The investigators found that children with acute respiratory infections were more likely to receive antibiotics and less likely to receive guideline concordant management at direct-to-consumer (DTC) telemedicine visits than when they were seen by their primary care physician or at an urgent care center.
In their discussion, the researchers note several possible explanations for the discrepancies they observed. DTC telemedicine visits are limited by the devices used by the families and physicians and generally lack availability of otoscopy and strep testing. The authors also wonder whether “there may be differential expectations for antibiotics among children and parents who use DTC telemedicine versus in person care.” Does this mean that families who utilize DTC telemedicine undervalue in-person care and/or are willing to compromise by accepting what they may suspect is substandard care for the convenience of DTC telemedicine?
Which brings me to my point. A physician who accepts the challenge of seeing pediatric patients with acute respiratory illnesses knowing that he or she will not be able to visualize tympanic membranes or perform strep testing also has accepted the fact that he or she will be compromising the principles of antibiotic stewardship he or she must have – or maybe should have – learned in medical school or residency.
We all occasionally compromise our principles when technology fails us or when the situations are extraordinary. But I am troubled that there some physicians who are willing to practice in an environment in which they are aware that they will be compromising their antibiotic stewardship on a daily or even hourly basis.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
It’s late on a Thursday afternoon. Even through the six walls that separate you from the waiting room you can feel the impatient throng of families as you struggle to see the tympanic membrane of a feverish and uncooperative 3-year-old. You already have scraped his auditory canal once with your curette. Your gut tells you that he must have an otitis but deeper in your soul there are other voices reminding you that to make the diagnosis you must visualize his ear drum. Your skill and the technology on hand has failed you.
It’s a Sunday morning, weekend hours, and you are seeing a 12-year-old with a sore throat and fever. Her physical exam suggests that she has strep pharyngitis but the team member in charge of restocking supplies has forgotten to reorder rapid strep kits and you used the last one yesterday afternoon.
Do you ignore your training and treat these sick children with antibiotics?
If you are someone who perceives the world in black and white, your response to these scenarios is simple because you NEVER prescribe antibiotics without seeing a tympanic membrane or confirming your suspicion with a rapid strep test. There are unrealistic solutions that could include requesting an immediate ear/nose/throat consult or sending the patient on an hour-long odyssey to the hospital lab. But for the rest of us who see in shades of gray, we may have to compromise our principles and temporarily become poor antibiotic stewards. The question is, how often do you compromise? Once a week, once a month, twice a year, or twice a day?
A study published in Pediatrics looks at the issue of antibiotic stewardship as it relates to telemedicine (“Antibiotic Prescribing During Pediatrics Direct-to-Consumer Telemedicine Visits,” Pediatrics. 2019 May. doi: 10.1542/peds.2018-2491).
The investigators found that children with acute respiratory infections were more likely to receive antibiotics and less likely to receive guideline concordant management at direct-to-consumer (DTC) telemedicine visits than when they were seen by their primary care physician or at an urgent care center.
In their discussion, the researchers note several possible explanations for the discrepancies they observed. DTC telemedicine visits are limited by the devices used by the families and physicians and generally lack availability of otoscopy and strep testing. The authors also wonder whether “there may be differential expectations for antibiotics among children and parents who use DTC telemedicine versus in person care.” Does this mean that families who utilize DTC telemedicine undervalue in-person care and/or are willing to compromise by accepting what they may suspect is substandard care for the convenience of DTC telemedicine?
Which brings me to my point. A physician who accepts the challenge of seeing pediatric patients with acute respiratory illnesses knowing that he or she will not be able to visualize tympanic membranes or perform strep testing also has accepted the fact that he or she will be compromising the principles of antibiotic stewardship he or she must have – or maybe should have – learned in medical school or residency.
We all occasionally compromise our principles when technology fails us or when the situations are extraordinary. But I am troubled that there some physicians who are willing to practice in an environment in which they are aware that they will be compromising their antibiotic stewardship on a daily or even hourly basis.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
It’s late on a Thursday afternoon. Even through the six walls that separate you from the waiting room you can feel the impatient throng of families as you struggle to see the tympanic membrane of a feverish and uncooperative 3-year-old. You already have scraped his auditory canal once with your curette. Your gut tells you that he must have an otitis but deeper in your soul there are other voices reminding you that to make the diagnosis you must visualize his ear drum. Your skill and the technology on hand has failed you.
It’s a Sunday morning, weekend hours, and you are seeing a 12-year-old with a sore throat and fever. Her physical exam suggests that she has strep pharyngitis but the team member in charge of restocking supplies has forgotten to reorder rapid strep kits and you used the last one yesterday afternoon.
Do you ignore your training and treat these sick children with antibiotics?
If you are someone who perceives the world in black and white, your response to these scenarios is simple because you NEVER prescribe antibiotics without seeing a tympanic membrane or confirming your suspicion with a rapid strep test. There are unrealistic solutions that could include requesting an immediate ear/nose/throat consult or sending the patient on an hour-long odyssey to the hospital lab. But for the rest of us who see in shades of gray, we may have to compromise our principles and temporarily become poor antibiotic stewards. The question is, how often do you compromise? Once a week, once a month, twice a year, or twice a day?
A study published in Pediatrics looks at the issue of antibiotic stewardship as it relates to telemedicine (“Antibiotic Prescribing During Pediatrics Direct-to-Consumer Telemedicine Visits,” Pediatrics. 2019 May. doi: 10.1542/peds.2018-2491).
The investigators found that children with acute respiratory infections were more likely to receive antibiotics and less likely to receive guideline concordant management at direct-to-consumer (DTC) telemedicine visits than when they were seen by their primary care physician or at an urgent care center.
In their discussion, the researchers note several possible explanations for the discrepancies they observed. DTC telemedicine visits are limited by the devices used by the families and physicians and generally lack availability of otoscopy and strep testing. The authors also wonder whether “there may be differential expectations for antibiotics among children and parents who use DTC telemedicine versus in person care.” Does this mean that families who utilize DTC telemedicine undervalue in-person care and/or are willing to compromise by accepting what they may suspect is substandard care for the convenience of DTC telemedicine?
Which brings me to my point. A physician who accepts the challenge of seeing pediatric patients with acute respiratory illnesses knowing that he or she will not be able to visualize tympanic membranes or perform strep testing also has accepted the fact that he or she will be compromising the principles of antibiotic stewardship he or she must have – or maybe should have – learned in medical school or residency.
We all occasionally compromise our principles when technology fails us or when the situations are extraordinary. But I am troubled that there some physicians who are willing to practice in an environment in which they are aware that they will be compromising their antibiotic stewardship on a daily or even hourly basis.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Blast crisis, no crisis? Caring for the apathetic patient
The diagnosis was straightforward. My patient’s reaction was not.
One Saturday evening, I receive a call from the emergency room about a man with a very high white blood cell count. For the past 7 years, he had chronic myeloid leukemia – a cancer, but one of the few that can be well controlled for years. The discovery of the medications that can do it revolutionized care for the disease.
For the last 7 years, Mr. C didn’t take that medication regularly. He was young, with no other medical problems, and this was the only medication he was supposed to take. But his use was sporadic at best.
What was it, I wondered? Cost? Side effects? Not understanding the seriousness of having leukemia? No, the medication was fully covered by his insurance. No, he tolerated it well. Instead, his on-and-off medication schedule came across as a strange sense of apathy. He didn’t seem to recognize his agency in his own life.
Now, not only is his white count extremely high, but the majority are the cancerous cells. I look at his blood under the microscope – blasts everywhere. He has progressed from a chronic, indolent disease that can be kept at bay into the dreaded blast crisis, which is essentially an acute leukemia but even more challenging to treat.
It is very serious. I tell him this. “I am worried your leukemia has progressed into what we call a blast crisis,” I say. “Has anyone ever talked to you about this before?”
“Hmm, I think Dr. M may have said something,” he says. His medical chart over the last 7 years was populated with notes from his hematologist documenting their discussions of this possibility.
“This is serious,” I continue. “You will need to come into the hospital and we need to start medication to lower your white count. Otherwise you could have a stroke.”
“Okay.”
“As the white count comes down, your cells will break open and the chemicals in them can make you very sick. So we will have to check your blood often to watch for this.”
“Got it.”
“And we will change your chemotherapy pill.” I pause, letting it sink in, then repeat for emphasis: “This is very serious.”
“Sure thing, Doc.”
“I know I’ve said a lot. What are your thoughts?”
He looks at his wife, then back at me. He seems unfazed. Just as unfazed as when his hematologist warned this could happen. Just as unfazed as the day he learned his diagnosis.
He smiles and shrugs. “What will be, will be.”
As I listened to him, I honestly couldn’t tell if this was the best coping mechanism I had ever seen or the worst.
On one hand, his apathy had hurt him, clearly and indisputably. Refusing to acknowledge his agency in his medical outcomes allowed him to be cavalier about taking the cure. The cure was in a bottle on his kitchen shelf, an arm’s reach away, and he chose to reach elsewhere.
On the other hand, it was unusual to see someone so at peace with being so critically ill. His acceptance of his new reality was refreshing. There were no heartbreaking questions about whether this was his fault. There was no agonizing over what could have been. His apathy gave him closure and his loved ones comfort.
I’ve written before about how a cancer diagnosis involves holding two seemingly competing ideas in one’s mind at once. Last month, I wrote about how it is possible to be realistic about a grim prognosis while retaining hope that a treatment may work. I discussed that realism and hopefulness are compatible beliefs, and it’s okay – preferred, even – to hold them at once.
Mr. C’s strange sense of apathy made me think about another mental limbo, this one involving control. As doctors and patients, we like when we have agency over outcomes. Take these medications, and you will be okay. Undergo this procedure, and you will reduce your risk of recurrence. At the same time, poor outcomes still occur when everything is done “right.” When that happens, it can be psychologically beneficial to relinquish control. Doing so discards the unhelpful emotions of guilt and blame in favor of acceptance.
Mr. C’s apathy seemed to be present from day 1. But now, in a dire blast crisis, what was once a harmful attitude actually became a helpful one.
His “what will be, will be” attitude wasn’t inherently maladaptive; it was ill timed. Under the right circumstances, well-placed apathy can be leveraged as a positive coping mechanism.
But alas, if only there were a switch to turn on the right emotion at the right time. There’s no right or wrong or sensible reaction to cancer. There’s only a swirl of messy, overwhelming feelings. It’s trying to bring effective emotions to light at the right time while playing whack-a-mole with the others. It’s cognitive dissonance. It’s exhausting. Cancer doesn’t create personalities; it surfaces them.
It’s the last day of Mr. C’s hospitalization. His blast crisis is amazingly under good control.
“So,” I say. “Will you take your medications now?”
“Sure,” he says instinctively. I look at him. “I mean, honestly, Doc? I’m not sure.”
As we shake hands, I wonder if I’ll ever truly understand Mr. C’s motivations. But I can’t wonder too long. I can only control my part: I hand him his medications and wish him luck.
Minor details of this story were changed to protect privacy.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz.
The diagnosis was straightforward. My patient’s reaction was not.
One Saturday evening, I receive a call from the emergency room about a man with a very high white blood cell count. For the past 7 years, he had chronic myeloid leukemia – a cancer, but one of the few that can be well controlled for years. The discovery of the medications that can do it revolutionized care for the disease.
For the last 7 years, Mr. C didn’t take that medication regularly. He was young, with no other medical problems, and this was the only medication he was supposed to take. But his use was sporadic at best.
What was it, I wondered? Cost? Side effects? Not understanding the seriousness of having leukemia? No, the medication was fully covered by his insurance. No, he tolerated it well. Instead, his on-and-off medication schedule came across as a strange sense of apathy. He didn’t seem to recognize his agency in his own life.
Now, not only is his white count extremely high, but the majority are the cancerous cells. I look at his blood under the microscope – blasts everywhere. He has progressed from a chronic, indolent disease that can be kept at bay into the dreaded blast crisis, which is essentially an acute leukemia but even more challenging to treat.
It is very serious. I tell him this. “I am worried your leukemia has progressed into what we call a blast crisis,” I say. “Has anyone ever talked to you about this before?”
“Hmm, I think Dr. M may have said something,” he says. His medical chart over the last 7 years was populated with notes from his hematologist documenting their discussions of this possibility.
“This is serious,” I continue. “You will need to come into the hospital and we need to start medication to lower your white count. Otherwise you could have a stroke.”
“Okay.”
“As the white count comes down, your cells will break open and the chemicals in them can make you very sick. So we will have to check your blood often to watch for this.”
“Got it.”
“And we will change your chemotherapy pill.” I pause, letting it sink in, then repeat for emphasis: “This is very serious.”
“Sure thing, Doc.”
“I know I’ve said a lot. What are your thoughts?”
He looks at his wife, then back at me. He seems unfazed. Just as unfazed as when his hematologist warned this could happen. Just as unfazed as the day he learned his diagnosis.
He smiles and shrugs. “What will be, will be.”
As I listened to him, I honestly couldn’t tell if this was the best coping mechanism I had ever seen or the worst.
On one hand, his apathy had hurt him, clearly and indisputably. Refusing to acknowledge his agency in his medical outcomes allowed him to be cavalier about taking the cure. The cure was in a bottle on his kitchen shelf, an arm’s reach away, and he chose to reach elsewhere.
On the other hand, it was unusual to see someone so at peace with being so critically ill. His acceptance of his new reality was refreshing. There were no heartbreaking questions about whether this was his fault. There was no agonizing over what could have been. His apathy gave him closure and his loved ones comfort.
I’ve written before about how a cancer diagnosis involves holding two seemingly competing ideas in one’s mind at once. Last month, I wrote about how it is possible to be realistic about a grim prognosis while retaining hope that a treatment may work. I discussed that realism and hopefulness are compatible beliefs, and it’s okay – preferred, even – to hold them at once.
Mr. C’s strange sense of apathy made me think about another mental limbo, this one involving control. As doctors and patients, we like when we have agency over outcomes. Take these medications, and you will be okay. Undergo this procedure, and you will reduce your risk of recurrence. At the same time, poor outcomes still occur when everything is done “right.” When that happens, it can be psychologically beneficial to relinquish control. Doing so discards the unhelpful emotions of guilt and blame in favor of acceptance.
Mr. C’s apathy seemed to be present from day 1. But now, in a dire blast crisis, what was once a harmful attitude actually became a helpful one.
His “what will be, will be” attitude wasn’t inherently maladaptive; it was ill timed. Under the right circumstances, well-placed apathy can be leveraged as a positive coping mechanism.
But alas, if only there were a switch to turn on the right emotion at the right time. There’s no right or wrong or sensible reaction to cancer. There’s only a swirl of messy, overwhelming feelings. It’s trying to bring effective emotions to light at the right time while playing whack-a-mole with the others. It’s cognitive dissonance. It’s exhausting. Cancer doesn’t create personalities; it surfaces them.
It’s the last day of Mr. C’s hospitalization. His blast crisis is amazingly under good control.
“So,” I say. “Will you take your medications now?”
“Sure,” he says instinctively. I look at him. “I mean, honestly, Doc? I’m not sure.”
As we shake hands, I wonder if I’ll ever truly understand Mr. C’s motivations. But I can’t wonder too long. I can only control my part: I hand him his medications and wish him luck.
Minor details of this story were changed to protect privacy.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz.
The diagnosis was straightforward. My patient’s reaction was not.
One Saturday evening, I receive a call from the emergency room about a man with a very high white blood cell count. For the past 7 years, he had chronic myeloid leukemia – a cancer, but one of the few that can be well controlled for years. The discovery of the medications that can do it revolutionized care for the disease.
For the last 7 years, Mr. C didn’t take that medication regularly. He was young, with no other medical problems, and this was the only medication he was supposed to take. But his use was sporadic at best.
What was it, I wondered? Cost? Side effects? Not understanding the seriousness of having leukemia? No, the medication was fully covered by his insurance. No, he tolerated it well. Instead, his on-and-off medication schedule came across as a strange sense of apathy. He didn’t seem to recognize his agency in his own life.
Now, not only is his white count extremely high, but the majority are the cancerous cells. I look at his blood under the microscope – blasts everywhere. He has progressed from a chronic, indolent disease that can be kept at bay into the dreaded blast crisis, which is essentially an acute leukemia but even more challenging to treat.
It is very serious. I tell him this. “I am worried your leukemia has progressed into what we call a blast crisis,” I say. “Has anyone ever talked to you about this before?”
“Hmm, I think Dr. M may have said something,” he says. His medical chart over the last 7 years was populated with notes from his hematologist documenting their discussions of this possibility.
“This is serious,” I continue. “You will need to come into the hospital and we need to start medication to lower your white count. Otherwise you could have a stroke.”
“Okay.”
“As the white count comes down, your cells will break open and the chemicals in them can make you very sick. So we will have to check your blood often to watch for this.”
“Got it.”
“And we will change your chemotherapy pill.” I pause, letting it sink in, then repeat for emphasis: “This is very serious.”
“Sure thing, Doc.”
“I know I’ve said a lot. What are your thoughts?”
He looks at his wife, then back at me. He seems unfazed. Just as unfazed as when his hematologist warned this could happen. Just as unfazed as the day he learned his diagnosis.
He smiles and shrugs. “What will be, will be.”
As I listened to him, I honestly couldn’t tell if this was the best coping mechanism I had ever seen or the worst.
On one hand, his apathy had hurt him, clearly and indisputably. Refusing to acknowledge his agency in his medical outcomes allowed him to be cavalier about taking the cure. The cure was in a bottle on his kitchen shelf, an arm’s reach away, and he chose to reach elsewhere.
On the other hand, it was unusual to see someone so at peace with being so critically ill. His acceptance of his new reality was refreshing. There were no heartbreaking questions about whether this was his fault. There was no agonizing over what could have been. His apathy gave him closure and his loved ones comfort.
I’ve written before about how a cancer diagnosis involves holding two seemingly competing ideas in one’s mind at once. Last month, I wrote about how it is possible to be realistic about a grim prognosis while retaining hope that a treatment may work. I discussed that realism and hopefulness are compatible beliefs, and it’s okay – preferred, even – to hold them at once.
Mr. C’s strange sense of apathy made me think about another mental limbo, this one involving control. As doctors and patients, we like when we have agency over outcomes. Take these medications, and you will be okay. Undergo this procedure, and you will reduce your risk of recurrence. At the same time, poor outcomes still occur when everything is done “right.” When that happens, it can be psychologically beneficial to relinquish control. Doing so discards the unhelpful emotions of guilt and blame in favor of acceptance.
Mr. C’s apathy seemed to be present from day 1. But now, in a dire blast crisis, what was once a harmful attitude actually became a helpful one.
His “what will be, will be” attitude wasn’t inherently maladaptive; it was ill timed. Under the right circumstances, well-placed apathy can be leveraged as a positive coping mechanism.
But alas, if only there were a switch to turn on the right emotion at the right time. There’s no right or wrong or sensible reaction to cancer. There’s only a swirl of messy, overwhelming feelings. It’s trying to bring effective emotions to light at the right time while playing whack-a-mole with the others. It’s cognitive dissonance. It’s exhausting. Cancer doesn’t create personalities; it surfaces them.
It’s the last day of Mr. C’s hospitalization. His blast crisis is amazingly under good control.
“So,” I say. “Will you take your medications now?”
“Sure,” he says instinctively. I look at him. “I mean, honestly, Doc? I’m not sure.”
As we shake hands, I wonder if I’ll ever truly understand Mr. C’s motivations. But I can’t wonder too long. I can only control my part: I hand him his medications and wish him luck.
Minor details of this story were changed to protect privacy.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz.
Rat race
My son and I used to play a game called CASHFLOW. It was invented by Robert Kiyosaki, the real estate magnate who originated the “Rich Dad Poor Dad” book series to educate the masses on the basics of real estate investing.
The object of the game was to acquire enough passive income to become independent of active income like salary. The hope was that by playing the game, participants would recognize the advantages of passive income and become entrepreneurs in real estate or business. The winner was no longer an employee, but happily self-employed and out of the rat race.
Alas, the lesson was lost on me and my son. Both of us are still very much in the rat race and dependent on salary.
But a rat race can be more than just a competitive quest for financial gain. In politics, the quest is more for power. In sports, the quest includes championships. In academic medicine – and hematology is usually practiced in an academic setting – the quest is often for power and prestige. Training for our hematologic quest began in high school.
In high school, superior grades were a given, but we also worked to excel in sports, extracurricular activities, and standardized tests in order to get into the best universities. The cycle was then repeated to allow entry into the best medical schools. The old adage that students who finished last in their medical school class are still addressed as “Doctor” notwithstanding, most of us pushed ourselves beyond good grades to volunteer work, research activities, and prestigious clerkships to ensure that we matched at the best residency programs. There, those inclined to hematology cozied up to influential faculty by helping with their research in order to obtain the cherished letter of recommendation that promised admission to the best fellowship program, where the cycle was again repeated in the hope of landing a position in the best academic medical center.
Through these pursuits, young recruits to medical academia are primed and ready to enter a rat race of individual accomplishment. The academic rat race is a particularly pernicious result of our training to be the best, and the “best” hematologists are found at the podium, not in the exam room.
Not content to be recognized for clinical excellence by their patients, academic hematologists often aspire more to be recognized for content expertise by their peers. Through the noble pursuit of advancing science, peer recognition bestows prestige and power in the form of promotions, grants, advisory boards, consultancies, and speaking opportunities all over the globe. For some, the academic rat race validates a life dedicated to being the best.
However, the demands of patient care can interfere with academic pursuits and stand as impediments to the march of science, with its attendant rewards in power and prestige. The most common complaint I get from my team is the inability to fully participate in all that is required to succeed academically because of clinical responsibilities. The difficulty is worsened when financial realities require even more time spent in the clinic to generate income. This makes it hard enough to keep a healthy balance between research and patient care. When the pressures of clinical and academic hematology are combined with the responsibility of family, the rat race can begin to lead to burnout.
A rat race forces us to compare ourselves to others, and we often find ourselves wanting. There is always someone who seems wealthier and wiser than we are. Our training often compels us to compete with whoever it is we are comparing ourselves to. That competition simultaneously drives us toward a laudable goal and away from a balanced, happy life.
Theodore Roosevelt said “Comparison is the thief of joy,” and that certainly seems to be the case among medical professionals. As physicians, we do not lack for wealth, unless we compare ourselves to those who have more. We do not lack for wisdom, unless we compare ourselves to those who have more. We’d see that we really lack very little and occupy a privileged place in society if we only took the time to be grateful for having had the talent and support to do so.
I enjoyed playing CASHFLOW when I was younger and naively thought that either my son or I might materially benefit from its lessons. I realize now that the real enjoyment of playing was not to win or to get rich, but rather to spend time with my son. Likewise, our training got us where we are, and it will sustain a happy fulfilling career, but it will also consume us if we let go of why we started playing the game in the first place.
Dr. Kalaycio is editor in chief of Hematology News. He chairs the department of hematology and medical oncology at Cleveland Clinic Taussig Cancer Institute. Contact him at [email protected].
My son and I used to play a game called CASHFLOW. It was invented by Robert Kiyosaki, the real estate magnate who originated the “Rich Dad Poor Dad” book series to educate the masses on the basics of real estate investing.
The object of the game was to acquire enough passive income to become independent of active income like salary. The hope was that by playing the game, participants would recognize the advantages of passive income and become entrepreneurs in real estate or business. The winner was no longer an employee, but happily self-employed and out of the rat race.
Alas, the lesson was lost on me and my son. Both of us are still very much in the rat race and dependent on salary.
But a rat race can be more than just a competitive quest for financial gain. In politics, the quest is more for power. In sports, the quest includes championships. In academic medicine – and hematology is usually practiced in an academic setting – the quest is often for power and prestige. Training for our hematologic quest began in high school.
In high school, superior grades were a given, but we also worked to excel in sports, extracurricular activities, and standardized tests in order to get into the best universities. The cycle was then repeated to allow entry into the best medical schools. The old adage that students who finished last in their medical school class are still addressed as “Doctor” notwithstanding, most of us pushed ourselves beyond good grades to volunteer work, research activities, and prestigious clerkships to ensure that we matched at the best residency programs. There, those inclined to hematology cozied up to influential faculty by helping with their research in order to obtain the cherished letter of recommendation that promised admission to the best fellowship program, where the cycle was again repeated in the hope of landing a position in the best academic medical center.
Through these pursuits, young recruits to medical academia are primed and ready to enter a rat race of individual accomplishment. The academic rat race is a particularly pernicious result of our training to be the best, and the “best” hematologists are found at the podium, not in the exam room.
Not content to be recognized for clinical excellence by their patients, academic hematologists often aspire more to be recognized for content expertise by their peers. Through the noble pursuit of advancing science, peer recognition bestows prestige and power in the form of promotions, grants, advisory boards, consultancies, and speaking opportunities all over the globe. For some, the academic rat race validates a life dedicated to being the best.
However, the demands of patient care can interfere with academic pursuits and stand as impediments to the march of science, with its attendant rewards in power and prestige. The most common complaint I get from my team is the inability to fully participate in all that is required to succeed academically because of clinical responsibilities. The difficulty is worsened when financial realities require even more time spent in the clinic to generate income. This makes it hard enough to keep a healthy balance between research and patient care. When the pressures of clinical and academic hematology are combined with the responsibility of family, the rat race can begin to lead to burnout.
A rat race forces us to compare ourselves to others, and we often find ourselves wanting. There is always someone who seems wealthier and wiser than we are. Our training often compels us to compete with whoever it is we are comparing ourselves to. That competition simultaneously drives us toward a laudable goal and away from a balanced, happy life.
Theodore Roosevelt said “Comparison is the thief of joy,” and that certainly seems to be the case among medical professionals. As physicians, we do not lack for wealth, unless we compare ourselves to those who have more. We do not lack for wisdom, unless we compare ourselves to those who have more. We’d see that we really lack very little and occupy a privileged place in society if we only took the time to be grateful for having had the talent and support to do so.
I enjoyed playing CASHFLOW when I was younger and naively thought that either my son or I might materially benefit from its lessons. I realize now that the real enjoyment of playing was not to win or to get rich, but rather to spend time with my son. Likewise, our training got us where we are, and it will sustain a happy fulfilling career, but it will also consume us if we let go of why we started playing the game in the first place.
Dr. Kalaycio is editor in chief of Hematology News. He chairs the department of hematology and medical oncology at Cleveland Clinic Taussig Cancer Institute. Contact him at [email protected].
My son and I used to play a game called CASHFLOW. It was invented by Robert Kiyosaki, the real estate magnate who originated the “Rich Dad Poor Dad” book series to educate the masses on the basics of real estate investing.
The object of the game was to acquire enough passive income to become independent of active income like salary. The hope was that by playing the game, participants would recognize the advantages of passive income and become entrepreneurs in real estate or business. The winner was no longer an employee, but happily self-employed and out of the rat race.
Alas, the lesson was lost on me and my son. Both of us are still very much in the rat race and dependent on salary.
But a rat race can be more than just a competitive quest for financial gain. In politics, the quest is more for power. In sports, the quest includes championships. In academic medicine – and hematology is usually practiced in an academic setting – the quest is often for power and prestige. Training for our hematologic quest began in high school.
In high school, superior grades were a given, but we also worked to excel in sports, extracurricular activities, and standardized tests in order to get into the best universities. The cycle was then repeated to allow entry into the best medical schools. The old adage that students who finished last in their medical school class are still addressed as “Doctor” notwithstanding, most of us pushed ourselves beyond good grades to volunteer work, research activities, and prestigious clerkships to ensure that we matched at the best residency programs. There, those inclined to hematology cozied up to influential faculty by helping with their research in order to obtain the cherished letter of recommendation that promised admission to the best fellowship program, where the cycle was again repeated in the hope of landing a position in the best academic medical center.
Through these pursuits, young recruits to medical academia are primed and ready to enter a rat race of individual accomplishment. The academic rat race is a particularly pernicious result of our training to be the best, and the “best” hematologists are found at the podium, not in the exam room.
Not content to be recognized for clinical excellence by their patients, academic hematologists often aspire more to be recognized for content expertise by their peers. Through the noble pursuit of advancing science, peer recognition bestows prestige and power in the form of promotions, grants, advisory boards, consultancies, and speaking opportunities all over the globe. For some, the academic rat race validates a life dedicated to being the best.
However, the demands of patient care can interfere with academic pursuits and stand as impediments to the march of science, with its attendant rewards in power and prestige. The most common complaint I get from my team is the inability to fully participate in all that is required to succeed academically because of clinical responsibilities. The difficulty is worsened when financial realities require even more time spent in the clinic to generate income. This makes it hard enough to keep a healthy balance between research and patient care. When the pressures of clinical and academic hematology are combined with the responsibility of family, the rat race can begin to lead to burnout.
A rat race forces us to compare ourselves to others, and we often find ourselves wanting. There is always someone who seems wealthier and wiser than we are. Our training often compels us to compete with whoever it is we are comparing ourselves to. That competition simultaneously drives us toward a laudable goal and away from a balanced, happy life.
Theodore Roosevelt said “Comparison is the thief of joy,” and that certainly seems to be the case among medical professionals. As physicians, we do not lack for wealth, unless we compare ourselves to those who have more. We do not lack for wisdom, unless we compare ourselves to those who have more. We’d see that we really lack very little and occupy a privileged place in society if we only took the time to be grateful for having had the talent and support to do so.
I enjoyed playing CASHFLOW when I was younger and naively thought that either my son or I might materially benefit from its lessons. I realize now that the real enjoyment of playing was not to win or to get rich, but rather to spend time with my son. Likewise, our training got us where we are, and it will sustain a happy fulfilling career, but it will also consume us if we let go of why we started playing the game in the first place.
Dr. Kalaycio is editor in chief of Hematology News. He chairs the department of hematology and medical oncology at Cleveland Clinic Taussig Cancer Institute. Contact him at [email protected].
Your patient’s brain is different at every visit
Unlike other organs in the human body, the brain is constantly changing. The main driver for this ongoing re-engineering across various neural circuits is “experiential neuroplasticity,” which creates billions of new synapses and dendrite spines as well as new connections. And as the brain reinvents itself from day to day, the mind evolves as well.
The neurobiologic re-sculpting of the brain’s complex innards continuously encodes memories of what we learn and experience during waking hours, including all that we see, hear, feel, think, contemplate, plan, and decide. However, in addition to the ongoing intrinsic neuroplasticity that records life’s experiences within neural circuits, there are many extrinsic factors that can further modify the brain and the “psyche” it generates via electrical, neurochemical, and physiological mechanisms. That’s why every patient a psychiatrist sees at follow-up visits will have a brain that will be different from the previous encounter.
Consider the following factors that can modify a patient’s brain (for better or worse) between sessions:
- Psychotherapy that the patient received at the last session will biologically modify his or her brain. Creating new insights and understanding of one’s behavior and “connecting the dots” of the past and present emotions and reactions are all associated with neuroplastic changes within the brain.
- Mood or psychotic episodes. Depressive, manic, or psychotic episodes are associated with neuroinflammation, oxidative stress, and apoptotic effects, which can disrupt the brain’s cytoarchitecture. That’s why psychiatrists must inquire about such episodes between visits and document the possible effects on the patient’s mental status.
- Psychotropic medications all bind to one or more brain receptors to exert therapeutic or adverse effects, both of which are associated with changes in neurotransmitter pathways. A key component of every follow-up visit is to gauge the risks and benefits of the pharmacotherapy prescribed at the prior visit.
- Nonpsychiatric prescription medications are often associated with iatrogenic effects on the brain apart from their intended target organs. These iatrogenic effects include anxiety, depression, mania, psychosis, and cognitive changes. That’s why during each visit, the physician or nurse practitioner must review all prescription medications and consider their potential effects on the patient’s mental status.
- Over-the-counter drugs and supplements may exert neurologic effects via histaminergic, muscarinic, glutamatergic, adrenergic, or serotonergic effects—all of which can alter brain chemistry and contribute to mental status changes. They can also inhibit or induce cytochrome enzymes and induce adverse effects or loss of efficacy of the primary psychotropic medication the patient takes.
- Medical illness, even as simple as an upper respiratory viral infection, can alter brain function due to illness-induced physiological aberrations, including pain and peripheral inflammation, with neurologic consequences. Common metabolic disorders such as diabetes, hyperlipidemia, and hypertension can exert mental status changes.
- Alcohol and drugs of abuse alter brain structure and function and can induce psychological and cognitive changes. Inquiring about the amount and frequency of alcohol and recreational drug use must be done in detail at every visit.
- Stressful events. It is almost impossible for a psychiatric patient not to encounter stressful life events between visits. Coping with any mental disorder can be quite stressful and challenging due to its social, vocational, or personal consequences. Stress increases cortisol, which is associated with deleterious inflammatory effects on the brain. Persistent stress can lead to hippocampal atrophy because of the abundance of glucocorticoid receptors in the hippocampus. Inquiry about stressors must be part of every psychiatric follow-up visit. Multiple psychological, physiological, and behavioral effects are well known to be generated by stress, especially in individuals already impaired by mental illness.
- Diet. What a patient eats (or avoids eating) can affect the brain. High-fat diets can be inflammatory, while a diet rich in fruits, vegetables, and nuts can be neuroprotective. The microbiota and the enteric brain—both in the gastrointestinal tract—have been reported to influence mood and behavior. (For more on this, see “Gut microbiota and its implications for psychiatry: A review of 3 studies” on page 40 and “It takes guts to be mentally ill: Microbiota and psychopathology,” From the Editor,
Current Psychiatry , September 2018, p. 4-6.) - Obesity is associated with brain atrophy as well as depression. Weight should be assessed at every visit and coupled with counseling about diet and exercise.
- Exercise, or the lack of it, can alter the brain in good or bad ways. Many studies have shown that regular exercise can induce hippocampal neurogenesis and sharpen memory and cognition. On the other hand, a sedentary lifestyle can be detrimental to the heart, bones, and brain, with an elevation in cerebrovascular and cardiovascular risks, both of which can progressively alter brain structure and function.
- Concussion, contusions, and traumatic brain injury obviously can activate the microglia and trigger neurologic sequelae and mental repercussions. At every visit, patients should be asked if they have experienced a mild or severe head injury, whether it is accidental or sports-related.
- Dehydration, especially on the day of the visit, can alter mental status in subtle ways. Cerebral ventricular volume has been shown to change with dehydration. Asking a patient about daily fluid intake should be a standard question, especially for older patients, who may experience hypotension and mental status changes due to hypovolemia.
- Sleep, whether too much or too little, is associated with brain effects and can impact cognition and behavior. Asking patients about sleep is important because it can affect the brain, and also can be a symptom of unresolved psychiatric disorders. Chronic sleep disorders are associated with neuroinflammation.
- Menstrual cycle. Various neurotransmitters fluctuate during a woman’s menstrual cycle. Her cognition becomes sharper around ovulation, and that may influence her mental status and perhaps the neuroplasticity of her brain.
- Pregnancy and its major hormone changes can change brain structure and function. Estrogen, progesterone, and prolactin have different structural effects on the brain that can help the future mother care for her dependent baby. Asking about missed periods and pregnancy during childbearing years can be useful during psychiatric encounters.
Continue to: In summary...
In summary, numerous variables can affect the patient’s brain between visits, influencing his or her mental status. The ever-changing brain can be challenging to assess, especially in brief 15- to 20-minute follow-up sessions that have become more common in psychiatry. Perhaps patients should help their psychiatrists or nurse practitioners by completing a checklist with all the above variables, either online on the day of their appointment or on a form in the waiting room immediately prior to the visit. This might also increase patients’ awareness of the importance of participating in monitoring themselves.
And finally, let’s not forget that the psychiatrist’s brain also changes continuously due to his or her own daily experiences, stresses, diet, lifestyle, medical illness, or medications. Thus, at every psychiatric session, the brains of both patient and psychiatrist are very different from the previous encounter!
To comment on this editorial or other topics of interest: [email protected].
Unlike other organs in the human body, the brain is constantly changing. The main driver for this ongoing re-engineering across various neural circuits is “experiential neuroplasticity,” which creates billions of new synapses and dendrite spines as well as new connections. And as the brain reinvents itself from day to day, the mind evolves as well.
The neurobiologic re-sculpting of the brain’s complex innards continuously encodes memories of what we learn and experience during waking hours, including all that we see, hear, feel, think, contemplate, plan, and decide. However, in addition to the ongoing intrinsic neuroplasticity that records life’s experiences within neural circuits, there are many extrinsic factors that can further modify the brain and the “psyche” it generates via electrical, neurochemical, and physiological mechanisms. That’s why every patient a psychiatrist sees at follow-up visits will have a brain that will be different from the previous encounter.
Consider the following factors that can modify a patient’s brain (for better or worse) between sessions:
- Psychotherapy that the patient received at the last session will biologically modify his or her brain. Creating new insights and understanding of one’s behavior and “connecting the dots” of the past and present emotions and reactions are all associated with neuroplastic changes within the brain.
- Mood or psychotic episodes. Depressive, manic, or psychotic episodes are associated with neuroinflammation, oxidative stress, and apoptotic effects, which can disrupt the brain’s cytoarchitecture. That’s why psychiatrists must inquire about such episodes between visits and document the possible effects on the patient’s mental status.
- Psychotropic medications all bind to one or more brain receptors to exert therapeutic or adverse effects, both of which are associated with changes in neurotransmitter pathways. A key component of every follow-up visit is to gauge the risks and benefits of the pharmacotherapy prescribed at the prior visit.
- Nonpsychiatric prescription medications are often associated with iatrogenic effects on the brain apart from their intended target organs. These iatrogenic effects include anxiety, depression, mania, psychosis, and cognitive changes. That’s why during each visit, the physician or nurse practitioner must review all prescription medications and consider their potential effects on the patient’s mental status.
- Over-the-counter drugs and supplements may exert neurologic effects via histaminergic, muscarinic, glutamatergic, adrenergic, or serotonergic effects—all of which can alter brain chemistry and contribute to mental status changes. They can also inhibit or induce cytochrome enzymes and induce adverse effects or loss of efficacy of the primary psychotropic medication the patient takes.
- Medical illness, even as simple as an upper respiratory viral infection, can alter brain function due to illness-induced physiological aberrations, including pain and peripheral inflammation, with neurologic consequences. Common metabolic disorders such as diabetes, hyperlipidemia, and hypertension can exert mental status changes.
- Alcohol and drugs of abuse alter brain structure and function and can induce psychological and cognitive changes. Inquiring about the amount and frequency of alcohol and recreational drug use must be done in detail at every visit.
- Stressful events. It is almost impossible for a psychiatric patient not to encounter stressful life events between visits. Coping with any mental disorder can be quite stressful and challenging due to its social, vocational, or personal consequences. Stress increases cortisol, which is associated with deleterious inflammatory effects on the brain. Persistent stress can lead to hippocampal atrophy because of the abundance of glucocorticoid receptors in the hippocampus. Inquiry about stressors must be part of every psychiatric follow-up visit. Multiple psychological, physiological, and behavioral effects are well known to be generated by stress, especially in individuals already impaired by mental illness.
- Diet. What a patient eats (or avoids eating) can affect the brain. High-fat diets can be inflammatory, while a diet rich in fruits, vegetables, and nuts can be neuroprotective. The microbiota and the enteric brain—both in the gastrointestinal tract—have been reported to influence mood and behavior. (For more on this, see “Gut microbiota and its implications for psychiatry: A review of 3 studies” on page 40 and “It takes guts to be mentally ill: Microbiota and psychopathology,” From the Editor,
Current Psychiatry , September 2018, p. 4-6.) - Obesity is associated with brain atrophy as well as depression. Weight should be assessed at every visit and coupled with counseling about diet and exercise.
- Exercise, or the lack of it, can alter the brain in good or bad ways. Many studies have shown that regular exercise can induce hippocampal neurogenesis and sharpen memory and cognition. On the other hand, a sedentary lifestyle can be detrimental to the heart, bones, and brain, with an elevation in cerebrovascular and cardiovascular risks, both of which can progressively alter brain structure and function.
- Concussion, contusions, and traumatic brain injury obviously can activate the microglia and trigger neurologic sequelae and mental repercussions. At every visit, patients should be asked if they have experienced a mild or severe head injury, whether it is accidental or sports-related.
- Dehydration, especially on the day of the visit, can alter mental status in subtle ways. Cerebral ventricular volume has been shown to change with dehydration. Asking a patient about daily fluid intake should be a standard question, especially for older patients, who may experience hypotension and mental status changes due to hypovolemia.
- Sleep, whether too much or too little, is associated with brain effects and can impact cognition and behavior. Asking patients about sleep is important because it can affect the brain, and also can be a symptom of unresolved psychiatric disorders. Chronic sleep disorders are associated with neuroinflammation.
- Menstrual cycle. Various neurotransmitters fluctuate during a woman’s menstrual cycle. Her cognition becomes sharper around ovulation, and that may influence her mental status and perhaps the neuroplasticity of her brain.
- Pregnancy and its major hormone changes can change brain structure and function. Estrogen, progesterone, and prolactin have different structural effects on the brain that can help the future mother care for her dependent baby. Asking about missed periods and pregnancy during childbearing years can be useful during psychiatric encounters.
Continue to: In summary...
In summary, numerous variables can affect the patient’s brain between visits, influencing his or her mental status. The ever-changing brain can be challenging to assess, especially in brief 15- to 20-minute follow-up sessions that have become more common in psychiatry. Perhaps patients should help their psychiatrists or nurse practitioners by completing a checklist with all the above variables, either online on the day of their appointment or on a form in the waiting room immediately prior to the visit. This might also increase patients’ awareness of the importance of participating in monitoring themselves.
And finally, let’s not forget that the psychiatrist’s brain also changes continuously due to his or her own daily experiences, stresses, diet, lifestyle, medical illness, or medications. Thus, at every psychiatric session, the brains of both patient and psychiatrist are very different from the previous encounter!
To comment on this editorial or other topics of interest: [email protected].
Unlike other organs in the human body, the brain is constantly changing. The main driver for this ongoing re-engineering across various neural circuits is “experiential neuroplasticity,” which creates billions of new synapses and dendrite spines as well as new connections. And as the brain reinvents itself from day to day, the mind evolves as well.
The neurobiologic re-sculpting of the brain’s complex innards continuously encodes memories of what we learn and experience during waking hours, including all that we see, hear, feel, think, contemplate, plan, and decide. However, in addition to the ongoing intrinsic neuroplasticity that records life’s experiences within neural circuits, there are many extrinsic factors that can further modify the brain and the “psyche” it generates via electrical, neurochemical, and physiological mechanisms. That’s why every patient a psychiatrist sees at follow-up visits will have a brain that will be different from the previous encounter.
Consider the following factors that can modify a patient’s brain (for better or worse) between sessions:
- Psychotherapy that the patient received at the last session will biologically modify his or her brain. Creating new insights and understanding of one’s behavior and “connecting the dots” of the past and present emotions and reactions are all associated with neuroplastic changes within the brain.
- Mood or psychotic episodes. Depressive, manic, or psychotic episodes are associated with neuroinflammation, oxidative stress, and apoptotic effects, which can disrupt the brain’s cytoarchitecture. That’s why psychiatrists must inquire about such episodes between visits and document the possible effects on the patient’s mental status.
- Psychotropic medications all bind to one or more brain receptors to exert therapeutic or adverse effects, both of which are associated with changes in neurotransmitter pathways. A key component of every follow-up visit is to gauge the risks and benefits of the pharmacotherapy prescribed at the prior visit.
- Nonpsychiatric prescription medications are often associated with iatrogenic effects on the brain apart from their intended target organs. These iatrogenic effects include anxiety, depression, mania, psychosis, and cognitive changes. That’s why during each visit, the physician or nurse practitioner must review all prescription medications and consider their potential effects on the patient’s mental status.
- Over-the-counter drugs and supplements may exert neurologic effects via histaminergic, muscarinic, glutamatergic, adrenergic, or serotonergic effects—all of which can alter brain chemistry and contribute to mental status changes. They can also inhibit or induce cytochrome enzymes and induce adverse effects or loss of efficacy of the primary psychotropic medication the patient takes.
- Medical illness, even as simple as an upper respiratory viral infection, can alter brain function due to illness-induced physiological aberrations, including pain and peripheral inflammation, with neurologic consequences. Common metabolic disorders such as diabetes, hyperlipidemia, and hypertension can exert mental status changes.
- Alcohol and drugs of abuse alter brain structure and function and can induce psychological and cognitive changes. Inquiring about the amount and frequency of alcohol and recreational drug use must be done in detail at every visit.
- Stressful events. It is almost impossible for a psychiatric patient not to encounter stressful life events between visits. Coping with any mental disorder can be quite stressful and challenging due to its social, vocational, or personal consequences. Stress increases cortisol, which is associated with deleterious inflammatory effects on the brain. Persistent stress can lead to hippocampal atrophy because of the abundance of glucocorticoid receptors in the hippocampus. Inquiry about stressors must be part of every psychiatric follow-up visit. Multiple psychological, physiological, and behavioral effects are well known to be generated by stress, especially in individuals already impaired by mental illness.
- Diet. What a patient eats (or avoids eating) can affect the brain. High-fat diets can be inflammatory, while a diet rich in fruits, vegetables, and nuts can be neuroprotective. The microbiota and the enteric brain—both in the gastrointestinal tract—have been reported to influence mood and behavior. (For more on this, see “Gut microbiota and its implications for psychiatry: A review of 3 studies” on page 40 and “It takes guts to be mentally ill: Microbiota and psychopathology,” From the Editor,
Current Psychiatry , September 2018, p. 4-6.) - Obesity is associated with brain atrophy as well as depression. Weight should be assessed at every visit and coupled with counseling about diet and exercise.
- Exercise, or the lack of it, can alter the brain in good or bad ways. Many studies have shown that regular exercise can induce hippocampal neurogenesis and sharpen memory and cognition. On the other hand, a sedentary lifestyle can be detrimental to the heart, bones, and brain, with an elevation in cerebrovascular and cardiovascular risks, both of which can progressively alter brain structure and function.
- Concussion, contusions, and traumatic brain injury obviously can activate the microglia and trigger neurologic sequelae and mental repercussions. At every visit, patients should be asked if they have experienced a mild or severe head injury, whether it is accidental or sports-related.
- Dehydration, especially on the day of the visit, can alter mental status in subtle ways. Cerebral ventricular volume has been shown to change with dehydration. Asking a patient about daily fluid intake should be a standard question, especially for older patients, who may experience hypotension and mental status changes due to hypovolemia.
- Sleep, whether too much or too little, is associated with brain effects and can impact cognition and behavior. Asking patients about sleep is important because it can affect the brain, and also can be a symptom of unresolved psychiatric disorders. Chronic sleep disorders are associated with neuroinflammation.
- Menstrual cycle. Various neurotransmitters fluctuate during a woman’s menstrual cycle. Her cognition becomes sharper around ovulation, and that may influence her mental status and perhaps the neuroplasticity of her brain.
- Pregnancy and its major hormone changes can change brain structure and function. Estrogen, progesterone, and prolactin have different structural effects on the brain that can help the future mother care for her dependent baby. Asking about missed periods and pregnancy during childbearing years can be useful during psychiatric encounters.
Continue to: In summary...
In summary, numerous variables can affect the patient’s brain between visits, influencing his or her mental status. The ever-changing brain can be challenging to assess, especially in brief 15- to 20-minute follow-up sessions that have become more common in psychiatry. Perhaps patients should help their psychiatrists or nurse practitioners by completing a checklist with all the above variables, either online on the day of their appointment or on a form in the waiting room immediately prior to the visit. This might also increase patients’ awareness of the importance of participating in monitoring themselves.
And finally, let’s not forget that the psychiatrist’s brain also changes continuously due to his or her own daily experiences, stresses, diet, lifestyle, medical illness, or medications. Thus, at every psychiatric session, the brains of both patient and psychiatrist are very different from the previous encounter!
To comment on this editorial or other topics of interest: [email protected].
Technology and the evolution of medical knowledge: What’s happening in the background
“Knowledge comes, but wisdom lingers. It may not be difficult to store up in the mind a vast quantity of facts within a comparatively short time, but the ability to form judgments requires the severe discipline of hard work and the tempering heat of experience and maturity.” – Calvin Coolidge
The information we use every day in patient care comes from one of two sources: personal experience (our own or that of another clinician) or a research study. Up until a hundred years ago, medicine was primarily a trade in which more experienced clinicians passed along their wisdom to younger clinicians, teaching them the things that they had learned during their long and difficult careers. Knowledge accrued slowly, influenced by the biased observations of each practicing doctor. People tended to remember their successes or unusual outcomes more than their failures or ordinary outcomes. Eventually, doctors realized that their knowledge base would be more accurate and accumulate more efficiently if they looked at the outcomes of many patients given the same treatment. Thus, the observational trial emerged.
As promising and important as the dawn of observational research was, it quickly became apparent that these trials had important limitations. The most notable limitations were the potential for bias and confounding variables to influence the results. Bias occurs when the opinion of the researcher influences how the result is interpreted. Confounders occur when an outcome is generated by some unexpected aspect of the patient, environment, or medication, rather than the thing that is being studied. An example of this might be a study that finds a higher mortality rate in a city by the sea than a city located inland. From these results, one might initially conclude that the sea is unhealthy. After realizing more retired people lived in the city by the sea; however, an individual would probably change his or her mind. In this example, the older age of this city’s population would be a confounding variable that drove the increased mortality in the city by the sea.
To solve the inherent problems with observational trials, the randomized, controlled trial was developed. Our reliance on information from RCTs runs so deep that it is hard to believe that the first modern clinical trial was not reported until 1948, in a paper on streptomycin in the treatment of pulmonary tuberculosis. It followed that faith in the randomized, controlled trial reached almost religious proportions, and the belief that information that does not come from an RCT should not be relied on was held by many, until recently. Why have things changed and what does this have to do with technology?
The first is an increasing recognition that, for all of their advantages, randomized trials have one nagging but critical limitation – generalizability. Randomized trials have strict inclusion and exclusion criteria. We do not have such inclusion and exclusion criteria when we take care of patients in our offices. For example, a recent trial published in the New England Journal of Medicine (2018 Dec 4. doi: 10.1056/NEJMoa1814468.), entitled “Apixaban to prevent venous thromboembolism in patients with cancer,” concluded that apixaban therapy resulted in a lower rate of venous thromboembolism than did placebo in patients starting chemotherapy for cancer. This was a large trial with more than 500 patients enrolled, and it reached an important conclusion with significant clinical implications. When you look at the details of the article, more than 1,800 patients were assessed to find the 500 patients who were eventually included in the trial. This is fairly typical of clinical trials and raises an important point: We need to be careful about how well the results of these clinical trials can be generalized to apply to the patient in front of us. This leads us to the second development that is something happening behind the scenes that each of us has contributed to.
Real-world research
As we see each patient and type information into the EHR, we add to an enormous database of medical information. That database is increasingly being used to advance our knowledge of how medicines actually work in the real world with real patients, and has already started providing answers that supplement, clarify, and even change our perspectives. The information will provide observations derived from real populations that have not been selected or influenced by the way in which a study is conducted. This new field of research is called “real-world research.”
An example of the difference between randomized controlled trial results and real-world research was published in Diabetes Care. This article examined the effectiveness of dipeptidyl peptidase 4 (DPP-4) inhibitors vs. glucagonlike peptide–1 receptor agonists (GLP-1 RAs) in the treatment of patients with diabetes. The goal of the study was to assess the difference in change in hemoglobin A1c between real-world evidence and randomized-trial evidence after initiation of a GLP-1 RA or a DPP-4 inhibitor. In RCTs, GLP-1 RAs decreased HbA1c by about 1.3% while DPP-4 inhibitors decreased HbA1c by about 0.68% (i.e., DPP-4 inhibitors were about half as effective). However, when the effects of these two diabetes drugs were examined using clinical databases in the real world, the two classes of medications had almost the same effect, each decreasing HbA1c by about 0.5%. This difference between RCT and real-world evidence might have been caused by the differential adherence to the two classes of medications, one being an injectable with significant GI side effects, and the other being a pill with few side effects.
The important take-home point is that we are now all contributing to a massive database that can be queried to give quicker, more accurate, more relevant information. Along with personal experience and randomized trials, this third source of clinical information, when used with wisdom, will provide us with the information we need to take ever better care of patients.
References
Carls GS et al. Understanding the gap between efficacy in randomized controlled trials and effectiveness in real-world use of GLP-1 RA and DPP-4 therapies in patients with type 2 diabetes. Diabetes Care. 2017;40:1469-78.
Blonde L et al. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018 Nov;35:1763-74.
“Knowledge comes, but wisdom lingers. It may not be difficult to store up in the mind a vast quantity of facts within a comparatively short time, but the ability to form judgments requires the severe discipline of hard work and the tempering heat of experience and maturity.” – Calvin Coolidge
The information we use every day in patient care comes from one of two sources: personal experience (our own or that of another clinician) or a research study. Up until a hundred years ago, medicine was primarily a trade in which more experienced clinicians passed along their wisdom to younger clinicians, teaching them the things that they had learned during their long and difficult careers. Knowledge accrued slowly, influenced by the biased observations of each practicing doctor. People tended to remember their successes or unusual outcomes more than their failures or ordinary outcomes. Eventually, doctors realized that their knowledge base would be more accurate and accumulate more efficiently if they looked at the outcomes of many patients given the same treatment. Thus, the observational trial emerged.
As promising and important as the dawn of observational research was, it quickly became apparent that these trials had important limitations. The most notable limitations were the potential for bias and confounding variables to influence the results. Bias occurs when the opinion of the researcher influences how the result is interpreted. Confounders occur when an outcome is generated by some unexpected aspect of the patient, environment, or medication, rather than the thing that is being studied. An example of this might be a study that finds a higher mortality rate in a city by the sea than a city located inland. From these results, one might initially conclude that the sea is unhealthy. After realizing more retired people lived in the city by the sea; however, an individual would probably change his or her mind. In this example, the older age of this city’s population would be a confounding variable that drove the increased mortality in the city by the sea.
To solve the inherent problems with observational trials, the randomized, controlled trial was developed. Our reliance on information from RCTs runs so deep that it is hard to believe that the first modern clinical trial was not reported until 1948, in a paper on streptomycin in the treatment of pulmonary tuberculosis. It followed that faith in the randomized, controlled trial reached almost religious proportions, and the belief that information that does not come from an RCT should not be relied on was held by many, until recently. Why have things changed and what does this have to do with technology?
The first is an increasing recognition that, for all of their advantages, randomized trials have one nagging but critical limitation – generalizability. Randomized trials have strict inclusion and exclusion criteria. We do not have such inclusion and exclusion criteria when we take care of patients in our offices. For example, a recent trial published in the New England Journal of Medicine (2018 Dec 4. doi: 10.1056/NEJMoa1814468.), entitled “Apixaban to prevent venous thromboembolism in patients with cancer,” concluded that apixaban therapy resulted in a lower rate of venous thromboembolism than did placebo in patients starting chemotherapy for cancer. This was a large trial with more than 500 patients enrolled, and it reached an important conclusion with significant clinical implications. When you look at the details of the article, more than 1,800 patients were assessed to find the 500 patients who were eventually included in the trial. This is fairly typical of clinical trials and raises an important point: We need to be careful about how well the results of these clinical trials can be generalized to apply to the patient in front of us. This leads us to the second development that is something happening behind the scenes that each of us has contributed to.
Real-world research
As we see each patient and type information into the EHR, we add to an enormous database of medical information. That database is increasingly being used to advance our knowledge of how medicines actually work in the real world with real patients, and has already started providing answers that supplement, clarify, and even change our perspectives. The information will provide observations derived from real populations that have not been selected or influenced by the way in which a study is conducted. This new field of research is called “real-world research.”
An example of the difference between randomized controlled trial results and real-world research was published in Diabetes Care. This article examined the effectiveness of dipeptidyl peptidase 4 (DPP-4) inhibitors vs. glucagonlike peptide–1 receptor agonists (GLP-1 RAs) in the treatment of patients with diabetes. The goal of the study was to assess the difference in change in hemoglobin A1c between real-world evidence and randomized-trial evidence after initiation of a GLP-1 RA or a DPP-4 inhibitor. In RCTs, GLP-1 RAs decreased HbA1c by about 1.3% while DPP-4 inhibitors decreased HbA1c by about 0.68% (i.e., DPP-4 inhibitors were about half as effective). However, when the effects of these two diabetes drugs were examined using clinical databases in the real world, the two classes of medications had almost the same effect, each decreasing HbA1c by about 0.5%. This difference between RCT and real-world evidence might have been caused by the differential adherence to the two classes of medications, one being an injectable with significant GI side effects, and the other being a pill with few side effects.
The important take-home point is that we are now all contributing to a massive database that can be queried to give quicker, more accurate, more relevant information. Along with personal experience and randomized trials, this third source of clinical information, when used with wisdom, will provide us with the information we need to take ever better care of patients.
References
Carls GS et al. Understanding the gap between efficacy in randomized controlled trials and effectiveness in real-world use of GLP-1 RA and DPP-4 therapies in patients with type 2 diabetes. Diabetes Care. 2017;40:1469-78.
Blonde L et al. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018 Nov;35:1763-74.
“Knowledge comes, but wisdom lingers. It may not be difficult to store up in the mind a vast quantity of facts within a comparatively short time, but the ability to form judgments requires the severe discipline of hard work and the tempering heat of experience and maturity.” – Calvin Coolidge
The information we use every day in patient care comes from one of two sources: personal experience (our own or that of another clinician) or a research study. Up until a hundred years ago, medicine was primarily a trade in which more experienced clinicians passed along their wisdom to younger clinicians, teaching them the things that they had learned during their long and difficult careers. Knowledge accrued slowly, influenced by the biased observations of each practicing doctor. People tended to remember their successes or unusual outcomes more than their failures or ordinary outcomes. Eventually, doctors realized that their knowledge base would be more accurate and accumulate more efficiently if they looked at the outcomes of many patients given the same treatment. Thus, the observational trial emerged.
As promising and important as the dawn of observational research was, it quickly became apparent that these trials had important limitations. The most notable limitations were the potential for bias and confounding variables to influence the results. Bias occurs when the opinion of the researcher influences how the result is interpreted. Confounders occur when an outcome is generated by some unexpected aspect of the patient, environment, or medication, rather than the thing that is being studied. An example of this might be a study that finds a higher mortality rate in a city by the sea than a city located inland. From these results, one might initially conclude that the sea is unhealthy. After realizing more retired people lived in the city by the sea; however, an individual would probably change his or her mind. In this example, the older age of this city’s population would be a confounding variable that drove the increased mortality in the city by the sea.
To solve the inherent problems with observational trials, the randomized, controlled trial was developed. Our reliance on information from RCTs runs so deep that it is hard to believe that the first modern clinical trial was not reported until 1948, in a paper on streptomycin in the treatment of pulmonary tuberculosis. It followed that faith in the randomized, controlled trial reached almost religious proportions, and the belief that information that does not come from an RCT should not be relied on was held by many, until recently. Why have things changed and what does this have to do with technology?
The first is an increasing recognition that, for all of their advantages, randomized trials have one nagging but critical limitation – generalizability. Randomized trials have strict inclusion and exclusion criteria. We do not have such inclusion and exclusion criteria when we take care of patients in our offices. For example, a recent trial published in the New England Journal of Medicine (2018 Dec 4. doi: 10.1056/NEJMoa1814468.), entitled “Apixaban to prevent venous thromboembolism in patients with cancer,” concluded that apixaban therapy resulted in a lower rate of venous thromboembolism than did placebo in patients starting chemotherapy for cancer. This was a large trial with more than 500 patients enrolled, and it reached an important conclusion with significant clinical implications. When you look at the details of the article, more than 1,800 patients were assessed to find the 500 patients who were eventually included in the trial. This is fairly typical of clinical trials and raises an important point: We need to be careful about how well the results of these clinical trials can be generalized to apply to the patient in front of us. This leads us to the second development that is something happening behind the scenes that each of us has contributed to.
Real-world research
As we see each patient and type information into the EHR, we add to an enormous database of medical information. That database is increasingly being used to advance our knowledge of how medicines actually work in the real world with real patients, and has already started providing answers that supplement, clarify, and even change our perspectives. The information will provide observations derived from real populations that have not been selected or influenced by the way in which a study is conducted. This new field of research is called “real-world research.”
An example of the difference between randomized controlled trial results and real-world research was published in Diabetes Care. This article examined the effectiveness of dipeptidyl peptidase 4 (DPP-4) inhibitors vs. glucagonlike peptide–1 receptor agonists (GLP-1 RAs) in the treatment of patients with diabetes. The goal of the study was to assess the difference in change in hemoglobin A1c between real-world evidence and randomized-trial evidence after initiation of a GLP-1 RA or a DPP-4 inhibitor. In RCTs, GLP-1 RAs decreased HbA1c by about 1.3% while DPP-4 inhibitors decreased HbA1c by about 0.68% (i.e., DPP-4 inhibitors were about half as effective). However, when the effects of these two diabetes drugs were examined using clinical databases in the real world, the two classes of medications had almost the same effect, each decreasing HbA1c by about 0.5%. This difference between RCT and real-world evidence might have been caused by the differential adherence to the two classes of medications, one being an injectable with significant GI side effects, and the other being a pill with few side effects.
The important take-home point is that we are now all contributing to a massive database that can be queried to give quicker, more accurate, more relevant information. Along with personal experience and randomized trials, this third source of clinical information, when used with wisdom, will provide us with the information we need to take ever better care of patients.
References
Carls GS et al. Understanding the gap between efficacy in randomized controlled trials and effectiveness in real-world use of GLP-1 RA and DPP-4 therapies in patients with type 2 diabetes. Diabetes Care. 2017;40:1469-78.
Blonde L et al. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018 Nov;35:1763-74.
Statute of limitations in malpractice actions
Question: Regarding the statute of limitations, which of the following is incorrect?
A. The statute stipulates the time period from knowledge of injury to when a lawsuit must be filed, beyond which it will be forever barred.
B. This time period is usually 2 years but varies somewhat from jurisdiction to jurisdiction.
C. It starts to “run” when the cause of action accrues, i.e., when the claimant knew or should have known of the injury, not when the negligent act took place.
D. In the case of minors, disability, and concealment, the statute may be tolled, thereby giving the plaintiff more time to file his/her claim.
E. In some U.S. jurisdictions, the judge may exercise discretion and waive the statutory time period.
Answer: E. At common law, there was no time limit that barred a plaintiff from bringing a claim, although there was a so-called “doctrine of laches” that foreclosed an action that had long lapsed. However, statutory changes in the law now require that complaints be brought in a timely manner so that the evidence remains fresh, accurate, and reliable. Another reason is to provide repose to the wrongdoer, i.e., relief from worrying for an indefinite period of time whether a lawsuit will be brought. It is 2 years for the tort of negligence in most jurisdictions, although states like California and Tennessee place a 1-year limit on medical malpractice claims under some circumstances. In England, actions for negligence-based personal injury have a limitation period of 3 years. Additionally, section 33 allows the court to use its discretion to extend this time period, something that is not available in other common law jurisdictions such as Singapore and the United States.
The statute of limitations does not start to run from the date of the negligent act or omission. For example, if there is a failure to timely diagnose and treat a cancerous condition and the patient suffers harm several years later, time starts to accrue from the date of discovering the injury, not the date of misdiagnosis. The term “discovery rule” defines the accrual period, which begins from the date the injury is discovered or should have been discovered if the party had exercised reasonable diligence. In cases of fraudulent concealment of a right of action, the statute may be tolled (halted) during the period of concealment. Tolling also may apply during legal disability.
In malpractice actions involving minors, the running of the time period may be tolled until the minor reaches a certain age, such as the age of majority, or by the minor’s 10th birthday (Hawaii law). Chaffin v. Nicosia1 dealt with such a situation. As the result of negligent forceps delivery, which injured the optic nerve, the plaintiff became blind in the right eye in early infancy. He brought suit when he was 22 years old. Indiana had two statutes on the issue, one requiring a malpractice suit to be brought within 2 years of the incident, and the other allowing a minor to sue no later than 2 years after reaching the age of 21. The Indiana Supreme Court allowed the case to go forward, reversing the lower court’s decision barring the action.
Courts are apt to closely scrutinize attempts to use the statute of limitations to prevent recovery as taking such actions could deprive the injured plaintiff of an otherwise legitimate claim. In one example, the defendants sought to dismiss the case (so-called motion for summary judgment) by arguing that the plaintiff filed suit some 32 months after she had developed Sheehan syndrome from postpartum hemorrhagic shock, and this exceeded the 2-year statute of limitations. The court ruled: “Since reasonable minds could differ as to when the injury and its operative cause should have been discovered by a reasonably diligent patient, the timeliness of the plaintiff’s claims should be decided by a jury and the motions for summary judgment will therefore be denied.”2
Two very recent cases are illustrative of litigation over statutes of limitations. In the first case, the District of Columbia’s highest court held that BKW, a patient-plaintiff, did not qualify for an extension and rejected his untimely suit against the hospital.3 The patient’s injuries stemmed from alleged unsuccessful venipunctures, and his complaint contained six causes of action, including negligent and intentional infliction of emotional distress and unnecessary pain, suffering, and bodily injury. In the District of Columbia, a plaintiff must serve the defendant with notice of intention to file suit (pre-suit notice) not less than 90 days prior to filing the action. The plaintiff must then file the complaint itself within the 3-year limitations period, with an extension allowed to take into account the 90-day pre-suit notice requirement. The case centered on the “within 90 days” requirement to trigger the statute of limitations extension. BKW, acting on one’s own behalf, conceded that the 3-year period applicable to his claims had lapsed, but because his complaint was filed “within 90 days” after the limitation period expired, it was eligible for an extension. The Court disagreed and dismissed the case, holding that to be eligible for the 90-day extension, a plaintiff must serve the pre-suit notice within 90 days before the limitation period expired.
The second case4 alleged malpractice in the care of a patient who died of anaphylaxis after a nurse infused him with iron dextran. The nurse had allegedly left the patient’s room too soon and did not adequately monitor his reaction to the drug. The patient was admitted to the hospital for removal of a colonic tumor and was to receive treatment for iron deficiency anemia. The nurse, identified in the chart as Agency Nurse RN 104, administered the prescribed intravenous 25-mg test-dose of iron dextran over a 5-minute period, but when the patient began having an anaphylactic-type allergic reaction, the nurse was allegedly not in the patient’s room. The plaintiff and her attorney attempted, on several occasions and without success, to discover the actual identity of the nurse from the hospital’s representatives. Consequently, the complaint designated the nurse as “Agency Nurse RN 104,” and the plaintiff did not provide the name of the nurse, even though doing so was legally required; the exclusion of the nurse’s name would have resulted in case dismissal since the statute of limitations had lapsed. However, the court ruled, “we are satisfied that plaintiff and her attorney acted with reasonable diligence in attempting – with no avail – to ascertain the true identity of “Agency Nurse RN 104” before filing suit and before the 2-year limitations statute ran ...”
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Portions of this article had been previously published in a 2010 issue of Internal Medicine News. For additional information, readers may contact the author at [email protected]
References
1. Chaffin v. Nicosia, 310 N.E.2d 867 (Ind. 1974).
2. Lomeo v. Davis, 53 Pa. D. & C. 4th 49 (Pa. Com. Pl. Jul 24, 2001).
3. Waugh v. Medstar Georgetown University Hospital, District of Columbia Court of Appeals No. 18-CV-329. Decided March 14, 2019.
4. Rosenberg v. Watts, Superior Court N.J. Appellate Div., Docket No. A-4525-16T4. Decided March 21, 2019.
Question: Regarding the statute of limitations, which of the following is incorrect?
A. The statute stipulates the time period from knowledge of injury to when a lawsuit must be filed, beyond which it will be forever barred.
B. This time period is usually 2 years but varies somewhat from jurisdiction to jurisdiction.
C. It starts to “run” when the cause of action accrues, i.e., when the claimant knew or should have known of the injury, not when the negligent act took place.
D. In the case of minors, disability, and concealment, the statute may be tolled, thereby giving the plaintiff more time to file his/her claim.
E. In some U.S. jurisdictions, the judge may exercise discretion and waive the statutory time period.
Answer: E. At common law, there was no time limit that barred a plaintiff from bringing a claim, although there was a so-called “doctrine of laches” that foreclosed an action that had long lapsed. However, statutory changes in the law now require that complaints be brought in a timely manner so that the evidence remains fresh, accurate, and reliable. Another reason is to provide repose to the wrongdoer, i.e., relief from worrying for an indefinite period of time whether a lawsuit will be brought. It is 2 years for the tort of negligence in most jurisdictions, although states like California and Tennessee place a 1-year limit on medical malpractice claims under some circumstances. In England, actions for negligence-based personal injury have a limitation period of 3 years. Additionally, section 33 allows the court to use its discretion to extend this time period, something that is not available in other common law jurisdictions such as Singapore and the United States.
The statute of limitations does not start to run from the date of the negligent act or omission. For example, if there is a failure to timely diagnose and treat a cancerous condition and the patient suffers harm several years later, time starts to accrue from the date of discovering the injury, not the date of misdiagnosis. The term “discovery rule” defines the accrual period, which begins from the date the injury is discovered or should have been discovered if the party had exercised reasonable diligence. In cases of fraudulent concealment of a right of action, the statute may be tolled (halted) during the period of concealment. Tolling also may apply during legal disability.
In malpractice actions involving minors, the running of the time period may be tolled until the minor reaches a certain age, such as the age of majority, or by the minor’s 10th birthday (Hawaii law). Chaffin v. Nicosia1 dealt with such a situation. As the result of negligent forceps delivery, which injured the optic nerve, the plaintiff became blind in the right eye in early infancy. He brought suit when he was 22 years old. Indiana had two statutes on the issue, one requiring a malpractice suit to be brought within 2 years of the incident, and the other allowing a minor to sue no later than 2 years after reaching the age of 21. The Indiana Supreme Court allowed the case to go forward, reversing the lower court’s decision barring the action.
Courts are apt to closely scrutinize attempts to use the statute of limitations to prevent recovery as taking such actions could deprive the injured plaintiff of an otherwise legitimate claim. In one example, the defendants sought to dismiss the case (so-called motion for summary judgment) by arguing that the plaintiff filed suit some 32 months after she had developed Sheehan syndrome from postpartum hemorrhagic shock, and this exceeded the 2-year statute of limitations. The court ruled: “Since reasonable minds could differ as to when the injury and its operative cause should have been discovered by a reasonably diligent patient, the timeliness of the plaintiff’s claims should be decided by a jury and the motions for summary judgment will therefore be denied.”2
Two very recent cases are illustrative of litigation over statutes of limitations. In the first case, the District of Columbia’s highest court held that BKW, a patient-plaintiff, did not qualify for an extension and rejected his untimely suit against the hospital.3 The patient’s injuries stemmed from alleged unsuccessful venipunctures, and his complaint contained six causes of action, including negligent and intentional infliction of emotional distress and unnecessary pain, suffering, and bodily injury. In the District of Columbia, a plaintiff must serve the defendant with notice of intention to file suit (pre-suit notice) not less than 90 days prior to filing the action. The plaintiff must then file the complaint itself within the 3-year limitations period, with an extension allowed to take into account the 90-day pre-suit notice requirement. The case centered on the “within 90 days” requirement to trigger the statute of limitations extension. BKW, acting on one’s own behalf, conceded that the 3-year period applicable to his claims had lapsed, but because his complaint was filed “within 90 days” after the limitation period expired, it was eligible for an extension. The Court disagreed and dismissed the case, holding that to be eligible for the 90-day extension, a plaintiff must serve the pre-suit notice within 90 days before the limitation period expired.
The second case4 alleged malpractice in the care of a patient who died of anaphylaxis after a nurse infused him with iron dextran. The nurse had allegedly left the patient’s room too soon and did not adequately monitor his reaction to the drug. The patient was admitted to the hospital for removal of a colonic tumor and was to receive treatment for iron deficiency anemia. The nurse, identified in the chart as Agency Nurse RN 104, administered the prescribed intravenous 25-mg test-dose of iron dextran over a 5-minute period, but when the patient began having an anaphylactic-type allergic reaction, the nurse was allegedly not in the patient’s room. The plaintiff and her attorney attempted, on several occasions and without success, to discover the actual identity of the nurse from the hospital’s representatives. Consequently, the complaint designated the nurse as “Agency Nurse RN 104,” and the plaintiff did not provide the name of the nurse, even though doing so was legally required; the exclusion of the nurse’s name would have resulted in case dismissal since the statute of limitations had lapsed. However, the court ruled, “we are satisfied that plaintiff and her attorney acted with reasonable diligence in attempting – with no avail – to ascertain the true identity of “Agency Nurse RN 104” before filing suit and before the 2-year limitations statute ran ...”
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Portions of this article had been previously published in a 2010 issue of Internal Medicine News. For additional information, readers may contact the author at [email protected]
References
1. Chaffin v. Nicosia, 310 N.E.2d 867 (Ind. 1974).
2. Lomeo v. Davis, 53 Pa. D. & C. 4th 49 (Pa. Com. Pl. Jul 24, 2001).
3. Waugh v. Medstar Georgetown University Hospital, District of Columbia Court of Appeals No. 18-CV-329. Decided March 14, 2019.
4. Rosenberg v. Watts, Superior Court N.J. Appellate Div., Docket No. A-4525-16T4. Decided March 21, 2019.
Question: Regarding the statute of limitations, which of the following is incorrect?
A. The statute stipulates the time period from knowledge of injury to when a lawsuit must be filed, beyond which it will be forever barred.
B. This time period is usually 2 years but varies somewhat from jurisdiction to jurisdiction.
C. It starts to “run” when the cause of action accrues, i.e., when the claimant knew or should have known of the injury, not when the negligent act took place.
D. In the case of minors, disability, and concealment, the statute may be tolled, thereby giving the plaintiff more time to file his/her claim.
E. In some U.S. jurisdictions, the judge may exercise discretion and waive the statutory time period.
Answer: E. At common law, there was no time limit that barred a plaintiff from bringing a claim, although there was a so-called “doctrine of laches” that foreclosed an action that had long lapsed. However, statutory changes in the law now require that complaints be brought in a timely manner so that the evidence remains fresh, accurate, and reliable. Another reason is to provide repose to the wrongdoer, i.e., relief from worrying for an indefinite period of time whether a lawsuit will be brought. It is 2 years for the tort of negligence in most jurisdictions, although states like California and Tennessee place a 1-year limit on medical malpractice claims under some circumstances. In England, actions for negligence-based personal injury have a limitation period of 3 years. Additionally, section 33 allows the court to use its discretion to extend this time period, something that is not available in other common law jurisdictions such as Singapore and the United States.
The statute of limitations does not start to run from the date of the negligent act or omission. For example, if there is a failure to timely diagnose and treat a cancerous condition and the patient suffers harm several years later, time starts to accrue from the date of discovering the injury, not the date of misdiagnosis. The term “discovery rule” defines the accrual period, which begins from the date the injury is discovered or should have been discovered if the party had exercised reasonable diligence. In cases of fraudulent concealment of a right of action, the statute may be tolled (halted) during the period of concealment. Tolling also may apply during legal disability.
In malpractice actions involving minors, the running of the time period may be tolled until the minor reaches a certain age, such as the age of majority, or by the minor’s 10th birthday (Hawaii law). Chaffin v. Nicosia1 dealt with such a situation. As the result of negligent forceps delivery, which injured the optic nerve, the plaintiff became blind in the right eye in early infancy. He brought suit when he was 22 years old. Indiana had two statutes on the issue, one requiring a malpractice suit to be brought within 2 years of the incident, and the other allowing a minor to sue no later than 2 years after reaching the age of 21. The Indiana Supreme Court allowed the case to go forward, reversing the lower court’s decision barring the action.
Courts are apt to closely scrutinize attempts to use the statute of limitations to prevent recovery as taking such actions could deprive the injured plaintiff of an otherwise legitimate claim. In one example, the defendants sought to dismiss the case (so-called motion for summary judgment) by arguing that the plaintiff filed suit some 32 months after she had developed Sheehan syndrome from postpartum hemorrhagic shock, and this exceeded the 2-year statute of limitations. The court ruled: “Since reasonable minds could differ as to when the injury and its operative cause should have been discovered by a reasonably diligent patient, the timeliness of the plaintiff’s claims should be decided by a jury and the motions for summary judgment will therefore be denied.”2
Two very recent cases are illustrative of litigation over statutes of limitations. In the first case, the District of Columbia’s highest court held that BKW, a patient-plaintiff, did not qualify for an extension and rejected his untimely suit against the hospital.3 The patient’s injuries stemmed from alleged unsuccessful venipunctures, and his complaint contained six causes of action, including negligent and intentional infliction of emotional distress and unnecessary pain, suffering, and bodily injury. In the District of Columbia, a plaintiff must serve the defendant with notice of intention to file suit (pre-suit notice) not less than 90 days prior to filing the action. The plaintiff must then file the complaint itself within the 3-year limitations period, with an extension allowed to take into account the 90-day pre-suit notice requirement. The case centered on the “within 90 days” requirement to trigger the statute of limitations extension. BKW, acting on one’s own behalf, conceded that the 3-year period applicable to his claims had lapsed, but because his complaint was filed “within 90 days” after the limitation period expired, it was eligible for an extension. The Court disagreed and dismissed the case, holding that to be eligible for the 90-day extension, a plaintiff must serve the pre-suit notice within 90 days before the limitation period expired.
The second case4 alleged malpractice in the care of a patient who died of anaphylaxis after a nurse infused him with iron dextran. The nurse had allegedly left the patient’s room too soon and did not adequately monitor his reaction to the drug. The patient was admitted to the hospital for removal of a colonic tumor and was to receive treatment for iron deficiency anemia. The nurse, identified in the chart as Agency Nurse RN 104, administered the prescribed intravenous 25-mg test-dose of iron dextran over a 5-minute period, but when the patient began having an anaphylactic-type allergic reaction, the nurse was allegedly not in the patient’s room. The plaintiff and her attorney attempted, on several occasions and without success, to discover the actual identity of the nurse from the hospital’s representatives. Consequently, the complaint designated the nurse as “Agency Nurse RN 104,” and the plaintiff did not provide the name of the nurse, even though doing so was legally required; the exclusion of the nurse’s name would have resulted in case dismissal since the statute of limitations had lapsed. However, the court ruled, “we are satisfied that plaintiff and her attorney acted with reasonable diligence in attempting – with no avail – to ascertain the true identity of “Agency Nurse RN 104” before filing suit and before the 2-year limitations statute ran ...”
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Portions of this article had been previously published in a 2010 issue of Internal Medicine News. For additional information, readers may contact the author at [email protected]
References
1. Chaffin v. Nicosia, 310 N.E.2d 867 (Ind. 1974).
2. Lomeo v. Davis, 53 Pa. D. & C. 4th 49 (Pa. Com. Pl. Jul 24, 2001).
3. Waugh v. Medstar Georgetown University Hospital, District of Columbia Court of Appeals No. 18-CV-329. Decided March 14, 2019.
4. Rosenberg v. Watts, Superior Court N.J. Appellate Div., Docket No. A-4525-16T4. Decided March 21, 2019.
Navigating the Oncology Care Model
Care of the cancer patient is complex and expensive. During 2001-2011, medical spending to treat cancer increased from $56.8 billion to $88.3 billion in the United States. During this time, ambulatory expenditures for care and treatment increased while inpatient hospital expenditures decreased.1,2 Treatments for cancer have advanced, but costs do not correlate with outcomes. Advanced payment models aimed at ensuring high quality while lowering costs may be the vehicle to help mitigate the financial burden of cancer treatment on patients and society at large.
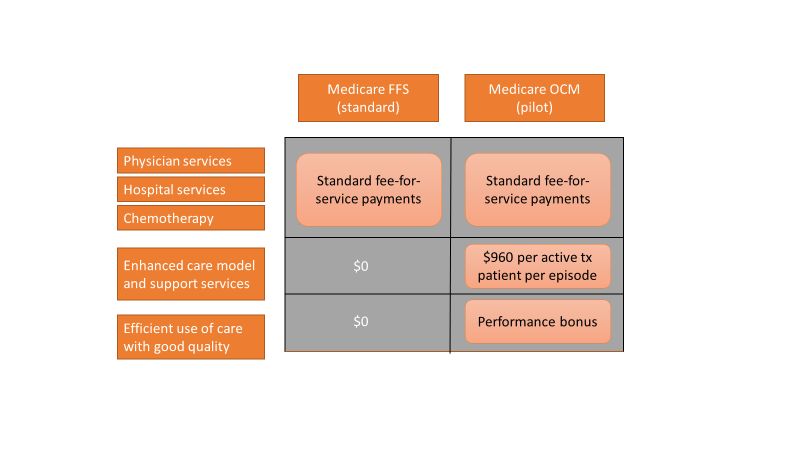
Oncology Care Model
The Center for Medicare and Medicaid Innovation designed the Oncology Care Model (OCM), which allows practices and payers in the United States to partner with the Centers for Medicare & Medicaid Services. The goal of the OCM is to provide high quality, highly coordinated cancer care at the same or lower cost. Practice partnerships with the CMS involve payment arrangements that include financial and performance accountability for episodes of cancer care surrounding chemotherapy delivery to patients.3
Practices that have been selected by the CMS have attested to providing a number of enhanced services from 24/7 patient access to an appropriate clinician who can access medical records to having a documented care plan for every patient.4
Payment methodology
An episode of care is defined as a 6-month period that starts at the time of chemotherapy administration. In addition to the standard fee-for-service payment, practices have the ability to earn two other types of payments during an oncology episode.
The per-beneficiary Monthly Enhanced Oncology Services payment is $960 for the entire episode but is paid to practices at $160 per month.
Practices have the potential to earn additional performance-based payments (PBP) based on the difference in cost between the projected and actual cost of the episode. The PBP also incorporates performance on quality metrics, based on Medicare claims and other information submitted by the practice. For example, claims-based measures include hospital, emergency department (ED), and hospice utilization.
To participate in the OCM, practices must choose either a one-sided or two-sided risk model. In the one-sided risk model, practices take on no downside risk but need to achieve a greater reduction in expenditures (4% below the benchmark price). In the two-side risk model, practices need only to reduce expenditures by 2.75% below the benchmark price. But if they fail to meet their savings goals, they must pay the difference to the CMS. The recoupment is capped at 20% of the benchmark amount.
Feedback reports
The CMS sends quarterly feedback reports that contain information on practice demographics, outcomes, expenditures, chemotherapy use, and patient satisfaction. The outcomes include the mortality rate for Medicare beneficiaries treated at the practice, compared with other practices nationally. In addition, the reports include end-of-life metrics and patient satisfaction, as well as details of expenditures on drugs, hospital use, imaging and laboratory services, and a description of chemotherapy usage.
These reports can be a helpful tool for measuring your own use of services, as well as benchmarking it against national figures.
Practice modifications
According to CMS feedback reports, the cost of care per beneficiary per month has increased across all practices since the inception of the OCM. However, there are practices that have been successful in reducing cost of care without negatively affecting mortality.
Drugs, hospital, and ED visits, along with imaging and laboratory evaluation, account for 75% of the cost. Some strategies to reduce expenditure involve targeting those areas.
Consider prescribing drugs conservatively without affecting outcomes. For instance, bisphosphonates for bone metastasis can be given every 12 weeks instead of 4 weeks.5 Similarly, adjuvant chemotherapy can be given for 3 months, instead of 6 months in appropriate stage 3 colon cancer patients.6
Another potential opportunity for savings is the judicious use of pertuzumab in early-stage breast cancer patients.7 These are all evidence-based recommendations with potential for cost savings. Clinical pathways can aid in this process, but physician buy-in is imperative.
In terms of imaging, avoid PET scans when they will not affect your clinical decision making, avoid staging scans in early-stage breast and prostate cancer patients, and avoid surveillance scans among early-stage breast cancer and lymphoma patients. The Choosing Wisely campaign can help guide some of these decisions.8
Another area where good care meets cost effective care is in the early engagement of palliative care. Several studies have shown that early involvement of palliative care improves survival and quality of life.9,10 Palliative care involvement also decreases the emotional burden for patients and oncologists. Appropriate symptom control, particularly of pain, decreases hospitalizations during treatment.
Investing in a robust supportive care team – financial advocates, social work, nutrition, behavioral health, as well as various community services – can help reduce the financial, physical, and emotional distress levels for patients. All of these services ultimately lead to reduced hospitalizations.11 The Monthly Enhanced Oncology Services payment can be put toward these expenses.
Care teams working at the highest level of competence and license can also save time and money. Consider using registered nurses to implement triage pathways to assess side effects and symptom management, or using nurse practitioners, registered nurses, and physician assistants for same-day appointments and to assess symptoms rather than referring patients to the emergency department.
Avoid the ED and hospitalizations by using the infusion center to provide hydration and blood transfusions in a timely fashion.
Telemedicine can be used for symptom management as well as leveraging supportive care services.
Cost for cancer care is very difficult to sustain. The OCM provides early insights into expenditures, challenges, and opportunities. Practices should use this information to build infrastructure and provide high quality, cost-effective care. Value-based cancer care should be the overarching goal for oncology practices and health care organizations.
Dr. Mahesh is the director of hematology-oncology and program director of the Oncology Care Model at Summa Health in Akron, Ohio.
References
1. Siegel RL et al. Cancer statistics, 2018. CA Cancer J Clin. 2018 Jan;68(1):7-30.
2. Medical Expenditure Panel Survey, Statistical Brief #443. 2014 Jun.
3. CMS: Oncology Care Model.
4. CMS: OCM Frequently Asked Questions.
5. Himelstein AL et al. Effect of longer-interval vs. standard dosing of zoledronic acid on skeletal events in patients with bone metastases. JAMA. 2017 Jan 3;317(1):48-58.
6. Grothey A et al. Duration of adjuvant chemotherapy for stage III colon cancer. N Engl J Med. 2018;378(13):1177-88.
7. Von Minckwitz G et al. Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer. N Engl J Med. 2017;377(2):122-31.
8. American Society of Clinical Oncology: Ten Things Physician and Patients Should Question.
9. Temel JS et al. Early palliative care for patients with metastatic non–small cell lung cancer. N Engl J Med. 2010;363(8):733-42.
10. Blayney DW et al. Critical lessons from high-value oncology practices. JAMA Oncol. 2018 Feb 1;4(2):164-71.
11. Sherman DE. Transforming practices through the oncology care model: financial toxicity and counseling. J Oncol Pract. 2017 Aug;13(8):519-22.
Care of the cancer patient is complex and expensive. During 2001-2011, medical spending to treat cancer increased from $56.8 billion to $88.3 billion in the United States. During this time, ambulatory expenditures for care and treatment increased while inpatient hospital expenditures decreased.1,2 Treatments for cancer have advanced, but costs do not correlate with outcomes. Advanced payment models aimed at ensuring high quality while lowering costs may be the vehicle to help mitigate the financial burden of cancer treatment on patients and society at large.
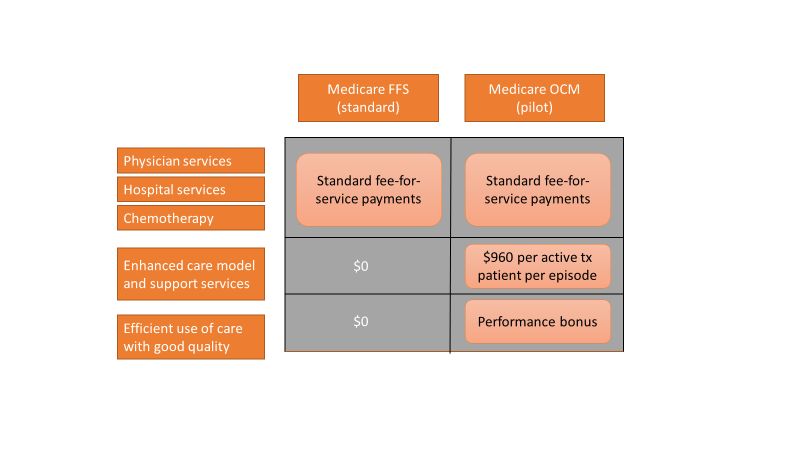
Oncology Care Model
The Center for Medicare and Medicaid Innovation designed the Oncology Care Model (OCM), which allows practices and payers in the United States to partner with the Centers for Medicare & Medicaid Services. The goal of the OCM is to provide high quality, highly coordinated cancer care at the same or lower cost. Practice partnerships with the CMS involve payment arrangements that include financial and performance accountability for episodes of cancer care surrounding chemotherapy delivery to patients.3
Practices that have been selected by the CMS have attested to providing a number of enhanced services from 24/7 patient access to an appropriate clinician who can access medical records to having a documented care plan for every patient.4
Payment methodology
An episode of care is defined as a 6-month period that starts at the time of chemotherapy administration. In addition to the standard fee-for-service payment, practices have the ability to earn two other types of payments during an oncology episode.
The per-beneficiary Monthly Enhanced Oncology Services payment is $960 for the entire episode but is paid to practices at $160 per month.
Practices have the potential to earn additional performance-based payments (PBP) based on the difference in cost between the projected and actual cost of the episode. The PBP also incorporates performance on quality metrics, based on Medicare claims and other information submitted by the practice. For example, claims-based measures include hospital, emergency department (ED), and hospice utilization.
To participate in the OCM, practices must choose either a one-sided or two-sided risk model. In the one-sided risk model, practices take on no downside risk but need to achieve a greater reduction in expenditures (4% below the benchmark price). In the two-side risk model, practices need only to reduce expenditures by 2.75% below the benchmark price. But if they fail to meet their savings goals, they must pay the difference to the CMS. The recoupment is capped at 20% of the benchmark amount.
Feedback reports
The CMS sends quarterly feedback reports that contain information on practice demographics, outcomes, expenditures, chemotherapy use, and patient satisfaction. The outcomes include the mortality rate for Medicare beneficiaries treated at the practice, compared with other practices nationally. In addition, the reports include end-of-life metrics and patient satisfaction, as well as details of expenditures on drugs, hospital use, imaging and laboratory services, and a description of chemotherapy usage.
These reports can be a helpful tool for measuring your own use of services, as well as benchmarking it against national figures.
Practice modifications
According to CMS feedback reports, the cost of care per beneficiary per month has increased across all practices since the inception of the OCM. However, there are practices that have been successful in reducing cost of care without negatively affecting mortality.
Drugs, hospital, and ED visits, along with imaging and laboratory evaluation, account for 75% of the cost. Some strategies to reduce expenditure involve targeting those areas.
Consider prescribing drugs conservatively without affecting outcomes. For instance, bisphosphonates for bone metastasis can be given every 12 weeks instead of 4 weeks.5 Similarly, adjuvant chemotherapy can be given for 3 months, instead of 6 months in appropriate stage 3 colon cancer patients.6
Another potential opportunity for savings is the judicious use of pertuzumab in early-stage breast cancer patients.7 These are all evidence-based recommendations with potential for cost savings. Clinical pathways can aid in this process, but physician buy-in is imperative.
In terms of imaging, avoid PET scans when they will not affect your clinical decision making, avoid staging scans in early-stage breast and prostate cancer patients, and avoid surveillance scans among early-stage breast cancer and lymphoma patients. The Choosing Wisely campaign can help guide some of these decisions.8
Another area where good care meets cost effective care is in the early engagement of palliative care. Several studies have shown that early involvement of palliative care improves survival and quality of life.9,10 Palliative care involvement also decreases the emotional burden for patients and oncologists. Appropriate symptom control, particularly of pain, decreases hospitalizations during treatment.
Investing in a robust supportive care team – financial advocates, social work, nutrition, behavioral health, as well as various community services – can help reduce the financial, physical, and emotional distress levels for patients. All of these services ultimately lead to reduced hospitalizations.11 The Monthly Enhanced Oncology Services payment can be put toward these expenses.
Care teams working at the highest level of competence and license can also save time and money. Consider using registered nurses to implement triage pathways to assess side effects and symptom management, or using nurse practitioners, registered nurses, and physician assistants for same-day appointments and to assess symptoms rather than referring patients to the emergency department.
Avoid the ED and hospitalizations by using the infusion center to provide hydration and blood transfusions in a timely fashion.
Telemedicine can be used for symptom management as well as leveraging supportive care services.
Cost for cancer care is very difficult to sustain. The OCM provides early insights into expenditures, challenges, and opportunities. Practices should use this information to build infrastructure and provide high quality, cost-effective care. Value-based cancer care should be the overarching goal for oncology practices and health care organizations.
Dr. Mahesh is the director of hematology-oncology and program director of the Oncology Care Model at Summa Health in Akron, Ohio.
References
1. Siegel RL et al. Cancer statistics, 2018. CA Cancer J Clin. 2018 Jan;68(1):7-30.
2. Medical Expenditure Panel Survey, Statistical Brief #443. 2014 Jun.
3. CMS: Oncology Care Model.
4. CMS: OCM Frequently Asked Questions.
5. Himelstein AL et al. Effect of longer-interval vs. standard dosing of zoledronic acid on skeletal events in patients with bone metastases. JAMA. 2017 Jan 3;317(1):48-58.
6. Grothey A et al. Duration of adjuvant chemotherapy for stage III colon cancer. N Engl J Med. 2018;378(13):1177-88.
7. Von Minckwitz G et al. Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer. N Engl J Med. 2017;377(2):122-31.
8. American Society of Clinical Oncology: Ten Things Physician and Patients Should Question.
9. Temel JS et al. Early palliative care for patients with metastatic non–small cell lung cancer. N Engl J Med. 2010;363(8):733-42.
10. Blayney DW et al. Critical lessons from high-value oncology practices. JAMA Oncol. 2018 Feb 1;4(2):164-71.
11. Sherman DE. Transforming practices through the oncology care model: financial toxicity and counseling. J Oncol Pract. 2017 Aug;13(8):519-22.
Care of the cancer patient is complex and expensive. During 2001-2011, medical spending to treat cancer increased from $56.8 billion to $88.3 billion in the United States. During this time, ambulatory expenditures for care and treatment increased while inpatient hospital expenditures decreased.1,2 Treatments for cancer have advanced, but costs do not correlate with outcomes. Advanced payment models aimed at ensuring high quality while lowering costs may be the vehicle to help mitigate the financial burden of cancer treatment on patients and society at large.
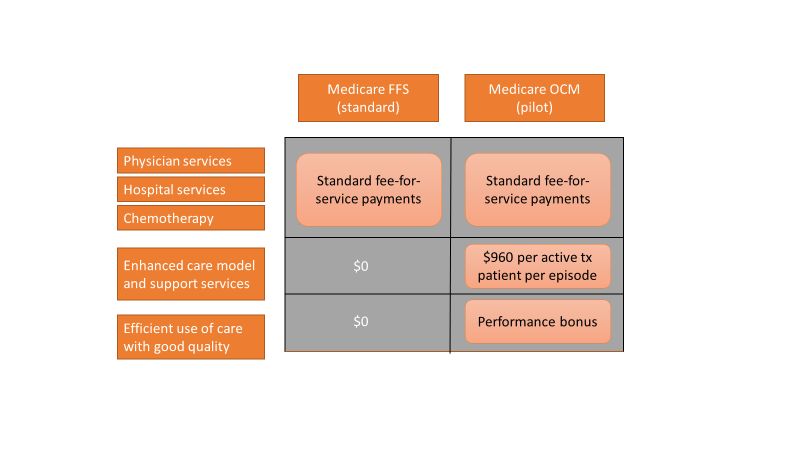
Oncology Care Model
The Center for Medicare and Medicaid Innovation designed the Oncology Care Model (OCM), which allows practices and payers in the United States to partner with the Centers for Medicare & Medicaid Services. The goal of the OCM is to provide high quality, highly coordinated cancer care at the same or lower cost. Practice partnerships with the CMS involve payment arrangements that include financial and performance accountability for episodes of cancer care surrounding chemotherapy delivery to patients.3
Practices that have been selected by the CMS have attested to providing a number of enhanced services from 24/7 patient access to an appropriate clinician who can access medical records to having a documented care plan for every patient.4
Payment methodology
An episode of care is defined as a 6-month period that starts at the time of chemotherapy administration. In addition to the standard fee-for-service payment, practices have the ability to earn two other types of payments during an oncology episode.
The per-beneficiary Monthly Enhanced Oncology Services payment is $960 for the entire episode but is paid to practices at $160 per month.
Practices have the potential to earn additional performance-based payments (PBP) based on the difference in cost between the projected and actual cost of the episode. The PBP also incorporates performance on quality metrics, based on Medicare claims and other information submitted by the practice. For example, claims-based measures include hospital, emergency department (ED), and hospice utilization.
To participate in the OCM, practices must choose either a one-sided or two-sided risk model. In the one-sided risk model, practices take on no downside risk but need to achieve a greater reduction in expenditures (4% below the benchmark price). In the two-side risk model, practices need only to reduce expenditures by 2.75% below the benchmark price. But if they fail to meet their savings goals, they must pay the difference to the CMS. The recoupment is capped at 20% of the benchmark amount.
Feedback reports
The CMS sends quarterly feedback reports that contain information on practice demographics, outcomes, expenditures, chemotherapy use, and patient satisfaction. The outcomes include the mortality rate for Medicare beneficiaries treated at the practice, compared with other practices nationally. In addition, the reports include end-of-life metrics and patient satisfaction, as well as details of expenditures on drugs, hospital use, imaging and laboratory services, and a description of chemotherapy usage.
These reports can be a helpful tool for measuring your own use of services, as well as benchmarking it against national figures.
Practice modifications
According to CMS feedback reports, the cost of care per beneficiary per month has increased across all practices since the inception of the OCM. However, there are practices that have been successful in reducing cost of care without negatively affecting mortality.
Drugs, hospital, and ED visits, along with imaging and laboratory evaluation, account for 75% of the cost. Some strategies to reduce expenditure involve targeting those areas.
Consider prescribing drugs conservatively without affecting outcomes. For instance, bisphosphonates for bone metastasis can be given every 12 weeks instead of 4 weeks.5 Similarly, adjuvant chemotherapy can be given for 3 months, instead of 6 months in appropriate stage 3 colon cancer patients.6
Another potential opportunity for savings is the judicious use of pertuzumab in early-stage breast cancer patients.7 These are all evidence-based recommendations with potential for cost savings. Clinical pathways can aid in this process, but physician buy-in is imperative.
In terms of imaging, avoid PET scans when they will not affect your clinical decision making, avoid staging scans in early-stage breast and prostate cancer patients, and avoid surveillance scans among early-stage breast cancer and lymphoma patients. The Choosing Wisely campaign can help guide some of these decisions.8
Another area where good care meets cost effective care is in the early engagement of palliative care. Several studies have shown that early involvement of palliative care improves survival and quality of life.9,10 Palliative care involvement also decreases the emotional burden for patients and oncologists. Appropriate symptom control, particularly of pain, decreases hospitalizations during treatment.
Investing in a robust supportive care team – financial advocates, social work, nutrition, behavioral health, as well as various community services – can help reduce the financial, physical, and emotional distress levels for patients. All of these services ultimately lead to reduced hospitalizations.11 The Monthly Enhanced Oncology Services payment can be put toward these expenses.
Care teams working at the highest level of competence and license can also save time and money. Consider using registered nurses to implement triage pathways to assess side effects and symptom management, or using nurse practitioners, registered nurses, and physician assistants for same-day appointments and to assess symptoms rather than referring patients to the emergency department.
Avoid the ED and hospitalizations by using the infusion center to provide hydration and blood transfusions in a timely fashion.
Telemedicine can be used for symptom management as well as leveraging supportive care services.
Cost for cancer care is very difficult to sustain. The OCM provides early insights into expenditures, challenges, and opportunities. Practices should use this information to build infrastructure and provide high quality, cost-effective care. Value-based cancer care should be the overarching goal for oncology practices and health care organizations.
Dr. Mahesh is the director of hematology-oncology and program director of the Oncology Care Model at Summa Health in Akron, Ohio.
References
1. Siegel RL et al. Cancer statistics, 2018. CA Cancer J Clin. 2018 Jan;68(1):7-30.
2. Medical Expenditure Panel Survey, Statistical Brief #443. 2014 Jun.
3. CMS: Oncology Care Model.
4. CMS: OCM Frequently Asked Questions.
5. Himelstein AL et al. Effect of longer-interval vs. standard dosing of zoledronic acid on skeletal events in patients with bone metastases. JAMA. 2017 Jan 3;317(1):48-58.
6. Grothey A et al. Duration of adjuvant chemotherapy for stage III colon cancer. N Engl J Med. 2018;378(13):1177-88.
7. Von Minckwitz G et al. Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer. N Engl J Med. 2017;377(2):122-31.
8. American Society of Clinical Oncology: Ten Things Physician and Patients Should Question.
9. Temel JS et al. Early palliative care for patients with metastatic non–small cell lung cancer. N Engl J Med. 2010;363(8):733-42.
10. Blayney DW et al. Critical lessons from high-value oncology practices. JAMA Oncol. 2018 Feb 1;4(2):164-71.
11. Sherman DE. Transforming practices through the oncology care model: financial toxicity and counseling. J Oncol Pract. 2017 Aug;13(8):519-22.
Lessons from KEYNOTE-158 and the role of R-CHOP
In this edition of “How I will treat my next patient,” I take a look at two recent trials – one offers potential in previously-treated cervical cancer patients with poor prognosis and the other confirms the role of R-CHOP as the standard of care in diffuse large B-cell lymphoma.
Pembrolizumab in KEYNOTE-158
In an international phase 2 “basket trial,” Hyun Cheol Chung, MD, PhD, and colleagues used pembrolizumab 200 mg every 3 weeks in 98 previously treated patients with advanced cervical cancer. Almost 84% of o the patients had PD-L1 positive tumors (greater than 1%). The authors said that viral induction of malignancy leads to antigen production and upregulation of PD-1. Therefore, advanced cervical cancer patients would likely express PD-L1 on tumor cells and respond to immune checkpoint inhibitor therapy.
In this interim report, there were 12 responses (all in PD-L1 positive patients), with three complete responses. Median response duration had not been reached at median follow-up of 10.2 months. Seven of 12 responses were ongoing at 12 months. There were grade 3-4 adverse events in 12.2% of patients and no treatment-related deaths.
The study – “Efficacy and Safety of Pembrolizumab in Previously Treated Advanced Cervical Cancer: Results From the Phase II KEYNOTE-158 Study” – was published in the Journal of Clinical Oncology (2019 April 3. doi: 10.1200/JCO.18.01265).
The encouraging results of pembrolizumab in this generally chemotherapy-refractory patient population were consistent with other small, early-phase studies investigating immune checkpoint inhibitors that led to the accelerated approval of pembrolizumab in previously treated PD-L1 advanced cervical cancer patients with progressive disease after chemotherapy.
What this means in practice
Although excitement should be tempered about an interim report of an organ-specific subset of a phase 2 international basket trial that was heavily populated by young PS 0-1 patients and generated an overall response rate of less than 15%, no conventional chemotherapy or biologic agent offers the potential of complete or prolonged response, and disease control rates of 30%.
Clinical trials should always be the first choice, but immune checkpoint inhibitors offer an attractive off-study option.
Among many single agents in National Comprehensive Cancer Network guidelines for recurrent advanced cervical cancer after first-line cisplatin-based chemotherapy, there is a reason why pembrolizumab is listed first. For patients with PD-L1 expressing tumors or MSI-H/dMMR tumors, I would use it.
Frontline therapy in DLBCL
In a large, randomized phase 3 trial, close to 500 stage III-IV patients with diffuse large B-cell lymphoma (DLBCL), including primary mediastinal B-cell lymphoma and intravascular large B-cell lymphoma, were assigned to receive either conventional R-CHOP chemotherapy or the more complex, more toxic DA-EPOCH-R regimen that appeared superior in single-institution studies and was feasible in multi-institutional phase 2 trials.
The study – “Dose-Adjusted EPOCH-R Compared With R-CHOP as Frontline Therapy for Diffuse Large B-Cell Lymphoma: Clinical Outcomes of the Phase III Intergroup Trial Alliance/CALGB 50303” – was published in the Journal of Clinical Oncology (2019 Apr 2. doi: 10.1200/JCO.18.01994).
In the study, progression-free survival and overall survival were no different for R-CHOP and DA-EPOCH-R, but – predictably – DA-EPOCH-R was more toxic and had more treatment discontinuations.
R-CHOP had better outcomes than expected. This suggests that patient-selection bias (more favorable histology, fewer high-risk subsets who required urgent therapy) may have been at work.
Further study of DA-EPOCH-R in higher IPI patients or in patients selected because of more adverse molecular features (DE phenotype, MYC+, double hit) is warranted given the poor outcomes with R-CHOP in high-risk patients, intriguing results in single institution trials of DA-EPOCH-R, and the underrepresentation of high-risk patients in the current study.
What this means in practice
Whether by virtue of the types of patients enrolled or because it is the best regimen in all DLBCL patients, R-CHOP remains the standard of care outside of a clinical trial.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers, and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I will treat my next patient,” I take a look at two recent trials – one offers potential in previously-treated cervical cancer patients with poor prognosis and the other confirms the role of R-CHOP as the standard of care in diffuse large B-cell lymphoma.
Pembrolizumab in KEYNOTE-158
In an international phase 2 “basket trial,” Hyun Cheol Chung, MD, PhD, and colleagues used pembrolizumab 200 mg every 3 weeks in 98 previously treated patients with advanced cervical cancer. Almost 84% of o the patients had PD-L1 positive tumors (greater than 1%). The authors said that viral induction of malignancy leads to antigen production and upregulation of PD-1. Therefore, advanced cervical cancer patients would likely express PD-L1 on tumor cells and respond to immune checkpoint inhibitor therapy.
In this interim report, there were 12 responses (all in PD-L1 positive patients), with three complete responses. Median response duration had not been reached at median follow-up of 10.2 months. Seven of 12 responses were ongoing at 12 months. There were grade 3-4 adverse events in 12.2% of patients and no treatment-related deaths.
The study – “Efficacy and Safety of Pembrolizumab in Previously Treated Advanced Cervical Cancer: Results From the Phase II KEYNOTE-158 Study” – was published in the Journal of Clinical Oncology (2019 April 3. doi: 10.1200/JCO.18.01265).
The encouraging results of pembrolizumab in this generally chemotherapy-refractory patient population were consistent with other small, early-phase studies investigating immune checkpoint inhibitors that led to the accelerated approval of pembrolizumab in previously treated PD-L1 advanced cervical cancer patients with progressive disease after chemotherapy.
What this means in practice
Although excitement should be tempered about an interim report of an organ-specific subset of a phase 2 international basket trial that was heavily populated by young PS 0-1 patients and generated an overall response rate of less than 15%, no conventional chemotherapy or biologic agent offers the potential of complete or prolonged response, and disease control rates of 30%.
Clinical trials should always be the first choice, but immune checkpoint inhibitors offer an attractive off-study option.
Among many single agents in National Comprehensive Cancer Network guidelines for recurrent advanced cervical cancer after first-line cisplatin-based chemotherapy, there is a reason why pembrolizumab is listed first. For patients with PD-L1 expressing tumors or MSI-H/dMMR tumors, I would use it.
Frontline therapy in DLBCL
In a large, randomized phase 3 trial, close to 500 stage III-IV patients with diffuse large B-cell lymphoma (DLBCL), including primary mediastinal B-cell lymphoma and intravascular large B-cell lymphoma, were assigned to receive either conventional R-CHOP chemotherapy or the more complex, more toxic DA-EPOCH-R regimen that appeared superior in single-institution studies and was feasible in multi-institutional phase 2 trials.
The study – “Dose-Adjusted EPOCH-R Compared With R-CHOP as Frontline Therapy for Diffuse Large B-Cell Lymphoma: Clinical Outcomes of the Phase III Intergroup Trial Alliance/CALGB 50303” – was published in the Journal of Clinical Oncology (2019 Apr 2. doi: 10.1200/JCO.18.01994).
In the study, progression-free survival and overall survival were no different for R-CHOP and DA-EPOCH-R, but – predictably – DA-EPOCH-R was more toxic and had more treatment discontinuations.
R-CHOP had better outcomes than expected. This suggests that patient-selection bias (more favorable histology, fewer high-risk subsets who required urgent therapy) may have been at work.
Further study of DA-EPOCH-R in higher IPI patients or in patients selected because of more adverse molecular features (DE phenotype, MYC+, double hit) is warranted given the poor outcomes with R-CHOP in high-risk patients, intriguing results in single institution trials of DA-EPOCH-R, and the underrepresentation of high-risk patients in the current study.
What this means in practice
Whether by virtue of the types of patients enrolled or because it is the best regimen in all DLBCL patients, R-CHOP remains the standard of care outside of a clinical trial.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers, and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I will treat my next patient,” I take a look at two recent trials – one offers potential in previously-treated cervical cancer patients with poor prognosis and the other confirms the role of R-CHOP as the standard of care in diffuse large B-cell lymphoma.
Pembrolizumab in KEYNOTE-158
In an international phase 2 “basket trial,” Hyun Cheol Chung, MD, PhD, and colleagues used pembrolizumab 200 mg every 3 weeks in 98 previously treated patients with advanced cervical cancer. Almost 84% of o the patients had PD-L1 positive tumors (greater than 1%). The authors said that viral induction of malignancy leads to antigen production and upregulation of PD-1. Therefore, advanced cervical cancer patients would likely express PD-L1 on tumor cells and respond to immune checkpoint inhibitor therapy.
In this interim report, there were 12 responses (all in PD-L1 positive patients), with three complete responses. Median response duration had not been reached at median follow-up of 10.2 months. Seven of 12 responses were ongoing at 12 months. There were grade 3-4 adverse events in 12.2% of patients and no treatment-related deaths.
The study – “Efficacy and Safety of Pembrolizumab in Previously Treated Advanced Cervical Cancer: Results From the Phase II KEYNOTE-158 Study” – was published in the Journal of Clinical Oncology (2019 April 3. doi: 10.1200/JCO.18.01265).
The encouraging results of pembrolizumab in this generally chemotherapy-refractory patient population were consistent with other small, early-phase studies investigating immune checkpoint inhibitors that led to the accelerated approval of pembrolizumab in previously treated PD-L1 advanced cervical cancer patients with progressive disease after chemotherapy.
What this means in practice
Although excitement should be tempered about an interim report of an organ-specific subset of a phase 2 international basket trial that was heavily populated by young PS 0-1 patients and generated an overall response rate of less than 15%, no conventional chemotherapy or biologic agent offers the potential of complete or prolonged response, and disease control rates of 30%.
Clinical trials should always be the first choice, but immune checkpoint inhibitors offer an attractive off-study option.
Among many single agents in National Comprehensive Cancer Network guidelines for recurrent advanced cervical cancer after first-line cisplatin-based chemotherapy, there is a reason why pembrolizumab is listed first. For patients with PD-L1 expressing tumors or MSI-H/dMMR tumors, I would use it.
Frontline therapy in DLBCL
In a large, randomized phase 3 trial, close to 500 stage III-IV patients with diffuse large B-cell lymphoma (DLBCL), including primary mediastinal B-cell lymphoma and intravascular large B-cell lymphoma, were assigned to receive either conventional R-CHOP chemotherapy or the more complex, more toxic DA-EPOCH-R regimen that appeared superior in single-institution studies and was feasible in multi-institutional phase 2 trials.
The study – “Dose-Adjusted EPOCH-R Compared With R-CHOP as Frontline Therapy for Diffuse Large B-Cell Lymphoma: Clinical Outcomes of the Phase III Intergroup Trial Alliance/CALGB 50303” – was published in the Journal of Clinical Oncology (2019 Apr 2. doi: 10.1200/JCO.18.01994).
In the study, progression-free survival and overall survival were no different for R-CHOP and DA-EPOCH-R, but – predictably – DA-EPOCH-R was more toxic and had more treatment discontinuations.
R-CHOP had better outcomes than expected. This suggests that patient-selection bias (more favorable histology, fewer high-risk subsets who required urgent therapy) may have been at work.
Further study of DA-EPOCH-R in higher IPI patients or in patients selected because of more adverse molecular features (DE phenotype, MYC+, double hit) is warranted given the poor outcomes with R-CHOP in high-risk patients, intriguing results in single institution trials of DA-EPOCH-R, and the underrepresentation of high-risk patients in the current study.
What this means in practice
Whether by virtue of the types of patients enrolled or because it is the best regimen in all DLBCL patients, R-CHOP remains the standard of care outside of a clinical trial.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers, and in expanding access to clinical trials to medically underserved populations.
Teen e-cigarette use: A public health crisis
After 2 decades of steady decline in adolescent and young adult use of tobacco products, e-cigarettes have dramatically altered the landscape of substance use in youth. E-cigarette use among teens has been on the rise for years but the recent exponential increase is unprecedented. From 2017 to 2018, adolescent e-cigarette use had the largest year-to-year increase (78%, from 12% to 21%) of any individual substance or class of substances at any time during the past 2 decades of nationwide monitoring.1 This has appropriately caught the nation’s attention. In 2016, Surgeon General Vivek H. Murthy, MD, commissioned an extensive report about electronic cigarettes, and in 2018 Surgeon General Jerome Adams, MD, MPH, issued an advisory declaring e-cigarettes a public health crisis for adolescents.2
E-cigarettes have received attention as a possible boon to adult cigarette smokers seeking a less hazardous product. We can consider the use of tobacco products along a continuum from smoked tobacco, dual use (both smoked tobacco and electronic nicotine delivery), electronic nicotine delivery only, and finally, nonuse. For some adults, transitioning from smoked tobacco products to electronic delivery systems has been a step toward less overall harm from substance use, with a small minority of that population going on to achieve abstinence from all nicotine products.3 For youth and teens, the story has been the opposite. With the rapid rise of e-cigarettes, adolescents overwhelmingly have been moving in the wrong direction at each potential step along this continuum.4 Less than 8% of teens who use e-cigarettes indicated that smoking cessation is a factor in their use.5 An estimated 1.3 million U.S. teens now are dependent or at high risk for dependence upon nicotine because of e-cigarette use. Furthermore, these teens are at a fourfold higher risk of progression to cigarette use, compared with their peers.6
One product in particular gives us information as to why this trend has accelerated so rapidly. Juul, now the sales leader among electronic nicotine delivery systems, rose from approximately 25% to a dominant 75% of market share in just over 1 fiscal year after a social media campaign targeted toward youth and young adults. The device is shaped like an elongated flash drive, is marketed as “sleek,” “looking cool,” and being “super easy” to use. This product touts its use of nicotine salts that can deliver higher concentrations of nicotine more rapidly to mimic the experience of smoking a cigarette as closely as possible. The fruity flavors in Juul “pods” and many other devices also appeal to teens. Many youth are left misinformed, thinking they are using a relatively harmless alternative to cigarettes.
E-cigarette use in youth carries many risks. Among the physical risks is exposure to harmful chemicals (even if less numerous than smoked tobacco products) such as diacetyl (a known cause of bronchiolitis obliterans, or “popcorn lung”), formaldehyde, acrolein, benzene, and metals such as nickel, tin and lead.7 “Safer than cigarettes” is a low bar indeed. Cognitive and emotional risks of early nicotine exposure include poor focus and attention, permanent lowering of impulse control, and a higher risk of mood and anxiety disorders.
Furthermore, nicotine is a gateway drug, with a clearly understood molecular basis for how it can potentiate the effects of later used substances, especially stimulants such as cocaine.8 The gateway and priming effect is compounded for youth because of ongoing brain development and plasticity during teen years. E-cigarette use also is associated with other risk behaviors including a manyfold higher likelihood of binge drinking, having multiple sexual partners in a short period of time, and using other substances such as cannabis, cocaine, methamphetamine, and heroin or nonprescribed opioids.9 An electronic system for vaporization also presents a risk for use of other substances. In just 1 year from 2017 to 2018, marijuana “vaping” increased by more than 50% among all ages surveyed.10
Pediatric health care providers are essential educators for both teens and parents regarding the risks of e-cigarette use. Many youth don’t know what they’re using; 66% of youth reported that the vapors they were inhaling contained only flavoring. Only 13% reported they were inhaling nicotine.10 In stark contrast to these self-reports, all Juul “pods” contain nicotine. As has been a pattern with nationwide surveys of substance use for decades, adolescent use is inversely correlated with perception of risk; 70% of 8th-12th graders do not foresee great harm in regular e-cigarette use. In addition, adolescents use substances less often when they know their parents disapprove. Parents also must be taught about the risks of e-cigarette use and can be provided with resources and taught effective strategies if they have difficulty communicating their disapproval to their children.
Age-appropriate screening in primary care settings must include specific language regarding the use of electronic cigarettes, with questions about “vaping” and “juuling.” Discussions with teens may be more effective with emphasis on issues that resonate with youth such as the financial cost, loss of freedom when dependence develops, and the fact that their generation is once again being targeted by the tobacco industry. Referral for further treatment, including individual and group therapy as well as family-focused interventions, should be considered for teens who use daily, use other substances regularly, or could benefit from treatment for co-occurring mental health disorders.
Electronic cigarette use should not be recommended as a smoking cessation strategy for teens.11 Pediatric health care providers must advocate for regulation of these products, including increasing the legal age of purchase and banning flavoring in e-cigarettes products, Internet sales, and advertisements targeted to youth.
The rapid rise in e-cigarette use among teens is of great concern. As with all classes of substances, early initiation of nicotine drastically increases the risk of developing a substance use disorder and portends a prolonged course and greater accumulation of adverse consequences. There is an urgent need for education, prevention, and early identification of e-cigarette use to protect the current and future well-being of children and adolescents.
Dr. Jackson is assistant professor of psychiatry at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email Dr. Jackson at [email protected].
References
1. MMWR Morb Mortal Wkly Rep. 2018;67:1276-7.
2. e-cigarettes.surgeongeneral.gov
3. N Engl J Med 2019;380:629-37.
4. Pediatrics. 2018 Dec; 142(6):e20180486.
5. MMWR Morb Mortal Wkly Rep 2018;67:196-200.
6. JAMA Pediatr. 2017 Aug 1;171(8):788-97.
7. “Public health consequences of e-cigarettes” (Washington, DC: National Academies Press, January 2018).
8. N Engl J Med 2014;371:932-43.
9. N Engl J Med 2019;380:689-90.
10. MMWR Morb Mortal Wkly Rep. 2016 Jan 8;64(52):1403-8.
11. Pediatrics. 2019 Feb;143(2). pii: e20183652.
After 2 decades of steady decline in adolescent and young adult use of tobacco products, e-cigarettes have dramatically altered the landscape of substance use in youth. E-cigarette use among teens has been on the rise for years but the recent exponential increase is unprecedented. From 2017 to 2018, adolescent e-cigarette use had the largest year-to-year increase (78%, from 12% to 21%) of any individual substance or class of substances at any time during the past 2 decades of nationwide monitoring.1 This has appropriately caught the nation’s attention. In 2016, Surgeon General Vivek H. Murthy, MD, commissioned an extensive report about electronic cigarettes, and in 2018 Surgeon General Jerome Adams, MD, MPH, issued an advisory declaring e-cigarettes a public health crisis for adolescents.2
E-cigarettes have received attention as a possible boon to adult cigarette smokers seeking a less hazardous product. We can consider the use of tobacco products along a continuum from smoked tobacco, dual use (both smoked tobacco and electronic nicotine delivery), electronic nicotine delivery only, and finally, nonuse. For some adults, transitioning from smoked tobacco products to electronic delivery systems has been a step toward less overall harm from substance use, with a small minority of that population going on to achieve abstinence from all nicotine products.3 For youth and teens, the story has been the opposite. With the rapid rise of e-cigarettes, adolescents overwhelmingly have been moving in the wrong direction at each potential step along this continuum.4 Less than 8% of teens who use e-cigarettes indicated that smoking cessation is a factor in their use.5 An estimated 1.3 million U.S. teens now are dependent or at high risk for dependence upon nicotine because of e-cigarette use. Furthermore, these teens are at a fourfold higher risk of progression to cigarette use, compared with their peers.6
One product in particular gives us information as to why this trend has accelerated so rapidly. Juul, now the sales leader among electronic nicotine delivery systems, rose from approximately 25% to a dominant 75% of market share in just over 1 fiscal year after a social media campaign targeted toward youth and young adults. The device is shaped like an elongated flash drive, is marketed as “sleek,” “looking cool,” and being “super easy” to use. This product touts its use of nicotine salts that can deliver higher concentrations of nicotine more rapidly to mimic the experience of smoking a cigarette as closely as possible. The fruity flavors in Juul “pods” and many other devices also appeal to teens. Many youth are left misinformed, thinking they are using a relatively harmless alternative to cigarettes.
E-cigarette use in youth carries many risks. Among the physical risks is exposure to harmful chemicals (even if less numerous than smoked tobacco products) such as diacetyl (a known cause of bronchiolitis obliterans, or “popcorn lung”), formaldehyde, acrolein, benzene, and metals such as nickel, tin and lead.7 “Safer than cigarettes” is a low bar indeed. Cognitive and emotional risks of early nicotine exposure include poor focus and attention, permanent lowering of impulse control, and a higher risk of mood and anxiety disorders.
Furthermore, nicotine is a gateway drug, with a clearly understood molecular basis for how it can potentiate the effects of later used substances, especially stimulants such as cocaine.8 The gateway and priming effect is compounded for youth because of ongoing brain development and plasticity during teen years. E-cigarette use also is associated with other risk behaviors including a manyfold higher likelihood of binge drinking, having multiple sexual partners in a short period of time, and using other substances such as cannabis, cocaine, methamphetamine, and heroin or nonprescribed opioids.9 An electronic system for vaporization also presents a risk for use of other substances. In just 1 year from 2017 to 2018, marijuana “vaping” increased by more than 50% among all ages surveyed.10
Pediatric health care providers are essential educators for both teens and parents regarding the risks of e-cigarette use. Many youth don’t know what they’re using; 66% of youth reported that the vapors they were inhaling contained only flavoring. Only 13% reported they were inhaling nicotine.10 In stark contrast to these self-reports, all Juul “pods” contain nicotine. As has been a pattern with nationwide surveys of substance use for decades, adolescent use is inversely correlated with perception of risk; 70% of 8th-12th graders do not foresee great harm in regular e-cigarette use. In addition, adolescents use substances less often when they know their parents disapprove. Parents also must be taught about the risks of e-cigarette use and can be provided with resources and taught effective strategies if they have difficulty communicating their disapproval to their children.
Age-appropriate screening in primary care settings must include specific language regarding the use of electronic cigarettes, with questions about “vaping” and “juuling.” Discussions with teens may be more effective with emphasis on issues that resonate with youth such as the financial cost, loss of freedom when dependence develops, and the fact that their generation is once again being targeted by the tobacco industry. Referral for further treatment, including individual and group therapy as well as family-focused interventions, should be considered for teens who use daily, use other substances regularly, or could benefit from treatment for co-occurring mental health disorders.
Electronic cigarette use should not be recommended as a smoking cessation strategy for teens.11 Pediatric health care providers must advocate for regulation of these products, including increasing the legal age of purchase and banning flavoring in e-cigarettes products, Internet sales, and advertisements targeted to youth.
The rapid rise in e-cigarette use among teens is of great concern. As with all classes of substances, early initiation of nicotine drastically increases the risk of developing a substance use disorder and portends a prolonged course and greater accumulation of adverse consequences. There is an urgent need for education, prevention, and early identification of e-cigarette use to protect the current and future well-being of children and adolescents.
Dr. Jackson is assistant professor of psychiatry at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email Dr. Jackson at [email protected].
References
1. MMWR Morb Mortal Wkly Rep. 2018;67:1276-7.
2. e-cigarettes.surgeongeneral.gov
3. N Engl J Med 2019;380:629-37.
4. Pediatrics. 2018 Dec; 142(6):e20180486.
5. MMWR Morb Mortal Wkly Rep 2018;67:196-200.
6. JAMA Pediatr. 2017 Aug 1;171(8):788-97.
7. “Public health consequences of e-cigarettes” (Washington, DC: National Academies Press, January 2018).
8. N Engl J Med 2014;371:932-43.
9. N Engl J Med 2019;380:689-90.
10. MMWR Morb Mortal Wkly Rep. 2016 Jan 8;64(52):1403-8.
11. Pediatrics. 2019 Feb;143(2). pii: e20183652.
After 2 decades of steady decline in adolescent and young adult use of tobacco products, e-cigarettes have dramatically altered the landscape of substance use in youth. E-cigarette use among teens has been on the rise for years but the recent exponential increase is unprecedented. From 2017 to 2018, adolescent e-cigarette use had the largest year-to-year increase (78%, from 12% to 21%) of any individual substance or class of substances at any time during the past 2 decades of nationwide monitoring.1 This has appropriately caught the nation’s attention. In 2016, Surgeon General Vivek H. Murthy, MD, commissioned an extensive report about electronic cigarettes, and in 2018 Surgeon General Jerome Adams, MD, MPH, issued an advisory declaring e-cigarettes a public health crisis for adolescents.2
E-cigarettes have received attention as a possible boon to adult cigarette smokers seeking a less hazardous product. We can consider the use of tobacco products along a continuum from smoked tobacco, dual use (both smoked tobacco and electronic nicotine delivery), electronic nicotine delivery only, and finally, nonuse. For some adults, transitioning from smoked tobacco products to electronic delivery systems has been a step toward less overall harm from substance use, with a small minority of that population going on to achieve abstinence from all nicotine products.3 For youth and teens, the story has been the opposite. With the rapid rise of e-cigarettes, adolescents overwhelmingly have been moving in the wrong direction at each potential step along this continuum.4 Less than 8% of teens who use e-cigarettes indicated that smoking cessation is a factor in their use.5 An estimated 1.3 million U.S. teens now are dependent or at high risk for dependence upon nicotine because of e-cigarette use. Furthermore, these teens are at a fourfold higher risk of progression to cigarette use, compared with their peers.6
One product in particular gives us information as to why this trend has accelerated so rapidly. Juul, now the sales leader among electronic nicotine delivery systems, rose from approximately 25% to a dominant 75% of market share in just over 1 fiscal year after a social media campaign targeted toward youth and young adults. The device is shaped like an elongated flash drive, is marketed as “sleek,” “looking cool,” and being “super easy” to use. This product touts its use of nicotine salts that can deliver higher concentrations of nicotine more rapidly to mimic the experience of smoking a cigarette as closely as possible. The fruity flavors in Juul “pods” and many other devices also appeal to teens. Many youth are left misinformed, thinking they are using a relatively harmless alternative to cigarettes.
E-cigarette use in youth carries many risks. Among the physical risks is exposure to harmful chemicals (even if less numerous than smoked tobacco products) such as diacetyl (a known cause of bronchiolitis obliterans, or “popcorn lung”), formaldehyde, acrolein, benzene, and metals such as nickel, tin and lead.7 “Safer than cigarettes” is a low bar indeed. Cognitive and emotional risks of early nicotine exposure include poor focus and attention, permanent lowering of impulse control, and a higher risk of mood and anxiety disorders.
Furthermore, nicotine is a gateway drug, with a clearly understood molecular basis for how it can potentiate the effects of later used substances, especially stimulants such as cocaine.8 The gateway and priming effect is compounded for youth because of ongoing brain development and plasticity during teen years. E-cigarette use also is associated with other risk behaviors including a manyfold higher likelihood of binge drinking, having multiple sexual partners in a short period of time, and using other substances such as cannabis, cocaine, methamphetamine, and heroin or nonprescribed opioids.9 An electronic system for vaporization also presents a risk for use of other substances. In just 1 year from 2017 to 2018, marijuana “vaping” increased by more than 50% among all ages surveyed.10
Pediatric health care providers are essential educators for both teens and parents regarding the risks of e-cigarette use. Many youth don’t know what they’re using; 66% of youth reported that the vapors they were inhaling contained only flavoring. Only 13% reported they were inhaling nicotine.10 In stark contrast to these self-reports, all Juul “pods” contain nicotine. As has been a pattern with nationwide surveys of substance use for decades, adolescent use is inversely correlated with perception of risk; 70% of 8th-12th graders do not foresee great harm in regular e-cigarette use. In addition, adolescents use substances less often when they know their parents disapprove. Parents also must be taught about the risks of e-cigarette use and can be provided with resources and taught effective strategies if they have difficulty communicating their disapproval to their children.
Age-appropriate screening in primary care settings must include specific language regarding the use of electronic cigarettes, with questions about “vaping” and “juuling.” Discussions with teens may be more effective with emphasis on issues that resonate with youth such as the financial cost, loss of freedom when dependence develops, and the fact that their generation is once again being targeted by the tobacco industry. Referral for further treatment, including individual and group therapy as well as family-focused interventions, should be considered for teens who use daily, use other substances regularly, or could benefit from treatment for co-occurring mental health disorders.
Electronic cigarette use should not be recommended as a smoking cessation strategy for teens.11 Pediatric health care providers must advocate for regulation of these products, including increasing the legal age of purchase and banning flavoring in e-cigarettes products, Internet sales, and advertisements targeted to youth.
The rapid rise in e-cigarette use among teens is of great concern. As with all classes of substances, early initiation of nicotine drastically increases the risk of developing a substance use disorder and portends a prolonged course and greater accumulation of adverse consequences. There is an urgent need for education, prevention, and early identification of e-cigarette use to protect the current and future well-being of children and adolescents.
Dr. Jackson is assistant professor of psychiatry at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email Dr. Jackson at [email protected].
References
1. MMWR Morb Mortal Wkly Rep. 2018;67:1276-7.
2. e-cigarettes.surgeongeneral.gov
3. N Engl J Med 2019;380:629-37.
4. Pediatrics. 2018 Dec; 142(6):e20180486.
5. MMWR Morb Mortal Wkly Rep 2018;67:196-200.
6. JAMA Pediatr. 2017 Aug 1;171(8):788-97.
7. “Public health consequences of e-cigarettes” (Washington, DC: National Academies Press, January 2018).
8. N Engl J Med 2014;371:932-43.
9. N Engl J Med 2019;380:689-90.
10. MMWR Morb Mortal Wkly Rep. 2016 Jan 8;64(52):1403-8.
11. Pediatrics. 2019 Feb;143(2). pii: e20183652.