User login
States move to curb insurers’ prior authorization requirements as federal reforms lag
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Common fracture risk predictors often fail for women of any race
according to a study published in JAMA Internal Medicine.
One of the screenings, the U.S. Fracture Risk Assessment Tool (FRAX), proved relatively ineffective at identifying women who developed osteoporosis. The other screening, the Osteoporosis Self-Assessment Tool (OST), excelled at identifying osteoporosis for women in every racial and ethnic group, but also failed at identifying who was most likely to experience a fracture. Osteoporosis experts say that primary care physicians should test for the condition in anyone with any risk factor for it, even if a screening tool suggests doing so is unnecessary.
The United States Preventive Services Task Force (USPSTF) recommends routine testing of bone mineral density in women age 65 years and older to detect risk of developing osteoporosis, which in turn leads to an increased risk for fractures of the hip, spine, shoulder, or forearm. For women aged 50-64, whether bone mineral density accurately reflects who will develop osteoporosis is less clear. In this age range, the USPSTF recommends using either FRAX or OST rather than routine bone mineral density tests.
“I have the utmost respect for the United States Preventive Services Task Force, which lists both of these as valid screening tools for younger postmenopausal women. What I hope this study does is to inform the next iteration of the screening guidelines,” by maintaining the recommendation to use the OST while not keeping FRAX, said Carolyn J. Crandall, MD, MS, an internal medicine physician and health services researcher at University of California, Los Angeles, who helped conduct the research.
The U.S. version of FRAX requires identifying someone’s race, height, and weight, then answering whether they have different risk factors for a fracture such as a previous fracture, rheumatoid arthritis, or smoking. The result was thought to indicate a cumulative risk for major fracture over the next 10 years. Patients at significant risk should then undergo a bone density test.
The tool can also incorporate information about bone mineral density, if available, but the FRAX analyses in Dr. Crandall’s study did not include those data because the study aimed to test the measure’s predictive ability in the absence of a bone scan.
The OST includes only two variables – weight and age – to calculate risk for osteoporosis, and generally takes seconds to complete. It does not include race. As with FRAX, anyone deemed at significant risk for developing osteoporosis should undergo a bone density test.
“OST is really simple; that makes it very appealing,” Dr. Crandall said. “OST could probably be automatically calculated in the electronic medical record.”
Using data from the Women’s Health Initiative, Dr. Crandall and colleagues tracked more than 67,000 women aged 50-64 years for 10 years following enrollment in the study to see who experienced a fracture or developed osteoporosis over that decade. The investigators found that neither FRAX nor OST was particularly good at predicting who went on to experience a fracture.
The accuracy of FRAX at fracture prediction peaked at 65% for Asian women (area under the receiver operating curve, 0.65; 95% confidence interval, 0.58-0.71), and was lowest for Black women (AUC 0.55; 95% CI, 0.52-0.59). OST also was most accurate for Asian women, but only up to 62% (AUC 0.62; 95% CI, 0.56-0.69), and was again lowest for Black women (AUC 0.53; 95% CI, 0.50 - 0.57)
“It is just very hard to predict fractures in this age group,” Dr. Crandall said, noting that more evidence exists about risk for fracture in people older than 65.
The story diverges with predicting risk of osteoporosis in the neck. The OST did this roughly 80% of the time, for all racial groups. That figure proved better than FRAX, without including race.
Treatment gap
“This evidence supports using OST instead of FRAX” for selecting younger postmenopausal women who should undergo a bone mineral density exam, said E. Michael Lewiecki, MD, director of the New Mexico Clinical Research & Osteoporosis Center in Albuquerque.

Dr. Lewiecki, who was not involved in the new study, noted that the U.S. version of FRAX specifies race because of some clinical evidence that different races have different rates of fracture. But he and Dr. Crandall said the validity of race-based algorithms to guide clinical care is a controversial and evolving topic in medicine. Dr. Lewiecki said the Canadian version of FRAX, which is similarly applied to a diverse population as in the United States, omits race and works as well as the U.S. version. Future iterations of the instrument in the United States may not include race, Dr. Lewiecki said.
“The study is perfectly valid as far as it goes. But the big gorilla in the room is that most patients who need a bone density test are not getting it,” Dr. Lewiecki added. Sometimes a patient might break a bone in their wrist, for example, and tell their primary care provider that anyone would have broken that bone because the fall was so hard. Even if that’s true, Dr. Lewiecki said, any woman older than 45 who has broken a bone should undergo a bone density test to determine if they have osteoporosis, even if it seems like there are other possible reasons for why the break occurred.
“Most of the clinical practice guidelines that are used by physicians recommend getting a bone density test in postmenopausal women under the age of 65 who have a risk factor for fracture,” Dr. Lewiecki said, with a primary risk factor being a prior fracture. Dr. Lewiecki said he would rather that anyone who could benefit from a bone density test receive it, rather than someone foregoing a scan based on a screening tool that may be flawed.
“Most patients – men and women – who have osteoporosis are currently not being identified. Even when they are being identified, they are commonly not being treated. And when they are started on treatment, many patients discontinue treatment before they’ve taken it long enough to benefit,” Dr. Lewiecki said.
Dr. Crandall and Dr. Lewiecki report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a study published in JAMA Internal Medicine.
One of the screenings, the U.S. Fracture Risk Assessment Tool (FRAX), proved relatively ineffective at identifying women who developed osteoporosis. The other screening, the Osteoporosis Self-Assessment Tool (OST), excelled at identifying osteoporosis for women in every racial and ethnic group, but also failed at identifying who was most likely to experience a fracture. Osteoporosis experts say that primary care physicians should test for the condition in anyone with any risk factor for it, even if a screening tool suggests doing so is unnecessary.
The United States Preventive Services Task Force (USPSTF) recommends routine testing of bone mineral density in women age 65 years and older to detect risk of developing osteoporosis, which in turn leads to an increased risk for fractures of the hip, spine, shoulder, or forearm. For women aged 50-64, whether bone mineral density accurately reflects who will develop osteoporosis is less clear. In this age range, the USPSTF recommends using either FRAX or OST rather than routine bone mineral density tests.
“I have the utmost respect for the United States Preventive Services Task Force, which lists both of these as valid screening tools for younger postmenopausal women. What I hope this study does is to inform the next iteration of the screening guidelines,” by maintaining the recommendation to use the OST while not keeping FRAX, said Carolyn J. Crandall, MD, MS, an internal medicine physician and health services researcher at University of California, Los Angeles, who helped conduct the research.
The U.S. version of FRAX requires identifying someone’s race, height, and weight, then answering whether they have different risk factors for a fracture such as a previous fracture, rheumatoid arthritis, or smoking. The result was thought to indicate a cumulative risk for major fracture over the next 10 years. Patients at significant risk should then undergo a bone density test.
The tool can also incorporate information about bone mineral density, if available, but the FRAX analyses in Dr. Crandall’s study did not include those data because the study aimed to test the measure’s predictive ability in the absence of a bone scan.
The OST includes only two variables – weight and age – to calculate risk for osteoporosis, and generally takes seconds to complete. It does not include race. As with FRAX, anyone deemed at significant risk for developing osteoporosis should undergo a bone density test.
“OST is really simple; that makes it very appealing,” Dr. Crandall said. “OST could probably be automatically calculated in the electronic medical record.”
Using data from the Women’s Health Initiative, Dr. Crandall and colleagues tracked more than 67,000 women aged 50-64 years for 10 years following enrollment in the study to see who experienced a fracture or developed osteoporosis over that decade. The investigators found that neither FRAX nor OST was particularly good at predicting who went on to experience a fracture.
The accuracy of FRAX at fracture prediction peaked at 65% for Asian women (area under the receiver operating curve, 0.65; 95% confidence interval, 0.58-0.71), and was lowest for Black women (AUC 0.55; 95% CI, 0.52-0.59). OST also was most accurate for Asian women, but only up to 62% (AUC 0.62; 95% CI, 0.56-0.69), and was again lowest for Black women (AUC 0.53; 95% CI, 0.50 - 0.57)
“It is just very hard to predict fractures in this age group,” Dr. Crandall said, noting that more evidence exists about risk for fracture in people older than 65.
The story diverges with predicting risk of osteoporosis in the neck. The OST did this roughly 80% of the time, for all racial groups. That figure proved better than FRAX, without including race.
Treatment gap
“This evidence supports using OST instead of FRAX” for selecting younger postmenopausal women who should undergo a bone mineral density exam, said E. Michael Lewiecki, MD, director of the New Mexico Clinical Research & Osteoporosis Center in Albuquerque.

Dr. Lewiecki, who was not involved in the new study, noted that the U.S. version of FRAX specifies race because of some clinical evidence that different races have different rates of fracture. But he and Dr. Crandall said the validity of race-based algorithms to guide clinical care is a controversial and evolving topic in medicine. Dr. Lewiecki said the Canadian version of FRAX, which is similarly applied to a diverse population as in the United States, omits race and works as well as the U.S. version. Future iterations of the instrument in the United States may not include race, Dr. Lewiecki said.
“The study is perfectly valid as far as it goes. But the big gorilla in the room is that most patients who need a bone density test are not getting it,” Dr. Lewiecki added. Sometimes a patient might break a bone in their wrist, for example, and tell their primary care provider that anyone would have broken that bone because the fall was so hard. Even if that’s true, Dr. Lewiecki said, any woman older than 45 who has broken a bone should undergo a bone density test to determine if they have osteoporosis, even if it seems like there are other possible reasons for why the break occurred.
“Most of the clinical practice guidelines that are used by physicians recommend getting a bone density test in postmenopausal women under the age of 65 who have a risk factor for fracture,” Dr. Lewiecki said, with a primary risk factor being a prior fracture. Dr. Lewiecki said he would rather that anyone who could benefit from a bone density test receive it, rather than someone foregoing a scan based on a screening tool that may be flawed.
“Most patients – men and women – who have osteoporosis are currently not being identified. Even when they are being identified, they are commonly not being treated. And when they are started on treatment, many patients discontinue treatment before they’ve taken it long enough to benefit,” Dr. Lewiecki said.
Dr. Crandall and Dr. Lewiecki report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a study published in JAMA Internal Medicine.
One of the screenings, the U.S. Fracture Risk Assessment Tool (FRAX), proved relatively ineffective at identifying women who developed osteoporosis. The other screening, the Osteoporosis Self-Assessment Tool (OST), excelled at identifying osteoporosis for women in every racial and ethnic group, but also failed at identifying who was most likely to experience a fracture. Osteoporosis experts say that primary care physicians should test for the condition in anyone with any risk factor for it, even if a screening tool suggests doing so is unnecessary.
The United States Preventive Services Task Force (USPSTF) recommends routine testing of bone mineral density in women age 65 years and older to detect risk of developing osteoporosis, which in turn leads to an increased risk for fractures of the hip, spine, shoulder, or forearm. For women aged 50-64, whether bone mineral density accurately reflects who will develop osteoporosis is less clear. In this age range, the USPSTF recommends using either FRAX or OST rather than routine bone mineral density tests.
“I have the utmost respect for the United States Preventive Services Task Force, which lists both of these as valid screening tools for younger postmenopausal women. What I hope this study does is to inform the next iteration of the screening guidelines,” by maintaining the recommendation to use the OST while not keeping FRAX, said Carolyn J. Crandall, MD, MS, an internal medicine physician and health services researcher at University of California, Los Angeles, who helped conduct the research.
The U.S. version of FRAX requires identifying someone’s race, height, and weight, then answering whether they have different risk factors for a fracture such as a previous fracture, rheumatoid arthritis, or smoking. The result was thought to indicate a cumulative risk for major fracture over the next 10 years. Patients at significant risk should then undergo a bone density test.
The tool can also incorporate information about bone mineral density, if available, but the FRAX analyses in Dr. Crandall’s study did not include those data because the study aimed to test the measure’s predictive ability in the absence of a bone scan.
The OST includes only two variables – weight and age – to calculate risk for osteoporosis, and generally takes seconds to complete. It does not include race. As with FRAX, anyone deemed at significant risk for developing osteoporosis should undergo a bone density test.
“OST is really simple; that makes it very appealing,” Dr. Crandall said. “OST could probably be automatically calculated in the electronic medical record.”
Using data from the Women’s Health Initiative, Dr. Crandall and colleagues tracked more than 67,000 women aged 50-64 years for 10 years following enrollment in the study to see who experienced a fracture or developed osteoporosis over that decade. The investigators found that neither FRAX nor OST was particularly good at predicting who went on to experience a fracture.
The accuracy of FRAX at fracture prediction peaked at 65% for Asian women (area under the receiver operating curve, 0.65; 95% confidence interval, 0.58-0.71), and was lowest for Black women (AUC 0.55; 95% CI, 0.52-0.59). OST also was most accurate for Asian women, but only up to 62% (AUC 0.62; 95% CI, 0.56-0.69), and was again lowest for Black women (AUC 0.53; 95% CI, 0.50 - 0.57)
“It is just very hard to predict fractures in this age group,” Dr. Crandall said, noting that more evidence exists about risk for fracture in people older than 65.
The story diverges with predicting risk of osteoporosis in the neck. The OST did this roughly 80% of the time, for all racial groups. That figure proved better than FRAX, without including race.
Treatment gap
“This evidence supports using OST instead of FRAX” for selecting younger postmenopausal women who should undergo a bone mineral density exam, said E. Michael Lewiecki, MD, director of the New Mexico Clinical Research & Osteoporosis Center in Albuquerque.

Dr. Lewiecki, who was not involved in the new study, noted that the U.S. version of FRAX specifies race because of some clinical evidence that different races have different rates of fracture. But he and Dr. Crandall said the validity of race-based algorithms to guide clinical care is a controversial and evolving topic in medicine. Dr. Lewiecki said the Canadian version of FRAX, which is similarly applied to a diverse population as in the United States, omits race and works as well as the U.S. version. Future iterations of the instrument in the United States may not include race, Dr. Lewiecki said.
“The study is perfectly valid as far as it goes. But the big gorilla in the room is that most patients who need a bone density test are not getting it,” Dr. Lewiecki added. Sometimes a patient might break a bone in their wrist, for example, and tell their primary care provider that anyone would have broken that bone because the fall was so hard. Even if that’s true, Dr. Lewiecki said, any woman older than 45 who has broken a bone should undergo a bone density test to determine if they have osteoporosis, even if it seems like there are other possible reasons for why the break occurred.
“Most of the clinical practice guidelines that are used by physicians recommend getting a bone density test in postmenopausal women under the age of 65 who have a risk factor for fracture,” Dr. Lewiecki said, with a primary risk factor being a prior fracture. Dr. Lewiecki said he would rather that anyone who could benefit from a bone density test receive it, rather than someone foregoing a scan based on a screening tool that may be flawed.
“Most patients – men and women – who have osteoporosis are currently not being identified. Even when they are being identified, they are commonly not being treated. And when they are started on treatment, many patients discontinue treatment before they’ve taken it long enough to benefit,” Dr. Lewiecki said.
Dr. Crandall and Dr. Lewiecki report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA INTERNAL MEDICINE
Youth-led sexual health program improves teen knowledge, autonomy
BALTIMORE – , according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
While the small pilot study focused primarily on assessing feasibility and effectiveness, the results suggest potential for scaling the program up to reach a larger audience and assessing the knowledge disseminated from direct youth participants.
“The good thing about this subject is that not a lot of it has to be context-specific,” Saumya Sao, a clinical researcher in gynecology and obstetrics at the Johns Hopkins University, Baltimore, and the study’s lead author, said in an interview. “A lot of it is just baseline information that everybody needs and doesn’t get.”
Jaime Friedman, MD, a pediatrician and director of marketing at Children’s Primary Care Medical Group in San Diego, was not involved in the study but was impressed with the program’s objectives and results so far.
“While education is massively important, teens don’t always want to hear it from their parents or other adults,” Dr. Friedman said in an interview. “Learning from their peers is one way to overcome this hurdle.”
Given the high rate of sexually transmitted infections and unintended pregnancies in youth, paired with low sexual and reproductive health literacy in this population, the researchers sought to learn whether a program focused on peer-to-peer health education on these topics was feasible. The goal was to increase youth sexual and reproductive health knowledge, self-efficacy, and autonomy using a youth-led intervention.
The researchers hosted nine monthly, interactive, youth-led sessions that lasted 2 hours over Zoom or in person. Incorporated into the meetings were principles from Youth Participatory Action Research (YPAR) and Positive Youth Development (PYD).
The major topics included the following: Use of social media, values and goal-setting, anatomy and menstrual health, risk factors of sexual activities , STI and HIV prevention, contraceptive methods, healthy relationships and consent, practice responding to unhealthy behavior, gender and sexuality, and social media and body image.
The 24 participants were provided with transportation to the study site at the researchers’ institution and received financial compensation for their participation. They were an average 15.8 years old, lived in the greater Baltimore area, and mostly self-identified as female. Eight percent identified as non-binary and half (50%) identified as LGBTQIA+. Just over half the participants (52%) were Black/African American, 28% were Asian/Asian American, 12% were White, and 8% were Hispanic. The participants attended an average 88% of the sessions throughout the full intervention.
For each of the nine sessions, more than 50% of participants reported that they “learned a lot,” and only one participant reported for one session (session 5) that they “didn’t learn” anything. The researchers assessed participants’ knowledge, self-efficacy, and sense of autonomy at baseline and after completion of the intervention. Significant improvements occurred across all areas.
The average score improved by 31% in sexual and reproductive health knowledge (P < .001), 33% in sexual and reproductive health services awareness (P = .002), 46% in advocacy and empowerment (P < .001), 16% in general perceived efficacy (P = .002), and 22% personal sexuality empowerment (P = .006).
Ms. Sao said she was very pleased to see that the improvements were significant in every domain they measured, which she attributed largely to the incorporation of YPAR and PYD into the program.
“We approached it using these two frameworks that really do focus on involving youth in the teaching themselves, so I think that’s what increased their general perceived efficacy and advocacy empowerment without us necessarily having to emphasize, ‘You are advocates,’” Ms. Sao said. “Those frameworks ask the youth for their opinions and then give the youth an opportunity in every single session to be teachers themselves, and I think that lends itself well to all of the domains.”
Ms. Sao was also pleasantly surprised at the high level of retention across the 9 months.
“Every single session was slotted for 2 hours, but they would want to stay for 3 hours. Eventually, we actually started meeting with them twice a month, just adding an extra session,” she said. “As they gained confidence, they were so excited to be peer educators and realized, ‘I can really do this. I can teach my peers. We’re not getting this from anywhere else.’ ”
Ms. Sao and another study author, Maclaine Barré-Quick, an undergraduate research assistant at Johns Hopkins University, said the participants quickly discovered how easy it was to have a non-stigmatizing conversation about many of the topics once a subject was brought up.
“They’re actively looking for that opportunity,” Ms. Barré-Quick said in an interview.
Dr. Friedman agreed that this type of program provides what many adolescents need in a way that they may welcome more than through other methods.
“Adolescents’ bodies are approaching adulthood and function like adults, but their brains are still developing. They don’t have the worldly experience and education of adults, but they think they know everything,” Dr. Friedman said. “They are a population known for their high risk behavior due to their natural impulsivity. This can be a scary combination, especially when it comes to sexual health.”
But if teens don’t want to hear some of the information they need from adults, they may be more open to hearing it from other teens, Dr. Friedman said.
“Using an evidence-based approach ensures the desired outcome of healthier habits, decreased STIs and decreased teen pregnancy,” Dr. Friedman said. “It also adds weight to the argument against abstinence-only education. Teens deserve accurate and evidence-based education about their own bodies.”
Ms. Sao said the next steps will be exploring ways to scale the program up, such as putting the curriculum resources into a bundle available to other educators. They’re also looking at ways to put it into an online platform that’s self-paced, though that requires solving the challenge of having synchronous meetings for youth-led discussion.
“There are certain kinks that we have to work out because there were some activities where I think the students really benefited from having those open discussions with each other, so [we need to determine] how to replicate that in an online format,” Ms. Sao said.
Dr. Friedman agreed that scalability appears to be the biggest challenge, along with funding programs. But if those obstacles can be overcome, such programs would complement and expand on the education she does currently with families.
“I don’t have time for a full sex ed course at each visit,” Dr. Friedman said. “I would like to be able to direct them to a program that I know works and would be easy for them to complete. Even better, this would be an amazing program to ‘sell’ to practices interested in hosting these sessions themselves.”
Ms. Sao said they also hope to assess the impact of the intervention on the participants’ peers to see how well the knowledge and self-efficacy spread through the youths’ teaching.
No external funding was noted. One author reported research support from Hologic and Merck. Dr. Friedman had no disclosures.
BALTIMORE – , according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
While the small pilot study focused primarily on assessing feasibility and effectiveness, the results suggest potential for scaling the program up to reach a larger audience and assessing the knowledge disseminated from direct youth participants.
“The good thing about this subject is that not a lot of it has to be context-specific,” Saumya Sao, a clinical researcher in gynecology and obstetrics at the Johns Hopkins University, Baltimore, and the study’s lead author, said in an interview. “A lot of it is just baseline information that everybody needs and doesn’t get.”
Jaime Friedman, MD, a pediatrician and director of marketing at Children’s Primary Care Medical Group in San Diego, was not involved in the study but was impressed with the program’s objectives and results so far.
“While education is massively important, teens don’t always want to hear it from their parents or other adults,” Dr. Friedman said in an interview. “Learning from their peers is one way to overcome this hurdle.”
Given the high rate of sexually transmitted infections and unintended pregnancies in youth, paired with low sexual and reproductive health literacy in this population, the researchers sought to learn whether a program focused on peer-to-peer health education on these topics was feasible. The goal was to increase youth sexual and reproductive health knowledge, self-efficacy, and autonomy using a youth-led intervention.
The researchers hosted nine monthly, interactive, youth-led sessions that lasted 2 hours over Zoom or in person. Incorporated into the meetings were principles from Youth Participatory Action Research (YPAR) and Positive Youth Development (PYD).
The major topics included the following: Use of social media, values and goal-setting, anatomy and menstrual health, risk factors of sexual activities , STI and HIV prevention, contraceptive methods, healthy relationships and consent, practice responding to unhealthy behavior, gender and sexuality, and social media and body image.
The 24 participants were provided with transportation to the study site at the researchers’ institution and received financial compensation for their participation. They were an average 15.8 years old, lived in the greater Baltimore area, and mostly self-identified as female. Eight percent identified as non-binary and half (50%) identified as LGBTQIA+. Just over half the participants (52%) were Black/African American, 28% were Asian/Asian American, 12% were White, and 8% were Hispanic. The participants attended an average 88% of the sessions throughout the full intervention.
For each of the nine sessions, more than 50% of participants reported that they “learned a lot,” and only one participant reported for one session (session 5) that they “didn’t learn” anything. The researchers assessed participants’ knowledge, self-efficacy, and sense of autonomy at baseline and after completion of the intervention. Significant improvements occurred across all areas.
The average score improved by 31% in sexual and reproductive health knowledge (P < .001), 33% in sexual and reproductive health services awareness (P = .002), 46% in advocacy and empowerment (P < .001), 16% in general perceived efficacy (P = .002), and 22% personal sexuality empowerment (P = .006).
Ms. Sao said she was very pleased to see that the improvements were significant in every domain they measured, which she attributed largely to the incorporation of YPAR and PYD into the program.
“We approached it using these two frameworks that really do focus on involving youth in the teaching themselves, so I think that’s what increased their general perceived efficacy and advocacy empowerment without us necessarily having to emphasize, ‘You are advocates,’” Ms. Sao said. “Those frameworks ask the youth for their opinions and then give the youth an opportunity in every single session to be teachers themselves, and I think that lends itself well to all of the domains.”
Ms. Sao was also pleasantly surprised at the high level of retention across the 9 months.
“Every single session was slotted for 2 hours, but they would want to stay for 3 hours. Eventually, we actually started meeting with them twice a month, just adding an extra session,” she said. “As they gained confidence, they were so excited to be peer educators and realized, ‘I can really do this. I can teach my peers. We’re not getting this from anywhere else.’ ”
Ms. Sao and another study author, Maclaine Barré-Quick, an undergraduate research assistant at Johns Hopkins University, said the participants quickly discovered how easy it was to have a non-stigmatizing conversation about many of the topics once a subject was brought up.
“They’re actively looking for that opportunity,” Ms. Barré-Quick said in an interview.
Dr. Friedman agreed that this type of program provides what many adolescents need in a way that they may welcome more than through other methods.
“Adolescents’ bodies are approaching adulthood and function like adults, but their brains are still developing. They don’t have the worldly experience and education of adults, but they think they know everything,” Dr. Friedman said. “They are a population known for their high risk behavior due to their natural impulsivity. This can be a scary combination, especially when it comes to sexual health.”
But if teens don’t want to hear some of the information they need from adults, they may be more open to hearing it from other teens, Dr. Friedman said.
“Using an evidence-based approach ensures the desired outcome of healthier habits, decreased STIs and decreased teen pregnancy,” Dr. Friedman said. “It also adds weight to the argument against abstinence-only education. Teens deserve accurate and evidence-based education about their own bodies.”
Ms. Sao said the next steps will be exploring ways to scale the program up, such as putting the curriculum resources into a bundle available to other educators. They’re also looking at ways to put it into an online platform that’s self-paced, though that requires solving the challenge of having synchronous meetings for youth-led discussion.
“There are certain kinks that we have to work out because there were some activities where I think the students really benefited from having those open discussions with each other, so [we need to determine] how to replicate that in an online format,” Ms. Sao said.
Dr. Friedman agreed that scalability appears to be the biggest challenge, along with funding programs. But if those obstacles can be overcome, such programs would complement and expand on the education she does currently with families.
“I don’t have time for a full sex ed course at each visit,” Dr. Friedman said. “I would like to be able to direct them to a program that I know works and would be easy for them to complete. Even better, this would be an amazing program to ‘sell’ to practices interested in hosting these sessions themselves.”
Ms. Sao said they also hope to assess the impact of the intervention on the participants’ peers to see how well the knowledge and self-efficacy spread through the youths’ teaching.
No external funding was noted. One author reported research support from Hologic and Merck. Dr. Friedman had no disclosures.
BALTIMORE – , according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
While the small pilot study focused primarily on assessing feasibility and effectiveness, the results suggest potential for scaling the program up to reach a larger audience and assessing the knowledge disseminated from direct youth participants.
“The good thing about this subject is that not a lot of it has to be context-specific,” Saumya Sao, a clinical researcher in gynecology and obstetrics at the Johns Hopkins University, Baltimore, and the study’s lead author, said in an interview. “A lot of it is just baseline information that everybody needs and doesn’t get.”
Jaime Friedman, MD, a pediatrician and director of marketing at Children’s Primary Care Medical Group in San Diego, was not involved in the study but was impressed with the program’s objectives and results so far.
“While education is massively important, teens don’t always want to hear it from their parents or other adults,” Dr. Friedman said in an interview. “Learning from their peers is one way to overcome this hurdle.”
Given the high rate of sexually transmitted infections and unintended pregnancies in youth, paired with low sexual and reproductive health literacy in this population, the researchers sought to learn whether a program focused on peer-to-peer health education on these topics was feasible. The goal was to increase youth sexual and reproductive health knowledge, self-efficacy, and autonomy using a youth-led intervention.
The researchers hosted nine monthly, interactive, youth-led sessions that lasted 2 hours over Zoom or in person. Incorporated into the meetings were principles from Youth Participatory Action Research (YPAR) and Positive Youth Development (PYD).
The major topics included the following: Use of social media, values and goal-setting, anatomy and menstrual health, risk factors of sexual activities , STI and HIV prevention, contraceptive methods, healthy relationships and consent, practice responding to unhealthy behavior, gender and sexuality, and social media and body image.
The 24 participants were provided with transportation to the study site at the researchers’ institution and received financial compensation for their participation. They were an average 15.8 years old, lived in the greater Baltimore area, and mostly self-identified as female. Eight percent identified as non-binary and half (50%) identified as LGBTQIA+. Just over half the participants (52%) were Black/African American, 28% were Asian/Asian American, 12% were White, and 8% were Hispanic. The participants attended an average 88% of the sessions throughout the full intervention.
For each of the nine sessions, more than 50% of participants reported that they “learned a lot,” and only one participant reported for one session (session 5) that they “didn’t learn” anything. The researchers assessed participants’ knowledge, self-efficacy, and sense of autonomy at baseline and after completion of the intervention. Significant improvements occurred across all areas.
The average score improved by 31% in sexual and reproductive health knowledge (P < .001), 33% in sexual and reproductive health services awareness (P = .002), 46% in advocacy and empowerment (P < .001), 16% in general perceived efficacy (P = .002), and 22% personal sexuality empowerment (P = .006).
Ms. Sao said she was very pleased to see that the improvements were significant in every domain they measured, which she attributed largely to the incorporation of YPAR and PYD into the program.
“We approached it using these two frameworks that really do focus on involving youth in the teaching themselves, so I think that’s what increased their general perceived efficacy and advocacy empowerment without us necessarily having to emphasize, ‘You are advocates,’” Ms. Sao said. “Those frameworks ask the youth for their opinions and then give the youth an opportunity in every single session to be teachers themselves, and I think that lends itself well to all of the domains.”
Ms. Sao was also pleasantly surprised at the high level of retention across the 9 months.
“Every single session was slotted for 2 hours, but they would want to stay for 3 hours. Eventually, we actually started meeting with them twice a month, just adding an extra session,” she said. “As they gained confidence, they were so excited to be peer educators and realized, ‘I can really do this. I can teach my peers. We’re not getting this from anywhere else.’ ”
Ms. Sao and another study author, Maclaine Barré-Quick, an undergraduate research assistant at Johns Hopkins University, said the participants quickly discovered how easy it was to have a non-stigmatizing conversation about many of the topics once a subject was brought up.
“They’re actively looking for that opportunity,” Ms. Barré-Quick said in an interview.
Dr. Friedman agreed that this type of program provides what many adolescents need in a way that they may welcome more than through other methods.
“Adolescents’ bodies are approaching adulthood and function like adults, but their brains are still developing. They don’t have the worldly experience and education of adults, but they think they know everything,” Dr. Friedman said. “They are a population known for their high risk behavior due to their natural impulsivity. This can be a scary combination, especially when it comes to sexual health.”
But if teens don’t want to hear some of the information they need from adults, they may be more open to hearing it from other teens, Dr. Friedman said.
“Using an evidence-based approach ensures the desired outcome of healthier habits, decreased STIs and decreased teen pregnancy,” Dr. Friedman said. “It also adds weight to the argument against abstinence-only education. Teens deserve accurate and evidence-based education about their own bodies.”
Ms. Sao said the next steps will be exploring ways to scale the program up, such as putting the curriculum resources into a bundle available to other educators. They’re also looking at ways to put it into an online platform that’s self-paced, though that requires solving the challenge of having synchronous meetings for youth-led discussion.
“There are certain kinks that we have to work out because there were some activities where I think the students really benefited from having those open discussions with each other, so [we need to determine] how to replicate that in an online format,” Ms. Sao said.
Dr. Friedman agreed that scalability appears to be the biggest challenge, along with funding programs. But if those obstacles can be overcome, such programs would complement and expand on the education she does currently with families.
“I don’t have time for a full sex ed course at each visit,” Dr. Friedman said. “I would like to be able to direct them to a program that I know works and would be easy for them to complete. Even better, this would be an amazing program to ‘sell’ to practices interested in hosting these sessions themselves.”
Ms. Sao said they also hope to assess the impact of the intervention on the participants’ peers to see how well the knowledge and self-efficacy spread through the youths’ teaching.
No external funding was noted. One author reported research support from Hologic and Merck. Dr. Friedman had no disclosures.
AT ACOG 2023
Circulatory support for RV failure caused by pulmonary embolism
A new review article highlights approaches for mechanical circulatory support in patients with high-risk acute pulmonary embolism (PE).
Pulmonary embolism with hemodynamic significance is widely underdiagnosed, and the mortality rate can be as high as 30%, but new therapeutic developments offer promise. “Over the past few years, a renewed interest in mechanical circulatory support (MCS; both percutaneous and surgical) for acute RVF has emerged, increasing viable treatment options for high-risk acute PE,” wrote the authors of the review, which was published online in Interventional Cardiology Clinics.
Poor outcomes are often driven by RVF, which is tricky to diagnose and manage, and it stems from a sudden increase in pulmonary vascular resistance (PVR) following PE. “The mechanism for increased PVR in acute PE is multifactorial, including direct blood flow impedance, local hypoxia-induced vasoconstriction, and platelet/thrombin-induced release of vasoactive peptides. The cascade of events that then leads to RVF includes decreased RV stoke volume, increased RV wall tension, and RV dilation,” the authors wrote.
The authors noted that diuretics help to correct changes to RV geometry and can improve left ventricle filling, which improves hemodynamics. Diuretics can be used in patients who are hypotensive and volume overloaded, but vasopressors should be employed to support blood pressure.
When using mechanical ventilation, strategies such as low tidal volumes, minimization of positive end expiratory pressure, and prevention of hypoxemia and acidemia should be employed to prevent an increase of pulmonary vascular resistance, which can worsen RV failure.
Pulmonary vasodilators aren’t recommended for acute PE, but inhaled pulmonary vasodilators may be considered in hemodynamically unstable patients.
Surgically implanted right ventricle assistance device are generally not used for acute RV failure in high-risk PE, unless the patient has not improved after medical management.
Percutaneous devices
Percutaneous mechanical circulatory support devices can be used for patients experiencing refractory shock. The review highlighted three such devices, including the Impella RP, tandem-heart right ventricular assist devices (TH-RVAD) or Protek Duo, and venoarterial extracorporeal membrane oxygenation (VA-ECMO), but they are not without limitations. “Challenges to using these devices in patients with acute PE include clot dislodgement, vascular complications, infections, device migration, and fracture of individual elements,” the authors wrote.
The Impella RP is easy to deploy and bypasses the RV, but it can’t provide blood oxygenation and may cause bleeding or hemolysis. TH-RVAD oxygenates the blood and bypasses the RV, but suffers from a large sheath size. VA-ECMO oxygenates the blood but may cause bleeding.
There are important differences among the mechanical support devices, according to Jonathan Ludmir, MD, who was asked to comment. “In reality, if someone has a large pulmonary embolism burden, to put in the Impella RP or the Protek Duo would be a little bit risky, because you’d be sometimes putting the device right where the clot is. At least what we do in our institution, when someone is in extremis despite using [intravenous] medications like vasopressors or inotropes, VA-ECMO is kind of the go to. This is both the quickest and probably most effective way to support the patient. I say the quickest because this is a procedure you can do at the bedside.”
Benefits of PERT
One message that the review only briefly mentions, but Dr. Ludmir believes is key, is employing a pulmonary embolism response team. “That’s been looked at extensively, and it’s a really key part of any decision-making. If someone presents to the emergency room or someone inside the hospital has an acute pulmonary embolism, you have a team of people that can respond and help assess the next step. Typically, that involves a cardiologist or an interventional cardiologist, a hematologist, vascular surgeon, often a cardiac surgeon, so it’s a whole slew of people. Based on the patient assessment they can quickly decide, can this patient just be okay with a blood thinner like heparin? Does this patient need something more aggressive, like a thrombectomy? Or is this a serious case where you involve the shock team or the ECMO team, and you have to stabilize the patient on mechanical circulatory support, so you can accomplish what you need to do to get rid of the pulmonary embolism,” said Dr. Ludmir, who is an assistant professor of medicine at Corrigan Minehan Heart Center at Massachusetts General Hospital and Harvard Medical School, both in Boston.
“Every case is individualized, hence the importance of having a team of a variety of different backgrounds and thoughts to approach it. And I think that’s kind of like the key takeaway. Yes, you have to be familiar with all the therapies, but at the end of the day, not every patient is going to fit into the algorithm for how you approach pulmonary embolism,” said Dr. Ludmir.
Dr. Ludmir has no relevant conflicts of interest.
A new review article highlights approaches for mechanical circulatory support in patients with high-risk acute pulmonary embolism (PE).
Pulmonary embolism with hemodynamic significance is widely underdiagnosed, and the mortality rate can be as high as 30%, but new therapeutic developments offer promise. “Over the past few years, a renewed interest in mechanical circulatory support (MCS; both percutaneous and surgical) for acute RVF has emerged, increasing viable treatment options for high-risk acute PE,” wrote the authors of the review, which was published online in Interventional Cardiology Clinics.
Poor outcomes are often driven by RVF, which is tricky to diagnose and manage, and it stems from a sudden increase in pulmonary vascular resistance (PVR) following PE. “The mechanism for increased PVR in acute PE is multifactorial, including direct blood flow impedance, local hypoxia-induced vasoconstriction, and platelet/thrombin-induced release of vasoactive peptides. The cascade of events that then leads to RVF includes decreased RV stoke volume, increased RV wall tension, and RV dilation,” the authors wrote.
The authors noted that diuretics help to correct changes to RV geometry and can improve left ventricle filling, which improves hemodynamics. Diuretics can be used in patients who are hypotensive and volume overloaded, but vasopressors should be employed to support blood pressure.
When using mechanical ventilation, strategies such as low tidal volumes, minimization of positive end expiratory pressure, and prevention of hypoxemia and acidemia should be employed to prevent an increase of pulmonary vascular resistance, which can worsen RV failure.
Pulmonary vasodilators aren’t recommended for acute PE, but inhaled pulmonary vasodilators may be considered in hemodynamically unstable patients.
Surgically implanted right ventricle assistance device are generally not used for acute RV failure in high-risk PE, unless the patient has not improved after medical management.
Percutaneous devices
Percutaneous mechanical circulatory support devices can be used for patients experiencing refractory shock. The review highlighted three such devices, including the Impella RP, tandem-heart right ventricular assist devices (TH-RVAD) or Protek Duo, and venoarterial extracorporeal membrane oxygenation (VA-ECMO), but they are not without limitations. “Challenges to using these devices in patients with acute PE include clot dislodgement, vascular complications, infections, device migration, and fracture of individual elements,” the authors wrote.
The Impella RP is easy to deploy and bypasses the RV, but it can’t provide blood oxygenation and may cause bleeding or hemolysis. TH-RVAD oxygenates the blood and bypasses the RV, but suffers from a large sheath size. VA-ECMO oxygenates the blood but may cause bleeding.
There are important differences among the mechanical support devices, according to Jonathan Ludmir, MD, who was asked to comment. “In reality, if someone has a large pulmonary embolism burden, to put in the Impella RP or the Protek Duo would be a little bit risky, because you’d be sometimes putting the device right where the clot is. At least what we do in our institution, when someone is in extremis despite using [intravenous] medications like vasopressors or inotropes, VA-ECMO is kind of the go to. This is both the quickest and probably most effective way to support the patient. I say the quickest because this is a procedure you can do at the bedside.”
Benefits of PERT
One message that the review only briefly mentions, but Dr. Ludmir believes is key, is employing a pulmonary embolism response team. “That’s been looked at extensively, and it’s a really key part of any decision-making. If someone presents to the emergency room or someone inside the hospital has an acute pulmonary embolism, you have a team of people that can respond and help assess the next step. Typically, that involves a cardiologist or an interventional cardiologist, a hematologist, vascular surgeon, often a cardiac surgeon, so it’s a whole slew of people. Based on the patient assessment they can quickly decide, can this patient just be okay with a blood thinner like heparin? Does this patient need something more aggressive, like a thrombectomy? Or is this a serious case where you involve the shock team or the ECMO team, and you have to stabilize the patient on mechanical circulatory support, so you can accomplish what you need to do to get rid of the pulmonary embolism,” said Dr. Ludmir, who is an assistant professor of medicine at Corrigan Minehan Heart Center at Massachusetts General Hospital and Harvard Medical School, both in Boston.
“Every case is individualized, hence the importance of having a team of a variety of different backgrounds and thoughts to approach it. And I think that’s kind of like the key takeaway. Yes, you have to be familiar with all the therapies, but at the end of the day, not every patient is going to fit into the algorithm for how you approach pulmonary embolism,” said Dr. Ludmir.
Dr. Ludmir has no relevant conflicts of interest.
A new review article highlights approaches for mechanical circulatory support in patients with high-risk acute pulmonary embolism (PE).
Pulmonary embolism with hemodynamic significance is widely underdiagnosed, and the mortality rate can be as high as 30%, but new therapeutic developments offer promise. “Over the past few years, a renewed interest in mechanical circulatory support (MCS; both percutaneous and surgical) for acute RVF has emerged, increasing viable treatment options for high-risk acute PE,” wrote the authors of the review, which was published online in Interventional Cardiology Clinics.
Poor outcomes are often driven by RVF, which is tricky to diagnose and manage, and it stems from a sudden increase in pulmonary vascular resistance (PVR) following PE. “The mechanism for increased PVR in acute PE is multifactorial, including direct blood flow impedance, local hypoxia-induced vasoconstriction, and platelet/thrombin-induced release of vasoactive peptides. The cascade of events that then leads to RVF includes decreased RV stoke volume, increased RV wall tension, and RV dilation,” the authors wrote.
The authors noted that diuretics help to correct changes to RV geometry and can improve left ventricle filling, which improves hemodynamics. Diuretics can be used in patients who are hypotensive and volume overloaded, but vasopressors should be employed to support blood pressure.
When using mechanical ventilation, strategies such as low tidal volumes, minimization of positive end expiratory pressure, and prevention of hypoxemia and acidemia should be employed to prevent an increase of pulmonary vascular resistance, which can worsen RV failure.
Pulmonary vasodilators aren’t recommended for acute PE, but inhaled pulmonary vasodilators may be considered in hemodynamically unstable patients.
Surgically implanted right ventricle assistance device are generally not used for acute RV failure in high-risk PE, unless the patient has not improved after medical management.
Percutaneous devices
Percutaneous mechanical circulatory support devices can be used for patients experiencing refractory shock. The review highlighted three such devices, including the Impella RP, tandem-heart right ventricular assist devices (TH-RVAD) or Protek Duo, and venoarterial extracorporeal membrane oxygenation (VA-ECMO), but they are not without limitations. “Challenges to using these devices in patients with acute PE include clot dislodgement, vascular complications, infections, device migration, and fracture of individual elements,” the authors wrote.
The Impella RP is easy to deploy and bypasses the RV, but it can’t provide blood oxygenation and may cause bleeding or hemolysis. TH-RVAD oxygenates the blood and bypasses the RV, but suffers from a large sheath size. VA-ECMO oxygenates the blood but may cause bleeding.
There are important differences among the mechanical support devices, according to Jonathan Ludmir, MD, who was asked to comment. “In reality, if someone has a large pulmonary embolism burden, to put in the Impella RP or the Protek Duo would be a little bit risky, because you’d be sometimes putting the device right where the clot is. At least what we do in our institution, when someone is in extremis despite using [intravenous] medications like vasopressors or inotropes, VA-ECMO is kind of the go to. This is both the quickest and probably most effective way to support the patient. I say the quickest because this is a procedure you can do at the bedside.”
Benefits of PERT
One message that the review only briefly mentions, but Dr. Ludmir believes is key, is employing a pulmonary embolism response team. “That’s been looked at extensively, and it’s a really key part of any decision-making. If someone presents to the emergency room or someone inside the hospital has an acute pulmonary embolism, you have a team of people that can respond and help assess the next step. Typically, that involves a cardiologist or an interventional cardiologist, a hematologist, vascular surgeon, often a cardiac surgeon, so it’s a whole slew of people. Based on the patient assessment they can quickly decide, can this patient just be okay with a blood thinner like heparin? Does this patient need something more aggressive, like a thrombectomy? Or is this a serious case where you involve the shock team or the ECMO team, and you have to stabilize the patient on mechanical circulatory support, so you can accomplish what you need to do to get rid of the pulmonary embolism,” said Dr. Ludmir, who is an assistant professor of medicine at Corrigan Minehan Heart Center at Massachusetts General Hospital and Harvard Medical School, both in Boston.
“Every case is individualized, hence the importance of having a team of a variety of different backgrounds and thoughts to approach it. And I think that’s kind of like the key takeaway. Yes, you have to be familiar with all the therapies, but at the end of the day, not every patient is going to fit into the algorithm for how you approach pulmonary embolism,” said Dr. Ludmir.
Dr. Ludmir has no relevant conflicts of interest.
FROM INTERVENTIONAL CARDIOLOGY CLINICS
Leadless dual-chamber pacemaker clears early safety, performance hurdles
Cardiology, well into the age of leadless pacemakers, could be headed for an age of leadless pacemaker systems in which various pacing functions are achieved by multiple implants that “talk” to each other.
Even now, a leadless two-part pacemaker system has shown it can safely achieve atrioventricular (AV) synchrony in patients with standard indications for a dual-chamber device, at least over the short term, suggests a prospective observational study. Currently available leadless pacemakers can stimulate only the right ventricle.
Experienced operators achieved a 98% implantation success rate in 300 patients who received an investigational dual-chamber leadless system, the AVEIR DR i2i (Abbott).
Its two separately implanted miniature pulse generators achieve AV synchrony via “beat-to-beat wireless bidirectional communication,” Daniel J. Cantillon, MD, said when presenting the study at the annual scientific sessions of the Heart Rhythm Societyin New Orleans.
The system seemed to work well regardless of the patient’s body orientation. “Sitting, supine, left lateral, right lateral, standing, normal walk, fast walk – we demonstrated robust AV synchrony in all of those positions and with movement,” said Dr. Cantillon, of the Cleveland Clinic.
Should the device be approved, it could “expand the use case for leadless cardiac pacing” to include atrial-only, ventricular-only, fully functional dual-chamber pacing scenarios.”
Dr. Cantillon is senior author on the study’s online publication in the New England Journal of Medicine, timed to coincide with his HRS presentation, with first author Reinoud E. Knops, MD, PhD, Amsterdam University Medical Center.
“The electrical performance of both the atrial and ventricular leadless pacemakers appears to be similar to that of transvenous dual-chamber pacemakers,” the published report states.
More data needed
The study is important and has “significant implications for our pacing field,” Jonathan P. Piccini, MD, MHS, said in an interview. It suggests that “dual-chamber pacing can be achieved with leadless technology” and “with a very high degree” of AV synchrony.
“Obviously, more data as the technology moves into clinical practice will be critical,” said Dr. Piccini, who directs cardiac electrophysiology at Duke University Medical Center, Durham, N.C. “We will also need to understand which patients are best served by leadless technology and which will be better served with traditional transvenous devices.”
The AVEIR DR i2i system consists of two leadless pulse generators for percutaneous implantation in the right atrium and right ventricle, respectively. They link like components of a wireless network to coordinate their separate sensing and rate-adaptive, AV-synchronous pacing functions.
The right ventricular implant “is physically identical to a commercially available single-chamber leadless pacemaker” from Abbott, the published report states.
Leadless pacemaker systems inherently avoid the two main sources of transvenous devices’ major complication – infection – by not requiring such leads or surgery for creating a pulse-generator subcutaneous pocket.
The first such systems consisted of one implant that could provide single-chamber ventricular pacing but not atrial pacing or AV synchronous pacing. The transcatheter single-chamber leadless Micra (Medtronic) for example, was approved in the United States in April 2016 for ventricular-only pacing.
A successor, the Micra AV, approved in 2020, was designed to simulate AV-synchronous pacing by stimulating the ventricle in sequence with mechanically sensed atrial contractions, as described by Dr. Cantillon and associates. But it could not directly pace the atrium, “rendering it inappropriate for patients with sinus-node dysfunction.”
The AVEIR DR i2i system doesn’t have those limitations. It was, however, associated with 35 device- or procedure-related complications in the study, of which the most common was procedural arrhythmia, “namely atrial fibrillation,” Dr. Cantillon said.
Atrial fibrillation can develop during implantation of pacemakers with transvenous leads but is generally terminated without being considered an important event. Yet the study classified it as a serious complication, inflating the complication rate, because “the patients had to be restored to sinus rhythm so we could assess the AV synchrony and also the atrial electrical performance,” he said.
Some of the devices dislodged from their implantation site within a month of the procedure, but “all of those patients were successfully managed percutaneously,” said Dr. Cantillon.
“The 1.7% dislodgement rate is something that we will need to keep an eye on, as embolization of devices is always a significant concern,” Dr. Piccini said. Still, the observed total complication rate “was certainly in line” with rates associated with conventional pacemaker implantation.
Reliable AV synchrony
Fred M. Kusumoto, MD, Mayo Clinic, Jacksonville, Fla., lauded what seems to be the system’s “incredibly reliable AV synchrony in different conditions, albeit in a very controlled environment.”
Of interest will be whether its performance, including maintenance of AV synchrony, holds up in “a more long-term evaluation in the outpatient setting,” said Dr. Kusumoto, speaking as the invited discussant for Dr. Cantillon’s presentation.
Also missing or in short supply from the study, he observed, are insights about long-term efficacy and complications, battery longevity, effectiveness of its rate-responsive capability, and any effect on clinical outcomes.
Local body network
Of the study’s 300 patients (mean age 69 years; 38% female) at 55 sites in Canada, Europe, and the United States, 63.3% had sinus-node dysfunction and 33.3% had AV block as their primary dual-chamber pacing indication; 298 were successfully implanted with both devices.
About 45% had a history of supraventricular arrhythmia, 4.3% had prior ventricular arrhythmia, and 20% had a history of arrhythmia ablation.
By 3 months, the group reported, the primary safety endpoint (freedom from device- or procedure-related serious adverse events) occurred in 90.3%, compared with the performance goal of 78% (P < .001).
The first of two primary performance endpoints (adequate atrial capture threshold and sensing amplitude by predefined criteria) was met in 90.2%, surpassing the 82.5% performance goal (P < .001).
The second primary performance goal (at least 70% AV synchrony with the patient sitting) was seen in 97.3% against the performance goal of 83% (P < .001).
What shouldn’t be “glossed over” from the study, Dr. Kusumoto offered, is that it’s possible to achieve a wireless connection “between two devices that are actually intracardiac.” That raises the prospect of a “local body network” that could be “expanded even more dramatically with other types of devices. I mean, think of the paradigm shift.”
The AVEIR DR i2i trial was funded by Abbott. Dr. Cantillon discloses receiving honoraria or fees for speaking or consulting from Abbott Laboratories, Boston Scientific, Biosense Webster, and Shockwave Medical, as well as holding royalty rights with AirStrip. Dr. Piccini has disclosed relationships with Abbott, Medtronic, Biotronik, Boston Scientific, and other drug and medical device companies. Dr. Kusumoto reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiology, well into the age of leadless pacemakers, could be headed for an age of leadless pacemaker systems in which various pacing functions are achieved by multiple implants that “talk” to each other.
Even now, a leadless two-part pacemaker system has shown it can safely achieve atrioventricular (AV) synchrony in patients with standard indications for a dual-chamber device, at least over the short term, suggests a prospective observational study. Currently available leadless pacemakers can stimulate only the right ventricle.
Experienced operators achieved a 98% implantation success rate in 300 patients who received an investigational dual-chamber leadless system, the AVEIR DR i2i (Abbott).
Its two separately implanted miniature pulse generators achieve AV synchrony via “beat-to-beat wireless bidirectional communication,” Daniel J. Cantillon, MD, said when presenting the study at the annual scientific sessions of the Heart Rhythm Societyin New Orleans.
The system seemed to work well regardless of the patient’s body orientation. “Sitting, supine, left lateral, right lateral, standing, normal walk, fast walk – we demonstrated robust AV synchrony in all of those positions and with movement,” said Dr. Cantillon, of the Cleveland Clinic.
Should the device be approved, it could “expand the use case for leadless cardiac pacing” to include atrial-only, ventricular-only, fully functional dual-chamber pacing scenarios.”
Dr. Cantillon is senior author on the study’s online publication in the New England Journal of Medicine, timed to coincide with his HRS presentation, with first author Reinoud E. Knops, MD, PhD, Amsterdam University Medical Center.
“The electrical performance of both the atrial and ventricular leadless pacemakers appears to be similar to that of transvenous dual-chamber pacemakers,” the published report states.
More data needed
The study is important and has “significant implications for our pacing field,” Jonathan P. Piccini, MD, MHS, said in an interview. It suggests that “dual-chamber pacing can be achieved with leadless technology” and “with a very high degree” of AV synchrony.
“Obviously, more data as the technology moves into clinical practice will be critical,” said Dr. Piccini, who directs cardiac electrophysiology at Duke University Medical Center, Durham, N.C. “We will also need to understand which patients are best served by leadless technology and which will be better served with traditional transvenous devices.”
The AVEIR DR i2i system consists of two leadless pulse generators for percutaneous implantation in the right atrium and right ventricle, respectively. They link like components of a wireless network to coordinate their separate sensing and rate-adaptive, AV-synchronous pacing functions.
The right ventricular implant “is physically identical to a commercially available single-chamber leadless pacemaker” from Abbott, the published report states.
Leadless pacemaker systems inherently avoid the two main sources of transvenous devices’ major complication – infection – by not requiring such leads or surgery for creating a pulse-generator subcutaneous pocket.
The first such systems consisted of one implant that could provide single-chamber ventricular pacing but not atrial pacing or AV synchronous pacing. The transcatheter single-chamber leadless Micra (Medtronic) for example, was approved in the United States in April 2016 for ventricular-only pacing.
A successor, the Micra AV, approved in 2020, was designed to simulate AV-synchronous pacing by stimulating the ventricle in sequence with mechanically sensed atrial contractions, as described by Dr. Cantillon and associates. But it could not directly pace the atrium, “rendering it inappropriate for patients with sinus-node dysfunction.”
The AVEIR DR i2i system doesn’t have those limitations. It was, however, associated with 35 device- or procedure-related complications in the study, of which the most common was procedural arrhythmia, “namely atrial fibrillation,” Dr. Cantillon said.
Atrial fibrillation can develop during implantation of pacemakers with transvenous leads but is generally terminated without being considered an important event. Yet the study classified it as a serious complication, inflating the complication rate, because “the patients had to be restored to sinus rhythm so we could assess the AV synchrony and also the atrial electrical performance,” he said.
Some of the devices dislodged from their implantation site within a month of the procedure, but “all of those patients were successfully managed percutaneously,” said Dr. Cantillon.
“The 1.7% dislodgement rate is something that we will need to keep an eye on, as embolization of devices is always a significant concern,” Dr. Piccini said. Still, the observed total complication rate “was certainly in line” with rates associated with conventional pacemaker implantation.
Reliable AV synchrony
Fred M. Kusumoto, MD, Mayo Clinic, Jacksonville, Fla., lauded what seems to be the system’s “incredibly reliable AV synchrony in different conditions, albeit in a very controlled environment.”
Of interest will be whether its performance, including maintenance of AV synchrony, holds up in “a more long-term evaluation in the outpatient setting,” said Dr. Kusumoto, speaking as the invited discussant for Dr. Cantillon’s presentation.
Also missing or in short supply from the study, he observed, are insights about long-term efficacy and complications, battery longevity, effectiveness of its rate-responsive capability, and any effect on clinical outcomes.
Local body network
Of the study’s 300 patients (mean age 69 years; 38% female) at 55 sites in Canada, Europe, and the United States, 63.3% had sinus-node dysfunction and 33.3% had AV block as their primary dual-chamber pacing indication; 298 were successfully implanted with both devices.
About 45% had a history of supraventricular arrhythmia, 4.3% had prior ventricular arrhythmia, and 20% had a history of arrhythmia ablation.
By 3 months, the group reported, the primary safety endpoint (freedom from device- or procedure-related serious adverse events) occurred in 90.3%, compared with the performance goal of 78% (P < .001).
The first of two primary performance endpoints (adequate atrial capture threshold and sensing amplitude by predefined criteria) was met in 90.2%, surpassing the 82.5% performance goal (P < .001).
The second primary performance goal (at least 70% AV synchrony with the patient sitting) was seen in 97.3% against the performance goal of 83% (P < .001).
What shouldn’t be “glossed over” from the study, Dr. Kusumoto offered, is that it’s possible to achieve a wireless connection “between two devices that are actually intracardiac.” That raises the prospect of a “local body network” that could be “expanded even more dramatically with other types of devices. I mean, think of the paradigm shift.”
The AVEIR DR i2i trial was funded by Abbott. Dr. Cantillon discloses receiving honoraria or fees for speaking or consulting from Abbott Laboratories, Boston Scientific, Biosense Webster, and Shockwave Medical, as well as holding royalty rights with AirStrip. Dr. Piccini has disclosed relationships with Abbott, Medtronic, Biotronik, Boston Scientific, and other drug and medical device companies. Dr. Kusumoto reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiology, well into the age of leadless pacemakers, could be headed for an age of leadless pacemaker systems in which various pacing functions are achieved by multiple implants that “talk” to each other.
Even now, a leadless two-part pacemaker system has shown it can safely achieve atrioventricular (AV) synchrony in patients with standard indications for a dual-chamber device, at least over the short term, suggests a prospective observational study. Currently available leadless pacemakers can stimulate only the right ventricle.
Experienced operators achieved a 98% implantation success rate in 300 patients who received an investigational dual-chamber leadless system, the AVEIR DR i2i (Abbott).
Its two separately implanted miniature pulse generators achieve AV synchrony via “beat-to-beat wireless bidirectional communication,” Daniel J. Cantillon, MD, said when presenting the study at the annual scientific sessions of the Heart Rhythm Societyin New Orleans.
The system seemed to work well regardless of the patient’s body orientation. “Sitting, supine, left lateral, right lateral, standing, normal walk, fast walk – we demonstrated robust AV synchrony in all of those positions and with movement,” said Dr. Cantillon, of the Cleveland Clinic.
Should the device be approved, it could “expand the use case for leadless cardiac pacing” to include atrial-only, ventricular-only, fully functional dual-chamber pacing scenarios.”
Dr. Cantillon is senior author on the study’s online publication in the New England Journal of Medicine, timed to coincide with his HRS presentation, with first author Reinoud E. Knops, MD, PhD, Amsterdam University Medical Center.
“The electrical performance of both the atrial and ventricular leadless pacemakers appears to be similar to that of transvenous dual-chamber pacemakers,” the published report states.
More data needed
The study is important and has “significant implications for our pacing field,” Jonathan P. Piccini, MD, MHS, said in an interview. It suggests that “dual-chamber pacing can be achieved with leadless technology” and “with a very high degree” of AV synchrony.
“Obviously, more data as the technology moves into clinical practice will be critical,” said Dr. Piccini, who directs cardiac electrophysiology at Duke University Medical Center, Durham, N.C. “We will also need to understand which patients are best served by leadless technology and which will be better served with traditional transvenous devices.”
The AVEIR DR i2i system consists of two leadless pulse generators for percutaneous implantation in the right atrium and right ventricle, respectively. They link like components of a wireless network to coordinate their separate sensing and rate-adaptive, AV-synchronous pacing functions.
The right ventricular implant “is physically identical to a commercially available single-chamber leadless pacemaker” from Abbott, the published report states.
Leadless pacemaker systems inherently avoid the two main sources of transvenous devices’ major complication – infection – by not requiring such leads or surgery for creating a pulse-generator subcutaneous pocket.
The first such systems consisted of one implant that could provide single-chamber ventricular pacing but not atrial pacing or AV synchronous pacing. The transcatheter single-chamber leadless Micra (Medtronic) for example, was approved in the United States in April 2016 for ventricular-only pacing.
A successor, the Micra AV, approved in 2020, was designed to simulate AV-synchronous pacing by stimulating the ventricle in sequence with mechanically sensed atrial contractions, as described by Dr. Cantillon and associates. But it could not directly pace the atrium, “rendering it inappropriate for patients with sinus-node dysfunction.”
The AVEIR DR i2i system doesn’t have those limitations. It was, however, associated with 35 device- or procedure-related complications in the study, of which the most common was procedural arrhythmia, “namely atrial fibrillation,” Dr. Cantillon said.
Atrial fibrillation can develop during implantation of pacemakers with transvenous leads but is generally terminated without being considered an important event. Yet the study classified it as a serious complication, inflating the complication rate, because “the patients had to be restored to sinus rhythm so we could assess the AV synchrony and also the atrial electrical performance,” he said.
Some of the devices dislodged from their implantation site within a month of the procedure, but “all of those patients were successfully managed percutaneously,” said Dr. Cantillon.
“The 1.7% dislodgement rate is something that we will need to keep an eye on, as embolization of devices is always a significant concern,” Dr. Piccini said. Still, the observed total complication rate “was certainly in line” with rates associated with conventional pacemaker implantation.
Reliable AV synchrony
Fred M. Kusumoto, MD, Mayo Clinic, Jacksonville, Fla., lauded what seems to be the system’s “incredibly reliable AV synchrony in different conditions, albeit in a very controlled environment.”
Of interest will be whether its performance, including maintenance of AV synchrony, holds up in “a more long-term evaluation in the outpatient setting,” said Dr. Kusumoto, speaking as the invited discussant for Dr. Cantillon’s presentation.
Also missing or in short supply from the study, he observed, are insights about long-term efficacy and complications, battery longevity, effectiveness of its rate-responsive capability, and any effect on clinical outcomes.
Local body network
Of the study’s 300 patients (mean age 69 years; 38% female) at 55 sites in Canada, Europe, and the United States, 63.3% had sinus-node dysfunction and 33.3% had AV block as their primary dual-chamber pacing indication; 298 were successfully implanted with both devices.
About 45% had a history of supraventricular arrhythmia, 4.3% had prior ventricular arrhythmia, and 20% had a history of arrhythmia ablation.
By 3 months, the group reported, the primary safety endpoint (freedom from device- or procedure-related serious adverse events) occurred in 90.3%, compared with the performance goal of 78% (P < .001).
The first of two primary performance endpoints (adequate atrial capture threshold and sensing amplitude by predefined criteria) was met in 90.2%, surpassing the 82.5% performance goal (P < .001).
The second primary performance goal (at least 70% AV synchrony with the patient sitting) was seen in 97.3% against the performance goal of 83% (P < .001).
What shouldn’t be “glossed over” from the study, Dr. Kusumoto offered, is that it’s possible to achieve a wireless connection “between two devices that are actually intracardiac.” That raises the prospect of a “local body network” that could be “expanded even more dramatically with other types of devices. I mean, think of the paradigm shift.”
The AVEIR DR i2i trial was funded by Abbott. Dr. Cantillon discloses receiving honoraria or fees for speaking or consulting from Abbott Laboratories, Boston Scientific, Biosense Webster, and Shockwave Medical, as well as holding royalty rights with AirStrip. Dr. Piccini has disclosed relationships with Abbott, Medtronic, Biotronik, Boston Scientific, and other drug and medical device companies. Dr. Kusumoto reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HRS 2023
Researchers locate signals in brain related to chronic pain
a new study in Nature Neuroscience concluded.
The researchers used the devices on four patients who had felt endless nerve pain for more than a year. The devices recorded several times a day, which could pave “the way for implanted devices to one day predict pain signals or even short-circuit them,” The New York Times reported.
The study says the pain “was associated with electrical fluctuations in the orbitofrontal cortex, an area involved in emotion regulation, self-evaluation, and decision-making,” The Times reported. “The research suggests that such patterns of brain activity could serve as biomarkers to guide diagnosis and treatment for millions of people with shooting or burning chronic pain linked to a damaged nervous system.”
Ajay Wasan, MD, and a pain specialist at the University of Pittsburgh who was not involved in the study praised it to the Times.
“The study really advances a whole generation of research that has shown that the functioning of the brain is really important to processing and perceiving pain,” he said.
Chronic pain is defined as persistent or recurring and lasting more than three months. The Centers for Disease Control and Prevention says about 20% of Americans experience it. It has been linked with depression, Alzheimer’s disease and other dementias, suicide, and substance use.
Yet, the study’s authors noted, “pain severity is often measured through subjective report, while objective biomarkers that may guide diagnosis and treatment are lacking.”
Medtronic provided devices for the study. The study authors reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
a new study in Nature Neuroscience concluded.
The researchers used the devices on four patients who had felt endless nerve pain for more than a year. The devices recorded several times a day, which could pave “the way for implanted devices to one day predict pain signals or even short-circuit them,” The New York Times reported.
The study says the pain “was associated with electrical fluctuations in the orbitofrontal cortex, an area involved in emotion regulation, self-evaluation, and decision-making,” The Times reported. “The research suggests that such patterns of brain activity could serve as biomarkers to guide diagnosis and treatment for millions of people with shooting or burning chronic pain linked to a damaged nervous system.”
Ajay Wasan, MD, and a pain specialist at the University of Pittsburgh who was not involved in the study praised it to the Times.
“The study really advances a whole generation of research that has shown that the functioning of the brain is really important to processing and perceiving pain,” he said.
Chronic pain is defined as persistent or recurring and lasting more than three months. The Centers for Disease Control and Prevention says about 20% of Americans experience it. It has been linked with depression, Alzheimer’s disease and other dementias, suicide, and substance use.
Yet, the study’s authors noted, “pain severity is often measured through subjective report, while objective biomarkers that may guide diagnosis and treatment are lacking.”
Medtronic provided devices for the study. The study authors reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
a new study in Nature Neuroscience concluded.
The researchers used the devices on four patients who had felt endless nerve pain for more than a year. The devices recorded several times a day, which could pave “the way for implanted devices to one day predict pain signals or even short-circuit them,” The New York Times reported.
The study says the pain “was associated with electrical fluctuations in the orbitofrontal cortex, an area involved in emotion regulation, self-evaluation, and decision-making,” The Times reported. “The research suggests that such patterns of brain activity could serve as biomarkers to guide diagnosis and treatment for millions of people with shooting or burning chronic pain linked to a damaged nervous system.”
Ajay Wasan, MD, and a pain specialist at the University of Pittsburgh who was not involved in the study praised it to the Times.
“The study really advances a whole generation of research that has shown that the functioning of the brain is really important to processing and perceiving pain,” he said.
Chronic pain is defined as persistent or recurring and lasting more than three months. The Centers for Disease Control and Prevention says about 20% of Americans experience it. It has been linked with depression, Alzheimer’s disease and other dementias, suicide, and substance use.
Yet, the study’s authors noted, “pain severity is often measured through subjective report, while objective biomarkers that may guide diagnosis and treatment are lacking.”
Medtronic provided devices for the study. The study authors reported no conflicts of interest.
A version of this article first appeared on WebMD.com.
FROM NATURE NEUROSCIENCE
ARNI bests ARB to reduce NT-proBNP in stabilized preserved-EF HF
Patients with an ejection fraction (EF) greater than 40% who were stabilized after recent worsening or de novo heart failure (HF) had a greater reduction in natriuretic peptides and less worsening renal function, but a higher rate of hypotension over 8 weeks with sacubitril-valsartan (Entresto) versus valsartan (Diovan) in the PARAGLIDE-HF trial.
A subgroup analysis showed evidence of a larger treatment effect among those with an EF of 60% or less, said Robert Mentz, MD, of the Duke Clinical Research Institute, Durham, N.C.
Dr. Mentz presented the findings at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) scientific sessions. The study was also published online simultaneously in the Journal of the American College of Cardiology.
“Next steps will involve further assessment of the cardiovascular and renal benefits, as well as further exploration of the symptomatic hypotension that we observed,” Dr. Mentz said in an interview.
Meanwhile, he said, “clinicians should be aware of these new data – specifically, the incremental reduction in natriuretic peptide level, compared with valsartan, and potential benefits on cardiovascular and renal events,” particularly in those with an EF greater than 40% to 60% or less.
Larger benefit for EF > 40% to < 60%
PARAGLIDE-HF was a double-blind, randomized controlled trial with 466 patients with EF greater than 40% enrolled within 30 days of a worsening HF event. The median age was 71 years, 52% were women, and 22% were Black.
The trial was a follow-up to PARAGON-HF, which had shown that, in patients with an EF of at least 45%, sacubitril-valsartan did not result in a significantly lower rate of total hospitalizations for HF or death from cardiovascular causes, compared with valsartan.
The primary endpoint for PARAGLIDE was the time-averaged proportional change in N-terminal of the prohormone brain natriuretic peptide (NT-proBNP) from baseline through weeks 4 and 8, as in the PIONEER-HF trial. That trial showed that among patients hospitalized for acute decompensated HF with reduced EF (< 40%), the angiotensin receptor/neprilysin inhibitor (ARNI) led to a greater reduction in NT-proBNP concentration than the angiotensin receptor blocker (ARB).
Similarly, for PARAGLIDE, the time-averaged reduction in NT-proBNP was greater with sacubitril-valsartan, with a change ratio of 0.85 (15% greater reduction).
A secondary hierarchical outcome for PARAGLIDE, using the win ratio, consisted of time to cardiovascular death, number and timing of HF hospitalizations, number and timing of urgent HF visits, and time-averaged proportional change in NT-proBNP from baseline to weeks 4 and 8.
The hierarchical outcome favored sacubitril-valsartan, but was not significant (unmatched win ratio, 1.19).
As noted, sacubitril-valsartan reduced worsening renal function, compared with valsartan (odds ratio, 0.61), but increased symptomatic hypotension (OR, 1.73).
“We will work to better characterize the hypotension events that were observed to help identify those patients at greater risk and to provide further clarity around the timing and implications of these events,” Dr. Mentz said in an interview.
The team hypothesized that such events may be prevented by optimizing volume status and background therapies commonly used to treat hypertension in these patients.
“For instance,” Dr. Mentz suggested, “calcium channel blockers like amlodipine could be dose reduced or discontinued in patients with lower baseline blood pressures to better support sacubitril/valsartan initiation and titration.”
He highlighted the subgroup analysis showing evidence of a larger treatment effect in study patients with an EF of 60% or less for the NT-proBNP change (0.78) and the hierarchical outcome (win ratio, 1.46).
“These data may influence future guidance for sacubitril-valsartan in HF with EF greater than 40%, regardless of HF chronicity [acute or chronic vs. de novo] and treatment setting [hospital vs. clinic],” Dr. Mentz concluded.
Data ‘far from conclusive’
In a comment, Sean Pinney, MD, chief of cardiology at Mount Sinai Morningside, New York, said that the study results “help expand the current evidence base supporting the use of an ARNI in patients” with an EF greater than 40% up to 60%, and “provide confidence that ARNIs help to lower natriuretic peptides.
“It comes as little surprise that not everyone was able to tolerate these medications due to intolerable side effects like dizziness or hypotension,” he said.
Nevertheless, he added, “hopefully, these trial data help strengthen clinicians’ resolve to prescribe sacubitril/valsartan to a growing population of vulnerable patients.”
In a related editorial, Hector O. Ventura, MD, of the Ochsner Clinical School–University of Queensland, New Orleans, and colleagues express several concerns about the study.
Although the trial achieved significance for the primary endpoint, the margin of benefit was less than expected and the magnitude of the NT-proBNP reduction may not have been enough to reach the threshold for clinical benefit, they wrote.
Diuretic dosing in the two groups was not reported, and between-group differences may have contributed to both the differential NT-proBNP reduction and the rates of hypotension.
Furthermore, the sacubitril-valsartan group had a higher proportion of missing NT-proBNP data, which may have biased the results.
“Clinicians who elect to use sacubitril-valsartan in this population should be mindful of the risk for hypotension and select patients carefully, while providing close ambulatory follow up to ensure stability and adherence,” they noted.
“This important trial provides some wins that support selective use of sacubitril-valsartan in HFpEF [as well as] observed losses, which too may help to define better implementation strategies in appropriately selected patients,” the editorialists concluded.
The study was funded by Novartis. Dr. Mentz and other coauthors have received fees from Novartis. Dr. Pinney, Dr. Ventura, and the other editorialists disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with an ejection fraction (EF) greater than 40% who were stabilized after recent worsening or de novo heart failure (HF) had a greater reduction in natriuretic peptides and less worsening renal function, but a higher rate of hypotension over 8 weeks with sacubitril-valsartan (Entresto) versus valsartan (Diovan) in the PARAGLIDE-HF trial.
A subgroup analysis showed evidence of a larger treatment effect among those with an EF of 60% or less, said Robert Mentz, MD, of the Duke Clinical Research Institute, Durham, N.C.
Dr. Mentz presented the findings at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) scientific sessions. The study was also published online simultaneously in the Journal of the American College of Cardiology.
“Next steps will involve further assessment of the cardiovascular and renal benefits, as well as further exploration of the symptomatic hypotension that we observed,” Dr. Mentz said in an interview.
Meanwhile, he said, “clinicians should be aware of these new data – specifically, the incremental reduction in natriuretic peptide level, compared with valsartan, and potential benefits on cardiovascular and renal events,” particularly in those with an EF greater than 40% to 60% or less.
Larger benefit for EF > 40% to < 60%
PARAGLIDE-HF was a double-blind, randomized controlled trial with 466 patients with EF greater than 40% enrolled within 30 days of a worsening HF event. The median age was 71 years, 52% were women, and 22% were Black.
The trial was a follow-up to PARAGON-HF, which had shown that, in patients with an EF of at least 45%, sacubitril-valsartan did not result in a significantly lower rate of total hospitalizations for HF or death from cardiovascular causes, compared with valsartan.
The primary endpoint for PARAGLIDE was the time-averaged proportional change in N-terminal of the prohormone brain natriuretic peptide (NT-proBNP) from baseline through weeks 4 and 8, as in the PIONEER-HF trial. That trial showed that among patients hospitalized for acute decompensated HF with reduced EF (< 40%), the angiotensin receptor/neprilysin inhibitor (ARNI) led to a greater reduction in NT-proBNP concentration than the angiotensin receptor blocker (ARB).
Similarly, for PARAGLIDE, the time-averaged reduction in NT-proBNP was greater with sacubitril-valsartan, with a change ratio of 0.85 (15% greater reduction).
A secondary hierarchical outcome for PARAGLIDE, using the win ratio, consisted of time to cardiovascular death, number and timing of HF hospitalizations, number and timing of urgent HF visits, and time-averaged proportional change in NT-proBNP from baseline to weeks 4 and 8.
The hierarchical outcome favored sacubitril-valsartan, but was not significant (unmatched win ratio, 1.19).
As noted, sacubitril-valsartan reduced worsening renal function, compared with valsartan (odds ratio, 0.61), but increased symptomatic hypotension (OR, 1.73).
“We will work to better characterize the hypotension events that were observed to help identify those patients at greater risk and to provide further clarity around the timing and implications of these events,” Dr. Mentz said in an interview.
The team hypothesized that such events may be prevented by optimizing volume status and background therapies commonly used to treat hypertension in these patients.
“For instance,” Dr. Mentz suggested, “calcium channel blockers like amlodipine could be dose reduced or discontinued in patients with lower baseline blood pressures to better support sacubitril/valsartan initiation and titration.”
He highlighted the subgroup analysis showing evidence of a larger treatment effect in study patients with an EF of 60% or less for the NT-proBNP change (0.78) and the hierarchical outcome (win ratio, 1.46).
“These data may influence future guidance for sacubitril-valsartan in HF with EF greater than 40%, regardless of HF chronicity [acute or chronic vs. de novo] and treatment setting [hospital vs. clinic],” Dr. Mentz concluded.
Data ‘far from conclusive’
In a comment, Sean Pinney, MD, chief of cardiology at Mount Sinai Morningside, New York, said that the study results “help expand the current evidence base supporting the use of an ARNI in patients” with an EF greater than 40% up to 60%, and “provide confidence that ARNIs help to lower natriuretic peptides.
“It comes as little surprise that not everyone was able to tolerate these medications due to intolerable side effects like dizziness or hypotension,” he said.
Nevertheless, he added, “hopefully, these trial data help strengthen clinicians’ resolve to prescribe sacubitril/valsartan to a growing population of vulnerable patients.”
In a related editorial, Hector O. Ventura, MD, of the Ochsner Clinical School–University of Queensland, New Orleans, and colleagues express several concerns about the study.
Although the trial achieved significance for the primary endpoint, the margin of benefit was less than expected and the magnitude of the NT-proBNP reduction may not have been enough to reach the threshold for clinical benefit, they wrote.
Diuretic dosing in the two groups was not reported, and between-group differences may have contributed to both the differential NT-proBNP reduction and the rates of hypotension.
Furthermore, the sacubitril-valsartan group had a higher proportion of missing NT-proBNP data, which may have biased the results.
“Clinicians who elect to use sacubitril-valsartan in this population should be mindful of the risk for hypotension and select patients carefully, while providing close ambulatory follow up to ensure stability and adherence,” they noted.
“This important trial provides some wins that support selective use of sacubitril-valsartan in HFpEF [as well as] observed losses, which too may help to define better implementation strategies in appropriately selected patients,” the editorialists concluded.
The study was funded by Novartis. Dr. Mentz and other coauthors have received fees from Novartis. Dr. Pinney, Dr. Ventura, and the other editorialists disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with an ejection fraction (EF) greater than 40% who were stabilized after recent worsening or de novo heart failure (HF) had a greater reduction in natriuretic peptides and less worsening renal function, but a higher rate of hypotension over 8 weeks with sacubitril-valsartan (Entresto) versus valsartan (Diovan) in the PARAGLIDE-HF trial.
A subgroup analysis showed evidence of a larger treatment effect among those with an EF of 60% or less, said Robert Mentz, MD, of the Duke Clinical Research Institute, Durham, N.C.
Dr. Mentz presented the findings at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) scientific sessions. The study was also published online simultaneously in the Journal of the American College of Cardiology.
“Next steps will involve further assessment of the cardiovascular and renal benefits, as well as further exploration of the symptomatic hypotension that we observed,” Dr. Mentz said in an interview.
Meanwhile, he said, “clinicians should be aware of these new data – specifically, the incremental reduction in natriuretic peptide level, compared with valsartan, and potential benefits on cardiovascular and renal events,” particularly in those with an EF greater than 40% to 60% or less.
Larger benefit for EF > 40% to < 60%
PARAGLIDE-HF was a double-blind, randomized controlled trial with 466 patients with EF greater than 40% enrolled within 30 days of a worsening HF event. The median age was 71 years, 52% were women, and 22% were Black.
The trial was a follow-up to PARAGON-HF, which had shown that, in patients with an EF of at least 45%, sacubitril-valsartan did not result in a significantly lower rate of total hospitalizations for HF or death from cardiovascular causes, compared with valsartan.
The primary endpoint for PARAGLIDE was the time-averaged proportional change in N-terminal of the prohormone brain natriuretic peptide (NT-proBNP) from baseline through weeks 4 and 8, as in the PIONEER-HF trial. That trial showed that among patients hospitalized for acute decompensated HF with reduced EF (< 40%), the angiotensin receptor/neprilysin inhibitor (ARNI) led to a greater reduction in NT-proBNP concentration than the angiotensin receptor blocker (ARB).
Similarly, for PARAGLIDE, the time-averaged reduction in NT-proBNP was greater with sacubitril-valsartan, with a change ratio of 0.85 (15% greater reduction).
A secondary hierarchical outcome for PARAGLIDE, using the win ratio, consisted of time to cardiovascular death, number and timing of HF hospitalizations, number and timing of urgent HF visits, and time-averaged proportional change in NT-proBNP from baseline to weeks 4 and 8.
The hierarchical outcome favored sacubitril-valsartan, but was not significant (unmatched win ratio, 1.19).
As noted, sacubitril-valsartan reduced worsening renal function, compared with valsartan (odds ratio, 0.61), but increased symptomatic hypotension (OR, 1.73).
“We will work to better characterize the hypotension events that were observed to help identify those patients at greater risk and to provide further clarity around the timing and implications of these events,” Dr. Mentz said in an interview.
The team hypothesized that such events may be prevented by optimizing volume status and background therapies commonly used to treat hypertension in these patients.
“For instance,” Dr. Mentz suggested, “calcium channel blockers like amlodipine could be dose reduced or discontinued in patients with lower baseline blood pressures to better support sacubitril/valsartan initiation and titration.”
He highlighted the subgroup analysis showing evidence of a larger treatment effect in study patients with an EF of 60% or less for the NT-proBNP change (0.78) and the hierarchical outcome (win ratio, 1.46).
“These data may influence future guidance for sacubitril-valsartan in HF with EF greater than 40%, regardless of HF chronicity [acute or chronic vs. de novo] and treatment setting [hospital vs. clinic],” Dr. Mentz concluded.
Data ‘far from conclusive’
In a comment, Sean Pinney, MD, chief of cardiology at Mount Sinai Morningside, New York, said that the study results “help expand the current evidence base supporting the use of an ARNI in patients” with an EF greater than 40% up to 60%, and “provide confidence that ARNIs help to lower natriuretic peptides.
“It comes as little surprise that not everyone was able to tolerate these medications due to intolerable side effects like dizziness or hypotension,” he said.
Nevertheless, he added, “hopefully, these trial data help strengthen clinicians’ resolve to prescribe sacubitril/valsartan to a growing population of vulnerable patients.”
In a related editorial, Hector O. Ventura, MD, of the Ochsner Clinical School–University of Queensland, New Orleans, and colleagues express several concerns about the study.
Although the trial achieved significance for the primary endpoint, the margin of benefit was less than expected and the magnitude of the NT-proBNP reduction may not have been enough to reach the threshold for clinical benefit, they wrote.
Diuretic dosing in the two groups was not reported, and between-group differences may have contributed to both the differential NT-proBNP reduction and the rates of hypotension.
Furthermore, the sacubitril-valsartan group had a higher proportion of missing NT-proBNP data, which may have biased the results.
“Clinicians who elect to use sacubitril-valsartan in this population should be mindful of the risk for hypotension and select patients carefully, while providing close ambulatory follow up to ensure stability and adherence,” they noted.
“This important trial provides some wins that support selective use of sacubitril-valsartan in HFpEF [as well as] observed losses, which too may help to define better implementation strategies in appropriately selected patients,” the editorialists concluded.
The study was funded by Novartis. Dr. Mentz and other coauthors have received fees from Novartis. Dr. Pinney, Dr. Ventura, and the other editorialists disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM ESC HEART FAILURE 2023
Adult tonsillectomies work and they’re cost effective
A new randomized trial offers rare insight into outcomes in adult tonsillectomy, a surgical procedure that’s commonly performed in the United States yet falling out of favor. Tonsillectomies are both clinically effective and cost-effective in adult patients with recurrent acute tonsillitis, a British team reports.
The researchers declined to weigh in on whether the procedure is actually better than nonsurgical management. Still, “here at last, we have a substantial piece of scientific evidence which shows that, compared with nonsurgical management, removal of tonsils has a significant impact on the number of sore throat days and on the cost of managing sore throat disease in adults,” said study lead author Janet A. Wilson, MBChB, MD, an emerita professor of otolaryngology at Newcastle University (England), in an interview.
The study was published in The Lancet.
Tonsillectomies have become much less common over the past several decades as questions have arisen about their value. In the United States, the number of procedures performed each year plunged from a high of 1.4 million in 1959 to an estimated 286,000 tonsillectomies performed in children under 15 and 120,000 in people aged 15 in 2010.
It’s harder for adults to tolerate tonsillectomies than children, Dr. Wilson said. In children, surgeons can easily remove tonsils by scraping them off the throat’s side walls. But, she said, “an adult tonsillectomy is more akin to taking off the skin of an unripe orange, so it’s harder work for the surgeon and more traumatizing for the wall of the adult patient’s pharynx. We can only assume that this greater amount of fibrous tissue reflects the cumulative effect of infections over a period of years.”
While tonsillectomies are still performed hundreds of times a day in adults in the United States, a 2014 Cochrane Library review found there’s “insufficient information “to support them versus nonsurgical care as treatments to reduce sore throats.”
For the new multicenter, open-label, randomized study, researchers randomly assigned patients aged 16 and older with recurrent acute tonsillitis to immediate tonsillectomy or nonsurgical management, which Dr. Wilson said can include cold fluids, honey, analgesics/anti-inflammatories. and anesthetic throat lozenges. The study was conducted between 2015 and 2018.
Ultimately, there were 224 and 204 patients, respectively, in the two groups (average age = 23, [19-30], 78% female, 90% White).
Patients who underwent tonsillectomies versus nonsurgical treatment had fewer sore throats over 2 years (median 23 days [IQR 11-46 days] vs. 30 days [14-65 days]) with an incident rate ratio of 0.53 (95% confidence interval, 0.43-0.65, P < 0.0001) after adjustment for clinic site and baseline severity.
The study also shows that “adults who have severe recurrent throat infections with a frequency of seven episodes within 1 year, five or more for 2 consecutive years, or three or more in 3 consecutive years will suffer fewer days of sore throat in the 2 years following tonsillectomy than if they had kept their tonsils,” Dr. Wilson said.
The study doesn’t examine longer-term consequences. A 2018 study of children linked tonsillectomies to “significantly increased relative risk of later respiratory, allergic, and infectious diseases.”
In the new study, nearly 4 in 10 (39%) of the tonsillectomy patients had adverse events linked to the surgeries, and bleeding (19%) was the most common adverse effect. The researchers also estimated that “tonsillectomy has a high probability of being considered cost-effective.”
“Whichever way the results were analyzed and confounding variables allowed for, the result always seems to be the same: Tonsillectomy applied using current qualifying criteria was a worthwhile procedure,” Dr. Wilson said.
Dr. Wilson noted that tonsillectomy patients will suffer a persistent sore throat after surgery, “about the same as a bad episode of tonsillitis.” And she said patients will need to adjust their diet for a few days and take 1-2 weeks off work.
In an interview, internal medicine physician Noel Deep, MD, of Antigo, Wisc., said antibiotics are a common treatment for tonsillitis in primary care clinics. According to him, the United States doesn’t have guidelines for tonsillectomies in adults. He believes they can be considered if tonsillitis keeps recurring three to five times a year and disrupts quality of life.
Dr. Deep said the new study “reinforces the benefit of tonsillectomies. Several studies from Germany, Sweden, Finland, and the United Kingdom have demonstrated benefits of tonsillectomies, but they were only for short periods of less than a year and lacked long-term data.”
He noted that “there is no clear evidence as to when to recommend tonsillectomies.” Clinicians should talk to patients about the potential that tonsillectomies will reduce sore throat episodes and cost the patient less in the long run, he said. It’s also important, he said, to make sure tonsillitis is bacterial before prescribing antibiotics.
The United Kingdom’s National Institute for Health Research funded the study. Dr. Wilson disclosed support for meetings/travel from ENT Scotland, and the other authors report various disclosures, including grants and contracts. Dr. Deep serves on the editorial advisory board of Internal Medicine News and is chair of the American Medical Association Council on Science and Public Health.
A new randomized trial offers rare insight into outcomes in adult tonsillectomy, a surgical procedure that’s commonly performed in the United States yet falling out of favor. Tonsillectomies are both clinically effective and cost-effective in adult patients with recurrent acute tonsillitis, a British team reports.
The researchers declined to weigh in on whether the procedure is actually better than nonsurgical management. Still, “here at last, we have a substantial piece of scientific evidence which shows that, compared with nonsurgical management, removal of tonsils has a significant impact on the number of sore throat days and on the cost of managing sore throat disease in adults,” said study lead author Janet A. Wilson, MBChB, MD, an emerita professor of otolaryngology at Newcastle University (England), in an interview.
The study was published in The Lancet.
Tonsillectomies have become much less common over the past several decades as questions have arisen about their value. In the United States, the number of procedures performed each year plunged from a high of 1.4 million in 1959 to an estimated 286,000 tonsillectomies performed in children under 15 and 120,000 in people aged 15 in 2010.
It’s harder for adults to tolerate tonsillectomies than children, Dr. Wilson said. In children, surgeons can easily remove tonsils by scraping them off the throat’s side walls. But, she said, “an adult tonsillectomy is more akin to taking off the skin of an unripe orange, so it’s harder work for the surgeon and more traumatizing for the wall of the adult patient’s pharynx. We can only assume that this greater amount of fibrous tissue reflects the cumulative effect of infections over a period of years.”
While tonsillectomies are still performed hundreds of times a day in adults in the United States, a 2014 Cochrane Library review found there’s “insufficient information “to support them versus nonsurgical care as treatments to reduce sore throats.”
For the new multicenter, open-label, randomized study, researchers randomly assigned patients aged 16 and older with recurrent acute tonsillitis to immediate tonsillectomy or nonsurgical management, which Dr. Wilson said can include cold fluids, honey, analgesics/anti-inflammatories. and anesthetic throat lozenges. The study was conducted between 2015 and 2018.
Ultimately, there were 224 and 204 patients, respectively, in the two groups (average age = 23, [19-30], 78% female, 90% White).
Patients who underwent tonsillectomies versus nonsurgical treatment had fewer sore throats over 2 years (median 23 days [IQR 11-46 days] vs. 30 days [14-65 days]) with an incident rate ratio of 0.53 (95% confidence interval, 0.43-0.65, P < 0.0001) after adjustment for clinic site and baseline severity.
The study also shows that “adults who have severe recurrent throat infections with a frequency of seven episodes within 1 year, five or more for 2 consecutive years, or three or more in 3 consecutive years will suffer fewer days of sore throat in the 2 years following tonsillectomy than if they had kept their tonsils,” Dr. Wilson said.
The study doesn’t examine longer-term consequences. A 2018 study of children linked tonsillectomies to “significantly increased relative risk of later respiratory, allergic, and infectious diseases.”
In the new study, nearly 4 in 10 (39%) of the tonsillectomy patients had adverse events linked to the surgeries, and bleeding (19%) was the most common adverse effect. The researchers also estimated that “tonsillectomy has a high probability of being considered cost-effective.”
“Whichever way the results were analyzed and confounding variables allowed for, the result always seems to be the same: Tonsillectomy applied using current qualifying criteria was a worthwhile procedure,” Dr. Wilson said.
Dr. Wilson noted that tonsillectomy patients will suffer a persistent sore throat after surgery, “about the same as a bad episode of tonsillitis.” And she said patients will need to adjust their diet for a few days and take 1-2 weeks off work.
In an interview, internal medicine physician Noel Deep, MD, of Antigo, Wisc., said antibiotics are a common treatment for tonsillitis in primary care clinics. According to him, the United States doesn’t have guidelines for tonsillectomies in adults. He believes they can be considered if tonsillitis keeps recurring three to five times a year and disrupts quality of life.
Dr. Deep said the new study “reinforces the benefit of tonsillectomies. Several studies from Germany, Sweden, Finland, and the United Kingdom have demonstrated benefits of tonsillectomies, but they were only for short periods of less than a year and lacked long-term data.”
He noted that “there is no clear evidence as to when to recommend tonsillectomies.” Clinicians should talk to patients about the potential that tonsillectomies will reduce sore throat episodes and cost the patient less in the long run, he said. It’s also important, he said, to make sure tonsillitis is bacterial before prescribing antibiotics.
The United Kingdom’s National Institute for Health Research funded the study. Dr. Wilson disclosed support for meetings/travel from ENT Scotland, and the other authors report various disclosures, including grants and contracts. Dr. Deep serves on the editorial advisory board of Internal Medicine News and is chair of the American Medical Association Council on Science and Public Health.
A new randomized trial offers rare insight into outcomes in adult tonsillectomy, a surgical procedure that’s commonly performed in the United States yet falling out of favor. Tonsillectomies are both clinically effective and cost-effective in adult patients with recurrent acute tonsillitis, a British team reports.
The researchers declined to weigh in on whether the procedure is actually better than nonsurgical management. Still, “here at last, we have a substantial piece of scientific evidence which shows that, compared with nonsurgical management, removal of tonsils has a significant impact on the number of sore throat days and on the cost of managing sore throat disease in adults,” said study lead author Janet A. Wilson, MBChB, MD, an emerita professor of otolaryngology at Newcastle University (England), in an interview.
The study was published in The Lancet.
Tonsillectomies have become much less common over the past several decades as questions have arisen about their value. In the United States, the number of procedures performed each year plunged from a high of 1.4 million in 1959 to an estimated 286,000 tonsillectomies performed in children under 15 and 120,000 in people aged 15 in 2010.
It’s harder for adults to tolerate tonsillectomies than children, Dr. Wilson said. In children, surgeons can easily remove tonsils by scraping them off the throat’s side walls. But, she said, “an adult tonsillectomy is more akin to taking off the skin of an unripe orange, so it’s harder work for the surgeon and more traumatizing for the wall of the adult patient’s pharynx. We can only assume that this greater amount of fibrous tissue reflects the cumulative effect of infections over a period of years.”
While tonsillectomies are still performed hundreds of times a day in adults in the United States, a 2014 Cochrane Library review found there’s “insufficient information “to support them versus nonsurgical care as treatments to reduce sore throats.”
For the new multicenter, open-label, randomized study, researchers randomly assigned patients aged 16 and older with recurrent acute tonsillitis to immediate tonsillectomy or nonsurgical management, which Dr. Wilson said can include cold fluids, honey, analgesics/anti-inflammatories. and anesthetic throat lozenges. The study was conducted between 2015 and 2018.
Ultimately, there were 224 and 204 patients, respectively, in the two groups (average age = 23, [19-30], 78% female, 90% White).
Patients who underwent tonsillectomies versus nonsurgical treatment had fewer sore throats over 2 years (median 23 days [IQR 11-46 days] vs. 30 days [14-65 days]) with an incident rate ratio of 0.53 (95% confidence interval, 0.43-0.65, P < 0.0001) after adjustment for clinic site and baseline severity.
The study also shows that “adults who have severe recurrent throat infections with a frequency of seven episodes within 1 year, five or more for 2 consecutive years, or three or more in 3 consecutive years will suffer fewer days of sore throat in the 2 years following tonsillectomy than if they had kept their tonsils,” Dr. Wilson said.
The study doesn’t examine longer-term consequences. A 2018 study of children linked tonsillectomies to “significantly increased relative risk of later respiratory, allergic, and infectious diseases.”
In the new study, nearly 4 in 10 (39%) of the tonsillectomy patients had adverse events linked to the surgeries, and bleeding (19%) was the most common adverse effect. The researchers also estimated that “tonsillectomy has a high probability of being considered cost-effective.”
“Whichever way the results were analyzed and confounding variables allowed for, the result always seems to be the same: Tonsillectomy applied using current qualifying criteria was a worthwhile procedure,” Dr. Wilson said.
Dr. Wilson noted that tonsillectomy patients will suffer a persistent sore throat after surgery, “about the same as a bad episode of tonsillitis.” And she said patients will need to adjust their diet for a few days and take 1-2 weeks off work.
In an interview, internal medicine physician Noel Deep, MD, of Antigo, Wisc., said antibiotics are a common treatment for tonsillitis in primary care clinics. According to him, the United States doesn’t have guidelines for tonsillectomies in adults. He believes they can be considered if tonsillitis keeps recurring three to five times a year and disrupts quality of life.
Dr. Deep said the new study “reinforces the benefit of tonsillectomies. Several studies from Germany, Sweden, Finland, and the United Kingdom have demonstrated benefits of tonsillectomies, but they were only for short periods of less than a year and lacked long-term data.”
He noted that “there is no clear evidence as to when to recommend tonsillectomies.” Clinicians should talk to patients about the potential that tonsillectomies will reduce sore throat episodes and cost the patient less in the long run, he said. It’s also important, he said, to make sure tonsillitis is bacterial before prescribing antibiotics.
The United Kingdom’s National Institute for Health Research funded the study. Dr. Wilson disclosed support for meetings/travel from ENT Scotland, and the other authors report various disclosures, including grants and contracts. Dr. Deep serves on the editorial advisory board of Internal Medicine News and is chair of the American Medical Association Council on Science and Public Health.
FROM THE LANCET
The weird world of hydrogels: How they’ll change health care
Imagine a day when a simple injection prompts a broken bone to heal. When tiny, ingestible devices linger in the body, unnoticed, tracking our health or delivering life-saving medications. When brain and heart implants mesh with flesh so seamlessly that the body thinks they’ve been there all along.
These are the dreams of materials scientists who have toiled for decades to mimic the complex architecture of the human body in hopes of replacing broken parts or treating disease.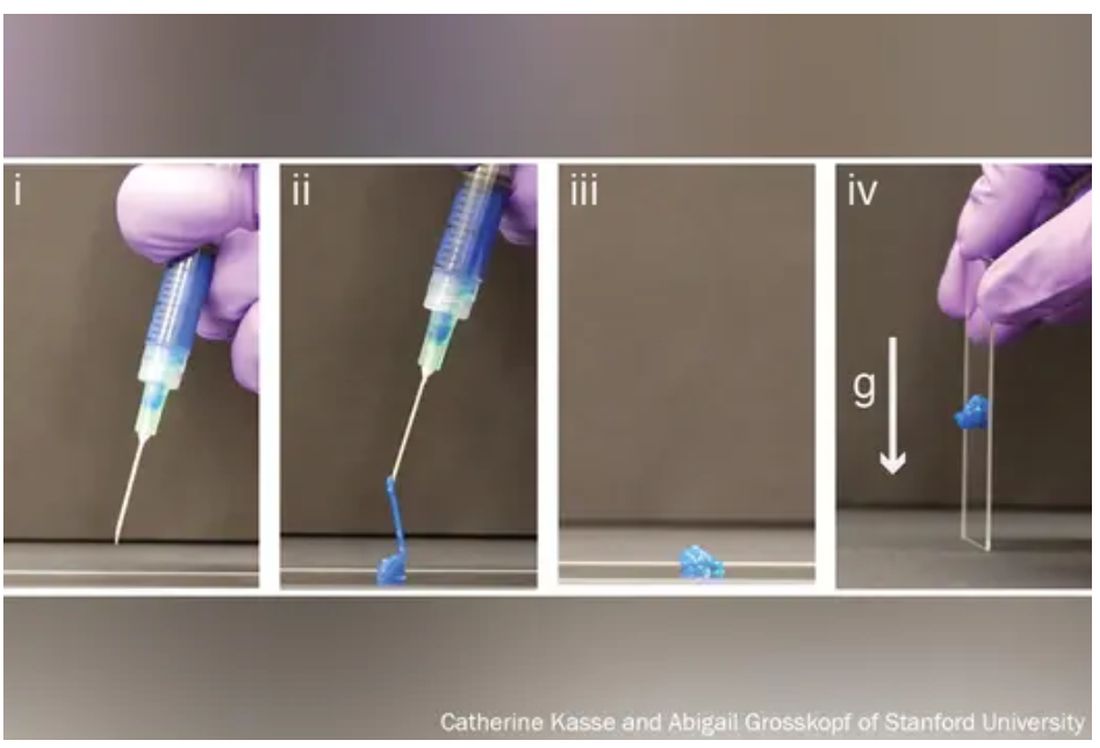
The problem, say bioengineers, is that most replacement and corrective parts – from prosthetics to pacemakers – are made of hard, dry, lifeless materials, like metal or plastic, while biological tissue is soft, wet, and living.
The body knows the difference and tends to reject imitations.
Enter hydrogels, three-dimensional networks of molecules swollen with – by definition – water.
First described in 1960 by creators of soft contact lenses, these weird, shape-shifting substances are able to morph from liquid to solid to a squishy in-between. (Early, simple uses include hair gel or Jell-O.). Slow to gain attention, growing to just 1,000 studies published by 1982, they’ve become the subject of intense study recently, with 100,000 papers published by 2020, and 3,800 already this year alone.
As chemists, biologists, and engineers begin to work more with one another and with medical doctors,
“We are, essentially, hydrogels,” said Benjamin Wiley, PhD, a chemistry professor at Duke University in Durham, N.C. “As people develop new hydrogels that more closely match the tissues in our body, we’ll be able to treat a whole host of ailments we couldn’t treat before.”
From contact lenses to brain implants
Put simply, a hydrogel is like a mesh bag of water.
The mesh is made of polymers, or spaghetti-like strands of molecules, stitched together in a repeating pattern and swollen with H2O, much like the way 3D matrixes in our body surround, support, and give structure to our cells and tissues.
“Imagine a soccer net, with all of these long fibers woven together to create the net,” said Eric Appel, PhD, associate professor of materials science and engineering at Stanford (Calif.) University.
While the broader category of “gels” could be filled with anything, including chemical solvents, water is the key ingredient that sets hydrogels apart, making them ideal for, as some scientists put it, “merging humans and machines.”
Human bones are about 25% water, while muscles hover around 70% and the brain is 85%. The precious liquid plays a host of critical roles, from shuttling nutrients in and waste out to helping cells talk to each other.
Lab-made hydrogels can be loaded with cargo (like a ball in the net), including cells or drugs that help mimic some of those functions.
Hydrogels are soft and pliable like flesh. So, if used in implants, they may be less likely to damage surrounding tissue.
“Think about a metal spoon in your bowl of pudding. As you’re shaking the bowl, the spoon doesn’t stay in place, and you get scarring around the spoon,” said Christina Tringides, PhD, a materials scientist who studies neural engineering. That, she says, is exactly what happens to brain implants when patients breathe or move. “It’s a mechanical mismatch. But with hydrogels, you could get perfect mechanical matching.”
Hydrogels also tend to be nontoxic, so the immune system may be less likely to attack them as foreign bodies.
All this has made hydrogels the new darling of the bioengineering world.
“There has been an absolute explosion of interest in these materials,” Dr. Appel said.
Smarter drug delivery and ingestible electronics
Early versions of hydrogels were thick and gooey, making it hard to get them inside the body.
“Think of a block of Jell-O. You couldn’t inject something like that,” Dr. Appel said.
But Dr. Appel, whose lab develops new drug delivery systems, has been tinkering with gel formulas for years in hopes that these high-tech globs could someday ferry timed-release drugs to just the right spot in the body.
His new hydrogels start as fully formed gels (which help preserve the drug contents) inside a syringe. But once the plunger is pushed, they magically shape-shift to a liquid thin enough to flow easily through a standard needle. Upon exit, they immediately reform into gels, protecting the inherent cargo from degrading.
This could be a game changer at a time when many cutting-edge drugs – think Humira for arthritis or Ozempic for type 2 diabetes – are made of quickly degrading proteins too large and complex to simply jam into a pill. Instead, they must be injected, often frequently.
“Because the gel takes months to dissolve, it slowly delivers the drug over time,” Dr. Appel said. “You could conceivably go from a shot once a week to once every 4 months.”
Such slow-release hydrogels could make vaccines last longer, in turn teaching the body to better resist emerging virus variants, and deliver tumor-busting therapies more precisely, said Dr. Appel, who has formed a startup and hopes to fast-track the first hydrogel drug delivery system to clinical trials within a few years.
Meanwhile, another team at the Massachusetts Institute of Technology has taken a different approach, developing a standard-sized ingestible hydrogel pill that swells up like a puffer fish in the stomach, lasting a month and slowly releasing drugs all the while. To remove the pill, a patient simply drinks a salt-based solution that shrivels the ping-pong ball–sized device so it can be passed out of the body.
In a paper in Nature Communications, the scientists showed the puffer fish pill could also be loaded with tiny cameras or monitors to track conditions like ulcers or cancer.
“The dream is to have a Jell-O-like smart pill that, once swallowed, stays in the stomach and monitors the patient’s health,” said Xuanhe Zhao, PhD, a researcher on the project and associate professor of mechanical engineering at MIT.
Building joints and regrowing bones
Since the 1970s, researchers have mulled using hydrogels to replace human cartilage, a remarkably strong and flexible tissue made of about 90% water but able to withstand the weight of a car on an area about the size of a coin.
Until recently, those efforts have largely failed. Meaning when knee cartilage wears down, things like cartilage transplants, drilling holes to stimulate new growth, or total joint replacements – all of which require lengthy rehab – are the only options.
But that may be about to change.
Dr. Wiley and his colleagues at Duke recently reported that they’d developed the first gel-based cartilage substitute even stronger and more durable than the real thing.
By attaching their hydrogel to a titanium backing to help stick it in place, they hope to repair damaged cartilage “much like a dentist fills a cavity” long before surgery is necessary.
They too have partnered with industry to bring their hydrogel to market – starting with knees.
“Ultimately, the goal is to do any joint – hips, ankles, fingers, and toes,” Dr. Wiley said.
At the University of Toronto, chemist Karina Carneiro, PhD, and dentist Christopher McCulloch, DDS, are also thinking big.
In a recent paper in Proceedings of the National Academy of Sciences, they describe a hydrogel, designed by Dr. Carneiro and made of DNA, that can be injected, migrate to a defect in bone – an irreparable break, hole from surgery, or jawbone withered by age – and fill in the gap like putty. But not only does it patch the hole, it prompts the bone to regenerate.
In rats with holes in their skulls due to surgery, they found that the treatment did not work as well as the existing gold standard for repairing holes in bone – grafting bone from elsewhere in the body. But it did work.
“These are very early days for DNA hydrogels,” cautioned Dr. McCulloch, a study coauthor and professor in the Faculty of Dentistry, noting that it will likely be a decade or more before such technology could be available to patients. “But there is the potential that DNA hydrogel could someday grow bone without having to have highly invasive surgical procedures. That’s a significant advancement.”
A sci-fi future
Perhaps the wildest, and weirdest, potential applications of hydrogels come in the realm of human-machine interaction.
Numerous companies are already dabbling in neural prosthetic or brain computer interfaces that might someday, for instance, let someone who is paralyzed and can’t speak write on a laptop using their thoughts.
The spoon-in-the-Jell-O problem has been a major stumbling block.
But Dr. Tringides, who recently earned her PhD in biophysics from Harvard, is working on it.
She and her team have developed a seaweed-based hydrogel loaded with tiny flecks of nanomaterials that can not only meld nicely into squishy brain tissue but also conduct electricity.
Within a decade, she says, this could replace the clunky platinum metal discs used for electrocorticography – recording electrical activity in the brain to identify where seizures start or doing precise brain surgery.
In 30 to 50 years? Let your imagination run wild.
“I’m a skeptic. I like to take research step by step,” she said. “But things are definitely progressing in an interesting direction.”
A version of this article first appeared on WebMD.com.
Imagine a day when a simple injection prompts a broken bone to heal. When tiny, ingestible devices linger in the body, unnoticed, tracking our health or delivering life-saving medications. When brain and heart implants mesh with flesh so seamlessly that the body thinks they’ve been there all along.
These are the dreams of materials scientists who have toiled for decades to mimic the complex architecture of the human body in hopes of replacing broken parts or treating disease.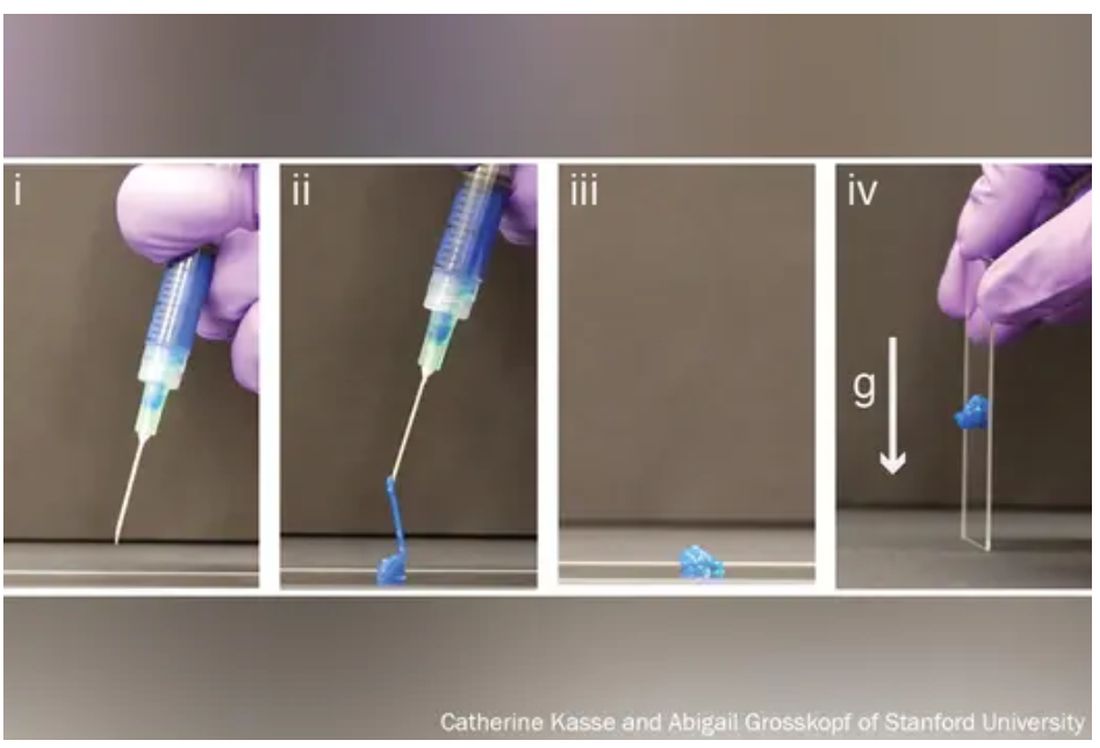
The problem, say bioengineers, is that most replacement and corrective parts – from prosthetics to pacemakers – are made of hard, dry, lifeless materials, like metal or plastic, while biological tissue is soft, wet, and living.
The body knows the difference and tends to reject imitations.
Enter hydrogels, three-dimensional networks of molecules swollen with – by definition – water.
First described in 1960 by creators of soft contact lenses, these weird, shape-shifting substances are able to morph from liquid to solid to a squishy in-between. (Early, simple uses include hair gel or Jell-O.). Slow to gain attention, growing to just 1,000 studies published by 1982, they’ve become the subject of intense study recently, with 100,000 papers published by 2020, and 3,800 already this year alone.
As chemists, biologists, and engineers begin to work more with one another and with medical doctors,
“We are, essentially, hydrogels,” said Benjamin Wiley, PhD, a chemistry professor at Duke University in Durham, N.C. “As people develop new hydrogels that more closely match the tissues in our body, we’ll be able to treat a whole host of ailments we couldn’t treat before.”
From contact lenses to brain implants
Put simply, a hydrogel is like a mesh bag of water.
The mesh is made of polymers, or spaghetti-like strands of molecules, stitched together in a repeating pattern and swollen with H2O, much like the way 3D matrixes in our body surround, support, and give structure to our cells and tissues.
“Imagine a soccer net, with all of these long fibers woven together to create the net,” said Eric Appel, PhD, associate professor of materials science and engineering at Stanford (Calif.) University.
While the broader category of “gels” could be filled with anything, including chemical solvents, water is the key ingredient that sets hydrogels apart, making them ideal for, as some scientists put it, “merging humans and machines.”
Human bones are about 25% water, while muscles hover around 70% and the brain is 85%. The precious liquid plays a host of critical roles, from shuttling nutrients in and waste out to helping cells talk to each other.
Lab-made hydrogels can be loaded with cargo (like a ball in the net), including cells or drugs that help mimic some of those functions.
Hydrogels are soft and pliable like flesh. So, if used in implants, they may be less likely to damage surrounding tissue.
“Think about a metal spoon in your bowl of pudding. As you’re shaking the bowl, the spoon doesn’t stay in place, and you get scarring around the spoon,” said Christina Tringides, PhD, a materials scientist who studies neural engineering. That, she says, is exactly what happens to brain implants when patients breathe or move. “It’s a mechanical mismatch. But with hydrogels, you could get perfect mechanical matching.”
Hydrogels also tend to be nontoxic, so the immune system may be less likely to attack them as foreign bodies.
All this has made hydrogels the new darling of the bioengineering world.
“There has been an absolute explosion of interest in these materials,” Dr. Appel said.
Smarter drug delivery and ingestible electronics
Early versions of hydrogels were thick and gooey, making it hard to get them inside the body.
“Think of a block of Jell-O. You couldn’t inject something like that,” Dr. Appel said.
But Dr. Appel, whose lab develops new drug delivery systems, has been tinkering with gel formulas for years in hopes that these high-tech globs could someday ferry timed-release drugs to just the right spot in the body.
His new hydrogels start as fully formed gels (which help preserve the drug contents) inside a syringe. But once the plunger is pushed, they magically shape-shift to a liquid thin enough to flow easily through a standard needle. Upon exit, they immediately reform into gels, protecting the inherent cargo from degrading.
This could be a game changer at a time when many cutting-edge drugs – think Humira for arthritis or Ozempic for type 2 diabetes – are made of quickly degrading proteins too large and complex to simply jam into a pill. Instead, they must be injected, often frequently.
“Because the gel takes months to dissolve, it slowly delivers the drug over time,” Dr. Appel said. “You could conceivably go from a shot once a week to once every 4 months.”
Such slow-release hydrogels could make vaccines last longer, in turn teaching the body to better resist emerging virus variants, and deliver tumor-busting therapies more precisely, said Dr. Appel, who has formed a startup and hopes to fast-track the first hydrogel drug delivery system to clinical trials within a few years.
Meanwhile, another team at the Massachusetts Institute of Technology has taken a different approach, developing a standard-sized ingestible hydrogel pill that swells up like a puffer fish in the stomach, lasting a month and slowly releasing drugs all the while. To remove the pill, a patient simply drinks a salt-based solution that shrivels the ping-pong ball–sized device so it can be passed out of the body.
In a paper in Nature Communications, the scientists showed the puffer fish pill could also be loaded with tiny cameras or monitors to track conditions like ulcers or cancer.
“The dream is to have a Jell-O-like smart pill that, once swallowed, stays in the stomach and monitors the patient’s health,” said Xuanhe Zhao, PhD, a researcher on the project and associate professor of mechanical engineering at MIT.
Building joints and regrowing bones
Since the 1970s, researchers have mulled using hydrogels to replace human cartilage, a remarkably strong and flexible tissue made of about 90% water but able to withstand the weight of a car on an area about the size of a coin.
Until recently, those efforts have largely failed. Meaning when knee cartilage wears down, things like cartilage transplants, drilling holes to stimulate new growth, or total joint replacements – all of which require lengthy rehab – are the only options.
But that may be about to change.
Dr. Wiley and his colleagues at Duke recently reported that they’d developed the first gel-based cartilage substitute even stronger and more durable than the real thing.
By attaching their hydrogel to a titanium backing to help stick it in place, they hope to repair damaged cartilage “much like a dentist fills a cavity” long before surgery is necessary.
They too have partnered with industry to bring their hydrogel to market – starting with knees.
“Ultimately, the goal is to do any joint – hips, ankles, fingers, and toes,” Dr. Wiley said.
At the University of Toronto, chemist Karina Carneiro, PhD, and dentist Christopher McCulloch, DDS, are also thinking big.
In a recent paper in Proceedings of the National Academy of Sciences, they describe a hydrogel, designed by Dr. Carneiro and made of DNA, that can be injected, migrate to a defect in bone – an irreparable break, hole from surgery, or jawbone withered by age – and fill in the gap like putty. But not only does it patch the hole, it prompts the bone to regenerate.
In rats with holes in their skulls due to surgery, they found that the treatment did not work as well as the existing gold standard for repairing holes in bone – grafting bone from elsewhere in the body. But it did work.
“These are very early days for DNA hydrogels,” cautioned Dr. McCulloch, a study coauthor and professor in the Faculty of Dentistry, noting that it will likely be a decade or more before such technology could be available to patients. “But there is the potential that DNA hydrogel could someday grow bone without having to have highly invasive surgical procedures. That’s a significant advancement.”
A sci-fi future
Perhaps the wildest, and weirdest, potential applications of hydrogels come in the realm of human-machine interaction.
Numerous companies are already dabbling in neural prosthetic or brain computer interfaces that might someday, for instance, let someone who is paralyzed and can’t speak write on a laptop using their thoughts.
The spoon-in-the-Jell-O problem has been a major stumbling block.
But Dr. Tringides, who recently earned her PhD in biophysics from Harvard, is working on it.
She and her team have developed a seaweed-based hydrogel loaded with tiny flecks of nanomaterials that can not only meld nicely into squishy brain tissue but also conduct electricity.
Within a decade, she says, this could replace the clunky platinum metal discs used for electrocorticography – recording electrical activity in the brain to identify where seizures start or doing precise brain surgery.
In 30 to 50 years? Let your imagination run wild.
“I’m a skeptic. I like to take research step by step,” she said. “But things are definitely progressing in an interesting direction.”
A version of this article first appeared on WebMD.com.
Imagine a day when a simple injection prompts a broken bone to heal. When tiny, ingestible devices linger in the body, unnoticed, tracking our health or delivering life-saving medications. When brain and heart implants mesh with flesh so seamlessly that the body thinks they’ve been there all along.
These are the dreams of materials scientists who have toiled for decades to mimic the complex architecture of the human body in hopes of replacing broken parts or treating disease.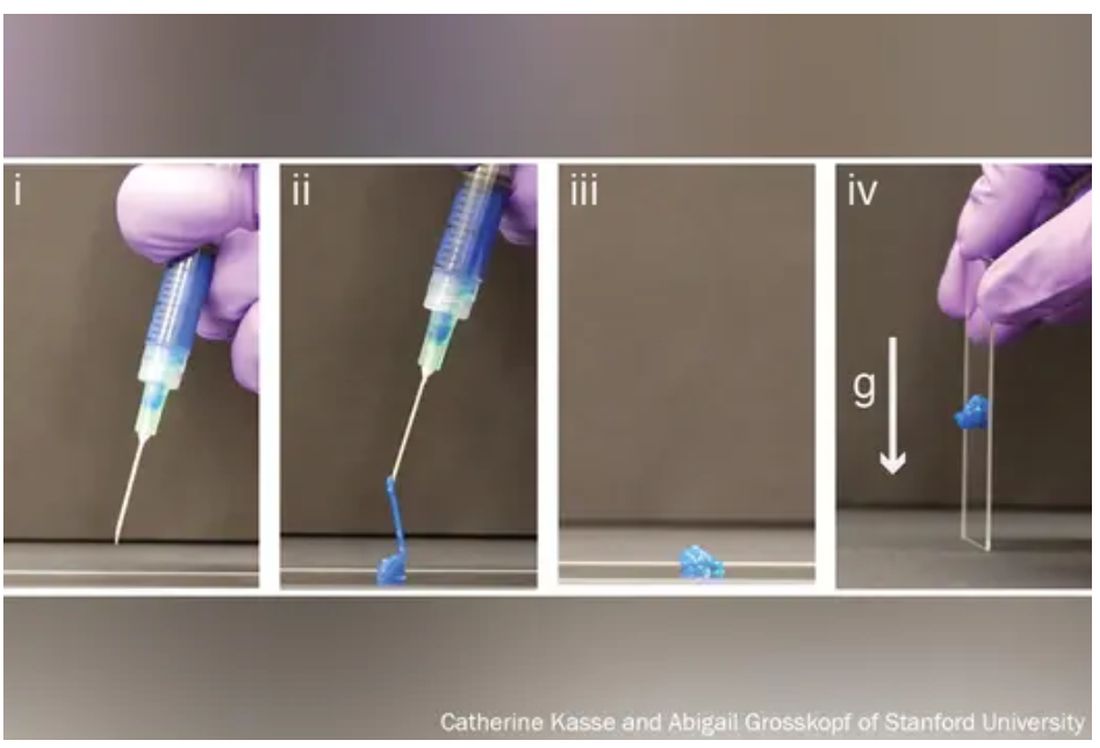
The problem, say bioengineers, is that most replacement and corrective parts – from prosthetics to pacemakers – are made of hard, dry, lifeless materials, like metal or plastic, while biological tissue is soft, wet, and living.
The body knows the difference and tends to reject imitations.
Enter hydrogels, three-dimensional networks of molecules swollen with – by definition – water.
First described in 1960 by creators of soft contact lenses, these weird, shape-shifting substances are able to morph from liquid to solid to a squishy in-between. (Early, simple uses include hair gel or Jell-O.). Slow to gain attention, growing to just 1,000 studies published by 1982, they’ve become the subject of intense study recently, with 100,000 papers published by 2020, and 3,800 already this year alone.
As chemists, biologists, and engineers begin to work more with one another and with medical doctors,
“We are, essentially, hydrogels,” said Benjamin Wiley, PhD, a chemistry professor at Duke University in Durham, N.C. “As people develop new hydrogels that more closely match the tissues in our body, we’ll be able to treat a whole host of ailments we couldn’t treat before.”
From contact lenses to brain implants
Put simply, a hydrogel is like a mesh bag of water.
The mesh is made of polymers, or spaghetti-like strands of molecules, stitched together in a repeating pattern and swollen with H2O, much like the way 3D matrixes in our body surround, support, and give structure to our cells and tissues.
“Imagine a soccer net, with all of these long fibers woven together to create the net,” said Eric Appel, PhD, associate professor of materials science and engineering at Stanford (Calif.) University.
While the broader category of “gels” could be filled with anything, including chemical solvents, water is the key ingredient that sets hydrogels apart, making them ideal for, as some scientists put it, “merging humans and machines.”
Human bones are about 25% water, while muscles hover around 70% and the brain is 85%. The precious liquid plays a host of critical roles, from shuttling nutrients in and waste out to helping cells talk to each other.
Lab-made hydrogels can be loaded with cargo (like a ball in the net), including cells or drugs that help mimic some of those functions.
Hydrogels are soft and pliable like flesh. So, if used in implants, they may be less likely to damage surrounding tissue.
“Think about a metal spoon in your bowl of pudding. As you’re shaking the bowl, the spoon doesn’t stay in place, and you get scarring around the spoon,” said Christina Tringides, PhD, a materials scientist who studies neural engineering. That, she says, is exactly what happens to brain implants when patients breathe or move. “It’s a mechanical mismatch. But with hydrogels, you could get perfect mechanical matching.”
Hydrogels also tend to be nontoxic, so the immune system may be less likely to attack them as foreign bodies.
All this has made hydrogels the new darling of the bioengineering world.
“There has been an absolute explosion of interest in these materials,” Dr. Appel said.
Smarter drug delivery and ingestible electronics
Early versions of hydrogels were thick and gooey, making it hard to get them inside the body.
“Think of a block of Jell-O. You couldn’t inject something like that,” Dr. Appel said.
But Dr. Appel, whose lab develops new drug delivery systems, has been tinkering with gel formulas for years in hopes that these high-tech globs could someday ferry timed-release drugs to just the right spot in the body.
His new hydrogels start as fully formed gels (which help preserve the drug contents) inside a syringe. But once the plunger is pushed, they magically shape-shift to a liquid thin enough to flow easily through a standard needle. Upon exit, they immediately reform into gels, protecting the inherent cargo from degrading.
This could be a game changer at a time when many cutting-edge drugs – think Humira for arthritis or Ozempic for type 2 diabetes – are made of quickly degrading proteins too large and complex to simply jam into a pill. Instead, they must be injected, often frequently.
“Because the gel takes months to dissolve, it slowly delivers the drug over time,” Dr. Appel said. “You could conceivably go from a shot once a week to once every 4 months.”
Such slow-release hydrogels could make vaccines last longer, in turn teaching the body to better resist emerging virus variants, and deliver tumor-busting therapies more precisely, said Dr. Appel, who has formed a startup and hopes to fast-track the first hydrogel drug delivery system to clinical trials within a few years.
Meanwhile, another team at the Massachusetts Institute of Technology has taken a different approach, developing a standard-sized ingestible hydrogel pill that swells up like a puffer fish in the stomach, lasting a month and slowly releasing drugs all the while. To remove the pill, a patient simply drinks a salt-based solution that shrivels the ping-pong ball–sized device so it can be passed out of the body.
In a paper in Nature Communications, the scientists showed the puffer fish pill could also be loaded with tiny cameras or monitors to track conditions like ulcers or cancer.
“The dream is to have a Jell-O-like smart pill that, once swallowed, stays in the stomach and monitors the patient’s health,” said Xuanhe Zhao, PhD, a researcher on the project and associate professor of mechanical engineering at MIT.
Building joints and regrowing bones
Since the 1970s, researchers have mulled using hydrogels to replace human cartilage, a remarkably strong and flexible tissue made of about 90% water but able to withstand the weight of a car on an area about the size of a coin.
Until recently, those efforts have largely failed. Meaning when knee cartilage wears down, things like cartilage transplants, drilling holes to stimulate new growth, or total joint replacements – all of which require lengthy rehab – are the only options.
But that may be about to change.
Dr. Wiley and his colleagues at Duke recently reported that they’d developed the first gel-based cartilage substitute even stronger and more durable than the real thing.
By attaching their hydrogel to a titanium backing to help stick it in place, they hope to repair damaged cartilage “much like a dentist fills a cavity” long before surgery is necessary.
They too have partnered with industry to bring their hydrogel to market – starting with knees.
“Ultimately, the goal is to do any joint – hips, ankles, fingers, and toes,” Dr. Wiley said.
At the University of Toronto, chemist Karina Carneiro, PhD, and dentist Christopher McCulloch, DDS, are also thinking big.
In a recent paper in Proceedings of the National Academy of Sciences, they describe a hydrogel, designed by Dr. Carneiro and made of DNA, that can be injected, migrate to a defect in bone – an irreparable break, hole from surgery, or jawbone withered by age – and fill in the gap like putty. But not only does it patch the hole, it prompts the bone to regenerate.
In rats with holes in their skulls due to surgery, they found that the treatment did not work as well as the existing gold standard for repairing holes in bone – grafting bone from elsewhere in the body. But it did work.
“These are very early days for DNA hydrogels,” cautioned Dr. McCulloch, a study coauthor and professor in the Faculty of Dentistry, noting that it will likely be a decade or more before such technology could be available to patients. “But there is the potential that DNA hydrogel could someday grow bone without having to have highly invasive surgical procedures. That’s a significant advancement.”
A sci-fi future
Perhaps the wildest, and weirdest, potential applications of hydrogels come in the realm of human-machine interaction.
Numerous companies are already dabbling in neural prosthetic or brain computer interfaces that might someday, for instance, let someone who is paralyzed and can’t speak write on a laptop using their thoughts.
The spoon-in-the-Jell-O problem has been a major stumbling block.
But Dr. Tringides, who recently earned her PhD in biophysics from Harvard, is working on it.
She and her team have developed a seaweed-based hydrogel loaded with tiny flecks of nanomaterials that can not only meld nicely into squishy brain tissue but also conduct electricity.
Within a decade, she says, this could replace the clunky platinum metal discs used for electrocorticography – recording electrical activity in the brain to identify where seizures start or doing precise brain surgery.
In 30 to 50 years? Let your imagination run wild.
“I’m a skeptic. I like to take research step by step,” she said. “But things are definitely progressing in an interesting direction.”
A version of this article first appeared on WebMD.com.
Should you prescribe bioidentical hormones for menopause?
BALTIMORE – according to an expert at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists (ACOG).
Clinicians write an estimated 26 to 33 million prescriptions for compounded bioidentical hormone therapy (cBHT) every year, and almost 41% of menopausal women who need treatment try cBHT during their lives. But these drugs lack the approval for this indication from the Food and Drug Administration.
“There is a public perception that this is natural, safer, and anti-aging,” said Robert Kauffman, MD, a professor of obstetrics and gynecology and assistant dean for research at Texas Tech University Health Sciences Center in Amarillo.
Following the 2002 Women’s Health Initiative report showing a link between hormone therapy (HT) and an increase in the incidence of breast cancer, medical schools have slowed or paused instructing trainees on the traditional treatment, Dr. Kauffman said. The association was later determined to be spurious: HT is not associated with a risk for all-cause mortality or deaths from cardiovascular disease or cancer. However, HT still is largely ignored by younger physicians, Dr. Kauffman said, because of unsubstantiated “dangers” such as heart attack, stroke, and deep vein thrombosis.
The lack of education on HT for medical school students and residents has “opened the door to unsubstantiated marketing claims and practices” for cBHT, Dr. Kauffman said. “Hence, the use of compounded bioidentical hormone therapy has increased” as clinicians look for alternatives.
Groups including ACOG, the North American Menopause Society (NAMS), and the U.S. Preventive Services Task Force recommend against the use of Non–FDA-approved therapies such as cBHT, except for narrow indications. Dr. Kauffman said that drug manufacturers have not conducted randomized controlled trials or observational studies on cBHT in treating menopause.
He cited studies showing quality problems with the compounding process of these drugs, and wide variations in the amount of actual ingredients from product labels. One 2021 study published in Menopause comparing patients taking cBHT or FDA-approved HT found that side effects were significantly higher in the cBHT group (57.6% vs. 14.8%; P < .0001).
But manufacturers of cBHT claim that their products prevent cardiovascular disease and Alzheimer’s disease and decrease the risk for breast cancer and stroke – assertions that are at best unproven, according to Dr. Kauffman.
The National Academies of Sciences, Engineering, and Medicine in 2020 said that clinicians have a duty to inform patients of the insufficient evidence to support clinical use of cBHT and should prescribe the products only to patients with documented allergies to an active ingredient in an FDA-approved agent or who require an alternative dosage.
Patients may also have to pay much more out of pocket for cBHT products because they often are not covered by insurance. Generic HT products, meanwhile, are relatively inexpensive and typically are covered, he noted.
“We have to be careful to avoid financial harm to patients by prescribing things, which are much more expensive than those which are usually available,” Dr. Kauffman said.
Prescribing any non–FDA-approved product, especially when biosimilars are available, places physicians at legal risk, Dr. Kauffman said. Physicians who recommend cBHT should inform patients that the products are not FDA approved and carefully document this discussion in the patient’s electronic health record. State boards of medicine can sanction physicians for “coercion” for prescribing cBHT products without mentioning alternatives, he added.
JoAnn Pinkerton, MD, professor of obstetrics and gynecology at the University of Virginia, Charlottesville, and executive director emeritus of NAMS, who attended the session, praised Dr. Kauffman for providing a balanced and evidence-based overview of the subject.
“There are issues concerning safety, contaminants, and not knowing exactly what dose you’re getting,” with compounded hormones, Dr. Pinkerton said. “They’re being hyped as safer and more effective when in reality, we don’t have any studies that show that information.”
Dr. Pinkerton noted that while a compounded form of physiological testosterone might be relatively reliable, “if you’re using something like a pellet that is super physiologic with incredibly high doses, that you really don’t have any information to stand on that it’s safe or effective ... it might be putting your license at risk.”
A version of this article first appeared on Medscape.com.
BALTIMORE – according to an expert at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists (ACOG).
Clinicians write an estimated 26 to 33 million prescriptions for compounded bioidentical hormone therapy (cBHT) every year, and almost 41% of menopausal women who need treatment try cBHT during their lives. But these drugs lack the approval for this indication from the Food and Drug Administration.
“There is a public perception that this is natural, safer, and anti-aging,” said Robert Kauffman, MD, a professor of obstetrics and gynecology and assistant dean for research at Texas Tech University Health Sciences Center in Amarillo.
Following the 2002 Women’s Health Initiative report showing a link between hormone therapy (HT) and an increase in the incidence of breast cancer, medical schools have slowed or paused instructing trainees on the traditional treatment, Dr. Kauffman said. The association was later determined to be spurious: HT is not associated with a risk for all-cause mortality or deaths from cardiovascular disease or cancer. However, HT still is largely ignored by younger physicians, Dr. Kauffman said, because of unsubstantiated “dangers” such as heart attack, stroke, and deep vein thrombosis.
The lack of education on HT for medical school students and residents has “opened the door to unsubstantiated marketing claims and practices” for cBHT, Dr. Kauffman said. “Hence, the use of compounded bioidentical hormone therapy has increased” as clinicians look for alternatives.
Groups including ACOG, the North American Menopause Society (NAMS), and the U.S. Preventive Services Task Force recommend against the use of Non–FDA-approved therapies such as cBHT, except for narrow indications. Dr. Kauffman said that drug manufacturers have not conducted randomized controlled trials or observational studies on cBHT in treating menopause.
He cited studies showing quality problems with the compounding process of these drugs, and wide variations in the amount of actual ingredients from product labels. One 2021 study published in Menopause comparing patients taking cBHT or FDA-approved HT found that side effects were significantly higher in the cBHT group (57.6% vs. 14.8%; P < .0001).
But manufacturers of cBHT claim that their products prevent cardiovascular disease and Alzheimer’s disease and decrease the risk for breast cancer and stroke – assertions that are at best unproven, according to Dr. Kauffman.
The National Academies of Sciences, Engineering, and Medicine in 2020 said that clinicians have a duty to inform patients of the insufficient evidence to support clinical use of cBHT and should prescribe the products only to patients with documented allergies to an active ingredient in an FDA-approved agent or who require an alternative dosage.
Patients may also have to pay much more out of pocket for cBHT products because they often are not covered by insurance. Generic HT products, meanwhile, are relatively inexpensive and typically are covered, he noted.
“We have to be careful to avoid financial harm to patients by prescribing things, which are much more expensive than those which are usually available,” Dr. Kauffman said.
Prescribing any non–FDA-approved product, especially when biosimilars are available, places physicians at legal risk, Dr. Kauffman said. Physicians who recommend cBHT should inform patients that the products are not FDA approved and carefully document this discussion in the patient’s electronic health record. State boards of medicine can sanction physicians for “coercion” for prescribing cBHT products without mentioning alternatives, he added.
JoAnn Pinkerton, MD, professor of obstetrics and gynecology at the University of Virginia, Charlottesville, and executive director emeritus of NAMS, who attended the session, praised Dr. Kauffman for providing a balanced and evidence-based overview of the subject.
“There are issues concerning safety, contaminants, and not knowing exactly what dose you’re getting,” with compounded hormones, Dr. Pinkerton said. “They’re being hyped as safer and more effective when in reality, we don’t have any studies that show that information.”
Dr. Pinkerton noted that while a compounded form of physiological testosterone might be relatively reliable, “if you’re using something like a pellet that is super physiologic with incredibly high doses, that you really don’t have any information to stand on that it’s safe or effective ... it might be putting your license at risk.”
A version of this article first appeared on Medscape.com.
BALTIMORE – according to an expert at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists (ACOG).
Clinicians write an estimated 26 to 33 million prescriptions for compounded bioidentical hormone therapy (cBHT) every year, and almost 41% of menopausal women who need treatment try cBHT during their lives. But these drugs lack the approval for this indication from the Food and Drug Administration.
“There is a public perception that this is natural, safer, and anti-aging,” said Robert Kauffman, MD, a professor of obstetrics and gynecology and assistant dean for research at Texas Tech University Health Sciences Center in Amarillo.
Following the 2002 Women’s Health Initiative report showing a link between hormone therapy (HT) and an increase in the incidence of breast cancer, medical schools have slowed or paused instructing trainees on the traditional treatment, Dr. Kauffman said. The association was later determined to be spurious: HT is not associated with a risk for all-cause mortality or deaths from cardiovascular disease or cancer. However, HT still is largely ignored by younger physicians, Dr. Kauffman said, because of unsubstantiated “dangers” such as heart attack, stroke, and deep vein thrombosis.
The lack of education on HT for medical school students and residents has “opened the door to unsubstantiated marketing claims and practices” for cBHT, Dr. Kauffman said. “Hence, the use of compounded bioidentical hormone therapy has increased” as clinicians look for alternatives.
Groups including ACOG, the North American Menopause Society (NAMS), and the U.S. Preventive Services Task Force recommend against the use of Non–FDA-approved therapies such as cBHT, except for narrow indications. Dr. Kauffman said that drug manufacturers have not conducted randomized controlled trials or observational studies on cBHT in treating menopause.
He cited studies showing quality problems with the compounding process of these drugs, and wide variations in the amount of actual ingredients from product labels. One 2021 study published in Menopause comparing patients taking cBHT or FDA-approved HT found that side effects were significantly higher in the cBHT group (57.6% vs. 14.8%; P < .0001).
But manufacturers of cBHT claim that their products prevent cardiovascular disease and Alzheimer’s disease and decrease the risk for breast cancer and stroke – assertions that are at best unproven, according to Dr. Kauffman.
The National Academies of Sciences, Engineering, and Medicine in 2020 said that clinicians have a duty to inform patients of the insufficient evidence to support clinical use of cBHT and should prescribe the products only to patients with documented allergies to an active ingredient in an FDA-approved agent or who require an alternative dosage.
Patients may also have to pay much more out of pocket for cBHT products because they often are not covered by insurance. Generic HT products, meanwhile, are relatively inexpensive and typically are covered, he noted.
“We have to be careful to avoid financial harm to patients by prescribing things, which are much more expensive than those which are usually available,” Dr. Kauffman said.
Prescribing any non–FDA-approved product, especially when biosimilars are available, places physicians at legal risk, Dr. Kauffman said. Physicians who recommend cBHT should inform patients that the products are not FDA approved and carefully document this discussion in the patient’s electronic health record. State boards of medicine can sanction physicians for “coercion” for prescribing cBHT products without mentioning alternatives, he added.
JoAnn Pinkerton, MD, professor of obstetrics and gynecology at the University of Virginia, Charlottesville, and executive director emeritus of NAMS, who attended the session, praised Dr. Kauffman for providing a balanced and evidence-based overview of the subject.
“There are issues concerning safety, contaminants, and not knowing exactly what dose you’re getting,” with compounded hormones, Dr. Pinkerton said. “They’re being hyped as safer and more effective when in reality, we don’t have any studies that show that information.”
Dr. Pinkerton noted that while a compounded form of physiological testosterone might be relatively reliable, “if you’re using something like a pellet that is super physiologic with incredibly high doses, that you really don’t have any information to stand on that it’s safe or effective ... it might be putting your license at risk.”
A version of this article first appeared on Medscape.com.
AT ACOG 2023










