User login
Poster ads don’t belong in the clinic
In the last few months, I’ve received several posters. They’re always delivered by UPS, and come in a solid cardboard box to keep them from being crushed.
The boxes get opened, and once I know what they are, the whole thing gets tossed in the office recycling.
I know they’re presented as helpful patient information, with some bullet lists and glossy graphics showing brains, nerve transmitters, or patients. But the basic reality is that they’re just advertisements. Like infomercials on TV, they come across as professional and interesting, but at their heart and soul are just selling something.
No thanks.
Years ago, a company sent me a poster listing the warning signs of stroke. Although it was still an advertisement, I decided to hang it up in my exam room as a sort of public service announcement. Unfortunately, I soon discovered that any patient left staring at it for more than 1-2 minutes would start to complain of at least two of the symptoms listed. It got taken down after a few days.
I have nothing against advertising. It pays for websites, television shows, sporting events, newspapers, and magazines.
But my exam room isn’t the place for it. Patients are bombarded with direct-to-consumer advertising for many drugs in every media outlet. The doctor’s discussion room shouldn’t be one of the them.
The meeting between me and a patient should be frank, honest assessments about what should be done and what, specifically, is best for their individual case. I don’t need marketing for a drug that may or may not be appropriate, or easily covered by insurance, staring back at them.
It’s a thin line. Obviously, magazines out in my lobby are full of pharmaceutical ads, and that doesn’t bother me. But once a patient crosses the line into my consultation area it should just be between me and them.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In the last few months, I’ve received several posters. They’re always delivered by UPS, and come in a solid cardboard box to keep them from being crushed.
The boxes get opened, and once I know what they are, the whole thing gets tossed in the office recycling.
I know they’re presented as helpful patient information, with some bullet lists and glossy graphics showing brains, nerve transmitters, or patients. But the basic reality is that they’re just advertisements. Like infomercials on TV, they come across as professional and interesting, but at their heart and soul are just selling something.
No thanks.
Years ago, a company sent me a poster listing the warning signs of stroke. Although it was still an advertisement, I decided to hang it up in my exam room as a sort of public service announcement. Unfortunately, I soon discovered that any patient left staring at it for more than 1-2 minutes would start to complain of at least two of the symptoms listed. It got taken down after a few days.
I have nothing against advertising. It pays for websites, television shows, sporting events, newspapers, and magazines.
But my exam room isn’t the place for it. Patients are bombarded with direct-to-consumer advertising for many drugs in every media outlet. The doctor’s discussion room shouldn’t be one of the them.
The meeting between me and a patient should be frank, honest assessments about what should be done and what, specifically, is best for their individual case. I don’t need marketing for a drug that may or may not be appropriate, or easily covered by insurance, staring back at them.
It’s a thin line. Obviously, magazines out in my lobby are full of pharmaceutical ads, and that doesn’t bother me. But once a patient crosses the line into my consultation area it should just be between me and them.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In the last few months, I’ve received several posters. They’re always delivered by UPS, and come in a solid cardboard box to keep them from being crushed.
The boxes get opened, and once I know what they are, the whole thing gets tossed in the office recycling.
I know they’re presented as helpful patient information, with some bullet lists and glossy graphics showing brains, nerve transmitters, or patients. But the basic reality is that they’re just advertisements. Like infomercials on TV, they come across as professional and interesting, but at their heart and soul are just selling something.
No thanks.
Years ago, a company sent me a poster listing the warning signs of stroke. Although it was still an advertisement, I decided to hang it up in my exam room as a sort of public service announcement. Unfortunately, I soon discovered that any patient left staring at it for more than 1-2 minutes would start to complain of at least two of the symptoms listed. It got taken down after a few days.
I have nothing against advertising. It pays for websites, television shows, sporting events, newspapers, and magazines.
But my exam room isn’t the place for it. Patients are bombarded with direct-to-consumer advertising for many drugs in every media outlet. The doctor’s discussion room shouldn’t be one of the them.
The meeting between me and a patient should be frank, honest assessments about what should be done and what, specifically, is best for their individual case. I don’t need marketing for a drug that may or may not be appropriate, or easily covered by insurance, staring back at them.
It’s a thin line. Obviously, magazines out in my lobby are full of pharmaceutical ads, and that doesn’t bother me. But once a patient crosses the line into my consultation area it should just be between me and them.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A chance to unite
Is America coming apart at the seams? According to the press, there are more things that divide us than bind us together. It’s red state versus blue state, it’s the privileged versus the disadvantaged, people of color versus the white majority. Could the great melting pot have cooled and its contents settled out into a dozen stratified layers?
Despite the image of a divided America that we see portrayed in the newspapers and on television, I continue to believe that there is more that we share in common than separate us, but it’s a struggle. The media operate on the assumption that conflict draws more readers than good news about cooperation and compromise. The situation is compounded by the apparent absence of a leader from either party who wants to unite us.
However, when one scratches the surface, there is surprising amount of agreement among Americans. For example, according to John Gramlich (“7 facts about guns in the U.S.,” Pew Research Center, Dec. 27, 2018), 89% of both Republicans and Democrats feel that people with mental illness should not be allowed to purchase a gun. And 79% of Republicans and 91% of Democrats favor background checks at gun shows and for private sales for purchase of a gun. As of 2018, 58% of Americans feel that abortion should be legal in all or most cases, and only 37% feel it should be illegal in all or most cases. (“Public Opinion on Abortion,” Pew Research Center, Oct. 15, 2018).
At the core of many of our struggles to unite is a question that has bedeviled democracies for millennia: How does one balance a citizen’s freedom of choice with the health and safety of the society in which that person lives? While resolutions on gun control and abortion seem unlikely in the foreseeable future, the current outbreaks of measles offer America a rare opportunity to unite on an issue that pits personal freedom against societal safety.
According to Virginia Villa (“5 facts about vaccines in the U.S.,” Pew Research Center, Mar. 19, 2019), 82% of adults in the United States believe that the MMR vaccine should be required for public school attendance, while only 17% believe that parents should be allowed to leave their child unvaccinated even if their decision creates a health risk for other children and adults.
Why should we expect the government to respond to protect the population from the risk posed by the unvaccinated minority when it has done very little to further gun control? Obviously a key difference is that the antivaccination minority lacks the financial resources and political muscle of a large organization such as the National Rifle Association. While we must never underestimate the power of social media, the publicity surfacing from the mainstream media as the measles outbreaks in the United States have continued has prompted several states to rethink their policies regarding vaccination requirements and school attendance. Here in Maine, there has been strong support among the legislature for eliminating exemptions for philosophic or religious exemptions.
It is probably unrealistic to expect the federal government to act on the health threat caused by the antivaccine movement. However, it is encouraging that, at least at the local level, there is hope for closing one of the wounds that divide us. As providers who care for children, we should seize this opportunity created by the measles outbreaks to promote legislation and policies that strike a sensible balance between the right of the individual and the safety of the society at large.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Is America coming apart at the seams? According to the press, there are more things that divide us than bind us together. It’s red state versus blue state, it’s the privileged versus the disadvantaged, people of color versus the white majority. Could the great melting pot have cooled and its contents settled out into a dozen stratified layers?
Despite the image of a divided America that we see portrayed in the newspapers and on television, I continue to believe that there is more that we share in common than separate us, but it’s a struggle. The media operate on the assumption that conflict draws more readers than good news about cooperation and compromise. The situation is compounded by the apparent absence of a leader from either party who wants to unite us.
However, when one scratches the surface, there is surprising amount of agreement among Americans. For example, according to John Gramlich (“7 facts about guns in the U.S.,” Pew Research Center, Dec. 27, 2018), 89% of both Republicans and Democrats feel that people with mental illness should not be allowed to purchase a gun. And 79% of Republicans and 91% of Democrats favor background checks at gun shows and for private sales for purchase of a gun. As of 2018, 58% of Americans feel that abortion should be legal in all or most cases, and only 37% feel it should be illegal in all or most cases. (“Public Opinion on Abortion,” Pew Research Center, Oct. 15, 2018).
At the core of many of our struggles to unite is a question that has bedeviled democracies for millennia: How does one balance a citizen’s freedom of choice with the health and safety of the society in which that person lives? While resolutions on gun control and abortion seem unlikely in the foreseeable future, the current outbreaks of measles offer America a rare opportunity to unite on an issue that pits personal freedom against societal safety.
According to Virginia Villa (“5 facts about vaccines in the U.S.,” Pew Research Center, Mar. 19, 2019), 82% of adults in the United States believe that the MMR vaccine should be required for public school attendance, while only 17% believe that parents should be allowed to leave their child unvaccinated even if their decision creates a health risk for other children and adults.
Why should we expect the government to respond to protect the population from the risk posed by the unvaccinated minority when it has done very little to further gun control? Obviously a key difference is that the antivaccination minority lacks the financial resources and political muscle of a large organization such as the National Rifle Association. While we must never underestimate the power of social media, the publicity surfacing from the mainstream media as the measles outbreaks in the United States have continued has prompted several states to rethink their policies regarding vaccination requirements and school attendance. Here in Maine, there has been strong support among the legislature for eliminating exemptions for philosophic or religious exemptions.
It is probably unrealistic to expect the federal government to act on the health threat caused by the antivaccine movement. However, it is encouraging that, at least at the local level, there is hope for closing one of the wounds that divide us. As providers who care for children, we should seize this opportunity created by the measles outbreaks to promote legislation and policies that strike a sensible balance between the right of the individual and the safety of the society at large.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Is America coming apart at the seams? According to the press, there are more things that divide us than bind us together. It’s red state versus blue state, it’s the privileged versus the disadvantaged, people of color versus the white majority. Could the great melting pot have cooled and its contents settled out into a dozen stratified layers?
Despite the image of a divided America that we see portrayed in the newspapers and on television, I continue to believe that there is more that we share in common than separate us, but it’s a struggle. The media operate on the assumption that conflict draws more readers than good news about cooperation and compromise. The situation is compounded by the apparent absence of a leader from either party who wants to unite us.
However, when one scratches the surface, there is surprising amount of agreement among Americans. For example, according to John Gramlich (“7 facts about guns in the U.S.,” Pew Research Center, Dec. 27, 2018), 89% of both Republicans and Democrats feel that people with mental illness should not be allowed to purchase a gun. And 79% of Republicans and 91% of Democrats favor background checks at gun shows and for private sales for purchase of a gun. As of 2018, 58% of Americans feel that abortion should be legal in all or most cases, and only 37% feel it should be illegal in all or most cases. (“Public Opinion on Abortion,” Pew Research Center, Oct. 15, 2018).
At the core of many of our struggles to unite is a question that has bedeviled democracies for millennia: How does one balance a citizen’s freedom of choice with the health and safety of the society in which that person lives? While resolutions on gun control and abortion seem unlikely in the foreseeable future, the current outbreaks of measles offer America a rare opportunity to unite on an issue that pits personal freedom against societal safety.
According to Virginia Villa (“5 facts about vaccines in the U.S.,” Pew Research Center, Mar. 19, 2019), 82% of adults in the United States believe that the MMR vaccine should be required for public school attendance, while only 17% believe that parents should be allowed to leave their child unvaccinated even if their decision creates a health risk for other children and adults.
Why should we expect the government to respond to protect the population from the risk posed by the unvaccinated minority when it has done very little to further gun control? Obviously a key difference is that the antivaccination minority lacks the financial resources and political muscle of a large organization such as the National Rifle Association. While we must never underestimate the power of social media, the publicity surfacing from the mainstream media as the measles outbreaks in the United States have continued has prompted several states to rethink their policies regarding vaccination requirements and school attendance. Here in Maine, there has been strong support among the legislature for eliminating exemptions for philosophic or religious exemptions.
It is probably unrealistic to expect the federal government to act on the health threat caused by the antivaccine movement. However, it is encouraging that, at least at the local level, there is hope for closing one of the wounds that divide us. As providers who care for children, we should seize this opportunity created by the measles outbreaks to promote legislation and policies that strike a sensible balance between the right of the individual and the safety of the society at large.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
A state of mind
Are you happy with your current situation? Do you enjoy your job and look forward to getting home at the end of the day? Or, do you find your work unrewarding? Do you consider your home simply a place to wait impatiently until you can hop on a plane for your next getaway vacation?
Maybe you should consider relocating to Montana. According to the headline in an article by Richard Franki in Pediatric News (“Montana named ‘best state to practice medicine’ in 2019,” Mar. 28, 2019) the Treasure State is currently the best state to practice medicine. Big Sky Country earned this distinction by outdistancing 49 states and Washington, D.C., in a ranking by WalletHub. The personal finance website used 18 metrics ranging from average annual wage adjusted for cost of living to malpractice award payment per capita. One category of metrics grouped data related to “competition and opportunity” and the other “medical environment.”
I suspect that you are as skeptical as I am of surveys that claim to rank complex entities across broad geographic landscapes. I hope you are neither depressed or elated when your alma mater moves three positions on U.S. News and World Report’s ranking of colleges and universities. However, there are a few pearls hidden in this WalletHub attempt at choosing the most physician-friendly states.
New York was again ranked the worst state to practice medicine, a distinction it had “earned” in 2017 with a highest cost of malpractice insurance. This consistency suggests that there is a litigious atmosphere, at least in some parts of New York, that could make forging a trusting doctor-patient relationship difficult. Heading off to work each morning under the dark cloud of malpractice must take a lot of the fun out of practicing medicine.
The other interesting association buried in the ranking is that Montana is at the top of the list because it also was the state with the highest percentage of “medical residents retained.” This concurrence suggests that living and working in Big Sky Country provided a balance that young physicians found not just tolerable but so enjoyable they wanted to stay. I have been unable to find a complete listing of the raw data, but I suspect that Maine also could boast a high percentage of medical residents who choose to remain at the end of their training. It has been and continues to be a wonderful place to live and raise a family.
While there may be days when you feel as though the practice of medicine has consumed your every waking moment, the truth is that there is more to life than being a physician. Of course, one must be able to earn enough to support oneself and family, but this survey that purports to rank the best place to practice is too heavily weighted to the financial side of the equation and ignores the more difficult to quantify lifestyle qualities.
You may have found a position that pays well enough but requires a time-gobbling and stress-inducing commute to a place you feel comfortable living. Or, you may like your work, but find the community where you have settled lacks the suite of recreational and/or cultural opportunities you enjoy. Not everyone gets it right the first time. Sometimes it is a matter of making compromises and then continuing to reassess whether these compromises have been the best ones.
Regardless of its ranking on any survey, every state has multiple communities in which a physician can have a satisfying career and a lifestyle he or she enjoys. However, achieving this balanced mix may require the physician to invest something of him or herself into making that community one that feels like home.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Are you happy with your current situation? Do you enjoy your job and look forward to getting home at the end of the day? Or, do you find your work unrewarding? Do you consider your home simply a place to wait impatiently until you can hop on a plane for your next getaway vacation?
Maybe you should consider relocating to Montana. According to the headline in an article by Richard Franki in Pediatric News (“Montana named ‘best state to practice medicine’ in 2019,” Mar. 28, 2019) the Treasure State is currently the best state to practice medicine. Big Sky Country earned this distinction by outdistancing 49 states and Washington, D.C., in a ranking by WalletHub. The personal finance website used 18 metrics ranging from average annual wage adjusted for cost of living to malpractice award payment per capita. One category of metrics grouped data related to “competition and opportunity” and the other “medical environment.”
I suspect that you are as skeptical as I am of surveys that claim to rank complex entities across broad geographic landscapes. I hope you are neither depressed or elated when your alma mater moves three positions on U.S. News and World Report’s ranking of colleges and universities. However, there are a few pearls hidden in this WalletHub attempt at choosing the most physician-friendly states.
New York was again ranked the worst state to practice medicine, a distinction it had “earned” in 2017 with a highest cost of malpractice insurance. This consistency suggests that there is a litigious atmosphere, at least in some parts of New York, that could make forging a trusting doctor-patient relationship difficult. Heading off to work each morning under the dark cloud of malpractice must take a lot of the fun out of practicing medicine.
The other interesting association buried in the ranking is that Montana is at the top of the list because it also was the state with the highest percentage of “medical residents retained.” This concurrence suggests that living and working in Big Sky Country provided a balance that young physicians found not just tolerable but so enjoyable they wanted to stay. I have been unable to find a complete listing of the raw data, but I suspect that Maine also could boast a high percentage of medical residents who choose to remain at the end of their training. It has been and continues to be a wonderful place to live and raise a family.
While there may be days when you feel as though the practice of medicine has consumed your every waking moment, the truth is that there is more to life than being a physician. Of course, one must be able to earn enough to support oneself and family, but this survey that purports to rank the best place to practice is too heavily weighted to the financial side of the equation and ignores the more difficult to quantify lifestyle qualities.
You may have found a position that pays well enough but requires a time-gobbling and stress-inducing commute to a place you feel comfortable living. Or, you may like your work, but find the community where you have settled lacks the suite of recreational and/or cultural opportunities you enjoy. Not everyone gets it right the first time. Sometimes it is a matter of making compromises and then continuing to reassess whether these compromises have been the best ones.
Regardless of its ranking on any survey, every state has multiple communities in which a physician can have a satisfying career and a lifestyle he or she enjoys. However, achieving this balanced mix may require the physician to invest something of him or herself into making that community one that feels like home.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Are you happy with your current situation? Do you enjoy your job and look forward to getting home at the end of the day? Or, do you find your work unrewarding? Do you consider your home simply a place to wait impatiently until you can hop on a plane for your next getaway vacation?
Maybe you should consider relocating to Montana. According to the headline in an article by Richard Franki in Pediatric News (“Montana named ‘best state to practice medicine’ in 2019,” Mar. 28, 2019) the Treasure State is currently the best state to practice medicine. Big Sky Country earned this distinction by outdistancing 49 states and Washington, D.C., in a ranking by WalletHub. The personal finance website used 18 metrics ranging from average annual wage adjusted for cost of living to malpractice award payment per capita. One category of metrics grouped data related to “competition and opportunity” and the other “medical environment.”
I suspect that you are as skeptical as I am of surveys that claim to rank complex entities across broad geographic landscapes. I hope you are neither depressed or elated when your alma mater moves three positions on U.S. News and World Report’s ranking of colleges and universities. However, there are a few pearls hidden in this WalletHub attempt at choosing the most physician-friendly states.
New York was again ranked the worst state to practice medicine, a distinction it had “earned” in 2017 with a highest cost of malpractice insurance. This consistency suggests that there is a litigious atmosphere, at least in some parts of New York, that could make forging a trusting doctor-patient relationship difficult. Heading off to work each morning under the dark cloud of malpractice must take a lot of the fun out of practicing medicine.
The other interesting association buried in the ranking is that Montana is at the top of the list because it also was the state with the highest percentage of “medical residents retained.” This concurrence suggests that living and working in Big Sky Country provided a balance that young physicians found not just tolerable but so enjoyable they wanted to stay. I have been unable to find a complete listing of the raw data, but I suspect that Maine also could boast a high percentage of medical residents who choose to remain at the end of their training. It has been and continues to be a wonderful place to live and raise a family.
While there may be days when you feel as though the practice of medicine has consumed your every waking moment, the truth is that there is more to life than being a physician. Of course, one must be able to earn enough to support oneself and family, but this survey that purports to rank the best place to practice is too heavily weighted to the financial side of the equation and ignores the more difficult to quantify lifestyle qualities.
You may have found a position that pays well enough but requires a time-gobbling and stress-inducing commute to a place you feel comfortable living. Or, you may like your work, but find the community where you have settled lacks the suite of recreational and/or cultural opportunities you enjoy. Not everyone gets it right the first time. Sometimes it is a matter of making compromises and then continuing to reassess whether these compromises have been the best ones.
Regardless of its ranking on any survey, every state has multiple communities in which a physician can have a satisfying career and a lifestyle he or she enjoys. However, achieving this balanced mix may require the physician to invest something of him or herself into making that community one that feels like home.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Is childhood cancer associated with assisted reproductive technology?
Recently, two studies were published addressing the potential association of childhood cancer and assisted reproductive technology. For more than a decade and a half, it has been acknowledged that ART is associated with increased concern both with structural birth defects, as well as imprinting disorders. As both of these issues have been linked to greater cancer risk in children, it is important to decipher the impact of ART on childhood cancer risk.
Published online April 1 in JAMA Pediatrics, the study, “Association of in vitro fertilization [IVF] with childhood cancer in the United States,”1 by LG Spector et al. looked retrospectively at birth and cancer registries in 14 states with 8 years of data on 275,686 children were conceived via ART through 2013, who were compared with 2,266,847 children selected randomly.
The overall cancer rate per 1,000,000 person-years was low in both groups: 252 for the IVF group and 193 for the control group, for an overall hazard risk of 1.17. Of note, the rate of hepatic tumors was higher among the IVF group than the non-IVF group (18 vs. 5.7; hazard ratio, 2.46). There appeared to be no association with specific IVF treatments, whether children were conceived by donor egg vs. autologous egg; frozen embryos vs. fresh embryos; use of intracytoplasmic sperm injection (ICSI) vs. none; assisted hatching vs. none; and day-3 vs. day-5 transfer. The researchers concluded that the “increased rate of embryonal cancers, particularly hepatic tumors, that could not be attributed to IVF rather than to underlying infertility.”
This first and largest cohort study of association between IVF and the risk of childhood cancer ever published showed little evidence of excess risk of most cancers, including more common cancers such as leukemia.
The authors did note limitations in their study. Mothers who conceived via IVF were more likely to be white, non-Hispanic, more educated, and older. Could this patient population undergoing ART be at greater risk of producing offspring with cancer concerns? If that were the case – and not great risk of childhood cancer in ART, per se – one therefore would extrapolate that couples undergoing ART vs. alternative infertility treatment should not show a treatment-biased risk (i.e., ART vs. non-ART).
This was demonstrated recently in the study, “Risk of cancer in children and young adults conceived by assisted reproductive technology.”2 This Dutch historical cohort study with prospective follow-up of a median 21 years evaluated 47,690 live-born children, of which 24,269 were ART conceived, 13,761 naturally conceived, and 9,660 conceived naturally or with fertility drugs but not by ART.
Overall, cancer risk was not increased in ART-conceived children, compared with naturally conceived subfertile women or even the general population. A nonsignificant increased risk was observed in children conceived by ICSI or cryopreservation.
On the basis of these two studies, there appears to be no significant increased risk of cancer in children conceived through fertility treatment, including ART.
Although these studies do not support the conclusion reached by a 2013 meta-analysis of 9 studies that specifically looked at ART and 16 other studies that looked at other types of medically assisted reproduction (such medically assisted reproduction as reproduction achieved through ovulation induction; controlled ovarian stimulation; ovulation triggering; intrauterine, intracervical, or intravaginal insemination) which reported a significant increased risk of overall cancers (1.33), including leukemia, CNS cancer, and neuroblastoma,3 they do agree more closely with two prospective studies conducted in the United Kingdom and Nordic countries.
In the U.K. study,4 there was no overall increased risk of cancer associated with ART, but two types of cancer were noted to be higher in the ART-conceived group – hepatoblastoma (3.27 risk) and rhabdomyosarcoma (2.62 risk) – but the absolute risk of these two types of cancer was small in this 17-year study of 106,013 children. This, of course, would be consistent with the JAMA Pediatrics study. In the Nordic study,5 similar to the Dutch Study, IVF was not associated with a significant increased risk of cancer (1.08). The Nordic study included 91,796 children born of ART-assisted pregnancies, compared with 358,419 children born after spontaneous conceptions.
The evidence so far shows that there appears to be no significant increased risk of cancer overall associated with fertility treatments, including IVF.
Dr. Miller is a clinical associate professor at the University of Illinois in Chicago and past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in metropolitan Chicago and the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. He also is a member of Ob.Gyn. News editorial advisory board. Dr. Miller disclosed that he is president of the Advanced IVF Institute in Park Ridge and Naperville, Ill.
References
1. JAMA Pediatr. 2019 Apr 1. doi: 10.1001/jamapediatrics.2019.0392.
2. Hum Reprod. 2019 Apr 1;34(4):740-50.
3. Fertil Steril. 2013 Jul. doi: 10.1016/j.fertnstert.2013.03.017.
4. N Engl J Med. 2013 Nov 7;369(19):1819-27.
5. Hum Reprod. 2014 Sep;29(9):2050-7.
Recently, two studies were published addressing the potential association of childhood cancer and assisted reproductive technology. For more than a decade and a half, it has been acknowledged that ART is associated with increased concern both with structural birth defects, as well as imprinting disorders. As both of these issues have been linked to greater cancer risk in children, it is important to decipher the impact of ART on childhood cancer risk.
Published online April 1 in JAMA Pediatrics, the study, “Association of in vitro fertilization [IVF] with childhood cancer in the United States,”1 by LG Spector et al. looked retrospectively at birth and cancer registries in 14 states with 8 years of data on 275,686 children were conceived via ART through 2013, who were compared with 2,266,847 children selected randomly.
The overall cancer rate per 1,000,000 person-years was low in both groups: 252 for the IVF group and 193 for the control group, for an overall hazard risk of 1.17. Of note, the rate of hepatic tumors was higher among the IVF group than the non-IVF group (18 vs. 5.7; hazard ratio, 2.46). There appeared to be no association with specific IVF treatments, whether children were conceived by donor egg vs. autologous egg; frozen embryos vs. fresh embryos; use of intracytoplasmic sperm injection (ICSI) vs. none; assisted hatching vs. none; and day-3 vs. day-5 transfer. The researchers concluded that the “increased rate of embryonal cancers, particularly hepatic tumors, that could not be attributed to IVF rather than to underlying infertility.”
This first and largest cohort study of association between IVF and the risk of childhood cancer ever published showed little evidence of excess risk of most cancers, including more common cancers such as leukemia.
The authors did note limitations in their study. Mothers who conceived via IVF were more likely to be white, non-Hispanic, more educated, and older. Could this patient population undergoing ART be at greater risk of producing offspring with cancer concerns? If that were the case – and not great risk of childhood cancer in ART, per se – one therefore would extrapolate that couples undergoing ART vs. alternative infertility treatment should not show a treatment-biased risk (i.e., ART vs. non-ART).
This was demonstrated recently in the study, “Risk of cancer in children and young adults conceived by assisted reproductive technology.”2 This Dutch historical cohort study with prospective follow-up of a median 21 years evaluated 47,690 live-born children, of which 24,269 were ART conceived, 13,761 naturally conceived, and 9,660 conceived naturally or with fertility drugs but not by ART.
Overall, cancer risk was not increased in ART-conceived children, compared with naturally conceived subfertile women or even the general population. A nonsignificant increased risk was observed in children conceived by ICSI or cryopreservation.
On the basis of these two studies, there appears to be no significant increased risk of cancer in children conceived through fertility treatment, including ART.
Although these studies do not support the conclusion reached by a 2013 meta-analysis of 9 studies that specifically looked at ART and 16 other studies that looked at other types of medically assisted reproduction (such medically assisted reproduction as reproduction achieved through ovulation induction; controlled ovarian stimulation; ovulation triggering; intrauterine, intracervical, or intravaginal insemination) which reported a significant increased risk of overall cancers (1.33), including leukemia, CNS cancer, and neuroblastoma,3 they do agree more closely with two prospective studies conducted in the United Kingdom and Nordic countries.
In the U.K. study,4 there was no overall increased risk of cancer associated with ART, but two types of cancer were noted to be higher in the ART-conceived group – hepatoblastoma (3.27 risk) and rhabdomyosarcoma (2.62 risk) – but the absolute risk of these two types of cancer was small in this 17-year study of 106,013 children. This, of course, would be consistent with the JAMA Pediatrics study. In the Nordic study,5 similar to the Dutch Study, IVF was not associated with a significant increased risk of cancer (1.08). The Nordic study included 91,796 children born of ART-assisted pregnancies, compared with 358,419 children born after spontaneous conceptions.
The evidence so far shows that there appears to be no significant increased risk of cancer overall associated with fertility treatments, including IVF.
Dr. Miller is a clinical associate professor at the University of Illinois in Chicago and past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in metropolitan Chicago and the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. He also is a member of Ob.Gyn. News editorial advisory board. Dr. Miller disclosed that he is president of the Advanced IVF Institute in Park Ridge and Naperville, Ill.
References
1. JAMA Pediatr. 2019 Apr 1. doi: 10.1001/jamapediatrics.2019.0392.
2. Hum Reprod. 2019 Apr 1;34(4):740-50.
3. Fertil Steril. 2013 Jul. doi: 10.1016/j.fertnstert.2013.03.017.
4. N Engl J Med. 2013 Nov 7;369(19):1819-27.
5. Hum Reprod. 2014 Sep;29(9):2050-7.
Recently, two studies were published addressing the potential association of childhood cancer and assisted reproductive technology. For more than a decade and a half, it has been acknowledged that ART is associated with increased concern both with structural birth defects, as well as imprinting disorders. As both of these issues have been linked to greater cancer risk in children, it is important to decipher the impact of ART on childhood cancer risk.
Published online April 1 in JAMA Pediatrics, the study, “Association of in vitro fertilization [IVF] with childhood cancer in the United States,”1 by LG Spector et al. looked retrospectively at birth and cancer registries in 14 states with 8 years of data on 275,686 children were conceived via ART through 2013, who were compared with 2,266,847 children selected randomly.
The overall cancer rate per 1,000,000 person-years was low in both groups: 252 for the IVF group and 193 for the control group, for an overall hazard risk of 1.17. Of note, the rate of hepatic tumors was higher among the IVF group than the non-IVF group (18 vs. 5.7; hazard ratio, 2.46). There appeared to be no association with specific IVF treatments, whether children were conceived by donor egg vs. autologous egg; frozen embryos vs. fresh embryos; use of intracytoplasmic sperm injection (ICSI) vs. none; assisted hatching vs. none; and day-3 vs. day-5 transfer. The researchers concluded that the “increased rate of embryonal cancers, particularly hepatic tumors, that could not be attributed to IVF rather than to underlying infertility.”
This first and largest cohort study of association between IVF and the risk of childhood cancer ever published showed little evidence of excess risk of most cancers, including more common cancers such as leukemia.
The authors did note limitations in their study. Mothers who conceived via IVF were more likely to be white, non-Hispanic, more educated, and older. Could this patient population undergoing ART be at greater risk of producing offspring with cancer concerns? If that were the case – and not great risk of childhood cancer in ART, per se – one therefore would extrapolate that couples undergoing ART vs. alternative infertility treatment should not show a treatment-biased risk (i.e., ART vs. non-ART).
This was demonstrated recently in the study, “Risk of cancer in children and young adults conceived by assisted reproductive technology.”2 This Dutch historical cohort study with prospective follow-up of a median 21 years evaluated 47,690 live-born children, of which 24,269 were ART conceived, 13,761 naturally conceived, and 9,660 conceived naturally or with fertility drugs but not by ART.
Overall, cancer risk was not increased in ART-conceived children, compared with naturally conceived subfertile women or even the general population. A nonsignificant increased risk was observed in children conceived by ICSI or cryopreservation.
On the basis of these two studies, there appears to be no significant increased risk of cancer in children conceived through fertility treatment, including ART.
Although these studies do not support the conclusion reached by a 2013 meta-analysis of 9 studies that specifically looked at ART and 16 other studies that looked at other types of medically assisted reproduction (such medically assisted reproduction as reproduction achieved through ovulation induction; controlled ovarian stimulation; ovulation triggering; intrauterine, intracervical, or intravaginal insemination) which reported a significant increased risk of overall cancers (1.33), including leukemia, CNS cancer, and neuroblastoma,3 they do agree more closely with two prospective studies conducted in the United Kingdom and Nordic countries.
In the U.K. study,4 there was no overall increased risk of cancer associated with ART, but two types of cancer were noted to be higher in the ART-conceived group – hepatoblastoma (3.27 risk) and rhabdomyosarcoma (2.62 risk) – but the absolute risk of these two types of cancer was small in this 17-year study of 106,013 children. This, of course, would be consistent with the JAMA Pediatrics study. In the Nordic study,5 similar to the Dutch Study, IVF was not associated with a significant increased risk of cancer (1.08). The Nordic study included 91,796 children born of ART-assisted pregnancies, compared with 358,419 children born after spontaneous conceptions.
The evidence so far shows that there appears to be no significant increased risk of cancer overall associated with fertility treatments, including IVF.
Dr. Miller is a clinical associate professor at the University of Illinois in Chicago and past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in metropolitan Chicago and the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. He also is a member of Ob.Gyn. News editorial advisory board. Dr. Miller disclosed that he is president of the Advanced IVF Institute in Park Ridge and Naperville, Ill.
References
1. JAMA Pediatr. 2019 Apr 1. doi: 10.1001/jamapediatrics.2019.0392.
2. Hum Reprod. 2019 Apr 1;34(4):740-50.
3. Fertil Steril. 2013 Jul. doi: 10.1016/j.fertnstert.2013.03.017.
4. N Engl J Med. 2013 Nov 7;369(19):1819-27.
5. Hum Reprod. 2014 Sep;29(9):2050-7.
“I go by thickness”
One of our favorite comics was Steven Wright, who made it to the Tonight Show with Johnny Carson. (Google him.)
Wright’s offbeat humor was quirky and a bit philosophical, and was delivered in a deadpan, mumbled monotone. For instance:
When I got to school, the teacher said, “The socks you’re wearing don’t match. They’re two different colors.”
I said, “I go by thickness.”
That punchline goes pop in your head, like a shy little firecracker: How come it never occurred to me to look at it that way?
I thought of Steven Wright recently while I was enrolling Stacy, a 20-year-old, in the iPledge program for a planned course of isotretinoin. Stacy told me she is sexually active and has an IUD.
“When you start the medicine next month,” I told her, “you’ll need to pick a second form of contraception.”
Stacy looked bewildered. When I’ve made that statement to a thousand previous patients, none of them ever looked bewildered.
“I mean,” I said, “besides the IUD, you’ll need to use a second type of contraception, to be sure you don’t get pregnant. You could choose condoms, or one of the other types listed in the booklet I gave you.”
That didn’t seem to help. Stacey hemmed a bit. “Does that mean I have to tell you ... ?”
“Yes, you have to pick another form of birth control and tell me which one it is.”
“I have to tell you every time?”
My go-by-thickness moment – I finally got it. “NO,” I said. “You do NOT have to tell me which second contraceptive you use every time you have sex!”
Steven Wright would be proud of Stacy. Isotretinoin came out in 1982, but nobody ever thought of “choose a second type of contraception” that way before. Stacy goes by retail.
That case reminded of another out-of-left field question I heard for the first – and only – time almost 40 years ago. I had prescribed a cream for a young man.
“Can I get it refilled?” he asked.
“Sure,” I said.
“How do I refill it?” he asked.
“You take it back to the pharmacy, and they refill it for you,” I said.
“But how do they refill it?”
“You show them what you need, and they refill it.”
“But how?”
“Why do you keep asking me that?”
“The tube is going to be all scrunched up from my squeezing it,” he said. “How do they get the new cream back in?”
Well son of a gun, “refill” could mean that, couldn’t it? If you go by thickness.
In idle moments I like to let novel perspectives such as those roll around in my head. The other day I accompanied a relative to an emergency department. While waiting in triage for 5 hours, I looked up and saw a sign on the wall, in big, blue letters: “Support ED Research!”
That puzzled me. I know it can be an important problem, but why the dickens would someone come to an emergency department for erectile dysfunction?
I go by acronyms.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
One of our favorite comics was Steven Wright, who made it to the Tonight Show with Johnny Carson. (Google him.)
Wright’s offbeat humor was quirky and a bit philosophical, and was delivered in a deadpan, mumbled monotone. For instance:
When I got to school, the teacher said, “The socks you’re wearing don’t match. They’re two different colors.”
I said, “I go by thickness.”
That punchline goes pop in your head, like a shy little firecracker: How come it never occurred to me to look at it that way?
I thought of Steven Wright recently while I was enrolling Stacy, a 20-year-old, in the iPledge program for a planned course of isotretinoin. Stacy told me she is sexually active and has an IUD.
“When you start the medicine next month,” I told her, “you’ll need to pick a second form of contraception.”
Stacy looked bewildered. When I’ve made that statement to a thousand previous patients, none of them ever looked bewildered.
“I mean,” I said, “besides the IUD, you’ll need to use a second type of contraception, to be sure you don’t get pregnant. You could choose condoms, or one of the other types listed in the booklet I gave you.”
That didn’t seem to help. Stacey hemmed a bit. “Does that mean I have to tell you ... ?”
“Yes, you have to pick another form of birth control and tell me which one it is.”
“I have to tell you every time?”
My go-by-thickness moment – I finally got it. “NO,” I said. “You do NOT have to tell me which second contraceptive you use every time you have sex!”
Steven Wright would be proud of Stacy. Isotretinoin came out in 1982, but nobody ever thought of “choose a second type of contraception” that way before. Stacy goes by retail.
That case reminded of another out-of-left field question I heard for the first – and only – time almost 40 years ago. I had prescribed a cream for a young man.
“Can I get it refilled?” he asked.
“Sure,” I said.
“How do I refill it?” he asked.
“You take it back to the pharmacy, and they refill it for you,” I said.
“But how do they refill it?”
“You show them what you need, and they refill it.”
“But how?”
“Why do you keep asking me that?”
“The tube is going to be all scrunched up from my squeezing it,” he said. “How do they get the new cream back in?”
Well son of a gun, “refill” could mean that, couldn’t it? If you go by thickness.
In idle moments I like to let novel perspectives such as those roll around in my head. The other day I accompanied a relative to an emergency department. While waiting in triage for 5 hours, I looked up and saw a sign on the wall, in big, blue letters: “Support ED Research!”
That puzzled me. I know it can be an important problem, but why the dickens would someone come to an emergency department for erectile dysfunction?
I go by acronyms.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
One of our favorite comics was Steven Wright, who made it to the Tonight Show with Johnny Carson. (Google him.)
Wright’s offbeat humor was quirky and a bit philosophical, and was delivered in a deadpan, mumbled monotone. For instance:
When I got to school, the teacher said, “The socks you’re wearing don’t match. They’re two different colors.”
I said, “I go by thickness.”
That punchline goes pop in your head, like a shy little firecracker: How come it never occurred to me to look at it that way?
I thought of Steven Wright recently while I was enrolling Stacy, a 20-year-old, in the iPledge program for a planned course of isotretinoin. Stacy told me she is sexually active and has an IUD.
“When you start the medicine next month,” I told her, “you’ll need to pick a second form of contraception.”
Stacy looked bewildered. When I’ve made that statement to a thousand previous patients, none of them ever looked bewildered.
“I mean,” I said, “besides the IUD, you’ll need to use a second type of contraception, to be sure you don’t get pregnant. You could choose condoms, or one of the other types listed in the booklet I gave you.”
That didn’t seem to help. Stacey hemmed a bit. “Does that mean I have to tell you ... ?”
“Yes, you have to pick another form of birth control and tell me which one it is.”
“I have to tell you every time?”
My go-by-thickness moment – I finally got it. “NO,” I said. “You do NOT have to tell me which second contraceptive you use every time you have sex!”
Steven Wright would be proud of Stacy. Isotretinoin came out in 1982, but nobody ever thought of “choose a second type of contraception” that way before. Stacy goes by retail.
That case reminded of another out-of-left field question I heard for the first – and only – time almost 40 years ago. I had prescribed a cream for a young man.
“Can I get it refilled?” he asked.
“Sure,” I said.
“How do I refill it?” he asked.
“You take it back to the pharmacy, and they refill it for you,” I said.
“But how do they refill it?”
“You show them what you need, and they refill it.”
“But how?”
“Why do you keep asking me that?”
“The tube is going to be all scrunched up from my squeezing it,” he said. “How do they get the new cream back in?”
Well son of a gun, “refill” could mean that, couldn’t it? If you go by thickness.
In idle moments I like to let novel perspectives such as those roll around in my head. The other day I accompanied a relative to an emergency department. While waiting in triage for 5 hours, I looked up and saw a sign on the wall, in big, blue letters: “Support ED Research!”
That puzzled me. I know it can be an important problem, but why the dickens would someone come to an emergency department for erectile dysfunction?
I go by acronyms.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
Doctor, will you please lie to me?
“Doctor, I have a question for you.”
“Yes?”
“Have you ever had a patient – I mean, someone like me, someone in my ... state ... get cured without any treatment?”
Mr. B thought he felt too well to have an aggressive cancer infiltrating his liver, abdominal wall, and lungs. He lived an active life, going to church, volunteering, and playing with his grandchildren. But the biopsy results were back. It wasn’t an infection. It wasn’t inflammation. It was stage 4 cancer.
And just like that, his life changed.
His prognosis was likely months, with a best case scenario of several years. But gone were the days of thinking 10, 20, and 30 years ahead.
Mr. B was a spiritual person. He told me this was God’s plan for him. He trusted God to get him through this, so he would not need chemotherapy.
Looking for hope in the face of terrible news is a common reaction. It’s natural. We tend to be optimists, and we look for a silver lining. We look for the “but.”
Patients and doctors alike do this.
“The cancer is metastatic ... but we have chemotherapy that can slow it down.”
“The doctor told me the median survival is 3 months ... but I plan to beat those odds.”
“Your mother is dying ... but we have good medicines to make her comfortable.”
It’s not a bad thing. It’s an adaptive mechanism and positive outlooks can even be associated with better medical outcomes. There’s almost always a “but” if you look hard enough. And in the face of life-changing news, we are incentivized to look really, really hard.
Yet Mr. B caught me off guard because he wasn’t asking me to maintain hope. He was pushing me one step further.
At one point in our conversation, he revealed this clearly. “Doctor, I don’t even care if it’s false hope – just tell me the cancer will disappear.”
Mr. B was asking me to lie to him.
The last thing I wanted was to take away hope, closing the door on a future that truly was clouded in uncertainty. But I also couldn’t look him in the eye and tell him his incurable disease was, in fact, curable.
That doesn’t mean there aren’t ways to phrase things kindly. Patients respond differently to “there’s a 90% chance of survival” and “there’s a 10% chance of death” even though the facts are identical.
When I sense a person like Mr. B is looking to me for hope, I try to frame that initial conversation in the style of the first statement. It’s not dishonest. With an already overwhelming piece of information, it’s choosing to share the most positive version of a narrative that can be told in many different ways and will evolve over time.
Moreover, being hopeful and realistic are not mutually exclusive. Just because someone is seeking the rare chance of a good outcome doesn’t mean he or she doesn’t understand the seriousness of the situation. It is possible to seek out experimental drugs while also considering hospice. It is possible to hope for a plan A while preparing for a plan B. Those are two compatible beliefs, and it’s OK – preferred, even – to hold them at once.
The challenge is avoiding getting pulled into an outlook that is not just positive, not just unlikely – but one with no basis in reality. There’s hope – and then there’s false hope. There’s a positive take – and then there’s lying. It can be a fine line, and with the intention of being kind it can be all too easy to “yes, but” our way into untruths.
The best we can do is set limits with compassion, and understand that telling the truth doesn’t always mean that someone hears it.
“Have you ever had a patient – I mean, someone like me, someone in my ... state ... get cured without any treatment?”
The chances of Mr. B’s cancer responding to chemotherapy were not good but hardly impossible. But without any therapy at all?
“I have not.”
“What about at other places ... in other states or countries. Have you ever heard of a person like me who was cured without treatment?”
“I have not.”
“I guess what I’m asking, Doctor, is ... have you ever seen where the cancer was there and then one day was not ... have you ever seen a miracle?”
Reaching. Grasping.
“I have not.”
“Well,” he said, “Maybe I will be the first.”
We look at each other, pondering this. In my silence is the answer.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz.
“Doctor, I have a question for you.”
“Yes?”
“Have you ever had a patient – I mean, someone like me, someone in my ... state ... get cured without any treatment?”
Mr. B thought he felt too well to have an aggressive cancer infiltrating his liver, abdominal wall, and lungs. He lived an active life, going to church, volunteering, and playing with his grandchildren. But the biopsy results were back. It wasn’t an infection. It wasn’t inflammation. It was stage 4 cancer.
And just like that, his life changed.
His prognosis was likely months, with a best case scenario of several years. But gone were the days of thinking 10, 20, and 30 years ahead.
Mr. B was a spiritual person. He told me this was God’s plan for him. He trusted God to get him through this, so he would not need chemotherapy.
Looking for hope in the face of terrible news is a common reaction. It’s natural. We tend to be optimists, and we look for a silver lining. We look for the “but.”
Patients and doctors alike do this.
“The cancer is metastatic ... but we have chemotherapy that can slow it down.”
“The doctor told me the median survival is 3 months ... but I plan to beat those odds.”
“Your mother is dying ... but we have good medicines to make her comfortable.”
It’s not a bad thing. It’s an adaptive mechanism and positive outlooks can even be associated with better medical outcomes. There’s almost always a “but” if you look hard enough. And in the face of life-changing news, we are incentivized to look really, really hard.
Yet Mr. B caught me off guard because he wasn’t asking me to maintain hope. He was pushing me one step further.
At one point in our conversation, he revealed this clearly. “Doctor, I don’t even care if it’s false hope – just tell me the cancer will disappear.”
Mr. B was asking me to lie to him.
The last thing I wanted was to take away hope, closing the door on a future that truly was clouded in uncertainty. But I also couldn’t look him in the eye and tell him his incurable disease was, in fact, curable.
That doesn’t mean there aren’t ways to phrase things kindly. Patients respond differently to “there’s a 90% chance of survival” and “there’s a 10% chance of death” even though the facts are identical.
When I sense a person like Mr. B is looking to me for hope, I try to frame that initial conversation in the style of the first statement. It’s not dishonest. With an already overwhelming piece of information, it’s choosing to share the most positive version of a narrative that can be told in many different ways and will evolve over time.
Moreover, being hopeful and realistic are not mutually exclusive. Just because someone is seeking the rare chance of a good outcome doesn’t mean he or she doesn’t understand the seriousness of the situation. It is possible to seek out experimental drugs while also considering hospice. It is possible to hope for a plan A while preparing for a plan B. Those are two compatible beliefs, and it’s OK – preferred, even – to hold them at once.
The challenge is avoiding getting pulled into an outlook that is not just positive, not just unlikely – but one with no basis in reality. There’s hope – and then there’s false hope. There’s a positive take – and then there’s lying. It can be a fine line, and with the intention of being kind it can be all too easy to “yes, but” our way into untruths.
The best we can do is set limits with compassion, and understand that telling the truth doesn’t always mean that someone hears it.
“Have you ever had a patient – I mean, someone like me, someone in my ... state ... get cured without any treatment?”
The chances of Mr. B’s cancer responding to chemotherapy were not good but hardly impossible. But without any therapy at all?
“I have not.”
“What about at other places ... in other states or countries. Have you ever heard of a person like me who was cured without treatment?”
“I have not.”
“I guess what I’m asking, Doctor, is ... have you ever seen where the cancer was there and then one day was not ... have you ever seen a miracle?”
Reaching. Grasping.
“I have not.”
“Well,” he said, “Maybe I will be the first.”
We look at each other, pondering this. In my silence is the answer.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz.
“Doctor, I have a question for you.”
“Yes?”
“Have you ever had a patient – I mean, someone like me, someone in my ... state ... get cured without any treatment?”
Mr. B thought he felt too well to have an aggressive cancer infiltrating his liver, abdominal wall, and lungs. He lived an active life, going to church, volunteering, and playing with his grandchildren. But the biopsy results were back. It wasn’t an infection. It wasn’t inflammation. It was stage 4 cancer.
And just like that, his life changed.
His prognosis was likely months, with a best case scenario of several years. But gone were the days of thinking 10, 20, and 30 years ahead.
Mr. B was a spiritual person. He told me this was God’s plan for him. He trusted God to get him through this, so he would not need chemotherapy.
Looking for hope in the face of terrible news is a common reaction. It’s natural. We tend to be optimists, and we look for a silver lining. We look for the “but.”
Patients and doctors alike do this.
“The cancer is metastatic ... but we have chemotherapy that can slow it down.”
“The doctor told me the median survival is 3 months ... but I plan to beat those odds.”
“Your mother is dying ... but we have good medicines to make her comfortable.”
It’s not a bad thing. It’s an adaptive mechanism and positive outlooks can even be associated with better medical outcomes. There’s almost always a “but” if you look hard enough. And in the face of life-changing news, we are incentivized to look really, really hard.
Yet Mr. B caught me off guard because he wasn’t asking me to maintain hope. He was pushing me one step further.
At one point in our conversation, he revealed this clearly. “Doctor, I don’t even care if it’s false hope – just tell me the cancer will disappear.”
Mr. B was asking me to lie to him.
The last thing I wanted was to take away hope, closing the door on a future that truly was clouded in uncertainty. But I also couldn’t look him in the eye and tell him his incurable disease was, in fact, curable.
That doesn’t mean there aren’t ways to phrase things kindly. Patients respond differently to “there’s a 90% chance of survival” and “there’s a 10% chance of death” even though the facts are identical.
When I sense a person like Mr. B is looking to me for hope, I try to frame that initial conversation in the style of the first statement. It’s not dishonest. With an already overwhelming piece of information, it’s choosing to share the most positive version of a narrative that can be told in many different ways and will evolve over time.
Moreover, being hopeful and realistic are not mutually exclusive. Just because someone is seeking the rare chance of a good outcome doesn’t mean he or she doesn’t understand the seriousness of the situation. It is possible to seek out experimental drugs while also considering hospice. It is possible to hope for a plan A while preparing for a plan B. Those are two compatible beliefs, and it’s OK – preferred, even – to hold them at once.
The challenge is avoiding getting pulled into an outlook that is not just positive, not just unlikely – but one with no basis in reality. There’s hope – and then there’s false hope. There’s a positive take – and then there’s lying. It can be a fine line, and with the intention of being kind it can be all too easy to “yes, but” our way into untruths.
The best we can do is set limits with compassion, and understand that telling the truth doesn’t always mean that someone hears it.
“Have you ever had a patient – I mean, someone like me, someone in my ... state ... get cured without any treatment?”
The chances of Mr. B’s cancer responding to chemotherapy were not good but hardly impossible. But without any therapy at all?
“I have not.”
“What about at other places ... in other states or countries. Have you ever heard of a person like me who was cured without treatment?”
“I have not.”
“I guess what I’m asking, Doctor, is ... have you ever seen where the cancer was there and then one day was not ... have you ever seen a miracle?”
Reaching. Grasping.
“I have not.”
“Well,” he said, “Maybe I will be the first.”
We look at each other, pondering this. In my silence is the answer.
Dr. Yurkiewicz is a fellow in hematology and oncology at Stanford (Calif.) University. Follow her on Twitter @ilanayurkiewicz.
Reframing the conversation around the ‘gender-reveal’ ultrasound
How revealing fetal anatomy, not gender, is inclusive
Every ob.gyn. expects that the topic of gender will come up at some point in a patient’s pregnancy. “When will I find out the gender?” asks the 24-year-old at her first prenatal visit. “We want the gender to be a surprise!” exclaims the couple at their anatomy scan for their second in vitro fertilization pregnancy. “Do you know what you’re having?” asks the obstetrician anticipating an imminent delivery.
The topic of gender is in fact so ingrained in our practice that we don’t bat an eye when approached with questions about fetal gender. But what exactly are we talking about when we discuss the gender of an unborn baby?
As we established in our previous column, gender identity is an internal experience of gender that one feels to be a part of oneself. So, then, what does an ultrasound actually reveal? Objectively, ultrasound can show the provider the presence or absence of a hyperechoic anatomical structure between the fetal legs that may become a penis, a vagina, or an ambiguous form of genitalia. While ultrasound is an incredible tool for anatomical and other forms of antenatal testing, ultrasound cannot detect identity characteristics because identities are, by definition, socially and internally experienced without respect to anatomy.
The distinction between gender identity and sex assigned at birth in discussions of antenatal ultrasonography is more than just a simple problem of semantics or vocabulary. To describe a fetus as a boy or a girl based on the presence/absence of a projection between the fetal legs seen on ultrasound is to reinforce the idea that gender identity and sex assigned at birth are equivalent. This conflation also erases nonbinary, genderqueer, and many other groups that identify with genders other than “boy” or “girl.” To be clear, unborn fetuses do not have a gender identity. Studies have shown that children begin to self-label their gender as early as 18-24 months of age, and similarly those who grow up to inhabit gender-nonconforming identities usually already are starting to show signs of their nonconformity starting at age 2 years.1 Some of the deepest traumas that trans and gender-nonconforming people experience are rated to the enforcement of unwritten gender laws during early childhood that are applied based on the sex assigned at birth.
Obstetricians can help to break the cycle of inappropriate gender assignment by correctly using the terms “gender” and “sex assigned at birth.” One opportunity for addressing patients’ questions about fetal gender might be to avoid the term “gender” altogether when discussing fetal sex assigned at birth, emphasizing instead what fetal ultrasound is actually able to do: Give us information about the appearance of external genitalia to help predict what sex will be assigned at birth.2 We have used this strategy when performing anatomy scans, and our experience has been that patients often will make their own assumptions about what it means to see certain external genitalia on ultrasound between the fetal legs. Motivated providers who want to go the extra mile may use a patient’s exclamation about their understanding of the fetus’s gender as an opportunity to educate the patient on the distinction between gender and sex assigned at birth, but even just smiling and moving onto the next part of the scan is an appropriate way of maintaining an atmosphere of inclusion and respect.
One of the roots of gender-based violence and gender dysphoria later in life is the conflation of gender and sex assigned at birth. While there is an entire social and political framework that enforces and polices gender after birth, the obstetrician can take steps to break the cycle starting before the birth has even occurred. Obstetricians are tasked with the unique challenge of providing care for the mother-fetus dyad, and much of the work is in setting up the fetus for the best possible life. Our scope of inclusion should be sufficiently wide to account for nonanatomical variations that could develop later in life in the infants we deliver.
Dr. Bahng is a PGY-1 resident physician in the gynecology & obstetrics residency program at Emory University, Atlanta. Dr. Bahng identifies as nonbinary and uses they/them/their as their personal pronouns. Dr. Joyner is an assistant professor at Emory University and is the director of gynecologic services in the Gender Center at Grady Memorial Hospital in Atlanta. Dr. Joyner identifies as a cisgender female and uses she/hers/her as her personal pronouns. Dr. Bahng and Dr. Joyner reported no financial disclosures.
References
1. Horm Behav. 2013 Jul;64(2):288-97.
2. Obstet Gynecol Surv. 2009 Jan;64(1):50-7.
How revealing fetal anatomy, not gender, is inclusive
How revealing fetal anatomy, not gender, is inclusive
Every ob.gyn. expects that the topic of gender will come up at some point in a patient’s pregnancy. “When will I find out the gender?” asks the 24-year-old at her first prenatal visit. “We want the gender to be a surprise!” exclaims the couple at their anatomy scan for their second in vitro fertilization pregnancy. “Do you know what you’re having?” asks the obstetrician anticipating an imminent delivery.
The topic of gender is in fact so ingrained in our practice that we don’t bat an eye when approached with questions about fetal gender. But what exactly are we talking about when we discuss the gender of an unborn baby?
As we established in our previous column, gender identity is an internal experience of gender that one feels to be a part of oneself. So, then, what does an ultrasound actually reveal? Objectively, ultrasound can show the provider the presence or absence of a hyperechoic anatomical structure between the fetal legs that may become a penis, a vagina, or an ambiguous form of genitalia. While ultrasound is an incredible tool for anatomical and other forms of antenatal testing, ultrasound cannot detect identity characteristics because identities are, by definition, socially and internally experienced without respect to anatomy.
The distinction between gender identity and sex assigned at birth in discussions of antenatal ultrasonography is more than just a simple problem of semantics or vocabulary. To describe a fetus as a boy or a girl based on the presence/absence of a projection between the fetal legs seen on ultrasound is to reinforce the idea that gender identity and sex assigned at birth are equivalent. This conflation also erases nonbinary, genderqueer, and many other groups that identify with genders other than “boy” or “girl.” To be clear, unborn fetuses do not have a gender identity. Studies have shown that children begin to self-label their gender as early as 18-24 months of age, and similarly those who grow up to inhabit gender-nonconforming identities usually already are starting to show signs of their nonconformity starting at age 2 years.1 Some of the deepest traumas that trans and gender-nonconforming people experience are rated to the enforcement of unwritten gender laws during early childhood that are applied based on the sex assigned at birth.
Obstetricians can help to break the cycle of inappropriate gender assignment by correctly using the terms “gender” and “sex assigned at birth.” One opportunity for addressing patients’ questions about fetal gender might be to avoid the term “gender” altogether when discussing fetal sex assigned at birth, emphasizing instead what fetal ultrasound is actually able to do: Give us information about the appearance of external genitalia to help predict what sex will be assigned at birth.2 We have used this strategy when performing anatomy scans, and our experience has been that patients often will make their own assumptions about what it means to see certain external genitalia on ultrasound between the fetal legs. Motivated providers who want to go the extra mile may use a patient’s exclamation about their understanding of the fetus’s gender as an opportunity to educate the patient on the distinction between gender and sex assigned at birth, but even just smiling and moving onto the next part of the scan is an appropriate way of maintaining an atmosphere of inclusion and respect.
One of the roots of gender-based violence and gender dysphoria later in life is the conflation of gender and sex assigned at birth. While there is an entire social and political framework that enforces and polices gender after birth, the obstetrician can take steps to break the cycle starting before the birth has even occurred. Obstetricians are tasked with the unique challenge of providing care for the mother-fetus dyad, and much of the work is in setting up the fetus for the best possible life. Our scope of inclusion should be sufficiently wide to account for nonanatomical variations that could develop later in life in the infants we deliver.
Dr. Bahng is a PGY-1 resident physician in the gynecology & obstetrics residency program at Emory University, Atlanta. Dr. Bahng identifies as nonbinary and uses they/them/their as their personal pronouns. Dr. Joyner is an assistant professor at Emory University and is the director of gynecologic services in the Gender Center at Grady Memorial Hospital in Atlanta. Dr. Joyner identifies as a cisgender female and uses she/hers/her as her personal pronouns. Dr. Bahng and Dr. Joyner reported no financial disclosures.
References
1. Horm Behav. 2013 Jul;64(2):288-97.
2. Obstet Gynecol Surv. 2009 Jan;64(1):50-7.
Every ob.gyn. expects that the topic of gender will come up at some point in a patient’s pregnancy. “When will I find out the gender?” asks the 24-year-old at her first prenatal visit. “We want the gender to be a surprise!” exclaims the couple at their anatomy scan for their second in vitro fertilization pregnancy. “Do you know what you’re having?” asks the obstetrician anticipating an imminent delivery.
The topic of gender is in fact so ingrained in our practice that we don’t bat an eye when approached with questions about fetal gender. But what exactly are we talking about when we discuss the gender of an unborn baby?
As we established in our previous column, gender identity is an internal experience of gender that one feels to be a part of oneself. So, then, what does an ultrasound actually reveal? Objectively, ultrasound can show the provider the presence or absence of a hyperechoic anatomical structure between the fetal legs that may become a penis, a vagina, or an ambiguous form of genitalia. While ultrasound is an incredible tool for anatomical and other forms of antenatal testing, ultrasound cannot detect identity characteristics because identities are, by definition, socially and internally experienced without respect to anatomy.
The distinction between gender identity and sex assigned at birth in discussions of antenatal ultrasonography is more than just a simple problem of semantics or vocabulary. To describe a fetus as a boy or a girl based on the presence/absence of a projection between the fetal legs seen on ultrasound is to reinforce the idea that gender identity and sex assigned at birth are equivalent. This conflation also erases nonbinary, genderqueer, and many other groups that identify with genders other than “boy” or “girl.” To be clear, unborn fetuses do not have a gender identity. Studies have shown that children begin to self-label their gender as early as 18-24 months of age, and similarly those who grow up to inhabit gender-nonconforming identities usually already are starting to show signs of their nonconformity starting at age 2 years.1 Some of the deepest traumas that trans and gender-nonconforming people experience are rated to the enforcement of unwritten gender laws during early childhood that are applied based on the sex assigned at birth.
Obstetricians can help to break the cycle of inappropriate gender assignment by correctly using the terms “gender” and “sex assigned at birth.” One opportunity for addressing patients’ questions about fetal gender might be to avoid the term “gender” altogether when discussing fetal sex assigned at birth, emphasizing instead what fetal ultrasound is actually able to do: Give us information about the appearance of external genitalia to help predict what sex will be assigned at birth.2 We have used this strategy when performing anatomy scans, and our experience has been that patients often will make their own assumptions about what it means to see certain external genitalia on ultrasound between the fetal legs. Motivated providers who want to go the extra mile may use a patient’s exclamation about their understanding of the fetus’s gender as an opportunity to educate the patient on the distinction between gender and sex assigned at birth, but even just smiling and moving onto the next part of the scan is an appropriate way of maintaining an atmosphere of inclusion and respect.
One of the roots of gender-based violence and gender dysphoria later in life is the conflation of gender and sex assigned at birth. While there is an entire social and political framework that enforces and polices gender after birth, the obstetrician can take steps to break the cycle starting before the birth has even occurred. Obstetricians are tasked with the unique challenge of providing care for the mother-fetus dyad, and much of the work is in setting up the fetus for the best possible life. Our scope of inclusion should be sufficiently wide to account for nonanatomical variations that could develop later in life in the infants we deliver.
Dr. Bahng is a PGY-1 resident physician in the gynecology & obstetrics residency program at Emory University, Atlanta. Dr. Bahng identifies as nonbinary and uses they/them/their as their personal pronouns. Dr. Joyner is an assistant professor at Emory University and is the director of gynecologic services in the Gender Center at Grady Memorial Hospital in Atlanta. Dr. Joyner identifies as a cisgender female and uses she/hers/her as her personal pronouns. Dr. Bahng and Dr. Joyner reported no financial disclosures.
References
1. Horm Behav. 2013 Jul;64(2):288-97.
2. Obstet Gynecol Surv. 2009 Jan;64(1):50-7.
Pimavanserin: A potentially safer alternative to clozapine for refractory hallucinations and delusions
Up to 30% of patients with schizophrenia do not respond to dopamine antagonists, which include all first- and second-generation antipsychotics. They are labeled as “treatment-resistant” if they have a partial response, or “treatment-refractory” if their hallucinations and/or delusions do not improve at all despite multiple trials of antipsychotics.
That’s why clozapine is considered a “lifesaver” for such patients, a last-resort medication that unshackles patients with refractory psychotic symptoms from the tyranny of auditory and/or visual hallucinations and the reality distortion of fixed false beliefs such as paranoid delusions.
Many long-suffering patients with refractory psychosis recover and return to their baseline, thanks to clozapine. In a past editorial, I discussed how one of my patients, Bethany, who had dropped out of college and became homeless for 4 years with refractory delusions and hallucinations, recovered completely when she received clozapine.1 She then returned to college, graduated with honors, and authored a book about her journey of recovery.2 She and I later established a nonprofit foundation we called CURESZ (Comprehensive Understanding via Research and Education in Schizophrenia), and assembled a panel of 80 clozapine experts across the country to provide access to clozapine for the hundreds of thousands of individuals with refractory psychosis who never received a trial of clozapine from their psychiatrists or psychiatric nurse practitioners. (Visit CURESZ.org for details.)
Bethany was very lucky to respond and recover completely, because only 40% of patients with refractory psychosis respond to clozapine. She does not mind having her blood drawn every week to measure her white blood cell count for early detection of potentially fatal agranulocytosis. Many refractory, often homeless patients with chronic schizophrenia refuse to have weekly phlebotomy and therefore are not treated with clozapine. Bethany was also fortunate to experience only 1 adverse effect of clozapine: extreme sedation that forced her to sleep up to 15 hours a day (this was reduced to 9 to 10 hours a day with adjunctive modafinil). Fortunately, she was spared the multiple other serious adverse effects of clozapine, which include excessive salivation, extreme weight gain, diabetes, hyperlipidemia, cardiomyopathy, pancreatitis, seizures, and ileus.3 Clozapine is also associated with sudden death more than any other antipsychotic agent.4
So, what can be done for patients with refractory hallucinations and delusions who are among the 60% who fail to respond to clozapine, or who experience intolerable adverse effects or safety problems, or who refuse to take clozapine and have their blood drawn every week? This is a desperately ill and seriously disabled group of patients who are deemed to be beyond the reach of medical intervention by psychiatry. They are often treated with various off-label medications as adjunctive therapy to clozapine, to which they failed to respond. This includes adding lamotrigine5 or benzoate,6 but none have been approved as an efficacious and safe monotherapy alternative to clozapine. So, what can be done for patients with refractory illness?
Enter pimavanserin. This new medication is an inverse agonist of serotonin 5-HT2A receptors and (to a lesser extent) serotonin 5-HT2C receptors. It was recently FDA-approved for treating the hallucinations and delusions of Parkinson’s disease psychosis,7 which is estimated to develop in up to 50% of individuals with Parkinson’s disease. It does not have any affinity to any dopamine receptors, which makes it an ideal antipsychotic for Parkinson’s disease, where any dopamine antagonism can worsen the motor symptoms (rigidity, hypokinesia, and tremors) associated with that movement disorder. Thus, pimavanserin became the first ever non-dopaminergic antipsychotic in the world and is indicated only for Parkinson’s disease psychosis.
Our clinical team made a serendipitous discovery about the efficacy of pimavanserin in patients with schizophrenia who failed to respond to clozapine therapy after several months at clinically adequate doses. Our findings were published online last month in the highly respected journal Schizophrenia Research.8 We reported the successful treatment with pimavanserin in 2 groups:
- patients who had not responded to clozapine received pimavanserin as an add-on to clozapine in doses of 34 mg/d, the same dose recommended for patients with Parkinson’s disease hallucinations and/or delusions.
- patients who had hallucinations and delusions that failed to respond to several non-clozapine antipsychotics received pimavanserin monotherapy instead of clozapine to avoid blood draws and serious adverse effects.
Continue to: Pimavanserin successfully treated...
Pimavanserin successfully treated the hallucinations and delusions of all 10 patients in both groups. Remission occurred within 1 month in most cases, and after 2 months in 1 patient. Those patients no longer required hospitalization as they did prior to taking pimavanserin, and they maintained their response for several months of follow-up. We were also pleased to note that most patients became more sociable and affable, with improved mood and affect, after their hallucinations and delusions disappeared with pimavanserin. We did have a few patients who did not respond to 34 mg/d of pimavanserin, and some who responded for several months but then showed signs of recurrence. We are considering increasing the dose to 68 mg/d in such patients because it is possible that a higher dose may be needed in some patients with refractory illness, who may vary in symptom severity or biology.
We are now planning to apply for a research grant to conduct a controlled trial to confirm our very encouraging clinical findings, and we hope other investigators will also conduct clinical trials in patients with refractory psychosis comparing pimavanserin with placebo or pimavanserin with clozapine in double-blind studies.
As a disclosure, our clinical findings were obtained without any knowledge of, or funding from, the company that makes pimavanserin (Acadia Pharmaceuticals Inc.). The company was informed of our findings only after our article was accepted for publication.
I hope this important finding of a potentially safer alternative to clozapine may address a major unmet need in psychiatry, involving the treatment of hundreds of thousands of patients with treatment-resistant or treatment-refractory psychosis, which includes patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder.
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Clozapine is a vastly underutilized, unique agent with multiple applications. Current Psychiatry. 2014;13(10):21, 24-25.
2. Yeiser B. Mind estranged: my journey from schizophrenia and homelessness to recovery. Seattle, WA: Amazon; 2014.
3. Raja M, Raja S. Clozapine safety, 40 years later. Curr Drug Saf. 2014;9(3):163-195.
4. Manu P, Kane JM, Corell CU. Sudden deaths in psychiatric patients. J Clin Psychiatry. 2011;72(7):936-941.
5. Tiihonen J, Wahlbeck K, Kiviniemi V. The efficacy of lamotrigine in clozapine-resistant schizophrenia: a systematic review and meta-analysis. Schizophrenia Research. 2009;109(1-3):10-14.
6. Lin CH, Lin CH, Chang YC, et al. Sodium benzoate, a D-amino acid oxidase inhibitor, added to clozapine for the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2017;84(6):422-432.
7. Ballard C, Banister C, Khan Z, et al; ADP Investigators. Evaluation of the safety, tolerability, and efficacy of pimavanserin versus placebo in p atients with Alzheimer’s disease psychosis: a phase 2, randomised, placebo-controlled, double-blind study. Lancet Neurol. 2018;17(3):213-222.
8. Nasrallah HA, Fedora R, Morton R. Successful treatment of clozapine-nonresponsive refractory hallucinations and delusions with pimavanserin, a serotonin 5HT-2A receptor inverse agonist [Epub ahead of print March 2, 2019]. Schizophrenia Res. 2019. doi: 10.1016/j.schres.2019.02.018.
Up to 30% of patients with schizophrenia do not respond to dopamine antagonists, which include all first- and second-generation antipsychotics. They are labeled as “treatment-resistant” if they have a partial response, or “treatment-refractory” if their hallucinations and/or delusions do not improve at all despite multiple trials of antipsychotics.
That’s why clozapine is considered a “lifesaver” for such patients, a last-resort medication that unshackles patients with refractory psychotic symptoms from the tyranny of auditory and/or visual hallucinations and the reality distortion of fixed false beliefs such as paranoid delusions.
Many long-suffering patients with refractory psychosis recover and return to their baseline, thanks to clozapine. In a past editorial, I discussed how one of my patients, Bethany, who had dropped out of college and became homeless for 4 years with refractory delusions and hallucinations, recovered completely when she received clozapine.1 She then returned to college, graduated with honors, and authored a book about her journey of recovery.2 She and I later established a nonprofit foundation we called CURESZ (Comprehensive Understanding via Research and Education in Schizophrenia), and assembled a panel of 80 clozapine experts across the country to provide access to clozapine for the hundreds of thousands of individuals with refractory psychosis who never received a trial of clozapine from their psychiatrists or psychiatric nurse practitioners. (Visit CURESZ.org for details.)
Bethany was very lucky to respond and recover completely, because only 40% of patients with refractory psychosis respond to clozapine. She does not mind having her blood drawn every week to measure her white blood cell count for early detection of potentially fatal agranulocytosis. Many refractory, often homeless patients with chronic schizophrenia refuse to have weekly phlebotomy and therefore are not treated with clozapine. Bethany was also fortunate to experience only 1 adverse effect of clozapine: extreme sedation that forced her to sleep up to 15 hours a day (this was reduced to 9 to 10 hours a day with adjunctive modafinil). Fortunately, she was spared the multiple other serious adverse effects of clozapine, which include excessive salivation, extreme weight gain, diabetes, hyperlipidemia, cardiomyopathy, pancreatitis, seizures, and ileus.3 Clozapine is also associated with sudden death more than any other antipsychotic agent.4
So, what can be done for patients with refractory hallucinations and delusions who are among the 60% who fail to respond to clozapine, or who experience intolerable adverse effects or safety problems, or who refuse to take clozapine and have their blood drawn every week? This is a desperately ill and seriously disabled group of patients who are deemed to be beyond the reach of medical intervention by psychiatry. They are often treated with various off-label medications as adjunctive therapy to clozapine, to which they failed to respond. This includes adding lamotrigine5 or benzoate,6 but none have been approved as an efficacious and safe monotherapy alternative to clozapine. So, what can be done for patients with refractory illness?
Enter pimavanserin. This new medication is an inverse agonist of serotonin 5-HT2A receptors and (to a lesser extent) serotonin 5-HT2C receptors. It was recently FDA-approved for treating the hallucinations and delusions of Parkinson’s disease psychosis,7 which is estimated to develop in up to 50% of individuals with Parkinson’s disease. It does not have any affinity to any dopamine receptors, which makes it an ideal antipsychotic for Parkinson’s disease, where any dopamine antagonism can worsen the motor symptoms (rigidity, hypokinesia, and tremors) associated with that movement disorder. Thus, pimavanserin became the first ever non-dopaminergic antipsychotic in the world and is indicated only for Parkinson’s disease psychosis.
Our clinical team made a serendipitous discovery about the efficacy of pimavanserin in patients with schizophrenia who failed to respond to clozapine therapy after several months at clinically adequate doses. Our findings were published online last month in the highly respected journal Schizophrenia Research.8 We reported the successful treatment with pimavanserin in 2 groups:
- patients who had not responded to clozapine received pimavanserin as an add-on to clozapine in doses of 34 mg/d, the same dose recommended for patients with Parkinson’s disease hallucinations and/or delusions.
- patients who had hallucinations and delusions that failed to respond to several non-clozapine antipsychotics received pimavanserin monotherapy instead of clozapine to avoid blood draws and serious adverse effects.
Continue to: Pimavanserin successfully treated...
Pimavanserin successfully treated the hallucinations and delusions of all 10 patients in both groups. Remission occurred within 1 month in most cases, and after 2 months in 1 patient. Those patients no longer required hospitalization as they did prior to taking pimavanserin, and they maintained their response for several months of follow-up. We were also pleased to note that most patients became more sociable and affable, with improved mood and affect, after their hallucinations and delusions disappeared with pimavanserin. We did have a few patients who did not respond to 34 mg/d of pimavanserin, and some who responded for several months but then showed signs of recurrence. We are considering increasing the dose to 68 mg/d in such patients because it is possible that a higher dose may be needed in some patients with refractory illness, who may vary in symptom severity or biology.
We are now planning to apply for a research grant to conduct a controlled trial to confirm our very encouraging clinical findings, and we hope other investigators will also conduct clinical trials in patients with refractory psychosis comparing pimavanserin with placebo or pimavanserin with clozapine in double-blind studies.
As a disclosure, our clinical findings were obtained without any knowledge of, or funding from, the company that makes pimavanserin (Acadia Pharmaceuticals Inc.). The company was informed of our findings only after our article was accepted for publication.
I hope this important finding of a potentially safer alternative to clozapine may address a major unmet need in psychiatry, involving the treatment of hundreds of thousands of patients with treatment-resistant or treatment-refractory psychosis, which includes patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder.
To comment on this editorial or other topics of interest: [email protected].
Up to 30% of patients with schizophrenia do not respond to dopamine antagonists, which include all first- and second-generation antipsychotics. They are labeled as “treatment-resistant” if they have a partial response, or “treatment-refractory” if their hallucinations and/or delusions do not improve at all despite multiple trials of antipsychotics.
That’s why clozapine is considered a “lifesaver” for such patients, a last-resort medication that unshackles patients with refractory psychotic symptoms from the tyranny of auditory and/or visual hallucinations and the reality distortion of fixed false beliefs such as paranoid delusions.
Many long-suffering patients with refractory psychosis recover and return to their baseline, thanks to clozapine. In a past editorial, I discussed how one of my patients, Bethany, who had dropped out of college and became homeless for 4 years with refractory delusions and hallucinations, recovered completely when she received clozapine.1 She then returned to college, graduated with honors, and authored a book about her journey of recovery.2 She and I later established a nonprofit foundation we called CURESZ (Comprehensive Understanding via Research and Education in Schizophrenia), and assembled a panel of 80 clozapine experts across the country to provide access to clozapine for the hundreds of thousands of individuals with refractory psychosis who never received a trial of clozapine from their psychiatrists or psychiatric nurse practitioners. (Visit CURESZ.org for details.)
Bethany was very lucky to respond and recover completely, because only 40% of patients with refractory psychosis respond to clozapine. She does not mind having her blood drawn every week to measure her white blood cell count for early detection of potentially fatal agranulocytosis. Many refractory, often homeless patients with chronic schizophrenia refuse to have weekly phlebotomy and therefore are not treated with clozapine. Bethany was also fortunate to experience only 1 adverse effect of clozapine: extreme sedation that forced her to sleep up to 15 hours a day (this was reduced to 9 to 10 hours a day with adjunctive modafinil). Fortunately, she was spared the multiple other serious adverse effects of clozapine, which include excessive salivation, extreme weight gain, diabetes, hyperlipidemia, cardiomyopathy, pancreatitis, seizures, and ileus.3 Clozapine is also associated with sudden death more than any other antipsychotic agent.4
So, what can be done for patients with refractory hallucinations and delusions who are among the 60% who fail to respond to clozapine, or who experience intolerable adverse effects or safety problems, or who refuse to take clozapine and have their blood drawn every week? This is a desperately ill and seriously disabled group of patients who are deemed to be beyond the reach of medical intervention by psychiatry. They are often treated with various off-label medications as adjunctive therapy to clozapine, to which they failed to respond. This includes adding lamotrigine5 or benzoate,6 but none have been approved as an efficacious and safe monotherapy alternative to clozapine. So, what can be done for patients with refractory illness?
Enter pimavanserin. This new medication is an inverse agonist of serotonin 5-HT2A receptors and (to a lesser extent) serotonin 5-HT2C receptors. It was recently FDA-approved for treating the hallucinations and delusions of Parkinson’s disease psychosis,7 which is estimated to develop in up to 50% of individuals with Parkinson’s disease. It does not have any affinity to any dopamine receptors, which makes it an ideal antipsychotic for Parkinson’s disease, where any dopamine antagonism can worsen the motor symptoms (rigidity, hypokinesia, and tremors) associated with that movement disorder. Thus, pimavanserin became the first ever non-dopaminergic antipsychotic in the world and is indicated only for Parkinson’s disease psychosis.
Our clinical team made a serendipitous discovery about the efficacy of pimavanserin in patients with schizophrenia who failed to respond to clozapine therapy after several months at clinically adequate doses. Our findings were published online last month in the highly respected journal Schizophrenia Research.8 We reported the successful treatment with pimavanserin in 2 groups:
- patients who had not responded to clozapine received pimavanserin as an add-on to clozapine in doses of 34 mg/d, the same dose recommended for patients with Parkinson’s disease hallucinations and/or delusions.
- patients who had hallucinations and delusions that failed to respond to several non-clozapine antipsychotics received pimavanserin monotherapy instead of clozapine to avoid blood draws and serious adverse effects.
Continue to: Pimavanserin successfully treated...
Pimavanserin successfully treated the hallucinations and delusions of all 10 patients in both groups. Remission occurred within 1 month in most cases, and after 2 months in 1 patient. Those patients no longer required hospitalization as they did prior to taking pimavanserin, and they maintained their response for several months of follow-up. We were also pleased to note that most patients became more sociable and affable, with improved mood and affect, after their hallucinations and delusions disappeared with pimavanserin. We did have a few patients who did not respond to 34 mg/d of pimavanserin, and some who responded for several months but then showed signs of recurrence. We are considering increasing the dose to 68 mg/d in such patients because it is possible that a higher dose may be needed in some patients with refractory illness, who may vary in symptom severity or biology.
We are now planning to apply for a research grant to conduct a controlled trial to confirm our very encouraging clinical findings, and we hope other investigators will also conduct clinical trials in patients with refractory psychosis comparing pimavanserin with placebo or pimavanserin with clozapine in double-blind studies.
As a disclosure, our clinical findings were obtained without any knowledge of, or funding from, the company that makes pimavanserin (Acadia Pharmaceuticals Inc.). The company was informed of our findings only after our article was accepted for publication.
I hope this important finding of a potentially safer alternative to clozapine may address a major unmet need in psychiatry, involving the treatment of hundreds of thousands of patients with treatment-resistant or treatment-refractory psychosis, which includes patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder.
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Clozapine is a vastly underutilized, unique agent with multiple applications. Current Psychiatry. 2014;13(10):21, 24-25.
2. Yeiser B. Mind estranged: my journey from schizophrenia and homelessness to recovery. Seattle, WA: Amazon; 2014.
3. Raja M, Raja S. Clozapine safety, 40 years later. Curr Drug Saf. 2014;9(3):163-195.
4. Manu P, Kane JM, Corell CU. Sudden deaths in psychiatric patients. J Clin Psychiatry. 2011;72(7):936-941.
5. Tiihonen J, Wahlbeck K, Kiviniemi V. The efficacy of lamotrigine in clozapine-resistant schizophrenia: a systematic review and meta-analysis. Schizophrenia Research. 2009;109(1-3):10-14.
6. Lin CH, Lin CH, Chang YC, et al. Sodium benzoate, a D-amino acid oxidase inhibitor, added to clozapine for the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2017;84(6):422-432.
7. Ballard C, Banister C, Khan Z, et al; ADP Investigators. Evaluation of the safety, tolerability, and efficacy of pimavanserin versus placebo in p atients with Alzheimer’s disease psychosis: a phase 2, randomised, placebo-controlled, double-blind study. Lancet Neurol. 2018;17(3):213-222.
8. Nasrallah HA, Fedora R, Morton R. Successful treatment of clozapine-nonresponsive refractory hallucinations and delusions with pimavanserin, a serotonin 5HT-2A receptor inverse agonist [Epub ahead of print March 2, 2019]. Schizophrenia Res. 2019. doi: 10.1016/j.schres.2019.02.018.
1. Nasrallah HA. Clozapine is a vastly underutilized, unique agent with multiple applications. Current Psychiatry. 2014;13(10):21, 24-25.
2. Yeiser B. Mind estranged: my journey from schizophrenia and homelessness to recovery. Seattle, WA: Amazon; 2014.
3. Raja M, Raja S. Clozapine safety, 40 years later. Curr Drug Saf. 2014;9(3):163-195.
4. Manu P, Kane JM, Corell CU. Sudden deaths in psychiatric patients. J Clin Psychiatry. 2011;72(7):936-941.
5. Tiihonen J, Wahlbeck K, Kiviniemi V. The efficacy of lamotrigine in clozapine-resistant schizophrenia: a systematic review and meta-analysis. Schizophrenia Research. 2009;109(1-3):10-14.
6. Lin CH, Lin CH, Chang YC, et al. Sodium benzoate, a D-amino acid oxidase inhibitor, added to clozapine for the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2017;84(6):422-432.
7. Ballard C, Banister C, Khan Z, et al; ADP Investigators. Evaluation of the safety, tolerability, and efficacy of pimavanserin versus placebo in p atients with Alzheimer’s disease psychosis: a phase 2, randomised, placebo-controlled, double-blind study. Lancet Neurol. 2018;17(3):213-222.
8. Nasrallah HA, Fedora R, Morton R. Successful treatment of clozapine-nonresponsive refractory hallucinations and delusions with pimavanserin, a serotonin 5HT-2A receptor inverse agonist [Epub ahead of print March 2, 2019]. Schizophrenia Res. 2019. doi: 10.1016/j.schres.2019.02.018.
Paraphilic disorders: A better understanding
In my role as the Director of The Johns Hopkins Sex and Gender Clinic, I have had the opportunity to provide care to 3 broad categories of patients: patients with sexual dysfunctions, patients experiencing gender dysphoria, and patients manifesting a paraphilic disorder. This article will not address sexual dysfunctions or gender dysphoria, but these terms are defined in the Box1-3 to clearly distinguish them from paraphilic disorders.
Box
Individuals with a sexual dysfunction (eg, erectile dysfunction or anorgasmia) generally experience conventional sexual feelings, but they may have difficulty performing sexually.1 Although ordinarily capable of adequate sexual performance, persons with a paraphilic disorder experience atypical erotic cravings.2 Such cravings can either be for an atypical or unacceptable category of potential partner (eg, animals or children), or for an atypical or unacceptable type of behavior (eg, crossdressing or public exhibitionism). Individuals with gender dysphoria frequently experience distress because their internal sense of feeling either male or female is not congruent with their external physical anatomy.3 The primary concerns of individuals experiencing gender dysphoria relate to feelings of gender identity, as opposed to problems involving erotic arousal.
Persons with paraphilic disorders (predominantly males) experience recurrent atypical sexual fantasies and urges that cause clinically significant impairment or distress.1 Those atypical fantasies and urges may be directed towards unacceptable partners such as animals or children, or towards unacceptable behaviors such as public exhibitionism. Table 11 lists the paraphilic disorders identified in DSM-5. This article focuses primarily, though not exclusively, upon pedophilic disorder, and its pharmacologic treatment. However, the rationale underlying such treatment is applicable across the paraphilic spectrum. Before providing such treatment, it is important for clinicians to have a clear conceptual understanding of paraphilic disorders.
When is a difference a disorder?
Cancer and respiration are 2 different biologic phenomenon. Cancer causes suffering and impairment, and as a consequence, we label it a disorder. We do so in the hope of learning more about it, and being able to successfully treat it. We do not classify respiration as a disorder because we do not consider it to be harmful.
The spectrum of human sexuality is quite broad, and psychiatry is generally not concerned with private sexual thoughts and behaviors involving consenting adults that do not cause suffering or impairment. When adults choose to engage in “kinky sex” that causes neither harm nor distress, so be it.
Some individuals may be privately aware of experiencing either an exclusive or nonexclusive sexual attraction to children. Some of these individuals may not be distressed by experiencing such attractions, and may be fully capable of resisting the temptation to enact them. In such an instance, even though an individual may be experiencing sexual attractions that are different from the norm, there may not be a sufficient basis for diagnosing pedophilic disorder. However, that difference in sexual phenomenology (ie, mental experience) could rise to the level of a diagnosable disorder if the individual in question expresses distress about experiencing such attractions, and/or if his capacity to resist acting upon them is impaired.4 Under such circumstances, treatment would be warranted.
Patients with paraphilic disorders deserve treatment
Prior to establishment of the Betty Ford Clinic in 1982, individuals who were drug- or alcohol-dependent were often portrayed in a negative light and referred to by derogatory pejoratives such as “bum” or “pothead.”5 Over time, society came to appreciate that good people, deserving of treatment, can become dependent upon substances, and in recent years there has been considerable support for related research initiatives and humane care. However, there has not been analogous support for individuals who manifest paraphilic disorders, especially those with pedophilic disorder. Instead, such individuals are often perceived as undeserving of mental health care and resources. This has been the case, even though successful treatment of a pedophilic disorder could help prevent the serious consequences of child molestation from occurring.
In contemporary society, the term pedophilia, which is a psychiatric specifier intended to guide research and treatment, has been hijacked by the nonmedical community and turned into a demeaning pejorative. In the collective consciousness of the public, the term pedophilia is routinely and mistakenly equated with the behavior of child molestation. Just as all alcoholics are not drunk drivers, all individuals with pedophilic disorder are not “child molesters.” Conversely, not all “child molesters” have pedophilic disorder.
Continue to: Individuals with other types...
Individuals with other types of paraphilic disorders are frequently similarly maligned and referred to as “perverts” or “deviants.” Public service announcements are frequently aired to reach out to individuals who are depressed, or drug- or alcohol-dependent, or suffering with other forms of mental disorders. When does one hear a public service announcement that encourages young people who may be experiencing disturbing or unacceptable sexual feelings to seek psychiatric treatment? There is a support group on the internet called Virtuous Pedophiles.6 That organization is unequivocally opposed to child molestation, while supporting efforts to improve the mental well-being of individuals who, through no fault of their own, experience unwanted pedophilic feelings.
Causes and noncauses
In attempting to elucidate etiology, researchers typically investigate nature (biology) and/or nurture (life experiences). In terms of the development of pedophilic disorder, there is evidence that both nature and nurture can play a role. Researchers have found that boys who are sexually abused are at increased risk for developing pedophilic disorder, and evidence of temporal lobe disturbances has also been documented in some instances.7,8
From clinical, societal, and forensic perspectives, it may be equally important to identify noncausal factors. Paraphilic disorders, including pedophilic disorder, do not develop as a consequence of volitional choice.9 For example, none of us decide which category, or categories, of potential partners are going to attract us sexually. Rather, in maturing we discover the nature of our own sexuality. Children do not ponder their options, somehow deciding while growing up to be attracted to the opposite sex (heterosexuality), the same sex (homosexuality), or both sexes (bisexuality). Similarly, in maturing into adulthood, individuals do not decide to become sexually attracted to prepubescent children. Who would decide to do that? Instead, unlike most of us, some individuals discover this about themselves; this often is a deeply disturbing insight.
It is not an individual’s fault that he or she has a paraphilic disorder. It is, however, his or her responsibility to do something about it. This may require accessing appropriate psychiatric care.
Why treatment may be needed
Sex is a powerful, biologically based appetite that recurrently craves satiation. God or nature has put that drive into all of us to ensure the survival of humanity. Even when that powerful biologic drive becomes misdirected (for example, towards children, or towards a desire to engage in public exhibitionism), it still recurrently craves satisfaction. It does not require mental health expertise to appreciate what a problematic situation this could become.
Continue to: Some individuals need help...
Some individuals need help in overcoming cravings related to nonsexual appetites. For example, Americans spend millions of dollars each year trying to diet; they often require some form of assistance in order to succeed. Individuals who crave drugs or alcohol often require mental health interventions to abstain because they are unable to consistently resist through willpower alone the powerful biologic urges that drive their actions.
The fundamental mental characteristic of any paraphilic disorder is the presence of intense, recurrent, sexual urges of an atypical nature. In the case of a pedophilic disorder, those urges involve sexual feelings about children.2 In the case of an exhibitionistic disorder, the afflicted individual experiences intense, recurrent sexual fantasies/urges related to exposing his genitals in public.1 Clearly, most men do not have to recurrently fight off the urge to act in such a fashion. Given the driven nature of intense erotic cravings, individuals who experience such cravings will frequently require access to competent mental health care.
Pharmacologic treatment of paraphilic disorders
In the future, we may develop a scientifically based understanding of the biologic factors that underlie qualitative differences in sexuality. At that point, it may become possible to intervene pharmacologically, changing the qualitative nature of a sexual urge with pharmacologic interventions. This cannot yet be done. H
In 1939, a Nobel Prize in Chemistry was awarded for the identification and isolation of the hormone testosterone, which energizes sexual drive.10 If an individual is hungering sexually to expose himself, to view child pornography, or to engage in sexual acts with children, the intensity of such hungers can be significantly reduced by lowering testosterone, thereby enhancing the capacity for successful sexual self-control.
A large body of scientific data has documented a marked decrease in sexually motivated behaviors when testosterone levels are significantly diminished.11 There is also evidence that recidivism rates of sexually motivated crimes can be significantly reduced when testosterone-lowering interventions are used.12
Continue to: Historically, removal of the testes...
Historically, removal of the testes (surgical castration) had been the only effective way to reliably lower testosterone. Today, this can be achieved pharmacologically. Use of a sex drive–lowering medication should be considered when either the clinician or the patient is concerned that a nonpharmacologic approach may be inadequate. In all instances, a patient with a paraphilic disorder should be informed that pharmacologic treatment is an option. A protocol for the pharmacologic treatment of paraphilic disorders that is based on my clinical experience is summarized in Table 2.
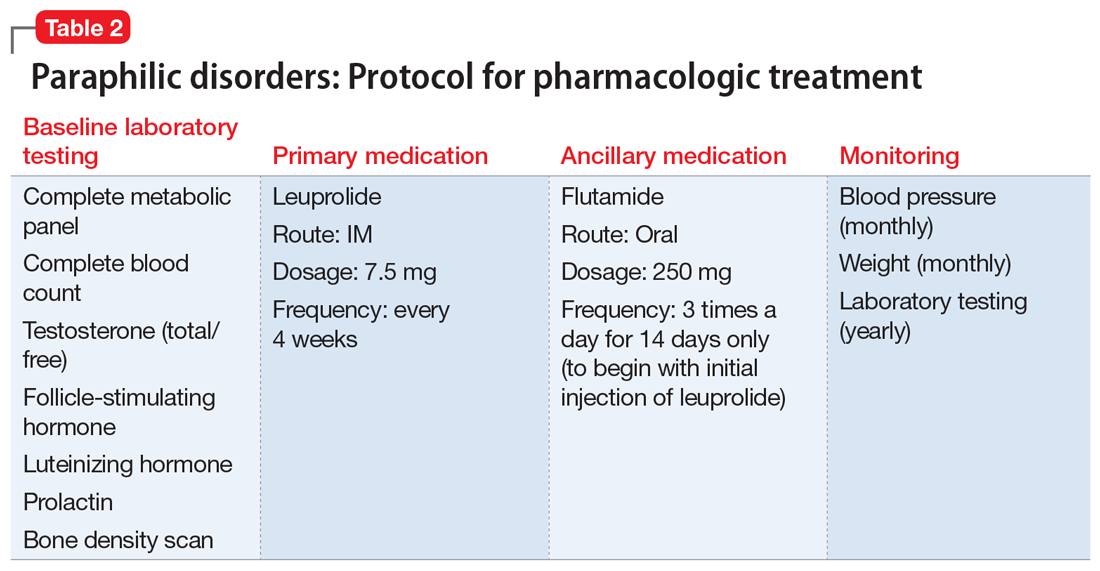
Leuprolide. A depot form of leuprolide is the most commonly employed agent to pharmacologically lower testosterone to treat a paraphilic disorder.13 When injected into muscle, leuprolide binds to it before gradually being released into the bloodstream. Previously, a depot medroxyprogesterone (a form of progesterone) had been used to treat paraphilic disorders.14 However, that had required weekly rather than monthly injections, and carried an increased risk of thrombotic emboli.
Prescribing leuprolide to treat a paraphilic disorder falls under FDA guidelines regarding the use of an approved drug for an “off-label” indication, and therefore is not considered investigational. For treating a paraphilic disorder, an effective dosage of leuprolide is 7.5 mg IM every 4 weeks. Long-term treatment is generally required, analogous to the management of diabetes. Because the initial injection of the series can cause a transient increase in testosterone (prior to its sustained decline), flutamide, a testosterone receptor blocking agent, is ordinarily prescribed for the first 14 days only, following initiation of treatment with depot leuprolide.15 Using flutamide in this fashion prevents the transient increase in testosterone from transiently increasing sexual drive. Flutamide should be discontinued after 14 days because long-term use can result in liver toxicity.
Some clinicians have been hesitant to prescribe leuprolide because of negative connotations associated with the term “chemical castration.” Unlike surgical castration, use of leuprolide is not a physically irreversible intervention, and does not result in sterility (although there may be an increase of atypical sperm and a decrease in total sperm production). The dosage can sometimes be titrated without a loss of efficacy.
In general, leuprolide’s safety protocol is well within the range associated with psychotropic medications.13 Low-risk adverse effects, such as hot flashes or cold sweats, may occur, especially during the period when hormone levels are in transition. There are no absolute contraindications to the use of leuprolide.
Continue to: Other medications
Other medications. Some researchers have suggested treating paraphilic disorders with psychotropic medications known to lower libido, such as selective serotonin reuptake inhibitors (SSRIs).16 However, leuprolide is far more reliable in consistently lowering testosterone and lowering the frequency and intensity of sexual urges. Although psychiatrists unfamiliar with treating paraphilic disorders may feel more comfortable initiating treatment with an SSRI, in my clinical experience, SSRIs have often proven inadequate for this purpose. When it comes to those paraphilic disorders in which treatment failure can result in significant harm (eg, pedophilic disorder), in my judgment, leuprolide should be the pharmacologic treatment of choice.
The opioid antagonist naltrexone has been used clinically to reduce cravings, primarily cravings for alcohol or drugs.17 However, I have not seen convincing evidence that it can be reliably beneficial in treating paraphilic disorders.
Tests to order before starting leuprolide
Long-term use of leuprolide can increase the risk of osteoporosis. Therefore, a baseline bone density scan should be performed before starting a patient on leuprolide. Baseline levels of testosterone, follicle-stimulating hormone, and luteinizing hormone also should be obtained. Patients should have yearly physical examinations, with accompanying laboratory testing. Hematocrit levels are often marginally low after beginning treatment, but not in a clinically significant way. Patients should also undergo routine monitoring for possible weight gain and the potential for associated hypertension. Treatment is predicated upon the known testosterone-suppressing effects of leuprolide, not upon routine monitoring of blood androgen levels.
Pharmacologic treatment of a paraphilic disorder should ordinarily occur in conjunction with nonpharmacologic modalities. One such modality would be group therapy, similar to the type frequently used to treat other craving disorders, such as drug or alcohol dependency.
In recent years, I have seen increasing numbers of patients presenting with a history of accessing and viewing child pornography. Once they have become more aware of the serious consequences of this behavior, most patients have been able to discontinue doing so without pharmacologic treatment. However, for patients in whom that behavior has seemed more driven (suggestive of a variant of voyeuristic disorder), prescription of leuprolide has been beneficial. Under such circumstances, I have diagnosed the patient’s condition as “other specified paraphilic disorder” with elements of pedophilia and voyeurism—the associated behaviors restricted to the voyeuristic viewing of child pornography.18
Continue to: Can treated patients still be sexual?
Can treated patients still be sexual?
If pharmacologic treatment of a paraphilic disorder results in erectile dysfunction, prescription of a medication such as sildenafil can be considered for patients who are in a consenting adult relationship, generally with the knowledge of their partner. Sildenafil can facilitate erectile capacity without increasing sexual drive. It can be helpful to explain to a patient that the purpose of pharmacologic treatment is not to prevent the enjoyment of sexual feelings within the context of a healthy, consenting, adult relationship, but instead to lower the intensity of problematic sexual urges, thereby facilitating sexual self-control. Just as lowering the appetite for food can make it easier to diet but not impossible to eat, lowering sexual appetite can facilitate successful self-control without necessarily interfering with erotic feelings experienced during sexual intimacy.
Bottom Line
Paraphilic disorders are not manifestations of a character flaw, but manifestations of unchosen qualitative differences in the nature of one’s sexual cravings. Not enough is yet known about the biology of sex to be able to pharmacologically alter its qualitative nature. However, pharmacologically lowering the intensity of a patient’s sexual drive can facilitate successful sexual self-regulation.
Related Resources
- LeVay S. Gay, straight and the reason why: the science of sexual orientation. London, UK: Oxford University Press; 2011.
- Rosler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998;338(7):416-422.
- Brown GR. Overview of paraphilic disorders (paraphilias). https://www.merckmanuals.com/professional/psychiatricdisorders/sexuality,-gender-dysphoria,-and-paraphilias/overview-of-paraphilic-disorders.
Drug Brand Names
Flutamide • Eulexin
Leuprolide injection •
Eligard, Lupron Depot
Medroxyprogesterone •
Provera
Naltrexone • Revia, Vivitrol
Progesterone • Prometrium
Sildenafil • Viagra
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:423-450.
2. Berlin FS. Pedophilia: criminal mind-set or mental disorder? A conceptual review. American Journal of Forensic Psychiatry. 2001;32(2):3-25.
3. Berlin FS. A conceptual overview and commentary on gender dysphoria. J Am Acad Psychiatry Law. 2016;44(2):246-252
4. Berlin FS. Pedophilia: when is a difference a disorder: Peer commentaries on Green (2002) and Schmidt (2002). Arch Sex Behav. 2002;31:1-2.
5. Ford B, Chase C. Betty: a glad awakening. New York, NY: Doubleday; 1987.
6. Virtuous Pedophiles. https://www.virped.org/. Accessed September 28, 2018.
7. Freund K, Kuban M. The basis of the abused abuser theory of pedophilia: A further elaboration of an earlier study. Arch Sex Behav. 1994;23(5):553-563.
8. Mendes MF, Chow T, Ringman T, et al. Pedophilia and temporal lobe disturbances. J Neuropsychiatry Clin Neurosci. 2000;12(1):71-76.
9. Money J. Love and love sickness: The science of sex, gender differences, and pair bonding. Baltimore, MD: Johns Hopkins University Press; 1980.
10. The Nobel Prize in Chemistry 1939. https://www.nobelprize.org/prizes/chemistry/1939/summary/. Accessed September 29, 2018.
11. Berlin FS. Commentary: The impact of surgical castration on sexual recidivism risk among civilly committed sex offenders. J Am Acad Psychiatry Law. 2005;33(1):37-41.
12. Hansen H. Treatment of dangerous sexual offenders. In: Seminar on Prison Health Services in Tampere, Finland. Helsinki, Finland: Ministry of Justice, Government Printing Centre; 1991:33-38.
13. Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. J Am Acad Psychiatry Law. 2009;37(1):59-62.
14. Berlin FS, Meinecke CF. Treatment of sex offenders with antiandrogenic medication: conceptualization, review of treatment modalities, and preliminary findings. Am J Psychiatry. 1981;138(5):601-607.
15. Neri R. Pharmacology and pharmacokinetics of flutamide. Urology. 1989;34(suppl 4):19-21; discussion 46-56.
16. Adi Y, Ashcroft D, Browne K, et al. Clinical effectiveness and cost consequences of selective serotonin receptor reuptake inhibitors in the treatment of sex offenders. Health Technol Assess. 2002;6(28):1-66.
17. Anton RF. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715-721.
18. Berlin FS. Commentary on pedophilia diagnostic criteria in DSM-5. J Am Acad Psychiatry Law. 2011;39(2):242-244.
In my role as the Director of The Johns Hopkins Sex and Gender Clinic, I have had the opportunity to provide care to 3 broad categories of patients: patients with sexual dysfunctions, patients experiencing gender dysphoria, and patients manifesting a paraphilic disorder. This article will not address sexual dysfunctions or gender dysphoria, but these terms are defined in the Box1-3 to clearly distinguish them from paraphilic disorders.
Box
Individuals with a sexual dysfunction (eg, erectile dysfunction or anorgasmia) generally experience conventional sexual feelings, but they may have difficulty performing sexually.1 Although ordinarily capable of adequate sexual performance, persons with a paraphilic disorder experience atypical erotic cravings.2 Such cravings can either be for an atypical or unacceptable category of potential partner (eg, animals or children), or for an atypical or unacceptable type of behavior (eg, crossdressing or public exhibitionism). Individuals with gender dysphoria frequently experience distress because their internal sense of feeling either male or female is not congruent with their external physical anatomy.3 The primary concerns of individuals experiencing gender dysphoria relate to feelings of gender identity, as opposed to problems involving erotic arousal.
Persons with paraphilic disorders (predominantly males) experience recurrent atypical sexual fantasies and urges that cause clinically significant impairment or distress.1 Those atypical fantasies and urges may be directed towards unacceptable partners such as animals or children, or towards unacceptable behaviors such as public exhibitionism. Table 11 lists the paraphilic disorders identified in DSM-5. This article focuses primarily, though not exclusively, upon pedophilic disorder, and its pharmacologic treatment. However, the rationale underlying such treatment is applicable across the paraphilic spectrum. Before providing such treatment, it is important for clinicians to have a clear conceptual understanding of paraphilic disorders.
When is a difference a disorder?
Cancer and respiration are 2 different biologic phenomenon. Cancer causes suffering and impairment, and as a consequence, we label it a disorder. We do so in the hope of learning more about it, and being able to successfully treat it. We do not classify respiration as a disorder because we do not consider it to be harmful.
The spectrum of human sexuality is quite broad, and psychiatry is generally not concerned with private sexual thoughts and behaviors involving consenting adults that do not cause suffering or impairment. When adults choose to engage in “kinky sex” that causes neither harm nor distress, so be it.
Some individuals may be privately aware of experiencing either an exclusive or nonexclusive sexual attraction to children. Some of these individuals may not be distressed by experiencing such attractions, and may be fully capable of resisting the temptation to enact them. In such an instance, even though an individual may be experiencing sexual attractions that are different from the norm, there may not be a sufficient basis for diagnosing pedophilic disorder. However, that difference in sexual phenomenology (ie, mental experience) could rise to the level of a diagnosable disorder if the individual in question expresses distress about experiencing such attractions, and/or if his capacity to resist acting upon them is impaired.4 Under such circumstances, treatment would be warranted.
Patients with paraphilic disorders deserve treatment
Prior to establishment of the Betty Ford Clinic in 1982, individuals who were drug- or alcohol-dependent were often portrayed in a negative light and referred to by derogatory pejoratives such as “bum” or “pothead.”5 Over time, society came to appreciate that good people, deserving of treatment, can become dependent upon substances, and in recent years there has been considerable support for related research initiatives and humane care. However, there has not been analogous support for individuals who manifest paraphilic disorders, especially those with pedophilic disorder. Instead, such individuals are often perceived as undeserving of mental health care and resources. This has been the case, even though successful treatment of a pedophilic disorder could help prevent the serious consequences of child molestation from occurring.
In contemporary society, the term pedophilia, which is a psychiatric specifier intended to guide research and treatment, has been hijacked by the nonmedical community and turned into a demeaning pejorative. In the collective consciousness of the public, the term pedophilia is routinely and mistakenly equated with the behavior of child molestation. Just as all alcoholics are not drunk drivers, all individuals with pedophilic disorder are not “child molesters.” Conversely, not all “child molesters” have pedophilic disorder.
Continue to: Individuals with other types...
Individuals with other types of paraphilic disorders are frequently similarly maligned and referred to as “perverts” or “deviants.” Public service announcements are frequently aired to reach out to individuals who are depressed, or drug- or alcohol-dependent, or suffering with other forms of mental disorders. When does one hear a public service announcement that encourages young people who may be experiencing disturbing or unacceptable sexual feelings to seek psychiatric treatment? There is a support group on the internet called Virtuous Pedophiles.6 That organization is unequivocally opposed to child molestation, while supporting efforts to improve the mental well-being of individuals who, through no fault of their own, experience unwanted pedophilic feelings.
Causes and noncauses
In attempting to elucidate etiology, researchers typically investigate nature (biology) and/or nurture (life experiences). In terms of the development of pedophilic disorder, there is evidence that both nature and nurture can play a role. Researchers have found that boys who are sexually abused are at increased risk for developing pedophilic disorder, and evidence of temporal lobe disturbances has also been documented in some instances.7,8
From clinical, societal, and forensic perspectives, it may be equally important to identify noncausal factors. Paraphilic disorders, including pedophilic disorder, do not develop as a consequence of volitional choice.9 For example, none of us decide which category, or categories, of potential partners are going to attract us sexually. Rather, in maturing we discover the nature of our own sexuality. Children do not ponder their options, somehow deciding while growing up to be attracted to the opposite sex (heterosexuality), the same sex (homosexuality), or both sexes (bisexuality). Similarly, in maturing into adulthood, individuals do not decide to become sexually attracted to prepubescent children. Who would decide to do that? Instead, unlike most of us, some individuals discover this about themselves; this often is a deeply disturbing insight.
It is not an individual’s fault that he or she has a paraphilic disorder. It is, however, his or her responsibility to do something about it. This may require accessing appropriate psychiatric care.
Why treatment may be needed
Sex is a powerful, biologically based appetite that recurrently craves satiation. God or nature has put that drive into all of us to ensure the survival of humanity. Even when that powerful biologic drive becomes misdirected (for example, towards children, or towards a desire to engage in public exhibitionism), it still recurrently craves satisfaction. It does not require mental health expertise to appreciate what a problematic situation this could become.
Continue to: Some individuals need help...
Some individuals need help in overcoming cravings related to nonsexual appetites. For example, Americans spend millions of dollars each year trying to diet; they often require some form of assistance in order to succeed. Individuals who crave drugs or alcohol often require mental health interventions to abstain because they are unable to consistently resist through willpower alone the powerful biologic urges that drive their actions.
The fundamental mental characteristic of any paraphilic disorder is the presence of intense, recurrent, sexual urges of an atypical nature. In the case of a pedophilic disorder, those urges involve sexual feelings about children.2 In the case of an exhibitionistic disorder, the afflicted individual experiences intense, recurrent sexual fantasies/urges related to exposing his genitals in public.1 Clearly, most men do not have to recurrently fight off the urge to act in such a fashion. Given the driven nature of intense erotic cravings, individuals who experience such cravings will frequently require access to competent mental health care.
Pharmacologic treatment of paraphilic disorders
In the future, we may develop a scientifically based understanding of the biologic factors that underlie qualitative differences in sexuality. At that point, it may become possible to intervene pharmacologically, changing the qualitative nature of a sexual urge with pharmacologic interventions. This cannot yet be done. H
In 1939, a Nobel Prize in Chemistry was awarded for the identification and isolation of the hormone testosterone, which energizes sexual drive.10 If an individual is hungering sexually to expose himself, to view child pornography, or to engage in sexual acts with children, the intensity of such hungers can be significantly reduced by lowering testosterone, thereby enhancing the capacity for successful sexual self-control.
A large body of scientific data has documented a marked decrease in sexually motivated behaviors when testosterone levels are significantly diminished.11 There is also evidence that recidivism rates of sexually motivated crimes can be significantly reduced when testosterone-lowering interventions are used.12
Continue to: Historically, removal of the testes...
Historically, removal of the testes (surgical castration) had been the only effective way to reliably lower testosterone. Today, this can be achieved pharmacologically. Use of a sex drive–lowering medication should be considered when either the clinician or the patient is concerned that a nonpharmacologic approach may be inadequate. In all instances, a patient with a paraphilic disorder should be informed that pharmacologic treatment is an option. A protocol for the pharmacologic treatment of paraphilic disorders that is based on my clinical experience is summarized in Table 2.
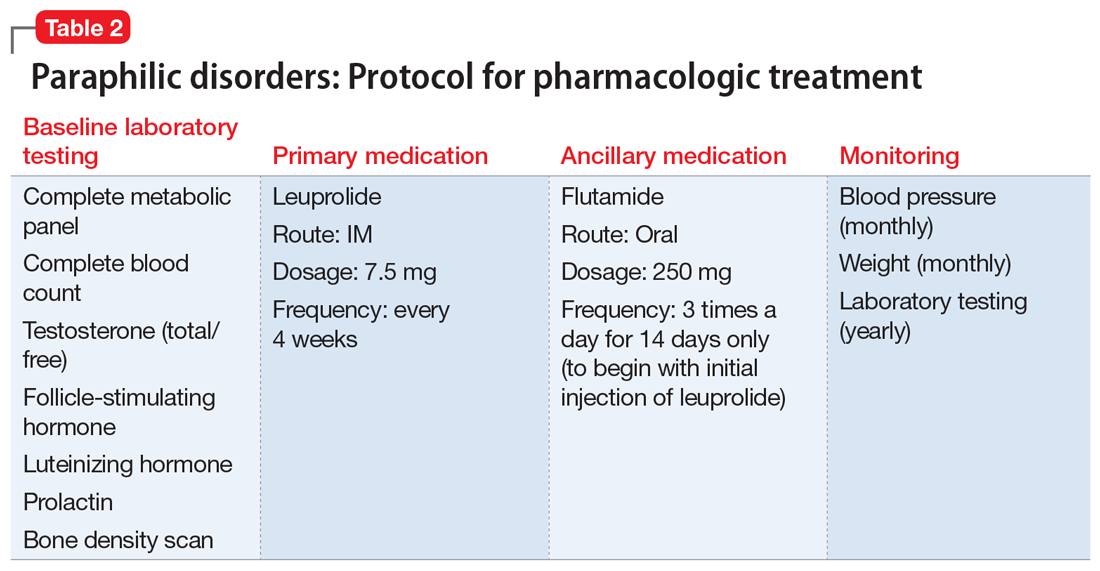
Leuprolide. A depot form of leuprolide is the most commonly employed agent to pharmacologically lower testosterone to treat a paraphilic disorder.13 When injected into muscle, leuprolide binds to it before gradually being released into the bloodstream. Previously, a depot medroxyprogesterone (a form of progesterone) had been used to treat paraphilic disorders.14 However, that had required weekly rather than monthly injections, and carried an increased risk of thrombotic emboli.
Prescribing leuprolide to treat a paraphilic disorder falls under FDA guidelines regarding the use of an approved drug for an “off-label” indication, and therefore is not considered investigational. For treating a paraphilic disorder, an effective dosage of leuprolide is 7.5 mg IM every 4 weeks. Long-term treatment is generally required, analogous to the management of diabetes. Because the initial injection of the series can cause a transient increase in testosterone (prior to its sustained decline), flutamide, a testosterone receptor blocking agent, is ordinarily prescribed for the first 14 days only, following initiation of treatment with depot leuprolide.15 Using flutamide in this fashion prevents the transient increase in testosterone from transiently increasing sexual drive. Flutamide should be discontinued after 14 days because long-term use can result in liver toxicity.
Some clinicians have been hesitant to prescribe leuprolide because of negative connotations associated with the term “chemical castration.” Unlike surgical castration, use of leuprolide is not a physically irreversible intervention, and does not result in sterility (although there may be an increase of atypical sperm and a decrease in total sperm production). The dosage can sometimes be titrated without a loss of efficacy.
In general, leuprolide’s safety protocol is well within the range associated with psychotropic medications.13 Low-risk adverse effects, such as hot flashes or cold sweats, may occur, especially during the period when hormone levels are in transition. There are no absolute contraindications to the use of leuprolide.
Continue to: Other medications
Other medications. Some researchers have suggested treating paraphilic disorders with psychotropic medications known to lower libido, such as selective serotonin reuptake inhibitors (SSRIs).16 However, leuprolide is far more reliable in consistently lowering testosterone and lowering the frequency and intensity of sexual urges. Although psychiatrists unfamiliar with treating paraphilic disorders may feel more comfortable initiating treatment with an SSRI, in my clinical experience, SSRIs have often proven inadequate for this purpose. When it comes to those paraphilic disorders in which treatment failure can result in significant harm (eg, pedophilic disorder), in my judgment, leuprolide should be the pharmacologic treatment of choice.
The opioid antagonist naltrexone has been used clinically to reduce cravings, primarily cravings for alcohol or drugs.17 However, I have not seen convincing evidence that it can be reliably beneficial in treating paraphilic disorders.
Tests to order before starting leuprolide
Long-term use of leuprolide can increase the risk of osteoporosis. Therefore, a baseline bone density scan should be performed before starting a patient on leuprolide. Baseline levels of testosterone, follicle-stimulating hormone, and luteinizing hormone also should be obtained. Patients should have yearly physical examinations, with accompanying laboratory testing. Hematocrit levels are often marginally low after beginning treatment, but not in a clinically significant way. Patients should also undergo routine monitoring for possible weight gain and the potential for associated hypertension. Treatment is predicated upon the known testosterone-suppressing effects of leuprolide, not upon routine monitoring of blood androgen levels.
Pharmacologic treatment of a paraphilic disorder should ordinarily occur in conjunction with nonpharmacologic modalities. One such modality would be group therapy, similar to the type frequently used to treat other craving disorders, such as drug or alcohol dependency.
In recent years, I have seen increasing numbers of patients presenting with a history of accessing and viewing child pornography. Once they have become more aware of the serious consequences of this behavior, most patients have been able to discontinue doing so without pharmacologic treatment. However, for patients in whom that behavior has seemed more driven (suggestive of a variant of voyeuristic disorder), prescription of leuprolide has been beneficial. Under such circumstances, I have diagnosed the patient’s condition as “other specified paraphilic disorder” with elements of pedophilia and voyeurism—the associated behaviors restricted to the voyeuristic viewing of child pornography.18
Continue to: Can treated patients still be sexual?
Can treated patients still be sexual?
If pharmacologic treatment of a paraphilic disorder results in erectile dysfunction, prescription of a medication such as sildenafil can be considered for patients who are in a consenting adult relationship, generally with the knowledge of their partner. Sildenafil can facilitate erectile capacity without increasing sexual drive. It can be helpful to explain to a patient that the purpose of pharmacologic treatment is not to prevent the enjoyment of sexual feelings within the context of a healthy, consenting, adult relationship, but instead to lower the intensity of problematic sexual urges, thereby facilitating sexual self-control. Just as lowering the appetite for food can make it easier to diet but not impossible to eat, lowering sexual appetite can facilitate successful self-control without necessarily interfering with erotic feelings experienced during sexual intimacy.
Bottom Line
Paraphilic disorders are not manifestations of a character flaw, but manifestations of unchosen qualitative differences in the nature of one’s sexual cravings. Not enough is yet known about the biology of sex to be able to pharmacologically alter its qualitative nature. However, pharmacologically lowering the intensity of a patient’s sexual drive can facilitate successful sexual self-regulation.
Related Resources
- LeVay S. Gay, straight and the reason why: the science of sexual orientation. London, UK: Oxford University Press; 2011.
- Rosler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998;338(7):416-422.
- Brown GR. Overview of paraphilic disorders (paraphilias). https://www.merckmanuals.com/professional/psychiatricdisorders/sexuality,-gender-dysphoria,-and-paraphilias/overview-of-paraphilic-disorders.
Drug Brand Names
Flutamide • Eulexin
Leuprolide injection •
Eligard, Lupron Depot
Medroxyprogesterone •
Provera
Naltrexone • Revia, Vivitrol
Progesterone • Prometrium
Sildenafil • Viagra
In my role as the Director of The Johns Hopkins Sex and Gender Clinic, I have had the opportunity to provide care to 3 broad categories of patients: patients with sexual dysfunctions, patients experiencing gender dysphoria, and patients manifesting a paraphilic disorder. This article will not address sexual dysfunctions or gender dysphoria, but these terms are defined in the Box1-3 to clearly distinguish them from paraphilic disorders.
Box
Individuals with a sexual dysfunction (eg, erectile dysfunction or anorgasmia) generally experience conventional sexual feelings, but they may have difficulty performing sexually.1 Although ordinarily capable of adequate sexual performance, persons with a paraphilic disorder experience atypical erotic cravings.2 Such cravings can either be for an atypical or unacceptable category of potential partner (eg, animals or children), or for an atypical or unacceptable type of behavior (eg, crossdressing or public exhibitionism). Individuals with gender dysphoria frequently experience distress because their internal sense of feeling either male or female is not congruent with their external physical anatomy.3 The primary concerns of individuals experiencing gender dysphoria relate to feelings of gender identity, as opposed to problems involving erotic arousal.
Persons with paraphilic disorders (predominantly males) experience recurrent atypical sexual fantasies and urges that cause clinically significant impairment or distress.1 Those atypical fantasies and urges may be directed towards unacceptable partners such as animals or children, or towards unacceptable behaviors such as public exhibitionism. Table 11 lists the paraphilic disorders identified in DSM-5. This article focuses primarily, though not exclusively, upon pedophilic disorder, and its pharmacologic treatment. However, the rationale underlying such treatment is applicable across the paraphilic spectrum. Before providing such treatment, it is important for clinicians to have a clear conceptual understanding of paraphilic disorders.
When is a difference a disorder?
Cancer and respiration are 2 different biologic phenomenon. Cancer causes suffering and impairment, and as a consequence, we label it a disorder. We do so in the hope of learning more about it, and being able to successfully treat it. We do not classify respiration as a disorder because we do not consider it to be harmful.
The spectrum of human sexuality is quite broad, and psychiatry is generally not concerned with private sexual thoughts and behaviors involving consenting adults that do not cause suffering or impairment. When adults choose to engage in “kinky sex” that causes neither harm nor distress, so be it.
Some individuals may be privately aware of experiencing either an exclusive or nonexclusive sexual attraction to children. Some of these individuals may not be distressed by experiencing such attractions, and may be fully capable of resisting the temptation to enact them. In such an instance, even though an individual may be experiencing sexual attractions that are different from the norm, there may not be a sufficient basis for diagnosing pedophilic disorder. However, that difference in sexual phenomenology (ie, mental experience) could rise to the level of a diagnosable disorder if the individual in question expresses distress about experiencing such attractions, and/or if his capacity to resist acting upon them is impaired.4 Under such circumstances, treatment would be warranted.
Patients with paraphilic disorders deserve treatment
Prior to establishment of the Betty Ford Clinic in 1982, individuals who were drug- or alcohol-dependent were often portrayed in a negative light and referred to by derogatory pejoratives such as “bum” or “pothead.”5 Over time, society came to appreciate that good people, deserving of treatment, can become dependent upon substances, and in recent years there has been considerable support for related research initiatives and humane care. However, there has not been analogous support for individuals who manifest paraphilic disorders, especially those with pedophilic disorder. Instead, such individuals are often perceived as undeserving of mental health care and resources. This has been the case, even though successful treatment of a pedophilic disorder could help prevent the serious consequences of child molestation from occurring.
In contemporary society, the term pedophilia, which is a psychiatric specifier intended to guide research and treatment, has been hijacked by the nonmedical community and turned into a demeaning pejorative. In the collective consciousness of the public, the term pedophilia is routinely and mistakenly equated with the behavior of child molestation. Just as all alcoholics are not drunk drivers, all individuals with pedophilic disorder are not “child molesters.” Conversely, not all “child molesters” have pedophilic disorder.
Continue to: Individuals with other types...
Individuals with other types of paraphilic disorders are frequently similarly maligned and referred to as “perverts” or “deviants.” Public service announcements are frequently aired to reach out to individuals who are depressed, or drug- or alcohol-dependent, or suffering with other forms of mental disorders. When does one hear a public service announcement that encourages young people who may be experiencing disturbing or unacceptable sexual feelings to seek psychiatric treatment? There is a support group on the internet called Virtuous Pedophiles.6 That organization is unequivocally opposed to child molestation, while supporting efforts to improve the mental well-being of individuals who, through no fault of their own, experience unwanted pedophilic feelings.
Causes and noncauses
In attempting to elucidate etiology, researchers typically investigate nature (biology) and/or nurture (life experiences). In terms of the development of pedophilic disorder, there is evidence that both nature and nurture can play a role. Researchers have found that boys who are sexually abused are at increased risk for developing pedophilic disorder, and evidence of temporal lobe disturbances has also been documented in some instances.7,8
From clinical, societal, and forensic perspectives, it may be equally important to identify noncausal factors. Paraphilic disorders, including pedophilic disorder, do not develop as a consequence of volitional choice.9 For example, none of us decide which category, or categories, of potential partners are going to attract us sexually. Rather, in maturing we discover the nature of our own sexuality. Children do not ponder their options, somehow deciding while growing up to be attracted to the opposite sex (heterosexuality), the same sex (homosexuality), or both sexes (bisexuality). Similarly, in maturing into adulthood, individuals do not decide to become sexually attracted to prepubescent children. Who would decide to do that? Instead, unlike most of us, some individuals discover this about themselves; this often is a deeply disturbing insight.
It is not an individual’s fault that he or she has a paraphilic disorder. It is, however, his or her responsibility to do something about it. This may require accessing appropriate psychiatric care.
Why treatment may be needed
Sex is a powerful, biologically based appetite that recurrently craves satiation. God or nature has put that drive into all of us to ensure the survival of humanity. Even when that powerful biologic drive becomes misdirected (for example, towards children, or towards a desire to engage in public exhibitionism), it still recurrently craves satisfaction. It does not require mental health expertise to appreciate what a problematic situation this could become.
Continue to: Some individuals need help...
Some individuals need help in overcoming cravings related to nonsexual appetites. For example, Americans spend millions of dollars each year trying to diet; they often require some form of assistance in order to succeed. Individuals who crave drugs or alcohol often require mental health interventions to abstain because they are unable to consistently resist through willpower alone the powerful biologic urges that drive their actions.
The fundamental mental characteristic of any paraphilic disorder is the presence of intense, recurrent, sexual urges of an atypical nature. In the case of a pedophilic disorder, those urges involve sexual feelings about children.2 In the case of an exhibitionistic disorder, the afflicted individual experiences intense, recurrent sexual fantasies/urges related to exposing his genitals in public.1 Clearly, most men do not have to recurrently fight off the urge to act in such a fashion. Given the driven nature of intense erotic cravings, individuals who experience such cravings will frequently require access to competent mental health care.
Pharmacologic treatment of paraphilic disorders
In the future, we may develop a scientifically based understanding of the biologic factors that underlie qualitative differences in sexuality. At that point, it may become possible to intervene pharmacologically, changing the qualitative nature of a sexual urge with pharmacologic interventions. This cannot yet be done. H
In 1939, a Nobel Prize in Chemistry was awarded for the identification and isolation of the hormone testosterone, which energizes sexual drive.10 If an individual is hungering sexually to expose himself, to view child pornography, or to engage in sexual acts with children, the intensity of such hungers can be significantly reduced by lowering testosterone, thereby enhancing the capacity for successful sexual self-control.
A large body of scientific data has documented a marked decrease in sexually motivated behaviors when testosterone levels are significantly diminished.11 There is also evidence that recidivism rates of sexually motivated crimes can be significantly reduced when testosterone-lowering interventions are used.12
Continue to: Historically, removal of the testes...
Historically, removal of the testes (surgical castration) had been the only effective way to reliably lower testosterone. Today, this can be achieved pharmacologically. Use of a sex drive–lowering medication should be considered when either the clinician or the patient is concerned that a nonpharmacologic approach may be inadequate. In all instances, a patient with a paraphilic disorder should be informed that pharmacologic treatment is an option. A protocol for the pharmacologic treatment of paraphilic disorders that is based on my clinical experience is summarized in Table 2.
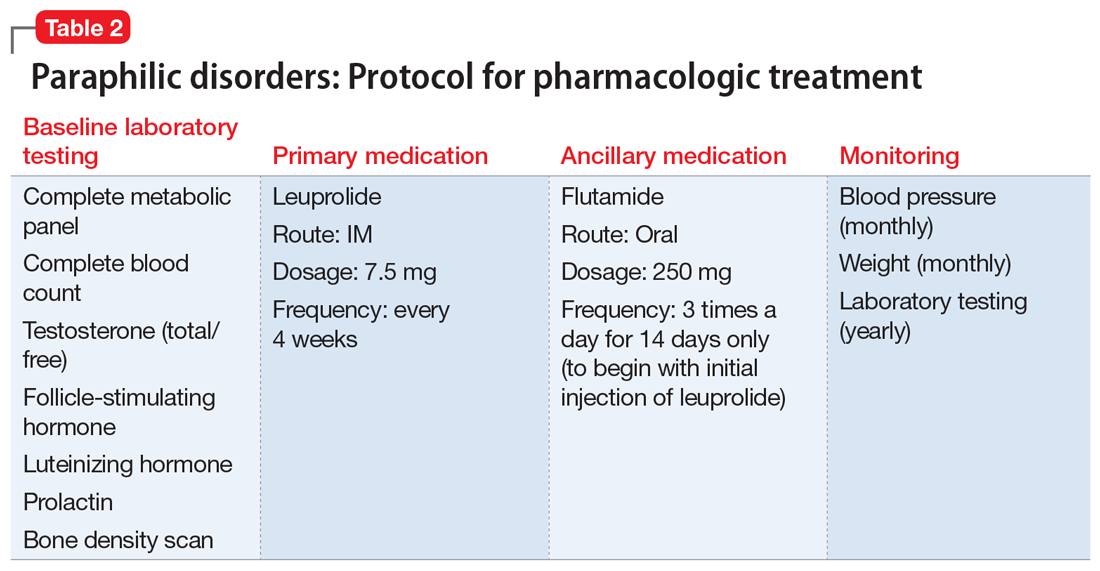
Leuprolide. A depot form of leuprolide is the most commonly employed agent to pharmacologically lower testosterone to treat a paraphilic disorder.13 When injected into muscle, leuprolide binds to it before gradually being released into the bloodstream. Previously, a depot medroxyprogesterone (a form of progesterone) had been used to treat paraphilic disorders.14 However, that had required weekly rather than monthly injections, and carried an increased risk of thrombotic emboli.
Prescribing leuprolide to treat a paraphilic disorder falls under FDA guidelines regarding the use of an approved drug for an “off-label” indication, and therefore is not considered investigational. For treating a paraphilic disorder, an effective dosage of leuprolide is 7.5 mg IM every 4 weeks. Long-term treatment is generally required, analogous to the management of diabetes. Because the initial injection of the series can cause a transient increase in testosterone (prior to its sustained decline), flutamide, a testosterone receptor blocking agent, is ordinarily prescribed for the first 14 days only, following initiation of treatment with depot leuprolide.15 Using flutamide in this fashion prevents the transient increase in testosterone from transiently increasing sexual drive. Flutamide should be discontinued after 14 days because long-term use can result in liver toxicity.
Some clinicians have been hesitant to prescribe leuprolide because of negative connotations associated with the term “chemical castration.” Unlike surgical castration, use of leuprolide is not a physically irreversible intervention, and does not result in sterility (although there may be an increase of atypical sperm and a decrease in total sperm production). The dosage can sometimes be titrated without a loss of efficacy.
In general, leuprolide’s safety protocol is well within the range associated with psychotropic medications.13 Low-risk adverse effects, such as hot flashes or cold sweats, may occur, especially during the period when hormone levels are in transition. There are no absolute contraindications to the use of leuprolide.
Continue to: Other medications
Other medications. Some researchers have suggested treating paraphilic disorders with psychotropic medications known to lower libido, such as selective serotonin reuptake inhibitors (SSRIs).16 However, leuprolide is far more reliable in consistently lowering testosterone and lowering the frequency and intensity of sexual urges. Although psychiatrists unfamiliar with treating paraphilic disorders may feel more comfortable initiating treatment with an SSRI, in my clinical experience, SSRIs have often proven inadequate for this purpose. When it comes to those paraphilic disorders in which treatment failure can result in significant harm (eg, pedophilic disorder), in my judgment, leuprolide should be the pharmacologic treatment of choice.
The opioid antagonist naltrexone has been used clinically to reduce cravings, primarily cravings for alcohol or drugs.17 However, I have not seen convincing evidence that it can be reliably beneficial in treating paraphilic disorders.
Tests to order before starting leuprolide
Long-term use of leuprolide can increase the risk of osteoporosis. Therefore, a baseline bone density scan should be performed before starting a patient on leuprolide. Baseline levels of testosterone, follicle-stimulating hormone, and luteinizing hormone also should be obtained. Patients should have yearly physical examinations, with accompanying laboratory testing. Hematocrit levels are often marginally low after beginning treatment, but not in a clinically significant way. Patients should also undergo routine monitoring for possible weight gain and the potential for associated hypertension. Treatment is predicated upon the known testosterone-suppressing effects of leuprolide, not upon routine monitoring of blood androgen levels.
Pharmacologic treatment of a paraphilic disorder should ordinarily occur in conjunction with nonpharmacologic modalities. One such modality would be group therapy, similar to the type frequently used to treat other craving disorders, such as drug or alcohol dependency.
In recent years, I have seen increasing numbers of patients presenting with a history of accessing and viewing child pornography. Once they have become more aware of the serious consequences of this behavior, most patients have been able to discontinue doing so without pharmacologic treatment. However, for patients in whom that behavior has seemed more driven (suggestive of a variant of voyeuristic disorder), prescription of leuprolide has been beneficial. Under such circumstances, I have diagnosed the patient’s condition as “other specified paraphilic disorder” with elements of pedophilia and voyeurism—the associated behaviors restricted to the voyeuristic viewing of child pornography.18
Continue to: Can treated patients still be sexual?
Can treated patients still be sexual?
If pharmacologic treatment of a paraphilic disorder results in erectile dysfunction, prescription of a medication such as sildenafil can be considered for patients who are in a consenting adult relationship, generally with the knowledge of their partner. Sildenafil can facilitate erectile capacity without increasing sexual drive. It can be helpful to explain to a patient that the purpose of pharmacologic treatment is not to prevent the enjoyment of sexual feelings within the context of a healthy, consenting, adult relationship, but instead to lower the intensity of problematic sexual urges, thereby facilitating sexual self-control. Just as lowering the appetite for food can make it easier to diet but not impossible to eat, lowering sexual appetite can facilitate successful self-control without necessarily interfering with erotic feelings experienced during sexual intimacy.
Bottom Line
Paraphilic disorders are not manifestations of a character flaw, but manifestations of unchosen qualitative differences in the nature of one’s sexual cravings. Not enough is yet known about the biology of sex to be able to pharmacologically alter its qualitative nature. However, pharmacologically lowering the intensity of a patient’s sexual drive can facilitate successful sexual self-regulation.
Related Resources
- LeVay S. Gay, straight and the reason why: the science of sexual orientation. London, UK: Oxford University Press; 2011.
- Rosler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998;338(7):416-422.
- Brown GR. Overview of paraphilic disorders (paraphilias). https://www.merckmanuals.com/professional/psychiatricdisorders/sexuality,-gender-dysphoria,-and-paraphilias/overview-of-paraphilic-disorders.
Drug Brand Names
Flutamide • Eulexin
Leuprolide injection •
Eligard, Lupron Depot
Medroxyprogesterone •
Provera
Naltrexone • Revia, Vivitrol
Progesterone • Prometrium
Sildenafil • Viagra
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:423-450.
2. Berlin FS. Pedophilia: criminal mind-set or mental disorder? A conceptual review. American Journal of Forensic Psychiatry. 2001;32(2):3-25.
3. Berlin FS. A conceptual overview and commentary on gender dysphoria. J Am Acad Psychiatry Law. 2016;44(2):246-252
4. Berlin FS. Pedophilia: when is a difference a disorder: Peer commentaries on Green (2002) and Schmidt (2002). Arch Sex Behav. 2002;31:1-2.
5. Ford B, Chase C. Betty: a glad awakening. New York, NY: Doubleday; 1987.
6. Virtuous Pedophiles. https://www.virped.org/. Accessed September 28, 2018.
7. Freund K, Kuban M. The basis of the abused abuser theory of pedophilia: A further elaboration of an earlier study. Arch Sex Behav. 1994;23(5):553-563.
8. Mendes MF, Chow T, Ringman T, et al. Pedophilia and temporal lobe disturbances. J Neuropsychiatry Clin Neurosci. 2000;12(1):71-76.
9. Money J. Love and love sickness: The science of sex, gender differences, and pair bonding. Baltimore, MD: Johns Hopkins University Press; 1980.
10. The Nobel Prize in Chemistry 1939. https://www.nobelprize.org/prizes/chemistry/1939/summary/. Accessed September 29, 2018.
11. Berlin FS. Commentary: The impact of surgical castration on sexual recidivism risk among civilly committed sex offenders. J Am Acad Psychiatry Law. 2005;33(1):37-41.
12. Hansen H. Treatment of dangerous sexual offenders. In: Seminar on Prison Health Services in Tampere, Finland. Helsinki, Finland: Ministry of Justice, Government Printing Centre; 1991:33-38.
13. Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. J Am Acad Psychiatry Law. 2009;37(1):59-62.
14. Berlin FS, Meinecke CF. Treatment of sex offenders with antiandrogenic medication: conceptualization, review of treatment modalities, and preliminary findings. Am J Psychiatry. 1981;138(5):601-607.
15. Neri R. Pharmacology and pharmacokinetics of flutamide. Urology. 1989;34(suppl 4):19-21; discussion 46-56.
16. Adi Y, Ashcroft D, Browne K, et al. Clinical effectiveness and cost consequences of selective serotonin receptor reuptake inhibitors in the treatment of sex offenders. Health Technol Assess. 2002;6(28):1-66.
17. Anton RF. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715-721.
18. Berlin FS. Commentary on pedophilia diagnostic criteria in DSM-5. J Am Acad Psychiatry Law. 2011;39(2):242-244.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:423-450.
2. Berlin FS. Pedophilia: criminal mind-set or mental disorder? A conceptual review. American Journal of Forensic Psychiatry. 2001;32(2):3-25.
3. Berlin FS. A conceptual overview and commentary on gender dysphoria. J Am Acad Psychiatry Law. 2016;44(2):246-252
4. Berlin FS. Pedophilia: when is a difference a disorder: Peer commentaries on Green (2002) and Schmidt (2002). Arch Sex Behav. 2002;31:1-2.
5. Ford B, Chase C. Betty: a glad awakening. New York, NY: Doubleday; 1987.
6. Virtuous Pedophiles. https://www.virped.org/. Accessed September 28, 2018.
7. Freund K, Kuban M. The basis of the abused abuser theory of pedophilia: A further elaboration of an earlier study. Arch Sex Behav. 1994;23(5):553-563.
8. Mendes MF, Chow T, Ringman T, et al. Pedophilia and temporal lobe disturbances. J Neuropsychiatry Clin Neurosci. 2000;12(1):71-76.
9. Money J. Love and love sickness: The science of sex, gender differences, and pair bonding. Baltimore, MD: Johns Hopkins University Press; 1980.
10. The Nobel Prize in Chemistry 1939. https://www.nobelprize.org/prizes/chemistry/1939/summary/. Accessed September 29, 2018.
11. Berlin FS. Commentary: The impact of surgical castration on sexual recidivism risk among civilly committed sex offenders. J Am Acad Psychiatry Law. 2005;33(1):37-41.
12. Hansen H. Treatment of dangerous sexual offenders. In: Seminar on Prison Health Services in Tampere, Finland. Helsinki, Finland: Ministry of Justice, Government Printing Centre; 1991:33-38.
13. Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. J Am Acad Psychiatry Law. 2009;37(1):59-62.
14. Berlin FS, Meinecke CF. Treatment of sex offenders with antiandrogenic medication: conceptualization, review of treatment modalities, and preliminary findings. Am J Psychiatry. 1981;138(5):601-607.
15. Neri R. Pharmacology and pharmacokinetics of flutamide. Urology. 1989;34(suppl 4):19-21; discussion 46-56.
16. Adi Y, Ashcroft D, Browne K, et al. Clinical effectiveness and cost consequences of selective serotonin receptor reuptake inhibitors in the treatment of sex offenders. Health Technol Assess. 2002;6(28):1-66.
17. Anton RF. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715-721.
18. Berlin FS. Commentary on pedophilia diagnostic criteria in DSM-5. J Am Acad Psychiatry Law. 2011;39(2):242-244.
Who’s increasing health care costs? Not us!
Determining who is responsible for the increase in health care cost in the United States has seemingly limitless possibilities. There are enough culprits to go around, but a recent analysis points a finger at hospital-based care (Health Aff. 2019 Feb;38[2]:184-9).
The authors of the paper found that, during the period from 2007 to 2014, inpatient hospital care for surgical procedures increased 42% and outpatient hospital care increased 25%. In the same period, physician care increased only 6%. Much of this increase in hospital costs was associated with hospital consolidations and mergers.
We have been led to believe that hospital mergers will cut costs by eliminating duplication of both physical and personnel overhead costs. In fact that doesn’t seem to happen. It appears that hospital mergers were associated with increased per patient costs and is a result of decrease in competition in local health care markets. This observation has been made in the past (Am Econ Rev. 2015 Jan;105:172-203), and was reiterated by the most recent report. If there were decreases in overhead observed in the mergers, they were not passed on to the patients or insurers.
There was a time when community hospitals, large and small, were run by community leaders and local doctors, often under the aegis of religious and social groups. I can remember the medical and community leadership in Utica, N.Y., where I grew up and where I worked in a hospital as a summer intern. Their goal was to provide quality health care. The financial success or failures of the hospitals were the responsibility of the local community, and the profits and losses were kept at a minimum.
Fast forward to the 21st century and health care in general, and hospital care in particular, has become a “cash cow.” Community leadership has been minimized, and where it exists, it is under constant pressure to make a profit. Hospital mergers, arranged under the guise of economy of size, are now controlled by hedge funds and large health care corporations.
The community board of trustees has been replaced by investors, whose main concern is the return on their investments regardless of quality of care or need. If those profits fail to materialize, the hospitals are taken over by another investor group. So much for quality. As the corporations grow, they buy up the competition, particularly small community hospitals leaving many, particularly in rural America, without medical support.
There seems to be little recourse to consumers or insurers to mitigate this process. Investors have a right to a return on their investment, but until we have governmental control of competition, that incentive remains. We can see similar price increases in the pharmaceutical marketplace, where Congress has limited competition to preserve the drug monopoly. Americans will be asked to pay more to maintain a system that is inherently on the road to bankruptcy and fails to provide either quality or fair drug and hospital charges.
But what do we care, we can afford it.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
Determining who is responsible for the increase in health care cost in the United States has seemingly limitless possibilities. There are enough culprits to go around, but a recent analysis points a finger at hospital-based care (Health Aff. 2019 Feb;38[2]:184-9).
The authors of the paper found that, during the period from 2007 to 2014, inpatient hospital care for surgical procedures increased 42% and outpatient hospital care increased 25%. In the same period, physician care increased only 6%. Much of this increase in hospital costs was associated with hospital consolidations and mergers.
We have been led to believe that hospital mergers will cut costs by eliminating duplication of both physical and personnel overhead costs. In fact that doesn’t seem to happen. It appears that hospital mergers were associated with increased per patient costs and is a result of decrease in competition in local health care markets. This observation has been made in the past (Am Econ Rev. 2015 Jan;105:172-203), and was reiterated by the most recent report. If there were decreases in overhead observed in the mergers, they were not passed on to the patients or insurers.
There was a time when community hospitals, large and small, were run by community leaders and local doctors, often under the aegis of religious and social groups. I can remember the medical and community leadership in Utica, N.Y., where I grew up and where I worked in a hospital as a summer intern. Their goal was to provide quality health care. The financial success or failures of the hospitals were the responsibility of the local community, and the profits and losses were kept at a minimum.
Fast forward to the 21st century and health care in general, and hospital care in particular, has become a “cash cow.” Community leadership has been minimized, and where it exists, it is under constant pressure to make a profit. Hospital mergers, arranged under the guise of economy of size, are now controlled by hedge funds and large health care corporations.
The community board of trustees has been replaced by investors, whose main concern is the return on their investments regardless of quality of care or need. If those profits fail to materialize, the hospitals are taken over by another investor group. So much for quality. As the corporations grow, they buy up the competition, particularly small community hospitals leaving many, particularly in rural America, without medical support.
There seems to be little recourse to consumers or insurers to mitigate this process. Investors have a right to a return on their investment, but until we have governmental control of competition, that incentive remains. We can see similar price increases in the pharmaceutical marketplace, where Congress has limited competition to preserve the drug monopoly. Americans will be asked to pay more to maintain a system that is inherently on the road to bankruptcy and fails to provide either quality or fair drug and hospital charges.
But what do we care, we can afford it.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
Determining who is responsible for the increase in health care cost in the United States has seemingly limitless possibilities. There are enough culprits to go around, but a recent analysis points a finger at hospital-based care (Health Aff. 2019 Feb;38[2]:184-9).
The authors of the paper found that, during the period from 2007 to 2014, inpatient hospital care for surgical procedures increased 42% and outpatient hospital care increased 25%. In the same period, physician care increased only 6%. Much of this increase in hospital costs was associated with hospital consolidations and mergers.
We have been led to believe that hospital mergers will cut costs by eliminating duplication of both physical and personnel overhead costs. In fact that doesn’t seem to happen. It appears that hospital mergers were associated with increased per patient costs and is a result of decrease in competition in local health care markets. This observation has been made in the past (Am Econ Rev. 2015 Jan;105:172-203), and was reiterated by the most recent report. If there were decreases in overhead observed in the mergers, they were not passed on to the patients or insurers.
There was a time when community hospitals, large and small, were run by community leaders and local doctors, often under the aegis of religious and social groups. I can remember the medical and community leadership in Utica, N.Y., where I grew up and where I worked in a hospital as a summer intern. Their goal was to provide quality health care. The financial success or failures of the hospitals were the responsibility of the local community, and the profits and losses were kept at a minimum.
Fast forward to the 21st century and health care in general, and hospital care in particular, has become a “cash cow.” Community leadership has been minimized, and where it exists, it is under constant pressure to make a profit. Hospital mergers, arranged under the guise of economy of size, are now controlled by hedge funds and large health care corporations.
The community board of trustees has been replaced by investors, whose main concern is the return on their investments regardless of quality of care or need. If those profits fail to materialize, the hospitals are taken over by another investor group. So much for quality. As the corporations grow, they buy up the competition, particularly small community hospitals leaving many, particularly in rural America, without medical support.
There seems to be little recourse to consumers or insurers to mitigate this process. Investors have a right to a return on their investment, but until we have governmental control of competition, that incentive remains. We can see similar price increases in the pharmaceutical marketplace, where Congress has limited competition to preserve the drug monopoly. Americans will be asked to pay more to maintain a system that is inherently on the road to bankruptcy and fails to provide either quality or fair drug and hospital charges.
But what do we care, we can afford it.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.